User login
Can aspirin prolong survival in patients with NSCLC?
(NSCLC), according to a new study from Taiwan.
The analysis, published online Nov. 22 in BMC Cancer , adds another data point to a small and inconsistent evidence base.
“Despite the need for future prospective randomized clinical trials, aspirin may be considered as an additional treatment for inoperable NSCLC patients,” Ming-Szu Hung, MD, of Chang-Gung University, Taoyuan City, and colleagues write.
The current literature suggests that the over-the-counter medication may help ward off various types of cancer, including lung cancer, but the various study findings do not always align. For lung-cancer survival, in particular, a few observational studies have found increased survival among aspirin users while others have not.
To help bring clarity to the literature, Dr. Hung’s team examined data from Taiwan’s National Health Insurance Research Database on more than 38,000 patients diagnosed with NSCLC between 2000 and 2012, almost 5,000 of whom were taking aspirin at the time of diagnosis.
The researchers found that aspirin users survived for a median of 1.73 years, compared with 1.30 years for nonusers. Taking the drug was associated with longer overall survival in time-varying covariate analysis (hazard ratio, 0.83; 95% CI, 0.80-0.86). This finding was confirmed in a propensity-score analysis of 4,932 matched pairs (HR, 0.79; 95% CI, 0.75-0.83).
“These results warrant further randomized clinical trials to evaluate the actual role of aspirin in the treatment of NSCLC patients,” the researchers conclude.
But Úna McMenamin, PhD, a cancer epidemiologist at Queen’s University Belfast, Ireland, was not convinced by the study’s methods.
While she praised its large size and use of population-based health registers, she expressed concern about the potential for reverse causation, “as it is unclear whether authors lagged the aspirin exposure in the cohort of lung cancer patients.”
There is evidence that common medications such as aspirin may be withdrawn from patients who are thought to be near the end of their life, Dr. McMenamin told this news organization. When not factored into the statistical analysis, aspirin may appear “to be spuriously associated with a reduced risk of death when, in fact, no association may be present.”
Previous studies of aspirin use in lung cancer patients that have included a lag, such as one Dr. McMenamin and colleagues conducted in 2015, have found no evidence of a protective effect.
That is why, according to Dr. McMenamin, “additional population-based studies, in diverse populations, are required to investigate the association between aspirin use and survival outcomes in lung-cancer patients to determine whether randomized controlled trials are warranted in this patient group.”
In addition, she noted, “any potential benefit of aspirin in lung cancer patients needs to be balanced against known adverse events associated with prolonged aspirin use, such as gastrointestinal bleeding.”
Dr. Hung did not reply to requests for comment.
The study had no funding, and the researchers report no conflicts of interest.
A version of this article first appeared on Medscape.com.
(NSCLC), according to a new study from Taiwan.
The analysis, published online Nov. 22 in BMC Cancer , adds another data point to a small and inconsistent evidence base.
“Despite the need for future prospective randomized clinical trials, aspirin may be considered as an additional treatment for inoperable NSCLC patients,” Ming-Szu Hung, MD, of Chang-Gung University, Taoyuan City, and colleagues write.
The current literature suggests that the over-the-counter medication may help ward off various types of cancer, including lung cancer, but the various study findings do not always align. For lung-cancer survival, in particular, a few observational studies have found increased survival among aspirin users while others have not.
To help bring clarity to the literature, Dr. Hung’s team examined data from Taiwan’s National Health Insurance Research Database on more than 38,000 patients diagnosed with NSCLC between 2000 and 2012, almost 5,000 of whom were taking aspirin at the time of diagnosis.
The researchers found that aspirin users survived for a median of 1.73 years, compared with 1.30 years for nonusers. Taking the drug was associated with longer overall survival in time-varying covariate analysis (hazard ratio, 0.83; 95% CI, 0.80-0.86). This finding was confirmed in a propensity-score analysis of 4,932 matched pairs (HR, 0.79; 95% CI, 0.75-0.83).
“These results warrant further randomized clinical trials to evaluate the actual role of aspirin in the treatment of NSCLC patients,” the researchers conclude.
But Úna McMenamin, PhD, a cancer epidemiologist at Queen’s University Belfast, Ireland, was not convinced by the study’s methods.
While she praised its large size and use of population-based health registers, she expressed concern about the potential for reverse causation, “as it is unclear whether authors lagged the aspirin exposure in the cohort of lung cancer patients.”
There is evidence that common medications such as aspirin may be withdrawn from patients who are thought to be near the end of their life, Dr. McMenamin told this news organization. When not factored into the statistical analysis, aspirin may appear “to be spuriously associated with a reduced risk of death when, in fact, no association may be present.”
Previous studies of aspirin use in lung cancer patients that have included a lag, such as one Dr. McMenamin and colleagues conducted in 2015, have found no evidence of a protective effect.
That is why, according to Dr. McMenamin, “additional population-based studies, in diverse populations, are required to investigate the association between aspirin use and survival outcomes in lung-cancer patients to determine whether randomized controlled trials are warranted in this patient group.”
In addition, she noted, “any potential benefit of aspirin in lung cancer patients needs to be balanced against known adverse events associated with prolonged aspirin use, such as gastrointestinal bleeding.”
Dr. Hung did not reply to requests for comment.
The study had no funding, and the researchers report no conflicts of interest.
A version of this article first appeared on Medscape.com.
(NSCLC), according to a new study from Taiwan.
The analysis, published online Nov. 22 in BMC Cancer , adds another data point to a small and inconsistent evidence base.
“Despite the need for future prospective randomized clinical trials, aspirin may be considered as an additional treatment for inoperable NSCLC patients,” Ming-Szu Hung, MD, of Chang-Gung University, Taoyuan City, and colleagues write.
The current literature suggests that the over-the-counter medication may help ward off various types of cancer, including lung cancer, but the various study findings do not always align. For lung-cancer survival, in particular, a few observational studies have found increased survival among aspirin users while others have not.
To help bring clarity to the literature, Dr. Hung’s team examined data from Taiwan’s National Health Insurance Research Database on more than 38,000 patients diagnosed with NSCLC between 2000 and 2012, almost 5,000 of whom were taking aspirin at the time of diagnosis.
The researchers found that aspirin users survived for a median of 1.73 years, compared with 1.30 years for nonusers. Taking the drug was associated with longer overall survival in time-varying covariate analysis (hazard ratio, 0.83; 95% CI, 0.80-0.86). This finding was confirmed in a propensity-score analysis of 4,932 matched pairs (HR, 0.79; 95% CI, 0.75-0.83).
“These results warrant further randomized clinical trials to evaluate the actual role of aspirin in the treatment of NSCLC patients,” the researchers conclude.
But Úna McMenamin, PhD, a cancer epidemiologist at Queen’s University Belfast, Ireland, was not convinced by the study’s methods.
While she praised its large size and use of population-based health registers, she expressed concern about the potential for reverse causation, “as it is unclear whether authors lagged the aspirin exposure in the cohort of lung cancer patients.”
There is evidence that common medications such as aspirin may be withdrawn from patients who are thought to be near the end of their life, Dr. McMenamin told this news organization. When not factored into the statistical analysis, aspirin may appear “to be spuriously associated with a reduced risk of death when, in fact, no association may be present.”
Previous studies of aspirin use in lung cancer patients that have included a lag, such as one Dr. McMenamin and colleagues conducted in 2015, have found no evidence of a protective effect.
That is why, according to Dr. McMenamin, “additional population-based studies, in diverse populations, are required to investigate the association between aspirin use and survival outcomes in lung-cancer patients to determine whether randomized controlled trials are warranted in this patient group.”
In addition, she noted, “any potential benefit of aspirin in lung cancer patients needs to be balanced against known adverse events associated with prolonged aspirin use, such as gastrointestinal bleeding.”
Dr. Hung did not reply to requests for comment.
The study had no funding, and the researchers report no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM BMC CANCER
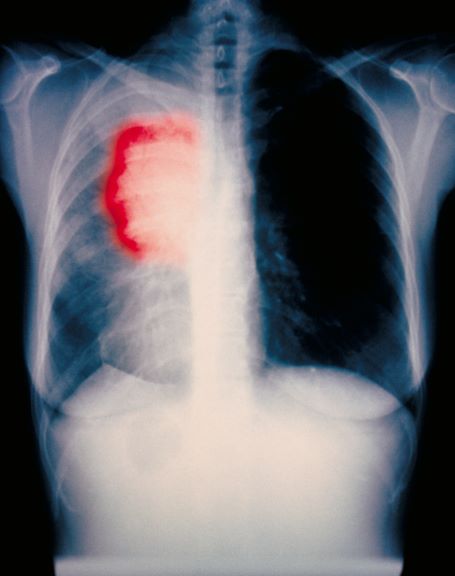
History of dysphagia and abdominal pain
The diagnosis is squamous cell carcinoma. A central or hilar mass is most likely to be a squamous cell carcinoma or a small cell tumor and less commonly an adenocarcinoma. Histologically, when there is lack of cohesion among the epithelial cells due to malignant changes, the cells get arranged in a concentric manner. The fate of a squamous cell is to form keratin, so these cells lay down keratin in a concentric manner and then appear as keratin pearls.
This patient's tumor is found to have programmed cell death–ligand 1 ≥ 1% and has no actionable molecular markers. The patient has a performance status score of 1. In a patient with advanced or metastatic squamous cell carcinoma with a performance status score of 1, the National Comprehensive Cancer Network recommends pembrolizumab/carboplatin/paclitaxel or pembrolizumab/carboplatin/albumin-bound paclitaxel as preferred regimens. The pembrolizumab component is based on the results of the KEYNOTE-407 trial. In patients with previously untreated metastatic, squamous non-small cell lung cancer, the addition of pembrolizumab to chemotherapy with carboplatin plus paclitaxel or nab-paclitaxel resulted in significantly longer overall survival and progression-free survival than chemotherapy alone.
Maurie Markman, MD, President, Department of Medical Oncology, Cancer Treatment Centers of America.
Maurie Markman, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Merck
Serve(d) as a speaker or a member of a speakers bureau for: AstraZeneca; Novis; Glaxo Smith Kline
Received research grant from: AstraZeneca; Novis; GSK; Merck
The diagnosis is squamous cell carcinoma. A central or hilar mass is most likely to be a squamous cell carcinoma or a small cell tumor and less commonly an adenocarcinoma. Histologically, when there is lack of cohesion among the epithelial cells due to malignant changes, the cells get arranged in a concentric manner. The fate of a squamous cell is to form keratin, so these cells lay down keratin in a concentric manner and then appear as keratin pearls.
This patient's tumor is found to have programmed cell death–ligand 1 ≥ 1% and has no actionable molecular markers. The patient has a performance status score of 1. In a patient with advanced or metastatic squamous cell carcinoma with a performance status score of 1, the National Comprehensive Cancer Network recommends pembrolizumab/carboplatin/paclitaxel or pembrolizumab/carboplatin/albumin-bound paclitaxel as preferred regimens. The pembrolizumab component is based on the results of the KEYNOTE-407 trial. In patients with previously untreated metastatic, squamous non-small cell lung cancer, the addition of pembrolizumab to chemotherapy with carboplatin plus paclitaxel or nab-paclitaxel resulted in significantly longer overall survival and progression-free survival than chemotherapy alone.
Maurie Markman, MD, President, Department of Medical Oncology, Cancer Treatment Centers of America.
Maurie Markman, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Merck
Serve(d) as a speaker or a member of a speakers bureau for: AstraZeneca; Novis; Glaxo Smith Kline
Received research grant from: AstraZeneca; Novis; GSK; Merck
The diagnosis is squamous cell carcinoma. A central or hilar mass is most likely to be a squamous cell carcinoma or a small cell tumor and less commonly an adenocarcinoma. Histologically, when there is lack of cohesion among the epithelial cells due to malignant changes, the cells get arranged in a concentric manner. The fate of a squamous cell is to form keratin, so these cells lay down keratin in a concentric manner and then appear as keratin pearls.
This patient's tumor is found to have programmed cell death–ligand 1 ≥ 1% and has no actionable molecular markers. The patient has a performance status score of 1. In a patient with advanced or metastatic squamous cell carcinoma with a performance status score of 1, the National Comprehensive Cancer Network recommends pembrolizumab/carboplatin/paclitaxel or pembrolizumab/carboplatin/albumin-bound paclitaxel as preferred regimens. The pembrolizumab component is based on the results of the KEYNOTE-407 trial. In patients with previously untreated metastatic, squamous non-small cell lung cancer, the addition of pembrolizumab to chemotherapy with carboplatin plus paclitaxel or nab-paclitaxel resulted in significantly longer overall survival and progression-free survival than chemotherapy alone.
Maurie Markman, MD, President, Department of Medical Oncology, Cancer Treatment Centers of America.
Maurie Markman, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Merck
Serve(d) as a speaker or a member of a speakers bureau for: AstraZeneca; Novis; Glaxo Smith Kline
Received research grant from: AstraZeneca; Novis; GSK; Merck
A 59-year-old woman presents with a 4-month history of dysphagia when eating solids in addition to nausea and abdominal pain. She also reports recent hemoptysis and the onset of hoarseness. She has had an unintentional 22-lb weight loss over the past 6 months. She has a history of emphysema. She takes no medication. She has a 26 pack-year history of cigarette smoking. She is 5 feet 4 in tall and weighs 105 lb, with a BMI of 18. Her vital signs are within normal limits. Chest auscultation reveals diminished breath sounds over the right lung fields. Chest radiography reveals a right-sided 6-cm hilar mass. Laboratory studies show a serum calcium level of 12 mg/dL (normal range, 8.5-10.5 mg/dL). A CT scan revealed a spiculated lesion and hepatic metastases. A biopsy was performed. Keratinization was found in the form of keratin pearls.
Three drugs go head-to-head in advanced lung cancer study
The findings were reported in JAMA Network Open.
“Until recently, chemotherapy with platinum doublet was the standard first-line option for most patients with advanced NSCLC who did not have these genetic drivers or were not tested for them and remains the first choice in many parts of the world,” wrote the authors of the study which was led by Sreeram Ramagopalan, PhD, of F. Hoffmann-La Roche in Switzerland which funded the study.
Atezolizumab (Tecentriq, Genentech), which was approved in October by the U.S. Food and Drug Administration, is a monoclonal antibody that targets programmed cell death ligand 1 (PD-L1). It is also approved as monotherapy for patients with advanced NSCLC whose disease progressed despite treatment with platinum-based chemotherapy.
This is the first-known analysis that compares atezolizumab, nivolumab (Opdivo, Bristol Myers Squibb), and docetaxel (Taxotere, Sanofi) in patients outside of clinical trials, said Vivek Subbiah, MD, of MD Anderson Cancer Center and the study’s first author. “We have several new immune checkpoint inhibitors approved for treatment for NSCLC. Head-to-head comparison of the effectiveness of these agents in the real world are lacking,” he said.
Treatment with immune checkpoint inhibitors has shown improvement in the survival of patients with advanced NSCLC who failed chemotherapy treatment.
This study included 3,336 patients (mean age 67 years, 54.6% men) with advanced NSCLC who were treated with platinum-based chemotherapy. Data were collected from more than 1,000 clinics in the United States. Of the patients, 206 received atezolizumab, 500 received docetaxel, and 2,630 received nivolumab.
Patients were followed between May 2011 and March 2020. Atezolizumab and nivolumab showed a similar overall survival in these patients, but atezolizumab showed a longer overall survival, compared with docetaxel.
“Compared with docetaxel, atezolizumab was associated with significantly longer survival in the overall population and across all subgroups analyzed,” including patients with stage IIIB or IV cancer at diagnosis and nonsquamous NSCLC, the authors wrote. “Atezolizumab was associated with longer overall survival compared with docetaxel and was on par with nivolumab, supporting current clinical guidelines for systemic therapy for patients with advanced NSCLC in the U.S.”
Limitations of the study included its observational design and a small number of patients receiving atezolizumab. The authors suggested that studies using larger sample sizes are needed.
This study was funded by F. Hoffmann-La Roche. Genentech is a subsidiary of F. Hoffmann-La Roche.
The findings were reported in JAMA Network Open.
“Until recently, chemotherapy with platinum doublet was the standard first-line option for most patients with advanced NSCLC who did not have these genetic drivers or were not tested for them and remains the first choice in many parts of the world,” wrote the authors of the study which was led by Sreeram Ramagopalan, PhD, of F. Hoffmann-La Roche in Switzerland which funded the study.
Atezolizumab (Tecentriq, Genentech), which was approved in October by the U.S. Food and Drug Administration, is a monoclonal antibody that targets programmed cell death ligand 1 (PD-L1). It is also approved as monotherapy for patients with advanced NSCLC whose disease progressed despite treatment with platinum-based chemotherapy.
This is the first-known analysis that compares atezolizumab, nivolumab (Opdivo, Bristol Myers Squibb), and docetaxel (Taxotere, Sanofi) in patients outside of clinical trials, said Vivek Subbiah, MD, of MD Anderson Cancer Center and the study’s first author. “We have several new immune checkpoint inhibitors approved for treatment for NSCLC. Head-to-head comparison of the effectiveness of these agents in the real world are lacking,” he said.
Treatment with immune checkpoint inhibitors has shown improvement in the survival of patients with advanced NSCLC who failed chemotherapy treatment.
This study included 3,336 patients (mean age 67 years, 54.6% men) with advanced NSCLC who were treated with platinum-based chemotherapy. Data were collected from more than 1,000 clinics in the United States. Of the patients, 206 received atezolizumab, 500 received docetaxel, and 2,630 received nivolumab.
Patients were followed between May 2011 and March 2020. Atezolizumab and nivolumab showed a similar overall survival in these patients, but atezolizumab showed a longer overall survival, compared with docetaxel.
“Compared with docetaxel, atezolizumab was associated with significantly longer survival in the overall population and across all subgroups analyzed,” including patients with stage IIIB or IV cancer at diagnosis and nonsquamous NSCLC, the authors wrote. “Atezolizumab was associated with longer overall survival compared with docetaxel and was on par with nivolumab, supporting current clinical guidelines for systemic therapy for patients with advanced NSCLC in the U.S.”
Limitations of the study included its observational design and a small number of patients receiving atezolizumab. The authors suggested that studies using larger sample sizes are needed.
This study was funded by F. Hoffmann-La Roche. Genentech is a subsidiary of F. Hoffmann-La Roche.
The findings were reported in JAMA Network Open.
“Until recently, chemotherapy with platinum doublet was the standard first-line option for most patients with advanced NSCLC who did not have these genetic drivers or were not tested for them and remains the first choice in many parts of the world,” wrote the authors of the study which was led by Sreeram Ramagopalan, PhD, of F. Hoffmann-La Roche in Switzerland which funded the study.
Atezolizumab (Tecentriq, Genentech), which was approved in October by the U.S. Food and Drug Administration, is a monoclonal antibody that targets programmed cell death ligand 1 (PD-L1). It is also approved as monotherapy for patients with advanced NSCLC whose disease progressed despite treatment with platinum-based chemotherapy.
This is the first-known analysis that compares atezolizumab, nivolumab (Opdivo, Bristol Myers Squibb), and docetaxel (Taxotere, Sanofi) in patients outside of clinical trials, said Vivek Subbiah, MD, of MD Anderson Cancer Center and the study’s first author. “We have several new immune checkpoint inhibitors approved for treatment for NSCLC. Head-to-head comparison of the effectiveness of these agents in the real world are lacking,” he said.
Treatment with immune checkpoint inhibitors has shown improvement in the survival of patients with advanced NSCLC who failed chemotherapy treatment.
This study included 3,336 patients (mean age 67 years, 54.6% men) with advanced NSCLC who were treated with platinum-based chemotherapy. Data were collected from more than 1,000 clinics in the United States. Of the patients, 206 received atezolizumab, 500 received docetaxel, and 2,630 received nivolumab.
Patients were followed between May 2011 and March 2020. Atezolizumab and nivolumab showed a similar overall survival in these patients, but atezolizumab showed a longer overall survival, compared with docetaxel.
“Compared with docetaxel, atezolizumab was associated with significantly longer survival in the overall population and across all subgroups analyzed,” including patients with stage IIIB or IV cancer at diagnosis and nonsquamous NSCLC, the authors wrote. “Atezolizumab was associated with longer overall survival compared with docetaxel and was on par with nivolumab, supporting current clinical guidelines for systemic therapy for patients with advanced NSCLC in the U.S.”
Limitations of the study included its observational design and a small number of patients receiving atezolizumab. The authors suggested that studies using larger sample sizes are needed.
This study was funded by F. Hoffmann-La Roche. Genentech is a subsidiary of F. Hoffmann-La Roche.
FROM JAMA NETWORK OPEN
Common lung cancer screening tool superior to alternatives
a Dutch clinical trial that measures nodule volume and growth rate instead of linear measurement of nodule size as done in Lung-RADs.
The study, published in the American Journal of Roentgenology on Nov. 10, 2021,was a retrospective study of 185 patients (100 women, 85 men; mean age, 66 years) who underwent lung cancer screening at a single health care system between July 2015 and August 2018. Using Lung-RADS, seven cancers were downgraded to category 2. The weighted cancer risk was 5% for new nodules, 1% for stable existing nodules, and 44% for growing existing nodules.
“Lung-RADS scores exhibited excellent sensitivity and specificity for cancer in existing nodules and excellent sensitivity in new nodules, though low specificity in new nodules,” wrote the authors, led by Mark M. Hammer, MD, a radiologist with Brigham and Women’s Hospital in Boston.
CT scans are increasingly used for lung cancer screening, so accuracy is essential in devising an appropriate treatment plan for patients. Nearly all centers in the United States use the American College of Radiology’s Lung-RADS for lung cancer screening. In Europe, many centers use the volumetric-based approach of NELSON.
Several studies have compared the performance of nodule risk assessment algorithms, but the findings are inconsistent. Lung-RADS was found to be inferior to the Vancouver risk calculator in predicting malignancy in the National Lung Screening Trial for total nodules. Dr. Hammer previously reported that subsolid nodules classified as Lung-RADS categories 2 and 3 have a higher risk of malignancy than reported. Meanwhile, a study that followed 13,195 men and 2,594 women at high risk of lung cancer found that lung cancer mortality was lower among participants who underwent volume CT screening than among those who underwent no screening.
The authors cited the retrospective design and the small sample size as study limitations. They added that pathological proof was not obtained from benign nodules, which may represent undiagnosed cancer.
The authors declared no conflict of interest.
a Dutch clinical trial that measures nodule volume and growth rate instead of linear measurement of nodule size as done in Lung-RADs.
The study, published in the American Journal of Roentgenology on Nov. 10, 2021,was a retrospective study of 185 patients (100 women, 85 men; mean age, 66 years) who underwent lung cancer screening at a single health care system between July 2015 and August 2018. Using Lung-RADS, seven cancers were downgraded to category 2. The weighted cancer risk was 5% for new nodules, 1% for stable existing nodules, and 44% for growing existing nodules.
“Lung-RADS scores exhibited excellent sensitivity and specificity for cancer in existing nodules and excellent sensitivity in new nodules, though low specificity in new nodules,” wrote the authors, led by Mark M. Hammer, MD, a radiologist with Brigham and Women’s Hospital in Boston.
CT scans are increasingly used for lung cancer screening, so accuracy is essential in devising an appropriate treatment plan for patients. Nearly all centers in the United States use the American College of Radiology’s Lung-RADS for lung cancer screening. In Europe, many centers use the volumetric-based approach of NELSON.
Several studies have compared the performance of nodule risk assessment algorithms, but the findings are inconsistent. Lung-RADS was found to be inferior to the Vancouver risk calculator in predicting malignancy in the National Lung Screening Trial for total nodules. Dr. Hammer previously reported that subsolid nodules classified as Lung-RADS categories 2 and 3 have a higher risk of malignancy than reported. Meanwhile, a study that followed 13,195 men and 2,594 women at high risk of lung cancer found that lung cancer mortality was lower among participants who underwent volume CT screening than among those who underwent no screening.
The authors cited the retrospective design and the small sample size as study limitations. They added that pathological proof was not obtained from benign nodules, which may represent undiagnosed cancer.
The authors declared no conflict of interest.
a Dutch clinical trial that measures nodule volume and growth rate instead of linear measurement of nodule size as done in Lung-RADs.
The study, published in the American Journal of Roentgenology on Nov. 10, 2021,was a retrospective study of 185 patients (100 women, 85 men; mean age, 66 years) who underwent lung cancer screening at a single health care system between July 2015 and August 2018. Using Lung-RADS, seven cancers were downgraded to category 2. The weighted cancer risk was 5% for new nodules, 1% for stable existing nodules, and 44% for growing existing nodules.
“Lung-RADS scores exhibited excellent sensitivity and specificity for cancer in existing nodules and excellent sensitivity in new nodules, though low specificity in new nodules,” wrote the authors, led by Mark M. Hammer, MD, a radiologist with Brigham and Women’s Hospital in Boston.
CT scans are increasingly used for lung cancer screening, so accuracy is essential in devising an appropriate treatment plan for patients. Nearly all centers in the United States use the American College of Radiology’s Lung-RADS for lung cancer screening. In Europe, many centers use the volumetric-based approach of NELSON.
Several studies have compared the performance of nodule risk assessment algorithms, but the findings are inconsistent. Lung-RADS was found to be inferior to the Vancouver risk calculator in predicting malignancy in the National Lung Screening Trial for total nodules. Dr. Hammer previously reported that subsolid nodules classified as Lung-RADS categories 2 and 3 have a higher risk of malignancy than reported. Meanwhile, a study that followed 13,195 men and 2,594 women at high risk of lung cancer found that lung cancer mortality was lower among participants who underwent volume CT screening than among those who underwent no screening.
The authors cited the retrospective design and the small sample size as study limitations. They added that pathological proof was not obtained from benign nodules, which may represent undiagnosed cancer.
The authors declared no conflict of interest.
FROM THE AMERICAN JOURNAL OF ROENTGENOLOGY
One-quarter of lung cancer patients alive at 5 years
In recent years, the survival rate for patients with lung cancer has increased to the point where now, almost one-quarter of patients with lung cancer are alive 5 years after being diagnosed.
This new statistic is highlighted in the State of Lung Cancer report from the American Lung Association (ALA), published online on Nov. 16.
“If you look back, the 5-year survival rate has been very slowly eking up at about 1% over the years,” Andrea McKee, MD, volunteer spokesperson at the ALA, told this news organization. “To see this big jump is truly remarkable, so that is something we are all celebrating,” she added.
“But we have to change the fatalistic thinking that both patients and primary care physicians still have about lung cancer. Most people say, ‘Everybody I know who had lung cancer died,’ and that was the way it used to be,” she commented, “but that has now changed. Lung cancer is highly curable in its early stages, and even if not early-stage, there are treatments that are making an impact now.”
“So we’ve got to change that perception, as it does exist, even on the part of primary care providers, too,” Dr. McKee emphasized.
Lung cancer decreasing but still being diagnosed late
The report notes that the risk of being diagnosed with lung cancer varies considerably across the United States. For example, rates of lung cancer diagnoses are almost 2.5 times higher in Kentucky than in Utah.
Overall, the incidence is decreasing. “Over the last 5 years, the rate of new cases decreased 10% nationally,” the authors point out.
However, in almost half of the cases, the disease is diagnosed in late stages.
When diagnosed at a late stage, the 5-year survival rate for lung cancer drops to only 6%, whereas when the disease is diagnosed early, the 5-year survival rate is 60%.
At present, around 24% of cases of lung cancer are diagnosed at early stages, the report notes, but again, this varies across the United States. The highest rate (30%) is in Massachusetts, and the lowest rate (19%) is in Hawaii.
The percentage of lung cancer cases diagnosed early has been steadily increasing, presumably in part because of the introduction of low-dose CT screening for individuals at highest risk (such as smokers).
However, across the nation, only 5.7% of individuals at high risk for lung cancer underwent annual low-dose CT screening, the report notes.
“CT screening is so powerful at saving lives that even with only 5.7% of people that we’ve been able to screen, I believe it’s making a difference,” Dr. McKee commented. That small national percentage still represents a considerable number of patients, she noted, “so even with what we’ve done so far, I believe that screening is making a difference, at least within my own practice, where I’m definitely seeing it,” Dr. McKee emphasized.
Recent changes to the recommendations as to who should undergo lung cancer screening “have almost doubled the size of the screening population in the U.S.,” Dr. McKee commented. “So there are now about 15 million people who need to get screened, and it again helps that primary care physicians know that screening is very powerful at detecting early-stage lung cancer,” she said.
In her hospital’s own screening program, among the individuals who regularly undergo screening, the majority (88%) of lung cancer cases are detected at stage I or II, for which the cure rate is approximately 90%, she noted.
Another misconception of primary care physicians is that lung cancer screening has an unacceptably high false positive rate. Previous reports in the medical literature suggested the rate could be as high as 96%. “This is absolutely, positively wrong. That is not the false positive rate; the false positive rate for lung cancer screening is less than 10%,” Dr. McKee emphasized.
“So we have to change that in the minds of primary care providers as well,” she underscored.
Report highlights racial disparities
The report also highlights the racial disparities that persist in all aspects of lung cancer management – early diagnosis, surgical treatment, lack of treatment, and survival.
For example, Black Americans are 18% less likely to be diagnosed with early-stage disease and are 23% less likely to receive surgical treatment than their White counterparts. They are also 9% more likely to receive no treatment at all, and mortality from lung cancer among Black patients is 21% worse than it is for White patients.
The same trend is seen among Latinx persons, although they are just as likely as White patients to undergo surgical treatment.
First and foremost, “we have to make sure that the [Black and Latinx persons] are screened in an equal fashion,” Dr. McKee said. Providing screening for communities of color is one strategy that might improve screening rates, she suggested.
So, too, can outreach programs in which lung cancer experts work with leaders within these communities, because people are more likely to listen to their leaders regarding the importance of screening for early detection of lung cancer.
Physicians also need to emphasize that even for people who quit smoking decades ago, once those persons are in their 70s, “there is a spike again in lung cancer diagnoses, and that is true for both Black and White patients,” Dr. McKee stressed.
“Again, this is something that many doctors are not aware of,” she emphasized.
Dr. McKee has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In recent years, the survival rate for patients with lung cancer has increased to the point where now, almost one-quarter of patients with lung cancer are alive 5 years after being diagnosed.
This new statistic is highlighted in the State of Lung Cancer report from the American Lung Association (ALA), published online on Nov. 16.
“If you look back, the 5-year survival rate has been very slowly eking up at about 1% over the years,” Andrea McKee, MD, volunteer spokesperson at the ALA, told this news organization. “To see this big jump is truly remarkable, so that is something we are all celebrating,” she added.
“But we have to change the fatalistic thinking that both patients and primary care physicians still have about lung cancer. Most people say, ‘Everybody I know who had lung cancer died,’ and that was the way it used to be,” she commented, “but that has now changed. Lung cancer is highly curable in its early stages, and even if not early-stage, there are treatments that are making an impact now.”
“So we’ve got to change that perception, as it does exist, even on the part of primary care providers, too,” Dr. McKee emphasized.
Lung cancer decreasing but still being diagnosed late
The report notes that the risk of being diagnosed with lung cancer varies considerably across the United States. For example, rates of lung cancer diagnoses are almost 2.5 times higher in Kentucky than in Utah.
Overall, the incidence is decreasing. “Over the last 5 years, the rate of new cases decreased 10% nationally,” the authors point out.
However, in almost half of the cases, the disease is diagnosed in late stages.
When diagnosed at a late stage, the 5-year survival rate for lung cancer drops to only 6%, whereas when the disease is diagnosed early, the 5-year survival rate is 60%.
At present, around 24% of cases of lung cancer are diagnosed at early stages, the report notes, but again, this varies across the United States. The highest rate (30%) is in Massachusetts, and the lowest rate (19%) is in Hawaii.
The percentage of lung cancer cases diagnosed early has been steadily increasing, presumably in part because of the introduction of low-dose CT screening for individuals at highest risk (such as smokers).
However, across the nation, only 5.7% of individuals at high risk for lung cancer underwent annual low-dose CT screening, the report notes.
“CT screening is so powerful at saving lives that even with only 5.7% of people that we’ve been able to screen, I believe it’s making a difference,” Dr. McKee commented. That small national percentage still represents a considerable number of patients, she noted, “so even with what we’ve done so far, I believe that screening is making a difference, at least within my own practice, where I’m definitely seeing it,” Dr. McKee emphasized.
Recent changes to the recommendations as to who should undergo lung cancer screening “have almost doubled the size of the screening population in the U.S.,” Dr. McKee commented. “So there are now about 15 million people who need to get screened, and it again helps that primary care physicians know that screening is very powerful at detecting early-stage lung cancer,” she said.
In her hospital’s own screening program, among the individuals who regularly undergo screening, the majority (88%) of lung cancer cases are detected at stage I or II, for which the cure rate is approximately 90%, she noted.
Another misconception of primary care physicians is that lung cancer screening has an unacceptably high false positive rate. Previous reports in the medical literature suggested the rate could be as high as 96%. “This is absolutely, positively wrong. That is not the false positive rate; the false positive rate for lung cancer screening is less than 10%,” Dr. McKee emphasized.
“So we have to change that in the minds of primary care providers as well,” she underscored.
Report highlights racial disparities
The report also highlights the racial disparities that persist in all aspects of lung cancer management – early diagnosis, surgical treatment, lack of treatment, and survival.
For example, Black Americans are 18% less likely to be diagnosed with early-stage disease and are 23% less likely to receive surgical treatment than their White counterparts. They are also 9% more likely to receive no treatment at all, and mortality from lung cancer among Black patients is 21% worse than it is for White patients.
The same trend is seen among Latinx persons, although they are just as likely as White patients to undergo surgical treatment.
First and foremost, “we have to make sure that the [Black and Latinx persons] are screened in an equal fashion,” Dr. McKee said. Providing screening for communities of color is one strategy that might improve screening rates, she suggested.
So, too, can outreach programs in which lung cancer experts work with leaders within these communities, because people are more likely to listen to their leaders regarding the importance of screening for early detection of lung cancer.
Physicians also need to emphasize that even for people who quit smoking decades ago, once those persons are in their 70s, “there is a spike again in lung cancer diagnoses, and that is true for both Black and White patients,” Dr. McKee stressed.
“Again, this is something that many doctors are not aware of,” she emphasized.
Dr. McKee has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In recent years, the survival rate for patients with lung cancer has increased to the point where now, almost one-quarter of patients with lung cancer are alive 5 years after being diagnosed.
This new statistic is highlighted in the State of Lung Cancer report from the American Lung Association (ALA), published online on Nov. 16.
“If you look back, the 5-year survival rate has been very slowly eking up at about 1% over the years,” Andrea McKee, MD, volunteer spokesperson at the ALA, told this news organization. “To see this big jump is truly remarkable, so that is something we are all celebrating,” she added.
“But we have to change the fatalistic thinking that both patients and primary care physicians still have about lung cancer. Most people say, ‘Everybody I know who had lung cancer died,’ and that was the way it used to be,” she commented, “but that has now changed. Lung cancer is highly curable in its early stages, and even if not early-stage, there are treatments that are making an impact now.”
“So we’ve got to change that perception, as it does exist, even on the part of primary care providers, too,” Dr. McKee emphasized.
Lung cancer decreasing but still being diagnosed late
The report notes that the risk of being diagnosed with lung cancer varies considerably across the United States. For example, rates of lung cancer diagnoses are almost 2.5 times higher in Kentucky than in Utah.
Overall, the incidence is decreasing. “Over the last 5 years, the rate of new cases decreased 10% nationally,” the authors point out.
However, in almost half of the cases, the disease is diagnosed in late stages.
When diagnosed at a late stage, the 5-year survival rate for lung cancer drops to only 6%, whereas when the disease is diagnosed early, the 5-year survival rate is 60%.
At present, around 24% of cases of lung cancer are diagnosed at early stages, the report notes, but again, this varies across the United States. The highest rate (30%) is in Massachusetts, and the lowest rate (19%) is in Hawaii.
The percentage of lung cancer cases diagnosed early has been steadily increasing, presumably in part because of the introduction of low-dose CT screening for individuals at highest risk (such as smokers).
However, across the nation, only 5.7% of individuals at high risk for lung cancer underwent annual low-dose CT screening, the report notes.
“CT screening is so powerful at saving lives that even with only 5.7% of people that we’ve been able to screen, I believe it’s making a difference,” Dr. McKee commented. That small national percentage still represents a considerable number of patients, she noted, “so even with what we’ve done so far, I believe that screening is making a difference, at least within my own practice, where I’m definitely seeing it,” Dr. McKee emphasized.
Recent changes to the recommendations as to who should undergo lung cancer screening “have almost doubled the size of the screening population in the U.S.,” Dr. McKee commented. “So there are now about 15 million people who need to get screened, and it again helps that primary care physicians know that screening is very powerful at detecting early-stage lung cancer,” she said.
In her hospital’s own screening program, among the individuals who regularly undergo screening, the majority (88%) of lung cancer cases are detected at stage I or II, for which the cure rate is approximately 90%, she noted.
Another misconception of primary care physicians is that lung cancer screening has an unacceptably high false positive rate. Previous reports in the medical literature suggested the rate could be as high as 96%. “This is absolutely, positively wrong. That is not the false positive rate; the false positive rate for lung cancer screening is less than 10%,” Dr. McKee emphasized.
“So we have to change that in the minds of primary care providers as well,” she underscored.
Report highlights racial disparities
The report also highlights the racial disparities that persist in all aspects of lung cancer management – early diagnosis, surgical treatment, lack of treatment, and survival.
For example, Black Americans are 18% less likely to be diagnosed with early-stage disease and are 23% less likely to receive surgical treatment than their White counterparts. They are also 9% more likely to receive no treatment at all, and mortality from lung cancer among Black patients is 21% worse than it is for White patients.
The same trend is seen among Latinx persons, although they are just as likely as White patients to undergo surgical treatment.
First and foremost, “we have to make sure that the [Black and Latinx persons] are screened in an equal fashion,” Dr. McKee said. Providing screening for communities of color is one strategy that might improve screening rates, she suggested.
So, too, can outreach programs in which lung cancer experts work with leaders within these communities, because people are more likely to listen to their leaders regarding the importance of screening for early detection of lung cancer.
Physicians also need to emphasize that even for people who quit smoking decades ago, once those persons are in their 70s, “there is a spike again in lung cancer diagnoses, and that is true for both Black and White patients,” Dr. McKee stressed.
“Again, this is something that many doctors are not aware of,” she emphasized.
Dr. McKee has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
EU panel endorses first-of-its-kind lung cancer drug
At its November meeting, the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) endorsed the novel oral therapy sotorasib (Lumykras). The indication is use in the treatment of adults with advanced NSCLC with a KRAS G12C mutation who have progressed after at least one prior line of systemic therapy.
Sotorasib is an inhibitor of KRAS G12C, an oncogenic driver of tumorigenesis. The drug blocks tumor cell signaling and survival, inhibits cell growth, and selectively promotes apoptosis in tumors harboring KRAS G12C, according to the CHMP.
KRAS mutations are the most common mutations in NSCLC tumors, but for a long time appeared to be resistant to drug therapy.
The KRAS G12C mutation occurs in about 13% of NSCLC mutations.
When clinical data on sotorasib were presented at the 2020 World Conference on Lung Cancer, lung cancer experts greeted the results enthusiastically.
“This is a historic milestone in lung cancer therapy. After four decades of scientific efforts in targeting KRAS, sotorasib has potential to be the first targeted treatment option for this patient population with a high unmet need,” Bob Li, MD, PhD, MPH, of Memorial Sloan Kettering Cancer Center in New York City, said at the time.
The drug was approved by the U.S. Food and Drug Administration in May based on a study of 124 patients with locally advanced or metastatic KRAS G12C-mutated NSCLC with disease progression after receiving an immune checkpoint inhibitor and/or platinum-based chemotherapy.
The FDA approval was based on an overall response rate of 36%, the study’s primary outcome. Of the patients who responded, 58% had a duration of response of 6 months or longer.
The EMA says its recommendation for approval is based on objective response rate and response duration data.
The most common side effects of sotorasib are diarrhea, nausea, fatigue, increased aspartate aminotransferase, and arthralgia said the CHMP.
A version of this article first appeared on Medscape.com.
At its November meeting, the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) endorsed the novel oral therapy sotorasib (Lumykras). The indication is use in the treatment of adults with advanced NSCLC with a KRAS G12C mutation who have progressed after at least one prior line of systemic therapy.
Sotorasib is an inhibitor of KRAS G12C, an oncogenic driver of tumorigenesis. The drug blocks tumor cell signaling and survival, inhibits cell growth, and selectively promotes apoptosis in tumors harboring KRAS G12C, according to the CHMP.
KRAS mutations are the most common mutations in NSCLC tumors, but for a long time appeared to be resistant to drug therapy.
The KRAS G12C mutation occurs in about 13% of NSCLC mutations.
When clinical data on sotorasib were presented at the 2020 World Conference on Lung Cancer, lung cancer experts greeted the results enthusiastically.
“This is a historic milestone in lung cancer therapy. After four decades of scientific efforts in targeting KRAS, sotorasib has potential to be the first targeted treatment option for this patient population with a high unmet need,” Bob Li, MD, PhD, MPH, of Memorial Sloan Kettering Cancer Center in New York City, said at the time.
The drug was approved by the U.S. Food and Drug Administration in May based on a study of 124 patients with locally advanced or metastatic KRAS G12C-mutated NSCLC with disease progression after receiving an immune checkpoint inhibitor and/or platinum-based chemotherapy.
The FDA approval was based on an overall response rate of 36%, the study’s primary outcome. Of the patients who responded, 58% had a duration of response of 6 months or longer.
The EMA says its recommendation for approval is based on objective response rate and response duration data.
The most common side effects of sotorasib are diarrhea, nausea, fatigue, increased aspartate aminotransferase, and arthralgia said the CHMP.
A version of this article first appeared on Medscape.com.
At its November meeting, the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) endorsed the novel oral therapy sotorasib (Lumykras). The indication is use in the treatment of adults with advanced NSCLC with a KRAS G12C mutation who have progressed after at least one prior line of systemic therapy.
Sotorasib is an inhibitor of KRAS G12C, an oncogenic driver of tumorigenesis. The drug blocks tumor cell signaling and survival, inhibits cell growth, and selectively promotes apoptosis in tumors harboring KRAS G12C, according to the CHMP.
KRAS mutations are the most common mutations in NSCLC tumors, but for a long time appeared to be resistant to drug therapy.
The KRAS G12C mutation occurs in about 13% of NSCLC mutations.
When clinical data on sotorasib were presented at the 2020 World Conference on Lung Cancer, lung cancer experts greeted the results enthusiastically.
“This is a historic milestone in lung cancer therapy. After four decades of scientific efforts in targeting KRAS, sotorasib has potential to be the first targeted treatment option for this patient population with a high unmet need,” Bob Li, MD, PhD, MPH, of Memorial Sloan Kettering Cancer Center in New York City, said at the time.
The drug was approved by the U.S. Food and Drug Administration in May based on a study of 124 patients with locally advanced or metastatic KRAS G12C-mutated NSCLC with disease progression after receiving an immune checkpoint inhibitor and/or platinum-based chemotherapy.
The FDA approval was based on an overall response rate of 36%, the study’s primary outcome. Of the patients who responded, 58% had a duration of response of 6 months or longer.
The EMA says its recommendation for approval is based on objective response rate and response duration data.
The most common side effects of sotorasib are diarrhea, nausea, fatigue, increased aspartate aminotransferase, and arthralgia said the CHMP.
A version of this article first appeared on Medscape.com.
Most oncology trainees encounter discrimination, don’t report it, survey finds
On day 1 of her fellowship, Francesca C. Duncan, MD, was blindsided by her first patient.
The patient, a White man who was accompanied by his wife, sat in the exam room with his sunglasses on.
“I remember him saying, ‘I need to take off my sunglasses so you don’t look so Black,’” said Dr. Duncan, a pulmonologist and intensivist at Indiana University, Indianapolis, who has a specialty in lung cancer disparities.
The patient proceeded to grill her about her experience and training. He asked where she attended college and mocked her degree from a historically Black university. His wife sat there, silent.
Dr. Duncan was shocked by the fact that she still had to defend her credentials.
“I just kind of felt like at that point in my training, my title would have earned me more respect,” said Dr. Duncan, now an assistant professor after recently completing a 3-year fellowship in pulmonary and critical care medicine. “I thought at some point [the racism and discrimination] would stop, but after all that training, all that late-night studying, I still had to prove myself.”
Unfortunately, Dr. Duncan’s experience in fellowship is not unique.
A recent survey of hematology and oncology fellows revealed that medical trainees routinely encounter discrimination during their training.
The 17 fellows who were anonymously interviewed in the survey all recalled experiencing or witnessing discriminatory behaviors during their fellowship, mostly from patients. These encounters rarely come to light. Only one respondent officially reported an incident.
The findings, published online November 8 in JAMA Network Open, underscore the need for graduate medical education programs to improve learning environments and support for trainees, lead author Rahma M. Warsame, MD, and colleagues say .
Discrimination at work
Initially, Dr. Warsame and co–principal investigator Katharine Price, MD, were tasked with developing strategies to mitigate instances of racism and bias that fellows encountered during training, but both felt it was critical to understand the experiences of their trainees first.
Out of 34 fellows and recent graduates of the hematology and oncology fellowship program of the Mayo Clinic, Rochester, Minn., 20 consented to participate in the study. Of those, 17 were interviewed between July and November 2018. Among the 17 interviewees, six were Asian, two were Black, three were Hispanic, two were multiracial, and four were White.
The majority of these offenses were committed by patients, not faculty or other employees. The researchers largely interpreted most of the incidents as microaggressions.
From the interviews, the researchers identified six central themes. Among them: foreign fellows and U.S.-born trainees being perceived or made to feel like outsiders; inappropriate comments being made toward female employees about their looks, credentials, or marital status; lack of action after reporting incidents or concerns that reporting such incidents would be futile; and strategies fellows used to cope after negative interactions.
One interviewee said, “I was fired by a patient because I have an accent.” Another said that when she is interviewing for jobs, she is always asked if she has children: “Maybe they’re asking in an innocuous manner, but I always feel like people worry. Is this person going to take maternity leave and be less available for work?”
For Dr. Warsame, “the idea that American citizens were frequently made to feel like they do not belong was surprising.”
Not surprising to Dr. Warsame, however, was the importance of fostering diversity and inclusion during fellowship years. Fellows often noted that greater diversity within the program helped create a more inclusive environment.
“[What’s] important to reinforce is the value of creating platforms for honest discussion and intentionally seeking fellows’ voices and perspectives, which in turn makes them feel like they belong,” Dr. Warsame said.
Still, the researchers found that fellows often did not report incidents of discrimination or bias. Only six trainees were aware of policies for reporting patient misconduct or discrimination, and only one ever reported an incident.
Where’s the support?
For Dr. Duncan, her encounter 3 years ago with the patient with sunglasses wasn’t her first experience of discrimination on the job — or her last.
Although hurtful in the moment, she had the wherewithal to report the incident to her attending physician, who was equally shocked. Initially unsure of how to handle it, the attending ultimately stepped up and provided “immense support,” Dr. Duncan said
The issue was brought to the attention of the program director, who took swift action. The patient was documented as “disruptive,” informed of that status in writing, and was banned from receiving treatment from trainees at the center, although Dr. Duncan noted he still received the medical care he needed.
Often, however, fellows who report incidents of discrimination and racism receive little support. According to Dr. Warsame and colleagues, most trainees don’t bother reporting these experiences because they believe that doing so would be futile.
“Concerns about reporting included jeopardizing future employability, risk of retaliation, and challenges reporting experiences that could be perceived as subjective and difficult to prove,” the authors write.
For instance, one interviewee said: “I’m afraid to report these things because there’s gonna be repercussions. There’s no way it’s gonna be anonymous.... I just have to toughen up and, you know, get used [to it].”
Dr. Warsame added, “A major challenge for trainees was that they often felt unheard, and at the time, there was no formal debrief regarding discrimination issues when they arose.”
These instances of bias have implications for trainee well-being. In a 2019 study, discrimination that physicians and students experienced during training had adverse effects on their emotional health. Responses from 50 trainees and physicians revealed a wide range of discriminatory experiences, including patients rejecting care and spewing racist, sexist, or homophobic epithets. Many physicians were uncertain about how to respond effectively and appropriately.
Since that study was published and after having completed her own fellowship, Dr. Duncan said she has seen some change for the better.
“There is a lot more awareness around this, and programs are trying to do better in recognizing and responding to incidents,” she said. She noted that it’s important to ensure that those who are directly affected by discriminatory behaviors aren’t left to do all of the “heavy lifting” of addressing and resolving the issues.
The weight of discriminatory incidents, from microaggressions to overt racism, is cumulative and can adversely affect a person’s career. “It’s exhausting -- we need support,” she said.
The Mayo Clinic is working to ensure that trainees receive support. “The study has prompted communication workshops and faculty development to better equip trainees with strategies to address [and report] patients who behave or display disrespectful or discriminatory behavior,” Dr. Warsame said.
She and her colleagues noted that the anonymous hotline used for the survey cultivated a safe environment for candid discussions and that such an approach is “feasible and effective to explore sensitive topics and scalable to various geographic locations and different medical specialties.”
“We recognize that our program must seek this feedback regularly and ensure we keep a finger on the pulse of our trainees,” Dr. Warsame added.
Dr. Warsame and Dr. Duncan have disclosed no relevant financial relationships. Dr. Duncan noted that her views and comments are her own and do not necessarily reflect those of her institution.
A version of this article first appeared on Medscape.com.
On day 1 of her fellowship, Francesca C. Duncan, MD, was blindsided by her first patient.
The patient, a White man who was accompanied by his wife, sat in the exam room with his sunglasses on.
“I remember him saying, ‘I need to take off my sunglasses so you don’t look so Black,’” said Dr. Duncan, a pulmonologist and intensivist at Indiana University, Indianapolis, who has a specialty in lung cancer disparities.
The patient proceeded to grill her about her experience and training. He asked where she attended college and mocked her degree from a historically Black university. His wife sat there, silent.
Dr. Duncan was shocked by the fact that she still had to defend her credentials.
“I just kind of felt like at that point in my training, my title would have earned me more respect,” said Dr. Duncan, now an assistant professor after recently completing a 3-year fellowship in pulmonary and critical care medicine. “I thought at some point [the racism and discrimination] would stop, but after all that training, all that late-night studying, I still had to prove myself.”
Unfortunately, Dr. Duncan’s experience in fellowship is not unique.
A recent survey of hematology and oncology fellows revealed that medical trainees routinely encounter discrimination during their training.
The 17 fellows who were anonymously interviewed in the survey all recalled experiencing or witnessing discriminatory behaviors during their fellowship, mostly from patients. These encounters rarely come to light. Only one respondent officially reported an incident.
The findings, published online November 8 in JAMA Network Open, underscore the need for graduate medical education programs to improve learning environments and support for trainees, lead author Rahma M. Warsame, MD, and colleagues say .
Discrimination at work
Initially, Dr. Warsame and co–principal investigator Katharine Price, MD, were tasked with developing strategies to mitigate instances of racism and bias that fellows encountered during training, but both felt it was critical to understand the experiences of their trainees first.
Out of 34 fellows and recent graduates of the hematology and oncology fellowship program of the Mayo Clinic, Rochester, Minn., 20 consented to participate in the study. Of those, 17 were interviewed between July and November 2018. Among the 17 interviewees, six were Asian, two were Black, three were Hispanic, two were multiracial, and four were White.
The majority of these offenses were committed by patients, not faculty or other employees. The researchers largely interpreted most of the incidents as microaggressions.
From the interviews, the researchers identified six central themes. Among them: foreign fellows and U.S.-born trainees being perceived or made to feel like outsiders; inappropriate comments being made toward female employees about their looks, credentials, or marital status; lack of action after reporting incidents or concerns that reporting such incidents would be futile; and strategies fellows used to cope after negative interactions.
One interviewee said, “I was fired by a patient because I have an accent.” Another said that when she is interviewing for jobs, she is always asked if she has children: “Maybe they’re asking in an innocuous manner, but I always feel like people worry. Is this person going to take maternity leave and be less available for work?”
For Dr. Warsame, “the idea that American citizens were frequently made to feel like they do not belong was surprising.”
Not surprising to Dr. Warsame, however, was the importance of fostering diversity and inclusion during fellowship years. Fellows often noted that greater diversity within the program helped create a more inclusive environment.
“[What’s] important to reinforce is the value of creating platforms for honest discussion and intentionally seeking fellows’ voices and perspectives, which in turn makes them feel like they belong,” Dr. Warsame said.
Still, the researchers found that fellows often did not report incidents of discrimination or bias. Only six trainees were aware of policies for reporting patient misconduct or discrimination, and only one ever reported an incident.
Where’s the support?
For Dr. Duncan, her encounter 3 years ago with the patient with sunglasses wasn’t her first experience of discrimination on the job — or her last.
Although hurtful in the moment, she had the wherewithal to report the incident to her attending physician, who was equally shocked. Initially unsure of how to handle it, the attending ultimately stepped up and provided “immense support,” Dr. Duncan said
The issue was brought to the attention of the program director, who took swift action. The patient was documented as “disruptive,” informed of that status in writing, and was banned from receiving treatment from trainees at the center, although Dr. Duncan noted he still received the medical care he needed.
Often, however, fellows who report incidents of discrimination and racism receive little support. According to Dr. Warsame and colleagues, most trainees don’t bother reporting these experiences because they believe that doing so would be futile.
“Concerns about reporting included jeopardizing future employability, risk of retaliation, and challenges reporting experiences that could be perceived as subjective and difficult to prove,” the authors write.
For instance, one interviewee said: “I’m afraid to report these things because there’s gonna be repercussions. There’s no way it’s gonna be anonymous.... I just have to toughen up and, you know, get used [to it].”
Dr. Warsame added, “A major challenge for trainees was that they often felt unheard, and at the time, there was no formal debrief regarding discrimination issues when they arose.”
These instances of bias have implications for trainee well-being. In a 2019 study, discrimination that physicians and students experienced during training had adverse effects on their emotional health. Responses from 50 trainees and physicians revealed a wide range of discriminatory experiences, including patients rejecting care and spewing racist, sexist, or homophobic epithets. Many physicians were uncertain about how to respond effectively and appropriately.
Since that study was published and after having completed her own fellowship, Dr. Duncan said she has seen some change for the better.
“There is a lot more awareness around this, and programs are trying to do better in recognizing and responding to incidents,” she said. She noted that it’s important to ensure that those who are directly affected by discriminatory behaviors aren’t left to do all of the “heavy lifting” of addressing and resolving the issues.
The weight of discriminatory incidents, from microaggressions to overt racism, is cumulative and can adversely affect a person’s career. “It’s exhausting -- we need support,” she said.
The Mayo Clinic is working to ensure that trainees receive support. “The study has prompted communication workshops and faculty development to better equip trainees with strategies to address [and report] patients who behave or display disrespectful or discriminatory behavior,” Dr. Warsame said.
She and her colleagues noted that the anonymous hotline used for the survey cultivated a safe environment for candid discussions and that such an approach is “feasible and effective to explore sensitive topics and scalable to various geographic locations and different medical specialties.”
“We recognize that our program must seek this feedback regularly and ensure we keep a finger on the pulse of our trainees,” Dr. Warsame added.
Dr. Warsame and Dr. Duncan have disclosed no relevant financial relationships. Dr. Duncan noted that her views and comments are her own and do not necessarily reflect those of her institution.
A version of this article first appeared on Medscape.com.
On day 1 of her fellowship, Francesca C. Duncan, MD, was blindsided by her first patient.
The patient, a White man who was accompanied by his wife, sat in the exam room with his sunglasses on.
“I remember him saying, ‘I need to take off my sunglasses so you don’t look so Black,’” said Dr. Duncan, a pulmonologist and intensivist at Indiana University, Indianapolis, who has a specialty in lung cancer disparities.
The patient proceeded to grill her about her experience and training. He asked where she attended college and mocked her degree from a historically Black university. His wife sat there, silent.
Dr. Duncan was shocked by the fact that she still had to defend her credentials.
“I just kind of felt like at that point in my training, my title would have earned me more respect,” said Dr. Duncan, now an assistant professor after recently completing a 3-year fellowship in pulmonary and critical care medicine. “I thought at some point [the racism and discrimination] would stop, but after all that training, all that late-night studying, I still had to prove myself.”
Unfortunately, Dr. Duncan’s experience in fellowship is not unique.
A recent survey of hematology and oncology fellows revealed that medical trainees routinely encounter discrimination during their training.
The 17 fellows who were anonymously interviewed in the survey all recalled experiencing or witnessing discriminatory behaviors during their fellowship, mostly from patients. These encounters rarely come to light. Only one respondent officially reported an incident.
The findings, published online November 8 in JAMA Network Open, underscore the need for graduate medical education programs to improve learning environments and support for trainees, lead author Rahma M. Warsame, MD, and colleagues say .
Discrimination at work
Initially, Dr. Warsame and co–principal investigator Katharine Price, MD, were tasked with developing strategies to mitigate instances of racism and bias that fellows encountered during training, but both felt it was critical to understand the experiences of their trainees first.
Out of 34 fellows and recent graduates of the hematology and oncology fellowship program of the Mayo Clinic, Rochester, Minn., 20 consented to participate in the study. Of those, 17 were interviewed between July and November 2018. Among the 17 interviewees, six were Asian, two were Black, three were Hispanic, two were multiracial, and four were White.
The majority of these offenses were committed by patients, not faculty or other employees. The researchers largely interpreted most of the incidents as microaggressions.
From the interviews, the researchers identified six central themes. Among them: foreign fellows and U.S.-born trainees being perceived or made to feel like outsiders; inappropriate comments being made toward female employees about their looks, credentials, or marital status; lack of action after reporting incidents or concerns that reporting such incidents would be futile; and strategies fellows used to cope after negative interactions.
One interviewee said, “I was fired by a patient because I have an accent.” Another said that when she is interviewing for jobs, she is always asked if she has children: “Maybe they’re asking in an innocuous manner, but I always feel like people worry. Is this person going to take maternity leave and be less available for work?”
For Dr. Warsame, “the idea that American citizens were frequently made to feel like they do not belong was surprising.”
Not surprising to Dr. Warsame, however, was the importance of fostering diversity and inclusion during fellowship years. Fellows often noted that greater diversity within the program helped create a more inclusive environment.
“[What’s] important to reinforce is the value of creating platforms for honest discussion and intentionally seeking fellows’ voices and perspectives, which in turn makes them feel like they belong,” Dr. Warsame said.
Still, the researchers found that fellows often did not report incidents of discrimination or bias. Only six trainees were aware of policies for reporting patient misconduct or discrimination, and only one ever reported an incident.
Where’s the support?
For Dr. Duncan, her encounter 3 years ago with the patient with sunglasses wasn’t her first experience of discrimination on the job — or her last.
Although hurtful in the moment, she had the wherewithal to report the incident to her attending physician, who was equally shocked. Initially unsure of how to handle it, the attending ultimately stepped up and provided “immense support,” Dr. Duncan said
The issue was brought to the attention of the program director, who took swift action. The patient was documented as “disruptive,” informed of that status in writing, and was banned from receiving treatment from trainees at the center, although Dr. Duncan noted he still received the medical care he needed.
Often, however, fellows who report incidents of discrimination and racism receive little support. According to Dr. Warsame and colleagues, most trainees don’t bother reporting these experiences because they believe that doing so would be futile.
“Concerns about reporting included jeopardizing future employability, risk of retaliation, and challenges reporting experiences that could be perceived as subjective and difficult to prove,” the authors write.
For instance, one interviewee said: “I’m afraid to report these things because there’s gonna be repercussions. There’s no way it’s gonna be anonymous.... I just have to toughen up and, you know, get used [to it].”
Dr. Warsame added, “A major challenge for trainees was that they often felt unheard, and at the time, there was no formal debrief regarding discrimination issues when they arose.”
These instances of bias have implications for trainee well-being. In a 2019 study, discrimination that physicians and students experienced during training had adverse effects on their emotional health. Responses from 50 trainees and physicians revealed a wide range of discriminatory experiences, including patients rejecting care and spewing racist, sexist, or homophobic epithets. Many physicians were uncertain about how to respond effectively and appropriately.
Since that study was published and after having completed her own fellowship, Dr. Duncan said she has seen some change for the better.
“There is a lot more awareness around this, and programs are trying to do better in recognizing and responding to incidents,” she said. She noted that it’s important to ensure that those who are directly affected by discriminatory behaviors aren’t left to do all of the “heavy lifting” of addressing and resolving the issues.
The weight of discriminatory incidents, from microaggressions to overt racism, is cumulative and can adversely affect a person’s career. “It’s exhausting -- we need support,” she said.
The Mayo Clinic is working to ensure that trainees receive support. “The study has prompted communication workshops and faculty development to better equip trainees with strategies to address [and report] patients who behave or display disrespectful or discriminatory behavior,” Dr. Warsame said.
She and her colleagues noted that the anonymous hotline used for the survey cultivated a safe environment for candid discussions and that such an approach is “feasible and effective to explore sensitive topics and scalable to various geographic locations and different medical specialties.”
“We recognize that our program must seek this feedback regularly and ensure we keep a finger on the pulse of our trainees,” Dr. Warsame added.
Dr. Warsame and Dr. Duncan have disclosed no relevant financial relationships. Dr. Duncan noted that her views and comments are her own and do not necessarily reflect those of her institution.
A version of this article first appeared on Medscape.com.
Substantial declines in mortality for most cancers
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis.
Researchers found that rates for all cancers combined declined by 27% overall between 1971 and 2019 and decreased significantly for 12 of the 15 top cancer sites analyzed.
The data revealed even greater mortality declines for certain cancers in particular years. For example, mortality from lung cancer was 44% lower in 2019, compared with its peak rate in 1993, whereas it was only 13% lower, compared with morality rates in 1971.
“The cancer mortality rate has reduced considerably since 1971 overall and for most cancer sites because of improvements in prevention, early detection, and treatment,” lead author Ahmedin Jemal, DVM, PhD, American Cancer Society, Kennesaw, Ga., and colleagues wrote.
Advances in surgery, radiotherapy, chemotherapy, precision medicine, and combinations therapies over the past 5 decades have contributed to these significant declines in mortality, Dr. Jemal and colleagues explained. The researchers also credit the “expanded investment” in the National Cancer Institute’s annual budget following the 1971 National Cancer Act, which increased the budget 25-fold from $227 million in 1971 to $6 billion in 2019.
The report, published online Nov. 11, 2021, in JAMA Oncology, analyzed mortality rates for all cancers as well as the top 15 sites using the National Center for Health Statistics.
The researchers found that, overall, deaths declined significantly for all cancers over the study period. Some of the biggest headway since 1971 occurred for stomach and cervical cancers – with 72% and 69% lower mortality rates, respectively – as well as colorectal cancer (56%), oral cavity and pharynx cancer (43%), and ovarian cancer (41%). Mortality rates of female breast cancer and prostate cancer also dropped considerably – both by 39%.
“The decline in mortality for female breast, cervical, colorectal, and prostate cancer in part reflects increased detection (and removal) of premalignant lesions and early-stage cancers,” Dr. Jemal and colleagues noted.
Data suggest that screening likely explains about half of the observed decline in mortality from colorectal cancer between 1975 and 2002. A 2018 study also found that the use of adjuvant chemotherapy was responsible for 63% of the decline in mortality from female breast cancer between 2000 and 2012.
In addition, the authors noted, “the decline in lung, oral cavity and bladder cancers largely reflects reductions in smoking because of enhanced public awareness of the health consequences, implementation of increased cigarette excise taxes, and comprehensive smoke-free laws.”
However, mortality did increase in a few categories. For instance, the mortality rate from pancreatic cancer increased by 3% between 1971 and 2019, and by 8% for both esophageal and brain cancers. Mortality rates from cancer were also greater for 29% of the U.S. counties included in the analysis, mostly those in the South.
The increase in mortality from pancreatic cancer likely reflects the growing rates of obesity in the United States, along with no real advances in pancreatic cancer prevention, early detection, or treatment, the authors suggested. In addition, lack of progress in regions of the south may be related to unequal access to improvements in treatment compared with other parts of the country.
“Improving equity through investment in the social determinants of health and implementation research is critical to furthering the national cancer-control agenda,” the authors concluded.
The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
Success in closing racial survival gap in lung and breast cancer
When barriers to completing radiation therapy were identified and addressed in a cohort of patients with early-stage lung and breast cancer, 5-year survival rates improved for all patients and closed the racial disparity gap, researchers reported at the annual meeting of the American Society for Radiation Oncology (ASTRO).
The findings come from the ACCURE clinical trial. This is the first prospective study designed to erase gaps in cancer treatment completion and survival among Black and White patient populations, explained lead author Matthew A. Manning, MD, a radiation oncologist and chief of oncology at Cone Health in Greensboro, N.C.
“Thousands of studies have looked at racial disparities in health care, but until recently, very few studies have implemented interventions to eliminate those disparities,” he said.
“This study shows that the implementation of ‘systems-change’ can eliminate racial disparities in cancer survival while improving survival for all,” he added.
“These results add to a growing body of evidence that health care disparities in cancer outcomes are eliminated or minimized by providing supportive, timely, and guideline-directed care,” said Lannis Hall, MD, MPH, director of radiation oncology, Siteman Cancer Center, and associate professor of radiation oncology at Washington University School of Medicine, St. Louis, who was approached for comment
“This research supports that access to care and timely treatment completion is critical to eliminating health care disparities,” she told this news organization. The system-based intervention in this trial was designed to reduce treatment delays and provide a supportive matrix for patients confronting real-world difficulties like transportation issues, childcare complications, and work absence, she explained.
Eliminating racial disparities
Previous findings from the ACCURE trial showed that it eliminated Black-White disparities in treatment completion rates, which was the study’s primary endpoint (Cancer Med. 2019;8:1095-1102). “It also improved treatment for all patients,” said Dr. Manning. “The current study is a follow-up on the survival of eligible patients treated during the ACCURE enrollment as compared to historical data.”
ACCURE was a multi-institutional trial designed to test a community-created intervention to reduce racial disparities. The intervention involved multiple changes to the way patients were supported while receiving cancer treatment and had four components:
- an electronic health record with automatic alerts to flag missed appointments or unmet milestones in expected care
- a nurse navigator trained in race-specific barriers to help patients overcome obstacles to care when alerts are flagged
- a physician champion to engage health care teams with race-related feedback on treatment completion
- regular health equity education training sessions for staff
The cohort was comprised of 1,413 patients with lung and breast cancer (stage 0-II) who were diagnosed from 2013-2015, and survival was compared to historical cases – 2,016 patients who had been treated from 2007-2011.
The results showed a significant improvement in survival for both Black and White patients with breast and lung cancer over time, and the racial gap in survival was reduced.
The 5-year survival rate for breast cancer increased from 91% for White patients and 89% in Black patients in historical cases, to 94% for both during the study period.
For patients with lung cancer, the 5-year survival rate improved from 43% in White patients and 37% in Black patients to 56% and 54%, respectively.
A subgroup analysis showed that patients with lung cancer who underwent surgery had 5-year survival rates of 78.5% for White and 70.1% for Black patients, whereas for those who underwent stereotactic body radiation therapy (SBRT) the rates were 41.9% and 50% respectively.
“We’ve shown it’s possible to eliminate disparities in cancer treatment completion and that this change has the potential to close cancer survival gaps downstream,” said Dr. Manning. “But we think the application can be much broader.”
The ACCURE study was sponsored by the National Institutes of Health. Dr. Manning and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When barriers to completing radiation therapy were identified and addressed in a cohort of patients with early-stage lung and breast cancer, 5-year survival rates improved for all patients and closed the racial disparity gap, researchers reported at the annual meeting of the American Society for Radiation Oncology (ASTRO).
The findings come from the ACCURE clinical trial. This is the first prospective study designed to erase gaps in cancer treatment completion and survival among Black and White patient populations, explained lead author Matthew A. Manning, MD, a radiation oncologist and chief of oncology at Cone Health in Greensboro, N.C.
“Thousands of studies have looked at racial disparities in health care, but until recently, very few studies have implemented interventions to eliminate those disparities,” he said.
“This study shows that the implementation of ‘systems-change’ can eliminate racial disparities in cancer survival while improving survival for all,” he added.
“These results add to a growing body of evidence that health care disparities in cancer outcomes are eliminated or minimized by providing supportive, timely, and guideline-directed care,” said Lannis Hall, MD, MPH, director of radiation oncology, Siteman Cancer Center, and associate professor of radiation oncology at Washington University School of Medicine, St. Louis, who was approached for comment
“This research supports that access to care and timely treatment completion is critical to eliminating health care disparities,” she told this news organization. The system-based intervention in this trial was designed to reduce treatment delays and provide a supportive matrix for patients confronting real-world difficulties like transportation issues, childcare complications, and work absence, she explained.
Eliminating racial disparities
Previous findings from the ACCURE trial showed that it eliminated Black-White disparities in treatment completion rates, which was the study’s primary endpoint (Cancer Med. 2019;8:1095-1102). “It also improved treatment for all patients,” said Dr. Manning. “The current study is a follow-up on the survival of eligible patients treated during the ACCURE enrollment as compared to historical data.”
ACCURE was a multi-institutional trial designed to test a community-created intervention to reduce racial disparities. The intervention involved multiple changes to the way patients were supported while receiving cancer treatment and had four components:
- an electronic health record with automatic alerts to flag missed appointments or unmet milestones in expected care
- a nurse navigator trained in race-specific barriers to help patients overcome obstacles to care when alerts are flagged
- a physician champion to engage health care teams with race-related feedback on treatment completion
- regular health equity education training sessions for staff
The cohort was comprised of 1,413 patients with lung and breast cancer (stage 0-II) who were diagnosed from 2013-2015, and survival was compared to historical cases – 2,016 patients who had been treated from 2007-2011.
The results showed a significant improvement in survival for both Black and White patients with breast and lung cancer over time, and the racial gap in survival was reduced.
The 5-year survival rate for breast cancer increased from 91% for White patients and 89% in Black patients in historical cases, to 94% for both during the study period.
For patients with lung cancer, the 5-year survival rate improved from 43% in White patients and 37% in Black patients to 56% and 54%, respectively.
A subgroup analysis showed that patients with lung cancer who underwent surgery had 5-year survival rates of 78.5% for White and 70.1% for Black patients, whereas for those who underwent stereotactic body radiation therapy (SBRT) the rates were 41.9% and 50% respectively.
“We’ve shown it’s possible to eliminate disparities in cancer treatment completion and that this change has the potential to close cancer survival gaps downstream,” said Dr. Manning. “But we think the application can be much broader.”
The ACCURE study was sponsored by the National Institutes of Health. Dr. Manning and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When barriers to completing radiation therapy were identified and addressed in a cohort of patients with early-stage lung and breast cancer, 5-year survival rates improved for all patients and closed the racial disparity gap, researchers reported at the annual meeting of the American Society for Radiation Oncology (ASTRO).
The findings come from the ACCURE clinical trial. This is the first prospective study designed to erase gaps in cancer treatment completion and survival among Black and White patient populations, explained lead author Matthew A. Manning, MD, a radiation oncologist and chief of oncology at Cone Health in Greensboro, N.C.
“Thousands of studies have looked at racial disparities in health care, but until recently, very few studies have implemented interventions to eliminate those disparities,” he said.
“This study shows that the implementation of ‘systems-change’ can eliminate racial disparities in cancer survival while improving survival for all,” he added.
“These results add to a growing body of evidence that health care disparities in cancer outcomes are eliminated or minimized by providing supportive, timely, and guideline-directed care,” said Lannis Hall, MD, MPH, director of radiation oncology, Siteman Cancer Center, and associate professor of radiation oncology at Washington University School of Medicine, St. Louis, who was approached for comment
“This research supports that access to care and timely treatment completion is critical to eliminating health care disparities,” she told this news organization. The system-based intervention in this trial was designed to reduce treatment delays and provide a supportive matrix for patients confronting real-world difficulties like transportation issues, childcare complications, and work absence, she explained.
Eliminating racial disparities
Previous findings from the ACCURE trial showed that it eliminated Black-White disparities in treatment completion rates, which was the study’s primary endpoint (Cancer Med. 2019;8:1095-1102). “It also improved treatment for all patients,” said Dr. Manning. “The current study is a follow-up on the survival of eligible patients treated during the ACCURE enrollment as compared to historical data.”
ACCURE was a multi-institutional trial designed to test a community-created intervention to reduce racial disparities. The intervention involved multiple changes to the way patients were supported while receiving cancer treatment and had four components:
- an electronic health record with automatic alerts to flag missed appointments or unmet milestones in expected care
- a nurse navigator trained in race-specific barriers to help patients overcome obstacles to care when alerts are flagged
- a physician champion to engage health care teams with race-related feedback on treatment completion
- regular health equity education training sessions for staff
The cohort was comprised of 1,413 patients with lung and breast cancer (stage 0-II) who were diagnosed from 2013-2015, and survival was compared to historical cases – 2,016 patients who had been treated from 2007-2011.
The results showed a significant improvement in survival for both Black and White patients with breast and lung cancer over time, and the racial gap in survival was reduced.
The 5-year survival rate for breast cancer increased from 91% for White patients and 89% in Black patients in historical cases, to 94% for both during the study period.
For patients with lung cancer, the 5-year survival rate improved from 43% in White patients and 37% in Black patients to 56% and 54%, respectively.
A subgroup analysis showed that patients with lung cancer who underwent surgery had 5-year survival rates of 78.5% for White and 70.1% for Black patients, whereas for those who underwent stereotactic body radiation therapy (SBRT) the rates were 41.9% and 50% respectively.
“We’ve shown it’s possible to eliminate disparities in cancer treatment completion and that this change has the potential to close cancer survival gaps downstream,” said Dr. Manning. “But we think the application can be much broader.”
The ACCURE study was sponsored by the National Institutes of Health. Dr. Manning and Dr. Hall have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ASTRO 2021
SBRT on oligoprogressive lesions: Benefit in lung cancer
Patients treated with SBRT had a median PFS of 44 weeks, compared with 9 weeks for those who received standard care.
However, no benefit was observed in patients with metastatic breast cancer. There was no significant difference in PFS between the two groups (18 weeks with SBRT vs. 19 weeks with standard care).
“In this preplanned interim analysis, we demonstrated the benefit of SBRT to sites of oligoprogression on overall progression-free survival, which was the primary endpoint,” said lead author C. Jillian Tsai, MD, PhD, a radiation oncologist and director of metastatic disease radiation oncology research at Memorial Sloan Kettering Cancer Center in New York. “The difference was driven by the substantial response in [this] NSCLC cohort.”
There was no benefit of SBRT seen in the breast cohort, she noted, and most breast patients developed new lesions upon further progression.
Dr. Tsai and colleagues are planning to close the trial early, after the interim analysis established the benefit of SBRT. They are now investigating why SBRT was beneficial in NSCLC but not in breast cancer.
The findings were presented at the American Society for Radiation Oncology (ASTRO) annual meeting.
Dr. Tsai explained that the current standard of care for patients with oligoprogressive metastatic NSCLC is to switch to a different targeted therapy or chemotherapy following progression, but options may be limited. Efficacy for second-line therapy can be poor, with PFS ranging from about 4 months to 10 months for NSCLC, “and after second line, efficacy for third and fourth lines is even poorer,” she said.
Similarly, for breast cancer, PFS ranges from about 9 months to 20 months for estrogen-receptor positive patients. “But for triple negative patients, there really is no standard of care and PFS is poor,” Dr. Tsai said.
SBRT superior to standard of care
The authors hypothesized that there is an oligoprogressive state in metastatic cancer, in which disease control can be improved by applying local therapy to progressive lesions only.
The cohort included 102 patients with metastatic NSCLC or breast cancer who had received one or more lines of systemic therapy and had oligoprogressive lesions amenable to SBRT. There was no upper limit of nonprogressive lesions.
Oligoprogression was defined as Response Evaluation or Positron Emission Tomography Response Criteria in Solid Tumors documented progression ≤5 individual lesions.
Patients were randomly assigned to receive either SBRT to all progressive sites plus palliative standard of care or systemic SOC only. Systemic therapy was per physician’s discretion.
There were 58 patients with NSCLC (30 in the SBRT group) and 44 patients with breast cancer (22 in each group).
Most patients (75%) had more than one site of oligoprogression and 47% had more than 5 total metastatic lesions. About half of patients (54%) had received immunotherapy and the majority of those with NSCLC (86%) did not harbor an actionable driver mutation. About one-third (32%) of the breast cancer cohort were triple negative.
Patients were followed for a median of 45 weeks (58 weeks for living patients), by which time 78 (74%) had experienced further tumor progression and 39 (37%) had died.
Median progression-free survival for the entire cohort was 31 weeks for SBRT and 11 weeks for palliative SOC (P = .002).
In multivariable analysis that stratified for factors including age, sex, lines of systemic therapy, and change of systemic therapy, the progression-free survival benefit of SBRT continued to remain substantial in the NSCLC cohort (hazard ratio: 0.38; P = .007).
Adverse events were higher in the SBRT group. Grade 2 or higher adverse events occurred in 23 (61%) of SBRT patients, and 15 (40%) of SOC patients (P = .13).
Hoped-for results, with a few caveats
Approached for comment on the new findings, Clifford Robinson, MD, professor of radiation oncology, chief of SBRT service, and director of clinical trials and informatics at Washington University, St. Louis, said the results tie in with previous findings.
There are multiple published or presented prospective randomized phase 2 and 3 trials in various disease sites that have explored the role of local therapy, including SBRT, for patients who present with oligometastatic disease.
“These studies have nearly uniformly shown improvements in progression-free and/or overall survival with the inclusion of local therapy,” he told this news organization. Dr. Robinson was not involved with the study.
He explained that relatively few patients present with oligometastatic disease. However, many patients present with more advanced disease, but after an initial course of systemic therapy, develop oligoprogression.
“There is tremendous appeal to using local therapy at the time of oligoprogression in lieu of switching systemic therapy,” said Dr. Robinson. “It allows patients to stay on systemic therapy that is otherwise effective for the remainder of their disease.”
First-line systemic therapies are the most effective and the most tolerable, he continued, and switching systemic therapy introduces the potential for more toxicity and less efficacy. Therefore, it has become increasingly popular to offer SBRT to one or a few sites of oligoprogressive disease based on the results of oligometastatic disease.
“However, there is no established prospective data to guide this practice,” he said. “This trial is the first to examine this carefully in lung and breast cancer patients, and this trial shows what we hoped to see – that use of SBRT after oligoprogression results in improved progression-free survival as compared with standard of care alone. And this was accomplished with limited toxicity.”
There are a few caveats, though, he pointed out. “Progression-free survival is defined as time to first progression or death,” he said. “Since we don’t know what the overall survival is in this abstract, it’s entirely possible that patients live for the same length of time, but just take longer to progress.”
Another caveat is that this was a planned interim analysis. “Typically, planned interim analyses occur to see if the trial should be stopped or to adjust the study based on results,” he said. “It’s unclear what the investigators will do with this information.”
“But overall, these are very exciting data and lend support to the increasingly common practice of treating oligoprogressive disease,” Dr. Robinson added. “Since most of the serious adverse events of SBRT occur later, longer follow-up is needed, although the median survival of patients may not reach that timepoint.”
“For now, practice should not be altered based on these interim results,” he added.
Dr. Tsai reported acting as a consultant/advisor for Varian and Galera and also receiving research funding from Varian. Dr. Robinson reports stock/ownership in Radialogica, acting as a consultant/advisor for Varian, AstraZeneca, EMD Serono, Quantitative Radiology Solutions, research funding from Varian and Merck, and owning patents on systems for cardiac arrhythmias and ablation.
A version of this article first appeared on Medscape.com.
Patients treated with SBRT had a median PFS of 44 weeks, compared with 9 weeks for those who received standard care.
However, no benefit was observed in patients with metastatic breast cancer. There was no significant difference in PFS between the two groups (18 weeks with SBRT vs. 19 weeks with standard care).
“In this preplanned interim analysis, we demonstrated the benefit of SBRT to sites of oligoprogression on overall progression-free survival, which was the primary endpoint,” said lead author C. Jillian Tsai, MD, PhD, a radiation oncologist and director of metastatic disease radiation oncology research at Memorial Sloan Kettering Cancer Center in New York. “The difference was driven by the substantial response in [this] NSCLC cohort.”
There was no benefit of SBRT seen in the breast cohort, she noted, and most breast patients developed new lesions upon further progression.
Dr. Tsai and colleagues are planning to close the trial early, after the interim analysis established the benefit of SBRT. They are now investigating why SBRT was beneficial in NSCLC but not in breast cancer.
The findings were presented at the American Society for Radiation Oncology (ASTRO) annual meeting.
Dr. Tsai explained that the current standard of care for patients with oligoprogressive metastatic NSCLC is to switch to a different targeted therapy or chemotherapy following progression, but options may be limited. Efficacy for second-line therapy can be poor, with PFS ranging from about 4 months to 10 months for NSCLC, “and after second line, efficacy for third and fourth lines is even poorer,” she said.
Similarly, for breast cancer, PFS ranges from about 9 months to 20 months for estrogen-receptor positive patients. “But for triple negative patients, there really is no standard of care and PFS is poor,” Dr. Tsai said.
SBRT superior to standard of care
The authors hypothesized that there is an oligoprogressive state in metastatic cancer, in which disease control can be improved by applying local therapy to progressive lesions only.
The cohort included 102 patients with metastatic NSCLC or breast cancer who had received one or more lines of systemic therapy and had oligoprogressive lesions amenable to SBRT. There was no upper limit of nonprogressive lesions.
Oligoprogression was defined as Response Evaluation or Positron Emission Tomography Response Criteria in Solid Tumors documented progression ≤5 individual lesions.
Patients were randomly assigned to receive either SBRT to all progressive sites plus palliative standard of care or systemic SOC only. Systemic therapy was per physician’s discretion.
There were 58 patients with NSCLC (30 in the SBRT group) and 44 patients with breast cancer (22 in each group).
Most patients (75%) had more than one site of oligoprogression and 47% had more than 5 total metastatic lesions. About half of patients (54%) had received immunotherapy and the majority of those with NSCLC (86%) did not harbor an actionable driver mutation. About one-third (32%) of the breast cancer cohort were triple negative.
Patients were followed for a median of 45 weeks (58 weeks for living patients), by which time 78 (74%) had experienced further tumor progression and 39 (37%) had died.
Median progression-free survival for the entire cohort was 31 weeks for SBRT and 11 weeks for palliative SOC (P = .002).
In multivariable analysis that stratified for factors including age, sex, lines of systemic therapy, and change of systemic therapy, the progression-free survival benefit of SBRT continued to remain substantial in the NSCLC cohort (hazard ratio: 0.38; P = .007).
Adverse events were higher in the SBRT group. Grade 2 or higher adverse events occurred in 23 (61%) of SBRT patients, and 15 (40%) of SOC patients (P = .13).
Hoped-for results, with a few caveats
Approached for comment on the new findings, Clifford Robinson, MD, professor of radiation oncology, chief of SBRT service, and director of clinical trials and informatics at Washington University, St. Louis, said the results tie in with previous findings.
There are multiple published or presented prospective randomized phase 2 and 3 trials in various disease sites that have explored the role of local therapy, including SBRT, for patients who present with oligometastatic disease.
“These studies have nearly uniformly shown improvements in progression-free and/or overall survival with the inclusion of local therapy,” he told this news organization. Dr. Robinson was not involved with the study.
He explained that relatively few patients present with oligometastatic disease. However, many patients present with more advanced disease, but after an initial course of systemic therapy, develop oligoprogression.
“There is tremendous appeal to using local therapy at the time of oligoprogression in lieu of switching systemic therapy,” said Dr. Robinson. “It allows patients to stay on systemic therapy that is otherwise effective for the remainder of their disease.”
First-line systemic therapies are the most effective and the most tolerable, he continued, and switching systemic therapy introduces the potential for more toxicity and less efficacy. Therefore, it has become increasingly popular to offer SBRT to one or a few sites of oligoprogressive disease based on the results of oligometastatic disease.
“However, there is no established prospective data to guide this practice,” he said. “This trial is the first to examine this carefully in lung and breast cancer patients, and this trial shows what we hoped to see – that use of SBRT after oligoprogression results in improved progression-free survival as compared with standard of care alone. And this was accomplished with limited toxicity.”
There are a few caveats, though, he pointed out. “Progression-free survival is defined as time to first progression or death,” he said. “Since we don’t know what the overall survival is in this abstract, it’s entirely possible that patients live for the same length of time, but just take longer to progress.”
Another caveat is that this was a planned interim analysis. “Typically, planned interim analyses occur to see if the trial should be stopped or to adjust the study based on results,” he said. “It’s unclear what the investigators will do with this information.”
“But overall, these are very exciting data and lend support to the increasingly common practice of treating oligoprogressive disease,” Dr. Robinson added. “Since most of the serious adverse events of SBRT occur later, longer follow-up is needed, although the median survival of patients may not reach that timepoint.”
“For now, practice should not be altered based on these interim results,” he added.
Dr. Tsai reported acting as a consultant/advisor for Varian and Galera and also receiving research funding from Varian. Dr. Robinson reports stock/ownership in Radialogica, acting as a consultant/advisor for Varian, AstraZeneca, EMD Serono, Quantitative Radiology Solutions, research funding from Varian and Merck, and owning patents on systems for cardiac arrhythmias and ablation.
A version of this article first appeared on Medscape.com.
Patients treated with SBRT had a median PFS of 44 weeks, compared with 9 weeks for those who received standard care.
However, no benefit was observed in patients with metastatic breast cancer. There was no significant difference in PFS between the two groups (18 weeks with SBRT vs. 19 weeks with standard care).
“In this preplanned interim analysis, we demonstrated the benefit of SBRT to sites of oligoprogression on overall progression-free survival, which was the primary endpoint,” said lead author C. Jillian Tsai, MD, PhD, a radiation oncologist and director of metastatic disease radiation oncology research at Memorial Sloan Kettering Cancer Center in New York. “The difference was driven by the substantial response in [this] NSCLC cohort.”
There was no benefit of SBRT seen in the breast cohort, she noted, and most breast patients developed new lesions upon further progression.
Dr. Tsai and colleagues are planning to close the trial early, after the interim analysis established the benefit of SBRT. They are now investigating why SBRT was beneficial in NSCLC but not in breast cancer.
The findings were presented at the American Society for Radiation Oncology (ASTRO) annual meeting.
Dr. Tsai explained that the current standard of care for patients with oligoprogressive metastatic NSCLC is to switch to a different targeted therapy or chemotherapy following progression, but options may be limited. Efficacy for second-line therapy can be poor, with PFS ranging from about 4 months to 10 months for NSCLC, “and after second line, efficacy for third and fourth lines is even poorer,” she said.
Similarly, for breast cancer, PFS ranges from about 9 months to 20 months for estrogen-receptor positive patients. “But for triple negative patients, there really is no standard of care and PFS is poor,” Dr. Tsai said.
SBRT superior to standard of care
The authors hypothesized that there is an oligoprogressive state in metastatic cancer, in which disease control can be improved by applying local therapy to progressive lesions only.
The cohort included 102 patients with metastatic NSCLC or breast cancer who had received one or more lines of systemic therapy and had oligoprogressive lesions amenable to SBRT. There was no upper limit of nonprogressive lesions.
Oligoprogression was defined as Response Evaluation or Positron Emission Tomography Response Criteria in Solid Tumors documented progression ≤5 individual lesions.
Patients were randomly assigned to receive either SBRT to all progressive sites plus palliative standard of care or systemic SOC only. Systemic therapy was per physician’s discretion.
There were 58 patients with NSCLC (30 in the SBRT group) and 44 patients with breast cancer (22 in each group).
Most patients (75%) had more than one site of oligoprogression and 47% had more than 5 total metastatic lesions. About half of patients (54%) had received immunotherapy and the majority of those with NSCLC (86%) did not harbor an actionable driver mutation. About one-third (32%) of the breast cancer cohort were triple negative.
Patients were followed for a median of 45 weeks (58 weeks for living patients), by which time 78 (74%) had experienced further tumor progression and 39 (37%) had died.
Median progression-free survival for the entire cohort was 31 weeks for SBRT and 11 weeks for palliative SOC (P = .002).
In multivariable analysis that stratified for factors including age, sex, lines of systemic therapy, and change of systemic therapy, the progression-free survival benefit of SBRT continued to remain substantial in the NSCLC cohort (hazard ratio: 0.38; P = .007).
Adverse events were higher in the SBRT group. Grade 2 or higher adverse events occurred in 23 (61%) of SBRT patients, and 15 (40%) of SOC patients (P = .13).
Hoped-for results, with a few caveats
Approached for comment on the new findings, Clifford Robinson, MD, professor of radiation oncology, chief of SBRT service, and director of clinical trials and informatics at Washington University, St. Louis, said the results tie in with previous findings.
There are multiple published or presented prospective randomized phase 2 and 3 trials in various disease sites that have explored the role of local therapy, including SBRT, for patients who present with oligometastatic disease.
“These studies have nearly uniformly shown improvements in progression-free and/or overall survival with the inclusion of local therapy,” he told this news organization. Dr. Robinson was not involved with the study.
He explained that relatively few patients present with oligometastatic disease. However, many patients present with more advanced disease, but after an initial course of systemic therapy, develop oligoprogression.
“There is tremendous appeal to using local therapy at the time of oligoprogression in lieu of switching systemic therapy,” said Dr. Robinson. “It allows patients to stay on systemic therapy that is otherwise effective for the remainder of their disease.”
First-line systemic therapies are the most effective and the most tolerable, he continued, and switching systemic therapy introduces the potential for more toxicity and less efficacy. Therefore, it has become increasingly popular to offer SBRT to one or a few sites of oligoprogressive disease based on the results of oligometastatic disease.
“However, there is no established prospective data to guide this practice,” he said. “This trial is the first to examine this carefully in lung and breast cancer patients, and this trial shows what we hoped to see – that use of SBRT after oligoprogression results in improved progression-free survival as compared with standard of care alone. And this was accomplished with limited toxicity.”
There are a few caveats, though, he pointed out. “Progression-free survival is defined as time to first progression or death,” he said. “Since we don’t know what the overall survival is in this abstract, it’s entirely possible that patients live for the same length of time, but just take longer to progress.”
Another caveat is that this was a planned interim analysis. “Typically, planned interim analyses occur to see if the trial should be stopped or to adjust the study based on results,” he said. “It’s unclear what the investigators will do with this information.”
“But overall, these are very exciting data and lend support to the increasingly common practice of treating oligoprogressive disease,” Dr. Robinson added. “Since most of the serious adverse events of SBRT occur later, longer follow-up is needed, although the median survival of patients may not reach that timepoint.”
“For now, practice should not be altered based on these interim results,” he added.
Dr. Tsai reported acting as a consultant/advisor for Varian and Galera and also receiving research funding from Varian. Dr. Robinson reports stock/ownership in Radialogica, acting as a consultant/advisor for Varian, AstraZeneca, EMD Serono, Quantitative Radiology Solutions, research funding from Varian and Merck, and owning patents on systems for cardiac arrhythmias and ablation.
A version of this article first appeared on Medscape.com.