User login
Climate Change May Bring More Skin Disease
LAS VEGAS - Some of the effects of climate change are beginning to appear in dermatologists' offices, and there may be more to come.
Expanded geographic ranges of tick and parasite vectors due to climate change already are pushing infectious diseases into unfamiliar territory, Dr. Sigfrid A. Muller said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
Lyme disease has spread well into Canada, and leishmaniasis is moving north from Mexico into Texas, Arizona, Oklahoma, and Ohio. Reports of Chagas disease are increasing in the United States and Central and South America. Peru and Ecuador are seeing more Carrion’s disease, he said.
Extreme heat, drought, and wide-scale fires, storms, and flooding, as well as other manifestations of climate change, will alter the incidence and severity of allergies, atopic dermatitis, and asthma, added Dr. Muller, a dermatologist in Las Vegas and chair of the International Society of Dermatology's Climate Change Task Force. The society, in 2009, declared climate change to be the defining dermatologic issue of the 21st century.
Global warming may be debated in the popular media, but there is little controversy about it in the scientific literature, he said. June 2010 was the warmest month on record (combining global land and ocean average surface temperatures) and the 304th consecutive month with a global temperature above the 20th-century average, according to the National Oceanic and Atmospheric Administration.
Scientists predict changes already underway will warm the planet at least 2 or 3 degrees Centigrade this century, and perhaps double or triple that if humans don't alter the behaviors that contribute to climate change. Current scientific estimates suggest that an increase of 2 degrees Centigrade may be the "tipping point" that triggers irreversible changes (such as methane release from melting permafrost) with unpredictable but severe consequences for the planet and its inhabitants, Dr. Muller said.
Some projected changes already are being seen in the extreme summer heat in western Russia, flooding in Pakistan, intense wildfires in Australia, and drought in regions of the United States and elsewhere. The patterns of resulting changes in some skin diseases from these conditions will vary regionally depending on altitude, latitude, storms, deforestation, desertification, urbanization, land use patterns, energy production, and transportation.
Dr. Muller highlighted changes in several diseases:
• Lyme disease. Lyme disease used to be limited to five U.S. geographic regions, but its geographic range has expanded into many areas of Canada as temperatures have become more hospitable to the rodents and deer that act as vectors and reservoirs, spreading into southern and northern Ontario, southern Québec, Manitoba, the Prairie Provinces, the Maritime Provinces, and British Columbia.
• Leishmaniasis. This vector-borne parasitic disease is endemic in most tropical regions of the world and has begun to expand northward as more habitats become suitable for the rodents and sand flies that act as vectors and reservoirs for Leishmaniasis. The parasite has been isolated from humans, dogs, rodents, and sand flies in Texas, Arizona, Oklahoma, and Ohio. Climate change will exacerbate this spread, especially into the east-central United States, Dr. Muller predicted.
• Chagas' disease. The protozoan that causes Chagas disease Trypanosoma cruzi is becoming more common in U.S. wildlife reservoirs, with prevalences increasing by 37% in opossums, by 47% in southeastern U.S. raccoons, and by 29% in Louisiana armadillos, he said. It is expected to spread into central U.S. regions if average temperatures rise by 1 degree Centigrade by 2030, as predicted. Few states require reporting of Chagas' disease, but the Food and Drug Administration in 2010 approved screening for the disease in blood, tissue, and organ donors.
• Carrion's disease. Children bear the brunt of this reemerging disease that has spread to new areas between the jungle and highlands of Peru and Ecuador. Changes in sea surface temperatures that triggered extreme seasonal rain patterns known as El Niño events in the 1980s and 1990s were associated with a nearly fourfold increase in Carrion's disease in Peru's Ancash region.
Dr. Muller urged dermatologists to join the International Society of Dermatology and attend its climate change conferences. Scientific, political, and public strategies are needed to help reduce human contributions to climate change and to plan adaptations to reduce damage caused by global warming, he said.
Dr. Muller said he has no relevant conflicts of interest.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Some of the effects of climate change are beginning to appear in dermatologists' offices, and there may be more to come.
Expanded geographic ranges of tick and parasite vectors due to climate change already are pushing infectious diseases into unfamiliar territory, Dr. Sigfrid A. Muller said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
Lyme disease has spread well into Canada, and leishmaniasis is moving north from Mexico into Texas, Arizona, Oklahoma, and Ohio. Reports of Chagas disease are increasing in the United States and Central and South America. Peru and Ecuador are seeing more Carrion’s disease, he said.
Extreme heat, drought, and wide-scale fires, storms, and flooding, as well as other manifestations of climate change, will alter the incidence and severity of allergies, atopic dermatitis, and asthma, added Dr. Muller, a dermatologist in Las Vegas and chair of the International Society of Dermatology's Climate Change Task Force. The society, in 2009, declared climate change to be the defining dermatologic issue of the 21st century.
Global warming may be debated in the popular media, but there is little controversy about it in the scientific literature, he said. June 2010 was the warmest month on record (combining global land and ocean average surface temperatures) and the 304th consecutive month with a global temperature above the 20th-century average, according to the National Oceanic and Atmospheric Administration.
Scientists predict changes already underway will warm the planet at least 2 or 3 degrees Centigrade this century, and perhaps double or triple that if humans don't alter the behaviors that contribute to climate change. Current scientific estimates suggest that an increase of 2 degrees Centigrade may be the "tipping point" that triggers irreversible changes (such as methane release from melting permafrost) with unpredictable but severe consequences for the planet and its inhabitants, Dr. Muller said.
Some projected changes already are being seen in the extreme summer heat in western Russia, flooding in Pakistan, intense wildfires in Australia, and drought in regions of the United States and elsewhere. The patterns of resulting changes in some skin diseases from these conditions will vary regionally depending on altitude, latitude, storms, deforestation, desertification, urbanization, land use patterns, energy production, and transportation.
Dr. Muller highlighted changes in several diseases:
• Lyme disease. Lyme disease used to be limited to five U.S. geographic regions, but its geographic range has expanded into many areas of Canada as temperatures have become more hospitable to the rodents and deer that act as vectors and reservoirs, spreading into southern and northern Ontario, southern Québec, Manitoba, the Prairie Provinces, the Maritime Provinces, and British Columbia.
• Leishmaniasis. This vector-borne parasitic disease is endemic in most tropical regions of the world and has begun to expand northward as more habitats become suitable for the rodents and sand flies that act as vectors and reservoirs for Leishmaniasis. The parasite has been isolated from humans, dogs, rodents, and sand flies in Texas, Arizona, Oklahoma, and Ohio. Climate change will exacerbate this spread, especially into the east-central United States, Dr. Muller predicted.
• Chagas' disease. The protozoan that causes Chagas disease Trypanosoma cruzi is becoming more common in U.S. wildlife reservoirs, with prevalences increasing by 37% in opossums, by 47% in southeastern U.S. raccoons, and by 29% in Louisiana armadillos, he said. It is expected to spread into central U.S. regions if average temperatures rise by 1 degree Centigrade by 2030, as predicted. Few states require reporting of Chagas' disease, but the Food and Drug Administration in 2010 approved screening for the disease in blood, tissue, and organ donors.
• Carrion's disease. Children bear the brunt of this reemerging disease that has spread to new areas between the jungle and highlands of Peru and Ecuador. Changes in sea surface temperatures that triggered extreme seasonal rain patterns known as El Niño events in the 1980s and 1990s were associated with a nearly fourfold increase in Carrion's disease in Peru's Ancash region.
Dr. Muller urged dermatologists to join the International Society of Dermatology and attend its climate change conferences. Scientific, political, and public strategies are needed to help reduce human contributions to climate change and to plan adaptations to reduce damage caused by global warming, he said.
Dr. Muller said he has no relevant conflicts of interest.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Some of the effects of climate change are beginning to appear in dermatologists' offices, and there may be more to come.
Expanded geographic ranges of tick and parasite vectors due to climate change already are pushing infectious diseases into unfamiliar territory, Dr. Sigfrid A. Muller said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
Lyme disease has spread well into Canada, and leishmaniasis is moving north from Mexico into Texas, Arizona, Oklahoma, and Ohio. Reports of Chagas disease are increasing in the United States and Central and South America. Peru and Ecuador are seeing more Carrion’s disease, he said.
Extreme heat, drought, and wide-scale fires, storms, and flooding, as well as other manifestations of climate change, will alter the incidence and severity of allergies, atopic dermatitis, and asthma, added Dr. Muller, a dermatologist in Las Vegas and chair of the International Society of Dermatology's Climate Change Task Force. The society, in 2009, declared climate change to be the defining dermatologic issue of the 21st century.
Global warming may be debated in the popular media, but there is little controversy about it in the scientific literature, he said. June 2010 was the warmest month on record (combining global land and ocean average surface temperatures) and the 304th consecutive month with a global temperature above the 20th-century average, according to the National Oceanic and Atmospheric Administration.
Scientists predict changes already underway will warm the planet at least 2 or 3 degrees Centigrade this century, and perhaps double or triple that if humans don't alter the behaviors that contribute to climate change. Current scientific estimates suggest that an increase of 2 degrees Centigrade may be the "tipping point" that triggers irreversible changes (such as methane release from melting permafrost) with unpredictable but severe consequences for the planet and its inhabitants, Dr. Muller said.
Some projected changes already are being seen in the extreme summer heat in western Russia, flooding in Pakistan, intense wildfires in Australia, and drought in regions of the United States and elsewhere. The patterns of resulting changes in some skin diseases from these conditions will vary regionally depending on altitude, latitude, storms, deforestation, desertification, urbanization, land use patterns, energy production, and transportation.
Dr. Muller highlighted changes in several diseases:
• Lyme disease. Lyme disease used to be limited to five U.S. geographic regions, but its geographic range has expanded into many areas of Canada as temperatures have become more hospitable to the rodents and deer that act as vectors and reservoirs, spreading into southern and northern Ontario, southern Québec, Manitoba, the Prairie Provinces, the Maritime Provinces, and British Columbia.
• Leishmaniasis. This vector-borne parasitic disease is endemic in most tropical regions of the world and has begun to expand northward as more habitats become suitable for the rodents and sand flies that act as vectors and reservoirs for Leishmaniasis. The parasite has been isolated from humans, dogs, rodents, and sand flies in Texas, Arizona, Oklahoma, and Ohio. Climate change will exacerbate this spread, especially into the east-central United States, Dr. Muller predicted.
• Chagas' disease. The protozoan that causes Chagas disease Trypanosoma cruzi is becoming more common in U.S. wildlife reservoirs, with prevalences increasing by 37% in opossums, by 47% in southeastern U.S. raccoons, and by 29% in Louisiana armadillos, he said. It is expected to spread into central U.S. regions if average temperatures rise by 1 degree Centigrade by 2030, as predicted. Few states require reporting of Chagas' disease, but the Food and Drug Administration in 2010 approved screening for the disease in blood, tissue, and organ donors.
• Carrion's disease. Children bear the brunt of this reemerging disease that has spread to new areas between the jungle and highlands of Peru and Ecuador. Changes in sea surface temperatures that triggered extreme seasonal rain patterns known as El Niño events in the 1980s and 1990s were associated with a nearly fourfold increase in Carrion's disease in Peru's Ancash region.
Dr. Muller urged dermatologists to join the International Society of Dermatology and attend its climate change conferences. Scientific, political, and public strategies are needed to help reduce human contributions to climate change and to plan adaptations to reduce damage caused by global warming, he said.
Dr. Muller said he has no relevant conflicts of interest.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Assess and Treat Cardiovascular Risk in Psoriasis
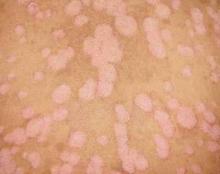
LAS VEGAS - Dermatologists may be doing patients with psoriasis a disservice if they don’t prescribe a good anti-inflammatory drug to reduce the risk of MI, according to Dr. Bruce E. Strober.
People with psoriasis are more likely to have comorbidities and behaviors associated with cardiovascular disease including smoking, alcohol misuse, hypertension, diabetes, dyslipidemia, and obesity. Dyslipidemia therapies that patients with psoriasis may take such as corticosteroids, acitretin, and cyclosporine can also increase cardiovascular risk.
Aside from these, psoriasis is independently associated with a higher risk for MI, stroke and death, probably due to the cardiovascular effects of uncontrolled inflammation, Dr. Strober said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
"You might say to a patient, this is a disease that has every bit as much an effect as hypertension on mortality. The data on hypertension are not even as impressive as this," said Dr. Strober of the department of dermatology at New York University. "Maybe this is a big deal that cardiologists need to think about. They are starting to catch on."
Rheumatoid arthritis studies show that methotrexate and tumor necrosis factor blockers reduce comorbid risks, and the same may be true for psoriasis. "That’s why I sometimes say methotrexate may have an overall net benefit when given to patients with severe psoriasis," he said. Any potential toxicity from methotrexate should be weighed against its potential cardiovascular advantages. A prospective, British population–based cohort study found that the incidence of MI was 3.6 per 1,000 patient-years among 556,995 control patients without psoriasis, 4.0 among 127,139 patients with mild psoriasis, and 5.1 among 3,837 patients with severe psoriasis after controlling for other cardiovascular risk factors (JAMA 2006;296:1735-41).
Younger patients with severe psoriasis had the greatest risk. The relative risk for MI with mild psoriasis was 1.3 in 30-year-olds and 1.1 in 60-year-olds. The relative risk for MI with severe psoriasis was 3.1 for 30-year-olds and 1.4 for 60-year-olds.
The study may have underestimated the cardiovascular risk of severe psoriasis by limiting the definition of severe disease to patients on systemic therapy, Dr. Strober added. Some with severe disease may have been assigned to the mild psoriasis category.
The most likely cause of this increased risk for MI is uncontrolled inflammation in systemic psoriasis, not unlike rheumatoid arthritis and lupus, which also are known to create MI risk, he said. Psoriasis has immune effects and creates a hyperinflammatory state. Uncontrolled inflammation leads to endothelial dysfunction and dyslipidemia.
A separate study of the same British database found that women and men with psoriasis died 3.5 years and 4.4 years, respectively, earlier than people without psoriasis after controlling for other risk factors for mortality (Arch. Dermatol. 2007;143:1493-99).
Other data sets have substantiated this concept in the Medicare population. "People with psoriasis die younger. We have to think of this as a disease that has a direct effect on mortality," Dr. Strober said.
Will dermatologists accept the role of primary screeners for comorbidities that increase the risk for cardiovascular disease and other problems? That remains to be seen, but the National Psoriasis Foundation’s 2008 clinical consensus statement provided guidance for dermatologists willing to screen (J. Am. Acad. Dermatol. 2008;58:1031-42).
Basic screening steps include assessing blood pressure and overweight or obese status and getting laboratory evaluations – a fasting comprehensive metabolic panel and fasting lipids. Physicians also should ask about use of alcohol, smoking, depression, and arthritis.
Comorbidities may make it harder to treat psoriasis, and vice versa, though data are sparse, Dr. Strober said. Obese patients, for example, may need larger doses of psoriasis medications. The hyperinflammatory state of psoriasis may make treating psoriasis difficult unless it's addressed, and conceivably make it more difficult to treat hypertension or dyslipidemia, but this has not been studied, he said.
Dr. Strober has received grants from or been a consultant, speaker or advisor for Abbott, Amgen, Centocor, Johnson & Johnson, Pfizer, and Celgene.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Dermatologists may be doing patients with psoriasis a disservice if they don’t prescribe a good anti-inflammatory drug to reduce the risk of MI, according to Dr. Bruce E. Strober.
People with psoriasis are more likely to have comorbidities and behaviors associated with cardiovascular disease including smoking, alcohol misuse, hypertension, diabetes, dyslipidemia, and obesity. Dyslipidemia therapies that patients with psoriasis may take such as corticosteroids, acitretin, and cyclosporine can also increase cardiovascular risk.
Aside from these, psoriasis is independently associated with a higher risk for MI, stroke and death, probably due to the cardiovascular effects of uncontrolled inflammation, Dr. Strober said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
"You might say to a patient, this is a disease that has every bit as much an effect as hypertension on mortality. The data on hypertension are not even as impressive as this," said Dr. Strober of the department of dermatology at New York University. "Maybe this is a big deal that cardiologists need to think about. They are starting to catch on."
Rheumatoid arthritis studies show that methotrexate and tumor necrosis factor blockers reduce comorbid risks, and the same may be true for psoriasis. "That’s why I sometimes say methotrexate may have an overall net benefit when given to patients with severe psoriasis," he said. Any potential toxicity from methotrexate should be weighed against its potential cardiovascular advantages. A prospective, British population–based cohort study found that the incidence of MI was 3.6 per 1,000 patient-years among 556,995 control patients without psoriasis, 4.0 among 127,139 patients with mild psoriasis, and 5.1 among 3,837 patients with severe psoriasis after controlling for other cardiovascular risk factors (JAMA 2006;296:1735-41).
Younger patients with severe psoriasis had the greatest risk. The relative risk for MI with mild psoriasis was 1.3 in 30-year-olds and 1.1 in 60-year-olds. The relative risk for MI with severe psoriasis was 3.1 for 30-year-olds and 1.4 for 60-year-olds.
The study may have underestimated the cardiovascular risk of severe psoriasis by limiting the definition of severe disease to patients on systemic therapy, Dr. Strober added. Some with severe disease may have been assigned to the mild psoriasis category.
The most likely cause of this increased risk for MI is uncontrolled inflammation in systemic psoriasis, not unlike rheumatoid arthritis and lupus, which also are known to create MI risk, he said. Psoriasis has immune effects and creates a hyperinflammatory state. Uncontrolled inflammation leads to endothelial dysfunction and dyslipidemia.
A separate study of the same British database found that women and men with psoriasis died 3.5 years and 4.4 years, respectively, earlier than people without psoriasis after controlling for other risk factors for mortality (Arch. Dermatol. 2007;143:1493-99).
Other data sets have substantiated this concept in the Medicare population. "People with psoriasis die younger. We have to think of this as a disease that has a direct effect on mortality," Dr. Strober said.
Will dermatologists accept the role of primary screeners for comorbidities that increase the risk for cardiovascular disease and other problems? That remains to be seen, but the National Psoriasis Foundation’s 2008 clinical consensus statement provided guidance for dermatologists willing to screen (J. Am. Acad. Dermatol. 2008;58:1031-42).
Basic screening steps include assessing blood pressure and overweight or obese status and getting laboratory evaluations – a fasting comprehensive metabolic panel and fasting lipids. Physicians also should ask about use of alcohol, smoking, depression, and arthritis.
Comorbidities may make it harder to treat psoriasis, and vice versa, though data are sparse, Dr. Strober said. Obese patients, for example, may need larger doses of psoriasis medications. The hyperinflammatory state of psoriasis may make treating psoriasis difficult unless it's addressed, and conceivably make it more difficult to treat hypertension or dyslipidemia, but this has not been studied, he said.
Dr. Strober has received grants from or been a consultant, speaker or advisor for Abbott, Amgen, Centocor, Johnson & Johnson, Pfizer, and Celgene.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Dermatologists may be doing patients with psoriasis a disservice if they don’t prescribe a good anti-inflammatory drug to reduce the risk of MI, according to Dr. Bruce E. Strober.
People with psoriasis are more likely to have comorbidities and behaviors associated with cardiovascular disease including smoking, alcohol misuse, hypertension, diabetes, dyslipidemia, and obesity. Dyslipidemia therapies that patients with psoriasis may take such as corticosteroids, acitretin, and cyclosporine can also increase cardiovascular risk.
Aside from these, psoriasis is independently associated with a higher risk for MI, stroke and death, probably due to the cardiovascular effects of uncontrolled inflammation, Dr. Strober said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
"You might say to a patient, this is a disease that has every bit as much an effect as hypertension on mortality. The data on hypertension are not even as impressive as this," said Dr. Strober of the department of dermatology at New York University. "Maybe this is a big deal that cardiologists need to think about. They are starting to catch on."
Rheumatoid arthritis studies show that methotrexate and tumor necrosis factor blockers reduce comorbid risks, and the same may be true for psoriasis. "That’s why I sometimes say methotrexate may have an overall net benefit when given to patients with severe psoriasis," he said. Any potential toxicity from methotrexate should be weighed against its potential cardiovascular advantages. A prospective, British population–based cohort study found that the incidence of MI was 3.6 per 1,000 patient-years among 556,995 control patients without psoriasis, 4.0 among 127,139 patients with mild psoriasis, and 5.1 among 3,837 patients with severe psoriasis after controlling for other cardiovascular risk factors (JAMA 2006;296:1735-41).
Younger patients with severe psoriasis had the greatest risk. The relative risk for MI with mild psoriasis was 1.3 in 30-year-olds and 1.1 in 60-year-olds. The relative risk for MI with severe psoriasis was 3.1 for 30-year-olds and 1.4 for 60-year-olds.
The study may have underestimated the cardiovascular risk of severe psoriasis by limiting the definition of severe disease to patients on systemic therapy, Dr. Strober added. Some with severe disease may have been assigned to the mild psoriasis category.
The most likely cause of this increased risk for MI is uncontrolled inflammation in systemic psoriasis, not unlike rheumatoid arthritis and lupus, which also are known to create MI risk, he said. Psoriasis has immune effects and creates a hyperinflammatory state. Uncontrolled inflammation leads to endothelial dysfunction and dyslipidemia.
A separate study of the same British database found that women and men with psoriasis died 3.5 years and 4.4 years, respectively, earlier than people without psoriasis after controlling for other risk factors for mortality (Arch. Dermatol. 2007;143:1493-99).
Other data sets have substantiated this concept in the Medicare population. "People with psoriasis die younger. We have to think of this as a disease that has a direct effect on mortality," Dr. Strober said.
Will dermatologists accept the role of primary screeners for comorbidities that increase the risk for cardiovascular disease and other problems? That remains to be seen, but the National Psoriasis Foundation’s 2008 clinical consensus statement provided guidance for dermatologists willing to screen (J. Am. Acad. Dermatol. 2008;58:1031-42).
Basic screening steps include assessing blood pressure and overweight or obese status and getting laboratory evaluations – a fasting comprehensive metabolic panel and fasting lipids. Physicians also should ask about use of alcohol, smoking, depression, and arthritis.
Comorbidities may make it harder to treat psoriasis, and vice versa, though data are sparse, Dr. Strober said. Obese patients, for example, may need larger doses of psoriasis medications. The hyperinflammatory state of psoriasis may make treating psoriasis difficult unless it's addressed, and conceivably make it more difficult to treat hypertension or dyslipidemia, but this has not been studied, he said.
Dr. Strober has received grants from or been a consultant, speaker or advisor for Abbott, Amgen, Centocor, Johnson & Johnson, Pfizer, and Celgene.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Assess and Treat Cardiovascular Risk in Psoriasis
LAS VEGAS – Dermatologists may be doing patients with psoriasis a disservice if they don’t prescribe a good anti-inflammatory drug to reduce the risk of MI, according to Dr. Bruce E. Strober.
People with psoriasis are more likely to have comorbidities and behaviors associated with cardiovascular disease including smoking, alcohol misuse, hypertension, diabetes, dyslipidemia, and obesity. Dyslipidemia therapies that patients with psoriasis may take such as corticosteroids, acitretin, and cyclosporine can also increase cardiovascular risk.
Aside from these, psoriasis is independently associated with a higher risk for MI, stroke and death, probably due to the cardiovascular effects of uncontrolled inflammation, Dr. Strober said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
"You might say to a patient, this is a disease that has every bit as much an effect as hypertension on mortality. The data on hypertension are not even as impressive as this," said Dr. Strober of the department of dermatology at New York University. "Maybe this is a big deal that cardiologists need to think about. They are starting to catch on."
Rheumatoid arthritis studies show that methotrexate and tumor necrosis factor blockers reduce comorbid risks, and the same may be true for psoriasis. "That’s why I sometimes say methotrexate may have an overall net benefit when given to patients with severe psoriasis," he said. Any potential toxicity from methotrexate should be weighed against its potential cardiovascular advantages. A prospective, British population–based cohort study found that the incidence of MI was 3.6 per 1,000 patient-years among 556,995 control patients without psoriasis, 4.0 among 127,139 patients with mild psoriasis, and 5.1 among 3,837 patients with severe psoriasis after controlling for other cardiovascular risk factors (JAMA 2006;296:1735-41).
Younger patients with severe psoriasis had the greatest risk. The relative risk for MI with mild psoriasis was 1.3 in 30-year-olds and 1.1 in 60-year-olds. The relative risk for MI with severe psoriasis was 3.1 for 30-year-olds and 1.4 for 60-year-olds.
The study may have underestimated the cardiovascular risk of severe psoriasis by limiting the definition of severe disease to patients on systemic therapy, Dr. Strober added. Some with severe disease may have been assigned to the mild psoriasis category.
The most likely cause of this increased risk for MI is uncontrolled inflammation in systemic psoriasis, not unlike rheumatoid arthritis and lupus, which also are known to create MI risk, he said. Psoriasis has immune effects and creates a hyperinflammatory state. Uncontrolled inflammation leads to endothelial dysfunction and dyslipidemia.
A separate study of the same British database found that women and men with psoriasis died 3.5 years and 4.4 years, respectively, earlier than people without psoriasis after controlling for other risk factors for mortality (Arch. Dermatol. 2007;143:1493-99).
Other data sets have substantiated this concept in the Medicare population. "People with psoriasis die younger. We have to think of this as a disease that has a direct effect on mortality," Dr. Strober said.
Will dermatologists accept the role of primary screeners for comorbidities that increase the risk for cardiovascular disease and other problems? That remains to be seen, but the National Psoriasis Foundation’s 2008 clinical consensus statement provided guidance for dermatologists willing to screen (J. Am. Acad. Dermatol. 2008;58:1031-42).
Basic screening steps include assessing blood pressure and overweight or obese status and getting laboratory evaluations – a fasting comprehensive metabolic panel and fasting lipids. Physicians also should ask about use of alcohol, smoking, depression, and arthritis.
Comorbidities may make it harder to treat psoriasis, and vice versa, though data are sparse, Dr. Strober said. Obese patients, for example, may need larger doses of psoriasis medications. The hyperinflammatory state of psoriasis may make treating psoriasis difficult unless it’s addressed, and conceivably make it more difficult to treat hypertension or dyslipidemia, but this has not been studied, he said.
Dr. Strober has received grants from or been a consultant, speaker or advisor for Abbott, Amgen, Centocor, Johnson & Johnson, Pfizer, and Celgene.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Dermatologists may be doing patients with psoriasis a disservice if they don’t prescribe a good anti-inflammatory drug to reduce the risk of MI, according to Dr. Bruce E. Strober.
People with psoriasis are more likely to have comorbidities and behaviors associated with cardiovascular disease including smoking, alcohol misuse, hypertension, diabetes, dyslipidemia, and obesity. Dyslipidemia therapies that patients with psoriasis may take such as corticosteroids, acitretin, and cyclosporine can also increase cardiovascular risk.
Aside from these, psoriasis is independently associated with a higher risk for MI, stroke and death, probably due to the cardiovascular effects of uncontrolled inflammation, Dr. Strober said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
"You might say to a patient, this is a disease that has every bit as much an effect as hypertension on mortality. The data on hypertension are not even as impressive as this," said Dr. Strober of the department of dermatology at New York University. "Maybe this is a big deal that cardiologists need to think about. They are starting to catch on."
Rheumatoid arthritis studies show that methotrexate and tumor necrosis factor blockers reduce comorbid risks, and the same may be true for psoriasis. "That’s why I sometimes say methotrexate may have an overall net benefit when given to patients with severe psoriasis," he said. Any potential toxicity from methotrexate should be weighed against its potential cardiovascular advantages. A prospective, British population–based cohort study found that the incidence of MI was 3.6 per 1,000 patient-years among 556,995 control patients without psoriasis, 4.0 among 127,139 patients with mild psoriasis, and 5.1 among 3,837 patients with severe psoriasis after controlling for other cardiovascular risk factors (JAMA 2006;296:1735-41).
Younger patients with severe psoriasis had the greatest risk. The relative risk for MI with mild psoriasis was 1.3 in 30-year-olds and 1.1 in 60-year-olds. The relative risk for MI with severe psoriasis was 3.1 for 30-year-olds and 1.4 for 60-year-olds.
The study may have underestimated the cardiovascular risk of severe psoriasis by limiting the definition of severe disease to patients on systemic therapy, Dr. Strober added. Some with severe disease may have been assigned to the mild psoriasis category.
The most likely cause of this increased risk for MI is uncontrolled inflammation in systemic psoriasis, not unlike rheumatoid arthritis and lupus, which also are known to create MI risk, he said. Psoriasis has immune effects and creates a hyperinflammatory state. Uncontrolled inflammation leads to endothelial dysfunction and dyslipidemia.
A separate study of the same British database found that women and men with psoriasis died 3.5 years and 4.4 years, respectively, earlier than people without psoriasis after controlling for other risk factors for mortality (Arch. Dermatol. 2007;143:1493-99).
Other data sets have substantiated this concept in the Medicare population. "People with psoriasis die younger. We have to think of this as a disease that has a direct effect on mortality," Dr. Strober said.
Will dermatologists accept the role of primary screeners for comorbidities that increase the risk for cardiovascular disease and other problems? That remains to be seen, but the National Psoriasis Foundation’s 2008 clinical consensus statement provided guidance for dermatologists willing to screen (J. Am. Acad. Dermatol. 2008;58:1031-42).
Basic screening steps include assessing blood pressure and overweight or obese status and getting laboratory evaluations – a fasting comprehensive metabolic panel and fasting lipids. Physicians also should ask about use of alcohol, smoking, depression, and arthritis.
Comorbidities may make it harder to treat psoriasis, and vice versa, though data are sparse, Dr. Strober said. Obese patients, for example, may need larger doses of psoriasis medications. The hyperinflammatory state of psoriasis may make treating psoriasis difficult unless it’s addressed, and conceivably make it more difficult to treat hypertension or dyslipidemia, but this has not been studied, he said.
Dr. Strober has received grants from or been a consultant, speaker or advisor for Abbott, Amgen, Centocor, Johnson & Johnson, Pfizer, and Celgene.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Dermatologists may be doing patients with psoriasis a disservice if they don’t prescribe a good anti-inflammatory drug to reduce the risk of MI, according to Dr. Bruce E. Strober.
People with psoriasis are more likely to have comorbidities and behaviors associated with cardiovascular disease including smoking, alcohol misuse, hypertension, diabetes, dyslipidemia, and obesity. Dyslipidemia therapies that patients with psoriasis may take such as corticosteroids, acitretin, and cyclosporine can also increase cardiovascular risk.
Aside from these, psoriasis is independently associated with a higher risk for MI, stroke and death, probably due to the cardiovascular effects of uncontrolled inflammation, Dr. Strober said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
"You might say to a patient, this is a disease that has every bit as much an effect as hypertension on mortality. The data on hypertension are not even as impressive as this," said Dr. Strober of the department of dermatology at New York University. "Maybe this is a big deal that cardiologists need to think about. They are starting to catch on."
Rheumatoid arthritis studies show that methotrexate and tumor necrosis factor blockers reduce comorbid risks, and the same may be true for psoriasis. "That’s why I sometimes say methotrexate may have an overall net benefit when given to patients with severe psoriasis," he said. Any potential toxicity from methotrexate should be weighed against its potential cardiovascular advantages. A prospective, British population–based cohort study found that the incidence of MI was 3.6 per 1,000 patient-years among 556,995 control patients without psoriasis, 4.0 among 127,139 patients with mild psoriasis, and 5.1 among 3,837 patients with severe psoriasis after controlling for other cardiovascular risk factors (JAMA 2006;296:1735-41).
Younger patients with severe psoriasis had the greatest risk. The relative risk for MI with mild psoriasis was 1.3 in 30-year-olds and 1.1 in 60-year-olds. The relative risk for MI with severe psoriasis was 3.1 for 30-year-olds and 1.4 for 60-year-olds.
The study may have underestimated the cardiovascular risk of severe psoriasis by limiting the definition of severe disease to patients on systemic therapy, Dr. Strober added. Some with severe disease may have been assigned to the mild psoriasis category.
The most likely cause of this increased risk for MI is uncontrolled inflammation in systemic psoriasis, not unlike rheumatoid arthritis and lupus, which also are known to create MI risk, he said. Psoriasis has immune effects and creates a hyperinflammatory state. Uncontrolled inflammation leads to endothelial dysfunction and dyslipidemia.
A separate study of the same British database found that women and men with psoriasis died 3.5 years and 4.4 years, respectively, earlier than people without psoriasis after controlling for other risk factors for mortality (Arch. Dermatol. 2007;143:1493-99).
Other data sets have substantiated this concept in the Medicare population. "People with psoriasis die younger. We have to think of this as a disease that has a direct effect on mortality," Dr. Strober said.
Will dermatologists accept the role of primary screeners for comorbidities that increase the risk for cardiovascular disease and other problems? That remains to be seen, but the National Psoriasis Foundation’s 2008 clinical consensus statement provided guidance for dermatologists willing to screen (J. Am. Acad. Dermatol. 2008;58:1031-42).
Basic screening steps include assessing blood pressure and overweight or obese status and getting laboratory evaluations – a fasting comprehensive metabolic panel and fasting lipids. Physicians also should ask about use of alcohol, smoking, depression, and arthritis.
Comorbidities may make it harder to treat psoriasis, and vice versa, though data are sparse, Dr. Strober said. Obese patients, for example, may need larger doses of psoriasis medications. The hyperinflammatory state of psoriasis may make treating psoriasis difficult unless it’s addressed, and conceivably make it more difficult to treat hypertension or dyslipidemia, but this has not been studied, he said.
Dr. Strober has received grants from or been a consultant, speaker or advisor for Abbott, Amgen, Centocor, Johnson & Johnson, Pfizer, and Celgene.
SDEF and this news organization are owned by Elsevier.
Climate Change May Result in More Skin Disease
LAS VEGAS – Some of the effects of climate change are beginning to appear in dermatologists’ offices, and there may be more to come.
Expanded geographic ranges of tick and parasite vectors due to climate change already are pushing infectious diseases into unfamiliar territory, Dr. Sigfrid A. Muller said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
Lyme disease has spread well into Canada, and leishmaniasis is moving north from Mexico into Texas, Arizona, Oklahoma, and Ohio. Reports of Chagas disease are increasing in the United States and Central and South America. Peru and Ecuador are seeing more Carrion’s disease, he said.
Extreme heat, drought, and wide-scale fires, storms, and flooding, as well as other manifestations of climate change, will alter the incidence and severity of allergies, atopic dermatitis, and asthma, added Dr. Muller, a dermatologist in Las Vegas and chair of the International Society of Dermatology’s Climate Change Task Force. The society, in 2009, declared climate change to be the defining dermatologic issue of the 21st century.
Global warming may be debated in the popular media, but there is little controversy about it in the scientific literature, he said. June 2010 was the warmest month on record (combining global land and ocean average surface temperatures) and the 304th consecutive month with a global temperature above the 20th-century average, according to the National Oceanic and Atmospheric Administration.
Scientists predict changes already underway will warm the planet at least 2 or 3 degrees Centigrade this century, and perhaps double or triple that if humans don’t alter the behaviors that contribute to climate change. Current scientific estimates suggest that an increase of 2 degrees Centigrade may be the "tipping point" that triggers irreversible changes (such as methane release from melting permafrost) with unpredictable but severe consequences for the planet and its inhabitants, Dr. Muller said.
Some projected changes already are being seen in the extreme summer heat in western Russia, flooding in Pakistan, intense wildfires in Australia, and drought in regions of the United States and elsewhere. The patterns of resulting changes in some skin diseases from these conditions will vary regionally depending on altitude, latitude, storms, deforestation, desertification, urbanization, land use patterns, energy production, and transportation.
Dr. Muller highlighted changes in several diseases:
• Lyme disease. Lyme disease used to be limited to five U.S. geographic regions, but its geographic range has expanded into many areas of Canada as temperatures have become more hospitable to the rodents and deer that act as vectors and reservoirs, spreading into southern and northern Ontario, southern Qu?bec, Manitoba, the Prairie Provinces, the Maritime Provinces, and British Columbia.
• Leishmaniasis. This vector-borne parasitic disease is endemic in most tropical regions of the world and has begun to expand northward as more habitats become suitable for the rodents and sand flies that act as vectors and reservoirs for Leishmaniasis. The parasite has been isolated from humans, dogs, rodents, and sand flies in Texas, Arizona, Oklahoma, and Ohio. Climate change will exacerbate this spread, especially into the east-central United States, Dr. Muller predicted.
• Chagas disease. The protozoan that causes Chagas disease Trypanosoma cruzi is becoming more common in U.S. wildlife reservoirs, with prevalences increasing by 37% in opossums, by 47% in southeastern U.S. raccoons, and by 29% in Louisiana armadillos, he said. It is expected to spread into central U.S. regions if average temperatures rise by 1 degree Centigrade by 2030, as predicted. Few states require reporting of Chagas disease, but the Food and Drug Administration in 2010 approved screening for the disease in blood, tissue, and organ donors.
• Carrion’s disease. Children bear the brunt of this reemerging disease that has spread to new areas between the jungle and highlands of Peru and Ecuador. Changes in sea surface temperatures that triggered extreme seasonal rain patterns known as El Niño events in the 1980s and 1990s were associated with a nearly fourfold increase in Carrion’s disease in Peru’s Ancash region.
Dr. Muller urged dermatologists to join the International Society of Dermatology and attend its climate change conferences. Scientific, political, and public strategies are needed to help reduce human contributions to climate change and to plan adaptations to reduce damage caused by global warming, he said.
Muller said he has no relevant conflicts of interest.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Some of the effects of climate change are beginning to appear in dermatologists’ offices, and there may be more to come.
Expanded geographic ranges of tick and parasite vectors due to climate change already are pushing infectious diseases into unfamiliar territory, Dr. Sigfrid A. Muller said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
Lyme disease has spread well into Canada, and leishmaniasis is moving north from Mexico into Texas, Arizona, Oklahoma, and Ohio. Reports of Chagas disease are increasing in the United States and Central and South America. Peru and Ecuador are seeing more Carrion’s disease, he said.
Extreme heat, drought, and wide-scale fires, storms, and flooding, as well as other manifestations of climate change, will alter the incidence and severity of allergies, atopic dermatitis, and asthma, added Dr. Muller, a dermatologist in Las Vegas and chair of the International Society of Dermatology’s Climate Change Task Force. The society, in 2009, declared climate change to be the defining dermatologic issue of the 21st century.
Global warming may be debated in the popular media, but there is little controversy about it in the scientific literature, he said. June 2010 was the warmest month on record (combining global land and ocean average surface temperatures) and the 304th consecutive month with a global temperature above the 20th-century average, according to the National Oceanic and Atmospheric Administration.
Scientists predict changes already underway will warm the planet at least 2 or 3 degrees Centigrade this century, and perhaps double or triple that if humans don’t alter the behaviors that contribute to climate change. Current scientific estimates suggest that an increase of 2 degrees Centigrade may be the "tipping point" that triggers irreversible changes (such as methane release from melting permafrost) with unpredictable but severe consequences for the planet and its inhabitants, Dr. Muller said.
Some projected changes already are being seen in the extreme summer heat in western Russia, flooding in Pakistan, intense wildfires in Australia, and drought in regions of the United States and elsewhere. The patterns of resulting changes in some skin diseases from these conditions will vary regionally depending on altitude, latitude, storms, deforestation, desertification, urbanization, land use patterns, energy production, and transportation.
Dr. Muller highlighted changes in several diseases:
• Lyme disease. Lyme disease used to be limited to five U.S. geographic regions, but its geographic range has expanded into many areas of Canada as temperatures have become more hospitable to the rodents and deer that act as vectors and reservoirs, spreading into southern and northern Ontario, southern Qu?bec, Manitoba, the Prairie Provinces, the Maritime Provinces, and British Columbia.
• Leishmaniasis. This vector-borne parasitic disease is endemic in most tropical regions of the world and has begun to expand northward as more habitats become suitable for the rodents and sand flies that act as vectors and reservoirs for Leishmaniasis. The parasite has been isolated from humans, dogs, rodents, and sand flies in Texas, Arizona, Oklahoma, and Ohio. Climate change will exacerbate this spread, especially into the east-central United States, Dr. Muller predicted.
• Chagas disease. The protozoan that causes Chagas disease Trypanosoma cruzi is becoming more common in U.S. wildlife reservoirs, with prevalences increasing by 37% in opossums, by 47% in southeastern U.S. raccoons, and by 29% in Louisiana armadillos, he said. It is expected to spread into central U.S. regions if average temperatures rise by 1 degree Centigrade by 2030, as predicted. Few states require reporting of Chagas disease, but the Food and Drug Administration in 2010 approved screening for the disease in blood, tissue, and organ donors.
• Carrion’s disease. Children bear the brunt of this reemerging disease that has spread to new areas between the jungle and highlands of Peru and Ecuador. Changes in sea surface temperatures that triggered extreme seasonal rain patterns known as El Niño events in the 1980s and 1990s were associated with a nearly fourfold increase in Carrion’s disease in Peru’s Ancash region.
Dr. Muller urged dermatologists to join the International Society of Dermatology and attend its climate change conferences. Scientific, political, and public strategies are needed to help reduce human contributions to climate change and to plan adaptations to reduce damage caused by global warming, he said.
Muller said he has no relevant conflicts of interest.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Some of the effects of climate change are beginning to appear in dermatologists’ offices, and there may be more to come.
Expanded geographic ranges of tick and parasite vectors due to climate change already are pushing infectious diseases into unfamiliar territory, Dr. Sigfrid A. Muller said at a dermatology seminar sponsored by Skin Disease Education Foundation (SDEF).
Lyme disease has spread well into Canada, and leishmaniasis is moving north from Mexico into Texas, Arizona, Oklahoma, and Ohio. Reports of Chagas disease are increasing in the United States and Central and South America. Peru and Ecuador are seeing more Carrion’s disease, he said.
Extreme heat, drought, and wide-scale fires, storms, and flooding, as well as other manifestations of climate change, will alter the incidence and severity of allergies, atopic dermatitis, and asthma, added Dr. Muller, a dermatologist in Las Vegas and chair of the International Society of Dermatology’s Climate Change Task Force. The society, in 2009, declared climate change to be the defining dermatologic issue of the 21st century.
Global warming may be debated in the popular media, but there is little controversy about it in the scientific literature, he said. June 2010 was the warmest month on record (combining global land and ocean average surface temperatures) and the 304th consecutive month with a global temperature above the 20th-century average, according to the National Oceanic and Atmospheric Administration.
Scientists predict changes already underway will warm the planet at least 2 or 3 degrees Centigrade this century, and perhaps double or triple that if humans don’t alter the behaviors that contribute to climate change. Current scientific estimates suggest that an increase of 2 degrees Centigrade may be the "tipping point" that triggers irreversible changes (such as methane release from melting permafrost) with unpredictable but severe consequences for the planet and its inhabitants, Dr. Muller said.
Some projected changes already are being seen in the extreme summer heat in western Russia, flooding in Pakistan, intense wildfires in Australia, and drought in regions of the United States and elsewhere. The patterns of resulting changes in some skin diseases from these conditions will vary regionally depending on altitude, latitude, storms, deforestation, desertification, urbanization, land use patterns, energy production, and transportation.
Dr. Muller highlighted changes in several diseases:
• Lyme disease. Lyme disease used to be limited to five U.S. geographic regions, but its geographic range has expanded into many areas of Canada as temperatures have become more hospitable to the rodents and deer that act as vectors and reservoirs, spreading into southern and northern Ontario, southern Qu?bec, Manitoba, the Prairie Provinces, the Maritime Provinces, and British Columbia.
• Leishmaniasis. This vector-borne parasitic disease is endemic in most tropical regions of the world and has begun to expand northward as more habitats become suitable for the rodents and sand flies that act as vectors and reservoirs for Leishmaniasis. The parasite has been isolated from humans, dogs, rodents, and sand flies in Texas, Arizona, Oklahoma, and Ohio. Climate change will exacerbate this spread, especially into the east-central United States, Dr. Muller predicted.
• Chagas disease. The protozoan that causes Chagas disease Trypanosoma cruzi is becoming more common in U.S. wildlife reservoirs, with prevalences increasing by 37% in opossums, by 47% in southeastern U.S. raccoons, and by 29% in Louisiana armadillos, he said. It is expected to spread into central U.S. regions if average temperatures rise by 1 degree Centigrade by 2030, as predicted. Few states require reporting of Chagas disease, but the Food and Drug Administration in 2010 approved screening for the disease in blood, tissue, and organ donors.
• Carrion’s disease. Children bear the brunt of this reemerging disease that has spread to new areas between the jungle and highlands of Peru and Ecuador. Changes in sea surface temperatures that triggered extreme seasonal rain patterns known as El Niño events in the 1980s and 1990s were associated with a nearly fourfold increase in Carrion’s disease in Peru’s Ancash region.
Dr. Muller urged dermatologists to join the International Society of Dermatology and attend its climate change conferences. Scientific, political, and public strategies are needed to help reduce human contributions to climate change and to plan adaptations to reduce damage caused by global warming, he said.
Muller said he has no relevant conflicts of interest.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Patch Testing Still Possible With Immunosuppressive Therapy
LAS VEGAS – Immunosuppressive drug therapy is not an absolute contraindication for allergy patch testing, according to Dr. Joseph F. Fowler Jr.
A recent report on 11 patients who underwent patch testing while on a variety of systemic immunosuppressive drugs suggested patch testing may be more successful than many clinicians think, Dr. Fowler said. Speaking at the seminar sponsored by Skin Disease Education Foundation (SDEF), he fleshed out the findings with advice from his own experience in patch testing patients on immunosuppressives.
The retrospective chart review included patients on prednisone, cyclosporine, mycophenolate mofetil, or infliximab (Dermatitis 2009;20:265-70).
All but one of the patients who were taking 10 mg/day of prednisone had positive patch test reactions, said Dr. Fowler of the University of Louisville (Ky.) and president of the North American Contact Dermatitis Group.
"In the past, we had thought that about 10 mg/day was the maximum" prednisone dose that could still allow successful patch testing, but this belief was based on extrapolations of animal studies and case reports, with no hard data, he said. "I have personally seen patients who are on higher doses of prednisone produce good positive reactions."
Ideally, though, it’s best to patch test when patients are off prednisone, or on doses of 10 mg/day or less, he added. "If you could get them on every-other-day prednisone dosing, that would be even better."
For an untreated patient with fairly bad dermatitis, especially on the back, Dr. Fowler may treat for 5-7 days with a corticosteroid, perhaps prednisone 40-60 mg/day with no taper, and then stop the corticosteroid for 2-3 days before patch testing. "That’s one way you can get a person clear enough to patch test them if they’re already broken out," he said.
If the patient already is on chronic corticosteroid therapy, he tries to reduce the dose to 10 mg/day or less for several weeks before patch testing.
Dr. Fowler was surprised patients in the report who were being treated with cyclosporine 200 or 300 mg/day all had positive reactions to patch testing. "Generally, we expect cyclosporine to reduce the likelihood of positive reactions because of its broad immunosuppressant effect," he said. "These folks were on relatively low doses, so maybe that was a factor." In his own experience, Dr. Fowler said he has rarely seen positive reactions to patch testing in patients on cyclosporine, "so I think that’s problematic," he added.
One patient on mycophenolate (CellCept) 2 g/day had a negative result when patch tested but then stopped the drug and had a positive reaction on repeat patch testing. "That would suggest that the CellCept suppressed reactions," Dr. Fowler said. He advised not patch testing patients who are on CellCept, cyclosporine, tacrolimus, or azathioprine if at all possible.
One patient on infliximab (Remicade) whose last infusion occurred 3 weeks before patch testing developed multiple positive reactions. "That mirrors what I’ve been perceiving in clinical practice," he said.
Use of methotrexate or tumor necrosis factor–alpha inhibitors such as Remicade or etanercept (Enbrel) should not prevent patch testing. "I’ve had no problem patch testing people on methotrexate," Dr. Fowler said.
The report did not include antihistamines, which also are not a barrier to patch testing. "Other docs, allergists especially, tell patients they can’t take antihistamines when they’re being patch tested," he explained. "They may not be able to take antihistamines and get a good scratch test result, but remember in patch testing you’re looking at a T cell–mediated process. Antihistamines have essentially no effect on that."
Dr. Fowler has been a consultant, speaker, or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova, Ranbaxy, Shire, Stiefel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Immunosuppressive drug therapy is not an absolute contraindication for allergy patch testing, according to Dr. Joseph F. Fowler Jr.
A recent report on 11 patients who underwent patch testing while on a variety of systemic immunosuppressive drugs suggested patch testing may be more successful than many clinicians think, Dr. Fowler said. Speaking at the seminar sponsored by Skin Disease Education Foundation (SDEF), he fleshed out the findings with advice from his own experience in patch testing patients on immunosuppressives.
The retrospective chart review included patients on prednisone, cyclosporine, mycophenolate mofetil, or infliximab (Dermatitis 2009;20:265-70).
All but one of the patients who were taking 10 mg/day of prednisone had positive patch test reactions, said Dr. Fowler of the University of Louisville (Ky.) and president of the North American Contact Dermatitis Group.
"In the past, we had thought that about 10 mg/day was the maximum" prednisone dose that could still allow successful patch testing, but this belief was based on extrapolations of animal studies and case reports, with no hard data, he said. "I have personally seen patients who are on higher doses of prednisone produce good positive reactions."
Ideally, though, it’s best to patch test when patients are off prednisone, or on doses of 10 mg/day or less, he added. "If you could get them on every-other-day prednisone dosing, that would be even better."
For an untreated patient with fairly bad dermatitis, especially on the back, Dr. Fowler may treat for 5-7 days with a corticosteroid, perhaps prednisone 40-60 mg/day with no taper, and then stop the corticosteroid for 2-3 days before patch testing. "That’s one way you can get a person clear enough to patch test them if they’re already broken out," he said.
If the patient already is on chronic corticosteroid therapy, he tries to reduce the dose to 10 mg/day or less for several weeks before patch testing.
Dr. Fowler was surprised patients in the report who were being treated with cyclosporine 200 or 300 mg/day all had positive reactions to patch testing. "Generally, we expect cyclosporine to reduce the likelihood of positive reactions because of its broad immunosuppressant effect," he said. "These folks were on relatively low doses, so maybe that was a factor." In his own experience, Dr. Fowler said he has rarely seen positive reactions to patch testing in patients on cyclosporine, "so I think that’s problematic," he added.
One patient on mycophenolate (CellCept) 2 g/day had a negative result when patch tested but then stopped the drug and had a positive reaction on repeat patch testing. "That would suggest that the CellCept suppressed reactions," Dr. Fowler said. He advised not patch testing patients who are on CellCept, cyclosporine, tacrolimus, or azathioprine if at all possible.
One patient on infliximab (Remicade) whose last infusion occurred 3 weeks before patch testing developed multiple positive reactions. "That mirrors what I’ve been perceiving in clinical practice," he said.
Use of methotrexate or tumor necrosis factor–alpha inhibitors such as Remicade or etanercept (Enbrel) should not prevent patch testing. "I’ve had no problem patch testing people on methotrexate," Dr. Fowler said.
The report did not include antihistamines, which also are not a barrier to patch testing. "Other docs, allergists especially, tell patients they can’t take antihistamines when they’re being patch tested," he explained. "They may not be able to take antihistamines and get a good scratch test result, but remember in patch testing you’re looking at a T cell–mediated process. Antihistamines have essentially no effect on that."
Dr. Fowler has been a consultant, speaker, or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova, Ranbaxy, Shire, Stiefel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Immunosuppressive drug therapy is not an absolute contraindication for allergy patch testing, according to Dr. Joseph F. Fowler Jr.
A recent report on 11 patients who underwent patch testing while on a variety of systemic immunosuppressive drugs suggested patch testing may be more successful than many clinicians think, Dr. Fowler said. Speaking at the seminar sponsored by Skin Disease Education Foundation (SDEF), he fleshed out the findings with advice from his own experience in patch testing patients on immunosuppressives.
The retrospective chart review included patients on prednisone, cyclosporine, mycophenolate mofetil, or infliximab (Dermatitis 2009;20:265-70).
All but one of the patients who were taking 10 mg/day of prednisone had positive patch test reactions, said Dr. Fowler of the University of Louisville (Ky.) and president of the North American Contact Dermatitis Group.
"In the past, we had thought that about 10 mg/day was the maximum" prednisone dose that could still allow successful patch testing, but this belief was based on extrapolations of animal studies and case reports, with no hard data, he said. "I have personally seen patients who are on higher doses of prednisone produce good positive reactions."
Ideally, though, it’s best to patch test when patients are off prednisone, or on doses of 10 mg/day or less, he added. "If you could get them on every-other-day prednisone dosing, that would be even better."
For an untreated patient with fairly bad dermatitis, especially on the back, Dr. Fowler may treat for 5-7 days with a corticosteroid, perhaps prednisone 40-60 mg/day with no taper, and then stop the corticosteroid for 2-3 days before patch testing. "That’s one way you can get a person clear enough to patch test them if they’re already broken out," he said.
If the patient already is on chronic corticosteroid therapy, he tries to reduce the dose to 10 mg/day or less for several weeks before patch testing.
Dr. Fowler was surprised patients in the report who were being treated with cyclosporine 200 or 300 mg/day all had positive reactions to patch testing. "Generally, we expect cyclosporine to reduce the likelihood of positive reactions because of its broad immunosuppressant effect," he said. "These folks were on relatively low doses, so maybe that was a factor." In his own experience, Dr. Fowler said he has rarely seen positive reactions to patch testing in patients on cyclosporine, "so I think that’s problematic," he added.
One patient on mycophenolate (CellCept) 2 g/day had a negative result when patch tested but then stopped the drug and had a positive reaction on repeat patch testing. "That would suggest that the CellCept suppressed reactions," Dr. Fowler said. He advised not patch testing patients who are on CellCept, cyclosporine, tacrolimus, or azathioprine if at all possible.
One patient on infliximab (Remicade) whose last infusion occurred 3 weeks before patch testing developed multiple positive reactions. "That mirrors what I’ve been perceiving in clinical practice," he said.
Use of methotrexate or tumor necrosis factor–alpha inhibitors such as Remicade or etanercept (Enbrel) should not prevent patch testing. "I’ve had no problem patch testing people on methotrexate," Dr. Fowler said.
The report did not include antihistamines, which also are not a barrier to patch testing. "Other docs, allergists especially, tell patients they can’t take antihistamines when they’re being patch tested," he explained. "They may not be able to take antihistamines and get a good scratch test result, but remember in patch testing you’re looking at a T cell–mediated process. Antihistamines have essentially no effect on that."
Dr. Fowler has been a consultant, speaker, or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova, Ranbaxy, Shire, Stiefel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Patch Testing Still Possible With Immunosuppressive Therapy
LAS VEGAS – Immunosuppressive drug therapy is not an absolute contraindication for allergy patch testing, according to Dr. Joseph F. Fowler Jr.
A recent report on 11 patients who underwent patch testing while on a variety of systemic immunosuppressive drugs suggested patch testing may be more successful than many clinicians think, Dr. Fowler said. Speaking at the seminar sponsored by Skin Disease Education Foundation (SDEF), he fleshed out the findings with advice from his own experience in patch testing patients on immunosuppressives.
The retrospective chart review included patients on prednisone, cyclosporine, mycophenolate mofetil, or infliximab (Dermatitis 2009;20:265-70).
All but one of the patients who were taking 10 mg/day of prednisone had positive patch test reactions, said Dr. Fowler of the University of Louisville (Ky.) and president of the North American Contact Dermatitis Group.
"In the past, we had thought that about 10 mg/day was the maximum" prednisone dose that could still allow successful patch testing, but this belief was based on extrapolations of animal studies and case reports, with no hard data, he said. "I have personally seen patients who are on higher doses of prednisone produce good positive reactions."
Ideally, though, it’s best to patch test when patients are off prednisone, or on doses of 10 mg/day or less, he added. "If you could get them on every-other-day prednisone dosing, that would be even better."
For an untreated patient with fairly bad dermatitis, especially on the back, Dr. Fowler may treat for 5-7 days with a corticosteroid, perhaps prednisone 40-60 mg/day with no taper, and then stop the corticosteroid for 2-3 days before patch testing. "That’s one way you can get a person clear enough to patch test them if they’re already broken out," he said.
If the patient already is on chronic corticosteroid therapy, he tries to reduce the dose to 10 mg/day or less for several weeks before patch testing.
Dr. Fowler was surprised patients in the report who were being treated with cyclosporine 200 or 300 mg/day all had positive reactions to patch testing. "Generally, we expect cyclosporine to reduce the likelihood of positive reactions because of its broad immunosuppressant effect," he said. "These folks were on relatively low doses, so maybe that was a factor." In his own experience, Dr. Fowler said he has rarely seen positive reactions to patch testing in patients on cyclosporine, "so I think that’s problematic," he added.
One patient on mycophenolate (CellCept) 2 g/day had a negative result when patch tested but then stopped the drug and had a positive reaction on repeat patch testing. "That would suggest that the CellCept suppressed reactions," Dr. Fowler said. He advised not patch testing patients who are on CellCept, cyclosporine, tacrolimus, or azathioprine if at all possible.
One patient on infliximab (Remicade) whose last infusion occurred 3 weeks before patch testing developed multiple positive reactions. "That mirrors what I’ve been perceiving in clinical practice," he said.
Use of methotrexate or tumor necrosis factor–alpha inhibitors such as Remicade or etanercept (Enbrel) should not prevent patch testing. "I’ve had no problem patch testing people on methotrexate," Dr. Fowler said.
The report did not include antihistamines, which also are not a barrier to patch testing. "Other docs, allergists especially, tell patients they can’t take antihistamines when they’re being patch tested," he explained. "They may not be able to take antihistamines and get a good scratch test result, but remember in patch testing you’re looking at a T cell–mediated process. Antihistamines have essentially no effect on that."
Dr. Fowler has been a consultant, speaker, or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova, Ranbaxy, Shire, Stiefel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Immunosuppressive drug therapy is not an absolute contraindication for allergy patch testing, according to Dr. Joseph F. Fowler Jr.
A recent report on 11 patients who underwent patch testing while on a variety of systemic immunosuppressive drugs suggested patch testing may be more successful than many clinicians think, Dr. Fowler said. Speaking at the seminar sponsored by Skin Disease Education Foundation (SDEF), he fleshed out the findings with advice from his own experience in patch testing patients on immunosuppressives.
The retrospective chart review included patients on prednisone, cyclosporine, mycophenolate mofetil, or infliximab (Dermatitis 2009;20:265-70).
All but one of the patients who were taking 10 mg/day of prednisone had positive patch test reactions, said Dr. Fowler of the University of Louisville (Ky.) and president of the North American Contact Dermatitis Group.
"In the past, we had thought that about 10 mg/day was the maximum" prednisone dose that could still allow successful patch testing, but this belief was based on extrapolations of animal studies and case reports, with no hard data, he said. "I have personally seen patients who are on higher doses of prednisone produce good positive reactions."
Ideally, though, it’s best to patch test when patients are off prednisone, or on doses of 10 mg/day or less, he added. "If you could get them on every-other-day prednisone dosing, that would be even better."
For an untreated patient with fairly bad dermatitis, especially on the back, Dr. Fowler may treat for 5-7 days with a corticosteroid, perhaps prednisone 40-60 mg/day with no taper, and then stop the corticosteroid for 2-3 days before patch testing. "That’s one way you can get a person clear enough to patch test them if they’re already broken out," he said.
If the patient already is on chronic corticosteroid therapy, he tries to reduce the dose to 10 mg/day or less for several weeks before patch testing.
Dr. Fowler was surprised patients in the report who were being treated with cyclosporine 200 or 300 mg/day all had positive reactions to patch testing. "Generally, we expect cyclosporine to reduce the likelihood of positive reactions because of its broad immunosuppressant effect," he said. "These folks were on relatively low doses, so maybe that was a factor." In his own experience, Dr. Fowler said he has rarely seen positive reactions to patch testing in patients on cyclosporine, "so I think that’s problematic," he added.
One patient on mycophenolate (CellCept) 2 g/day had a negative result when patch tested but then stopped the drug and had a positive reaction on repeat patch testing. "That would suggest that the CellCept suppressed reactions," Dr. Fowler said. He advised not patch testing patients who are on CellCept, cyclosporine, tacrolimus, or azathioprine if at all possible.
One patient on infliximab (Remicade) whose last infusion occurred 3 weeks before patch testing developed multiple positive reactions. "That mirrors what I’ve been perceiving in clinical practice," he said.
Use of methotrexate or tumor necrosis factor–alpha inhibitors such as Remicade or etanercept (Enbrel) should not prevent patch testing. "I’ve had no problem patch testing people on methotrexate," Dr. Fowler said.
The report did not include antihistamines, which also are not a barrier to patch testing. "Other docs, allergists especially, tell patients they can’t take antihistamines when they’re being patch tested," he explained. "They may not be able to take antihistamines and get a good scratch test result, but remember in patch testing you’re looking at a T cell–mediated process. Antihistamines have essentially no effect on that."
Dr. Fowler has been a consultant, speaker, or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova, Ranbaxy, Shire, Stiefel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Immunosuppressive drug therapy is not an absolute contraindication for allergy patch testing, according to Dr. Joseph F. Fowler Jr.
A recent report on 11 patients who underwent patch testing while on a variety of systemic immunosuppressive drugs suggested patch testing may be more successful than many clinicians think, Dr. Fowler said. Speaking at the seminar sponsored by Skin Disease Education Foundation (SDEF), he fleshed out the findings with advice from his own experience in patch testing patients on immunosuppressives.
The retrospective chart review included patients on prednisone, cyclosporine, mycophenolate mofetil, or infliximab (Dermatitis 2009;20:265-70).
All but one of the patients who were taking 10 mg/day of prednisone had positive patch test reactions, said Dr. Fowler of the University of Louisville (Ky.) and president of the North American Contact Dermatitis Group.
"In the past, we had thought that about 10 mg/day was the maximum" prednisone dose that could still allow successful patch testing, but this belief was based on extrapolations of animal studies and case reports, with no hard data, he said. "I have personally seen patients who are on higher doses of prednisone produce good positive reactions."
Ideally, though, it’s best to patch test when patients are off prednisone, or on doses of 10 mg/day or less, he added. "If you could get them on every-other-day prednisone dosing, that would be even better."
For an untreated patient with fairly bad dermatitis, especially on the back, Dr. Fowler may treat for 5-7 days with a corticosteroid, perhaps prednisone 40-60 mg/day with no taper, and then stop the corticosteroid for 2-3 days before patch testing. "That’s one way you can get a person clear enough to patch test them if they’re already broken out," he said.
If the patient already is on chronic corticosteroid therapy, he tries to reduce the dose to 10 mg/day or less for several weeks before patch testing.
Dr. Fowler was surprised patients in the report who were being treated with cyclosporine 200 or 300 mg/day all had positive reactions to patch testing. "Generally, we expect cyclosporine to reduce the likelihood of positive reactions because of its broad immunosuppressant effect," he said. "These folks were on relatively low doses, so maybe that was a factor." In his own experience, Dr. Fowler said he has rarely seen positive reactions to patch testing in patients on cyclosporine, "so I think that’s problematic," he added.
One patient on mycophenolate (CellCept) 2 g/day had a negative result when patch tested but then stopped the drug and had a positive reaction on repeat patch testing. "That would suggest that the CellCept suppressed reactions," Dr. Fowler said. He advised not patch testing patients who are on CellCept, cyclosporine, tacrolimus, or azathioprine if at all possible.
One patient on infliximab (Remicade) whose last infusion occurred 3 weeks before patch testing developed multiple positive reactions. "That mirrors what I’ve been perceiving in clinical practice," he said.
Use of methotrexate or tumor necrosis factor–alpha inhibitors such as Remicade or etanercept (Enbrel) should not prevent patch testing. "I’ve had no problem patch testing people on methotrexate," Dr. Fowler said.
The report did not include antihistamines, which also are not a barrier to patch testing. "Other docs, allergists especially, tell patients they can’t take antihistamines when they’re being patch tested," he explained. "They may not be able to take antihistamines and get a good scratch test result, but remember in patch testing you’re looking at a T cell–mediated process. Antihistamines have essentially no effect on that."
Dr. Fowler has been a consultant, speaker, or researcher for Coria, Galderma, Graceway, Hyland, Johnson & Johnson, Quinnova, Ranbaxy, Shire, Stiefel, Triax, UCB, Medicis, Novartis, Abbott, Taro, Allerderm, Allergan, Amgen, Astellas, Centocor, Dermik, Dow, Genentech, Taisho, and 3M.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Take the Phototherapy for Psoriasis Quiz
LAS VEGAS - Practical phototherapy means not thinking strictly in terms of protocols, according to Dr. Kenneth B. Gordon.
Many protocols have been published for psoriasis phototherapy, and good ones were published by the American Academy of Dermatology in early 2010 (J. Amer. Acad. Dermatol. 2010;62:114-35), said Dr. Gordon of the University of Chicago. The guidelines emphasize tailoring therapy to meet the individual patient’s needs, and physicians should consider the best treatment for each patient.
"Simple, published protocols are not sufficient if you really do phototherapy," Dr. Gordon said.
He challenged the audience members with a quiz to test their knowledge of practical phototherapy in particular cases. The cases excluded patients with psoriatic arthritis.
"There are no right answers to these questions," Dr. Gordon said. "There are some wrong answers to these questions, however."
The Quiz Cases
– Case 1: What method of phototherapy would you use to treat a young woman with limited plaque psoriasis, primarily on her elbows? (a) Whole-body narrow-band UVB, (b) Targeted narrow-band-UVB with excimer laser, or (c) Topical psoralen plus long-wave UVA (PUVA).
– Case 2: What type of phototherapy would you use for a 50-year-old woman with extensive plaque psoriasis and type II skin who has not responded to topical therapy? She lives across the street from your office, can come for treatment in the middle of the day, and has no copay on her insurance. (a) Targeted narrow-band UVB, (b) Broad-band UVB, (c) Narrow-band UVB, (d) Retinoids plus UVB, or (e) PUVA.
– Case 3: How would you treat an 18-year-old man having an acute outbreak of guttate psoriasis, with explosive small plaques all over the body? (a) Narrow-band UVB with expectation for short-term treatment, (b) Narrow-band UVB with expectation of long-term maintenance, (c) PUVA, or (d) Biologic immunotherapy.
– Case 4: What’s the best phototherapy for a 59-year-old woman with palmar psoriasis that is interfering with her family business, a packing company? (a) Targeted narrow-band UVB phototherapy using an excimer laser, (b) Phototherapy using a using a hand-foot narrow-band UVB unit, (c) Oral PUVA with a hand-foot UVA unit, or (d) Topical PUVA with a hand-foot UVA unit.
– Case 5: Which phototherapy would you choose for a 53-year-old man with extensive plaque psoriasis with big, thick plaques, including many on his back? (a) Targeted UVB with excimer laser, (b) Narrow-band UVB, (c) Retinoids plus narrow-band UVB, or (d) PUVA.
– Case 6: How would you treat a 52-year-old man with type I skin who has had plaque psoriasis for years but has become erythrodermic over the past 6 months? (a) Narrow-band UVB, (b) Retinoids plus UVB, (c) PUVA, (d) Targeted phototherapy with excimer laser, or (e) None of the above.
Answers
– Case 1: Dr. Gordon said he would choose (b) Targeted narrow-band UVB with excimer laser, although topical PUVA may be the solution sometimes, he added.
Targeted narrow-band UVB with excimer laser is "not so easy," he cautioned. On the plus side, two or three treatments per week for 6-12 weeks have a high chance of success, with more than 75% of patients achieving a Psoriasis Area and Severity Index (PASI) score of 75, or even better if you treat with higher-than-usual fluences. This method only treats involved areas and avoids treating normal skin. Perhaps more than half of patients will have long-term clearing of those limited areas at 1 year after treatment.
On the down side, severe and permanent hyperpigmentation is always a risk with the excimer laser, particularly when higher fluences are used, so it’s important to discuss this with patients when considering targeted UVB therapy. There also may be temporary blistering and pain.
"Application to extensive body surface areas is, in a scientific word, silly," Dr. Gordon said. "I bring that up because I have people in our community who are using it for people who have 20%-30% body surface area involved in psoriasis." In those cases, it’s better to refer the patient for other therapy or consider alternatives such as topical treatments or intralesional injections.
– Case 2: Broad-band UVB may be effective for this patient, though not as effective as narrow-band UVB. Retinoids plus UVB is a reasonable option in a postmenopausal 50-year-old woman. He does not use PUVA therapy "because of biases that I developed during my residency," he said.
Narrow-band UVB (c) would be Dr. Gordon’s choice, although other answers are reasonable. A clearly wrong answer is (a) Targeted narrow-band UVB, which should not be used for extensive psoriasis.
He said that he would begin treating the patient with narrow-band UVB three times per week. Some published protocols suggest starting at 400 mJ/cm2, but based on her type II skin, he said he would start at 200 mJ/m2 and increase the dose by 25-mJ increments over time. "Why 200 mJ instead of 220 mJ? The math is easier. For the people who work with me, I want the math to be really easy," he said.
Applying petrolatum or mineral oil before phototherapy can eliminate the reflectiveness of the scale to help the light penetrate, but make sure the patient is willing to do this for every treatment. "If they don’t have it as you’re building up the dose, and then they start using it, that’s when people get burned," he explained. "You just have to be consistent."
Four to 6 weeks of thrice-weekly treatments should produce a good response. There’s a dearth of data to help clinicians decide what to do after that. Some reports suggest more patients will remain clear at 1 year if treatment is decreased to twice weekly for 4 weeks and then once weekly instead of stopping phototherapy. Ultimately, this may entail fewer phototherapy sessions than stopping phototherapy and having to resume thrice-weekly sessions if the psoriasis flares again.
"Maintenance therapy is a real way to make life easier for patients with phototherapy. I think it’s a very underused process," he said. Dr. Gordon does not decrease the dose when shifting to maintenance phototherapy, but others recommend decreasing the dose by 25% during once-weekly sessions.
Data on the safety of long-term narrow-band UVB in patients with psoriasis are insufficient, but European studies suggest it does not significantly increase the incidence of nonmelanoma skin cancer. "I leave it up to the patient" to decide if this is acceptable, he said.
– Case 3: Dr. Gordon chose (a) Narrow-band UVB with expectation for short-term treatment. Unlike chronic psoriasis, guttate psoriasis is basically a self-limited disease, so short-term phototherapy is more appropriate than chronic therapy or biologics. Patients tend to respond quickly to narrow-band UVB therapy. PUVA therapy also might be a reasonable treatment, but Dr. Gordon said he has not used it for guttate psoriasis.
"Later on in life, many of these patients will come back and have plaque psoriasis," and then other treatments may be appropriate, he noted.
– Case 4: There’s no clear answer for this case because of a lack of data, according to Dr. Gordon, but he would choose (d) Topical PUVA with a hand-foot UVA unit. "The decision rests on what you sense is best for the patient," but this method is most effective in his experience, he said.
His second choice would be targeted narrow-band UVB with excimer laser, which may be effective at higher fluences but carries the risk of hyperpigmentation. The hand-foot narrow-band UVB unit also is somewhat effective. With limited disease such as this palmar psoriasis, he tries to avoid use of oral psoralen, so would not choose oral PUVA with a hand-foot UVA unit.
– Case 5: For this patient, Dr. Gordon would choose (c) Retinoids plus narrow-band UVB. Erythrodermic psoriasis features inflamed, fine-scaled skin, which is distinct from extensive plaque psoriasis. The patient’s extensive disease needs a high rate of response, so Dr. Gordon would add a retinoid to the UVB to try to boost the treatment benefit.
He advised starting acitretin first for about 1 month to make sure the patient tolerates it and to see if the disease clears on the retinoid alone, without the need for phototherapy. The protocol for UVB should account for the addition of this photosensitizing agent. Dr. Gordon usually decreases the phototherapy dose by one skin type to account for the retinoid. Others suggest decreasing the dose by 25-50 mJ/cm2.
– Case 6: No one in the audience at the meeting picked the correct answer, (d) None of the above. Phototherapy often will worsen erythrodermic psoriasis in people with light skin. Avoid phototherapy in these patients. "If you put somebody like this in a light box, you’ll be in real trouble," he warned. This patient responded well to biologic therapy.
Dr. Gordon has been a consultant for or received grants from Abbott, Amgen, Centocor, Galderma, Lilly, Pfizer, Celgene, and Merck. Also, a partner in his practice derives income from phototherapy.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Practical phototherapy means not thinking strictly in terms of protocols, according to Dr. Kenneth B. Gordon.
Many protocols have been published for psoriasis phototherapy, and good ones were published by the American Academy of Dermatology in early 2010 (J. Amer. Acad. Dermatol. 2010;62:114-35), said Dr. Gordon of the University of Chicago. The guidelines emphasize tailoring therapy to meet the individual patient’s needs, and physicians should consider the best treatment for each patient.
"Simple, published protocols are not sufficient if you really do phototherapy," Dr. Gordon said.
He challenged the audience members with a quiz to test their knowledge of practical phototherapy in particular cases. The cases excluded patients with psoriatic arthritis.
"There are no right answers to these questions," Dr. Gordon said. "There are some wrong answers to these questions, however."
The Quiz Cases
– Case 1: What method of phototherapy would you use to treat a young woman with limited plaque psoriasis, primarily on her elbows? (a) Whole-body narrow-band UVB, (b) Targeted narrow-band-UVB with excimer laser, or (c) Topical psoralen plus long-wave UVA (PUVA).
– Case 2: What type of phototherapy would you use for a 50-year-old woman with extensive plaque psoriasis and type II skin who has not responded to topical therapy? She lives across the street from your office, can come for treatment in the middle of the day, and has no copay on her insurance. (a) Targeted narrow-band UVB, (b) Broad-band UVB, (c) Narrow-band UVB, (d) Retinoids plus UVB, or (e) PUVA.
– Case 3: How would you treat an 18-year-old man having an acute outbreak of guttate psoriasis, with explosive small plaques all over the body? (a) Narrow-band UVB with expectation for short-term treatment, (b) Narrow-band UVB with expectation of long-term maintenance, (c) PUVA, or (d) Biologic immunotherapy.
– Case 4: What’s the best phototherapy for a 59-year-old woman with palmar psoriasis that is interfering with her family business, a packing company? (a) Targeted narrow-band UVB phototherapy using an excimer laser, (b) Phototherapy using a using a hand-foot narrow-band UVB unit, (c) Oral PUVA with a hand-foot UVA unit, or (d) Topical PUVA with a hand-foot UVA unit.
– Case 5: Which phototherapy would you choose for a 53-year-old man with extensive plaque psoriasis with big, thick plaques, including many on his back? (a) Targeted UVB with excimer laser, (b) Narrow-band UVB, (c) Retinoids plus narrow-band UVB, or (d) PUVA.
– Case 6: How would you treat a 52-year-old man with type I skin who has had plaque psoriasis for years but has become erythrodermic over the past 6 months? (a) Narrow-band UVB, (b) Retinoids plus UVB, (c) PUVA, (d) Targeted phototherapy with excimer laser, or (e) None of the above.
Answers
– Case 1: Dr. Gordon said he would choose (b) Targeted narrow-band UVB with excimer laser, although topical PUVA may be the solution sometimes, he added.
Targeted narrow-band UVB with excimer laser is "not so easy," he cautioned. On the plus side, two or three treatments per week for 6-12 weeks have a high chance of success, with more than 75% of patients achieving a Psoriasis Area and Severity Index (PASI) score of 75, or even better if you treat with higher-than-usual fluences. This method only treats involved areas and avoids treating normal skin. Perhaps more than half of patients will have long-term clearing of those limited areas at 1 year after treatment.
On the down side, severe and permanent hyperpigmentation is always a risk with the excimer laser, particularly when higher fluences are used, so it’s important to discuss this with patients when considering targeted UVB therapy. There also may be temporary blistering and pain.
"Application to extensive body surface areas is, in a scientific word, silly," Dr. Gordon said. "I bring that up because I have people in our community who are using it for people who have 20%-30% body surface area involved in psoriasis." In those cases, it’s better to refer the patient for other therapy or consider alternatives such as topical treatments or intralesional injections.
– Case 2: Broad-band UVB may be effective for this patient, though not as effective as narrow-band UVB. Retinoids plus UVB is a reasonable option in a postmenopausal 50-year-old woman. He does not use PUVA therapy "because of biases that I developed during my residency," he said.
Narrow-band UVB (c) would be Dr. Gordon’s choice, although other answers are reasonable. A clearly wrong answer is (a) Targeted narrow-band UVB, which should not be used for extensive psoriasis.
He said that he would begin treating the patient with narrow-band UVB three times per week. Some published protocols suggest starting at 400 mJ/cm2, but based on her type II skin, he said he would start at 200 mJ/m2 and increase the dose by 25-mJ increments over time. "Why 200 mJ instead of 220 mJ? The math is easier. For the people who work with me, I want the math to be really easy," he said.
Applying petrolatum or mineral oil before phototherapy can eliminate the reflectiveness of the scale to help the light penetrate, but make sure the patient is willing to do this for every treatment. "If they don’t have it as you’re building up the dose, and then they start using it, that’s when people get burned," he explained. "You just have to be consistent."
Four to 6 weeks of thrice-weekly treatments should produce a good response. There’s a dearth of data to help clinicians decide what to do after that. Some reports suggest more patients will remain clear at 1 year if treatment is decreased to twice weekly for 4 weeks and then once weekly instead of stopping phototherapy. Ultimately, this may entail fewer phototherapy sessions than stopping phototherapy and having to resume thrice-weekly sessions if the psoriasis flares again.
"Maintenance therapy is a real way to make life easier for patients with phototherapy. I think it’s a very underused process," he said. Dr. Gordon does not decrease the dose when shifting to maintenance phototherapy, but others recommend decreasing the dose by 25% during once-weekly sessions.
Data on the safety of long-term narrow-band UVB in patients with psoriasis are insufficient, but European studies suggest it does not significantly increase the incidence of nonmelanoma skin cancer. "I leave it up to the patient" to decide if this is acceptable, he said.
– Case 3: Dr. Gordon chose (a) Narrow-band UVB with expectation for short-term treatment. Unlike chronic psoriasis, guttate psoriasis is basically a self-limited disease, so short-term phototherapy is more appropriate than chronic therapy or biologics. Patients tend to respond quickly to narrow-band UVB therapy. PUVA therapy also might be a reasonable treatment, but Dr. Gordon said he has not used it for guttate psoriasis.
"Later on in life, many of these patients will come back and have plaque psoriasis," and then other treatments may be appropriate, he noted.
– Case 4: There’s no clear answer for this case because of a lack of data, according to Dr. Gordon, but he would choose (d) Topical PUVA with a hand-foot UVA unit. "The decision rests on what you sense is best for the patient," but this method is most effective in his experience, he said.
His second choice would be targeted narrow-band UVB with excimer laser, which may be effective at higher fluences but carries the risk of hyperpigmentation. The hand-foot narrow-band UVB unit also is somewhat effective. With limited disease such as this palmar psoriasis, he tries to avoid use of oral psoralen, so would not choose oral PUVA with a hand-foot UVA unit.
– Case 5: For this patient, Dr. Gordon would choose (c) Retinoids plus narrow-band UVB. Erythrodermic psoriasis features inflamed, fine-scaled skin, which is distinct from extensive plaque psoriasis. The patient’s extensive disease needs a high rate of response, so Dr. Gordon would add a retinoid to the UVB to try to boost the treatment benefit.
He advised starting acitretin first for about 1 month to make sure the patient tolerates it and to see if the disease clears on the retinoid alone, without the need for phototherapy. The protocol for UVB should account for the addition of this photosensitizing agent. Dr. Gordon usually decreases the phototherapy dose by one skin type to account for the retinoid. Others suggest decreasing the dose by 25-50 mJ/cm2.
– Case 6: No one in the audience at the meeting picked the correct answer, (d) None of the above. Phototherapy often will worsen erythrodermic psoriasis in people with light skin. Avoid phototherapy in these patients. "If you put somebody like this in a light box, you’ll be in real trouble," he warned. This patient responded well to biologic therapy.
Dr. Gordon has been a consultant for or received grants from Abbott, Amgen, Centocor, Galderma, Lilly, Pfizer, Celgene, and Merck. Also, a partner in his practice derives income from phototherapy.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Practical phototherapy means not thinking strictly in terms of protocols, according to Dr. Kenneth B. Gordon.
Many protocols have been published for psoriasis phototherapy, and good ones were published by the American Academy of Dermatology in early 2010 (J. Amer. Acad. Dermatol. 2010;62:114-35), said Dr. Gordon of the University of Chicago. The guidelines emphasize tailoring therapy to meet the individual patient’s needs, and physicians should consider the best treatment for each patient.
"Simple, published protocols are not sufficient if you really do phototherapy," Dr. Gordon said.
He challenged the audience members with a quiz to test their knowledge of practical phototherapy in particular cases. The cases excluded patients with psoriatic arthritis.
"There are no right answers to these questions," Dr. Gordon said. "There are some wrong answers to these questions, however."
The Quiz Cases
– Case 1: What method of phototherapy would you use to treat a young woman with limited plaque psoriasis, primarily on her elbows? (a) Whole-body narrow-band UVB, (b) Targeted narrow-band-UVB with excimer laser, or (c) Topical psoralen plus long-wave UVA (PUVA).
– Case 2: What type of phototherapy would you use for a 50-year-old woman with extensive plaque psoriasis and type II skin who has not responded to topical therapy? She lives across the street from your office, can come for treatment in the middle of the day, and has no copay on her insurance. (a) Targeted narrow-band UVB, (b) Broad-band UVB, (c) Narrow-band UVB, (d) Retinoids plus UVB, or (e) PUVA.
– Case 3: How would you treat an 18-year-old man having an acute outbreak of guttate psoriasis, with explosive small plaques all over the body? (a) Narrow-band UVB with expectation for short-term treatment, (b) Narrow-band UVB with expectation of long-term maintenance, (c) PUVA, or (d) Biologic immunotherapy.
– Case 4: What’s the best phototherapy for a 59-year-old woman with palmar psoriasis that is interfering with her family business, a packing company? (a) Targeted narrow-band UVB phototherapy using an excimer laser, (b) Phototherapy using a using a hand-foot narrow-band UVB unit, (c) Oral PUVA with a hand-foot UVA unit, or (d) Topical PUVA with a hand-foot UVA unit.
– Case 5: Which phototherapy would you choose for a 53-year-old man with extensive plaque psoriasis with big, thick plaques, including many on his back? (a) Targeted UVB with excimer laser, (b) Narrow-band UVB, (c) Retinoids plus narrow-band UVB, or (d) PUVA.
– Case 6: How would you treat a 52-year-old man with type I skin who has had plaque psoriasis for years but has become erythrodermic over the past 6 months? (a) Narrow-band UVB, (b) Retinoids plus UVB, (c) PUVA, (d) Targeted phototherapy with excimer laser, or (e) None of the above.
Answers
– Case 1: Dr. Gordon said he would choose (b) Targeted narrow-band UVB with excimer laser, although topical PUVA may be the solution sometimes, he added.
Targeted narrow-band UVB with excimer laser is "not so easy," he cautioned. On the plus side, two or three treatments per week for 6-12 weeks have a high chance of success, with more than 75% of patients achieving a Psoriasis Area and Severity Index (PASI) score of 75, or even better if you treat with higher-than-usual fluences. This method only treats involved areas and avoids treating normal skin. Perhaps more than half of patients will have long-term clearing of those limited areas at 1 year after treatment.
On the down side, severe and permanent hyperpigmentation is always a risk with the excimer laser, particularly when higher fluences are used, so it’s important to discuss this with patients when considering targeted UVB therapy. There also may be temporary blistering and pain.
"Application to extensive body surface areas is, in a scientific word, silly," Dr. Gordon said. "I bring that up because I have people in our community who are using it for people who have 20%-30% body surface area involved in psoriasis." In those cases, it’s better to refer the patient for other therapy or consider alternatives such as topical treatments or intralesional injections.
– Case 2: Broad-band UVB may be effective for this patient, though not as effective as narrow-band UVB. Retinoids plus UVB is a reasonable option in a postmenopausal 50-year-old woman. He does not use PUVA therapy "because of biases that I developed during my residency," he said.
Narrow-band UVB (c) would be Dr. Gordon’s choice, although other answers are reasonable. A clearly wrong answer is (a) Targeted narrow-band UVB, which should not be used for extensive psoriasis.
He said that he would begin treating the patient with narrow-band UVB three times per week. Some published protocols suggest starting at 400 mJ/cm2, but based on her type II skin, he said he would start at 200 mJ/m2 and increase the dose by 25-mJ increments over time. "Why 200 mJ instead of 220 mJ? The math is easier. For the people who work with me, I want the math to be really easy," he said.
Applying petrolatum or mineral oil before phototherapy can eliminate the reflectiveness of the scale to help the light penetrate, but make sure the patient is willing to do this for every treatment. "If they don’t have it as you’re building up the dose, and then they start using it, that’s when people get burned," he explained. "You just have to be consistent."
Four to 6 weeks of thrice-weekly treatments should produce a good response. There’s a dearth of data to help clinicians decide what to do after that. Some reports suggest more patients will remain clear at 1 year if treatment is decreased to twice weekly for 4 weeks and then once weekly instead of stopping phototherapy. Ultimately, this may entail fewer phototherapy sessions than stopping phototherapy and having to resume thrice-weekly sessions if the psoriasis flares again.
"Maintenance therapy is a real way to make life easier for patients with phototherapy. I think it’s a very underused process," he said. Dr. Gordon does not decrease the dose when shifting to maintenance phototherapy, but others recommend decreasing the dose by 25% during once-weekly sessions.
Data on the safety of long-term narrow-band UVB in patients with psoriasis are insufficient, but European studies suggest it does not significantly increase the incidence of nonmelanoma skin cancer. "I leave it up to the patient" to decide if this is acceptable, he said.
– Case 3: Dr. Gordon chose (a) Narrow-band UVB with expectation for short-term treatment. Unlike chronic psoriasis, guttate psoriasis is basically a self-limited disease, so short-term phototherapy is more appropriate than chronic therapy or biologics. Patients tend to respond quickly to narrow-band UVB therapy. PUVA therapy also might be a reasonable treatment, but Dr. Gordon said he has not used it for guttate psoriasis.
"Later on in life, many of these patients will come back and have plaque psoriasis," and then other treatments may be appropriate, he noted.
– Case 4: There’s no clear answer for this case because of a lack of data, according to Dr. Gordon, but he would choose (d) Topical PUVA with a hand-foot UVA unit. "The decision rests on what you sense is best for the patient," but this method is most effective in his experience, he said.
His second choice would be targeted narrow-band UVB with excimer laser, which may be effective at higher fluences but carries the risk of hyperpigmentation. The hand-foot narrow-band UVB unit also is somewhat effective. With limited disease such as this palmar psoriasis, he tries to avoid use of oral psoralen, so would not choose oral PUVA with a hand-foot UVA unit.
– Case 5: For this patient, Dr. Gordon would choose (c) Retinoids plus narrow-band UVB. Erythrodermic psoriasis features inflamed, fine-scaled skin, which is distinct from extensive plaque psoriasis. The patient’s extensive disease needs a high rate of response, so Dr. Gordon would add a retinoid to the UVB to try to boost the treatment benefit.
He advised starting acitretin first for about 1 month to make sure the patient tolerates it and to see if the disease clears on the retinoid alone, without the need for phototherapy. The protocol for UVB should account for the addition of this photosensitizing agent. Dr. Gordon usually decreases the phototherapy dose by one skin type to account for the retinoid. Others suggest decreasing the dose by 25-50 mJ/cm2.
– Case 6: No one in the audience at the meeting picked the correct answer, (d) None of the above. Phototherapy often will worsen erythrodermic psoriasis in people with light skin. Avoid phototherapy in these patients. "If you put somebody like this in a light box, you’ll be in real trouble," he warned. This patient responded well to biologic therapy.
Dr. Gordon has been a consultant for or received grants from Abbott, Amgen, Centocor, Galderma, Lilly, Pfizer, Celgene, and Merck. Also, a partner in his practice derives income from phototherapy.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Take the Phototherapy for Psoriasis Quiz
LAS VEGAS - Practical phototherapy means not thinking strictly in terms of protocols, according to Dr. Kenneth B. Gordon.
Many protocols have been published for psoriasis phototherapy, and good ones were published by the American Academy of Dermatology in early 2010 (J. Amer. Acad. Dermatol. 2010;62:114-35), said Dr. Gordon of the University of Chicago. The guidelines emphasize tailoring therapy to meet the individual patient’s needs, and physicians should consider the best treatment for each patient.
"Simple, published protocols are not sufficient if you really do phototherapy," Dr. Gordon said.
He challenged the audience members with a quiz to test their knowledge of practical phototherapy in particular cases. The cases excluded patients with psoriatic arthritis.
"There are no right answers to these questions," Dr. Gordon said. "There are some wrong answers to these questions, however."
The Quiz Cases
– Case 1: What method of phototherapy would you use to treat a young woman with limited plaque psoriasis, primarily on her elbows? (a) Whole-body narrow-band UVB, (b) Targeted narrow-band-UVB with excimer laser, or (c) Topical psoralen plus long-wave UVA (PUVA).
– Case 2: What type of phototherapy would you use for a 50-year-old woman with extensive plaque psoriasis and type II skin who has not responded to topical therapy? She lives across the street from your office, can come for treatment in the middle of the day, and has no copay on her insurance. (a) Targeted narrow-band UVB, (b) Broad-band UVB, (c) Narrow-band UVB, (d) Retinoids plus UVB, or (e) PUVA.
– Case 3: How would you treat an 18-year-old man having an acute outbreak of guttate psoriasis, with explosive small plaques all over the body? (a) Narrow-band UVB with expectation for short-term treatment, (b) Narrow-band UVB with expectation of long-term maintenance, (c) PUVA, or (d) Biologic immunotherapy.
– Case 4: What’s the best phototherapy for a 59-year-old woman with palmar psoriasis that is interfering with her family business, a packing company? (a) Targeted narrow-band UVB phototherapy using an excimer laser, (b) Phototherapy using a using a hand-foot narrow-band UVB unit, (c) Oral PUVA with a hand-foot UVA unit, or (d) Topical PUVA with a hand-foot UVA unit.
– Case 5: Which phototherapy would you choose for a 53-year-old man with extensive plaque psoriasis with big, thick plaques, including many on his back? (a) Targeted UVB with excimer laser, (b) Narrow-band UVB, (c) Retinoids plus narrow-band UVB, or (d) PUVA.
– Case 6: How would you treat a 52-year-old man with type I skin who has had plaque psoriasis for years but has become erythrodermic over the past 6 months? (a) Narrow-band UVB, (b) Retinoids plus UVB, (c) PUVA, (d) Targeted phototherapy with excimer laser, or (e) None of the above.
Answers
– Case 1: Dr. Gordon said he would choose (b) Targeted narrow-band UVB with excimer laser, although topical PUVA may be the solution sometimes, he added.
Targeted narrow-band UVB with excimer laser is "not so easy," he cautioned. On the plus side, two or three treatments per week for 6-12 weeks have a high chance of success, with more than 75% of patients achieving a Psoriasis Area and Severity Index (PASI) score of 75, or even better if you treat with higher-than-usual fluences. This method only treats involved areas and avoids treating normal skin. Perhaps more than half of patients will have long-term clearing of those limited areas at 1 year after treatment.
On the down side, severe and permanent hyperpigmentation is always a risk with the excimer laser, particularly when higher fluences are used, so it’s important to discuss this with patients when considering targeted UVB therapy. There also may be temporary blistering and pain.
"Application to extensive body surface areas is, in a scientific word, silly," Dr. Gordon said. "I bring that up because I have people in our community who are using it for people who have 20%-30% body surface area involved in psoriasis." In those cases, it’s better to refer the patient for other therapy or consider alternatives such as topical treatments or intralesional injections.
– Case 2: Broad-band UVB may be effective for this patient, though not as effective as narrow-band UVB. Retinoids plus UVB is a reasonable option in a postmenopausal 50-year-old woman. He does not use PUVA therapy "because of biases that I developed during my residency," he said.
Narrow-band UVB (c) would be Dr. Gordon’s choice, although other answers are reasonable. A clearly wrong answer is (a) Targeted narrow-band UVB, which should not be used for extensive psoriasis.
He said that he would begin treating the patient with narrow-band UVB three times per week. Some published protocols suggest starting at 400 mJ/cm2, but based on her type II skin, he said he would start at 200 mJ/m2 and increase the dose by 25-mJ increments over time. "Why 200 mJ instead of 220 mJ? The math is easier. For the people who work with me, I want the math to be really easy," he said.
Applying petrolatum or mineral oil before phototherapy can eliminate the reflectiveness of the scale to help the light penetrate, but make sure the patient is willing to do this for every treatment. "If they don’t have it as you’re building up the dose, and then they start using it, that’s when people get burned," he explained. "You just have to be consistent."
Four to 6 weeks of thrice-weekly treatments should produce a good response. There’s a dearth of data to help clinicians decide what to do after that. Some reports suggest more patients will remain clear at 1 year if treatment is decreased to twice weekly for 4 weeks and then once weekly instead of stopping phototherapy. Ultimately, this may entail fewer phototherapy sessions than stopping phototherapy and having to resume thrice-weekly sessions if the psoriasis flares again.
"Maintenance therapy is a real way to make life easier for patients with phototherapy. I think it’s a very underused process," he said. Dr. Gordon does not decrease the dose when shifting to maintenance phototherapy, but others recommend decreasing the dose by 25% during once-weekly sessions.
Data on the safety of long-term narrow-band UVB in patients with psoriasis are insufficient, but European studies suggest it does not significantly increase the incidence of nonmelanoma skin cancer. "I leave it up to the patient" to decide if this is acceptable, he said.
– Case 3: Dr. Gordon chose (a) Narrow-band UVB with expectation for short-term treatment. Unlike chronic psoriasis, guttate psoriasis is basically a self-limited disease, so short-term phototherapy is more appropriate than chronic therapy or biologics. Patients tend to respond quickly to narrow-band UVB therapy. PUVA therapy also might be a reasonable treatment, but Dr. Gordon said he has not used it for guttate psoriasis.
"Later on in life, many of these patients will come back and have plaque psoriasis," and then other treatments may be appropriate, he noted.
– Case 4: There’s no clear answer for this case because of a lack of data, according to Dr. Gordon, but he would choose (d) Topical PUVA with a hand-foot UVA unit. "The decision rests on what you sense is best for the patient," but this method is most effective in his experience, he said.
His second choice would be targeted narrow-band UVB with excimer laser, which may be effective at higher fluences but carries the risk of hyperpigmentation. The hand-foot narrow-band UVB unit also is somewhat effective. With limited disease such as this palmar psoriasis, he tries to avoid use of oral psoralen, so would not choose oral PUVA with a hand-foot UVA unit.
– Case 5: For this patient, Dr. Gordon would choose (c) Retinoids plus narrow-band UVB. Erythrodermic psoriasis features inflamed, fine-scaled skin, which is distinct from extensive plaque psoriasis. The patient’s extensive disease needs a high rate of response, so Dr. Gordon would add a retinoid to the UVB to try to boost the treatment benefit.
He advised starting acitretin first for about 1 month to make sure the patient tolerates it and to see if the disease clears on the retinoid alone, without the need for phototherapy. The protocol for UVB should account for the addition of this photosensitizing agent. Dr. Gordon usually decreases the phototherapy dose by one skin type to account for the retinoid. Others suggest decreasing the dose by 25-50 mJ/cm2.
– Case 6: No one in the audience at the meeting picked the correct answer, (d) None of the above. Phototherapy often will worsen erythrodermic psoriasis in people with light skin. Avoid phototherapy in these patients. "If you put somebody like this in a light box, you’ll be in real trouble," he warned. This patient responded well to biologic therapy.
Dr. Gordon has been a consultant for or received grants from Abbott, Amgen, Centocor, Galderma, Lilly, Pfizer, Celgene, and Merck. Also, a partner in his practice derives income from phototherapy.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Practical phototherapy means not thinking strictly in terms of protocols, according to Dr. Kenneth B. Gordon.
Many protocols have been published for psoriasis phototherapy, and good ones were published by the American Academy of Dermatology in early 2010 (J. Amer. Acad. Dermatol. 2010;62:114-35), said Dr. Gordon of the University of Chicago. The guidelines emphasize tailoring therapy to meet the individual patient’s needs, and physicians should consider the best treatment for each patient.
"Simple, published protocols are not sufficient if you really do phototherapy," Dr. Gordon said.
He challenged the audience members with a quiz to test their knowledge of practical phototherapy in particular cases. The cases excluded patients with psoriatic arthritis.
"There are no right answers to these questions," Dr. Gordon said. "There are some wrong answers to these questions, however."
The Quiz Cases
– Case 1: What method of phototherapy would you use to treat a young woman with limited plaque psoriasis, primarily on her elbows? (a) Whole-body narrow-band UVB, (b) Targeted narrow-band-UVB with excimer laser, or (c) Topical psoralen plus long-wave UVA (PUVA).
– Case 2: What type of phototherapy would you use for a 50-year-old woman with extensive plaque psoriasis and type II skin who has not responded to topical therapy? She lives across the street from your office, can come for treatment in the middle of the day, and has no copay on her insurance. (a) Targeted narrow-band UVB, (b) Broad-band UVB, (c) Narrow-band UVB, (d) Retinoids plus UVB, or (e) PUVA.
– Case 3: How would you treat an 18-year-old man having an acute outbreak of guttate psoriasis, with explosive small plaques all over the body? (a) Narrow-band UVB with expectation for short-term treatment, (b) Narrow-band UVB with expectation of long-term maintenance, (c) PUVA, or (d) Biologic immunotherapy.
– Case 4: What’s the best phototherapy for a 59-year-old woman with palmar psoriasis that is interfering with her family business, a packing company? (a) Targeted narrow-band UVB phototherapy using an excimer laser, (b) Phototherapy using a using a hand-foot narrow-band UVB unit, (c) Oral PUVA with a hand-foot UVA unit, or (d) Topical PUVA with a hand-foot UVA unit.
– Case 5: Which phototherapy would you choose for a 53-year-old man with extensive plaque psoriasis with big, thick plaques, including many on his back? (a) Targeted UVB with excimer laser, (b) Narrow-band UVB, (c) Retinoids plus narrow-band UVB, or (d) PUVA.
– Case 6: How would you treat a 52-year-old man with type I skin who has had plaque psoriasis for years but has become erythrodermic over the past 6 months? (a) Narrow-band UVB, (b) Retinoids plus UVB, (c) PUVA, (d) Targeted phototherapy with excimer laser, or (e) None of the above.
Answers
– Case 1: Dr. Gordon said he would choose (b) Targeted narrow-band UVB with excimer laser, although topical PUVA may be the solution sometimes, he added.
Targeted narrow-band UVB with excimer laser is "not so easy," he cautioned. On the plus side, two or three treatments per week for 6-12 weeks have a high chance of success, with more than 75% of patients achieving a Psoriasis Area and Severity Index (PASI) score of 75, or even better if you treat with higher-than-usual fluences. This method only treats involved areas and avoids treating normal skin. Perhaps more than half of patients will have long-term clearing of those limited areas at 1 year after treatment.
On the down side, severe and permanent hyperpigmentation is always a risk with the excimer laser, particularly when higher fluences are used, so it’s important to discuss this with patients when considering targeted UVB therapy. There also may be temporary blistering and pain.
"Application to extensive body surface areas is, in a scientific word, silly," Dr. Gordon said. "I bring that up because I have people in our community who are using it for people who have 20%-30% body surface area involved in psoriasis." In those cases, it’s better to refer the patient for other therapy or consider alternatives such as topical treatments or intralesional injections.
– Case 2: Broad-band UVB may be effective for this patient, though not as effective as narrow-band UVB. Retinoids plus UVB is a reasonable option in a postmenopausal 50-year-old woman. He does not use PUVA therapy "because of biases that I developed during my residency," he said.
Narrow-band UVB (c) would be Dr. Gordon’s choice, although other answers are reasonable. A clearly wrong answer is (a) Targeted narrow-band UVB, which should not be used for extensive psoriasis.
He said that he would begin treating the patient with narrow-band UVB three times per week. Some published protocols suggest starting at 400 mJ/cm2, but based on her type II skin, he said he would start at 200 mJ/m2 and increase the dose by 25-mJ increments over time. "Why 200 mJ instead of 220 mJ? The math is easier. For the people who work with me, I want the math to be really easy," he said.
Applying petrolatum or mineral oil before phototherapy can eliminate the reflectiveness of the scale to help the light penetrate, but make sure the patient is willing to do this for every treatment. "If they don’t have it as you’re building up the dose, and then they start using it, that’s when people get burned," he explained. "You just have to be consistent."
Four to 6 weeks of thrice-weekly treatments should produce a good response. There’s a dearth of data to help clinicians decide what to do after that. Some reports suggest more patients will remain clear at 1 year if treatment is decreased to twice weekly for 4 weeks and then once weekly instead of stopping phototherapy. Ultimately, this may entail fewer phototherapy sessions than stopping phototherapy and having to resume thrice-weekly sessions if the psoriasis flares again.
"Maintenance therapy is a real way to make life easier for patients with phototherapy. I think it’s a very underused process," he said. Dr. Gordon does not decrease the dose when shifting to maintenance phototherapy, but others recommend decreasing the dose by 25% during once-weekly sessions.
Data on the safety of long-term narrow-band UVB in patients with psoriasis are insufficient, but European studies suggest it does not significantly increase the incidence of nonmelanoma skin cancer. "I leave it up to the patient" to decide if this is acceptable, he said.
– Case 3: Dr. Gordon chose (a) Narrow-band UVB with expectation for short-term treatment. Unlike chronic psoriasis, guttate psoriasis is basically a self-limited disease, so short-term phototherapy is more appropriate than chronic therapy or biologics. Patients tend to respond quickly to narrow-band UVB therapy. PUVA therapy also might be a reasonable treatment, but Dr. Gordon said he has not used it for guttate psoriasis.
"Later on in life, many of these patients will come back and have plaque psoriasis," and then other treatments may be appropriate, he noted.
– Case 4: There’s no clear answer for this case because of a lack of data, according to Dr. Gordon, but he would choose (d) Topical PUVA with a hand-foot UVA unit. "The decision rests on what you sense is best for the patient," but this method is most effective in his experience, he said.
His second choice would be targeted narrow-band UVB with excimer laser, which may be effective at higher fluences but carries the risk of hyperpigmentation. The hand-foot narrow-band UVB unit also is somewhat effective. With limited disease such as this palmar psoriasis, he tries to avoid use of oral psoralen, so would not choose oral PUVA with a hand-foot UVA unit.
– Case 5: For this patient, Dr. Gordon would choose (c) Retinoids plus narrow-band UVB. Erythrodermic psoriasis features inflamed, fine-scaled skin, which is distinct from extensive plaque psoriasis. The patient’s extensive disease needs a high rate of response, so Dr. Gordon would add a retinoid to the UVB to try to boost the treatment benefit.
He advised starting acitretin first for about 1 month to make sure the patient tolerates it and to see if the disease clears on the retinoid alone, without the need for phototherapy. The protocol for UVB should account for the addition of this photosensitizing agent. Dr. Gordon usually decreases the phototherapy dose by one skin type to account for the retinoid. Others suggest decreasing the dose by 25-50 mJ/cm2.
– Case 6: No one in the audience at the meeting picked the correct answer, (d) None of the above. Phototherapy often will worsen erythrodermic psoriasis in people with light skin. Avoid phototherapy in these patients. "If you put somebody like this in a light box, you’ll be in real trouble," he warned. This patient responded well to biologic therapy.
Dr. Gordon has been a consultant for or received grants from Abbott, Amgen, Centocor, Galderma, Lilly, Pfizer, Celgene, and Merck. Also, a partner in his practice derives income from phototherapy.
SDEF and this news organization are owned by Elsevier.
LAS VEGAS - Practical phototherapy means not thinking strictly in terms of protocols, according to Dr. Kenneth B. Gordon.
Many protocols have been published for psoriasis phototherapy, and good ones were published by the American Academy of Dermatology in early 2010 (J. Amer. Acad. Dermatol. 2010;62:114-35), said Dr. Gordon of the University of Chicago. The guidelines emphasize tailoring therapy to meet the individual patient’s needs, and physicians should consider the best treatment for each patient.
"Simple, published protocols are not sufficient if you really do phototherapy," Dr. Gordon said.
He challenged the audience members with a quiz to test their knowledge of practical phototherapy in particular cases. The cases excluded patients with psoriatic arthritis.
"There are no right answers to these questions," Dr. Gordon said. "There are some wrong answers to these questions, however."
The Quiz Cases
– Case 1: What method of phototherapy would you use to treat a young woman with limited plaque psoriasis, primarily on her elbows? (a) Whole-body narrow-band UVB, (b) Targeted narrow-band-UVB with excimer laser, or (c) Topical psoralen plus long-wave UVA (PUVA).
– Case 2: What type of phototherapy would you use for a 50-year-old woman with extensive plaque psoriasis and type II skin who has not responded to topical therapy? She lives across the street from your office, can come for treatment in the middle of the day, and has no copay on her insurance. (a) Targeted narrow-band UVB, (b) Broad-band UVB, (c) Narrow-band UVB, (d) Retinoids plus UVB, or (e) PUVA.
– Case 3: How would you treat an 18-year-old man having an acute outbreak of guttate psoriasis, with explosive small plaques all over the body? (a) Narrow-band UVB with expectation for short-term treatment, (b) Narrow-band UVB with expectation of long-term maintenance, (c) PUVA, or (d) Biologic immunotherapy.
– Case 4: What’s the best phototherapy for a 59-year-old woman with palmar psoriasis that is interfering with her family business, a packing company? (a) Targeted narrow-band UVB phototherapy using an excimer laser, (b) Phototherapy using a using a hand-foot narrow-band UVB unit, (c) Oral PUVA with a hand-foot UVA unit, or (d) Topical PUVA with a hand-foot UVA unit.
– Case 5: Which phototherapy would you choose for a 53-year-old man with extensive plaque psoriasis with big, thick plaques, including many on his back? (a) Targeted UVB with excimer laser, (b) Narrow-band UVB, (c) Retinoids plus narrow-band UVB, or (d) PUVA.
– Case 6: How would you treat a 52-year-old man with type I skin who has had plaque psoriasis for years but has become erythrodermic over the past 6 months? (a) Narrow-band UVB, (b) Retinoids plus UVB, (c) PUVA, (d) Targeted phototherapy with excimer laser, or (e) None of the above.
Answers
– Case 1: Dr. Gordon said he would choose (b) Targeted narrow-band UVB with excimer laser, although topical PUVA may be the solution sometimes, he added.
Targeted narrow-band UVB with excimer laser is "not so easy," he cautioned. On the plus side, two or three treatments per week for 6-12 weeks have a high chance of success, with more than 75% of patients achieving a Psoriasis Area and Severity Index (PASI) score of 75, or even better if you treat with higher-than-usual fluences. This method only treats involved areas and avoids treating normal skin. Perhaps more than half of patients will have long-term clearing of those limited areas at 1 year after treatment.
On the down side, severe and permanent hyperpigmentation is always a risk with the excimer laser, particularly when higher fluences are used, so it’s important to discuss this with patients when considering targeted UVB therapy. There also may be temporary blistering and pain.
"Application to extensive body surface areas is, in a scientific word, silly," Dr. Gordon said. "I bring that up because I have people in our community who are using it for people who have 20%-30% body surface area involved in psoriasis." In those cases, it’s better to refer the patient for other therapy or consider alternatives such as topical treatments or intralesional injections.
– Case 2: Broad-band UVB may be effective for this patient, though not as effective as narrow-band UVB. Retinoids plus UVB is a reasonable option in a postmenopausal 50-year-old woman. He does not use PUVA therapy "because of biases that I developed during my residency," he said.
Narrow-band UVB (c) would be Dr. Gordon’s choice, although other answers are reasonable. A clearly wrong answer is (a) Targeted narrow-band UVB, which should not be used for extensive psoriasis.
He said that he would begin treating the patient with narrow-band UVB three times per week. Some published protocols suggest starting at 400 mJ/cm2, but based on her type II skin, he said he would start at 200 mJ/m2 and increase the dose by 25-mJ increments over time. "Why 200 mJ instead of 220 mJ? The math is easier. For the people who work with me, I want the math to be really easy," he said.
Applying petrolatum or mineral oil before phototherapy can eliminate the reflectiveness of the scale to help the light penetrate, but make sure the patient is willing to do this for every treatment. "If they don’t have it as you’re building up the dose, and then they start using it, that’s when people get burned," he explained. "You just have to be consistent."
Four to 6 weeks of thrice-weekly treatments should produce a good response. There’s a dearth of data to help clinicians decide what to do after that. Some reports suggest more patients will remain clear at 1 year if treatment is decreased to twice weekly for 4 weeks and then once weekly instead of stopping phototherapy. Ultimately, this may entail fewer phototherapy sessions than stopping phototherapy and having to resume thrice-weekly sessions if the psoriasis flares again.
"Maintenance therapy is a real way to make life easier for patients with phototherapy. I think it’s a very underused process," he said. Dr. Gordon does not decrease the dose when shifting to maintenance phototherapy, but others recommend decreasing the dose by 25% during once-weekly sessions.
Data on the safety of long-term narrow-band UVB in patients with psoriasis are insufficient, but European studies suggest it does not significantly increase the incidence of nonmelanoma skin cancer. "I leave it up to the patient" to decide if this is acceptable, he said.
– Case 3: Dr. Gordon chose (a) Narrow-band UVB with expectation for short-term treatment. Unlike chronic psoriasis, guttate psoriasis is basically a self-limited disease, so short-term phototherapy is more appropriate than chronic therapy or biologics. Patients tend to respond quickly to narrow-band UVB therapy. PUVA therapy also might be a reasonable treatment, but Dr. Gordon said he has not used it for guttate psoriasis.
"Later on in life, many of these patients will come back and have plaque psoriasis," and then other treatments may be appropriate, he noted.
– Case 4: There’s no clear answer for this case because of a lack of data, according to Dr. Gordon, but he would choose (d) Topical PUVA with a hand-foot UVA unit. "The decision rests on what you sense is best for the patient," but this method is most effective in his experience, he said.
His second choice would be targeted narrow-band UVB with excimer laser, which may be effective at higher fluences but carries the risk of hyperpigmentation. The hand-foot narrow-band UVB unit also is somewhat effective. With limited disease such as this palmar psoriasis, he tries to avoid use of oral psoralen, so would not choose oral PUVA with a hand-foot UVA unit.
– Case 5: For this patient, Dr. Gordon would choose (c) Retinoids plus narrow-band UVB. Erythrodermic psoriasis features inflamed, fine-scaled skin, which is distinct from extensive plaque psoriasis. The patient’s extensive disease needs a high rate of response, so Dr. Gordon would add a retinoid to the UVB to try to boost the treatment benefit.
He advised starting acitretin first for about 1 month to make sure the patient tolerates it and to see if the disease clears on the retinoid alone, without the need for phototherapy. The protocol for UVB should account for the addition of this photosensitizing agent. Dr. Gordon usually decreases the phototherapy dose by one skin type to account for the retinoid. Others suggest decreasing the dose by 25-50 mJ/cm2.
– Case 6: No one in the audience at the meeting picked the correct answer, (d) None of the above. Phototherapy often will worsen erythrodermic psoriasis in people with light skin. Avoid phototherapy in these patients. "If you put somebody like this in a light box, you’ll be in real trouble," he warned. This patient responded well to biologic therapy.
Dr. Gordon has been a consultant for or received grants from Abbott, Amgen, Centocor, Galderma, Lilly, Pfizer, Celgene, and Merck. Also, a partner in his practice derives income from phototherapy.
SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Expert: Cellulite Treatment Effectiveness Unproven, Studies Flawed
LAS VEGAS – Treatment for cellulite is a multibillion dollar industry of unproved therapies, according to Dr. Mathew M. Avram.
Some treatments that claim to lessen cellulite may have produced minor, temporary improvements in flawed studies, but none has been proven to be truly effective, said Dr. Avram of Harvard University and director of Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center, Boston.
There is no medical reason to treat cellulite, which is normal in the female dermis and is not associated with morbidity or mortality. Many women care about it anyway "because every tabloid likes to show celebrities and their cellulite running around in Hawaii," he said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Many physicians and patients misunderstand cellulite, which is simply gender-related differences in the structure of subcutaneous fat lobules and the connective tissue septae that divide them, usually in the thigh area, Dr. Avram said. The treatment industry capitalizes on this ignorance.
"We need to educate our patients that cellulite is a totally normal condition" and treatments are at best mildly helpful for a short period of time, he said. "We need to be skeptical as well. There is a consistent history of inflated and unsubstantiated claims of success."
Fat removal technologies have no effect on cellulite because fat and cellulite are distinct. Weight and cellulite are unrelated. Cellulite is nearly universal in postpubertal females even if they are lean, but most obese males do not have cellulite unless they have androgen deficiency. "Exercise doesn’t really help it," he explained.
There is no good evidence for invasive treatments such as liposuction, subcision, mesotherapy, or carboxytherapy. Most data on noninvasive treatments measure results by body circumference, "which isn’t relevant to cellulite, so it’s hard to know whether or not there is improvement," he noted.
Flawed studies of treatments such as noninvasive Endermologie (mechanical cell stimulation), unipolar and bipolar radiofrequency, devices combining lasers and light sources, and topical treatments show modest, temporary benefit, he said.
Nearly 2 decades ago, a study of topical retinoids for cellulite showed some improvements, but this may have just been temporary improvements in inflammation, Dr. Avram said. Multiple expensive topical formulations have shown no significant efficacy, including xanthines, lactic acid, and aminophylline.
At least three laser devices that are cleared by the Food and Drug Administration are used to treat cellulite, but these devices only needed to prove safety, not efficacy, to achieve clearance, noted Dr. Avram, who is a lawyer as well as a physician. Studies of two of the laser devices suggested that they may produce temporary and limited decreases in limb circumference, which is a poor measure of cellulite.
A study of the third device treated 17 patients twice weekly for 4 weeks with a dual wavelength laser system with vacuum suction and mechanical massage (Plast. Reconstr. Surg. 2010;125:1788-96). The study suggested that 14 patients (82%) showed "improvement" at 1 month as measured by VECTRA 3-D photographs, but initial cellulite irregularities and any possible improvements were more difficult to see by conventional digital photography. The study did not define "improvement" and included no control sites or histology to assess improvement, noted Dr. Avram.
"This is really a flawed study," he said.
A separate study of a unipolar radiofrequency device for treating cellulite in 30 patients reported a mean 2.45-cm improvement in thigh circumference in 27 patients at 6 months with changes in upper dermis fibrosis on histology (Dermatol. Surg. 2008;34:204-9). However, circumference is an inherently imprecise measure that is irrelevant to cellulite, Dr. Avram noted.
"We need a set of criteria by which we can assess the efficacy of these technologies," he said. Photography is difficult and easily manipulated to exaggerate results. Ultrasound is imprecise and user dependent. MRI is expensive and requires specific coils for fat and 3-D imaging systems.
"At a minimum we need to have untreated controls, weight maintenance during studies, and laboratory data to confirm safety," Dr. Avram said. "We must hold our industry and our colleagues to high standards" and demand proof of scientifically important efficacy.
Physicians also should question whether the postulated mechanisms of action for these new technologies make sense with regard to cellulite. Any study without a histology report, for example, has no basis for a claim of efficacy in treating cellulite, he said.
Dr. Avram holds stock options in Zeltiq Aesthetics. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Treatment for cellulite is a multibillion dollar industry of unproved therapies, according to Dr. Mathew M. Avram.
Some treatments that claim to lessen cellulite may have produced minor, temporary improvements in flawed studies, but none has been proven to be truly effective, said Dr. Avram of Harvard University and director of Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center, Boston.
There is no medical reason to treat cellulite, which is normal in the female dermis and is not associated with morbidity or mortality. Many women care about it anyway "because every tabloid likes to show celebrities and their cellulite running around in Hawaii," he said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Many physicians and patients misunderstand cellulite, which is simply gender-related differences in the structure of subcutaneous fat lobules and the connective tissue septae that divide them, usually in the thigh area, Dr. Avram said. The treatment industry capitalizes on this ignorance.
"We need to educate our patients that cellulite is a totally normal condition" and treatments are at best mildly helpful for a short period of time, he said. "We need to be skeptical as well. There is a consistent history of inflated and unsubstantiated claims of success."
Fat removal technologies have no effect on cellulite because fat and cellulite are distinct. Weight and cellulite are unrelated. Cellulite is nearly universal in postpubertal females even if they are lean, but most obese males do not have cellulite unless they have androgen deficiency. "Exercise doesn’t really help it," he explained.
There is no good evidence for invasive treatments such as liposuction, subcision, mesotherapy, or carboxytherapy. Most data on noninvasive treatments measure results by body circumference, "which isn’t relevant to cellulite, so it’s hard to know whether or not there is improvement," he noted.
Flawed studies of treatments such as noninvasive Endermologie (mechanical cell stimulation), unipolar and bipolar radiofrequency, devices combining lasers and light sources, and topical treatments show modest, temporary benefit, he said.
Nearly 2 decades ago, a study of topical retinoids for cellulite showed some improvements, but this may have just been temporary improvements in inflammation, Dr. Avram said. Multiple expensive topical formulations have shown no significant efficacy, including xanthines, lactic acid, and aminophylline.
At least three laser devices that are cleared by the Food and Drug Administration are used to treat cellulite, but these devices only needed to prove safety, not efficacy, to achieve clearance, noted Dr. Avram, who is a lawyer as well as a physician. Studies of two of the laser devices suggested that they may produce temporary and limited decreases in limb circumference, which is a poor measure of cellulite.
A study of the third device treated 17 patients twice weekly for 4 weeks with a dual wavelength laser system with vacuum suction and mechanical massage (Plast. Reconstr. Surg. 2010;125:1788-96). The study suggested that 14 patients (82%) showed "improvement" at 1 month as measured by VECTRA 3-D photographs, but initial cellulite irregularities and any possible improvements were more difficult to see by conventional digital photography. The study did not define "improvement" and included no control sites or histology to assess improvement, noted Dr. Avram.
"This is really a flawed study," he said.
A separate study of a unipolar radiofrequency device for treating cellulite in 30 patients reported a mean 2.45-cm improvement in thigh circumference in 27 patients at 6 months with changes in upper dermis fibrosis on histology (Dermatol. Surg. 2008;34:204-9). However, circumference is an inherently imprecise measure that is irrelevant to cellulite, Dr. Avram noted.
"We need a set of criteria by which we can assess the efficacy of these technologies," he said. Photography is difficult and easily manipulated to exaggerate results. Ultrasound is imprecise and user dependent. MRI is expensive and requires specific coils for fat and 3-D imaging systems.
"At a minimum we need to have untreated controls, weight maintenance during studies, and laboratory data to confirm safety," Dr. Avram said. "We must hold our industry and our colleagues to high standards" and demand proof of scientifically important efficacy.
Physicians also should question whether the postulated mechanisms of action for these new technologies make sense with regard to cellulite. Any study without a histology report, for example, has no basis for a claim of efficacy in treating cellulite, he said.
Dr. Avram holds stock options in Zeltiq Aesthetics. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Treatment for cellulite is a multibillion dollar industry of unproved therapies, according to Dr. Mathew M. Avram.
Some treatments that claim to lessen cellulite may have produced minor, temporary improvements in flawed studies, but none has been proven to be truly effective, said Dr. Avram of Harvard University and director of Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center, Boston.
There is no medical reason to treat cellulite, which is normal in the female dermis and is not associated with morbidity or mortality. Many women care about it anyway "because every tabloid likes to show celebrities and their cellulite running around in Hawaii," he said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Many physicians and patients misunderstand cellulite, which is simply gender-related differences in the structure of subcutaneous fat lobules and the connective tissue septae that divide them, usually in the thigh area, Dr. Avram said. The treatment industry capitalizes on this ignorance.
"We need to educate our patients that cellulite is a totally normal condition" and treatments are at best mildly helpful for a short period of time, he said. "We need to be skeptical as well. There is a consistent history of inflated and unsubstantiated claims of success."
Fat removal technologies have no effect on cellulite because fat and cellulite are distinct. Weight and cellulite are unrelated. Cellulite is nearly universal in postpubertal females even if they are lean, but most obese males do not have cellulite unless they have androgen deficiency. "Exercise doesn’t really help it," he explained.
There is no good evidence for invasive treatments such as liposuction, subcision, mesotherapy, or carboxytherapy. Most data on noninvasive treatments measure results by body circumference, "which isn’t relevant to cellulite, so it’s hard to know whether or not there is improvement," he noted.
Flawed studies of treatments such as noninvasive Endermologie (mechanical cell stimulation), unipolar and bipolar radiofrequency, devices combining lasers and light sources, and topical treatments show modest, temporary benefit, he said.
Nearly 2 decades ago, a study of topical retinoids for cellulite showed some improvements, but this may have just been temporary improvements in inflammation, Dr. Avram said. Multiple expensive topical formulations have shown no significant efficacy, including xanthines, lactic acid, and aminophylline.
At least three laser devices that are cleared by the Food and Drug Administration are used to treat cellulite, but these devices only needed to prove safety, not efficacy, to achieve clearance, noted Dr. Avram, who is a lawyer as well as a physician. Studies of two of the laser devices suggested that they may produce temporary and limited decreases in limb circumference, which is a poor measure of cellulite.
A study of the third device treated 17 patients twice weekly for 4 weeks with a dual wavelength laser system with vacuum suction and mechanical massage (Plast. Reconstr. Surg. 2010;125:1788-96). The study suggested that 14 patients (82%) showed "improvement" at 1 month as measured by VECTRA 3-D photographs, but initial cellulite irregularities and any possible improvements were more difficult to see by conventional digital photography. The study did not define "improvement" and included no control sites or histology to assess improvement, noted Dr. Avram.
"This is really a flawed study," he said.
A separate study of a unipolar radiofrequency device for treating cellulite in 30 patients reported a mean 2.45-cm improvement in thigh circumference in 27 patients at 6 months with changes in upper dermis fibrosis on histology (Dermatol. Surg. 2008;34:204-9). However, circumference is an inherently imprecise measure that is irrelevant to cellulite, Dr. Avram noted.
"We need a set of criteria by which we can assess the efficacy of these technologies," he said. Photography is difficult and easily manipulated to exaggerate results. Ultrasound is imprecise and user dependent. MRI is expensive and requires specific coils for fat and 3-D imaging systems.
"At a minimum we need to have untreated controls, weight maintenance during studies, and laboratory data to confirm safety," Dr. Avram said. "We must hold our industry and our colleagues to high standards" and demand proof of scientifically important efficacy.
Physicians also should question whether the postulated mechanisms of action for these new technologies make sense with regard to cellulite. Any study without a histology report, for example, has no basis for a claim of efficacy in treating cellulite, he said.
Dr. Avram holds stock options in Zeltiq Aesthetics. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR
Expert: Cellulite Treatment Effectiveness Unproven, Studies Flawed
LAS VEGAS – Treatment for cellulite is a multibillion dollar industry of unproved therapies, according to Dr. Matthew M. Avram.
Some treatments that claim to lessen cellulite may have produced minor, temporary improvements in flawed studies, but none has been proven to be truly effective, said Dr. Avram of Harvard University and director of Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center, Boston.
There is no medical reason to treat cellulite, which is normal in the female dermis and is not associated with morbidity or mortality. Many women care about it anyway "because every tabloid likes to show celebrities and their cellulite running around in Hawaii," he said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Many physicians and patients misunderstand cellulite, which is simply gender-related differences in the structure of subcutaneous fat lobules and the connective tissue septae that divide them, usually in the thigh area, Dr. Avram said. The treatment industry capitalizes on this ignorance.
"We need to educate our patients that cellulite is a totally normal condition" and treatments are at best mildly helpful for a short period of time, he said. "We need to be skeptical as well. There is a consistent history of inflated and unsubstantiated claims of success."
Fat removal technologies have no effect on cellulite because fat and cellulite are distinct. Weight and cellulite are unrelated. Cellulite is nearly universal in postpubertal females even if they are lean, but most obese males do not have cellulite unless they have androgen deficiency. "Exercise doesn’t really help it," he explained.
There is no good evidence for invasive treatments such as liposuction, subcision, mesotherapy, or carboxytherapy. Most data on noninvasive treatments measure results by body circumference, "which isn’t relevant to cellulite, so it’s hard to know whether or not there is improvement," he noted.
Flawed studies of treatments such as noninvasive Endermologie (mechanical cell stimulation), unipolar and bipolar radiofrequency, devices combining lasers and light sources, and topical treatments show modest, temporary benefit, he said.
Nearly 2 decades ago, a study of topical retinoids for cellulite showed some improvements, but this may have just been temporary improvements in inflammation, Dr. Avram said. Multiple expensive topical formulations have shown no significant efficacy, including xanthines, lactic acid, and aminophylline.
At least three laser devices that are cleared by the Food and Drug Administration are used to treat cellulite, but these devices only needed to prove safety, not efficacy, to achieve clearance, noted Dr. Avram, who is a lawyer as well as a physician. Studies of two of the laser devices suggested that they may produce temporary and limited decreases in limb circumference, which is a poor measure of cellulite.
A study of the third device treated 17 patients twice weekly for 4 weeks with a dual wavelength laser system with vacuum suction and mechanical massage (Plast. Reconstr. Surg. 2010;125:1788-96). The study suggested that 14 patients (82%) showed "improvement" at 1 month as measured by VECTRA 3-D photographs, but initial cellulite irregularities and any possible improvements were more difficult to see by conventional digital photography. The study did not define "improvement" and included no control sites or histology to assess improvement, noted Dr. Avram.
"This is really a flawed study," he said.
A separate study of a unipolar radiofrequency device for treating cellulite in 30 patients reported a mean 2.45-cm improvement in thigh circumference in 27 patients at 6 months with changes in upper dermis fibrosis on histology (Dermatol. Surg. 2008;34:204-9). However, circumference is an inherently imprecise measure that is irrelevant to cellulite, Dr. Avram noted.
"We need a set of criteria by which we can assess the efficacy of these technologies," he said. Photography is difficult and easily manipulated to exaggerate results. Ultrasound is imprecise and user dependent. MRI is expensive and requires specific coils for fat and 3-D imaging systems.
"At a minimum we need to have untreated controls, weight maintenance during studies, and laboratory data to confirm safety," Dr. Avram said. "We must hold our industry and our colleagues to high standards" and demand proof of scientifically important efficacy.
Physicians also should question whether the postulated mechanisms of action for these new technologies make sense with regard to cellulite. Any study without a histology report, for example, has no basis for a claim of efficacy in treating cellulite, he said.
Dr. Avram holds stock options in Zeltiq Aesthetics. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Treatment for cellulite is a multibillion dollar industry of unproved therapies, according to Dr. Matthew M. Avram.
Some treatments that claim to lessen cellulite may have produced minor, temporary improvements in flawed studies, but none has been proven to be truly effective, said Dr. Avram of Harvard University and director of Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center, Boston.
There is no medical reason to treat cellulite, which is normal in the female dermis and is not associated with morbidity or mortality. Many women care about it anyway "because every tabloid likes to show celebrities and their cellulite running around in Hawaii," he said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Many physicians and patients misunderstand cellulite, which is simply gender-related differences in the structure of subcutaneous fat lobules and the connective tissue septae that divide them, usually in the thigh area, Dr. Avram said. The treatment industry capitalizes on this ignorance.
"We need to educate our patients that cellulite is a totally normal condition" and treatments are at best mildly helpful for a short period of time, he said. "We need to be skeptical as well. There is a consistent history of inflated and unsubstantiated claims of success."
Fat removal technologies have no effect on cellulite because fat and cellulite are distinct. Weight and cellulite are unrelated. Cellulite is nearly universal in postpubertal females even if they are lean, but most obese males do not have cellulite unless they have androgen deficiency. "Exercise doesn’t really help it," he explained.
There is no good evidence for invasive treatments such as liposuction, subcision, mesotherapy, or carboxytherapy. Most data on noninvasive treatments measure results by body circumference, "which isn’t relevant to cellulite, so it’s hard to know whether or not there is improvement," he noted.
Flawed studies of treatments such as noninvasive Endermologie (mechanical cell stimulation), unipolar and bipolar radiofrequency, devices combining lasers and light sources, and topical treatments show modest, temporary benefit, he said.
Nearly 2 decades ago, a study of topical retinoids for cellulite showed some improvements, but this may have just been temporary improvements in inflammation, Dr. Avram said. Multiple expensive topical formulations have shown no significant efficacy, including xanthines, lactic acid, and aminophylline.
At least three laser devices that are cleared by the Food and Drug Administration are used to treat cellulite, but these devices only needed to prove safety, not efficacy, to achieve clearance, noted Dr. Avram, who is a lawyer as well as a physician. Studies of two of the laser devices suggested that they may produce temporary and limited decreases in limb circumference, which is a poor measure of cellulite.
A study of the third device treated 17 patients twice weekly for 4 weeks with a dual wavelength laser system with vacuum suction and mechanical massage (Plast. Reconstr. Surg. 2010;125:1788-96). The study suggested that 14 patients (82%) showed "improvement" at 1 month as measured by VECTRA 3-D photographs, but initial cellulite irregularities and any possible improvements were more difficult to see by conventional digital photography. The study did not define "improvement" and included no control sites or histology to assess improvement, noted Dr. Avram.
"This is really a flawed study," he said.
A separate study of a unipolar radiofrequency device for treating cellulite in 30 patients reported a mean 2.45-cm improvement in thigh circumference in 27 patients at 6 months with changes in upper dermis fibrosis on histology (Dermatol. Surg. 2008;34:204-9). However, circumference is an inherently imprecise measure that is irrelevant to cellulite, Dr. Avram noted.
"We need a set of criteria by which we can assess the efficacy of these technologies," he said. Photography is difficult and easily manipulated to exaggerate results. Ultrasound is imprecise and user dependent. MRI is expensive and requires specific coils for fat and 3-D imaging systems.
"At a minimum we need to have untreated controls, weight maintenance during studies, and laboratory data to confirm safety," Dr. Avram said. "We must hold our industry and our colleagues to high standards" and demand proof of scientifically important efficacy.
Physicians also should question whether the postulated mechanisms of action for these new technologies make sense with regard to cellulite. Any study without a histology report, for example, has no basis for a claim of efficacy in treating cellulite, he said.
Dr. Avram holds stock options in Zeltiq Aesthetics. SDEF and this news organization are owned by Elsevier.
LAS VEGAS – Treatment for cellulite is a multibillion dollar industry of unproved therapies, according to Dr. Matthew M. Avram.
Some treatments that claim to lessen cellulite may have produced minor, temporary improvements in flawed studies, but none has been proven to be truly effective, said Dr. Avram of Harvard University and director of Massachusetts General Hospital’s Dermatology Laser and Cosmetic Center, Boston.
There is no medical reason to treat cellulite, which is normal in the female dermis and is not associated with morbidity or mortality. Many women care about it anyway "because every tabloid likes to show celebrities and their cellulite running around in Hawaii," he said at the seminar sponsored by Skin Disease Education Foundation (SDEF).
Many physicians and patients misunderstand cellulite, which is simply gender-related differences in the structure of subcutaneous fat lobules and the connective tissue septae that divide them, usually in the thigh area, Dr. Avram said. The treatment industry capitalizes on this ignorance.
"We need to educate our patients that cellulite is a totally normal condition" and treatments are at best mildly helpful for a short period of time, he said. "We need to be skeptical as well. There is a consistent history of inflated and unsubstantiated claims of success."
Fat removal technologies have no effect on cellulite because fat and cellulite are distinct. Weight and cellulite are unrelated. Cellulite is nearly universal in postpubertal females even if they are lean, but most obese males do not have cellulite unless they have androgen deficiency. "Exercise doesn’t really help it," he explained.
There is no good evidence for invasive treatments such as liposuction, subcision, mesotherapy, or carboxytherapy. Most data on noninvasive treatments measure results by body circumference, "which isn’t relevant to cellulite, so it’s hard to know whether or not there is improvement," he noted.
Flawed studies of treatments such as noninvasive Endermologie (mechanical cell stimulation), unipolar and bipolar radiofrequency, devices combining lasers and light sources, and topical treatments show modest, temporary benefit, he said.
Nearly 2 decades ago, a study of topical retinoids for cellulite showed some improvements, but this may have just been temporary improvements in inflammation, Dr. Avram said. Multiple expensive topical formulations have shown no significant efficacy, including xanthines, lactic acid, and aminophylline.
At least three laser devices that are cleared by the Food and Drug Administration are used to treat cellulite, but these devices only needed to prove safety, not efficacy, to achieve clearance, noted Dr. Avram, who is a lawyer as well as a physician. Studies of two of the laser devices suggested that they may produce temporary and limited decreases in limb circumference, which is a poor measure of cellulite.
A study of the third device treated 17 patients twice weekly for 4 weeks with a dual wavelength laser system with vacuum suction and mechanical massage (Plast. Reconstr. Surg. 2010;125:1788-96). The study suggested that 14 patients (82%) showed "improvement" at 1 month as measured by VECTRA 3-D photographs, but initial cellulite irregularities and any possible improvements were more difficult to see by conventional digital photography. The study did not define "improvement" and included no control sites or histology to assess improvement, noted Dr. Avram.
"This is really a flawed study," he said.
A separate study of a unipolar radiofrequency device for treating cellulite in 30 patients reported a mean 2.45-cm improvement in thigh circumference in 27 patients at 6 months with changes in upper dermis fibrosis on histology (Dermatol. Surg. 2008;34:204-9). However, circumference is an inherently imprecise measure that is irrelevant to cellulite, Dr. Avram noted.
"We need a set of criteria by which we can assess the efficacy of these technologies," he said. Photography is difficult and easily manipulated to exaggerate results. Ultrasound is imprecise and user dependent. MRI is expensive and requires specific coils for fat and 3-D imaging systems.
"At a minimum we need to have untreated controls, weight maintenance during studies, and laboratory data to confirm safety," Dr. Avram said. "We must hold our industry and our colleagues to high standards" and demand proof of scientifically important efficacy.
Physicians also should question whether the postulated mechanisms of action for these new technologies make sense with regard to cellulite. Any study without a histology report, for example, has no basis for a claim of efficacy in treating cellulite, he said.
Dr. Avram holds stock options in Zeltiq Aesthetics. SDEF and this news organization are owned by Elsevier.
EXPERT ANALYSIS FROM A DERMATOLOGY SEMINAR