User login
Ustekinumab again linked to cardiovascular events
WAIKOLOA, HAWAII – The anti-interleukin-12/23 biologic agents ustekinumab and briakinumab were associated with a statistically significant 4.23-fold increased risk of major adverse cardiac events in the latest meta-analysis of placebo-controlled clinical trials conducted in patients with chronic plaque psoriasis.
"What are the implications? It’s probably a class effect. That’s the way I practice. I think there is a slightly increased risk of myocardial infarction in our anti-IL-12/23-treated patients. So I think you should consider all of your options when selecting a biologic therapy. We know that our psoriasis patients typically have multiple cardiac risk factors, and that TNF antagonists are cardioprotective," Dr. Craig L. Leonardi said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
The latest industry-independent meta-analysis (J. Eur. Acad. Dermatol. Venereol. 2013;27:622-7), led by dermatologists at Dessau (Germany) Medical Center, examined the same nine phase-II and phase-III placebo-controlled randomized trials scrutinized in an earlier meta-analysis, also industry independent, carried out by Dr. Leonardi and coinvestigators (JAMA 2011;306:864-71).
The earlier meta-analysis identified 10 major adverse cardiovascular events (MACE) in 3,179 IL-12/23-treated subjects and none among 1,474 placebo-treated controls. This signal was deemed not statistically significant, although Dr. Leonardi and coworkers noted that their meta-analysis may have been underpowered to detect a small increase in risk.
Given that the two meta-analyses relied upon essentially the same data, how did they reach such different conclusions? It’s all in the statistical methods. Without getting geeky about the statistical fine points, Dr. Leonardi noted that his group used the Mantel-Haenszel fixed-effects model, while the Dessau group employed the Peto method, which their statisticians deemed more appropriate on the basis of its previously established superior performance in detecting rare events.
The Peto method is named for Sir Richard Peto, a renowned University of Oxford epidemiologist knighted for his statistical contributions.
Dr. Leonardi, a dermatologist in private practice in St. Louis and a clinical professor of dermatology at Saint Louis University, wasn’t about to quibble about statistics. Taken together, he said, the story conveyed by the two meta-analyses is one of a small but real increase in the absolute risk of MACE in psoriasis patients exposed to anti-IL-12/23 biologics. Based upon this evidence, when he starts a psoriasis patient on ustekinumab (Stelara), he now generally does so at the lower 45-mg dose regardless of the patient’s weight, even though the 90-mg dose is approved for use in patients weighing more than 100 kg.
"And I’m placing my patients on aspirin at 81 mg/day while we await further data," he added.
He anticipates that clinically meaningful data will eventually come from the Psoriasis Longitudinal Assessment and Registry (PSOLAR) study, an ongoing observational registry that has enrolled nearly 12,000 psoriasis patients for a planned follow-up period of at least 8 years at 266 investigative sites in 15 countries. The Janssen-funded registry includes roughly 3,800 patients on ustekinumab, lesser numbers on the other biologics, as well as a large group on phototherapy and no biologics.
Dr. Leonardi presented an early interim analysis in which the rate of MACE in the ustekinumab group was 0.28 per 100 patient-years. This was numerically slightly lower than but still comparable to the rates observed with infliximab and other biologics, and half the rate in patients on no biologics. He stressed, however, that these are unadjusted rates. Planned formal comparisons will require longer follow-up periods, more MACE, and multivariate analysis to control for baseline differences in comorbid conditions and cardiovascular risk factors. The no-biologics group, for example, was significantly older than patients on biologic agents, because once patients become Medicare eligible it is quite difficult to get a prescription for a biologic. And of course cardiovascular risk climbs with advancing age.
Dr. Leonardi is a PSOLAR coinvestigator, and a big fan of the project’s potential.
"Don’t wait for an NIH-sponsored disease-specific registry. The fact is the government is not going to fund it, so we have to do the best we can with the tools we have. PSOLAR is the largest psoriasis registry in the world. It will allow us to answer questions about the emergence of comorbid diseases like psoriatic arthritis and cardiovascular disease, and treatment-specific questions like rates of infection, cancer, and MACE, as well as unanticipated issues nobody knew about," he said.
Dr. Leonardi disclosed ties with Janssen and nearly two dozen other pharmaceutical companies.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – The anti-interleukin-12/23 biologic agents ustekinumab and briakinumab were associated with a statistically significant 4.23-fold increased risk of major adverse cardiac events in the latest meta-analysis of placebo-controlled clinical trials conducted in patients with chronic plaque psoriasis.
"What are the implications? It’s probably a class effect. That’s the way I practice. I think there is a slightly increased risk of myocardial infarction in our anti-IL-12/23-treated patients. So I think you should consider all of your options when selecting a biologic therapy. We know that our psoriasis patients typically have multiple cardiac risk factors, and that TNF antagonists are cardioprotective," Dr. Craig L. Leonardi said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
The latest industry-independent meta-analysis (J. Eur. Acad. Dermatol. Venereol. 2013;27:622-7), led by dermatologists at Dessau (Germany) Medical Center, examined the same nine phase-II and phase-III placebo-controlled randomized trials scrutinized in an earlier meta-analysis, also industry independent, carried out by Dr. Leonardi and coinvestigators (JAMA 2011;306:864-71).
The earlier meta-analysis identified 10 major adverse cardiovascular events (MACE) in 3,179 IL-12/23-treated subjects and none among 1,474 placebo-treated controls. This signal was deemed not statistically significant, although Dr. Leonardi and coworkers noted that their meta-analysis may have been underpowered to detect a small increase in risk.
Given that the two meta-analyses relied upon essentially the same data, how did they reach such different conclusions? It’s all in the statistical methods. Without getting geeky about the statistical fine points, Dr. Leonardi noted that his group used the Mantel-Haenszel fixed-effects model, while the Dessau group employed the Peto method, which their statisticians deemed more appropriate on the basis of its previously established superior performance in detecting rare events.
The Peto method is named for Sir Richard Peto, a renowned University of Oxford epidemiologist knighted for his statistical contributions.
Dr. Leonardi, a dermatologist in private practice in St. Louis and a clinical professor of dermatology at Saint Louis University, wasn’t about to quibble about statistics. Taken together, he said, the story conveyed by the two meta-analyses is one of a small but real increase in the absolute risk of MACE in psoriasis patients exposed to anti-IL-12/23 biologics. Based upon this evidence, when he starts a psoriasis patient on ustekinumab (Stelara), he now generally does so at the lower 45-mg dose regardless of the patient’s weight, even though the 90-mg dose is approved for use in patients weighing more than 100 kg.
"And I’m placing my patients on aspirin at 81 mg/day while we await further data," he added.
He anticipates that clinically meaningful data will eventually come from the Psoriasis Longitudinal Assessment and Registry (PSOLAR) study, an ongoing observational registry that has enrolled nearly 12,000 psoriasis patients for a planned follow-up period of at least 8 years at 266 investigative sites in 15 countries. The Janssen-funded registry includes roughly 3,800 patients on ustekinumab, lesser numbers on the other biologics, as well as a large group on phototherapy and no biologics.
Dr. Leonardi presented an early interim analysis in which the rate of MACE in the ustekinumab group was 0.28 per 100 patient-years. This was numerically slightly lower than but still comparable to the rates observed with infliximab and other biologics, and half the rate in patients on no biologics. He stressed, however, that these are unadjusted rates. Planned formal comparisons will require longer follow-up periods, more MACE, and multivariate analysis to control for baseline differences in comorbid conditions and cardiovascular risk factors. The no-biologics group, for example, was significantly older than patients on biologic agents, because once patients become Medicare eligible it is quite difficult to get a prescription for a biologic. And of course cardiovascular risk climbs with advancing age.
Dr. Leonardi is a PSOLAR coinvestigator, and a big fan of the project’s potential.
"Don’t wait for an NIH-sponsored disease-specific registry. The fact is the government is not going to fund it, so we have to do the best we can with the tools we have. PSOLAR is the largest psoriasis registry in the world. It will allow us to answer questions about the emergence of comorbid diseases like psoriatic arthritis and cardiovascular disease, and treatment-specific questions like rates of infection, cancer, and MACE, as well as unanticipated issues nobody knew about," he said.
Dr. Leonardi disclosed ties with Janssen and nearly two dozen other pharmaceutical companies.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – The anti-interleukin-12/23 biologic agents ustekinumab and briakinumab were associated with a statistically significant 4.23-fold increased risk of major adverse cardiac events in the latest meta-analysis of placebo-controlled clinical trials conducted in patients with chronic plaque psoriasis.
"What are the implications? It’s probably a class effect. That’s the way I practice. I think there is a slightly increased risk of myocardial infarction in our anti-IL-12/23-treated patients. So I think you should consider all of your options when selecting a biologic therapy. We know that our psoriasis patients typically have multiple cardiac risk factors, and that TNF antagonists are cardioprotective," Dr. Craig L. Leonardi said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
The latest industry-independent meta-analysis (J. Eur. Acad. Dermatol. Venereol. 2013;27:622-7), led by dermatologists at Dessau (Germany) Medical Center, examined the same nine phase-II and phase-III placebo-controlled randomized trials scrutinized in an earlier meta-analysis, also industry independent, carried out by Dr. Leonardi and coinvestigators (JAMA 2011;306:864-71).
The earlier meta-analysis identified 10 major adverse cardiovascular events (MACE) in 3,179 IL-12/23-treated subjects and none among 1,474 placebo-treated controls. This signal was deemed not statistically significant, although Dr. Leonardi and coworkers noted that their meta-analysis may have been underpowered to detect a small increase in risk.
Given that the two meta-analyses relied upon essentially the same data, how did they reach such different conclusions? It’s all in the statistical methods. Without getting geeky about the statistical fine points, Dr. Leonardi noted that his group used the Mantel-Haenszel fixed-effects model, while the Dessau group employed the Peto method, which their statisticians deemed more appropriate on the basis of its previously established superior performance in detecting rare events.
The Peto method is named for Sir Richard Peto, a renowned University of Oxford epidemiologist knighted for his statistical contributions.
Dr. Leonardi, a dermatologist in private practice in St. Louis and a clinical professor of dermatology at Saint Louis University, wasn’t about to quibble about statistics. Taken together, he said, the story conveyed by the two meta-analyses is one of a small but real increase in the absolute risk of MACE in psoriasis patients exposed to anti-IL-12/23 biologics. Based upon this evidence, when he starts a psoriasis patient on ustekinumab (Stelara), he now generally does so at the lower 45-mg dose regardless of the patient’s weight, even though the 90-mg dose is approved for use in patients weighing more than 100 kg.
"And I’m placing my patients on aspirin at 81 mg/day while we await further data," he added.
He anticipates that clinically meaningful data will eventually come from the Psoriasis Longitudinal Assessment and Registry (PSOLAR) study, an ongoing observational registry that has enrolled nearly 12,000 psoriasis patients for a planned follow-up period of at least 8 years at 266 investigative sites in 15 countries. The Janssen-funded registry includes roughly 3,800 patients on ustekinumab, lesser numbers on the other biologics, as well as a large group on phototherapy and no biologics.
Dr. Leonardi presented an early interim analysis in which the rate of MACE in the ustekinumab group was 0.28 per 100 patient-years. This was numerically slightly lower than but still comparable to the rates observed with infliximab and other biologics, and half the rate in patients on no biologics. He stressed, however, that these are unadjusted rates. Planned formal comparisons will require longer follow-up periods, more MACE, and multivariate analysis to control for baseline differences in comorbid conditions and cardiovascular risk factors. The no-biologics group, for example, was significantly older than patients on biologic agents, because once patients become Medicare eligible it is quite difficult to get a prescription for a biologic. And of course cardiovascular risk climbs with advancing age.
Dr. Leonardi is a PSOLAR coinvestigator, and a big fan of the project’s potential.
"Don’t wait for an NIH-sponsored disease-specific registry. The fact is the government is not going to fund it, so we have to do the best we can with the tools we have. PSOLAR is the largest psoriasis registry in the world. It will allow us to answer questions about the emergence of comorbid diseases like psoriatic arthritis and cardiovascular disease, and treatment-specific questions like rates of infection, cancer, and MACE, as well as unanticipated issues nobody knew about," he said.
Dr. Leonardi disclosed ties with Janssen and nearly two dozen other pharmaceutical companies.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Simple smell test may predict donepezil response
ORLANDO – Predicting whether add-on donepezil will improve residual cognitive deficits in an elderly patient on adequate antidepressant therapy may be as plain as the nose on the patient’s face.
Compared with the olfaction-intact patient, those with baseline deficits in sense of smell on a simple scratch-and-sniff test had significantly more improvements in episodic memory after 12 weeks of donepezil (Aricept) in a placebo-controlled, double-blind randomized pilot study, Dr. Gregory H. Pelton reported at the annual meeting of the American Association for Geriatric Psychiatry.
"One’s ability to smell may be a predictor of Alzheimer’s disease pathology that will respond to acetylcholinesterase inhibitor therapy. That’s the logic here," explained Dr. Pelton, a psychiatrist at Columbia University, New York.
Patients with late-life depression and cognitive impairment are known to be at even greater risk for progression to dementia than are patients with mild cognitive impairment. Donepezil is approved for improving cognition in patients with Alzheimer’s disease but not in those with mild cognitive impairment, where the evidence of benefit has been equivocal. Since the distinctive neurobiologic abnormalities of Alzheimer’s disease are known to be present for many years before the disease is diagnosed, Dr. Pelton and his coworkers reasoned that a low score on a test of olfactory identification might be a biomarker for donepezil responsiveness in these patients.
"The olfactory system is a very old evolutionary system. Since it projects directly to the entorhinal cortex, which then goes to the hippocampus, it’s actually directly involved in memory. Everybody has these flashes of old memories that arise with olfactory stimuli," Dr. Pelton said in an interview. The nose is an expressway to memory.
Deficits in olfactory identification as assessed by the commercially available, 40-item, multiple-choice, scratch-and-sniff University of Pennsylvania Smell Identification Test (UPSIT) have been shown to be associated with an increased rate of conversion from mild cognitive impairment to Alzheimer’s disease (Am. J. Psychiatry 2000;157:1399-405).
The pilot study included 18 patients with late-life depression and cognitive impairment with a Mini Mental State Exam score above 20 out of a possible 30. All participants received 8 weeks of open-label antidepressant therapy followed by 12 weeks of donepezil or placebo in the trial. The primary outcome was the change in episodic verbal memory between weeks 8 and 20 as reflected in the Selective Reminding Test immediate total recall score.
Five patients had a low baseline UPSIT score, meaning they correctly identified fewer than 30 of the 40 scratch-and-sniff items. Patients with a low UPSIT score who were assigned to donepezil showed a mean 10.4-point improvement on the Selective Reminding Test, while those with an UPSIT score of 30 or more showed a 2.7-point improvement in response to the acetylcholinesterase inhibitor.
Based upon these encouraging pilot study results, Dr. Pelton is now conducting a larger, confirmatory randomized trial funded by the National Institutes of Health.
"If the finding of olfactory deficits predicting acetylcholinesterase inhibitor response is replicated in larger samples, utilizing this simple, reliable, and inexpensive approach may improve the selection of patients with late-life depression and cognitive impairment, and possibly also those with mild cognitive impairment or Alzheimer’s disease, who are likely to respond to acetylcholinesterase inhibitor therapy," he noted.
The study was funded by the Alzheimer’s Association, federal research grants, and Pfizer. Dr. Pelton is a consultant to the company.
ORLANDO – Predicting whether add-on donepezil will improve residual cognitive deficits in an elderly patient on adequate antidepressant therapy may be as plain as the nose on the patient’s face.
Compared with the olfaction-intact patient, those with baseline deficits in sense of smell on a simple scratch-and-sniff test had significantly more improvements in episodic memory after 12 weeks of donepezil (Aricept) in a placebo-controlled, double-blind randomized pilot study, Dr. Gregory H. Pelton reported at the annual meeting of the American Association for Geriatric Psychiatry.
"One’s ability to smell may be a predictor of Alzheimer’s disease pathology that will respond to acetylcholinesterase inhibitor therapy. That’s the logic here," explained Dr. Pelton, a psychiatrist at Columbia University, New York.
Patients with late-life depression and cognitive impairment are known to be at even greater risk for progression to dementia than are patients with mild cognitive impairment. Donepezil is approved for improving cognition in patients with Alzheimer’s disease but not in those with mild cognitive impairment, where the evidence of benefit has been equivocal. Since the distinctive neurobiologic abnormalities of Alzheimer’s disease are known to be present for many years before the disease is diagnosed, Dr. Pelton and his coworkers reasoned that a low score on a test of olfactory identification might be a biomarker for donepezil responsiveness in these patients.
"The olfactory system is a very old evolutionary system. Since it projects directly to the entorhinal cortex, which then goes to the hippocampus, it’s actually directly involved in memory. Everybody has these flashes of old memories that arise with olfactory stimuli," Dr. Pelton said in an interview. The nose is an expressway to memory.
Deficits in olfactory identification as assessed by the commercially available, 40-item, multiple-choice, scratch-and-sniff University of Pennsylvania Smell Identification Test (UPSIT) have been shown to be associated with an increased rate of conversion from mild cognitive impairment to Alzheimer’s disease (Am. J. Psychiatry 2000;157:1399-405).
The pilot study included 18 patients with late-life depression and cognitive impairment with a Mini Mental State Exam score above 20 out of a possible 30. All participants received 8 weeks of open-label antidepressant therapy followed by 12 weeks of donepezil or placebo in the trial. The primary outcome was the change in episodic verbal memory between weeks 8 and 20 as reflected in the Selective Reminding Test immediate total recall score.
Five patients had a low baseline UPSIT score, meaning they correctly identified fewer than 30 of the 40 scratch-and-sniff items. Patients with a low UPSIT score who were assigned to donepezil showed a mean 10.4-point improvement on the Selective Reminding Test, while those with an UPSIT score of 30 or more showed a 2.7-point improvement in response to the acetylcholinesterase inhibitor.
Based upon these encouraging pilot study results, Dr. Pelton is now conducting a larger, confirmatory randomized trial funded by the National Institutes of Health.
"If the finding of olfactory deficits predicting acetylcholinesterase inhibitor response is replicated in larger samples, utilizing this simple, reliable, and inexpensive approach may improve the selection of patients with late-life depression and cognitive impairment, and possibly also those with mild cognitive impairment or Alzheimer’s disease, who are likely to respond to acetylcholinesterase inhibitor therapy," he noted.
The study was funded by the Alzheimer’s Association, federal research grants, and Pfizer. Dr. Pelton is a consultant to the company.
ORLANDO – Predicting whether add-on donepezil will improve residual cognitive deficits in an elderly patient on adequate antidepressant therapy may be as plain as the nose on the patient’s face.
Compared with the olfaction-intact patient, those with baseline deficits in sense of smell on a simple scratch-and-sniff test had significantly more improvements in episodic memory after 12 weeks of donepezil (Aricept) in a placebo-controlled, double-blind randomized pilot study, Dr. Gregory H. Pelton reported at the annual meeting of the American Association for Geriatric Psychiatry.
"One’s ability to smell may be a predictor of Alzheimer’s disease pathology that will respond to acetylcholinesterase inhibitor therapy. That’s the logic here," explained Dr. Pelton, a psychiatrist at Columbia University, New York.
Patients with late-life depression and cognitive impairment are known to be at even greater risk for progression to dementia than are patients with mild cognitive impairment. Donepezil is approved for improving cognition in patients with Alzheimer’s disease but not in those with mild cognitive impairment, where the evidence of benefit has been equivocal. Since the distinctive neurobiologic abnormalities of Alzheimer’s disease are known to be present for many years before the disease is diagnosed, Dr. Pelton and his coworkers reasoned that a low score on a test of olfactory identification might be a biomarker for donepezil responsiveness in these patients.
"The olfactory system is a very old evolutionary system. Since it projects directly to the entorhinal cortex, which then goes to the hippocampus, it’s actually directly involved in memory. Everybody has these flashes of old memories that arise with olfactory stimuli," Dr. Pelton said in an interview. The nose is an expressway to memory.
Deficits in olfactory identification as assessed by the commercially available, 40-item, multiple-choice, scratch-and-sniff University of Pennsylvania Smell Identification Test (UPSIT) have been shown to be associated with an increased rate of conversion from mild cognitive impairment to Alzheimer’s disease (Am. J. Psychiatry 2000;157:1399-405).
The pilot study included 18 patients with late-life depression and cognitive impairment with a Mini Mental State Exam score above 20 out of a possible 30. All participants received 8 weeks of open-label antidepressant therapy followed by 12 weeks of donepezil or placebo in the trial. The primary outcome was the change in episodic verbal memory between weeks 8 and 20 as reflected in the Selective Reminding Test immediate total recall score.
Five patients had a low baseline UPSIT score, meaning they correctly identified fewer than 30 of the 40 scratch-and-sniff items. Patients with a low UPSIT score who were assigned to donepezil showed a mean 10.4-point improvement on the Selective Reminding Test, while those with an UPSIT score of 30 or more showed a 2.7-point improvement in response to the acetylcholinesterase inhibitor.
Based upon these encouraging pilot study results, Dr. Pelton is now conducting a larger, confirmatory randomized trial funded by the National Institutes of Health.
"If the finding of olfactory deficits predicting acetylcholinesterase inhibitor response is replicated in larger samples, utilizing this simple, reliable, and inexpensive approach may improve the selection of patients with late-life depression and cognitive impairment, and possibly also those with mild cognitive impairment or Alzheimer’s disease, who are likely to respond to acetylcholinesterase inhibitor therapy," he noted.
The study was funded by the Alzheimer’s Association, federal research grants, and Pfizer. Dr. Pelton is a consultant to the company.
AT THE AAGP ANNUAL MEETING
Major finding: Patients with a low UPSIT score who were assigned to donepezil showed a mean 10.4-point improvement on the Selective Reminding Test, while those with an UPSIT score of 30 or more showed a 2.7-point improvement in response to the acetylcholinesterase inhibitor.
Data source: This was a pilot study involving 18 patients with late-life depression and cognitive impairment who received 8 weeks of antidepressant therapy, and then were randomized double-blind to 12 weeks of donepezil or placebo.
Disclosures: The study was funded by the Alzheimer’s Association, federal research grants, and Pfizer. Dr. Pelton is a consultant to the company.
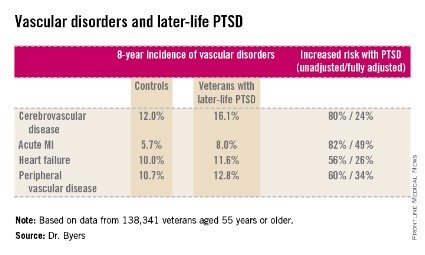
Later-life PTSD boosts vascular risk
ORLANDO – Military veterans aged 55 years or older with current posttraumatic stress disorder are at significantly higher risk of developing new-onset vascular disease than those without PTSD, according to a very large national longitudinal study.
"This study suggests the need for greater monitoring and treatment of PTSD in older veterans to assist in the prevention of vascular disorders over the long term," Amy L. Byers, Ph.D., asserted at the annual meeting of the American Association for Geriatric Psychiatry.
She reported on 138,341 veterans aged 55 years or older, all of whom were free of known vascular disease at baseline. During 8 years of follow-up, the subjects with PTSD had significantly higher rates of incident cerebrovascular disease, acute myocardial infarction, heart failure, and peripheral vascular disease than those without a current diagnosis of PTSD.
This remained the case even after controlling for numerous potential confounders in multivariate analysis, including demographics and comorbid diabetes, hypertension, cancer, chronic obstructive pulmonary disease, renal disease, traumatic brain injury, dementia, substance use disorders, and psychiatric diagnoses. The fully adjusted increased risk of each of the forms of vascular disease under study still remained significant at the P less than .001 level, noted Dr. Byers, an epidemiologist in the psychiatry department at the University of California, San Francisco.
These findings are neither generalizable to veterans under age 55 with PTSD nor generalizable to civilians, she said. But a separate, newly published study in which Dr. Byers was the lead author did show that PTSD in the general population with onset prior to age 55 and persistence beyond age 55 is a powerful independent predictor of global disability.
Dr. Byers’ study of older veterans was funded by the Department of Defense. She reported having no financial conflicts.
ORLANDO – Military veterans aged 55 years or older with current posttraumatic stress disorder are at significantly higher risk of developing new-onset vascular disease than those without PTSD, according to a very large national longitudinal study.
"This study suggests the need for greater monitoring and treatment of PTSD in older veterans to assist in the prevention of vascular disorders over the long term," Amy L. Byers, Ph.D., asserted at the annual meeting of the American Association for Geriatric Psychiatry.
She reported on 138,341 veterans aged 55 years or older, all of whom were free of known vascular disease at baseline. During 8 years of follow-up, the subjects with PTSD had significantly higher rates of incident cerebrovascular disease, acute myocardial infarction, heart failure, and peripheral vascular disease than those without a current diagnosis of PTSD.
This remained the case even after controlling for numerous potential confounders in multivariate analysis, including demographics and comorbid diabetes, hypertension, cancer, chronic obstructive pulmonary disease, renal disease, traumatic brain injury, dementia, substance use disorders, and psychiatric diagnoses. The fully adjusted increased risk of each of the forms of vascular disease under study still remained significant at the P less than .001 level, noted Dr. Byers, an epidemiologist in the psychiatry department at the University of California, San Francisco.
These findings are neither generalizable to veterans under age 55 with PTSD nor generalizable to civilians, she said. But a separate, newly published study in which Dr. Byers was the lead author did show that PTSD in the general population with onset prior to age 55 and persistence beyond age 55 is a powerful independent predictor of global disability.
Dr. Byers’ study of older veterans was funded by the Department of Defense. She reported having no financial conflicts.
ORLANDO – Military veterans aged 55 years or older with current posttraumatic stress disorder are at significantly higher risk of developing new-onset vascular disease than those without PTSD, according to a very large national longitudinal study.
"This study suggests the need for greater monitoring and treatment of PTSD in older veterans to assist in the prevention of vascular disorders over the long term," Amy L. Byers, Ph.D., asserted at the annual meeting of the American Association for Geriatric Psychiatry.
She reported on 138,341 veterans aged 55 years or older, all of whom were free of known vascular disease at baseline. During 8 years of follow-up, the subjects with PTSD had significantly higher rates of incident cerebrovascular disease, acute myocardial infarction, heart failure, and peripheral vascular disease than those without a current diagnosis of PTSD.
This remained the case even after controlling for numerous potential confounders in multivariate analysis, including demographics and comorbid diabetes, hypertension, cancer, chronic obstructive pulmonary disease, renal disease, traumatic brain injury, dementia, substance use disorders, and psychiatric diagnoses. The fully adjusted increased risk of each of the forms of vascular disease under study still remained significant at the P less than .001 level, noted Dr. Byers, an epidemiologist in the psychiatry department at the University of California, San Francisco.
These findings are neither generalizable to veterans under age 55 with PTSD nor generalizable to civilians, she said. But a separate, newly published study in which Dr. Byers was the lead author did show that PTSD in the general population with onset prior to age 55 and persistence beyond age 55 is a powerful independent predictor of global disability.
Dr. Byers’ study of older veterans was funded by the Department of Defense. She reported having no financial conflicts.
AT THE AAGP ANNUAL MEETING
Major finding: Military veterans with late-life posttraumatic stress disorder were 80% more likely to develop new-onset cerebrovascular disease during 8 years of follow-up than were those without PTSD. They were also 82% more likely to have a first acute myocardial infarction, 56% more likely to develop heart failure, and 60% more likely to be diagnosed with peripheral vascular disease.
Data source: This was a longitudinal observational study in 138,341 veterans aged 55 years or older who were free of known vascular disease at baseline and were followed for 8 years.
Disclosures: Dr. Byers’ study of older veterans was funded by the Department of Defense. She reported having no financial conflicts.
ECT quells dementia-associated agitation
ORLANDO – Electroconvulsive therapy was safe and effective for treatment of refractory agitation in patients with dementia, including those with multiple medical comorbidities, in the largest case series reported to date.
"This was true at least in the short term. Long term, there are no data," Dr. Yilang Tang noted at the annual meeting of the American Association for Geriatric Psychiatry.
He presented a retrospective chart review of the 38 patients with dementia who received ECT for agitation at Emory University’s Wesley Woods Geriatric Hospital in Atlanta during 2012.
On admission, patients were on an average of six psychotropic medications, including two or more antipsychotic agents in half of cases. The subjects averaged 6.2 Axis III diagnoses. Patients received a mean of 10.2 and median of 6 ECT treatments. The ECT was performed initially with right unilateral electrode placement in 35 of 38 patients; however, 6 patients were switched to bifrontal placement after four to six sessions because of poor response.
The mean baseline total Pittsburgh Agitation Scale score was 9.2. At discharge, after an average length of stay of 26 days, all patients demonstrated a significant reduction in their agitation score, with a median 8-point drop from baseline. Two patients had transient increases in their agitation score, from 7 points to 11 in one case and from 3 points to 7 in the other, but they improved with maintenance ECT after their acute course of therapy. In addition, patients went from an average of six psychotropic medications at admission to five at discharge, according to Dr. Tang, a psychiatric resident at Emory University in Atlanta.
Most patients were discharged after four to six ECT sessions, although seven patients received more than 12 treatments, mostly delivered as outpatient maintenance therapy.
One patient experienced transient ECT-related delirium. Yet no major treatment-related medical complications occurred, even though 7 patients had coronary artery disease, 24 were hypertensive, 3 had a history of stroke, and 3 patients had heart failure.
Only 2 of 38 patients were readmitted within 1 year after discharge, one of whom got another course of ECT. Although the possibility of readmission at other facilities can’t be ruled out, it seems unlikely that this occurred often, since patients’ surrogates were pleased with the post-ECT clinical improvement, Dr. Tang observed.
Agitation is one of the most distressing behavioral manifestations of dementia for patients, caregivers, and hospital staff. No medication has demonstrated effectiveness in treating this condition.
Subsequent to Dr. Tang’s presentation, two distinguished senior geriatric psychiatrists weighed in on the question of whether ECT has a legitimate role in treating agitation and other behavioral disturbances associated with dementia.
"It’s an unconventional use of the therapy. I would say it would be a fairly rare occurrence. It should not be something that is done commonly," asserted Dr. W. Vaughn McCall, professor of psychiatry and health behavior at the Medical College of Georgia, Augusta.
"Remember, the FDA indication for ECT does not include that particular use, although like with medications, you have the right to use a device off label if you can justify it. I would say the key in justifying it is to make sure you’re treating the patient’s distress and [you’re not using it] for the benefit of the nursing home staff. If you’re going to use ECT for a patient with dementia-associated agitation, it needs to be crystal clear that this is being done for the benefit of the patient, that the patient is in distress, and if you can also make the case that there is a concurrent depression along with the major neurocognitive disorder, then possibly you could justify using ECT if all other options have been exhausted," he added.
His fellow panelist Dr. George T. Grossberg took a more expansive view of ECT in patients with dementia.
"We do recommend ECT for patients with major neurocognitive disorders, either in instances where they have severe or treatment-resistant depression in the context of Alzheimer’s disease – where they tend to respond very well – or on rare occasions in treatment-resistant agitation. After we’ve tried everything else possible and they’re just really difficult to manage, I think a trial of ECT may be warranted. It has a calming, dampening effect on agitation and irritability," said Dr. Grossberg, professor of psychiatry, anatomy, neurobiology, and internal medicine at Saint Louis University.
"One thing it’s important to keep in mind is that if you have depression in the context of Alzheimer’s disease, and you decide to go with ECT because the depression is so severe or refractory, cognition will actually improve. When the depression starts to lift with the ECT, confusion and cognitive impairment will also improve. So I would keep ECT on the agenda," the geriatric psychiatrist added.
Dr. Tang reported having no financial conflicts of interest.
ORLANDO – Electroconvulsive therapy was safe and effective for treatment of refractory agitation in patients with dementia, including those with multiple medical comorbidities, in the largest case series reported to date.
"This was true at least in the short term. Long term, there are no data," Dr. Yilang Tang noted at the annual meeting of the American Association for Geriatric Psychiatry.
He presented a retrospective chart review of the 38 patients with dementia who received ECT for agitation at Emory University’s Wesley Woods Geriatric Hospital in Atlanta during 2012.
On admission, patients were on an average of six psychotropic medications, including two or more antipsychotic agents in half of cases. The subjects averaged 6.2 Axis III diagnoses. Patients received a mean of 10.2 and median of 6 ECT treatments. The ECT was performed initially with right unilateral electrode placement in 35 of 38 patients; however, 6 patients were switched to bifrontal placement after four to six sessions because of poor response.
The mean baseline total Pittsburgh Agitation Scale score was 9.2. At discharge, after an average length of stay of 26 days, all patients demonstrated a significant reduction in their agitation score, with a median 8-point drop from baseline. Two patients had transient increases in their agitation score, from 7 points to 11 in one case and from 3 points to 7 in the other, but they improved with maintenance ECT after their acute course of therapy. In addition, patients went from an average of six psychotropic medications at admission to five at discharge, according to Dr. Tang, a psychiatric resident at Emory University in Atlanta.
Most patients were discharged after four to six ECT sessions, although seven patients received more than 12 treatments, mostly delivered as outpatient maintenance therapy.
One patient experienced transient ECT-related delirium. Yet no major treatment-related medical complications occurred, even though 7 patients had coronary artery disease, 24 were hypertensive, 3 had a history of stroke, and 3 patients had heart failure.
Only 2 of 38 patients were readmitted within 1 year after discharge, one of whom got another course of ECT. Although the possibility of readmission at other facilities can’t be ruled out, it seems unlikely that this occurred often, since patients’ surrogates were pleased with the post-ECT clinical improvement, Dr. Tang observed.
Agitation is one of the most distressing behavioral manifestations of dementia for patients, caregivers, and hospital staff. No medication has demonstrated effectiveness in treating this condition.
Subsequent to Dr. Tang’s presentation, two distinguished senior geriatric psychiatrists weighed in on the question of whether ECT has a legitimate role in treating agitation and other behavioral disturbances associated with dementia.
"It’s an unconventional use of the therapy. I would say it would be a fairly rare occurrence. It should not be something that is done commonly," asserted Dr. W. Vaughn McCall, professor of psychiatry and health behavior at the Medical College of Georgia, Augusta.
"Remember, the FDA indication for ECT does not include that particular use, although like with medications, you have the right to use a device off label if you can justify it. I would say the key in justifying it is to make sure you’re treating the patient’s distress and [you’re not using it] for the benefit of the nursing home staff. If you’re going to use ECT for a patient with dementia-associated agitation, it needs to be crystal clear that this is being done for the benefit of the patient, that the patient is in distress, and if you can also make the case that there is a concurrent depression along with the major neurocognitive disorder, then possibly you could justify using ECT if all other options have been exhausted," he added.
His fellow panelist Dr. George T. Grossberg took a more expansive view of ECT in patients with dementia.
"We do recommend ECT for patients with major neurocognitive disorders, either in instances where they have severe or treatment-resistant depression in the context of Alzheimer’s disease – where they tend to respond very well – or on rare occasions in treatment-resistant agitation. After we’ve tried everything else possible and they’re just really difficult to manage, I think a trial of ECT may be warranted. It has a calming, dampening effect on agitation and irritability," said Dr. Grossberg, professor of psychiatry, anatomy, neurobiology, and internal medicine at Saint Louis University.
"One thing it’s important to keep in mind is that if you have depression in the context of Alzheimer’s disease, and you decide to go with ECT because the depression is so severe or refractory, cognition will actually improve. When the depression starts to lift with the ECT, confusion and cognitive impairment will also improve. So I would keep ECT on the agenda," the geriatric psychiatrist added.
Dr. Tang reported having no financial conflicts of interest.
ORLANDO – Electroconvulsive therapy was safe and effective for treatment of refractory agitation in patients with dementia, including those with multiple medical comorbidities, in the largest case series reported to date.
"This was true at least in the short term. Long term, there are no data," Dr. Yilang Tang noted at the annual meeting of the American Association for Geriatric Psychiatry.
He presented a retrospective chart review of the 38 patients with dementia who received ECT for agitation at Emory University’s Wesley Woods Geriatric Hospital in Atlanta during 2012.
On admission, patients were on an average of six psychotropic medications, including two or more antipsychotic agents in half of cases. The subjects averaged 6.2 Axis III diagnoses. Patients received a mean of 10.2 and median of 6 ECT treatments. The ECT was performed initially with right unilateral electrode placement in 35 of 38 patients; however, 6 patients were switched to bifrontal placement after four to six sessions because of poor response.
The mean baseline total Pittsburgh Agitation Scale score was 9.2. At discharge, after an average length of stay of 26 days, all patients demonstrated a significant reduction in their agitation score, with a median 8-point drop from baseline. Two patients had transient increases in their agitation score, from 7 points to 11 in one case and from 3 points to 7 in the other, but they improved with maintenance ECT after their acute course of therapy. In addition, patients went from an average of six psychotropic medications at admission to five at discharge, according to Dr. Tang, a psychiatric resident at Emory University in Atlanta.
Most patients were discharged after four to six ECT sessions, although seven patients received more than 12 treatments, mostly delivered as outpatient maintenance therapy.
One patient experienced transient ECT-related delirium. Yet no major treatment-related medical complications occurred, even though 7 patients had coronary artery disease, 24 were hypertensive, 3 had a history of stroke, and 3 patients had heart failure.
Only 2 of 38 patients were readmitted within 1 year after discharge, one of whom got another course of ECT. Although the possibility of readmission at other facilities can’t be ruled out, it seems unlikely that this occurred often, since patients’ surrogates were pleased with the post-ECT clinical improvement, Dr. Tang observed.
Agitation is one of the most distressing behavioral manifestations of dementia for patients, caregivers, and hospital staff. No medication has demonstrated effectiveness in treating this condition.
Subsequent to Dr. Tang’s presentation, two distinguished senior geriatric psychiatrists weighed in on the question of whether ECT has a legitimate role in treating agitation and other behavioral disturbances associated with dementia.
"It’s an unconventional use of the therapy. I would say it would be a fairly rare occurrence. It should not be something that is done commonly," asserted Dr. W. Vaughn McCall, professor of psychiatry and health behavior at the Medical College of Georgia, Augusta.
"Remember, the FDA indication for ECT does not include that particular use, although like with medications, you have the right to use a device off label if you can justify it. I would say the key in justifying it is to make sure you’re treating the patient’s distress and [you’re not using it] for the benefit of the nursing home staff. If you’re going to use ECT for a patient with dementia-associated agitation, it needs to be crystal clear that this is being done for the benefit of the patient, that the patient is in distress, and if you can also make the case that there is a concurrent depression along with the major neurocognitive disorder, then possibly you could justify using ECT if all other options have been exhausted," he added.
His fellow panelist Dr. George T. Grossberg took a more expansive view of ECT in patients with dementia.
"We do recommend ECT for patients with major neurocognitive disorders, either in instances where they have severe or treatment-resistant depression in the context of Alzheimer’s disease – where they tend to respond very well – or on rare occasions in treatment-resistant agitation. After we’ve tried everything else possible and they’re just really difficult to manage, I think a trial of ECT may be warranted. It has a calming, dampening effect on agitation and irritability," said Dr. Grossberg, professor of psychiatry, anatomy, neurobiology, and internal medicine at Saint Louis University.
"One thing it’s important to keep in mind is that if you have depression in the context of Alzheimer’s disease, and you decide to go with ECT because the depression is so severe or refractory, cognition will actually improve. When the depression starts to lift with the ECT, confusion and cognitive impairment will also improve. So I would keep ECT on the agenda," the geriatric psychiatrist added.
Dr. Tang reported having no financial conflicts of interest.
AT THE AAGP ANNUAL MEETING
Major finding: Patients responded to ECT for agitation as a symptom of dementia with an average 8-point drop on the Pittsburgh Agitation Scale from a baseline of 9.2.
Data source: A retrospective study of the 38 patients discharged from one geriatric hospital in 2012 following ECT for dementia-associated agitation.
Disclosures: This was a university-funded study. The presenter reported having no financial conflicts.
Vortioxetine establishes credentials for late-life depression
ORLANDO – The novel antidepressant vortioxetine proved safe, effective, and well tolerated for treatment of major depressive disorder specifically in elderly patients in a combined analysis of nine randomized, placebo-controlled clinical trials.
Only one of the trials was restricted to patients aged 65 years or older. This 8-week, double-blind study included 302 patients (mean age, 71 years) randomized to vortioxetine (Brintellix) at 5 mg once daily or placebo. From a baseline mean Hamilton Rating Scale-Depression score of 29.0, scores in the vortioxetine group fell by an average of 3.3 more points than in controls at 8 weeks. The response rate, defined as at least a 50% reduction in depression scores compared with baseline, was 53% in the vortioxetine group, compared with 35% with placebo.
Similarly, scores on the Montgomery-Åsberg Depression Rating Scale dropped by an average of 15.5 points in vortioxetine-treated patients, a significantly better performance than the 11.2-point reduction with placebo, Dr. Atul R. Mahableshwarkar reported at the annual meeting of the American Association for Geriatric Psychiatry.
The safety analysis incorporated the limited numbers of elderly patients in the other eight randomized, placebo-controlled, short-term studies. There were 286 patients over age 65 who received vortioxetine at 5-20 mg/day and 212 placebo-treated controls. The only side effect significantly more common in vortioxetine-treated patients than in controls was nausea, by a margin of 22.4% to 7.5%. There were no instances of treatment-emergent sexual dysfunction and no signal of increased suicidal ideation in these elderly patients on vortioxetine, according to Dr. Mahableshwarkar, senior medical director at Takeda Pharmaceuticals in Deerfield, Ill.
A clinical efficacy analysis couldn’t be done in any meaningful way for the nine-study overview because the patient numbers on any given dose were too small. While laboratory studies indicated that drug exposure was increased up to 30% in elderly patients, the wide therapeutic index of vortioxetine should make dose adjustments unnecessary, he added.
Vortioxetine at 5-20 mg/day received Food and Drug Administration marketing approval for treatment of major depressive disorder last fall. The drug has multimodal mechanisms of action, directly modulating the activity of the serotonin 5-HT3, 5-HT7, 5-HT1D, 5-HT1B, and 5-HT1A receptors while also inhibiting the 5-HT transporter.
In a separate session on late-life depression held during the AAGP annual meeting, Dr. J. Craig Nelson commented that he considers vortioxetine to be first and foremost a selective serotonin reuptake inhibitor.
"This is a new agent for many of us. We’ll need to get more experience with it to see how important these secondary and tertiary effects really are and at what doses they come into play," said Dr. Nelson, professor of psychiatry at the University of California, San Francisco.
One particularly intriguing feature of vortioxetine is that in the elderly-specific randomized trial, it showed evidence of beneficial effects on cognition as expressed in scoring on tests of processing speed, verbal learning, and memory. There are also supportive animal studies.
"This finding will need to be replicated. It’ll be interesting to see how this plays out. It certainly would be nice to have something for depression that’s also perhaps effective for cognitive impairment," he added.
Dr. Mahableshwarkar is an employee of Takeda, which sponsored the nine randomized trials. Dr. Nelson serves as a consultant to Bristol-Myers Squibb, Eli Lilly, and other companies.
ORLANDO – The novel antidepressant vortioxetine proved safe, effective, and well tolerated for treatment of major depressive disorder specifically in elderly patients in a combined analysis of nine randomized, placebo-controlled clinical trials.
Only one of the trials was restricted to patients aged 65 years or older. This 8-week, double-blind study included 302 patients (mean age, 71 years) randomized to vortioxetine (Brintellix) at 5 mg once daily or placebo. From a baseline mean Hamilton Rating Scale-Depression score of 29.0, scores in the vortioxetine group fell by an average of 3.3 more points than in controls at 8 weeks. The response rate, defined as at least a 50% reduction in depression scores compared with baseline, was 53% in the vortioxetine group, compared with 35% with placebo.
Similarly, scores on the Montgomery-Åsberg Depression Rating Scale dropped by an average of 15.5 points in vortioxetine-treated patients, a significantly better performance than the 11.2-point reduction with placebo, Dr. Atul R. Mahableshwarkar reported at the annual meeting of the American Association for Geriatric Psychiatry.
The safety analysis incorporated the limited numbers of elderly patients in the other eight randomized, placebo-controlled, short-term studies. There were 286 patients over age 65 who received vortioxetine at 5-20 mg/day and 212 placebo-treated controls. The only side effect significantly more common in vortioxetine-treated patients than in controls was nausea, by a margin of 22.4% to 7.5%. There were no instances of treatment-emergent sexual dysfunction and no signal of increased suicidal ideation in these elderly patients on vortioxetine, according to Dr. Mahableshwarkar, senior medical director at Takeda Pharmaceuticals in Deerfield, Ill.
A clinical efficacy analysis couldn’t be done in any meaningful way for the nine-study overview because the patient numbers on any given dose were too small. While laboratory studies indicated that drug exposure was increased up to 30% in elderly patients, the wide therapeutic index of vortioxetine should make dose adjustments unnecessary, he added.
Vortioxetine at 5-20 mg/day received Food and Drug Administration marketing approval for treatment of major depressive disorder last fall. The drug has multimodal mechanisms of action, directly modulating the activity of the serotonin 5-HT3, 5-HT7, 5-HT1D, 5-HT1B, and 5-HT1A receptors while also inhibiting the 5-HT transporter.
In a separate session on late-life depression held during the AAGP annual meeting, Dr. J. Craig Nelson commented that he considers vortioxetine to be first and foremost a selective serotonin reuptake inhibitor.
"This is a new agent for many of us. We’ll need to get more experience with it to see how important these secondary and tertiary effects really are and at what doses they come into play," said Dr. Nelson, professor of psychiatry at the University of California, San Francisco.
One particularly intriguing feature of vortioxetine is that in the elderly-specific randomized trial, it showed evidence of beneficial effects on cognition as expressed in scoring on tests of processing speed, verbal learning, and memory. There are also supportive animal studies.
"This finding will need to be replicated. It’ll be interesting to see how this plays out. It certainly would be nice to have something for depression that’s also perhaps effective for cognitive impairment," he added.
Dr. Mahableshwarkar is an employee of Takeda, which sponsored the nine randomized trials. Dr. Nelson serves as a consultant to Bristol-Myers Squibb, Eli Lilly, and other companies.
ORLANDO – The novel antidepressant vortioxetine proved safe, effective, and well tolerated for treatment of major depressive disorder specifically in elderly patients in a combined analysis of nine randomized, placebo-controlled clinical trials.
Only one of the trials was restricted to patients aged 65 years or older. This 8-week, double-blind study included 302 patients (mean age, 71 years) randomized to vortioxetine (Brintellix) at 5 mg once daily or placebo. From a baseline mean Hamilton Rating Scale-Depression score of 29.0, scores in the vortioxetine group fell by an average of 3.3 more points than in controls at 8 weeks. The response rate, defined as at least a 50% reduction in depression scores compared with baseline, was 53% in the vortioxetine group, compared with 35% with placebo.
Similarly, scores on the Montgomery-Åsberg Depression Rating Scale dropped by an average of 15.5 points in vortioxetine-treated patients, a significantly better performance than the 11.2-point reduction with placebo, Dr. Atul R. Mahableshwarkar reported at the annual meeting of the American Association for Geriatric Psychiatry.
The safety analysis incorporated the limited numbers of elderly patients in the other eight randomized, placebo-controlled, short-term studies. There were 286 patients over age 65 who received vortioxetine at 5-20 mg/day and 212 placebo-treated controls. The only side effect significantly more common in vortioxetine-treated patients than in controls was nausea, by a margin of 22.4% to 7.5%. There were no instances of treatment-emergent sexual dysfunction and no signal of increased suicidal ideation in these elderly patients on vortioxetine, according to Dr. Mahableshwarkar, senior medical director at Takeda Pharmaceuticals in Deerfield, Ill.
A clinical efficacy analysis couldn’t be done in any meaningful way for the nine-study overview because the patient numbers on any given dose were too small. While laboratory studies indicated that drug exposure was increased up to 30% in elderly patients, the wide therapeutic index of vortioxetine should make dose adjustments unnecessary, he added.
Vortioxetine at 5-20 mg/day received Food and Drug Administration marketing approval for treatment of major depressive disorder last fall. The drug has multimodal mechanisms of action, directly modulating the activity of the serotonin 5-HT3, 5-HT7, 5-HT1D, 5-HT1B, and 5-HT1A receptors while also inhibiting the 5-HT transporter.
In a separate session on late-life depression held during the AAGP annual meeting, Dr. J. Craig Nelson commented that he considers vortioxetine to be first and foremost a selective serotonin reuptake inhibitor.
"This is a new agent for many of us. We’ll need to get more experience with it to see how important these secondary and tertiary effects really are and at what doses they come into play," said Dr. Nelson, professor of psychiatry at the University of California, San Francisco.
One particularly intriguing feature of vortioxetine is that in the elderly-specific randomized trial, it showed evidence of beneficial effects on cognition as expressed in scoring on tests of processing speed, verbal learning, and memory. There are also supportive animal studies.
"This finding will need to be replicated. It’ll be interesting to see how this plays out. It certainly would be nice to have something for depression that’s also perhaps effective for cognitive impairment," he added.
Dr. Mahableshwarkar is an employee of Takeda, which sponsored the nine randomized trials. Dr. Nelson serves as a consultant to Bristol-Myers Squibb, Eli Lilly, and other companies.
AT THE AAGP ANNUAL MEETING
Major finding: Hamilton Rating Scale–Depression scores among those in the vortioxetine group fell by an average of 3.3 more points than in controls at 8 weeks. The response rate, defined as at least a 50% reduction in depression scores compared with baseline, was 53% in the vortioxetine group, compared to 35% with placebo.
Data source: This was an analysis of the 498 patients over age 65 with major depressive disorder who participated in nine randomized, placebo-controlled clinical trials.
Disclosures: Dr. Mahableshwarkar is an employee of Takeda, which sponsored the nine randomized trials. Dr. Nelson serves as a consultant to Bristol-Myers Squibb, Eli Lilly, and other companies.
Later-life PTSD linked to global disability
SAN FRANCISCO – Posttraumatic stress disorder that persists into later life was associated with more than a threefold increased risk of functional disability compared with that of individuals with no history of PTSD, according to a first-of-its-kind national study.
The study included a nationally representative sample of Americans aged 55 years or older. The group consisted of 3,287 participants (mean age, 66 years) in the Collaborative Psychiatric Epidemiology Surveys.
Eighty-eight subjects had been diagnosed with PTSD by DSM-IV (Diagnostic and Statistical Manual of Mental Disorders-IV) criteria before age 55 but no longer met diagnostic criteria for the disorder by age 55. An additional 68 were diagnosed with PTSD before age 55, and the anxiety disorder persisted beyond that age. The remaining 3,131 no-PTSD subjects served as controls.
The study endpoint was the presence and degree of disability within the past 30 days as defined by the World Health Organization Disability Assessment Schedule. This instrument evaluates disability in five domains: self-care, mobility, cognition, social, and out-of-role, which is measured by the number of days in the past month a participant was completely unable to work or do their normal activities because of physical or mental problems.
The frequency of any of the WHO disability domains in the 30 days prior to evaluation was 36.9% in the no-PTSD controls, 69.6% in those with PTSD that began and ended before age 55, and 79.7% in those with persistent later-life PTSD, according to Amy L. Byers, Ph.D., an epidemiologist in the psychiatry department at the University of California, San Francisco.
In a multivariate analysis adjusted for demographics, comorbid medical conditions, depression, generalized anxiety disorder, substance use disorders, and smoking, study participants with persistent PTSD beyond age 55 were 3.2-fold more likely to have any form of disability than controls. This sharply increased risk extended to each of the five domains of disability. The group with PTSD diagnosed before age 55 but without PTSD after age 55 had a statistically nonsignificant 1.99-fold increased risk. Thus, this study shows that persistence of PTSD in later life is a potent predictor of disability independent of other psychiatric issues and medical conditions. The results are clinically relevant and generalizable to the burgeoning population of older Americans.
"These findings suggest that, if left unresolved, PTSD in older adults will have significant functional consequences," Dr. Byers said. "Our study emphasizes the importance of improving the monitoring and treatment of PTSD over the long term."
One possible mechanism for the strong association between persistent later-life PTSD and disability is that exposure to trauma results in dysregulation of the hypothalamic-pituitary-adrenocortical axis, leading to increased glucocorticoid levels and hippocampal degeneration, she surmised (JAMA Psychiatry 2014 March 19 [doi: 10.1001/jamapsychiatry.2014.5]).
The study was funded by the Department of Defense. Dr. Byers reported having no financial conflicts of interest.
SAN FRANCISCO – Posttraumatic stress disorder that persists into later life was associated with more than a threefold increased risk of functional disability compared with that of individuals with no history of PTSD, according to a first-of-its-kind national study.
The study included a nationally representative sample of Americans aged 55 years or older. The group consisted of 3,287 participants (mean age, 66 years) in the Collaborative Psychiatric Epidemiology Surveys.
Eighty-eight subjects had been diagnosed with PTSD by DSM-IV (Diagnostic and Statistical Manual of Mental Disorders-IV) criteria before age 55 but no longer met diagnostic criteria for the disorder by age 55. An additional 68 were diagnosed with PTSD before age 55, and the anxiety disorder persisted beyond that age. The remaining 3,131 no-PTSD subjects served as controls.
The study endpoint was the presence and degree of disability within the past 30 days as defined by the World Health Organization Disability Assessment Schedule. This instrument evaluates disability in five domains: self-care, mobility, cognition, social, and out-of-role, which is measured by the number of days in the past month a participant was completely unable to work or do their normal activities because of physical or mental problems.
The frequency of any of the WHO disability domains in the 30 days prior to evaluation was 36.9% in the no-PTSD controls, 69.6% in those with PTSD that began and ended before age 55, and 79.7% in those with persistent later-life PTSD, according to Amy L. Byers, Ph.D., an epidemiologist in the psychiatry department at the University of California, San Francisco.
In a multivariate analysis adjusted for demographics, comorbid medical conditions, depression, generalized anxiety disorder, substance use disorders, and smoking, study participants with persistent PTSD beyond age 55 were 3.2-fold more likely to have any form of disability than controls. This sharply increased risk extended to each of the five domains of disability. The group with PTSD diagnosed before age 55 but without PTSD after age 55 had a statistically nonsignificant 1.99-fold increased risk. Thus, this study shows that persistence of PTSD in later life is a potent predictor of disability independent of other psychiatric issues and medical conditions. The results are clinically relevant and generalizable to the burgeoning population of older Americans.
"These findings suggest that, if left unresolved, PTSD in older adults will have significant functional consequences," Dr. Byers said. "Our study emphasizes the importance of improving the monitoring and treatment of PTSD over the long term."
One possible mechanism for the strong association between persistent later-life PTSD and disability is that exposure to trauma results in dysregulation of the hypothalamic-pituitary-adrenocortical axis, leading to increased glucocorticoid levels and hippocampal degeneration, she surmised (JAMA Psychiatry 2014 March 19 [doi: 10.1001/jamapsychiatry.2014.5]).
The study was funded by the Department of Defense. Dr. Byers reported having no financial conflicts of interest.
SAN FRANCISCO – Posttraumatic stress disorder that persists into later life was associated with more than a threefold increased risk of functional disability compared with that of individuals with no history of PTSD, according to a first-of-its-kind national study.
The study included a nationally representative sample of Americans aged 55 years or older. The group consisted of 3,287 participants (mean age, 66 years) in the Collaborative Psychiatric Epidemiology Surveys.
Eighty-eight subjects had been diagnosed with PTSD by DSM-IV (Diagnostic and Statistical Manual of Mental Disorders-IV) criteria before age 55 but no longer met diagnostic criteria for the disorder by age 55. An additional 68 were diagnosed with PTSD before age 55, and the anxiety disorder persisted beyond that age. The remaining 3,131 no-PTSD subjects served as controls.
The study endpoint was the presence and degree of disability within the past 30 days as defined by the World Health Organization Disability Assessment Schedule. This instrument evaluates disability in five domains: self-care, mobility, cognition, social, and out-of-role, which is measured by the number of days in the past month a participant was completely unable to work or do their normal activities because of physical or mental problems.
The frequency of any of the WHO disability domains in the 30 days prior to evaluation was 36.9% in the no-PTSD controls, 69.6% in those with PTSD that began and ended before age 55, and 79.7% in those with persistent later-life PTSD, according to Amy L. Byers, Ph.D., an epidemiologist in the psychiatry department at the University of California, San Francisco.
In a multivariate analysis adjusted for demographics, comorbid medical conditions, depression, generalized anxiety disorder, substance use disorders, and smoking, study participants with persistent PTSD beyond age 55 were 3.2-fold more likely to have any form of disability than controls. This sharply increased risk extended to each of the five domains of disability. The group with PTSD diagnosed before age 55 but without PTSD after age 55 had a statistically nonsignificant 1.99-fold increased risk. Thus, this study shows that persistence of PTSD in later life is a potent predictor of disability independent of other psychiatric issues and medical conditions. The results are clinically relevant and generalizable to the burgeoning population of older Americans.
"These findings suggest that, if left unresolved, PTSD in older adults will have significant functional consequences," Dr. Byers said. "Our study emphasizes the importance of improving the monitoring and treatment of PTSD over the long term."
One possible mechanism for the strong association between persistent later-life PTSD and disability is that exposure to trauma results in dysregulation of the hypothalamic-pituitary-adrenocortical axis, leading to increased glucocorticoid levels and hippocampal degeneration, she surmised (JAMA Psychiatry 2014 March 19 [doi: 10.1001/jamapsychiatry.2014.5]).
The study was funded by the Department of Defense. Dr. Byers reported having no financial conflicts of interest.
FROM JAMA PSYCHIATRY
Major finding: Older Americans with persistent posttraumatic stress disorder beyond age 55 were an adjusted 3.2-fold more likely than no-PTSD controls to have significant disability.
Data source: This study involved a structured disability assessment conducted in a nationally representative sample composed of 3,287 subjects aged 55 years or older, 68 of whom were diagnosed with PTSD prior to age 55 and had persistent PTSD beyond that age.
Disclosures: The study was funded by the Department of Defense. Dr. Byers reported having no financial conflicts.
Sinus surgery: new rigor in research
KEYSTONE, COLO. – Research-minded otolaryngologists have gotten serious about conducting high-quality, patient-centered outcomes studies of endoscopic sinus surgery for chronic rhinosinusitis, which more than 250,000 Americans undergo each year. And the results are eye opening.
Mounting evidence documents that endoscopic sinus surgery (ESS) in properly selected patients with chronic rhinosinusitis (CRS) results in markedly improved quality of life, functional status, and reduced use of medications, compared with medical management, Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
These studies utilize validated measures of patient-centered quality of life and symptoms. They are nothing like the lightweight, less-than-persuasive ESS research published in the 1990s, which reported glowing ‘success’ rates of 80%-97% in single-institution retrospective studies using variable inclusion criteria and often-sketchy definitions of success.
"Those data are not acceptable, but that’s what we had. This was before evidence-based medicine with an emphasis on rigorously designed studies took hold," explained Dr. Kingdom, professor and vice chairman of the department of otolaryngology – head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
Current research emphasizes the use of modern, validated patient-centered quality of life tools and symptom scores because CRS is a symptom-based diagnosis and it is symptom severity that drives patients to seek treatment. Also, objective measures, such as the Lund-Mackay CT staging system, fail to capture the full experience of disease burden. Nor do objective measures necessarily correlate with patient symptoms, according to the otolaryngologist.
A low point in the field of sinus surgery, in Dr. Kingdom’s view, was the 2006 Cochrane systematic review which concluded ESS "has not been demonstrated to confer additional benefit to that obtained by medical therapy" (Cochrane Database Syst. Rev. 2006:CD004458).
"This review was a disservice," he asserted.
The review was based entirely on three older randomized trials, which not only did not use current treatment paradigms but also did not study the key research question, which Dr. Kingdom believes is this: What’s the comparative effectiveness of ESS vs. continued medical therapy in patients who’ve failed initial medical therapy?
He offered as an example of the contemporary approach to comparative outcomes research in the field of ESS a recent multicenter prospective study led by otolaryngologists at Oregon Health and Science University, Portland. It involved 1 year of prospective follow-up of patients with CRS who had failed initial medical therapy, at which point they elected to undergo ESS or further medical management.
The 65 patients who opted for ESS and the 50 whose chose more medical management were comparable in terms of baseline CRS severity and comorbidities. Both groups showed durable improvement at 12 months, compared with baseline. But ESS was the clear winner, with a mean 71% improvement in the validated Chronic Sinusitis Survey total score, compared with a 46% improvement in the medically managed group. Moreover, during the year of follow-up 17 patients switched over from medical management to ESS and they, too, showed significantly greater improvement than those who remained on medical management (Int. Forum Allergy Rhinol. 2013;3:236-41).
An earlier interim report featuring 6 months of followup showed the surgical group experienced roughly twofold greater improvement, compared with the medical cohort in endpoints including number of days on oral antibiotics or oral corticosteroids and missed days of work or school (Int. Forum Allergy Rhinol. 2011;1:235-41).
Cost-effectiveness studies by various research groups are in the pipeline. The early indication is that the data will show an economic advantage for ESS over medical therapy in patients with recalcitrant disease, according to Dr. Kingdom.
The next research frontier in surgical outcomes in CRS is identification of cellular and molecular markers of disease activity and their genetic underpinnings, which it’s hoped can be used to select the best candidates for ESS, he added.
Dr. Kingdom reported having no financial conflicts of interest.
KEYSTONE, COLO. – Research-minded otolaryngologists have gotten serious about conducting high-quality, patient-centered outcomes studies of endoscopic sinus surgery for chronic rhinosinusitis, which more than 250,000 Americans undergo each year. And the results are eye opening.
Mounting evidence documents that endoscopic sinus surgery (ESS) in properly selected patients with chronic rhinosinusitis (CRS) results in markedly improved quality of life, functional status, and reduced use of medications, compared with medical management, Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
These studies utilize validated measures of patient-centered quality of life and symptoms. They are nothing like the lightweight, less-than-persuasive ESS research published in the 1990s, which reported glowing ‘success’ rates of 80%-97% in single-institution retrospective studies using variable inclusion criteria and often-sketchy definitions of success.
"Those data are not acceptable, but that’s what we had. This was before evidence-based medicine with an emphasis on rigorously designed studies took hold," explained Dr. Kingdom, professor and vice chairman of the department of otolaryngology – head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
Current research emphasizes the use of modern, validated patient-centered quality of life tools and symptom scores because CRS is a symptom-based diagnosis and it is symptom severity that drives patients to seek treatment. Also, objective measures, such as the Lund-Mackay CT staging system, fail to capture the full experience of disease burden. Nor do objective measures necessarily correlate with patient symptoms, according to the otolaryngologist.
A low point in the field of sinus surgery, in Dr. Kingdom’s view, was the 2006 Cochrane systematic review which concluded ESS "has not been demonstrated to confer additional benefit to that obtained by medical therapy" (Cochrane Database Syst. Rev. 2006:CD004458).
"This review was a disservice," he asserted.
The review was based entirely on three older randomized trials, which not only did not use current treatment paradigms but also did not study the key research question, which Dr. Kingdom believes is this: What’s the comparative effectiveness of ESS vs. continued medical therapy in patients who’ve failed initial medical therapy?
He offered as an example of the contemporary approach to comparative outcomes research in the field of ESS a recent multicenter prospective study led by otolaryngologists at Oregon Health and Science University, Portland. It involved 1 year of prospective follow-up of patients with CRS who had failed initial medical therapy, at which point they elected to undergo ESS or further medical management.
The 65 patients who opted for ESS and the 50 whose chose more medical management were comparable in terms of baseline CRS severity and comorbidities. Both groups showed durable improvement at 12 months, compared with baseline. But ESS was the clear winner, with a mean 71% improvement in the validated Chronic Sinusitis Survey total score, compared with a 46% improvement in the medically managed group. Moreover, during the year of follow-up 17 patients switched over from medical management to ESS and they, too, showed significantly greater improvement than those who remained on medical management (Int. Forum Allergy Rhinol. 2013;3:236-41).
An earlier interim report featuring 6 months of followup showed the surgical group experienced roughly twofold greater improvement, compared with the medical cohort in endpoints including number of days on oral antibiotics or oral corticosteroids and missed days of work or school (Int. Forum Allergy Rhinol. 2011;1:235-41).
Cost-effectiveness studies by various research groups are in the pipeline. The early indication is that the data will show an economic advantage for ESS over medical therapy in patients with recalcitrant disease, according to Dr. Kingdom.
The next research frontier in surgical outcomes in CRS is identification of cellular and molecular markers of disease activity and their genetic underpinnings, which it’s hoped can be used to select the best candidates for ESS, he added.
Dr. Kingdom reported having no financial conflicts of interest.
KEYSTONE, COLO. – Research-minded otolaryngologists have gotten serious about conducting high-quality, patient-centered outcomes studies of endoscopic sinus surgery for chronic rhinosinusitis, which more than 250,000 Americans undergo each year. And the results are eye opening.
Mounting evidence documents that endoscopic sinus surgery (ESS) in properly selected patients with chronic rhinosinusitis (CRS) results in markedly improved quality of life, functional status, and reduced use of medications, compared with medical management, Dr. Todd T. Kingdom said at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
These studies utilize validated measures of patient-centered quality of life and symptoms. They are nothing like the lightweight, less-than-persuasive ESS research published in the 1990s, which reported glowing ‘success’ rates of 80%-97% in single-institution retrospective studies using variable inclusion criteria and often-sketchy definitions of success.
"Those data are not acceptable, but that’s what we had. This was before evidence-based medicine with an emphasis on rigorously designed studies took hold," explained Dr. Kingdom, professor and vice chairman of the department of otolaryngology – head and neck surgery, at the University of Colorado, Denver, and immediate past president of the American Rhinologic Society.
Current research emphasizes the use of modern, validated patient-centered quality of life tools and symptom scores because CRS is a symptom-based diagnosis and it is symptom severity that drives patients to seek treatment. Also, objective measures, such as the Lund-Mackay CT staging system, fail to capture the full experience of disease burden. Nor do objective measures necessarily correlate with patient symptoms, according to the otolaryngologist.
A low point in the field of sinus surgery, in Dr. Kingdom’s view, was the 2006 Cochrane systematic review which concluded ESS "has not been demonstrated to confer additional benefit to that obtained by medical therapy" (Cochrane Database Syst. Rev. 2006:CD004458).
"This review was a disservice," he asserted.
The review was based entirely on three older randomized trials, which not only did not use current treatment paradigms but also did not study the key research question, which Dr. Kingdom believes is this: What’s the comparative effectiveness of ESS vs. continued medical therapy in patients who’ve failed initial medical therapy?
He offered as an example of the contemporary approach to comparative outcomes research in the field of ESS a recent multicenter prospective study led by otolaryngologists at Oregon Health and Science University, Portland. It involved 1 year of prospective follow-up of patients with CRS who had failed initial medical therapy, at which point they elected to undergo ESS or further medical management.
The 65 patients who opted for ESS and the 50 whose chose more medical management were comparable in terms of baseline CRS severity and comorbidities. Both groups showed durable improvement at 12 months, compared with baseline. But ESS was the clear winner, with a mean 71% improvement in the validated Chronic Sinusitis Survey total score, compared with a 46% improvement in the medically managed group. Moreover, during the year of follow-up 17 patients switched over from medical management to ESS and they, too, showed significantly greater improvement than those who remained on medical management (Int. Forum Allergy Rhinol. 2013;3:236-41).
An earlier interim report featuring 6 months of followup showed the surgical group experienced roughly twofold greater improvement, compared with the medical cohort in endpoints including number of days on oral antibiotics or oral corticosteroids and missed days of work or school (Int. Forum Allergy Rhinol. 2011;1:235-41).
Cost-effectiveness studies by various research groups are in the pipeline. The early indication is that the data will show an economic advantage for ESS over medical therapy in patients with recalcitrant disease, according to Dr. Kingdom.
The next research frontier in surgical outcomes in CRS is identification of cellular and molecular markers of disease activity and their genetic underpinnings, which it’s hoped can be used to select the best candidates for ESS, he added.
Dr. Kingdom reported having no financial conflicts of interest.
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE
Say goodbye to ‘dementia’
ORLANDO – This May, the hallowed term "dementia" is supposed to be tossed onto the scrapheap of discarded psychiatric nomenclature, replaced by "major neurocognitive disorder."
When the DSM-5 was released in May 2013, the American Psychiatric Association gave a year’s grace period for the world to absorb the changes before they take effect. "Dementia" was replaced in the DSM-5 because the term was deemed stigmatizing; the rough translation from the Latin roots is "loss of mind." Acknowledging that old habits die hard, however, the DSM-5 also states that use of the term is not precluded "where that term is standard."
The old DSM-IV category of delirium, dementia, and amnestic and other cognitive disorders has been replaced in the DSM-5 by the neurocognitive disorders category. Major or mild neurocognitive disorder from Alzheimer’s disease is included under this new category. At the annual meeting of the American Association for Geriatric Psychiatry, Dr. W. Vaughn McCall and Dr. George T. Grossberg highlighted the changes.
"Major neurocognitive disorder" is a syndrome, which includes what was formerly known as dementia. The distinction between it and the new "mild neurocognitive disorder," previously known as mild cognitive impairment or MCI, is necessarily somewhat arbitrary. Major neurocognitive disorder requires "significant" cognitive decline in one or more cognitive domains as noted by the patient, family member, or clinician along with objective evidence of "substantial" impaired cognition compared to normative test values.
"In contrast, the requirements for mild neurocognitive disorder are ‘mild’ cognitive decline observed by patient, family member, or clinician and ‘modest’ impairment on testing, explained Dr. McCall, professor of psychiatry and health behavior at the Medical College of Georgia, Augusta.
Dr. Grossberg offered two practical tips in drawing the distinction between major and mild neurocognitive disorder. One is whether the cognitive deficits are sufficiently limited in scope that the patient is still able to function independently in everyday activities.
"If they’re not, I’m moving from [mild] to major," said Dr. Grossberg, professor of psychiatry, neurobiology, and internal medicine at Saint Louis University.
Also, if neuropsychologic testing focusing on memory is performed, Dr. Grossberg wants to see at least a one standard deviation below the expected age- and education-adjusted norms before calling it objective evidence of "substantial" impaired cognition rising to the level of major neurocognitive disorder.
Since major neurocognitive disorder is a syndrome, Dr. McCall said, it’s important to try to specify its nature. For the condition to qualify as major neurocognitive disorder from Alzheimer’s disease under the DSM-5, the impairment in cognition must be insidious in onset and gradual in progression. The patient must either have a causative Alzheimer’s disease mutation, which is present in less than 1% of all cases of the disease, or else the patient must meet three criteria: a decline in memory and learning, plus at least one additional cognitive domain; a steady decline without extended plateaus; and no evidence of mixed etiology involving cardiovascular disease or other disorders.
"There’s no requirement that memory impairment be the first affected domain. That’s a bit of a change," the psychiatrist noted.
The office-based assessment of neurocognitive disorders as recommended in the DSM-5 includes a careful history and an objective measure of cognitive function such as the Montreal Cognitive Assessment, the Saint Louis University Mental Status Evaluation, and the Mini-Mental State Examination. The patient’s ability to perform activities of daily living should be objectively evaluated, as by the Katz Index of Activities of Daily Living scale or the Barthel Index. A screening neurologic exam should be part of the work-up; this can be performed by a primary care physician or a neurologist if the psychiatrist prefers. Since major neurocognitive disorder is a syndrome, the DSM-5 does not require imaging via MRI or CT, although both Dr. McCall and Dr. Grossberg said this was a controversial issue during the creation of the DSM-5, and they recommend one-time baseline neuroimaging in order to rule out a tumor, old stroke, or frontotemporal atrophy.
Laboratory tests deemed an essential part of the work-up are a complete metabolic profile, thyroid stimulating hormone, a complete blood count, urinalysis, and folate.
In addition, Dr. Grossberg said, many memory clinics now routinely include measurements of vitamin D level, homocysteine, and C-reactive protein in the work-up.
"Vitamin D deficiency is extremely common. We’re finding in St. Louis – and I don’t think it’s a whole lot different among the elderly even in Florida, where there’s a lot of sun – that people are afraid of the sun now so they put on a whole lot of sunscreen, preventing vitamin D absorption. We check vitamin D levels routinely in our clinic, and maybe two out of every three older adults we test are low in vitamin D. More and more research shows that deficiency may be related to depression and may also have an effect on cognition. It’s something that’s easily remediable. We give 50,000 IU orally per week for 8 weeks, then a maintenance dose of 1,000-2,000 IU/day," Dr. Grossman said.
Elevated homocysteine and C-reactive protein levels are implicated in cardiovascular disease and also increasingly under scrutiny in Alzheimer’s disease. High homocysteine levels can readily be lowered with folate, and 81 mg/day of aspirin may be sufficient to reduce C-reactive protein, he added.
"Delirium" is the one neurocognitive disorder that’s essentially unchanged from the DSM-IV, according to Dr. McCall and Dr. Grossberg. This condition is characterized by rapid onset and fluctuations in severity during the day and must be linked to the physiologic consequences of a medical condition.
Dr. McCall reported receiving research grants from the National Institute of Mental Health and Merck. Dr. Grossberg serves as a consultant to Forest Laboratories, Lundbeck, Novartis, Otsuka, and Takeda.
ORLANDO – This May, the hallowed term "dementia" is supposed to be tossed onto the scrapheap of discarded psychiatric nomenclature, replaced by "major neurocognitive disorder."
When the DSM-5 was released in May 2013, the American Psychiatric Association gave a year’s grace period for the world to absorb the changes before they take effect. "Dementia" was replaced in the DSM-5 because the term was deemed stigmatizing; the rough translation from the Latin roots is "loss of mind." Acknowledging that old habits die hard, however, the DSM-5 also states that use of the term is not precluded "where that term is standard."
The old DSM-IV category of delirium, dementia, and amnestic and other cognitive disorders has been replaced in the DSM-5 by the neurocognitive disorders category. Major or mild neurocognitive disorder from Alzheimer’s disease is included under this new category. At the annual meeting of the American Association for Geriatric Psychiatry, Dr. W. Vaughn McCall and Dr. George T. Grossberg highlighted the changes.
"Major neurocognitive disorder" is a syndrome, which includes what was formerly known as dementia. The distinction between it and the new "mild neurocognitive disorder," previously known as mild cognitive impairment or MCI, is necessarily somewhat arbitrary. Major neurocognitive disorder requires "significant" cognitive decline in one or more cognitive domains as noted by the patient, family member, or clinician along with objective evidence of "substantial" impaired cognition compared to normative test values.
"In contrast, the requirements for mild neurocognitive disorder are ‘mild’ cognitive decline observed by patient, family member, or clinician and ‘modest’ impairment on testing, explained Dr. McCall, professor of psychiatry and health behavior at the Medical College of Georgia, Augusta.
Dr. Grossberg offered two practical tips in drawing the distinction between major and mild neurocognitive disorder. One is whether the cognitive deficits are sufficiently limited in scope that the patient is still able to function independently in everyday activities.
"If they’re not, I’m moving from [mild] to major," said Dr. Grossberg, professor of psychiatry, neurobiology, and internal medicine at Saint Louis University.
Also, if neuropsychologic testing focusing on memory is performed, Dr. Grossberg wants to see at least a one standard deviation below the expected age- and education-adjusted norms before calling it objective evidence of "substantial" impaired cognition rising to the level of major neurocognitive disorder.
Since major neurocognitive disorder is a syndrome, Dr. McCall said, it’s important to try to specify its nature. For the condition to qualify as major neurocognitive disorder from Alzheimer’s disease under the DSM-5, the impairment in cognition must be insidious in onset and gradual in progression. The patient must either have a causative Alzheimer’s disease mutation, which is present in less than 1% of all cases of the disease, or else the patient must meet three criteria: a decline in memory and learning, plus at least one additional cognitive domain; a steady decline without extended plateaus; and no evidence of mixed etiology involving cardiovascular disease or other disorders.
"There’s no requirement that memory impairment be the first affected domain. That’s a bit of a change," the psychiatrist noted.
The office-based assessment of neurocognitive disorders as recommended in the DSM-5 includes a careful history and an objective measure of cognitive function such as the Montreal Cognitive Assessment, the Saint Louis University Mental Status Evaluation, and the Mini-Mental State Examination. The patient’s ability to perform activities of daily living should be objectively evaluated, as by the Katz Index of Activities of Daily Living scale or the Barthel Index. A screening neurologic exam should be part of the work-up; this can be performed by a primary care physician or a neurologist if the psychiatrist prefers. Since major neurocognitive disorder is a syndrome, the DSM-5 does not require imaging via MRI or CT, although both Dr. McCall and Dr. Grossberg said this was a controversial issue during the creation of the DSM-5, and they recommend one-time baseline neuroimaging in order to rule out a tumor, old stroke, or frontotemporal atrophy.
Laboratory tests deemed an essential part of the work-up are a complete metabolic profile, thyroid stimulating hormone, a complete blood count, urinalysis, and folate.
In addition, Dr. Grossberg said, many memory clinics now routinely include measurements of vitamin D level, homocysteine, and C-reactive protein in the work-up.
"Vitamin D deficiency is extremely common. We’re finding in St. Louis – and I don’t think it’s a whole lot different among the elderly even in Florida, where there’s a lot of sun – that people are afraid of the sun now so they put on a whole lot of sunscreen, preventing vitamin D absorption. We check vitamin D levels routinely in our clinic, and maybe two out of every three older adults we test are low in vitamin D. More and more research shows that deficiency may be related to depression and may also have an effect on cognition. It’s something that’s easily remediable. We give 50,000 IU orally per week for 8 weeks, then a maintenance dose of 1,000-2,000 IU/day," Dr. Grossman said.
Elevated homocysteine and C-reactive protein levels are implicated in cardiovascular disease and also increasingly under scrutiny in Alzheimer’s disease. High homocysteine levels can readily be lowered with folate, and 81 mg/day of aspirin may be sufficient to reduce C-reactive protein, he added.
"Delirium" is the one neurocognitive disorder that’s essentially unchanged from the DSM-IV, according to Dr. McCall and Dr. Grossberg. This condition is characterized by rapid onset and fluctuations in severity during the day and must be linked to the physiologic consequences of a medical condition.
Dr. McCall reported receiving research grants from the National Institute of Mental Health and Merck. Dr. Grossberg serves as a consultant to Forest Laboratories, Lundbeck, Novartis, Otsuka, and Takeda.
ORLANDO – This May, the hallowed term "dementia" is supposed to be tossed onto the scrapheap of discarded psychiatric nomenclature, replaced by "major neurocognitive disorder."
When the DSM-5 was released in May 2013, the American Psychiatric Association gave a year’s grace period for the world to absorb the changes before they take effect. "Dementia" was replaced in the DSM-5 because the term was deemed stigmatizing; the rough translation from the Latin roots is "loss of mind." Acknowledging that old habits die hard, however, the DSM-5 also states that use of the term is not precluded "where that term is standard."
The old DSM-IV category of delirium, dementia, and amnestic and other cognitive disorders has been replaced in the DSM-5 by the neurocognitive disorders category. Major or mild neurocognitive disorder from Alzheimer’s disease is included under this new category. At the annual meeting of the American Association for Geriatric Psychiatry, Dr. W. Vaughn McCall and Dr. George T. Grossberg highlighted the changes.
"Major neurocognitive disorder" is a syndrome, which includes what was formerly known as dementia. The distinction between it and the new "mild neurocognitive disorder," previously known as mild cognitive impairment or MCI, is necessarily somewhat arbitrary. Major neurocognitive disorder requires "significant" cognitive decline in one or more cognitive domains as noted by the patient, family member, or clinician along with objective evidence of "substantial" impaired cognition compared to normative test values.
"In contrast, the requirements for mild neurocognitive disorder are ‘mild’ cognitive decline observed by patient, family member, or clinician and ‘modest’ impairment on testing, explained Dr. McCall, professor of psychiatry and health behavior at the Medical College of Georgia, Augusta.
Dr. Grossberg offered two practical tips in drawing the distinction between major and mild neurocognitive disorder. One is whether the cognitive deficits are sufficiently limited in scope that the patient is still able to function independently in everyday activities.
"If they’re not, I’m moving from [mild] to major," said Dr. Grossberg, professor of psychiatry, neurobiology, and internal medicine at Saint Louis University.
Also, if neuropsychologic testing focusing on memory is performed, Dr. Grossberg wants to see at least a one standard deviation below the expected age- and education-adjusted norms before calling it objective evidence of "substantial" impaired cognition rising to the level of major neurocognitive disorder.
Since major neurocognitive disorder is a syndrome, Dr. McCall said, it’s important to try to specify its nature. For the condition to qualify as major neurocognitive disorder from Alzheimer’s disease under the DSM-5, the impairment in cognition must be insidious in onset and gradual in progression. The patient must either have a causative Alzheimer’s disease mutation, which is present in less than 1% of all cases of the disease, or else the patient must meet three criteria: a decline in memory and learning, plus at least one additional cognitive domain; a steady decline without extended plateaus; and no evidence of mixed etiology involving cardiovascular disease or other disorders.
"There’s no requirement that memory impairment be the first affected domain. That’s a bit of a change," the psychiatrist noted.
The office-based assessment of neurocognitive disorders as recommended in the DSM-5 includes a careful history and an objective measure of cognitive function such as the Montreal Cognitive Assessment, the Saint Louis University Mental Status Evaluation, and the Mini-Mental State Examination. The patient’s ability to perform activities of daily living should be objectively evaluated, as by the Katz Index of Activities of Daily Living scale or the Barthel Index. A screening neurologic exam should be part of the work-up; this can be performed by a primary care physician or a neurologist if the psychiatrist prefers. Since major neurocognitive disorder is a syndrome, the DSM-5 does not require imaging via MRI or CT, although both Dr. McCall and Dr. Grossberg said this was a controversial issue during the creation of the DSM-5, and they recommend one-time baseline neuroimaging in order to rule out a tumor, old stroke, or frontotemporal atrophy.
Laboratory tests deemed an essential part of the work-up are a complete metabolic profile, thyroid stimulating hormone, a complete blood count, urinalysis, and folate.
In addition, Dr. Grossberg said, many memory clinics now routinely include measurements of vitamin D level, homocysteine, and C-reactive protein in the work-up.
"Vitamin D deficiency is extremely common. We’re finding in St. Louis – and I don’t think it’s a whole lot different among the elderly even in Florida, where there’s a lot of sun – that people are afraid of the sun now so they put on a whole lot of sunscreen, preventing vitamin D absorption. We check vitamin D levels routinely in our clinic, and maybe two out of every three older adults we test are low in vitamin D. More and more research shows that deficiency may be related to depression and may also have an effect on cognition. It’s something that’s easily remediable. We give 50,000 IU orally per week for 8 weeks, then a maintenance dose of 1,000-2,000 IU/day," Dr. Grossman said.
Elevated homocysteine and C-reactive protein levels are implicated in cardiovascular disease and also increasingly under scrutiny in Alzheimer’s disease. High homocysteine levels can readily be lowered with folate, and 81 mg/day of aspirin may be sufficient to reduce C-reactive protein, he added.
"Delirium" is the one neurocognitive disorder that’s essentially unchanged from the DSM-IV, according to Dr. McCall and Dr. Grossberg. This condition is characterized by rapid onset and fluctuations in severity during the day and must be linked to the physiologic consequences of a medical condition.
Dr. McCall reported receiving research grants from the National Institute of Mental Health and Merck. Dr. Grossberg serves as a consultant to Forest Laboratories, Lundbeck, Novartis, Otsuka, and Takeda.
EXPERT ANALYSIS FROM THE AAGP ANNUAL MEETING
Late-life depression can be dementia prodrome
ORLANDO – Elderly patients with acute depression who show deficits on brief structured tests of memory and executive function are at high risk for developing Alzheimer’s disease within the next few years, mounting evidence indicates.
"Our study suggests that late-life depression with documented memory and executive function impairment is just the tip of a very bad neuropsychiatric iceberg and that there is more to come," Dr. David C. Steffens said at the annual meeting of the American Association for Geriatric Psychiatry (AAGP).
It’s unclear as yet whether depression in the elderly is a risk factor for dementia or a prodrome of the disorder. That’s an ongoing debate in the field. The two possibilities are not mutually exclusive, according to Dr. Steffens, professor and chairman of the psychiatry department at the University of Connecticut, Farmington.
What is clear is that the subsequent course of elderly depressed patients with comorbid mild cognitive impairment is highly variable, as illustrated in a study in which Dr. Steffens and his colleagues followed 69 such patients for 2 years. Seventeen ended up cognitively unimpaired, 6 developed subsyndromal Alzheimer’s disease, 6 had possible Alzheimer’s disease, 2 had probable Alzheimer’s, 2 had dementia of undetermined etiology, 13 still met criteria for mild cognitive impairment without dementia, and 23 had cognitive impairment which during follow-up became attributable to a more specific cause, such as cerebrovascular disease or another medical condition (J. Geriatr. Psychiatry Neurol. 2009;22:52-61).
In an effort to find a means of predicting which patients with late-life major depressive disorder are most likely to go on to develop dementia, the investigators turned to baseline neuropsychologic testing. Dr. Steffens presented recently published highlights of the NCODE (Neurocognitive Outcomes of Depression in the Elderly) trial, a longitudinal outpatient depression treatment study. In this phase of NCODE, 179 nondemented, acutely depressed older adults underwent baseline neuropsychologic testing, received active treatment for their depression, and were followed for a mean of 5.5 years. During follow-up, Dr. Steffens and his coinvestigators diagnosed 30 subjects as having incident dementia, while the other 149 were deemed cognitively normal.
Of course, completing an extensive battery of neuropsychologic tests is a lot to ask of an elderly patient with late-life depression. Fortunately, two of the neuropsychologic tests – the CERAD (Consortium to Establish a Registry of Alzheimer’s Disease) Recognition Memory and the Trail Making B – proved to be the best predictors of subsequent conversion to dementia. That’s good news, because focusing on just two tests for prognostication is practical in everyday clinical practice, whereas administering a lengthy battery of neuropsychologic tests really isn’t, observed Dr. Steffens, who is AAGP president.
In a multivariate analysis, deficits on CERAD Recognition Memory and Trail Making B were associated with a 6.8-fold increased risk of developing dementia during follow-up, compared with elderly acutely depressed patients who scored in the normal range. The two tests correctly classified 91.6% of NCODE participants, with false-positive and false-negative rates of 5.9% and 8.6%, respectively (Am J. Geriatr. Psychiatry 2013;21:297-306).
"As more and more data accumulate, I think the field is moving to a point where we can say that as part of our assessment, if you focus on one or two tests, that may actually prognosticate better," the psychiatrist observed.
The NCODE study was supported by the National Institute of Mental Health. Dr. Steffens reported having no financial conflicts of interest.
ORLANDO – Elderly patients with acute depression who show deficits on brief structured tests of memory and executive function are at high risk for developing Alzheimer’s disease within the next few years, mounting evidence indicates.
"Our study suggests that late-life depression with documented memory and executive function impairment is just the tip of a very bad neuropsychiatric iceberg and that there is more to come," Dr. David C. Steffens said at the annual meeting of the American Association for Geriatric Psychiatry (AAGP).
It’s unclear as yet whether depression in the elderly is a risk factor for dementia or a prodrome of the disorder. That’s an ongoing debate in the field. The two possibilities are not mutually exclusive, according to Dr. Steffens, professor and chairman of the psychiatry department at the University of Connecticut, Farmington.
What is clear is that the subsequent course of elderly depressed patients with comorbid mild cognitive impairment is highly variable, as illustrated in a study in which Dr. Steffens and his colleagues followed 69 such patients for 2 years. Seventeen ended up cognitively unimpaired, 6 developed subsyndromal Alzheimer’s disease, 6 had possible Alzheimer’s disease, 2 had probable Alzheimer’s, 2 had dementia of undetermined etiology, 13 still met criteria for mild cognitive impairment without dementia, and 23 had cognitive impairment which during follow-up became attributable to a more specific cause, such as cerebrovascular disease or another medical condition (J. Geriatr. Psychiatry Neurol. 2009;22:52-61).
In an effort to find a means of predicting which patients with late-life major depressive disorder are most likely to go on to develop dementia, the investigators turned to baseline neuropsychologic testing. Dr. Steffens presented recently published highlights of the NCODE (Neurocognitive Outcomes of Depression in the Elderly) trial, a longitudinal outpatient depression treatment study. In this phase of NCODE, 179 nondemented, acutely depressed older adults underwent baseline neuropsychologic testing, received active treatment for their depression, and were followed for a mean of 5.5 years. During follow-up, Dr. Steffens and his coinvestigators diagnosed 30 subjects as having incident dementia, while the other 149 were deemed cognitively normal.
Of course, completing an extensive battery of neuropsychologic tests is a lot to ask of an elderly patient with late-life depression. Fortunately, two of the neuropsychologic tests – the CERAD (Consortium to Establish a Registry of Alzheimer’s Disease) Recognition Memory and the Trail Making B – proved to be the best predictors of subsequent conversion to dementia. That’s good news, because focusing on just two tests for prognostication is practical in everyday clinical practice, whereas administering a lengthy battery of neuropsychologic tests really isn’t, observed Dr. Steffens, who is AAGP president.
In a multivariate analysis, deficits on CERAD Recognition Memory and Trail Making B were associated with a 6.8-fold increased risk of developing dementia during follow-up, compared with elderly acutely depressed patients who scored in the normal range. The two tests correctly classified 91.6% of NCODE participants, with false-positive and false-negative rates of 5.9% and 8.6%, respectively (Am J. Geriatr. Psychiatry 2013;21:297-306).
"As more and more data accumulate, I think the field is moving to a point where we can say that as part of our assessment, if you focus on one or two tests, that may actually prognosticate better," the psychiatrist observed.
The NCODE study was supported by the National Institute of Mental Health. Dr. Steffens reported having no financial conflicts of interest.
ORLANDO – Elderly patients with acute depression who show deficits on brief structured tests of memory and executive function are at high risk for developing Alzheimer’s disease within the next few years, mounting evidence indicates.
"Our study suggests that late-life depression with documented memory and executive function impairment is just the tip of a very bad neuropsychiatric iceberg and that there is more to come," Dr. David C. Steffens said at the annual meeting of the American Association for Geriatric Psychiatry (AAGP).
It’s unclear as yet whether depression in the elderly is a risk factor for dementia or a prodrome of the disorder. That’s an ongoing debate in the field. The two possibilities are not mutually exclusive, according to Dr. Steffens, professor and chairman of the psychiatry department at the University of Connecticut, Farmington.
What is clear is that the subsequent course of elderly depressed patients with comorbid mild cognitive impairment is highly variable, as illustrated in a study in which Dr. Steffens and his colleagues followed 69 such patients for 2 years. Seventeen ended up cognitively unimpaired, 6 developed subsyndromal Alzheimer’s disease, 6 had possible Alzheimer’s disease, 2 had probable Alzheimer’s, 2 had dementia of undetermined etiology, 13 still met criteria for mild cognitive impairment without dementia, and 23 had cognitive impairment which during follow-up became attributable to a more specific cause, such as cerebrovascular disease or another medical condition (J. Geriatr. Psychiatry Neurol. 2009;22:52-61).
In an effort to find a means of predicting which patients with late-life major depressive disorder are most likely to go on to develop dementia, the investigators turned to baseline neuropsychologic testing. Dr. Steffens presented recently published highlights of the NCODE (Neurocognitive Outcomes of Depression in the Elderly) trial, a longitudinal outpatient depression treatment study. In this phase of NCODE, 179 nondemented, acutely depressed older adults underwent baseline neuropsychologic testing, received active treatment for their depression, and were followed for a mean of 5.5 years. During follow-up, Dr. Steffens and his coinvestigators diagnosed 30 subjects as having incident dementia, while the other 149 were deemed cognitively normal.
Of course, completing an extensive battery of neuropsychologic tests is a lot to ask of an elderly patient with late-life depression. Fortunately, two of the neuropsychologic tests – the CERAD (Consortium to Establish a Registry of Alzheimer’s Disease) Recognition Memory and the Trail Making B – proved to be the best predictors of subsequent conversion to dementia. That’s good news, because focusing on just two tests for prognostication is practical in everyday clinical practice, whereas administering a lengthy battery of neuropsychologic tests really isn’t, observed Dr. Steffens, who is AAGP president.
In a multivariate analysis, deficits on CERAD Recognition Memory and Trail Making B were associated with a 6.8-fold increased risk of developing dementia during follow-up, compared with elderly acutely depressed patients who scored in the normal range. The two tests correctly classified 91.6% of NCODE participants, with false-positive and false-negative rates of 5.9% and 8.6%, respectively (Am J. Geriatr. Psychiatry 2013;21:297-306).
"As more and more data accumulate, I think the field is moving to a point where we can say that as part of our assessment, if you focus on one or two tests, that may actually prognosticate better," the psychiatrist observed.
The NCODE study was supported by the National Institute of Mental Health. Dr. Steffens reported having no financial conflicts of interest.
AT THE AAGP ANNUAL MEETING
Major finding: Deficits on two tests – CERAD Recognition Memory and Trail Making B – were associated with a 6.8-fold increased risk of developing dementia during follow-up, compared with elderly acutely depressed patients who scored in the normal range.
Data source: This was a single-center study in which 179 elderly patients with major depressive disorder completed a baseline battery of neuropsychologic tests, received active treatment for depression, and were followed for an average of 5.5 years, during which 30 patients developed dementia.
Disclosures: The study was supported by the National Institute of Mental Health. Dr. Steffens reported having no relevant financial interests.
Hoarding: Not just a symptom of OCD
ORLANDO – Compulsive hoarding traditionally has been considered virtually synonymous with obsessive-compulsive disorder, but its reach actually extends far beyond.
Indeed, hoarding turns out to be is highly prevalent across a broad span of psychiatric disorders, including bipolar disorder.
In a random sample of 165 psychiatric inpatients with a variety of diagnoses who were screened using the Hoarding Rating Scale, 70 (42%) showed evidence of clinically significant compulsive hoarding, Dr. Nidhi Goel reported at the annual meeting of the American Association for Geriatric Psychiatry.
Clinically significant hoarding as defined by a score of 14 or more was present in half of patients hospitalized with bipolar disorder, 41% of those with substance use disorders, close to 40% of those diagnosed with schizophrenia or schizoaffective disorder, more than one-third of patients hospitalized for major depression, and 28% with other psychotic spectrum disorders, noted Dr. Goel, director of inpatient psychiatric services at Maimonides Medical Center in Brooklyn, N.Y.
The clinical implication is clear, she added: Hoarding disorder – newly upgraded to a full-blown diagnostic category in the DSM-5 – needs to be brought up onto more psychiatrists’ radars.
"Patients come in with depression, substance use problems, and all sorts of Axis I diagnoses where we just forget to assess the hoarding problem. Then when they’re ready to be discharged, a family member mentions, ‘We cannot even get into their apartment because of all the stuff that has piled up.’ This disorder negatively [affects] our patients’ quality of life quite a lot," Dr. Goel continued.
"My thinking is that if hoarding is so common in all of these disorders, could treating hoarding prevent some of these other disorders? We don’t know. It hasn’t been studied," Dr. Goel said in an interview.
In the DSM-5, hoarding disorder is for the first time categorized as a distinct entity. It is listed under the chapter heading Obsessive-Compulsive and Related Disorders. Before the DSM-5, there was no "hoarding disorder." Rather, hoarding was merely considered a symptom of OCD. And OCD was included in the chapter on anxiety disorders. Now OCD and Related Disorders have their own chapter and are no longer considered anxiety disorders.
The DSM-5 fact sheet on hoarding disorder states, "Creating a unique diagnosis in DSM-5 will increase public awareness, improve identification of cases, and stimulate both research and the development of specific treatments for hoarding disorder. This is particularly important, as studies show that the prevalence of hoarding disorder is estimated at approximately 2%-5% of the population. These behaviors can often be quite severe and even threatening."
Hoarding disorder and its attendant clutter also create a significant public health problem, according to Dr. Goel, who noted that hoarding-related complaints to urban public health departments occur at a rate of 26/100,000 population per 5 years.
One of the features of the DSM-5 diagnostic category of hoarding disorder Dr. Goel considers a big step forward is the inclusion of specifiers regarding insight and delusional beliefs. Patients with hoarding disorder can be categorized as having good or fair insight, poor insight, or absent insight with delusional beliefs.
"Let’s say, for example, that a patient comes in who has been diagnosed with schizophrenia just because there is some delusional component attached. I’m now thinking maybe this patient may not have schizophrenia. Maybe it’s just hoarding disorder with delusions, or delusional disorder [not otherwise specified]," she said.
The Hoarding Rating Scale assesses difficulty in using living spaces because of clutter, the inability to get rid of possessions, the excessive acquisition of objects, and hoarding behavior–related functional impairment and emotional distress.
Dr. Goel reported having no financial conflicts with regard to this study.
ORLANDO – Compulsive hoarding traditionally has been considered virtually synonymous with obsessive-compulsive disorder, but its reach actually extends far beyond.
Indeed, hoarding turns out to be is highly prevalent across a broad span of psychiatric disorders, including bipolar disorder.
In a random sample of 165 psychiatric inpatients with a variety of diagnoses who were screened using the Hoarding Rating Scale, 70 (42%) showed evidence of clinically significant compulsive hoarding, Dr. Nidhi Goel reported at the annual meeting of the American Association for Geriatric Psychiatry.
Clinically significant hoarding as defined by a score of 14 or more was present in half of patients hospitalized with bipolar disorder, 41% of those with substance use disorders, close to 40% of those diagnosed with schizophrenia or schizoaffective disorder, more than one-third of patients hospitalized for major depression, and 28% with other psychotic spectrum disorders, noted Dr. Goel, director of inpatient psychiatric services at Maimonides Medical Center in Brooklyn, N.Y.
The clinical implication is clear, she added: Hoarding disorder – newly upgraded to a full-blown diagnostic category in the DSM-5 – needs to be brought up onto more psychiatrists’ radars.
"Patients come in with depression, substance use problems, and all sorts of Axis I diagnoses where we just forget to assess the hoarding problem. Then when they’re ready to be discharged, a family member mentions, ‘We cannot even get into their apartment because of all the stuff that has piled up.’ This disorder negatively [affects] our patients’ quality of life quite a lot," Dr. Goel continued.
"My thinking is that if hoarding is so common in all of these disorders, could treating hoarding prevent some of these other disorders? We don’t know. It hasn’t been studied," Dr. Goel said in an interview.
In the DSM-5, hoarding disorder is for the first time categorized as a distinct entity. It is listed under the chapter heading Obsessive-Compulsive and Related Disorders. Before the DSM-5, there was no "hoarding disorder." Rather, hoarding was merely considered a symptom of OCD. And OCD was included in the chapter on anxiety disorders. Now OCD and Related Disorders have their own chapter and are no longer considered anxiety disorders.
The DSM-5 fact sheet on hoarding disorder states, "Creating a unique diagnosis in DSM-5 will increase public awareness, improve identification of cases, and stimulate both research and the development of specific treatments for hoarding disorder. This is particularly important, as studies show that the prevalence of hoarding disorder is estimated at approximately 2%-5% of the population. These behaviors can often be quite severe and even threatening."
Hoarding disorder and its attendant clutter also create a significant public health problem, according to Dr. Goel, who noted that hoarding-related complaints to urban public health departments occur at a rate of 26/100,000 population per 5 years.
One of the features of the DSM-5 diagnostic category of hoarding disorder Dr. Goel considers a big step forward is the inclusion of specifiers regarding insight and delusional beliefs. Patients with hoarding disorder can be categorized as having good or fair insight, poor insight, or absent insight with delusional beliefs.
"Let’s say, for example, that a patient comes in who has been diagnosed with schizophrenia just because there is some delusional component attached. I’m now thinking maybe this patient may not have schizophrenia. Maybe it’s just hoarding disorder with delusions, or delusional disorder [not otherwise specified]," she said.
The Hoarding Rating Scale assesses difficulty in using living spaces because of clutter, the inability to get rid of possessions, the excessive acquisition of objects, and hoarding behavior–related functional impairment and emotional distress.
Dr. Goel reported having no financial conflicts with regard to this study.
ORLANDO – Compulsive hoarding traditionally has been considered virtually synonymous with obsessive-compulsive disorder, but its reach actually extends far beyond.
Indeed, hoarding turns out to be is highly prevalent across a broad span of psychiatric disorders, including bipolar disorder.
In a random sample of 165 psychiatric inpatients with a variety of diagnoses who were screened using the Hoarding Rating Scale, 70 (42%) showed evidence of clinically significant compulsive hoarding, Dr. Nidhi Goel reported at the annual meeting of the American Association for Geriatric Psychiatry.
Clinically significant hoarding as defined by a score of 14 or more was present in half of patients hospitalized with bipolar disorder, 41% of those with substance use disorders, close to 40% of those diagnosed with schizophrenia or schizoaffective disorder, more than one-third of patients hospitalized for major depression, and 28% with other psychotic spectrum disorders, noted Dr. Goel, director of inpatient psychiatric services at Maimonides Medical Center in Brooklyn, N.Y.
The clinical implication is clear, she added: Hoarding disorder – newly upgraded to a full-blown diagnostic category in the DSM-5 – needs to be brought up onto more psychiatrists’ radars.
"Patients come in with depression, substance use problems, and all sorts of Axis I diagnoses where we just forget to assess the hoarding problem. Then when they’re ready to be discharged, a family member mentions, ‘We cannot even get into their apartment because of all the stuff that has piled up.’ This disorder negatively [affects] our patients’ quality of life quite a lot," Dr. Goel continued.
"My thinking is that if hoarding is so common in all of these disorders, could treating hoarding prevent some of these other disorders? We don’t know. It hasn’t been studied," Dr. Goel said in an interview.
In the DSM-5, hoarding disorder is for the first time categorized as a distinct entity. It is listed under the chapter heading Obsessive-Compulsive and Related Disorders. Before the DSM-5, there was no "hoarding disorder." Rather, hoarding was merely considered a symptom of OCD. And OCD was included in the chapter on anxiety disorders. Now OCD and Related Disorders have their own chapter and are no longer considered anxiety disorders.
The DSM-5 fact sheet on hoarding disorder states, "Creating a unique diagnosis in DSM-5 will increase public awareness, improve identification of cases, and stimulate both research and the development of specific treatments for hoarding disorder. This is particularly important, as studies show that the prevalence of hoarding disorder is estimated at approximately 2%-5% of the population. These behaviors can often be quite severe and even threatening."
Hoarding disorder and its attendant clutter also create a significant public health problem, according to Dr. Goel, who noted that hoarding-related complaints to urban public health departments occur at a rate of 26/100,000 population per 5 years.
One of the features of the DSM-5 diagnostic category of hoarding disorder Dr. Goel considers a big step forward is the inclusion of specifiers regarding insight and delusional beliefs. Patients with hoarding disorder can be categorized as having good or fair insight, poor insight, or absent insight with delusional beliefs.
"Let’s say, for example, that a patient comes in who has been diagnosed with schizophrenia just because there is some delusional component attached. I’m now thinking maybe this patient may not have schizophrenia. Maybe it’s just hoarding disorder with delusions, or delusional disorder [not otherwise specified]," she said.
The Hoarding Rating Scale assesses difficulty in using living spaces because of clutter, the inability to get rid of possessions, the excessive acquisition of objects, and hoarding behavior–related functional impairment and emotional distress.
Dr. Goel reported having no financial conflicts with regard to this study.
AT THE AAGP ANNUAL MEETING
Major finding: Seventy of 165 adult psychiatric inpatients screened for compulsive hoarding displayed evidence of a clinically significant hoarding problem. Hoarding was highly prevalent among patients hospitalized for depression, schizophrenia, bipolar disorder, substance use, and a variety of diagnoses other than obsessive-compulsive disorder.
Data source: This was a cross-sectional study in which inpatients with a broad array of psychiatric diagnoses were screened for compulsive hoarding using the Hoarding Rating Scale.
Disclosures: The study presenter reported having no financial conflicts of interest.