User login
Studies reveal pregnancy trends in American women with MS
New evidence provides estimates of the pregnancy rates for American women with multiple sclerosis (MS), their complication rates, and the rates of relapse and disease-modifying drug treatment during different phases before and after pregnancy.
The two new studies, conducted by Maria K. Houtchens, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, and her colleagues involved retrospective mining of U.S. commercial health plan data in the IQVIA Real-World Data Adjudicated Claims–U.S. database between Jan. 1, 2006, and June 30, 2015.
The mean age of pregnant women in the nine annual cohorts during that period was just over 32 years for those with MS and just over 29 years for those without. The percentage of women without MS who had a pregnancy-related claim in the database declined from 8.83% in 2006 to 7.75% in 2014 after adjusting for age, region, payer, and Charlson Comorbidity Index score, whereas the percentage increased in women with MS during the same period, from 7.91% to 9.47%. The investigators matched 2,115 women with MS and 2,115 without MS who had live births for a variety of variables and found that women with MS had higher rates of premature labor (31.4% vs. 27.4%; P = .005), infection in pregnancy (13.3% vs. 10.9%; P = .016), maternal cardiovascular disease (3.0% vs. 1.9%; P = .028), anemia or acquired coagulation disorder (2.5% vs. 1.3%; P = .007), neurologic complications in pregnancy (1.6% vs. 0.6%; P = .005), and sexually transmitted diseases in pregnancy (0.4% vs. 0%; P = .045). During labor and delivery, women with MS who had a live birth more often had a claim for acquired damage to the fetus (27.8% vs. 23.5%; P = .002) and congenital fetal malformations (13.2% vs. 10.3%; P = .004) than did women without MS.
In the second study, Dr. Houtchens and two coauthors from the first study of the database reported on a set of 2,158 women who had a live birth during the study period and had 1 year of continuous insurance eligibility before and after pregnancy. The odds for having an MS relapse declined during pregnancy (odds ratio, 0.623; 95% confidence interval, 0.521-0.744), rose during the 6-week postpartum puerperium (OR, 1.710; 95% CI, 1.358-2.152), and leveled off during the last three postpartum quarters to remain at a higher level than before pregnancy (OR, 1.216; 95% CI, 1.052-1.406). Disease-modifying drug treatment followed the same pattern with 20% using it before pregnancy, dropping to about 2% in the second trimester, and peaking in about a quarter of all patients 9-12 months post partum.
SOURCES: Houtchens MK et al. Neurology. 2018 Sep 28. doi: 10.1212/WNL.0000000000006382; Houtchens MK et al. Neurology. 2018 Sep 28. doi: 10.1212/WNL.0000000000006384.
New evidence provides estimates of the pregnancy rates for American women with multiple sclerosis (MS), their complication rates, and the rates of relapse and disease-modifying drug treatment during different phases before and after pregnancy.
The two new studies, conducted by Maria K. Houtchens, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, and her colleagues involved retrospective mining of U.S. commercial health plan data in the IQVIA Real-World Data Adjudicated Claims–U.S. database between Jan. 1, 2006, and June 30, 2015.
The mean age of pregnant women in the nine annual cohorts during that period was just over 32 years for those with MS and just over 29 years for those without. The percentage of women without MS who had a pregnancy-related claim in the database declined from 8.83% in 2006 to 7.75% in 2014 after adjusting for age, region, payer, and Charlson Comorbidity Index score, whereas the percentage increased in women with MS during the same period, from 7.91% to 9.47%. The investigators matched 2,115 women with MS and 2,115 without MS who had live births for a variety of variables and found that women with MS had higher rates of premature labor (31.4% vs. 27.4%; P = .005), infection in pregnancy (13.3% vs. 10.9%; P = .016), maternal cardiovascular disease (3.0% vs. 1.9%; P = .028), anemia or acquired coagulation disorder (2.5% vs. 1.3%; P = .007), neurologic complications in pregnancy (1.6% vs. 0.6%; P = .005), and sexually transmitted diseases in pregnancy (0.4% vs. 0%; P = .045). During labor and delivery, women with MS who had a live birth more often had a claim for acquired damage to the fetus (27.8% vs. 23.5%; P = .002) and congenital fetal malformations (13.2% vs. 10.3%; P = .004) than did women without MS.
In the second study, Dr. Houtchens and two coauthors from the first study of the database reported on a set of 2,158 women who had a live birth during the study period and had 1 year of continuous insurance eligibility before and after pregnancy. The odds for having an MS relapse declined during pregnancy (odds ratio, 0.623; 95% confidence interval, 0.521-0.744), rose during the 6-week postpartum puerperium (OR, 1.710; 95% CI, 1.358-2.152), and leveled off during the last three postpartum quarters to remain at a higher level than before pregnancy (OR, 1.216; 95% CI, 1.052-1.406). Disease-modifying drug treatment followed the same pattern with 20% using it before pregnancy, dropping to about 2% in the second trimester, and peaking in about a quarter of all patients 9-12 months post partum.
SOURCES: Houtchens MK et al. Neurology. 2018 Sep 28. doi: 10.1212/WNL.0000000000006382; Houtchens MK et al. Neurology. 2018 Sep 28. doi: 10.1212/WNL.0000000000006384.
New evidence provides estimates of the pregnancy rates for American women with multiple sclerosis (MS), their complication rates, and the rates of relapse and disease-modifying drug treatment during different phases before and after pregnancy.
The two new studies, conducted by Maria K. Houtchens, MD, of Brigham and Women’s Hospital and Harvard Medical School, Boston, and her colleagues involved retrospective mining of U.S. commercial health plan data in the IQVIA Real-World Data Adjudicated Claims–U.S. database between Jan. 1, 2006, and June 30, 2015.
The mean age of pregnant women in the nine annual cohorts during that period was just over 32 years for those with MS and just over 29 years for those without. The percentage of women without MS who had a pregnancy-related claim in the database declined from 8.83% in 2006 to 7.75% in 2014 after adjusting for age, region, payer, and Charlson Comorbidity Index score, whereas the percentage increased in women with MS during the same period, from 7.91% to 9.47%. The investigators matched 2,115 women with MS and 2,115 without MS who had live births for a variety of variables and found that women with MS had higher rates of premature labor (31.4% vs. 27.4%; P = .005), infection in pregnancy (13.3% vs. 10.9%; P = .016), maternal cardiovascular disease (3.0% vs. 1.9%; P = .028), anemia or acquired coagulation disorder (2.5% vs. 1.3%; P = .007), neurologic complications in pregnancy (1.6% vs. 0.6%; P = .005), and sexually transmitted diseases in pregnancy (0.4% vs. 0%; P = .045). During labor and delivery, women with MS who had a live birth more often had a claim for acquired damage to the fetus (27.8% vs. 23.5%; P = .002) and congenital fetal malformations (13.2% vs. 10.3%; P = .004) than did women without MS.
In the second study, Dr. Houtchens and two coauthors from the first study of the database reported on a set of 2,158 women who had a live birth during the study period and had 1 year of continuous insurance eligibility before and after pregnancy. The odds for having an MS relapse declined during pregnancy (odds ratio, 0.623; 95% confidence interval, 0.521-0.744), rose during the 6-week postpartum puerperium (OR, 1.710; 95% CI, 1.358-2.152), and leveled off during the last three postpartum quarters to remain at a higher level than before pregnancy (OR, 1.216; 95% CI, 1.052-1.406). Disease-modifying drug treatment followed the same pattern with 20% using it before pregnancy, dropping to about 2% in the second trimester, and peaking in about a quarter of all patients 9-12 months post partum.
SOURCES: Houtchens MK et al. Neurology. 2018 Sep 28. doi: 10.1212/WNL.0000000000006382; Houtchens MK et al. Neurology. 2018 Sep 28. doi: 10.1212/WNL.0000000000006384.
FROM NEUROLOGY
MBC care causes more money problems for uninsured – but more financial stress for the insured
PHOENIX – Metastatic breast cancer care may be a bigger financial burden for uninsured patients, but it’s actually causing more financial distress for the insured, results of a recent survey suggest.
The uninsured more often reported material burdens, such as lack of savings or refusing treatment because of cost, according to survey results reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
By contrast, the insured reported more worry, distress, and frustration related to financial problems, reported Stephanie B. Wheeler, PhD, MPH, of the Gillings School of Global Public Health, University of North Carolina at Chapel Hill.
That divide suggests increased health insurance coverage is not enough to tackle the problem of cancer-related financial harm, said Dr. Wheeler.
“Health insurance expansion is important,” she said, “but it’s going to be ultimately inadequate in solving the problem of financial distress in our cancer patients. We really need to be thinking about other types of interventions that can do a better job of meeting patients where they are.”
Regardless of insurance status, this survey showed an “unprecedented” high level of cancer-related financial harm in metastatic breast cancer patients as compared with previous studies of early-stage cancer patients, Dr. Wheeler said.
The online survey was completed by 1,054 individuals who were members of the Metastatic Breast Cancer Network, a patient advocacy group. Approximately 30% of participants were uninsured, Dr. Wheeler reported.
Overall, 56% of respondents reported not having enough savings to cover costs of care, while 54% stopped or refused treatment because of cost, and 49% said they had been contacted by collection agencies, survey results show.
These material burdens were “perhaps not surprisingly” significantly more often reported by the uninsured respondents, Dr. Wheeler said. What may be surprising, she added, is that psychosocial burdens were more frequently reported by the insured respondents.
The most frequently reported psychosocial burden was worry about cancer-related financial problems, reported by 68% of respondents overall, but nearly 80% of insured and around 45% of uninsured respondents (P less than .001), Dr. Wheeler said.
The least often reported psychosocial issue was worry about the effects of financial stress on the family, at 31% of all respondents. Even so, there was a significant difference in response by insurance status, with the percentage approaching 40% for the insured, but less than 20% for the uninsured (P less than .001).
This high level of worry and distress may indicate that insured cancer patients may be expecting their insurance to cover more that it does, but ultimately, it is inadequate to meet their needs, Dr. Wheeler said.
“It’s also possible that because insured participants are more often affluent – they more often have retirement and other savings to draw down – that they actually have more to lose,” she added, “and when it comes to the legacy that they leave behind for their family, that creates additional stress – not just for them as an individual, but for their entire household.”
Previous research shows that the adverse financial impacts of cancer, also referred to as financial toxicity, affect about 30% of cancer patients, Dr. Wheeler said in her presentation.
Dr. Wheeler had no relationships to disclose. Funding for the project was provided from the National Comprehensive Cancer Network and Pfizer Independent Grants for Learning & Change.
SOURCE: Wheeler SB et al. Quality Care Symposium, Abstract 32.
PHOENIX – Metastatic breast cancer care may be a bigger financial burden for uninsured patients, but it’s actually causing more financial distress for the insured, results of a recent survey suggest.
The uninsured more often reported material burdens, such as lack of savings or refusing treatment because of cost, according to survey results reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
By contrast, the insured reported more worry, distress, and frustration related to financial problems, reported Stephanie B. Wheeler, PhD, MPH, of the Gillings School of Global Public Health, University of North Carolina at Chapel Hill.
That divide suggests increased health insurance coverage is not enough to tackle the problem of cancer-related financial harm, said Dr. Wheeler.
“Health insurance expansion is important,” she said, “but it’s going to be ultimately inadequate in solving the problem of financial distress in our cancer patients. We really need to be thinking about other types of interventions that can do a better job of meeting patients where they are.”
Regardless of insurance status, this survey showed an “unprecedented” high level of cancer-related financial harm in metastatic breast cancer patients as compared with previous studies of early-stage cancer patients, Dr. Wheeler said.
The online survey was completed by 1,054 individuals who were members of the Metastatic Breast Cancer Network, a patient advocacy group. Approximately 30% of participants were uninsured, Dr. Wheeler reported.
Overall, 56% of respondents reported not having enough savings to cover costs of care, while 54% stopped or refused treatment because of cost, and 49% said they had been contacted by collection agencies, survey results show.
These material burdens were “perhaps not surprisingly” significantly more often reported by the uninsured respondents, Dr. Wheeler said. What may be surprising, she added, is that psychosocial burdens were more frequently reported by the insured respondents.
The most frequently reported psychosocial burden was worry about cancer-related financial problems, reported by 68% of respondents overall, but nearly 80% of insured and around 45% of uninsured respondents (P less than .001), Dr. Wheeler said.
The least often reported psychosocial issue was worry about the effects of financial stress on the family, at 31% of all respondents. Even so, there was a significant difference in response by insurance status, with the percentage approaching 40% for the insured, but less than 20% for the uninsured (P less than .001).
This high level of worry and distress may indicate that insured cancer patients may be expecting their insurance to cover more that it does, but ultimately, it is inadequate to meet their needs, Dr. Wheeler said.
“It’s also possible that because insured participants are more often affluent – they more often have retirement and other savings to draw down – that they actually have more to lose,” she added, “and when it comes to the legacy that they leave behind for their family, that creates additional stress – not just for them as an individual, but for their entire household.”
Previous research shows that the adverse financial impacts of cancer, also referred to as financial toxicity, affect about 30% of cancer patients, Dr. Wheeler said in her presentation.
Dr. Wheeler had no relationships to disclose. Funding for the project was provided from the National Comprehensive Cancer Network and Pfizer Independent Grants for Learning & Change.
SOURCE: Wheeler SB et al. Quality Care Symposium, Abstract 32.
PHOENIX – Metastatic breast cancer care may be a bigger financial burden for uninsured patients, but it’s actually causing more financial distress for the insured, results of a recent survey suggest.
The uninsured more often reported material burdens, such as lack of savings or refusing treatment because of cost, according to survey results reported at a symposium on quality care sponsored by the American Society of Clinical Oncology.
By contrast, the insured reported more worry, distress, and frustration related to financial problems, reported Stephanie B. Wheeler, PhD, MPH, of the Gillings School of Global Public Health, University of North Carolina at Chapel Hill.
That divide suggests increased health insurance coverage is not enough to tackle the problem of cancer-related financial harm, said Dr. Wheeler.
“Health insurance expansion is important,” she said, “but it’s going to be ultimately inadequate in solving the problem of financial distress in our cancer patients. We really need to be thinking about other types of interventions that can do a better job of meeting patients where they are.”
Regardless of insurance status, this survey showed an “unprecedented” high level of cancer-related financial harm in metastatic breast cancer patients as compared with previous studies of early-stage cancer patients, Dr. Wheeler said.
The online survey was completed by 1,054 individuals who were members of the Metastatic Breast Cancer Network, a patient advocacy group. Approximately 30% of participants were uninsured, Dr. Wheeler reported.
Overall, 56% of respondents reported not having enough savings to cover costs of care, while 54% stopped or refused treatment because of cost, and 49% said they had been contacted by collection agencies, survey results show.
These material burdens were “perhaps not surprisingly” significantly more often reported by the uninsured respondents, Dr. Wheeler said. What may be surprising, she added, is that psychosocial burdens were more frequently reported by the insured respondents.
The most frequently reported psychosocial burden was worry about cancer-related financial problems, reported by 68% of respondents overall, but nearly 80% of insured and around 45% of uninsured respondents (P less than .001), Dr. Wheeler said.
The least often reported psychosocial issue was worry about the effects of financial stress on the family, at 31% of all respondents. Even so, there was a significant difference in response by insurance status, with the percentage approaching 40% for the insured, but less than 20% for the uninsured (P less than .001).
This high level of worry and distress may indicate that insured cancer patients may be expecting their insurance to cover more that it does, but ultimately, it is inadequate to meet their needs, Dr. Wheeler said.
“It’s also possible that because insured participants are more often affluent – they more often have retirement and other savings to draw down – that they actually have more to lose,” she added, “and when it comes to the legacy that they leave behind for their family, that creates additional stress – not just for them as an individual, but for their entire household.”
Previous research shows that the adverse financial impacts of cancer, also referred to as financial toxicity, affect about 30% of cancer patients, Dr. Wheeler said in her presentation.
Dr. Wheeler had no relationships to disclose. Funding for the project was provided from the National Comprehensive Cancer Network and Pfizer Independent Grants for Learning & Change.
SOURCE: Wheeler SB et al. Quality Care Symposium, Abstract 32.
REPORTING FROM THE QUALITY CARE SYMPOSIUM
Key clinical point: Survey results suggest that metastatic breast cancer care is a bigger financial burden for uninsured patients vs insured patients, though the insured have more financial distress related to that care.
Major finding: Overall, 68% of respondents said they worried about cancer-related financial problems, and significantly more insured individuals reported this worry (P less than .001).
Study details: Analysis of survey responses from 1,054 members of the Metastatic Breast Cancer Network, of whom about 30% were uninsured.
Disclosures: Funding for the project was provided from the National Comprehensive Cancer Network and Pfizer Independent Grants for Learning & Change.
Source: Wheeler SB et al. Quality Care Symposium, Abstract 32.
Investigators identify 21 genomic “hotspots” in breast cancers
Cancer geneticists have identified 21 clusters of complex chromosomal rearrangements in breast cancers that contain both known oncogenes and potential new driver loci.
A systematic analysis of chromosomal rearrangements in tissues from 560 patients with breast cancer identified 21 “hotspots,” some of which contain known oncogene chromosomal loci, and others of which contain genes not typically associated with breast cancer, reported Serena Nik-Zainal, PhD, of the University of Cambridge, England, and her colleagues.
“Detailed analysis of rearrangements at these hotspots highlights chromosomal aberrations likely driven by selection, and reveal underlying mutational processes,” they wrote in a study published online in Annals of Oncology.
The investigators sought insight into mutational mechanisms of gene amplifications by examining clustered rearrangements – somatic breakpoints occurring in high densities – in individual patients.
To see whether these rearrangements were associated with breast cancer, they identified the aforementioned chromosomal hotspots where clustered rearrangements were seen in samples from different patients.
They identified 624 cluster rearrangements in the 560 breast cancer genomes, including 17,247 within-chromosome rearrangements, and 6,509 between-chromosome translocations.
Of the 560 samples, 372 had at least one rearrangement cluster, with the frequency of clusters similar between some breast cancer types. For example, there were 0.96 rearrangements clusters per sample from patients with triple negative breast cancers, and 1.00 per sample from women with estrogen receptor–positive tumors.
“To identify loci where clusters of rearrangements recur across multiple independent tumor samples, we pooled all breakpoints in the ‘clustered’ category and sorted them according to position in the reference genome,” the investigators explained.
They used a Piecewise-Constant-Fitting algorithm to identify genome sequences where there were short inter-mutation distances between rearrangement clusters, suggesting the presence of hotspots.
In the 21 hotspots they identified, they found, as expected, common driver amplification regions (e.g., CCND1, ERBB2, ZNF217, chr8:ZNF703/FGFR1, IGF1R, and MYC), but also several hotspots near oncogenes that are not typically associated with breast cancer.
Notably, they saw simultaneous amplification of regions on chromosomes 8 and 11 (chr8:ZNF703/FGFR1 and chr11:CCND1). Amplification of these regions are frequent in estrogen receptor–positive breast cancers. The investigators propose a pathogenic model in which a chromosome 8 to chromosome 11 translocation is an early, critical event leading to breast tumor development.
“Clustered rearrangements are common in breast cancer genomes, and often associated with gene amplifications that drive oncogenesis. Understanding the process of amplicon formation, an example of which we present here for the chr8:ZNF703/FGFR1 and chr11:CCND1 co-amplifications, will be important for our understanding of the origins of a subset of breast cancers,” they concluded.
The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
SOURCE: Glodzik D et al. Ann Oncol. 2018 Sept 25. doi: 10.1093/annonc/mdy404.
Cancer geneticists have identified 21 clusters of complex chromosomal rearrangements in breast cancers that contain both known oncogenes and potential new driver loci.
A systematic analysis of chromosomal rearrangements in tissues from 560 patients with breast cancer identified 21 “hotspots,” some of which contain known oncogene chromosomal loci, and others of which contain genes not typically associated with breast cancer, reported Serena Nik-Zainal, PhD, of the University of Cambridge, England, and her colleagues.
“Detailed analysis of rearrangements at these hotspots highlights chromosomal aberrations likely driven by selection, and reveal underlying mutational processes,” they wrote in a study published online in Annals of Oncology.
The investigators sought insight into mutational mechanisms of gene amplifications by examining clustered rearrangements – somatic breakpoints occurring in high densities – in individual patients.
To see whether these rearrangements were associated with breast cancer, they identified the aforementioned chromosomal hotspots where clustered rearrangements were seen in samples from different patients.
They identified 624 cluster rearrangements in the 560 breast cancer genomes, including 17,247 within-chromosome rearrangements, and 6,509 between-chromosome translocations.
Of the 560 samples, 372 had at least one rearrangement cluster, with the frequency of clusters similar between some breast cancer types. For example, there were 0.96 rearrangements clusters per sample from patients with triple negative breast cancers, and 1.00 per sample from women with estrogen receptor–positive tumors.
“To identify loci where clusters of rearrangements recur across multiple independent tumor samples, we pooled all breakpoints in the ‘clustered’ category and sorted them according to position in the reference genome,” the investigators explained.
They used a Piecewise-Constant-Fitting algorithm to identify genome sequences where there were short inter-mutation distances between rearrangement clusters, suggesting the presence of hotspots.
In the 21 hotspots they identified, they found, as expected, common driver amplification regions (e.g., CCND1, ERBB2, ZNF217, chr8:ZNF703/FGFR1, IGF1R, and MYC), but also several hotspots near oncogenes that are not typically associated with breast cancer.
Notably, they saw simultaneous amplification of regions on chromosomes 8 and 11 (chr8:ZNF703/FGFR1 and chr11:CCND1). Amplification of these regions are frequent in estrogen receptor–positive breast cancers. The investigators propose a pathogenic model in which a chromosome 8 to chromosome 11 translocation is an early, critical event leading to breast tumor development.
“Clustered rearrangements are common in breast cancer genomes, and often associated with gene amplifications that drive oncogenesis. Understanding the process of amplicon formation, an example of which we present here for the chr8:ZNF703/FGFR1 and chr11:CCND1 co-amplifications, will be important for our understanding of the origins of a subset of breast cancers,” they concluded.
The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
SOURCE: Glodzik D et al. Ann Oncol. 2018 Sept 25. doi: 10.1093/annonc/mdy404.
Cancer geneticists have identified 21 clusters of complex chromosomal rearrangements in breast cancers that contain both known oncogenes and potential new driver loci.
A systematic analysis of chromosomal rearrangements in tissues from 560 patients with breast cancer identified 21 “hotspots,” some of which contain known oncogene chromosomal loci, and others of which contain genes not typically associated with breast cancer, reported Serena Nik-Zainal, PhD, of the University of Cambridge, England, and her colleagues.
“Detailed analysis of rearrangements at these hotspots highlights chromosomal aberrations likely driven by selection, and reveal underlying mutational processes,” they wrote in a study published online in Annals of Oncology.
The investigators sought insight into mutational mechanisms of gene amplifications by examining clustered rearrangements – somatic breakpoints occurring in high densities – in individual patients.
To see whether these rearrangements were associated with breast cancer, they identified the aforementioned chromosomal hotspots where clustered rearrangements were seen in samples from different patients.
They identified 624 cluster rearrangements in the 560 breast cancer genomes, including 17,247 within-chromosome rearrangements, and 6,509 between-chromosome translocations.
Of the 560 samples, 372 had at least one rearrangement cluster, with the frequency of clusters similar between some breast cancer types. For example, there were 0.96 rearrangements clusters per sample from patients with triple negative breast cancers, and 1.00 per sample from women with estrogen receptor–positive tumors.
“To identify loci where clusters of rearrangements recur across multiple independent tumor samples, we pooled all breakpoints in the ‘clustered’ category and sorted them according to position in the reference genome,” the investigators explained.
They used a Piecewise-Constant-Fitting algorithm to identify genome sequences where there were short inter-mutation distances between rearrangement clusters, suggesting the presence of hotspots.
In the 21 hotspots they identified, they found, as expected, common driver amplification regions (e.g., CCND1, ERBB2, ZNF217, chr8:ZNF703/FGFR1, IGF1R, and MYC), but also several hotspots near oncogenes that are not typically associated with breast cancer.
Notably, they saw simultaneous amplification of regions on chromosomes 8 and 11 (chr8:ZNF703/FGFR1 and chr11:CCND1). Amplification of these regions are frequent in estrogen receptor–positive breast cancers. The investigators propose a pathogenic model in which a chromosome 8 to chromosome 11 translocation is an early, critical event leading to breast tumor development.
“Clustered rearrangements are common in breast cancer genomes, and often associated with gene amplifications that drive oncogenesis. Understanding the process of amplicon formation, an example of which we present here for the chr8:ZNF703/FGFR1 and chr11:CCND1 co-amplifications, will be important for our understanding of the origins of a subset of breast cancers,” they concluded.
The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
SOURCE: Glodzik D et al. Ann Oncol. 2018 Sept 25. doi: 10.1093/annonc/mdy404.
FROM ANNALS OF ONCOLOGY
Key clinical point: Chromosomal rearrangement “hotspots” contain both known breast cancer oncogenes and potential new loci that may explain the mechanism of deleterious gene amplifications.
Major finding: A chromosome 8 to 11 translocation may be the initiating event for some breast cancer subtypes.
Study details: Genomic analysis of samples from 560 patients with breast cancer.
Disclosures: The study was supported by an award from the Wellcome Trust. Dr. Nik-Zainal and coauthor Dominik Glodzik are inventors on several patent applications. All remaining authors declared no conflicts of interest.
Source: Glodzik D et al. Ann Oncol. 2018 Sep 25. doi: 10.1093/annonc/mdy404.
Mobile App Rankings in Dermatology
As technology continues to advance, so too does its accessibility to the general population. In 2013, 56% of Americans owned a smartphone versus 77% in 2017.1With the increase in mobile applications (apps) available, it is no surprise that the market has extended into the medical field, with dermatology being no exception.2 The majority of dermatology apps can be classified as teledermatology apps, followed by self-surveillance, disease guide, and reference apps. Additional types of dermatology apps include dermoscopy, conference, education, photograph storage and sharing, and journal apps, and others.2 In this study, we examined Apple App Store rankings to determine the types of dermatology apps that are most popular among patients and physicians.
METHODS
A popular app rankings analyzer (App Annie) was used to search for dermatology apps along with their App Store rankings.3 Although iOS is not the most popular mobile device operating system, we chose to evaluate app rankings via the App Store because iPhones are the top-selling individual phones of any kind in the United States.4
We performed our analysis on a single day (July 14, 2018) given that app rankings can change daily. We incorporated the following keywords, which were commonly used in other dermatology app studies: dermatology, psoriasis, rosacea, acne, skin cancer, melanoma, eczema, and teledermatology. The category ranking was defined as the rank of a free or paid app in the App Store’s top charts for the selected country (United States), market (Apple), and device (iPhone) within their app category (Medical). Inclusion criteria required a ranking in the top 1500 Medical apps and being categorized in the App Store as a Medical app. Exclusion criteria included apps that focused on cosmetics, private practice, direct advertisements, photograph editing, or claims to cure skin disease, as well as non–English-language apps. The App Store descriptions were assessed to determine the type of each app (eg, teledermatology, disease guide) and target audience (patient, physician, or both).
Another search was performed using the same keywords but within the Health and Fitness category to capture potentially more highly ranked apps among patients. We also conducted separate searches within the Medical category using the keywords billing, coding, and ICD (International Classification of Diseases) to evaluate rankings for billing/coding apps, as well as EMR and electronic medical records for electronic medical record (EMR) apps.
RESULTS
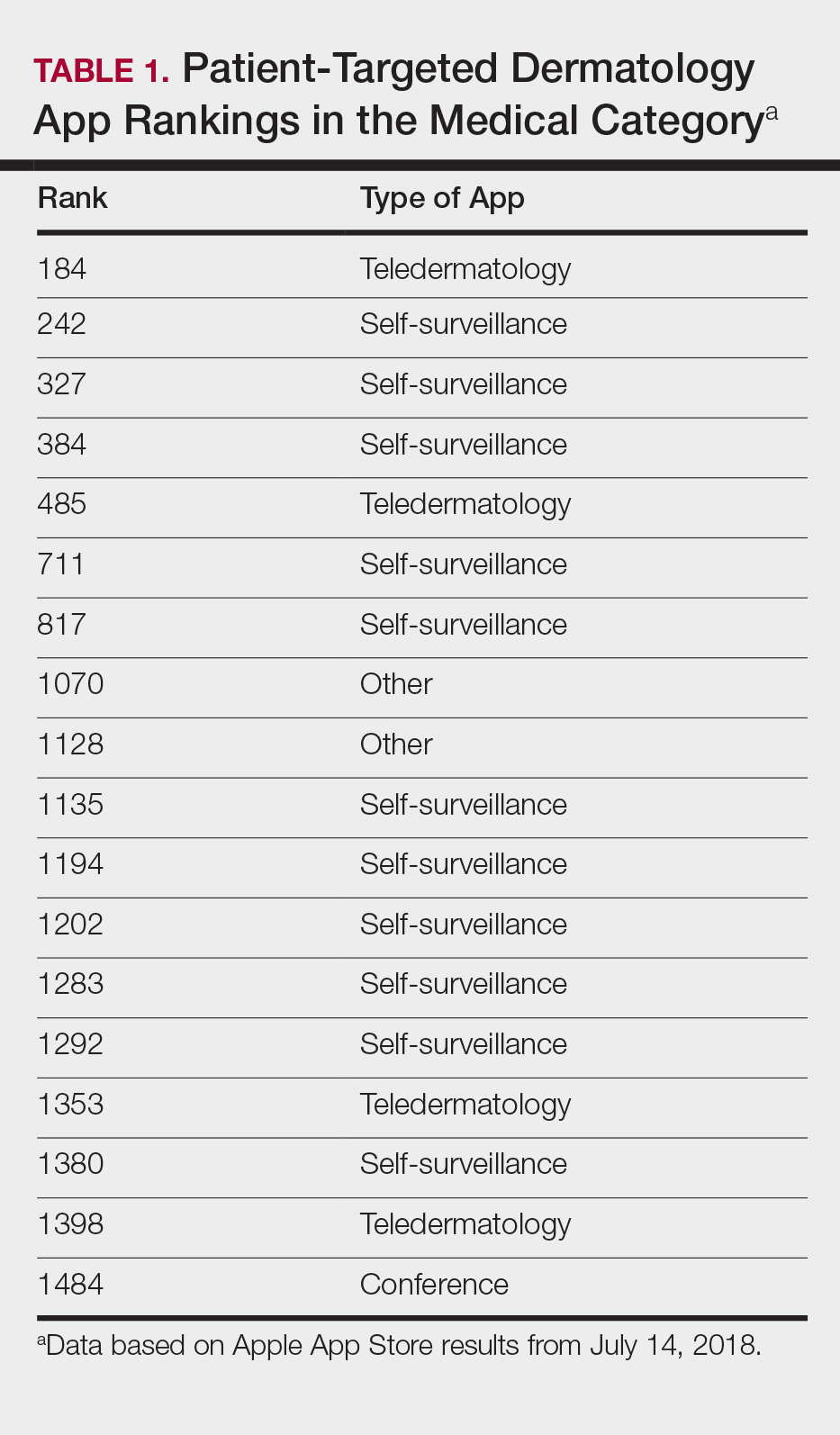
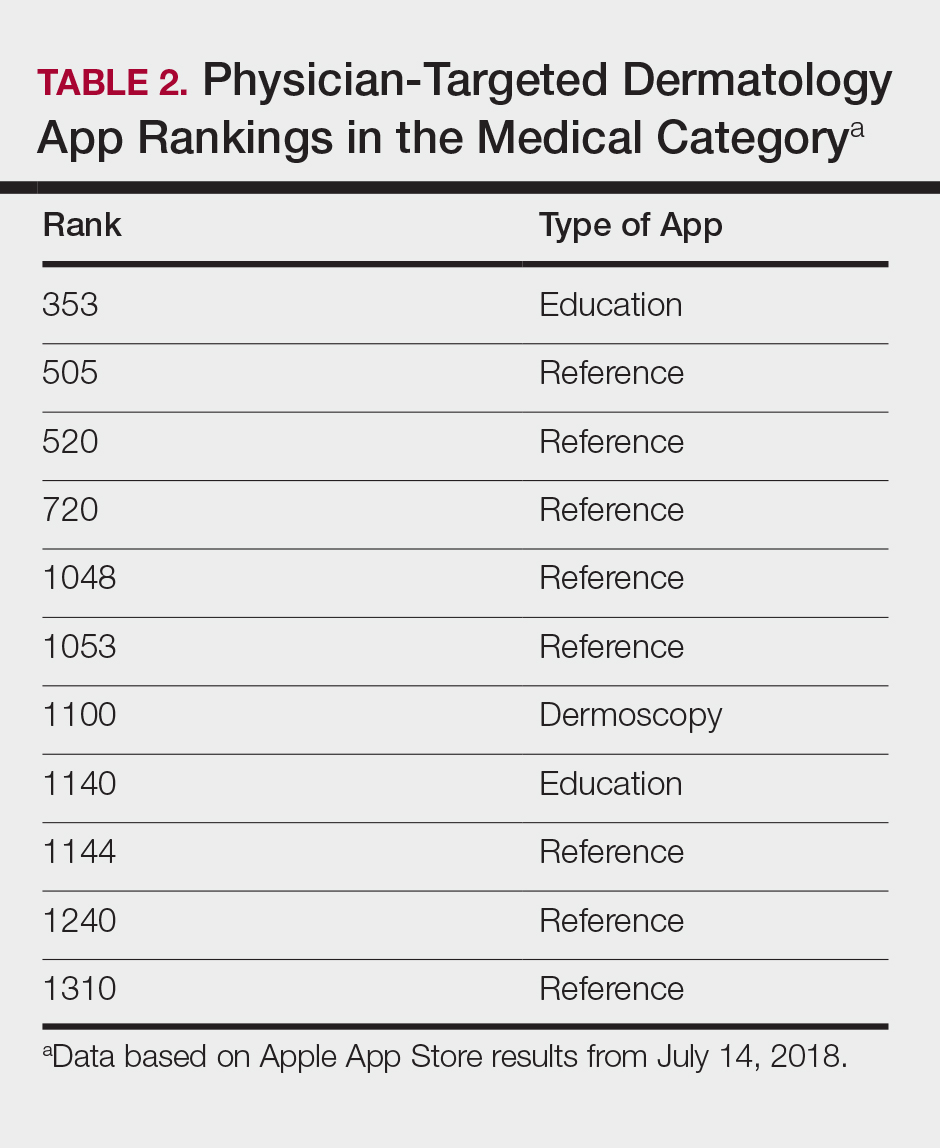
The initial search yielded 851 results, which was narrowed down to 29 apps after applying the exclusion criteria. Of note, prior to application of the exclusion criteria, one dermatology app that was considered to be a direct advertisement app claiming to cure acne was ranked fourth of 1500 apps in the Medical category. However, the majority of the search results were excluded because they were not popular enough to be ranked among the top 1500 apps. There were more ranked dermatology apps in the Medical category targeting patients than physicians; 18 of 29 (62%) qualifying apps targeted patients and 11 (38%) targeted physicians (Tables 1 and 2). No apps targeted both groups. The most common type of ranked app targeting patients was self-surveillance (11/18), and the most common type targeting physicians was reference (8/11). The highest ranked app targeting patients was a teledermatology app with a ranking of 184, and the highest ranked app targeting physicians was educational, ranked 353. The least common type of ranked apps targeting patients were “other” (2/18 [11%]; 1 prescription and 1 UV monitor app) and conference (1/18 [6%]). The least common type of ranked apps targeting physicians were education (2/11 [18%]) and dermoscopy (1/11 [9%]).
Our search of the Health and Fitness category yielded 6 apps, all targeting patients; 3 (50%) were self-surveillance apps, and 3 (50%) were classified as other (2 UV monitors and a conferencing app for cancer emotional support)(Table 3).
Our search of the Medical category for billing/coding and EMR apps yielded 232 and 164 apps, respectively; of them, 49 (21%) and 54 (33%) apps were ranked. These apps did not overlap with the dermatology-related search criteria; thus, we were not able to ascertain how many of these apps were used specifically by health care providers in dermatology.
COMMENT
Patient Apps
The most common apps used by patients are fitness and nutrition tracker apps categorized as Health and Fitness5,6; however, the majority of ranked dermatology apps are categorized as Medical per our findings. In a study of 557 dermatology patients, it was found that among the health-related apps they used, the most common apps after fitness/nutrition were references, followed by patient portals, self-surveillance, and emotional assistance apps.6 Our search was consistent with these findings, suggesting that the most desired dermatology apps by patients are those that allow them to be proactive with their health. It is no surprise that the top-ranked app targeting patients was a teledermatology app, followed by multiple self-surveillance apps. The highest ranked self-surveillance app in the Health and Fitness category focused on monitoring the effects of nutrition on symptoms of diseases including skin disorders, while the highest ranked (as well as the majority of) self-surveillance apps in the Medical category encompassed mole monitoring and cancer risk calculators.
Benefits of the ranked dermatology apps in the Medical and Health and Fitness categories targeting patients include more immediate access to health care and education. Despite this popularity among patients, Masud et al7 demonstrated that only 20.5% (9/44) of dermatology apps targeting patients may be reliable resources based on a rubric created by the investigators. Overall, there remains a research gap for a standardized scientific approach to evaluating app validity and reliability.
Teledermatology
Teledermatology apps are the most common dermatology apps,2 allowing for remote evaluation of patients through either live consultations or transmittance of medical information for later review by board-certified physicians.8 Features common to many teledermatology apps include accessibility on Android (Google Inc) and iOS as well as a web version. Security and Health Insurance Portability and Accountability Act compliance is especially important and is enforced through user authentications, data encryption, and automatic logout features. Data is not stored locally and is secured on a private server with backup. Referring providers and consultants often can communicate within the app. Insurance providers also may cover teledermatology services, and if not, the out-of-pocket costs often are affordable.
The highest-ranked patient app (ranked 184 in the Medical category) was a teledermatology app that did not meet the American Telemedicine Association standards for teledermatology apps.9 The popularity of this app among patients may have been attributable to multiple ease-of-use and turnaround time features. The user interface was simplistic, and the design was appealing to the eye. The entry field options were minimal to avoid confusion. The turnaround time to receive a diagnosis depended on 1 of 3 options, including a more rapid response for an increased cost. Ease of use was the highlight of this app at the cost of accuracy, as the limited amount of information that users were required to provide physicians compromised diagnostic accuracy in this app.
For comparison, we chose a nonranked (and thus less frequently used) teledermatology app that had previously undergone scientific evaluation using 13 evaluation criteria specific to teledermatology.10 The app also met the American Telemedicine Association standard for teledermatology apps.9 The app was originally a broader telemedicine app but featured a section specific to teledermatology. The user interface was simple but professional, almost resembling an EMR. The input fields included a comprehensive history that permitted a better evaluation of a lesion but might be tedious for users. This app boasted professionalism and accuracy, but from a user standpoint, it may have been too time-consuming.
Striking a balance between ensuring proper care versus appealing to patients is a difficult but important task. Based on this study, it appears that popular patient apps may in fact have less scientific rationale and therefore potentially less accuracy.
Self-surveillance
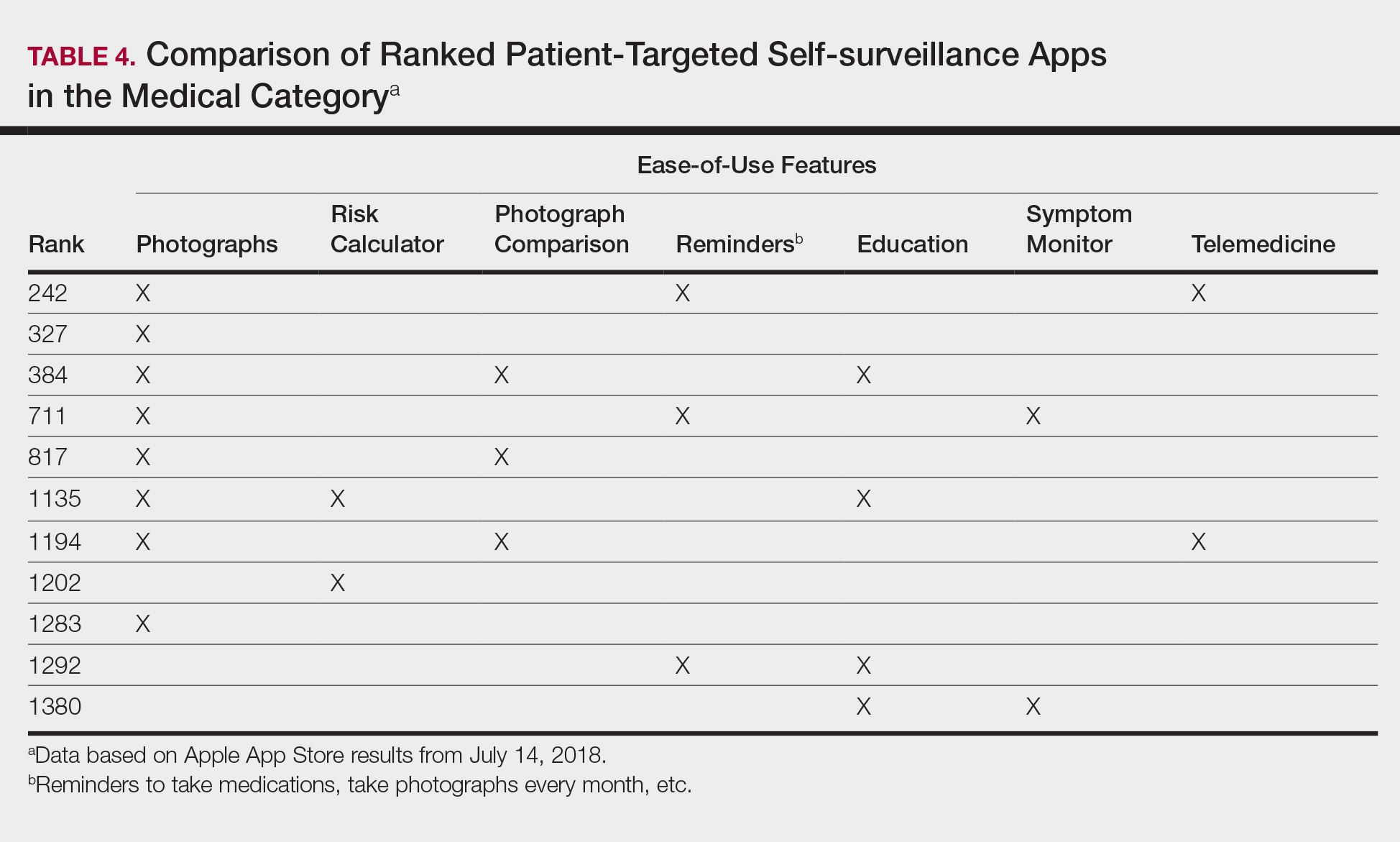
Although self-surveillance apps did not account for the highest-ranked app, they were the most frequently ranked app type in our study. Most of the ranked self-surveillance apps in the Medical category were for monitoring lesions over time to assess for changes. These apps help users take photographs that are well organized in a single, easy-to-find location. Some apps were risk calculators that assessed the risk for malignancies using a questionnaire. The majority of these self-surveillance apps were specific to skin cancer detection. Of note, one of the ranked self-surveillance apps assessed drug effectiveness by monitoring clinical appearance and symptoms. The lowest ranked self-surveillance app in the top 1500 ranked Medical apps in our search monitored cancer symptoms not specific to dermatology. Although this app had a low ranking (1380/1500), it received a high number of reviews and was well rated at 4.8 out of 5 stars; therefore, it seemed more helpful than the other higher-ranked apps targeting patients, which had higher rankings but minimal to no reviews or ratings. A comparison of the ease-of-use features of all the ranked patient-targeted self-surveillance apps in the Medical category is provided in Table 4.
Physician Apps
After examining the results of apps targeting physicians, we realized that the data may be accurate but may not be as representative of all currently practicing dermatology providers. Given the increased usage of apps among younger age groups,11 our data may be skewed toward medical students and residents, supported by the fact that the top-ranked physician app in our study was an education app and the majority were reference apps. Future studies are needed to reexamine app ranking as this age group transitions from entry-level health care providers in the next 5 to 10 years. These findings also suggest less frequent app use among more veteran health care providers within our specific search parameters. Therefore, we decided to do subsequent searches for available billing/coding and EMR apps, which were many, but as mentioned above, none were specific to dermatology.
General Dermatology References
Most of the dermatology reference apps were formatted as e-books; however, other apps such as the Amazon Kindle app (categorized under Books) providing access to multiple e-books within one app were not included. Some apps included study aid features (eg, flash cards, quizzes), and topics spanned both dermatology and dermatopathology. Apps provide a unique way for on-the-go studying for dermatologists in training, and if the usage continues to grow, there may be a need for increased formal integration in dermatology education in the future.
Journals
Journal apps were not among those listed in the top-ranked apps we evaluated, which we suspect may be because journals were categorized differently from one journal to the next; for example, the Journal of the American Academy of Dermatology was ranked 1168 in the Magazines and Newspapers category. On the other hand, Dermatology World was ranked 1363 in the Reference category. An article’s citation affects the publishing journal’s impact factor, which is one of the most important variables in measuring a journal’s influence. In the future, there may be other variables that could aid in understanding journal impact as it relates to the journal’s accessibility.
Limitations
Our study did not look at Android apps. The top chart apps in the Android and Apple App Stores use undisclosed algorithms likely involving different characteristics such as number of downloads, frequency of updates, number of reviews, ratings, and more. Thus, the rankings across these different markets would not be comparable. Although our choice of keywords stemmed from the majority of prior studies looking at dermatology apps, our search was limited due to the use of these specific keywords. To avoid skewing data by cross-comparison of noncomparable categories, we could not compare apps in the Medical category versus those in other categories.
CONCLUSION
There seems to be a disconnect between the apps that are popular among patients and the scientific validity of the apps. As app usage increases among dermatology providers, whose demographic is shifting younger and younger, apps may become more incorporated in our education, and as such, it will become more critical to develop formal scientific standards. Given these future trends, we may need to increase our current literature and understanding of apps in dermatology with regard to their impact on both patients and health care providers.
- Poushter J, Bishop C, Chwe H. Social media use continues to rise in developing countries but plateaus across developed ones. Pew Research Center website. http://www.pewglobal.org/2018/06/19/social-media-use-continues-to-rise-in-developing-countries-but-plateaus-across-developed-ones/#table. Published June 19, 2018. Accessed August 28, 2018.
- Flaten HK, St Claire C, Schlager E, et al. Growth of mobile applications in dermatology—2017 update. Dermatol Online J. 2018;24. pii:13030/qt3hs7n9z6.
- App Annie website. https://www.appannie.com/top/. Accessed August 28, 2018.
- Number of iPhone users in the United States from 2012 to 2016 (in millions). Statista website. https://www.statista.com/statistics/232790/forecast-of-apple-users-in-the-us/. Accessed August 28, 2018.
- Burkhart C. Medical mobile apps and dermatology. Cutis. 2012;90:278-281.
- Wolf JA, Moreau JF, Patton TJ, et al. Prevalence and impact of health-related internet and smartphone use among dermatology patients. Cutis. 2015;95:323-328.
- Masud A, Shafi S, Rao BK. Mobile medical apps for patient education: a graded review of available dermatology apps. Cutis. 2018;101:141-144.
- Walocko FM, Tejasvi T. Teledermatology applications in skin cancer diagnosis. Dermatol Clin. 2017;35:559-563.
- Krupinski E, Burdick A, Pak H, et al. American Telemedicine Association’s practice guidelines for teledermatology. Telemed J E Health. 2008;14:289-302.
- Ho B, Lee M, Armstrong AW. Evaluation criteria for mobile teledermatology applications and comparison of major mobile teledermatology applications. Telemed J E Health. 2013;19:678-682.
- Number of mobile app hours per smartphone and tablet app user in the United States in June 2016, by age group. Statista website. https://www.statista.com/statistics/323522/us-user-mobile-app-engagement-age/. Accessed September 18, 2018.
As technology continues to advance, so too does its accessibility to the general population. In 2013, 56% of Americans owned a smartphone versus 77% in 2017.1With the increase in mobile applications (apps) available, it is no surprise that the market has extended into the medical field, with dermatology being no exception.2 The majority of dermatology apps can be classified as teledermatology apps, followed by self-surveillance, disease guide, and reference apps. Additional types of dermatology apps include dermoscopy, conference, education, photograph storage and sharing, and journal apps, and others.2 In this study, we examined Apple App Store rankings to determine the types of dermatology apps that are most popular among patients and physicians.
METHODS
A popular app rankings analyzer (App Annie) was used to search for dermatology apps along with their App Store rankings.3 Although iOS is not the most popular mobile device operating system, we chose to evaluate app rankings via the App Store because iPhones are the top-selling individual phones of any kind in the United States.4
We performed our analysis on a single day (July 14, 2018) given that app rankings can change daily. We incorporated the following keywords, which were commonly used in other dermatology app studies: dermatology, psoriasis, rosacea, acne, skin cancer, melanoma, eczema, and teledermatology. The category ranking was defined as the rank of a free or paid app in the App Store’s top charts for the selected country (United States), market (Apple), and device (iPhone) within their app category (Medical). Inclusion criteria required a ranking in the top 1500 Medical apps and being categorized in the App Store as a Medical app. Exclusion criteria included apps that focused on cosmetics, private practice, direct advertisements, photograph editing, or claims to cure skin disease, as well as non–English-language apps. The App Store descriptions were assessed to determine the type of each app (eg, teledermatology, disease guide) and target audience (patient, physician, or both).
Another search was performed using the same keywords but within the Health and Fitness category to capture potentially more highly ranked apps among patients. We also conducted separate searches within the Medical category using the keywords billing, coding, and ICD (International Classification of Diseases) to evaluate rankings for billing/coding apps, as well as EMR and electronic medical records for electronic medical record (EMR) apps.
RESULTS
The initial search yielded 851 results, which was narrowed down to 29 apps after applying the exclusion criteria. Of note, prior to application of the exclusion criteria, one dermatology app that was considered to be a direct advertisement app claiming to cure acne was ranked fourth of 1500 apps in the Medical category. However, the majority of the search results were excluded because they were not popular enough to be ranked among the top 1500 apps. There were more ranked dermatology apps in the Medical category targeting patients than physicians; 18 of 29 (62%) qualifying apps targeted patients and 11 (38%) targeted physicians (Tables 1 and 2). No apps targeted both groups. The most common type of ranked app targeting patients was self-surveillance (11/18), and the most common type targeting physicians was reference (8/11). The highest ranked app targeting patients was a teledermatology app with a ranking of 184, and the highest ranked app targeting physicians was educational, ranked 353. The least common type of ranked apps targeting patients were “other” (2/18 [11%]; 1 prescription and 1 UV monitor app) and conference (1/18 [6%]). The least common type of ranked apps targeting physicians were education (2/11 [18%]) and dermoscopy (1/11 [9%]).
Our search of the Health and Fitness category yielded 6 apps, all targeting patients; 3 (50%) were self-surveillance apps, and 3 (50%) were classified as other (2 UV monitors and a conferencing app for cancer emotional support)(Table 3).
Our search of the Medical category for billing/coding and EMR apps yielded 232 and 164 apps, respectively; of them, 49 (21%) and 54 (33%) apps were ranked. These apps did not overlap with the dermatology-related search criteria; thus, we were not able to ascertain how many of these apps were used specifically by health care providers in dermatology.
COMMENT
Patient Apps
The most common apps used by patients are fitness and nutrition tracker apps categorized as Health and Fitness5,6; however, the majority of ranked dermatology apps are categorized as Medical per our findings. In a study of 557 dermatology patients, it was found that among the health-related apps they used, the most common apps after fitness/nutrition were references, followed by patient portals, self-surveillance, and emotional assistance apps.6 Our search was consistent with these findings, suggesting that the most desired dermatology apps by patients are those that allow them to be proactive with their health. It is no surprise that the top-ranked app targeting patients was a teledermatology app, followed by multiple self-surveillance apps. The highest ranked self-surveillance app in the Health and Fitness category focused on monitoring the effects of nutrition on symptoms of diseases including skin disorders, while the highest ranked (as well as the majority of) self-surveillance apps in the Medical category encompassed mole monitoring and cancer risk calculators.
Benefits of the ranked dermatology apps in the Medical and Health and Fitness categories targeting patients include more immediate access to health care and education. Despite this popularity among patients, Masud et al7 demonstrated that only 20.5% (9/44) of dermatology apps targeting patients may be reliable resources based on a rubric created by the investigators. Overall, there remains a research gap for a standardized scientific approach to evaluating app validity and reliability.
Teledermatology
Teledermatology apps are the most common dermatology apps,2 allowing for remote evaluation of patients through either live consultations or transmittance of medical information for later review by board-certified physicians.8 Features common to many teledermatology apps include accessibility on Android (Google Inc) and iOS as well as a web version. Security and Health Insurance Portability and Accountability Act compliance is especially important and is enforced through user authentications, data encryption, and automatic logout features. Data is not stored locally and is secured on a private server with backup. Referring providers and consultants often can communicate within the app. Insurance providers also may cover teledermatology services, and if not, the out-of-pocket costs often are affordable.
The highest-ranked patient app (ranked 184 in the Medical category) was a teledermatology app that did not meet the American Telemedicine Association standards for teledermatology apps.9 The popularity of this app among patients may have been attributable to multiple ease-of-use and turnaround time features. The user interface was simplistic, and the design was appealing to the eye. The entry field options were minimal to avoid confusion. The turnaround time to receive a diagnosis depended on 1 of 3 options, including a more rapid response for an increased cost. Ease of use was the highlight of this app at the cost of accuracy, as the limited amount of information that users were required to provide physicians compromised diagnostic accuracy in this app.
For comparison, we chose a nonranked (and thus less frequently used) teledermatology app that had previously undergone scientific evaluation using 13 evaluation criteria specific to teledermatology.10 The app also met the American Telemedicine Association standard for teledermatology apps.9 The app was originally a broader telemedicine app but featured a section specific to teledermatology. The user interface was simple but professional, almost resembling an EMR. The input fields included a comprehensive history that permitted a better evaluation of a lesion but might be tedious for users. This app boasted professionalism and accuracy, but from a user standpoint, it may have been too time-consuming.
Striking a balance between ensuring proper care versus appealing to patients is a difficult but important task. Based on this study, it appears that popular patient apps may in fact have less scientific rationale and therefore potentially less accuracy.
Self-surveillance
Although self-surveillance apps did not account for the highest-ranked app, they were the most frequently ranked app type in our study. Most of the ranked self-surveillance apps in the Medical category were for monitoring lesions over time to assess for changes. These apps help users take photographs that are well organized in a single, easy-to-find location. Some apps were risk calculators that assessed the risk for malignancies using a questionnaire. The majority of these self-surveillance apps were specific to skin cancer detection. Of note, one of the ranked self-surveillance apps assessed drug effectiveness by monitoring clinical appearance and symptoms. The lowest ranked self-surveillance app in the top 1500 ranked Medical apps in our search monitored cancer symptoms not specific to dermatology. Although this app had a low ranking (1380/1500), it received a high number of reviews and was well rated at 4.8 out of 5 stars; therefore, it seemed more helpful than the other higher-ranked apps targeting patients, which had higher rankings but minimal to no reviews or ratings. A comparison of the ease-of-use features of all the ranked patient-targeted self-surveillance apps in the Medical category is provided in Table 4.
Physician Apps
After examining the results of apps targeting physicians, we realized that the data may be accurate but may not be as representative of all currently practicing dermatology providers. Given the increased usage of apps among younger age groups,11 our data may be skewed toward medical students and residents, supported by the fact that the top-ranked physician app in our study was an education app and the majority were reference apps. Future studies are needed to reexamine app ranking as this age group transitions from entry-level health care providers in the next 5 to 10 years. These findings also suggest less frequent app use among more veteran health care providers within our specific search parameters. Therefore, we decided to do subsequent searches for available billing/coding and EMR apps, which were many, but as mentioned above, none were specific to dermatology.
General Dermatology References
Most of the dermatology reference apps were formatted as e-books; however, other apps such as the Amazon Kindle app (categorized under Books) providing access to multiple e-books within one app were not included. Some apps included study aid features (eg, flash cards, quizzes), and topics spanned both dermatology and dermatopathology. Apps provide a unique way for on-the-go studying for dermatologists in training, and if the usage continues to grow, there may be a need for increased formal integration in dermatology education in the future.
Journals
Journal apps were not among those listed in the top-ranked apps we evaluated, which we suspect may be because journals were categorized differently from one journal to the next; for example, the Journal of the American Academy of Dermatology was ranked 1168 in the Magazines and Newspapers category. On the other hand, Dermatology World was ranked 1363 in the Reference category. An article’s citation affects the publishing journal’s impact factor, which is one of the most important variables in measuring a journal’s influence. In the future, there may be other variables that could aid in understanding journal impact as it relates to the journal’s accessibility.
Limitations
Our study did not look at Android apps. The top chart apps in the Android and Apple App Stores use undisclosed algorithms likely involving different characteristics such as number of downloads, frequency of updates, number of reviews, ratings, and more. Thus, the rankings across these different markets would not be comparable. Although our choice of keywords stemmed from the majority of prior studies looking at dermatology apps, our search was limited due to the use of these specific keywords. To avoid skewing data by cross-comparison of noncomparable categories, we could not compare apps in the Medical category versus those in other categories.
CONCLUSION
There seems to be a disconnect between the apps that are popular among patients and the scientific validity of the apps. As app usage increases among dermatology providers, whose demographic is shifting younger and younger, apps may become more incorporated in our education, and as such, it will become more critical to develop formal scientific standards. Given these future trends, we may need to increase our current literature and understanding of apps in dermatology with regard to their impact on both patients and health care providers.
As technology continues to advance, so too does its accessibility to the general population. In 2013, 56% of Americans owned a smartphone versus 77% in 2017.1With the increase in mobile applications (apps) available, it is no surprise that the market has extended into the medical field, with dermatology being no exception.2 The majority of dermatology apps can be classified as teledermatology apps, followed by self-surveillance, disease guide, and reference apps. Additional types of dermatology apps include dermoscopy, conference, education, photograph storage and sharing, and journal apps, and others.2 In this study, we examined Apple App Store rankings to determine the types of dermatology apps that are most popular among patients and physicians.
METHODS
A popular app rankings analyzer (App Annie) was used to search for dermatology apps along with their App Store rankings.3 Although iOS is not the most popular mobile device operating system, we chose to evaluate app rankings via the App Store because iPhones are the top-selling individual phones of any kind in the United States.4
We performed our analysis on a single day (July 14, 2018) given that app rankings can change daily. We incorporated the following keywords, which were commonly used in other dermatology app studies: dermatology, psoriasis, rosacea, acne, skin cancer, melanoma, eczema, and teledermatology. The category ranking was defined as the rank of a free or paid app in the App Store’s top charts for the selected country (United States), market (Apple), and device (iPhone) within their app category (Medical). Inclusion criteria required a ranking in the top 1500 Medical apps and being categorized in the App Store as a Medical app. Exclusion criteria included apps that focused on cosmetics, private practice, direct advertisements, photograph editing, or claims to cure skin disease, as well as non–English-language apps. The App Store descriptions were assessed to determine the type of each app (eg, teledermatology, disease guide) and target audience (patient, physician, or both).
Another search was performed using the same keywords but within the Health and Fitness category to capture potentially more highly ranked apps among patients. We also conducted separate searches within the Medical category using the keywords billing, coding, and ICD (International Classification of Diseases) to evaluate rankings for billing/coding apps, as well as EMR and electronic medical records for electronic medical record (EMR) apps.
RESULTS
The initial search yielded 851 results, which was narrowed down to 29 apps after applying the exclusion criteria. Of note, prior to application of the exclusion criteria, one dermatology app that was considered to be a direct advertisement app claiming to cure acne was ranked fourth of 1500 apps in the Medical category. However, the majority of the search results were excluded because they were not popular enough to be ranked among the top 1500 apps. There were more ranked dermatology apps in the Medical category targeting patients than physicians; 18 of 29 (62%) qualifying apps targeted patients and 11 (38%) targeted physicians (Tables 1 and 2). No apps targeted both groups. The most common type of ranked app targeting patients was self-surveillance (11/18), and the most common type targeting physicians was reference (8/11). The highest ranked app targeting patients was a teledermatology app with a ranking of 184, and the highest ranked app targeting physicians was educational, ranked 353. The least common type of ranked apps targeting patients were “other” (2/18 [11%]; 1 prescription and 1 UV monitor app) and conference (1/18 [6%]). The least common type of ranked apps targeting physicians were education (2/11 [18%]) and dermoscopy (1/11 [9%]).
Our search of the Health and Fitness category yielded 6 apps, all targeting patients; 3 (50%) were self-surveillance apps, and 3 (50%) were classified as other (2 UV monitors and a conferencing app for cancer emotional support)(Table 3).
Our search of the Medical category for billing/coding and EMR apps yielded 232 and 164 apps, respectively; of them, 49 (21%) and 54 (33%) apps were ranked. These apps did not overlap with the dermatology-related search criteria; thus, we were not able to ascertain how many of these apps were used specifically by health care providers in dermatology.
COMMENT
Patient Apps
The most common apps used by patients are fitness and nutrition tracker apps categorized as Health and Fitness5,6; however, the majority of ranked dermatology apps are categorized as Medical per our findings. In a study of 557 dermatology patients, it was found that among the health-related apps they used, the most common apps after fitness/nutrition were references, followed by patient portals, self-surveillance, and emotional assistance apps.6 Our search was consistent with these findings, suggesting that the most desired dermatology apps by patients are those that allow them to be proactive with their health. It is no surprise that the top-ranked app targeting patients was a teledermatology app, followed by multiple self-surveillance apps. The highest ranked self-surveillance app in the Health and Fitness category focused on monitoring the effects of nutrition on symptoms of diseases including skin disorders, while the highest ranked (as well as the majority of) self-surveillance apps in the Medical category encompassed mole monitoring and cancer risk calculators.
Benefits of the ranked dermatology apps in the Medical and Health and Fitness categories targeting patients include more immediate access to health care and education. Despite this popularity among patients, Masud et al7 demonstrated that only 20.5% (9/44) of dermatology apps targeting patients may be reliable resources based on a rubric created by the investigators. Overall, there remains a research gap for a standardized scientific approach to evaluating app validity and reliability.
Teledermatology
Teledermatology apps are the most common dermatology apps,2 allowing for remote evaluation of patients through either live consultations or transmittance of medical information for later review by board-certified physicians.8 Features common to many teledermatology apps include accessibility on Android (Google Inc) and iOS as well as a web version. Security and Health Insurance Portability and Accountability Act compliance is especially important and is enforced through user authentications, data encryption, and automatic logout features. Data is not stored locally and is secured on a private server with backup. Referring providers and consultants often can communicate within the app. Insurance providers also may cover teledermatology services, and if not, the out-of-pocket costs often are affordable.
The highest-ranked patient app (ranked 184 in the Medical category) was a teledermatology app that did not meet the American Telemedicine Association standards for teledermatology apps.9 The popularity of this app among patients may have been attributable to multiple ease-of-use and turnaround time features. The user interface was simplistic, and the design was appealing to the eye. The entry field options were minimal to avoid confusion. The turnaround time to receive a diagnosis depended on 1 of 3 options, including a more rapid response for an increased cost. Ease of use was the highlight of this app at the cost of accuracy, as the limited amount of information that users were required to provide physicians compromised diagnostic accuracy in this app.
For comparison, we chose a nonranked (and thus less frequently used) teledermatology app that had previously undergone scientific evaluation using 13 evaluation criteria specific to teledermatology.10 The app also met the American Telemedicine Association standard for teledermatology apps.9 The app was originally a broader telemedicine app but featured a section specific to teledermatology. The user interface was simple but professional, almost resembling an EMR. The input fields included a comprehensive history that permitted a better evaluation of a lesion but might be tedious for users. This app boasted professionalism and accuracy, but from a user standpoint, it may have been too time-consuming.
Striking a balance between ensuring proper care versus appealing to patients is a difficult but important task. Based on this study, it appears that popular patient apps may in fact have less scientific rationale and therefore potentially less accuracy.
Self-surveillance
Although self-surveillance apps did not account for the highest-ranked app, they were the most frequently ranked app type in our study. Most of the ranked self-surveillance apps in the Medical category were for monitoring lesions over time to assess for changes. These apps help users take photographs that are well organized in a single, easy-to-find location. Some apps were risk calculators that assessed the risk for malignancies using a questionnaire. The majority of these self-surveillance apps were specific to skin cancer detection. Of note, one of the ranked self-surveillance apps assessed drug effectiveness by monitoring clinical appearance and symptoms. The lowest ranked self-surveillance app in the top 1500 ranked Medical apps in our search monitored cancer symptoms not specific to dermatology. Although this app had a low ranking (1380/1500), it received a high number of reviews and was well rated at 4.8 out of 5 stars; therefore, it seemed more helpful than the other higher-ranked apps targeting patients, which had higher rankings but minimal to no reviews or ratings. A comparison of the ease-of-use features of all the ranked patient-targeted self-surveillance apps in the Medical category is provided in Table 4.
Physician Apps
After examining the results of apps targeting physicians, we realized that the data may be accurate but may not be as representative of all currently practicing dermatology providers. Given the increased usage of apps among younger age groups,11 our data may be skewed toward medical students and residents, supported by the fact that the top-ranked physician app in our study was an education app and the majority were reference apps. Future studies are needed to reexamine app ranking as this age group transitions from entry-level health care providers in the next 5 to 10 years. These findings also suggest less frequent app use among more veteran health care providers within our specific search parameters. Therefore, we decided to do subsequent searches for available billing/coding and EMR apps, which were many, but as mentioned above, none were specific to dermatology.
General Dermatology References
Most of the dermatology reference apps were formatted as e-books; however, other apps such as the Amazon Kindle app (categorized under Books) providing access to multiple e-books within one app were not included. Some apps included study aid features (eg, flash cards, quizzes), and topics spanned both dermatology and dermatopathology. Apps provide a unique way for on-the-go studying for dermatologists in training, and if the usage continues to grow, there may be a need for increased formal integration in dermatology education in the future.
Journals
Journal apps were not among those listed in the top-ranked apps we evaluated, which we suspect may be because journals were categorized differently from one journal to the next; for example, the Journal of the American Academy of Dermatology was ranked 1168 in the Magazines and Newspapers category. On the other hand, Dermatology World was ranked 1363 in the Reference category. An article’s citation affects the publishing journal’s impact factor, which is one of the most important variables in measuring a journal’s influence. In the future, there may be other variables that could aid in understanding journal impact as it relates to the journal’s accessibility.
Limitations
Our study did not look at Android apps. The top chart apps in the Android and Apple App Stores use undisclosed algorithms likely involving different characteristics such as number of downloads, frequency of updates, number of reviews, ratings, and more. Thus, the rankings across these different markets would not be comparable. Although our choice of keywords stemmed from the majority of prior studies looking at dermatology apps, our search was limited due to the use of these specific keywords. To avoid skewing data by cross-comparison of noncomparable categories, we could not compare apps in the Medical category versus those in other categories.
CONCLUSION
There seems to be a disconnect between the apps that are popular among patients and the scientific validity of the apps. As app usage increases among dermatology providers, whose demographic is shifting younger and younger, apps may become more incorporated in our education, and as such, it will become more critical to develop formal scientific standards. Given these future trends, we may need to increase our current literature and understanding of apps in dermatology with regard to their impact on both patients and health care providers.
- Poushter J, Bishop C, Chwe H. Social media use continues to rise in developing countries but plateaus across developed ones. Pew Research Center website. http://www.pewglobal.org/2018/06/19/social-media-use-continues-to-rise-in-developing-countries-but-plateaus-across-developed-ones/#table. Published June 19, 2018. Accessed August 28, 2018.
- Flaten HK, St Claire C, Schlager E, et al. Growth of mobile applications in dermatology—2017 update. Dermatol Online J. 2018;24. pii:13030/qt3hs7n9z6.
- App Annie website. https://www.appannie.com/top/. Accessed August 28, 2018.
- Number of iPhone users in the United States from 2012 to 2016 (in millions). Statista website. https://www.statista.com/statistics/232790/forecast-of-apple-users-in-the-us/. Accessed August 28, 2018.
- Burkhart C. Medical mobile apps and dermatology. Cutis. 2012;90:278-281.
- Wolf JA, Moreau JF, Patton TJ, et al. Prevalence and impact of health-related internet and smartphone use among dermatology patients. Cutis. 2015;95:323-328.
- Masud A, Shafi S, Rao BK. Mobile medical apps for patient education: a graded review of available dermatology apps. Cutis. 2018;101:141-144.
- Walocko FM, Tejasvi T. Teledermatology applications in skin cancer diagnosis. Dermatol Clin. 2017;35:559-563.
- Krupinski E, Burdick A, Pak H, et al. American Telemedicine Association’s practice guidelines for teledermatology. Telemed J E Health. 2008;14:289-302.
- Ho B, Lee M, Armstrong AW. Evaluation criteria for mobile teledermatology applications and comparison of major mobile teledermatology applications. Telemed J E Health. 2013;19:678-682.
- Number of mobile app hours per smartphone and tablet app user in the United States in June 2016, by age group. Statista website. https://www.statista.com/statistics/323522/us-user-mobile-app-engagement-age/. Accessed September 18, 2018.
- Poushter J, Bishop C, Chwe H. Social media use continues to rise in developing countries but plateaus across developed ones. Pew Research Center website. http://www.pewglobal.org/2018/06/19/social-media-use-continues-to-rise-in-developing-countries-but-plateaus-across-developed-ones/#table. Published June 19, 2018. Accessed August 28, 2018.
- Flaten HK, St Claire C, Schlager E, et al. Growth of mobile applications in dermatology—2017 update. Dermatol Online J. 2018;24. pii:13030/qt3hs7n9z6.
- App Annie website. https://www.appannie.com/top/. Accessed August 28, 2018.
- Number of iPhone users in the United States from 2012 to 2016 (in millions). Statista website. https://www.statista.com/statistics/232790/forecast-of-apple-users-in-the-us/. Accessed August 28, 2018.
- Burkhart C. Medical mobile apps and dermatology. Cutis. 2012;90:278-281.
- Wolf JA, Moreau JF, Patton TJ, et al. Prevalence and impact of health-related internet and smartphone use among dermatology patients. Cutis. 2015;95:323-328.
- Masud A, Shafi S, Rao BK. Mobile medical apps for patient education: a graded review of available dermatology apps. Cutis. 2018;101:141-144.
- Walocko FM, Tejasvi T. Teledermatology applications in skin cancer diagnosis. Dermatol Clin. 2017;35:559-563.
- Krupinski E, Burdick A, Pak H, et al. American Telemedicine Association’s practice guidelines for teledermatology. Telemed J E Health. 2008;14:289-302.
- Ho B, Lee M, Armstrong AW. Evaluation criteria for mobile teledermatology applications and comparison of major mobile teledermatology applications. Telemed J E Health. 2013;19:678-682.
- Number of mobile app hours per smartphone and tablet app user in the United States in June 2016, by age group. Statista website. https://www.statista.com/statistics/323522/us-user-mobile-app-engagement-age/. Accessed September 18, 2018.
Practice Points
- As mobile application (app) usage increases among dermatology providers, whose demographic is shifting younger and younger, apps may become more incorporated in dermatology education. As such, it will become more critical to develop formal scientific standards.
- The most desired dermatology apps for patients were apps that allowed them to be proactive with their health.
- There seems to be a disconnect between the apps that are popular among patients and the scientific validity of the apps.
Breast cancer risk in type 2 diabetes related to adiposity
ORLANDO – findings from meta-analyses suggest.
In one meta-analysis of data from 21 prospective studies with a total of nearly 15.2 million women, 325,117 breast cancer cases, and a mean follow-up time of 8 years (nearly 33 million person-years), the risk of breast cancer was significantly greater among patients with diabetes than it was among patients without diabetes (summary relative risk, 1.11), Maria Bota reported at the annual scientific sessions of the American Diabetes Association.
However, there was substantial unexplained heterogeneity of results across the individual studies (I2 = 82%), said Ms. Bota, a faculty member at the International Prevention Research Institute, Lyon, France.
“When the analysis was restricted to the 12 studies that adjusted for [body mass index], the summary relative risk decreased to 1.09 and the heterogeneity also decreased to a moderate value of 32%; when the analysis was restricted to the 9 studies that did not adjust for BMI, the summary relative risk increased to 1.14 again, and the heterogeneity increased even more to 91%,” she said.
In an analysis that combined the results of the nine studies that did not adjust for BMI along with crude relative risks from studies that reported both crude and BMI-adjusted relative risks (17 studies in all), the SRR was 1.12, and heterogeneity among the studies was high at 84%.
Additionally, an analysis by menopausal status based on four studies that reported breast cancer in both pre- and postmenopausal women showed SRRs for breast cancer of 0.97 (a 3% decrease in risk) and 1.14 among diabetic vs. nondiabetic premenopausal women and postmenopausal women, respectively, she said, noting that heterogeneity was low (I2 = 0%) among the premenopausal breast cancer study groups and high (I2 = 70%) among the postmenopausal study groups.
The findings provide evidence for a moderately increased risk of breast cancer in women with T2DM, Ms. Bota said.
“However, the effect of the adjustment or lack of adjustment on the heterogeneity suggests that the higher risk of breast cancer in women with diabetes may not be due to diabetes itself, but to adiposity,” she said, adding that “this hypothesis is equally supported by our subgroup analysis according to menopausal status because we saw that the risk of breast cancer was only associated with diabetes in postmenopausal women and this pattern resembles the pattern of the risk of breast cancer associated with adiposity, which is also only increased in postmenopausal women.”
This study was limited by insufficient data for investigating the sources of heterogeneity, she said.
“Therefore we propose ... future pooled analyses based on individual data from good quality prospective studies in order to increase the study power and to do some detailed analysis of the links between adiposity, diabetes, and breast cancer,” she concluded, adding that new studies to examine those relationships only in premenopausal women are also needed
In a separate meta-analysis, she and her colleagues, including Peter Boyle, PhD, president of the International Prevention Research Institute, assessed the association between insulin treatment and breast cancer risk in patients with diabetes.
“The long-acting insulin analogues glargine and detemir have been shown in some studies to be associated with increased risk of breast cancer, and other studies have shown no association between the use of these two compounds and the risk of breast cancer,” Dr. Boyle said in a separate presentation at the ADA meeting. “It was important to sort out a little bit what was going on in the literature.”
Overall, the meta-analysis of data from 12 longitudinal cohort studies – including more than 6,000 cases of breast cancer – showed a slight increase in breast cancer risk in patients taking long-acting insulin (SRR, 1.13) with “a relatively reasonable” level of heterogeneity (I2 = 23%).
“But we see that the story is not that simple,” he said.
For example, some studies included only patients who were prescribed insulin for the first time after the study began (new users), some included only patients who were prescribed insulin before the study began (prevalent users), and some included both (ever users), which may have introduced bias in the results, he explained.
Studies of glargine included 4,168 breast cancer cases over a total of 1,418,743 person-years of observation, and studies of detemir included fewer than 2,047 breast cancer cases (not all studies reported case numbers). Among both new users of glargine and detemir, the SRR was 1.12, suggesting no real association between either glargine or detemir use and breast cancer, he said.
“One important take-home message is that you have to be careful that these pharmaco-epidemiological studies, even when working with the same database, may have conflicting results ... so we still need more robust standards in methods for [such] studies,” he concluded.
Ms. Bota reported having no disclosures. The study presented by Dr. Boyle was funded by Sanofi. Dr. Boyle is president of a charity that has received donations from Pfizer, Roche, Novartis, and Lilly.
SOURCE: Bota M. ADA 2018, Abstract 180-OR; Boyle P. ADA 2018, Abstract 133-OR.
ORLANDO – findings from meta-analyses suggest.
In one meta-analysis of data from 21 prospective studies with a total of nearly 15.2 million women, 325,117 breast cancer cases, and a mean follow-up time of 8 years (nearly 33 million person-years), the risk of breast cancer was significantly greater among patients with diabetes than it was among patients without diabetes (summary relative risk, 1.11), Maria Bota reported at the annual scientific sessions of the American Diabetes Association.
However, there was substantial unexplained heterogeneity of results across the individual studies (I2 = 82%), said Ms. Bota, a faculty member at the International Prevention Research Institute, Lyon, France.
“When the analysis was restricted to the 12 studies that adjusted for [body mass index], the summary relative risk decreased to 1.09 and the heterogeneity also decreased to a moderate value of 32%; when the analysis was restricted to the 9 studies that did not adjust for BMI, the summary relative risk increased to 1.14 again, and the heterogeneity increased even more to 91%,” she said.
In an analysis that combined the results of the nine studies that did not adjust for BMI along with crude relative risks from studies that reported both crude and BMI-adjusted relative risks (17 studies in all), the SRR was 1.12, and heterogeneity among the studies was high at 84%.
Additionally, an analysis by menopausal status based on four studies that reported breast cancer in both pre- and postmenopausal women showed SRRs for breast cancer of 0.97 (a 3% decrease in risk) and 1.14 among diabetic vs. nondiabetic premenopausal women and postmenopausal women, respectively, she said, noting that heterogeneity was low (I2 = 0%) among the premenopausal breast cancer study groups and high (I2 = 70%) among the postmenopausal study groups.
The findings provide evidence for a moderately increased risk of breast cancer in women with T2DM, Ms. Bota said.
“However, the effect of the adjustment or lack of adjustment on the heterogeneity suggests that the higher risk of breast cancer in women with diabetes may not be due to diabetes itself, but to adiposity,” she said, adding that “this hypothesis is equally supported by our subgroup analysis according to menopausal status because we saw that the risk of breast cancer was only associated with diabetes in postmenopausal women and this pattern resembles the pattern of the risk of breast cancer associated with adiposity, which is also only increased in postmenopausal women.”
This study was limited by insufficient data for investigating the sources of heterogeneity, she said.
“Therefore we propose ... future pooled analyses based on individual data from good quality prospective studies in order to increase the study power and to do some detailed analysis of the links between adiposity, diabetes, and breast cancer,” she concluded, adding that new studies to examine those relationships only in premenopausal women are also needed
In a separate meta-analysis, she and her colleagues, including Peter Boyle, PhD, president of the International Prevention Research Institute, assessed the association between insulin treatment and breast cancer risk in patients with diabetes.
“The long-acting insulin analogues glargine and detemir have been shown in some studies to be associated with increased risk of breast cancer, and other studies have shown no association between the use of these two compounds and the risk of breast cancer,” Dr. Boyle said in a separate presentation at the ADA meeting. “It was important to sort out a little bit what was going on in the literature.”
Overall, the meta-analysis of data from 12 longitudinal cohort studies – including more than 6,000 cases of breast cancer – showed a slight increase in breast cancer risk in patients taking long-acting insulin (SRR, 1.13) with “a relatively reasonable” level of heterogeneity (I2 = 23%).
“But we see that the story is not that simple,” he said.
For example, some studies included only patients who were prescribed insulin for the first time after the study began (new users), some included only patients who were prescribed insulin before the study began (prevalent users), and some included both (ever users), which may have introduced bias in the results, he explained.
Studies of glargine included 4,168 breast cancer cases over a total of 1,418,743 person-years of observation, and studies of detemir included fewer than 2,047 breast cancer cases (not all studies reported case numbers). Among both new users of glargine and detemir, the SRR was 1.12, suggesting no real association between either glargine or detemir use and breast cancer, he said.
“One important take-home message is that you have to be careful that these pharmaco-epidemiological studies, even when working with the same database, may have conflicting results ... so we still need more robust standards in methods for [such] studies,” he concluded.
Ms. Bota reported having no disclosures. The study presented by Dr. Boyle was funded by Sanofi. Dr. Boyle is president of a charity that has received donations from Pfizer, Roche, Novartis, and Lilly.
SOURCE: Bota M. ADA 2018, Abstract 180-OR; Boyle P. ADA 2018, Abstract 133-OR.
ORLANDO – findings from meta-analyses suggest.
In one meta-analysis of data from 21 prospective studies with a total of nearly 15.2 million women, 325,117 breast cancer cases, and a mean follow-up time of 8 years (nearly 33 million person-years), the risk of breast cancer was significantly greater among patients with diabetes than it was among patients without diabetes (summary relative risk, 1.11), Maria Bota reported at the annual scientific sessions of the American Diabetes Association.
However, there was substantial unexplained heterogeneity of results across the individual studies (I2 = 82%), said Ms. Bota, a faculty member at the International Prevention Research Institute, Lyon, France.
“When the analysis was restricted to the 12 studies that adjusted for [body mass index], the summary relative risk decreased to 1.09 and the heterogeneity also decreased to a moderate value of 32%; when the analysis was restricted to the 9 studies that did not adjust for BMI, the summary relative risk increased to 1.14 again, and the heterogeneity increased even more to 91%,” she said.
In an analysis that combined the results of the nine studies that did not adjust for BMI along with crude relative risks from studies that reported both crude and BMI-adjusted relative risks (17 studies in all), the SRR was 1.12, and heterogeneity among the studies was high at 84%.
Additionally, an analysis by menopausal status based on four studies that reported breast cancer in both pre- and postmenopausal women showed SRRs for breast cancer of 0.97 (a 3% decrease in risk) and 1.14 among diabetic vs. nondiabetic premenopausal women and postmenopausal women, respectively, she said, noting that heterogeneity was low (I2 = 0%) among the premenopausal breast cancer study groups and high (I2 = 70%) among the postmenopausal study groups.
The findings provide evidence for a moderately increased risk of breast cancer in women with T2DM, Ms. Bota said.
“However, the effect of the adjustment or lack of adjustment on the heterogeneity suggests that the higher risk of breast cancer in women with diabetes may not be due to diabetes itself, but to adiposity,” she said, adding that “this hypothesis is equally supported by our subgroup analysis according to menopausal status because we saw that the risk of breast cancer was only associated with diabetes in postmenopausal women and this pattern resembles the pattern of the risk of breast cancer associated with adiposity, which is also only increased in postmenopausal women.”
This study was limited by insufficient data for investigating the sources of heterogeneity, she said.
“Therefore we propose ... future pooled analyses based on individual data from good quality prospective studies in order to increase the study power and to do some detailed analysis of the links between adiposity, diabetes, and breast cancer,” she concluded, adding that new studies to examine those relationships only in premenopausal women are also needed
In a separate meta-analysis, she and her colleagues, including Peter Boyle, PhD, president of the International Prevention Research Institute, assessed the association between insulin treatment and breast cancer risk in patients with diabetes.
“The long-acting insulin analogues glargine and detemir have been shown in some studies to be associated with increased risk of breast cancer, and other studies have shown no association between the use of these two compounds and the risk of breast cancer,” Dr. Boyle said in a separate presentation at the ADA meeting. “It was important to sort out a little bit what was going on in the literature.”
Overall, the meta-analysis of data from 12 longitudinal cohort studies – including more than 6,000 cases of breast cancer – showed a slight increase in breast cancer risk in patients taking long-acting insulin (SRR, 1.13) with “a relatively reasonable” level of heterogeneity (I2 = 23%).
“But we see that the story is not that simple,” he said.
For example, some studies included only patients who were prescribed insulin for the first time after the study began (new users), some included only patients who were prescribed insulin before the study began (prevalent users), and some included both (ever users), which may have introduced bias in the results, he explained.
Studies of glargine included 4,168 breast cancer cases over a total of 1,418,743 person-years of observation, and studies of detemir included fewer than 2,047 breast cancer cases (not all studies reported case numbers). Among both new users of glargine and detemir, the SRR was 1.12, suggesting no real association between either glargine or detemir use and breast cancer, he said.
“One important take-home message is that you have to be careful that these pharmaco-epidemiological studies, even when working with the same database, may have conflicting results ... so we still need more robust standards in methods for [such] studies,” he concluded.
Ms. Bota reported having no disclosures. The study presented by Dr. Boyle was funded by Sanofi. Dr. Boyle is president of a charity that has received donations from Pfizer, Roche, Novartis, and Lilly.
SOURCE: Bota M. ADA 2018, Abstract 180-OR; Boyle P. ADA 2018, Abstract 133-OR.
REPORTING FROM ADA 2018
Key clinical point: Adiposity accounts for the increased risk of breast cancer among women with diabetes.
Major finding: An analysis of 12 studies that adjusted for BMI showed a summary relative risk for breast cancer of 1.09 in diabetic versus nondiabetic women, with moderate study heterogeneity.
Study details: Meta-analyses including 21 and 12 studies, respectively.
Disclosures: Ms. Bota reported having no disclosures. The study presented by Dr. Boyle was funded by Sanofi. Dr. Boyle is president of a charity that has received donations from Pfizer, Roche, Novartis, and Lilly.
Source: Bota M. ADA 2018, Abstract 180-OR; Boyle P. ADA 2018, Abstract 133-OR.
Agrees that OC use clearly reduces mortality
Agrees that OC use clearly reduces mortality
Recent evidence from long-term observations of hundreds of thousands of women, in 10 European countries, clearly demonstrated that the use of oral contraceptives (OCs) reduced mortality by roughly 10%.1,2 Newer OCs increase women’s overall survival.
In comparison, reducing obesity by 5 body mass index points would reduce mortality by only 5%, from 1.05 to 1.3
Dr. Stavros Saripanidis
Thessaloniki, Greece
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition: a cohort study. BMC Med. 2015;13:252.
- Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216(6):580.e1–580.e9.
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
Agrees that OC use clearly reduces mortality
Recent evidence from long-term observations of hundreds of thousands of women, in 10 European countries, clearly demonstrated that the use of oral contraceptives (OCs) reduced mortality by roughly 10%.1,2 Newer OCs increase women’s overall survival.
In comparison, reducing obesity by 5 body mass index points would reduce mortality by only 5%, from 1.05 to 1.3
Dr. Stavros Saripanidis
Thessaloniki, Greece
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Agrees that OC use clearly reduces mortality
Recent evidence from long-term observations of hundreds of thousands of women, in 10 European countries, clearly demonstrated that the use of oral contraceptives (OCs) reduced mortality by roughly 10%.1,2 Newer OCs increase women’s overall survival.
In comparison, reducing obesity by 5 body mass index points would reduce mortality by only 5%, from 1.05 to 1.3
Dr. Stavros Saripanidis
Thessaloniki, Greece
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition: a cohort study. BMC Med. 2015;13:252.
- Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216(6):580.e1–580.e9.
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
- Merritt MA, Riboli E, Murphy N, et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition: a cohort study. BMC Med. 2015;13:252.
- Iversen L, Sivasubramaniam S, Lee AJ, Fielding S, Hannaford PC. Lifetime cancer risk and combined oral contraceptives: the Royal College of General Practitioners’ Oral Contraception Study. Am J Obstet Gynecol. 2017;216(6):580.e1–580.e9.
- Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156.
FDA Approves Galcanezumab for Migraine Prevention
The treatment is the third anti-CGRP antibody to receive regulatory approval.
ROCKVILLE, MD—The FDA has approved galcanezumab-gnlm (Emgality) for the preventive treatment of migraine in adults. Eli Lilly and Company manufactures the therapy. Emgality is the third calcitonin gene-related peptide (CGRP) antagonist to receive regulatory approval.
The approval is based on the results of three phase III clinical trials: EVOLVE-1, EVOLVE-2, and REGAIN. EVOLVE-1 and EVOLVE-2 were six-month, double-blind, placebo-controlled studies that included adults with episodic migraine. REGAIN was a three-month, double-blind, placebo-controlled study of adults with chronic migraine. The primary end point of all three trials was mean change from baseline in the number of monthly headache days.
In all trials, patients received either placebo, 120 mg of galcanezumab-gnlm after an initial loading dose of 240 mg, or 240 mg of galcanezumab-gnlm. In EVOLVE-1 and EVOLVE-2, people who received galcanezumab-gnlm had significantly fewer headache days per month than people who received placebo, and those who received galcanezumab-gnlm were also more likely to achieve a 50%, 75%, and 100% reduction in headache days.
In REGAIN, patients who received galcanezumab-gnlm experienced fewer monthly headache days than those who received placebo and were more likely to achieve a 50% reduction in headache days. There was no difference between groups in the likelihood of achieving a 75% or 100% reduction.
The recommended dosage, according to the label, is a monthly, 120-mg subcutaneous injection with an initial loading dose of 240 mg. The most common adverse event associated with galcanezumab-gnlm is injection-site reaction.
Galcanezumab-gnlm is under final review by the European Commission for approval in Europe.
—Lucas Franki
The treatment is the third anti-CGRP antibody to receive regulatory approval.
The treatment is the third anti-CGRP antibody to receive regulatory approval.
ROCKVILLE, MD—The FDA has approved galcanezumab-gnlm (Emgality) for the preventive treatment of migraine in adults. Eli Lilly and Company manufactures the therapy. Emgality is the third calcitonin gene-related peptide (CGRP) antagonist to receive regulatory approval.
The approval is based on the results of three phase III clinical trials: EVOLVE-1, EVOLVE-2, and REGAIN. EVOLVE-1 and EVOLVE-2 were six-month, double-blind, placebo-controlled studies that included adults with episodic migraine. REGAIN was a three-month, double-blind, placebo-controlled study of adults with chronic migraine. The primary end point of all three trials was mean change from baseline in the number of monthly headache days.
In all trials, patients received either placebo, 120 mg of galcanezumab-gnlm after an initial loading dose of 240 mg, or 240 mg of galcanezumab-gnlm. In EVOLVE-1 and EVOLVE-2, people who received galcanezumab-gnlm had significantly fewer headache days per month than people who received placebo, and those who received galcanezumab-gnlm were also more likely to achieve a 50%, 75%, and 100% reduction in headache days.
In REGAIN, patients who received galcanezumab-gnlm experienced fewer monthly headache days than those who received placebo and were more likely to achieve a 50% reduction in headache days. There was no difference between groups in the likelihood of achieving a 75% or 100% reduction.
The recommended dosage, according to the label, is a monthly, 120-mg subcutaneous injection with an initial loading dose of 240 mg. The most common adverse event associated with galcanezumab-gnlm is injection-site reaction.
Galcanezumab-gnlm is under final review by the European Commission for approval in Europe.
—Lucas Franki
ROCKVILLE, MD—The FDA has approved galcanezumab-gnlm (Emgality) for the preventive treatment of migraine in adults. Eli Lilly and Company manufactures the therapy. Emgality is the third calcitonin gene-related peptide (CGRP) antagonist to receive regulatory approval.
The approval is based on the results of three phase III clinical trials: EVOLVE-1, EVOLVE-2, and REGAIN. EVOLVE-1 and EVOLVE-2 were six-month, double-blind, placebo-controlled studies that included adults with episodic migraine. REGAIN was a three-month, double-blind, placebo-controlled study of adults with chronic migraine. The primary end point of all three trials was mean change from baseline in the number of monthly headache days.
In all trials, patients received either placebo, 120 mg of galcanezumab-gnlm after an initial loading dose of 240 mg, or 240 mg of galcanezumab-gnlm. In EVOLVE-1 and EVOLVE-2, people who received galcanezumab-gnlm had significantly fewer headache days per month than people who received placebo, and those who received galcanezumab-gnlm were also more likely to achieve a 50%, 75%, and 100% reduction in headache days.
In REGAIN, patients who received galcanezumab-gnlm experienced fewer monthly headache days than those who received placebo and were more likely to achieve a 50% reduction in headache days. There was no difference between groups in the likelihood of achieving a 75% or 100% reduction.
The recommended dosage, according to the label, is a monthly, 120-mg subcutaneous injection with an initial loading dose of 240 mg. The most common adverse event associated with galcanezumab-gnlm is injection-site reaction.
Galcanezumab-gnlm is under final review by the European Commission for approval in Europe.
—Lucas Franki
New MS Subtype Shows Absence of Cerebral White Matter Demyelination
A new subtype of multiple sclerosis (MS) called myelocortical MS is characterized by demyelination only in the spinal cord and cerebral cortex and not in the cerebral white matter, according to a study published online ahead of print August 21 in Lancet Neurology. The findings are based on an examination of the brains and spinal cords of 100 patients who died of MS.
Bruce D. Trapp, PhD, the Morris R. and Ruth V. Graham Endowed Chair in Biomedical Research at the Lerner Research Institute at the Cleveland Clinic in Ohio, and his coauthors said that while the demyelination of cerebral white matter is a pathologic hallmark of MS, previous research has found that only around half of cerebral T2-weighted hyperintense white matter lesions are demyelinated, and these lesions account for less than a third of variance in the rate of brain atrophy.
“In the absence of specific MRI metrics for demyelination, the relationship between cerebral white-matter demyelination and neurodegeneration remains speculative,” they said.
In this study, researchers scanned the brains with MRI before autopsy, then took centimeter-thick hemispheric slices to study the white-matter lesions. They identified 12 individuals as having what they describe as myelocortical MS, characterized by the absence of areas of cerebral white-matter discoloration indicative of demyelinated lesions.
The authors then compared these individuals with 12 individuals with typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration, and Expanded Disability Status Scale score.
Not Typical MS
They found that while individuals with myelocortical MS did not have demyelinated lesions in the cerebral white matter, they had areas of demyelinated lesions in the cerebral cortex similar to those of individuals with typical MS (median 4.45% vs 9.74%, respectively). However, the individuals with myelocortical MS had a significantly smaller area of spinal cord demyelination (median 3.81% vs 13.81%).
Individuals with myelocortical MS also had significantly lower mean cortical neuronal densities, compared with healthy control brains, in layer III, layer V, and layer VI. But individuals with typical MS only had a lower cortical neuronal density in layer V when compared with controls.
Dr. Trapp and colleagues also saw that in typical MS, neuronal density decreased as the area of brain white-matter demyelination increased. However, this negative linear correlation was not seen in myelocortical MS.
On MRI, researchers were still able to see abnormalities in the cerebral white matter in individuals with myelocortical MS, in T2-weighted, T1-weighted, and magnetization transfer ratios (MTR) images. They also found similar total T2-weighted and T1-weighted lesion volumes in individuals with myelocortical MS and those with typical MS, although individuals with typical MS had significantly greater MTR lesion volumes.
The Hallmarks of Myelocortical MS
“We propose that myelocortical MS is characterized by spinal cord demyelination, subpial cortical demyelination, and an absence of cerebral white-matter demyelination,” Dr. Trapp and colleagues wrote. “Our findings indicate that abnormal cerebral white-matter T2-T1-MTR regions of interest are not always demyelinated, and this pathologic evidence suggests that cerebral white-matter demyelination and cortical neuronal degeneration can be independent events in myelocortical MS.”
The authors acknowledged that one limitation of their study may have been selection bias, as all the patients in the study died from complications of advanced MS. They suggested that it was therefore not appropriate to conclude that the prevalence of myelocortical MS seen in their sample would be similar across the entire MS population, nor were the findings likely to apply to pateints with earlier stage disease.
The study received funding from the NIH and the National MS Society. One author is an employee of Renovo Neural, and three authors are employees of Biogen. One author declared a pending patent related to automated lesion segmentation from MRI images, and four authors declared funding, fees, and nonfinancial support from pharmaceutical companies.
—Bianca Nogrady
Suggested Reading
Trapp BD, Vignos M, Dudman J, et al. Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study. Lancet Neurol. 2018 Aug 21 [Epub ahead of print].
A new subtype of multiple sclerosis (MS) called myelocortical MS is characterized by demyelination only in the spinal cord and cerebral cortex and not in the cerebral white matter, according to a study published online ahead of print August 21 in Lancet Neurology. The findings are based on an examination of the brains and spinal cords of 100 patients who died of MS.
Bruce D. Trapp, PhD, the Morris R. and Ruth V. Graham Endowed Chair in Biomedical Research at the Lerner Research Institute at the Cleveland Clinic in Ohio, and his coauthors said that while the demyelination of cerebral white matter is a pathologic hallmark of MS, previous research has found that only around half of cerebral T2-weighted hyperintense white matter lesions are demyelinated, and these lesions account for less than a third of variance in the rate of brain atrophy.
“In the absence of specific MRI metrics for demyelination, the relationship between cerebral white-matter demyelination and neurodegeneration remains speculative,” they said.
In this study, researchers scanned the brains with MRI before autopsy, then took centimeter-thick hemispheric slices to study the white-matter lesions. They identified 12 individuals as having what they describe as myelocortical MS, characterized by the absence of areas of cerebral white-matter discoloration indicative of demyelinated lesions.
The authors then compared these individuals with 12 individuals with typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration, and Expanded Disability Status Scale score.
Not Typical MS
They found that while individuals with myelocortical MS did not have demyelinated lesions in the cerebral white matter, they had areas of demyelinated lesions in the cerebral cortex similar to those of individuals with typical MS (median 4.45% vs 9.74%, respectively). However, the individuals with myelocortical MS had a significantly smaller area of spinal cord demyelination (median 3.81% vs 13.81%).
Individuals with myelocortical MS also had significantly lower mean cortical neuronal densities, compared with healthy control brains, in layer III, layer V, and layer VI. But individuals with typical MS only had a lower cortical neuronal density in layer V when compared with controls.
Dr. Trapp and colleagues also saw that in typical MS, neuronal density decreased as the area of brain white-matter demyelination increased. However, this negative linear correlation was not seen in myelocortical MS.
On MRI, researchers were still able to see abnormalities in the cerebral white matter in individuals with myelocortical MS, in T2-weighted, T1-weighted, and magnetization transfer ratios (MTR) images. They also found similar total T2-weighted and T1-weighted lesion volumes in individuals with myelocortical MS and those with typical MS, although individuals with typical MS had significantly greater MTR lesion volumes.
The Hallmarks of Myelocortical MS
“We propose that myelocortical MS is characterized by spinal cord demyelination, subpial cortical demyelination, and an absence of cerebral white-matter demyelination,” Dr. Trapp and colleagues wrote. “Our findings indicate that abnormal cerebral white-matter T2-T1-MTR regions of interest are not always demyelinated, and this pathologic evidence suggests that cerebral white-matter demyelination and cortical neuronal degeneration can be independent events in myelocortical MS.”
The authors acknowledged that one limitation of their study may have been selection bias, as all the patients in the study died from complications of advanced MS. They suggested that it was therefore not appropriate to conclude that the prevalence of myelocortical MS seen in their sample would be similar across the entire MS population, nor were the findings likely to apply to pateints with earlier stage disease.
The study received funding from the NIH and the National MS Society. One author is an employee of Renovo Neural, and three authors are employees of Biogen. One author declared a pending patent related to automated lesion segmentation from MRI images, and four authors declared funding, fees, and nonfinancial support from pharmaceutical companies.
—Bianca Nogrady
Suggested Reading
Trapp BD, Vignos M, Dudman J, et al. Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study. Lancet Neurol. 2018 Aug 21 [Epub ahead of print].
A new subtype of multiple sclerosis (MS) called myelocortical MS is characterized by demyelination only in the spinal cord and cerebral cortex and not in the cerebral white matter, according to a study published online ahead of print August 21 in Lancet Neurology. The findings are based on an examination of the brains and spinal cords of 100 patients who died of MS.
Bruce D. Trapp, PhD, the Morris R. and Ruth V. Graham Endowed Chair in Biomedical Research at the Lerner Research Institute at the Cleveland Clinic in Ohio, and his coauthors said that while the demyelination of cerebral white matter is a pathologic hallmark of MS, previous research has found that only around half of cerebral T2-weighted hyperintense white matter lesions are demyelinated, and these lesions account for less than a third of variance in the rate of brain atrophy.
“In the absence of specific MRI metrics for demyelination, the relationship between cerebral white-matter demyelination and neurodegeneration remains speculative,” they said.
In this study, researchers scanned the brains with MRI before autopsy, then took centimeter-thick hemispheric slices to study the white-matter lesions. They identified 12 individuals as having what they describe as myelocortical MS, characterized by the absence of areas of cerebral white-matter discoloration indicative of demyelinated lesions.
The authors then compared these individuals with 12 individuals with typical MS matched by age, sex, MRI protocol, MS disease subtype, disease duration, and Expanded Disability Status Scale score.
Not Typical MS
They found that while individuals with myelocortical MS did not have demyelinated lesions in the cerebral white matter, they had areas of demyelinated lesions in the cerebral cortex similar to those of individuals with typical MS (median 4.45% vs 9.74%, respectively). However, the individuals with myelocortical MS had a significantly smaller area of spinal cord demyelination (median 3.81% vs 13.81%).
Individuals with myelocortical MS also had significantly lower mean cortical neuronal densities, compared with healthy control brains, in layer III, layer V, and layer VI. But individuals with typical MS only had a lower cortical neuronal density in layer V when compared with controls.
Dr. Trapp and colleagues also saw that in typical MS, neuronal density decreased as the area of brain white-matter demyelination increased. However, this negative linear correlation was not seen in myelocortical MS.
On MRI, researchers were still able to see abnormalities in the cerebral white matter in individuals with myelocortical MS, in T2-weighted, T1-weighted, and magnetization transfer ratios (MTR) images. They also found similar total T2-weighted and T1-weighted lesion volumes in individuals with myelocortical MS and those with typical MS, although individuals with typical MS had significantly greater MTR lesion volumes.
The Hallmarks of Myelocortical MS
“We propose that myelocortical MS is characterized by spinal cord demyelination, subpial cortical demyelination, and an absence of cerebral white-matter demyelination,” Dr. Trapp and colleagues wrote. “Our findings indicate that abnormal cerebral white-matter T2-T1-MTR regions of interest are not always demyelinated, and this pathologic evidence suggests that cerebral white-matter demyelination and cortical neuronal degeneration can be independent events in myelocortical MS.”
The authors acknowledged that one limitation of their study may have been selection bias, as all the patients in the study died from complications of advanced MS. They suggested that it was therefore not appropriate to conclude that the prevalence of myelocortical MS seen in their sample would be similar across the entire MS population, nor were the findings likely to apply to pateints with earlier stage disease.
The study received funding from the NIH and the National MS Society. One author is an employee of Renovo Neural, and three authors are employees of Biogen. One author declared a pending patent related to automated lesion segmentation from MRI images, and four authors declared funding, fees, and nonfinancial support from pharmaceutical companies.
—Bianca Nogrady
Suggested Reading
Trapp BD, Vignos M, Dudman J, et al. Cortical neuronal densities and cerebral white matter demyelination in multiple sclerosis: a retrospective study. Lancet Neurol. 2018 Aug 21 [Epub ahead of print].
Cardiovascular Health and Cognitive Decline: What Is the Connection?
Maintaining cardiovascular health may reduce white matter hyperintensities and decrease the risk of dementia.
Optimal measures of cardiovascular health are associated with brain health in adults, according to two studies published in the August 21 issue of JAMA.
In a French population-based cohort study, adults ages 65 and older with more cardiovascular health measures at ideal levels had a lower risk of dementia and lower rates of cognitive decline than did those with fewer optimal cardiovascular measures, such as blood pressure and physical activity.
In addition, a preliminary, cross-sectional study of younger adults found that the number of modifiable cardiovascular risk factors at recommended levels was associated with brain vessel structure and function and the number of white matter hyperintensities.
“These two studies convey an immediately actionable message to clinicians, policy makers, and patients,” said Jeffrey L. Saver, MD, and Mary Cushman, MD, in an accompanying editorial. “Available evidence indicates that to achieve a lifetime of robust brain health free of dementia, it is never too early or too late to strive for attainment of ideal cardiovascular health.” Dr. Saver is a Professor of Neurology and Director of the Stroke Center at the University of California, Los Angeles. Dr. Cushman is a Professor of Medicine and Pathology at Larner College of Medicine at the University of Vermont in Burlington.
Cardiovascular Health in Older Age
Vascular dementia is the second most common neuropathologic basis of dementia, after Alzheimer’s disease, and “most cases of dementia arise from a combination of [Alzheimer’s disease] and cerebrovascular pathology,” the editorialists noted. Studies have suggested a connection between cardiovascular health and dementia, but the evidence is limited.
Cécilia Samieri, PhD, a Senior Researcher at the Bordeaux Population Health Research Center at the Université de Bordeaux in France, and colleagues studied people age 65 and older from Bordeaux, Dijon, and Montpellier, France, to examine the association between cardiovascular health level and risk of dementia and cognitive decline in older adults.
The study included 6,626 people without a history of cardiovascular disease or dementia at baseline. Participants underwent in-person neuropsychologic testing between January 1999 and July 2016 and systematic detection of incident dementia. Participants had a mean age of 73.7, and 63.4% were women.
The investigators defined cardiovascular health using a seven-item tool from the American Heart Association (AHA). They determined the number of the AHA’s Life’s Simple Seven metrics that were at recommended levels (ie, nonsmoking, BMI < 25, regular physical activity, eating fish at least twice per week and fruits and vegetables at least three times per day, cholesterol < 200 mg/dL [untreated], fasting glucose < 100 mg/dL [untreated], and blood pressure < 120/80 mm Hg [untreated]).
Approximately 36.5% of the cohort had zero, one, or two optimal health metrics, 57.1% had three or four optimal health metrics, and 6.5% had five, six, or seven optimal health metrics.
During an average follow-up of 8.5 years, 745 participants developed dementia. Among participants with zero or one health metrics at optimal levels at baseline, the incidence rate of dementia was 1.76 per 100 person-years. Compared with this rate, the incidence rate per 100 person-years was 0.26 lower for participants with two optimal health metrics, 0.59 lower for participants with three optimal health metrics, 0.43 lower for participants with four optimal health metrics, 0.93 lower for participants with five optimal health metrics, and 0.96 lower for participants with six or seven optimal health metrics.
“In multivariable models, the hazard ratios for dementia were 0.90 per additional optimal metric,” the investigators said. “The study results support the recent recommendations of the AHA and the American Stroke Association for the promotion of the Life’s Simple Seven tool.”
Cerebrovascular Structure and Function in Young Adults
Wilby Williamson, BMBS
The researchers assessed patients’ cerebral vessel density, caliber, and tortuosity and brain white matter hyperintensity lesion count. In a subgroup of 52 participants, they assessed cerebral blood flow.
The researchers determined for each participant how many of eight modifiable risk factors were at recommended levels (ie, BMI < 25, highest tertile of cardiovascular fitness or physical activity, alcohol consumption < eight drinks per week, nonsmoker for more than six months, blood pressure on awake ambulatory monitoring < 130/80 mm Hg, a nonhypertensive diastolic response to exercise [ie, peak diastolic blood pressure < 90 mm Hg], total cholesterol < 200 mg/dL, and fasting glucose < 100 mg/dL).
On average, participants had six of the eight modifiable cardiovascular risk factors at recommended levels.
In multivariable models, cardiovascular risk factors were associated with cerebrovascular structure and the number of white matter hyperintensities. “For each additional modifiable risk factor categorized as healthy, vessel density was greater by 0.3 vessels/cm3, vessel caliber was greater by 8 μm, and white matter hyperintensity lesions were fewer by 1.6 lesions. Among the 52 participants with available data, cerebral blood flow varied with vessel density and was 2.5 mL/100 g/min higher for each healthier category of a modifiable risk factor,” Dr. Williamson and colleagues said.
The findings suggest that “some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood,” the researchers said. The study was exploratory, however, and follow-up studies are needed to determine the clinical significance of these findings, they said.
“The magnitude of changes was generally much less than would be expected to produce clinical symptoms such as cognitive impairment or gait difficulty,” said Drs. Saver and Cushman. The changes, however, “may portend more substantial abnormalities later in life,” they said. “Even during the late-life period, when septuagenarians become octogenarians, cardiovascular health is associated with substantial differences in cognitive trajectory and dementia onset.”
—Jake Remaly
Suggested Reading
Samieri C, Perier MC, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657-664.
Saver JL, Cushman M. Striving for ideal cardiovascular and brain health: It is never too early or too late. JAMA. 2018; 320(7):645-647.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of cardiovascular risk factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665-673.
Maintaining cardiovascular health may reduce white matter hyperintensities and decrease the risk of dementia.
Maintaining cardiovascular health may reduce white matter hyperintensities and decrease the risk of dementia.
Optimal measures of cardiovascular health are associated with brain health in adults, according to two studies published in the August 21 issue of JAMA.
In a French population-based cohort study, adults ages 65 and older with more cardiovascular health measures at ideal levels had a lower risk of dementia and lower rates of cognitive decline than did those with fewer optimal cardiovascular measures, such as blood pressure and physical activity.
In addition, a preliminary, cross-sectional study of younger adults found that the number of modifiable cardiovascular risk factors at recommended levels was associated with brain vessel structure and function and the number of white matter hyperintensities.
“These two studies convey an immediately actionable message to clinicians, policy makers, and patients,” said Jeffrey L. Saver, MD, and Mary Cushman, MD, in an accompanying editorial. “Available evidence indicates that to achieve a lifetime of robust brain health free of dementia, it is never too early or too late to strive for attainment of ideal cardiovascular health.” Dr. Saver is a Professor of Neurology and Director of the Stroke Center at the University of California, Los Angeles. Dr. Cushman is a Professor of Medicine and Pathology at Larner College of Medicine at the University of Vermont in Burlington.
Cardiovascular Health in Older Age
Vascular dementia is the second most common neuropathologic basis of dementia, after Alzheimer’s disease, and “most cases of dementia arise from a combination of [Alzheimer’s disease] and cerebrovascular pathology,” the editorialists noted. Studies have suggested a connection between cardiovascular health and dementia, but the evidence is limited.
Cécilia Samieri, PhD, a Senior Researcher at the Bordeaux Population Health Research Center at the Université de Bordeaux in France, and colleagues studied people age 65 and older from Bordeaux, Dijon, and Montpellier, France, to examine the association between cardiovascular health level and risk of dementia and cognitive decline in older adults.
The study included 6,626 people without a history of cardiovascular disease or dementia at baseline. Participants underwent in-person neuropsychologic testing between January 1999 and July 2016 and systematic detection of incident dementia. Participants had a mean age of 73.7, and 63.4% were women.
The investigators defined cardiovascular health using a seven-item tool from the American Heart Association (AHA). They determined the number of the AHA’s Life’s Simple Seven metrics that were at recommended levels (ie, nonsmoking, BMI < 25, regular physical activity, eating fish at least twice per week and fruits and vegetables at least three times per day, cholesterol < 200 mg/dL [untreated], fasting glucose < 100 mg/dL [untreated], and blood pressure < 120/80 mm Hg [untreated]).
Approximately 36.5% of the cohort had zero, one, or two optimal health metrics, 57.1% had three or four optimal health metrics, and 6.5% had five, six, or seven optimal health metrics.
During an average follow-up of 8.5 years, 745 participants developed dementia. Among participants with zero or one health metrics at optimal levels at baseline, the incidence rate of dementia was 1.76 per 100 person-years. Compared with this rate, the incidence rate per 100 person-years was 0.26 lower for participants with two optimal health metrics, 0.59 lower for participants with three optimal health metrics, 0.43 lower for participants with four optimal health metrics, 0.93 lower for participants with five optimal health metrics, and 0.96 lower for participants with six or seven optimal health metrics.
“In multivariable models, the hazard ratios for dementia were 0.90 per additional optimal metric,” the investigators said. “The study results support the recent recommendations of the AHA and the American Stroke Association for the promotion of the Life’s Simple Seven tool.”
Cerebrovascular Structure and Function in Young Adults
Wilby Williamson, BMBS
The researchers assessed patients’ cerebral vessel density, caliber, and tortuosity and brain white matter hyperintensity lesion count. In a subgroup of 52 participants, they assessed cerebral blood flow.
The researchers determined for each participant how many of eight modifiable risk factors were at recommended levels (ie, BMI < 25, highest tertile of cardiovascular fitness or physical activity, alcohol consumption < eight drinks per week, nonsmoker for more than six months, blood pressure on awake ambulatory monitoring < 130/80 mm Hg, a nonhypertensive diastolic response to exercise [ie, peak diastolic blood pressure < 90 mm Hg], total cholesterol < 200 mg/dL, and fasting glucose < 100 mg/dL).
On average, participants had six of the eight modifiable cardiovascular risk factors at recommended levels.
In multivariable models, cardiovascular risk factors were associated with cerebrovascular structure and the number of white matter hyperintensities. “For each additional modifiable risk factor categorized as healthy, vessel density was greater by 0.3 vessels/cm3, vessel caliber was greater by 8 μm, and white matter hyperintensity lesions were fewer by 1.6 lesions. Among the 52 participants with available data, cerebral blood flow varied with vessel density and was 2.5 mL/100 g/min higher for each healthier category of a modifiable risk factor,” Dr. Williamson and colleagues said.
The findings suggest that “some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood,” the researchers said. The study was exploratory, however, and follow-up studies are needed to determine the clinical significance of these findings, they said.
“The magnitude of changes was generally much less than would be expected to produce clinical symptoms such as cognitive impairment or gait difficulty,” said Drs. Saver and Cushman. The changes, however, “may portend more substantial abnormalities later in life,” they said. “Even during the late-life period, when septuagenarians become octogenarians, cardiovascular health is associated with substantial differences in cognitive trajectory and dementia onset.”
—Jake Remaly
Suggested Reading
Samieri C, Perier MC, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657-664.
Saver JL, Cushman M. Striving for ideal cardiovascular and brain health: It is never too early or too late. JAMA. 2018; 320(7):645-647.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of cardiovascular risk factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665-673.
Optimal measures of cardiovascular health are associated with brain health in adults, according to two studies published in the August 21 issue of JAMA.
In a French population-based cohort study, adults ages 65 and older with more cardiovascular health measures at ideal levels had a lower risk of dementia and lower rates of cognitive decline than did those with fewer optimal cardiovascular measures, such as blood pressure and physical activity.
In addition, a preliminary, cross-sectional study of younger adults found that the number of modifiable cardiovascular risk factors at recommended levels was associated with brain vessel structure and function and the number of white matter hyperintensities.
“These two studies convey an immediately actionable message to clinicians, policy makers, and patients,” said Jeffrey L. Saver, MD, and Mary Cushman, MD, in an accompanying editorial. “Available evidence indicates that to achieve a lifetime of robust brain health free of dementia, it is never too early or too late to strive for attainment of ideal cardiovascular health.” Dr. Saver is a Professor of Neurology and Director of the Stroke Center at the University of California, Los Angeles. Dr. Cushman is a Professor of Medicine and Pathology at Larner College of Medicine at the University of Vermont in Burlington.
Cardiovascular Health in Older Age
Vascular dementia is the second most common neuropathologic basis of dementia, after Alzheimer’s disease, and “most cases of dementia arise from a combination of [Alzheimer’s disease] and cerebrovascular pathology,” the editorialists noted. Studies have suggested a connection between cardiovascular health and dementia, but the evidence is limited.
Cécilia Samieri, PhD, a Senior Researcher at the Bordeaux Population Health Research Center at the Université de Bordeaux in France, and colleagues studied people age 65 and older from Bordeaux, Dijon, and Montpellier, France, to examine the association between cardiovascular health level and risk of dementia and cognitive decline in older adults.
The study included 6,626 people without a history of cardiovascular disease or dementia at baseline. Participants underwent in-person neuropsychologic testing between January 1999 and July 2016 and systematic detection of incident dementia. Participants had a mean age of 73.7, and 63.4% were women.
The investigators defined cardiovascular health using a seven-item tool from the American Heart Association (AHA). They determined the number of the AHA’s Life’s Simple Seven metrics that were at recommended levels (ie, nonsmoking, BMI < 25, regular physical activity, eating fish at least twice per week and fruits and vegetables at least three times per day, cholesterol < 200 mg/dL [untreated], fasting glucose < 100 mg/dL [untreated], and blood pressure < 120/80 mm Hg [untreated]).
Approximately 36.5% of the cohort had zero, one, or two optimal health metrics, 57.1% had three or four optimal health metrics, and 6.5% had five, six, or seven optimal health metrics.
During an average follow-up of 8.5 years, 745 participants developed dementia. Among participants with zero or one health metrics at optimal levels at baseline, the incidence rate of dementia was 1.76 per 100 person-years. Compared with this rate, the incidence rate per 100 person-years was 0.26 lower for participants with two optimal health metrics, 0.59 lower for participants with three optimal health metrics, 0.43 lower for participants with four optimal health metrics, 0.93 lower for participants with five optimal health metrics, and 0.96 lower for participants with six or seven optimal health metrics.
“In multivariable models, the hazard ratios for dementia were 0.90 per additional optimal metric,” the investigators said. “The study results support the recent recommendations of the AHA and the American Stroke Association for the promotion of the Life’s Simple Seven tool.”
Cerebrovascular Structure and Function in Young Adults
Wilby Williamson, BMBS
The researchers assessed patients’ cerebral vessel density, caliber, and tortuosity and brain white matter hyperintensity lesion count. In a subgroup of 52 participants, they assessed cerebral blood flow.
The researchers determined for each participant how many of eight modifiable risk factors were at recommended levels (ie, BMI < 25, highest tertile of cardiovascular fitness or physical activity, alcohol consumption < eight drinks per week, nonsmoker for more than six months, blood pressure on awake ambulatory monitoring < 130/80 mm Hg, a nonhypertensive diastolic response to exercise [ie, peak diastolic blood pressure < 90 mm Hg], total cholesterol < 200 mg/dL, and fasting glucose < 100 mg/dL).
On average, participants had six of the eight modifiable cardiovascular risk factors at recommended levels.
In multivariable models, cardiovascular risk factors were associated with cerebrovascular structure and the number of white matter hyperintensities. “For each additional modifiable risk factor categorized as healthy, vessel density was greater by 0.3 vessels/cm3, vessel caliber was greater by 8 μm, and white matter hyperintensity lesions were fewer by 1.6 lesions. Among the 52 participants with available data, cerebral blood flow varied with vessel density and was 2.5 mL/100 g/min higher for each healthier category of a modifiable risk factor,” Dr. Williamson and colleagues said.
The findings suggest that “some individuals may be starting to diverge to different risk trajectories for brain vascular health in early adulthood,” the researchers said. The study was exploratory, however, and follow-up studies are needed to determine the clinical significance of these findings, they said.
“The magnitude of changes was generally much less than would be expected to produce clinical symptoms such as cognitive impairment or gait difficulty,” said Drs. Saver and Cushman. The changes, however, “may portend more substantial abnormalities later in life,” they said. “Even during the late-life period, when septuagenarians become octogenarians, cardiovascular health is associated with substantial differences in cognitive trajectory and dementia onset.”
—Jake Remaly
Suggested Reading
Samieri C, Perier MC, Gaye B, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657-664.
Saver JL, Cushman M. Striving for ideal cardiovascular and brain health: It is never too early or too late. JAMA. 2018; 320(7):645-647.
Williamson W, Lewandowski AJ, Forkert ND, et al. Association of cardiovascular risk factors with MRI indices of cerebrovascular structure and function and white matter hyperintensities in young adults. JAMA. 2018;320(7):665-673.
Alan M. Rapoport, MD, on Medication Overuse Headache
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center (mrc@mdedge.com) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center (mrc@mdedge.com) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California
Neurology Reviews recently shared two poll questions with our Facebook followers about treatment medication overuse headache (MOH). I was very interested to see the results of our poll. While the number of responses was somewhat low, we do get some sense of what respondents are saying. In this commentary, I will first tell you my perspective on the answers and then we will see what some other headache specialists say about the answers to these questions.
Poll Results:
Can MOH be treated with preventive medications without detoxification?
33 votes
YES, 39%
NO, 61%
Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor) without detoxification?
26 votes
YES, 38%
NO, 62%
My Commentary:
Let me explain in more detail my thoughts on the first question, “Can MOH be treated with preventive medications without detoxification?”
If a patient had the diagnosis of MOH – meaning 15 or more headache days per month for at least 3 months, with use of stronger medications (triptans, ergots, opiates, butalbital-containing medications) for 10 days per month or milder treatment (aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs [NSAIDs]) for 15 days per month – can they improve by being put on a traditional preventive medication without intentionally reducing their overused acute medications by a detoxification protocol ordered by a doctor or nurse?
Only 39% of our audience said yes. Yet some studies have shown that patients placed on onabotulinumtoxinA or topiramate might improve without them going through a detoxification of the overused medications. As a physician, I would suggest simultaneously decreasing in their acute medications. I think in some cases this approach creates additional improvement and makes the patient feel better. It would be better for their quality of life, as well as for their kidneys and possibly even their brains.
Here are my thoughts on the second question, “Can MOH be treated with the new preventive medications (the monoclonal antibodies to CGRP ligand or receptor), without detoxification?”
If a patient has MOH, can you expect them to improve after being placed on 1 of the 4 monoclonal antibodies to CGRP ligand or its receptor – all of which are either recently approved or currently in development – without suggesting that they decrease their overused acute care medications? Note that erenumab (Aimovig-aaoe) has been approved by the FDA and marketed as of the time of this writing; we expect 2 more products to be approved very soon.
Almost an identical percentage of our audience (38%) said yes. There is evidence in published clinical trials that those patients given these new medications did about as well with or without the presence of MOH, and both groups did better than the placebo patients. Note that most trials prohibited overuse of opiates and butalbital.
I am a firm believer of detoxifying patients from their overused over-the-counter (OTC) or prescription medications. I believe that opiates and butalbital-containing medications, when overused, are worse for patients than OTCs, NSAIDs, ergot and triptans, but all of these can cause MOH. There are many studies showing that both inpatient and outpatient detoxification alone can really help. However, it is difficult to detoxify patients and some refuse to try this approach.
So, what should we do as physicians? If a patient has MOH, I educate them, try to detoxify them slowly on an outpatient basis, and if I feel it will help, start them on a preventive medication, even before the detoxification begins so they can reach therapeutic levels. In the future, will I use one of the standard preventives, approved or off-label, for migraine prevention (beta blockers, topiramate and other anticonvulsants, antidepressants, angiotensin receptor blockers, onabotulinumtoxinA and others)? It remains to be seen. I am leaning towards the anti CGRP ligand and receptor monoclonal antibodies and preventive small molecule oral CGRP receptor blockers. While that might be enough to start with, I will continue explaining to my patients why they should actively begin a slow detoxification.
Let us see what some headache specialists said about both questions.
Robert Cowan, MD, FAAN:
There have been studies that show migraine can improve without the discontinuation of medication overuse. But that is not what the question asks. The question as posed is whether MOH can be treated with a preventive medication without detoxification. Since the diagnosis of MOH has, in the past, required the cessation of overuse leading to an improvement in the underlying headache, then technically, the answer would be “no.” But that being said, there is ample evidence that the number of headache days/months and other measures of headache can, in fact, improve with the introduction of a preventive, along with other measures such as lifestyle modification. The other ambiguity in the question has to do with what is meant by “detoxification.” Is this a hospital-based detox, or is a gradual decrease in the offending medicine in combination with the addition of a preventive, still considered “detoxification?” Also, does the response imply a sequential relationship between the detoxification and initiation of the preventive? Without further clarification, this response ratio to the question is very difficult to interpret.
There is animal data that suggests acute migraine medications may promote MOH in susceptible individuals through CGRP-dependent mechanisms and anti-CGRP antibodies may be useful for the MOH (Cephalalgia. 2017;37(6):560-570. doi: 10.1177/0333102416650702). While there are no published CGRP antibody studies that did not exclude MOH patients to my knowledge, an abstract by Silberstein et al at the recent AHS Scientific Meeting reported decreased use of overused medication with fremanazumab (Headache. 2018;58(S2):76-78).
Ira Turner, MD
There is clear data to suggest that it is not necessary to detoxify these patients before starting preventive therapy. This is true for the older and newer medications. In fact, not only do these preventive therapies still work in the presence of medication overuse, but they also help to reduce medication overuse. The one caveat that must be mentioned is that this may not apply to opiate overuse. Opiate over-users were excluded from these studies.
While it is of course our goal to reduce and stop acute medication overuse, it should not be done at the expense of delaying preventive therapy. In fact, it is desirable to do both simultaneously. This applies to oral preventive medications, botulinum toxin and CGRP monoclonal antibodies.
In view of this well-established data, it was quite surprising to me to see the results of the 2 polls cited. It seems as if we still have a lot of educating to do regarding migraine prevention in general and with medication overuse in migraine in particular.
Stewart Tepper, MD
Dr. Tepper did not have time to comment, but suggested we show you an abstract presented at the recent AHS meeting. It shows that erenumab-aaoe helps patients with MOH who have not been detoxified (Headache. 2018;58(S2):160-162).
###
Please write to us at Neurology Reviews Migraine Resource Center (mrc@mdedge.com) with your opinions.
Alan M. Rapoport, MD
Editor-in-Chief
Migraine Resource Center
Clinical Professor of Neurology
The David Geffen School of Medicine at UCLA
Los Angeles, California