User login
Experts debate fecal transplants as first-line therapy for CDI
SAN DIEGO – Fecal microbiota transplantation (FMT) is now first-line therapy for Clostridium difficile infection (CDI) in much of Scandinavia. At an annual conference on infectious diseases, two specialists debated whether that should be the case in the United States, too.
The epidemiology of CDI has changed greatly in the past decade, as other researchers have noted (Infect Drug Resist. 2014;7:63-72). Incidence, severity, and case-fatality rates have risen substantially, and individuals who lack the usual risk factors for CDI are now acquiring it in community settings. Moreover, CDI adds about 5-6 days to a patient’s average hospital stay, and almost one in three affected patients is rehospitalized (Am J Infect Control. 2015 Apr 1;43[4]:314-7.) – most often within a week of discharge, said Dr. Thomas Moore, who is at the University of Kansas, Wichita.
“Should FMT be used as first-line therapy? Not just yes, but hell, yes! It has superior efficacy,” Dr. Moore said.
He pointed to the recent landmark study (N Engl J Med. 2013;368:407-15) of CDI in which duodenal infusions of donor feces more than tripled the rates of relapse-free cure, compared with vancomycin monotherapy or vancomycin with bowel lavage (P less than .001 for both comparisons). Moreover, diarrhea resolved for 81% of patients after the first fecal infusion, and the observed superiority over the vancomycin regimens was so marked that investigators stopped the study after the interim analysis.
Evidence suggests FMT is safe as well as effective, said Dr. Moore. Centers in Norway, Sweden, Denmark, Finland, and Holland have treated at least 900 patients with no reported adverse effects and with cure rates of about 90%, he noted. Of more than 1,000 published FMT studies worldwide, there has been one only report of peritonitis after colonoscopy, one case of irritable bowel syndrome, three reports of mild enteritis, one case of upper gastrointestinal bleeding, one death from sepsis from a dislodged gastrostomy tube, and one case of new-onset obesity, which occurred after a patient received fecal microbiota donated by an obese relative, he added (Open Forum Infect Dis. 2015 Feb 1. doi: 10.1093/ofid/ofv004). Patients now receive fecal microbiota donations from normal-weight individuals, he noted (http://www.openbiome.org/stool-donation/).
“Fecal microbiota transplantation could save lives,” Dr. Moore concluded. Donor material is “cheap and unlimited, the procedure is cost-effective, easy to perform, can even be done at home, and patient satisfaction is very high.”
But Dr. Johan S. Bakken, an infectious disease specialist at St. Luke’s Hospital in Duluth, Minn., argued that FMT is not ready for first-line use for CDI in the United States. “There are no published FMT practice guidelines for initial therapy, even in Scandinavia, and no randomized controlled trials of FMT conducted anywhere,” said Dr. Bakken. He noted that because the Food and Drug Administration has not approved FMT for first-line use in CDI, utilization could require an approved Investigational New Drug application, leading to “unavoidable” treatment delays.
Clinicians also should not gloss over concerns about adverse effects with FMT, Dr. Bakken said. In addition to the case of new-onset obesity, there are risks of aspirating fecal material or perforating hollow viscera. Furthermore, the potential long-term adverse consequences of FMT are unknown, he said.
In contrast, the rate of resolution of initial CDI with per oral vancomycin or fidaxomicin is more than 80%, Dr. Bakken said. Moreover, liquid vancomycin at an appropriate dose and frequency for CDI costs about $4.25 per day in Duluth, he added. “No comparative outcomes data are available for FMT, but it is more costly than vancomycin, may not be locally available, and requires several days or weeks of planning,” he emphasized.
Cost-reimbursement issues with third-party payers are also likely with FMT, according to Dr. Bakken. “There also are potential or perceived medicolegal issues with FMT,” he said. “Keep in mind that about 80% of the world’s lawyers work and practice in the U.S.A.”
Dr. Moore had no disclosures. Dr. Bakken reported being an advisory board member of Rebiotix, which is developing a biologic drug to treat recurrent CDI.
 |
| Dr. Christina Surawicz |
Fecal microbiota transplant is the best treatment for multiple recurrences of C. difficile infection that have not responded to standard therapy including a good pulse and taper course of vancomycin. There is such enthusiasm for FMT because of its simplicity and the ready availability of stool, which is a natural product. Why use an antibiotic to treat an illness that is usually a result of antibiotics? Is FMT therefore the best treatment for a primary infection of C. difficile infection? While treatment for recurrent C. difficile infection is supported by several randomized, controlled trials, including comparison with vancomycin, gut lavage, and sham colonoscopy, there are no randomized, controlled trials for FMT as a treatment of first episodes of CDI. Moreover, 80% of people with their first infection respond to standard antibiotic therapy. In addition, we are learning how important the microbiome is but we do not know the long-term consequences of FMT on an individual. I must agree with Dr. Bakken, it is not wise at this time to use FMT for first episodes of uncomplicated CDI.
Dr. Christina Surawicz is a professor of medicine at University of Washington, Seattle. She has no conflicts of interest.
 |
| Dr. Christina Surawicz |
Fecal microbiota transplant is the best treatment for multiple recurrences of C. difficile infection that have not responded to standard therapy including a good pulse and taper course of vancomycin. There is such enthusiasm for FMT because of its simplicity and the ready availability of stool, which is a natural product. Why use an antibiotic to treat an illness that is usually a result of antibiotics? Is FMT therefore the best treatment for a primary infection of C. difficile infection? While treatment for recurrent C. difficile infection is supported by several randomized, controlled trials, including comparison with vancomycin, gut lavage, and sham colonoscopy, there are no randomized, controlled trials for FMT as a treatment of first episodes of CDI. Moreover, 80% of people with their first infection respond to standard antibiotic therapy. In addition, we are learning how important the microbiome is but we do not know the long-term consequences of FMT on an individual. I must agree with Dr. Bakken, it is not wise at this time to use FMT for first episodes of uncomplicated CDI.
Dr. Christina Surawicz is a professor of medicine at University of Washington, Seattle. She has no conflicts of interest.
 |
| Dr. Christina Surawicz |
Fecal microbiota transplant is the best treatment for multiple recurrences of C. difficile infection that have not responded to standard therapy including a good pulse and taper course of vancomycin. There is such enthusiasm for FMT because of its simplicity and the ready availability of stool, which is a natural product. Why use an antibiotic to treat an illness that is usually a result of antibiotics? Is FMT therefore the best treatment for a primary infection of C. difficile infection? While treatment for recurrent C. difficile infection is supported by several randomized, controlled trials, including comparison with vancomycin, gut lavage, and sham colonoscopy, there are no randomized, controlled trials for FMT as a treatment of first episodes of CDI. Moreover, 80% of people with their first infection respond to standard antibiotic therapy. In addition, we are learning how important the microbiome is but we do not know the long-term consequences of FMT on an individual. I must agree with Dr. Bakken, it is not wise at this time to use FMT for first episodes of uncomplicated CDI.
Dr. Christina Surawicz is a professor of medicine at University of Washington, Seattle. She has no conflicts of interest.
SAN DIEGO – Fecal microbiota transplantation (FMT) is now first-line therapy for Clostridium difficile infection (CDI) in much of Scandinavia. At an annual conference on infectious diseases, two specialists debated whether that should be the case in the United States, too.
The epidemiology of CDI has changed greatly in the past decade, as other researchers have noted (Infect Drug Resist. 2014;7:63-72). Incidence, severity, and case-fatality rates have risen substantially, and individuals who lack the usual risk factors for CDI are now acquiring it in community settings. Moreover, CDI adds about 5-6 days to a patient’s average hospital stay, and almost one in three affected patients is rehospitalized (Am J Infect Control. 2015 Apr 1;43[4]:314-7.) – most often within a week of discharge, said Dr. Thomas Moore, who is at the University of Kansas, Wichita.
“Should FMT be used as first-line therapy? Not just yes, but hell, yes! It has superior efficacy,” Dr. Moore said.
He pointed to the recent landmark study (N Engl J Med. 2013;368:407-15) of CDI in which duodenal infusions of donor feces more than tripled the rates of relapse-free cure, compared with vancomycin monotherapy or vancomycin with bowel lavage (P less than .001 for both comparisons). Moreover, diarrhea resolved for 81% of patients after the first fecal infusion, and the observed superiority over the vancomycin regimens was so marked that investigators stopped the study after the interim analysis.
Evidence suggests FMT is safe as well as effective, said Dr. Moore. Centers in Norway, Sweden, Denmark, Finland, and Holland have treated at least 900 patients with no reported adverse effects and with cure rates of about 90%, he noted. Of more than 1,000 published FMT studies worldwide, there has been one only report of peritonitis after colonoscopy, one case of irritable bowel syndrome, three reports of mild enteritis, one case of upper gastrointestinal bleeding, one death from sepsis from a dislodged gastrostomy tube, and one case of new-onset obesity, which occurred after a patient received fecal microbiota donated by an obese relative, he added (Open Forum Infect Dis. 2015 Feb 1. doi: 10.1093/ofid/ofv004). Patients now receive fecal microbiota donations from normal-weight individuals, he noted (http://www.openbiome.org/stool-donation/).
“Fecal microbiota transplantation could save lives,” Dr. Moore concluded. Donor material is “cheap and unlimited, the procedure is cost-effective, easy to perform, can even be done at home, and patient satisfaction is very high.”
But Dr. Johan S. Bakken, an infectious disease specialist at St. Luke’s Hospital in Duluth, Minn., argued that FMT is not ready for first-line use for CDI in the United States. “There are no published FMT practice guidelines for initial therapy, even in Scandinavia, and no randomized controlled trials of FMT conducted anywhere,” said Dr. Bakken. He noted that because the Food and Drug Administration has not approved FMT for first-line use in CDI, utilization could require an approved Investigational New Drug application, leading to “unavoidable” treatment delays.
Clinicians also should not gloss over concerns about adverse effects with FMT, Dr. Bakken said. In addition to the case of new-onset obesity, there are risks of aspirating fecal material or perforating hollow viscera. Furthermore, the potential long-term adverse consequences of FMT are unknown, he said.
In contrast, the rate of resolution of initial CDI with per oral vancomycin or fidaxomicin is more than 80%, Dr. Bakken said. Moreover, liquid vancomycin at an appropriate dose and frequency for CDI costs about $4.25 per day in Duluth, he added. “No comparative outcomes data are available for FMT, but it is more costly than vancomycin, may not be locally available, and requires several days or weeks of planning,” he emphasized.
Cost-reimbursement issues with third-party payers are also likely with FMT, according to Dr. Bakken. “There also are potential or perceived medicolegal issues with FMT,” he said. “Keep in mind that about 80% of the world’s lawyers work and practice in the U.S.A.”
Dr. Moore had no disclosures. Dr. Bakken reported being an advisory board member of Rebiotix, which is developing a biologic drug to treat recurrent CDI.
SAN DIEGO – Fecal microbiota transplantation (FMT) is now first-line therapy for Clostridium difficile infection (CDI) in much of Scandinavia. At an annual conference on infectious diseases, two specialists debated whether that should be the case in the United States, too.
The epidemiology of CDI has changed greatly in the past decade, as other researchers have noted (Infect Drug Resist. 2014;7:63-72). Incidence, severity, and case-fatality rates have risen substantially, and individuals who lack the usual risk factors for CDI are now acquiring it in community settings. Moreover, CDI adds about 5-6 days to a patient’s average hospital stay, and almost one in three affected patients is rehospitalized (Am J Infect Control. 2015 Apr 1;43[4]:314-7.) – most often within a week of discharge, said Dr. Thomas Moore, who is at the University of Kansas, Wichita.
“Should FMT be used as first-line therapy? Not just yes, but hell, yes! It has superior efficacy,” Dr. Moore said.
He pointed to the recent landmark study (N Engl J Med. 2013;368:407-15) of CDI in which duodenal infusions of donor feces more than tripled the rates of relapse-free cure, compared with vancomycin monotherapy or vancomycin with bowel lavage (P less than .001 for both comparisons). Moreover, diarrhea resolved for 81% of patients after the first fecal infusion, and the observed superiority over the vancomycin regimens was so marked that investigators stopped the study after the interim analysis.
Evidence suggests FMT is safe as well as effective, said Dr. Moore. Centers in Norway, Sweden, Denmark, Finland, and Holland have treated at least 900 patients with no reported adverse effects and with cure rates of about 90%, he noted. Of more than 1,000 published FMT studies worldwide, there has been one only report of peritonitis after colonoscopy, one case of irritable bowel syndrome, three reports of mild enteritis, one case of upper gastrointestinal bleeding, one death from sepsis from a dislodged gastrostomy tube, and one case of new-onset obesity, which occurred after a patient received fecal microbiota donated by an obese relative, he added (Open Forum Infect Dis. 2015 Feb 1. doi: 10.1093/ofid/ofv004). Patients now receive fecal microbiota donations from normal-weight individuals, he noted (http://www.openbiome.org/stool-donation/).
“Fecal microbiota transplantation could save lives,” Dr. Moore concluded. Donor material is “cheap and unlimited, the procedure is cost-effective, easy to perform, can even be done at home, and patient satisfaction is very high.”
But Dr. Johan S. Bakken, an infectious disease specialist at St. Luke’s Hospital in Duluth, Minn., argued that FMT is not ready for first-line use for CDI in the United States. “There are no published FMT practice guidelines for initial therapy, even in Scandinavia, and no randomized controlled trials of FMT conducted anywhere,” said Dr. Bakken. He noted that because the Food and Drug Administration has not approved FMT for first-line use in CDI, utilization could require an approved Investigational New Drug application, leading to “unavoidable” treatment delays.
Clinicians also should not gloss over concerns about adverse effects with FMT, Dr. Bakken said. In addition to the case of new-onset obesity, there are risks of aspirating fecal material or perforating hollow viscera. Furthermore, the potential long-term adverse consequences of FMT are unknown, he said.
In contrast, the rate of resolution of initial CDI with per oral vancomycin or fidaxomicin is more than 80%, Dr. Bakken said. Moreover, liquid vancomycin at an appropriate dose and frequency for CDI costs about $4.25 per day in Duluth, he added. “No comparative outcomes data are available for FMT, but it is more costly than vancomycin, may not be locally available, and requires several days or weeks of planning,” he emphasized.
Cost-reimbursement issues with third-party payers are also likely with FMT, according to Dr. Bakken. “There also are potential or perceived medicolegal issues with FMT,” he said. “Keep in mind that about 80% of the world’s lawyers work and practice in the U.S.A.”
Dr. Moore had no disclosures. Dr. Bakken reported being an advisory board member of Rebiotix, which is developing a biologic drug to treat recurrent CDI.
EXPERT ANALYSIS AT IDWEEK 2015
C. difficile risk score identifies high-risk patients
Researchers have created a risk score to help identify patients at high risk for Clostridium difficile infection after hospitalization, for future use in vaccine trials, according to a new study.
C. difficile is the most common pathogen type in health care–associated infections and the leading cause of enterocolitis-associated deaths. Identification of patients who are at high risk for C. difficile is important in the development of future vaccines.
Dr. James Baggs, epidemiologist at the Centers for Disease Control and Prevention, and his colleagues conducted a retrospective cohort study to identify groups at high risk for C. difficile infection (CDI) for future vaccine trials. Their results were published in Vaccine online Oct. 9.
Data on medications and discharge were obtained from two large academic medical centers in Connecticut and New York. This information was linked to surveillance data from the Emerging Infections Program on active population-based CDIs. Participants were included if they had a hospital stay without a history of CDI with a primary outcome of infection 28 days or more after discharge.
To identify predictors of CDI after discharge, the investigators used a backward elimination employing a Cox proportional hazards model. They then created a CDI risk index based on the predictors.
During the study period, a total of 35,186 index hospitalizations were identified in Connecticut and New York. CDI diagnosis 28 days or more after discharge was observed in 288 patients (0.82%).
Initial models did not perform well in cross-site validation; however, a combined model that included age, past hospitalizations, use of 3rd/4th generation cephalosporin, clindamycin, or fluoroquinolone antibiotics was developed. This validation cohort resulted in a risk score that was predictive (P less than .001).
Finally, the study participants were divided into high-risk and low-risk groups based on the distribution of scores in the cohort. The low-risk group experienced CDI diagnosis 28 days or more after hospitalization at a rate of 0.3% versus 1.6% in the high-risk group.
“Our study identified specific parameters for a risk index that can be applied at hospital discharge to identify a patient population with increased risk of CDI [greater than or equal to] 28 days after discharge that could be targeted for vaccine trials,” Dr. Braggs and his coauthors wrote.
The authors noted several limitations to the study. For example, they indicated that data was obtained from two hospitals which may not represent some minority populations. Therefore, data from other hospitals may be able to help identify if the risk index is generalizable.
No conflicts of interest were reported. The study was partially funded by GlaxoSmithKline through the CDC Foundation, and GSK had the opportunity to review the preliminary manuscript.
Researchers have created a risk score to help identify patients at high risk for Clostridium difficile infection after hospitalization, for future use in vaccine trials, according to a new study.
C. difficile is the most common pathogen type in health care–associated infections and the leading cause of enterocolitis-associated deaths. Identification of patients who are at high risk for C. difficile is important in the development of future vaccines.
Dr. James Baggs, epidemiologist at the Centers for Disease Control and Prevention, and his colleagues conducted a retrospective cohort study to identify groups at high risk for C. difficile infection (CDI) for future vaccine trials. Their results were published in Vaccine online Oct. 9.
Data on medications and discharge were obtained from two large academic medical centers in Connecticut and New York. This information was linked to surveillance data from the Emerging Infections Program on active population-based CDIs. Participants were included if they had a hospital stay without a history of CDI with a primary outcome of infection 28 days or more after discharge.
To identify predictors of CDI after discharge, the investigators used a backward elimination employing a Cox proportional hazards model. They then created a CDI risk index based on the predictors.
During the study period, a total of 35,186 index hospitalizations were identified in Connecticut and New York. CDI diagnosis 28 days or more after discharge was observed in 288 patients (0.82%).
Initial models did not perform well in cross-site validation; however, a combined model that included age, past hospitalizations, use of 3rd/4th generation cephalosporin, clindamycin, or fluoroquinolone antibiotics was developed. This validation cohort resulted in a risk score that was predictive (P less than .001).
Finally, the study participants were divided into high-risk and low-risk groups based on the distribution of scores in the cohort. The low-risk group experienced CDI diagnosis 28 days or more after hospitalization at a rate of 0.3% versus 1.6% in the high-risk group.
“Our study identified specific parameters for a risk index that can be applied at hospital discharge to identify a patient population with increased risk of CDI [greater than or equal to] 28 days after discharge that could be targeted for vaccine trials,” Dr. Braggs and his coauthors wrote.
The authors noted several limitations to the study. For example, they indicated that data was obtained from two hospitals which may not represent some minority populations. Therefore, data from other hospitals may be able to help identify if the risk index is generalizable.
No conflicts of interest were reported. The study was partially funded by GlaxoSmithKline through the CDC Foundation, and GSK had the opportunity to review the preliminary manuscript.
Researchers have created a risk score to help identify patients at high risk for Clostridium difficile infection after hospitalization, for future use in vaccine trials, according to a new study.
C. difficile is the most common pathogen type in health care–associated infections and the leading cause of enterocolitis-associated deaths. Identification of patients who are at high risk for C. difficile is important in the development of future vaccines.
Dr. James Baggs, epidemiologist at the Centers for Disease Control and Prevention, and his colleagues conducted a retrospective cohort study to identify groups at high risk for C. difficile infection (CDI) for future vaccine trials. Their results were published in Vaccine online Oct. 9.
Data on medications and discharge were obtained from two large academic medical centers in Connecticut and New York. This information was linked to surveillance data from the Emerging Infections Program on active population-based CDIs. Participants were included if they had a hospital stay without a history of CDI with a primary outcome of infection 28 days or more after discharge.
To identify predictors of CDI after discharge, the investigators used a backward elimination employing a Cox proportional hazards model. They then created a CDI risk index based on the predictors.
During the study period, a total of 35,186 index hospitalizations were identified in Connecticut and New York. CDI diagnosis 28 days or more after discharge was observed in 288 patients (0.82%).
Initial models did not perform well in cross-site validation; however, a combined model that included age, past hospitalizations, use of 3rd/4th generation cephalosporin, clindamycin, or fluoroquinolone antibiotics was developed. This validation cohort resulted in a risk score that was predictive (P less than .001).
Finally, the study participants were divided into high-risk and low-risk groups based on the distribution of scores in the cohort. The low-risk group experienced CDI diagnosis 28 days or more after hospitalization at a rate of 0.3% versus 1.6% in the high-risk group.
“Our study identified specific parameters for a risk index that can be applied at hospital discharge to identify a patient population with increased risk of CDI [greater than or equal to] 28 days after discharge that could be targeted for vaccine trials,” Dr. Braggs and his coauthors wrote.
The authors noted several limitations to the study. For example, they indicated that data was obtained from two hospitals which may not represent some minority populations. Therefore, data from other hospitals may be able to help identify if the risk index is generalizable.
No conflicts of interest were reported. The study was partially funded by GlaxoSmithKline through the CDC Foundation, and GSK had the opportunity to review the preliminary manuscript.
FROM VACCINE
Key clinical point: Researchers have created a risk score identifying patients at high risk for C. difficile infection after hospitalization, for future use in vaccine trials.
Major finding: A combined model which included age, past hospitalizations, use of 3rd/4th generation cephalosporin, clindamycin, or fluoroquinolone antibiotics resulted in a predictive risk score (P less than .001).
Data source: A retrospective cohort study with data from two large academic medical centers in Connecticut and New York which was linked to surveillance data from the Emerging Infections Program.
Disclosures: No conflicts of interest were reported. The study was partially funded by GlaxoSmithKline through the CDC Foundation, and GSK had the opportunity to review the preliminary manuscript.
IDWeek: Testing delays linked to misclassification of hospital-onset C. difficile
SAN DIEGO – Delays in laboratory testing led a hospital to misclassify the origin of nearly a quarter of Clostridium difficile infections, Dr. Christopher Polage said at an annual scientific meeting on infectious diseases.
“Many patients with symptoms and risk factors are not being tested within 3 days of admission, leading to overreporting of hospital-onset [Clostridium difficile infections] and underreporting of community-onset CDI,” said Dr. Polage of the UC Davis (Calif.) Health System. By testing patients who have diarrhea and risk factors for CDI sooner after admission, hospitals can prevent outbreaks and improve their standardized infection ratio for CDI, he added.
Clostridium difficile is implicated in about 29,000 deaths every year in the United States. The vast majority of such cases are classified as hospital onset, based on the “3-day rule,” meaning that patients were tested more than 3 days after admission. “This is the preventable hospital outcome that we’re all trying to bring down,” Dr. Polage said.
As part of that effort, he and his colleagues studied 11 hospital units that were considered high risk for CDI. To identify toxigenic C. difficile, they performed culture and polymerase chain reaction testing on perianal swabs collected from all adult patients admitted to these units. They also analyzed toxin immunoassays of stool samples when physicians requested them for patients with diarrhea.
“The question was, how often was misclassification happening?” said Dr. Polage. Among 48 cases that the laboratory reported as hospital onset, based on the “3-day rule,” close to half (44%) actually had CD-positive perianal swabs when admitted, he said. And half of these swab-positive patients waited more than 3 days for a CD stool test even though they had current or recent diarrhea, he added. In fact, swab-positive patients with diarrhea went a median of 6 days without a CD stool test, and some went untested for 10 days, Dr. Polage said.
“Anyone who has tried to determine if a hospitalized patient is having diarrhea knows that this can be very hard to pin down,” Dr. Polage noted. But some patients with positive swabs on admission met three different definitions for diarrhea, “making it pretty clear that they had community-onset CDI,” he said. This most conservative approach found that 23% of “hospital-onset” cases were actually community onset, he said.
Thus far, UC Davis Health System seems not to have had an increase in antibiotic prescriptions in response to greater detection of community-onset CDI, Dr. Polage said. “This is not something we take lightly,” he added. “We put together a lot of educational materials for patients, physicians, and providers, and work with our antibiotic stewardship team. We found that we might be able to focus on patients who had CDI at time of admission, and intervene with them individually to more carefully monitor what antibiotic they were using.”
Dr. Polage reported these findings at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The Gordon and Betty Moore Foundation helped fund the study. Dr. Polage reported having received research materials or honoraria from Cepheid, TechLab, Alere, Meridian, and ACEA Biosciences.
SAN DIEGO – Delays in laboratory testing led a hospital to misclassify the origin of nearly a quarter of Clostridium difficile infections, Dr. Christopher Polage said at an annual scientific meeting on infectious diseases.
“Many patients with symptoms and risk factors are not being tested within 3 days of admission, leading to overreporting of hospital-onset [Clostridium difficile infections] and underreporting of community-onset CDI,” said Dr. Polage of the UC Davis (Calif.) Health System. By testing patients who have diarrhea and risk factors for CDI sooner after admission, hospitals can prevent outbreaks and improve their standardized infection ratio for CDI, he added.
Clostridium difficile is implicated in about 29,000 deaths every year in the United States. The vast majority of such cases are classified as hospital onset, based on the “3-day rule,” meaning that patients were tested more than 3 days after admission. “This is the preventable hospital outcome that we’re all trying to bring down,” Dr. Polage said.
As part of that effort, he and his colleagues studied 11 hospital units that were considered high risk for CDI. To identify toxigenic C. difficile, they performed culture and polymerase chain reaction testing on perianal swabs collected from all adult patients admitted to these units. They also analyzed toxin immunoassays of stool samples when physicians requested them for patients with diarrhea.
“The question was, how often was misclassification happening?” said Dr. Polage. Among 48 cases that the laboratory reported as hospital onset, based on the “3-day rule,” close to half (44%) actually had CD-positive perianal swabs when admitted, he said. And half of these swab-positive patients waited more than 3 days for a CD stool test even though they had current or recent diarrhea, he added. In fact, swab-positive patients with diarrhea went a median of 6 days without a CD stool test, and some went untested for 10 days, Dr. Polage said.
“Anyone who has tried to determine if a hospitalized patient is having diarrhea knows that this can be very hard to pin down,” Dr. Polage noted. But some patients with positive swabs on admission met three different definitions for diarrhea, “making it pretty clear that they had community-onset CDI,” he said. This most conservative approach found that 23% of “hospital-onset” cases were actually community onset, he said.
Thus far, UC Davis Health System seems not to have had an increase in antibiotic prescriptions in response to greater detection of community-onset CDI, Dr. Polage said. “This is not something we take lightly,” he added. “We put together a lot of educational materials for patients, physicians, and providers, and work with our antibiotic stewardship team. We found that we might be able to focus on patients who had CDI at time of admission, and intervene with them individually to more carefully monitor what antibiotic they were using.”
Dr. Polage reported these findings at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The Gordon and Betty Moore Foundation helped fund the study. Dr. Polage reported having received research materials or honoraria from Cepheid, TechLab, Alere, Meridian, and ACEA Biosciences.
SAN DIEGO – Delays in laboratory testing led a hospital to misclassify the origin of nearly a quarter of Clostridium difficile infections, Dr. Christopher Polage said at an annual scientific meeting on infectious diseases.
“Many patients with symptoms and risk factors are not being tested within 3 days of admission, leading to overreporting of hospital-onset [Clostridium difficile infections] and underreporting of community-onset CDI,” said Dr. Polage of the UC Davis (Calif.) Health System. By testing patients who have diarrhea and risk factors for CDI sooner after admission, hospitals can prevent outbreaks and improve their standardized infection ratio for CDI, he added.
Clostridium difficile is implicated in about 29,000 deaths every year in the United States. The vast majority of such cases are classified as hospital onset, based on the “3-day rule,” meaning that patients were tested more than 3 days after admission. “This is the preventable hospital outcome that we’re all trying to bring down,” Dr. Polage said.
As part of that effort, he and his colleagues studied 11 hospital units that were considered high risk for CDI. To identify toxigenic C. difficile, they performed culture and polymerase chain reaction testing on perianal swabs collected from all adult patients admitted to these units. They also analyzed toxin immunoassays of stool samples when physicians requested them for patients with diarrhea.
“The question was, how often was misclassification happening?” said Dr. Polage. Among 48 cases that the laboratory reported as hospital onset, based on the “3-day rule,” close to half (44%) actually had CD-positive perianal swabs when admitted, he said. And half of these swab-positive patients waited more than 3 days for a CD stool test even though they had current or recent diarrhea, he added. In fact, swab-positive patients with diarrhea went a median of 6 days without a CD stool test, and some went untested for 10 days, Dr. Polage said.
“Anyone who has tried to determine if a hospitalized patient is having diarrhea knows that this can be very hard to pin down,” Dr. Polage noted. But some patients with positive swabs on admission met three different definitions for diarrhea, “making it pretty clear that they had community-onset CDI,” he said. This most conservative approach found that 23% of “hospital-onset” cases were actually community onset, he said.
Thus far, UC Davis Health System seems not to have had an increase in antibiotic prescriptions in response to greater detection of community-onset CDI, Dr. Polage said. “This is not something we take lightly,” he added. “We put together a lot of educational materials for patients, physicians, and providers, and work with our antibiotic stewardship team. We found that we might be able to focus on patients who had CDI at time of admission, and intervene with them individually to more carefully monitor what antibiotic they were using.”
Dr. Polage reported these findings at IDWeek, the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
The Gordon and Betty Moore Foundation helped fund the study. Dr. Polage reported having received research materials or honoraria from Cepheid, TechLab, Alere, Meridian, and ACEA Biosciences.
AT IDWEEK 2015
Key clinical point: Delays in laboratory testing led to misclassification of Clostridium difficile infections.
Major finding: At least 23% of cases that were reported as hospital onset were actually community onset.
Data source: An analysis of 12 months of C. difficile infection surveillance data from one academic medical center.
Disclosures: The Gordon and Betty Moore Foundation helped fund the study. Dr. Polage reported having received research materials or honoraria from Cepheid, TechLab, Alere, Meridian, and ACEA Biosciences.
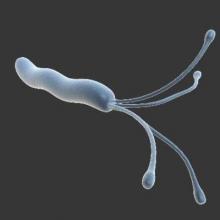
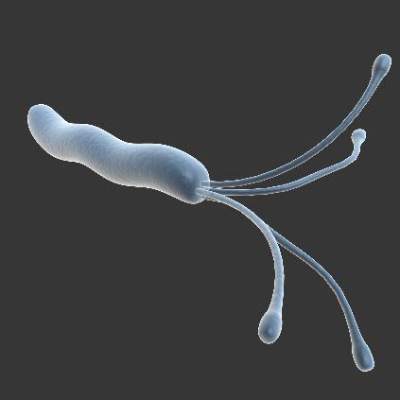
Oral H. pylori vaccine found effective, safe
For the first time, an oral vaccine against Helicobacter pylori infection proved effective and safe in a phase III trial involving nearly 4,500 children in China, according to a report published in the Oct. 10 issue of the Lancet.
The vaccine’s efficacy waned somewhat after the first year but still significantly reduced H. pylori infection in approximately 1,000 of the recipients followed for the entire 3-year study period. This suggests that it could substantially reduce the rates of gastritis, peptic ulcer, gastric adenocarcinoma, and lymphoma associated with the infection, which currently affects more than half the world’s population, including more than 600 million in China, said Ming Zeng, Ph.D., of the Chinese National Institute for Food and Drug Control, Beijing, and associates.
Researchers at Third Military Medical University, Chongqing and Chongqing Kangwei Biotechnology, both in China, developed the new vaccine using DNA recombination technology to fuse urease B subunit proteins (gene derived from H. pylori) with heat-labile enterotoxin B subunit proteins (gene derived from E. coli). The vaccine was designed to be administered in three oral doses given 2 weeks apart, after study subjects fasted for at least 2 hours and then drank an 80-mL buffer solution containing sodium bicarbonate and sodium citrate.
Dr. Zeng and associates compared the vaccine (2,232 participants) against an identical placebo (2,232 participants) in the single-center, double-blind, randomized trial, which involved children aged 6-15 years recruited from 12 schools in Ganyu County in eastern China. All the study participants were healthy and tested negative for past or present H. pylori infection at baseline.
The primary endpoint – the development of H. pylori infection within the first year after vaccination – occurred in 14 children who received the vaccine, which was significantly fewer than the 50 children who received placebo. This yielded a vaccine efficacy rate of 71.8% at 1 year. During extended follow-up of a subset of 3,014 participants at 2 years, 10 H. pylori infections developed in the vaccine group and 22 in the placebo group, for a vaccine efficacy of 55.0%. Similarly, at 3-year follow-up of 1,946 participants, vaccine efficacy was 55.8%, the investigators said (Lancet 2015 Oct 10;386:1457-64).
“The event rate of the placebo group varied from 2.4 to 1.4 per 100 person-years, whereas that of the vaccine group remained around 0.7/100 person-years” throughout the 3-year study period, they added.
The vaccine elicited a significantly greater immune response than did the placebo, as measured in serum IgG and salivary IgA. The geometric mean titer was 389.4 in vaccine recipients, compared with only 72.2 in the placebo group, and the seroconversion rate was 86.1% for the vaccine, compared with 4.6% for placebo. The “mild” waning trend in vaccine-elicited antibodies suggests that a booster dose may be necessary in later years, Dr. Zeng and associates wrote.
The incidence of adverse reactions to the vaccine was identical in the two study groups, at 7%. All adverse reactions were mild and resolved within 24 hours. The most frequent was vomiting, followed by fever and headache. No serious adverse events were considered to be related to the study drug. “However, the number of participants in this study might not be enough to identify rare vaccine-related adverse events. Longer-term follow-up is needed in much larger populations” and in more ethnically and demographically diverse groups to identify such rare reactions, they noted.
A game changer for H. pylori infection?
Prevention of H. pylori infection through low-cost vaccination is appealing to reduce the global gastric cancer burden. While effective vaccines are available for other cancer-causing infections such as hepatitis B and human papillomavirus, vaccine development for H. pylori has been disappointing. In the October issue of the Lancet, a new study by Zheng and colleagues offers renewed optimism for preventative vaccination strategies aimed at H. pylori. The study reports the results of a large double-blind, randomized placebo-controlled oral vaccine trial in China in nearly 4,500 children (aged 5-16).
 |
| Dr. Nicola L. Jones |
The primary endpoint was H. pylori infection at 1 year. Fourteen children developed infection in the vaccine group versus 50 in the placebo group, providing a vaccine efficacy of approximately 70%. No serious adverse events were reported and minor adverse events were comparable between the groups. The trial was extended to allow long-term follow-up to 3 years in a large subset of children. Although the vaccine continued to offer protection, vaccine efficacy was 50.8% at the 3-year time point suggesting a waning of protective effect and need for optimization.
The promising results of this study suggest that reduction of the world-wide burden of H. pylori-related disease through preventative vaccination is attainable.
Nicola L. Jones, M.D., FRCPC, Ph.D., is professor of paediatrics and physiology, University of Toronto; division of gastroenterology, hepatology, and nutrition, Sickkids Hospital, Toronto. She has no conflicts of interest.
A game changer for H. pylori infection?
Prevention of H. pylori infection through low-cost vaccination is appealing to reduce the global gastric cancer burden. While effective vaccines are available for other cancer-causing infections such as hepatitis B and human papillomavirus, vaccine development for H. pylori has been disappointing. In the October issue of the Lancet, a new study by Zheng and colleagues offers renewed optimism for preventative vaccination strategies aimed at H. pylori. The study reports the results of a large double-blind, randomized placebo-controlled oral vaccine trial in China in nearly 4,500 children (aged 5-16).
 |
| Dr. Nicola L. Jones |
The primary endpoint was H. pylori infection at 1 year. Fourteen children developed infection in the vaccine group versus 50 in the placebo group, providing a vaccine efficacy of approximately 70%. No serious adverse events were reported and minor adverse events were comparable between the groups. The trial was extended to allow long-term follow-up to 3 years in a large subset of children. Although the vaccine continued to offer protection, vaccine efficacy was 50.8% at the 3-year time point suggesting a waning of protective effect and need for optimization.
The promising results of this study suggest that reduction of the world-wide burden of H. pylori-related disease through preventative vaccination is attainable.
Nicola L. Jones, M.D., FRCPC, Ph.D., is professor of paediatrics and physiology, University of Toronto; division of gastroenterology, hepatology, and nutrition, Sickkids Hospital, Toronto. She has no conflicts of interest.
A game changer for H. pylori infection?
Prevention of H. pylori infection through low-cost vaccination is appealing to reduce the global gastric cancer burden. While effective vaccines are available for other cancer-causing infections such as hepatitis B and human papillomavirus, vaccine development for H. pylori has been disappointing. In the October issue of the Lancet, a new study by Zheng and colleagues offers renewed optimism for preventative vaccination strategies aimed at H. pylori. The study reports the results of a large double-blind, randomized placebo-controlled oral vaccine trial in China in nearly 4,500 children (aged 5-16).
 |
| Dr. Nicola L. Jones |
The primary endpoint was H. pylori infection at 1 year. Fourteen children developed infection in the vaccine group versus 50 in the placebo group, providing a vaccine efficacy of approximately 70%. No serious adverse events were reported and minor adverse events were comparable between the groups. The trial was extended to allow long-term follow-up to 3 years in a large subset of children. Although the vaccine continued to offer protection, vaccine efficacy was 50.8% at the 3-year time point suggesting a waning of protective effect and need for optimization.
The promising results of this study suggest that reduction of the world-wide burden of H. pylori-related disease through preventative vaccination is attainable.
Nicola L. Jones, M.D., FRCPC, Ph.D., is professor of paediatrics and physiology, University of Toronto; division of gastroenterology, hepatology, and nutrition, Sickkids Hospital, Toronto. She has no conflicts of interest.
For the first time, an oral vaccine against Helicobacter pylori infection proved effective and safe in a phase III trial involving nearly 4,500 children in China, according to a report published in the Oct. 10 issue of the Lancet.
The vaccine’s efficacy waned somewhat after the first year but still significantly reduced H. pylori infection in approximately 1,000 of the recipients followed for the entire 3-year study period. This suggests that it could substantially reduce the rates of gastritis, peptic ulcer, gastric adenocarcinoma, and lymphoma associated with the infection, which currently affects more than half the world’s population, including more than 600 million in China, said Ming Zeng, Ph.D., of the Chinese National Institute for Food and Drug Control, Beijing, and associates.
Researchers at Third Military Medical University, Chongqing and Chongqing Kangwei Biotechnology, both in China, developed the new vaccine using DNA recombination technology to fuse urease B subunit proteins (gene derived from H. pylori) with heat-labile enterotoxin B subunit proteins (gene derived from E. coli). The vaccine was designed to be administered in three oral doses given 2 weeks apart, after study subjects fasted for at least 2 hours and then drank an 80-mL buffer solution containing sodium bicarbonate and sodium citrate.
Dr. Zeng and associates compared the vaccine (2,232 participants) against an identical placebo (2,232 participants) in the single-center, double-blind, randomized trial, which involved children aged 6-15 years recruited from 12 schools in Ganyu County in eastern China. All the study participants were healthy and tested negative for past or present H. pylori infection at baseline.
The primary endpoint – the development of H. pylori infection within the first year after vaccination – occurred in 14 children who received the vaccine, which was significantly fewer than the 50 children who received placebo. This yielded a vaccine efficacy rate of 71.8% at 1 year. During extended follow-up of a subset of 3,014 participants at 2 years, 10 H. pylori infections developed in the vaccine group and 22 in the placebo group, for a vaccine efficacy of 55.0%. Similarly, at 3-year follow-up of 1,946 participants, vaccine efficacy was 55.8%, the investigators said (Lancet 2015 Oct 10;386:1457-64).
“The event rate of the placebo group varied from 2.4 to 1.4 per 100 person-years, whereas that of the vaccine group remained around 0.7/100 person-years” throughout the 3-year study period, they added.
The vaccine elicited a significantly greater immune response than did the placebo, as measured in serum IgG and salivary IgA. The geometric mean titer was 389.4 in vaccine recipients, compared with only 72.2 in the placebo group, and the seroconversion rate was 86.1% for the vaccine, compared with 4.6% for placebo. The “mild” waning trend in vaccine-elicited antibodies suggests that a booster dose may be necessary in later years, Dr. Zeng and associates wrote.
The incidence of adverse reactions to the vaccine was identical in the two study groups, at 7%. All adverse reactions were mild and resolved within 24 hours. The most frequent was vomiting, followed by fever and headache. No serious adverse events were considered to be related to the study drug. “However, the number of participants in this study might not be enough to identify rare vaccine-related adverse events. Longer-term follow-up is needed in much larger populations” and in more ethnically and demographically diverse groups to identify such rare reactions, they noted.
For the first time, an oral vaccine against Helicobacter pylori infection proved effective and safe in a phase III trial involving nearly 4,500 children in China, according to a report published in the Oct. 10 issue of the Lancet.
The vaccine’s efficacy waned somewhat after the first year but still significantly reduced H. pylori infection in approximately 1,000 of the recipients followed for the entire 3-year study period. This suggests that it could substantially reduce the rates of gastritis, peptic ulcer, gastric adenocarcinoma, and lymphoma associated with the infection, which currently affects more than half the world’s population, including more than 600 million in China, said Ming Zeng, Ph.D., of the Chinese National Institute for Food and Drug Control, Beijing, and associates.
Researchers at Third Military Medical University, Chongqing and Chongqing Kangwei Biotechnology, both in China, developed the new vaccine using DNA recombination technology to fuse urease B subunit proteins (gene derived from H. pylori) with heat-labile enterotoxin B subunit proteins (gene derived from E. coli). The vaccine was designed to be administered in three oral doses given 2 weeks apart, after study subjects fasted for at least 2 hours and then drank an 80-mL buffer solution containing sodium bicarbonate and sodium citrate.
Dr. Zeng and associates compared the vaccine (2,232 participants) against an identical placebo (2,232 participants) in the single-center, double-blind, randomized trial, which involved children aged 6-15 years recruited from 12 schools in Ganyu County in eastern China. All the study participants were healthy and tested negative for past or present H. pylori infection at baseline.
The primary endpoint – the development of H. pylori infection within the first year after vaccination – occurred in 14 children who received the vaccine, which was significantly fewer than the 50 children who received placebo. This yielded a vaccine efficacy rate of 71.8% at 1 year. During extended follow-up of a subset of 3,014 participants at 2 years, 10 H. pylori infections developed in the vaccine group and 22 in the placebo group, for a vaccine efficacy of 55.0%. Similarly, at 3-year follow-up of 1,946 participants, vaccine efficacy was 55.8%, the investigators said (Lancet 2015 Oct 10;386:1457-64).
“The event rate of the placebo group varied from 2.4 to 1.4 per 100 person-years, whereas that of the vaccine group remained around 0.7/100 person-years” throughout the 3-year study period, they added.
The vaccine elicited a significantly greater immune response than did the placebo, as measured in serum IgG and salivary IgA. The geometric mean titer was 389.4 in vaccine recipients, compared with only 72.2 in the placebo group, and the seroconversion rate was 86.1% for the vaccine, compared with 4.6% for placebo. The “mild” waning trend in vaccine-elicited antibodies suggests that a booster dose may be necessary in later years, Dr. Zeng and associates wrote.
The incidence of adverse reactions to the vaccine was identical in the two study groups, at 7%. All adverse reactions were mild and resolved within 24 hours. The most frequent was vomiting, followed by fever and headache. No serious adverse events were considered to be related to the study drug. “However, the number of participants in this study might not be enough to identify rare vaccine-related adverse events. Longer-term follow-up is needed in much larger populations” and in more ethnically and demographically diverse groups to identify such rare reactions, they noted.
FROM LANCET
Key clinical point: For the first time, an oral vaccine against H. pylori infection proved effective and safe in a phase III trial.
Major finding: The primary endpoint – the development of H. pylori infection within the first year after vaccination – occurred in 14 children who received the vaccine and 50 children who received placebo, for a vaccine efficacy rate of 71.8%.
Data source: A single-center, randomized, placebo-controlled, phase III trial involving 4,464 children aged 6-15 years residing in China.
Disclosures: This study was funded by Chongqing Kangwei Biotechnology. Dr. Zeng reported having no relevant financial disclosures; one associate reported being employed by Chongqing Kangwei.
Chinese herbs bring relief from IBS constipation
A Chinese herbal medicine preparation may offer relief from constipation symptoms in individuals with irritable bowel syndrome.
A randomized, placebo-controlled trial in 125 individuals with constipation-predominant irritable bowel syndrome (IBS-C) showed the preparation was associated with significant improvements, compared with placebo.
In the per-protocol analysis, 68% of patients given the herbal medicine reported achieving adequate relief from their symptoms, compared with 43% of the placebo group (P = .10), according to a paper published online in Clinical Gastroenterology and Hepatology.
Patients were randomized to receive either a standardized extract of seven Chinese herbal medicine ingredients in capsule form – five capsules taken twice daily – or a taste- and color-matched placebo for 8 weeks, with further follow-up at 16 weeks.
The herbal ingredients included extracts of Chinese peony (Paeonia lactiflora), Seville orange (Citrus aurantium), Magnolia officinalis, and Chinese licorice (Glycyrrhiza uralensis), which were used for their antispasmodic effects, as intestinal muscle relaxants, and as myorelaxants.
The authors commented that while there are recent advances in the treatment of irritable bowel syndrome – such as the serotonergic agent prucalopride, chloride channel activator lubiprostone, and guanylate cyclase–C activator linaclotide – there is not yet a single drug regimen that shows efficacy for the many symptoms of IBS or addresses the high rate of symptom return.
In the study, patients treated with the herbal preparation showed improved bowel habits at the end of treatment, including significantly lower IBS Symptom Severity Scale scores, reduced straining during defecation, a decrease in hard, lumpy stools, and increased stool consistency.
“Although there were significant results for participants in the treatment group, to gain adequate benefit they needed to remain on treatment,” wrote Dr. Alan Bensoussan of the National Institute of Complementary Medicine at the University of Western Sydney (Australia) and his coauthors.
However, the study did not find any statistically significant differences between the intervention and placebo arm in overall IBS-related quality of life, abdominal pain, or bloating at the end of treatment (Clin. Gastroenterol. Hepatol. 2015 Jun 29. doi:10.1016/j.cgh.2015.06.022).
“Thus, IBS-C participants appeared to interpret more normal bowel functions as a significant improvement in the condition, but [quality of life] may only improve when pain and bloating are also substantially ameliorated,” the authors wrote.
Researchers said this finding supports recently published data suggesting that improving bowel movements is a higher priority for patients with IBS-C than pain relief.
Although patients were asked to discontinue related treatment such as anticholinergic agents, opioid analgesics, and regular laxatives, they were allowed some rescue medication.
There was a nonsignificantly greater use of bulking agents in the Chinese herbal medicine group, and stimulant laxative use in the placebo group.
The study medication was generally well tolerated, although there were twice as many gastrointestinal adverse events reported in the intervention group as in the control group.
Overall, there were 19 withdrawals from the study, 6 of which were potentially associated with the study drug; the reasons included diarrhea, blood in the urine, increased bloating, and dizziness.
The study was supported by the National Health and Medical Research Council, and there were no conflicts of interest reported.
Chinese herbal medicine has yet to gain widespread endorsement from the larger medical community, due to concerns regarding the relatively dearth and low rigor of previous clinical trials, unknown safety of some CHM constituents, and the lack of readily reproducible standardized formulations. While the report by Bensoussan and colleagues raises the bar compared to many previous clinical trials of CHM, their results should be carefully assessed in terms of their significance and applicability to current clinical practi
 |
| Dr. Brooks Cash, AGAF |
The overall treatment period was short, comprising only 8 weeks, with an additional 8 weeks of observation and the therapy intake burden was high at 10 capsules per day. Additionally, the final study enrollment was underpowered and required 2.5 years, suggesting potential difficulties in recruitment. An intention to treat (ITT) analysis is required by regulatory bodies (as opposed to a per protocol analysis), and the ITT analysis failed to demonstrate that CHM was significantly better than placebo at achieving the primary endpoint of adequate relief. In fact, the symptoms that did appear to improve with CHM were primarily centered around defecation and did not include the important viscerosensory symptoms of IBS-C.
At the final analysis, the current report suggests that this formulation of CHM may have some beneficial laxative effects, but is not sufficiently convincing to embrace CHM as an alternative to currently approved IBS-C therapies that have been subjected to rigorous, randomized controlled trials that demonstrate statistically significant improvement per regulatory endpoints as well as global and individual IBS-C symptoms.
Dr. Brooks D. Cash, AGAF, FACG, FASGE. is professor of medicine, director of the physiology laboratory, division of gastroenterology, University of South Alabama, Mobile. He has consulted or worked for the speaker’s bureau for Ironwood, Allergan, IM HealthScience, and Takeda.
Chinese herbal medicine has yet to gain widespread endorsement from the larger medical community, due to concerns regarding the relatively dearth and low rigor of previous clinical trials, unknown safety of some CHM constituents, and the lack of readily reproducible standardized formulations. While the report by Bensoussan and colleagues raises the bar compared to many previous clinical trials of CHM, their results should be carefully assessed in terms of their significance and applicability to current clinical practi
 |
| Dr. Brooks Cash, AGAF |
The overall treatment period was short, comprising only 8 weeks, with an additional 8 weeks of observation and the therapy intake burden was high at 10 capsules per day. Additionally, the final study enrollment was underpowered and required 2.5 years, suggesting potential difficulties in recruitment. An intention to treat (ITT) analysis is required by regulatory bodies (as opposed to a per protocol analysis), and the ITT analysis failed to demonstrate that CHM was significantly better than placebo at achieving the primary endpoint of adequate relief. In fact, the symptoms that did appear to improve with CHM were primarily centered around defecation and did not include the important viscerosensory symptoms of IBS-C.
At the final analysis, the current report suggests that this formulation of CHM may have some beneficial laxative effects, but is not sufficiently convincing to embrace CHM as an alternative to currently approved IBS-C therapies that have been subjected to rigorous, randomized controlled trials that demonstrate statistically significant improvement per regulatory endpoints as well as global and individual IBS-C symptoms.
Dr. Brooks D. Cash, AGAF, FACG, FASGE. is professor of medicine, director of the physiology laboratory, division of gastroenterology, University of South Alabama, Mobile. He has consulted or worked for the speaker’s bureau for Ironwood, Allergan, IM HealthScience, and Takeda.
Chinese herbal medicine has yet to gain widespread endorsement from the larger medical community, due to concerns regarding the relatively dearth and low rigor of previous clinical trials, unknown safety of some CHM constituents, and the lack of readily reproducible standardized formulations. While the report by Bensoussan and colleagues raises the bar compared to many previous clinical trials of CHM, their results should be carefully assessed in terms of their significance and applicability to current clinical practi
 |
| Dr. Brooks Cash, AGAF |
The overall treatment period was short, comprising only 8 weeks, with an additional 8 weeks of observation and the therapy intake burden was high at 10 capsules per day. Additionally, the final study enrollment was underpowered and required 2.5 years, suggesting potential difficulties in recruitment. An intention to treat (ITT) analysis is required by regulatory bodies (as opposed to a per protocol analysis), and the ITT analysis failed to demonstrate that CHM was significantly better than placebo at achieving the primary endpoint of adequate relief. In fact, the symptoms that did appear to improve with CHM were primarily centered around defecation and did not include the important viscerosensory symptoms of IBS-C.
At the final analysis, the current report suggests that this formulation of CHM may have some beneficial laxative effects, but is not sufficiently convincing to embrace CHM as an alternative to currently approved IBS-C therapies that have been subjected to rigorous, randomized controlled trials that demonstrate statistically significant improvement per regulatory endpoints as well as global and individual IBS-C symptoms.
Dr. Brooks D. Cash, AGAF, FACG, FASGE. is professor of medicine, director of the physiology laboratory, division of gastroenterology, University of South Alabama, Mobile. He has consulted or worked for the speaker’s bureau for Ironwood, Allergan, IM HealthScience, and Takeda.
A Chinese herbal medicine preparation may offer relief from constipation symptoms in individuals with irritable bowel syndrome.
A randomized, placebo-controlled trial in 125 individuals with constipation-predominant irritable bowel syndrome (IBS-C) showed the preparation was associated with significant improvements, compared with placebo.
In the per-protocol analysis, 68% of patients given the herbal medicine reported achieving adequate relief from their symptoms, compared with 43% of the placebo group (P = .10), according to a paper published online in Clinical Gastroenterology and Hepatology.
Patients were randomized to receive either a standardized extract of seven Chinese herbal medicine ingredients in capsule form – five capsules taken twice daily – or a taste- and color-matched placebo for 8 weeks, with further follow-up at 16 weeks.
The herbal ingredients included extracts of Chinese peony (Paeonia lactiflora), Seville orange (Citrus aurantium), Magnolia officinalis, and Chinese licorice (Glycyrrhiza uralensis), which were used for their antispasmodic effects, as intestinal muscle relaxants, and as myorelaxants.
The authors commented that while there are recent advances in the treatment of irritable bowel syndrome – such as the serotonergic agent prucalopride, chloride channel activator lubiprostone, and guanylate cyclase–C activator linaclotide – there is not yet a single drug regimen that shows efficacy for the many symptoms of IBS or addresses the high rate of symptom return.
In the study, patients treated with the herbal preparation showed improved bowel habits at the end of treatment, including significantly lower IBS Symptom Severity Scale scores, reduced straining during defecation, a decrease in hard, lumpy stools, and increased stool consistency.
“Although there were significant results for participants in the treatment group, to gain adequate benefit they needed to remain on treatment,” wrote Dr. Alan Bensoussan of the National Institute of Complementary Medicine at the University of Western Sydney (Australia) and his coauthors.
However, the study did not find any statistically significant differences between the intervention and placebo arm in overall IBS-related quality of life, abdominal pain, or bloating at the end of treatment (Clin. Gastroenterol. Hepatol. 2015 Jun 29. doi:10.1016/j.cgh.2015.06.022).
“Thus, IBS-C participants appeared to interpret more normal bowel functions as a significant improvement in the condition, but [quality of life] may only improve when pain and bloating are also substantially ameliorated,” the authors wrote.
Researchers said this finding supports recently published data suggesting that improving bowel movements is a higher priority for patients with IBS-C than pain relief.
Although patients were asked to discontinue related treatment such as anticholinergic agents, opioid analgesics, and regular laxatives, they were allowed some rescue medication.
There was a nonsignificantly greater use of bulking agents in the Chinese herbal medicine group, and stimulant laxative use in the placebo group.
The study medication was generally well tolerated, although there were twice as many gastrointestinal adverse events reported in the intervention group as in the control group.
Overall, there were 19 withdrawals from the study, 6 of which were potentially associated with the study drug; the reasons included diarrhea, blood in the urine, increased bloating, and dizziness.
The study was supported by the National Health and Medical Research Council, and there were no conflicts of interest reported.
A Chinese herbal medicine preparation may offer relief from constipation symptoms in individuals with irritable bowel syndrome.
A randomized, placebo-controlled trial in 125 individuals with constipation-predominant irritable bowel syndrome (IBS-C) showed the preparation was associated with significant improvements, compared with placebo.
In the per-protocol analysis, 68% of patients given the herbal medicine reported achieving adequate relief from their symptoms, compared with 43% of the placebo group (P = .10), according to a paper published online in Clinical Gastroenterology and Hepatology.
Patients were randomized to receive either a standardized extract of seven Chinese herbal medicine ingredients in capsule form – five capsules taken twice daily – or a taste- and color-matched placebo for 8 weeks, with further follow-up at 16 weeks.
The herbal ingredients included extracts of Chinese peony (Paeonia lactiflora), Seville orange (Citrus aurantium), Magnolia officinalis, and Chinese licorice (Glycyrrhiza uralensis), which were used for their antispasmodic effects, as intestinal muscle relaxants, and as myorelaxants.
The authors commented that while there are recent advances in the treatment of irritable bowel syndrome – such as the serotonergic agent prucalopride, chloride channel activator lubiprostone, and guanylate cyclase–C activator linaclotide – there is not yet a single drug regimen that shows efficacy for the many symptoms of IBS or addresses the high rate of symptom return.
In the study, patients treated with the herbal preparation showed improved bowel habits at the end of treatment, including significantly lower IBS Symptom Severity Scale scores, reduced straining during defecation, a decrease in hard, lumpy stools, and increased stool consistency.
“Although there were significant results for participants in the treatment group, to gain adequate benefit they needed to remain on treatment,” wrote Dr. Alan Bensoussan of the National Institute of Complementary Medicine at the University of Western Sydney (Australia) and his coauthors.
However, the study did not find any statistically significant differences between the intervention and placebo arm in overall IBS-related quality of life, abdominal pain, or bloating at the end of treatment (Clin. Gastroenterol. Hepatol. 2015 Jun 29. doi:10.1016/j.cgh.2015.06.022).
“Thus, IBS-C participants appeared to interpret more normal bowel functions as a significant improvement in the condition, but [quality of life] may only improve when pain and bloating are also substantially ameliorated,” the authors wrote.
Researchers said this finding supports recently published data suggesting that improving bowel movements is a higher priority for patients with IBS-C than pain relief.
Although patients were asked to discontinue related treatment such as anticholinergic agents, opioid analgesics, and regular laxatives, they were allowed some rescue medication.
There was a nonsignificantly greater use of bulking agents in the Chinese herbal medicine group, and stimulant laxative use in the placebo group.
The study medication was generally well tolerated, although there were twice as many gastrointestinal adverse events reported in the intervention group as in the control group.
Overall, there were 19 withdrawals from the study, 6 of which were potentially associated with the study drug; the reasons included diarrhea, blood in the urine, increased bloating, and dizziness.
The study was supported by the National Health and Medical Research Council, and there were no conflicts of interest reported.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point:A Chinese herbal medicine preparation may offer relief from constipation symptoms in individuals with irritable bowel syndrome.
Major finding: Individuals treated with a Chinese herbal medicine preparation showed significant relief from symptoms and improved bowel movements, compared with individuals given placebo.
Data source: A randomized, placebo-controlled trial in 125 individuals with constipation-predominant irritable bowel syndrome.
Disclosures: The study was supported by the National Health and Medical Research Council, and there were no conflicts of interest reported.
Hospitals report inadequate duodenoscope reprocessing practices
SAN DIEGO – Less than a third of hospitals reprocessed duodenoscopes adequately to prevent potential transmission of carbapenem-resistant Enterobacteriaceae (CRE) and other pathogens, investigators reported at an annual scientific meeting on infectious diseases.
Moreover, only a third of facilities had conducted active surveillance for multidrug-resistant infections related to use of their duodenoscopes in the past year, reported Susan Beekmann of the Emerging Infections Network of the Infectious Diseases Society of America. “These findings suggest that endemic bacterial transmission associated with duodenoscopy may occur and may go unrecognized,” said Ms. Beekmann, program coordinator for EIN at the University of Iowa Carver College of Medicine in Iowa City.
Duodenoscopes, which are used in endoscopic retrograde cholangiopancreatography (ERCP), became a hot topic earlier this year after causing outbreaks of fatal CRE infections in Los Angeles County. The Food and Drug Administration has acknowledged that the “complex design of the devices makes it difficult to remove contaminants compared to other types of endoscopes,” and both the CDC and the FDA have recommended specific reprocessing and surveillance steps to reduce the chances that the scopes transmit serious infections.
To understand how hospitals were actually reprocessing and culturing the scopes at the time CDC released its guidance, Ms. Beekmann and her colleagues electronically surveyed 740 hospital epidemiologists through IDSA-EIN. They received responses from 378 physicians (52%), of which half said their facilities used duodenoscopes, Ms. Beekmann reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Only 55 (29%) of these respondents said their facilities reprocessed duodenoscopes to an extent that the IDSA researchers defined as adequate – that is, manual reprocessing with high-level disinfection, either alone or in combination with other options, Ms. Beekmann said. Furthermore, only a third of facilities had cultured their duodenoscopes or done any other surveillance for bacterial transmission after duodenoscopy in the past year, even though most said they reviewed their reprocessing policies and procedures more often than once a year.
Respondents also described widely varying methodologies for sampling and culturing, Ms. Beekmann said. “Although we did not ask about them, ten respondents mentioned ATP bioluminescence assays,” she added. Based on the findings, better reprocessing technologies and consistent, real-time strategies to monitor the effectiveness of scope reprocessing are “urgent patient safety needs,” she and her colleagues concluded.
Ms. Beekmann and her associates reported no relevant financial disclosures.
SAN DIEGO – Less than a third of hospitals reprocessed duodenoscopes adequately to prevent potential transmission of carbapenem-resistant Enterobacteriaceae (CRE) and other pathogens, investigators reported at an annual scientific meeting on infectious diseases.
Moreover, only a third of facilities had conducted active surveillance for multidrug-resistant infections related to use of their duodenoscopes in the past year, reported Susan Beekmann of the Emerging Infections Network of the Infectious Diseases Society of America. “These findings suggest that endemic bacterial transmission associated with duodenoscopy may occur and may go unrecognized,” said Ms. Beekmann, program coordinator for EIN at the University of Iowa Carver College of Medicine in Iowa City.
Duodenoscopes, which are used in endoscopic retrograde cholangiopancreatography (ERCP), became a hot topic earlier this year after causing outbreaks of fatal CRE infections in Los Angeles County. The Food and Drug Administration has acknowledged that the “complex design of the devices makes it difficult to remove contaminants compared to other types of endoscopes,” and both the CDC and the FDA have recommended specific reprocessing and surveillance steps to reduce the chances that the scopes transmit serious infections.
To understand how hospitals were actually reprocessing and culturing the scopes at the time CDC released its guidance, Ms. Beekmann and her colleagues electronically surveyed 740 hospital epidemiologists through IDSA-EIN. They received responses from 378 physicians (52%), of which half said their facilities used duodenoscopes, Ms. Beekmann reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Only 55 (29%) of these respondents said their facilities reprocessed duodenoscopes to an extent that the IDSA researchers defined as adequate – that is, manual reprocessing with high-level disinfection, either alone or in combination with other options, Ms. Beekmann said. Furthermore, only a third of facilities had cultured their duodenoscopes or done any other surveillance for bacterial transmission after duodenoscopy in the past year, even though most said they reviewed their reprocessing policies and procedures more often than once a year.
Respondents also described widely varying methodologies for sampling and culturing, Ms. Beekmann said. “Although we did not ask about them, ten respondents mentioned ATP bioluminescence assays,” she added. Based on the findings, better reprocessing technologies and consistent, real-time strategies to monitor the effectiveness of scope reprocessing are “urgent patient safety needs,” she and her colleagues concluded.
Ms. Beekmann and her associates reported no relevant financial disclosures.
SAN DIEGO – Less than a third of hospitals reprocessed duodenoscopes adequately to prevent potential transmission of carbapenem-resistant Enterobacteriaceae (CRE) and other pathogens, investigators reported at an annual scientific meeting on infectious diseases.
Moreover, only a third of facilities had conducted active surveillance for multidrug-resistant infections related to use of their duodenoscopes in the past year, reported Susan Beekmann of the Emerging Infections Network of the Infectious Diseases Society of America. “These findings suggest that endemic bacterial transmission associated with duodenoscopy may occur and may go unrecognized,” said Ms. Beekmann, program coordinator for EIN at the University of Iowa Carver College of Medicine in Iowa City.
Duodenoscopes, which are used in endoscopic retrograde cholangiopancreatography (ERCP), became a hot topic earlier this year after causing outbreaks of fatal CRE infections in Los Angeles County. The Food and Drug Administration has acknowledged that the “complex design of the devices makes it difficult to remove contaminants compared to other types of endoscopes,” and both the CDC and the FDA have recommended specific reprocessing and surveillance steps to reduce the chances that the scopes transmit serious infections.
To understand how hospitals were actually reprocessing and culturing the scopes at the time CDC released its guidance, Ms. Beekmann and her colleagues electronically surveyed 740 hospital epidemiologists through IDSA-EIN. They received responses from 378 physicians (52%), of which half said their facilities used duodenoscopes, Ms. Beekmann reported at the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Only 55 (29%) of these respondents said their facilities reprocessed duodenoscopes to an extent that the IDSA researchers defined as adequate – that is, manual reprocessing with high-level disinfection, either alone or in combination with other options, Ms. Beekmann said. Furthermore, only a third of facilities had cultured their duodenoscopes or done any other surveillance for bacterial transmission after duodenoscopy in the past year, even though most said they reviewed their reprocessing policies and procedures more often than once a year.
Respondents also described widely varying methodologies for sampling and culturing, Ms. Beekmann said. “Although we did not ask about them, ten respondents mentioned ATP bioluminescence assays,” she added. Based on the findings, better reprocessing technologies and consistent, real-time strategies to monitor the effectiveness of scope reprocessing are “urgent patient safety needs,” she and her colleagues concluded.
Ms. Beekmann and her associates reported no relevant financial disclosures.
AT IDWEEK 2015
Key clinical point: Most hospitals did not reprocess duodenoscopes in a way that the Infectious Diseases Society of America considers adequate.
Major finding: Only 29% of facilities followed the minimum adequate practices.
Data source: A cross-sectional electronic survey of 378 physician members of the Emerging Infections Network of the Infectious Diseases Society of America.
Disclosures: Susan Beekmann reported no relevant financial disclosures.
Hepatitis C drove steep rises in cirrhosis, HCC, and related deaths
Cirrhosis nearly doubled among Veterans Affairs patients between 2001 and 2013, while cirrhosis-related mortality rose by about 50% and deaths from hepatocellular carcinoma almost tripled, investigators reported in the November issue of Gastroenterology.
Hepatitis C virus infection was “the overwhelming driver of these trends, with smaller contributions from alcoholic liver disease, nonalcoholic fatty liver disease, and other liver diseases,” said Dr. Lauren Beste of the University of Washington, Seattle, and her associates. Based on their data, the prevalence of cirrhosis in the United States will peak in 2021, they said. “In contrast, the incidence of HCC continues to increase, confirming worrisome predictions of rapid growth put forward by work (Gastroenterology. 2010;138[2]:513-21) conducted” in the early 2000s.
New HCV infections have dropped sharply in the United States since about 1990, but cases of HCV-related cirrhosis and HCC continue to rise as chronically infected patients age and their liver disease progresses. Although the burden of cirrhosis and HCC due to HCV infection is expected to peak in about the year 2020, the population-level effects of nonalcoholic fatty liver disease, alcoholic liver disease, and hepatitis B virus infection remained unclear, the investigators said. Therefore, they retrospectively studied underlying etiologies among a national cohort of almost 130,000 Veterans Affairs patients with cirrhosis and more than 21,000 patients with HCC between 2001 and 2013 (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
In 2013, the VA cared for more than 5.7 million patients, including about 1% with cirrhosis and 0.13% with HCC. Between 2001 and 2013, the prevalence of cirrhosis almost doubled, rising from 664 to 1,058 cases for every 100,000 patients. Deaths among cirrhotic patients also increased by about half, rising from 83 to 126 for every 100,000 patient-years. These liver-related deaths were mainly caused by HCC, whose incidence rose about 2.5 times from 17 to 45 per 100,000 patient-years, Dr. Beste and her associates reported.
Notably, deaths due to liver cancer rose threefold – from 13 to 37 per 100,000 patient-years between 2001 and 2013, “driven overwhelmingly by HCV with much smaller contributions from NAFLD and alcoholic liver disease,” said the researchers. By 2013, almost half of cirrhosis cases and related deaths occurred among HCV-infected patients, as did 67% of HCC cases and related deaths, they noted.
About 60% of patients with cirrhosis and HCV infection also had a longstanding history of alcohol use, the researchers noted. Addressing both factors, as well as diabetes, obesity, and other drivers of nonalcoholic fatty liver disease, could help ease the national burden of liver disease and liver-related mortality among U.S. veterans and other groups, they added. “The increasing burden of cirrhosis and HCC highlights the need for greater efforts to address their causes at a population level,” Dr. Beste and her associates wrote. “Health care systems will need to accommodate rising numbers of patients with cirrhosis and HCC.”
The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Despite recent advances in hepatitis C virus treatment, many infected patients have preexisting liver fibrosis that puts them at risk for cirrhosis and hepatocellular carcinoma. Meanwhile, risk factors for nonalcoholic fatty liver disease (NAFLD) are increasingly prevalent. In this study, the investigators sought to understand the contribution of liver disease etiology to trends in adverse liver outcomes (the prevalence, incidence, and mortality of cirrhosis and HCC). They identified all VA health care users from 2001 to 2013 with diagnoses of cirrhosis (n = 129,998) or HCC (n = 21,326) and their liver disease etiology, and compared outcomes by calendar year.
 |
Dr. Barry Schlansky |
Over the study period, marked increases in cirrhosis prevalence (59%), cirrhosis mortality (52%), HCC incidence (164%), and HCC mortality (185%) were observed in this national VA cohort. The increasing prevalence of cirrhosis was mainly driven by increasing contributions from HCV or NAFLD liver disease, but rises in mortality from cirrhosis and both incidence and mortality from HCC were almost entirely due to HCV. Based on these trends, the researchers forecasted that the prevalence of cirrhosis will plateau and begin to decline in 2021 (2020 in the HCV subgroup), but rates of HCC will continue to surge.
Although these results differ from two recent analyses of the national cancer surveillance registry (SEER) that found decelerations in HCC incidence and mortality in recent years, the current study included methodologic features (stratification by liver disease etiology and absence of age standardization) that likely facilitated more accurate estimates of HCC incidence and mortality. The generalizability of VA data to the general population is always debated (the former is nearly exclusively men with a higher prevalence of HCV infection and other liver disease risk factors, all of whom have access to medical care), yet the researchers rightly note that the time trends in cirrhosis and HCC outcomes (rather than absolute numbers) are still applicable to the non-VA population, particularly men. This study highlights the dramatic rise in cirrhosis and HCC, and associated deaths from these conditions, over the last decade. In addition to aggressive treatment of the underlying cause of liver disease, meaningful reductions in the burden of advanced liver disease will require a renewed focus on measures to improve adherence with maintenance care for cirrhotic patients, especially liver cancer screening.
Dr. Barry Schlansky is assistant professor, division of gastroenterology and hepatology, department of medicine, Oregon Health and Science University, Portland. He has no conflicts of interest.
Despite recent advances in hepatitis C virus treatment, many infected patients have preexisting liver fibrosis that puts them at risk for cirrhosis and hepatocellular carcinoma. Meanwhile, risk factors for nonalcoholic fatty liver disease (NAFLD) are increasingly prevalent. In this study, the investigators sought to understand the contribution of liver disease etiology to trends in adverse liver outcomes (the prevalence, incidence, and mortality of cirrhosis and HCC). They identified all VA health care users from 2001 to 2013 with diagnoses of cirrhosis (n = 129,998) or HCC (n = 21,326) and their liver disease etiology, and compared outcomes by calendar year.
 |
Dr. Barry Schlansky |
Over the study period, marked increases in cirrhosis prevalence (59%), cirrhosis mortality (52%), HCC incidence (164%), and HCC mortality (185%) were observed in this national VA cohort. The increasing prevalence of cirrhosis was mainly driven by increasing contributions from HCV or NAFLD liver disease, but rises in mortality from cirrhosis and both incidence and mortality from HCC were almost entirely due to HCV. Based on these trends, the researchers forecasted that the prevalence of cirrhosis will plateau and begin to decline in 2021 (2020 in the HCV subgroup), but rates of HCC will continue to surge.
Although these results differ from two recent analyses of the national cancer surveillance registry (SEER) that found decelerations in HCC incidence and mortality in recent years, the current study included methodologic features (stratification by liver disease etiology and absence of age standardization) that likely facilitated more accurate estimates of HCC incidence and mortality. The generalizability of VA data to the general population is always debated (the former is nearly exclusively men with a higher prevalence of HCV infection and other liver disease risk factors, all of whom have access to medical care), yet the researchers rightly note that the time trends in cirrhosis and HCC outcomes (rather than absolute numbers) are still applicable to the non-VA population, particularly men. This study highlights the dramatic rise in cirrhosis and HCC, and associated deaths from these conditions, over the last decade. In addition to aggressive treatment of the underlying cause of liver disease, meaningful reductions in the burden of advanced liver disease will require a renewed focus on measures to improve adherence with maintenance care for cirrhotic patients, especially liver cancer screening.
Dr. Barry Schlansky is assistant professor, division of gastroenterology and hepatology, department of medicine, Oregon Health and Science University, Portland. He has no conflicts of interest.
Despite recent advances in hepatitis C virus treatment, many infected patients have preexisting liver fibrosis that puts them at risk for cirrhosis and hepatocellular carcinoma. Meanwhile, risk factors for nonalcoholic fatty liver disease (NAFLD) are increasingly prevalent. In this study, the investigators sought to understand the contribution of liver disease etiology to trends in adverse liver outcomes (the prevalence, incidence, and mortality of cirrhosis and HCC). They identified all VA health care users from 2001 to 2013 with diagnoses of cirrhosis (n = 129,998) or HCC (n = 21,326) and their liver disease etiology, and compared outcomes by calendar year.
 |
Dr. Barry Schlansky |
Over the study period, marked increases in cirrhosis prevalence (59%), cirrhosis mortality (52%), HCC incidence (164%), and HCC mortality (185%) were observed in this national VA cohort. The increasing prevalence of cirrhosis was mainly driven by increasing contributions from HCV or NAFLD liver disease, but rises in mortality from cirrhosis and both incidence and mortality from HCC were almost entirely due to HCV. Based on these trends, the researchers forecasted that the prevalence of cirrhosis will plateau and begin to decline in 2021 (2020 in the HCV subgroup), but rates of HCC will continue to surge.
Although these results differ from two recent analyses of the national cancer surveillance registry (SEER) that found decelerations in HCC incidence and mortality in recent years, the current study included methodologic features (stratification by liver disease etiology and absence of age standardization) that likely facilitated more accurate estimates of HCC incidence and mortality. The generalizability of VA data to the general population is always debated (the former is nearly exclusively men with a higher prevalence of HCV infection and other liver disease risk factors, all of whom have access to medical care), yet the researchers rightly note that the time trends in cirrhosis and HCC outcomes (rather than absolute numbers) are still applicable to the non-VA population, particularly men. This study highlights the dramatic rise in cirrhosis and HCC, and associated deaths from these conditions, over the last decade. In addition to aggressive treatment of the underlying cause of liver disease, meaningful reductions in the burden of advanced liver disease will require a renewed focus on measures to improve adherence with maintenance care for cirrhotic patients, especially liver cancer screening.
Dr. Barry Schlansky is assistant professor, division of gastroenterology and hepatology, department of medicine, Oregon Health and Science University, Portland. He has no conflicts of interest.
Cirrhosis nearly doubled among Veterans Affairs patients between 2001 and 2013, while cirrhosis-related mortality rose by about 50% and deaths from hepatocellular carcinoma almost tripled, investigators reported in the November issue of Gastroenterology.
Hepatitis C virus infection was “the overwhelming driver of these trends, with smaller contributions from alcoholic liver disease, nonalcoholic fatty liver disease, and other liver diseases,” said Dr. Lauren Beste of the University of Washington, Seattle, and her associates. Based on their data, the prevalence of cirrhosis in the United States will peak in 2021, they said. “In contrast, the incidence of HCC continues to increase, confirming worrisome predictions of rapid growth put forward by work (Gastroenterology. 2010;138[2]:513-21) conducted” in the early 2000s.
New HCV infections have dropped sharply in the United States since about 1990, but cases of HCV-related cirrhosis and HCC continue to rise as chronically infected patients age and their liver disease progresses. Although the burden of cirrhosis and HCC due to HCV infection is expected to peak in about the year 2020, the population-level effects of nonalcoholic fatty liver disease, alcoholic liver disease, and hepatitis B virus infection remained unclear, the investigators said. Therefore, they retrospectively studied underlying etiologies among a national cohort of almost 130,000 Veterans Affairs patients with cirrhosis and more than 21,000 patients with HCC between 2001 and 2013 (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
In 2013, the VA cared for more than 5.7 million patients, including about 1% with cirrhosis and 0.13% with HCC. Between 2001 and 2013, the prevalence of cirrhosis almost doubled, rising from 664 to 1,058 cases for every 100,000 patients. Deaths among cirrhotic patients also increased by about half, rising from 83 to 126 for every 100,000 patient-years. These liver-related deaths were mainly caused by HCC, whose incidence rose about 2.5 times from 17 to 45 per 100,000 patient-years, Dr. Beste and her associates reported.
Notably, deaths due to liver cancer rose threefold – from 13 to 37 per 100,000 patient-years between 2001 and 2013, “driven overwhelmingly by HCV with much smaller contributions from NAFLD and alcoholic liver disease,” said the researchers. By 2013, almost half of cirrhosis cases and related deaths occurred among HCV-infected patients, as did 67% of HCC cases and related deaths, they noted.
About 60% of patients with cirrhosis and HCV infection also had a longstanding history of alcohol use, the researchers noted. Addressing both factors, as well as diabetes, obesity, and other drivers of nonalcoholic fatty liver disease, could help ease the national burden of liver disease and liver-related mortality among U.S. veterans and other groups, they added. “The increasing burden of cirrhosis and HCC highlights the need for greater efforts to address their causes at a population level,” Dr. Beste and her associates wrote. “Health care systems will need to accommodate rising numbers of patients with cirrhosis and HCC.”
The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Cirrhosis nearly doubled among Veterans Affairs patients between 2001 and 2013, while cirrhosis-related mortality rose by about 50% and deaths from hepatocellular carcinoma almost tripled, investigators reported in the November issue of Gastroenterology.
Hepatitis C virus infection was “the overwhelming driver of these trends, with smaller contributions from alcoholic liver disease, nonalcoholic fatty liver disease, and other liver diseases,” said Dr. Lauren Beste of the University of Washington, Seattle, and her associates. Based on their data, the prevalence of cirrhosis in the United States will peak in 2021, they said. “In contrast, the incidence of HCC continues to increase, confirming worrisome predictions of rapid growth put forward by work (Gastroenterology. 2010;138[2]:513-21) conducted” in the early 2000s.
New HCV infections have dropped sharply in the United States since about 1990, but cases of HCV-related cirrhosis and HCC continue to rise as chronically infected patients age and their liver disease progresses. Although the burden of cirrhosis and HCC due to HCV infection is expected to peak in about the year 2020, the population-level effects of nonalcoholic fatty liver disease, alcoholic liver disease, and hepatitis B virus infection remained unclear, the investigators said. Therefore, they retrospectively studied underlying etiologies among a national cohort of almost 130,000 Veterans Affairs patients with cirrhosis and more than 21,000 patients with HCC between 2001 and 2013 (Gastroenterology 2015. doi: 10.1053/j.gastro.2015.07.056).
In 2013, the VA cared for more than 5.7 million patients, including about 1% with cirrhosis and 0.13% with HCC. Between 2001 and 2013, the prevalence of cirrhosis almost doubled, rising from 664 to 1,058 cases for every 100,000 patients. Deaths among cirrhotic patients also increased by about half, rising from 83 to 126 for every 100,000 patient-years. These liver-related deaths were mainly caused by HCC, whose incidence rose about 2.5 times from 17 to 45 per 100,000 patient-years, Dr. Beste and her associates reported.
Notably, deaths due to liver cancer rose threefold – from 13 to 37 per 100,000 patient-years between 2001 and 2013, “driven overwhelmingly by HCV with much smaller contributions from NAFLD and alcoholic liver disease,” said the researchers. By 2013, almost half of cirrhosis cases and related deaths occurred among HCV-infected patients, as did 67% of HCC cases and related deaths, they noted.
About 60% of patients with cirrhosis and HCV infection also had a longstanding history of alcohol use, the researchers noted. Addressing both factors, as well as diabetes, obesity, and other drivers of nonalcoholic fatty liver disease, could help ease the national burden of liver disease and liver-related mortality among U.S. veterans and other groups, they added. “The increasing burden of cirrhosis and HCC highlights the need for greater efforts to address their causes at a population level,” Dr. Beste and her associates wrote. “Health care systems will need to accommodate rising numbers of patients with cirrhosis and HCC.”
The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
FROM GASTROENTEROLOGY
Key clinical point: Cirrhosis, hepatocellular carcinoma, and liver-related mortality rose substantially among Veterans Affairs patients over the past 12 years, mainly driven by HCV infection.
Major finding: The prevalence of cirrhosis nearly doubled between 2001 and 2013, while cirrhosis-related deaths rose by about 50% and the incidence of hepatocellular carcinoma almost tripled.
Data source: A retrospective cohort study of 129,998 Veterans Affairs patients with cirrhosis and 21,326 VA patients with HCC between 2001 and 2013.
Disclosures: The Department of Veterans Affairs and the Veterans Health Administration funded the study. The investigators declared no competing interests.
Lavage does not reduce severe complications in perforated diverticulitis
Patients needing emergency surgery for perforated diverticulitis saw no decrease in serious complications when treated with laparoscopic lavage, a minimally invasive procedure, than with primary resection of the colon, according to results from a randomized multicenter trial in Scandinavia.
Likelihood of reoperation also was significantly higher among patients undergoing laparoscopic lavage, and more sigmoid carcinomas were missed.
For their research, published Oct. 6 in JAMA (2015;314:1364-75), a group led by Dr. Johannes Kurt Schultz of the Akershus University Hospital in Lørenskog, Norway, and the University of Oslo sought to eliminate the selection bias that may have contributed to more favorable outcomes associated with laparoscopic lavage in observational studies.
Dr. Schultz and colleagues randomized patients with suspected perforated diverticulitis from 21 centers in Sweden and Norway to laparoscopic peritoneal lavage (n = 101) or colon resection (n = 98), with the choice of open or laparoscopic approach used for resection, as well as the option of colorectal anastomosis, left to the surgeon.
The study did not use laparoscopic Hinchey staging to classify the severity of the perforation prior to treatment assignment as a way of reducing the selection bias that may have occurred in observational studies.
The preoperative randomization resulted in both groups having similar rates of feculent peritonitis and incorrect preoperative diagnoses. Patients assigned to laparoscopic lavage were treated instead with resection if they were found to have fecal peritonitis. Also, patients in both groups whose pathology required additional treatment were treated at surgeon discretion. This left 74 patients randomized to lavage who received it as assigned and 70 patients undergoing resection per assigned protocol. In the intention-to-treat analysis, 31% of patients in the lavage group and 26% of patients in the resection group saw severe postoperative complications within 90 days, a difference of 4.7% that did not reach statistical significance (95% confidence interval, −7.9% to 17%; P = .53). Severe postoperative complications were defined as any complications resulting in a reintervention requiring general anesthesia, a life-threatening organ dysfunction, or death.
Of the patients treated as assigned with lavage, about 20% (n = 15) required reoperation, compared with 6% (n = 4) in the resection arm, a difference of about 14.6% (95% CI, 3.5% to 25.6%; P =.01).
The main reasons for reoperation were secondary peritonitis in the lavage group and wound rupture in the resection group. Intra-abdominal infections were more frequent in the laparoscopic lavage group, Dr. Schultz and colleagues found.
Also in the lavage group, four carcinomas were missed, compared with two in the resection group. “Because of the relatively high rate of missed colon carcinomas in the lavage group, it was essential to perform a colonoscopy after a patient recovered from the perforation,” the researchers wrote in their analysis.
Although patients in the laparoscopic lavage group had significantly shorter operating times, less blood loss, and lower incidence of stoma at 3 months, the researchers concluded that, based on these results, laparoscopic lavage could not be supported in perforated diverticulitis.
Dr. Schultz and colleagues had planned to enroll about half of eligible patients at the study sites. They noted as a limitation of their study that those not enrolled had more severe disease and worse postoperative outcomes, raising the possibility that the results “may not pertain to patients with perforated diverticulitis who are very ill.”
The study was funded by the South-Eastern Norway Regional Health Authority and Akershus University Hospital. None of its authors reported conflicts of interest.
Dr. Schultz and associates detail findings from a randomized, multicenter clinical trial conducted in Scandinavia designed to assess the superiority of laparoscopic lavage plus drainage, compared with laparoscopic or open resection with or without anastomosis for diverticulitis (Hinchey grades I-III) requiring urgent surgery.
The primary outcome was the incidence of severe complications (Clavien-Dindo classification IIIb-V). Of 144 patients, 74 were randomized to receive laparoscopic lavage and 70 to resection. The two groups were similar in characteristics, although significantly fewer of the lavage procedures were performed by a specialty-trained surgeon. Severe complications occurred in 25.7% of patients in the lavage group and 14.3% in the resection group (difference, 11.4%; 95% CI, −1.8 to 24.1), and significantly more patients in the lavage group developed secondary peritonitis (12% vs. 0%) or returned to the operating room (20% vs. 6%). The hospital mortality rates and follow-up quality-of-life scores were comparable between the groups (3% vs. 4% and 0.75 vs. 0.73, respectively). Somewhat worrisome is that four colon cancers were initially missed in patients treated by laparoscopic lavage alone.
Performing laparoscopic lavage is more difficult than merely irrigating the abdomen and placing drains within the pelvis. Surgeons vary in their attitudes related to concomitant adhesiolysis or debridement, and consensus about these procedures is lacking. Furthermore, subjective signs and objective criteria that identify patients at risk for secondary peritonitis or reoperation must be studied, and risk models should be validated to determine which patients are best suited for this less invasive approach. The utility of less intrusive strategies and minimally invasive approaches will undoubtedly expand as technologies evolve, but they must be responsibly incorporated into surgical practice based on evidence rather than subjective reasons.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University, Chicago. These comments were taken from an accompanying editorial (JAMA 2015;314[13]:1343-5). They declared no conflicts of interest.
Dr. Schultz and associates detail findings from a randomized, multicenter clinical trial conducted in Scandinavia designed to assess the superiority of laparoscopic lavage plus drainage, compared with laparoscopic or open resection with or without anastomosis for diverticulitis (Hinchey grades I-III) requiring urgent surgery.
The primary outcome was the incidence of severe complications (Clavien-Dindo classification IIIb-V). Of 144 patients, 74 were randomized to receive laparoscopic lavage and 70 to resection. The two groups were similar in characteristics, although significantly fewer of the lavage procedures were performed by a specialty-trained surgeon. Severe complications occurred in 25.7% of patients in the lavage group and 14.3% in the resection group (difference, 11.4%; 95% CI, −1.8 to 24.1), and significantly more patients in the lavage group developed secondary peritonitis (12% vs. 0%) or returned to the operating room (20% vs. 6%). The hospital mortality rates and follow-up quality-of-life scores were comparable between the groups (3% vs. 4% and 0.75 vs. 0.73, respectively). Somewhat worrisome is that four colon cancers were initially missed in patients treated by laparoscopic lavage alone.
Performing laparoscopic lavage is more difficult than merely irrigating the abdomen and placing drains within the pelvis. Surgeons vary in their attitudes related to concomitant adhesiolysis or debridement, and consensus about these procedures is lacking. Furthermore, subjective signs and objective criteria that identify patients at risk for secondary peritonitis or reoperation must be studied, and risk models should be validated to determine which patients are best suited for this less invasive approach. The utility of less intrusive strategies and minimally invasive approaches will undoubtedly expand as technologies evolve, but they must be responsibly incorporated into surgical practice based on evidence rather than subjective reasons.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University, Chicago. These comments were taken from an accompanying editorial (JAMA 2015;314[13]:1343-5). They declared no conflicts of interest.
Dr. Schultz and associates detail findings from a randomized, multicenter clinical trial conducted in Scandinavia designed to assess the superiority of laparoscopic lavage plus drainage, compared with laparoscopic or open resection with or without anastomosis for diverticulitis (Hinchey grades I-III) requiring urgent surgery.
The primary outcome was the incidence of severe complications (Clavien-Dindo classification IIIb-V). Of 144 patients, 74 were randomized to receive laparoscopic lavage and 70 to resection. The two groups were similar in characteristics, although significantly fewer of the lavage procedures were performed by a specialty-trained surgeon. Severe complications occurred in 25.7% of patients in the lavage group and 14.3% in the resection group (difference, 11.4%; 95% CI, −1.8 to 24.1), and significantly more patients in the lavage group developed secondary peritonitis (12% vs. 0%) or returned to the operating room (20% vs. 6%). The hospital mortality rates and follow-up quality-of-life scores were comparable between the groups (3% vs. 4% and 0.75 vs. 0.73, respectively). Somewhat worrisome is that four colon cancers were initially missed in patients treated by laparoscopic lavage alone.
Performing laparoscopic lavage is more difficult than merely irrigating the abdomen and placing drains within the pelvis. Surgeons vary in their attitudes related to concomitant adhesiolysis or debridement, and consensus about these procedures is lacking. Furthermore, subjective signs and objective criteria that identify patients at risk for secondary peritonitis or reoperation must be studied, and risk models should be validated to determine which patients are best suited for this less invasive approach. The utility of less intrusive strategies and minimally invasive approaches will undoubtedly expand as technologies evolve, but they must be responsibly incorporated into surgical practice based on evidence rather than subjective reasons.
Dr. Scott A. Strong and Dr. Nathaniel J. Soper are with Northwestern University, Chicago. These comments were taken from an accompanying editorial (JAMA 2015;314[13]:1343-5). They declared no conflicts of interest.
Patients needing emergency surgery for perforated diverticulitis saw no decrease in serious complications when treated with laparoscopic lavage, a minimally invasive procedure, than with primary resection of the colon, according to results from a randomized multicenter trial in Scandinavia.
Likelihood of reoperation also was significantly higher among patients undergoing laparoscopic lavage, and more sigmoid carcinomas were missed.
For their research, published Oct. 6 in JAMA (2015;314:1364-75), a group led by Dr. Johannes Kurt Schultz of the Akershus University Hospital in Lørenskog, Norway, and the University of Oslo sought to eliminate the selection bias that may have contributed to more favorable outcomes associated with laparoscopic lavage in observational studies.
Dr. Schultz and colleagues randomized patients with suspected perforated diverticulitis from 21 centers in Sweden and Norway to laparoscopic peritoneal lavage (n = 101) or colon resection (n = 98), with the choice of open or laparoscopic approach used for resection, as well as the option of colorectal anastomosis, left to the surgeon.
The study did not use laparoscopic Hinchey staging to classify the severity of the perforation prior to treatment assignment as a way of reducing the selection bias that may have occurred in observational studies.
The preoperative randomization resulted in both groups having similar rates of feculent peritonitis and incorrect preoperative diagnoses. Patients assigned to laparoscopic lavage were treated instead with resection if they were found to have fecal peritonitis. Also, patients in both groups whose pathology required additional treatment were treated at surgeon discretion. This left 74 patients randomized to lavage who received it as assigned and 70 patients undergoing resection per assigned protocol. In the intention-to-treat analysis, 31% of patients in the lavage group and 26% of patients in the resection group saw severe postoperative complications within 90 days, a difference of 4.7% that did not reach statistical significance (95% confidence interval, −7.9% to 17%; P = .53). Severe postoperative complications were defined as any complications resulting in a reintervention requiring general anesthesia, a life-threatening organ dysfunction, or death.
Of the patients treated as assigned with lavage, about 20% (n = 15) required reoperation, compared with 6% (n = 4) in the resection arm, a difference of about 14.6% (95% CI, 3.5% to 25.6%; P =.01).
The main reasons for reoperation were secondary peritonitis in the lavage group and wound rupture in the resection group. Intra-abdominal infections were more frequent in the laparoscopic lavage group, Dr. Schultz and colleagues found.
Also in the lavage group, four carcinomas were missed, compared with two in the resection group. “Because of the relatively high rate of missed colon carcinomas in the lavage group, it was essential to perform a colonoscopy after a patient recovered from the perforation,” the researchers wrote in their analysis.
Although patients in the laparoscopic lavage group had significantly shorter operating times, less blood loss, and lower incidence of stoma at 3 months, the researchers concluded that, based on these results, laparoscopic lavage could not be supported in perforated diverticulitis.
Dr. Schultz and colleagues had planned to enroll about half of eligible patients at the study sites. They noted as a limitation of their study that those not enrolled had more severe disease and worse postoperative outcomes, raising the possibility that the results “may not pertain to patients with perforated diverticulitis who are very ill.”
The study was funded by the South-Eastern Norway Regional Health Authority and Akershus University Hospital. None of its authors reported conflicts of interest.
Patients needing emergency surgery for perforated diverticulitis saw no decrease in serious complications when treated with laparoscopic lavage, a minimally invasive procedure, than with primary resection of the colon, according to results from a randomized multicenter trial in Scandinavia.
Likelihood of reoperation also was significantly higher among patients undergoing laparoscopic lavage, and more sigmoid carcinomas were missed.
For their research, published Oct. 6 in JAMA (2015;314:1364-75), a group led by Dr. Johannes Kurt Schultz of the Akershus University Hospital in Lørenskog, Norway, and the University of Oslo sought to eliminate the selection bias that may have contributed to more favorable outcomes associated with laparoscopic lavage in observational studies.
Dr. Schultz and colleagues randomized patients with suspected perforated diverticulitis from 21 centers in Sweden and Norway to laparoscopic peritoneal lavage (n = 101) or colon resection (n = 98), with the choice of open or laparoscopic approach used for resection, as well as the option of colorectal anastomosis, left to the surgeon.
The study did not use laparoscopic Hinchey staging to classify the severity of the perforation prior to treatment assignment as a way of reducing the selection bias that may have occurred in observational studies.
The preoperative randomization resulted in both groups having similar rates of feculent peritonitis and incorrect preoperative diagnoses. Patients assigned to laparoscopic lavage were treated instead with resection if they were found to have fecal peritonitis. Also, patients in both groups whose pathology required additional treatment were treated at surgeon discretion. This left 74 patients randomized to lavage who received it as assigned and 70 patients undergoing resection per assigned protocol. In the intention-to-treat analysis, 31% of patients in the lavage group and 26% of patients in the resection group saw severe postoperative complications within 90 days, a difference of 4.7% that did not reach statistical significance (95% confidence interval, −7.9% to 17%; P = .53). Severe postoperative complications were defined as any complications resulting in a reintervention requiring general anesthesia, a life-threatening organ dysfunction, or death.
Of the patients treated as assigned with lavage, about 20% (n = 15) required reoperation, compared with 6% (n = 4) in the resection arm, a difference of about 14.6% (95% CI, 3.5% to 25.6%; P =.01).
The main reasons for reoperation were secondary peritonitis in the lavage group and wound rupture in the resection group. Intra-abdominal infections were more frequent in the laparoscopic lavage group, Dr. Schultz and colleagues found.
Also in the lavage group, four carcinomas were missed, compared with two in the resection group. “Because of the relatively high rate of missed colon carcinomas in the lavage group, it was essential to perform a colonoscopy after a patient recovered from the perforation,” the researchers wrote in their analysis.
Although patients in the laparoscopic lavage group had significantly shorter operating times, less blood loss, and lower incidence of stoma at 3 months, the researchers concluded that, based on these results, laparoscopic lavage could not be supported in perforated diverticulitis.
Dr. Schultz and colleagues had planned to enroll about half of eligible patients at the study sites. They noted as a limitation of their study that those not enrolled had more severe disease and worse postoperative outcomes, raising the possibility that the results “may not pertain to patients with perforated diverticulitis who are very ill.”
The study was funded by the South-Eastern Norway Regional Health Authority and Akershus University Hospital. None of its authors reported conflicts of interest.
FROM JAMA
Key clinical point: Laparoscopic lavage carries risks of severe postoperative complications similar to colon resection in people presenting with suspected perforated diverticulitis requiring emergency surgery.
Major finding: Mortality and severe complications did not differ significantly at 90 days postoperation between intention-to-treat groups, while reoperation was significantly higher among patients treated with lavage (5.7% for resection vs. 20.3% for lavage, P < .01).
Data source: A multicenter, open-label randomized trial in which patients presenting with likely perforated diverticulitis were randomized to lavage (n = 74) or resection (n = 70).
Disclosures: The study was sponsored by investigator institutions and Norwegian regional government grants. No conflicts of interest were reported.
Anti-TNFs for IBD may double relative risk of demyelinating diseases
Anti-TNF therapy for inflammatory bowel disease appears to double the relative risk of developing central demyelinating disease, though the absolute risk remains small, according to a preliminary report published online Oct. 5 in JAMA Internal Medicine.
Previous case reports have suggested a possible association between anti-TNF agents taken for IBD and later development of demyelinating diseases, but a definitive link has been difficult to establish because of the rarity of these disorders and the suspicion that there already may be an underlying association between IBD and demyelinating disease.
So researchers examined the issue by analyzing data from nationwide Danish health registries for IBD patients and medication exposure. They identified 4,504 patients treated during a 14-year period who had IBD and took anti-TNF agents, and 16,429 IBD patients matched for sex, age, and IBD duration who did not take the medications, according to Dr. Nynne Nyboe Andersen, of the department of epidemiology research, Statens Serum Institut, Copenhagen, and her associates.
Eleven patients in the exposed group had central demyelinating events: multiple sclerosis (2 patients), optic neuritis (5 patients), or other central demyelinating disease (4 patients). For exposed patients, there were 7.5 events per 10,000 person-years.
In comparison, 17 patients in the unexposed group had central demyelinating events: multiple sclerosis (5 patients), optic neuritis (6 patients), transverse myelitis (1 patient), or other central demyelinating disease (5 patients). In this group there were 3.3 events per 10,000 person-years.
The hazard ratio for developing central demyelinating disease after exposure to anti-TNF agents was 2.19, the investigators wrote (JAMA Intern Med. 2015 Oct 5, doi:10.1001/jamainternmed.2015.5396.).
These preliminary findings represent the first report of this association and must be confirmed in future studies, according to the researchers.
“If true, the observed association could either be attributed to the unmasking of a latent demyelinating disease or to the emergence of a de novo demyelinating disease,” Dr. Nyboe Andersen and her associates wrote in the research letter.
The study was supported by the Lundbeck Foundation, Women in Science, the Beckett Foundation, the Danish Colitis Crohn Association, and the Danish Council for Independent Research. Dr. Nyboe Andersen reported receiving travel and speaking fees from MSD and speaking fees from Ferring, and one of her associates reported receiving travel and speaking fees from AbbVie.
Anti-TNF therapy for inflammatory bowel disease appears to double the relative risk of developing central demyelinating disease, though the absolute risk remains small, according to a preliminary report published online Oct. 5 in JAMA Internal Medicine.
Previous case reports have suggested a possible association between anti-TNF agents taken for IBD and later development of demyelinating diseases, but a definitive link has been difficult to establish because of the rarity of these disorders and the suspicion that there already may be an underlying association between IBD and demyelinating disease.
So researchers examined the issue by analyzing data from nationwide Danish health registries for IBD patients and medication exposure. They identified 4,504 patients treated during a 14-year period who had IBD and took anti-TNF agents, and 16,429 IBD patients matched for sex, age, and IBD duration who did not take the medications, according to Dr. Nynne Nyboe Andersen, of the department of epidemiology research, Statens Serum Institut, Copenhagen, and her associates.
Eleven patients in the exposed group had central demyelinating events: multiple sclerosis (2 patients), optic neuritis (5 patients), or other central demyelinating disease (4 patients). For exposed patients, there were 7.5 events per 10,000 person-years.
In comparison, 17 patients in the unexposed group had central demyelinating events: multiple sclerosis (5 patients), optic neuritis (6 patients), transverse myelitis (1 patient), or other central demyelinating disease (5 patients). In this group there were 3.3 events per 10,000 person-years.
The hazard ratio for developing central demyelinating disease after exposure to anti-TNF agents was 2.19, the investigators wrote (JAMA Intern Med. 2015 Oct 5, doi:10.1001/jamainternmed.2015.5396.).
These preliminary findings represent the first report of this association and must be confirmed in future studies, according to the researchers.
“If true, the observed association could either be attributed to the unmasking of a latent demyelinating disease or to the emergence of a de novo demyelinating disease,” Dr. Nyboe Andersen and her associates wrote in the research letter.
The study was supported by the Lundbeck Foundation, Women in Science, the Beckett Foundation, the Danish Colitis Crohn Association, and the Danish Council for Independent Research. Dr. Nyboe Andersen reported receiving travel and speaking fees from MSD and speaking fees from Ferring, and one of her associates reported receiving travel and speaking fees from AbbVie.
Anti-TNF therapy for inflammatory bowel disease appears to double the relative risk of developing central demyelinating disease, though the absolute risk remains small, according to a preliminary report published online Oct. 5 in JAMA Internal Medicine.
Previous case reports have suggested a possible association between anti-TNF agents taken for IBD and later development of demyelinating diseases, but a definitive link has been difficult to establish because of the rarity of these disorders and the suspicion that there already may be an underlying association between IBD and demyelinating disease.
So researchers examined the issue by analyzing data from nationwide Danish health registries for IBD patients and medication exposure. They identified 4,504 patients treated during a 14-year period who had IBD and took anti-TNF agents, and 16,429 IBD patients matched for sex, age, and IBD duration who did not take the medications, according to Dr. Nynne Nyboe Andersen, of the department of epidemiology research, Statens Serum Institut, Copenhagen, and her associates.
Eleven patients in the exposed group had central demyelinating events: multiple sclerosis (2 patients), optic neuritis (5 patients), or other central demyelinating disease (4 patients). For exposed patients, there were 7.5 events per 10,000 person-years.
In comparison, 17 patients in the unexposed group had central demyelinating events: multiple sclerosis (5 patients), optic neuritis (6 patients), transverse myelitis (1 patient), or other central demyelinating disease (5 patients). In this group there were 3.3 events per 10,000 person-years.
The hazard ratio for developing central demyelinating disease after exposure to anti-TNF agents was 2.19, the investigators wrote (JAMA Intern Med. 2015 Oct 5, doi:10.1001/jamainternmed.2015.5396.).
These preliminary findings represent the first report of this association and must be confirmed in future studies, according to the researchers.
“If true, the observed association could either be attributed to the unmasking of a latent demyelinating disease or to the emergence of a de novo demyelinating disease,” Dr. Nyboe Andersen and her associates wrote in the research letter.
The study was supported by the Lundbeck Foundation, Women in Science, the Beckett Foundation, the Danish Colitis Crohn Association, and the Danish Council for Independent Research. Dr. Nyboe Andersen reported receiving travel and speaking fees from MSD and speaking fees from Ferring, and one of her associates reported receiving travel and speaking fees from AbbVie.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Anti-TNF therapy for inflammatory bowel disease may double the risk of developing central demyelinating diseases.
Major finding: There were 7.5 central demyelinating events per 10,000 person-years in exposed IBD patients, compared with 3.3 cases in unexposed patients (hazard ratio, 2.19).
Data source: A Danish population-based cohort study involving 4,504 IBD patients exposed to and 16,429 not exposed to anti-TNF agents during a 14-year period.
Disclosures: The study was supported by the Lundbeck Foundation, Women in Science, the Beckett Foundation, the Danish Colitis Crohn Association, and the Danish Council for Independent Research. Dr. Nyboe Andersen reported receiving travel and speaking fees from MSD and speaking fees from Ferring, and one of her associates reported receiving travel and speaking fees from AbbVie.
High death rates for IBD patients who underwent emergency resections
Patients with inflammatory bowel disease (IBD) were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery, a large meta-analysis found.
Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis (UC) and 3.6% for patients with Crohn’s disease (CD), said Dr. Sunny Singh and his associates at the University of Calgary in Alberta, Canada. In contrast, only 0.6%-0.7% of patients died after elective resection, the researchers reported in the October issue of Gastroenterology (2015 Jun 5. doi: 10.1053/j.gastro.2015.06.001).
Source: American Gastroenterological AssociationClinicians should optimize medical management to avoid emergency resection, seek ways to reduce associated mortality, and use the data when counseling patients and weighing medical and surgical management options, they added.
Intestinal resection is less common among patients with IBD than in decades past, but almost half of CD patients undergo the surgery within 10 years of diagnosis, as do 16% of UC patients, according to another meta-analysis (Gastroenterology 2013;145:996-1006). Past studies have reported divergent rates of death after these surgeries, the researchers noted. To better understand mortality rates and relevant risk factors, they reviewed 18 original research articles and three abstracts published between 1990 and 2015, all of which were indexed in Medline, EMBASE, or PubMed. The studies included 67,057 UC patients and 75,971 CD patients from 15 countries.
Rates of mortality after elective resection were significantly lower than after emergency resection, whether patients had CD (elective, 0.6%; 95% confidence interval, 0.2%-1.7%; emergency, 3.6%; 1.8%-6.9%) or UC (elective, 0.7%; 0.6%-0.9%; emergency, 5.3%; 3.8%-7.3%), the researchers found. Death rates did not significantly differ based on disease type. Postoperative mortality dropped significantly after the 1990s among CD patients only, perhaps because emergency surgery has become less common in Calgary since 1997, the researchers said. However, they were unable to compare changes in death rates over time by surgery type, they said.
Several factors could explain the high fatality rates after emergency intestinal resection, the researchers said. Patients tended to have worse disease activity and higher rates of intestinal obstruction, intra-abdominal abscess, toxic megacolon, preoperative clostridial diarrhea, venous thromboembolism, malnourishment, or prolonged treatment with intravenous corticosteroids, they said. General surgeons are more likely to perform emergency resections than elective cases, which are typically handled by more experienced colorectal surgeons, they added. Emergency resections also are less likely to be performed laparoscopically than are elective resections, they noted. “The low risk of death associated with elective intestinal resections for CD and UC could be used as a quality assurance benchmark to compare outcomes between hospitals and surgeons,” they added.
The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
Patients with inflammatory bowel disease (IBD) were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery, a large meta-analysis found.
Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis (UC) and 3.6% for patients with Crohn’s disease (CD), said Dr. Sunny Singh and his associates at the University of Calgary in Alberta, Canada. In contrast, only 0.6%-0.7% of patients died after elective resection, the researchers reported in the October issue of Gastroenterology (2015 Jun 5. doi: 10.1053/j.gastro.2015.06.001).
Source: American Gastroenterological AssociationClinicians should optimize medical management to avoid emergency resection, seek ways to reduce associated mortality, and use the data when counseling patients and weighing medical and surgical management options, they added.
Intestinal resection is less common among patients with IBD than in decades past, but almost half of CD patients undergo the surgery within 10 years of diagnosis, as do 16% of UC patients, according to another meta-analysis (Gastroenterology 2013;145:996-1006). Past studies have reported divergent rates of death after these surgeries, the researchers noted. To better understand mortality rates and relevant risk factors, they reviewed 18 original research articles and three abstracts published between 1990 and 2015, all of which were indexed in Medline, EMBASE, or PubMed. The studies included 67,057 UC patients and 75,971 CD patients from 15 countries.
Rates of mortality after elective resection were significantly lower than after emergency resection, whether patients had CD (elective, 0.6%; 95% confidence interval, 0.2%-1.7%; emergency, 3.6%; 1.8%-6.9%) or UC (elective, 0.7%; 0.6%-0.9%; emergency, 5.3%; 3.8%-7.3%), the researchers found. Death rates did not significantly differ based on disease type. Postoperative mortality dropped significantly after the 1990s among CD patients only, perhaps because emergency surgery has become less common in Calgary since 1997, the researchers said. However, they were unable to compare changes in death rates over time by surgery type, they said.
Several factors could explain the high fatality rates after emergency intestinal resection, the researchers said. Patients tended to have worse disease activity and higher rates of intestinal obstruction, intra-abdominal abscess, toxic megacolon, preoperative clostridial diarrhea, venous thromboembolism, malnourishment, or prolonged treatment with intravenous corticosteroids, they said. General surgeons are more likely to perform emergency resections than elective cases, which are typically handled by more experienced colorectal surgeons, they added. Emergency resections also are less likely to be performed laparoscopically than are elective resections, they noted. “The low risk of death associated with elective intestinal resections for CD and UC could be used as a quality assurance benchmark to compare outcomes between hospitals and surgeons,” they added.
The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
Patients with inflammatory bowel disease (IBD) were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery, a large meta-analysis found.
Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis (UC) and 3.6% for patients with Crohn’s disease (CD), said Dr. Sunny Singh and his associates at the University of Calgary in Alberta, Canada. In contrast, only 0.6%-0.7% of patients died after elective resection, the researchers reported in the October issue of Gastroenterology (2015 Jun 5. doi: 10.1053/j.gastro.2015.06.001).
Source: American Gastroenterological AssociationClinicians should optimize medical management to avoid emergency resection, seek ways to reduce associated mortality, and use the data when counseling patients and weighing medical and surgical management options, they added.
Intestinal resection is less common among patients with IBD than in decades past, but almost half of CD patients undergo the surgery within 10 years of diagnosis, as do 16% of UC patients, according to another meta-analysis (Gastroenterology 2013;145:996-1006). Past studies have reported divergent rates of death after these surgeries, the researchers noted. To better understand mortality rates and relevant risk factors, they reviewed 18 original research articles and three abstracts published between 1990 and 2015, all of which were indexed in Medline, EMBASE, or PubMed. The studies included 67,057 UC patients and 75,971 CD patients from 15 countries.
Rates of mortality after elective resection were significantly lower than after emergency resection, whether patients had CD (elective, 0.6%; 95% confidence interval, 0.2%-1.7%; emergency, 3.6%; 1.8%-6.9%) or UC (elective, 0.7%; 0.6%-0.9%; emergency, 5.3%; 3.8%-7.3%), the researchers found. Death rates did not significantly differ based on disease type. Postoperative mortality dropped significantly after the 1990s among CD patients only, perhaps because emergency surgery has become less common in Calgary since 1997, the researchers said. However, they were unable to compare changes in death rates over time by surgery type, they said.
Several factors could explain the high fatality rates after emergency intestinal resection, the researchers said. Patients tended to have worse disease activity and higher rates of intestinal obstruction, intra-abdominal abscess, toxic megacolon, preoperative clostridial diarrhea, venous thromboembolism, malnourishment, or prolonged treatment with intravenous corticosteroids, they said. General surgeons are more likely to perform emergency resections than elective cases, which are typically handled by more experienced colorectal surgeons, they added. Emergency resections also are less likely to be performed laparoscopically than are elective resections, they noted. “The low risk of death associated with elective intestinal resections for CD and UC could be used as a quality assurance benchmark to compare outcomes between hospitals and surgeons,” they added.
The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.
FROM GASTROENTEROLOGY
Key clinical point: Patients with IBD were about five to eight times more likely to die after emergency intestinal resection as opposed to elective surgery.
Major finding: Overall mortality rates after emergency intestinal resection were 5.3% for patients with ulcerative colitis and 3.6% for Crohn’s disease; mortality rates after elective surgery were 0.7% and 0.6%, respectively.
Data source: Meta-analysis of 18 original research studies and three abstracts published between 1990 and 2015.
Disclosures: The research was funded by the Canadian Institute of Health Research, Alberta-Innovates Health-Solutions, the Alberta IBD Consortium. Dr. Singh reported no conflicts of interest. Senior author Dr. Gilaad Kaplan and four coauthors disclosed speaker, advisory board, and funding relationships with a number of pharmaceutical companies.