User login
Transfusion errors more common in kids than adults, study suggests
BOSTON—Even the most vigilant hospitals experience transfusion errors and problems with blood storage, according to researchers.
A review of data from 32 U.S. hospitals showed that pediatric transfusions were associated with a higher rate of safety problems than adult transfusions, with errors differing by age group.
The most common error in the pediatric population was failure to follow protocol, and the most common error in the adult population was that scheduled transfusions were not performed.
Sarah Vossoughi, MD, of Columbia University and New York–Presbyterian Hospital in New York, described these findings at AABB 2018 (abstract QT4).
To evaluate patient safety events related to blood transfusions, Dr. Vossoughi and her colleagues reviewed data on events reported by three children’s hospitals and 29 adult hospitals. Events were reported to either the AABB Center for Patient Safety or the medical center’s own adverse event reporting system from January 2010 through September 2017.
The researchers identified a total of 1,806 reports associated with approximately 1,088,884 transfusions.
There were 249 reports associated with 99,064 pediatric transfusions and 1,577 reports associated with 989,820 adult transfusions. So the reporting rate was 251 per 100,000 transfusions for the pediatric population and 157 per 100,000 transfusions for the adult population (P<0.001).
The most common error for pediatric patients—failure to follow the transfusion protocol—made up 31% of the pediatric errors.
“In a lot of the pediatric hospitals, it’s kind of like the Wild West,” Dr. Vossoughi said. “People say, ‘Well, I know it’s the hospital policy, but this child is special, so I’m going to do it this way, this time.’ That seems to be a culture in pediatrics, whereas, on the adult side, [clinicians] seem to be much less likely to just deviate from the protocol.”
Among adults, the most common error was “transfusion not performed,” which accounted for 43% of the adult errors. Dr. Vossoughi said transfusions may be skipped due to a bungled patient hand-off during a shift change or when a patient is being moved from one unit to another.
“The next day, they’ll check the patient’s CBC [complete blood count] and realize that the patient didn’t respond to the infusion that it turned out they never got, and then the product will be found on the floor, expired,” Dr. Vossoughi said.
She and her colleagues also found that 20% of pediatric errors and 24% of adult errors were associated with incorrect storage of blood products on the patient floor.
“It’s very common for blood banks to find platelets in the refrigerator,” Dr. Vossoughi said. “It doesn’t matter how old you are or what type of hospital you’re at. Everyone’s putting platelets in the fridge.”
Dr. Vossoughi and her colleagues believe these findings could help inpatient blood management programs target education and interventions to providers who commit similar errors.
“If you know that a particular provider group has problems following the protocol, maybe you can make the protocol a little simpler to follow or make the checklist less cumbersome, and then maybe they’ll follow them more often,” Dr. Vossoughi said.
This research was supported by the AABB Center for Patient Safety and University of Vermont Medical Center. The researchers reported no conflicts of interest.
BOSTON—Even the most vigilant hospitals experience transfusion errors and problems with blood storage, according to researchers.
A review of data from 32 U.S. hospitals showed that pediatric transfusions were associated with a higher rate of safety problems than adult transfusions, with errors differing by age group.
The most common error in the pediatric population was failure to follow protocol, and the most common error in the adult population was that scheduled transfusions were not performed.
Sarah Vossoughi, MD, of Columbia University and New York–Presbyterian Hospital in New York, described these findings at AABB 2018 (abstract QT4).
To evaluate patient safety events related to blood transfusions, Dr. Vossoughi and her colleagues reviewed data on events reported by three children’s hospitals and 29 adult hospitals. Events were reported to either the AABB Center for Patient Safety or the medical center’s own adverse event reporting system from January 2010 through September 2017.
The researchers identified a total of 1,806 reports associated with approximately 1,088,884 transfusions.
There were 249 reports associated with 99,064 pediatric transfusions and 1,577 reports associated with 989,820 adult transfusions. So the reporting rate was 251 per 100,000 transfusions for the pediatric population and 157 per 100,000 transfusions for the adult population (P<0.001).
The most common error for pediatric patients—failure to follow the transfusion protocol—made up 31% of the pediatric errors.
“In a lot of the pediatric hospitals, it’s kind of like the Wild West,” Dr. Vossoughi said. “People say, ‘Well, I know it’s the hospital policy, but this child is special, so I’m going to do it this way, this time.’ That seems to be a culture in pediatrics, whereas, on the adult side, [clinicians] seem to be much less likely to just deviate from the protocol.”
Among adults, the most common error was “transfusion not performed,” which accounted for 43% of the adult errors. Dr. Vossoughi said transfusions may be skipped due to a bungled patient hand-off during a shift change or when a patient is being moved from one unit to another.
“The next day, they’ll check the patient’s CBC [complete blood count] and realize that the patient didn’t respond to the infusion that it turned out they never got, and then the product will be found on the floor, expired,” Dr. Vossoughi said.
She and her colleagues also found that 20% of pediatric errors and 24% of adult errors were associated with incorrect storage of blood products on the patient floor.
“It’s very common for blood banks to find platelets in the refrigerator,” Dr. Vossoughi said. “It doesn’t matter how old you are or what type of hospital you’re at. Everyone’s putting platelets in the fridge.”
Dr. Vossoughi and her colleagues believe these findings could help inpatient blood management programs target education and interventions to providers who commit similar errors.
“If you know that a particular provider group has problems following the protocol, maybe you can make the protocol a little simpler to follow or make the checklist less cumbersome, and then maybe they’ll follow them more often,” Dr. Vossoughi said.
This research was supported by the AABB Center for Patient Safety and University of Vermont Medical Center. The researchers reported no conflicts of interest.
BOSTON—Even the most vigilant hospitals experience transfusion errors and problems with blood storage, according to researchers.
A review of data from 32 U.S. hospitals showed that pediatric transfusions were associated with a higher rate of safety problems than adult transfusions, with errors differing by age group.
The most common error in the pediatric population was failure to follow protocol, and the most common error in the adult population was that scheduled transfusions were not performed.
Sarah Vossoughi, MD, of Columbia University and New York–Presbyterian Hospital in New York, described these findings at AABB 2018 (abstract QT4).
To evaluate patient safety events related to blood transfusions, Dr. Vossoughi and her colleagues reviewed data on events reported by three children’s hospitals and 29 adult hospitals. Events were reported to either the AABB Center for Patient Safety or the medical center’s own adverse event reporting system from January 2010 through September 2017.
The researchers identified a total of 1,806 reports associated with approximately 1,088,884 transfusions.
There were 249 reports associated with 99,064 pediatric transfusions and 1,577 reports associated with 989,820 adult transfusions. So the reporting rate was 251 per 100,000 transfusions for the pediatric population and 157 per 100,000 transfusions for the adult population (P<0.001).
The most common error for pediatric patients—failure to follow the transfusion protocol—made up 31% of the pediatric errors.
“In a lot of the pediatric hospitals, it’s kind of like the Wild West,” Dr. Vossoughi said. “People say, ‘Well, I know it’s the hospital policy, but this child is special, so I’m going to do it this way, this time.’ That seems to be a culture in pediatrics, whereas, on the adult side, [clinicians] seem to be much less likely to just deviate from the protocol.”
Among adults, the most common error was “transfusion not performed,” which accounted for 43% of the adult errors. Dr. Vossoughi said transfusions may be skipped due to a bungled patient hand-off during a shift change or when a patient is being moved from one unit to another.
“The next day, they’ll check the patient’s CBC [complete blood count] and realize that the patient didn’t respond to the infusion that it turned out they never got, and then the product will be found on the floor, expired,” Dr. Vossoughi said.
She and her colleagues also found that 20% of pediatric errors and 24% of adult errors were associated with incorrect storage of blood products on the patient floor.
“It’s very common for blood banks to find platelets in the refrigerator,” Dr. Vossoughi said. “It doesn’t matter how old you are or what type of hospital you’re at. Everyone’s putting platelets in the fridge.”
Dr. Vossoughi and her colleagues believe these findings could help inpatient blood management programs target education and interventions to providers who commit similar errors.
“If you know that a particular provider group has problems following the protocol, maybe you can make the protocol a little simpler to follow or make the checklist less cumbersome, and then maybe they’ll follow them more often,” Dr. Vossoughi said.
This research was supported by the AABB Center for Patient Safety and University of Vermont Medical Center. The researchers reported no conflicts of interest.
Protocol violations, missed transfusions among blood delivery errors
BOSTON – Even the most vigilant hospitals experience problems with blood storage and delivery on the patient floor, particularly in pediatric units, investigators cautioned.
A review of patient safety incidents that occurred surrounding more than 1 million transfusions in U.S. hospitals showed that pediatric transfusions were associated with a higher rate of safety problems compared with adult transfusions, with errors differing by age group.
“We just looked at units transfused [and] incidents that occurred during product administration and we found that the highest incident in the pediatric population is that the protocol is not being followed, and the highest incident in the adult population is that the transfusion is not performed, in error, at all,” said Sarah Vossoughi, MD, of Columbia University and New York–Presbyterian Hospital, New York.
In both settings, the investigators observed problems with product storage on the patient floor. “It’s very common for blood banks to find platelets in the refrigerator. It doesn’t matter how old you are or what type of hospital you’re at – everyone’s putting platelets in the fridge,” she said in an interview at AABB 2018, the annual meeting of the organization formerly known as the American Association of Blood Banks.
Dr. Vossoughi and her colleagues in New York and at the University of Vermont in Burlington noted that the National Patient Safety Foundation, now a part of the Institute for Healthcare Improvement, declared preventable medical harm to be a public health crisis. In a paper published in the BMJ in 2016, researchers estimated that medical errors were the third leading cause of death in the United States, accounting for more than 250,000 fatalities annually.
Dr. Vossoughi also pointed to a study suggesting that the incidence of nonlethal medical errors may be 10- to 20-fold higher than the number of fatal errors (J Patient Saf. 2013 Sep;9[3]:122-8).
To evaluate patient safety events related to blood transfusions, Dr. Vossoughi and her colleagues drew data on events reported by three children’s hospitals and 29 adult hospitals to either the AABB Center for Patient Safety or the medical center’s own adverse event reporting system from January 2010 through September 2017.
They identified a total of 1,806 reports associated with approximately 1,088.884 transfusions. Of these reports, 249 were associated with 99,064 pediatric transfusions, and 1,577 were reported in association with 989,820 adult transfusions.
In all, 31% of the pediatric events were failure to follow the transfusion protocol.
“In a lot of the pediatric hospitals, it’s kind of like the Wild West. People say, ‘well I know it’s the hospital policy, but this child is special, so I’m going to do it this way, this time.’ That seems to be a culture in pediatrics, whereas on the adult side [clinicians] seem to be much less likely to just deviate from the protocol,” Dr. Vossoughi said.
Among adults, 43% of the errors were “transfusion not performed,” which may occur because of a bungled patient hand-off during a shift change, or when a patient is being moved from one unit to another.
“The next day, they’ll check the patient’s CBC and realize that the patient didn’t respond to the infusion that it turned out they never got, and then the product will be found on the floor, expired,” Dr. Vossoughi said.
In all, 20% of pediatric errors and 24% of adult errors were associated with incorrect storage of blood products on the patient floor.
The information they presented could help inpatient blood management programs target education and interventions to providers who commit similar errors.
“If you know that a particular provider group has problems following the protocol, maybe you can make the protocol a little simpler to follow, or make the checklist less cumbersome, and then maybe they’ll follow them more often,” she said.
The study was supported by the AABB Center for Patient Safety and University of Vermont Medical Center. The authors reported no conflicts of interest.
SOURCE: Vossoughi S et al. AABB 2018, Abstract QT4.
BOSTON – Even the most vigilant hospitals experience problems with blood storage and delivery on the patient floor, particularly in pediatric units, investigators cautioned.
A review of patient safety incidents that occurred surrounding more than 1 million transfusions in U.S. hospitals showed that pediatric transfusions were associated with a higher rate of safety problems compared with adult transfusions, with errors differing by age group.
“We just looked at units transfused [and] incidents that occurred during product administration and we found that the highest incident in the pediatric population is that the protocol is not being followed, and the highest incident in the adult population is that the transfusion is not performed, in error, at all,” said Sarah Vossoughi, MD, of Columbia University and New York–Presbyterian Hospital, New York.
In both settings, the investigators observed problems with product storage on the patient floor. “It’s very common for blood banks to find platelets in the refrigerator. It doesn’t matter how old you are or what type of hospital you’re at – everyone’s putting platelets in the fridge,” she said in an interview at AABB 2018, the annual meeting of the organization formerly known as the American Association of Blood Banks.
Dr. Vossoughi and her colleagues in New York and at the University of Vermont in Burlington noted that the National Patient Safety Foundation, now a part of the Institute for Healthcare Improvement, declared preventable medical harm to be a public health crisis. In a paper published in the BMJ in 2016, researchers estimated that medical errors were the third leading cause of death in the United States, accounting for more than 250,000 fatalities annually.
Dr. Vossoughi also pointed to a study suggesting that the incidence of nonlethal medical errors may be 10- to 20-fold higher than the number of fatal errors (J Patient Saf. 2013 Sep;9[3]:122-8).
To evaluate patient safety events related to blood transfusions, Dr. Vossoughi and her colleagues drew data on events reported by three children’s hospitals and 29 adult hospitals to either the AABB Center for Patient Safety or the medical center’s own adverse event reporting system from January 2010 through September 2017.
They identified a total of 1,806 reports associated with approximately 1,088.884 transfusions. Of these reports, 249 were associated with 99,064 pediatric transfusions, and 1,577 were reported in association with 989,820 adult transfusions.
In all, 31% of the pediatric events were failure to follow the transfusion protocol.
“In a lot of the pediatric hospitals, it’s kind of like the Wild West. People say, ‘well I know it’s the hospital policy, but this child is special, so I’m going to do it this way, this time.’ That seems to be a culture in pediatrics, whereas on the adult side [clinicians] seem to be much less likely to just deviate from the protocol,” Dr. Vossoughi said.
Among adults, 43% of the errors were “transfusion not performed,” which may occur because of a bungled patient hand-off during a shift change, or when a patient is being moved from one unit to another.
“The next day, they’ll check the patient’s CBC and realize that the patient didn’t respond to the infusion that it turned out they never got, and then the product will be found on the floor, expired,” Dr. Vossoughi said.
In all, 20% of pediatric errors and 24% of adult errors were associated with incorrect storage of blood products on the patient floor.
The information they presented could help inpatient blood management programs target education and interventions to providers who commit similar errors.
“If you know that a particular provider group has problems following the protocol, maybe you can make the protocol a little simpler to follow, or make the checklist less cumbersome, and then maybe they’ll follow them more often,” she said.
The study was supported by the AABB Center for Patient Safety and University of Vermont Medical Center. The authors reported no conflicts of interest.
SOURCE: Vossoughi S et al. AABB 2018, Abstract QT4.
BOSTON – Even the most vigilant hospitals experience problems with blood storage and delivery on the patient floor, particularly in pediatric units, investigators cautioned.
A review of patient safety incidents that occurred surrounding more than 1 million transfusions in U.S. hospitals showed that pediatric transfusions were associated with a higher rate of safety problems compared with adult transfusions, with errors differing by age group.
“We just looked at units transfused [and] incidents that occurred during product administration and we found that the highest incident in the pediatric population is that the protocol is not being followed, and the highest incident in the adult population is that the transfusion is not performed, in error, at all,” said Sarah Vossoughi, MD, of Columbia University and New York–Presbyterian Hospital, New York.
In both settings, the investigators observed problems with product storage on the patient floor. “It’s very common for blood banks to find platelets in the refrigerator. It doesn’t matter how old you are or what type of hospital you’re at – everyone’s putting platelets in the fridge,” she said in an interview at AABB 2018, the annual meeting of the organization formerly known as the American Association of Blood Banks.
Dr. Vossoughi and her colleagues in New York and at the University of Vermont in Burlington noted that the National Patient Safety Foundation, now a part of the Institute for Healthcare Improvement, declared preventable medical harm to be a public health crisis. In a paper published in the BMJ in 2016, researchers estimated that medical errors were the third leading cause of death in the United States, accounting for more than 250,000 fatalities annually.
Dr. Vossoughi also pointed to a study suggesting that the incidence of nonlethal medical errors may be 10- to 20-fold higher than the number of fatal errors (J Patient Saf. 2013 Sep;9[3]:122-8).
To evaluate patient safety events related to blood transfusions, Dr. Vossoughi and her colleagues drew data on events reported by three children’s hospitals and 29 adult hospitals to either the AABB Center for Patient Safety or the medical center’s own adverse event reporting system from January 2010 through September 2017.
They identified a total of 1,806 reports associated with approximately 1,088.884 transfusions. Of these reports, 249 were associated with 99,064 pediatric transfusions, and 1,577 were reported in association with 989,820 adult transfusions.
In all, 31% of the pediatric events were failure to follow the transfusion protocol.
“In a lot of the pediatric hospitals, it’s kind of like the Wild West. People say, ‘well I know it’s the hospital policy, but this child is special, so I’m going to do it this way, this time.’ That seems to be a culture in pediatrics, whereas on the adult side [clinicians] seem to be much less likely to just deviate from the protocol,” Dr. Vossoughi said.
Among adults, 43% of the errors were “transfusion not performed,” which may occur because of a bungled patient hand-off during a shift change, or when a patient is being moved from one unit to another.
“The next day, they’ll check the patient’s CBC and realize that the patient didn’t respond to the infusion that it turned out they never got, and then the product will be found on the floor, expired,” Dr. Vossoughi said.
In all, 20% of pediatric errors and 24% of adult errors were associated with incorrect storage of blood products on the patient floor.
The information they presented could help inpatient blood management programs target education and interventions to providers who commit similar errors.
“If you know that a particular provider group has problems following the protocol, maybe you can make the protocol a little simpler to follow, or make the checklist less cumbersome, and then maybe they’ll follow them more often,” she said.
The study was supported by the AABB Center for Patient Safety and University of Vermont Medical Center. The authors reported no conflicts of interest.
SOURCE: Vossoughi S et al. AABB 2018, Abstract QT4.
REPORTING FROM AABB 2018
Key clinical point:
Major finding: In all, 31% of pediatric errors were due to protocol violation, and 43% of adult errors were due to an ordered transfusion not being performed.
Study details: Descriptive study of data from 32 U.S. hospitals that reported transfusion safety events.
Disclosures: The study was supported by the AABB Center for Patient Safety and University of Vermont. The authors reported no conflicts of interest.
Source: Vossoughi S et al. AABB 2018, Abstract QT4.
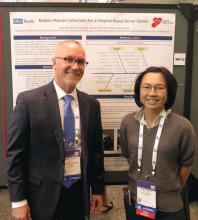
Team reports success with mobile platelet collection
BOSTON—If donors can’t get to the apheresis center, bring the apheresis center to the donors.
Researchers have found that apheresis platelet collection in the field is practical with proper planning and support.
A team at the University of California at Los Angeles (UCLA) Blood and Platelet Center explored adding mobile apheresis units to their existing community blood drives.
They found that, with careful planning and coordination, they could augment their supply of blood products and introduce potential new donors to the idea of apheresis donations at the hospital.
The researchers reported these findings in a poster presentation at AABB 2018 (poster BBC 135).
It all started with a needs drive for an oncology patient at UCLA, explained David Anthony, manager of the UCLA Blood and Platelet Center.
“She wanted to bring in donors and had her whole community behind her,” Anthony said. “And we thought, well, she’s an oncology patient, and she uses platelets, and we had talked about doing platelets out in the field rather than just at fixed sites, and we thought that this would be a good chance to try it.”
Until the mobile unit was established, apheresis platelet collections for the hospital-based donor center were limited to two fixed collection sites, with mobile units used only for collection of whole blood.
To see whether concurrent whole blood and platelet community drives were practical, the center’s blood donor field recruiter requested to schedule a community drive in a region of the county where potential donors had expressed a high level of interest in apheresis platelet donations.
Operations staff visited the site to assess its suitability, including appropriate space for donor registration and history taking, separate areas for whole blood and apheresis donations, and a donor recovery area. The assessment included ensuring there were suitable electrical outlets, space, and support for apheresis machines.
“Over about 2 weeks, we discussed with our medical directors, [infusion technicians], and our mobile people what we would need to do it,” Anthony said. “The recruiter out in the field was able to go to a high school drive out in that area, recruit donors, and get [platelet] precounts from them so that we could find out who was a good candidate.”
Once they had platelet counts from potential apheresis donors, 10 donors were prescreened based on their eligibility to donate multiple products, history of donations and red blood cell loss, and, for women who had previously had more than one pregnancy, favorable human leukocyte antigen test results.
Four of the prescreened donors were scheduled to donate platelets, and the time slot also included two backup donors, one of whom ultimately donated platelets.
The first drive resulted in the collection of seven platelet products, including three double products and one single product.
The donated products resulted in about a $3,000 cost savings by obviating the need for purchasing products from an outside supplier and bolstered the blood bank’s inventory on a normally low collection day, the researchers reported.
“We’ve had two more apheresis drives since then, and we’ll have another one in 3 weeks,” Anthony said.
He acknowledged that it is more challenging to recruit, educate, and retain donors in the field than in the brick-and-mortar hospital setting.
“We have to make sure that they’re going to show up if we’re going to make the effort to take a machine out there, whereas, at our centers, we have regular donors who come in every 2 weeks,” Anthony said. “It’s easy for them to make an appointment, and they know where we are.”
The center plans to continue concurrent monthly whole blood and platelet collection drives, he added.
This pilot program was internally funded. The researchers reported having no relevant conflicts of interest.
BOSTON—If donors can’t get to the apheresis center, bring the apheresis center to the donors.
Researchers have found that apheresis platelet collection in the field is practical with proper planning and support.
A team at the University of California at Los Angeles (UCLA) Blood and Platelet Center explored adding mobile apheresis units to their existing community blood drives.
They found that, with careful planning and coordination, they could augment their supply of blood products and introduce potential new donors to the idea of apheresis donations at the hospital.
The researchers reported these findings in a poster presentation at AABB 2018 (poster BBC 135).
It all started with a needs drive for an oncology patient at UCLA, explained David Anthony, manager of the UCLA Blood and Platelet Center.
“She wanted to bring in donors and had her whole community behind her,” Anthony said. “And we thought, well, she’s an oncology patient, and she uses platelets, and we had talked about doing platelets out in the field rather than just at fixed sites, and we thought that this would be a good chance to try it.”
Until the mobile unit was established, apheresis platelet collections for the hospital-based donor center were limited to two fixed collection sites, with mobile units used only for collection of whole blood.
To see whether concurrent whole blood and platelet community drives were practical, the center’s blood donor field recruiter requested to schedule a community drive in a region of the county where potential donors had expressed a high level of interest in apheresis platelet donations.
Operations staff visited the site to assess its suitability, including appropriate space for donor registration and history taking, separate areas for whole blood and apheresis donations, and a donor recovery area. The assessment included ensuring there were suitable electrical outlets, space, and support for apheresis machines.
“Over about 2 weeks, we discussed with our medical directors, [infusion technicians], and our mobile people what we would need to do it,” Anthony said. “The recruiter out in the field was able to go to a high school drive out in that area, recruit donors, and get [platelet] precounts from them so that we could find out who was a good candidate.”
Once they had platelet counts from potential apheresis donors, 10 donors were prescreened based on their eligibility to donate multiple products, history of donations and red blood cell loss, and, for women who had previously had more than one pregnancy, favorable human leukocyte antigen test results.
Four of the prescreened donors were scheduled to donate platelets, and the time slot also included two backup donors, one of whom ultimately donated platelets.
The first drive resulted in the collection of seven platelet products, including three double products and one single product.
The donated products resulted in about a $3,000 cost savings by obviating the need for purchasing products from an outside supplier and bolstered the blood bank’s inventory on a normally low collection day, the researchers reported.
“We’ve had two more apheresis drives since then, and we’ll have another one in 3 weeks,” Anthony said.
He acknowledged that it is more challenging to recruit, educate, and retain donors in the field than in the brick-and-mortar hospital setting.
“We have to make sure that they’re going to show up if we’re going to make the effort to take a machine out there, whereas, at our centers, we have regular donors who come in every 2 weeks,” Anthony said. “It’s easy for them to make an appointment, and they know where we are.”
The center plans to continue concurrent monthly whole blood and platelet collection drives, he added.
This pilot program was internally funded. The researchers reported having no relevant conflicts of interest.
BOSTON—If donors can’t get to the apheresis center, bring the apheresis center to the donors.
Researchers have found that apheresis platelet collection in the field is practical with proper planning and support.
A team at the University of California at Los Angeles (UCLA) Blood and Platelet Center explored adding mobile apheresis units to their existing community blood drives.
They found that, with careful planning and coordination, they could augment their supply of blood products and introduce potential new donors to the idea of apheresis donations at the hospital.
The researchers reported these findings in a poster presentation at AABB 2018 (poster BBC 135).
It all started with a needs drive for an oncology patient at UCLA, explained David Anthony, manager of the UCLA Blood and Platelet Center.
“She wanted to bring in donors and had her whole community behind her,” Anthony said. “And we thought, well, she’s an oncology patient, and she uses platelets, and we had talked about doing platelets out in the field rather than just at fixed sites, and we thought that this would be a good chance to try it.”
Until the mobile unit was established, apheresis platelet collections for the hospital-based donor center were limited to two fixed collection sites, with mobile units used only for collection of whole blood.
To see whether concurrent whole blood and platelet community drives were practical, the center’s blood donor field recruiter requested to schedule a community drive in a region of the county where potential donors had expressed a high level of interest in apheresis platelet donations.
Operations staff visited the site to assess its suitability, including appropriate space for donor registration and history taking, separate areas for whole blood and apheresis donations, and a donor recovery area. The assessment included ensuring there were suitable electrical outlets, space, and support for apheresis machines.
“Over about 2 weeks, we discussed with our medical directors, [infusion technicians], and our mobile people what we would need to do it,” Anthony said. “The recruiter out in the field was able to go to a high school drive out in that area, recruit donors, and get [platelet] precounts from them so that we could find out who was a good candidate.”
Once they had platelet counts from potential apheresis donors, 10 donors were prescreened based on their eligibility to donate multiple products, history of donations and red blood cell loss, and, for women who had previously had more than one pregnancy, favorable human leukocyte antigen test results.
Four of the prescreened donors were scheduled to donate platelets, and the time slot also included two backup donors, one of whom ultimately donated platelets.
The first drive resulted in the collection of seven platelet products, including three double products and one single product.
The donated products resulted in about a $3,000 cost savings by obviating the need for purchasing products from an outside supplier and bolstered the blood bank’s inventory on a normally low collection day, the researchers reported.
“We’ve had two more apheresis drives since then, and we’ll have another one in 3 weeks,” Anthony said.
He acknowledged that it is more challenging to recruit, educate, and retain donors in the field than in the brick-and-mortar hospital setting.
“We have to make sure that they’re going to show up if we’re going to make the effort to take a machine out there, whereas, at our centers, we have regular donors who come in every 2 weeks,” Anthony said. “It’s easy for them to make an appointment, and they know where we are.”
The center plans to continue concurrent monthly whole blood and platelet collection drives, he added.
This pilot program was internally funded. The researchers reported having no relevant conflicts of interest.
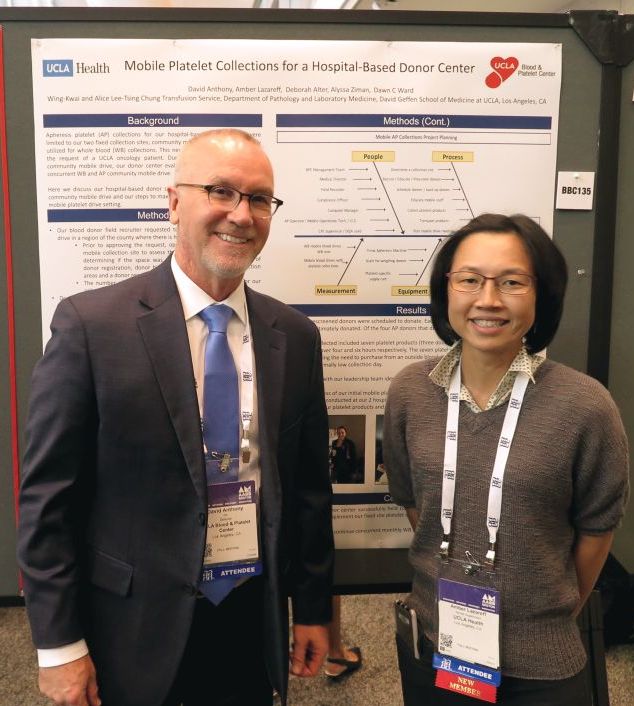
Have apheresis units, will travel
BOSTON – If donors can’t get to the apheresis center, bring the apheresis center to the donors.
Responding to the request of a patient with cancer, David Anthony, Amber Lazareff, RN, and their colleagues at the University of California at Los Angeles Blood and Platelet Center explored adding mobile apheresis units to their existing community blood drives. They found that, with careful planning and coordination, they could augment their supply of vital blood products and introduce potential new donors to the idea of apheresis donations at the hospital.
“There was a needs drive for an oncology patient at UCLA. She wanted to bring in donors and had her whole community behind her, and we thought well, she’s an oncology patient and she uses platelets, and we had talked about doing platelets out in the field rather than just at fixed sites, and we thought that this would be a good chance to try it,” Mr. Anthony said in an interview at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Until the mobile unit was established, apheresis platelet collections for the hospital-based donor center were limited to two fixed collection sites, with mobile units used only for collection of whole blood.
To see whether concurrent whole blood and platelet community drives were practical, the center’s blood donor field recruiter requested to schedule a community drive in a region of the county where potential donors had expressed a high level of interest in apheresis platelet donations.
Operations staff visited the site to assess its suitability, including appropriate space for donor registration and history taking, separate areas for whole blood and apheresis donations, and a donor recovery area. The assessment included ensuring that there were suitable electrical outlets, space, and support for apheresis machines.
“Over about 2 weeks we discussed with our medical directors, [infusion technicians], and our mobile people what we would need to do it. The recruiter out in the field was able to go to a high school drive out in that area, recruit donors, and get [platelet] precounts from them so that we could find out who was a good candidate,” Mr. Anthony said.
Once they had platelet counts from potential apheresis donors, 10 donors were prescreened based on their eligibility to donate multiple products, history of donations and red blood cell loss, and, for women who had previously had more than one pregnancy, favorable HLA test results.
Four of the prescreened donors were scheduled to donate platelets, and the time slot also included two backup donors, one of whom ultimately donated platelets. Of the four apheresis donors, three were first-time platelet donors.
The first drive collected seven platelet products, including three double products and one single product.
The donated products resulted in about a $3,000 cost savings by obviating the need for purchasing products from an outside supplier, and bolstered the blood bank’s inventory on a normally low collection day, the authors reported.
“We’ve had two more apheresis drives since then, and we’ll have another one in 3 weeks,” Mr. Anthony said.
He acknowledged that it is more challenging to recruit, educate, and ideally retain donors in the field than in the brick-and-mortar hospital setting.
“We have to make sure that they’re going to show up if we’re going to make the effort to take a machine out there, whereas at our centers, we have regular donors who come in every 2 weeks, it’s easy for them to make an appointment, and they know where we are,” he said.
The center plans to continue concurrent monthly whole blood and platelet collection drives, he added.
The pilot program was internally funded. The authors reported having no relevant conflicts of interest.
SOURCE: Anthony D et al., AABB 2018, Poster BBC 135.
BOSTON – If donors can’t get to the apheresis center, bring the apheresis center to the donors.
Responding to the request of a patient with cancer, David Anthony, Amber Lazareff, RN, and their colleagues at the University of California at Los Angeles Blood and Platelet Center explored adding mobile apheresis units to their existing community blood drives. They found that, with careful planning and coordination, they could augment their supply of vital blood products and introduce potential new donors to the idea of apheresis donations at the hospital.
“There was a needs drive for an oncology patient at UCLA. She wanted to bring in donors and had her whole community behind her, and we thought well, she’s an oncology patient and she uses platelets, and we had talked about doing platelets out in the field rather than just at fixed sites, and we thought that this would be a good chance to try it,” Mr. Anthony said in an interview at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Until the mobile unit was established, apheresis platelet collections for the hospital-based donor center were limited to two fixed collection sites, with mobile units used only for collection of whole blood.
To see whether concurrent whole blood and platelet community drives were practical, the center’s blood donor field recruiter requested to schedule a community drive in a region of the county where potential donors had expressed a high level of interest in apheresis platelet donations.
Operations staff visited the site to assess its suitability, including appropriate space for donor registration and history taking, separate areas for whole blood and apheresis donations, and a donor recovery area. The assessment included ensuring that there were suitable electrical outlets, space, and support for apheresis machines.
“Over about 2 weeks we discussed with our medical directors, [infusion technicians], and our mobile people what we would need to do it. The recruiter out in the field was able to go to a high school drive out in that area, recruit donors, and get [platelet] precounts from them so that we could find out who was a good candidate,” Mr. Anthony said.
Once they had platelet counts from potential apheresis donors, 10 donors were prescreened based on their eligibility to donate multiple products, history of donations and red blood cell loss, and, for women who had previously had more than one pregnancy, favorable HLA test results.
Four of the prescreened donors were scheduled to donate platelets, and the time slot also included two backup donors, one of whom ultimately donated platelets. Of the four apheresis donors, three were first-time platelet donors.
The first drive collected seven platelet products, including three double products and one single product.
The donated products resulted in about a $3,000 cost savings by obviating the need for purchasing products from an outside supplier, and bolstered the blood bank’s inventory on a normally low collection day, the authors reported.
“We’ve had two more apheresis drives since then, and we’ll have another one in 3 weeks,” Mr. Anthony said.
He acknowledged that it is more challenging to recruit, educate, and ideally retain donors in the field than in the brick-and-mortar hospital setting.
“We have to make sure that they’re going to show up if we’re going to make the effort to take a machine out there, whereas at our centers, we have regular donors who come in every 2 weeks, it’s easy for them to make an appointment, and they know where we are,” he said.
The center plans to continue concurrent monthly whole blood and platelet collection drives, he added.
The pilot program was internally funded. The authors reported having no relevant conflicts of interest.
SOURCE: Anthony D et al., AABB 2018, Poster BBC 135.
BOSTON – If donors can’t get to the apheresis center, bring the apheresis center to the donors.
Responding to the request of a patient with cancer, David Anthony, Amber Lazareff, RN, and their colleagues at the University of California at Los Angeles Blood and Platelet Center explored adding mobile apheresis units to their existing community blood drives. They found that, with careful planning and coordination, they could augment their supply of vital blood products and introduce potential new donors to the idea of apheresis donations at the hospital.
“There was a needs drive for an oncology patient at UCLA. She wanted to bring in donors and had her whole community behind her, and we thought well, she’s an oncology patient and she uses platelets, and we had talked about doing platelets out in the field rather than just at fixed sites, and we thought that this would be a good chance to try it,” Mr. Anthony said in an interview at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Until the mobile unit was established, apheresis platelet collections for the hospital-based donor center were limited to two fixed collection sites, with mobile units used only for collection of whole blood.
To see whether concurrent whole blood and platelet community drives were practical, the center’s blood donor field recruiter requested to schedule a community drive in a region of the county where potential donors had expressed a high level of interest in apheresis platelet donations.
Operations staff visited the site to assess its suitability, including appropriate space for donor registration and history taking, separate areas for whole blood and apheresis donations, and a donor recovery area. The assessment included ensuring that there were suitable electrical outlets, space, and support for apheresis machines.
“Over about 2 weeks we discussed with our medical directors, [infusion technicians], and our mobile people what we would need to do it. The recruiter out in the field was able to go to a high school drive out in that area, recruit donors, and get [platelet] precounts from them so that we could find out who was a good candidate,” Mr. Anthony said.
Once they had platelet counts from potential apheresis donors, 10 donors were prescreened based on their eligibility to donate multiple products, history of donations and red blood cell loss, and, for women who had previously had more than one pregnancy, favorable HLA test results.
Four of the prescreened donors were scheduled to donate platelets, and the time slot also included two backup donors, one of whom ultimately donated platelets. Of the four apheresis donors, three were first-time platelet donors.
The first drive collected seven platelet products, including three double products and one single product.
The donated products resulted in about a $3,000 cost savings by obviating the need for purchasing products from an outside supplier, and bolstered the blood bank’s inventory on a normally low collection day, the authors reported.
“We’ve had two more apheresis drives since then, and we’ll have another one in 3 weeks,” Mr. Anthony said.
He acknowledged that it is more challenging to recruit, educate, and ideally retain donors in the field than in the brick-and-mortar hospital setting.
“We have to make sure that they’re going to show up if we’re going to make the effort to take a machine out there, whereas at our centers, we have regular donors who come in every 2 weeks, it’s easy for them to make an appointment, and they know where we are,” he said.
The center plans to continue concurrent monthly whole blood and platelet collection drives, he added.
The pilot program was internally funded. The authors reported having no relevant conflicts of interest.
SOURCE: Anthony D et al., AABB 2018, Poster BBC 135.
AT AABB 2018
Key clinical point:
Major finding: Field-based collection of platelet products saved costs and augmented the hospital’s supply on a normally low collection day.
Study details: Pilot program testing apheresis platelet donations during community blood drives.
Disclosures: The pilot program was internally funded. The authors reported having no relevant conflicts of interest.
Source: Anthony D et al. AABB 2018, Poster BBC 135.
Drones can deliver blood products, but hurdles remain
BOSTON—Drone-delivered blood products may be coming soon to a hospital near you, experts said at AABB 2018.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries,” Kenney said. “That’s almost 20,000 units of blood.”
One-third of all deliveries are needed for urgent, life-saving interventions, he added.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, according to Kenney.
How it works
Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section.
The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products, which can be done by text message or via WhatsApp, a free messaging and voiceover IP calling service.
After the order was placed, Zipline was able to deliver blood products using multiple drone launches over the course of 90 minutes. The deliveries consisted of 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15 to 25 minutes by air, Kenney said.
The drones—more formally known as “unmanned aerial vehicles”—fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters, and drop the package, which has a parachute attached.
Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Kenney said.
“The whole process is 100% autonomous,” he noted. “The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package.”
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are significantly cheaper than ground-based services for local delivery, according to Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold cited statistics suggesting the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more. However, drone delivery could be as cheap as 5 cents per mile.
Barriers to drone delivery
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, according to Dr. Eastvold.
He described the hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters in the United States.
Dr. Eastvold said the barriers to adoption of drone-based delivery systems include differences in state laws about when, where, and how drones can be used and who can operate them as well as Federal Aviation Administration (FAA) airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation for most drone operators, meaning the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery.
In 2015, Johns Hopkins researchers reported that transporting blood samples on hobby-sized drones did not affect the results of common and routine blood tests.
In 2016, the researchers showed that large bags of blood products can maintain temperature and cellular integrity when transported by drones.
In 2017, the researchers demonstrated that a drone could deliver blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Kenney said his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
BOSTON—Drone-delivered blood products may be coming soon to a hospital near you, experts said at AABB 2018.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries,” Kenney said. “That’s almost 20,000 units of blood.”
One-third of all deliveries are needed for urgent, life-saving interventions, he added.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, according to Kenney.
How it works
Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section.
The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products, which can be done by text message or via WhatsApp, a free messaging and voiceover IP calling service.
After the order was placed, Zipline was able to deliver blood products using multiple drone launches over the course of 90 minutes. The deliveries consisted of 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15 to 25 minutes by air, Kenney said.
The drones—more formally known as “unmanned aerial vehicles”—fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters, and drop the package, which has a parachute attached.
Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Kenney said.
“The whole process is 100% autonomous,” he noted. “The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package.”
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are significantly cheaper than ground-based services for local delivery, according to Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold cited statistics suggesting the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more. However, drone delivery could be as cheap as 5 cents per mile.
Barriers to drone delivery
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, according to Dr. Eastvold.
He described the hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters in the United States.
Dr. Eastvold said the barriers to adoption of drone-based delivery systems include differences in state laws about when, where, and how drones can be used and who can operate them as well as Federal Aviation Administration (FAA) airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation for most drone operators, meaning the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery.
In 2015, Johns Hopkins researchers reported that transporting blood samples on hobby-sized drones did not affect the results of common and routine blood tests.
In 2016, the researchers showed that large bags of blood products can maintain temperature and cellular integrity when transported by drones.
In 2017, the researchers demonstrated that a drone could deliver blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Kenney said his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
BOSTON—Drone-delivered blood products may be coming soon to a hospital near you, experts said at AABB 2018.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries,” Kenney said. “That’s almost 20,000 units of blood.”
One-third of all deliveries are needed for urgent, life-saving interventions, he added.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, according to Kenney.
How it works
Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section.
The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products, which can be done by text message or via WhatsApp, a free messaging and voiceover IP calling service.
After the order was placed, Zipline was able to deliver blood products using multiple drone launches over the course of 90 minutes. The deliveries consisted of 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15 to 25 minutes by air, Kenney said.
The drones—more formally known as “unmanned aerial vehicles”—fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters, and drop the package, which has a parachute attached.
Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Kenney said.
“The whole process is 100% autonomous,” he noted. “The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package.”
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are significantly cheaper than ground-based services for local delivery, according to Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold cited statistics suggesting the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more. However, drone delivery could be as cheap as 5 cents per mile.
Barriers to drone delivery
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, according to Dr. Eastvold.
He described the hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters in the United States.
Dr. Eastvold said the barriers to adoption of drone-based delivery systems include differences in state laws about when, where, and how drones can be used and who can operate them as well as Federal Aviation Administration (FAA) airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation for most drone operators, meaning the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery.
In 2015, Johns Hopkins researchers reported that transporting blood samples on hobby-sized drones did not affect the results of common and routine blood tests.
In 2016, the researchers showed that large bags of blood products can maintain temperature and cellular integrity when transported by drones.
In 2017, the researchers demonstrated that a drone could deliver blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Kenney said his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
Need blood STAT? Call for a drone
BOSTON – While Amazon and other retailers are experimenting with drones to deliver toasters and toilet seats to your doorstep, drone-delivered platelets and fresh frozen plasma may be coming soon to a hospital near you, experts said at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries – that’s almost 20,000 units of blood,” he said.
One-third of all deliveries are needed for urgent, life-saving interventions, he said.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, Mr. Kenney said.
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, however, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, said Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold, who is also a private pilot, described the regulatory hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters are currently. He added, however, “I can guarantee you that in the future this is going to be an applicable technology to our industry in one way, shape, or another.”
Fast and cheap
Speed and cost are two of the most compelling arguments for blood banks to use drones. Mr. Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section. The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products – ordering can be done by text message or via WhatsApp, a free, cross-platform messaging and voiceover IP calling service – and over the course of 90 minutes Zipline was able to deliver, using multiple drone launches, 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15-25 minutes by air, Mr. Kenney said.
The drones – more formally known as “unmanned aerial vehicles” (UAVs) – fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters and drop the package, which has a parachute attached. Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Mr. Kenney said.
“The whole process is 100% autonomous. The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package,” he explained.
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are also significantly cheaper than ground-based services for local delivery, Dr. Eastvold noted. He cited a study showing that the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more, drones could be as cheap as 5 cents per mile with delivery within about 30 minutes, he said.
The fly in the ointment
Dr. Eastvold outlined the significant barriers to adoption of drone-based delivery systems in the United States, ranging from differences in state laws about when, where, and how drones can be used and who can operate them, to Federal Aviation Administration airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation only for most drone operators, meaning that the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 years old or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery. In 2017, they demonstrated that a drone could successfully deliver human blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Mr. Kenney said that his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
BOSTON – While Amazon and other retailers are experimenting with drones to deliver toasters and toilet seats to your doorstep, drone-delivered platelets and fresh frozen plasma may be coming soon to a hospital near you, experts said at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries – that’s almost 20,000 units of blood,” he said.
One-third of all deliveries are needed for urgent, life-saving interventions, he said.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, Mr. Kenney said.
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, however, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, said Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold, who is also a private pilot, described the regulatory hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters are currently. He added, however, “I can guarantee you that in the future this is going to be an applicable technology to our industry in one way, shape, or another.”
Fast and cheap
Speed and cost are two of the most compelling arguments for blood banks to use drones. Mr. Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section. The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products – ordering can be done by text message or via WhatsApp, a free, cross-platform messaging and voiceover IP calling service – and over the course of 90 minutes Zipline was able to deliver, using multiple drone launches, 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15-25 minutes by air, Mr. Kenney said.
The drones – more formally known as “unmanned aerial vehicles” (UAVs) – fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters and drop the package, which has a parachute attached. Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Mr. Kenney said.
“The whole process is 100% autonomous. The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package,” he explained.
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are also significantly cheaper than ground-based services for local delivery, Dr. Eastvold noted. He cited a study showing that the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more, drones could be as cheap as 5 cents per mile with delivery within about 30 minutes, he said.
The fly in the ointment
Dr. Eastvold outlined the significant barriers to adoption of drone-based delivery systems in the United States, ranging from differences in state laws about when, where, and how drones can be used and who can operate them, to Federal Aviation Administration airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation only for most drone operators, meaning that the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 years old or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery. In 2017, they demonstrated that a drone could successfully deliver human blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Mr. Kenney said that his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
BOSTON – While Amazon and other retailers are experimenting with drones to deliver toasters and toilet seats to your doorstep, drone-delivered platelets and fresh frozen plasma may be coming soon to a hospital near you, experts said at AABB 2018, the annual meeting of the group formerly known as the American Association of Blood Banks.
Using a system of completely autonomous delivery drones launched from a central location, U.S.-based Zipline International delivers blood products to treat postpartum hemorrhage, trauma, malaria, and other life-threatening conditions to patients in rural Rwanda, according to company spokesman Chris Kenney.
“In less than 2 years in Rwanda, we’ve made almost 10,000 deliveries – that’s almost 20,000 units of blood,” he said.
One-third of all deliveries are needed for urgent, life-saving interventions, he said.
The system, which delivers 30% of all blood products used in Rwanda outside the capital Kigali, has resulted in 100% availability of blood products when needed, a 98% reduction in waste (i.e., when unused blood products are discarded because of age), and a 175% increase in the use of platelets and fresh frozen plasma, Mr. Kenney said.
Setting up an airborne delivery network in the largely unregulated and uncrowded Rwandan airspace was a relatively simple process, however, compared with the myriad challenges of establishing a similar system for deliveries to urban medical centers in Boston, Chicago, New York, or Los Angeles, said Paul Eastvold, MD, chief medical officer at Vitalant, a nonprofit network of community blood banks headquartered in Spokane, Wash.
Dr. Eastvold, who is also a private pilot, described the regulatory hurdles that will need to be surmounted before blood-delivery drones are as common a sight as traffic helicopters are currently. He added, however, “I can guarantee you that in the future this is going to be an applicable technology to our industry in one way, shape, or another.”
Fast and cheap
Speed and cost are two of the most compelling arguments for blood banks to use drones. Mr. Kenney described the case of a 24-year-old Rwandan woman who had uncontrolled bleeding from complications following a cesarean section. The clinicians treating her opted to give her an immediate red blood cell transfusion, but she continued to bleed, and the hospital ran out of red blood cells in about 15 minutes.
They placed an order for more blood products – ordering can be done by text message or via WhatsApp, a free, cross-platform messaging and voiceover IP calling service – and over the course of 90 minutes Zipline was able to deliver, using multiple drone launches, 7 units of red blood cells, 4 units of plasma, and 2 units of platelets, all of which were transfused into the patient and allowed her condition to stabilize.
Deliveries that would take a minimum of 3 hours by road can be accomplished in about 15-25 minutes by air, Mr. Kenney said.
The drones – more formally known as “unmanned aerial vehicles” (UAVs) – fly a loop starting at the distribution center, find their target, descend to a height of about 10 meters and drop the package, which has a parachute attached. Packages can be delivered within a drop zone the size of two parking spaces, even in gale-force winds, Mr. Kenney said.
“The whole process is 100% autonomous. The aircraft knows where it’s going, it knows what conditions [are], it knows what its payload characteristics are and flies to the delivery point and drops its package,” he explained.
As drones return to the distribution center, they are snared from the air with a wire that catches a small tail hook on the fuselage.
Airborne deliveries are also significantly cheaper than ground-based services for local delivery, Dr. Eastvold noted. He cited a study showing that the cost of ground shipping from a local warehouse by carriers such as UPS or FedEx could be $6 or more, drones could be as cheap as 5 cents per mile with delivery within about 30 minutes, he said.
The fly in the ointment
Dr. Eastvold outlined the significant barriers to adoption of drone-based delivery systems in the United States, ranging from differences in state laws about when, where, and how drones can be used and who can operate them, to Federal Aviation Administration airspace restrictions and regulations.
For example, the FAA currently requires “line-of-sight” operation only for most drone operators, meaning that the operator must have visual contact with the drone at all times. The FAA will, however, grant waivers to individual operators for specified flying conditions on a case-by-case basis, if compelling need or extenuating circumstances can be satisfactorily explained.
In addition, federal regulations require commercial drone pilots to be 16 years old or older, be fluent in English, be in a physical and mental condition that would not interfere with safe operation of a drone, pass an aeronautical knowledge exam at an FAA-approved testing center, and undergo a Transportation Safety Administration background security screening.
Despite these challenges, at least one U.S. medical center, Johns Hopkins University, is testing the use of drones for blood delivery. In 2017, they demonstrated that a drone could successfully deliver human blood samples in temperature-controlled conditions across 161 miles of Arizona desert, in a flight lasting 3 hours.
Mr. Kenney said that his company is developing a second distribution center in Rwanda that will expand coverage to the entire country and is also working with the FAA, federal regulators, and the state of North Carolina to develop a drone-based blood delivery system in the United States.
AT AABB 2018
Primary, metastatic ccRCC share mutational features
A comparison of the genomic landscapes of both primary and metastatic clear cell renal cell carcinoma (ccRCC) found no significant differences in gene expression or mutational burden between the disease states, suggesting that there is no single genetic driver of metastases, investigators reported.
An analysis of targeted next-generation sequencing of both primary tumors and metastases in two independent patient cohorts showed that only the gene encoding for the tumor suppressor TP53 was significantly more frequently mutated in metastases, compared with primary tumors, but this finding did not pass a false positive test (false discovery rate), noted Toni K. Choueiri, MD, from the Dana-Farber Cancer Institute in Boston, and his colleagues, in the British Journal of Cancer.
“No other gene had significant difference in the cohort frequency of mutations between the metastases and primary tumors. Mutation burden was not significantly different between the metastases and primary tumors or between metastatic sites,” they wrote.
Frequently mutated genes in ccRCC include VHL, the gene encoding for von Hippel–Lindau syndrome, as well as tumor suppressor genes such as PBRM1, SEDT2, BAP1 and KDM5C, but few mutations are clinically actionable, the investigators noted. “However, the value of genomic alterations will be determined by understanding the interactions between acquired genetic alterations, treatments received, heterogeneity, and the dynamics of mutations during evolution of disease.”
To see whether they could improve understanding of the genomic differences between primary and metastatic ccRCC and potentially develop personalized therapies, the investigators studied targeted next-generation sequencing data from two separate cohorts.
The first cohort included data on 349 ccRCC primary tumors and 229 unmatched cases of metastatic ccRCC from the Foundation Medicine database. The second, a validation cohort, included data on 177 ccRCC primary tumors and 80 metastases from patients treated at Dana-Farber. In each cohort, sequencing was performed on 275 genes and intronic regions in 30 genes for a total of 282 unique genes.
In cohort 1, which included tumor samples from 417 men and 169 women with a median age of 58 years, the frequency of mutations was similar in primary tumors and metastases. As noted before, mutations in TP53 were significantly more frequent in metastases than in primary tumors, detected in 14.85% versus 8.90% of samples, respectively (P = .031). This difference did not, however, pass the false discovery rate test (q = 0.21). Two other tumor suppressor genes, PBRM1 and KDM5C, were numerically but not significantly more frequent in metastases.
There were no differences in median tumor mutational burden between primary and metastatic samples and no difference in either mutations or mutational burden across different metastatic sites.
In cohort 2 there were no significantly different mutational frequencies between primary and metastatic samples for any gene and no differences in median tumor mutational burden.
An analysis comparing the frequency of gene mutations in primary tumors of patients in this cohort who went on to develop metastatic disease versus those of patients with only localized disease showed that, after a median follow-up of 21.9 months, there were no significant differences in either mutational frequency or tumor mutational burden.
“It is currently unknown if cohortwide genomic alterations in RCC metastases have a different genomic profile, including potential actionable mutations, compared to samples derived from the primary site. To our knowledge, our analysis is the largest genomic ccRCC study that compares cohortwide mutational differences between metastases and primary tumors,” the investigators wrote.
They acknowledged that because they did not match primary tumors with metastatic tumors in the same patients they were unable to evaluate how individual tumors evolve over time or how systemic therapies may alter the tumor genomic landscape.
Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors declared no competing interests.
SOURCE: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
A comparison of the genomic landscapes of both primary and metastatic clear cell renal cell carcinoma (ccRCC) found no significant differences in gene expression or mutational burden between the disease states, suggesting that there is no single genetic driver of metastases, investigators reported.
An analysis of targeted next-generation sequencing of both primary tumors and metastases in two independent patient cohorts showed that only the gene encoding for the tumor suppressor TP53 was significantly more frequently mutated in metastases, compared with primary tumors, but this finding did not pass a false positive test (false discovery rate), noted Toni K. Choueiri, MD, from the Dana-Farber Cancer Institute in Boston, and his colleagues, in the British Journal of Cancer.
“No other gene had significant difference in the cohort frequency of mutations between the metastases and primary tumors. Mutation burden was not significantly different between the metastases and primary tumors or between metastatic sites,” they wrote.
Frequently mutated genes in ccRCC include VHL, the gene encoding for von Hippel–Lindau syndrome, as well as tumor suppressor genes such as PBRM1, SEDT2, BAP1 and KDM5C, but few mutations are clinically actionable, the investigators noted. “However, the value of genomic alterations will be determined by understanding the interactions between acquired genetic alterations, treatments received, heterogeneity, and the dynamics of mutations during evolution of disease.”
To see whether they could improve understanding of the genomic differences between primary and metastatic ccRCC and potentially develop personalized therapies, the investigators studied targeted next-generation sequencing data from two separate cohorts.
The first cohort included data on 349 ccRCC primary tumors and 229 unmatched cases of metastatic ccRCC from the Foundation Medicine database. The second, a validation cohort, included data on 177 ccRCC primary tumors and 80 metastases from patients treated at Dana-Farber. In each cohort, sequencing was performed on 275 genes and intronic regions in 30 genes for a total of 282 unique genes.
In cohort 1, which included tumor samples from 417 men and 169 women with a median age of 58 years, the frequency of mutations was similar in primary tumors and metastases. As noted before, mutations in TP53 were significantly more frequent in metastases than in primary tumors, detected in 14.85% versus 8.90% of samples, respectively (P = .031). This difference did not, however, pass the false discovery rate test (q = 0.21). Two other tumor suppressor genes, PBRM1 and KDM5C, were numerically but not significantly more frequent in metastases.
There were no differences in median tumor mutational burden between primary and metastatic samples and no difference in either mutations or mutational burden across different metastatic sites.
In cohort 2 there were no significantly different mutational frequencies between primary and metastatic samples for any gene and no differences in median tumor mutational burden.
An analysis comparing the frequency of gene mutations in primary tumors of patients in this cohort who went on to develop metastatic disease versus those of patients with only localized disease showed that, after a median follow-up of 21.9 months, there were no significant differences in either mutational frequency or tumor mutational burden.
“It is currently unknown if cohortwide genomic alterations in RCC metastases have a different genomic profile, including potential actionable mutations, compared to samples derived from the primary site. To our knowledge, our analysis is the largest genomic ccRCC study that compares cohortwide mutational differences between metastases and primary tumors,” the investigators wrote.
They acknowledged that because they did not match primary tumors with metastatic tumors in the same patients they were unable to evaluate how individual tumors evolve over time or how systemic therapies may alter the tumor genomic landscape.
Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors declared no competing interests.
SOURCE: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
A comparison of the genomic landscapes of both primary and metastatic clear cell renal cell carcinoma (ccRCC) found no significant differences in gene expression or mutational burden between the disease states, suggesting that there is no single genetic driver of metastases, investigators reported.
An analysis of targeted next-generation sequencing of both primary tumors and metastases in two independent patient cohorts showed that only the gene encoding for the tumor suppressor TP53 was significantly more frequently mutated in metastases, compared with primary tumors, but this finding did not pass a false positive test (false discovery rate), noted Toni K. Choueiri, MD, from the Dana-Farber Cancer Institute in Boston, and his colleagues, in the British Journal of Cancer.
“No other gene had significant difference in the cohort frequency of mutations between the metastases and primary tumors. Mutation burden was not significantly different between the metastases and primary tumors or between metastatic sites,” they wrote.
Frequently mutated genes in ccRCC include VHL, the gene encoding for von Hippel–Lindau syndrome, as well as tumor suppressor genes such as PBRM1, SEDT2, BAP1 and KDM5C, but few mutations are clinically actionable, the investigators noted. “However, the value of genomic alterations will be determined by understanding the interactions between acquired genetic alterations, treatments received, heterogeneity, and the dynamics of mutations during evolution of disease.”
To see whether they could improve understanding of the genomic differences between primary and metastatic ccRCC and potentially develop personalized therapies, the investigators studied targeted next-generation sequencing data from two separate cohorts.
The first cohort included data on 349 ccRCC primary tumors and 229 unmatched cases of metastatic ccRCC from the Foundation Medicine database. The second, a validation cohort, included data on 177 ccRCC primary tumors and 80 metastases from patients treated at Dana-Farber. In each cohort, sequencing was performed on 275 genes and intronic regions in 30 genes for a total of 282 unique genes.
In cohort 1, which included tumor samples from 417 men and 169 women with a median age of 58 years, the frequency of mutations was similar in primary tumors and metastases. As noted before, mutations in TP53 were significantly more frequent in metastases than in primary tumors, detected in 14.85% versus 8.90% of samples, respectively (P = .031). This difference did not, however, pass the false discovery rate test (q = 0.21). Two other tumor suppressor genes, PBRM1 and KDM5C, were numerically but not significantly more frequent in metastases.
There were no differences in median tumor mutational burden between primary and metastatic samples and no difference in either mutations or mutational burden across different metastatic sites.
In cohort 2 there were no significantly different mutational frequencies between primary and metastatic samples for any gene and no differences in median tumor mutational burden.
An analysis comparing the frequency of gene mutations in primary tumors of patients in this cohort who went on to develop metastatic disease versus those of patients with only localized disease showed that, after a median follow-up of 21.9 months, there were no significant differences in either mutational frequency or tumor mutational burden.
“It is currently unknown if cohortwide genomic alterations in RCC metastases have a different genomic profile, including potential actionable mutations, compared to samples derived from the primary site. To our knowledge, our analysis is the largest genomic ccRCC study that compares cohortwide mutational differences between metastases and primary tumors,” the investigators wrote.
They acknowledged that because they did not match primary tumors with metastatic tumors in the same patients they were unable to evaluate how individual tumors evolve over time or how systemic therapies may alter the tumor genomic landscape.
Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors declared no competing interests.
SOURCE: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
FROM THE BRITISH JOURNAL OF CANCER
Key clinical point: There does not appear to be a single-gene driver of metastases in patients with clear cell renal cell carcinoma.
Major finding: There were no significant differences in mutational frequency or tumor mutational burden between primary and metastatic clear cell renal cell carcinoma.
Study details: A targeted next-generation sequencing analysis of data from two independent patient cohorts.
Disclosures: Dr. Choueri is supported in part by the Dana-Farber/Harvard Cancer Center Kidney SPORE, the Kohlberg Chair at Harvard Medical School and the Trust Family, Michael Brigham, and Loker Pinard Funds for Kidney Cancer Research at the Dana-Farber Cancer Institute. Six of the study’s coauthors are employed by Foundation Medicine. The remaining authors reported no competing interests.
Source: Choueiri TK et al. Br J Cancer. 2018 May;118(9):1238-42.
5-year remission rates with combo prove durable in MCL
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Long-term results of a phase 2 clinical trial of the lenalidomide and rituximab combination as first-line therapy for mantle cell lymphoma (MCL) show continued durable responses with manageable toxicities after 5 years.
With a median follow-up of 64 months, 21 of 33 patients with initial responses remained in durable, minimal residual disease (MRD)-negative remission following induction with lenalidomide and rituximab and maintenance with those same two agents for at least 3 years.
The patients with durable responses included five who opted to discontinue maintenance after 3 years, reported Jia Ruan, MD, PhD, of Cornell University in New York, and her colleagues.
“Our long-term data provide proof of concept that an outpatient-based induction and maintenance strategy free of conventional chemotherapy is effective, safe, and feasible as first-line therapy for MCL,” they wrote.
Their report was published in Blood.
In the multicenter, phase 2 single-arm study (NCT01472562), 38 patients with untreated MCL were enrolled and treated with lenalidomide 20 mg daily on days 1-21 of each 28-day cycle for 12 cycles during induction, followed by dose reduction to 15 mg during the maintenance phase.
Patients also received standard dose rituximab 375 mg/m2 weekly for 4 weeks during cycle 1, then once every other cycle.
Patients remained on treatment until disease progression, unacceptable toxicities, or study withdrawal. Patients who remained in remission after 3 years, based on routine surveillance CT scans, had the option to discontinue maintenance.
Results
Of the original 38 patients enrolled, 36 were evaluable for response, including 23 with a complete response (CR) and 10 with a partial response.
At the 64-month median follow-up, neither the median progression-free survival (PFS) nor duration of response had been reached.
Overall, 21 of the 33 patients with responses (64%) had ongoing responses, including six patients with responses beyond 6 years.
Estimated 3-year and 5-year PFS rates were 80.3% and 63.9%, respectively. Respective estimated 3- and 5-year overall survival rates were 89.5% and 77.4%.
Mantle cell lymphoma international prognostic index (MIPI) scores were not associated with either response or PFS rates, but patients with high-risk MIPI scores were significantly more likely to have worse overall survival (P=0.04).
Safety
Grade 3 or greater hematologic toxicities included neutropenia in 42% of patients in both induction and maintenance, anemia in 8% and 3%, thrombocytopenia in 11% and 5%, and febrile neutropenia in 3% and 5%.
Secondary primary malignancies occurred in six patients. These included five noninvasive skin cancers requiring only local therapy without the need for study interruption.
Two patients, including one with a skin cancer, died from the secondary malignancies, including one from Merkel cell carcinoma and one from pancreatic cancer.
“The efficacy and survival outcome observed in our study compared favorably to those reported with lenalidomide either as single agent, or in combination with rituximab in relapsed and refractory setting,” the investigators wrote, “lending support for prioritizing novel agents such as lenalidomide early in the treatment sequence, to compare to conventional chemotherapy-based approach.”
The study was supported in part by Celgene Corporation, a Clinical Translational Science Center grant, and the Lymphoma Foundation.
Investigators identify 21 genomic “hotspots” in breast cancers
Cancer geneticists have identified 21 clusters of complex chromosomal rearrangements in breast cancers that contain both known oncogenes and potential new driver loci.
A systematic analysis of chromosomal rearrangements in tissues from 560 patients with breast cancer identified 21 “hotspots,” some of which contain known oncogene chromosomal loci, and others of which contain genes not typically associated with breast cancer, reported Serena Nik-Zainal, PhD, of the University of Cambridge, England, and her colleagues.
“Detailed analysis of rearrangements at these hotspots highlights chromosomal aberrations likely driven by selection, and reveal underlying mutational processes,” they wrote in a study published online in Annals of Oncology.
The investigators sought insight into mutational mechanisms of gene amplifications by examining clustered rearrangements – somatic breakpoints occurring in high densities – in individual patients.
To see whether these rearrangements were associated with breast cancer, they identified the aforementioned chromosomal hotspots where clustered rearrangements were seen in samples from different patients.
They identified 624 cluster rearrangements in the 560 breast cancer genomes, including 17,247 within-chromosome rearrangements, and 6,509 between-chromosome translocations.
Of the 560 samples, 372 had at least one rearrangement cluster, with the frequency of clusters similar between some breast cancer types. For example, there were 0.96 rearrangements clusters per sample from patients with triple negative breast cancers, and 1.00 per sample from women with estrogen receptor–positive tumors.
“To identify loci where clusters of rearrangements recur across multiple independent tumor samples, we pooled all breakpoints in the ‘clustered’ category and sorted them according to position in the reference genome,” the investigators explained.
They used a Piecewise-Constant-Fitting algorithm to identify genome sequences where there were short inter-mutation distances between rearrangement clusters, suggesting the presence of hotspots.
In the 21 hotspots they identified, they found, as expected, common driver amplification regions (e.g., CCND1, ERBB2, ZNF217, chr8:ZNF703/FGFR1, IGF1R, and MYC), but also several hotspots near oncogenes that are not typically associated with breast cancer.
Notably, they saw simultaneous amplification of regions on chromosomes 8 and 11 (chr8:ZNF703/FGFR1 and chr11:CCND1). Amplification of these regions are frequent in estrogen receptor–positive breast cancers. The investigators propose a pathogenic model in which a chromosome 8 to chromosome 11 translocation is an early, critical event leading to breast tumor development.
“Clustered rearrangements are common in breast cancer genomes, and often associated with gene amplifications that drive oncogenesis. Understanding the process of amplicon formation, an example of which we present here for the chr8:ZNF703/FGFR1 and chr11:CCND1 co-amplifications, will be important for our understanding of the origins of a subset of breast cancers,” they concluded.
The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
SOURCE: Glodzik D et al. Ann Oncol. 2018 Sept 25. doi: 10.1093/annonc/mdy404.
Cancer geneticists have identified 21 clusters of complex chromosomal rearrangements in breast cancers that contain both known oncogenes and potential new driver loci.
A systematic analysis of chromosomal rearrangements in tissues from 560 patients with breast cancer identified 21 “hotspots,” some of which contain known oncogene chromosomal loci, and others of which contain genes not typically associated with breast cancer, reported Serena Nik-Zainal, PhD, of the University of Cambridge, England, and her colleagues.
“Detailed analysis of rearrangements at these hotspots highlights chromosomal aberrations likely driven by selection, and reveal underlying mutational processes,” they wrote in a study published online in Annals of Oncology.
The investigators sought insight into mutational mechanisms of gene amplifications by examining clustered rearrangements – somatic breakpoints occurring in high densities – in individual patients.
To see whether these rearrangements were associated with breast cancer, they identified the aforementioned chromosomal hotspots where clustered rearrangements were seen in samples from different patients.
They identified 624 cluster rearrangements in the 560 breast cancer genomes, including 17,247 within-chromosome rearrangements, and 6,509 between-chromosome translocations.
Of the 560 samples, 372 had at least one rearrangement cluster, with the frequency of clusters similar between some breast cancer types. For example, there were 0.96 rearrangements clusters per sample from patients with triple negative breast cancers, and 1.00 per sample from women with estrogen receptor–positive tumors.
“To identify loci where clusters of rearrangements recur across multiple independent tumor samples, we pooled all breakpoints in the ‘clustered’ category and sorted them according to position in the reference genome,” the investigators explained.
They used a Piecewise-Constant-Fitting algorithm to identify genome sequences where there were short inter-mutation distances between rearrangement clusters, suggesting the presence of hotspots.
In the 21 hotspots they identified, they found, as expected, common driver amplification regions (e.g., CCND1, ERBB2, ZNF217, chr8:ZNF703/FGFR1, IGF1R, and MYC), but also several hotspots near oncogenes that are not typically associated with breast cancer.
Notably, they saw simultaneous amplification of regions on chromosomes 8 and 11 (chr8:ZNF703/FGFR1 and chr11:CCND1). Amplification of these regions are frequent in estrogen receptor–positive breast cancers. The investigators propose a pathogenic model in which a chromosome 8 to chromosome 11 translocation is an early, critical event leading to breast tumor development.
“Clustered rearrangements are common in breast cancer genomes, and often associated with gene amplifications that drive oncogenesis. Understanding the process of amplicon formation, an example of which we present here for the chr8:ZNF703/FGFR1 and chr11:CCND1 co-amplifications, will be important for our understanding of the origins of a subset of breast cancers,” they concluded.
The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
SOURCE: Glodzik D et al. Ann Oncol. 2018 Sept 25. doi: 10.1093/annonc/mdy404.
Cancer geneticists have identified 21 clusters of complex chromosomal rearrangements in breast cancers that contain both known oncogenes and potential new driver loci.
A systematic analysis of chromosomal rearrangements in tissues from 560 patients with breast cancer identified 21 “hotspots,” some of which contain known oncogene chromosomal loci, and others of which contain genes not typically associated with breast cancer, reported Serena Nik-Zainal, PhD, of the University of Cambridge, England, and her colleagues.
“Detailed analysis of rearrangements at these hotspots highlights chromosomal aberrations likely driven by selection, and reveal underlying mutational processes,” they wrote in a study published online in Annals of Oncology.
The investigators sought insight into mutational mechanisms of gene amplifications by examining clustered rearrangements – somatic breakpoints occurring in high densities – in individual patients.
To see whether these rearrangements were associated with breast cancer, they identified the aforementioned chromosomal hotspots where clustered rearrangements were seen in samples from different patients.
They identified 624 cluster rearrangements in the 560 breast cancer genomes, including 17,247 within-chromosome rearrangements, and 6,509 between-chromosome translocations.
Of the 560 samples, 372 had at least one rearrangement cluster, with the frequency of clusters similar between some breast cancer types. For example, there were 0.96 rearrangements clusters per sample from patients with triple negative breast cancers, and 1.00 per sample from women with estrogen receptor–positive tumors.
“To identify loci where clusters of rearrangements recur across multiple independent tumor samples, we pooled all breakpoints in the ‘clustered’ category and sorted them according to position in the reference genome,” the investigators explained.
They used a Piecewise-Constant-Fitting algorithm to identify genome sequences where there were short inter-mutation distances between rearrangement clusters, suggesting the presence of hotspots.
In the 21 hotspots they identified, they found, as expected, common driver amplification regions (e.g., CCND1, ERBB2, ZNF217, chr8:ZNF703/FGFR1, IGF1R, and MYC), but also several hotspots near oncogenes that are not typically associated with breast cancer.
Notably, they saw simultaneous amplification of regions on chromosomes 8 and 11 (chr8:ZNF703/FGFR1 and chr11:CCND1). Amplification of these regions are frequent in estrogen receptor–positive breast cancers. The investigators propose a pathogenic model in which a chromosome 8 to chromosome 11 translocation is an early, critical event leading to breast tumor development.
“Clustered rearrangements are common in breast cancer genomes, and often associated with gene amplifications that drive oncogenesis. Understanding the process of amplicon formation, an example of which we present here for the chr8:ZNF703/FGFR1 and chr11:CCND1 co-amplifications, will be important for our understanding of the origins of a subset of breast cancers,” they concluded.
The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
SOURCE: Glodzik D et al. Ann Oncol. 2018 Sept 25. doi: 10.1093/annonc/mdy404.
FROM ANNALS OF ONCOLOGY
Key clinical point: Chromosomal rearrangement “hotspots” contain both known breast cancer oncogenes and potential new loci that may explain the mechanism of deleterious gene amplifications.
Major finding: A chromosome 8 to 11 translocation may be the initiating event for some breast cancer subtypes.
Study details: Genomic analysis of samples from 560 patients with breast cancer.
Disclosures: The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
Source: Glodzik D et al. Ann Oncol. 2018 Sep 25. doi: 10.1093/annonc/mdy404.
Better therapy, not earlier diagnosis, explains improved RCC survival
Credit improvements in therapy rather than diagnosis at an earlier stage for improved survival of renal cell carcinoma in recent years, investigators say.
A review of records on nearly 263,000 patients diagnosed with renal cell carcinoma (RCC ) from 2004 through 2015 showed that better 5-year overall survival (OS) in later years was likely attributable to better treatments rather than an uptick in detection of cancers at an earlier stage, a trend known as “stage migration,” reported Hiten D. Patel, MD, of the Brady Urological Institute at Johns Hopkins Medicine in Baltimore, and his colleagues.
“While survival has improved over time when considering all RCC patients, the primary benefit was observed in advanced RCC (stage III–IV), with 5-year survival increasing from 9.8% in 2004 to 13.2% in 2010 for patients with distant metastatic disease. The results indicate that stage migration no longer contributes to improvements in survival for RCC, and additional gains reflect improvements in advanced treatment options,” they wrote in European Urology Oncology.
Dr. Patel and colleagues noted that the incidence of RCC has been on the rise worldwide for nearly 3 decades because of both environmental risk factors and improvements in medical imaging that have resulted in an increase in incidental cancers.
“Data from the National Cancer Database (NCDB) indicated an increase in the proportion of patients presenting with cT1 RCC from 40% before 1993 to 60% through 2004. However, it is unknown if clinical stage migration has continued into recent years, which has implications for patient outcomes,” they wrote.
To try to answer this question, they sifted through data on 262,597 patients diagnosed with RCC from 2004 through 2015 at more than 1,500 facilities covered by the U.S. National Cancer Database.
They found that, up to 2007, there were statistically significant trends toward more frequent diagnosis of clinical stage I disease (70% of cases) and less frequent diagnoses of stage III (8%) and stage IV (11%; P less than .001 for all comparisons). From 2008 through 2015, however, the respective rates stabilized.
They also noticed a trend throughout the study period for decreased size of localized tumors at diagnosis, with a mean decrease of 0.22 cm for stage I lesions, and 1.24 cm for stage II tumors.
When they looked at 5-year overall survival by Kaplan-Meier analysis, they saw that it improved from 67.9% in 2004 to 72.3% in 2010. As noted before, most of the benefit was attributable to gains in survival among patients with stage III or IV disease.
In multivariable Cox proportional hazard models, diagnosis in recent years was a statistically significant predictor of improved survival, even after adjustment for stage distribution. In addition, receipt of systemic therapy was associated with improved survival, with a hazard ratio of 0.811 (P less than .001).
The authors acknowledged that a limitation of the findings is the reliance on the NCDB, which includes data on most cancer diagnoses in the United States, but is not a population-based sample.
No study funding source was reported. Dr. Patel and coauthors reported having no conflicts of interest to disclose.
SOURCE: Patel HD et al. Eur Urol Oncol. 2018 Sep 25. doi: 10.1016/j.euo.2018.08.023.
Credit improvements in therapy rather than diagnosis at an earlier stage for improved survival of renal cell carcinoma in recent years, investigators say.
A review of records on nearly 263,000 patients diagnosed with renal cell carcinoma (RCC ) from 2004 through 2015 showed that better 5-year overall survival (OS) in later years was likely attributable to better treatments rather than an uptick in detection of cancers at an earlier stage, a trend known as “stage migration,” reported Hiten D. Patel, MD, of the Brady Urological Institute at Johns Hopkins Medicine in Baltimore, and his colleagues.
“While survival has improved over time when considering all RCC patients, the primary benefit was observed in advanced RCC (stage III–IV), with 5-year survival increasing from 9.8% in 2004 to 13.2% in 2010 for patients with distant metastatic disease. The results indicate that stage migration no longer contributes to improvements in survival for RCC, and additional gains reflect improvements in advanced treatment options,” they wrote in European Urology Oncology.
Dr. Patel and colleagues noted that the incidence of RCC has been on the rise worldwide for nearly 3 decades because of both environmental risk factors and improvements in medical imaging that have resulted in an increase in incidental cancers.
“Data from the National Cancer Database (NCDB) indicated an increase in the proportion of patients presenting with cT1 RCC from 40% before 1993 to 60% through 2004. However, it is unknown if clinical stage migration has continued into recent years, which has implications for patient outcomes,” they wrote.
To try to answer this question, they sifted through data on 262,597 patients diagnosed with RCC from 2004 through 2015 at more than 1,500 facilities covered by the U.S. National Cancer Database.
They found that, up to 2007, there were statistically significant trends toward more frequent diagnosis of clinical stage I disease (70% of cases) and less frequent diagnoses of stage III (8%) and stage IV (11%; P less than .001 for all comparisons). From 2008 through 2015, however, the respective rates stabilized.
They also noticed a trend throughout the study period for decreased size of localized tumors at diagnosis, with a mean decrease of 0.22 cm for stage I lesions, and 1.24 cm for stage II tumors.
When they looked at 5-year overall survival by Kaplan-Meier analysis, they saw that it improved from 67.9% in 2004 to 72.3% in 2010. As noted before, most of the benefit was attributable to gains in survival among patients with stage III or IV disease.
In multivariable Cox proportional hazard models, diagnosis in recent years was a statistically significant predictor of improved survival, even after adjustment for stage distribution. In addition, receipt of systemic therapy was associated with improved survival, with a hazard ratio of 0.811 (P less than .001).
The authors acknowledged that a limitation of the findings is the reliance on the NCDB, which includes data on most cancer diagnoses in the United States, but is not a population-based sample.
No study funding source was reported. Dr. Patel and coauthors reported having no conflicts of interest to disclose.
SOURCE: Patel HD et al. Eur Urol Oncol. 2018 Sep 25. doi: 10.1016/j.euo.2018.08.023.
Credit improvements in therapy rather than diagnosis at an earlier stage for improved survival of renal cell carcinoma in recent years, investigators say.
A review of records on nearly 263,000 patients diagnosed with renal cell carcinoma (RCC ) from 2004 through 2015 showed that better 5-year overall survival (OS) in later years was likely attributable to better treatments rather than an uptick in detection of cancers at an earlier stage, a trend known as “stage migration,” reported Hiten D. Patel, MD, of the Brady Urological Institute at Johns Hopkins Medicine in Baltimore, and his colleagues.
“While survival has improved over time when considering all RCC patients, the primary benefit was observed in advanced RCC (stage III–IV), with 5-year survival increasing from 9.8% in 2004 to 13.2% in 2010 for patients with distant metastatic disease. The results indicate that stage migration no longer contributes to improvements in survival for RCC, and additional gains reflect improvements in advanced treatment options,” they wrote in European Urology Oncology.
Dr. Patel and colleagues noted that the incidence of RCC has been on the rise worldwide for nearly 3 decades because of both environmental risk factors and improvements in medical imaging that have resulted in an increase in incidental cancers.
“Data from the National Cancer Database (NCDB) indicated an increase in the proportion of patients presenting with cT1 RCC from 40% before 1993 to 60% through 2004. However, it is unknown if clinical stage migration has continued into recent years, which has implications for patient outcomes,” they wrote.
To try to answer this question, they sifted through data on 262,597 patients diagnosed with RCC from 2004 through 2015 at more than 1,500 facilities covered by the U.S. National Cancer Database.
They found that, up to 2007, there were statistically significant trends toward more frequent diagnosis of clinical stage I disease (70% of cases) and less frequent diagnoses of stage III (8%) and stage IV (11%; P less than .001 for all comparisons). From 2008 through 2015, however, the respective rates stabilized.
They also noticed a trend throughout the study period for decreased size of localized tumors at diagnosis, with a mean decrease of 0.22 cm for stage I lesions, and 1.24 cm for stage II tumors.
When they looked at 5-year overall survival by Kaplan-Meier analysis, they saw that it improved from 67.9% in 2004 to 72.3% in 2010. As noted before, most of the benefit was attributable to gains in survival among patients with stage III or IV disease.
In multivariable Cox proportional hazard models, diagnosis in recent years was a statistically significant predictor of improved survival, even after adjustment for stage distribution. In addition, receipt of systemic therapy was associated with improved survival, with a hazard ratio of 0.811 (P less than .001).
The authors acknowledged that a limitation of the findings is the reliance on the NCDB, which includes data on most cancer diagnoses in the United States, but is not a population-based sample.
No study funding source was reported. Dr. Patel and coauthors reported having no conflicts of interest to disclose.
SOURCE: Patel HD et al. Eur Urol Oncol. 2018 Sep 25. doi: 10.1016/j.euo.2018.08.023.
FROM EUROPEAN UROLOGY ONCOLOGY
Key clinical point: Improved renal cell carcinoma survival appears to be attributable to improvements in therapy rather than increased diagnosis of early-stage disease.
Major finding: 5-year survival increased from 9.8% in 2004 to 13.2% in 2010 for patients with distant metastatic disease.
Study details: Retrospective analysis of data from the National Cancer Database on 262,597 patients diagnosed with RCC from 2004 through 2015.
Disclosures: No study funding source was reported. Dr. Patel and coauthors reported having no conflicts of interest to disclose.
Source: Patel HD et al. Eur Urol Oncol. 2018 Sep 25. doi: 10.1016/j.euo.2018.08.023.