User login
Controversies in dual antiplatelet therapy post PCI
SNOWMASS, COLO. – Wide local variation in the guideline-recommended use of low-dose aspirin as part of dual antiplatelet therapy after coronary stent implantation appears to be a prime target for a quality improvement effort.
American College of Cardiology/American Heart Association guidelines recommend aspirin at 81 mg/day along with an oral thienopyridine for maintenance therapy after percutaneous coronary intervention (PCI). This Class IIa/Level of Evidence B recommendation for preferential use of low- rather than high-dose aspirin is based upon the results of the OASIS 7 study (N. Engl. J. Med. 2010;354:1706-17) and other randomized trials that demonstrate that low- and high-dose aspirin (300-325 mg/day) are equally effective in reducing ischemic complications after PCI but that high-dose aspirin is associated with an increased risk of bleeding, Dr. Patrick T. O’Gara noted at the Annual Cardiovascular Conference at Snowmass.
Yet in a contemporary series of more than 23,000 U.S. patients enrolled in the major ongoing Dual Antiplatelet Therapy Study, only 28% were placed on low-dose aspirin at discharge after PCI; the rest got high-dose aspirin as part of their dual antiplatelet therapy (DAPT). In contrast, 90% of study participants from other countries got low-dose aspirin for their DAPT, commented Dr. O’Gara, who is ACC president-elect and professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, both in Boston.
The DAPT Study investigators determined that patient characteristics explained a mere 1.6% of the total variation in aspirin dosing. Site of enrollment accounted for 46% of the unexplained variation (Am. J. Cardiol. 201;113:1146-52).
The optimal duration of DAPT after PCI with placement of a drug-eluting stent remains unclear. Current guidelines call for at least 12 months of DAPT. The massive DAPT Study is designed to learn whether longer than 12 months is better. Participants were placed on 12 months of aspirin plus a thienopyridine, then randomized to an additional 18 months of DAPT or to aspirin plus placebo. The trial includes a variety of stents and indications for implantation. Results are expected later this year.
In the meantime, Dr. O’Gara said, the use of more than 12 months of DAPT is highly variable around the world. Studies suggest that at 3 years post-PCI, 40%-50% of North American patients remain on DAPT compared to about 10% of patients in Europe and elsewhere.
The ACC/AHA guidelines state as a relatively weak Class IIb/Level of Evidence C recommendation that continuation of DAPT beyond 12 months "may be considered" in drug-eluting stent recipients. Until the results of the DAPT Study become available to provide further guidance, however, Dr. O’Gara urged his colleagues to weigh this decision carefully on a case by case basis.
"The duration of DAPT is uncertain, but if you choose to continue therapy beyond 12 months, I think you need to be aware of the increasing number of trials that show no benefit of doing that – and an excess hazard of bleeding by doing so," he cautioned.
Dr. O’Gara cited three such major randomized trials totaling more than 6,100 patients: the Italian PRODIGY trial (Circulation 2012;125:2015-26), in which patients had near-identical rates of the 2-year composite of all-cause mortality, MI, or cerebrovascular accident regardless of whether they were randomized to 6 or 24 months of DAPT; the Korean combined REAL-LATE and ZEST-LATE trials (N. Engl. J. Med. 2010;362:1374-82), in which 12 and 24 months of DAPT resulted in similar rates of MI or cardiac death at 2 years; and EXCELLENT, in which 12 months of DAPT proved no better than 6 in terms of the combined endpoint of cardiac death, MI, or target vessel revascularization (Circulation 2012;125:505-13).
Moreover, a secondary analysis of the Korean trials found a 2.96-fold increased risk of Thrombosis in Myocardial Infarction major bleeding in patients on DAPT for longer than 12 months. And PRODIGY investigators found a 2.7-fold increased major bleeding risk with 24 as compared to 6 months of DAPT.
Further uncertainty regarding the optimal duration of DAPT comes from the OPTIMIZE trial, in which 3,119 Brazilian patients with low-risk acute coronary syndrome or stable coronary artery disease received a zotarolimus-eluting stent and were randomized to 3 or 12 months of DAPT. There was no difference between the two groups in the combined endpoint of all-cause mortality, MI, stroke, or major bleeding (JAMA 2013;310:2510-22).
"Interestingly enough, in Europe the zotarolimus-eluting stent has achieved approval for a 3-month course of dual antiplatelet therapy," Dr. O’Gara said.
He reported having no financial conflicts.
SNOWMASS, COLO. – Wide local variation in the guideline-recommended use of low-dose aspirin as part of dual antiplatelet therapy after coronary stent implantation appears to be a prime target for a quality improvement effort.
American College of Cardiology/American Heart Association guidelines recommend aspirin at 81 mg/day along with an oral thienopyridine for maintenance therapy after percutaneous coronary intervention (PCI). This Class IIa/Level of Evidence B recommendation for preferential use of low- rather than high-dose aspirin is based upon the results of the OASIS 7 study (N. Engl. J. Med. 2010;354:1706-17) and other randomized trials that demonstrate that low- and high-dose aspirin (300-325 mg/day) are equally effective in reducing ischemic complications after PCI but that high-dose aspirin is associated with an increased risk of bleeding, Dr. Patrick T. O’Gara noted at the Annual Cardiovascular Conference at Snowmass.
Yet in a contemporary series of more than 23,000 U.S. patients enrolled in the major ongoing Dual Antiplatelet Therapy Study, only 28% were placed on low-dose aspirin at discharge after PCI; the rest got high-dose aspirin as part of their dual antiplatelet therapy (DAPT). In contrast, 90% of study participants from other countries got low-dose aspirin for their DAPT, commented Dr. O’Gara, who is ACC president-elect and professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, both in Boston.
The DAPT Study investigators determined that patient characteristics explained a mere 1.6% of the total variation in aspirin dosing. Site of enrollment accounted for 46% of the unexplained variation (Am. J. Cardiol. 201;113:1146-52).
The optimal duration of DAPT after PCI with placement of a drug-eluting stent remains unclear. Current guidelines call for at least 12 months of DAPT. The massive DAPT Study is designed to learn whether longer than 12 months is better. Participants were placed on 12 months of aspirin plus a thienopyridine, then randomized to an additional 18 months of DAPT or to aspirin plus placebo. The trial includes a variety of stents and indications for implantation. Results are expected later this year.
In the meantime, Dr. O’Gara said, the use of more than 12 months of DAPT is highly variable around the world. Studies suggest that at 3 years post-PCI, 40%-50% of North American patients remain on DAPT compared to about 10% of patients in Europe and elsewhere.
The ACC/AHA guidelines state as a relatively weak Class IIb/Level of Evidence C recommendation that continuation of DAPT beyond 12 months "may be considered" in drug-eluting stent recipients. Until the results of the DAPT Study become available to provide further guidance, however, Dr. O’Gara urged his colleagues to weigh this decision carefully on a case by case basis.
"The duration of DAPT is uncertain, but if you choose to continue therapy beyond 12 months, I think you need to be aware of the increasing number of trials that show no benefit of doing that – and an excess hazard of bleeding by doing so," he cautioned.
Dr. O’Gara cited three such major randomized trials totaling more than 6,100 patients: the Italian PRODIGY trial (Circulation 2012;125:2015-26), in which patients had near-identical rates of the 2-year composite of all-cause mortality, MI, or cerebrovascular accident regardless of whether they were randomized to 6 or 24 months of DAPT; the Korean combined REAL-LATE and ZEST-LATE trials (N. Engl. J. Med. 2010;362:1374-82), in which 12 and 24 months of DAPT resulted in similar rates of MI or cardiac death at 2 years; and EXCELLENT, in which 12 months of DAPT proved no better than 6 in terms of the combined endpoint of cardiac death, MI, or target vessel revascularization (Circulation 2012;125:505-13).
Moreover, a secondary analysis of the Korean trials found a 2.96-fold increased risk of Thrombosis in Myocardial Infarction major bleeding in patients on DAPT for longer than 12 months. And PRODIGY investigators found a 2.7-fold increased major bleeding risk with 24 as compared to 6 months of DAPT.
Further uncertainty regarding the optimal duration of DAPT comes from the OPTIMIZE trial, in which 3,119 Brazilian patients with low-risk acute coronary syndrome or stable coronary artery disease received a zotarolimus-eluting stent and were randomized to 3 or 12 months of DAPT. There was no difference between the two groups in the combined endpoint of all-cause mortality, MI, stroke, or major bleeding (JAMA 2013;310:2510-22).
"Interestingly enough, in Europe the zotarolimus-eluting stent has achieved approval for a 3-month course of dual antiplatelet therapy," Dr. O’Gara said.
He reported having no financial conflicts.
SNOWMASS, COLO. – Wide local variation in the guideline-recommended use of low-dose aspirin as part of dual antiplatelet therapy after coronary stent implantation appears to be a prime target for a quality improvement effort.
American College of Cardiology/American Heart Association guidelines recommend aspirin at 81 mg/day along with an oral thienopyridine for maintenance therapy after percutaneous coronary intervention (PCI). This Class IIa/Level of Evidence B recommendation for preferential use of low- rather than high-dose aspirin is based upon the results of the OASIS 7 study (N. Engl. J. Med. 2010;354:1706-17) and other randomized trials that demonstrate that low- and high-dose aspirin (300-325 mg/day) are equally effective in reducing ischemic complications after PCI but that high-dose aspirin is associated with an increased risk of bleeding, Dr. Patrick T. O’Gara noted at the Annual Cardiovascular Conference at Snowmass.
Yet in a contemporary series of more than 23,000 U.S. patients enrolled in the major ongoing Dual Antiplatelet Therapy Study, only 28% were placed on low-dose aspirin at discharge after PCI; the rest got high-dose aspirin as part of their dual antiplatelet therapy (DAPT). In contrast, 90% of study participants from other countries got low-dose aspirin for their DAPT, commented Dr. O’Gara, who is ACC president-elect and professor of medicine at Harvard Medical School and director of clinical cardiology at Brigham and Women’s Hospital, both in Boston.
The DAPT Study investigators determined that patient characteristics explained a mere 1.6% of the total variation in aspirin dosing. Site of enrollment accounted for 46% of the unexplained variation (Am. J. Cardiol. 201;113:1146-52).
The optimal duration of DAPT after PCI with placement of a drug-eluting stent remains unclear. Current guidelines call for at least 12 months of DAPT. The massive DAPT Study is designed to learn whether longer than 12 months is better. Participants were placed on 12 months of aspirin plus a thienopyridine, then randomized to an additional 18 months of DAPT or to aspirin plus placebo. The trial includes a variety of stents and indications for implantation. Results are expected later this year.
In the meantime, Dr. O’Gara said, the use of more than 12 months of DAPT is highly variable around the world. Studies suggest that at 3 years post-PCI, 40%-50% of North American patients remain on DAPT compared to about 10% of patients in Europe and elsewhere.
The ACC/AHA guidelines state as a relatively weak Class IIb/Level of Evidence C recommendation that continuation of DAPT beyond 12 months "may be considered" in drug-eluting stent recipients. Until the results of the DAPT Study become available to provide further guidance, however, Dr. O’Gara urged his colleagues to weigh this decision carefully on a case by case basis.
"The duration of DAPT is uncertain, but if you choose to continue therapy beyond 12 months, I think you need to be aware of the increasing number of trials that show no benefit of doing that – and an excess hazard of bleeding by doing so," he cautioned.
Dr. O’Gara cited three such major randomized trials totaling more than 6,100 patients: the Italian PRODIGY trial (Circulation 2012;125:2015-26), in which patients had near-identical rates of the 2-year composite of all-cause mortality, MI, or cerebrovascular accident regardless of whether they were randomized to 6 or 24 months of DAPT; the Korean combined REAL-LATE and ZEST-LATE trials (N. Engl. J. Med. 2010;362:1374-82), in which 12 and 24 months of DAPT resulted in similar rates of MI or cardiac death at 2 years; and EXCELLENT, in which 12 months of DAPT proved no better than 6 in terms of the combined endpoint of cardiac death, MI, or target vessel revascularization (Circulation 2012;125:505-13).
Moreover, a secondary analysis of the Korean trials found a 2.96-fold increased risk of Thrombosis in Myocardial Infarction major bleeding in patients on DAPT for longer than 12 months. And PRODIGY investigators found a 2.7-fold increased major bleeding risk with 24 as compared to 6 months of DAPT.
Further uncertainty regarding the optimal duration of DAPT comes from the OPTIMIZE trial, in which 3,119 Brazilian patients with low-risk acute coronary syndrome or stable coronary artery disease received a zotarolimus-eluting stent and were randomized to 3 or 12 months of DAPT. There was no difference between the two groups in the combined endpoint of all-cause mortality, MI, stroke, or major bleeding (JAMA 2013;310:2510-22).
"Interestingly enough, in Europe the zotarolimus-eluting stent has achieved approval for a 3-month course of dual antiplatelet therapy," Dr. O’Gara said.
He reported having no financial conflicts.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Be wary of asthma’s masqueraders
KEYSTONE, COLO. – The diagnosis of asthma isn’t as simple as it may seem.
Asthma is a clinical syndrome with no specific diagnostic test. So, the response to therapy becomes a key element in finalizing the diagnosis, Dr. Gary R. Cott emphasized at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
"If you have features that make you think of asthma, particularly mild to moderate asthma, and you initiate therapy, you should expect a therapeutic response in 80%-85% of cases. If you don’t get a response, step back and think about whether you made the right diagnosis before you start escalating care," advised Dr. Cott, a pulmonologist and executive vice president of medical and clinical services at National Jewish Health, Denver.
How often do physicians on the front lines get the diagnosis of asthma wrong? The National Jewish experience is illuminating.
In a series of 305 consecutive patients referred to the tertiary center with a preestablished diagnosis of asthma, all of whom were already on treatment for the disease, fully 25% didn’t have asthma at all. A mere 5% were found to have asthma only. A total of 38% had asthma plus an associated contributory respiratory condition, such as allergic rhinitis, rhinosinusitis, or aspirin sensitivity. Another 32% had asthma plus a cardiopulmonary condition that contributed to their symptoms, such as valvular dysfunction, a vascular ring, or pulmonary embolus.
"This experience has been duplicated at other specialty centers. It’s not unique to what we see," according to Dr. Cott.
He defined asthma as a syndrome characterized by increased airway responsiveness to various stimuli, along with variable obstruction of expiratory flow. It’s a physiologic definition. Four elements are essential in establishing the diagnosis: the history, physical exam, spirometry, and response to therapy. A variety of other tests are often helpful in narrowing the differential diagnosis – for example, chest imaging, blood eosinophil measurement, allergy testing, bronchial challenges, diffusing capacity of the lung for carbon monoxide, lung volumes, and elasticity. But they’re not specific for asthma.
"All that wheezes is not asthma. But most is," Dr. Cott observed. "I must say, I’m not very critical of the outside docs who send patients in and say, ‘I think they have asthma,’ and we then say, ‘No, they’ve got something else.’ Asthma is a common disorder. In Colorado, as much as 11% of the population can have asthma. It’s probably the most common thing that will cause an otherwise healthy individual to present with recurring or persistent symptoms.
"I think that sometimes leads us down a path – not always incorrect – of thinking, ‘Let’s try treating for asthma,’ " Dr. Cott noted. "The problem is that when they’re not responding, it’s time to rethink the differential carefully."
The list of disorders involving lower airways obstruction that can mimic asthma is extensive. The top two masqueraders are emphysema and chronic bronchitis. What’s more, asthma, emphysema, and chronic bronchitis aren’t mutually exclusive diseases. A given patient can have any two or even all three.
In contrast to asthma, which is defined physiologically, chronic bronchitis has a historical definition: It’s a condition involving cough with excessive sputum production for at least 3 months per year in at least 2 consecutive years. And emphysema is defined anatomically: permanent enlargement of air spaces distal to the terminal bronchiole with alveolar septae destruction.
It’s important to differentiate these conditions, because their guideline-recommended management strategies differ, as do their prognoses, Dr. Cott continued.
In addition to emphysema and chronic bronchitis, other lower airways disorders that can mimic asthma include infection, sarcoidosis, interstitial lung disease, cystic fibrosis, a tumor or foreign body, and bronchiolitis.
The list of upper airways disorders that can be mistaken for asthma includes vocal cord dysfunction, infection, laryngeal spasm, and laryngeal edema secondary to angioedema. The most useful spirometric clue to upper airways obstruction, in Dr. Cott’s view, is a ratio of the forced expiratory flow at 50% volume to forced inspiratory volume at 50% of 1 or greater.
"That’s virtually always present with upper airway or extrathoracic airways obstruction," he said.
Dr. Cott reported having no conflicts of interest.
KEYSTONE, COLO. – The diagnosis of asthma isn’t as simple as it may seem.
Asthma is a clinical syndrome with no specific diagnostic test. So, the response to therapy becomes a key element in finalizing the diagnosis, Dr. Gary R. Cott emphasized at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
"If you have features that make you think of asthma, particularly mild to moderate asthma, and you initiate therapy, you should expect a therapeutic response in 80%-85% of cases. If you don’t get a response, step back and think about whether you made the right diagnosis before you start escalating care," advised Dr. Cott, a pulmonologist and executive vice president of medical and clinical services at National Jewish Health, Denver.
How often do physicians on the front lines get the diagnosis of asthma wrong? The National Jewish experience is illuminating.
In a series of 305 consecutive patients referred to the tertiary center with a preestablished diagnosis of asthma, all of whom were already on treatment for the disease, fully 25% didn’t have asthma at all. A mere 5% were found to have asthma only. A total of 38% had asthma plus an associated contributory respiratory condition, such as allergic rhinitis, rhinosinusitis, or aspirin sensitivity. Another 32% had asthma plus a cardiopulmonary condition that contributed to their symptoms, such as valvular dysfunction, a vascular ring, or pulmonary embolus.
"This experience has been duplicated at other specialty centers. It’s not unique to what we see," according to Dr. Cott.
He defined asthma as a syndrome characterized by increased airway responsiveness to various stimuli, along with variable obstruction of expiratory flow. It’s a physiologic definition. Four elements are essential in establishing the diagnosis: the history, physical exam, spirometry, and response to therapy. A variety of other tests are often helpful in narrowing the differential diagnosis – for example, chest imaging, blood eosinophil measurement, allergy testing, bronchial challenges, diffusing capacity of the lung for carbon monoxide, lung volumes, and elasticity. But they’re not specific for asthma.
"All that wheezes is not asthma. But most is," Dr. Cott observed. "I must say, I’m not very critical of the outside docs who send patients in and say, ‘I think they have asthma,’ and we then say, ‘No, they’ve got something else.’ Asthma is a common disorder. In Colorado, as much as 11% of the population can have asthma. It’s probably the most common thing that will cause an otherwise healthy individual to present with recurring or persistent symptoms.
"I think that sometimes leads us down a path – not always incorrect – of thinking, ‘Let’s try treating for asthma,’ " Dr. Cott noted. "The problem is that when they’re not responding, it’s time to rethink the differential carefully."
The list of disorders involving lower airways obstruction that can mimic asthma is extensive. The top two masqueraders are emphysema and chronic bronchitis. What’s more, asthma, emphysema, and chronic bronchitis aren’t mutually exclusive diseases. A given patient can have any two or even all three.
In contrast to asthma, which is defined physiologically, chronic bronchitis has a historical definition: It’s a condition involving cough with excessive sputum production for at least 3 months per year in at least 2 consecutive years. And emphysema is defined anatomically: permanent enlargement of air spaces distal to the terminal bronchiole with alveolar septae destruction.
It’s important to differentiate these conditions, because their guideline-recommended management strategies differ, as do their prognoses, Dr. Cott continued.
In addition to emphysema and chronic bronchitis, other lower airways disorders that can mimic asthma include infection, sarcoidosis, interstitial lung disease, cystic fibrosis, a tumor or foreign body, and bronchiolitis.
The list of upper airways disorders that can be mistaken for asthma includes vocal cord dysfunction, infection, laryngeal spasm, and laryngeal edema secondary to angioedema. The most useful spirometric clue to upper airways obstruction, in Dr. Cott’s view, is a ratio of the forced expiratory flow at 50% volume to forced inspiratory volume at 50% of 1 or greater.
"That’s virtually always present with upper airway or extrathoracic airways obstruction," he said.
Dr. Cott reported having no conflicts of interest.
KEYSTONE, COLO. – The diagnosis of asthma isn’t as simple as it may seem.
Asthma is a clinical syndrome with no specific diagnostic test. So, the response to therapy becomes a key element in finalizing the diagnosis, Dr. Gary R. Cott emphasized at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
"If you have features that make you think of asthma, particularly mild to moderate asthma, and you initiate therapy, you should expect a therapeutic response in 80%-85% of cases. If you don’t get a response, step back and think about whether you made the right diagnosis before you start escalating care," advised Dr. Cott, a pulmonologist and executive vice president of medical and clinical services at National Jewish Health, Denver.
How often do physicians on the front lines get the diagnosis of asthma wrong? The National Jewish experience is illuminating.
In a series of 305 consecutive patients referred to the tertiary center with a preestablished diagnosis of asthma, all of whom were already on treatment for the disease, fully 25% didn’t have asthma at all. A mere 5% were found to have asthma only. A total of 38% had asthma plus an associated contributory respiratory condition, such as allergic rhinitis, rhinosinusitis, or aspirin sensitivity. Another 32% had asthma plus a cardiopulmonary condition that contributed to their symptoms, such as valvular dysfunction, a vascular ring, or pulmonary embolus.
"This experience has been duplicated at other specialty centers. It’s not unique to what we see," according to Dr. Cott.
He defined asthma as a syndrome characterized by increased airway responsiveness to various stimuli, along with variable obstruction of expiratory flow. It’s a physiologic definition. Four elements are essential in establishing the diagnosis: the history, physical exam, spirometry, and response to therapy. A variety of other tests are often helpful in narrowing the differential diagnosis – for example, chest imaging, blood eosinophil measurement, allergy testing, bronchial challenges, diffusing capacity of the lung for carbon monoxide, lung volumes, and elasticity. But they’re not specific for asthma.
"All that wheezes is not asthma. But most is," Dr. Cott observed. "I must say, I’m not very critical of the outside docs who send patients in and say, ‘I think they have asthma,’ and we then say, ‘No, they’ve got something else.’ Asthma is a common disorder. In Colorado, as much as 11% of the population can have asthma. It’s probably the most common thing that will cause an otherwise healthy individual to present with recurring or persistent symptoms.
"I think that sometimes leads us down a path – not always incorrect – of thinking, ‘Let’s try treating for asthma,’ " Dr. Cott noted. "The problem is that when they’re not responding, it’s time to rethink the differential carefully."
The list of disorders involving lower airways obstruction that can mimic asthma is extensive. The top two masqueraders are emphysema and chronic bronchitis. What’s more, asthma, emphysema, and chronic bronchitis aren’t mutually exclusive diseases. A given patient can have any two or even all three.
In contrast to asthma, which is defined physiologically, chronic bronchitis has a historical definition: It’s a condition involving cough with excessive sputum production for at least 3 months per year in at least 2 consecutive years. And emphysema is defined anatomically: permanent enlargement of air spaces distal to the terminal bronchiole with alveolar septae destruction.
It’s important to differentiate these conditions, because their guideline-recommended management strategies differ, as do their prognoses, Dr. Cott continued.
In addition to emphysema and chronic bronchitis, other lower airways disorders that can mimic asthma include infection, sarcoidosis, interstitial lung disease, cystic fibrosis, a tumor or foreign body, and bronchiolitis.
The list of upper airways disorders that can be mistaken for asthma includes vocal cord dysfunction, infection, laryngeal spasm, and laryngeal edema secondary to angioedema. The most useful spirometric clue to upper airways obstruction, in Dr. Cott’s view, is a ratio of the forced expiratory flow at 50% volume to forced inspiratory volume at 50% of 1 or greater.
"That’s virtually always present with upper airway or extrathoracic airways obstruction," he said.
Dr. Cott reported having no conflicts of interest.
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE
Plugging the practice gaps in pediatric acne therapy
WAIKOLOA, HAWAII – A major impetus behind the first-ever evidence-based guidelines on the management of pediatric acne was to close significant practice gaps identified between what the acne experts recommend and what many clinicians do, according to the lead author of the guidelines.
"One of the points we wanted both dermatologists and primary care physicians to be aware of is that when you see acne in a 7- to 10-year-old, it’s predictive of much worse acne years later. That has been underappreciated," Dr. Lawrence F. Eichenfield said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation (SDEF).
"It used to be said that you didn’t need to start worrying about acne until age 12, but the data shows that acne is now incredibly common in 8-, 9-, and 10-year-olds. There is clear evidence that puberty is occurring earlier, and acne is, too. Acne can be the first sign of normal puberty, starting as young as 7 years of age," he observed.
Another point the guidelines panel sought to publicize: While the traditional view has been that scarring acne comes from deep nodular and nodulocystic lesions, new data suggest that’s not the case. Plenty of patients with acne scars never had nodulocystic acne, nor did they pick at their lesions, Dr. Eichenfield said. Serial imaging studies demonstrate that acne scars don’t necessarily even come from inflammatory acne lesions. Instead, many such scars arise from erythematous red spots, simple papules, or even closed comedones. And scarring isn’t always an adult process; it can occur in pediatric patients.
"If you see evidence of scarring, that may move you to be much more aggressive in your acne therapy. It’s still easier for us to prevent acne scarring than it is to fix it. Prevention is clearly the way to go," observed Dr. Eichenfield, chief of pediatric and adolescent dermatology at Rady Children’s Hospital and professor of clinical pediatrics and medicine at the University of California, San Diego.
He noted that one significant practice gap in acne therapy highlighted in a recent national study involves underutilization of topical retinoids. Investigators analyzed data from the National Ambulatory Medical Care Survey for 2005-2010 and determined that a topical retinoid was prescribed in 41% of acne-related physician visits. Moreover, patients who saw a pediatrician or family physician were 77% less likely to get a prescription for a topical retinoid than those who visited a dermatologist. Older age, male gender, and being on Medicaid were other factors associated with a significantly lower likelihood of receiving a prescription for a topical retinoid (J. Dermatol. Treat. 2014; 25:110-4).
That 41% rate for topical retinoids is much too low, according to Dr. Eichenfield. The recent guidelines emphasize that topical retinoids are useful as monotherapy or in fixed-combination products in treating acne of all types and severities in children and adolescents of all ages.
Another recent study that focused on national treatment patterns for acne in 7- to 12-year-olds, found striking differences according to physician specialty. The top three medications prescribed by dermatologists in these preadolescent patients were the topical retinoid adapalene in 35.9%, benzoyl peroxide in 16.9%, and the topical retinoid tretinoin in 16.1%. In contrast, the top three prescribed by pediatricians and family physicians were minocycline in 13.4%, oral clindamycin in 10.5%, and tretinoin in 10.5% (Pediatr. Dermatol. 2013;30:689-94). The fairly common use of oral clindamycin for acne documented in this study is disturbing; acne experts almost never use that drug because there are other oral antibiotic options with much better safety profiles, Dr. Eichenfield said.
The guidelines (Pediatrics 2013;131:S163-86), which were developed by the American Acne and Rosacea Society and endorsed by the American Academy of Pediatrics, contain detailed acne treatment algorithms. Among the key points:
• Topical antibiotics are not recommended as monotherapy for acne for longer than a few weeks because of the risk of inducing bacterial resistance. Beyond several weeks, topical benzoyl peroxide should be added, because it has a potent antimicrobial effect across a broad range of organisms and it does not promote bacterial resistance.
• The guidelines recommend oral antibiotics as appropriate for moderate to severe acne at any age, but not as monotherapy because of the growing threat posed by global antibiotic resistance. Instead, oral antibiotics should always be used with topical retinoids and usually in conjunction with benzoyl peroxide. The patient should be using the retinoid when starting the oral antibiotic so that when the oral antibiotic is discontinued, usually after a few months, the topical agent can assume a key role in maintaining remission.
• The second-generation oral tetracyclines, doxycycline and minocycline, are sometimes preferable to tetracycline because of their greater ease of use, better absorption, and less frequent dosing. But none of these drugs should be used in children under age 8, for whom the options are erythromycin, azithromycin, and trimethoprim/sulfamethoxazole.
• Combined oral contraceptives are useful as second-line therapy in pubertal girls with moderate to severe acne after assessment for tobacco use and family history of thromboembolic events. Because of concerns about possible deleterious effects on growth and bone density, however, it’s worth considering withholding oral contraceptives for acne until 1 year after onset of menstruation.
• First-line therapy for severe acne is an oral antibiotic in combination with a topical retinoid, benzoyl peroxide, and sometimes a topical antibiotic as well.
"I know there’s a practice gap there because some dermatologists like to go straight to oral isotretinoin. But many acne experts feel that the use of an oral cycline-based antibiotic is highly useful prior to initiating isotretinoin, because the anti-inflammatory effect helps minimize the severe flares we sometimes get with initiation of isotretinoin," Dr. Eichenfield explained.
SDEF and this news organization are owned by the same parent company.
Dr. Eichenfield reported having served as a clinical investigator and/or consultant to Allergan, Galderma, GlaxoSmithKline (Stiefel), and Medicis/Valeant.
WAIKOLOA, HAWAII – A major impetus behind the first-ever evidence-based guidelines on the management of pediatric acne was to close significant practice gaps identified between what the acne experts recommend and what many clinicians do, according to the lead author of the guidelines.
"One of the points we wanted both dermatologists and primary care physicians to be aware of is that when you see acne in a 7- to 10-year-old, it’s predictive of much worse acne years later. That has been underappreciated," Dr. Lawrence F. Eichenfield said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation (SDEF).
"It used to be said that you didn’t need to start worrying about acne until age 12, but the data shows that acne is now incredibly common in 8-, 9-, and 10-year-olds. There is clear evidence that puberty is occurring earlier, and acne is, too. Acne can be the first sign of normal puberty, starting as young as 7 years of age," he observed.
Another point the guidelines panel sought to publicize: While the traditional view has been that scarring acne comes from deep nodular and nodulocystic lesions, new data suggest that’s not the case. Plenty of patients with acne scars never had nodulocystic acne, nor did they pick at their lesions, Dr. Eichenfield said. Serial imaging studies demonstrate that acne scars don’t necessarily even come from inflammatory acne lesions. Instead, many such scars arise from erythematous red spots, simple papules, or even closed comedones. And scarring isn’t always an adult process; it can occur in pediatric patients.
"If you see evidence of scarring, that may move you to be much more aggressive in your acne therapy. It’s still easier for us to prevent acne scarring than it is to fix it. Prevention is clearly the way to go," observed Dr. Eichenfield, chief of pediatric and adolescent dermatology at Rady Children’s Hospital and professor of clinical pediatrics and medicine at the University of California, San Diego.
He noted that one significant practice gap in acne therapy highlighted in a recent national study involves underutilization of topical retinoids. Investigators analyzed data from the National Ambulatory Medical Care Survey for 2005-2010 and determined that a topical retinoid was prescribed in 41% of acne-related physician visits. Moreover, patients who saw a pediatrician or family physician were 77% less likely to get a prescription for a topical retinoid than those who visited a dermatologist. Older age, male gender, and being on Medicaid were other factors associated with a significantly lower likelihood of receiving a prescription for a topical retinoid (J. Dermatol. Treat. 2014; 25:110-4).
That 41% rate for topical retinoids is much too low, according to Dr. Eichenfield. The recent guidelines emphasize that topical retinoids are useful as monotherapy or in fixed-combination products in treating acne of all types and severities in children and adolescents of all ages.
Another recent study that focused on national treatment patterns for acne in 7- to 12-year-olds, found striking differences according to physician specialty. The top three medications prescribed by dermatologists in these preadolescent patients were the topical retinoid adapalene in 35.9%, benzoyl peroxide in 16.9%, and the topical retinoid tretinoin in 16.1%. In contrast, the top three prescribed by pediatricians and family physicians were minocycline in 13.4%, oral clindamycin in 10.5%, and tretinoin in 10.5% (Pediatr. Dermatol. 2013;30:689-94). The fairly common use of oral clindamycin for acne documented in this study is disturbing; acne experts almost never use that drug because there are other oral antibiotic options with much better safety profiles, Dr. Eichenfield said.
The guidelines (Pediatrics 2013;131:S163-86), which were developed by the American Acne and Rosacea Society and endorsed by the American Academy of Pediatrics, contain detailed acne treatment algorithms. Among the key points:
• Topical antibiotics are not recommended as monotherapy for acne for longer than a few weeks because of the risk of inducing bacterial resistance. Beyond several weeks, topical benzoyl peroxide should be added, because it has a potent antimicrobial effect across a broad range of organisms and it does not promote bacterial resistance.
• The guidelines recommend oral antibiotics as appropriate for moderate to severe acne at any age, but not as monotherapy because of the growing threat posed by global antibiotic resistance. Instead, oral antibiotics should always be used with topical retinoids and usually in conjunction with benzoyl peroxide. The patient should be using the retinoid when starting the oral antibiotic so that when the oral antibiotic is discontinued, usually after a few months, the topical agent can assume a key role in maintaining remission.
• The second-generation oral tetracyclines, doxycycline and minocycline, are sometimes preferable to tetracycline because of their greater ease of use, better absorption, and less frequent dosing. But none of these drugs should be used in children under age 8, for whom the options are erythromycin, azithromycin, and trimethoprim/sulfamethoxazole.
• Combined oral contraceptives are useful as second-line therapy in pubertal girls with moderate to severe acne after assessment for tobacco use and family history of thromboembolic events. Because of concerns about possible deleterious effects on growth and bone density, however, it’s worth considering withholding oral contraceptives for acne until 1 year after onset of menstruation.
• First-line therapy for severe acne is an oral antibiotic in combination with a topical retinoid, benzoyl peroxide, and sometimes a topical antibiotic as well.
"I know there’s a practice gap there because some dermatologists like to go straight to oral isotretinoin. But many acne experts feel that the use of an oral cycline-based antibiotic is highly useful prior to initiating isotretinoin, because the anti-inflammatory effect helps minimize the severe flares we sometimes get with initiation of isotretinoin," Dr. Eichenfield explained.
SDEF and this news organization are owned by the same parent company.
Dr. Eichenfield reported having served as a clinical investigator and/or consultant to Allergan, Galderma, GlaxoSmithKline (Stiefel), and Medicis/Valeant.
WAIKOLOA, HAWAII – A major impetus behind the first-ever evidence-based guidelines on the management of pediatric acne was to close significant practice gaps identified between what the acne experts recommend and what many clinicians do, according to the lead author of the guidelines.
"One of the points we wanted both dermatologists and primary care physicians to be aware of is that when you see acne in a 7- to 10-year-old, it’s predictive of much worse acne years later. That has been underappreciated," Dr. Lawrence F. Eichenfield said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation (SDEF).
"It used to be said that you didn’t need to start worrying about acne until age 12, but the data shows that acne is now incredibly common in 8-, 9-, and 10-year-olds. There is clear evidence that puberty is occurring earlier, and acne is, too. Acne can be the first sign of normal puberty, starting as young as 7 years of age," he observed.
Another point the guidelines panel sought to publicize: While the traditional view has been that scarring acne comes from deep nodular and nodulocystic lesions, new data suggest that’s not the case. Plenty of patients with acne scars never had nodulocystic acne, nor did they pick at their lesions, Dr. Eichenfield said. Serial imaging studies demonstrate that acne scars don’t necessarily even come from inflammatory acne lesions. Instead, many such scars arise from erythematous red spots, simple papules, or even closed comedones. And scarring isn’t always an adult process; it can occur in pediatric patients.
"If you see evidence of scarring, that may move you to be much more aggressive in your acne therapy. It’s still easier for us to prevent acne scarring than it is to fix it. Prevention is clearly the way to go," observed Dr. Eichenfield, chief of pediatric and adolescent dermatology at Rady Children’s Hospital and professor of clinical pediatrics and medicine at the University of California, San Diego.
He noted that one significant practice gap in acne therapy highlighted in a recent national study involves underutilization of topical retinoids. Investigators analyzed data from the National Ambulatory Medical Care Survey for 2005-2010 and determined that a topical retinoid was prescribed in 41% of acne-related physician visits. Moreover, patients who saw a pediatrician or family physician were 77% less likely to get a prescription for a topical retinoid than those who visited a dermatologist. Older age, male gender, and being on Medicaid were other factors associated with a significantly lower likelihood of receiving a prescription for a topical retinoid (J. Dermatol. Treat. 2014; 25:110-4).
That 41% rate for topical retinoids is much too low, according to Dr. Eichenfield. The recent guidelines emphasize that topical retinoids are useful as monotherapy or in fixed-combination products in treating acne of all types and severities in children and adolescents of all ages.
Another recent study that focused on national treatment patterns for acne in 7- to 12-year-olds, found striking differences according to physician specialty. The top three medications prescribed by dermatologists in these preadolescent patients were the topical retinoid adapalene in 35.9%, benzoyl peroxide in 16.9%, and the topical retinoid tretinoin in 16.1%. In contrast, the top three prescribed by pediatricians and family physicians were minocycline in 13.4%, oral clindamycin in 10.5%, and tretinoin in 10.5% (Pediatr. Dermatol. 2013;30:689-94). The fairly common use of oral clindamycin for acne documented in this study is disturbing; acne experts almost never use that drug because there are other oral antibiotic options with much better safety profiles, Dr. Eichenfield said.
The guidelines (Pediatrics 2013;131:S163-86), which were developed by the American Acne and Rosacea Society and endorsed by the American Academy of Pediatrics, contain detailed acne treatment algorithms. Among the key points:
• Topical antibiotics are not recommended as monotherapy for acne for longer than a few weeks because of the risk of inducing bacterial resistance. Beyond several weeks, topical benzoyl peroxide should be added, because it has a potent antimicrobial effect across a broad range of organisms and it does not promote bacterial resistance.
• The guidelines recommend oral antibiotics as appropriate for moderate to severe acne at any age, but not as monotherapy because of the growing threat posed by global antibiotic resistance. Instead, oral antibiotics should always be used with topical retinoids and usually in conjunction with benzoyl peroxide. The patient should be using the retinoid when starting the oral antibiotic so that when the oral antibiotic is discontinued, usually after a few months, the topical agent can assume a key role in maintaining remission.
• The second-generation oral tetracyclines, doxycycline and minocycline, are sometimes preferable to tetracycline because of their greater ease of use, better absorption, and less frequent dosing. But none of these drugs should be used in children under age 8, for whom the options are erythromycin, azithromycin, and trimethoprim/sulfamethoxazole.
• Combined oral contraceptives are useful as second-line therapy in pubertal girls with moderate to severe acne after assessment for tobacco use and family history of thromboembolic events. Because of concerns about possible deleterious effects on growth and bone density, however, it’s worth considering withholding oral contraceptives for acne until 1 year after onset of menstruation.
• First-line therapy for severe acne is an oral antibiotic in combination with a topical retinoid, benzoyl peroxide, and sometimes a topical antibiotic as well.
"I know there’s a practice gap there because some dermatologists like to go straight to oral isotretinoin. But many acne experts feel that the use of an oral cycline-based antibiotic is highly useful prior to initiating isotretinoin, because the anti-inflammatory effect helps minimize the severe flares we sometimes get with initiation of isotretinoin," Dr. Eichenfield explained.
SDEF and this news organization are owned by the same parent company.
Dr. Eichenfield reported having served as a clinical investigator and/or consultant to Allergan, Galderma, GlaxoSmithKline (Stiefel), and Medicis/Valeant.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Frailty assessment central to TAVR decision
SNOWMASS, COLO. – Transcatheter aortic valve replacement in nonsurgical candidates with severe symptomatic aortic stenosis carries a hefty price tag of $116,500 per quality-adjusted life-year gained over medical management.
That’s the bottom line in a cost-effectiveness study led by cardiologist Dr. Mark A. Hlatky. The investigators applied data on the costs and benefits of transfemoral transcatheter aortic valve replacement (TAVR) as documented in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial in their Markov model involving a hypothetical patient cohort. The estimated incremental cost-effectiveness of $116,500 per quality-adjusted life-year gained is well in excess of the $50,000 figure widely accepted by health policy makers as defining a cutoff for cost-effective therapy.
In this cost-effectiveness analysis (Circ. Cardiovasc. Qual. Outcomes 2013;6:419-28), TAVR boosted life expectancy by roughly 11 months, from 2.08 years with medical therapy to 2.93 years. Quality-adjusted life expectancy rose from 1.19 to 1.93 years. TAVR also resulted in 1.4 fewer hospitalizations than with medical management. However, undergoing TAVR rather than medical management raised the lifetime stroke risk from 1% to 11% and increased lifetime health care costs from $83,600 to $169,100, reported the group led by Dr. Hlatky, professor of health research and policy and also professor of medicine at Stanford (Calif.) University.
"This is a fascinating study," Dr. Karen P. Alexander said at the Annual Cardiovascular Conference at Snowmass. "I think the lesson here is that futility from a cost perspective is also something that should be in the discussion" regarding TAVR vs. medical therapy in patients with inoperable aortic stenosis.
She highlighted the Hlatky study in discussing the key role frailty assessment plays in considering TAVR. The study showed that the cost-effectiveness of TAVR is greater in patients with a lower burden of noncardiac disease, which is another way saying "those who are less frail."
This conclusion underscores a statement in the 2012 American College of Cardiology/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons expert consensus document on TAVR paraphrased by Dr. Alexander: Frailty will assume central importance in patient selection for TAVR by virtue of the extensive comorbidities in this population. Existing models do not have predictive variables of interest in high-risk patients. (J. Am. Coll. Cardiol. 2012;59:1200-54).
Dr. Alexander of Duke University in Durham, N.C., said frailty is important when considering TAVR because it has been shown to be associated with increased rates of post-TAVR 30-day morbidity and mortality, prolonged hospital length of stay, and 1-year mortality.
She defined frailty as a multisystem impairment resulting in reduced physiologic reserve and increased vulnerability to stress. Frailty is a physiologic phenotype associated with slow gait, weakness, weight loss, exhaustion, and a low daily activity level.
While the degree of a patient’s frailty is an important consideration in deciding on TAVR vs. medical management, frailty per se is no contraindication to the procedure. Indeed, the prevalence of frailty as defined simply by a baseline 5-meter walk time in excess of 6 seconds was 72% among the 7,710 TAVR patients, mean age 84 years, included in the recent first report of the comprehensive national STS/ACC Transcatheter Valve Therapy Registry (JAMA 2013;310:2069-77). That’s nearly twice the 38% prevalence among community-dwelling 85-year-olds, Dr. Alexander noted, citing data from the Canadian Study of Health and Aging (CMAJ 2011;183:e487-94).
More than 20 different frailty risk scores are now in circulation. Dr. Alexander is particularly enthusiastic about the frailty risk tool developed as part of the ACC’s new Championing Care for the Patient With Aortic Stenosis Initiative. It efficiently assesses five domains of frailty – slowness, weakness, malnutrition, inactivity with loss of independence, and malnutrition – and generates a clinically useful qualitative frailty rating. A patient with a high frailty score may not have sufficient life expectancy to obtain the benefits of TAVR.
With regard to treatment futility, Dr. Alexander observed that it can be defined as either lack of medical efficacy as judged by physicians or as lack of meaningful survival as judged by a patient’s personal values. Yet one in four Americans aged 75 years or older has given little or no thought to their own wishes for end-of-life medical therapy, according to a recent Pew Research Center survey.
The telephone survey, conducted last spring, included a representative sample of 1,994 U.S. adults. While 47% of respondents aged 75 years or older indicated they had given their own wishes for end-of-life medical care a great deal of thought, 25% said they had given the matter "not much or none." Reflection on those personal wishes needs to be part of the physician/patient discussion about TAVR, according to Dr. Alexander.
With regard to general views on end-of-life therapy, 74% of surveyed individuals age 75 and up declared there should be circumstances in which a patient should be allowed to die. Another 22% said medical staff should do everything possible to save a patient’s life under all circumstances.
Dr. Alexander reported serving as a consultant to Gilead and Pozen.
SNOWMASS, COLO. – Transcatheter aortic valve replacement in nonsurgical candidates with severe symptomatic aortic stenosis carries a hefty price tag of $116,500 per quality-adjusted life-year gained over medical management.
That’s the bottom line in a cost-effectiveness study led by cardiologist Dr. Mark A. Hlatky. The investigators applied data on the costs and benefits of transfemoral transcatheter aortic valve replacement (TAVR) as documented in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial in their Markov model involving a hypothetical patient cohort. The estimated incremental cost-effectiveness of $116,500 per quality-adjusted life-year gained is well in excess of the $50,000 figure widely accepted by health policy makers as defining a cutoff for cost-effective therapy.
In this cost-effectiveness analysis (Circ. Cardiovasc. Qual. Outcomes 2013;6:419-28), TAVR boosted life expectancy by roughly 11 months, from 2.08 years with medical therapy to 2.93 years. Quality-adjusted life expectancy rose from 1.19 to 1.93 years. TAVR also resulted in 1.4 fewer hospitalizations than with medical management. However, undergoing TAVR rather than medical management raised the lifetime stroke risk from 1% to 11% and increased lifetime health care costs from $83,600 to $169,100, reported the group led by Dr. Hlatky, professor of health research and policy and also professor of medicine at Stanford (Calif.) University.
"This is a fascinating study," Dr. Karen P. Alexander said at the Annual Cardiovascular Conference at Snowmass. "I think the lesson here is that futility from a cost perspective is also something that should be in the discussion" regarding TAVR vs. medical therapy in patients with inoperable aortic stenosis.
She highlighted the Hlatky study in discussing the key role frailty assessment plays in considering TAVR. The study showed that the cost-effectiveness of TAVR is greater in patients with a lower burden of noncardiac disease, which is another way saying "those who are less frail."
This conclusion underscores a statement in the 2012 American College of Cardiology/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons expert consensus document on TAVR paraphrased by Dr. Alexander: Frailty will assume central importance in patient selection for TAVR by virtue of the extensive comorbidities in this population. Existing models do not have predictive variables of interest in high-risk patients. (J. Am. Coll. Cardiol. 2012;59:1200-54).
Dr. Alexander of Duke University in Durham, N.C., said frailty is important when considering TAVR because it has been shown to be associated with increased rates of post-TAVR 30-day morbidity and mortality, prolonged hospital length of stay, and 1-year mortality.
She defined frailty as a multisystem impairment resulting in reduced physiologic reserve and increased vulnerability to stress. Frailty is a physiologic phenotype associated with slow gait, weakness, weight loss, exhaustion, and a low daily activity level.
While the degree of a patient’s frailty is an important consideration in deciding on TAVR vs. medical management, frailty per se is no contraindication to the procedure. Indeed, the prevalence of frailty as defined simply by a baseline 5-meter walk time in excess of 6 seconds was 72% among the 7,710 TAVR patients, mean age 84 years, included in the recent first report of the comprehensive national STS/ACC Transcatheter Valve Therapy Registry (JAMA 2013;310:2069-77). That’s nearly twice the 38% prevalence among community-dwelling 85-year-olds, Dr. Alexander noted, citing data from the Canadian Study of Health and Aging (CMAJ 2011;183:e487-94).
More than 20 different frailty risk scores are now in circulation. Dr. Alexander is particularly enthusiastic about the frailty risk tool developed as part of the ACC’s new Championing Care for the Patient With Aortic Stenosis Initiative. It efficiently assesses five domains of frailty – slowness, weakness, malnutrition, inactivity with loss of independence, and malnutrition – and generates a clinically useful qualitative frailty rating. A patient with a high frailty score may not have sufficient life expectancy to obtain the benefits of TAVR.
With regard to treatment futility, Dr. Alexander observed that it can be defined as either lack of medical efficacy as judged by physicians or as lack of meaningful survival as judged by a patient’s personal values. Yet one in four Americans aged 75 years or older has given little or no thought to their own wishes for end-of-life medical therapy, according to a recent Pew Research Center survey.
The telephone survey, conducted last spring, included a representative sample of 1,994 U.S. adults. While 47% of respondents aged 75 years or older indicated they had given their own wishes for end-of-life medical care a great deal of thought, 25% said they had given the matter "not much or none." Reflection on those personal wishes needs to be part of the physician/patient discussion about TAVR, according to Dr. Alexander.
With regard to general views on end-of-life therapy, 74% of surveyed individuals age 75 and up declared there should be circumstances in which a patient should be allowed to die. Another 22% said medical staff should do everything possible to save a patient’s life under all circumstances.
Dr. Alexander reported serving as a consultant to Gilead and Pozen.
SNOWMASS, COLO. – Transcatheter aortic valve replacement in nonsurgical candidates with severe symptomatic aortic stenosis carries a hefty price tag of $116,500 per quality-adjusted life-year gained over medical management.
That’s the bottom line in a cost-effectiveness study led by cardiologist Dr. Mark A. Hlatky. The investigators applied data on the costs and benefits of transfemoral transcatheter aortic valve replacement (TAVR) as documented in the landmark PARTNER (Placement of Aortic Transcatheter Valves) trial in their Markov model involving a hypothetical patient cohort. The estimated incremental cost-effectiveness of $116,500 per quality-adjusted life-year gained is well in excess of the $50,000 figure widely accepted by health policy makers as defining a cutoff for cost-effective therapy.
In this cost-effectiveness analysis (Circ. Cardiovasc. Qual. Outcomes 2013;6:419-28), TAVR boosted life expectancy by roughly 11 months, from 2.08 years with medical therapy to 2.93 years. Quality-adjusted life expectancy rose from 1.19 to 1.93 years. TAVR also resulted in 1.4 fewer hospitalizations than with medical management. However, undergoing TAVR rather than medical management raised the lifetime stroke risk from 1% to 11% and increased lifetime health care costs from $83,600 to $169,100, reported the group led by Dr. Hlatky, professor of health research and policy and also professor of medicine at Stanford (Calif.) University.
"This is a fascinating study," Dr. Karen P. Alexander said at the Annual Cardiovascular Conference at Snowmass. "I think the lesson here is that futility from a cost perspective is also something that should be in the discussion" regarding TAVR vs. medical therapy in patients with inoperable aortic stenosis.
She highlighted the Hlatky study in discussing the key role frailty assessment plays in considering TAVR. The study showed that the cost-effectiveness of TAVR is greater in patients with a lower burden of noncardiac disease, which is another way saying "those who are less frail."
This conclusion underscores a statement in the 2012 American College of Cardiology/American Association for Thoracic Surgery/Society for Cardiovascular Angiography and Interventions/Society of Thoracic Surgeons expert consensus document on TAVR paraphrased by Dr. Alexander: Frailty will assume central importance in patient selection for TAVR by virtue of the extensive comorbidities in this population. Existing models do not have predictive variables of interest in high-risk patients. (J. Am. Coll. Cardiol. 2012;59:1200-54).
Dr. Alexander of Duke University in Durham, N.C., said frailty is important when considering TAVR because it has been shown to be associated with increased rates of post-TAVR 30-day morbidity and mortality, prolonged hospital length of stay, and 1-year mortality.
She defined frailty as a multisystem impairment resulting in reduced physiologic reserve and increased vulnerability to stress. Frailty is a physiologic phenotype associated with slow gait, weakness, weight loss, exhaustion, and a low daily activity level.
While the degree of a patient’s frailty is an important consideration in deciding on TAVR vs. medical management, frailty per se is no contraindication to the procedure. Indeed, the prevalence of frailty as defined simply by a baseline 5-meter walk time in excess of 6 seconds was 72% among the 7,710 TAVR patients, mean age 84 years, included in the recent first report of the comprehensive national STS/ACC Transcatheter Valve Therapy Registry (JAMA 2013;310:2069-77). That’s nearly twice the 38% prevalence among community-dwelling 85-year-olds, Dr. Alexander noted, citing data from the Canadian Study of Health and Aging (CMAJ 2011;183:e487-94).
More than 20 different frailty risk scores are now in circulation. Dr. Alexander is particularly enthusiastic about the frailty risk tool developed as part of the ACC’s new Championing Care for the Patient With Aortic Stenosis Initiative. It efficiently assesses five domains of frailty – slowness, weakness, malnutrition, inactivity with loss of independence, and malnutrition – and generates a clinically useful qualitative frailty rating. A patient with a high frailty score may not have sufficient life expectancy to obtain the benefits of TAVR.
With regard to treatment futility, Dr. Alexander observed that it can be defined as either lack of medical efficacy as judged by physicians or as lack of meaningful survival as judged by a patient’s personal values. Yet one in four Americans aged 75 years or older has given little or no thought to their own wishes for end-of-life medical therapy, according to a recent Pew Research Center survey.
The telephone survey, conducted last spring, included a representative sample of 1,994 U.S. adults. While 47% of respondents aged 75 years or older indicated they had given their own wishes for end-of-life medical care a great deal of thought, 25% said they had given the matter "not much or none." Reflection on those personal wishes needs to be part of the physician/patient discussion about TAVR, according to Dr. Alexander.
With regard to general views on end-of-life therapy, 74% of surveyed individuals age 75 and up declared there should be circumstances in which a patient should be allowed to die. Another 22% said medical staff should do everything possible to save a patient’s life under all circumstances.
Dr. Alexander reported serving as a consultant to Gilead and Pozen.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
What’s new in non-STEMI management
SNOWMASS, COLO. – An early invasive strategy is particularly beneficial in octogenarians with non–ST-segment elevation myocardial infarction, according to a recent study involving close to 1 million NSTEMI patients aged 80 years or older.
The very eldest are an understudied segment of the NSTEMI population, for whom an initial conservative strategy has been the dominant approach in daily practice.
"This is an important study. We can see that as you get older and older, by virtue of the fact that you have more and more coronary disease, probably you’re going to be better off with an invasive strategy, all other things being equal," Dr. David R. Holmes Jr. commented in highlighting the study at the Annual Cardiovascular Conference at Snowmass.
The study included 968,542 octogenarians hospitalized with NSTEMI during 2003-2010 and entered into the Nationwide Inpatient Sample. Eighty-three percent were managed via an initial conservative approach, with coronary angiography performed only in the event of hemodynamic or electrical instability, refractory angina despite optimal medical therapy, or a test result indicative of high risk. The other 17% underwent an early invasive approach, with angiography within 48 hours of presentation.
Octogenarians managed via an early invasive strategy were more often younger, obese, smokers, dyslipidemic, hypertensive, white, and male, and more likely to have known vascular disease. In a multivariate analysis adjusted for potential confounders, the early invasive strategy group had a 34% reduction in in-hospital mortality compared with the conservatively managed group. They also had a 37% lower rate of acute ischemic stroke, a 40% reduction in intracranial hemorrhage, a 37% lower risk of gastrointestinal bleeding, and a shorter length of stay by an average of half a day. On the other side of the ledger, they had a 2.1-fold increased rate of cardiogenic shock (Am. J. Med. 2013;126:1076-83).
Does time to cath lab matter?
Another recent study looked at the optimal time frame for taking an NSTEMI patient to the cardiac catheterization laboratory as part of an invasive strategy. This was a meta-analysis of seven randomized controlled trials totaling 5,370 NSTEMI patients, along with four observational studies with more than 77,000 NSTEMI patients. The conclusion: There is as yet no persuasive evidence that the time interval makes a difference in outcomes (Ann. Intern. Med. 2013;158:261-70).
"That’s the data that’s available. It doesn’t matter how quickly you get the patient to the cath lab within that first period of time. You just need to take them, whether it’s in 2 hours, 6 hours, or 18 hours," Dr. Holmes said.
This has important implications as we think about systems of care. If somebody comes into the hospital late on a Friday night, do you have to take them to the cath lab Friday night, or can you wait electively and take them tomorrow or potentially even Monday morning when everybody’s there?" commented Dr. Holmes, professor of medicine at the Mayo Clinic in Rochester, Minn.
GRACE and CRUSADE
The cornerstone of decision making as to whether to opt for an invasive versus a conservative strategy in a given NSTEMI patient involves application of a formal risk score. A plethora of these risk scoring systems are in use today. Which is the best choice for a cardiologist as an aid to decision making? A meta-analysis involving 36 studies with nearly 117,000 NSTEMI patients has concluded that the GRACE (Global Registry of Acute Cardiac Events) risk score (JAMA 2004;291:2727-33) is the best of the pack. It significantly outperformed the TIMI score, which is the other widely used scoring system, as well as others less widely known (Contemp. Clin. Trials 2012:33:507-14).
"GRACE looks like it performs better. We’ll need better ones in the future, of course. But at the present time, select GRACE for risk stratification," advised the cardiologist, adding that a Grace score app is available.
Despite the fact that physicians are diagnosing and treating NSTEMI earlier in its course, in large part because of the widespread use of troponin assays in the emergency department, NSTEMI is still associated with substantial long-term morbidity and mortality, particularly in the elderly. This was underscored in a recent analysis of 19,336 NSTEMI patients aged 65 years or older who underwent early catheterization and were included in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry.
Twenty-one percent of patients received medical management alone, 60.8% underwent percutaneous coronary intervention, and 18.2% had coronary artery bypass graft surgery. The 5-year unadjusted all-cause mortality rate was 50% in the medically managed group, 33.5% in older patients who underwent PCI, and 24.2% in those who underwent CABG surgery. The unadjusted 5-year rate of a composite of death, readmission for MI, or readmission for stroke was 62.4% with medical management, 44.9% with PCI, and 33% with CABG. The investigators concluded that long-term outcomes in elderly NSTEMI patients appear to be better in this large registry when revascularization is accomplished via CABG than with PCI. This sets the stage for future confirmatory trials (Circ. Cardiovasc. Qual. Outcomes 2013;6:323-32).
Dr. Holmes noted that the incidence of NSTEMI has climbed steadily while that of STEMI has declined over the past couple of decades, not just in the United States but worldwide. In Australia, for example, during 1993-2010 the adjusted incidence of NSTEMI increased by a whopping 315%, from 67 to 182 cases per 100,000 person-years, while the adjusted incidence of STEMI fell by 30% (Am. J. Cardiol. 2013;112:169-73).
"NSTEMI is clearly an annuity for all of cardiology," Dr. Holmes said. "The growth rate is increasing and it will continue to increase as we get older."
He reported having no conflicts of interest.
These studies collectively offer guidance in key management decisions for an invasive strategy for our NSTEMI patients, namely, the factor of age, the impact of timing, and risk stratification scores. Currently, the "less is more" approach is often taken for octogenarians, but a large sample size from this registry shows better results across a spectrum of outcomes even while adjusting for cofounders. This should prompt a reevaluation of current practice. Although the timing of an invasive approach in STEMI is defined in prior studies, this large meta-analysis tells us that timing in NSTEMI does not correlate with outcomes as long as angiography is pursued at some point in time, a very important conclusion.
Finally, although TIMI scoring systems are used at most institutions, the GRACE score performed even better, a surprising finding.
Taken in sum, these key studies should be followed up by randomized controlled trials to definitively answer these important questions for our NSTEMI patients.
Dr. Hiren Shah is an assistant professor of medicine in the Feinberg School of Medicine, Northwestern University, Chicago, and a medical director of the Medicine and Cardiac Telemetry Hospitalist Unit at Northwestern Memorial Hospital. He is on the advisory board of Hospitalist News.
These studies collectively offer guidance in key management decisions for an invasive strategy for our NSTEMI patients, namely, the factor of age, the impact of timing, and risk stratification scores. Currently, the "less is more" approach is often taken for octogenarians, but a large sample size from this registry shows better results across a spectrum of outcomes even while adjusting for cofounders. This should prompt a reevaluation of current practice. Although the timing of an invasive approach in STEMI is defined in prior studies, this large meta-analysis tells us that timing in NSTEMI does not correlate with outcomes as long as angiography is pursued at some point in time, a very important conclusion.
Finally, although TIMI scoring systems are used at most institutions, the GRACE score performed even better, a surprising finding.
Taken in sum, these key studies should be followed up by randomized controlled trials to definitively answer these important questions for our NSTEMI patients.
Dr. Hiren Shah is an assistant professor of medicine in the Feinberg School of Medicine, Northwestern University, Chicago, and a medical director of the Medicine and Cardiac Telemetry Hospitalist Unit at Northwestern Memorial Hospital. He is on the advisory board of Hospitalist News.
These studies collectively offer guidance in key management decisions for an invasive strategy for our NSTEMI patients, namely, the factor of age, the impact of timing, and risk stratification scores. Currently, the "less is more" approach is often taken for octogenarians, but a large sample size from this registry shows better results across a spectrum of outcomes even while adjusting for cofounders. This should prompt a reevaluation of current practice. Although the timing of an invasive approach in STEMI is defined in prior studies, this large meta-analysis tells us that timing in NSTEMI does not correlate with outcomes as long as angiography is pursued at some point in time, a very important conclusion.
Finally, although TIMI scoring systems are used at most institutions, the GRACE score performed even better, a surprising finding.
Taken in sum, these key studies should be followed up by randomized controlled trials to definitively answer these important questions for our NSTEMI patients.
Dr. Hiren Shah is an assistant professor of medicine in the Feinberg School of Medicine, Northwestern University, Chicago, and a medical director of the Medicine and Cardiac Telemetry Hospitalist Unit at Northwestern Memorial Hospital. He is on the advisory board of Hospitalist News.
SNOWMASS, COLO. – An early invasive strategy is particularly beneficial in octogenarians with non–ST-segment elevation myocardial infarction, according to a recent study involving close to 1 million NSTEMI patients aged 80 years or older.
The very eldest are an understudied segment of the NSTEMI population, for whom an initial conservative strategy has been the dominant approach in daily practice.
"This is an important study. We can see that as you get older and older, by virtue of the fact that you have more and more coronary disease, probably you’re going to be better off with an invasive strategy, all other things being equal," Dr. David R. Holmes Jr. commented in highlighting the study at the Annual Cardiovascular Conference at Snowmass.
The study included 968,542 octogenarians hospitalized with NSTEMI during 2003-2010 and entered into the Nationwide Inpatient Sample. Eighty-three percent were managed via an initial conservative approach, with coronary angiography performed only in the event of hemodynamic or electrical instability, refractory angina despite optimal medical therapy, or a test result indicative of high risk. The other 17% underwent an early invasive approach, with angiography within 48 hours of presentation.
Octogenarians managed via an early invasive strategy were more often younger, obese, smokers, dyslipidemic, hypertensive, white, and male, and more likely to have known vascular disease. In a multivariate analysis adjusted for potential confounders, the early invasive strategy group had a 34% reduction in in-hospital mortality compared with the conservatively managed group. They also had a 37% lower rate of acute ischemic stroke, a 40% reduction in intracranial hemorrhage, a 37% lower risk of gastrointestinal bleeding, and a shorter length of stay by an average of half a day. On the other side of the ledger, they had a 2.1-fold increased rate of cardiogenic shock (Am. J. Med. 2013;126:1076-83).
Does time to cath lab matter?
Another recent study looked at the optimal time frame for taking an NSTEMI patient to the cardiac catheterization laboratory as part of an invasive strategy. This was a meta-analysis of seven randomized controlled trials totaling 5,370 NSTEMI patients, along with four observational studies with more than 77,000 NSTEMI patients. The conclusion: There is as yet no persuasive evidence that the time interval makes a difference in outcomes (Ann. Intern. Med. 2013;158:261-70).
"That’s the data that’s available. It doesn’t matter how quickly you get the patient to the cath lab within that first period of time. You just need to take them, whether it’s in 2 hours, 6 hours, or 18 hours," Dr. Holmes said.
This has important implications as we think about systems of care. If somebody comes into the hospital late on a Friday night, do you have to take them to the cath lab Friday night, or can you wait electively and take them tomorrow or potentially even Monday morning when everybody’s there?" commented Dr. Holmes, professor of medicine at the Mayo Clinic in Rochester, Minn.
GRACE and CRUSADE
The cornerstone of decision making as to whether to opt for an invasive versus a conservative strategy in a given NSTEMI patient involves application of a formal risk score. A plethora of these risk scoring systems are in use today. Which is the best choice for a cardiologist as an aid to decision making? A meta-analysis involving 36 studies with nearly 117,000 NSTEMI patients has concluded that the GRACE (Global Registry of Acute Cardiac Events) risk score (JAMA 2004;291:2727-33) is the best of the pack. It significantly outperformed the TIMI score, which is the other widely used scoring system, as well as others less widely known (Contemp. Clin. Trials 2012:33:507-14).
"GRACE looks like it performs better. We’ll need better ones in the future, of course. But at the present time, select GRACE for risk stratification," advised the cardiologist, adding that a Grace score app is available.
Despite the fact that physicians are diagnosing and treating NSTEMI earlier in its course, in large part because of the widespread use of troponin assays in the emergency department, NSTEMI is still associated with substantial long-term morbidity and mortality, particularly in the elderly. This was underscored in a recent analysis of 19,336 NSTEMI patients aged 65 years or older who underwent early catheterization and were included in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry.
Twenty-one percent of patients received medical management alone, 60.8% underwent percutaneous coronary intervention, and 18.2% had coronary artery bypass graft surgery. The 5-year unadjusted all-cause mortality rate was 50% in the medically managed group, 33.5% in older patients who underwent PCI, and 24.2% in those who underwent CABG surgery. The unadjusted 5-year rate of a composite of death, readmission for MI, or readmission for stroke was 62.4% with medical management, 44.9% with PCI, and 33% with CABG. The investigators concluded that long-term outcomes in elderly NSTEMI patients appear to be better in this large registry when revascularization is accomplished via CABG than with PCI. This sets the stage for future confirmatory trials (Circ. Cardiovasc. Qual. Outcomes 2013;6:323-32).
Dr. Holmes noted that the incidence of NSTEMI has climbed steadily while that of STEMI has declined over the past couple of decades, not just in the United States but worldwide. In Australia, for example, during 1993-2010 the adjusted incidence of NSTEMI increased by a whopping 315%, from 67 to 182 cases per 100,000 person-years, while the adjusted incidence of STEMI fell by 30% (Am. J. Cardiol. 2013;112:169-73).
"NSTEMI is clearly an annuity for all of cardiology," Dr. Holmes said. "The growth rate is increasing and it will continue to increase as we get older."
He reported having no conflicts of interest.
SNOWMASS, COLO. – An early invasive strategy is particularly beneficial in octogenarians with non–ST-segment elevation myocardial infarction, according to a recent study involving close to 1 million NSTEMI patients aged 80 years or older.
The very eldest are an understudied segment of the NSTEMI population, for whom an initial conservative strategy has been the dominant approach in daily practice.
"This is an important study. We can see that as you get older and older, by virtue of the fact that you have more and more coronary disease, probably you’re going to be better off with an invasive strategy, all other things being equal," Dr. David R. Holmes Jr. commented in highlighting the study at the Annual Cardiovascular Conference at Snowmass.
The study included 968,542 octogenarians hospitalized with NSTEMI during 2003-2010 and entered into the Nationwide Inpatient Sample. Eighty-three percent were managed via an initial conservative approach, with coronary angiography performed only in the event of hemodynamic or electrical instability, refractory angina despite optimal medical therapy, or a test result indicative of high risk. The other 17% underwent an early invasive approach, with angiography within 48 hours of presentation.
Octogenarians managed via an early invasive strategy were more often younger, obese, smokers, dyslipidemic, hypertensive, white, and male, and more likely to have known vascular disease. In a multivariate analysis adjusted for potential confounders, the early invasive strategy group had a 34% reduction in in-hospital mortality compared with the conservatively managed group. They also had a 37% lower rate of acute ischemic stroke, a 40% reduction in intracranial hemorrhage, a 37% lower risk of gastrointestinal bleeding, and a shorter length of stay by an average of half a day. On the other side of the ledger, they had a 2.1-fold increased rate of cardiogenic shock (Am. J. Med. 2013;126:1076-83).
Does time to cath lab matter?
Another recent study looked at the optimal time frame for taking an NSTEMI patient to the cardiac catheterization laboratory as part of an invasive strategy. This was a meta-analysis of seven randomized controlled trials totaling 5,370 NSTEMI patients, along with four observational studies with more than 77,000 NSTEMI patients. The conclusion: There is as yet no persuasive evidence that the time interval makes a difference in outcomes (Ann. Intern. Med. 2013;158:261-70).
"That’s the data that’s available. It doesn’t matter how quickly you get the patient to the cath lab within that first period of time. You just need to take them, whether it’s in 2 hours, 6 hours, or 18 hours," Dr. Holmes said.
This has important implications as we think about systems of care. If somebody comes into the hospital late on a Friday night, do you have to take them to the cath lab Friday night, or can you wait electively and take them tomorrow or potentially even Monday morning when everybody’s there?" commented Dr. Holmes, professor of medicine at the Mayo Clinic in Rochester, Minn.
GRACE and CRUSADE
The cornerstone of decision making as to whether to opt for an invasive versus a conservative strategy in a given NSTEMI patient involves application of a formal risk score. A plethora of these risk scoring systems are in use today. Which is the best choice for a cardiologist as an aid to decision making? A meta-analysis involving 36 studies with nearly 117,000 NSTEMI patients has concluded that the GRACE (Global Registry of Acute Cardiac Events) risk score (JAMA 2004;291:2727-33) is the best of the pack. It significantly outperformed the TIMI score, which is the other widely used scoring system, as well as others less widely known (Contemp. Clin. Trials 2012:33:507-14).
"GRACE looks like it performs better. We’ll need better ones in the future, of course. But at the present time, select GRACE for risk stratification," advised the cardiologist, adding that a Grace score app is available.
Despite the fact that physicians are diagnosing and treating NSTEMI earlier in its course, in large part because of the widespread use of troponin assays in the emergency department, NSTEMI is still associated with substantial long-term morbidity and mortality, particularly in the elderly. This was underscored in a recent analysis of 19,336 NSTEMI patients aged 65 years or older who underwent early catheterization and were included in the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry.
Twenty-one percent of patients received medical management alone, 60.8% underwent percutaneous coronary intervention, and 18.2% had coronary artery bypass graft surgery. The 5-year unadjusted all-cause mortality rate was 50% in the medically managed group, 33.5% in older patients who underwent PCI, and 24.2% in those who underwent CABG surgery. The unadjusted 5-year rate of a composite of death, readmission for MI, or readmission for stroke was 62.4% with medical management, 44.9% with PCI, and 33% with CABG. The investigators concluded that long-term outcomes in elderly NSTEMI patients appear to be better in this large registry when revascularization is accomplished via CABG than with PCI. This sets the stage for future confirmatory trials (Circ. Cardiovasc. Qual. Outcomes 2013;6:323-32).
Dr. Holmes noted that the incidence of NSTEMI has climbed steadily while that of STEMI has declined over the past couple of decades, not just in the United States but worldwide. In Australia, for example, during 1993-2010 the adjusted incidence of NSTEMI increased by a whopping 315%, from 67 to 182 cases per 100,000 person-years, while the adjusted incidence of STEMI fell by 30% (Am. J. Cardiol. 2013;112:169-73).
"NSTEMI is clearly an annuity for all of cardiology," Dr. Holmes said. "The growth rate is increasing and it will continue to increase as we get older."
He reported having no conflicts of interest.
EXPERT ANALYSIS FROM THE CARDIOVASCULAR CONFERENCE AT SNOWMASS
Pseudobulbar affect: More common than you’d think
ORLANDO – The prevalence of pseudobulbar affect symptoms – that is, uncontrollable, disruptive outbursts of crying and/or laughing – is considerably greater across a range of neurologic disorders than previously appreciated, according to the largest-ever study to screen for this condition.
Pseudobulbar affect (PBA) symptoms were found in the study to be more common among neurology patients under age 65; however, the adverse impact of PBA symptoms upon quality of life was greater in the elderly, Dr. David W. Crumpacker reported at the annual meeting of the American Association for Geriatric Psychiatry.
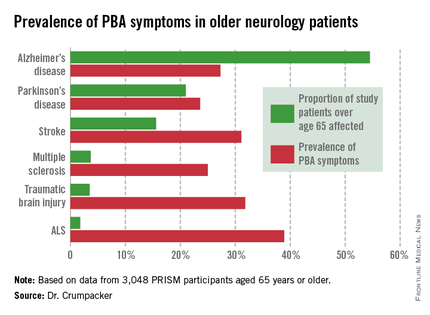
He presented the results of the PRISM (PBA Registry Series) study, which enrolled 5,290 patients on the basis of having any of six neurologic disorders: Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), multiple sclerosis, Parkinson’s disease, stroke, or traumatic brain injury. They were screened for the presence of PBA symptoms using the validated Center for Neurologic Study–Lability Scale (CNS-LS). A score of 13 or more was deemed positive, based upon its demonstrated good predictive value for physician diagnosis of PBA in patients with ALS.
The CNS-LS is a simple test that can be completed quickly by either the patient or caregiver. The test is well-suited for routine use in clinical practice, noted Dr. W. Crumpacker, a psychiatrist at Baylor University Medical Center, Dallas.
The overall prevalence of PBA symptoms among the 3,048 PRISM participants aged 65 years or older was 27.4%, with the highest rate seen in patients having ALS (see chart). In contrast, the prevalence of PBA symptoms among patients under age 65 years was 49.5%, with the highest rate – 56.9% – being seen in traumatic brain injury patients.
Patients or caregivers were asked to rate on a 0-10 scale the impact their primary neurologic disease has had on their quality of life. Patients 65 years and older with PBA symptoms reported a significantly greater negative impact than did those without PBA symptoms, with mean scores on the quality of life impact scale of 6.3 vs. 4.6. The quality of life difference between those with PBA symptoms and those without was significant for patients with each of the neurologic diseases except for ALS.
As another measure of the adverse impact of having PBA symptoms, 56% of affected older patients were on at least one antipsychotic or antidepressant, compared with 35% of older patients without PBA symptoms.
PBA is thought to result from injury to neurologic pathways that regulate emotional expression as a secondary consequence of a variety of neurologic disorders.
In an interview, Dr. Crumpacker said PBA is greatly underdiagnosed and often gets misdiagnosed as depression.
"The symptoms are extremely disturbing to others, and patients are acutely aware of that. I tell my friends in neurology, it’s the psychiatric pathology that causes people problems in their lives. No one gets divorced over neurologic pathology, they get divorced over psychiatric pathology. It’s not, ‘I got a divorce because he had a stroke.’ " "It’s "We got divorced because he had a stroke and it changed his personality; he was a different person and I couldn’t be around him anymore,’ " the psychiatrist said.
PBA became a diagnosable disorder with its own ICD-9 code, albeit a diagnosis that can’t be made in the absence of neurologic pathology, at the behest of the Food and Drug Administration, Dr. Crumpacker explained. The impetus was the discovery of an effective treatment, dextromethorphan HBr and quinidine sulfate (Nuedexta), which received FDA approval for PBA 3 years ago.
Nuedexta’s development as the sole medication indicated for PBA was serendipitous, according to Dr. Crumpacker.
"The drug was being tested in Alzheimer’s disease. The jury is still out on whether it helps. But families of study participants came back saying, ‘You know that stuff dad used to do – the crying, the inappropriate laughter, the anger? He doesn’t do those kinds of things anymore,’ " Dr. Crumpacker recalled.
He reported serving on a scientific advisory board for Avanir Pharmaceuticals, which markets Nuedexta.
ORLANDO – The prevalence of pseudobulbar affect symptoms – that is, uncontrollable, disruptive outbursts of crying and/or laughing – is considerably greater across a range of neurologic disorders than previously appreciated, according to the largest-ever study to screen for this condition.
Pseudobulbar affect (PBA) symptoms were found in the study to be more common among neurology patients under age 65; however, the adverse impact of PBA symptoms upon quality of life was greater in the elderly, Dr. David W. Crumpacker reported at the annual meeting of the American Association for Geriatric Psychiatry.
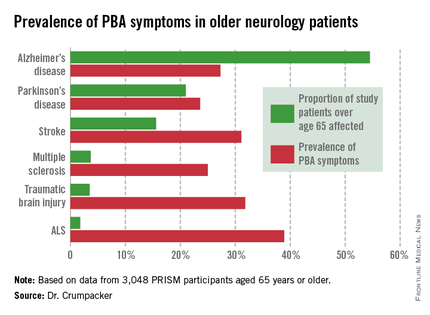
He presented the results of the PRISM (PBA Registry Series) study, which enrolled 5,290 patients on the basis of having any of six neurologic disorders: Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), multiple sclerosis, Parkinson’s disease, stroke, or traumatic brain injury. They were screened for the presence of PBA symptoms using the validated Center for Neurologic Study–Lability Scale (CNS-LS). A score of 13 or more was deemed positive, based upon its demonstrated good predictive value for physician diagnosis of PBA in patients with ALS.
The CNS-LS is a simple test that can be completed quickly by either the patient or caregiver. The test is well-suited for routine use in clinical practice, noted Dr. W. Crumpacker, a psychiatrist at Baylor University Medical Center, Dallas.
The overall prevalence of PBA symptoms among the 3,048 PRISM participants aged 65 years or older was 27.4%, with the highest rate seen in patients having ALS (see chart). In contrast, the prevalence of PBA symptoms among patients under age 65 years was 49.5%, with the highest rate – 56.9% – being seen in traumatic brain injury patients.
Patients or caregivers were asked to rate on a 0-10 scale the impact their primary neurologic disease has had on their quality of life. Patients 65 years and older with PBA symptoms reported a significantly greater negative impact than did those without PBA symptoms, with mean scores on the quality of life impact scale of 6.3 vs. 4.6. The quality of life difference between those with PBA symptoms and those without was significant for patients with each of the neurologic diseases except for ALS.
As another measure of the adverse impact of having PBA symptoms, 56% of affected older patients were on at least one antipsychotic or antidepressant, compared with 35% of older patients without PBA symptoms.
PBA is thought to result from injury to neurologic pathways that regulate emotional expression as a secondary consequence of a variety of neurologic disorders.
In an interview, Dr. Crumpacker said PBA is greatly underdiagnosed and often gets misdiagnosed as depression.
"The symptoms are extremely disturbing to others, and patients are acutely aware of that. I tell my friends in neurology, it’s the psychiatric pathology that causes people problems in their lives. No one gets divorced over neurologic pathology, they get divorced over psychiatric pathology. It’s not, ‘I got a divorce because he had a stroke.’ " "It’s "We got divorced because he had a stroke and it changed his personality; he was a different person and I couldn’t be around him anymore,’ " the psychiatrist said.
PBA became a diagnosable disorder with its own ICD-9 code, albeit a diagnosis that can’t be made in the absence of neurologic pathology, at the behest of the Food and Drug Administration, Dr. Crumpacker explained. The impetus was the discovery of an effective treatment, dextromethorphan HBr and quinidine sulfate (Nuedexta), which received FDA approval for PBA 3 years ago.
Nuedexta’s development as the sole medication indicated for PBA was serendipitous, according to Dr. Crumpacker.
"The drug was being tested in Alzheimer’s disease. The jury is still out on whether it helps. But families of study participants came back saying, ‘You know that stuff dad used to do – the crying, the inappropriate laughter, the anger? He doesn’t do those kinds of things anymore,’ " Dr. Crumpacker recalled.
He reported serving on a scientific advisory board for Avanir Pharmaceuticals, which markets Nuedexta.
ORLANDO – The prevalence of pseudobulbar affect symptoms – that is, uncontrollable, disruptive outbursts of crying and/or laughing – is considerably greater across a range of neurologic disorders than previously appreciated, according to the largest-ever study to screen for this condition.
Pseudobulbar affect (PBA) symptoms were found in the study to be more common among neurology patients under age 65; however, the adverse impact of PBA symptoms upon quality of life was greater in the elderly, Dr. David W. Crumpacker reported at the annual meeting of the American Association for Geriatric Psychiatry.
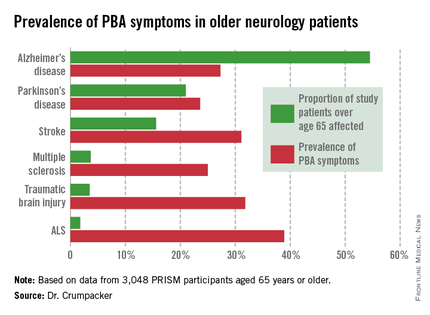
He presented the results of the PRISM (PBA Registry Series) study, which enrolled 5,290 patients on the basis of having any of six neurologic disorders: Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), multiple sclerosis, Parkinson’s disease, stroke, or traumatic brain injury. They were screened for the presence of PBA symptoms using the validated Center for Neurologic Study–Lability Scale (CNS-LS). A score of 13 or more was deemed positive, based upon its demonstrated good predictive value for physician diagnosis of PBA in patients with ALS.
The CNS-LS is a simple test that can be completed quickly by either the patient or caregiver. The test is well-suited for routine use in clinical practice, noted Dr. W. Crumpacker, a psychiatrist at Baylor University Medical Center, Dallas.
The overall prevalence of PBA symptoms among the 3,048 PRISM participants aged 65 years or older was 27.4%, with the highest rate seen in patients having ALS (see chart). In contrast, the prevalence of PBA symptoms among patients under age 65 years was 49.5%, with the highest rate – 56.9% – being seen in traumatic brain injury patients.
Patients or caregivers were asked to rate on a 0-10 scale the impact their primary neurologic disease has had on their quality of life. Patients 65 years and older with PBA symptoms reported a significantly greater negative impact than did those without PBA symptoms, with mean scores on the quality of life impact scale of 6.3 vs. 4.6. The quality of life difference between those with PBA symptoms and those without was significant for patients with each of the neurologic diseases except for ALS.
As another measure of the adverse impact of having PBA symptoms, 56% of affected older patients were on at least one antipsychotic or antidepressant, compared with 35% of older patients without PBA symptoms.
PBA is thought to result from injury to neurologic pathways that regulate emotional expression as a secondary consequence of a variety of neurologic disorders.
In an interview, Dr. Crumpacker said PBA is greatly underdiagnosed and often gets misdiagnosed as depression.
"The symptoms are extremely disturbing to others, and patients are acutely aware of that. I tell my friends in neurology, it’s the psychiatric pathology that causes people problems in their lives. No one gets divorced over neurologic pathology, they get divorced over psychiatric pathology. It’s not, ‘I got a divorce because he had a stroke.’ " "It’s "We got divorced because he had a stroke and it changed his personality; he was a different person and I couldn’t be around him anymore,’ " the psychiatrist said.
PBA became a diagnosable disorder with its own ICD-9 code, albeit a diagnosis that can’t be made in the absence of neurologic pathology, at the behest of the Food and Drug Administration, Dr. Crumpacker explained. The impetus was the discovery of an effective treatment, dextromethorphan HBr and quinidine sulfate (Nuedexta), which received FDA approval for PBA 3 years ago.
Nuedexta’s development as the sole medication indicated for PBA was serendipitous, according to Dr. Crumpacker.
"The drug was being tested in Alzheimer’s disease. The jury is still out on whether it helps. But families of study participants came back saying, ‘You know that stuff dad used to do – the crying, the inappropriate laughter, the anger? He doesn’t do those kinds of things anymore,’ " Dr. Crumpacker recalled.
He reported serving on a scientific advisory board for Avanir Pharmaceuticals, which markets Nuedexta.
AT THE AAGP ANNUAL MEETING
Major finding: The prevalence of PBA symptoms among patients over age 65 years with any of six underlying neurologic disorders was 27.4%. That was significantly less than in younger patients with the same disorders, but the adverse effect of having PBA symptoms upon quality of life was markedly greater in the older group.
Data source: The PRISM study included 5,290 patients with Alzheimer’s disease or any of five other less common neurologic disorders, all of whom were screened for the presence of PBA symptoms using a brief validated measure.
Disclosures: The presenter serves on a scientific advisory board for Avanir Pharmaceuticals, which funded the PRISM study.
Abdominal pain during aspirin desensitization? Think pancreatitis
KEYSTONE, COLO – Pancreatitis may be a rare complication of aspirin desensitization therapy – and perhaps actually not so rare – in patients with aspirin-exacerbated respiratory disease.
"Be aware: If you’re doing desensitization and a patient reports severe abdominal pain, please check the pancreatic enzyme levels," Dr. Rohit K. Katial urged at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
He and his coworkers were the first to describe this novel complication in a report detailing three cases. Two occurred during the 2-day aspirin desensitization procedure, with pancreatic lipase levels of 425 and 789 U/L, respectively, with normal defined as 13-63 U/L. The third involved a subacute presentation beginning 4 days after finishing desensitization, with a lipase level of 207 U/L while the patient was on standard postdensensitization high-dose aspirin therapy at 650 mg b.i.d. (J. Allergy Clin. Immunol. 2012;129:1684-6).
Gallbladder disease, alcohol, drugs, and other secondary causes of pancreatitis were ruled out in all three cases, noted Dr. Katial, professor of medicine at the University of Colorado, Denver, and director of allergy and immunology clinical services at National Jewish Health.
This previously unreported close temporal association between pancreatitis and aspirin desensitization is of particular interest because it may actually not be all that uncommon. Indeed, other investigators, in a study of 172 aspirin-desensitized patients, reported that 27% of them discontinued high-dose maintenance aspirin therapy during the first year. The most common reason for doing so was the emergence of epigastric pain, accounting for 14 discontinuations. Another two patients discontinued therapy because of GI bleeding (J. Allergy Clin. Immunol. 2003;111:180-6).
These gastrointestinal reactions weren’t extensively investigated, since it’s well known that high-dose aspirin is associated with gastritis and peptic ulcer disease. So it’s quite possible that some of these cases of what was classified clinically as gastritis were actually pancreatitis, according to Dr. Katial.
The mechanism involved in pancreatitis in the setting of aspirin desensitization is unknown. Animal studies suggest the marked increase in leukotriene levels occurring during aspirin desensitization may play a role. Even though all three patients were on prophylactic montelukast (Singulair) at the time of aspirin challenge, the leukotriene receptor antagonist may not provide complete protection in a subset of vulnerable patients.
Dr. Katial reported serving as an adviser to and on the speakers bureau for Teva Pharmaceuticals.
KEYSTONE, COLO – Pancreatitis may be a rare complication of aspirin desensitization therapy – and perhaps actually not so rare – in patients with aspirin-exacerbated respiratory disease.
"Be aware: If you’re doing desensitization and a patient reports severe abdominal pain, please check the pancreatic enzyme levels," Dr. Rohit K. Katial urged at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
He and his coworkers were the first to describe this novel complication in a report detailing three cases. Two occurred during the 2-day aspirin desensitization procedure, with pancreatic lipase levels of 425 and 789 U/L, respectively, with normal defined as 13-63 U/L. The third involved a subacute presentation beginning 4 days after finishing desensitization, with a lipase level of 207 U/L while the patient was on standard postdensensitization high-dose aspirin therapy at 650 mg b.i.d. (J. Allergy Clin. Immunol. 2012;129:1684-6).
Gallbladder disease, alcohol, drugs, and other secondary causes of pancreatitis were ruled out in all three cases, noted Dr. Katial, professor of medicine at the University of Colorado, Denver, and director of allergy and immunology clinical services at National Jewish Health.
This previously unreported close temporal association between pancreatitis and aspirin desensitization is of particular interest because it may actually not be all that uncommon. Indeed, other investigators, in a study of 172 aspirin-desensitized patients, reported that 27% of them discontinued high-dose maintenance aspirin therapy during the first year. The most common reason for doing so was the emergence of epigastric pain, accounting for 14 discontinuations. Another two patients discontinued therapy because of GI bleeding (J. Allergy Clin. Immunol. 2003;111:180-6).
These gastrointestinal reactions weren’t extensively investigated, since it’s well known that high-dose aspirin is associated with gastritis and peptic ulcer disease. So it’s quite possible that some of these cases of what was classified clinically as gastritis were actually pancreatitis, according to Dr. Katial.
The mechanism involved in pancreatitis in the setting of aspirin desensitization is unknown. Animal studies suggest the marked increase in leukotriene levels occurring during aspirin desensitization may play a role. Even though all three patients were on prophylactic montelukast (Singulair) at the time of aspirin challenge, the leukotriene receptor antagonist may not provide complete protection in a subset of vulnerable patients.
Dr. Katial reported serving as an adviser to and on the speakers bureau for Teva Pharmaceuticals.
KEYSTONE, COLO – Pancreatitis may be a rare complication of aspirin desensitization therapy – and perhaps actually not so rare – in patients with aspirin-exacerbated respiratory disease.
"Be aware: If you’re doing desensitization and a patient reports severe abdominal pain, please check the pancreatic enzyme levels," Dr. Rohit K. Katial urged at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
He and his coworkers were the first to describe this novel complication in a report detailing three cases. Two occurred during the 2-day aspirin desensitization procedure, with pancreatic lipase levels of 425 and 789 U/L, respectively, with normal defined as 13-63 U/L. The third involved a subacute presentation beginning 4 days after finishing desensitization, with a lipase level of 207 U/L while the patient was on standard postdensensitization high-dose aspirin therapy at 650 mg b.i.d. (J. Allergy Clin. Immunol. 2012;129:1684-6).
Gallbladder disease, alcohol, drugs, and other secondary causes of pancreatitis were ruled out in all three cases, noted Dr. Katial, professor of medicine at the University of Colorado, Denver, and director of allergy and immunology clinical services at National Jewish Health.
This previously unreported close temporal association between pancreatitis and aspirin desensitization is of particular interest because it may actually not be all that uncommon. Indeed, other investigators, in a study of 172 aspirin-desensitized patients, reported that 27% of them discontinued high-dose maintenance aspirin therapy during the first year. The most common reason for doing so was the emergence of epigastric pain, accounting for 14 discontinuations. Another two patients discontinued therapy because of GI bleeding (J. Allergy Clin. Immunol. 2003;111:180-6).
These gastrointestinal reactions weren’t extensively investigated, since it’s well known that high-dose aspirin is associated with gastritis and peptic ulcer disease. So it’s quite possible that some of these cases of what was classified clinically as gastritis were actually pancreatitis, according to Dr. Katial.
The mechanism involved in pancreatitis in the setting of aspirin desensitization is unknown. Animal studies suggest the marked increase in leukotriene levels occurring during aspirin desensitization may play a role. Even though all three patients were on prophylactic montelukast (Singulair) at the time of aspirin challenge, the leukotriene receptor antagonist may not provide complete protection in a subset of vulnerable patients.
Dr. Katial reported serving as an adviser to and on the speakers bureau for Teva Pharmaceuticals.
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE
How an expert uses Voluma
WAIKOLOA, HAWAII – A key point to understand about Juvederm Voluma XC, the recently approved filler for age-related midface volume deficit, is that it’s a pillar or lift product, according to Dr. Sue Ellen Cox.
"Voluma loves to lift. It works great when placed on bone, such as the malar bone. With a supraperiosteal vertical puncture, you’ll see the skin lift right in front of your eyes," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill and principal investigator in the pivotal clinical trial that led to Food and Drug Administration approval of Voluma.
This characteristic of the highly cohesive 20-mg/mL hyaluronic acid filler has important implications for the product’s optimal use and achieving maximal patient satisfaction. For one, Voluma absolutely should not be used for patients with thin skin. For these patients, a more effective option is a product containing monophasic monodensified hyaluronic acids, such as Juvederm Ultra or Ultra Plus, Dr. Cox said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
As a rule of thumb, approximately 40% of Voluma is needed compared with the amount of monophasic monodensified hyaluronic acid fillers dermatologists are accustomed to working with, she said.
It’s crucial to inject Voluma extremely slowly, Dr. Cox emphasized. She advised scheduling 30 minutes for a patient’s first volumizing session. It’s also important to avoid using a large bolus, and be sure not to overcorrect. Voluma loves water and will draw it from tissue, Dr. Cox noted. Therefore it’s important to use the exact correction. Remember that at 9 months post treatment, 50% or more of the original correction will remain, so the 9-month mark is a good time to schedule a touch-up, she added.
Another pearl: Inject struts or pillars from the periostium; then blend and mold them, Dr. Cox continued.
She urged her colleagues to be conservative in using Voluma around the eyes. In her experience, too much Voluma in this area causes the product to migrate anteriorly on the cheek, which could result in an unwelcome doughy appearance.
To achieve improvement in the submalar area, it’s best to utilize tangential microdroplets of Voluma after reconstitution with saline so the filler doesn’t affect the nerve and cause a lip drop, according to Dr. Cox.
Should it become necessary to dissolve Voluma, use twice as much hyaluronidase (Hylenex).
Dr. Cox reported serving as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – A key point to understand about Juvederm Voluma XC, the recently approved filler for age-related midface volume deficit, is that it’s a pillar or lift product, according to Dr. Sue Ellen Cox.
"Voluma loves to lift. It works great when placed on bone, such as the malar bone. With a supraperiosteal vertical puncture, you’ll see the skin lift right in front of your eyes," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill and principal investigator in the pivotal clinical trial that led to Food and Drug Administration approval of Voluma.
This characteristic of the highly cohesive 20-mg/mL hyaluronic acid filler has important implications for the product’s optimal use and achieving maximal patient satisfaction. For one, Voluma absolutely should not be used for patients with thin skin. For these patients, a more effective option is a product containing monophasic monodensified hyaluronic acids, such as Juvederm Ultra or Ultra Plus, Dr. Cox said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
As a rule of thumb, approximately 40% of Voluma is needed compared with the amount of monophasic monodensified hyaluronic acid fillers dermatologists are accustomed to working with, she said.
It’s crucial to inject Voluma extremely slowly, Dr. Cox emphasized. She advised scheduling 30 minutes for a patient’s first volumizing session. It’s also important to avoid using a large bolus, and be sure not to overcorrect. Voluma loves water and will draw it from tissue, Dr. Cox noted. Therefore it’s important to use the exact correction. Remember that at 9 months post treatment, 50% or more of the original correction will remain, so the 9-month mark is a good time to schedule a touch-up, she added.
Another pearl: Inject struts or pillars from the periostium; then blend and mold them, Dr. Cox continued.
She urged her colleagues to be conservative in using Voluma around the eyes. In her experience, too much Voluma in this area causes the product to migrate anteriorly on the cheek, which could result in an unwelcome doughy appearance.
To achieve improvement in the submalar area, it’s best to utilize tangential microdroplets of Voluma after reconstitution with saline so the filler doesn’t affect the nerve and cause a lip drop, according to Dr. Cox.
Should it become necessary to dissolve Voluma, use twice as much hyaluronidase (Hylenex).
Dr. Cox reported serving as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – A key point to understand about Juvederm Voluma XC, the recently approved filler for age-related midface volume deficit, is that it’s a pillar or lift product, according to Dr. Sue Ellen Cox.
"Voluma loves to lift. It works great when placed on bone, such as the malar bone. With a supraperiosteal vertical puncture, you’ll see the skin lift right in front of your eyes," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill and principal investigator in the pivotal clinical trial that led to Food and Drug Administration approval of Voluma.
This characteristic of the highly cohesive 20-mg/mL hyaluronic acid filler has important implications for the product’s optimal use and achieving maximal patient satisfaction. For one, Voluma absolutely should not be used for patients with thin skin. For these patients, a more effective option is a product containing monophasic monodensified hyaluronic acids, such as Juvederm Ultra or Ultra Plus, Dr. Cox said at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
As a rule of thumb, approximately 40% of Voluma is needed compared with the amount of monophasic monodensified hyaluronic acid fillers dermatologists are accustomed to working with, she said.
It’s crucial to inject Voluma extremely slowly, Dr. Cox emphasized. She advised scheduling 30 minutes for a patient’s first volumizing session. It’s also important to avoid using a large bolus, and be sure not to overcorrect. Voluma loves water and will draw it from tissue, Dr. Cox noted. Therefore it’s important to use the exact correction. Remember that at 9 months post treatment, 50% or more of the original correction will remain, so the 9-month mark is a good time to schedule a touch-up, she added.
Another pearl: Inject struts or pillars from the periostium; then blend and mold them, Dr. Cox continued.
She urged her colleagues to be conservative in using Voluma around the eyes. In her experience, too much Voluma in this area causes the product to migrate anteriorly on the cheek, which could result in an unwelcome doughy appearance.
To achieve improvement in the submalar area, it’s best to utilize tangential microdroplets of Voluma after reconstitution with saline so the filler doesn’t affect the nerve and cause a lip drop, according to Dr. Cox.
Should it become necessary to dissolve Voluma, use twice as much hyaluronidase (Hylenex).
Dr. Cox reported serving as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Midface filler Voluma provides long-lasting patient satisfaction
WAIKOLOA, HAWAII – Juvederm Voluma XC continues to show significant results in extended follow-up data from the pivotal phase III trial that earned the product marketing approval from the Food and Drug Administration late last year as the first filler indicated specifically for treating age-related midface volume deficit.
One of the notable new findings: At 6 months post treatment, 73% of Voluma-treated study participants rated themselves as looking younger than at baseline – and by an average of 5 years less than their mean baseline chronologic age of 56 years. Moreover, at 24 months, 55% of patients said they felt that they still looked younger by an average of 3 years, Dr. Sue Ellen Cox reported at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
"The improvement was really profound. What was also profound was how long it lasted. I’m now 3 years out seeing these patients and they still have retention of their product. So I am a believer," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill, who was principal investigator in the pivotal phase III trial.
Dr. Cox shared highlights of the extended follow-up data, along with her personal observations regarding how to use Voluma most effectively.
Voluma XC is a highly cohesive volumizing hyaluronic acid filler formulated at a concentration of 20 mg/mL. It fills what has been widely regarded as a major unmet need in aesthetic dermatology, said Dr. Cox
"It’s a wonderful filler we’re all really going to enjoy using. I think it’s going to prove to be everything we want it to be," she said.
The pivotal data reviewed by the FDA came from a 15-center, randomized, single-blind clinical trial including 235 Voluma-treated patients and 47 no-treatment controls. All patients had moderate or severe baseline midface volume deficits as reflected by scores of 3-5 on a standardized 0-5 scoring system. The active treatment group received one treatment with the option of a touch-up session a month later.
The primary study endpoint prespecified by the FDA was an improvement of at least 1 point between baseline and 6 months on the Mid-Facial Volume Deficit Scale (MFVDS). This endpoint was achieved in 86% of the Voluma group and 39% of controls. Moreover, 51% of the active treatment group had an improvement of 2 points or greater compared with 11% of controls. And 26% of the Voluma group, but none of the controls, showed a 2.5-point improvement or better.
The durability of the treatment response was noteworthy, Dr. Cox added. At 2 years, 67% of patients in the Voluma group maintained a clinically significant improvement based upon MFVDS scores.
Every 3 months for the 2 years of follow-up, patients were asked how they felt about their appearance. As Dr. Cox noted, this is the true litmus test for any aesthetic dermatology procedure. At 6 months, 90% of patients pronounced themselves satisfied with the improvement in their facial appearance. At 12 months, 82% said they were satisfied; and at 2 years post treatment, 76% of patients remained satisfied with their facial appearance.
At baseline, 67% of patients rated their midface appearance as making them look "very much" older; at 6 months post treatment, only 12% of patients felt that way. Similarly, at baseline 55%-66% of patients characterized their midface appearance as variously "very much" unattractive, sad, and/or tired; at 6 months post treatment, only 9%-11% of subjects did so.
Treatment of the nasolabial folds and tear ducts was not permitted in the pivotal trial. Yet by investigator assessment at 6 months’ follow-up 32% of the active treatment group had a clinically meaningful improvement of at least 1 point on the 5-point Nasolabial Fold Photo Severity Scale, compared with 8% of controls, said Dr. Cox. Moreover, 54% of Voluma-treated patients rated themselves as moderately, very much, or completely satisfied with the appearance of their tear trough area, a marked improvement over the 17% rate at baseline. These findings underscore the point that effectively reinflating the midface and reestablishing optimal proportion provides ancillary benefits that may render treatment of the tear troughs and nasolabial folds unnecessary, she said.
Common treatment side effects consisted of mild to moderate injection site tenderness, swelling, bruising, lumps and bumps, and pain. All cases of side effects resolved within 30 days, and most resolved within 2 weeks.
Dr. Cox reported acting as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Juvederm Voluma XC continues to show significant results in extended follow-up data from the pivotal phase III trial that earned the product marketing approval from the Food and Drug Administration late last year as the first filler indicated specifically for treating age-related midface volume deficit.
One of the notable new findings: At 6 months post treatment, 73% of Voluma-treated study participants rated themselves as looking younger than at baseline – and by an average of 5 years less than their mean baseline chronologic age of 56 years. Moreover, at 24 months, 55% of patients said they felt that they still looked younger by an average of 3 years, Dr. Sue Ellen Cox reported at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
"The improvement was really profound. What was also profound was how long it lasted. I’m now 3 years out seeing these patients and they still have retention of their product. So I am a believer," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill, who was principal investigator in the pivotal phase III trial.
Dr. Cox shared highlights of the extended follow-up data, along with her personal observations regarding how to use Voluma most effectively.
Voluma XC is a highly cohesive volumizing hyaluronic acid filler formulated at a concentration of 20 mg/mL. It fills what has been widely regarded as a major unmet need in aesthetic dermatology, said Dr. Cox
"It’s a wonderful filler we’re all really going to enjoy using. I think it’s going to prove to be everything we want it to be," she said.
The pivotal data reviewed by the FDA came from a 15-center, randomized, single-blind clinical trial including 235 Voluma-treated patients and 47 no-treatment controls. All patients had moderate or severe baseline midface volume deficits as reflected by scores of 3-5 on a standardized 0-5 scoring system. The active treatment group received one treatment with the option of a touch-up session a month later.
The primary study endpoint prespecified by the FDA was an improvement of at least 1 point between baseline and 6 months on the Mid-Facial Volume Deficit Scale (MFVDS). This endpoint was achieved in 86% of the Voluma group and 39% of controls. Moreover, 51% of the active treatment group had an improvement of 2 points or greater compared with 11% of controls. And 26% of the Voluma group, but none of the controls, showed a 2.5-point improvement or better.
The durability of the treatment response was noteworthy, Dr. Cox added. At 2 years, 67% of patients in the Voluma group maintained a clinically significant improvement based upon MFVDS scores.
Every 3 months for the 2 years of follow-up, patients were asked how they felt about their appearance. As Dr. Cox noted, this is the true litmus test for any aesthetic dermatology procedure. At 6 months, 90% of patients pronounced themselves satisfied with the improvement in their facial appearance. At 12 months, 82% said they were satisfied; and at 2 years post treatment, 76% of patients remained satisfied with their facial appearance.
At baseline, 67% of patients rated their midface appearance as making them look "very much" older; at 6 months post treatment, only 12% of patients felt that way. Similarly, at baseline 55%-66% of patients characterized their midface appearance as variously "very much" unattractive, sad, and/or tired; at 6 months post treatment, only 9%-11% of subjects did so.
Treatment of the nasolabial folds and tear ducts was not permitted in the pivotal trial. Yet by investigator assessment at 6 months’ follow-up 32% of the active treatment group had a clinically meaningful improvement of at least 1 point on the 5-point Nasolabial Fold Photo Severity Scale, compared with 8% of controls, said Dr. Cox. Moreover, 54% of Voluma-treated patients rated themselves as moderately, very much, or completely satisfied with the appearance of their tear trough area, a marked improvement over the 17% rate at baseline. These findings underscore the point that effectively reinflating the midface and reestablishing optimal proportion provides ancillary benefits that may render treatment of the tear troughs and nasolabial folds unnecessary, she said.
Common treatment side effects consisted of mild to moderate injection site tenderness, swelling, bruising, lumps and bumps, and pain. All cases of side effects resolved within 30 days, and most resolved within 2 weeks.
Dr. Cox reported acting as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – Juvederm Voluma XC continues to show significant results in extended follow-up data from the pivotal phase III trial that earned the product marketing approval from the Food and Drug Administration late last year as the first filler indicated specifically for treating age-related midface volume deficit.
One of the notable new findings: At 6 months post treatment, 73% of Voluma-treated study participants rated themselves as looking younger than at baseline – and by an average of 5 years less than their mean baseline chronologic age of 56 years. Moreover, at 24 months, 55% of patients said they felt that they still looked younger by an average of 3 years, Dr. Sue Ellen Cox reported at the Hawaii Dermatology Seminar sponsored by Global Academy for Medical Education/Skin Disease Education Foundation.
"The improvement was really profound. What was also profound was how long it lasted. I’m now 3 years out seeing these patients and they still have retention of their product. So I am a believer," said Dr. Cox, a dermatologist at the University of North Carolina at Chapel Hill, who was principal investigator in the pivotal phase III trial.
Dr. Cox shared highlights of the extended follow-up data, along with her personal observations regarding how to use Voluma most effectively.
Voluma XC is a highly cohesive volumizing hyaluronic acid filler formulated at a concentration of 20 mg/mL. It fills what has been widely regarded as a major unmet need in aesthetic dermatology, said Dr. Cox
"It’s a wonderful filler we’re all really going to enjoy using. I think it’s going to prove to be everything we want it to be," she said.
The pivotal data reviewed by the FDA came from a 15-center, randomized, single-blind clinical trial including 235 Voluma-treated patients and 47 no-treatment controls. All patients had moderate or severe baseline midface volume deficits as reflected by scores of 3-5 on a standardized 0-5 scoring system. The active treatment group received one treatment with the option of a touch-up session a month later.
The primary study endpoint prespecified by the FDA was an improvement of at least 1 point between baseline and 6 months on the Mid-Facial Volume Deficit Scale (MFVDS). This endpoint was achieved in 86% of the Voluma group and 39% of controls. Moreover, 51% of the active treatment group had an improvement of 2 points or greater compared with 11% of controls. And 26% of the Voluma group, but none of the controls, showed a 2.5-point improvement or better.
The durability of the treatment response was noteworthy, Dr. Cox added. At 2 years, 67% of patients in the Voluma group maintained a clinically significant improvement based upon MFVDS scores.
Every 3 months for the 2 years of follow-up, patients were asked how they felt about their appearance. As Dr. Cox noted, this is the true litmus test for any aesthetic dermatology procedure. At 6 months, 90% of patients pronounced themselves satisfied with the improvement in their facial appearance. At 12 months, 82% said they were satisfied; and at 2 years post treatment, 76% of patients remained satisfied with their facial appearance.
At baseline, 67% of patients rated their midface appearance as making them look "very much" older; at 6 months post treatment, only 12% of patients felt that way. Similarly, at baseline 55%-66% of patients characterized their midface appearance as variously "very much" unattractive, sad, and/or tired; at 6 months post treatment, only 9%-11% of subjects did so.
Treatment of the nasolabial folds and tear ducts was not permitted in the pivotal trial. Yet by investigator assessment at 6 months’ follow-up 32% of the active treatment group had a clinically meaningful improvement of at least 1 point on the 5-point Nasolabial Fold Photo Severity Scale, compared with 8% of controls, said Dr. Cox. Moreover, 54% of Voluma-treated patients rated themselves as moderately, very much, or completely satisfied with the appearance of their tear trough area, a marked improvement over the 17% rate at baseline. These findings underscore the point that effectively reinflating the midface and reestablishing optimal proportion provides ancillary benefits that may render treatment of the tear troughs and nasolabial folds unnecessary, she said.
Common treatment side effects consisted of mild to moderate injection site tenderness, swelling, bruising, lumps and bumps, and pain. All cases of side effects resolved within 30 days, and most resolved within 2 weeks.
Dr. Cox reported acting as a consultant to Allergan and Medicis and serving as principal investigator in trials funded by those companies, as well as in studies funded by Revance and Kythera.
SDEF and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Exhaled nitric oxide’s merits in childhood asthma
KEYSTONE, COLO. – Fractional exhaled nitric oxide as a tool for patient care in pediatric asthma has often gotten a bad rap, according to a long-time researcher in the field.
"You’re either an exhaled nitric oxide fan or you’re not, it seems like, in the medical community. Some people expect it to be all things when in fact it’s just one measure. It measures atopic eosinophilic inflammation. We know that asthma is more than one disease, so we need more than one tool. This is a tool that’s useful in a subgroup of asthmatics, but I think the subgroup it’s useful in is big enough that it’s a valuable tool," Dr. Joseph D. Spahn declared at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
The pediatric allergist published his first study demonstrating the clinical benefits of measuring fractional exhaled nitric oxide (FeNO) well before the technology won Food and Drug Administration approval and became commercially available.
An American Thoracic Society clinical practice guideline addressing the clinical utility of the test was a long time coming. Finally, several years ago, the ATS issued an official guideline declaring "FeNO offers added advantages for patient care" over conventional tests for asthma, such as FEV1 [forced expiratory volume in 1 second] reversibility and provocation tests (Am. J. Respir. Crit. Care Med. 2011;184:602-15).
The guideline describes three major clinical uses for FeNO testing: diagnosing asthma, predicting response to inhaled corticosteroids, and monitoring adherence to this cornerstone therapy.
FeNO’s role in diagnosing asthma
FeNO is significantly elevated in allergic asthma but not in other neutrophilic diseases that can masquerade as asthma, including primary immunodeficiencies, bronchopulmonary dysplasia, alpha-1antitrypsin deficiency, and cystic fibrosis, all of which feature either low or normal FeNO levels.
But it’s important to understand where the test is most likely to prove useful.
"FeNO is the only noninvasive tool we have for assessing airway inflammation. It’s a marker of atopic and Th2-driven inflammation. Many severe adult asthmatics don’t seem to have a Th2-driven disease process. Many little kids with nonatopic asthma and viral-induced wheezing don’t have Th2-driven inflammation. As a result, FeNO is not going to be a great tool in those situations. But for those individuals in which atopy plays a role, it’s a great measure of active airway inflammation," explained Dr. Spahn of the University of Colorado, Denver, and National Jewish Health.
In one representative head-to-head comparative study, a 15% or greater improvement in FEV1 in response to an inhaled corticosteroid – widely considered a gold standard test in support of a diagnosis of asthma – had a 12% sensitivity for the diagnosis, while a reduction of greater than 20 ppb in FeNO had an 88% sensitivity (Am. J. Respir. Crit. Care Med. 2004;169:473-8).
Predicting response to steroid therapy
The ATS guidelines state that symptomatic patients who present initially with a high FeNO – more than 35 ppb in children or 50 ppb in adults – are likely to benefit from a trial of inhaled corticosteroids, and that it’s appropriate to probe for allergen exposure in such patients. The guidelines further recommend that patients with a low baseline FeNO of less than 20 ppb in children or 25 ppb in adults are less likely to have eosinophilic inflammation and are unlikely to benefit from inhaled corticosteroid therapy. Consideration of a therapeutic trial with serial FeNO monitoring is recommended in patients with intermediate levels.
Years ago, Dr. Spahn and his coworkers showed in a double-blind, randomized, crossover study that FeNO values could predict whether children with mild to moderate asthma were more likely to respond to fluticasone (Flonase) or montelukast (Singulair); the higher the initial FeNO, the more likely fluticasone was the more effective option (J. Allergy Clin. Immunol. 2005;115:233-42).
Dr. Spahn also finds FeNO results helpful in combating parental steroid phobia. "Steroid phobia still exists in the pediatric world. I know we as health care providers don’t really worry about inhaled corticosteroids having significant side effects, but parents do," he observed.
He shared a story of a 10-year-old with a severe chronic cough and newly diagnosed asthma.
"This kid was extremely disabled from his cough. If you’re coughing every 30 seconds, it’s not going to be easy for you to function normally in school. But when I mentioned that he needed to be on inhaled corticosteroid therapy, the mom acted like I’d just given her kid a death sentence. So the FeNO was a tool that I used to help convince her that there was inflammation in his airways and the way to treat it was with an inhaled corticosteroid.
"After spending half an hour convincing her of the benefits and safety of inhaled corticosteroids, she agreed. I saw him back 6 weeks later. His cough was pretty much gone, his lung function was completely normalized, and his FeNO had fallen 90%. That’s my record: A 90% reduction is about as good as it gets," Dr. Spahn said.
Assessing steroid adherence
Placing an allergic asthma patient on inhaled corticosteroid therapy should result in at least a 50% reduction in an elevated baseline FeNO. A lesser response, or an increasing FeNO during follow-up visits, is an indicator of an adherence problem.
"I like to tell people who’ve been in practice 20 years or longer that FeNO is to inhaled steroids as the theophylline blood level was to theophylline therapy. Back in the day when we used theophylline, our measure of adherence was checking someone’s theophylline level. If it was low and the patient was poorly controlled, we could blame their poor control on their poor adherence to theophylline. Up until FeNO, we didn’t have that ability with inhaled steroids. We can’t measure inhaled steroid levels due to the fact that they’re so small in the bloodstream," Dr. Spahn explained.
He reported receiving honoraria from GlaxoSmithKline as well as from Aerocrine, which markets an FeNO analyzer.
KEYSTONE, COLO. – Fractional exhaled nitric oxide as a tool for patient care in pediatric asthma has often gotten a bad rap, according to a long-time researcher in the field.
"You’re either an exhaled nitric oxide fan or you’re not, it seems like, in the medical community. Some people expect it to be all things when in fact it’s just one measure. It measures atopic eosinophilic inflammation. We know that asthma is more than one disease, so we need more than one tool. This is a tool that’s useful in a subgroup of asthmatics, but I think the subgroup it’s useful in is big enough that it’s a valuable tool," Dr. Joseph D. Spahn declared at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
The pediatric allergist published his first study demonstrating the clinical benefits of measuring fractional exhaled nitric oxide (FeNO) well before the technology won Food and Drug Administration approval and became commercially available.
An American Thoracic Society clinical practice guideline addressing the clinical utility of the test was a long time coming. Finally, several years ago, the ATS issued an official guideline declaring "FeNO offers added advantages for patient care" over conventional tests for asthma, such as FEV1 [forced expiratory volume in 1 second] reversibility and provocation tests (Am. J. Respir. Crit. Care Med. 2011;184:602-15).
The guideline describes three major clinical uses for FeNO testing: diagnosing asthma, predicting response to inhaled corticosteroids, and monitoring adherence to this cornerstone therapy.
FeNO’s role in diagnosing asthma
FeNO is significantly elevated in allergic asthma but not in other neutrophilic diseases that can masquerade as asthma, including primary immunodeficiencies, bronchopulmonary dysplasia, alpha-1antitrypsin deficiency, and cystic fibrosis, all of which feature either low or normal FeNO levels.
But it’s important to understand where the test is most likely to prove useful.
"FeNO is the only noninvasive tool we have for assessing airway inflammation. It’s a marker of atopic and Th2-driven inflammation. Many severe adult asthmatics don’t seem to have a Th2-driven disease process. Many little kids with nonatopic asthma and viral-induced wheezing don’t have Th2-driven inflammation. As a result, FeNO is not going to be a great tool in those situations. But for those individuals in which atopy plays a role, it’s a great measure of active airway inflammation," explained Dr. Spahn of the University of Colorado, Denver, and National Jewish Health.
In one representative head-to-head comparative study, a 15% or greater improvement in FEV1 in response to an inhaled corticosteroid – widely considered a gold standard test in support of a diagnosis of asthma – had a 12% sensitivity for the diagnosis, while a reduction of greater than 20 ppb in FeNO had an 88% sensitivity (Am. J. Respir. Crit. Care Med. 2004;169:473-8).
Predicting response to steroid therapy
The ATS guidelines state that symptomatic patients who present initially with a high FeNO – more than 35 ppb in children or 50 ppb in adults – are likely to benefit from a trial of inhaled corticosteroids, and that it’s appropriate to probe for allergen exposure in such patients. The guidelines further recommend that patients with a low baseline FeNO of less than 20 ppb in children or 25 ppb in adults are less likely to have eosinophilic inflammation and are unlikely to benefit from inhaled corticosteroid therapy. Consideration of a therapeutic trial with serial FeNO monitoring is recommended in patients with intermediate levels.
Years ago, Dr. Spahn and his coworkers showed in a double-blind, randomized, crossover study that FeNO values could predict whether children with mild to moderate asthma were more likely to respond to fluticasone (Flonase) or montelukast (Singulair); the higher the initial FeNO, the more likely fluticasone was the more effective option (J. Allergy Clin. Immunol. 2005;115:233-42).
Dr. Spahn also finds FeNO results helpful in combating parental steroid phobia. "Steroid phobia still exists in the pediatric world. I know we as health care providers don’t really worry about inhaled corticosteroids having significant side effects, but parents do," he observed.
He shared a story of a 10-year-old with a severe chronic cough and newly diagnosed asthma.
"This kid was extremely disabled from his cough. If you’re coughing every 30 seconds, it’s not going to be easy for you to function normally in school. But when I mentioned that he needed to be on inhaled corticosteroid therapy, the mom acted like I’d just given her kid a death sentence. So the FeNO was a tool that I used to help convince her that there was inflammation in his airways and the way to treat it was with an inhaled corticosteroid.
"After spending half an hour convincing her of the benefits and safety of inhaled corticosteroids, she agreed. I saw him back 6 weeks later. His cough was pretty much gone, his lung function was completely normalized, and his FeNO had fallen 90%. That’s my record: A 90% reduction is about as good as it gets," Dr. Spahn said.
Assessing steroid adherence
Placing an allergic asthma patient on inhaled corticosteroid therapy should result in at least a 50% reduction in an elevated baseline FeNO. A lesser response, or an increasing FeNO during follow-up visits, is an indicator of an adherence problem.
"I like to tell people who’ve been in practice 20 years or longer that FeNO is to inhaled steroids as the theophylline blood level was to theophylline therapy. Back in the day when we used theophylline, our measure of adherence was checking someone’s theophylline level. If it was low and the patient was poorly controlled, we could blame their poor control on their poor adherence to theophylline. Up until FeNO, we didn’t have that ability with inhaled steroids. We can’t measure inhaled steroid levels due to the fact that they’re so small in the bloodstream," Dr. Spahn explained.
He reported receiving honoraria from GlaxoSmithKline as well as from Aerocrine, which markets an FeNO analyzer.
KEYSTONE, COLO. – Fractional exhaled nitric oxide as a tool for patient care in pediatric asthma has often gotten a bad rap, according to a long-time researcher in the field.
"You’re either an exhaled nitric oxide fan or you’re not, it seems like, in the medical community. Some people expect it to be all things when in fact it’s just one measure. It measures atopic eosinophilic inflammation. We know that asthma is more than one disease, so we need more than one tool. This is a tool that’s useful in a subgroup of asthmatics, but I think the subgroup it’s useful in is big enough that it’s a valuable tool," Dr. Joseph D. Spahn declared at a meeting on allergy and respiratory diseases sponsored by National Jewish Health.
The pediatric allergist published his first study demonstrating the clinical benefits of measuring fractional exhaled nitric oxide (FeNO) well before the technology won Food and Drug Administration approval and became commercially available.
An American Thoracic Society clinical practice guideline addressing the clinical utility of the test was a long time coming. Finally, several years ago, the ATS issued an official guideline declaring "FeNO offers added advantages for patient care" over conventional tests for asthma, such as FEV1 [forced expiratory volume in 1 second] reversibility and provocation tests (Am. J. Respir. Crit. Care Med. 2011;184:602-15).
The guideline describes three major clinical uses for FeNO testing: diagnosing asthma, predicting response to inhaled corticosteroids, and monitoring adherence to this cornerstone therapy.
FeNO’s role in diagnosing asthma
FeNO is significantly elevated in allergic asthma but not in other neutrophilic diseases that can masquerade as asthma, including primary immunodeficiencies, bronchopulmonary dysplasia, alpha-1antitrypsin deficiency, and cystic fibrosis, all of which feature either low or normal FeNO levels.
But it’s important to understand where the test is most likely to prove useful.
"FeNO is the only noninvasive tool we have for assessing airway inflammation. It’s a marker of atopic and Th2-driven inflammation. Many severe adult asthmatics don’t seem to have a Th2-driven disease process. Many little kids with nonatopic asthma and viral-induced wheezing don’t have Th2-driven inflammation. As a result, FeNO is not going to be a great tool in those situations. But for those individuals in which atopy plays a role, it’s a great measure of active airway inflammation," explained Dr. Spahn of the University of Colorado, Denver, and National Jewish Health.
In one representative head-to-head comparative study, a 15% or greater improvement in FEV1 in response to an inhaled corticosteroid – widely considered a gold standard test in support of a diagnosis of asthma – had a 12% sensitivity for the diagnosis, while a reduction of greater than 20 ppb in FeNO had an 88% sensitivity (Am. J. Respir. Crit. Care Med. 2004;169:473-8).
Predicting response to steroid therapy
The ATS guidelines state that symptomatic patients who present initially with a high FeNO – more than 35 ppb in children or 50 ppb in adults – are likely to benefit from a trial of inhaled corticosteroids, and that it’s appropriate to probe for allergen exposure in such patients. The guidelines further recommend that patients with a low baseline FeNO of less than 20 ppb in children or 25 ppb in adults are less likely to have eosinophilic inflammation and are unlikely to benefit from inhaled corticosteroid therapy. Consideration of a therapeutic trial with serial FeNO monitoring is recommended in patients with intermediate levels.
Years ago, Dr. Spahn and his coworkers showed in a double-blind, randomized, crossover study that FeNO values could predict whether children with mild to moderate asthma were more likely to respond to fluticasone (Flonase) or montelukast (Singulair); the higher the initial FeNO, the more likely fluticasone was the more effective option (J. Allergy Clin. Immunol. 2005;115:233-42).
Dr. Spahn also finds FeNO results helpful in combating parental steroid phobia. "Steroid phobia still exists in the pediatric world. I know we as health care providers don’t really worry about inhaled corticosteroids having significant side effects, but parents do," he observed.
He shared a story of a 10-year-old with a severe chronic cough and newly diagnosed asthma.
"This kid was extremely disabled from his cough. If you’re coughing every 30 seconds, it’s not going to be easy for you to function normally in school. But when I mentioned that he needed to be on inhaled corticosteroid therapy, the mom acted like I’d just given her kid a death sentence. So the FeNO was a tool that I used to help convince her that there was inflammation in his airways and the way to treat it was with an inhaled corticosteroid.
"After spending half an hour convincing her of the benefits and safety of inhaled corticosteroids, she agreed. I saw him back 6 weeks later. His cough was pretty much gone, his lung function was completely normalized, and his FeNO had fallen 90%. That’s my record: A 90% reduction is about as good as it gets," Dr. Spahn said.
Assessing steroid adherence
Placing an allergic asthma patient on inhaled corticosteroid therapy should result in at least a 50% reduction in an elevated baseline FeNO. A lesser response, or an increasing FeNO during follow-up visits, is an indicator of an adherence problem.
"I like to tell people who’ve been in practice 20 years or longer that FeNO is to inhaled steroids as the theophylline blood level was to theophylline therapy. Back in the day when we used theophylline, our measure of adherence was checking someone’s theophylline level. If it was low and the patient was poorly controlled, we could blame their poor control on their poor adherence to theophylline. Up until FeNO, we didn’t have that ability with inhaled steroids. We can’t measure inhaled steroid levels due to the fact that they’re so small in the bloodstream," Dr. Spahn explained.
He reported receiving honoraria from GlaxoSmithKline as well as from Aerocrine, which markets an FeNO analyzer.
EXPERT ANALYSIS FROM THE PULMONARY AND ALLERGY UPDATE