User login
EULAR issues guidelines on managing rheumatic complications of cancer immunotherapies
MADRID – EULAR has issued recommendations to help rheumatologists address the increasingly common clinical issue of diagnosing and managing rheumatic-related adverse events associated with cancer immunotherapy.
“The rheumatic adverse events associated with immunotherapy represent a spectrum of new clinical entities, and they are challenging because they can be difficult to control while attempting to preserve the antitumor effects of oncological drugs,” Marie Kostine, MD, of the Centre Universitaire Hospitalier, Bordeaux, France, explained at the European Congress of Rheumatology.
The recommendations were drawn from the deliberations of an expert task force that identified the clinical issues to address and then developed a consensus about best practice recommendations. In addition to rheumatologists with expertise in this field, the task force included oncologists, allied health personnel, and two patient representatives.
The recommendations include four overarching principles and 10 recommendations.
“One of the overarching principles regards the importance of shared decision making between rheumatologists, oncologists, and patients,” Dr. Kostine said. Because of the expertise of rheumatologists in employing immunomodulatory therapies as they pertain to inflammation of the joints, the recommendations emphasize the value of their collaboration in clinical decisions.
The recommendations address patient referral, the assessment of preexisting rheumatic conditions, diagnosis, and therapeutic strategies.
“Rheumatologists should make themselves aware of the wide spectrum of potential clinical presentations of rheumatic adverse events following the initiation of immunotherapy,” Dr. Kostine said. While rheumatoid arthritis–like symptoms are common, the immune activation produced by checkpoint inhibitors and other immunotherapies can affect nearly every organ in the body, which includes diverse involvement of joint tissues.
In addition to joint pain, which has occurred in up to 40% of patients receiving a checkpoint inhibitor in some series, rheumatology-related events can include vasculitis, systemic sclerosis, and lupus. When associated with immunotherapy, these events sometimes develop in the absence of inflammatory markers or autoantibodies.
The new consensus guidelines emphasize that glucocorticoids can be “considered” to control rheumatic-related adverse events despite their immunosuppressive effect. However, because of their potential to attenuate the benefit of immune activation for treatment of the oncologic disease, such drugs, if used, “should be tapered to the lowest effective dose.”
The consensus recommendations were based on an extensive literature review, but Dr. Kostine acknowledged that prospective studies regarding the best practices for managing rheumatic-related adverse events of immunotherapies remain limited. She suggested that this knowledge gap was one reason for creating an expert task force.
“There has been an immunotherapy revolution, such that rheumatologists who have not yet seen these adverse events soon will,” said Dr. Kostine, noting that the number of approved immunotherapies and their clinical indications have been increasing rapidly.
The EULAR recommendations were created specifically for rheumatologists. In addition to guiding them toward best practice, the report from the task force provides background on the clinical issues raised by therapies that cause inflammatory side effects while stimulating immune function to treat malignancy.
MADRID – EULAR has issued recommendations to help rheumatologists address the increasingly common clinical issue of diagnosing and managing rheumatic-related adverse events associated with cancer immunotherapy.
“The rheumatic adverse events associated with immunotherapy represent a spectrum of new clinical entities, and they are challenging because they can be difficult to control while attempting to preserve the antitumor effects of oncological drugs,” Marie Kostine, MD, of the Centre Universitaire Hospitalier, Bordeaux, France, explained at the European Congress of Rheumatology.
The recommendations were drawn from the deliberations of an expert task force that identified the clinical issues to address and then developed a consensus about best practice recommendations. In addition to rheumatologists with expertise in this field, the task force included oncologists, allied health personnel, and two patient representatives.
The recommendations include four overarching principles and 10 recommendations.
“One of the overarching principles regards the importance of shared decision making between rheumatologists, oncologists, and patients,” Dr. Kostine said. Because of the expertise of rheumatologists in employing immunomodulatory therapies as they pertain to inflammation of the joints, the recommendations emphasize the value of their collaboration in clinical decisions.
The recommendations address patient referral, the assessment of preexisting rheumatic conditions, diagnosis, and therapeutic strategies.
“Rheumatologists should make themselves aware of the wide spectrum of potential clinical presentations of rheumatic adverse events following the initiation of immunotherapy,” Dr. Kostine said. While rheumatoid arthritis–like symptoms are common, the immune activation produced by checkpoint inhibitors and other immunotherapies can affect nearly every organ in the body, which includes diverse involvement of joint tissues.
In addition to joint pain, which has occurred in up to 40% of patients receiving a checkpoint inhibitor in some series, rheumatology-related events can include vasculitis, systemic sclerosis, and lupus. When associated with immunotherapy, these events sometimes develop in the absence of inflammatory markers or autoantibodies.
The new consensus guidelines emphasize that glucocorticoids can be “considered” to control rheumatic-related adverse events despite their immunosuppressive effect. However, because of their potential to attenuate the benefit of immune activation for treatment of the oncologic disease, such drugs, if used, “should be tapered to the lowest effective dose.”
The consensus recommendations were based on an extensive literature review, but Dr. Kostine acknowledged that prospective studies regarding the best practices for managing rheumatic-related adverse events of immunotherapies remain limited. She suggested that this knowledge gap was one reason for creating an expert task force.
“There has been an immunotherapy revolution, such that rheumatologists who have not yet seen these adverse events soon will,” said Dr. Kostine, noting that the number of approved immunotherapies and their clinical indications have been increasing rapidly.
The EULAR recommendations were created specifically for rheumatologists. In addition to guiding them toward best practice, the report from the task force provides background on the clinical issues raised by therapies that cause inflammatory side effects while stimulating immune function to treat malignancy.
MADRID – EULAR has issued recommendations to help rheumatologists address the increasingly common clinical issue of diagnosing and managing rheumatic-related adverse events associated with cancer immunotherapy.
“The rheumatic adverse events associated with immunotherapy represent a spectrum of new clinical entities, and they are challenging because they can be difficult to control while attempting to preserve the antitumor effects of oncological drugs,” Marie Kostine, MD, of the Centre Universitaire Hospitalier, Bordeaux, France, explained at the European Congress of Rheumatology.
The recommendations were drawn from the deliberations of an expert task force that identified the clinical issues to address and then developed a consensus about best practice recommendations. In addition to rheumatologists with expertise in this field, the task force included oncologists, allied health personnel, and two patient representatives.
The recommendations include four overarching principles and 10 recommendations.
“One of the overarching principles regards the importance of shared decision making between rheumatologists, oncologists, and patients,” Dr. Kostine said. Because of the expertise of rheumatologists in employing immunomodulatory therapies as they pertain to inflammation of the joints, the recommendations emphasize the value of their collaboration in clinical decisions.
The recommendations address patient referral, the assessment of preexisting rheumatic conditions, diagnosis, and therapeutic strategies.
“Rheumatologists should make themselves aware of the wide spectrum of potential clinical presentations of rheumatic adverse events following the initiation of immunotherapy,” Dr. Kostine said. While rheumatoid arthritis–like symptoms are common, the immune activation produced by checkpoint inhibitors and other immunotherapies can affect nearly every organ in the body, which includes diverse involvement of joint tissues.
In addition to joint pain, which has occurred in up to 40% of patients receiving a checkpoint inhibitor in some series, rheumatology-related events can include vasculitis, systemic sclerosis, and lupus. When associated with immunotherapy, these events sometimes develop in the absence of inflammatory markers or autoantibodies.
The new consensus guidelines emphasize that glucocorticoids can be “considered” to control rheumatic-related adverse events despite their immunosuppressive effect. However, because of their potential to attenuate the benefit of immune activation for treatment of the oncologic disease, such drugs, if used, “should be tapered to the lowest effective dose.”
The consensus recommendations were based on an extensive literature review, but Dr. Kostine acknowledged that prospective studies regarding the best practices for managing rheumatic-related adverse events of immunotherapies remain limited. She suggested that this knowledge gap was one reason for creating an expert task force.
“There has been an immunotherapy revolution, such that rheumatologists who have not yet seen these adverse events soon will,” said Dr. Kostine, noting that the number of approved immunotherapies and their clinical indications have been increasing rapidly.
The EULAR recommendations were created specifically for rheumatologists. In addition to guiding them toward best practice, the report from the task force provides background on the clinical issues raised by therapies that cause inflammatory side effects while stimulating immune function to treat malignancy.
REPORTING FROM EULAR 2019 CONGRESS
Adding ipilimumab to nivolumab provides no benefit in SCC trial
CHICAGO – Phase 3 results suggest ipilimumab plus nivolumab is no more effective than nivolumab alone in previously treated patients with metastatic squamous cell lung cancer and no matching biomarker.
However, there is evidence to suggest that patients with a high tumor mutational burden (TMB) and low programmed death–ligand 1 (PD-L1) tumor proportion score (TPS) may derive a benefit from the combination.
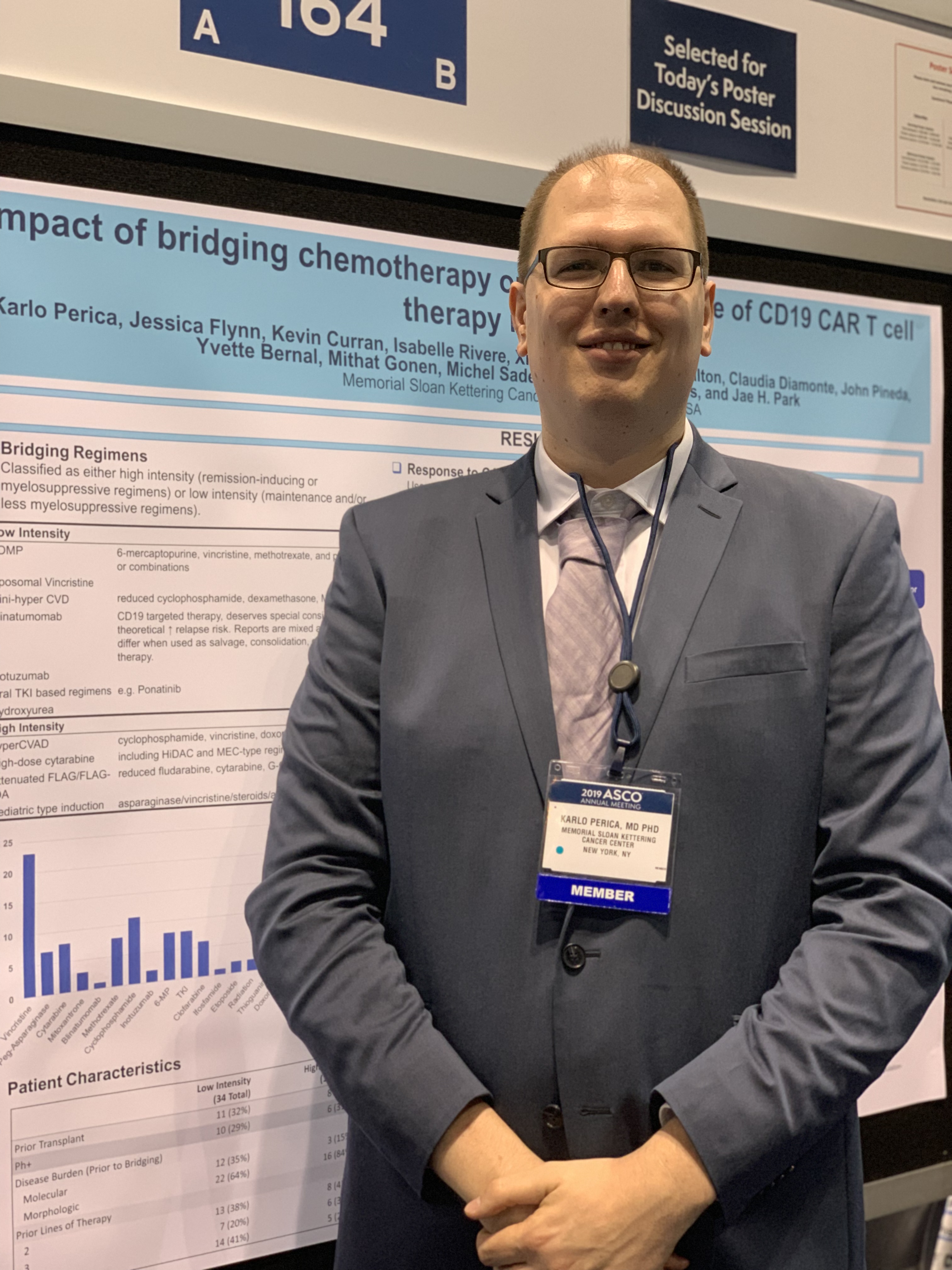
Lyudmila Bazhenova, MD, of the University of California, San Diego, and her colleagues presented results from this trial (NCT02785952) in a poster at the annual meeting of the American Society for Clinical Oncology. Kathryn C. Arbour, MD, of Memorial Sloan Kettering Cancer Center in New York reviewed the data in a poster discussion session.
Patients and treatment
The researchers reported on 275 previously treated patients with stage IV or recurrent squamous cell lung cancer who were naive to checkpoint inhibitors. Patients were randomized to receive nivolumab (nivo) at 3 mg/m2 once every 2 weeks (n = 137) or the same dose of nivolumab plus ipilimumab (ipi + nivo) at 1 mg/m2 once every 6 weeks (n = 138).
The patients were stratified by gender and number of prior therapies (one vs. two or more), but they were not stratified by TMB or PD-L1 expression.
The PD-L1 TPS was unknown in 36% of patients, less than 5% in 57%, and 5% or greater in 43% of patients. TMB was unknown in 8% of patients, less than 10 mutations per megabase in 52%, and 10 mutations per megabase or greater in 48%.
Baseline characteristics were similar between the treatment arms. The median age was 67.5 years (range, 42-83 years) in the ipi + nivo arm and 68.1 years (range, 49-90 years) in the nivo arm. Most patients had received only one prior therapy – 85% and 83%, respectively – and most had a performance status of 1 – 71% and 72%, respectively.
Efficacy
There were no significant differences in outcomes between the treatment arms, and the study was closed early for futility.
The overall response rate was 18% in the ipi + nivo arm and 17% in the nivo arm, with one complete response occurring in each arm. The median duration of response was 9.1 months in the ipi + nivo arm and 8.6 months in the nivo arm.
The median progression-free survival was 3.8 months in the ipi + nivo arm and 2.9 months in the nivo arm (hazard ratio, 0.84; P = .19). The 24-month progression-free survival was 8.2% and 5.9%, respectively.
The median overall survival was 10.0 months in the ipi + nivo arm and 11.0 months in the nivo arm (HR, 0.97; P = .82). The 24-month overall survival was 27.6% and 20.1%, respectively.
There were no significant differences in outcomes by TMB or PD-L1 with the cutoffs used in this study, according to Dr. Bazhenova and colleagues, but different cutoffs are being explored.
The median progression-free survival was 4.4 months in TMB-high/PD-L1-low patients in the ipi + nivo arm, compared with 1.7 months in the TMB-high/PD-L1-low patients in the nivo arm. The median overall survival was 15.9 months and 10.3 months, respectively.
“It is slightly challenging to interpret the results without knowing the PD-L1 data of all patients in the cohort, and biomarker selection remains crucial for this combination,” Dr. Arbour said.
Safety
There were no differences in individual toxicities between the treatment arms, but cumulative toxicities were higher in the combination arm, according to the researchers.
The incidence of treatment-related adverse events (AEs) was 88% in the ipi + nivo arm and 90% in the nivo arm. The incidence of grade 3-5 treatment-related AEs was 39% and 31%, respectively.
The incidence of immune-mediated AEs was 65% in the ipi + nivo arm and 57% in the nivo arm. The incidence of immune-mediated grade 3-5 AEs was 20% and 11%, respectively.
There were six AEs leading to death in the ipi + nivo arm – two due to dyspnea, one due to colitis, and one due to respiratory failure. The attribution of one death is under review. For the remaining death, the exact cause is unknown.
There were two AEs leading to death in the nivo arm, both due to pneumonitis.
This study was supported by grants from the National Institutes of Health and by AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Genentech, and Pfizer through the Foundation for the National Institutes of Health in partnership with Friends of Cancer Research.
Dr. Bazhenova reported relationships with Epic Sciences, AbbVie, AstraZeneca, Boston Biomedical, Genentech/Roche, Lilly, Loxo, Pfizer, Takeda, and BeyondSpring Pharmaceuticals. Her colleagues reported relationships with these and other companies. Dr. Arbour reported a relationship with AstraZeneca.
SOURCE: Bazhenova L et al. ASCO 2019, Abstract 9014.
CHICAGO – Phase 3 results suggest ipilimumab plus nivolumab is no more effective than nivolumab alone in previously treated patients with metastatic squamous cell lung cancer and no matching biomarker.
However, there is evidence to suggest that patients with a high tumor mutational burden (TMB) and low programmed death–ligand 1 (PD-L1) tumor proportion score (TPS) may derive a benefit from the combination.
Lyudmila Bazhenova, MD, of the University of California, San Diego, and her colleagues presented results from this trial (NCT02785952) in a poster at the annual meeting of the American Society for Clinical Oncology. Kathryn C. Arbour, MD, of Memorial Sloan Kettering Cancer Center in New York reviewed the data in a poster discussion session.
Patients and treatment
The researchers reported on 275 previously treated patients with stage IV or recurrent squamous cell lung cancer who were naive to checkpoint inhibitors. Patients were randomized to receive nivolumab (nivo) at 3 mg/m2 once every 2 weeks (n = 137) or the same dose of nivolumab plus ipilimumab (ipi + nivo) at 1 mg/m2 once every 6 weeks (n = 138).
The patients were stratified by gender and number of prior therapies (one vs. two or more), but they were not stratified by TMB or PD-L1 expression.
The PD-L1 TPS was unknown in 36% of patients, less than 5% in 57%, and 5% or greater in 43% of patients. TMB was unknown in 8% of patients, less than 10 mutations per megabase in 52%, and 10 mutations per megabase or greater in 48%.
Baseline characteristics were similar between the treatment arms. The median age was 67.5 years (range, 42-83 years) in the ipi + nivo arm and 68.1 years (range, 49-90 years) in the nivo arm. Most patients had received only one prior therapy – 85% and 83%, respectively – and most had a performance status of 1 – 71% and 72%, respectively.
Efficacy
There were no significant differences in outcomes between the treatment arms, and the study was closed early for futility.
The overall response rate was 18% in the ipi + nivo arm and 17% in the nivo arm, with one complete response occurring in each arm. The median duration of response was 9.1 months in the ipi + nivo arm and 8.6 months in the nivo arm.
The median progression-free survival was 3.8 months in the ipi + nivo arm and 2.9 months in the nivo arm (hazard ratio, 0.84; P = .19). The 24-month progression-free survival was 8.2% and 5.9%, respectively.
The median overall survival was 10.0 months in the ipi + nivo arm and 11.0 months in the nivo arm (HR, 0.97; P = .82). The 24-month overall survival was 27.6% and 20.1%, respectively.
There were no significant differences in outcomes by TMB or PD-L1 with the cutoffs used in this study, according to Dr. Bazhenova and colleagues, but different cutoffs are being explored.
The median progression-free survival was 4.4 months in TMB-high/PD-L1-low patients in the ipi + nivo arm, compared with 1.7 months in the TMB-high/PD-L1-low patients in the nivo arm. The median overall survival was 15.9 months and 10.3 months, respectively.
“It is slightly challenging to interpret the results without knowing the PD-L1 data of all patients in the cohort, and biomarker selection remains crucial for this combination,” Dr. Arbour said.
Safety
There were no differences in individual toxicities between the treatment arms, but cumulative toxicities were higher in the combination arm, according to the researchers.
The incidence of treatment-related adverse events (AEs) was 88% in the ipi + nivo arm and 90% in the nivo arm. The incidence of grade 3-5 treatment-related AEs was 39% and 31%, respectively.
The incidence of immune-mediated AEs was 65% in the ipi + nivo arm and 57% in the nivo arm. The incidence of immune-mediated grade 3-5 AEs was 20% and 11%, respectively.
There were six AEs leading to death in the ipi + nivo arm – two due to dyspnea, one due to colitis, and one due to respiratory failure. The attribution of one death is under review. For the remaining death, the exact cause is unknown.
There were two AEs leading to death in the nivo arm, both due to pneumonitis.
This study was supported by grants from the National Institutes of Health and by AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Genentech, and Pfizer through the Foundation for the National Institutes of Health in partnership with Friends of Cancer Research.
Dr. Bazhenova reported relationships with Epic Sciences, AbbVie, AstraZeneca, Boston Biomedical, Genentech/Roche, Lilly, Loxo, Pfizer, Takeda, and BeyondSpring Pharmaceuticals. Her colleagues reported relationships with these and other companies. Dr. Arbour reported a relationship with AstraZeneca.
SOURCE: Bazhenova L et al. ASCO 2019, Abstract 9014.
CHICAGO – Phase 3 results suggest ipilimumab plus nivolumab is no more effective than nivolumab alone in previously treated patients with metastatic squamous cell lung cancer and no matching biomarker.
However, there is evidence to suggest that patients with a high tumor mutational burden (TMB) and low programmed death–ligand 1 (PD-L1) tumor proportion score (TPS) may derive a benefit from the combination.
Lyudmila Bazhenova, MD, of the University of California, San Diego, and her colleagues presented results from this trial (NCT02785952) in a poster at the annual meeting of the American Society for Clinical Oncology. Kathryn C. Arbour, MD, of Memorial Sloan Kettering Cancer Center in New York reviewed the data in a poster discussion session.
Patients and treatment
The researchers reported on 275 previously treated patients with stage IV or recurrent squamous cell lung cancer who were naive to checkpoint inhibitors. Patients were randomized to receive nivolumab (nivo) at 3 mg/m2 once every 2 weeks (n = 137) or the same dose of nivolumab plus ipilimumab (ipi + nivo) at 1 mg/m2 once every 6 weeks (n = 138).
The patients were stratified by gender and number of prior therapies (one vs. two or more), but they were not stratified by TMB or PD-L1 expression.
The PD-L1 TPS was unknown in 36% of patients, less than 5% in 57%, and 5% or greater in 43% of patients. TMB was unknown in 8% of patients, less than 10 mutations per megabase in 52%, and 10 mutations per megabase or greater in 48%.
Baseline characteristics were similar between the treatment arms. The median age was 67.5 years (range, 42-83 years) in the ipi + nivo arm and 68.1 years (range, 49-90 years) in the nivo arm. Most patients had received only one prior therapy – 85% and 83%, respectively – and most had a performance status of 1 – 71% and 72%, respectively.
Efficacy
There were no significant differences in outcomes between the treatment arms, and the study was closed early for futility.
The overall response rate was 18% in the ipi + nivo arm and 17% in the nivo arm, with one complete response occurring in each arm. The median duration of response was 9.1 months in the ipi + nivo arm and 8.6 months in the nivo arm.
The median progression-free survival was 3.8 months in the ipi + nivo arm and 2.9 months in the nivo arm (hazard ratio, 0.84; P = .19). The 24-month progression-free survival was 8.2% and 5.9%, respectively.
The median overall survival was 10.0 months in the ipi + nivo arm and 11.0 months in the nivo arm (HR, 0.97; P = .82). The 24-month overall survival was 27.6% and 20.1%, respectively.
There were no significant differences in outcomes by TMB or PD-L1 with the cutoffs used in this study, according to Dr. Bazhenova and colleagues, but different cutoffs are being explored.
The median progression-free survival was 4.4 months in TMB-high/PD-L1-low patients in the ipi + nivo arm, compared with 1.7 months in the TMB-high/PD-L1-low patients in the nivo arm. The median overall survival was 15.9 months and 10.3 months, respectively.
“It is slightly challenging to interpret the results without knowing the PD-L1 data of all patients in the cohort, and biomarker selection remains crucial for this combination,” Dr. Arbour said.
Safety
There were no differences in individual toxicities between the treatment arms, but cumulative toxicities were higher in the combination arm, according to the researchers.
The incidence of treatment-related adverse events (AEs) was 88% in the ipi + nivo arm and 90% in the nivo arm. The incidence of grade 3-5 treatment-related AEs was 39% and 31%, respectively.
The incidence of immune-mediated AEs was 65% in the ipi + nivo arm and 57% in the nivo arm. The incidence of immune-mediated grade 3-5 AEs was 20% and 11%, respectively.
There were six AEs leading to death in the ipi + nivo arm – two due to dyspnea, one due to colitis, and one due to respiratory failure. The attribution of one death is under review. For the remaining death, the exact cause is unknown.
There were two AEs leading to death in the nivo arm, both due to pneumonitis.
This study was supported by grants from the National Institutes of Health and by AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Genentech, and Pfizer through the Foundation for the National Institutes of Health in partnership with Friends of Cancer Research.
Dr. Bazhenova reported relationships with Epic Sciences, AbbVie, AstraZeneca, Boston Biomedical, Genentech/Roche, Lilly, Loxo, Pfizer, Takeda, and BeyondSpring Pharmaceuticals. Her colleagues reported relationships with these and other companies. Dr. Arbour reported a relationship with AstraZeneca.
SOURCE: Bazhenova L et al. ASCO 2019, Abstract 9014.
REPORTING FROM ASCO 2019
Key clinical point: Ipilimumab plus nivolumab appears no more effective than nivolumab alone in previously treated patients with metastatic squamous cell lung cancer and no matching biomarker.
Major finding: The median progression-free survival was 3.8 months in the ipilimumab plus nivolumab arm and 2.9 months in the nivolumab arm (P = .19). The median overall survival was 10.0 months and 11.0 months, respectively (P = .82).
Study details: A phase 3 trial of 275 previously treated patients with stage IV or recurrent squamous cell lung cancer.
Disclosures: This study was supported by grants from the National Institutes of Health and by AbbVie, Amgen, AstraZeneca, Bristol-Myers Squibb, Genentech, and Pfizer through the Foundation for the National Institutes of Health in partnership with Friends of Cancer Research. The researchers reported relationships with a range of companies. Source: Bazhenova L et al. ASCO 2019, Abstract 9014.
Adjuvant immunotherapy results ‘encouraging’ in early NSCLC
CHICAGO – Neoadjuvant monotherapy with the immune checkpoint inhibitor atezolizumab is associated with “encouraging” responses with no new safety signals for patients with non–small cell lung cancer (NSCLC), an interim analysis of a multicenter phase 2 trial suggests.
Among 77 of a planned 180 patients with resectable NSCLC enrolled in the LCMC3 (Lung Cancer Mutation Consortium 3) trial, the pathological complete response (pCR) rate following two cycles of neoadjuvant atezolizumab (Tecentriq) and surgery was 5%, and the major pathological response (MPR) rate was 19%, reported David J. Kwiatkowski, MD, PhD, of the Dana-Farber Cancer Institute in Boston.
“Pathological regression moderately correlated with target lesions’ measurements by RECIST [Response Evaluation Criteria in Solid Tumors] and MPR was observed irrespective of PD-L1 expression, although there was some correlation,” he said at the annual meeting of the American Society of Clinical Oncology.
The study was designed to test whether preoperative immunotherapy with an immune checkpoint inhibitor could have additional clinical benefits for patients with early-stage NSCLC.
Investigators are enrolling patients with stage IB, II, IIIA, or selected IIIB resectable, previously untreated NSCLC. Patients receive 1,200 mg atezolizumab on days 1 and 22 (two cycles), followed by surgery on or about day 40.
The primary endpoint, MPR, “means that at the time of surgical resection, all of the samples of the tumor that are cut into sections are reviewed by a pathologist, and an aggregate score of a percent of viable tumor cells is determined based on a comparison of viable tumor cells and necrotic tumor cells and stroma,” Dr. Kwiatkowski said.
The threshold for MPR was 10% or fewer viable tumor cells at the time of resection.
Following surgery, patients received standard-of-care adjuvant chemotherapy and could receive optional continued atezolizumab for an additional 12 months.
At the time of this interim analysis, with a data cutoff of Sept. 5, 2018, 101 patients had been enrolled and were included in the interim safety analysis. Of this group, 11 did not undergo surgery, because of progressive disease, withdrawal of consent, failed echocardiogram (1 patient), or pulmonary artery involvement (1) patient.
Of the 10 patients with either progressive disease and no surgery or unresectable disease at surgery, 8 had stage IIIA tumors and 2 had stage IIIB tumors. All patients with stage I or II disease underwent resection.
Dr. Kwiatkowski presented interim data on 90 patients intended for surgery, of whom 84 had assessment of the primary endpoint, including 7 positive for EGFR and/or ALK, and 77 whose tumors were either EGFR/ALK negative or had unknown status. These 77 patients were the primary efficacy population.
As noted before, among the 77 in the primary efficacy population, 15 (19%) had a MPR, and 4 patients (5%) had a pCR. In addition, 38 patients (49%) had pathological regression of tumor of 50% or greater. Pathological regression correlated significantly with change in tumor lesion size (P less than .001).
Tumor mutational burden, however, was not significantly correlated with MPR or pathological regression.
Among the 101 patients in the safety population, there were two deaths deemed not related to study treatment: one cardiac death post surgical resection, and one from disease progression. Treatment-related adverse events occurred in 57% of patients, including 6% that were grade 3 or greater. Adverse events leading to treatment withdrawal occurred in 5% of patients.
The efficacy interim analysis passed the prespecified futility boundary, and investigators are continuing to enroll patients.
Invited discussant Maximilian Diehn, MD, PhD, of Stanford (Calif.) University commented that neoadjuvant immunotherapy for NSCLC is promising, but added that the MPR endpoint still needs validation.
“Currently, it is not considered a validated surrogate endpoint for survival and therefore is not currently used for drug approvals. Secondly, the optimal cut point may differ by histology, such as being different for adenocarcinoma and squamous cell carcinoma. And this has potential implications for using this in trials that enroll patients of both histologies. And, third, there are some emerging data that MPR may need to measured somewhat differently after immunotherapy than after chemotherapy,” he said.
The study is supported by Genentech. Dr. Kwiatkowski disclosed research funding and a consulting or advisory role for the company. Dr. Diehn reported stock ownership, consulting, research funding, and travel expenses from various companies.
SOURCE: Kwiatkowski DJ et al. ASCO 2019, Abstract 8503.
CHICAGO – Neoadjuvant monotherapy with the immune checkpoint inhibitor atezolizumab is associated with “encouraging” responses with no new safety signals for patients with non–small cell lung cancer (NSCLC), an interim analysis of a multicenter phase 2 trial suggests.
Among 77 of a planned 180 patients with resectable NSCLC enrolled in the LCMC3 (Lung Cancer Mutation Consortium 3) trial, the pathological complete response (pCR) rate following two cycles of neoadjuvant atezolizumab (Tecentriq) and surgery was 5%, and the major pathological response (MPR) rate was 19%, reported David J. Kwiatkowski, MD, PhD, of the Dana-Farber Cancer Institute in Boston.
“Pathological regression moderately correlated with target lesions’ measurements by RECIST [Response Evaluation Criteria in Solid Tumors] and MPR was observed irrespective of PD-L1 expression, although there was some correlation,” he said at the annual meeting of the American Society of Clinical Oncology.
The study was designed to test whether preoperative immunotherapy with an immune checkpoint inhibitor could have additional clinical benefits for patients with early-stage NSCLC.
Investigators are enrolling patients with stage IB, II, IIIA, or selected IIIB resectable, previously untreated NSCLC. Patients receive 1,200 mg atezolizumab on days 1 and 22 (two cycles), followed by surgery on or about day 40.
The primary endpoint, MPR, “means that at the time of surgical resection, all of the samples of the tumor that are cut into sections are reviewed by a pathologist, and an aggregate score of a percent of viable tumor cells is determined based on a comparison of viable tumor cells and necrotic tumor cells and stroma,” Dr. Kwiatkowski said.
The threshold for MPR was 10% or fewer viable tumor cells at the time of resection.
Following surgery, patients received standard-of-care adjuvant chemotherapy and could receive optional continued atezolizumab for an additional 12 months.
At the time of this interim analysis, with a data cutoff of Sept. 5, 2018, 101 patients had been enrolled and were included in the interim safety analysis. Of this group, 11 did not undergo surgery, because of progressive disease, withdrawal of consent, failed echocardiogram (1 patient), or pulmonary artery involvement (1) patient.
Of the 10 patients with either progressive disease and no surgery or unresectable disease at surgery, 8 had stage IIIA tumors and 2 had stage IIIB tumors. All patients with stage I or II disease underwent resection.
Dr. Kwiatkowski presented interim data on 90 patients intended for surgery, of whom 84 had assessment of the primary endpoint, including 7 positive for EGFR and/or ALK, and 77 whose tumors were either EGFR/ALK negative or had unknown status. These 77 patients were the primary efficacy population.
As noted before, among the 77 in the primary efficacy population, 15 (19%) had a MPR, and 4 patients (5%) had a pCR. In addition, 38 patients (49%) had pathological regression of tumor of 50% or greater. Pathological regression correlated significantly with change in tumor lesion size (P less than .001).
Tumor mutational burden, however, was not significantly correlated with MPR or pathological regression.
Among the 101 patients in the safety population, there were two deaths deemed not related to study treatment: one cardiac death post surgical resection, and one from disease progression. Treatment-related adverse events occurred in 57% of patients, including 6% that were grade 3 or greater. Adverse events leading to treatment withdrawal occurred in 5% of patients.
The efficacy interim analysis passed the prespecified futility boundary, and investigators are continuing to enroll patients.
Invited discussant Maximilian Diehn, MD, PhD, of Stanford (Calif.) University commented that neoadjuvant immunotherapy for NSCLC is promising, but added that the MPR endpoint still needs validation.
“Currently, it is not considered a validated surrogate endpoint for survival and therefore is not currently used for drug approvals. Secondly, the optimal cut point may differ by histology, such as being different for adenocarcinoma and squamous cell carcinoma. And this has potential implications for using this in trials that enroll patients of both histologies. And, third, there are some emerging data that MPR may need to measured somewhat differently after immunotherapy than after chemotherapy,” he said.
The study is supported by Genentech. Dr. Kwiatkowski disclosed research funding and a consulting or advisory role for the company. Dr. Diehn reported stock ownership, consulting, research funding, and travel expenses from various companies.
SOURCE: Kwiatkowski DJ et al. ASCO 2019, Abstract 8503.
CHICAGO – Neoadjuvant monotherapy with the immune checkpoint inhibitor atezolizumab is associated with “encouraging” responses with no new safety signals for patients with non–small cell lung cancer (NSCLC), an interim analysis of a multicenter phase 2 trial suggests.
Among 77 of a planned 180 patients with resectable NSCLC enrolled in the LCMC3 (Lung Cancer Mutation Consortium 3) trial, the pathological complete response (pCR) rate following two cycles of neoadjuvant atezolizumab (Tecentriq) and surgery was 5%, and the major pathological response (MPR) rate was 19%, reported David J. Kwiatkowski, MD, PhD, of the Dana-Farber Cancer Institute in Boston.
“Pathological regression moderately correlated with target lesions’ measurements by RECIST [Response Evaluation Criteria in Solid Tumors] and MPR was observed irrespective of PD-L1 expression, although there was some correlation,” he said at the annual meeting of the American Society of Clinical Oncology.
The study was designed to test whether preoperative immunotherapy with an immune checkpoint inhibitor could have additional clinical benefits for patients with early-stage NSCLC.
Investigators are enrolling patients with stage IB, II, IIIA, or selected IIIB resectable, previously untreated NSCLC. Patients receive 1,200 mg atezolizumab on days 1 and 22 (two cycles), followed by surgery on or about day 40.
The primary endpoint, MPR, “means that at the time of surgical resection, all of the samples of the tumor that are cut into sections are reviewed by a pathologist, and an aggregate score of a percent of viable tumor cells is determined based on a comparison of viable tumor cells and necrotic tumor cells and stroma,” Dr. Kwiatkowski said.
The threshold for MPR was 10% or fewer viable tumor cells at the time of resection.
Following surgery, patients received standard-of-care adjuvant chemotherapy and could receive optional continued atezolizumab for an additional 12 months.
At the time of this interim analysis, with a data cutoff of Sept. 5, 2018, 101 patients had been enrolled and were included in the interim safety analysis. Of this group, 11 did not undergo surgery, because of progressive disease, withdrawal of consent, failed echocardiogram (1 patient), or pulmonary artery involvement (1) patient.
Of the 10 patients with either progressive disease and no surgery or unresectable disease at surgery, 8 had stage IIIA tumors and 2 had stage IIIB tumors. All patients with stage I or II disease underwent resection.
Dr. Kwiatkowski presented interim data on 90 patients intended for surgery, of whom 84 had assessment of the primary endpoint, including 7 positive for EGFR and/or ALK, and 77 whose tumors were either EGFR/ALK negative or had unknown status. These 77 patients were the primary efficacy population.
As noted before, among the 77 in the primary efficacy population, 15 (19%) had a MPR, and 4 patients (5%) had a pCR. In addition, 38 patients (49%) had pathological regression of tumor of 50% or greater. Pathological regression correlated significantly with change in tumor lesion size (P less than .001).
Tumor mutational burden, however, was not significantly correlated with MPR or pathological regression.
Among the 101 patients in the safety population, there were two deaths deemed not related to study treatment: one cardiac death post surgical resection, and one from disease progression. Treatment-related adverse events occurred in 57% of patients, including 6% that were grade 3 or greater. Adverse events leading to treatment withdrawal occurred in 5% of patients.
The efficacy interim analysis passed the prespecified futility boundary, and investigators are continuing to enroll patients.
Invited discussant Maximilian Diehn, MD, PhD, of Stanford (Calif.) University commented that neoadjuvant immunotherapy for NSCLC is promising, but added that the MPR endpoint still needs validation.
“Currently, it is not considered a validated surrogate endpoint for survival and therefore is not currently used for drug approvals. Secondly, the optimal cut point may differ by histology, such as being different for adenocarcinoma and squamous cell carcinoma. And this has potential implications for using this in trials that enroll patients of both histologies. And, third, there are some emerging data that MPR may need to measured somewhat differently after immunotherapy than after chemotherapy,” he said.
The study is supported by Genentech. Dr. Kwiatkowski disclosed research funding and a consulting or advisory role for the company. Dr. Diehn reported stock ownership, consulting, research funding, and travel expenses from various companies.
SOURCE: Kwiatkowski DJ et al. ASCO 2019, Abstract 8503.
REPORTING FROM ASCO 2019
Nivo/ipi shrinks early NSCLC before surgery
CHICAGO – Two immune checkpoint inhibitors were better than one as neoadjuvant therapy for patients with resectable early-stage non–small cell lung cancer (NSCLC) in the phase 2 NEOSTAR trial.
Among 44 patients with stage I-IIIA NSCLC who were randomized to either a combination of nivolumab (Opdivo) and ipilimumab (Yervoy) or to nivolumab alone, the combination was associated with higher rates of the primary endpoint of major pathological response (MPR), defined as a reduction in viable tumors cells to 10% or less, reported Tina Cascone, MD, PhD, from the University of Texas MD Anderson Cancer Center in Houston.
“Nivolumab/ipilimumab induced a 44% MPR rate in resected patients, met the trial prespecified boundary with seven MPRs in the intention-to-treat population, and induced pathologic complete responses in 38% of resected patients,” she said at the annual meeting of the American Society of Clinical Oncology.
To test whether neoadjuvant monotherapy or combination therapy could improve outcomes of standard induction chemotherapy, NEOSTAR investigators enrolled patients with NSCLC stage I-IIIA, including patients with a single involved mediastinal node (N2 single station) who were eligible for surgical resection.
The patients were randomized on a 1:1 basis to receive nivolumab 3 mg/kg on days 1, 15 and 29 alone or in combination with ipilimumab delivered 1 mg/kg on day 1, followed by surgery 3-6 weeks after the last study dose and then postoperative standard-of-care chemotherapy.
Of 53 patients screened, 44 were eligible, with 23 randomized to nivolumab monotherapy and 21 randomized to nivolumab/ipilimumab. Of this group, five did not proceed to surgery (one in the monotherapy arm, four in the combination arm) because of either high surgical risk, lack of respectability, or refusal of surgery. The mean age at randomization was 65.6 years. In all, 18% were never smokers, and the remaining 82% were former or current smokers.
The MPR rate in the intention-to-treat population – the primary endpoint – was reached in four patients (17%) in the monotherapy arm and in seven patients (33%) in the combination arm. As noted, the combination arm reached the prespecified boundary of six or more patients with an MPR. All patients in each arm who had an MPR also had a pathologic complete responses.
Of the 39 patients who went on to resection, 37 were evaluable, and in these patients the respective MPR rates were 19% and 44%. Two patients on nivolumab alone and six on nivolumab plus ipilimumab had 0% viable tumor detectable at the time of surgery. Radiographic responses included one complete response in the combination arm and eight total partial responses, in five and three patients, respectively. The objective response rated was 20%. The responses, assessed by Response Evaluation Criteria in Solid Tumors (RECIST) were positively associated with MPR, Dr. Cascone said.
In 11% of patients, the investigators observed apparent radiographic progression after neoadjuvant immune checkpoint inhibitors in mediastinal and or in nonregional nodes. However, pathological assessment and evaluation of the flaring nodes did not reveal evidence of disease, but instead showed noncaseating granulomas that were not present at baseline.
“Awareness of this phenomenon, which we named the ‘nodal immune flare,’ is of critical importance, as if the clinician fails to distinguish the nodal immune flare from disease progression, potential curative surgery for these patients could be avoided,” she said.
Grade 1 or 2 treatment-related adverse events included rash, itching, fatigue, anemia, cough, and diarrhea. Grade 3 or greater treatment-related adverse events included hypoxia, pneumonia, and pneumonitis in the nivolumab monotherapy arm and diarrhea and hyponatremia in the combination group. One patient treated with nivolumab monotherapy, who had achieved 0% viable tumor, had grade 3 pneumonia and pneumonitis, which was treated with steroids that impeded the healing of a bronchopleural fistula and subsequent empyema. Other surgical complications included air leaks, which occurred in five patients in the nivolumab group and three in the nivolumab plus ipilimumab arm.
Two patients died, one in the monotherapy arm from steroid-treated pneumonitis 4.1 months after randomization and one in the combination arm who had progressive disease 2 months after randomization, and died from the disease 15 months later.
Invited discussant Maximilian Diehn, MD, PhD, from Stanford (California) University School of Medicine, commented that the choice of neoadjuvant immunotherapy was not based on molecular markers, “and I think we have a major unmet need for developing biomarkers for personalized treatment in this area.
“Ideally, the biomarkers that we would have in this setting would, A, allow us to identify which patients have micrometastatic disease and therefore are likely to benefit from the upfront systemic therapy and, secondly, also could tell us which neoadjuvant therapy they would respond to, be it immunotherapy, chemotherapy, or the combination,” he added.
The study was supported by Bristol-Myers Squibb. Dr. Cascone disclosed honoraria from the company. Dr. Diehn reported stock ownership, consulting, research funding and travel expenses from various companies.
SOURCE: Cascone T. et al. ASCO 2019, Abstract 8504.
CHICAGO – Two immune checkpoint inhibitors were better than one as neoadjuvant therapy for patients with resectable early-stage non–small cell lung cancer (NSCLC) in the phase 2 NEOSTAR trial.
Among 44 patients with stage I-IIIA NSCLC who were randomized to either a combination of nivolumab (Opdivo) and ipilimumab (Yervoy) or to nivolumab alone, the combination was associated with higher rates of the primary endpoint of major pathological response (MPR), defined as a reduction in viable tumors cells to 10% or less, reported Tina Cascone, MD, PhD, from the University of Texas MD Anderson Cancer Center in Houston.
“Nivolumab/ipilimumab induced a 44% MPR rate in resected patients, met the trial prespecified boundary with seven MPRs in the intention-to-treat population, and induced pathologic complete responses in 38% of resected patients,” she said at the annual meeting of the American Society of Clinical Oncology.
To test whether neoadjuvant monotherapy or combination therapy could improve outcomes of standard induction chemotherapy, NEOSTAR investigators enrolled patients with NSCLC stage I-IIIA, including patients with a single involved mediastinal node (N2 single station) who were eligible for surgical resection.
The patients were randomized on a 1:1 basis to receive nivolumab 3 mg/kg on days 1, 15 and 29 alone or in combination with ipilimumab delivered 1 mg/kg on day 1, followed by surgery 3-6 weeks after the last study dose and then postoperative standard-of-care chemotherapy.
Of 53 patients screened, 44 were eligible, with 23 randomized to nivolumab monotherapy and 21 randomized to nivolumab/ipilimumab. Of this group, five did not proceed to surgery (one in the monotherapy arm, four in the combination arm) because of either high surgical risk, lack of respectability, or refusal of surgery. The mean age at randomization was 65.6 years. In all, 18% were never smokers, and the remaining 82% were former or current smokers.
The MPR rate in the intention-to-treat population – the primary endpoint – was reached in four patients (17%) in the monotherapy arm and in seven patients (33%) in the combination arm. As noted, the combination arm reached the prespecified boundary of six or more patients with an MPR. All patients in each arm who had an MPR also had a pathologic complete responses.
Of the 39 patients who went on to resection, 37 were evaluable, and in these patients the respective MPR rates were 19% and 44%. Two patients on nivolumab alone and six on nivolumab plus ipilimumab had 0% viable tumor detectable at the time of surgery. Radiographic responses included one complete response in the combination arm and eight total partial responses, in five and three patients, respectively. The objective response rated was 20%. The responses, assessed by Response Evaluation Criteria in Solid Tumors (RECIST) were positively associated with MPR, Dr. Cascone said.
In 11% of patients, the investigators observed apparent radiographic progression after neoadjuvant immune checkpoint inhibitors in mediastinal and or in nonregional nodes. However, pathological assessment and evaluation of the flaring nodes did not reveal evidence of disease, but instead showed noncaseating granulomas that were not present at baseline.
“Awareness of this phenomenon, which we named the ‘nodal immune flare,’ is of critical importance, as if the clinician fails to distinguish the nodal immune flare from disease progression, potential curative surgery for these patients could be avoided,” she said.
Grade 1 or 2 treatment-related adverse events included rash, itching, fatigue, anemia, cough, and diarrhea. Grade 3 or greater treatment-related adverse events included hypoxia, pneumonia, and pneumonitis in the nivolumab monotherapy arm and diarrhea and hyponatremia in the combination group. One patient treated with nivolumab monotherapy, who had achieved 0% viable tumor, had grade 3 pneumonia and pneumonitis, which was treated with steroids that impeded the healing of a bronchopleural fistula and subsequent empyema. Other surgical complications included air leaks, which occurred in five patients in the nivolumab group and three in the nivolumab plus ipilimumab arm.
Two patients died, one in the monotherapy arm from steroid-treated pneumonitis 4.1 months after randomization and one in the combination arm who had progressive disease 2 months after randomization, and died from the disease 15 months later.
Invited discussant Maximilian Diehn, MD, PhD, from Stanford (California) University School of Medicine, commented that the choice of neoadjuvant immunotherapy was not based on molecular markers, “and I think we have a major unmet need for developing biomarkers for personalized treatment in this area.
“Ideally, the biomarkers that we would have in this setting would, A, allow us to identify which patients have micrometastatic disease and therefore are likely to benefit from the upfront systemic therapy and, secondly, also could tell us which neoadjuvant therapy they would respond to, be it immunotherapy, chemotherapy, or the combination,” he added.
The study was supported by Bristol-Myers Squibb. Dr. Cascone disclosed honoraria from the company. Dr. Diehn reported stock ownership, consulting, research funding and travel expenses from various companies.
SOURCE: Cascone T. et al. ASCO 2019, Abstract 8504.
CHICAGO – Two immune checkpoint inhibitors were better than one as neoadjuvant therapy for patients with resectable early-stage non–small cell lung cancer (NSCLC) in the phase 2 NEOSTAR trial.
Among 44 patients with stage I-IIIA NSCLC who were randomized to either a combination of nivolumab (Opdivo) and ipilimumab (Yervoy) or to nivolumab alone, the combination was associated with higher rates of the primary endpoint of major pathological response (MPR), defined as a reduction in viable tumors cells to 10% or less, reported Tina Cascone, MD, PhD, from the University of Texas MD Anderson Cancer Center in Houston.
“Nivolumab/ipilimumab induced a 44% MPR rate in resected patients, met the trial prespecified boundary with seven MPRs in the intention-to-treat population, and induced pathologic complete responses in 38% of resected patients,” she said at the annual meeting of the American Society of Clinical Oncology.
To test whether neoadjuvant monotherapy or combination therapy could improve outcomes of standard induction chemotherapy, NEOSTAR investigators enrolled patients with NSCLC stage I-IIIA, including patients with a single involved mediastinal node (N2 single station) who were eligible for surgical resection.
The patients were randomized on a 1:1 basis to receive nivolumab 3 mg/kg on days 1, 15 and 29 alone or in combination with ipilimumab delivered 1 mg/kg on day 1, followed by surgery 3-6 weeks after the last study dose and then postoperative standard-of-care chemotherapy.
Of 53 patients screened, 44 were eligible, with 23 randomized to nivolumab monotherapy and 21 randomized to nivolumab/ipilimumab. Of this group, five did not proceed to surgery (one in the monotherapy arm, four in the combination arm) because of either high surgical risk, lack of respectability, or refusal of surgery. The mean age at randomization was 65.6 years. In all, 18% were never smokers, and the remaining 82% were former or current smokers.
The MPR rate in the intention-to-treat population – the primary endpoint – was reached in four patients (17%) in the monotherapy arm and in seven patients (33%) in the combination arm. As noted, the combination arm reached the prespecified boundary of six or more patients with an MPR. All patients in each arm who had an MPR also had a pathologic complete responses.
Of the 39 patients who went on to resection, 37 were evaluable, and in these patients the respective MPR rates were 19% and 44%. Two patients on nivolumab alone and six on nivolumab plus ipilimumab had 0% viable tumor detectable at the time of surgery. Radiographic responses included one complete response in the combination arm and eight total partial responses, in five and three patients, respectively. The objective response rated was 20%. The responses, assessed by Response Evaluation Criteria in Solid Tumors (RECIST) were positively associated with MPR, Dr. Cascone said.
In 11% of patients, the investigators observed apparent radiographic progression after neoadjuvant immune checkpoint inhibitors in mediastinal and or in nonregional nodes. However, pathological assessment and evaluation of the flaring nodes did not reveal evidence of disease, but instead showed noncaseating granulomas that were not present at baseline.
“Awareness of this phenomenon, which we named the ‘nodal immune flare,’ is of critical importance, as if the clinician fails to distinguish the nodal immune flare from disease progression, potential curative surgery for these patients could be avoided,” she said.
Grade 1 or 2 treatment-related adverse events included rash, itching, fatigue, anemia, cough, and diarrhea. Grade 3 or greater treatment-related adverse events included hypoxia, pneumonia, and pneumonitis in the nivolumab monotherapy arm and diarrhea and hyponatremia in the combination group. One patient treated with nivolumab monotherapy, who had achieved 0% viable tumor, had grade 3 pneumonia and pneumonitis, which was treated with steroids that impeded the healing of a bronchopleural fistula and subsequent empyema. Other surgical complications included air leaks, which occurred in five patients in the nivolumab group and three in the nivolumab plus ipilimumab arm.
Two patients died, one in the monotherapy arm from steroid-treated pneumonitis 4.1 months after randomization and one in the combination arm who had progressive disease 2 months after randomization, and died from the disease 15 months later.
Invited discussant Maximilian Diehn, MD, PhD, from Stanford (California) University School of Medicine, commented that the choice of neoadjuvant immunotherapy was not based on molecular markers, “and I think we have a major unmet need for developing biomarkers for personalized treatment in this area.
“Ideally, the biomarkers that we would have in this setting would, A, allow us to identify which patients have micrometastatic disease and therefore are likely to benefit from the upfront systemic therapy and, secondly, also could tell us which neoadjuvant therapy they would respond to, be it immunotherapy, chemotherapy, or the combination,” he added.
The study was supported by Bristol-Myers Squibb. Dr. Cascone disclosed honoraria from the company. Dr. Diehn reported stock ownership, consulting, research funding and travel expenses from various companies.
SOURCE: Cascone T. et al. ASCO 2019, Abstract 8504.
REPORTING FROM ASCO 2019
Checkpoint inhibitor rechallenge is possible for select patients
Rechallenge resulted in the recurrence of a grade 2 or higher immune-related adverse event (irAE) in 55% of rechallenged patients, but no deaths occurred, according to Audrey Simonaggio, MD, of the department of drug development at Gustave Roussy, Villejuif, France, and colleagues.
In those rechallenged patients who had a second irAE, the second event was not more severe than the first. “The rechallenge should first be assessed in a multidisciplinary team meeting with regard to each patient’s individual risk-reward ratio. ... We recommend close monitoring,” the researchers wrote in a study published in JAMA Oncology.
As there are no specific recommendations to guide the decision to rechallenge, the usefulness of the rechallenge was considered. The readministration could be delayed if the patient was in complete or excellent partial response. The existence of other therapeutic alternatives was also important as was the patient’s clinical state. Rechallenge was considered possible only after the grade of the initial irAE returned to 0 or 1.
“Because of life-threatening risk, we did not support rechallenge for cardiac (myocarditis) and neurologic irAEs [such] as Guillain-Barré syndrome, encephalitis, and severe myositis,” they said. CT scans were used to guide the decision to rechallenge in those with initial lung adverse events.
The cohort study included 93 consecutive adult patients who were referred over an 18-month period to the ImmunoTOX assessment board at the Gustave Roussy cancer center and followed for at least 1 year. The cohort was balanced for gender and ranged in age from 33 to 85 years, with a median age of 62.5 years. Melanoma was the predominant tumor (33%), followed by lung (16%), colorectal (9%), and lymphoma (9%).
The initial immune-related adverse event was a grade 2 event in 46% of patients, grade 3 in 39%, and grade 4 in 15%. Events included hepatitis (18%), skin toxicity (15%), pneumonitis (14%), colitis (12%), and arthralgia (7.5%). A rechallenge with the same anti–PD-1 or anti–PD-L1 was conducted in 43% of patients.
When compared with patients who were not rechallenged, there was no difference in median patient age, time to initial immune-related adverse event (five vs. three treatment cycles), event severity, or steroid use. With a median follow-up period of 14 months, the same or a different immune-related adverse event occurred in 22 patients (55%). A shorter time to the initial event was linked to the occurrence of a second event (9 vs. 15 weeks; P = .04).
“However, we did observe a trend toward a higher recurrence rate after a more severe initial irAE and a trend toward more frequent recurrence in patients treated with corticosteroids after the initial irAE,” the researchers wrote. “An anti–PD-1or anti–PD-L1 rechallenge after a grade 4 irAE should always be considered with caution.” Three of the five patients with these events were being treated for lymphoma, they said.
“As long as patients are closely monitored, anti–PD-1 or anti–PD-L1 rechallenge appears to have an acceptable toxic effect profile. Myocarditis and neurologic toxic effect should remain a contraindication. Rechallenge conditions require further investigation in a prospective clinical trial. ... Well-powered, prospective studies with a larger number of patients would be required to generate information on putative risk factors for the recurrence of irAEs. Our results highlighted the value of a review board, like ImmunoTOX, with intention to build a large irAE database and then establish evidence-based guidelines on the safety of a rechallenge,” the researchers concluded.
The study was supported by the Gustave Roussy cancer center and the Gustave Roussy immunotherapy program. Dr. Simonaggio had no relevant disclosures; several coauthors reported consultancy fees and research support from multiple drug companies.
SOURCE: Simonaggio A et al. JAMA Oncol. 2019 Jun 6. doi:10.1001/jamaoncol.2019.1022.
Rechallenge resulted in the recurrence of a grade 2 or higher immune-related adverse event (irAE) in 55% of rechallenged patients, but no deaths occurred, according to Audrey Simonaggio, MD, of the department of drug development at Gustave Roussy, Villejuif, France, and colleagues.
In those rechallenged patients who had a second irAE, the second event was not more severe than the first. “The rechallenge should first be assessed in a multidisciplinary team meeting with regard to each patient’s individual risk-reward ratio. ... We recommend close monitoring,” the researchers wrote in a study published in JAMA Oncology.
As there are no specific recommendations to guide the decision to rechallenge, the usefulness of the rechallenge was considered. The readministration could be delayed if the patient was in complete or excellent partial response. The existence of other therapeutic alternatives was also important as was the patient’s clinical state. Rechallenge was considered possible only after the grade of the initial irAE returned to 0 or 1.
“Because of life-threatening risk, we did not support rechallenge for cardiac (myocarditis) and neurologic irAEs [such] as Guillain-Barré syndrome, encephalitis, and severe myositis,” they said. CT scans were used to guide the decision to rechallenge in those with initial lung adverse events.
The cohort study included 93 consecutive adult patients who were referred over an 18-month period to the ImmunoTOX assessment board at the Gustave Roussy cancer center and followed for at least 1 year. The cohort was balanced for gender and ranged in age from 33 to 85 years, with a median age of 62.5 years. Melanoma was the predominant tumor (33%), followed by lung (16%), colorectal (9%), and lymphoma (9%).
The initial immune-related adverse event was a grade 2 event in 46% of patients, grade 3 in 39%, and grade 4 in 15%. Events included hepatitis (18%), skin toxicity (15%), pneumonitis (14%), colitis (12%), and arthralgia (7.5%). A rechallenge with the same anti–PD-1 or anti–PD-L1 was conducted in 43% of patients.
When compared with patients who were not rechallenged, there was no difference in median patient age, time to initial immune-related adverse event (five vs. three treatment cycles), event severity, or steroid use. With a median follow-up period of 14 months, the same or a different immune-related adverse event occurred in 22 patients (55%). A shorter time to the initial event was linked to the occurrence of a second event (9 vs. 15 weeks; P = .04).
“However, we did observe a trend toward a higher recurrence rate after a more severe initial irAE and a trend toward more frequent recurrence in patients treated with corticosteroids after the initial irAE,” the researchers wrote. “An anti–PD-1or anti–PD-L1 rechallenge after a grade 4 irAE should always be considered with caution.” Three of the five patients with these events were being treated for lymphoma, they said.
“As long as patients are closely monitored, anti–PD-1 or anti–PD-L1 rechallenge appears to have an acceptable toxic effect profile. Myocarditis and neurologic toxic effect should remain a contraindication. Rechallenge conditions require further investigation in a prospective clinical trial. ... Well-powered, prospective studies with a larger number of patients would be required to generate information on putative risk factors for the recurrence of irAEs. Our results highlighted the value of a review board, like ImmunoTOX, with intention to build a large irAE database and then establish evidence-based guidelines on the safety of a rechallenge,” the researchers concluded.
The study was supported by the Gustave Roussy cancer center and the Gustave Roussy immunotherapy program. Dr. Simonaggio had no relevant disclosures; several coauthors reported consultancy fees and research support from multiple drug companies.
SOURCE: Simonaggio A et al. JAMA Oncol. 2019 Jun 6. doi:10.1001/jamaoncol.2019.1022.
Rechallenge resulted in the recurrence of a grade 2 or higher immune-related adverse event (irAE) in 55% of rechallenged patients, but no deaths occurred, according to Audrey Simonaggio, MD, of the department of drug development at Gustave Roussy, Villejuif, France, and colleagues.
In those rechallenged patients who had a second irAE, the second event was not more severe than the first. “The rechallenge should first be assessed in a multidisciplinary team meeting with regard to each patient’s individual risk-reward ratio. ... We recommend close monitoring,” the researchers wrote in a study published in JAMA Oncology.
As there are no specific recommendations to guide the decision to rechallenge, the usefulness of the rechallenge was considered. The readministration could be delayed if the patient was in complete or excellent partial response. The existence of other therapeutic alternatives was also important as was the patient’s clinical state. Rechallenge was considered possible only after the grade of the initial irAE returned to 0 or 1.
“Because of life-threatening risk, we did not support rechallenge for cardiac (myocarditis) and neurologic irAEs [such] as Guillain-Barré syndrome, encephalitis, and severe myositis,” they said. CT scans were used to guide the decision to rechallenge in those with initial lung adverse events.
The cohort study included 93 consecutive adult patients who were referred over an 18-month period to the ImmunoTOX assessment board at the Gustave Roussy cancer center and followed for at least 1 year. The cohort was balanced for gender and ranged in age from 33 to 85 years, with a median age of 62.5 years. Melanoma was the predominant tumor (33%), followed by lung (16%), colorectal (9%), and lymphoma (9%).
The initial immune-related adverse event was a grade 2 event in 46% of patients, grade 3 in 39%, and grade 4 in 15%. Events included hepatitis (18%), skin toxicity (15%), pneumonitis (14%), colitis (12%), and arthralgia (7.5%). A rechallenge with the same anti–PD-1 or anti–PD-L1 was conducted in 43% of patients.
When compared with patients who were not rechallenged, there was no difference in median patient age, time to initial immune-related adverse event (five vs. three treatment cycles), event severity, or steroid use. With a median follow-up period of 14 months, the same or a different immune-related adverse event occurred in 22 patients (55%). A shorter time to the initial event was linked to the occurrence of a second event (9 vs. 15 weeks; P = .04).
“However, we did observe a trend toward a higher recurrence rate after a more severe initial irAE and a trend toward more frequent recurrence in patients treated with corticosteroids after the initial irAE,” the researchers wrote. “An anti–PD-1or anti–PD-L1 rechallenge after a grade 4 irAE should always be considered with caution.” Three of the five patients with these events were being treated for lymphoma, they said.
“As long as patients are closely monitored, anti–PD-1 or anti–PD-L1 rechallenge appears to have an acceptable toxic effect profile. Myocarditis and neurologic toxic effect should remain a contraindication. Rechallenge conditions require further investigation in a prospective clinical trial. ... Well-powered, prospective studies with a larger number of patients would be required to generate information on putative risk factors for the recurrence of irAEs. Our results highlighted the value of a review board, like ImmunoTOX, with intention to build a large irAE database and then establish evidence-based guidelines on the safety of a rechallenge,” the researchers concluded.
The study was supported by the Gustave Roussy cancer center and the Gustave Roussy immunotherapy program. Dr. Simonaggio had no relevant disclosures; several coauthors reported consultancy fees and research support from multiple drug companies.
SOURCE: Simonaggio A et al. JAMA Oncol. 2019 Jun 6. doi:10.1001/jamaoncol.2019.1022.
FROM JAMA ONCOLOGY
Pembrolizumab improves 5-year OS in advanced NSCLC
CHICAGO – New data suggest pembrolizumab can increase 5-year overall survival (OS) for patients with advanced non–small cell lung cancer (NSCLC).
In the phase 1b KEYNOTE-001 trial, the 5-year OS rate was 23.2% in treatment-naive patients and 15.5% in previously treated patients. This is in comparison to the 5.5% average 5-year OS rate observed in NSCLC patients who receive standard chemotherapy (Noone AM et al. SEER Cancer Statistics Review, 1975-2015).
“In total, the data confirm that pembrolizumab has the potential to improve long-term outcomes for both treatment-naive and previously treated patients with advanced non–small cell lung cancer,” said Edward B. Garon, MD, of the University of California, Los Angeles.
Dr. Garon and colleagues presented these results in a poster at the annual meeting of the American Society for Clinical Oncology, and the data were simultaneously published in the Journal of Clinical Oncology.
KEYNOTE-001 (NCT01295827) enrolled 550 patients with advanced NSCLC who had received no prior therapy (n = 101) or at least one prior line of therapy (n = 449). Initially, patients received pembrolizumab at varying doses depending on body weight, but the protocol was changed to a single dose of pembrolizumab at 200 mg every 3 weeks.
At a median follow-up of 60.6 months, 100 patients were still alive. Sixty patients had received at least 2 years of pembrolizumab, 14 of whom were treatment-naive at baseline, and 46 of whom were previously treated at baseline.
Five-year OS rates were best among patients who had high PD-L1 expression, which was defined as 50% or greater.
Among treatment-naive patients, the 5-year OS rate was 29.6% in PD-L1–high patients and 15.7% in PD-L1–low patients (expression of 1% to 49%). The median OS was 35.4 months and 19.5 months, respectively.
Among previously treated patients, the 5-year OS rate was 25.0% in PD-L1–high patients, 12.6% in patients with PD-L1 expression of 1%-49%, and 3.5% in patients with PD-L1 expression less than 1%. The median OS was 15.4 months, 8.5 months, and 8.6 months, respectively.
Among patients who received at least 2 years of pembrolizumab, the 5-year OS rate was 78.6% in the treatment-naive group and 75.8% in the previously treated group. The objective response rate was 86% and 91%, respectively. The rate of ongoing response at the data cutoff was 58% and 71%, respectively.
“The safety data did not show any unanticipated late toxicity, which I consider encouraging,” Dr. Garon noted.
He said rates of immune-mediated adverse events were similar at 3 years and 5 years of follow-up. At 5 years, 17% of patients (n = 92) had experienced an immune-related adverse event, the most common of which were hypothyroidism (9%), pneumonitis (5%), and hyperthyroidism (2%).
Dr. Garon disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Dracen, Dynavax, Genentech, Iovance Biotherapeutics, Lilly, Merck, Mirati Therapeutics, Neon Therapeutics, and Novartis. KEYNOTE-001 was sponsored by Merck Sharp & Dohme Corp.
SOURCES: Garon E. et al. ASCO 2019, Abstract LBA9015; J Clin Oncol. 2019 June 2. doi: 10.1200/JCO.19.00934
CHICAGO – New data suggest pembrolizumab can increase 5-year overall survival (OS) for patients with advanced non–small cell lung cancer (NSCLC).
In the phase 1b KEYNOTE-001 trial, the 5-year OS rate was 23.2% in treatment-naive patients and 15.5% in previously treated patients. This is in comparison to the 5.5% average 5-year OS rate observed in NSCLC patients who receive standard chemotherapy (Noone AM et al. SEER Cancer Statistics Review, 1975-2015).
“In total, the data confirm that pembrolizumab has the potential to improve long-term outcomes for both treatment-naive and previously treated patients with advanced non–small cell lung cancer,” said Edward B. Garon, MD, of the University of California, Los Angeles.
Dr. Garon and colleagues presented these results in a poster at the annual meeting of the American Society for Clinical Oncology, and the data were simultaneously published in the Journal of Clinical Oncology.
KEYNOTE-001 (NCT01295827) enrolled 550 patients with advanced NSCLC who had received no prior therapy (n = 101) or at least one prior line of therapy (n = 449). Initially, patients received pembrolizumab at varying doses depending on body weight, but the protocol was changed to a single dose of pembrolizumab at 200 mg every 3 weeks.
At a median follow-up of 60.6 months, 100 patients were still alive. Sixty patients had received at least 2 years of pembrolizumab, 14 of whom were treatment-naive at baseline, and 46 of whom were previously treated at baseline.
Five-year OS rates were best among patients who had high PD-L1 expression, which was defined as 50% or greater.
Among treatment-naive patients, the 5-year OS rate was 29.6% in PD-L1–high patients and 15.7% in PD-L1–low patients (expression of 1% to 49%). The median OS was 35.4 months and 19.5 months, respectively.
Among previously treated patients, the 5-year OS rate was 25.0% in PD-L1–high patients, 12.6% in patients with PD-L1 expression of 1%-49%, and 3.5% in patients with PD-L1 expression less than 1%. The median OS was 15.4 months, 8.5 months, and 8.6 months, respectively.
Among patients who received at least 2 years of pembrolizumab, the 5-year OS rate was 78.6% in the treatment-naive group and 75.8% in the previously treated group. The objective response rate was 86% and 91%, respectively. The rate of ongoing response at the data cutoff was 58% and 71%, respectively.
“The safety data did not show any unanticipated late toxicity, which I consider encouraging,” Dr. Garon noted.
He said rates of immune-mediated adverse events were similar at 3 years and 5 years of follow-up. At 5 years, 17% of patients (n = 92) had experienced an immune-related adverse event, the most common of which were hypothyroidism (9%), pneumonitis (5%), and hyperthyroidism (2%).
Dr. Garon disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Dracen, Dynavax, Genentech, Iovance Biotherapeutics, Lilly, Merck, Mirati Therapeutics, Neon Therapeutics, and Novartis. KEYNOTE-001 was sponsored by Merck Sharp & Dohme Corp.
SOURCES: Garon E. et al. ASCO 2019, Abstract LBA9015; J Clin Oncol. 2019 June 2. doi: 10.1200/JCO.19.00934
CHICAGO – New data suggest pembrolizumab can increase 5-year overall survival (OS) for patients with advanced non–small cell lung cancer (NSCLC).
In the phase 1b KEYNOTE-001 trial, the 5-year OS rate was 23.2% in treatment-naive patients and 15.5% in previously treated patients. This is in comparison to the 5.5% average 5-year OS rate observed in NSCLC patients who receive standard chemotherapy (Noone AM et al. SEER Cancer Statistics Review, 1975-2015).
“In total, the data confirm that pembrolizumab has the potential to improve long-term outcomes for both treatment-naive and previously treated patients with advanced non–small cell lung cancer,” said Edward B. Garon, MD, of the University of California, Los Angeles.
Dr. Garon and colleagues presented these results in a poster at the annual meeting of the American Society for Clinical Oncology, and the data were simultaneously published in the Journal of Clinical Oncology.
KEYNOTE-001 (NCT01295827) enrolled 550 patients with advanced NSCLC who had received no prior therapy (n = 101) or at least one prior line of therapy (n = 449). Initially, patients received pembrolizumab at varying doses depending on body weight, but the protocol was changed to a single dose of pembrolizumab at 200 mg every 3 weeks.
At a median follow-up of 60.6 months, 100 patients were still alive. Sixty patients had received at least 2 years of pembrolizumab, 14 of whom were treatment-naive at baseline, and 46 of whom were previously treated at baseline.
Five-year OS rates were best among patients who had high PD-L1 expression, which was defined as 50% or greater.
Among treatment-naive patients, the 5-year OS rate was 29.6% in PD-L1–high patients and 15.7% in PD-L1–low patients (expression of 1% to 49%). The median OS was 35.4 months and 19.5 months, respectively.
Among previously treated patients, the 5-year OS rate was 25.0% in PD-L1–high patients, 12.6% in patients with PD-L1 expression of 1%-49%, and 3.5% in patients with PD-L1 expression less than 1%. The median OS was 15.4 months, 8.5 months, and 8.6 months, respectively.
Among patients who received at least 2 years of pembrolizumab, the 5-year OS rate was 78.6% in the treatment-naive group and 75.8% in the previously treated group. The objective response rate was 86% and 91%, respectively. The rate of ongoing response at the data cutoff was 58% and 71%, respectively.
“The safety data did not show any unanticipated late toxicity, which I consider encouraging,” Dr. Garon noted.
He said rates of immune-mediated adverse events were similar at 3 years and 5 years of follow-up. At 5 years, 17% of patients (n = 92) had experienced an immune-related adverse event, the most common of which were hypothyroidism (9%), pneumonitis (5%), and hyperthyroidism (2%).
Dr. Garon disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Dracen, Dynavax, Genentech, Iovance Biotherapeutics, Lilly, Merck, Mirati Therapeutics, Neon Therapeutics, and Novartis. KEYNOTE-001 was sponsored by Merck Sharp & Dohme Corp.
SOURCES: Garon E. et al. ASCO 2019, Abstract LBA9015; J Clin Oncol. 2019 June 2. doi: 10.1200/JCO.19.00934
REPORTING FROM ASCO 2019
Pembro as good as chemo for gastric cancers with less toxicity
CHICAGO – In gastric and gastroesophageal junction (GEJ) cancers, positive for PD-L1, treatment with the PD-1 inhibitor pembrolizumab offered comparable survival with fewer side effects, according to results of a phase 3 randomized clinical trial.
The checkpoint inhibitor also demonstrated a clinically meaningful improvement in patients who had high levels of PD-L1 expression, with a 2-year survival rate of 39% versus 22% for patients receiving the standard chemotherapy, which consisted of a platinum and a fluoropyrimidine, according to Josep Tabernero, MD, PhD, lead author of the KEYNOTE-062 study.
By contrast, the study failed to demonstrate that pembrolizumab immunotherapy combined with that chemotherapy backbone was superior to chemotherapy alone on survival endpoints, said Dr. Tabernero, Head of the Medical Oncology Department at the Vall d’Hebron Barcelona University Hospital and Institute of Oncology, Spain.
“There are several factors we are evaluating,” Dr. Tabernero said here in a press conference at the annual meeting of the American Society of Clinical Oncology (ASCO). “We still have to do more studies to understand why, with this chemotherapy backbone, we don’t see a clear synergistic effect for superiority in overall survival.”
Nevertheless, these findings make pembrolizumab a “preferred treatment” for many patients, particularly in light of its “substantially improved safety profile” versus chemotherapy, said ASCO Senior Vice President and Chief Medical Officer Richard L. Schilsky, MD.
“What I take away from this study is that for patients with advanced gastric and gastroesophageal cancer, pembrolizumab should really in many cases replace chemotherapy as a first-line treatment for this population,” Dr. Schilsky said in a press conference. “It’s certainly not worse, and it may well be better.”
The KEYNOTE-062 study included 763 patients with HER2-negative, PD-L1-positive advanced gastric or GEJ cancers randomized to one of three arms: pembrolizumab alone for up to 35 cycles, pembrolizumab for up to 35 cycles plus chemotherapy, or placebo plus chemotherapy.
Pembrolizumab alone was not inferior compared to chemotherapy, with median overall survival rates of 10.5 and 11.1 months, respectively (HR, 0.91; 99.2% CI, 0.69-1.18), Dr. Tabernero reported.
Overall survival appeared to be prolonged in patients with high levels of PD-L1 expression, defined as a combined positive score (CPS) of 10 or greater. The median survival in that subgroup was 17.4 months for those receiving pembrolizumab, and just 10.8 months for chemotherapy. However, the design of the study precluded an analysis of statistical significance for this finding, according to Dr. Tabernero.
Looking at the overall study population, pembrolizumab plus chemotherapy did not improve survival versus chemotherapy alone, he added, reporting median overall survivals of 12.5 and 11.1 months, respectively (P = .046).
Subgroup analysis suggested that Asian patients derived particular benefit from pembrolizumab as compared to chemotherapy, though Dr. Tabernero cautioned against overinterpretation of the finding, saying that it could be due to biology, or could be a statistical anomaly.
Funding for the study came from Merck & Co., Inc. Dr. Tabernero reported disclosures related to Bayer, Boehringer Ingelheim, Lilly, MSD, Merck Serono, Novartis, Sanofi, and others.
SOURCE: Tabernero J, et al. ASCO 2019. Abstract LBA4007.
CHICAGO – In gastric and gastroesophageal junction (GEJ) cancers, positive for PD-L1, treatment with the PD-1 inhibitor pembrolizumab offered comparable survival with fewer side effects, according to results of a phase 3 randomized clinical trial.
The checkpoint inhibitor also demonstrated a clinically meaningful improvement in patients who had high levels of PD-L1 expression, with a 2-year survival rate of 39% versus 22% for patients receiving the standard chemotherapy, which consisted of a platinum and a fluoropyrimidine, according to Josep Tabernero, MD, PhD, lead author of the KEYNOTE-062 study.
By contrast, the study failed to demonstrate that pembrolizumab immunotherapy combined with that chemotherapy backbone was superior to chemotherapy alone on survival endpoints, said Dr. Tabernero, Head of the Medical Oncology Department at the Vall d’Hebron Barcelona University Hospital and Institute of Oncology, Spain.
“There are several factors we are evaluating,” Dr. Tabernero said here in a press conference at the annual meeting of the American Society of Clinical Oncology (ASCO). “We still have to do more studies to understand why, with this chemotherapy backbone, we don’t see a clear synergistic effect for superiority in overall survival.”
Nevertheless, these findings make pembrolizumab a “preferred treatment” for many patients, particularly in light of its “substantially improved safety profile” versus chemotherapy, said ASCO Senior Vice President and Chief Medical Officer Richard L. Schilsky, MD.
“What I take away from this study is that for patients with advanced gastric and gastroesophageal cancer, pembrolizumab should really in many cases replace chemotherapy as a first-line treatment for this population,” Dr. Schilsky said in a press conference. “It’s certainly not worse, and it may well be better.”
The KEYNOTE-062 study included 763 patients with HER2-negative, PD-L1-positive advanced gastric or GEJ cancers randomized to one of three arms: pembrolizumab alone for up to 35 cycles, pembrolizumab for up to 35 cycles plus chemotherapy, or placebo plus chemotherapy.
Pembrolizumab alone was not inferior compared to chemotherapy, with median overall survival rates of 10.5 and 11.1 months, respectively (HR, 0.91; 99.2% CI, 0.69-1.18), Dr. Tabernero reported.
Overall survival appeared to be prolonged in patients with high levels of PD-L1 expression, defined as a combined positive score (CPS) of 10 or greater. The median survival in that subgroup was 17.4 months for those receiving pembrolizumab, and just 10.8 months for chemotherapy. However, the design of the study precluded an analysis of statistical significance for this finding, according to Dr. Tabernero.
Looking at the overall study population, pembrolizumab plus chemotherapy did not improve survival versus chemotherapy alone, he added, reporting median overall survivals of 12.5 and 11.1 months, respectively (P = .046).
Subgroup analysis suggested that Asian patients derived particular benefit from pembrolizumab as compared to chemotherapy, though Dr. Tabernero cautioned against overinterpretation of the finding, saying that it could be due to biology, or could be a statistical anomaly.
Funding for the study came from Merck & Co., Inc. Dr. Tabernero reported disclosures related to Bayer, Boehringer Ingelheim, Lilly, MSD, Merck Serono, Novartis, Sanofi, and others.
SOURCE: Tabernero J, et al. ASCO 2019. Abstract LBA4007.
CHICAGO – In gastric and gastroesophageal junction (GEJ) cancers, positive for PD-L1, treatment with the PD-1 inhibitor pembrolizumab offered comparable survival with fewer side effects, according to results of a phase 3 randomized clinical trial.
The checkpoint inhibitor also demonstrated a clinically meaningful improvement in patients who had high levels of PD-L1 expression, with a 2-year survival rate of 39% versus 22% for patients receiving the standard chemotherapy, which consisted of a platinum and a fluoropyrimidine, according to Josep Tabernero, MD, PhD, lead author of the KEYNOTE-062 study.
By contrast, the study failed to demonstrate that pembrolizumab immunotherapy combined with that chemotherapy backbone was superior to chemotherapy alone on survival endpoints, said Dr. Tabernero, Head of the Medical Oncology Department at the Vall d’Hebron Barcelona University Hospital and Institute of Oncology, Spain.
“There are several factors we are evaluating,” Dr. Tabernero said here in a press conference at the annual meeting of the American Society of Clinical Oncology (ASCO). “We still have to do more studies to understand why, with this chemotherapy backbone, we don’t see a clear synergistic effect for superiority in overall survival.”
Nevertheless, these findings make pembrolizumab a “preferred treatment” for many patients, particularly in light of its “substantially improved safety profile” versus chemotherapy, said ASCO Senior Vice President and Chief Medical Officer Richard L. Schilsky, MD.
“What I take away from this study is that for patients with advanced gastric and gastroesophageal cancer, pembrolizumab should really in many cases replace chemotherapy as a first-line treatment for this population,” Dr. Schilsky said in a press conference. “It’s certainly not worse, and it may well be better.”
The KEYNOTE-062 study included 763 patients with HER2-negative, PD-L1-positive advanced gastric or GEJ cancers randomized to one of three arms: pembrolizumab alone for up to 35 cycles, pembrolizumab for up to 35 cycles plus chemotherapy, or placebo plus chemotherapy.
Pembrolizumab alone was not inferior compared to chemotherapy, with median overall survival rates of 10.5 and 11.1 months, respectively (HR, 0.91; 99.2% CI, 0.69-1.18), Dr. Tabernero reported.
Overall survival appeared to be prolonged in patients with high levels of PD-L1 expression, defined as a combined positive score (CPS) of 10 or greater. The median survival in that subgroup was 17.4 months for those receiving pembrolizumab, and just 10.8 months for chemotherapy. However, the design of the study precluded an analysis of statistical significance for this finding, according to Dr. Tabernero.
Looking at the overall study population, pembrolizumab plus chemotherapy did not improve survival versus chemotherapy alone, he added, reporting median overall survivals of 12.5 and 11.1 months, respectively (P = .046).
Subgroup analysis suggested that Asian patients derived particular benefit from pembrolizumab as compared to chemotherapy, though Dr. Tabernero cautioned against overinterpretation of the finding, saying that it could be due to biology, or could be a statistical anomaly.
Funding for the study came from Merck & Co., Inc. Dr. Tabernero reported disclosures related to Bayer, Boehringer Ingelheim, Lilly, MSD, Merck Serono, Novartis, Sanofi, and others.
SOURCE: Tabernero J, et al. ASCO 2019. Abstract LBA4007.
REPORTING FROM ASCO 2019
Low intensity bridging may be best path to CAR T in adult ALL
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
CHICAGO – A low intensity chemotherapy regimen may be the best approach to bridge patients waiting for chimeric antigen receptor (CAR) T-cell therapy, according to a retrospective analysis of adults with acute lymphoblastic leukemia (ALL).
Investigators found that high intensity bridging regimens provided no clear outcome benefit, but did produce a greater number of infections.
But the decision on the type of regimen is very much dependent on the individual patient, Karlo Perica, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York, said at the annual meeting of the American Society of Clinical Oncology.
Dr. Perica and his colleagues at Memorial Sloan Kettering examined the effectiveness and toxicity of bridging therapies provided to relapsed or refractory ALL patients waiting to receive CD19 CAR T-cell therapy as part of a phase 1 trial (N Engl J Med. 2018 Feb 1;378[5]:449-59).
Bridging therapy was defined as any therapy given from leukapheresis to cell infusion.
The low-intensity regimens included POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone, or combinations), liposomal vincristine, mini-hyper CVD (reduced cyclophosphamide, dexamethasone, methotrexate, Ara-C), blinatumomab, inotuzumab, oral tyrosine kinase inhibitor-based regimens, or hydroxyurea.
The high-intensity regimens included hyper-CVAD (cyclophosphamide, vincristine, doxorubicin, dexamethasone), high-dose cytarabine, attenuated FLAG/FLAG-IDA (reduced fludarabine, cytarabine, G-CSF plus or minus idarubicin), and pediatric-type induction.
Of the 53 patients who were ultimately infused with CAR T cells, 19 received some type of high intensity regimen, 29 received low intensity regimens, and 5 received no bridging treatment. The group overall was heavily pretreated. Nearly a third of the low intensity and no bridging patients and 42% of the high intensity patients had previously undergone transplant. More than 40% of the low intensity and no bridging patients and about a quarter of the high intensity bridging group had four or more prior lines of therapy.
The use of high intensity bridging therapy was not associated with improved overall response or relapse-free survival to CAR T-cell therapy, the investigators reported. In a subgroup with 23 high disease burden patients with greater than 20% blasts, there was no difference in MRD-negative complete response by intensity (75% versus 60%, Fisher’s P = .65).
High intensity bridging was also not associated with successful CAR T-cell infusion, versus low intensity regimens (63% versus 79%, P greater than .05) or a combined endpoint of CAR T-cell infusion plus transplant or alternative treatment (80% versus 86%, P greater than .05).
In terms of toxicity, the high intensity bridging regimens were associated with a higher rate of grade 3 or 4 infections – 15 versus 11 infections (Fisher’s P = .002). But there was no association with post-infusion grade 3 or 4 cytokine release syndrome or neurotoxicity.
Dr. Perica said the results reflect that the real goal of bridging is not to reduce disease burden but instead to successfully bring patients to the next phase of their treatment. “The goal of the bridging therapy is to get the patient to the CAR infusion,” he said.
Due to the retrospective nature of the study, Dr. Perica said he can’t recommend any single bridging regimen and he emphasized that the decisions are patient-specific.
The original study was funded by several foundations and Juno Therapeutics. Dr. Perica reported royalties from technology licensed to Neximmune.
SOURCE: Perica K et al. ASCO 2019, Abstract 2520.
FROM ASCO 2019
Pembro with or without chemo superior to EXTREME for advanced HNSCC
CHICAGO – Pembrolizumab with and without chemotherapy proved superior for overall survival compared with the EXTREME regimen when used first line in certain subgroups of patients with recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC), according to “practice-changing” final results from the randomized phase 3 KEYNOTE-048 study.
Compared with 300 patients randomized to receive the EXTREME regimen (a certuximab loading dose followed by carboplatin or cisplatin and 5-fluorouracil), 281 who received pembrolizumab plus chemotherapy (P+C) had superior overall survival (OS) with comparable safety–including both those with programmed death-Ligand 1 (PD-L1) combined positive score (CPS) of 20 or greater (median 14.7 vs 11.0 months; hazard ratio, 0.60) and with CPS of 1 or greater (median, 13.6 vs. 10.4 months; HR, 0.65), Danny Rischin, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The differences were highly statistically significant, said Dr. Rischin, a professor and director of the Division of Cancer Medicine and head of the Department of Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia.
“And this benefit in overall survival in CPS greater than or equal to 20 and greater than or equal to 1 appeared to be present across all the subgroups that we looked at,” he added.
The response rates did not differ between P+C and EXTREME groups, but the median duration of response was significantly greater with P+C vs. EXTREME in both the CPS of 20 or greater and 1 or greater (7.1 vs. 4.2 months and 6.7 vs. 4.3 months, respectively).
Additionally, the final results of the study showed an OS benefit with P+C vs. EXTREME in the total population (13.0 vs. 10.7 months; HR, 0.72), Dr. Rischin said.
The difference between the groups with respect to progression-free survival (PFS), however, was not statistically significant and did not reach the superiority threshold, he noted.
In the 301 patients who received pembrolizumab alone, OS was superior in the CPS 20 or greater and 1 or greater populations (median, 14.8 vs. 10.7 months; HR, 0.58 and 12.4 vs. 10.3 months; HR, 0.74, respectively), compared with EXTREME, but was noninferior in the total population (median 11.5 vs. 10.7 months; HR, 0.83), and safety was favorable .
Again, PFS did not differ between the groups (median, 2.3 vs. 5.2 months; HR, 1.34), and while the overall response rates did not differ significantly, the median duration of response was substantially longer with pembrolizumab at 22.6 vs. 4.5 months with EXTREME, he said.
Study participants had locally incurable R/M HNSCC and no prior systemic therapy in the R/M setting. Those in he P+C arm received pembrolizumab at 200 mg plus 6 cycles of cisplatin at 100 mg/m2 or carboplatin AUC 5, and 5-fluorouracil at a dose of 1000 mg/m2/day for 4 days every 3 weeks; those in the pembrolizumab alone arm received 200 mg every 3 weeks for up to 35 cycles, and those in the EXTREME arm received certuximab at a 400 mg/m2 loading dose followed by 250 mg/m2 weekly with carboplatin AUC 5 or cisplatin at 100 mg/m2, and 5-FU at 1000 mg/m2/day for 4 days for 6 cycles.
“The data from KEYNOTE-048 support pembrolizumab plus platinum-based chemotherapy and pembrolizumab monotherapy as new standard of care monotherapies for recurrent/metastatic head and neck squamous cell carcinoma,” he concluded.
Discussant Vanita Noronha, MD, a professor in the Department of Medical Oncology at Tata Memorial Hospital in Mumbai, India, said that while the findings are practice changing, they also raise a number of questions, such as which patients should get pembrolizumab and which should get P+C, why there is a differential effect of pembrolizumab based on PD-L1 by CPS–and what about those with CPS of 0 or 1-20, and why the response rates and PFS rates were not improved in the pembrolizumab groups.
Other important questions include whether there are predictive biomarkers for response, and whether sequential therapy would be of benefit, she added.
While these and other questions remain to be addressed, the KEYNOTE-048 findings have implications for practice going forward; based on the current data, her approach to treating patients with R/M HNSCC not amenable to radical therapy is to treat with pembrolizumab alone in those with disease-free interval of 6 months or less, she said.
For those with disease-free interval greater than 6 months and good performance status who have controlled comorbidities, are platinum eligible, and for whom the treatment is reimbursable/affordable, treatment depends on symptom severity; she would treat those with mild/moderate symptoms and CPS of 20 or greater with pembrolizumab alone, those with CPS of 1 or greater with P+C or pembrolizumab alone, and those with CPS of 0 or unknown CPS with EXTREME or a similar regimen or with P+C, and she would treat those with severe symptoms with P+C.
“If the patient were a bit borderline, had multiple comorbidities, could not receive platinum, or had financial constraints, I would treat the patient with singe-agent intravenous chemotherapy or with oral metronomic chemotherapy, single-agent targeted therapy or with best supportive care,” she said.
Dr. Rischin has received research funding from Amgen, Bristol-Myers Squibb, Genentech/Roche, GSK, Merck, and Regeneron. Dr. Noronha has received research funding (to her institution) from Amgen,and Sanofi Aventis.
SOURCE: D Rischin et al., ASCO 2019: Abstract 6000.
CHICAGO – Pembrolizumab with and without chemotherapy proved superior for overall survival compared with the EXTREME regimen when used first line in certain subgroups of patients with recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC), according to “practice-changing” final results from the randomized phase 3 KEYNOTE-048 study.
Compared with 300 patients randomized to receive the EXTREME regimen (a certuximab loading dose followed by carboplatin or cisplatin and 5-fluorouracil), 281 who received pembrolizumab plus chemotherapy (P+C) had superior overall survival (OS) with comparable safety–including both those with programmed death-Ligand 1 (PD-L1) combined positive score (CPS) of 20 or greater (median 14.7 vs 11.0 months; hazard ratio, 0.60) and with CPS of 1 or greater (median, 13.6 vs. 10.4 months; HR, 0.65), Danny Rischin, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The differences were highly statistically significant, said Dr. Rischin, a professor and director of the Division of Cancer Medicine and head of the Department of Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia.
“And this benefit in overall survival in CPS greater than or equal to 20 and greater than or equal to 1 appeared to be present across all the subgroups that we looked at,” he added.
The response rates did not differ between P+C and EXTREME groups, but the median duration of response was significantly greater with P+C vs. EXTREME in both the CPS of 20 or greater and 1 or greater (7.1 vs. 4.2 months and 6.7 vs. 4.3 months, respectively).
Additionally, the final results of the study showed an OS benefit with P+C vs. EXTREME in the total population (13.0 vs. 10.7 months; HR, 0.72), Dr. Rischin said.
The difference between the groups with respect to progression-free survival (PFS), however, was not statistically significant and did not reach the superiority threshold, he noted.
In the 301 patients who received pembrolizumab alone, OS was superior in the CPS 20 or greater and 1 or greater populations (median, 14.8 vs. 10.7 months; HR, 0.58 and 12.4 vs. 10.3 months; HR, 0.74, respectively), compared with EXTREME, but was noninferior in the total population (median 11.5 vs. 10.7 months; HR, 0.83), and safety was favorable .
Again, PFS did not differ between the groups (median, 2.3 vs. 5.2 months; HR, 1.34), and while the overall response rates did not differ significantly, the median duration of response was substantially longer with pembrolizumab at 22.6 vs. 4.5 months with EXTREME, he said.
Study participants had locally incurable R/M HNSCC and no prior systemic therapy in the R/M setting. Those in he P+C arm received pembrolizumab at 200 mg plus 6 cycles of cisplatin at 100 mg/m2 or carboplatin AUC 5, and 5-fluorouracil at a dose of 1000 mg/m2/day for 4 days every 3 weeks; those in the pembrolizumab alone arm received 200 mg every 3 weeks for up to 35 cycles, and those in the EXTREME arm received certuximab at a 400 mg/m2 loading dose followed by 250 mg/m2 weekly with carboplatin AUC 5 or cisplatin at 100 mg/m2, and 5-FU at 1000 mg/m2/day for 4 days for 6 cycles.
“The data from KEYNOTE-048 support pembrolizumab plus platinum-based chemotherapy and pembrolizumab monotherapy as new standard of care monotherapies for recurrent/metastatic head and neck squamous cell carcinoma,” he concluded.
Discussant Vanita Noronha, MD, a professor in the Department of Medical Oncology at Tata Memorial Hospital in Mumbai, India, said that while the findings are practice changing, they also raise a number of questions, such as which patients should get pembrolizumab and which should get P+C, why there is a differential effect of pembrolizumab based on PD-L1 by CPS–and what about those with CPS of 0 or 1-20, and why the response rates and PFS rates were not improved in the pembrolizumab groups.
Other important questions include whether there are predictive biomarkers for response, and whether sequential therapy would be of benefit, she added.
While these and other questions remain to be addressed, the KEYNOTE-048 findings have implications for practice going forward; based on the current data, her approach to treating patients with R/M HNSCC not amenable to radical therapy is to treat with pembrolizumab alone in those with disease-free interval of 6 months or less, she said.
For those with disease-free interval greater than 6 months and good performance status who have controlled comorbidities, are platinum eligible, and for whom the treatment is reimbursable/affordable, treatment depends on symptom severity; she would treat those with mild/moderate symptoms and CPS of 20 or greater with pembrolizumab alone, those with CPS of 1 or greater with P+C or pembrolizumab alone, and those with CPS of 0 or unknown CPS with EXTREME or a similar regimen or with P+C, and she would treat those with severe symptoms with P+C.
“If the patient were a bit borderline, had multiple comorbidities, could not receive platinum, or had financial constraints, I would treat the patient with singe-agent intravenous chemotherapy or with oral metronomic chemotherapy, single-agent targeted therapy or with best supportive care,” she said.
Dr. Rischin has received research funding from Amgen, Bristol-Myers Squibb, Genentech/Roche, GSK, Merck, and Regeneron. Dr. Noronha has received research funding (to her institution) from Amgen,and Sanofi Aventis.
SOURCE: D Rischin et al., ASCO 2019: Abstract 6000.
CHICAGO – Pembrolizumab with and without chemotherapy proved superior for overall survival compared with the EXTREME regimen when used first line in certain subgroups of patients with recurrent/metastatic head and neck squamous cell carcinoma (R/M HNSCC), according to “practice-changing” final results from the randomized phase 3 KEYNOTE-048 study.
Compared with 300 patients randomized to receive the EXTREME regimen (a certuximab loading dose followed by carboplatin or cisplatin and 5-fluorouracil), 281 who received pembrolizumab plus chemotherapy (P+C) had superior overall survival (OS) with comparable safety–including both those with programmed death-Ligand 1 (PD-L1) combined positive score (CPS) of 20 or greater (median 14.7 vs 11.0 months; hazard ratio, 0.60) and with CPS of 1 or greater (median, 13.6 vs. 10.4 months; HR, 0.65), Danny Rischin, MD, reported at the annual meeting of the American Society of Clinical Oncology.
The differences were highly statistically significant, said Dr. Rischin, a professor and director of the Division of Cancer Medicine and head of the Department of Medical Oncology at Peter MacCallum Cancer Centre, Melbourne, Australia.
“And this benefit in overall survival in CPS greater than or equal to 20 and greater than or equal to 1 appeared to be present across all the subgroups that we looked at,” he added.
The response rates did not differ between P+C and EXTREME groups, but the median duration of response was significantly greater with P+C vs. EXTREME in both the CPS of 20 or greater and 1 or greater (7.1 vs. 4.2 months and 6.7 vs. 4.3 months, respectively).
Additionally, the final results of the study showed an OS benefit with P+C vs. EXTREME in the total population (13.0 vs. 10.7 months; HR, 0.72), Dr. Rischin said.
The difference between the groups with respect to progression-free survival (PFS), however, was not statistically significant and did not reach the superiority threshold, he noted.
In the 301 patients who received pembrolizumab alone, OS was superior in the CPS 20 or greater and 1 or greater populations (median, 14.8 vs. 10.7 months; HR, 0.58 and 12.4 vs. 10.3 months; HR, 0.74, respectively), compared with EXTREME, but was noninferior in the total population (median 11.5 vs. 10.7 months; HR, 0.83), and safety was favorable .
Again, PFS did not differ between the groups (median, 2.3 vs. 5.2 months; HR, 1.34), and while the overall response rates did not differ significantly, the median duration of response was substantially longer with pembrolizumab at 22.6 vs. 4.5 months with EXTREME, he said.
Study participants had locally incurable R/M HNSCC and no prior systemic therapy in the R/M setting. Those in he P+C arm received pembrolizumab at 200 mg plus 6 cycles of cisplatin at 100 mg/m2 or carboplatin AUC 5, and 5-fluorouracil at a dose of 1000 mg/m2/day for 4 days every 3 weeks; those in the pembrolizumab alone arm received 200 mg every 3 weeks for up to 35 cycles, and those in the EXTREME arm received certuximab at a 400 mg/m2 loading dose followed by 250 mg/m2 weekly with carboplatin AUC 5 or cisplatin at 100 mg/m2, and 5-FU at 1000 mg/m2/day for 4 days for 6 cycles.
“The data from KEYNOTE-048 support pembrolizumab plus platinum-based chemotherapy and pembrolizumab monotherapy as new standard of care monotherapies for recurrent/metastatic head and neck squamous cell carcinoma,” he concluded.
Discussant Vanita Noronha, MD, a professor in the Department of Medical Oncology at Tata Memorial Hospital in Mumbai, India, said that while the findings are practice changing, they also raise a number of questions, such as which patients should get pembrolizumab and which should get P+C, why there is a differential effect of pembrolizumab based on PD-L1 by CPS–and what about those with CPS of 0 or 1-20, and why the response rates and PFS rates were not improved in the pembrolizumab groups.
Other important questions include whether there are predictive biomarkers for response, and whether sequential therapy would be of benefit, she added.
While these and other questions remain to be addressed, the KEYNOTE-048 findings have implications for practice going forward; based on the current data, her approach to treating patients with R/M HNSCC not amenable to radical therapy is to treat with pembrolizumab alone in those with disease-free interval of 6 months or less, she said.
For those with disease-free interval greater than 6 months and good performance status who have controlled comorbidities, are platinum eligible, and for whom the treatment is reimbursable/affordable, treatment depends on symptom severity; she would treat those with mild/moderate symptoms and CPS of 20 or greater with pembrolizumab alone, those with CPS of 1 or greater with P+C or pembrolizumab alone, and those with CPS of 0 or unknown CPS with EXTREME or a similar regimen or with P+C, and she would treat those with severe symptoms with P+C.
“If the patient were a bit borderline, had multiple comorbidities, could not receive platinum, or had financial constraints, I would treat the patient with singe-agent intravenous chemotherapy or with oral metronomic chemotherapy, single-agent targeted therapy or with best supportive care,” she said.
Dr. Rischin has received research funding from Amgen, Bristol-Myers Squibb, Genentech/Roche, GSK, Merck, and Regeneron. Dr. Noronha has received research funding (to her institution) from Amgen,and Sanofi Aventis.
SOURCE: D Rischin et al., ASCO 2019: Abstract 6000.
REPORTING FROM ASCO 2019
Novel anti-PD-1 antibody can be given subcutaneously
based on results from an ongoing phase 1 trial.
“We assessed feasibility of monthly subcutaneous administration of PF-06801591, a humanized immunoglobulin G4 monoclonal antibody that binds to the programmed cell death [PD-1] receptor,” Melissa L. Johnson, MD, of the Sarah Cannon Research Institute, Nashville, Tenn., and colleagues wrote in JAMA Oncology. “Subcutaneous administration of an anti-PD-1 antibody in patients with advanced solid tumors appears to be feasible.”
The researchers evaluated the efficacy, safety, and pharmacokinetics of the novel anti-PD-1 therapy in a group of 40 patients with locally advanced or metastatic solid tumors. The antibody was administered in both subcutaneous and intravenous forms.
Study participants were administered the subcutaneous form of the antibody at 300 mg every 4 weeks or the intravenous form at 0.5, 1, 3, or 10 mg/kg every 3 weeks.
“Dose escalation occurred after two to four patients were enrolled per dose level, with additional patients enrolled in each cohort for further assessment,” the researchers wrote.
The primary endpoints were safety and dose-limiting adverse effects. Efficacy, immunogenicity, pharmacokinetics, and PD-1 receptor occupancy were secondary endpoints.
After analysis, Dr. Johnson and colleagues reported that the overall response rate was 18.4%. In addition, no dose-limiting toxicities were detected in both intravenous and subcutaneous groups, but grade 3 or greater adverse events were reported in 6.7% and 16% of patients treated with subcutaneous and intravenous dosage forms, respectively.
“No dose–adverse event associations were observed during intravenous dose escalation, and no serious skin toxic effects occurred with subcutaneous delivery,” they reported.
Based on the findings, the team selected the subcutaneous form (300 mg) of the therapy for additional assessment in the second half of this ongoing trial.
The study was funded by Pfizer. The authors reported financial affiliations with BerGenBio, EMD Serono, Janssen, Mirati Therapeutics, Pfizer, and several others.
SOURCE: Johnson ML et al. JAMA Oncol. 2019 May 30. doi: 10.1001/jamaoncol.2019.0836.
based on results from an ongoing phase 1 trial.
“We assessed feasibility of monthly subcutaneous administration of PF-06801591, a humanized immunoglobulin G4 monoclonal antibody that binds to the programmed cell death [PD-1] receptor,” Melissa L. Johnson, MD, of the Sarah Cannon Research Institute, Nashville, Tenn., and colleagues wrote in JAMA Oncology. “Subcutaneous administration of an anti-PD-1 antibody in patients with advanced solid tumors appears to be feasible.”
The researchers evaluated the efficacy, safety, and pharmacokinetics of the novel anti-PD-1 therapy in a group of 40 patients with locally advanced or metastatic solid tumors. The antibody was administered in both subcutaneous and intravenous forms.
Study participants were administered the subcutaneous form of the antibody at 300 mg every 4 weeks or the intravenous form at 0.5, 1, 3, or 10 mg/kg every 3 weeks.
“Dose escalation occurred after two to four patients were enrolled per dose level, with additional patients enrolled in each cohort for further assessment,” the researchers wrote.
The primary endpoints were safety and dose-limiting adverse effects. Efficacy, immunogenicity, pharmacokinetics, and PD-1 receptor occupancy were secondary endpoints.
After analysis, Dr. Johnson and colleagues reported that the overall response rate was 18.4%. In addition, no dose-limiting toxicities were detected in both intravenous and subcutaneous groups, but grade 3 or greater adverse events were reported in 6.7% and 16% of patients treated with subcutaneous and intravenous dosage forms, respectively.
“No dose–adverse event associations were observed during intravenous dose escalation, and no serious skin toxic effects occurred with subcutaneous delivery,” they reported.
Based on the findings, the team selected the subcutaneous form (300 mg) of the therapy for additional assessment in the second half of this ongoing trial.
The study was funded by Pfizer. The authors reported financial affiliations with BerGenBio, EMD Serono, Janssen, Mirati Therapeutics, Pfizer, and several others.
SOURCE: Johnson ML et al. JAMA Oncol. 2019 May 30. doi: 10.1001/jamaoncol.2019.0836.
based on results from an ongoing phase 1 trial.
“We assessed feasibility of monthly subcutaneous administration of PF-06801591, a humanized immunoglobulin G4 monoclonal antibody that binds to the programmed cell death [PD-1] receptor,” Melissa L. Johnson, MD, of the Sarah Cannon Research Institute, Nashville, Tenn., and colleagues wrote in JAMA Oncology. “Subcutaneous administration of an anti-PD-1 antibody in patients with advanced solid tumors appears to be feasible.”
The researchers evaluated the efficacy, safety, and pharmacokinetics of the novel anti-PD-1 therapy in a group of 40 patients with locally advanced or metastatic solid tumors. The antibody was administered in both subcutaneous and intravenous forms.
Study participants were administered the subcutaneous form of the antibody at 300 mg every 4 weeks or the intravenous form at 0.5, 1, 3, or 10 mg/kg every 3 weeks.
“Dose escalation occurred after two to four patients were enrolled per dose level, with additional patients enrolled in each cohort for further assessment,” the researchers wrote.
The primary endpoints were safety and dose-limiting adverse effects. Efficacy, immunogenicity, pharmacokinetics, and PD-1 receptor occupancy were secondary endpoints.
After analysis, Dr. Johnson and colleagues reported that the overall response rate was 18.4%. In addition, no dose-limiting toxicities were detected in both intravenous and subcutaneous groups, but grade 3 or greater adverse events were reported in 6.7% and 16% of patients treated with subcutaneous and intravenous dosage forms, respectively.
“No dose–adverse event associations were observed during intravenous dose escalation, and no serious skin toxic effects occurred with subcutaneous delivery,” they reported.
Based on the findings, the team selected the subcutaneous form (300 mg) of the therapy for additional assessment in the second half of this ongoing trial.
The study was funded by Pfizer. The authors reported financial affiliations with BerGenBio, EMD Serono, Janssen, Mirati Therapeutics, Pfizer, and several others.
SOURCE: Johnson ML et al. JAMA Oncol. 2019 May 30. doi: 10.1001/jamaoncol.2019.0836.
FROM JAMA ONCOLOGY