User login
Higher Mortality Seen in Women With Diabetes, Depression
The combination of type 2 diabetes and depression doubled the overall risk of death and nearly tripled the likelihood of dying of cardiovascular disease within 6 years, an analysis of data on 78,282 women found.
Previous studies have shown an association between depression or diabetes and increased risk of death from any cause or from cardiovascular disease, but the combined effects of these diseases on mortality have not been well studied, especially in women. Earlier studies also tended to be smaller and to have shorter follow-up.
An Pan, Ph.D., of the Harvard School of Public Health, Boston, and his associates analyzed data on participants in the prospective Nurses’ Health Study who were 54-79 years of age in 2000 and who were followed until 2006. There were 979 deaths from cardiovascular disease and 4,654 deaths from any cause during that time.
Compared with the 80% of women who developed neither diabetes nor depression, the age-adjusted relative risk of death was 1.71 in the 5% of women with diabetes alone, 1.76 in the 14% of women with depression alone, and 3.11 in the 1% of women with both diseases. The relative risk of death from cardiovascular disease was 1.67 in women with depression alone, 1.37 in women with depression alone, and 2.72 in those with both diabetes and depression. The results were released online on Jan. 3 and will appear in January issue of Archives of General Psychiatry (2011;68:42-50).
The increased risks with either diabetes or depression were statistically significant, and the higher risks with both diseases were significant compared with either disease alone, even after adjustment for the effects of age, family history of diabetes and cancer, history of myocardial infarction, current marital status, ethnicity, body mass index, alcohol consumption, smoking status, current multivitamin use, estrogen hormone use, current aspirin use, and major comorbidities including hypertension, hypercholesterolemia, heart disease, stroke, and cancer.
The highest risks were seen in women with depression combined with more severe diabetes, indicated by a longer duration of diabetes or treatment with oral medication or insulin. Death from cardiovascular disease was three times more likely in depressed women who had had diabetes for more than 10 years, and four times more likely in depressed women who received insulin therapy for diabetes, compared with women who had neither depression nor diabetes.
The greater likelihood of death or of death from cardiovascular disease in women with both diabetes and depression deserves greater attention, especially considering that 20%-25% of people with diabetes are depressed, the investigators suggested. An estimated 24 million U.S. adults have diabetes and 15 million U.S. adults are depressed. Adults with diabetes are twice as likely to be depressed, compared with those without diabetes.
In general, physicians don’t do a great job of recognizing major depression, and the United States can claim a relatively high prevalence of untreated mental disorders, they added. Better strategies may be needed to provide adequate psychological management and support for people with diabetes. In addition, the co-existence of depression and diabetes should identify women who are at particularly high risk, the investigators concluded.
The underlying mechanisms of the association between increased mortality and depression in women with diabetes are unknown.
The Nurses’ Health Study, ongoing since 1976, has followed a large cohort of female nurses every 2 years with mailed questionnaires (and phone calls if necessary), and had better than a 94% follow-up rate through 2006. Deaths were identified by the next of kin, postal authorities, or National Death Index. The investigators obtained the medical records and death certificates of those who died to determine the cause of death.
The current analysis excluded participants with a history of gestational diabetes, type 1 diabetes, secondary diabetes, or missing data regarding depression or diabetes.
The investigators reported having no conflicts of interest. The study was funded by the National Institutes of Health, the National Alliance for Research on Schizophrenia and Depression, and the Fonds de Recherche en Santé du Québec.
The study shows that the risks of death in women with diabetes or depression are additive in those who have both diseases, but it doesn’t establish a synergistic effect between the two diseases, Dr. Elizabeth Murphy said in an interview.
"Given the increasing evidence establishing a link between diabetes and depression, this article should provide an important reminder for clinicians to be vigilant about screening and treating depression in patients with diabetes," commented Dr. Murphy, who was not involved in the study.
Perhaps more interesting is a previous report by Dr. Pan and associates that established a bidirectional association between type 2 diabetes and depression, Dr. Murphy added. Women who developed either disease were at increased risk for developing the other (Arch. Intern. Med. 2010;170:1884-91).
That report also drew from the Nurses’ Health Study, analyzing data on 65,381 women aged 50-75 years who had neither diabetes nor depression in 1996. During 10 years of follow-up, 2,844 developed type 2 diabetes, and 7,415 developed clinical depression.
Depressed mood was associated with a 17% increased risk for developing diabetes, and use of antidepressants was associated with a 25% higher risk for diabetes, compared with women with the best depressive symptom scores. Women who developed diabetes were 24%-53% more likely to develop depression, depending on the severity of the diabetes.
Dr. Murphy is chief of endocrinology at San Francisco General Hospital.
The study shows that the risks of death in women with diabetes or depression are additive in those who have both diseases, but it doesn’t establish a synergistic effect between the two diseases, Dr. Elizabeth Murphy said in an interview.
"Given the increasing evidence establishing a link between diabetes and depression, this article should provide an important reminder for clinicians to be vigilant about screening and treating depression in patients with diabetes," commented Dr. Murphy, who was not involved in the study.
Perhaps more interesting is a previous report by Dr. Pan and associates that established a bidirectional association between type 2 diabetes and depression, Dr. Murphy added. Women who developed either disease were at increased risk for developing the other (Arch. Intern. Med. 2010;170:1884-91).
That report also drew from the Nurses’ Health Study, analyzing data on 65,381 women aged 50-75 years who had neither diabetes nor depression in 1996. During 10 years of follow-up, 2,844 developed type 2 diabetes, and 7,415 developed clinical depression.
Depressed mood was associated with a 17% increased risk for developing diabetes, and use of antidepressants was associated with a 25% higher risk for diabetes, compared with women with the best depressive symptom scores. Women who developed diabetes were 24%-53% more likely to develop depression, depending on the severity of the diabetes.
Dr. Murphy is chief of endocrinology at San Francisco General Hospital.
The study shows that the risks of death in women with diabetes or depression are additive in those who have both diseases, but it doesn’t establish a synergistic effect between the two diseases, Dr. Elizabeth Murphy said in an interview.
"Given the increasing evidence establishing a link between diabetes and depression, this article should provide an important reminder for clinicians to be vigilant about screening and treating depression in patients with diabetes," commented Dr. Murphy, who was not involved in the study.
Perhaps more interesting is a previous report by Dr. Pan and associates that established a bidirectional association between type 2 diabetes and depression, Dr. Murphy added. Women who developed either disease were at increased risk for developing the other (Arch. Intern. Med. 2010;170:1884-91).
That report also drew from the Nurses’ Health Study, analyzing data on 65,381 women aged 50-75 years who had neither diabetes nor depression in 1996. During 10 years of follow-up, 2,844 developed type 2 diabetes, and 7,415 developed clinical depression.
Depressed mood was associated with a 17% increased risk for developing diabetes, and use of antidepressants was associated with a 25% higher risk for diabetes, compared with women with the best depressive symptom scores. Women who developed diabetes were 24%-53% more likely to develop depression, depending on the severity of the diabetes.
Dr. Murphy is chief of endocrinology at San Francisco General Hospital.
The combination of type 2 diabetes and depression doubled the overall risk of death and nearly tripled the likelihood of dying of cardiovascular disease within 6 years, an analysis of data on 78,282 women found.
Previous studies have shown an association between depression or diabetes and increased risk of death from any cause or from cardiovascular disease, but the combined effects of these diseases on mortality have not been well studied, especially in women. Earlier studies also tended to be smaller and to have shorter follow-up.
An Pan, Ph.D., of the Harvard School of Public Health, Boston, and his associates analyzed data on participants in the prospective Nurses’ Health Study who were 54-79 years of age in 2000 and who were followed until 2006. There were 979 deaths from cardiovascular disease and 4,654 deaths from any cause during that time.
Compared with the 80% of women who developed neither diabetes nor depression, the age-adjusted relative risk of death was 1.71 in the 5% of women with diabetes alone, 1.76 in the 14% of women with depression alone, and 3.11 in the 1% of women with both diseases. The relative risk of death from cardiovascular disease was 1.67 in women with depression alone, 1.37 in women with depression alone, and 2.72 in those with both diabetes and depression. The results were released online on Jan. 3 and will appear in January issue of Archives of General Psychiatry (2011;68:42-50).
The increased risks with either diabetes or depression were statistically significant, and the higher risks with both diseases were significant compared with either disease alone, even after adjustment for the effects of age, family history of diabetes and cancer, history of myocardial infarction, current marital status, ethnicity, body mass index, alcohol consumption, smoking status, current multivitamin use, estrogen hormone use, current aspirin use, and major comorbidities including hypertension, hypercholesterolemia, heart disease, stroke, and cancer.
The highest risks were seen in women with depression combined with more severe diabetes, indicated by a longer duration of diabetes or treatment with oral medication or insulin. Death from cardiovascular disease was three times more likely in depressed women who had had diabetes for more than 10 years, and four times more likely in depressed women who received insulin therapy for diabetes, compared with women who had neither depression nor diabetes.
The greater likelihood of death or of death from cardiovascular disease in women with both diabetes and depression deserves greater attention, especially considering that 20%-25% of people with diabetes are depressed, the investigators suggested. An estimated 24 million U.S. adults have diabetes and 15 million U.S. adults are depressed. Adults with diabetes are twice as likely to be depressed, compared with those without diabetes.
In general, physicians don’t do a great job of recognizing major depression, and the United States can claim a relatively high prevalence of untreated mental disorders, they added. Better strategies may be needed to provide adequate psychological management and support for people with diabetes. In addition, the co-existence of depression and diabetes should identify women who are at particularly high risk, the investigators concluded.
The underlying mechanisms of the association between increased mortality and depression in women with diabetes are unknown.
The Nurses’ Health Study, ongoing since 1976, has followed a large cohort of female nurses every 2 years with mailed questionnaires (and phone calls if necessary), and had better than a 94% follow-up rate through 2006. Deaths were identified by the next of kin, postal authorities, or National Death Index. The investigators obtained the medical records and death certificates of those who died to determine the cause of death.
The current analysis excluded participants with a history of gestational diabetes, type 1 diabetes, secondary diabetes, or missing data regarding depression or diabetes.
The investigators reported having no conflicts of interest. The study was funded by the National Institutes of Health, the National Alliance for Research on Schizophrenia and Depression, and the Fonds de Recherche en Santé du Québec.
The combination of type 2 diabetes and depression doubled the overall risk of death and nearly tripled the likelihood of dying of cardiovascular disease within 6 years, an analysis of data on 78,282 women found.
Previous studies have shown an association between depression or diabetes and increased risk of death from any cause or from cardiovascular disease, but the combined effects of these diseases on mortality have not been well studied, especially in women. Earlier studies also tended to be smaller and to have shorter follow-up.
An Pan, Ph.D., of the Harvard School of Public Health, Boston, and his associates analyzed data on participants in the prospective Nurses’ Health Study who were 54-79 years of age in 2000 and who were followed until 2006. There were 979 deaths from cardiovascular disease and 4,654 deaths from any cause during that time.
Compared with the 80% of women who developed neither diabetes nor depression, the age-adjusted relative risk of death was 1.71 in the 5% of women with diabetes alone, 1.76 in the 14% of women with depression alone, and 3.11 in the 1% of women with both diseases. The relative risk of death from cardiovascular disease was 1.67 in women with depression alone, 1.37 in women with depression alone, and 2.72 in those with both diabetes and depression. The results were released online on Jan. 3 and will appear in January issue of Archives of General Psychiatry (2011;68:42-50).
The increased risks with either diabetes or depression were statistically significant, and the higher risks with both diseases were significant compared with either disease alone, even after adjustment for the effects of age, family history of diabetes and cancer, history of myocardial infarction, current marital status, ethnicity, body mass index, alcohol consumption, smoking status, current multivitamin use, estrogen hormone use, current aspirin use, and major comorbidities including hypertension, hypercholesterolemia, heart disease, stroke, and cancer.
The highest risks were seen in women with depression combined with more severe diabetes, indicated by a longer duration of diabetes or treatment with oral medication or insulin. Death from cardiovascular disease was three times more likely in depressed women who had had diabetes for more than 10 years, and four times more likely in depressed women who received insulin therapy for diabetes, compared with women who had neither depression nor diabetes.
The greater likelihood of death or of death from cardiovascular disease in women with both diabetes and depression deserves greater attention, especially considering that 20%-25% of people with diabetes are depressed, the investigators suggested. An estimated 24 million U.S. adults have diabetes and 15 million U.S. adults are depressed. Adults with diabetes are twice as likely to be depressed, compared with those without diabetes.
In general, physicians don’t do a great job of recognizing major depression, and the United States can claim a relatively high prevalence of untreated mental disorders, they added. Better strategies may be needed to provide adequate psychological management and support for people with diabetes. In addition, the co-existence of depression and diabetes should identify women who are at particularly high risk, the investigators concluded.
The underlying mechanisms of the association between increased mortality and depression in women with diabetes are unknown.
The Nurses’ Health Study, ongoing since 1976, has followed a large cohort of female nurses every 2 years with mailed questionnaires (and phone calls if necessary), and had better than a 94% follow-up rate through 2006. Deaths were identified by the next of kin, postal authorities, or National Death Index. The investigators obtained the medical records and death certificates of those who died to determine the cause of death.
The current analysis excluded participants with a history of gestational diabetes, type 1 diabetes, secondary diabetes, or missing data regarding depression or diabetes.
The investigators reported having no conflicts of interest. The study was funded by the National Institutes of Health, the National Alliance for Research on Schizophrenia and Depression, and the Fonds de Recherche en Santé du Québec.
Major Finding: Women with type 2 diabetes and depression were twice as likely to die within 6 years and nearly three times as likely to die of cardiovascular disease, compared with women with neither diabetes nor depression.
Data Source: Data from 6 years of follow-up on 78,282 women in the Nurses’ Health Study.
Disclosures: The investigators reported having no conflicts of interest. The study was funded by the National Institutes of Health, the National Alliance for Research on Schizophrenia and Depression, and the Fonds de Recherche en Sant? du Qu?bec.
Get Neurologist Consult for Neuropathic Itch
LAS VEGAS – If a patient complains of an itch that is "too deep to scratch," and the skin doesn’t show a cause, refer the patient to a neurologist, said Dr. Timothy G. Berger.
"The only thing I want the neurologist to tell me is that the patient doesn’t have multiple sclerosis," said Dr. Berger of the University of California, San Francisco.
There have been numerous reports of patients presenting with signs and symptoms of neuropathic itch who subsequently are diagnosed with multiple sclerosis. Dr. Berger commonly sees patients who are referred to him because treatment of their itching did not help, and they have neuropathic itch.
What does neuropathic itch look like? "The way to think about this is itch with other sensory findings," such as hypesthesia, he suggested at the seminar sponsored by Skin Disease Education Foundation. "We often have patients who’ve had neural or back injury" and develop itch with hypesthesia.
Many patients will say the "itch is too deep to scratch," he said. Or, the itch may be accompanied by burning or pain. There may be no primary lesion, or only erythema, in the itch area. The patient may describe the itch as sharp spasms of itch, or formication of skin (a crawling itch). Plenty of reports in the medical literature describe patients who present with delusions of parasitosis or formication who turn out to have multiple sclerosis, he noted.
A different CNS problem also can cause neuropathic pruritus: progressive multifocal leukoencephalopathy. Peripheral causes of neuropathic itch include brachioradial pruritus, notalgia paresthetica, or postherpetic neuralgia. In addition, prurigo nodularis or lichen simplex chronicus can produce neuropathic itch.
Spinal cord tumor or cervical spine disease with nerve entrapment are two of three important differential diagnoses when you see a patient with neuropathic itching on the extensor forearms, elbows, and arms that is typical of brachioradial pruritus. Consider also the possibility of polymorphous light eruption (sun allergy), Dr. Berger said. Sun exposure worsens all of these, making them difficult to distinguish clinically.
Referring patients with brachioradial pruritus to a physical medicine department or a spine center may help make the diagnosis and provide treatment and support, Dr. Berger suggested.
The itching from brachioradial pruritus tends to be worst with late-summer sun exposure and may clear in the winter. In contrast, polymorphous light eruption tends to be worst in the spring. Brachioradial pruritus is severe and causes potentially disabling itch, most commonly affecting white, middle-aged, affluent women with chronic sun damage.
Patients often use ice to stop the itching because little else seems to help. Sun protection and topical steroids may provide some relief. Lidoderm patches may also help. Some clinicians have prescribed topical Sinequan or capsaicin for brachioradial pruritus. Wrapping up the itching area in Unna’s boot occlusion for a few weeks may break the itch-scratch cycle, Dr. Berger suggested.
Other treatments that have been tried include gabapentin, paroxetine, mirtazapine, acupuncture, physical therapy, spinal cord manipulation, and transcutaneous electrical nerve stimulation (20 minutes per day for 5 weeks).
Thalidomide (25-200 mg nightly) is particularly effective for neuropathic pruritus, especially brachioradial pruritus, prurigo nodularis, or photodermatoses, but doses greater than 100 mg/day increase risk for deep vein thromboses and stroke.
Two of Dr. Berger’s patients on thalidomide for prurigo nodularis developed stroke. "Both of those patients are back on thalidomide after their stroke even though they know that thalidomide caused their stroke, because this is the only thing that stops their itch," he said.
Thalidomide also can cause neuropathy at doses greater than 25 mg/day, "so I start everybody at 50 mg every other day" and titrate up, he said. The drug also can cause constipation, weight gain, and sedation. Its slow onset of action can take weeks to show any benefit. "You have to hang in there," he added.
Dr. Joseph F. Fowler Jr., who moderated a question-and-answer session after Dr. Berger’s presentation, echoed his advice to send patients with neuropathic pruritus to neurologists.
"I see a lot of people who itch who come to me for patch testing as a kind of last resort," and only one or two had relevant patch test results when no skin disease was visible as a potential cause of itch, said Dr. Fowler of the University of Louisville (Ky.) "It can happen, but it’s not terribly common."
More commonly, if he doesn’t see much on the skin besides secondary lesions from scratching, "I immediately send them" to a neurologist, he added.
The neurologists aren’t always impressed. Dr. Fowler recalled a neurologist who was amused by the referral until imaging showed a tumor in the cervical spinal cord that was at risk of imminently severing the spinal cord and was causing referred itching.
Among other types of neuropathic itch, notalgia paresthetica has been treated with capsaicin 0.025% applied up to four times daily, or with acupuncture, or occlusion, he added.
Dr. Berger had no conflicts of interest. All the medications for itching that he discussed are used off-label.
Dr. Fowler has been a consultant, speaker or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova Ranbaxy Shire, Steifel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – If a patient complains of an itch that is "too deep to scratch," and the skin doesn’t show a cause, refer the patient to a neurologist, said Dr. Timothy G. Berger.
"The only thing I want the neurologist to tell me is that the patient doesn’t have multiple sclerosis," said Dr. Berger of the University of California, San Francisco.
There have been numerous reports of patients presenting with signs and symptoms of neuropathic itch who subsequently are diagnosed with multiple sclerosis. Dr. Berger commonly sees patients who are referred to him because treatment of their itching did not help, and they have neuropathic itch.
What does neuropathic itch look like? "The way to think about this is itch with other sensory findings," such as hypesthesia, he suggested at the seminar sponsored by Skin Disease Education Foundation. "We often have patients who’ve had neural or back injury" and develop itch with hypesthesia.
Many patients will say the "itch is too deep to scratch," he said. Or, the itch may be accompanied by burning or pain. There may be no primary lesion, or only erythema, in the itch area. The patient may describe the itch as sharp spasms of itch, or formication of skin (a crawling itch). Plenty of reports in the medical literature describe patients who present with delusions of parasitosis or formication who turn out to have multiple sclerosis, he noted.
A different CNS problem also can cause neuropathic pruritus: progressive multifocal leukoencephalopathy. Peripheral causes of neuropathic itch include brachioradial pruritus, notalgia paresthetica, or postherpetic neuralgia. In addition, prurigo nodularis or lichen simplex chronicus can produce neuropathic itch.
Spinal cord tumor or cervical spine disease with nerve entrapment are two of three important differential diagnoses when you see a patient with neuropathic itching on the extensor forearms, elbows, and arms that is typical of brachioradial pruritus. Consider also the possibility of polymorphous light eruption (sun allergy), Dr. Berger said. Sun exposure worsens all of these, making them difficult to distinguish clinically.
Referring patients with brachioradial pruritus to a physical medicine department or a spine center may help make the diagnosis and provide treatment and support, Dr. Berger suggested.
The itching from brachioradial pruritus tends to be worst with late-summer sun exposure and may clear in the winter. In contrast, polymorphous light eruption tends to be worst in the spring. Brachioradial pruritus is severe and causes potentially disabling itch, most commonly affecting white, middle-aged, affluent women with chronic sun damage.
Patients often use ice to stop the itching because little else seems to help. Sun protection and topical steroids may provide some relief. Lidoderm patches may also help. Some clinicians have prescribed topical Sinequan or capsaicin for brachioradial pruritus. Wrapping up the itching area in Unna’s boot occlusion for a few weeks may break the itch-scratch cycle, Dr. Berger suggested.
Other treatments that have been tried include gabapentin, paroxetine, mirtazapine, acupuncture, physical therapy, spinal cord manipulation, and transcutaneous electrical nerve stimulation (20 minutes per day for 5 weeks).
Thalidomide (25-200 mg nightly) is particularly effective for neuropathic pruritus, especially brachioradial pruritus, prurigo nodularis, or photodermatoses, but doses greater than 100 mg/day increase risk for deep vein thromboses and stroke.
Two of Dr. Berger’s patients on thalidomide for prurigo nodularis developed stroke. "Both of those patients are back on thalidomide after their stroke even though they know that thalidomide caused their stroke, because this is the only thing that stops their itch," he said.
Thalidomide also can cause neuropathy at doses greater than 25 mg/day, "so I start everybody at 50 mg every other day" and titrate up, he said. The drug also can cause constipation, weight gain, and sedation. Its slow onset of action can take weeks to show any benefit. "You have to hang in there," he added.
Dr. Joseph F. Fowler Jr., who moderated a question-and-answer session after Dr. Berger’s presentation, echoed his advice to send patients with neuropathic pruritus to neurologists.
"I see a lot of people who itch who come to me for patch testing as a kind of last resort," and only one or two had relevant patch test results when no skin disease was visible as a potential cause of itch, said Dr. Fowler of the University of Louisville (Ky.) "It can happen, but it’s not terribly common."
More commonly, if he doesn’t see much on the skin besides secondary lesions from scratching, "I immediately send them" to a neurologist, he added.
The neurologists aren’t always impressed. Dr. Fowler recalled a neurologist who was amused by the referral until imaging showed a tumor in the cervical spinal cord that was at risk of imminently severing the spinal cord and was causing referred itching.
Among other types of neuropathic itch, notalgia paresthetica has been treated with capsaicin 0.025% applied up to four times daily, or with acupuncture, or occlusion, he added.
Dr. Berger had no conflicts of interest. All the medications for itching that he discussed are used off-label.
Dr. Fowler has been a consultant, speaker or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova Ranbaxy Shire, Steifel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – If a patient complains of an itch that is "too deep to scratch," and the skin doesn’t show a cause, refer the patient to a neurologist, said Dr. Timothy G. Berger.
"The only thing I want the neurologist to tell me is that the patient doesn’t have multiple sclerosis," said Dr. Berger of the University of California, San Francisco.
There have been numerous reports of patients presenting with signs and symptoms of neuropathic itch who subsequently are diagnosed with multiple sclerosis. Dr. Berger commonly sees patients who are referred to him because treatment of their itching did not help, and they have neuropathic itch.
What does neuropathic itch look like? "The way to think about this is itch with other sensory findings," such as hypesthesia, he suggested at the seminar sponsored by Skin Disease Education Foundation. "We often have patients who’ve had neural or back injury" and develop itch with hypesthesia.
Many patients will say the "itch is too deep to scratch," he said. Or, the itch may be accompanied by burning or pain. There may be no primary lesion, or only erythema, in the itch area. The patient may describe the itch as sharp spasms of itch, or formication of skin (a crawling itch). Plenty of reports in the medical literature describe patients who present with delusions of parasitosis or formication who turn out to have multiple sclerosis, he noted.
A different CNS problem also can cause neuropathic pruritus: progressive multifocal leukoencephalopathy. Peripheral causes of neuropathic itch include brachioradial pruritus, notalgia paresthetica, or postherpetic neuralgia. In addition, prurigo nodularis or lichen simplex chronicus can produce neuropathic itch.
Spinal cord tumor or cervical spine disease with nerve entrapment are two of three important differential diagnoses when you see a patient with neuropathic itching on the extensor forearms, elbows, and arms that is typical of brachioradial pruritus. Consider also the possibility of polymorphous light eruption (sun allergy), Dr. Berger said. Sun exposure worsens all of these, making them difficult to distinguish clinically.
Referring patients with brachioradial pruritus to a physical medicine department or a spine center may help make the diagnosis and provide treatment and support, Dr. Berger suggested.
The itching from brachioradial pruritus tends to be worst with late-summer sun exposure and may clear in the winter. In contrast, polymorphous light eruption tends to be worst in the spring. Brachioradial pruritus is severe and causes potentially disabling itch, most commonly affecting white, middle-aged, affluent women with chronic sun damage.
Patients often use ice to stop the itching because little else seems to help. Sun protection and topical steroids may provide some relief. Lidoderm patches may also help. Some clinicians have prescribed topical Sinequan or capsaicin for brachioradial pruritus. Wrapping up the itching area in Unna’s boot occlusion for a few weeks may break the itch-scratch cycle, Dr. Berger suggested.
Other treatments that have been tried include gabapentin, paroxetine, mirtazapine, acupuncture, physical therapy, spinal cord manipulation, and transcutaneous electrical nerve stimulation (20 minutes per day for 5 weeks).
Thalidomide (25-200 mg nightly) is particularly effective for neuropathic pruritus, especially brachioradial pruritus, prurigo nodularis, or photodermatoses, but doses greater than 100 mg/day increase risk for deep vein thromboses and stroke.
Two of Dr. Berger’s patients on thalidomide for prurigo nodularis developed stroke. "Both of those patients are back on thalidomide after their stroke even though they know that thalidomide caused their stroke, because this is the only thing that stops their itch," he said.
Thalidomide also can cause neuropathy at doses greater than 25 mg/day, "so I start everybody at 50 mg every other day" and titrate up, he said. The drug also can cause constipation, weight gain, and sedation. Its slow onset of action can take weeks to show any benefit. "You have to hang in there," he added.
Dr. Joseph F. Fowler Jr., who moderated a question-and-answer session after Dr. Berger’s presentation, echoed his advice to send patients with neuropathic pruritus to neurologists.
"I see a lot of people who itch who come to me for patch testing as a kind of last resort," and only one or two had relevant patch test results when no skin disease was visible as a potential cause of itch, said Dr. Fowler of the University of Louisville (Ky.) "It can happen, but it’s not terribly common."
More commonly, if he doesn’t see much on the skin besides secondary lesions from scratching, "I immediately send them" to a neurologist, he added.
The neurologists aren’t always impressed. Dr. Fowler recalled a neurologist who was amused by the referral until imaging showed a tumor in the cervical spinal cord that was at risk of imminently severing the spinal cord and was causing referred itching.
Among other types of neuropathic itch, notalgia paresthetica has been treated with capsaicin 0.025% applied up to four times daily, or with acupuncture, or occlusion, he added.
Dr. Berger had no conflicts of interest. All the medications for itching that he discussed are used off-label.
Dr. Fowler has been a consultant, speaker or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova Ranbaxy Shire, Steifel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Diagnostic Challenge: Cutaneous Colon Cancer
What’s Your Diagnosis?
A 57-year-old woman hospitalized for nausea and hyponatremia reported having a pruritic groin rash for a week. Topical triamcinolone prescribed by her primary care physician had not helped the rash. She had a history of hereditary nonpolyposis colon cancer with metastases and stage IIa endometrial cancer. On her lower abdomen and inguinal region, clinicians could see peristomal, indurated, smooth, light pink papules and nodules coalescing into plaques.
Diagnosis: Cutaneous Colon Cancer
The patient’s history of metastatic colon cancer should have been a clue to prevent clinicians from mistaking her rash for eczema and prescribing triamcinolone.
Cutaneous metastases from internal malignancies account for approximately 2% of all skin tumors and are the first sign of internal disease in up to 22% of cases, noted Dr. Jamie Zussman, who submitted the case for discussion at the annual meeting of the Pacific Dermatologic Association.
Colon cancer is believed to metastasize to the skin in 4% of cases, which is what happened in this patient.
A preponderance of skin changes adjacent to the patient’s abdominal incision from previous surgery raises the possibility of direct inoculation of tumor cells during her surgical resection, added Dr. Zussman of the University of California, Los Angeles.
This case illustrates the importance of primary care physicians consulting early with dermatologists when unusual skin eruptions appear in ill patients, she said.
Dr. Scott Binder, who discussed the case at the meeting, put it more bluntly. "People weren’t paying attention to the clinical history," said Dr. Binder also of UCLA. "This woman had a complicated history, but if someone had read her history, they would have figured it out."
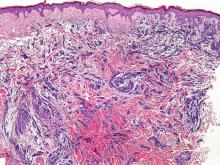
Finally, a dermatologist took a biopsy of the rash. Hematoxylin and eosin (H&E) staining showed dermis and subcutis localization, epithelial cells forming glandular structures, and perineural invasion. Cellular pleomorphism also could be seen, plus hyperchromatic, mitotically active atypical nuclei.
Immunohistochemistry showed reactivity for cytokeratin (CK) 20 and CDX2 protein, but was negative for CK7. "CDX2 is an extremely specific marker for colon cancer or GI cancers in general. A case that’s negative for CK7 and positive for CK20 is most likely colon carcinoma until proven otherwise," Dr. Binder said.
Two other immunostains have made a huge difference in the past 3-4 years in differentiating primary cutaneous carcinoma from other tumors, he added. "Immunostains for CK 5/6 and p63 have changed my practice. Get to know them," Dr. Binder said. Almost all metastases stain negative for CK 5/6 and p63, so if CK 5/6 and p63 are positive, it is probably primary skin carcinoma.
"This has been a revolution for dermatopathology," Dr. Binder said. "I talked to people at other cancer centers, and they’re finding that this is indeed useful," he added.
Breast cancer is the most common internal malignancy to metastasize to the skin, followed by lung cancer, colorectal cancer, and others. Approximately 4% of colon cancers metastasize to the skin, most frequently at abdominal sites or the hair-bearing areas of the scalp, neck, or face.
Cutaneous metastases can be classified as locoregional, in-transit, or distant. They may occur through direct invasion, lymphatic or hematogenous spread, or inoculation during surgical procedures.
Now that patients with internal malignancies are living longer and their treatment is more successful (at least in the short and intermediate term), approximately 5%-10% are developing cutaneous metastases, Dr. Binder said.
"I’ve seen two cases in the last year of metastatic renal cell carcinoma that have classically metastasized to the head and neck and that was the first diagnosis. I’ve also seen a case of metastatic lung carcinoma that metastasized to the chest wall that was also not suspected," he said.
Cutaneous metastases confer a poor prognosis and should trigger additional studies to look for metastatic disease in other organs, Dr. Zussman noted. Treatment is mainly palliative, and expectation of survival drops below 1 year once cutaneous metastases of internal malignancy appears.
Dr. Zussman and Dr. Binder reported having no pertinent conflicts of interest.
What’s Your Diagnosis?
A 57-year-old woman hospitalized for nausea and hyponatremia reported having a pruritic groin rash for a week. Topical triamcinolone prescribed by her primary care physician had not helped the rash. She had a history of hereditary nonpolyposis colon cancer with metastases and stage IIa endometrial cancer. On her lower abdomen and inguinal region, clinicians could see peristomal, indurated, smooth, light pink papules and nodules coalescing into plaques.
Diagnosis: Cutaneous Colon Cancer
The patient’s history of metastatic colon cancer should have been a clue to prevent clinicians from mistaking her rash for eczema and prescribing triamcinolone.
Cutaneous metastases from internal malignancies account for approximately 2% of all skin tumors and are the first sign of internal disease in up to 22% of cases, noted Dr. Jamie Zussman, who submitted the case for discussion at the annual meeting of the Pacific Dermatologic Association.
Colon cancer is believed to metastasize to the skin in 4% of cases, which is what happened in this patient.
A preponderance of skin changes adjacent to the patient’s abdominal incision from previous surgery raises the possibility of direct inoculation of tumor cells during her surgical resection, added Dr. Zussman of the University of California, Los Angeles.
This case illustrates the importance of primary care physicians consulting early with dermatologists when unusual skin eruptions appear in ill patients, she said.
Dr. Scott Binder, who discussed the case at the meeting, put it more bluntly. "People weren’t paying attention to the clinical history," said Dr. Binder also of UCLA. "This woman had a complicated history, but if someone had read her history, they would have figured it out."
Finally, a dermatologist took a biopsy of the rash. Hematoxylin and eosin (H&E) staining showed dermis and subcutis localization, epithelial cells forming glandular structures, and perineural invasion. Cellular pleomorphism also could be seen, plus hyperchromatic, mitotically active atypical nuclei.
Immunohistochemistry showed reactivity for cytokeratin (CK) 20 and CDX2 protein, but was negative for CK7. "CDX2 is an extremely specific marker for colon cancer or GI cancers in general. A case that’s negative for CK7 and positive for CK20 is most likely colon carcinoma until proven otherwise," Dr. Binder said.
Two other immunostains have made a huge difference in the past 3-4 years in differentiating primary cutaneous carcinoma from other tumors, he added. "Immunostains for CK 5/6 and p63 have changed my practice. Get to know them," Dr. Binder said. Almost all metastases stain negative for CK 5/6 and p63, so if CK 5/6 and p63 are positive, it is probably primary skin carcinoma.
"This has been a revolution for dermatopathology," Dr. Binder said. "I talked to people at other cancer centers, and they’re finding that this is indeed useful," he added.
Breast cancer is the most common internal malignancy to metastasize to the skin, followed by lung cancer, colorectal cancer, and others. Approximately 4% of colon cancers metastasize to the skin, most frequently at abdominal sites or the hair-bearing areas of the scalp, neck, or face.
Cutaneous metastases can be classified as locoregional, in-transit, or distant. They may occur through direct invasion, lymphatic or hematogenous spread, or inoculation during surgical procedures.
Now that patients with internal malignancies are living longer and their treatment is more successful (at least in the short and intermediate term), approximately 5%-10% are developing cutaneous metastases, Dr. Binder said.
"I’ve seen two cases in the last year of metastatic renal cell carcinoma that have classically metastasized to the head and neck and that was the first diagnosis. I’ve also seen a case of metastatic lung carcinoma that metastasized to the chest wall that was also not suspected," he said.
Cutaneous metastases confer a poor prognosis and should trigger additional studies to look for metastatic disease in other organs, Dr. Zussman noted. Treatment is mainly palliative, and expectation of survival drops below 1 year once cutaneous metastases of internal malignancy appears.
Dr. Zussman and Dr. Binder reported having no pertinent conflicts of interest.
What’s Your Diagnosis?
A 57-year-old woman hospitalized for nausea and hyponatremia reported having a pruritic groin rash for a week. Topical triamcinolone prescribed by her primary care physician had not helped the rash. She had a history of hereditary nonpolyposis colon cancer with metastases and stage IIa endometrial cancer. On her lower abdomen and inguinal region, clinicians could see peristomal, indurated, smooth, light pink papules and nodules coalescing into plaques.
Diagnosis: Cutaneous Colon Cancer
The patient’s history of metastatic colon cancer should have been a clue to prevent clinicians from mistaking her rash for eczema and prescribing triamcinolone.
Cutaneous metastases from internal malignancies account for approximately 2% of all skin tumors and are the first sign of internal disease in up to 22% of cases, noted Dr. Jamie Zussman, who submitted the case for discussion at the annual meeting of the Pacific Dermatologic Association.
Colon cancer is believed to metastasize to the skin in 4% of cases, which is what happened in this patient.
A preponderance of skin changes adjacent to the patient’s abdominal incision from previous surgery raises the possibility of direct inoculation of tumor cells during her surgical resection, added Dr. Zussman of the University of California, Los Angeles.
This case illustrates the importance of primary care physicians consulting early with dermatologists when unusual skin eruptions appear in ill patients, she said.
Dr. Scott Binder, who discussed the case at the meeting, put it more bluntly. "People weren’t paying attention to the clinical history," said Dr. Binder also of UCLA. "This woman had a complicated history, but if someone had read her history, they would have figured it out."
Finally, a dermatologist took a biopsy of the rash. Hematoxylin and eosin (H&E) staining showed dermis and subcutis localization, epithelial cells forming glandular structures, and perineural invasion. Cellular pleomorphism also could be seen, plus hyperchromatic, mitotically active atypical nuclei.
Immunohistochemistry showed reactivity for cytokeratin (CK) 20 and CDX2 protein, but was negative for CK7. "CDX2 is an extremely specific marker for colon cancer or GI cancers in general. A case that’s negative for CK7 and positive for CK20 is most likely colon carcinoma until proven otherwise," Dr. Binder said.
Two other immunostains have made a huge difference in the past 3-4 years in differentiating primary cutaneous carcinoma from other tumors, he added. "Immunostains for CK 5/6 and p63 have changed my practice. Get to know them," Dr. Binder said. Almost all metastases stain negative for CK 5/6 and p63, so if CK 5/6 and p63 are positive, it is probably primary skin carcinoma.
"This has been a revolution for dermatopathology," Dr. Binder said. "I talked to people at other cancer centers, and they’re finding that this is indeed useful," he added.
Breast cancer is the most common internal malignancy to metastasize to the skin, followed by lung cancer, colorectal cancer, and others. Approximately 4% of colon cancers metastasize to the skin, most frequently at abdominal sites or the hair-bearing areas of the scalp, neck, or face.
Cutaneous metastases can be classified as locoregional, in-transit, or distant. They may occur through direct invasion, lymphatic or hematogenous spread, or inoculation during surgical procedures.
Now that patients with internal malignancies are living longer and their treatment is more successful (at least in the short and intermediate term), approximately 5%-10% are developing cutaneous metastases, Dr. Binder said.
"I’ve seen two cases in the last year of metastatic renal cell carcinoma that have classically metastasized to the head and neck and that was the first diagnosis. I’ve also seen a case of metastatic lung carcinoma that metastasized to the chest wall that was also not suspected," he said.
Cutaneous metastases confer a poor prognosis and should trigger additional studies to look for metastatic disease in other organs, Dr. Zussman noted. Treatment is mainly palliative, and expectation of survival drops below 1 year once cutaneous metastases of internal malignancy appears.
Dr. Zussman and Dr. Binder reported having no pertinent conflicts of interest.
New Device Speeds Coagulation Test Results
SAN DIEGO – A device recently approved in the United States could greatly speed decisions about transfusion and coagulation management in patients undergoing noncardiac surgery or liver transplantation, according to Dr. Klaus Görlinger.
Conventional coagulation tests can take 20-30 minutes to produce results, he said at the annual meeting of the American Society of Anesthesiologists. "This is too long for us to make our decisions," said Dr. Görlinger of University Hospital, Essen, Germany.
He and his associates retrospectively analyzed data on 866 patients who underwent liver transplantation, visceral surgery, trauma surgery, or neurosurgery that included blood analysis using the ROTEM rotational thromboelastometry device. They looked at whether maximum clot firmness could be predicted by the amplitude of clot firmness at 5, 10, or 15 minutes after clotting time or by clot formation time, to shorten time to treatment when necessary.
The amplitude of clot firmness at 10 minutes after clotting time showed excellent correlation with maximum clot firmness and was superior to using clot formation time. "So, 12-15 minutes after starting the test, we can make our decisions about what to do in our patients," he said.
A comparison of results using various assays with the ROTEM showed that the extrinsically activated test produced useful results slightly faster than did the intrinsically activated test, which takes a bit longer to start. Both showed excellent correlation with maximum clot firmness and were superior to using clot formation time.
The Food and Drug Administration cleared the ROTEM for use in early 2010, but "only the intrinsically activated tests are FDA approved. We hope all of them will be soon," commented Dr. Linda Shore-Lesserson, comoderator of the session at the meeting. "This is really useful, not having to wait 20-25 minutes for information," said Dr. Shore-Lesserson of Montefiore Medical Center, New York.
And in situations requiring even faster decisions on transfusion and coagulation management, the 5-minute amplitude of clot firmness also provides good predictive value for the maximum clot firmness, "so we can start our specific intervention 10-12 minutes after blood sampling," Dr. Görlinger added.
At his facility, eight ROTEM devices are used in operating rooms, one in the liver transplant ICU, and one in the cardiac ICU. "We can take the device on small trolleys with us to the OR. We have four channels [on the device] and different tests we can use to differentiate what kind of problem we have in our patients," he said.
Dr. Stanley Brauer, another speaker at the session, said he was impressed by Dr. Görlinger’s findings. "After seeing your presentation, I plan to go back to my hospital administrators and ask them to order the ROTEM," said Dr. Brauer, professor of anesthesiology, Loma Linda (Calif.) University.
The study excluded ROTEM analyses that had a run time shorter than 35 minutes and perhaps hadn’t reached a maximum amplitude of clot firmness, Dr. Görlinger said. The study also excluded patients with signs of hyperfibrinolysis. It included patients regardless of whether they had been treated prior to ROTEM analysis of their blood.
Dr. Görlinger said he has received consulting fees and honoraria from Tem Innovations GmbH, which makes the ROTEM device, and CSL Behring GmbH. Two of his coinvestigators have received speaking fees from CSL Behring.
SAN DIEGO – A device recently approved in the United States could greatly speed decisions about transfusion and coagulation management in patients undergoing noncardiac surgery or liver transplantation, according to Dr. Klaus Görlinger.
Conventional coagulation tests can take 20-30 minutes to produce results, he said at the annual meeting of the American Society of Anesthesiologists. "This is too long for us to make our decisions," said Dr. Görlinger of University Hospital, Essen, Germany.
He and his associates retrospectively analyzed data on 866 patients who underwent liver transplantation, visceral surgery, trauma surgery, or neurosurgery that included blood analysis using the ROTEM rotational thromboelastometry device. They looked at whether maximum clot firmness could be predicted by the amplitude of clot firmness at 5, 10, or 15 minutes after clotting time or by clot formation time, to shorten time to treatment when necessary.
The amplitude of clot firmness at 10 minutes after clotting time showed excellent correlation with maximum clot firmness and was superior to using clot formation time. "So, 12-15 minutes after starting the test, we can make our decisions about what to do in our patients," he said.
A comparison of results using various assays with the ROTEM showed that the extrinsically activated test produced useful results slightly faster than did the intrinsically activated test, which takes a bit longer to start. Both showed excellent correlation with maximum clot firmness and were superior to using clot formation time.
The Food and Drug Administration cleared the ROTEM for use in early 2010, but "only the intrinsically activated tests are FDA approved. We hope all of them will be soon," commented Dr. Linda Shore-Lesserson, comoderator of the session at the meeting. "This is really useful, not having to wait 20-25 minutes for information," said Dr. Shore-Lesserson of Montefiore Medical Center, New York.
And in situations requiring even faster decisions on transfusion and coagulation management, the 5-minute amplitude of clot firmness also provides good predictive value for the maximum clot firmness, "so we can start our specific intervention 10-12 minutes after blood sampling," Dr. Görlinger added.
At his facility, eight ROTEM devices are used in operating rooms, one in the liver transplant ICU, and one in the cardiac ICU. "We can take the device on small trolleys with us to the OR. We have four channels [on the device] and different tests we can use to differentiate what kind of problem we have in our patients," he said.
Dr. Stanley Brauer, another speaker at the session, said he was impressed by Dr. Görlinger’s findings. "After seeing your presentation, I plan to go back to my hospital administrators and ask them to order the ROTEM," said Dr. Brauer, professor of anesthesiology, Loma Linda (Calif.) University.
The study excluded ROTEM analyses that had a run time shorter than 35 minutes and perhaps hadn’t reached a maximum amplitude of clot firmness, Dr. Görlinger said. The study also excluded patients with signs of hyperfibrinolysis. It included patients regardless of whether they had been treated prior to ROTEM analysis of their blood.
Dr. Görlinger said he has received consulting fees and honoraria from Tem Innovations GmbH, which makes the ROTEM device, and CSL Behring GmbH. Two of his coinvestigators have received speaking fees from CSL Behring.
SAN DIEGO – A device recently approved in the United States could greatly speed decisions about transfusion and coagulation management in patients undergoing noncardiac surgery or liver transplantation, according to Dr. Klaus Görlinger.
Conventional coagulation tests can take 20-30 minutes to produce results, he said at the annual meeting of the American Society of Anesthesiologists. "This is too long for us to make our decisions," said Dr. Görlinger of University Hospital, Essen, Germany.
He and his associates retrospectively analyzed data on 866 patients who underwent liver transplantation, visceral surgery, trauma surgery, or neurosurgery that included blood analysis using the ROTEM rotational thromboelastometry device. They looked at whether maximum clot firmness could be predicted by the amplitude of clot firmness at 5, 10, or 15 minutes after clotting time or by clot formation time, to shorten time to treatment when necessary.
The amplitude of clot firmness at 10 minutes after clotting time showed excellent correlation with maximum clot firmness and was superior to using clot formation time. "So, 12-15 minutes after starting the test, we can make our decisions about what to do in our patients," he said.
A comparison of results using various assays with the ROTEM showed that the extrinsically activated test produced useful results slightly faster than did the intrinsically activated test, which takes a bit longer to start. Both showed excellent correlation with maximum clot firmness and were superior to using clot formation time.
The Food and Drug Administration cleared the ROTEM for use in early 2010, but "only the intrinsically activated tests are FDA approved. We hope all of them will be soon," commented Dr. Linda Shore-Lesserson, comoderator of the session at the meeting. "This is really useful, not having to wait 20-25 minutes for information," said Dr. Shore-Lesserson of Montefiore Medical Center, New York.
And in situations requiring even faster decisions on transfusion and coagulation management, the 5-minute amplitude of clot firmness also provides good predictive value for the maximum clot firmness, "so we can start our specific intervention 10-12 minutes after blood sampling," Dr. Görlinger added.
At his facility, eight ROTEM devices are used in operating rooms, one in the liver transplant ICU, and one in the cardiac ICU. "We can take the device on small trolleys with us to the OR. We have four channels [on the device] and different tests we can use to differentiate what kind of problem we have in our patients," he said.
Dr. Stanley Brauer, another speaker at the session, said he was impressed by Dr. Görlinger’s findings. "After seeing your presentation, I plan to go back to my hospital administrators and ask them to order the ROTEM," said Dr. Brauer, professor of anesthesiology, Loma Linda (Calif.) University.
The study excluded ROTEM analyses that had a run time shorter than 35 minutes and perhaps hadn’t reached a maximum amplitude of clot firmness, Dr. Görlinger said. The study also excluded patients with signs of hyperfibrinolysis. It included patients regardless of whether they had been treated prior to ROTEM analysis of their blood.
Dr. Görlinger said he has received consulting fees and honoraria from Tem Innovations GmbH, which makes the ROTEM device, and CSL Behring GmbH. Two of his coinvestigators have received speaking fees from CSL Behring.
FROM THE ANNUAL MEETING OF THE AMERICAN SOCIETY OF ANESTHESIOLOGISTS
Major Finding: The amplitude of clot firmness 10 minutes after clotting time reported by a rotational thromboelastometry device correlated highly with maximum clot firmness, which could speed management decisions.
Data Source: Retrospective analysis of data from 866 patients undergoing liver transplantation or noncardiac surgery whose blood was analyzed by ROTEM.
Disclosures: Dr. Görlinger said he has received consulting fees and honoraria from Tem Innovations GmbH, which makes the ROTEM device, and CSL Behring GmbH. Two of his coinvestigators have received speaking fees from CSL Behring.
Role of Perioperative Oxygen Unclear in Wound Infections
SAN DIEGO – The benefit of giving a high perioperative oxygen fraction during surgery to prevent wound infections is not clear cut, judging by conflicting data from several studies.
Surgical site infections occur in 2%-3% of surgical patients. "They’re serious – the average infected patient stays in the hospital longer than they would otherwise" and the risk of being admitted to the ICU or dying doubles if surgical sites become infected, said Dr. Daniel I. Sessler said at a meeting of the American Society of Anesthesiologists.
High tissue oxygenation reduces the risk of wound infection by improving the efficacy of neutrophils to kill bacteria, so surgical patients often receive extra inspired oxygen to boost tissue oxygen. However, different results were seen in four randomized, controlled studies comparing surgical patients given a high inspiratory oxygen fraction (80%) with those who received a more conventional, lower oxygen fraction (30%) during surgery and for 2 hours afterward, said Dr. Sessler, professor and chair of outcomes research at the Cleveland Clinic.
One study randomized 500 patients undergoing colorectal resection and found surgical wound infections in 5% of the 80% oxygen group, less than half the 11% infection rate in the 30% oxygen group (New Engl. J. Med. 2000;342:161-7).
A separate study of 165 surgical patients reported that the wound infection rate more than doubled in the 80% oxygen group, compared with the 30% oxygen group – 25% vs. 11%, respectively (JAMA 2004;291:79-87).
In a separate study of 291 patients undergoing colorectal surgery, the surgical wound infection rate was lower in the 80% oxygen group than in the 30% oxygen group – 15% vs. 24%, respectively (JAMA 2005;294:2035-42).
The differences between groups in those studies were statistically significant, but no significant difference in infection rates between groups was seen in the most recent study, the PROXI trial. Among 1,386 adult patients undergoing abdominal surgery (acute or elective laparotomy) wound infection rates were 19% in the 80% oxygen group and 20% in the 30% oxygen group (JAMA 2009;302:1543-50).
"There are differences among the trials" Dr. Sessler noted. In the PROXI trial, for example, the investigators gave very little fluid to patients, so patients may have been well oxygenated but not well perfused. Factors like this may help explain their conflicting results.
"But, basically, we don’t know why this difference exists, and clearly additional research is necessary," he added.
Improving postanesthesia outcomes such as wound infections is an important goal, especially since the risk of mortality is so rare, Dr. Sessler said. "Twenty-five years ago, when I was an anesthesiology resident, anesthetic mortality was about 1 in 10,000 people, making anesthesia more dangerous than surgery in most cases," he recalled. "Now, preventable anesthetic mortality is probably about 1 in 100,000 cases," thanks to improvements in equipment, drugs and training.
Dr. Sessler has had financial relationships with Arizant, Dynatherm, Aspect Medical System (Covidien), Hutchinson Technology, Merck Pharmaceuticals, Cardinal Health, King Systems, and Velomedix.
SAN DIEGO – The benefit of giving a high perioperative oxygen fraction during surgery to prevent wound infections is not clear cut, judging by conflicting data from several studies.
Surgical site infections occur in 2%-3% of surgical patients. "They’re serious – the average infected patient stays in the hospital longer than they would otherwise" and the risk of being admitted to the ICU or dying doubles if surgical sites become infected, said Dr. Daniel I. Sessler said at a meeting of the American Society of Anesthesiologists.
High tissue oxygenation reduces the risk of wound infection by improving the efficacy of neutrophils to kill bacteria, so surgical patients often receive extra inspired oxygen to boost tissue oxygen. However, different results were seen in four randomized, controlled studies comparing surgical patients given a high inspiratory oxygen fraction (80%) with those who received a more conventional, lower oxygen fraction (30%) during surgery and for 2 hours afterward, said Dr. Sessler, professor and chair of outcomes research at the Cleveland Clinic.
One study randomized 500 patients undergoing colorectal resection and found surgical wound infections in 5% of the 80% oxygen group, less than half the 11% infection rate in the 30% oxygen group (New Engl. J. Med. 2000;342:161-7).
A separate study of 165 surgical patients reported that the wound infection rate more than doubled in the 80% oxygen group, compared with the 30% oxygen group – 25% vs. 11%, respectively (JAMA 2004;291:79-87).
In a separate study of 291 patients undergoing colorectal surgery, the surgical wound infection rate was lower in the 80% oxygen group than in the 30% oxygen group – 15% vs. 24%, respectively (JAMA 2005;294:2035-42).
The differences between groups in those studies were statistically significant, but no significant difference in infection rates between groups was seen in the most recent study, the PROXI trial. Among 1,386 adult patients undergoing abdominal surgery (acute or elective laparotomy) wound infection rates were 19% in the 80% oxygen group and 20% in the 30% oxygen group (JAMA 2009;302:1543-50).
"There are differences among the trials" Dr. Sessler noted. In the PROXI trial, for example, the investigators gave very little fluid to patients, so patients may have been well oxygenated but not well perfused. Factors like this may help explain their conflicting results.
"But, basically, we don’t know why this difference exists, and clearly additional research is necessary," he added.
Improving postanesthesia outcomes such as wound infections is an important goal, especially since the risk of mortality is so rare, Dr. Sessler said. "Twenty-five years ago, when I was an anesthesiology resident, anesthetic mortality was about 1 in 10,000 people, making anesthesia more dangerous than surgery in most cases," he recalled. "Now, preventable anesthetic mortality is probably about 1 in 100,000 cases," thanks to improvements in equipment, drugs and training.
Dr. Sessler has had financial relationships with Arizant, Dynatherm, Aspect Medical System (Covidien), Hutchinson Technology, Merck Pharmaceuticals, Cardinal Health, King Systems, and Velomedix.
SAN DIEGO – The benefit of giving a high perioperative oxygen fraction during surgery to prevent wound infections is not clear cut, judging by conflicting data from several studies.
Surgical site infections occur in 2%-3% of surgical patients. "They’re serious – the average infected patient stays in the hospital longer than they would otherwise" and the risk of being admitted to the ICU or dying doubles if surgical sites become infected, said Dr. Daniel I. Sessler said at a meeting of the American Society of Anesthesiologists.
High tissue oxygenation reduces the risk of wound infection by improving the efficacy of neutrophils to kill bacteria, so surgical patients often receive extra inspired oxygen to boost tissue oxygen. However, different results were seen in four randomized, controlled studies comparing surgical patients given a high inspiratory oxygen fraction (80%) with those who received a more conventional, lower oxygen fraction (30%) during surgery and for 2 hours afterward, said Dr. Sessler, professor and chair of outcomes research at the Cleveland Clinic.
One study randomized 500 patients undergoing colorectal resection and found surgical wound infections in 5% of the 80% oxygen group, less than half the 11% infection rate in the 30% oxygen group (New Engl. J. Med. 2000;342:161-7).
A separate study of 165 surgical patients reported that the wound infection rate more than doubled in the 80% oxygen group, compared with the 30% oxygen group – 25% vs. 11%, respectively (JAMA 2004;291:79-87).
In a separate study of 291 patients undergoing colorectal surgery, the surgical wound infection rate was lower in the 80% oxygen group than in the 30% oxygen group – 15% vs. 24%, respectively (JAMA 2005;294:2035-42).
The differences between groups in those studies were statistically significant, but no significant difference in infection rates between groups was seen in the most recent study, the PROXI trial. Among 1,386 adult patients undergoing abdominal surgery (acute or elective laparotomy) wound infection rates were 19% in the 80% oxygen group and 20% in the 30% oxygen group (JAMA 2009;302:1543-50).
"There are differences among the trials" Dr. Sessler noted. In the PROXI trial, for example, the investigators gave very little fluid to patients, so patients may have been well oxygenated but not well perfused. Factors like this may help explain their conflicting results.
"But, basically, we don’t know why this difference exists, and clearly additional research is necessary," he added.
Improving postanesthesia outcomes such as wound infections is an important goal, especially since the risk of mortality is so rare, Dr. Sessler said. "Twenty-five years ago, when I was an anesthesiology resident, anesthetic mortality was about 1 in 10,000 people, making anesthesia more dangerous than surgery in most cases," he recalled. "Now, preventable anesthetic mortality is probably about 1 in 100,000 cases," thanks to improvements in equipment, drugs and training.
Dr. Sessler has had financial relationships with Arizant, Dynatherm, Aspect Medical System (Covidien), Hutchinson Technology, Merck Pharmaceuticals, Cardinal Health, King Systems, and Velomedix.
ANNUAL MEETING OF THE AMERICAN SOCIETY OF ANESTHESIOLOGISTS
Itch Centers May Be Coming
LAS VEGAS - Improved understanding of itching and best practices in management of the condition may lead to U.S. medical centers specializing in treating pruritus.
A recent gathering of experts convened by the National Institutes of Health (NIH) may be the first step in this direction, Dr. Timothy G. Berger said at a dermatology seminar sponsored by Skin Disease Education Foundation.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) pulled together 50 physicians on Oct. 29, 2010, to discuss the topic of pruritus. One of a series of roundtable discussions held by NIAMS, this was the first to focus on itching. A summary of the meeting and a list of attendees will be posted on the NIAMS website by the end of 2010, NIAMS media liaison Trish Reynolds said in an interview.
“These things are usually followed by calls for proposals,” said Dr. Berger of the University of California, San Francisco (UCSF), who did not attend the roundtable discussion. “The NIH is moving to a model of having major itch referral centers at several sites.”
Patients with itch would be referred to a center where their tissue samples and data could be stored and analyzed while they get expert treatment. “There will be direct translational benefits” from this approach, he predicted.
These centers would be patterned after two models – referral centers for pain, and European itch centers. The U.S. itch centers might first appear at UCSF; Washington University, St. Louis; and Harvard University, Boston, he said.
“In Europe, every patient with itch goes to a medical center for itch, is seen in a standard way, and has a defined database established about that patient. They now have tens of thousands of itch patients of various types logged into this database,” and data it provides are helping to build greater understanding of the problem of itching, Dr. Berger said.
One of the key insights into itching in recent years has been the understanding that chronic itch is like chronic pain. Chronic itch is thought to begin peripherally but then trigger anatomic changes in the CNS that make treatment much more difficult. “This suggests that we will have agents that will act both peripherally and centrally” to ease itching, he said. “We’re now at the verge of being able to do something about itching.”
Chronic itching should be treated aggressively because once central sensitization occurs, it is very, very hard to manage, he advised. Chronic itching has a huge impact on quality of life, earning the same scores by patients as the reduced quality of life reported by patients with chronic renal failure on dialysis.
Once itch is chronic, the threshold for sensation of itch is reduced. “Even if you make their rash better, they still itch,” he said. Itch intensity increases with chronicity, producing more itch from the same rash. Even when the skin is clear, patients may have short bursts of spontaneous itch. In atopic dermatitis and perhaps some other forms of itchy lesions, patients may scratch themselves raw because inflammatory mediators of pain are perceived as itch.
“This whole system is miswired” in chronic itch, Dr. Berger said.
Perceived itch is a delicate interaction between the skin, nerves, and immune system, and treatments may target or more of these pathways. The most common medication for chronic itch is second-generation antihistamines, in higher doses than used for the approved indication of allergic rhinitis. “These substances also block other inflammatory mediators that may be important for itch, so they may have benefit beyond what we know,” Dr. Berger said.
Neuroleptic medications for itch include amitriptyline or other tricyclic antidepressants, gabapentin, pregabalin, duloxetine, or thalidomide for prurigo nodularis. “These act primarily on the neural axis,” he said.
Central-acting agents include paroxetine, amitriptyline, doxepin, or mirtazapine. In a large European cohort, 6-9 months of treatment with paroxetine reduced chronic itch by 75% in 70% of patients. “It’s now become one of our drugs to treat itch, and is the treatment of choice for itch in polycythemia vera,” he said.
Research has shown that patients with liver disease can develop itch caused by abnormalities in opiate metabolism, leading some clinicians to treat chronic itch with naltrexone, butorphanol or other agents that act on the opiate pathway.
Phototherapy also has been used to treat chronic itch, including narrow-band UVB, psoralen plus UVA, or broadband UVB for itch associated with renal disease. “Phototherapy probably has an immunomodulatory effect that can benefit itch,” Dr. Berger said.
Several European itch centers incorporate a biopsychosocial approach to managing itch. As with chronic pain, focusing on the itch through education and support from nurses helps reduce the itch and decrease feelings of helplessness or inability to cope. Patients miss less work and report more low-itch days and improved quality of life. “So, there’s a biopsychosocial aspect that probably will need to be addressed,” he said. Some U.S. centers have employed this approach in managing atopic dermatitis.
Dr. Berger has been a consultant for Prescription Solutions and received research funding from GlaxoSmithKline, Clinsys Clinical Research, Merz Pharmaceuticals, and Pharmanet, none of which is relevant to this topic, he said. All the medications for itching that he discussed are used off-label. SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Improved understanding of itching and best practices in management of the condition may lead to U.S. medical centers specializing in treating pruritus.
A recent gathering of experts convened by the National Institutes of Health (NIH) may be the first step in this direction, Dr. Timothy G. Berger said at a dermatology seminar sponsored by Skin Disease Education Foundation.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) pulled together 50 physicians on Oct. 29, 2010, to discuss the topic of pruritus. One of a series of roundtable discussions held by NIAMS, this was the first to focus on itching. A summary of the meeting and a list of attendees will be posted on the NIAMS website by the end of 2010, NIAMS media liaison Trish Reynolds said in an interview.
“These things are usually followed by calls for proposals,” said Dr. Berger of the University of California, San Francisco (UCSF), who did not attend the roundtable discussion. “The NIH is moving to a model of having major itch referral centers at several sites.”
Patients with itch would be referred to a center where their tissue samples and data could be stored and analyzed while they get expert treatment. “There will be direct translational benefits” from this approach, he predicted.
These centers would be patterned after two models – referral centers for pain, and European itch centers. The U.S. itch centers might first appear at UCSF; Washington University, St. Louis; and Harvard University, Boston, he said.
“In Europe, every patient with itch goes to a medical center for itch, is seen in a standard way, and has a defined database established about that patient. They now have tens of thousands of itch patients of various types logged into this database,” and data it provides are helping to build greater understanding of the problem of itching, Dr. Berger said.
One of the key insights into itching in recent years has been the understanding that chronic itch is like chronic pain. Chronic itch is thought to begin peripherally but then trigger anatomic changes in the CNS that make treatment much more difficult. “This suggests that we will have agents that will act both peripherally and centrally” to ease itching, he said. “We’re now at the verge of being able to do something about itching.”
Chronic itching should be treated aggressively because once central sensitization occurs, it is very, very hard to manage, he advised. Chronic itching has a huge impact on quality of life, earning the same scores by patients as the reduced quality of life reported by patients with chronic renal failure on dialysis.
Once itch is chronic, the threshold for sensation of itch is reduced. “Even if you make their rash better, they still itch,” he said. Itch intensity increases with chronicity, producing more itch from the same rash. Even when the skin is clear, patients may have short bursts of spontaneous itch. In atopic dermatitis and perhaps some other forms of itchy lesions, patients may scratch themselves raw because inflammatory mediators of pain are perceived as itch.
“This whole system is miswired” in chronic itch, Dr. Berger said.
Perceived itch is a delicate interaction between the skin, nerves, and immune system, and treatments may target or more of these pathways. The most common medication for chronic itch is second-generation antihistamines, in higher doses than used for the approved indication of allergic rhinitis. “These substances also block other inflammatory mediators that may be important for itch, so they may have benefit beyond what we know,” Dr. Berger said.
Neuroleptic medications for itch include amitriptyline or other tricyclic antidepressants, gabapentin, pregabalin, duloxetine, or thalidomide for prurigo nodularis. “These act primarily on the neural axis,” he said.
Central-acting agents include paroxetine, amitriptyline, doxepin, or mirtazapine. In a large European cohort, 6-9 months of treatment with paroxetine reduced chronic itch by 75% in 70% of patients. “It’s now become one of our drugs to treat itch, and is the treatment of choice for itch in polycythemia vera,” he said.
Research has shown that patients with liver disease can develop itch caused by abnormalities in opiate metabolism, leading some clinicians to treat chronic itch with naltrexone, butorphanol or other agents that act on the opiate pathway.
Phototherapy also has been used to treat chronic itch, including narrow-band UVB, psoralen plus UVA, or broadband UVB for itch associated with renal disease. “Phototherapy probably has an immunomodulatory effect that can benefit itch,” Dr. Berger said.
Several European itch centers incorporate a biopsychosocial approach to managing itch. As with chronic pain, focusing on the itch through education and support from nurses helps reduce the itch and decrease feelings of helplessness or inability to cope. Patients miss less work and report more low-itch days and improved quality of life. “So, there’s a biopsychosocial aspect that probably will need to be addressed,” he said. Some U.S. centers have employed this approach in managing atopic dermatitis.
Dr. Berger has been a consultant for Prescription Solutions and received research funding from GlaxoSmithKline, Clinsys Clinical Research, Merz Pharmaceuticals, and Pharmanet, none of which is relevant to this topic, he said. All the medications for itching that he discussed are used off-label. SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Improved understanding of itching and best practices in management of the condition may lead to U.S. medical centers specializing in treating pruritus.
A recent gathering of experts convened by the National Institutes of Health (NIH) may be the first step in this direction, Dr. Timothy G. Berger said at a dermatology seminar sponsored by Skin Disease Education Foundation.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) pulled together 50 physicians on Oct. 29, 2010, to discuss the topic of pruritus. One of a series of roundtable discussions held by NIAMS, this was the first to focus on itching. A summary of the meeting and a list of attendees will be posted on the NIAMS website by the end of 2010, NIAMS media liaison Trish Reynolds said in an interview.
“These things are usually followed by calls for proposals,” said Dr. Berger of the University of California, San Francisco (UCSF), who did not attend the roundtable discussion. “The NIH is moving to a model of having major itch referral centers at several sites.”
Patients with itch would be referred to a center where their tissue samples and data could be stored and analyzed while they get expert treatment. “There will be direct translational benefits” from this approach, he predicted.
These centers would be patterned after two models – referral centers for pain, and European itch centers. The U.S. itch centers might first appear at UCSF; Washington University, St. Louis; and Harvard University, Boston, he said.
“In Europe, every patient with itch goes to a medical center for itch, is seen in a standard way, and has a defined database established about that patient. They now have tens of thousands of itch patients of various types logged into this database,” and data it provides are helping to build greater understanding of the problem of itching, Dr. Berger said.
One of the key insights into itching in recent years has been the understanding that chronic itch is like chronic pain. Chronic itch is thought to begin peripherally but then trigger anatomic changes in the CNS that make treatment much more difficult. “This suggests that we will have agents that will act both peripherally and centrally” to ease itching, he said. “We’re now at the verge of being able to do something about itching.”
Chronic itching should be treated aggressively because once central sensitization occurs, it is very, very hard to manage, he advised. Chronic itching has a huge impact on quality of life, earning the same scores by patients as the reduced quality of life reported by patients with chronic renal failure on dialysis.
Once itch is chronic, the threshold for sensation of itch is reduced. “Even if you make their rash better, they still itch,” he said. Itch intensity increases with chronicity, producing more itch from the same rash. Even when the skin is clear, patients may have short bursts of spontaneous itch. In atopic dermatitis and perhaps some other forms of itchy lesions, patients may scratch themselves raw because inflammatory mediators of pain are perceived as itch.
“This whole system is miswired” in chronic itch, Dr. Berger said.
Perceived itch is a delicate interaction between the skin, nerves, and immune system, and treatments may target or more of these pathways. The most common medication for chronic itch is second-generation antihistamines, in higher doses than used for the approved indication of allergic rhinitis. “These substances also block other inflammatory mediators that may be important for itch, so they may have benefit beyond what we know,” Dr. Berger said.
Neuroleptic medications for itch include amitriptyline or other tricyclic antidepressants, gabapentin, pregabalin, duloxetine, or thalidomide for prurigo nodularis. “These act primarily on the neural axis,” he said.
Central-acting agents include paroxetine, amitriptyline, doxepin, or mirtazapine. In a large European cohort, 6-9 months of treatment with paroxetine reduced chronic itch by 75% in 70% of patients. “It’s now become one of our drugs to treat itch, and is the treatment of choice for itch in polycythemia vera,” he said.
Research has shown that patients with liver disease can develop itch caused by abnormalities in opiate metabolism, leading some clinicians to treat chronic itch with naltrexone, butorphanol or other agents that act on the opiate pathway.
Phototherapy also has been used to treat chronic itch, including narrow-band UVB, psoralen plus UVA, or broadband UVB for itch associated with renal disease. “Phototherapy probably has an immunomodulatory effect that can benefit itch,” Dr. Berger said.
Several European itch centers incorporate a biopsychosocial approach to managing itch. As with chronic pain, focusing on the itch through education and support from nurses helps reduce the itch and decrease feelings of helplessness or inability to cope. Patients miss less work and report more low-itch days and improved quality of life. “So, there’s a biopsychosocial aspect that probably will need to be addressed,” he said. Some U.S. centers have employed this approach in managing atopic dermatitis.
Dr. Berger has been a consultant for Prescription Solutions and received research funding from GlaxoSmithKline, Clinsys Clinical Research, Merz Pharmaceuticals, and Pharmanet, none of which is relevant to this topic, he said. All the medications for itching that he discussed are used off-label. SDEF and this news organization are owned by Elsevier.
Itch Centers May Be Coming
LAS VEGAS - Improved understanding of itching and best practices in management of the condition may lead to U.S. medical centers specializing in treating pruritus.
A recent gathering of experts convened by the National Institutes of Health (NIH) may be the first step in this direction, Dr. Timothy G. Berger said at a dermatology seminar sponsored by Skin Disease Education Foundation.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) pulled together 50 physicians on Oct. 29, 2010, to discuss the topic of pruritus. One of a series of roundtable discussions held by NIAMS, this was the first to focus on itching. A summary of the meeting and a list of attendees will be posted on the NIAMS website by the end of 2010, NIAMS media liaison Trish Reynolds said in an interview.
“These things are usually followed by calls for proposals,” said Dr. Berger of the University of California, San Francisco (UCSF), who did not attend the roundtable discussion. “The NIH is moving to a model of having major itch referral centers at several sites.”
Patients with itch would be referred to a center where their tissue samples and data could be stored and analyzed while they get expert treatment. “There will be direct translational benefits” from this approach, he predicted.
These centers would be patterned after two models – referral centers for pain, and European itch centers. The U.S. itch centers might first appear at UCSF; Washington University, St. Louis; and Harvard University, Boston, he said.
“In Europe, every patient with itch goes to a medical center for itch, is seen in a standard way, and has a defined database established about that patient. They now have tens of thousands of itch patients of various types logged into this database,” and data it provides are helping to build greater understanding of the problem of itching, Dr. Berger said.
One of the key insights into itching in recent years has been the understanding that chronic itch is like chronic pain. Chronic itch is thought to begin peripherally but then trigger anatomic changes in the CNS that make treatment much more difficult. “This suggests that we will have agents that will act both peripherally and centrally” to ease itching, he said. “We’re now at the verge of being able to do something about itching.”
Chronic itching should be treated aggressively because once central sensitization occurs, it is very, very hard to manage, he advised. Chronic itching has a huge impact on quality of life, earning the same scores by patients as the reduced quality of life reported by patients with chronic renal failure on dialysis.
Once itch is chronic, the threshold for sensation of itch is reduced. “Even if you make their rash better, they still itch,” he said. Itch intensity increases with chronicity, producing more itch from the same rash. Even when the skin is clear, patients may have short bursts of spontaneous itch. In atopic dermatitis and perhaps some other forms of itchy lesions, patients may scratch themselves raw because inflammatory mediators of pain are perceived as itch.
“This whole system is miswired” in chronic itch, Dr. Berger said.
Perceived itch is a delicate interaction between the skin, nerves, and immune system, and treatments may target or more of these pathways. The most common medication for chronic itch is second-generation antihistamines, in higher doses than used for the approved indication of allergic rhinitis. “These substances also block other inflammatory mediators that may be important for itch, so they may have benefit beyond what we know,” Dr. Berger said.
Neuroleptic medications for itch include amitriptyline or other tricyclic antidepressants, gabapentin, pregabalin, duloxetine, or thalidomide for prurigo nodularis. “These act primarily on the neural axis,” he said.
Central-acting agents include paroxetine, amitriptyline, doxepin, or mirtazapine. In a large European cohort, 6-9 months of treatment with paroxetine reduced chronic itch by 75% in 70% of patients. “It’s now become one of our drugs to treat itch, and is the treatment of choice for itch in polycythemia vera,” he said.
Research has shown that patients with liver disease can develop itch caused by abnormalities in opiate metabolism, leading some clinicians to treat chronic itch with naltrexone, butorphanol or other agents that act on the opiate pathway.
Phototherapy also has been used to treat chronic itch, including narrow-band UVB, psoralen plus UVA, or broadband UVB for itch associated with renal disease. “Phototherapy probably has an immunomodulatory effect that can benefit itch,” Dr. Berger said.
Several European itch centers incorporate a biopsychosocial approach to managing itch. As with chronic pain, focusing on the itch through education and support from nurses helps reduce the itch and decrease feelings of helplessness or inability to cope. Patients miss less work and report more low-itch days and improved quality of life. “So, there’s a biopsychosocial aspect that probably will need to be addressed,” he said. Some U.S. centers have employed this approach in managing atopic dermatitis.
Dr. Berger has been a consultant for Prescription Solutions and received research funding from GlaxoSmithKline, Clinsys Clinical Research, Merz Pharmaceuticals, and Pharmanet, none of which is relevant to this topic, he said. All the medications for itching that he discussed are used off-label. SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Improved understanding of itching and best practices in management of the condition may lead to U.S. medical centers specializing in treating pruritus.
A recent gathering of experts convened by the National Institutes of Health (NIH) may be the first step in this direction, Dr. Timothy G. Berger said at a dermatology seminar sponsored by Skin Disease Education Foundation.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) pulled together 50 physicians on Oct. 29, 2010, to discuss the topic of pruritus. One of a series of roundtable discussions held by NIAMS, this was the first to focus on itching. A summary of the meeting and a list of attendees will be posted on the NIAMS website by the end of 2010, NIAMS media liaison Trish Reynolds said in an interview.
“These things are usually followed by calls for proposals,” said Dr. Berger of the University of California, San Francisco (UCSF), who did not attend the roundtable discussion. “The NIH is moving to a model of having major itch referral centers at several sites.”
Patients with itch would be referred to a center where their tissue samples and data could be stored and analyzed while they get expert treatment. “There will be direct translational benefits” from this approach, he predicted.
These centers would be patterned after two models – referral centers for pain, and European itch centers. The U.S. itch centers might first appear at UCSF; Washington University, St. Louis; and Harvard University, Boston, he said.
“In Europe, every patient with itch goes to a medical center for itch, is seen in a standard way, and has a defined database established about that patient. They now have tens of thousands of itch patients of various types logged into this database,” and data it provides are helping to build greater understanding of the problem of itching, Dr. Berger said.
One of the key insights into itching in recent years has been the understanding that chronic itch is like chronic pain. Chronic itch is thought to begin peripherally but then trigger anatomic changes in the CNS that make treatment much more difficult. “This suggests that we will have agents that will act both peripherally and centrally” to ease itching, he said. “We’re now at the verge of being able to do something about itching.”
Chronic itching should be treated aggressively because once central sensitization occurs, it is very, very hard to manage, he advised. Chronic itching has a huge impact on quality of life, earning the same scores by patients as the reduced quality of life reported by patients with chronic renal failure on dialysis.
Once itch is chronic, the threshold for sensation of itch is reduced. “Even if you make their rash better, they still itch,” he said. Itch intensity increases with chronicity, producing more itch from the same rash. Even when the skin is clear, patients may have short bursts of spontaneous itch. In atopic dermatitis and perhaps some other forms of itchy lesions, patients may scratch themselves raw because inflammatory mediators of pain are perceived as itch.
“This whole system is miswired” in chronic itch, Dr. Berger said.
Perceived itch is a delicate interaction between the skin, nerves, and immune system, and treatments may target or more of these pathways. The most common medication for chronic itch is second-generation antihistamines, in higher doses than used for the approved indication of allergic rhinitis. “These substances also block other inflammatory mediators that may be important for itch, so they may have benefit beyond what we know,” Dr. Berger said.
Neuroleptic medications for itch include amitriptyline or other tricyclic antidepressants, gabapentin, pregabalin, duloxetine, or thalidomide for prurigo nodularis. “These act primarily on the neural axis,” he said.
Central-acting agents include paroxetine, amitriptyline, doxepin, or mirtazapine. In a large European cohort, 6-9 months of treatment with paroxetine reduced chronic itch by 75% in 70% of patients. “It’s now become one of our drugs to treat itch, and is the treatment of choice for itch in polycythemia vera,” he said.
Research has shown that patients with liver disease can develop itch caused by abnormalities in opiate metabolism, leading some clinicians to treat chronic itch with naltrexone, butorphanol or other agents that act on the opiate pathway.
Phototherapy also has been used to treat chronic itch, including narrow-band UVB, psoralen plus UVA, or broadband UVB for itch associated with renal disease. “Phototherapy probably has an immunomodulatory effect that can benefit itch,” Dr. Berger said.
Several European itch centers incorporate a biopsychosocial approach to managing itch. As with chronic pain, focusing on the itch through education and support from nurses helps reduce the itch and decrease feelings of helplessness or inability to cope. Patients miss less work and report more low-itch days and improved quality of life. “So, there’s a biopsychosocial aspect that probably will need to be addressed,” he said. Some U.S. centers have employed this approach in managing atopic dermatitis.
Dr. Berger has been a consultant for Prescription Solutions and received research funding from GlaxoSmithKline, Clinsys Clinical Research, Merz Pharmaceuticals, and Pharmanet, none of which is relevant to this topic, he said. All the medications for itching that he discussed are used off-label. SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Improved understanding of itching and best practices in management of the condition may lead to U.S. medical centers specializing in treating pruritus.
A recent gathering of experts convened by the National Institutes of Health (NIH) may be the first step in this direction, Dr. Timothy G. Berger said at a dermatology seminar sponsored by Skin Disease Education Foundation.
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) pulled together 50 physicians on Oct. 29, 2010, to discuss the topic of pruritus. One of a series of roundtable discussions held by NIAMS, this was the first to focus on itching. A summary of the meeting and a list of attendees will be posted on the NIAMS website by the end of 2010, NIAMS media liaison Trish Reynolds said in an interview.
“These things are usually followed by calls for proposals,” said Dr. Berger of the University of California, San Francisco (UCSF), who did not attend the roundtable discussion. “The NIH is moving to a model of having major itch referral centers at several sites.”
Patients with itch would be referred to a center where their tissue samples and data could be stored and analyzed while they get expert treatment. “There will be direct translational benefits” from this approach, he predicted.
These centers would be patterned after two models – referral centers for pain, and European itch centers. The U.S. itch centers might first appear at UCSF; Washington University, St. Louis; and Harvard University, Boston, he said.
“In Europe, every patient with itch goes to a medical center for itch, is seen in a standard way, and has a defined database established about that patient. They now have tens of thousands of itch patients of various types logged into this database,” and data it provides are helping to build greater understanding of the problem of itching, Dr. Berger said.
One of the key insights into itching in recent years has been the understanding that chronic itch is like chronic pain. Chronic itch is thought to begin peripherally but then trigger anatomic changes in the CNS that make treatment much more difficult. “This suggests that we will have agents that will act both peripherally and centrally” to ease itching, he said. “We’re now at the verge of being able to do something about itching.”
Chronic itching should be treated aggressively because once central sensitization occurs, it is very, very hard to manage, he advised. Chronic itching has a huge impact on quality of life, earning the same scores by patients as the reduced quality of life reported by patients with chronic renal failure on dialysis.
Once itch is chronic, the threshold for sensation of itch is reduced. “Even if you make their rash better, they still itch,” he said. Itch intensity increases with chronicity, producing more itch from the same rash. Even when the skin is clear, patients may have short bursts of spontaneous itch. In atopic dermatitis and perhaps some other forms of itchy lesions, patients may scratch themselves raw because inflammatory mediators of pain are perceived as itch.
“This whole system is miswired” in chronic itch, Dr. Berger said.
Perceived itch is a delicate interaction between the skin, nerves, and immune system, and treatments may target or more of these pathways. The most common medication for chronic itch is second-generation antihistamines, in higher doses than used for the approved indication of allergic rhinitis. “These substances also block other inflammatory mediators that may be important for itch, so they may have benefit beyond what we know,” Dr. Berger said.
Neuroleptic medications for itch include amitriptyline or other tricyclic antidepressants, gabapentin, pregabalin, duloxetine, or thalidomide for prurigo nodularis. “These act primarily on the neural axis,” he said.
Central-acting agents include paroxetine, amitriptyline, doxepin, or mirtazapine. In a large European cohort, 6-9 months of treatment with paroxetine reduced chronic itch by 75% in 70% of patients. “It’s now become one of our drugs to treat itch, and is the treatment of choice for itch in polycythemia vera,” he said.
Research has shown that patients with liver disease can develop itch caused by abnormalities in opiate metabolism, leading some clinicians to treat chronic itch with naltrexone, butorphanol or other agents that act on the opiate pathway.
Phototherapy also has been used to treat chronic itch, including narrow-band UVB, psoralen plus UVA, or broadband UVB for itch associated with renal disease. “Phototherapy probably has an immunomodulatory effect that can benefit itch,” Dr. Berger said.
Several European itch centers incorporate a biopsychosocial approach to managing itch. As with chronic pain, focusing on the itch through education and support from nurses helps reduce the itch and decrease feelings of helplessness or inability to cope. Patients miss less work and report more low-itch days and improved quality of life. “So, there’s a biopsychosocial aspect that probably will need to be addressed,” he said. Some U.S. centers have employed this approach in managing atopic dermatitis.
Dr. Berger has been a consultant for Prescription Solutions and received research funding from GlaxoSmithKline, Clinsys Clinical Research, Merz Pharmaceuticals, and Pharmanet, none of which is relevant to this topic, he said. All the medications for itching that he discussed are used off-label. SDEF and this news organization are owned by Elsevier.
Take Steps to Protect Your Online Reputation
MONTEREY, CALIF. — Have you searched for your name on the Internet? Your patients have.
“Your patients are Googling you,” and some of them probably are rating your performance as a doctor on one of the many physician-rating sites or generic rating sites, Dr. Clifford Warren Lober said.
Here's the problem: The patients most likely to rate you are those who are livid at you, or those who think you walk on water.
And it's not just patients who are posting comments about you, but previous patients, ex-employees, former spouses, or anyone else who knows you, said Dr. Lober, a dermatologist and attorney in Kissimmee, Fla.
Online comments may be made anonymously, persist for years on the Internet, be accessed by anyone with a computer, and be replicated on other Web sites beyond the original.
If you discover comments about you that you think are harmful to your reputation, your attempts to remedy the situation may backfire and instead “optimize” the content by bringing more attention to the posted statement, amplifying its negativity, the physician said.
Legal remedies are few and complicated. “There is a morass of legal defenses and privileges that protect the offending person,” Dr. Lober said.
So how best to manage your online reputation?
One strategy is to minimize the impact of negative online information through search-engine optimization, he suggested.
In practice, this means blitzing the Web with your own content to crowd out comments by others. “You want to occupy the first three pages of the rating sites” and the search-engine results pages if possible, Dr. Lober said, adding that most people don't look beyond the first three pages of results.
This can be done by establishing multiple Web sites, each with numerous internal page links, external high-traffic links, significant content on each of your home pages, and other features that make these the sites that show up when someone searches your name.
Establishing a deep social network presence helps, too. Create accounts on Facebook, Twitter, LinkedIn, ZoomInfo, Connectbeam, Yahoo Profile, Google Profile, MSN Profile, Wetpaint, Naymz, Jigsaw, Ning, and others, he suggested. Ideally, get on sites that feature RSS (Really Simple Syndication) feeds so that information posted on one site transfers to others.
Other prongs in this strategy include issuing press releases by using Internet publication sites, establishing one or more blogs in your name, and using pay-per-click advertising.
Sound overwhelming? Innovative entrepreneurs thought that it might, so a number of Internet reputation-management companies have formed to do some of this work for you—for a fee, of course. These include companies like Reputation Repair & Management, Internet Reputation Management, and ReputationDefender, Dr. Lober said.
If, instead, you want to try to get a specific offensive statement removed from the Web, seek legal counsel to guide you, he advised.
First, the statement must be determined to meet the legal definition of defamation. If it does, the next step is to determine if the person who wrote it is covered by any one of several standard legal defenses.
If that's not an issue, check the terms and conditions listed by the Internet service provider (ISP) of the site where the comment appeared, to see if the ISP made any promises or assurances about the content on the site. If you contact the ISP, it may take the comment down.
Normally, ISPs are immune from lawsuits over statements made by others on its service; they resemble telephone companies more than newspapers in that respect, he said.
You or your lawyer can request that the courts issue a subpoena to try to compel the person who made the statement (even an anonymous poster) to remedy the situation, but this process is time consuming and expensive, and the person who posted the comment may be difficult to locate, Dr. Lober cautioned.
And if you sue, the defendant may try to frame your action as a SLAPP (strategic litigation against public participation) suit intended to muzzle critics and restrict freedom of speech.
Some states have anti-SLAPP laws that could leave you paying the defendant's attorney fees and costs, and make you vulnerable to a countersuit by the defendant.
Better to try to “manage” your online reputation than to try to legally defend it, he suggested.
Dr. Lober reported having no pertinent conflicts of interest.
MONTEREY, CALIF. — Have you searched for your name on the Internet? Your patients have.
“Your patients are Googling you,” and some of them probably are rating your performance as a doctor on one of the many physician-rating sites or generic rating sites, Dr. Clifford Warren Lober said.
Here's the problem: The patients most likely to rate you are those who are livid at you, or those who think you walk on water.
And it's not just patients who are posting comments about you, but previous patients, ex-employees, former spouses, or anyone else who knows you, said Dr. Lober, a dermatologist and attorney in Kissimmee, Fla.
Online comments may be made anonymously, persist for years on the Internet, be accessed by anyone with a computer, and be replicated on other Web sites beyond the original.
If you discover comments about you that you think are harmful to your reputation, your attempts to remedy the situation may backfire and instead “optimize” the content by bringing more attention to the posted statement, amplifying its negativity, the physician said.
Legal remedies are few and complicated. “There is a morass of legal defenses and privileges that protect the offending person,” Dr. Lober said.
So how best to manage your online reputation?
One strategy is to minimize the impact of negative online information through search-engine optimization, he suggested.
In practice, this means blitzing the Web with your own content to crowd out comments by others. “You want to occupy the first three pages of the rating sites” and the search-engine results pages if possible, Dr. Lober said, adding that most people don't look beyond the first three pages of results.
This can be done by establishing multiple Web sites, each with numerous internal page links, external high-traffic links, significant content on each of your home pages, and other features that make these the sites that show up when someone searches your name.
Establishing a deep social network presence helps, too. Create accounts on Facebook, Twitter, LinkedIn, ZoomInfo, Connectbeam, Yahoo Profile, Google Profile, MSN Profile, Wetpaint, Naymz, Jigsaw, Ning, and others, he suggested. Ideally, get on sites that feature RSS (Really Simple Syndication) feeds so that information posted on one site transfers to others.
Other prongs in this strategy include issuing press releases by using Internet publication sites, establishing one or more blogs in your name, and using pay-per-click advertising.
Sound overwhelming? Innovative entrepreneurs thought that it might, so a number of Internet reputation-management companies have formed to do some of this work for you—for a fee, of course. These include companies like Reputation Repair & Management, Internet Reputation Management, and ReputationDefender, Dr. Lober said.
If, instead, you want to try to get a specific offensive statement removed from the Web, seek legal counsel to guide you, he advised.
First, the statement must be determined to meet the legal definition of defamation. If it does, the next step is to determine if the person who wrote it is covered by any one of several standard legal defenses.
If that's not an issue, check the terms and conditions listed by the Internet service provider (ISP) of the site where the comment appeared, to see if the ISP made any promises or assurances about the content on the site. If you contact the ISP, it may take the comment down.
Normally, ISPs are immune from lawsuits over statements made by others on its service; they resemble telephone companies more than newspapers in that respect, he said.
You or your lawyer can request that the courts issue a subpoena to try to compel the person who made the statement (even an anonymous poster) to remedy the situation, but this process is time consuming and expensive, and the person who posted the comment may be difficult to locate, Dr. Lober cautioned.
And if you sue, the defendant may try to frame your action as a SLAPP (strategic litigation against public participation) suit intended to muzzle critics and restrict freedom of speech.
Some states have anti-SLAPP laws that could leave you paying the defendant's attorney fees and costs, and make you vulnerable to a countersuit by the defendant.
Better to try to “manage” your online reputation than to try to legally defend it, he suggested.
Dr. Lober reported having no pertinent conflicts of interest.
MONTEREY, CALIF. — Have you searched for your name on the Internet? Your patients have.
“Your patients are Googling you,” and some of them probably are rating your performance as a doctor on one of the many physician-rating sites or generic rating sites, Dr. Clifford Warren Lober said.
Here's the problem: The patients most likely to rate you are those who are livid at you, or those who think you walk on water.
And it's not just patients who are posting comments about you, but previous patients, ex-employees, former spouses, or anyone else who knows you, said Dr. Lober, a dermatologist and attorney in Kissimmee, Fla.
Online comments may be made anonymously, persist for years on the Internet, be accessed by anyone with a computer, and be replicated on other Web sites beyond the original.
If you discover comments about you that you think are harmful to your reputation, your attempts to remedy the situation may backfire and instead “optimize” the content by bringing more attention to the posted statement, amplifying its negativity, the physician said.
Legal remedies are few and complicated. “There is a morass of legal defenses and privileges that protect the offending person,” Dr. Lober said.
So how best to manage your online reputation?
One strategy is to minimize the impact of negative online information through search-engine optimization, he suggested.
In practice, this means blitzing the Web with your own content to crowd out comments by others. “You want to occupy the first three pages of the rating sites” and the search-engine results pages if possible, Dr. Lober said, adding that most people don't look beyond the first three pages of results.
This can be done by establishing multiple Web sites, each with numerous internal page links, external high-traffic links, significant content on each of your home pages, and other features that make these the sites that show up when someone searches your name.
Establishing a deep social network presence helps, too. Create accounts on Facebook, Twitter, LinkedIn, ZoomInfo, Connectbeam, Yahoo Profile, Google Profile, MSN Profile, Wetpaint, Naymz, Jigsaw, Ning, and others, he suggested. Ideally, get on sites that feature RSS (Really Simple Syndication) feeds so that information posted on one site transfers to others.
Other prongs in this strategy include issuing press releases by using Internet publication sites, establishing one or more blogs in your name, and using pay-per-click advertising.
Sound overwhelming? Innovative entrepreneurs thought that it might, so a number of Internet reputation-management companies have formed to do some of this work for you—for a fee, of course. These include companies like Reputation Repair & Management, Internet Reputation Management, and ReputationDefender, Dr. Lober said.
If, instead, you want to try to get a specific offensive statement removed from the Web, seek legal counsel to guide you, he advised.
First, the statement must be determined to meet the legal definition of defamation. If it does, the next step is to determine if the person who wrote it is covered by any one of several standard legal defenses.
If that's not an issue, check the terms and conditions listed by the Internet service provider (ISP) of the site where the comment appeared, to see if the ISP made any promises or assurances about the content on the site. If you contact the ISP, it may take the comment down.
Normally, ISPs are immune from lawsuits over statements made by others on its service; they resemble telephone companies more than newspapers in that respect, he said.
You or your lawyer can request that the courts issue a subpoena to try to compel the person who made the statement (even an anonymous poster) to remedy the situation, but this process is time consuming and expensive, and the person who posted the comment may be difficult to locate, Dr. Lober cautioned.
And if you sue, the defendant may try to frame your action as a SLAPP (strategic litigation against public participation) suit intended to muzzle critics and restrict freedom of speech.
Some states have anti-SLAPP laws that could leave you paying the defendant's attorney fees and costs, and make you vulnerable to a countersuit by the defendant.
Better to try to “manage” your online reputation than to try to legally defend it, he suggested.
Dr. Lober reported having no pertinent conflicts of interest.
Expert Opinion from the Annual Meeting of the American Society for Mohs Surgery
Blitz Web With Content to Protect Your Online Reputation
MONTEREY, CALIF. — Have you searched for your name on the Internet? Your patients have.
“Your patients are Googling you,” and some of them probably are rating your performance as a doctor on one of the many physician-rating sites or generic rating sites, Dr. Clifford Warren Lober said. H
Here's the problem: The patients most likely to rate you are those who are livid at you, or those who think you walk on water. And it's not just patients who are posting comments about you, but previous patients, ex-employees, former spouses, or anyone else who knows you, said Dr. Lober, a dermatologist and attorney in Kissimmee, Fla.
Online comments may be made anonymously, persist for years on the Internet, be accessed by anyone with a computer, and be replicated on other Web sites beyond the original. If you discover comments about you that you think are harmful to your reputation, your attempts to remedy the situation may backfire and instead “optimize” the content by bringing more attention to the posted statement, amplifying its negativity, he said.
Legal remedies are few and complicated. “There is a morass of legal defenses and privileges that protect the offending person,” Dr. Lober said.
So how best to manage your online reputation? One strategy is to minimize the impact of negative online information by using search-engine optimization.
In practice, this means blitzing the Web with your own content to crowd out comments by others. “You want to occupy the first three pages of the rating sites” and the search-engine results pages if possible, Dr. Lober said, adding that most people don't look beyond the first three pages of results.
This can be done by establishing multiple Web sites, each with numerous internal page links, external high-traffic links, significant content on each of your home pages, and other features that make these the sites that show up when someone searches your name.
Establishing a deep social network presence helps, too. Create accounts on Facebook, Twitter, LinkedIn, ZoomInfo, Connectbeam, Yahoo Profile, Google Profile, MSN Profile, Wetpaint, Naymz, Jigsaw, Ning, and others, he suggested. Ideally, get on sites that feature RSS (Really Simple Syndication) feeds so that information posted on one site transfers to others.
Other prongs in this strategy include issuing press releases by using Internet publication sites, establishing one or more blogs in your name, and using pay-per-click advertising.
Sound overwhelming? Innovative entrepreneurs thought that it might, so a number of Internet reputation-management companies have formed to do some of this work for you'for a fee, of course. These include companies like Reputation Repair & Management, Internet Reputation Management, and ReputationDefender, Dr. Lober said.
If, instead, you want to try to get a specific offensive statement removed from the Web, seek legal counsel for guidance, Dr. Lober advised. First, the statement must be determined to meet the legal definition of defamation. If it does, the next step is to determine if the person who wrote it is covered by any one of several standard legal defenses. If that's not an issue, check the terms and conditions listed by the Internet service provider (ISP) of the site where the comment appeared, to see if the ISP made any promises or assurances about the content on the site. If you contact the ISP, it may take the comment down.
Normally, ISPs are immune from lawsuits over statements made by others on its service; they resemble telephone companies more than newspapers in that respect, he said.
You or your lawyer can request that the courts issue a subpoena to try to compel the person who made the statement (even an anonymous poster) to remedy the situation, but this process is time consuming and expensive, and the person who posted the comment may be difficult to locate, Dr. Lober cautioned.
And if you sue, the defendant may try to frame your action as a SLAPP (strategic litigation against public participation) suit intended to muzzle critics and restrict freedom of speech. Some states have anti-SLAPP laws that could leave you paying the defendant's attorney fees and costs, and make you vulnerable to a countersuit by the defendant. Better to try to “manage” your
Better to try to “manage” your online reputation than to try to legally defend it, he suggested.
Dr. Lober reported having no pertinent conflicts of interest.
MONTEREY, CALIF. — Have you searched for your name on the Internet? Your patients have.
“Your patients are Googling you,” and some of them probably are rating your performance as a doctor on one of the many physician-rating sites or generic rating sites, Dr. Clifford Warren Lober said. H
Here's the problem: The patients most likely to rate you are those who are livid at you, or those who think you walk on water. And it's not just patients who are posting comments about you, but previous patients, ex-employees, former spouses, or anyone else who knows you, said Dr. Lober, a dermatologist and attorney in Kissimmee, Fla.
Online comments may be made anonymously, persist for years on the Internet, be accessed by anyone with a computer, and be replicated on other Web sites beyond the original. If you discover comments about you that you think are harmful to your reputation, your attempts to remedy the situation may backfire and instead “optimize” the content by bringing more attention to the posted statement, amplifying its negativity, he said.
Legal remedies are few and complicated. “There is a morass of legal defenses and privileges that protect the offending person,” Dr. Lober said.
So how best to manage your online reputation? One strategy is to minimize the impact of negative online information by using search-engine optimization.
In practice, this means blitzing the Web with your own content to crowd out comments by others. “You want to occupy the first three pages of the rating sites” and the search-engine results pages if possible, Dr. Lober said, adding that most people don't look beyond the first three pages of results.
This can be done by establishing multiple Web sites, each with numerous internal page links, external high-traffic links, significant content on each of your home pages, and other features that make these the sites that show up when someone searches your name.
Establishing a deep social network presence helps, too. Create accounts on Facebook, Twitter, LinkedIn, ZoomInfo, Connectbeam, Yahoo Profile, Google Profile, MSN Profile, Wetpaint, Naymz, Jigsaw, Ning, and others, he suggested. Ideally, get on sites that feature RSS (Really Simple Syndication) feeds so that information posted on one site transfers to others.
Other prongs in this strategy include issuing press releases by using Internet publication sites, establishing one or more blogs in your name, and using pay-per-click advertising.
Sound overwhelming? Innovative entrepreneurs thought that it might, so a number of Internet reputation-management companies have formed to do some of this work for you'for a fee, of course. These include companies like Reputation Repair & Management, Internet Reputation Management, and ReputationDefender, Dr. Lober said.
If, instead, you want to try to get a specific offensive statement removed from the Web, seek legal counsel for guidance, Dr. Lober advised. First, the statement must be determined to meet the legal definition of defamation. If it does, the next step is to determine if the person who wrote it is covered by any one of several standard legal defenses. If that's not an issue, check the terms and conditions listed by the Internet service provider (ISP) of the site where the comment appeared, to see if the ISP made any promises or assurances about the content on the site. If you contact the ISP, it may take the comment down.
Normally, ISPs are immune from lawsuits over statements made by others on its service; they resemble telephone companies more than newspapers in that respect, he said.
You or your lawyer can request that the courts issue a subpoena to try to compel the person who made the statement (even an anonymous poster) to remedy the situation, but this process is time consuming and expensive, and the person who posted the comment may be difficult to locate, Dr. Lober cautioned.
And if you sue, the defendant may try to frame your action as a SLAPP (strategic litigation against public participation) suit intended to muzzle critics and restrict freedom of speech. Some states have anti-SLAPP laws that could leave you paying the defendant's attorney fees and costs, and make you vulnerable to a countersuit by the defendant. Better to try to “manage” your
Better to try to “manage” your online reputation than to try to legally defend it, he suggested.
Dr. Lober reported having no pertinent conflicts of interest.
MONTEREY, CALIF. — Have you searched for your name on the Internet? Your patients have.
“Your patients are Googling you,” and some of them probably are rating your performance as a doctor on one of the many physician-rating sites or generic rating sites, Dr. Clifford Warren Lober said. H
Here's the problem: The patients most likely to rate you are those who are livid at you, or those who think you walk on water. And it's not just patients who are posting comments about you, but previous patients, ex-employees, former spouses, or anyone else who knows you, said Dr. Lober, a dermatologist and attorney in Kissimmee, Fla.
Online comments may be made anonymously, persist for years on the Internet, be accessed by anyone with a computer, and be replicated on other Web sites beyond the original. If you discover comments about you that you think are harmful to your reputation, your attempts to remedy the situation may backfire and instead “optimize” the content by bringing more attention to the posted statement, amplifying its negativity, he said.
Legal remedies are few and complicated. “There is a morass of legal defenses and privileges that protect the offending person,” Dr. Lober said.
So how best to manage your online reputation? One strategy is to minimize the impact of negative online information by using search-engine optimization.
In practice, this means blitzing the Web with your own content to crowd out comments by others. “You want to occupy the first three pages of the rating sites” and the search-engine results pages if possible, Dr. Lober said, adding that most people don't look beyond the first three pages of results.
This can be done by establishing multiple Web sites, each with numerous internal page links, external high-traffic links, significant content on each of your home pages, and other features that make these the sites that show up when someone searches your name.
Establishing a deep social network presence helps, too. Create accounts on Facebook, Twitter, LinkedIn, ZoomInfo, Connectbeam, Yahoo Profile, Google Profile, MSN Profile, Wetpaint, Naymz, Jigsaw, Ning, and others, he suggested. Ideally, get on sites that feature RSS (Really Simple Syndication) feeds so that information posted on one site transfers to others.
Other prongs in this strategy include issuing press releases by using Internet publication sites, establishing one or more blogs in your name, and using pay-per-click advertising.
Sound overwhelming? Innovative entrepreneurs thought that it might, so a number of Internet reputation-management companies have formed to do some of this work for you'for a fee, of course. These include companies like Reputation Repair & Management, Internet Reputation Management, and ReputationDefender, Dr. Lober said.
If, instead, you want to try to get a specific offensive statement removed from the Web, seek legal counsel for guidance, Dr. Lober advised. First, the statement must be determined to meet the legal definition of defamation. If it does, the next step is to determine if the person who wrote it is covered by any one of several standard legal defenses. If that's not an issue, check the terms and conditions listed by the Internet service provider (ISP) of the site where the comment appeared, to see if the ISP made any promises or assurances about the content on the site. If you contact the ISP, it may take the comment down.
Normally, ISPs are immune from lawsuits over statements made by others on its service; they resemble telephone companies more than newspapers in that respect, he said.
You or your lawyer can request that the courts issue a subpoena to try to compel the person who made the statement (even an anonymous poster) to remedy the situation, but this process is time consuming and expensive, and the person who posted the comment may be difficult to locate, Dr. Lober cautioned.
And if you sue, the defendant may try to frame your action as a SLAPP (strategic litigation against public participation) suit intended to muzzle critics and restrict freedom of speech. Some states have anti-SLAPP laws that could leave you paying the defendant's attorney fees and costs, and make you vulnerable to a countersuit by the defendant. Better to try to “manage” your
Better to try to “manage” your online reputation than to try to legally defend it, he suggested.
Dr. Lober reported having no pertinent conflicts of interest.
Medical Home Payment Models to Be Tested
SAN FRANCISCO — Beginning in January 2011, federal agencies will identify and test various models of paying for health services in a patient-centered medical home.
The Centers for Medicaid and Medicare Services is charged by the 2010 Affordable Care Act to test innovative payment and service delivery models to reduce program spending while promoting quality care. The health care reform act specifies that models of care be chosen based on their ability to improve the coordination, quality, and efficiency of services, Dr. Xavier Sevilla said at the meeting.
The patient-centered medical home is one of the models to be tested, and the challenge lies in figuring out payment methods that will enable physician practices to provide comprehensive primary care that is accessible, continuous, family centered, coordinated with other caregivers, compassionate, and culturally effective, he said.
“I don't think we're going to see the private payers move until CMS does,” added Dr. Sevilla, chief of pediatrics for Manatee County Rural Health Services, Bradenton, Fla. He serves as the AAPcs representative to the National Committee for Quality Assurance Advisory Panel on the Physician Practice Connections – Patient-Centered Medical Home.
Today, however, the most common “resolution kit” available to physicians trying to resolve payment issues for the different kinds of work they do in patient-centered medical homes is a homemade sign with a circle around the words “Bang head here,” he joked. Current payment systems encourage quantity over quality and reward procedures over evaluation and management of patients, he said. Payments are made only for services administered by clinicians and cover only services performed in the office setting when the patient is present, which ignores care coordination and nonoffice communications with patients, such as e-mail.
The ideal payment system would incentivize care coordination and quality of care improvement. It would support the transformation of practices from individual to population-based care, from physician-provided to team-based care, and from episodic to continuous care, Dr. Sevilla said.
He described several payment proposals that could be tested in the demonstration programs, some of which already are underway in pilot projects.
One model retains existing fee-for-service contracts and adds a per-member-per-month case-management fee and pay-for-performance reimbursements using nationally validated quality measures of process and outcome. A Colorado-based pilot is testing this model in a Multistate Patient Centered Medical Home program.
This model could improve office efficiency and access, depending on the pay-for-performance measures, Dr. Sevilla said. The management fee supports non-office communications and nonphysician care, and allows the practice team to concentrate on the whole practice population. Fundamental practice changes are unlikely unless the management fee and payments for performance are large enough, he added. The management fee could allow small practices to join together to share costs. This payment model could bereasy to implement, because itsidds to the existing payment system.
Another model would keep the fee-for-service system but develop new CPT codes for medical home activities that currently are not reimbursed, such as phone and e-mail consultations, after-hours services, phone calls with specialists, and more. Currently, Blue Cross and Blue Shield of Michigan pays for practice-based care management, and Horizon Blue Cross and Blue Shield of New Jersey pays for phone calls to patients and specialists.
This model does not incentivize quality of care improvement or population-based care, hand the new CPT codes would need to include tasks performed by non-physicians to support a team approach. Many of the CPT codes needed for patient-centered medical homes exist, but are not recognized by most payeors, including the CMS. Adding more codes to the 8,000-code CPT system would increase complexity, and costs may not decrease if the codes are overused, Dr. Sevilla said.
A third model would provide monthly comprehensive payments based on yearly per-patient risk-adjusted calculations of per-patient-per-month reimbursements. Practices would receive up to 25% risk-adjusted bonuses for achieving goals in quality, cost, and patient experience.
To make this work, we'd need a validated actuarial model that predicts a patient's need for primary care and that provides a relative risk based on demographics and billing diagnoses, he said. The guaranteed monthly payment would cover the multidisciplinary team, technological infrastructure, and non–face-to-face communications.
“This would require a major culture change by payers and physicians,” Dr. Sevilla noted. Payeors would need to make up-front investments and change their basis for payment. The Capital District Physicians Health Plan in Albany, N.Y., is trying this payment model, he added.
Pediatricians can help move the medical system toward patient-centered medical homes by advocating for payment methods that support the medical home, lobbying the AAP to prioritize research on the value of pediatricians, and participating in one of the demonstrations of new payment methods, said Dr. Sevilla, who noted that he had no conflicts of interest.
SAN FRANCISCO — Beginning in January 2011, federal agencies will identify and test various models of paying for health services in a patient-centered medical home.
The Centers for Medicaid and Medicare Services is charged by the 2010 Affordable Care Act to test innovative payment and service delivery models to reduce program spending while promoting quality care. The health care reform act specifies that models of care be chosen based on their ability to improve the coordination, quality, and efficiency of services, Dr. Xavier Sevilla said at the meeting.
The patient-centered medical home is one of the models to be tested, and the challenge lies in figuring out payment methods that will enable physician practices to provide comprehensive primary care that is accessible, continuous, family centered, coordinated with other caregivers, compassionate, and culturally effective, he said.
“I don't think we're going to see the private payers move until CMS does,” added Dr. Sevilla, chief of pediatrics for Manatee County Rural Health Services, Bradenton, Fla. He serves as the AAPcs representative to the National Committee for Quality Assurance Advisory Panel on the Physician Practice Connections – Patient-Centered Medical Home.
Today, however, the most common “resolution kit” available to physicians trying to resolve payment issues for the different kinds of work they do in patient-centered medical homes is a homemade sign with a circle around the words “Bang head here,” he joked. Current payment systems encourage quantity over quality and reward procedures over evaluation and management of patients, he said. Payments are made only for services administered by clinicians and cover only services performed in the office setting when the patient is present, which ignores care coordination and nonoffice communications with patients, such as e-mail.
The ideal payment system would incentivize care coordination and quality of care improvement. It would support the transformation of practices from individual to population-based care, from physician-provided to team-based care, and from episodic to continuous care, Dr. Sevilla said.
He described several payment proposals that could be tested in the demonstration programs, some of which already are underway in pilot projects.
One model retains existing fee-for-service contracts and adds a per-member-per-month case-management fee and pay-for-performance reimbursements using nationally validated quality measures of process and outcome. A Colorado-based pilot is testing this model in a Multistate Patient Centered Medical Home program.
This model could improve office efficiency and access, depending on the pay-for-performance measures, Dr. Sevilla said. The management fee supports non-office communications and nonphysician care, and allows the practice team to concentrate on the whole practice population. Fundamental practice changes are unlikely unless the management fee and payments for performance are large enough, he added. The management fee could allow small practices to join together to share costs. This payment model could bereasy to implement, because itsidds to the existing payment system.
Another model would keep the fee-for-service system but develop new CPT codes for medical home activities that currently are not reimbursed, such as phone and e-mail consultations, after-hours services, phone calls with specialists, and more. Currently, Blue Cross and Blue Shield of Michigan pays for practice-based care management, and Horizon Blue Cross and Blue Shield of New Jersey pays for phone calls to patients and specialists.
This model does not incentivize quality of care improvement or population-based care, hand the new CPT codes would need to include tasks performed by non-physicians to support a team approach. Many of the CPT codes needed for patient-centered medical homes exist, but are not recognized by most payeors, including the CMS. Adding more codes to the 8,000-code CPT system would increase complexity, and costs may not decrease if the codes are overused, Dr. Sevilla said.
A third model would provide monthly comprehensive payments based on yearly per-patient risk-adjusted calculations of per-patient-per-month reimbursements. Practices would receive up to 25% risk-adjusted bonuses for achieving goals in quality, cost, and patient experience.
To make this work, we'd need a validated actuarial model that predicts a patient's need for primary care and that provides a relative risk based on demographics and billing diagnoses, he said. The guaranteed monthly payment would cover the multidisciplinary team, technological infrastructure, and non–face-to-face communications.
“This would require a major culture change by payers and physicians,” Dr. Sevilla noted. Payeors would need to make up-front investments and change their basis for payment. The Capital District Physicians Health Plan in Albany, N.Y., is trying this payment model, he added.
Pediatricians can help move the medical system toward patient-centered medical homes by advocating for payment methods that support the medical home, lobbying the AAP to prioritize research on the value of pediatricians, and participating in one of the demonstrations of new payment methods, said Dr. Sevilla, who noted that he had no conflicts of interest.
SAN FRANCISCO — Beginning in January 2011, federal agencies will identify and test various models of paying for health services in a patient-centered medical home.
The Centers for Medicaid and Medicare Services is charged by the 2010 Affordable Care Act to test innovative payment and service delivery models to reduce program spending while promoting quality care. The health care reform act specifies that models of care be chosen based on their ability to improve the coordination, quality, and efficiency of services, Dr. Xavier Sevilla said at the meeting.
The patient-centered medical home is one of the models to be tested, and the challenge lies in figuring out payment methods that will enable physician practices to provide comprehensive primary care that is accessible, continuous, family centered, coordinated with other caregivers, compassionate, and culturally effective, he said.
“I don't think we're going to see the private payers move until CMS does,” added Dr. Sevilla, chief of pediatrics for Manatee County Rural Health Services, Bradenton, Fla. He serves as the AAPcs representative to the National Committee for Quality Assurance Advisory Panel on the Physician Practice Connections – Patient-Centered Medical Home.
Today, however, the most common “resolution kit” available to physicians trying to resolve payment issues for the different kinds of work they do in patient-centered medical homes is a homemade sign with a circle around the words “Bang head here,” he joked. Current payment systems encourage quantity over quality and reward procedures over evaluation and management of patients, he said. Payments are made only for services administered by clinicians and cover only services performed in the office setting when the patient is present, which ignores care coordination and nonoffice communications with patients, such as e-mail.
The ideal payment system would incentivize care coordination and quality of care improvement. It would support the transformation of practices from individual to population-based care, from physician-provided to team-based care, and from episodic to continuous care, Dr. Sevilla said.
He described several payment proposals that could be tested in the demonstration programs, some of which already are underway in pilot projects.
One model retains existing fee-for-service contracts and adds a per-member-per-month case-management fee and pay-for-performance reimbursements using nationally validated quality measures of process and outcome. A Colorado-based pilot is testing this model in a Multistate Patient Centered Medical Home program.
This model could improve office efficiency and access, depending on the pay-for-performance measures, Dr. Sevilla said. The management fee supports non-office communications and nonphysician care, and allows the practice team to concentrate on the whole practice population. Fundamental practice changes are unlikely unless the management fee and payments for performance are large enough, he added. The management fee could allow small practices to join together to share costs. This payment model could bereasy to implement, because itsidds to the existing payment system.
Another model would keep the fee-for-service system but develop new CPT codes for medical home activities that currently are not reimbursed, such as phone and e-mail consultations, after-hours services, phone calls with specialists, and more. Currently, Blue Cross and Blue Shield of Michigan pays for practice-based care management, and Horizon Blue Cross and Blue Shield of New Jersey pays for phone calls to patients and specialists.
This model does not incentivize quality of care improvement or population-based care, hand the new CPT codes would need to include tasks performed by non-physicians to support a team approach. Many of the CPT codes needed for patient-centered medical homes exist, but are not recognized by most payeors, including the CMS. Adding more codes to the 8,000-code CPT system would increase complexity, and costs may not decrease if the codes are overused, Dr. Sevilla said.
A third model would provide monthly comprehensive payments based on yearly per-patient risk-adjusted calculations of per-patient-per-month reimbursements. Practices would receive up to 25% risk-adjusted bonuses for achieving goals in quality, cost, and patient experience.
To make this work, we'd need a validated actuarial model that predicts a patient's need for primary care and that provides a relative risk based on demographics and billing diagnoses, he said. The guaranteed monthly payment would cover the multidisciplinary team, technological infrastructure, and non–face-to-face communications.
“This would require a major culture change by payers and physicians,” Dr. Sevilla noted. Payeors would need to make up-front investments and change their basis for payment. The Capital District Physicians Health Plan in Albany, N.Y., is trying this payment model, he added.
Pediatricians can help move the medical system toward patient-centered medical homes by advocating for payment methods that support the medical home, lobbying the AAP to prioritize research on the value of pediatricians, and participating in one of the demonstrations of new payment methods, said Dr. Sevilla, who noted that he had no conflicts of interest.