User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
Opioid use higher in adults with health conditions
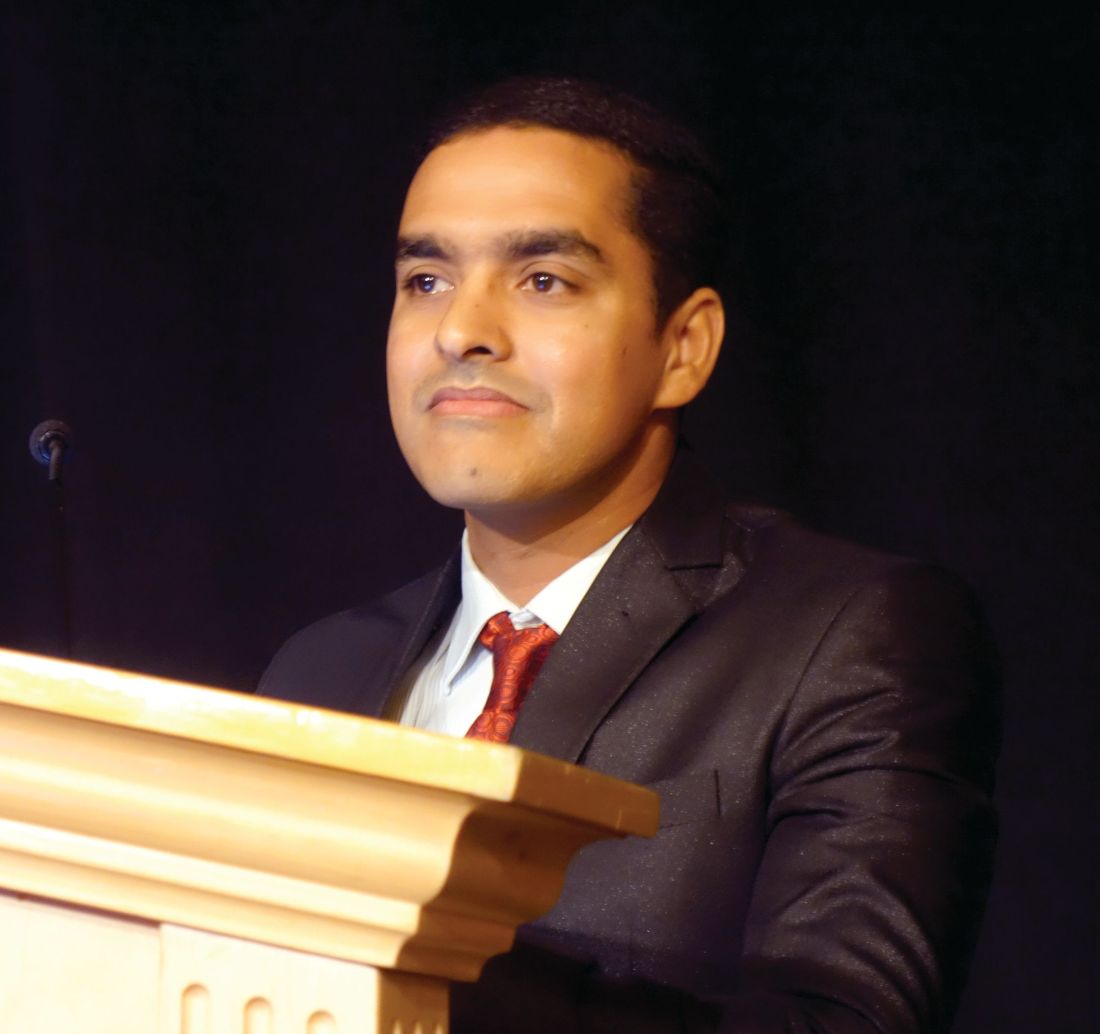
Use of prescription opioids is higher among adults with health conditions such as cirrhosis and diabetes, compared with those who do not have the conditions, according to an analysis of national survey data.
In 2015, reported use of opioids was 71.7% in adults with cirrhosis, compared with 37.8% for those who did not have cirrhosis. That is the largest difference among any of the various health conditions included in a report by Beth Han, MD, PhD, of the Substance Abuse and Mental Health Services Administration in Rockville, Md., which conducts the ongoing survey, and her associates (Ann Intern Med. 2017 July 31. doi: 10.7326/M17-0865).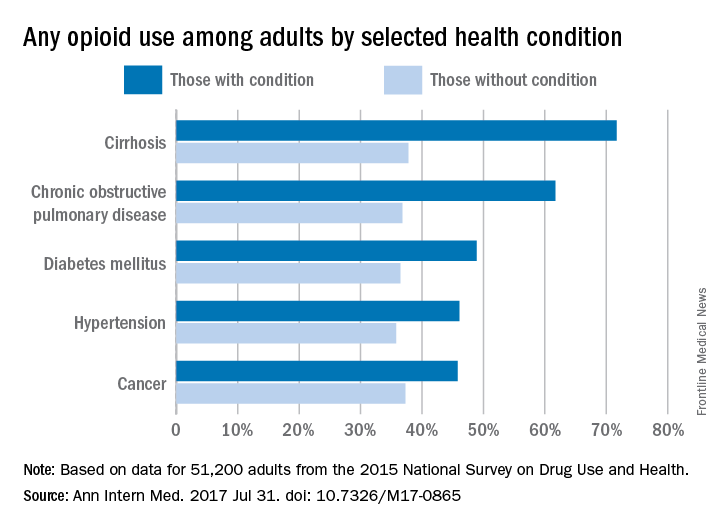
Of those with cirrhosis who reported any use of prescription opioids, 86.1% said that they did so without misuse, while the other four conditions had rates ranging from 91.3% to 93.9%. Among those with chronic obstructive pulmonary disease, 6.2% misused opioids without use disorder, and 2.5% had opioid use disorder. These estimates were not available for cirrhosis because of low statistical precision, but the corresponding figures were 6.9% and 1.5% for diabetes, 6% and 2.1% for hypertension, and 5.3% and 0.8% for cancer, the investigators said.
Overall prescription opioid use in 2015 was 37.8% for the civilian, noninstitutionalized adult population, about 91.8 million individuals. Estimates suggest that 4.7% (1.5 million) of all adults misused them in some way, and that 0.8% (1.9 million) had a use disorder, they reported.
“Among adults with misuse of prescription opioids, 59.9% used them without a prescription at least once in 2015, and 40.8% obtained them from friends or relatives for free for their most recent episode of misuse. Such widespread social availability of prescription opioids suggests that they are commonly dispensed in amounts not fully consumed by the patients to whom they are prescribed,” the authors wrote.
Funding for the study came from the Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the Office of the Assistant Secretary for Planning and Evaluation of the Department of Health and Human Services. One investigator reported stock holdings in 3M, General Electric, and Pfizer, and another reported stock holdings in Eli Lilly, General Electric, and Sanofi. Dr. Han and the other three investigators disclosed that they had no conflicts of interest.
Talk to any busy full-time primary care physician, and it becomes evident that writing an opioid prescription is much easier than exploring other options for addressing chronic pain in the course of a 15-minute visit. The same stressful work conditions likely also make it difficult for primary care providers to appropriately monitor patients who take opioids in the long term with urine drug tests and pill counts to assess for opioid diversion or other substance use.
A potential solution to the problem of the overburdened primary care physician is to distribute some of the work to other members of the health care team. Indeed, we have found that using a nurse care manager with a registry increased receipt of guideline-concordant care (urine drug testing and patient-provider agreements) among patients receiving long-term opioid therapy. The intervention also resulted in reductions in opioid doses at a large urban safety-net hospital and three community health centers.
Karen E. Lasser, MD, is with Boston Medical Center and Boston University. Her remarks are excerpted from an editorial response (Ann Intern Med. 2017 Jul 31. doi: 10.7326/M17-1559) to Dr. Han’s study.
Talk to any busy full-time primary care physician, and it becomes evident that writing an opioid prescription is much easier than exploring other options for addressing chronic pain in the course of a 15-minute visit. The same stressful work conditions likely also make it difficult for primary care providers to appropriately monitor patients who take opioids in the long term with urine drug tests and pill counts to assess for opioid diversion or other substance use.
A potential solution to the problem of the overburdened primary care physician is to distribute some of the work to other members of the health care team. Indeed, we have found that using a nurse care manager with a registry increased receipt of guideline-concordant care (urine drug testing and patient-provider agreements) among patients receiving long-term opioid therapy. The intervention also resulted in reductions in opioid doses at a large urban safety-net hospital and three community health centers.
Karen E. Lasser, MD, is with Boston Medical Center and Boston University. Her remarks are excerpted from an editorial response (Ann Intern Med. 2017 Jul 31. doi: 10.7326/M17-1559) to Dr. Han’s study.
Talk to any busy full-time primary care physician, and it becomes evident that writing an opioid prescription is much easier than exploring other options for addressing chronic pain in the course of a 15-minute visit. The same stressful work conditions likely also make it difficult for primary care providers to appropriately monitor patients who take opioids in the long term with urine drug tests and pill counts to assess for opioid diversion or other substance use.
A potential solution to the problem of the overburdened primary care physician is to distribute some of the work to other members of the health care team. Indeed, we have found that using a nurse care manager with a registry increased receipt of guideline-concordant care (urine drug testing and patient-provider agreements) among patients receiving long-term opioid therapy. The intervention also resulted in reductions in opioid doses at a large urban safety-net hospital and three community health centers.
Karen E. Lasser, MD, is with Boston Medical Center and Boston University. Her remarks are excerpted from an editorial response (Ann Intern Med. 2017 Jul 31. doi: 10.7326/M17-1559) to Dr. Han’s study.
Use of prescription opioids is higher among adults with health conditions such as cirrhosis and diabetes, compared with those who do not have the conditions, according to an analysis of national survey data.
In 2015, reported use of opioids was 71.7% in adults with cirrhosis, compared with 37.8% for those who did not have cirrhosis. That is the largest difference among any of the various health conditions included in a report by Beth Han, MD, PhD, of the Substance Abuse and Mental Health Services Administration in Rockville, Md., which conducts the ongoing survey, and her associates (Ann Intern Med. 2017 July 31. doi: 10.7326/M17-0865).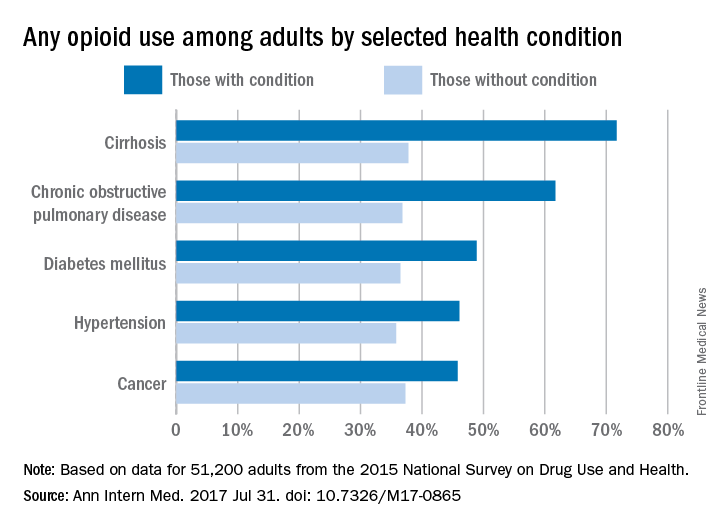
Of those with cirrhosis who reported any use of prescription opioids, 86.1% said that they did so without misuse, while the other four conditions had rates ranging from 91.3% to 93.9%. Among those with chronic obstructive pulmonary disease, 6.2% misused opioids without use disorder, and 2.5% had opioid use disorder. These estimates were not available for cirrhosis because of low statistical precision, but the corresponding figures were 6.9% and 1.5% for diabetes, 6% and 2.1% for hypertension, and 5.3% and 0.8% for cancer, the investigators said.
Overall prescription opioid use in 2015 was 37.8% for the civilian, noninstitutionalized adult population, about 91.8 million individuals. Estimates suggest that 4.7% (1.5 million) of all adults misused them in some way, and that 0.8% (1.9 million) had a use disorder, they reported.
“Among adults with misuse of prescription opioids, 59.9% used them without a prescription at least once in 2015, and 40.8% obtained them from friends or relatives for free for their most recent episode of misuse. Such widespread social availability of prescription opioids suggests that they are commonly dispensed in amounts not fully consumed by the patients to whom they are prescribed,” the authors wrote.
Funding for the study came from the Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the Office of the Assistant Secretary for Planning and Evaluation of the Department of Health and Human Services. One investigator reported stock holdings in 3M, General Electric, and Pfizer, and another reported stock holdings in Eli Lilly, General Electric, and Sanofi. Dr. Han and the other three investigators disclosed that they had no conflicts of interest.
Use of prescription opioids is higher among adults with health conditions such as cirrhosis and diabetes, compared with those who do not have the conditions, according to an analysis of national survey data.
In 2015, reported use of opioids was 71.7% in adults with cirrhosis, compared with 37.8% for those who did not have cirrhosis. That is the largest difference among any of the various health conditions included in a report by Beth Han, MD, PhD, of the Substance Abuse and Mental Health Services Administration in Rockville, Md., which conducts the ongoing survey, and her associates (Ann Intern Med. 2017 July 31. doi: 10.7326/M17-0865).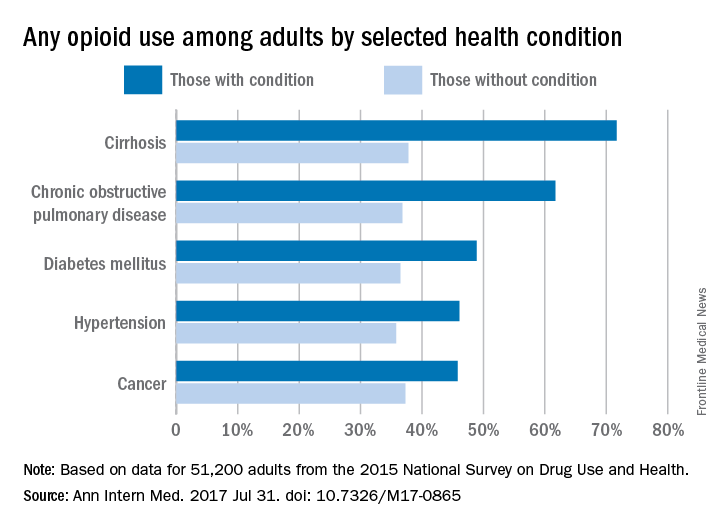
Of those with cirrhosis who reported any use of prescription opioids, 86.1% said that they did so without misuse, while the other four conditions had rates ranging from 91.3% to 93.9%. Among those with chronic obstructive pulmonary disease, 6.2% misused opioids without use disorder, and 2.5% had opioid use disorder. These estimates were not available for cirrhosis because of low statistical precision, but the corresponding figures were 6.9% and 1.5% for diabetes, 6% and 2.1% for hypertension, and 5.3% and 0.8% for cancer, the investigators said.
Overall prescription opioid use in 2015 was 37.8% for the civilian, noninstitutionalized adult population, about 91.8 million individuals. Estimates suggest that 4.7% (1.5 million) of all adults misused them in some way, and that 0.8% (1.9 million) had a use disorder, they reported.
“Among adults with misuse of prescription opioids, 59.9% used them without a prescription at least once in 2015, and 40.8% obtained them from friends or relatives for free for their most recent episode of misuse. Such widespread social availability of prescription opioids suggests that they are commonly dispensed in amounts not fully consumed by the patients to whom they are prescribed,” the authors wrote.
Funding for the study came from the Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the Office of the Assistant Secretary for Planning and Evaluation of the Department of Health and Human Services. One investigator reported stock holdings in 3M, General Electric, and Pfizer, and another reported stock holdings in Eli Lilly, General Electric, and Sanofi. Dr. Han and the other three investigators disclosed that they had no conflicts of interest.
FROM ANNALS OF INTERNAL MEDICINE
Better bariatric surgery outcomes with lower preoperative BMI
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according to a paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
The authors’ conclusion that bariatric surgery should be more liberally applied to patients with less severe obesity is consistent with multiple reports of improved control of type 2 diabetes, if not remission, among lower-BMI patient populations following MBS [metabolic and bariatric surgery]. However, these reports generally do not refute the importance of weight loss in achieving important clinical benefit among patients with obesity-related comorbid disease.
One strength of the present study is that it is a clinical database. However, 50% attrition of the follow-up weight loss data at 1 year is potentially problematic.
Bruce M. Wolfe, MD, FACS, and Elizaveta Walker, MPH, are in the division of bariatric surgery, department of surgery, at Oregon Health & Science University, Portland. These comments are taken from an accompanying editorial (JAMA Surgery 2017 Jul 26. doi: 10.1001/jamasurg.2017.2349). No conflicts of interest were declared.
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according to a paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Delaying bariatric surgery until body mass index is highly elevated may reduce the likelihood of achieving a BMI of less than 30 within a year, according to a paper published online July 26 in JAMA Surgery.
A retrospective study using prospectively gathered clinical data of 27,320 adults who underwent bariatric surgery in Michigan showed around one in three (36%) achieved a BMI below 30 within a year after surgery (JAMA Surgery 2017, July 26. doi: 10.1001/jamasurg.2017.2348). But obese patients with a body mass index of less than 40 kg/m2 before undergoing bariatric surgery are significantly more likely to achieve a postoperative BMI of under 30.
Individuals who had a preoperative BMI of less than 40 had a 12-fold higher chance of getting their BMI below 30, compared to those whose preoperative BMI was 40 or above (95% confidence interval 1.71-14.16, P less than .001). Only 8.5% of individuals with a BMI at or above 50 achieved a postoperative BMI below 30.
The likelihood of getting below 30 within a year was eightfold higher in patients who had a sleeve gastrectomy, 21 times greater in those who underwent Roux-en-Y bypass, and 82 times higher in those who had a duodenal switch, compared with patients who had adjustable gastric banding (P less than .001).
The researchers also compared other outcomes in individuals whose BMI dropped below 30 and in those who did not achieve this degree of weight loss. The analysis showed that those with a BMI below 30 after 1 year had at least a twofold greater chance of discontinuing cholesterol-lowering medications, insulin, diabetes medications, antihypertensives, and CPAP for sleep apnea, compared with those whose BMI remained at 30 or above. They were also more than three times more likely to report being ‘very satisfied’ with the outcomes of surgery.
The authors noted that the cohort’s mean BMI was 48, which was above the established threshold for bariatric surgery, namely a BMI of 40, or 35 with weight-related comorbidities.
“Our results suggest that patients with morbid obesity should be targeted for surgery when their BMI is still less than 40, as these patients are more likely to achieve a target BMI that results in substantial reduction in weight-related comorbidities,” the authors wrote.
However, they stressed that their findings should not be taken as a reason to exclude patients with a BMI above 40 from surgery, pointing out that even for patients with higher preoperative BMIs, bariatric surgery offered substantial health and quality of life benefits.
They also acknowledged that 1-year weight data was available for around 50% of patients in the registry, which may have led to selection bias.
“Policies and practice patterns that delay or incentivize patients to pursue bariatric surgery only once the BMI is highly elevated can result in inferior outcomes,” the investigators concluded.
Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
FROM JAMA SURGERY
Key clinical point: A BMI below 40 prior to undergoing bariatric surgery gives patients a significantly better chance of achieving a 1-year postoperative BMI under 30.
Major finding: Obese patients with a BMI less than 40 before undergoing bariatric surgery are more than 12 times more likely to achieve a postoperative BMI of under 30.
Data source: A retrospective study using prospectively gathered clinical data of 27, 320 adults who underwent bariatric surgery.
Disclosures: Blue Cross Blue Shield of Michigan/Blue Care Network funded the study. Three authors had received salary support from Blue Cross Blue Shield. No other conflicts of interest were declared.
Exercise, CBT linked to higher drop in depression in type 2 diabetes
SAN DIEGO – The odds of full remission from clinically diagnosed major depression greatly improved in patients with type 2 diabetes who took part in 12-week supervised exercise and cognitive behavioral therapy (CBT). By the end of the study, 96% of the CBT participants no longer met diagnostic criteria for major depression, compared with just 65% of those on usual care, judging from the findings of a new study.
Another approach – a combination treatment of both exercise and CBT therapies – did not show a statistically significant effect on full remission rates but showed improvement in some other areas.
Dr. De Groot and her colleagues recruited 140 adults – mean age 57 years, 77% female, 71% white, 52% married – who had a diagnosis of both type 2 diabetes and diagnosed clinical depression. They came from three states and had various levels of income and educational background.
The researchers randomly assigned the participants to usual care, 12 weeks of exercise with a personal trainer, 10 individual CBT sessions, or a combination of both exercise and CBT therapies. There were 34-36 participants in each group.
The researchers found improvements in depressive symptoms (P less than .05); negative automatic thoughts (P less than .03), and diabetes distress (P less than .01) and physical quality of life (P less than .03 for all except P greater than 0.1 for CBT) for all three intervention groups compared with usual care. Diabetes-specific quality of life improved in the exercise and combination groups only (P less than .01).
The researchers calculated odds ratios of full or partial remission as 12.4 (CBT) and 5.8 (exercise) compared to usual care (P less than .03), controlling for changes in antidepressant drugs. However, the odds ratio for combination therapy was 2.3 and not deemed statistically significant (P = .218).
The researchers also examined results in subjects with a baseline hemoglobin A1c of 7% or higher and found evidence linking the exercise therapy to clinically meaningful 0.7% improvements in HbA1c (P less than .04).
It’s also not clear whether the interventions will hold up over the long term.
The National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Diseases funded the study. Dr. De Groot reported no relevant disclosures.
SAN DIEGO – The odds of full remission from clinically diagnosed major depression greatly improved in patients with type 2 diabetes who took part in 12-week supervised exercise and cognitive behavioral therapy (CBT). By the end of the study, 96% of the CBT participants no longer met diagnostic criteria for major depression, compared with just 65% of those on usual care, judging from the findings of a new study.
Another approach – a combination treatment of both exercise and CBT therapies – did not show a statistically significant effect on full remission rates but showed improvement in some other areas.
Dr. De Groot and her colleagues recruited 140 adults – mean age 57 years, 77% female, 71% white, 52% married – who had a diagnosis of both type 2 diabetes and diagnosed clinical depression. They came from three states and had various levels of income and educational background.
The researchers randomly assigned the participants to usual care, 12 weeks of exercise with a personal trainer, 10 individual CBT sessions, or a combination of both exercise and CBT therapies. There were 34-36 participants in each group.
The researchers found improvements in depressive symptoms (P less than .05); negative automatic thoughts (P less than .03), and diabetes distress (P less than .01) and physical quality of life (P less than .03 for all except P greater than 0.1 for CBT) for all three intervention groups compared with usual care. Diabetes-specific quality of life improved in the exercise and combination groups only (P less than .01).
The researchers calculated odds ratios of full or partial remission as 12.4 (CBT) and 5.8 (exercise) compared to usual care (P less than .03), controlling for changes in antidepressant drugs. However, the odds ratio for combination therapy was 2.3 and not deemed statistically significant (P = .218).
The researchers also examined results in subjects with a baseline hemoglobin A1c of 7% or higher and found evidence linking the exercise therapy to clinically meaningful 0.7% improvements in HbA1c (P less than .04).
It’s also not clear whether the interventions will hold up over the long term.
The National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Diseases funded the study. Dr. De Groot reported no relevant disclosures.
SAN DIEGO – The odds of full remission from clinically diagnosed major depression greatly improved in patients with type 2 diabetes who took part in 12-week supervised exercise and cognitive behavioral therapy (CBT). By the end of the study, 96% of the CBT participants no longer met diagnostic criteria for major depression, compared with just 65% of those on usual care, judging from the findings of a new study.
Another approach – a combination treatment of both exercise and CBT therapies – did not show a statistically significant effect on full remission rates but showed improvement in some other areas.
Dr. De Groot and her colleagues recruited 140 adults – mean age 57 years, 77% female, 71% white, 52% married – who had a diagnosis of both type 2 diabetes and diagnosed clinical depression. They came from three states and had various levels of income and educational background.
The researchers randomly assigned the participants to usual care, 12 weeks of exercise with a personal trainer, 10 individual CBT sessions, or a combination of both exercise and CBT therapies. There were 34-36 participants in each group.
The researchers found improvements in depressive symptoms (P less than .05); negative automatic thoughts (P less than .03), and diabetes distress (P less than .01) and physical quality of life (P less than .03 for all except P greater than 0.1 for CBT) for all three intervention groups compared with usual care. Diabetes-specific quality of life improved in the exercise and combination groups only (P less than .01).
The researchers calculated odds ratios of full or partial remission as 12.4 (CBT) and 5.8 (exercise) compared to usual care (P less than .03), controlling for changes in antidepressant drugs. However, the odds ratio for combination therapy was 2.3 and not deemed statistically significant (P = .218).
The researchers also examined results in subjects with a baseline hemoglobin A1c of 7% or higher and found evidence linking the exercise therapy to clinically meaningful 0.7% improvements in HbA1c (P less than .04).
It’s also not clear whether the interventions will hold up over the long term.
The National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Diseases funded the study. Dr. De Groot reported no relevant disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Supervised exercise and cognitive behavioral therapies are linked to higher rates of recovery from major depression at 12 weeks in patients with type 2 diabetes.
Major finding: Full or partial remission was more likely in CBT and exercise groups compared with usual care after researchers controlled for changes in antidepressant drugs.
Data source: Prospective study of 140 adults with type 2 diabetes randomly assigned to 12 weeks of exercise with a physical trainer, 10 individual CBT sessions, a combination of the two therapies, or usual care.
Disclosures: The National Institutes of Health–National Institute of Diabetes and Digestive and Kidney Diseases funded the study.
Meta-analysis shows correlation between diabetes and erectile dysfunction
WASHINGTON – More than half of men with type 1 or type 2 diabetes develop erectile dysfunction, making them more than three times as likely to develop ED, compared with healthy men, according to a systematic review of diabetes studies.
Data on the exact prevalence of erectile dysfunction in this population has been lacking until now. More precise figures are available from a meta-analysis of 145 studies taken from international diabetes databases.
In terms of risk, men with diabetes were 3.62 (95% CI, 2.53-5.16; P less than .0001) times more likely to develop ED, compared with healthy controls, according to investigators (Diabet Med. 2017 Jul 18. doi: 10.1111/dme.13403).
“Regarding sexual activity and the psychological impact of erectile dysfunction in men with diabetes mellitus, significant and positive associations have been found between depressive symptoms and erectile dysfunction,” said Youssef Kouidrat, MD, PhD, of the department of psychosis studies, Institute of Psychiatry, King’s College London, and his fellow researchers. “Therefore, early detection of erectile dysfunction is essential to improve the psychological health and men’s quality of life.”
Given ED’s serious effects on patients’ physical and emotional well being, it is essential for physicians to have a better understanding of the root causes of the condition in order to help patients as soon as possible, wrote the investigators.
The studies included in the meta-analysis represented a population of 88.755 men with an average age of 56 years, with dates of the studies ranging from the inception of the databases they were taken from up until November 2016.
A majority of the studies included were conducted in Asia (61), followed by Europe (48), North America (17), Africa (15), and Oceania, South America, and multiple continents (4 in total).
South America reported the highest prevalence of ED (74.6%), while the lowest prevalence reported was among studies in North America (34.5%).
Patients who were assessed using the Sexual Health Inventory for Men (SHIM) score reported a higher ED prevalence (82.2%), as did men above the age of 60 years old (62.2%).
With ED correlated to cardiovascular health and mortality, investigators advise physicians to keep testing in mind when assessing patients’ cardiovascular risk.
This study was limited by incomplete data from studies included, which made it difficult to determine prevalence by certain categories.
Other limitations included the lack of separation between type 1 and type 2 diabetes among many of the studies analyzed, as well as a lack of information from the studies analyzed on other risk factors concerning diabetes-related erectile dysfunction.
Investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
WASHINGTON – More than half of men with type 1 or type 2 diabetes develop erectile dysfunction, making them more than three times as likely to develop ED, compared with healthy men, according to a systematic review of diabetes studies.
Data on the exact prevalence of erectile dysfunction in this population has been lacking until now. More precise figures are available from a meta-analysis of 145 studies taken from international diabetes databases.
In terms of risk, men with diabetes were 3.62 (95% CI, 2.53-5.16; P less than .0001) times more likely to develop ED, compared with healthy controls, according to investigators (Diabet Med. 2017 Jul 18. doi: 10.1111/dme.13403).
“Regarding sexual activity and the psychological impact of erectile dysfunction in men with diabetes mellitus, significant and positive associations have been found between depressive symptoms and erectile dysfunction,” said Youssef Kouidrat, MD, PhD, of the department of psychosis studies, Institute of Psychiatry, King’s College London, and his fellow researchers. “Therefore, early detection of erectile dysfunction is essential to improve the psychological health and men’s quality of life.”
Given ED’s serious effects on patients’ physical and emotional well being, it is essential for physicians to have a better understanding of the root causes of the condition in order to help patients as soon as possible, wrote the investigators.
The studies included in the meta-analysis represented a population of 88.755 men with an average age of 56 years, with dates of the studies ranging from the inception of the databases they were taken from up until November 2016.
A majority of the studies included were conducted in Asia (61), followed by Europe (48), North America (17), Africa (15), and Oceania, South America, and multiple continents (4 in total).
South America reported the highest prevalence of ED (74.6%), while the lowest prevalence reported was among studies in North America (34.5%).
Patients who were assessed using the Sexual Health Inventory for Men (SHIM) score reported a higher ED prevalence (82.2%), as did men above the age of 60 years old (62.2%).
With ED correlated to cardiovascular health and mortality, investigators advise physicians to keep testing in mind when assessing patients’ cardiovascular risk.
This study was limited by incomplete data from studies included, which made it difficult to determine prevalence by certain categories.
Other limitations included the lack of separation between type 1 and type 2 diabetes among many of the studies analyzed, as well as a lack of information from the studies analyzed on other risk factors concerning diabetes-related erectile dysfunction.
Investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
WASHINGTON – More than half of men with type 1 or type 2 diabetes develop erectile dysfunction, making them more than three times as likely to develop ED, compared with healthy men, according to a systematic review of diabetes studies.
Data on the exact prevalence of erectile dysfunction in this population has been lacking until now. More precise figures are available from a meta-analysis of 145 studies taken from international diabetes databases.
In terms of risk, men with diabetes were 3.62 (95% CI, 2.53-5.16; P less than .0001) times more likely to develop ED, compared with healthy controls, according to investigators (Diabet Med. 2017 Jul 18. doi: 10.1111/dme.13403).
“Regarding sexual activity and the psychological impact of erectile dysfunction in men with diabetes mellitus, significant and positive associations have been found between depressive symptoms and erectile dysfunction,” said Youssef Kouidrat, MD, PhD, of the department of psychosis studies, Institute of Psychiatry, King’s College London, and his fellow researchers. “Therefore, early detection of erectile dysfunction is essential to improve the psychological health and men’s quality of life.”
Given ED’s serious effects on patients’ physical and emotional well being, it is essential for physicians to have a better understanding of the root causes of the condition in order to help patients as soon as possible, wrote the investigators.
The studies included in the meta-analysis represented a population of 88.755 men with an average age of 56 years, with dates of the studies ranging from the inception of the databases they were taken from up until November 2016.
A majority of the studies included were conducted in Asia (61), followed by Europe (48), North America (17), Africa (15), and Oceania, South America, and multiple continents (4 in total).
South America reported the highest prevalence of ED (74.6%), while the lowest prevalence reported was among studies in North America (34.5%).
Patients who were assessed using the Sexual Health Inventory for Men (SHIM) score reported a higher ED prevalence (82.2%), as did men above the age of 60 years old (62.2%).
With ED correlated to cardiovascular health and mortality, investigators advise physicians to keep testing in mind when assessing patients’ cardiovascular risk.
This study was limited by incomplete data from studies included, which made it difficult to determine prevalence by certain categories.
Other limitations included the lack of separation between type 1 and type 2 diabetes among many of the studies analyzed, as well as a lack of information from the studies analyzed on other risk factors concerning diabetes-related erectile dysfunction.
Investigators reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
FROM DIABETIC MEDICINE
Key clinical point:
Major finding: Men with diabetes showed an odds ratio of 3.62 (95% CI, 2.53-5.16; P less than .0001) of developing erectile dysfunction, compared with healthy controls.
Data source: An analysis of 145 studies representing 88,577 men from international databases spanning from creation of the database to November 2016.
Disclosures: Investigators report no relevant financial disclosures.
Life-long risk reduction could cut late-life dementia by up to 35%
LONDON – As many as a third of dementia cases could be prevented worldwide if society could adopt a life course–focused approach of supporting brain health with mostly common-sense measures.
Improving childhood education, controlling blood pressure and cholesterol, keeping socially and intellectually active, exercising, and ceasing tobacco use are among the recommendations to reduce the incidence of dementia made by a worldwide panel of expert clinicians and researchers.
The findings are part of an exhaustive report commission by The Lancet and released at the Alzheimer’s Association International Conference. The report has concluded that nine lifestyle factors, most of which are modifiable from childhood though middle age, account for 35% of dementia that strikes elderly persons, Gillian Livingston, MD, said at the conference. The report was simultaneously published.
Being homozygous for the ApoE4 allele confers about an immutable 7% increased chance of developing Alzheimer’s disease. But two of the other factors identified in the Lancet report, low education in childhood and hearing loss at middle age, confer even higher individual risks of 8% and 9%. And when combined with other mid-life risks of hypertension and obesity, and late-life risks imposed by smoking, depression, inactivity, social isolation, and diabetes, these factors not only dwarf the potential impact of ApoE4, but offer a lifelong chance to forestall or even prevent dementia.
The findings, all gathered from an exhaustive literature review, bolster the notion that public health interventions could block the tsunami of dementia cases that threaten to overwhelm the world’s health care resources by 2050, Dr. Livingston said.
“While public health interventions won’t prevent or cure all potentially modifiable dementia, intervention for cardiovascular risk factors, mental health, and hearing may push back the onset in many people for years. Even if only some of this promise is realized, it could make a huge difference. We have, in fact, already seen that in some populations dementia is being delayed for years. If we could achieve an overall delay of onset by 5 years, we could cut the global prevalence by half.”
The Lancet commissioned the panel of global dementia experts to review the extant literature and construct a lifespan-focused risk model. In addition to examining risk and making recommendations to ameliorate it, the panel issued recommendations about treating cognition and psychiatric and behavioral problems; protecting dementia patients in both home and long-term care settings; supporting the family members who provide most of the care for dementia patients; and helping patients and families navigate end-of-life situations.
The literature review identified nine modifiable risk factors that account for 35% of dementia risk worldwide:
• Education in youth. Less education in childhood, which the commission identified as a lack of secondary schooling, increased the risk of dementia by 8%. Improving education at this age would remove this portion of the population attributable risk factor (PAF), Dr. Livingston said.
This finding represents an enormous opportunity for improvement: The decline in dementia incidence seen in some populations occurs mostly among the better-educated. “The mechanism of prevention here appears to be increasing brain resilience,” said Lon Schneider, MD, a member of the Lancet panel.
Tackling poor childhood education is a daunting task and requires commitment from both public and private sectors, the report noted, but its importance cannot be overstated.
• Hearing loss at mid-life. This emerged as the most powerful risk factor in the analysis, conferring an independent 9% increased risk of dementia, “a relatively new idea that has not been included in previous calculations of population attributable factors,” the commission wrote. The mechanism of increased risk isn’t clear, but may be a combination of neurodegeneration and social isolation imposed by being shut out of easy communication. It’s unclear whether hearing aids can mitigate the effects of hearing loss on dementia risk, the report noted.
• Hypertension, obesity, and diabetes. Respectively, these accounted for 2%, 1%, and 1% of the PAF. Obesity is linked to prediabetes and diabetes, which are in turn linked to insulin resistance, decreased brain amyloid clearance, high blood glucose, and inflammation – all risks for Alzheimer’s disease.
The report recommends that anyone aged 45-65 years who has hypertension should be actively treated for the disorder.
• Smoking. At 5%, smoking posted the third-highest PAF. The risk is probably mediated through smoking’s detrimental effects on cardiovascular health. But the report noted that tobacco smoke contains known neurotoxins as well.
Preventing the smoking/dementia connection is simple, Dr. Livingston said. “Simply stop smoking. If you’re smoking, just stop. Please.”
• Depression. Depression in late life imposed a 4% PAF. The evidence reviewed suggested that depression is not, in fact, linked to dementia when experienced at mid-life. But late-life depression may be a prodromal symptom of dementia and biologically linked to increased stress hormones, decreased neuronal growth factors, and decreased hippocampal volume. The commission noted animal models that suggest some antidepressants, including citalopram, decrease amyloid progression.
• Social isolation. Associated with a 2% PAF, social isolation may, like depression, be a prodromal symptom. But, the report said, there is growing evidence that it actually is an independent risk factor as well. It has been shown to also increase the risk of hypertension, cardiovascular disease, and depression, all dementia risk factors in their own right.
Longitudinal studies suggest that social activities and personal connections may prevent or delay dementia, although top-grade evidence is lacking. Still, maintaining a rich social network not only reduces the chance of isolation, but helps prevent depression as well.
• Physical inactivity. Sedentary lifestyle carried a 3% PAF for dementia. Older adults who maintain physical activity are more likely to remain cognitively intact. Physical exercise improves mood, reduces the risk of falls, and maintains normal physical function. The report cited a meta-analysis of 16 studies and almost 164,000 participants without dementia; it concluded that those in the highest level of activity had a 25% decreased risk of all-cause dementia and a 45% decreased risk of Alzheimer’s disease.
The strongest evidence for exercise’s benefit on cognition may be from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Patients with a high risk of dementia who completed the lifestyle modification program of healthy diet cognitive training, vascular risk factor management, and aerobic exercise showed a slowing of cognitive decline and improvements in executive function and processing speed.
Becoming aware of the risk factors is one thing, the report said. Doing something about them is another. In general, the first step is to “be ambitious” about prevention.
“Prevention is always better than treatment,” Dr. Livingston said in an interview. “We need to start thinking about dementia not as something that simply happens outside our control, but as something that we can have an effect on.”
The Lancet commissioned the report. Dr. Livingston did not have any financial declarations but many of the other authors reported multiple relationships with pharmaceutical companies.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
LONDON – As many as a third of dementia cases could be prevented worldwide if society could adopt a life course–focused approach of supporting brain health with mostly common-sense measures.
Improving childhood education, controlling blood pressure and cholesterol, keeping socially and intellectually active, exercising, and ceasing tobacco use are among the recommendations to reduce the incidence of dementia made by a worldwide panel of expert clinicians and researchers.
The findings are part of an exhaustive report commission by The Lancet and released at the Alzheimer’s Association International Conference. The report has concluded that nine lifestyle factors, most of which are modifiable from childhood though middle age, account for 35% of dementia that strikes elderly persons, Gillian Livingston, MD, said at the conference. The report was simultaneously published.
Being homozygous for the ApoE4 allele confers about an immutable 7% increased chance of developing Alzheimer’s disease. But two of the other factors identified in the Lancet report, low education in childhood and hearing loss at middle age, confer even higher individual risks of 8% and 9%. And when combined with other mid-life risks of hypertension and obesity, and late-life risks imposed by smoking, depression, inactivity, social isolation, and diabetes, these factors not only dwarf the potential impact of ApoE4, but offer a lifelong chance to forestall or even prevent dementia.
The findings, all gathered from an exhaustive literature review, bolster the notion that public health interventions could block the tsunami of dementia cases that threaten to overwhelm the world’s health care resources by 2050, Dr. Livingston said.
“While public health interventions won’t prevent or cure all potentially modifiable dementia, intervention for cardiovascular risk factors, mental health, and hearing may push back the onset in many people for years. Even if only some of this promise is realized, it could make a huge difference. We have, in fact, already seen that in some populations dementia is being delayed for years. If we could achieve an overall delay of onset by 5 years, we could cut the global prevalence by half.”
The Lancet commissioned the panel of global dementia experts to review the extant literature and construct a lifespan-focused risk model. In addition to examining risk and making recommendations to ameliorate it, the panel issued recommendations about treating cognition and psychiatric and behavioral problems; protecting dementia patients in both home and long-term care settings; supporting the family members who provide most of the care for dementia patients; and helping patients and families navigate end-of-life situations.
The literature review identified nine modifiable risk factors that account for 35% of dementia risk worldwide:
• Education in youth. Less education in childhood, which the commission identified as a lack of secondary schooling, increased the risk of dementia by 8%. Improving education at this age would remove this portion of the population attributable risk factor (PAF), Dr. Livingston said.
This finding represents an enormous opportunity for improvement: The decline in dementia incidence seen in some populations occurs mostly among the better-educated. “The mechanism of prevention here appears to be increasing brain resilience,” said Lon Schneider, MD, a member of the Lancet panel.
Tackling poor childhood education is a daunting task and requires commitment from both public and private sectors, the report noted, but its importance cannot be overstated.
• Hearing loss at mid-life. This emerged as the most powerful risk factor in the analysis, conferring an independent 9% increased risk of dementia, “a relatively new idea that has not been included in previous calculations of population attributable factors,” the commission wrote. The mechanism of increased risk isn’t clear, but may be a combination of neurodegeneration and social isolation imposed by being shut out of easy communication. It’s unclear whether hearing aids can mitigate the effects of hearing loss on dementia risk, the report noted.
• Hypertension, obesity, and diabetes. Respectively, these accounted for 2%, 1%, and 1% of the PAF. Obesity is linked to prediabetes and diabetes, which are in turn linked to insulin resistance, decreased brain amyloid clearance, high blood glucose, and inflammation – all risks for Alzheimer’s disease.
The report recommends that anyone aged 45-65 years who has hypertension should be actively treated for the disorder.
• Smoking. At 5%, smoking posted the third-highest PAF. The risk is probably mediated through smoking’s detrimental effects on cardiovascular health. But the report noted that tobacco smoke contains known neurotoxins as well.
Preventing the smoking/dementia connection is simple, Dr. Livingston said. “Simply stop smoking. If you’re smoking, just stop. Please.”
• Depression. Depression in late life imposed a 4% PAF. The evidence reviewed suggested that depression is not, in fact, linked to dementia when experienced at mid-life. But late-life depression may be a prodromal symptom of dementia and biologically linked to increased stress hormones, decreased neuronal growth factors, and decreased hippocampal volume. The commission noted animal models that suggest some antidepressants, including citalopram, decrease amyloid progression.
• Social isolation. Associated with a 2% PAF, social isolation may, like depression, be a prodromal symptom. But, the report said, there is growing evidence that it actually is an independent risk factor as well. It has been shown to also increase the risk of hypertension, cardiovascular disease, and depression, all dementia risk factors in their own right.
Longitudinal studies suggest that social activities and personal connections may prevent or delay dementia, although top-grade evidence is lacking. Still, maintaining a rich social network not only reduces the chance of isolation, but helps prevent depression as well.
• Physical inactivity. Sedentary lifestyle carried a 3% PAF for dementia. Older adults who maintain physical activity are more likely to remain cognitively intact. Physical exercise improves mood, reduces the risk of falls, and maintains normal physical function. The report cited a meta-analysis of 16 studies and almost 164,000 participants without dementia; it concluded that those in the highest level of activity had a 25% decreased risk of all-cause dementia and a 45% decreased risk of Alzheimer’s disease.
The strongest evidence for exercise’s benefit on cognition may be from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Patients with a high risk of dementia who completed the lifestyle modification program of healthy diet cognitive training, vascular risk factor management, and aerobic exercise showed a slowing of cognitive decline and improvements in executive function and processing speed.
Becoming aware of the risk factors is one thing, the report said. Doing something about them is another. In general, the first step is to “be ambitious” about prevention.
“Prevention is always better than treatment,” Dr. Livingston said in an interview. “We need to start thinking about dementia not as something that simply happens outside our control, but as something that we can have an effect on.”
The Lancet commissioned the report. Dr. Livingston did not have any financial declarations but many of the other authors reported multiple relationships with pharmaceutical companies.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
LONDON – As many as a third of dementia cases could be prevented worldwide if society could adopt a life course–focused approach of supporting brain health with mostly common-sense measures.
Improving childhood education, controlling blood pressure and cholesterol, keeping socially and intellectually active, exercising, and ceasing tobacco use are among the recommendations to reduce the incidence of dementia made by a worldwide panel of expert clinicians and researchers.
The findings are part of an exhaustive report commission by The Lancet and released at the Alzheimer’s Association International Conference. The report has concluded that nine lifestyle factors, most of which are modifiable from childhood though middle age, account for 35% of dementia that strikes elderly persons, Gillian Livingston, MD, said at the conference. The report was simultaneously published.
Being homozygous for the ApoE4 allele confers about an immutable 7% increased chance of developing Alzheimer’s disease. But two of the other factors identified in the Lancet report, low education in childhood and hearing loss at middle age, confer even higher individual risks of 8% and 9%. And when combined with other mid-life risks of hypertension and obesity, and late-life risks imposed by smoking, depression, inactivity, social isolation, and diabetes, these factors not only dwarf the potential impact of ApoE4, but offer a lifelong chance to forestall or even prevent dementia.
The findings, all gathered from an exhaustive literature review, bolster the notion that public health interventions could block the tsunami of dementia cases that threaten to overwhelm the world’s health care resources by 2050, Dr. Livingston said.
“While public health interventions won’t prevent or cure all potentially modifiable dementia, intervention for cardiovascular risk factors, mental health, and hearing may push back the onset in many people for years. Even if only some of this promise is realized, it could make a huge difference. We have, in fact, already seen that in some populations dementia is being delayed for years. If we could achieve an overall delay of onset by 5 years, we could cut the global prevalence by half.”
The Lancet commissioned the panel of global dementia experts to review the extant literature and construct a lifespan-focused risk model. In addition to examining risk and making recommendations to ameliorate it, the panel issued recommendations about treating cognition and psychiatric and behavioral problems; protecting dementia patients in both home and long-term care settings; supporting the family members who provide most of the care for dementia patients; and helping patients and families navigate end-of-life situations.
The literature review identified nine modifiable risk factors that account for 35% of dementia risk worldwide:
• Education in youth. Less education in childhood, which the commission identified as a lack of secondary schooling, increased the risk of dementia by 8%. Improving education at this age would remove this portion of the population attributable risk factor (PAF), Dr. Livingston said.
This finding represents an enormous opportunity for improvement: The decline in dementia incidence seen in some populations occurs mostly among the better-educated. “The mechanism of prevention here appears to be increasing brain resilience,” said Lon Schneider, MD, a member of the Lancet panel.
Tackling poor childhood education is a daunting task and requires commitment from both public and private sectors, the report noted, but its importance cannot be overstated.
• Hearing loss at mid-life. This emerged as the most powerful risk factor in the analysis, conferring an independent 9% increased risk of dementia, “a relatively new idea that has not been included in previous calculations of population attributable factors,” the commission wrote. The mechanism of increased risk isn’t clear, but may be a combination of neurodegeneration and social isolation imposed by being shut out of easy communication. It’s unclear whether hearing aids can mitigate the effects of hearing loss on dementia risk, the report noted.
• Hypertension, obesity, and diabetes. Respectively, these accounted for 2%, 1%, and 1% of the PAF. Obesity is linked to prediabetes and diabetes, which are in turn linked to insulin resistance, decreased brain amyloid clearance, high blood glucose, and inflammation – all risks for Alzheimer’s disease.
The report recommends that anyone aged 45-65 years who has hypertension should be actively treated for the disorder.
• Smoking. At 5%, smoking posted the third-highest PAF. The risk is probably mediated through smoking’s detrimental effects on cardiovascular health. But the report noted that tobacco smoke contains known neurotoxins as well.
Preventing the smoking/dementia connection is simple, Dr. Livingston said. “Simply stop smoking. If you’re smoking, just stop. Please.”
• Depression. Depression in late life imposed a 4% PAF. The evidence reviewed suggested that depression is not, in fact, linked to dementia when experienced at mid-life. But late-life depression may be a prodromal symptom of dementia and biologically linked to increased stress hormones, decreased neuronal growth factors, and decreased hippocampal volume. The commission noted animal models that suggest some antidepressants, including citalopram, decrease amyloid progression.
• Social isolation. Associated with a 2% PAF, social isolation may, like depression, be a prodromal symptom. But, the report said, there is growing evidence that it actually is an independent risk factor as well. It has been shown to also increase the risk of hypertension, cardiovascular disease, and depression, all dementia risk factors in their own right.
Longitudinal studies suggest that social activities and personal connections may prevent or delay dementia, although top-grade evidence is lacking. Still, maintaining a rich social network not only reduces the chance of isolation, but helps prevent depression as well.
• Physical inactivity. Sedentary lifestyle carried a 3% PAF for dementia. Older adults who maintain physical activity are more likely to remain cognitively intact. Physical exercise improves mood, reduces the risk of falls, and maintains normal physical function. The report cited a meta-analysis of 16 studies and almost 164,000 participants without dementia; it concluded that those in the highest level of activity had a 25% decreased risk of all-cause dementia and a 45% decreased risk of Alzheimer’s disease.
The strongest evidence for exercise’s benefit on cognition may be from the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER). Patients with a high risk of dementia who completed the lifestyle modification program of healthy diet cognitive training, vascular risk factor management, and aerobic exercise showed a slowing of cognitive decline and improvements in executive function and processing speed.
Becoming aware of the risk factors is one thing, the report said. Doing something about them is another. In general, the first step is to “be ambitious” about prevention.
“Prevention is always better than treatment,” Dr. Livingston said in an interview. “We need to start thinking about dementia not as something that simply happens outside our control, but as something that we can have an effect on.”
The Lancet commissioned the report. Dr. Livingston did not have any financial declarations but many of the other authors reported multiple relationships with pharmaceutical companies.
msullivan@frontlinemedcom.com
On Twitter @alz_gal
AT AAIC 2017
Over 45% of American adults have type 2 diabetes mellitus or prediabetes
More than 114 million American adults have type 2 diabetes mellitus or prediabetes, according to estimates from the Centers for Disease Control and Prevention.
As of 2015, the combined prevalence of diabetes and prediabetes was 45.4% among adults in the United States: 11.5% (30.3 million) have diabetes and 33.9% have prediabetes, representing 84.1 million people who could develop type 2 diabetes within 5 years, the CDC said in the National Diabetes Statistics Report, 2017.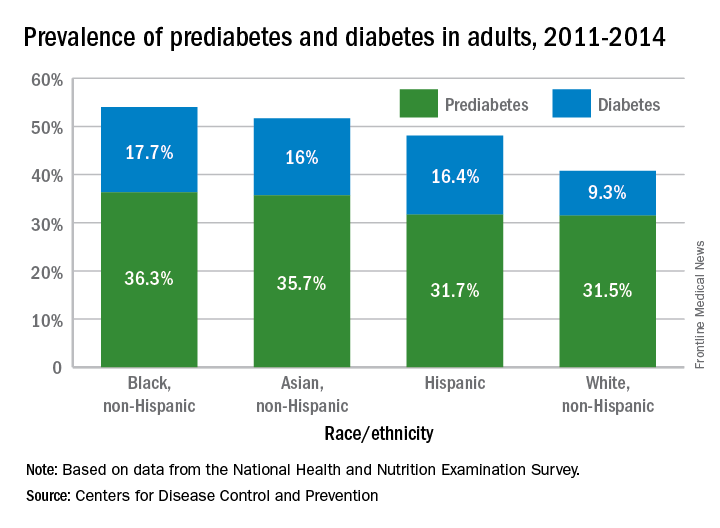
Lack of knowledge about having the disease was common: Almost a quarter (23.8%) of adults with diabetes didn’t know they had it, and the number jumped to 88% for those with prediabetes, based on data from the National Health and Nutrition Examination Survey, which included a blood test for fasting plasma glucose or hemoglobin A1c.
“More than a third of U.S. adults have prediabetes, and the majority don’t know it. Now, more than ever, we must step up our efforts to reduce the burden of this serious disease,” CDC Director Brenda Fitzgerald, MD, said in a statement.
“Diabetes and prediabetes remain serious threats for more than one-third of Americans – the statistics are staggering,” William T. Cefalu, MD, chief scientific, medical, and mission officer of the American Diabetes Association, said in a written statement.
“We must continue to innovate in scientific research and to translate findings to the clinical level to decrease the prevalence of diabetes. These data clearly confirm it is critical for us to continue to provide the education and support needed to improve health outcomes and decrease the daily burden of diabetes. We must reduce the incidence of diabetes and its enormous costs, including both the financial costs and the human toll of lost quality of life,” he said.
“Diabetes and prediabetes remain serious threats for more than one-third of Americans – the statistics are staggering,” William T. Cefalu, MD, chief scientific, medical, and mission officer of the American Diabetes Association, said in a written statement.
“We must continue to innovate in scientific research and to translate findings to the clinical level to decrease the prevalence of diabetes. These data clearly confirm it is critical for us to continue to provide the education and support needed to improve health outcomes and decrease the daily burden of diabetes. We must reduce the incidence of diabetes and its enormous costs, including both the financial costs and the human toll of lost quality of life,” he said.
“Diabetes and prediabetes remain serious threats for more than one-third of Americans – the statistics are staggering,” William T. Cefalu, MD, chief scientific, medical, and mission officer of the American Diabetes Association, said in a written statement.
“We must continue to innovate in scientific research and to translate findings to the clinical level to decrease the prevalence of diabetes. These data clearly confirm it is critical for us to continue to provide the education and support needed to improve health outcomes and decrease the daily burden of diabetes. We must reduce the incidence of diabetes and its enormous costs, including both the financial costs and the human toll of lost quality of life,” he said.
More than 114 million American adults have type 2 diabetes mellitus or prediabetes, according to estimates from the Centers for Disease Control and Prevention.
As of 2015, the combined prevalence of diabetes and prediabetes was 45.4% among adults in the United States: 11.5% (30.3 million) have diabetes and 33.9% have prediabetes, representing 84.1 million people who could develop type 2 diabetes within 5 years, the CDC said in the National Diabetes Statistics Report, 2017.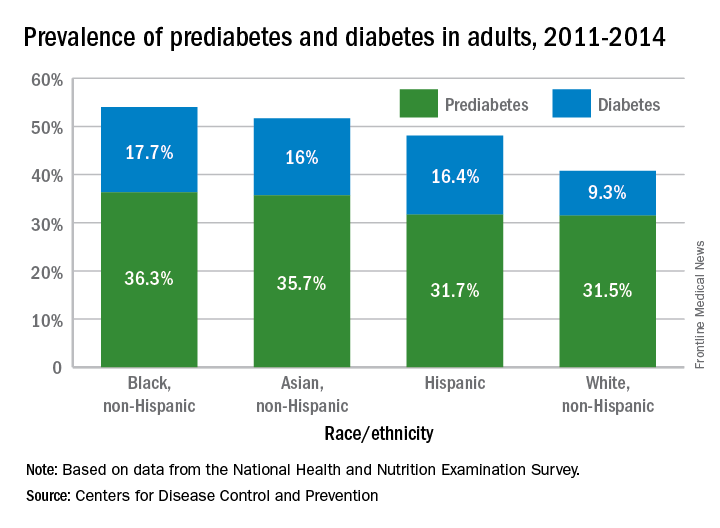
Lack of knowledge about having the disease was common: Almost a quarter (23.8%) of adults with diabetes didn’t know they had it, and the number jumped to 88% for those with prediabetes, based on data from the National Health and Nutrition Examination Survey, which included a blood test for fasting plasma glucose or hemoglobin A1c.
“More than a third of U.S. adults have prediabetes, and the majority don’t know it. Now, more than ever, we must step up our efforts to reduce the burden of this serious disease,” CDC Director Brenda Fitzgerald, MD, said in a statement.
More than 114 million American adults have type 2 diabetes mellitus or prediabetes, according to estimates from the Centers for Disease Control and Prevention.
As of 2015, the combined prevalence of diabetes and prediabetes was 45.4% among adults in the United States: 11.5% (30.3 million) have diabetes and 33.9% have prediabetes, representing 84.1 million people who could develop type 2 diabetes within 5 years, the CDC said in the National Diabetes Statistics Report, 2017.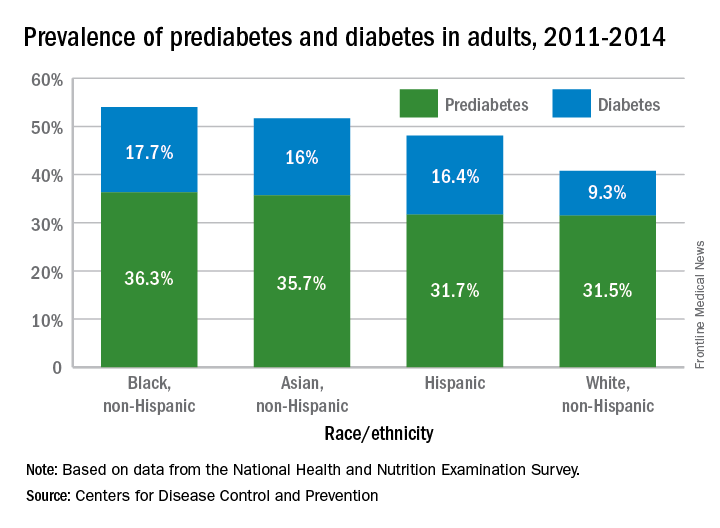
Lack of knowledge about having the disease was common: Almost a quarter (23.8%) of adults with diabetes didn’t know they had it, and the number jumped to 88% for those with prediabetes, based on data from the National Health and Nutrition Examination Survey, which included a blood test for fasting plasma glucose or hemoglobin A1c.
“More than a third of U.S. adults have prediabetes, and the majority don’t know it. Now, more than ever, we must step up our efforts to reduce the burden of this serious disease,” CDC Director Brenda Fitzgerald, MD, said in a statement.
Even a few middle age pounds are dangerous
Gaining just 5-22 pounds in the first half of adulthood significantly increases the risk of chronic disease in the second half, especially the likelihood of type 2 diabetes, gallstones, and hypertension, according to investigators.
They looked at how much 92,837 women in the Nurses’ Health Study remembered weighing when they were 18 years old, and how much 25,303 men in the Health Professionals Follow-Up Study recalled weighing at age 21. The Harvard team matched those weights to how much their subjects actually weighed at age 55, and then followed the women out to a median of 73 years and the men out to a median of 69 years to see how their weight changes in early adulthood affected their health later on (JAMA. 2017;318[3]:255-269. doi: 10.1001/jama.2017.7092).
The investigators found that even a moderate gain of up to 10 kg increased the risk of major chronic diseases and early death. “Maintaining a healthy weight throughout early and middle adulthood is associated with overall health ... These findings may help counsel patients regarding the risks of weight gain,” wrote the investigators, led by Yan Zheng, MD, PhD, of the department of nutrition, Harvard T. H. Chan School of Public Health, Boston.
It’s not news that packing on a few pounds with age isn’t healthy, but quantifying the effects of early adulthood weight gain is novel. “The advantage of focusing on weight gain throughout” the first half of adult life “is that it primarily reflects the accumulation of excess adiposity from early to middle adulthood, which is often ignored by individuals and their physicians because the consequences of modest weight accumulation may not yet be apparent,” the investigators noted.
Specifically, they found that compared to participants who maintained a stable weight – no more than 2.5 kg either way – people who gained up to 10 kg had an increased incidence of not only type 2 diabetes, gallstones, and hypertension, but also cardiovascular disease, cataracts, severe osteoarthritis, and death, and added weight increased health risks in a dose-dependent manner. People who gained more than 10 kg from their high school years fared worse, even if they started out as obese.
The adjusted incidence per 100,000 person-years for type 2 diabetes rose from 110 cases to 207 cases per 100,000 person-years among women 55 years old who weighed up to 22 pounds more than they did in high school; it was similar for men, with a rise from 147 cases to 258 cases per 100,000 person-years. Weight gain up to 10 kg boosted the incidence of hypertension from 2,754 cases to 3,415 cases per 100,000 person-years for women and from 2,366 cases to 2,861 cases for men.
Results were similar for cardiovascular disease and obesity-related cancers, particularly breast cancer among women and colorectal and prostate cancer among men. Higher amounts of weight gain were also associated with a lower likelihood of healthy aging, a composite score of the absence of multiple chronic diseases, cognitive decline, and physical limitations.
However, the investigators noted that “considering that individuals tend to underreport their weight, it is possible that our findings might have exaggerated the true risks associated with the measured weight change from early to middle adulthood.”
Also, “participants were all health professionals and were mostly white ... the results might not be generalizable to all populations,” they said.
The National Institutes of Health and American Diabetes Association funded the work. The researchers reported no conflicts of interest.
The prevalence of obesity emphasizes that it will not be possible to provide effective treatment for all of those affected. Therefore, efforts to prevent and control this widespread disease must be renewed. Reducing and preventing obesity and excessive weight gain in young adults provides a new target, and one that could offer an effective transgenerational approach for prevention.
Broader venues for intervention efforts could include a supplemental nutrition plan for the Women, Infants, and Children program that provides nutritional counseling for pregnant women and women, infants, and children up to the age of 4 years. Sustained productivity and reduced absenteeism among employees with healthy weights might motivate employers with long-term work forces to invest in prevention efforts directed at families. Beyond clinical interventions, identification and implementation of environmental changes that effectively promote weight maintenance are essential for population-based efforts.
William Dietz, MD, PhD, is the director of the Redstone Global Center for Prevention and Wellness at The George Washington University in Washington, D.C. He is an adviser for Weight Watchers and RTI, and has grant support from Bridgespan. Dr. Dietz’s remarks came from an editorial accompanying the research report ( JAMA. 2017;318[3]:241-2 ).
The prevalence of obesity emphasizes that it will not be possible to provide effective treatment for all of those affected. Therefore, efforts to prevent and control this widespread disease must be renewed. Reducing and preventing obesity and excessive weight gain in young adults provides a new target, and one that could offer an effective transgenerational approach for prevention.
Broader venues for intervention efforts could include a supplemental nutrition plan for the Women, Infants, and Children program that provides nutritional counseling for pregnant women and women, infants, and children up to the age of 4 years. Sustained productivity and reduced absenteeism among employees with healthy weights might motivate employers with long-term work forces to invest in prevention efforts directed at families. Beyond clinical interventions, identification and implementation of environmental changes that effectively promote weight maintenance are essential for population-based efforts.
William Dietz, MD, PhD, is the director of the Redstone Global Center for Prevention and Wellness at The George Washington University in Washington, D.C. He is an adviser for Weight Watchers and RTI, and has grant support from Bridgespan. Dr. Dietz’s remarks came from an editorial accompanying the research report ( JAMA. 2017;318[3]:241-2 ).
The prevalence of obesity emphasizes that it will not be possible to provide effective treatment for all of those affected. Therefore, efforts to prevent and control this widespread disease must be renewed. Reducing and preventing obesity and excessive weight gain in young adults provides a new target, and one that could offer an effective transgenerational approach for prevention.
Broader venues for intervention efforts could include a supplemental nutrition plan for the Women, Infants, and Children program that provides nutritional counseling for pregnant women and women, infants, and children up to the age of 4 years. Sustained productivity and reduced absenteeism among employees with healthy weights might motivate employers with long-term work forces to invest in prevention efforts directed at families. Beyond clinical interventions, identification and implementation of environmental changes that effectively promote weight maintenance are essential for population-based efforts.
William Dietz, MD, PhD, is the director of the Redstone Global Center for Prevention and Wellness at The George Washington University in Washington, D.C. He is an adviser for Weight Watchers and RTI, and has grant support from Bridgespan. Dr. Dietz’s remarks came from an editorial accompanying the research report ( JAMA. 2017;318[3]:241-2 ).
Gaining just 5-22 pounds in the first half of adulthood significantly increases the risk of chronic disease in the second half, especially the likelihood of type 2 diabetes, gallstones, and hypertension, according to investigators.
They looked at how much 92,837 women in the Nurses’ Health Study remembered weighing when they were 18 years old, and how much 25,303 men in the Health Professionals Follow-Up Study recalled weighing at age 21. The Harvard team matched those weights to how much their subjects actually weighed at age 55, and then followed the women out to a median of 73 years and the men out to a median of 69 years to see how their weight changes in early adulthood affected their health later on (JAMA. 2017;318[3]:255-269. doi: 10.1001/jama.2017.7092).
The investigators found that even a moderate gain of up to 10 kg increased the risk of major chronic diseases and early death. “Maintaining a healthy weight throughout early and middle adulthood is associated with overall health ... These findings may help counsel patients regarding the risks of weight gain,” wrote the investigators, led by Yan Zheng, MD, PhD, of the department of nutrition, Harvard T. H. Chan School of Public Health, Boston.
It’s not news that packing on a few pounds with age isn’t healthy, but quantifying the effects of early adulthood weight gain is novel. “The advantage of focusing on weight gain throughout” the first half of adult life “is that it primarily reflects the accumulation of excess adiposity from early to middle adulthood, which is often ignored by individuals and their physicians because the consequences of modest weight accumulation may not yet be apparent,” the investigators noted.
Specifically, they found that compared to participants who maintained a stable weight – no more than 2.5 kg either way – people who gained up to 10 kg had an increased incidence of not only type 2 diabetes, gallstones, and hypertension, but also cardiovascular disease, cataracts, severe osteoarthritis, and death, and added weight increased health risks in a dose-dependent manner. People who gained more than 10 kg from their high school years fared worse, even if they started out as obese.
The adjusted incidence per 100,000 person-years for type 2 diabetes rose from 110 cases to 207 cases per 100,000 person-years among women 55 years old who weighed up to 22 pounds more than they did in high school; it was similar for men, with a rise from 147 cases to 258 cases per 100,000 person-years. Weight gain up to 10 kg boosted the incidence of hypertension from 2,754 cases to 3,415 cases per 100,000 person-years for women and from 2,366 cases to 2,861 cases for men.
Results were similar for cardiovascular disease and obesity-related cancers, particularly breast cancer among women and colorectal and prostate cancer among men. Higher amounts of weight gain were also associated with a lower likelihood of healthy aging, a composite score of the absence of multiple chronic diseases, cognitive decline, and physical limitations.
However, the investigators noted that “considering that individuals tend to underreport their weight, it is possible that our findings might have exaggerated the true risks associated with the measured weight change from early to middle adulthood.”
Also, “participants were all health professionals and were mostly white ... the results might not be generalizable to all populations,” they said.
The National Institutes of Health and American Diabetes Association funded the work. The researchers reported no conflicts of interest.
Gaining just 5-22 pounds in the first half of adulthood significantly increases the risk of chronic disease in the second half, especially the likelihood of type 2 diabetes, gallstones, and hypertension, according to investigators.
They looked at how much 92,837 women in the Nurses’ Health Study remembered weighing when they were 18 years old, and how much 25,303 men in the Health Professionals Follow-Up Study recalled weighing at age 21. The Harvard team matched those weights to how much their subjects actually weighed at age 55, and then followed the women out to a median of 73 years and the men out to a median of 69 years to see how their weight changes in early adulthood affected their health later on (JAMA. 2017;318[3]:255-269. doi: 10.1001/jama.2017.7092).
The investigators found that even a moderate gain of up to 10 kg increased the risk of major chronic diseases and early death. “Maintaining a healthy weight throughout early and middle adulthood is associated with overall health ... These findings may help counsel patients regarding the risks of weight gain,” wrote the investigators, led by Yan Zheng, MD, PhD, of the department of nutrition, Harvard T. H. Chan School of Public Health, Boston.
It’s not news that packing on a few pounds with age isn’t healthy, but quantifying the effects of early adulthood weight gain is novel. “The advantage of focusing on weight gain throughout” the first half of adult life “is that it primarily reflects the accumulation of excess adiposity from early to middle adulthood, which is often ignored by individuals and their physicians because the consequences of modest weight accumulation may not yet be apparent,” the investigators noted.
Specifically, they found that compared to participants who maintained a stable weight – no more than 2.5 kg either way – people who gained up to 10 kg had an increased incidence of not only type 2 diabetes, gallstones, and hypertension, but also cardiovascular disease, cataracts, severe osteoarthritis, and death, and added weight increased health risks in a dose-dependent manner. People who gained more than 10 kg from their high school years fared worse, even if they started out as obese.
The adjusted incidence per 100,000 person-years for type 2 diabetes rose from 110 cases to 207 cases per 100,000 person-years among women 55 years old who weighed up to 22 pounds more than they did in high school; it was similar for men, with a rise from 147 cases to 258 cases per 100,000 person-years. Weight gain up to 10 kg boosted the incidence of hypertension from 2,754 cases to 3,415 cases per 100,000 person-years for women and from 2,366 cases to 2,861 cases for men.
Results were similar for cardiovascular disease and obesity-related cancers, particularly breast cancer among women and colorectal and prostate cancer among men. Higher amounts of weight gain were also associated with a lower likelihood of healthy aging, a composite score of the absence of multiple chronic diseases, cognitive decline, and physical limitations.
However, the investigators noted that “considering that individuals tend to underreport their weight, it is possible that our findings might have exaggerated the true risks associated with the measured weight change from early to middle adulthood.”
Also, “participants were all health professionals and were mostly white ... the results might not be generalizable to all populations,” they said.
The National Institutes of Health and American Diabetes Association funded the work. The researchers reported no conflicts of interest.
FROM JAMA
Key clinical point:
Major finding: The adjusted incidence per 100,000 person-years for type 2 diabetes rose from 110 cases to 207 cases per 100,000 person-years among women 55 years old who weighed up to 22 pounds more than they did in high school; it was similar for men, with a rise from 147 cases to 258 cases per 100,000 person-years.
Data source: Review of data on 92,837 women in the Nurses’ Health Study and 25,303 men in the Health Professionals Follow-Up Study.
Disclosures: The National Institutes of Health and American Diabetes Association funded the work. The researchers reported no conflicts of interest.
Statins linked to fewer deaths, slightly higher HbA1c in T2DM
SAN DIEGO – Findings from a study of 12,725 new insulin users with type 2 diabetes mellitus (T2DM) show that those who did not take statins were slightly better able to control their blood sugar, but those who used the cholesterol-lowering drugs lived longer and had fewer cardiac events.
“It is clear that, in this high-risk population, the benefits of statins on cardiovascular outcomes outweigh the small adverse metabolic effects on glycemic control,” study lead author Uche Anyanwagu, MBBS, MSc, a graduate student and research fellow at the University of Nottingham (England), said in an interview about his data presented in a poster at the annual scientific sessions of the American Diabetes Association.
However, “there remain great concerns about statins and their modest adverse effects on glucose and insulin metabolism in increasing the risk of new-onset diabetes or worsening glycemic control, especially in higher doses and with the more potent statins,” Dr. Anyanwagu said. “Very little is known about the relationship between statin use and glycemic control in patients with established T2DM.”
The study authors retrospectively analyzed medical records of 12,725 new insulin users with T2DM from a British primary care database. “The commencement of insulin represents a group of patients with T2DM with longer disease duration and more complex needs, many of whom have other comorbid illnesses,” Dr. Anyanwagu said.
The average age of the subjects was 58.6 years (standard deviation, 13.8), and 50% were female (P less than 0.001 for both). Their average HbA1c level was 8.7 (SD, 1.8; P = .556), and 63% were obese.
The numbers of statin users and nonstatin users were 10,682 and 2,043, respectively. Researchers found that the statin users performed better in measures of all-cause mortality, nonfatal stroke, and a composite outcome measure but not in acute myocardial infarction.
In all-cause mortality, the absolute rate over 5 years was 9.5 deaths per 1,000 person years (95% confidence interval, 8.7-10.5) for statin users and 24.9 (95% CI, 21.5-28.9) for nonusers. After adjustment for age, gender, duration of insulin use, albumin, glomerular filtration rate, lipid profile, and coronary heart disease, the hazard ratio was 1.89 (95% CI, 1.51-2.37) for nonusers, compared with a reference of 1 for users. (P less than .0001).
The absolute rate for a composite outcome – encompassing measures of all-cause mortality, nonfatal acute myocardial infarction, and nonfatal stroke – was 20.7 (95% CI, 19.3-22.1) for statin users and 30.9 (95% CI , 27-35.3) for nonusers (P less than .0001).
As for HbA1c levels, at 12 months, they’d fallen by an average of 0.29% in the statin group and 0.37% in the nonuser group (P = .021). At 36 months, there was a smaller difference (–0.31% vs. –0.35%, respectively), and it wasn’t statistically significant (P = .344).
The study was funded by the University of Nottingham. (England). Dr. Anyanwagu reports no relevant disclosures.
SAN DIEGO – Findings from a study of 12,725 new insulin users with type 2 diabetes mellitus (T2DM) show that those who did not take statins were slightly better able to control their blood sugar, but those who used the cholesterol-lowering drugs lived longer and had fewer cardiac events.
“It is clear that, in this high-risk population, the benefits of statins on cardiovascular outcomes outweigh the small adverse metabolic effects on glycemic control,” study lead author Uche Anyanwagu, MBBS, MSc, a graduate student and research fellow at the University of Nottingham (England), said in an interview about his data presented in a poster at the annual scientific sessions of the American Diabetes Association.
However, “there remain great concerns about statins and their modest adverse effects on glucose and insulin metabolism in increasing the risk of new-onset diabetes or worsening glycemic control, especially in higher doses and with the more potent statins,” Dr. Anyanwagu said. “Very little is known about the relationship between statin use and glycemic control in patients with established T2DM.”
The study authors retrospectively analyzed medical records of 12,725 new insulin users with T2DM from a British primary care database. “The commencement of insulin represents a group of patients with T2DM with longer disease duration and more complex needs, many of whom have other comorbid illnesses,” Dr. Anyanwagu said.
The average age of the subjects was 58.6 years (standard deviation, 13.8), and 50% were female (P less than 0.001 for both). Their average HbA1c level was 8.7 (SD, 1.8; P = .556), and 63% were obese.
The numbers of statin users and nonstatin users were 10,682 and 2,043, respectively. Researchers found that the statin users performed better in measures of all-cause mortality, nonfatal stroke, and a composite outcome measure but not in acute myocardial infarction.
In all-cause mortality, the absolute rate over 5 years was 9.5 deaths per 1,000 person years (95% confidence interval, 8.7-10.5) for statin users and 24.9 (95% CI, 21.5-28.9) for nonusers. After adjustment for age, gender, duration of insulin use, albumin, glomerular filtration rate, lipid profile, and coronary heart disease, the hazard ratio was 1.89 (95% CI, 1.51-2.37) for nonusers, compared with a reference of 1 for users. (P less than .0001).
The absolute rate for a composite outcome – encompassing measures of all-cause mortality, nonfatal acute myocardial infarction, and nonfatal stroke – was 20.7 (95% CI, 19.3-22.1) for statin users and 30.9 (95% CI , 27-35.3) for nonusers (P less than .0001).
As for HbA1c levels, at 12 months, they’d fallen by an average of 0.29% in the statin group and 0.37% in the nonuser group (P = .021). At 36 months, there was a smaller difference (–0.31% vs. –0.35%, respectively), and it wasn’t statistically significant (P = .344).
The study was funded by the University of Nottingham. (England). Dr. Anyanwagu reports no relevant disclosures.
SAN DIEGO – Findings from a study of 12,725 new insulin users with type 2 diabetes mellitus (T2DM) show that those who did not take statins were slightly better able to control their blood sugar, but those who used the cholesterol-lowering drugs lived longer and had fewer cardiac events.
“It is clear that, in this high-risk population, the benefits of statins on cardiovascular outcomes outweigh the small adverse metabolic effects on glycemic control,” study lead author Uche Anyanwagu, MBBS, MSc, a graduate student and research fellow at the University of Nottingham (England), said in an interview about his data presented in a poster at the annual scientific sessions of the American Diabetes Association.
However, “there remain great concerns about statins and their modest adverse effects on glucose and insulin metabolism in increasing the risk of new-onset diabetes or worsening glycemic control, especially in higher doses and with the more potent statins,” Dr. Anyanwagu said. “Very little is known about the relationship between statin use and glycemic control in patients with established T2DM.”
The study authors retrospectively analyzed medical records of 12,725 new insulin users with T2DM from a British primary care database. “The commencement of insulin represents a group of patients with T2DM with longer disease duration and more complex needs, many of whom have other comorbid illnesses,” Dr. Anyanwagu said.
The average age of the subjects was 58.6 years (standard deviation, 13.8), and 50% were female (P less than 0.001 for both). Their average HbA1c level was 8.7 (SD, 1.8; P = .556), and 63% were obese.
The numbers of statin users and nonstatin users were 10,682 and 2,043, respectively. Researchers found that the statin users performed better in measures of all-cause mortality, nonfatal stroke, and a composite outcome measure but not in acute myocardial infarction.
In all-cause mortality, the absolute rate over 5 years was 9.5 deaths per 1,000 person years (95% confidence interval, 8.7-10.5) for statin users and 24.9 (95% CI, 21.5-28.9) for nonusers. After adjustment for age, gender, duration of insulin use, albumin, glomerular filtration rate, lipid profile, and coronary heart disease, the hazard ratio was 1.89 (95% CI, 1.51-2.37) for nonusers, compared with a reference of 1 for users. (P less than .0001).
The absolute rate for a composite outcome – encompassing measures of all-cause mortality, nonfatal acute myocardial infarction, and nonfatal stroke – was 20.7 (95% CI, 19.3-22.1) for statin users and 30.9 (95% CI , 27-35.3) for nonusers (P less than .0001).
As for HbA1c levels, at 12 months, they’d fallen by an average of 0.29% in the statin group and 0.37% in the nonuser group (P = .021). At 36 months, there was a smaller difference (–0.31% vs. –0.35%, respectively), and it wasn’t statistically significant (P = .344).
The study was funded by the University of Nottingham. (England). Dr. Anyanwagu reports no relevant disclosures.
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: In new insulin users with T2DM, statin use appears to slightly lower the decline in HbA1c, compared with nonuse, but the drug improved all-cause mortality.
Major finding: The adjusted hazard ratio of 5-year all-cause mortality was 1.89 in nonstatin users, vs. a reference of 1 for statin users. At 12 months, HbA1c fell by an average of 0.29% in the statin group and 0.37% in the nonuser group, but the difference wasn’t statistically significant at 36 months.
Data source: A retrospective study of 10,682 stain users and 2,043 nonusers, all of whom were new insulin users, from a British primary care database.
Disclosures: The study was funded by the University of Nottingham (England).
Target childhood obesity now to prevent knee OA later
LAS VEGAS – Childhood overweight was associated with increased risk of patellar cartilage defects in young adulthood independent of adult weight status in what’s believed to be the first long-term prospective study to address the issue using informative MRI imaging.
“Our data indicate the importance of intervening in childhood obesity for adult joint health,” Benny E. Antony, MD, reported at the World Congress on Osteoarthritis, sponsored by the Osteoarthritis Research Society International.
He presented the 25-year prospective follow-up from the population-based Childhood Determinants of Adult Knee Cartilage Study, a substudy of the Australian Schools Health and Fitness Survey of 1985. The analysis included 322 nationally representative participants who were 7-15 years old at enrollment and 31-41 years old at follow-up, when they underwent screening MRI knee scans in which cartilage defects in the tibial, femoral, and patellar zones were rated by a modified Outerbridge scoring system.
The increased prevalence of patellar compared with tibiofemoral cartilage defects is consistent with growing evidence that knee OA typically starts in the patellar region and then spreads through the knee over time, according to Dr. Antony of the University of Tasmania in Hobart, Australia.
Among the other key findings:
• Women had a higher prevalence of cartilage defects: 43% in the whole knee and 30% at the patella, compared with rates of 34% and 20%, respectively, in men.
• The prevalence of patellar cartilage defects in young adulthood was 24.2% in those who had a normal weight both as children and young adults compared with 40% in participants who were overweight at both time points, for an adjusted 1.77-fold increased risk in subjects who were overweight across the decades, .
• Excess childhood weight per kilogram, fat mass per kilogram, and body mass per unit were each associated with 5%-12% increased risks of patellar cartilage defects 25 years later, independent of adult body weight status, in an analysis adjusted for childhood age, sex, height, duration of follow-up, and history of pediatric or adult knee injury.
• A dose-response relationship was evident between the degree of childhood overweight and the severity of cartilage defects as young adults on a 0-4 rating scale.
Dr. Antony reported having no financial conflicts of interest regarding the study, which was supported by the National Health and Medical Research Council of Australia.
LAS VEGAS – Childhood overweight was associated with increased risk of patellar cartilage defects in young adulthood independent of adult weight status in what’s believed to be the first long-term prospective study to address the issue using informative MRI imaging.
“Our data indicate the importance of intervening in childhood obesity for adult joint health,” Benny E. Antony, MD, reported at the World Congress on Osteoarthritis, sponsored by the Osteoarthritis Research Society International.
He presented the 25-year prospective follow-up from the population-based Childhood Determinants of Adult Knee Cartilage Study, a substudy of the Australian Schools Health and Fitness Survey of 1985. The analysis included 322 nationally representative participants who were 7-15 years old at enrollment and 31-41 years old at follow-up, when they underwent screening MRI knee scans in which cartilage defects in the tibial, femoral, and patellar zones were rated by a modified Outerbridge scoring system.
The increased prevalence of patellar compared with tibiofemoral cartilage defects is consistent with growing evidence that knee OA typically starts in the patellar region and then spreads through the knee over time, according to Dr. Antony of the University of Tasmania in Hobart, Australia.
Among the other key findings:
• Women had a higher prevalence of cartilage defects: 43% in the whole knee and 30% at the patella, compared with rates of 34% and 20%, respectively, in men.
• The prevalence of patellar cartilage defects in young adulthood was 24.2% in those who had a normal weight both as children and young adults compared with 40% in participants who were overweight at both time points, for an adjusted 1.77-fold increased risk in subjects who were overweight across the decades, .
• Excess childhood weight per kilogram, fat mass per kilogram, and body mass per unit were each associated with 5%-12% increased risks of patellar cartilage defects 25 years later, independent of adult body weight status, in an analysis adjusted for childhood age, sex, height, duration of follow-up, and history of pediatric or adult knee injury.
• A dose-response relationship was evident between the degree of childhood overweight and the severity of cartilage defects as young adults on a 0-4 rating scale.
Dr. Antony reported having no financial conflicts of interest regarding the study, which was supported by the National Health and Medical Research Council of Australia.
LAS VEGAS – Childhood overweight was associated with increased risk of patellar cartilage defects in young adulthood independent of adult weight status in what’s believed to be the first long-term prospective study to address the issue using informative MRI imaging.
“Our data indicate the importance of intervening in childhood obesity for adult joint health,” Benny E. Antony, MD, reported at the World Congress on Osteoarthritis, sponsored by the Osteoarthritis Research Society International.
He presented the 25-year prospective follow-up from the population-based Childhood Determinants of Adult Knee Cartilage Study, a substudy of the Australian Schools Health and Fitness Survey of 1985. The analysis included 322 nationally representative participants who were 7-15 years old at enrollment and 31-41 years old at follow-up, when they underwent screening MRI knee scans in which cartilage defects in the tibial, femoral, and patellar zones were rated by a modified Outerbridge scoring system.
The increased prevalence of patellar compared with tibiofemoral cartilage defects is consistent with growing evidence that knee OA typically starts in the patellar region and then spreads through the knee over time, according to Dr. Antony of the University of Tasmania in Hobart, Australia.
Among the other key findings:
• Women had a higher prevalence of cartilage defects: 43% in the whole knee and 30% at the patella, compared with rates of 34% and 20%, respectively, in men.
• The prevalence of patellar cartilage defects in young adulthood was 24.2% in those who had a normal weight both as children and young adults compared with 40% in participants who were overweight at both time points, for an adjusted 1.77-fold increased risk in subjects who were overweight across the decades, .
• Excess childhood weight per kilogram, fat mass per kilogram, and body mass per unit were each associated with 5%-12% increased risks of patellar cartilage defects 25 years later, independent of adult body weight status, in an analysis adjusted for childhood age, sex, height, duration of follow-up, and history of pediatric or adult knee injury.
• A dose-response relationship was evident between the degree of childhood overweight and the severity of cartilage defects as young adults on a 0-4 rating scale.
Dr. Antony reported having no financial conflicts of interest regarding the study, which was supported by the National Health and Medical Research Council of Australia.
AT OARSI 2017
Key clinical point:
Major finding: The prevalence of patellar cartilage defects in young adults was 24.2% in those who were normal weight both as children and young adults, compared with 40% in subjects who were overweight at both time points.
Data source: A prospective population-based cohort study of 322 subjects followed from childhood to age 31-41 years, when they were assessed via MRI for knee cartilage defects.
Disclosures: The National Health and Medical Research Council of Australia supported the study. The presenter reported having no financial conflicts.
Adult diabetes up 35% over 25 years
The overall prevalence of diabetes increased 35% from 1988-1994 to 2011-2014 among adults aged 20 years and over, according the National Center for Health Statistics.
During 2011-2014, the age-adjusted prevalence of diabetes was 11.9% in adults aged 20 years and over, compared with 8.8% in 1988-1994. That 35% increase came despite a decrease in undiagnosed diabetes from 3.6% to 2.9% over that time period, which was not enough to offset a jump in physician-diagnosed disease from 5.2% to 9%, the NCHS reported in “Health, United States, 2016.”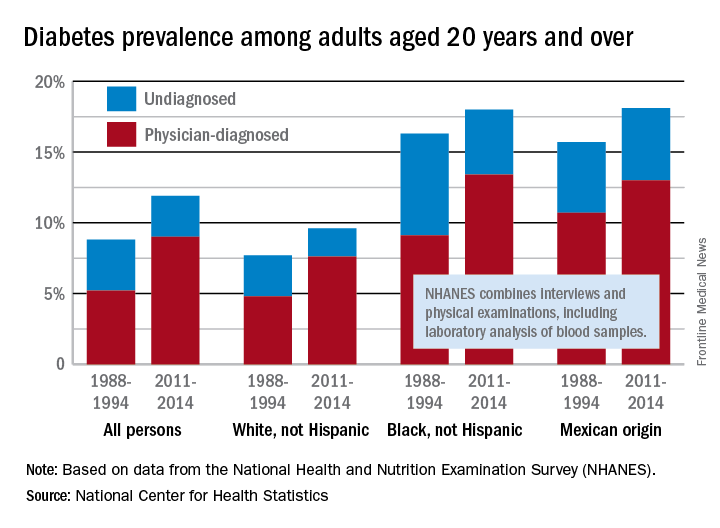
Undiagnosed diabetes dropped from 2.9% to 2% in whites and from 7.2% to 4.6% in blacks, but adults of Mexican origin saw a slight increase from 5% in 1988-1994 to 5.1% in 2011-2014. The physician-diagnosed side of the equation rose from 4.8% to 7.6% in whites, 9.1% to 13.4% in blacks, and 10.7% to 13% in those of Mexican origin, according to data from the National Health and Nutrition Examination Survey, which combines interviews and physical examinations, including laboratory analysis of blood samples.
The overall prevalence of diabetes increased 35% from 1988-1994 to 2011-2014 among adults aged 20 years and over, according the National Center for Health Statistics.
During 2011-2014, the age-adjusted prevalence of diabetes was 11.9% in adults aged 20 years and over, compared with 8.8% in 1988-1994. That 35% increase came despite a decrease in undiagnosed diabetes from 3.6% to 2.9% over that time period, which was not enough to offset a jump in physician-diagnosed disease from 5.2% to 9%, the NCHS reported in “Health, United States, 2016.”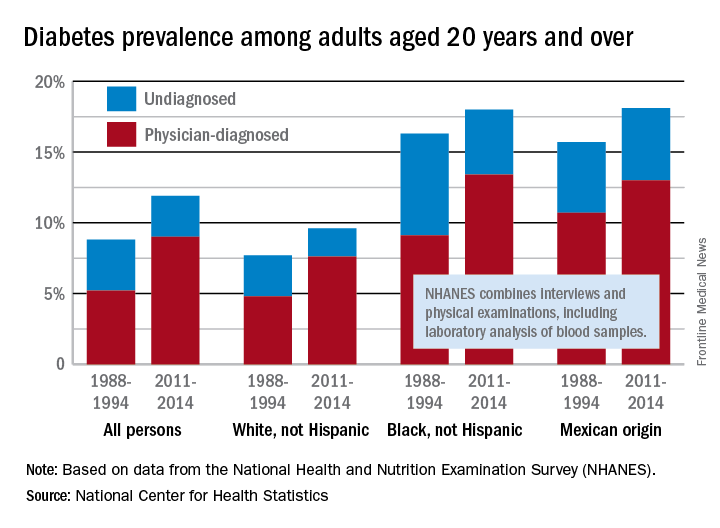
Undiagnosed diabetes dropped from 2.9% to 2% in whites and from 7.2% to 4.6% in blacks, but adults of Mexican origin saw a slight increase from 5% in 1988-1994 to 5.1% in 2011-2014. The physician-diagnosed side of the equation rose from 4.8% to 7.6% in whites, 9.1% to 13.4% in blacks, and 10.7% to 13% in those of Mexican origin, according to data from the National Health and Nutrition Examination Survey, which combines interviews and physical examinations, including laboratory analysis of blood samples.
The overall prevalence of diabetes increased 35% from 1988-1994 to 2011-2014 among adults aged 20 years and over, according the National Center for Health Statistics.
During 2011-2014, the age-adjusted prevalence of diabetes was 11.9% in adults aged 20 years and over, compared with 8.8% in 1988-1994. That 35% increase came despite a decrease in undiagnosed diabetes from 3.6% to 2.9% over that time period, which was not enough to offset a jump in physician-diagnosed disease from 5.2% to 9%, the NCHS reported in “Health, United States, 2016.”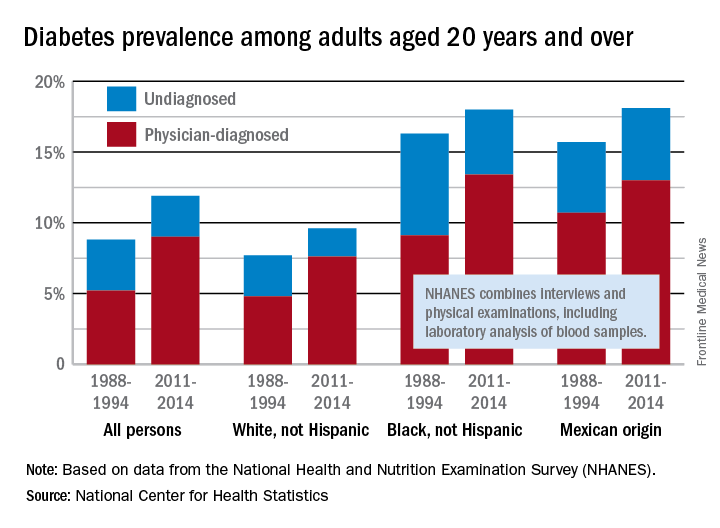
Undiagnosed diabetes dropped from 2.9% to 2% in whites and from 7.2% to 4.6% in blacks, but adults of Mexican origin saw a slight increase from 5% in 1988-1994 to 5.1% in 2011-2014. The physician-diagnosed side of the equation rose from 4.8% to 7.6% in whites, 9.1% to 13.4% in blacks, and 10.7% to 13% in those of Mexican origin, according to data from the National Health and Nutrition Examination Survey, which combines interviews and physical examinations, including laboratory analysis of blood samples.