User login
Talking with vaccine-hesitant parents takes training and finesse
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
CHICAGO – Addressing vaccine-hesitant parents can cause physicians considerable stress. However, they can feel more confident by adopting one of two communication strategies after gauging the strength of antivaccine beliefs, results of a pilot study suggest.
“We found that physicians frequently feel anxious and uncomfortable when confronted with parents who are strongly vaccine hesitant. They frequently lack confidence in dispelling the various safety concerns raised by parents and find themselves frequently combating an internal desire to just avoid the conflict,” said Paul J. Carson, MD, an expert in infectious diseases in the department of public health at North Dakota State University in Fargo.
The AAP suggests pediatricians adopt the “CASE method,” which stands for Corroborate parents’ concern, talk About me, describe the Science, and Explain/advise why they should vaccinate. The academy also recommends motivational interviewing as an additional tool to achieve vaccine acceptance. Ms. Dybsand, Dr. Carson, and their colleagues examined these two different approaches after training five pediatric providers. They also assessed physician perceptions about confidence and satisfaction regarding each method.
The pediatric providers were trained during a 7-hour retreat and 10 subsequent 1-hour training/debriefing sessions over 9 months. Explanations of vaccine safety and efficacy, vaccine licensure, how to refute common vaccine myths, and the two differing communication strategies were included in the training. Participants implemented the presumptive/CASE approach for 4 months then crossed over and used motivational interviewing for an additional 4 months.
“Some intensive training and education on the vaccine safety process and scientific evidence dispelling the common myths about vaccine safety were very helpful in boosting provider confidence,” Dr. Carson said.
“We want to be able to give them the tools to approach these conversations in an educated manner. We want them to feel like they have some ammunition behind the conversation,” said Ms. Dybsand, a graduate research assistant at the university.
The study revealed that the CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent. However, the investigators found the pediatricians perceived motivational interviewing as useful for the more strongly resistant parent. “For those really resistant parents who have looked at all the websites and are very concerned about vaccines, maybe motivational interviewing is the way to go,” Ms. Dybsand said. The goal of motivational interviewing is to build a trusting relationship over time. “You may not be giving that vaccine today, but you may be able to convince them in the future to vaccinate.”
The frequency and duration of training may be essential to success. “We didn’t really set out to find this, but it really takes more than 1 day of training to get providers to make a meaningful change in their communication strategies,” Ms. Dybsand said. When asked how long it might take the average pediatrician to become proficient in both techniques, she said that likely is a focus of future study.
The investigators plan to build on the success of the pilot study by expanding the research to multiple sites. In addition, they want to go beyond assessing provider perceptions of the communication techniques. Dr. Carson said, “These strategies need to be tested in formal clinical trials to see what is successful in actually increasing vaccine acceptance.”
Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Pediatricians can use tactics to help reduce the anxiety of discussing the importance of immunization with vaccine-hesitant parents.
Major finding: The CASE approach was easier to learn and used more readily when pediatricians encountered a moderately hesitant parent, but pediatricians perceived motivational interviewing as useful for the more strongly resistant parent.
Data source: Pilot study of five pediatric providers who received comprehensive training and ongoing support using different communication techniques.
Disclosures: Ms. Dybsand and Dr. Carson had no relevant financial disclosures.
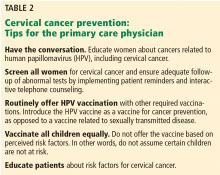
Disparities in cervical cancer in African American women: What primary care physicians can do
African American, Hispanic, American Indian, and Alaskan Native women continue to be disproportionately affected by cervical cancer compared with white women. From 2006 to 2010, the incidence of cervical cancer in African American women was 10.3 per 100,000; in white women it was 7.2.1 The mortality rate from cervical cancer in African American women is twice that in white women.1 Although cervical cancer rates have decreased nationwide, significant racial health disparities persist.
As the first-line healthcare providers for many women, the primary care physician and the general obstetrician-gynecologist are optimally positioned to reduce these disparities.
Cervical cancer is the third most common gynecologic cancer, after uterine and ovarian cancer. Nearly 13,000 new cases are diagnosed each year in the United States, and more than 4,000 women die of it.2 Fortunately, cervical cancer can be significantly prevented with adequate screening and vaccination against human papillomavirus (HPV).
WHY ARE BLACK WOMEN MORE LIKELY TO DIE OF CERVICAL CANCER?
Later stage at diagnosis. African American women are more likely to present with advanced cervical cancer than non-Hispanic white women.3–6
Less-aggressive treatment. African American women are more likely to receive no treatment after a cancer diagnosis.6 Differences in treatment may be attributed to comorbid conditions, stage at cancer diagnosis, and patient refusal.5,7
Less access to care. A study from the Surveillance, Epidemiology, and End Results program of the National Cancer Institute looked at 7,267 women (4,431 non-Hispanic white women, 1,830 Hispanic white women, and 1,006 non-Hispanic African American women) who were diagnosed with primary invasive cervical cancer from 1992 to 1996 and followed through 2000. African American women had a 19% higher mortality rate compared with non-Hispanic white women during follow-up despite adjusting for age, stage, histology, and time of first treatment.8
However, a later study from the same program found no such difference after 1995, when the data were adjusted for marital status, disease stage, age, treatment, grade, and histology.6
Equal access to healthcare may eliminate most of the disparity.7 A study in women with cervical cancer who sought treatment within the United States military healthcare system found no difference in treatment or 5- and 10-year survival rates between African American and white women.5 Equal access to comprehensive healthcare eliminated any disparity once cervical cancer was diagnosed.
CERVICAL CANCER SCREENING
The value of cervical cancer screening and prevention is well established. In 1941, Papanicolau reported that cervical cancer could be detected from vaginal smears.9 Since the development and widespread implementation of the “Pap” smear, cervical cancer rates have decreased dramatically in the United States.
Another major advance was the discovery that persistent infection with HPV is necessary for the development of cervical cancer, precancerous lesions, and genital warts.10
With advancing research, guidelines for cervical cancer screening have changed considerably over the years. Today, combined cervical cytologic and HPV testing is the mainstay. (Isolated HPV testing is generally not available outside clinical trials.)
Who should be screened?
Previous recommendations called for women to undergo Pap testing when they first became sexually active and then every year. However, cervical lesions are likely to regress in young women.11 One study found that 28% of cervical intimal neoplasia (CIN) grade 2 and 3 lesions spontaneously regressed by 15 weeks, although lesions associated with HPV 16 infection were less likely to regress than with other HPV types.12 A study of college women found that HPV infection persisted in only 9% of women after 24 months.13
To minimize unnecessary treatment of young women with dysplasia, the American Society for Colposcopy and Cervical Pathology in 2012 recommended cytologic screening for all women 21 years or older, regardless of age at first sexual encounter.14 Screening intervals were changed from every year to every 3 years until age 30, at which time cotesting with cytology and HPV testing is performed every 5 years. Routine cotesting is not recommended for women younger than 30, who have a high likelihood of HPV infection and spontaneous regression.
In 2014, the US Food and Drug Administration approved primary HPV screening (ie, testing for HPV first, and then performing cytology in samples that test positive) for women age 25 and older.15
Patients who need further evaluation and testing should be referred for colposcopy. The current guidelines for patients who have abnormal results on cervical cancer screening16 can be reviewed at www.asccp.org/asccp-guidelines.
As screening guidelines continue to evolve, primary care physicians will need to stay current and also help educate their patients. For example, many of our patients have undergone annual Pap screening for most of their lives and may not yet know about the new testing intervals.
Are there disparities in screening and follow-up?
Disparities in screening and follow-up may exist, but the evidence is not clear-cut.
In a 2013 National Health Interview Survey report, the rates of cervical cancer screening with Pap tests did not differ between African American and white women.17 However, the information on Pap testing was based on a single question asking participants if they had had a Pap test in the last 3 years. In our experience, patients may confuse Pap tests with speculum examinations.
Once women are screened, adequate and timely follow-up of abnormal results is key.
In a study from the National Breast and Cervical Cancer Early Detection Program,18 women who had cytology findings of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesions were to undergo repeat Pap testing every 4 to 6 months for 2 years. African American women were the least likely to have a follow-up Pap smear compared with other racial groups.
On the other hand, there was no difference related to race in follow-up rates of abnormal Pap tests in women ages 47 to 64 in the South Carolina Breast and Cervical Cancer Early Detection Program.19
In a study in an urban population (predominantly African African), the overall follow-up rate was only 26% at 12 months from an initial abnormal Pap smear. This study did not find any differences in follow-up according to race or ethnicity; however, it had insufficient power to detect a difference because only 15% of the study participants were white.20
What is in a genotype?
HPV is implicated in progression to both squamous cell carcinoma and adenocarcinoma of the cervix. Worldwide, HPV genotypes 16 and 18 are associated with 73% of cases of invasive cervical cancer; most of the remainder are associated with, in order of decreasing prevalence, genotypes 58, 33, 45, 31, 52, 35, 59, 39, 51, and 56.21
High-grade cervical lesions in African American women may less often be positive for HPV 16 and 18 than in white women.22,23 On the other hand, the proportion of non-Hispanic black women infected with HPV 35 and 58 was significantly higher than in non-Hispanic white women.22 Regardless, HPV screening is recommended for women of all races and ethnicities.
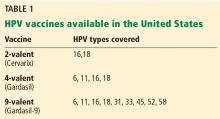
The 2-valent and 4-valent HPV vaccines do not cover HPV 35 or 58. The newer 9-valent vaccine covers HPV 58 (but not 35) and so may in theory decrease any potential disparity related to infection with a specific oncogenic subtype.
THE ROLE OF PREVENTION
HPV vaccination
The Females United to Unilaterally Reduce Endo/Ectocervical Disease study demonstrated that the 4-valent vaccine was highly effective against cervical intraepithelial neoplasia due to HPV 16 and 18.24 In another study, the 2-valent vaccine reduced the incidence of CIN 3 or higher by 87% in women who received all 3 doses and who had no evidence of HPV infection at baseline.25
HPV vaccination is expensive. Each shot costs about $130, plus the cost of administering it. Although the Vaccines for Children program covers the HPV vaccine for uninsured and underinsured children and adolescents under age 19, Medicaid coverage varies from state to state for adults over age 21.
The Advisory Committee on Immunization Practices (ACIP)26 recommends routine vaccination for:
- Males 11 or 12 years old
- Females ages 9 to 26.
In October 2016, the ACIP approved a 2-dose series given 6 to 12 months apart for patients starting vaccination at ages 9 through 14 years who are not immunocompromised. Others should receive a 3-dose series, with the second dose given 1 to 2 months after the first dose and the third dose given 6 months after the first dose.27 Previously, 3 doses were recommended for everyone.
Disparities in HPV vaccination rates
HPV vaccination rates among adolescents in the United States increased from 33.6% in 2013 to 41.7% in 2014.28 However, HPV vaccination rates continue to lag behind those of other routine vaccines, such as Tdap and meningococcal conjugate.
Reagan-Steiner et al28 reported that more black than white girls age 13 through 17 received at least 1 dose of a 3-dose HPV vaccination series, but more white girls received all 3 doses (70.6% vs 61.6%). In contrast, a meta-analysis by Fisher et al29 found African American and uninsured women generally less likely to initiate the HPV vaccination series. Kessels et al30 reported similar findings.
Barriers to HPV vaccination
Barriers to HPV vaccination can be provider-dependent, parental, or institutional.
Malo et al31 surveyed Florida Medicaid providers and found that those who participated in the Vaccines for Children program were less likely to cite lack of reimbursement as a barrier to vaccination.
Meites et al32 surveyed sexually transmitted disease clinics and found that common reasons for not offering HPV vaccine were cost, staff time, and difficulty coordinating follow-up visits to complete the series.
Providers report lack of urgency or lack of perception of cervical cancer as a true public health threat, safety concerns regarding the vaccine, and the inability to coadminister vaccines as barriers.33
Studies have shown that relatively few parents (up to 18%) of parents are concerned about the effect of the vaccine on sexual activity.34 Rather, they are most likely to cite lack of information regarding the vaccine, lack of physician recommendation, and not knowing where to receive the vaccine as barriers.35,36
Guerry et al37 determined that the single most important factor in vaccine initiation was physician recommendation, a finding reiterated in other studies.35,38 A study in North Carolina identified failure of physician recommendation as one of the missed opportunities for vaccination of young women.39
Therefore, the primary care physician, as the initial contact with the child or young adult, holds a responsibility to narrow this gap. In simply discussing and recommending the vaccine, physicians could increase vaccination rates.
REPRODUCTIVE HEALTH
Although 80% of women will be infected with HPV in their lifetime, only a small proportion will develop cervical cancer, suggesting there are other cofactors in the progression to cervical cancer.40
Given the infectious etiology of cervical cancer, other contributing reproductive health factors have been described. As expected, the number of sexual partners correlates with HPV infection.41,42 Younger age at first intercourse has been linked to development of cervical neoplasia, consistent with persistent infection leading to neoplasia.41,42
Primary care physicians should provide timely and comprehensive sexual education, including information on safe sexual practices and pregnancy prevention.
Human immunodeficiency virus
In 2010, the estimated rate of new human immunodeficiency virus (HIV) infections in African American women was nearly 20 times greater than in white women.43 Previous studies have shown a clear relationship between HIV and HPV-associated cancers, including cervical neoplasia and invasive cervical cancer.44,45
Women with HIV should receive screening for cervical cancer at the time of diagnosis, 6 months after the initial diagnosis, and annually thereafter.46
Conflicting evidence exists regarding the effect of highly active antiretroviral therapy on the incidence of HPV-related disease, so aggressive screening and management of cervical neoplasia is recommended for women with HIV, regardless of CD4+ levels or viral load.47–49
Additional infectious culprits
Coinfection with other sexually transmitted infections, specifically Chlamydia, herpes, and HIV, has been associated with cervical neoplasia and invasive cervical cancer. A positive linear association exists between the number of sexually transmitted infections and cervical neoplasia.50
C trachomatis is the most common sexually transmitted infection in the United States, with a 6-times higher rate in African American women.51 Women who are seropositive for C trachomatis are at twofold higher risk of developing squamous cell cervical cancer.52,53 Women who are seropositive for Chlamydia infection, herpes virus 2, or HPV are at markedly increased risk of invasive cervical cancer.50
Tobacco use
The negative impact of smoking on numerous other cancers resulted in investigation of its role in cervical cancer.
Early case-control studies found an association between cervical cancer and smoking,54 but because these studies did not account for HPV infection status, they could not establish causality. Subsequently, several studies did control for HPV infection; the risk of squamous cervical cancer was twice as high in women who had ever smoked.55 Furthermore, the more cigarettes smoked per day, the higher the risk of cervical neoplasia.41,56
According to the US Centers for Disease Control and Prevention in 2014, the highest prevalence of smoking was among American Indian and Alaskan Native women, 32.5% of whom said they smoked every day, compared with 17.2% of white women and 13.7% of African American women.57
HOW CAN PRIMARY CARE PHYSICIANS CLOSE THE GAP?
By promoting HPV vaccination to children and young adults, primary care physicians can help prevent cervical cancer. Moreover, primary care physicians will see most adolescents for a nonpreventive health visit, an optimal opportunity to discuss sexual activity practices and HPV vaccination.58 Including the HPV vaccine as routine with other vaccinations can close the gap.38
Screening and treatment of sexually transmitted infection during these visits can affect the risk that future HPV infection will progress to neoplasia or cancer. Persistent lifestyle modification counseling, especially smoking cessation through motivational interviewing, can lessen the risk of cervical cancer neoplasia progression.
Additionally, in light of recent changes in cervical cancer screening guidelines, the primary care physician’s role as educator is of utmost importance. In one study, although 99% of women had received a Pap test, 87% could not identify the purpose of the Pap test.59 The primary care physician’s role is perhaps the most influential in preventing disease and, as such, has the greatest impact on a patient’s disease process.
- Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin 2014; 64:9–29.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015; 65:5–29.
- Koh WJ, Greer BE, Abu-Rustum NR, et al. Cervical cancer, version 2.2015. J Natl Compr Canc Netw 2015; 13:395-404.
- Farley J, Risinger JI, Rose GS, Maxwell GL. Racial disparities in blacks with gynecologic cancers. Cancer 2007; 110:234–243.
- Farley JH, Hines JF, Taylor RR, et al. Equal care ensures equal survival for African-American women with cervical carcinoma. Cancer 2001; 91:869–873.
- Rauh-Hain JA, Clemmer JT, Bradford LS, et al. Racial disparities in cervical cancer survival over time. Cancer 2013; 119:3644–3652.
- Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: a report from the Health Disparities Taskforce of the Society of Gynecologic Oncology. Gynecol Oncol 2014; 133:353–361.
- Patel DA, Barnholtz-Sloan JS, Patel MK, Malone JM Jr, Chuba PJ, Schwartz K. A population-based study of racial and ethnic differences in survival among women with invasive cervical cancer: analysis of surveillance, epidemiology, and end results data. Gynecol Oncol 2005; 97:550–558.
- Papanicolaou GN, Traut HF. The diagnostic value of vaginal smears in carcinoma of the uterus. 1941. Arch Pathol Lab Med 1997; 121:211–224.
- Walboomers JM, Jacobs M V, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999; 189:12–19.
- Moscicki AB, Shiboski S, Hills NK, et al. Regression of low-grade squamous intra-epithelial lesions in young women. Lancet 2004; 364:1678–1683.
- Trimble CL, Piantadosi S, Gravitt P, et al. Spontaneous regression of high-grade cervical dysplasia: effects of human papillomavirus type and HLA phenotype. Clin Cancer Res 2005; 11:4717–4723.
- Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998; 338:423-428.
- Saslow D, Solomon D, Lawson HW, et al; ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin 2012; 62:147–172.
- Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Obstet Gynecol 2015; 125:330–337.
- Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 2013; 17(suppl 1):S1–S27.
- Sabatino SA, White MC, Thompson TD, Klabunde CN. Cancer screening test use—United States, 2013. MMWR 2015; 64:464–468.
- Benard VB, Lawson HW, Eheman CR, Anderson C, Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstet Gynecol 2005; 105:1323–1328.
- Eggleston KS, Coker AL, Luchok KJ, Meyer TE. Adherence to recommendations for follow-up to abnormal Pap tests. Obstet Gynecol 2007; 109:1332–1341.
- Peterson NB, Han J, Freund KM. Inadequate follow-up for abnormal Pap smears in an urban population. J Natl Med Assoc 2003; 95:825–832.
- Li N, Franceschi S, Howell-Jones R, Snijders PJ, Clifford GM. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: variation by geographical region, histological type and year of publication. Int J Cancer 2011; 128:927–935.
- Hariri S, Unger ER, Powell SE, et al; HPV-IMPACT Working Group. Human papillomavirus genotypes in high-grade cervical lesions in the United States. J Infect Dis 2012; 206:1878–1886.
- Niccolai LM, Russ C, Julian PJ, et al. Individual and geographic disparities in human papillomavirus types 16/18 in high-grade cervical lesions: associations with race, ethnicity, and poverty. Cancer 2013; 119:3052–3058.
- FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 2007; 356:1915–1927.
- Paavonen J, Naud P, Salmerón J, et al; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 2009; 374:301–314.
- Centers for Disease Control and Prevention (CDC). Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep 2011; 60:1705–1708.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65:1405–1408.
- Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2014. MMWR Morb Mortal Wkly Rep 2015; 64:784–792.
- Fisher H, Trotter CL, Audrey S, MacDonald-Wallis K, Hickman M. Inequalities in the uptake of human papillomavirus vaccination: a systematic review and meta-analysis. Int J Epidemiol 2013; 42:896–908.
- Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine 2012; 30:3546–3556.
- Malo TL, Hassani D, Staras SA, Shenkman EA, Giuliano AR, Vadaparampil ST. Do Florida Medicaid providers’ barriers to HPV vaccination vary based on VFC program participation? Matern Child Health J 2013; 17:609–615.
- Meites E, Llata E, Hariri S, et al. HPV vaccine implementation in STD clinics—STD Surveillance Network. Sex Transm Dis 2012; 39:32–34.
- Perkins RB, Clark JA. What affects human papillomavirus vaccination rates? A qualitative analysis of providers’ perceptions. Womens Health Issues 2012; 22:e379–e386.
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014; 168:76–82.
- Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008–2009. Pediatrics 2011; 128:830–839.
- Bastani R, Glenn BA, Tsui J, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomarkers Prev 2011; 20:1463–1472.
- Guerry SL, De Rosa CJ, Markowitz LE, et al. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 2011; 29:2235–2241.
- Hull PC, Williams EA, Khabele D, Dean C, Bond B, Sanderson M. HPV vaccine use among African American girls: qualitative formative research using a participatory social marketing approach. Gynecol Oncol 2014; 132(suppl 1):S13–S20.
- Brewer NT, Gottlieb SL, Reiter PL, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis 2011; 38:197–204.
- Wang SS, Zuna RE, Wentzensen N, et al. Human papillomavirus cofactors by disease progression and human papillomavirus types in the study to understand cervical cancer early endpoints and determinants. Cancer Epidemiol Biomarkers Prev 2009; 18:113–120.
- Deacon JM, Evans CD, Yule R, et al. Sexual behaviour and smoking as determinants of cervical HPV infection and of CIN3 among those infected: a case-control study nested within the Manchester cohort. Br J Cancer 2000; 83:1565–1572.
- International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and sexual behavior: collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol Biomarkers Prev 2009; 18:1060–1069.
- Centers for Disease Control and Prevention (CDC). Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012; 17(No. 4). https://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. Accessed September 12, 2017.
- Frisch M, Biggar RJ, Goedert JJ. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst 2000; 92:1500–1510.
- Schäfer A, Friedmann W, Mielke M, Schwartländer B, Koch MA. The increased frequency of cervical dysplasia-neoplasia in women infected with the human immunodeficiency virus is related to the degree of immunosuppression. Am J Obstet Gynecol 1991; 164:593–599.
- Phillips AA, Justman JE. Screening HIV-infected patients for non-AIDS-defining malignancies. Curr HIV/AIDS Rep 2009; 6:83–92.
- De Vuyst H, Lillo F, Broutet N, Smith JS. HIV, human papillomavirus, and cervical neoplasia and cancer in the era of highly active antiretroviral therapy. Eur J Cancer Prev 2008; 17:545–554.
- Palefsky JM. Cervical human papillomavirus infection and cervical intraepithelial neoplasia in women positive for human immunodeficiency virus in the era of highly active antiretroviral therapy. Curr Opin Oncol 2003; 15:382–388.
- Adler DH. The impact of HAART on HPV-related cervical disease. Curr HIV Res 2010; 8:493–497.
- Castellsagué X, Pawlita M, Roura E, et al. Prospective seroepidemiologic study on the role of human papillomavirus and other infections in cervical carcinogenesis: evidence from the EPIC cohort. Int J Cancer 2014; 135:440–452.
- Centers for Disease Control and Prevention (CDC). 2013 sexually transmitted disease surveillance. www.cdc.gov/std/stats13/exordium.htm. Accessed September 12, 2017.
- Smith JS, Bosetti C, Muñoz N, et al; IARC multicentric case-control study. Chlamydia trachomatis and invasive cervical cancer: a pooled analysis of the IARC multicentric case-control study. Int J Cancer 2004; 111:431–439.
- Koskela P, Anttila T, Bjørge T, et al. Chlamydia trachomatis infection as a risk factor for invasive cervical cancer. Int J Cancer 2000; 85:35–39.
- Office on Smoking and Health (US). Women and smoking: a report of the Surgeon General: Chapter 3. Health consequences of tobacco use among women. http://www.ncbi.nlm.nih.gov/books/NBK44312. Accessed September 12, 2017.
- Plummer M, Herrero R, Franceschi S, et al; IARC Multi-centre Cervical Cancer Study Group. Smoking and cervical cancer: pooled analysis of the IARC multi-centric case—control study. Cancer Causes Control 2003; 14:805–814.
- Ho GY, Kadish AS, Burk RD, et al. HPV 16 and cigarette smoking as risk factors for high-grade cervical intra-epithelial neoplasia. Int J Cancer 1998; 78:281–285.
- Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults - United States, 2005-2014. MMWR Morb Mortal Wkly Rep 2015; 64:1233–1240.
- Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med 2010; 8:511–516.
- Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol 2002; 186:938–943.
African American, Hispanic, American Indian, and Alaskan Native women continue to be disproportionately affected by cervical cancer compared with white women. From 2006 to 2010, the incidence of cervical cancer in African American women was 10.3 per 100,000; in white women it was 7.2.1 The mortality rate from cervical cancer in African American women is twice that in white women.1 Although cervical cancer rates have decreased nationwide, significant racial health disparities persist.
As the first-line healthcare providers for many women, the primary care physician and the general obstetrician-gynecologist are optimally positioned to reduce these disparities.
Cervical cancer is the third most common gynecologic cancer, after uterine and ovarian cancer. Nearly 13,000 new cases are diagnosed each year in the United States, and more than 4,000 women die of it.2 Fortunately, cervical cancer can be significantly prevented with adequate screening and vaccination against human papillomavirus (HPV).
WHY ARE BLACK WOMEN MORE LIKELY TO DIE OF CERVICAL CANCER?
Later stage at diagnosis. African American women are more likely to present with advanced cervical cancer than non-Hispanic white women.3–6
Less-aggressive treatment. African American women are more likely to receive no treatment after a cancer diagnosis.6 Differences in treatment may be attributed to comorbid conditions, stage at cancer diagnosis, and patient refusal.5,7
Less access to care. A study from the Surveillance, Epidemiology, and End Results program of the National Cancer Institute looked at 7,267 women (4,431 non-Hispanic white women, 1,830 Hispanic white women, and 1,006 non-Hispanic African American women) who were diagnosed with primary invasive cervical cancer from 1992 to 1996 and followed through 2000. African American women had a 19% higher mortality rate compared with non-Hispanic white women during follow-up despite adjusting for age, stage, histology, and time of first treatment.8
However, a later study from the same program found no such difference after 1995, when the data were adjusted for marital status, disease stage, age, treatment, grade, and histology.6
Equal access to healthcare may eliminate most of the disparity.7 A study in women with cervical cancer who sought treatment within the United States military healthcare system found no difference in treatment or 5- and 10-year survival rates between African American and white women.5 Equal access to comprehensive healthcare eliminated any disparity once cervical cancer was diagnosed.
CERVICAL CANCER SCREENING
The value of cervical cancer screening and prevention is well established. In 1941, Papanicolau reported that cervical cancer could be detected from vaginal smears.9 Since the development and widespread implementation of the “Pap” smear, cervical cancer rates have decreased dramatically in the United States.
Another major advance was the discovery that persistent infection with HPV is necessary for the development of cervical cancer, precancerous lesions, and genital warts.10
With advancing research, guidelines for cervical cancer screening have changed considerably over the years. Today, combined cervical cytologic and HPV testing is the mainstay. (Isolated HPV testing is generally not available outside clinical trials.)
Who should be screened?
Previous recommendations called for women to undergo Pap testing when they first became sexually active and then every year. However, cervical lesions are likely to regress in young women.11 One study found that 28% of cervical intimal neoplasia (CIN) grade 2 and 3 lesions spontaneously regressed by 15 weeks, although lesions associated with HPV 16 infection were less likely to regress than with other HPV types.12 A study of college women found that HPV infection persisted in only 9% of women after 24 months.13
To minimize unnecessary treatment of young women with dysplasia, the American Society for Colposcopy and Cervical Pathology in 2012 recommended cytologic screening for all women 21 years or older, regardless of age at first sexual encounter.14 Screening intervals were changed from every year to every 3 years until age 30, at which time cotesting with cytology and HPV testing is performed every 5 years. Routine cotesting is not recommended for women younger than 30, who have a high likelihood of HPV infection and spontaneous regression.
In 2014, the US Food and Drug Administration approved primary HPV screening (ie, testing for HPV first, and then performing cytology in samples that test positive) for women age 25 and older.15
Patients who need further evaluation and testing should be referred for colposcopy. The current guidelines for patients who have abnormal results on cervical cancer screening16 can be reviewed at www.asccp.org/asccp-guidelines.
As screening guidelines continue to evolve, primary care physicians will need to stay current and also help educate their patients. For example, many of our patients have undergone annual Pap screening for most of their lives and may not yet know about the new testing intervals.
Are there disparities in screening and follow-up?
Disparities in screening and follow-up may exist, but the evidence is not clear-cut.
In a 2013 National Health Interview Survey report, the rates of cervical cancer screening with Pap tests did not differ between African American and white women.17 However, the information on Pap testing was based on a single question asking participants if they had had a Pap test in the last 3 years. In our experience, patients may confuse Pap tests with speculum examinations.
Once women are screened, adequate and timely follow-up of abnormal results is key.
In a study from the National Breast and Cervical Cancer Early Detection Program,18 women who had cytology findings of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesions were to undergo repeat Pap testing every 4 to 6 months for 2 years. African American women were the least likely to have a follow-up Pap smear compared with other racial groups.
On the other hand, there was no difference related to race in follow-up rates of abnormal Pap tests in women ages 47 to 64 in the South Carolina Breast and Cervical Cancer Early Detection Program.19
In a study in an urban population (predominantly African African), the overall follow-up rate was only 26% at 12 months from an initial abnormal Pap smear. This study did not find any differences in follow-up according to race or ethnicity; however, it had insufficient power to detect a difference because only 15% of the study participants were white.20
What is in a genotype?
HPV is implicated in progression to both squamous cell carcinoma and adenocarcinoma of the cervix. Worldwide, HPV genotypes 16 and 18 are associated with 73% of cases of invasive cervical cancer; most of the remainder are associated with, in order of decreasing prevalence, genotypes 58, 33, 45, 31, 52, 35, 59, 39, 51, and 56.21
High-grade cervical lesions in African American women may less often be positive for HPV 16 and 18 than in white women.22,23 On the other hand, the proportion of non-Hispanic black women infected with HPV 35 and 58 was significantly higher than in non-Hispanic white women.22 Regardless, HPV screening is recommended for women of all races and ethnicities.
The 2-valent and 4-valent HPV vaccines do not cover HPV 35 or 58. The newer 9-valent vaccine covers HPV 58 (but not 35) and so may in theory decrease any potential disparity related to infection with a specific oncogenic subtype.
THE ROLE OF PREVENTION
HPV vaccination
The Females United to Unilaterally Reduce Endo/Ectocervical Disease study demonstrated that the 4-valent vaccine was highly effective against cervical intraepithelial neoplasia due to HPV 16 and 18.24 In another study, the 2-valent vaccine reduced the incidence of CIN 3 or higher by 87% in women who received all 3 doses and who had no evidence of HPV infection at baseline.25
HPV vaccination is expensive. Each shot costs about $130, plus the cost of administering it. Although the Vaccines for Children program covers the HPV vaccine for uninsured and underinsured children and adolescents under age 19, Medicaid coverage varies from state to state for adults over age 21.
The Advisory Committee on Immunization Practices (ACIP)26 recommends routine vaccination for:
- Males 11 or 12 years old
- Females ages 9 to 26.
In October 2016, the ACIP approved a 2-dose series given 6 to 12 months apart for patients starting vaccination at ages 9 through 14 years who are not immunocompromised. Others should receive a 3-dose series, with the second dose given 1 to 2 months after the first dose and the third dose given 6 months after the first dose.27 Previously, 3 doses were recommended for everyone.
Disparities in HPV vaccination rates
HPV vaccination rates among adolescents in the United States increased from 33.6% in 2013 to 41.7% in 2014.28 However, HPV vaccination rates continue to lag behind those of other routine vaccines, such as Tdap and meningococcal conjugate.
Reagan-Steiner et al28 reported that more black than white girls age 13 through 17 received at least 1 dose of a 3-dose HPV vaccination series, but more white girls received all 3 doses (70.6% vs 61.6%). In contrast, a meta-analysis by Fisher et al29 found African American and uninsured women generally less likely to initiate the HPV vaccination series. Kessels et al30 reported similar findings.
Barriers to HPV vaccination
Barriers to HPV vaccination can be provider-dependent, parental, or institutional.
Malo et al31 surveyed Florida Medicaid providers and found that those who participated in the Vaccines for Children program were less likely to cite lack of reimbursement as a barrier to vaccination.
Meites et al32 surveyed sexually transmitted disease clinics and found that common reasons for not offering HPV vaccine were cost, staff time, and difficulty coordinating follow-up visits to complete the series.
Providers report lack of urgency or lack of perception of cervical cancer as a true public health threat, safety concerns regarding the vaccine, and the inability to coadminister vaccines as barriers.33
Studies have shown that relatively few parents (up to 18%) of parents are concerned about the effect of the vaccine on sexual activity.34 Rather, they are most likely to cite lack of information regarding the vaccine, lack of physician recommendation, and not knowing where to receive the vaccine as barriers.35,36
Guerry et al37 determined that the single most important factor in vaccine initiation was physician recommendation, a finding reiterated in other studies.35,38 A study in North Carolina identified failure of physician recommendation as one of the missed opportunities for vaccination of young women.39
Therefore, the primary care physician, as the initial contact with the child or young adult, holds a responsibility to narrow this gap. In simply discussing and recommending the vaccine, physicians could increase vaccination rates.
REPRODUCTIVE HEALTH
Although 80% of women will be infected with HPV in their lifetime, only a small proportion will develop cervical cancer, suggesting there are other cofactors in the progression to cervical cancer.40
Given the infectious etiology of cervical cancer, other contributing reproductive health factors have been described. As expected, the number of sexual partners correlates with HPV infection.41,42 Younger age at first intercourse has been linked to development of cervical neoplasia, consistent with persistent infection leading to neoplasia.41,42
Primary care physicians should provide timely and comprehensive sexual education, including information on safe sexual practices and pregnancy prevention.
Human immunodeficiency virus
In 2010, the estimated rate of new human immunodeficiency virus (HIV) infections in African American women was nearly 20 times greater than in white women.43 Previous studies have shown a clear relationship between HIV and HPV-associated cancers, including cervical neoplasia and invasive cervical cancer.44,45
Women with HIV should receive screening for cervical cancer at the time of diagnosis, 6 months after the initial diagnosis, and annually thereafter.46
Conflicting evidence exists regarding the effect of highly active antiretroviral therapy on the incidence of HPV-related disease, so aggressive screening and management of cervical neoplasia is recommended for women with HIV, regardless of CD4+ levels or viral load.47–49
Additional infectious culprits
Coinfection with other sexually transmitted infections, specifically Chlamydia, herpes, and HIV, has been associated with cervical neoplasia and invasive cervical cancer. A positive linear association exists between the number of sexually transmitted infections and cervical neoplasia.50
C trachomatis is the most common sexually transmitted infection in the United States, with a 6-times higher rate in African American women.51 Women who are seropositive for C trachomatis are at twofold higher risk of developing squamous cell cervical cancer.52,53 Women who are seropositive for Chlamydia infection, herpes virus 2, or HPV are at markedly increased risk of invasive cervical cancer.50
Tobacco use
The negative impact of smoking on numerous other cancers resulted in investigation of its role in cervical cancer.
Early case-control studies found an association between cervical cancer and smoking,54 but because these studies did not account for HPV infection status, they could not establish causality. Subsequently, several studies did control for HPV infection; the risk of squamous cervical cancer was twice as high in women who had ever smoked.55 Furthermore, the more cigarettes smoked per day, the higher the risk of cervical neoplasia.41,56
According to the US Centers for Disease Control and Prevention in 2014, the highest prevalence of smoking was among American Indian and Alaskan Native women, 32.5% of whom said they smoked every day, compared with 17.2% of white women and 13.7% of African American women.57
HOW CAN PRIMARY CARE PHYSICIANS CLOSE THE GAP?
By promoting HPV vaccination to children and young adults, primary care physicians can help prevent cervical cancer. Moreover, primary care physicians will see most adolescents for a nonpreventive health visit, an optimal opportunity to discuss sexual activity practices and HPV vaccination.58 Including the HPV vaccine as routine with other vaccinations can close the gap.38
Screening and treatment of sexually transmitted infection during these visits can affect the risk that future HPV infection will progress to neoplasia or cancer. Persistent lifestyle modification counseling, especially smoking cessation through motivational interviewing, can lessen the risk of cervical cancer neoplasia progression.
Additionally, in light of recent changes in cervical cancer screening guidelines, the primary care physician’s role as educator is of utmost importance. In one study, although 99% of women had received a Pap test, 87% could not identify the purpose of the Pap test.59 The primary care physician’s role is perhaps the most influential in preventing disease and, as such, has the greatest impact on a patient’s disease process.
African American, Hispanic, American Indian, and Alaskan Native women continue to be disproportionately affected by cervical cancer compared with white women. From 2006 to 2010, the incidence of cervical cancer in African American women was 10.3 per 100,000; in white women it was 7.2.1 The mortality rate from cervical cancer in African American women is twice that in white women.1 Although cervical cancer rates have decreased nationwide, significant racial health disparities persist.
As the first-line healthcare providers for many women, the primary care physician and the general obstetrician-gynecologist are optimally positioned to reduce these disparities.
Cervical cancer is the third most common gynecologic cancer, after uterine and ovarian cancer. Nearly 13,000 new cases are diagnosed each year in the United States, and more than 4,000 women die of it.2 Fortunately, cervical cancer can be significantly prevented with adequate screening and vaccination against human papillomavirus (HPV).
WHY ARE BLACK WOMEN MORE LIKELY TO DIE OF CERVICAL CANCER?
Later stage at diagnosis. African American women are more likely to present with advanced cervical cancer than non-Hispanic white women.3–6
Less-aggressive treatment. African American women are more likely to receive no treatment after a cancer diagnosis.6 Differences in treatment may be attributed to comorbid conditions, stage at cancer diagnosis, and patient refusal.5,7
Less access to care. A study from the Surveillance, Epidemiology, and End Results program of the National Cancer Institute looked at 7,267 women (4,431 non-Hispanic white women, 1,830 Hispanic white women, and 1,006 non-Hispanic African American women) who were diagnosed with primary invasive cervical cancer from 1992 to 1996 and followed through 2000. African American women had a 19% higher mortality rate compared with non-Hispanic white women during follow-up despite adjusting for age, stage, histology, and time of first treatment.8
However, a later study from the same program found no such difference after 1995, when the data were adjusted for marital status, disease stage, age, treatment, grade, and histology.6
Equal access to healthcare may eliminate most of the disparity.7 A study in women with cervical cancer who sought treatment within the United States military healthcare system found no difference in treatment or 5- and 10-year survival rates between African American and white women.5 Equal access to comprehensive healthcare eliminated any disparity once cervical cancer was diagnosed.
CERVICAL CANCER SCREENING
The value of cervical cancer screening and prevention is well established. In 1941, Papanicolau reported that cervical cancer could be detected from vaginal smears.9 Since the development and widespread implementation of the “Pap” smear, cervical cancer rates have decreased dramatically in the United States.
Another major advance was the discovery that persistent infection with HPV is necessary for the development of cervical cancer, precancerous lesions, and genital warts.10
With advancing research, guidelines for cervical cancer screening have changed considerably over the years. Today, combined cervical cytologic and HPV testing is the mainstay. (Isolated HPV testing is generally not available outside clinical trials.)
Who should be screened?
Previous recommendations called for women to undergo Pap testing when they first became sexually active and then every year. However, cervical lesions are likely to regress in young women.11 One study found that 28% of cervical intimal neoplasia (CIN) grade 2 and 3 lesions spontaneously regressed by 15 weeks, although lesions associated with HPV 16 infection were less likely to regress than with other HPV types.12 A study of college women found that HPV infection persisted in only 9% of women after 24 months.13
To minimize unnecessary treatment of young women with dysplasia, the American Society for Colposcopy and Cervical Pathology in 2012 recommended cytologic screening for all women 21 years or older, regardless of age at first sexual encounter.14 Screening intervals were changed from every year to every 3 years until age 30, at which time cotesting with cytology and HPV testing is performed every 5 years. Routine cotesting is not recommended for women younger than 30, who have a high likelihood of HPV infection and spontaneous regression.
In 2014, the US Food and Drug Administration approved primary HPV screening (ie, testing for HPV first, and then performing cytology in samples that test positive) for women age 25 and older.15
Patients who need further evaluation and testing should be referred for colposcopy. The current guidelines for patients who have abnormal results on cervical cancer screening16 can be reviewed at www.asccp.org/asccp-guidelines.
As screening guidelines continue to evolve, primary care physicians will need to stay current and also help educate their patients. For example, many of our patients have undergone annual Pap screening for most of their lives and may not yet know about the new testing intervals.
Are there disparities in screening and follow-up?
Disparities in screening and follow-up may exist, but the evidence is not clear-cut.
In a 2013 National Health Interview Survey report, the rates of cervical cancer screening with Pap tests did not differ between African American and white women.17 However, the information on Pap testing was based on a single question asking participants if they had had a Pap test in the last 3 years. In our experience, patients may confuse Pap tests with speculum examinations.
Once women are screened, adequate and timely follow-up of abnormal results is key.
In a study from the National Breast and Cervical Cancer Early Detection Program,18 women who had cytology findings of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesions were to undergo repeat Pap testing every 4 to 6 months for 2 years. African American women were the least likely to have a follow-up Pap smear compared with other racial groups.
On the other hand, there was no difference related to race in follow-up rates of abnormal Pap tests in women ages 47 to 64 in the South Carolina Breast and Cervical Cancer Early Detection Program.19
In a study in an urban population (predominantly African African), the overall follow-up rate was only 26% at 12 months from an initial abnormal Pap smear. This study did not find any differences in follow-up according to race or ethnicity; however, it had insufficient power to detect a difference because only 15% of the study participants were white.20
What is in a genotype?
HPV is implicated in progression to both squamous cell carcinoma and adenocarcinoma of the cervix. Worldwide, HPV genotypes 16 and 18 are associated with 73% of cases of invasive cervical cancer; most of the remainder are associated with, in order of decreasing prevalence, genotypes 58, 33, 45, 31, 52, 35, 59, 39, 51, and 56.21
High-grade cervical lesions in African American women may less often be positive for HPV 16 and 18 than in white women.22,23 On the other hand, the proportion of non-Hispanic black women infected with HPV 35 and 58 was significantly higher than in non-Hispanic white women.22 Regardless, HPV screening is recommended for women of all races and ethnicities.
The 2-valent and 4-valent HPV vaccines do not cover HPV 35 or 58. The newer 9-valent vaccine covers HPV 58 (but not 35) and so may in theory decrease any potential disparity related to infection with a specific oncogenic subtype.
THE ROLE OF PREVENTION
HPV vaccination
The Females United to Unilaterally Reduce Endo/Ectocervical Disease study demonstrated that the 4-valent vaccine was highly effective against cervical intraepithelial neoplasia due to HPV 16 and 18.24 In another study, the 2-valent vaccine reduced the incidence of CIN 3 or higher by 87% in women who received all 3 doses and who had no evidence of HPV infection at baseline.25
HPV vaccination is expensive. Each shot costs about $130, plus the cost of administering it. Although the Vaccines for Children program covers the HPV vaccine for uninsured and underinsured children and adolescents under age 19, Medicaid coverage varies from state to state for adults over age 21.
The Advisory Committee on Immunization Practices (ACIP)26 recommends routine vaccination for:
- Males 11 or 12 years old
- Females ages 9 to 26.
In October 2016, the ACIP approved a 2-dose series given 6 to 12 months apart for patients starting vaccination at ages 9 through 14 years who are not immunocompromised. Others should receive a 3-dose series, with the second dose given 1 to 2 months after the first dose and the third dose given 6 months after the first dose.27 Previously, 3 doses were recommended for everyone.
Disparities in HPV vaccination rates
HPV vaccination rates among adolescents in the United States increased from 33.6% in 2013 to 41.7% in 2014.28 However, HPV vaccination rates continue to lag behind those of other routine vaccines, such as Tdap and meningococcal conjugate.
Reagan-Steiner et al28 reported that more black than white girls age 13 through 17 received at least 1 dose of a 3-dose HPV vaccination series, but more white girls received all 3 doses (70.6% vs 61.6%). In contrast, a meta-analysis by Fisher et al29 found African American and uninsured women generally less likely to initiate the HPV vaccination series. Kessels et al30 reported similar findings.
Barriers to HPV vaccination
Barriers to HPV vaccination can be provider-dependent, parental, or institutional.
Malo et al31 surveyed Florida Medicaid providers and found that those who participated in the Vaccines for Children program were less likely to cite lack of reimbursement as a barrier to vaccination.
Meites et al32 surveyed sexually transmitted disease clinics and found that common reasons for not offering HPV vaccine were cost, staff time, and difficulty coordinating follow-up visits to complete the series.
Providers report lack of urgency or lack of perception of cervical cancer as a true public health threat, safety concerns regarding the vaccine, and the inability to coadminister vaccines as barriers.33
Studies have shown that relatively few parents (up to 18%) of parents are concerned about the effect of the vaccine on sexual activity.34 Rather, they are most likely to cite lack of information regarding the vaccine, lack of physician recommendation, and not knowing where to receive the vaccine as barriers.35,36
Guerry et al37 determined that the single most important factor in vaccine initiation was physician recommendation, a finding reiterated in other studies.35,38 A study in North Carolina identified failure of physician recommendation as one of the missed opportunities for vaccination of young women.39
Therefore, the primary care physician, as the initial contact with the child or young adult, holds a responsibility to narrow this gap. In simply discussing and recommending the vaccine, physicians could increase vaccination rates.
REPRODUCTIVE HEALTH
Although 80% of women will be infected with HPV in their lifetime, only a small proportion will develop cervical cancer, suggesting there are other cofactors in the progression to cervical cancer.40
Given the infectious etiology of cervical cancer, other contributing reproductive health factors have been described. As expected, the number of sexual partners correlates with HPV infection.41,42 Younger age at first intercourse has been linked to development of cervical neoplasia, consistent with persistent infection leading to neoplasia.41,42
Primary care physicians should provide timely and comprehensive sexual education, including information on safe sexual practices and pregnancy prevention.
Human immunodeficiency virus
In 2010, the estimated rate of new human immunodeficiency virus (HIV) infections in African American women was nearly 20 times greater than in white women.43 Previous studies have shown a clear relationship between HIV and HPV-associated cancers, including cervical neoplasia and invasive cervical cancer.44,45
Women with HIV should receive screening for cervical cancer at the time of diagnosis, 6 months after the initial diagnosis, and annually thereafter.46
Conflicting evidence exists regarding the effect of highly active antiretroviral therapy on the incidence of HPV-related disease, so aggressive screening and management of cervical neoplasia is recommended for women with HIV, regardless of CD4+ levels or viral load.47–49
Additional infectious culprits
Coinfection with other sexually transmitted infections, specifically Chlamydia, herpes, and HIV, has been associated with cervical neoplasia and invasive cervical cancer. A positive linear association exists between the number of sexually transmitted infections and cervical neoplasia.50
C trachomatis is the most common sexually transmitted infection in the United States, with a 6-times higher rate in African American women.51 Women who are seropositive for C trachomatis are at twofold higher risk of developing squamous cell cervical cancer.52,53 Women who are seropositive for Chlamydia infection, herpes virus 2, or HPV are at markedly increased risk of invasive cervical cancer.50
Tobacco use
The negative impact of smoking on numerous other cancers resulted in investigation of its role in cervical cancer.
Early case-control studies found an association between cervical cancer and smoking,54 but because these studies did not account for HPV infection status, they could not establish causality. Subsequently, several studies did control for HPV infection; the risk of squamous cervical cancer was twice as high in women who had ever smoked.55 Furthermore, the more cigarettes smoked per day, the higher the risk of cervical neoplasia.41,56
According to the US Centers for Disease Control and Prevention in 2014, the highest prevalence of smoking was among American Indian and Alaskan Native women, 32.5% of whom said they smoked every day, compared with 17.2% of white women and 13.7% of African American women.57
HOW CAN PRIMARY CARE PHYSICIANS CLOSE THE GAP?
By promoting HPV vaccination to children and young adults, primary care physicians can help prevent cervical cancer. Moreover, primary care physicians will see most adolescents for a nonpreventive health visit, an optimal opportunity to discuss sexual activity practices and HPV vaccination.58 Including the HPV vaccine as routine with other vaccinations can close the gap.38
Screening and treatment of sexually transmitted infection during these visits can affect the risk that future HPV infection will progress to neoplasia or cancer. Persistent lifestyle modification counseling, especially smoking cessation through motivational interviewing, can lessen the risk of cervical cancer neoplasia progression.
Additionally, in light of recent changes in cervical cancer screening guidelines, the primary care physician’s role as educator is of utmost importance. In one study, although 99% of women had received a Pap test, 87% could not identify the purpose of the Pap test.59 The primary care physician’s role is perhaps the most influential in preventing disease and, as such, has the greatest impact on a patient’s disease process.
- Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin 2014; 64:9–29.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015; 65:5–29.
- Koh WJ, Greer BE, Abu-Rustum NR, et al. Cervical cancer, version 2.2015. J Natl Compr Canc Netw 2015; 13:395-404.
- Farley J, Risinger JI, Rose GS, Maxwell GL. Racial disparities in blacks with gynecologic cancers. Cancer 2007; 110:234–243.
- Farley JH, Hines JF, Taylor RR, et al. Equal care ensures equal survival for African-American women with cervical carcinoma. Cancer 2001; 91:869–873.
- Rauh-Hain JA, Clemmer JT, Bradford LS, et al. Racial disparities in cervical cancer survival over time. Cancer 2013; 119:3644–3652.
- Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: a report from the Health Disparities Taskforce of the Society of Gynecologic Oncology. Gynecol Oncol 2014; 133:353–361.
- Patel DA, Barnholtz-Sloan JS, Patel MK, Malone JM Jr, Chuba PJ, Schwartz K. A population-based study of racial and ethnic differences in survival among women with invasive cervical cancer: analysis of surveillance, epidemiology, and end results data. Gynecol Oncol 2005; 97:550–558.
- Papanicolaou GN, Traut HF. The diagnostic value of vaginal smears in carcinoma of the uterus. 1941. Arch Pathol Lab Med 1997; 121:211–224.
- Walboomers JM, Jacobs M V, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999; 189:12–19.
- Moscicki AB, Shiboski S, Hills NK, et al. Regression of low-grade squamous intra-epithelial lesions in young women. Lancet 2004; 364:1678–1683.
- Trimble CL, Piantadosi S, Gravitt P, et al. Spontaneous regression of high-grade cervical dysplasia: effects of human papillomavirus type and HLA phenotype. Clin Cancer Res 2005; 11:4717–4723.
- Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998; 338:423-428.
- Saslow D, Solomon D, Lawson HW, et al; ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin 2012; 62:147–172.
- Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Obstet Gynecol 2015; 125:330–337.
- Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 2013; 17(suppl 1):S1–S27.
- Sabatino SA, White MC, Thompson TD, Klabunde CN. Cancer screening test use—United States, 2013. MMWR 2015; 64:464–468.
- Benard VB, Lawson HW, Eheman CR, Anderson C, Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstet Gynecol 2005; 105:1323–1328.
- Eggleston KS, Coker AL, Luchok KJ, Meyer TE. Adherence to recommendations for follow-up to abnormal Pap tests. Obstet Gynecol 2007; 109:1332–1341.
- Peterson NB, Han J, Freund KM. Inadequate follow-up for abnormal Pap smears in an urban population. J Natl Med Assoc 2003; 95:825–832.
- Li N, Franceschi S, Howell-Jones R, Snijders PJ, Clifford GM. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: variation by geographical region, histological type and year of publication. Int J Cancer 2011; 128:927–935.
- Hariri S, Unger ER, Powell SE, et al; HPV-IMPACT Working Group. Human papillomavirus genotypes in high-grade cervical lesions in the United States. J Infect Dis 2012; 206:1878–1886.
- Niccolai LM, Russ C, Julian PJ, et al. Individual and geographic disparities in human papillomavirus types 16/18 in high-grade cervical lesions: associations with race, ethnicity, and poverty. Cancer 2013; 119:3052–3058.
- FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 2007; 356:1915–1927.
- Paavonen J, Naud P, Salmerón J, et al; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 2009; 374:301–314.
- Centers for Disease Control and Prevention (CDC). Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep 2011; 60:1705–1708.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65:1405–1408.
- Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2014. MMWR Morb Mortal Wkly Rep 2015; 64:784–792.
- Fisher H, Trotter CL, Audrey S, MacDonald-Wallis K, Hickman M. Inequalities in the uptake of human papillomavirus vaccination: a systematic review and meta-analysis. Int J Epidemiol 2013; 42:896–908.
- Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine 2012; 30:3546–3556.
- Malo TL, Hassani D, Staras SA, Shenkman EA, Giuliano AR, Vadaparampil ST. Do Florida Medicaid providers’ barriers to HPV vaccination vary based on VFC program participation? Matern Child Health J 2013; 17:609–615.
- Meites E, Llata E, Hariri S, et al. HPV vaccine implementation in STD clinics—STD Surveillance Network. Sex Transm Dis 2012; 39:32–34.
- Perkins RB, Clark JA. What affects human papillomavirus vaccination rates? A qualitative analysis of providers’ perceptions. Womens Health Issues 2012; 22:e379–e386.
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014; 168:76–82.
- Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008–2009. Pediatrics 2011; 128:830–839.
- Bastani R, Glenn BA, Tsui J, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomarkers Prev 2011; 20:1463–1472.
- Guerry SL, De Rosa CJ, Markowitz LE, et al. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 2011; 29:2235–2241.
- Hull PC, Williams EA, Khabele D, Dean C, Bond B, Sanderson M. HPV vaccine use among African American girls: qualitative formative research using a participatory social marketing approach. Gynecol Oncol 2014; 132(suppl 1):S13–S20.
- Brewer NT, Gottlieb SL, Reiter PL, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis 2011; 38:197–204.
- Wang SS, Zuna RE, Wentzensen N, et al. Human papillomavirus cofactors by disease progression and human papillomavirus types in the study to understand cervical cancer early endpoints and determinants. Cancer Epidemiol Biomarkers Prev 2009; 18:113–120.
- Deacon JM, Evans CD, Yule R, et al. Sexual behaviour and smoking as determinants of cervical HPV infection and of CIN3 among those infected: a case-control study nested within the Manchester cohort. Br J Cancer 2000; 83:1565–1572.
- International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and sexual behavior: collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol Biomarkers Prev 2009; 18:1060–1069.
- Centers for Disease Control and Prevention (CDC). Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012; 17(No. 4). https://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. Accessed September 12, 2017.
- Frisch M, Biggar RJ, Goedert JJ. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst 2000; 92:1500–1510.
- Schäfer A, Friedmann W, Mielke M, Schwartländer B, Koch MA. The increased frequency of cervical dysplasia-neoplasia in women infected with the human immunodeficiency virus is related to the degree of immunosuppression. Am J Obstet Gynecol 1991; 164:593–599.
- Phillips AA, Justman JE. Screening HIV-infected patients for non-AIDS-defining malignancies. Curr HIV/AIDS Rep 2009; 6:83–92.
- De Vuyst H, Lillo F, Broutet N, Smith JS. HIV, human papillomavirus, and cervical neoplasia and cancer in the era of highly active antiretroviral therapy. Eur J Cancer Prev 2008; 17:545–554.
- Palefsky JM. Cervical human papillomavirus infection and cervical intraepithelial neoplasia in women positive for human immunodeficiency virus in the era of highly active antiretroviral therapy. Curr Opin Oncol 2003; 15:382–388.
- Adler DH. The impact of HAART on HPV-related cervical disease. Curr HIV Res 2010; 8:493–497.
- Castellsagué X, Pawlita M, Roura E, et al. Prospective seroepidemiologic study on the role of human papillomavirus and other infections in cervical carcinogenesis: evidence from the EPIC cohort. Int J Cancer 2014; 135:440–452.
- Centers for Disease Control and Prevention (CDC). 2013 sexually transmitted disease surveillance. www.cdc.gov/std/stats13/exordium.htm. Accessed September 12, 2017.
- Smith JS, Bosetti C, Muñoz N, et al; IARC multicentric case-control study. Chlamydia trachomatis and invasive cervical cancer: a pooled analysis of the IARC multicentric case-control study. Int J Cancer 2004; 111:431–439.
- Koskela P, Anttila T, Bjørge T, et al. Chlamydia trachomatis infection as a risk factor for invasive cervical cancer. Int J Cancer 2000; 85:35–39.
- Office on Smoking and Health (US). Women and smoking: a report of the Surgeon General: Chapter 3. Health consequences of tobacco use among women. http://www.ncbi.nlm.nih.gov/books/NBK44312. Accessed September 12, 2017.
- Plummer M, Herrero R, Franceschi S, et al; IARC Multi-centre Cervical Cancer Study Group. Smoking and cervical cancer: pooled analysis of the IARC multi-centric case—control study. Cancer Causes Control 2003; 14:805–814.
- Ho GY, Kadish AS, Burk RD, et al. HPV 16 and cigarette smoking as risk factors for high-grade cervical intra-epithelial neoplasia. Int J Cancer 1998; 78:281–285.
- Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults - United States, 2005-2014. MMWR Morb Mortal Wkly Rep 2015; 64:1233–1240.
- Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med 2010; 8:511–516.
- Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol 2002; 186:938–943.
- Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin 2014; 64:9–29.
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015; 65:5–29.
- Koh WJ, Greer BE, Abu-Rustum NR, et al. Cervical cancer, version 2.2015. J Natl Compr Canc Netw 2015; 13:395-404.
- Farley J, Risinger JI, Rose GS, Maxwell GL. Racial disparities in blacks with gynecologic cancers. Cancer 2007; 110:234–243.
- Farley JH, Hines JF, Taylor RR, et al. Equal care ensures equal survival for African-American women with cervical carcinoma. Cancer 2001; 91:869–873.
- Rauh-Hain JA, Clemmer JT, Bradford LS, et al. Racial disparities in cervical cancer survival over time. Cancer 2013; 119:3644–3652.
- Collins Y, Holcomb K, Chapman-Davis E, Khabele D, Farley JH. Gynecologic cancer disparities: a report from the Health Disparities Taskforce of the Society of Gynecologic Oncology. Gynecol Oncol 2014; 133:353–361.
- Patel DA, Barnholtz-Sloan JS, Patel MK, Malone JM Jr, Chuba PJ, Schwartz K. A population-based study of racial and ethnic differences in survival among women with invasive cervical cancer: analysis of surveillance, epidemiology, and end results data. Gynecol Oncol 2005; 97:550–558.
- Papanicolaou GN, Traut HF. The diagnostic value of vaginal smears in carcinoma of the uterus. 1941. Arch Pathol Lab Med 1997; 121:211–224.
- Walboomers JM, Jacobs M V, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999; 189:12–19.
- Moscicki AB, Shiboski S, Hills NK, et al. Regression of low-grade squamous intra-epithelial lesions in young women. Lancet 2004; 364:1678–1683.
- Trimble CL, Piantadosi S, Gravitt P, et al. Spontaneous regression of high-grade cervical dysplasia: effects of human papillomavirus type and HLA phenotype. Clin Cancer Res 2005; 11:4717–4723.
- Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998; 338:423-428.
- Saslow D, Solomon D, Lawson HW, et al; ACS-ASCCP-ASCP Cervical Cancer Guideline Committee. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin 2012; 62:147–172.
- Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Obstet Gynecol 2015; 125:330–337.
- Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 2013; 17(suppl 1):S1–S27.
- Sabatino SA, White MC, Thompson TD, Klabunde CN. Cancer screening test use—United States, 2013. MMWR 2015; 64:464–468.
- Benard VB, Lawson HW, Eheman CR, Anderson C, Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstet Gynecol 2005; 105:1323–1328.
- Eggleston KS, Coker AL, Luchok KJ, Meyer TE. Adherence to recommendations for follow-up to abnormal Pap tests. Obstet Gynecol 2007; 109:1332–1341.
- Peterson NB, Han J, Freund KM. Inadequate follow-up for abnormal Pap smears in an urban population. J Natl Med Assoc 2003; 95:825–832.
- Li N, Franceschi S, Howell-Jones R, Snijders PJ, Clifford GM. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: variation by geographical region, histological type and year of publication. Int J Cancer 2011; 128:927–935.
- Hariri S, Unger ER, Powell SE, et al; HPV-IMPACT Working Group. Human papillomavirus genotypes in high-grade cervical lesions in the United States. J Infect Dis 2012; 206:1878–1886.
- Niccolai LM, Russ C, Julian PJ, et al. Individual and geographic disparities in human papillomavirus types 16/18 in high-grade cervical lesions: associations with race, ethnicity, and poverty. Cancer 2013; 119:3052–3058.
- FUTURE II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 2007; 356:1915–1927.
- Paavonen J, Naud P, Salmerón J, et al; HPV PATRICIA Study Group. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 2009; 374:301–314.
- Centers for Disease Control and Prevention (CDC). Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep 2011; 60:1705–1708.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65:1405–1408.
- Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2014. MMWR Morb Mortal Wkly Rep 2015; 64:784–792.
- Fisher H, Trotter CL, Audrey S, MacDonald-Wallis K, Hickman M. Inequalities in the uptake of human papillomavirus vaccination: a systematic review and meta-analysis. Int J Epidemiol 2013; 42:896–908.
- Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine 2012; 30:3546–3556.
- Malo TL, Hassani D, Staras SA, Shenkman EA, Giuliano AR, Vadaparampil ST. Do Florida Medicaid providers’ barriers to HPV vaccination vary based on VFC program participation? Matern Child Health J 2013; 17:609–615.
- Meites E, Llata E, Hariri S, et al. HPV vaccine implementation in STD clinics—STD Surveillance Network. Sex Transm Dis 2012; 39:32–34.
- Perkins RB, Clark JA. What affects human papillomavirus vaccination rates? A qualitative analysis of providers’ perceptions. Womens Health Issues 2012; 22:e379–e386.
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014; 168:76–82.
- Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008–2009. Pediatrics 2011; 128:830–839.
- Bastani R, Glenn BA, Tsui J, et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomarkers Prev 2011; 20:1463–1472.
- Guerry SL, De Rosa CJ, Markowitz LE, et al. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 2011; 29:2235–2241.
- Hull PC, Williams EA, Khabele D, Dean C, Bond B, Sanderson M. HPV vaccine use among African American girls: qualitative formative research using a participatory social marketing approach. Gynecol Oncol 2014; 132(suppl 1):S13–S20.
- Brewer NT, Gottlieb SL, Reiter PL, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis 2011; 38:197–204.
- Wang SS, Zuna RE, Wentzensen N, et al. Human papillomavirus cofactors by disease progression and human papillomavirus types in the study to understand cervical cancer early endpoints and determinants. Cancer Epidemiol Biomarkers Prev 2009; 18:113–120.
- Deacon JM, Evans CD, Yule R, et al. Sexual behaviour and smoking as determinants of cervical HPV infection and of CIN3 among those infected: a case-control study nested within the Manchester cohort. Br J Cancer 2000; 83:1565–1572.
- International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and sexual behavior: collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol Biomarkers Prev 2009; 18:1060–1069.
- Centers for Disease Control and Prevention (CDC). Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012; 17(No. 4). https://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. Accessed September 12, 2017.
- Frisch M, Biggar RJ, Goedert JJ. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst 2000; 92:1500–1510.
- Schäfer A, Friedmann W, Mielke M, Schwartländer B, Koch MA. The increased frequency of cervical dysplasia-neoplasia in women infected with the human immunodeficiency virus is related to the degree of immunosuppression. Am J Obstet Gynecol 1991; 164:593–599.
- Phillips AA, Justman JE. Screening HIV-infected patients for non-AIDS-defining malignancies. Curr HIV/AIDS Rep 2009; 6:83–92.
- De Vuyst H, Lillo F, Broutet N, Smith JS. HIV, human papillomavirus, and cervical neoplasia and cancer in the era of highly active antiretroviral therapy. Eur J Cancer Prev 2008; 17:545–554.
- Palefsky JM. Cervical human papillomavirus infection and cervical intraepithelial neoplasia in women positive for human immunodeficiency virus in the era of highly active antiretroviral therapy. Curr Opin Oncol 2003; 15:382–388.
- Adler DH. The impact of HAART on HPV-related cervical disease. Curr HIV Res 2010; 8:493–497.
- Castellsagué X, Pawlita M, Roura E, et al. Prospective seroepidemiologic study on the role of human papillomavirus and other infections in cervical carcinogenesis: evidence from the EPIC cohort. Int J Cancer 2014; 135:440–452.
- Centers for Disease Control and Prevention (CDC). 2013 sexually transmitted disease surveillance. www.cdc.gov/std/stats13/exordium.htm. Accessed September 12, 2017.
- Smith JS, Bosetti C, Muñoz N, et al; IARC multicentric case-control study. Chlamydia trachomatis and invasive cervical cancer: a pooled analysis of the IARC multicentric case-control study. Int J Cancer 2004; 111:431–439.
- Koskela P, Anttila T, Bjørge T, et al. Chlamydia trachomatis infection as a risk factor for invasive cervical cancer. Int J Cancer 2000; 85:35–39.
- Office on Smoking and Health (US). Women and smoking: a report of the Surgeon General: Chapter 3. Health consequences of tobacco use among women. http://www.ncbi.nlm.nih.gov/books/NBK44312. Accessed September 12, 2017.
- Plummer M, Herrero R, Franceschi S, et al; IARC Multi-centre Cervical Cancer Study Group. Smoking and cervical cancer: pooled analysis of the IARC multi-centric case—control study. Cancer Causes Control 2003; 14:805–814.
- Ho GY, Kadish AS, Burk RD, et al. HPV 16 and cigarette smoking as risk factors for high-grade cervical intra-epithelial neoplasia. Int J Cancer 1998; 78:281–285.
- Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults - United States, 2005-2014. MMWR Morb Mortal Wkly Rep 2015; 64:1233–1240.
- Nordin JD, Solberg LI, Parker ED. Adolescent primary care visit patterns. Ann Fam Med 2010; 8:511–516.
- Lindau ST, Tomori C, Lyons T, Langseth L, Bennett CL, Garcia P. The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. Am J Obstet Gynecol 2002; 186:938–943.
Cervical cancer in African American women: Optimizing prevention to reduce disparities
Primary care providers play a crucial role in cancer control, including screening and follow-up.1,2 In particular, they are often responsible for performing the initial screening and, when necessary, discussing appropriate treatment options. However, cancer screening practices in primary care can vary significantly, leading to disparities in access to these services.3
Arvizo and Mahdi,4 in this issue of the Journal, discuss disparities in cervical cancer screening, noting that African American women have a higher risk of developing and dying of cervical cancer than white women, possibly because they are diagnosed at a later stage and have lower stage-specific survival rates. The authors state that equal access to healthcare may help mitigate these factors, and they also discuss how primary care providers can reduce these disparities.
PRIORITIZING CERVICAL CANCER SCREENING
Even in patients who have access to regular primary care, other barriers to cancer screening may exist. A 2014 study used self-reported data from the Behavioral Risk Factor Surveillance System survey to assess barriers to cervical cancer screening in older women (ages 40 to 65) who reported having health insurance and a personal healthcare provider.5 Those who were never or rarely screened for cervical cancer were more likely than those who were regularly screened to have a chronic condition, such as heart disease, chronic obstructive pulmonary disease, arthritis, depression, kidney disease, or diabetes.
This finding suggests that cancer screening may be a low priority during an adult primary care visit in which multiple chronic diseases must be addressed. To reduce disparities in cancer screening, primary care systems need to be designed to optimize delivery of preventive care and disease management using a team approach.
SYSTEMATIC FOLLOW-UP
Arvizo and Mahdi also discuss the follow-up of abnormal screening Papanicolaou (Pap) smears. While appropriate follow-up is a key factor in the management of cervical dysplasia, follow-up rates vary among African American women. System-level interventions such as the use of an electronic medical record-based tracking system in primary care settings6 with established protocols for follow-up may be effective.
But even with such systems in place, patients may face psychosocial barriers (eg, lack of health literacy, distress after receiving an abnormal cervical cytology test result7) that prevent them from seeking additional care. To improve follow-up rates, providers must be aware of these barriers and know how to address them through effective communication.
VACCINATION FOR HPV
Finally, the association between human papilloma virus (HPV) infection and cervical cancer makes HPV vaccination a crucial step in cervical cancer prevention. Continued provider education regarding HPV vaccination can improve knowledge about the HPV vaccine,8 as well as improve vaccination rates.9 The recent approval of a 2-dose vaccine schedule for younger girls10 may also help improve vaccine series completion rates.
The authors also suggest that primary care providers counsel all patients about risk factors for cervical cancer, including unsafe sex practices and tobacco use.
OPTIMIZING SCREENING AND PREVENTION
I commend the authors for their discussion of cervical cancer disparities and for raising awareness of the important role primary care providers play in reducing these disparities. Improving cervical cancer screening rates and follow-up will require providers and patients to be aware of cervical cancer risk factors. Further, system-level practice interventions will optimize primary care providers’ ability to engage patients in cancer screening conversations and ensure timely follow-up of screening tests.
- Emery JD, Shaw K, Williams B, et al. The role of primary care in early detection and follow-up of cancer. Nat Rev Clin Oncol 2014; 11:38–48.
- Rubin G, Berendsen A, Crawford SM, et al. The expanding role of primary care in cancer control. Lancet Oncol 2015; 16:1231–1272.
- Martires KJ, Kurlander DE, Minwell GJ, Dahms EB, Bordeaux JS. Patterns of cancer screening in primary care from 2005 to 2010. Cancer 2014; 120:253–261.
- Arvizo C, Mahdi H. Disparities in cervical cancer in African-American women: what primary care physicians can do. Cleve Clin J Med 2017; 84:788–794.
- Crawford A, Benard V, King J, Thomas CC. Understanding barriers to cervical cancer screening in women with access to care, behavioral risk factor surveillance system, 2014. Prev Chronic Dis 2016; 13:E154.
- Dupuis EA, White HF, Newman D, Sobieraj JE, Gokhale M, Freund KM. Tracking abnormal cervical cancer screening: evaluation of an EMR-based intervention. J Gen Intern Med 2010; 25:575–580.
- Hui SK, Miller SM, Wen KY, et al. Psychosocial barriers to follow-up adherence after an abnormal cervical cytology test result among low-income, inner-city women. J Prim Care Community Health 2014; 5:234–241.
- Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers’ human papillomavirus vaccine knowledge. Hum Vaccin Immunother 2015; 11:1331–1336.
- Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine 2015; 33:1223–1229.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65:1405–1408.
Primary care providers play a crucial role in cancer control, including screening and follow-up.1,2 In particular, they are often responsible for performing the initial screening and, when necessary, discussing appropriate treatment options. However, cancer screening practices in primary care can vary significantly, leading to disparities in access to these services.3
Arvizo and Mahdi,4 in this issue of the Journal, discuss disparities in cervical cancer screening, noting that African American women have a higher risk of developing and dying of cervical cancer than white women, possibly because they are diagnosed at a later stage and have lower stage-specific survival rates. The authors state that equal access to healthcare may help mitigate these factors, and they also discuss how primary care providers can reduce these disparities.
PRIORITIZING CERVICAL CANCER SCREENING
Even in patients who have access to regular primary care, other barriers to cancer screening may exist. A 2014 study used self-reported data from the Behavioral Risk Factor Surveillance System survey to assess barriers to cervical cancer screening in older women (ages 40 to 65) who reported having health insurance and a personal healthcare provider.5 Those who were never or rarely screened for cervical cancer were more likely than those who were regularly screened to have a chronic condition, such as heart disease, chronic obstructive pulmonary disease, arthritis, depression, kidney disease, or diabetes.
This finding suggests that cancer screening may be a low priority during an adult primary care visit in which multiple chronic diseases must be addressed. To reduce disparities in cancer screening, primary care systems need to be designed to optimize delivery of preventive care and disease management using a team approach.
SYSTEMATIC FOLLOW-UP
Arvizo and Mahdi also discuss the follow-up of abnormal screening Papanicolaou (Pap) smears. While appropriate follow-up is a key factor in the management of cervical dysplasia, follow-up rates vary among African American women. System-level interventions such as the use of an electronic medical record-based tracking system in primary care settings6 with established protocols for follow-up may be effective.
But even with such systems in place, patients may face psychosocial barriers (eg, lack of health literacy, distress after receiving an abnormal cervical cytology test result7) that prevent them from seeking additional care. To improve follow-up rates, providers must be aware of these barriers and know how to address them through effective communication.
VACCINATION FOR HPV
Finally, the association between human papilloma virus (HPV) infection and cervical cancer makes HPV vaccination a crucial step in cervical cancer prevention. Continued provider education regarding HPV vaccination can improve knowledge about the HPV vaccine,8 as well as improve vaccination rates.9 The recent approval of a 2-dose vaccine schedule for younger girls10 may also help improve vaccine series completion rates.
The authors also suggest that primary care providers counsel all patients about risk factors for cervical cancer, including unsafe sex practices and tobacco use.
OPTIMIZING SCREENING AND PREVENTION
I commend the authors for their discussion of cervical cancer disparities and for raising awareness of the important role primary care providers play in reducing these disparities. Improving cervical cancer screening rates and follow-up will require providers and patients to be aware of cervical cancer risk factors. Further, system-level practice interventions will optimize primary care providers’ ability to engage patients in cancer screening conversations and ensure timely follow-up of screening tests.
Primary care providers play a crucial role in cancer control, including screening and follow-up.1,2 In particular, they are often responsible for performing the initial screening and, when necessary, discussing appropriate treatment options. However, cancer screening practices in primary care can vary significantly, leading to disparities in access to these services.3
Arvizo and Mahdi,4 in this issue of the Journal, discuss disparities in cervical cancer screening, noting that African American women have a higher risk of developing and dying of cervical cancer than white women, possibly because they are diagnosed at a later stage and have lower stage-specific survival rates. The authors state that equal access to healthcare may help mitigate these factors, and they also discuss how primary care providers can reduce these disparities.
PRIORITIZING CERVICAL CANCER SCREENING
Even in patients who have access to regular primary care, other barriers to cancer screening may exist. A 2014 study used self-reported data from the Behavioral Risk Factor Surveillance System survey to assess barriers to cervical cancer screening in older women (ages 40 to 65) who reported having health insurance and a personal healthcare provider.5 Those who were never or rarely screened for cervical cancer were more likely than those who were regularly screened to have a chronic condition, such as heart disease, chronic obstructive pulmonary disease, arthritis, depression, kidney disease, or diabetes.
This finding suggests that cancer screening may be a low priority during an adult primary care visit in which multiple chronic diseases must be addressed. To reduce disparities in cancer screening, primary care systems need to be designed to optimize delivery of preventive care and disease management using a team approach.
SYSTEMATIC FOLLOW-UP
Arvizo and Mahdi also discuss the follow-up of abnormal screening Papanicolaou (Pap) smears. While appropriate follow-up is a key factor in the management of cervical dysplasia, follow-up rates vary among African American women. System-level interventions such as the use of an electronic medical record-based tracking system in primary care settings6 with established protocols for follow-up may be effective.
But even with such systems in place, patients may face psychosocial barriers (eg, lack of health literacy, distress after receiving an abnormal cervical cytology test result7) that prevent them from seeking additional care. To improve follow-up rates, providers must be aware of these barriers and know how to address them through effective communication.
VACCINATION FOR HPV
Finally, the association between human papilloma virus (HPV) infection and cervical cancer makes HPV vaccination a crucial step in cervical cancer prevention. Continued provider education regarding HPV vaccination can improve knowledge about the HPV vaccine,8 as well as improve vaccination rates.9 The recent approval of a 2-dose vaccine schedule for younger girls10 may also help improve vaccine series completion rates.
The authors also suggest that primary care providers counsel all patients about risk factors for cervical cancer, including unsafe sex practices and tobacco use.
OPTIMIZING SCREENING AND PREVENTION
I commend the authors for their discussion of cervical cancer disparities and for raising awareness of the important role primary care providers play in reducing these disparities. Improving cervical cancer screening rates and follow-up will require providers and patients to be aware of cervical cancer risk factors. Further, system-level practice interventions will optimize primary care providers’ ability to engage patients in cancer screening conversations and ensure timely follow-up of screening tests.
- Emery JD, Shaw K, Williams B, et al. The role of primary care in early detection and follow-up of cancer. Nat Rev Clin Oncol 2014; 11:38–48.
- Rubin G, Berendsen A, Crawford SM, et al. The expanding role of primary care in cancer control. Lancet Oncol 2015; 16:1231–1272.
- Martires KJ, Kurlander DE, Minwell GJ, Dahms EB, Bordeaux JS. Patterns of cancer screening in primary care from 2005 to 2010. Cancer 2014; 120:253–261.
- Arvizo C, Mahdi H. Disparities in cervical cancer in African-American women: what primary care physicians can do. Cleve Clin J Med 2017; 84:788–794.
- Crawford A, Benard V, King J, Thomas CC. Understanding barriers to cervical cancer screening in women with access to care, behavioral risk factor surveillance system, 2014. Prev Chronic Dis 2016; 13:E154.
- Dupuis EA, White HF, Newman D, Sobieraj JE, Gokhale M, Freund KM. Tracking abnormal cervical cancer screening: evaluation of an EMR-based intervention. J Gen Intern Med 2010; 25:575–580.
- Hui SK, Miller SM, Wen KY, et al. Psychosocial barriers to follow-up adherence after an abnormal cervical cytology test result among low-income, inner-city women. J Prim Care Community Health 2014; 5:234–241.
- Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers’ human papillomavirus vaccine knowledge. Hum Vaccin Immunother 2015; 11:1331–1336.
- Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine 2015; 33:1223–1229.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65:1405–1408.
- Emery JD, Shaw K, Williams B, et al. The role of primary care in early detection and follow-up of cancer. Nat Rev Clin Oncol 2014; 11:38–48.
- Rubin G, Berendsen A, Crawford SM, et al. The expanding role of primary care in cancer control. Lancet Oncol 2015; 16:1231–1272.
- Martires KJ, Kurlander DE, Minwell GJ, Dahms EB, Bordeaux JS. Patterns of cancer screening in primary care from 2005 to 2010. Cancer 2014; 120:253–261.
- Arvizo C, Mahdi H. Disparities in cervical cancer in African-American women: what primary care physicians can do. Cleve Clin J Med 2017; 84:788–794.
- Crawford A, Benard V, King J, Thomas CC. Understanding barriers to cervical cancer screening in women with access to care, behavioral risk factor surveillance system, 2014. Prev Chronic Dis 2016; 13:E154.
- Dupuis EA, White HF, Newman D, Sobieraj JE, Gokhale M, Freund KM. Tracking abnormal cervical cancer screening: evaluation of an EMR-based intervention. J Gen Intern Med 2010; 25:575–580.
- Hui SK, Miller SM, Wen KY, et al. Psychosocial barriers to follow-up adherence after an abnormal cervical cytology test result among low-income, inner-city women. J Prim Care Community Health 2014; 5:234–241.
- Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers’ human papillomavirus vaccine knowledge. Hum Vaccin Immunother 2015; 11:1331–1336.
- Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine 2015; 33:1223–1229.
- Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep 2016; 65:1405–1408.
Insist on flu vaccination for all, say experts
sponsored by the National Foundation for Infectious Diseases.
Some good news about the flu – vaccination rates increased slightly last year, compared with the previous year among all individuals aged 6 months and older without contraindications, according to data from the Centers for Disease Control and Prevention.
Experts continue to recommend annual influenza vaccination for all persons aged 6 months and older, but they emphasize the need to identify those at risk of not getting vaccinated and develop strategies to increase vaccination coverage.
“Vaccines are among the greatest public health achievements of modern times, but they are only as useful as we as a society take advantage of them,” Secretary of Health & Human Services Thomas E. Price, MD, said at the briefing.
Overall flu vaccination in the United States was 47% for the 2016-2017 season, compared with 46% during the 2015-2016 season, according to data from the Centers for Disease Control and Prevention.
Dr. Price emphasized that vaccination is only part of a successful flu prevention strategy. Stay home when you are sick to help avoid spreading germs to others and take antiviral drugs if a doctor prescribes them to help reduce and avoid complications from flu, he said.
Children aged 6-23 months were the only population subgroup to meet the 70% Healthy People 2020 goal last year, with a rate of 73%, said Patricia A. Stinchfield, RN, CPNP, senior director of infection prevention and control at Children’s Hospital Minnesota, Minneapolis.
“Our goal is to increase coverage for children of all ages,” she said. But it’s not just about the kids themselves, she emphasized.
“If your child gets the flu, they expose babies, grandparents, pregnant women. We need to vaccinate children to protect the public at large,” she said. In addition, health care professionals must be clear about recommending vaccination. The research shows that a specific recommendation often makes the difference for vaccinating families.
Pregnant women are among those who can and should safely be vaccinated, Ms. Stinchfield emphasized. Flu vaccination among pregnant women was 54% in 2016-2017, similar to the past three flu seasons, and approximately two-thirds (67%) of pregnant women in 2016-2017 reported that a health care provider recommended and offered flu vaccination, according to CDC data.
Older adults also are important targets for flu vaccination, noted Kathleen M. Neuzil, MD, director of the Center for Vaccine Development at the University of Maryland, Baltimore. Last year, approximately 65% of U.S. adults aged 65 years and older were vaccinated, which was the largest subgroup of adults aged 18 years and older, she said. Older adults may be caring for frail spouses or infant grandchildren, so protecting others should be a motivating factor in continuing to encourage vaccination in this age group, she noted.
The flu vaccine supply is plentiful going into the start of the 2016-2017 flu season, with an estimated 166 million doses available in several formulations, said Daniel B. Jernigan, MD, director of the CDC’s Influenza Division.
Options for vaccination include the standard vaccine, a cell-based vaccine, and a recombinant vaccine. In addition, an adjuvanted vaccine and a high-dose vaccine are available specifically for adults aged 65 years and older; these vaccines are designed to provoke a stronger immune response, Dr. Jernigan said.
However, the briefing participants agreed that the best strategy is to get vaccinated as soon as possible, rather than postponing vaccination in order to secure a particular vaccine type.
Clinicians should not underestimate the power of leading by example when it comes to flu vaccination, Dr. Schaffner noted. Support from the highest levels of administration is important to help overcome barriers to vaccination coverage for health care workers by making vaccination easy and accessible, he said.
The overall influenza vaccination coverage estimate among health care providers was 79% for the 2016-2017 season, similar to the 2014-2015 and 2015-2016 seasons, but representing a 15% increase since 2010-2011. Vaccination coverage was highest among health care personnel whose workplaces required it.
Complete data on 2016-2017 vaccination coverage in health care workers and in pregnant women were published in the CDC’s Morbidity and Mortality Weekly Report on Sept. 29.
The CDC’s complete flu vaccination recommendations are available online.
The briefing participants had no relevant financial conflicts to disclose.
sponsored by the National Foundation for Infectious Diseases.
Some good news about the flu – vaccination rates increased slightly last year, compared with the previous year among all individuals aged 6 months and older without contraindications, according to data from the Centers for Disease Control and Prevention.
Experts continue to recommend annual influenza vaccination for all persons aged 6 months and older, but they emphasize the need to identify those at risk of not getting vaccinated and develop strategies to increase vaccination coverage.
“Vaccines are among the greatest public health achievements of modern times, but they are only as useful as we as a society take advantage of them,” Secretary of Health & Human Services Thomas E. Price, MD, said at the briefing.
Overall flu vaccination in the United States was 47% for the 2016-2017 season, compared with 46% during the 2015-2016 season, according to data from the Centers for Disease Control and Prevention.
Dr. Price emphasized that vaccination is only part of a successful flu prevention strategy. Stay home when you are sick to help avoid spreading germs to others and take antiviral drugs if a doctor prescribes them to help reduce and avoid complications from flu, he said.
Children aged 6-23 months were the only population subgroup to meet the 70% Healthy People 2020 goal last year, with a rate of 73%, said Patricia A. Stinchfield, RN, CPNP, senior director of infection prevention and control at Children’s Hospital Minnesota, Minneapolis.
“Our goal is to increase coverage for children of all ages,” she said. But it’s not just about the kids themselves, she emphasized.
“If your child gets the flu, they expose babies, grandparents, pregnant women. We need to vaccinate children to protect the public at large,” she said. In addition, health care professionals must be clear about recommending vaccination. The research shows that a specific recommendation often makes the difference for vaccinating families.
Pregnant women are among those who can and should safely be vaccinated, Ms. Stinchfield emphasized. Flu vaccination among pregnant women was 54% in 2016-2017, similar to the past three flu seasons, and approximately two-thirds (67%) of pregnant women in 2016-2017 reported that a health care provider recommended and offered flu vaccination, according to CDC data.
Older adults also are important targets for flu vaccination, noted Kathleen M. Neuzil, MD, director of the Center for Vaccine Development at the University of Maryland, Baltimore. Last year, approximately 65% of U.S. adults aged 65 years and older were vaccinated, which was the largest subgroup of adults aged 18 years and older, she said. Older adults may be caring for frail spouses or infant grandchildren, so protecting others should be a motivating factor in continuing to encourage vaccination in this age group, she noted.
The flu vaccine supply is plentiful going into the start of the 2016-2017 flu season, with an estimated 166 million doses available in several formulations, said Daniel B. Jernigan, MD, director of the CDC’s Influenza Division.
Options for vaccination include the standard vaccine, a cell-based vaccine, and a recombinant vaccine. In addition, an adjuvanted vaccine and a high-dose vaccine are available specifically for adults aged 65 years and older; these vaccines are designed to provoke a stronger immune response, Dr. Jernigan said.
However, the briefing participants agreed that the best strategy is to get vaccinated as soon as possible, rather than postponing vaccination in order to secure a particular vaccine type.
Clinicians should not underestimate the power of leading by example when it comes to flu vaccination, Dr. Schaffner noted. Support from the highest levels of administration is important to help overcome barriers to vaccination coverage for health care workers by making vaccination easy and accessible, he said.
The overall influenza vaccination coverage estimate among health care providers was 79% for the 2016-2017 season, similar to the 2014-2015 and 2015-2016 seasons, but representing a 15% increase since 2010-2011. Vaccination coverage was highest among health care personnel whose workplaces required it.
Complete data on 2016-2017 vaccination coverage in health care workers and in pregnant women were published in the CDC’s Morbidity and Mortality Weekly Report on Sept. 29.
The CDC’s complete flu vaccination recommendations are available online.
The briefing participants had no relevant financial conflicts to disclose.
sponsored by the National Foundation for Infectious Diseases.
Some good news about the flu – vaccination rates increased slightly last year, compared with the previous year among all individuals aged 6 months and older without contraindications, according to data from the Centers for Disease Control and Prevention.
Experts continue to recommend annual influenza vaccination for all persons aged 6 months and older, but they emphasize the need to identify those at risk of not getting vaccinated and develop strategies to increase vaccination coverage.
“Vaccines are among the greatest public health achievements of modern times, but they are only as useful as we as a society take advantage of them,” Secretary of Health & Human Services Thomas E. Price, MD, said at the briefing.
Overall flu vaccination in the United States was 47% for the 2016-2017 season, compared with 46% during the 2015-2016 season, according to data from the Centers for Disease Control and Prevention.
Dr. Price emphasized that vaccination is only part of a successful flu prevention strategy. Stay home when you are sick to help avoid spreading germs to others and take antiviral drugs if a doctor prescribes them to help reduce and avoid complications from flu, he said.
Children aged 6-23 months were the only population subgroup to meet the 70% Healthy People 2020 goal last year, with a rate of 73%, said Patricia A. Stinchfield, RN, CPNP, senior director of infection prevention and control at Children’s Hospital Minnesota, Minneapolis.
“Our goal is to increase coverage for children of all ages,” she said. But it’s not just about the kids themselves, she emphasized.
“If your child gets the flu, they expose babies, grandparents, pregnant women. We need to vaccinate children to protect the public at large,” she said. In addition, health care professionals must be clear about recommending vaccination. The research shows that a specific recommendation often makes the difference for vaccinating families.
Pregnant women are among those who can and should safely be vaccinated, Ms. Stinchfield emphasized. Flu vaccination among pregnant women was 54% in 2016-2017, similar to the past three flu seasons, and approximately two-thirds (67%) of pregnant women in 2016-2017 reported that a health care provider recommended and offered flu vaccination, according to CDC data.
Older adults also are important targets for flu vaccination, noted Kathleen M. Neuzil, MD, director of the Center for Vaccine Development at the University of Maryland, Baltimore. Last year, approximately 65% of U.S. adults aged 65 years and older were vaccinated, which was the largest subgroup of adults aged 18 years and older, she said. Older adults may be caring for frail spouses or infant grandchildren, so protecting others should be a motivating factor in continuing to encourage vaccination in this age group, she noted.
The flu vaccine supply is plentiful going into the start of the 2016-2017 flu season, with an estimated 166 million doses available in several formulations, said Daniel B. Jernigan, MD, director of the CDC’s Influenza Division.
Options for vaccination include the standard vaccine, a cell-based vaccine, and a recombinant vaccine. In addition, an adjuvanted vaccine and a high-dose vaccine are available specifically for adults aged 65 years and older; these vaccines are designed to provoke a stronger immune response, Dr. Jernigan said.
However, the briefing participants agreed that the best strategy is to get vaccinated as soon as possible, rather than postponing vaccination in order to secure a particular vaccine type.
Clinicians should not underestimate the power of leading by example when it comes to flu vaccination, Dr. Schaffner noted. Support from the highest levels of administration is important to help overcome barriers to vaccination coverage for health care workers by making vaccination easy and accessible, he said.
The overall influenza vaccination coverage estimate among health care providers was 79% for the 2016-2017 season, similar to the 2014-2015 and 2015-2016 seasons, but representing a 15% increase since 2010-2011. Vaccination coverage was highest among health care personnel whose workplaces required it.
Complete data on 2016-2017 vaccination coverage in health care workers and in pregnant women were published in the CDC’s Morbidity and Mortality Weekly Report on Sept. 29.
The CDC’s complete flu vaccination recommendations are available online.
The briefing participants had no relevant financial conflicts to disclose.
Clinicians: Be clear about flu vaccine’s value
WASHINGTON – Flu vaccination rates remain below the 70% Healthy People 2020 goal for most of the U.S. population, but data show that a recommendation from a clinician can encourage individuals to get vaccinated and to vaccinate their children, according to a panel of experts who spoke at a press briefing sponsored by the National Foundation for Infectious Diseases.
“Annual vaccination is our first line of defense against the flu,” William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., said at the briefing. The unpredictable nature of the flu makes annual vaccination even more important – and the earlier, the better, said Dr. Schaffner. “If you have seen one flu season, you have seen ... one flu season.”
In a video interview at the briefing, experts emphasized the safety and effectiveness of the flu vaccine for a range of populations, including children, pregnant women, and older adults. And they offered tips to convince patients of the importance of vaccination, as well as the need to make sure health care staff are protected.
Briefing participants included former Department of Health and Human Services Secretary Thomas A. Price, MD; Patricia A. Stinchfield, RN, MS, CPNP, CIC of Children’s Hospitals and Clinics of Minnesota, St. Paul; Kathleen M. Neuzil, MD, of the University of Maryland; and Daniel B. Jernigan, MD, of the Centers for Disease Control and Prevention.
The clinicians interviewed had no financial conflicts to disclose.
WASHINGTON – Flu vaccination rates remain below the 70% Healthy People 2020 goal for most of the U.S. population, but data show that a recommendation from a clinician can encourage individuals to get vaccinated and to vaccinate their children, according to a panel of experts who spoke at a press briefing sponsored by the National Foundation for Infectious Diseases.
“Annual vaccination is our first line of defense against the flu,” William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., said at the briefing. The unpredictable nature of the flu makes annual vaccination even more important – and the earlier, the better, said Dr. Schaffner. “If you have seen one flu season, you have seen ... one flu season.”
In a video interview at the briefing, experts emphasized the safety and effectiveness of the flu vaccine for a range of populations, including children, pregnant women, and older adults. And they offered tips to convince patients of the importance of vaccination, as well as the need to make sure health care staff are protected.
Briefing participants included former Department of Health and Human Services Secretary Thomas A. Price, MD; Patricia A. Stinchfield, RN, MS, CPNP, CIC of Children’s Hospitals and Clinics of Minnesota, St. Paul; Kathleen M. Neuzil, MD, of the University of Maryland; and Daniel B. Jernigan, MD, of the Centers for Disease Control and Prevention.
The clinicians interviewed had no financial conflicts to disclose.
WASHINGTON – Flu vaccination rates remain below the 70% Healthy People 2020 goal for most of the U.S. population, but data show that a recommendation from a clinician can encourage individuals to get vaccinated and to vaccinate their children, according to a panel of experts who spoke at a press briefing sponsored by the National Foundation for Infectious Diseases.
“Annual vaccination is our first line of defense against the flu,” William Schaffner, MD, of Vanderbilt University, Nashville, Tenn., said at the briefing. The unpredictable nature of the flu makes annual vaccination even more important – and the earlier, the better, said Dr. Schaffner. “If you have seen one flu season, you have seen ... one flu season.”
In a video interview at the briefing, experts emphasized the safety and effectiveness of the flu vaccine for a range of populations, including children, pregnant women, and older adults. And they offered tips to convince patients of the importance of vaccination, as well as the need to make sure health care staff are protected.
Briefing participants included former Department of Health and Human Services Secretary Thomas A. Price, MD; Patricia A. Stinchfield, RN, MS, CPNP, CIC of Children’s Hospitals and Clinics of Minnesota, St. Paul; Kathleen M. Neuzil, MD, of the University of Maryland; and Daniel B. Jernigan, MD, of the Centers for Disease Control and Prevention.
The clinicians interviewed had no financial conflicts to disclose.
AT A PRESS BRIEFING BY THE NATIONAL FOUNDATION FOR INFECTIOUS DISEASES
New AAP policy recommends flu vaccination regardless of egg allergy
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
CHICAGO – The American Academy of Pediatrics has released a new policy statement that in part suggests that physicians can administer influenza vaccine to children and teenagers with egg allergies without any special precautions beyond those that apply to other vaccines.
This is some “egg-citing news,” said Mary Ann Jackson, MD. “In 28 studies with 4,315 egg allergic subjects, 656 of whom had severe allergies, there were no serious allergic reactions.” In other words, there was no respiratory distress or hypotension observed after participants received the influenza vaccine in these studies, she added.
Officially, the policy statement from the academy’s Committee on Infectious Diseases reads: “All children with egg allergy of any severity can receive influenza vaccine without any additional precautions beyond those recommended for any vaccine. Special precautions for egg-allergic recipients of IIV [inactivated influenza vaccine] are not warranted, as the rate of anaphylaxis after IIV administration is no greater in egg-allergic than non–egg-allergic recipients or from other universally recommended vaccines. Standard vaccination practice for all vaccines in children should include the ability to respond to rare acute hypersensitivity reactions.” The full policy statement was published online in the journal Pediatrics (2017 Sep. 6; doi: 10.1542/peds.2017-2550.)
This new policy “makes your life so much easier … and allows you to continue to recommend the vaccine strongly,” said Dr. Jackson, division director of infectious diseases at Children’s Mercy Hospital and professor of pediatrics at the University of Missouri at Kansas City.
Other reasons to recommend flu vaccination
Dr. Jackson also gave an overview of influenza epidemiology and why ongoing education of patients and families remains essential. “It’s almost flu season now. It’s inevitable – like RSV [respiratory syncytial virus] is inevitable – but when the seasons starts is unknown,” she said. “How severe and long the season will be is also unpredictable.” Which viruses are spread and whether there is a good match between circulating virus and the vaccine are additional unknowns each year.
Patient and family education are important for these reasons, and because “it’s the most likely vaccine to be opted out of by the otherwise fully immunized,” she noted.
The lowest covered population are individuals between 18 years and 49 years, Dr. Jackson said. “My young adult son did not think he needed to worry about flu for himself; he said he was healthy and well. But it’s a bummer when your mom is an ID doctor who likes vaccines, because I made it happen for him.”
Dr. Jackson had no relevant financial disclosures.
AT AAP 2017
With inpatient flu shots, providers’ attitude problem may outweigh parents’
reported Suchitra Rao, MD, of the University of Colorado, Aurora, and her colleagues.
Surveys assessing attitudes toward inpatient influenza vaccination were given to parents/caregivers of general pediatric inpatients and to inpatient physicians, residents, nurses, physician assistants, and nurse practitioners at Children’s Hospital Colorado in Aurora between October 2014 and March 2015. Response rates were 95% of the 1,053 parents/caregivers and 58% of the 339 providers.
The parents agreed that the flu is a serious disease (92%), that flu vaccines work (58%), that flu vaccines are safe (76%), and that the vaccines are needed annually (76%), the Dr. Rao and her colleagues found.
The providers thought the most common barriers to vaccination were parental refusal because of child illness (80%) and family misconceptions about the vaccine (74%). Also, 54% of providers forgot to ask about flu vaccination status and 46% forgot to order flu vaccines.
When asked what interventions might increase flu vaccination rates in the inpatient setting, 73% of providers agreed that personal reminders might help increase vaccination rates, but only 48% thought that provider education might help do so.
Read more in the journal Influenza and Other Respiratory Viruses (2017 Sep 5. doi: 10.1111/irv.12482.)
reported Suchitra Rao, MD, of the University of Colorado, Aurora, and her colleagues.
Surveys assessing attitudes toward inpatient influenza vaccination were given to parents/caregivers of general pediatric inpatients and to inpatient physicians, residents, nurses, physician assistants, and nurse practitioners at Children’s Hospital Colorado in Aurora between October 2014 and March 2015. Response rates were 95% of the 1,053 parents/caregivers and 58% of the 339 providers.
The parents agreed that the flu is a serious disease (92%), that flu vaccines work (58%), that flu vaccines are safe (76%), and that the vaccines are needed annually (76%), the Dr. Rao and her colleagues found.
The providers thought the most common barriers to vaccination were parental refusal because of child illness (80%) and family misconceptions about the vaccine (74%). Also, 54% of providers forgot to ask about flu vaccination status and 46% forgot to order flu vaccines.
When asked what interventions might increase flu vaccination rates in the inpatient setting, 73% of providers agreed that personal reminders might help increase vaccination rates, but only 48% thought that provider education might help do so.
Read more in the journal Influenza and Other Respiratory Viruses (2017 Sep 5. doi: 10.1111/irv.12482.)
reported Suchitra Rao, MD, of the University of Colorado, Aurora, and her colleagues.
Surveys assessing attitudes toward inpatient influenza vaccination were given to parents/caregivers of general pediatric inpatients and to inpatient physicians, residents, nurses, physician assistants, and nurse practitioners at Children’s Hospital Colorado in Aurora between October 2014 and March 2015. Response rates were 95% of the 1,053 parents/caregivers and 58% of the 339 providers.
The parents agreed that the flu is a serious disease (92%), that flu vaccines work (58%), that flu vaccines are safe (76%), and that the vaccines are needed annually (76%), the Dr. Rao and her colleagues found.
The providers thought the most common barriers to vaccination were parental refusal because of child illness (80%) and family misconceptions about the vaccine (74%). Also, 54% of providers forgot to ask about flu vaccination status and 46% forgot to order flu vaccines.
When asked what interventions might increase flu vaccination rates in the inpatient setting, 73% of providers agreed that personal reminders might help increase vaccination rates, but only 48% thought that provider education might help do so.
Read more in the journal Influenza and Other Respiratory Viruses (2017 Sep 5. doi: 10.1111/irv.12482.)
Combo vaccines improve compliance
, reported Samantha K. Kurosky of RTI Health Solutions, Research Triangle Park, N.C., and her colleagues.
Data from the 2012 National Immunization Survey was used to assess vaccination completion and compliance in 11,561 children age 24-35 months. Most children had providers who were in private practice (58%); about half of the children were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).
Completion of the full 4:3:1:3:3:1:4 vaccine series (4 DTaP, 3 inactivated polio vaccine [IPV], 1 MMR, 3 or 4 Haemophilus influenzae type b [Hib], 3 hepatitis B, 1 varicella, and 4 pneumococcal conjugate vaccine) was better among those who received combination vaccines, at 69%, compared with children who received single-antigen vaccine only (50%).
Children receiving combination vaccines also had a significantly higher compliance rate for the 4:3:1:3:3:1:4 series, at 24%, compared with those receiving single-antigen vaccines only, at 13% (P less than .001). Of children who received at least one vaccine by 24 months, 86% received at least one combo vaccine.
Children getting at least one combo vaccine were 2.2 times more likely to get all vaccines on time, and 2.4 times more likely to spend less time undervaccinated (less than 7 months), compared with those receiving single-antigen vaccines only, Ms. Kurosky and her associates said.
Previous studies have found that parents who refuse or intentionally delay vaccines often have higher income and are married mothers with college educations. In this study, parents with these demographics tended to have children who received single-antigen–only vaccines – that is, children who were less likely to complete a full vaccine series or have a high compliance rate, they said.
GlaxoSmithKline funded the research.
Read more at Human Vaccines & Immunotherapeutics (2017 Sep 7. doi: 10.1080/21645515.2017.1362515).
, reported Samantha K. Kurosky of RTI Health Solutions, Research Triangle Park, N.C., and her colleagues.
Data from the 2012 National Immunization Survey was used to assess vaccination completion and compliance in 11,561 children age 24-35 months. Most children had providers who were in private practice (58%); about half of the children were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).
Completion of the full 4:3:1:3:3:1:4 vaccine series (4 DTaP, 3 inactivated polio vaccine [IPV], 1 MMR, 3 or 4 Haemophilus influenzae type b [Hib], 3 hepatitis B, 1 varicella, and 4 pneumococcal conjugate vaccine) was better among those who received combination vaccines, at 69%, compared with children who received single-antigen vaccine only (50%).
Children receiving combination vaccines also had a significantly higher compliance rate for the 4:3:1:3:3:1:4 series, at 24%, compared with those receiving single-antigen vaccines only, at 13% (P less than .001). Of children who received at least one vaccine by 24 months, 86% received at least one combo vaccine.
Children getting at least one combo vaccine were 2.2 times more likely to get all vaccines on time, and 2.4 times more likely to spend less time undervaccinated (less than 7 months), compared with those receiving single-antigen vaccines only, Ms. Kurosky and her associates said.
Previous studies have found that parents who refuse or intentionally delay vaccines often have higher income and are married mothers with college educations. In this study, parents with these demographics tended to have children who received single-antigen–only vaccines – that is, children who were less likely to complete a full vaccine series or have a high compliance rate, they said.
GlaxoSmithKline funded the research.
Read more at Human Vaccines & Immunotherapeutics (2017 Sep 7. doi: 10.1080/21645515.2017.1362515).
, reported Samantha K. Kurosky of RTI Health Solutions, Research Triangle Park, N.C., and her colleagues.
Data from the 2012 National Immunization Survey was used to assess vaccination completion and compliance in 11,561 children age 24-35 months. Most children had providers who were in private practice (58%); about half of the children were enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).
Completion of the full 4:3:1:3:3:1:4 vaccine series (4 DTaP, 3 inactivated polio vaccine [IPV], 1 MMR, 3 or 4 Haemophilus influenzae type b [Hib], 3 hepatitis B, 1 varicella, and 4 pneumococcal conjugate vaccine) was better among those who received combination vaccines, at 69%, compared with children who received single-antigen vaccine only (50%).
Children receiving combination vaccines also had a significantly higher compliance rate for the 4:3:1:3:3:1:4 series, at 24%, compared with those receiving single-antigen vaccines only, at 13% (P less than .001). Of children who received at least one vaccine by 24 months, 86% received at least one combo vaccine.
Children getting at least one combo vaccine were 2.2 times more likely to get all vaccines on time, and 2.4 times more likely to spend less time undervaccinated (less than 7 months), compared with those receiving single-antigen vaccines only, Ms. Kurosky and her associates said.
Previous studies have found that parents who refuse or intentionally delay vaccines often have higher income and are married mothers with college educations. In this study, parents with these demographics tended to have children who received single-antigen–only vaccines – that is, children who were less likely to complete a full vaccine series or have a high compliance rate, they said.
GlaxoSmithKline funded the research.
Read more at Human Vaccines & Immunotherapeutics (2017 Sep 7. doi: 10.1080/21645515.2017.1362515).
FROM HUMAN VACCINES & IMMUNOTHERAPEUTICS
EMR pop-up aims to boost HPV vaccination rates
An electronic pop-up placed on clinicians’ electronic medical record may have had a positive impact on the human papillomavirus vaccination rates in a Texas pediatric clinic, according to a study presented at the annual meeting of the American Academy of Pediatrics.

HPV vaccination rates grew from 34% before the installation of the reminder to 53% afterwards. “We’ve had a lot of success in increasing the rates,” said lead researcher Kimberly Ferris, a fourth-year medical student at Texas Tech’s Paul L. Foster School of Medicine.
Ms. Ferris said that the medical center is located near Mexico, and the patient population includes children and adolescents from Juarez. “We still have a lot of young women who are dying from cervical cancer. Really honing in on this population will have a long term effect. ...Pediatrics is really where it starts. This is where you want to capture them.”
The plan is to keep the pop-up reminder in place and continue its use to educate staff and families, said co-author Maria Theresa Villanos, MD, director of ambulatory pediatrics at Texas Tech. Part of the success of their project is “there is no missed opportunity. This pop-up reminder appears during well child visits as well as any time a child comes in sick or for acute care,” she said.
“The major barrier that needs to be addressed is probably pop-up fatigue,” Ms. Ferris said. Because the prompt is new, people are still reading it each time it comes up, but that behavior could wane over time, she said. “It would be interesting to look at long-term vaccination rates and whether the numbers stay the same or if there is a decline.”
Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
An electronic pop-up placed on clinicians’ electronic medical record may have had a positive impact on the human papillomavirus vaccination rates in a Texas pediatric clinic, according to a study presented at the annual meeting of the American Academy of Pediatrics.

HPV vaccination rates grew from 34% before the installation of the reminder to 53% afterwards. “We’ve had a lot of success in increasing the rates,” said lead researcher Kimberly Ferris, a fourth-year medical student at Texas Tech’s Paul L. Foster School of Medicine.
Ms. Ferris said that the medical center is located near Mexico, and the patient population includes children and adolescents from Juarez. “We still have a lot of young women who are dying from cervical cancer. Really honing in on this population will have a long term effect. ...Pediatrics is really where it starts. This is where you want to capture them.”
The plan is to keep the pop-up reminder in place and continue its use to educate staff and families, said co-author Maria Theresa Villanos, MD, director of ambulatory pediatrics at Texas Tech. Part of the success of their project is “there is no missed opportunity. This pop-up reminder appears during well child visits as well as any time a child comes in sick or for acute care,” she said.
“The major barrier that needs to be addressed is probably pop-up fatigue,” Ms. Ferris said. Because the prompt is new, people are still reading it each time it comes up, but that behavior could wane over time, she said. “It would be interesting to look at long-term vaccination rates and whether the numbers stay the same or if there is a decline.”
Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
An electronic pop-up placed on clinicians’ electronic medical record may have had a positive impact on the human papillomavirus vaccination rates in a Texas pediatric clinic, according to a study presented at the annual meeting of the American Academy of Pediatrics.

HPV vaccination rates grew from 34% before the installation of the reminder to 53% afterwards. “We’ve had a lot of success in increasing the rates,” said lead researcher Kimberly Ferris, a fourth-year medical student at Texas Tech’s Paul L. Foster School of Medicine.
Ms. Ferris said that the medical center is located near Mexico, and the patient population includes children and adolescents from Juarez. “We still have a lot of young women who are dying from cervical cancer. Really honing in on this population will have a long term effect. ...Pediatrics is really where it starts. This is where you want to capture them.”
The plan is to keep the pop-up reminder in place and continue its use to educate staff and families, said co-author Maria Theresa Villanos, MD, director of ambulatory pediatrics at Texas Tech. Part of the success of their project is “there is no missed opportunity. This pop-up reminder appears during well child visits as well as any time a child comes in sick or for acute care,” she said.
“The major barrier that needs to be addressed is probably pop-up fatigue,” Ms. Ferris said. Because the prompt is new, people are still reading it each time it comes up, but that behavior could wane over time, she said. “It would be interesting to look at long-term vaccination rates and whether the numbers stay the same or if there is a decline.”
Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
AT AAP 2017
Key clinical point: Vaccination of patients for HPV jumped nearly 20% following the installation of a reminder to an electronic medical record system.
Major finding: HPV vaccination rates jumped from 33.5% to 52.9% after addition of a pop-up reminder.
Data source: Random chart audit comparing periods before and after intervention.
Disclosures: Ms. Ferris and Dr. Villanos had no relevant financial disclosures.
HPV vaccine pioneers win 2017 Lasker-DeBakey Clinical Medical Research Award
Douglas R. Lowy, MD, and John T. Schiller, PhD, received the 2017 Lasker-DeBakey Clinical Medical Research Award for their development of the virus-like particle technology used to create the human papillomavirus (HPV) vaccine. Their team discovered that proteins making up the outer shell of HPV could form virus-like particles that closely resemble the original virus but are not infectious, and these particles could trigger the immune system to produce protective antibodies that could neutralize HPV in a later infection. These particles eventually became the basis of the HPV vaccines Gardasil, Gardasil 9, and Cervarix.

HPV causes cervical cancer and other cancers such as cancer of the vulva, vagina, penis, or anus, as well as oropharyngeal cancer. Two of the high-risk types of HPV – HPV-16 and HPV-18 – cause about 70% of cervical cancers worldwide; it ranks 14th in frequency in the United States, according to the National Cancer Institute. The HPV vaccines are very effective in preventing persistent infections with HPV-16 and HPV-18. The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices continues to recommend routine HPV vaccination for girls and boys at age 11 or 12 years, with a second vaccine given 6-12 months later.
Douglas R. Lowy, MD, and John T. Schiller, PhD, received the 2017 Lasker-DeBakey Clinical Medical Research Award for their development of the virus-like particle technology used to create the human papillomavirus (HPV) vaccine. Their team discovered that proteins making up the outer shell of HPV could form virus-like particles that closely resemble the original virus but are not infectious, and these particles could trigger the immune system to produce protective antibodies that could neutralize HPV in a later infection. These particles eventually became the basis of the HPV vaccines Gardasil, Gardasil 9, and Cervarix.

HPV causes cervical cancer and other cancers such as cancer of the vulva, vagina, penis, or anus, as well as oropharyngeal cancer. Two of the high-risk types of HPV – HPV-16 and HPV-18 – cause about 70% of cervical cancers worldwide; it ranks 14th in frequency in the United States, according to the National Cancer Institute. The HPV vaccines are very effective in preventing persistent infections with HPV-16 and HPV-18. The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices continues to recommend routine HPV vaccination for girls and boys at age 11 or 12 years, with a second vaccine given 6-12 months later.
Douglas R. Lowy, MD, and John T. Schiller, PhD, received the 2017 Lasker-DeBakey Clinical Medical Research Award for their development of the virus-like particle technology used to create the human papillomavirus (HPV) vaccine. Their team discovered that proteins making up the outer shell of HPV could form virus-like particles that closely resemble the original virus but are not infectious, and these particles could trigger the immune system to produce protective antibodies that could neutralize HPV in a later infection. These particles eventually became the basis of the HPV vaccines Gardasil, Gardasil 9, and Cervarix.

HPV causes cervical cancer and other cancers such as cancer of the vulva, vagina, penis, or anus, as well as oropharyngeal cancer. Two of the high-risk types of HPV – HPV-16 and HPV-18 – cause about 70% of cervical cancers worldwide; it ranks 14th in frequency in the United States, according to the National Cancer Institute. The HPV vaccines are very effective in preventing persistent infections with HPV-16 and HPV-18. The Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices continues to recommend routine HPV vaccination for girls and boys at age 11 or 12 years, with a second vaccine given 6-12 months later.