User login
Neurology Reviews covers innovative and emerging news in neurology and neuroscience every month, with a focus on practical approaches to treating Parkinson's disease, epilepsy, headache, stroke, multiple sclerosis, Alzheimer's disease, and other neurologic disorders.
PML
Progressive multifocal leukoencephalopathy
Rituxan
The leading independent newspaper covering neurology news and commentary.
Medication overuse headache a pain to treat
BARCELONA, SPAIN — Around half of all patients with chronic headache or migraine overuse their medication, leading to aggravated or new types of headaches. “Medication overuse headache” is the third most frequent type of headache, affecting some 60 million people or around 1% of the world’s population.
“It’s a big problem,” Sait Ashina, MD, of Beth Israel Deaconess Medical Center, Boston, Massachusetts, told the audience in an opening plenary at the 17th European Headache Congress in Barcelona.
Medication overuse headache is characterized by an increasing headache frequency and progressive use of short-term medication and is recognized as a major factor in the shift from episodic to chronic headache.
It is often underrecognized; however, educating doctors and patients is a crucial element of effective treatment. Recognition that headache medication is being overused is a crucial first step to treatment, followed by advising the patient to discontinue the medication. But this poses its own problems, as it can cause withdrawal symptoms.
According to a longitudinal population-based study published in 2008, most patients overuse acetaminophen or paracetamol, followed by nonsteroidal anti-inflammatory drugs and 5-hydroxytriptamine agonists (triptans) and, in the United States, barbiturates and opioids.
What’s the Best Treatment Strategy?
Medication overuse headache is often treated by complete withdrawal from medication, but the withdrawal symptoms can be severe. They include nausea and vomiting, arterial hypertension, tachycardia, sleep disturbances, anxiety, and restlessness, with their duration and severity depending solely on the type of headache medication that has been overused.
There is, however, no consensus on how best to treat medication overuse headache — withdrawal plus preventive treatment, preventive treatment without withdrawal, and withdrawal with optional preventive treatment 2 months after withdrawal. The findings showed that all three strategies were effective. But the research team concluded that withdrawal combined with preventive medication from the start of withdrawal was the recommended approach.
The electronic headache diary has proved to be very useful, as it can aid accurate diagnosis by providing clear insights into a patient’s condition. Information from the diary is more reliable than self-reports because patients often underestimate the frequency of their headaches, migraines, and use of medication.
Patients who are treated for medication overuse headache tend to have a high relapse rate. So, the electronic headache diary can also be very useful for follow-up by alerting patients and clinicians when headaches and medication overuse are increasing again.
“After diagnosing medication overuse or medication overuse headache, we advise our patients to discontinue the medication,” said Judith Pijpers of Leiden University Medical School, the Netherlands. “This provides clinically relevant improvements in headache frequency in a majority of patients and a significant reduction in headache days.”
In 2019, Dr. Pijpers and her colleagues published the results of a double-blind randomized controlled trial showing that botulinum toxin A, which is widely used to treat chronic migraine, has no additional benefit over acute withdrawal in patients with chronic migraine and medication overuse.
“We saw no difference between the groups during both the double-blind and the open label phase,” said Dr. Pijpers. “And that is why we do not give patients botulinum toxin A during withdrawal.”
A further trial within the botox study showed modest benefits for behavioral intervention by a headache nurse comprising education, motivational interviewing, and value-based activity planning during withdrawal therapy.
Patients can be stratified to some extent based on the type of headache they have and the medication they are taking for it.
“You can predict [a patient’s response] to some extent from the type of medication they overuse and the type of underlying primary headache,” Dr. Pijpers said in an interview.
“Those with underlying tension-type headache have different withdrawal symptoms than those with underlying migraine, and the withdrawal symptoms tend to be somewhat shorter if a patient overuses triptans compared to analgesics.”
Predicting Patients’ Responses to Migraine Medication
Dr. Pijpers and her colleagues recently published the results of a cohort study suggesting that cutaneous allodynia may predict how patients with migraine respond to withdrawal therapy. Nearly 75% of the 173 patients enrolled in the study reported experiencing allodynia — pain caused by a stimulus that does not normally cause pain. The study showed that absence of allodynia was predictive of a good outcome for patients after withdrawal therapy and of reversion from chronic to episodic migraine.
The ability to accurately predict patients’ responses could pave the way for personalized treatments of medication overuse headache.
A version of this article appeared in Medscape.com.
BARCELONA, SPAIN — Around half of all patients with chronic headache or migraine overuse their medication, leading to aggravated or new types of headaches. “Medication overuse headache” is the third most frequent type of headache, affecting some 60 million people or around 1% of the world’s population.
“It’s a big problem,” Sait Ashina, MD, of Beth Israel Deaconess Medical Center, Boston, Massachusetts, told the audience in an opening plenary at the 17th European Headache Congress in Barcelona.
Medication overuse headache is characterized by an increasing headache frequency and progressive use of short-term medication and is recognized as a major factor in the shift from episodic to chronic headache.
It is often underrecognized; however, educating doctors and patients is a crucial element of effective treatment. Recognition that headache medication is being overused is a crucial first step to treatment, followed by advising the patient to discontinue the medication. But this poses its own problems, as it can cause withdrawal symptoms.
According to a longitudinal population-based study published in 2008, most patients overuse acetaminophen or paracetamol, followed by nonsteroidal anti-inflammatory drugs and 5-hydroxytriptamine agonists (triptans) and, in the United States, barbiturates and opioids.
What’s the Best Treatment Strategy?
Medication overuse headache is often treated by complete withdrawal from medication, but the withdrawal symptoms can be severe. They include nausea and vomiting, arterial hypertension, tachycardia, sleep disturbances, anxiety, and restlessness, with their duration and severity depending solely on the type of headache medication that has been overused.
There is, however, no consensus on how best to treat medication overuse headache — withdrawal plus preventive treatment, preventive treatment without withdrawal, and withdrawal with optional preventive treatment 2 months after withdrawal. The findings showed that all three strategies were effective. But the research team concluded that withdrawal combined with preventive medication from the start of withdrawal was the recommended approach.
The electronic headache diary has proved to be very useful, as it can aid accurate diagnosis by providing clear insights into a patient’s condition. Information from the diary is more reliable than self-reports because patients often underestimate the frequency of their headaches, migraines, and use of medication.
Patients who are treated for medication overuse headache tend to have a high relapse rate. So, the electronic headache diary can also be very useful for follow-up by alerting patients and clinicians when headaches and medication overuse are increasing again.
“After diagnosing medication overuse or medication overuse headache, we advise our patients to discontinue the medication,” said Judith Pijpers of Leiden University Medical School, the Netherlands. “This provides clinically relevant improvements in headache frequency in a majority of patients and a significant reduction in headache days.”
In 2019, Dr. Pijpers and her colleagues published the results of a double-blind randomized controlled trial showing that botulinum toxin A, which is widely used to treat chronic migraine, has no additional benefit over acute withdrawal in patients with chronic migraine and medication overuse.
“We saw no difference between the groups during both the double-blind and the open label phase,” said Dr. Pijpers. “And that is why we do not give patients botulinum toxin A during withdrawal.”
A further trial within the botox study showed modest benefits for behavioral intervention by a headache nurse comprising education, motivational interviewing, and value-based activity planning during withdrawal therapy.
Patients can be stratified to some extent based on the type of headache they have and the medication they are taking for it.
“You can predict [a patient’s response] to some extent from the type of medication they overuse and the type of underlying primary headache,” Dr. Pijpers said in an interview.
“Those with underlying tension-type headache have different withdrawal symptoms than those with underlying migraine, and the withdrawal symptoms tend to be somewhat shorter if a patient overuses triptans compared to analgesics.”
Predicting Patients’ Responses to Migraine Medication
Dr. Pijpers and her colleagues recently published the results of a cohort study suggesting that cutaneous allodynia may predict how patients with migraine respond to withdrawal therapy. Nearly 75% of the 173 patients enrolled in the study reported experiencing allodynia — pain caused by a stimulus that does not normally cause pain. The study showed that absence of allodynia was predictive of a good outcome for patients after withdrawal therapy and of reversion from chronic to episodic migraine.
The ability to accurately predict patients’ responses could pave the way for personalized treatments of medication overuse headache.
A version of this article appeared in Medscape.com.
BARCELONA, SPAIN — Around half of all patients with chronic headache or migraine overuse their medication, leading to aggravated or new types of headaches. “Medication overuse headache” is the third most frequent type of headache, affecting some 60 million people or around 1% of the world’s population.
“It’s a big problem,” Sait Ashina, MD, of Beth Israel Deaconess Medical Center, Boston, Massachusetts, told the audience in an opening plenary at the 17th European Headache Congress in Barcelona.
Medication overuse headache is characterized by an increasing headache frequency and progressive use of short-term medication and is recognized as a major factor in the shift from episodic to chronic headache.
It is often underrecognized; however, educating doctors and patients is a crucial element of effective treatment. Recognition that headache medication is being overused is a crucial first step to treatment, followed by advising the patient to discontinue the medication. But this poses its own problems, as it can cause withdrawal symptoms.
According to a longitudinal population-based study published in 2008, most patients overuse acetaminophen or paracetamol, followed by nonsteroidal anti-inflammatory drugs and 5-hydroxytriptamine agonists (triptans) and, in the United States, barbiturates and opioids.
What’s the Best Treatment Strategy?
Medication overuse headache is often treated by complete withdrawal from medication, but the withdrawal symptoms can be severe. They include nausea and vomiting, arterial hypertension, tachycardia, sleep disturbances, anxiety, and restlessness, with their duration and severity depending solely on the type of headache medication that has been overused.
There is, however, no consensus on how best to treat medication overuse headache — withdrawal plus preventive treatment, preventive treatment without withdrawal, and withdrawal with optional preventive treatment 2 months after withdrawal. The findings showed that all three strategies were effective. But the research team concluded that withdrawal combined with preventive medication from the start of withdrawal was the recommended approach.
The electronic headache diary has proved to be very useful, as it can aid accurate diagnosis by providing clear insights into a patient’s condition. Information from the diary is more reliable than self-reports because patients often underestimate the frequency of their headaches, migraines, and use of medication.
Patients who are treated for medication overuse headache tend to have a high relapse rate. So, the electronic headache diary can also be very useful for follow-up by alerting patients and clinicians when headaches and medication overuse are increasing again.
“After diagnosing medication overuse or medication overuse headache, we advise our patients to discontinue the medication,” said Judith Pijpers of Leiden University Medical School, the Netherlands. “This provides clinically relevant improvements in headache frequency in a majority of patients and a significant reduction in headache days.”
In 2019, Dr. Pijpers and her colleagues published the results of a double-blind randomized controlled trial showing that botulinum toxin A, which is widely used to treat chronic migraine, has no additional benefit over acute withdrawal in patients with chronic migraine and medication overuse.
“We saw no difference between the groups during both the double-blind and the open label phase,” said Dr. Pijpers. “And that is why we do not give patients botulinum toxin A during withdrawal.”
A further trial within the botox study showed modest benefits for behavioral intervention by a headache nurse comprising education, motivational interviewing, and value-based activity planning during withdrawal therapy.
Patients can be stratified to some extent based on the type of headache they have and the medication they are taking for it.
“You can predict [a patient’s response] to some extent from the type of medication they overuse and the type of underlying primary headache,” Dr. Pijpers said in an interview.
“Those with underlying tension-type headache have different withdrawal symptoms than those with underlying migraine, and the withdrawal symptoms tend to be somewhat shorter if a patient overuses triptans compared to analgesics.”
Predicting Patients’ Responses to Migraine Medication
Dr. Pijpers and her colleagues recently published the results of a cohort study suggesting that cutaneous allodynia may predict how patients with migraine respond to withdrawal therapy. Nearly 75% of the 173 patients enrolled in the study reported experiencing allodynia — pain caused by a stimulus that does not normally cause pain. The study showed that absence of allodynia was predictive of a good outcome for patients after withdrawal therapy and of reversion from chronic to episodic migraine.
The ability to accurately predict patients’ responses could pave the way for personalized treatments of medication overuse headache.
A version of this article appeared in Medscape.com.
FROM EHC 2023
Sleep disorders linked to increased mortality risk in epilepsy
ORLANDO — , new research shows.
SUDEP is a major concern for patients with epilepsy, said study investigator Marion Lazaj, MSc, Center for Neuroscience Studies, Queen’s University, Kingston, Ontario, Canada, but she believes that SUDEP risk assessment is overly focused on seizure control.
“We want to push the idea that this mortality risk assessment needs to be widened to include sleep factors, and not just sleep disorders but even sleep disturbances,” said Ms. Lazaj.
She also believes physicians should routinely discuss SUDEP with their patients with epilepsy. Given that the incidence of SUDEP is only about 1%, many clinicians don’t want to unduly frighten their patients, she added.
The findings were presented at the annual meeting of the American Epilepsy Society (AES).
The retrospective study included chart data from 1,506 consecutive patients diagnosed with epilepsy at a single center over 4 years. The mean age of participants was about 37 years but there was a large age range, said Ms. Lazaj.
The cohort was divided into two groups. Group 1 included 1130 patients without a comorbid sleep disorder, and Group 2 had 376 patients with a primary comorbid sleep disorder, mostly obstructive sleep apnea (OSA) but also restless leg syndrome or insomnia.
They gathered demographic information including age, sex, employment status, education, and epilepsy-related data such as epilepsy type, duration, the number of anti-seizure medications and relevant information from hospital and emergency room (ER) records.
SUDEP Inventory
Researchers assessed SUDEP risk using the revised SUDEP-7 risk inventory. The first four items on this inventory focus on generalized tonic clonic seizure activity and occurrence while others assess the number of antiseizure medicines, epilepsy duration, and the presence of other developmental delays.
Investigators then stratified patients into high risk (score on the SUDEP-7 of 5 or greater) and low mortality risk (score less than 5).
Results showed a significant association between a high mortality risk and having a comorbid sleep disorder (P = .033). Researchers also looked at all-cause mortality, including drownings and suicides, and found a similar significant association (P = .026). There was also an association between high risk and accidents and trauma (P = .042).
The researchers had access to overnight diagnostic polysomnography data for a smaller group of patients. Here, they found decreased sleep efficiency (P =.0098), increased spontaneous arousal index (P = .034), and prolonged sleep onset latency (P = .0000052) were all significantly associated with high SUDEP risk.
From the polysomnographic data, researchers found high SUDEP risk was significantly associated with a diagnosis of OSA (P = .034).
Powerful Study
Commenting on the findings, Gordon F. Buchanan, MD, PhD, Beth L. Tross epilepsy associate professor, Department of Neurology, University of Iowa Carver College of Medicine, Iowa City, said he was “very excited” by the research.
“That this study attempts to look through data in a retrospective way and see if there’s additional risk with having comorbid sleep disorders is really interesting and I think really powerful,” he said.
Sleep disorders “are potentially a really simple thing that we can screen for and test for,” he added. He also noted that additional research is needed to replicate the findings.
Dr. Buchanan acknowledged that the SUDEP-7 inventory is not a particularly good tool and said there is a need for a better means of assessment that includes sleep disorders and other factors like sleep states and circadian rhythm, which he said affect SUDEP risk.
Ms. Lazaj and Dr. Buchanan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ORLANDO — , new research shows.
SUDEP is a major concern for patients with epilepsy, said study investigator Marion Lazaj, MSc, Center for Neuroscience Studies, Queen’s University, Kingston, Ontario, Canada, but she believes that SUDEP risk assessment is overly focused on seizure control.
“We want to push the idea that this mortality risk assessment needs to be widened to include sleep factors, and not just sleep disorders but even sleep disturbances,” said Ms. Lazaj.
She also believes physicians should routinely discuss SUDEP with their patients with epilepsy. Given that the incidence of SUDEP is only about 1%, many clinicians don’t want to unduly frighten their patients, she added.
The findings were presented at the annual meeting of the American Epilepsy Society (AES).
The retrospective study included chart data from 1,506 consecutive patients diagnosed with epilepsy at a single center over 4 years. The mean age of participants was about 37 years but there was a large age range, said Ms. Lazaj.
The cohort was divided into two groups. Group 1 included 1130 patients without a comorbid sleep disorder, and Group 2 had 376 patients with a primary comorbid sleep disorder, mostly obstructive sleep apnea (OSA) but also restless leg syndrome or insomnia.
They gathered demographic information including age, sex, employment status, education, and epilepsy-related data such as epilepsy type, duration, the number of anti-seizure medications and relevant information from hospital and emergency room (ER) records.
SUDEP Inventory
Researchers assessed SUDEP risk using the revised SUDEP-7 risk inventory. The first four items on this inventory focus on generalized tonic clonic seizure activity and occurrence while others assess the number of antiseizure medicines, epilepsy duration, and the presence of other developmental delays.
Investigators then stratified patients into high risk (score on the SUDEP-7 of 5 or greater) and low mortality risk (score less than 5).
Results showed a significant association between a high mortality risk and having a comorbid sleep disorder (P = .033). Researchers also looked at all-cause mortality, including drownings and suicides, and found a similar significant association (P = .026). There was also an association between high risk and accidents and trauma (P = .042).
The researchers had access to overnight diagnostic polysomnography data for a smaller group of patients. Here, they found decreased sleep efficiency (P =.0098), increased spontaneous arousal index (P = .034), and prolonged sleep onset latency (P = .0000052) were all significantly associated with high SUDEP risk.
From the polysomnographic data, researchers found high SUDEP risk was significantly associated with a diagnosis of OSA (P = .034).
Powerful Study
Commenting on the findings, Gordon F. Buchanan, MD, PhD, Beth L. Tross epilepsy associate professor, Department of Neurology, University of Iowa Carver College of Medicine, Iowa City, said he was “very excited” by the research.
“That this study attempts to look through data in a retrospective way and see if there’s additional risk with having comorbid sleep disorders is really interesting and I think really powerful,” he said.
Sleep disorders “are potentially a really simple thing that we can screen for and test for,” he added. He also noted that additional research is needed to replicate the findings.
Dr. Buchanan acknowledged that the SUDEP-7 inventory is not a particularly good tool and said there is a need for a better means of assessment that includes sleep disorders and other factors like sleep states and circadian rhythm, which he said affect SUDEP risk.
Ms. Lazaj and Dr. Buchanan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ORLANDO — , new research shows.
SUDEP is a major concern for patients with epilepsy, said study investigator Marion Lazaj, MSc, Center for Neuroscience Studies, Queen’s University, Kingston, Ontario, Canada, but she believes that SUDEP risk assessment is overly focused on seizure control.
“We want to push the idea that this mortality risk assessment needs to be widened to include sleep factors, and not just sleep disorders but even sleep disturbances,” said Ms. Lazaj.
She also believes physicians should routinely discuss SUDEP with their patients with epilepsy. Given that the incidence of SUDEP is only about 1%, many clinicians don’t want to unduly frighten their patients, she added.
The findings were presented at the annual meeting of the American Epilepsy Society (AES).
The retrospective study included chart data from 1,506 consecutive patients diagnosed with epilepsy at a single center over 4 years. The mean age of participants was about 37 years but there was a large age range, said Ms. Lazaj.
The cohort was divided into two groups. Group 1 included 1130 patients without a comorbid sleep disorder, and Group 2 had 376 patients with a primary comorbid sleep disorder, mostly obstructive sleep apnea (OSA) but also restless leg syndrome or insomnia.
They gathered demographic information including age, sex, employment status, education, and epilepsy-related data such as epilepsy type, duration, the number of anti-seizure medications and relevant information from hospital and emergency room (ER) records.
SUDEP Inventory
Researchers assessed SUDEP risk using the revised SUDEP-7 risk inventory. The first four items on this inventory focus on generalized tonic clonic seizure activity and occurrence while others assess the number of antiseizure medicines, epilepsy duration, and the presence of other developmental delays.
Investigators then stratified patients into high risk (score on the SUDEP-7 of 5 or greater) and low mortality risk (score less than 5).
Results showed a significant association between a high mortality risk and having a comorbid sleep disorder (P = .033). Researchers also looked at all-cause mortality, including drownings and suicides, and found a similar significant association (P = .026). There was also an association between high risk and accidents and trauma (P = .042).
The researchers had access to overnight diagnostic polysomnography data for a smaller group of patients. Here, they found decreased sleep efficiency (P =.0098), increased spontaneous arousal index (P = .034), and prolonged sleep onset latency (P = .0000052) were all significantly associated with high SUDEP risk.
From the polysomnographic data, researchers found high SUDEP risk was significantly associated with a diagnosis of OSA (P = .034).
Powerful Study
Commenting on the findings, Gordon F. Buchanan, MD, PhD, Beth L. Tross epilepsy associate professor, Department of Neurology, University of Iowa Carver College of Medicine, Iowa City, said he was “very excited” by the research.
“That this study attempts to look through data in a retrospective way and see if there’s additional risk with having comorbid sleep disorders is really interesting and I think really powerful,” he said.
Sleep disorders “are potentially a really simple thing that we can screen for and test for,” he added. He also noted that additional research is needed to replicate the findings.
Dr. Buchanan acknowledged that the SUDEP-7 inventory is not a particularly good tool and said there is a need for a better means of assessment that includes sleep disorders and other factors like sleep states and circadian rhythm, which he said affect SUDEP risk.
Ms. Lazaj and Dr. Buchanan report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AES 2023
EMRs: gumming up the works
I don’t like EMR systems, with all their requirements, click boxes, endless cut & paste abuse, and 20-page notes that say nothing.
But I am a fan of what computers have brought to medical charts.
When I started out in 2000, I had no patients, hence no charts. I had the advantage of being able to start from scratch — there was nothing to convert to digital. So, from the beginning, that’s how I went. Back then, of course, everything came to the office as paper. It had to be scanned in, then named, then placed in the right computer file.
But it was still easier than amassing paper records. At that time I subleased from a doc who’d been in practice for 15 years. His charts were all paper. Charts were neatly filed on shelves, everything was initialed, hole-punched, and put in the right section (which involved pulling out other stuff and putting it back). A few times a year, his staff would comb through the charts in front, and anyone who hadn’t been seen in 2 years would have their chart moved to a storage room in the back. Once a year they’d pull the charts of anyone not seen in 7 years and a company would come in and shred those records.
After 23 years, I still have it all. The whole thing takes up a little over 50 gigabytes on a hard drive, which realistically is nothing these days. Electrons don’t take up much space.
The majority of the charts — those that are more than 7 years old — I’ll probably never need to access, but it still happens sometimes. People call in and say they’ve moved back to Phoenix, or need to see a neurologist again, or need the records for insurance reasons, or whatever. My staff is also spared from moving charts to a storage room, then to shredding. Since they don’t take up any physical space, it’s no effort to keep everything.
And they aren’t just at my office. They’re at home, on my phone, wherever I am. If I get called from an ER, I can pull them up quickly. If I travel, they’re with me. My memory is good, but not that good, and I’d rather be able to look things up than guess.
This, at least to me, is the advantage of computers. Their data storage and retrieval advantages far exceed that of paper. In my opinion EMRs, while well-intentioned, have taken these benefits and twisted them into something cumbersome, geared more to meet nonmedical requirements and billing purposes.
In the process they’ve lost sight of our age-old job of caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t like EMR systems, with all their requirements, click boxes, endless cut & paste abuse, and 20-page notes that say nothing.
But I am a fan of what computers have brought to medical charts.
When I started out in 2000, I had no patients, hence no charts. I had the advantage of being able to start from scratch — there was nothing to convert to digital. So, from the beginning, that’s how I went. Back then, of course, everything came to the office as paper. It had to be scanned in, then named, then placed in the right computer file.
But it was still easier than amassing paper records. At that time I subleased from a doc who’d been in practice for 15 years. His charts were all paper. Charts were neatly filed on shelves, everything was initialed, hole-punched, and put in the right section (which involved pulling out other stuff and putting it back). A few times a year, his staff would comb through the charts in front, and anyone who hadn’t been seen in 2 years would have their chart moved to a storage room in the back. Once a year they’d pull the charts of anyone not seen in 7 years and a company would come in and shred those records.
After 23 years, I still have it all. The whole thing takes up a little over 50 gigabytes on a hard drive, which realistically is nothing these days. Electrons don’t take up much space.
The majority of the charts — those that are more than 7 years old — I’ll probably never need to access, but it still happens sometimes. People call in and say they’ve moved back to Phoenix, or need to see a neurologist again, or need the records for insurance reasons, or whatever. My staff is also spared from moving charts to a storage room, then to shredding. Since they don’t take up any physical space, it’s no effort to keep everything.
And they aren’t just at my office. They’re at home, on my phone, wherever I am. If I get called from an ER, I can pull them up quickly. If I travel, they’re with me. My memory is good, but not that good, and I’d rather be able to look things up than guess.
This, at least to me, is the advantage of computers. Their data storage and retrieval advantages far exceed that of paper. In my opinion EMRs, while well-intentioned, have taken these benefits and twisted them into something cumbersome, geared more to meet nonmedical requirements and billing purposes.
In the process they’ve lost sight of our age-old job of caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t like EMR systems, with all their requirements, click boxes, endless cut & paste abuse, and 20-page notes that say nothing.
But I am a fan of what computers have brought to medical charts.
When I started out in 2000, I had no patients, hence no charts. I had the advantage of being able to start from scratch — there was nothing to convert to digital. So, from the beginning, that’s how I went. Back then, of course, everything came to the office as paper. It had to be scanned in, then named, then placed in the right computer file.
But it was still easier than amassing paper records. At that time I subleased from a doc who’d been in practice for 15 years. His charts were all paper. Charts were neatly filed on shelves, everything was initialed, hole-punched, and put in the right section (which involved pulling out other stuff and putting it back). A few times a year, his staff would comb through the charts in front, and anyone who hadn’t been seen in 2 years would have their chart moved to a storage room in the back. Once a year they’d pull the charts of anyone not seen in 7 years and a company would come in and shred those records.
After 23 years, I still have it all. The whole thing takes up a little over 50 gigabytes on a hard drive, which realistically is nothing these days. Electrons don’t take up much space.
The majority of the charts — those that are more than 7 years old — I’ll probably never need to access, but it still happens sometimes. People call in and say they’ve moved back to Phoenix, or need to see a neurologist again, or need the records for insurance reasons, or whatever. My staff is also spared from moving charts to a storage room, then to shredding. Since they don’t take up any physical space, it’s no effort to keep everything.
And they aren’t just at my office. They’re at home, on my phone, wherever I am. If I get called from an ER, I can pull them up quickly. If I travel, they’re with me. My memory is good, but not that good, and I’d rather be able to look things up than guess.
This, at least to me, is the advantage of computers. Their data storage and retrieval advantages far exceed that of paper. In my opinion EMRs, while well-intentioned, have taken these benefits and twisted them into something cumbersome, geared more to meet nonmedical requirements and billing purposes.
In the process they’ve lost sight of our age-old job of caring for patients.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Are you sure your patient is alive?
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
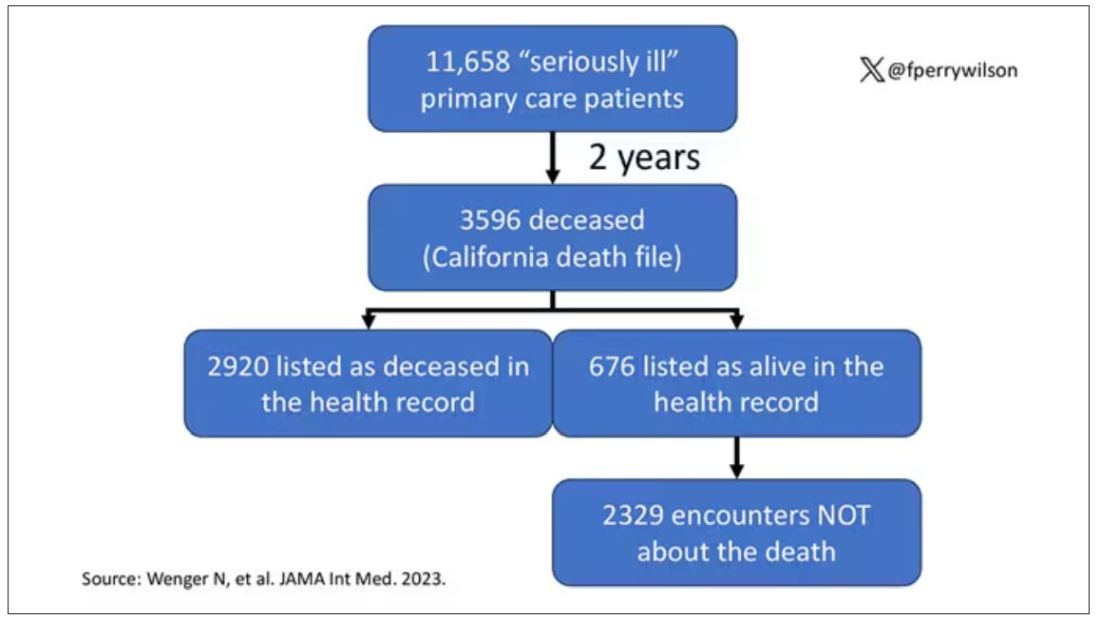
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.
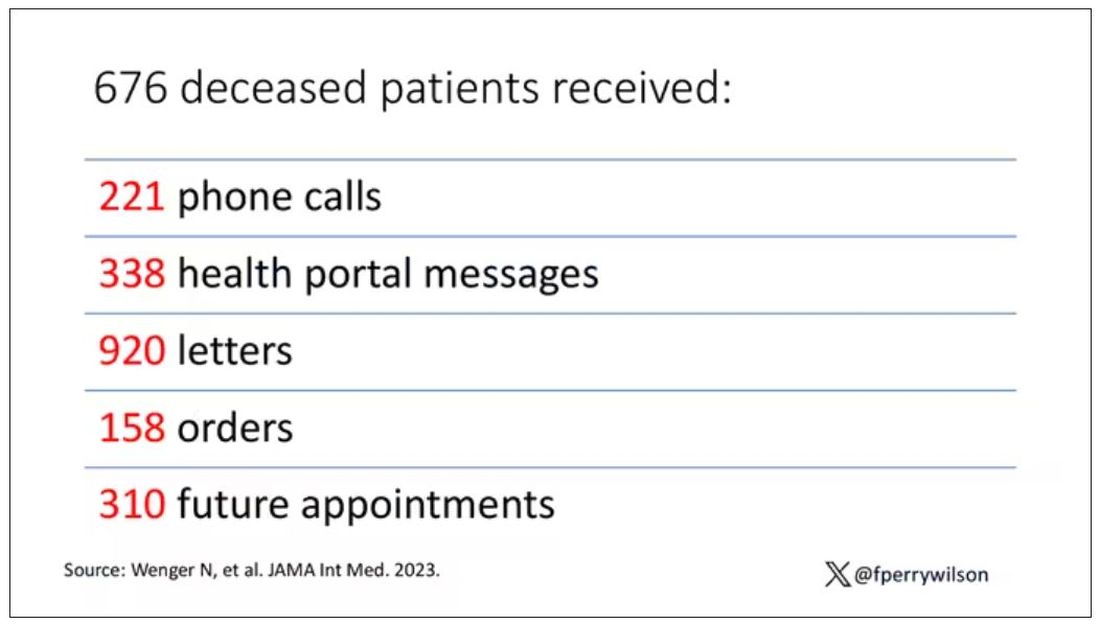
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
Experimental Therapy Restores Cognitive Function in Chronic TBI
(msTBI) and chronic sequelae.
Participants in this first-in-humans trial experienced brain injuries between 3-18 years before the study that left them with persistent neuropsychological impairment and a range of functional disabilities.
This is the first time a DBS device has been implanted in the central thalamus in humans, an area of the brain measuring only a few millimeters wide that helps regulate consciousness.
Placing the electrodes required a novel surgical technique developed by the investigators that included virtual models of each participant’s brain, microelectrode recording, and neuroimaging to identify neuronal circuits affected by the TBI.
After 3 months of 12-hour daily DBS treatments, participants’ performance on cognitive tests improved by an average of 32% from baseline. Participants were able to read books, watch TV shows, play video games, complete schoolwork, and felt significantly less fatigued during the day.
Although the small trial only included five patients, the work is already being hailed by other experts as significant.“We were looking for partial restoration of executive attention and expected [the treatment] would have an effect, but I wouldn’t have anticipated the effect size we saw,” co-lead investigator Nicholas Schiff, MD, professor of neuroscience at Weill Cornell Medical College, New York City, said in an interview.
The findings were published online Dec. 4 in Nature Medicine.
“No Trivial Feat”
An estimated 5.3 million children and adults are living with a permanent TBI-related disability in the US today. There currently is no effective therapy for impaired attention, executive function, working memory or information-processing speed caused by the initial injury.
Previous research suggests that a loss of activity in key brain circuits in the thalamus may be associated with a loss of cognitive function.
The investigators recruited six adults (four men and two women) between the ages of 22 and 60 years with a history of msTBI and chronic neuropsychological impairment and functional disability. One participant was later withdrawn from the trial for protocol noncompliance.
Participants completed a range of questionnaires and tests to establish baseline cognitive, psychological, and quality-of-life status.
To restore lost executive functioning in the brain, investigators had to target not only the central lateral nucleus, but also the neuronal network connected to the region that reaches other parts of the brain.
“To do both of those things we had to develop a whole toolset in order to model both the target and trajectory, which had to be right to make it work properly,” co-lead investigator Jaimie Henderson, MD, professor of neurosurgery at Stanford University College of Medicine, Stanford, California, said in an interview. “That gave us a pretty narrow window in which to work and getting an electrode accurately to this target is not a trivial feat.”
“A Moving Target”
Each participant’s brain physiology was slightly different, meaning the path that worked for one individual might not work for another. The surgery was further complicated by shifting in the brain that occurred as individual electrodes were placed.
“It was a literal moving target,” Dr. Henderson said.
In the beginning, investigators used microelectrode recording to “listen” to individual neurons to see which ones weren’t firing correctly.
When that method failed to offer the precise information needed for electrode placement, the investigators switched to neuroimaging, which allowed them to complete the surgery more quickly and accurately.
Participants remained in the hospital 1-2 days after surgery. They returned for postoperative imaging 30 days after surgery and were randomly assigned to different schedules for a 14-day titration period to optimize DBS stimulation.
The primary outcome was a 10% improvement on part B of the trail-making test, a neuropsychological test that measures executive functioning.
After 90 days of 12-hour daily DBS treatments, participants’ scores increased 15%–52% (average 32%) from baseline. Participants also reported an average of 33% decline in fatigue, one of the most common side effects of msTBI, and an average 80% improvement in attention.
The main safety risk during the 3- to-4-hour procedure is bleeding, which didn’t affect any of the participants in this study. One participant developed a surgical site infection, but all other side effects were mild.
After the 90-day treatment period, the study plan called for patients to be randomly assigned to a blinded withdrawal of treatment, with the DBS turned off for 21 days. Two of the patients declined to be randomized. DBS was turned off in one participant while the other two continued as normal.
After 3 weeks, the patient whose DBS was turned off showed a 34% decline on cognitive tests. The device was reactivated after the study and that participant has since reported improvements.
The DBS devices continue to function in all participants. Although their performance is not being measured as part of the study, anecdotal reports indicate sustained improvement in executive functioning.
“The brain injury causes this global down-regulation of brain function and what we think that this is doing is turning that back up again,” Dr. Henderson said. “At a very simplistic level, what we’re trying to do is turn the lights back up after the dimmer switch is switched down from the injury.”
New Hope
TBI patients are usually treated aggressively during the first year, when significant improvements are most likely, but there are few therapeutic options beyond that time, said neurologist Javier Cardenas, MD, who commented on the findings for this article.
“Many providers throw their hands up after a year in terms of intervention and then we’re always looking at potential declines over time,” said Dr. Cardenas, director of the Concussion and Brain Injury Center at the Rockefeller Neuroscience Institution, West Virginia University, Morgantown. “Most people plateau and don’t decline but we’re always worried about a secondary decline in traumatic brain injury.”Surgery is usually only employed immediately following the brain injury. The notion of surgery as a therapeutic option years after the initial assault on the brain is novel, said Jimmy Yang, MD, assistant professor of neurologic surgery at Ohio State University College of Medicine, Columbus, who commented on the findings for this article.
“While deep brain stimulation surgery in clinical practice is specifically tailored to each patient we treat, this study goes a step further by integrating research tools that have not yet made it to the clinical realm,” Dr. Yang said. “As a result, while these methods are not commonly used in clinical care, the overall strategy highlights how research advances are linked to clinical advances.”
Investigators are working to secure funding for a larger phase 2 trial.
“With millions of people affected by traumatic brain injury but without effective therapies, this study brings hope that options are on the horizon to help these patients,” Dr. Yang said.
The study was supported by funding from the National Institute of Health BRAIN Initiative and a grant from the Translational Science Center at Weill Cornell Medical College. Surgical implants were provided by Medtronic. Dr. Henderson and Dr. Schiff are listed as inventors on several patent applications for the experimental DBS therapy described in the study. Dr. Cardenas and Dr. Yang report no relevant financial relationships.
A version of this article first appeared on Medscape.com .
(msTBI) and chronic sequelae.
Participants in this first-in-humans trial experienced brain injuries between 3-18 years before the study that left them with persistent neuropsychological impairment and a range of functional disabilities.
This is the first time a DBS device has been implanted in the central thalamus in humans, an area of the brain measuring only a few millimeters wide that helps regulate consciousness.
Placing the electrodes required a novel surgical technique developed by the investigators that included virtual models of each participant’s brain, microelectrode recording, and neuroimaging to identify neuronal circuits affected by the TBI.
After 3 months of 12-hour daily DBS treatments, participants’ performance on cognitive tests improved by an average of 32% from baseline. Participants were able to read books, watch TV shows, play video games, complete schoolwork, and felt significantly less fatigued during the day.
Although the small trial only included five patients, the work is already being hailed by other experts as significant.“We were looking for partial restoration of executive attention and expected [the treatment] would have an effect, but I wouldn’t have anticipated the effect size we saw,” co-lead investigator Nicholas Schiff, MD, professor of neuroscience at Weill Cornell Medical College, New York City, said in an interview.
The findings were published online Dec. 4 in Nature Medicine.
“No Trivial Feat”
An estimated 5.3 million children and adults are living with a permanent TBI-related disability in the US today. There currently is no effective therapy for impaired attention, executive function, working memory or information-processing speed caused by the initial injury.
Previous research suggests that a loss of activity in key brain circuits in the thalamus may be associated with a loss of cognitive function.
The investigators recruited six adults (four men and two women) between the ages of 22 and 60 years with a history of msTBI and chronic neuropsychological impairment and functional disability. One participant was later withdrawn from the trial for protocol noncompliance.
Participants completed a range of questionnaires and tests to establish baseline cognitive, psychological, and quality-of-life status.
To restore lost executive functioning in the brain, investigators had to target not only the central lateral nucleus, but also the neuronal network connected to the region that reaches other parts of the brain.
“To do both of those things we had to develop a whole toolset in order to model both the target and trajectory, which had to be right to make it work properly,” co-lead investigator Jaimie Henderson, MD, professor of neurosurgery at Stanford University College of Medicine, Stanford, California, said in an interview. “That gave us a pretty narrow window in which to work and getting an electrode accurately to this target is not a trivial feat.”
“A Moving Target”
Each participant’s brain physiology was slightly different, meaning the path that worked for one individual might not work for another. The surgery was further complicated by shifting in the brain that occurred as individual electrodes were placed.
“It was a literal moving target,” Dr. Henderson said.
In the beginning, investigators used microelectrode recording to “listen” to individual neurons to see which ones weren’t firing correctly.
When that method failed to offer the precise information needed for electrode placement, the investigators switched to neuroimaging, which allowed them to complete the surgery more quickly and accurately.
Participants remained in the hospital 1-2 days after surgery. They returned for postoperative imaging 30 days after surgery and were randomly assigned to different schedules for a 14-day titration period to optimize DBS stimulation.
The primary outcome was a 10% improvement on part B of the trail-making test, a neuropsychological test that measures executive functioning.
After 90 days of 12-hour daily DBS treatments, participants’ scores increased 15%–52% (average 32%) from baseline. Participants also reported an average of 33% decline in fatigue, one of the most common side effects of msTBI, and an average 80% improvement in attention.
The main safety risk during the 3- to-4-hour procedure is bleeding, which didn’t affect any of the participants in this study. One participant developed a surgical site infection, but all other side effects were mild.
After the 90-day treatment period, the study plan called for patients to be randomly assigned to a blinded withdrawal of treatment, with the DBS turned off for 21 days. Two of the patients declined to be randomized. DBS was turned off in one participant while the other two continued as normal.
After 3 weeks, the patient whose DBS was turned off showed a 34% decline on cognitive tests. The device was reactivated after the study and that participant has since reported improvements.
The DBS devices continue to function in all participants. Although their performance is not being measured as part of the study, anecdotal reports indicate sustained improvement in executive functioning.
“The brain injury causes this global down-regulation of brain function and what we think that this is doing is turning that back up again,” Dr. Henderson said. “At a very simplistic level, what we’re trying to do is turn the lights back up after the dimmer switch is switched down from the injury.”
New Hope
TBI patients are usually treated aggressively during the first year, when significant improvements are most likely, but there are few therapeutic options beyond that time, said neurologist Javier Cardenas, MD, who commented on the findings for this article.
“Many providers throw their hands up after a year in terms of intervention and then we’re always looking at potential declines over time,” said Dr. Cardenas, director of the Concussion and Brain Injury Center at the Rockefeller Neuroscience Institution, West Virginia University, Morgantown. “Most people plateau and don’t decline but we’re always worried about a secondary decline in traumatic brain injury.”Surgery is usually only employed immediately following the brain injury. The notion of surgery as a therapeutic option years after the initial assault on the brain is novel, said Jimmy Yang, MD, assistant professor of neurologic surgery at Ohio State University College of Medicine, Columbus, who commented on the findings for this article.
“While deep brain stimulation surgery in clinical practice is specifically tailored to each patient we treat, this study goes a step further by integrating research tools that have not yet made it to the clinical realm,” Dr. Yang said. “As a result, while these methods are not commonly used in clinical care, the overall strategy highlights how research advances are linked to clinical advances.”
Investigators are working to secure funding for a larger phase 2 trial.
“With millions of people affected by traumatic brain injury but without effective therapies, this study brings hope that options are on the horizon to help these patients,” Dr. Yang said.
The study was supported by funding from the National Institute of Health BRAIN Initiative and a grant from the Translational Science Center at Weill Cornell Medical College. Surgical implants were provided by Medtronic. Dr. Henderson and Dr. Schiff are listed as inventors on several patent applications for the experimental DBS therapy described in the study. Dr. Cardenas and Dr. Yang report no relevant financial relationships.
A version of this article first appeared on Medscape.com .
(msTBI) and chronic sequelae.
Participants in this first-in-humans trial experienced brain injuries between 3-18 years before the study that left them with persistent neuropsychological impairment and a range of functional disabilities.
This is the first time a DBS device has been implanted in the central thalamus in humans, an area of the brain measuring only a few millimeters wide that helps regulate consciousness.
Placing the electrodes required a novel surgical technique developed by the investigators that included virtual models of each participant’s brain, microelectrode recording, and neuroimaging to identify neuronal circuits affected by the TBI.
After 3 months of 12-hour daily DBS treatments, participants’ performance on cognitive tests improved by an average of 32% from baseline. Participants were able to read books, watch TV shows, play video games, complete schoolwork, and felt significantly less fatigued during the day.
Although the small trial only included five patients, the work is already being hailed by other experts as significant.“We were looking for partial restoration of executive attention and expected [the treatment] would have an effect, but I wouldn’t have anticipated the effect size we saw,” co-lead investigator Nicholas Schiff, MD, professor of neuroscience at Weill Cornell Medical College, New York City, said in an interview.
The findings were published online Dec. 4 in Nature Medicine.
“No Trivial Feat”
An estimated 5.3 million children and adults are living with a permanent TBI-related disability in the US today. There currently is no effective therapy for impaired attention, executive function, working memory or information-processing speed caused by the initial injury.
Previous research suggests that a loss of activity in key brain circuits in the thalamus may be associated with a loss of cognitive function.
The investigators recruited six adults (four men and two women) between the ages of 22 and 60 years with a history of msTBI and chronic neuropsychological impairment and functional disability. One participant was later withdrawn from the trial for protocol noncompliance.
Participants completed a range of questionnaires and tests to establish baseline cognitive, psychological, and quality-of-life status.
To restore lost executive functioning in the brain, investigators had to target not only the central lateral nucleus, but also the neuronal network connected to the region that reaches other parts of the brain.
“To do both of those things we had to develop a whole toolset in order to model both the target and trajectory, which had to be right to make it work properly,” co-lead investigator Jaimie Henderson, MD, professor of neurosurgery at Stanford University College of Medicine, Stanford, California, said in an interview. “That gave us a pretty narrow window in which to work and getting an electrode accurately to this target is not a trivial feat.”
“A Moving Target”
Each participant’s brain physiology was slightly different, meaning the path that worked for one individual might not work for another. The surgery was further complicated by shifting in the brain that occurred as individual electrodes were placed.
“It was a literal moving target,” Dr. Henderson said.
In the beginning, investigators used microelectrode recording to “listen” to individual neurons to see which ones weren’t firing correctly.
When that method failed to offer the precise information needed for electrode placement, the investigators switched to neuroimaging, which allowed them to complete the surgery more quickly and accurately.
Participants remained in the hospital 1-2 days after surgery. They returned for postoperative imaging 30 days after surgery and were randomly assigned to different schedules for a 14-day titration period to optimize DBS stimulation.
The primary outcome was a 10% improvement on part B of the trail-making test, a neuropsychological test that measures executive functioning.
After 90 days of 12-hour daily DBS treatments, participants’ scores increased 15%–52% (average 32%) from baseline. Participants also reported an average of 33% decline in fatigue, one of the most common side effects of msTBI, and an average 80% improvement in attention.
The main safety risk during the 3- to-4-hour procedure is bleeding, which didn’t affect any of the participants in this study. One participant developed a surgical site infection, but all other side effects were mild.
After the 90-day treatment period, the study plan called for patients to be randomly assigned to a blinded withdrawal of treatment, with the DBS turned off for 21 days. Two of the patients declined to be randomized. DBS was turned off in one participant while the other two continued as normal.
After 3 weeks, the patient whose DBS was turned off showed a 34% decline on cognitive tests. The device was reactivated after the study and that participant has since reported improvements.
The DBS devices continue to function in all participants. Although their performance is not being measured as part of the study, anecdotal reports indicate sustained improvement in executive functioning.
“The brain injury causes this global down-regulation of brain function and what we think that this is doing is turning that back up again,” Dr. Henderson said. “At a very simplistic level, what we’re trying to do is turn the lights back up after the dimmer switch is switched down from the injury.”
New Hope
TBI patients are usually treated aggressively during the first year, when significant improvements are most likely, but there are few therapeutic options beyond that time, said neurologist Javier Cardenas, MD, who commented on the findings for this article.
“Many providers throw their hands up after a year in terms of intervention and then we’re always looking at potential declines over time,” said Dr. Cardenas, director of the Concussion and Brain Injury Center at the Rockefeller Neuroscience Institution, West Virginia University, Morgantown. “Most people plateau and don’t decline but we’re always worried about a secondary decline in traumatic brain injury.”Surgery is usually only employed immediately following the brain injury. The notion of surgery as a therapeutic option years after the initial assault on the brain is novel, said Jimmy Yang, MD, assistant professor of neurologic surgery at Ohio State University College of Medicine, Columbus, who commented on the findings for this article.
“While deep brain stimulation surgery in clinical practice is specifically tailored to each patient we treat, this study goes a step further by integrating research tools that have not yet made it to the clinical realm,” Dr. Yang said. “As a result, while these methods are not commonly used in clinical care, the overall strategy highlights how research advances are linked to clinical advances.”
Investigators are working to secure funding for a larger phase 2 trial.
“With millions of people affected by traumatic brain injury but without effective therapies, this study brings hope that options are on the horizon to help these patients,” Dr. Yang said.
The study was supported by funding from the National Institute of Health BRAIN Initiative and a grant from the Translational Science Center at Weill Cornell Medical College. Surgical implants were provided by Medtronic. Dr. Henderson and Dr. Schiff are listed as inventors on several patent applications for the experimental DBS therapy described in the study. Dr. Cardenas and Dr. Yang report no relevant financial relationships.
A version of this article first appeared on Medscape.com .
PFO closure may reduce migraine days and prevent stroke
, according to a discussion at the 2023 Scottsdale Headache Symposium.
In two clinical trials evaluating whether PFO closure reduces migraine risk, the primary endpoints were not met, but a signal of benefit on secondary endpoints and the association between PFO, migraine, and stroke are among the reasons that PFO closure should be reevaluated, according to Andrew Charles MD, Director of the Goldberg Migraine Program, University of California, Los Angeles.
Other right-to-left shunt defects have also been associated with both migraine and stroke, leading Dr. Charles to suggest these defects are more a common denominator.
“Stroke during a migraine is, in fact, very uncommon,” Dr. Charles said. “This raises the possibility that it is not the migraine causing the stroke but rather there is a shared risk factor for stroke and migraine,” said Dr. Charles, referring to PFO as well as other right-to-left shunt defects, such as hereditary hemorrhaging telangiectasia in the lungs.
One Intervention, Two Potential Benefits
Fixing these defects is therefore at least theoretically attractive for preventing both migraine and stroke, but Dr. Charles said the opportunity for preventing both migraine and stroke is most attractive in migraine patients who have additional stroke risk factors.
Use of oral contraceptives, which produce a hypercoagulable state, is an example.
“Are these the people we should really be thinking about if they have PFO and migraine, particularly migraine with aura?” Dr. Charles asked.
The association between right-to-left shunts and migraine is strong. Although PFO is common, presenting in 20%-25% of the adult population, it has been found in up to 50% of individuals who have migraine with aura. In patients with migraine but no aura, the prevalence of PFO has been estimated to be approximately 35% or still somewhat elevated relative to the general population.
Primary Endpoint Missed in Clinical Trials
The question of whether risk of migraine can be reduced with repair of PFO or other right-to-left shunts remains unresolved. In two high-quality randomized trials undertaken in PFO repair, neither met its primary endpoint. In one of these, called PRIMA, which was terminated early for slow enrollment, the reduction in mean headache attacks was not significant relative to medical therapy.
In the second, called PREMIUM, device closure of PFO also failed to significantly reduce migraine attacks over sham procedure although it was associated with complete migraine remission (10% vs 1%).
A pooled analysis of these two studies that was conducted subsequently concluded that PFO closure reduces mean monthly migraine days (-3.1 vs. -1.9 days; P = -.02) and increases the likelihood of complete migraine cessation (9% vs. 0.7%; P < .001), but Dr. Charles pointed out the primary endpoint was migraine attacks not migraine days, so other analyses can only be considered hypothesis-generating.
There are several reasons to relook at the relationship between migraine and PFO but the potential to prevent both migraine and stroke with PFO closure could be one of the most important.
Several years ago, Dr. Charles and his coinvestigators from UCLA evaluated more than 700 ischemic strokes. Of these, 127 strokes were characterized as cryptogenic because of lack of another identifiable etiology. While 59% of these patients had PFO, which is several times higher than the general population, the prevalence of PFO in patients with a cryptogenic stroke and a history of migraine was 79% in this published study.
“So, in this group of patients who did not have any other clear cause for a stroke, a diagnosis of PFO was very much overrepresented,” Dr. Charles said.
Migraine Days Might Be a Better Endpoint
For patients with migraine who have risk factors for stroke, this makes PFO closure an attractive intervention, but a positive randomized trial is needed. Several are underway. Importantly, the trials now enrolling are using migraine days, which was significantly reduced in both PREMIUM and PRIMA, rather than migraine attacks as the primary endpoint.
“Migraine days is now accepted by the Food and Drug Administration as a criterion of benefit,” reported Jonathan Tobis, MD, Research Director, Interventional Cardiology, UCLA David Geffen School of Medicine, Los Angeles.
He explained that the FDA insisted on migraine attacks as the endpoint for the PREMIUM trial, but this was a far more challenging endpoint on which to show a statistical benefit. He emphasized that a new set of trials will now test efficacy on the basis of migraine days.
One of these trials, called RELIEF, which is randomizing patients to device closure of PFO or a sham procedure. Both groups are receiving clopidogrel or prasugrel based on a previous observation that patients who respond to these drugs are also more likely to respond to PFO closure.
Another trial, called COMPETE-2, is comparing PFO closure with a device to aspirin plus a sham closure. This trial is ongoing in China.
Stroke is not being evaluated as an endpoint in either trial, but Dr. Charles suggested that this does warrant attention.
“I would also just put it out there that, apart from simply migraine, this is a therapeutic approach that we might actually think about in terms of helping to prevent stroke in our migraine patients,” he said.
Senior author of a recent meta-analysis of trials evaluating PFO closure and control of migraine, Ling Liu, MD, Department of Neurology, University of Sichuan, Chengdu, China, agreed that PFO closure for the treatment of migraine deserves “a reevaluation.”
In his meta-analysis of three randomized trials, one pooled study, and eight retrospective case series with 1,165 patients, PFO closure was associated with a nearly 75% reduction (odds ratio [OR], 0.259; P = .0048) reduction in migraine days and 50% increase in resolution of migraine in patients with a history of migraine with aura (OR, 1.586; P = .227).
The incidence of stroke was not evaluated in this meta-analysis, but Dr. Liu believes that the evidence of reducing the burden of migraine with PFO closure is compelling. Given the evidence from this meta-analysis that PFO closure is safe, Dr. Liu maintained that a definitive trial is needed “especially for migraine with frequent aura.”
As an interventional cardiologist, Dr. Tobis said that when PFO closures is performed for prevention of stroke in patients with migraine, it often leads to reduced migraine activity and, in some cases, elimination of migraine. Like others, he believes new analyses should be conducted.
“Everyone involved in this field believes there is something there,” Dr. Tobis said. The missing link is a clinical trial to confirm it.
Dr. Charles and Dr. Liu report no potential conflicts of interest. Dr. Tobis reports a financial relationship with Holistick Medical.
, according to a discussion at the 2023 Scottsdale Headache Symposium.
In two clinical trials evaluating whether PFO closure reduces migraine risk, the primary endpoints were not met, but a signal of benefit on secondary endpoints and the association between PFO, migraine, and stroke are among the reasons that PFO closure should be reevaluated, according to Andrew Charles MD, Director of the Goldberg Migraine Program, University of California, Los Angeles.
Other right-to-left shunt defects have also been associated with both migraine and stroke, leading Dr. Charles to suggest these defects are more a common denominator.
“Stroke during a migraine is, in fact, very uncommon,” Dr. Charles said. “This raises the possibility that it is not the migraine causing the stroke but rather there is a shared risk factor for stroke and migraine,” said Dr. Charles, referring to PFO as well as other right-to-left shunt defects, such as hereditary hemorrhaging telangiectasia in the lungs.
One Intervention, Two Potential Benefits
Fixing these defects is therefore at least theoretically attractive for preventing both migraine and stroke, but Dr. Charles said the opportunity for preventing both migraine and stroke is most attractive in migraine patients who have additional stroke risk factors.
Use of oral contraceptives, which produce a hypercoagulable state, is an example.
“Are these the people we should really be thinking about if they have PFO and migraine, particularly migraine with aura?” Dr. Charles asked.
The association between right-to-left shunts and migraine is strong. Although PFO is common, presenting in 20%-25% of the adult population, it has been found in up to 50% of individuals who have migraine with aura. In patients with migraine but no aura, the prevalence of PFO has been estimated to be approximately 35% or still somewhat elevated relative to the general population.
Primary Endpoint Missed in Clinical Trials
The question of whether risk of migraine can be reduced with repair of PFO or other right-to-left shunts remains unresolved. In two high-quality randomized trials undertaken in PFO repair, neither met its primary endpoint. In one of these, called PRIMA, which was terminated early for slow enrollment, the reduction in mean headache attacks was not significant relative to medical therapy.
In the second, called PREMIUM, device closure of PFO also failed to significantly reduce migraine attacks over sham procedure although it was associated with complete migraine remission (10% vs 1%).
A pooled analysis of these two studies that was conducted subsequently concluded that PFO closure reduces mean monthly migraine days (-3.1 vs. -1.9 days; P = -.02) and increases the likelihood of complete migraine cessation (9% vs. 0.7%; P < .001), but Dr. Charles pointed out the primary endpoint was migraine attacks not migraine days, so other analyses can only be considered hypothesis-generating.
There are several reasons to relook at the relationship between migraine and PFO but the potential to prevent both migraine and stroke with PFO closure could be one of the most important.
Several years ago, Dr. Charles and his coinvestigators from UCLA evaluated more than 700 ischemic strokes. Of these, 127 strokes were characterized as cryptogenic because of lack of another identifiable etiology. While 59% of these patients had PFO, which is several times higher than the general population, the prevalence of PFO in patients with a cryptogenic stroke and a history of migraine was 79% in this published study.
“So, in this group of patients who did not have any other clear cause for a stroke, a diagnosis of PFO was very much overrepresented,” Dr. Charles said.
Migraine Days Might Be a Better Endpoint
For patients with migraine who have risk factors for stroke, this makes PFO closure an attractive intervention, but a positive randomized trial is needed. Several are underway. Importantly, the trials now enrolling are using migraine days, which was significantly reduced in both PREMIUM and PRIMA, rather than migraine attacks as the primary endpoint.
“Migraine days is now accepted by the Food and Drug Administration as a criterion of benefit,” reported Jonathan Tobis, MD, Research Director, Interventional Cardiology, UCLA David Geffen School of Medicine, Los Angeles.
He explained that the FDA insisted on migraine attacks as the endpoint for the PREMIUM trial, but this was a far more challenging endpoint on which to show a statistical benefit. He emphasized that a new set of trials will now test efficacy on the basis of migraine days.
One of these trials, called RELIEF, which is randomizing patients to device closure of PFO or a sham procedure. Both groups are receiving clopidogrel or prasugrel based on a previous observation that patients who respond to these drugs are also more likely to respond to PFO closure.
Another trial, called COMPETE-2, is comparing PFO closure with a device to aspirin plus a sham closure. This trial is ongoing in China.
Stroke is not being evaluated as an endpoint in either trial, but Dr. Charles suggested that this does warrant attention.
“I would also just put it out there that, apart from simply migraine, this is a therapeutic approach that we might actually think about in terms of helping to prevent stroke in our migraine patients,” he said.
Senior author of a recent meta-analysis of trials evaluating PFO closure and control of migraine, Ling Liu, MD, Department of Neurology, University of Sichuan, Chengdu, China, agreed that PFO closure for the treatment of migraine deserves “a reevaluation.”
In his meta-analysis of three randomized trials, one pooled study, and eight retrospective case series with 1,165 patients, PFO closure was associated with a nearly 75% reduction (odds ratio [OR], 0.259; P = .0048) reduction in migraine days and 50% increase in resolution of migraine in patients with a history of migraine with aura (OR, 1.586; P = .227).
The incidence of stroke was not evaluated in this meta-analysis, but Dr. Liu believes that the evidence of reducing the burden of migraine with PFO closure is compelling. Given the evidence from this meta-analysis that PFO closure is safe, Dr. Liu maintained that a definitive trial is needed “especially for migraine with frequent aura.”
As an interventional cardiologist, Dr. Tobis said that when PFO closures is performed for prevention of stroke in patients with migraine, it often leads to reduced migraine activity and, in some cases, elimination of migraine. Like others, he believes new analyses should be conducted.
“Everyone involved in this field believes there is something there,” Dr. Tobis said. The missing link is a clinical trial to confirm it.
Dr. Charles and Dr. Liu report no potential conflicts of interest. Dr. Tobis reports a financial relationship with Holistick Medical.
, according to a discussion at the 2023 Scottsdale Headache Symposium.
In two clinical trials evaluating whether PFO closure reduces migraine risk, the primary endpoints were not met, but a signal of benefit on secondary endpoints and the association between PFO, migraine, and stroke are among the reasons that PFO closure should be reevaluated, according to Andrew Charles MD, Director of the Goldberg Migraine Program, University of California, Los Angeles.
Other right-to-left shunt defects have also been associated with both migraine and stroke, leading Dr. Charles to suggest these defects are more a common denominator.
“Stroke during a migraine is, in fact, very uncommon,” Dr. Charles said. “This raises the possibility that it is not the migraine causing the stroke but rather there is a shared risk factor for stroke and migraine,” said Dr. Charles, referring to PFO as well as other right-to-left shunt defects, such as hereditary hemorrhaging telangiectasia in the lungs.
One Intervention, Two Potential Benefits
Fixing these defects is therefore at least theoretically attractive for preventing both migraine and stroke, but Dr. Charles said the opportunity for preventing both migraine and stroke is most attractive in migraine patients who have additional stroke risk factors.
Use of oral contraceptives, which produce a hypercoagulable state, is an example.
“Are these the people we should really be thinking about if they have PFO and migraine, particularly migraine with aura?” Dr. Charles asked.
The association between right-to-left shunts and migraine is strong. Although PFO is common, presenting in 20%-25% of the adult population, it has been found in up to 50% of individuals who have migraine with aura. In patients with migraine but no aura, the prevalence of PFO has been estimated to be approximately 35% or still somewhat elevated relative to the general population.
Primary Endpoint Missed in Clinical Trials
The question of whether risk of migraine can be reduced with repair of PFO or other right-to-left shunts remains unresolved. In two high-quality randomized trials undertaken in PFO repair, neither met its primary endpoint. In one of these, called PRIMA, which was terminated early for slow enrollment, the reduction in mean headache attacks was not significant relative to medical therapy.
In the second, called PREMIUM, device closure of PFO also failed to significantly reduce migraine attacks over sham procedure although it was associated with complete migraine remission (10% vs 1%).
A pooled analysis of these two studies that was conducted subsequently concluded that PFO closure reduces mean monthly migraine days (-3.1 vs. -1.9 days; P = -.02) and increases the likelihood of complete migraine cessation (9% vs. 0.7%; P < .001), but Dr. Charles pointed out the primary endpoint was migraine attacks not migraine days, so other analyses can only be considered hypothesis-generating.
There are several reasons to relook at the relationship between migraine and PFO but the potential to prevent both migraine and stroke with PFO closure could be one of the most important.
Several years ago, Dr. Charles and his coinvestigators from UCLA evaluated more than 700 ischemic strokes. Of these, 127 strokes were characterized as cryptogenic because of lack of another identifiable etiology. While 59% of these patients had PFO, which is several times higher than the general population, the prevalence of PFO in patients with a cryptogenic stroke and a history of migraine was 79% in this published study.
“So, in this group of patients who did not have any other clear cause for a stroke, a diagnosis of PFO was very much overrepresented,” Dr. Charles said.
Migraine Days Might Be a Better Endpoint
For patients with migraine who have risk factors for stroke, this makes PFO closure an attractive intervention, but a positive randomized trial is needed. Several are underway. Importantly, the trials now enrolling are using migraine days, which was significantly reduced in both PREMIUM and PRIMA, rather than migraine attacks as the primary endpoint.
“Migraine days is now accepted by the Food and Drug Administration as a criterion of benefit,” reported Jonathan Tobis, MD, Research Director, Interventional Cardiology, UCLA David Geffen School of Medicine, Los Angeles.
He explained that the FDA insisted on migraine attacks as the endpoint for the PREMIUM trial, but this was a far more challenging endpoint on which to show a statistical benefit. He emphasized that a new set of trials will now test efficacy on the basis of migraine days.
One of these trials, called RELIEF, which is randomizing patients to device closure of PFO or a sham procedure. Both groups are receiving clopidogrel or prasugrel based on a previous observation that patients who respond to these drugs are also more likely to respond to PFO closure.
Another trial, called COMPETE-2, is comparing PFO closure with a device to aspirin plus a sham closure. This trial is ongoing in China.
Stroke is not being evaluated as an endpoint in either trial, but Dr. Charles suggested that this does warrant attention.
“I would also just put it out there that, apart from simply migraine, this is a therapeutic approach that we might actually think about in terms of helping to prevent stroke in our migraine patients,” he said.
Senior author of a recent meta-analysis of trials evaluating PFO closure and control of migraine, Ling Liu, MD, Department of Neurology, University of Sichuan, Chengdu, China, agreed that PFO closure for the treatment of migraine deserves “a reevaluation.”
In his meta-analysis of three randomized trials, one pooled study, and eight retrospective case series with 1,165 patients, PFO closure was associated with a nearly 75% reduction (odds ratio [OR], 0.259; P = .0048) reduction in migraine days and 50% increase in resolution of migraine in patients with a history of migraine with aura (OR, 1.586; P = .227).
The incidence of stroke was not evaluated in this meta-analysis, but Dr. Liu believes that the evidence of reducing the burden of migraine with PFO closure is compelling. Given the evidence from this meta-analysis that PFO closure is safe, Dr. Liu maintained that a definitive trial is needed “especially for migraine with frequent aura.”
As an interventional cardiologist, Dr. Tobis said that when PFO closures is performed for prevention of stroke in patients with migraine, it often leads to reduced migraine activity and, in some cases, elimination of migraine. Like others, he believes new analyses should be conducted.
“Everyone involved in this field believes there is something there,” Dr. Tobis said. The missing link is a clinical trial to confirm it.
Dr. Charles and Dr. Liu report no potential conflicts of interest. Dr. Tobis reports a financial relationship with Holistick Medical.
FROM THE 2023 SCOTTSDALE HEADACHE SYMPOSIUM
Secondhand smoke exposure linked to migraine, severe headache
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
, with effects of exposure varying depending on body mass index (BMI) and level of physical activity, new research shows.
METHODOLOGY:
Investigators analyzed data on 4,560 participants (median age, 43 years; 60% female; 71.5% White) from the 1999-2004 National Health and Nutrition Examination Survey.
Participants were aged 20 years or older and had never smoked.
Migraine headache status was determined by asking whether participants experienced severe headaches or migraines during the previous 3 months.
SHS exposure was categorized as unexposed (serum cotinine levels <0.05 ng/mL and no smoker in the home), low (0.05 ng/mL ≤ serum cotinine level <1 ng/mL), or heavy (1 ng/mL ≤ serum cotinine level ≤ 10 ng/mL).
TAKEAWAY:
In all, 919 (20%) participants had severe headaches or migraines.
After adjustment for demographic and lifestyle factors (including medication use), heavy SHS exposure was positively associated with severe headache or migraine (adjusted odds ratio [aOR], 2.02; 95% CI, 1.19-3.43).
No significant association was found between low SHS exposure and severe headaches or migraine (aOR, 1.15; 95% CI, 0.91-1.47).
In participants who were sedentary (P=.016) and those with a BMI <25 (P=.001), significant associations between SHS and severe headache or migraine were observed.
IN PRACTICE:
Noting a linear dose-response relationship between cotinine and severe headaches or migraine, the investigators write, “These findings underscore the need for stronger regulation of tobacco exposure, particularly in homes and public places.”
SOURCE:
Junpeng Wu, MMc, and Haitang Wang, MD, of Southern Medical University in Guangzhou, China, and their colleagues conducted the study. It was published online in Headache.
LIMITATIONS:
The study could not establish causal relationships between SHS and migraine or severe headache. In addition, the half-life of serum cotinine is 15-40 hours and thus this measure can reflect only recent SHS exposure.
DISCLOSURES:
The study was not funded. The investigators reported no disclosures.
A version of this article appeared on Medscape.com.
New tests may finally diagnose long COVID
One of the biggest challenges facing clinicians who treat long COVID is a lack of consensus when it comes to recognizing and diagnosing the condition. But
Effective diagnostic testing would be a game-changer in the long COVID fight, for it’s not just the fatigue, brain fog, heart palpitations, and other persistent symptoms that affect patients. Two out of three people with long COVID also suffer mental health challenges like depression and anxiety. Some patients say their symptoms are not taken seriously by their doctors. And as many as 12% of long COVID patients are unemployed because of the severity of their illness and their employers may be skeptical of their condition.
Quick, accurate diagnosis would eliminate all that. Now a new preprint study suggests that the elevation of certain immune system proteins are a commonality in long COVID patients and identifying them may be an accurate way to diagnose the condition.
Researchers at Cardiff (Wales) University, tracked 166 patients, 79 of whom had been diagnosed with long COVID and 87 who had not. All participants had recovered from a severe bout of acute COVID-19.
In an analysis of the blood plasma of the study participants, researchers found elevated levels of certain components. Four proteins in particular – Ba, iC3b, C5a, and TCC – predicted the presence of long COVID with 78.5% accuracy.
“I was gobsmacked by the results. We’re seeing a massive dysregulation in those four biomarkers,” says study author Wioleta Zelek, PhD, a research fellow at Cardiff University. “It’s a combination that we showed was predictive of long COVID.”
The study revealed that long COVID was associated with inflammation of the immune system causing these complement proteins to remain dysregulated. Proteins like C3, C4, and C5 are important parts of the immune system because they recruit phagocytes, cells that attack and engulf bacteria and viruses at the site of infection to destroy pathogens like SARS-coV-2.
In the case of long COVID, these proteins remain chronically elevated. While the symptoms of long COVID have seemed largely unrelated to one another, researchers point to elevated inflammation as a connecting factor that causes various systems in the body to go haywire.
“Anything that could help to better diagnose patients with long COVID is research we’re greatly appreciative of within the clinical community,” said Nisha Viswanathan, MD, director of the University of California, Los Angeles, Long COVID program at UCLA Health.
Testing for biomarkers highlighted in the study, as well as others like serotonin and cortisol, may help doctors separate patients who have long COVID from patients who have similar symptoms caused by other conditions, said Dr. Viswanathan. For example, a recent study published in the journal Cell found lower serotonin levels in long COVID patients, compared with patients who were diagnosed with acute COVID-19 but recovered from the condition.
Dr. Viswanathan cautions that the biomarker test does not answer all the questions about diagnosing long COVID. For example, Dr. Viswanathan said scientists don’t know whether complement dysregulation is caused by long COVID and not another underlying medical issue that patients had prior to infection, because “we don’t know where patients’ levels were prior to developing long COVID.” For example, those with autoimmune issues are more likely to develop long COVID, which means their levels could have been elevated prior to a COVID infection.
It is increasingly likely, said Dr. Viswanathan, that long COVID is an umbrella term for a host of conditions that could be caused by different impacts of the virus. Other research has pointed to the different phenotypes of long COVID. For example, some are focused on cardiopulmonary issues and others on fatigue and gastrointestinal problems.
“It looks like these different phenotypes have a different mechanism for disease,” she said. This means that it’s less likely to be a one-size-fits-all condition and the next step in the research should be identifying which biomarker is aligned with which phenotype of the disease.
Better diagnostics will open the door to better treatments, Dr. Zelek said. The more doctors understand about the mechanism causing immune dysregulation in long COVID patients, the more they can treat it with existing medications. Dr. Zelek’s lab has been studying certain medications like pegcetacoplan (C3 blocker), danicopan (anti-factor D), and iptacopan (anti-factor B) that can be used to break the body’s cycle of inflammation and reduce symptoms experienced in those with long COVID.
These drugs are approved by the U.S. Food and Drug Administration for the treatment of a rare blood disease called paroxysmal nocturnal hemoglobinuria. The C5 inhibitor zilucoplan has also been used in patients hospitalized with COVID-19 and researchers have found that the drug lowered serum C5 and interleukin-8 concentration in the blood, seeming to reduce certain aspects of the immune system’s inflammatory response to the virus.
The Cardiff University research is one of the most detailed studies to highlight long COVID biomarkers to date, said infectious disease specialist Grace McComsey, MD, who leads the long COVID RECOVER study at University Hospitals Health System in Cleveland, Ohio. The research needs to be duplicated in a larger study population that might include the other biomarkers like serotonin and cortisol to see if they’re related, she said.
Researchers are learning more everyday about the various biomarkers that may be linked to long COVID, she added. This Cardiff study showed that a huge percentage of those patients had elevated levels of certain complements. The next step, said Dr. McComsey, “is to put all these puzzle pieces together” so that clinicians have a common diagnostic tool or tools that provide patients with some peace of mind in starting their road to recovery.
A version of this article first appeared on Medscape.com.
One of the biggest challenges facing clinicians who treat long COVID is a lack of consensus when it comes to recognizing and diagnosing the condition. But
Effective diagnostic testing would be a game-changer in the long COVID fight, for it’s not just the fatigue, brain fog, heart palpitations, and other persistent symptoms that affect patients. Two out of three people with long COVID also suffer mental health challenges like depression and anxiety. Some patients say their symptoms are not taken seriously by their doctors. And as many as 12% of long COVID patients are unemployed because of the severity of their illness and their employers may be skeptical of their condition.
Quick, accurate diagnosis would eliminate all that. Now a new preprint study suggests that the elevation of certain immune system proteins are a commonality in long COVID patients and identifying them may be an accurate way to diagnose the condition.
Researchers at Cardiff (Wales) University, tracked 166 patients, 79 of whom had been diagnosed with long COVID and 87 who had not. All participants had recovered from a severe bout of acute COVID-19.
In an analysis of the blood plasma of the study participants, researchers found elevated levels of certain components. Four proteins in particular – Ba, iC3b, C5a, and TCC – predicted the presence of long COVID with 78.5% accuracy.
“I was gobsmacked by the results. We’re seeing a massive dysregulation in those four biomarkers,” says study author Wioleta Zelek, PhD, a research fellow at Cardiff University. “It’s a combination that we showed was predictive of long COVID.”
The study revealed that long COVID was associated with inflammation of the immune system causing these complement proteins to remain dysregulated. Proteins like C3, C4, and C5 are important parts of the immune system because they recruit phagocytes, cells that attack and engulf bacteria and viruses at the site of infection to destroy pathogens like SARS-coV-2.
In the case of long COVID, these proteins remain chronically elevated. While the symptoms of long COVID have seemed largely unrelated to one another, researchers point to elevated inflammation as a connecting factor that causes various systems in the body to go haywire.
“Anything that could help to better diagnose patients with long COVID is research we’re greatly appreciative of within the clinical community,” said Nisha Viswanathan, MD, director of the University of California, Los Angeles, Long COVID program at UCLA Health.
Testing for biomarkers highlighted in the study, as well as others like serotonin and cortisol, may help doctors separate patients who have long COVID from patients who have similar symptoms caused by other conditions, said Dr. Viswanathan. For example, a recent study published in the journal Cell found lower serotonin levels in long COVID patients, compared with patients who were diagnosed with acute COVID-19 but recovered from the condition.
Dr. Viswanathan cautions that the biomarker test does not answer all the questions about diagnosing long COVID. For example, Dr. Viswanathan said scientists don’t know whether complement dysregulation is caused by long COVID and not another underlying medical issue that patients had prior to infection, because “we don’t know where patients’ levels were prior to developing long COVID.” For example, those with autoimmune issues are more likely to develop long COVID, which means their levels could have been elevated prior to a COVID infection.
It is increasingly likely, said Dr. Viswanathan, that long COVID is an umbrella term for a host of conditions that could be caused by different impacts of the virus. Other research has pointed to the different phenotypes of long COVID. For example, some are focused on cardiopulmonary issues and others on fatigue and gastrointestinal problems.
“It looks like these different phenotypes have a different mechanism for disease,” she said. This means that it’s less likely to be a one-size-fits-all condition and the next step in the research should be identifying which biomarker is aligned with which phenotype of the disease.
Better diagnostics will open the door to better treatments, Dr. Zelek said. The more doctors understand about the mechanism causing immune dysregulation in long COVID patients, the more they can treat it with existing medications. Dr. Zelek’s lab has been studying certain medications like pegcetacoplan (C3 blocker), danicopan (anti-factor D), and iptacopan (anti-factor B) that can be used to break the body’s cycle of inflammation and reduce symptoms experienced in those with long COVID.
These drugs are approved by the U.S. Food and Drug Administration for the treatment of a rare blood disease called paroxysmal nocturnal hemoglobinuria. The C5 inhibitor zilucoplan has also been used in patients hospitalized with COVID-19 and researchers have found that the drug lowered serum C5 and interleukin-8 concentration in the blood, seeming to reduce certain aspects of the immune system’s inflammatory response to the virus.
The Cardiff University research is one of the most detailed studies to highlight long COVID biomarkers to date, said infectious disease specialist Grace McComsey, MD, who leads the long COVID RECOVER study at University Hospitals Health System in Cleveland, Ohio. The research needs to be duplicated in a larger study population that might include the other biomarkers like serotonin and cortisol to see if they’re related, she said.
Researchers are learning more everyday about the various biomarkers that may be linked to long COVID, she added. This Cardiff study showed that a huge percentage of those patients had elevated levels of certain complements. The next step, said Dr. McComsey, “is to put all these puzzle pieces together” so that clinicians have a common diagnostic tool or tools that provide patients with some peace of mind in starting their road to recovery.
A version of this article first appeared on Medscape.com.
One of the biggest challenges facing clinicians who treat long COVID is a lack of consensus when it comes to recognizing and diagnosing the condition. But
Effective diagnostic testing would be a game-changer in the long COVID fight, for it’s not just the fatigue, brain fog, heart palpitations, and other persistent symptoms that affect patients. Two out of three people with long COVID also suffer mental health challenges like depression and anxiety. Some patients say their symptoms are not taken seriously by their doctors. And as many as 12% of long COVID patients are unemployed because of the severity of their illness and their employers may be skeptical of their condition.
Quick, accurate diagnosis would eliminate all that. Now a new preprint study suggests that the elevation of certain immune system proteins are a commonality in long COVID patients and identifying them may be an accurate way to diagnose the condition.
Researchers at Cardiff (Wales) University, tracked 166 patients, 79 of whom had been diagnosed with long COVID and 87 who had not. All participants had recovered from a severe bout of acute COVID-19.
In an analysis of the blood plasma of the study participants, researchers found elevated levels of certain components. Four proteins in particular – Ba, iC3b, C5a, and TCC – predicted the presence of long COVID with 78.5% accuracy.
“I was gobsmacked by the results. We’re seeing a massive dysregulation in those four biomarkers,” says study author Wioleta Zelek, PhD, a research fellow at Cardiff University. “It’s a combination that we showed was predictive of long COVID.”
The study revealed that long COVID was associated with inflammation of the immune system causing these complement proteins to remain dysregulated. Proteins like C3, C4, and C5 are important parts of the immune system because they recruit phagocytes, cells that attack and engulf bacteria and viruses at the site of infection to destroy pathogens like SARS-coV-2.
In the case of long COVID, these proteins remain chronically elevated. While the symptoms of long COVID have seemed largely unrelated to one another, researchers point to elevated inflammation as a connecting factor that causes various systems in the body to go haywire.
“Anything that could help to better diagnose patients with long COVID is research we’re greatly appreciative of within the clinical community,” said Nisha Viswanathan, MD, director of the University of California, Los Angeles, Long COVID program at UCLA Health.
Testing for biomarkers highlighted in the study, as well as others like serotonin and cortisol, may help doctors separate patients who have long COVID from patients who have similar symptoms caused by other conditions, said Dr. Viswanathan. For example, a recent study published in the journal Cell found lower serotonin levels in long COVID patients, compared with patients who were diagnosed with acute COVID-19 but recovered from the condition.
Dr. Viswanathan cautions that the biomarker test does not answer all the questions about diagnosing long COVID. For example, Dr. Viswanathan said scientists don’t know whether complement dysregulation is caused by long COVID and not another underlying medical issue that patients had prior to infection, because “we don’t know where patients’ levels were prior to developing long COVID.” For example, those with autoimmune issues are more likely to develop long COVID, which means their levels could have been elevated prior to a COVID infection.
It is increasingly likely, said Dr. Viswanathan, that long COVID is an umbrella term for a host of conditions that could be caused by different impacts of the virus. Other research has pointed to the different phenotypes of long COVID. For example, some are focused on cardiopulmonary issues and others on fatigue and gastrointestinal problems.
“It looks like these different phenotypes have a different mechanism for disease,” she said. This means that it’s less likely to be a one-size-fits-all condition and the next step in the research should be identifying which biomarker is aligned with which phenotype of the disease.
Better diagnostics will open the door to better treatments, Dr. Zelek said. The more doctors understand about the mechanism causing immune dysregulation in long COVID patients, the more they can treat it with existing medications. Dr. Zelek’s lab has been studying certain medications like pegcetacoplan (C3 blocker), danicopan (anti-factor D), and iptacopan (anti-factor B) that can be used to break the body’s cycle of inflammation and reduce symptoms experienced in those with long COVID.
These drugs are approved by the U.S. Food and Drug Administration for the treatment of a rare blood disease called paroxysmal nocturnal hemoglobinuria. The C5 inhibitor zilucoplan has also been used in patients hospitalized with COVID-19 and researchers have found that the drug lowered serum C5 and interleukin-8 concentration in the blood, seeming to reduce certain aspects of the immune system’s inflammatory response to the virus.
The Cardiff University research is one of the most detailed studies to highlight long COVID biomarkers to date, said infectious disease specialist Grace McComsey, MD, who leads the long COVID RECOVER study at University Hospitals Health System in Cleveland, Ohio. The research needs to be duplicated in a larger study population that might include the other biomarkers like serotonin and cortisol to see if they’re related, she said.
Researchers are learning more everyday about the various biomarkers that may be linked to long COVID, she added. This Cardiff study showed that a huge percentage of those patients had elevated levels of certain complements. The next step, said Dr. McComsey, “is to put all these puzzle pieces together” so that clinicians have a common diagnostic tool or tools that provide patients with some peace of mind in starting their road to recovery.
A version of this article first appeared on Medscape.com.
FROM MEDRXIV
Food insecurity a dementia risk factor?
TOPLINE:
Food insecurity among older adults is associated with increased dementia risk, poorer memory function, and faster memory decline, new research indicates.
METHODOLOGY:
- Researchers analyzed data on 7,012 adults (mean age, 67 years; 59% women) from the U.S. Health and Retirement Study.
- Food security status was assessed in 2013 using a validated survey, with cognitive outcomes evaluated between 2014 and 2018.
- Analyses were adjusted for demographics, socioeconomics, and health factors.
TAKEAWAY:
- About 18% of adults were food insecure, with 10% reporting low food security and 8% very low food security. About 11% of those aged 65+ in 2013 were food insecure.
- The odds of dementia were 38% higher (odds ratio, 1.38; 95% confidence interval [CI], 1.15-1.67) in adults with low food security and 37% higher (OR, 1.37; 95% CI, 1.11-1.59) in those with very low food security, compared with food-secure adults.
- Translated to years of excess cognitive aging, food insecurity was associated with increased dementia risk equivalent to roughly 1.3 excess years of aging.
- Low and very low food security were also associated with lower memory levels and faster age-related memory decline.
IN PRACTICE:
“Our study contributes to a limited literature by capitalizing on a large and diverse sample, validated exposure and outcome measures, and longitudinal data to robustly evaluate these associations, providing evidence in support of the connection between food insecurity in older adulthood and subsequent brain health,” the authors wrote. “Our findings highlight the need to improve food security in older adults and that doing so may protect individuals from cognitive decline and dementia.”
SOURCE:
The study, with first author Haobing Qian, PhD, with the University of California, San Francisco, was published online in JAMA Network Open.
LIMITATIONS:
Residual confounding cannot be ruled out. Food insecurity was not assessed prior to 2013. The researchers lacked information on clinical dementia diagnoses.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health. The authors reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
Food insecurity among older adults is associated with increased dementia risk, poorer memory function, and faster memory decline, new research indicates.
METHODOLOGY:
- Researchers analyzed data on 7,012 adults (mean age, 67 years; 59% women) from the U.S. Health and Retirement Study.
- Food security status was assessed in 2013 using a validated survey, with cognitive outcomes evaluated between 2014 and 2018.
- Analyses were adjusted for demographics, socioeconomics, and health factors.
TAKEAWAY:
- About 18% of adults were food insecure, with 10% reporting low food security and 8% very low food security. About 11% of those aged 65+ in 2013 were food insecure.
- The odds of dementia were 38% higher (odds ratio, 1.38; 95% confidence interval [CI], 1.15-1.67) in adults with low food security and 37% higher (OR, 1.37; 95% CI, 1.11-1.59) in those with very low food security, compared with food-secure adults.
- Translated to years of excess cognitive aging, food insecurity was associated with increased dementia risk equivalent to roughly 1.3 excess years of aging.
- Low and very low food security were also associated with lower memory levels and faster age-related memory decline.
IN PRACTICE:
“Our study contributes to a limited literature by capitalizing on a large and diverse sample, validated exposure and outcome measures, and longitudinal data to robustly evaluate these associations, providing evidence in support of the connection between food insecurity in older adulthood and subsequent brain health,” the authors wrote. “Our findings highlight the need to improve food security in older adults and that doing so may protect individuals from cognitive decline and dementia.”
SOURCE:
The study, with first author Haobing Qian, PhD, with the University of California, San Francisco, was published online in JAMA Network Open.
LIMITATIONS:
Residual confounding cannot be ruled out. Food insecurity was not assessed prior to 2013. The researchers lacked information on clinical dementia diagnoses.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health. The authors reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
Food insecurity among older adults is associated with increased dementia risk, poorer memory function, and faster memory decline, new research indicates.
METHODOLOGY:
- Researchers analyzed data on 7,012 adults (mean age, 67 years; 59% women) from the U.S. Health and Retirement Study.
- Food security status was assessed in 2013 using a validated survey, with cognitive outcomes evaluated between 2014 and 2018.
- Analyses were adjusted for demographics, socioeconomics, and health factors.
TAKEAWAY:
- About 18% of adults were food insecure, with 10% reporting low food security and 8% very low food security. About 11% of those aged 65+ in 2013 were food insecure.
- The odds of dementia were 38% higher (odds ratio, 1.38; 95% confidence interval [CI], 1.15-1.67) in adults with low food security and 37% higher (OR, 1.37; 95% CI, 1.11-1.59) in those with very low food security, compared with food-secure adults.
- Translated to years of excess cognitive aging, food insecurity was associated with increased dementia risk equivalent to roughly 1.3 excess years of aging.
- Low and very low food security were also associated with lower memory levels and faster age-related memory decline.
IN PRACTICE:
“Our study contributes to a limited literature by capitalizing on a large and diverse sample, validated exposure and outcome measures, and longitudinal data to robustly evaluate these associations, providing evidence in support of the connection between food insecurity in older adulthood and subsequent brain health,” the authors wrote. “Our findings highlight the need to improve food security in older adults and that doing so may protect individuals from cognitive decline and dementia.”
SOURCE:
The study, with first author Haobing Qian, PhD, with the University of California, San Francisco, was published online in JAMA Network Open.
LIMITATIONS:
Residual confounding cannot be ruled out. Food insecurity was not assessed prior to 2013. The researchers lacked information on clinical dementia diagnoses.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health. The authors reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Exercise improves physical and cognitive health in Down syndrome
In the first study of its kind, U.K. and French researchers reported that exercise positively affected physical and cognitive health in persons with Down syndrome. “The findings are significant and offer a crucial challenge to the [Down syndrome] and wider societies,” wrote a team led by Dan Gordon, PhD, associate professor of cardiorespiratory exercise physiology at Anglia Ruskin University in Cambridge, England. “Impact of Prescribed Exercise on the Physical and Cognitive Health of Adults with Down Syndrome: The MinDSets Study” was published in the International Journal of Environmental Research and Public Health.
“Through the simple application of walking, a form of exercise which requires little to no equipment or expense, there were significant increases in cognitive and executive function, reflecting improved capabilities in key attributes of information processing, vigilance, and selective attention,” the researchers wrote.
“Increased cognitive function will help foster increased societal integration and quality of life, which, given that this is the first generation of those with [Down syndrome] to outlive their parents and caregivers, is of importance,” they wrote.
For example, those in an exercise-only intervention arm had an 11.4% improvement on the distance covered in the Six-Minute Walk Test, going from a mean of 498.8 meters before intervention to 522.1 meters afterward. Those in a group that combined group exercise with cognitive training increased the distance walked by 9.9%, or 49.2 meters. Groups that got cognitive training only or no intervention showed no significant changes.
In measures of cognitive function, the exercise group showed a 38% increase in selective attention, with the cognitive and combined groups showing changes for the same measure of 16.5% and 55.3%, respectively. The changes for concentration in the exercise-alone group was 31.5%, while those receiving cognitive training alone or combined exercise plus cognitive training showed improvements in concentration of 21% and 15%, respectively.
Asked why a combination intervention was not superior to exercise alone, Dr. Gordon said in an interview, “Something we’re looking at in the data but can’t fully confirm is that the combined group started to become fatigued due to the double dose of the intervention, and this prevented them in the final tests from doing quite so well as the exercise-alone group. Irrespective of the magnitude of change, any cognitive adaptation observed will be beneficial to this population.”
The evidence for the benefits of exercise on both physical and cognitive health in a non–Down syndrome population are well established, he said, but there were few data on its effect on the Down syndrome population.
One small study showed physical and neurocognitive benefits with resistance training.
“The evidence from previous studies showed increased levels of inactivity and sitting time in Down syndrome individuals compared with non–[Down syndrome] controls, so we hypothesized that exercise, albeit small amounts, would increase their physical fitness,” Dr. Gordon said.
His team also hypothesized that walking would stimulate cognitive development since it requires heightened cognitive engagement compared with inactivity. “What surprised us was the degree of improvement,” Dr. Gordon said.
The process of walking requires the brain to interpret information on a real-time basis from both internal and external cues, he continued. “For most of us this process requires low-level cognitive engagement. However, in the [Down syndrome] population, where motor control is impaired and accompanied by poor muscle tone, walking imposes a heightened cognitive load.” It requires them to concentrate on the action, be aware of their surroundings, and make the right decisions, all of which stimulate areas of the brain that control these functions.
Study details
Eighty-three adult participants were available for final analysis – 67 from North America, 8 from Europe, 5 from Africa, 2 from Asia, and 1 from Australia. The mean age of participants was 27.1 years, 40 were female, and all had caregiver support during the study.
Those unable to visualize information on computer and mobile/tablet screens or to listen to instructions/auditory cues were excluded. All were provided with instructions and a mobile monitoring tool set to record steps completed, distances covered, speeds, and heart rate.
Each was assigned to one of four groups. Exercise intervention-only consisted of 8 weeks of cardiorespiratory exercise defined as either walking or jogging three times a week for 30 minutes. Cognitive training included eight levels (about 20 minutes) of cognitive and executive function exercises six times per week. The combined group completed both the cardiorespiratory and cognitive interventions, while the fourth group acted as controls with no intervention.
According to the authors, the study offers a real-life scenario that can be readily adopted within the Down syndrome community.
This study was commissioned by the Canadian Down Syndrome Society. The authors had no conflicts of interest to declare.
In the first study of its kind, U.K. and French researchers reported that exercise positively affected physical and cognitive health in persons with Down syndrome. “The findings are significant and offer a crucial challenge to the [Down syndrome] and wider societies,” wrote a team led by Dan Gordon, PhD, associate professor of cardiorespiratory exercise physiology at Anglia Ruskin University in Cambridge, England. “Impact of Prescribed Exercise on the Physical and Cognitive Health of Adults with Down Syndrome: The MinDSets Study” was published in the International Journal of Environmental Research and Public Health.
“Through the simple application of walking, a form of exercise which requires little to no equipment or expense, there were significant increases in cognitive and executive function, reflecting improved capabilities in key attributes of information processing, vigilance, and selective attention,” the researchers wrote.
“Increased cognitive function will help foster increased societal integration and quality of life, which, given that this is the first generation of those with [Down syndrome] to outlive their parents and caregivers, is of importance,” they wrote.
For example, those in an exercise-only intervention arm had an 11.4% improvement on the distance covered in the Six-Minute Walk Test, going from a mean of 498.8 meters before intervention to 522.1 meters afterward. Those in a group that combined group exercise with cognitive training increased the distance walked by 9.9%, or 49.2 meters. Groups that got cognitive training only or no intervention showed no significant changes.
In measures of cognitive function, the exercise group showed a 38% increase in selective attention, with the cognitive and combined groups showing changes for the same measure of 16.5% and 55.3%, respectively. The changes for concentration in the exercise-alone group was 31.5%, while those receiving cognitive training alone or combined exercise plus cognitive training showed improvements in concentration of 21% and 15%, respectively.
Asked why a combination intervention was not superior to exercise alone, Dr. Gordon said in an interview, “Something we’re looking at in the data but can’t fully confirm is that the combined group started to become fatigued due to the double dose of the intervention, and this prevented them in the final tests from doing quite so well as the exercise-alone group. Irrespective of the magnitude of change, any cognitive adaptation observed will be beneficial to this population.”
The evidence for the benefits of exercise on both physical and cognitive health in a non–Down syndrome population are well established, he said, but there were few data on its effect on the Down syndrome population.
One small study showed physical and neurocognitive benefits with resistance training.
“The evidence from previous studies showed increased levels of inactivity and sitting time in Down syndrome individuals compared with non–[Down syndrome] controls, so we hypothesized that exercise, albeit small amounts, would increase their physical fitness,” Dr. Gordon said.
His team also hypothesized that walking would stimulate cognitive development since it requires heightened cognitive engagement compared with inactivity. “What surprised us was the degree of improvement,” Dr. Gordon said.
The process of walking requires the brain to interpret information on a real-time basis from both internal and external cues, he continued. “For most of us this process requires low-level cognitive engagement. However, in the [Down syndrome] population, where motor control is impaired and accompanied by poor muscle tone, walking imposes a heightened cognitive load.” It requires them to concentrate on the action, be aware of their surroundings, and make the right decisions, all of which stimulate areas of the brain that control these functions.
Study details
Eighty-three adult participants were available for final analysis – 67 from North America, 8 from Europe, 5 from Africa, 2 from Asia, and 1 from Australia. The mean age of participants was 27.1 years, 40 were female, and all had caregiver support during the study.
Those unable to visualize information on computer and mobile/tablet screens or to listen to instructions/auditory cues were excluded. All were provided with instructions and a mobile monitoring tool set to record steps completed, distances covered, speeds, and heart rate.
Each was assigned to one of four groups. Exercise intervention-only consisted of 8 weeks of cardiorespiratory exercise defined as either walking or jogging three times a week for 30 minutes. Cognitive training included eight levels (about 20 minutes) of cognitive and executive function exercises six times per week. The combined group completed both the cardiorespiratory and cognitive interventions, while the fourth group acted as controls with no intervention.
According to the authors, the study offers a real-life scenario that can be readily adopted within the Down syndrome community.
This study was commissioned by the Canadian Down Syndrome Society. The authors had no conflicts of interest to declare.
In the first study of its kind, U.K. and French researchers reported that exercise positively affected physical and cognitive health in persons with Down syndrome. “The findings are significant and offer a crucial challenge to the [Down syndrome] and wider societies,” wrote a team led by Dan Gordon, PhD, associate professor of cardiorespiratory exercise physiology at Anglia Ruskin University in Cambridge, England. “Impact of Prescribed Exercise on the Physical and Cognitive Health of Adults with Down Syndrome: The MinDSets Study” was published in the International Journal of Environmental Research and Public Health.
“Through the simple application of walking, a form of exercise which requires little to no equipment or expense, there were significant increases in cognitive and executive function, reflecting improved capabilities in key attributes of information processing, vigilance, and selective attention,” the researchers wrote.
“Increased cognitive function will help foster increased societal integration and quality of life, which, given that this is the first generation of those with [Down syndrome] to outlive their parents and caregivers, is of importance,” they wrote.
For example, those in an exercise-only intervention arm had an 11.4% improvement on the distance covered in the Six-Minute Walk Test, going from a mean of 498.8 meters before intervention to 522.1 meters afterward. Those in a group that combined group exercise with cognitive training increased the distance walked by 9.9%, or 49.2 meters. Groups that got cognitive training only or no intervention showed no significant changes.
In measures of cognitive function, the exercise group showed a 38% increase in selective attention, with the cognitive and combined groups showing changes for the same measure of 16.5% and 55.3%, respectively. The changes for concentration in the exercise-alone group was 31.5%, while those receiving cognitive training alone or combined exercise plus cognitive training showed improvements in concentration of 21% and 15%, respectively.
Asked why a combination intervention was not superior to exercise alone, Dr. Gordon said in an interview, “Something we’re looking at in the data but can’t fully confirm is that the combined group started to become fatigued due to the double dose of the intervention, and this prevented them in the final tests from doing quite so well as the exercise-alone group. Irrespective of the magnitude of change, any cognitive adaptation observed will be beneficial to this population.”
The evidence for the benefits of exercise on both physical and cognitive health in a non–Down syndrome population are well established, he said, but there were few data on its effect on the Down syndrome population.
One small study showed physical and neurocognitive benefits with resistance training.
“The evidence from previous studies showed increased levels of inactivity and sitting time in Down syndrome individuals compared with non–[Down syndrome] controls, so we hypothesized that exercise, albeit small amounts, would increase their physical fitness,” Dr. Gordon said.
His team also hypothesized that walking would stimulate cognitive development since it requires heightened cognitive engagement compared with inactivity. “What surprised us was the degree of improvement,” Dr. Gordon said.
The process of walking requires the brain to interpret information on a real-time basis from both internal and external cues, he continued. “For most of us this process requires low-level cognitive engagement. However, in the [Down syndrome] population, where motor control is impaired and accompanied by poor muscle tone, walking imposes a heightened cognitive load.” It requires them to concentrate on the action, be aware of their surroundings, and make the right decisions, all of which stimulate areas of the brain that control these functions.
Study details
Eighty-three adult participants were available for final analysis – 67 from North America, 8 from Europe, 5 from Africa, 2 from Asia, and 1 from Australia. The mean age of participants was 27.1 years, 40 were female, and all had caregiver support during the study.
Those unable to visualize information on computer and mobile/tablet screens or to listen to instructions/auditory cues were excluded. All were provided with instructions and a mobile monitoring tool set to record steps completed, distances covered, speeds, and heart rate.
Each was assigned to one of four groups. Exercise intervention-only consisted of 8 weeks of cardiorespiratory exercise defined as either walking or jogging three times a week for 30 minutes. Cognitive training included eight levels (about 20 minutes) of cognitive and executive function exercises six times per week. The combined group completed both the cardiorespiratory and cognitive interventions, while the fourth group acted as controls with no intervention.
According to the authors, the study offers a real-life scenario that can be readily adopted within the Down syndrome community.
This study was commissioned by the Canadian Down Syndrome Society. The authors had no conflicts of interest to declare.
FROM INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH