User login
Sandoz halts pursuit of U.S. approval for rituximab biosimilar
.
Sandoz, a division of Novartis, was seeking Food and Drug Administration approval of GP2013 for all the same indications as the reference product – B-cell non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, microscopic polyangiitis, and pemphigus vulgaris.
GP2013 already is approved in the European Union and elsewhere.
The FDA had accepted the biologics license application (BLA) for GP2013 in September 2017. In May 2018, the agency issued a complete response letter saying it could not approve GP2013. The agency also requested additional information to complement the BLA submission.
At the time of the complete response letter, Sandoz said it was still committed to bringing GP2013 to the U.S. market.
“We appreciate the important conversations with the FDA, which have provided specific requirements for our potential U.S. biosimilar rituximab but believe the patient and marketplace needs in the U.S. will be satisfied before we can generate the data required,” Stefan Hendriks, global head of biopharmaceuticals at Sandoz, said in a statement.
“We are disappointed to have to make this decision and stand behind the safety, efficacy, and quality of our medicine, which met the stringent criteria for approval in the European Union, Switzerland, Japan, New Zealand, and Australia.”
The BLA for GP2013 was supported, in part, by results from the ASSIST-FL trial, in which researchers compared GP2013 with the reference product (Lancet Haematol. 2017 Aug;4[8]:e350-61).
The phase 3 trial included adults with previously untreated, advanced-stage follicular lymphoma. Patients received eight cycles of cyclophosphamide, vincristine, and prednisone with either GP2013 or reference rituximab. Responders then received GP2013 or rituximab monotherapy as maintenance for up to 2 years.
At a median follow-up of 11.6 months, the overall response rate was 87% in the GP2013 arm and 88% in the rituximab arm.
.
Sandoz, a division of Novartis, was seeking Food and Drug Administration approval of GP2013 for all the same indications as the reference product – B-cell non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, microscopic polyangiitis, and pemphigus vulgaris.
GP2013 already is approved in the European Union and elsewhere.
The FDA had accepted the biologics license application (BLA) for GP2013 in September 2017. In May 2018, the agency issued a complete response letter saying it could not approve GP2013. The agency also requested additional information to complement the BLA submission.
At the time of the complete response letter, Sandoz said it was still committed to bringing GP2013 to the U.S. market.
“We appreciate the important conversations with the FDA, which have provided specific requirements for our potential U.S. biosimilar rituximab but believe the patient and marketplace needs in the U.S. will be satisfied before we can generate the data required,” Stefan Hendriks, global head of biopharmaceuticals at Sandoz, said in a statement.
“We are disappointed to have to make this decision and stand behind the safety, efficacy, and quality of our medicine, which met the stringent criteria for approval in the European Union, Switzerland, Japan, New Zealand, and Australia.”
The BLA for GP2013 was supported, in part, by results from the ASSIST-FL trial, in which researchers compared GP2013 with the reference product (Lancet Haematol. 2017 Aug;4[8]:e350-61).
The phase 3 trial included adults with previously untreated, advanced-stage follicular lymphoma. Patients received eight cycles of cyclophosphamide, vincristine, and prednisone with either GP2013 or reference rituximab. Responders then received GP2013 or rituximab monotherapy as maintenance for up to 2 years.
At a median follow-up of 11.6 months, the overall response rate was 87% in the GP2013 arm and 88% in the rituximab arm.
.
Sandoz, a division of Novartis, was seeking Food and Drug Administration approval of GP2013 for all the same indications as the reference product – B-cell non-Hodgkin lymphoma, chronic lymphocytic leukemia, rheumatoid arthritis, granulomatosis with polyangiitis, microscopic polyangiitis, and pemphigus vulgaris.
GP2013 already is approved in the European Union and elsewhere.
The FDA had accepted the biologics license application (BLA) for GP2013 in September 2017. In May 2018, the agency issued a complete response letter saying it could not approve GP2013. The agency also requested additional information to complement the BLA submission.
At the time of the complete response letter, Sandoz said it was still committed to bringing GP2013 to the U.S. market.
“We appreciate the important conversations with the FDA, which have provided specific requirements for our potential U.S. biosimilar rituximab but believe the patient and marketplace needs in the U.S. will be satisfied before we can generate the data required,” Stefan Hendriks, global head of biopharmaceuticals at Sandoz, said in a statement.
“We are disappointed to have to make this decision and stand behind the safety, efficacy, and quality of our medicine, which met the stringent criteria for approval in the European Union, Switzerland, Japan, New Zealand, and Australia.”
The BLA for GP2013 was supported, in part, by results from the ASSIST-FL trial, in which researchers compared GP2013 with the reference product (Lancet Haematol. 2017 Aug;4[8]:e350-61).
The phase 3 trial included adults with previously untreated, advanced-stage follicular lymphoma. Patients received eight cycles of cyclophosphamide, vincristine, and prednisone with either GP2013 or reference rituximab. Responders then received GP2013 or rituximab monotherapy as maintenance for up to 2 years.
At a median follow-up of 11.6 months, the overall response rate was 87% in the GP2013 arm and 88% in the rituximab arm.
FDA and EC approve pegfilgrastim biosimilar
The U.S. Food and Drug Administration (FDA) and European Commission (EC) have approved Coherus BioSciences, Inc.’s pegfilgrastim-cbqv (Udenyca™), a biosimilar of Amgen’s pegfilgrastim product (Neulasta).
Both agencies approved pegfilgrastim-cbqv (formerly CHS-1701) for cancer patients receiving myelosuppressive chemotherapy.
Pegfilgrastim-cbqv is FDA-approved “to decrease the incidence of infection, as manifested by febrile neutropenia, in patients with non-myeloid malignancies receiving myelosuppressive anticancer drugs associated with a clinically significant incidence of febrile neutropenia.”
The product is EC-approved to reduce “the duration of neutropenia and the incidence of febrile neutropenia in adult patients treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).”
The U.S. prescribing information for pegfilgrastim-cbqv is available at www.UDENYCA.com, and the European summary of product characteristics is available on the European Medicines Agency’s website.
The FDA and EC approvals of pegfilgrastim-cbqv were supported by analyses establishing biosimilarity as well as pharmacokinetic, pharmacodynamic, and immunogenicity studies of healthy subjects (NCT02650973, NCT02385851, and NCT02418104).
Results from one of these studies (NCT02650973) were presented at the 2017 ASCO Annual Meeting.
“Udenyca’s robust clinical package includes a dedicated immunogenicity similarity study in over 300 healthy subjects,” said Barbara Finck, MD, chief medical officer of Coherus BioSciences.
“In support of that study, and as part of our commitment to ensuring patient safety, we deployed a battery of sensitive immunogenicity assays. This effort not only supported the biosimilarity of Udenyca but also advanced the understanding of the immunogenic response of pegfilgrastim products.”
The U.S. Food and Drug Administration (FDA) and European Commission (EC) have approved Coherus BioSciences, Inc.’s pegfilgrastim-cbqv (Udenyca™), a biosimilar of Amgen’s pegfilgrastim product (Neulasta).
Both agencies approved pegfilgrastim-cbqv (formerly CHS-1701) for cancer patients receiving myelosuppressive chemotherapy.
Pegfilgrastim-cbqv is FDA-approved “to decrease the incidence of infection, as manifested by febrile neutropenia, in patients with non-myeloid malignancies receiving myelosuppressive anticancer drugs associated with a clinically significant incidence of febrile neutropenia.”
The product is EC-approved to reduce “the duration of neutropenia and the incidence of febrile neutropenia in adult patients treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).”
The U.S. prescribing information for pegfilgrastim-cbqv is available at www.UDENYCA.com, and the European summary of product characteristics is available on the European Medicines Agency’s website.
The FDA and EC approvals of pegfilgrastim-cbqv were supported by analyses establishing biosimilarity as well as pharmacokinetic, pharmacodynamic, and immunogenicity studies of healthy subjects (NCT02650973, NCT02385851, and NCT02418104).
Results from one of these studies (NCT02650973) were presented at the 2017 ASCO Annual Meeting.
“Udenyca’s robust clinical package includes a dedicated immunogenicity similarity study in over 300 healthy subjects,” said Barbara Finck, MD, chief medical officer of Coherus BioSciences.
“In support of that study, and as part of our commitment to ensuring patient safety, we deployed a battery of sensitive immunogenicity assays. This effort not only supported the biosimilarity of Udenyca but also advanced the understanding of the immunogenic response of pegfilgrastim products.”
The U.S. Food and Drug Administration (FDA) and European Commission (EC) have approved Coherus BioSciences, Inc.’s pegfilgrastim-cbqv (Udenyca™), a biosimilar of Amgen’s pegfilgrastim product (Neulasta).
Both agencies approved pegfilgrastim-cbqv (formerly CHS-1701) for cancer patients receiving myelosuppressive chemotherapy.
Pegfilgrastim-cbqv is FDA-approved “to decrease the incidence of infection, as manifested by febrile neutropenia, in patients with non-myeloid malignancies receiving myelosuppressive anticancer drugs associated with a clinically significant incidence of febrile neutropenia.”
The product is EC-approved to reduce “the duration of neutropenia and the incidence of febrile neutropenia in adult patients treated with cytotoxic chemotherapy for malignancy (with the exception of chronic myeloid leukemia and myelodysplastic syndromes).”
The U.S. prescribing information for pegfilgrastim-cbqv is available at www.UDENYCA.com, and the European summary of product characteristics is available on the European Medicines Agency’s website.
The FDA and EC approvals of pegfilgrastim-cbqv were supported by analyses establishing biosimilarity as well as pharmacokinetic, pharmacodynamic, and immunogenicity studies of healthy subjects (NCT02650973, NCT02385851, and NCT02418104).
Results from one of these studies (NCT02650973) were presented at the 2017 ASCO Annual Meeting.
“Udenyca’s robust clinical package includes a dedicated immunogenicity similarity study in over 300 healthy subjects,” said Barbara Finck, MD, chief medical officer of Coherus BioSciences.
“In support of that study, and as part of our commitment to ensuring patient safety, we deployed a battery of sensitive immunogenicity assays. This effort not only supported the biosimilarity of Udenyca but also advanced the understanding of the immunogenic response of pegfilgrastim products.”
Haploidentical transplantation holds promise in relapsed myeloma
, investigators have reported.
The rate of non-relapse mortality at one year was 21% in the retrospective analysis of 96 patients, recently reported in the journal Biology of Blood and Marrow Transplantation.
Haploidentical allogeneic hematopoietic stem cell transplant (allo-HCT) is currently limited in use due to a high rate of relapse, but may hold potential promise for future applications, according to Firoozeh Sahebi, MD, a hematologist with the City of Hope Medical Center, Duarte, Calif., and colleagues. “Our results demonstrate that haploidentical allo-HCT can be safely performed in appropriate patients with MM who lack on HLA-matched sibling or unrelated donor.”
“The allo-HCT platform can be used in the context of other post-transplantation immune-based strategies, such as donor-derived chimeric antigen receptor T cells and natural killer cell infusions, newer immunomodulatory drugs or proteasome inhibitors, bispecific T cell engagers, and bispecific killer cell engagers, to further enhance antitumor effects and ultimately improve survival in an appropriate patient population,” Dr. Sahebi and colleagues said in their report.
The investigators reported results of a retrospective analysis including 96 patients with relapsed multiple myeloma who had failed at least one previous autologous HCT. They underwent haploidentical allo-HCT at European Society for Blood and Marrow Transplantation/Center for International Blood and Marrow Transplant Research centers between 2008 and 2016.
Median follow-up in the analysis was 24 months. Almost all patients (97%) achieved neutrophil engraftment by day 28, while 75% had recovery of platelets by day 60, Dr. Sahebi and co-investigators reported.
The 1-year nonrelapse mortality rate was 21%, but the cumulative risk of relapse and progression at 2 years was 56%, according to the study results. Two-year progression-free survival was reported to be 17%, while overall survival was 48%.
Acute graft-versus-host-disease (GVHD) of grades II-IV occurred in 39% by 100 days, while chronic GVHD was seen in 46% at 2 years, the report shows.
Factors linked to improved overall survival at 2 years included use of bone marrow as the source of stem cells, and the use of cyclophosphamide after transplantation, according to Dr. Sahebi and co-authors.
By contrast, factors that had no impact on overall survival, progression-free survival, or non-relapse mortality included disease status (ie, degree of response), gender, conditioning regimen intensity, presence of cytomegalovirus in the blood, or donor-recipient sex mismatch.
This analysis was conducted in part due to the limited availability of matched donors, along with the promising results of allo-HCT in other malignancies, according to investigators.
There were no conflicts of interest to report related to this research, Dr. Sahebi and colleagues reported in the journal.
SOURCE: Sahebi F, et al. Biol Blood Marrow Transplant. 2018 Sep 20. pii: S1083-8791(18)30575-5.
, investigators have reported.
The rate of non-relapse mortality at one year was 21% in the retrospective analysis of 96 patients, recently reported in the journal Biology of Blood and Marrow Transplantation.
Haploidentical allogeneic hematopoietic stem cell transplant (allo-HCT) is currently limited in use due to a high rate of relapse, but may hold potential promise for future applications, according to Firoozeh Sahebi, MD, a hematologist with the City of Hope Medical Center, Duarte, Calif., and colleagues. “Our results demonstrate that haploidentical allo-HCT can be safely performed in appropriate patients with MM who lack on HLA-matched sibling or unrelated donor.”
“The allo-HCT platform can be used in the context of other post-transplantation immune-based strategies, such as donor-derived chimeric antigen receptor T cells and natural killer cell infusions, newer immunomodulatory drugs or proteasome inhibitors, bispecific T cell engagers, and bispecific killer cell engagers, to further enhance antitumor effects and ultimately improve survival in an appropriate patient population,” Dr. Sahebi and colleagues said in their report.
The investigators reported results of a retrospective analysis including 96 patients with relapsed multiple myeloma who had failed at least one previous autologous HCT. They underwent haploidentical allo-HCT at European Society for Blood and Marrow Transplantation/Center for International Blood and Marrow Transplant Research centers between 2008 and 2016.
Median follow-up in the analysis was 24 months. Almost all patients (97%) achieved neutrophil engraftment by day 28, while 75% had recovery of platelets by day 60, Dr. Sahebi and co-investigators reported.
The 1-year nonrelapse mortality rate was 21%, but the cumulative risk of relapse and progression at 2 years was 56%, according to the study results. Two-year progression-free survival was reported to be 17%, while overall survival was 48%.
Acute graft-versus-host-disease (GVHD) of grades II-IV occurred in 39% by 100 days, while chronic GVHD was seen in 46% at 2 years, the report shows.
Factors linked to improved overall survival at 2 years included use of bone marrow as the source of stem cells, and the use of cyclophosphamide after transplantation, according to Dr. Sahebi and co-authors.
By contrast, factors that had no impact on overall survival, progression-free survival, or non-relapse mortality included disease status (ie, degree of response), gender, conditioning regimen intensity, presence of cytomegalovirus in the blood, or donor-recipient sex mismatch.
This analysis was conducted in part due to the limited availability of matched donors, along with the promising results of allo-HCT in other malignancies, according to investigators.
There were no conflicts of interest to report related to this research, Dr. Sahebi and colleagues reported in the journal.
SOURCE: Sahebi F, et al. Biol Blood Marrow Transplant. 2018 Sep 20. pii: S1083-8791(18)30575-5.
, investigators have reported.
The rate of non-relapse mortality at one year was 21% in the retrospective analysis of 96 patients, recently reported in the journal Biology of Blood and Marrow Transplantation.
Haploidentical allogeneic hematopoietic stem cell transplant (allo-HCT) is currently limited in use due to a high rate of relapse, but may hold potential promise for future applications, according to Firoozeh Sahebi, MD, a hematologist with the City of Hope Medical Center, Duarte, Calif., and colleagues. “Our results demonstrate that haploidentical allo-HCT can be safely performed in appropriate patients with MM who lack on HLA-matched sibling or unrelated donor.”
“The allo-HCT platform can be used in the context of other post-transplantation immune-based strategies, such as donor-derived chimeric antigen receptor T cells and natural killer cell infusions, newer immunomodulatory drugs or proteasome inhibitors, bispecific T cell engagers, and bispecific killer cell engagers, to further enhance antitumor effects and ultimately improve survival in an appropriate patient population,” Dr. Sahebi and colleagues said in their report.
The investigators reported results of a retrospective analysis including 96 patients with relapsed multiple myeloma who had failed at least one previous autologous HCT. They underwent haploidentical allo-HCT at European Society for Blood and Marrow Transplantation/Center for International Blood and Marrow Transplant Research centers between 2008 and 2016.
Median follow-up in the analysis was 24 months. Almost all patients (97%) achieved neutrophil engraftment by day 28, while 75% had recovery of platelets by day 60, Dr. Sahebi and co-investigators reported.
The 1-year nonrelapse mortality rate was 21%, but the cumulative risk of relapse and progression at 2 years was 56%, according to the study results. Two-year progression-free survival was reported to be 17%, while overall survival was 48%.
Acute graft-versus-host-disease (GVHD) of grades II-IV occurred in 39% by 100 days, while chronic GVHD was seen in 46% at 2 years, the report shows.
Factors linked to improved overall survival at 2 years included use of bone marrow as the source of stem cells, and the use of cyclophosphamide after transplantation, according to Dr. Sahebi and co-authors.
By contrast, factors that had no impact on overall survival, progression-free survival, or non-relapse mortality included disease status (ie, degree of response), gender, conditioning regimen intensity, presence of cytomegalovirus in the blood, or donor-recipient sex mismatch.
This analysis was conducted in part due to the limited availability of matched donors, along with the promising results of allo-HCT in other malignancies, according to investigators.
There were no conflicts of interest to report related to this research, Dr. Sahebi and colleagues reported in the journal.
SOURCE: Sahebi F, et al. Biol Blood Marrow Transplant. 2018 Sep 20. pii: S1083-8791(18)30575-5.
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Key clinical point: Haploidentical allogeneic transplantation is feasible and had an acceptable rate of non-relapse mortality, setting the stage for its use in future combination strategies.
Major finding: The cumulative risk of relapse and progression at 2 years was 56%, and the 1-year nonrelapse mortality was 21%.
Study details: A retrospective analysis including 96 patients who underwent haploidentical allogeneic hematopoietic stem cell transplantation between 2008 and 2016.
Disclosures: Authors reported no conflicts of interest.
Source: Sahebi F, et al. Biol Blood Marrow Transplant. 2018 Sep 20. pii: S1083-8791(18)30575-5.
Health Canada approves pralatrexate for rel/ref PTCL
Health Canada has granted conditional approval for pralatrexate (Folotyn®) to treat relapsed or refractory peripheral T-cell lymphoma (PTCL).
Pralatrexate received a Notice of Compliance with Conditions (NOC/c), which is an approval granted on the basis of promising evidence of clinical effectiveness that must be verified in additional clinical trials.
To be approved under Health Canada’s NOC/c policy, a product must be intended for the treatment, prevention, or diagnosis of a serious, life-threatening, or severely debilitating illness.
In addition, the product must have demonstrated promising benefit, be of high quality, have an acceptable safety profile based on a benefit/risk assessment, and either respond to a serious unmet need or provide a significant improvement over existing therapies.
The NOC/c for pralatrexate is based on response rates in the single-arm, phase 2 PROPEL trial. Results from PROPEL were published in the Journal of Clinical Oncology in 2011.
The trial enrolled 115 patients with relapsed or refractory PTCL who had received a median of three (range, 1-12) prior systemic therapies.
The patients received pralatrexate once weekly at a dose of 30 mg/m2 for 6 weeks in 7-week cycles until disease progression or unacceptable toxicity.
In the 109 evaluable patients, the response rate was 29% (32/109). The complete response rate was 11% (n=12), and the partial response rate was 18% (n=20).
The median duration of response was 10.1 months, the median progression-free survival was 3.5 months, and the median overall survival was 14.5 months.
The most common adverse events (AEs) were mucositis (71%), thrombocytopenia (41%), nausea (41%), fatigue (36%), pyrexia (34%), anemia (34%), constipation (34%), edema (31%), cough (29%), epistaxis (26%), vomiting (25%), neutropenia (25%), and diarrhea (23%).
The most common grade 3/4 AEs were thrombocytopenia (32%), mucositis (22%), neutropenia (22%), and anemia (18%).
The product monograph for pralatrexate contains a boxed warning highlighting the risk of AEs associated with pralatrexate use, including dermatologic reactions, bone marrow suppression, infection, mucosal inflammation, tumor lysis syndrome, potential fetal harm, and pulmonary toxicity.
The product monograph is available for download from the website of Servier Canada, the company marketing pralatrexate in Canada.
Health Canada has granted conditional approval for pralatrexate (Folotyn®) to treat relapsed or refractory peripheral T-cell lymphoma (PTCL).
Pralatrexate received a Notice of Compliance with Conditions (NOC/c), which is an approval granted on the basis of promising evidence of clinical effectiveness that must be verified in additional clinical trials.
To be approved under Health Canada’s NOC/c policy, a product must be intended for the treatment, prevention, or diagnosis of a serious, life-threatening, or severely debilitating illness.
In addition, the product must have demonstrated promising benefit, be of high quality, have an acceptable safety profile based on a benefit/risk assessment, and either respond to a serious unmet need or provide a significant improvement over existing therapies.
The NOC/c for pralatrexate is based on response rates in the single-arm, phase 2 PROPEL trial. Results from PROPEL were published in the Journal of Clinical Oncology in 2011.
The trial enrolled 115 patients with relapsed or refractory PTCL who had received a median of three (range, 1-12) prior systemic therapies.
The patients received pralatrexate once weekly at a dose of 30 mg/m2 for 6 weeks in 7-week cycles until disease progression or unacceptable toxicity.
In the 109 evaluable patients, the response rate was 29% (32/109). The complete response rate was 11% (n=12), and the partial response rate was 18% (n=20).
The median duration of response was 10.1 months, the median progression-free survival was 3.5 months, and the median overall survival was 14.5 months.
The most common adverse events (AEs) were mucositis (71%), thrombocytopenia (41%), nausea (41%), fatigue (36%), pyrexia (34%), anemia (34%), constipation (34%), edema (31%), cough (29%), epistaxis (26%), vomiting (25%), neutropenia (25%), and diarrhea (23%).
The most common grade 3/4 AEs were thrombocytopenia (32%), mucositis (22%), neutropenia (22%), and anemia (18%).
The product monograph for pralatrexate contains a boxed warning highlighting the risk of AEs associated with pralatrexate use, including dermatologic reactions, bone marrow suppression, infection, mucosal inflammation, tumor lysis syndrome, potential fetal harm, and pulmonary toxicity.
The product monograph is available for download from the website of Servier Canada, the company marketing pralatrexate in Canada.
Health Canada has granted conditional approval for pralatrexate (Folotyn®) to treat relapsed or refractory peripheral T-cell lymphoma (PTCL).
Pralatrexate received a Notice of Compliance with Conditions (NOC/c), which is an approval granted on the basis of promising evidence of clinical effectiveness that must be verified in additional clinical trials.
To be approved under Health Canada’s NOC/c policy, a product must be intended for the treatment, prevention, or diagnosis of a serious, life-threatening, or severely debilitating illness.
In addition, the product must have demonstrated promising benefit, be of high quality, have an acceptable safety profile based on a benefit/risk assessment, and either respond to a serious unmet need or provide a significant improvement over existing therapies.
The NOC/c for pralatrexate is based on response rates in the single-arm, phase 2 PROPEL trial. Results from PROPEL were published in the Journal of Clinical Oncology in 2011.
The trial enrolled 115 patients with relapsed or refractory PTCL who had received a median of three (range, 1-12) prior systemic therapies.
The patients received pralatrexate once weekly at a dose of 30 mg/m2 for 6 weeks in 7-week cycles until disease progression or unacceptable toxicity.
In the 109 evaluable patients, the response rate was 29% (32/109). The complete response rate was 11% (n=12), and the partial response rate was 18% (n=20).
The median duration of response was 10.1 months, the median progression-free survival was 3.5 months, and the median overall survival was 14.5 months.
The most common adverse events (AEs) were mucositis (71%), thrombocytopenia (41%), nausea (41%), fatigue (36%), pyrexia (34%), anemia (34%), constipation (34%), edema (31%), cough (29%), epistaxis (26%), vomiting (25%), neutropenia (25%), and diarrhea (23%).
The most common grade 3/4 AEs were thrombocytopenia (32%), mucositis (22%), neutropenia (22%), and anemia (18%).
The product monograph for pralatrexate contains a boxed warning highlighting the risk of AEs associated with pralatrexate use, including dermatologic reactions, bone marrow suppression, infection, mucosal inflammation, tumor lysis syndrome, potential fetal harm, and pulmonary toxicity.
The product monograph is available for download from the website of Servier Canada, the company marketing pralatrexate in Canada.
EC approves venetoclax in combo with rituximab
The European Commission (EC) has approved a new indication for venetoclax (Venclyxto®).
The drug is now approved for use in combination with rituximab to treat patients with relapsed/refractory chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.
The approval is valid in all member states of the European Union as well as Iceland, Liechtenstein, and Norway.
The EC’s approval is based on results from the phase 3 MURANO trial, which were published in The New England Journal of Medicine in March.
The trial included 389 CLL patients who were randomized to receive venetoclax plus rituximab (VEN+R) or bendamustine plus rituximab (B+R). The median follow-up was 23.8 months.
According to an independent review committee, the overall response rate was 92.3% in the VEN+R arm and 72.3% in the B+R arm. The investigator-assessed overall response rates were 93.3% and 67.7%, respectively.
According to investigators, the median progression-free survival (PFS) was not reached in the VEN+R arm and was 17.0 months in the B+R arm (hazard ratio [HR]=0.17; P<0.0001).
According to the independent review committee, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (HR=0.20; P<0.0001).
Investigators said the 2-year PFS rate was 84.9% in the VEN+R arm and 36.3% in the B+R arm.
They said the 2-year overall survival rates were 91.9% and 86.6%, respectively (HR=0.48; P<0.0001). The median overall survival was not reached in either arm.
Grade 3/4 adverse events (AEs) with at least a 2% difference in incidence between the treatment arms (in the VEN+R and B+R arms, respectively) included:
- Neutropenia (57.7% and 38.8%)
- Infections and infestations (17.5% and 21.8%)
- Anemia (10.8% and 13.8%)
- Thrombocytopenia (5.7% and 10.1%)
- Febrile neutropenia (3.6% and 9.6%)
- Pneumonia (5.2% and 8.0%)
- Infusion-related reactions (1.5% and 5.3%)
- Tumor lysis syndrome (3.1% and 1.1%)
- Hypotension (0% and 2.7%)
- Hyperglycemia (2.1% and 0%)
- Hypogammaglobulinemia (2.1% and 0%).
Serious AEs with at least a 2% difference in incidence between the arms (in the VEN+R and B+R arms, respectively) were:
- Pneumonia (8.2% and 8.0%)
- Febrile neutropenia (3.6% and 8.5%)
- Pyrexia (2.6% and 6.9%)
- Anemia (1.5% and 2.7%)
- Infusion-related reactions (0.5% and 3.2%)
- Sepsis (0.5% and 2.1%)
- Tumor lysis syndrome (2.1% and 0.5%)
- Hypotension (0% and 2.7%).
Fatal AEs occurred in 5.2% of patients in the VEN+R arm and 5.9% in the B+R arm.
Fatal AEs in the VEN+R arm included pneumonia (n=3), sepsis (n=1), thrombocytopenia (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1). Two cases of pneumonia occurred in the setting of progression/Richter’s transformation.
The European Commission (EC) has approved a new indication for venetoclax (Venclyxto®).
The drug is now approved for use in combination with rituximab to treat patients with relapsed/refractory chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.
The approval is valid in all member states of the European Union as well as Iceland, Liechtenstein, and Norway.
The EC’s approval is based on results from the phase 3 MURANO trial, which were published in The New England Journal of Medicine in March.
The trial included 389 CLL patients who were randomized to receive venetoclax plus rituximab (VEN+R) or bendamustine plus rituximab (B+R). The median follow-up was 23.8 months.
According to an independent review committee, the overall response rate was 92.3% in the VEN+R arm and 72.3% in the B+R arm. The investigator-assessed overall response rates were 93.3% and 67.7%, respectively.
According to investigators, the median progression-free survival (PFS) was not reached in the VEN+R arm and was 17.0 months in the B+R arm (hazard ratio [HR]=0.17; P<0.0001).
According to the independent review committee, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (HR=0.20; P<0.0001).
Investigators said the 2-year PFS rate was 84.9% in the VEN+R arm and 36.3% in the B+R arm.
They said the 2-year overall survival rates were 91.9% and 86.6%, respectively (HR=0.48; P<0.0001). The median overall survival was not reached in either arm.
Grade 3/4 adverse events (AEs) with at least a 2% difference in incidence between the treatment arms (in the VEN+R and B+R arms, respectively) included:
- Neutropenia (57.7% and 38.8%)
- Infections and infestations (17.5% and 21.8%)
- Anemia (10.8% and 13.8%)
- Thrombocytopenia (5.7% and 10.1%)
- Febrile neutropenia (3.6% and 9.6%)
- Pneumonia (5.2% and 8.0%)
- Infusion-related reactions (1.5% and 5.3%)
- Tumor lysis syndrome (3.1% and 1.1%)
- Hypotension (0% and 2.7%)
- Hyperglycemia (2.1% and 0%)
- Hypogammaglobulinemia (2.1% and 0%).
Serious AEs with at least a 2% difference in incidence between the arms (in the VEN+R and B+R arms, respectively) were:
- Pneumonia (8.2% and 8.0%)
- Febrile neutropenia (3.6% and 8.5%)
- Pyrexia (2.6% and 6.9%)
- Anemia (1.5% and 2.7%)
- Infusion-related reactions (0.5% and 3.2%)
- Sepsis (0.5% and 2.1%)
- Tumor lysis syndrome (2.1% and 0.5%)
- Hypotension (0% and 2.7%).
Fatal AEs occurred in 5.2% of patients in the VEN+R arm and 5.9% in the B+R arm.
Fatal AEs in the VEN+R arm included pneumonia (n=3), sepsis (n=1), thrombocytopenia (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1). Two cases of pneumonia occurred in the setting of progression/Richter’s transformation.
The European Commission (EC) has approved a new indication for venetoclax (Venclyxto®).
The drug is now approved for use in combination with rituximab to treat patients with relapsed/refractory chronic lymphocytic leukemia (CLL) who have received at least one prior therapy.
The approval is valid in all member states of the European Union as well as Iceland, Liechtenstein, and Norway.
The EC’s approval is based on results from the phase 3 MURANO trial, which were published in The New England Journal of Medicine in March.
The trial included 389 CLL patients who were randomized to receive venetoclax plus rituximab (VEN+R) or bendamustine plus rituximab (B+R). The median follow-up was 23.8 months.
According to an independent review committee, the overall response rate was 92.3% in the VEN+R arm and 72.3% in the B+R arm. The investigator-assessed overall response rates were 93.3% and 67.7%, respectively.
According to investigators, the median progression-free survival (PFS) was not reached in the VEN+R arm and was 17.0 months in the B+R arm (hazard ratio [HR]=0.17; P<0.0001).
According to the independent review committee, the median PFS was not reached in the VEN+R arm and was 18.1 months in the B+R arm (HR=0.20; P<0.0001).
Investigators said the 2-year PFS rate was 84.9% in the VEN+R arm and 36.3% in the B+R arm.
They said the 2-year overall survival rates were 91.9% and 86.6%, respectively (HR=0.48; P<0.0001). The median overall survival was not reached in either arm.
Grade 3/4 adverse events (AEs) with at least a 2% difference in incidence between the treatment arms (in the VEN+R and B+R arms, respectively) included:
- Neutropenia (57.7% and 38.8%)
- Infections and infestations (17.5% and 21.8%)
- Anemia (10.8% and 13.8%)
- Thrombocytopenia (5.7% and 10.1%)
- Febrile neutropenia (3.6% and 9.6%)
- Pneumonia (5.2% and 8.0%)
- Infusion-related reactions (1.5% and 5.3%)
- Tumor lysis syndrome (3.1% and 1.1%)
- Hypotension (0% and 2.7%)
- Hyperglycemia (2.1% and 0%)
- Hypogammaglobulinemia (2.1% and 0%).
Serious AEs with at least a 2% difference in incidence between the arms (in the VEN+R and B+R arms, respectively) were:
- Pneumonia (8.2% and 8.0%)
- Febrile neutropenia (3.6% and 8.5%)
- Pyrexia (2.6% and 6.9%)
- Anemia (1.5% and 2.7%)
- Infusion-related reactions (0.5% and 3.2%)
- Sepsis (0.5% and 2.1%)
- Tumor lysis syndrome (2.1% and 0.5%)
- Hypotension (0% and 2.7%).
Fatal AEs occurred in 5.2% of patients in the VEN+R arm and 5.9% in the B+R arm.
Fatal AEs in the VEN+R arm included pneumonia (n=3), sepsis (n=1), thrombocytopenia (n=1), cardiac failure (n=1), myocardial infarction (n=1), sudden cardiac death (n=1), colorectal cancer (n=1), status epilepticus (n=1), and acute respiratory failure (n=1). Two cases of pneumonia occurred in the setting of progression/Richter’s transformation.
Genomic abnormalities shed light on racial disparity in myeloma
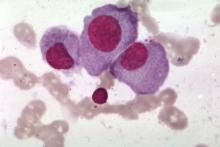
Researchers say they may have determined why African Americans have a two- to threefold increased risk of multiple myeloma (MM), compared with European Americans.
The team genotyped 881 MM samples from various racial groups and identified three gene subtypes – t(11;14), t(14;16), and t(14;20) – that explain the racial disparity.
They found that patients with African ancestry of 80% or more had a significantly higher occurrence of these subtypes, compared with individuals with African ancestry of less than 0.1%.
And these subtypes are driving the disparity in MM diagnoses between the populations.
Previous attempts to explain the disparity relied on self-reported race rather than quantitatively measured genetic ancestry, which could result in bias, Vincent Rajkumar, MD, of the Mayo Clinic in Rochester, Minn., and his colleagues reported in Blood Cancer Journal.
“A major new aspect of this study is that we identified the ancestry of each patient through DNA sequencing, which allowed us to determine ancestry more accurately,” Dr. Rajkumar said in a statement.
All 881 samples had abnormal plasma cell FISH, 851 had a normal chromosome study, and 30 had an abnormal study.
Median age for the entire group was 64 years. More samples were from men (54.3%) than women (45.7%). Researchers observed no significant difference between men and women in the proportion of primary cytogenetic abnormalities.
Of the 881 samples, the median African ancestry was 2.3%, the median European ancestry was 64.7%, and Northern European ancestry was 26.6%.
Thirty percent of the entire cohort had less than 0.1% African ancestry, and 13.6% had 80% or greater African ancestry.
Using a logistic regression model, the researchers determined that a 10% increase in the percentage of African ancestry was associated with a 6% increase in the odds of detecting t(11;14), t(14;16), or t(14;20) odds ratio, 1.06; 95% confidence interval, 1.02-1.11; P = .05).
The researchers plotted the probability of observing these cytogenetic abnormalities with the percentage of African ancestry and found the differences were most striking in the extreme populations – individuals with 80% or greater African ancestry and individuals with less than 0.1% African ancestry.
Upon further analysis, the team found a significantly higher prevalence of t(11;14), t(14;16), and t(14;20) in the group of patients with the greatest proportion of African ancestry (P = .008), compared with the European cohort.
The differences emerged in only the highest and lowest cohorts, they noted. Most patients (60%) were not included in these extreme populations because they had mixed ancestry.
The team observed no significant differences when the cutoff for African ancestry was greater than 50%.
The research was supported by the National Cancer Institute and the Mayo Clinic. One study author reported relationships with Celgene, Takeda, Prothena, Janssen, Pfizer, Alnylam, and GSK. Two authors reported relationships with the DNA Diagnostics Center.
SOURCE: Baughn LB et al. Blood Cancer J. 2018 Oct 10;8(10):96.
Researchers say they may have determined why African Americans have a two- to threefold increased risk of multiple myeloma (MM), compared with European Americans.
The team genotyped 881 MM samples from various racial groups and identified three gene subtypes – t(11;14), t(14;16), and t(14;20) – that explain the racial disparity.
They found that patients with African ancestry of 80% or more had a significantly higher occurrence of these subtypes, compared with individuals with African ancestry of less than 0.1%.
And these subtypes are driving the disparity in MM diagnoses between the populations.
Previous attempts to explain the disparity relied on self-reported race rather than quantitatively measured genetic ancestry, which could result in bias, Vincent Rajkumar, MD, of the Mayo Clinic in Rochester, Minn., and his colleagues reported in Blood Cancer Journal.
“A major new aspect of this study is that we identified the ancestry of each patient through DNA sequencing, which allowed us to determine ancestry more accurately,” Dr. Rajkumar said in a statement.
All 881 samples had abnormal plasma cell FISH, 851 had a normal chromosome study, and 30 had an abnormal study.
Median age for the entire group was 64 years. More samples were from men (54.3%) than women (45.7%). Researchers observed no significant difference between men and women in the proportion of primary cytogenetic abnormalities.
Of the 881 samples, the median African ancestry was 2.3%, the median European ancestry was 64.7%, and Northern European ancestry was 26.6%.
Thirty percent of the entire cohort had less than 0.1% African ancestry, and 13.6% had 80% or greater African ancestry.
Using a logistic regression model, the researchers determined that a 10% increase in the percentage of African ancestry was associated with a 6% increase in the odds of detecting t(11;14), t(14;16), or t(14;20) odds ratio, 1.06; 95% confidence interval, 1.02-1.11; P = .05).
The researchers plotted the probability of observing these cytogenetic abnormalities with the percentage of African ancestry and found the differences were most striking in the extreme populations – individuals with 80% or greater African ancestry and individuals with less than 0.1% African ancestry.
Upon further analysis, the team found a significantly higher prevalence of t(11;14), t(14;16), and t(14;20) in the group of patients with the greatest proportion of African ancestry (P = .008), compared with the European cohort.
The differences emerged in only the highest and lowest cohorts, they noted. Most patients (60%) were not included in these extreme populations because they had mixed ancestry.
The team observed no significant differences when the cutoff for African ancestry was greater than 50%.
The research was supported by the National Cancer Institute and the Mayo Clinic. One study author reported relationships with Celgene, Takeda, Prothena, Janssen, Pfizer, Alnylam, and GSK. Two authors reported relationships with the DNA Diagnostics Center.
SOURCE: Baughn LB et al. Blood Cancer J. 2018 Oct 10;8(10):96.
Researchers say they may have determined why African Americans have a two- to threefold increased risk of multiple myeloma (MM), compared with European Americans.
The team genotyped 881 MM samples from various racial groups and identified three gene subtypes – t(11;14), t(14;16), and t(14;20) – that explain the racial disparity.
They found that patients with African ancestry of 80% or more had a significantly higher occurrence of these subtypes, compared with individuals with African ancestry of less than 0.1%.
And these subtypes are driving the disparity in MM diagnoses between the populations.
Previous attempts to explain the disparity relied on self-reported race rather than quantitatively measured genetic ancestry, which could result in bias, Vincent Rajkumar, MD, of the Mayo Clinic in Rochester, Minn., and his colleagues reported in Blood Cancer Journal.
“A major new aspect of this study is that we identified the ancestry of each patient through DNA sequencing, which allowed us to determine ancestry more accurately,” Dr. Rajkumar said in a statement.
All 881 samples had abnormal plasma cell FISH, 851 had a normal chromosome study, and 30 had an abnormal study.
Median age for the entire group was 64 years. More samples were from men (54.3%) than women (45.7%). Researchers observed no significant difference between men and women in the proportion of primary cytogenetic abnormalities.
Of the 881 samples, the median African ancestry was 2.3%, the median European ancestry was 64.7%, and Northern European ancestry was 26.6%.
Thirty percent of the entire cohort had less than 0.1% African ancestry, and 13.6% had 80% or greater African ancestry.
Using a logistic regression model, the researchers determined that a 10% increase in the percentage of African ancestry was associated with a 6% increase in the odds of detecting t(11;14), t(14;16), or t(14;20) odds ratio, 1.06; 95% confidence interval, 1.02-1.11; P = .05).
The researchers plotted the probability of observing these cytogenetic abnormalities with the percentage of African ancestry and found the differences were most striking in the extreme populations – individuals with 80% or greater African ancestry and individuals with less than 0.1% African ancestry.
Upon further analysis, the team found a significantly higher prevalence of t(11;14), t(14;16), and t(14;20) in the group of patients with the greatest proportion of African ancestry (P = .008), compared with the European cohort.
The differences emerged in only the highest and lowest cohorts, they noted. Most patients (60%) were not included in these extreme populations because they had mixed ancestry.
The team observed no significant differences when the cutoff for African ancestry was greater than 50%.
The research was supported by the National Cancer Institute and the Mayo Clinic. One study author reported relationships with Celgene, Takeda, Prothena, Janssen, Pfizer, Alnylam, and GSK. Two authors reported relationships with the DNA Diagnostics Center.
SOURCE: Baughn LB et al. Blood Cancer J. 2018 Oct 10;8(10):96.
FROM BLOOD CANCER JOURNAL
Key clinical point:
Major finding: There was a significantly higher prevalence of t(11;14), t(14;16), and t(14:20) in patients with 80% or greater African ancestry, compared with the European cohort (P = .008).
Study details: The study included 881 samples from patients with an abnormal plasma cell proliferative disorder FISH result and concurrent conventional G-banded chromosome evaluation.
Disclosures: The research was supported by the National Cancer Institute and the Mayo Clinic. One study author reported relationships with Celgene, Takeda, Prothena, Janssen, Pfizer, Alnylam, and GSK. Two authors reported relationships with the DNA Diagnostics Center.
Source: Baughn LB et al. Blood Cancer J. 2018 Oct 10;8(10):96.
Novel risk factors for febrile neutropenia in NHL, other cancers
A retrospective study has revealed new potential risk factors for chemotherapy-induced febrile neutropenia (FN) in patients with solid tumors and non-Hodgkin lymphoma (NHL).
Researchers found the timing and duration of corticosteroid use were both associated with FN.
The team also observed “marginal” associations between FN and certain dermatologic and mucosal conditions as well as the use of intravenous (IV) antibiotics before chemotherapy.
On the other hand, there was no association between oral antibiotic use and FN or between radiation therapy (RT) and FN.
Chun Rebecca Chao, PhD, of Kaiser Permanente Southern California in Pasadena, and her colleagues reported these findings in JNCCN.
“Febrile neutropenia is life-threatening and often requires hospitalization,” Dr. Chao noted. “Furthermore, FN can lead to chemotherapy dose delay and dose reduction, which, in turn, negatively impacts antitumor efficacy. However, it can be prevented if high-risk individuals are identified and treated prophylactically.”
With this in mind, Dr. Chao and her colleagues set out to identify novel risk factors for FN by analyzing 15,971 patients who were treated with myelosuppressive chemotherapy at Kaiser Permanente Southern California between 2000 and 2009.
Patients had been diagnosed with NHL (n=1,617) or breast (n=6,323), lung (n=3,584), colorectal (n=3,062), ovarian (n=924), or gastric (n=461) cancers.
In all, 4.3% of patients developed FN during their first cycle of chemotherapy.
Corticosteroid use
The researchers found corticosteroid use was associated with an increased risk of FN in a propensity score-adjusted (PSA) model (adjusted for age, sex, socioeconomic factors, comorbidities, etc.). The hazard ratio (HR) was 1.53 (95% CI, 1.17-1.98; P<0.01) for patients who received corticosteroids.
A longer duration of corticosteroid use was associated with a greater risk of FN. The adjusted HR (compared to no corticosteroid use) was:
- 1.78 for corticosteroid treatment lasting less than 15 days (P<0.01)
- 1.84 for treatment lasting 15 to 29 days (P<0.01)
- 2.27 for treatment lasting 30 to 44 days (P<0.01)
- 2.86 for treatment lasting 45 to 90 days (P<0.01).
More recent corticosteroid use was associated with a greater risk of FN as well. The adjusted HR was:
- 1.88 for corticosteroid treatment less than 15 days before chemotherapy (P<0.01)
- 1.13 for treatment 15 to 29 days before chemotherapy (P=0.72)
- 1.22 for treatment 30 to 44 days before chemotherapy (P=0.66)
- 1.41 for treatment 45 to 90 days before chemotherapy (P=0.32).
“One way to reduce the incidence rate for FN could be to schedule prior corticosteroid use and subsequent chemotherapy with at least 2 weeks between them, given the magnitude of the risk increase and prevalence of this risk factor,” Dr. Chao said.
Other potential risk factors
The researchers found a “marginally” increased risk of FN in patients with certain dermatologic conditions (dermatitis, psoriasis, pruritus, etc.) and mucosal conditions (gastritis, stomatitis, mucositis, etc.).
In the PSA model, the HR was 1.40 (95% CI, 0.98-1.93; P=0.05) for patients with these conditions.
IV antibiotic use was also found to be marginally associated with an increased risk of FN in a restricted analysis covering patients treated in 2008 and 2009. In the PSA model, the HR was 1.35 (95% CI, 0.97-1.87; P=0.08).
On the other hand, there was no association between FN and oral antibiotic use in the restricted analysis. In the PSA model, the HR was 1.07 (95% CI, 0.77-1.48; P=0.70) for patients who received oral antibiotics.
Dr. Chao and her colleagues said these results suggest IV antibiotics may have a more profound impact than oral antibiotics on the balance of bacterial flora and other immune functions. Another possible explanation is that patients who received IV antibiotics were generally sicker and more prone to severe infection than patients who received oral antibiotics.
As with oral antibiotics, the researchers found no association between FN and the following factors (with the PSA model):
- Prior surgery (HR=0.89; 95% CI, 0.72-1.11; P=0.30)
- Prior RT (HR=0.91; 95% CI, 0.64-1.27; P=0.61)
- Concurrent RT (HR=1.32; 95% CI, 0.69-2.37; P=0.37).
The researchers noted that they did not account for radiation field or dose in this study, so additional evaluation of RT as a risk factor is needed.
In closing, Dr. Chao and her colleagues said these results suggest corticosteroid use, IV antibiotics, and certain dermatologic and mucosal conditions should be taken into consideration when monitoring patients receiving myelosuppressive chemotherapy and when evaluating the need for prophylactic granulocyte colony-stimulating factor or chemotherapy dose reduction.
Dr. Chao and her colleagues received funding from Amgen, Inc., to perform this study.
A retrospective study has revealed new potential risk factors for chemotherapy-induced febrile neutropenia (FN) in patients with solid tumors and non-Hodgkin lymphoma (NHL).
Researchers found the timing and duration of corticosteroid use were both associated with FN.
The team also observed “marginal” associations between FN and certain dermatologic and mucosal conditions as well as the use of intravenous (IV) antibiotics before chemotherapy.
On the other hand, there was no association between oral antibiotic use and FN or between radiation therapy (RT) and FN.
Chun Rebecca Chao, PhD, of Kaiser Permanente Southern California in Pasadena, and her colleagues reported these findings in JNCCN.
“Febrile neutropenia is life-threatening and often requires hospitalization,” Dr. Chao noted. “Furthermore, FN can lead to chemotherapy dose delay and dose reduction, which, in turn, negatively impacts antitumor efficacy. However, it can be prevented if high-risk individuals are identified and treated prophylactically.”
With this in mind, Dr. Chao and her colleagues set out to identify novel risk factors for FN by analyzing 15,971 patients who were treated with myelosuppressive chemotherapy at Kaiser Permanente Southern California between 2000 and 2009.
Patients had been diagnosed with NHL (n=1,617) or breast (n=6,323), lung (n=3,584), colorectal (n=3,062), ovarian (n=924), or gastric (n=461) cancers.
In all, 4.3% of patients developed FN during their first cycle of chemotherapy.
Corticosteroid use
The researchers found corticosteroid use was associated with an increased risk of FN in a propensity score-adjusted (PSA) model (adjusted for age, sex, socioeconomic factors, comorbidities, etc.). The hazard ratio (HR) was 1.53 (95% CI, 1.17-1.98; P<0.01) for patients who received corticosteroids.
A longer duration of corticosteroid use was associated with a greater risk of FN. The adjusted HR (compared to no corticosteroid use) was:
- 1.78 for corticosteroid treatment lasting less than 15 days (P<0.01)
- 1.84 for treatment lasting 15 to 29 days (P<0.01)
- 2.27 for treatment lasting 30 to 44 days (P<0.01)
- 2.86 for treatment lasting 45 to 90 days (P<0.01).
More recent corticosteroid use was associated with a greater risk of FN as well. The adjusted HR was:
- 1.88 for corticosteroid treatment less than 15 days before chemotherapy (P<0.01)
- 1.13 for treatment 15 to 29 days before chemotherapy (P=0.72)
- 1.22 for treatment 30 to 44 days before chemotherapy (P=0.66)
- 1.41 for treatment 45 to 90 days before chemotherapy (P=0.32).
“One way to reduce the incidence rate for FN could be to schedule prior corticosteroid use and subsequent chemotherapy with at least 2 weeks between them, given the magnitude of the risk increase and prevalence of this risk factor,” Dr. Chao said.
Other potential risk factors
The researchers found a “marginally” increased risk of FN in patients with certain dermatologic conditions (dermatitis, psoriasis, pruritus, etc.) and mucosal conditions (gastritis, stomatitis, mucositis, etc.).
In the PSA model, the HR was 1.40 (95% CI, 0.98-1.93; P=0.05) for patients with these conditions.
IV antibiotic use was also found to be marginally associated with an increased risk of FN in a restricted analysis covering patients treated in 2008 and 2009. In the PSA model, the HR was 1.35 (95% CI, 0.97-1.87; P=0.08).
On the other hand, there was no association between FN and oral antibiotic use in the restricted analysis. In the PSA model, the HR was 1.07 (95% CI, 0.77-1.48; P=0.70) for patients who received oral antibiotics.
Dr. Chao and her colleagues said these results suggest IV antibiotics may have a more profound impact than oral antibiotics on the balance of bacterial flora and other immune functions. Another possible explanation is that patients who received IV antibiotics were generally sicker and more prone to severe infection than patients who received oral antibiotics.
As with oral antibiotics, the researchers found no association between FN and the following factors (with the PSA model):
- Prior surgery (HR=0.89; 95% CI, 0.72-1.11; P=0.30)
- Prior RT (HR=0.91; 95% CI, 0.64-1.27; P=0.61)
- Concurrent RT (HR=1.32; 95% CI, 0.69-2.37; P=0.37).
The researchers noted that they did not account for radiation field or dose in this study, so additional evaluation of RT as a risk factor is needed.
In closing, Dr. Chao and her colleagues said these results suggest corticosteroid use, IV antibiotics, and certain dermatologic and mucosal conditions should be taken into consideration when monitoring patients receiving myelosuppressive chemotherapy and when evaluating the need for prophylactic granulocyte colony-stimulating factor or chemotherapy dose reduction.
Dr. Chao and her colleagues received funding from Amgen, Inc., to perform this study.
A retrospective study has revealed new potential risk factors for chemotherapy-induced febrile neutropenia (FN) in patients with solid tumors and non-Hodgkin lymphoma (NHL).
Researchers found the timing and duration of corticosteroid use were both associated with FN.
The team also observed “marginal” associations between FN and certain dermatologic and mucosal conditions as well as the use of intravenous (IV) antibiotics before chemotherapy.
On the other hand, there was no association between oral antibiotic use and FN or between radiation therapy (RT) and FN.
Chun Rebecca Chao, PhD, of Kaiser Permanente Southern California in Pasadena, and her colleagues reported these findings in JNCCN.
“Febrile neutropenia is life-threatening and often requires hospitalization,” Dr. Chao noted. “Furthermore, FN can lead to chemotherapy dose delay and dose reduction, which, in turn, negatively impacts antitumor efficacy. However, it can be prevented if high-risk individuals are identified and treated prophylactically.”
With this in mind, Dr. Chao and her colleagues set out to identify novel risk factors for FN by analyzing 15,971 patients who were treated with myelosuppressive chemotherapy at Kaiser Permanente Southern California between 2000 and 2009.
Patients had been diagnosed with NHL (n=1,617) or breast (n=6,323), lung (n=3,584), colorectal (n=3,062), ovarian (n=924), or gastric (n=461) cancers.
In all, 4.3% of patients developed FN during their first cycle of chemotherapy.
Corticosteroid use
The researchers found corticosteroid use was associated with an increased risk of FN in a propensity score-adjusted (PSA) model (adjusted for age, sex, socioeconomic factors, comorbidities, etc.). The hazard ratio (HR) was 1.53 (95% CI, 1.17-1.98; P<0.01) for patients who received corticosteroids.
A longer duration of corticosteroid use was associated with a greater risk of FN. The adjusted HR (compared to no corticosteroid use) was:
- 1.78 for corticosteroid treatment lasting less than 15 days (P<0.01)
- 1.84 for treatment lasting 15 to 29 days (P<0.01)
- 2.27 for treatment lasting 30 to 44 days (P<0.01)
- 2.86 for treatment lasting 45 to 90 days (P<0.01).
More recent corticosteroid use was associated with a greater risk of FN as well. The adjusted HR was:
- 1.88 for corticosteroid treatment less than 15 days before chemotherapy (P<0.01)
- 1.13 for treatment 15 to 29 days before chemotherapy (P=0.72)
- 1.22 for treatment 30 to 44 days before chemotherapy (P=0.66)
- 1.41 for treatment 45 to 90 days before chemotherapy (P=0.32).
“One way to reduce the incidence rate for FN could be to schedule prior corticosteroid use and subsequent chemotherapy with at least 2 weeks between them, given the magnitude of the risk increase and prevalence of this risk factor,” Dr. Chao said.
Other potential risk factors
The researchers found a “marginally” increased risk of FN in patients with certain dermatologic conditions (dermatitis, psoriasis, pruritus, etc.) and mucosal conditions (gastritis, stomatitis, mucositis, etc.).
In the PSA model, the HR was 1.40 (95% CI, 0.98-1.93; P=0.05) for patients with these conditions.
IV antibiotic use was also found to be marginally associated with an increased risk of FN in a restricted analysis covering patients treated in 2008 and 2009. In the PSA model, the HR was 1.35 (95% CI, 0.97-1.87; P=0.08).
On the other hand, there was no association between FN and oral antibiotic use in the restricted analysis. In the PSA model, the HR was 1.07 (95% CI, 0.77-1.48; P=0.70) for patients who received oral antibiotics.
Dr. Chao and her colleagues said these results suggest IV antibiotics may have a more profound impact than oral antibiotics on the balance of bacterial flora and other immune functions. Another possible explanation is that patients who received IV antibiotics were generally sicker and more prone to severe infection than patients who received oral antibiotics.
As with oral antibiotics, the researchers found no association between FN and the following factors (with the PSA model):
- Prior surgery (HR=0.89; 95% CI, 0.72-1.11; P=0.30)
- Prior RT (HR=0.91; 95% CI, 0.64-1.27; P=0.61)
- Concurrent RT (HR=1.32; 95% CI, 0.69-2.37; P=0.37).
The researchers noted that they did not account for radiation field or dose in this study, so additional evaluation of RT as a risk factor is needed.
In closing, Dr. Chao and her colleagues said these results suggest corticosteroid use, IV antibiotics, and certain dermatologic and mucosal conditions should be taken into consideration when monitoring patients receiving myelosuppressive chemotherapy and when evaluating the need for prophylactic granulocyte colony-stimulating factor or chemotherapy dose reduction.
Dr. Chao and her colleagues received funding from Amgen, Inc., to perform this study.
Palliative care guidelines relevant for hematologists, doc says
The latest edition of the national palliative care guidelines provides new clinical strategies relevant to hematology practice in the United States, according to a physician-researcher specializing in hematology.
The Clinical Practice Guidelines for Quality Palliative Care, 4th edition, represents a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, a physician-researcher at Duke University School of Medicine in Durham, North Carolina.
However, unlike previous editions, this update to the guidelines emphasizes the importance of palliative care provided by both primary care and specialty care clinicians.
“Part of this report is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” Dr. LeBlanc said.
The latest edition helps establish a foundation for gold standard palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to The National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology.
One key reason for the update, according to NCP, was to acknowledge that today’s healthcare system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on clinicians who don’t practice palliative care to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
That differs from the way palliative care is traditionally practiced, in which specially trained doctors, nurses, and other specialists provide that support.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who really needs us the most and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said.
That’s a major driver behind the emphasis in the latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, Dr. LeBlanc added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
The latest edition of the national palliative care guidelines provides new clinical strategies relevant to hematology practice in the United States, according to a physician-researcher specializing in hematology.
The Clinical Practice Guidelines for Quality Palliative Care, 4th edition, represents a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, a physician-researcher at Duke University School of Medicine in Durham, North Carolina.
However, unlike previous editions, this update to the guidelines emphasizes the importance of palliative care provided by both primary care and specialty care clinicians.
“Part of this report is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” Dr. LeBlanc said.
The latest edition helps establish a foundation for gold standard palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to The National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology.
One key reason for the update, according to NCP, was to acknowledge that today’s healthcare system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on clinicians who don’t practice palliative care to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
That differs from the way palliative care is traditionally practiced, in which specially trained doctors, nurses, and other specialists provide that support.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who really needs us the most and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said.
That’s a major driver behind the emphasis in the latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, Dr. LeBlanc added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
The latest edition of the national palliative care guidelines provides new clinical strategies relevant to hematology practice in the United States, according to a physician-researcher specializing in hematology.
The Clinical Practice Guidelines for Quality Palliative Care, 4th edition, represents a “blueprint for what it looks like to provide high-quality, comprehensive palliative care to people with serious illness,” said Thomas W. LeBlanc, MD, a physician-researcher at Duke University School of Medicine in Durham, North Carolina.
However, unlike previous editions, this update to the guidelines emphasizes the importance of palliative care provided by both primary care and specialty care clinicians.
“Part of this report is about trying to raise the game of everybody in medicine and provide a higher basic level of primary palliative care to all people with serious illness, but then also to figure out who has higher levels of needs where the specialists should be applied, since they are a scarce resource,” Dr. LeBlanc said.
The latest edition helps establish a foundation for gold standard palliative care for people living with serious illness, regardless of diagnosis, prognosis, setting, or age, according to The National Coalition for Hospice and Palliative Care, which published the clinical practice guidelines.
The update was developed by the National Consensus Project for Quality Palliative Care (NCP), which includes 16 national organizations with palliative care and hospice expertise, and is endorsed by more than 80 national organizations, including the American Society of Hematology.
One key reason for the update, according to NCP, was to acknowledge that today’s healthcare system may not be meeting patients’ palliative care needs.
Specifically, the guidelines call on clinicians who don’t practice palliative care to integrate palliative care principles into their routine assessment of seriously ill patients with conditions such as heart failure, lung disease, and cancer.
That differs from the way palliative care is traditionally practiced, in which specially trained doctors, nurses, and other specialists provide that support.
An issue with that traditional model is a shortage of specialized clinicians to meet palliative care needs, said Dr. LeBlanc, whose clinical practice and research focuses on palliative care needs of patients with hematologic malignancies.
“Palliative care has matured as a field such that we are now actually facing workforce shortage issues and really fundamental questions about who really needs us the most and how we increase our reach to improve the lives of more patients and families facing serious illness,” he said.
That’s a major driver behind the emphasis in the latest guidelines on providing palliative care in the community, coordinating care, and dealing with care transitions, Dr. LeBlanc added.
“I hope that this document will help to demonstrate the value and the need for palliative care specialists and for improvements in primary care in the care of patients with hematologic diseases in general,” he said. “To me, this adds increasing legitimacy to this whole field.”
Checkpoint inhibitor plus rituximab is active in non-Hodgkin lymphoma
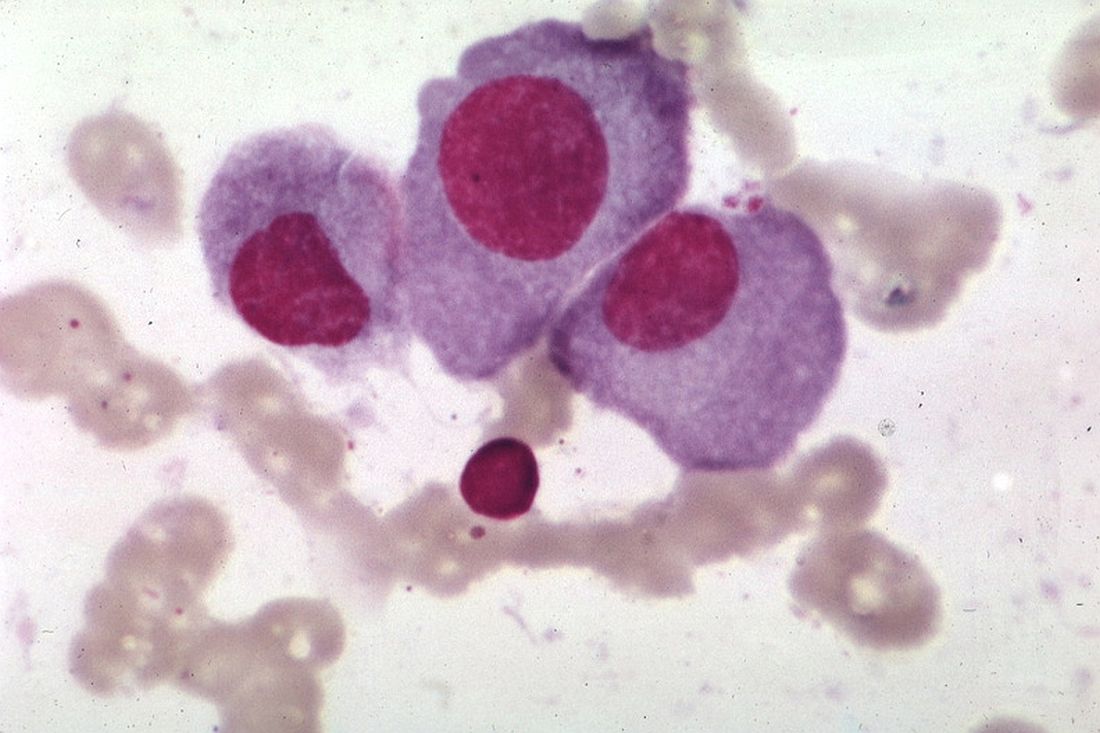
A macrophage-activating immune checkpoint inhibitor, combined with rituximab therapy, was safe and produced durable complete responses in patients with relapsed or refractory non-Hodgkin lymphoma, according to results of a phase 1b study.
Mainly low-grade toxic effects were seen on treatment with Hu5F9-G4 (5F9) and rituximab, which induced responses in more than half of patients, of which more than one-third were complete responses, the study investigators reported.
Most of the responses were ongoing at the time of data cutoff, suggesting durable responses with the combination of rituximab and 5F9 – a humanized monoclonal antibody that blocks CD47, an antiphagocytic or “do not eat me” signal overexpressed by most cancers, Ranjana Advani, MD, of Stanford (Calif.) University, and her coauthors wrote.
“The macrophage-mediated activity of 5F9 plus rituximab may serve as an effective new immunotherapy for stimulating the innate immune system,” Dr. Advani and her colleagues reported in the New England Journal of Medicine.
The study included 22 patients, including 15 with diffuse large B-cell lymphoma (DLBCL) and 7 with follicular lymphoma, who had received a median of four prior therapies. Almost all of the non-Hodgkin lymphomas (21, or 95%) were refractory to rituximab.
All patients received intravenous 5F9 starting with a priming dose of 1 mg/kg followed by weekly maintenance doses of 10-30 mg/kg in three dose-escalation cohorts, given until disease progression or lack of clinical benefit. Intravenous rituximab at 375 mg/m2 weekly was started on the second week of the first cycle, and then monthly for cycles 2 through 6.
“Substantial antitumor activity” was seen with this chemotherapy-free regimen in a group of heavily pretreated, largely rituximab-refractory patients, Dr. Advani and her coauthors wrote in their report.
The objective response rate was 50%, including a 36% complete response rate in the intent-to-treat analysis. For DLBCL, the rates of objective and complete responses were 40% and 33%, while for follicular lymphoma, they were 71% and 43%.
The median duration of response was not reached in either disease cohort with a median follow-up of 6.2 months for DLBCL and 8.1 months for follicular lymphoma. Of the 11 patients who responded, 10 (91%) were still in response at the time of data cutoff. “Longer follow-up is needed,” the investigators wrote.
Most adverse events were seen within the first few weeks of treatment and mainly included anemia and infusion-related reactions. The anemia was an expected, on-target effect of 5F9 because of selective clearance of older red cells, which was predictable, transient, and mitigated by the maintenance dosing strategy employed in this phase 1b trial.
“As red cells age, they lose CD47 expression and gain expression of prophagocytic signals, leading to homeostatic clearance,” they wrote.
The activity of 5F9 and rituximab is “synergistic” based on the results of previous, preclinical investigations in models of lymphoma, Dr. Advani and her coauthors added.
A phase 2 trial of 5F9 plus rituximab in relapsed or refractory B-cell non-Hodgkin lymphoma is ongoing, according to their report.
The study was supported by Forty Seven and the Leukemia & Lymphoma Society. Dr. Advani reported disclosures related to Forty Seven, Bristol-Myers Squibb, Pharmacyclics, Seattle Genetics, and Roche/Genentech, among others.
SOURCE: Advani R et al. N Engl J Med. 2018;379:1711-21.
A macrophage-activating immune checkpoint inhibitor, combined with rituximab therapy, was safe and produced durable complete responses in patients with relapsed or refractory non-Hodgkin lymphoma, according to results of a phase 1b study.
Mainly low-grade toxic effects were seen on treatment with Hu5F9-G4 (5F9) and rituximab, which induced responses in more than half of patients, of which more than one-third were complete responses, the study investigators reported.
Most of the responses were ongoing at the time of data cutoff, suggesting durable responses with the combination of rituximab and 5F9 – a humanized monoclonal antibody that blocks CD47, an antiphagocytic or “do not eat me” signal overexpressed by most cancers, Ranjana Advani, MD, of Stanford (Calif.) University, and her coauthors wrote.
“The macrophage-mediated activity of 5F9 plus rituximab may serve as an effective new immunotherapy for stimulating the innate immune system,” Dr. Advani and her colleagues reported in the New England Journal of Medicine.
The study included 22 patients, including 15 with diffuse large B-cell lymphoma (DLBCL) and 7 with follicular lymphoma, who had received a median of four prior therapies. Almost all of the non-Hodgkin lymphomas (21, or 95%) were refractory to rituximab.
All patients received intravenous 5F9 starting with a priming dose of 1 mg/kg followed by weekly maintenance doses of 10-30 mg/kg in three dose-escalation cohorts, given until disease progression or lack of clinical benefit. Intravenous rituximab at 375 mg/m2 weekly was started on the second week of the first cycle, and then monthly for cycles 2 through 6.
“Substantial antitumor activity” was seen with this chemotherapy-free regimen in a group of heavily pretreated, largely rituximab-refractory patients, Dr. Advani and her coauthors wrote in their report.
The objective response rate was 50%, including a 36% complete response rate in the intent-to-treat analysis. For DLBCL, the rates of objective and complete responses were 40% and 33%, while for follicular lymphoma, they were 71% and 43%.
The median duration of response was not reached in either disease cohort with a median follow-up of 6.2 months for DLBCL and 8.1 months for follicular lymphoma. Of the 11 patients who responded, 10 (91%) were still in response at the time of data cutoff. “Longer follow-up is needed,” the investigators wrote.
Most adverse events were seen within the first few weeks of treatment and mainly included anemia and infusion-related reactions. The anemia was an expected, on-target effect of 5F9 because of selective clearance of older red cells, which was predictable, transient, and mitigated by the maintenance dosing strategy employed in this phase 1b trial.
“As red cells age, they lose CD47 expression and gain expression of prophagocytic signals, leading to homeostatic clearance,” they wrote.
The activity of 5F9 and rituximab is “synergistic” based on the results of previous, preclinical investigations in models of lymphoma, Dr. Advani and her coauthors added.
A phase 2 trial of 5F9 plus rituximab in relapsed or refractory B-cell non-Hodgkin lymphoma is ongoing, according to their report.
The study was supported by Forty Seven and the Leukemia & Lymphoma Society. Dr. Advani reported disclosures related to Forty Seven, Bristol-Myers Squibb, Pharmacyclics, Seattle Genetics, and Roche/Genentech, among others.
SOURCE: Advani R et al. N Engl J Med. 2018;379:1711-21.
A macrophage-activating immune checkpoint inhibitor, combined with rituximab therapy, was safe and produced durable complete responses in patients with relapsed or refractory non-Hodgkin lymphoma, according to results of a phase 1b study.
Mainly low-grade toxic effects were seen on treatment with Hu5F9-G4 (5F9) and rituximab, which induced responses in more than half of patients, of which more than one-third were complete responses, the study investigators reported.
Most of the responses were ongoing at the time of data cutoff, suggesting durable responses with the combination of rituximab and 5F9 – a humanized monoclonal antibody that blocks CD47, an antiphagocytic or “do not eat me” signal overexpressed by most cancers, Ranjana Advani, MD, of Stanford (Calif.) University, and her coauthors wrote.
“The macrophage-mediated activity of 5F9 plus rituximab may serve as an effective new immunotherapy for stimulating the innate immune system,” Dr. Advani and her colleagues reported in the New England Journal of Medicine.
The study included 22 patients, including 15 with diffuse large B-cell lymphoma (DLBCL) and 7 with follicular lymphoma, who had received a median of four prior therapies. Almost all of the non-Hodgkin lymphomas (21, or 95%) were refractory to rituximab.
All patients received intravenous 5F9 starting with a priming dose of 1 mg/kg followed by weekly maintenance doses of 10-30 mg/kg in three dose-escalation cohorts, given until disease progression or lack of clinical benefit. Intravenous rituximab at 375 mg/m2 weekly was started on the second week of the first cycle, and then monthly for cycles 2 through 6.
“Substantial antitumor activity” was seen with this chemotherapy-free regimen in a group of heavily pretreated, largely rituximab-refractory patients, Dr. Advani and her coauthors wrote in their report.
The objective response rate was 50%, including a 36% complete response rate in the intent-to-treat analysis. For DLBCL, the rates of objective and complete responses were 40% and 33%, while for follicular lymphoma, they were 71% and 43%.
The median duration of response was not reached in either disease cohort with a median follow-up of 6.2 months for DLBCL and 8.1 months for follicular lymphoma. Of the 11 patients who responded, 10 (91%) were still in response at the time of data cutoff. “Longer follow-up is needed,” the investigators wrote.
Most adverse events were seen within the first few weeks of treatment and mainly included anemia and infusion-related reactions. The anemia was an expected, on-target effect of 5F9 because of selective clearance of older red cells, which was predictable, transient, and mitigated by the maintenance dosing strategy employed in this phase 1b trial.
“As red cells age, they lose CD47 expression and gain expression of prophagocytic signals, leading to homeostatic clearance,” they wrote.
The activity of 5F9 and rituximab is “synergistic” based on the results of previous, preclinical investigations in models of lymphoma, Dr. Advani and her coauthors added.
A phase 2 trial of 5F9 plus rituximab in relapsed or refractory B-cell non-Hodgkin lymphoma is ongoing, according to their report.
The study was supported by Forty Seven and the Leukemia & Lymphoma Society. Dr. Advani reported disclosures related to Forty Seven, Bristol-Myers Squibb, Pharmacyclics, Seattle Genetics, and Roche/Genentech, among others.
SOURCE: Advani R et al. N Engl J Med. 2018;379:1711-21.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Rates of overall and complete responses were 50% and 36%, respectively, with most responses ongoing at the time of data cutoff.
Study details: A phase 1b study of 22 patients, including 15 with diffuse large B-cell lymphoma and 7 with follicular lymphoma.
Disclosures: The study was supported by Forty Seven and the Leukemia & Lymphoma Society. Study authors reported disclosures related to Forty Seven, Bristol-Myers Squibb, Pharmacyclics, Seattle Genetics, and Roche/Genentech, among others.
Source: Advani R et al. N Engl J Med. 2018;379:1711-21.
Venetoclax approved to treat CLL patients regardless of genotype
The approval of Bcl-2 inhibitor venetoclax was expanded by the US Food and Drug Administration in June 2018 to include the treatment of patients with chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL), regardless of their genotype, who have received at least 1 prior therapy.1 It was previously approved in 2016 for the treatment of patients who had a chromosome 17p deletion, which leads to loss of the tumor-suppressor gene TP53.
Approval was based on the positive results of the phase 3, randomized, multicenter, open-label MURANO trial in which 389 patients were randomized 1:1 to receive a combination of venetoclax and the CD20-targeting monoclonal antibody rituximab (venetoclax–rituximab) or bendamustine in combination with rituximab (bendamustine–rituximab).
Eligible patients were 18 years of age or older, had been diagnosed with relapsed/refractory CLL that required treatment, had received 1-3 prior therapies (including at least 1 chemotherapy regimen), had an Eastern Cooperative Oncology Group performance status of 0 or 1 (on a 5-point scale, with 5 indicating the greatest level of disability), and had adequate bone marrow, renal, and hepatic function.
Patients who had received prior bendamustine treatment were eligible for the trial provided they had experienced a duration of response of 24 months or longer. However, patients with transformed CLL, central nervous system involvement, prior treatment with allogeneic or autologous stem cell transplant, major organ dysfunction, other active malignancy, or who were pregnant or breastfeeding, were excluded from the study.
Patients in the venetoclax arm received a 5-week ramp-up schedule, followed by a dose of 400 mg once daily for 24 months. Rituximab treatment started at the end of the venetoclax ramp-up period and was administered at a dose of 375 mg/m2 intravenously on cycle 1 day 1 and 500 mg/m2 on day 1 of cycles 2-6. In the control arm, patients received 6 cycles with the same rituxima
The primary endpoint was progression-free survival (PFS), as assessed by an independent review committee over a median follow-up of 23 months. Median PFS was significantly improved in the venetoclax arm (not yet reached versus 18.1 months in the bendamustine arm [HR, 0.19; P < .001]). In addition, objective response rate (ORR) and event-free survival (EFS) also favored the venetoclax arm; ORR was 92% compared with 72%, respectively, and 2-year EFS was 84.9% compared with 34.8%. There was also a trend toward improved 24-month overall survival (OS) rate (91.9% vs 86.6%), however this did not achieve statistical significance, nor did median OS.
The most common adverse events (AEs) in patients treated with venetoclax were neutropenia, diarrhea, upper-respiratory tract infection, fatigue, cough, and nausea. Grade 3/4 neutropenia occurred in 64% of patients, and serious AEs in 46% of patients. Serious infections occurred in 21% of patients, most commonly pneumonia. Ten deaths in the venetoclax arm were attributed to treatment, compared with 11 deaths in the bendamustine arm.2
The prescribing information details warnings and precautions relating to the risk of tumor lysis syndrome, which is increased in patients with higher tumor burden, reduced renal function, or in receipt of strong or moderate CYP3A inhibitors or P-gp inhibitors during the ramp-up stage. Patients should receive appropriate preventive strategies, including hydration and antihyperuricemics, blood chemistry should be monitored and abnormalities managed promptly, and dosing should be interrupted or adjusted as necessary.
Other warnings relate to neutropenia (complete blood counts should be monitored throughout treatment and venetoclax treatment interrupted or dose reduced for severe neutropenia, alongside possible use of supportive measures), immunization (live vaccines should not be administered before or during treatment or after treatment until B-cell recovery, and patients should be advised of the potentially reduced efficacy of vaccines), and embryofetal toxicity (patients should be advised of the risks and the need for effective contraception during and after treatment). Venetoclax is marketed as Venclexta by Genentech.3
1. US Food and Drug Administration website. FDA approves venetoclax for CLL or SLL, with or without 17p deletion, after one prior therapy. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm610308.htm. Last updated June 8, 2018. Accessed July 29, 2018.
2. Seymour JF, Kipps TJ, Eichhorst B, et al. Venetoclax-rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378:1107-1120.
3. Venclexta (venetoclax tablets) for oral use. Prescribing information. Genentech USA, Inc. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208573s000lbl.pdf. Last updated June 2018. Accessed July 29, 2018.
The approval of Bcl-2 inhibitor venetoclax was expanded by the US Food and Drug Administration in June 2018 to include the treatment of patients with chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL), regardless of their genotype, who have received at least 1 prior therapy.1 It was previously approved in 2016 for the treatment of patients who had a chromosome 17p deletion, which leads to loss of the tumor-suppressor gene TP53.
Approval was based on the positive results of the phase 3, randomized, multicenter, open-label MURANO trial in which 389 patients were randomized 1:1 to receive a combination of venetoclax and the CD20-targeting monoclonal antibody rituximab (venetoclax–rituximab) or bendamustine in combination with rituximab (bendamustine–rituximab).
Eligible patients were 18 years of age or older, had been diagnosed with relapsed/refractory CLL that required treatment, had received 1-3 prior therapies (including at least 1 chemotherapy regimen), had an Eastern Cooperative Oncology Group performance status of 0 or 1 (on a 5-point scale, with 5 indicating the greatest level of disability), and had adequate bone marrow, renal, and hepatic function.
Patients who had received prior bendamustine treatment were eligible for the trial provided they had experienced a duration of response of 24 months or longer. However, patients with transformed CLL, central nervous system involvement, prior treatment with allogeneic or autologous stem cell transplant, major organ dysfunction, other active malignancy, or who were pregnant or breastfeeding, were excluded from the study.
Patients in the venetoclax arm received a 5-week ramp-up schedule, followed by a dose of 400 mg once daily for 24 months. Rituximab treatment started at the end of the venetoclax ramp-up period and was administered at a dose of 375 mg/m2 intravenously on cycle 1 day 1 and 500 mg/m2 on day 1 of cycles 2-6. In the control arm, patients received 6 cycles with the same rituxima
The primary endpoint was progression-free survival (PFS), as assessed by an independent review committee over a median follow-up of 23 months. Median PFS was significantly improved in the venetoclax arm (not yet reached versus 18.1 months in the bendamustine arm [HR, 0.19; P < .001]). In addition, objective response rate (ORR) and event-free survival (EFS) also favored the venetoclax arm; ORR was 92% compared with 72%, respectively, and 2-year EFS was 84.9% compared with 34.8%. There was also a trend toward improved 24-month overall survival (OS) rate (91.9% vs 86.6%), however this did not achieve statistical significance, nor did median OS.
The most common adverse events (AEs) in patients treated with venetoclax were neutropenia, diarrhea, upper-respiratory tract infection, fatigue, cough, and nausea. Grade 3/4 neutropenia occurred in 64% of patients, and serious AEs in 46% of patients. Serious infections occurred in 21% of patients, most commonly pneumonia. Ten deaths in the venetoclax arm were attributed to treatment, compared with 11 deaths in the bendamustine arm.2
The prescribing information details warnings and precautions relating to the risk of tumor lysis syndrome, which is increased in patients with higher tumor burden, reduced renal function, or in receipt of strong or moderate CYP3A inhibitors or P-gp inhibitors during the ramp-up stage. Patients should receive appropriate preventive strategies, including hydration and antihyperuricemics, blood chemistry should be monitored and abnormalities managed promptly, and dosing should be interrupted or adjusted as necessary.
Other warnings relate to neutropenia (complete blood counts should be monitored throughout treatment and venetoclax treatment interrupted or dose reduced for severe neutropenia, alongside possible use of supportive measures), immunization (live vaccines should not be administered before or during treatment or after treatment until B-cell recovery, and patients should be advised of the potentially reduced efficacy of vaccines), and embryofetal toxicity (patients should be advised of the risks and the need for effective contraception during and after treatment). Venetoclax is marketed as Venclexta by Genentech.3
The approval of Bcl-2 inhibitor venetoclax was expanded by the US Food and Drug Administration in June 2018 to include the treatment of patients with chronic lymphocytic leukemia (CLL) or small lymphocytic leukemia (SLL), regardless of their genotype, who have received at least 1 prior therapy.1 It was previously approved in 2016 for the treatment of patients who had a chromosome 17p deletion, which leads to loss of the tumor-suppressor gene TP53.
Approval was based on the positive results of the phase 3, randomized, multicenter, open-label MURANO trial in which 389 patients were randomized 1:1 to receive a combination of venetoclax and the CD20-targeting monoclonal antibody rituximab (venetoclax–rituximab) or bendamustine in combination with rituximab (bendamustine–rituximab).
Eligible patients were 18 years of age or older, had been diagnosed with relapsed/refractory CLL that required treatment, had received 1-3 prior therapies (including at least 1 chemotherapy regimen), had an Eastern Cooperative Oncology Group performance status of 0 or 1 (on a 5-point scale, with 5 indicating the greatest level of disability), and had adequate bone marrow, renal, and hepatic function.
Patients who had received prior bendamustine treatment were eligible for the trial provided they had experienced a duration of response of 24 months or longer. However, patients with transformed CLL, central nervous system involvement, prior treatment with allogeneic or autologous stem cell transplant, major organ dysfunction, other active malignancy, or who were pregnant or breastfeeding, were excluded from the study.
Patients in the venetoclax arm received a 5-week ramp-up schedule, followed by a dose of 400 mg once daily for 24 months. Rituximab treatment started at the end of the venetoclax ramp-up period and was administered at a dose of 375 mg/m2 intravenously on cycle 1 day 1 and 500 mg/m2 on day 1 of cycles 2-6. In the control arm, patients received 6 cycles with the same rituxima
The primary endpoint was progression-free survival (PFS), as assessed by an independent review committee over a median follow-up of 23 months. Median PFS was significantly improved in the venetoclax arm (not yet reached versus 18.1 months in the bendamustine arm [HR, 0.19; P < .001]). In addition, objective response rate (ORR) and event-free survival (EFS) also favored the venetoclax arm; ORR was 92% compared with 72%, respectively, and 2-year EFS was 84.9% compared with 34.8%. There was also a trend toward improved 24-month overall survival (OS) rate (91.9% vs 86.6%), however this did not achieve statistical significance, nor did median OS.
The most common adverse events (AEs) in patients treated with venetoclax were neutropenia, diarrhea, upper-respiratory tract infection, fatigue, cough, and nausea. Grade 3/4 neutropenia occurred in 64% of patients, and serious AEs in 46% of patients. Serious infections occurred in 21% of patients, most commonly pneumonia. Ten deaths in the venetoclax arm were attributed to treatment, compared with 11 deaths in the bendamustine arm.2
The prescribing information details warnings and precautions relating to the risk of tumor lysis syndrome, which is increased in patients with higher tumor burden, reduced renal function, or in receipt of strong or moderate CYP3A inhibitors or P-gp inhibitors during the ramp-up stage. Patients should receive appropriate preventive strategies, including hydration and antihyperuricemics, blood chemistry should be monitored and abnormalities managed promptly, and dosing should be interrupted or adjusted as necessary.
Other warnings relate to neutropenia (complete blood counts should be monitored throughout treatment and venetoclax treatment interrupted or dose reduced for severe neutropenia, alongside possible use of supportive measures), immunization (live vaccines should not be administered before or during treatment or after treatment until B-cell recovery, and patients should be advised of the potentially reduced efficacy of vaccines), and embryofetal toxicity (patients should be advised of the risks and the need for effective contraception during and after treatment). Venetoclax is marketed as Venclexta by Genentech.3
1. US Food and Drug Administration website. FDA approves venetoclax for CLL or SLL, with or without 17p deletion, after one prior therapy. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm610308.htm. Last updated June 8, 2018. Accessed July 29, 2018.
2. Seymour JF, Kipps TJ, Eichhorst B, et al. Venetoclax-rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378:1107-1120.
3. Venclexta (venetoclax tablets) for oral use. Prescribing information. Genentech USA, Inc. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208573s000lbl.pdf. Last updated June 2018. Accessed July 29, 2018.
1. US Food and Drug Administration website. FDA approves venetoclax for CLL or SLL, with or without 17p deletion, after one prior therapy. https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm610308.htm. Last updated June 8, 2018. Accessed July 29, 2018.
2. Seymour JF, Kipps TJ, Eichhorst B, et al. Venetoclax-rituximab in relapsed or refractory chronic lymphocytic leukemia. N Engl J Med. 2018;378:1107-1120.
3. Venclexta (venetoclax tablets) for oral use. Prescribing information. Genentech USA, Inc. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208573s000lbl.pdf. Last updated June 2018. Accessed July 29, 2018.