User login
Serum biomarker predicts radiographic progression in spondyloarthritis
MADRID – Elevated serum levels of vascular endothelial growth factor may be predictive of radiographic progression in the spine, according to data from a German study of patients with spondyloarthritis.
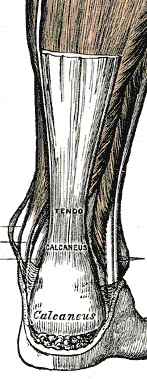
The cutoff point appears to be at 600 pg/mL, with the effects particularly strong in patients who also develop syndesmophytes, which are bony growths that develop within ligaments.
"In patients with syndesmophytes, VEGF [vascular endothelial growth factor], as a predictor of radiographic progression, performed better than CRP [C-reactive protein]," reported Dr. Denis Poddubnyy at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72:125).
"We all know that radiographic progression varies substantially among patients with spondyloarthritis," Dr. Poddubnyy observed. "Until recently there was only one strong predictor of radiographic progression: the presence of syndesmophytes at baseline," he added.
Last year, however, Dr. Poddubnyy of Charité Universitätsmedizin Berlin, Germany, and his associates published the findings of a study involving 210 patients with early axial spondyloarthritis (axSpA) who were recruited from the German Spondyloarthritis Inception Cohort (GESPIC). This study looked at baseline predictors of spinal radiographic progression over 2 years and found that in addition to radiographic damage, elevated CRP levels and cigarette smoking were independently predictive (Arthritis Rheum. 2012;64:1388-98).
The team’s research also suggested that there could be a few serum biomarkers, including VEGF, that could be predictive, so the investigators conducted a larger study in 172 patients with definite (n = 95) or nonradiographic (n = 77) axSpA to look specifically at the possible association.
Radiographs of the spine taken at baseline and at 2 years’ follow-up were reviewed independently by two readers, who used the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) to record the extent of radiographic progression. If there was a worsening of 2 units or more in mSASSS and the formation of new or increased growth of syndesmophytes, radiographic progression had occurred.
In total, 22 patients had radiographic progression, including 18 with new formation or growth of syndesmophytes.
Baseline VEGF was measured in the serum at baseline and was significantly higher in patients who developed radiographic progression at 2 years than in those who did not (562 plus or minus 357 pg/mL vs. 402 plus or minus 309 pg/mL; P = .027).
Serum VEGF levels were also significantly higher in the patients who had developed new syndesmophytes at 2 years when compared with those who had not (579 plus or minus 386 pg/mL vs. 404 plus or minus 307 pg/mL; P = .041).
"Patients with elevated VEGF had an odds ratio of 2.9 for [radiographic] progression and 3.1 for syndesmophyte formation," Dr. Poddubnyy reported. This was a little disappointing, he noted, as CRP and the erythrocyte sedimentation rate had similar predictive power.
However, in patients at high risk of progression, namely those with syndesmophytes already present at baseline, VEGF was significantly better than CRP at predicting both radiographic progression and new syndesmophyte formation or growth.
Patients with elevated VEGF at baseline were 36.6 times more likely to have radiographic progression and 13.6 times more likely to have new syndesmophyte formation or growth at 2 years than were those with levels below 600 pg/mL. In comparison, elevated CRP levels increased the risks by only 2.4 and 2.5 times, respectively.
VEGF is an essential mediator of angiogenesis and endochondral ossification, Dr. Poddubnyy observed. It’s been shown to have "a chemoattractive effect on osteoblasts and mesenchymal progenitor cells," he added, and also stimulate osteoblast differentiation and bone turnover.
While the results are very promising, further research is of course required. The possible predictive value of VEGF in relation to spinal radiographic progression in patients treated with tumor necrosis factor–alpha inhibitors remains to be seen, for example, and future studies should perhaps look at this question.
"With VEGF we are probably able to improve our prediction of spinal progression in patients with axSpA," Dr. Poddubnyy said in an interview. This is addition to assessing "classical factors," such as syndesmophytes, CRP, and smoking status.
Dr. Poddubnyy had no disclosures.
MADRID – Elevated serum levels of vascular endothelial growth factor may be predictive of radiographic progression in the spine, according to data from a German study of patients with spondyloarthritis.
The cutoff point appears to be at 600 pg/mL, with the effects particularly strong in patients who also develop syndesmophytes, which are bony growths that develop within ligaments.
"In patients with syndesmophytes, VEGF [vascular endothelial growth factor], as a predictor of radiographic progression, performed better than CRP [C-reactive protein]," reported Dr. Denis Poddubnyy at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72:125).
"We all know that radiographic progression varies substantially among patients with spondyloarthritis," Dr. Poddubnyy observed. "Until recently there was only one strong predictor of radiographic progression: the presence of syndesmophytes at baseline," he added.
Last year, however, Dr. Poddubnyy of Charité Universitätsmedizin Berlin, Germany, and his associates published the findings of a study involving 210 patients with early axial spondyloarthritis (axSpA) who were recruited from the German Spondyloarthritis Inception Cohort (GESPIC). This study looked at baseline predictors of spinal radiographic progression over 2 years and found that in addition to radiographic damage, elevated CRP levels and cigarette smoking were independently predictive (Arthritis Rheum. 2012;64:1388-98).
The team’s research also suggested that there could be a few serum biomarkers, including VEGF, that could be predictive, so the investigators conducted a larger study in 172 patients with definite (n = 95) or nonradiographic (n = 77) axSpA to look specifically at the possible association.
Radiographs of the spine taken at baseline and at 2 years’ follow-up were reviewed independently by two readers, who used the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) to record the extent of radiographic progression. If there was a worsening of 2 units or more in mSASSS and the formation of new or increased growth of syndesmophytes, radiographic progression had occurred.
In total, 22 patients had radiographic progression, including 18 with new formation or growth of syndesmophytes.
Baseline VEGF was measured in the serum at baseline and was significantly higher in patients who developed radiographic progression at 2 years than in those who did not (562 plus or minus 357 pg/mL vs. 402 plus or minus 309 pg/mL; P = .027).
Serum VEGF levels were also significantly higher in the patients who had developed new syndesmophytes at 2 years when compared with those who had not (579 plus or minus 386 pg/mL vs. 404 plus or minus 307 pg/mL; P = .041).
"Patients with elevated VEGF had an odds ratio of 2.9 for [radiographic] progression and 3.1 for syndesmophyte formation," Dr. Poddubnyy reported. This was a little disappointing, he noted, as CRP and the erythrocyte sedimentation rate had similar predictive power.
However, in patients at high risk of progression, namely those with syndesmophytes already present at baseline, VEGF was significantly better than CRP at predicting both radiographic progression and new syndesmophyte formation or growth.
Patients with elevated VEGF at baseline were 36.6 times more likely to have radiographic progression and 13.6 times more likely to have new syndesmophyte formation or growth at 2 years than were those with levels below 600 pg/mL. In comparison, elevated CRP levels increased the risks by only 2.4 and 2.5 times, respectively.
VEGF is an essential mediator of angiogenesis and endochondral ossification, Dr. Poddubnyy observed. It’s been shown to have "a chemoattractive effect on osteoblasts and mesenchymal progenitor cells," he added, and also stimulate osteoblast differentiation and bone turnover.
While the results are very promising, further research is of course required. The possible predictive value of VEGF in relation to spinal radiographic progression in patients treated with tumor necrosis factor–alpha inhibitors remains to be seen, for example, and future studies should perhaps look at this question.
"With VEGF we are probably able to improve our prediction of spinal progression in patients with axSpA," Dr. Poddubnyy said in an interview. This is addition to assessing "classical factors," such as syndesmophytes, CRP, and smoking status.
Dr. Poddubnyy had no disclosures.
MADRID – Elevated serum levels of vascular endothelial growth factor may be predictive of radiographic progression in the spine, according to data from a German study of patients with spondyloarthritis.
The cutoff point appears to be at 600 pg/mL, with the effects particularly strong in patients who also develop syndesmophytes, which are bony growths that develop within ligaments.
"In patients with syndesmophytes, VEGF [vascular endothelial growth factor], as a predictor of radiographic progression, performed better than CRP [C-reactive protein]," reported Dr. Denis Poddubnyy at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72:125).
"We all know that radiographic progression varies substantially among patients with spondyloarthritis," Dr. Poddubnyy observed. "Until recently there was only one strong predictor of radiographic progression: the presence of syndesmophytes at baseline," he added.
Last year, however, Dr. Poddubnyy of Charité Universitätsmedizin Berlin, Germany, and his associates published the findings of a study involving 210 patients with early axial spondyloarthritis (axSpA) who were recruited from the German Spondyloarthritis Inception Cohort (GESPIC). This study looked at baseline predictors of spinal radiographic progression over 2 years and found that in addition to radiographic damage, elevated CRP levels and cigarette smoking were independently predictive (Arthritis Rheum. 2012;64:1388-98).
The team’s research also suggested that there could be a few serum biomarkers, including VEGF, that could be predictive, so the investigators conducted a larger study in 172 patients with definite (n = 95) or nonradiographic (n = 77) axSpA to look specifically at the possible association.
Radiographs of the spine taken at baseline and at 2 years’ follow-up were reviewed independently by two readers, who used the modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS) to record the extent of radiographic progression. If there was a worsening of 2 units or more in mSASSS and the formation of new or increased growth of syndesmophytes, radiographic progression had occurred.
In total, 22 patients had radiographic progression, including 18 with new formation or growth of syndesmophytes.
Baseline VEGF was measured in the serum at baseline and was significantly higher in patients who developed radiographic progression at 2 years than in those who did not (562 plus or minus 357 pg/mL vs. 402 plus or minus 309 pg/mL; P = .027).
Serum VEGF levels were also significantly higher in the patients who had developed new syndesmophytes at 2 years when compared with those who had not (579 plus or minus 386 pg/mL vs. 404 plus or minus 307 pg/mL; P = .041).
"Patients with elevated VEGF had an odds ratio of 2.9 for [radiographic] progression and 3.1 for syndesmophyte formation," Dr. Poddubnyy reported. This was a little disappointing, he noted, as CRP and the erythrocyte sedimentation rate had similar predictive power.
However, in patients at high risk of progression, namely those with syndesmophytes already present at baseline, VEGF was significantly better than CRP at predicting both radiographic progression and new syndesmophyte formation or growth.
Patients with elevated VEGF at baseline were 36.6 times more likely to have radiographic progression and 13.6 times more likely to have new syndesmophyte formation or growth at 2 years than were those with levels below 600 pg/mL. In comparison, elevated CRP levels increased the risks by only 2.4 and 2.5 times, respectively.
VEGF is an essential mediator of angiogenesis and endochondral ossification, Dr. Poddubnyy observed. It’s been shown to have "a chemoattractive effect on osteoblasts and mesenchymal progenitor cells," he added, and also stimulate osteoblast differentiation and bone turnover.
While the results are very promising, further research is of course required. The possible predictive value of VEGF in relation to spinal radiographic progression in patients treated with tumor necrosis factor–alpha inhibitors remains to be seen, for example, and future studies should perhaps look at this question.
"With VEGF we are probably able to improve our prediction of spinal progression in patients with axSpA," Dr. Poddubnyy said in an interview. This is addition to assessing "classical factors," such as syndesmophytes, CRP, and smoking status.
Dr. Poddubnyy had no disclosures.
AT THE EULAR CONGRESS 2013
Major finding: Baseline serum VEGF levels were 562 plus or minus 357 pg/mL vs. 402 plus or minus 309 pg/mL in patients with and without radiographic progression, respectively, at 2 years (P = .027).
Data source: Study of 95 patients with definite axial spondyloarthritis (axSpA) and 77 with nonradiographic axSpA recruited from the German Spondyloarthritis Inception Cohort (GESPIC).
Disclosures: Dr. Poddubnyy had no disclosures.
Expert panel sets broad SpA treat-to-target goals
MADRID – A panel of clinicians with expertise in the management of patients with spondyloarthritis took another step toward better defining this disease category and the goals of its treatment by producing the first "treat-to-target" recommendations for spondyloarthritis.
The new recommendations will "guide physicians, patients, and other stakeholders on how to optimize reduction of signs and symptoms and, ideally, outcomes, and will drive" the current research agenda, Dr. Josef S. Smolen said while presenting the panel’s recommendations at the annual European Congress of Rheumatology.
"Treat to target proposes a stepwise approach to achieving optimal outcomes based on available evidence and expert opinion. Treat to target has been successfully applied to management of diabetes, hypertension, hyperlipidemia, and rheumatoid arthritis," and the new task force set out to address whether it could be used when treating patients with spondyloarthritis (SpA), a question that required the expert task force to review the evidence for setting specific treatment goals for patients with SpA, said Dr. Smolen, professor of medicine at the Medical University of Vienna.
The task force eventually decided that the treat-to-target concept was applicable to SpA, but that the data available so far prevented the task force from setting specific treatment goals. While the recommendations underscore the importance of treating SpA patients with a goal of remission or inactive disease, and failing that, at least low disease activity, they fall short of giving clinicians guidance on how to best measure and define remission or low disease activity or how to achieve these goals.
For example, for axial SpA – the subtype that received the most specific recommendations – the panel advised clinicians to guide treatment decisions by using a "validated composite measure of disease activity" such as the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) plus acute phase reactants, or the Ankylosing Spondylitis Disease Activity Score (ASDAS) with or without functional measures such as the Bath Ankylosing Spondylitis Functional Index (BASFI). But the recommendations say nothing about what scores by these measures would define remission or low disease activity. The recommendations also talk about using other factors to further gauge axial SpA disease activity such as MRI analysis of inflammation and radiographic progression, but again Dr. Smolen provided no specific targets when using these measures.
For other, less well studied types of SpA, the new recommendations were even more nebulous. For psoriatic arthritis, the panel indicated that "validated measures of musculoskeletal disease activity" should be "performed and documented regularly" as should other factors such as spinal and extraarticular manifestations, imaging findings, and comorbidities, but the recommendations gave no specifics on what any of these measures might be or what level might equal remission or low disease. The same held true for peripheral SpA.
Other factors touched on by the new recommendations include the need for individualized and shared decision making between physicians and patients, the need for coordination of care among rheumatologists and other medical specialists who treat SpA patients (dermatologists, gastroenterologists, and ophthalmologists), and the need to take into account extraarticular manifestations of SpA diseases, comorbidities, and treatment risks along with the goal of low disease activity.
"I think it was important to document that there is a paucity of trials that have looked at strategies to treat" SpA. "For rheumatoid arthritis we have strategies, but not in spondyloarthritis, and I think it is important to say that," said Dr. Jürgen Braun, medical director of Rheumazentrum Ruhrgebiet in Herne, Germany.
SpA also lags behind rheumatoid arthritis by not having any treatments proven to slow radiographic progression. "Although we say that it is presumably important to treat inflammation [in patients with SpA], we are not sure," said Dr. Braun, who served as a member of the treat-to-target task force.
Even though the task force’s report highlights the absence of evidence for most facets of SpA management, "in the absence of evidence you need eminence, and that’s what was produced." Dr. Braun predicted that rheumatologists and other clinicians who care for patients with SpA would welcome these new recommendations despite their shortcomings. "What we say is what clinicians feel: If a patient’s CRP is elevated we must do something about it, but the evidence supporting this is limited. Presumably, it is important to treat inflammation, but we are not yet sure," he said in an interview.
"We don’t have trial results yet where you set up a quantifiable endpoint as your target, but that is coming," said Dr. Philip J. Mease, director of the rheumatology clinical research division at Swedish Medical Center in Seattle and a member of the task force. For example, the results from the Tight Control of Psoriatic Arthritis (TICOPA) trial "will tell us whether more aggressive treatment to a quantifiable target is appropriate and makes a difference. We anticipate that it will, but evidence is currently lacking." The primary endpoint of the TICOPA trial is change in the ACR20 response, but the trial includes several other clinical measures as secondary endpoints, including the Assessment in Ankylosing Spondylitis (ASAS), the BASDAI, and the psoriasis area severity index (PASI).
"The rheumatoid model is prompting us to develop quantifiable measures like the ASDAS and the new Psoriatic Arthritis Disease Activity Score (PASDAS) that we’ll start to see used. I just spoke with a colleague about the need to also develop a similar measure for peripheral SpA," Dr. Mease said in an interview.
The task force that developed the treat-to-target recommendations included 16 physicians and patients on its steering committee and 16 on an advisory committee. The majority came from various European locations, but about a quarter of the task force members were from the United States. To arrive at its recommendations, the task force used a comprehensive literature review that identified 22 published reports that addressed treatment targets for SpA (Ann. Rheum. Dis. 2013 June 10 [doi:10.1136/annrheumdis-2013-203860]). The treat-to-target recommendations were published online a few days before Dr. Smolen’s presentation at the meeting (Ann. Rheum. Dis. 2013 June 8 [doi:10.1136/annrheumdis-2013-203419]).
Dr. Smolen, Dr. Braun, and Dr. Mease said that they had no disclosures relevant to the topic.
On Twitter @mitchelzoler
MADRID – A panel of clinicians with expertise in the management of patients with spondyloarthritis took another step toward better defining this disease category and the goals of its treatment by producing the first "treat-to-target" recommendations for spondyloarthritis.
The new recommendations will "guide physicians, patients, and other stakeholders on how to optimize reduction of signs and symptoms and, ideally, outcomes, and will drive" the current research agenda, Dr. Josef S. Smolen said while presenting the panel’s recommendations at the annual European Congress of Rheumatology.
"Treat to target proposes a stepwise approach to achieving optimal outcomes based on available evidence and expert opinion. Treat to target has been successfully applied to management of diabetes, hypertension, hyperlipidemia, and rheumatoid arthritis," and the new task force set out to address whether it could be used when treating patients with spondyloarthritis (SpA), a question that required the expert task force to review the evidence for setting specific treatment goals for patients with SpA, said Dr. Smolen, professor of medicine at the Medical University of Vienna.
The task force eventually decided that the treat-to-target concept was applicable to SpA, but that the data available so far prevented the task force from setting specific treatment goals. While the recommendations underscore the importance of treating SpA patients with a goal of remission or inactive disease, and failing that, at least low disease activity, they fall short of giving clinicians guidance on how to best measure and define remission or low disease activity or how to achieve these goals.
For example, for axial SpA – the subtype that received the most specific recommendations – the panel advised clinicians to guide treatment decisions by using a "validated composite measure of disease activity" such as the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) plus acute phase reactants, or the Ankylosing Spondylitis Disease Activity Score (ASDAS) with or without functional measures such as the Bath Ankylosing Spondylitis Functional Index (BASFI). But the recommendations say nothing about what scores by these measures would define remission or low disease activity. The recommendations also talk about using other factors to further gauge axial SpA disease activity such as MRI analysis of inflammation and radiographic progression, but again Dr. Smolen provided no specific targets when using these measures.
For other, less well studied types of SpA, the new recommendations were even more nebulous. For psoriatic arthritis, the panel indicated that "validated measures of musculoskeletal disease activity" should be "performed and documented regularly" as should other factors such as spinal and extraarticular manifestations, imaging findings, and comorbidities, but the recommendations gave no specifics on what any of these measures might be or what level might equal remission or low disease. The same held true for peripheral SpA.
Other factors touched on by the new recommendations include the need for individualized and shared decision making between physicians and patients, the need for coordination of care among rheumatologists and other medical specialists who treat SpA patients (dermatologists, gastroenterologists, and ophthalmologists), and the need to take into account extraarticular manifestations of SpA diseases, comorbidities, and treatment risks along with the goal of low disease activity.
"I think it was important to document that there is a paucity of trials that have looked at strategies to treat" SpA. "For rheumatoid arthritis we have strategies, but not in spondyloarthritis, and I think it is important to say that," said Dr. Jürgen Braun, medical director of Rheumazentrum Ruhrgebiet in Herne, Germany.
SpA also lags behind rheumatoid arthritis by not having any treatments proven to slow radiographic progression. "Although we say that it is presumably important to treat inflammation [in patients with SpA], we are not sure," said Dr. Braun, who served as a member of the treat-to-target task force.
Even though the task force’s report highlights the absence of evidence for most facets of SpA management, "in the absence of evidence you need eminence, and that’s what was produced." Dr. Braun predicted that rheumatologists and other clinicians who care for patients with SpA would welcome these new recommendations despite their shortcomings. "What we say is what clinicians feel: If a patient’s CRP is elevated we must do something about it, but the evidence supporting this is limited. Presumably, it is important to treat inflammation, but we are not yet sure," he said in an interview.
"We don’t have trial results yet where you set up a quantifiable endpoint as your target, but that is coming," said Dr. Philip J. Mease, director of the rheumatology clinical research division at Swedish Medical Center in Seattle and a member of the task force. For example, the results from the Tight Control of Psoriatic Arthritis (TICOPA) trial "will tell us whether more aggressive treatment to a quantifiable target is appropriate and makes a difference. We anticipate that it will, but evidence is currently lacking." The primary endpoint of the TICOPA trial is change in the ACR20 response, but the trial includes several other clinical measures as secondary endpoints, including the Assessment in Ankylosing Spondylitis (ASAS), the BASDAI, and the psoriasis area severity index (PASI).
"The rheumatoid model is prompting us to develop quantifiable measures like the ASDAS and the new Psoriatic Arthritis Disease Activity Score (PASDAS) that we’ll start to see used. I just spoke with a colleague about the need to also develop a similar measure for peripheral SpA," Dr. Mease said in an interview.
The task force that developed the treat-to-target recommendations included 16 physicians and patients on its steering committee and 16 on an advisory committee. The majority came from various European locations, but about a quarter of the task force members were from the United States. To arrive at its recommendations, the task force used a comprehensive literature review that identified 22 published reports that addressed treatment targets for SpA (Ann. Rheum. Dis. 2013 June 10 [doi:10.1136/annrheumdis-2013-203860]). The treat-to-target recommendations were published online a few days before Dr. Smolen’s presentation at the meeting (Ann. Rheum. Dis. 2013 June 8 [doi:10.1136/annrheumdis-2013-203419]).
Dr. Smolen, Dr. Braun, and Dr. Mease said that they had no disclosures relevant to the topic.
On Twitter @mitchelzoler
MADRID – A panel of clinicians with expertise in the management of patients with spondyloarthritis took another step toward better defining this disease category and the goals of its treatment by producing the first "treat-to-target" recommendations for spondyloarthritis.
The new recommendations will "guide physicians, patients, and other stakeholders on how to optimize reduction of signs and symptoms and, ideally, outcomes, and will drive" the current research agenda, Dr. Josef S. Smolen said while presenting the panel’s recommendations at the annual European Congress of Rheumatology.
"Treat to target proposes a stepwise approach to achieving optimal outcomes based on available evidence and expert opinion. Treat to target has been successfully applied to management of diabetes, hypertension, hyperlipidemia, and rheumatoid arthritis," and the new task force set out to address whether it could be used when treating patients with spondyloarthritis (SpA), a question that required the expert task force to review the evidence for setting specific treatment goals for patients with SpA, said Dr. Smolen, professor of medicine at the Medical University of Vienna.
The task force eventually decided that the treat-to-target concept was applicable to SpA, but that the data available so far prevented the task force from setting specific treatment goals. While the recommendations underscore the importance of treating SpA patients with a goal of remission or inactive disease, and failing that, at least low disease activity, they fall short of giving clinicians guidance on how to best measure and define remission or low disease activity or how to achieve these goals.
For example, for axial SpA – the subtype that received the most specific recommendations – the panel advised clinicians to guide treatment decisions by using a "validated composite measure of disease activity" such as the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) plus acute phase reactants, or the Ankylosing Spondylitis Disease Activity Score (ASDAS) with or without functional measures such as the Bath Ankylosing Spondylitis Functional Index (BASFI). But the recommendations say nothing about what scores by these measures would define remission or low disease activity. The recommendations also talk about using other factors to further gauge axial SpA disease activity such as MRI analysis of inflammation and radiographic progression, but again Dr. Smolen provided no specific targets when using these measures.
For other, less well studied types of SpA, the new recommendations were even more nebulous. For psoriatic arthritis, the panel indicated that "validated measures of musculoskeletal disease activity" should be "performed and documented regularly" as should other factors such as spinal and extraarticular manifestations, imaging findings, and comorbidities, but the recommendations gave no specifics on what any of these measures might be or what level might equal remission or low disease. The same held true for peripheral SpA.
Other factors touched on by the new recommendations include the need for individualized and shared decision making between physicians and patients, the need for coordination of care among rheumatologists and other medical specialists who treat SpA patients (dermatologists, gastroenterologists, and ophthalmologists), and the need to take into account extraarticular manifestations of SpA diseases, comorbidities, and treatment risks along with the goal of low disease activity.
"I think it was important to document that there is a paucity of trials that have looked at strategies to treat" SpA. "For rheumatoid arthritis we have strategies, but not in spondyloarthritis, and I think it is important to say that," said Dr. Jürgen Braun, medical director of Rheumazentrum Ruhrgebiet in Herne, Germany.
SpA also lags behind rheumatoid arthritis by not having any treatments proven to slow radiographic progression. "Although we say that it is presumably important to treat inflammation [in patients with SpA], we are not sure," said Dr. Braun, who served as a member of the treat-to-target task force.
Even though the task force’s report highlights the absence of evidence for most facets of SpA management, "in the absence of evidence you need eminence, and that’s what was produced." Dr. Braun predicted that rheumatologists and other clinicians who care for patients with SpA would welcome these new recommendations despite their shortcomings. "What we say is what clinicians feel: If a patient’s CRP is elevated we must do something about it, but the evidence supporting this is limited. Presumably, it is important to treat inflammation, but we are not yet sure," he said in an interview.
"We don’t have trial results yet where you set up a quantifiable endpoint as your target, but that is coming," said Dr. Philip J. Mease, director of the rheumatology clinical research division at Swedish Medical Center in Seattle and a member of the task force. For example, the results from the Tight Control of Psoriatic Arthritis (TICOPA) trial "will tell us whether more aggressive treatment to a quantifiable target is appropriate and makes a difference. We anticipate that it will, but evidence is currently lacking." The primary endpoint of the TICOPA trial is change in the ACR20 response, but the trial includes several other clinical measures as secondary endpoints, including the Assessment in Ankylosing Spondylitis (ASAS), the BASDAI, and the psoriasis area severity index (PASI).
"The rheumatoid model is prompting us to develop quantifiable measures like the ASDAS and the new Psoriatic Arthritis Disease Activity Score (PASDAS) that we’ll start to see used. I just spoke with a colleague about the need to also develop a similar measure for peripheral SpA," Dr. Mease said in an interview.
The task force that developed the treat-to-target recommendations included 16 physicians and patients on its steering committee and 16 on an advisory committee. The majority came from various European locations, but about a quarter of the task force members were from the United States. To arrive at its recommendations, the task force used a comprehensive literature review that identified 22 published reports that addressed treatment targets for SpA (Ann. Rheum. Dis. 2013 June 10 [doi:10.1136/annrheumdis-2013-203860]). The treat-to-target recommendations were published online a few days before Dr. Smolen’s presentation at the meeting (Ann. Rheum. Dis. 2013 June 8 [doi:10.1136/annrheumdis-2013-203419]).
Dr. Smolen, Dr. Braun, and Dr. Mease said that they had no disclosures relevant to the topic.
On Twitter @mitchelzoler
AT THE EULAR CONGRESS 2013
Spinal MRI does not enhance spondyloarthropathy diagnosis
MADRID – There is no added benefit of performing spinal MRI in the diagnosis of spondyloarthritis, the results of an international, multicenter study suggest.
Around one-quarter of patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had a negative MRI scan of the sacroiliac joints (SIJs) were reclassified as being positive for SpA by a combined evaluation of SIJ MRI and spinal MRI scans.
However, 17.5% of healthy volunteers and up to 26.8% of patients with mechanical back pain who had a negative SIJ MRI were also reclassified as having SpA. This false-positive result balances out the value of combined spinal and SIJ MRI.
"Combined MRI added little incremental value compared to SIJ MRI alone for diagnosis of nr-axSpA," said Dr. Ulrich Weber, who presented the findings at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72:145).
"Although you get about 20% more patients – which is the good news – we found about the same magnitude of false-positive controls," he said in an interview. He added that he "was very disappointed with this result, and these data need confirming." Dr. Weber collected data for the study while at the Balgrist University Clinic in Zurich, and also as a visiting professor in the rheumatology department at the University of Alberta, Edmonton.
SIJ MRI is a major criterion of the Assessment of SpondyloArthritis classification criteria for ankylosing spondylitis (AS). If a patient is strongly suspected of having early SpA, but this is not yet visible on radiographs, then an SIJ MRI is often the next step. If this is negative, however, it may be unclear what to do next.
"Our question was, ‘Would it help to order an additional spinal MRI in this situation?’ " Dr. Weber explained. These data suggest that it is not.
The collaborative study included 130 individuals with newly diagnosed back pain and aged 50 years or younger who were recruited from clinics based in Canada, China, Denmark, and Switzerland, as well as 20 healthy control individuals in whom MRI scans of the SIJ and spine were available.
The investigators used a clinical examination and pelvic radiography to stratify patients into groups, with 50 found to have nr-axSpA, 33 with AS, and 47 with mechanical back pain.
Three separate researchers blinded to the initial stratification read the MRI of the SIJ. An MRI of the spine was then performed 6 months later, with a combined SIJ/spinal scan done 1-12 months later. The presence or absence of SpA was determined in these scans, and comparisons were made between the results for MRI of the SIJ alone versus spinal MRI alone, as well as for the SIJ alone versus a combined read of both the spinal and SIJ MRI scans.
Dr. Weber noted that he would not recommend changing current practice as a result of this study. Further data are eagerly awaited from an ongoing Danish initiative that hopes to scan and assess around 2,000 whole-body MRIs in patients with suspected spondyloarthropathy by the end of the year. "This study will be very informative and very important for us because this is a large sample size. Preliminary data on about 1,000 MRIs point in the same direction," he observed.
Other data from the study, which Dr. Weber presented separately at the meeting, looked at the frequency and possible reasons for false-positive results with spinal MRI in the control groups (Ann. Rheum. Dis. 2013;72:125).
"Patients with mechanical back pain and healthy volunteers may show spinal MRI lesions suggestive of spondyloarthritis, such as corner inflammatory lesions or corner fat lesions," he explained. "We found that about 30% of those controls were misclassified as having spondyloarthritis by evaluation of the spinal MRI alone, so without SIJ MRI," said Dr. Weber. Bone marrow edema and fat infiltration were the MRI lesions largely responsible for this misclassification.
Dr. Weber said that, at least in Switzerland, general practitioners were more likely to order a spinal MRI than an SIJ MRI to assess a young patient with nonspecific back pain. "We think that caution is needed if a classification of SpA is based on MRI of the spine alone," he concluded.
Dr. Weber had no disclosures.
MADRID – There is no added benefit of performing spinal MRI in the diagnosis of spondyloarthritis, the results of an international, multicenter study suggest.
Around one-quarter of patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had a negative MRI scan of the sacroiliac joints (SIJs) were reclassified as being positive for SpA by a combined evaluation of SIJ MRI and spinal MRI scans.
However, 17.5% of healthy volunteers and up to 26.8% of patients with mechanical back pain who had a negative SIJ MRI were also reclassified as having SpA. This false-positive result balances out the value of combined spinal and SIJ MRI.
"Combined MRI added little incremental value compared to SIJ MRI alone for diagnosis of nr-axSpA," said Dr. Ulrich Weber, who presented the findings at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72:145).
"Although you get about 20% more patients – which is the good news – we found about the same magnitude of false-positive controls," he said in an interview. He added that he "was very disappointed with this result, and these data need confirming." Dr. Weber collected data for the study while at the Balgrist University Clinic in Zurich, and also as a visiting professor in the rheumatology department at the University of Alberta, Edmonton.
SIJ MRI is a major criterion of the Assessment of SpondyloArthritis classification criteria for ankylosing spondylitis (AS). If a patient is strongly suspected of having early SpA, but this is not yet visible on radiographs, then an SIJ MRI is often the next step. If this is negative, however, it may be unclear what to do next.
"Our question was, ‘Would it help to order an additional spinal MRI in this situation?’ " Dr. Weber explained. These data suggest that it is not.
The collaborative study included 130 individuals with newly diagnosed back pain and aged 50 years or younger who were recruited from clinics based in Canada, China, Denmark, and Switzerland, as well as 20 healthy control individuals in whom MRI scans of the SIJ and spine were available.
The investigators used a clinical examination and pelvic radiography to stratify patients into groups, with 50 found to have nr-axSpA, 33 with AS, and 47 with mechanical back pain.
Three separate researchers blinded to the initial stratification read the MRI of the SIJ. An MRI of the spine was then performed 6 months later, with a combined SIJ/spinal scan done 1-12 months later. The presence or absence of SpA was determined in these scans, and comparisons were made between the results for MRI of the SIJ alone versus spinal MRI alone, as well as for the SIJ alone versus a combined read of both the spinal and SIJ MRI scans.
Dr. Weber noted that he would not recommend changing current practice as a result of this study. Further data are eagerly awaited from an ongoing Danish initiative that hopes to scan and assess around 2,000 whole-body MRIs in patients with suspected spondyloarthropathy by the end of the year. "This study will be very informative and very important for us because this is a large sample size. Preliminary data on about 1,000 MRIs point in the same direction," he observed.
Other data from the study, which Dr. Weber presented separately at the meeting, looked at the frequency and possible reasons for false-positive results with spinal MRI in the control groups (Ann. Rheum. Dis. 2013;72:125).
"Patients with mechanical back pain and healthy volunteers may show spinal MRI lesions suggestive of spondyloarthritis, such as corner inflammatory lesions or corner fat lesions," he explained. "We found that about 30% of those controls were misclassified as having spondyloarthritis by evaluation of the spinal MRI alone, so without SIJ MRI," said Dr. Weber. Bone marrow edema and fat infiltration were the MRI lesions largely responsible for this misclassification.
Dr. Weber said that, at least in Switzerland, general practitioners were more likely to order a spinal MRI than an SIJ MRI to assess a young patient with nonspecific back pain. "We think that caution is needed if a classification of SpA is based on MRI of the spine alone," he concluded.
Dr. Weber had no disclosures.
MADRID – There is no added benefit of performing spinal MRI in the diagnosis of spondyloarthritis, the results of an international, multicenter study suggest.
Around one-quarter of patients with nonradiographic axial spondyloarthritis (nr-axSpA) who had a negative MRI scan of the sacroiliac joints (SIJs) were reclassified as being positive for SpA by a combined evaluation of SIJ MRI and spinal MRI scans.
However, 17.5% of healthy volunteers and up to 26.8% of patients with mechanical back pain who had a negative SIJ MRI were also reclassified as having SpA. This false-positive result balances out the value of combined spinal and SIJ MRI.
"Combined MRI added little incremental value compared to SIJ MRI alone for diagnosis of nr-axSpA," said Dr. Ulrich Weber, who presented the findings at the annual European Congress of Rheumatology (Ann. Rheum. Dis. 2013;72:145).
"Although you get about 20% more patients – which is the good news – we found about the same magnitude of false-positive controls," he said in an interview. He added that he "was very disappointed with this result, and these data need confirming." Dr. Weber collected data for the study while at the Balgrist University Clinic in Zurich, and also as a visiting professor in the rheumatology department at the University of Alberta, Edmonton.
SIJ MRI is a major criterion of the Assessment of SpondyloArthritis classification criteria for ankylosing spondylitis (AS). If a patient is strongly suspected of having early SpA, but this is not yet visible on radiographs, then an SIJ MRI is often the next step. If this is negative, however, it may be unclear what to do next.
"Our question was, ‘Would it help to order an additional spinal MRI in this situation?’ " Dr. Weber explained. These data suggest that it is not.
The collaborative study included 130 individuals with newly diagnosed back pain and aged 50 years or younger who were recruited from clinics based in Canada, China, Denmark, and Switzerland, as well as 20 healthy control individuals in whom MRI scans of the SIJ and spine were available.
The investigators used a clinical examination and pelvic radiography to stratify patients into groups, with 50 found to have nr-axSpA, 33 with AS, and 47 with mechanical back pain.
Three separate researchers blinded to the initial stratification read the MRI of the SIJ. An MRI of the spine was then performed 6 months later, with a combined SIJ/spinal scan done 1-12 months later. The presence or absence of SpA was determined in these scans, and comparisons were made between the results for MRI of the SIJ alone versus spinal MRI alone, as well as for the SIJ alone versus a combined read of both the spinal and SIJ MRI scans.
Dr. Weber noted that he would not recommend changing current practice as a result of this study. Further data are eagerly awaited from an ongoing Danish initiative that hopes to scan and assess around 2,000 whole-body MRIs in patients with suspected spondyloarthropathy by the end of the year. "This study will be very informative and very important for us because this is a large sample size. Preliminary data on about 1,000 MRIs point in the same direction," he observed.
Other data from the study, which Dr. Weber presented separately at the meeting, looked at the frequency and possible reasons for false-positive results with spinal MRI in the control groups (Ann. Rheum. Dis. 2013;72:125).
"Patients with mechanical back pain and healthy volunteers may show spinal MRI lesions suggestive of spondyloarthritis, such as corner inflammatory lesions or corner fat lesions," he explained. "We found that about 30% of those controls were misclassified as having spondyloarthritis by evaluation of the spinal MRI alone, so without SIJ MRI," said Dr. Weber. Bone marrow edema and fat infiltration were the MRI lesions largely responsible for this misclassification.
Dr. Weber said that, at least in Switzerland, general practitioners were more likely to order a spinal MRI than an SIJ MRI to assess a young patient with nonspecific back pain. "We think that caution is needed if a classification of SpA is based on MRI of the spine alone," he concluded.
Dr. Weber had no disclosures.
AT THE EULAR CONGRESS 2013
Major finding: More than 25% of patients with nonradiographic axial spondyloarthritis who had a negative MRI scan of the sacroiliac joints (SIJs) were reclassified as being positive for spondyloarthritis by a combined evaluation of SIJ MRI and spinal MRI scans, but this was balanced by a similarly high rate of false-positive results.
Data source: An international, multicenter study of combined SIJ and spinal MRI in 130 patients with newly diagnosed back pain and 20 healthy controls.
Disclosures: Dr. Weber had no disclosures.
New spondyloarthropathy index measures patient-relevant outcomes
MADRID – An international team has developed a new composite health index specifically for use in patients with ankylosing spondylitis.
The Assessment of SpondyloArthritis International Society Health Index (ASAS HI) is based on the ICF (International Classification of Functioning, Disability and Health) and includes 17 dichotomous items that ask about patients’ levels of pain, emotional functioning, sleep habits, sexual function, mobility, self-care, life in the community, and employment. The ICF is a comprehensive and already well-recognized and validated means of classifying and describing functioning, disability, and health in a systematic way,
The tool has yet to be "field tested" to see if it can measure changes in health status in response to treatment, Dr. Uta Kiltz said at the annual European Congress of Rheumatology.
Dr. Kiltz, of Rheumazentrum Ruhrgebiet, Herne, Germany, noted that the development of the tool involved five key stages. These have been outlined previously (Rheumatology 2011;50:894-8) and included a preparatory stage in which potential items for inclusion were identified. Dr. Kiltz and her colleagues considered a total of 251 items obtained from more than 60 existing questionnaires, such as the BASFI (Bath Ankylosing Spondylitis Functional Index), the Dougados Functional Index, and the AS Quality of Life Questionnaire.
The investigators then conducted an international, cross-sectional study involving 1,915 patients with AS (mean age, 51 years). In this second phase, they sent a postal survey to patients to ask about various parameters. An expert committee then assessed the results in the third phase and selected 50 items for possible inclusion in the final model. The penultimate stage in the development process involved sending a second postal survey to 628 patients with AS (mean age, 48.5 years).
In the final stage, an expert consensus meeting was held in which the final 17-item tool was agreed upon (Ann. Rheum. Dis. 2013;72:124).
"ASAS HI is a new composite index that captures relevant information on the health status of patients with AS," Dr. Kiltz said. "It is the first disease-specific index which is based on the ICF, and the items represent a whole range of abilities as defined by the ICF."
ASAS HI could eventually be used in clinical trials and clinical practice as a new composite index that captures relevant information on the health status of patients, Dr. Kiltz suggested.
"We are now doing a field test to test the 17 items in a wider range of patients," she said. After this is completed, the specifics of the tool will be published.
Dr. Kiltz had no conflicts of interest.
MADRID – An international team has developed a new composite health index specifically for use in patients with ankylosing spondylitis.
The Assessment of SpondyloArthritis International Society Health Index (ASAS HI) is based on the ICF (International Classification of Functioning, Disability and Health) and includes 17 dichotomous items that ask about patients’ levels of pain, emotional functioning, sleep habits, sexual function, mobility, self-care, life in the community, and employment. The ICF is a comprehensive and already well-recognized and validated means of classifying and describing functioning, disability, and health in a systematic way,
The tool has yet to be "field tested" to see if it can measure changes in health status in response to treatment, Dr. Uta Kiltz said at the annual European Congress of Rheumatology.
Dr. Kiltz, of Rheumazentrum Ruhrgebiet, Herne, Germany, noted that the development of the tool involved five key stages. These have been outlined previously (Rheumatology 2011;50:894-8) and included a preparatory stage in which potential items for inclusion were identified. Dr. Kiltz and her colleagues considered a total of 251 items obtained from more than 60 existing questionnaires, such as the BASFI (Bath Ankylosing Spondylitis Functional Index), the Dougados Functional Index, and the AS Quality of Life Questionnaire.
The investigators then conducted an international, cross-sectional study involving 1,915 patients with AS (mean age, 51 years). In this second phase, they sent a postal survey to patients to ask about various parameters. An expert committee then assessed the results in the third phase and selected 50 items for possible inclusion in the final model. The penultimate stage in the development process involved sending a second postal survey to 628 patients with AS (mean age, 48.5 years).
In the final stage, an expert consensus meeting was held in which the final 17-item tool was agreed upon (Ann. Rheum. Dis. 2013;72:124).
"ASAS HI is a new composite index that captures relevant information on the health status of patients with AS," Dr. Kiltz said. "It is the first disease-specific index which is based on the ICF, and the items represent a whole range of abilities as defined by the ICF."
ASAS HI could eventually be used in clinical trials and clinical practice as a new composite index that captures relevant information on the health status of patients, Dr. Kiltz suggested.
"We are now doing a field test to test the 17 items in a wider range of patients," she said. After this is completed, the specifics of the tool will be published.
Dr. Kiltz had no conflicts of interest.
MADRID – An international team has developed a new composite health index specifically for use in patients with ankylosing spondylitis.
The Assessment of SpondyloArthritis International Society Health Index (ASAS HI) is based on the ICF (International Classification of Functioning, Disability and Health) and includes 17 dichotomous items that ask about patients’ levels of pain, emotional functioning, sleep habits, sexual function, mobility, self-care, life in the community, and employment. The ICF is a comprehensive and already well-recognized and validated means of classifying and describing functioning, disability, and health in a systematic way,
The tool has yet to be "field tested" to see if it can measure changes in health status in response to treatment, Dr. Uta Kiltz said at the annual European Congress of Rheumatology.
Dr. Kiltz, of Rheumazentrum Ruhrgebiet, Herne, Germany, noted that the development of the tool involved five key stages. These have been outlined previously (Rheumatology 2011;50:894-8) and included a preparatory stage in which potential items for inclusion were identified. Dr. Kiltz and her colleagues considered a total of 251 items obtained from more than 60 existing questionnaires, such as the BASFI (Bath Ankylosing Spondylitis Functional Index), the Dougados Functional Index, and the AS Quality of Life Questionnaire.
The investigators then conducted an international, cross-sectional study involving 1,915 patients with AS (mean age, 51 years). In this second phase, they sent a postal survey to patients to ask about various parameters. An expert committee then assessed the results in the third phase and selected 50 items for possible inclusion in the final model. The penultimate stage in the development process involved sending a second postal survey to 628 patients with AS (mean age, 48.5 years).
In the final stage, an expert consensus meeting was held in which the final 17-item tool was agreed upon (Ann. Rheum. Dis. 2013;72:124).
"ASAS HI is a new composite index that captures relevant information on the health status of patients with AS," Dr. Kiltz said. "It is the first disease-specific index which is based on the ICF, and the items represent a whole range of abilities as defined by the ICF."
ASAS HI could eventually be used in clinical trials and clinical practice as a new composite index that captures relevant information on the health status of patients, Dr. Kiltz suggested.
"We are now doing a field test to test the 17 items in a wider range of patients," she said. After this is completed, the specifics of the tool will be published.
Dr. Kiltz had no conflicts of interest.
AT THE EULAR CONGRESS 2013
High ankylosing spondylitis activity linked to cardiovascular risk
MADRID – High baseline disease activity and serum C-reactive protein levels may be a means of predicting which patients with spondyloarthropathy are likely to develop cardiovascular disease.
Both were linked to arterial stiffness, a surrogate marker for heart disease, in a 5-year follow-up study of 103 hospital-recruited patients with ankylosing spondylitis (Ann. Rheum. Dis 2013;72[Suppls3]:125).
"Reducing disease activity may [therefore] be a viable way of reducing excess cardiovascular disease [CVD] in ankylosing spondylitis [AS]," study investigator Dr. Inger Jorid Berg said at the annual European Congress of Rheumatology.
Baseline disease severity was measured with the ankylosing spondylitis disease activity score (ASDAS) and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, only ASDAS predicted the development of increased arterial stiffness from high baseline disease activity.
"Several studies have shown that patients with ankylosing spondylitis have [an] increased [risk] of cardiovascular disease," noted Dr. Berg, a consultant rheumatologist at Diakonhjemmet Hospital in Oslo. This includes atherosclerotic CVD, she observed, which previous research has linked to having a high ASDAS.
The present investigation explored whether high baseline ASDAS could be used to predict increased arterial stiffness as measured with the Augmentation Index (AIx). The investigators measured arterial stiffness using the SphygmoCor apparatus, a noninvasive system that involves placement of a probe at the radial artery.
Patients included in the study had AS confirmed via modified New York criteria and had undergone assessments in 2003 and again in 2008-2009. The assessments included clinical examinations and questionnaires to assess baseline disease severity and blood tests to measure C-reactive protein (CRP) levels and the erythrocyte sedimentation rate (ESR).
At the baseline assessment in 2003, the patients (56% men) had a mean age of 48 years, and a mean body mass index of 24.4 kg/m2. A quarter of the patients were smokers. Their mean ASDAS was 2.5 and their mean BASDAI was 4.1, indicating moderate disease activity. There were only a few known cardiovascular comorbidities present, which included hypertension (5%) and diabetes (3%), although there were more patients with comorbidities at the later assessment. Most (83%) patients were taking nonsteroidal antiinflammatory drugs. Another 17% were using disease-modifying antirheumatic drugs, and very few (2%) were using tumor necrosis factor inhibitors.
"There was a clear trend in increasing CRP values, ESR values, and ASDAS," Dr. Berg said. This was significant for CRP (P = .004) and ASDAS (P = .01), and borderline significant for ESR (P = .05).
Multivariate analysis showed that CRP and ASDAS were independent predictors of increasing AIx, with an odds ratio of 2.09 (P = .02) for the latter.
"The strengths of this study are its longitudinal design and a representative cohort reflecting a range of disease activity," Dr. Berg observed. "Limitations are the low number of patients and that there might be a selection bias when inviting patients to examinations." Traditional risk factors were also not recorded during the 2003 assessment, so the effect of these variables could not be evaluated.
What these data show, however, are that inflammation signaled by elevated CRP and high disease activity measured by ASDAS predict future arterial stiffness, indicating that both are risk factors of CVD in AS. As such, better control of both of these parameters might be a way to reduce risk for CVD in this patient population.
Dr. Berg did not have any conflicts of interest to disclose.
MADRID – High baseline disease activity and serum C-reactive protein levels may be a means of predicting which patients with spondyloarthropathy are likely to develop cardiovascular disease.
Both were linked to arterial stiffness, a surrogate marker for heart disease, in a 5-year follow-up study of 103 hospital-recruited patients with ankylosing spondylitis (Ann. Rheum. Dis 2013;72[Suppls3]:125).
"Reducing disease activity may [therefore] be a viable way of reducing excess cardiovascular disease [CVD] in ankylosing spondylitis [AS]," study investigator Dr. Inger Jorid Berg said at the annual European Congress of Rheumatology.
Baseline disease severity was measured with the ankylosing spondylitis disease activity score (ASDAS) and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, only ASDAS predicted the development of increased arterial stiffness from high baseline disease activity.
"Several studies have shown that patients with ankylosing spondylitis have [an] increased [risk] of cardiovascular disease," noted Dr. Berg, a consultant rheumatologist at Diakonhjemmet Hospital in Oslo. This includes atherosclerotic CVD, she observed, which previous research has linked to having a high ASDAS.
The present investigation explored whether high baseline ASDAS could be used to predict increased arterial stiffness as measured with the Augmentation Index (AIx). The investigators measured arterial stiffness using the SphygmoCor apparatus, a noninvasive system that involves placement of a probe at the radial artery.
Patients included in the study had AS confirmed via modified New York criteria and had undergone assessments in 2003 and again in 2008-2009. The assessments included clinical examinations and questionnaires to assess baseline disease severity and blood tests to measure C-reactive protein (CRP) levels and the erythrocyte sedimentation rate (ESR).
At the baseline assessment in 2003, the patients (56% men) had a mean age of 48 years, and a mean body mass index of 24.4 kg/m2. A quarter of the patients were smokers. Their mean ASDAS was 2.5 and their mean BASDAI was 4.1, indicating moderate disease activity. There were only a few known cardiovascular comorbidities present, which included hypertension (5%) and diabetes (3%), although there were more patients with comorbidities at the later assessment. Most (83%) patients were taking nonsteroidal antiinflammatory drugs. Another 17% were using disease-modifying antirheumatic drugs, and very few (2%) were using tumor necrosis factor inhibitors.
"There was a clear trend in increasing CRP values, ESR values, and ASDAS," Dr. Berg said. This was significant for CRP (P = .004) and ASDAS (P = .01), and borderline significant for ESR (P = .05).
Multivariate analysis showed that CRP and ASDAS were independent predictors of increasing AIx, with an odds ratio of 2.09 (P = .02) for the latter.
"The strengths of this study are its longitudinal design and a representative cohort reflecting a range of disease activity," Dr. Berg observed. "Limitations are the low number of patients and that there might be a selection bias when inviting patients to examinations." Traditional risk factors were also not recorded during the 2003 assessment, so the effect of these variables could not be evaluated.
What these data show, however, are that inflammation signaled by elevated CRP and high disease activity measured by ASDAS predict future arterial stiffness, indicating that both are risk factors of CVD in AS. As such, better control of both of these parameters might be a way to reduce risk for CVD in this patient population.
Dr. Berg did not have any conflicts of interest to disclose.
MADRID – High baseline disease activity and serum C-reactive protein levels may be a means of predicting which patients with spondyloarthropathy are likely to develop cardiovascular disease.
Both were linked to arterial stiffness, a surrogate marker for heart disease, in a 5-year follow-up study of 103 hospital-recruited patients with ankylosing spondylitis (Ann. Rheum. Dis 2013;72[Suppls3]:125).
"Reducing disease activity may [therefore] be a viable way of reducing excess cardiovascular disease [CVD] in ankylosing spondylitis [AS]," study investigator Dr. Inger Jorid Berg said at the annual European Congress of Rheumatology.
Baseline disease severity was measured with the ankylosing spondylitis disease activity score (ASDAS) and the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI). However, only ASDAS predicted the development of increased arterial stiffness from high baseline disease activity.
"Several studies have shown that patients with ankylosing spondylitis have [an] increased [risk] of cardiovascular disease," noted Dr. Berg, a consultant rheumatologist at Diakonhjemmet Hospital in Oslo. This includes atherosclerotic CVD, she observed, which previous research has linked to having a high ASDAS.
The present investigation explored whether high baseline ASDAS could be used to predict increased arterial stiffness as measured with the Augmentation Index (AIx). The investigators measured arterial stiffness using the SphygmoCor apparatus, a noninvasive system that involves placement of a probe at the radial artery.
Patients included in the study had AS confirmed via modified New York criteria and had undergone assessments in 2003 and again in 2008-2009. The assessments included clinical examinations and questionnaires to assess baseline disease severity and blood tests to measure C-reactive protein (CRP) levels and the erythrocyte sedimentation rate (ESR).
At the baseline assessment in 2003, the patients (56% men) had a mean age of 48 years, and a mean body mass index of 24.4 kg/m2. A quarter of the patients were smokers. Their mean ASDAS was 2.5 and their mean BASDAI was 4.1, indicating moderate disease activity. There were only a few known cardiovascular comorbidities present, which included hypertension (5%) and diabetes (3%), although there were more patients with comorbidities at the later assessment. Most (83%) patients were taking nonsteroidal antiinflammatory drugs. Another 17% were using disease-modifying antirheumatic drugs, and very few (2%) were using tumor necrosis factor inhibitors.
"There was a clear trend in increasing CRP values, ESR values, and ASDAS," Dr. Berg said. This was significant for CRP (P = .004) and ASDAS (P = .01), and borderline significant for ESR (P = .05).
Multivariate analysis showed that CRP and ASDAS were independent predictors of increasing AIx, with an odds ratio of 2.09 (P = .02) for the latter.
"The strengths of this study are its longitudinal design and a representative cohort reflecting a range of disease activity," Dr. Berg observed. "Limitations are the low number of patients and that there might be a selection bias when inviting patients to examinations." Traditional risk factors were also not recorded during the 2003 assessment, so the effect of these variables could not be evaluated.
What these data show, however, are that inflammation signaled by elevated CRP and high disease activity measured by ASDAS predict future arterial stiffness, indicating that both are risk factors of CVD in AS. As such, better control of both of these parameters might be a way to reduce risk for CVD in this patient population.
Dr. Berg did not have any conflicts of interest to disclose.
AT THE EULAR CONGRESS 2013
Evidence grows for TNF inhibitors in spondyloarthritis
MADRID – Tumor necrosis factor inhibitors are further solidifying their position as the go-to drug class for patients with spondyloarthritis who fail to adequately respond to treatment with nonsteroidal anti-inflammatory drugs.
Results from a series of reports at the annual European Congress of Rheumatology gave further support for the safety and efficacy of tumor necrosis factor (TNF) inhibitors for treating axial spondyloarthritis (SpA), and another report at the meeting provided some of the first evidence for efficacy of the TNF inhibitor class in patients with the less-studied variant, peripheral SpA.
TNF inhibitors "work well for symptoms, and are the gold standard for treating active axial SpA," said Dr. Philip J. Mease, a rheumatologist at Swedish Medical Center in Seattle. He reported evidence for the efficacy of a TNF inhibitor in patients with peripheral SpA without psoriatic involvement, a form of SpA that he said is increasingly being diagnosed after it was first defined a few years ago. The study that Dr. Mease reported on was the first to use the diagnostic criteria for peripheral SpA published by the Assessment of Spondyloarthritis International Society (ASAS) in 2011 (Ann. Rheum. Dis. 2011;70:25-31). Although several TNF inhibitors now have labeling for treating axial SpA and psoriatic arthritis, none currently have U.S. approval for treating peripheral SpA.
The ABILITY-2 (Study of Adalimumab in Subjects With Peripheral Spondyloarthritis) study enrolled patients in the United States, Canada, and several European countries. Patients either had an inadequate response to at least two different nonsteroidal anti-inflammatory drugs (NSAIDs) or were intolerant of or had contraindications for these drugs. Study participants received either 40 mg of adalimumab (Humira) subcutaneously every other week or placebo for 12 weeks.
The study’s primary endpoint was the percentage of patients achieving the peripheral SpA response criteria 40 at 12 weeks, a composite endpoint that requires at least a 40% improvement on each of three measures: patient global assessment of disease activity; patient global assessment of disease pain; and swollen and tender joint count, enthesitis count, or dactylitis count.
The rate of patients fulfilling the primary endpoint was 39% in 84 patients treated with adalimumab and 20% in 81 patients on placebo, a significant difference. Treatment with adalimumab also was linked to "substantial" and statistically significant improvements after 12 weeks in physical function, health-related quality of life, and work productivity, Dr. Mease reported.
Reports on using TNF inhibitors to treat axial SpA at the congress included results from the first randomized, controlled, phase III trial of a TNF inhibitor to enroll patients from the full range of axial SpA, including roughly equal numbers of patients with ankylosing spondylitis and patients diagnosed with axial SpA but without radiographic changes. The phase III RAPID-axSpA (Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Evaluate Efficacy and Safety of Certolizumab Pegol in Subjects with Active Axial Spondyloarthritis) trial included 325 patients enrolled at 104 sites in the United States and several other countries. The study enrolled patients who had an elevated blood level of C-reactive protein, evidence of sacroiliitis on an MRI scan, or both, and had failed to adequately respond to treatment with at least one NSAID.
Researchers randomized patients to receive either 200 mg of certolizumab pegol (Cimzia) subcutaneously every 2 weeks, 400 mg of certolizumab pegol subcutaneously every 4 weeks, or placebo. All patients randomized to receive certolizumab pegol began with three subcutaneous loading doses of 400 mg administered at the study’s start and after 2 and 4 weeks. Currently, certolizumab pegol has no labeling for treating patients with axial SpA, unlike several other TNF inhibitors such as adalimumab and etanercept (Enbrel).
The study’s primary endpoint was the percentage of patients achieving an ASAS 20 response after 12 weeks of treatment, which requires at least a 20% improvement in at least three of these four criteria: patient global assessment, spinal pain assessment, function, and inflammation. This endpoint was reached by 38% of the 107 placebo patients, 58% of the 111 patients who received certolizumab pegol every 2 weeks, and 64% of those who received certolizumab pegol every 4 weeks, showing statistically significant differences in favor of the active treatment, reported Dr. Robert B.M. Landewé at the congress.
Response rates were similar among the patients with ankylosing spondylitis and those with no radiographic pathology. After 24 weeks of treatment, the rate of ASAS 20 responders fell to 29% of the placebo patients, compared with increases to 67% of patients receiving certolizumab pegol every 2 weeks and to 70% in those getting the drug every 4 weeks.
Dr. Landewé, who is a professor of rheumatology at the Academic Medical Center in Amsterdam, also presented results for several other secondary measures of response. One of these, the Ankylosing Spondylitis Disease Activity Score (ASDAS), showed that inactive disease developed after 24 weeks of treatment in 4% of the placebo-treated patients, 30% of the patients who received certolizumab pegol every 2 weeks, and 31% of patients who received the drug every 4 weeks. The results also showed no new signals of adverse effects, compared with several prior pivotal trials of certolizumab pegol.
Another set of measures in the same study focused on the impact of 24 weeks of treatment on work and household productivity and participation in social activities. Among the 69% of patients in the study who were employed, treatment with either dosage of certolizumab pegol was associated with an average of 10 more productive days of paid work per patient, compared with placebo, reported Dr. Désirée van der Heijde, professor of rheumatology at Leiden University in the Netherlands. During the 24 weeks of treatment, the active regimens also resulted in an added 13-17 days of productive household work and an average of about 10 added days of social or leisure activities, compared with placebo-treated patients.
Results from a third study reported at the meeting included outcomes from patients with axial SpA and objective evidence of inflammation at entry who remained on treatment with adalimumab during 2 years of follow-up in the ABILITY-1 study. This trial’s primary-endpoint results, which were recently published (Ann. Rheum. Dis. 2013;72:815-22), showed that 40 mg of adalimumab administered every other week was significantly better than placebo for reducing disease activity after 12 weeks of treatment. The new results came from 107 patients who remained in the study and received 104 weeks of adalimumab treatment.
After 2 years, 66% of patients showed ASAS 40 responses, and 44% had inactive disease based on their ASDAS, reported Dr. Joachim Sieper, professor and chief of rheumatology at Charité University Hospital in Berlin. Most of the patients in remission at 104 weeks had also been in remission after 52 and 80 weeks of treatment. In addition, the 2-year data showed no new safety concerns, compared with several other prior reports of long-term treatment with adalimumab, he said.
The ABILITY-1 and ABILITY-2 trials were sponsored by AbbVie, which markets adalimumab. Dr. Mease has been a consultant to and has received research support from AbbVie and other companies. Dr. Sieper has been a consultant to and has received research support from Abbott (from which AbbVie was created) as well as Merck, Pfizer, and UCB. The RAPID-axSpA trial was sponsored by UCB, which markets certolizumab. Dr. Landewé has been a consultant to and has received research support from UCB and other companies. Dr. van der Heijde has been a consultant to and has received grant support from UCB and other companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Tumor necrosis factor inhibitors are further solidifying their position as the go-to drug class for patients with spondyloarthritis who fail to adequately respond to treatment with nonsteroidal anti-inflammatory drugs.
Results from a series of reports at the annual European Congress of Rheumatology gave further support for the safety and efficacy of tumor necrosis factor (TNF) inhibitors for treating axial spondyloarthritis (SpA), and another report at the meeting provided some of the first evidence for efficacy of the TNF inhibitor class in patients with the less-studied variant, peripheral SpA.
TNF inhibitors "work well for symptoms, and are the gold standard for treating active axial SpA," said Dr. Philip J. Mease, a rheumatologist at Swedish Medical Center in Seattle. He reported evidence for the efficacy of a TNF inhibitor in patients with peripheral SpA without psoriatic involvement, a form of SpA that he said is increasingly being diagnosed after it was first defined a few years ago. The study that Dr. Mease reported on was the first to use the diagnostic criteria for peripheral SpA published by the Assessment of Spondyloarthritis International Society (ASAS) in 2011 (Ann. Rheum. Dis. 2011;70:25-31). Although several TNF inhibitors now have labeling for treating axial SpA and psoriatic arthritis, none currently have U.S. approval for treating peripheral SpA.
The ABILITY-2 (Study of Adalimumab in Subjects With Peripheral Spondyloarthritis) study enrolled patients in the United States, Canada, and several European countries. Patients either had an inadequate response to at least two different nonsteroidal anti-inflammatory drugs (NSAIDs) or were intolerant of or had contraindications for these drugs. Study participants received either 40 mg of adalimumab (Humira) subcutaneously every other week or placebo for 12 weeks.
The study’s primary endpoint was the percentage of patients achieving the peripheral SpA response criteria 40 at 12 weeks, a composite endpoint that requires at least a 40% improvement on each of three measures: patient global assessment of disease activity; patient global assessment of disease pain; and swollen and tender joint count, enthesitis count, or dactylitis count.
The rate of patients fulfilling the primary endpoint was 39% in 84 patients treated with adalimumab and 20% in 81 patients on placebo, a significant difference. Treatment with adalimumab also was linked to "substantial" and statistically significant improvements after 12 weeks in physical function, health-related quality of life, and work productivity, Dr. Mease reported.
Reports on using TNF inhibitors to treat axial SpA at the congress included results from the first randomized, controlled, phase III trial of a TNF inhibitor to enroll patients from the full range of axial SpA, including roughly equal numbers of patients with ankylosing spondylitis and patients diagnosed with axial SpA but without radiographic changes. The phase III RAPID-axSpA (Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Evaluate Efficacy and Safety of Certolizumab Pegol in Subjects with Active Axial Spondyloarthritis) trial included 325 patients enrolled at 104 sites in the United States and several other countries. The study enrolled patients who had an elevated blood level of C-reactive protein, evidence of sacroiliitis on an MRI scan, or both, and had failed to adequately respond to treatment with at least one NSAID.
Researchers randomized patients to receive either 200 mg of certolizumab pegol (Cimzia) subcutaneously every 2 weeks, 400 mg of certolizumab pegol subcutaneously every 4 weeks, or placebo. All patients randomized to receive certolizumab pegol began with three subcutaneous loading doses of 400 mg administered at the study’s start and after 2 and 4 weeks. Currently, certolizumab pegol has no labeling for treating patients with axial SpA, unlike several other TNF inhibitors such as adalimumab and etanercept (Enbrel).
The study’s primary endpoint was the percentage of patients achieving an ASAS 20 response after 12 weeks of treatment, which requires at least a 20% improvement in at least three of these four criteria: patient global assessment, spinal pain assessment, function, and inflammation. This endpoint was reached by 38% of the 107 placebo patients, 58% of the 111 patients who received certolizumab pegol every 2 weeks, and 64% of those who received certolizumab pegol every 4 weeks, showing statistically significant differences in favor of the active treatment, reported Dr. Robert B.M. Landewé at the congress.
Response rates were similar among the patients with ankylosing spondylitis and those with no radiographic pathology. After 24 weeks of treatment, the rate of ASAS 20 responders fell to 29% of the placebo patients, compared with increases to 67% of patients receiving certolizumab pegol every 2 weeks and to 70% in those getting the drug every 4 weeks.
Dr. Landewé, who is a professor of rheumatology at the Academic Medical Center in Amsterdam, also presented results for several other secondary measures of response. One of these, the Ankylosing Spondylitis Disease Activity Score (ASDAS), showed that inactive disease developed after 24 weeks of treatment in 4% of the placebo-treated patients, 30% of the patients who received certolizumab pegol every 2 weeks, and 31% of patients who received the drug every 4 weeks. The results also showed no new signals of adverse effects, compared with several prior pivotal trials of certolizumab pegol.
Another set of measures in the same study focused on the impact of 24 weeks of treatment on work and household productivity and participation in social activities. Among the 69% of patients in the study who were employed, treatment with either dosage of certolizumab pegol was associated with an average of 10 more productive days of paid work per patient, compared with placebo, reported Dr. Désirée van der Heijde, professor of rheumatology at Leiden University in the Netherlands. During the 24 weeks of treatment, the active regimens also resulted in an added 13-17 days of productive household work and an average of about 10 added days of social or leisure activities, compared with placebo-treated patients.
Results from a third study reported at the meeting included outcomes from patients with axial SpA and objective evidence of inflammation at entry who remained on treatment with adalimumab during 2 years of follow-up in the ABILITY-1 study. This trial’s primary-endpoint results, which were recently published (Ann. Rheum. Dis. 2013;72:815-22), showed that 40 mg of adalimumab administered every other week was significantly better than placebo for reducing disease activity after 12 weeks of treatment. The new results came from 107 patients who remained in the study and received 104 weeks of adalimumab treatment.
After 2 years, 66% of patients showed ASAS 40 responses, and 44% had inactive disease based on their ASDAS, reported Dr. Joachim Sieper, professor and chief of rheumatology at Charité University Hospital in Berlin. Most of the patients in remission at 104 weeks had also been in remission after 52 and 80 weeks of treatment. In addition, the 2-year data showed no new safety concerns, compared with several other prior reports of long-term treatment with adalimumab, he said.
The ABILITY-1 and ABILITY-2 trials were sponsored by AbbVie, which markets adalimumab. Dr. Mease has been a consultant to and has received research support from AbbVie and other companies. Dr. Sieper has been a consultant to and has received research support from Abbott (from which AbbVie was created) as well as Merck, Pfizer, and UCB. The RAPID-axSpA trial was sponsored by UCB, which markets certolizumab. Dr. Landewé has been a consultant to and has received research support from UCB and other companies. Dr. van der Heijde has been a consultant to and has received grant support from UCB and other companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
MADRID – Tumor necrosis factor inhibitors are further solidifying their position as the go-to drug class for patients with spondyloarthritis who fail to adequately respond to treatment with nonsteroidal anti-inflammatory drugs.
Results from a series of reports at the annual European Congress of Rheumatology gave further support for the safety and efficacy of tumor necrosis factor (TNF) inhibitors for treating axial spondyloarthritis (SpA), and another report at the meeting provided some of the first evidence for efficacy of the TNF inhibitor class in patients with the less-studied variant, peripheral SpA.
TNF inhibitors "work well for symptoms, and are the gold standard for treating active axial SpA," said Dr. Philip J. Mease, a rheumatologist at Swedish Medical Center in Seattle. He reported evidence for the efficacy of a TNF inhibitor in patients with peripheral SpA without psoriatic involvement, a form of SpA that he said is increasingly being diagnosed after it was first defined a few years ago. The study that Dr. Mease reported on was the first to use the diagnostic criteria for peripheral SpA published by the Assessment of Spondyloarthritis International Society (ASAS) in 2011 (Ann. Rheum. Dis. 2011;70:25-31). Although several TNF inhibitors now have labeling for treating axial SpA and psoriatic arthritis, none currently have U.S. approval for treating peripheral SpA.
The ABILITY-2 (Study of Adalimumab in Subjects With Peripheral Spondyloarthritis) study enrolled patients in the United States, Canada, and several European countries. Patients either had an inadequate response to at least two different nonsteroidal anti-inflammatory drugs (NSAIDs) or were intolerant of or had contraindications for these drugs. Study participants received either 40 mg of adalimumab (Humira) subcutaneously every other week or placebo for 12 weeks.
The study’s primary endpoint was the percentage of patients achieving the peripheral SpA response criteria 40 at 12 weeks, a composite endpoint that requires at least a 40% improvement on each of three measures: patient global assessment of disease activity; patient global assessment of disease pain; and swollen and tender joint count, enthesitis count, or dactylitis count.
The rate of patients fulfilling the primary endpoint was 39% in 84 patients treated with adalimumab and 20% in 81 patients on placebo, a significant difference. Treatment with adalimumab also was linked to "substantial" and statistically significant improvements after 12 weeks in physical function, health-related quality of life, and work productivity, Dr. Mease reported.
Reports on using TNF inhibitors to treat axial SpA at the congress included results from the first randomized, controlled, phase III trial of a TNF inhibitor to enroll patients from the full range of axial SpA, including roughly equal numbers of patients with ankylosing spondylitis and patients diagnosed with axial SpA but without radiographic changes. The phase III RAPID-axSpA (Multicenter, Randomized, Double-Blind, Placebo-Controlled Study to Evaluate Efficacy and Safety of Certolizumab Pegol in Subjects with Active Axial Spondyloarthritis) trial included 325 patients enrolled at 104 sites in the United States and several other countries. The study enrolled patients who had an elevated blood level of C-reactive protein, evidence of sacroiliitis on an MRI scan, or both, and had failed to adequately respond to treatment with at least one NSAID.
Researchers randomized patients to receive either 200 mg of certolizumab pegol (Cimzia) subcutaneously every 2 weeks, 400 mg of certolizumab pegol subcutaneously every 4 weeks, or placebo. All patients randomized to receive certolizumab pegol began with three subcutaneous loading doses of 400 mg administered at the study’s start and after 2 and 4 weeks. Currently, certolizumab pegol has no labeling for treating patients with axial SpA, unlike several other TNF inhibitors such as adalimumab and etanercept (Enbrel).
The study’s primary endpoint was the percentage of patients achieving an ASAS 20 response after 12 weeks of treatment, which requires at least a 20% improvement in at least three of these four criteria: patient global assessment, spinal pain assessment, function, and inflammation. This endpoint was reached by 38% of the 107 placebo patients, 58% of the 111 patients who received certolizumab pegol every 2 weeks, and 64% of those who received certolizumab pegol every 4 weeks, showing statistically significant differences in favor of the active treatment, reported Dr. Robert B.M. Landewé at the congress.
Response rates were similar among the patients with ankylosing spondylitis and those with no radiographic pathology. After 24 weeks of treatment, the rate of ASAS 20 responders fell to 29% of the placebo patients, compared with increases to 67% of patients receiving certolizumab pegol every 2 weeks and to 70% in those getting the drug every 4 weeks.
Dr. Landewé, who is a professor of rheumatology at the Academic Medical Center in Amsterdam, also presented results for several other secondary measures of response. One of these, the Ankylosing Spondylitis Disease Activity Score (ASDAS), showed that inactive disease developed after 24 weeks of treatment in 4% of the placebo-treated patients, 30% of the patients who received certolizumab pegol every 2 weeks, and 31% of patients who received the drug every 4 weeks. The results also showed no new signals of adverse effects, compared with several prior pivotal trials of certolizumab pegol.
Another set of measures in the same study focused on the impact of 24 weeks of treatment on work and household productivity and participation in social activities. Among the 69% of patients in the study who were employed, treatment with either dosage of certolizumab pegol was associated with an average of 10 more productive days of paid work per patient, compared with placebo, reported Dr. Désirée van der Heijde, professor of rheumatology at Leiden University in the Netherlands. During the 24 weeks of treatment, the active regimens also resulted in an added 13-17 days of productive household work and an average of about 10 added days of social or leisure activities, compared with placebo-treated patients.
Results from a third study reported at the meeting included outcomes from patients with axial SpA and objective evidence of inflammation at entry who remained on treatment with adalimumab during 2 years of follow-up in the ABILITY-1 study. This trial’s primary-endpoint results, which were recently published (Ann. Rheum. Dis. 2013;72:815-22), showed that 40 mg of adalimumab administered every other week was significantly better than placebo for reducing disease activity after 12 weeks of treatment. The new results came from 107 patients who remained in the study and received 104 weeks of adalimumab treatment.
After 2 years, 66% of patients showed ASAS 40 responses, and 44% had inactive disease based on their ASDAS, reported Dr. Joachim Sieper, professor and chief of rheumatology at Charité University Hospital in Berlin. Most of the patients in remission at 104 weeks had also been in remission after 52 and 80 weeks of treatment. In addition, the 2-year data showed no new safety concerns, compared with several other prior reports of long-term treatment with adalimumab, he said.
The ABILITY-1 and ABILITY-2 trials were sponsored by AbbVie, which markets adalimumab. Dr. Mease has been a consultant to and has received research support from AbbVie and other companies. Dr. Sieper has been a consultant to and has received research support from Abbott (from which AbbVie was created) as well as Merck, Pfizer, and UCB. The RAPID-axSpA trial was sponsored by UCB, which markets certolizumab. Dr. Landewé has been a consultant to and has received research support from UCB and other companies. Dr. van der Heijde has been a consultant to and has received grant support from UCB and other companies.
mzoler@frontlinemedcom.com
On Twitter @mitchelzoler
AT THE EULAR CONGRESS 2013
Improved definition boosts peripheral spondyloarthritis diagnoses
Spondyloarthritis became, in 2009, a much better defined disease, and partly as a result it is something that physicians increasingly see the more they look for it. That’s especially true for peripheral spondyloarthritis, historically ill defined and rarely diagnosed.
The prevalence of recognized cases of peripheral spondyloarthritis (SpA) and its more common sister disease axial SpA began rising when the Assessment of Spondyloarthritis International Society released new criteria in 2009 for diagnosing both axial and peripheral SpA. The consequence of the new peripheral SpA definitions has been increased diagnostic awareness over the ensuing 4 years.
"The nonaxial, nonpsoriatic peripheral SpA population is unique, and we increasingly find these patients as we have started to look for them," Seattle rheumatologist Dr. Philip Mease told me in June at the annual European Congress of Rheumatology in Madrid.
These patients often are initially misdiagnosed and unrecognized as peripheral SpA cases with presumed "fibromyalgia or nonspecific aches and pains" under the care of an orthopedist, physiatrist, or primary care physician. But more recently such patients "are starting to surface with evidence of elevated CRP [C-reactive protein] and inflammatory symptoms," including morning stiffness, back pain, and symptoms at the peripheral entheses that start at a relatively young age. Dr. Mease suggested that these "entry point" clinicians be on the lookout for "puzzlingly persistent pain in peripheral joint or tendon-insertion sites," along with subtle clues like an old episode of uveitis or a family history of psoriasis, all signals of a possible case of peripheral SpA. On further examination, patients with symptoms such as persistent Achilles tendonitis show elevated CRP levels, and an "MRI scan that lights up where the Achilles tendon inserts."
Dr. Mease told me that he sees growing awareness among primary care clinicians in the community about these symptoms and the fact that they flag an inflammatory, rheumatologic process that’s best managed by anti-inflammatory treatments, such as tumor necrosis factor inhibitors and newer drugs now receiving approval for rheumatic diseases.
"There is such a rising tide of interest in SpA in general," he said, a tide traceable back to the landmark definitions of 2009.
–By Mitchel L. Zoler
On Twitter @mitchelzoler
Spondyloarthritis became, in 2009, a much better defined disease, and partly as a result it is something that physicians increasingly see the more they look for it. That’s especially true for peripheral spondyloarthritis, historically ill defined and rarely diagnosed.
The prevalence of recognized cases of peripheral spondyloarthritis (SpA) and its more common sister disease axial SpA began rising when the Assessment of Spondyloarthritis International Society released new criteria in 2009 for diagnosing both axial and peripheral SpA. The consequence of the new peripheral SpA definitions has been increased diagnostic awareness over the ensuing 4 years.
"The nonaxial, nonpsoriatic peripheral SpA population is unique, and we increasingly find these patients as we have started to look for them," Seattle rheumatologist Dr. Philip Mease told me in June at the annual European Congress of Rheumatology in Madrid.
These patients often are initially misdiagnosed and unrecognized as peripheral SpA cases with presumed "fibromyalgia or nonspecific aches and pains" under the care of an orthopedist, physiatrist, or primary care physician. But more recently such patients "are starting to surface with evidence of elevated CRP [C-reactive protein] and inflammatory symptoms," including morning stiffness, back pain, and symptoms at the peripheral entheses that start at a relatively young age. Dr. Mease suggested that these "entry point" clinicians be on the lookout for "puzzlingly persistent pain in peripheral joint or tendon-insertion sites," along with subtle clues like an old episode of uveitis or a family history of psoriasis, all signals of a possible case of peripheral SpA. On further examination, patients with symptoms such as persistent Achilles tendonitis show elevated CRP levels, and an "MRI scan that lights up where the Achilles tendon inserts."
Dr. Mease told me that he sees growing awareness among primary care clinicians in the community about these symptoms and the fact that they flag an inflammatory, rheumatologic process that’s best managed by anti-inflammatory treatments, such as tumor necrosis factor inhibitors and newer drugs now receiving approval for rheumatic diseases.
"There is such a rising tide of interest in SpA in general," he said, a tide traceable back to the landmark definitions of 2009.
–By Mitchel L. Zoler
On Twitter @mitchelzoler
Spondyloarthritis became, in 2009, a much better defined disease, and partly as a result it is something that physicians increasingly see the more they look for it. That’s especially true for peripheral spondyloarthritis, historically ill defined and rarely diagnosed.
The prevalence of recognized cases of peripheral spondyloarthritis (SpA) and its more common sister disease axial SpA began rising when the Assessment of Spondyloarthritis International Society released new criteria in 2009 for diagnosing both axial and peripheral SpA. The consequence of the new peripheral SpA definitions has been increased diagnostic awareness over the ensuing 4 years.
"The nonaxial, nonpsoriatic peripheral SpA population is unique, and we increasingly find these patients as we have started to look for them," Seattle rheumatologist Dr. Philip Mease told me in June at the annual European Congress of Rheumatology in Madrid.
These patients often are initially misdiagnosed and unrecognized as peripheral SpA cases with presumed "fibromyalgia or nonspecific aches and pains" under the care of an orthopedist, physiatrist, or primary care physician. But more recently such patients "are starting to surface with evidence of elevated CRP [C-reactive protein] and inflammatory symptoms," including morning stiffness, back pain, and symptoms at the peripheral entheses that start at a relatively young age. Dr. Mease suggested that these "entry point" clinicians be on the lookout for "puzzlingly persistent pain in peripheral joint or tendon-insertion sites," along with subtle clues like an old episode of uveitis or a family history of psoriasis, all signals of a possible case of peripheral SpA. On further examination, patients with symptoms such as persistent Achilles tendonitis show elevated CRP levels, and an "MRI scan that lights up where the Achilles tendon inserts."
Dr. Mease told me that he sees growing awareness among primary care clinicians in the community about these symptoms and the fact that they flag an inflammatory, rheumatologic process that’s best managed by anti-inflammatory treatments, such as tumor necrosis factor inhibitors and newer drugs now receiving approval for rheumatic diseases.
"There is such a rising tide of interest in SpA in general," he said, a tide traceable back to the landmark definitions of 2009.
–By Mitchel L. Zoler
On Twitter @mitchelzoler
Apremilast effects sustained at 1 year in psoriatic arthritis
MADRID – Apremilast improves the signs and symptoms of psoriatic arthritis in about 60% of patients at 1 year, according to long-term data from the PALACE 1 trial.
At week 52, a 20% improvement in disease symptoms according to American College of Rheumatology (ACR 20) response criteria was achieved by 57%-63% of patients treated with apremilast, providing evidence of sustained treatment effects.
The PALACE 1 trial’s primary endpoint of an ACR 20 at 16 weeks, already reported last year, was achieved by 31% of patients treated with apremilast 20 mg and 40% of those given apremilast 30 mg, compared with 19% of those given placebo.
"Oral apremilast demonstrated long-term efficacy, including improvement in signs and symptoms and physical function, and skin manifestations," Dr. Arthur Kavanaugh, professor of medicine at the University of California, San Diego, said at the annual European Congress of Rheumatology.
Apremilast is an oral phosphodiesterase 4 inhibitor under investigation as a treatment for active psoriatic arthritis (PsA). It is being evaluated as a possible treatment for skin psoriasis, ankylosing spondylitis, rheumatoid arthritis, and Behçet’s disease.
PALACE 1 was a phase III, multicenter, double-blind, placebo-controlled study of apremilast for the treatment of active PsA. A total of 504 patients with a documented diagnosis of PsA for at least 6 months were recruited into the study (Ann. Rheum. Dis. 2013;72[Suppls3]:163).
Functional outcomes improved
Physical function improved according to measurements on the Health Assessment Questionnaire–Disability Index (HAQ-DI). At baseline, HAQ-DI scores were 1.21, and "we saw that patients improved by –0.35, which is certainly the level that patients can say, ‘I feel better and I can do my daily activities better,’ " Dr. Kavanaugh said.
Additionally, 25% and 37% of patients treated with apremilast 20 mg and 30 mg, respectively, achieved a 75% improvement in the Psoriasis Area and Severity Index at 52 weeks, which is a "very high bar" to achieve, he noted.
The main side effect seen was diarrhea, affecting 11%-19% of patients given apremilast and 2.4% given placebo. However, diarrhea occurred mainly in the first 6 months of therapy and could be managed by taking appropriate measures on an individual patient basis, Dr. Kavanaugh said. This might include prescription of an antidiarrheal agent.
"Prolonged exposure to apremilast did not result in any unexpected increased incidence of adverse events or laboratory abnormalities," he noted. The latter could mean that, if approved, apremilast might not need routine laboratory monitoring.
The PALACE development program
PALACE 1 is one of several clinical trials that have investigated the efficacy and safety of apremilast in active PsA. In these studies, 24 weeks’ treatment with one of two oral doses (20 mg or 30 mg twice daily) of apremilast was compared to placebo. The primary endpoint of the studies was the percentage of patients achieving ACR 20 at 16 weeks.
For inclusion in the trials, patients had to have active disease despite prior therapy with disease-modifying antirheumatic drugs (DMARDs), biologic agents, or both. Dr. Kavanaugh noted that the majority of patients had failed DMARD therapy in PALACE 1, with almost one-quarter receiving prior biologic therapy.
Patients who had a less than 20% reduction from baseline in swollen/tender joint counts at 16 weeks were re-randomized to receive apremilast 20 mg or 30 mg if they had originally been treated with placebo, while patients originally randomized to active treatment stayed on their initial dose if they failed to respond significantly. At the end of the planned 24-week treatment period, all remaining patients on placebo were re-randomized to apremilast 20 mg or 30 mg until 1 year of follow up.
PALACE 3 data also reported
The results of PALACE 3 and combined 6-month safety data from the PALACE 1, PALACE 2, and PALACE 3 trials were also reported at the congress.
In PALACE 3 (Ann. Rheum. Dis. 2013;72[Suppl. 3]:685), significantly more patients achieved the primary endpoint of an ACR 20 at 16 weeks if they were treated with either the 20-mg dose (29.4%, P = .02) or 30-mg dose (42.8%, P less than .0001) of apremilast, compared with those given placebo (18.9%). There was also statistically significant and "clinically meaningful" improvement in physical function and pain. "The results of PALACE 3 support the efficacy and safety findings of the PALACE 1 study and help establish the profile of apremilast in PsA," the PALACE 3 investigators concluded.
The pooled safety findings revealed no new safety concerns and showed apremilast was generally well tolerated (Ann. Rheum. Dis. 2013;72[Suppl. 3]:85). Rates of diarrhea at 24 weeks were 12.6% and 16.5% for the 20-mg and 30-mg doses of apremilast, and 2.8% for placebo, respectively. Other side effects of note included nausea (10% and 16.1% vs. 4.6%), headache (8.4% and 11.5% vs. 4.6%), and upper respiratory tract infection (7% and 6% vs. 3%).
Time for regulatory approval
Based on the positive findings of the PALACE 1, 2, and 3 studies, apremilast’s developer, Celgene, is expected to file for regulatory approval in the treatment of active PsA. In doing so, apremilast will join another novel agent, ustekinumab, in the queue for approval for this indication.
Ustekinumab is a human interleukin-12 and -23 antagonist produced by Janssen that is already approved in Europe and in the United States for skin psoriasis. One-year data also show that it is effective and well tolerated for PsA. It is given subcutaneously, whereas apremilast is an oral agent.
Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
MADRID – Apremilast improves the signs and symptoms of psoriatic arthritis in about 60% of patients at 1 year, according to long-term data from the PALACE 1 trial.
At week 52, a 20% improvement in disease symptoms according to American College of Rheumatology (ACR 20) response criteria was achieved by 57%-63% of patients treated with apremilast, providing evidence of sustained treatment effects.
The PALACE 1 trial’s primary endpoint of an ACR 20 at 16 weeks, already reported last year, was achieved by 31% of patients treated with apremilast 20 mg and 40% of those given apremilast 30 mg, compared with 19% of those given placebo.
"Oral apremilast demonstrated long-term efficacy, including improvement in signs and symptoms and physical function, and skin manifestations," Dr. Arthur Kavanaugh, professor of medicine at the University of California, San Diego, said at the annual European Congress of Rheumatology.
Apremilast is an oral phosphodiesterase 4 inhibitor under investigation as a treatment for active psoriatic arthritis (PsA). It is being evaluated as a possible treatment for skin psoriasis, ankylosing spondylitis, rheumatoid arthritis, and Behçet’s disease.
PALACE 1 was a phase III, multicenter, double-blind, placebo-controlled study of apremilast for the treatment of active PsA. A total of 504 patients with a documented diagnosis of PsA for at least 6 months were recruited into the study (Ann. Rheum. Dis. 2013;72[Suppls3]:163).
Functional outcomes improved
Physical function improved according to measurements on the Health Assessment Questionnaire–Disability Index (HAQ-DI). At baseline, HAQ-DI scores were 1.21, and "we saw that patients improved by –0.35, which is certainly the level that patients can say, ‘I feel better and I can do my daily activities better,’ " Dr. Kavanaugh said.
Additionally, 25% and 37% of patients treated with apremilast 20 mg and 30 mg, respectively, achieved a 75% improvement in the Psoriasis Area and Severity Index at 52 weeks, which is a "very high bar" to achieve, he noted.
The main side effect seen was diarrhea, affecting 11%-19% of patients given apremilast and 2.4% given placebo. However, diarrhea occurred mainly in the first 6 months of therapy and could be managed by taking appropriate measures on an individual patient basis, Dr. Kavanaugh said. This might include prescription of an antidiarrheal agent.
"Prolonged exposure to apremilast did not result in any unexpected increased incidence of adverse events or laboratory abnormalities," he noted. The latter could mean that, if approved, apremilast might not need routine laboratory monitoring.
The PALACE development program
PALACE 1 is one of several clinical trials that have investigated the efficacy and safety of apremilast in active PsA. In these studies, 24 weeks’ treatment with one of two oral doses (20 mg or 30 mg twice daily) of apremilast was compared to placebo. The primary endpoint of the studies was the percentage of patients achieving ACR 20 at 16 weeks.
For inclusion in the trials, patients had to have active disease despite prior therapy with disease-modifying antirheumatic drugs (DMARDs), biologic agents, or both. Dr. Kavanaugh noted that the majority of patients had failed DMARD therapy in PALACE 1, with almost one-quarter receiving prior biologic therapy.
Patients who had a less than 20% reduction from baseline in swollen/tender joint counts at 16 weeks were re-randomized to receive apremilast 20 mg or 30 mg if they had originally been treated with placebo, while patients originally randomized to active treatment stayed on their initial dose if they failed to respond significantly. At the end of the planned 24-week treatment period, all remaining patients on placebo were re-randomized to apremilast 20 mg or 30 mg until 1 year of follow up.
PALACE 3 data also reported
The results of PALACE 3 and combined 6-month safety data from the PALACE 1, PALACE 2, and PALACE 3 trials were also reported at the congress.
In PALACE 3 (Ann. Rheum. Dis. 2013;72[Suppl. 3]:685), significantly more patients achieved the primary endpoint of an ACR 20 at 16 weeks if they were treated with either the 20-mg dose (29.4%, P = .02) or 30-mg dose (42.8%, P less than .0001) of apremilast, compared with those given placebo (18.9%). There was also statistically significant and "clinically meaningful" improvement in physical function and pain. "The results of PALACE 3 support the efficacy and safety findings of the PALACE 1 study and help establish the profile of apremilast in PsA," the PALACE 3 investigators concluded.
The pooled safety findings revealed no new safety concerns and showed apremilast was generally well tolerated (Ann. Rheum. Dis. 2013;72[Suppl. 3]:85). Rates of diarrhea at 24 weeks were 12.6% and 16.5% for the 20-mg and 30-mg doses of apremilast, and 2.8% for placebo, respectively. Other side effects of note included nausea (10% and 16.1% vs. 4.6%), headache (8.4% and 11.5% vs. 4.6%), and upper respiratory tract infection (7% and 6% vs. 3%).
Time for regulatory approval
Based on the positive findings of the PALACE 1, 2, and 3 studies, apremilast’s developer, Celgene, is expected to file for regulatory approval in the treatment of active PsA. In doing so, apremilast will join another novel agent, ustekinumab, in the queue for approval for this indication.
Ustekinumab is a human interleukin-12 and -23 antagonist produced by Janssen that is already approved in Europe and in the United States for skin psoriasis. One-year data also show that it is effective and well tolerated for PsA. It is given subcutaneously, whereas apremilast is an oral agent.
Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
MADRID – Apremilast improves the signs and symptoms of psoriatic arthritis in about 60% of patients at 1 year, according to long-term data from the PALACE 1 trial.
At week 52, a 20% improvement in disease symptoms according to American College of Rheumatology (ACR 20) response criteria was achieved by 57%-63% of patients treated with apremilast, providing evidence of sustained treatment effects.
The PALACE 1 trial’s primary endpoint of an ACR 20 at 16 weeks, already reported last year, was achieved by 31% of patients treated with apremilast 20 mg and 40% of those given apremilast 30 mg, compared with 19% of those given placebo.
"Oral apremilast demonstrated long-term efficacy, including improvement in signs and symptoms and physical function, and skin manifestations," Dr. Arthur Kavanaugh, professor of medicine at the University of California, San Diego, said at the annual European Congress of Rheumatology.
Apremilast is an oral phosphodiesterase 4 inhibitor under investigation as a treatment for active psoriatic arthritis (PsA). It is being evaluated as a possible treatment for skin psoriasis, ankylosing spondylitis, rheumatoid arthritis, and Behçet’s disease.
PALACE 1 was a phase III, multicenter, double-blind, placebo-controlled study of apremilast for the treatment of active PsA. A total of 504 patients with a documented diagnosis of PsA for at least 6 months were recruited into the study (Ann. Rheum. Dis. 2013;72[Suppls3]:163).
Functional outcomes improved
Physical function improved according to measurements on the Health Assessment Questionnaire–Disability Index (HAQ-DI). At baseline, HAQ-DI scores were 1.21, and "we saw that patients improved by –0.35, which is certainly the level that patients can say, ‘I feel better and I can do my daily activities better,’ " Dr. Kavanaugh said.
Additionally, 25% and 37% of patients treated with apremilast 20 mg and 30 mg, respectively, achieved a 75% improvement in the Psoriasis Area and Severity Index at 52 weeks, which is a "very high bar" to achieve, he noted.
The main side effect seen was diarrhea, affecting 11%-19% of patients given apremilast and 2.4% given placebo. However, diarrhea occurred mainly in the first 6 months of therapy and could be managed by taking appropriate measures on an individual patient basis, Dr. Kavanaugh said. This might include prescription of an antidiarrheal agent.
"Prolonged exposure to apremilast did not result in any unexpected increased incidence of adverse events or laboratory abnormalities," he noted. The latter could mean that, if approved, apremilast might not need routine laboratory monitoring.
The PALACE development program
PALACE 1 is one of several clinical trials that have investigated the efficacy and safety of apremilast in active PsA. In these studies, 24 weeks’ treatment with one of two oral doses (20 mg or 30 mg twice daily) of apremilast was compared to placebo. The primary endpoint of the studies was the percentage of patients achieving ACR 20 at 16 weeks.
For inclusion in the trials, patients had to have active disease despite prior therapy with disease-modifying antirheumatic drugs (DMARDs), biologic agents, or both. Dr. Kavanaugh noted that the majority of patients had failed DMARD therapy in PALACE 1, with almost one-quarter receiving prior biologic therapy.
Patients who had a less than 20% reduction from baseline in swollen/tender joint counts at 16 weeks were re-randomized to receive apremilast 20 mg or 30 mg if they had originally been treated with placebo, while patients originally randomized to active treatment stayed on their initial dose if they failed to respond significantly. At the end of the planned 24-week treatment period, all remaining patients on placebo were re-randomized to apremilast 20 mg or 30 mg until 1 year of follow up.
PALACE 3 data also reported
The results of PALACE 3 and combined 6-month safety data from the PALACE 1, PALACE 2, and PALACE 3 trials were also reported at the congress.
In PALACE 3 (Ann. Rheum. Dis. 2013;72[Suppl. 3]:685), significantly more patients achieved the primary endpoint of an ACR 20 at 16 weeks if they were treated with either the 20-mg dose (29.4%, P = .02) or 30-mg dose (42.8%, P less than .0001) of apremilast, compared with those given placebo (18.9%). There was also statistically significant and "clinically meaningful" improvement in physical function and pain. "The results of PALACE 3 support the efficacy and safety findings of the PALACE 1 study and help establish the profile of apremilast in PsA," the PALACE 3 investigators concluded.
The pooled safety findings revealed no new safety concerns and showed apremilast was generally well tolerated (Ann. Rheum. Dis. 2013;72[Suppl. 3]:85). Rates of diarrhea at 24 weeks were 12.6% and 16.5% for the 20-mg and 30-mg doses of apremilast, and 2.8% for placebo, respectively. Other side effects of note included nausea (10% and 16.1% vs. 4.6%), headache (8.4% and 11.5% vs. 4.6%), and upper respiratory tract infection (7% and 6% vs. 3%).
Time for regulatory approval
Based on the positive findings of the PALACE 1, 2, and 3 studies, apremilast’s developer, Celgene, is expected to file for regulatory approval in the treatment of active PsA. In doing so, apremilast will join another novel agent, ustekinumab, in the queue for approval for this indication.
Ustekinumab is a human interleukin-12 and -23 antagonist produced by Janssen that is already approved in Europe and in the United States for skin psoriasis. One-year data also show that it is effective and well tolerated for PsA. It is given subcutaneously, whereas apremilast is an oral agent.
Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
AT THE EULAR CONGRESS 2013
Major finding: ACR 20 response at 1 year was 57%-63% for patients given apremilast.
Data source: PALACE 1, a 504-patient, phase III, multicenter, double blind, placebo-controlled study of apremilast for the treatment of active psoriatic arthritis.
Disclosures: Celgene funded the study. Dr. Kavanaugh has provided expert advice to and/or received research grants from the following companies: AstraZeneca, Bristol-Myers Squibb, Celgene, Centocor-Janssen, Pfizer, Roche, and UCB.
Exercise program improved strength, walking in AS
Patients with ankylosing spondylitis who participated in a progressive muscle strengthening program gained significant improvements in muscle strength and walking performance after 4 months, compared with those who did not participate, Dr. Fabio Jennings reported at the annual European Congress of Rheumatology.
The exercise program, which involved resistance training with the Swiss ball, was also well tolerated and was not associated with negative effects on disease activity, said Dr. Jennings of the rheumatology division at the Federal University of Sao Paulo, Brazil.
Dr. Jennings and his colleagues performed a randomized, controlled, single-blind, prospective trial of 60 patients with ankylosing spondylitis (AS).
Exercise is recommended for people with AS, but the benefits of a specific exercise program have not been well defined, Dr. Jennings noted.
In the study, 30 patients were randomized to the supervised exercise program, which entailed eight resistance exercises using free weights on a Swiss ball twice a week for 16 weeks, with increases in load every 4 weeks. The 30 patients in the control group continued regular treatment with medications, with no exercise. Demographics, clinical features, and medications were similar in the two groups at baseline.
The impact of the exercise on functional capacity, quality of life, muscle strength, and mobility was evaluated using the BASFI (Bath Ankylosing Spondylitis Functional Index), HAQ-S (Health Assessment Questionnaire for Spondyloarthropathies), the 6-minute walk test, and other assessment tools, every 4 weeks. Disease activity was measured with the BASDAI (Bath Ankylosing Spondylitis Disease Activity Index), erythrocyte sedimentation rate (ESR), and C-reactive protein levels.
After 4 months, there were statistically significant differences between the two groups in the strengths of the muscles used in performing the exercises (abdominal, squat, triceps, reverse fly, and rowing exercises), favoring the intervention group. These patients also had significant improvements in the 6-minute walk test; and they were satisfied with the treatment, as reflected by significant differences between the two groups in the Likert scale used to assess patient satisfaction at all time points measured.
In addition, disease activity – as measured by BASDAI, ESR, and C-reactive protein – did not worsen among those who participated in the exercise program.
The study showed that this type of exercise program, using a Swiss ball to improve muscle strength, "is a beneficial and safe intervention" in people with AS, lead author Mr. Marcelo Cardoso de Souza, a physiotherapist and member of a multidisciplinary rehabilitation team at the university, said in an interview. For these patients, improvement in muscular performance and functional capacity is important, he said, noting that before clinicians refer patients to such a program, patients should undergo a medical evaluation, and the program should be provided by an experienced professional.
None of the investigators had relevant financial conflicts of interest.
Patients with ankylosing spondylitis who participated in a progressive muscle strengthening program gained significant improvements in muscle strength and walking performance after 4 months, compared with those who did not participate, Dr. Fabio Jennings reported at the annual European Congress of Rheumatology.
The exercise program, which involved resistance training with the Swiss ball, was also well tolerated and was not associated with negative effects on disease activity, said Dr. Jennings of the rheumatology division at the Federal University of Sao Paulo, Brazil.
Dr. Jennings and his colleagues performed a randomized, controlled, single-blind, prospective trial of 60 patients with ankylosing spondylitis (AS).
Exercise is recommended for people with AS, but the benefits of a specific exercise program have not been well defined, Dr. Jennings noted.
In the study, 30 patients were randomized to the supervised exercise program, which entailed eight resistance exercises using free weights on a Swiss ball twice a week for 16 weeks, with increases in load every 4 weeks. The 30 patients in the control group continued regular treatment with medications, with no exercise. Demographics, clinical features, and medications were similar in the two groups at baseline.
The impact of the exercise on functional capacity, quality of life, muscle strength, and mobility was evaluated using the BASFI (Bath Ankylosing Spondylitis Functional Index), HAQ-S (Health Assessment Questionnaire for Spondyloarthropathies), the 6-minute walk test, and other assessment tools, every 4 weeks. Disease activity was measured with the BASDAI (Bath Ankylosing Spondylitis Disease Activity Index), erythrocyte sedimentation rate (ESR), and C-reactive protein levels.
After 4 months, there were statistically significant differences between the two groups in the strengths of the muscles used in performing the exercises (abdominal, squat, triceps, reverse fly, and rowing exercises), favoring the intervention group. These patients also had significant improvements in the 6-minute walk test; and they were satisfied with the treatment, as reflected by significant differences between the two groups in the Likert scale used to assess patient satisfaction at all time points measured.
In addition, disease activity – as measured by BASDAI, ESR, and C-reactive protein – did not worsen among those who participated in the exercise program.
The study showed that this type of exercise program, using a Swiss ball to improve muscle strength, "is a beneficial and safe intervention" in people with AS, lead author Mr. Marcelo Cardoso de Souza, a physiotherapist and member of a multidisciplinary rehabilitation team at the university, said in an interview. For these patients, improvement in muscular performance and functional capacity is important, he said, noting that before clinicians refer patients to such a program, patients should undergo a medical evaluation, and the program should be provided by an experienced professional.
None of the investigators had relevant financial conflicts of interest.
Patients with ankylosing spondylitis who participated in a progressive muscle strengthening program gained significant improvements in muscle strength and walking performance after 4 months, compared with those who did not participate, Dr. Fabio Jennings reported at the annual European Congress of Rheumatology.
The exercise program, which involved resistance training with the Swiss ball, was also well tolerated and was not associated with negative effects on disease activity, said Dr. Jennings of the rheumatology division at the Federal University of Sao Paulo, Brazil.
Dr. Jennings and his colleagues performed a randomized, controlled, single-blind, prospective trial of 60 patients with ankylosing spondylitis (AS).
Exercise is recommended for people with AS, but the benefits of a specific exercise program have not been well defined, Dr. Jennings noted.
In the study, 30 patients were randomized to the supervised exercise program, which entailed eight resistance exercises using free weights on a Swiss ball twice a week for 16 weeks, with increases in load every 4 weeks. The 30 patients in the control group continued regular treatment with medications, with no exercise. Demographics, clinical features, and medications were similar in the two groups at baseline.
The impact of the exercise on functional capacity, quality of life, muscle strength, and mobility was evaluated using the BASFI (Bath Ankylosing Spondylitis Functional Index), HAQ-S (Health Assessment Questionnaire for Spondyloarthropathies), the 6-minute walk test, and other assessment tools, every 4 weeks. Disease activity was measured with the BASDAI (Bath Ankylosing Spondylitis Disease Activity Index), erythrocyte sedimentation rate (ESR), and C-reactive protein levels.
After 4 months, there were statistically significant differences between the two groups in the strengths of the muscles used in performing the exercises (abdominal, squat, triceps, reverse fly, and rowing exercises), favoring the intervention group. These patients also had significant improvements in the 6-minute walk test; and they were satisfied with the treatment, as reflected by significant differences between the two groups in the Likert scale used to assess patient satisfaction at all time points measured.
In addition, disease activity – as measured by BASDAI, ESR, and C-reactive protein – did not worsen among those who participated in the exercise program.
The study showed that this type of exercise program, using a Swiss ball to improve muscle strength, "is a beneficial and safe intervention" in people with AS, lead author Mr. Marcelo Cardoso de Souza, a physiotherapist and member of a multidisciplinary rehabilitation team at the university, said in an interview. For these patients, improvement in muscular performance and functional capacity is important, he said, noting that before clinicians refer patients to such a program, patients should undergo a medical evaluation, and the program should be provided by an experienced professional.
None of the investigators had relevant financial conflicts of interest.
FROM THE EULAR CONGRESS 2013