User login
Tapering Corticosteroids in Severe Alcohol-Associated Hepatitis Appears Safe
SAN DIEGO — , according to new research.
“Although several drugs have been evaluated for severe alcohol-associated hepatitis, none have succeeded in practice. Corticosteroids remain the mainstay of treatment; however, infections remain a major concern in 25%-40% of cases,” said Anand Kulkarni, MD, senior consultant and director of critical care hepatology at the Asian Institute of Gastroenterology in Hyderabad, India.
“There are no standard society guidelines for steroid dosing, and our current practices stem from studies in the 1970s, so there’s a major knowledge gap around optimal dosing and if stepwise tapering helps,” said Kulkarni, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Assessing Tapered Doses
In a multicenter, open-label randomized controlled trial, 254 patients with SAH from four Indian centers and one Canadian center were randomized to receive either a fixed or tapering dose of 40 mg prednisolone daily for 4 weeks. The patients in the tapering group received a starting dose of 40 mg, which was reduced by 10 mg weekly over 4 weeks.
While taking corticosteroids, 66% of those in the fixed dose group and 55% of those in the tapering group also received prophylactic antibiotics.
The mean age of participants was 41.1 years, the median Model For End-Stage Liver Disease score was 25.6, and 98.4% were men.
The primary objective was to compare the incidence of drug-related adverse events, infections, hospitalization, and mortality through day 90.
The duration of corticosteroid therapy was 22 days in the fixed dose group and 23 days in the tapering dose group.
Overall, the proportion of steroid responders was similar in both groups, at 80.3% in the fixed dose group and 82.5% in the tapering dose group.
However, the incidence of drug-related adverse events was significantly higher in the fixed dose group (52%) than in the tapering dose group (36.2%). The most common adverse events in both groups were infection, hyperglycemia, and hematochezia.
At 90 days, the incidence of infection was significantly lower in the tapering group (19.7%) than in the fixed dose group (33.1%). In both groups, the most common infection sites were the lungs (28.3%) and urinary tract (22.4%).
In terms of liver-related outcomes, some patients developed hepatic encephalopathy (11.8% in fixed dose vs 6.3% in tapering dose) and acute variceal bleed (3.1% in each group), as well as acute kidney injury (26.8% in fixed dose vs 18.9% in tapering dose).
Hospitalization within 90 days was required in 44.1% of the fixed dose group and 33.1% of the tapering dose group.
Survival at day 90 was 83.5% in the fixed dose group and 86.6% in the tapering dose group. Four patients in the fixed dose group and three patients in the tapering dose group underwent living donor liver transplantation by day 90.
Relapse of alcohol use by day 90 occurred in 13.4% of the fixed dose group and 12.6% of the tapering dose group.
“Rapid tapering in severe alcohol-associated hepatitis reduces infections and hospitalizations but doesn’t have a significant impact on survival,” Kulkarni concluded.
Considering Alternative Therapies
Given the high risk for infection in patients with SAH and limited certainty around benefits, the data may also call into question whether to give steroids to these patients at all, said session co-moderator Aleksander Krag, MD, professor of clinical medicine at the University of Southern Denmark, Odense, Denmark, and secretary general of the European Association for the Study of Liver 2023-2025.
“Since there are no other treatments available as of now, we’ll still continue to give steroids,” Kulkarni noted. But “tapering the dose should be beneficial.”
Although steroid therapy has been considered the “mainstay treatment” for SAH for 50 years, it doesn’t always lead to long-term improvement in liver values or survival, said Prasun Jalal, MD, the Stan and Sue Partee Endowed Chair in Hepatology at Baylor College of Medicine, Houston, who wasn’t involved with the study.
Researchers are looking to other connections, such as the gut microbiome, to find treatments for advanced alcoholic liver disease, Jalal said in an interview. In a small pilot study, he and colleagues found that intestinal microbiota transplantation (IMT) appears to be safe and effective for these patients.
“Early analyses suggest that IMT has a favorable outcome on the prognosis of patients with severe alcohol-associated hepatitis and is safe,” Jalal said. “A longer follow-up study with a larger sample size is in progress.”
Kulkarni and Krag reported no relevant disclosures. Jalal has speaking and teaching relationships with AbbVie and Madrigal.
A version of this article appeared on Medscape.com.
SAN DIEGO — , according to new research.
“Although several drugs have been evaluated for severe alcohol-associated hepatitis, none have succeeded in practice. Corticosteroids remain the mainstay of treatment; however, infections remain a major concern in 25%-40% of cases,” said Anand Kulkarni, MD, senior consultant and director of critical care hepatology at the Asian Institute of Gastroenterology in Hyderabad, India.
“There are no standard society guidelines for steroid dosing, and our current practices stem from studies in the 1970s, so there’s a major knowledge gap around optimal dosing and if stepwise tapering helps,” said Kulkarni, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Assessing Tapered Doses
In a multicenter, open-label randomized controlled trial, 254 patients with SAH from four Indian centers and one Canadian center were randomized to receive either a fixed or tapering dose of 40 mg prednisolone daily for 4 weeks. The patients in the tapering group received a starting dose of 40 mg, which was reduced by 10 mg weekly over 4 weeks.
While taking corticosteroids, 66% of those in the fixed dose group and 55% of those in the tapering group also received prophylactic antibiotics.
The mean age of participants was 41.1 years, the median Model For End-Stage Liver Disease score was 25.6, and 98.4% were men.
The primary objective was to compare the incidence of drug-related adverse events, infections, hospitalization, and mortality through day 90.
The duration of corticosteroid therapy was 22 days in the fixed dose group and 23 days in the tapering dose group.
Overall, the proportion of steroid responders was similar in both groups, at 80.3% in the fixed dose group and 82.5% in the tapering dose group.
However, the incidence of drug-related adverse events was significantly higher in the fixed dose group (52%) than in the tapering dose group (36.2%). The most common adverse events in both groups were infection, hyperglycemia, and hematochezia.
At 90 days, the incidence of infection was significantly lower in the tapering group (19.7%) than in the fixed dose group (33.1%). In both groups, the most common infection sites were the lungs (28.3%) and urinary tract (22.4%).
In terms of liver-related outcomes, some patients developed hepatic encephalopathy (11.8% in fixed dose vs 6.3% in tapering dose) and acute variceal bleed (3.1% in each group), as well as acute kidney injury (26.8% in fixed dose vs 18.9% in tapering dose).
Hospitalization within 90 days was required in 44.1% of the fixed dose group and 33.1% of the tapering dose group.
Survival at day 90 was 83.5% in the fixed dose group and 86.6% in the tapering dose group. Four patients in the fixed dose group and three patients in the tapering dose group underwent living donor liver transplantation by day 90.
Relapse of alcohol use by day 90 occurred in 13.4% of the fixed dose group and 12.6% of the tapering dose group.
“Rapid tapering in severe alcohol-associated hepatitis reduces infections and hospitalizations but doesn’t have a significant impact on survival,” Kulkarni concluded.
Considering Alternative Therapies
Given the high risk for infection in patients with SAH and limited certainty around benefits, the data may also call into question whether to give steroids to these patients at all, said session co-moderator Aleksander Krag, MD, professor of clinical medicine at the University of Southern Denmark, Odense, Denmark, and secretary general of the European Association for the Study of Liver 2023-2025.
“Since there are no other treatments available as of now, we’ll still continue to give steroids,” Kulkarni noted. But “tapering the dose should be beneficial.”
Although steroid therapy has been considered the “mainstay treatment” for SAH for 50 years, it doesn’t always lead to long-term improvement in liver values or survival, said Prasun Jalal, MD, the Stan and Sue Partee Endowed Chair in Hepatology at Baylor College of Medicine, Houston, who wasn’t involved with the study.
Researchers are looking to other connections, such as the gut microbiome, to find treatments for advanced alcoholic liver disease, Jalal said in an interview. In a small pilot study, he and colleagues found that intestinal microbiota transplantation (IMT) appears to be safe and effective for these patients.
“Early analyses suggest that IMT has a favorable outcome on the prognosis of patients with severe alcohol-associated hepatitis and is safe,” Jalal said. “A longer follow-up study with a larger sample size is in progress.”
Kulkarni and Krag reported no relevant disclosures. Jalal has speaking and teaching relationships with AbbVie and Madrigal.
A version of this article appeared on Medscape.com.
SAN DIEGO — , according to new research.
“Although several drugs have been evaluated for severe alcohol-associated hepatitis, none have succeeded in practice. Corticosteroids remain the mainstay of treatment; however, infections remain a major concern in 25%-40% of cases,” said Anand Kulkarni, MD, senior consultant and director of critical care hepatology at the Asian Institute of Gastroenterology in Hyderabad, India.
“There are no standard society guidelines for steroid dosing, and our current practices stem from studies in the 1970s, so there’s a major knowledge gap around optimal dosing and if stepwise tapering helps,” said Kulkarni, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Assessing Tapered Doses
In a multicenter, open-label randomized controlled trial, 254 patients with SAH from four Indian centers and one Canadian center were randomized to receive either a fixed or tapering dose of 40 mg prednisolone daily for 4 weeks. The patients in the tapering group received a starting dose of 40 mg, which was reduced by 10 mg weekly over 4 weeks.
While taking corticosteroids, 66% of those in the fixed dose group and 55% of those in the tapering group also received prophylactic antibiotics.
The mean age of participants was 41.1 years, the median Model For End-Stage Liver Disease score was 25.6, and 98.4% were men.
The primary objective was to compare the incidence of drug-related adverse events, infections, hospitalization, and mortality through day 90.
The duration of corticosteroid therapy was 22 days in the fixed dose group and 23 days in the tapering dose group.
Overall, the proportion of steroid responders was similar in both groups, at 80.3% in the fixed dose group and 82.5% in the tapering dose group.
However, the incidence of drug-related adverse events was significantly higher in the fixed dose group (52%) than in the tapering dose group (36.2%). The most common adverse events in both groups were infection, hyperglycemia, and hematochezia.
At 90 days, the incidence of infection was significantly lower in the tapering group (19.7%) than in the fixed dose group (33.1%). In both groups, the most common infection sites were the lungs (28.3%) and urinary tract (22.4%).
In terms of liver-related outcomes, some patients developed hepatic encephalopathy (11.8% in fixed dose vs 6.3% in tapering dose) and acute variceal bleed (3.1% in each group), as well as acute kidney injury (26.8% in fixed dose vs 18.9% in tapering dose).
Hospitalization within 90 days was required in 44.1% of the fixed dose group and 33.1% of the tapering dose group.
Survival at day 90 was 83.5% in the fixed dose group and 86.6% in the tapering dose group. Four patients in the fixed dose group and three patients in the tapering dose group underwent living donor liver transplantation by day 90.
Relapse of alcohol use by day 90 occurred in 13.4% of the fixed dose group and 12.6% of the tapering dose group.
“Rapid tapering in severe alcohol-associated hepatitis reduces infections and hospitalizations but doesn’t have a significant impact on survival,” Kulkarni concluded.
Considering Alternative Therapies
Given the high risk for infection in patients with SAH and limited certainty around benefits, the data may also call into question whether to give steroids to these patients at all, said session co-moderator Aleksander Krag, MD, professor of clinical medicine at the University of Southern Denmark, Odense, Denmark, and secretary general of the European Association for the Study of Liver 2023-2025.
“Since there are no other treatments available as of now, we’ll still continue to give steroids,” Kulkarni noted. But “tapering the dose should be beneficial.”
Although steroid therapy has been considered the “mainstay treatment” for SAH for 50 years, it doesn’t always lead to long-term improvement in liver values or survival, said Prasun Jalal, MD, the Stan and Sue Partee Endowed Chair in Hepatology at Baylor College of Medicine, Houston, who wasn’t involved with the study.
Researchers are looking to other connections, such as the gut microbiome, to find treatments for advanced alcoholic liver disease, Jalal said in an interview. In a small pilot study, he and colleagues found that intestinal microbiota transplantation (IMT) appears to be safe and effective for these patients.
“Early analyses suggest that IMT has a favorable outcome on the prognosis of patients with severe alcohol-associated hepatitis and is safe,” Jalal said. “A longer follow-up study with a larger sample size is in progress.”
Kulkarni and Krag reported no relevant disclosures. Jalal has speaking and teaching relationships with AbbVie and Madrigal.
A version of this article appeared on Medscape.com.
FROM AASLD 2024
Bariatric Surgery Better Than Obesity Drugs for Some Patients With MASLD
SAN DIEGO — , new study results showed.
In a separate analysis of data from the same study, researchers also found that bariatric surgery alone had lower risks for major adverse cardiovascular events (MACEs) than GLP-1 or SGLT2 inhibitor use or a combination of surgery and medications.
“While weight loss medications have demonstrated notable success, especially in managing diabetes and aiding weight loss, bariatric surgery offers more significant and varied benefits for weight and metabolic health, making it a better option for some patients,” said Leith Ghani, DO, an internal medicine resident at The University of Arizona College of Medicine – Phoenix.
Ghani presented the findings about mortality at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD). His co-author and fellow internal medicine resident Qumber Ali, DO, presented the findings about MACEs.
These findings highlight “the need for personalized treatment plans, allowing the decision between surgery and medication to be customized according to each patient’s specific situation and health goals,” Ghani said. “It also emphasizes the importance of a multidisciplinary approach to patient management.”
Comparing Bariatric Interventions and Pharmacologic Treatments
The retrospective, multicenter study of hospital admissions data from the Banner Health system in Phoenix included more than 8600 patients who had MASLD-related diagnostic codes and metabolic criteria. Patients were divided into four groups according to the treatment they received: Bariatric surgery alone (5.8%), GLP-1 medications (39.3%), SGLT2 inhibitor medications (23.4%), or a combination of surgery and medications (31.5%).
In the mortality analysis, Ghani and colleagues looked at data for patients who died between 12 and 60 months after surgery or starting medication. They found that patients who underwent bariatric surgery had a significantly higher chance of survival at 5 years.
When compared to bariatric surgery, the adjusted hazard ratio (aHR) for GLP-1 medications was 2.99, followed by an aHR of 2.96 for SGLT2 inhibitor medications, and an aHR of 1.78 for a combination of treatments.
In the MACE analysis, Ali and colleagues looked at data for patients who were followed for 12 months or more after intervention or initiation of treatment, identifying MACE diagnostic codes for coronary artery disease, cerebrovascular disease, and congestive heart failure. They found that patients who underwent bariatric surgery alone had a significantly lower rate of MACEs.
When compared to bariatric surgery, the aHR was 1.83 for GLP-1 medications, 1.72 for SGLT2 inhibitor medications, and 1.91 for a combination of treatments.
Regarding both analyses, patients taking GLP-1 or SGLT2 inhibitor medications may face higher risks for mortality or serious heart problems due to existing metabolic disorders or heart disease, Ali said.
Future studies could look at other risk factors that make these patients more vulnerable, he added. For instance, factors related to body mass index, glucose control, other medications, different clinical settings, and race/ethnicity can contribute to different treatment responses, as could the decision to take medication or undergo surgery in the first place.
“This emphasizes the need for additional, prospective randomized clinical trial research to explore why these differences exist,” Ali said. “While progress has been made, there is still much to learn about the optimal management of patients with metabolic and cardiovascular disorders.”
Considering a Multidisciplinary Approach to MASLD Treatment
Ghani and Ali also called for personalized treatment plans for metabolic-related disorders such as MASLD, as well as strong communication among specialists and with patients about the benefits and risks of choosing certain medications and procedures.
“Bariatric surgery is not a universal solution, and not all patients are suitable for surgery,” Ghani said. “We also can’t say at this point that drug treatments are worse than bariatric surgery. The effectiveness of these therapies can vary greatly depending on a patient’s health, lifestyle, and preferences.”
Looking ahead, MASLD studies should investigate long-term weight loss seen with bariatric surgery and different medications, said Katherine Schwenger, PhD, RD, a scientific associate at Toronto General Hospital in Toronto, Ontario, Canada.
“GLP-1s are a hot topic right now,” said Schwenger, who wasn’t involved with the study. But “we need to look at factors such as the longevity of weight loss. It’s hard to beat the success and sustainability of bariatric surgery.”
Ghani, Ali, and Schwenger reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
SAN DIEGO — , new study results showed.
In a separate analysis of data from the same study, researchers also found that bariatric surgery alone had lower risks for major adverse cardiovascular events (MACEs) than GLP-1 or SGLT2 inhibitor use or a combination of surgery and medications.
“While weight loss medications have demonstrated notable success, especially in managing diabetes and aiding weight loss, bariatric surgery offers more significant and varied benefits for weight and metabolic health, making it a better option for some patients,” said Leith Ghani, DO, an internal medicine resident at The University of Arizona College of Medicine – Phoenix.
Ghani presented the findings about mortality at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD). His co-author and fellow internal medicine resident Qumber Ali, DO, presented the findings about MACEs.
These findings highlight “the need for personalized treatment plans, allowing the decision between surgery and medication to be customized according to each patient’s specific situation and health goals,” Ghani said. “It also emphasizes the importance of a multidisciplinary approach to patient management.”
Comparing Bariatric Interventions and Pharmacologic Treatments
The retrospective, multicenter study of hospital admissions data from the Banner Health system in Phoenix included more than 8600 patients who had MASLD-related diagnostic codes and metabolic criteria. Patients were divided into four groups according to the treatment they received: Bariatric surgery alone (5.8%), GLP-1 medications (39.3%), SGLT2 inhibitor medications (23.4%), or a combination of surgery and medications (31.5%).
In the mortality analysis, Ghani and colleagues looked at data for patients who died between 12 and 60 months after surgery or starting medication. They found that patients who underwent bariatric surgery had a significantly higher chance of survival at 5 years.
When compared to bariatric surgery, the adjusted hazard ratio (aHR) for GLP-1 medications was 2.99, followed by an aHR of 2.96 for SGLT2 inhibitor medications, and an aHR of 1.78 for a combination of treatments.
In the MACE analysis, Ali and colleagues looked at data for patients who were followed for 12 months or more after intervention or initiation of treatment, identifying MACE diagnostic codes for coronary artery disease, cerebrovascular disease, and congestive heart failure. They found that patients who underwent bariatric surgery alone had a significantly lower rate of MACEs.
When compared to bariatric surgery, the aHR was 1.83 for GLP-1 medications, 1.72 for SGLT2 inhibitor medications, and 1.91 for a combination of treatments.
Regarding both analyses, patients taking GLP-1 or SGLT2 inhibitor medications may face higher risks for mortality or serious heart problems due to existing metabolic disorders or heart disease, Ali said.
Future studies could look at other risk factors that make these patients more vulnerable, he added. For instance, factors related to body mass index, glucose control, other medications, different clinical settings, and race/ethnicity can contribute to different treatment responses, as could the decision to take medication or undergo surgery in the first place.
“This emphasizes the need for additional, prospective randomized clinical trial research to explore why these differences exist,” Ali said. “While progress has been made, there is still much to learn about the optimal management of patients with metabolic and cardiovascular disorders.”
Considering a Multidisciplinary Approach to MASLD Treatment
Ghani and Ali also called for personalized treatment plans for metabolic-related disorders such as MASLD, as well as strong communication among specialists and with patients about the benefits and risks of choosing certain medications and procedures.
“Bariatric surgery is not a universal solution, and not all patients are suitable for surgery,” Ghani said. “We also can’t say at this point that drug treatments are worse than bariatric surgery. The effectiveness of these therapies can vary greatly depending on a patient’s health, lifestyle, and preferences.”
Looking ahead, MASLD studies should investigate long-term weight loss seen with bariatric surgery and different medications, said Katherine Schwenger, PhD, RD, a scientific associate at Toronto General Hospital in Toronto, Ontario, Canada.
“GLP-1s are a hot topic right now,” said Schwenger, who wasn’t involved with the study. But “we need to look at factors such as the longevity of weight loss. It’s hard to beat the success and sustainability of bariatric surgery.”
Ghani, Ali, and Schwenger reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
SAN DIEGO — , new study results showed.
In a separate analysis of data from the same study, researchers also found that bariatric surgery alone had lower risks for major adverse cardiovascular events (MACEs) than GLP-1 or SGLT2 inhibitor use or a combination of surgery and medications.
“While weight loss medications have demonstrated notable success, especially in managing diabetes and aiding weight loss, bariatric surgery offers more significant and varied benefits for weight and metabolic health, making it a better option for some patients,” said Leith Ghani, DO, an internal medicine resident at The University of Arizona College of Medicine – Phoenix.
Ghani presented the findings about mortality at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD). His co-author and fellow internal medicine resident Qumber Ali, DO, presented the findings about MACEs.
These findings highlight “the need for personalized treatment plans, allowing the decision between surgery and medication to be customized according to each patient’s specific situation and health goals,” Ghani said. “It also emphasizes the importance of a multidisciplinary approach to patient management.”
Comparing Bariatric Interventions and Pharmacologic Treatments
The retrospective, multicenter study of hospital admissions data from the Banner Health system in Phoenix included more than 8600 patients who had MASLD-related diagnostic codes and metabolic criteria. Patients were divided into four groups according to the treatment they received: Bariatric surgery alone (5.8%), GLP-1 medications (39.3%), SGLT2 inhibitor medications (23.4%), or a combination of surgery and medications (31.5%).
In the mortality analysis, Ghani and colleagues looked at data for patients who died between 12 and 60 months after surgery or starting medication. They found that patients who underwent bariatric surgery had a significantly higher chance of survival at 5 years.
When compared to bariatric surgery, the adjusted hazard ratio (aHR) for GLP-1 medications was 2.99, followed by an aHR of 2.96 for SGLT2 inhibitor medications, and an aHR of 1.78 for a combination of treatments.
In the MACE analysis, Ali and colleagues looked at data for patients who were followed for 12 months or more after intervention or initiation of treatment, identifying MACE diagnostic codes for coronary artery disease, cerebrovascular disease, and congestive heart failure. They found that patients who underwent bariatric surgery alone had a significantly lower rate of MACEs.
When compared to bariatric surgery, the aHR was 1.83 for GLP-1 medications, 1.72 for SGLT2 inhibitor medications, and 1.91 for a combination of treatments.
Regarding both analyses, patients taking GLP-1 or SGLT2 inhibitor medications may face higher risks for mortality or serious heart problems due to existing metabolic disorders or heart disease, Ali said.
Future studies could look at other risk factors that make these patients more vulnerable, he added. For instance, factors related to body mass index, glucose control, other medications, different clinical settings, and race/ethnicity can contribute to different treatment responses, as could the decision to take medication or undergo surgery in the first place.
“This emphasizes the need for additional, prospective randomized clinical trial research to explore why these differences exist,” Ali said. “While progress has been made, there is still much to learn about the optimal management of patients with metabolic and cardiovascular disorders.”
Considering a Multidisciplinary Approach to MASLD Treatment
Ghani and Ali also called for personalized treatment plans for metabolic-related disorders such as MASLD, as well as strong communication among specialists and with patients about the benefits and risks of choosing certain medications and procedures.
“Bariatric surgery is not a universal solution, and not all patients are suitable for surgery,” Ghani said. “We also can’t say at this point that drug treatments are worse than bariatric surgery. The effectiveness of these therapies can vary greatly depending on a patient’s health, lifestyle, and preferences.”
Looking ahead, MASLD studies should investigate long-term weight loss seen with bariatric surgery and different medications, said Katherine Schwenger, PhD, RD, a scientific associate at Toronto General Hospital in Toronto, Ontario, Canada.
“GLP-1s are a hot topic right now,” said Schwenger, who wasn’t involved with the study. But “we need to look at factors such as the longevity of weight loss. It’s hard to beat the success and sustainability of bariatric surgery.”
Ghani, Ali, and Schwenger reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM AASLD 2024
Digestive Disease Mortality Higher for US Indigenous Communities
which experience the highest death rates and ongoing increases, according to a recent study.
Policymakers, healthcare providers, and communities need to respond with targeted interventions and collaborative efforts that address these inequities and advance digestive health equity, lead author Wafa A. Aldhaleei, MD, of Mayo Clinic, Rochester, Minnesota, and colleagues reported.
“Several studies have reported the epidemiological characteristics of certain digestive diseases such as pancreatitis, liver and biliary diseases, and inflammatory bowel disease,” the investigators wrote in Clinical Gastroenterology and Hepatology. “These studies provide insights into the US burden by sex and racial and ethnic disparities of various digestive diseases individually. However, little is known about racial disparities in the United States digestive diseases mortality burden.”
As part of the Global Burden of Disease Study, the investigators analyzed data from the Institute of Health Metrics and Evaluation Global Health Data Exchange, including age-standardized digestive disease mortality rates for five racial and ethnic groups (Black, White, American Indian and Alaska Native, Asian and Pacific Islander, and Latino) between 2000 and 2019, with further subgroups based on sex, state, and county. Joinpoint regression analysis was employed to determine overall temporal trends by demography.
Results showed striking mortality rate differences across racial and ethnic groups. In 2019, digestive disease mortality rates were highest among American Indian and Alaska Native individuals, reaching 86.2 per 100,000 — over twice the rate seen in White (35.5 per 100,000), Black (33.6 per 100,000), and Latino (33.6 per 100,000) populations, and more than five times higher than in Asian and Pacific Islander individuals (15.6 per 100,000). Over the study period, American Indian and Alaska Native individuals experienced a significant 0.87% average annual increase in mortality rates, while White individuals saw a smaller increase of 0.12% annually. In contrast, Latino, Black, and Asian and Pacific Islander individuals had declining average annual rates.
Geographic disparities in digestive disease mortality were significant, with West Virginia recording the highest state-level rate in 2019 at 44.8 deaths per 100,000, well above the national rate of 34.5 per 100,000. Certain regions with high concentrations of American Indian and Alaska Native populations, such as the Southwest Tribes service area (including Arizona and New Mexico) and the Plain Indians service area (spanning Montana, North Dakota, and South Dakota), reported mortality rates exceeding 70 per 100,000, more than double the national average. In Alaska, the American Indian and Alaska Native population’s mortality rate surged with annual increases of up to 3.53% during some periods.
Analyses also revealed some notable sex-based trends. Among American Indian and Alaska Native individuals, males experienced a mortality rate increase of 0.87% annually, reaching 93.5 per 100,000 by 2019, while females saw an even sharper rise at 1.11% per year, with a mortality rate of 79.6 per 100,000 in 2019. For White individuals, the average annual percentage increase was 0.12% for males, bringing their rate to 40.2 per 100,000, and 0.30% for females, with a rate of 31.0 per 100,000 in 2019.
“Our study reveals persistent racial, ethnic, and geographic disparities in digestive diseases mortality in the United States,” the investigators concluded. “Targeted interventions and further research are needed to address these disparities and promote digestive health equity. Collaboration among researchers, policymakers, healthcare providers, and communities is essential to achieve this goal.”This research was conducted as part of Global Burden of Disease, Injuries and Risk Factors Study, coordinated by the Institute of Health Metrics and Evaluation. The investigators disclosed no conflicts of interest.
which experience the highest death rates and ongoing increases, according to a recent study.
Policymakers, healthcare providers, and communities need to respond with targeted interventions and collaborative efforts that address these inequities and advance digestive health equity, lead author Wafa A. Aldhaleei, MD, of Mayo Clinic, Rochester, Minnesota, and colleagues reported.
“Several studies have reported the epidemiological characteristics of certain digestive diseases such as pancreatitis, liver and biliary diseases, and inflammatory bowel disease,” the investigators wrote in Clinical Gastroenterology and Hepatology. “These studies provide insights into the US burden by sex and racial and ethnic disparities of various digestive diseases individually. However, little is known about racial disparities in the United States digestive diseases mortality burden.”
As part of the Global Burden of Disease Study, the investigators analyzed data from the Institute of Health Metrics and Evaluation Global Health Data Exchange, including age-standardized digestive disease mortality rates for five racial and ethnic groups (Black, White, American Indian and Alaska Native, Asian and Pacific Islander, and Latino) between 2000 and 2019, with further subgroups based on sex, state, and county. Joinpoint regression analysis was employed to determine overall temporal trends by demography.
Results showed striking mortality rate differences across racial and ethnic groups. In 2019, digestive disease mortality rates were highest among American Indian and Alaska Native individuals, reaching 86.2 per 100,000 — over twice the rate seen in White (35.5 per 100,000), Black (33.6 per 100,000), and Latino (33.6 per 100,000) populations, and more than five times higher than in Asian and Pacific Islander individuals (15.6 per 100,000). Over the study period, American Indian and Alaska Native individuals experienced a significant 0.87% average annual increase in mortality rates, while White individuals saw a smaller increase of 0.12% annually. In contrast, Latino, Black, and Asian and Pacific Islander individuals had declining average annual rates.
Geographic disparities in digestive disease mortality were significant, with West Virginia recording the highest state-level rate in 2019 at 44.8 deaths per 100,000, well above the national rate of 34.5 per 100,000. Certain regions with high concentrations of American Indian and Alaska Native populations, such as the Southwest Tribes service area (including Arizona and New Mexico) and the Plain Indians service area (spanning Montana, North Dakota, and South Dakota), reported mortality rates exceeding 70 per 100,000, more than double the national average. In Alaska, the American Indian and Alaska Native population’s mortality rate surged with annual increases of up to 3.53% during some periods.
Analyses also revealed some notable sex-based trends. Among American Indian and Alaska Native individuals, males experienced a mortality rate increase of 0.87% annually, reaching 93.5 per 100,000 by 2019, while females saw an even sharper rise at 1.11% per year, with a mortality rate of 79.6 per 100,000 in 2019. For White individuals, the average annual percentage increase was 0.12% for males, bringing their rate to 40.2 per 100,000, and 0.30% for females, with a rate of 31.0 per 100,000 in 2019.
“Our study reveals persistent racial, ethnic, and geographic disparities in digestive diseases mortality in the United States,” the investigators concluded. “Targeted interventions and further research are needed to address these disparities and promote digestive health equity. Collaboration among researchers, policymakers, healthcare providers, and communities is essential to achieve this goal.”This research was conducted as part of Global Burden of Disease, Injuries and Risk Factors Study, coordinated by the Institute of Health Metrics and Evaluation. The investigators disclosed no conflicts of interest.
which experience the highest death rates and ongoing increases, according to a recent study.
Policymakers, healthcare providers, and communities need to respond with targeted interventions and collaborative efforts that address these inequities and advance digestive health equity, lead author Wafa A. Aldhaleei, MD, of Mayo Clinic, Rochester, Minnesota, and colleagues reported.
“Several studies have reported the epidemiological characteristics of certain digestive diseases such as pancreatitis, liver and biliary diseases, and inflammatory bowel disease,” the investigators wrote in Clinical Gastroenterology and Hepatology. “These studies provide insights into the US burden by sex and racial and ethnic disparities of various digestive diseases individually. However, little is known about racial disparities in the United States digestive diseases mortality burden.”
As part of the Global Burden of Disease Study, the investigators analyzed data from the Institute of Health Metrics and Evaluation Global Health Data Exchange, including age-standardized digestive disease mortality rates for five racial and ethnic groups (Black, White, American Indian and Alaska Native, Asian and Pacific Islander, and Latino) between 2000 and 2019, with further subgroups based on sex, state, and county. Joinpoint regression analysis was employed to determine overall temporal trends by demography.
Results showed striking mortality rate differences across racial and ethnic groups. In 2019, digestive disease mortality rates were highest among American Indian and Alaska Native individuals, reaching 86.2 per 100,000 — over twice the rate seen in White (35.5 per 100,000), Black (33.6 per 100,000), and Latino (33.6 per 100,000) populations, and more than five times higher than in Asian and Pacific Islander individuals (15.6 per 100,000). Over the study period, American Indian and Alaska Native individuals experienced a significant 0.87% average annual increase in mortality rates, while White individuals saw a smaller increase of 0.12% annually. In contrast, Latino, Black, and Asian and Pacific Islander individuals had declining average annual rates.
Geographic disparities in digestive disease mortality were significant, with West Virginia recording the highest state-level rate in 2019 at 44.8 deaths per 100,000, well above the national rate of 34.5 per 100,000. Certain regions with high concentrations of American Indian and Alaska Native populations, such as the Southwest Tribes service area (including Arizona and New Mexico) and the Plain Indians service area (spanning Montana, North Dakota, and South Dakota), reported mortality rates exceeding 70 per 100,000, more than double the national average. In Alaska, the American Indian and Alaska Native population’s mortality rate surged with annual increases of up to 3.53% during some periods.
Analyses also revealed some notable sex-based trends. Among American Indian and Alaska Native individuals, males experienced a mortality rate increase of 0.87% annually, reaching 93.5 per 100,000 by 2019, while females saw an even sharper rise at 1.11% per year, with a mortality rate of 79.6 per 100,000 in 2019. For White individuals, the average annual percentage increase was 0.12% for males, bringing their rate to 40.2 per 100,000, and 0.30% for females, with a rate of 31.0 per 100,000 in 2019.
“Our study reveals persistent racial, ethnic, and geographic disparities in digestive diseases mortality in the United States,” the investigators concluded. “Targeted interventions and further research are needed to address these disparities and promote digestive health equity. Collaboration among researchers, policymakers, healthcare providers, and communities is essential to achieve this goal.”This research was conducted as part of Global Burden of Disease, Injuries and Risk Factors Study, coordinated by the Institute of Health Metrics and Evaluation. The investigators disclosed no conflicts of interest.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
AI Tool Identifies Undiagnosed Early-Stage MASLD
SAN DIEGO — according to new research.
Among the patients identified by the algorithm as meeting the criteria for MASLD, only a small percentage had an MASLD-associated diagnostic code.
“A significant portion of patients who meet criteria for MASLD go undiagnosed, which can lead to delays in care and progression to advanced liver disease,” said lead author Ariana Stuart, MD, an internal medicine resident at the University of Washington, Seattle, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
“However, people shouldn’t interpret our findings as a lack of primary care training or management,” she said. “Instead, this study indicates that AI can complement physician workflow and address the limitations of traditional clinical practice.”
Developing an MASLD Algorithm
Typically, the identification of MASLD has relied on clinician recognition and descriptions in chart notes, Stuart said. Early-stage disease often goes unnoticed, particularly if patients remain asymptomatic, until cirrhosis develops.
To address this, Stuart and colleagues created a machine learning, natural language processing AI algorithm on the basis of MASLD criteria from AASLD: Hepatic steatosis on imaging and at least one metabolic factor (elevated body mass index, hypertension, prediabetes or diabetes, or dyslipidemia). The model was validated by two physicians, who manually reviewed monthly cohorts generated by the algorithm.
Between December 2023 and May 2024, the researchers used the algorithm to analyze an MASLD cohort from medical centers in the Seattle area. The mean age was 51 years, 44% were women, and 68% were White. Those with alcohol-associated liver disease, metastatic malignancy, and autoimmune, genetic, and infectious causes of liver disease were excluded.
The algorithm identified 957 patients with imaging that matched MASLD criteria.
Among those, 137 patients (17%) identified by the algorithm had an MASLD-associated diagnostic code. For these patients, the mean time from initial imaging with steatosis to diagnosis was 33 days, according to patient records.
An additional 26 patients received an MASLD diagnosis during the study period, with a mean time to diagnosis of 56.2 days.
In terms of patient management, 245 patients (26%) had contact with a gastroenterologist or hepatologist based on documentation of a letter, phone call, or office visit. In addition, 546 patients (57%) were screened for hepatitis C.
After adjusting for an over-inclusion error rate of 12.8% and an overdiagnosis rate of 0.02%, the research team found 697 patients (83%) lacked a relevant diagnosis. After multiple iterations, the algorithm achieved an accuracy of about 88%, Stuart said.
Considering Future AI Use
Stuart and colleagues are now testing the algorithm in larger groups and across longer periods.
After that, they intend to implement a quality improvement program to increase awareness for clinicians and primary care providers, as well as train users on how to interpret and move forward with findings of hepatic steatosis in patient records.
For instance, future AI models could flag patients for additional testing, improve chart review, and aid in research efforts around cardiometabolic comorbidities associated with MASLD, she said.
Looking ahead, AI tools such as these represent what’s possible for advancements in research, patient care, and clinical workflows, said Ashley Spann, MD, assistant professor and transplant hepatologist at Vanderbilt University, Nashville, Tennessee, and director of clinical research informatics for Vanderbilt’s Gastroenterology Division.
“AI, in my view, is actually augmented intelligence,” she added. “We need to think about the people and processes involved.”
Spann, who spoke about the use of AI tools in medicine in general, stressed the need for transparency in AI use, careful validation of input-output data, frameworks for machine learning models in medicine, and standardization across institutions.
“What we ultimately need is an infrastructure that supports the simultaneous deployment and evaluation of these models,” she said. “We all need to be on the same page and make sure our models work in multiple settings and make adjustments based on algorithmovigilance afterward.”
Stuart reported no relevant disclosures. Spann serves on Epic’s hepatology steering board, which has focused on how to use AI tools in electronic medical records.
A version of this article appeared on Medscape.com.
SAN DIEGO — according to new research.
Among the patients identified by the algorithm as meeting the criteria for MASLD, only a small percentage had an MASLD-associated diagnostic code.
“A significant portion of patients who meet criteria for MASLD go undiagnosed, which can lead to delays in care and progression to advanced liver disease,” said lead author Ariana Stuart, MD, an internal medicine resident at the University of Washington, Seattle, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
“However, people shouldn’t interpret our findings as a lack of primary care training or management,” she said. “Instead, this study indicates that AI can complement physician workflow and address the limitations of traditional clinical practice.”
Developing an MASLD Algorithm
Typically, the identification of MASLD has relied on clinician recognition and descriptions in chart notes, Stuart said. Early-stage disease often goes unnoticed, particularly if patients remain asymptomatic, until cirrhosis develops.
To address this, Stuart and colleagues created a machine learning, natural language processing AI algorithm on the basis of MASLD criteria from AASLD: Hepatic steatosis on imaging and at least one metabolic factor (elevated body mass index, hypertension, prediabetes or diabetes, or dyslipidemia). The model was validated by two physicians, who manually reviewed monthly cohorts generated by the algorithm.
Between December 2023 and May 2024, the researchers used the algorithm to analyze an MASLD cohort from medical centers in the Seattle area. The mean age was 51 years, 44% were women, and 68% were White. Those with alcohol-associated liver disease, metastatic malignancy, and autoimmune, genetic, and infectious causes of liver disease were excluded.
The algorithm identified 957 patients with imaging that matched MASLD criteria.
Among those, 137 patients (17%) identified by the algorithm had an MASLD-associated diagnostic code. For these patients, the mean time from initial imaging with steatosis to diagnosis was 33 days, according to patient records.
An additional 26 patients received an MASLD diagnosis during the study period, with a mean time to diagnosis of 56.2 days.
In terms of patient management, 245 patients (26%) had contact with a gastroenterologist or hepatologist based on documentation of a letter, phone call, or office visit. In addition, 546 patients (57%) were screened for hepatitis C.
After adjusting for an over-inclusion error rate of 12.8% and an overdiagnosis rate of 0.02%, the research team found 697 patients (83%) lacked a relevant diagnosis. After multiple iterations, the algorithm achieved an accuracy of about 88%, Stuart said.
Considering Future AI Use
Stuart and colleagues are now testing the algorithm in larger groups and across longer periods.
After that, they intend to implement a quality improvement program to increase awareness for clinicians and primary care providers, as well as train users on how to interpret and move forward with findings of hepatic steatosis in patient records.
For instance, future AI models could flag patients for additional testing, improve chart review, and aid in research efforts around cardiometabolic comorbidities associated with MASLD, she said.
Looking ahead, AI tools such as these represent what’s possible for advancements in research, patient care, and clinical workflows, said Ashley Spann, MD, assistant professor and transplant hepatologist at Vanderbilt University, Nashville, Tennessee, and director of clinical research informatics for Vanderbilt’s Gastroenterology Division.
“AI, in my view, is actually augmented intelligence,” she added. “We need to think about the people and processes involved.”
Spann, who spoke about the use of AI tools in medicine in general, stressed the need for transparency in AI use, careful validation of input-output data, frameworks for machine learning models in medicine, and standardization across institutions.
“What we ultimately need is an infrastructure that supports the simultaneous deployment and evaluation of these models,” she said. “We all need to be on the same page and make sure our models work in multiple settings and make adjustments based on algorithmovigilance afterward.”
Stuart reported no relevant disclosures. Spann serves on Epic’s hepatology steering board, which has focused on how to use AI tools in electronic medical records.
A version of this article appeared on Medscape.com.
SAN DIEGO — according to new research.
Among the patients identified by the algorithm as meeting the criteria for MASLD, only a small percentage had an MASLD-associated diagnostic code.
“A significant portion of patients who meet criteria for MASLD go undiagnosed, which can lead to delays in care and progression to advanced liver disease,” said lead author Ariana Stuart, MD, an internal medicine resident at the University of Washington, Seattle, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
“However, people shouldn’t interpret our findings as a lack of primary care training or management,” she said. “Instead, this study indicates that AI can complement physician workflow and address the limitations of traditional clinical practice.”
Developing an MASLD Algorithm
Typically, the identification of MASLD has relied on clinician recognition and descriptions in chart notes, Stuart said. Early-stage disease often goes unnoticed, particularly if patients remain asymptomatic, until cirrhosis develops.
To address this, Stuart and colleagues created a machine learning, natural language processing AI algorithm on the basis of MASLD criteria from AASLD: Hepatic steatosis on imaging and at least one metabolic factor (elevated body mass index, hypertension, prediabetes or diabetes, or dyslipidemia). The model was validated by two physicians, who manually reviewed monthly cohorts generated by the algorithm.
Between December 2023 and May 2024, the researchers used the algorithm to analyze an MASLD cohort from medical centers in the Seattle area. The mean age was 51 years, 44% were women, and 68% were White. Those with alcohol-associated liver disease, metastatic malignancy, and autoimmune, genetic, and infectious causes of liver disease were excluded.
The algorithm identified 957 patients with imaging that matched MASLD criteria.
Among those, 137 patients (17%) identified by the algorithm had an MASLD-associated diagnostic code. For these patients, the mean time from initial imaging with steatosis to diagnosis was 33 days, according to patient records.
An additional 26 patients received an MASLD diagnosis during the study period, with a mean time to diagnosis of 56.2 days.
In terms of patient management, 245 patients (26%) had contact with a gastroenterologist or hepatologist based on documentation of a letter, phone call, or office visit. In addition, 546 patients (57%) were screened for hepatitis C.
After adjusting for an over-inclusion error rate of 12.8% and an overdiagnosis rate of 0.02%, the research team found 697 patients (83%) lacked a relevant diagnosis. After multiple iterations, the algorithm achieved an accuracy of about 88%, Stuart said.
Considering Future AI Use
Stuart and colleagues are now testing the algorithm in larger groups and across longer periods.
After that, they intend to implement a quality improvement program to increase awareness for clinicians and primary care providers, as well as train users on how to interpret and move forward with findings of hepatic steatosis in patient records.
For instance, future AI models could flag patients for additional testing, improve chart review, and aid in research efforts around cardiometabolic comorbidities associated with MASLD, she said.
Looking ahead, AI tools such as these represent what’s possible for advancements in research, patient care, and clinical workflows, said Ashley Spann, MD, assistant professor and transplant hepatologist at Vanderbilt University, Nashville, Tennessee, and director of clinical research informatics for Vanderbilt’s Gastroenterology Division.
“AI, in my view, is actually augmented intelligence,” she added. “We need to think about the people and processes involved.”
Spann, who spoke about the use of AI tools in medicine in general, stressed the need for transparency in AI use, careful validation of input-output data, frameworks for machine learning models in medicine, and standardization across institutions.
“What we ultimately need is an infrastructure that supports the simultaneous deployment and evaluation of these models,” she said. “We all need to be on the same page and make sure our models work in multiple settings and make adjustments based on algorithmovigilance afterward.”
Stuart reported no relevant disclosures. Spann serves on Epic’s hepatology steering board, which has focused on how to use AI tools in electronic medical records.
A version of this article appeared on Medscape.com.
FROM AASLD 24
MELD 3.0 Reduces Sex-Based Liver Transplant Disparities
SAN DIEGO — , according to new research.
In particular, women are now more likely to be added to the waitlist for a liver transplant, more likely to receive a transplant, and less likely to fall off the waitlist because of death.
“MELD 3.0 improved access to transplantation for women, and now waitlist mortality and transplant rates for women more closely approximate the rates for men,” said lead author Allison Kwong, MD, assistant professor of medicine and transplant hepatologist at Stanford Medicine in California.
“Overall transplant outcomes have also improved year over year,” said Kwong, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Changes in MELD and Transplant Numbers
MELD, which estimates liver failure severity and short-term survival in patients with chronic liver disease, has been used since 2002 to determine organ allocation priority for patients in the United States awaiting liver transplantation. Originally, the score incorporated three variables: creatinine, bilirubin, and the international normalized ratio (INR). MELDNa1, or MELD 2.0, was adopted in 2016 to add sodium.
“Under this system, however, there have been sex-based disparities” with women receiving lower priority scores despite similar disease severity, said Kwong.
“This has been attributed to several factors, such as the creatinine term in the MELD score underestimating renal dysfunction in women, height and body size differences, and differences in disease etiology, and how we’ve assigned exception points historically,” she reported.
Men have had a lower pretransplant mortality rate and higher deceased donor transplant rates, she added.
MELD 3.0 was developed to address these gender differences and other determinants of waitlist outcomes. The updated equation added 1.33 points for women, as well as adding other variables, such as albumin, interactions between bilirubin and sodium, and interactions between albumin and creatinine, to increase prediction accuracy.
To observe the effects of the new system, Kwong and colleagues analyzed OPTN data for patients aged 12 years or older, focusing on the records of more than 20,300 newly registered liver transplant candidates, and about 18,700 transplant recipients, during the 12 months before and 12 months after MELD 3.0 was implemented.
After the switch, 43.7% of newly registered liver transplant candidates were women, compared with 40.4% before the switch. At registration, the median age was 55, both before and after the change in policy, and the median MELD score changed from 23 to 22 after implementation.
In addition, 42.1% of transplants occurred among women after MELD 3.0 implementation, as compared with 37.3% before. Overall, deceased donor transplant rates were similar for men and women after MELD 3.0 implementation.
The 90-day waitlist dropout rate — patients who died or became too sick to receive a transplant — decreased from 13.5% to 9.1% among women, which may be partially attributable to MELD 3.0, said Kwong.
However, waitlist dropout rates also decreased among men, from 9.8% to 7.4%, probably because of improvements in technology, such as machine perfusion, which have increased the number of available livers, she added.
Disparities Continue to Exist
Some disparities still exist. Although the total median MELD score at transplant decreased from 29 to 27, women still had a higher median score of 29 at transplant, compared with a median score of 27 among men.
“This indicates that there may still be differences in transplant access between the sexes,” Kwong said. “There are still body size differences that can affect the probability of transplant, and this would not be addressed by MELD 3.0.”
Additional transplant disparities exist related to other patient characteristics, such as age, race, and ethnicity.
Future versions of MELD could potentially consider these factors, said session moderator Aleksander Krag, MD, PhD, MBA, professor of clinical medicine at the University of Southern Denmark, Odense, and secretary general of the European Association for the Study of the Liver, 2023-2025.
“There are infinite versions of MELD that can be made,” Kwong said. “It’s still early to see how MELD 3.0 will serve the system, but so far, so good.”
In a comment, Tamar Taddei, MD, professor of medicine in digestive diseases at Yale School of Medicine, New Haven, Connecticut, who comoderated the session, noted the importance of using a MELD score that considers sex-based differences.
This study brings MELD 3.0 to its fruition by reducing the disparities experienced by women who were underserved by the previous scoring systems, she said.
It was lovely to see that MELD 3.0 reduced the disparities with transplants, and also that the waitlist dropout was reduced — for both men and women,” Taddei said. “This change is a no-brainer.”
Kwong, Krag, and Taddei reported no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — , according to new research.
In particular, women are now more likely to be added to the waitlist for a liver transplant, more likely to receive a transplant, and less likely to fall off the waitlist because of death.
“MELD 3.0 improved access to transplantation for women, and now waitlist mortality and transplant rates for women more closely approximate the rates for men,” said lead author Allison Kwong, MD, assistant professor of medicine and transplant hepatologist at Stanford Medicine in California.
“Overall transplant outcomes have also improved year over year,” said Kwong, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Changes in MELD and Transplant Numbers
MELD, which estimates liver failure severity and short-term survival in patients with chronic liver disease, has been used since 2002 to determine organ allocation priority for patients in the United States awaiting liver transplantation. Originally, the score incorporated three variables: creatinine, bilirubin, and the international normalized ratio (INR). MELDNa1, or MELD 2.0, was adopted in 2016 to add sodium.
“Under this system, however, there have been sex-based disparities” with women receiving lower priority scores despite similar disease severity, said Kwong.
“This has been attributed to several factors, such as the creatinine term in the MELD score underestimating renal dysfunction in women, height and body size differences, and differences in disease etiology, and how we’ve assigned exception points historically,” she reported.
Men have had a lower pretransplant mortality rate and higher deceased donor transplant rates, she added.
MELD 3.0 was developed to address these gender differences and other determinants of waitlist outcomes. The updated equation added 1.33 points for women, as well as adding other variables, such as albumin, interactions between bilirubin and sodium, and interactions between albumin and creatinine, to increase prediction accuracy.
To observe the effects of the new system, Kwong and colleagues analyzed OPTN data for patients aged 12 years or older, focusing on the records of more than 20,300 newly registered liver transplant candidates, and about 18,700 transplant recipients, during the 12 months before and 12 months after MELD 3.0 was implemented.
After the switch, 43.7% of newly registered liver transplant candidates were women, compared with 40.4% before the switch. At registration, the median age was 55, both before and after the change in policy, and the median MELD score changed from 23 to 22 after implementation.
In addition, 42.1% of transplants occurred among women after MELD 3.0 implementation, as compared with 37.3% before. Overall, deceased donor transplant rates were similar for men and women after MELD 3.0 implementation.
The 90-day waitlist dropout rate — patients who died or became too sick to receive a transplant — decreased from 13.5% to 9.1% among women, which may be partially attributable to MELD 3.0, said Kwong.
However, waitlist dropout rates also decreased among men, from 9.8% to 7.4%, probably because of improvements in technology, such as machine perfusion, which have increased the number of available livers, she added.
Disparities Continue to Exist
Some disparities still exist. Although the total median MELD score at transplant decreased from 29 to 27, women still had a higher median score of 29 at transplant, compared with a median score of 27 among men.
“This indicates that there may still be differences in transplant access between the sexes,” Kwong said. “There are still body size differences that can affect the probability of transplant, and this would not be addressed by MELD 3.0.”
Additional transplant disparities exist related to other patient characteristics, such as age, race, and ethnicity.
Future versions of MELD could potentially consider these factors, said session moderator Aleksander Krag, MD, PhD, MBA, professor of clinical medicine at the University of Southern Denmark, Odense, and secretary general of the European Association for the Study of the Liver, 2023-2025.
“There are infinite versions of MELD that can be made,” Kwong said. “It’s still early to see how MELD 3.0 will serve the system, but so far, so good.”
In a comment, Tamar Taddei, MD, professor of medicine in digestive diseases at Yale School of Medicine, New Haven, Connecticut, who comoderated the session, noted the importance of using a MELD score that considers sex-based differences.
This study brings MELD 3.0 to its fruition by reducing the disparities experienced by women who were underserved by the previous scoring systems, she said.
It was lovely to see that MELD 3.0 reduced the disparities with transplants, and also that the waitlist dropout was reduced — for both men and women,” Taddei said. “This change is a no-brainer.”
Kwong, Krag, and Taddei reported no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — , according to new research.
In particular, women are now more likely to be added to the waitlist for a liver transplant, more likely to receive a transplant, and less likely to fall off the waitlist because of death.
“MELD 3.0 improved access to transplantation for women, and now waitlist mortality and transplant rates for women more closely approximate the rates for men,” said lead author Allison Kwong, MD, assistant professor of medicine and transplant hepatologist at Stanford Medicine in California.
“Overall transplant outcomes have also improved year over year,” said Kwong, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Changes in MELD and Transplant Numbers
MELD, which estimates liver failure severity and short-term survival in patients with chronic liver disease, has been used since 2002 to determine organ allocation priority for patients in the United States awaiting liver transplantation. Originally, the score incorporated three variables: creatinine, bilirubin, and the international normalized ratio (INR). MELDNa1, or MELD 2.0, was adopted in 2016 to add sodium.
“Under this system, however, there have been sex-based disparities” with women receiving lower priority scores despite similar disease severity, said Kwong.
“This has been attributed to several factors, such as the creatinine term in the MELD score underestimating renal dysfunction in women, height and body size differences, and differences in disease etiology, and how we’ve assigned exception points historically,” she reported.
Men have had a lower pretransplant mortality rate and higher deceased donor transplant rates, she added.
MELD 3.0 was developed to address these gender differences and other determinants of waitlist outcomes. The updated equation added 1.33 points for women, as well as adding other variables, such as albumin, interactions between bilirubin and sodium, and interactions between albumin and creatinine, to increase prediction accuracy.
To observe the effects of the new system, Kwong and colleagues analyzed OPTN data for patients aged 12 years or older, focusing on the records of more than 20,300 newly registered liver transplant candidates, and about 18,700 transplant recipients, during the 12 months before and 12 months after MELD 3.0 was implemented.
After the switch, 43.7% of newly registered liver transplant candidates were women, compared with 40.4% before the switch. At registration, the median age was 55, both before and after the change in policy, and the median MELD score changed from 23 to 22 after implementation.
In addition, 42.1% of transplants occurred among women after MELD 3.0 implementation, as compared with 37.3% before. Overall, deceased donor transplant rates were similar for men and women after MELD 3.0 implementation.
The 90-day waitlist dropout rate — patients who died or became too sick to receive a transplant — decreased from 13.5% to 9.1% among women, which may be partially attributable to MELD 3.0, said Kwong.
However, waitlist dropout rates also decreased among men, from 9.8% to 7.4%, probably because of improvements in technology, such as machine perfusion, which have increased the number of available livers, she added.
Disparities Continue to Exist
Some disparities still exist. Although the total median MELD score at transplant decreased from 29 to 27, women still had a higher median score of 29 at transplant, compared with a median score of 27 among men.
“This indicates that there may still be differences in transplant access between the sexes,” Kwong said. “There are still body size differences that can affect the probability of transplant, and this would not be addressed by MELD 3.0.”
Additional transplant disparities exist related to other patient characteristics, such as age, race, and ethnicity.
Future versions of MELD could potentially consider these factors, said session moderator Aleksander Krag, MD, PhD, MBA, professor of clinical medicine at the University of Southern Denmark, Odense, and secretary general of the European Association for the Study of the Liver, 2023-2025.
“There are infinite versions of MELD that can be made,” Kwong said. “It’s still early to see how MELD 3.0 will serve the system, but so far, so good.”
In a comment, Tamar Taddei, MD, professor of medicine in digestive diseases at Yale School of Medicine, New Haven, Connecticut, who comoderated the session, noted the importance of using a MELD score that considers sex-based differences.
This study brings MELD 3.0 to its fruition by reducing the disparities experienced by women who were underserved by the previous scoring systems, she said.
It was lovely to see that MELD 3.0 reduced the disparities with transplants, and also that the waitlist dropout was reduced — for both men and women,” Taddei said. “This change is a no-brainer.”
Kwong, Krag, and Taddei reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AASLD 24
‘Watershed Moment’: Semaglutide Shown to Be Effective in MASH
SAN DIEGO — according to interim results from a phase 3 trial.
At 72 weeks, a 2.4-mg once-weekly subcutaneous dose of semaglutide demonstrated superiority, compared with placebo, for the two primary endpoints: Resolution of steatohepatitis with no worsening of fibrosis and improvement in liver fibrosis with no worsening of steatohepatitis.
“It’s been a long journey. I’ve been working with GLP-1s for 16 years, and it’s great to be able to report the first GLP-1 receptor agonist to demonstrate efficacy in a phase 3 trial for MASH,” said lead author Philip Newsome, MD, PhD, director of the Roger Williams Institute of Liver Studies at King’s College London in England.
“There were also improvements in a slew of other noninvasive markers,” said Newsome, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Although already seen in a broader context, “it’s nice to see a demonstration of the cardiometabolic benefits in the context of MASH and a reassuring safety profile,” he added.
Interim ESSENCE Trial Analysis
ESSENCE (NCT04822181) is an ongoing multicenter, phase 3 randomized, double-blind, placebo-controlled outcome trial studying semaglutide for the potential treatment of MASH.
The trial includes 1200 participants with biopsy-defined MASH and fibrosis, stages F2 and F3, who were randomized 2:1 to a once-weekly subcutaneous injection of 2.4 mg of semaglutide or placebo for 240 weeks. After initiation, the semaglutide dosage was increased every 4 weeks up to 16 weeks when the full dose (2.4 mg) was reached.
In a planned interim analysis, the trial investigators evaluated the primary endpoints at week 72 for the first 800 participants, with biopsies taken at weeks 1 and 72.
A total of 534 people were randomized to the semaglutide group, including 169 with F2 fibrosis and 365 with F3 fibrosis. Among the 266 participants randomized to placebo, 81 had F2 fibrosis and 185 had F3 fibrosis.
At baseline, the patient characteristics were similar between the groups (mean age, 56 years; body mass index, 34.6). A majority of participants also were White (67.5%), women (57.1%), had type 2 diabetes (55.9%), F3 fibrosis (68.8%), and enhanced liver fibrosis (ELF) scores around 10 (55.5%).
For the first primary endpoint, 62.9% of those in the semaglutide group and 34.1% of those in the placebo group reached resolution of steatohepatitis with no worsening of fibrosis. This represented an estimated difference in responder proportions (EDP) of 28.9%.
In addition, 37% of those in the semaglutide group and 22.5% of those in the placebo group met the second primary endpoint of improvement in liver fibrosis with no worsening of steatohepatitis (EDP, 14.4%).
Among the secondary endpoints, combined resolution of steatohepatitis with a one-stage improvement in liver fibrosis occurred in 32.8% of the semaglutide group and 16.2% of the placebo group (EDP, 16.6%).
In additional analyses, Newsome and colleagues found 20%-40% improvements in liver enzymes and noninvasive fibrosis markers, such as ELF and vibration-controlled transient elastography liver stiffness.
Weight loss was also significant, with a 10.5% reduction in the semaglutide group compared with a 2% reduction in the placebo group.
Cardiometabolic risk factors improved as well, with changes in blood pressure measurements, hemoglobin A1c scores, and cholesterol values.
Although not considered statistically significant, patients in the semaglutide group also reported greater reductions in body pain.
In a safety analysis of 1195 participants at 96 weeks, adverse events, severe adverse events, and discontinuations were similar in both groups. Not surprisingly, gastrointestinal side effects were more commonly reported in the semaglutide group, Newsome said.
Highly Anticipated Results
After Newsome’s presentation, attendees applauded.
Rohit Loomba, MD, a gastroenterologist at the University of California, San Diego, who was not involved with the study, called the results the “highlight of the meeting.”
This sentiment was echoed by Naga Chalasani, MD, AGAF, a gastroenterologist at Indiana University Medical Center, Indianapolis, who called the results a “watershed moment in the MASH field” with “terrific data.”
Based on questions after the presentation, Newsome indicated that future ESSENCE reports would look at certain aspects of the results, such as the 10% weight loss among those in the semaglutide group, as well as the mechanisms of histological and fibrosis improvement.
“We know from other GLP-1 trials that more weight loss occurs in those who don’t have type 2 diabetes, and we’re still running those analyses,” he said. “Weight loss is clearly a major contributor to MASH improvement, but there seem to be some weight-independent effects here, which are likely linked to insulin sensitivity or inflammation. We look forward to presenting those analyses in due course.”
In a comment, Kimberly Ann Brown, MD, AGAF, chief of gastroenterology and hepatology at Henry Ford Health System in Detroit, Michigan, AASLD Foundation chair, and comoderator of the late-breaking abstract session, spoke about the highly anticipated presentation.
“This study was really the pinnacle of this meeting. We’ve all been waiting for this data, in large part because many of our patients are already using these medications,” Brown said. “Seeing the benefit for the liver, as well as lipids and other cardiovascular measures, is so important. Having this confirmatory study will hopefully lead to the availability of the medication for this indication among our patients.”
Newsome reported numerous disclosures, including consultant relationships with pharmaceutical companies, such as Novo Nordisk, Boehringer Ingelheim, and Madrigal Pharmaceuticals. Loomba has research grant relationships with numerous companies, including Hanmi, Gilead, Galmed Pharmaceuticals, Galectin Therapeutics, Eli Lilly, Bristol-Myers Squibb, and Boehringer Ingelheim. Chalasani has consultant relationships with Ipsen, Pfizer, Merck, Altimmune, GSK, Madrigal Pharmaceuticals, and Zydus. Brown reported no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — according to interim results from a phase 3 trial.
At 72 weeks, a 2.4-mg once-weekly subcutaneous dose of semaglutide demonstrated superiority, compared with placebo, for the two primary endpoints: Resolution of steatohepatitis with no worsening of fibrosis and improvement in liver fibrosis with no worsening of steatohepatitis.
“It’s been a long journey. I’ve been working with GLP-1s for 16 years, and it’s great to be able to report the first GLP-1 receptor agonist to demonstrate efficacy in a phase 3 trial for MASH,” said lead author Philip Newsome, MD, PhD, director of the Roger Williams Institute of Liver Studies at King’s College London in England.
“There were also improvements in a slew of other noninvasive markers,” said Newsome, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Although already seen in a broader context, “it’s nice to see a demonstration of the cardiometabolic benefits in the context of MASH and a reassuring safety profile,” he added.
Interim ESSENCE Trial Analysis
ESSENCE (NCT04822181) is an ongoing multicenter, phase 3 randomized, double-blind, placebo-controlled outcome trial studying semaglutide for the potential treatment of MASH.
The trial includes 1200 participants with biopsy-defined MASH and fibrosis, stages F2 and F3, who were randomized 2:1 to a once-weekly subcutaneous injection of 2.4 mg of semaglutide or placebo for 240 weeks. After initiation, the semaglutide dosage was increased every 4 weeks up to 16 weeks when the full dose (2.4 mg) was reached.
In a planned interim analysis, the trial investigators evaluated the primary endpoints at week 72 for the first 800 participants, with biopsies taken at weeks 1 and 72.
A total of 534 people were randomized to the semaglutide group, including 169 with F2 fibrosis and 365 with F3 fibrosis. Among the 266 participants randomized to placebo, 81 had F2 fibrosis and 185 had F3 fibrosis.
At baseline, the patient characteristics were similar between the groups (mean age, 56 years; body mass index, 34.6). A majority of participants also were White (67.5%), women (57.1%), had type 2 diabetes (55.9%), F3 fibrosis (68.8%), and enhanced liver fibrosis (ELF) scores around 10 (55.5%).
For the first primary endpoint, 62.9% of those in the semaglutide group and 34.1% of those in the placebo group reached resolution of steatohepatitis with no worsening of fibrosis. This represented an estimated difference in responder proportions (EDP) of 28.9%.
In addition, 37% of those in the semaglutide group and 22.5% of those in the placebo group met the second primary endpoint of improvement in liver fibrosis with no worsening of steatohepatitis (EDP, 14.4%).
Among the secondary endpoints, combined resolution of steatohepatitis with a one-stage improvement in liver fibrosis occurred in 32.8% of the semaglutide group and 16.2% of the placebo group (EDP, 16.6%).
In additional analyses, Newsome and colleagues found 20%-40% improvements in liver enzymes and noninvasive fibrosis markers, such as ELF and vibration-controlled transient elastography liver stiffness.
Weight loss was also significant, with a 10.5% reduction in the semaglutide group compared with a 2% reduction in the placebo group.
Cardiometabolic risk factors improved as well, with changes in blood pressure measurements, hemoglobin A1c scores, and cholesterol values.
Although not considered statistically significant, patients in the semaglutide group also reported greater reductions in body pain.
In a safety analysis of 1195 participants at 96 weeks, adverse events, severe adverse events, and discontinuations were similar in both groups. Not surprisingly, gastrointestinal side effects were more commonly reported in the semaglutide group, Newsome said.
Highly Anticipated Results
After Newsome’s presentation, attendees applauded.
Rohit Loomba, MD, a gastroenterologist at the University of California, San Diego, who was not involved with the study, called the results the “highlight of the meeting.”
This sentiment was echoed by Naga Chalasani, MD, AGAF, a gastroenterologist at Indiana University Medical Center, Indianapolis, who called the results a “watershed moment in the MASH field” with “terrific data.”
Based on questions after the presentation, Newsome indicated that future ESSENCE reports would look at certain aspects of the results, such as the 10% weight loss among those in the semaglutide group, as well as the mechanisms of histological and fibrosis improvement.
“We know from other GLP-1 trials that more weight loss occurs in those who don’t have type 2 diabetes, and we’re still running those analyses,” he said. “Weight loss is clearly a major contributor to MASH improvement, but there seem to be some weight-independent effects here, which are likely linked to insulin sensitivity or inflammation. We look forward to presenting those analyses in due course.”
In a comment, Kimberly Ann Brown, MD, AGAF, chief of gastroenterology and hepatology at Henry Ford Health System in Detroit, Michigan, AASLD Foundation chair, and comoderator of the late-breaking abstract session, spoke about the highly anticipated presentation.
“This study was really the pinnacle of this meeting. We’ve all been waiting for this data, in large part because many of our patients are already using these medications,” Brown said. “Seeing the benefit for the liver, as well as lipids and other cardiovascular measures, is so important. Having this confirmatory study will hopefully lead to the availability of the medication for this indication among our patients.”
Newsome reported numerous disclosures, including consultant relationships with pharmaceutical companies, such as Novo Nordisk, Boehringer Ingelheim, and Madrigal Pharmaceuticals. Loomba has research grant relationships with numerous companies, including Hanmi, Gilead, Galmed Pharmaceuticals, Galectin Therapeutics, Eli Lilly, Bristol-Myers Squibb, and Boehringer Ingelheim. Chalasani has consultant relationships with Ipsen, Pfizer, Merck, Altimmune, GSK, Madrigal Pharmaceuticals, and Zydus. Brown reported no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — according to interim results from a phase 3 trial.
At 72 weeks, a 2.4-mg once-weekly subcutaneous dose of semaglutide demonstrated superiority, compared with placebo, for the two primary endpoints: Resolution of steatohepatitis with no worsening of fibrosis and improvement in liver fibrosis with no worsening of steatohepatitis.
“It’s been a long journey. I’ve been working with GLP-1s for 16 years, and it’s great to be able to report the first GLP-1 receptor agonist to demonstrate efficacy in a phase 3 trial for MASH,” said lead author Philip Newsome, MD, PhD, director of the Roger Williams Institute of Liver Studies at King’s College London in England.
“There were also improvements in a slew of other noninvasive markers,” said Newsome, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
Although already seen in a broader context, “it’s nice to see a demonstration of the cardiometabolic benefits in the context of MASH and a reassuring safety profile,” he added.
Interim ESSENCE Trial Analysis
ESSENCE (NCT04822181) is an ongoing multicenter, phase 3 randomized, double-blind, placebo-controlled outcome trial studying semaglutide for the potential treatment of MASH.
The trial includes 1200 participants with biopsy-defined MASH and fibrosis, stages F2 and F3, who were randomized 2:1 to a once-weekly subcutaneous injection of 2.4 mg of semaglutide or placebo for 240 weeks. After initiation, the semaglutide dosage was increased every 4 weeks up to 16 weeks when the full dose (2.4 mg) was reached.
In a planned interim analysis, the trial investigators evaluated the primary endpoints at week 72 for the first 800 participants, with biopsies taken at weeks 1 and 72.
A total of 534 people were randomized to the semaglutide group, including 169 with F2 fibrosis and 365 with F3 fibrosis. Among the 266 participants randomized to placebo, 81 had F2 fibrosis and 185 had F3 fibrosis.
At baseline, the patient characteristics were similar between the groups (mean age, 56 years; body mass index, 34.6). A majority of participants also were White (67.5%), women (57.1%), had type 2 diabetes (55.9%), F3 fibrosis (68.8%), and enhanced liver fibrosis (ELF) scores around 10 (55.5%).
For the first primary endpoint, 62.9% of those in the semaglutide group and 34.1% of those in the placebo group reached resolution of steatohepatitis with no worsening of fibrosis. This represented an estimated difference in responder proportions (EDP) of 28.9%.
In addition, 37% of those in the semaglutide group and 22.5% of those in the placebo group met the second primary endpoint of improvement in liver fibrosis with no worsening of steatohepatitis (EDP, 14.4%).
Among the secondary endpoints, combined resolution of steatohepatitis with a one-stage improvement in liver fibrosis occurred in 32.8% of the semaglutide group and 16.2% of the placebo group (EDP, 16.6%).
In additional analyses, Newsome and colleagues found 20%-40% improvements in liver enzymes and noninvasive fibrosis markers, such as ELF and vibration-controlled transient elastography liver stiffness.
Weight loss was also significant, with a 10.5% reduction in the semaglutide group compared with a 2% reduction in the placebo group.
Cardiometabolic risk factors improved as well, with changes in blood pressure measurements, hemoglobin A1c scores, and cholesterol values.
Although not considered statistically significant, patients in the semaglutide group also reported greater reductions in body pain.
In a safety analysis of 1195 participants at 96 weeks, adverse events, severe adverse events, and discontinuations were similar in both groups. Not surprisingly, gastrointestinal side effects were more commonly reported in the semaglutide group, Newsome said.
Highly Anticipated Results
After Newsome’s presentation, attendees applauded.
Rohit Loomba, MD, a gastroenterologist at the University of California, San Diego, who was not involved with the study, called the results the “highlight of the meeting.”
This sentiment was echoed by Naga Chalasani, MD, AGAF, a gastroenterologist at Indiana University Medical Center, Indianapolis, who called the results a “watershed moment in the MASH field” with “terrific data.”
Based on questions after the presentation, Newsome indicated that future ESSENCE reports would look at certain aspects of the results, such as the 10% weight loss among those in the semaglutide group, as well as the mechanisms of histological and fibrosis improvement.
“We know from other GLP-1 trials that more weight loss occurs in those who don’t have type 2 diabetes, and we’re still running those analyses,” he said. “Weight loss is clearly a major contributor to MASH improvement, but there seem to be some weight-independent effects here, which are likely linked to insulin sensitivity or inflammation. We look forward to presenting those analyses in due course.”
In a comment, Kimberly Ann Brown, MD, AGAF, chief of gastroenterology and hepatology at Henry Ford Health System in Detroit, Michigan, AASLD Foundation chair, and comoderator of the late-breaking abstract session, spoke about the highly anticipated presentation.
“This study was really the pinnacle of this meeting. We’ve all been waiting for this data, in large part because many of our patients are already using these medications,” Brown said. “Seeing the benefit for the liver, as well as lipids and other cardiovascular measures, is so important. Having this confirmatory study will hopefully lead to the availability of the medication for this indication among our patients.”
Newsome reported numerous disclosures, including consultant relationships with pharmaceutical companies, such as Novo Nordisk, Boehringer Ingelheim, and Madrigal Pharmaceuticals. Loomba has research grant relationships with numerous companies, including Hanmi, Gilead, Galmed Pharmaceuticals, Galectin Therapeutics, Eli Lilly, Bristol-Myers Squibb, and Boehringer Ingelheim. Chalasani has consultant relationships with Ipsen, Pfizer, Merck, Altimmune, GSK, Madrigal Pharmaceuticals, and Zydus. Brown reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AASLD 24
How to Discuss Lifestyle Modifications in MASLD
Metabolic dysfunction–associated steatotic liver disease (MASLD) is a spectrum of hepatic disorders closely linked to insulin resistance, dyslipidemia, hypertension, and obesity.1 An increasingly prevalent cause of liver disease and liver-related deaths worldwide, MASLD affects at least 38% of the global population.2 The immense burden of MASLD and its complications demands attention and action from the medical community.
Lifestyle modifications involving weight management and dietary composition adjustments are the foundation of addressing MASLD, with a critical emphasis on early intervention.3 Healthy dietary indices and weight loss can lower enzyme levels, reduce hepatic fat content, improve insulin resistance, and overall, reduce the risk of MASLD.3 Given the abundance of literature that exists on the benefits of lifestyle modifications on liver and general health outcomes, clinicians should be prepared to have informed, individualized, and culturally concordant conversations with their patients about these modifications. This Short Clinical Review aims to
Initiate the Conversation
Conversations about lifestyle modifications can be challenging and complex. If patients themselves are not initiating conversations about dietary composition and physical activity, then it is important for clinicians to start a productive discussion.
The use of non-stigmatizing, open-ended questions can begin this process. For example, clinicians can consider asking patients: “How would you describe your lifestyle habits, such as foods you usually eat and your physical activity levels? What do you usually look for when you are grocery shopping or thinking of a meal to cook? Are there ways in which you stay physically active throughout the day or week?”4 (see Table 1).
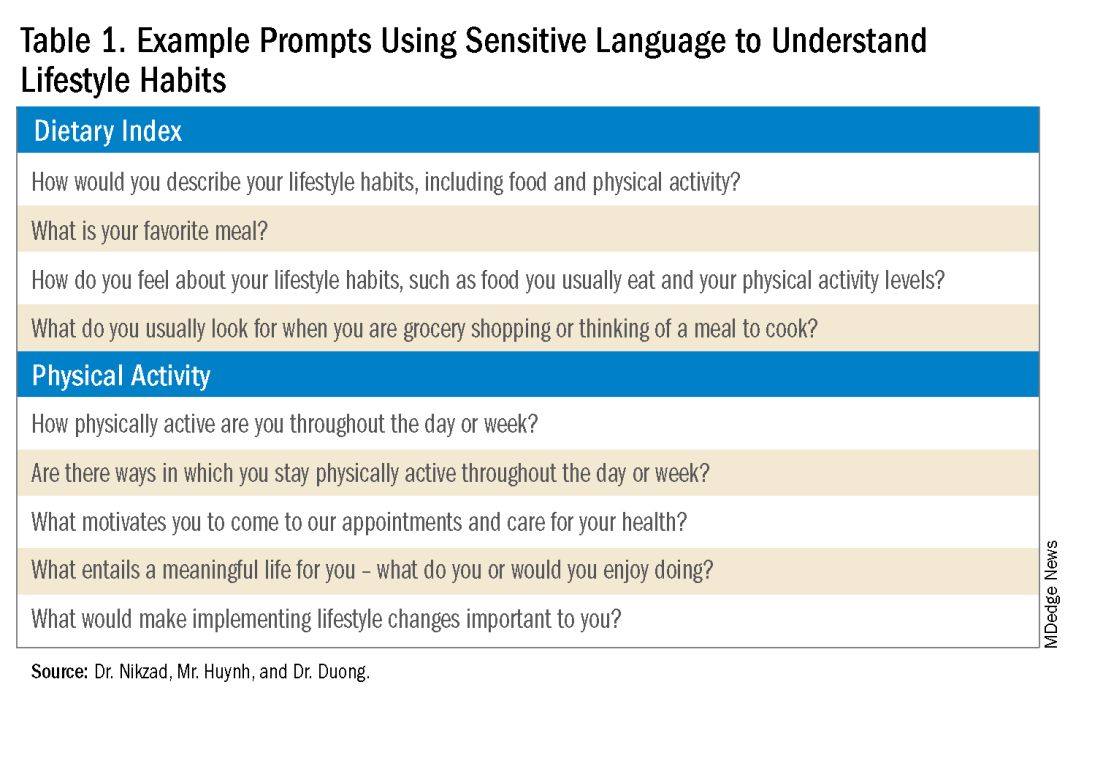
Such questions can provide significant insight into patients’ activity and eating patterns. They also eliminate the utilization of words such as “diet” or “exercise” that may have associated stigma, pressure, or negative connotations.4
Regardless, some patients may not feel prepared or willing to discuss lifestyle modifications during a visit, especially if it is the first clinical encounter when rapport has yet to even be established.4 Lifestyle modifications are implemented at various paces, and patients have their individual timelines for achieving these adjustments. Building rapport with patients and creating spaces in which they feel safe discussing and incorporating changes to various components of their lives can take time. Patients want to trust their providers while being vulnerable. They want to trust that their providers will guide them in what can sometimes be a life altering journey. It is important for clinicians to acknowledge and respect this reality when caring for patients with MASLD. Dr. Duong often utilizes this phrase, “It may seem like you are about to walk through fire, but we are here to walk with you. Remember, what doesn’t challenge you, doesn’t change you.”
Identify Motivators of Engagement
Identifying patients’ motivators of engagement will allow clinicians to guide patients through not only the introduction, but also the maintenance of such changes. Improvements in dietary composition and physical activity are often recommended by clinicians who are inevitably and understandably concerned about the consequences of MASLD. Liver diseases, specifically cirrhosis and hepatocellular carcinoma, as well as associated metabolic disorders, are consequences that could result from poorly controlled MASLD. Though these consequences should be conveyed to patients, this tactic may not always serve as an impetus for patients to engage in behavioral changes.5
Clinicians can shed light on motivators by utilizing these suggested prompts: “What motivates you to come to our appointments and care for your health? What entails a meaningful life for you — what do or would you enjoy doing? What would make implementing lifestyle changes important to you?” Patient goals may include “being able to keep up with their grandchildren,” “becoming a runner,” or “providing healthy meals for their families.”5,6 Engagement is more likely to be feasible and sustainable when lifestyle modifications are tied to goals that are personally meaningful and relevant to patients.
Within the realm of physical activity specifically, exercise can be individualized to optimize motivation as well. Both aerobic exercise and resistance training are associated independently with benefits such as weight loss and decreased hepatic adipose content.3 Currently, there is no consensus regarding the optimal type of physical activity for patients with MASLD; therefore, clinicians should encourage patients to personalize physical activity.3 While some patients may prefer aerobic activities such as running and swimming, others may find more fulfillment in weightlifting or high intensity interval training. Furthermore, patients with cardiopulmonary or musculoskeletal health contraindications may be limited to specific types of exercise. It is appropriate and helpful for clinicians to ask patients, “What types of physical activity feel achievable and realistic for you at this time?” If physicians can guide patients with MASLD in identifying types of exercise that are safe and enjoyable, their patients may be more motivated to implement such lifestyle changes.
It is also crucial to recognize that lifestyle changes demand active effort from patients. While sustained improvements in body weight and dietary composition are the foundation of MASLD management, they can initially feel cumbersome and abstract to patients. Physicians can help their patients remain motivated by developing small, tangible goals such as “reducing daily caloric intake by 500 kcal” or “participating in three 30-minute fitness classes per week.” These goals should be developed jointly with patients, primarily to ensure that they are tangible, feasible, and productive.
A Culturally Safe Approach
Additionally, acknowledging a patient’s cultural background can be conducive to incorporating patient-specific care into MASLD management. For example, qualitative studies have shown that people from Mexican heritage traditionally complement dinners with soft drinks. While meal portion sizes vary amongst households, families of Mexican origin believe larger portion sizes may be perceived as healthier than Western diets since their cuisine incorporates more vegetables into each dish.7
Eating rituals should also be considered since some families expect the absence of leftovers on the plate.7 Therefore, it is appropriate to consider questions such as, “What are common ingredients in your culture? What are some of your family traditions when it comes to meals?” By integrating cultural considerations, clinicians can adopt a culturally safe approach, empowering patients to make lifestyle modifications tailored toward their unique social identities. Clinicians should avoid generalizations or stereotypes about cultural values regarding lifestyle practices, as these can vary among individuals.
Identify Barriers to Lifestyle Changes and Social Determinants of Health
Even with delicate language from providers and immense motivation from patients, barriers to lifestyle changes persist. Studies have shown that patients with MASLD perceive a lack of self-efficacy and knowledge as major barriers to adopting lifestyle modifications.8,9 Patients have reported challenges in interpreting nutritional data, identifying caloric intake and portion sizes. Physicians can effectively guide patients through lifestyle changes by identifying each patient’s unique knowledge gap and determining the most effective, accessible form of education. For example, some patients may benefit from jointly interpreting a nutritional label with their healthcare providers, while others may require educational materials and interventions provided by a registered dietitian.
Understanding patients’ professional or other commitments can help physicians further individualize recommendations. Questions such as, “Do you have work or other responsibilities that take up some of your time during the day?” minimize presumptive language about employment status. It can reveal whether patients have schedules that make certain lifestyle changes more challenging than others. For example, a patient who is an overnight delivery associate at a warehouse may have a different routine from another patient who is a family member’s caretaker. This framework allows physicians to build rapport with their patients and ultimately, make lifestyle recommendations that are more accessible.
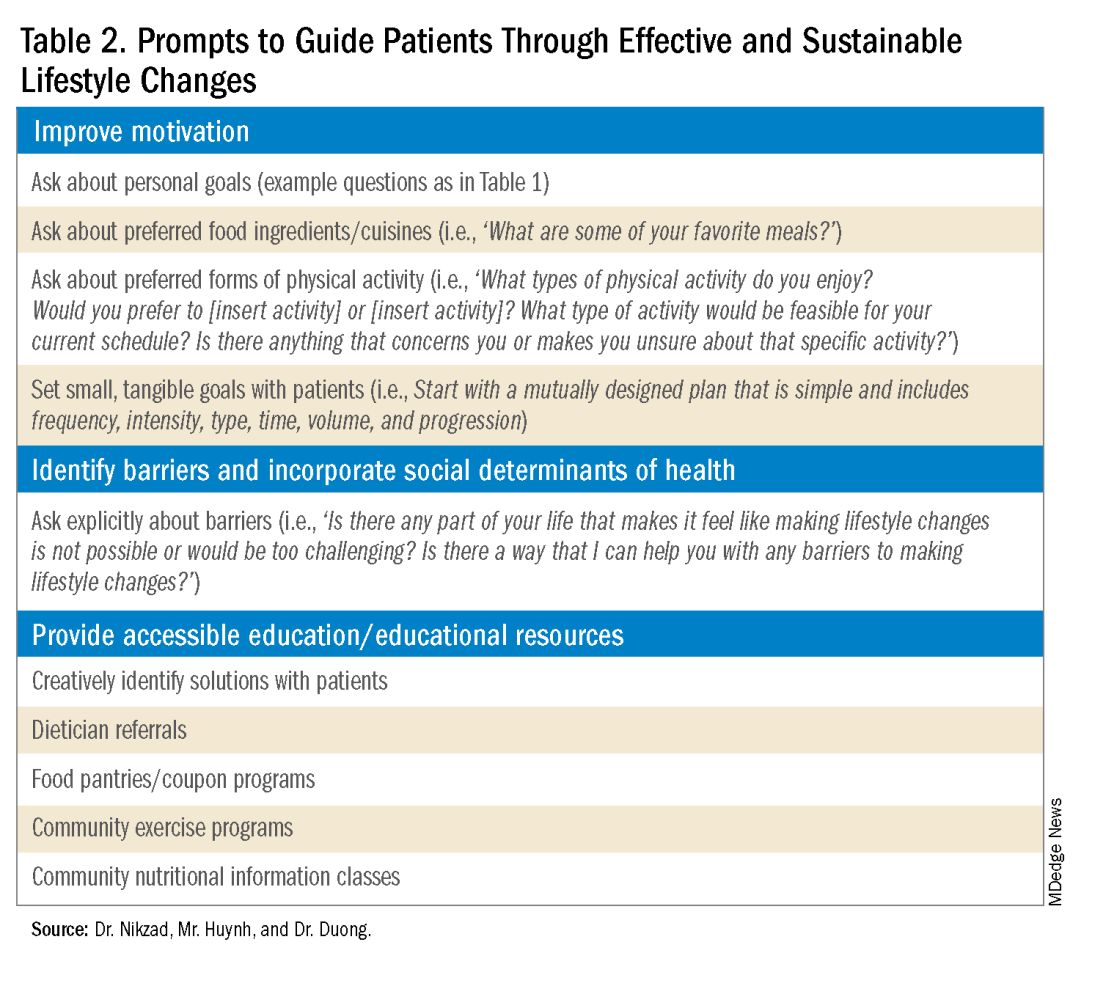
Though MASLD is driven by inflammation and metabolic dysregulation, social determinants of health play an equally important role in disease development and progression.10 As previously discussed, health literacy can deeply influence patients’ abilities to implement lifestyle changes. Furthermore, economic stability, neighborhood and built environment (i.e., access to fresh produce and sidewalks), community, and social support also impact lifestyle modifications. It is paramount to understand the tangible social factors in which patients live. Such factors can be ascertained by beginning the dialogue with “Which grocery stores do you find most convenient? How do you travel to obtain food/attend community exercise programs?” These questions may offer insight into physical barriers to lifestyle changes. Physicians must utilize an intersectional lens that incorporates patients’ unique circumstances of existence into their individualized health care plans to address MASLD.
Summary
- Communication preferences, cultural backgrounds, and sociocultural contexts of patient existence must be considered when treating a patient with MASLD.
- The utilization of an intersectional and culturally safe approach to communication with patients can lead to more sustainable lifestyle changes and improved health outcomes.
- Equipping and empowering physicians to have meaningful discussions about MASLD is crucial to combating a spectrum of diseases that is rapidly affecting a substantial proportion of patients worldwide.
Dr. Nikzad is based in the Department of Internal Medicine at University of Chicago Medicine (@NewshaN27). Mr. Huynh is a medical student at Stony Brook University Renaissance School of Medicine, Stony Brook, N.Y. (@danielhuynhhh). Dr. Duong is an assistant professor of medicine and transplant hepatologist at Stanford University, Palo Alto, Calif. (@doctornikkid). They have no conflicts of interest to declare.
References
1. Mohanty A. MASLD/MASH and Weight Loss. GI & Hepatology News. 2023 Oct. Data Trends 2023:9-13.
2. Wong VW, et al. Changing epidemiology, global trends and implications for outcomes of NAFLD. J Hepatol. 2023 Sep. doi: 10.1016/j.jhep.2023.04.036.
3. Zeng J, et al. Therapeutic management of metabolic dysfunction associated steatotic liver disease. United European Gastroenterol J. 2024 Mar. doi: 10.1002/ueg2.12525.
4. Berg S. How patients can start—and stick with—key lifestyle changes. AMA Public Health. 2020 Jan.
5. Berg S. 3 ways to get patients engaged in lasting lifestyle change. AMA Diabetes. 2019 Jan.
6. Teixeira PJ, et al. Motivation, self-determination, and long-term weight control. Int J Behav Nutr Phys Act. 2012 Mar. doi: 10.1186/1479-5868-9-22.
7. Aceves-Martins M, et al. Cultural factors related to childhood and adolescent obesity in Mexico: A systematic review of qualitative studies. Obes Rev. 2022 Sep. doi: 10.1111/obr.13461.
8. Figueroa G, et al. Low health literacy, lack of knowledge, and self-control hinder healthy lifestyles in diverse patients with steatotic liver disease. Dig Dis Sci. 2024 Feb. doi: 10.1007/s10620-023-08212-9.
9. Wang L, et al. Factors influencing adherence to lifestyle prescriptions among patients with nonalcoholic fatty liver disease: A qualitative study using the health action process approach framework. Front Public Health. 2023 Mar. doi: 10.3389/fpubh.2023.1131827.
10. Andermann A, CLEAR Collaboration. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016 Dec. doi: 10.1503/cmaj.160177.
Metabolic dysfunction–associated steatotic liver disease (MASLD) is a spectrum of hepatic disorders closely linked to insulin resistance, dyslipidemia, hypertension, and obesity.1 An increasingly prevalent cause of liver disease and liver-related deaths worldwide, MASLD affects at least 38% of the global population.2 The immense burden of MASLD and its complications demands attention and action from the medical community.
Lifestyle modifications involving weight management and dietary composition adjustments are the foundation of addressing MASLD, with a critical emphasis on early intervention.3 Healthy dietary indices and weight loss can lower enzyme levels, reduce hepatic fat content, improve insulin resistance, and overall, reduce the risk of MASLD.3 Given the abundance of literature that exists on the benefits of lifestyle modifications on liver and general health outcomes, clinicians should be prepared to have informed, individualized, and culturally concordant conversations with their patients about these modifications. This Short Clinical Review aims to
Initiate the Conversation
Conversations about lifestyle modifications can be challenging and complex. If patients themselves are not initiating conversations about dietary composition and physical activity, then it is important for clinicians to start a productive discussion.
The use of non-stigmatizing, open-ended questions can begin this process. For example, clinicians can consider asking patients: “How would you describe your lifestyle habits, such as foods you usually eat and your physical activity levels? What do you usually look for when you are grocery shopping or thinking of a meal to cook? Are there ways in which you stay physically active throughout the day or week?”4 (see Table 1).
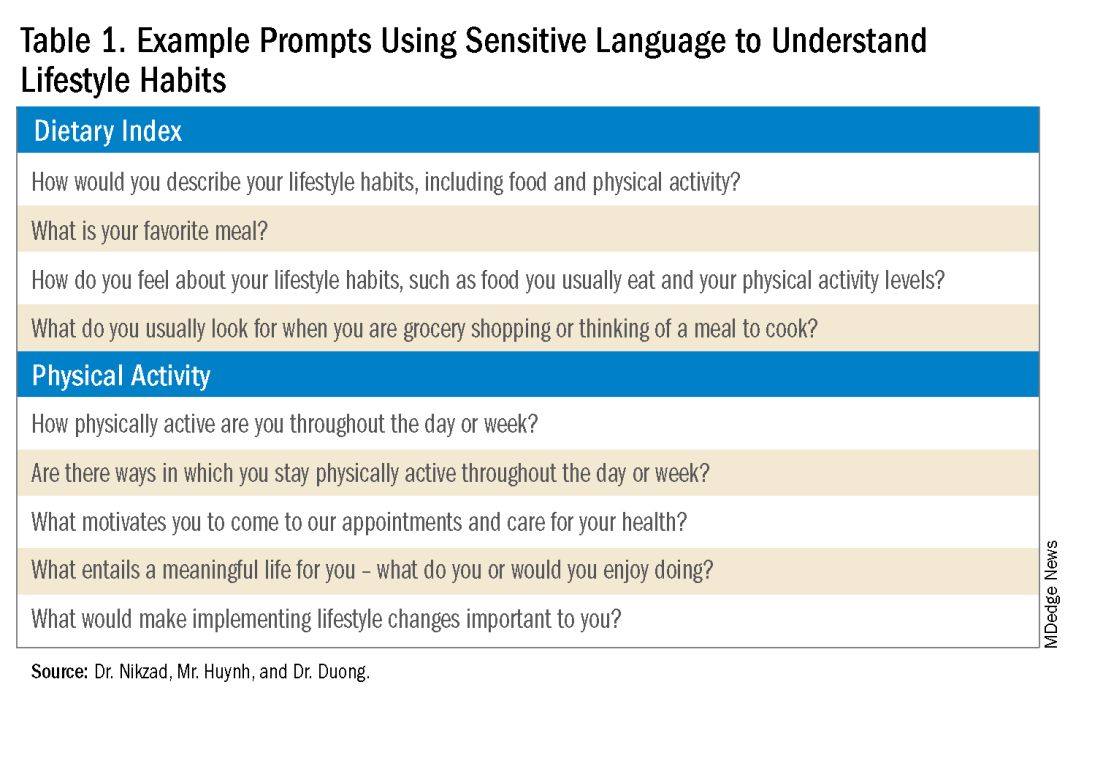
Such questions can provide significant insight into patients’ activity and eating patterns. They also eliminate the utilization of words such as “diet” or “exercise” that may have associated stigma, pressure, or negative connotations.4
Regardless, some patients may not feel prepared or willing to discuss lifestyle modifications during a visit, especially if it is the first clinical encounter when rapport has yet to even be established.4 Lifestyle modifications are implemented at various paces, and patients have their individual timelines for achieving these adjustments. Building rapport with patients and creating spaces in which they feel safe discussing and incorporating changes to various components of their lives can take time. Patients want to trust their providers while being vulnerable. They want to trust that their providers will guide them in what can sometimes be a life altering journey. It is important for clinicians to acknowledge and respect this reality when caring for patients with MASLD. Dr. Duong often utilizes this phrase, “It may seem like you are about to walk through fire, but we are here to walk with you. Remember, what doesn’t challenge you, doesn’t change you.”
Identify Motivators of Engagement
Identifying patients’ motivators of engagement will allow clinicians to guide patients through not only the introduction, but also the maintenance of such changes. Improvements in dietary composition and physical activity are often recommended by clinicians who are inevitably and understandably concerned about the consequences of MASLD. Liver diseases, specifically cirrhosis and hepatocellular carcinoma, as well as associated metabolic disorders, are consequences that could result from poorly controlled MASLD. Though these consequences should be conveyed to patients, this tactic may not always serve as an impetus for patients to engage in behavioral changes.5
Clinicians can shed light on motivators by utilizing these suggested prompts: “What motivates you to come to our appointments and care for your health? What entails a meaningful life for you — what do or would you enjoy doing? What would make implementing lifestyle changes important to you?” Patient goals may include “being able to keep up with their grandchildren,” “becoming a runner,” or “providing healthy meals for their families.”5,6 Engagement is more likely to be feasible and sustainable when lifestyle modifications are tied to goals that are personally meaningful and relevant to patients.
Within the realm of physical activity specifically, exercise can be individualized to optimize motivation as well. Both aerobic exercise and resistance training are associated independently with benefits such as weight loss and decreased hepatic adipose content.3 Currently, there is no consensus regarding the optimal type of physical activity for patients with MASLD; therefore, clinicians should encourage patients to personalize physical activity.3 While some patients may prefer aerobic activities such as running and swimming, others may find more fulfillment in weightlifting or high intensity interval training. Furthermore, patients with cardiopulmonary or musculoskeletal health contraindications may be limited to specific types of exercise. It is appropriate and helpful for clinicians to ask patients, “What types of physical activity feel achievable and realistic for you at this time?” If physicians can guide patients with MASLD in identifying types of exercise that are safe and enjoyable, their patients may be more motivated to implement such lifestyle changes.
It is also crucial to recognize that lifestyle changes demand active effort from patients. While sustained improvements in body weight and dietary composition are the foundation of MASLD management, they can initially feel cumbersome and abstract to patients. Physicians can help their patients remain motivated by developing small, tangible goals such as “reducing daily caloric intake by 500 kcal” or “participating in three 30-minute fitness classes per week.” These goals should be developed jointly with patients, primarily to ensure that they are tangible, feasible, and productive.
A Culturally Safe Approach
Additionally, acknowledging a patient’s cultural background can be conducive to incorporating patient-specific care into MASLD management. For example, qualitative studies have shown that people from Mexican heritage traditionally complement dinners with soft drinks. While meal portion sizes vary amongst households, families of Mexican origin believe larger portion sizes may be perceived as healthier than Western diets since their cuisine incorporates more vegetables into each dish.7
Eating rituals should also be considered since some families expect the absence of leftovers on the plate.7 Therefore, it is appropriate to consider questions such as, “What are common ingredients in your culture? What are some of your family traditions when it comes to meals?” By integrating cultural considerations, clinicians can adopt a culturally safe approach, empowering patients to make lifestyle modifications tailored toward their unique social identities. Clinicians should avoid generalizations or stereotypes about cultural values regarding lifestyle practices, as these can vary among individuals.
Identify Barriers to Lifestyle Changes and Social Determinants of Health
Even with delicate language from providers and immense motivation from patients, barriers to lifestyle changes persist. Studies have shown that patients with MASLD perceive a lack of self-efficacy and knowledge as major barriers to adopting lifestyle modifications.8,9 Patients have reported challenges in interpreting nutritional data, identifying caloric intake and portion sizes. Physicians can effectively guide patients through lifestyle changes by identifying each patient’s unique knowledge gap and determining the most effective, accessible form of education. For example, some patients may benefit from jointly interpreting a nutritional label with their healthcare providers, while others may require educational materials and interventions provided by a registered dietitian.
Understanding patients’ professional or other commitments can help physicians further individualize recommendations. Questions such as, “Do you have work or other responsibilities that take up some of your time during the day?” minimize presumptive language about employment status. It can reveal whether patients have schedules that make certain lifestyle changes more challenging than others. For example, a patient who is an overnight delivery associate at a warehouse may have a different routine from another patient who is a family member’s caretaker. This framework allows physicians to build rapport with their patients and ultimately, make lifestyle recommendations that are more accessible.
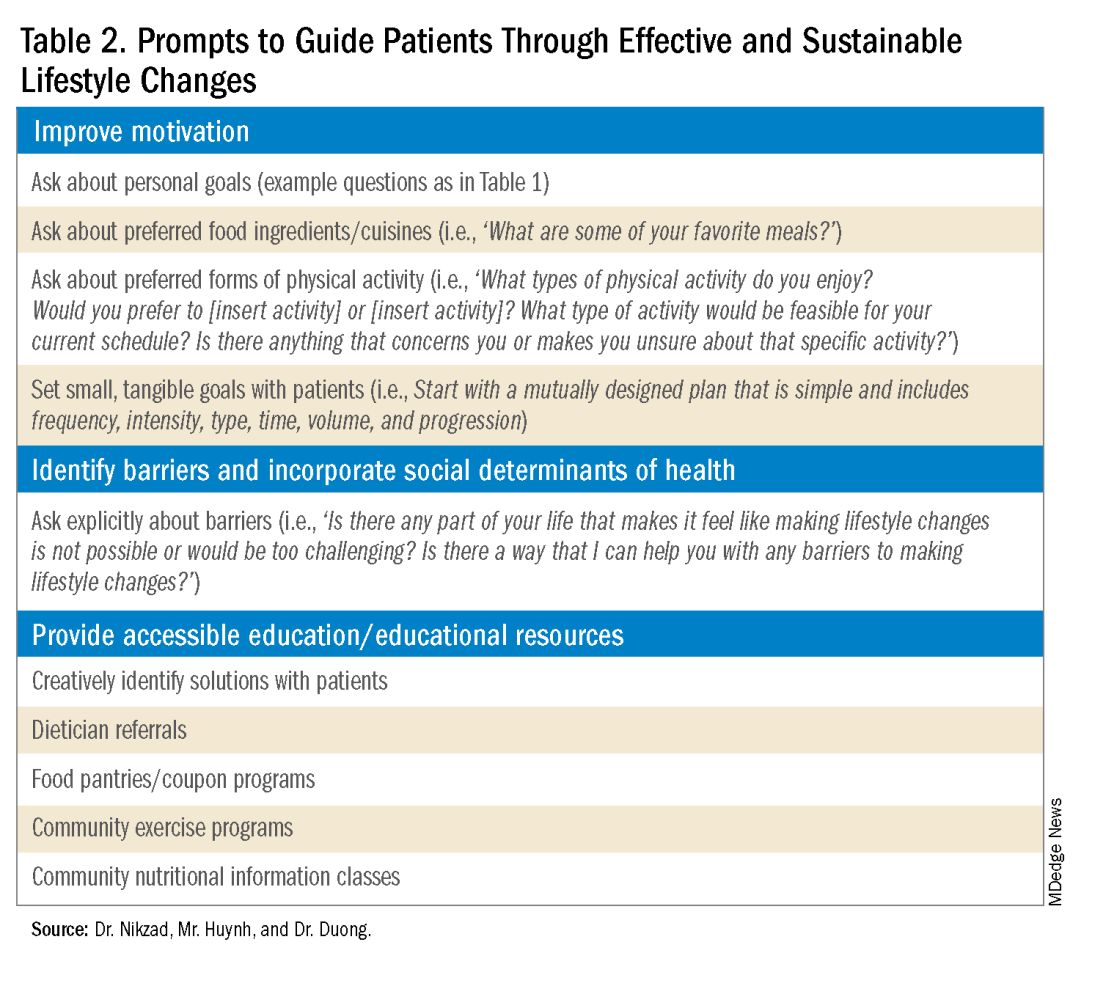
Though MASLD is driven by inflammation and metabolic dysregulation, social determinants of health play an equally important role in disease development and progression.10 As previously discussed, health literacy can deeply influence patients’ abilities to implement lifestyle changes. Furthermore, economic stability, neighborhood and built environment (i.e., access to fresh produce and sidewalks), community, and social support also impact lifestyle modifications. It is paramount to understand the tangible social factors in which patients live. Such factors can be ascertained by beginning the dialogue with “Which grocery stores do you find most convenient? How do you travel to obtain food/attend community exercise programs?” These questions may offer insight into physical barriers to lifestyle changes. Physicians must utilize an intersectional lens that incorporates patients’ unique circumstances of existence into their individualized health care plans to address MASLD.
Summary
- Communication preferences, cultural backgrounds, and sociocultural contexts of patient existence must be considered when treating a patient with MASLD.
- The utilization of an intersectional and culturally safe approach to communication with patients can lead to more sustainable lifestyle changes and improved health outcomes.
- Equipping and empowering physicians to have meaningful discussions about MASLD is crucial to combating a spectrum of diseases that is rapidly affecting a substantial proportion of patients worldwide.
Dr. Nikzad is based in the Department of Internal Medicine at University of Chicago Medicine (@NewshaN27). Mr. Huynh is a medical student at Stony Brook University Renaissance School of Medicine, Stony Brook, N.Y. (@danielhuynhhh). Dr. Duong is an assistant professor of medicine and transplant hepatologist at Stanford University, Palo Alto, Calif. (@doctornikkid). They have no conflicts of interest to declare.
References
1. Mohanty A. MASLD/MASH and Weight Loss. GI & Hepatology News. 2023 Oct. Data Trends 2023:9-13.
2. Wong VW, et al. Changing epidemiology, global trends and implications for outcomes of NAFLD. J Hepatol. 2023 Sep. doi: 10.1016/j.jhep.2023.04.036.
3. Zeng J, et al. Therapeutic management of metabolic dysfunction associated steatotic liver disease. United European Gastroenterol J. 2024 Mar. doi: 10.1002/ueg2.12525.
4. Berg S. How patients can start—and stick with—key lifestyle changes. AMA Public Health. 2020 Jan.
5. Berg S. 3 ways to get patients engaged in lasting lifestyle change. AMA Diabetes. 2019 Jan.
6. Teixeira PJ, et al. Motivation, self-determination, and long-term weight control. Int J Behav Nutr Phys Act. 2012 Mar. doi: 10.1186/1479-5868-9-22.
7. Aceves-Martins M, et al. Cultural factors related to childhood and adolescent obesity in Mexico: A systematic review of qualitative studies. Obes Rev. 2022 Sep. doi: 10.1111/obr.13461.
8. Figueroa G, et al. Low health literacy, lack of knowledge, and self-control hinder healthy lifestyles in diverse patients with steatotic liver disease. Dig Dis Sci. 2024 Feb. doi: 10.1007/s10620-023-08212-9.
9. Wang L, et al. Factors influencing adherence to lifestyle prescriptions among patients with nonalcoholic fatty liver disease: A qualitative study using the health action process approach framework. Front Public Health. 2023 Mar. doi: 10.3389/fpubh.2023.1131827.
10. Andermann A, CLEAR Collaboration. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016 Dec. doi: 10.1503/cmaj.160177.
Metabolic dysfunction–associated steatotic liver disease (MASLD) is a spectrum of hepatic disorders closely linked to insulin resistance, dyslipidemia, hypertension, and obesity.1 An increasingly prevalent cause of liver disease and liver-related deaths worldwide, MASLD affects at least 38% of the global population.2 The immense burden of MASLD and its complications demands attention and action from the medical community.
Lifestyle modifications involving weight management and dietary composition adjustments are the foundation of addressing MASLD, with a critical emphasis on early intervention.3 Healthy dietary indices and weight loss can lower enzyme levels, reduce hepatic fat content, improve insulin resistance, and overall, reduce the risk of MASLD.3 Given the abundance of literature that exists on the benefits of lifestyle modifications on liver and general health outcomes, clinicians should be prepared to have informed, individualized, and culturally concordant conversations with their patients about these modifications. This Short Clinical Review aims to
Initiate the Conversation
Conversations about lifestyle modifications can be challenging and complex. If patients themselves are not initiating conversations about dietary composition and physical activity, then it is important for clinicians to start a productive discussion.
The use of non-stigmatizing, open-ended questions can begin this process. For example, clinicians can consider asking patients: “How would you describe your lifestyle habits, such as foods you usually eat and your physical activity levels? What do you usually look for when you are grocery shopping or thinking of a meal to cook? Are there ways in which you stay physically active throughout the day or week?”4 (see Table 1).
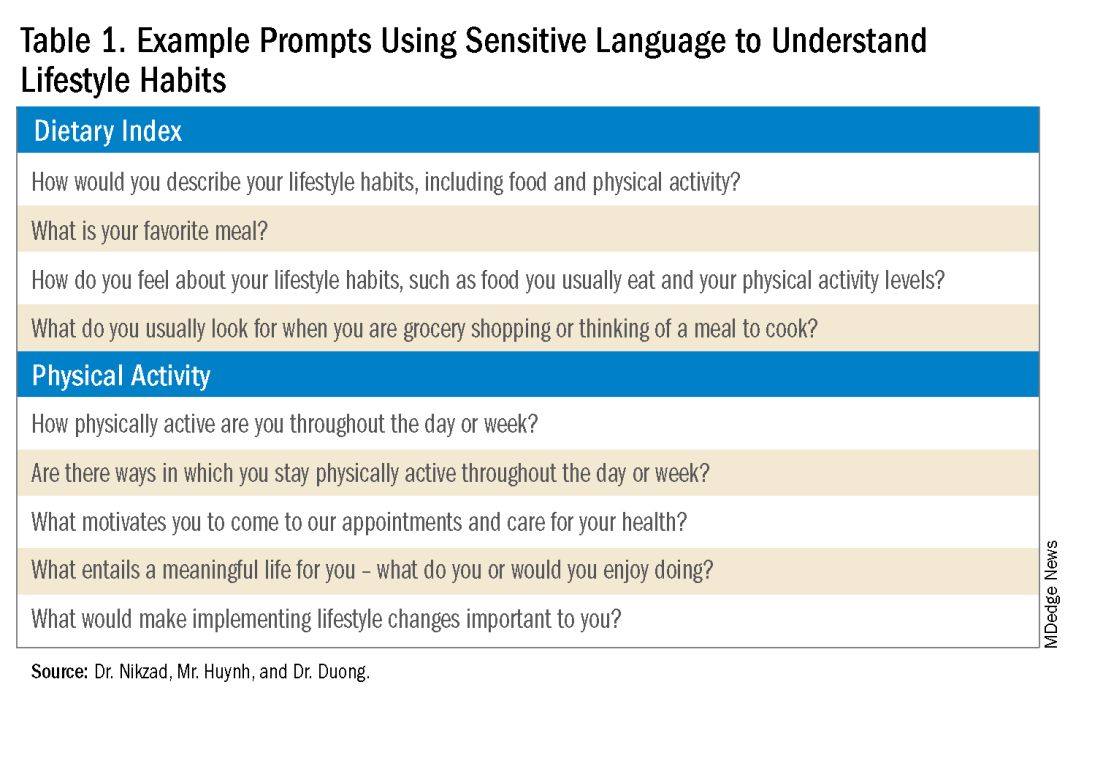
Such questions can provide significant insight into patients’ activity and eating patterns. They also eliminate the utilization of words such as “diet” or “exercise” that may have associated stigma, pressure, or negative connotations.4
Regardless, some patients may not feel prepared or willing to discuss lifestyle modifications during a visit, especially if it is the first clinical encounter when rapport has yet to even be established.4 Lifestyle modifications are implemented at various paces, and patients have their individual timelines for achieving these adjustments. Building rapport with patients and creating spaces in which they feel safe discussing and incorporating changes to various components of their lives can take time. Patients want to trust their providers while being vulnerable. They want to trust that their providers will guide them in what can sometimes be a life altering journey. It is important for clinicians to acknowledge and respect this reality when caring for patients with MASLD. Dr. Duong often utilizes this phrase, “It may seem like you are about to walk through fire, but we are here to walk with you. Remember, what doesn’t challenge you, doesn’t change you.”
Identify Motivators of Engagement
Identifying patients’ motivators of engagement will allow clinicians to guide patients through not only the introduction, but also the maintenance of such changes. Improvements in dietary composition and physical activity are often recommended by clinicians who are inevitably and understandably concerned about the consequences of MASLD. Liver diseases, specifically cirrhosis and hepatocellular carcinoma, as well as associated metabolic disorders, are consequences that could result from poorly controlled MASLD. Though these consequences should be conveyed to patients, this tactic may not always serve as an impetus for patients to engage in behavioral changes.5
Clinicians can shed light on motivators by utilizing these suggested prompts: “What motivates you to come to our appointments and care for your health? What entails a meaningful life for you — what do or would you enjoy doing? What would make implementing lifestyle changes important to you?” Patient goals may include “being able to keep up with their grandchildren,” “becoming a runner,” or “providing healthy meals for their families.”5,6 Engagement is more likely to be feasible and sustainable when lifestyle modifications are tied to goals that are personally meaningful and relevant to patients.
Within the realm of physical activity specifically, exercise can be individualized to optimize motivation as well. Both aerobic exercise and resistance training are associated independently with benefits such as weight loss and decreased hepatic adipose content.3 Currently, there is no consensus regarding the optimal type of physical activity for patients with MASLD; therefore, clinicians should encourage patients to personalize physical activity.3 While some patients may prefer aerobic activities such as running and swimming, others may find more fulfillment in weightlifting or high intensity interval training. Furthermore, patients with cardiopulmonary or musculoskeletal health contraindications may be limited to specific types of exercise. It is appropriate and helpful for clinicians to ask patients, “What types of physical activity feel achievable and realistic for you at this time?” If physicians can guide patients with MASLD in identifying types of exercise that are safe and enjoyable, their patients may be more motivated to implement such lifestyle changes.
It is also crucial to recognize that lifestyle changes demand active effort from patients. While sustained improvements in body weight and dietary composition are the foundation of MASLD management, they can initially feel cumbersome and abstract to patients. Physicians can help their patients remain motivated by developing small, tangible goals such as “reducing daily caloric intake by 500 kcal” or “participating in three 30-minute fitness classes per week.” These goals should be developed jointly with patients, primarily to ensure that they are tangible, feasible, and productive.
A Culturally Safe Approach
Additionally, acknowledging a patient’s cultural background can be conducive to incorporating patient-specific care into MASLD management. For example, qualitative studies have shown that people from Mexican heritage traditionally complement dinners with soft drinks. While meal portion sizes vary amongst households, families of Mexican origin believe larger portion sizes may be perceived as healthier than Western diets since their cuisine incorporates more vegetables into each dish.7
Eating rituals should also be considered since some families expect the absence of leftovers on the plate.7 Therefore, it is appropriate to consider questions such as, “What are common ingredients in your culture? What are some of your family traditions when it comes to meals?” By integrating cultural considerations, clinicians can adopt a culturally safe approach, empowering patients to make lifestyle modifications tailored toward their unique social identities. Clinicians should avoid generalizations or stereotypes about cultural values regarding lifestyle practices, as these can vary among individuals.
Identify Barriers to Lifestyle Changes and Social Determinants of Health
Even with delicate language from providers and immense motivation from patients, barriers to lifestyle changes persist. Studies have shown that patients with MASLD perceive a lack of self-efficacy and knowledge as major barriers to adopting lifestyle modifications.8,9 Patients have reported challenges in interpreting nutritional data, identifying caloric intake and portion sizes. Physicians can effectively guide patients through lifestyle changes by identifying each patient’s unique knowledge gap and determining the most effective, accessible form of education. For example, some patients may benefit from jointly interpreting a nutritional label with their healthcare providers, while others may require educational materials and interventions provided by a registered dietitian.
Understanding patients’ professional or other commitments can help physicians further individualize recommendations. Questions such as, “Do you have work or other responsibilities that take up some of your time during the day?” minimize presumptive language about employment status. It can reveal whether patients have schedules that make certain lifestyle changes more challenging than others. For example, a patient who is an overnight delivery associate at a warehouse may have a different routine from another patient who is a family member’s caretaker. This framework allows physicians to build rapport with their patients and ultimately, make lifestyle recommendations that are more accessible.
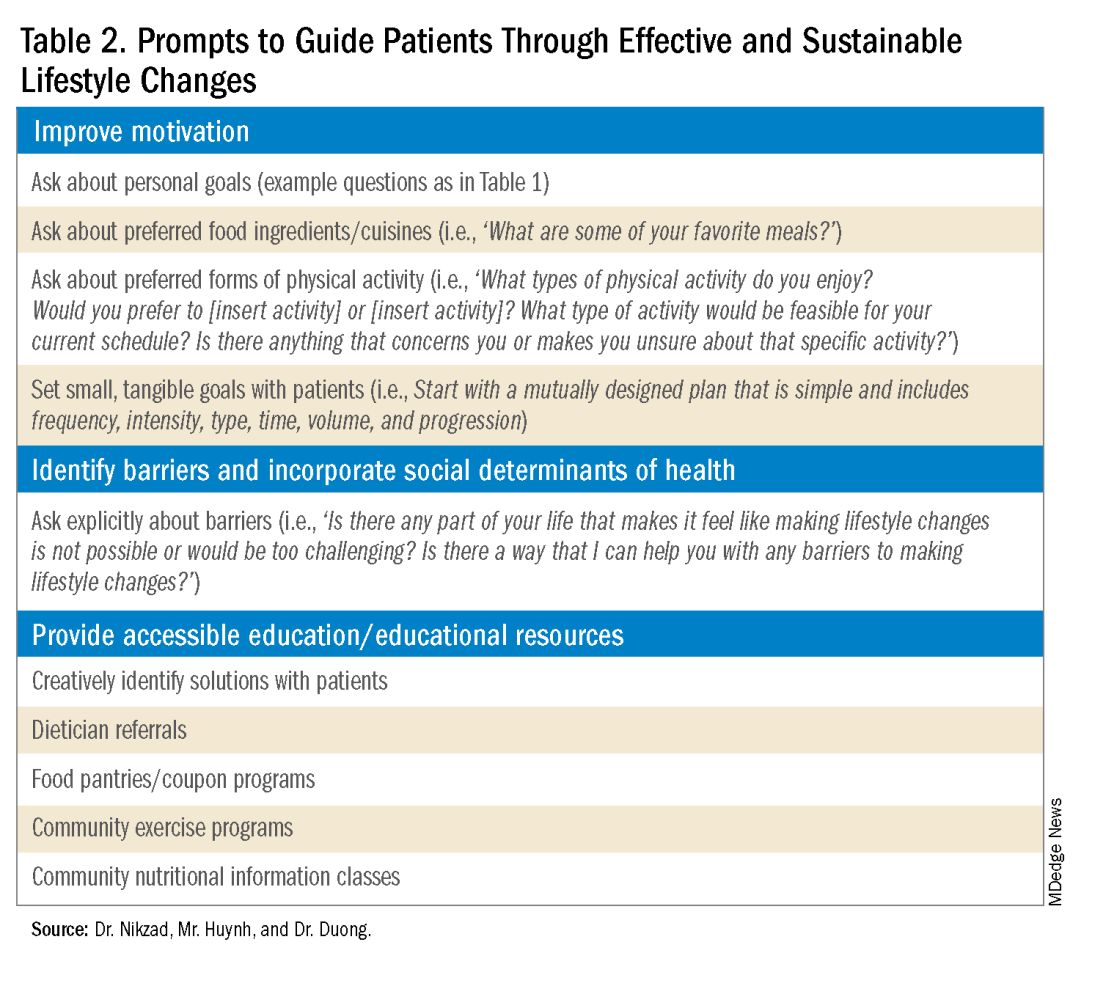
Though MASLD is driven by inflammation and metabolic dysregulation, social determinants of health play an equally important role in disease development and progression.10 As previously discussed, health literacy can deeply influence patients’ abilities to implement lifestyle changes. Furthermore, economic stability, neighborhood and built environment (i.e., access to fresh produce and sidewalks), community, and social support also impact lifestyle modifications. It is paramount to understand the tangible social factors in which patients live. Such factors can be ascertained by beginning the dialogue with “Which grocery stores do you find most convenient? How do you travel to obtain food/attend community exercise programs?” These questions may offer insight into physical barriers to lifestyle changes. Physicians must utilize an intersectional lens that incorporates patients’ unique circumstances of existence into their individualized health care plans to address MASLD.
Summary
- Communication preferences, cultural backgrounds, and sociocultural contexts of patient existence must be considered when treating a patient with MASLD.
- The utilization of an intersectional and culturally safe approach to communication with patients can lead to more sustainable lifestyle changes and improved health outcomes.
- Equipping and empowering physicians to have meaningful discussions about MASLD is crucial to combating a spectrum of diseases that is rapidly affecting a substantial proportion of patients worldwide.
Dr. Nikzad is based in the Department of Internal Medicine at University of Chicago Medicine (@NewshaN27). Mr. Huynh is a medical student at Stony Brook University Renaissance School of Medicine, Stony Brook, N.Y. (@danielhuynhhh). Dr. Duong is an assistant professor of medicine and transplant hepatologist at Stanford University, Palo Alto, Calif. (@doctornikkid). They have no conflicts of interest to declare.
References
1. Mohanty A. MASLD/MASH and Weight Loss. GI & Hepatology News. 2023 Oct. Data Trends 2023:9-13.
2. Wong VW, et al. Changing epidemiology, global trends and implications for outcomes of NAFLD. J Hepatol. 2023 Sep. doi: 10.1016/j.jhep.2023.04.036.
3. Zeng J, et al. Therapeutic management of metabolic dysfunction associated steatotic liver disease. United European Gastroenterol J. 2024 Mar. doi: 10.1002/ueg2.12525.
4. Berg S. How patients can start—and stick with—key lifestyle changes. AMA Public Health. 2020 Jan.
5. Berg S. 3 ways to get patients engaged in lasting lifestyle change. AMA Diabetes. 2019 Jan.
6. Teixeira PJ, et al. Motivation, self-determination, and long-term weight control. Int J Behav Nutr Phys Act. 2012 Mar. doi: 10.1186/1479-5868-9-22.
7. Aceves-Martins M, et al. Cultural factors related to childhood and adolescent obesity in Mexico: A systematic review of qualitative studies. Obes Rev. 2022 Sep. doi: 10.1111/obr.13461.
8. Figueroa G, et al. Low health literacy, lack of knowledge, and self-control hinder healthy lifestyles in diverse patients with steatotic liver disease. Dig Dis Sci. 2024 Feb. doi: 10.1007/s10620-023-08212-9.
9. Wang L, et al. Factors influencing adherence to lifestyle prescriptions among patients with nonalcoholic fatty liver disease: A qualitative study using the health action process approach framework. Front Public Health. 2023 Mar. doi: 10.3389/fpubh.2023.1131827.
10. Andermann A, CLEAR Collaboration. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016 Dec. doi: 10.1503/cmaj.160177.
Journal Highlights: Sept.-Oct. 2024
Upper GI
Levinthal DJ et al. AGA Clinical Practice Update on Diagnosis and Management of Cyclic Vomiting Syndrome: Commentary. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.05.031.
Geeratragool T et al. Comparison of Vonoprazan Versus Intravenous Proton Pump Inhibitor for Prevention of High-Risk Peptic Ulcers Rebleeding After Successful Endoscopic Hemostasis: A Multicenter Randomized Noninferiority Trial. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.03.036.
Goodoory VC et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology. 2024 Oct. doi: 10.1053/j.gastro.2024.05.010.
Kurlander JE et al; Gastrointestinal Bleeding Working Group. Prescribing of Proton Pump Inhibitors for Prevention of Upper Gastrointestinal Bleeding in US Outpatient Visits. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.01.047.
Oliva S et al. Crafting a Therapeutic Pyramid for Eosinophilic Esophagitis in the Age of Biologics. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.020.
Lower GI
Redd WD et al. Follow-Up Colonoscopy for Detection of Missed Colorectal Cancer After Diverticulitis. Clin Gastroenterol Hepatol. 2024 Oct. doi: 10.1016/j.cgh.2024.03.036.
Peyrin-Biroulet L et al. Upadacitinib Achieves Clinical and Endoscopic Outcomes in Crohn’s Disease Regardless of Prior Biologic Exposure. Clin Gastroenterol Hepatol. 2024 Oct. doi: 10.1016/j.cgh.2024.02.026.
Chang PW et al. ChatGPT4 Outperforms Endoscopists for Determination of Postcolonoscopy Rescreening and Surveillance Recommendations. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.022.
Liver
Wang L et al. Association of GLP-1 Receptor Agonists and Hepatocellular Carcinoma Incidence and Hepatic Decompensation in Patients With Type 2 Diabetes. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.04.029.
Bajaj JS et al. Serum Ammonia Levels Do Not Correlate With Overt Hepatic Encephalopathy Severity in Hospitalized Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.02.015.
Endoscopy
Steinbrück I, et al. Cold Versus Hot Snare Endoscopic Resection of Large Nonpedunculated Colorectal Polyps: Randomized Controlled German CHRONICLE Trial. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.05.013.
Misc.
Kothari S et al. AGA Clinical Practice Update on Pregnancy-Related Gastrointestinal and Liver Disease: Expert Review. Gastroenterology. 2024 Oct. doi: 10.1053/j.gastro.2024.06.014.
Chavannes M et al. AGA Clinical Practice Update on the Role of Intestinal Ultrasound in Inflammatory Bowel Disease: Commentary. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.039.
Dr. Trieu is assistant professor of medicine, interventional endoscopy, in the Division of Gastroenterology at Washington University in St. Louis School of Medicine, Missouri.
Upper GI
Levinthal DJ et al. AGA Clinical Practice Update on Diagnosis and Management of Cyclic Vomiting Syndrome: Commentary. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.05.031.
Geeratragool T et al. Comparison of Vonoprazan Versus Intravenous Proton Pump Inhibitor for Prevention of High-Risk Peptic Ulcers Rebleeding After Successful Endoscopic Hemostasis: A Multicenter Randomized Noninferiority Trial. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.03.036.
Goodoory VC et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology. 2024 Oct. doi: 10.1053/j.gastro.2024.05.010.
Kurlander JE et al; Gastrointestinal Bleeding Working Group. Prescribing of Proton Pump Inhibitors for Prevention of Upper Gastrointestinal Bleeding in US Outpatient Visits. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.01.047.
Oliva S et al. Crafting a Therapeutic Pyramid for Eosinophilic Esophagitis in the Age of Biologics. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.020.
Lower GI
Redd WD et al. Follow-Up Colonoscopy for Detection of Missed Colorectal Cancer After Diverticulitis. Clin Gastroenterol Hepatol. 2024 Oct. doi: 10.1016/j.cgh.2024.03.036.
Peyrin-Biroulet L et al. Upadacitinib Achieves Clinical and Endoscopic Outcomes in Crohn’s Disease Regardless of Prior Biologic Exposure. Clin Gastroenterol Hepatol. 2024 Oct. doi: 10.1016/j.cgh.2024.02.026.
Chang PW et al. ChatGPT4 Outperforms Endoscopists for Determination of Postcolonoscopy Rescreening and Surveillance Recommendations. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.022.
Liver
Wang L et al. Association of GLP-1 Receptor Agonists and Hepatocellular Carcinoma Incidence and Hepatic Decompensation in Patients With Type 2 Diabetes. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.04.029.
Bajaj JS et al. Serum Ammonia Levels Do Not Correlate With Overt Hepatic Encephalopathy Severity in Hospitalized Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.02.015.
Endoscopy
Steinbrück I, et al. Cold Versus Hot Snare Endoscopic Resection of Large Nonpedunculated Colorectal Polyps: Randomized Controlled German CHRONICLE Trial. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.05.013.
Misc.
Kothari S et al. AGA Clinical Practice Update on Pregnancy-Related Gastrointestinal and Liver Disease: Expert Review. Gastroenterology. 2024 Oct. doi: 10.1053/j.gastro.2024.06.014.
Chavannes M et al. AGA Clinical Practice Update on the Role of Intestinal Ultrasound in Inflammatory Bowel Disease: Commentary. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.039.
Dr. Trieu is assistant professor of medicine, interventional endoscopy, in the Division of Gastroenterology at Washington University in St. Louis School of Medicine, Missouri.
Upper GI
Levinthal DJ et al. AGA Clinical Practice Update on Diagnosis and Management of Cyclic Vomiting Syndrome: Commentary. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.05.031.
Geeratragool T et al. Comparison of Vonoprazan Versus Intravenous Proton Pump Inhibitor for Prevention of High-Risk Peptic Ulcers Rebleeding After Successful Endoscopic Hemostasis: A Multicenter Randomized Noninferiority Trial. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.03.036.
Goodoory VC et al. Effect of Brain-Gut Behavioral Treatments on Abdominal Pain in Irritable Bowel Syndrome: Systematic Review and Network Meta-Analysis. Gastroenterology. 2024 Oct. doi: 10.1053/j.gastro.2024.05.010.
Kurlander JE et al; Gastrointestinal Bleeding Working Group. Prescribing of Proton Pump Inhibitors for Prevention of Upper Gastrointestinal Bleeding in US Outpatient Visits. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.01.047.
Oliva S et al. Crafting a Therapeutic Pyramid for Eosinophilic Esophagitis in the Age of Biologics. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.020.
Lower GI
Redd WD et al. Follow-Up Colonoscopy for Detection of Missed Colorectal Cancer After Diverticulitis. Clin Gastroenterol Hepatol. 2024 Oct. doi: 10.1016/j.cgh.2024.03.036.
Peyrin-Biroulet L et al. Upadacitinib Achieves Clinical and Endoscopic Outcomes in Crohn’s Disease Regardless of Prior Biologic Exposure. Clin Gastroenterol Hepatol. 2024 Oct. doi: 10.1016/j.cgh.2024.02.026.
Chang PW et al. ChatGPT4 Outperforms Endoscopists for Determination of Postcolonoscopy Rescreening and Surveillance Recommendations. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.022.
Liver
Wang L et al. Association of GLP-1 Receptor Agonists and Hepatocellular Carcinoma Incidence and Hepatic Decompensation in Patients With Type 2 Diabetes. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.04.029.
Bajaj JS et al. Serum Ammonia Levels Do Not Correlate With Overt Hepatic Encephalopathy Severity in Hospitalized Patients With Cirrhosis. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.02.015.
Endoscopy
Steinbrück I, et al. Cold Versus Hot Snare Endoscopic Resection of Large Nonpedunculated Colorectal Polyps: Randomized Controlled German CHRONICLE Trial. Gastroenterology. 2024 Sep. doi: 10.1053/j.gastro.2024.05.013.
Misc.
Kothari S et al. AGA Clinical Practice Update on Pregnancy-Related Gastrointestinal and Liver Disease: Expert Review. Gastroenterology. 2024 Oct. doi: 10.1053/j.gastro.2024.06.014.
Chavannes M et al. AGA Clinical Practice Update on the Role of Intestinal Ultrasound in Inflammatory Bowel Disease: Commentary. Clin Gastroenterol Hepatol. 2024 Sep. doi: 10.1016/j.cgh.2024.04.039.
Dr. Trieu is assistant professor of medicine, interventional endoscopy, in the Division of Gastroenterology at Washington University in St. Louis School of Medicine, Missouri.
Alcohol-Associated Liver Disease and Alcohol Use Disorder on the Rise in Older Adults
SAN DIEGO — according to the results of a new study.
Even as mortality rates decline globally, AUD deaths rose in the United States, increasing 1.63% per year between 2010 and 2019. Deaths from cirrhosis increased by 0.56% each year, and deaths from primary liver cancer associated with alcohol increased by 3.09% per year.
Several factors, such as an aging US population and increasing alcohol consumption, play a major role in the uptick in mortality, said lead author Pojsakorn Danpanichkul, MD, an internal medicine resident at Texas Tech University Health Sciences Center, Lubbock, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
“Healthcare providers should increase screening for alcohol use among older adults and consider the added risks of alcohol consumption. Public health strategies should target alcohol prevention and treatment programs tailored to older adults,” he said.
“Older adults are more vulnerable to the harmful effects of alcohol due to natural declines in liver function and metabolism, leading to a higher risk of liver disease and complications,” he explained. However, “little research has focused on this issue.”
Trends in US Not Seen Globally
Danpanichkul and colleagues analyzed data from the Global Burden of Disease Study for 2010-2019, calculating the annual percent change for the burden of AUD, ALD, and liver cancer from alcohol in patients age 70 and older. The research team then compared data in the United States to global estimates for these same diseases.
In 2019, there were 556,340 cases of AUD, 112,560 cases of ALD, and 3720 cases of liver cancer from alcohol in older adults in the United States. In addition, there were 1750 deaths attributed to AUD, 4860 deaths from ALD, and 3010 deaths caused by primary liver cancer from alcohol.
The age-standardized prevalence rates (ASPRs) per 100,000 people were 1547 cases of AUD, 313 cases of ALD, and 10 cases of primary liver cancer caused by alcohol.
The age-standardized death rates (ASDRs) per 100,000 people were 4.88 for AUD, 13.52 for ALD, and 8.38 for primary liver cancer.
During the time period studied, upward trends occurred in the United States, with annual ASPRs increasing by 2.52% for AUD, 1.78% for ALD, and 3.31% for primary liver cancer due to alcohol. Globally, the trends were lower, with annual increases of 0.2% for AUD, 0.38% for ALD, and 0.67% for primary liver cancer from alcohol.
During the same time, ASDRs also increased in all three categories in the United States, while global trends showed a 0.91% decline in AUD deaths and 0.6% decline in ALD deaths. Liver cancer deaths, however, increased by 0.3% worldwide.
Targeted strategies are essential to reduce this growing health burden, especially in an aging population, Danpanichkul said. “These interventions should focus on early detection, intervention, and management for individuals at risk or already affected by ALD and AUD.”
Future studies should investigate alcohol consumption and mortality trends in other age groups, including by sex, location (such as state or territory), and race and ethnicity, he said. Data for more recent years would be compelling as well.
Increased Alcohol Use During and After Pandemic
Numerous studies have indicated that alcohol use increased in 2020 during the COVID-19 pandemic and has remained elevated since then.
In a study published in the Annals of Internal Medicine, for instance, alcohol use per 100 people increased 2.69% in 2020 and 2.96% in 2022, as compared with 2018. Increases occurred across all subgroups, including age, sex, race, ethnicity, and US region.
“During the COVID-19 pandemic, many people stayed at home, watched the television, and increased their alcohol intake” — in the United States and also in Japan — said Hisanori Muto, MD, senior assistant professor of gastroenterology at Fujita Health University in Nagoya, Japan, who wasn’t involved with this study.
“Although the global numbers may appear lower, we’re also seeing an increase in AUD and ALD in Japan, similar to the United States,” he said. “It’s very important to watch these trends and address these diseases.”
Danpanichkul and Muto reported no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — according to the results of a new study.
Even as mortality rates decline globally, AUD deaths rose in the United States, increasing 1.63% per year between 2010 and 2019. Deaths from cirrhosis increased by 0.56% each year, and deaths from primary liver cancer associated with alcohol increased by 3.09% per year.
Several factors, such as an aging US population and increasing alcohol consumption, play a major role in the uptick in mortality, said lead author Pojsakorn Danpanichkul, MD, an internal medicine resident at Texas Tech University Health Sciences Center, Lubbock, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
“Healthcare providers should increase screening for alcohol use among older adults and consider the added risks of alcohol consumption. Public health strategies should target alcohol prevention and treatment programs tailored to older adults,” he said.
“Older adults are more vulnerable to the harmful effects of alcohol due to natural declines in liver function and metabolism, leading to a higher risk of liver disease and complications,” he explained. However, “little research has focused on this issue.”
Trends in US Not Seen Globally
Danpanichkul and colleagues analyzed data from the Global Burden of Disease Study for 2010-2019, calculating the annual percent change for the burden of AUD, ALD, and liver cancer from alcohol in patients age 70 and older. The research team then compared data in the United States to global estimates for these same diseases.
In 2019, there were 556,340 cases of AUD, 112,560 cases of ALD, and 3720 cases of liver cancer from alcohol in older adults in the United States. In addition, there were 1750 deaths attributed to AUD, 4860 deaths from ALD, and 3010 deaths caused by primary liver cancer from alcohol.
The age-standardized prevalence rates (ASPRs) per 100,000 people were 1547 cases of AUD, 313 cases of ALD, and 10 cases of primary liver cancer caused by alcohol.
The age-standardized death rates (ASDRs) per 100,000 people were 4.88 for AUD, 13.52 for ALD, and 8.38 for primary liver cancer.
During the time period studied, upward trends occurred in the United States, with annual ASPRs increasing by 2.52% for AUD, 1.78% for ALD, and 3.31% for primary liver cancer due to alcohol. Globally, the trends were lower, with annual increases of 0.2% for AUD, 0.38% for ALD, and 0.67% for primary liver cancer from alcohol.
During the same time, ASDRs also increased in all three categories in the United States, while global trends showed a 0.91% decline in AUD deaths and 0.6% decline in ALD deaths. Liver cancer deaths, however, increased by 0.3% worldwide.
Targeted strategies are essential to reduce this growing health burden, especially in an aging population, Danpanichkul said. “These interventions should focus on early detection, intervention, and management for individuals at risk or already affected by ALD and AUD.”
Future studies should investigate alcohol consumption and mortality trends in other age groups, including by sex, location (such as state or territory), and race and ethnicity, he said. Data for more recent years would be compelling as well.
Increased Alcohol Use During and After Pandemic
Numerous studies have indicated that alcohol use increased in 2020 during the COVID-19 pandemic and has remained elevated since then.
In a study published in the Annals of Internal Medicine, for instance, alcohol use per 100 people increased 2.69% in 2020 and 2.96% in 2022, as compared with 2018. Increases occurred across all subgroups, including age, sex, race, ethnicity, and US region.
“During the COVID-19 pandemic, many people stayed at home, watched the television, and increased their alcohol intake” — in the United States and also in Japan — said Hisanori Muto, MD, senior assistant professor of gastroenterology at Fujita Health University in Nagoya, Japan, who wasn’t involved with this study.
“Although the global numbers may appear lower, we’re also seeing an increase in AUD and ALD in Japan, similar to the United States,” he said. “It’s very important to watch these trends and address these diseases.”
Danpanichkul and Muto reported no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — according to the results of a new study.
Even as mortality rates decline globally, AUD deaths rose in the United States, increasing 1.63% per year between 2010 and 2019. Deaths from cirrhosis increased by 0.56% each year, and deaths from primary liver cancer associated with alcohol increased by 3.09% per year.
Several factors, such as an aging US population and increasing alcohol consumption, play a major role in the uptick in mortality, said lead author Pojsakorn Danpanichkul, MD, an internal medicine resident at Texas Tech University Health Sciences Center, Lubbock, who presented the findings at The Liver Meeting 2024: American Association for the Study of Liver Diseases (AASLD).
“Healthcare providers should increase screening for alcohol use among older adults and consider the added risks of alcohol consumption. Public health strategies should target alcohol prevention and treatment programs tailored to older adults,” he said.
“Older adults are more vulnerable to the harmful effects of alcohol due to natural declines in liver function and metabolism, leading to a higher risk of liver disease and complications,” he explained. However, “little research has focused on this issue.”
Trends in US Not Seen Globally
Danpanichkul and colleagues analyzed data from the Global Burden of Disease Study for 2010-2019, calculating the annual percent change for the burden of AUD, ALD, and liver cancer from alcohol in patients age 70 and older. The research team then compared data in the United States to global estimates for these same diseases.
In 2019, there were 556,340 cases of AUD, 112,560 cases of ALD, and 3720 cases of liver cancer from alcohol in older adults in the United States. In addition, there were 1750 deaths attributed to AUD, 4860 deaths from ALD, and 3010 deaths caused by primary liver cancer from alcohol.
The age-standardized prevalence rates (ASPRs) per 100,000 people were 1547 cases of AUD, 313 cases of ALD, and 10 cases of primary liver cancer caused by alcohol.
The age-standardized death rates (ASDRs) per 100,000 people were 4.88 for AUD, 13.52 for ALD, and 8.38 for primary liver cancer.
During the time period studied, upward trends occurred in the United States, with annual ASPRs increasing by 2.52% for AUD, 1.78% for ALD, and 3.31% for primary liver cancer due to alcohol. Globally, the trends were lower, with annual increases of 0.2% for AUD, 0.38% for ALD, and 0.67% for primary liver cancer from alcohol.
During the same time, ASDRs also increased in all three categories in the United States, while global trends showed a 0.91% decline in AUD deaths and 0.6% decline in ALD deaths. Liver cancer deaths, however, increased by 0.3% worldwide.
Targeted strategies are essential to reduce this growing health burden, especially in an aging population, Danpanichkul said. “These interventions should focus on early detection, intervention, and management for individuals at risk or already affected by ALD and AUD.”
Future studies should investigate alcohol consumption and mortality trends in other age groups, including by sex, location (such as state or territory), and race and ethnicity, he said. Data for more recent years would be compelling as well.
Increased Alcohol Use During and After Pandemic
Numerous studies have indicated that alcohol use increased in 2020 during the COVID-19 pandemic and has remained elevated since then.
In a study published in the Annals of Internal Medicine, for instance, alcohol use per 100 people increased 2.69% in 2020 and 2.96% in 2022, as compared with 2018. Increases occurred across all subgroups, including age, sex, race, ethnicity, and US region.
“During the COVID-19 pandemic, many people stayed at home, watched the television, and increased their alcohol intake” — in the United States and also in Japan — said Hisanori Muto, MD, senior assistant professor of gastroenterology at Fujita Health University in Nagoya, Japan, who wasn’t involved with this study.
“Although the global numbers may appear lower, we’re also seeing an increase in AUD and ALD in Japan, similar to the United States,” he said. “It’s very important to watch these trends and address these diseases.”
Danpanichkul and Muto reported no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AASLD 2024
Alcohol Use Disorder Therapy Remains Underutilized in Alcohol-Associated Liver Disease
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In an analysis of commercially insured Americans, AUD medications were prescribed to only 1 in 50 patients with ALD and about 1 in 10 patients with acute alcohol-associated hepatitis (AAH).
“Providers caring for these patients should consider early initiation of this therapy in select cases,” said lead author Alex R. Jones, MD, chief resident of internal medicine at the University of Texas Southwestern Medical Center in Dallas.
“Based on additional analyses looking at the prescriber subspecialty, we didn’t identify any gastroenterologists or hepatologists who prescribed pharmacotherapy,” he said. “This could be a great opportunity for hepatologists to engage in the pharmacologic treatment of AUD.”
Jones and colleagues analyzed 2006-2021 data from IQVIA PharMetrics Plus for Academics, a nationally representative database of commercially insured patients in the United States. They looked for AUD pharmacologic treatment at any time after AUD diagnosis, including prescriptions for gabapentin, naltrexone, topiramate, acamprosate, baclofen, and disulfiram.
Among 28,625 patients with AUD (defined as at least two outpatient codes or at least one inpatient code), 1201 had ALD with cirrhosis and 439 had AAH.
Pharmacologic therapy was prescribed in 3924 (14.5%) patients without ALD, 28 (2.3%) with ALD, and 42 (9.8%) with AAH.
In addition, one-time prescriptions were observed in 1113 (28.4%) patients without ALD, three patients (10.7%) with ALD, and eight patients (18.6%) with AAH.
Overall, 64.5% of the general population consisted of men. About 46% had a psychiatric diagnosis other than substance use disorder (SUD), and 35.7% had a non-AUD SUD.
Patients who received AUD pharmacotherapy tended to be older, at a median age of 45 years, than those aged 42 years without a prescription.
The median time to prescription was 302 days, with no significant differences based on the presence of liver disease.
By medication, gabapentin was prescribed most often (9.4%), followed by oral naltrexone (2.6%) and topiramate (2%). Oral naltrexone was prescribed at a lower rate in patients with ALD and at a higher rate in patients with AAH than in patients without ALD. Baclofen was also prescribed at lower rates in patients with ALD and AAH.
In a multivariable logistic regression analysis, several characteristics were more significantly associated with pharmacologic therapy, such as age ≥ 50 years (adjusted odds ratio [aOR], 1.33), female sex (aOR, 1.31), a non-liver Charlson Comorbidity Index ≥ 3 (aOR, 2.21), and psychiatric comorbidities (aOR, 2.76).
On the other hand, the presence of hepatic decompensation — defined as ascites, hepatic encephalopathy, or bleeding varices — was associated with lower odds of receiving pharmacotherapy (aOR, 0.08). ALD cirrhosis (non-AAH) also had lower odds (aOR, 0.24).
The study was limited by only incorporating patients with commercial insurance, lacking demographic details related to race or ethnicity, and potentially misclassifying patients despite validated definitions of ALD and AUD, Jones said.
As the study couldn’t determine the indications for prescriptions, such as gabapentin use for migraines or diabetes-associated neuropathy, for instance, future studies could look at these precise details, he added.
“It’s important to know we’re underutilizing therapies that we have a lot of information about, such as gabapentin, which is an old medication that we should feel fairly comfortable using,” said Patricia Jones, MD, a hepatologist and associate professor of clinical medicine at the University of Miami Miller School of Medicine, in Florida. Patricia Jones comoderated the plenary session on small intestine, functional, and liver research.
“I also expect that, if a future study reviewed this data and excluded people with valid indications, such as migraines or diabetic neuropathy, we’d see even lower rates of prescription,” she said.
From a clinical perspective, patient communication and clinical decision-making are key, Patricia Jones added, particularly when clinical gastroenterologists and hepatologists may not offer this type of therapy or patients refuse this type of therapy.
“We need to think about our practice patterns and how we can offer therapy,” she said. “In general, we know these medications are very safe. Even though they’re not widely used in people with cirrhosis, there’s not enough evidence to suggest we shouldn’t use them.”
Alex Jones and Patricia Jones reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In an analysis of commercially insured Americans, AUD medications were prescribed to only 1 in 50 patients with ALD and about 1 in 10 patients with acute alcohol-associated hepatitis (AAH).
“Providers caring for these patients should consider early initiation of this therapy in select cases,” said lead author Alex R. Jones, MD, chief resident of internal medicine at the University of Texas Southwestern Medical Center in Dallas.
“Based on additional analyses looking at the prescriber subspecialty, we didn’t identify any gastroenterologists or hepatologists who prescribed pharmacotherapy,” he said. “This could be a great opportunity for hepatologists to engage in the pharmacologic treatment of AUD.”
Jones and colleagues analyzed 2006-2021 data from IQVIA PharMetrics Plus for Academics, a nationally representative database of commercially insured patients in the United States. They looked for AUD pharmacologic treatment at any time after AUD diagnosis, including prescriptions for gabapentin, naltrexone, topiramate, acamprosate, baclofen, and disulfiram.
Among 28,625 patients with AUD (defined as at least two outpatient codes or at least one inpatient code), 1201 had ALD with cirrhosis and 439 had AAH.
Pharmacologic therapy was prescribed in 3924 (14.5%) patients without ALD, 28 (2.3%) with ALD, and 42 (9.8%) with AAH.
In addition, one-time prescriptions were observed in 1113 (28.4%) patients without ALD, three patients (10.7%) with ALD, and eight patients (18.6%) with AAH.
Overall, 64.5% of the general population consisted of men. About 46% had a psychiatric diagnosis other than substance use disorder (SUD), and 35.7% had a non-AUD SUD.
Patients who received AUD pharmacotherapy tended to be older, at a median age of 45 years, than those aged 42 years without a prescription.
The median time to prescription was 302 days, with no significant differences based on the presence of liver disease.
By medication, gabapentin was prescribed most often (9.4%), followed by oral naltrexone (2.6%) and topiramate (2%). Oral naltrexone was prescribed at a lower rate in patients with ALD and at a higher rate in patients with AAH than in patients without ALD. Baclofen was also prescribed at lower rates in patients with ALD and AAH.
In a multivariable logistic regression analysis, several characteristics were more significantly associated with pharmacologic therapy, such as age ≥ 50 years (adjusted odds ratio [aOR], 1.33), female sex (aOR, 1.31), a non-liver Charlson Comorbidity Index ≥ 3 (aOR, 2.21), and psychiatric comorbidities (aOR, 2.76).
On the other hand, the presence of hepatic decompensation — defined as ascites, hepatic encephalopathy, or bleeding varices — was associated with lower odds of receiving pharmacotherapy (aOR, 0.08). ALD cirrhosis (non-AAH) also had lower odds (aOR, 0.24).
The study was limited by only incorporating patients with commercial insurance, lacking demographic details related to race or ethnicity, and potentially misclassifying patients despite validated definitions of ALD and AUD, Jones said.
As the study couldn’t determine the indications for prescriptions, such as gabapentin use for migraines or diabetes-associated neuropathy, for instance, future studies could look at these precise details, he added.
“It’s important to know we’re underutilizing therapies that we have a lot of information about, such as gabapentin, which is an old medication that we should feel fairly comfortable using,” said Patricia Jones, MD, a hepatologist and associate professor of clinical medicine at the University of Miami Miller School of Medicine, in Florida. Patricia Jones comoderated the plenary session on small intestine, functional, and liver research.
“I also expect that, if a future study reviewed this data and excluded people with valid indications, such as migraines or diabetic neuropathy, we’d see even lower rates of prescription,” she said.
From a clinical perspective, patient communication and clinical decision-making are key, Patricia Jones added, particularly when clinical gastroenterologists and hepatologists may not offer this type of therapy or patients refuse this type of therapy.
“We need to think about our practice patterns and how we can offer therapy,” she said. “In general, we know these medications are very safe. Even though they’re not widely used in people with cirrhosis, there’s not enough evidence to suggest we shouldn’t use them.”
Alex Jones and Patricia Jones reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
PHILADELPHIA — according to a study presented at the American College of Gastroenterology (ACG) 2024 Annual Scientific Meeting.
In an analysis of commercially insured Americans, AUD medications were prescribed to only 1 in 50 patients with ALD and about 1 in 10 patients with acute alcohol-associated hepatitis (AAH).
“Providers caring for these patients should consider early initiation of this therapy in select cases,” said lead author Alex R. Jones, MD, chief resident of internal medicine at the University of Texas Southwestern Medical Center in Dallas.
“Based on additional analyses looking at the prescriber subspecialty, we didn’t identify any gastroenterologists or hepatologists who prescribed pharmacotherapy,” he said. “This could be a great opportunity for hepatologists to engage in the pharmacologic treatment of AUD.”
Jones and colleagues analyzed 2006-2021 data from IQVIA PharMetrics Plus for Academics, a nationally representative database of commercially insured patients in the United States. They looked for AUD pharmacologic treatment at any time after AUD diagnosis, including prescriptions for gabapentin, naltrexone, topiramate, acamprosate, baclofen, and disulfiram.
Among 28,625 patients with AUD (defined as at least two outpatient codes or at least one inpatient code), 1201 had ALD with cirrhosis and 439 had AAH.
Pharmacologic therapy was prescribed in 3924 (14.5%) patients without ALD, 28 (2.3%) with ALD, and 42 (9.8%) with AAH.
In addition, one-time prescriptions were observed in 1113 (28.4%) patients without ALD, three patients (10.7%) with ALD, and eight patients (18.6%) with AAH.
Overall, 64.5% of the general population consisted of men. About 46% had a psychiatric diagnosis other than substance use disorder (SUD), and 35.7% had a non-AUD SUD.
Patients who received AUD pharmacotherapy tended to be older, at a median age of 45 years, than those aged 42 years without a prescription.
The median time to prescription was 302 days, with no significant differences based on the presence of liver disease.
By medication, gabapentin was prescribed most often (9.4%), followed by oral naltrexone (2.6%) and topiramate (2%). Oral naltrexone was prescribed at a lower rate in patients with ALD and at a higher rate in patients with AAH than in patients without ALD. Baclofen was also prescribed at lower rates in patients with ALD and AAH.
In a multivariable logistic regression analysis, several characteristics were more significantly associated with pharmacologic therapy, such as age ≥ 50 years (adjusted odds ratio [aOR], 1.33), female sex (aOR, 1.31), a non-liver Charlson Comorbidity Index ≥ 3 (aOR, 2.21), and psychiatric comorbidities (aOR, 2.76).
On the other hand, the presence of hepatic decompensation — defined as ascites, hepatic encephalopathy, or bleeding varices — was associated with lower odds of receiving pharmacotherapy (aOR, 0.08). ALD cirrhosis (non-AAH) also had lower odds (aOR, 0.24).
The study was limited by only incorporating patients with commercial insurance, lacking demographic details related to race or ethnicity, and potentially misclassifying patients despite validated definitions of ALD and AUD, Jones said.
As the study couldn’t determine the indications for prescriptions, such as gabapentin use for migraines or diabetes-associated neuropathy, for instance, future studies could look at these precise details, he added.
“It’s important to know we’re underutilizing therapies that we have a lot of information about, such as gabapentin, which is an old medication that we should feel fairly comfortable using,” said Patricia Jones, MD, a hepatologist and associate professor of clinical medicine at the University of Miami Miller School of Medicine, in Florida. Patricia Jones comoderated the plenary session on small intestine, functional, and liver research.
“I also expect that, if a future study reviewed this data and excluded people with valid indications, such as migraines or diabetic neuropathy, we’d see even lower rates of prescription,” she said.
From a clinical perspective, patient communication and clinical decision-making are key, Patricia Jones added, particularly when clinical gastroenterologists and hepatologists may not offer this type of therapy or patients refuse this type of therapy.
“We need to think about our practice patterns and how we can offer therapy,” she said. “In general, we know these medications are very safe. Even though they’re not widely used in people with cirrhosis, there’s not enough evidence to suggest we shouldn’t use them.”
Alex Jones and Patricia Jones reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ACG 2024







