User login
Product Update: PICO NPWT; Encision; TimerCap; AMA
SURGICAL SITE WOUND THERAPY
PICO NPWT is a negative-pressure wound therapy device to treat surgical site infection (SSI). According to Smith & Nephew, a new meta-analysis demonstrates that the prophylactic application of PICO with AIRLOCK™ Technology significantly reduces surgical site complications by 58%, the rate of dehiscence by 26%, and length of stay by one-half day when compared with standard care.
The PICO System is canister-free and disposable. Patients can be discharged safely with PICO in place. Seven days of therapy are provided in each kit, with 1 pump, 2 dressings, and fixation strips to allow for a dressing change.
PICO uses a 4-layer multifunction dressing design in which the layers work together to ensure that negative pressure is delivered to the wound bed and exudate is removed through absorption and evaporation. Approximately 20% of fluid still remains in the dressing. The top film layer has a high-moisture vapor transmission rate to transpire as much as 80% of the exudate, says Smith & Nephew.
FOR MORE INFORMATION, VISIT: http://www.smith-nephew.com/
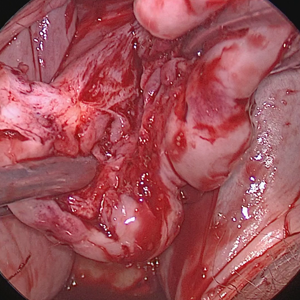
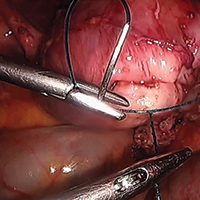
SHIELDED LAPAROSCOPIC INSTRUMENTS PREVENT BURNS
Encision’s patented Active Electrode Monitoring (AEM®) Shielded Laparoscopic Instruments eliminate patient burns and the associated complications.
Every 90 minutes in the United States, a patient is severely injured from a stray energy burn during laparoscopic surgery, according to Encision. The AEM® Shielded Instruments are designed to eliminate burns caused by monopolar energy insulation failure and capacitive coupling, reducing complications and re-admissions.
In addition to helping health care professionals improve patient safety in line with a recent FDA safety communication, Active Electrode Monitoring is a recommended practice of AORN and AAGL.
Encision offers a complete line of premium laparoscopic monopolar surgical instruments with integrated AEM® technology as well as complimentary products to improve clinical effectiveness and patient safety, including bipolar and cold instrumentation.
FOR MORE INFORMATION, VISIT: https://www.encision.com/
iSORT: 7-DAY BLUETOOTH PILLBOX
TimerCap has a new Bluetooth-enabled 7-day pill box called the iSort that sends reminders to take medication to a patient’s phone using a free TimerCap App found at the AppStore and Android Market.
The iSort automatically records and stores the times when each door/slot is opened and closed. It knows which door has been used and seamlessly updates the TimerCap App. The app will notify the patient and, if designated, a caregiver, whenever a dose is due or missed using pictures to show what and how many meds are scheduled. More than one iSort box can be used with the app.
iSort provides reminders that help improve adherence to medication dosing instructions and eliminates annoying false alarms, double entries, and unnecessary reminders when pills already have been taken. The portable iSort uses 2 AA batteries that need to be changed about once per year.
FOR MORE INFORMATION, VISIT: https://www.timercap.com/isort
PLATFORM TO COORDINATE HEALTH AND TECHNOLOGY
The American Medical Association (AMA) recently has established a new initiative that introduces a solution to improve, organize, and share health care information. The Integrated Health Model Initiative (IHMI) is a platform that coordinates the health and technology sectors around a common data model. IHMI fills the national imperative to pioneer a shared framework for organizing health data, emphasizing patient-centric information, and refining data elements to those most predictive of better outcomes. The AMA says that evolving available health data to depict a complete picture of a patient’s journey from wellness to illness to treatment and beyond allows health care delivery to fully focus on patient outcomes, goals, and wellness. Participation in IHMI is open to all health care and technology stakeholders.
FOR MORE INFORMATION, VISIT: www.ama-assn.org/ihmi
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
SURGICAL SITE WOUND THERAPY
PICO NPWT is a negative-pressure wound therapy device to treat surgical site infection (SSI). According to Smith & Nephew, a new meta-analysis demonstrates that the prophylactic application of PICO with AIRLOCK™ Technology significantly reduces surgical site complications by 58%, the rate of dehiscence by 26%, and length of stay by one-half day when compared with standard care.
The PICO System is canister-free and disposable. Patients can be discharged safely with PICO in place. Seven days of therapy are provided in each kit, with 1 pump, 2 dressings, and fixation strips to allow for a dressing change.
PICO uses a 4-layer multifunction dressing design in which the layers work together to ensure that negative pressure is delivered to the wound bed and exudate is removed through absorption and evaporation. Approximately 20% of fluid still remains in the dressing. The top film layer has a high-moisture vapor transmission rate to transpire as much as 80% of the exudate, says Smith & Nephew.
FOR MORE INFORMATION, VISIT: http://www.smith-nephew.com/
SHIELDED LAPAROSCOPIC INSTRUMENTS PREVENT BURNS
Encision’s patented Active Electrode Monitoring (AEM®) Shielded Laparoscopic Instruments eliminate patient burns and the associated complications.
Every 90 minutes in the United States, a patient is severely injured from a stray energy burn during laparoscopic surgery, according to Encision. The AEM® Shielded Instruments are designed to eliminate burns caused by monopolar energy insulation failure and capacitive coupling, reducing complications and re-admissions.
In addition to helping health care professionals improve patient safety in line with a recent FDA safety communication, Active Electrode Monitoring is a recommended practice of AORN and AAGL.
Encision offers a complete line of premium laparoscopic monopolar surgical instruments with integrated AEM® technology as well as complimentary products to improve clinical effectiveness and patient safety, including bipolar and cold instrumentation.
FOR MORE INFORMATION, VISIT: https://www.encision.com/
iSORT: 7-DAY BLUETOOTH PILLBOX
TimerCap has a new Bluetooth-enabled 7-day pill box called the iSort that sends reminders to take medication to a patient’s phone using a free TimerCap App found at the AppStore and Android Market.
The iSort automatically records and stores the times when each door/slot is opened and closed. It knows which door has been used and seamlessly updates the TimerCap App. The app will notify the patient and, if designated, a caregiver, whenever a dose is due or missed using pictures to show what and how many meds are scheduled. More than one iSort box can be used with the app.
iSort provides reminders that help improve adherence to medication dosing instructions and eliminates annoying false alarms, double entries, and unnecessary reminders when pills already have been taken. The portable iSort uses 2 AA batteries that need to be changed about once per year.
FOR MORE INFORMATION, VISIT: https://www.timercap.com/isort
PLATFORM TO COORDINATE HEALTH AND TECHNOLOGY
The American Medical Association (AMA) recently has established a new initiative that introduces a solution to improve, organize, and share health care information. The Integrated Health Model Initiative (IHMI) is a platform that coordinates the health and technology sectors around a common data model. IHMI fills the national imperative to pioneer a shared framework for organizing health data, emphasizing patient-centric information, and refining data elements to those most predictive of better outcomes. The AMA says that evolving available health data to depict a complete picture of a patient’s journey from wellness to illness to treatment and beyond allows health care delivery to fully focus on patient outcomes, goals, and wellness. Participation in IHMI is open to all health care and technology stakeholders.
FOR MORE INFORMATION, VISIT: www.ama-assn.org/ihmi
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
SURGICAL SITE WOUND THERAPY
PICO NPWT is a negative-pressure wound therapy device to treat surgical site infection (SSI). According to Smith & Nephew, a new meta-analysis demonstrates that the prophylactic application of PICO with AIRLOCK™ Technology significantly reduces surgical site complications by 58%, the rate of dehiscence by 26%, and length of stay by one-half day when compared with standard care.
The PICO System is canister-free and disposable. Patients can be discharged safely with PICO in place. Seven days of therapy are provided in each kit, with 1 pump, 2 dressings, and fixation strips to allow for a dressing change.
PICO uses a 4-layer multifunction dressing design in which the layers work together to ensure that negative pressure is delivered to the wound bed and exudate is removed through absorption and evaporation. Approximately 20% of fluid still remains in the dressing. The top film layer has a high-moisture vapor transmission rate to transpire as much as 80% of the exudate, says Smith & Nephew.
FOR MORE INFORMATION, VISIT: http://www.smith-nephew.com/
SHIELDED LAPAROSCOPIC INSTRUMENTS PREVENT BURNS
Encision’s patented Active Electrode Monitoring (AEM®) Shielded Laparoscopic Instruments eliminate patient burns and the associated complications.
Every 90 minutes in the United States, a patient is severely injured from a stray energy burn during laparoscopic surgery, according to Encision. The AEM® Shielded Instruments are designed to eliminate burns caused by monopolar energy insulation failure and capacitive coupling, reducing complications and re-admissions.
In addition to helping health care professionals improve patient safety in line with a recent FDA safety communication, Active Electrode Monitoring is a recommended practice of AORN and AAGL.
Encision offers a complete line of premium laparoscopic monopolar surgical instruments with integrated AEM® technology as well as complimentary products to improve clinical effectiveness and patient safety, including bipolar and cold instrumentation.
FOR MORE INFORMATION, VISIT: https://www.encision.com/
iSORT: 7-DAY BLUETOOTH PILLBOX
TimerCap has a new Bluetooth-enabled 7-day pill box called the iSort that sends reminders to take medication to a patient’s phone using a free TimerCap App found at the AppStore and Android Market.
The iSort automatically records and stores the times when each door/slot is opened and closed. It knows which door has been used and seamlessly updates the TimerCap App. The app will notify the patient and, if designated, a caregiver, whenever a dose is due or missed using pictures to show what and how many meds are scheduled. More than one iSort box can be used with the app.
iSort provides reminders that help improve adherence to medication dosing instructions and eliminates annoying false alarms, double entries, and unnecessary reminders when pills already have been taken. The portable iSort uses 2 AA batteries that need to be changed about once per year.
FOR MORE INFORMATION, VISIT: https://www.timercap.com/isort
PLATFORM TO COORDINATE HEALTH AND TECHNOLOGY
The American Medical Association (AMA) recently has established a new initiative that introduces a solution to improve, organize, and share health care information. The Integrated Health Model Initiative (IHMI) is a platform that coordinates the health and technology sectors around a common data model. IHMI fills the national imperative to pioneer a shared framework for organizing health data, emphasizing patient-centric information, and refining data elements to those most predictive of better outcomes. The AMA says that evolving available health data to depict a complete picture of a patient’s journey from wellness to illness to treatment and beyond allows health care delivery to fully focus on patient outcomes, goals, and wellness. Participation in IHMI is open to all health care and technology stakeholders.
FOR MORE INFORMATION, VISIT: www.ama-assn.org/ihmi
Share your thoughts! Send your Letter to the Editor to rbarbieri@mdedge.com. Please include your name and the city and state in which you practice.
Study examines POEM learning curve
Technical failures or adverse events complicated 4% of peroral endoscopic myotomies (POEMs) in a large single-center retrospective study.
Individual predictors of this composite negative outcome included case number, full-thickness myotomy, and procedure time, Zuqiang Liu, PhD, and his associates at Fudan University, Shanghai, China, wrote in the September issue of Clinical Gastroenterology and Hepatology.
After controlling for these risk factors, the composite rate of adverse events and technical failures dropped gradually after an endoscopist had performed his or her first 100 cases, according to the researchers. “Technical proficiency, demonstrated by plateauing of the procedure time, could be achieved after 70 cases,” they wrote. “The volume of cases required to manage challenging situations and prevent adverse events was thus higher than that needed for simple technical proficiency.” The experience of the training surgeon helped trainees gain technical proficiency faster, they added.
Peroral endoscopic myotomy (POEM) is minimally invasive and effectively treats spastic esophageal motility disorders. However, it is also a challenging procedure, and little is known about its learning curve. For the study, the researchers retrospectively reviewed technical failures and adverse events among 1,346 POEMs performed for achalasia at a single hospital in China between August 2010 and July 2015. They also assessed procedure time and a secondary composite outcome consisting of technical failure, adverse events, and clinical failure (further symptoms) for the first 192 cases performed by the original training surgeon.
There were 10 technical failures and 44 adverse events affecting a total of 54 patients (4%). Case number (P = .010), full-thickness myotomy (P = .002), and procedure time (P = .001) independently predicted this primary composite outcome. Adjusted cumulative sum analysis showed that the rate of this composite outcome decreased gradually after a surgeon had performed his or her first 100 cases. “The procedure time was high during the first few cases and decreased after endoscopists performed 70 cases,” indicating technical proficiency, the investigators wrote. The rate of the secondary composite outcome also fell gradually after the primary surgeon had performed between 90 and 100 cases.
For the first 192 cases performed by the lead surgeon, postprocedural follow-up time was typically 59 months, with a range of 3-71 months. Clinical failures occurred in 20 cases (10%). Rates of clinical failure were 6% at 1 year, 8% at 2 years, and 10% at 3 years.
This is the first study and the largest POEM database so far to assess the learning curve for this procedure by evaluating adverse events and clinical and technical failure, said the researchers. Previous studies consisted of small cases, usually of less than 100 patients each, they added. Such studies would inherently be biased because the smaller the caseload, the longer it might take for the learning curves of surgeons to plateau, they added.
Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest.
SOURCE: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
Determining competency in endoscopic procedures has been a vexing challenge since the introduction of flexible endoscopy. Traditionally, procedure volume has been used as a surrogate for technical competence. However, each endoscopist has their own learning curve. Furthermore, that curve is influenced by both the endoscopist and the characteristics of each patient. Thus, relying on procedure volume or length of time are likely inadequate markers of the true learning process. It has become more important to rely on more sophisticated measurements of competence, as illustrated in this study by Liu et al.
By using a large database of patients undergoing POEM, the authors applied risk-adjusted cumulative sum and moving averages (CUSUM) analysis to develop individual learning curves of six training endoscopists. The primary outcomes used to develop the curve were technical failure and adverse effects (likely the two outcomes patients are most concerned about). The analysis was adjusted for case complexity as well, reflecting that not all training episodes are the same. The results reveal that, although trainee endoscopists were able to perform POEM “quickly” by 70 cases, they did not achieve the more important primary outcomes of technical success and low adverse events until at least 100 procedures. This is akin to the difference between getting to the cecum quickly and having a high adenoma detection rate in colonoscopy.
Moving forward, using sophisticated measurement of individual endoscopists’ learning curves will allow maximal effectiveness of routine procedures such as colonoscopy.
Kal Patel, MD, is associate professor of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Determining competency in endoscopic procedures has been a vexing challenge since the introduction of flexible endoscopy. Traditionally, procedure volume has been used as a surrogate for technical competence. However, each endoscopist has their own learning curve. Furthermore, that curve is influenced by both the endoscopist and the characteristics of each patient. Thus, relying on procedure volume or length of time are likely inadequate markers of the true learning process. It has become more important to rely on more sophisticated measurements of competence, as illustrated in this study by Liu et al.
By using a large database of patients undergoing POEM, the authors applied risk-adjusted cumulative sum and moving averages (CUSUM) analysis to develop individual learning curves of six training endoscopists. The primary outcomes used to develop the curve were technical failure and adverse effects (likely the two outcomes patients are most concerned about). The analysis was adjusted for case complexity as well, reflecting that not all training episodes are the same. The results reveal that, although trainee endoscopists were able to perform POEM “quickly” by 70 cases, they did not achieve the more important primary outcomes of technical success and low adverse events until at least 100 procedures. This is akin to the difference between getting to the cecum quickly and having a high adenoma detection rate in colonoscopy.
Moving forward, using sophisticated measurement of individual endoscopists’ learning curves will allow maximal effectiveness of routine procedures such as colonoscopy.
Kal Patel, MD, is associate professor of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Determining competency in endoscopic procedures has been a vexing challenge since the introduction of flexible endoscopy. Traditionally, procedure volume has been used as a surrogate for technical competence. However, each endoscopist has their own learning curve. Furthermore, that curve is influenced by both the endoscopist and the characteristics of each patient. Thus, relying on procedure volume or length of time are likely inadequate markers of the true learning process. It has become more important to rely on more sophisticated measurements of competence, as illustrated in this study by Liu et al.
By using a large database of patients undergoing POEM, the authors applied risk-adjusted cumulative sum and moving averages (CUSUM) analysis to develop individual learning curves of six training endoscopists. The primary outcomes used to develop the curve were technical failure and adverse effects (likely the two outcomes patients are most concerned about). The analysis was adjusted for case complexity as well, reflecting that not all training episodes are the same. The results reveal that, although trainee endoscopists were able to perform POEM “quickly” by 70 cases, they did not achieve the more important primary outcomes of technical success and low adverse events until at least 100 procedures. This is akin to the difference between getting to the cecum quickly and having a high adenoma detection rate in colonoscopy.
Moving forward, using sophisticated measurement of individual endoscopists’ learning curves will allow maximal effectiveness of routine procedures such as colonoscopy.
Kal Patel, MD, is associate professor of medicine, Baylor College of Medicine, Houston. He has no conflicts of interest.
Technical failures or adverse events complicated 4% of peroral endoscopic myotomies (POEMs) in a large single-center retrospective study.
Individual predictors of this composite negative outcome included case number, full-thickness myotomy, and procedure time, Zuqiang Liu, PhD, and his associates at Fudan University, Shanghai, China, wrote in the September issue of Clinical Gastroenterology and Hepatology.
After controlling for these risk factors, the composite rate of adverse events and technical failures dropped gradually after an endoscopist had performed his or her first 100 cases, according to the researchers. “Technical proficiency, demonstrated by plateauing of the procedure time, could be achieved after 70 cases,” they wrote. “The volume of cases required to manage challenging situations and prevent adverse events was thus higher than that needed for simple technical proficiency.” The experience of the training surgeon helped trainees gain technical proficiency faster, they added.
Peroral endoscopic myotomy (POEM) is minimally invasive and effectively treats spastic esophageal motility disorders. However, it is also a challenging procedure, and little is known about its learning curve. For the study, the researchers retrospectively reviewed technical failures and adverse events among 1,346 POEMs performed for achalasia at a single hospital in China between August 2010 and July 2015. They also assessed procedure time and a secondary composite outcome consisting of technical failure, adverse events, and clinical failure (further symptoms) for the first 192 cases performed by the original training surgeon.
There were 10 technical failures and 44 adverse events affecting a total of 54 patients (4%). Case number (P = .010), full-thickness myotomy (P = .002), and procedure time (P = .001) independently predicted this primary composite outcome. Adjusted cumulative sum analysis showed that the rate of this composite outcome decreased gradually after a surgeon had performed his or her first 100 cases. “The procedure time was high during the first few cases and decreased after endoscopists performed 70 cases,” indicating technical proficiency, the investigators wrote. The rate of the secondary composite outcome also fell gradually after the primary surgeon had performed between 90 and 100 cases.
For the first 192 cases performed by the lead surgeon, postprocedural follow-up time was typically 59 months, with a range of 3-71 months. Clinical failures occurred in 20 cases (10%). Rates of clinical failure were 6% at 1 year, 8% at 2 years, and 10% at 3 years.
This is the first study and the largest POEM database so far to assess the learning curve for this procedure by evaluating adverse events and clinical and technical failure, said the researchers. Previous studies consisted of small cases, usually of less than 100 patients each, they added. Such studies would inherently be biased because the smaller the caseload, the longer it might take for the learning curves of surgeons to plateau, they added.
Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest.
SOURCE: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
Technical failures or adverse events complicated 4% of peroral endoscopic myotomies (POEMs) in a large single-center retrospective study.
Individual predictors of this composite negative outcome included case number, full-thickness myotomy, and procedure time, Zuqiang Liu, PhD, and his associates at Fudan University, Shanghai, China, wrote in the September issue of Clinical Gastroenterology and Hepatology.
After controlling for these risk factors, the composite rate of adverse events and technical failures dropped gradually after an endoscopist had performed his or her first 100 cases, according to the researchers. “Technical proficiency, demonstrated by plateauing of the procedure time, could be achieved after 70 cases,” they wrote. “The volume of cases required to manage challenging situations and prevent adverse events was thus higher than that needed for simple technical proficiency.” The experience of the training surgeon helped trainees gain technical proficiency faster, they added.
Peroral endoscopic myotomy (POEM) is minimally invasive and effectively treats spastic esophageal motility disorders. However, it is also a challenging procedure, and little is known about its learning curve. For the study, the researchers retrospectively reviewed technical failures and adverse events among 1,346 POEMs performed for achalasia at a single hospital in China between August 2010 and July 2015. They also assessed procedure time and a secondary composite outcome consisting of technical failure, adverse events, and clinical failure (further symptoms) for the first 192 cases performed by the original training surgeon.
There were 10 technical failures and 44 adverse events affecting a total of 54 patients (4%). Case number (P = .010), full-thickness myotomy (P = .002), and procedure time (P = .001) independently predicted this primary composite outcome. Adjusted cumulative sum analysis showed that the rate of this composite outcome decreased gradually after a surgeon had performed his or her first 100 cases. “The procedure time was high during the first few cases and decreased after endoscopists performed 70 cases,” indicating technical proficiency, the investigators wrote. The rate of the secondary composite outcome also fell gradually after the primary surgeon had performed between 90 and 100 cases.
For the first 192 cases performed by the lead surgeon, postprocedural follow-up time was typically 59 months, with a range of 3-71 months. Clinical failures occurred in 20 cases (10%). Rates of clinical failure were 6% at 1 year, 8% at 2 years, and 10% at 3 years.
This is the first study and the largest POEM database so far to assess the learning curve for this procedure by evaluating adverse events and clinical and technical failure, said the researchers. Previous studies consisted of small cases, usually of less than 100 patients each, they added. Such studies would inherently be biased because the smaller the caseload, the longer it might take for the learning curves of surgeons to plateau, they added.
Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest.
SOURCE: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: One hundred cases was the typical learning curve for peroral endoscopic myotomy (POEM).
Major finding: The composite rate of technical failure or adverse events was 4%. An adjusted analysis showed that the rate of this negative composite outcome fell gradually after an endoscopist had performed his or her first 100 cases.
Study details: Single-center retrospective study of 1,346 patients undergoing POEM.
Disclosures: Funders included the National Natural Science Foundation of China, the Major Project of Shanghai Municipal Science and Technology Committee, the Chen Guang Program of Shanghai Municipal Education Commission, and the Outstanding Young Doctor Training Project of Shanghai Municipal Commission of Health and Family Planning. The investigators reported having no relevant conflicts of interest..
Source: Zuqiang L et al. Clin Gastroenterol Hepatol. 2017 Dec 5. doi: 10.1016/j.cgh.2017.11.048.
Excision of a Bartholin gland cyst
Bartholin gland cysts comprise up to 2% of all outpatient gynecology visits each year1 and are a common consult for trainees in obstetrics and gynecology. Although excision of a Bartholin gland cyst is a procedure performed infrequently, knowledge of its anatomy and physiology is important for ObGyn trainees and practicing gynecologists, especially when attempts at conservative management have been exhausted.
Before proceeding with surgical excision, it is important to understand the basics of Bartholin gland anatomy, pathologies, and treatment options. This video demonstrates the excisional technique for a 46-year-old woman with a recurrent, symptomatic Bartholin gland cyst who failed prior conservative management. I hope that you will find this video from my colleagues beneficial to your clinical practice.

- Marzano DA, Haefner HK. The bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8(3):195–204.
Bartholin gland cysts comprise up to 2% of all outpatient gynecology visits each year1 and are a common consult for trainees in obstetrics and gynecology. Although excision of a Bartholin gland cyst is a procedure performed infrequently, knowledge of its anatomy and physiology is important for ObGyn trainees and practicing gynecologists, especially when attempts at conservative management have been exhausted.
Before proceeding with surgical excision, it is important to understand the basics of Bartholin gland anatomy, pathologies, and treatment options. This video demonstrates the excisional technique for a 46-year-old woman with a recurrent, symptomatic Bartholin gland cyst who failed prior conservative management. I hope that you will find this video from my colleagues beneficial to your clinical practice.

Bartholin gland cysts comprise up to 2% of all outpatient gynecology visits each year1 and are a common consult for trainees in obstetrics and gynecology. Although excision of a Bartholin gland cyst is a procedure performed infrequently, knowledge of its anatomy and physiology is important for ObGyn trainees and practicing gynecologists, especially when attempts at conservative management have been exhausted.
Before proceeding with surgical excision, it is important to understand the basics of Bartholin gland anatomy, pathologies, and treatment options. This video demonstrates the excisional technique for a 46-year-old woman with a recurrent, symptomatic Bartholin gland cyst who failed prior conservative management. I hope that you will find this video from my colleagues beneficial to your clinical practice.

- Marzano DA, Haefner HK. The bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8(3):195–204.
- Marzano DA, Haefner HK. The bartholin gland cyst: past, present, and future. J Low Genit Tract Dis. 2004;8(3):195–204.
Morcellation at the time of vaginal hysterectomy

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:

Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
This video is brought to you by
Sexual minorities seeking abortion report high levels of male violence
Pregnant lesbian and bisexual women who seek abortions are more likely than are their heterosexual counterparts to be the victims of violence by the men who impregnated them, a new study finds.
Rachel K. Jones, PhD, of the Guttmacher Institute, New York, and her associates also found that these sexual minority women, plus a group of individuals who described their sexual orientation as “something else,” were much more likely to report exposure to sexual and physical violence.
“No patient should be presumed to be heterosexual for any reason, including a pregnancy history. All pregnancies – like all patients – should be treated as unique and operating within the dynamic and interconnected circumstances of peoples’ lives, which may encompass differences in sexual orientation and exposure to violence,” the researchers wrote. Their report is in Obstetrics & Gynecology.
Previous research has suggested that nonheterosexual women are more likely than are straight women to become pregnant unintentionally. There also are signs suggesting that they have more abortions, too, although the findings are iffy, the study authors wrote.
For this study, Dr. Jones and her associates examined questionnaire answers of 8,380 women who responded to the Guttmacher Institute’s 2014 Abortion Patient Survey. All were undergoing abortions at 87 U.S. nonhospital facilities that performed 30 or more abortions each per year.
Of the sample, about 9% declined to describe their sexual orientation. Of the rest, 94% described themselves as heterosexual; of those, 41% were white, 28% were black, and 22% were Hispanic. Most were in their 20s, 47% were never married, and 48% had incomes below the federal poverty level.
Women also described themselves as bisexual (4%), “something else” (1%), and lesbian (0.4%). All these groups were more likely than were heterosexuals to be below the federal poverty level; more than half of the lesbian and bisexual respondents said they had previously given birth.
Fifteen percent of lesbians said their current pregnancy was caused by forced sex, compared with 1% of heterosexuals and 3% of bisexuals. (P less than .001).
Bisexuals (9%) and lesbians (33%) were more likely than were heterosexuals (4%) to say the men who impregnated them had physically abused them. The same was true for sexual abuse, which was reported by 7% of bisexuals, 35% of lesbians, and 2% of heterosexuals. After the researchers controlled for various factors including age and race, lesbians remained much more likely to report physical abuse, sexual abuse, and forced sex at the hands of the men who impregnated them (odds ratios = 15, 25, and 10, respectively, P less than .001).
“Exposure to physical and sexual violence was substantially higher among each of the sexual minority groups compared with their heterosexual counterparts, sometimes by a factor of 15 or more,” the study authors wrote. “We found that lesbian respondents had the highest levels of exposure to violence, perhaps because this population was more likely to have had sex with a man only in the context of forced sex.”
The researchers noted that their study has various limitations, such as low numbers of sexual minority women and the 4-year gap since the data were collected.
Still, Dr. Jones and her associates wrote, the study has strengths. “Health care providers, including those working in abortion settings, need to be aware that a proportion of their patient population identifies as something other than heterosexual,” they wrote.
The study was funded by the Susan Thompson Buffett Foundation with support from the National Institutes of Health via a grant to the Guttmacher Center for Population Research Innovation and Dissemination. The study authors reported no relevant financial disclosures.
SOURCE: Jones R et al. Obstet Gynecol. 2018 Sep;132(3):605-11.
Pregnant lesbian and bisexual women who seek abortions are more likely than are their heterosexual counterparts to be the victims of violence by the men who impregnated them, a new study finds.
Rachel K. Jones, PhD, of the Guttmacher Institute, New York, and her associates also found that these sexual minority women, plus a group of individuals who described their sexual orientation as “something else,” were much more likely to report exposure to sexual and physical violence.
“No patient should be presumed to be heterosexual for any reason, including a pregnancy history. All pregnancies – like all patients – should be treated as unique and operating within the dynamic and interconnected circumstances of peoples’ lives, which may encompass differences in sexual orientation and exposure to violence,” the researchers wrote. Their report is in Obstetrics & Gynecology.
Previous research has suggested that nonheterosexual women are more likely than are straight women to become pregnant unintentionally. There also are signs suggesting that they have more abortions, too, although the findings are iffy, the study authors wrote.
For this study, Dr. Jones and her associates examined questionnaire answers of 8,380 women who responded to the Guttmacher Institute’s 2014 Abortion Patient Survey. All were undergoing abortions at 87 U.S. nonhospital facilities that performed 30 or more abortions each per year.
Of the sample, about 9% declined to describe their sexual orientation. Of the rest, 94% described themselves as heterosexual; of those, 41% were white, 28% were black, and 22% were Hispanic. Most were in their 20s, 47% were never married, and 48% had incomes below the federal poverty level.
Women also described themselves as bisexual (4%), “something else” (1%), and lesbian (0.4%). All these groups were more likely than were heterosexuals to be below the federal poverty level; more than half of the lesbian and bisexual respondents said they had previously given birth.
Fifteen percent of lesbians said their current pregnancy was caused by forced sex, compared with 1% of heterosexuals and 3% of bisexuals. (P less than .001).
Bisexuals (9%) and lesbians (33%) were more likely than were heterosexuals (4%) to say the men who impregnated them had physically abused them. The same was true for sexual abuse, which was reported by 7% of bisexuals, 35% of lesbians, and 2% of heterosexuals. After the researchers controlled for various factors including age and race, lesbians remained much more likely to report physical abuse, sexual abuse, and forced sex at the hands of the men who impregnated them (odds ratios = 15, 25, and 10, respectively, P less than .001).
“Exposure to physical and sexual violence was substantially higher among each of the sexual minority groups compared with their heterosexual counterparts, sometimes by a factor of 15 or more,” the study authors wrote. “We found that lesbian respondents had the highest levels of exposure to violence, perhaps because this population was more likely to have had sex with a man only in the context of forced sex.”
The researchers noted that their study has various limitations, such as low numbers of sexual minority women and the 4-year gap since the data were collected.
Still, Dr. Jones and her associates wrote, the study has strengths. “Health care providers, including those working in abortion settings, need to be aware that a proportion of their patient population identifies as something other than heterosexual,” they wrote.
The study was funded by the Susan Thompson Buffett Foundation with support from the National Institutes of Health via a grant to the Guttmacher Center for Population Research Innovation and Dissemination. The study authors reported no relevant financial disclosures.
SOURCE: Jones R et al. Obstet Gynecol. 2018 Sep;132(3):605-11.
Pregnant lesbian and bisexual women who seek abortions are more likely than are their heterosexual counterparts to be the victims of violence by the men who impregnated them, a new study finds.
Rachel K. Jones, PhD, of the Guttmacher Institute, New York, and her associates also found that these sexual minority women, plus a group of individuals who described their sexual orientation as “something else,” were much more likely to report exposure to sexual and physical violence.
“No patient should be presumed to be heterosexual for any reason, including a pregnancy history. All pregnancies – like all patients – should be treated as unique and operating within the dynamic and interconnected circumstances of peoples’ lives, which may encompass differences in sexual orientation and exposure to violence,” the researchers wrote. Their report is in Obstetrics & Gynecology.
Previous research has suggested that nonheterosexual women are more likely than are straight women to become pregnant unintentionally. There also are signs suggesting that they have more abortions, too, although the findings are iffy, the study authors wrote.
For this study, Dr. Jones and her associates examined questionnaire answers of 8,380 women who responded to the Guttmacher Institute’s 2014 Abortion Patient Survey. All were undergoing abortions at 87 U.S. nonhospital facilities that performed 30 or more abortions each per year.
Of the sample, about 9% declined to describe their sexual orientation. Of the rest, 94% described themselves as heterosexual; of those, 41% were white, 28% were black, and 22% were Hispanic. Most were in their 20s, 47% were never married, and 48% had incomes below the federal poverty level.
Women also described themselves as bisexual (4%), “something else” (1%), and lesbian (0.4%). All these groups were more likely than were heterosexuals to be below the federal poverty level; more than half of the lesbian and bisexual respondents said they had previously given birth.
Fifteen percent of lesbians said their current pregnancy was caused by forced sex, compared with 1% of heterosexuals and 3% of bisexuals. (P less than .001).
Bisexuals (9%) and lesbians (33%) were more likely than were heterosexuals (4%) to say the men who impregnated them had physically abused them. The same was true for sexual abuse, which was reported by 7% of bisexuals, 35% of lesbians, and 2% of heterosexuals. After the researchers controlled for various factors including age and race, lesbians remained much more likely to report physical abuse, sexual abuse, and forced sex at the hands of the men who impregnated them (odds ratios = 15, 25, and 10, respectively, P less than .001).
“Exposure to physical and sexual violence was substantially higher among each of the sexual minority groups compared with their heterosexual counterparts, sometimes by a factor of 15 or more,” the study authors wrote. “We found that lesbian respondents had the highest levels of exposure to violence, perhaps because this population was more likely to have had sex with a man only in the context of forced sex.”
The researchers noted that their study has various limitations, such as low numbers of sexual minority women and the 4-year gap since the data were collected.
Still, Dr. Jones and her associates wrote, the study has strengths. “Health care providers, including those working in abortion settings, need to be aware that a proportion of their patient population identifies as something other than heterosexual,” they wrote.
The study was funded by the Susan Thompson Buffett Foundation with support from the National Institutes of Health via a grant to the Guttmacher Center for Population Research Innovation and Dissemination. The study authors reported no relevant financial disclosures.
SOURCE: Jones R et al. Obstet Gynecol. 2018 Sep;132(3):605-11.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point:
Major finding: Fifteen percent of lesbians said their current pregnancy was caused by forced sex, compared with 1% of heterosexuals (P less than .001), and 3% of bisexuals. Lesbians (33%) were more likely than were heterosexuals (4%) to say the man who impregnated them had physically and/or sexually abused them.
Study details: A 2014 survey of 8,380 women seeking abortions at 87 U.S. nonhospital facilities.
Disclosures: The study was funded by the Susan Thompson Buffett Foundation with support from the National Institutes of Health via a grant to the Guttmacher Center for Population Research Innovation and Dissemination. The study authors reported no relevant financial disclosures.
Source: Jones R et al. Obstet Gynecol. 2018 Sep;132(3):605-11.
Discharge opioid prescriptions for many surgical hospitalizations may be unnecessary
Background: Prescription opioids play a significant role in the current opioid epidemic. Opioids used for nonmedical purposes often are obtained from the prescription of friends and family members, and a majority of heroin users report that their first opioid exposure was via a prescription opioid. Prescription of opioids following low-risk surgical procedures has increased over the past decade.
Study design: Cross-sectional study.
Setting: Two Boston-area acute care hospitals from May 2014 to September 2016.
Synopsis: The authors identified 6,548 inpatient surgical hospitalizations lasting longer than 1 day with a discharge to home in which the patient used no opioid medications in the final 24 hours prior to discharge. Of these, 43.7% received an opioid prescription at discharge. The mean prescription morphine milligram equivalents (MME) provided to this group was 343. The authors identified these cases as instances in which overprescription of opiates may have occurred. Surgical services that tended to have more patients still using opioids at the time of discharge had a higher likelihood of potential overprescription. For patients who used opioids during the final 24 hours of their hospitalization and received an opioid prescription at discharge, inpatient MME use and prescription MME were only weakly correlated (R2 = 0.112). The retrospective two-site design of this study may limit its generalizability.
Bottom line: In postoperative surgical patients, overprescription of opioid medications may occur frequently.
Citation: Chen EY et al. Correlation between 24-hour predischarge opioid use and amount of opioids prescribed at hospital discharge. JAMA Surg. 2018;153(2):e174859.
Dr. Salber is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Background: Prescription opioids play a significant role in the current opioid epidemic. Opioids used for nonmedical purposes often are obtained from the prescription of friends and family members, and a majority of heroin users report that their first opioid exposure was via a prescription opioid. Prescription of opioids following low-risk surgical procedures has increased over the past decade.
Study design: Cross-sectional study.
Setting: Two Boston-area acute care hospitals from May 2014 to September 2016.
Synopsis: The authors identified 6,548 inpatient surgical hospitalizations lasting longer than 1 day with a discharge to home in which the patient used no opioid medications in the final 24 hours prior to discharge. Of these, 43.7% received an opioid prescription at discharge. The mean prescription morphine milligram equivalents (MME) provided to this group was 343. The authors identified these cases as instances in which overprescription of opiates may have occurred. Surgical services that tended to have more patients still using opioids at the time of discharge had a higher likelihood of potential overprescription. For patients who used opioids during the final 24 hours of their hospitalization and received an opioid prescription at discharge, inpatient MME use and prescription MME were only weakly correlated (R2 = 0.112). The retrospective two-site design of this study may limit its generalizability.
Bottom line: In postoperative surgical patients, overprescription of opioid medications may occur frequently.
Citation: Chen EY et al. Correlation between 24-hour predischarge opioid use and amount of opioids prescribed at hospital discharge. JAMA Surg. 2018;153(2):e174859.
Dr. Salber is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Background: Prescription opioids play a significant role in the current opioid epidemic. Opioids used for nonmedical purposes often are obtained from the prescription of friends and family members, and a majority of heroin users report that their first opioid exposure was via a prescription opioid. Prescription of opioids following low-risk surgical procedures has increased over the past decade.
Study design: Cross-sectional study.
Setting: Two Boston-area acute care hospitals from May 2014 to September 2016.
Synopsis: The authors identified 6,548 inpatient surgical hospitalizations lasting longer than 1 day with a discharge to home in which the patient used no opioid medications in the final 24 hours prior to discharge. Of these, 43.7% received an opioid prescription at discharge. The mean prescription morphine milligram equivalents (MME) provided to this group was 343. The authors identified these cases as instances in which overprescription of opiates may have occurred. Surgical services that tended to have more patients still using opioids at the time of discharge had a higher likelihood of potential overprescription. For patients who used opioids during the final 24 hours of their hospitalization and received an opioid prescription at discharge, inpatient MME use and prescription MME were only weakly correlated (R2 = 0.112). The retrospective two-site design of this study may limit its generalizability.
Bottom line: In postoperative surgical patients, overprescription of opioid medications may occur frequently.
Citation: Chen EY et al. Correlation between 24-hour predischarge opioid use and amount of opioids prescribed at hospital discharge. JAMA Surg. 2018;153(2):e174859.
Dr. Salber is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, Boston.
Osteochondritis Dissecans Lesion of the Radial Head
ABSTRACT
This case shows an atypical presentation of an osteochondritis dissecans (OCD) lesion of the radial head with detachment diagnosed on plain radiographs and magnetic resonance imaging (MRI). OCD lesions are rather uncommon in the elbow joint; however, when present, these lesions are typically seen in throwing athletes or gymnasts who engage in activities involving repetitive trauma to the elbow. Involvement of the radial head is extremely rare, accounting for <5% of all elbow OCD lesions. Conventional radiographs have low sensitivity for detecting OCD lesions and may frequently miss these lesions in the early stages. MRI, the imaging modality of choice, can detect these lesions at the earliest stage and provide a clear picture of the involved articular cartilage and underlying bone. Treatment options can vary between nonoperative and operative management depending on several factors, including age and activity level of the patient, size and type of lesion, and clinical presentation. This case represents a radial head OCD lesion managed by arthroscopic débridement alone, resulting in a positive outcome.
Continue to: Case Report...
CASE REPORT
A healthy, 14-year-old, left-hand-dominant adolescent boy presented to the office with a chief complaint of pain localized to the posterolateral aspect of his elbow. He described an injury where he felt a “pop” in his elbow followed by immediate pain in the posterolateral elbow after throwing a pitch during a baseball game. Since the injury, the patient had experienced difficulty extending his elbow and a sharp, throbbing pain during forearm rotation. The patient also reported an intermittent clicking feeling in the elbow. Prior to this injury, he had no elbow pain. He presented in an otherwise normal state of health with no reported past medical or surgical history and no previous trauma to the left upper extremity.
Physical examination demonstrated a mild effusion of the left elbow in the region of the posterolateral corner or “soft spot” with tenderness to palpation over the radial head. The patient had restricted elbow motion with 30° to 135° of flexion. He had 90° of pronation and supination. Ligamentous examination revealed stability of the elbow to both varus and valgus stress at 30° of flexion. No deficits were observed upon upper-extremity neurovascular examination.
Plain radiographs of the left elbow were initially taken. Anteroposterior, lateral, and Greenspan views revealed evidence of a displaced osteochondral fragment of the radial head in this skeletally immature patient. No involvement of the capitellum was apparent (Figures 1A-1C). Non-contrast magnetic resonance imaging (MRI) of the left elbow was subsequently obtained to evaluate the lesion further, and the images confirmed an unstable osteochondritis dissecans (OCD) lesion of the radial head with a detached fragment entrapped within the elbow joint (Figures 2A-2E).


Elbow arthroscopy was performed to evaluate the extent of the OCD lesion to enable determination of the integrity of the cartilaginous surface and remove the loose body entrapped within the elbow joint. Multiple loose bodies (all <5 mm in size) were removed from the elbow joint. Visualization of the radiocapitellar joint revealed extensive cartilage damage to the radial head with multiple areas of denuded cartilage and exposed bone. The main chondral defect measured approximately 4 mm in size. Probing of the lesion confirmed no stable edge; thus, abrasion arthroplasty was performed to stabilize the lesion and stimulate future fibrous cartilage growth (Figures 3A, 3B).

The patient was started on physical therapy consisting of active and active-assisted elbow ranges of motion on postoperative day 10. At the 6-week follow up, the patient presented to the office with pain-free motion of the left elbow ranging from −5° to 135° of flexion. He maintained full pronation and supination. At this point, the patient was advised to begin a throwing program. Three months after treatment, the patient resumed baseball activities, including throwing, with pain-free, full range of motion of the elbow. The patient and the patient’s parents provided written informed consent for print and electronic publication of this case report.
Continue to: Discussion...
DISCUSSION
Elbow pain is a common complaint among young baseball players. OCD lesions, however, are an uncommon entity associated with elbow pathology.1 The overall incidence of OCD lesions is between 15 to 30 per 100,000 people.2-3 Specifically in patients aged 2 to 19 years, the incidence of elbow OCD lesions is 2.2 per 100,000 patients and 3.8 and 0.6 per 100,000 for males and females, respectively.4 Radial head OCD lesions are extremely rare, occurring in <5% of all elbow OCD cases.1 The majority of these lesions are asymptomatic and typically seen in patients who engage in repetitive overhead and upper-extremity weight-bearing activities. Reports indicate that the incidence of these lesions is on the rise and the age of presentation is decreasing, likely because of increased awareness of the disease and increasing involvement of young athletes in competitive athletics.4-5 Most patients with elbow OCD have a history of repetitive overuse of the elbow, as seen in baseball players, leading to excessive compressive and shear forces across the radiocapitellar joint and progression of the dissecans lesion.6
Patients with OCD lesions of the elbow typically present with inflammatory type symptoms and lateral elbow pain. The pain tends to be mild at rest and becomes more pronounced with activity. Patients often wait until mechanical symptoms ensue (eg, clicking, catching, or locking) before presenting to the office. On physical examination, pain in the region of the OCD lesion is usually accompanied by a mild effusion. Stiffness, particularly a loss of terminal extension, may accompany the mechanical symptoms on range of motion testing.7
Workup of elbow OCD lesions begins with obtaining plain radiographs of the elbow. Plain films are of limited use in evaluating these lesions but can help determine separation and the approximate size of the fragment.8 Further work-up must include MRI sequences, which allow for the best evaluation of the articular cartilage, underlying bone, and, specifically, the size and degree of separation of the OCD lesion.9
Nonoperative treatment of OCD lesions is usually successful if diagnosed early. Such treatment consists of activity modification, rest, anti-inflammatory medications, and a gradual return to athletic activities over the next 3 to 6 months provided the symptoms abate.10-11 During this interval, physical therapy may be employed to preserve or regain range of motion in the elbow. Clinical evidence has demonstrated improved outcomes in younger athletes with open physes.12 Returning to athletic activities is advised only when complete resolution of symptoms has been achieved and full motion about the elbow and shoulder girdle has been regained.6
If symptoms persist despite nonoperative management, or if evidence of an unstable lesion (ie, detached fragment) is obtained, operative intervention is appropriate. Operative management includes diagnostic arthroscopy of the entire elbow, removal of any small, loose bodies, and synovectomy as needed. Thereafter, the OCD lesion must be addressed. In cases of capitellar OCD lesions, if the articular cartilage surface is intact, antegrade or retrograde drilling of the subchondral bone is appropriate and will likely result in a good-to-excellent functional outcome.13-14 If disruption to the articular cartilage fissures is found or the lesion appears to be separating from the native bone, fixation of the fragment can be attempted, provided an adequate portion of the subchondral bone remains attached to the OCD lesion.6,14 Oftentimes, the bony bed must be prepared prior to fixation by removal of any fibrous tissue overlying the subchondral bone and ensuring adequate bleeding across the entire bed. Care should be taken to remove any fibrous tissue underlying the OCD lesion. If the OCD lesion is completely loose and/or the bone stock is insufficient or fragmented, arthroscopic removal of the OCD lesion followed by débridement and abrasion arthroplasty of subchondral bone is recommended.15 Improved functional outcomes from this procedure can be expected in contained lesions.15 If the patient continues to be symptomatic, osteochondral autograft or allograft procedures can be attempted depending on the size of the remaining defect.16-18
Other cases of radial head OCD lesions have been reported in the literature.19-20 In 2009, Dotzis and colleagues19 reported a case of an OCD lesion that was managed nonsurgically with observation alone as the lesion was stable and non-detached. Tatebe and colleagues20 reported 4 cases in which OCD involved the radial head and was accompanied by radial head subluxation. All lesions were located at the posteromedial aspect of the radial head with anterior subluxation of the radial head.20 Three of the cases were managed surgically via ulnar osteotomy (2 cases) and fragment removal (1 case).20 All except the 1 case treated by fragment excision revealed a good outcome.20 The patient in this case presented with a detached lesion, confirmed on MRI, with pain, mechanical symptoms, and of loss of terminal extension. Given the chronicity of the injury and the presence of mechanical symptoms, the decision was made to proceed with operative intervention. During elbow arthroscopy, multiple loose bodies were removed from the elbow joint, and inspection of the radiocapitellar joint revealed extensive cartilage damage to the radial head with multiple areas of denuded cartilage and exposed bone. Since the OCD lesion was completely loose and the bone stock was insufficient and too fragmented to attempt fixation, abrasion arthroplasty was performed to stabilize the lesion and stimulate future fibrous cartilage growth. At the 6-week follow up, the patient regained full range of motion of this elbow with no complaints of pain. At the 3-month follow up, the patient reported no pain after returning to throwing and all baseball-related activities.
CONCLUSION
This report presents an extremely rare case of an OCD lesion involving the radial head. Diagnosis and treatment of this lesion followed a protocol similar to that used for the management of capitellar OCD lesions. When dealing with elbow OCD lesions, especially in the skeletally immature patient population, nonsurgical management and a gradual return to activities should be attempted. If symptoms persist despite nonoperative management or evidence of an unstable lesion (as presented in this case) is obtained, operative intervention is appropriate.
- Jans LB, Ditchfield M, Anna G, Jaremko JL, Verstraete KL. MR imaging findings and MR criteria for instability in osteochondritis dissecans of the elbow in children. Eur J Radiol. 2012;81(6):1306-1310. doi:10.1016/j.ejrad.2011.01.007.
- Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg. 1984;66(9):1340-1348. doi:10.2106/00004623-198466090-00003.
- Lindén B. The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand. 1976;47(6):664-667. doi:10.3109/17453677608988756.
- Kessler JI, Nikizad H, Shea KG, Jacobs JC, Bebchuk JD, Weiss JM. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med. 2014;42(2):320-326. doi:10.1177/0363546513510390.
- Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current Concepts Review. Am J Sports Med. 2006;34(7):1181-1191. doi:10.1177/0363546506290127.
- Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89(6):1205-1214. doi:10.2106/JBJS.F.00622.
- Takahara M, Ogino T, Takagi M, Tsuchida H, Orui H, Nambu T. Natural progression of osteo Chondritis dissecans of the humeral capitellum: initial observations. Radiology. 2000;216(1):207-212. doi:10.1148/radiology.216.1.r00jl29207.
- Kijowski R, De Smet AA. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34(5):266-271. doi:10.1007/s00256-005-0899-6.
- Kijowski R, De Smet AA. MRI findings of osteochondritis dissecans of the capitellum with surgical correlation. AJR Am J Roentgenol. 2005;185:1453-1459. doi:10.2214/AJR.04.1570.
- Takahara M, Ogino T, Fukushima S, Tsuchida H, Kaneda K. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am J Sports Med. 1999;27(6):728-732. doi:10.1177/03635465990270060701.
- Takahara M, Ogino T, Sasaki I, Kato H, Minami A, Kaneda K. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res. 1999;363(363):108-115. doi:10.1097/00003086-199906000-00014.
- Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM. Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop. 2003;23(1):102-108. doi:10.1097/01241398-200301000-00021.
- Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19(1):31-37. doi:10.1016/j.jse.2009.04.007.
- Byrd JWT, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30(4):474-478. doi:10.1177/03635465020300040401.
- Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: report of 5 female athletes. Arthroscopy. 2003;19(2):210-214. doi:10.1053/jars.2003.50052.
- Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19(1):31-37. doi:10.1016/j.jse.2009.04.007.
- Yamamoto Y, Ishibashi Y, Tsuda E, Sato H, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):714-720. doi:10.1177/0363546505282620.
- Ahmad CS, ElAttrache NS. Mosaicplasty for capitellar osteochondritis dissecans. In: Yamaguchi K, O'Driscoll S, King G, McKee M, eds. [In press] Advanced Reconstruction Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons.
- Dotzis A, Galissier B, Peyrou P, Longis B, Moulies D. Osteochondritis dissecans of the radial head: a case report. J Shoulder Elbow Surg. 2009;18(1):e18-e21. doi:10.1016/j.jse.2008.04.009.
- Tatebe M, Hirata H, Shinohara T, Yamamoto M, Morita A, Horii E. Pathomechanical significance of radial head subluxation in the onset of osteochondritis dissecans of the radial head. J Orthop Trauma. 2012;26(1):e4-e6. doi:10.1097/BOT.0b013e318214d678.
ABSTRACT
This case shows an atypical presentation of an osteochondritis dissecans (OCD) lesion of the radial head with detachment diagnosed on plain radiographs and magnetic resonance imaging (MRI). OCD lesions are rather uncommon in the elbow joint; however, when present, these lesions are typically seen in throwing athletes or gymnasts who engage in activities involving repetitive trauma to the elbow. Involvement of the radial head is extremely rare, accounting for <5% of all elbow OCD lesions. Conventional radiographs have low sensitivity for detecting OCD lesions and may frequently miss these lesions in the early stages. MRI, the imaging modality of choice, can detect these lesions at the earliest stage and provide a clear picture of the involved articular cartilage and underlying bone. Treatment options can vary between nonoperative and operative management depending on several factors, including age and activity level of the patient, size and type of lesion, and clinical presentation. This case represents a radial head OCD lesion managed by arthroscopic débridement alone, resulting in a positive outcome.
Continue to: Case Report...
CASE REPORT
A healthy, 14-year-old, left-hand-dominant adolescent boy presented to the office with a chief complaint of pain localized to the posterolateral aspect of his elbow. He described an injury where he felt a “pop” in his elbow followed by immediate pain in the posterolateral elbow after throwing a pitch during a baseball game. Since the injury, the patient had experienced difficulty extending his elbow and a sharp, throbbing pain during forearm rotation. The patient also reported an intermittent clicking feeling in the elbow. Prior to this injury, he had no elbow pain. He presented in an otherwise normal state of health with no reported past medical or surgical history and no previous trauma to the left upper extremity.
Physical examination demonstrated a mild effusion of the left elbow in the region of the posterolateral corner or “soft spot” with tenderness to palpation over the radial head. The patient had restricted elbow motion with 30° to 135° of flexion. He had 90° of pronation and supination. Ligamentous examination revealed stability of the elbow to both varus and valgus stress at 30° of flexion. No deficits were observed upon upper-extremity neurovascular examination.
Plain radiographs of the left elbow were initially taken. Anteroposterior, lateral, and Greenspan views revealed evidence of a displaced osteochondral fragment of the radial head in this skeletally immature patient. No involvement of the capitellum was apparent (Figures 1A-1C). Non-contrast magnetic resonance imaging (MRI) of the left elbow was subsequently obtained to evaluate the lesion further, and the images confirmed an unstable osteochondritis dissecans (OCD) lesion of the radial head with a detached fragment entrapped within the elbow joint (Figures 2A-2E).


Elbow arthroscopy was performed to evaluate the extent of the OCD lesion to enable determination of the integrity of the cartilaginous surface and remove the loose body entrapped within the elbow joint. Multiple loose bodies (all <5 mm in size) were removed from the elbow joint. Visualization of the radiocapitellar joint revealed extensive cartilage damage to the radial head with multiple areas of denuded cartilage and exposed bone. The main chondral defect measured approximately 4 mm in size. Probing of the lesion confirmed no stable edge; thus, abrasion arthroplasty was performed to stabilize the lesion and stimulate future fibrous cartilage growth (Figures 3A, 3B).

The patient was started on physical therapy consisting of active and active-assisted elbow ranges of motion on postoperative day 10. At the 6-week follow up, the patient presented to the office with pain-free motion of the left elbow ranging from −5° to 135° of flexion. He maintained full pronation and supination. At this point, the patient was advised to begin a throwing program. Three months after treatment, the patient resumed baseball activities, including throwing, with pain-free, full range of motion of the elbow. The patient and the patient’s parents provided written informed consent for print and electronic publication of this case report.
Continue to: Discussion...
DISCUSSION
Elbow pain is a common complaint among young baseball players. OCD lesions, however, are an uncommon entity associated with elbow pathology.1 The overall incidence of OCD lesions is between 15 to 30 per 100,000 people.2-3 Specifically in patients aged 2 to 19 years, the incidence of elbow OCD lesions is 2.2 per 100,000 patients and 3.8 and 0.6 per 100,000 for males and females, respectively.4 Radial head OCD lesions are extremely rare, occurring in <5% of all elbow OCD cases.1 The majority of these lesions are asymptomatic and typically seen in patients who engage in repetitive overhead and upper-extremity weight-bearing activities. Reports indicate that the incidence of these lesions is on the rise and the age of presentation is decreasing, likely because of increased awareness of the disease and increasing involvement of young athletes in competitive athletics.4-5 Most patients with elbow OCD have a history of repetitive overuse of the elbow, as seen in baseball players, leading to excessive compressive and shear forces across the radiocapitellar joint and progression of the dissecans lesion.6
Patients with OCD lesions of the elbow typically present with inflammatory type symptoms and lateral elbow pain. The pain tends to be mild at rest and becomes more pronounced with activity. Patients often wait until mechanical symptoms ensue (eg, clicking, catching, or locking) before presenting to the office. On physical examination, pain in the region of the OCD lesion is usually accompanied by a mild effusion. Stiffness, particularly a loss of terminal extension, may accompany the mechanical symptoms on range of motion testing.7
Workup of elbow OCD lesions begins with obtaining plain radiographs of the elbow. Plain films are of limited use in evaluating these lesions but can help determine separation and the approximate size of the fragment.8 Further work-up must include MRI sequences, which allow for the best evaluation of the articular cartilage, underlying bone, and, specifically, the size and degree of separation of the OCD lesion.9
Nonoperative treatment of OCD lesions is usually successful if diagnosed early. Such treatment consists of activity modification, rest, anti-inflammatory medications, and a gradual return to athletic activities over the next 3 to 6 months provided the symptoms abate.10-11 During this interval, physical therapy may be employed to preserve or regain range of motion in the elbow. Clinical evidence has demonstrated improved outcomes in younger athletes with open physes.12 Returning to athletic activities is advised only when complete resolution of symptoms has been achieved and full motion about the elbow and shoulder girdle has been regained.6
If symptoms persist despite nonoperative management, or if evidence of an unstable lesion (ie, detached fragment) is obtained, operative intervention is appropriate. Operative management includes diagnostic arthroscopy of the entire elbow, removal of any small, loose bodies, and synovectomy as needed. Thereafter, the OCD lesion must be addressed. In cases of capitellar OCD lesions, if the articular cartilage surface is intact, antegrade or retrograde drilling of the subchondral bone is appropriate and will likely result in a good-to-excellent functional outcome.13-14 If disruption to the articular cartilage fissures is found or the lesion appears to be separating from the native bone, fixation of the fragment can be attempted, provided an adequate portion of the subchondral bone remains attached to the OCD lesion.6,14 Oftentimes, the bony bed must be prepared prior to fixation by removal of any fibrous tissue overlying the subchondral bone and ensuring adequate bleeding across the entire bed. Care should be taken to remove any fibrous tissue underlying the OCD lesion. If the OCD lesion is completely loose and/or the bone stock is insufficient or fragmented, arthroscopic removal of the OCD lesion followed by débridement and abrasion arthroplasty of subchondral bone is recommended.15 Improved functional outcomes from this procedure can be expected in contained lesions.15 If the patient continues to be symptomatic, osteochondral autograft or allograft procedures can be attempted depending on the size of the remaining defect.16-18
Other cases of radial head OCD lesions have been reported in the literature.19-20 In 2009, Dotzis and colleagues19 reported a case of an OCD lesion that was managed nonsurgically with observation alone as the lesion was stable and non-detached. Tatebe and colleagues20 reported 4 cases in which OCD involved the radial head and was accompanied by radial head subluxation. All lesions were located at the posteromedial aspect of the radial head with anterior subluxation of the radial head.20 Three of the cases were managed surgically via ulnar osteotomy (2 cases) and fragment removal (1 case).20 All except the 1 case treated by fragment excision revealed a good outcome.20 The patient in this case presented with a detached lesion, confirmed on MRI, with pain, mechanical symptoms, and of loss of terminal extension. Given the chronicity of the injury and the presence of mechanical symptoms, the decision was made to proceed with operative intervention. During elbow arthroscopy, multiple loose bodies were removed from the elbow joint, and inspection of the radiocapitellar joint revealed extensive cartilage damage to the radial head with multiple areas of denuded cartilage and exposed bone. Since the OCD lesion was completely loose and the bone stock was insufficient and too fragmented to attempt fixation, abrasion arthroplasty was performed to stabilize the lesion and stimulate future fibrous cartilage growth. At the 6-week follow up, the patient regained full range of motion of this elbow with no complaints of pain. At the 3-month follow up, the patient reported no pain after returning to throwing and all baseball-related activities.
CONCLUSION
This report presents an extremely rare case of an OCD lesion involving the radial head. Diagnosis and treatment of this lesion followed a protocol similar to that used for the management of capitellar OCD lesions. When dealing with elbow OCD lesions, especially in the skeletally immature patient population, nonsurgical management and a gradual return to activities should be attempted. If symptoms persist despite nonoperative management or evidence of an unstable lesion (as presented in this case) is obtained, operative intervention is appropriate.
ABSTRACT
This case shows an atypical presentation of an osteochondritis dissecans (OCD) lesion of the radial head with detachment diagnosed on plain radiographs and magnetic resonance imaging (MRI). OCD lesions are rather uncommon in the elbow joint; however, when present, these lesions are typically seen in throwing athletes or gymnasts who engage in activities involving repetitive trauma to the elbow. Involvement of the radial head is extremely rare, accounting for <5% of all elbow OCD lesions. Conventional radiographs have low sensitivity for detecting OCD lesions and may frequently miss these lesions in the early stages. MRI, the imaging modality of choice, can detect these lesions at the earliest stage and provide a clear picture of the involved articular cartilage and underlying bone. Treatment options can vary between nonoperative and operative management depending on several factors, including age and activity level of the patient, size and type of lesion, and clinical presentation. This case represents a radial head OCD lesion managed by arthroscopic débridement alone, resulting in a positive outcome.
Continue to: Case Report...
CASE REPORT
A healthy, 14-year-old, left-hand-dominant adolescent boy presented to the office with a chief complaint of pain localized to the posterolateral aspect of his elbow. He described an injury where he felt a “pop” in his elbow followed by immediate pain in the posterolateral elbow after throwing a pitch during a baseball game. Since the injury, the patient had experienced difficulty extending his elbow and a sharp, throbbing pain during forearm rotation. The patient also reported an intermittent clicking feeling in the elbow. Prior to this injury, he had no elbow pain. He presented in an otherwise normal state of health with no reported past medical or surgical history and no previous trauma to the left upper extremity.
Physical examination demonstrated a mild effusion of the left elbow in the region of the posterolateral corner or “soft spot” with tenderness to palpation over the radial head. The patient had restricted elbow motion with 30° to 135° of flexion. He had 90° of pronation and supination. Ligamentous examination revealed stability of the elbow to both varus and valgus stress at 30° of flexion. No deficits were observed upon upper-extremity neurovascular examination.
Plain radiographs of the left elbow were initially taken. Anteroposterior, lateral, and Greenspan views revealed evidence of a displaced osteochondral fragment of the radial head in this skeletally immature patient. No involvement of the capitellum was apparent (Figures 1A-1C). Non-contrast magnetic resonance imaging (MRI) of the left elbow was subsequently obtained to evaluate the lesion further, and the images confirmed an unstable osteochondritis dissecans (OCD) lesion of the radial head with a detached fragment entrapped within the elbow joint (Figures 2A-2E).


Elbow arthroscopy was performed to evaluate the extent of the OCD lesion to enable determination of the integrity of the cartilaginous surface and remove the loose body entrapped within the elbow joint. Multiple loose bodies (all <5 mm in size) were removed from the elbow joint. Visualization of the radiocapitellar joint revealed extensive cartilage damage to the radial head with multiple areas of denuded cartilage and exposed bone. The main chondral defect measured approximately 4 mm in size. Probing of the lesion confirmed no stable edge; thus, abrasion arthroplasty was performed to stabilize the lesion and stimulate future fibrous cartilage growth (Figures 3A, 3B).

The patient was started on physical therapy consisting of active and active-assisted elbow ranges of motion on postoperative day 10. At the 6-week follow up, the patient presented to the office with pain-free motion of the left elbow ranging from −5° to 135° of flexion. He maintained full pronation and supination. At this point, the patient was advised to begin a throwing program. Three months after treatment, the patient resumed baseball activities, including throwing, with pain-free, full range of motion of the elbow. The patient and the patient’s parents provided written informed consent for print and electronic publication of this case report.
Continue to: Discussion...
DISCUSSION
Elbow pain is a common complaint among young baseball players. OCD lesions, however, are an uncommon entity associated with elbow pathology.1 The overall incidence of OCD lesions is between 15 to 30 per 100,000 people.2-3 Specifically in patients aged 2 to 19 years, the incidence of elbow OCD lesions is 2.2 per 100,000 patients and 3.8 and 0.6 per 100,000 for males and females, respectively.4 Radial head OCD lesions are extremely rare, occurring in <5% of all elbow OCD cases.1 The majority of these lesions are asymptomatic and typically seen in patients who engage in repetitive overhead and upper-extremity weight-bearing activities. Reports indicate that the incidence of these lesions is on the rise and the age of presentation is decreasing, likely because of increased awareness of the disease and increasing involvement of young athletes in competitive athletics.4-5 Most patients with elbow OCD have a history of repetitive overuse of the elbow, as seen in baseball players, leading to excessive compressive and shear forces across the radiocapitellar joint and progression of the dissecans lesion.6
Patients with OCD lesions of the elbow typically present with inflammatory type symptoms and lateral elbow pain. The pain tends to be mild at rest and becomes more pronounced with activity. Patients often wait until mechanical symptoms ensue (eg, clicking, catching, or locking) before presenting to the office. On physical examination, pain in the region of the OCD lesion is usually accompanied by a mild effusion. Stiffness, particularly a loss of terminal extension, may accompany the mechanical symptoms on range of motion testing.7
Workup of elbow OCD lesions begins with obtaining plain radiographs of the elbow. Plain films are of limited use in evaluating these lesions but can help determine separation and the approximate size of the fragment.8 Further work-up must include MRI sequences, which allow for the best evaluation of the articular cartilage, underlying bone, and, specifically, the size and degree of separation of the OCD lesion.9
Nonoperative treatment of OCD lesions is usually successful if diagnosed early. Such treatment consists of activity modification, rest, anti-inflammatory medications, and a gradual return to athletic activities over the next 3 to 6 months provided the symptoms abate.10-11 During this interval, physical therapy may be employed to preserve or regain range of motion in the elbow. Clinical evidence has demonstrated improved outcomes in younger athletes with open physes.12 Returning to athletic activities is advised only when complete resolution of symptoms has been achieved and full motion about the elbow and shoulder girdle has been regained.6
If symptoms persist despite nonoperative management, or if evidence of an unstable lesion (ie, detached fragment) is obtained, operative intervention is appropriate. Operative management includes diagnostic arthroscopy of the entire elbow, removal of any small, loose bodies, and synovectomy as needed. Thereafter, the OCD lesion must be addressed. In cases of capitellar OCD lesions, if the articular cartilage surface is intact, antegrade or retrograde drilling of the subchondral bone is appropriate and will likely result in a good-to-excellent functional outcome.13-14 If disruption to the articular cartilage fissures is found or the lesion appears to be separating from the native bone, fixation of the fragment can be attempted, provided an adequate portion of the subchondral bone remains attached to the OCD lesion.6,14 Oftentimes, the bony bed must be prepared prior to fixation by removal of any fibrous tissue overlying the subchondral bone and ensuring adequate bleeding across the entire bed. Care should be taken to remove any fibrous tissue underlying the OCD lesion. If the OCD lesion is completely loose and/or the bone stock is insufficient or fragmented, arthroscopic removal of the OCD lesion followed by débridement and abrasion arthroplasty of subchondral bone is recommended.15 Improved functional outcomes from this procedure can be expected in contained lesions.15 If the patient continues to be symptomatic, osteochondral autograft or allograft procedures can be attempted depending on the size of the remaining defect.16-18
Other cases of radial head OCD lesions have been reported in the literature.19-20 In 2009, Dotzis and colleagues19 reported a case of an OCD lesion that was managed nonsurgically with observation alone as the lesion was stable and non-detached. Tatebe and colleagues20 reported 4 cases in which OCD involved the radial head and was accompanied by radial head subluxation. All lesions were located at the posteromedial aspect of the radial head with anterior subluxation of the radial head.20 Three of the cases were managed surgically via ulnar osteotomy (2 cases) and fragment removal (1 case).20 All except the 1 case treated by fragment excision revealed a good outcome.20 The patient in this case presented with a detached lesion, confirmed on MRI, with pain, mechanical symptoms, and of loss of terminal extension. Given the chronicity of the injury and the presence of mechanical symptoms, the decision was made to proceed with operative intervention. During elbow arthroscopy, multiple loose bodies were removed from the elbow joint, and inspection of the radiocapitellar joint revealed extensive cartilage damage to the radial head with multiple areas of denuded cartilage and exposed bone. Since the OCD lesion was completely loose and the bone stock was insufficient and too fragmented to attempt fixation, abrasion arthroplasty was performed to stabilize the lesion and stimulate future fibrous cartilage growth. At the 6-week follow up, the patient regained full range of motion of this elbow with no complaints of pain. At the 3-month follow up, the patient reported no pain after returning to throwing and all baseball-related activities.
CONCLUSION
This report presents an extremely rare case of an OCD lesion involving the radial head. Diagnosis and treatment of this lesion followed a protocol similar to that used for the management of capitellar OCD lesions. When dealing with elbow OCD lesions, especially in the skeletally immature patient population, nonsurgical management and a gradual return to activities should be attempted. If symptoms persist despite nonoperative management or evidence of an unstable lesion (as presented in this case) is obtained, operative intervention is appropriate.
- Jans LB, Ditchfield M, Anna G, Jaremko JL, Verstraete KL. MR imaging findings and MR criteria for instability in osteochondritis dissecans of the elbow in children. Eur J Radiol. 2012;81(6):1306-1310. doi:10.1016/j.ejrad.2011.01.007.
- Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg. 1984;66(9):1340-1348. doi:10.2106/00004623-198466090-00003.
- Lindén B. The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand. 1976;47(6):664-667. doi:10.3109/17453677608988756.
- Kessler JI, Nikizad H, Shea KG, Jacobs JC, Bebchuk JD, Weiss JM. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med. 2014;42(2):320-326. doi:10.1177/0363546513510390.
- Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current Concepts Review. Am J Sports Med. 2006;34(7):1181-1191. doi:10.1177/0363546506290127.
- Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89(6):1205-1214. doi:10.2106/JBJS.F.00622.
- Takahara M, Ogino T, Takagi M, Tsuchida H, Orui H, Nambu T. Natural progression of osteo Chondritis dissecans of the humeral capitellum: initial observations. Radiology. 2000;216(1):207-212. doi:10.1148/radiology.216.1.r00jl29207.
- Kijowski R, De Smet AA. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34(5):266-271. doi:10.1007/s00256-005-0899-6.
- Kijowski R, De Smet AA. MRI findings of osteochondritis dissecans of the capitellum with surgical correlation. AJR Am J Roentgenol. 2005;185:1453-1459. doi:10.2214/AJR.04.1570.
- Takahara M, Ogino T, Fukushima S, Tsuchida H, Kaneda K. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am J Sports Med. 1999;27(6):728-732. doi:10.1177/03635465990270060701.
- Takahara M, Ogino T, Sasaki I, Kato H, Minami A, Kaneda K. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res. 1999;363(363):108-115. doi:10.1097/00003086-199906000-00014.
- Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM. Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop. 2003;23(1):102-108. doi:10.1097/01241398-200301000-00021.
- Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19(1):31-37. doi:10.1016/j.jse.2009.04.007.
- Byrd JWT, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30(4):474-478. doi:10.1177/03635465020300040401.
- Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: report of 5 female athletes. Arthroscopy. 2003;19(2):210-214. doi:10.1053/jars.2003.50052.
- Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19(1):31-37. doi:10.1016/j.jse.2009.04.007.
- Yamamoto Y, Ishibashi Y, Tsuda E, Sato H, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):714-720. doi:10.1177/0363546505282620.
- Ahmad CS, ElAttrache NS. Mosaicplasty for capitellar osteochondritis dissecans. In: Yamaguchi K, O'Driscoll S, King G, McKee M, eds. [In press] Advanced Reconstruction Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons.
- Dotzis A, Galissier B, Peyrou P, Longis B, Moulies D. Osteochondritis dissecans of the radial head: a case report. J Shoulder Elbow Surg. 2009;18(1):e18-e21. doi:10.1016/j.jse.2008.04.009.
- Tatebe M, Hirata H, Shinohara T, Yamamoto M, Morita A, Horii E. Pathomechanical significance of radial head subluxation in the onset of osteochondritis dissecans of the radial head. J Orthop Trauma. 2012;26(1):e4-e6. doi:10.1097/BOT.0b013e318214d678.
- Jans LB, Ditchfield M, Anna G, Jaremko JL, Verstraete KL. MR imaging findings and MR criteria for instability in osteochondritis dissecans of the elbow in children. Eur J Radiol. 2012;81(6):1306-1310. doi:10.1016/j.ejrad.2011.01.007.
- Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg. 1984;66(9):1340-1348. doi:10.2106/00004623-198466090-00003.
- Lindén B. The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand. 1976;47(6):664-667. doi:10.3109/17453677608988756.
- Kessler JI, Nikizad H, Shea KG, Jacobs JC, Bebchuk JD, Weiss JM. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med. 2014;42(2):320-326. doi:10.1177/0363546513510390.
- Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current Concepts Review. Am J Sports Med. 2006;34(7):1181-1191. doi:10.1177/0363546506290127.
- Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89(6):1205-1214. doi:10.2106/JBJS.F.00622.
- Takahara M, Ogino T, Takagi M, Tsuchida H, Orui H, Nambu T. Natural progression of osteo Chondritis dissecans of the humeral capitellum: initial observations. Radiology. 2000;216(1):207-212. doi:10.1148/radiology.216.1.r00jl29207.
- Kijowski R, De Smet AA. Radiography of the elbow for evaluation of patients with osteochondritis dissecans of the capitellum. Skeletal Radiol. 2005;34(5):266-271. doi:10.1007/s00256-005-0899-6.
- Kijowski R, De Smet AA. MRI findings of osteochondritis dissecans of the capitellum with surgical correlation. AJR Am J Roentgenol. 2005;185:1453-1459. doi:10.2214/AJR.04.1570.
- Takahara M, Ogino T, Fukushima S, Tsuchida H, Kaneda K. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am J Sports Med. 1999;27(6):728-732. doi:10.1177/03635465990270060701.
- Takahara M, Ogino T, Sasaki I, Kato H, Minami A, Kaneda K. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin Orthop Relat Res. 1999;363(363):108-115. doi:10.1097/00003086-199906000-00014.
- Pill SG, Ganley TJ, Milam RA, Lou JE, Meyer JS, Flynn JM. Role of magnetic resonance imaging and clinical criteria in predicting successful nonoperative treatment of osteochondritis dissecans in children. J Pediatr Orthop. 2003;23(1):102-108. doi:10.1097/01241398-200301000-00021.
- Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19(1):31-37. doi:10.1016/j.jse.2009.04.007.
- Byrd JWT, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30(4):474-478. doi:10.1177/03635465020300040401.
- Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: report of 5 female athletes. Arthroscopy. 2003;19(2):210-214. doi:10.1053/jars.2003.50052.
- Mihara K, Suzuki K, Makiuchi D, Nishinaka N, Yamaguchi K, Tsutsui H. Surgical treatment for osteochondritis dissecans of the humeral capitellum. J Shoulder Elbow Surg. 2010;19(1):31-37. doi:10.1016/j.jse.2009.04.007.
- Yamamoto Y, Ishibashi Y, Tsuda E, Sato H, Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: minimum 2-year follow-up. Am J Sports Med. 2006;34(5):714-720. doi:10.1177/0363546505282620.
- Ahmad CS, ElAttrache NS. Mosaicplasty for capitellar osteochondritis dissecans. In: Yamaguchi K, O'Driscoll S, King G, McKee M, eds. [In press] Advanced Reconstruction Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons.
- Dotzis A, Galissier B, Peyrou P, Longis B, Moulies D. Osteochondritis dissecans of the radial head: a case report. J Shoulder Elbow Surg. 2009;18(1):e18-e21. doi:10.1016/j.jse.2008.04.009.
- Tatebe M, Hirata H, Shinohara T, Yamamoto M, Morita A, Horii E. Pathomechanical significance of radial head subluxation in the onset of osteochondritis dissecans of the radial head. J Orthop Trauma. 2012;26(1):e4-e6. doi:10.1097/BOT.0b013e318214d678.
TAKE-HOME POINTS
- Radial Head OCD lesions are uncommon.
- Typically present in athletes that engage in repetitive trauma to elbow (throwers, gymnasts).
- MRI is the best modality for making diagnosis.
- Attempt nonsurgical treatment initially, especially in skeletally immature patients.
- If nonsurgical fails or there is an unstable lesion, consider operative intervention.
Surgical management of non-tubal ectopic pregnancies
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Additional videos from SGS are available here, including these recent offerings:
This video is brought to you by
Pediatric appendectomy fast track reduced LoS, narcotic use
Orlando – A significantly reduced length of stay and improved other measures of quality care, according to results from a recent single-center quality improvement project.
After implementation of the multidisciplinary clinical pathway, postoperative narcotic use decreased, while use of a standard antibiotic regimen increased, said Angela M. Kao, MD, a surgical resident with Carolinas Medical Center, Charlotte, N.C.
Of the patients treated according to the fast-track pathway, 90% were discharged within 8 hours of surgery or immediately after morning rounds with no increase in complications or readmissions, said Dr. Kao, who was named the Trainee Abstract Competition Winner based on this research presented at the American College of Surgeons Quality and Safety Conference.
While same-day discharge after laparoscopic appendectomy is safe for most children with nonperforated acute appendicitis, there is wide variability in its perioperative management, Dr. Kao said in an oral abstract presentation.
“At our institution, we noted that no standardized protocol existed for patients with noncomplicated appendicitis, leading to wide variations in postoperative length of stay,” she said.
In addition, preoperative antibiotics and postoperative pain regimens were largely based on provider preference, she added.
Accordingly, a multidisciplinary team used information from the American College of Surgeons National Surgical Quality Improvement Program Pediatric (NSQIP-P) to identify areas for improvement, including multimodal analgesia, standardization of antibiotics, early mobilization, and discharge initiated by nursing.
They also created a designated pre- and postoperative unit staffed by nurses trained in ERAS (Enhanced Recovery After Surgery), which greatly facilitated the goals of the project, Dr. Kao and her coauthors said.
The study results included 61 patients with noncomplicated acute appendicitis who underwent laparoscopic appendectomy after implementation of the fast-track pathway initiative. They were compared with a historical cohort of 58 patients treated in the year leading up to implementation of the pathway.
Dr. Kao and her colleagues found that 87% of fast-track patients received the standard recommended dosing of a third-generation cephalosporin and metronidazole, compared with just 13.8% among those in the period before the fast track’s implementation. In addition, duplicate antibiotic dosing was seen in 6.6% of cases, down from 49%.
Postoperative nausea was minimal, with 9% of fast-tracked patients requiring antiemetic, down from 18.9% in the previous period.
Postoperative IV narcotic use decreased from 86% to 54% because of the use of multimodal analgesia, Dr. Kao added.
Total hospital length of stay decreased 43% to a mean of 16 hours, and the postoperative length of stay decreased by 60% to a mean of 8 hours with no differences in complications or readmission, compared with the period before the fast track’s implementation, according to Dr. Kao.
Almost all of the fast-track patients (90.2%) were discharged within 8 hours or, in the case of procedures performed between midnight and 7 a.m., discharged immediately after morning rounds, according to data presented by the investigators.
“At our institution, a transition from patients discharged by the surgical team to nursing-initiated recovery and discharge was a key component,” Dr. Kao said at the meeting. “Earlier discharge was largely facilitated by nursing-initiated discharge, which allowed for more frequent evaluation of discharge readiness, compared to surgeon providers.”
Dr. Kao had no disclosures relevant to her presentation.
Orlando – A significantly reduced length of stay and improved other measures of quality care, according to results from a recent single-center quality improvement project.
After implementation of the multidisciplinary clinical pathway, postoperative narcotic use decreased, while use of a standard antibiotic regimen increased, said Angela M. Kao, MD, a surgical resident with Carolinas Medical Center, Charlotte, N.C.
Of the patients treated according to the fast-track pathway, 90% were discharged within 8 hours of surgery or immediately after morning rounds with no increase in complications or readmissions, said Dr. Kao, who was named the Trainee Abstract Competition Winner based on this research presented at the American College of Surgeons Quality and Safety Conference.
While same-day discharge after laparoscopic appendectomy is safe for most children with nonperforated acute appendicitis, there is wide variability in its perioperative management, Dr. Kao said in an oral abstract presentation.
“At our institution, we noted that no standardized protocol existed for patients with noncomplicated appendicitis, leading to wide variations in postoperative length of stay,” she said.
In addition, preoperative antibiotics and postoperative pain regimens were largely based on provider preference, she added.
Accordingly, a multidisciplinary team used information from the American College of Surgeons National Surgical Quality Improvement Program Pediatric (NSQIP-P) to identify areas for improvement, including multimodal analgesia, standardization of antibiotics, early mobilization, and discharge initiated by nursing.
They also created a designated pre- and postoperative unit staffed by nurses trained in ERAS (Enhanced Recovery After Surgery), which greatly facilitated the goals of the project, Dr. Kao and her coauthors said.
The study results included 61 patients with noncomplicated acute appendicitis who underwent laparoscopic appendectomy after implementation of the fast-track pathway initiative. They were compared with a historical cohort of 58 patients treated in the year leading up to implementation of the pathway.
Dr. Kao and her colleagues found that 87% of fast-track patients received the standard recommended dosing of a third-generation cephalosporin and metronidazole, compared with just 13.8% among those in the period before the fast track’s implementation. In addition, duplicate antibiotic dosing was seen in 6.6% of cases, down from 49%.
Postoperative nausea was minimal, with 9% of fast-tracked patients requiring antiemetic, down from 18.9% in the previous period.
Postoperative IV narcotic use decreased from 86% to 54% because of the use of multimodal analgesia, Dr. Kao added.
Total hospital length of stay decreased 43% to a mean of 16 hours, and the postoperative length of stay decreased by 60% to a mean of 8 hours with no differences in complications or readmission, compared with the period before the fast track’s implementation, according to Dr. Kao.
Almost all of the fast-track patients (90.2%) were discharged within 8 hours or, in the case of procedures performed between midnight and 7 a.m., discharged immediately after morning rounds, according to data presented by the investigators.
“At our institution, a transition from patients discharged by the surgical team to nursing-initiated recovery and discharge was a key component,” Dr. Kao said at the meeting. “Earlier discharge was largely facilitated by nursing-initiated discharge, which allowed for more frequent evaluation of discharge readiness, compared to surgeon providers.”
Dr. Kao had no disclosures relevant to her presentation.
Orlando – A significantly reduced length of stay and improved other measures of quality care, according to results from a recent single-center quality improvement project.
After implementation of the multidisciplinary clinical pathway, postoperative narcotic use decreased, while use of a standard antibiotic regimen increased, said Angela M. Kao, MD, a surgical resident with Carolinas Medical Center, Charlotte, N.C.
Of the patients treated according to the fast-track pathway, 90% were discharged within 8 hours of surgery or immediately after morning rounds with no increase in complications or readmissions, said Dr. Kao, who was named the Trainee Abstract Competition Winner based on this research presented at the American College of Surgeons Quality and Safety Conference.
While same-day discharge after laparoscopic appendectomy is safe for most children with nonperforated acute appendicitis, there is wide variability in its perioperative management, Dr. Kao said in an oral abstract presentation.
“At our institution, we noted that no standardized protocol existed for patients with noncomplicated appendicitis, leading to wide variations in postoperative length of stay,” she said.
In addition, preoperative antibiotics and postoperative pain regimens were largely based on provider preference, she added.
Accordingly, a multidisciplinary team used information from the American College of Surgeons National Surgical Quality Improvement Program Pediatric (NSQIP-P) to identify areas for improvement, including multimodal analgesia, standardization of antibiotics, early mobilization, and discharge initiated by nursing.
They also created a designated pre- and postoperative unit staffed by nurses trained in ERAS (Enhanced Recovery After Surgery), which greatly facilitated the goals of the project, Dr. Kao and her coauthors said.
The study results included 61 patients with noncomplicated acute appendicitis who underwent laparoscopic appendectomy after implementation of the fast-track pathway initiative. They were compared with a historical cohort of 58 patients treated in the year leading up to implementation of the pathway.
Dr. Kao and her colleagues found that 87% of fast-track patients received the standard recommended dosing of a third-generation cephalosporin and metronidazole, compared with just 13.8% among those in the period before the fast track’s implementation. In addition, duplicate antibiotic dosing was seen in 6.6% of cases, down from 49%.
Postoperative nausea was minimal, with 9% of fast-tracked patients requiring antiemetic, down from 18.9% in the previous period.
Postoperative IV narcotic use decreased from 86% to 54% because of the use of multimodal analgesia, Dr. Kao added.
Total hospital length of stay decreased 43% to a mean of 16 hours, and the postoperative length of stay decreased by 60% to a mean of 8 hours with no differences in complications or readmission, compared with the period before the fast track’s implementation, according to Dr. Kao.
Almost all of the fast-track patients (90.2%) were discharged within 8 hours or, in the case of procedures performed between midnight and 7 a.m., discharged immediately after morning rounds, according to data presented by the investigators.
“At our institution, a transition from patients discharged by the surgical team to nursing-initiated recovery and discharge was a key component,” Dr. Kao said at the meeting. “Earlier discharge was largely facilitated by nursing-initiated discharge, which allowed for more frequent evaluation of discharge readiness, compared to surgeon providers.”
Dr. Kao had no disclosures relevant to her presentation.
REPORTING FROM ACSQSC 2018
Enhanced recovery initiative improved bariatric length of stay
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
REPORTING FROM ACSQSC 2018
Key clinical point: An evidence-based enhanced recovery protocol reduced length of stay for bariatric surgery patients.
Major finding: Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers.
Study details: Data on 36 bariatric surgery centers and 4,700 patients who underwent procedures in the first 6 months of the data collection period.
Disclosures: Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.