User login
Infection Risk With Biologic Therapy for Psoriasis: Report From the AAD Meeting
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
David Hafler, MD
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
VIDEO: Don’t overlook psychosocial concerns of vitiligo patients
ORLANDO – There are ways to assess the psychosocial needs of your patients with vitiligo, even if you don’t believe you have the necessary skills to do a complete mental health work-up, according to Seemal R. Desai, MD.
In an interview recorded at this year’s annual meeting of the American Academy of Dermatology, Dr. Desai, an assistant clinical professor of dermatology at the University of Texas, Dallas, shares his ideas for how to have casual conversations with patients that can help reveal important clues to psychosocial stress patients with this serious medical skin condition might be facing.
“There are subtle clues to look for to know that these patients are uncomfortable with others seeing their skin,” says Dr. Desai.
In the video interview, he also covers taking a multidisciplinary approach to caring for these patients, what treatments are available to those who are suffering psychosocial stress after having failed several interventions, and how patients from many Asian and African counties are especially at risk for ostracization.
“It’s important to let your patients know that you understand this is really affecting them psychosocially, and that you care,” says Dr. Desai.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
ORLANDO – There are ways to assess the psychosocial needs of your patients with vitiligo, even if you don’t believe you have the necessary skills to do a complete mental health work-up, according to Seemal R. Desai, MD.
In an interview recorded at this year’s annual meeting of the American Academy of Dermatology, Dr. Desai, an assistant clinical professor of dermatology at the University of Texas, Dallas, shares his ideas for how to have casual conversations with patients that can help reveal important clues to psychosocial stress patients with this serious medical skin condition might be facing.
“There are subtle clues to look for to know that these patients are uncomfortable with others seeing their skin,” says Dr. Desai.
In the video interview, he also covers taking a multidisciplinary approach to caring for these patients, what treatments are available to those who are suffering psychosocial stress after having failed several interventions, and how patients from many Asian and African counties are especially at risk for ostracization.
“It’s important to let your patients know that you understand this is really affecting them psychosocially, and that you care,” says Dr. Desai.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
ORLANDO – There are ways to assess the psychosocial needs of your patients with vitiligo, even if you don’t believe you have the necessary skills to do a complete mental health work-up, according to Seemal R. Desai, MD.
In an interview recorded at this year’s annual meeting of the American Academy of Dermatology, Dr. Desai, an assistant clinical professor of dermatology at the University of Texas, Dallas, shares his ideas for how to have casual conversations with patients that can help reveal important clues to psychosocial stress patients with this serious medical skin condition might be facing.
“There are subtle clues to look for to know that these patients are uncomfortable with others seeing their skin,” says Dr. Desai.
In the video interview, he also covers taking a multidisciplinary approach to caring for these patients, what treatments are available to those who are suffering psychosocial stress after having failed several interventions, and how patients from many Asian and African counties are especially at risk for ostracization.
“It’s important to let your patients know that you understand this is really affecting them psychosocially, and that you care,” says Dr. Desai.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
wmcknight@frontlinemedcom.com
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM AAD 17
VIDEO: Despite promises of abstinence, isotretinoin-exposed pregnancies still occur
ORLANDO – Pregnancy prevention remains a challenge when prescribing isotretinoin to women of childbearing years with acne, Megha M. Tollefson, MD, said at the annual meeting of the American Academy of Dermatology.
Like so many promises having to do with love, a promise of sexual abstinence, however earnest, may at some point fall by the wayside, said Dr. Tollefson of the Mayo Clinic, Rochester, Minn., in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Despite the promises, the education, and the allegiance to the iPLEDGE program, exposed pregnancies still occur. iPLEDGE, with a 2.67 rate of fetal exposure over 1,000 treatment courses, was no more effective than its predecessor, SMART, with a 3.11 exposure rate. Altogether, there are still about 150 exposed pregnancies every year; 18 babies were exposed to the drug during SMART and 11 during iPLEDGE.
An anonymous survey of 75 iPLEDGE participants disclosed that 19% of those who chose abstinence were not, and that 34% of those who were sexually active did not comply with the promise to use two forms of birth control.
For some patients, Dr. Tollefson said, the best choice is a patient-independent form of birth control. That’s not an easy conversation to have sometimes, especially when parents are involved, but it’s an important one to have.
Dr. Tollefson had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
ORLANDO – Pregnancy prevention remains a challenge when prescribing isotretinoin to women of childbearing years with acne, Megha M. Tollefson, MD, said at the annual meeting of the American Academy of Dermatology.
Like so many promises having to do with love, a promise of sexual abstinence, however earnest, may at some point fall by the wayside, said Dr. Tollefson of the Mayo Clinic, Rochester, Minn., in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Despite the promises, the education, and the allegiance to the iPLEDGE program, exposed pregnancies still occur. iPLEDGE, with a 2.67 rate of fetal exposure over 1,000 treatment courses, was no more effective than its predecessor, SMART, with a 3.11 exposure rate. Altogether, there are still about 150 exposed pregnancies every year; 18 babies were exposed to the drug during SMART and 11 during iPLEDGE.
An anonymous survey of 75 iPLEDGE participants disclosed that 19% of those who chose abstinence were not, and that 34% of those who were sexually active did not comply with the promise to use two forms of birth control.
For some patients, Dr. Tollefson said, the best choice is a patient-independent form of birth control. That’s not an easy conversation to have sometimes, especially when parents are involved, but it’s an important one to have.
Dr. Tollefson had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
ORLANDO – Pregnancy prevention remains a challenge when prescribing isotretinoin to women of childbearing years with acne, Megha M. Tollefson, MD, said at the annual meeting of the American Academy of Dermatology.
Like so many promises having to do with love, a promise of sexual abstinence, however earnest, may at some point fall by the wayside, said Dr. Tollefson of the Mayo Clinic, Rochester, Minn., in a video interview.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Despite the promises, the education, and the allegiance to the iPLEDGE program, exposed pregnancies still occur. iPLEDGE, with a 2.67 rate of fetal exposure over 1,000 treatment courses, was no more effective than its predecessor, SMART, with a 3.11 exposure rate. Altogether, there are still about 150 exposed pregnancies every year; 18 babies were exposed to the drug during SMART and 11 during iPLEDGE.
An anonymous survey of 75 iPLEDGE participants disclosed that 19% of those who chose abstinence were not, and that 34% of those who were sexually active did not comply with the promise to use two forms of birth control.
For some patients, Dr. Tollefson said, the best choice is a patient-independent form of birth control. That’s not an easy conversation to have sometimes, especially when parents are involved, but it’s an important one to have.
Dr. Tollefson had no financial disclosures.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
AT AAD 17
VIDEO: Gold nanoparticles target laser acne therapy
ORLANDO – There may soon be a new gold standard in acne therapy – gold nanoparticles.
Evidence is mounting that the combination of a laser and a topical suspension of gold- or silver-coated silica nanoparticles can ablate the inner lining of the pilosebaceous unit, dramatically reducing or eliminating acne.
The system is still investigational in the United States, but shows great promise, Gilly Munavalli, MD, said in a video interview at the annual meeting of the American Academy of Dermatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Munavalli, medical director and founder of Dermatology, Laser, and Vein Specialists of the Carolinas, Charlotte, N.C., described how the system works, and some of the evidence supporting it.
“Basically what we’re doing is creating a chromophore for the laser to target,” he said. Just as a laser won’t work on light hair, it can’t target the colorless sebum inside the gland. The colored particles absorb the laser energy, vibrate, and create the locally destructive heat.
The particles are about 150 nm in diameter. They are designed to absorb infrared and near-infrared irradiation. A nanoparticle solution is applied to the affected area. Dr. Munavalli uses an ultrasound paddle to drive the particles into the sebaceous gland, and then removes any solution left on the skin.
He passes a hand-held, 800-nm laser over the skin. The laser activates the particles, generating heat that disrupts the lining of the pilosebaceous unit.
In 2014, Sebacia (Duluth, Ga.), which is developing the technology, reported positive results from two small European trials enrolling a total of 97 patients with acne. The patients were randomized to the gold nanoparticles or to a control group of, in the first study, an over-the-counter face wash and later, the vehicle solution minus the gold nanoparticles.
At 12 weeks’ follow-up, there was a significant reduction in inflammatory lesions and in the Investigator’s Global Assessment score. Treatment was well tolerated and results were durable at 6 months. At that time, the inflammatory lesion count was still 60% below baseline. Side effects were transient erythema and mild edema.
Dr. Munavalli serves as a scientific advisor for Sebacia.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
ORLANDO – There may soon be a new gold standard in acne therapy – gold nanoparticles.
Evidence is mounting that the combination of a laser and a topical suspension of gold- or silver-coated silica nanoparticles can ablate the inner lining of the pilosebaceous unit, dramatically reducing or eliminating acne.
The system is still investigational in the United States, but shows great promise, Gilly Munavalli, MD, said in a video interview at the annual meeting of the American Academy of Dermatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Munavalli, medical director and founder of Dermatology, Laser, and Vein Specialists of the Carolinas, Charlotte, N.C., described how the system works, and some of the evidence supporting it.
“Basically what we’re doing is creating a chromophore for the laser to target,” he said. Just as a laser won’t work on light hair, it can’t target the colorless sebum inside the gland. The colored particles absorb the laser energy, vibrate, and create the locally destructive heat.
The particles are about 150 nm in diameter. They are designed to absorb infrared and near-infrared irradiation. A nanoparticle solution is applied to the affected area. Dr. Munavalli uses an ultrasound paddle to drive the particles into the sebaceous gland, and then removes any solution left on the skin.
He passes a hand-held, 800-nm laser over the skin. The laser activates the particles, generating heat that disrupts the lining of the pilosebaceous unit.
In 2014, Sebacia (Duluth, Ga.), which is developing the technology, reported positive results from two small European trials enrolling a total of 97 patients with acne. The patients were randomized to the gold nanoparticles or to a control group of, in the first study, an over-the-counter face wash and later, the vehicle solution minus the gold nanoparticles.
At 12 weeks’ follow-up, there was a significant reduction in inflammatory lesions and in the Investigator’s Global Assessment score. Treatment was well tolerated and results were durable at 6 months. At that time, the inflammatory lesion count was still 60% below baseline. Side effects were transient erythema and mild edema.
Dr. Munavalli serves as a scientific advisor for Sebacia.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
ORLANDO – There may soon be a new gold standard in acne therapy – gold nanoparticles.
Evidence is mounting that the combination of a laser and a topical suspension of gold- or silver-coated silica nanoparticles can ablate the inner lining of the pilosebaceous unit, dramatically reducing or eliminating acne.
The system is still investigational in the United States, but shows great promise, Gilly Munavalli, MD, said in a video interview at the annual meeting of the American Academy of Dermatology.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Munavalli, medical director and founder of Dermatology, Laser, and Vein Specialists of the Carolinas, Charlotte, N.C., described how the system works, and some of the evidence supporting it.
“Basically what we’re doing is creating a chromophore for the laser to target,” he said. Just as a laser won’t work on light hair, it can’t target the colorless sebum inside the gland. The colored particles absorb the laser energy, vibrate, and create the locally destructive heat.
The particles are about 150 nm in diameter. They are designed to absorb infrared and near-infrared irradiation. A nanoparticle solution is applied to the affected area. Dr. Munavalli uses an ultrasound paddle to drive the particles into the sebaceous gland, and then removes any solution left on the skin.
He passes a hand-held, 800-nm laser over the skin. The laser activates the particles, generating heat that disrupts the lining of the pilosebaceous unit.
In 2014, Sebacia (Duluth, Ga.), which is developing the technology, reported positive results from two small European trials enrolling a total of 97 patients with acne. The patients were randomized to the gold nanoparticles or to a control group of, in the first study, an over-the-counter face wash and later, the vehicle solution minus the gold nanoparticles.
At 12 weeks’ follow-up, there was a significant reduction in inflammatory lesions and in the Investigator’s Global Assessment score. Treatment was well tolerated and results were durable at 6 months. At that time, the inflammatory lesion count was still 60% below baseline. Side effects were transient erythema and mild edema.
Dr. Munavalli serves as a scientific advisor for Sebacia.
msullivan@frontlinemedcom.com
On Twitter @Alz_Gal
AT AAD 17
VIDEO: Updating the rule of threes for melanoma gene testing
ORLANDO – The rule of threes that has been used to identify patients at risk of hereditary melanoma who may be candidates for genetic testing may be modified soon, according to Sancy Leachman, MD, PhD, professor and chair of the department of dermatology, Oregon Health and Science University, Portland.
Dr. Leachman was the author of a 2009 study that listed three factors as criteria for identifying melanoma: a personal history of at least three invasive melanomas, a combination of at least three melanomas in the individual and in first-degree and second-degree blood relatives – or, in first- or second-degree relatives, a total of at least three diagnoses of melanoma or pancreatic cancer or astrocytoma, which also have been associated with a known susceptibility gene, p16 (J Am Acad Dermatol. 2009 Oct;61[4]:677.e1-14).
But with more genetic testing, it is becoming clear that there are other cancers associated with an increased risk of hereditary melanoma, she explained in a video interview at the annual meeting of the American Academy of Dermatology. “The genes are a little bit different, but if you could identify those patients, you could potentially then screen them for those other cancers,” said Dr. Leachman, who is also director of the melanoma research program at Knight Cancer Institute at OHSU.
In the interview, she discussed a soon-to-be-published literature review that builds upon the rule of threes and suggests a strategy for deciding which patients should be considered for genetic testing, and includes “a suggested list of genes” that should be used in these different subsets of patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Leachman had no relevant disclosures.
ORLANDO – The rule of threes that has been used to identify patients at risk of hereditary melanoma who may be candidates for genetic testing may be modified soon, according to Sancy Leachman, MD, PhD, professor and chair of the department of dermatology, Oregon Health and Science University, Portland.
Dr. Leachman was the author of a 2009 study that listed three factors as criteria for identifying melanoma: a personal history of at least three invasive melanomas, a combination of at least three melanomas in the individual and in first-degree and second-degree blood relatives – or, in first- or second-degree relatives, a total of at least three diagnoses of melanoma or pancreatic cancer or astrocytoma, which also have been associated with a known susceptibility gene, p16 (J Am Acad Dermatol. 2009 Oct;61[4]:677.e1-14).
But with more genetic testing, it is becoming clear that there are other cancers associated with an increased risk of hereditary melanoma, she explained in a video interview at the annual meeting of the American Academy of Dermatology. “The genes are a little bit different, but if you could identify those patients, you could potentially then screen them for those other cancers,” said Dr. Leachman, who is also director of the melanoma research program at Knight Cancer Institute at OHSU.
In the interview, she discussed a soon-to-be-published literature review that builds upon the rule of threes and suggests a strategy for deciding which patients should be considered for genetic testing, and includes “a suggested list of genes” that should be used in these different subsets of patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Leachman had no relevant disclosures.
ORLANDO – The rule of threes that has been used to identify patients at risk of hereditary melanoma who may be candidates for genetic testing may be modified soon, according to Sancy Leachman, MD, PhD, professor and chair of the department of dermatology, Oregon Health and Science University, Portland.
Dr. Leachman was the author of a 2009 study that listed three factors as criteria for identifying melanoma: a personal history of at least three invasive melanomas, a combination of at least three melanomas in the individual and in first-degree and second-degree blood relatives – or, in first- or second-degree relatives, a total of at least three diagnoses of melanoma or pancreatic cancer or astrocytoma, which also have been associated with a known susceptibility gene, p16 (J Am Acad Dermatol. 2009 Oct;61[4]:677.e1-14).
But with more genetic testing, it is becoming clear that there are other cancers associated with an increased risk of hereditary melanoma, she explained in a video interview at the annual meeting of the American Academy of Dermatology. “The genes are a little bit different, but if you could identify those patients, you could potentially then screen them for those other cancers,” said Dr. Leachman, who is also director of the melanoma research program at Knight Cancer Institute at OHSU.
In the interview, she discussed a soon-to-be-published literature review that builds upon the rule of threes and suggests a strategy for deciding which patients should be considered for genetic testing, and includes “a suggested list of genes” that should be used in these different subsets of patients.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Leachman had no relevant disclosures.
AT AAD 17
VIDEO: Tips for performing contained power morcellation
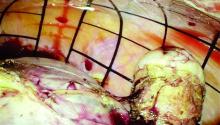
Experience with electromechanical power morcellation in a bag has advanced in the last several years in an effort to achieve safe tissue removal for minimally invasive procedures such as myomectomy, laparoscopic supracervical hysterectomy, or total hysterectomy of a large uterus.
Tissue extraction using contained power morcellation has become favored over contained morcellation using a scalpel – not only because the latter approach is cumbersome but because of the risk of bag puncture and subsequent organ injury. Surgeons have experimented with various sizes and types of retrieval bags and with various techniques for contained power morcellation.
The PneumoLiner carries the same restrictions as do other laparoscopic power morcellation systems – namely that it should not be used in surgery in which the tissue to be morcellated is known or suspected to contain malignancy, and that it should not be used in women who are peri- or postmenopausal. Moreover, to further enhance safety, physicians must have successfully completed the FDA-required validated training program run by Advanced Surgical Concepts and Olympus in order to use the device.
The FDA reviewed the PneumoLiner through a regulatory process known as the de novo classification process. This regulatory process is for first of its kind, low- to moderate-risk medical devices. The PneumoLiner was tested in laboratory conditions to ensure that it could withstand stress force in excess of the normal forces of surgery, and was found to be impervious to substances similar in molecular size to tissues, cells, and body fluids. There could be no cellular migration or leakage.
As surgeons were advancing the idea of inflated bag morcellation, one promising adaptation was to puncture the inflated bag to place accessory ports. However, recent research has shown that contained morcellation involving intentional bag puncture with a trocar may result in tissue or fluid leakage.
Spillage was noted in 7 of 76 cases (9.2%) in a multicenter prospective cohort of women who underwent hysterectomy or myomectomy using a contained power morcellation technique that involved perforation of the containment bag with a balloon-tipped lateral trocar. Investigators had injected blue dye into the bag prior to morcellation and examined the abdomen and pelvis after removing the bag for signs of spillage of dye, fluid, or tissue. In all cases, the containment bags were intact (Am J Obstet Gynecol. 2016 Feb;214[2]:257.e1-6).
The authors prematurely closed this study and recommended against this puncture technique. For complete containment, it appears to be important that we morcellate using a bag that has a single opening and is not punctured with accessory trocars.
The technique
The PneumoLiner comes loaded in an insertion tube for placement. It has a plunger to deploy the device and a retrieval lanyard that closes the bag around the specimen, enabling retrieval of the neck of the bag outside the abdomen.
Included with the PneumoLiner is a multi-instrument port that can be used during the laparoscopic procedure and then converted to the active port for morcellation. The port has an opening for the laparoscope (either a 5-mm 30-degree straight or a 5-mm articulating laparoscope) and an opening for the morcellator, as well as two small openings for insufflation and for smoke exhaustion.
Surgery may be performed using this single-port or a multiport laparoscopic or robotic approach. For morcellation, the approach converts to a single-site technique that involves only one entry point for all instruments and no perforation of the bag.
At the beginning of the procedure (or at the end of the case if preferred), a 25-mm incision is made in the umbilicus and the system’s port is inserted and trimmed. The port cap is placed, the abdomen is insufflated, and the laparoscope is inserted. If placed at the beginning of the case, this port can be used as a camera or accessory port.
Before deployment of the PneumoLiner, the uterus or target tissue is placed out of the way; I recommend the upper right quadrant. The PneumoLiner is then inserted with its directional tab pointing upward, and the system’s plunger is depressed while the sleeve is pulled back. In essence, the PneumoLiner is advanced while the sleeve is simultaneously withdrawn, laying it flat in the pelvis.
With an atraumatic grasper, the uterus is placed within the opening of the bag, and the bag is grasped at the collar and elevated up and around the specimen. When full containment of the specimen is visualized, the retrieval lanyard is withdrawn until an opening ring partially protrudes outside the port. All lateral trocars must have been withdrawn prior to inflation of the bag to prevent it from being damaged.
At this point, the port cap is removed and the PneumoLiner neck is withdrawn until a black grid pattern on the bag is visible. The surgeon should then ensure there are no twists in the bag before replacing the port cap and insufflating the bag to a pressure of 15 mm Hg.*
The bag must be correctly in place and fully insufflated before the laparoscope is inserted. The laparoscope must be inserted prior to the morcellator. When the morcellator is inserted, care must be taken to ensure that the morcellator probe is in place.
Once the morcellator is placed, the probe is withdrawn and a closed tenaculum is placed. With the closed tenaculum, the surgeon can manipulate tissue and gauge depth and bearings without inadvertently grabbing the bag. The black grid pattern on the bag assists with estimation of tissue fragment size; morcellation proceeds under direct vision until the tissue fragments are smaller than four printed grids.
Instrumentation is removed in a set order, with the morcellator first and the laparoscope last. The port cap is detached and the PneumoLiner is removed while allowing fumes to escape. The morcellator, camera, tenaculum, and port cap are considered contaminated at this point and should not re-enter the field.
Pearls for morcellation
- The single-site nature of the procedure can sometimes be challenging. If you’ve placed your laparoscope and are having difficulty locating the morcellator, bring your laparoscope and morcellator shaft in parallel to each other, and you’ll be able to better orient yourself.
- To enlarge your field of view after you’ve inflated the PneumoLiner and captured the tissue within the bag, level the patient a bit and move the tissue further away from the laparoscope.
- If the morcellator tube is limiting visualization of the tenaculum tip, slide the morcellator back while leaving the tenaculum in a fixed position.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Courtesy Dr. Tony Shibley and Olympus
Dr. Shibley is an ob.gyn. in private practice in the Minneapolis area. He receives royalties from Advanced Surgical Concepts and serves as a consultant for Olympus.
*Correction 3/8/17: An earlier version of this article misstated the name of the Pneumoliner device in a photo caption. The pressure of the morcellation bag also was misstated.
Experience with electromechanical power morcellation in a bag has advanced in the last several years in an effort to achieve safe tissue removal for minimally invasive procedures such as myomectomy, laparoscopic supracervical hysterectomy, or total hysterectomy of a large uterus.
Tissue extraction using contained power morcellation has become favored over contained morcellation using a scalpel – not only because the latter approach is cumbersome but because of the risk of bag puncture and subsequent organ injury. Surgeons have experimented with various sizes and types of retrieval bags and with various techniques for contained power morcellation.
The PneumoLiner carries the same restrictions as do other laparoscopic power morcellation systems – namely that it should not be used in surgery in which the tissue to be morcellated is known or suspected to contain malignancy, and that it should not be used in women who are peri- or postmenopausal. Moreover, to further enhance safety, physicians must have successfully completed the FDA-required validated training program run by Advanced Surgical Concepts and Olympus in order to use the device.
The FDA reviewed the PneumoLiner through a regulatory process known as the de novo classification process. This regulatory process is for first of its kind, low- to moderate-risk medical devices. The PneumoLiner was tested in laboratory conditions to ensure that it could withstand stress force in excess of the normal forces of surgery, and was found to be impervious to substances similar in molecular size to tissues, cells, and body fluids. There could be no cellular migration or leakage.
As surgeons were advancing the idea of inflated bag morcellation, one promising adaptation was to puncture the inflated bag to place accessory ports. However, recent research has shown that contained morcellation involving intentional bag puncture with a trocar may result in tissue or fluid leakage.
Spillage was noted in 7 of 76 cases (9.2%) in a multicenter prospective cohort of women who underwent hysterectomy or myomectomy using a contained power morcellation technique that involved perforation of the containment bag with a balloon-tipped lateral trocar. Investigators had injected blue dye into the bag prior to morcellation and examined the abdomen and pelvis after removing the bag for signs of spillage of dye, fluid, or tissue. In all cases, the containment bags were intact (Am J Obstet Gynecol. 2016 Feb;214[2]:257.e1-6).
The authors prematurely closed this study and recommended against this puncture technique. For complete containment, it appears to be important that we morcellate using a bag that has a single opening and is not punctured with accessory trocars.
The technique
The PneumoLiner comes loaded in an insertion tube for placement. It has a plunger to deploy the device and a retrieval lanyard that closes the bag around the specimen, enabling retrieval of the neck of the bag outside the abdomen.
Included with the PneumoLiner is a multi-instrument port that can be used during the laparoscopic procedure and then converted to the active port for morcellation. The port has an opening for the laparoscope (either a 5-mm 30-degree straight or a 5-mm articulating laparoscope) and an opening for the morcellator, as well as two small openings for insufflation and for smoke exhaustion.
Surgery may be performed using this single-port or a multiport laparoscopic or robotic approach. For morcellation, the approach converts to a single-site technique that involves only one entry point for all instruments and no perforation of the bag.
At the beginning of the procedure (or at the end of the case if preferred), a 25-mm incision is made in the umbilicus and the system’s port is inserted and trimmed. The port cap is placed, the abdomen is insufflated, and the laparoscope is inserted. If placed at the beginning of the case, this port can be used as a camera or accessory port.
Before deployment of the PneumoLiner, the uterus or target tissue is placed out of the way; I recommend the upper right quadrant. The PneumoLiner is then inserted with its directional tab pointing upward, and the system’s plunger is depressed while the sleeve is pulled back. In essence, the PneumoLiner is advanced while the sleeve is simultaneously withdrawn, laying it flat in the pelvis.
With an atraumatic grasper, the uterus is placed within the opening of the bag, and the bag is grasped at the collar and elevated up and around the specimen. When full containment of the specimen is visualized, the retrieval lanyard is withdrawn until an opening ring partially protrudes outside the port. All lateral trocars must have been withdrawn prior to inflation of the bag to prevent it from being damaged.
At this point, the port cap is removed and the PneumoLiner neck is withdrawn until a black grid pattern on the bag is visible. The surgeon should then ensure there are no twists in the bag before replacing the port cap and insufflating the bag to a pressure of 15 mm Hg.*
The bag must be correctly in place and fully insufflated before the laparoscope is inserted. The laparoscope must be inserted prior to the morcellator. When the morcellator is inserted, care must be taken to ensure that the morcellator probe is in place.
Once the morcellator is placed, the probe is withdrawn and a closed tenaculum is placed. With the closed tenaculum, the surgeon can manipulate tissue and gauge depth and bearings without inadvertently grabbing the bag. The black grid pattern on the bag assists with estimation of tissue fragment size; morcellation proceeds under direct vision until the tissue fragments are smaller than four printed grids.
Instrumentation is removed in a set order, with the morcellator first and the laparoscope last. The port cap is detached and the PneumoLiner is removed while allowing fumes to escape. The morcellator, camera, tenaculum, and port cap are considered contaminated at this point and should not re-enter the field.
Pearls for morcellation
- The single-site nature of the procedure can sometimes be challenging. If you’ve placed your laparoscope and are having difficulty locating the morcellator, bring your laparoscope and morcellator shaft in parallel to each other, and you’ll be able to better orient yourself.
- To enlarge your field of view after you’ve inflated the PneumoLiner and captured the tissue within the bag, level the patient a bit and move the tissue further away from the laparoscope.
- If the morcellator tube is limiting visualization of the tenaculum tip, slide the morcellator back while leaving the tenaculum in a fixed position.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Courtesy Dr. Tony Shibley and Olympus
Dr. Shibley is an ob.gyn. in private practice in the Minneapolis area. He receives royalties from Advanced Surgical Concepts and serves as a consultant for Olympus.
*Correction 3/8/17: An earlier version of this article misstated the name of the Pneumoliner device in a photo caption. The pressure of the morcellation bag also was misstated.
Experience with electromechanical power morcellation in a bag has advanced in the last several years in an effort to achieve safe tissue removal for minimally invasive procedures such as myomectomy, laparoscopic supracervical hysterectomy, or total hysterectomy of a large uterus.
Tissue extraction using contained power morcellation has become favored over contained morcellation using a scalpel – not only because the latter approach is cumbersome but because of the risk of bag puncture and subsequent organ injury. Surgeons have experimented with various sizes and types of retrieval bags and with various techniques for contained power morcellation.
The PneumoLiner carries the same restrictions as do other laparoscopic power morcellation systems – namely that it should not be used in surgery in which the tissue to be morcellated is known or suspected to contain malignancy, and that it should not be used in women who are peri- or postmenopausal. Moreover, to further enhance safety, physicians must have successfully completed the FDA-required validated training program run by Advanced Surgical Concepts and Olympus in order to use the device.
The FDA reviewed the PneumoLiner through a regulatory process known as the de novo classification process. This regulatory process is for first of its kind, low- to moderate-risk medical devices. The PneumoLiner was tested in laboratory conditions to ensure that it could withstand stress force in excess of the normal forces of surgery, and was found to be impervious to substances similar in molecular size to tissues, cells, and body fluids. There could be no cellular migration or leakage.
As surgeons were advancing the idea of inflated bag morcellation, one promising adaptation was to puncture the inflated bag to place accessory ports. However, recent research has shown that contained morcellation involving intentional bag puncture with a trocar may result in tissue or fluid leakage.
Spillage was noted in 7 of 76 cases (9.2%) in a multicenter prospective cohort of women who underwent hysterectomy or myomectomy using a contained power morcellation technique that involved perforation of the containment bag with a balloon-tipped lateral trocar. Investigators had injected blue dye into the bag prior to morcellation and examined the abdomen and pelvis after removing the bag for signs of spillage of dye, fluid, or tissue. In all cases, the containment bags were intact (Am J Obstet Gynecol. 2016 Feb;214[2]:257.e1-6).
The authors prematurely closed this study and recommended against this puncture technique. For complete containment, it appears to be important that we morcellate using a bag that has a single opening and is not punctured with accessory trocars.
The technique
The PneumoLiner comes loaded in an insertion tube for placement. It has a plunger to deploy the device and a retrieval lanyard that closes the bag around the specimen, enabling retrieval of the neck of the bag outside the abdomen.
Included with the PneumoLiner is a multi-instrument port that can be used during the laparoscopic procedure and then converted to the active port for morcellation. The port has an opening for the laparoscope (either a 5-mm 30-degree straight or a 5-mm articulating laparoscope) and an opening for the morcellator, as well as two small openings for insufflation and for smoke exhaustion.
Surgery may be performed using this single-port or a multiport laparoscopic or robotic approach. For morcellation, the approach converts to a single-site technique that involves only one entry point for all instruments and no perforation of the bag.
At the beginning of the procedure (or at the end of the case if preferred), a 25-mm incision is made in the umbilicus and the system’s port is inserted and trimmed. The port cap is placed, the abdomen is insufflated, and the laparoscope is inserted. If placed at the beginning of the case, this port can be used as a camera or accessory port.
Before deployment of the PneumoLiner, the uterus or target tissue is placed out of the way; I recommend the upper right quadrant. The PneumoLiner is then inserted with its directional tab pointing upward, and the system’s plunger is depressed while the sleeve is pulled back. In essence, the PneumoLiner is advanced while the sleeve is simultaneously withdrawn, laying it flat in the pelvis.
With an atraumatic grasper, the uterus is placed within the opening of the bag, and the bag is grasped at the collar and elevated up and around the specimen. When full containment of the specimen is visualized, the retrieval lanyard is withdrawn until an opening ring partially protrudes outside the port. All lateral trocars must have been withdrawn prior to inflation of the bag to prevent it from being damaged.
At this point, the port cap is removed and the PneumoLiner neck is withdrawn until a black grid pattern on the bag is visible. The surgeon should then ensure there are no twists in the bag before replacing the port cap and insufflating the bag to a pressure of 15 mm Hg.*
The bag must be correctly in place and fully insufflated before the laparoscope is inserted. The laparoscope must be inserted prior to the morcellator. When the morcellator is inserted, care must be taken to ensure that the morcellator probe is in place.
Once the morcellator is placed, the probe is withdrawn and a closed tenaculum is placed. With the closed tenaculum, the surgeon can manipulate tissue and gauge depth and bearings without inadvertently grabbing the bag. The black grid pattern on the bag assists with estimation of tissue fragment size; morcellation proceeds under direct vision until the tissue fragments are smaller than four printed grids.
Instrumentation is removed in a set order, with the morcellator first and the laparoscope last. The port cap is detached and the PneumoLiner is removed while allowing fumes to escape. The morcellator, camera, tenaculum, and port cap are considered contaminated at this point and should not re-enter the field.
Pearls for morcellation
- The single-site nature of the procedure can sometimes be challenging. If you’ve placed your laparoscope and are having difficulty locating the morcellator, bring your laparoscope and morcellator shaft in parallel to each other, and you’ll be able to better orient yourself.
- To enlarge your field of view after you’ve inflated the PneumoLiner and captured the tissue within the bag, level the patient a bit and move the tissue further away from the laparoscope.
- If the morcellator tube is limiting visualization of the tenaculum tip, slide the morcellator back while leaving the tenaculum in a fixed position.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Courtesy Dr. Tony Shibley and Olympus
Dr. Shibley is an ob.gyn. in private practice in the Minneapolis area. He receives royalties from Advanced Surgical Concepts and serves as a consultant for Olympus.
*Correction 3/8/17: An earlier version of this article misstated the name of the Pneumoliner device in a photo caption. The pressure of the morcellation bag also was misstated.