User login
Precocious puberty – how early is too soon?
A 6-year-old girl presents with breast development. Her medical history is unremarkable. The parents are of average height, and the mother reports her thelarche was age 11 years. The girl is at the 97th percentile for her height and 90th percentile for her weight. She has Tanner stage 3 breast development and Tanner stage 2 pubic hair development. She has grown slightly more than 3 inches over the past year. How should she be evaluated and managed (N Engl J Med. 2008;358:2366-77)?
The premature onset of puberty, i.e., precocious puberty (PP), can be an emotionally traumatic event for the child and parents. Over the past century, improvements in public health and nutrition, and, more recently, increased obesity, have been associated with earlier puberty and the dominant factor has been attributed to genetics (Curr Opin Endocrinol Diabetes Obes. 2018;25[1]:49-54). This month’s article will focus on understanding what is considered “early” puberty, evaluating for causes, and managing precocious puberty.
More commonly seen in girls than boys, PP is defined as the onset of secondary sexual characteristics before age 7.5 years in Black and Hispanic girls, and prior to 8 years in White girls, which is 2-2.5 standard deviations below the average age of pubertal onset in healthy children (J Pediatr Adolesc Gynecol. 2019;32:455-9). As a comparison, PP is diagnosed with onset before age 9 years in boys. For White compared with Black girls, the average timing of thelarche is age 10 vs. 9.5 years, peak growth velocity is age 11.5, menarche is age 12.5 vs. 12, while completion of puberty is near age 14.5 vs. 13.5, respectively (J Pediatr. 1985;107:317). Fortunately, most girls with PP have common variants rather than serious pathology.
Classification: Central (CPP) vs. peripheral (PPP)
CPP is gonadotropin dependent, meaning the hypothalamic-pituitary-ovarian axis (HPO) is prematurely activated resulting in the normal progression of puberty.
PPP is gonadotropin independent, caused by sex steroid secretion from any source – ovaries, adrenal gland, exogenous or ectopic production, e.g., germ-cell tumor. This results in a disordered progression of pubertal milestones.
Whereas CPP is typically isosexual development, i.e., consistent with the child’s gender, PPP can be isosexual or contrasexual, e.g., virilization of girls. A third classification is “benign or nonprogressive pubertal variants” manifesting as isolated premature thelarche or adrenarche.
Causes (see table)
CPP. Idiopathic causes account for 80%-90% of presentations in girls and 25%-80% in boys. Remarkably, international and domestic adoption, as well as a family history of PP increases the likelihood of CPP in girls. Other etiologies include CNS lesions, e.g., hamartomas, which are the most common cause of PP in young children. MRI with contrast has been the traditional mode of diagnosis for CNS tumors, yet the yield is dubious in girls above age 6. Genetic causes are found in only a small percentage of PP cases. Rarely, CPP can result from gonadotropin-secreting tumors because of elevated luteinizing hormone levels.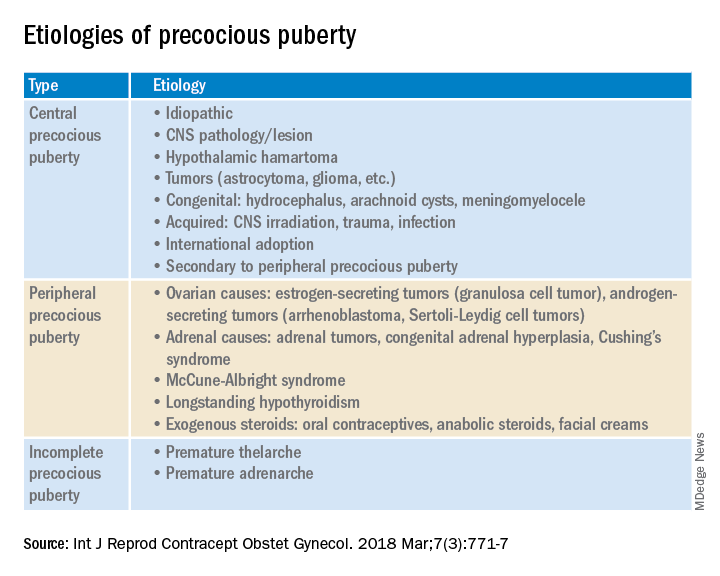
PPP. As a result of sex steroid secretion, peripheral causes of PPP include ovarian cysts and ovarian tumors that increase circulating estradiol, such as granulosa cell tumors, which would cause isosexual PPP and Sertoli-Leydig cell tumors that secrete testosterone, which can result in contrasexual PPP. Mild congenital adrenal hyperplasia can result in PPP with virilization (contrasexual) and markedly advanced bone age.
McCune-Albright syndrome is rare and presents with the classic triad of PPP, skin pigmentation called café-au-lait, and fibrous dysplasia of bone. The pathophysiology of McCune-Albright syndrome is autoactivation of the G-protein leading to activation of ovarian tissue that results in formation of large ovarian cysts and extreme elevations in serum estradiol as well as the potential production of other hormones, e.g., thyrotoxicosis, excess growth hormone (acromegaly), and Cushing syndrome.
Premature thelarche. Premature thelarche typically occurs in girls between the ages of 1 and 3 years and is limited to breast enlargement. While no cause has been determined, the plausible explanations include partial activation of the HPO axis, endocrine-disrupting chemicals (EDCs), or a genetic origin. A small percentage of these girls progress to CPP.
EDCs have been considered as potential influencers of early puberty, but no consensus has been established. (Examples of EDCs in the environment include air, soil, or water supply along with food sources, personal care products, and manufactured products that can affect the endocrine system.)
Premature adenarche. Premature adrenarche presents with adult body odor and/or body hair (pubic and/or axillary) in girls who have an elevated body mass index, most commonly at the ages of 6-7 years. The presumed mechanism is normal maturation of the adrenal gland with resultant elevation of circulating androgens. Bone age may be mildly accelerated and DHEAS is prematurely elevated for age. These girls appear to be at increased risk for polycystic ovary syndrome.
Evaluation
The initial step in the evaluation of PP is to determine whether the cause is CPP or PPP; the latter includes distinguishing isosexual from contrasexual development. A thorough history (growth, headaches, behavior or visual change, seizures, abdominal pain), physical exam, including Tanner staging, and bone age is required. However, with isolated premature thelarche or adrenarche, a bone age may not be necessary, as initial close clinical observation for pubertal progression is likely sufficient.
For CPP, the diagnosis is based on serum LH, whether random levels or elevations follow GnRH stimulation. Puberty milestones progress normally although adrenarche is not consistently apparent. For girls younger than age 6, a brain MRI is recommended but not in asymptomatic older girls with CPP. LH and FSH along with estradiol or testosterone, the latter especially in boys, are the first line of serum testing. Serum TSH is recommended for suspicion of primary hypothyroidism. In girls with premature adrenarche, a bone age, testosterone, DHEAS, and 17-OHP to rule out adrenal hyperplasia should be obtained. Pelvic ultrasound may be a useful adjunct to assess uterine volume and/or ovarian cysts/tumors.
Rapidity of onset can also lead the evaluation since a normal growth chart and skeletal maturation suggests a benign pubertal variant whereas a more rapid rate can signal CPP or PPP. Of note, health care providers should ensure prescription, over-the-counter oral or topical sources of hormones, and EDCs are ruled out.
Consequences
An association between childhood sexual abuse and earlier pubertal onset has been cited. These girls may be at increased risk for psychosocial difficulties, menstrual and fertility problems, and even reproductive cancers because of prolonged exposure to sex hormones (J Adolesc Health. 2016;60[1]:65-71).
Treatment
The mainstay of CPP treatment is maximizing adult height, typically through the use of a GnRH agonist for HPO suppression from pituitary downregulation. For girls above age 8 years, attempts at improving adult height have not shown a benefit.
In girls with PPP, treatment is directed at the prevailing pathology. Interestingly, early PPP can activate the HPO axis thereby converting to “secondary” CPP. In PPP, McCune-Albright syndrome treatment targets reducing circulating estrogens through letrozole or tamoxifen as well as addressing other autoactivated hormone production. Ovarian and adrenal tumors, albeit rare, can cause PP; therefore, surgical excision is the goal of treatment.
PP should be approached with equal concerns about the physical and emotional effects while including the family to help them understand the pathophysiology and psychosocial risks.
Dr. Mark P. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
A 6-year-old girl presents with breast development. Her medical history is unremarkable. The parents are of average height, and the mother reports her thelarche was age 11 years. The girl is at the 97th percentile for her height and 90th percentile for her weight. She has Tanner stage 3 breast development and Tanner stage 2 pubic hair development. She has grown slightly more than 3 inches over the past year. How should she be evaluated and managed (N Engl J Med. 2008;358:2366-77)?
The premature onset of puberty, i.e., precocious puberty (PP), can be an emotionally traumatic event for the child and parents. Over the past century, improvements in public health and nutrition, and, more recently, increased obesity, have been associated with earlier puberty and the dominant factor has been attributed to genetics (Curr Opin Endocrinol Diabetes Obes. 2018;25[1]:49-54). This month’s article will focus on understanding what is considered “early” puberty, evaluating for causes, and managing precocious puberty.
More commonly seen in girls than boys, PP is defined as the onset of secondary sexual characteristics before age 7.5 years in Black and Hispanic girls, and prior to 8 years in White girls, which is 2-2.5 standard deviations below the average age of pubertal onset in healthy children (J Pediatr Adolesc Gynecol. 2019;32:455-9). As a comparison, PP is diagnosed with onset before age 9 years in boys. For White compared with Black girls, the average timing of thelarche is age 10 vs. 9.5 years, peak growth velocity is age 11.5, menarche is age 12.5 vs. 12, while completion of puberty is near age 14.5 vs. 13.5, respectively (J Pediatr. 1985;107:317). Fortunately, most girls with PP have common variants rather than serious pathology.
Classification: Central (CPP) vs. peripheral (PPP)
CPP is gonadotropin dependent, meaning the hypothalamic-pituitary-ovarian axis (HPO) is prematurely activated resulting in the normal progression of puberty.
PPP is gonadotropin independent, caused by sex steroid secretion from any source – ovaries, adrenal gland, exogenous or ectopic production, e.g., germ-cell tumor. This results in a disordered progression of pubertal milestones.
Whereas CPP is typically isosexual development, i.e., consistent with the child’s gender, PPP can be isosexual or contrasexual, e.g., virilization of girls. A third classification is “benign or nonprogressive pubertal variants” manifesting as isolated premature thelarche or adrenarche.
Causes (see table)
CPP. Idiopathic causes account for 80%-90% of presentations in girls and 25%-80% in boys. Remarkably, international and domestic adoption, as well as a family history of PP increases the likelihood of CPP in girls. Other etiologies include CNS lesions, e.g., hamartomas, which are the most common cause of PP in young children. MRI with contrast has been the traditional mode of diagnosis for CNS tumors, yet the yield is dubious in girls above age 6. Genetic causes are found in only a small percentage of PP cases. Rarely, CPP can result from gonadotropin-secreting tumors because of elevated luteinizing hormone levels.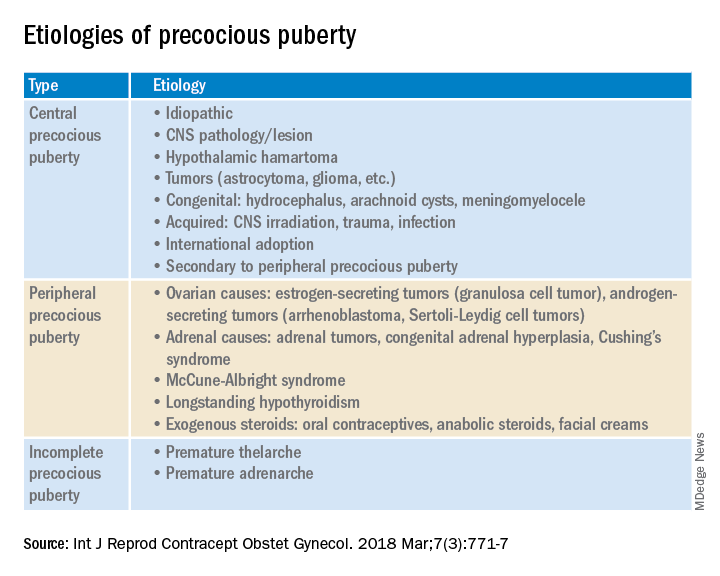
PPP. As a result of sex steroid secretion, peripheral causes of PPP include ovarian cysts and ovarian tumors that increase circulating estradiol, such as granulosa cell tumors, which would cause isosexual PPP and Sertoli-Leydig cell tumors that secrete testosterone, which can result in contrasexual PPP. Mild congenital adrenal hyperplasia can result in PPP with virilization (contrasexual) and markedly advanced bone age.
McCune-Albright syndrome is rare and presents with the classic triad of PPP, skin pigmentation called café-au-lait, and fibrous dysplasia of bone. The pathophysiology of McCune-Albright syndrome is autoactivation of the G-protein leading to activation of ovarian tissue that results in formation of large ovarian cysts and extreme elevations in serum estradiol as well as the potential production of other hormones, e.g., thyrotoxicosis, excess growth hormone (acromegaly), and Cushing syndrome.
Premature thelarche. Premature thelarche typically occurs in girls between the ages of 1 and 3 years and is limited to breast enlargement. While no cause has been determined, the plausible explanations include partial activation of the HPO axis, endocrine-disrupting chemicals (EDCs), or a genetic origin. A small percentage of these girls progress to CPP.
EDCs have been considered as potential influencers of early puberty, but no consensus has been established. (Examples of EDCs in the environment include air, soil, or water supply along with food sources, personal care products, and manufactured products that can affect the endocrine system.)
Premature adenarche. Premature adrenarche presents with adult body odor and/or body hair (pubic and/or axillary) in girls who have an elevated body mass index, most commonly at the ages of 6-7 years. The presumed mechanism is normal maturation of the adrenal gland with resultant elevation of circulating androgens. Bone age may be mildly accelerated and DHEAS is prematurely elevated for age. These girls appear to be at increased risk for polycystic ovary syndrome.
Evaluation
The initial step in the evaluation of PP is to determine whether the cause is CPP or PPP; the latter includes distinguishing isosexual from contrasexual development. A thorough history (growth, headaches, behavior or visual change, seizures, abdominal pain), physical exam, including Tanner staging, and bone age is required. However, with isolated premature thelarche or adrenarche, a bone age may not be necessary, as initial close clinical observation for pubertal progression is likely sufficient.
For CPP, the diagnosis is based on serum LH, whether random levels or elevations follow GnRH stimulation. Puberty milestones progress normally although adrenarche is not consistently apparent. For girls younger than age 6, a brain MRI is recommended but not in asymptomatic older girls with CPP. LH and FSH along with estradiol or testosterone, the latter especially in boys, are the first line of serum testing. Serum TSH is recommended for suspicion of primary hypothyroidism. In girls with premature adrenarche, a bone age, testosterone, DHEAS, and 17-OHP to rule out adrenal hyperplasia should be obtained. Pelvic ultrasound may be a useful adjunct to assess uterine volume and/or ovarian cysts/tumors.
Rapidity of onset can also lead the evaluation since a normal growth chart and skeletal maturation suggests a benign pubertal variant whereas a more rapid rate can signal CPP or PPP. Of note, health care providers should ensure prescription, over-the-counter oral or topical sources of hormones, and EDCs are ruled out.
Consequences
An association between childhood sexual abuse and earlier pubertal onset has been cited. These girls may be at increased risk for psychosocial difficulties, menstrual and fertility problems, and even reproductive cancers because of prolonged exposure to sex hormones (J Adolesc Health. 2016;60[1]:65-71).
Treatment
The mainstay of CPP treatment is maximizing adult height, typically through the use of a GnRH agonist for HPO suppression from pituitary downregulation. For girls above age 8 years, attempts at improving adult height have not shown a benefit.
In girls with PPP, treatment is directed at the prevailing pathology. Interestingly, early PPP can activate the HPO axis thereby converting to “secondary” CPP. In PPP, McCune-Albright syndrome treatment targets reducing circulating estrogens through letrozole or tamoxifen as well as addressing other autoactivated hormone production. Ovarian and adrenal tumors, albeit rare, can cause PP; therefore, surgical excision is the goal of treatment.
PP should be approached with equal concerns about the physical and emotional effects while including the family to help them understand the pathophysiology and psychosocial risks.
Dr. Mark P. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
A 6-year-old girl presents with breast development. Her medical history is unremarkable. The parents are of average height, and the mother reports her thelarche was age 11 years. The girl is at the 97th percentile for her height and 90th percentile for her weight. She has Tanner stage 3 breast development and Tanner stage 2 pubic hair development. She has grown slightly more than 3 inches over the past year. How should she be evaluated and managed (N Engl J Med. 2008;358:2366-77)?
The premature onset of puberty, i.e., precocious puberty (PP), can be an emotionally traumatic event for the child and parents. Over the past century, improvements in public health and nutrition, and, more recently, increased obesity, have been associated with earlier puberty and the dominant factor has been attributed to genetics (Curr Opin Endocrinol Diabetes Obes. 2018;25[1]:49-54). This month’s article will focus on understanding what is considered “early” puberty, evaluating for causes, and managing precocious puberty.
More commonly seen in girls than boys, PP is defined as the onset of secondary sexual characteristics before age 7.5 years in Black and Hispanic girls, and prior to 8 years in White girls, which is 2-2.5 standard deviations below the average age of pubertal onset in healthy children (J Pediatr Adolesc Gynecol. 2019;32:455-9). As a comparison, PP is diagnosed with onset before age 9 years in boys. For White compared with Black girls, the average timing of thelarche is age 10 vs. 9.5 years, peak growth velocity is age 11.5, menarche is age 12.5 vs. 12, while completion of puberty is near age 14.5 vs. 13.5, respectively (J Pediatr. 1985;107:317). Fortunately, most girls with PP have common variants rather than serious pathology.
Classification: Central (CPP) vs. peripheral (PPP)
CPP is gonadotropin dependent, meaning the hypothalamic-pituitary-ovarian axis (HPO) is prematurely activated resulting in the normal progression of puberty.
PPP is gonadotropin independent, caused by sex steroid secretion from any source – ovaries, adrenal gland, exogenous or ectopic production, e.g., germ-cell tumor. This results in a disordered progression of pubertal milestones.
Whereas CPP is typically isosexual development, i.e., consistent with the child’s gender, PPP can be isosexual or contrasexual, e.g., virilization of girls. A third classification is “benign or nonprogressive pubertal variants” manifesting as isolated premature thelarche or adrenarche.
Causes (see table)
CPP. Idiopathic causes account for 80%-90% of presentations in girls and 25%-80% in boys. Remarkably, international and domestic adoption, as well as a family history of PP increases the likelihood of CPP in girls. Other etiologies include CNS lesions, e.g., hamartomas, which are the most common cause of PP in young children. MRI with contrast has been the traditional mode of diagnosis for CNS tumors, yet the yield is dubious in girls above age 6. Genetic causes are found in only a small percentage of PP cases. Rarely, CPP can result from gonadotropin-secreting tumors because of elevated luteinizing hormone levels.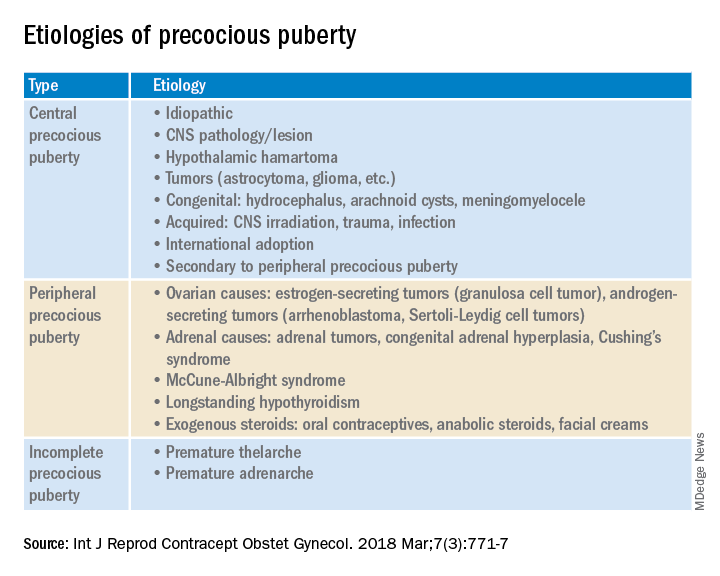
PPP. As a result of sex steroid secretion, peripheral causes of PPP include ovarian cysts and ovarian tumors that increase circulating estradiol, such as granulosa cell tumors, which would cause isosexual PPP and Sertoli-Leydig cell tumors that secrete testosterone, which can result in contrasexual PPP. Mild congenital adrenal hyperplasia can result in PPP with virilization (contrasexual) and markedly advanced bone age.
McCune-Albright syndrome is rare and presents with the classic triad of PPP, skin pigmentation called café-au-lait, and fibrous dysplasia of bone. The pathophysiology of McCune-Albright syndrome is autoactivation of the G-protein leading to activation of ovarian tissue that results in formation of large ovarian cysts and extreme elevations in serum estradiol as well as the potential production of other hormones, e.g., thyrotoxicosis, excess growth hormone (acromegaly), and Cushing syndrome.
Premature thelarche. Premature thelarche typically occurs in girls between the ages of 1 and 3 years and is limited to breast enlargement. While no cause has been determined, the plausible explanations include partial activation of the HPO axis, endocrine-disrupting chemicals (EDCs), or a genetic origin. A small percentage of these girls progress to CPP.
EDCs have been considered as potential influencers of early puberty, but no consensus has been established. (Examples of EDCs in the environment include air, soil, or water supply along with food sources, personal care products, and manufactured products that can affect the endocrine system.)
Premature adenarche. Premature adrenarche presents with adult body odor and/or body hair (pubic and/or axillary) in girls who have an elevated body mass index, most commonly at the ages of 6-7 years. The presumed mechanism is normal maturation of the adrenal gland with resultant elevation of circulating androgens. Bone age may be mildly accelerated and DHEAS is prematurely elevated for age. These girls appear to be at increased risk for polycystic ovary syndrome.
Evaluation
The initial step in the evaluation of PP is to determine whether the cause is CPP or PPP; the latter includes distinguishing isosexual from contrasexual development. A thorough history (growth, headaches, behavior or visual change, seizures, abdominal pain), physical exam, including Tanner staging, and bone age is required. However, with isolated premature thelarche or adrenarche, a bone age may not be necessary, as initial close clinical observation for pubertal progression is likely sufficient.
For CPP, the diagnosis is based on serum LH, whether random levels or elevations follow GnRH stimulation. Puberty milestones progress normally although adrenarche is not consistently apparent. For girls younger than age 6, a brain MRI is recommended but not in asymptomatic older girls with CPP. LH and FSH along with estradiol or testosterone, the latter especially in boys, are the first line of serum testing. Serum TSH is recommended for suspicion of primary hypothyroidism. In girls with premature adrenarche, a bone age, testosterone, DHEAS, and 17-OHP to rule out adrenal hyperplasia should be obtained. Pelvic ultrasound may be a useful adjunct to assess uterine volume and/or ovarian cysts/tumors.
Rapidity of onset can also lead the evaluation since a normal growth chart and skeletal maturation suggests a benign pubertal variant whereas a more rapid rate can signal CPP or PPP. Of note, health care providers should ensure prescription, over-the-counter oral or topical sources of hormones, and EDCs are ruled out.
Consequences
An association between childhood sexual abuse and earlier pubertal onset has been cited. These girls may be at increased risk for psychosocial difficulties, menstrual and fertility problems, and even reproductive cancers because of prolonged exposure to sex hormones (J Adolesc Health. 2016;60[1]:65-71).
Treatment
The mainstay of CPP treatment is maximizing adult height, typically through the use of a GnRH agonist for HPO suppression from pituitary downregulation. For girls above age 8 years, attempts at improving adult height have not shown a benefit.
In girls with PPP, treatment is directed at the prevailing pathology. Interestingly, early PPP can activate the HPO axis thereby converting to “secondary” CPP. In PPP, McCune-Albright syndrome treatment targets reducing circulating estrogens through letrozole or tamoxifen as well as addressing other autoactivated hormone production. Ovarian and adrenal tumors, albeit rare, can cause PP; therefore, surgical excision is the goal of treatment.
PP should be approached with equal concerns about the physical and emotional effects while including the family to help them understand the pathophysiology and psychosocial risks.
Dr. Mark P. Trolice is director of The IVF Center in Winter Park, Fla., and professor of obstetrics and gynecology at the University of Central Florida, Orlando.
Hard habit to break
“I love practicing medicine.”
The speaker was one of my patients. A distinguished, friendly, gentleman in his mid-to-late 70s, here to see me for a minor problem. He still practices medicine part time.
Since his neurologic issue was simple, we spent a fair amount of the time chatting. We’d both seen changes in medicine over time, he more than I, obviously.
Some good, some bad. Fancier toys, better drugs, more paperwork (even if it’s not all on paper anymore).
But we both still like what we do, and have no plans to give it up anytime soon.
Some doctors end up hating their jobs and leave the field. I understand that, and I don’t blame them. It’s not an easy one.
But I still enjoy the job. I look forward to seeing patients each day, turning over their cases, trying to figure them out, and doing what I can to help people.
I see that it is similar with attorneys. Maybe it’s part of the time and commitment you put into getting to a job that makes it hard to walk away as you get older. Or maybe (probably more likely) it’s some intrinsic part of the personality that drove you to get there.
I’m roughly two-thirds of the way through my career, but still don’t have any plans to close down. Granted, that’s practical – I have kids in college, a mortgage, and office overhead. My colleague across the desk can stop practicing whenever he wants, but gets satisfaction, validation, and enjoyment from doing the same job. At this point in his life that’s more important than the money.
I hope to someday feel that same way. I don’t want to always work the 80-90 hours a week I do now, but I can’t imagine not doing this, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I love practicing medicine.”
The speaker was one of my patients. A distinguished, friendly, gentleman in his mid-to-late 70s, here to see me for a minor problem. He still practices medicine part time.
Since his neurologic issue was simple, we spent a fair amount of the time chatting. We’d both seen changes in medicine over time, he more than I, obviously.
Some good, some bad. Fancier toys, better drugs, more paperwork (even if it’s not all on paper anymore).
But we both still like what we do, and have no plans to give it up anytime soon.
Some doctors end up hating their jobs and leave the field. I understand that, and I don’t blame them. It’s not an easy one.
But I still enjoy the job. I look forward to seeing patients each day, turning over their cases, trying to figure them out, and doing what I can to help people.
I see that it is similar with attorneys. Maybe it’s part of the time and commitment you put into getting to a job that makes it hard to walk away as you get older. Or maybe (probably more likely) it’s some intrinsic part of the personality that drove you to get there.
I’m roughly two-thirds of the way through my career, but still don’t have any plans to close down. Granted, that’s practical – I have kids in college, a mortgage, and office overhead. My colleague across the desk can stop practicing whenever he wants, but gets satisfaction, validation, and enjoyment from doing the same job. At this point in his life that’s more important than the money.
I hope to someday feel that same way. I don’t want to always work the 80-90 hours a week I do now, but I can’t imagine not doing this, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I love practicing medicine.”
The speaker was one of my patients. A distinguished, friendly, gentleman in his mid-to-late 70s, here to see me for a minor problem. He still practices medicine part time.
Since his neurologic issue was simple, we spent a fair amount of the time chatting. We’d both seen changes in medicine over time, he more than I, obviously.
Some good, some bad. Fancier toys, better drugs, more paperwork (even if it’s not all on paper anymore).
But we both still like what we do, and have no plans to give it up anytime soon.
Some doctors end up hating their jobs and leave the field. I understand that, and I don’t blame them. It’s not an easy one.
But I still enjoy the job. I look forward to seeing patients each day, turning over their cases, trying to figure them out, and doing what I can to help people.
I see that it is similar with attorneys. Maybe it’s part of the time and commitment you put into getting to a job that makes it hard to walk away as you get older. Or maybe (probably more likely) it’s some intrinsic part of the personality that drove you to get there.
I’m roughly two-thirds of the way through my career, but still don’t have any plans to close down. Granted, that’s practical – I have kids in college, a mortgage, and office overhead. My colleague across the desk can stop practicing whenever he wants, but gets satisfaction, validation, and enjoyment from doing the same job. At this point in his life that’s more important than the money.
I hope to someday feel that same way. I don’t want to always work the 80-90 hours a week I do now, but I can’t imagine not doing this, either.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Bored? Change the world or read a book
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do (like payroll and paying bills), legal cases to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
So this weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon. Which is rare, usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do.
Boredom is one of the odder human conditions. Certainly, there are more ways to waste time now than there ever have been. TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. (Fortunately, he wasn’t hit by a car in the process.)
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most other mammals tend to doze off. But not us. It’s always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.”
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we’re here. The mind that keeps working is a powerful tool, driving us forward in all walks of life. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
Perhaps it’s the real reason we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do (like payroll and paying bills), legal cases to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
So this weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon. Which is rare, usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do.
Boredom is one of the odder human conditions. Certainly, there are more ways to waste time now than there ever have been. TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. (Fortunately, he wasn’t hit by a car in the process.)
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most other mammals tend to doze off. But not us. It’s always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.”
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we’re here. The mind that keeps working is a powerful tool, driving us forward in all walks of life. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
Perhaps it’s the real reason we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
A weekend, for most of us in solo practice, doesn’t really signify time off from work. It just means we’re not seeing patients at the office.
There’s always business stuff to do (like payroll and paying bills), legal cases to review, the never-ending forms for a million things, and all the other stuff there never seems to be enough time to do on weekdays.
So this weekend I started attacking the pile after dinner on Friday and found myself done by Saturday afternoon. Which is rare, usually I spend the better part of a weekend at my desk.
And then, unexpectedly faced with an empty desk, I found myself wondering what to do.
Boredom is one of the odder human conditions. Certainly, there are more ways to waste time now than there ever have been. TV, Netflix, phone games, TikTok, books, just to name a few.
But do we always have to be entertained? Many great scientists have said that world-changing ideas have come to them when they weren’t working, such as while showering or riding to work. Leo Szilard was crossing a London street in 1933 when he suddenly saw how a nuclear chain reaction would be self-sustaining once initiated. (Fortunately, he wasn’t hit by a car in the process.)
But I’m not Szilard. So I rationalized a reason not to exercise and sat on the couch with a book.
The remarkable human brain doesn’t shut down easily. With nothing else to do, most other mammals tend to doze off. But not us. It’s always on, trying to think of the next goal, the next move, the next whatever.
Having nothing to do sounds like a great idea, until you have nothing to do. It may be fine for a few days, but after a while you realize there’s only so long you can stare at the waves or mountains before your mind turns back to “what’s next.”
This isn’t a bad thing. Being bored is probably constructive. Without realizing it we use it to form new ideas and start new plans.
Maybe this is why we’re here. The mind that keeps working is a powerful tool, driving us forward in all walks of life. Perhaps it’s this feature that pushed the development of intelligence further and led us to form civilizations.
Perhaps it’s the real reason we keep moving forward.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Book Review: Quality improvement in mental health care
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
Sunil Khushalani and Antonio DePaolo,
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare”
(London: Routledge, Taylor & Francis, 2022)
Since the publication of our book, “Lean Behavioral Health: The Kings County Hospital Story” (Oxford, England: Oxford University Press, 2014) almost a decade ago, “Transforming Mental Healthcare” is the first major book published about the use of a system for quality improvement across the health care continuum. That it has taken this long is probably surprising to those of us who have spent careers on trying to improve what is universally described as a system that is “broken” and in need of a major overhaul.
Every news cycle that reports mass violence typically spends a good bit of time talking about the failures of the mental health care system. One important lesson I learned when taking over the beleaguered Kings County (N.Y.) psychiatry service in 2009 (a department that has made extraordinary improvements over the years and is now exclaimed by the U.S. Department of Justice as “a model program”), is that the employees on the front line are often erroneously blamed for such failures.
The failure is systemic and usually starts at the top of the table of organization, not at the bottom. Dr. Khushalani and Dr. DePaolo have produced an excellent volume that should be purchased by every mental health care CEO and given “with thanks” to the local leaders overseeing the direct care of some of our nation’s most vulnerable patient populations.
The first part of “Transforming Mental Healthcare” provides an excellent overview of the current state of our mental health care system and its too numerous to name problems. This section could be a primer for all our legislators so their eyes can be opened to the failures on the ground that require their help in correcting. Many of the “failures” of our mental health care are societal failures – lack of affordable housing, access to care, reimbursement for care, gun access, etc. – and cannot be “fixed” by providers of care. Such problems are societal problems that call for societal and governmental solutions, and not only at the local level but from coast to coast.
The remainder of this easy to read and follow text provides many rich resources for the deliverers of mental health care. (e.g., plan-do-act, standard work, and A3 thinking).
The closing section focuses on leadership and culture – often overlooked to the detriment of any organization that doesn’t pay close attention to supporting both. Culture is cultivated and nourished by the organization’s leaders. Culture empowers staff to become problem solvers and agents of improvement. Empowered staff support and enrich their culture. Together a workplace that brings out the best of all its people is created, and burnout is held at bay.
“Transforming Mental Healthcare: Applying Performance Improvement Methods to Mental Healthcare” is a welcome and essential addition to the current morass, which is our mental health care delivery system, an oasis in the desert from which perhaps the lotus flower can emerge.
Dr. Merlino is emeritus professor of psychiatry, SUNY Downstate College of Medicine, Rhinebeck, N.Y., and formerly director of psychiatry at Kings County Hospital Center, Brooklyn, NY. He is the coauthor of “Lean Behavioral Health: The Kings County Hospital Story.” .
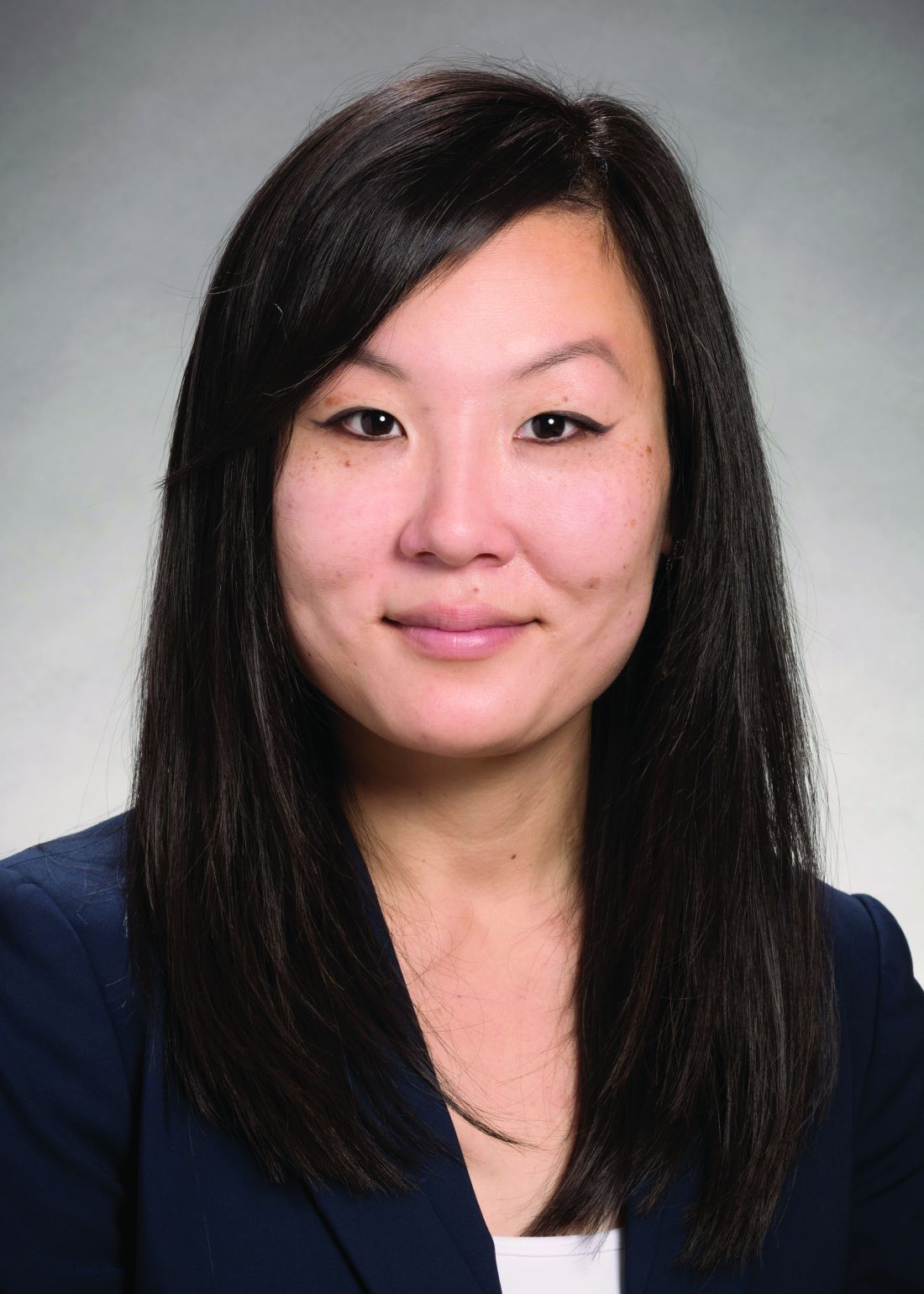
What is palliative care and what’s new in practicing this type of medicine?
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
Caring for the young elite athlete
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
The mother’s double jeopardy
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
For the Fourth of July, a neuroscientist reflects on patriotism
This week, we celebrate our nation’s birth in a national and individual display of our patriotic attachment to this country. — which includes our self-definition as Americans.
For each of us, personhood is an almost miraculous product of our brain’s plasticity — the brain’s ability to change chemically, structurally, and functionally, based on our life experiences — arising from near countless moments of change in the wiring of our brain.
The incredibly complex remodeling that created “you” is a product, of course, of your very complicated, unique passage in life. You have a repertoire of skills and ability; you have stories and understanding and a history of sensing and acting and thinking in the world that is, in detail, unique only to you and your experiences.
As your brain created its model of your world by recording “what goes with what” at each brief moment of time, your brain — that most complicated and wonderful of “machines” on planet Earth — also associated billions of moments of feeling and action and thought with their source, your Self.
Because we primarily construct our model of the world through our eyes and ears, it’s not surprising that the emergent Self that is located somewhere in the center of your head behind your eyes and between your ears. Through billions of contacts with the surfaces of your hide and sensory organs, you have embodied yourself.
Your sense of ‘us’
These same neurologic processes extend beyond our physical beings to incorporate other contributors to our well-being into our personhoods. Loving parents, siblings, friends — and others in your clans and tribes and nations — literally grow into your personhood by these same self-associating processes. These relationships are supported in mutual identity by all of the tokens and icons and charms and customs that collectively define you and enable a sense of “us.”
Put another way, Mother Nature (or, in another cultural perspective, our Creator) has designed our brains to incorporate all of those who are close to us — and more broadly, other individuals in our clan or tribe or nation — to be a part of each of us.
Humans are highly social creatures. When we rise up and risk our lives to defend our friends, family, or cultural “in-groups,” we are literally fighting to defend ourselves — because those other individuals have grown into our very being. In defending them, we are literally defending a part of ourselves.
From one human perspective, this attachment to family and clan and tribe and nation is obviously key for our survival. We are an individually vulnerable but collectively powerful species, and attachment and mutual support are a key to our personal and collective successes in life.
From another perspective, there is also a dark side to this “gift of nature.”
We draw lines in substantially arbitrary locations across the surface of planet Earth, or we may define our self as belonging to a group in a political or social or religious context, or sect. Our tribalism can support a generally strong level of support and succor for fellow humans on our side of that line, while we regard those just across the line as undeserving of our support. If they offend us, they may become targets of our capacity for cruelty.
Our allegiances can be both wonderful and harmful.
The individuality of us
As we celebrate this holiday — a favorite day on my personal calendar — I am compelled to reflect on the fact that America was designed to be fractious. We Americans are not required to all operate like “peas in the pod.”
While we, as a nation, often fail to live up to our ideals, when we pursue the highest standards of liberty, we celebrate diversity, difference, and the ability of each member of our tribe to find their own path.
In a very real sense, the great American “invention” was to create a nation in which we could all find a wonderful place of our own, with the sympathy and protection of fellow citizens, and with liberty and justice for all.
Happy Independence Day to my American tribe!
Michael Merzenich, PhD, is often credited with discovering lifelong plasticity, with being the first to harness plasticity for human benefit (in his co-invention of the cochlear implant), and for pioneering the field of plasticity-based computerized brain exercise. He is professor emeritus at UCSF and a Kavli Laureate in Neuroscience, and he has been honored by each of the US National Academies of Sciences, Engineering, and Medicine. He may be most widely known for a series of specials on the brain on public television. His current focus is BrainHQ, a brain exercise app. He has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Posit Science Corporation; Stronger Brains Inc. Serve(d) as a speaker or a member of a speakers bureau for: Posit Science Corporation; Stronger Brains Inc. Received research grant from: National Institutes of Health Have a 5% or greater equity interest in: Posit Science Corporation; Stronger Brains Inc. Received income in an amount equal to or greater than $250 from: Posit Science Corporation; Stronger Brains Inc.; National Institutes of Health.
A version of this article first appeared on Medscape.com.
This week, we celebrate our nation’s birth in a national and individual display of our patriotic attachment to this country. — which includes our self-definition as Americans.
For each of us, personhood is an almost miraculous product of our brain’s plasticity — the brain’s ability to change chemically, structurally, and functionally, based on our life experiences — arising from near countless moments of change in the wiring of our brain.
The incredibly complex remodeling that created “you” is a product, of course, of your very complicated, unique passage in life. You have a repertoire of skills and ability; you have stories and understanding and a history of sensing and acting and thinking in the world that is, in detail, unique only to you and your experiences.
As your brain created its model of your world by recording “what goes with what” at each brief moment of time, your brain — that most complicated and wonderful of “machines” on planet Earth — also associated billions of moments of feeling and action and thought with their source, your Self.
Because we primarily construct our model of the world through our eyes and ears, it’s not surprising that the emergent Self that is located somewhere in the center of your head behind your eyes and between your ears. Through billions of contacts with the surfaces of your hide and sensory organs, you have embodied yourself.
Your sense of ‘us’
These same neurologic processes extend beyond our physical beings to incorporate other contributors to our well-being into our personhoods. Loving parents, siblings, friends — and others in your clans and tribes and nations — literally grow into your personhood by these same self-associating processes. These relationships are supported in mutual identity by all of the tokens and icons and charms and customs that collectively define you and enable a sense of “us.”
Put another way, Mother Nature (or, in another cultural perspective, our Creator) has designed our brains to incorporate all of those who are close to us — and more broadly, other individuals in our clan or tribe or nation — to be a part of each of us.
Humans are highly social creatures. When we rise up and risk our lives to defend our friends, family, or cultural “in-groups,” we are literally fighting to defend ourselves — because those other individuals have grown into our very being. In defending them, we are literally defending a part of ourselves.
From one human perspective, this attachment to family and clan and tribe and nation is obviously key for our survival. We are an individually vulnerable but collectively powerful species, and attachment and mutual support are a key to our personal and collective successes in life.
From another perspective, there is also a dark side to this “gift of nature.”
We draw lines in substantially arbitrary locations across the surface of planet Earth, or we may define our self as belonging to a group in a political or social or religious context, or sect. Our tribalism can support a generally strong level of support and succor for fellow humans on our side of that line, while we regard those just across the line as undeserving of our support. If they offend us, they may become targets of our capacity for cruelty.
Our allegiances can be both wonderful and harmful.
The individuality of us
As we celebrate this holiday — a favorite day on my personal calendar — I am compelled to reflect on the fact that America was designed to be fractious. We Americans are not required to all operate like “peas in the pod.”
While we, as a nation, often fail to live up to our ideals, when we pursue the highest standards of liberty, we celebrate diversity, difference, and the ability of each member of our tribe to find their own path.
In a very real sense, the great American “invention” was to create a nation in which we could all find a wonderful place of our own, with the sympathy and protection of fellow citizens, and with liberty and justice for all.
Happy Independence Day to my American tribe!
Michael Merzenich, PhD, is often credited with discovering lifelong plasticity, with being the first to harness plasticity for human benefit (in his co-invention of the cochlear implant), and for pioneering the field of plasticity-based computerized brain exercise. He is professor emeritus at UCSF and a Kavli Laureate in Neuroscience, and he has been honored by each of the US National Academies of Sciences, Engineering, and Medicine. He may be most widely known for a series of specials on the brain on public television. His current focus is BrainHQ, a brain exercise app. He has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Posit Science Corporation; Stronger Brains Inc. Serve(d) as a speaker or a member of a speakers bureau for: Posit Science Corporation; Stronger Brains Inc. Received research grant from: National Institutes of Health Have a 5% or greater equity interest in: Posit Science Corporation; Stronger Brains Inc. Received income in an amount equal to or greater than $250 from: Posit Science Corporation; Stronger Brains Inc.; National Institutes of Health.
A version of this article first appeared on Medscape.com.
This week, we celebrate our nation’s birth in a national and individual display of our patriotic attachment to this country. — which includes our self-definition as Americans.
For each of us, personhood is an almost miraculous product of our brain’s plasticity — the brain’s ability to change chemically, structurally, and functionally, based on our life experiences — arising from near countless moments of change in the wiring of our brain.
The incredibly complex remodeling that created “you” is a product, of course, of your very complicated, unique passage in life. You have a repertoire of skills and ability; you have stories and understanding and a history of sensing and acting and thinking in the world that is, in detail, unique only to you and your experiences.
As your brain created its model of your world by recording “what goes with what” at each brief moment of time, your brain — that most complicated and wonderful of “machines” on planet Earth — also associated billions of moments of feeling and action and thought with their source, your Self.
Because we primarily construct our model of the world through our eyes and ears, it’s not surprising that the emergent Self that is located somewhere in the center of your head behind your eyes and between your ears. Through billions of contacts with the surfaces of your hide and sensory organs, you have embodied yourself.
Your sense of ‘us’
These same neurologic processes extend beyond our physical beings to incorporate other contributors to our well-being into our personhoods. Loving parents, siblings, friends — and others in your clans and tribes and nations — literally grow into your personhood by these same self-associating processes. These relationships are supported in mutual identity by all of the tokens and icons and charms and customs that collectively define you and enable a sense of “us.”
Put another way, Mother Nature (or, in another cultural perspective, our Creator) has designed our brains to incorporate all of those who are close to us — and more broadly, other individuals in our clan or tribe or nation — to be a part of each of us.
Humans are highly social creatures. When we rise up and risk our lives to defend our friends, family, or cultural “in-groups,” we are literally fighting to defend ourselves — because those other individuals have grown into our very being. In defending them, we are literally defending a part of ourselves.
From one human perspective, this attachment to family and clan and tribe and nation is obviously key for our survival. We are an individually vulnerable but collectively powerful species, and attachment and mutual support are a key to our personal and collective successes in life.
From another perspective, there is also a dark side to this “gift of nature.”
We draw lines in substantially arbitrary locations across the surface of planet Earth, or we may define our self as belonging to a group in a political or social or religious context, or sect. Our tribalism can support a generally strong level of support and succor for fellow humans on our side of that line, while we regard those just across the line as undeserving of our support. If they offend us, they may become targets of our capacity for cruelty.
Our allegiances can be both wonderful and harmful.
The individuality of us
As we celebrate this holiday — a favorite day on my personal calendar — I am compelled to reflect on the fact that America was designed to be fractious. We Americans are not required to all operate like “peas in the pod.”
While we, as a nation, often fail to live up to our ideals, when we pursue the highest standards of liberty, we celebrate diversity, difference, and the ability of each member of our tribe to find their own path.
In a very real sense, the great American “invention” was to create a nation in which we could all find a wonderful place of our own, with the sympathy and protection of fellow citizens, and with liberty and justice for all.
Happy Independence Day to my American tribe!
Michael Merzenich, PhD, is often credited with discovering lifelong plasticity, with being the first to harness plasticity for human benefit (in his co-invention of the cochlear implant), and for pioneering the field of plasticity-based computerized brain exercise. He is professor emeritus at UCSF and a Kavli Laureate in Neuroscience, and he has been honored by each of the US National Academies of Sciences, Engineering, and Medicine. He may be most widely known for a series of specials on the brain on public television. His current focus is BrainHQ, a brain exercise app. He has disclosed the following relevant financial relationships: Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: Posit Science Corporation; Stronger Brains Inc. Serve(d) as a speaker or a member of a speakers bureau for: Posit Science Corporation; Stronger Brains Inc. Received research grant from: National Institutes of Health Have a 5% or greater equity interest in: Posit Science Corporation; Stronger Brains Inc. Received income in an amount equal to or greater than $250 from: Posit Science Corporation; Stronger Brains Inc.; National Institutes of Health.
A version of this article first appeared on Medscape.com.
Then and Now: A ‘lifetime’ of advancement in upper GI tract
Fifteen years is a lifetime for the advancement of medical research. This seems particularly true for upper GI tract disorders.
In 2007, eosinophilic esophagitis was a rare disease; limited clinical data were available describing the symptoms, demographic characteristics, and endoscopic findings. Treatment was guided mostly by uncontrolled patient series for topical steroids and comprehensive diet exclusion therapy. Today, the molecular, genetic, and evolving microbiome’s contributions to EoE are being elucidated. EoE is recognized as one of the most common diseases in our practice, and rigorously performed controlled trials of steroids and biologics (including Food and Drug Administration–approved dupilumab) guide our treatment. Diet has also become easier with the identification of a single food antigen as the cause in 40% of EoE patients. The most pressing need is for a test that’s reliable and less invasive than endoscopy to assess and monitor treatment.
Barrett’s esophagus was of great concern 15 years ago and has surged in importance because of the increasing incidence of Barrett’s and esophageal adenocarcinoma, likely emphasized by the obesity epidemic. Sadly, survival with esophageal adenocarcinoma has changed little because most patients present with advanced stages. Multiple studies are questioning guideline recommendations because of their low yield and high expense. Fortunately, a range of easier screening tools is being tested, including sponge on string devices, video capsules, transnasal endoscopy, and the electronic “nose.” These can provide more widespread screening in broader populations of patients at risk who may lack heartburn or classic demographics. In 2007 there was little endoscopic therapy; now, the gastroenterologist has a robust armamentarium with multiple methods for mucosal ablation and resection achieving cure and sparing the patient an esophagectomy. Tissue biomarkers continue to be elucidated and are being applied to clinical practice.
For esophageal motility disorders, manometric data were obtained through a primitive water-infused system. With high-resolution manometry, the Chicago Classification, and impedance planimetry, our ability to precisely define, understand, and treat these disorders has been greatly enhanced.
In prior decades, the association of H. pylori to gastric cancer was noted but landmark trials and meta-analyses have strongly linked eradication of H. pylori with reduction in gastric cancer. These include broad population studies from Taiwan and the U.S. Veterans Health Administration, as well as a Cochrane review. These data have reinforced the need to search for and eradicate H. pylori infection. Although antibiotic resistance is rampant, newer antibiotic combinations including nitazoxanide, levofloxacin, rifabutin, and tinidazole have been proven effective. Potassium-competitive acid blockers may also augment effective eradication.
Endoscopy itself is one of the greatest areas of advancement in upper GI disease since 2007. What was once limited to biopsy, removal of polyps, and control of gastrointestinal bleeding, now has a breathtaking range of diagnostic and therapeutic capabilities. Who could imagine being able to perform bariatric procedures, create a gastrojejunostomy, treat a Zenker’s diverticulum, or drain extraluminal abscesses through an endoscope? With description of the technique of submucosal tunneling, endoscopic mucosal resection has been extended to submucosal dissection for more advanced cancers and benign tumors. This technique has also revolutionized the treatment of achalasia with peroral endoscopic myotomy, a procedure found equivalent to laparoscopic myotomy in controlled trials. Finally, artificial intelligence has taken endoscopic imaging by storm, and the accuracy with which we will diagnose premalignant lesions of the esophagus and stomach should significantly increase our abilities to prevent and treat early cancers.
Dr. Katzka is professor of medicine at Columbia University, New York. He reports consulting for Takeda and Celgene.
This article was updated July 7, 2022.
Fifteen years is a lifetime for the advancement of medical research. This seems particularly true for upper GI tract disorders.
In 2007, eosinophilic esophagitis was a rare disease; limited clinical data were available describing the symptoms, demographic characteristics, and endoscopic findings. Treatment was guided mostly by uncontrolled patient series for topical steroids and comprehensive diet exclusion therapy. Today, the molecular, genetic, and evolving microbiome’s contributions to EoE are being elucidated. EoE is recognized as one of the most common diseases in our practice, and rigorously performed controlled trials of steroids and biologics (including Food and Drug Administration–approved dupilumab) guide our treatment. Diet has also become easier with the identification of a single food antigen as the cause in 40% of EoE patients. The most pressing need is for a test that’s reliable and less invasive than endoscopy to assess and monitor treatment.
Barrett’s esophagus was of great concern 15 years ago and has surged in importance because of the increasing incidence of Barrett’s and esophageal adenocarcinoma, likely emphasized by the obesity epidemic. Sadly, survival with esophageal adenocarcinoma has changed little because most patients present with advanced stages. Multiple studies are questioning guideline recommendations because of their low yield and high expense. Fortunately, a range of easier screening tools is being tested, including sponge on string devices, video capsules, transnasal endoscopy, and the electronic “nose.” These can provide more widespread screening in broader populations of patients at risk who may lack heartburn or classic demographics. In 2007 there was little endoscopic therapy; now, the gastroenterologist has a robust armamentarium with multiple methods for mucosal ablation and resection achieving cure and sparing the patient an esophagectomy. Tissue biomarkers continue to be elucidated and are being applied to clinical practice.
For esophageal motility disorders, manometric data were obtained through a primitive water-infused system. With high-resolution manometry, the Chicago Classification, and impedance planimetry, our ability to precisely define, understand, and treat these disorders has been greatly enhanced.
In prior decades, the association of H. pylori to gastric cancer was noted but landmark trials and meta-analyses have strongly linked eradication of H. pylori with reduction in gastric cancer. These include broad population studies from Taiwan and the U.S. Veterans Health Administration, as well as a Cochrane review. These data have reinforced the need to search for and eradicate H. pylori infection. Although antibiotic resistance is rampant, newer antibiotic combinations including nitazoxanide, levofloxacin, rifabutin, and tinidazole have been proven effective. Potassium-competitive acid blockers may also augment effective eradication.
Endoscopy itself is one of the greatest areas of advancement in upper GI disease since 2007. What was once limited to biopsy, removal of polyps, and control of gastrointestinal bleeding, now has a breathtaking range of diagnostic and therapeutic capabilities. Who could imagine being able to perform bariatric procedures, create a gastrojejunostomy, treat a Zenker’s diverticulum, or drain extraluminal abscesses through an endoscope? With description of the technique of submucosal tunneling, endoscopic mucosal resection has been extended to submucosal dissection for more advanced cancers and benign tumors. This technique has also revolutionized the treatment of achalasia with peroral endoscopic myotomy, a procedure found equivalent to laparoscopic myotomy in controlled trials. Finally, artificial intelligence has taken endoscopic imaging by storm, and the accuracy with which we will diagnose premalignant lesions of the esophagus and stomach should significantly increase our abilities to prevent and treat early cancers.
Dr. Katzka is professor of medicine at Columbia University, New York. He reports consulting for Takeda and Celgene.
This article was updated July 7, 2022.
Fifteen years is a lifetime for the advancement of medical research. This seems particularly true for upper GI tract disorders.
In 2007, eosinophilic esophagitis was a rare disease; limited clinical data were available describing the symptoms, demographic characteristics, and endoscopic findings. Treatment was guided mostly by uncontrolled patient series for topical steroids and comprehensive diet exclusion therapy. Today, the molecular, genetic, and evolving microbiome’s contributions to EoE are being elucidated. EoE is recognized as one of the most common diseases in our practice, and rigorously performed controlled trials of steroids and biologics (including Food and Drug Administration–approved dupilumab) guide our treatment. Diet has also become easier with the identification of a single food antigen as the cause in 40% of EoE patients. The most pressing need is for a test that’s reliable and less invasive than endoscopy to assess and monitor treatment.
Barrett’s esophagus was of great concern 15 years ago and has surged in importance because of the increasing incidence of Barrett’s and esophageal adenocarcinoma, likely emphasized by the obesity epidemic. Sadly, survival with esophageal adenocarcinoma has changed little because most patients present with advanced stages. Multiple studies are questioning guideline recommendations because of their low yield and high expense. Fortunately, a range of easier screening tools is being tested, including sponge on string devices, video capsules, transnasal endoscopy, and the electronic “nose.” These can provide more widespread screening in broader populations of patients at risk who may lack heartburn or classic demographics. In 2007 there was little endoscopic therapy; now, the gastroenterologist has a robust armamentarium with multiple methods for mucosal ablation and resection achieving cure and sparing the patient an esophagectomy. Tissue biomarkers continue to be elucidated and are being applied to clinical practice.
For esophageal motility disorders, manometric data were obtained through a primitive water-infused system. With high-resolution manometry, the Chicago Classification, and impedance planimetry, our ability to precisely define, understand, and treat these disorders has been greatly enhanced.
In prior decades, the association of H. pylori to gastric cancer was noted but landmark trials and meta-analyses have strongly linked eradication of H. pylori with reduction in gastric cancer. These include broad population studies from Taiwan and the U.S. Veterans Health Administration, as well as a Cochrane review. These data have reinforced the need to search for and eradicate H. pylori infection. Although antibiotic resistance is rampant, newer antibiotic combinations including nitazoxanide, levofloxacin, rifabutin, and tinidazole have been proven effective. Potassium-competitive acid blockers may also augment effective eradication.
Endoscopy itself is one of the greatest areas of advancement in upper GI disease since 2007. What was once limited to biopsy, removal of polyps, and control of gastrointestinal bleeding, now has a breathtaking range of diagnostic and therapeutic capabilities. Who could imagine being able to perform bariatric procedures, create a gastrojejunostomy, treat a Zenker’s diverticulum, or drain extraluminal abscesses through an endoscope? With description of the technique of submucosal tunneling, endoscopic mucosal resection has been extended to submucosal dissection for more advanced cancers and benign tumors. This technique has also revolutionized the treatment of achalasia with peroral endoscopic myotomy, a procedure found equivalent to laparoscopic myotomy in controlled trials. Finally, artificial intelligence has taken endoscopic imaging by storm, and the accuracy with which we will diagnose premalignant lesions of the esophagus and stomach should significantly increase our abilities to prevent and treat early cancers.
Dr. Katzka is professor of medicine at Columbia University, New York. He reports consulting for Takeda and Celgene.
This article was updated July 7, 2022.
Will ESD replace EMR for large colorectal polyps?
Dear colleagues,
Resection of polyps is the bread and butter of endoscopy. Advances in technology have enabled us to tackle larger and more complex lesions throughout the gastrointestinal tract, especially through endoscopic mucosal resection (EMR). Endoscopic submucosal dissection (ESD) is another technique that offers much promise for complex colorectal polyps and is being rapidly adopted in the West. But do its benefits outweigh the costs in time, money and additional training needed for successful ESD? How can we justify higher recurrence rates with EMR when ESD is available? Will reimbursement continue to favor EMR? In this issue of Perspectives, Dr. Alexis Bayudan and Dr. Craig A. Munroe make the case for adopting ESD, while Dr. Sumeet Tewani highlights all the benefits of EMR. I invite you to a great debate and look forward to hearing your own thoughts on Twitter @AGA_GIHN and by email at ginews@gastro.org.
Gyanprakash A. Ketwaroo, MD, MSc, is assistant professor of medicine at Baylor College of Medicine, Houston. He is an associate editor for GI & Hepatology News.
The future standard of care
BY ALEXIS BAYUDAN, MD, AND CRAIG A. MUNROE, MD
Endoscopic submucosal dissection (ESD) is a minimally invasive, organ-sparing, flexible endoscopic technique used to treat advanced neoplasia of the digestive tract, with the goal of en bloc resection for accurate histologic assessment. ESD was introduced over 25 years ago in Japan by a small group of innovative endoscopists.1 After its initial adoption and success with removing gastric lesions, ESD later evolved as a technique used for complete resection of lesions throughout the gastrointestinal tract.
The intent of ESD is to achieve clear pathologic evaluation of deep and lateral margins, which is generally lost when piecemeal EMR (pEMR) is performed on lesions larger than 2 cm. With growing global experience, the evidence is clear that ESD is advantageous when compared to pEMR in the resection of large colorectal lesions en bloc, leading to improved curative resection rates and less local recurrence.
From our own experience, and from the results of many studies, we know that although procedure time in ESD can be longer, the rate of complete resection is far superior. ESD was previously cited as having a 10% risk of perforation in the 1990s and early 2000s, but current rates are closer to 4.5%, as noted by Nimii et al., with nearly complete successful treatment with endoscopic closure.1 In a 2021 meta-analysis reviewing a total of 21 studies, Lim et. al demonstrate that, although there is an increased risk of perforation with ESD compared to EMR (risk ratio, 7.597; 95% confidence interval, 4.281-13.479; P < .001), there is no significant difference in bleeding risk between the two techniques (RR, 7.597; 95% CI, 4.281-13.479; P < .001).2
Since its inception, many refinements of the ESD technique have occurred through technology, and better understanding of anatomy and disease states. These include, but are not limited to, improvements in hemostatic and closure techniques, electrosurgical equipment, resection and traction devices, the use of carbon dioxide, the ability to perform full-thickness endoscopic surgery, and submucosal lifting.1 The realm of endoscopic innovation is moving at a rapid pace within commercial and noncommercial entities, and advancements in ESD devices will allow for further improvements in procedure times and decreased procedural complications. Conversely, there have been few advancements in EMR technique in decades.
Further developments in ESD will continue to democratize this intervention, so that it can be practiced in all medical centers, not just expert centers. However, for ESD to become standard of care in the Western world, it will require more exposure and training. ESD has rapidly spread throughout Japan because of the master-mentor relationship that fosters safe learning, in addition to an abundance of highly skilled EMR-experienced physicians who went on to acquire their skills under the supervision of ESD experts. Current methods of teaching ESD, such as using pig models to practice specific steps of the procedure, can be implemented in Western gastroenterology training programs and through GI and surgical society training programs to learn safe operation in the third space. Mentorship and proctorship are also mandatory. The incorporation of ESD into standard practice over pEMR is very akin to laparoscopic cholecystectomy revolutionizing gallbladder surgery, even though open cholecystectomy was known to be effective.
A major limitation in the adoption of ESD in the West is reimbursement. Despite mounting evidence of the superiority of ESD in well-trained hands, and the additional training needed to safely perform these procedures, there had not been a pathway forward for payment for the increased requirements needed to perform these procedures safely.3 This leads to more endoscopists performing pEMR in the West which is anti-innovative. In October 2021, the Centers for Medicare and Medicaid Services expanded the reimbursement for ESD (Healthcare Common Procedure Coding System C9779). The availability of billing codes paves the way for increasing patient access to these therapies. Hopefully, additional codes will follow.
With the mounting evidence demonstrating ESD is superior to pEMR in terms of curative resection and recurrence rates, we think it is time for ESD to be incorporated widely into Western practice. ESD is still evolving and improving; ESD will become both safer and more effective. ESD has revolutionized endoscopic resection, and we are just beginning to see the possibilities and value of these techniques.
Dr. Baydan is a second-year fellow, and Dr. Munroe is an associate professor, both at the University of California, San Francisco. They have no relevant conflicts of interest.
References
1. Ferreira J et al. Clin Colon Rectal Surg. 2015 Sep; 28(3):146-151.
2. Lim X et al. World J Gastroenterol. 2021 Jul 7;27(25):3925-39.
3. Iqbal S et al. World J Gastrointest Endosc. 2020 Jan 16; 12(1):49-52.
More investment than payoff
Most large colorectal polyps are best managed by endoscopic mucosal resection (EMR) and do not require endoscopic submucosal dissection (ESD). EMR can provide complete, safe, and effective removal, preventing colorectal cancer while avoiding the risks of surgery or ESD. EMR has several advantages over ESD. It is minimally invasive, low cost, well tolerated, and allows excellent histopathologic examination. It is performed during colonoscopy in an outpatient endoscopy lab or ambulatory surgery center. There are several techniques that can be performed safely and efficiently using accessories that are readily available. It is easier to learn and perform, with lower risks and fewer resources. Endoscopists can effectively integrate EMR into a busy practice, without making significant additional investments.
EMR of large adenomas has improved morbidity, mortality, and cost compared to surgery.1-3 I first carefully inspect the lesion to plan the approach and exclude submucosal invasion, which should be referred for ESD or surgery instead. This includes understanding the size, location, morphology, and surface characteristics, using high-definition and narrow-band imaging or Fujinon intelligent chromoendoscopy. Conventional EMR utilizes submucosal injection to lift the polyp away from the underlying muscle layer before hot snare resection. Injection needles and snares of various shapes, sizes, and stiffness are available in most endoscopy labs. The goal is en bloc resection to achieve potential cure with complete histological assessment and low rate of recurrence. This can be achieved for lesions up to 2 cm in size, although larger lesions require piecemeal resection, which limits accurate histopathology and carries a recurrence rate up to 25%.1 Thermal ablation of the resection margins with argon plasma coagulation or snare-tip soft coagulation can reduce the rate of recurrence. Additionally, most recurrences are identified during early surveillance within 6 months and managed endoscopically. The rates of adverse events, including bleeding (6%-15%), perforation (1%-2%), and postpolypectomy syndrome (< 1%) remain at acceptable low levels.1,4
For many polyps, saline injection is safe, effective, and inexpensive, but it dissipates rapidly with limited duration of effect. Alternative agents can improve the lift, at additional cost.4 I prefer adding dye, such as methylene blue, to differentiate the submucosa from the muscularis, demarcate the lesion margins, and allow easier inspection of the defect. Dilute epinephrine can also be added to reduce intraprocedural bleeding and maintain a clean resection field. I reserve this for the duodenum, but it can be an important adjunct for some colorectal polyps. Submucosal injection also allows assessment for a “nonlifting sign,” which raises suspicion for invasive carcinoma but can also occur with benign submucosal fibrosis from previous biopsy, partial resection, or adjacent tattoo. In these cases, effective management can still be achieved using EMR in combination with avulsion and thermal ablation techniques.
Alternative techniques include cold EMR and underwater EMR.1,4 These are gaining popularity because of their excellent safety profile and favorable outcomes. Cold EMR involves submucosal injection followed by cold-snare resection, eliminating the use of cautery and its associated risks. Cold EMR is very safe and effective for small polyps, and we use this for progressively larger polyps given the low complication rate. Despite the need for piecemeal resection of polyps larger than 10 mm, local recurrence rates are comparable to conventional EMR. Sessile serrated polyps are especially ideal for piecemeal cold EMR. Meanwhile, underwater EMR eliminates the need for submucosal injection by utilizing water immersion, which elevates the mucosal lesion away from the muscularis layer. Either hot or cold snare resection can be performed. Benefits include reduced procedure time and cost, and relatively low complication and recurrence rates, compared with conventional EMR. I find this to be a nice option for laterally spreading polyps, with potentially higher rates of en bloc resection.1,4
ESD involves similar techniques but includes careful dissection of the submucosal layer beneath the lesion. In addition to the tools for EMR, a specialized electrosurgical knife is necessary, as well as dedicated training and mentorship that can be difficult to accommodate for an active endoscopist in practice. The primary advantage of ESD is higher en bloc resection rates for larger and potentially deeper lesions, with accurate histologic assessment and staging, and very low recurrence rates.1,4,5 However, ESD is more complex, technically challenging, and time and resource intensive, with higher risk of complications. Intraprocedural bleeding is common and requires immediate management. Additional risks include 2% risk of delayed bleeding and 5% risk of perforation.1,5 ESD involves an operating room, longer procedure times, and higher cost including surgical, anesthesia, and nursing costs. Some of this may be balanced by reduced frequency of surveillance and therapeutic procedures. While both EMR and ESD carry significant cost savings, compared with surgery, ESD is additionally disadvantaged by lack of reimbursement.
Regardless of the technique, EMR is easier to learn and perform than ESD, uses a limited number of devices that are readily available, and carries lower cost-burden. EMR is successful for most colorectal polyps, with the primary disadvantage being piecemeal resection of larger polyps. The rates of adverse events are lower, and appropriate surveillance is essential to ensuring complete resection and eliminating recurrence. Japanese and European guidelines endorse ESD for lesions that have a high likelihood of cancer invading the submucosa and for lesions that cannot be removed by EMR because of submucosal fibrosis. Ultimately, patients need to be treated individually with the most appropriate technique.
Dr. Tewani of Rockford Gastroenterology Associates is clinical assistant professor of medicine at the University of Illinois, Rockford. He has no relevant conflicts of interest to disclose.
References
1. Rashid MU et al. Surg Oncol. 2022 Mar 18;101742.
2. Law R et al. Gastrointest Endosc. 2016 Jun;83(6):1248-57.
3. Backes Y et al. BMC Gastroenterol. 2016 May 26;16(1):56.
4. Thiruvengadam SS et al. Gastroenterol Hepatol. 2022 Mar;18(3):133-44.
5. Wang J et al. World J Gastroenterol. 2014 Jul 7;20(25):8282-7l.
Dear colleagues,
Resection of polyps is the bread and butter of endoscopy. Advances in technology have enabled us to tackle larger and more complex lesions throughout the gastrointestinal tract, especially through endoscopic mucosal resection (EMR). Endoscopic submucosal dissection (ESD) is another technique that offers much promise for complex colorectal polyps and is being rapidly adopted in the West. But do its benefits outweigh the costs in time, money and additional training needed for successful ESD? How can we justify higher recurrence rates with EMR when ESD is available? Will reimbursement continue to favor EMR? In this issue of Perspectives, Dr. Alexis Bayudan and Dr. Craig A. Munroe make the case for adopting ESD, while Dr. Sumeet Tewani highlights all the benefits of EMR. I invite you to a great debate and look forward to hearing your own thoughts on Twitter @AGA_GIHN and by email at ginews@gastro.org.
Gyanprakash A. Ketwaroo, MD, MSc, is assistant professor of medicine at Baylor College of Medicine, Houston. He is an associate editor for GI & Hepatology News.
The future standard of care
BY ALEXIS BAYUDAN, MD, AND CRAIG A. MUNROE, MD
Endoscopic submucosal dissection (ESD) is a minimally invasive, organ-sparing, flexible endoscopic technique used to treat advanced neoplasia of the digestive tract, with the goal of en bloc resection for accurate histologic assessment. ESD was introduced over 25 years ago in Japan by a small group of innovative endoscopists.1 After its initial adoption and success with removing gastric lesions, ESD later evolved as a technique used for complete resection of lesions throughout the gastrointestinal tract.
The intent of ESD is to achieve clear pathologic evaluation of deep and lateral margins, which is generally lost when piecemeal EMR (pEMR) is performed on lesions larger than 2 cm. With growing global experience, the evidence is clear that ESD is advantageous when compared to pEMR in the resection of large colorectal lesions en bloc, leading to improved curative resection rates and less local recurrence.
From our own experience, and from the results of many studies, we know that although procedure time in ESD can be longer, the rate of complete resection is far superior. ESD was previously cited as having a 10% risk of perforation in the 1990s and early 2000s, but current rates are closer to 4.5%, as noted by Nimii et al., with nearly complete successful treatment with endoscopic closure.1 In a 2021 meta-analysis reviewing a total of 21 studies, Lim et. al demonstrate that, although there is an increased risk of perforation with ESD compared to EMR (risk ratio, 7.597; 95% confidence interval, 4.281-13.479; P < .001), there is no significant difference in bleeding risk between the two techniques (RR, 7.597; 95% CI, 4.281-13.479; P < .001).2
Since its inception, many refinements of the ESD technique have occurred through technology, and better understanding of anatomy and disease states. These include, but are not limited to, improvements in hemostatic and closure techniques, electrosurgical equipment, resection and traction devices, the use of carbon dioxide, the ability to perform full-thickness endoscopic surgery, and submucosal lifting.1 The realm of endoscopic innovation is moving at a rapid pace within commercial and noncommercial entities, and advancements in ESD devices will allow for further improvements in procedure times and decreased procedural complications. Conversely, there have been few advancements in EMR technique in decades.
Further developments in ESD will continue to democratize this intervention, so that it can be practiced in all medical centers, not just expert centers. However, for ESD to become standard of care in the Western world, it will require more exposure and training. ESD has rapidly spread throughout Japan because of the master-mentor relationship that fosters safe learning, in addition to an abundance of highly skilled EMR-experienced physicians who went on to acquire their skills under the supervision of ESD experts. Current methods of teaching ESD, such as using pig models to practice specific steps of the procedure, can be implemented in Western gastroenterology training programs and through GI and surgical society training programs to learn safe operation in the third space. Mentorship and proctorship are also mandatory. The incorporation of ESD into standard practice over pEMR is very akin to laparoscopic cholecystectomy revolutionizing gallbladder surgery, even though open cholecystectomy was known to be effective.
A major limitation in the adoption of ESD in the West is reimbursement. Despite mounting evidence of the superiority of ESD in well-trained hands, and the additional training needed to safely perform these procedures, there had not been a pathway forward for payment for the increased requirements needed to perform these procedures safely.3 This leads to more endoscopists performing pEMR in the West which is anti-innovative. In October 2021, the Centers for Medicare and Medicaid Services expanded the reimbursement for ESD (Healthcare Common Procedure Coding System C9779). The availability of billing codes paves the way for increasing patient access to these therapies. Hopefully, additional codes will follow.
With the mounting evidence demonstrating ESD is superior to pEMR in terms of curative resection and recurrence rates, we think it is time for ESD to be incorporated widely into Western practice. ESD is still evolving and improving; ESD will become both safer and more effective. ESD has revolutionized endoscopic resection, and we are just beginning to see the possibilities and value of these techniques.
Dr. Baydan is a second-year fellow, and Dr. Munroe is an associate professor, both at the University of California, San Francisco. They have no relevant conflicts of interest.
References
1. Ferreira J et al. Clin Colon Rectal Surg. 2015 Sep; 28(3):146-151.
2. Lim X et al. World J Gastroenterol. 2021 Jul 7;27(25):3925-39.
3. Iqbal S et al. World J Gastrointest Endosc. 2020 Jan 16; 12(1):49-52.
More investment than payoff
Most large colorectal polyps are best managed by endoscopic mucosal resection (EMR) and do not require endoscopic submucosal dissection (ESD). EMR can provide complete, safe, and effective removal, preventing colorectal cancer while avoiding the risks of surgery or ESD. EMR has several advantages over ESD. It is minimally invasive, low cost, well tolerated, and allows excellent histopathologic examination. It is performed during colonoscopy in an outpatient endoscopy lab or ambulatory surgery center. There are several techniques that can be performed safely and efficiently using accessories that are readily available. It is easier to learn and perform, with lower risks and fewer resources. Endoscopists can effectively integrate EMR into a busy practice, without making significant additional investments.
EMR of large adenomas has improved morbidity, mortality, and cost compared to surgery.1-3 I first carefully inspect the lesion to plan the approach and exclude submucosal invasion, which should be referred for ESD or surgery instead. This includes understanding the size, location, morphology, and surface characteristics, using high-definition and narrow-band imaging or Fujinon intelligent chromoendoscopy. Conventional EMR utilizes submucosal injection to lift the polyp away from the underlying muscle layer before hot snare resection. Injection needles and snares of various shapes, sizes, and stiffness are available in most endoscopy labs. The goal is en bloc resection to achieve potential cure with complete histological assessment and low rate of recurrence. This can be achieved for lesions up to 2 cm in size, although larger lesions require piecemeal resection, which limits accurate histopathology and carries a recurrence rate up to 25%.1 Thermal ablation of the resection margins with argon plasma coagulation or snare-tip soft coagulation can reduce the rate of recurrence. Additionally, most recurrences are identified during early surveillance within 6 months and managed endoscopically. The rates of adverse events, including bleeding (6%-15%), perforation (1%-2%), and postpolypectomy syndrome (< 1%) remain at acceptable low levels.1,4
For many polyps, saline injection is safe, effective, and inexpensive, but it dissipates rapidly with limited duration of effect. Alternative agents can improve the lift, at additional cost.4 I prefer adding dye, such as methylene blue, to differentiate the submucosa from the muscularis, demarcate the lesion margins, and allow easier inspection of the defect. Dilute epinephrine can also be added to reduce intraprocedural bleeding and maintain a clean resection field. I reserve this for the duodenum, but it can be an important adjunct for some colorectal polyps. Submucosal injection also allows assessment for a “nonlifting sign,” which raises suspicion for invasive carcinoma but can also occur with benign submucosal fibrosis from previous biopsy, partial resection, or adjacent tattoo. In these cases, effective management can still be achieved using EMR in combination with avulsion and thermal ablation techniques.
Alternative techniques include cold EMR and underwater EMR.1,4 These are gaining popularity because of their excellent safety profile and favorable outcomes. Cold EMR involves submucosal injection followed by cold-snare resection, eliminating the use of cautery and its associated risks. Cold EMR is very safe and effective for small polyps, and we use this for progressively larger polyps given the low complication rate. Despite the need for piecemeal resection of polyps larger than 10 mm, local recurrence rates are comparable to conventional EMR. Sessile serrated polyps are especially ideal for piecemeal cold EMR. Meanwhile, underwater EMR eliminates the need for submucosal injection by utilizing water immersion, which elevates the mucosal lesion away from the muscularis layer. Either hot or cold snare resection can be performed. Benefits include reduced procedure time and cost, and relatively low complication and recurrence rates, compared with conventional EMR. I find this to be a nice option for laterally spreading polyps, with potentially higher rates of en bloc resection.1,4
ESD involves similar techniques but includes careful dissection of the submucosal layer beneath the lesion. In addition to the tools for EMR, a specialized electrosurgical knife is necessary, as well as dedicated training and mentorship that can be difficult to accommodate for an active endoscopist in practice. The primary advantage of ESD is higher en bloc resection rates for larger and potentially deeper lesions, with accurate histologic assessment and staging, and very low recurrence rates.1,4,5 However, ESD is more complex, technically challenging, and time and resource intensive, with higher risk of complications. Intraprocedural bleeding is common and requires immediate management. Additional risks include 2% risk of delayed bleeding and 5% risk of perforation.1,5 ESD involves an operating room, longer procedure times, and higher cost including surgical, anesthesia, and nursing costs. Some of this may be balanced by reduced frequency of surveillance and therapeutic procedures. While both EMR and ESD carry significant cost savings, compared with surgery, ESD is additionally disadvantaged by lack of reimbursement.
Regardless of the technique, EMR is easier to learn and perform than ESD, uses a limited number of devices that are readily available, and carries lower cost-burden. EMR is successful for most colorectal polyps, with the primary disadvantage being piecemeal resection of larger polyps. The rates of adverse events are lower, and appropriate surveillance is essential to ensuring complete resection and eliminating recurrence. Japanese and European guidelines endorse ESD for lesions that have a high likelihood of cancer invading the submucosa and for lesions that cannot be removed by EMR because of submucosal fibrosis. Ultimately, patients need to be treated individually with the most appropriate technique.
Dr. Tewani of Rockford Gastroenterology Associates is clinical assistant professor of medicine at the University of Illinois, Rockford. He has no relevant conflicts of interest to disclose.
References
1. Rashid MU et al. Surg Oncol. 2022 Mar 18;101742.
2. Law R et al. Gastrointest Endosc. 2016 Jun;83(6):1248-57.
3. Backes Y et al. BMC Gastroenterol. 2016 May 26;16(1):56.
4. Thiruvengadam SS et al. Gastroenterol Hepatol. 2022 Mar;18(3):133-44.
5. Wang J et al. World J Gastroenterol. 2014 Jul 7;20(25):8282-7l.
Dear colleagues,
Resection of polyps is the bread and butter of endoscopy. Advances in technology have enabled us to tackle larger and more complex lesions throughout the gastrointestinal tract, especially through endoscopic mucosal resection (EMR). Endoscopic submucosal dissection (ESD) is another technique that offers much promise for complex colorectal polyps and is being rapidly adopted in the West. But do its benefits outweigh the costs in time, money and additional training needed for successful ESD? How can we justify higher recurrence rates with EMR when ESD is available? Will reimbursement continue to favor EMR? In this issue of Perspectives, Dr. Alexis Bayudan and Dr. Craig A. Munroe make the case for adopting ESD, while Dr. Sumeet Tewani highlights all the benefits of EMR. I invite you to a great debate and look forward to hearing your own thoughts on Twitter @AGA_GIHN and by email at ginews@gastro.org.
Gyanprakash A. Ketwaroo, MD, MSc, is assistant professor of medicine at Baylor College of Medicine, Houston. He is an associate editor for GI & Hepatology News.
The future standard of care
BY ALEXIS BAYUDAN, MD, AND CRAIG A. MUNROE, MD
Endoscopic submucosal dissection (ESD) is a minimally invasive, organ-sparing, flexible endoscopic technique used to treat advanced neoplasia of the digestive tract, with the goal of en bloc resection for accurate histologic assessment. ESD was introduced over 25 years ago in Japan by a small group of innovative endoscopists.1 After its initial adoption and success with removing gastric lesions, ESD later evolved as a technique used for complete resection of lesions throughout the gastrointestinal tract.
The intent of ESD is to achieve clear pathologic evaluation of deep and lateral margins, which is generally lost when piecemeal EMR (pEMR) is performed on lesions larger than 2 cm. With growing global experience, the evidence is clear that ESD is advantageous when compared to pEMR in the resection of large colorectal lesions en bloc, leading to improved curative resection rates and less local recurrence.
From our own experience, and from the results of many studies, we know that although procedure time in ESD can be longer, the rate of complete resection is far superior. ESD was previously cited as having a 10% risk of perforation in the 1990s and early 2000s, but current rates are closer to 4.5%, as noted by Nimii et al., with nearly complete successful treatment with endoscopic closure.1 In a 2021 meta-analysis reviewing a total of 21 studies, Lim et. al demonstrate that, although there is an increased risk of perforation with ESD compared to EMR (risk ratio, 7.597; 95% confidence interval, 4.281-13.479; P < .001), there is no significant difference in bleeding risk between the two techniques (RR, 7.597; 95% CI, 4.281-13.479; P < .001).2
Since its inception, many refinements of the ESD technique have occurred through technology, and better understanding of anatomy and disease states. These include, but are not limited to, improvements in hemostatic and closure techniques, electrosurgical equipment, resection and traction devices, the use of carbon dioxide, the ability to perform full-thickness endoscopic surgery, and submucosal lifting.1 The realm of endoscopic innovation is moving at a rapid pace within commercial and noncommercial entities, and advancements in ESD devices will allow for further improvements in procedure times and decreased procedural complications. Conversely, there have been few advancements in EMR technique in decades.
Further developments in ESD will continue to democratize this intervention, so that it can be practiced in all medical centers, not just expert centers. However, for ESD to become standard of care in the Western world, it will require more exposure and training. ESD has rapidly spread throughout Japan because of the master-mentor relationship that fosters safe learning, in addition to an abundance of highly skilled EMR-experienced physicians who went on to acquire their skills under the supervision of ESD experts. Current methods of teaching ESD, such as using pig models to practice specific steps of the procedure, can be implemented in Western gastroenterology training programs and through GI and surgical society training programs to learn safe operation in the third space. Mentorship and proctorship are also mandatory. The incorporation of ESD into standard practice over pEMR is very akin to laparoscopic cholecystectomy revolutionizing gallbladder surgery, even though open cholecystectomy was known to be effective.
A major limitation in the adoption of ESD in the West is reimbursement. Despite mounting evidence of the superiority of ESD in well-trained hands, and the additional training needed to safely perform these procedures, there had not been a pathway forward for payment for the increased requirements needed to perform these procedures safely.3 This leads to more endoscopists performing pEMR in the West which is anti-innovative. In October 2021, the Centers for Medicare and Medicaid Services expanded the reimbursement for ESD (Healthcare Common Procedure Coding System C9779). The availability of billing codes paves the way for increasing patient access to these therapies. Hopefully, additional codes will follow.
With the mounting evidence demonstrating ESD is superior to pEMR in terms of curative resection and recurrence rates, we think it is time for ESD to be incorporated widely into Western practice. ESD is still evolving and improving; ESD will become both safer and more effective. ESD has revolutionized endoscopic resection, and we are just beginning to see the possibilities and value of these techniques.
Dr. Baydan is a second-year fellow, and Dr. Munroe is an associate professor, both at the University of California, San Francisco. They have no relevant conflicts of interest.
References
1. Ferreira J et al. Clin Colon Rectal Surg. 2015 Sep; 28(3):146-151.
2. Lim X et al. World J Gastroenterol. 2021 Jul 7;27(25):3925-39.
3. Iqbal S et al. World J Gastrointest Endosc. 2020 Jan 16; 12(1):49-52.
More investment than payoff
Most large colorectal polyps are best managed by endoscopic mucosal resection (EMR) and do not require endoscopic submucosal dissection (ESD). EMR can provide complete, safe, and effective removal, preventing colorectal cancer while avoiding the risks of surgery or ESD. EMR has several advantages over ESD. It is minimally invasive, low cost, well tolerated, and allows excellent histopathologic examination. It is performed during colonoscopy in an outpatient endoscopy lab or ambulatory surgery center. There are several techniques that can be performed safely and efficiently using accessories that are readily available. It is easier to learn and perform, with lower risks and fewer resources. Endoscopists can effectively integrate EMR into a busy practice, without making significant additional investments.
EMR of large adenomas has improved morbidity, mortality, and cost compared to surgery.1-3 I first carefully inspect the lesion to plan the approach and exclude submucosal invasion, which should be referred for ESD or surgery instead. This includes understanding the size, location, morphology, and surface characteristics, using high-definition and narrow-band imaging or Fujinon intelligent chromoendoscopy. Conventional EMR utilizes submucosal injection to lift the polyp away from the underlying muscle layer before hot snare resection. Injection needles and snares of various shapes, sizes, and stiffness are available in most endoscopy labs. The goal is en bloc resection to achieve potential cure with complete histological assessment and low rate of recurrence. This can be achieved for lesions up to 2 cm in size, although larger lesions require piecemeal resection, which limits accurate histopathology and carries a recurrence rate up to 25%.1 Thermal ablation of the resection margins with argon plasma coagulation or snare-tip soft coagulation can reduce the rate of recurrence. Additionally, most recurrences are identified during early surveillance within 6 months and managed endoscopically. The rates of adverse events, including bleeding (6%-15%), perforation (1%-2%), and postpolypectomy syndrome (< 1%) remain at acceptable low levels.1,4
For many polyps, saline injection is safe, effective, and inexpensive, but it dissipates rapidly with limited duration of effect. Alternative agents can improve the lift, at additional cost.4 I prefer adding dye, such as methylene blue, to differentiate the submucosa from the muscularis, demarcate the lesion margins, and allow easier inspection of the defect. Dilute epinephrine can also be added to reduce intraprocedural bleeding and maintain a clean resection field. I reserve this for the duodenum, but it can be an important adjunct for some colorectal polyps. Submucosal injection also allows assessment for a “nonlifting sign,” which raises suspicion for invasive carcinoma but can also occur with benign submucosal fibrosis from previous biopsy, partial resection, or adjacent tattoo. In these cases, effective management can still be achieved using EMR in combination with avulsion and thermal ablation techniques.
Alternative techniques include cold EMR and underwater EMR.1,4 These are gaining popularity because of their excellent safety profile and favorable outcomes. Cold EMR involves submucosal injection followed by cold-snare resection, eliminating the use of cautery and its associated risks. Cold EMR is very safe and effective for small polyps, and we use this for progressively larger polyps given the low complication rate. Despite the need for piecemeal resection of polyps larger than 10 mm, local recurrence rates are comparable to conventional EMR. Sessile serrated polyps are especially ideal for piecemeal cold EMR. Meanwhile, underwater EMR eliminates the need for submucosal injection by utilizing water immersion, which elevates the mucosal lesion away from the muscularis layer. Either hot or cold snare resection can be performed. Benefits include reduced procedure time and cost, and relatively low complication and recurrence rates, compared with conventional EMR. I find this to be a nice option for laterally spreading polyps, with potentially higher rates of en bloc resection.1,4
ESD involves similar techniques but includes careful dissection of the submucosal layer beneath the lesion. In addition to the tools for EMR, a specialized electrosurgical knife is necessary, as well as dedicated training and mentorship that can be difficult to accommodate for an active endoscopist in practice. The primary advantage of ESD is higher en bloc resection rates for larger and potentially deeper lesions, with accurate histologic assessment and staging, and very low recurrence rates.1,4,5 However, ESD is more complex, technically challenging, and time and resource intensive, with higher risk of complications. Intraprocedural bleeding is common and requires immediate management. Additional risks include 2% risk of delayed bleeding and 5% risk of perforation.1,5 ESD involves an operating room, longer procedure times, and higher cost including surgical, anesthesia, and nursing costs. Some of this may be balanced by reduced frequency of surveillance and therapeutic procedures. While both EMR and ESD carry significant cost savings, compared with surgery, ESD is additionally disadvantaged by lack of reimbursement.
Regardless of the technique, EMR is easier to learn and perform than ESD, uses a limited number of devices that are readily available, and carries lower cost-burden. EMR is successful for most colorectal polyps, with the primary disadvantage being piecemeal resection of larger polyps. The rates of adverse events are lower, and appropriate surveillance is essential to ensuring complete resection and eliminating recurrence. Japanese and European guidelines endorse ESD for lesions that have a high likelihood of cancer invading the submucosa and for lesions that cannot be removed by EMR because of submucosal fibrosis. Ultimately, patients need to be treated individually with the most appropriate technique.
Dr. Tewani of Rockford Gastroenterology Associates is clinical assistant professor of medicine at the University of Illinois, Rockford. He has no relevant conflicts of interest to disclose.
References
1. Rashid MU et al. Surg Oncol. 2022 Mar 18;101742.
2. Law R et al. Gastrointest Endosc. 2016 Jun;83(6):1248-57.
3. Backes Y et al. BMC Gastroenterol. 2016 May 26;16(1):56.
4. Thiruvengadam SS et al. Gastroenterol Hepatol. 2022 Mar;18(3):133-44.
5. Wang J et al. World J Gastroenterol. 2014 Jul 7;20(25):8282-7l.