User login
Uncorking the negative emotions of IBS
CHICAGO – For patients with irritable bowel syndrome, expressing rather than bottling up negative emotions may be just what the doctor ordered, according to Elyse R. Thakur, Ph.D.
A novel psychological intervention designed to elicit negative emotions was associated with a significantly greater reduction in IBS symptom severity at 4 weeks than standard medical care (mean, 3.62 vs. 4.68; P = .004) and reductions similar to those seen with relaxation training (mean, 3.62 vs. 4.16; P = .126).
By 12 weeks, there were no differences between groups, and all patients continued to improve, Dr. Thakur of the DeBakey VA Medical Center and Baylor College of Medicine in Houston reported at the meeting sponsored by the American Gastroenterological Association.
One patient who had IBS-related nausea off and on for years wrote after Emotional Awareness and Expression Training (EAET): “I feel lighter, and after the exercise to deal with a particularly traumatic event, I feel less angry and less tense. I can’t say that my IBS is completely gone, but the symptoms have definitely gotten better.”
Psychological interventions for IBS have traditionally emphasized suppressing negative emotions such as anxiety and sadness through psychophysiologic strategies such as relaxation training (RT).
Recent research, however, suggests this suppression may be counterproductive. In a study involving 47 healthy controls, self-reported anger suppression predicted greater pain intensity in response to the cold pressor ice water immersion test (Ann Behav Med. 2010 Jun;39[3]:211-21).
While at the Wayne State University stress and health lab in Detroit, Dr. Thakur and her then graduate school adviser Mark Lumley, Ph.D., opted to take a different tact and developed the EAET based on the principle that emotional awareness and suppression can lead to stress-related symptoms and a dysregulated brain-gut system.
The goal of the intervention is to help patients reduce stress by having them learn about connections between stressful life experiences and physical symptoms; by teaching them to identify, experience, and express their emotions related to these stressful situations; and by encouraging them to engage in healthy emotional and interpersonal behaviors in their daily lives, including assertive and genuine communication, Dr. Thakur explained.
To facilitate this process, patients undergo a life-history interview, which helps them connect their IBS episodes to their life experiences. The therapist then conducts experiential exercises such as role playing and imagery to help patients engage with their avoided feelings, behaviors, memories, and relationships through their tone of voice, words, and body language. Finally, patients are encouraged to communicate more genuinely in their relationships, she said.
To evaluate the intervention, 106 patients who met the Rome III IBS diagnostic criteria were recruited from the community and gastroenterologic clinics, and evenly randomized to standard medical care or three 50-minute individualized sessions per week of EAET or RT including progressive muscle relaxation, relaxed breathing skills, and guided imagery. Patients had to have at least moderately severe IBS symptoms at least 2 days per week at the time of screening. Their mean age was 36 years, 80.2% were female, and 65% were of European-American descent.
Outcomes were measured at 4 and 12 weeks by using the IBS Symptom Severity Scale, Brief Symptom Inventory, and IBS Quality of Life questionnaire.
At 4 weeks, EAET and RT significantly reduced anxiety (mean, 0.71 and 0.62 vs. 1.16; P = .003 and P = .001, respectively) and hostility (mean, 0.56 and 0.60 vs. 0.89; P = .013 and P = .029, respectively), compared with controls, Dr. Thakur reported in a poster at the meeting.
“These findings suggest that techniques that enhance awareness, experiencing, and expression of negative emotions resulting from life stress and psychological conflicts are as effective in reducing anxiety and hostility as somatic control techniques,” she said in an interview.
RT significantly reduced depression, compared with standard care (mean, 0.52 vs. 1.02; P = .002), while EAET did not (mean, 0.77 vs. 1.02; P = .119).
This finding was unexpected, “albeit in retrospect, not surprising because emotional processing interventions often negatively impact the moods of people, at least in the short term, as they deal with the newfound awareness of their conflicts,” Dr. Thakur explained.
At 12 weeks, EAET and relaxation training maintained the improvements in anxiety and hostility, but the differences were no longer statistically significant because the standard care group improved, she noted.
Poor quality of life was significantly less common among patients receiving EAET and RT than standard medical care at 4 weeks (mean, 2.12 vs. 2.22 vs. 2.61; both P values less than .001) and 12 weeks (mean, 1.98 vs. 2.04 vs. 2.39; P = .004 and P = .016, respectively).
“These findings have broadened my conceptualization of IBS patients and provided me with a viable treatment alternative for those patients who have difficulties with emotional awareness and expression,” Dr. Thakur said in the interview.
Future research goals are to determine the types of patients for whom EAET is best suited, explore whether EAET and RT work best when integrated, and identify the best ways to implement brief, psychological interventions in routine practice settings, she said.
The study was funded by Blue Cross Blue Shied of Michigan, American Psychological Association, and Wayne State University. Dr. Thakur reported having no financial disclosures.
On Twitter @pwendl
CHICAGO – For patients with irritable bowel syndrome, expressing rather than bottling up negative emotions may be just what the doctor ordered, according to Elyse R. Thakur, Ph.D.
A novel psychological intervention designed to elicit negative emotions was associated with a significantly greater reduction in IBS symptom severity at 4 weeks than standard medical care (mean, 3.62 vs. 4.68; P = .004) and reductions similar to those seen with relaxation training (mean, 3.62 vs. 4.16; P = .126).
By 12 weeks, there were no differences between groups, and all patients continued to improve, Dr. Thakur of the DeBakey VA Medical Center and Baylor College of Medicine in Houston reported at the meeting sponsored by the American Gastroenterological Association.
One patient who had IBS-related nausea off and on for years wrote after Emotional Awareness and Expression Training (EAET): “I feel lighter, and after the exercise to deal with a particularly traumatic event, I feel less angry and less tense. I can’t say that my IBS is completely gone, but the symptoms have definitely gotten better.”
Psychological interventions for IBS have traditionally emphasized suppressing negative emotions such as anxiety and sadness through psychophysiologic strategies such as relaxation training (RT).
Recent research, however, suggests this suppression may be counterproductive. In a study involving 47 healthy controls, self-reported anger suppression predicted greater pain intensity in response to the cold pressor ice water immersion test (Ann Behav Med. 2010 Jun;39[3]:211-21).
While at the Wayne State University stress and health lab in Detroit, Dr. Thakur and her then graduate school adviser Mark Lumley, Ph.D., opted to take a different tact and developed the EAET based on the principle that emotional awareness and suppression can lead to stress-related symptoms and a dysregulated brain-gut system.
The goal of the intervention is to help patients reduce stress by having them learn about connections between stressful life experiences and physical symptoms; by teaching them to identify, experience, and express their emotions related to these stressful situations; and by encouraging them to engage in healthy emotional and interpersonal behaviors in their daily lives, including assertive and genuine communication, Dr. Thakur explained.
To facilitate this process, patients undergo a life-history interview, which helps them connect their IBS episodes to their life experiences. The therapist then conducts experiential exercises such as role playing and imagery to help patients engage with their avoided feelings, behaviors, memories, and relationships through their tone of voice, words, and body language. Finally, patients are encouraged to communicate more genuinely in their relationships, she said.
To evaluate the intervention, 106 patients who met the Rome III IBS diagnostic criteria were recruited from the community and gastroenterologic clinics, and evenly randomized to standard medical care or three 50-minute individualized sessions per week of EAET or RT including progressive muscle relaxation, relaxed breathing skills, and guided imagery. Patients had to have at least moderately severe IBS symptoms at least 2 days per week at the time of screening. Their mean age was 36 years, 80.2% were female, and 65% were of European-American descent.
Outcomes were measured at 4 and 12 weeks by using the IBS Symptom Severity Scale, Brief Symptom Inventory, and IBS Quality of Life questionnaire.
At 4 weeks, EAET and RT significantly reduced anxiety (mean, 0.71 and 0.62 vs. 1.16; P = .003 and P = .001, respectively) and hostility (mean, 0.56 and 0.60 vs. 0.89; P = .013 and P = .029, respectively), compared with controls, Dr. Thakur reported in a poster at the meeting.
“These findings suggest that techniques that enhance awareness, experiencing, and expression of negative emotions resulting from life stress and psychological conflicts are as effective in reducing anxiety and hostility as somatic control techniques,” she said in an interview.
RT significantly reduced depression, compared with standard care (mean, 0.52 vs. 1.02; P = .002), while EAET did not (mean, 0.77 vs. 1.02; P = .119).
This finding was unexpected, “albeit in retrospect, not surprising because emotional processing interventions often negatively impact the moods of people, at least in the short term, as they deal with the newfound awareness of their conflicts,” Dr. Thakur explained.
At 12 weeks, EAET and relaxation training maintained the improvements in anxiety and hostility, but the differences were no longer statistically significant because the standard care group improved, she noted.
Poor quality of life was significantly less common among patients receiving EAET and RT than standard medical care at 4 weeks (mean, 2.12 vs. 2.22 vs. 2.61; both P values less than .001) and 12 weeks (mean, 1.98 vs. 2.04 vs. 2.39; P = .004 and P = .016, respectively).
“These findings have broadened my conceptualization of IBS patients and provided me with a viable treatment alternative for those patients who have difficulties with emotional awareness and expression,” Dr. Thakur said in the interview.
Future research goals are to determine the types of patients for whom EAET is best suited, explore whether EAET and RT work best when integrated, and identify the best ways to implement brief, psychological interventions in routine practice settings, she said.
The study was funded by Blue Cross Blue Shied of Michigan, American Psychological Association, and Wayne State University. Dr. Thakur reported having no financial disclosures.
On Twitter @pwendl
CHICAGO – For patients with irritable bowel syndrome, expressing rather than bottling up negative emotions may be just what the doctor ordered, according to Elyse R. Thakur, Ph.D.
A novel psychological intervention designed to elicit negative emotions was associated with a significantly greater reduction in IBS symptom severity at 4 weeks than standard medical care (mean, 3.62 vs. 4.68; P = .004) and reductions similar to those seen with relaxation training (mean, 3.62 vs. 4.16; P = .126).
By 12 weeks, there were no differences between groups, and all patients continued to improve, Dr. Thakur of the DeBakey VA Medical Center and Baylor College of Medicine in Houston reported at the meeting sponsored by the American Gastroenterological Association.
One patient who had IBS-related nausea off and on for years wrote after Emotional Awareness and Expression Training (EAET): “I feel lighter, and after the exercise to deal with a particularly traumatic event, I feel less angry and less tense. I can’t say that my IBS is completely gone, but the symptoms have definitely gotten better.”
Psychological interventions for IBS have traditionally emphasized suppressing negative emotions such as anxiety and sadness through psychophysiologic strategies such as relaxation training (RT).
Recent research, however, suggests this suppression may be counterproductive. In a study involving 47 healthy controls, self-reported anger suppression predicted greater pain intensity in response to the cold pressor ice water immersion test (Ann Behav Med. 2010 Jun;39[3]:211-21).
While at the Wayne State University stress and health lab in Detroit, Dr. Thakur and her then graduate school adviser Mark Lumley, Ph.D., opted to take a different tact and developed the EAET based on the principle that emotional awareness and suppression can lead to stress-related symptoms and a dysregulated brain-gut system.
The goal of the intervention is to help patients reduce stress by having them learn about connections between stressful life experiences and physical symptoms; by teaching them to identify, experience, and express their emotions related to these stressful situations; and by encouraging them to engage in healthy emotional and interpersonal behaviors in their daily lives, including assertive and genuine communication, Dr. Thakur explained.
To facilitate this process, patients undergo a life-history interview, which helps them connect their IBS episodes to their life experiences. The therapist then conducts experiential exercises such as role playing and imagery to help patients engage with their avoided feelings, behaviors, memories, and relationships through their tone of voice, words, and body language. Finally, patients are encouraged to communicate more genuinely in their relationships, she said.
To evaluate the intervention, 106 patients who met the Rome III IBS diagnostic criteria were recruited from the community and gastroenterologic clinics, and evenly randomized to standard medical care or three 50-minute individualized sessions per week of EAET or RT including progressive muscle relaxation, relaxed breathing skills, and guided imagery. Patients had to have at least moderately severe IBS symptoms at least 2 days per week at the time of screening. Their mean age was 36 years, 80.2% were female, and 65% were of European-American descent.
Outcomes were measured at 4 and 12 weeks by using the IBS Symptom Severity Scale, Brief Symptom Inventory, and IBS Quality of Life questionnaire.
At 4 weeks, EAET and RT significantly reduced anxiety (mean, 0.71 and 0.62 vs. 1.16; P = .003 and P = .001, respectively) and hostility (mean, 0.56 and 0.60 vs. 0.89; P = .013 and P = .029, respectively), compared with controls, Dr. Thakur reported in a poster at the meeting.
“These findings suggest that techniques that enhance awareness, experiencing, and expression of negative emotions resulting from life stress and psychological conflicts are as effective in reducing anxiety and hostility as somatic control techniques,” she said in an interview.
RT significantly reduced depression, compared with standard care (mean, 0.52 vs. 1.02; P = .002), while EAET did not (mean, 0.77 vs. 1.02; P = .119).
This finding was unexpected, “albeit in retrospect, not surprising because emotional processing interventions often negatively impact the moods of people, at least in the short term, as they deal with the newfound awareness of their conflicts,” Dr. Thakur explained.
At 12 weeks, EAET and relaxation training maintained the improvements in anxiety and hostility, but the differences were no longer statistically significant because the standard care group improved, she noted.
Poor quality of life was significantly less common among patients receiving EAET and RT than standard medical care at 4 weeks (mean, 2.12 vs. 2.22 vs. 2.61; both P values less than .001) and 12 weeks (mean, 1.98 vs. 2.04 vs. 2.39; P = .004 and P = .016, respectively).
“These findings have broadened my conceptualization of IBS patients and provided me with a viable treatment alternative for those patients who have difficulties with emotional awareness and expression,” Dr. Thakur said in the interview.
Future research goals are to determine the types of patients for whom EAET is best suited, explore whether EAET and RT work best when integrated, and identify the best ways to implement brief, psychological interventions in routine practice settings, she said.
The study was funded by Blue Cross Blue Shied of Michigan, American Psychological Association, and Wayne State University. Dr. Thakur reported having no financial disclosures.
On Twitter @pwendl
AT THE 2015 JAMES W. FRESTON CONFERENCE
Key clinical point: A psychological intervention designed to elicit negative emotions may have therapeutic advantages over somatic control techniques in patients with IBS.
Major finding: Emotional Awareness and Expression Training was associated with a significantly greater reduction in IBS symptom severity at 4 weeks than treatment as usual (mean, 3.62 vs. 4.68; P = .004) and reductions similar to those seen with relaxation training (mean, 3.62 vs. 4.16; P = .126).
Data source: A randomized clinical trial in 106 patients with IBS.
Disclosures: The study was funded by Blue Cross Blue Shield of Michigan, American Psychological Association, and Wayne State University. Dr. Thakur reported having no financial disclosures.
Symptom-based diagnostic criteria: A work in progress in IBS
CHICAGO – Symptom-based criteria provide a substrate to diagnose patients with irritable bowel syndrome, but these criteria have their own distinct limitations, according to Dr. Douglas Drossman.
They’re too cumbersome for clinical diagnosis, they don’t help clinicians determine the diagnostic pathway, and their time frame and frequency criteria prevent treatment of subthreshold symptoms, Dr. Drossman said at the meeting sponsored by the American Gastroenterological Association.
They’re also not precise enough to identify meaningful physiologic subgroups that might lead to more targeted treatment and don’t fully characterize the complex variability in clinical presentation.
“A patient with IBS in primary care is going to be very different than the patient with IBS in the referral setting. They oversimplify the dimensionality of the illness by just using criteria,” he added.
The Rome IV diagnostic criteria, which are due out in spring 2016, try to address some of these limitations by further simplifying some of the 2006 Rome III diagnostic criteria and creating clinical algorithms that provide clinicians with a pathway leading to diagnosis and subtyping.
To address the severity and variability of clinical presentation, a Multi-Dimensional Clinical Profile (MDCP) system has been created that incorporates diagnostic criteria with additional clinical, quality of life, psychosocial, and physiologic parameters to help create a more precise, individualized treatment plan for patients with functional gastrointestinal disorders, Dr. Drossman, president of the Rome Foundation, said.
“The rationale is that with the Rome criteria, you either have it or you don’t,” he explained. “It’s a categorical classification system. The MDCP augments the criteria by providing patient-specific information.”
The MDCP has five categories beginning with the diagnosis (category A), which can be made using traditional symptom-based criteria like the Rome diagnostic criteria, but may also include physiologic criteria.
Category B is the clinical modifiers that are not part of the diagnostic criteria such as IBS-C (constipation); IBS-D (diarrhea); IBS-M (mixed); postinfective IBS; sphincter of Oddi dysfunction I, II, or III; or FODMAP (fermentable, oligosaccharides, disaccharides, monosaccharides, and polyols) sensitivity.
“This is going to help you in terms of treatment by drilling down a bit on the symptoms,” Dr. Drossman said.
Category C is essentially a single quality of life question: “How do your symptoms interfere with life?” that results in a rating of mild, moderate, or severe.
Category D is psychosocial modifiers or comorbidities. They may be categorical like a DSM-IV diagnosis of anxiety or depression, dimensional like a Rome psychosocial red flag, or patient reported such as a history of abuse. But all can impact outcome and symptom presentation, Dr. Drossman said.
Category E is physiologic modifiers, like motility, that can alter the clinical expression of the condition, and also will include validated biomarkers that will allow clinicians to subspecify patients for a particular type of treatment.
Dr. Drossman provided several case examples to illustrate how the MDCP might play out in practice and observed that a free primer on the MDCP, which includes cases, is now downloadable from the Rome Foundation website.
Finally, the Rome Foundation formed a partnership with LogicNets to develop and deliver an online decision support system for the next generation of MDCP protocols. The interactive system will guide practitioners through the decision-making pathways of the MDCP and allow gastroenterology experts worldwide to weigh in on cases, he said. The target launch date for the new platform is planned to coincide with release of the second edition of the MDCP containing the Rome IV diagnostic criteria and diagnostic algorithms.
Dr. Drossman reported having no financial conflicts of interest.
On Twitter @pwendl
CHICAGO – Symptom-based criteria provide a substrate to diagnose patients with irritable bowel syndrome, but these criteria have their own distinct limitations, according to Dr. Douglas Drossman.
They’re too cumbersome for clinical diagnosis, they don’t help clinicians determine the diagnostic pathway, and their time frame and frequency criteria prevent treatment of subthreshold symptoms, Dr. Drossman said at the meeting sponsored by the American Gastroenterological Association.
They’re also not precise enough to identify meaningful physiologic subgroups that might lead to more targeted treatment and don’t fully characterize the complex variability in clinical presentation.
“A patient with IBS in primary care is going to be very different than the patient with IBS in the referral setting. They oversimplify the dimensionality of the illness by just using criteria,” he added.
The Rome IV diagnostic criteria, which are due out in spring 2016, try to address some of these limitations by further simplifying some of the 2006 Rome III diagnostic criteria and creating clinical algorithms that provide clinicians with a pathway leading to diagnosis and subtyping.
To address the severity and variability of clinical presentation, a Multi-Dimensional Clinical Profile (MDCP) system has been created that incorporates diagnostic criteria with additional clinical, quality of life, psychosocial, and physiologic parameters to help create a more precise, individualized treatment plan for patients with functional gastrointestinal disorders, Dr. Drossman, president of the Rome Foundation, said.
“The rationale is that with the Rome criteria, you either have it or you don’t,” he explained. “It’s a categorical classification system. The MDCP augments the criteria by providing patient-specific information.”
The MDCP has five categories beginning with the diagnosis (category A), which can be made using traditional symptom-based criteria like the Rome diagnostic criteria, but may also include physiologic criteria.
Category B is the clinical modifiers that are not part of the diagnostic criteria such as IBS-C (constipation); IBS-D (diarrhea); IBS-M (mixed); postinfective IBS; sphincter of Oddi dysfunction I, II, or III; or FODMAP (fermentable, oligosaccharides, disaccharides, monosaccharides, and polyols) sensitivity.
“This is going to help you in terms of treatment by drilling down a bit on the symptoms,” Dr. Drossman said.
Category C is essentially a single quality of life question: “How do your symptoms interfere with life?” that results in a rating of mild, moderate, or severe.
Category D is psychosocial modifiers or comorbidities. They may be categorical like a DSM-IV diagnosis of anxiety or depression, dimensional like a Rome psychosocial red flag, or patient reported such as a history of abuse. But all can impact outcome and symptom presentation, Dr. Drossman said.
Category E is physiologic modifiers, like motility, that can alter the clinical expression of the condition, and also will include validated biomarkers that will allow clinicians to subspecify patients for a particular type of treatment.
Dr. Drossman provided several case examples to illustrate how the MDCP might play out in practice and observed that a free primer on the MDCP, which includes cases, is now downloadable from the Rome Foundation website.
Finally, the Rome Foundation formed a partnership with LogicNets to develop and deliver an online decision support system for the next generation of MDCP protocols. The interactive system will guide practitioners through the decision-making pathways of the MDCP and allow gastroenterology experts worldwide to weigh in on cases, he said. The target launch date for the new platform is planned to coincide with release of the second edition of the MDCP containing the Rome IV diagnostic criteria and diagnostic algorithms.
Dr. Drossman reported having no financial conflicts of interest.
On Twitter @pwendl
CHICAGO – Symptom-based criteria provide a substrate to diagnose patients with irritable bowel syndrome, but these criteria have their own distinct limitations, according to Dr. Douglas Drossman.
They’re too cumbersome for clinical diagnosis, they don’t help clinicians determine the diagnostic pathway, and their time frame and frequency criteria prevent treatment of subthreshold symptoms, Dr. Drossman said at the meeting sponsored by the American Gastroenterological Association.
They’re also not precise enough to identify meaningful physiologic subgroups that might lead to more targeted treatment and don’t fully characterize the complex variability in clinical presentation.
“A patient with IBS in primary care is going to be very different than the patient with IBS in the referral setting. They oversimplify the dimensionality of the illness by just using criteria,” he added.
The Rome IV diagnostic criteria, which are due out in spring 2016, try to address some of these limitations by further simplifying some of the 2006 Rome III diagnostic criteria and creating clinical algorithms that provide clinicians with a pathway leading to diagnosis and subtyping.
To address the severity and variability of clinical presentation, a Multi-Dimensional Clinical Profile (MDCP) system has been created that incorporates diagnostic criteria with additional clinical, quality of life, psychosocial, and physiologic parameters to help create a more precise, individualized treatment plan for patients with functional gastrointestinal disorders, Dr. Drossman, president of the Rome Foundation, said.
“The rationale is that with the Rome criteria, you either have it or you don’t,” he explained. “It’s a categorical classification system. The MDCP augments the criteria by providing patient-specific information.”
The MDCP has five categories beginning with the diagnosis (category A), which can be made using traditional symptom-based criteria like the Rome diagnostic criteria, but may also include physiologic criteria.
Category B is the clinical modifiers that are not part of the diagnostic criteria such as IBS-C (constipation); IBS-D (diarrhea); IBS-M (mixed); postinfective IBS; sphincter of Oddi dysfunction I, II, or III; or FODMAP (fermentable, oligosaccharides, disaccharides, monosaccharides, and polyols) sensitivity.
“This is going to help you in terms of treatment by drilling down a bit on the symptoms,” Dr. Drossman said.
Category C is essentially a single quality of life question: “How do your symptoms interfere with life?” that results in a rating of mild, moderate, or severe.
Category D is psychosocial modifiers or comorbidities. They may be categorical like a DSM-IV diagnosis of anxiety or depression, dimensional like a Rome psychosocial red flag, or patient reported such as a history of abuse. But all can impact outcome and symptom presentation, Dr. Drossman said.
Category E is physiologic modifiers, like motility, that can alter the clinical expression of the condition, and also will include validated biomarkers that will allow clinicians to subspecify patients for a particular type of treatment.
Dr. Drossman provided several case examples to illustrate how the MDCP might play out in practice and observed that a free primer on the MDCP, which includes cases, is now downloadable from the Rome Foundation website.
Finally, the Rome Foundation formed a partnership with LogicNets to develop and deliver an online decision support system for the next generation of MDCP protocols. The interactive system will guide practitioners through the decision-making pathways of the MDCP and allow gastroenterology experts worldwide to weigh in on cases, he said. The target launch date for the new platform is planned to coincide with release of the second edition of the MDCP containing the Rome IV diagnostic criteria and diagnostic algorithms.
Dr. Drossman reported having no financial conflicts of interest.
On Twitter @pwendl
EXPERT ANALYSIS FROM THE 2015 JAMES W. FRESTON CONFERENCE
H. pylori resistance highlights need for guided therapy
Only half of Helicobacter pylori strains were pansusceptible, and almost one in three was resistant to at least one antibiotic, according to a single-center study of U.S. veterans published in Clinical Gastroenterology and Hepatology.
The analysis is the first published report of H. pylori resistance in more than a decade, said Dr. Seiji Shiota at the Michael E. DeBakey Veterans Affairs Medical Center and the Baylor College of Medicine, Houston, and his associates. “Clarithromycin, metronidazole, and levofloxacin resistances were all high among untreated patients, suggesting that they all should be avoided as components of empiric triple therapy [consisting of a] proton pump inhibitor, amoxicillin, plus a third antibiotic,” said the researchers. “The four-drug concomitant therapy and bismuth quadruple therapy, or antibiotic susceptibility–guided therapy, are likely be the best strategies locally and are recommended for previously untreated patients with H. pylori infection.”
The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. About 90% of patients were male, and patients ranged in age from 40 to 79 years old, with an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline. (Clin Gastroenterol Hepatol. 2015 Feb 11. pii: S1542-3565(15)00122-6).
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers. The extent of levofloxacin resistance was a “new and concerning finding” that was linked in the multivariable analysis with past fluoroquinolone treatment, reflecting the rising use of fluoroquinolones in community practice, they said. “Levofloxacin has been recommended as a rescue drug to eradicate H. pylori in patients who fail first-line therapy,” they added. “Locally, it would seem to be a poor choice on the basis of the high resistance rate (31.9%), which is higher than the 10% limit suggested as a cutoff for use of fluoroquinolone-containing triple therapy for H. pylori.”
Clarithromycin resistance also rose during the study period, probably because of the rising use of macrolides in respiratory and otorhinolaryngology, the investigators noted. Patients who had been treated before for helicobacteriosis were significantly more likely to have clarithromycin-resistant H. pylori infections even after accounting for demographic factors, smoking status, gastroesophageal reflux disease, and past use of macrolides and fluoroquinolones, they said. Based on that result, patients with a history of prior helicobacteriosis should not receive clarithromycin as part of triple therapy, they emphasized.
Resistance to metronidazole also remained high, but only 1.8% of isolates were resistant to both metronidazole and clarithromycin, making combination therapy with a proton pump inhibitor, clarithromycin, metronidazole, and amoxicillin “an excellent choice as an empiric therapy,” added Dr. Shiota and his associates. Furthermore, the study might have overestimated the rate of metronidazole resistance because the E test yielded significantly higher minimum inhibitory concentration values than did agar dilution, they noted. The study cohort also was demographically dissimilar to that of the United States and might have reflected selection bias, because patients with a history of helicobacteriosis would be more likely to be referred for endoscopy, they said.
The National Institutes of Health and the Veterans Affairs Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
Antimicrobial-resistant strains of H. pylori are increasing in prevalence in the United States. In the study described here, only half of H. pylori strains were susceptible to commonly used antibiotics and approximately one in three were resistant to at least one antibiotic, according to a single-center study of U.S. veterans. The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. Patients were mostly male and had an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline.
 |
Dr. Nimish Vakil |
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers.
The study mirrors findings in Europe where similar rates of resistance have been reported. European studies have also shown that levofloxacin resistance rises rapidly when it becomes widely used in the community, The study described here is not population based and consists mostly of male subjects and therefore may not be generalizable to the rest to the rest of the United States. As culture and antimicrobial sensitivity testing is not available to most gastroenterologists, the initial treatment chosen should reflect resistance data in the community. Given the rising rates of resistance, it is important that eradication be confirmed 4 weeks or more after eradication therapy ends using a stool antigen test or a breath test. Clinicians should be prepared to re-treat patients if necessary.
Dr. Nimish Vakil, AGAF, is clinical professor of medicine at the University of Wisconsin School of Medicine and Public Health in Madison. He has no conflicts of interest.
Antimicrobial-resistant strains of H. pylori are increasing in prevalence in the United States. In the study described here, only half of H. pylori strains were susceptible to commonly used antibiotics and approximately one in three were resistant to at least one antibiotic, according to a single-center study of U.S. veterans. The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. Patients were mostly male and had an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline.
 |
Dr. Nimish Vakil |
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers.
The study mirrors findings in Europe where similar rates of resistance have been reported. European studies have also shown that levofloxacin resistance rises rapidly when it becomes widely used in the community, The study described here is not population based and consists mostly of male subjects and therefore may not be generalizable to the rest to the rest of the United States. As culture and antimicrobial sensitivity testing is not available to most gastroenterologists, the initial treatment chosen should reflect resistance data in the community. Given the rising rates of resistance, it is important that eradication be confirmed 4 weeks or more after eradication therapy ends using a stool antigen test or a breath test. Clinicians should be prepared to re-treat patients if necessary.
Dr. Nimish Vakil, AGAF, is clinical professor of medicine at the University of Wisconsin School of Medicine and Public Health in Madison. He has no conflicts of interest.
Antimicrobial-resistant strains of H. pylori are increasing in prevalence in the United States. In the study described here, only half of H. pylori strains were susceptible to commonly used antibiotics and approximately one in three were resistant to at least one antibiotic, according to a single-center study of U.S. veterans. The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. Patients were mostly male and had an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline.
 |
Dr. Nimish Vakil |
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers.
The study mirrors findings in Europe where similar rates of resistance have been reported. European studies have also shown that levofloxacin resistance rises rapidly when it becomes widely used in the community, The study described here is not population based and consists mostly of male subjects and therefore may not be generalizable to the rest to the rest of the United States. As culture and antimicrobial sensitivity testing is not available to most gastroenterologists, the initial treatment chosen should reflect resistance data in the community. Given the rising rates of resistance, it is important that eradication be confirmed 4 weeks or more after eradication therapy ends using a stool antigen test or a breath test. Clinicians should be prepared to re-treat patients if necessary.
Dr. Nimish Vakil, AGAF, is clinical professor of medicine at the University of Wisconsin School of Medicine and Public Health in Madison. He has no conflicts of interest.
Only half of Helicobacter pylori strains were pansusceptible, and almost one in three was resistant to at least one antibiotic, according to a single-center study of U.S. veterans published in Clinical Gastroenterology and Hepatology.
The analysis is the first published report of H. pylori resistance in more than a decade, said Dr. Seiji Shiota at the Michael E. DeBakey Veterans Affairs Medical Center and the Baylor College of Medicine, Houston, and his associates. “Clarithromycin, metronidazole, and levofloxacin resistances were all high among untreated patients, suggesting that they all should be avoided as components of empiric triple therapy [consisting of a] proton pump inhibitor, amoxicillin, plus a third antibiotic,” said the researchers. “The four-drug concomitant therapy and bismuth quadruple therapy, or antibiotic susceptibility–guided therapy, are likely be the best strategies locally and are recommended for previously untreated patients with H. pylori infection.”
The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. About 90% of patients were male, and patients ranged in age from 40 to 79 years old, with an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline. (Clin Gastroenterol Hepatol. 2015 Feb 11. pii: S1542-3565(15)00122-6).
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers. The extent of levofloxacin resistance was a “new and concerning finding” that was linked in the multivariable analysis with past fluoroquinolone treatment, reflecting the rising use of fluoroquinolones in community practice, they said. “Levofloxacin has been recommended as a rescue drug to eradicate H. pylori in patients who fail first-line therapy,” they added. “Locally, it would seem to be a poor choice on the basis of the high resistance rate (31.9%), which is higher than the 10% limit suggested as a cutoff for use of fluoroquinolone-containing triple therapy for H. pylori.”
Clarithromycin resistance also rose during the study period, probably because of the rising use of macrolides in respiratory and otorhinolaryngology, the investigators noted. Patients who had been treated before for helicobacteriosis were significantly more likely to have clarithromycin-resistant H. pylori infections even after accounting for demographic factors, smoking status, gastroesophageal reflux disease, and past use of macrolides and fluoroquinolones, they said. Based on that result, patients with a history of prior helicobacteriosis should not receive clarithromycin as part of triple therapy, they emphasized.
Resistance to metronidazole also remained high, but only 1.8% of isolates were resistant to both metronidazole and clarithromycin, making combination therapy with a proton pump inhibitor, clarithromycin, metronidazole, and amoxicillin “an excellent choice as an empiric therapy,” added Dr. Shiota and his associates. Furthermore, the study might have overestimated the rate of metronidazole resistance because the E test yielded significantly higher minimum inhibitory concentration values than did agar dilution, they noted. The study cohort also was demographically dissimilar to that of the United States and might have reflected selection bias, because patients with a history of helicobacteriosis would be more likely to be referred for endoscopy, they said.
The National Institutes of Health and the Veterans Affairs Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
Only half of Helicobacter pylori strains were pansusceptible, and almost one in three was resistant to at least one antibiotic, according to a single-center study of U.S. veterans published in Clinical Gastroenterology and Hepatology.
The analysis is the first published report of H. pylori resistance in more than a decade, said Dr. Seiji Shiota at the Michael E. DeBakey Veterans Affairs Medical Center and the Baylor College of Medicine, Houston, and his associates. “Clarithromycin, metronidazole, and levofloxacin resistances were all high among untreated patients, suggesting that they all should be avoided as components of empiric triple therapy [consisting of a] proton pump inhibitor, amoxicillin, plus a third antibiotic,” said the researchers. “The four-drug concomitant therapy and bismuth quadruple therapy, or antibiotic susceptibility–guided therapy, are likely be the best strategies locally and are recommended for previously untreated patients with H. pylori infection.”
The study assessed 656 gastric biopsies randomly selected from a cohort of 1,559 patients who underwent esophagogastroduodenoscopy at the Houston VA Medical Center between 2009 and 2013. About 90% of patients were male, and patients ranged in age from 40 to 79 years old, with an average age of 60 years. The researchers cultured tissue samples and used the E test to assess minimum inhibitory concentrations for amoxicillin, clarithromycin, metronidazole, levofloxacin, and tetracycline. (Clin Gastroenterol Hepatol. 2015 Feb 11. pii: S1542-3565(15)00122-6).
A total of 135 (20.6%) of the biopsies cultured H. pylori, of which half (65 strains) were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin (95% confidence interval, 23%-39%), 20% were resistant to metronidazole (95% CI, 13%-27%), 16% were resistant to clarithromycin (95% CI, 10%-23%), 0.8% were resistant to tetracycline (95% CI, 0%-2%), and none were resistant to amoxicillin, said the researchers. The extent of levofloxacin resistance was a “new and concerning finding” that was linked in the multivariable analysis with past fluoroquinolone treatment, reflecting the rising use of fluoroquinolones in community practice, they said. “Levofloxacin has been recommended as a rescue drug to eradicate H. pylori in patients who fail first-line therapy,” they added. “Locally, it would seem to be a poor choice on the basis of the high resistance rate (31.9%), which is higher than the 10% limit suggested as a cutoff for use of fluoroquinolone-containing triple therapy for H. pylori.”
Clarithromycin resistance also rose during the study period, probably because of the rising use of macrolides in respiratory and otorhinolaryngology, the investigators noted. Patients who had been treated before for helicobacteriosis were significantly more likely to have clarithromycin-resistant H. pylori infections even after accounting for demographic factors, smoking status, gastroesophageal reflux disease, and past use of macrolides and fluoroquinolones, they said. Based on that result, patients with a history of prior helicobacteriosis should not receive clarithromycin as part of triple therapy, they emphasized.
Resistance to metronidazole also remained high, but only 1.8% of isolates were resistant to both metronidazole and clarithromycin, making combination therapy with a proton pump inhibitor, clarithromycin, metronidazole, and amoxicillin “an excellent choice as an empiric therapy,” added Dr. Shiota and his associates. Furthermore, the study might have overestimated the rate of metronidazole resistance because the E test yielded significantly higher minimum inhibitory concentration values than did agar dilution, they noted. The study cohort also was demographically dissimilar to that of the United States and might have reflected selection bias, because patients with a history of helicobacteriosis would be more likely to be referred for endoscopy, they said.
The National Institutes of Health and the Veterans Affairs Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Because H. pylori showed high rates of resistance to clarithromycin, metronidazole, and levofloxacin, they should be excluded from triple therapy regimens for helicobacteriosis.
Major finding: Half of strains were susceptible to all five antibiotics tested, 31% were resistant to levofloxacin, 20% were resistant to metronidazole, 16% were resistant to clarithromycin, 0.8% were resistant to tetracycline, and none were resistant to amoxicillin.
Data source: Analysis of gastric biopsies from 656 U.S. veterans who underwent esophagogastroduodenoscopy in Texas between 2009 and 2013.
Disclosures: The National Institutes of Health and the VA Health Services Research & Development Center for Innovations in Quality, Effectiveness, and Safety supported the study. The researchers reported having no conflicts of interest.
Gluten exposure tied to worsened GI and extraintestinal symptoms in gluten sensitivity
Consuming the equivalent of two slices of bread a day for just 1 week significantly worsened abdominal pain, bloating, foggy mind, depression, and aphthous stomatitis among patients with self-diagnosed gluten intolerance, according to a double-blind, placebo-controlled, crossover study reported in the September issue of Clinical Gastroenterology and Hepatology.
The study is unique because its patients were referred for intestinal and extraintestinal symptoms of gluten sensitivity, rather than irritable bowel syndrome, said Dr. Antonio Di Sabatino at the University of Pavia (Italy) and his associates. The study also used gluten capsules that had been shown to be indistinguishable from placebo, excluded patients with minimal baseline symptoms, and used global response as the primary outcome measure because that is patients’ major concern, the investigators said.
The existence and definition of nonceliac gluten sensitivity (NCGS) remains debatable even as patients in “crowded online forums” diagnose themselves with it, the researchers noted.
To test if NCGS exists and if so, the amount of gluten needed to cause symptoms, they conducted a randomized, double-blind, placebo-controlled trial of 61 self-diagnosed patients with no history of wheat allergy or celiac disease. Patients ingested either 4.375 g of gluten – the equivalent of two slices of wheat bread – or placebo rice starch in capsule form every day for 1 week. Then they followed a gluten-free diet for a week before crossing over to the other study arm. Each day, patients were asked to grade 15 intestinal symptoms and 13 extraintestinal symptoms on a scale of 0 (absent) to 3 (severe and interfering with daily activities). The group averaged 39 years of age, and 87% were female, the investigators said (Clin Gastroenterol Hepatol. 2015 doi: 10.1016/j.cgh.2015.01.029).
Among 59 patients who finished the trial, gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034), said the researchers. Patients also reported significantly worse abdominal bloating (P = .04), abdominal pain (P = .047), aphthous stomatitis (P = .025), foggy mind (P = .019), and depression (P = .02) when they ingested gluten, compared with placebo.
“The observation that short-term exposure to gluten induced depression is remarkable,” Dr. Di Sabatino and his associates commented. “This result was supported by a recent double-blind, placebo-controlled, crossover study in which depression was assessed by an ad hoc psychiatric score (Aliment Pharmacol Ther. 2014 May;39:1104-12). The direct, highly significant correlation between symptom score and symptom prevalence at both the intestinal and extraintestinal levels is indirect proof of the validity of our findings.”
The study did not yield data on identifiable biomarkers, nor did it pinpoint pathogenic mechanisms for NCGS, the investigators acknowledged.
“Self-prescription of gluten withdrawal is becoming increasingly common, but this behavior should be strongly discouraged because it may lead to the consequent preclusion of a proper diagnosis of celiac disease and to a high and unjustified economic burden,” they emphasized. “Because a reliable marker of NCGS is not readily available at present, double-blind, placebo-controlled trials are mandatory to ascertain this condition.” Their laboratory is working to identify cytokines in the duodenal mucosa of patients in the trial, and early results have not implicated innate or adaptive immune mechanisms for NCGS, they said.
St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
Consuming the equivalent of two slices of bread a day for just 1 week significantly worsened abdominal pain, bloating, foggy mind, depression, and aphthous stomatitis among patients with self-diagnosed gluten intolerance, according to a double-blind, placebo-controlled, crossover study reported in the September issue of Clinical Gastroenterology and Hepatology.
The study is unique because its patients were referred for intestinal and extraintestinal symptoms of gluten sensitivity, rather than irritable bowel syndrome, said Dr. Antonio Di Sabatino at the University of Pavia (Italy) and his associates. The study also used gluten capsules that had been shown to be indistinguishable from placebo, excluded patients with minimal baseline symptoms, and used global response as the primary outcome measure because that is patients’ major concern, the investigators said.
The existence and definition of nonceliac gluten sensitivity (NCGS) remains debatable even as patients in “crowded online forums” diagnose themselves with it, the researchers noted.
To test if NCGS exists and if so, the amount of gluten needed to cause symptoms, they conducted a randomized, double-blind, placebo-controlled trial of 61 self-diagnosed patients with no history of wheat allergy or celiac disease. Patients ingested either 4.375 g of gluten – the equivalent of two slices of wheat bread – or placebo rice starch in capsule form every day for 1 week. Then they followed a gluten-free diet for a week before crossing over to the other study arm. Each day, patients were asked to grade 15 intestinal symptoms and 13 extraintestinal symptoms on a scale of 0 (absent) to 3 (severe and interfering with daily activities). The group averaged 39 years of age, and 87% were female, the investigators said (Clin Gastroenterol Hepatol. 2015 doi: 10.1016/j.cgh.2015.01.029).
Among 59 patients who finished the trial, gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034), said the researchers. Patients also reported significantly worse abdominal bloating (P = .04), abdominal pain (P = .047), aphthous stomatitis (P = .025), foggy mind (P = .019), and depression (P = .02) when they ingested gluten, compared with placebo.
“The observation that short-term exposure to gluten induced depression is remarkable,” Dr. Di Sabatino and his associates commented. “This result was supported by a recent double-blind, placebo-controlled, crossover study in which depression was assessed by an ad hoc psychiatric score (Aliment Pharmacol Ther. 2014 May;39:1104-12). The direct, highly significant correlation between symptom score and symptom prevalence at both the intestinal and extraintestinal levels is indirect proof of the validity of our findings.”
The study did not yield data on identifiable biomarkers, nor did it pinpoint pathogenic mechanisms for NCGS, the investigators acknowledged.
“Self-prescription of gluten withdrawal is becoming increasingly common, but this behavior should be strongly discouraged because it may lead to the consequent preclusion of a proper diagnosis of celiac disease and to a high and unjustified economic burden,” they emphasized. “Because a reliable marker of NCGS is not readily available at present, double-blind, placebo-controlled trials are mandatory to ascertain this condition.” Their laboratory is working to identify cytokines in the duodenal mucosa of patients in the trial, and early results have not implicated innate or adaptive immune mechanisms for NCGS, they said.
St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
Consuming the equivalent of two slices of bread a day for just 1 week significantly worsened abdominal pain, bloating, foggy mind, depression, and aphthous stomatitis among patients with self-diagnosed gluten intolerance, according to a double-blind, placebo-controlled, crossover study reported in the September issue of Clinical Gastroenterology and Hepatology.
The study is unique because its patients were referred for intestinal and extraintestinal symptoms of gluten sensitivity, rather than irritable bowel syndrome, said Dr. Antonio Di Sabatino at the University of Pavia (Italy) and his associates. The study also used gluten capsules that had been shown to be indistinguishable from placebo, excluded patients with minimal baseline symptoms, and used global response as the primary outcome measure because that is patients’ major concern, the investigators said.
The existence and definition of nonceliac gluten sensitivity (NCGS) remains debatable even as patients in “crowded online forums” diagnose themselves with it, the researchers noted.
To test if NCGS exists and if so, the amount of gluten needed to cause symptoms, they conducted a randomized, double-blind, placebo-controlled trial of 61 self-diagnosed patients with no history of wheat allergy or celiac disease. Patients ingested either 4.375 g of gluten – the equivalent of two slices of wheat bread – or placebo rice starch in capsule form every day for 1 week. Then they followed a gluten-free diet for a week before crossing over to the other study arm. Each day, patients were asked to grade 15 intestinal symptoms and 13 extraintestinal symptoms on a scale of 0 (absent) to 3 (severe and interfering with daily activities). The group averaged 39 years of age, and 87% were female, the investigators said (Clin Gastroenterol Hepatol. 2015 doi: 10.1016/j.cgh.2015.01.029).
Among 59 patients who finished the trial, gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034), said the researchers. Patients also reported significantly worse abdominal bloating (P = .04), abdominal pain (P = .047), aphthous stomatitis (P = .025), foggy mind (P = .019), and depression (P = .02) when they ingested gluten, compared with placebo.
“The observation that short-term exposure to gluten induced depression is remarkable,” Dr. Di Sabatino and his associates commented. “This result was supported by a recent double-blind, placebo-controlled, crossover study in which depression was assessed by an ad hoc psychiatric score (Aliment Pharmacol Ther. 2014 May;39:1104-12). The direct, highly significant correlation between symptom score and symptom prevalence at both the intestinal and extraintestinal levels is indirect proof of the validity of our findings.”
The study did not yield data on identifiable biomarkers, nor did it pinpoint pathogenic mechanisms for NCGS, the investigators acknowledged.
“Self-prescription of gluten withdrawal is becoming increasingly common, but this behavior should be strongly discouraged because it may lead to the consequent preclusion of a proper diagnosis of celiac disease and to a high and unjustified economic burden,” they emphasized. “Because a reliable marker of NCGS is not readily available at present, double-blind, placebo-controlled trials are mandatory to ascertain this condition.” Their laboratory is working to identify cytokines in the duodenal mucosa of patients in the trial, and early results have not implicated innate or adaptive immune mechanisms for NCGS, they said.
St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Patients with self-diagnosed gluten sensitivity reported significantly worse intestinal and extraintestinal symptoms when ingesting small amounts of gluten, compared with placebo.
Major finding: Gluten intake was tied to significantly higher overall symptom scores, compared with placebo (median score, 55 vs. 33; P = .034).
Data source: Double-blind, placebo-controlled, crossover trial of 61 patients with self-diagnosed gluten sensitivity.
Disclosures: St. Matteo Hospital Foundation supported the research, and Giuliani Pharma provided the capsules used in the study. The investigators reported having no conflicts of interest.
IBD surveillance: Quality not quantity
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
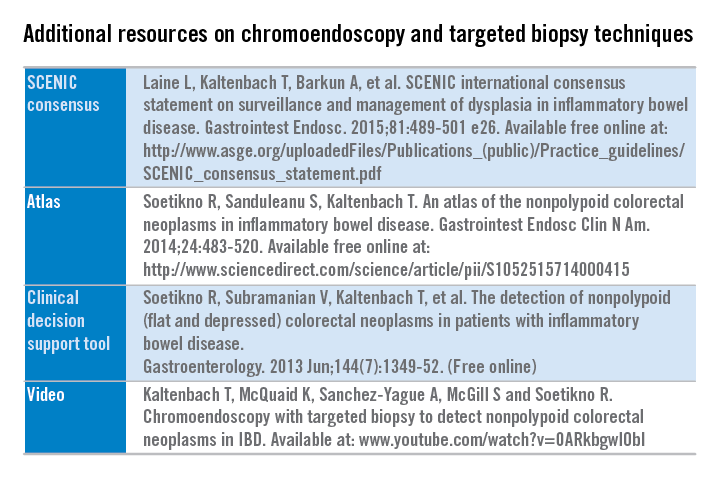
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
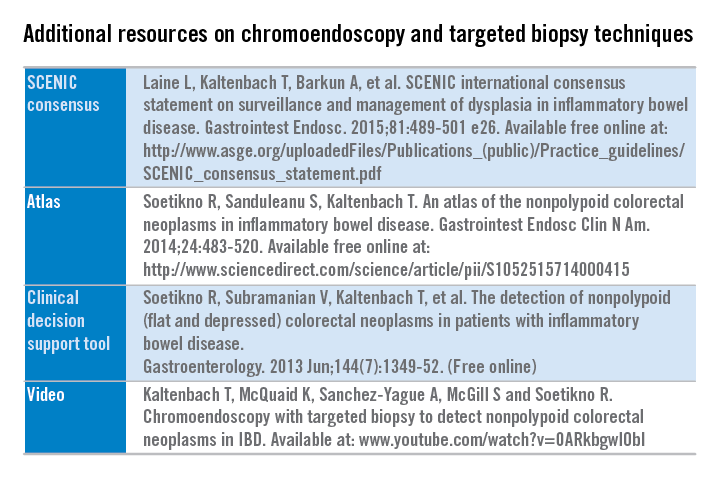
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Optimizing colonoscopy quality in patients with ulcerative colitis or Crohn’s disease involving the colon is important. Their risk for the development of colorectal cancer (CRC) and of interval CRC is significantly higher compared with the non–inflammatory bowel disease (IBD) population.
Most CRC cases in IBD are believed to arise from dysplasia, and thus, surveillance colonoscopy is recommended to detect dysplasia. Key factors that influence the success of surveillance colonoscopy in IBD patients include: 1) endoscopic recognition of dysplasia, 2) adequacy of mucosal sampling, 3) awareness of interfering anatomy, such as strictures and pseudopolyps, 4) appropriate differentiation of dysplastic lesions as endoscopically resectable, 5) complete removal of endoscopically resectable dysplasia, and 6) patient compliance.
Over a decade ago, we learned that most dysplasia discovered in patients with IBD is actually visible. The use of high-definition video-endoscopy and newer methods, such as chromoendoscopy with mucosal dye spraying, enhance the detection of dysplasia. Today, with the widespread use of newer technologies and techniques, the literature indicates that targeted biopsies of visible lesions account for approximately 90% of cases, whereas random biopsy (resulting in detection of an endoscopically invisible lesion) accounts for only 10% of cases of identified dysplasia.
The endoscopic recognition of dysplastic colorectal lesions may have important implications for the surveillance and management of dysplasia, and shift it away from the traditional random biopsy technique, where less than 0.1% of the colonic mucosal surface area is sampled, and from colectomy for any diagnosis of dysplasia.
Enhanced endoscopy techniques such as chromoendoscopy can have a substantial impact upon IBD surveillance, increasing the dysplasia detection rates, as well as informing management decisions. Chromoendoscopy, using a dye solution of either methylene blue or indigo carmine applied onto the colonic mucosa to enhance contrast during surveillance colonoscopy, is performed either in a pancolonic fashion to detect lesions or in a targeted fashion to allow for detailed viewing of an identified lesion (Figure 1).
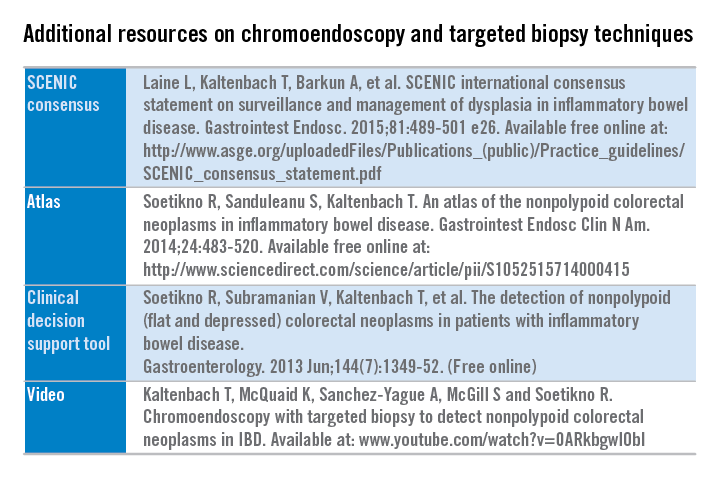
Additional resources are freely available detailing the technique and suggested steps to implement chromoendoscopy into practice. (See additional resources on chromoendoscopy and targeted biopsy techniques.)
An international multidisciplinary group, SCENIC (Surveillance for Colorectal Endoscopic Neoplasia Detection and Management in Inflammatory Bowel Disease Patients: International Consensus), which represents a wide spectrum of stakeholders and attitudes regarding IBD surveillance, sought to develop unifying consensus recommendations addressing two issues: 1) how should surveillance colonoscopy to detect dysplasia be performed, and 2) how should dysplasia identified at colonoscopy be managed. The SCENIC group adhered to suggested standards for guideline development from the Institute of Medicine and others and that incorporated the GRADE methodology. A systematic review was performed for each focused clinical question, followed by a review of a full synthesis of evidence by panelists.
SCENIC key summary recommendations
Detection
• High definition is recommended over standard definition for performance of surveillance colonoscopy.
• Routine performance of chromoendoscopy during IBD surveillance is suggested as an adjunct to high-definition colonoscopy.
• Narrowband imaging is not recommended as an alternative for high-definition, white-light colonoscopy or chromoendoscopy.
• No specific recommendation on performance of random biopsies was made in patients undergoing high-definition, white-light colonoscopy plus chromoendoscopy. The panel did not reach consensus on this topic because 60% of the panel members disagreed with performing random biopsies during chromoendoscopy, and a recommendation required 80% agreement or disagreement.
Management
• When dysplasia is detected, it should be characterized as “endoscopically resectable” or “nonendoscopically resectable” (The terms “dysplasia-associated lesion or mass (DALM),” “adenoma-like,” and “nonadenoma-like” should be abandoned).
• Visible dysplasia should be characterized according to the Paris classification polypoid or nonpolypoid, with modifications including the addition of terms for ulceration and border of the lesion.
• The term endoscopically resectable indicates that 1) distinct margins of the lesion could be identified, 2) the lesion appears to be completely removed on visual inspection after endoscopic resection, 3) histologic examination of the resected specimen is consistent with complete removal, and 4) biopsy specimens taken from mucosa immediately adjacent to the resection site are free of dysplasia on histologic examination.
• After complete removal of endoscopically resectable polypoid or nonpolypoid dysplasia, surveillance colonoscopy is recommended rather than colectomy.
• For patients with endoscopically invisible dysplasia (confirmed by a GI pathologist), referral is suggested to an endoscopist with expertise in IBD surveillance using chromoendoscopy with high-definition colonoscopy.
The SCENIC recommendations aim to optimize the detection and management of dysplasia in IBD patients. Future research in IBD surveillance should assess the potential for chromoendoscopy to improve risk stratification to elucidate optimal surveillance intervals, and the impact on CRC incidence and mortality. In addition, the role of resection of nonpolypoid dysplasia in the reduction in CRC incidence or need for colectomy requires further investigation.
Dr. Kaltenbach is a gastroenterologist at Veterans Affairs, and a clinical assistant professor of medicine at Stanford (Calif.) University. She has no conflicts of interest. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Bugs and drugs in inflammatory bowel disease
Important new themes are whether we can actually find a cure for inflammatory bowel disease and, in particular, whether there are common pathogenetic mechanisms leading to Crohn’s disease and ulcerative colitis. Are Crohn’s and ulcerative colitis infectious diseases? If the answer to that question is ‘yes,’ then eliminating that “pathogen” would turn off the immune response. Crohn’s disease and ulcerative colitis share common genetic origins with the majority of genes shared between both disorders. Indeed, 110 of the 163 confirmed loci in IBD are common between the two disorders (Nature 2012;491:119–24).
In addition to there being many genes contributing even a small amount to the development of IBD, there are also some genetic pathways that have a far more impactful role in IBD. By studying very-early-onset IBD, we have discovered that the IL-10 receptor pathway is very important in controlling intestinal inflammation, such that if you have a mutation in the receptor for IL-10 it can lead to very-early-onset IBD. Children who are born with these disorders can be treated with a hematopoietic bone marrow transplant. At this year’s Digestive Disease Week (DDW) in fact, there was the presentation of the ASTIC trial; it described patients having a prolonged remission after an autologous hematopoietic stem cell transplant.
One of the big advances that has been made in terms of the treatment of IBD is based on an understanding of the pathogenetic pathways; in particular, there has been an increase in the number of medications that are currently available to treat IBD from a variety of different avenues. There was a recent publication describing an anti-sense treatment against SMAD7 in restoring TGF-beta signaling that produced a very rapid and profound improvement in the clinical symptoms of Crohn’s disease. We await more data on that particular compound.
We now know that an antibody against P40, which is the common subunit between IL-12 and IL-23, is effective in the treatment of Crohn’s disease and is commercially available as ustekinumab. At this year’s DDW we heard about an antibody that is specific for anti-IL-23 since it only antagonizes the P19 subunit of the cytokine; it also shows great promise for treating IBD. At DDW 2014, vedolizumab had just obtained approval for the treatment of ulcerative colitis and Crohn’s disease and that has been a big advance in treating patients. On its heels are a variety of other compounds that work by a similar mechanism by inhibiting the trafficking of effector lymphocytes to the intestine; these include anti-beta7 strategies and anti-MAdCAM. Both of these have been shown to be more effective in ulcerative colitis than in Crohn’s disease, as has been a common theme.
The other important presentation that took place at DDW 2015 is the use of ozanimod to treat ulcerative colitis; again, this is an oral agent that has a very dramatic effect in treating ulcerative colitis in a very short period of time by inhibiting the exit of effector T cells from lymph nodes. This tells us about the host immune response. We can now sequence all the bacteria that are present in the gut and using that approach we have found broad patterns of decreased diversity in patients who have IBD, although we have not identified a particular pathogen or pathogens.
The laboratory of Dr. Richard Flavell used a strategy in which they identified bacteria that were IgA coated and reasoned that IgA-coated bacteria were more likely to be pathogens (Cell. 2014 Aug 28;158(5):1000-1010). Indeed, by giving mice these IgA-coated bacteria found in IBD patients, the mice were more likely to develop colitis than if you gave non–IgA-coated bacteria to the same mice.
Another very important observation was in a study that was published in Nature, which demonstrated that emulsifiers really changed the relationship between the host and the microbiome. In particular, the investigators found that interactions with the microbiota led to metabolic syndrome. They also found that with dietary emulsifiers there is encroachment of the epithelium because of a thinning of the mucous layer and the study animals were more susceptible to developing colitis. I think that this is a sign to our patients that it is better to avoid processed foods.
Dr. Abreu is professor of medicine, professor of microbiology and immunology, chief of the division of gastroenterology, the Martin Kalser Chair in gastroenterology, and the director, Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She consults for AbbVie, Focus Medical Communications, GSK, and many other biopharmaceutical companies. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Important new themes are whether we can actually find a cure for inflammatory bowel disease and, in particular, whether there are common pathogenetic mechanisms leading to Crohn’s disease and ulcerative colitis. Are Crohn’s and ulcerative colitis infectious diseases? If the answer to that question is ‘yes,’ then eliminating that “pathogen” would turn off the immune response. Crohn’s disease and ulcerative colitis share common genetic origins with the majority of genes shared between both disorders. Indeed, 110 of the 163 confirmed loci in IBD are common between the two disorders (Nature 2012;491:119–24).
In addition to there being many genes contributing even a small amount to the development of IBD, there are also some genetic pathways that have a far more impactful role in IBD. By studying very-early-onset IBD, we have discovered that the IL-10 receptor pathway is very important in controlling intestinal inflammation, such that if you have a mutation in the receptor for IL-10 it can lead to very-early-onset IBD. Children who are born with these disorders can be treated with a hematopoietic bone marrow transplant. At this year’s Digestive Disease Week (DDW) in fact, there was the presentation of the ASTIC trial; it described patients having a prolonged remission after an autologous hematopoietic stem cell transplant.
One of the big advances that has been made in terms of the treatment of IBD is based on an understanding of the pathogenetic pathways; in particular, there has been an increase in the number of medications that are currently available to treat IBD from a variety of different avenues. There was a recent publication describing an anti-sense treatment against SMAD7 in restoring TGF-beta signaling that produced a very rapid and profound improvement in the clinical symptoms of Crohn’s disease. We await more data on that particular compound.
We now know that an antibody against P40, which is the common subunit between IL-12 and IL-23, is effective in the treatment of Crohn’s disease and is commercially available as ustekinumab. At this year’s DDW we heard about an antibody that is specific for anti-IL-23 since it only antagonizes the P19 subunit of the cytokine; it also shows great promise for treating IBD. At DDW 2014, vedolizumab had just obtained approval for the treatment of ulcerative colitis and Crohn’s disease and that has been a big advance in treating patients. On its heels are a variety of other compounds that work by a similar mechanism by inhibiting the trafficking of effector lymphocytes to the intestine; these include anti-beta7 strategies and anti-MAdCAM. Both of these have been shown to be more effective in ulcerative colitis than in Crohn’s disease, as has been a common theme.
The other important presentation that took place at DDW 2015 is the use of ozanimod to treat ulcerative colitis; again, this is an oral agent that has a very dramatic effect in treating ulcerative colitis in a very short period of time by inhibiting the exit of effector T cells from lymph nodes. This tells us about the host immune response. We can now sequence all the bacteria that are present in the gut and using that approach we have found broad patterns of decreased diversity in patients who have IBD, although we have not identified a particular pathogen or pathogens.
The laboratory of Dr. Richard Flavell used a strategy in which they identified bacteria that were IgA coated and reasoned that IgA-coated bacteria were more likely to be pathogens (Cell. 2014 Aug 28;158(5):1000-1010). Indeed, by giving mice these IgA-coated bacteria found in IBD patients, the mice were more likely to develop colitis than if you gave non–IgA-coated bacteria to the same mice.
Another very important observation was in a study that was published in Nature, which demonstrated that emulsifiers really changed the relationship between the host and the microbiome. In particular, the investigators found that interactions with the microbiota led to metabolic syndrome. They also found that with dietary emulsifiers there is encroachment of the epithelium because of a thinning of the mucous layer and the study animals were more susceptible to developing colitis. I think that this is a sign to our patients that it is better to avoid processed foods.
Dr. Abreu is professor of medicine, professor of microbiology and immunology, chief of the division of gastroenterology, the Martin Kalser Chair in gastroenterology, and the director, Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She consults for AbbVie, Focus Medical Communications, GSK, and many other biopharmaceutical companies. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Important new themes are whether we can actually find a cure for inflammatory bowel disease and, in particular, whether there are common pathogenetic mechanisms leading to Crohn’s disease and ulcerative colitis. Are Crohn’s and ulcerative colitis infectious diseases? If the answer to that question is ‘yes,’ then eliminating that “pathogen” would turn off the immune response. Crohn’s disease and ulcerative colitis share common genetic origins with the majority of genes shared between both disorders. Indeed, 110 of the 163 confirmed loci in IBD are common between the two disorders (Nature 2012;491:119–24).
In addition to there being many genes contributing even a small amount to the development of IBD, there are also some genetic pathways that have a far more impactful role in IBD. By studying very-early-onset IBD, we have discovered that the IL-10 receptor pathway is very important in controlling intestinal inflammation, such that if you have a mutation in the receptor for IL-10 it can lead to very-early-onset IBD. Children who are born with these disorders can be treated with a hematopoietic bone marrow transplant. At this year’s Digestive Disease Week (DDW) in fact, there was the presentation of the ASTIC trial; it described patients having a prolonged remission after an autologous hematopoietic stem cell transplant.
One of the big advances that has been made in terms of the treatment of IBD is based on an understanding of the pathogenetic pathways; in particular, there has been an increase in the number of medications that are currently available to treat IBD from a variety of different avenues. There was a recent publication describing an anti-sense treatment against SMAD7 in restoring TGF-beta signaling that produced a very rapid and profound improvement in the clinical symptoms of Crohn’s disease. We await more data on that particular compound.
We now know that an antibody against P40, which is the common subunit between IL-12 and IL-23, is effective in the treatment of Crohn’s disease and is commercially available as ustekinumab. At this year’s DDW we heard about an antibody that is specific for anti-IL-23 since it only antagonizes the P19 subunit of the cytokine; it also shows great promise for treating IBD. At DDW 2014, vedolizumab had just obtained approval for the treatment of ulcerative colitis and Crohn’s disease and that has been a big advance in treating patients. On its heels are a variety of other compounds that work by a similar mechanism by inhibiting the trafficking of effector lymphocytes to the intestine; these include anti-beta7 strategies and anti-MAdCAM. Both of these have been shown to be more effective in ulcerative colitis than in Crohn’s disease, as has been a common theme.
The other important presentation that took place at DDW 2015 is the use of ozanimod to treat ulcerative colitis; again, this is an oral agent that has a very dramatic effect in treating ulcerative colitis in a very short period of time by inhibiting the exit of effector T cells from lymph nodes. This tells us about the host immune response. We can now sequence all the bacteria that are present in the gut and using that approach we have found broad patterns of decreased diversity in patients who have IBD, although we have not identified a particular pathogen or pathogens.
The laboratory of Dr. Richard Flavell used a strategy in which they identified bacteria that were IgA coated and reasoned that IgA-coated bacteria were more likely to be pathogens (Cell. 2014 Aug 28;158(5):1000-1010). Indeed, by giving mice these IgA-coated bacteria found in IBD patients, the mice were more likely to develop colitis than if you gave non–IgA-coated bacteria to the same mice.
Another very important observation was in a study that was published in Nature, which demonstrated that emulsifiers really changed the relationship between the host and the microbiome. In particular, the investigators found that interactions with the microbiota led to metabolic syndrome. They also found that with dietary emulsifiers there is encroachment of the epithelium because of a thinning of the mucous layer and the study animals were more susceptible to developing colitis. I think that this is a sign to our patients that it is better to avoid processed foods.
Dr. Abreu is professor of medicine, professor of microbiology and immunology, chief of the division of gastroenterology, the Martin Kalser Chair in gastroenterology, and the director, Crohn’s & Colitis Center at the University of Miami Miller School of Medicine. She consults for AbbVie, Focus Medical Communications, GSK, and many other biopharmaceutical companies. Her comments were made during the ASGE and AGA joint Presidential Plenary at the annual Digestive Disease Week.
Intestinal obstruction risk increased in some childhood cancer survivors
Childhood cancer survivors are at an increased risk for developing an intestinal obstruction requiring surgery (IOS) 5 or more years after the initial cancer diagnosis, according to a study based on data from the Childhood Cancer Survivor Study.
The risk was greater among those who had a pelvic or abdominal tumor and had been exposed to pelvic or abdominal radiotherapy, reported the authors, who pointed out that no study has “rigorously” investigated the incidence of intestinal obstruction in childhood cancer survivors. The study appeared online in the Journal of Clinical Oncology (2015 Aug 10 doi: 10.1200/JCO.2015.61.5070).
The subjects in the study had been diagnosed with cancer before age 21 years between 1970 and 1986 and were followed longitudinally in the CCSS. The sample included 12,316 childhood cancer survivors who had survived at least 5 years from the time they were diagnosed with cancer and 4,023 of their siblings.
The cumulative incidence of “late” IOS (occurring at least 5 years after the cancer diagnosis) was 5.8% among those who had an abdominopelvic tumor and 1% among those who had other types of cancer, compared with 0.3% among siblings, who served as controls in the study. After adjusting for year of diagnosis, age at diagnosis, cancer type, radiotherapy, surgery, and other confounding factors, the risk of late IOS was significantly increased among those who had an abdominopelvic tumor (3.6 times greater) and those who had received abdominal/pelvic radiotherapy (2.4 times greater). Mortality was also almost twofold higher among those who developed late IOS when adjusted for the same factors, but there was no association with chemotherapy, cyclophosphamide equivalent dose, or platinum agent score and late IOS.
“The risk of IOS extends for decades beyond cancer diagnosis, implying the need for long-term vigilance, especially among survivors with abdominal or pelvic tumors and survivors who have undergone treatment with abdominal or pelvic surgery or radiotherapy,” concluded lead author Dr. Arin Madenci of Boston Children’s Hospital and his coauthors.
“Widespread awareness of the signs and symptoms of IOS will facilitate timely presentation and effective management of this complication. Although prevention of IOS is not currently possible, education of survivors of cancer, their families, and their health care providers is critical,” they added.
The study was supported by grants from the National Cancer Institute and Cancer Center Support (Centers of Research Excellence) and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
Childhood cancer survivors are at an increased risk for developing an intestinal obstruction requiring surgery (IOS) 5 or more years after the initial cancer diagnosis, according to a study based on data from the Childhood Cancer Survivor Study.
The risk was greater among those who had a pelvic or abdominal tumor and had been exposed to pelvic or abdominal radiotherapy, reported the authors, who pointed out that no study has “rigorously” investigated the incidence of intestinal obstruction in childhood cancer survivors. The study appeared online in the Journal of Clinical Oncology (2015 Aug 10 doi: 10.1200/JCO.2015.61.5070).
The subjects in the study had been diagnosed with cancer before age 21 years between 1970 and 1986 and were followed longitudinally in the CCSS. The sample included 12,316 childhood cancer survivors who had survived at least 5 years from the time they were diagnosed with cancer and 4,023 of their siblings.
The cumulative incidence of “late” IOS (occurring at least 5 years after the cancer diagnosis) was 5.8% among those who had an abdominopelvic tumor and 1% among those who had other types of cancer, compared with 0.3% among siblings, who served as controls in the study. After adjusting for year of diagnosis, age at diagnosis, cancer type, radiotherapy, surgery, and other confounding factors, the risk of late IOS was significantly increased among those who had an abdominopelvic tumor (3.6 times greater) and those who had received abdominal/pelvic radiotherapy (2.4 times greater). Mortality was also almost twofold higher among those who developed late IOS when adjusted for the same factors, but there was no association with chemotherapy, cyclophosphamide equivalent dose, or platinum agent score and late IOS.
“The risk of IOS extends for decades beyond cancer diagnosis, implying the need for long-term vigilance, especially among survivors with abdominal or pelvic tumors and survivors who have undergone treatment with abdominal or pelvic surgery or radiotherapy,” concluded lead author Dr. Arin Madenci of Boston Children’s Hospital and his coauthors.
“Widespread awareness of the signs and symptoms of IOS will facilitate timely presentation and effective management of this complication. Although prevention of IOS is not currently possible, education of survivors of cancer, their families, and their health care providers is critical,” they added.
The study was supported by grants from the National Cancer Institute and Cancer Center Support (Centers of Research Excellence) and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
Childhood cancer survivors are at an increased risk for developing an intestinal obstruction requiring surgery (IOS) 5 or more years after the initial cancer diagnosis, according to a study based on data from the Childhood Cancer Survivor Study.
The risk was greater among those who had a pelvic or abdominal tumor and had been exposed to pelvic or abdominal radiotherapy, reported the authors, who pointed out that no study has “rigorously” investigated the incidence of intestinal obstruction in childhood cancer survivors. The study appeared online in the Journal of Clinical Oncology (2015 Aug 10 doi: 10.1200/JCO.2015.61.5070).
The subjects in the study had been diagnosed with cancer before age 21 years between 1970 and 1986 and were followed longitudinally in the CCSS. The sample included 12,316 childhood cancer survivors who had survived at least 5 years from the time they were diagnosed with cancer and 4,023 of their siblings.
The cumulative incidence of “late” IOS (occurring at least 5 years after the cancer diagnosis) was 5.8% among those who had an abdominopelvic tumor and 1% among those who had other types of cancer, compared with 0.3% among siblings, who served as controls in the study. After adjusting for year of diagnosis, age at diagnosis, cancer type, radiotherapy, surgery, and other confounding factors, the risk of late IOS was significantly increased among those who had an abdominopelvic tumor (3.6 times greater) and those who had received abdominal/pelvic radiotherapy (2.4 times greater). Mortality was also almost twofold higher among those who developed late IOS when adjusted for the same factors, but there was no association with chemotherapy, cyclophosphamide equivalent dose, or platinum agent score and late IOS.
“The risk of IOS extends for decades beyond cancer diagnosis, implying the need for long-term vigilance, especially among survivors with abdominal or pelvic tumors and survivors who have undergone treatment with abdominal or pelvic surgery or radiotherapy,” concluded lead author Dr. Arin Madenci of Boston Children’s Hospital and his coauthors.
“Widespread awareness of the signs and symptoms of IOS will facilitate timely presentation and effective management of this complication. Although prevention of IOS is not currently possible, education of survivors of cancer, their families, and their health care providers is critical,” they added.
The study was supported by grants from the National Cancer Institute and Cancer Center Support (Centers of Research Excellence) and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Some childhood cancer survivors are at a significantly increased risk of developing an intestinal obstruction requiring surgery (IOS), which should be considered in their long-term follow-up.
Major finding: The cumulative incidence of IOS occurring at least 5 years after the cancer diagnosis was 5.8% among those who had an abdominopelvic tumor and 1% among those who did not have an abdominopelvic tumor, compared with 0.3% among sibling controls in the study, and late IOS was associated with increased mortality.
Data source: A retrospective cohort study involving 12,316 childhood cancer survivors who had survived at least 5 years and 4,023 of their siblings, who served as controls, from the Childhood Cancer Survivor Study.
Disclosures: The study was supported by National Cancer Institute and Cancer Center Support (Centers of Research Excellence) grants, and by the American Lebanese Syrian Associated Charities. Dr. Madenci and nine other authors had no disclosures. The remaining three authors had disclosures that included receiving honoraria, travel, and expenses from Sandoz, holding stock or other ownership in Pfizer and Novartis, serving as a consultant or advisor to United Therapeutics, and having an immediate family member with stock or other ownership in several pharmaceutical companies.
Cut to the chase: Admitting patients with ASBO directly to surgical service
Patients with suspected adhesive small bowel obstruction have shorter hospitalization times and fewer complications when admitted directly to a surgical service, rather than being admitted to the medical hospitalist service, according to researchers at Virginia Mason Medical Center in Seattle.
Although adhesive small bowel obstruction (ASBO) is a potential surgical emergency, it is increasingly managed by medical hospitalists because of the presumption that these patients will probably not require surgery. Dr. Phillip A. Bilderback and his colleagues investigated whether the value of care delivered in the medical hospital service (MHS) was comparable to the value of care delivered in the surgical service (SS) (J Am Coll Surg. 2015;221[1]:7-13).
The researchers reviewed 555 consecutive admissions with presumed ASBO from 2008 to 2012, grouping them according to admitting service (MHS vs. SS) and whether surgery had been performed. Group medians were then compared using multivariate analysis to identify variables independently associated with increased length of stay (LOS), time to operation (TTO), and hospital charges.
Median LOS among patients whose ASBO resolved nonoperatively was similar for those on SS and MHS (2.85 days vs. 2.98 days; P = .49). But patients requiring surgery who were admitted to MHS had longer median LOS, compared with those admitted to SS (9.57 days vs. 6.99 days; P = .002), and higher median charges ($38,800 vs. $30,100; P = .025). Operative MHS patients also had a greater median TTO than did operative SS patients (51.72 hours vs. 8.4 hours; P less than .001).
The researchers noted that a possible explanation for this observed different in outcomes included variability in the knowledge and experience of providers in managing ASBO and in the use of modern processes of care. “For example, surgeons may make timelier decisions to operate based on the findings of CT scans or response to a water-soluble contrast medium challenge than do internists, who may tend to rely on outdated processes of care, such as repeated abdominal radiographs,” they suggested.
In the absence of findings suggestive of ischemia or strangulation, recent evidence points to the safety of nonoperative management of patients with ASBO, even in the setting of high-grade or complete obstruction, they noted. Accordingly, there has been a shift toward initial admission of patients with ASBO to medical hospitalist services. But although this approach is equally safe, in terms of clinical outcomes, ASBO is “managed in a more cost-effective fashion with primary admission to an SS, particularly if the patients require an operation,” the researchers stated.
The researchers concluded that “admitting all patients suspected of having an ASBO to the SS or implementing an institution-wide pathway that defines appropriate triage and elements of care has the potential to dramatically reduce LOS and reduce waste in those requiring operation, thereby reducing overall health care expenditures and improving value for patients and the health care system as a whole.”
The study authors had no relevant financial conflicts.
Patients with suspected adhesive small bowel obstruction have shorter hospitalization times and fewer complications when admitted directly to a surgical service, rather than being admitted to the medical hospitalist service, according to researchers at Virginia Mason Medical Center in Seattle.
Although adhesive small bowel obstruction (ASBO) is a potential surgical emergency, it is increasingly managed by medical hospitalists because of the presumption that these patients will probably not require surgery. Dr. Phillip A. Bilderback and his colleagues investigated whether the value of care delivered in the medical hospital service (MHS) was comparable to the value of care delivered in the surgical service (SS) (J Am Coll Surg. 2015;221[1]:7-13).
The researchers reviewed 555 consecutive admissions with presumed ASBO from 2008 to 2012, grouping them according to admitting service (MHS vs. SS) and whether surgery had been performed. Group medians were then compared using multivariate analysis to identify variables independently associated with increased length of stay (LOS), time to operation (TTO), and hospital charges.
Median LOS among patients whose ASBO resolved nonoperatively was similar for those on SS and MHS (2.85 days vs. 2.98 days; P = .49). But patients requiring surgery who were admitted to MHS had longer median LOS, compared with those admitted to SS (9.57 days vs. 6.99 days; P = .002), and higher median charges ($38,800 vs. $30,100; P = .025). Operative MHS patients also had a greater median TTO than did operative SS patients (51.72 hours vs. 8.4 hours; P less than .001).
The researchers noted that a possible explanation for this observed different in outcomes included variability in the knowledge and experience of providers in managing ASBO and in the use of modern processes of care. “For example, surgeons may make timelier decisions to operate based on the findings of CT scans or response to a water-soluble contrast medium challenge than do internists, who may tend to rely on outdated processes of care, such as repeated abdominal radiographs,” they suggested.
In the absence of findings suggestive of ischemia or strangulation, recent evidence points to the safety of nonoperative management of patients with ASBO, even in the setting of high-grade or complete obstruction, they noted. Accordingly, there has been a shift toward initial admission of patients with ASBO to medical hospitalist services. But although this approach is equally safe, in terms of clinical outcomes, ASBO is “managed in a more cost-effective fashion with primary admission to an SS, particularly if the patients require an operation,” the researchers stated.
The researchers concluded that “admitting all patients suspected of having an ASBO to the SS or implementing an institution-wide pathway that defines appropriate triage and elements of care has the potential to dramatically reduce LOS and reduce waste in those requiring operation, thereby reducing overall health care expenditures and improving value for patients and the health care system as a whole.”
The study authors had no relevant financial conflicts.
Patients with suspected adhesive small bowel obstruction have shorter hospitalization times and fewer complications when admitted directly to a surgical service, rather than being admitted to the medical hospitalist service, according to researchers at Virginia Mason Medical Center in Seattle.
Although adhesive small bowel obstruction (ASBO) is a potential surgical emergency, it is increasingly managed by medical hospitalists because of the presumption that these patients will probably not require surgery. Dr. Phillip A. Bilderback and his colleagues investigated whether the value of care delivered in the medical hospital service (MHS) was comparable to the value of care delivered in the surgical service (SS) (J Am Coll Surg. 2015;221[1]:7-13).
The researchers reviewed 555 consecutive admissions with presumed ASBO from 2008 to 2012, grouping them according to admitting service (MHS vs. SS) and whether surgery had been performed. Group medians were then compared using multivariate analysis to identify variables independently associated with increased length of stay (LOS), time to operation (TTO), and hospital charges.
Median LOS among patients whose ASBO resolved nonoperatively was similar for those on SS and MHS (2.85 days vs. 2.98 days; P = .49). But patients requiring surgery who were admitted to MHS had longer median LOS, compared with those admitted to SS (9.57 days vs. 6.99 days; P = .002), and higher median charges ($38,800 vs. $30,100; P = .025). Operative MHS patients also had a greater median TTO than did operative SS patients (51.72 hours vs. 8.4 hours; P less than .001).
The researchers noted that a possible explanation for this observed different in outcomes included variability in the knowledge and experience of providers in managing ASBO and in the use of modern processes of care. “For example, surgeons may make timelier decisions to operate based on the findings of CT scans or response to a water-soluble contrast medium challenge than do internists, who may tend to rely on outdated processes of care, such as repeated abdominal radiographs,” they suggested.
In the absence of findings suggestive of ischemia or strangulation, recent evidence points to the safety of nonoperative management of patients with ASBO, even in the setting of high-grade or complete obstruction, they noted. Accordingly, there has been a shift toward initial admission of patients with ASBO to medical hospitalist services. But although this approach is equally safe, in terms of clinical outcomes, ASBO is “managed in a more cost-effective fashion with primary admission to an SS, particularly if the patients require an operation,” the researchers stated.
The researchers concluded that “admitting all patients suspected of having an ASBO to the SS or implementing an institution-wide pathway that defines appropriate triage and elements of care has the potential to dramatically reduce LOS and reduce waste in those requiring operation, thereby reducing overall health care expenditures and improving value for patients and the health care system as a whole.”
The study authors had no relevant financial conflicts.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF SURGEONS
Key clinical point: Patients who needed surgery for suspected adhesive small bowel obstruction had shorter hospital stays and lower costs if they went straight to surgical services instead of medical hospital services.
Major finding: ASBO patients requiring surgery who were admitted to the medical hospitalist service had longer median hospital stays, compared with those admitted to the surgical service (9.57 days vs. 6.99 days) and higher median charges ($38,800 vs. $30,100).
Data source: Data from 555 consecutive admissions with presumed adhesive small bowel obstruction from 2008 to 2012.
Disclosures: The study authors had no relevant financial conflicts.
CDC: Coordinated strategy will curb resistant infections
A coordinated approach to infection control and antibiotic stewardship would dramatically reduce the number of people affected by antibiotic-resistant pathogens and health care–associated infections (HAIs), saving tens of thousands of lives and billions of dollars over the next 5 years, according to a federal report.
With a nationwide prevention and antibiotic stewardship program, the total number of HAIs could be reduced by 619,000 over the next 5 years, saving 37,000 lives and reducing direct medical costs by $7.7 billion, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention (CDC), said in a telebriefing sponsored by the agency.
The coordinated approach requires both a public health tracking and alerting system and robust interfacility infection control practices. “Facilities that go it alone can’t effectively protect their own patients,” he said.
A CDC Vital Signs report projected outcomes for institution-based versus coordinated responses to antibiotic-resistant infections, predicting infections and deaths from 2014-2019 in a series of three scenarios.
Rachel Slayton, Ph.D., of the Center for Emerging and Zoonotic Infectious Diseases, used carbapenem-resistant Enterobacteriaceae (CRE) as the test case to determine the effect size of coordinated compared with institution-based infection control and alerting practices.*
She and her coauthors projected that the number of health care-associated CRE infections would rise about 10% over the next 5 years, from 310,000 to 340,000, under current practices. Using these prevalence figures, a coordinated approach would result in CRE prevalence within a health care network of just 2% after 5 years, compared with a 12% baseline prevalence and an 8.6% prevalence with augmented individual efforts.
“Two percent is still two percent too much, but it’s still a whole lot better than 12%,” said Dr. Frieden.
Infection control practices that are enhanced by interfacility coordination may include maintaining regional databases that permit alerts when an individual with an HAI transfers from one facility to the other; having inter-institution agreement about best practices for gowning, gloving, and isolation; and commencing enhanced screening for HAIs when public health officials identify a potential outbreak. Antibiotic stewardship is also enhanced when institutions explicitly agree to follow best prescribing practices.
Implementation of the coordinated approach would be supported by the CDC’s Antibiotic Resistance Solutions Initiative, with $264 million requested in the federal fiscal year 2016 budget for a broad set of programs. Part of this amount would provide for funding of a coordinated prevention approach in all 50 states, with support for state and local health departments, and a network of laboratory facilities for improved surveillance for resistant pathogens.
On Twitter: @karioakes
*CORRECTION 8/9/2015: The original version of this story misidentified the test case organism.
A coordinated approach to infection control and antibiotic stewardship would dramatically reduce the number of people affected by antibiotic-resistant pathogens and health care–associated infections (HAIs), saving tens of thousands of lives and billions of dollars over the next 5 years, according to a federal report.
With a nationwide prevention and antibiotic stewardship program, the total number of HAIs could be reduced by 619,000 over the next 5 years, saving 37,000 lives and reducing direct medical costs by $7.7 billion, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention (CDC), said in a telebriefing sponsored by the agency.
The coordinated approach requires both a public health tracking and alerting system and robust interfacility infection control practices. “Facilities that go it alone can’t effectively protect their own patients,” he said.
A CDC Vital Signs report projected outcomes for institution-based versus coordinated responses to antibiotic-resistant infections, predicting infections and deaths from 2014-2019 in a series of three scenarios.
Rachel Slayton, Ph.D., of the Center for Emerging and Zoonotic Infectious Diseases, used carbapenem-resistant Enterobacteriaceae (CRE) as the test case to determine the effect size of coordinated compared with institution-based infection control and alerting practices.*
She and her coauthors projected that the number of health care-associated CRE infections would rise about 10% over the next 5 years, from 310,000 to 340,000, under current practices. Using these prevalence figures, a coordinated approach would result in CRE prevalence within a health care network of just 2% after 5 years, compared with a 12% baseline prevalence and an 8.6% prevalence with augmented individual efforts.
“Two percent is still two percent too much, but it’s still a whole lot better than 12%,” said Dr. Frieden.
Infection control practices that are enhanced by interfacility coordination may include maintaining regional databases that permit alerts when an individual with an HAI transfers from one facility to the other; having inter-institution agreement about best practices for gowning, gloving, and isolation; and commencing enhanced screening for HAIs when public health officials identify a potential outbreak. Antibiotic stewardship is also enhanced when institutions explicitly agree to follow best prescribing practices.
Implementation of the coordinated approach would be supported by the CDC’s Antibiotic Resistance Solutions Initiative, with $264 million requested in the federal fiscal year 2016 budget for a broad set of programs. Part of this amount would provide for funding of a coordinated prevention approach in all 50 states, with support for state and local health departments, and a network of laboratory facilities for improved surveillance for resistant pathogens.
On Twitter: @karioakes
*CORRECTION 8/9/2015: The original version of this story misidentified the test case organism.
A coordinated approach to infection control and antibiotic stewardship would dramatically reduce the number of people affected by antibiotic-resistant pathogens and health care–associated infections (HAIs), saving tens of thousands of lives and billions of dollars over the next 5 years, according to a federal report.
With a nationwide prevention and antibiotic stewardship program, the total number of HAIs could be reduced by 619,000 over the next 5 years, saving 37,000 lives and reducing direct medical costs by $7.7 billion, Dr. Thomas Frieden, director of the Centers for Disease Control and Prevention (CDC), said in a telebriefing sponsored by the agency.
The coordinated approach requires both a public health tracking and alerting system and robust interfacility infection control practices. “Facilities that go it alone can’t effectively protect their own patients,” he said.
A CDC Vital Signs report projected outcomes for institution-based versus coordinated responses to antibiotic-resistant infections, predicting infections and deaths from 2014-2019 in a series of three scenarios.
Rachel Slayton, Ph.D., of the Center for Emerging and Zoonotic Infectious Diseases, used carbapenem-resistant Enterobacteriaceae (CRE) as the test case to determine the effect size of coordinated compared with institution-based infection control and alerting practices.*
She and her coauthors projected that the number of health care-associated CRE infections would rise about 10% over the next 5 years, from 310,000 to 340,000, under current practices. Using these prevalence figures, a coordinated approach would result in CRE prevalence within a health care network of just 2% after 5 years, compared with a 12% baseline prevalence and an 8.6% prevalence with augmented individual efforts.
“Two percent is still two percent too much, but it’s still a whole lot better than 12%,” said Dr. Frieden.
Infection control practices that are enhanced by interfacility coordination may include maintaining regional databases that permit alerts when an individual with an HAI transfers from one facility to the other; having inter-institution agreement about best practices for gowning, gloving, and isolation; and commencing enhanced screening for HAIs when public health officials identify a potential outbreak. Antibiotic stewardship is also enhanced when institutions explicitly agree to follow best prescribing practices.
Implementation of the coordinated approach would be supported by the CDC’s Antibiotic Resistance Solutions Initiative, with $264 million requested in the federal fiscal year 2016 budget for a broad set of programs. Part of this amount would provide for funding of a coordinated prevention approach in all 50 states, with support for state and local health departments, and a network of laboratory facilities for improved surveillance for resistant pathogens.
On Twitter: @karioakes
*CORRECTION 8/9/2015: The original version of this story misidentified the test case organism.
Key clinical point: A coordinated U.S. strategy is needed to stem the tide of antibiotic-resistant and health care–associated infections.
Major finding: A coordinated 5-year approach would prevent more than 600,000 infections and save more than 37,000 lives in the United States.
Data source: Centers for Disease Control and Prevention Vital Signs report modeling coordinated strategies to combat antibiotic resistant and health care–associated infections.
Disclosures: The study was sponsored by the Centers for Disease Control and Prevention, with assistance from Emerging Infectious Programs participants, the Agency for Healthcare Research and Quality, University of Pittsburgh Center for Simulation and Modeling, and the VA Salt Lake City Health Care System.
No link found between vaccinations, IBD
Neither childhood immunizations nor H1N1 influenza vaccination increased the risk of inflammatory bowel disease, according to a meta-analysis of 11 studies in the August issue of Clinical Gastroenterology and Hepatology published online (2015 [doi:10.1016/j.cgh.2015.04.179]).
“Overall, our results did not find any significant increased risk of developing IBD after childhood immunization with BCG [bacille Calmette-Guérin], diphtheria, tetanus, poliomyelitis, smallpox, pertussis, measles, mumps, and rubella-containing vaccines,” said Dr. Guillaume Pineton de Chambrun of Lille (France) University Hospital and his associates. “The results of this meta-analysis are globally reassuring regarding the risk of developing IBD after childhood vaccination. Vaccines that are developed to protect against an infectious disease or its consequences are, for the majority, not a risk for the subsequent development of intestinal inflammatory disease.”
Besides the childhood vaccines, H1N1 vaccination was not linked to IBD in a single large study of adults (risk ratio, 1.13; 95% confidence interval, 0.97-1.32), the investigators said.
Controversies about immunizations and IBD date to at least 1995, when a report by Thompson et al. linked live measles vaccine to the disease (Lancet 1995;345:1071-4), said the investigators. “However, many publications after this report investigating vaccination with measles-containing vaccines did not show any association between immunization and IBD,” they emphasized. “Epidemiologic studies also investigated other vaccines such as BCG, diphtheria, tetanus, poliomyelitis, smallpox, pertussis, rubella, and mumps, reporting conflicting results.”
To further clarify the issue, they compared rates of IBD, Crohn’s disease, and ulcerative colitis among vaccinated and unvaccinated patients from eight case-control and three cohort studies published between 1970 and June 2014. When looking at IBD overall, 95% CIs for RRs all crossed 1.0, indicating no significant associations, they said. A subgroup analysis did link poliomyelitis vaccination with increased risk of developing Crohn’s disease (RR, 2.28; 95% CI, 1.12-4.63) or ulcerative colitis (RR, 3.48; 95% CI, 1.2-9.71), but the studies were dissimilar enough that the results need to be interpreted cautiously, they added.
To find the studies, the researchers searched MEDLINE, EMBASE, and the Cochrane central trials registry for randomized controlled trials, controlled clinical trials, cohort studies, and case-control studies published in any language and that included the terms ulcerative colitis, Crohn’s disease, inflammatory bowel disease, colitis, or ileitis. This approach yielded six population-based and two hospital-based case-control studies, and three population-based cohort studies. The studies of childhood immunizations included 2,399 patients with IBD and 33,747 controls, and the H1N1 study included 14,842 patients with IBD and almost 2 million controls, said the investigators.
The studies were “extremely heterogeneous” in terms of design, sample size, geographic location, and methods used to help patients recall their vaccination history, the investigators noted. “Vaccination protocols varied between countries and evolved through the years, with different types of vaccines and schedules leading to difficulties in risk evaluation,” they said. “Moreover, some vaccines used were live attenuated vaccines such as measles, oral poliomyelitis, or whole-cell pertussis vaccines, and may have a different effect on immune system activation and dysregulation, compared with other inactivated acellular vaccines.”
The Digitscience Foundation supported the research. The researchers declared having no conflicts of interest.
Neither childhood immunizations nor H1N1 influenza vaccination increased the risk of inflammatory bowel disease, according to a meta-analysis of 11 studies in the August issue of Clinical Gastroenterology and Hepatology published online (2015 [doi:10.1016/j.cgh.2015.04.179]).
“Overall, our results did not find any significant increased risk of developing IBD after childhood immunization with BCG [bacille Calmette-Guérin], diphtheria, tetanus, poliomyelitis, smallpox, pertussis, measles, mumps, and rubella-containing vaccines,” said Dr. Guillaume Pineton de Chambrun of Lille (France) University Hospital and his associates. “The results of this meta-analysis are globally reassuring regarding the risk of developing IBD after childhood vaccination. Vaccines that are developed to protect against an infectious disease or its consequences are, for the majority, not a risk for the subsequent development of intestinal inflammatory disease.”
Besides the childhood vaccines, H1N1 vaccination was not linked to IBD in a single large study of adults (risk ratio, 1.13; 95% confidence interval, 0.97-1.32), the investigators said.
Controversies about immunizations and IBD date to at least 1995, when a report by Thompson et al. linked live measles vaccine to the disease (Lancet 1995;345:1071-4), said the investigators. “However, many publications after this report investigating vaccination with measles-containing vaccines did not show any association between immunization and IBD,” they emphasized. “Epidemiologic studies also investigated other vaccines such as BCG, diphtheria, tetanus, poliomyelitis, smallpox, pertussis, rubella, and mumps, reporting conflicting results.”
To further clarify the issue, they compared rates of IBD, Crohn’s disease, and ulcerative colitis among vaccinated and unvaccinated patients from eight case-control and three cohort studies published between 1970 and June 2014. When looking at IBD overall, 95% CIs for RRs all crossed 1.0, indicating no significant associations, they said. A subgroup analysis did link poliomyelitis vaccination with increased risk of developing Crohn’s disease (RR, 2.28; 95% CI, 1.12-4.63) or ulcerative colitis (RR, 3.48; 95% CI, 1.2-9.71), but the studies were dissimilar enough that the results need to be interpreted cautiously, they added.
To find the studies, the researchers searched MEDLINE, EMBASE, and the Cochrane central trials registry for randomized controlled trials, controlled clinical trials, cohort studies, and case-control studies published in any language and that included the terms ulcerative colitis, Crohn’s disease, inflammatory bowel disease, colitis, or ileitis. This approach yielded six population-based and two hospital-based case-control studies, and three population-based cohort studies. The studies of childhood immunizations included 2,399 patients with IBD and 33,747 controls, and the H1N1 study included 14,842 patients with IBD and almost 2 million controls, said the investigators.
The studies were “extremely heterogeneous” in terms of design, sample size, geographic location, and methods used to help patients recall their vaccination history, the investigators noted. “Vaccination protocols varied between countries and evolved through the years, with different types of vaccines and schedules leading to difficulties in risk evaluation,” they said. “Moreover, some vaccines used were live attenuated vaccines such as measles, oral poliomyelitis, or whole-cell pertussis vaccines, and may have a different effect on immune system activation and dysregulation, compared with other inactivated acellular vaccines.”
The Digitscience Foundation supported the research. The researchers declared having no conflicts of interest.
Neither childhood immunizations nor H1N1 influenza vaccination increased the risk of inflammatory bowel disease, according to a meta-analysis of 11 studies in the August issue of Clinical Gastroenterology and Hepatology published online (2015 [doi:10.1016/j.cgh.2015.04.179]).
“Overall, our results did not find any significant increased risk of developing IBD after childhood immunization with BCG [bacille Calmette-Guérin], diphtheria, tetanus, poliomyelitis, smallpox, pertussis, measles, mumps, and rubella-containing vaccines,” said Dr. Guillaume Pineton de Chambrun of Lille (France) University Hospital and his associates. “The results of this meta-analysis are globally reassuring regarding the risk of developing IBD after childhood vaccination. Vaccines that are developed to protect against an infectious disease or its consequences are, for the majority, not a risk for the subsequent development of intestinal inflammatory disease.”
Besides the childhood vaccines, H1N1 vaccination was not linked to IBD in a single large study of adults (risk ratio, 1.13; 95% confidence interval, 0.97-1.32), the investigators said.
Controversies about immunizations and IBD date to at least 1995, when a report by Thompson et al. linked live measles vaccine to the disease (Lancet 1995;345:1071-4), said the investigators. “However, many publications after this report investigating vaccination with measles-containing vaccines did not show any association between immunization and IBD,” they emphasized. “Epidemiologic studies also investigated other vaccines such as BCG, diphtheria, tetanus, poliomyelitis, smallpox, pertussis, rubella, and mumps, reporting conflicting results.”
To further clarify the issue, they compared rates of IBD, Crohn’s disease, and ulcerative colitis among vaccinated and unvaccinated patients from eight case-control and three cohort studies published between 1970 and June 2014. When looking at IBD overall, 95% CIs for RRs all crossed 1.0, indicating no significant associations, they said. A subgroup analysis did link poliomyelitis vaccination with increased risk of developing Crohn’s disease (RR, 2.28; 95% CI, 1.12-4.63) or ulcerative colitis (RR, 3.48; 95% CI, 1.2-9.71), but the studies were dissimilar enough that the results need to be interpreted cautiously, they added.
To find the studies, the researchers searched MEDLINE, EMBASE, and the Cochrane central trials registry for randomized controlled trials, controlled clinical trials, cohort studies, and case-control studies published in any language and that included the terms ulcerative colitis, Crohn’s disease, inflammatory bowel disease, colitis, or ileitis. This approach yielded six population-based and two hospital-based case-control studies, and three population-based cohort studies. The studies of childhood immunizations included 2,399 patients with IBD and 33,747 controls, and the H1N1 study included 14,842 patients with IBD and almost 2 million controls, said the investigators.
The studies were “extremely heterogeneous” in terms of design, sample size, geographic location, and methods used to help patients recall their vaccination history, the investigators noted. “Vaccination protocols varied between countries and evolved through the years, with different types of vaccines and schedules leading to difficulties in risk evaluation,” they said. “Moreover, some vaccines used were live attenuated vaccines such as measles, oral poliomyelitis, or whole-cell pertussis vaccines, and may have a different effect on immune system activation and dysregulation, compared with other inactivated acellular vaccines.”
The Digitscience Foundation supported the research. The researchers declared having no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: A meta-analysis found no link between childhood vaccinations or H1N1 immunization in adults and inflammatory bowel disease.
Major finding: Risk ratios showed no significant associations between IBD and vaccines for BCG infection, diphtheria, tetanus, smallpox, poliomyelitis, measles, rubella, mumps, or H1N1 influenza.
Data source: Systematic review and meta-analysis of eight case-control studies and three cohort studies, encompassing 50,988 total patients.
Disclosures: The Digitscience Foundation supported the research. The researchers declared having no conflicts of interest.