User login
Washington State grapples with coronavirus outbreak
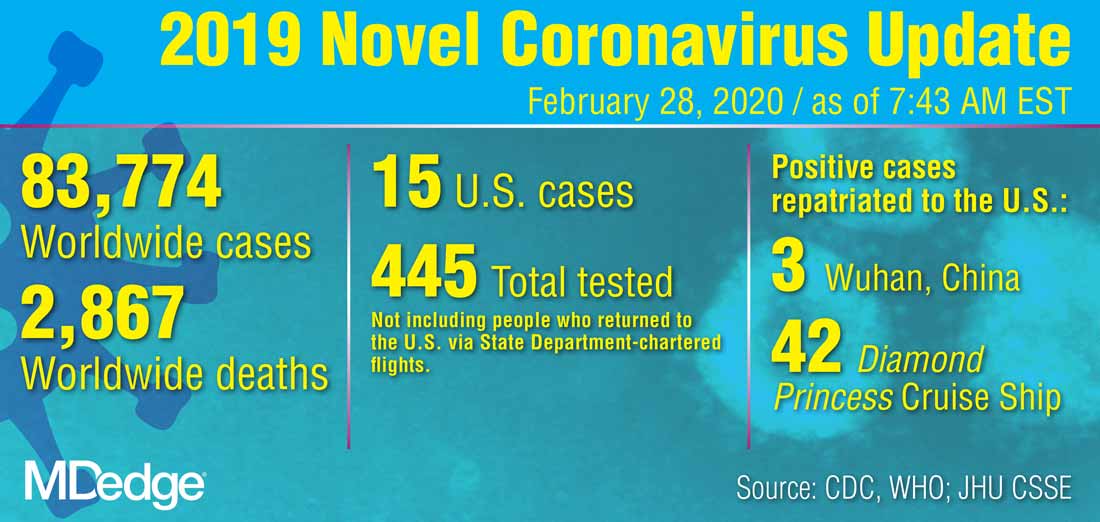
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
As the first COVID-19 outbreak in the United States emerges in Washington State, the city of Seattle, King County, and Washington State health officials provided the beginnings of a roadmap for how the region will address the rapidly evolving health crisis.
Health officials announced that four new cases were reported over the weekend in King County, Wash. There have now been 10 hospitalizations and 6 COVID-19 deaths at Evergreen Health, Kirkland, Wash. Of the deaths, five were King County residents and one was a resident of Snohomish County. Three patients died on March 1; all were in their 70s or 80s with comorbidities. Two had been residents of the Life Care senior residential facility that is at the center of the Kirkland outbreak. The number of cases in Washington now totals 18, with four cases in Snohomish County and the balance in neighboring King County.
Approximately 29 cases are under investigation with test results pending; a Centers for Disease Control and Prevention (CDC) team is on-site.
Speaking at a news conference March 2, officials sought to strike a balance between giving the community a realistic appraisal of the likely scope of the COVID-19 outbreak and avoiding sparking a panic.
“This is a complex and unprecedented challenge nationally, globally, and locally. The vast majority of the infected have mild or moderate disease and do not need hospitalization,” said Jeffrey Duchin, MD, health officer and chief, Communicable Disease EPI/Immunization Section, Public Health, Seattle and King County, and a professor of infectious diseases at the University of Washington, Seattle. “On the other hand, it’s obvious that this infection can cause very serious disease in people who are older and have underlying health conditions. We expect cases to continue to increase. We are taking the situation extremely seriously; the risk for all of us becoming infected is increasing. ...There is the potential for many to become ill at the same time.”
Among the measures being taken immediately are the purchase by King County of a hotel to house individuals who require isolation and those who are convalescing from the virus. Officials are also placing a number of prefabricated stand-alone housing units on public grounds in Seattle, with the recognition that the area has a large transient and homeless community. The stand-alone units will house homeless individuals who need isolation, treatment, or recuperation but who aren’t ill enough to be hospitalized.
Dr. Duchin said that testing capacity is ramping up rapidly in Washington State: The state lab can now accommodate up to about 200 tests daily, and expects to be able to do up to 1,000 daily soon. The University of Washington’s testing capacity will come online March 2 or 3 as a testing facility with similar initial and future peak testing capacities.
The testing strategy will continue to include very ill individuals with pneumonia or other respiratory illness of unknown etiology, but will also expand to include less ill people. This shift is being made in accordance with a shift in CDC guidelines, because of increased testing capacity, and to provide a better picture of the severity, scope, geography, and timing of the current COVID-19 outbreak in the greater Seattle area.
No school closures or cancellation of gatherings are currently recommended by public health authorities. There are currently no COVID-19 cases in Washington schools. The expectation is that any recommendations regarding closures will be re-evaluated as the outbreak progresses.
Repeatedly, officials asked the general public to employ basic measures such as handwashing and avoidance of touching the face, and to spare masks for the ill and for those who care for them. “The vast majority of people will not have serious illness. In turn we need to do everything we can to help those health care workers. I’m asking the public to do things like save the masks for our health care workers. …We need assets for our front-line health care workers and also for those who may be needing them,” said King County Health Department director Patty Hayes, RN, MN.
Now is also the time for households to initiate basic emergency preparedness measures, such as having adequate food and medication, and to make arrangements for childcare in the event of school closures, said several officials.
“We can decrease the impact on our health care system by reducing our individual risk. We are making individual- and community-level recommendations to limit the spread of disease. These are very similar to what we recommend for influenza,” said Dr. Duchin.
Ettore Palazzo, MD, chief medical and quality officer at EvergreenHealth, gave a sense of how the hospital is coping with being Ground Zero for COVID-19 in the United States. “We have made adjustments for airborne precautions,” he said, including transforming the entire critical care unit to a negative pressure unit. “We have these capabilities in other parts of the hospital as well.” Staff are working hard, but thus far staffing has kept pace with demand, he said, but all are feeling the strain already.
Dr. Duchin made the point that Washington is relatively well equipped to handle the increasingly likely scenario of a large spike in coronavirus cases, since it’s part of the Northwest Healthcare Response Network. The network is planning for sharing resources such as staff, respirators, and intensive care unit beds as circumstances warrant.
“What you just heard illustrates the challenge of this disease,” said Dr. Duchin, summing up. “The public health service and clinical health care delivery systems don’t have the capacity to track down every case in the community. I’m guessing we will see more cases of coronavirus than we see of influenza. At some point we will be shifting from counting every case” to focusing on outbreaks and the critically ill in hospitals, he said.
“We are still trying to contain the outbreak, but we are at the same time pivoting to a more community-based approach,” similar to the approach with influenza, said Dr. Duchin.
A summary of deaths and ongoing cases, drawn from the press release, is below:
The four new cases are:
• A male in his 50s, hospitalized at Highline Hospital. He has no known exposures. He is in stable but critical condition. He had no underlying health conditions.
• A male in his 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The man had underlying health conditions, and died March 1.
• A female in her 70s, a resident of Life Care, hospitalized at EvergreenHealth in Kirkland. The woman had underlying health conditions, and died March 1.
• A female in her 80s, a resident of Life Care, was hospitalized at EvergreenHealth. She is in critical condition.
In addition, a woman in her 80s, who was already reported as in critical condition at Evergreen, has died. She died on March 1.
Ten other cases, already reported earlier by Public Health, include:
• A female in her 80s, hospitalized at EvergreenHealth in Kirkland. This person has now died, and is reported as such above.
• A female in her 90s, hospitalized at EvergreenHealth in Kirkland. The woman has underlying health conditions, and is in critical condition.
• A male in his 70s, hospitalized at EvergreenHealth in Kirkland. The man has underlying health conditions, and is in critical condition.
• A male in his 70s was hospitalized at EvergreenHealth. He had underlying health conditions and died on Feb. 29.
• A man in his 60s, hospitalized at Valley Medical Center in Renton.
• A man in 60s, hospitalized at Virginia Mason Medical Center.
• A woman in her 50s, who had traveled to South Korea; recovering at home.
• A woman in her 70s, who was a resident of Life Care in Kirkland, hospitalized at EvergreenHealth.
• A woman in her 40s, employed by Life Care, who is hospitalized at Overlake Medical Center.
• A man in his 50s, who was hospitalized and died at EvergreenHealth.
FROM A KING COUNTY, WASH. NEWS BRIEFING
In gestational diabetes, early postpartum glucose testing is a winner
GRAPEVINE, TEX. – Early postpartum glucose tolerance testing for women with gestational diabetes resulted in a 99% adherence rate, with similar sensitivity and specificity as the currently recommended 4- to 12-week postpartum testing schedule.
“Two-day postpartum glucose tolerance testing has similar diagnostic utility as the 4- to 12-week postpartum glucose tolerance test to identify impaired glucose metabolism and diabetes at 1 year postpartum,” said Erika Werner, MD, speaking at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Overall, 29% of women studied had impaired glucose metabolism at 2 days postpartum, as did 25% in the 4- to 12-weeks postpartum window. At 1 year, that figure was 35%. The number of women meeting diagnostic criteria for diabetes held steady at 4% for all three time points.
The findings warrant “consideration for the 2-day postpartum glucose tolerance test (GTT) as the initial postpartum test for women who have gestational diabetes, with repeat testing at 1 year,” said Dr. Werner, a maternal-fetal medicine physician at Brown University, Providence, R.I.
Glucose testing for women with gestational diabetes mellitus (GDM) is recommended at 4-12 weeks postpartum by both the American Diabetes Association and the American College of Obstetricians and Gynecologists.
Testing can allow detection and treatment of impaired glucose metabolism, seen in 15%-40% of women with a history of GDM. Up to 1 in 20 women with GDM will receive a postpartum diagnosis of type 2 diabetes.
However, fewer than one in five women will actually have postpartum glucose testing, representing a large missed opportunity, said Dr. Werner.
Several factors likely contribute to those screening failures, she added. In addition to the potential for public insurance to lapse at 6 weeks postpartum, the logistical realities and time demands of parenting a newborn are themselves a significant barrier.
“What if we changed the timing?” and shifted glucose testing to the early postpartum days, before hospital discharge, asked Dr. Werner. Several pilot studies had already compared glucose screening in the first few days postpartum with the routine schedule, finding good correlation between the early and routine GTT schedule.
Importantly, the earlier studies achieved an adherence rate of more than 90% for early GTT. By contrast, fewer than half of the participants in the usual-care arms actually returned for postpartum GTT in the 4- to 12-week postpartum window, even under the optimized conditions associated with a medical study.
The single-center prospective cohort study conducted by Dr. Werner and collaborators enrolled 300 women with GDM. Women agreed to participate in glucose tolerance testing as inpatients, at 2 days postpartum, in addition to receiving a GTT between 4 and 12 weeks postpartum, and additional screening that included a glycosylated hemoglobin (HbA1c) test at 1 year postpartum.
The investigators obtained postpartum day 2 GTTs for all but four of the patients. A total of 201 patients returned in the 4- to 12-week postpartum window, and 168 of those participants returned for HbA1c testing at 1 year. Of the 95 patients who didn’t come back for the 4- to 12-week test, 33 did return at 1 year for HbA1c testing.
Dr. Werner and her coinvestigators included adult women who spoke either fluent Spanish or English and had GDM diagnosed by the Carpenter-Coustan criteria, or by having a blood glucose level of 200 mg/dL or more in a 1-hour glucose challenge test.
The early GTT results weren’t shared with patients or their health care providers. For outpatient visits, participants were offered financial incentives and received multiple reminder phone calls and the offer of free transportation.
For the purposes of the study, impaired glucose metabolism was defined as fasting blood glucose of 100 mg/dL or greater, a 2-hour GTT blood glucose level of 140 mg/dL or greater, or HbA1c of 5.7% or greater.
Participants were diagnosed with diabetes if they had a fasting blood glucose of 126 mg/dL or greater, a 2-hour GTT blood glucose level of 200 mg/dL or greater, or HbA1c of 6.5% or greater.
Dr. Werner and colleagues conducted two analyses of their results. In the first, they included only women in both arms who had complete data. In the second analysis, they looked at all women who had data for the 1-year postpartum mark, assuming that interval GTTs were negative for women who were missing these values.
The statistical analysis showed that, for women with complete data, both early and later postpartum GTTs were similar in predicting impaired glucose metabolism at 1 year postpartum (areas under the receiver operating curve [AUC], 0.63 and 0.60, respectively).
For identifying diabetes at 1 year, both early and late testing had high negative predictive value (98% and 99%, respectively), but the later testing strategy had higher sensitivity and specificity, yielding an AUC of 0.83, compared with 0.65 for early testing.
Turning to the second analysis that included all women who had 1-year postpartum HbA1c values, negative predictive values for diabetes were similarly high (98%) for both the early and late testing strategies. For identifying impaired glucose metabolism at 1 year in this group, both the positive and negative predictive value of the early and late strategies were similar.
Patients were about 32 years old at baseline, with a mean body mass index of 31.7 kg/m2. More than half of patients (52.3%) had private insurance, and 22% had GDM in a pregnancy prior to the index pregnancy. Black patients made up about 9% of the study population; 54% of participants were white, and 23% Hispanic. About one-third of patients were nulliparous, and two-thirds had education beyond high school.
During their pregnancies, about 44% of patients managed GDM by diet alone, 40% required insulin, with an additional 1% also requiring an oral agent. The remainder required oral agents alone. Patients delivered at a mean 38.3 weeks gestation, with about 40% receiving cesarean deliveries.
Some of the study’s strengths included its prospective nature, the diverse population recruited, and the fact that participants and providers were both blinded to the 2-day GTT results. Although more than half of participants completed the study – besting the previous pilots – 44% of patients still had incomplete data, noted Dr. Werner.
The American Diabetes Association sponsored the study. Dr. Werner reported no other conflicts of interest.
SOURCE: Werner E et al. SMFM 2020. Abstract 72.
GRAPEVINE, TEX. – Early postpartum glucose tolerance testing for women with gestational diabetes resulted in a 99% adherence rate, with similar sensitivity and specificity as the currently recommended 4- to 12-week postpartum testing schedule.
“Two-day postpartum glucose tolerance testing has similar diagnostic utility as the 4- to 12-week postpartum glucose tolerance test to identify impaired glucose metabolism and diabetes at 1 year postpartum,” said Erika Werner, MD, speaking at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Overall, 29% of women studied had impaired glucose metabolism at 2 days postpartum, as did 25% in the 4- to 12-weeks postpartum window. At 1 year, that figure was 35%. The number of women meeting diagnostic criteria for diabetes held steady at 4% for all three time points.
The findings warrant “consideration for the 2-day postpartum glucose tolerance test (GTT) as the initial postpartum test for women who have gestational diabetes, with repeat testing at 1 year,” said Dr. Werner, a maternal-fetal medicine physician at Brown University, Providence, R.I.
Glucose testing for women with gestational diabetes mellitus (GDM) is recommended at 4-12 weeks postpartum by both the American Diabetes Association and the American College of Obstetricians and Gynecologists.
Testing can allow detection and treatment of impaired glucose metabolism, seen in 15%-40% of women with a history of GDM. Up to 1 in 20 women with GDM will receive a postpartum diagnosis of type 2 diabetes.
However, fewer than one in five women will actually have postpartum glucose testing, representing a large missed opportunity, said Dr. Werner.
Several factors likely contribute to those screening failures, she added. In addition to the potential for public insurance to lapse at 6 weeks postpartum, the logistical realities and time demands of parenting a newborn are themselves a significant barrier.
“What if we changed the timing?” and shifted glucose testing to the early postpartum days, before hospital discharge, asked Dr. Werner. Several pilot studies had already compared glucose screening in the first few days postpartum with the routine schedule, finding good correlation between the early and routine GTT schedule.
Importantly, the earlier studies achieved an adherence rate of more than 90% for early GTT. By contrast, fewer than half of the participants in the usual-care arms actually returned for postpartum GTT in the 4- to 12-week postpartum window, even under the optimized conditions associated with a medical study.
The single-center prospective cohort study conducted by Dr. Werner and collaborators enrolled 300 women with GDM. Women agreed to participate in glucose tolerance testing as inpatients, at 2 days postpartum, in addition to receiving a GTT between 4 and 12 weeks postpartum, and additional screening that included a glycosylated hemoglobin (HbA1c) test at 1 year postpartum.
The investigators obtained postpartum day 2 GTTs for all but four of the patients. A total of 201 patients returned in the 4- to 12-week postpartum window, and 168 of those participants returned for HbA1c testing at 1 year. Of the 95 patients who didn’t come back for the 4- to 12-week test, 33 did return at 1 year for HbA1c testing.
Dr. Werner and her coinvestigators included adult women who spoke either fluent Spanish or English and had GDM diagnosed by the Carpenter-Coustan criteria, or by having a blood glucose level of 200 mg/dL or more in a 1-hour glucose challenge test.
The early GTT results weren’t shared with patients or their health care providers. For outpatient visits, participants were offered financial incentives and received multiple reminder phone calls and the offer of free transportation.
For the purposes of the study, impaired glucose metabolism was defined as fasting blood glucose of 100 mg/dL or greater, a 2-hour GTT blood glucose level of 140 mg/dL or greater, or HbA1c of 5.7% or greater.
Participants were diagnosed with diabetes if they had a fasting blood glucose of 126 mg/dL or greater, a 2-hour GTT blood glucose level of 200 mg/dL or greater, or HbA1c of 6.5% or greater.
Dr. Werner and colleagues conducted two analyses of their results. In the first, they included only women in both arms who had complete data. In the second analysis, they looked at all women who had data for the 1-year postpartum mark, assuming that interval GTTs were negative for women who were missing these values.
The statistical analysis showed that, for women with complete data, both early and later postpartum GTTs were similar in predicting impaired glucose metabolism at 1 year postpartum (areas under the receiver operating curve [AUC], 0.63 and 0.60, respectively).
For identifying diabetes at 1 year, both early and late testing had high negative predictive value (98% and 99%, respectively), but the later testing strategy had higher sensitivity and specificity, yielding an AUC of 0.83, compared with 0.65 for early testing.
Turning to the second analysis that included all women who had 1-year postpartum HbA1c values, negative predictive values for diabetes were similarly high (98%) for both the early and late testing strategies. For identifying impaired glucose metabolism at 1 year in this group, both the positive and negative predictive value of the early and late strategies were similar.
Patients were about 32 years old at baseline, with a mean body mass index of 31.7 kg/m2. More than half of patients (52.3%) had private insurance, and 22% had GDM in a pregnancy prior to the index pregnancy. Black patients made up about 9% of the study population; 54% of participants were white, and 23% Hispanic. About one-third of patients were nulliparous, and two-thirds had education beyond high school.
During their pregnancies, about 44% of patients managed GDM by diet alone, 40% required insulin, with an additional 1% also requiring an oral agent. The remainder required oral agents alone. Patients delivered at a mean 38.3 weeks gestation, with about 40% receiving cesarean deliveries.
Some of the study’s strengths included its prospective nature, the diverse population recruited, and the fact that participants and providers were both blinded to the 2-day GTT results. Although more than half of participants completed the study – besting the previous pilots – 44% of patients still had incomplete data, noted Dr. Werner.
The American Diabetes Association sponsored the study. Dr. Werner reported no other conflicts of interest.
SOURCE: Werner E et al. SMFM 2020. Abstract 72.
GRAPEVINE, TEX. – Early postpartum glucose tolerance testing for women with gestational diabetes resulted in a 99% adherence rate, with similar sensitivity and specificity as the currently recommended 4- to 12-week postpartum testing schedule.
“Two-day postpartum glucose tolerance testing has similar diagnostic utility as the 4- to 12-week postpartum glucose tolerance test to identify impaired glucose metabolism and diabetes at 1 year postpartum,” said Erika Werner, MD, speaking at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Overall, 29% of women studied had impaired glucose metabolism at 2 days postpartum, as did 25% in the 4- to 12-weeks postpartum window. At 1 year, that figure was 35%. The number of women meeting diagnostic criteria for diabetes held steady at 4% for all three time points.
The findings warrant “consideration for the 2-day postpartum glucose tolerance test (GTT) as the initial postpartum test for women who have gestational diabetes, with repeat testing at 1 year,” said Dr. Werner, a maternal-fetal medicine physician at Brown University, Providence, R.I.
Glucose testing for women with gestational diabetes mellitus (GDM) is recommended at 4-12 weeks postpartum by both the American Diabetes Association and the American College of Obstetricians and Gynecologists.
Testing can allow detection and treatment of impaired glucose metabolism, seen in 15%-40% of women with a history of GDM. Up to 1 in 20 women with GDM will receive a postpartum diagnosis of type 2 diabetes.
However, fewer than one in five women will actually have postpartum glucose testing, representing a large missed opportunity, said Dr. Werner.
Several factors likely contribute to those screening failures, she added. In addition to the potential for public insurance to lapse at 6 weeks postpartum, the logistical realities and time demands of parenting a newborn are themselves a significant barrier.
“What if we changed the timing?” and shifted glucose testing to the early postpartum days, before hospital discharge, asked Dr. Werner. Several pilot studies had already compared glucose screening in the first few days postpartum with the routine schedule, finding good correlation between the early and routine GTT schedule.
Importantly, the earlier studies achieved an adherence rate of more than 90% for early GTT. By contrast, fewer than half of the participants in the usual-care arms actually returned for postpartum GTT in the 4- to 12-week postpartum window, even under the optimized conditions associated with a medical study.
The single-center prospective cohort study conducted by Dr. Werner and collaborators enrolled 300 women with GDM. Women agreed to participate in glucose tolerance testing as inpatients, at 2 days postpartum, in addition to receiving a GTT between 4 and 12 weeks postpartum, and additional screening that included a glycosylated hemoglobin (HbA1c) test at 1 year postpartum.
The investigators obtained postpartum day 2 GTTs for all but four of the patients. A total of 201 patients returned in the 4- to 12-week postpartum window, and 168 of those participants returned for HbA1c testing at 1 year. Of the 95 patients who didn’t come back for the 4- to 12-week test, 33 did return at 1 year for HbA1c testing.
Dr. Werner and her coinvestigators included adult women who spoke either fluent Spanish or English and had GDM diagnosed by the Carpenter-Coustan criteria, or by having a blood glucose level of 200 mg/dL or more in a 1-hour glucose challenge test.
The early GTT results weren’t shared with patients or their health care providers. For outpatient visits, participants were offered financial incentives and received multiple reminder phone calls and the offer of free transportation.
For the purposes of the study, impaired glucose metabolism was defined as fasting blood glucose of 100 mg/dL or greater, a 2-hour GTT blood glucose level of 140 mg/dL or greater, or HbA1c of 5.7% or greater.
Participants were diagnosed with diabetes if they had a fasting blood glucose of 126 mg/dL or greater, a 2-hour GTT blood glucose level of 200 mg/dL or greater, or HbA1c of 6.5% or greater.
Dr. Werner and colleagues conducted two analyses of their results. In the first, they included only women in both arms who had complete data. In the second analysis, they looked at all women who had data for the 1-year postpartum mark, assuming that interval GTTs were negative for women who were missing these values.
The statistical analysis showed that, for women with complete data, both early and later postpartum GTTs were similar in predicting impaired glucose metabolism at 1 year postpartum (areas under the receiver operating curve [AUC], 0.63 and 0.60, respectively).
For identifying diabetes at 1 year, both early and late testing had high negative predictive value (98% and 99%, respectively), but the later testing strategy had higher sensitivity and specificity, yielding an AUC of 0.83, compared with 0.65 for early testing.
Turning to the second analysis that included all women who had 1-year postpartum HbA1c values, negative predictive values for diabetes were similarly high (98%) for both the early and late testing strategies. For identifying impaired glucose metabolism at 1 year in this group, both the positive and negative predictive value of the early and late strategies were similar.
Patients were about 32 years old at baseline, with a mean body mass index of 31.7 kg/m2. More than half of patients (52.3%) had private insurance, and 22% had GDM in a pregnancy prior to the index pregnancy. Black patients made up about 9% of the study population; 54% of participants were white, and 23% Hispanic. About one-third of patients were nulliparous, and two-thirds had education beyond high school.
During their pregnancies, about 44% of patients managed GDM by diet alone, 40% required insulin, with an additional 1% also requiring an oral agent. The remainder required oral agents alone. Patients delivered at a mean 38.3 weeks gestation, with about 40% receiving cesarean deliveries.
Some of the study’s strengths included its prospective nature, the diverse population recruited, and the fact that participants and providers were both blinded to the 2-day GTT results. Although more than half of participants completed the study – besting the previous pilots – 44% of patients still had incomplete data, noted Dr. Werner.
The American Diabetes Association sponsored the study. Dr. Werner reported no other conflicts of interest.
SOURCE: Werner E et al. SMFM 2020. Abstract 72.
REPORTING FROM THE PREGNANCY MEETING
CDC revises COVID-19 test kits, broadens ‘person under investigation’ definition
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
In a telebriefing on the COVID-19 outbreak, Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at .
The definition has been revised “to meet the needs of this rapidly evolving situation,” she said. The new PUI definition includes travel to more geographic areas to reflect this past week’s marked uptick in coronavirus activity in Italy and Iran. In addition to these countries and China, recent travel to Japan or South Korea also constitutes an epidemiologic risk factor which, in conjunction with clinical features, warrant an individual being classified as a PUI. These five countries each now have widespread person-to-person transmission of the virus.
Dr. Messonnier left open the possibility that the PUI definition would continue to evolve if such transmission within communities becomes more common. Asked whether the small number of U.S. cases thus might be an artifact of low test volumes, she said, “We aggressively controlled our borders to slow the spread. This was an intentional U.S. strategy. The CDC has always had the capacity to test rapidly from the time the sequence was available. ...We have been testing aggressively.”
The original PUI definition, she explained, emphasized individuals with fever, cough, or trouble breathing who had traveled recently from areas with COVID-19 activity, in particular China’s Hubei province. “We have been most focused on symptomatic people who are closely linked to, or who had, travel history, but our criteria also allow for clinical discretion,” she said. “There is no substitute for an astute clinician on the front lines of patient care.”
The first COVID-19 case from person-to-person spread was reported on Feb. 27. “At this time, we don’t know how or where this person became infected,” said Dr. Messonnier, although investigations are still underway. She responded to a question about whether the CDC delayed allowing COVID-19 testing for the patient for several days, as was reported in some media accounts. “According to CDC records, the first call we got was Feb. 23,” when public health officials in California reported a severely ill person with no travel abroad and no known contacts with individuals that would trigger suspicions for coronavirus. The CDC recommended COVID-19 testing on that day, she said.
Dr. Messonnier declined to answer questions about a whistleblower report alleging improper training and inadequate protective measures for Department of Health & Human Services workers at the quarantine center at Travis Air Force Base, Calif.
Dr. Messonnier said that the CDC has been working closely with the Food and Drug Administration to address problems with the COVID-19 test kits that were unusable because of a large number of indeterminate results. The two agencies together have determined that of the three reactions that were initially deemed necessary for a definitive COVID-19 diagnosis, just two are sufficient, so new kits that omit the problematic chemical are being manufactured and distributed.
These new kits are rapidly being made available; the goal, said Dr. Messonnier, is to have to state and local public health departments equipped with test kits by about March 7.
As local tests become available, the most updated information will be coming from state and local public health departments, she stressed, adding that the CDC would continue to update case counts on Monday, Wednesday, and Friday of each week. Procedures are being developed for the management of patients presumed to have COVID-19, where local health departments see positive tests but the mandatory CDC confirmatory test hasn’t been completed.
While new cases emerge across Europe and Asia, China’s earlier COVID-19 explosion seems to be slowing. “It’s really good news that the case counts in China are decreasing,” both for the well-being of that country’s citizens, and as a sign of the disease’s potential global effects, said Dr. Messonnier. She added that epidemiologists and mathematical modelers are parsing case fatality rates as well.
She advised health care providers and public health officials to keep abreast of changes in CDC guidance by checking frequently at https://www.cdc.gov/coronavirus/2019-ncov/index.html.
REPORTING FROM A CDC BRIEFING
Community-wide initiative ups teen LARC adoption sixfold
In Rochester, N.Y., a comprehensive community initiative that raised awareness about and delivered training in the use of long-acting reversible contraceptives (LARCs) significantly upped LARC adoption among sexually active female high schoolers.
Over the course of the 3-year project, LARC use rose from about 4% to 24% in this group, a statistically significant increase (P less than .0001). During the same time period, LARC use increased nationally, as well, but at a lower rate, rising from 2% to 5% for the same population, while New York state saw LARC use rise from 2% to 5%.
In New York City, where an unrelated LARC awareness campaign was conducted, LARC use went from 3% to 5% over the study period for sexually active female high school students. Comparing the trend in LARC use in Rochester to the secular trend in these control groups showed significantly higher uptake over time in Rochester (P less than .0001).
Through a series of lunch-and-learn talks given to adults who work with adolescents in community-based settings and in medical settings, the Greater Rochester LARC Initiative reached more than 1,300 individuals during July 2014-June 2017, C. Andrew Aligne, MD, MPH, of the University of Rochester (N.Y.), and coauthors reported in the American Journal of Obstetrics and Gynecology.
Of the 81 total talks delivered, 50 were in medical settings, reaching 703 attendees ranging from front-office personnel to primary care physicians, advanced practice clinicians, and nurses; the talks in community-based settings reached 662 attendees.
“We use the term ‘community detailing’ to describe the design of the intervention because it was an innovative hybrid of academic detailing and community health education,” explained Dr. Aligne and colleagues. This approach is a unique, feasible, and effective approach to unintended adolescent pregnancy programs. “The community detailing approach could be a useful complement to programs for preventing unintended adolescent pregnancy.”
The study’s primary outcome measure was LARC use among sexually active female high school students as identified by responses on the U.S. Centers for Disease Control and Statistics’ Youth Risk Behavior Survey (YRBS).
YRBS data were examined for the years 2013, 2015, and 2017, spanning the period before and after the LARC initiative was begun. A separate question about LARC use wasn’t included in the 2013 YRBS survey, so the investigators used a generous estimate that two-thirds of respondents who reported using the “other” contraceptive category for that year were using LARCs. That category was chosen by a total of 6% of respondents, and encompassed LARC use along with use of the patch, ring, diaphragm, and fertility awareness, explained Dr. Aligne and collaborators.
Addressing the problem of failure to use a condom with LARC use, Dr. Aligne and collaborators found overall low rates of dual-method use, but higher rates in Rochester than in the comparison groups. In Rochester, 78% of respondents reported that they also did not use condoms. This figure was lower than the 91% reported for the United States as a whole, and also was lower than the 93% reported in New York City and the 85% reported in New York state. No increase in sexually transmitted infections was seen in Rochester’s sexually active high school females during the study period.
“Our main finding of increased LARC use is consistent with the literature demonstrating that many sexually active young women, including adolescents, will choose LARC if they are given access not only to birth control itself, but also to accurate information about various contraceptive methods,” concluded Dr. Aligne and his associates.
A practical strength of the Greater Rochester LARC initiative was that it capitalized on existing resources, such as New York state’s preexisting program for free access to contraception and similar provisions in the Affordable Care Act. Also, local Title X clinics that were enrolled in New York’s free contraception initiative already had practitioners who were trained and able to provide same-day LARC insertion.
Pediatricians engaged in the initiative were able to receive free training from LARC manufacturers, as mandated by the Food and Drug Administration. Through collaboration with implant manufacturers, Rochester LARC Initiative staff were able to piggyback on training sessions to add education about contraception counseling and the importance of offering access to all contraception methods.
Taken as a whole, the LARC Initiative could be scaled up, wrote Dr. Aligne and his coauthors, a potential boon in the 21 states where qualifying individuals younger than 19 years of age are eligible for Medicaid reimbursement for family planning services. “Even though easy LARC access is far from universal, there are vast areas of the nation where cost need not be seen as an insurmountable barrier.” Dr. Aligne and coauthors also addressed the fraught history of reproductive justice in the United States, cautioning that universal LARC adoption was not – and should not be – the goal of such initiatives. “There is a history of reproductive coercion in the U.S. including forced sterilization of women of color; therefore, it is critical that LARC methods not be imposed on any particular group. On the other hand, LARC should not be withheld deliberately from adolescents who want it, as this is another form of injustice,” they wrote. “The goal should be to empower individuals to decide what is right for them in a context of social and reproductive justice.”
Using the nationally administered YRBS was a significant strength of the study, commented Dr. Aligne and his collaborators. “This allowed us to employ the study design of pre-post with a nonrandomized control group,” the investigators noted, adding that the “relatively rigorous” methodology reduced the risk of problems with internal validity, and also allowed comparisons between changes in Rochester and those at the state and national level.
However, the researchers acknowledged that the study was not a randomized trial, and there’s always the possibility of unknown confounders contributing to LARC uptake during the study period. Also, the YRBS is a self-report instrument and only includes those enrolled in school.
Dr. Aligne reported that his spouse received compensation for providing contraceptive implant insertion training, as did two coauthors. The LARC initiative was supported by a grant from the Greater Rochester Health Foundation.
SOURCE: Aligne CA et al. Am J Obstet Gynecol. 2020 Jan 22. doi: 10.1016/j.ajog.2020.01.029.
In Rochester, N.Y., a comprehensive community initiative that raised awareness about and delivered training in the use of long-acting reversible contraceptives (LARCs) significantly upped LARC adoption among sexually active female high schoolers.
Over the course of the 3-year project, LARC use rose from about 4% to 24% in this group, a statistically significant increase (P less than .0001). During the same time period, LARC use increased nationally, as well, but at a lower rate, rising from 2% to 5% for the same population, while New York state saw LARC use rise from 2% to 5%.
In New York City, where an unrelated LARC awareness campaign was conducted, LARC use went from 3% to 5% over the study period for sexually active female high school students. Comparing the trend in LARC use in Rochester to the secular trend in these control groups showed significantly higher uptake over time in Rochester (P less than .0001).
Through a series of lunch-and-learn talks given to adults who work with adolescents in community-based settings and in medical settings, the Greater Rochester LARC Initiative reached more than 1,300 individuals during July 2014-June 2017, C. Andrew Aligne, MD, MPH, of the University of Rochester (N.Y.), and coauthors reported in the American Journal of Obstetrics and Gynecology.
Of the 81 total talks delivered, 50 were in medical settings, reaching 703 attendees ranging from front-office personnel to primary care physicians, advanced practice clinicians, and nurses; the talks in community-based settings reached 662 attendees.
“We use the term ‘community detailing’ to describe the design of the intervention because it was an innovative hybrid of academic detailing and community health education,” explained Dr. Aligne and colleagues. This approach is a unique, feasible, and effective approach to unintended adolescent pregnancy programs. “The community detailing approach could be a useful complement to programs for preventing unintended adolescent pregnancy.”
The study’s primary outcome measure was LARC use among sexually active female high school students as identified by responses on the U.S. Centers for Disease Control and Statistics’ Youth Risk Behavior Survey (YRBS).
YRBS data were examined for the years 2013, 2015, and 2017, spanning the period before and after the LARC initiative was begun. A separate question about LARC use wasn’t included in the 2013 YRBS survey, so the investigators used a generous estimate that two-thirds of respondents who reported using the “other” contraceptive category for that year were using LARCs. That category was chosen by a total of 6% of respondents, and encompassed LARC use along with use of the patch, ring, diaphragm, and fertility awareness, explained Dr. Aligne and collaborators.
Addressing the problem of failure to use a condom with LARC use, Dr. Aligne and collaborators found overall low rates of dual-method use, but higher rates in Rochester than in the comparison groups. In Rochester, 78% of respondents reported that they also did not use condoms. This figure was lower than the 91% reported for the United States as a whole, and also was lower than the 93% reported in New York City and the 85% reported in New York state. No increase in sexually transmitted infections was seen in Rochester’s sexually active high school females during the study period.
“Our main finding of increased LARC use is consistent with the literature demonstrating that many sexually active young women, including adolescents, will choose LARC if they are given access not only to birth control itself, but also to accurate information about various contraceptive methods,” concluded Dr. Aligne and his associates.
A practical strength of the Greater Rochester LARC initiative was that it capitalized on existing resources, such as New York state’s preexisting program for free access to contraception and similar provisions in the Affordable Care Act. Also, local Title X clinics that were enrolled in New York’s free contraception initiative already had practitioners who were trained and able to provide same-day LARC insertion.
Pediatricians engaged in the initiative were able to receive free training from LARC manufacturers, as mandated by the Food and Drug Administration. Through collaboration with implant manufacturers, Rochester LARC Initiative staff were able to piggyback on training sessions to add education about contraception counseling and the importance of offering access to all contraception methods.
Taken as a whole, the LARC Initiative could be scaled up, wrote Dr. Aligne and his coauthors, a potential boon in the 21 states where qualifying individuals younger than 19 years of age are eligible for Medicaid reimbursement for family planning services. “Even though easy LARC access is far from universal, there are vast areas of the nation where cost need not be seen as an insurmountable barrier.” Dr. Aligne and coauthors also addressed the fraught history of reproductive justice in the United States, cautioning that universal LARC adoption was not – and should not be – the goal of such initiatives. “There is a history of reproductive coercion in the U.S. including forced sterilization of women of color; therefore, it is critical that LARC methods not be imposed on any particular group. On the other hand, LARC should not be withheld deliberately from adolescents who want it, as this is another form of injustice,” they wrote. “The goal should be to empower individuals to decide what is right for them in a context of social and reproductive justice.”
Using the nationally administered YRBS was a significant strength of the study, commented Dr. Aligne and his collaborators. “This allowed us to employ the study design of pre-post with a nonrandomized control group,” the investigators noted, adding that the “relatively rigorous” methodology reduced the risk of problems with internal validity, and also allowed comparisons between changes in Rochester and those at the state and national level.
However, the researchers acknowledged that the study was not a randomized trial, and there’s always the possibility of unknown confounders contributing to LARC uptake during the study period. Also, the YRBS is a self-report instrument and only includes those enrolled in school.
Dr. Aligne reported that his spouse received compensation for providing contraceptive implant insertion training, as did two coauthors. The LARC initiative was supported by a grant from the Greater Rochester Health Foundation.
SOURCE: Aligne CA et al. Am J Obstet Gynecol. 2020 Jan 22. doi: 10.1016/j.ajog.2020.01.029.
In Rochester, N.Y., a comprehensive community initiative that raised awareness about and delivered training in the use of long-acting reversible contraceptives (LARCs) significantly upped LARC adoption among sexually active female high schoolers.
Over the course of the 3-year project, LARC use rose from about 4% to 24% in this group, a statistically significant increase (P less than .0001). During the same time period, LARC use increased nationally, as well, but at a lower rate, rising from 2% to 5% for the same population, while New York state saw LARC use rise from 2% to 5%.
In New York City, where an unrelated LARC awareness campaign was conducted, LARC use went from 3% to 5% over the study period for sexually active female high school students. Comparing the trend in LARC use in Rochester to the secular trend in these control groups showed significantly higher uptake over time in Rochester (P less than .0001).
Through a series of lunch-and-learn talks given to adults who work with adolescents in community-based settings and in medical settings, the Greater Rochester LARC Initiative reached more than 1,300 individuals during July 2014-June 2017, C. Andrew Aligne, MD, MPH, of the University of Rochester (N.Y.), and coauthors reported in the American Journal of Obstetrics and Gynecology.
Of the 81 total talks delivered, 50 were in medical settings, reaching 703 attendees ranging from front-office personnel to primary care physicians, advanced practice clinicians, and nurses; the talks in community-based settings reached 662 attendees.
“We use the term ‘community detailing’ to describe the design of the intervention because it was an innovative hybrid of academic detailing and community health education,” explained Dr. Aligne and colleagues. This approach is a unique, feasible, and effective approach to unintended adolescent pregnancy programs. “The community detailing approach could be a useful complement to programs for preventing unintended adolescent pregnancy.”
The study’s primary outcome measure was LARC use among sexually active female high school students as identified by responses on the U.S. Centers for Disease Control and Statistics’ Youth Risk Behavior Survey (YRBS).
YRBS data were examined for the years 2013, 2015, and 2017, spanning the period before and after the LARC initiative was begun. A separate question about LARC use wasn’t included in the 2013 YRBS survey, so the investigators used a generous estimate that two-thirds of respondents who reported using the “other” contraceptive category for that year were using LARCs. That category was chosen by a total of 6% of respondents, and encompassed LARC use along with use of the patch, ring, diaphragm, and fertility awareness, explained Dr. Aligne and collaborators.
Addressing the problem of failure to use a condom with LARC use, Dr. Aligne and collaborators found overall low rates of dual-method use, but higher rates in Rochester than in the comparison groups. In Rochester, 78% of respondents reported that they also did not use condoms. This figure was lower than the 91% reported for the United States as a whole, and also was lower than the 93% reported in New York City and the 85% reported in New York state. No increase in sexually transmitted infections was seen in Rochester’s sexually active high school females during the study period.
“Our main finding of increased LARC use is consistent with the literature demonstrating that many sexually active young women, including adolescents, will choose LARC if they are given access not only to birth control itself, but also to accurate information about various contraceptive methods,” concluded Dr. Aligne and his associates.
A practical strength of the Greater Rochester LARC initiative was that it capitalized on existing resources, such as New York state’s preexisting program for free access to contraception and similar provisions in the Affordable Care Act. Also, local Title X clinics that were enrolled in New York’s free contraception initiative already had practitioners who were trained and able to provide same-day LARC insertion.
Pediatricians engaged in the initiative were able to receive free training from LARC manufacturers, as mandated by the Food and Drug Administration. Through collaboration with implant manufacturers, Rochester LARC Initiative staff were able to piggyback on training sessions to add education about contraception counseling and the importance of offering access to all contraception methods.
Taken as a whole, the LARC Initiative could be scaled up, wrote Dr. Aligne and his coauthors, a potential boon in the 21 states where qualifying individuals younger than 19 years of age are eligible for Medicaid reimbursement for family planning services. “Even though easy LARC access is far from universal, there are vast areas of the nation where cost need not be seen as an insurmountable barrier.” Dr. Aligne and coauthors also addressed the fraught history of reproductive justice in the United States, cautioning that universal LARC adoption was not – and should not be – the goal of such initiatives. “There is a history of reproductive coercion in the U.S. including forced sterilization of women of color; therefore, it is critical that LARC methods not be imposed on any particular group. On the other hand, LARC should not be withheld deliberately from adolescents who want it, as this is another form of injustice,” they wrote. “The goal should be to empower individuals to decide what is right for them in a context of social and reproductive justice.”
Using the nationally administered YRBS was a significant strength of the study, commented Dr. Aligne and his collaborators. “This allowed us to employ the study design of pre-post with a nonrandomized control group,” the investigators noted, adding that the “relatively rigorous” methodology reduced the risk of problems with internal validity, and also allowed comparisons between changes in Rochester and those at the state and national level.
However, the researchers acknowledged that the study was not a randomized trial, and there’s always the possibility of unknown confounders contributing to LARC uptake during the study period. Also, the YRBS is a self-report instrument and only includes those enrolled in school.
Dr. Aligne reported that his spouse received compensation for providing contraceptive implant insertion training, as did two coauthors. The LARC initiative was supported by a grant from the Greater Rochester Health Foundation.
SOURCE: Aligne CA et al. Am J Obstet Gynecol. 2020 Jan 22. doi: 10.1016/j.ajog.2020.01.029.
FROM AJOG
Genetic risk score may flag post-GDM incidence of type 2 disease
Women who had gestational diabetes mellitus had an increased risk for later type 2 diabetes if they carried certain genetic risk factors for the disease, according to a new analysis in BMJ Open Diabetes Research & Care of data from two independent populations.
A higher genetic risk score (GRS) had a modest association with developing type 2 diabetes, but a healthier diet may mitigate this risk, as Mengying Li, PhD, and her colleagues found for participants in the Nurses’ Health Study and members of the Danish National Birth Cohort who developed gestational diabetes mellitus (GDM).
Of 1,884 white women with a history of GDM in the Nurses’ Health Study II (NHSII), 446 (23.7%) went on to develop type 2 diabetes, and of the 550 women who had GDM in the Danish National Birth Cohort (DNBC), 155 (28.2%) developed the disease. The researchers calculated a GRS for type 2 diabetes for the full cohort. Genome-wide association studies completed in European populations were used to identify 59 single-nucleotide polymorphisms (SNPs) associated with the disease.
Dr. Li, an epidemiologist and postdoctoral researcher at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md., and her coauthors found that women whose GRS was in the highest quartile had a relative risk of 1.19 for type 2 diabetes. The relative risks for the three lower quartiles were 1.25, 0.97, and 1.00, respectively (P value for trend = .02). For each increase of five risk alleles in the GRS, NHSII participants had a 7% increased risk for type 2 diabetes, and DNBC participants saw a 9% increased risk.
Comparing these findings with other studies looking at genetic risk and type 2 diabetes in the general population, Dr. Li and her coauthors noted that the increase in relative risk for type 2 disease with increase in GRS was actually slightly weaker in the GDM cohort they studied. “The smaller effect size among women with GDM likely reflects an already higher baseline genetic risk for [type 2 diabetes] than the general population, as we have demonstrated,” they explained.
Though 11 individual SNPs had a significant individual association with the risk for type 2 diabetes initially, that association disappeared after correction for a false-discovery rate. Dr. Li and her coinvestigators conducted a sensitivity analysis that included only 42 SNPs that were later definitively associated with type 2 disease and they saw essentially unchanged results.
The researchers also investigated how dietary quality affected the GRS–type 2 diabetes association by dichotomizing self-reported diet quality in both cohorts into healthier diet quality and less healthy diet quality. They found a tighter association between GRS and type 2 diabetes for women with diet quality below the median, whereas women with higher diet quality did not have such a strong association between GRS and type 2 disease. The researchers wrote that there was “suggestive evidence that a healthful diet might mitigate the excessive risk of T2D [type 2 diabetes] related to greater genetic susceptibility, which supports public health efforts of encouraging a healthful diet” for diabetes prevention in this high-risk population.
Patients in the NHSII were followed for a mean 21.3 years, and those in the DNBC were followed for a mean 12.7 years. Mean age at index pregnancy was 30.5 years for the NHSII cohort and 31.7 for the DNBC cohort. In the NHSII cohort, just 8.4% of participants reported smoking before pregnancy, compared with 26.4% of those in the DNBC cohort. The NHSII cohort participants, wrote Dr. Li and her coauthors, “were also less likely to have a family history of diabetes, less likely to smoke, and be leaner than women in the DNBC.”
Dr. Li and her coauthors noted that, “despite being the largest genetic study by far on [type 2 diabetes] among women with GDM, our study may not be sufficiently powered to examine the associations of individual T2D SNPs in relation to the risk of developing T2D.” Another limitation was that for the Danish cohort, information about diet was drawn from a one-time questionnaire administered between 9 and 16 years after the index pregnancy, so full data about dietary quality over time was not available. Also of note is that the study included only white participants, limiting generalizability to women of color. The authors called for expanding this research into more racially diverse populations.
The study was supported by the National Institutes of Health. The authors reported that they had no conflicts of interest.
SOURCE: Li M et al. BMJ Open Diab Res Care. 2020 Feb 13. doi: 10.1136/bmjdrc-2019-000850.
Women who had gestational diabetes mellitus had an increased risk for later type 2 diabetes if they carried certain genetic risk factors for the disease, according to a new analysis in BMJ Open Diabetes Research & Care of data from two independent populations.
A higher genetic risk score (GRS) had a modest association with developing type 2 diabetes, but a healthier diet may mitigate this risk, as Mengying Li, PhD, and her colleagues found for participants in the Nurses’ Health Study and members of the Danish National Birth Cohort who developed gestational diabetes mellitus (GDM).
Of 1,884 white women with a history of GDM in the Nurses’ Health Study II (NHSII), 446 (23.7%) went on to develop type 2 diabetes, and of the 550 women who had GDM in the Danish National Birth Cohort (DNBC), 155 (28.2%) developed the disease. The researchers calculated a GRS for type 2 diabetes for the full cohort. Genome-wide association studies completed in European populations were used to identify 59 single-nucleotide polymorphisms (SNPs) associated with the disease.
Dr. Li, an epidemiologist and postdoctoral researcher at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md., and her coauthors found that women whose GRS was in the highest quartile had a relative risk of 1.19 for type 2 diabetes. The relative risks for the three lower quartiles were 1.25, 0.97, and 1.00, respectively (P value for trend = .02). For each increase of five risk alleles in the GRS, NHSII participants had a 7% increased risk for type 2 diabetes, and DNBC participants saw a 9% increased risk.
Comparing these findings with other studies looking at genetic risk and type 2 diabetes in the general population, Dr. Li and her coauthors noted that the increase in relative risk for type 2 disease with increase in GRS was actually slightly weaker in the GDM cohort they studied. “The smaller effect size among women with GDM likely reflects an already higher baseline genetic risk for [type 2 diabetes] than the general population, as we have demonstrated,” they explained.
Though 11 individual SNPs had a significant individual association with the risk for type 2 diabetes initially, that association disappeared after correction for a false-discovery rate. Dr. Li and her coinvestigators conducted a sensitivity analysis that included only 42 SNPs that were later definitively associated with type 2 disease and they saw essentially unchanged results.
The researchers also investigated how dietary quality affected the GRS–type 2 diabetes association by dichotomizing self-reported diet quality in both cohorts into healthier diet quality and less healthy diet quality. They found a tighter association between GRS and type 2 diabetes for women with diet quality below the median, whereas women with higher diet quality did not have such a strong association between GRS and type 2 disease. The researchers wrote that there was “suggestive evidence that a healthful diet might mitigate the excessive risk of T2D [type 2 diabetes] related to greater genetic susceptibility, which supports public health efforts of encouraging a healthful diet” for diabetes prevention in this high-risk population.
Patients in the NHSII were followed for a mean 21.3 years, and those in the DNBC were followed for a mean 12.7 years. Mean age at index pregnancy was 30.5 years for the NHSII cohort and 31.7 for the DNBC cohort. In the NHSII cohort, just 8.4% of participants reported smoking before pregnancy, compared with 26.4% of those in the DNBC cohort. The NHSII cohort participants, wrote Dr. Li and her coauthors, “were also less likely to have a family history of diabetes, less likely to smoke, and be leaner than women in the DNBC.”
Dr. Li and her coauthors noted that, “despite being the largest genetic study by far on [type 2 diabetes] among women with GDM, our study may not be sufficiently powered to examine the associations of individual T2D SNPs in relation to the risk of developing T2D.” Another limitation was that for the Danish cohort, information about diet was drawn from a one-time questionnaire administered between 9 and 16 years after the index pregnancy, so full data about dietary quality over time was not available. Also of note is that the study included only white participants, limiting generalizability to women of color. The authors called for expanding this research into more racially diverse populations.
The study was supported by the National Institutes of Health. The authors reported that they had no conflicts of interest.
SOURCE: Li M et al. BMJ Open Diab Res Care. 2020 Feb 13. doi: 10.1136/bmjdrc-2019-000850.
Women who had gestational diabetes mellitus had an increased risk for later type 2 diabetes if they carried certain genetic risk factors for the disease, according to a new analysis in BMJ Open Diabetes Research & Care of data from two independent populations.
A higher genetic risk score (GRS) had a modest association with developing type 2 diabetes, but a healthier diet may mitigate this risk, as Mengying Li, PhD, and her colleagues found for participants in the Nurses’ Health Study and members of the Danish National Birth Cohort who developed gestational diabetes mellitus (GDM).
Of 1,884 white women with a history of GDM in the Nurses’ Health Study II (NHSII), 446 (23.7%) went on to develop type 2 diabetes, and of the 550 women who had GDM in the Danish National Birth Cohort (DNBC), 155 (28.2%) developed the disease. The researchers calculated a GRS for type 2 diabetes for the full cohort. Genome-wide association studies completed in European populations were used to identify 59 single-nucleotide polymorphisms (SNPs) associated with the disease.
Dr. Li, an epidemiologist and postdoctoral researcher at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, Md., and her coauthors found that women whose GRS was in the highest quartile had a relative risk of 1.19 for type 2 diabetes. The relative risks for the three lower quartiles were 1.25, 0.97, and 1.00, respectively (P value for trend = .02). For each increase of five risk alleles in the GRS, NHSII participants had a 7% increased risk for type 2 diabetes, and DNBC participants saw a 9% increased risk.
Comparing these findings with other studies looking at genetic risk and type 2 diabetes in the general population, Dr. Li and her coauthors noted that the increase in relative risk for type 2 disease with increase in GRS was actually slightly weaker in the GDM cohort they studied. “The smaller effect size among women with GDM likely reflects an already higher baseline genetic risk for [type 2 diabetes] than the general population, as we have demonstrated,” they explained.
Though 11 individual SNPs had a significant individual association with the risk for type 2 diabetes initially, that association disappeared after correction for a false-discovery rate. Dr. Li and her coinvestigators conducted a sensitivity analysis that included only 42 SNPs that were later definitively associated with type 2 disease and they saw essentially unchanged results.
The researchers also investigated how dietary quality affected the GRS–type 2 diabetes association by dichotomizing self-reported diet quality in both cohorts into healthier diet quality and less healthy diet quality. They found a tighter association between GRS and type 2 diabetes for women with diet quality below the median, whereas women with higher diet quality did not have such a strong association between GRS and type 2 disease. The researchers wrote that there was “suggestive evidence that a healthful diet might mitigate the excessive risk of T2D [type 2 diabetes] related to greater genetic susceptibility, which supports public health efforts of encouraging a healthful diet” for diabetes prevention in this high-risk population.
Patients in the NHSII were followed for a mean 21.3 years, and those in the DNBC were followed for a mean 12.7 years. Mean age at index pregnancy was 30.5 years for the NHSII cohort and 31.7 for the DNBC cohort. In the NHSII cohort, just 8.4% of participants reported smoking before pregnancy, compared with 26.4% of those in the DNBC cohort. The NHSII cohort participants, wrote Dr. Li and her coauthors, “were also less likely to have a family history of diabetes, less likely to smoke, and be leaner than women in the DNBC.”
Dr. Li and her coauthors noted that, “despite being the largest genetic study by far on [type 2 diabetes] among women with GDM, our study may not be sufficiently powered to examine the associations of individual T2D SNPs in relation to the risk of developing T2D.” Another limitation was that for the Danish cohort, information about diet was drawn from a one-time questionnaire administered between 9 and 16 years after the index pregnancy, so full data about dietary quality over time was not available. Also of note is that the study included only white participants, limiting generalizability to women of color. The authors called for expanding this research into more racially diverse populations.
The study was supported by the National Institutes of Health. The authors reported that they had no conflicts of interest.
SOURCE: Li M et al. BMJ Open Diab Res Care. 2020 Feb 13. doi: 10.1136/bmjdrc-2019-000850.
FROM BMJ OPEN DIABETES RESEARCH & CARE
Fast-track surgery for hip fracture does not reduce mortality
An accelerated path to surgery after hip fracture did not improve mortality or major complications, according to a new international randomized trial. However, a fast track to surgery hastened mobilization, weight-bearing, and hospital discharge, and reduced the risk of urinary tract infection and delirium.
The HIP ATTACK (Hip Fracture Accelerated Surgical Treatment and Care Track) study enrolled 2,970 patients (median age, 79 years; 69% women) during March 2014-May 2019. The study excluded patients younger than 45 years, as well as those who were on nonreversible anticoagulation and who had high-energy or more complex hip fractures. In all, 1,487 patients were randomly assigned to the accelerated-surgery group, which received early medical evaluation with a goal of heading to surgery within 6 hours of a hip fracture diagnosis. The goal was achieved, with patients in the intervention arm receiving care at a median 6 hours after diagnosis. Patients in the 69 participating hospitals in 17 countries who were assigned to standard of care received surgery at a median 24 hours after diagnosis (P less than .001).
“Observational data, clinical experience, and biological rationale suggest that the longer a patient is immobile and lying in a bed, the higher the risk of poor outcomes,” wrote principal investigators Philip J. Devereaux, MD, PhD, and Mohit Bhandari, MD, PhD, of McMaster University, Hamilton, Ont., and their colleagues on the HIP ATTACK writing committee.
The study was the first large, randomized trial that directly compared accelerated surgery with standard of care, noted the authors. Previous observational studies had shown worse outcomes for those usual-care patients who waited longer for surgery.
In HIP ATTACK, there was no difference in the primary outcome measures of 90-day mortality and major complications for patients receiving surgery within 6 hours after hip fracture diagnosis, compared with those who received surgery within 24 hours. The coprimary outcome measures included serious complications, such as MI, stroke, venous thromboembolism, sepsis, pneumonia, and life-threatening or major bleeding.
In practice, the researchers found that patients in the accelerated-surgery group received medical clearance in a median time of 2 hours after a diagnosis of hip fracture, whereas the standard of care group was cleared in 4 hours.
At 90 days, 9% of patients in the accelerated-surgery group and 10% of those in the usual-care group had died, a nonsignificant difference between the two groups. In both groups, 22% of patients experienced a major complication. A post hoc analysis that looked for any site-clustering effects did not detect different outcomes, the investigators wrote.
Delirium occurred in 132 patients (9%) of the accelerated-surgery group and in 175 patients (12%) in the usual-care group (odds ratio, 0.72; 95% confidence interval, 0.58-0.92). Infection without sepsis and urinary tract infection were both less common in the accelerated-surgery group (hazard ratio, 0.80 and 0.78, respectively).
The authors noted that the potential benefits of a speedy course to surgery, including reduced immobility and less pain, could be negated if physicians had less time to optimize medical care for older patients with multiple comorbidities and who make up a significant proportion of those who sustain low-energy hip fractures. However, medical complications, such as MI and new-onset atrial fibrillation, were not seen more frequently in the accelerated-surgery group.
In an editorial accompanying the study, Alejandro Lizaur-Utrilla, MD, and Fernando Lopez-Prats, MD, of the Universidad Miguel Hernández, Alicante, Spain, observed that the 6-hour window for hip fracture surgery may be difficult to achieve given clinical practicalities and that, in some cases, the 6-hour window might be unavoidable if severe comorbidities and overall poor health make early surgery inadvisable.
They also expressed concern that, despite the lack of harm shown in the patients who underwent accelerated surgery, the surgery “might negatively affect patients’ outcomes by preventing or limiting the opportunity for optimization of patients’ medical conditions before surgery.” They called for further study to delineate how fitness for surgery affects outcomes in accelerated surgery and to further examine whether the better outcomes are associated with improved cost-effectiveness.
Multiple HIP ATTACK coinvestigators reported relationships with pharmaceutical and medical device companies, including companies that manufacture hip prosthesis and orthopedic surgical devices and implants. The study was sponsored by the Canadian Population Health Research Institute, the Ontario Strategy for Patient Oriented Research Support Unit, the Ontario Ministry of Health and Long-Term Care, the Hamilton Health Sciences Foundation, Physicians’ Services Incorporated Foundation, Michael G. DeGroote Institute for Pain Research and Care, Smith & Nephew (to recruit patients in Spain), and Indiegogo Crowdfunding.
SOURCE: Borges F et al. Lancet. 2020 Feb. 9. doi: 10.1016/S0140-6736(20)30058-1.
An accelerated path to surgery after hip fracture did not improve mortality or major complications, according to a new international randomized trial. However, a fast track to surgery hastened mobilization, weight-bearing, and hospital discharge, and reduced the risk of urinary tract infection and delirium.
The HIP ATTACK (Hip Fracture Accelerated Surgical Treatment and Care Track) study enrolled 2,970 patients (median age, 79 years; 69% women) during March 2014-May 2019. The study excluded patients younger than 45 years, as well as those who were on nonreversible anticoagulation and who had high-energy or more complex hip fractures. In all, 1,487 patients were randomly assigned to the accelerated-surgery group, which received early medical evaluation with a goal of heading to surgery within 6 hours of a hip fracture diagnosis. The goal was achieved, with patients in the intervention arm receiving care at a median 6 hours after diagnosis. Patients in the 69 participating hospitals in 17 countries who were assigned to standard of care received surgery at a median 24 hours after diagnosis (P less than .001).
“Observational data, clinical experience, and biological rationale suggest that the longer a patient is immobile and lying in a bed, the higher the risk of poor outcomes,” wrote principal investigators Philip J. Devereaux, MD, PhD, and Mohit Bhandari, MD, PhD, of McMaster University, Hamilton, Ont., and their colleagues on the HIP ATTACK writing committee.
The study was the first large, randomized trial that directly compared accelerated surgery with standard of care, noted the authors. Previous observational studies had shown worse outcomes for those usual-care patients who waited longer for surgery.
In HIP ATTACK, there was no difference in the primary outcome measures of 90-day mortality and major complications for patients receiving surgery within 6 hours after hip fracture diagnosis, compared with those who received surgery within 24 hours. The coprimary outcome measures included serious complications, such as MI, stroke, venous thromboembolism, sepsis, pneumonia, and life-threatening or major bleeding.
In practice, the researchers found that patients in the accelerated-surgery group received medical clearance in a median time of 2 hours after a diagnosis of hip fracture, whereas the standard of care group was cleared in 4 hours.
At 90 days, 9% of patients in the accelerated-surgery group and 10% of those in the usual-care group had died, a nonsignificant difference between the two groups. In both groups, 22% of patients experienced a major complication. A post hoc analysis that looked for any site-clustering effects did not detect different outcomes, the investigators wrote.
Delirium occurred in 132 patients (9%) of the accelerated-surgery group and in 175 patients (12%) in the usual-care group (odds ratio, 0.72; 95% confidence interval, 0.58-0.92). Infection without sepsis and urinary tract infection were both less common in the accelerated-surgery group (hazard ratio, 0.80 and 0.78, respectively).
The authors noted that the potential benefits of a speedy course to surgery, including reduced immobility and less pain, could be negated if physicians had less time to optimize medical care for older patients with multiple comorbidities and who make up a significant proportion of those who sustain low-energy hip fractures. However, medical complications, such as MI and new-onset atrial fibrillation, were not seen more frequently in the accelerated-surgery group.
In an editorial accompanying the study, Alejandro Lizaur-Utrilla, MD, and Fernando Lopez-Prats, MD, of the Universidad Miguel Hernández, Alicante, Spain, observed that the 6-hour window for hip fracture surgery may be difficult to achieve given clinical practicalities and that, in some cases, the 6-hour window might be unavoidable if severe comorbidities and overall poor health make early surgery inadvisable.
They also expressed concern that, despite the lack of harm shown in the patients who underwent accelerated surgery, the surgery “might negatively affect patients’ outcomes by preventing or limiting the opportunity for optimization of patients’ medical conditions before surgery.” They called for further study to delineate how fitness for surgery affects outcomes in accelerated surgery and to further examine whether the better outcomes are associated with improved cost-effectiveness.
Multiple HIP ATTACK coinvestigators reported relationships with pharmaceutical and medical device companies, including companies that manufacture hip prosthesis and orthopedic surgical devices and implants. The study was sponsored by the Canadian Population Health Research Institute, the Ontario Strategy for Patient Oriented Research Support Unit, the Ontario Ministry of Health and Long-Term Care, the Hamilton Health Sciences Foundation, Physicians’ Services Incorporated Foundation, Michael G. DeGroote Institute for Pain Research and Care, Smith & Nephew (to recruit patients in Spain), and Indiegogo Crowdfunding.
SOURCE: Borges F et al. Lancet. 2020 Feb. 9. doi: 10.1016/S0140-6736(20)30058-1.
An accelerated path to surgery after hip fracture did not improve mortality or major complications, according to a new international randomized trial. However, a fast track to surgery hastened mobilization, weight-bearing, and hospital discharge, and reduced the risk of urinary tract infection and delirium.
The HIP ATTACK (Hip Fracture Accelerated Surgical Treatment and Care Track) study enrolled 2,970 patients (median age, 79 years; 69% women) during March 2014-May 2019. The study excluded patients younger than 45 years, as well as those who were on nonreversible anticoagulation and who had high-energy or more complex hip fractures. In all, 1,487 patients were randomly assigned to the accelerated-surgery group, which received early medical evaluation with a goal of heading to surgery within 6 hours of a hip fracture diagnosis. The goal was achieved, with patients in the intervention arm receiving care at a median 6 hours after diagnosis. Patients in the 69 participating hospitals in 17 countries who were assigned to standard of care received surgery at a median 24 hours after diagnosis (P less than .001).
“Observational data, clinical experience, and biological rationale suggest that the longer a patient is immobile and lying in a bed, the higher the risk of poor outcomes,” wrote principal investigators Philip J. Devereaux, MD, PhD, and Mohit Bhandari, MD, PhD, of McMaster University, Hamilton, Ont., and their colleagues on the HIP ATTACK writing committee.
The study was the first large, randomized trial that directly compared accelerated surgery with standard of care, noted the authors. Previous observational studies had shown worse outcomes for those usual-care patients who waited longer for surgery.
In HIP ATTACK, there was no difference in the primary outcome measures of 90-day mortality and major complications for patients receiving surgery within 6 hours after hip fracture diagnosis, compared with those who received surgery within 24 hours. The coprimary outcome measures included serious complications, such as MI, stroke, venous thromboembolism, sepsis, pneumonia, and life-threatening or major bleeding.
In practice, the researchers found that patients in the accelerated-surgery group received medical clearance in a median time of 2 hours after a diagnosis of hip fracture, whereas the standard of care group was cleared in 4 hours.
At 90 days, 9% of patients in the accelerated-surgery group and 10% of those in the usual-care group had died, a nonsignificant difference between the two groups. In both groups, 22% of patients experienced a major complication. A post hoc analysis that looked for any site-clustering effects did not detect different outcomes, the investigators wrote.
Delirium occurred in 132 patients (9%) of the accelerated-surgery group and in 175 patients (12%) in the usual-care group (odds ratio, 0.72; 95% confidence interval, 0.58-0.92). Infection without sepsis and urinary tract infection were both less common in the accelerated-surgery group (hazard ratio, 0.80 and 0.78, respectively).
The authors noted that the potential benefits of a speedy course to surgery, including reduced immobility and less pain, could be negated if physicians had less time to optimize medical care for older patients with multiple comorbidities and who make up a significant proportion of those who sustain low-energy hip fractures. However, medical complications, such as MI and new-onset atrial fibrillation, were not seen more frequently in the accelerated-surgery group.
In an editorial accompanying the study, Alejandro Lizaur-Utrilla, MD, and Fernando Lopez-Prats, MD, of the Universidad Miguel Hernández, Alicante, Spain, observed that the 6-hour window for hip fracture surgery may be difficult to achieve given clinical practicalities and that, in some cases, the 6-hour window might be unavoidable if severe comorbidities and overall poor health make early surgery inadvisable.
They also expressed concern that, despite the lack of harm shown in the patients who underwent accelerated surgery, the surgery “might negatively affect patients’ outcomes by preventing or limiting the opportunity for optimization of patients’ medical conditions before surgery.” They called for further study to delineate how fitness for surgery affects outcomes in accelerated surgery and to further examine whether the better outcomes are associated with improved cost-effectiveness.
Multiple HIP ATTACK coinvestigators reported relationships with pharmaceutical and medical device companies, including companies that manufacture hip prosthesis and orthopedic surgical devices and implants. The study was sponsored by the Canadian Population Health Research Institute, the Ontario Strategy for Patient Oriented Research Support Unit, the Ontario Ministry of Health and Long-Term Care, the Hamilton Health Sciences Foundation, Physicians’ Services Incorporated Foundation, Michael G. DeGroote Institute for Pain Research and Care, Smith & Nephew (to recruit patients in Spain), and Indiegogo Crowdfunding.
SOURCE: Borges F et al. Lancet. 2020 Feb. 9. doi: 10.1016/S0140-6736(20)30058-1.
Consider PET/CT when infectious source is a puzzler
CHICAGO – Dual positron emission tomography-computed tomography (PET/CT) scans changed the treatment course of nearly half of patients whose scans were positive for infection. In a single-center systematic review of 18fluorodeoxyglucose (FDG)–PET/CT scans, 55 of the 138 scans (40%) changed clinical management.
Presenting the findings at the annual meeting of the Radiological Society of North America, Benjamin Viglianti, MD, PhD, said that PET/CT had particular utility in cases of bacteremia and endocarditis, in which the scans changed treatment in 46% of those cases.
Dr. Viglianti, a radiologist at the University of Michigan, Ann Arbor, explained that medical student and first author Anitha Menon, himself, and their collaborators deliberately used a broad definition of clinical management change. The management course was considered to change not only if an unknown infection site was discovered or if a new intervention was initiated after the scan, but also if antibiotic choice or duration was changed or an additional specialty was consulted.
Scans were included in the study if an infectious etiology was found in the scan and if the patient received an infectious disease consult. Bacteremia and endocarditis were the most frequent indications for scans and also the indications for which management was most frequently changed. When a vascular cause was the indication for the scan, management changed 41% of the time. For fevers of unknown origin, the scan changed management in 30% of the cases, while for osteomyelitis, management was changed for 28% of patients.
The investigators identified several broad themes from their review that pointed toward when clinicians might consider FDG-PET/CT imaging in infectious disease management.
The first, said Dr. Viglianti, was that “for patients with suspected vascular graft infection, PET/CT using FDG may be a good first-choice imaging modality.” He pointed to an illustrative case of a patient who was 1 month out from open repair of a thoracoabdominal aortic aneurysm. The patient had abdominal pain, epigastric tenderness and nausea, as well as an erythematous incision site. A CT scan just revealed an abdominal fluid collection, but the PET/CT scan showed radiotracer uptake at the prior repair site, indicating infection.
For patients with bacteremia, the investigators judged that FDG-PET/CT might be particularly useful in patients who have a graft, prosthetic valve, or cardiac device. Here, Dr. Viglianti and his collaborators highlighted the scan of a woman with DiGeorge syndrome who had received aortic root replacement for truncus arteriosis. She had been found to have persistent enterococcal bacteremia at high levels, but had been symptom free. To take a close look at the suspected infectious nidus, a transesophageal echocardiogram had been obtained, but this study didn’t turn up any clear masses or vegetations. The PET/CT scan, though, revealed avid FDG uptake in the area of the prosthesis.
Management course was not likely to be changed for patients with fever of unknown origin, but the investigators did note that whole-body PET/CT was useful to distinguish infectious etiologies from hematologic and oncologic processes. Their review included a patient who had Crohn’s disease and fever, myalgias, and upper abdominal pain, as well as liver enzyme elevation. The PET/CT showed radiotracer uptake within the spleen, which was enlarged. The scan also showed bone marrow uptake; these findings pointed toward hemophagocytic lymphohistiocytosis rather than an infectious etiology.
For osteomyelitis, said Dr. Viglianti, FDG-PET may have limited utility; it might be most useful when MRI is contraindicated. Within the study population, the investigators identified a patient who had chills and fever along with focal tenderness over the lumbar spine in the context of recent pyelonephritis of a graft kidney. Here, MRI findings were suspicious for osteomyelitis and diskitis, and the FDG uptake at the L4-L5 vertebral levels confirmed the MRI results.
When a patient with a prosthetic valve is suspected of having endocarditis, “cardiac PET/CT may be of high diagnostic value,” said Dr. Viglianti. For patients with endocarditis of native valves, though, a full-body FDG-PET/CT scan may spot septic emboli. A patient identified in the investigators’ review had been admitted for methicillin-resistant Staphylococcus aureus endocarditis. The patient, who had a history of intravenous drug use, received a transesophageal echocardiogram that found severe tricuspid valve regurgitation and vegetations. The whole-body PET/CT scan, though, revealed avid uptake in both buttocks, as well as thigh, ankle and calf muscles – a pattern “suspicious for infectious myositis,” said the researchers.
In discussion during the poster session, Dr. Viglianti said that, although reimbursement for PET/CT scans for infectious etiologies might not be feasible, it can still be a reasonable and even cost-effective choice. At his institution, he said, the requisite radioisotope is made in-house, twice daily, so it’s relatively easy to arrange scans. Since PET/CT scans can be acquired relatively quickly and there’s no delay while waiting for radiotracer uptake, clinical decisions can be made more quickly than when waiting for bone uptake for a technetium-99 scan, he said. This can have the effect of saving a night of hospitalization in many cases.
Dr. Viglianti and Ms. Menon reported that they had no relevant conflicts of interest. No outside sources of funding were reported.
SOURCE: Menon A et al. RSNA 2019, Abstract NM203-SDSUB1.
CHICAGO – Dual positron emission tomography-computed tomography (PET/CT) scans changed the treatment course of nearly half of patients whose scans were positive for infection. In a single-center systematic review of 18fluorodeoxyglucose (FDG)–PET/CT scans, 55 of the 138 scans (40%) changed clinical management.
Presenting the findings at the annual meeting of the Radiological Society of North America, Benjamin Viglianti, MD, PhD, said that PET/CT had particular utility in cases of bacteremia and endocarditis, in which the scans changed treatment in 46% of those cases.
Dr. Viglianti, a radiologist at the University of Michigan, Ann Arbor, explained that medical student and first author Anitha Menon, himself, and their collaborators deliberately used a broad definition of clinical management change. The management course was considered to change not only if an unknown infection site was discovered or if a new intervention was initiated after the scan, but also if antibiotic choice or duration was changed or an additional specialty was consulted.
Scans were included in the study if an infectious etiology was found in the scan and if the patient received an infectious disease consult. Bacteremia and endocarditis were the most frequent indications for scans and also the indications for which management was most frequently changed. When a vascular cause was the indication for the scan, management changed 41% of the time. For fevers of unknown origin, the scan changed management in 30% of the cases, while for osteomyelitis, management was changed for 28% of patients.
The investigators identified several broad themes from their review that pointed toward when clinicians might consider FDG-PET/CT imaging in infectious disease management.
The first, said Dr. Viglianti, was that “for patients with suspected vascular graft infection, PET/CT using FDG may be a good first-choice imaging modality.” He pointed to an illustrative case of a patient who was 1 month out from open repair of a thoracoabdominal aortic aneurysm. The patient had abdominal pain, epigastric tenderness and nausea, as well as an erythematous incision site. A CT scan just revealed an abdominal fluid collection, but the PET/CT scan showed radiotracer uptake at the prior repair site, indicating infection.
For patients with bacteremia, the investigators judged that FDG-PET/CT might be particularly useful in patients who have a graft, prosthetic valve, or cardiac device. Here, Dr. Viglianti and his collaborators highlighted the scan of a woman with DiGeorge syndrome who had received aortic root replacement for truncus arteriosis. She had been found to have persistent enterococcal bacteremia at high levels, but had been symptom free. To take a close look at the suspected infectious nidus, a transesophageal echocardiogram had been obtained, but this study didn’t turn up any clear masses or vegetations. The PET/CT scan, though, revealed avid FDG uptake in the area of the prosthesis.
Management course was not likely to be changed for patients with fever of unknown origin, but the investigators did note that whole-body PET/CT was useful to distinguish infectious etiologies from hematologic and oncologic processes. Their review included a patient who had Crohn’s disease and fever, myalgias, and upper abdominal pain, as well as liver enzyme elevation. The PET/CT showed radiotracer uptake within the spleen, which was enlarged. The scan also showed bone marrow uptake; these findings pointed toward hemophagocytic lymphohistiocytosis rather than an infectious etiology.
For osteomyelitis, said Dr. Viglianti, FDG-PET may have limited utility; it might be most useful when MRI is contraindicated. Within the study population, the investigators identified a patient who had chills and fever along with focal tenderness over the lumbar spine in the context of recent pyelonephritis of a graft kidney. Here, MRI findings were suspicious for osteomyelitis and diskitis, and the FDG uptake at the L4-L5 vertebral levels confirmed the MRI results.
When a patient with a prosthetic valve is suspected of having endocarditis, “cardiac PET/CT may be of high diagnostic value,” said Dr. Viglianti. For patients with endocarditis of native valves, though, a full-body FDG-PET/CT scan may spot septic emboli. A patient identified in the investigators’ review had been admitted for methicillin-resistant Staphylococcus aureus endocarditis. The patient, who had a history of intravenous drug use, received a transesophageal echocardiogram that found severe tricuspid valve regurgitation and vegetations. The whole-body PET/CT scan, though, revealed avid uptake in both buttocks, as well as thigh, ankle and calf muscles – a pattern “suspicious for infectious myositis,” said the researchers.
In discussion during the poster session, Dr. Viglianti said that, although reimbursement for PET/CT scans for infectious etiologies might not be feasible, it can still be a reasonable and even cost-effective choice. At his institution, he said, the requisite radioisotope is made in-house, twice daily, so it’s relatively easy to arrange scans. Since PET/CT scans can be acquired relatively quickly and there’s no delay while waiting for radiotracer uptake, clinical decisions can be made more quickly than when waiting for bone uptake for a technetium-99 scan, he said. This can have the effect of saving a night of hospitalization in many cases.
Dr. Viglianti and Ms. Menon reported that they had no relevant conflicts of interest. No outside sources of funding were reported.
SOURCE: Menon A et al. RSNA 2019, Abstract NM203-SDSUB1.
CHICAGO – Dual positron emission tomography-computed tomography (PET/CT) scans changed the treatment course of nearly half of patients whose scans were positive for infection. In a single-center systematic review of 18fluorodeoxyglucose (FDG)–PET/CT scans, 55 of the 138 scans (40%) changed clinical management.
Presenting the findings at the annual meeting of the Radiological Society of North America, Benjamin Viglianti, MD, PhD, said that PET/CT had particular utility in cases of bacteremia and endocarditis, in which the scans changed treatment in 46% of those cases.
Dr. Viglianti, a radiologist at the University of Michigan, Ann Arbor, explained that medical student and first author Anitha Menon, himself, and their collaborators deliberately used a broad definition of clinical management change. The management course was considered to change not only if an unknown infection site was discovered or if a new intervention was initiated after the scan, but also if antibiotic choice or duration was changed or an additional specialty was consulted.
Scans were included in the study if an infectious etiology was found in the scan and if the patient received an infectious disease consult. Bacteremia and endocarditis were the most frequent indications for scans and also the indications for which management was most frequently changed. When a vascular cause was the indication for the scan, management changed 41% of the time. For fevers of unknown origin, the scan changed management in 30% of the cases, while for osteomyelitis, management was changed for 28% of patients.
The investigators identified several broad themes from their review that pointed toward when clinicians might consider FDG-PET/CT imaging in infectious disease management.
The first, said Dr. Viglianti, was that “for patients with suspected vascular graft infection, PET/CT using FDG may be a good first-choice imaging modality.” He pointed to an illustrative case of a patient who was 1 month out from open repair of a thoracoabdominal aortic aneurysm. The patient had abdominal pain, epigastric tenderness and nausea, as well as an erythematous incision site. A CT scan just revealed an abdominal fluid collection, but the PET/CT scan showed radiotracer uptake at the prior repair site, indicating infection.
For patients with bacteremia, the investigators judged that FDG-PET/CT might be particularly useful in patients who have a graft, prosthetic valve, or cardiac device. Here, Dr. Viglianti and his collaborators highlighted the scan of a woman with DiGeorge syndrome who had received aortic root replacement for truncus arteriosis. She had been found to have persistent enterococcal bacteremia at high levels, but had been symptom free. To take a close look at the suspected infectious nidus, a transesophageal echocardiogram had been obtained, but this study didn’t turn up any clear masses or vegetations. The PET/CT scan, though, revealed avid FDG uptake in the area of the prosthesis.
Management course was not likely to be changed for patients with fever of unknown origin, but the investigators did note that whole-body PET/CT was useful to distinguish infectious etiologies from hematologic and oncologic processes. Their review included a patient who had Crohn’s disease and fever, myalgias, and upper abdominal pain, as well as liver enzyme elevation. The PET/CT showed radiotracer uptake within the spleen, which was enlarged. The scan also showed bone marrow uptake; these findings pointed toward hemophagocytic lymphohistiocytosis rather than an infectious etiology.
For osteomyelitis, said Dr. Viglianti, FDG-PET may have limited utility; it might be most useful when MRI is contraindicated. Within the study population, the investigators identified a patient who had chills and fever along with focal tenderness over the lumbar spine in the context of recent pyelonephritis of a graft kidney. Here, MRI findings were suspicious for osteomyelitis and diskitis, and the FDG uptake at the L4-L5 vertebral levels confirmed the MRI results.
When a patient with a prosthetic valve is suspected of having endocarditis, “cardiac PET/CT may be of high diagnostic value,” said Dr. Viglianti. For patients with endocarditis of native valves, though, a full-body FDG-PET/CT scan may spot septic emboli. A patient identified in the investigators’ review had been admitted for methicillin-resistant Staphylococcus aureus endocarditis. The patient, who had a history of intravenous drug use, received a transesophageal echocardiogram that found severe tricuspid valve regurgitation and vegetations. The whole-body PET/CT scan, though, revealed avid uptake in both buttocks, as well as thigh, ankle and calf muscles – a pattern “suspicious for infectious myositis,” said the researchers.
In discussion during the poster session, Dr. Viglianti said that, although reimbursement for PET/CT scans for infectious etiologies might not be feasible, it can still be a reasonable and even cost-effective choice. At his institution, he said, the requisite radioisotope is made in-house, twice daily, so it’s relatively easy to arrange scans. Since PET/CT scans can be acquired relatively quickly and there’s no delay while waiting for radiotracer uptake, clinical decisions can be made more quickly than when waiting for bone uptake for a technetium-99 scan, he said. This can have the effect of saving a night of hospitalization in many cases.
Dr. Viglianti and Ms. Menon reported that they had no relevant conflicts of interest. No outside sources of funding were reported.
SOURCE: Menon A et al. RSNA 2019, Abstract NM203-SDSUB1.
REPORTING FROM RSNA 2019
Abbreviated MRI equals standard protocol for high-risk breast cancer screens
CHICAGO – An abbreviated magnetic resonance imaging (MRI) protocol for screening individuals at high risk for breast cancer performed as well as a standard protocol, in about half the time and with greater patient satisfaction.
The abbreviated protocol also resulted in fewer false positive findings, with 5% fewer patients receiving biopsies for benign lesions than with a standard protocol (8.4% versus 13.7%, P less than .001).
Findings from the prospective 10-month trial conducted in the province of Ontario were presented by Jean Seely, MD, professor of radiology at the University of Ottawa, at the annual meeting of the Radiological Society of North America.
“The abbreviated protocol was shown to be as effective as the standard protocol in high-risk screening breast MRI, supporting previous studies,” said Dr. Seely. The shorter protocol took 16.3 minutes on average, compared with 27 minutes for the standard MRI protocol. This difference resulted in a 50% increase in institutional capacity, or a jump from two to three patients screened per hour.
In the province of Ontario, said Dr. Seely, women assessed at being at a 25% or greater lifetime risk of breast cancer receive MRIs as part of the Ontario Breast Screening Program (OBSP), which calculates risk by using the International Breast Cancer Intervention Study model.
For high-risk patients, the OBSP model provides annual mammography and an MRI for women between the ages of 30 and 60 years. Not only is the half-hour duration of the standard protocol resource-intensive, especially in regions with limited scanner availability, but patients may either be reluctant to undergo a half-hour scan, or not tolerate a lengthy scan very well.
Dr. Seely cited previous work (J Clin Oncol. 2014 Aug 1;32[22]:2304-10) showing that an abbreviated MRI protocol has similar accuracy as the full standard protocol. With the foundation of evidence from this study, Dr. Seely and her collaborators compared outcomes for high-risk patients who were screened with an abbreviated versus a standard protocol.
The abbreviated protocol, approved by the American College of Radiology, omits a final round of image acquisition sequences at the 9-minute mark after gadolinium administration, instead performing acquisition at 1, 2, 3, and 4 minutes after contrast delivery. Total time required for this protocol is just over 13 minutes, said Dr. Seely, and additional diagnostic MRIs were not required.
The trial was constructed so that the abbreviated protocol was used for the entire OBSP cohort for 10 months in 2018. Results were compared with those from the 12 previous months, when OBSP patients’ MRIs were performed using the standard protocol.
A total of 881 patients received standard-protocol MRIs; about three quarters (651) of those patients had previous MRI screening, while the remaining 230 patients had a baseline screen via the standard protocol.
Of the 658 patients in the abbreviated protocol group, 135, or about 20%, received the briefer scans as a baseline screen; the remast of the patients in this arm had received earlier MRI screening.
In addition to tracking scanning times, Dr. Seely and her collaborators also compared cancer detection rates, Breast Imaging Reporting and Data System (BI-RADS) assessment categories, positive predictive values, and the abnormal interpretation rate – that is, how many scans fell into BI-RADS categories 0, 4, and 5.
No significant difference was found between the rates of BI-RADs 0, 3, or 5 studies between the groups. Significantly fewer abbreviated scans fell into the BI-RADS 4 category, however (9.3% vs. 14.9%; P less than .001).
Similarly, the abnormal interpretation rate was 12.5% for the abbreviated protocol, compared with 17.5% for the standard protocol (P less than .007), with a correspondingly lower biopsy rate of 8.4% for the abbreviated protocol, compared with 13.7% for the standard protocol (P less than .001). The overall cancer detection rate did not differ between groups.
She and her colleagues will continue to track outcomes for those receiving abbreviated screening within the province of Ontario to track performance over time.
Dr. Seely reported that she had no relevant conflicts of interest. She reported no funding source beyond the province of Ontario.
koakes@mdedge.com
SOURCE: Seely J et al. RSNA 2019, Session RC-215-04.
CHICAGO – An abbreviated magnetic resonance imaging (MRI) protocol for screening individuals at high risk for breast cancer performed as well as a standard protocol, in about half the time and with greater patient satisfaction.
The abbreviated protocol also resulted in fewer false positive findings, with 5% fewer patients receiving biopsies for benign lesions than with a standard protocol (8.4% versus 13.7%, P less than .001).
Findings from the prospective 10-month trial conducted in the province of Ontario were presented by Jean Seely, MD, professor of radiology at the University of Ottawa, at the annual meeting of the Radiological Society of North America.
“The abbreviated protocol was shown to be as effective as the standard protocol in high-risk screening breast MRI, supporting previous studies,” said Dr. Seely. The shorter protocol took 16.3 minutes on average, compared with 27 minutes for the standard MRI protocol. This difference resulted in a 50% increase in institutional capacity, or a jump from two to three patients screened per hour.
In the province of Ontario, said Dr. Seely, women assessed at being at a 25% or greater lifetime risk of breast cancer receive MRIs as part of the Ontario Breast Screening Program (OBSP), which calculates risk by using the International Breast Cancer Intervention Study model.
For high-risk patients, the OBSP model provides annual mammography and an MRI for women between the ages of 30 and 60 years. Not only is the half-hour duration of the standard protocol resource-intensive, especially in regions with limited scanner availability, but patients may either be reluctant to undergo a half-hour scan, or not tolerate a lengthy scan very well.
Dr. Seely cited previous work (J Clin Oncol. 2014 Aug 1;32[22]:2304-10) showing that an abbreviated MRI protocol has similar accuracy as the full standard protocol. With the foundation of evidence from this study, Dr. Seely and her collaborators compared outcomes for high-risk patients who were screened with an abbreviated versus a standard protocol.
The abbreviated protocol, approved by the American College of Radiology, omits a final round of image acquisition sequences at the 9-minute mark after gadolinium administration, instead performing acquisition at 1, 2, 3, and 4 minutes after contrast delivery. Total time required for this protocol is just over 13 minutes, said Dr. Seely, and additional diagnostic MRIs were not required.
The trial was constructed so that the abbreviated protocol was used for the entire OBSP cohort for 10 months in 2018. Results were compared with those from the 12 previous months, when OBSP patients’ MRIs were performed using the standard protocol.
A total of 881 patients received standard-protocol MRIs; about three quarters (651) of those patients had previous MRI screening, while the remaining 230 patients had a baseline screen via the standard protocol.
Of the 658 patients in the abbreviated protocol group, 135, or about 20%, received the briefer scans as a baseline screen; the remast of the patients in this arm had received earlier MRI screening.
In addition to tracking scanning times, Dr. Seely and her collaborators also compared cancer detection rates, Breast Imaging Reporting and Data System (BI-RADS) assessment categories, positive predictive values, and the abnormal interpretation rate – that is, how many scans fell into BI-RADS categories 0, 4, and 5.
No significant difference was found between the rates of BI-RADs 0, 3, or 5 studies between the groups. Significantly fewer abbreviated scans fell into the BI-RADS 4 category, however (9.3% vs. 14.9%; P less than .001).
Similarly, the abnormal interpretation rate was 12.5% for the abbreviated protocol, compared with 17.5% for the standard protocol (P less than .007), with a correspondingly lower biopsy rate of 8.4% for the abbreviated protocol, compared with 13.7% for the standard protocol (P less than .001). The overall cancer detection rate did not differ between groups.
She and her colleagues will continue to track outcomes for those receiving abbreviated screening within the province of Ontario to track performance over time.
Dr. Seely reported that she had no relevant conflicts of interest. She reported no funding source beyond the province of Ontario.
koakes@mdedge.com
SOURCE: Seely J et al. RSNA 2019, Session RC-215-04.
CHICAGO – An abbreviated magnetic resonance imaging (MRI) protocol for screening individuals at high risk for breast cancer performed as well as a standard protocol, in about half the time and with greater patient satisfaction.
The abbreviated protocol also resulted in fewer false positive findings, with 5% fewer patients receiving biopsies for benign lesions than with a standard protocol (8.4% versus 13.7%, P less than .001).
Findings from the prospective 10-month trial conducted in the province of Ontario were presented by Jean Seely, MD, professor of radiology at the University of Ottawa, at the annual meeting of the Radiological Society of North America.
“The abbreviated protocol was shown to be as effective as the standard protocol in high-risk screening breast MRI, supporting previous studies,” said Dr. Seely. The shorter protocol took 16.3 minutes on average, compared with 27 minutes for the standard MRI protocol. This difference resulted in a 50% increase in institutional capacity, or a jump from two to three patients screened per hour.
In the province of Ontario, said Dr. Seely, women assessed at being at a 25% or greater lifetime risk of breast cancer receive MRIs as part of the Ontario Breast Screening Program (OBSP), which calculates risk by using the International Breast Cancer Intervention Study model.
For high-risk patients, the OBSP model provides annual mammography and an MRI for women between the ages of 30 and 60 years. Not only is the half-hour duration of the standard protocol resource-intensive, especially in regions with limited scanner availability, but patients may either be reluctant to undergo a half-hour scan, or not tolerate a lengthy scan very well.
Dr. Seely cited previous work (J Clin Oncol. 2014 Aug 1;32[22]:2304-10) showing that an abbreviated MRI protocol has similar accuracy as the full standard protocol. With the foundation of evidence from this study, Dr. Seely and her collaborators compared outcomes for high-risk patients who were screened with an abbreviated versus a standard protocol.
The abbreviated protocol, approved by the American College of Radiology, omits a final round of image acquisition sequences at the 9-minute mark after gadolinium administration, instead performing acquisition at 1, 2, 3, and 4 minutes after contrast delivery. Total time required for this protocol is just over 13 minutes, said Dr. Seely, and additional diagnostic MRIs were not required.
The trial was constructed so that the abbreviated protocol was used for the entire OBSP cohort for 10 months in 2018. Results were compared with those from the 12 previous months, when OBSP patients’ MRIs were performed using the standard protocol.
A total of 881 patients received standard-protocol MRIs; about three quarters (651) of those patients had previous MRI screening, while the remaining 230 patients had a baseline screen via the standard protocol.
Of the 658 patients in the abbreviated protocol group, 135, or about 20%, received the briefer scans as a baseline screen; the remast of the patients in this arm had received earlier MRI screening.
In addition to tracking scanning times, Dr. Seely and her collaborators also compared cancer detection rates, Breast Imaging Reporting and Data System (BI-RADS) assessment categories, positive predictive values, and the abnormal interpretation rate – that is, how many scans fell into BI-RADS categories 0, 4, and 5.
No significant difference was found between the rates of BI-RADs 0, 3, or 5 studies between the groups. Significantly fewer abbreviated scans fell into the BI-RADS 4 category, however (9.3% vs. 14.9%; P less than .001).
Similarly, the abnormal interpretation rate was 12.5% for the abbreviated protocol, compared with 17.5% for the standard protocol (P less than .007), with a correspondingly lower biopsy rate of 8.4% for the abbreviated protocol, compared with 13.7% for the standard protocol (P less than .001). The overall cancer detection rate did not differ between groups.
She and her colleagues will continue to track outcomes for those receiving abbreviated screening within the province of Ontario to track performance over time.
Dr. Seely reported that she had no relevant conflicts of interest. She reported no funding source beyond the province of Ontario.
koakes@mdedge.com
SOURCE: Seely J et al. RSNA 2019, Session RC-215-04.
REPORTING FROM RSNA 2019
Racial disparities persist in preterm birth risk
Education, status are not protective for non-Hispanic black women
GRAPEVINE, TEX. – College education and high socioeconomic status do not erase U.S. racial disparities in birth outcomes, according to a new analysis of all U.S. live births from 2015-2017.
Very early preterm birth – birth before 28 weeks gestational age – was five times more likely to occur in non-Hispanic black women of high socioeconomic status as similarly situated white women, even after statistical adjustment for a host of potentially confounding factors.
Being of non-Hispanic black race was the single strongest predictor of preterm birth (PTB) at less than 28 weeks’ gestation. The adjusted odds ratio (aOR) of 4.99 surpassed an interpregnancy interval under 1 year (aOR, 4.47), chronic hypertension (aOR, 2.84), and prior history of preterm birth (aOR, 2.81).
“Even among college-educated women with private insurance who are not receiving (Women, Infants, and Children support), racial disparities in prematurity persist. These results suggest that factors other than sociodemographics are important in the underlying pathogenesis of PTB and in etiologies of racial disparities,” wrote Jasmine Johnson, MD, and her coauthors in the abstract accompanying the presentation at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The analysis that Dr. Johnson and her coinvestigators used, she explained during her plenary session presentation, still found significantly elevated risks for preterm birth for non-Hispanic black women after accounting for marital status, prior history of preterm birth, tobacco use, an interpregnancy interval of fewer than 12 months, and carrying a male fetus.
“Birth certificates do not inform the lived experiences of one’s self-identified race, and how that experience – or possibly just one’s identification with a particular racial group – may positively or negatively affect their clinical risk of preterm birth,” said Dr. Johnson. “In this study, as in others, race is a social construct. It’s a surrogate for social and societal racism that disproportionately affects birth outcomes of women of color.”
Using non-Hispanic white (NHW) women as a reference, women who described themselves as non-Hispanic black (NHB) had increased odds of preterm birth at 34 and 37 weeks gestation as well. Women identifying as both NHB and NHW had numerically elevated odds for preterm birth at all time points as well, but the odds at 37 weeks didn’t reach statistical significance.
The results were based on a retrospective population-based study of a cohort drawn from the National Vital Statistics birth certificate data of all live births in the United States between 2015 and 2017, explained Dr. Johnson, a maternal-fetal medicine fellow at the University of North Carolina, Chapel Hill. Drawing from a nationally representative sample and having a population-level design drawn were strengths of the study, she said.
Women with singleton pregnancies without anomalies who identified as NHB, NHW, or as both NHB and NHW were included if they also had high socioeconomic status. Including women who identify as both black and white was another strength of the study, Dr. Johnson added.
She explained that, for the purposes of the study, high socioeconomic status was defined as having 16 or more years of education and private insurance, and not receiving WIC benefits.
In addition to the primary outcome measure of preterm birth at fewer than 37 weeks gestation, secondary outcomes included preterm birth at fewer than 34 and fewer than 28 weeks’ gestation, as well as low birthweight (LBW) and very low birthweight (VLBW).
About 11.8 million live births occurred during the study period, and 11.3 million of those were singleton pregnancies without fetal anomaly. After excluding women who did not meet the racial self-identification or socioeconomic status inclusion criteria, the investigators arrived at the final study population of 2,170,688 individuals.
Of those, 2,017,470, or 92.9%, were non-Hispanic white, while 144,612, or 6.7%, were non-Hispanic black. The remaining 8,604 participants, or 0.4%, identified their race as non-Hispanic black and non-Hispanic white.
The groups identified in the study differed significantly in demographic characteristics, Dr. Johnson said. Women in the NHB and NHB + NHW groups were less likely to be married than NHW women – about 75% of the former two groups were married, compared with 92.5% of NHW women. This difference was statistically significant with a P value of .001, as were all the differences Dr. Johnson reported.
Pre-pregnancy body mass index (BMI) was highest in NHB women at 27.1 kg/m sq, followed by NHB = NHW women at 25.7 kg/m sq, with NHW women having the lowest BMI at 23.8 kg/m sq.
Prior preterm birth of 37 weeks’ gestation or less was more common in NHB women and NHB + NHW women, as was an interpregnancy interval of fewer than 12 months.
Chronic hypertension was more than twice as common in NHB women than in either NHB = NHW or NHW women, occurring in 3.9%, 1.8%, and 1.4% of participants, respectively.
Pregestational diabetes was about twice as common in NHB women than NHW women, occurring in 1% and 0.52% of those groups, respectively. Prevalence of pregestational diabetes was intermediate in NHB = NHW women, at 0.72%.
Tobacco use was rare overall, and less common in NHB women than NHB + NHW and NHW women.
In terms of pregnancy characteristics, though 85% of NHB women initiated prenatal care in the first trimester, they were less likely to have done so than either of the other two groups. Few women overall had no prenatal care, but 0.7% of NHB women fell into this category, more than the 0.4% and 0.3% reported for NHB + NHW and NHW women, respectively.
During their pregnancies, NHB women were more likely to develop gestational hypertension and/or pre-eclampsia as well as gestational diabetes than either of the other two groups (7.6% compared with 6% for the other two groups). Of the NHB women, 5.9% developed gestational diabetes, compared with 4.8% of NHB + NHW and 4.8% of NHW women.
Delivering a baby with a birthweight less than the 10th percentile was twice as common for NHB, compared with NHW women (7.2% versus 3.4%). The risk for NHB + NHW women was intermediate, at 4.7%.
Dr. Johnson said she and her team performed further analyses, including using initiation of prenatal care in the first trimester of pregnancy as a surrogate for high socioeconomic status; the association of race and risk for preterm birth persisted.
The study had the usual limitations of using National Vital Statistics data, such as the inability to evaluate underlying etiologies for preterm birth.
However, Dr. Johnson highlighted additional limitations that pertain to the experience of race in 21st century America. “Our definition of high socioeconomic status does not guarantee that all women in this analysis have financial stability,” she said, pointing out that the study’s definition of high socioeconomic status was insensitive to wealth accumulation. She also noted that high educational attainment does not necessarily correlate with high income. Hence, the potential burden of economic stressors could not fully be captured.
The study was supported by the National Institutes of Health. Dr. Johnson reported no conflicts of interest.
SOURCE: Johnson J et al. Obstet Gynecol. 2020 Jan;222(1):S-37-8, Abstract 44.
Education, status are not protective for non-Hispanic black women
Education, status are not protective for non-Hispanic black women
GRAPEVINE, TEX. – College education and high socioeconomic status do not erase U.S. racial disparities in birth outcomes, according to a new analysis of all U.S. live births from 2015-2017.
Very early preterm birth – birth before 28 weeks gestational age – was five times more likely to occur in non-Hispanic black women of high socioeconomic status as similarly situated white women, even after statistical adjustment for a host of potentially confounding factors.
Being of non-Hispanic black race was the single strongest predictor of preterm birth (PTB) at less than 28 weeks’ gestation. The adjusted odds ratio (aOR) of 4.99 surpassed an interpregnancy interval under 1 year (aOR, 4.47), chronic hypertension (aOR, 2.84), and prior history of preterm birth (aOR, 2.81).
“Even among college-educated women with private insurance who are not receiving (Women, Infants, and Children support), racial disparities in prematurity persist. These results suggest that factors other than sociodemographics are important in the underlying pathogenesis of PTB and in etiologies of racial disparities,” wrote Jasmine Johnson, MD, and her coauthors in the abstract accompanying the presentation at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The analysis that Dr. Johnson and her coinvestigators used, she explained during her plenary session presentation, still found significantly elevated risks for preterm birth for non-Hispanic black women after accounting for marital status, prior history of preterm birth, tobacco use, an interpregnancy interval of fewer than 12 months, and carrying a male fetus.
“Birth certificates do not inform the lived experiences of one’s self-identified race, and how that experience – or possibly just one’s identification with a particular racial group – may positively or negatively affect their clinical risk of preterm birth,” said Dr. Johnson. “In this study, as in others, race is a social construct. It’s a surrogate for social and societal racism that disproportionately affects birth outcomes of women of color.”
Using non-Hispanic white (NHW) women as a reference, women who described themselves as non-Hispanic black (NHB) had increased odds of preterm birth at 34 and 37 weeks gestation as well. Women identifying as both NHB and NHW had numerically elevated odds for preterm birth at all time points as well, but the odds at 37 weeks didn’t reach statistical significance.
The results were based on a retrospective population-based study of a cohort drawn from the National Vital Statistics birth certificate data of all live births in the United States between 2015 and 2017, explained Dr. Johnson, a maternal-fetal medicine fellow at the University of North Carolina, Chapel Hill. Drawing from a nationally representative sample and having a population-level design drawn were strengths of the study, she said.
Women with singleton pregnancies without anomalies who identified as NHB, NHW, or as both NHB and NHW were included if they also had high socioeconomic status. Including women who identify as both black and white was another strength of the study, Dr. Johnson added.
She explained that, for the purposes of the study, high socioeconomic status was defined as having 16 or more years of education and private insurance, and not receiving WIC benefits.
In addition to the primary outcome measure of preterm birth at fewer than 37 weeks gestation, secondary outcomes included preterm birth at fewer than 34 and fewer than 28 weeks’ gestation, as well as low birthweight (LBW) and very low birthweight (VLBW).
About 11.8 million live births occurred during the study period, and 11.3 million of those were singleton pregnancies without fetal anomaly. After excluding women who did not meet the racial self-identification or socioeconomic status inclusion criteria, the investigators arrived at the final study population of 2,170,688 individuals.
Of those, 2,017,470, or 92.9%, were non-Hispanic white, while 144,612, or 6.7%, were non-Hispanic black. The remaining 8,604 participants, or 0.4%, identified their race as non-Hispanic black and non-Hispanic white.
The groups identified in the study differed significantly in demographic characteristics, Dr. Johnson said. Women in the NHB and NHB + NHW groups were less likely to be married than NHW women – about 75% of the former two groups were married, compared with 92.5% of NHW women. This difference was statistically significant with a P value of .001, as were all the differences Dr. Johnson reported.
Pre-pregnancy body mass index (BMI) was highest in NHB women at 27.1 kg/m sq, followed by NHB = NHW women at 25.7 kg/m sq, with NHW women having the lowest BMI at 23.8 kg/m sq.
Prior preterm birth of 37 weeks’ gestation or less was more common in NHB women and NHB + NHW women, as was an interpregnancy interval of fewer than 12 months.
Chronic hypertension was more than twice as common in NHB women than in either NHB = NHW or NHW women, occurring in 3.9%, 1.8%, and 1.4% of participants, respectively.
Pregestational diabetes was about twice as common in NHB women than NHW women, occurring in 1% and 0.52% of those groups, respectively. Prevalence of pregestational diabetes was intermediate in NHB = NHW women, at 0.72%.
Tobacco use was rare overall, and less common in NHB women than NHB + NHW and NHW women.
In terms of pregnancy characteristics, though 85% of NHB women initiated prenatal care in the first trimester, they were less likely to have done so than either of the other two groups. Few women overall had no prenatal care, but 0.7% of NHB women fell into this category, more than the 0.4% and 0.3% reported for NHB + NHW and NHW women, respectively.
During their pregnancies, NHB women were more likely to develop gestational hypertension and/or pre-eclampsia as well as gestational diabetes than either of the other two groups (7.6% compared with 6% for the other two groups). Of the NHB women, 5.9% developed gestational diabetes, compared with 4.8% of NHB + NHW and 4.8% of NHW women.
Delivering a baby with a birthweight less than the 10th percentile was twice as common for NHB, compared with NHW women (7.2% versus 3.4%). The risk for NHB + NHW women was intermediate, at 4.7%.
Dr. Johnson said she and her team performed further analyses, including using initiation of prenatal care in the first trimester of pregnancy as a surrogate for high socioeconomic status; the association of race and risk for preterm birth persisted.
The study had the usual limitations of using National Vital Statistics data, such as the inability to evaluate underlying etiologies for preterm birth.
However, Dr. Johnson highlighted additional limitations that pertain to the experience of race in 21st century America. “Our definition of high socioeconomic status does not guarantee that all women in this analysis have financial stability,” she said, pointing out that the study’s definition of high socioeconomic status was insensitive to wealth accumulation. She also noted that high educational attainment does not necessarily correlate with high income. Hence, the potential burden of economic stressors could not fully be captured.
The study was supported by the National Institutes of Health. Dr. Johnson reported no conflicts of interest.
SOURCE: Johnson J et al. Obstet Gynecol. 2020 Jan;222(1):S-37-8, Abstract 44.
GRAPEVINE, TEX. – College education and high socioeconomic status do not erase U.S. racial disparities in birth outcomes, according to a new analysis of all U.S. live births from 2015-2017.
Very early preterm birth – birth before 28 weeks gestational age – was five times more likely to occur in non-Hispanic black women of high socioeconomic status as similarly situated white women, even after statistical adjustment for a host of potentially confounding factors.
Being of non-Hispanic black race was the single strongest predictor of preterm birth (PTB) at less than 28 weeks’ gestation. The adjusted odds ratio (aOR) of 4.99 surpassed an interpregnancy interval under 1 year (aOR, 4.47), chronic hypertension (aOR, 2.84), and prior history of preterm birth (aOR, 2.81).
“Even among college-educated women with private insurance who are not receiving (Women, Infants, and Children support), racial disparities in prematurity persist. These results suggest that factors other than sociodemographics are important in the underlying pathogenesis of PTB and in etiologies of racial disparities,” wrote Jasmine Johnson, MD, and her coauthors in the abstract accompanying the presentation at the meeting sponsored by the Society for Maternal-Fetal Medicine.
The analysis that Dr. Johnson and her coinvestigators used, she explained during her plenary session presentation, still found significantly elevated risks for preterm birth for non-Hispanic black women after accounting for marital status, prior history of preterm birth, tobacco use, an interpregnancy interval of fewer than 12 months, and carrying a male fetus.
“Birth certificates do not inform the lived experiences of one’s self-identified race, and how that experience – or possibly just one’s identification with a particular racial group – may positively or negatively affect their clinical risk of preterm birth,” said Dr. Johnson. “In this study, as in others, race is a social construct. It’s a surrogate for social and societal racism that disproportionately affects birth outcomes of women of color.”
Using non-Hispanic white (NHW) women as a reference, women who described themselves as non-Hispanic black (NHB) had increased odds of preterm birth at 34 and 37 weeks gestation as well. Women identifying as both NHB and NHW had numerically elevated odds for preterm birth at all time points as well, but the odds at 37 weeks didn’t reach statistical significance.
The results were based on a retrospective population-based study of a cohort drawn from the National Vital Statistics birth certificate data of all live births in the United States between 2015 and 2017, explained Dr. Johnson, a maternal-fetal medicine fellow at the University of North Carolina, Chapel Hill. Drawing from a nationally representative sample and having a population-level design drawn were strengths of the study, she said.
Women with singleton pregnancies without anomalies who identified as NHB, NHW, or as both NHB and NHW were included if they also had high socioeconomic status. Including women who identify as both black and white was another strength of the study, Dr. Johnson added.
She explained that, for the purposes of the study, high socioeconomic status was defined as having 16 or more years of education and private insurance, and not receiving WIC benefits.
In addition to the primary outcome measure of preterm birth at fewer than 37 weeks gestation, secondary outcomes included preterm birth at fewer than 34 and fewer than 28 weeks’ gestation, as well as low birthweight (LBW) and very low birthweight (VLBW).
About 11.8 million live births occurred during the study period, and 11.3 million of those were singleton pregnancies without fetal anomaly. After excluding women who did not meet the racial self-identification or socioeconomic status inclusion criteria, the investigators arrived at the final study population of 2,170,688 individuals.
Of those, 2,017,470, or 92.9%, were non-Hispanic white, while 144,612, or 6.7%, were non-Hispanic black. The remaining 8,604 participants, or 0.4%, identified their race as non-Hispanic black and non-Hispanic white.
The groups identified in the study differed significantly in demographic characteristics, Dr. Johnson said. Women in the NHB and NHB + NHW groups were less likely to be married than NHW women – about 75% of the former two groups were married, compared with 92.5% of NHW women. This difference was statistically significant with a P value of .001, as were all the differences Dr. Johnson reported.
Pre-pregnancy body mass index (BMI) was highest in NHB women at 27.1 kg/m sq, followed by NHB = NHW women at 25.7 kg/m sq, with NHW women having the lowest BMI at 23.8 kg/m sq.
Prior preterm birth of 37 weeks’ gestation or less was more common in NHB women and NHB + NHW women, as was an interpregnancy interval of fewer than 12 months.
Chronic hypertension was more than twice as common in NHB women than in either NHB = NHW or NHW women, occurring in 3.9%, 1.8%, and 1.4% of participants, respectively.
Pregestational diabetes was about twice as common in NHB women than NHW women, occurring in 1% and 0.52% of those groups, respectively. Prevalence of pregestational diabetes was intermediate in NHB = NHW women, at 0.72%.
Tobacco use was rare overall, and less common in NHB women than NHB + NHW and NHW women.
In terms of pregnancy characteristics, though 85% of NHB women initiated prenatal care in the first trimester, they were less likely to have done so than either of the other two groups. Few women overall had no prenatal care, but 0.7% of NHB women fell into this category, more than the 0.4% and 0.3% reported for NHB + NHW and NHW women, respectively.
During their pregnancies, NHB women were more likely to develop gestational hypertension and/or pre-eclampsia as well as gestational diabetes than either of the other two groups (7.6% compared with 6% for the other two groups). Of the NHB women, 5.9% developed gestational diabetes, compared with 4.8% of NHB + NHW and 4.8% of NHW women.
Delivering a baby with a birthweight less than the 10th percentile was twice as common for NHB, compared with NHW women (7.2% versus 3.4%). The risk for NHB + NHW women was intermediate, at 4.7%.
Dr. Johnson said she and her team performed further analyses, including using initiation of prenatal care in the first trimester of pregnancy as a surrogate for high socioeconomic status; the association of race and risk for preterm birth persisted.
The study had the usual limitations of using National Vital Statistics data, such as the inability to evaluate underlying etiologies for preterm birth.
However, Dr. Johnson highlighted additional limitations that pertain to the experience of race in 21st century America. “Our definition of high socioeconomic status does not guarantee that all women in this analysis have financial stability,” she said, pointing out that the study’s definition of high socioeconomic status was insensitive to wealth accumulation. She also noted that high educational attainment does not necessarily correlate with high income. Hence, the potential burden of economic stressors could not fully be captured.
The study was supported by the National Institutes of Health. Dr. Johnson reported no conflicts of interest.
SOURCE: Johnson J et al. Obstet Gynecol. 2020 Jan;222(1):S-37-8, Abstract 44.
AT THE PREGNANCY MEETING
Primary care can embrace gender-affirming policies, approaches
In a new “blueprint” for practices planning to implement a transgender care program, Anna M. Morenz, MD, and her coauthors emphasized that more than technical skills are needed to build an effective and welcoming transgender health practice.
All patient-facing staff – from schedulers and receptionists to nurses and billers – should “receive a foundational level of training in cultural sensitivity and effective communication with transgender and gender-diverse persons,” they wrote. In addition, they emphasized, “the workplace culture must ensure that chatter behind closed doors does not differ from patient-facing language.”
One thing that’s become clear over time, noted the authors of the blueprint, is that transgender care is no longer limited to the endocrinologist’s office. “After years of referring transgender and gender-diverse patients to specialty clinics and endocrinologists, transgender health experts have come to agree that gender-affirming hormone therapy can be safely delivered as part of routine care by a trained primary care clinician,” wrote Dr. Morenz, an internal medicine resident at the University of Washington, Seattle, and her coauthors.
Nor do most adults receiving gender-affirming care require mental health services, unless the patient or the primary care clinician sees a need or utility for psychological care. The blueprint was published in the Annals of Family Medicine.
The first step to setting up transgender services within a primary care practice is to conduct a needs assessment, suggested Dr. Morenz and her colleagues. Whether in-person focus groups or online surveys or questionnaires are best might depend on the community climate, they wrote. When stigma is high, the opportunity for anonymity might provide more robust results. Other considerations include whether there’s a concentration of transgender people with particularly high need or risk in the community – for example, transgender women of color, who might be at higher risk of HIV/AIDS than the general population. Depending on the needs of a particular community, initial transgender care efforts may have a focus on such a population.
A practice also should conduct a realistic appraisal of its own strengths and areas of weakness: Is signage inclusive? Do intake forms afford flexibility in gender and pronoun preference? Are front office staff comfortable greeting members of the lesbian-gay-bisexual-transgender-queer-intersex-asexual (LGBTQIA) community? What about restroom signage – is there a gender-inclusive option?
Competent provision of trauma-informed care goes hand in hand with assessment and preparation for providing transgender care, noted the blueprint authors, because “transgender and gender-diverse people experience high levels of trauma and stress related to minority status.”
Performing outreach within an organization and community also can unearth existing services, so that a primary care transgender practice dovetails with and complements those ongoing efforts, avoiding unnecessarily duplicative services. “All transgender health programs can benefit from developing broad relationships with external agencies, community-based organizatons, and individual practitioners who provide a range of services and can function as a network for knowledge-sharing and referrals,” noted Dr. Morenz and her coauthors.
“Starting a new program, especially one focused on a stigmatized population, can generate staff concerns and resistance,” acknowledged Dr. Morenz and her colleagues. Efforts at getting organizational buy-in can emphasize that providing transgender care helps meet ethical obligations within medicine. Emphasizing that making such care available is really at the vanguard of best practices might help overcome some resistance, they said.
, with at least one champion having a leadership role within the organization, wrote Dr. Morenz and her colleagues.
A variety of care models can work when a practice is initiating transgender care, depending on community needs, internal resources, and the commitment level of various stakeholders. An evening clinic staffed by a small number of clinicians can be a good way to test the waters in some cases. Other facilities might wish to identify clinicians who are competent to offer hormone therapy, while still other clinics might be able to incorporate transgender care more globally within their practice. Regardless of which service model a practice opts for, however, it’s crucial to have staff members who are savvy navigators of insurance reimbursement for gender-affirming care.
And when transgender care is nested within a practice, those patients must not feel like second-class citizens of the clinic, or that they’re receiving care that’s somehow different or substandard. For example, wrote Dr. Morenz and her coauthors, a facility must consider what will happen when a transgender patient presents for urgent health needs and the primary care clinician is not available.
The nuts and bolts of providing safe and effective gender-affirming hormone therapy, said the blueprint authors, can be mastered with training and practice. “Despite common concerns that transgender health care is complicated, it is in fact as straightforward as managing common chronic diseases.”
The first step, they said, is providing risk-benefit education and counseling to patients, and reviewing fertility preservation considerations and options. Then, either estradiol or testosterone is initiated; Further suppression of endogenous hormones also might be indicated in feminization therapy in particular. The authors provided several continuing education resources for clinicians and other health care team members, and noted that a “train the trainer” model can prove effective, with a core team training others once they’ve become comfortable with the ins and outs of hormone prescribing and monitoring.
Having a staff that looks like the patient panel can go a long way toward promoting authentic inclusivity, but Dr. Morenz and her colleagues cautioned against hiring practices that amount to tokenism, or expecting transgender or gender-diverse staff to be ambassadors or spokespeople for others.
Taken together, the start-up costs for providing transgender care can be “minimal,” wrote the blueprint authors, because many free and low-cost educational resources are available. Some of the only real outlays may come from altering restroom signage and tweaking the electronic health record to accommodate gender diversity.
A practice that goes forward with transgender care, they conclude, “will provide a unique opportunity to holistically improve wellness and quality of life for transgender and gender-diverse people,” joining the “growing and passionate network of clinical practice teams who are committed to health care, innovation, and equity for transgender and gender-diverse communities.”
Dr. Morenz reported no outside sources of funding and reported that she has no relevant conflicts of interest.
SOURCE: Morenz AM et al. Ann Fam Med. 2020 Jan;18(1):73-9.
In a new “blueprint” for practices planning to implement a transgender care program, Anna M. Morenz, MD, and her coauthors emphasized that more than technical skills are needed to build an effective and welcoming transgender health practice.
All patient-facing staff – from schedulers and receptionists to nurses and billers – should “receive a foundational level of training in cultural sensitivity and effective communication with transgender and gender-diverse persons,” they wrote. In addition, they emphasized, “the workplace culture must ensure that chatter behind closed doors does not differ from patient-facing language.”
One thing that’s become clear over time, noted the authors of the blueprint, is that transgender care is no longer limited to the endocrinologist’s office. “After years of referring transgender and gender-diverse patients to specialty clinics and endocrinologists, transgender health experts have come to agree that gender-affirming hormone therapy can be safely delivered as part of routine care by a trained primary care clinician,” wrote Dr. Morenz, an internal medicine resident at the University of Washington, Seattle, and her coauthors.
Nor do most adults receiving gender-affirming care require mental health services, unless the patient or the primary care clinician sees a need or utility for psychological care. The blueprint was published in the Annals of Family Medicine.
The first step to setting up transgender services within a primary care practice is to conduct a needs assessment, suggested Dr. Morenz and her colleagues. Whether in-person focus groups or online surveys or questionnaires are best might depend on the community climate, they wrote. When stigma is high, the opportunity for anonymity might provide more robust results. Other considerations include whether there’s a concentration of transgender people with particularly high need or risk in the community – for example, transgender women of color, who might be at higher risk of HIV/AIDS than the general population. Depending on the needs of a particular community, initial transgender care efforts may have a focus on such a population.
A practice also should conduct a realistic appraisal of its own strengths and areas of weakness: Is signage inclusive? Do intake forms afford flexibility in gender and pronoun preference? Are front office staff comfortable greeting members of the lesbian-gay-bisexual-transgender-queer-intersex-asexual (LGBTQIA) community? What about restroom signage – is there a gender-inclusive option?
Competent provision of trauma-informed care goes hand in hand with assessment and preparation for providing transgender care, noted the blueprint authors, because “transgender and gender-diverse people experience high levels of trauma and stress related to minority status.”
Performing outreach within an organization and community also can unearth existing services, so that a primary care transgender practice dovetails with and complements those ongoing efforts, avoiding unnecessarily duplicative services. “All transgender health programs can benefit from developing broad relationships with external agencies, community-based organizatons, and individual practitioners who provide a range of services and can function as a network for knowledge-sharing and referrals,” noted Dr. Morenz and her coauthors.
“Starting a new program, especially one focused on a stigmatized population, can generate staff concerns and resistance,” acknowledged Dr. Morenz and her colleagues. Efforts at getting organizational buy-in can emphasize that providing transgender care helps meet ethical obligations within medicine. Emphasizing that making such care available is really at the vanguard of best practices might help overcome some resistance, they said.
, with at least one champion having a leadership role within the organization, wrote Dr. Morenz and her colleagues.
A variety of care models can work when a practice is initiating transgender care, depending on community needs, internal resources, and the commitment level of various stakeholders. An evening clinic staffed by a small number of clinicians can be a good way to test the waters in some cases. Other facilities might wish to identify clinicians who are competent to offer hormone therapy, while still other clinics might be able to incorporate transgender care more globally within their practice. Regardless of which service model a practice opts for, however, it’s crucial to have staff members who are savvy navigators of insurance reimbursement for gender-affirming care.
And when transgender care is nested within a practice, those patients must not feel like second-class citizens of the clinic, or that they’re receiving care that’s somehow different or substandard. For example, wrote Dr. Morenz and her coauthors, a facility must consider what will happen when a transgender patient presents for urgent health needs and the primary care clinician is not available.
The nuts and bolts of providing safe and effective gender-affirming hormone therapy, said the blueprint authors, can be mastered with training and practice. “Despite common concerns that transgender health care is complicated, it is in fact as straightforward as managing common chronic diseases.”
The first step, they said, is providing risk-benefit education and counseling to patients, and reviewing fertility preservation considerations and options. Then, either estradiol or testosterone is initiated; Further suppression of endogenous hormones also might be indicated in feminization therapy in particular. The authors provided several continuing education resources for clinicians and other health care team members, and noted that a “train the trainer” model can prove effective, with a core team training others once they’ve become comfortable with the ins and outs of hormone prescribing and monitoring.
Having a staff that looks like the patient panel can go a long way toward promoting authentic inclusivity, but Dr. Morenz and her colleagues cautioned against hiring practices that amount to tokenism, or expecting transgender or gender-diverse staff to be ambassadors or spokespeople for others.
Taken together, the start-up costs for providing transgender care can be “minimal,” wrote the blueprint authors, because many free and low-cost educational resources are available. Some of the only real outlays may come from altering restroom signage and tweaking the electronic health record to accommodate gender diversity.
A practice that goes forward with transgender care, they conclude, “will provide a unique opportunity to holistically improve wellness and quality of life for transgender and gender-diverse people,” joining the “growing and passionate network of clinical practice teams who are committed to health care, innovation, and equity for transgender and gender-diverse communities.”
Dr. Morenz reported no outside sources of funding and reported that she has no relevant conflicts of interest.
SOURCE: Morenz AM et al. Ann Fam Med. 2020 Jan;18(1):73-9.
In a new “blueprint” for practices planning to implement a transgender care program, Anna M. Morenz, MD, and her coauthors emphasized that more than technical skills are needed to build an effective and welcoming transgender health practice.
All patient-facing staff – from schedulers and receptionists to nurses and billers – should “receive a foundational level of training in cultural sensitivity and effective communication with transgender and gender-diverse persons,” they wrote. In addition, they emphasized, “the workplace culture must ensure that chatter behind closed doors does not differ from patient-facing language.”
One thing that’s become clear over time, noted the authors of the blueprint, is that transgender care is no longer limited to the endocrinologist’s office. “After years of referring transgender and gender-diverse patients to specialty clinics and endocrinologists, transgender health experts have come to agree that gender-affirming hormone therapy can be safely delivered as part of routine care by a trained primary care clinician,” wrote Dr. Morenz, an internal medicine resident at the University of Washington, Seattle, and her coauthors.
Nor do most adults receiving gender-affirming care require mental health services, unless the patient or the primary care clinician sees a need or utility for psychological care. The blueprint was published in the Annals of Family Medicine.
The first step to setting up transgender services within a primary care practice is to conduct a needs assessment, suggested Dr. Morenz and her colleagues. Whether in-person focus groups or online surveys or questionnaires are best might depend on the community climate, they wrote. When stigma is high, the opportunity for anonymity might provide more robust results. Other considerations include whether there’s a concentration of transgender people with particularly high need or risk in the community – for example, transgender women of color, who might be at higher risk of HIV/AIDS than the general population. Depending on the needs of a particular community, initial transgender care efforts may have a focus on such a population.
A practice also should conduct a realistic appraisal of its own strengths and areas of weakness: Is signage inclusive? Do intake forms afford flexibility in gender and pronoun preference? Are front office staff comfortable greeting members of the lesbian-gay-bisexual-transgender-queer-intersex-asexual (LGBTQIA) community? What about restroom signage – is there a gender-inclusive option?
Competent provision of trauma-informed care goes hand in hand with assessment and preparation for providing transgender care, noted the blueprint authors, because “transgender and gender-diverse people experience high levels of trauma and stress related to minority status.”
Performing outreach within an organization and community also can unearth existing services, so that a primary care transgender practice dovetails with and complements those ongoing efforts, avoiding unnecessarily duplicative services. “All transgender health programs can benefit from developing broad relationships with external agencies, community-based organizatons, and individual practitioners who provide a range of services and can function as a network for knowledge-sharing and referrals,” noted Dr. Morenz and her coauthors.
“Starting a new program, especially one focused on a stigmatized population, can generate staff concerns and resistance,” acknowledged Dr. Morenz and her colleagues. Efforts at getting organizational buy-in can emphasize that providing transgender care helps meet ethical obligations within medicine. Emphasizing that making such care available is really at the vanguard of best practices might help overcome some resistance, they said.
, with at least one champion having a leadership role within the organization, wrote Dr. Morenz and her colleagues.
A variety of care models can work when a practice is initiating transgender care, depending on community needs, internal resources, and the commitment level of various stakeholders. An evening clinic staffed by a small number of clinicians can be a good way to test the waters in some cases. Other facilities might wish to identify clinicians who are competent to offer hormone therapy, while still other clinics might be able to incorporate transgender care more globally within their practice. Regardless of which service model a practice opts for, however, it’s crucial to have staff members who are savvy navigators of insurance reimbursement for gender-affirming care.
And when transgender care is nested within a practice, those patients must not feel like second-class citizens of the clinic, or that they’re receiving care that’s somehow different or substandard. For example, wrote Dr. Morenz and her coauthors, a facility must consider what will happen when a transgender patient presents for urgent health needs and the primary care clinician is not available.
The nuts and bolts of providing safe and effective gender-affirming hormone therapy, said the blueprint authors, can be mastered with training and practice. “Despite common concerns that transgender health care is complicated, it is in fact as straightforward as managing common chronic diseases.”
The first step, they said, is providing risk-benefit education and counseling to patients, and reviewing fertility preservation considerations and options. Then, either estradiol or testosterone is initiated; Further suppression of endogenous hormones also might be indicated in feminization therapy in particular. The authors provided several continuing education resources for clinicians and other health care team members, and noted that a “train the trainer” model can prove effective, with a core team training others once they’ve become comfortable with the ins and outs of hormone prescribing and monitoring.
Having a staff that looks like the patient panel can go a long way toward promoting authentic inclusivity, but Dr. Morenz and her colleagues cautioned against hiring practices that amount to tokenism, or expecting transgender or gender-diverse staff to be ambassadors or spokespeople for others.
Taken together, the start-up costs for providing transgender care can be “minimal,” wrote the blueprint authors, because many free and low-cost educational resources are available. Some of the only real outlays may come from altering restroom signage and tweaking the electronic health record to accommodate gender diversity.
A practice that goes forward with transgender care, they conclude, “will provide a unique opportunity to holistically improve wellness and quality of life for transgender and gender-diverse people,” joining the “growing and passionate network of clinical practice teams who are committed to health care, innovation, and equity for transgender and gender-diverse communities.”
Dr. Morenz reported no outside sources of funding and reported that she has no relevant conflicts of interest.
SOURCE: Morenz AM et al. Ann Fam Med. 2020 Jan;18(1):73-9.
FROM THE ANNALS OF FAMILY MEDICINE