User login
VIDEO: Survival improves when cancer patients self-report symptoms
CHICAGO – Patients with metastatic cancer who self-reported symptoms during routine cancer treatment experienced a number of benefits, including a statistically significant improvement in overall survival, according to findings from a randomized, controlled clinical trial.
The median overall survival among 441 patients receiving treatment for metastatic breast, lung, genitourinary, or gynecologic cancer who were randomized to the intervention arm was more than 5 months longer – a nearly 20% increase – than in 325 patients who received standard care (31.2 vs. 26 months), Ethan Basch, MD, reported at the annual meeting of the American Society of Clinical Oncology.
Additionally, 31% of patients in the intervention arm had better quality of life/physical functioning, compared with those in the control arm, and 7% fewer patients in the intervention arm visited an emergency room during the course of the study. The duration of potentially life-prolonging chemotherapy was increased by an average of 2 months in the intervention arm, he said.
The findings were simultaneously published online in a research letter in JAMA (2017 Jun 4. doi: 10.1001/jama.2017.7156).
Symptoms such as nausea, pain, and fatigue are common among patients with metastatic cancer, Dr. Basch said. “Unfortunately, they often go undetected by doctors and nurses until they become severe and physically debilitating,” he added, explaining that patients are often hesitant to call the office to report symptoms between visits.
Even at office visits, competing topics can interfere with communication about symptoms, he noted.
He and his colleagues hypothesized that self-reporting of patient symptoms between visits or prior to a visit while in the clinic waiting area would prompt earlier intervention and improve symptom control and outcomes.
Study subjects were patients at Memorial Sloan Kettering Cancer Center who had advanced solid genitourinary, gynecologic, breast, or lung tumors and who were receiving outpatient chemotherapy. Those assigned to the intervention group used tablet computers and an online web survey system to report on 12 symptoms commonly experienced during chemotherapy. The system triggers an alert to a nurse when a severe or worsening symptom is reported. Patients in the usual care group discussed symptoms during office visits and were encouraged to call the office between visits if they experienced concerning symptoms.
Patients remained on the study until discontinuation of all cancer treatment, hospice, or death.
One possible explanation for the findings is that this self-reporting approach prompts clinicians to manage symptoms before they cause serious downstream complications, Dr. Basch said.
The approach may also keep patients more physically functional, which is known from prior studies to have a strong association with better survival, and the approach may also improve management of chemotherapy side effects, enabling longer duration of beneficial cancer treatment, he said, explaining that, “in oncology, we often are limited in our ability to give life-prolonging treatment because people don’t tolerate it well.”
“This approach should be considered for inclusion in standard symptoms management as a component of high quality cancer care,” he concluded, noting that efforts are underway to test the next generation of systems to improve communication between patients and care teams and to figure out how best to integrate these tools into oncology practice.
The system used in the this study was designed for research, but a number of companies have tools currently available for patient-reported outcomes, and others are being developed, Dr. Basch said, noting that a National Cancer Institute questionnaire – the PRO-CTCAE – is publicly available and could be loaded into patients’ electronic health records for this purpose as well.
ASCO’s chief medical officer, Richard L. Schilsky, MD, said the findings demonstrate that “these frequent touches between the patient and their health care providers obviously can make a huge difference in their outcomes.”
Additionally, ASCO expert Harold J. Burstein, MD, of Dana-Farber Cancer Institute, Boston, said this “exciting and compelling study” validates the feeling among many clinicians that patient-focused, team-based care can improve outcomes in a meaningful way for patients. In a video interview, he further discusses the challenges with implementing a system like this and particularly with obtaining funding to support implementation.
“If this was a drug, if it was iPad-olizumab, it would be worth tens, if not hundreds of thousands, of dollars per year to have something that improved overall survival. We don’t have those same kinds of dollars to help implement these into our electronic health records or our systems. We need to find ways to support that and make it happen,” he said.
This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr. Basch and Dr. Burstein each reported having no disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – Patients with metastatic cancer who self-reported symptoms during routine cancer treatment experienced a number of benefits, including a statistically significant improvement in overall survival, according to findings from a randomized, controlled clinical trial.
The median overall survival among 441 patients receiving treatment for metastatic breast, lung, genitourinary, or gynecologic cancer who were randomized to the intervention arm was more than 5 months longer – a nearly 20% increase – than in 325 patients who received standard care (31.2 vs. 26 months), Ethan Basch, MD, reported at the annual meeting of the American Society of Clinical Oncology.
Additionally, 31% of patients in the intervention arm had better quality of life/physical functioning, compared with those in the control arm, and 7% fewer patients in the intervention arm visited an emergency room during the course of the study. The duration of potentially life-prolonging chemotherapy was increased by an average of 2 months in the intervention arm, he said.
The findings were simultaneously published online in a research letter in JAMA (2017 Jun 4. doi: 10.1001/jama.2017.7156).
Symptoms such as nausea, pain, and fatigue are common among patients with metastatic cancer, Dr. Basch said. “Unfortunately, they often go undetected by doctors and nurses until they become severe and physically debilitating,” he added, explaining that patients are often hesitant to call the office to report symptoms between visits.
Even at office visits, competing topics can interfere with communication about symptoms, he noted.
He and his colleagues hypothesized that self-reporting of patient symptoms between visits or prior to a visit while in the clinic waiting area would prompt earlier intervention and improve symptom control and outcomes.
Study subjects were patients at Memorial Sloan Kettering Cancer Center who had advanced solid genitourinary, gynecologic, breast, or lung tumors and who were receiving outpatient chemotherapy. Those assigned to the intervention group used tablet computers and an online web survey system to report on 12 symptoms commonly experienced during chemotherapy. The system triggers an alert to a nurse when a severe or worsening symptom is reported. Patients in the usual care group discussed symptoms during office visits and were encouraged to call the office between visits if they experienced concerning symptoms.
Patients remained on the study until discontinuation of all cancer treatment, hospice, or death.
One possible explanation for the findings is that this self-reporting approach prompts clinicians to manage symptoms before they cause serious downstream complications, Dr. Basch said.
The approach may also keep patients more physically functional, which is known from prior studies to have a strong association with better survival, and the approach may also improve management of chemotherapy side effects, enabling longer duration of beneficial cancer treatment, he said, explaining that, “in oncology, we often are limited in our ability to give life-prolonging treatment because people don’t tolerate it well.”
“This approach should be considered for inclusion in standard symptoms management as a component of high quality cancer care,” he concluded, noting that efforts are underway to test the next generation of systems to improve communication between patients and care teams and to figure out how best to integrate these tools into oncology practice.
The system used in the this study was designed for research, but a number of companies have tools currently available for patient-reported outcomes, and others are being developed, Dr. Basch said, noting that a National Cancer Institute questionnaire – the PRO-CTCAE – is publicly available and could be loaded into patients’ electronic health records for this purpose as well.
ASCO’s chief medical officer, Richard L. Schilsky, MD, said the findings demonstrate that “these frequent touches between the patient and their health care providers obviously can make a huge difference in their outcomes.”
Additionally, ASCO expert Harold J. Burstein, MD, of Dana-Farber Cancer Institute, Boston, said this “exciting and compelling study” validates the feeling among many clinicians that patient-focused, team-based care can improve outcomes in a meaningful way for patients. In a video interview, he further discusses the challenges with implementing a system like this and particularly with obtaining funding to support implementation.
“If this was a drug, if it was iPad-olizumab, it would be worth tens, if not hundreds of thousands, of dollars per year to have something that improved overall survival. We don’t have those same kinds of dollars to help implement these into our electronic health records or our systems. We need to find ways to support that and make it happen,” he said.
This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr. Basch and Dr. Burstein each reported having no disclosures.
CHICAGO – Patients with metastatic cancer who self-reported symptoms during routine cancer treatment experienced a number of benefits, including a statistically significant improvement in overall survival, according to findings from a randomized, controlled clinical trial.
The median overall survival among 441 patients receiving treatment for metastatic breast, lung, genitourinary, or gynecologic cancer who were randomized to the intervention arm was more than 5 months longer – a nearly 20% increase – than in 325 patients who received standard care (31.2 vs. 26 months), Ethan Basch, MD, reported at the annual meeting of the American Society of Clinical Oncology.
Additionally, 31% of patients in the intervention arm had better quality of life/physical functioning, compared with those in the control arm, and 7% fewer patients in the intervention arm visited an emergency room during the course of the study. The duration of potentially life-prolonging chemotherapy was increased by an average of 2 months in the intervention arm, he said.
The findings were simultaneously published online in a research letter in JAMA (2017 Jun 4. doi: 10.1001/jama.2017.7156).
Symptoms such as nausea, pain, and fatigue are common among patients with metastatic cancer, Dr. Basch said. “Unfortunately, they often go undetected by doctors and nurses until they become severe and physically debilitating,” he added, explaining that patients are often hesitant to call the office to report symptoms between visits.
Even at office visits, competing topics can interfere with communication about symptoms, he noted.
He and his colleagues hypothesized that self-reporting of patient symptoms between visits or prior to a visit while in the clinic waiting area would prompt earlier intervention and improve symptom control and outcomes.
Study subjects were patients at Memorial Sloan Kettering Cancer Center who had advanced solid genitourinary, gynecologic, breast, or lung tumors and who were receiving outpatient chemotherapy. Those assigned to the intervention group used tablet computers and an online web survey system to report on 12 symptoms commonly experienced during chemotherapy. The system triggers an alert to a nurse when a severe or worsening symptom is reported. Patients in the usual care group discussed symptoms during office visits and were encouraged to call the office between visits if they experienced concerning symptoms.
Patients remained on the study until discontinuation of all cancer treatment, hospice, or death.
One possible explanation for the findings is that this self-reporting approach prompts clinicians to manage symptoms before they cause serious downstream complications, Dr. Basch said.
The approach may also keep patients more physically functional, which is known from prior studies to have a strong association with better survival, and the approach may also improve management of chemotherapy side effects, enabling longer duration of beneficial cancer treatment, he said, explaining that, “in oncology, we often are limited in our ability to give life-prolonging treatment because people don’t tolerate it well.”
“This approach should be considered for inclusion in standard symptoms management as a component of high quality cancer care,” he concluded, noting that efforts are underway to test the next generation of systems to improve communication between patients and care teams and to figure out how best to integrate these tools into oncology practice.
The system used in the this study was designed for research, but a number of companies have tools currently available for patient-reported outcomes, and others are being developed, Dr. Basch said, noting that a National Cancer Institute questionnaire – the PRO-CTCAE – is publicly available and could be loaded into patients’ electronic health records for this purpose as well.
ASCO’s chief medical officer, Richard L. Schilsky, MD, said the findings demonstrate that “these frequent touches between the patient and their health care providers obviously can make a huge difference in their outcomes.”
Additionally, ASCO expert Harold J. Burstein, MD, of Dana-Farber Cancer Institute, Boston, said this “exciting and compelling study” validates the feeling among many clinicians that patient-focused, team-based care can improve outcomes in a meaningful way for patients. In a video interview, he further discusses the challenges with implementing a system like this and particularly with obtaining funding to support implementation.
“If this was a drug, if it was iPad-olizumab, it would be worth tens, if not hundreds of thousands, of dollars per year to have something that improved overall survival. We don’t have those same kinds of dollars to help implement these into our electronic health records or our systems. We need to find ways to support that and make it happen,” he said.
This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr. Basch and Dr. Burstein each reported having no disclosures.
AT THE 2017 ASCO ANNUAL MEETING
Key clinical point:
Major finding: Median overall survival was 31.2, vs. 26 months, with self-reporting of symptoms, vs. usual care.
Data source: A randomized controlled clinical trial of 766 patients.
Disclosures: This study was supported by the National Institutes of Health and the Conquer Cancer Foundation of the American Society of Clinical Oncology. Dr. Basch and Dr. Burstein each reported having no disclosures.
Test goes wide and deep to detect free tumor DNA in blood
CHICAGO – An experimental liquid biopsy method plumbs the depths of the genome to detect a broad array of mutations in blood samples that closely correspond to variants in tumors.
The high-intensity method for detecting circulating free DNA (cfDNA) in plasma detected at least one significant genetic variant in samples from 89% of patients with advanced breast, lung, and prostate cancers.
If validated in further studies, the technique could inform more accurate drug selection in patients with refractory disease and eventually may form the basis for plasma-based assays to detect early-stage cancers, said Pedram Razavi, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
“This novel, high-intensity sequencing assay incorporates an unprecedented combination of depth and breadth of coverage compared to previous assays. High levels of concordance for variants between plasma and tissue provide strong evidence for high rates of tumor DNA detection in plasma,” he said at a press briefing at the annual meeting of the American Society of Clinical Oncology.
The technique also provides important insights into tumor biology, “including first exploration of mutational signatures in the plasma,” he added.
Deep scanning
The high-intensity sequencing method scans for 508 genes in a 2 million base-pair swath of genome, performing 60,000 repeat reads on each genome region to improve the assay’s sensitivity, and deep sequencing allows for detection of rare “needle-in-a-haystack” variants.
Dr. Razavi and his colleagues examined prospectively collected blood and tissues from 161 patients, 124 of whom had samples sufficient for concordance studies.
The samples were collected within 6 weeks of a de novo cancer diagnosis or evidence of disease progression, before the initiation of therapy.
Both cfDNA and genomic data from white blood cells (WBCs) of each patient were sequenced with the aforementioned 508-gene panel covering a broad range of known cancer variants and mutations.
Tumor tissues were sequenced with MSK-IMPACT, a 410 gene assay, with blinding of results in regard to plasma and WBC sequencing. Variants were classified as clonal or subclonal based on tumor sequencing in breast cancer and non–small cell lung cancer (NSCLC).
As noted before, 89% of patients had at least one genetic variant detected in both the tumor and in plasma, including 97% of patients with metastatic breast cancer, 85% of those with NSCLC, and 84% of patients with metastatic prostate cancer.
The investigators identified 864 clonal or subclonal variants in tissue samples from all three of these cancers, and 627 of the variants also were found in plasma.
In addition, 76% of clinically actionable somatic mutations identified in tumors also were found in plasma, which suggests that the high-intensity sequencing technique may be able to identify tumor heterogeneity that is not always evident in single tumor biopsies, Dr. Razavi said.
‘A clear advance’
“The work by Dr. Razavi and colleagues is a clear advance in the field because it surveys for the first time a much broader panel of genes – 508 genes in this case – and it does it with much deeper sequencing, which means it can detect much rarer alterations,” commented ASCO expert John Heymach, MD, PhD, from the University of Texas MD Anderson Cancer Center in Houston.
The study “helps illuminate a path toward a day when we will be using circulating tumor DNA assays for early detection of cancer, and not just for selecting certain therapies,” he added.
“We’re a long way from utilizing liquid biopsy for detecting cancers; already though, we’re seeing some utility of circulating tumor DNA in the domain of identifying novel alterations as a means of segmentation clinical trials,” commented ASCO expert Sumanta Kumar Pal, MD, from City of Hope in Duarte, Calif.
Dr. Heymach and Dr. Pal were not involved in the study, but were invited discussants at the briefing.
The study was funded in part by GRAIL. Dr. Razavi reported institutional research funding from the company. Multiple coauthors are employees of the company.
CHICAGO – An experimental liquid biopsy method plumbs the depths of the genome to detect a broad array of mutations in blood samples that closely correspond to variants in tumors.
The high-intensity method for detecting circulating free DNA (cfDNA) in plasma detected at least one significant genetic variant in samples from 89% of patients with advanced breast, lung, and prostate cancers.
If validated in further studies, the technique could inform more accurate drug selection in patients with refractory disease and eventually may form the basis for plasma-based assays to detect early-stage cancers, said Pedram Razavi, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
“This novel, high-intensity sequencing assay incorporates an unprecedented combination of depth and breadth of coverage compared to previous assays. High levels of concordance for variants between plasma and tissue provide strong evidence for high rates of tumor DNA detection in plasma,” he said at a press briefing at the annual meeting of the American Society of Clinical Oncology.
The technique also provides important insights into tumor biology, “including first exploration of mutational signatures in the plasma,” he added.
Deep scanning
The high-intensity sequencing method scans for 508 genes in a 2 million base-pair swath of genome, performing 60,000 repeat reads on each genome region to improve the assay’s sensitivity, and deep sequencing allows for detection of rare “needle-in-a-haystack” variants.
Dr. Razavi and his colleagues examined prospectively collected blood and tissues from 161 patients, 124 of whom had samples sufficient for concordance studies.
The samples were collected within 6 weeks of a de novo cancer diagnosis or evidence of disease progression, before the initiation of therapy.
Both cfDNA and genomic data from white blood cells (WBCs) of each patient were sequenced with the aforementioned 508-gene panel covering a broad range of known cancer variants and mutations.
Tumor tissues were sequenced with MSK-IMPACT, a 410 gene assay, with blinding of results in regard to plasma and WBC sequencing. Variants were classified as clonal or subclonal based on tumor sequencing in breast cancer and non–small cell lung cancer (NSCLC).
As noted before, 89% of patients had at least one genetic variant detected in both the tumor and in plasma, including 97% of patients with metastatic breast cancer, 85% of those with NSCLC, and 84% of patients with metastatic prostate cancer.
The investigators identified 864 clonal or subclonal variants in tissue samples from all three of these cancers, and 627 of the variants also were found in plasma.
In addition, 76% of clinically actionable somatic mutations identified in tumors also were found in plasma, which suggests that the high-intensity sequencing technique may be able to identify tumor heterogeneity that is not always evident in single tumor biopsies, Dr. Razavi said.
‘A clear advance’
“The work by Dr. Razavi and colleagues is a clear advance in the field because it surveys for the first time a much broader panel of genes – 508 genes in this case – and it does it with much deeper sequencing, which means it can detect much rarer alterations,” commented ASCO expert John Heymach, MD, PhD, from the University of Texas MD Anderson Cancer Center in Houston.
The study “helps illuminate a path toward a day when we will be using circulating tumor DNA assays for early detection of cancer, and not just for selecting certain therapies,” he added.
“We’re a long way from utilizing liquid biopsy for detecting cancers; already though, we’re seeing some utility of circulating tumor DNA in the domain of identifying novel alterations as a means of segmentation clinical trials,” commented ASCO expert Sumanta Kumar Pal, MD, from City of Hope in Duarte, Calif.
Dr. Heymach and Dr. Pal were not involved in the study, but were invited discussants at the briefing.
The study was funded in part by GRAIL. Dr. Razavi reported institutional research funding from the company. Multiple coauthors are employees of the company.
CHICAGO – An experimental liquid biopsy method plumbs the depths of the genome to detect a broad array of mutations in blood samples that closely correspond to variants in tumors.
The high-intensity method for detecting circulating free DNA (cfDNA) in plasma detected at least one significant genetic variant in samples from 89% of patients with advanced breast, lung, and prostate cancers.
If validated in further studies, the technique could inform more accurate drug selection in patients with refractory disease and eventually may form the basis for plasma-based assays to detect early-stage cancers, said Pedram Razavi, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
“This novel, high-intensity sequencing assay incorporates an unprecedented combination of depth and breadth of coverage compared to previous assays. High levels of concordance for variants between plasma and tissue provide strong evidence for high rates of tumor DNA detection in plasma,” he said at a press briefing at the annual meeting of the American Society of Clinical Oncology.
The technique also provides important insights into tumor biology, “including first exploration of mutational signatures in the plasma,” he added.
Deep scanning
The high-intensity sequencing method scans for 508 genes in a 2 million base-pair swath of genome, performing 60,000 repeat reads on each genome region to improve the assay’s sensitivity, and deep sequencing allows for detection of rare “needle-in-a-haystack” variants.
Dr. Razavi and his colleagues examined prospectively collected blood and tissues from 161 patients, 124 of whom had samples sufficient for concordance studies.
The samples were collected within 6 weeks of a de novo cancer diagnosis or evidence of disease progression, before the initiation of therapy.
Both cfDNA and genomic data from white blood cells (WBCs) of each patient were sequenced with the aforementioned 508-gene panel covering a broad range of known cancer variants and mutations.
Tumor tissues were sequenced with MSK-IMPACT, a 410 gene assay, with blinding of results in regard to plasma and WBC sequencing. Variants were classified as clonal or subclonal based on tumor sequencing in breast cancer and non–small cell lung cancer (NSCLC).
As noted before, 89% of patients had at least one genetic variant detected in both the tumor and in plasma, including 97% of patients with metastatic breast cancer, 85% of those with NSCLC, and 84% of patients with metastatic prostate cancer.
The investigators identified 864 clonal or subclonal variants in tissue samples from all three of these cancers, and 627 of the variants also were found in plasma.
In addition, 76% of clinically actionable somatic mutations identified in tumors also were found in plasma, which suggests that the high-intensity sequencing technique may be able to identify tumor heterogeneity that is not always evident in single tumor biopsies, Dr. Razavi said.
‘A clear advance’
“The work by Dr. Razavi and colleagues is a clear advance in the field because it surveys for the first time a much broader panel of genes – 508 genes in this case – and it does it with much deeper sequencing, which means it can detect much rarer alterations,” commented ASCO expert John Heymach, MD, PhD, from the University of Texas MD Anderson Cancer Center in Houston.
The study “helps illuminate a path toward a day when we will be using circulating tumor DNA assays for early detection of cancer, and not just for selecting certain therapies,” he added.
“We’re a long way from utilizing liquid biopsy for detecting cancers; already though, we’re seeing some utility of circulating tumor DNA in the domain of identifying novel alterations as a means of segmentation clinical trials,” commented ASCO expert Sumanta Kumar Pal, MD, from City of Hope in Duarte, Calif.
Dr. Heymach and Dr. Pal were not involved in the study, but were invited discussants at the briefing.
The study was funded in part by GRAIL. Dr. Razavi reported institutional research funding from the company. Multiple coauthors are employees of the company.
AT ASCO 2017
Key clinical point: High-intensity sequencing of plasma samples appears capable of detecting actionable tumor mutations in a large proportion of samples.
Major finding: In 89% of patients with advanced cancers, genetic variants were identified in both tumor samples and circulating free DNA testing.
Data source: Prospective study of tissue and plasma samples from 124 patients with non–small cell lung cancer or metastatic breast and prostate cancers.
Disclosures: The study was funded in part by GRAIL. Dr. Razavi reported institutional research funding from the company. Multiple coauthors are employees of the company.
VIDEO: TRK inhibitor shows 76% ORR across diverse cancers harboring TRK fusions
CHICAGO – An integrated analysis of three trials has shown that larotrectinib, an oral selective inhibitor of tropomyosin receptor kinase (TRK), has durable efficacy across diverse adult and pediatric cancers harboring TRK fusions, netting an impressive 76% overall response rate.
Lead study author David Hyman, MD, chief of early drug development at Memorial Sloan Kettering Cancer Center in New York, discussed highlights of the analysis, larotrectinib’s regulatory status, and implications for TRK fusion testing in clinical care at the annual meeting of the American Society of Clinical Oncology.
Dr. Hyman disclosed that he has a consulting or advisory role with Atara Biotherapeutics, Chugai Pharma, and CytomX Therapeutics, and that he receives research funding from AstraZeneca and Puma Biotechnology. The study was funded by Loxo Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – An integrated analysis of three trials has shown that larotrectinib, an oral selective inhibitor of tropomyosin receptor kinase (TRK), has durable efficacy across diverse adult and pediatric cancers harboring TRK fusions, netting an impressive 76% overall response rate.
Lead study author David Hyman, MD, chief of early drug development at Memorial Sloan Kettering Cancer Center in New York, discussed highlights of the analysis, larotrectinib’s regulatory status, and implications for TRK fusion testing in clinical care at the annual meeting of the American Society of Clinical Oncology.
Dr. Hyman disclosed that he has a consulting or advisory role with Atara Biotherapeutics, Chugai Pharma, and CytomX Therapeutics, and that he receives research funding from AstraZeneca and Puma Biotechnology. The study was funded by Loxo Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
CHICAGO – An integrated analysis of three trials has shown that larotrectinib, an oral selective inhibitor of tropomyosin receptor kinase (TRK), has durable efficacy across diverse adult and pediatric cancers harboring TRK fusions, netting an impressive 76% overall response rate.
Lead study author David Hyman, MD, chief of early drug development at Memorial Sloan Kettering Cancer Center in New York, discussed highlights of the analysis, larotrectinib’s regulatory status, and implications for TRK fusion testing in clinical care at the annual meeting of the American Society of Clinical Oncology.
Dr. Hyman disclosed that he has a consulting or advisory role with Atara Biotherapeutics, Chugai Pharma, and CytomX Therapeutics, and that he receives research funding from AstraZeneca and Puma Biotechnology. The study was funded by Loxo Oncology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT ASCO 2017
VIDEO: Wedge resection offers higher survival for NSCLC
BOSTON – High quality wedge resection results in higher survival for patients with early stage non–small cell lung cancer when compared with stereotactic body radiation therapy, according to new research.
The analysis, reported at the annual meeting of the American Association for Thoracic Surgery, evaluated the treatment of 7,337 patients in the National Cancer Database with clinical T1-T2, N0, M0 non–small cell lung cancer who were treated with either wedge resection or stereotactic body radiation therapy from 2005 to 2012.
In this video, Varun Puri, MD, of Washington University, St. Louis, discusses the study and the significance of the findings.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
agallegos@frontlinemedcom.com
On Twitter @legal_med
BOSTON – High quality wedge resection results in higher survival for patients with early stage non–small cell lung cancer when compared with stereotactic body radiation therapy, according to new research.
The analysis, reported at the annual meeting of the American Association for Thoracic Surgery, evaluated the treatment of 7,337 patients in the National Cancer Database with clinical T1-T2, N0, M0 non–small cell lung cancer who were treated with either wedge resection or stereotactic body radiation therapy from 2005 to 2012.
In this video, Varun Puri, MD, of Washington University, St. Louis, discusses the study and the significance of the findings.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
agallegos@frontlinemedcom.com
On Twitter @legal_med
BOSTON – High quality wedge resection results in higher survival for patients with early stage non–small cell lung cancer when compared with stereotactic body radiation therapy, according to new research.
The analysis, reported at the annual meeting of the American Association for Thoracic Surgery, evaluated the treatment of 7,337 patients in the National Cancer Database with clinical T1-T2, N0, M0 non–small cell lung cancer who were treated with either wedge resection or stereotactic body radiation therapy from 2005 to 2012.
In this video, Varun Puri, MD, of Washington University, St. Louis, discusses the study and the significance of the findings.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
agallegos@frontlinemedcom.com
On Twitter @legal_med
AT THE AATS ANNUAL MEETING
Gefitinib bests chemo as adjuvant therapy for early EGFR-mutant NSCLC
The targeted agent gefitinib is superior to the standard of care chemotherapy for treating resected early non–small cell lung cancer (NSCLC) harboring an epidermal growth factor receptor (EGFR) activating mutation, finds the phase III randomized Chinese ADJUVANT trial.
Gefitinib, an oral tyrosine kinase inhibitor that targets the EGFR kinase among others, is already approved by the Food and Drug Administration for treatment of locally advanced or metastatic disease having mutations in the gene for this receptor.
Trial results reported in a presscast leading up to the annual meeting of the American Society of Clinical Oncology showed that compared with vinorelbine and cisplatin combination chemotherapy, 2 years of gefitinib prolonged the time to recurrence or death by more than 10 months, reducing risk of these events by a significant 40%. Gefitinib also was better tolerated: The rate of grade 3 or worse adverse events with the targeted agent was one-fourth that seen with the chemotherapy.
“Targeted therapy can delay recurrence of intermediate-stage lung cancer after surgery. Two-year treatment duration of gefitinib is efficacious and tolerated well,” said lead study author Yi-Long Wu, MD, director of the Guangdong Lung Cancer Institute, Guangdong General Hospital, Guangzhou, China. “Adjuvant gefitinib should be considered as an important option for stage II to IIIA lung cancer patients with an activating EGFR mutation.”
Clinical implications
The improved disease-free survival seen with gefitinib in ADJUVANT is “encouraging,” according to ASCO President-Elect Bruce E. Johnson, MD, chief clinical research officer and an Institute Physician at the Dana-Farber Cancer Institute in Boston.
Longer follow-up will be needed to obtain a full picture as the horizon for events in the adjuvant setting is more on the order of years, and the disease-free survival curves began converging over time, he noted. “We will ultimately be interested in seeing whether this actually prolongs survival in a longer follow-up study, which Dr. Wu’s group is planning to do.
“I haven’t changed my approach yet for the patients with EGFR-mutant lung cancer,” Dr. Johnson concluded. “But I will be following this [trial] very closely to see what happens to the survival.”
The new data from ADJUVANT will likely have several effects on the clinical management of NSCLC, according to presscast moderator and ASCO Chief Medical Officer Richard L. Schilsky, MD.
“I suspect that many doctors will begin testing these lung cancer tumors right after surgery, to see if they actually have an EGFR mutation. That is not currently standard of care in the U.S.; typically the testing doesn’t take place until the cancer recurs or becomes metastatic,” he said. “So that way, doctors and patients will know whether or not treatment with an EGFR inhibitor is even an option.
“If it is an option, then many factors will likely come into play, and most importantly we will be waiting for the survival data,” said Dr. Schilsky, professor emeritus at the University of Chicago. Another consideration is that the trial compared 12 weeks of chemotherapy with 2 years of continuous gefitinib therapy, the latter of which requires a long-term commitment to adherence by patients and carries much greater cost.
“At the end of the day, I think that once the survival data is known in particular, doctors and patients are going to have to have very thoughtful discussions about what is the magnitude of the survival benefit; what is the burden on the patient to take either cytotoxic chemotherapy for 12 weeks or 2 years of an oral treatment, which, while it is less toxic, is not without toxicity; and what’s the financial burden of that treatment choice going to be for the patient,” he concluded.
Study details
Eligibility for the ADJUVANT trial required completely resected pathological stage II-IIIA (N1-N2) NSCLC with an EGFR-activating mutation. In all, 220 patients were randomized evenly to receive gefitinib (Iressa) once daily for 24 months or vinorelbine plus cisplatin every 3 weeks for 4 cycles.
Results showed that median disease-free survival – the trial’s primary endpoint—was 28.7 months with gefitinib compared with 18.0 months with chemotherapy (hazard ratio, 0.60; P = .005), Dr. Wu reported in the presscast. Corresponding 3-year disease-free survival rates were 34% and 27%.
The rate of grade 3 or worse adverse events was 12.3% in the gefitinib group, compared with 48.3% in the chemotherapy group. Most types of events were less common with the tyrosine kinase inhibitor, with the exception of rash, diarrhea, and elevation of liver enzymes.
Dr. Wu disclosed ties with AstraZeneca, Roche, Merck, Boehringer Ingelheim; Lilly, Pierre Fabre, Pfizer, and Sanofi. The Chinese Thoracic Oncology Group and AstraZeneca Chin funded the trial.
The targeted agent gefitinib is superior to the standard of care chemotherapy for treating resected early non–small cell lung cancer (NSCLC) harboring an epidermal growth factor receptor (EGFR) activating mutation, finds the phase III randomized Chinese ADJUVANT trial.
Gefitinib, an oral tyrosine kinase inhibitor that targets the EGFR kinase among others, is already approved by the Food and Drug Administration for treatment of locally advanced or metastatic disease having mutations in the gene for this receptor.
Trial results reported in a presscast leading up to the annual meeting of the American Society of Clinical Oncology showed that compared with vinorelbine and cisplatin combination chemotherapy, 2 years of gefitinib prolonged the time to recurrence or death by more than 10 months, reducing risk of these events by a significant 40%. Gefitinib also was better tolerated: The rate of grade 3 or worse adverse events with the targeted agent was one-fourth that seen with the chemotherapy.
“Targeted therapy can delay recurrence of intermediate-stage lung cancer after surgery. Two-year treatment duration of gefitinib is efficacious and tolerated well,” said lead study author Yi-Long Wu, MD, director of the Guangdong Lung Cancer Institute, Guangdong General Hospital, Guangzhou, China. “Adjuvant gefitinib should be considered as an important option for stage II to IIIA lung cancer patients with an activating EGFR mutation.”
Clinical implications
The improved disease-free survival seen with gefitinib in ADJUVANT is “encouraging,” according to ASCO President-Elect Bruce E. Johnson, MD, chief clinical research officer and an Institute Physician at the Dana-Farber Cancer Institute in Boston.
Longer follow-up will be needed to obtain a full picture as the horizon for events in the adjuvant setting is more on the order of years, and the disease-free survival curves began converging over time, he noted. “We will ultimately be interested in seeing whether this actually prolongs survival in a longer follow-up study, which Dr. Wu’s group is planning to do.
“I haven’t changed my approach yet for the patients with EGFR-mutant lung cancer,” Dr. Johnson concluded. “But I will be following this [trial] very closely to see what happens to the survival.”
The new data from ADJUVANT will likely have several effects on the clinical management of NSCLC, according to presscast moderator and ASCO Chief Medical Officer Richard L. Schilsky, MD.
“I suspect that many doctors will begin testing these lung cancer tumors right after surgery, to see if they actually have an EGFR mutation. That is not currently standard of care in the U.S.; typically the testing doesn’t take place until the cancer recurs or becomes metastatic,” he said. “So that way, doctors and patients will know whether or not treatment with an EGFR inhibitor is even an option.
“If it is an option, then many factors will likely come into play, and most importantly we will be waiting for the survival data,” said Dr. Schilsky, professor emeritus at the University of Chicago. Another consideration is that the trial compared 12 weeks of chemotherapy with 2 years of continuous gefitinib therapy, the latter of which requires a long-term commitment to adherence by patients and carries much greater cost.
“At the end of the day, I think that once the survival data is known in particular, doctors and patients are going to have to have very thoughtful discussions about what is the magnitude of the survival benefit; what is the burden on the patient to take either cytotoxic chemotherapy for 12 weeks or 2 years of an oral treatment, which, while it is less toxic, is not without toxicity; and what’s the financial burden of that treatment choice going to be for the patient,” he concluded.
Study details
Eligibility for the ADJUVANT trial required completely resected pathological stage II-IIIA (N1-N2) NSCLC with an EGFR-activating mutation. In all, 220 patients were randomized evenly to receive gefitinib (Iressa) once daily for 24 months or vinorelbine plus cisplatin every 3 weeks for 4 cycles.
Results showed that median disease-free survival – the trial’s primary endpoint—was 28.7 months with gefitinib compared with 18.0 months with chemotherapy (hazard ratio, 0.60; P = .005), Dr. Wu reported in the presscast. Corresponding 3-year disease-free survival rates were 34% and 27%.
The rate of grade 3 or worse adverse events was 12.3% in the gefitinib group, compared with 48.3% in the chemotherapy group. Most types of events were less common with the tyrosine kinase inhibitor, with the exception of rash, diarrhea, and elevation of liver enzymes.
Dr. Wu disclosed ties with AstraZeneca, Roche, Merck, Boehringer Ingelheim; Lilly, Pierre Fabre, Pfizer, and Sanofi. The Chinese Thoracic Oncology Group and AstraZeneca Chin funded the trial.
The targeted agent gefitinib is superior to the standard of care chemotherapy for treating resected early non–small cell lung cancer (NSCLC) harboring an epidermal growth factor receptor (EGFR) activating mutation, finds the phase III randomized Chinese ADJUVANT trial.
Gefitinib, an oral tyrosine kinase inhibitor that targets the EGFR kinase among others, is already approved by the Food and Drug Administration for treatment of locally advanced or metastatic disease having mutations in the gene for this receptor.
Trial results reported in a presscast leading up to the annual meeting of the American Society of Clinical Oncology showed that compared with vinorelbine and cisplatin combination chemotherapy, 2 years of gefitinib prolonged the time to recurrence or death by more than 10 months, reducing risk of these events by a significant 40%. Gefitinib also was better tolerated: The rate of grade 3 or worse adverse events with the targeted agent was one-fourth that seen with the chemotherapy.
“Targeted therapy can delay recurrence of intermediate-stage lung cancer after surgery. Two-year treatment duration of gefitinib is efficacious and tolerated well,” said lead study author Yi-Long Wu, MD, director of the Guangdong Lung Cancer Institute, Guangdong General Hospital, Guangzhou, China. “Adjuvant gefitinib should be considered as an important option for stage II to IIIA lung cancer patients with an activating EGFR mutation.”
Clinical implications
The improved disease-free survival seen with gefitinib in ADJUVANT is “encouraging,” according to ASCO President-Elect Bruce E. Johnson, MD, chief clinical research officer and an Institute Physician at the Dana-Farber Cancer Institute in Boston.
Longer follow-up will be needed to obtain a full picture as the horizon for events in the adjuvant setting is more on the order of years, and the disease-free survival curves began converging over time, he noted. “We will ultimately be interested in seeing whether this actually prolongs survival in a longer follow-up study, which Dr. Wu’s group is planning to do.
“I haven’t changed my approach yet for the patients with EGFR-mutant lung cancer,” Dr. Johnson concluded. “But I will be following this [trial] very closely to see what happens to the survival.”
The new data from ADJUVANT will likely have several effects on the clinical management of NSCLC, according to presscast moderator and ASCO Chief Medical Officer Richard L. Schilsky, MD.
“I suspect that many doctors will begin testing these lung cancer tumors right after surgery, to see if they actually have an EGFR mutation. That is not currently standard of care in the U.S.; typically the testing doesn’t take place until the cancer recurs or becomes metastatic,” he said. “So that way, doctors and patients will know whether or not treatment with an EGFR inhibitor is even an option.
“If it is an option, then many factors will likely come into play, and most importantly we will be waiting for the survival data,” said Dr. Schilsky, professor emeritus at the University of Chicago. Another consideration is that the trial compared 12 weeks of chemotherapy with 2 years of continuous gefitinib therapy, the latter of which requires a long-term commitment to adherence by patients and carries much greater cost.
“At the end of the day, I think that once the survival data is known in particular, doctors and patients are going to have to have very thoughtful discussions about what is the magnitude of the survival benefit; what is the burden on the patient to take either cytotoxic chemotherapy for 12 weeks or 2 years of an oral treatment, which, while it is less toxic, is not without toxicity; and what’s the financial burden of that treatment choice going to be for the patient,” he concluded.
Study details
Eligibility for the ADJUVANT trial required completely resected pathological stage II-IIIA (N1-N2) NSCLC with an EGFR-activating mutation. In all, 220 patients were randomized evenly to receive gefitinib (Iressa) once daily for 24 months or vinorelbine plus cisplatin every 3 weeks for 4 cycles.
Results showed that median disease-free survival – the trial’s primary endpoint—was 28.7 months with gefitinib compared with 18.0 months with chemotherapy (hazard ratio, 0.60; P = .005), Dr. Wu reported in the presscast. Corresponding 3-year disease-free survival rates were 34% and 27%.
The rate of grade 3 or worse adverse events was 12.3% in the gefitinib group, compared with 48.3% in the chemotherapy group. Most types of events were less common with the tyrosine kinase inhibitor, with the exception of rash, diarrhea, and elevation of liver enzymes.
Dr. Wu disclosed ties with AstraZeneca, Roche, Merck, Boehringer Ingelheim; Lilly, Pierre Fabre, Pfizer, and Sanofi. The Chinese Thoracic Oncology Group and AstraZeneca Chin funded the trial.
FROM THE 2017 ASCO ANNUAL MEETING
Key clinical point:
Major finding: Patients in the gefitinib group had a sharply reduced risk of recurrence or death relative to peers in the vinorelbine-cisplatin group (hazard ratio, 0.60; P = .005).
Data source: ADJUVANT, a phase III randomized controlled study of 220 patients with completely resected EGFR-mutant pathological stage II-IIIA (N1-N2) NSCLC.
Disclosures: Dr. Wu disclosed ties with AstraZeneca, Roche, Merck, Boehringer Ingelheim; Lilly, Pierre Fabre, Pfizer, and Sanofi. The Chinese Thoracic Oncology Group and AstraZeneca Chin funded the trial.
More early-stage cancer diagnosis since ACA implementation
Implementation of the Affordable Care Act (ACA) has been associated with a shift toward earlier stage at diagnosis for common screenable cancers, finds an analysis of nearly 273,000 patients reported in a presscast leading up to the annual meeting of the American Society of Clinical Oncology.
“Extensive evidence has shown that people without insurance are more likely to be diagnosed at later stage, especially for the cancers that can be detected earlier through screening or symptoms,” said lead study author Xuesong Han, PhD, strategic director of health policy and health care delivery research at the American Cancer Society in Atlanta. “In 2014, two major components of the Affordable Care Act – Medicaid expansion and marketplace exchange – were implemented. As a result, insurance coverage has substantially increased for nonelderly Americans.”
Study findings showed that, for four of five screenable cancers – breast and cervical cancer in women and lung and colorectal cancer in both sexes combined – the proportion of cancers that were stage I at diagnosis, and hence most curable, increased by an absolute 1% or so after the ACA was implemented. Prostate cancer was the outlier: the value for this malignancy decreased by 1%.
“The increases for the first four cancers were consistent with our hypothesis, with more people gaining insurance and access to screening services or access to physicians to detect early symptoms,” Dr. Han summarized. “But what about prostate cancer? We think [that pattern] may reflect the recent USPSTF recommendations against routine prostate cancer screening.”
“We think that this is an important study,” commented ASCO president-elect Bruce E. Johnson, MD, who is also chief clinical research officer and an institute physician at the Dana-Farber Cancer Institute in Boston. “Obviously, the changes are not enormous; they are not dramatic. But … because the uptake of screening is relatively slow, this is certainly consistent with the idea that, by doing additional screening, you can potentially find more stage I patients, and, the earlier the stage, the more likely one is to be cured.”
“The other important thing is that ASCO strongly supports the relative ease of access to screening capabilities, and that’s one of the characteristics of the Affordable Care Act, that most of the cancer screening is covered,” he further stated. “Whatever form our health care takes over the next several years, we advocate for patients to have early access to screening, which can identify cancers at an earlier stage in their more curable forms.”
Study details
For the study, the investigators used the National Cancer Database – which captures 70% of newly diagnosed cases in the United States – to identify patients younger than 65 who were eligible for cancer screening and who received a diagnosis of any of the five screenable cancers in 2013 or 2014. They compared stage distribution before ACA implementation (first nine months of 2013) and afterward (last nine months of 2014).
Analyses were based on data from 121,402 female breast cancer patients aged 40-64 years, 39,418 colorectal cancer patients aged 50-64 years, 11,190 cervical cancer patients aged 21-64 years, 59,210 prostate cancer patients aged 50-64 years, and 41,436 lung cancer patients aged 55-64 years.
Results showed that the proportion of cancers that were stage I at diagnosis increased after ACA implementation from 47.8% to 48.9% for breast cancer (adjusted prevalence ratio, 1.02) and from 47.3% to 48.8% for cervical cancer (APR, 1.02) in women, and from 16.6% to 17.7% for lung cancer (APR, 1.07) and from 22.8% to 23.7% for colorectal cancer (APR, 1.04) in men and women combined, Dr. Han reported.
Prostate cancer was the exception, with the proportion of cases that were stage I at diagnosis falling from 18.5% to 17.2% (APR, 0.93).
In a stratified analysis, the significant downshift in lung and colorectal cancer stage were seen only in states that had actually adopted the Medicaid expansion component of the ACA, which covers low-income individuals, according to Dr. Han. The downshift in female breast cancer stage and upshift in prostate cancer stage occurred regardless of whether states had done so.
Implementation of the Affordable Care Act (ACA) has been associated with a shift toward earlier stage at diagnosis for common screenable cancers, finds an analysis of nearly 273,000 patients reported in a presscast leading up to the annual meeting of the American Society of Clinical Oncology.
“Extensive evidence has shown that people without insurance are more likely to be diagnosed at later stage, especially for the cancers that can be detected earlier through screening or symptoms,” said lead study author Xuesong Han, PhD, strategic director of health policy and health care delivery research at the American Cancer Society in Atlanta. “In 2014, two major components of the Affordable Care Act – Medicaid expansion and marketplace exchange – were implemented. As a result, insurance coverage has substantially increased for nonelderly Americans.”
Study findings showed that, for four of five screenable cancers – breast and cervical cancer in women and lung and colorectal cancer in both sexes combined – the proportion of cancers that were stage I at diagnosis, and hence most curable, increased by an absolute 1% or so after the ACA was implemented. Prostate cancer was the outlier: the value for this malignancy decreased by 1%.
“The increases for the first four cancers were consistent with our hypothesis, with more people gaining insurance and access to screening services or access to physicians to detect early symptoms,” Dr. Han summarized. “But what about prostate cancer? We think [that pattern] may reflect the recent USPSTF recommendations against routine prostate cancer screening.”
“We think that this is an important study,” commented ASCO president-elect Bruce E. Johnson, MD, who is also chief clinical research officer and an institute physician at the Dana-Farber Cancer Institute in Boston. “Obviously, the changes are not enormous; they are not dramatic. But … because the uptake of screening is relatively slow, this is certainly consistent with the idea that, by doing additional screening, you can potentially find more stage I patients, and, the earlier the stage, the more likely one is to be cured.”
“The other important thing is that ASCO strongly supports the relative ease of access to screening capabilities, and that’s one of the characteristics of the Affordable Care Act, that most of the cancer screening is covered,” he further stated. “Whatever form our health care takes over the next several years, we advocate for patients to have early access to screening, which can identify cancers at an earlier stage in their more curable forms.”
Study details
For the study, the investigators used the National Cancer Database – which captures 70% of newly diagnosed cases in the United States – to identify patients younger than 65 who were eligible for cancer screening and who received a diagnosis of any of the five screenable cancers in 2013 or 2014. They compared stage distribution before ACA implementation (first nine months of 2013) and afterward (last nine months of 2014).
Analyses were based on data from 121,402 female breast cancer patients aged 40-64 years, 39,418 colorectal cancer patients aged 50-64 years, 11,190 cervical cancer patients aged 21-64 years, 59,210 prostate cancer patients aged 50-64 years, and 41,436 lung cancer patients aged 55-64 years.
Results showed that the proportion of cancers that were stage I at diagnosis increased after ACA implementation from 47.8% to 48.9% for breast cancer (adjusted prevalence ratio, 1.02) and from 47.3% to 48.8% for cervical cancer (APR, 1.02) in women, and from 16.6% to 17.7% for lung cancer (APR, 1.07) and from 22.8% to 23.7% for colorectal cancer (APR, 1.04) in men and women combined, Dr. Han reported.
Prostate cancer was the exception, with the proportion of cases that were stage I at diagnosis falling from 18.5% to 17.2% (APR, 0.93).
In a stratified analysis, the significant downshift in lung and colorectal cancer stage were seen only in states that had actually adopted the Medicaid expansion component of the ACA, which covers low-income individuals, according to Dr. Han. The downshift in female breast cancer stage and upshift in prostate cancer stage occurred regardless of whether states had done so.
Implementation of the Affordable Care Act (ACA) has been associated with a shift toward earlier stage at diagnosis for common screenable cancers, finds an analysis of nearly 273,000 patients reported in a presscast leading up to the annual meeting of the American Society of Clinical Oncology.
“Extensive evidence has shown that people without insurance are more likely to be diagnosed at later stage, especially for the cancers that can be detected earlier through screening or symptoms,” said lead study author Xuesong Han, PhD, strategic director of health policy and health care delivery research at the American Cancer Society in Atlanta. “In 2014, two major components of the Affordable Care Act – Medicaid expansion and marketplace exchange – were implemented. As a result, insurance coverage has substantially increased for nonelderly Americans.”
Study findings showed that, for four of five screenable cancers – breast and cervical cancer in women and lung and colorectal cancer in both sexes combined – the proportion of cancers that were stage I at diagnosis, and hence most curable, increased by an absolute 1% or so after the ACA was implemented. Prostate cancer was the outlier: the value for this malignancy decreased by 1%.
“The increases for the first four cancers were consistent with our hypothesis, with more people gaining insurance and access to screening services or access to physicians to detect early symptoms,” Dr. Han summarized. “But what about prostate cancer? We think [that pattern] may reflect the recent USPSTF recommendations against routine prostate cancer screening.”
“We think that this is an important study,” commented ASCO president-elect Bruce E. Johnson, MD, who is also chief clinical research officer and an institute physician at the Dana-Farber Cancer Institute in Boston. “Obviously, the changes are not enormous; they are not dramatic. But … because the uptake of screening is relatively slow, this is certainly consistent with the idea that, by doing additional screening, you can potentially find more stage I patients, and, the earlier the stage, the more likely one is to be cured.”
“The other important thing is that ASCO strongly supports the relative ease of access to screening capabilities, and that’s one of the characteristics of the Affordable Care Act, that most of the cancer screening is covered,” he further stated. “Whatever form our health care takes over the next several years, we advocate for patients to have early access to screening, which can identify cancers at an earlier stage in their more curable forms.”
Study details
For the study, the investigators used the National Cancer Database – which captures 70% of newly diagnosed cases in the United States – to identify patients younger than 65 who were eligible for cancer screening and who received a diagnosis of any of the five screenable cancers in 2013 or 2014. They compared stage distribution before ACA implementation (first nine months of 2013) and afterward (last nine months of 2014).
Analyses were based on data from 121,402 female breast cancer patients aged 40-64 years, 39,418 colorectal cancer patients aged 50-64 years, 11,190 cervical cancer patients aged 21-64 years, 59,210 prostate cancer patients aged 50-64 years, and 41,436 lung cancer patients aged 55-64 years.
Results showed that the proportion of cancers that were stage I at diagnosis increased after ACA implementation from 47.8% to 48.9% for breast cancer (adjusted prevalence ratio, 1.02) and from 47.3% to 48.8% for cervical cancer (APR, 1.02) in women, and from 16.6% to 17.7% for lung cancer (APR, 1.07) and from 22.8% to 23.7% for colorectal cancer (APR, 1.04) in men and women combined, Dr. Han reported.
Prostate cancer was the exception, with the proportion of cases that were stage I at diagnosis falling from 18.5% to 17.2% (APR, 0.93).
In a stratified analysis, the significant downshift in lung and colorectal cancer stage were seen only in states that had actually adopted the Medicaid expansion component of the ACA, which covers low-income individuals, according to Dr. Han. The downshift in female breast cancer stage and upshift in prostate cancer stage occurred regardless of whether states had done so.
FROM THE 2017 ASCO ANNUAL MEETING
Key clinical point:
Major finding: The proportion of cancers that were stage I when diagnosed increased by about 1% after ACA implementation for breast, cervical, lung, and colorectal cancer, while it decreased by 1% for prostate cancer.
Data source: A cohort study of 272,656 patients with these five cancers from the National Cancer Database.
Disclosures: Dr. Han reported that she had no disclosures.
Pulmonary sarcomatoid carcinoma presenting as a necrotizing cavitary lung lesion: diagnostic dilemma
Pulmonary sarcomatoid carcinoma (PSC) is a rare histological subtype that has an aggressive course with average survival of 11-13 months.1 In clinical practice, the possible presentations of this rare cancer are not widely known, resulting in a misdiagnosis. That is what happened with our patient, who presented with necrotizing cavitary lung lesion and soft tissue necrotizing lymphadenitis. The clinical picture was reminiscent of tuberculosis or granulomatosis with polyangiitis and was further confounded by negative computed-tomography (CT)-guided biopsy and bronchoscopy findings, which added to the delay in diagnosis. With the currently available knowledge, the diagnosis of PSC depends largely on evaluation of the surgically resected specimen, which in most cases is avoided until there is a high suspicion of PSC. Biopsy is not useful due to extensive necrosis, as will be seen in our case. Consequently, most of the data in the literature is based on case series of autopsy specimen, and the clinical characteristics of PSC remain unclear. The rarity of PSC has prevented its characterization in literature. We report here a rare presentation of PSC with necrotizing lung lesion, to add to the paucity of the current data.
Case presentation and summary
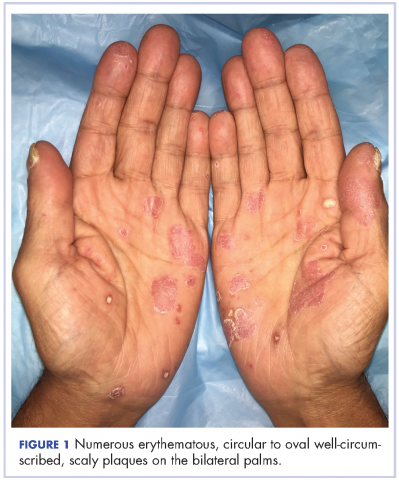
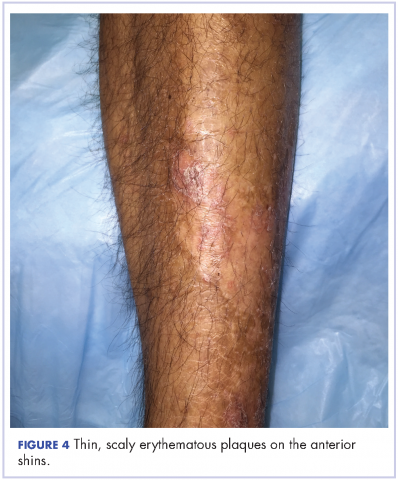
A 58-year-old homeless man presented to the Upstate University Hospital, Syracuse, New York, with a 25-pound weight loss during the previous month and associated productive cough and hemoptysis for a week and a painful mass in the nape of his neck. He denied any fever, chest pain, sick contacts, or joint pain. He had a history of about 40 pack-years of smoking, and his brother had recently been diagnosed with lung cancer. A tender fluctuant mass was detected in the nape of his neck on examination (Figure 1).
The patient had presented 9 months earlier with persistent cough and hemoptysis, and at that visit was found to have a cavitary lesion in the right lung measuring 2 cm (0.8 in). He had undergone a computed-tomograpghy (CT)-guided biopsy of the lesion, which had shown acute and chronic inflammation with fibrosis, and he had negative bronchoscopy findings. The patient tested negative for tuberculosis during the first visit but he left the hospital against the medical advice of the physicians and he was lost to follow-up until his re-presentation.
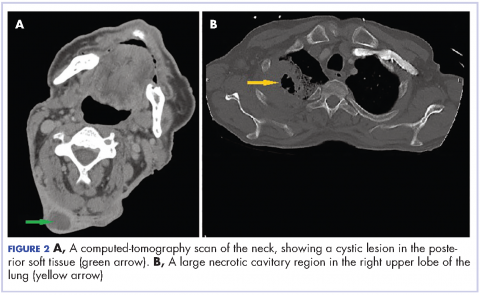
On physical examination at his re-presentation, the patient seemed cachectic, with a blood pressure of 94/62 mm of Hg. The mass in the nape of his neck was about 3 cm (1.2 in) long, with erythema of the surrounding skin (Figure 1). Bronchial breath sounds were heard in the right upper lobe of the lung, likely due to the underlying cavitary lesion (Figure 2).
Given the patient’s advanced disease, he was started on palliative radiotherapy with radiosensitizing chemotherapy with carboplatin (target AUC 6) and paclitaxel (135 mg/m2 over 24 hours). His symptoms of hemoptysis improved transiently after the first cycle, but he became hypotensive and drowsy during the second cycle of therapy, and the family decided to make the patient comfort care and withdraw all further treatment. He was discharged to hospice.
Discussion
PSC is a rare variant of non-small-cell carcinoma lung cancer, accounting for up to 0.4% of lung malignancy.1 It was recently subtyped by the World Health Organization as a non-small cell lung carcinoma with certain amount of differentiation resembling sarcoma or containing elements of sarcoma.2-4 It is not known why both elements co-exist in the tumor, but Franks and colleagues some theories have been postulated in the literature, including possible origin from a single, aberrant stem cell with progenies differentiating in two separate pathways.3
Sarcomatoid carcinoma consists of spectrum of tumors including pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and blastoma.3,4 It usually shows male preponderance, and association with smoking.3 The diagnosis commonly occurs in the sixth decade of life, except for pulmonary blastoma, which is more common in the fourth decade and with equal gender distribution.4
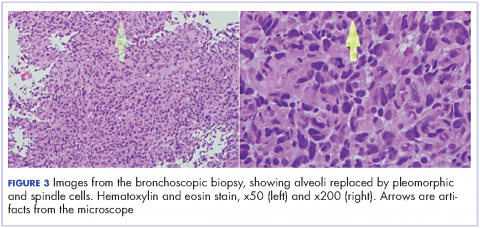
The presenting symptoms can be variable and nonspecific, but predominantly include chest pain, cough, hemoptysis, and/or weight loss.5 Radiologically, pulmonary sarcomatoid cancer presenting as a necrotizing cavitary lesion in the lung is a rare finding, seldom reported in the past.6,7 The presentation in our case, with necrotizing lymphadenitis, was reminiscent of an infectious or autoimmune etiology such as tuberculosis or granulomatosis with polyangiitis. The presence of extensive necrosis in the lesion and the characteristic heterogeneity of the tumor had resulted in inconclusive biopsy findings during the previous presentation. In clinical practice, there is over-reliance on biopsy findings to make the distinction between cancer and other mimicking conditions. This is especially true for rare tumors such as PSC, which often results in misdiagnosis and a delay in administering the proper treatment.
Transbronchial biopsy in cases such as the present case, carries little benefit because the diagnosis depends on the site from which the biopsy is taken and whether the biopsied tissue is representative of the entire mass. The diagnosis can be suspected based on the clinical and radiological findings but confirmation requires a surgical resection to delineate the accurate cytology and architecture.5,6,8 Huang and colleagues showed a misdiagnosis rate of PSC of >70% preoperatively.4 Resective surgery is feasible only in patients with high index of suspicion for a malignancy, which in most cases requires previous confirmation with a biopsy. The rarity of this cancer, its unusual presentations, and the lack of specific testing preclude early diagnosis and timely treatment of this fatal condition.
Initial treatment options for localized or with limited spread disease is resective surgery. The role of chemo- or radiation therapy is not known, but they have not previously shown promising results,6,8 except in some cases when they are used as postoperative adjuvant chemotherapy4 or in bulky, locally invasive tumors.1 The recurrence rate after surgery is very high, resulting in a poor 5-year survival rate.1,8 Experimental therapies, such as antibodies that target epidermal growth factor receptor mutations, have not shown much success either.8 In conclusion, the outlook for patients with PSC with the current available knowledge and treatment protocols, is dismal.
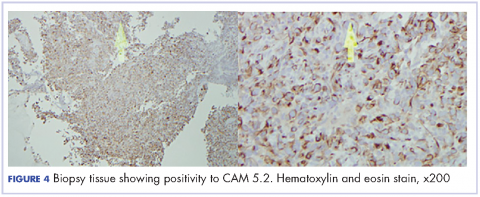
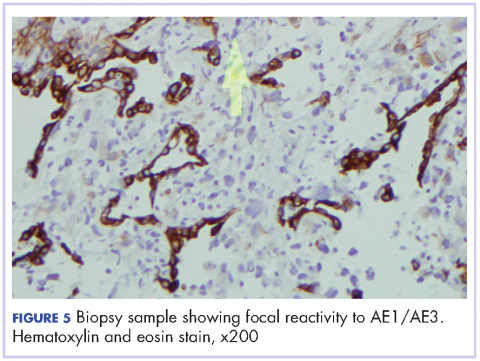
Most of the current knowledge and data in the literature is based on cases from autopsy or early-stage surgical resections rather than on patients with advanced cancer.5 Moreover, the role of surgical resection in PSC is questionable, given the high recurrence rate. Subsequently, the clinical and pathological manifestations have yet to be well characterized.4 There has been advance with the publication of more studies recently. Cytokeratin markers such as CAM 5.2 and AE1/AE3 are commonly useful to support the diagnosis when suspected.3 Other markers, including the carcinoembryonic antigen, CD15, and thyroid transcription factor-1 may be variably positive, based on the differentiation of the cancer. Other exciting prospects in the study of PSC include the suggestion of a modified vimentin histologic score for better characterization of the cancer and the discovery of high platelet-derived growth factor receptor beta immunohistochemistry expression in PSC as a potential target for future therapy.
Conclusion
Pulmonary sarcomatoid lung cancer can present with a predominant necrotizing picture that mimics diseases such as tuberculosis. In such case, transbronchial biopsy carries little benefit because the diagnosis depends on whether the biopsied tissue is representative of the entire mass, often confounded by the extensive necrosis. More data is needed to determine prognostic factors and appropriate therapeutic strategies.
1. Martin LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007;84(3):973-980.
2. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18(6):1059-1068.
3. Franks TJ, Galvin JR. Sarcomatoid carcinoma of the lung: histologic criteria and common lesions in the differential diagnosis. Arch Pathol Lab Med. 2010;134(1):49-54.
4. Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. http://wjso.biomedcentral.com/articles/10.1186/1477-7819-11-252. Published 2013. Accessed March 12, 2017.
5. Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134(11):1645-1658.
6. Pelosi G, Sonzogni A, De Pas T, et al. Review article: pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol. 2010;18(2):103-120.
7. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34(1):91-97.
8. Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3-4):206-213.
Pulmonary sarcomatoid carcinoma (PSC) is a rare histological subtype that has an aggressive course with average survival of 11-13 months.1 In clinical practice, the possible presentations of this rare cancer are not widely known, resulting in a misdiagnosis. That is what happened with our patient, who presented with necrotizing cavitary lung lesion and soft tissue necrotizing lymphadenitis. The clinical picture was reminiscent of tuberculosis or granulomatosis with polyangiitis and was further confounded by negative computed-tomography (CT)-guided biopsy and bronchoscopy findings, which added to the delay in diagnosis. With the currently available knowledge, the diagnosis of PSC depends largely on evaluation of the surgically resected specimen, which in most cases is avoided until there is a high suspicion of PSC. Biopsy is not useful due to extensive necrosis, as will be seen in our case. Consequently, most of the data in the literature is based on case series of autopsy specimen, and the clinical characteristics of PSC remain unclear. The rarity of PSC has prevented its characterization in literature. We report here a rare presentation of PSC with necrotizing lung lesion, to add to the paucity of the current data.
Case presentation and summary
A 58-year-old homeless man presented to the Upstate University Hospital, Syracuse, New York, with a 25-pound weight loss during the previous month and associated productive cough and hemoptysis for a week and a painful mass in the nape of his neck. He denied any fever, chest pain, sick contacts, or joint pain. He had a history of about 40 pack-years of smoking, and his brother had recently been diagnosed with lung cancer. A tender fluctuant mass was detected in the nape of his neck on examination (Figure 1).
The patient had presented 9 months earlier with persistent cough and hemoptysis, and at that visit was found to have a cavitary lesion in the right lung measuring 2 cm (0.8 in). He had undergone a computed-tomograpghy (CT)-guided biopsy of the lesion, which had shown acute and chronic inflammation with fibrosis, and he had negative bronchoscopy findings. The patient tested negative for tuberculosis during the first visit but he left the hospital against the medical advice of the physicians and he was lost to follow-up until his re-presentation.
On physical examination at his re-presentation, the patient seemed cachectic, with a blood pressure of 94/62 mm of Hg. The mass in the nape of his neck was about 3 cm (1.2 in) long, with erythema of the surrounding skin (Figure 1). Bronchial breath sounds were heard in the right upper lobe of the lung, likely due to the underlying cavitary lesion (Figure 2).
Given the patient’s advanced disease, he was started on palliative radiotherapy with radiosensitizing chemotherapy with carboplatin (target AUC 6) and paclitaxel (135 mg/m2 over 24 hours). His symptoms of hemoptysis improved transiently after the first cycle, but he became hypotensive and drowsy during the second cycle of therapy, and the family decided to make the patient comfort care and withdraw all further treatment. He was discharged to hospice.
Discussion
PSC is a rare variant of non-small-cell carcinoma lung cancer, accounting for up to 0.4% of lung malignancy.1 It was recently subtyped by the World Health Organization as a non-small cell lung carcinoma with certain amount of differentiation resembling sarcoma or containing elements of sarcoma.2-4 It is not known why both elements co-exist in the tumor, but Franks and colleagues some theories have been postulated in the literature, including possible origin from a single, aberrant stem cell with progenies differentiating in two separate pathways.3
Sarcomatoid carcinoma consists of spectrum of tumors including pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and blastoma.3,4 It usually shows male preponderance, and association with smoking.3 The diagnosis commonly occurs in the sixth decade of life, except for pulmonary blastoma, which is more common in the fourth decade and with equal gender distribution.4
The presenting symptoms can be variable and nonspecific, but predominantly include chest pain, cough, hemoptysis, and/or weight loss.5 Radiologically, pulmonary sarcomatoid cancer presenting as a necrotizing cavitary lesion in the lung is a rare finding, seldom reported in the past.6,7 The presentation in our case, with necrotizing lymphadenitis, was reminiscent of an infectious or autoimmune etiology such as tuberculosis or granulomatosis with polyangiitis. The presence of extensive necrosis in the lesion and the characteristic heterogeneity of the tumor had resulted in inconclusive biopsy findings during the previous presentation. In clinical practice, there is over-reliance on biopsy findings to make the distinction between cancer and other mimicking conditions. This is especially true for rare tumors such as PSC, which often results in misdiagnosis and a delay in administering the proper treatment.
Transbronchial biopsy in cases such as the present case, carries little benefit because the diagnosis depends on the site from which the biopsy is taken and whether the biopsied tissue is representative of the entire mass. The diagnosis can be suspected based on the clinical and radiological findings but confirmation requires a surgical resection to delineate the accurate cytology and architecture.5,6,8 Huang and colleagues showed a misdiagnosis rate of PSC of >70% preoperatively.4 Resective surgery is feasible only in patients with high index of suspicion for a malignancy, which in most cases requires previous confirmation with a biopsy. The rarity of this cancer, its unusual presentations, and the lack of specific testing preclude early diagnosis and timely treatment of this fatal condition.
Initial treatment options for localized or with limited spread disease is resective surgery. The role of chemo- or radiation therapy is not known, but they have not previously shown promising results,6,8 except in some cases when they are used as postoperative adjuvant chemotherapy4 or in bulky, locally invasive tumors.1 The recurrence rate after surgery is very high, resulting in a poor 5-year survival rate.1,8 Experimental therapies, such as antibodies that target epidermal growth factor receptor mutations, have not shown much success either.8 In conclusion, the outlook for patients with PSC with the current available knowledge and treatment protocols, is dismal.
Most of the current knowledge and data in the literature is based on cases from autopsy or early-stage surgical resections rather than on patients with advanced cancer.5 Moreover, the role of surgical resection in PSC is questionable, given the high recurrence rate. Subsequently, the clinical and pathological manifestations have yet to be well characterized.4 There has been advance with the publication of more studies recently. Cytokeratin markers such as CAM 5.2 and AE1/AE3 are commonly useful to support the diagnosis when suspected.3 Other markers, including the carcinoembryonic antigen, CD15, and thyroid transcription factor-1 may be variably positive, based on the differentiation of the cancer. Other exciting prospects in the study of PSC include the suggestion of a modified vimentin histologic score for better characterization of the cancer and the discovery of high platelet-derived growth factor receptor beta immunohistochemistry expression in PSC as a potential target for future therapy.
Conclusion
Pulmonary sarcomatoid lung cancer can present with a predominant necrotizing picture that mimics diseases such as tuberculosis. In such case, transbronchial biopsy carries little benefit because the diagnosis depends on whether the biopsied tissue is representative of the entire mass, often confounded by the extensive necrosis. More data is needed to determine prognostic factors and appropriate therapeutic strategies.
Pulmonary sarcomatoid carcinoma (PSC) is a rare histological subtype that has an aggressive course with average survival of 11-13 months.1 In clinical practice, the possible presentations of this rare cancer are not widely known, resulting in a misdiagnosis. That is what happened with our patient, who presented with necrotizing cavitary lung lesion and soft tissue necrotizing lymphadenitis. The clinical picture was reminiscent of tuberculosis or granulomatosis with polyangiitis and was further confounded by negative computed-tomography (CT)-guided biopsy and bronchoscopy findings, which added to the delay in diagnosis. With the currently available knowledge, the diagnosis of PSC depends largely on evaluation of the surgically resected specimen, which in most cases is avoided until there is a high suspicion of PSC. Biopsy is not useful due to extensive necrosis, as will be seen in our case. Consequently, most of the data in the literature is based on case series of autopsy specimen, and the clinical characteristics of PSC remain unclear. The rarity of PSC has prevented its characterization in literature. We report here a rare presentation of PSC with necrotizing lung lesion, to add to the paucity of the current data.
Case presentation and summary
A 58-year-old homeless man presented to the Upstate University Hospital, Syracuse, New York, with a 25-pound weight loss during the previous month and associated productive cough and hemoptysis for a week and a painful mass in the nape of his neck. He denied any fever, chest pain, sick contacts, or joint pain. He had a history of about 40 pack-years of smoking, and his brother had recently been diagnosed with lung cancer. A tender fluctuant mass was detected in the nape of his neck on examination (Figure 1).
The patient had presented 9 months earlier with persistent cough and hemoptysis, and at that visit was found to have a cavitary lesion in the right lung measuring 2 cm (0.8 in). He had undergone a computed-tomograpghy (CT)-guided biopsy of the lesion, which had shown acute and chronic inflammation with fibrosis, and he had negative bronchoscopy findings. The patient tested negative for tuberculosis during the first visit but he left the hospital against the medical advice of the physicians and he was lost to follow-up until his re-presentation.
On physical examination at his re-presentation, the patient seemed cachectic, with a blood pressure of 94/62 mm of Hg. The mass in the nape of his neck was about 3 cm (1.2 in) long, with erythema of the surrounding skin (Figure 1). Bronchial breath sounds were heard in the right upper lobe of the lung, likely due to the underlying cavitary lesion (Figure 2).
Given the patient’s advanced disease, he was started on palliative radiotherapy with radiosensitizing chemotherapy with carboplatin (target AUC 6) and paclitaxel (135 mg/m2 over 24 hours). His symptoms of hemoptysis improved transiently after the first cycle, but he became hypotensive and drowsy during the second cycle of therapy, and the family decided to make the patient comfort care and withdraw all further treatment. He was discharged to hospice.
Discussion
PSC is a rare variant of non-small-cell carcinoma lung cancer, accounting for up to 0.4% of lung malignancy.1 It was recently subtyped by the World Health Organization as a non-small cell lung carcinoma with certain amount of differentiation resembling sarcoma or containing elements of sarcoma.2-4 It is not known why both elements co-exist in the tumor, but Franks and colleagues some theories have been postulated in the literature, including possible origin from a single, aberrant stem cell with progenies differentiating in two separate pathways.3
Sarcomatoid carcinoma consists of spectrum of tumors including pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and blastoma.3,4 It usually shows male preponderance, and association with smoking.3 The diagnosis commonly occurs in the sixth decade of life, except for pulmonary blastoma, which is more common in the fourth decade and with equal gender distribution.4
The presenting symptoms can be variable and nonspecific, but predominantly include chest pain, cough, hemoptysis, and/or weight loss.5 Radiologically, pulmonary sarcomatoid cancer presenting as a necrotizing cavitary lesion in the lung is a rare finding, seldom reported in the past.6,7 The presentation in our case, with necrotizing lymphadenitis, was reminiscent of an infectious or autoimmune etiology such as tuberculosis or granulomatosis with polyangiitis. The presence of extensive necrosis in the lesion and the characteristic heterogeneity of the tumor had resulted in inconclusive biopsy findings during the previous presentation. In clinical practice, there is over-reliance on biopsy findings to make the distinction between cancer and other mimicking conditions. This is especially true for rare tumors such as PSC, which often results in misdiagnosis and a delay in administering the proper treatment.
Transbronchial biopsy in cases such as the present case, carries little benefit because the diagnosis depends on the site from which the biopsy is taken and whether the biopsied tissue is representative of the entire mass. The diagnosis can be suspected based on the clinical and radiological findings but confirmation requires a surgical resection to delineate the accurate cytology and architecture.5,6,8 Huang and colleagues showed a misdiagnosis rate of PSC of >70% preoperatively.4 Resective surgery is feasible only in patients with high index of suspicion for a malignancy, which in most cases requires previous confirmation with a biopsy. The rarity of this cancer, its unusual presentations, and the lack of specific testing preclude early diagnosis and timely treatment of this fatal condition.
Initial treatment options for localized or with limited spread disease is resective surgery. The role of chemo- or radiation therapy is not known, but they have not previously shown promising results,6,8 except in some cases when they are used as postoperative adjuvant chemotherapy4 or in bulky, locally invasive tumors.1 The recurrence rate after surgery is very high, resulting in a poor 5-year survival rate.1,8 Experimental therapies, such as antibodies that target epidermal growth factor receptor mutations, have not shown much success either.8 In conclusion, the outlook for patients with PSC with the current available knowledge and treatment protocols, is dismal.
Most of the current knowledge and data in the literature is based on cases from autopsy or early-stage surgical resections rather than on patients with advanced cancer.5 Moreover, the role of surgical resection in PSC is questionable, given the high recurrence rate. Subsequently, the clinical and pathological manifestations have yet to be well characterized.4 There has been advance with the publication of more studies recently. Cytokeratin markers such as CAM 5.2 and AE1/AE3 are commonly useful to support the diagnosis when suspected.3 Other markers, including the carcinoembryonic antigen, CD15, and thyroid transcription factor-1 may be variably positive, based on the differentiation of the cancer. Other exciting prospects in the study of PSC include the suggestion of a modified vimentin histologic score for better characterization of the cancer and the discovery of high platelet-derived growth factor receptor beta immunohistochemistry expression in PSC as a potential target for future therapy.
Conclusion
Pulmonary sarcomatoid lung cancer can present with a predominant necrotizing picture that mimics diseases such as tuberculosis. In such case, transbronchial biopsy carries little benefit because the diagnosis depends on whether the biopsied tissue is representative of the entire mass, often confounded by the extensive necrosis. More data is needed to determine prognostic factors and appropriate therapeutic strategies.
1. Martin LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007;84(3):973-980.
2. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18(6):1059-1068.
3. Franks TJ, Galvin JR. Sarcomatoid carcinoma of the lung: histologic criteria and common lesions in the differential diagnosis. Arch Pathol Lab Med. 2010;134(1):49-54.
4. Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. http://wjso.biomedcentral.com/articles/10.1186/1477-7819-11-252. Published 2013. Accessed March 12, 2017.
5. Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134(11):1645-1658.
6. Pelosi G, Sonzogni A, De Pas T, et al. Review article: pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol. 2010;18(2):103-120.
7. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34(1):91-97.
8. Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3-4):206-213.
1. Martin LW, Correa AM, Ordonez NG, et al. Sarcomatoid carcinoma of the lung: a predictor of poor prognosis. Ann Thorac Surg. 2007;84(3):973-980.
2. Brambilla E, Travis WD, Colby TV, Corrin B, Shimosato Y. The new World Health Organization classification of lung tumours. Eur Respir J. 2001;18(6):1059-1068.
3. Franks TJ, Galvin JR. Sarcomatoid carcinoma of the lung: histologic criteria and common lesions in the differential diagnosis. Arch Pathol Lab Med. 2010;134(1):49-54.
4. Huang SY, Shen SJ, Li XY. Pulmonary sarcomatoid carcinoma: a clinicopathologic study and prognostic analysis of 51 cases. http://wjso.biomedcentral.com/articles/10.1186/1477-7819-11-252. Published 2013. Accessed March 12, 2017.
5. Travis WD. Sarcomatoid neoplasms of the lung and pleura. Arch Pathol Lab Med. 2010;134(11):1645-1658.
6. Pelosi G, Sonzogni A, De Pas T, et al. Review article: pulmonary sarcomatoid carcinomas: a practical overview. Int J Surg Pathol. 2010;18(2):103-120.
7. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34(1):91-97.
8. Park JS, Lee Y, Han J, et al. Clinicopathologic outcomes of curative resection for sarcomatoid carcinoma of the lung. Oncology. 2011;81(3-4):206-213.
Palmoplantar exacerbation of psoriasis after nivolumab for lung cancer
Nivolumab is a full human immunoglobulin antibody to the programmed cell death 1 (PD-1) immune checkpoint receptor on T cells. This programmed cell death inhibitor is a targeted immunotherapy used to treat patients with melanoma, among other malignancies.1 More recently, nivolumab has been used for advanced non-small-cell lung cancer (NSCLC) after failure of previous chemotherapeutic agents. It was approved by the US Food and Drug Administration for the NSCLC indication in 2015.2
PD-1 inhibitors are efficacious in treating advanced malignancies, although their immune-mediated functions can lead to undesirable side effects. Patients treated with nivolumab have been reported to develop thyroid disease,1,3,4 diabetes,3 hypophysitis,1,3 hypopituitarism,3 and pneumonitis,4,2 as well as other autoimmune conditions.3 Although nivolumab is often used to treat skin diseases such as melanoma, it can have many cutaneous side effects including pruritus,1,3-6 rash,1,3,4,6,7 vitiligo,1,3,7,6 mouth sores,3 injection site reactions,3,6 and alopecia.5 Herein, we describe a patient who was treated with nivolumab and developed an exacerbation of pre-existing psoriasis.
Case presentation and summary
A 57-year-old man with metastatic NSCLC and a history of plaque psoriasis presented to the dermatology clinic for evaluation of new lesions on his palms and soles. The patient had been previously treated with numerous therapies for NSCLC, including chemotherapy and radiation. Previous chemotherapeutic agents included the cisplatin plus etoposide combination, with doxetaxel and pemetrexed. The patient was not able to tolerate the chemotherapy and instead opted for hospice care. After several months, he chose to restart therapy, and was started on the programmed cell death (PD)-1 inhibitor, nivolumab, at a dose of 3 mg/kg for a total of 6 cycles. He received his first dose 5 weeks before his current presentation to the clinic, and his second dose 2 weeks before.
The patient reported a 20-year history of plaque psoriasis, characterized by psoriatic plaques on the elbows and shins and for which he was treated with topical therapies with good effect. Every few months, he would develop one or two small plaques of psoriasis on his palms and soles. The lesions were inconsequential to the patient, as he never experienced more than one or two small palmoplantar lesions at a time. One week after his second cycle of nivolumab, the patient developed an eruption of lesions on his palms and soles. He observed that the lesions seemed to be similar to his previous palmoplantar psoriatic plaques but with significantly greater skin involvement. The patient denied any new-onset joint pain.
The results of a physical examination revealed a cachectic man in no acute distress, with more than 30 erythematous circular to oval circumscribed plaques with yellow to whitish scales on the bilateral palms (Figure 1) and soles (Figure 2).
The patient also had well-demarcated, thick oval erythematous plaques with micaceous scales on the bilateral elbows (Figure 3), and thin scaly erythematous plaques on the anterior shins (Figure 4). There were no psoriatic plaques on the remainder of the trunk or extremities. Mucosal surfaces, scalp, and nails were uninvolved.
A clinical diagnosis of exacerbation of pre-existing psoriasis owing to nivolumab therapy was made. The patient was started on clobetasol 0.05% ointment twice daily under occlusion with plastic wrap to the affected areas, and he was continued on nivolumab for his NSCLC.
Discussion
Treatment with nivolumab can lead to a range of autoimmune side effects, and as shown in this case, psoriasis is one of the cutaneous findings that could be exacerbated by treatment with nivolumab. To date, two cases of exacerbation of psoriasis in patients treated with nivolumab for melanoma have been reported in the literature.8,9 In the first case, the patient had well-controlled plaque psoriasis at baseline and he subsequently developed psoriatic plaques on the trunk and extremities after the second infusion of nivolumab for metastatic melanoma. A biopsy showed regular acanthosis with hyperkeratosis and parakeratosis in addition to dilated vessels in the papillary dermis.8 In the second case, the patient had a history of psoriasis vulgaris with no active lesions. Three weeks after his first course of nivolumab for metastatic oral mucosal melanoma, he developed new, well-circumscribed erythematous scaly plaques on the trunk and extremities that were clinically diagnosed as psoriasis.9 In a third case, a patient without a prior history of psoriasis experienced a psoriasiform eruption on the trunk and extremities after the fourth dose of nivolumab for oral mucosal melanoma.10 Thus, our case is the third reported case of exacerbation of preexisting psoriasis in a patient treated with nivolumab. Furthermore, our patient is the first reported case of a patient treated with nivolumab for NSCLC to develop this adverse event. Whereas the previously reported cases were characterized by widespread trunk and extremity involvement, our patient developed focal exacerbation of the palmoplantar areas.
Additional studies are needed to more clearly characterize the specific cutaneous toxicities of nivolumab and to determine if particular skin reactions may indicate a better response to the anticancer agent. Side effects such as psoriasis can often be managed with topical therapies and may not require withdrawal of the medication. We encourage the collaboration of dermatologists and oncologists to enhance the diagnosis and management of these cutaneous side effects in cancer patients.
1. Larkin J, Lao CD, Urba WJ, et al. Efficacy and safety of Nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433-440.
2. Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004-2012.
3. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
4. Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257-265.
5. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
6. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311-4318.
7. Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber J. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2015.
8. Matsumura N, Ohtsuka M, Kikuchi N, Yamamoto T. Exacerbation of psoriasis during nivolumab therapy for metastatic melanoma. Acta Derm Venereol. 2016;96(2):259-260.
9. Kato Y, Otsuka A, Miyachi Y, Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30(10):e89-e91.
10. Ohtsuka M, Miura T, Mori T, Ishikawa M, Yamamoto T. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol. 2015;151(7):797-799.
Nivolumab is a full human immunoglobulin antibody to the programmed cell death 1 (PD-1) immune checkpoint receptor on T cells. This programmed cell death inhibitor is a targeted immunotherapy used to treat patients with melanoma, among other malignancies.1 More recently, nivolumab has been used for advanced non-small-cell lung cancer (NSCLC) after failure of previous chemotherapeutic agents. It was approved by the US Food and Drug Administration for the NSCLC indication in 2015.2
PD-1 inhibitors are efficacious in treating advanced malignancies, although their immune-mediated functions can lead to undesirable side effects. Patients treated with nivolumab have been reported to develop thyroid disease,1,3,4 diabetes,3 hypophysitis,1,3 hypopituitarism,3 and pneumonitis,4,2 as well as other autoimmune conditions.3 Although nivolumab is often used to treat skin diseases such as melanoma, it can have many cutaneous side effects including pruritus,1,3-6 rash,1,3,4,6,7 vitiligo,1,3,7,6 mouth sores,3 injection site reactions,3,6 and alopecia.5 Herein, we describe a patient who was treated with nivolumab and developed an exacerbation of pre-existing psoriasis.
Case presentation and summary
A 57-year-old man with metastatic NSCLC and a history of plaque psoriasis presented to the dermatology clinic for evaluation of new lesions on his palms and soles. The patient had been previously treated with numerous therapies for NSCLC, including chemotherapy and radiation. Previous chemotherapeutic agents included the cisplatin plus etoposide combination, with doxetaxel and pemetrexed. The patient was not able to tolerate the chemotherapy and instead opted for hospice care. After several months, he chose to restart therapy, and was started on the programmed cell death (PD)-1 inhibitor, nivolumab, at a dose of 3 mg/kg for a total of 6 cycles. He received his first dose 5 weeks before his current presentation to the clinic, and his second dose 2 weeks before.
The patient reported a 20-year history of plaque psoriasis, characterized by psoriatic plaques on the elbows and shins and for which he was treated with topical therapies with good effect. Every few months, he would develop one or two small plaques of psoriasis on his palms and soles. The lesions were inconsequential to the patient, as he never experienced more than one or two small palmoplantar lesions at a time. One week after his second cycle of nivolumab, the patient developed an eruption of lesions on his palms and soles. He observed that the lesions seemed to be similar to his previous palmoplantar psoriatic plaques but with significantly greater skin involvement. The patient denied any new-onset joint pain.
The results of a physical examination revealed a cachectic man in no acute distress, with more than 30 erythematous circular to oval circumscribed plaques with yellow to whitish scales on the bilateral palms (Figure 1) and soles (Figure 2).
The patient also had well-demarcated, thick oval erythematous plaques with micaceous scales on the bilateral elbows (Figure 3), and thin scaly erythematous plaques on the anterior shins (Figure 4). There were no psoriatic plaques on the remainder of the trunk or extremities. Mucosal surfaces, scalp, and nails were uninvolved.
A clinical diagnosis of exacerbation of pre-existing psoriasis owing to nivolumab therapy was made. The patient was started on clobetasol 0.05% ointment twice daily under occlusion with plastic wrap to the affected areas, and he was continued on nivolumab for his NSCLC.
Discussion
Treatment with nivolumab can lead to a range of autoimmune side effects, and as shown in this case, psoriasis is one of the cutaneous findings that could be exacerbated by treatment with nivolumab. To date, two cases of exacerbation of psoriasis in patients treated with nivolumab for melanoma have been reported in the literature.8,9 In the first case, the patient had well-controlled plaque psoriasis at baseline and he subsequently developed psoriatic plaques on the trunk and extremities after the second infusion of nivolumab for metastatic melanoma. A biopsy showed regular acanthosis with hyperkeratosis and parakeratosis in addition to dilated vessels in the papillary dermis.8 In the second case, the patient had a history of psoriasis vulgaris with no active lesions. Three weeks after his first course of nivolumab for metastatic oral mucosal melanoma, he developed new, well-circumscribed erythematous scaly plaques on the trunk and extremities that were clinically diagnosed as psoriasis.9 In a third case, a patient without a prior history of psoriasis experienced a psoriasiform eruption on the trunk and extremities after the fourth dose of nivolumab for oral mucosal melanoma.10 Thus, our case is the third reported case of exacerbation of preexisting psoriasis in a patient treated with nivolumab. Furthermore, our patient is the first reported case of a patient treated with nivolumab for NSCLC to develop this adverse event. Whereas the previously reported cases were characterized by widespread trunk and extremity involvement, our patient developed focal exacerbation of the palmoplantar areas.
Additional studies are needed to more clearly characterize the specific cutaneous toxicities of nivolumab and to determine if particular skin reactions may indicate a better response to the anticancer agent. Side effects such as psoriasis can often be managed with topical therapies and may not require withdrawal of the medication. We encourage the collaboration of dermatologists and oncologists to enhance the diagnosis and management of these cutaneous side effects in cancer patients.
Nivolumab is a full human immunoglobulin antibody to the programmed cell death 1 (PD-1) immune checkpoint receptor on T cells. This programmed cell death inhibitor is a targeted immunotherapy used to treat patients with melanoma, among other malignancies.1 More recently, nivolumab has been used for advanced non-small-cell lung cancer (NSCLC) after failure of previous chemotherapeutic agents. It was approved by the US Food and Drug Administration for the NSCLC indication in 2015.2
PD-1 inhibitors are efficacious in treating advanced malignancies, although their immune-mediated functions can lead to undesirable side effects. Patients treated with nivolumab have been reported to develop thyroid disease,1,3,4 diabetes,3 hypophysitis,1,3 hypopituitarism,3 and pneumonitis,4,2 as well as other autoimmune conditions.3 Although nivolumab is often used to treat skin diseases such as melanoma, it can have many cutaneous side effects including pruritus,1,3-6 rash,1,3,4,6,7 vitiligo,1,3,7,6 mouth sores,3 injection site reactions,3,6 and alopecia.5 Herein, we describe a patient who was treated with nivolumab and developed an exacerbation of pre-existing psoriasis.
Case presentation and summary
A 57-year-old man with metastatic NSCLC and a history of plaque psoriasis presented to the dermatology clinic for evaluation of new lesions on his palms and soles. The patient had been previously treated with numerous therapies for NSCLC, including chemotherapy and radiation. Previous chemotherapeutic agents included the cisplatin plus etoposide combination, with doxetaxel and pemetrexed. The patient was not able to tolerate the chemotherapy and instead opted for hospice care. After several months, he chose to restart therapy, and was started on the programmed cell death (PD)-1 inhibitor, nivolumab, at a dose of 3 mg/kg for a total of 6 cycles. He received his first dose 5 weeks before his current presentation to the clinic, and his second dose 2 weeks before.
The patient reported a 20-year history of plaque psoriasis, characterized by psoriatic plaques on the elbows and shins and for which he was treated with topical therapies with good effect. Every few months, he would develop one or two small plaques of psoriasis on his palms and soles. The lesions were inconsequential to the patient, as he never experienced more than one or two small palmoplantar lesions at a time. One week after his second cycle of nivolumab, the patient developed an eruption of lesions on his palms and soles. He observed that the lesions seemed to be similar to his previous palmoplantar psoriatic plaques but with significantly greater skin involvement. The patient denied any new-onset joint pain.
The results of a physical examination revealed a cachectic man in no acute distress, with more than 30 erythematous circular to oval circumscribed plaques with yellow to whitish scales on the bilateral palms (Figure 1) and soles (Figure 2).
The patient also had well-demarcated, thick oval erythematous plaques with micaceous scales on the bilateral elbows (Figure 3), and thin scaly erythematous plaques on the anterior shins (Figure 4). There were no psoriatic plaques on the remainder of the trunk or extremities. Mucosal surfaces, scalp, and nails were uninvolved.
A clinical diagnosis of exacerbation of pre-existing psoriasis owing to nivolumab therapy was made. The patient was started on clobetasol 0.05% ointment twice daily under occlusion with plastic wrap to the affected areas, and he was continued on nivolumab for his NSCLC.
Discussion
Treatment with nivolumab can lead to a range of autoimmune side effects, and as shown in this case, psoriasis is one of the cutaneous findings that could be exacerbated by treatment with nivolumab. To date, two cases of exacerbation of psoriasis in patients treated with nivolumab for melanoma have been reported in the literature.8,9 In the first case, the patient had well-controlled plaque psoriasis at baseline and he subsequently developed psoriatic plaques on the trunk and extremities after the second infusion of nivolumab for metastatic melanoma. A biopsy showed regular acanthosis with hyperkeratosis and parakeratosis in addition to dilated vessels in the papillary dermis.8 In the second case, the patient had a history of psoriasis vulgaris with no active lesions. Three weeks after his first course of nivolumab for metastatic oral mucosal melanoma, he developed new, well-circumscribed erythematous scaly plaques on the trunk and extremities that were clinically diagnosed as psoriasis.9 In a third case, a patient without a prior history of psoriasis experienced a psoriasiform eruption on the trunk and extremities after the fourth dose of nivolumab for oral mucosal melanoma.10 Thus, our case is the third reported case of exacerbation of preexisting psoriasis in a patient treated with nivolumab. Furthermore, our patient is the first reported case of a patient treated with nivolumab for NSCLC to develop this adverse event. Whereas the previously reported cases were characterized by widespread trunk and extremity involvement, our patient developed focal exacerbation of the palmoplantar areas.
Additional studies are needed to more clearly characterize the specific cutaneous toxicities of nivolumab and to determine if particular skin reactions may indicate a better response to the anticancer agent. Side effects such as psoriasis can often be managed with topical therapies and may not require withdrawal of the medication. We encourage the collaboration of dermatologists and oncologists to enhance the diagnosis and management of these cutaneous side effects in cancer patients.
1. Larkin J, Lao CD, Urba WJ, et al. Efficacy and safety of Nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433-440.
2. Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004-2012.
3. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
4. Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257-265.
5. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
6. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311-4318.
7. Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber J. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2015.
8. Matsumura N, Ohtsuka M, Kikuchi N, Yamamoto T. Exacerbation of psoriasis during nivolumab therapy for metastatic melanoma. Acta Derm Venereol. 2016;96(2):259-260.
9. Kato Y, Otsuka A, Miyachi Y, Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30(10):e89-e91.
10. Ohtsuka M, Miura T, Mori T, Ishikawa M, Yamamoto T. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol. 2015;151(7):797-799.
1. Larkin J, Lao CD, Urba WJ, et al. Efficacy and safety of Nivolumab in patients with BRAF V600 mutant and BRAF wild-type advanced melanoma: a pooled analysis of 4 clinical trials. JAMA Oncol. 2015;1(4):433-440.
2. Gettinger SN, Horn L, Gandhi L, et al. Overall survival and long-term safety of nivolumab (anti-programmed death 1 antibody, BMS-936558, ONO-4538) in patients with previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2015;33(18):2004-2012.
3. Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443-2454.
4. Rizvi NA, Mazieres J, Planchard D, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257-265.
5. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375-384.
6. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311-4318.
7. Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber J. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2015.
8. Matsumura N, Ohtsuka M, Kikuchi N, Yamamoto T. Exacerbation of psoriasis during nivolumab therapy for metastatic melanoma. Acta Derm Venereol. 2016;96(2):259-260.
9. Kato Y, Otsuka A, Miyachi Y, Kabashima K. Exacerbation of psoriasis vulgaris during nivolumab for oral mucosal melanoma. J Eur Acad Dermatol Venereol. 2016;30(10):e89-e91.
10. Ohtsuka M, Miura T, Mori T, Ishikawa M, Yamamoto T. Occurrence of psoriasiform eruption during nivolumab therapy for primary oral mucosal melanoma. JAMA Dermatol. 2015;151(7):797-799.
Consider invasive mediastinal staging in higher risk NSCLC patients, despite guidelines
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) appears to be cost effective for use in non–small cell lung cancer (NSCLC) staging if the prevalence of mediastinal lymph node metastasis (MLNM) is greater than or equal to 2.5%, according to the results of single institution modeling study. In addition, the study found that confirmatory mediastinoscopy should be performed in high-risk patients in cases of negative EBUS-TBNA.
Katarzyna Czarnecka-Kujawa, MD, of the University of Toronto and Toronto General Hospital, and her colleagues performed a decision analysis to compare health outcomes and costs of four mediastinal staging strategies. They assessed the following: no invasive staging, endobronchial ultrasound-guided transbronchial need aspiration (EBUS-TBNA), mediastinoscopy, and EBUS-TBNA followed by mediastinoscopy if EBUS-TBNA results were negative. They determined incremental cost-effectiveness ratios (ICER) for all strategies and performed comprehensive sensitivity analyses using a willingness to pay threshold of $80,000 [Canadian]/quality adjusted life-year (QALY).
They used data obtained for staging, outcomes, and costs from the patients in the lung cancer program at the Toronto General Hospital from Jan. 1, 2005 to Dec. 31, 2014, as detailed in a report published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2017. doi: 10.1016/j.jtcvs.2016.12.048).
After exclusions, they utilized a final case count of 499 cases for developing their surgical and procedure cost analysis, and a total of 750 cases in their endoscopy database for endoscopy analysis. For the base-case analysis, they assumed a prevalence of mediastinal metastasis of 9%, and obtained the prevalence of a pathologic lymph nodal stage disease following EBUS-TBNA from their institutional data.
Their results showed that EBUS-TBNA followed by mediastinoscopy was the strategy that resulted in the highest QALYs, but that it had a prohibitive ICER of greater than $1.4 million/QALY. Accordingly, it may not be justifiable to use mediastinoscopy after negative EBUS-TBNA in all patients, the researchers noted. However, the researchers’ data suggest that invasive screening may be justified in a very-low-risk population (MLNM above 2.5%).
In addition, the researchers stated that “[the] benefit conveyed by detecting mediastinal metastatic disease becomes more apparent as the prevalence of MLNM increases, with confirmatory mediastinoscopy becoming cost effective in cases of negative EBUS-TBNA in patients with moderate to high probability of MLNM” (greater than 57%).
Our model points out that there is a well-defined role for the use of different modalities, including mediastinoscopy. This stresses the need for ongoing focus on maintenance of competency and skill acquisition in mediastinoscopy and EBUS-TBNA by currently practicing and future thoracic surgeons respectively,” the researchers concluded.
Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
The authors make a compelling argument for invasive mediastinal staging in patients with clinical stage I non–small cell lung cancer and acknowledge that this conflicts with current guidelines, according to Biniam Kidane, MD, of the University of Manitoba, Winnipeg, in his invited comments on the study in the Journal of Thoracic and Cardiovascular Surgery (2017 Mar 10. doi: 10.1016/j.jtcvs.2017.02.051).
Their single-payer system is likely to have a different willingness-to-pay threshold, compared with those in other countries, especially the United States, where the EBUS-TBNA strategy without invasive staging is likely to remain the cost-effective choice.
“Cost-economic analyses such as these provide a window into the factors necessary to bridge guidelines from the realm of the abstract to the realm of local reality. When interpreting these findings, clinicians should consider: 1) What EBUS resources are available? (2) What is your local EBUS sensitivity? 3) What is the prevalence of MLNM?” Dr. Kidane concluded, with the caveat that such studies are not infallible and models are based on assumptions and must be treated with care.
Dr. Kidane reported no disclosures with regard to commercial support.
The authors make a compelling argument for invasive mediastinal staging in patients with clinical stage I non–small cell lung cancer and acknowledge that this conflicts with current guidelines, according to Biniam Kidane, MD, of the University of Manitoba, Winnipeg, in his invited comments on the study in the Journal of Thoracic and Cardiovascular Surgery (2017 Mar 10. doi: 10.1016/j.jtcvs.2017.02.051).
Their single-payer system is likely to have a different willingness-to-pay threshold, compared with those in other countries, especially the United States, where the EBUS-TBNA strategy without invasive staging is likely to remain the cost-effective choice.
“Cost-economic analyses such as these provide a window into the factors necessary to bridge guidelines from the realm of the abstract to the realm of local reality. When interpreting these findings, clinicians should consider: 1) What EBUS resources are available? (2) What is your local EBUS sensitivity? 3) What is the prevalence of MLNM?” Dr. Kidane concluded, with the caveat that such studies are not infallible and models are based on assumptions and must be treated with care.
Dr. Kidane reported no disclosures with regard to commercial support.
The authors make a compelling argument for invasive mediastinal staging in patients with clinical stage I non–small cell lung cancer and acknowledge that this conflicts with current guidelines, according to Biniam Kidane, MD, of the University of Manitoba, Winnipeg, in his invited comments on the study in the Journal of Thoracic and Cardiovascular Surgery (2017 Mar 10. doi: 10.1016/j.jtcvs.2017.02.051).
Their single-payer system is likely to have a different willingness-to-pay threshold, compared with those in other countries, especially the United States, where the EBUS-TBNA strategy without invasive staging is likely to remain the cost-effective choice.
“Cost-economic analyses such as these provide a window into the factors necessary to bridge guidelines from the realm of the abstract to the realm of local reality. When interpreting these findings, clinicians should consider: 1) What EBUS resources are available? (2) What is your local EBUS sensitivity? 3) What is the prevalence of MLNM?” Dr. Kidane concluded, with the caveat that such studies are not infallible and models are based on assumptions and must be treated with care.
Dr. Kidane reported no disclosures with regard to commercial support.
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) appears to be cost effective for use in non–small cell lung cancer (NSCLC) staging if the prevalence of mediastinal lymph node metastasis (MLNM) is greater than or equal to 2.5%, according to the results of single institution modeling study. In addition, the study found that confirmatory mediastinoscopy should be performed in high-risk patients in cases of negative EBUS-TBNA.
Katarzyna Czarnecka-Kujawa, MD, of the University of Toronto and Toronto General Hospital, and her colleagues performed a decision analysis to compare health outcomes and costs of four mediastinal staging strategies. They assessed the following: no invasive staging, endobronchial ultrasound-guided transbronchial need aspiration (EBUS-TBNA), mediastinoscopy, and EBUS-TBNA followed by mediastinoscopy if EBUS-TBNA results were negative. They determined incremental cost-effectiveness ratios (ICER) for all strategies and performed comprehensive sensitivity analyses using a willingness to pay threshold of $80,000 [Canadian]/quality adjusted life-year (QALY).
They used data obtained for staging, outcomes, and costs from the patients in the lung cancer program at the Toronto General Hospital from Jan. 1, 2005 to Dec. 31, 2014, as detailed in a report published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2017. doi: 10.1016/j.jtcvs.2016.12.048).
After exclusions, they utilized a final case count of 499 cases for developing their surgical and procedure cost analysis, and a total of 750 cases in their endoscopy database for endoscopy analysis. For the base-case analysis, they assumed a prevalence of mediastinal metastasis of 9%, and obtained the prevalence of a pathologic lymph nodal stage disease following EBUS-TBNA from their institutional data.
Their results showed that EBUS-TBNA followed by mediastinoscopy was the strategy that resulted in the highest QALYs, but that it had a prohibitive ICER of greater than $1.4 million/QALY. Accordingly, it may not be justifiable to use mediastinoscopy after negative EBUS-TBNA in all patients, the researchers noted. However, the researchers’ data suggest that invasive screening may be justified in a very-low-risk population (MLNM above 2.5%).
In addition, the researchers stated that “[the] benefit conveyed by detecting mediastinal metastatic disease becomes more apparent as the prevalence of MLNM increases, with confirmatory mediastinoscopy becoming cost effective in cases of negative EBUS-TBNA in patients with moderate to high probability of MLNM” (greater than 57%).
Our model points out that there is a well-defined role for the use of different modalities, including mediastinoscopy. This stresses the need for ongoing focus on maintenance of competency and skill acquisition in mediastinoscopy and EBUS-TBNA by currently practicing and future thoracic surgeons respectively,” the researchers concluded.
Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
Endobronchial ultrasound transbronchial needle aspiration (EBUS-TBNA) appears to be cost effective for use in non–small cell lung cancer (NSCLC) staging if the prevalence of mediastinal lymph node metastasis (MLNM) is greater than or equal to 2.5%, according to the results of single institution modeling study. In addition, the study found that confirmatory mediastinoscopy should be performed in high-risk patients in cases of negative EBUS-TBNA.
Katarzyna Czarnecka-Kujawa, MD, of the University of Toronto and Toronto General Hospital, and her colleagues performed a decision analysis to compare health outcomes and costs of four mediastinal staging strategies. They assessed the following: no invasive staging, endobronchial ultrasound-guided transbronchial need aspiration (EBUS-TBNA), mediastinoscopy, and EBUS-TBNA followed by mediastinoscopy if EBUS-TBNA results were negative. They determined incremental cost-effectiveness ratios (ICER) for all strategies and performed comprehensive sensitivity analyses using a willingness to pay threshold of $80,000 [Canadian]/quality adjusted life-year (QALY).
They used data obtained for staging, outcomes, and costs from the patients in the lung cancer program at the Toronto General Hospital from Jan. 1, 2005 to Dec. 31, 2014, as detailed in a report published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2017. doi: 10.1016/j.jtcvs.2016.12.048).
After exclusions, they utilized a final case count of 499 cases for developing their surgical and procedure cost analysis, and a total of 750 cases in their endoscopy database for endoscopy analysis. For the base-case analysis, they assumed a prevalence of mediastinal metastasis of 9%, and obtained the prevalence of a pathologic lymph nodal stage disease following EBUS-TBNA from their institutional data.
Their results showed that EBUS-TBNA followed by mediastinoscopy was the strategy that resulted in the highest QALYs, but that it had a prohibitive ICER of greater than $1.4 million/QALY. Accordingly, it may not be justifiable to use mediastinoscopy after negative EBUS-TBNA in all patients, the researchers noted. However, the researchers’ data suggest that invasive screening may be justified in a very-low-risk population (MLNM above 2.5%).
In addition, the researchers stated that “[the] benefit conveyed by detecting mediastinal metastatic disease becomes more apparent as the prevalence of MLNM increases, with confirmatory mediastinoscopy becoming cost effective in cases of negative EBUS-TBNA in patients with moderate to high probability of MLNM” (greater than 57%).
Our model points out that there is a well-defined role for the use of different modalities, including mediastinoscopy. This stresses the need for ongoing focus on maintenance of competency and skill acquisition in mediastinoscopy and EBUS-TBNA by currently practicing and future thoracic surgeons respectively,” the researchers concluded.
Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point:
Major finding: Once the pathologic lymph nodal stage reaches 57%, EBUS-TBNA followed by mediastinoscopy is cost effective.
Data source: A model of health care outcomes and costs was developed from data obtained from patients treated over a 10-year period at a single institution.
Disclosures: Dr. Czarnecka-Kujawa disclosed that she is a research consultant with Olympus America. The study was funded in part by agencies of the Austrian government.
Salvage chemo for NSCLC more effective after PD-1/PD-L1 inhibitors
GENEVA – Patients with stage IV non–small cell lung cancer (NSCLC) who have disease progression following treatment with an immune checkpoint inhibitor have a 30% better chance of achieving at least a partial response with salvage chemotherapy compared with patients who had received prior chemotherapy but not immunotherapy, according to Swiss and U.S. investigators.
In a study of 82 patients with advanced NSCLC, 18 of 67 patients (27%) who had progressed on an inhibitor of programmed death-1 (PD-1) or programmed death ligand-1 (PD-L1) had a partial response to combination chemotherapy, compared with just 1 of 15 (7%) of patients who had not received a checkpoint inhibitor, reported Sacha Rothschild, MD, PhD, of University Hospital Basel, Switzerland, and colleagues.
“The odds of achieving a partial response to salvage chemotherapy were significantly higher in patients with prior exposure to PD-1/PD-L1 inhibitors. This observed difference, however, warrants confirmation in larger cohorts. Ongoing investigations include the duration of response as well as evaluation of toxicity,” the researchers wrote in a scientific poster presented at the European Lung Cancer Conference.
Immune checkpoint inhibitors have been shown to be active in patients with late-stage NSCLC who have experienced disease progression following chemotherapy. To see whether salvage chemotherapy could offer any additional benefit to patients who had disease progression on immunotherapy, the investigators conducted a retrospective case-control study. They reviewed 355 patient records, and identified 82 patients – 46 men and 36 women – who met the study criteria.
Of this group, 67 patients had received a PD-1/PD-L1 checkpoint inhibitor, either nivolumab (Opdivo, 56 patients), pembrolizumab (Keytruda, 7), or atezolizumab (Tecentriq, 4). These patients were designated as cases. The remaining 15 patients, who had received prior chemotherapy or chemoradiotherapy only, were designated as controls.
Of all 82 patients, 63 (77%) had adenocarcinomas, 18 (22%) had squamous cell carcinomas, and 1 (1%) had a large-cell carcinoma.
Cases had a mean of 2.37 chemotherapy regimens prior to salvage chemotherapy, and controls had a mean of 1.93. Drugs used in the salvage regimens were docetaxel in 62% of patients, pemetrexed in 20%, gemcitabine in 12%, and paclitaxel in 6%.
The odds ratio for achieving a partial response was 0.30 (95% confidence interval, 0.18-0.50, P less than .0001).
In a multiple logistic regression model, neither age, sex, number of prior chemotherapy regimens, tumor histology, smoking status, nor type of salvage chemotherapy regimen were significantly associated with the likelihood of achieving a partial response.
In a poster discussion session, Simon Ekman, MD, of Karolinska Institute in Stockholm, Sweden, the invited discussant, said that the data from the study are convincing, and raise the question of what to do next.
“The question is how do we combine immunotherapy with chemotherapy? Should we use the immune therapy first, like in this trial, or vice versa, or should we combine concurrently” he said.
The strategy of chemotherapy first is supported by research showing that neoantigens crucial for the immune response are released during chemotherapy and radiotherapy, enabling immunotherapeutic agents to work better, he said.
The study was internally funded. Dr. Rothschild and Dr. Ekman reported no conflicts relevant to the research.
GENEVA – Patients with stage IV non–small cell lung cancer (NSCLC) who have disease progression following treatment with an immune checkpoint inhibitor have a 30% better chance of achieving at least a partial response with salvage chemotherapy compared with patients who had received prior chemotherapy but not immunotherapy, according to Swiss and U.S. investigators.
In a study of 82 patients with advanced NSCLC, 18 of 67 patients (27%) who had progressed on an inhibitor of programmed death-1 (PD-1) or programmed death ligand-1 (PD-L1) had a partial response to combination chemotherapy, compared with just 1 of 15 (7%) of patients who had not received a checkpoint inhibitor, reported Sacha Rothschild, MD, PhD, of University Hospital Basel, Switzerland, and colleagues.
“The odds of achieving a partial response to salvage chemotherapy were significantly higher in patients with prior exposure to PD-1/PD-L1 inhibitors. This observed difference, however, warrants confirmation in larger cohorts. Ongoing investigations include the duration of response as well as evaluation of toxicity,” the researchers wrote in a scientific poster presented at the European Lung Cancer Conference.
Immune checkpoint inhibitors have been shown to be active in patients with late-stage NSCLC who have experienced disease progression following chemotherapy. To see whether salvage chemotherapy could offer any additional benefit to patients who had disease progression on immunotherapy, the investigators conducted a retrospective case-control study. They reviewed 355 patient records, and identified 82 patients – 46 men and 36 women – who met the study criteria.
Of this group, 67 patients had received a PD-1/PD-L1 checkpoint inhibitor, either nivolumab (Opdivo, 56 patients), pembrolizumab (Keytruda, 7), or atezolizumab (Tecentriq, 4). These patients were designated as cases. The remaining 15 patients, who had received prior chemotherapy or chemoradiotherapy only, were designated as controls.
Of all 82 patients, 63 (77%) had adenocarcinomas, 18 (22%) had squamous cell carcinomas, and 1 (1%) had a large-cell carcinoma.
Cases had a mean of 2.37 chemotherapy regimens prior to salvage chemotherapy, and controls had a mean of 1.93. Drugs used in the salvage regimens were docetaxel in 62% of patients, pemetrexed in 20%, gemcitabine in 12%, and paclitaxel in 6%.
The odds ratio for achieving a partial response was 0.30 (95% confidence interval, 0.18-0.50, P less than .0001).
In a multiple logistic regression model, neither age, sex, number of prior chemotherapy regimens, tumor histology, smoking status, nor type of salvage chemotherapy regimen were significantly associated with the likelihood of achieving a partial response.
In a poster discussion session, Simon Ekman, MD, of Karolinska Institute in Stockholm, Sweden, the invited discussant, said that the data from the study are convincing, and raise the question of what to do next.
“The question is how do we combine immunotherapy with chemotherapy? Should we use the immune therapy first, like in this trial, or vice versa, or should we combine concurrently” he said.
The strategy of chemotherapy first is supported by research showing that neoantigens crucial for the immune response are released during chemotherapy and radiotherapy, enabling immunotherapeutic agents to work better, he said.
The study was internally funded. Dr. Rothschild and Dr. Ekman reported no conflicts relevant to the research.
GENEVA – Patients with stage IV non–small cell lung cancer (NSCLC) who have disease progression following treatment with an immune checkpoint inhibitor have a 30% better chance of achieving at least a partial response with salvage chemotherapy compared with patients who had received prior chemotherapy but not immunotherapy, according to Swiss and U.S. investigators.
In a study of 82 patients with advanced NSCLC, 18 of 67 patients (27%) who had progressed on an inhibitor of programmed death-1 (PD-1) or programmed death ligand-1 (PD-L1) had a partial response to combination chemotherapy, compared with just 1 of 15 (7%) of patients who had not received a checkpoint inhibitor, reported Sacha Rothschild, MD, PhD, of University Hospital Basel, Switzerland, and colleagues.
“The odds of achieving a partial response to salvage chemotherapy were significantly higher in patients with prior exposure to PD-1/PD-L1 inhibitors. This observed difference, however, warrants confirmation in larger cohorts. Ongoing investigations include the duration of response as well as evaluation of toxicity,” the researchers wrote in a scientific poster presented at the European Lung Cancer Conference.
Immune checkpoint inhibitors have been shown to be active in patients with late-stage NSCLC who have experienced disease progression following chemotherapy. To see whether salvage chemotherapy could offer any additional benefit to patients who had disease progression on immunotherapy, the investigators conducted a retrospective case-control study. They reviewed 355 patient records, and identified 82 patients – 46 men and 36 women – who met the study criteria.
Of this group, 67 patients had received a PD-1/PD-L1 checkpoint inhibitor, either nivolumab (Opdivo, 56 patients), pembrolizumab (Keytruda, 7), or atezolizumab (Tecentriq, 4). These patients were designated as cases. The remaining 15 patients, who had received prior chemotherapy or chemoradiotherapy only, were designated as controls.
Of all 82 patients, 63 (77%) had adenocarcinomas, 18 (22%) had squamous cell carcinomas, and 1 (1%) had a large-cell carcinoma.
Cases had a mean of 2.37 chemotherapy regimens prior to salvage chemotherapy, and controls had a mean of 1.93. Drugs used in the salvage regimens were docetaxel in 62% of patients, pemetrexed in 20%, gemcitabine in 12%, and paclitaxel in 6%.
The odds ratio for achieving a partial response was 0.30 (95% confidence interval, 0.18-0.50, P less than .0001).
In a multiple logistic regression model, neither age, sex, number of prior chemotherapy regimens, tumor histology, smoking status, nor type of salvage chemotherapy regimen were significantly associated with the likelihood of achieving a partial response.
In a poster discussion session, Simon Ekman, MD, of Karolinska Institute in Stockholm, Sweden, the invited discussant, said that the data from the study are convincing, and raise the question of what to do next.
“The question is how do we combine immunotherapy with chemotherapy? Should we use the immune therapy first, like in this trial, or vice versa, or should we combine concurrently” he said.
The strategy of chemotherapy first is supported by research showing that neoantigens crucial for the immune response are released during chemotherapy and radiotherapy, enabling immunotherapeutic agents to work better, he said.
The study was internally funded. Dr. Rothschild and Dr. Ekman reported no conflicts relevant to the research.
FROM ELCC
Key clinical point: Salvage chemotherapy was more effective among patients who had disease progression following immunotherapy in the second line than among patients who received only chemotherapy.
Major finding: Among patients with disease progression while on a checkpoint inhibitor, 18 of 67 had a partial response to salvage chemotherapy, compared with just 1 of 15 controls.
Data source: Retrospective case-control study of 82 patients with advanced NSCLC.
Disclosures: The study was internally funded. Dr. Rothschild and Dr. Ekman reported no conflicts relevant to the research.