User login
Complex trauma in the perinatal period
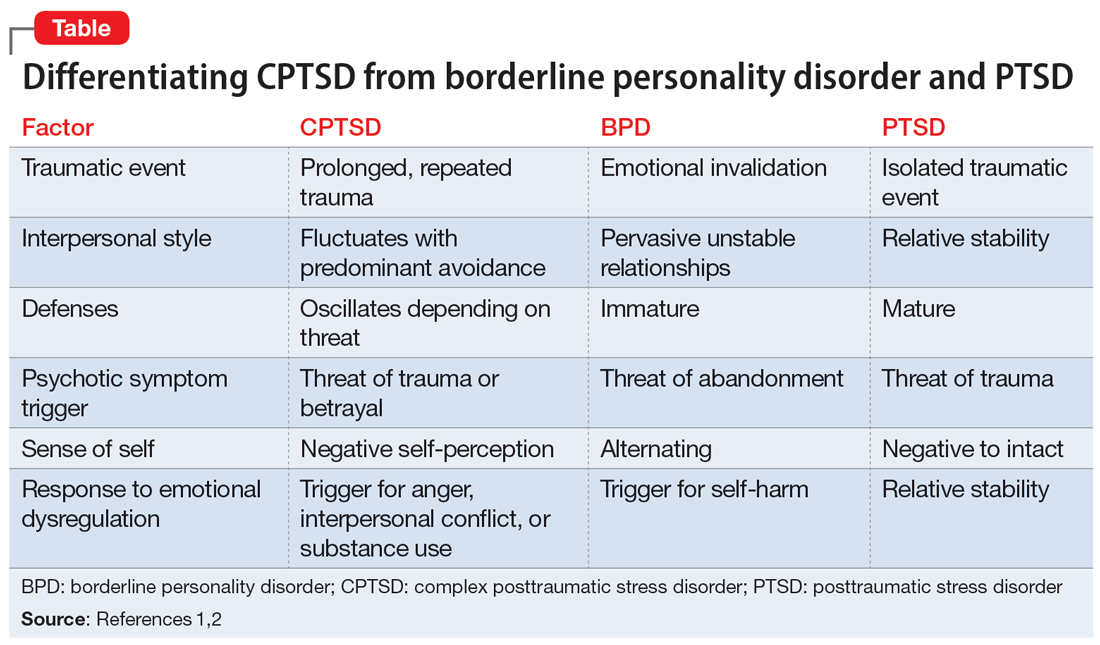
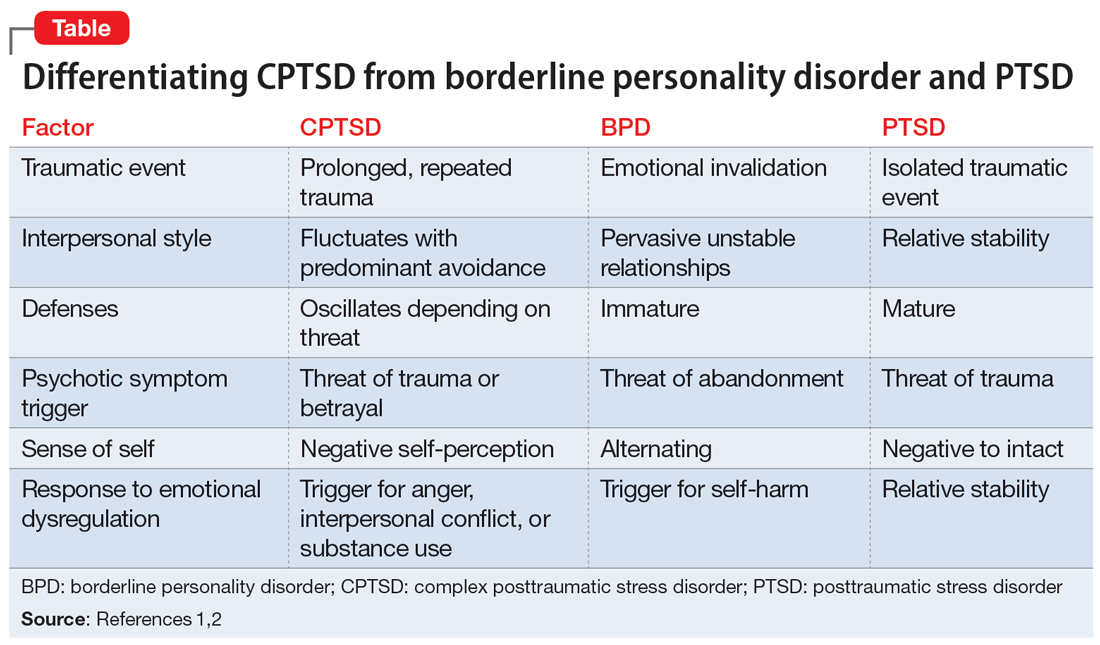
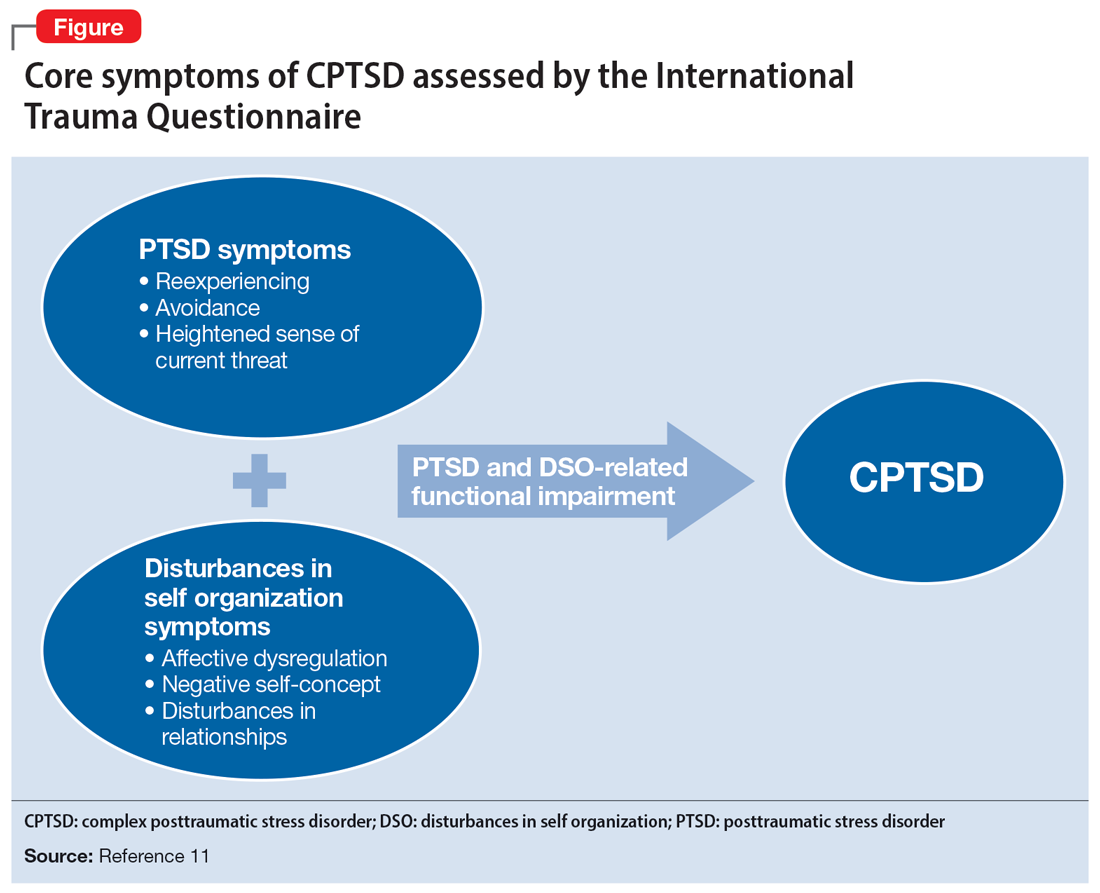
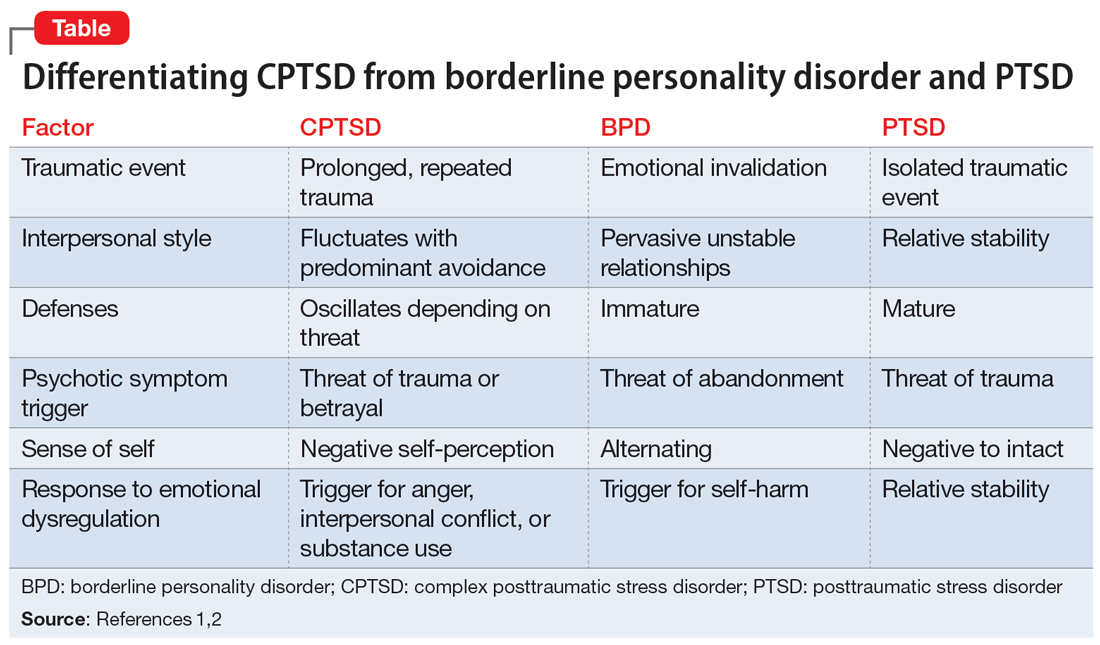
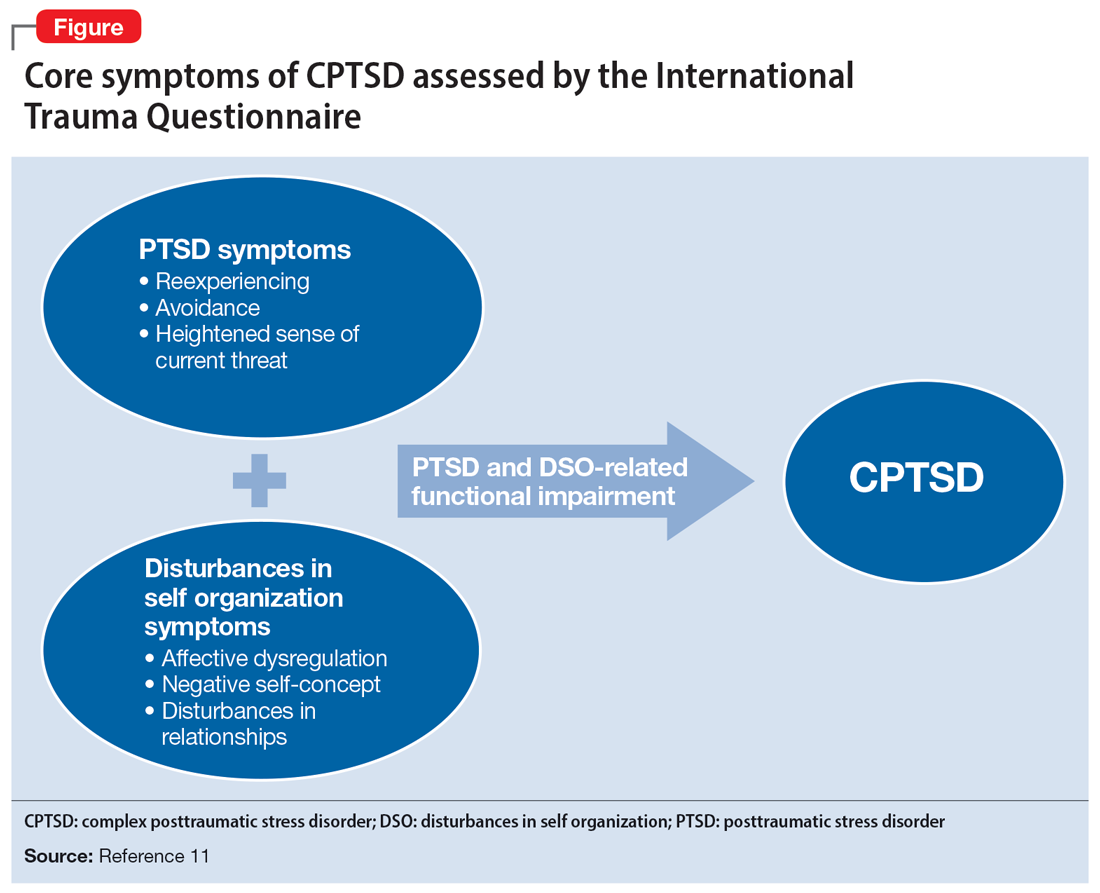
Complex posttraumatic stress disorder (CPTSD) is a condition characterized by classic trauma-related symptoms in addition to disturbances in self organization (DSO).1-3 DSO symptoms include negative self-concept, emotional dysregulation, and interpersonal problems. CPTSD differs from PTSD in that it includes symptoms of DSO, and differs from borderline personality disorder (BPD) in that it does not include extreme self-injurious behavior, a complete lack of sense of self, and avoidance of rejection or abandonment (Table1,2). The maladaptive traits of CPTSD are often the result of a chronic lack of safety in early childhood, particularly childhood sexual abuse (CSA). CSA may affect up to 20% of women and is defined by the CDC as “any completed or attempted sexual act, sexual contact with, or exploitation of a child by a caregiver.”4,5
Maternal lifetime trauma is more common among women who are in low-income minority groups and can lead to adverse birth outcomes in this vulnerable patient population.6 Recent research has found that trauma can increase cortisol levels during pregnancy, leading to increased placental permeability, inflammatory response, and longstanding alterations in the fetal hypothalamic-pituitary adrenal axis.6 A CPTSD diagnosis is of particular interest during the perinatal period because CPTSD is often a response to interpersonal trauma and attachment adversity, which can be reactivated during the perinatal period.7 CPTSD in survivors of CSA can be exacerbated due to feelings of disempowerment secondary to loss of bodily control throughout pregnancy, childbirth, breastfeeding, and obstetrical exams.5,8 Little is known about perinatal CPTSD, but we can extrapolate from trauma research that it is likely associated with the worsening of other maternal mental health conditions, suicidality, physical complaints, quality of life, maternal-child bonding outcomes, and low birth weight in offspring.5,9,10
Although there are no consensus guidelines on how to diagnose and treat CPTSD during the perinatal period, or how to promote family functioning thereafter, there are many opportunities for intervention. Mental health clinicians are in a particularly important position to care for women in the perinatal period, as collaborative work with obstetricians, pediatricians, and social services can have long-lasting effects.
In this article, we present cases of 3 CSA survivors who experienced worsening of CPTSD symptoms during the perinatal period and received psychiatric care via telehealth during the COVID-19 pandemic. We also identify best practice approaches and highlight areas for future research.
Case descriptions
Case 1
Ms. A, age 33, is married, has 3 children, has asthma, and is vaccinated against COVID-19. Her psychiatric history includes self-reported dissociative identity disorder and bulimia nervosa. At 2 months postpartum following an unplanned yet desired pregnancy, Ms. A presents to the outpatient clinic after a violent episode toward her husband during sexual intercourse. Since the first trimester of her pregnancy, she has expressed increased anxiety and difficulty sleeping, hypervigilance, intimacy avoidance, and negative views of herself and the world, yet she denies persistent depressive, manic, or psychotic symptoms, other maladaptive personality traits, or substance use. She recalls experiencing similar symptoms during her 2 previous peripartum periods, and attributes it to worsening memories of sexual abuse during childhood. Ms. A has a history of psychiatric hospitalizations during adolescence and young adulthood for suicidal ideation. She had been treated with various medications, including chlorpromazine, lamotrigine, carbamazepine, and clonazepam, but self-discontinued these medications in 2016 because she felt they were ineffective. Since becoming a mother, she has consistently denied depressive symptoms or suicidal ideation, and intermittently engaged in interpersonal psychotherapy targeting her conflictual relationship with her husband and parenting struggles.
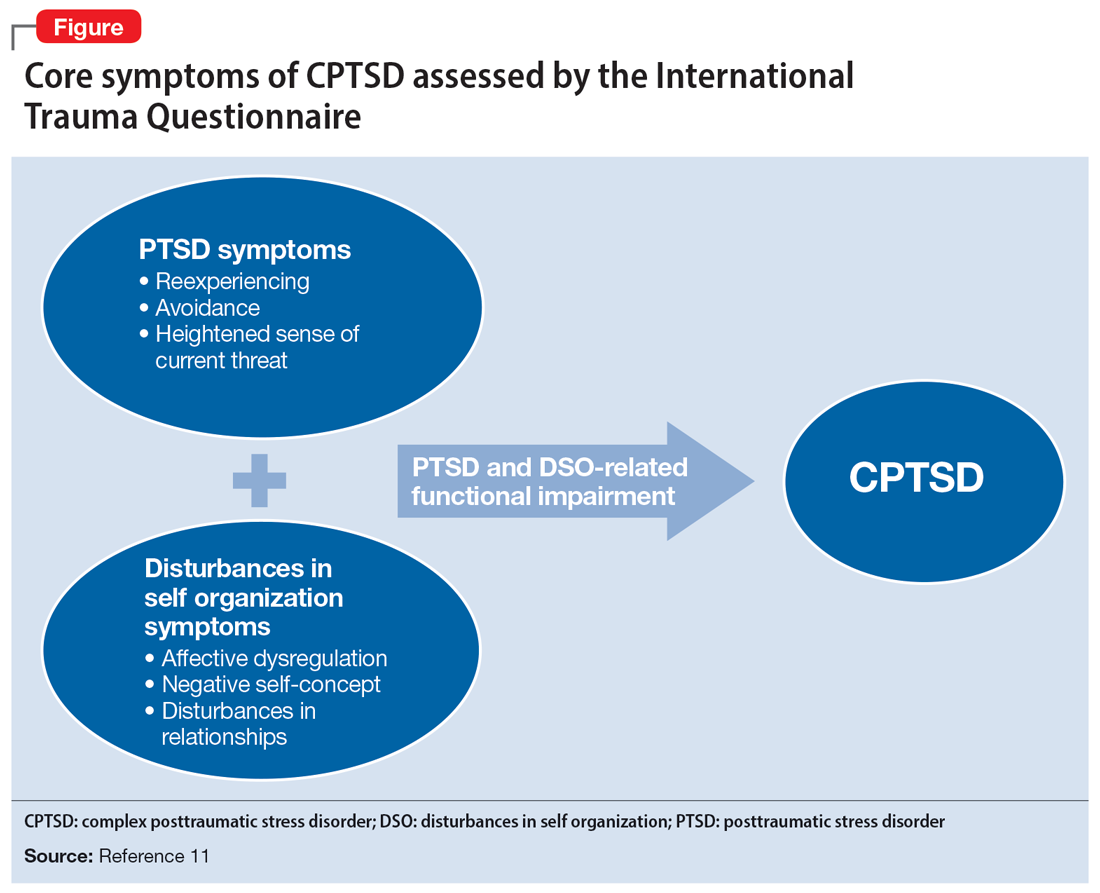
Ms. A underwent an induced vaginal delivery at 36 weeks gestation due to preeclampsia and had success with breastfeeding. While engaging in sexual activity for the first time postpartum, she dissociated and later learned she had forcefully grabbed her husband’s neck for several seconds but did not cause any longstanding physical damage. Upon learning of this episode, Ms. A’s psychiatrist asks her to complete the International Trauma Questionnaire (ITQ), a brief self-report measure developed for the assessment of the ICD-11 diagnosis of CPTSD (Figure11). Ms. A also completes the PTSD Checklist for DSM-5 (PCL-5), the Dissociative Experiences Scale, and the Edinburgh Postnatal Depression Scale (EPDS) to assist with assessing her symptoms.12-15 The psychiatrist uses ICD-11 criteria to diagnose Ms. A with CPTSD, given her functional impairment associated with both PTSD and DSO symptoms, which have acutely worsened during the perinatal period.
Ms. A initially engages in extensive trauma psychoeducation and supportive psychotherapy for 3 months. She later pursues prolonged exposure psychotherapy targeting intimacy, and after 6 months of treatment, improves her avoidance behaviors and marriage.
Continue to: Case 2
Case 2
Ms. R, age 35, is a partnered mother expecting her third child. She has no relevant medical history and is not vaccinated against COVID-19. Her psychiatric history includes self-reported panic attacks and bipolar affective disorder (BPAD). During the second trimester of a desired, unplanned pregnancy, Ms. R presents to an outpatient psychiatry clinic with symptoms of worsening dysphoria and insomnia. She endorses frequent nightmares and flashbacks of CSA as well as remote intimate partner violence. These symptoms, along with hypervigilance, insomnia, anxiety, dysphoria, negative views of herself and her surroundings, and hallucinations of a shadow that whispers “come” when she is alone, worsened during the first trimester of her pregnancy. She recalls experiencing similar trauma-related symptoms during a previous pregnancy but denies a history of pervasive depressive, manic, or psychotic symptoms. She has no other maladaptive personality traits, denies prior substance use or suicidal behavior, and has never been psychiatrically hospitalized or taken psychotropic medications.
Ms. R completes the PCL-5, ITQ, EPDS, and Mood Disorder Questionnaire (MDQ). The results are notable for significant functional impairment related to PTSD and DSO symptoms with minimal concern for BPAD symptoms. The psychiatrist uses ICD-11 criteria to diagnose Ms. R with CPTSD and discusses treatment options with her and her obstetrician. Ms. R is reluctant to take medication until she delivers her baby. She intermittently attends supportive therapy while pregnant. Her pregnancy is complicated by gestational diabetes, and she often misses appointments with her obstetrician and nutritionist.
Ms. R has an uncomplicated vaginal delivery at 38 weeks gestation and success with breastfeeding, but continues to have CPTSD symptoms. She is prescribed quetiapine 25 mg/d for anxiety, insomnia, mood, and psychotic symptoms, but stops taking the medication after 3 days due to excessive sedation. Ms. R is then prescribed sertraline 50 mg/d, which she finds helpful, but has intermittent adherence. She misses multiple virtual appointments with the psychiatrist and does not want to attend in-person sessions due to fear of contracting COVID-19. The psychiatrist encourages Ms. R to get vaccinated, focuses on organizational skills during sessions to promote attendance, and recommends in-person appointments to increase her motivation for treatment and alliance building. Despite numerous outreach attempts, Ms. R is lost to follow-up at 10 months postpartum.
Case 3
Ms. S, age 29, is a partnered mother expecting her fourth child. Her medical history includes chronic back pain. She is not vaccinated against COVID-19, and her psychiatric history includes BPAD. During the first trimester of an undesired, unplanned pregnancy, Ms. S presents to an outpatient psychiatric clinic following an episode where she held a knife over her gravid abdomen during a fight with her partner. She recounts that she became dysregulated and held a knife to her body to communicate her distress, but she did not cut herself, and adamantly denies wanting to hurt herself or the fetus. Ms. S struggles with affective instability, poor frustration tolerance, and irritability. After 1 month of treatment, she discloses surviving prolonged CSA that led to her current nightmares and flashbacks. She also endorses impaired sleep, intimacy avoidance, hypervigilance, impulsive reckless behaviors (including excessive gambling), and negative views about herself and the world that worsened since she learned she was pregnant. Ms. S reports that these same symptoms were aggravated during prior perinatal periods and recalls 2 episodes of severe dysregulation that led to an interrupted suicide attempt and a violent episode toward a loved one. She denies other self-harm behaviors, substance use, or psychotic symptoms, and denies having a history of psychiatric hospitalizations. Ms. S recalls receiving a brief trial of topiramate for BPAD and migraine when she was last in outpatient psychiatric care 8 years ago.
Her psychiatrist administers the PCL-5, ITQ, MDQ, EPDS, and Borderline Symptoms List 23 (BLS-23). The results are notable for significant PTSD and DSO symptoms.16 The psychiatrist diagnoses Ms. S with CPTSD and bipolar II disorder, exacerbated during the peripartum period. Throughout the remainder of her pregnancy, she endorses mood instability with significant irritability but declines pharmacotherapy. Ms. S intermittently engages in psychotherapy using dialectical behavioral therapy (DBT) focusing on distress tolerance because she is unable to tolerate trauma-focused psychotherapy.
Continue to: Ms. S maintains the pregnancy...
Ms. S maintains the pregnancy without any additional complications and has a vaginal delivery at 39 weeks gestation. She initiates breastfeeding but chooses not to continue after 1 month due to fatigue, insomnia, and worsening mood. Her psychiatrist wants to contact Ms. S’s partner to discuss childcare support at night to promote better sleep conditions for Ms. S, but Ms. S declines. Ms. S intermittently attends virtual appointments, adamantly refuses the COVID-19 vaccine, and is fearful of starting a mood stabilizer despite extensive psychoeducation. At 5 months postpartum, Ms. S reports that she is in a worse mood and does not want to continue the appointment or further treatment, and abruptly ends the telepsychiatry session. Her psychiatrist reaches out the following week to schedule an in-person session if Ms. S agrees to wear personal protective equipment, which she is amenable to. During that appointment, the psychiatrist discusses the risks of bipolar depression and CPTSD on both her and her childrens’ development, against the risk of lamotrigine. Ms. S begins taking lamotrigine, which she tolerates without adverse effects, and quickly notices improvement in her mood as the medication is titrated up slowly to 200 mg/d. Ms. S then engages more consistently in psychotherapy and her CPTSD and bipolar II disorder symptoms much improve at 9 months postpartum.
Ensuring an accurate CPTSD diagnosis
These 3 cases illustrate the diversity and complexity of presentations for perinatal CPTSD following CSA. A CPTSD diagnosis is complicated because the differential is broad for those reporting PTSD and DSO symptoms, and CPTSD is commonly comorbid with other disorders such as anxiety and depression.17 While various scales can facilitate PTSD screening, the ITQ is helpful because it catalogs the symptoms of disturbances in self organization and functional impairment inherent in CPTSD. The ITQ can help clinicians and patients conceptualize symptoms and track progress (Figure11).
Once a patient screens positive, a CPTSD diagnosis is best made by the clinician after a full psychiatric interview, similar to other diagnoses. Psychiatrists must use ICD-11 criteria,1 as currently there are no formal DSM-5 criteria for CPTSD.2 Additional scales facilitate CPTSD symptom inventory, such as the PCL-5 to screen and monitor for PTSD symptoms and the BLS-23 to delineate between BPD or DSO symptoms.18 Furthermore, clinicians should screen for other comorbid conditions using additional scales such as the MDQ for BPAD and the EPDS for perinatal mood and anxiety disorders. Sharing a CPTSD diagnosis with a patient is an essential step when initiating treatment. Sensitive psychoeducation on the condition and its application to the perinatal period is key to establishing safety and trust, while also empowering survivors to make their own choices regarding treatment, all essential elements to trauma-informed care.19
A range of treatment options
Once CPTSD is appropriately diagnosed, clinicians must determine whether to use pharmacotherapy, psychotherapy, or both. A meta-analysis by Coventry et al20 sought to determine the best treatment strategies for complex traumatic events such as CSA, Multicomponent interventions were most promising, and psychological interventions were associated with larger effect sizes than pharmacologic interventions for managing PTSD, mood, and sleep. Therapeutic targets include trauma memory processing, self-perception, and dissociation, along with emotion, interpersonal, and somatic regulation.21
Psychotherapy. While there are no standardized guidelines for treating CPTSD, PTSD guidelines suggest using trauma-focused cognitive-behavioral therapy (TF-CBT) as a first-line therapy, though a longer course may be needed to resolve CPTSD symptoms compared to PTSD symptoms.3 DBT for PTSD can be particularly helpful in targeting DSO symptoms.22 Narrative therapy focused on identity, embodiment, and parenting has also shown to be effective for survivors of CSA in the perinatal period, specifically with the goal of meaning-making.5 Therapy can also be effective in a group setting (ie, a “Victim to Survivor” TF-CBT group).23 Sex and couples therapy may be indicated to reestablish trust, especially when it is evident there is sexual inhibition from trauma that influences the relationship, as seen in Case 1.24
Continue to: Pharmacotherapy
Pharmacotherapy. Case 2 and Case 3 both demonstrate that while the peripartum period presents an increased risk for exacerbation of psychiatric symptoms, patients and clinicians may be reluctant to start medications due to concerns for safety during pregnancy or lactation.25 Clinicians must weigh the risks of medication exposure against the risks of exposing the fetus or newborn to untreated psychiatric disease and consult an expert in reproductive psychiatry if questions or concerns arise.26
Adverse effects of psychotropic medications must be considered, especially sedation. Medications that lead to sedation may not be safe or feasible for a mother following delivery, especially if she is breastfeeding. This was exemplified in Case 2, when Ms. R was having troubling hallucinations for which the clinician prescribed quetiapine. The medication resulted in excessive sedation and Ms. R did not feel comfortable performing childcare duties while taking the medication, which greatly influenced future therapy decisions.
Making the decision to prescribe a certain medication for CPTSD is highly influenced by the patient’s most troubling symptoms and their comorbid diagnoses. Selective serotonin reuptake inhibitors (SSRIs) generally are considered safe during pregnancy and breastfeeding, and should be considered as a first-line intervention for PTSD, mood disorders, and anxiety disorders during the perinatal period.27 While prazosin is effective for PTSD symptoms outside of pregnancy, there is limited data regarding its safety during pregnancy and lactation, and it may lead to maternal hypotension and subsequent fetal adverse effects.28
Many patients with a history of CSA experience hallucinations and dissociative symptoms, as demonstrated by Case 1 and Case 2.29 In Case 3, Ms. S displayed features of BPAD with significant hypomanic symptoms and worsening suicidality during prior postpartum periods. The clinician felt comfortable prescribing lamotrigine, a relatively safe medication during the perinatal period compared to other mood stabilizers. Ms. S was amenable to taking lamotrigine, and her clinician avoided the use of an SSRI due to a concern of worsening a bipolar diathesis in this high-risk case.30 Case 2 and Case 3 both highlight the need to closely screen for comorbid conditions such as BPAD and using caution when considering an SSRI in light of the risk of precipitating mania, especially as the patient population is younger and at higher risk for antidepressant-associated mania.31,32
Help patients tap into their sources for strength
Other therapeutic strategies when treating patients with perinatal CPTSD include encouraging survivors to mobilize their support network and sources for strength. Chamberlain et al8 suggest incorporating socioecological and cultural contexts when considering outlets for social support systems and encourage collaborating with families, especially partners, along with community and spiritual networks. As seen in Case 3, clinicians should attempt to speak to family members on behalf of their patients to promote better sleeping conditions, which can greatly alleviate CPTSD and comorbid mood symptoms, and thus reduce suicide risk.33 Sources for strength should be accentuated and clinicians may need to advocate with child protective services to support parenting rights. As demonstrated in Case 1, motherhood can greatly reduce suicide risk, and should be promoted if a child’s safety is not in danger.34
Continue to: Clinicians must recognize...
Clinicians must recognize that patients in the perinatal period face barriers to obtaining health care, especially those with CPTSD, as these patients can be difficult to engage and retain. Each case described in this article challenged the psychiatrist with engagement and alliance-building, stemming from the patient’s CPTSD symptoms of interpersonal difficulties and negative views of surroundings. Case 2 demonstrates how the diagnosis can prevent patients from receiving appropriate prenatal care, while Case 3 shows how clinicians may need more flexible attendance policies and assertive outreach attempts to deliver the mental health care these patients deserve.
These vignettes highlight the psychosocial barriers women face during the perinatal period, such as caring for their child, financial stressors, and COVID-19 pandemic–related factors that can hinder treatment, which can be compounded by trauma. The uncertainty, unpredictability, loss of control, and loss of support structures collectively experienced during the pandemic can be triggering and precipitate worsening CPTSD symptoms.35 Women who experience trauma are less likely to obtain the COVID-19 vaccine for themselves or their children, and this hesitancy is often driven by institutional distrust.36 Policy leaders and clinicians should consider these factors to promote trauma-informed COVID-19 vaccine initiatives and expand mental health access using less orthodox treatment settings, such as telepsychiatry. Telepsychiatry can serve as a bridge to in-person care as patients may feel a higher sense of control when in a familiar home environment. Case 2 and Case 3 exemplify the difficulties of delivering mental health care to perinatal women with CPTSD during the pandemic, especially those who are vaccine-hesitant, and illustrate the importance of adapting a patient’s treatment plan in a personalized and trauma-informed way.
Psychiatrists can help obstetricians and pediatricians by explaining that avoidance patterns and distrust in the clinical setting may be related to trauma and are not grounds for conscious or subconscious punishment or abandonment. Educating other clinicians about trauma-informed care, precautions to use for perinatal patients, and ways to effectively support survivors of CSA can greatly improve health outcomes for perinatal women and their offspring.37
Bottom Line
Complex posttraumatic stress disorder (CPTSD) is characterized by classic PTSD symptoms as well as disturbances in self organization, which can include mood symptoms, psychotic symptoms, and maladaptive personality traits. CPTSD resulting from childhood sexual abuse is of particular concern for women, especially during the perinatal period. Clinicians must know how to recognize the signs and symptoms of CPTSD so they can tailor a trauma-informed treatment plan and promote treatment access in this highly vulnerable patient population.
Related Resources
- Tillman B, Sloan N, Westmoreland P. How COVID-19 affects peripartum women’s mental health. Current Psychiatry. 2021;20(6):18-22. doi:10.12788/cp.0129
- Keswani M, Nemcek S, Rashid N. Is it bipolar disorder, or a complex form of PTSD? Current Psychiatry. 2021;20(12):42-49. doi:10.12788/cp.0188
Drug Brand Names
Carbamazepine • Carbatrol
Clonazepam • Klonopin
Lamotrigine • Lamictal
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
Topiramate • Topamax
1. World Health Organization. International Classification of Diseases, 11th Revision (ICD-11). Complex posttraumatic stress disorder. Accessed November 6, 2021. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/585833559
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Cloitre M, Garvert DW, Brewin CR, et al. Evidence for proposed ICD-11 PTSD and complexPTSD: a latent profile analysis. Eur J Psychotraumatol. 2013;4:10.3402/ejpt.v4i0.20706. doi:10.3402/ejpt.v4i0.20706
4. Leeb RT, Paulozzi LJ, Melanson C, et al. Child Maltreatment Surveillance: Uniform Definitions for Public Health and Recommended Data Elements, Version 1.0. Centers for Disease Control and Prevention, Department of Health & Human Services; 2008. Accessed August 24, 2022. https://www.cdc.gov/violenceprevention/pdf/cm_surveillance-a.pdf
5. Byrne J, Smart C, Watson G. “I felt like I was being abused all over again”: how survivors of child sexual abuse make sense of the perinatal period through their narratives. J Child Sex Abus. 2017;26(4):465-486. doi:10.1080/10538712.2017.1297880
6. Flom JD, Chiu YM, Hsu HL, et al. Maternal lifetime trauma and birthweight: effect modification by in utero cortisol and child sex. J Pediatr. 2018;203:301-308. doi:10.1016/j.jpeds.2018.07.069
7. Spinazzola J, van der Kolk B, Ford JD. When nowhere is safe: interpersonal trauma and attachment adversity as antecedents of posttraumatic stress disorder and developmental trauma disorder. J Trauma Stress. 2018;31(5):631-642. doi:10.1002/jts.22320
8. Chamberlain C, Gee G, Harfield S, et al. Parenting after a history of childhood maltreatment: a scoping review and map of evidence in the perinatal period. PloS One. 2019;14(3):e0213460. doi:10.1371/journal.pone.0213460
9. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18-31. doi:10.1016/j.jad.2017.07.045
10. Gavin AR, Morris J. The association between maternal early life forced sexual intercourse and offspring birth weight: the role of socioeconomic status. J Womens Health (Larchmt). 2017;26(5):442-449. doi:10.1089/jwh.2016.5789
11. Cloitre M, Shevlin M, Brewin CR, et al. The international trauma questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr Scand. 2018;138(6):536-546.
12. Cloitre M, Hyland P, Prins A, et al. The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. Eur J Psychotraumatol. 2021;12(1):1930961. doi:10.1080/20008198.2021.1930961
13. Weathers FW, Litz BT, Keane TM, et al. PTSD Checklist for DSM-5 (PCL-5). US Department of Veterans Affairs. April 11, 2018. Accessed November 25, 2021. https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.PDF
14. Dissociative Experiences Scale – II. TraumaDissociation.com. Accessed November 25, 2021. http://traumadissociation.com/des
15. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782-786. doi:10.1192/bjp.150.6.782
16. Mood Disorder Questionnaire (MDQ). Oregon Health & Science University. Accessed November 7, 2021. https://www.ohsu.edu/sites/default/files/2019-06/cms-quality-bipolar_disorder_mdq_screener.pdf
17. Karatzias T, Hyland P, Bradley A, et al. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress Anxiety. 2019;36(9):887-894. doi:10.1002/da.22934
18. Bohus M, Kleindienst N, Limberger MF, et al. The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology. 2009;42(1):32-39.
19. Fallot RD, Harris M. A trauma-informed approach to screening and assessment. New Dir Ment Health Serv. 2001;(89):23-31. doi:10.1002/yd.23320018904
20. Coventry PA, Meader N, Melton H, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLoS Med. 2020;17(8):e1003262. doi:10.1371/journal.pmed.1003262
21. Ford JD. Progress and limitations in the treatment of complex PTSD and developmental trauma disorder. Curr Treat Options Psychiatry. 2021;8:1-17. doi:10.1007/s40501-020-00236-6
22. Becker-Sadzio J, Gundel F, Kroczek A, et al. Trauma exposure therapy in a pregnant woman suffering from complex posttraumatic stress disorder after childhood sexual abuse: risk or benefit? Eur J Psychotraumatol. 2020;11(1):1697581. doi:10.1080/20008198.2019.1697581
23. Mendelsohn M, Zachary RS, Harney PA. Group therapy as an ecological bridge to new community for trauma survivors. J Aggress Maltreat Trauma. 2007;14(1-2):227-243. doi:10.1300/J146v14n01_12
24. Macintosh HB, Vaillancourt-Morel MP, Bergeron S. Sex and couple therapy with survivors of childhood trauma. In: Hall KS, Binik YM, eds. Principles and Practice of Sex Therapy. 6th ed. Guilford Press; 2020.
25. Dresner N, Byatt N, Gopalan P, et al. Psychiatric care of peripartum women. Psychiatric Times. 2015;32(12).
26. Zagorski N. How to manage meds before, during, and after pregnancy. Psychiatric News. 2019;54(14):13. https://doi.org/10.1176/APPI.PN.2019.6B36
27. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370:2397-2407. doi:10.1056/NEJMoa1312828
28. Davidson AD, Bhat A, Chu F, et al. A systematic review of the use of prazosin in pregnancy and lactation. Gen Hosp Psychiatry. 2021;71:134-136. doi:10.1016/j.genhosppsych.2021.03.012
29. Shinn AK, Wolff JD, Hwang M, et al. Assessing voice hearing in trauma spectrum disorders: a comparison of two measures and a review of the literature. Front Psychiatry. 2020;10:1011. doi:10.3389/fpsyt.2019.01011
30. Raffi ER, Nonacs R, Cohen LS. Safety of psychotropic medications during pregnancy. Clin Perinatol. 2019;46(2):215-234. doi:10.1016/j.clp.2019.02.004
31. Martin A, Young C, Leckman JF, et al. Age effects on antidepressant-induced manic conversion. Arch Pediatr Adoles Med. 2004;158(8):773-780. doi:10.1001/archpedi.158.8.773
32. Gill N, Bayes A, Parker G. A review of antidepressant-associated hypomania in those diagnosed with unipolar depression-risk factors, conceptual models, and management. Curr Psychiatry Rep. 2020;22(4):20. doi:10.1007/s11920-020-01143-6
33. Harris LM, Huang X, Linthicum KP, et al. Sleep disturbances as risk factors for suicidal thoughts and behaviours: a meta-analysis of longitudinal studies. Sci Rep. 2020;10(1):13888. doi:10.1038/s41598-020-70866-6
34. Dehara M, Wells MB, Sjöqvist H, et al. Parenthood is associated with lower suicide risk: a register-based cohort study of 1.5 million Swedes. Acta Psychiatr Scand. 2021;143(3):206-215. doi:10.1111/acps.13240
35. Iyengar U, Jaiprakash B, Haitsuka H, et al. One year into the pandemic: a systematic review of perinatal mental health outcomes during COVID-19. Front Psychiatry. 2021;12:674194. doi:10.3389/fpsyt.2021.674194
36. Milan S, Dáu ALBT. The role of trauma in mothers’ COVID-19 vaccine beliefs and intentions. J Pediatr Psychol. 2021;46(5):526-535. doi:10.1093/jpepsy/jsab043
37. Coles J, Jones K. “Universal precautions”: perinatal touch and examination after childhood sexual abuse. Birth. 2009;36(3):230-236. doi:10.1111/j.1523-536X.2009.00327
Complex posttraumatic stress disorder (CPTSD) is a condition characterized by classic trauma-related symptoms in addition to disturbances in self organization (DSO).1-3 DSO symptoms include negative self-concept, emotional dysregulation, and interpersonal problems. CPTSD differs from PTSD in that it includes symptoms of DSO, and differs from borderline personality disorder (BPD) in that it does not include extreme self-injurious behavior, a complete lack of sense of self, and avoidance of rejection or abandonment (Table1,2). The maladaptive traits of CPTSD are often the result of a chronic lack of safety in early childhood, particularly childhood sexual abuse (CSA). CSA may affect up to 20% of women and is defined by the CDC as “any completed or attempted sexual act, sexual contact with, or exploitation of a child by a caregiver.”4,5
Maternal lifetime trauma is more common among women who are in low-income minority groups and can lead to adverse birth outcomes in this vulnerable patient population.6 Recent research has found that trauma can increase cortisol levels during pregnancy, leading to increased placental permeability, inflammatory response, and longstanding alterations in the fetal hypothalamic-pituitary adrenal axis.6 A CPTSD diagnosis is of particular interest during the perinatal period because CPTSD is often a response to interpersonal trauma and attachment adversity, which can be reactivated during the perinatal period.7 CPTSD in survivors of CSA can be exacerbated due to feelings of disempowerment secondary to loss of bodily control throughout pregnancy, childbirth, breastfeeding, and obstetrical exams.5,8 Little is known about perinatal CPTSD, but we can extrapolate from trauma research that it is likely associated with the worsening of other maternal mental health conditions, suicidality, physical complaints, quality of life, maternal-child bonding outcomes, and low birth weight in offspring.5,9,10
Although there are no consensus guidelines on how to diagnose and treat CPTSD during the perinatal period, or how to promote family functioning thereafter, there are many opportunities for intervention. Mental health clinicians are in a particularly important position to care for women in the perinatal period, as collaborative work with obstetricians, pediatricians, and social services can have long-lasting effects.
In this article, we present cases of 3 CSA survivors who experienced worsening of CPTSD symptoms during the perinatal period and received psychiatric care via telehealth during the COVID-19 pandemic. We also identify best practice approaches and highlight areas for future research.
Case descriptions
Case 1
Ms. A, age 33, is married, has 3 children, has asthma, and is vaccinated against COVID-19. Her psychiatric history includes self-reported dissociative identity disorder and bulimia nervosa. At 2 months postpartum following an unplanned yet desired pregnancy, Ms. A presents to the outpatient clinic after a violent episode toward her husband during sexual intercourse. Since the first trimester of her pregnancy, she has expressed increased anxiety and difficulty sleeping, hypervigilance, intimacy avoidance, and negative views of herself and the world, yet she denies persistent depressive, manic, or psychotic symptoms, other maladaptive personality traits, or substance use. She recalls experiencing similar symptoms during her 2 previous peripartum periods, and attributes it to worsening memories of sexual abuse during childhood. Ms. A has a history of psychiatric hospitalizations during adolescence and young adulthood for suicidal ideation. She had been treated with various medications, including chlorpromazine, lamotrigine, carbamazepine, and clonazepam, but self-discontinued these medications in 2016 because she felt they were ineffective. Since becoming a mother, she has consistently denied depressive symptoms or suicidal ideation, and intermittently engaged in interpersonal psychotherapy targeting her conflictual relationship with her husband and parenting struggles.
Ms. A underwent an induced vaginal delivery at 36 weeks gestation due to preeclampsia and had success with breastfeeding. While engaging in sexual activity for the first time postpartum, she dissociated and later learned she had forcefully grabbed her husband’s neck for several seconds but did not cause any longstanding physical damage. Upon learning of this episode, Ms. A’s psychiatrist asks her to complete the International Trauma Questionnaire (ITQ), a brief self-report measure developed for the assessment of the ICD-11 diagnosis of CPTSD (Figure11). Ms. A also completes the PTSD Checklist for DSM-5 (PCL-5), the Dissociative Experiences Scale, and the Edinburgh Postnatal Depression Scale (EPDS) to assist with assessing her symptoms.12-15 The psychiatrist uses ICD-11 criteria to diagnose Ms. A with CPTSD, given her functional impairment associated with both PTSD and DSO symptoms, which have acutely worsened during the perinatal period.
Ms. A initially engages in extensive trauma psychoeducation and supportive psychotherapy for 3 months. She later pursues prolonged exposure psychotherapy targeting intimacy, and after 6 months of treatment, improves her avoidance behaviors and marriage.
Continue to: Case 2
Case 2
Ms. R, age 35, is a partnered mother expecting her third child. She has no relevant medical history and is not vaccinated against COVID-19. Her psychiatric history includes self-reported panic attacks and bipolar affective disorder (BPAD). During the second trimester of a desired, unplanned pregnancy, Ms. R presents to an outpatient psychiatry clinic with symptoms of worsening dysphoria and insomnia. She endorses frequent nightmares and flashbacks of CSA as well as remote intimate partner violence. These symptoms, along with hypervigilance, insomnia, anxiety, dysphoria, negative views of herself and her surroundings, and hallucinations of a shadow that whispers “come” when she is alone, worsened during the first trimester of her pregnancy. She recalls experiencing similar trauma-related symptoms during a previous pregnancy but denies a history of pervasive depressive, manic, or psychotic symptoms. She has no other maladaptive personality traits, denies prior substance use or suicidal behavior, and has never been psychiatrically hospitalized or taken psychotropic medications.
Ms. R completes the PCL-5, ITQ, EPDS, and Mood Disorder Questionnaire (MDQ). The results are notable for significant functional impairment related to PTSD and DSO symptoms with minimal concern for BPAD symptoms. The psychiatrist uses ICD-11 criteria to diagnose Ms. R with CPTSD and discusses treatment options with her and her obstetrician. Ms. R is reluctant to take medication until she delivers her baby. She intermittently attends supportive therapy while pregnant. Her pregnancy is complicated by gestational diabetes, and she often misses appointments with her obstetrician and nutritionist.
Ms. R has an uncomplicated vaginal delivery at 38 weeks gestation and success with breastfeeding, but continues to have CPTSD symptoms. She is prescribed quetiapine 25 mg/d for anxiety, insomnia, mood, and psychotic symptoms, but stops taking the medication after 3 days due to excessive sedation. Ms. R is then prescribed sertraline 50 mg/d, which she finds helpful, but has intermittent adherence. She misses multiple virtual appointments with the psychiatrist and does not want to attend in-person sessions due to fear of contracting COVID-19. The psychiatrist encourages Ms. R to get vaccinated, focuses on organizational skills during sessions to promote attendance, and recommends in-person appointments to increase her motivation for treatment and alliance building. Despite numerous outreach attempts, Ms. R is lost to follow-up at 10 months postpartum.
Case 3
Ms. S, age 29, is a partnered mother expecting her fourth child. Her medical history includes chronic back pain. She is not vaccinated against COVID-19, and her psychiatric history includes BPAD. During the first trimester of an undesired, unplanned pregnancy, Ms. S presents to an outpatient psychiatric clinic following an episode where she held a knife over her gravid abdomen during a fight with her partner. She recounts that she became dysregulated and held a knife to her body to communicate her distress, but she did not cut herself, and adamantly denies wanting to hurt herself or the fetus. Ms. S struggles with affective instability, poor frustration tolerance, and irritability. After 1 month of treatment, she discloses surviving prolonged CSA that led to her current nightmares and flashbacks. She also endorses impaired sleep, intimacy avoidance, hypervigilance, impulsive reckless behaviors (including excessive gambling), and negative views about herself and the world that worsened since she learned she was pregnant. Ms. S reports that these same symptoms were aggravated during prior perinatal periods and recalls 2 episodes of severe dysregulation that led to an interrupted suicide attempt and a violent episode toward a loved one. She denies other self-harm behaviors, substance use, or psychotic symptoms, and denies having a history of psychiatric hospitalizations. Ms. S recalls receiving a brief trial of topiramate for BPAD and migraine when she was last in outpatient psychiatric care 8 years ago.
Her psychiatrist administers the PCL-5, ITQ, MDQ, EPDS, and Borderline Symptoms List 23 (BLS-23). The results are notable for significant PTSD and DSO symptoms.16 The psychiatrist diagnoses Ms. S with CPTSD and bipolar II disorder, exacerbated during the peripartum period. Throughout the remainder of her pregnancy, she endorses mood instability with significant irritability but declines pharmacotherapy. Ms. S intermittently engages in psychotherapy using dialectical behavioral therapy (DBT) focusing on distress tolerance because she is unable to tolerate trauma-focused psychotherapy.
Continue to: Ms. S maintains the pregnancy...
Ms. S maintains the pregnancy without any additional complications and has a vaginal delivery at 39 weeks gestation. She initiates breastfeeding but chooses not to continue after 1 month due to fatigue, insomnia, and worsening mood. Her psychiatrist wants to contact Ms. S’s partner to discuss childcare support at night to promote better sleep conditions for Ms. S, but Ms. S declines. Ms. S intermittently attends virtual appointments, adamantly refuses the COVID-19 vaccine, and is fearful of starting a mood stabilizer despite extensive psychoeducation. At 5 months postpartum, Ms. S reports that she is in a worse mood and does not want to continue the appointment or further treatment, and abruptly ends the telepsychiatry session. Her psychiatrist reaches out the following week to schedule an in-person session if Ms. S agrees to wear personal protective equipment, which she is amenable to. During that appointment, the psychiatrist discusses the risks of bipolar depression and CPTSD on both her and her childrens’ development, against the risk of lamotrigine. Ms. S begins taking lamotrigine, which she tolerates without adverse effects, and quickly notices improvement in her mood as the medication is titrated up slowly to 200 mg/d. Ms. S then engages more consistently in psychotherapy and her CPTSD and bipolar II disorder symptoms much improve at 9 months postpartum.
Ensuring an accurate CPTSD diagnosis
These 3 cases illustrate the diversity and complexity of presentations for perinatal CPTSD following CSA. A CPTSD diagnosis is complicated because the differential is broad for those reporting PTSD and DSO symptoms, and CPTSD is commonly comorbid with other disorders such as anxiety and depression.17 While various scales can facilitate PTSD screening, the ITQ is helpful because it catalogs the symptoms of disturbances in self organization and functional impairment inherent in CPTSD. The ITQ can help clinicians and patients conceptualize symptoms and track progress (Figure11).
Once a patient screens positive, a CPTSD diagnosis is best made by the clinician after a full psychiatric interview, similar to other diagnoses. Psychiatrists must use ICD-11 criteria,1 as currently there are no formal DSM-5 criteria for CPTSD.2 Additional scales facilitate CPTSD symptom inventory, such as the PCL-5 to screen and monitor for PTSD symptoms and the BLS-23 to delineate between BPD or DSO symptoms.18 Furthermore, clinicians should screen for other comorbid conditions using additional scales such as the MDQ for BPAD and the EPDS for perinatal mood and anxiety disorders. Sharing a CPTSD diagnosis with a patient is an essential step when initiating treatment. Sensitive psychoeducation on the condition and its application to the perinatal period is key to establishing safety and trust, while also empowering survivors to make their own choices regarding treatment, all essential elements to trauma-informed care.19
A range of treatment options
Once CPTSD is appropriately diagnosed, clinicians must determine whether to use pharmacotherapy, psychotherapy, or both. A meta-analysis by Coventry et al20 sought to determine the best treatment strategies for complex traumatic events such as CSA, Multicomponent interventions were most promising, and psychological interventions were associated with larger effect sizes than pharmacologic interventions for managing PTSD, mood, and sleep. Therapeutic targets include trauma memory processing, self-perception, and dissociation, along with emotion, interpersonal, and somatic regulation.21
Psychotherapy. While there are no standardized guidelines for treating CPTSD, PTSD guidelines suggest using trauma-focused cognitive-behavioral therapy (TF-CBT) as a first-line therapy, though a longer course may be needed to resolve CPTSD symptoms compared to PTSD symptoms.3 DBT for PTSD can be particularly helpful in targeting DSO symptoms.22 Narrative therapy focused on identity, embodiment, and parenting has also shown to be effective for survivors of CSA in the perinatal period, specifically with the goal of meaning-making.5 Therapy can also be effective in a group setting (ie, a “Victim to Survivor” TF-CBT group).23 Sex and couples therapy may be indicated to reestablish trust, especially when it is evident there is sexual inhibition from trauma that influences the relationship, as seen in Case 1.24
Continue to: Pharmacotherapy
Pharmacotherapy. Case 2 and Case 3 both demonstrate that while the peripartum period presents an increased risk for exacerbation of psychiatric symptoms, patients and clinicians may be reluctant to start medications due to concerns for safety during pregnancy or lactation.25 Clinicians must weigh the risks of medication exposure against the risks of exposing the fetus or newborn to untreated psychiatric disease and consult an expert in reproductive psychiatry if questions or concerns arise.26
Adverse effects of psychotropic medications must be considered, especially sedation. Medications that lead to sedation may not be safe or feasible for a mother following delivery, especially if she is breastfeeding. This was exemplified in Case 2, when Ms. R was having troubling hallucinations for which the clinician prescribed quetiapine. The medication resulted in excessive sedation and Ms. R did not feel comfortable performing childcare duties while taking the medication, which greatly influenced future therapy decisions.
Making the decision to prescribe a certain medication for CPTSD is highly influenced by the patient’s most troubling symptoms and their comorbid diagnoses. Selective serotonin reuptake inhibitors (SSRIs) generally are considered safe during pregnancy and breastfeeding, and should be considered as a first-line intervention for PTSD, mood disorders, and anxiety disorders during the perinatal period.27 While prazosin is effective for PTSD symptoms outside of pregnancy, there is limited data regarding its safety during pregnancy and lactation, and it may lead to maternal hypotension and subsequent fetal adverse effects.28
Many patients with a history of CSA experience hallucinations and dissociative symptoms, as demonstrated by Case 1 and Case 2.29 In Case 3, Ms. S displayed features of BPAD with significant hypomanic symptoms and worsening suicidality during prior postpartum periods. The clinician felt comfortable prescribing lamotrigine, a relatively safe medication during the perinatal period compared to other mood stabilizers. Ms. S was amenable to taking lamotrigine, and her clinician avoided the use of an SSRI due to a concern of worsening a bipolar diathesis in this high-risk case.30 Case 2 and Case 3 both highlight the need to closely screen for comorbid conditions such as BPAD and using caution when considering an SSRI in light of the risk of precipitating mania, especially as the patient population is younger and at higher risk for antidepressant-associated mania.31,32
Help patients tap into their sources for strength
Other therapeutic strategies when treating patients with perinatal CPTSD include encouraging survivors to mobilize their support network and sources for strength. Chamberlain et al8 suggest incorporating socioecological and cultural contexts when considering outlets for social support systems and encourage collaborating with families, especially partners, along with community and spiritual networks. As seen in Case 3, clinicians should attempt to speak to family members on behalf of their patients to promote better sleeping conditions, which can greatly alleviate CPTSD and comorbid mood symptoms, and thus reduce suicide risk.33 Sources for strength should be accentuated and clinicians may need to advocate with child protective services to support parenting rights. As demonstrated in Case 1, motherhood can greatly reduce suicide risk, and should be promoted if a child’s safety is not in danger.34
Continue to: Clinicians must recognize...
Clinicians must recognize that patients in the perinatal period face barriers to obtaining health care, especially those with CPTSD, as these patients can be difficult to engage and retain. Each case described in this article challenged the psychiatrist with engagement and alliance-building, stemming from the patient’s CPTSD symptoms of interpersonal difficulties and negative views of surroundings. Case 2 demonstrates how the diagnosis can prevent patients from receiving appropriate prenatal care, while Case 3 shows how clinicians may need more flexible attendance policies and assertive outreach attempts to deliver the mental health care these patients deserve.
These vignettes highlight the psychosocial barriers women face during the perinatal period, such as caring for their child, financial stressors, and COVID-19 pandemic–related factors that can hinder treatment, which can be compounded by trauma. The uncertainty, unpredictability, loss of control, and loss of support structures collectively experienced during the pandemic can be triggering and precipitate worsening CPTSD symptoms.35 Women who experience trauma are less likely to obtain the COVID-19 vaccine for themselves or their children, and this hesitancy is often driven by institutional distrust.36 Policy leaders and clinicians should consider these factors to promote trauma-informed COVID-19 vaccine initiatives and expand mental health access using less orthodox treatment settings, such as telepsychiatry. Telepsychiatry can serve as a bridge to in-person care as patients may feel a higher sense of control when in a familiar home environment. Case 2 and Case 3 exemplify the difficulties of delivering mental health care to perinatal women with CPTSD during the pandemic, especially those who are vaccine-hesitant, and illustrate the importance of adapting a patient’s treatment plan in a personalized and trauma-informed way.
Psychiatrists can help obstetricians and pediatricians by explaining that avoidance patterns and distrust in the clinical setting may be related to trauma and are not grounds for conscious or subconscious punishment or abandonment. Educating other clinicians about trauma-informed care, precautions to use for perinatal patients, and ways to effectively support survivors of CSA can greatly improve health outcomes for perinatal women and their offspring.37
Bottom Line
Complex posttraumatic stress disorder (CPTSD) is characterized by classic PTSD symptoms as well as disturbances in self organization, which can include mood symptoms, psychotic symptoms, and maladaptive personality traits. CPTSD resulting from childhood sexual abuse is of particular concern for women, especially during the perinatal period. Clinicians must know how to recognize the signs and symptoms of CPTSD so they can tailor a trauma-informed treatment plan and promote treatment access in this highly vulnerable patient population.
Related Resources
- Tillman B, Sloan N, Westmoreland P. How COVID-19 affects peripartum women’s mental health. Current Psychiatry. 2021;20(6):18-22. doi:10.12788/cp.0129
- Keswani M, Nemcek S, Rashid N. Is it bipolar disorder, or a complex form of PTSD? Current Psychiatry. 2021;20(12):42-49. doi:10.12788/cp.0188
Drug Brand Names
Carbamazepine • Carbatrol
Clonazepam • Klonopin
Lamotrigine • Lamictal
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
Topiramate • Topamax
Complex posttraumatic stress disorder (CPTSD) is a condition characterized by classic trauma-related symptoms in addition to disturbances in self organization (DSO).1-3 DSO symptoms include negative self-concept, emotional dysregulation, and interpersonal problems. CPTSD differs from PTSD in that it includes symptoms of DSO, and differs from borderline personality disorder (BPD) in that it does not include extreme self-injurious behavior, a complete lack of sense of self, and avoidance of rejection or abandonment (Table1,2). The maladaptive traits of CPTSD are often the result of a chronic lack of safety in early childhood, particularly childhood sexual abuse (CSA). CSA may affect up to 20% of women and is defined by the CDC as “any completed or attempted sexual act, sexual contact with, or exploitation of a child by a caregiver.”4,5
Maternal lifetime trauma is more common among women who are in low-income minority groups and can lead to adverse birth outcomes in this vulnerable patient population.6 Recent research has found that trauma can increase cortisol levels during pregnancy, leading to increased placental permeability, inflammatory response, and longstanding alterations in the fetal hypothalamic-pituitary adrenal axis.6 A CPTSD diagnosis is of particular interest during the perinatal period because CPTSD is often a response to interpersonal trauma and attachment adversity, which can be reactivated during the perinatal period.7 CPTSD in survivors of CSA can be exacerbated due to feelings of disempowerment secondary to loss of bodily control throughout pregnancy, childbirth, breastfeeding, and obstetrical exams.5,8 Little is known about perinatal CPTSD, but we can extrapolate from trauma research that it is likely associated with the worsening of other maternal mental health conditions, suicidality, physical complaints, quality of life, maternal-child bonding outcomes, and low birth weight in offspring.5,9,10
Although there are no consensus guidelines on how to diagnose and treat CPTSD during the perinatal period, or how to promote family functioning thereafter, there are many opportunities for intervention. Mental health clinicians are in a particularly important position to care for women in the perinatal period, as collaborative work with obstetricians, pediatricians, and social services can have long-lasting effects.
In this article, we present cases of 3 CSA survivors who experienced worsening of CPTSD symptoms during the perinatal period and received psychiatric care via telehealth during the COVID-19 pandemic. We also identify best practice approaches and highlight areas for future research.
Case descriptions
Case 1
Ms. A, age 33, is married, has 3 children, has asthma, and is vaccinated against COVID-19. Her psychiatric history includes self-reported dissociative identity disorder and bulimia nervosa. At 2 months postpartum following an unplanned yet desired pregnancy, Ms. A presents to the outpatient clinic after a violent episode toward her husband during sexual intercourse. Since the first trimester of her pregnancy, she has expressed increased anxiety and difficulty sleeping, hypervigilance, intimacy avoidance, and negative views of herself and the world, yet she denies persistent depressive, manic, or psychotic symptoms, other maladaptive personality traits, or substance use. She recalls experiencing similar symptoms during her 2 previous peripartum periods, and attributes it to worsening memories of sexual abuse during childhood. Ms. A has a history of psychiatric hospitalizations during adolescence and young adulthood for suicidal ideation. She had been treated with various medications, including chlorpromazine, lamotrigine, carbamazepine, and clonazepam, but self-discontinued these medications in 2016 because she felt they were ineffective. Since becoming a mother, she has consistently denied depressive symptoms or suicidal ideation, and intermittently engaged in interpersonal psychotherapy targeting her conflictual relationship with her husband and parenting struggles.
Ms. A underwent an induced vaginal delivery at 36 weeks gestation due to preeclampsia and had success with breastfeeding. While engaging in sexual activity for the first time postpartum, she dissociated and later learned she had forcefully grabbed her husband’s neck for several seconds but did not cause any longstanding physical damage. Upon learning of this episode, Ms. A’s psychiatrist asks her to complete the International Trauma Questionnaire (ITQ), a brief self-report measure developed for the assessment of the ICD-11 diagnosis of CPTSD (Figure11). Ms. A also completes the PTSD Checklist for DSM-5 (PCL-5), the Dissociative Experiences Scale, and the Edinburgh Postnatal Depression Scale (EPDS) to assist with assessing her symptoms.12-15 The psychiatrist uses ICD-11 criteria to diagnose Ms. A with CPTSD, given her functional impairment associated with both PTSD and DSO symptoms, which have acutely worsened during the perinatal period.
Ms. A initially engages in extensive trauma psychoeducation and supportive psychotherapy for 3 months. She later pursues prolonged exposure psychotherapy targeting intimacy, and after 6 months of treatment, improves her avoidance behaviors and marriage.
Continue to: Case 2
Case 2
Ms. R, age 35, is a partnered mother expecting her third child. She has no relevant medical history and is not vaccinated against COVID-19. Her psychiatric history includes self-reported panic attacks and bipolar affective disorder (BPAD). During the second trimester of a desired, unplanned pregnancy, Ms. R presents to an outpatient psychiatry clinic with symptoms of worsening dysphoria and insomnia. She endorses frequent nightmares and flashbacks of CSA as well as remote intimate partner violence. These symptoms, along with hypervigilance, insomnia, anxiety, dysphoria, negative views of herself and her surroundings, and hallucinations of a shadow that whispers “come” when she is alone, worsened during the first trimester of her pregnancy. She recalls experiencing similar trauma-related symptoms during a previous pregnancy but denies a history of pervasive depressive, manic, or psychotic symptoms. She has no other maladaptive personality traits, denies prior substance use or suicidal behavior, and has never been psychiatrically hospitalized or taken psychotropic medications.
Ms. R completes the PCL-5, ITQ, EPDS, and Mood Disorder Questionnaire (MDQ). The results are notable for significant functional impairment related to PTSD and DSO symptoms with minimal concern for BPAD symptoms. The psychiatrist uses ICD-11 criteria to diagnose Ms. R with CPTSD and discusses treatment options with her and her obstetrician. Ms. R is reluctant to take medication until she delivers her baby. She intermittently attends supportive therapy while pregnant. Her pregnancy is complicated by gestational diabetes, and she often misses appointments with her obstetrician and nutritionist.
Ms. R has an uncomplicated vaginal delivery at 38 weeks gestation and success with breastfeeding, but continues to have CPTSD symptoms. She is prescribed quetiapine 25 mg/d for anxiety, insomnia, mood, and psychotic symptoms, but stops taking the medication after 3 days due to excessive sedation. Ms. R is then prescribed sertraline 50 mg/d, which she finds helpful, but has intermittent adherence. She misses multiple virtual appointments with the psychiatrist and does not want to attend in-person sessions due to fear of contracting COVID-19. The psychiatrist encourages Ms. R to get vaccinated, focuses on organizational skills during sessions to promote attendance, and recommends in-person appointments to increase her motivation for treatment and alliance building. Despite numerous outreach attempts, Ms. R is lost to follow-up at 10 months postpartum.
Case 3
Ms. S, age 29, is a partnered mother expecting her fourth child. Her medical history includes chronic back pain. She is not vaccinated against COVID-19, and her psychiatric history includes BPAD. During the first trimester of an undesired, unplanned pregnancy, Ms. S presents to an outpatient psychiatric clinic following an episode where she held a knife over her gravid abdomen during a fight with her partner. She recounts that she became dysregulated and held a knife to her body to communicate her distress, but she did not cut herself, and adamantly denies wanting to hurt herself or the fetus. Ms. S struggles with affective instability, poor frustration tolerance, and irritability. After 1 month of treatment, she discloses surviving prolonged CSA that led to her current nightmares and flashbacks. She also endorses impaired sleep, intimacy avoidance, hypervigilance, impulsive reckless behaviors (including excessive gambling), and negative views about herself and the world that worsened since she learned she was pregnant. Ms. S reports that these same symptoms were aggravated during prior perinatal periods and recalls 2 episodes of severe dysregulation that led to an interrupted suicide attempt and a violent episode toward a loved one. She denies other self-harm behaviors, substance use, or psychotic symptoms, and denies having a history of psychiatric hospitalizations. Ms. S recalls receiving a brief trial of topiramate for BPAD and migraine when she was last in outpatient psychiatric care 8 years ago.
Her psychiatrist administers the PCL-5, ITQ, MDQ, EPDS, and Borderline Symptoms List 23 (BLS-23). The results are notable for significant PTSD and DSO symptoms.16 The psychiatrist diagnoses Ms. S with CPTSD and bipolar II disorder, exacerbated during the peripartum period. Throughout the remainder of her pregnancy, she endorses mood instability with significant irritability but declines pharmacotherapy. Ms. S intermittently engages in psychotherapy using dialectical behavioral therapy (DBT) focusing on distress tolerance because she is unable to tolerate trauma-focused psychotherapy.
Continue to: Ms. S maintains the pregnancy...
Ms. S maintains the pregnancy without any additional complications and has a vaginal delivery at 39 weeks gestation. She initiates breastfeeding but chooses not to continue after 1 month due to fatigue, insomnia, and worsening mood. Her psychiatrist wants to contact Ms. S’s partner to discuss childcare support at night to promote better sleep conditions for Ms. S, but Ms. S declines. Ms. S intermittently attends virtual appointments, adamantly refuses the COVID-19 vaccine, and is fearful of starting a mood stabilizer despite extensive psychoeducation. At 5 months postpartum, Ms. S reports that she is in a worse mood and does not want to continue the appointment or further treatment, and abruptly ends the telepsychiatry session. Her psychiatrist reaches out the following week to schedule an in-person session if Ms. S agrees to wear personal protective equipment, which she is amenable to. During that appointment, the psychiatrist discusses the risks of bipolar depression and CPTSD on both her and her childrens’ development, against the risk of lamotrigine. Ms. S begins taking lamotrigine, which she tolerates without adverse effects, and quickly notices improvement in her mood as the medication is titrated up slowly to 200 mg/d. Ms. S then engages more consistently in psychotherapy and her CPTSD and bipolar II disorder symptoms much improve at 9 months postpartum.
Ensuring an accurate CPTSD diagnosis
These 3 cases illustrate the diversity and complexity of presentations for perinatal CPTSD following CSA. A CPTSD diagnosis is complicated because the differential is broad for those reporting PTSD and DSO symptoms, and CPTSD is commonly comorbid with other disorders such as anxiety and depression.17 While various scales can facilitate PTSD screening, the ITQ is helpful because it catalogs the symptoms of disturbances in self organization and functional impairment inherent in CPTSD. The ITQ can help clinicians and patients conceptualize symptoms and track progress (Figure11).
Once a patient screens positive, a CPTSD diagnosis is best made by the clinician after a full psychiatric interview, similar to other diagnoses. Psychiatrists must use ICD-11 criteria,1 as currently there are no formal DSM-5 criteria for CPTSD.2 Additional scales facilitate CPTSD symptom inventory, such as the PCL-5 to screen and monitor for PTSD symptoms and the BLS-23 to delineate between BPD or DSO symptoms.18 Furthermore, clinicians should screen for other comorbid conditions using additional scales such as the MDQ for BPAD and the EPDS for perinatal mood and anxiety disorders. Sharing a CPTSD diagnosis with a patient is an essential step when initiating treatment. Sensitive psychoeducation on the condition and its application to the perinatal period is key to establishing safety and trust, while also empowering survivors to make their own choices regarding treatment, all essential elements to trauma-informed care.19
A range of treatment options
Once CPTSD is appropriately diagnosed, clinicians must determine whether to use pharmacotherapy, psychotherapy, or both. A meta-analysis by Coventry et al20 sought to determine the best treatment strategies for complex traumatic events such as CSA, Multicomponent interventions were most promising, and psychological interventions were associated with larger effect sizes than pharmacologic interventions for managing PTSD, mood, and sleep. Therapeutic targets include trauma memory processing, self-perception, and dissociation, along with emotion, interpersonal, and somatic regulation.21
Psychotherapy. While there are no standardized guidelines for treating CPTSD, PTSD guidelines suggest using trauma-focused cognitive-behavioral therapy (TF-CBT) as a first-line therapy, though a longer course may be needed to resolve CPTSD symptoms compared to PTSD symptoms.3 DBT for PTSD can be particularly helpful in targeting DSO symptoms.22 Narrative therapy focused on identity, embodiment, and parenting has also shown to be effective for survivors of CSA in the perinatal period, specifically with the goal of meaning-making.5 Therapy can also be effective in a group setting (ie, a “Victim to Survivor” TF-CBT group).23 Sex and couples therapy may be indicated to reestablish trust, especially when it is evident there is sexual inhibition from trauma that influences the relationship, as seen in Case 1.24
Continue to: Pharmacotherapy
Pharmacotherapy. Case 2 and Case 3 both demonstrate that while the peripartum period presents an increased risk for exacerbation of psychiatric symptoms, patients and clinicians may be reluctant to start medications due to concerns for safety during pregnancy or lactation.25 Clinicians must weigh the risks of medication exposure against the risks of exposing the fetus or newborn to untreated psychiatric disease and consult an expert in reproductive psychiatry if questions or concerns arise.26
Adverse effects of psychotropic medications must be considered, especially sedation. Medications that lead to sedation may not be safe or feasible for a mother following delivery, especially if she is breastfeeding. This was exemplified in Case 2, when Ms. R was having troubling hallucinations for which the clinician prescribed quetiapine. The medication resulted in excessive sedation and Ms. R did not feel comfortable performing childcare duties while taking the medication, which greatly influenced future therapy decisions.
Making the decision to prescribe a certain medication for CPTSD is highly influenced by the patient’s most troubling symptoms and their comorbid diagnoses. Selective serotonin reuptake inhibitors (SSRIs) generally are considered safe during pregnancy and breastfeeding, and should be considered as a first-line intervention for PTSD, mood disorders, and anxiety disorders during the perinatal period.27 While prazosin is effective for PTSD symptoms outside of pregnancy, there is limited data regarding its safety during pregnancy and lactation, and it may lead to maternal hypotension and subsequent fetal adverse effects.28
Many patients with a history of CSA experience hallucinations and dissociative symptoms, as demonstrated by Case 1 and Case 2.29 In Case 3, Ms. S displayed features of BPAD with significant hypomanic symptoms and worsening suicidality during prior postpartum periods. The clinician felt comfortable prescribing lamotrigine, a relatively safe medication during the perinatal period compared to other mood stabilizers. Ms. S was amenable to taking lamotrigine, and her clinician avoided the use of an SSRI due to a concern of worsening a bipolar diathesis in this high-risk case.30 Case 2 and Case 3 both highlight the need to closely screen for comorbid conditions such as BPAD and using caution when considering an SSRI in light of the risk of precipitating mania, especially as the patient population is younger and at higher risk for antidepressant-associated mania.31,32
Help patients tap into their sources for strength
Other therapeutic strategies when treating patients with perinatal CPTSD include encouraging survivors to mobilize their support network and sources for strength. Chamberlain et al8 suggest incorporating socioecological and cultural contexts when considering outlets for social support systems and encourage collaborating with families, especially partners, along with community and spiritual networks. As seen in Case 3, clinicians should attempt to speak to family members on behalf of their patients to promote better sleeping conditions, which can greatly alleviate CPTSD and comorbid mood symptoms, and thus reduce suicide risk.33 Sources for strength should be accentuated and clinicians may need to advocate with child protective services to support parenting rights. As demonstrated in Case 1, motherhood can greatly reduce suicide risk, and should be promoted if a child’s safety is not in danger.34
Continue to: Clinicians must recognize...
Clinicians must recognize that patients in the perinatal period face barriers to obtaining health care, especially those with CPTSD, as these patients can be difficult to engage and retain. Each case described in this article challenged the psychiatrist with engagement and alliance-building, stemming from the patient’s CPTSD symptoms of interpersonal difficulties and negative views of surroundings. Case 2 demonstrates how the diagnosis can prevent patients from receiving appropriate prenatal care, while Case 3 shows how clinicians may need more flexible attendance policies and assertive outreach attempts to deliver the mental health care these patients deserve.
These vignettes highlight the psychosocial barriers women face during the perinatal period, such as caring for their child, financial stressors, and COVID-19 pandemic–related factors that can hinder treatment, which can be compounded by trauma. The uncertainty, unpredictability, loss of control, and loss of support structures collectively experienced during the pandemic can be triggering and precipitate worsening CPTSD symptoms.35 Women who experience trauma are less likely to obtain the COVID-19 vaccine for themselves or their children, and this hesitancy is often driven by institutional distrust.36 Policy leaders and clinicians should consider these factors to promote trauma-informed COVID-19 vaccine initiatives and expand mental health access using less orthodox treatment settings, such as telepsychiatry. Telepsychiatry can serve as a bridge to in-person care as patients may feel a higher sense of control when in a familiar home environment. Case 2 and Case 3 exemplify the difficulties of delivering mental health care to perinatal women with CPTSD during the pandemic, especially those who are vaccine-hesitant, and illustrate the importance of adapting a patient’s treatment plan in a personalized and trauma-informed way.
Psychiatrists can help obstetricians and pediatricians by explaining that avoidance patterns and distrust in the clinical setting may be related to trauma and are not grounds for conscious or subconscious punishment or abandonment. Educating other clinicians about trauma-informed care, precautions to use for perinatal patients, and ways to effectively support survivors of CSA can greatly improve health outcomes for perinatal women and their offspring.37
Bottom Line
Complex posttraumatic stress disorder (CPTSD) is characterized by classic PTSD symptoms as well as disturbances in self organization, which can include mood symptoms, psychotic symptoms, and maladaptive personality traits. CPTSD resulting from childhood sexual abuse is of particular concern for women, especially during the perinatal period. Clinicians must know how to recognize the signs and symptoms of CPTSD so they can tailor a trauma-informed treatment plan and promote treatment access in this highly vulnerable patient population.
Related Resources
- Tillman B, Sloan N, Westmoreland P. How COVID-19 affects peripartum women’s mental health. Current Psychiatry. 2021;20(6):18-22. doi:10.12788/cp.0129
- Keswani M, Nemcek S, Rashid N. Is it bipolar disorder, or a complex form of PTSD? Current Psychiatry. 2021;20(12):42-49. doi:10.12788/cp.0188
Drug Brand Names
Carbamazepine • Carbatrol
Clonazepam • Klonopin
Lamotrigine • Lamictal
Prazosin • Minipress
Quetiapine • Seroquel
Sertraline • Zoloft
Topiramate • Topamax
1. World Health Organization. International Classification of Diseases, 11th Revision (ICD-11). Complex posttraumatic stress disorder. Accessed November 6, 2021. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/585833559
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Cloitre M, Garvert DW, Brewin CR, et al. Evidence for proposed ICD-11 PTSD and complexPTSD: a latent profile analysis. Eur J Psychotraumatol. 2013;4:10.3402/ejpt.v4i0.20706. doi:10.3402/ejpt.v4i0.20706
4. Leeb RT, Paulozzi LJ, Melanson C, et al. Child Maltreatment Surveillance: Uniform Definitions for Public Health and Recommended Data Elements, Version 1.0. Centers for Disease Control and Prevention, Department of Health & Human Services; 2008. Accessed August 24, 2022. https://www.cdc.gov/violenceprevention/pdf/cm_surveillance-a.pdf
5. Byrne J, Smart C, Watson G. “I felt like I was being abused all over again”: how survivors of child sexual abuse make sense of the perinatal period through their narratives. J Child Sex Abus. 2017;26(4):465-486. doi:10.1080/10538712.2017.1297880
6. Flom JD, Chiu YM, Hsu HL, et al. Maternal lifetime trauma and birthweight: effect modification by in utero cortisol and child sex. J Pediatr. 2018;203:301-308. doi:10.1016/j.jpeds.2018.07.069
7. Spinazzola J, van der Kolk B, Ford JD. When nowhere is safe: interpersonal trauma and attachment adversity as antecedents of posttraumatic stress disorder and developmental trauma disorder. J Trauma Stress. 2018;31(5):631-642. doi:10.1002/jts.22320
8. Chamberlain C, Gee G, Harfield S, et al. Parenting after a history of childhood maltreatment: a scoping review and map of evidence in the perinatal period. PloS One. 2019;14(3):e0213460. doi:10.1371/journal.pone.0213460
9. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18-31. doi:10.1016/j.jad.2017.07.045
10. Gavin AR, Morris J. The association between maternal early life forced sexual intercourse and offspring birth weight: the role of socioeconomic status. J Womens Health (Larchmt). 2017;26(5):442-449. doi:10.1089/jwh.2016.5789
11. Cloitre M, Shevlin M, Brewin CR, et al. The international trauma questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr Scand. 2018;138(6):536-546.
12. Cloitre M, Hyland P, Prins A, et al. The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. Eur J Psychotraumatol. 2021;12(1):1930961. doi:10.1080/20008198.2021.1930961
13. Weathers FW, Litz BT, Keane TM, et al. PTSD Checklist for DSM-5 (PCL-5). US Department of Veterans Affairs. April 11, 2018. Accessed November 25, 2021. https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.PDF
14. Dissociative Experiences Scale – II. TraumaDissociation.com. Accessed November 25, 2021. http://traumadissociation.com/des
15. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782-786. doi:10.1192/bjp.150.6.782
16. Mood Disorder Questionnaire (MDQ). Oregon Health & Science University. Accessed November 7, 2021. https://www.ohsu.edu/sites/default/files/2019-06/cms-quality-bipolar_disorder_mdq_screener.pdf
17. Karatzias T, Hyland P, Bradley A, et al. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress Anxiety. 2019;36(9):887-894. doi:10.1002/da.22934
18. Bohus M, Kleindienst N, Limberger MF, et al. The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology. 2009;42(1):32-39.
19. Fallot RD, Harris M. A trauma-informed approach to screening and assessment. New Dir Ment Health Serv. 2001;(89):23-31. doi:10.1002/yd.23320018904
20. Coventry PA, Meader N, Melton H, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLoS Med. 2020;17(8):e1003262. doi:10.1371/journal.pmed.1003262
21. Ford JD. Progress and limitations in the treatment of complex PTSD and developmental trauma disorder. Curr Treat Options Psychiatry. 2021;8:1-17. doi:10.1007/s40501-020-00236-6
22. Becker-Sadzio J, Gundel F, Kroczek A, et al. Trauma exposure therapy in a pregnant woman suffering from complex posttraumatic stress disorder after childhood sexual abuse: risk or benefit? Eur J Psychotraumatol. 2020;11(1):1697581. doi:10.1080/20008198.2019.1697581
23. Mendelsohn M, Zachary RS, Harney PA. Group therapy as an ecological bridge to new community for trauma survivors. J Aggress Maltreat Trauma. 2007;14(1-2):227-243. doi:10.1300/J146v14n01_12
24. Macintosh HB, Vaillancourt-Morel MP, Bergeron S. Sex and couple therapy with survivors of childhood trauma. In: Hall KS, Binik YM, eds. Principles and Practice of Sex Therapy. 6th ed. Guilford Press; 2020.
25. Dresner N, Byatt N, Gopalan P, et al. Psychiatric care of peripartum women. Psychiatric Times. 2015;32(12).
26. Zagorski N. How to manage meds before, during, and after pregnancy. Psychiatric News. 2019;54(14):13. https://doi.org/10.1176/APPI.PN.2019.6B36
27. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370:2397-2407. doi:10.1056/NEJMoa1312828
28. Davidson AD, Bhat A, Chu F, et al. A systematic review of the use of prazosin in pregnancy and lactation. Gen Hosp Psychiatry. 2021;71:134-136. doi:10.1016/j.genhosppsych.2021.03.012
29. Shinn AK, Wolff JD, Hwang M, et al. Assessing voice hearing in trauma spectrum disorders: a comparison of two measures and a review of the literature. Front Psychiatry. 2020;10:1011. doi:10.3389/fpsyt.2019.01011
30. Raffi ER, Nonacs R, Cohen LS. Safety of psychotropic medications during pregnancy. Clin Perinatol. 2019;46(2):215-234. doi:10.1016/j.clp.2019.02.004
31. Martin A, Young C, Leckman JF, et al. Age effects on antidepressant-induced manic conversion. Arch Pediatr Adoles Med. 2004;158(8):773-780. doi:10.1001/archpedi.158.8.773
32. Gill N, Bayes A, Parker G. A review of antidepressant-associated hypomania in those diagnosed with unipolar depression-risk factors, conceptual models, and management. Curr Psychiatry Rep. 2020;22(4):20. doi:10.1007/s11920-020-01143-6
33. Harris LM, Huang X, Linthicum KP, et al. Sleep disturbances as risk factors for suicidal thoughts and behaviours: a meta-analysis of longitudinal studies. Sci Rep. 2020;10(1):13888. doi:10.1038/s41598-020-70866-6
34. Dehara M, Wells MB, Sjöqvist H, et al. Parenthood is associated with lower suicide risk: a register-based cohort study of 1.5 million Swedes. Acta Psychiatr Scand. 2021;143(3):206-215. doi:10.1111/acps.13240
35. Iyengar U, Jaiprakash B, Haitsuka H, et al. One year into the pandemic: a systematic review of perinatal mental health outcomes during COVID-19. Front Psychiatry. 2021;12:674194. doi:10.3389/fpsyt.2021.674194
36. Milan S, Dáu ALBT. The role of trauma in mothers’ COVID-19 vaccine beliefs and intentions. J Pediatr Psychol. 2021;46(5):526-535. doi:10.1093/jpepsy/jsab043
37. Coles J, Jones K. “Universal precautions”: perinatal touch and examination after childhood sexual abuse. Birth. 2009;36(3):230-236. doi:10.1111/j.1523-536X.2009.00327
1. World Health Organization. International Classification of Diseases, 11th Revision (ICD-11). Complex posttraumatic stress disorder. Accessed November 6, 2021. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/585833559
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013.
3. Cloitre M, Garvert DW, Brewin CR, et al. Evidence for proposed ICD-11 PTSD and complexPTSD: a latent profile analysis. Eur J Psychotraumatol. 2013;4:10.3402/ejpt.v4i0.20706. doi:10.3402/ejpt.v4i0.20706
4. Leeb RT, Paulozzi LJ, Melanson C, et al. Child Maltreatment Surveillance: Uniform Definitions for Public Health and Recommended Data Elements, Version 1.0. Centers for Disease Control and Prevention, Department of Health & Human Services; 2008. Accessed August 24, 2022. https://www.cdc.gov/violenceprevention/pdf/cm_surveillance-a.pdf
5. Byrne J, Smart C, Watson G. “I felt like I was being abused all over again”: how survivors of child sexual abuse make sense of the perinatal period through their narratives. J Child Sex Abus. 2017;26(4):465-486. doi:10.1080/10538712.2017.1297880
6. Flom JD, Chiu YM, Hsu HL, et al. Maternal lifetime trauma and birthweight: effect modification by in utero cortisol and child sex. J Pediatr. 2018;203:301-308. doi:10.1016/j.jpeds.2018.07.069
7. Spinazzola J, van der Kolk B, Ford JD. When nowhere is safe: interpersonal trauma and attachment adversity as antecedents of posttraumatic stress disorder and developmental trauma disorder. J Trauma Stress. 2018;31(5):631-642. doi:10.1002/jts.22320
8. Chamberlain C, Gee G, Harfield S, et al. Parenting after a history of childhood maltreatment: a scoping review and map of evidence in the perinatal period. PloS One. 2019;14(3):e0213460. doi:10.1371/journal.pone.0213460
9. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18-31. doi:10.1016/j.jad.2017.07.045
10. Gavin AR, Morris J. The association between maternal early life forced sexual intercourse and offspring birth weight: the role of socioeconomic status. J Womens Health (Larchmt). 2017;26(5):442-449. doi:10.1089/jwh.2016.5789
11. Cloitre M, Shevlin M, Brewin CR, et al. The international trauma questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatr Scand. 2018;138(6):536-546.
12. Cloitre M, Hyland P, Prins A, et al. The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. Eur J Psychotraumatol. 2021;12(1):1930961. doi:10.1080/20008198.2021.1930961
13. Weathers FW, Litz BT, Keane TM, et al. PTSD Checklist for DSM-5 (PCL-5). US Department of Veterans Affairs. April 11, 2018. Accessed November 25, 2021. https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.PDF
14. Dissociative Experiences Scale – II. TraumaDissociation.com. Accessed November 25, 2021. http://traumadissociation.com/des
15. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782-786. doi:10.1192/bjp.150.6.782
16. Mood Disorder Questionnaire (MDQ). Oregon Health & Science University. Accessed November 7, 2021. https://www.ohsu.edu/sites/default/files/2019-06/cms-quality-bipolar_disorder_mdq_screener.pdf
17. Karatzias T, Hyland P, Bradley A, et al. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress Anxiety. 2019;36(9):887-894. doi:10.1002/da.22934
18. Bohus M, Kleindienst N, Limberger MF, et al. The short version of the Borderline Symptom List (BSL-23): development and initial data on psychometric properties. Psychopathology. 2009;42(1):32-39.
19. Fallot RD, Harris M. A trauma-informed approach to screening and assessment. New Dir Ment Health Serv. 2001;(89):23-31. doi:10.1002/yd.23320018904
20. Coventry PA, Meader N, Melton H, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLoS Med. 2020;17(8):e1003262. doi:10.1371/journal.pmed.1003262
21. Ford JD. Progress and limitations in the treatment of complex PTSD and developmental trauma disorder. Curr Treat Options Psychiatry. 2021;8:1-17. doi:10.1007/s40501-020-00236-6
22. Becker-Sadzio J, Gundel F, Kroczek A, et al. Trauma exposure therapy in a pregnant woman suffering from complex posttraumatic stress disorder after childhood sexual abuse: risk or benefit? Eur J Psychotraumatol. 2020;11(1):1697581. doi:10.1080/20008198.2019.1697581
23. Mendelsohn M, Zachary RS, Harney PA. Group therapy as an ecological bridge to new community for trauma survivors. J Aggress Maltreat Trauma. 2007;14(1-2):227-243. doi:10.1300/J146v14n01_12
24. Macintosh HB, Vaillancourt-Morel MP, Bergeron S. Sex and couple therapy with survivors of childhood trauma. In: Hall KS, Binik YM, eds. Principles and Practice of Sex Therapy. 6th ed. Guilford Press; 2020.
25. Dresner N, Byatt N, Gopalan P, et al. Psychiatric care of peripartum women. Psychiatric Times. 2015;32(12).
26. Zagorski N. How to manage meds before, during, and after pregnancy. Psychiatric News. 2019;54(14):13. https://doi.org/10.1176/APPI.PN.2019.6B36
27. Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370:2397-2407. doi:10.1056/NEJMoa1312828
28. Davidson AD, Bhat A, Chu F, et al. A systematic review of the use of prazosin in pregnancy and lactation. Gen Hosp Psychiatry. 2021;71:134-136. doi:10.1016/j.genhosppsych.2021.03.012
29. Shinn AK, Wolff JD, Hwang M, et al. Assessing voice hearing in trauma spectrum disorders: a comparison of two measures and a review of the literature. Front Psychiatry. 2020;10:1011. doi:10.3389/fpsyt.2019.01011
30. Raffi ER, Nonacs R, Cohen LS. Safety of psychotropic medications during pregnancy. Clin Perinatol. 2019;46(2):215-234. doi:10.1016/j.clp.2019.02.004
31. Martin A, Young C, Leckman JF, et al. Age effects on antidepressant-induced manic conversion. Arch Pediatr Adoles Med. 2004;158(8):773-780. doi:10.1001/archpedi.158.8.773
32. Gill N, Bayes A, Parker G. A review of antidepressant-associated hypomania in those diagnosed with unipolar depression-risk factors, conceptual models, and management. Curr Psychiatry Rep. 2020;22(4):20. doi:10.1007/s11920-020-01143-6
33. Harris LM, Huang X, Linthicum KP, et al. Sleep disturbances as risk factors for suicidal thoughts and behaviours: a meta-analysis of longitudinal studies. Sci Rep. 2020;10(1):13888. doi:10.1038/s41598-020-70866-6
34. Dehara M, Wells MB, Sjöqvist H, et al. Parenthood is associated with lower suicide risk: a register-based cohort study of 1.5 million Swedes. Acta Psychiatr Scand. 2021;143(3):206-215. doi:10.1111/acps.13240
35. Iyengar U, Jaiprakash B, Haitsuka H, et al. One year into the pandemic: a systematic review of perinatal mental health outcomes during COVID-19. Front Psychiatry. 2021;12:674194. doi:10.3389/fpsyt.2021.674194
36. Milan S, Dáu ALBT. The role of trauma in mothers’ COVID-19 vaccine beliefs and intentions. J Pediatr Psychol. 2021;46(5):526-535. doi:10.1093/jpepsy/jsab043
37. Coles J, Jones K. “Universal precautions”: perinatal touch and examination after childhood sexual abuse. Birth. 2009;36(3):230-236. doi:10.1111/j.1523-536X.2009.00327
Sleep kits help foster children manage effects of trauma
A stuffed animal, aromatherapy, a night light. A kit containing these and other items can help children in foster care who have experienced trauma sleep more soundly, a critical step in helping them cope with their emotional distress.
In a new study, researchers at the Children’s Hospital of Philadelphia reported that sleep kits specially tailored to foster children appeared to be helpful in most cases. The kits can be distributed by pediatricians in the office or clinic setting.
“Children who have experienced trauma can have issues with behavior, it can impact their school, and they have difficulties sleeping,” said Kristine Fortin, MD, MPH, director of the fostering health program at Safe Place: Center for Child Protection and Health at CHOP. “I thought, what could a pediatrician do in the office in one visit to help children with sleep?”
Dr. Fortin and colleagues designed sleep kits for both younger children and adolescents.
The version for teenagers contained a sound machine, aromatherapy spray, and a sleep mask. The kits for younger children contained matching stuffed toys to share with someone they felt connected to, and a rechargeable night-light. All kits included written materials about sleep hygiene, a journal, and directions for downloading a free age-appropriate relaxation app for belly breathing or a PTSD Coach app from the Department of Veterans Affairs to manage symptoms of trauma.
In a pilot study presented at the annual meeting of the American Academy of Pediatrics, Dr. Fortin and colleagues surveyed caregivers in foster homes about their use of the kits.
Of the 20 foster parents who responded to the survey, 11 said the kits helped “very much,” 5 others reported they helped “somewhat,” another 2 reported no improvements in sleep, and 2 said they didn’t know the effect. The children for whom results were unknown moved from the home without the sleep kit or had difficulties communicating with the foster parents, resulting in incomplete assessment, according to the researchers.
Night-lights were used most in the kits, followed by the stuffed toys, sound machines, and sleep journals.
Dr. Fortin said existing resources like sleep therapy or medication can be costly or difficult to find, and many pediatricians don’t have enough time during wellness visits to address symptoms like sleep deprivation. She said the sleep kits could be an alternative to other forms of sleep therapy. “If these sleep kits were effective, and could really help them sleep, then maybe less children would need something like medication.”
Dr. Fortin said the kits her group has designed are tailored specifically for children with symptoms of trauma, or with difficult emotions associated with foster care.
“We’ve tried to design something that can be really practical and easy to use in a pediatric visit, where there’s a lot of written information that can be discussed with the child and their family,” Dr. Fortin said.
She added that she would like to see clinicians give out the sleep kits during in-office visits.
“These sleep issues are common in foster children,” she said. “We felt it was important to do an intervention.”
Kristina Lenker, PhD, a sleep psychologist at Penn State Health, Hershey, said children in foster care often struggle with falling or staying asleep, an inability to sleep alone, nightmares, and bed wetting.
“Sleep kits can be particularly helpful for these children, given how they can help caregivers to provide a safe sleep environment and predictable routine, and send messages of safety and comfort at bedtime, with tangible objects, and enable children to feel a sense of control,” she said.
Charitable organizations like Pajama Program and Sleeping Children Around the World provide sleep kits to children from underserved backgrounds. But Candice Alfano, PhD, director of the University of Houston’s Sleep and Anxiety Center of Houston, said the CHOP kits are the first to specifically target sleeping difficulties in foster children.
“Sleep is a largely neglected yet essential area of health, development, and well-being in this highly-vulnerable population of youth, so I am very excited to see this work being done,” Dr. Alfano said in an interview.
Dr. Fortin and Dr. Lenker reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A stuffed animal, aromatherapy, a night light. A kit containing these and other items can help children in foster care who have experienced trauma sleep more soundly, a critical step in helping them cope with their emotional distress.
In a new study, researchers at the Children’s Hospital of Philadelphia reported that sleep kits specially tailored to foster children appeared to be helpful in most cases. The kits can be distributed by pediatricians in the office or clinic setting.
“Children who have experienced trauma can have issues with behavior, it can impact their school, and they have difficulties sleeping,” said Kristine Fortin, MD, MPH, director of the fostering health program at Safe Place: Center for Child Protection and Health at CHOP. “I thought, what could a pediatrician do in the office in one visit to help children with sleep?”
Dr. Fortin and colleagues designed sleep kits for both younger children and adolescents.
The version for teenagers contained a sound machine, aromatherapy spray, and a sleep mask. The kits for younger children contained matching stuffed toys to share with someone they felt connected to, and a rechargeable night-light. All kits included written materials about sleep hygiene, a journal, and directions for downloading a free age-appropriate relaxation app for belly breathing or a PTSD Coach app from the Department of Veterans Affairs to manage symptoms of trauma.
In a pilot study presented at the annual meeting of the American Academy of Pediatrics, Dr. Fortin and colleagues surveyed caregivers in foster homes about their use of the kits.
Of the 20 foster parents who responded to the survey, 11 said the kits helped “very much,” 5 others reported they helped “somewhat,” another 2 reported no improvements in sleep, and 2 said they didn’t know the effect. The children for whom results were unknown moved from the home without the sleep kit or had difficulties communicating with the foster parents, resulting in incomplete assessment, according to the researchers.
Night-lights were used most in the kits, followed by the stuffed toys, sound machines, and sleep journals.
Dr. Fortin said existing resources like sleep therapy or medication can be costly or difficult to find, and many pediatricians don’t have enough time during wellness visits to address symptoms like sleep deprivation. She said the sleep kits could be an alternative to other forms of sleep therapy. “If these sleep kits were effective, and could really help them sleep, then maybe less children would need something like medication.”
Dr. Fortin said the kits her group has designed are tailored specifically for children with symptoms of trauma, or with difficult emotions associated with foster care.
“We’ve tried to design something that can be really practical and easy to use in a pediatric visit, where there’s a lot of written information that can be discussed with the child and their family,” Dr. Fortin said.
She added that she would like to see clinicians give out the sleep kits during in-office visits.
“These sleep issues are common in foster children,” she said. “We felt it was important to do an intervention.”
Kristina Lenker, PhD, a sleep psychologist at Penn State Health, Hershey, said children in foster care often struggle with falling or staying asleep, an inability to sleep alone, nightmares, and bed wetting.
“Sleep kits can be particularly helpful for these children, given how they can help caregivers to provide a safe sleep environment and predictable routine, and send messages of safety and comfort at bedtime, with tangible objects, and enable children to feel a sense of control,” she said.
Charitable organizations like Pajama Program and Sleeping Children Around the World provide sleep kits to children from underserved backgrounds. But Candice Alfano, PhD, director of the University of Houston’s Sleep and Anxiety Center of Houston, said the CHOP kits are the first to specifically target sleeping difficulties in foster children.
“Sleep is a largely neglected yet essential area of health, development, and well-being in this highly-vulnerable population of youth, so I am very excited to see this work being done,” Dr. Alfano said in an interview.
Dr. Fortin and Dr. Lenker reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A stuffed animal, aromatherapy, a night light. A kit containing these and other items can help children in foster care who have experienced trauma sleep more soundly, a critical step in helping them cope with their emotional distress.
In a new study, researchers at the Children’s Hospital of Philadelphia reported that sleep kits specially tailored to foster children appeared to be helpful in most cases. The kits can be distributed by pediatricians in the office or clinic setting.
“Children who have experienced trauma can have issues with behavior, it can impact their school, and they have difficulties sleeping,” said Kristine Fortin, MD, MPH, director of the fostering health program at Safe Place: Center for Child Protection and Health at CHOP. “I thought, what could a pediatrician do in the office in one visit to help children with sleep?”
Dr. Fortin and colleagues designed sleep kits for both younger children and adolescents.
The version for teenagers contained a sound machine, aromatherapy spray, and a sleep mask. The kits for younger children contained matching stuffed toys to share with someone they felt connected to, and a rechargeable night-light. All kits included written materials about sleep hygiene, a journal, and directions for downloading a free age-appropriate relaxation app for belly breathing or a PTSD Coach app from the Department of Veterans Affairs to manage symptoms of trauma.
In a pilot study presented at the annual meeting of the American Academy of Pediatrics, Dr. Fortin and colleagues surveyed caregivers in foster homes about their use of the kits.
Of the 20 foster parents who responded to the survey, 11 said the kits helped “very much,” 5 others reported they helped “somewhat,” another 2 reported no improvements in sleep, and 2 said they didn’t know the effect. The children for whom results were unknown moved from the home without the sleep kit or had difficulties communicating with the foster parents, resulting in incomplete assessment, according to the researchers.
Night-lights were used most in the kits, followed by the stuffed toys, sound machines, and sleep journals.
Dr. Fortin said existing resources like sleep therapy or medication can be costly or difficult to find, and many pediatricians don’t have enough time during wellness visits to address symptoms like sleep deprivation. She said the sleep kits could be an alternative to other forms of sleep therapy. “If these sleep kits were effective, and could really help them sleep, then maybe less children would need something like medication.”
Dr. Fortin said the kits her group has designed are tailored specifically for children with symptoms of trauma, or with difficult emotions associated with foster care.
“We’ve tried to design something that can be really practical and easy to use in a pediatric visit, where there’s a lot of written information that can be discussed with the child and their family,” Dr. Fortin said.
She added that she would like to see clinicians give out the sleep kits during in-office visits.
“These sleep issues are common in foster children,” she said. “We felt it was important to do an intervention.”
Kristina Lenker, PhD, a sleep psychologist at Penn State Health, Hershey, said children in foster care often struggle with falling or staying asleep, an inability to sleep alone, nightmares, and bed wetting.
“Sleep kits can be particularly helpful for these children, given how they can help caregivers to provide a safe sleep environment and predictable routine, and send messages of safety and comfort at bedtime, with tangible objects, and enable children to feel a sense of control,” she said.
Charitable organizations like Pajama Program and Sleeping Children Around the World provide sleep kits to children from underserved backgrounds. But Candice Alfano, PhD, director of the University of Houston’s Sleep and Anxiety Center of Houston, said the CHOP kits are the first to specifically target sleeping difficulties in foster children.
“Sleep is a largely neglected yet essential area of health, development, and well-being in this highly-vulnerable population of youth, so I am very excited to see this work being done,” Dr. Alfano said in an interview.
Dr. Fortin and Dr. Lenker reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAP 2022
‘Disturbing’ lack of follow-up care after psychiatric crises
There is a concerning lack of follow-up care for young people who experience a mental health crisis, new research suggests.
The follow-up rate was less than 30% for those who had visited an ED.
The strongest predictor of follow-up was having received both primary and mental health care during the 6 months prior to using the acute service.
“For people discharging folks after a psychiatric crisis, whether it be in a hospital or emergency room setting, connecting them with their outpatient provider to ensure the transfer of care and continuity of care is vitally important to reduce risks for this population,” coinvestigator Brian Skehan, MD, PhD, assistant professor and psychiatrist, University of Massachusetts, Worcester, said during a press briefing.
If these discharged patients do not have a provider, “make sure they get one,” Lisa Dixon, MD, editor-in-chief of Psychiatric Services, added during the same briefing. “That’s the gift of life potentially for these young people.”
The findings were published online in Psychiatric Services.
Alarming trends
The alarming suicide trends among youths were exacerbated by the COVID-19 pandemic, Dr. Skehan noted.
He cited a 2021 study that showed more than 44% of high school students experienced persistent sadness or hopelessness over the previous year, 1 in 5 seriously considered suicide, and almost 1 in 10 actually attempted suicide.
“When we look at the number of young adults and adolescents struggling with behavioral health issues, the data trend is disturbing nationwide,” Dr. Skehan said.
The current study included participants aged 12-27 years who had private insurance. Many youth in this age category are experiencing significant changes, such as moving from high school to college and from pediatric providers to adult providers – and some “get lost in this transition,” said Dr. Skehan.
He noted many inpatient psychiatric units are not geared to young adults. “They may miss out on some aspects of inpatient care because it’s not geared to their developmental stage,” he said.
Assessing U.S. patient data in the IBM MarketScan commercial database (2013-2018), the researchers created two study samples: 95,153 inpatients and 108,576 patients who used the ED. All had an acute event stemming from a mental health condition.
The investigators explored the role of “established” outpatient care, defined as having had at least one visit with a provider of primary or mental health care in the 6 months prior to the acute psychiatric event.
Covariates included age at time of service (aged 12-17 years or 18-27 years), gender, health care plan type, psychiatric diagnosis, whether the acute event was self-harm or suicide related, and medical complexity.
Low follow-up rates
In the inpatient group, the average age was 18.9 years, the most common length of hospital stay was 4-6 days, and 1.5% left against medical advice. The most common primary diagnosis was major depression (53.7%), followed by bipolar disorder (22.3%). The least common disorders were PTSD, comorbid eating disorders, and disruptive disorders.
About one-third of participants had used both primary and mental health care during the 6 months before hospitalization, whereas 22.8% had no established outpatient care. Established care was most common among those with comorbid eating disorders and least common among those with psychotic disorders.
Results showed 42.7% of the hospitalized patients received follow up within 7 days and 67.4% received follow up within 30 days.
The strongest predictor of mental health follow-up care was established outpatient care. Compared with those who had no such care, those who had received both primary care and mental health care before the acute event had the highest odds of receiving follow-up (within 7 days, adjusted odds ratio, 2.81; 95% confidence interval, 2.68-2.94).
Older age and leaving against medical advice were associated with decreased likelihood of follow-up. Female sex, hospitalizations related to self-harm or suicidality, and longer length of stay were associated with increased likelihood of mental health follow-up care.
Compared with those hospitalized for major depression, those hospitalized for schizophrenia, bipolar disorder, PTSD, disruptive disorders, or comorbid substance use disorder were less likely to receive mental health follow-up. For example, only 23.7% of youth with comorbid substance use discharged from the hospital had follow-up within 7 days.
Similar patterns were observed for 30-day follow-up care.
‘Accessible and appealing’ options needed
In the ED-visit group, the average age was 19.5 years (58% female). Most (70.4%) had no chronic health conditions other than a psychiatric disorder. The primary diagnoses were anxiety disorders or phobias (44.1%) and major depression (23%).
One in four visits included a code for self-harm, suicidal ideation, or suicide attempt. And almost one third lacked established outpatient care before the ED visit.
Results showed 28.6% of the ED group received mental health care follow-up within 7 days and 46.4% received it within 30 days.
Again, the strongest predictor of mental health follow-up was prior outpatient care. For example, compared with participants with no established outpatient care, those with both primary care and mental health care were the most likely to receive follow-up within 7 days (aOR, 4.06; 95% CI, 3.72-4.42).
These numbers “are far from the goal of making sure everybody is getting follow-up care within 7 days of an acute psychiatric event,” Dr. Skehan said.
He stressed the need for “accessible and appealing options for youth.” These could include telehealth services, improved communication among health care providers in the ED, and reducing barriers to access follow-up care.
“This probably highlights the need to have more case management and referral services, and maybe make sure patients have a follow-up appointment before they leave the emergency room,” said Dr. Skehan. “This doesn’t necessarily guarantee they’ll get there but hopefully it makes it more likely they will have that access should they need it.”
The study was funded by grants from the National Institute of General Medical Sciences and the National Center for Advancing Translational Sciences, from the National Institutes of Health. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There is a concerning lack of follow-up care for young people who experience a mental health crisis, new research suggests.
The follow-up rate was less than 30% for those who had visited an ED.
The strongest predictor of follow-up was having received both primary and mental health care during the 6 months prior to using the acute service.
“For people discharging folks after a psychiatric crisis, whether it be in a hospital or emergency room setting, connecting them with their outpatient provider to ensure the transfer of care and continuity of care is vitally important to reduce risks for this population,” coinvestigator Brian Skehan, MD, PhD, assistant professor and psychiatrist, University of Massachusetts, Worcester, said during a press briefing.
If these discharged patients do not have a provider, “make sure they get one,” Lisa Dixon, MD, editor-in-chief of Psychiatric Services, added during the same briefing. “That’s the gift of life potentially for these young people.”
The findings were published online in Psychiatric Services.
Alarming trends
The alarming suicide trends among youths were exacerbated by the COVID-19 pandemic, Dr. Skehan noted.
He cited a 2021 study that showed more than 44% of high school students experienced persistent sadness or hopelessness over the previous year, 1 in 5 seriously considered suicide, and almost 1 in 10 actually attempted suicide.
“When we look at the number of young adults and adolescents struggling with behavioral health issues, the data trend is disturbing nationwide,” Dr. Skehan said.
The current study included participants aged 12-27 years who had private insurance. Many youth in this age category are experiencing significant changes, such as moving from high school to college and from pediatric providers to adult providers – and some “get lost in this transition,” said Dr. Skehan.
He noted many inpatient psychiatric units are not geared to young adults. “They may miss out on some aspects of inpatient care because it’s not geared to their developmental stage,” he said.
Assessing U.S. patient data in the IBM MarketScan commercial database (2013-2018), the researchers created two study samples: 95,153 inpatients and 108,576 patients who used the ED. All had an acute event stemming from a mental health condition.
The investigators explored the role of “established” outpatient care, defined as having had at least one visit with a provider of primary or mental health care in the 6 months prior to the acute psychiatric event.
Covariates included age at time of service (aged 12-17 years or 18-27 years), gender, health care plan type, psychiatric diagnosis, whether the acute event was self-harm or suicide related, and medical complexity.
Low follow-up rates
In the inpatient group, the average age was 18.9 years, the most common length of hospital stay was 4-6 days, and 1.5% left against medical advice. The most common primary diagnosis was major depression (53.7%), followed by bipolar disorder (22.3%). The least common disorders were PTSD, comorbid eating disorders, and disruptive disorders.
About one-third of participants had used both primary and mental health care during the 6 months before hospitalization, whereas 22.8% had no established outpatient care. Established care was most common among those with comorbid eating disorders and least common among those with psychotic disorders.
Results showed 42.7% of the hospitalized patients received follow up within 7 days and 67.4% received follow up within 30 days.
The strongest predictor of mental health follow-up care was established outpatient care. Compared with those who had no such care, those who had received both primary care and mental health care before the acute event had the highest odds of receiving follow-up (within 7 days, adjusted odds ratio, 2.81; 95% confidence interval, 2.68-2.94).
Older age and leaving against medical advice were associated with decreased likelihood of follow-up. Female sex, hospitalizations related to self-harm or suicidality, and longer length of stay were associated with increased likelihood of mental health follow-up care.
Compared with those hospitalized for major depression, those hospitalized for schizophrenia, bipolar disorder, PTSD, disruptive disorders, or comorbid substance use disorder were less likely to receive mental health follow-up. For example, only 23.7% of youth with comorbid substance use discharged from the hospital had follow-up within 7 days.
Similar patterns were observed for 30-day follow-up care.
‘Accessible and appealing’ options needed
In the ED-visit group, the average age was 19.5 years (58% female). Most (70.4%) had no chronic health conditions other than a psychiatric disorder. The primary diagnoses were anxiety disorders or phobias (44.1%) and major depression (23%).
One in four visits included a code for self-harm, suicidal ideation, or suicide attempt. And almost one third lacked established outpatient care before the ED visit.
Results showed 28.6% of the ED group received mental health care follow-up within 7 days and 46.4% received it within 30 days.
Again, the strongest predictor of mental health follow-up was prior outpatient care. For example, compared with participants with no established outpatient care, those with both primary care and mental health care were the most likely to receive follow-up within 7 days (aOR, 4.06; 95% CI, 3.72-4.42).
These numbers “are far from the goal of making sure everybody is getting follow-up care within 7 days of an acute psychiatric event,” Dr. Skehan said.
He stressed the need for “accessible and appealing options for youth.” These could include telehealth services, improved communication among health care providers in the ED, and reducing barriers to access follow-up care.
“This probably highlights the need to have more case management and referral services, and maybe make sure patients have a follow-up appointment before they leave the emergency room,” said Dr. Skehan. “This doesn’t necessarily guarantee they’ll get there but hopefully it makes it more likely they will have that access should they need it.”
The study was funded by grants from the National Institute of General Medical Sciences and the National Center for Advancing Translational Sciences, from the National Institutes of Health. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
There is a concerning lack of follow-up care for young people who experience a mental health crisis, new research suggests.
The follow-up rate was less than 30% for those who had visited an ED.
The strongest predictor of follow-up was having received both primary and mental health care during the 6 months prior to using the acute service.
“For people discharging folks after a psychiatric crisis, whether it be in a hospital or emergency room setting, connecting them with their outpatient provider to ensure the transfer of care and continuity of care is vitally important to reduce risks for this population,” coinvestigator Brian Skehan, MD, PhD, assistant professor and psychiatrist, University of Massachusetts, Worcester, said during a press briefing.
If these discharged patients do not have a provider, “make sure they get one,” Lisa Dixon, MD, editor-in-chief of Psychiatric Services, added during the same briefing. “That’s the gift of life potentially for these young people.”
The findings were published online in Psychiatric Services.
Alarming trends
The alarming suicide trends among youths were exacerbated by the COVID-19 pandemic, Dr. Skehan noted.
He cited a 2021 study that showed more than 44% of high school students experienced persistent sadness or hopelessness over the previous year, 1 in 5 seriously considered suicide, and almost 1 in 10 actually attempted suicide.
“When we look at the number of young adults and adolescents struggling with behavioral health issues, the data trend is disturbing nationwide,” Dr. Skehan said.
The current study included participants aged 12-27 years who had private insurance. Many youth in this age category are experiencing significant changes, such as moving from high school to college and from pediatric providers to adult providers – and some “get lost in this transition,” said Dr. Skehan.
He noted many inpatient psychiatric units are not geared to young adults. “They may miss out on some aspects of inpatient care because it’s not geared to their developmental stage,” he said.
Assessing U.S. patient data in the IBM MarketScan commercial database (2013-2018), the researchers created two study samples: 95,153 inpatients and 108,576 patients who used the ED. All had an acute event stemming from a mental health condition.
The investigators explored the role of “established” outpatient care, defined as having had at least one visit with a provider of primary or mental health care in the 6 months prior to the acute psychiatric event.
Covariates included age at time of service (aged 12-17 years or 18-27 years), gender, health care plan type, psychiatric diagnosis, whether the acute event was self-harm or suicide related, and medical complexity.
Low follow-up rates
In the inpatient group, the average age was 18.9 years, the most common length of hospital stay was 4-6 days, and 1.5% left against medical advice. The most common primary diagnosis was major depression (53.7%), followed by bipolar disorder (22.3%). The least common disorders were PTSD, comorbid eating disorders, and disruptive disorders.
About one-third of participants had used both primary and mental health care during the 6 months before hospitalization, whereas 22.8% had no established outpatient care. Established care was most common among those with comorbid eating disorders and least common among those with psychotic disorders.
Results showed 42.7% of the hospitalized patients received follow up within 7 days and 67.4% received follow up within 30 days.
The strongest predictor of mental health follow-up care was established outpatient care. Compared with those who had no such care, those who had received both primary care and mental health care before the acute event had the highest odds of receiving follow-up (within 7 days, adjusted odds ratio, 2.81; 95% confidence interval, 2.68-2.94).
Older age and leaving against medical advice were associated with decreased likelihood of follow-up. Female sex, hospitalizations related to self-harm or suicidality, and longer length of stay were associated with increased likelihood of mental health follow-up care.
Compared with those hospitalized for major depression, those hospitalized for schizophrenia, bipolar disorder, PTSD, disruptive disorders, or comorbid substance use disorder were less likely to receive mental health follow-up. For example, only 23.7% of youth with comorbid substance use discharged from the hospital had follow-up within 7 days.
Similar patterns were observed for 30-day follow-up care.
‘Accessible and appealing’ options needed
In the ED-visit group, the average age was 19.5 years (58% female). Most (70.4%) had no chronic health conditions other than a psychiatric disorder. The primary diagnoses were anxiety disorders or phobias (44.1%) and major depression (23%).
One in four visits included a code for self-harm, suicidal ideation, or suicide attempt. And almost one third lacked established outpatient care before the ED visit.
Results showed 28.6% of the ED group received mental health care follow-up within 7 days and 46.4% received it within 30 days.
Again, the strongest predictor of mental health follow-up was prior outpatient care. For example, compared with participants with no established outpatient care, those with both primary care and mental health care were the most likely to receive follow-up within 7 days (aOR, 4.06; 95% CI, 3.72-4.42).
These numbers “are far from the goal of making sure everybody is getting follow-up care within 7 days of an acute psychiatric event,” Dr. Skehan said.
He stressed the need for “accessible and appealing options for youth.” These could include telehealth services, improved communication among health care providers in the ED, and reducing barriers to access follow-up care.
“This probably highlights the need to have more case management and referral services, and maybe make sure patients have a follow-up appointment before they leave the emergency room,” said Dr. Skehan. “This doesn’t necessarily guarantee they’ll get there but hopefully it makes it more likely they will have that access should they need it.”
The study was funded by grants from the National Institute of General Medical Sciences and the National Center for Advancing Translational Sciences, from the National Institutes of Health. The investigators reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PSYCHIATRIC SERVICES
Support for Policy Changes for Therapy Related to Homefront Missions
Recent natural disasters, civil disorder, and the COVID-19 pandemic response created an unprecedented demand for the US National Guard and Reserve components as well as active-duty personnel to serve on homefront missions critical to our nation. At times, those serving in these capacities are front and center to the most tragic events confronting our nation, and they frequently encounter tremendous suffering.
Recognizing the potential for these missions to create psychological sequela for those who serve on them, the authority for the Veterans Health Administration (VHA) vet centers to provide readjustment counseling services was broadened on December 30, 2021. Vet centers are community-based counseling centers that have traditionally served combat veterans, and broadening services reflects a major change in mission. Revised VHA Directive 1500(2) specifies that those who “served on active duty in response to a national emergency or major disaster declared by the President” or “served on active duty in the National Guard of a State under orders of the chief executive of that State in response to a disaster or civil disorder in such State” may now receive therapy at vet centers.1,2
As a result of this recent policy change, National Guard and active-duty Reserve service members now have parity with combat veterans to obtain therapy for symptoms arising as a result of their activation for service on homefront missions. As they seek care, we need to be ready so that these service members can obtain the best therapy services possible. Soldiers who served on homefront missions comprise a new cohort of service members now eligible for vet center therapy. Soldiers who served on homefront missions may present with issues that differ from those of combat veterans and veterans who have experienced military sexual trauma (MST), the populations treated by vet centers and other VHA mental health care clinics prior to this broadened authority. This article highlights some suggestions for service delivery to best meet the needs of this population.
Discussion
Available evidence-based therapies to treat posttraumatic stress disorder (PTSD) are effective regardless of whether the trauma occurred in combat, on the homefront, or in a civilian setting. The vet centers and VHA mental health services already have staff trained to deliver these therapy modalities and, in this sense, are ready to provide trauma-focused therapy treatment to soldiers with PTSD who served on homefront missions.
The broadened authority for the vet centers to provide readjustment services is necessary, as it corrects for a critical gap in services, but the importance of ensuring adequate staffing to meet the expected increased demand for services cannot be underscored. According to clinical practice guidelines for the treatment of PTSD, developed by the US Department of Veterans Affairs (VA) and the US Department of Defense (DoD), the therapies with the strongest evidence-based backing are prolonged exposure-based therapy (PE), cognitive processing therapy (CPT), and eye movement and desensitization reprocessing (EMDR).3 These therapy modalities, based on findings from clinical trials, are predicated on seeing a client for a sufficient number of sessions. Attendance at these sessions is recommended at least weekly to ensure adequate intensity of service delivery.4-7 According to the National Center for PTSD, PE typically involves 8 to 15 weekly or twice weekly sessions; CPT requires 8 to 14 or more weekly sessions, and EMDR is usually 4 to 12 weekly sessions.4-7
Ensuring adequate staffing is critical to offer these therapies at least weekly as the efficacies of these therapies are otherwise not proven if return session visits are stretched out over multiple weeks or months. The most recent clinical research has demonstrated that PTSD recovery can be expedited and there are lower patient dropout rates when sessions are massed or compressed so that multiple sessions are administered over 1 week.8-12 Providing these therapies in a massed format has shown to be as effective as when these therapies are provided weekly.
As the authority to treat soldiers serving on homefront missions is new, epidemiologic data do not yet exist to estimate the proportion of this population who will need treatment or present with PTSD, depression, anxiety, a substance use disorder, and/or comorbid conditions. Those with PTSD can benefit from PTSD evidence-based therapies already available for treatment. Others may benefit from treatments that are proven effective for their mental health diagnoses.
Therapists with experience primarily treating patients with PTSD related to combat or MST will need to be sensitive to the unique experiences of the National Guard and Reserve service members. For example, this component of soldiers served on COVID-19–related missions that provided food service support to nursing homes residents who were locked down from family members. As a result, they developed bonds with residents who later died. This may have been the first time that these soldiers witnessed death. If such a soldier is assessed and does not have PTSD but is nonetheless distressed, then the soldier may need alternate therapies, such as grief counseling. This need may be more pronounced for those soldiers who lost loved ones to COVID-19 while they served on these missions.
New Jersey Army National Guard soldiers provided food service support at the Woodland Behavioral and Nursing Center in Andover, New Jersey. These soldiers witnessed the unfortunate conditions in this facility, which included stacked bodies in a makeshift morgue during the height of the pandemic; however, they did not have the ability to make changes. The facility is under investigation for abuse and neglect of its residents.13
New Jersey National Guard soldiers supporting that facility and similar ones may have experienced moral injury, defined as “…perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.”14 Importantly, when these soldiers present for therapy and express moral injury, their therapists need to be open to spiritual discourse. However, vet centers do not have chaplains on staff, so therapists must refer patients to chaplaincy services.
Among therapists with existing cultural competency for treating members of the military, some nuances exist for National Guard and Reserve service members. National Guard and Reserve component personnel already may feel that their problems are less important than those experienced by active-duty service members. Now that these soldiers have the eligibility to receive therapy, therapists may have to make extra efforts to both reassure this population that they are welcomed and to validate their need for services.
Special outreach efforts to those who served on historical National Guard and active-duty Reserve missions are a way to show good faith in serving these soldiers because they may have untreated PTSD or other undiagnosed mental health disorders related to earlier deployments, such as hurricane recovery missions. A study of disaster survivors found that the prevalence rate of severe and very severe psychological impact after a natural disaster was about 34%.15 Another epidemiologic study found that the prevalence rate of PTSD was 10% to 20% among disaster rescue workers.16 Specific data about the psychological problems of National Guard and Reserve components serving in disaster recovery are unavailable but is an area for future research.
Therapists who have treated active-duty service members and veterans who worked in mortuary services in a combat zone are used to hearing graphic details of horrifying scenes, but homefront experiences are different. Soldiers on homefront mortuary-based missions frequently reported being unable to forget the faces or the smell of dead bodies as they were stacked up and overwhelming the systems. Experienced vet center therapists should be prepared for the challenges in treating this new cohort of patients.
Conclusions
Now that National Guard and Reserve component soldiers who have responded to national and local emergencies are eligible for therapy, we need to be prepared to provide these services. In addition to addressing systemic staffing concerns, therapists need to be aware of the unique challenges faced by those who have served on homefront missions. These homefront missions have the potential to hit home for therapists.
1. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1550(2): readjustment counseling service. January 26, 2021. Accessed September 1, 2022. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=9168
2. US Department of Veterans Affairs. Vet centers (readjustment counseling: vet center eligibility. Updated January 3, 2022. Accessed September 1, 2022. https://www.vetcenter.va.gov/eligibility.asp
3. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction, version 3.0, 2017. Accessed September 1, 2022. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf
4. US Department of Veterans Affairs, National Center for PTSD. Prolonged exposure (PE) therapy. Updated August 10, 2022. Accessed September 1, 2022. https://www.ptsd.va.gov/understand_tx/prolonged_exposure.asp
5. US Department of Veterans Affairs, National Center for PTSD. Cognitive processing therapy (CPT) for PTSD: how to help your loved one during treatment. Accessed September 1, 2022. https://www.ptsd.va.gov/publications/print/CPT_familyhandout.pdf
6. US Department of Veterans Affairs, National Center for PTSD. A provider’s guide to brief cognitive behavioral therapy. Accessed September 1, 2022. https://www.mirecc.va.gov/visn16/docs/Therapists_Guide_to_Brief_CBTManual.pdf
7. US Department of Veterans Affairs, National Center for PTSD. Eye movement desensitization and reprocessing (EMDR) for PTSD. Accessed September 1, 2022. https://www.ptsd.va.gov/understand_tx/emdr.asp
8. Wachen JS, Dondanville KA, Evans WR, Morris K, Cole A. Adjusting the timeframe of evidence-based therapies for PTSD-massed treatments. Curr Treat Options Psych. 2019;6(2):107-118. doi:10.1007/s40501-019-00169-9
9. Dell L, Sbisa AM, Forbes A, et al. Effect of massed v. standard prolonged exposure therapy on PTSD in military personnel and veterans: a non-inferiority randomised controlled trial [published online ahead of print, 2022 Apr 20]. Psychol Med. 2022;1-8. doi:10.1017/S0033291722000927
10. Held P, Kovacevic M, Petrey K, et al. Treating posttraumatic stress disorder at home in a single week using 1-week virtual massed cognitive processing therapy. J Trauma Stress. 2022;35(4):1215-1225. doi:10.1002/jts.22831
11. Yamokoski C, Flores H, Facemire V, Maieritsch K, Perez S, Fedynich A. Feasibility of an intensive outpatient treatment program for posttraumatic stress disorder within the veterans health care administration [published online ahead of print, 2022 Mar 7]. Psychol Serv. 2022;10.1037/ser0000628. doi:10.1037/ser0000628
12. Galovski TE, Werner KB, Weaver TL, et al. Massed cognitive processing therapy for posttraumatic stress disorder in women survivors of intimate partner violence. Psychol Trauma. 2022;14(5):769-779. doi:10.1037/tra0001100
13. Fallon S. NJ to send monitors into troubled nursing home that stacked bodies in makeshift morgue. Updated March 10, 2022. Accessed September 1, 2022. https://www.northjersey.com/story/news/health/2022/03/09/sussex-county-nj-nursing-home-monitors-covid-morgue/9447243002/
14. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003009
15. Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207-239. doi:10.1521/psyc.65.3.207.20173
16. Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78-91. doi:10.1093/epirev/mxi003
Recent natural disasters, civil disorder, and the COVID-19 pandemic response created an unprecedented demand for the US National Guard and Reserve components as well as active-duty personnel to serve on homefront missions critical to our nation. At times, those serving in these capacities are front and center to the most tragic events confronting our nation, and they frequently encounter tremendous suffering.
Recognizing the potential for these missions to create psychological sequela for those who serve on them, the authority for the Veterans Health Administration (VHA) vet centers to provide readjustment counseling services was broadened on December 30, 2021. Vet centers are community-based counseling centers that have traditionally served combat veterans, and broadening services reflects a major change in mission. Revised VHA Directive 1500(2) specifies that those who “served on active duty in response to a national emergency or major disaster declared by the President” or “served on active duty in the National Guard of a State under orders of the chief executive of that State in response to a disaster or civil disorder in such State” may now receive therapy at vet centers.1,2
As a result of this recent policy change, National Guard and active-duty Reserve service members now have parity with combat veterans to obtain therapy for symptoms arising as a result of their activation for service on homefront missions. As they seek care, we need to be ready so that these service members can obtain the best therapy services possible. Soldiers who served on homefront missions comprise a new cohort of service members now eligible for vet center therapy. Soldiers who served on homefront missions may present with issues that differ from those of combat veterans and veterans who have experienced military sexual trauma (MST), the populations treated by vet centers and other VHA mental health care clinics prior to this broadened authority. This article highlights some suggestions for service delivery to best meet the needs of this population.
Discussion
Available evidence-based therapies to treat posttraumatic stress disorder (PTSD) are effective regardless of whether the trauma occurred in combat, on the homefront, or in a civilian setting. The vet centers and VHA mental health services already have staff trained to deliver these therapy modalities and, in this sense, are ready to provide trauma-focused therapy treatment to soldiers with PTSD who served on homefront missions.
The broadened authority for the vet centers to provide readjustment services is necessary, as it corrects for a critical gap in services, but the importance of ensuring adequate staffing to meet the expected increased demand for services cannot be underscored. According to clinical practice guidelines for the treatment of PTSD, developed by the US Department of Veterans Affairs (VA) and the US Department of Defense (DoD), the therapies with the strongest evidence-based backing are prolonged exposure-based therapy (PE), cognitive processing therapy (CPT), and eye movement and desensitization reprocessing (EMDR).3 These therapy modalities, based on findings from clinical trials, are predicated on seeing a client for a sufficient number of sessions. Attendance at these sessions is recommended at least weekly to ensure adequate intensity of service delivery.4-7 According to the National Center for PTSD, PE typically involves 8 to 15 weekly or twice weekly sessions; CPT requires 8 to 14 or more weekly sessions, and EMDR is usually 4 to 12 weekly sessions.4-7
Ensuring adequate staffing is critical to offer these therapies at least weekly as the efficacies of these therapies are otherwise not proven if return session visits are stretched out over multiple weeks or months. The most recent clinical research has demonstrated that PTSD recovery can be expedited and there are lower patient dropout rates when sessions are massed or compressed so that multiple sessions are administered over 1 week.8-12 Providing these therapies in a massed format has shown to be as effective as when these therapies are provided weekly.
As the authority to treat soldiers serving on homefront missions is new, epidemiologic data do not yet exist to estimate the proportion of this population who will need treatment or present with PTSD, depression, anxiety, a substance use disorder, and/or comorbid conditions. Those with PTSD can benefit from PTSD evidence-based therapies already available for treatment. Others may benefit from treatments that are proven effective for their mental health diagnoses.
Therapists with experience primarily treating patients with PTSD related to combat or MST will need to be sensitive to the unique experiences of the National Guard and Reserve service members. For example, this component of soldiers served on COVID-19–related missions that provided food service support to nursing homes residents who were locked down from family members. As a result, they developed bonds with residents who later died. This may have been the first time that these soldiers witnessed death. If such a soldier is assessed and does not have PTSD but is nonetheless distressed, then the soldier may need alternate therapies, such as grief counseling. This need may be more pronounced for those soldiers who lost loved ones to COVID-19 while they served on these missions.
New Jersey Army National Guard soldiers provided food service support at the Woodland Behavioral and Nursing Center in Andover, New Jersey. These soldiers witnessed the unfortunate conditions in this facility, which included stacked bodies in a makeshift morgue during the height of the pandemic; however, they did not have the ability to make changes. The facility is under investigation for abuse and neglect of its residents.13
New Jersey National Guard soldiers supporting that facility and similar ones may have experienced moral injury, defined as “…perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.”14 Importantly, when these soldiers present for therapy and express moral injury, their therapists need to be open to spiritual discourse. However, vet centers do not have chaplains on staff, so therapists must refer patients to chaplaincy services.
Among therapists with existing cultural competency for treating members of the military, some nuances exist for National Guard and Reserve service members. National Guard and Reserve component personnel already may feel that their problems are less important than those experienced by active-duty service members. Now that these soldiers have the eligibility to receive therapy, therapists may have to make extra efforts to both reassure this population that they are welcomed and to validate their need for services.
Special outreach efforts to those who served on historical National Guard and active-duty Reserve missions are a way to show good faith in serving these soldiers because they may have untreated PTSD or other undiagnosed mental health disorders related to earlier deployments, such as hurricane recovery missions. A study of disaster survivors found that the prevalence rate of severe and very severe psychological impact after a natural disaster was about 34%.15 Another epidemiologic study found that the prevalence rate of PTSD was 10% to 20% among disaster rescue workers.16 Specific data about the psychological problems of National Guard and Reserve components serving in disaster recovery are unavailable but is an area for future research.
Therapists who have treated active-duty service members and veterans who worked in mortuary services in a combat zone are used to hearing graphic details of horrifying scenes, but homefront experiences are different. Soldiers on homefront mortuary-based missions frequently reported being unable to forget the faces or the smell of dead bodies as they were stacked up and overwhelming the systems. Experienced vet center therapists should be prepared for the challenges in treating this new cohort of patients.
Conclusions
Now that National Guard and Reserve component soldiers who have responded to national and local emergencies are eligible for therapy, we need to be prepared to provide these services. In addition to addressing systemic staffing concerns, therapists need to be aware of the unique challenges faced by those who have served on homefront missions. These homefront missions have the potential to hit home for therapists.
Recent natural disasters, civil disorder, and the COVID-19 pandemic response created an unprecedented demand for the US National Guard and Reserve components as well as active-duty personnel to serve on homefront missions critical to our nation. At times, those serving in these capacities are front and center to the most tragic events confronting our nation, and they frequently encounter tremendous suffering.
Recognizing the potential for these missions to create psychological sequela for those who serve on them, the authority for the Veterans Health Administration (VHA) vet centers to provide readjustment counseling services was broadened on December 30, 2021. Vet centers are community-based counseling centers that have traditionally served combat veterans, and broadening services reflects a major change in mission. Revised VHA Directive 1500(2) specifies that those who “served on active duty in response to a national emergency or major disaster declared by the President” or “served on active duty in the National Guard of a State under orders of the chief executive of that State in response to a disaster or civil disorder in such State” may now receive therapy at vet centers.1,2
As a result of this recent policy change, National Guard and active-duty Reserve service members now have parity with combat veterans to obtain therapy for symptoms arising as a result of their activation for service on homefront missions. As they seek care, we need to be ready so that these service members can obtain the best therapy services possible. Soldiers who served on homefront missions comprise a new cohort of service members now eligible for vet center therapy. Soldiers who served on homefront missions may present with issues that differ from those of combat veterans and veterans who have experienced military sexual trauma (MST), the populations treated by vet centers and other VHA mental health care clinics prior to this broadened authority. This article highlights some suggestions for service delivery to best meet the needs of this population.
Discussion
Available evidence-based therapies to treat posttraumatic stress disorder (PTSD) are effective regardless of whether the trauma occurred in combat, on the homefront, or in a civilian setting. The vet centers and VHA mental health services already have staff trained to deliver these therapy modalities and, in this sense, are ready to provide trauma-focused therapy treatment to soldiers with PTSD who served on homefront missions.
The broadened authority for the vet centers to provide readjustment services is necessary, as it corrects for a critical gap in services, but the importance of ensuring adequate staffing to meet the expected increased demand for services cannot be underscored. According to clinical practice guidelines for the treatment of PTSD, developed by the US Department of Veterans Affairs (VA) and the US Department of Defense (DoD), the therapies with the strongest evidence-based backing are prolonged exposure-based therapy (PE), cognitive processing therapy (CPT), and eye movement and desensitization reprocessing (EMDR).3 These therapy modalities, based on findings from clinical trials, are predicated on seeing a client for a sufficient number of sessions. Attendance at these sessions is recommended at least weekly to ensure adequate intensity of service delivery.4-7 According to the National Center for PTSD, PE typically involves 8 to 15 weekly or twice weekly sessions; CPT requires 8 to 14 or more weekly sessions, and EMDR is usually 4 to 12 weekly sessions.4-7
Ensuring adequate staffing is critical to offer these therapies at least weekly as the efficacies of these therapies are otherwise not proven if return session visits are stretched out over multiple weeks or months. The most recent clinical research has demonstrated that PTSD recovery can be expedited and there are lower patient dropout rates when sessions are massed or compressed so that multiple sessions are administered over 1 week.8-12 Providing these therapies in a massed format has shown to be as effective as when these therapies are provided weekly.
As the authority to treat soldiers serving on homefront missions is new, epidemiologic data do not yet exist to estimate the proportion of this population who will need treatment or present with PTSD, depression, anxiety, a substance use disorder, and/or comorbid conditions. Those with PTSD can benefit from PTSD evidence-based therapies already available for treatment. Others may benefit from treatments that are proven effective for their mental health diagnoses.
Therapists with experience primarily treating patients with PTSD related to combat or MST will need to be sensitive to the unique experiences of the National Guard and Reserve service members. For example, this component of soldiers served on COVID-19–related missions that provided food service support to nursing homes residents who were locked down from family members. As a result, they developed bonds with residents who later died. This may have been the first time that these soldiers witnessed death. If such a soldier is assessed and does not have PTSD but is nonetheless distressed, then the soldier may need alternate therapies, such as grief counseling. This need may be more pronounced for those soldiers who lost loved ones to COVID-19 while they served on these missions.
New Jersey Army National Guard soldiers provided food service support at the Woodland Behavioral and Nursing Center in Andover, New Jersey. These soldiers witnessed the unfortunate conditions in this facility, which included stacked bodies in a makeshift morgue during the height of the pandemic; however, they did not have the ability to make changes. The facility is under investigation for abuse and neglect of its residents.13
New Jersey National Guard soldiers supporting that facility and similar ones may have experienced moral injury, defined as “…perpetrating, failing to prevent, or bearing witness to acts that transgress deeply held moral beliefs and expectations.”14 Importantly, when these soldiers present for therapy and express moral injury, their therapists need to be open to spiritual discourse. However, vet centers do not have chaplains on staff, so therapists must refer patients to chaplaincy services.
Among therapists with existing cultural competency for treating members of the military, some nuances exist for National Guard and Reserve service members. National Guard and Reserve component personnel already may feel that their problems are less important than those experienced by active-duty service members. Now that these soldiers have the eligibility to receive therapy, therapists may have to make extra efforts to both reassure this population that they are welcomed and to validate their need for services.
Special outreach efforts to those who served on historical National Guard and active-duty Reserve missions are a way to show good faith in serving these soldiers because they may have untreated PTSD or other undiagnosed mental health disorders related to earlier deployments, such as hurricane recovery missions. A study of disaster survivors found that the prevalence rate of severe and very severe psychological impact after a natural disaster was about 34%.15 Another epidemiologic study found that the prevalence rate of PTSD was 10% to 20% among disaster rescue workers.16 Specific data about the psychological problems of National Guard and Reserve components serving in disaster recovery are unavailable but is an area for future research.
Therapists who have treated active-duty service members and veterans who worked in mortuary services in a combat zone are used to hearing graphic details of horrifying scenes, but homefront experiences are different. Soldiers on homefront mortuary-based missions frequently reported being unable to forget the faces or the smell of dead bodies as they were stacked up and overwhelming the systems. Experienced vet center therapists should be prepared for the challenges in treating this new cohort of patients.
Conclusions
Now that National Guard and Reserve component soldiers who have responded to national and local emergencies are eligible for therapy, we need to be prepared to provide these services. In addition to addressing systemic staffing concerns, therapists need to be aware of the unique challenges faced by those who have served on homefront missions. These homefront missions have the potential to hit home for therapists.
1. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1550(2): readjustment counseling service. January 26, 2021. Accessed September 1, 2022. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=9168
2. US Department of Veterans Affairs. Vet centers (readjustment counseling: vet center eligibility. Updated January 3, 2022. Accessed September 1, 2022. https://www.vetcenter.va.gov/eligibility.asp
3. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction, version 3.0, 2017. Accessed September 1, 2022. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf
4. US Department of Veterans Affairs, National Center for PTSD. Prolonged exposure (PE) therapy. Updated August 10, 2022. Accessed September 1, 2022. https://www.ptsd.va.gov/understand_tx/prolonged_exposure.asp
5. US Department of Veterans Affairs, National Center for PTSD. Cognitive processing therapy (CPT) for PTSD: how to help your loved one during treatment. Accessed September 1, 2022. https://www.ptsd.va.gov/publications/print/CPT_familyhandout.pdf
6. US Department of Veterans Affairs, National Center for PTSD. A provider’s guide to brief cognitive behavioral therapy. Accessed September 1, 2022. https://www.mirecc.va.gov/visn16/docs/Therapists_Guide_to_Brief_CBTManual.pdf
7. US Department of Veterans Affairs, National Center for PTSD. Eye movement desensitization and reprocessing (EMDR) for PTSD. Accessed September 1, 2022. https://www.ptsd.va.gov/understand_tx/emdr.asp
8. Wachen JS, Dondanville KA, Evans WR, Morris K, Cole A. Adjusting the timeframe of evidence-based therapies for PTSD-massed treatments. Curr Treat Options Psych. 2019;6(2):107-118. doi:10.1007/s40501-019-00169-9
9. Dell L, Sbisa AM, Forbes A, et al. Effect of massed v. standard prolonged exposure therapy on PTSD in military personnel and veterans: a non-inferiority randomised controlled trial [published online ahead of print, 2022 Apr 20]. Psychol Med. 2022;1-8. doi:10.1017/S0033291722000927
10. Held P, Kovacevic M, Petrey K, et al. Treating posttraumatic stress disorder at home in a single week using 1-week virtual massed cognitive processing therapy. J Trauma Stress. 2022;35(4):1215-1225. doi:10.1002/jts.22831
11. Yamokoski C, Flores H, Facemire V, Maieritsch K, Perez S, Fedynich A. Feasibility of an intensive outpatient treatment program for posttraumatic stress disorder within the veterans health care administration [published online ahead of print, 2022 Mar 7]. Psychol Serv. 2022;10.1037/ser0000628. doi:10.1037/ser0000628
12. Galovski TE, Werner KB, Weaver TL, et al. Massed cognitive processing therapy for posttraumatic stress disorder in women survivors of intimate partner violence. Psychol Trauma. 2022;14(5):769-779. doi:10.1037/tra0001100
13. Fallon S. NJ to send monitors into troubled nursing home that stacked bodies in makeshift morgue. Updated March 10, 2022. Accessed September 1, 2022. https://www.northjersey.com/story/news/health/2022/03/09/sussex-county-nj-nursing-home-monitors-covid-morgue/9447243002/
14. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003009
15. Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207-239. doi:10.1521/psyc.65.3.207.20173
16. Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78-91. doi:10.1093/epirev/mxi003
1. US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1550(2): readjustment counseling service. January 26, 2021. Accessed September 1, 2022. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=9168
2. US Department of Veterans Affairs. Vet centers (readjustment counseling: vet center eligibility. Updated January 3, 2022. Accessed September 1, 2022. https://www.vetcenter.va.gov/eligibility.asp
3. US Department of Defense, US Department of Veterans Affairs. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress reaction, version 3.0, 2017. Accessed September 1, 2022. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf
4. US Department of Veterans Affairs, National Center for PTSD. Prolonged exposure (PE) therapy. Updated August 10, 2022. Accessed September 1, 2022. https://www.ptsd.va.gov/understand_tx/prolonged_exposure.asp
5. US Department of Veterans Affairs, National Center for PTSD. Cognitive processing therapy (CPT) for PTSD: how to help your loved one during treatment. Accessed September 1, 2022. https://www.ptsd.va.gov/publications/print/CPT_familyhandout.pdf
6. US Department of Veterans Affairs, National Center for PTSD. A provider’s guide to brief cognitive behavioral therapy. Accessed September 1, 2022. https://www.mirecc.va.gov/visn16/docs/Therapists_Guide_to_Brief_CBTManual.pdf
7. US Department of Veterans Affairs, National Center for PTSD. Eye movement desensitization and reprocessing (EMDR) for PTSD. Accessed September 1, 2022. https://www.ptsd.va.gov/understand_tx/emdr.asp
8. Wachen JS, Dondanville KA, Evans WR, Morris K, Cole A. Adjusting the timeframe of evidence-based therapies for PTSD-massed treatments. Curr Treat Options Psych. 2019;6(2):107-118. doi:10.1007/s40501-019-00169-9
9. Dell L, Sbisa AM, Forbes A, et al. Effect of massed v. standard prolonged exposure therapy on PTSD in military personnel and veterans: a non-inferiority randomised controlled trial [published online ahead of print, 2022 Apr 20]. Psychol Med. 2022;1-8. doi:10.1017/S0033291722000927
10. Held P, Kovacevic M, Petrey K, et al. Treating posttraumatic stress disorder at home in a single week using 1-week virtual massed cognitive processing therapy. J Trauma Stress. 2022;35(4):1215-1225. doi:10.1002/jts.22831
11. Yamokoski C, Flores H, Facemire V, Maieritsch K, Perez S, Fedynich A. Feasibility of an intensive outpatient treatment program for posttraumatic stress disorder within the veterans health care administration [published online ahead of print, 2022 Mar 7]. Psychol Serv. 2022;10.1037/ser0000628. doi:10.1037/ser0000628
12. Galovski TE, Werner KB, Weaver TL, et al. Massed cognitive processing therapy for posttraumatic stress disorder in women survivors of intimate partner violence. Psychol Trauma. 2022;14(5):769-779. doi:10.1037/tra0001100
13. Fallon S. NJ to send monitors into troubled nursing home that stacked bodies in makeshift morgue. Updated March 10, 2022. Accessed September 1, 2022. https://www.northjersey.com/story/news/health/2022/03/09/sussex-county-nj-nursing-home-monitors-covid-morgue/9447243002/
14. Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695-706. doi:10.1016/j.cpr.2009.07.003009
15. Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207-239. doi:10.1521/psyc.65.3.207.20173
16. Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78-91. doi:10.1093/epirev/mxi003
Urgent need for research into psychedelic therapy for older adults
new research shows.
“Geriatric psychiatrists and others caring for older adults are interested in how much is known about psychedelic use in older adults,” study investigator C. Bree Johnston, MD, MPH, University of Arizona, Tucson, told this news organization.
“A major concern is how safe psychedelic-assisted therapy is for patients with heart disease, hypertension, neurological disorders, and multimorbidity,” Dr. Johnston said.
The study is published online in the American Journal of Geriatric Psychiatry.
‘Groundswell’ of research
The past few years have brought a “groundswell” of interest and promising research into the potential therapeutic benefit of psychedelic-assisted therapy for a variety of conditions affecting adults, the researchers noted.
They include psilocybin-assisted therapy for the distress associated with a terminal diagnosis, depression, and addiction, and MDMA-assisted therapy for PTSD.
However, in most studies, psychedelic therapy has been tested in relatively young healthy adults, raising the question of how generalizable the study results are for the patients that most geropsychiatrists will be treating, the investigators noted.
They reviewed “the most important” research studies on psilocybin- and MDMA-assisted therapies published over the past 2 decades that are likely to be relevant for geriatric psychiatrists and other professionals caring for older adults.
The researchers point out that psychedelics and related compounds have shown efficacy for the treatment of a number of conditions that are common among older adults, including mood disorders, distress associated with a serious medical illness, PTSD, substance use problems, and prolonged grief.
Psychedelics also have properties that may provide for cognitive impairment and dementia and promote personal growth among healthy older adults.
Research has shown that psychedelics can be safely administered to healthy adults in controlled conditions.
However, both psilocybin and MDMA can increase blood pressure and heart rate, which could be a concern if used in older adults with cardiovascular disease, the investigators noted.
“Healthy older adults are likely to face similar risks when undergoing psychedelic-assisted therapy as healthy younger adults,” said Dr. Johnston.
“In carefully selected adults, those risks appear to be minor when psychedelics are administered in controlled conditions under the guidance of a skilled therapist,” she added.
Given the potential of psychedelic compounds to benefit older adults, the authors call for more research to establish the safety and efficacy among older adults, particularly those with multiple comorbidities.
Pressing knowledge gaps
The exclusion of older adults from clinical trials of novel treatments is “one of contemporary psychiatry’s more pressing problems – one that extends beyond psychedelics,” Ipsit V. Vahia, MD, associate chief of the division of geriatric psychiatry, McLean Hospital, Belmont, Mass., who wasn’t involved in the review, told this news organization.
“Currently, there is little evidence that clinicians can lean on while considering the use of psychedelics in older adults,” Dr. Vahia said.
This paper highlights “the most pressing gaps in the evidence that bear addressing in order to develop more substantial best practices around the use of these drugs,” he added.
For example, little is known about appropriate dosing, pharmacokinetics, and pharmacodynamics of psychedelics in older adults, Dr. Vahia said.
“Their risks, particularly cardiovascular risks, are barely studied, and almost nothing is known about how these drugs may impact those in their 80s or older, or those with serious medical comorbidities who use multiple medications,” Dr. Vahia said. “The majority of the existing literature has excluded older adults, and the extremely limited evidence that does exist has been collected in relatively healthy, and relatively young (aged below 75) persons.”
Dr. Vahia noted that, before psychedelics as a class can be considered viable treatment options for a broader group of older adults, “more research is needed, particularly to establish safety.”
This research had no specific funding. Dr. Johnston and Dr. Vahia have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
new research shows.
“Geriatric psychiatrists and others caring for older adults are interested in how much is known about psychedelic use in older adults,” study investigator C. Bree Johnston, MD, MPH, University of Arizona, Tucson, told this news organization.
“A major concern is how safe psychedelic-assisted therapy is for patients with heart disease, hypertension, neurological disorders, and multimorbidity,” Dr. Johnston said.
The study is published online in the American Journal of Geriatric Psychiatry.
‘Groundswell’ of research
The past few years have brought a “groundswell” of interest and promising research into the potential therapeutic benefit of psychedelic-assisted therapy for a variety of conditions affecting adults, the researchers noted.
They include psilocybin-assisted therapy for the distress associated with a terminal diagnosis, depression, and addiction, and MDMA-assisted therapy for PTSD.
However, in most studies, psychedelic therapy has been tested in relatively young healthy adults, raising the question of how generalizable the study results are for the patients that most geropsychiatrists will be treating, the investigators noted.
They reviewed “the most important” research studies on psilocybin- and MDMA-assisted therapies published over the past 2 decades that are likely to be relevant for geriatric psychiatrists and other professionals caring for older adults.
The researchers point out that psychedelics and related compounds have shown efficacy for the treatment of a number of conditions that are common among older adults, including mood disorders, distress associated with a serious medical illness, PTSD, substance use problems, and prolonged grief.
Psychedelics also have properties that may provide for cognitive impairment and dementia and promote personal growth among healthy older adults.
Research has shown that psychedelics can be safely administered to healthy adults in controlled conditions.
However, both psilocybin and MDMA can increase blood pressure and heart rate, which could be a concern if used in older adults with cardiovascular disease, the investigators noted.
“Healthy older adults are likely to face similar risks when undergoing psychedelic-assisted therapy as healthy younger adults,” said Dr. Johnston.
“In carefully selected adults, those risks appear to be minor when psychedelics are administered in controlled conditions under the guidance of a skilled therapist,” she added.
Given the potential of psychedelic compounds to benefit older adults, the authors call for more research to establish the safety and efficacy among older adults, particularly those with multiple comorbidities.
Pressing knowledge gaps
The exclusion of older adults from clinical trials of novel treatments is “one of contemporary psychiatry’s more pressing problems – one that extends beyond psychedelics,” Ipsit V. Vahia, MD, associate chief of the division of geriatric psychiatry, McLean Hospital, Belmont, Mass., who wasn’t involved in the review, told this news organization.
“Currently, there is little evidence that clinicians can lean on while considering the use of psychedelics in older adults,” Dr. Vahia said.
This paper highlights “the most pressing gaps in the evidence that bear addressing in order to develop more substantial best practices around the use of these drugs,” he added.
For example, little is known about appropriate dosing, pharmacokinetics, and pharmacodynamics of psychedelics in older adults, Dr. Vahia said.
“Their risks, particularly cardiovascular risks, are barely studied, and almost nothing is known about how these drugs may impact those in their 80s or older, or those with serious medical comorbidities who use multiple medications,” Dr. Vahia said. “The majority of the existing literature has excluded older adults, and the extremely limited evidence that does exist has been collected in relatively healthy, and relatively young (aged below 75) persons.”
Dr. Vahia noted that, before psychedelics as a class can be considered viable treatment options for a broader group of older adults, “more research is needed, particularly to establish safety.”
This research had no specific funding. Dr. Johnston and Dr. Vahia have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
new research shows.
“Geriatric psychiatrists and others caring for older adults are interested in how much is known about psychedelic use in older adults,” study investigator C. Bree Johnston, MD, MPH, University of Arizona, Tucson, told this news organization.
“A major concern is how safe psychedelic-assisted therapy is for patients with heart disease, hypertension, neurological disorders, and multimorbidity,” Dr. Johnston said.
The study is published online in the American Journal of Geriatric Psychiatry.
‘Groundswell’ of research
The past few years have brought a “groundswell” of interest and promising research into the potential therapeutic benefit of psychedelic-assisted therapy for a variety of conditions affecting adults, the researchers noted.
They include psilocybin-assisted therapy for the distress associated with a terminal diagnosis, depression, and addiction, and MDMA-assisted therapy for PTSD.
However, in most studies, psychedelic therapy has been tested in relatively young healthy adults, raising the question of how generalizable the study results are for the patients that most geropsychiatrists will be treating, the investigators noted.
They reviewed “the most important” research studies on psilocybin- and MDMA-assisted therapies published over the past 2 decades that are likely to be relevant for geriatric psychiatrists and other professionals caring for older adults.
The researchers point out that psychedelics and related compounds have shown efficacy for the treatment of a number of conditions that are common among older adults, including mood disorders, distress associated with a serious medical illness, PTSD, substance use problems, and prolonged grief.
Psychedelics also have properties that may provide for cognitive impairment and dementia and promote personal growth among healthy older adults.
Research has shown that psychedelics can be safely administered to healthy adults in controlled conditions.
However, both psilocybin and MDMA can increase blood pressure and heart rate, which could be a concern if used in older adults with cardiovascular disease, the investigators noted.
“Healthy older adults are likely to face similar risks when undergoing psychedelic-assisted therapy as healthy younger adults,” said Dr. Johnston.
“In carefully selected adults, those risks appear to be minor when psychedelics are administered in controlled conditions under the guidance of a skilled therapist,” she added.
Given the potential of psychedelic compounds to benefit older adults, the authors call for more research to establish the safety and efficacy among older adults, particularly those with multiple comorbidities.
Pressing knowledge gaps
The exclusion of older adults from clinical trials of novel treatments is “one of contemporary psychiatry’s more pressing problems – one that extends beyond psychedelics,” Ipsit V. Vahia, MD, associate chief of the division of geriatric psychiatry, McLean Hospital, Belmont, Mass., who wasn’t involved in the review, told this news organization.
“Currently, there is little evidence that clinicians can lean on while considering the use of psychedelics in older adults,” Dr. Vahia said.
This paper highlights “the most pressing gaps in the evidence that bear addressing in order to develop more substantial best practices around the use of these drugs,” he added.
For example, little is known about appropriate dosing, pharmacokinetics, and pharmacodynamics of psychedelics in older adults, Dr. Vahia said.
“Their risks, particularly cardiovascular risks, are barely studied, and almost nothing is known about how these drugs may impact those in their 80s or older, or those with serious medical comorbidities who use multiple medications,” Dr. Vahia said. “The majority of the existing literature has excluded older adults, and the extremely limited evidence that does exist has been collected in relatively healthy, and relatively young (aged below 75) persons.”
Dr. Vahia noted that, before psychedelics as a class can be considered viable treatment options for a broader group of older adults, “more research is needed, particularly to establish safety.”
This research had no specific funding. Dr. Johnston and Dr. Vahia have no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY
Detachment predicts worse posttraumatic outcomes
The results highlight the importance of screening for dissociation in patients who have experienced trauma, study investigator Lauren A.M. Lebois, PhD, director of the dissociative disorders and trauma research program at McLean Hospital in Belmont, Mass., told this news organization.
“Clinicians could identify individuals potentially at risk of a chronic, more severe psychiatric course before these people go down that road, and they have the opportunity to connect folks with a phased trauma treatment approach to speed their recovery,” said Dr. Lebois, who is also an assistant professor of psychiatry at Harvard Medical School, Boston.
The study was published in the American Journal of Psychiatry.
Underdiagnosed
Feelings of detachment or derealization are a type of dissociation. Patients with the syndrome report feeling foggy or as if they are in a dream. Dissociative diagnoses are not rare and, in fact, are more prevalent than schizophrenia.
Research supports a powerful relationship between dissociation and traumatic experiences. However, dissociation is among the most stigmatized of psychiatric conditions. Even among clinicians and researchers, beliefs about dissociation are often not based on the scientific literature, said Dr. Lebois.
“For instance, skepticism, misunderstanding, and lack of professional education about dissociation all contribute to striking rates of underdiagnosis and misdiagnoses,” she said.
Dr. Lebois and colleagues used data from the larger Advancing Understanding of Recovery After Trauma (AURORA) study and included 1,464 adults, mean age 35 years, appearing at 22 U.S. emergency departments. Patients experienced a traumatic event such as a motor vehicle crash or physical or sexual assault.
About 2 weeks after the trauma, participants reported symptoms of derealization as measured by a two-item version of the Brief Dissociative Experiences Scale.
Brain imaging data
A subset of 145 patients underwent functional MRI (fMRI), during which they completed an emotion reactivity task (viewing fearful-looking human faces) and a resting-state scan.
In addition to measuring history of childhood maltreatment, researchers assessed posttraumatic stress symptom severity at 2 weeks and again at 3 months using the posttraumatic stress disorder checklist. Also at 3 months, they measured depression and anxiety symptoms, pain, and functional impairment.
About 55% of self-report participants and 50% of MRI participants endorsed some level of persistent derealization at 2 weeks.
After controlling for potential confounders, including sex, age, childhood maltreatment, and current posttraumatic stress symptoms, researchers found persistent derealization was associated with increased ventromedial prefrontal cortex (vmPFC) activity while viewing fearful faces.
The vmPFC helps to regulate emotional and physical reactions. “This region puts the ‘brakes’ on your emotional and physical reactivity – helping you to calm down” after a threatening or stressful experience has passed, said Dr. Lebois.
Researchers also found an association between higher self-reported derealization and decreased resting-state connectivity between the vmPFC and the orbitofrontal cortex and right lobule VIIIa – a region of the cerebellum involved in sensorimotor function.
“This may contribute to perceptual and affective distortions experienced during derealization – for example, feelings that surroundings are fading away, unreal, or strange,” said Dr. Lebois.
More pain, depression, anxiety
Higher levels of self-reported derealization at 2 weeks post trauma predicted higher levels of PTSD, anxiety, and depression as well as more bodily pain and impairment in work, family, and social life at 3 months.
“When we accounted for baseline levels of posttraumatic stress symptoms and trauma history, higher levels of self-reported derealization still predicted higher posttraumatic stress disorder and depression symptoms at 3 months,” said Dr. Lebois.
Additional adjusted analyses showed increased vmPFC activity during the fearful face task predicted 3-month self-reported PTSD symptoms.
Dr. Lebois “highly recommends” clinicians screen for dissociative symptoms, including derealization, in patients with trauma. Self-report screening tools are freely available online.
She noted patients with significant dissociative symptoms often do better with a “phase-oriented” approach to trauma treatment.
“In phase one, they learn emotional regulation skills to help them take more control over when they dissociate. Then they can successfully move on to trauma processing in phase two, which can involve exposure to trauma details.”
Although the field is not yet ready to use brain scans to diagnose dissociative symptoms, the new results “take us one step closer to being able to use objective neuroimaging biomarkers of derealization to augment subjective self-report measures,” said Dr. Lebois.
A limitation of the study was it could not determine a causal relationship, as some derealization may have been present before the traumatic event. The findings may not generalize to other types of dissociation, and the derealization assessment was measured only through a self-report 2 weeks after the trauma.
Another limitation was exclusion of patients with self-inflicted injuries or who were involved in domestic violence. The researchers noted the prevalence of derealization might have been even higher if such individuals were included.
An important investigation
In an accompanying editorial, Lisa M. Shin, PhD, department of psychology, Tufts University, and department of psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, notes having both clinical and neuroimaging variables as well as a large sample size makes the study “an important investigation” into predictors of psychiatric symptoms post-trauma.
Investigating a specific subtype of dissociation – persistent derealization – adds to the “novelty” of the study, she said.
The new findings “are certainly exciting for their potential clinical relevance and contributions to neurocircuitry models of PTSD,” she writes.
Some may argue administering a short, self-report measure of derealization “is far more efficient, cost-effective, and inclusive than conducting a specialized and expensive fMRI scan that is unlikely to be available to everyone,” notes Dr. Shin.
However, she added, a potential benefit of such a scan is identification of specific brain regions as potential targets for intervention. “For example, the results of this and other studies suggest that the vmPFC is a reasonable target for transcranial magnetic stimulation or its variants.”
The new results need to be replicated in a large, independent sample, said Dr. Shin. She added it would be helpful to know if other types of dissociation, and activation in other subregions of the vmPFC, also predict psychiatric outcomes after a trauma.
The study was supported by National Institute of Mental Health grants, the U.S. Army Medical Research and Material Command, One Mind, and the Mayday Fund. Dr. Lebois has received grant support from NIMH, and her spouse receives payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals. Dr. Shin receives textbook-related royalties from Pearson.
A version of this article first appeared on Medscape.com.
The results highlight the importance of screening for dissociation in patients who have experienced trauma, study investigator Lauren A.M. Lebois, PhD, director of the dissociative disorders and trauma research program at McLean Hospital in Belmont, Mass., told this news organization.
“Clinicians could identify individuals potentially at risk of a chronic, more severe psychiatric course before these people go down that road, and they have the opportunity to connect folks with a phased trauma treatment approach to speed their recovery,” said Dr. Lebois, who is also an assistant professor of psychiatry at Harvard Medical School, Boston.
The study was published in the American Journal of Psychiatry.
Underdiagnosed
Feelings of detachment or derealization are a type of dissociation. Patients with the syndrome report feeling foggy or as if they are in a dream. Dissociative diagnoses are not rare and, in fact, are more prevalent than schizophrenia.
Research supports a powerful relationship between dissociation and traumatic experiences. However, dissociation is among the most stigmatized of psychiatric conditions. Even among clinicians and researchers, beliefs about dissociation are often not based on the scientific literature, said Dr. Lebois.
“For instance, skepticism, misunderstanding, and lack of professional education about dissociation all contribute to striking rates of underdiagnosis and misdiagnoses,” she said.
Dr. Lebois and colleagues used data from the larger Advancing Understanding of Recovery After Trauma (AURORA) study and included 1,464 adults, mean age 35 years, appearing at 22 U.S. emergency departments. Patients experienced a traumatic event such as a motor vehicle crash or physical or sexual assault.
About 2 weeks after the trauma, participants reported symptoms of derealization as measured by a two-item version of the Brief Dissociative Experiences Scale.
Brain imaging data
A subset of 145 patients underwent functional MRI (fMRI), during which they completed an emotion reactivity task (viewing fearful-looking human faces) and a resting-state scan.
In addition to measuring history of childhood maltreatment, researchers assessed posttraumatic stress symptom severity at 2 weeks and again at 3 months using the posttraumatic stress disorder checklist. Also at 3 months, they measured depression and anxiety symptoms, pain, and functional impairment.
About 55% of self-report participants and 50% of MRI participants endorsed some level of persistent derealization at 2 weeks.
After controlling for potential confounders, including sex, age, childhood maltreatment, and current posttraumatic stress symptoms, researchers found persistent derealization was associated with increased ventromedial prefrontal cortex (vmPFC) activity while viewing fearful faces.
The vmPFC helps to regulate emotional and physical reactions. “This region puts the ‘brakes’ on your emotional and physical reactivity – helping you to calm down” after a threatening or stressful experience has passed, said Dr. Lebois.
Researchers also found an association between higher self-reported derealization and decreased resting-state connectivity between the vmPFC and the orbitofrontal cortex and right lobule VIIIa – a region of the cerebellum involved in sensorimotor function.
“This may contribute to perceptual and affective distortions experienced during derealization – for example, feelings that surroundings are fading away, unreal, or strange,” said Dr. Lebois.
More pain, depression, anxiety
Higher levels of self-reported derealization at 2 weeks post trauma predicted higher levels of PTSD, anxiety, and depression as well as more bodily pain and impairment in work, family, and social life at 3 months.
“When we accounted for baseline levels of posttraumatic stress symptoms and trauma history, higher levels of self-reported derealization still predicted higher posttraumatic stress disorder and depression symptoms at 3 months,” said Dr. Lebois.
Additional adjusted analyses showed increased vmPFC activity during the fearful face task predicted 3-month self-reported PTSD symptoms.
Dr. Lebois “highly recommends” clinicians screen for dissociative symptoms, including derealization, in patients with trauma. Self-report screening tools are freely available online.
She noted patients with significant dissociative symptoms often do better with a “phase-oriented” approach to trauma treatment.
“In phase one, they learn emotional regulation skills to help them take more control over when they dissociate. Then they can successfully move on to trauma processing in phase two, which can involve exposure to trauma details.”
Although the field is not yet ready to use brain scans to diagnose dissociative symptoms, the new results “take us one step closer to being able to use objective neuroimaging biomarkers of derealization to augment subjective self-report measures,” said Dr. Lebois.
A limitation of the study was it could not determine a causal relationship, as some derealization may have been present before the traumatic event. The findings may not generalize to other types of dissociation, and the derealization assessment was measured only through a self-report 2 weeks after the trauma.
Another limitation was exclusion of patients with self-inflicted injuries or who were involved in domestic violence. The researchers noted the prevalence of derealization might have been even higher if such individuals were included.
An important investigation
In an accompanying editorial, Lisa M. Shin, PhD, department of psychology, Tufts University, and department of psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, notes having both clinical and neuroimaging variables as well as a large sample size makes the study “an important investigation” into predictors of psychiatric symptoms post-trauma.
Investigating a specific subtype of dissociation – persistent derealization – adds to the “novelty” of the study, she said.
The new findings “are certainly exciting for their potential clinical relevance and contributions to neurocircuitry models of PTSD,” she writes.
Some may argue administering a short, self-report measure of derealization “is far more efficient, cost-effective, and inclusive than conducting a specialized and expensive fMRI scan that is unlikely to be available to everyone,” notes Dr. Shin.
However, she added, a potential benefit of such a scan is identification of specific brain regions as potential targets for intervention. “For example, the results of this and other studies suggest that the vmPFC is a reasonable target for transcranial magnetic stimulation or its variants.”
The new results need to be replicated in a large, independent sample, said Dr. Shin. She added it would be helpful to know if other types of dissociation, and activation in other subregions of the vmPFC, also predict psychiatric outcomes after a trauma.
The study was supported by National Institute of Mental Health grants, the U.S. Army Medical Research and Material Command, One Mind, and the Mayday Fund. Dr. Lebois has received grant support from NIMH, and her spouse receives payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals. Dr. Shin receives textbook-related royalties from Pearson.
A version of this article first appeared on Medscape.com.
The results highlight the importance of screening for dissociation in patients who have experienced trauma, study investigator Lauren A.M. Lebois, PhD, director of the dissociative disorders and trauma research program at McLean Hospital in Belmont, Mass., told this news organization.
“Clinicians could identify individuals potentially at risk of a chronic, more severe psychiatric course before these people go down that road, and they have the opportunity to connect folks with a phased trauma treatment approach to speed their recovery,” said Dr. Lebois, who is also an assistant professor of psychiatry at Harvard Medical School, Boston.
The study was published in the American Journal of Psychiatry.
Underdiagnosed
Feelings of detachment or derealization are a type of dissociation. Patients with the syndrome report feeling foggy or as if they are in a dream. Dissociative diagnoses are not rare and, in fact, are more prevalent than schizophrenia.
Research supports a powerful relationship between dissociation and traumatic experiences. However, dissociation is among the most stigmatized of psychiatric conditions. Even among clinicians and researchers, beliefs about dissociation are often not based on the scientific literature, said Dr. Lebois.
“For instance, skepticism, misunderstanding, and lack of professional education about dissociation all contribute to striking rates of underdiagnosis and misdiagnoses,” she said.
Dr. Lebois and colleagues used data from the larger Advancing Understanding of Recovery After Trauma (AURORA) study and included 1,464 adults, mean age 35 years, appearing at 22 U.S. emergency departments. Patients experienced a traumatic event such as a motor vehicle crash or physical or sexual assault.
About 2 weeks after the trauma, participants reported symptoms of derealization as measured by a two-item version of the Brief Dissociative Experiences Scale.
Brain imaging data
A subset of 145 patients underwent functional MRI (fMRI), during which they completed an emotion reactivity task (viewing fearful-looking human faces) and a resting-state scan.
In addition to measuring history of childhood maltreatment, researchers assessed posttraumatic stress symptom severity at 2 weeks and again at 3 months using the posttraumatic stress disorder checklist. Also at 3 months, they measured depression and anxiety symptoms, pain, and functional impairment.
About 55% of self-report participants and 50% of MRI participants endorsed some level of persistent derealization at 2 weeks.
After controlling for potential confounders, including sex, age, childhood maltreatment, and current posttraumatic stress symptoms, researchers found persistent derealization was associated with increased ventromedial prefrontal cortex (vmPFC) activity while viewing fearful faces.
The vmPFC helps to regulate emotional and physical reactions. “This region puts the ‘brakes’ on your emotional and physical reactivity – helping you to calm down” after a threatening or stressful experience has passed, said Dr. Lebois.
Researchers also found an association between higher self-reported derealization and decreased resting-state connectivity between the vmPFC and the orbitofrontal cortex and right lobule VIIIa – a region of the cerebellum involved in sensorimotor function.
“This may contribute to perceptual and affective distortions experienced during derealization – for example, feelings that surroundings are fading away, unreal, or strange,” said Dr. Lebois.
More pain, depression, anxiety
Higher levels of self-reported derealization at 2 weeks post trauma predicted higher levels of PTSD, anxiety, and depression as well as more bodily pain and impairment in work, family, and social life at 3 months.
“When we accounted for baseline levels of posttraumatic stress symptoms and trauma history, higher levels of self-reported derealization still predicted higher posttraumatic stress disorder and depression symptoms at 3 months,” said Dr. Lebois.
Additional adjusted analyses showed increased vmPFC activity during the fearful face task predicted 3-month self-reported PTSD symptoms.
Dr. Lebois “highly recommends” clinicians screen for dissociative symptoms, including derealization, in patients with trauma. Self-report screening tools are freely available online.
She noted patients with significant dissociative symptoms often do better with a “phase-oriented” approach to trauma treatment.
“In phase one, they learn emotional regulation skills to help them take more control over when they dissociate. Then they can successfully move on to trauma processing in phase two, which can involve exposure to trauma details.”
Although the field is not yet ready to use brain scans to diagnose dissociative symptoms, the new results “take us one step closer to being able to use objective neuroimaging biomarkers of derealization to augment subjective self-report measures,” said Dr. Lebois.
A limitation of the study was it could not determine a causal relationship, as some derealization may have been present before the traumatic event. The findings may not generalize to other types of dissociation, and the derealization assessment was measured only through a self-report 2 weeks after the trauma.
Another limitation was exclusion of patients with self-inflicted injuries or who were involved in domestic violence. The researchers noted the prevalence of derealization might have been even higher if such individuals were included.
An important investigation
In an accompanying editorial, Lisa M. Shin, PhD, department of psychology, Tufts University, and department of psychiatry, Massachusetts General Hospital and Harvard Medical School, Boston, notes having both clinical and neuroimaging variables as well as a large sample size makes the study “an important investigation” into predictors of psychiatric symptoms post-trauma.
Investigating a specific subtype of dissociation – persistent derealization – adds to the “novelty” of the study, she said.
The new findings “are certainly exciting for their potential clinical relevance and contributions to neurocircuitry models of PTSD,” she writes.
Some may argue administering a short, self-report measure of derealization “is far more efficient, cost-effective, and inclusive than conducting a specialized and expensive fMRI scan that is unlikely to be available to everyone,” notes Dr. Shin.
However, she added, a potential benefit of such a scan is identification of specific brain regions as potential targets for intervention. “For example, the results of this and other studies suggest that the vmPFC is a reasonable target for transcranial magnetic stimulation or its variants.”
The new results need to be replicated in a large, independent sample, said Dr. Shin. She added it would be helpful to know if other types of dissociation, and activation in other subregions of the vmPFC, also predict psychiatric outcomes after a trauma.
The study was supported by National Institute of Mental Health grants, the U.S. Army Medical Research and Material Command, One Mind, and the Mayday Fund. Dr. Lebois has received grant support from NIMH, and her spouse receives payments from Vanderbilt University for technology licensed to Acadia Pharmaceuticals. Dr. Shin receives textbook-related royalties from Pearson.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF PSYCHIATRY
Hepatitis C meds linked to improved PTSD symptoms
The combination of the two antiviral medications glecaprevir and pibrentasvir (Mavyret) is linked to improved symptoms in posttraumatic stress disorder, new research suggests.
A national cohort study of U.S. Veterans Affairs patients included more than 250 participants with PTSD and comorbid hepatitis C virus.
Results showed in the study, including ledipasvir/sofosbuvir.
“While there are great treatments available for PTSD, there’s a lot of desire in the field to find a new medication that will be helpful,” lead author Brian Shiner, MD, acting associate chief of staff for research, VA Medical Center, White River Junction, Vt., told this news organization.
“We had a great opportunity to use a novel data mining method to look in a wonderful database for a new treatment and we found something very promising,” said Dr. Shiner, who is also an associate professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H.
The findings were published online in the American Journal of Epidemiology.
Common psychiatric disorder
PTSD is one of the most common psychiatric disorders, with an estimated lifetime prevalence of 6.4% in the United States. Yet only two drugs, the SSRIs sertraline (Zoloft) and paroxetine (Paxil), have been approved by the Food and Drug Administration to treat PTSD.
The VA recommends trauma-based psychotherapy, such as prolonged exposure and cognitive processing therapy, as first-line treatments for PTSD. However, not all patents respond to or have access to these approaches, said Dr. Shiner.
The investigators wanted to examine whether existing medications might reduce PTSD symptoms. Their previous exploratory study used “data mining” of national VA medical records.
Results from that study showed the three hepatitis C antivirals of GLE (an NS3/4A protease inhibitor), PIB (a NS5A protein inhibitor), and velpatasvir (another NS5A protein inhibitor) were associated with more than double the expected number of patients experiencing a clinically meaningful improvement in PTSD symptoms.
Sertraline was associated with only a slightly higher than expected improvement.
“SSRIs are effective, better than placebo, but the effects are not as good as we would hope,” Dr. Shiner said.
He noted that GLE and PIB are always prescribed together (Mavyret), whereas velpatasvir is commonly prescribed with the NS5B polymerase inhibitor sofosbuvir under the brand name Epclusa. Sofosbuvir is also commonly prescribed with the NS5A protein inhibitor ledipasvir under the brand name Harvoni.
Strong association
The new study included 253 VA users with a diagnosis of PTSD and hepatitis C. Of these, 54 were receiving GLE/PIB, 145 were receiving ledipasvir/sofosbuvir, and 54 were receiving sofosbuvir/velpatasvir.
Researchers compared the groups with respect to change over 8-12 weeks on the PTSD Checklist (PCL), a 20-item self-report scale.
In adjusted analyses, the largest mean improvement on the PCL was 14.9 points for the GLE/PIB group and the smallest adjusted mean improvement on the PCL was 7.5 points for the ledipasvir/sofosbuvir group (mean difference, 7.34 points; 95% confidence interval, 1.05-13.63).
The adjusted proportion of patients improving by 15 points or more on the PCL was highest for the GLE/PIB group at 43.6% and lowest for the ledipasvir/sofosbuvir group at 26.3%.
Even when accounting for patients receiving trauma-based therapy or SSRIs, “it still looks like there’s a strong association of the hepatitis C antivirals with PTSD symptom improvement,” said Dr. Shiner.
Researchers also carried out a sensitivity analysis among only patients who were cured of HCV (over 90% of the total sample), defined as having an undetectable HCV viral load up to a year after completion of therapy. The analysis showed PTSD outcomes were still superior for participants receiving GLE/PIB.
“The sensitivity analysis was not that robust because almost everyone was cured, so it included almost everybody, but it didn’t point us away from the possibility of an off-target effect,” Dr. Shiner said.
Why antivirals may improve PTSD symptoms is not clear, but they may affect the immune response in patients with hepatitis C – and there may also be an immune response in PTSD, he noted. “Some of those factors may be shared, and that could explain some of the off-target effect.”
However, he noted the GLE/PIB drug combination is costly and patients with PTSD can probably access it only through enrolling in a study.
“We are not recommending that people go out and purchase this very expensive drug to treat their PTSD at this point,” Dr. Shiner said.
He added that the research team has now received funding from the Department of Defense to conduct a randomized, placebo-controlled trial of GLE/PIB as a potential treatment for PTSD.
Promising potential treatment
PTSD expert Elspeth Cameron Ritchie, MD, chief of psychiatry at Medstar Washington Hospital Center, Washington, D.C., said the results suggest GLE/PIB is a promising potential treatment for PTSD.
“I definitely think this should be looked at further,” said Dr. Ritchie, who was not involved with the research.
She noted that current PTSD therapies have drawbacks. SSRIs have side effects, the most “troubling” being sexual dysfunction. And although cognitive-behavioral therapy is effective, “people have to stick with it” and studies show about two thirds of patients drop out, she said.
Potentially effective PTSD treatment approaches include “self-soothing” or “self-regulating” techniques such as exercise, meditation, yoga, and working with animals, she added.
Dr. Ritchie pointed out the numbers of participants in the study were relatively small, including two groups that had only 54 patients each.
And while the GLE/PIB combination should be explored further, cost, availability, and side effects of this medication need to be taken into consideration, she said.
Dr. Ritchie added she is not overly concerned that the mechanism of action for the combination on PTSD may not be well understood. She noted several psychiatric medications fall into that category, including electroconvulsive therapy and lithium.
“When lithium was first found to be effective against bipolar disorder, we had no clue why,” she said. “So I would not discount the antiviral based on us not knowing how it works.”
However, “we’re a long way off” from starting a patient with PTSD on an antiviral, said Dr. Ritchie, adding there are “a lot of steps to go through” to get FDA approval.
The study was funded by the National Institute of Mental Health. The cohort used for this study was developed through support from the Department of Defense. Dr. Shiner is a coinventor on a provisional patent application covering the use of glecaprevir, pibrentasvir, and velpatasvir for PTSD and other psychiatric indications. Dr. Ritchie reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The combination of the two antiviral medications glecaprevir and pibrentasvir (Mavyret) is linked to improved symptoms in posttraumatic stress disorder, new research suggests.
A national cohort study of U.S. Veterans Affairs patients included more than 250 participants with PTSD and comorbid hepatitis C virus.
Results showed in the study, including ledipasvir/sofosbuvir.
“While there are great treatments available for PTSD, there’s a lot of desire in the field to find a new medication that will be helpful,” lead author Brian Shiner, MD, acting associate chief of staff for research, VA Medical Center, White River Junction, Vt., told this news organization.
“We had a great opportunity to use a novel data mining method to look in a wonderful database for a new treatment and we found something very promising,” said Dr. Shiner, who is also an associate professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H.
The findings were published online in the American Journal of Epidemiology.
Common psychiatric disorder
PTSD is one of the most common psychiatric disorders, with an estimated lifetime prevalence of 6.4% in the United States. Yet only two drugs, the SSRIs sertraline (Zoloft) and paroxetine (Paxil), have been approved by the Food and Drug Administration to treat PTSD.
The VA recommends trauma-based psychotherapy, such as prolonged exposure and cognitive processing therapy, as first-line treatments for PTSD. However, not all patents respond to or have access to these approaches, said Dr. Shiner.
The investigators wanted to examine whether existing medications might reduce PTSD symptoms. Their previous exploratory study used “data mining” of national VA medical records.
Results from that study showed the three hepatitis C antivirals of GLE (an NS3/4A protease inhibitor), PIB (a NS5A protein inhibitor), and velpatasvir (another NS5A protein inhibitor) were associated with more than double the expected number of patients experiencing a clinically meaningful improvement in PTSD symptoms.
Sertraline was associated with only a slightly higher than expected improvement.
“SSRIs are effective, better than placebo, but the effects are not as good as we would hope,” Dr. Shiner said.
He noted that GLE and PIB are always prescribed together (Mavyret), whereas velpatasvir is commonly prescribed with the NS5B polymerase inhibitor sofosbuvir under the brand name Epclusa. Sofosbuvir is also commonly prescribed with the NS5A protein inhibitor ledipasvir under the brand name Harvoni.
Strong association
The new study included 253 VA users with a diagnosis of PTSD and hepatitis C. Of these, 54 were receiving GLE/PIB, 145 were receiving ledipasvir/sofosbuvir, and 54 were receiving sofosbuvir/velpatasvir.
Researchers compared the groups with respect to change over 8-12 weeks on the PTSD Checklist (PCL), a 20-item self-report scale.
In adjusted analyses, the largest mean improvement on the PCL was 14.9 points for the GLE/PIB group and the smallest adjusted mean improvement on the PCL was 7.5 points for the ledipasvir/sofosbuvir group (mean difference, 7.34 points; 95% confidence interval, 1.05-13.63).
The adjusted proportion of patients improving by 15 points or more on the PCL was highest for the GLE/PIB group at 43.6% and lowest for the ledipasvir/sofosbuvir group at 26.3%.
Even when accounting for patients receiving trauma-based therapy or SSRIs, “it still looks like there’s a strong association of the hepatitis C antivirals with PTSD symptom improvement,” said Dr. Shiner.
Researchers also carried out a sensitivity analysis among only patients who were cured of HCV (over 90% of the total sample), defined as having an undetectable HCV viral load up to a year after completion of therapy. The analysis showed PTSD outcomes were still superior for participants receiving GLE/PIB.
“The sensitivity analysis was not that robust because almost everyone was cured, so it included almost everybody, but it didn’t point us away from the possibility of an off-target effect,” Dr. Shiner said.
Why antivirals may improve PTSD symptoms is not clear, but they may affect the immune response in patients with hepatitis C – and there may also be an immune response in PTSD, he noted. “Some of those factors may be shared, and that could explain some of the off-target effect.”
However, he noted the GLE/PIB drug combination is costly and patients with PTSD can probably access it only through enrolling in a study.
“We are not recommending that people go out and purchase this very expensive drug to treat their PTSD at this point,” Dr. Shiner said.
He added that the research team has now received funding from the Department of Defense to conduct a randomized, placebo-controlled trial of GLE/PIB as a potential treatment for PTSD.
Promising potential treatment
PTSD expert Elspeth Cameron Ritchie, MD, chief of psychiatry at Medstar Washington Hospital Center, Washington, D.C., said the results suggest GLE/PIB is a promising potential treatment for PTSD.
“I definitely think this should be looked at further,” said Dr. Ritchie, who was not involved with the research.
She noted that current PTSD therapies have drawbacks. SSRIs have side effects, the most “troubling” being sexual dysfunction. And although cognitive-behavioral therapy is effective, “people have to stick with it” and studies show about two thirds of patients drop out, she said.
Potentially effective PTSD treatment approaches include “self-soothing” or “self-regulating” techniques such as exercise, meditation, yoga, and working with animals, she added.
Dr. Ritchie pointed out the numbers of participants in the study were relatively small, including two groups that had only 54 patients each.
And while the GLE/PIB combination should be explored further, cost, availability, and side effects of this medication need to be taken into consideration, she said.
Dr. Ritchie added she is not overly concerned that the mechanism of action for the combination on PTSD may not be well understood. She noted several psychiatric medications fall into that category, including electroconvulsive therapy and lithium.
“When lithium was first found to be effective against bipolar disorder, we had no clue why,” she said. “So I would not discount the antiviral based on us not knowing how it works.”
However, “we’re a long way off” from starting a patient with PTSD on an antiviral, said Dr. Ritchie, adding there are “a lot of steps to go through” to get FDA approval.
The study was funded by the National Institute of Mental Health. The cohort used for this study was developed through support from the Department of Defense. Dr. Shiner is a coinventor on a provisional patent application covering the use of glecaprevir, pibrentasvir, and velpatasvir for PTSD and other psychiatric indications. Dr. Ritchie reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The combination of the two antiviral medications glecaprevir and pibrentasvir (Mavyret) is linked to improved symptoms in posttraumatic stress disorder, new research suggests.
A national cohort study of U.S. Veterans Affairs patients included more than 250 participants with PTSD and comorbid hepatitis C virus.
Results showed in the study, including ledipasvir/sofosbuvir.
“While there are great treatments available for PTSD, there’s a lot of desire in the field to find a new medication that will be helpful,” lead author Brian Shiner, MD, acting associate chief of staff for research, VA Medical Center, White River Junction, Vt., told this news organization.
“We had a great opportunity to use a novel data mining method to look in a wonderful database for a new treatment and we found something very promising,” said Dr. Shiner, who is also an associate professor of psychiatry at the Geisel School of Medicine at Dartmouth, Hanover, N.H.
The findings were published online in the American Journal of Epidemiology.
Common psychiatric disorder
PTSD is one of the most common psychiatric disorders, with an estimated lifetime prevalence of 6.4% in the United States. Yet only two drugs, the SSRIs sertraline (Zoloft) and paroxetine (Paxil), have been approved by the Food and Drug Administration to treat PTSD.
The VA recommends trauma-based psychotherapy, such as prolonged exposure and cognitive processing therapy, as first-line treatments for PTSD. However, not all patents respond to or have access to these approaches, said Dr. Shiner.
The investigators wanted to examine whether existing medications might reduce PTSD symptoms. Their previous exploratory study used “data mining” of national VA medical records.
Results from that study showed the three hepatitis C antivirals of GLE (an NS3/4A protease inhibitor), PIB (a NS5A protein inhibitor), and velpatasvir (another NS5A protein inhibitor) were associated with more than double the expected number of patients experiencing a clinically meaningful improvement in PTSD symptoms.
Sertraline was associated with only a slightly higher than expected improvement.
“SSRIs are effective, better than placebo, but the effects are not as good as we would hope,” Dr. Shiner said.
He noted that GLE and PIB are always prescribed together (Mavyret), whereas velpatasvir is commonly prescribed with the NS5B polymerase inhibitor sofosbuvir under the brand name Epclusa. Sofosbuvir is also commonly prescribed with the NS5A protein inhibitor ledipasvir under the brand name Harvoni.
Strong association
The new study included 253 VA users with a diagnosis of PTSD and hepatitis C. Of these, 54 were receiving GLE/PIB, 145 were receiving ledipasvir/sofosbuvir, and 54 were receiving sofosbuvir/velpatasvir.
Researchers compared the groups with respect to change over 8-12 weeks on the PTSD Checklist (PCL), a 20-item self-report scale.
In adjusted analyses, the largest mean improvement on the PCL was 14.9 points for the GLE/PIB group and the smallest adjusted mean improvement on the PCL was 7.5 points for the ledipasvir/sofosbuvir group (mean difference, 7.34 points; 95% confidence interval, 1.05-13.63).
The adjusted proportion of patients improving by 15 points or more on the PCL was highest for the GLE/PIB group at 43.6% and lowest for the ledipasvir/sofosbuvir group at 26.3%.
Even when accounting for patients receiving trauma-based therapy or SSRIs, “it still looks like there’s a strong association of the hepatitis C antivirals with PTSD symptom improvement,” said Dr. Shiner.
Researchers also carried out a sensitivity analysis among only patients who were cured of HCV (over 90% of the total sample), defined as having an undetectable HCV viral load up to a year after completion of therapy. The analysis showed PTSD outcomes were still superior for participants receiving GLE/PIB.
“The sensitivity analysis was not that robust because almost everyone was cured, so it included almost everybody, but it didn’t point us away from the possibility of an off-target effect,” Dr. Shiner said.
Why antivirals may improve PTSD symptoms is not clear, but they may affect the immune response in patients with hepatitis C – and there may also be an immune response in PTSD, he noted. “Some of those factors may be shared, and that could explain some of the off-target effect.”
However, he noted the GLE/PIB drug combination is costly and patients with PTSD can probably access it only through enrolling in a study.
“We are not recommending that people go out and purchase this very expensive drug to treat their PTSD at this point,” Dr. Shiner said.
He added that the research team has now received funding from the Department of Defense to conduct a randomized, placebo-controlled trial of GLE/PIB as a potential treatment for PTSD.
Promising potential treatment
PTSD expert Elspeth Cameron Ritchie, MD, chief of psychiatry at Medstar Washington Hospital Center, Washington, D.C., said the results suggest GLE/PIB is a promising potential treatment for PTSD.
“I definitely think this should be looked at further,” said Dr. Ritchie, who was not involved with the research.
She noted that current PTSD therapies have drawbacks. SSRIs have side effects, the most “troubling” being sexual dysfunction. And although cognitive-behavioral therapy is effective, “people have to stick with it” and studies show about two thirds of patients drop out, she said.
Potentially effective PTSD treatment approaches include “self-soothing” or “self-regulating” techniques such as exercise, meditation, yoga, and working with animals, she added.
Dr. Ritchie pointed out the numbers of participants in the study were relatively small, including two groups that had only 54 patients each.
And while the GLE/PIB combination should be explored further, cost, availability, and side effects of this medication need to be taken into consideration, she said.
Dr. Ritchie added she is not overly concerned that the mechanism of action for the combination on PTSD may not be well understood. She noted several psychiatric medications fall into that category, including electroconvulsive therapy and lithium.
“When lithium was first found to be effective against bipolar disorder, we had no clue why,” she said. “So I would not discount the antiviral based on us not knowing how it works.”
However, “we’re a long way off” from starting a patient with PTSD on an antiviral, said Dr. Ritchie, adding there are “a lot of steps to go through” to get FDA approval.
The study was funded by the National Institute of Mental Health. The cohort used for this study was developed through support from the Department of Defense. Dr. Shiner is a coinventor on a provisional patent application covering the use of glecaprevir, pibrentasvir, and velpatasvir for PTSD and other psychiatric indications. Dr. Ritchie reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Which factors fuel sexual violence in health care?
At the beginning of July, Brazilians across the country were appalled when they heard that an anesthesiologist was accused of sexually abusing a woman he had been treating during cesarean delivery. The incident was recorded on video by nurses and nurse technicians who, having become suspicious of the excessive amount of sedatives given to mothers-to-be by this particular anesthesiologist, decided to film him during a procedure. To do this, they made a last-minute change, switching delivery rooms to one in which they had hidden a cell phone in a cabinet.
What the footage showed was horrifying and the assailant, Giovanni Quintella Bezerra, was arrested on the spot. He’s a 32-year-old, White, successful physician, and he’s now accused of rape. The authorities are looking into whether there are more victims, others who may have been abused by the physician. The police are investigating about 40 surgeries in which Dr. Bezerra participated. That same month saw the arrest of another physician, gynecologist Ricardo Teles Martins, who was arrested after being accused of sexually harassing and abusing several women in Hidrolândia, in the northeastern state of Ceará.
In gathering information about these incidents, this news organization interviewed four Brazilian specialists to get their insights on the issues that have been brought to light by these recent cases and the factors that play a role in these kinds of criminal acts. Claudio Cohen, MD, PhD, is a psychiatrist, bioethicist, and professor at the University of São Paulo in Brazil. Daniela Pedroso, MA, is a psychologist who has 25 years’ experience working with victims of sexual violence. Gynecologist and obstetrician Jefferson Drezett, MD, PhD, is a professor in the field of population genetics and reproductive and sexual health at the Federal University of ABC, São Paulo, and in the department of health, life cycles, and society at the University of São Paulo School of Public Health. Maria Alice Scardoelli, MD, is a psychiatrist who also serves as vice-chair of the São Paulo Regional Council of Medicine (Cremesp).
Accusations and investigations
Not all incidents of sexual violence in health care institutions are reported, and precise numbers are difficult to obtain. The fact that there are any cases at all is troubling. In 2019, journalists from The Intercept found that over a period of 6 years (2014-2019), 1,734 such attacks were recorded in nine Brazilian states. They were able to get that information from the states’ Public Security Secretariats by using the Information Access Act, a law that regulates the right to access public information.
Efforts to determine how widespread this type of sexual violence is are further complicated by the difficulties in collating the accusations filed at each state’s regional council of medicine, police stations, and public prosecutor’s office. Which investigative steps are taken depends upon where the report was filed, and only occasionally do these entities communicate with each other. According to its data, Cremesp received 78 accusations in 2019. In 2020, that number increased to 84. In 2021, it was 83; these types of attacks were the seventh most common among the investigations opened that year. In the first 6 months of 2022, there were 36 complaints. The number includes investigations opened on the basis of press reports. In such cases, enough information must be available in the press reports make it possible to initiate an evaluation and assessment of the matter. There is no information about how many accusations became the subject of professional ethics proceedings and how many were formally adjudicated.
“Each accusation received is investigated by a technical committee made up of professionals from various specialties. There really needs to be a rigorous evaluation and assessment during the investigation. We cannot be unfair: It may turn out that there was no truth to the accusation after all, and yet someone’s career may already have been destroyed,” explained Dr. Scardoelli.
After the accusation is investigated and accepted by Cremesp, there is no deadline by which the proceedings must end. They can take up to 5 years, and sometimes longer. Since March, however, a deadline for the investigation period has been in effect, after which the proceedings can commence.
“We now have 90 days to make an evaluation and assessment in the investigation phase; that time period can be extended by 3 months, starting from the date the accusation is submitted to the council. If the case is accepted, then the proceedings are opened,” Dr. Scardoelli said.
Some incidents are not reported by victims. And there are incidents that are reported only after many years have passed. This was the case with Nina Marqueti, the actress at the center of #OndeDói — “Where It Hurts” — a campaign that was launched to raise awareness about sexual violence committed by health care professionals. When she was 16, her pediatrician sexually abused her. It wasn’t until 2019, more than a decade later, that she felt able to make this accusation known publicly.
Almost immediately, the campaign received over 4,000 posts online. Most of them were people’s accounts of acts of violence committed by physicians during appointments in their offices or during treatment in a hospital. These are available on Twitter under the hashtag #ondedoi.
Inadequate sex education?
News reports about physicians who abuse patients have a tremendous impact on the public. People are genuinely surprised when they hear the words “health care professional” and “sex attack” in the same sentence. “One of the most disturbing aspects is that health care professionals are committing these acts of violence against women who are in a vulnerable state, typically when they’re under anesthesia, they’ve fallen ill, or when the health care professional introduces an element of deception into the procedure so as to create the opportunity to abuse the patient in some way,” said Dr. Drezett.
As Dr. Cohen sees it, to perpetrate these acts of sexual violence, physicians – as well as lawyers, religious leaders, judges, politicians, police officers, and other persons in a position of trust – make use of their power to take advantage of a person’s vulnerability. “Physicians, lawyers, police officers, religious leaders, dads, bosses, husbands – the people who commit sexual abuse all have something in common,” he said. “In terms of the emotional aspect, all of them are taking advantage of both the power that their position holds in society and the asymmetrical power dynamics that exist between them and the other person.”
Indeed, anyone who knocks on a physician’s door seeking a diagnosis or treatment, anyone who knocks on a lawyer’s door seeking assistance, is putting themselves in a fragile situation. “The abuser considers the other person an object, not a human being who has rights,” said Dr. Cohen. People who fit the psychological and behavioral profile of a sexual assailant find in these “powerful” professions and in the circumstances and opportunities these professions provide a means to fulfill their desires. In medicine, however, there is yet another imbalance, one involving consent to touch a person’s body.
The age of the recently arrested anesthesiologist is something that caught Dr. Cohen’s attention. As noted in one of his many books, Bioética e Sexualidade nas Relações Profissionais [Bioethics and Sexuality in Professional Relationships], published in 1999 by the São Paulo Medical Association, age is a characteristic that repeatedly came up in his analysis of 150 sexual abuse proceedings handled by Cremesp.
“When I looked over the cases, I saw that most of the abusers were not right out of med school in their twenties – a time when sex is at the forefront of one’s life – nor were the abusers on the older end of the age spectrum. The abusers were, in fact, those who had already had several years of experience – as was the case with this 32-year-old anesthesiologist who, at a particular moment in time, breached all prohibitions and betrayed the expectations that society had of him as a physician: to care for people’s well-being and to alleviate their suffering. There was nothing that could hold him back from fulfilling his desire, not even the presence of nurses and other physicians in the operating room.” As for the findings of Dr. Cohen’s review, the majority of the 150 cases were dismissed because of lack of evidence.
To Ms. Pedroso, who has treated more than 12,000 victims of sexual harassment, it’s the questioning and intimidation that women feel in relationship to the male physician – a person who is viewed as holding knowledge about her body – that leaves them vulnerable and more subject to acts of violence, especially in more remote places. “We’re speaking, yet again, about rape culture. Not many people know what that term means, but, generally speaking, it has to do with the objectification of women’s bodies and the issue of boys growing up thinking they have the right to touch girls and women and that they will go unpunished for doing so.”
The lack of sex education and efforts to prevent sexual abuse are contributing factors for why the situation remains unchanged. “We are long overdue. We live in a country where there’s this completely mistaken belief that talking about sex education involves teaching children how to have sex, as opposed to teaching them how to protect themselves. We teach girls that they have to protect themselves from being raped, but we don’t teach boys not to rape.”
Another point highlighted by Ms. Pedroso is the fact that to carry out their actions, sexual assailants seek out-of-the-way places, places where they believe the rules can be bent and where they won’t be caught. This is what may have happened with Dr. Bezerra. During a recent press conference, the coordinator of the Health Section of the Rio de Janeiro Public Defender’s Office, Thaísa Guerreiro, stated that although the Women’s Hospital in São João do Meriti – one of the places where the assailant worked as an anesthesiologist – had adopted protocols to protect patients, it failed to enforce them. Another observation was that the health care professionals normalized violations of a woman’s right to have a companion present throughout labor and delivery, a right guaranteed by federal law. Ms. Guerreiro went on to say that the hospital’s chief of anesthesia and the state’s health coordination office did not question this, nor did they find it strange or surprising. According to witness statements, Dr. Bezerra would ask the patients’ husbands to leave the room in the middle of the procedure.
It should be clarified, Dr. Drezett mentioned, that although obstetric violence and sexual abuse overlap in places, they do not have the same root cause or definition. “There are two sets of situations that we term ‘obstetric violence.’ One involves any type of disrespectful treatment, whether comments or neglect, during pregnancy, delivery, or the postpartum period. The other refers to health care professionals’ attitudes in imposing inadequate and outdated medical procedures at the time of birth, such as keeping the woman fasting, having her pubic hair removed, and inducing labor or speeding up the delivery with oxytocin and [routine] episiotomy, among other things.”
Early education crucial
How are health care institutions dealing with this problem? “Very poorly. Sexual violence perpetrated by physicians and other health care professionals is a taboo subject that people are still afraid to talk about,” Dr. Cohen observed. “Regrettably, sexual violence happens all too often. Before, maybe we weren’t talking about it much because, from our viewpoint, health care professionals, such as physicians and nurses, weren’t likely to commit acts of violence while performing their duties,” noted Dr. Drezett.
Dr. Drezett also spoke about schools and what role they can play. “Of course, schools should discuss violence against women, especially in the field of health care. This has been done for a long time now, though it’s not in every curriculum in every medical school or nursing school, nor in every school of social work or of psychology,” said Dr. Drezett. For example, in the bioethics classes taken in the third and fourth years of the University of São Paolo’s medical degree program, Dr. Cohen asks students to reflect on the significance of being in a position where you ask a patient you’ve never met to undress so you can perform an exam, and the patient promptly and readily complies. “This is not about the physician, it’s about the power of the institution,” the professor pointed out. Sexual violence is a problem on the university campus as well. Another front in the battle has formed across various schools, where groups of students have created feminist collectives to have sexual violence and other issues related to gender-based violence added to the agenda.
Dr. Drezett said it’s very unlikely that efforts made during a degree program are going to succeed in preventing students who are prone to commit sexual violence from engaging in such behavior. “We’re talking about gender-specific lessons, where discussions about gender-based violence should be started much, much earlier – parents talking to their children, teachers talking to their pupils.” He also doesn’t believe that the molesters are dissuaded by the fact that these accusations get publicized in the media. “If they were, the Roger Abdelmassih case would have done away with the problem.”
On the other hand, Dr. Drezett suggested, publicizing these stories can help to bring very positive issues out into the open. What the Bezerra case made clear was that laws were not followed and rights were not protected. An environment was thus created in which the sexual crime could be perpetrated, with nurses coming to suspect acts of obstetric violence, such as use of sedation, which prevented the woman from having skin-to-skin contact with the newborn and from breastfeeding within the first few hours of birth – two clinical practices that are recommended the world over.
“Health care professionals who act properly, in accordance with best practices for interacting with others and performing daily duties, at all times, in public or private practice – they remove themselves from situations like those described in the Bezerra case; they don’t practice medicine in a reckless manner,” said Dr. Drezett.
Another negative aspect of all this, he said, is that the suspicion and wariness that patients feel may spread far and wide. “Among my colleagues are anesthetists and anesthesiologists with impeccable ethical and professional records. They are very upset that people are now regarding them with doubt and uncertainty. We need to make it clear that those horrifying cases are the exceptions, not the rule,” he said. There is also a need to correct the misconception that such abuse is always in some way associated with obstetrics and gynecology.
“This is not true. These incidents can happen in any doctor’s office. It all depends on the physician – whether he or she has designs on committing a criminal act,” Dr. Drezett noted. He did point out that there are few sexual molesters among health care professionals, though there are numerous cases. Yet this in no way diminishes the seriousness of the incidents. “Of course, we’re speaking again about the exceptions, but in my experience of treating victims, I’ve seen, for example, more cases where it’s been a police officer, not a physician, committing an act of sexual violence against a woman,” he stated.
The nurses and nurse technicians at São João do Meriti Hospital who reported the abuser acted very assertively. If they hadn’t gathered the evidence to back up their accusations, it’s possible that the physician wouldn’t have been caught in the act and that the case would have taken a different course – including pressure being put on them and their becoming the target of retaliation.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape Portuguese edition.
At the beginning of July, Brazilians across the country were appalled when they heard that an anesthesiologist was accused of sexually abusing a woman he had been treating during cesarean delivery. The incident was recorded on video by nurses and nurse technicians who, having become suspicious of the excessive amount of sedatives given to mothers-to-be by this particular anesthesiologist, decided to film him during a procedure. To do this, they made a last-minute change, switching delivery rooms to one in which they had hidden a cell phone in a cabinet.
What the footage showed was horrifying and the assailant, Giovanni Quintella Bezerra, was arrested on the spot. He’s a 32-year-old, White, successful physician, and he’s now accused of rape. The authorities are looking into whether there are more victims, others who may have been abused by the physician. The police are investigating about 40 surgeries in which Dr. Bezerra participated. That same month saw the arrest of another physician, gynecologist Ricardo Teles Martins, who was arrested after being accused of sexually harassing and abusing several women in Hidrolândia, in the northeastern state of Ceará.
In gathering information about these incidents, this news organization interviewed four Brazilian specialists to get their insights on the issues that have been brought to light by these recent cases and the factors that play a role in these kinds of criminal acts. Claudio Cohen, MD, PhD, is a psychiatrist, bioethicist, and professor at the University of São Paulo in Brazil. Daniela Pedroso, MA, is a psychologist who has 25 years’ experience working with victims of sexual violence. Gynecologist and obstetrician Jefferson Drezett, MD, PhD, is a professor in the field of population genetics and reproductive and sexual health at the Federal University of ABC, São Paulo, and in the department of health, life cycles, and society at the University of São Paulo School of Public Health. Maria Alice Scardoelli, MD, is a psychiatrist who also serves as vice-chair of the São Paulo Regional Council of Medicine (Cremesp).
Accusations and investigations
Not all incidents of sexual violence in health care institutions are reported, and precise numbers are difficult to obtain. The fact that there are any cases at all is troubling. In 2019, journalists from The Intercept found that over a period of 6 years (2014-2019), 1,734 such attacks were recorded in nine Brazilian states. They were able to get that information from the states’ Public Security Secretariats by using the Information Access Act, a law that regulates the right to access public information.
Efforts to determine how widespread this type of sexual violence is are further complicated by the difficulties in collating the accusations filed at each state’s regional council of medicine, police stations, and public prosecutor’s office. Which investigative steps are taken depends upon where the report was filed, and only occasionally do these entities communicate with each other. According to its data, Cremesp received 78 accusations in 2019. In 2020, that number increased to 84. In 2021, it was 83; these types of attacks were the seventh most common among the investigations opened that year. In the first 6 months of 2022, there were 36 complaints. The number includes investigations opened on the basis of press reports. In such cases, enough information must be available in the press reports make it possible to initiate an evaluation and assessment of the matter. There is no information about how many accusations became the subject of professional ethics proceedings and how many were formally adjudicated.
“Each accusation received is investigated by a technical committee made up of professionals from various specialties. There really needs to be a rigorous evaluation and assessment during the investigation. We cannot be unfair: It may turn out that there was no truth to the accusation after all, and yet someone’s career may already have been destroyed,” explained Dr. Scardoelli.
After the accusation is investigated and accepted by Cremesp, there is no deadline by which the proceedings must end. They can take up to 5 years, and sometimes longer. Since March, however, a deadline for the investigation period has been in effect, after which the proceedings can commence.
“We now have 90 days to make an evaluation and assessment in the investigation phase; that time period can be extended by 3 months, starting from the date the accusation is submitted to the council. If the case is accepted, then the proceedings are opened,” Dr. Scardoelli said.
Some incidents are not reported by victims. And there are incidents that are reported only after many years have passed. This was the case with Nina Marqueti, the actress at the center of #OndeDói — “Where It Hurts” — a campaign that was launched to raise awareness about sexual violence committed by health care professionals. When she was 16, her pediatrician sexually abused her. It wasn’t until 2019, more than a decade later, that she felt able to make this accusation known publicly.
Almost immediately, the campaign received over 4,000 posts online. Most of them were people’s accounts of acts of violence committed by physicians during appointments in their offices or during treatment in a hospital. These are available on Twitter under the hashtag #ondedoi.
Inadequate sex education?
News reports about physicians who abuse patients have a tremendous impact on the public. People are genuinely surprised when they hear the words “health care professional” and “sex attack” in the same sentence. “One of the most disturbing aspects is that health care professionals are committing these acts of violence against women who are in a vulnerable state, typically when they’re under anesthesia, they’ve fallen ill, or when the health care professional introduces an element of deception into the procedure so as to create the opportunity to abuse the patient in some way,” said Dr. Drezett.
As Dr. Cohen sees it, to perpetrate these acts of sexual violence, physicians – as well as lawyers, religious leaders, judges, politicians, police officers, and other persons in a position of trust – make use of their power to take advantage of a person’s vulnerability. “Physicians, lawyers, police officers, religious leaders, dads, bosses, husbands – the people who commit sexual abuse all have something in common,” he said. “In terms of the emotional aspect, all of them are taking advantage of both the power that their position holds in society and the asymmetrical power dynamics that exist between them and the other person.”
Indeed, anyone who knocks on a physician’s door seeking a diagnosis or treatment, anyone who knocks on a lawyer’s door seeking assistance, is putting themselves in a fragile situation. “The abuser considers the other person an object, not a human being who has rights,” said Dr. Cohen. People who fit the psychological and behavioral profile of a sexual assailant find in these “powerful” professions and in the circumstances and opportunities these professions provide a means to fulfill their desires. In medicine, however, there is yet another imbalance, one involving consent to touch a person’s body.
The age of the recently arrested anesthesiologist is something that caught Dr. Cohen’s attention. As noted in one of his many books, Bioética e Sexualidade nas Relações Profissionais [Bioethics and Sexuality in Professional Relationships], published in 1999 by the São Paulo Medical Association, age is a characteristic that repeatedly came up in his analysis of 150 sexual abuse proceedings handled by Cremesp.
“When I looked over the cases, I saw that most of the abusers were not right out of med school in their twenties – a time when sex is at the forefront of one’s life – nor were the abusers on the older end of the age spectrum. The abusers were, in fact, those who had already had several years of experience – as was the case with this 32-year-old anesthesiologist who, at a particular moment in time, breached all prohibitions and betrayed the expectations that society had of him as a physician: to care for people’s well-being and to alleviate their suffering. There was nothing that could hold him back from fulfilling his desire, not even the presence of nurses and other physicians in the operating room.” As for the findings of Dr. Cohen’s review, the majority of the 150 cases were dismissed because of lack of evidence.
To Ms. Pedroso, who has treated more than 12,000 victims of sexual harassment, it’s the questioning and intimidation that women feel in relationship to the male physician – a person who is viewed as holding knowledge about her body – that leaves them vulnerable and more subject to acts of violence, especially in more remote places. “We’re speaking, yet again, about rape culture. Not many people know what that term means, but, generally speaking, it has to do with the objectification of women’s bodies and the issue of boys growing up thinking they have the right to touch girls and women and that they will go unpunished for doing so.”
The lack of sex education and efforts to prevent sexual abuse are contributing factors for why the situation remains unchanged. “We are long overdue. We live in a country where there’s this completely mistaken belief that talking about sex education involves teaching children how to have sex, as opposed to teaching them how to protect themselves. We teach girls that they have to protect themselves from being raped, but we don’t teach boys not to rape.”
Another point highlighted by Ms. Pedroso is the fact that to carry out their actions, sexual assailants seek out-of-the-way places, places where they believe the rules can be bent and where they won’t be caught. This is what may have happened with Dr. Bezerra. During a recent press conference, the coordinator of the Health Section of the Rio de Janeiro Public Defender’s Office, Thaísa Guerreiro, stated that although the Women’s Hospital in São João do Meriti – one of the places where the assailant worked as an anesthesiologist – had adopted protocols to protect patients, it failed to enforce them. Another observation was that the health care professionals normalized violations of a woman’s right to have a companion present throughout labor and delivery, a right guaranteed by federal law. Ms. Guerreiro went on to say that the hospital’s chief of anesthesia and the state’s health coordination office did not question this, nor did they find it strange or surprising. According to witness statements, Dr. Bezerra would ask the patients’ husbands to leave the room in the middle of the procedure.
It should be clarified, Dr. Drezett mentioned, that although obstetric violence and sexual abuse overlap in places, they do not have the same root cause or definition. “There are two sets of situations that we term ‘obstetric violence.’ One involves any type of disrespectful treatment, whether comments or neglect, during pregnancy, delivery, or the postpartum period. The other refers to health care professionals’ attitudes in imposing inadequate and outdated medical procedures at the time of birth, such as keeping the woman fasting, having her pubic hair removed, and inducing labor or speeding up the delivery with oxytocin and [routine] episiotomy, among other things.”
Early education crucial
How are health care institutions dealing with this problem? “Very poorly. Sexual violence perpetrated by physicians and other health care professionals is a taboo subject that people are still afraid to talk about,” Dr. Cohen observed. “Regrettably, sexual violence happens all too often. Before, maybe we weren’t talking about it much because, from our viewpoint, health care professionals, such as physicians and nurses, weren’t likely to commit acts of violence while performing their duties,” noted Dr. Drezett.
Dr. Drezett also spoke about schools and what role they can play. “Of course, schools should discuss violence against women, especially in the field of health care. This has been done for a long time now, though it’s not in every curriculum in every medical school or nursing school, nor in every school of social work or of psychology,” said Dr. Drezett. For example, in the bioethics classes taken in the third and fourth years of the University of São Paolo’s medical degree program, Dr. Cohen asks students to reflect on the significance of being in a position where you ask a patient you’ve never met to undress so you can perform an exam, and the patient promptly and readily complies. “This is not about the physician, it’s about the power of the institution,” the professor pointed out. Sexual violence is a problem on the university campus as well. Another front in the battle has formed across various schools, where groups of students have created feminist collectives to have sexual violence and other issues related to gender-based violence added to the agenda.
Dr. Drezett said it’s very unlikely that efforts made during a degree program are going to succeed in preventing students who are prone to commit sexual violence from engaging in such behavior. “We’re talking about gender-specific lessons, where discussions about gender-based violence should be started much, much earlier – parents talking to their children, teachers talking to their pupils.” He also doesn’t believe that the molesters are dissuaded by the fact that these accusations get publicized in the media. “If they were, the Roger Abdelmassih case would have done away with the problem.”
On the other hand, Dr. Drezett suggested, publicizing these stories can help to bring very positive issues out into the open. What the Bezerra case made clear was that laws were not followed and rights were not protected. An environment was thus created in which the sexual crime could be perpetrated, with nurses coming to suspect acts of obstetric violence, such as use of sedation, which prevented the woman from having skin-to-skin contact with the newborn and from breastfeeding within the first few hours of birth – two clinical practices that are recommended the world over.
“Health care professionals who act properly, in accordance with best practices for interacting with others and performing daily duties, at all times, in public or private practice – they remove themselves from situations like those described in the Bezerra case; they don’t practice medicine in a reckless manner,” said Dr. Drezett.
Another negative aspect of all this, he said, is that the suspicion and wariness that patients feel may spread far and wide. “Among my colleagues are anesthetists and anesthesiologists with impeccable ethical and professional records. They are very upset that people are now regarding them with doubt and uncertainty. We need to make it clear that those horrifying cases are the exceptions, not the rule,” he said. There is also a need to correct the misconception that such abuse is always in some way associated with obstetrics and gynecology.
“This is not true. These incidents can happen in any doctor’s office. It all depends on the physician – whether he or she has designs on committing a criminal act,” Dr. Drezett noted. He did point out that there are few sexual molesters among health care professionals, though there are numerous cases. Yet this in no way diminishes the seriousness of the incidents. “Of course, we’re speaking again about the exceptions, but in my experience of treating victims, I’ve seen, for example, more cases where it’s been a police officer, not a physician, committing an act of sexual violence against a woman,” he stated.
The nurses and nurse technicians at São João do Meriti Hospital who reported the abuser acted very assertively. If they hadn’t gathered the evidence to back up their accusations, it’s possible that the physician wouldn’t have been caught in the act and that the case would have taken a different course – including pressure being put on them and their becoming the target of retaliation.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape Portuguese edition.
At the beginning of July, Brazilians across the country were appalled when they heard that an anesthesiologist was accused of sexually abusing a woman he had been treating during cesarean delivery. The incident was recorded on video by nurses and nurse technicians who, having become suspicious of the excessive amount of sedatives given to mothers-to-be by this particular anesthesiologist, decided to film him during a procedure. To do this, they made a last-minute change, switching delivery rooms to one in which they had hidden a cell phone in a cabinet.
What the footage showed was horrifying and the assailant, Giovanni Quintella Bezerra, was arrested on the spot. He’s a 32-year-old, White, successful physician, and he’s now accused of rape. The authorities are looking into whether there are more victims, others who may have been abused by the physician. The police are investigating about 40 surgeries in which Dr. Bezerra participated. That same month saw the arrest of another physician, gynecologist Ricardo Teles Martins, who was arrested after being accused of sexually harassing and abusing several women in Hidrolândia, in the northeastern state of Ceará.
In gathering information about these incidents, this news organization interviewed four Brazilian specialists to get their insights on the issues that have been brought to light by these recent cases and the factors that play a role in these kinds of criminal acts. Claudio Cohen, MD, PhD, is a psychiatrist, bioethicist, and professor at the University of São Paulo in Brazil. Daniela Pedroso, MA, is a psychologist who has 25 years’ experience working with victims of sexual violence. Gynecologist and obstetrician Jefferson Drezett, MD, PhD, is a professor in the field of population genetics and reproductive and sexual health at the Federal University of ABC, São Paulo, and in the department of health, life cycles, and society at the University of São Paulo School of Public Health. Maria Alice Scardoelli, MD, is a psychiatrist who also serves as vice-chair of the São Paulo Regional Council of Medicine (Cremesp).
Accusations and investigations
Not all incidents of sexual violence in health care institutions are reported, and precise numbers are difficult to obtain. The fact that there are any cases at all is troubling. In 2019, journalists from The Intercept found that over a period of 6 years (2014-2019), 1,734 such attacks were recorded in nine Brazilian states. They were able to get that information from the states’ Public Security Secretariats by using the Information Access Act, a law that regulates the right to access public information.
Efforts to determine how widespread this type of sexual violence is are further complicated by the difficulties in collating the accusations filed at each state’s regional council of medicine, police stations, and public prosecutor’s office. Which investigative steps are taken depends upon where the report was filed, and only occasionally do these entities communicate with each other. According to its data, Cremesp received 78 accusations in 2019. In 2020, that number increased to 84. In 2021, it was 83; these types of attacks were the seventh most common among the investigations opened that year. In the first 6 months of 2022, there were 36 complaints. The number includes investigations opened on the basis of press reports. In such cases, enough information must be available in the press reports make it possible to initiate an evaluation and assessment of the matter. There is no information about how many accusations became the subject of professional ethics proceedings and how many were formally adjudicated.
“Each accusation received is investigated by a technical committee made up of professionals from various specialties. There really needs to be a rigorous evaluation and assessment during the investigation. We cannot be unfair: It may turn out that there was no truth to the accusation after all, and yet someone’s career may already have been destroyed,” explained Dr. Scardoelli.
After the accusation is investigated and accepted by Cremesp, there is no deadline by which the proceedings must end. They can take up to 5 years, and sometimes longer. Since March, however, a deadline for the investigation period has been in effect, after which the proceedings can commence.
“We now have 90 days to make an evaluation and assessment in the investigation phase; that time period can be extended by 3 months, starting from the date the accusation is submitted to the council. If the case is accepted, then the proceedings are opened,” Dr. Scardoelli said.
Some incidents are not reported by victims. And there are incidents that are reported only after many years have passed. This was the case with Nina Marqueti, the actress at the center of #OndeDói — “Where It Hurts” — a campaign that was launched to raise awareness about sexual violence committed by health care professionals. When she was 16, her pediatrician sexually abused her. It wasn’t until 2019, more than a decade later, that she felt able to make this accusation known publicly.
Almost immediately, the campaign received over 4,000 posts online. Most of them were people’s accounts of acts of violence committed by physicians during appointments in their offices or during treatment in a hospital. These are available on Twitter under the hashtag #ondedoi.
Inadequate sex education?
News reports about physicians who abuse patients have a tremendous impact on the public. People are genuinely surprised when they hear the words “health care professional” and “sex attack” in the same sentence. “One of the most disturbing aspects is that health care professionals are committing these acts of violence against women who are in a vulnerable state, typically when they’re under anesthesia, they’ve fallen ill, or when the health care professional introduces an element of deception into the procedure so as to create the opportunity to abuse the patient in some way,” said Dr. Drezett.
As Dr. Cohen sees it, to perpetrate these acts of sexual violence, physicians – as well as lawyers, religious leaders, judges, politicians, police officers, and other persons in a position of trust – make use of their power to take advantage of a person’s vulnerability. “Physicians, lawyers, police officers, religious leaders, dads, bosses, husbands – the people who commit sexual abuse all have something in common,” he said. “In terms of the emotional aspect, all of them are taking advantage of both the power that their position holds in society and the asymmetrical power dynamics that exist between them and the other person.”
Indeed, anyone who knocks on a physician’s door seeking a diagnosis or treatment, anyone who knocks on a lawyer’s door seeking assistance, is putting themselves in a fragile situation. “The abuser considers the other person an object, not a human being who has rights,” said Dr. Cohen. People who fit the psychological and behavioral profile of a sexual assailant find in these “powerful” professions and in the circumstances and opportunities these professions provide a means to fulfill their desires. In medicine, however, there is yet another imbalance, one involving consent to touch a person’s body.
The age of the recently arrested anesthesiologist is something that caught Dr. Cohen’s attention. As noted in one of his many books, Bioética e Sexualidade nas Relações Profissionais [Bioethics and Sexuality in Professional Relationships], published in 1999 by the São Paulo Medical Association, age is a characteristic that repeatedly came up in his analysis of 150 sexual abuse proceedings handled by Cremesp.
“When I looked over the cases, I saw that most of the abusers were not right out of med school in their twenties – a time when sex is at the forefront of one’s life – nor were the abusers on the older end of the age spectrum. The abusers were, in fact, those who had already had several years of experience – as was the case with this 32-year-old anesthesiologist who, at a particular moment in time, breached all prohibitions and betrayed the expectations that society had of him as a physician: to care for people’s well-being and to alleviate their suffering. There was nothing that could hold him back from fulfilling his desire, not even the presence of nurses and other physicians in the operating room.” As for the findings of Dr. Cohen’s review, the majority of the 150 cases were dismissed because of lack of evidence.
To Ms. Pedroso, who has treated more than 12,000 victims of sexual harassment, it’s the questioning and intimidation that women feel in relationship to the male physician – a person who is viewed as holding knowledge about her body – that leaves them vulnerable and more subject to acts of violence, especially in more remote places. “We’re speaking, yet again, about rape culture. Not many people know what that term means, but, generally speaking, it has to do with the objectification of women’s bodies and the issue of boys growing up thinking they have the right to touch girls and women and that they will go unpunished for doing so.”
The lack of sex education and efforts to prevent sexual abuse are contributing factors for why the situation remains unchanged. “We are long overdue. We live in a country where there’s this completely mistaken belief that talking about sex education involves teaching children how to have sex, as opposed to teaching them how to protect themselves. We teach girls that they have to protect themselves from being raped, but we don’t teach boys not to rape.”
Another point highlighted by Ms. Pedroso is the fact that to carry out their actions, sexual assailants seek out-of-the-way places, places where they believe the rules can be bent and where they won’t be caught. This is what may have happened with Dr. Bezerra. During a recent press conference, the coordinator of the Health Section of the Rio de Janeiro Public Defender’s Office, Thaísa Guerreiro, stated that although the Women’s Hospital in São João do Meriti – one of the places where the assailant worked as an anesthesiologist – had adopted protocols to protect patients, it failed to enforce them. Another observation was that the health care professionals normalized violations of a woman’s right to have a companion present throughout labor and delivery, a right guaranteed by federal law. Ms. Guerreiro went on to say that the hospital’s chief of anesthesia and the state’s health coordination office did not question this, nor did they find it strange or surprising. According to witness statements, Dr. Bezerra would ask the patients’ husbands to leave the room in the middle of the procedure.
It should be clarified, Dr. Drezett mentioned, that although obstetric violence and sexual abuse overlap in places, they do not have the same root cause or definition. “There are two sets of situations that we term ‘obstetric violence.’ One involves any type of disrespectful treatment, whether comments or neglect, during pregnancy, delivery, or the postpartum period. The other refers to health care professionals’ attitudes in imposing inadequate and outdated medical procedures at the time of birth, such as keeping the woman fasting, having her pubic hair removed, and inducing labor or speeding up the delivery with oxytocin and [routine] episiotomy, among other things.”
Early education crucial
How are health care institutions dealing with this problem? “Very poorly. Sexual violence perpetrated by physicians and other health care professionals is a taboo subject that people are still afraid to talk about,” Dr. Cohen observed. “Regrettably, sexual violence happens all too often. Before, maybe we weren’t talking about it much because, from our viewpoint, health care professionals, such as physicians and nurses, weren’t likely to commit acts of violence while performing their duties,” noted Dr. Drezett.
Dr. Drezett also spoke about schools and what role they can play. “Of course, schools should discuss violence against women, especially in the field of health care. This has been done for a long time now, though it’s not in every curriculum in every medical school or nursing school, nor in every school of social work or of psychology,” said Dr. Drezett. For example, in the bioethics classes taken in the third and fourth years of the University of São Paolo’s medical degree program, Dr. Cohen asks students to reflect on the significance of being in a position where you ask a patient you’ve never met to undress so you can perform an exam, and the patient promptly and readily complies. “This is not about the physician, it’s about the power of the institution,” the professor pointed out. Sexual violence is a problem on the university campus as well. Another front in the battle has formed across various schools, where groups of students have created feminist collectives to have sexual violence and other issues related to gender-based violence added to the agenda.
Dr. Drezett said it’s very unlikely that efforts made during a degree program are going to succeed in preventing students who are prone to commit sexual violence from engaging in such behavior. “We’re talking about gender-specific lessons, where discussions about gender-based violence should be started much, much earlier – parents talking to their children, teachers talking to their pupils.” He also doesn’t believe that the molesters are dissuaded by the fact that these accusations get publicized in the media. “If they were, the Roger Abdelmassih case would have done away with the problem.”
On the other hand, Dr. Drezett suggested, publicizing these stories can help to bring very positive issues out into the open. What the Bezerra case made clear was that laws were not followed and rights were not protected. An environment was thus created in which the sexual crime could be perpetrated, with nurses coming to suspect acts of obstetric violence, such as use of sedation, which prevented the woman from having skin-to-skin contact with the newborn and from breastfeeding within the first few hours of birth – two clinical practices that are recommended the world over.
“Health care professionals who act properly, in accordance with best practices for interacting with others and performing daily duties, at all times, in public or private practice – they remove themselves from situations like those described in the Bezerra case; they don’t practice medicine in a reckless manner,” said Dr. Drezett.
Another negative aspect of all this, he said, is that the suspicion and wariness that patients feel may spread far and wide. “Among my colleagues are anesthetists and anesthesiologists with impeccable ethical and professional records. They are very upset that people are now regarding them with doubt and uncertainty. We need to make it clear that those horrifying cases are the exceptions, not the rule,” he said. There is also a need to correct the misconception that such abuse is always in some way associated with obstetrics and gynecology.
“This is not true. These incidents can happen in any doctor’s office. It all depends on the physician – whether he or she has designs on committing a criminal act,” Dr. Drezett noted. He did point out that there are few sexual molesters among health care professionals, though there are numerous cases. Yet this in no way diminishes the seriousness of the incidents. “Of course, we’re speaking again about the exceptions, but in my experience of treating victims, I’ve seen, for example, more cases where it’s been a police officer, not a physician, committing an act of sexual violence against a woman,” he stated.
The nurses and nurse technicians at São João do Meriti Hospital who reported the abuser acted very assertively. If they hadn’t gathered the evidence to back up their accusations, it’s possible that the physician wouldn’t have been caught in the act and that the case would have taken a different course – including pressure being put on them and their becoming the target of retaliation.
A version of this article first appeared on Medscape.com. This article was translated from the Medscape Portuguese edition.
Federal Health Care Data Trends 2022
Federal Health Care Data Trends (click to view the digital edition) is a special supplement to Federal Practitioner highlighting the latest research and study outcomes related to the health of veteran and active-duty populations.
In this issue:
- Vaccinations
- Mental Health and Related Disorders
- LGBTQ+ Veterans
- Military Sexual Trauma
- Sleep Disorders
- Respiratory Illnesses
- HIV Care in the VA
- Rheumatologic Diseases
- The Cancer-Obesity Connection
- Skin Health for Active-Duty Personnel
- Contraception
- Chronic Kidney Disease
- Cardiovascular Diseases
- Neurologic Disorders
- Hearing, Vision, and Balance
Federal Practitioner would like to thank the following experts for their review of content and helpful guidance in developing this issue:
Kelvin N.V. Bush, MD, FACC, CCDS; Sonya Borrero, MD, MS; Kenneth L. Cameron, PhD, MPH, ATC, FNATA; Jason DeViva, PhD; Ellen Lockard Edens, MD; Leonard E. Egede, MD, MS; Amy Justice, MD, PhD; Stephanie Knudson, MD; Willis H. Lyford, MD; Sarah O. Meadows, PhD; Tamara Schult, PhD, MPH; Eric L. Singman, MD, PhD; Art Wallace, MD, PhD; Elizabeth Waterhouse, MD, FAAN
Federal Health Care Data Trends (click to view the digital edition) is a special supplement to Federal Practitioner highlighting the latest research and study outcomes related to the health of veteran and active-duty populations.
In this issue:
- Vaccinations
- Mental Health and Related Disorders
- LGBTQ+ Veterans
- Military Sexual Trauma
- Sleep Disorders
- Respiratory Illnesses
- HIV Care in the VA
- Rheumatologic Diseases
- The Cancer-Obesity Connection
- Skin Health for Active-Duty Personnel
- Contraception
- Chronic Kidney Disease
- Cardiovascular Diseases
- Neurologic Disorders
- Hearing, Vision, and Balance
Federal Practitioner would like to thank the following experts for their review of content and helpful guidance in developing this issue:
Kelvin N.V. Bush, MD, FACC, CCDS; Sonya Borrero, MD, MS; Kenneth L. Cameron, PhD, MPH, ATC, FNATA; Jason DeViva, PhD; Ellen Lockard Edens, MD; Leonard E. Egede, MD, MS; Amy Justice, MD, PhD; Stephanie Knudson, MD; Willis H. Lyford, MD; Sarah O. Meadows, PhD; Tamara Schult, PhD, MPH; Eric L. Singman, MD, PhD; Art Wallace, MD, PhD; Elizabeth Waterhouse, MD, FAAN
Federal Health Care Data Trends (click to view the digital edition) is a special supplement to Federal Practitioner highlighting the latest research and study outcomes related to the health of veteran and active-duty populations.
In this issue:
- Vaccinations
- Mental Health and Related Disorders
- LGBTQ+ Veterans
- Military Sexual Trauma
- Sleep Disorders
- Respiratory Illnesses
- HIV Care in the VA
- Rheumatologic Diseases
- The Cancer-Obesity Connection
- Skin Health for Active-Duty Personnel
- Contraception
- Chronic Kidney Disease
- Cardiovascular Diseases
- Neurologic Disorders
- Hearing, Vision, and Balance
Federal Practitioner would like to thank the following experts for their review of content and helpful guidance in developing this issue:
Kelvin N.V. Bush, MD, FACC, CCDS; Sonya Borrero, MD, MS; Kenneth L. Cameron, PhD, MPH, ATC, FNATA; Jason DeViva, PhD; Ellen Lockard Edens, MD; Leonard E. Egede, MD, MS; Amy Justice, MD, PhD; Stephanie Knudson, MD; Willis H. Lyford, MD; Sarah O. Meadows, PhD; Tamara Schult, PhD, MPH; Eric L. Singman, MD, PhD; Art Wallace, MD, PhD; Elizabeth Waterhouse, MD, FAAN
University to train ‘trip facilitators’ for psychedelic therapy
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.
The UC Berkeley Center for the Science of Psychedelics (BCSP) training program aims to create a cadre of facilitators who will be ready to help if, and when, substances such as psilocybin, MDMA, and LSD are approved in the United States, Tina Trujillo, PhD, an associate professor at UC Berkeley’s School of Education, told reporters at a press briefing.
Hallucinogenic drugs are on the Drug Enforcement Administration’s (DEA) Schedule I list because they are considered to have no currently accepted medical use and high abuse potential. But there has been an explosion of research into psychedelics – combined with therapy – as treatment for severe depression, posttraumatic stress disorder, substance-use disorder, and other mental health conditions. Some 100 clinical trials are underway.
“The estimates are that we’re going to need 100,000 trained psychedelic facilitators once psilocybin and MDMA are approved by the [U.S. Food and Drug Administration] FDA, which is expected to happen within the next 5 years or so,” said Michael Pollan, co-founder of the BCSP. He is author of “How to Change Your Mind,” a 2018 book about psychedelics, which has been adapted into a four-part docuseries currently streaming on Netflix.
Nine-month program
The first 24 trainees – a mix of physicians, nurses, psychotherapists, and social workers – will undergo 9 months of education and preparation in “the technical, the cultural, the mystical, and the ethical dimensions of psychedelic facilitation,” said Dr. Trujillo.
The BCSP’s Certificate Program in Psychedelic Facilitation will have “an emphasis on both western science and spiritual care traditions,” she said.
Trainees will receive 150 instructional hours and a 25-hour practicum and will take part in a final 5-day retreat. The program will initially focus only on psilocybin, in part because the BCSP is involved in several FDA-approved trials testing the drug.
In one study – which aims to enroll participants in the fall – researchers will use functional MRI to examine the neural correlates of the psychedelic experience in individuals receiving low-dose psilocybin.
Eligible trainees will have an opportunity to participate in the Berkeley psilocybin trials and “increase their first-hand knowledge,” Dr. Trujillo said.
At the conclusion of the training, students will receive a certificate, “not a license or sanction to go off and practice,” she said. She noted that eventually, when facilitation is legal, certificate holders will be able to practice in clinical research settings or in health care settings.
Growing acceptance in psychiatry
Mr. Pollan said there has been a radical change in acceptance of psychedelics as potential therapies.
“The shift from destroyer of young minds in the ‘60s to effective medicine in the 2020s is as sudden as it is confusing for many people,” he said. He noted that the Berkeley center hopes to provide evidence-based information for journalists, the public, and clinicians.
He said that after his book was released, he expected pushback from “mainstream psychiatry.” Instead, he was invited to give grand rounds talks. Psychiatrists are “very open to the potential of psychedelics,” Mr. Pollan said.
“The reason for that, quite frankly, is because they are desperate,” he said. “The tools of conventional psychiatry to deal with things like depression and anxiety and addiction are not very good, and some of them are failing,” he said.
Mr. Pollan cited some other indicators of acceptance. In Oregon, beginning in 2023, psilocybin will be available to anyone older than 21 years but only for use in licensed facilities with licensed facilitators, and the substance must be produced by a licensed manufacturer.
In November, Colorado will ask voters whether they want to follow the Oregon model and legalize psilocybin. If approved, another Colorado ballot initiative would decriminalize possession.
Mr. Pollan noted that Cory Booker, the Democratic Senator from New Jersey, and Rand Paul, a conservative Republican Senator from Kentucky, have found a common cause, introducing legislation to let select terminally ill patients have access to psychedelics and other Schedule I drugs.
Some 400 companies are conducting research on psychedelics. Researchers must have a license from the DEA to obtain and study the substances, Andrea Gomez, assistant professor of neurobiology at UC Berkeley, told reporters.
She said growing interest in the potential of these drugs might lead more researchers to “jump through the hoops” to get the licenses. The floodgates would truly open if the National Institutes of Health started funding studies, she said.
A version of this article first appeared on Medscape.com.