User login
EUS and MRCP as complementary studies in the etiologic diagnosis of idiopathic acute pancreatitis
Background: Approximately 10%-30% of patients with acute pancreatitis do not have an established etiology after routine investigation with imaging. These patients are classified as IAP. Less invasive tests, such as EUS, MRCP, and secretin stimulation MRCP (S-MRCP) have been used to further explore IAP, but their comparison in the etiologic diagnosis of idiopathic acute pancreatitis is lacking.
Study design: Meta-analysis involving 34 studies that investigated the etiology of IAP with MRCP and/or S-MRCP and/or EUS.
Setting: Brazil, Canada, China, France, Hong Kong, India, Italy, Korea, Spain, the United Kingdom, and the United States.
Synopsis: When EUS was compared with MRCP, the diagnostic yield of EUS (153/239 patients; 64%) was higher than that of MRCP (82/238 patients; 34%; P less than .01). Specifically, EUS seemed to have a significant benefit in detecting biliary disease, compared with MRCP. In the subgroup analysis, the diagnostic yield of EUS was higher than that of MRCP for detecting parenchymal changes suggestive of chronic pancreatitis (10% vs. 1%). S-MRCP was superior to EUS and MRCP (12% vs. 2% vs. 2%, respectively) in diagnosing pancreatic divisum, a congenital anomaly that is prevalent in 5%-14% of the population and an etiology of IAP.
A limitation in this meta-analysis was that EUS was used in seven times as many studies as was MRCP, which may have influenced the overall results.
Bottom line: Less invasive modalities, such as EUS and S-MRCP, used together could improve the diagnostic yield in evaluating the etiology of AIP.
Citation: Wang J et al. Comparison of EUS with MRCP in idiopathic acute pancreatitis: A systemic review and meta-analysis. Gastrointest Endosc. 2017 Dec 7. doi: 10.1016/j.gie.2017.11.028.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Background: Approximately 10%-30% of patients with acute pancreatitis do not have an established etiology after routine investigation with imaging. These patients are classified as IAP. Less invasive tests, such as EUS, MRCP, and secretin stimulation MRCP (S-MRCP) have been used to further explore IAP, but their comparison in the etiologic diagnosis of idiopathic acute pancreatitis is lacking.
Study design: Meta-analysis involving 34 studies that investigated the etiology of IAP with MRCP and/or S-MRCP and/or EUS.
Setting: Brazil, Canada, China, France, Hong Kong, India, Italy, Korea, Spain, the United Kingdom, and the United States.
Synopsis: When EUS was compared with MRCP, the diagnostic yield of EUS (153/239 patients; 64%) was higher than that of MRCP (82/238 patients; 34%; P less than .01). Specifically, EUS seemed to have a significant benefit in detecting biliary disease, compared with MRCP. In the subgroup analysis, the diagnostic yield of EUS was higher than that of MRCP for detecting parenchymal changes suggestive of chronic pancreatitis (10% vs. 1%). S-MRCP was superior to EUS and MRCP (12% vs. 2% vs. 2%, respectively) in diagnosing pancreatic divisum, a congenital anomaly that is prevalent in 5%-14% of the population and an etiology of IAP.
A limitation in this meta-analysis was that EUS was used in seven times as many studies as was MRCP, which may have influenced the overall results.
Bottom line: Less invasive modalities, such as EUS and S-MRCP, used together could improve the diagnostic yield in evaluating the etiology of AIP.
Citation: Wang J et al. Comparison of EUS with MRCP in idiopathic acute pancreatitis: A systemic review and meta-analysis. Gastrointest Endosc. 2017 Dec 7. doi: 10.1016/j.gie.2017.11.028.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Background: Approximately 10%-30% of patients with acute pancreatitis do not have an established etiology after routine investigation with imaging. These patients are classified as IAP. Less invasive tests, such as EUS, MRCP, and secretin stimulation MRCP (S-MRCP) have been used to further explore IAP, but their comparison in the etiologic diagnosis of idiopathic acute pancreatitis is lacking.
Study design: Meta-analysis involving 34 studies that investigated the etiology of IAP with MRCP and/or S-MRCP and/or EUS.
Setting: Brazil, Canada, China, France, Hong Kong, India, Italy, Korea, Spain, the United Kingdom, and the United States.
Synopsis: When EUS was compared with MRCP, the diagnostic yield of EUS (153/239 patients; 64%) was higher than that of MRCP (82/238 patients; 34%; P less than .01). Specifically, EUS seemed to have a significant benefit in detecting biliary disease, compared with MRCP. In the subgroup analysis, the diagnostic yield of EUS was higher than that of MRCP for detecting parenchymal changes suggestive of chronic pancreatitis (10% vs. 1%). S-MRCP was superior to EUS and MRCP (12% vs. 2% vs. 2%, respectively) in diagnosing pancreatic divisum, a congenital anomaly that is prevalent in 5%-14% of the population and an etiology of IAP.
A limitation in this meta-analysis was that EUS was used in seven times as many studies as was MRCP, which may have influenced the overall results.
Bottom line: Less invasive modalities, such as EUS and S-MRCP, used together could improve the diagnostic yield in evaluating the etiology of AIP.
Citation: Wang J et al. Comparison of EUS with MRCP in idiopathic acute pancreatitis: A systemic review and meta-analysis. Gastrointest Endosc. 2017 Dec 7. doi: 10.1016/j.gie.2017.11.028.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Patients With Concussions Aren’t Getting Enough Follow-Up
Many patients with traumatic brain injury (TBI) may not be receiving follow-up care, according to findings from Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI), a long-term NIH-funded study.
Of 831 patients who completed questionnaires 2 weeks and 3 months after sustaining TBI, 44% reported seeing a health care provider within 3 months. Of those, 15% visited a clinic that specialized in head injury. Approximately half saw a general practitioner; close to a third reported seeing ≥ 1 type of doctor.
Among the 279 patients with ≥ 3 symptoms of moderate to severe postconcussion, 41% had not had a follow-up visit at 3 months. Moreover, half of the patients were discharged without TBI educational materials.
Rates and components of follow-up care varied widely from institution to institution even among patients with the same initial degree of injury.
Many patients with traumatic brain injury (TBI) may not be receiving follow-up care, according to findings from Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI), a long-term NIH-funded study.
Of 831 patients who completed questionnaires 2 weeks and 3 months after sustaining TBI, 44% reported seeing a health care provider within 3 months. Of those, 15% visited a clinic that specialized in head injury. Approximately half saw a general practitioner; close to a third reported seeing ≥ 1 type of doctor.
Among the 279 patients with ≥ 3 symptoms of moderate to severe postconcussion, 41% had not had a follow-up visit at 3 months. Moreover, half of the patients were discharged without TBI educational materials.
Rates and components of follow-up care varied widely from institution to institution even among patients with the same initial degree of injury.
Many patients with traumatic brain injury (TBI) may not be receiving follow-up care, according to findings from Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI), a long-term NIH-funded study.
Of 831 patients who completed questionnaires 2 weeks and 3 months after sustaining TBI, 44% reported seeing a health care provider within 3 months. Of those, 15% visited a clinic that specialized in head injury. Approximately half saw a general practitioner; close to a third reported seeing ≥ 1 type of doctor.
Among the 279 patients with ≥ 3 symptoms of moderate to severe postconcussion, 41% had not had a follow-up visit at 3 months. Moreover, half of the patients were discharged without TBI educational materials.
Rates and components of follow-up care varied widely from institution to institution even among patients with the same initial degree of injury.
Talk Therapy—Without Words
Many forms of therapy rely on the patient being able to verbally communicate thoughts and feelings. Arts-based therapies, however, can help people explore sensitive and controversial topics that might be hard to talk about.
Body mapping, which has been in use for more than 30 years, is an interesting, revealing, and productive way of using art to help patients “talk” about their thoughts and feelings. Several studies have used body maps as therapy for patients with HIV/AIDS, but researchers from University of New South Wales, Sydney, theorized that it could be particularly helpful for patients with cognitive disability who have complex support needs as well as those who are socially marginalized.
In body-mapping sessions, participants trace outlines of their bodies and then “populate” the outlines with drawings, magazine photos, symbols, words, and other visual representations of the experience they are investigating. It is a form of storytelling that allows the participant to engage physically, visually, verbally, and relationally (through dialogue and interaction with the researcher).
The researchers used body mapping in 2 studies, first with 29 adults with cognitive disability and complex support needs, such as mental illness and sensory impairment, to explore experiences of support planning. In the second study, one of the researchers used body mapping with 13 teens and young adults with complex support needs (eg, drug and alcohol misuse) to explore support they received during a life transition.
The body-mapping technique, the researchers say, shifts the power balance between researcher and participant, because the patient is in control of the images used and where they are placed on the map. Patients could decide not only how they spoke about the topic, but also which topic they spoke about. The researchers say, “we were often taken to surprising places” that might not have come up in an interview, as when participants used images to reveal aspects of cultural heritage and sexual orientation that had not come up in conversation. For example, a transsexual woman in the second study was uncomfortable with the process until she covered her incorrectly gendered body with another piece of paper on which she could redraw her body as she wished.
Body mapping does not suit everyone, the researchers acknowledge. Participants need to be able to engage in a level of abstraction and reflection about personal experiences. It is important to have other methods available for those who do not want to take part. The researchers say one way they protected patients was by recruiting through service providers so support could be “embedded in existing relationships.” The potential vulnerabilities of the patients mean researchers need to be flexible, they add, and allow the method to evolve, much like the patients’ personal stories.
Source:
Dew A, Smith L, Collings S, Savage ID. FQS. 2018;19(2).
doi: http://dx.doi.org/10.17169/fqs-19.2.2929.
Many forms of therapy rely on the patient being able to verbally communicate thoughts and feelings. Arts-based therapies, however, can help people explore sensitive and controversial topics that might be hard to talk about.
Body mapping, which has been in use for more than 30 years, is an interesting, revealing, and productive way of using art to help patients “talk” about their thoughts and feelings. Several studies have used body maps as therapy for patients with HIV/AIDS, but researchers from University of New South Wales, Sydney, theorized that it could be particularly helpful for patients with cognitive disability who have complex support needs as well as those who are socially marginalized.
In body-mapping sessions, participants trace outlines of their bodies and then “populate” the outlines with drawings, magazine photos, symbols, words, and other visual representations of the experience they are investigating. It is a form of storytelling that allows the participant to engage physically, visually, verbally, and relationally (through dialogue and interaction with the researcher).
The researchers used body mapping in 2 studies, first with 29 adults with cognitive disability and complex support needs, such as mental illness and sensory impairment, to explore experiences of support planning. In the second study, one of the researchers used body mapping with 13 teens and young adults with complex support needs (eg, drug and alcohol misuse) to explore support they received during a life transition.
The body-mapping technique, the researchers say, shifts the power balance between researcher and participant, because the patient is in control of the images used and where they are placed on the map. Patients could decide not only how they spoke about the topic, but also which topic they spoke about. The researchers say, “we were often taken to surprising places” that might not have come up in an interview, as when participants used images to reveal aspects of cultural heritage and sexual orientation that had not come up in conversation. For example, a transsexual woman in the second study was uncomfortable with the process until she covered her incorrectly gendered body with another piece of paper on which she could redraw her body as she wished.
Body mapping does not suit everyone, the researchers acknowledge. Participants need to be able to engage in a level of abstraction and reflection about personal experiences. It is important to have other methods available for those who do not want to take part. The researchers say one way they protected patients was by recruiting through service providers so support could be “embedded in existing relationships.” The potential vulnerabilities of the patients mean researchers need to be flexible, they add, and allow the method to evolve, much like the patients’ personal stories.
Source:
Dew A, Smith L, Collings S, Savage ID. FQS. 2018;19(2).
doi: http://dx.doi.org/10.17169/fqs-19.2.2929.
Many forms of therapy rely on the patient being able to verbally communicate thoughts and feelings. Arts-based therapies, however, can help people explore sensitive and controversial topics that might be hard to talk about.
Body mapping, which has been in use for more than 30 years, is an interesting, revealing, and productive way of using art to help patients “talk” about their thoughts and feelings. Several studies have used body maps as therapy for patients with HIV/AIDS, but researchers from University of New South Wales, Sydney, theorized that it could be particularly helpful for patients with cognitive disability who have complex support needs as well as those who are socially marginalized.
In body-mapping sessions, participants trace outlines of their bodies and then “populate” the outlines with drawings, magazine photos, symbols, words, and other visual representations of the experience they are investigating. It is a form of storytelling that allows the participant to engage physically, visually, verbally, and relationally (through dialogue and interaction with the researcher).
The researchers used body mapping in 2 studies, first with 29 adults with cognitive disability and complex support needs, such as mental illness and sensory impairment, to explore experiences of support planning. In the second study, one of the researchers used body mapping with 13 teens and young adults with complex support needs (eg, drug and alcohol misuse) to explore support they received during a life transition.
The body-mapping technique, the researchers say, shifts the power balance between researcher and participant, because the patient is in control of the images used and where they are placed on the map. Patients could decide not only how they spoke about the topic, but also which topic they spoke about. The researchers say, “we were often taken to surprising places” that might not have come up in an interview, as when participants used images to reveal aspects of cultural heritage and sexual orientation that had not come up in conversation. For example, a transsexual woman in the second study was uncomfortable with the process until she covered her incorrectly gendered body with another piece of paper on which she could redraw her body as she wished.
Body mapping does not suit everyone, the researchers acknowledge. Participants need to be able to engage in a level of abstraction and reflection about personal experiences. It is important to have other methods available for those who do not want to take part. The researchers say one way they protected patients was by recruiting through service providers so support could be “embedded in existing relationships.” The potential vulnerabilities of the patients mean researchers need to be flexible, they add, and allow the method to evolve, much like the patients’ personal stories.
Source:
Dew A, Smith L, Collings S, Savage ID. FQS. 2018;19(2).
doi: http://dx.doi.org/10.17169/fqs-19.2.2929.
EC approves new use, formulation of dasatinib
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
The European Commission (EC) has expanded the marketing authorization for dasatinib (Sprycel).
The drug is now approved to treat patients ages 1 to 18 with Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in chronic phase (CP).
The EC has also approved a new formulation of dasatinib—a powder for oral suspension (PFOS) intended for patients who cannot swallow tablets whole or who weigh 10 kg or less.
Dasatinib is also EC-approved to treat adults with:
- Newly diagnosed Ph+ CML-CP
- Chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy, including imatinib
- Ph+ acute lymphoblastic leukemia and lymphoid blast CML with resistance or intolerance to prior therapy.
The EC’s latest approval of dasatinib is supported by results from a phase 2 trial (NCT00777036), which were published in the Journal of Clinical Oncology in March.
The trial included 29 patients with imatinib-resistant/intolerant CML-CP and 84 patients with newly diagnosed CML-CP.
The previously treated patients received dasatinib tablets. Newly diagnosed patients were treated with dasatinib tablets (n=51) or PFOS (n=33).
Patients who started on PFOS could switch to tablets after receiving PFOS for at least 1 year. Sixty-seven percent of patients on PFOS switched to tablets due to patient preference.
The average daily dose of dasatinib was 58.18 mg/m2 in the previously treated patients and 59.84 mg/m2 in the newly diagnosed patients (for both tablets and PFOS). The median duration of treatment was 49.91 months (range, 1.9 to 90.2) and 42.30 months (range, 0.1 to 75.2), respectively.
Rates of confirmed complete hematologic response (CHR) at any time were 93% in the previously treated patients and 96% in the newly diagnosed patients.
At 12 months, previously treated patients had a major molecular response (MMR) rate of 41% and a complete molecular response (CMR) rate of 7%. In newly diagnosed patients, MMR was 52%, and CMR was 8%.
At 24 months, previously treated patients had an MMR rate of 55% and a CMR rate of 17%. In the newly diagnosed patients, MMR was 70%, and CMR was 21%.
The rate of major cytogenetic response (MCyR) at any time was 89.7% in all previously treated patients and 90% when the researchers excluded patients with MCyR or unknown cytogenetic status at baseline.
The rate of complete cytogenetic response (CCyR) at any time was 94% in all newly diagnosed patients and 93.9% when the researchers excluded patients with CCyR or unknown cytogenetic status at baseline.
The median progression-free survival and overall survival had not been reached at last follow-up.
The estimated 48-month progression-free survival was 78% in the previously treated patients and 93% in the newly diagnosed patients. The estimated 48-month overall survival was 96% and 100%, respectively.
Dasatinib-related adverse events (AEs) occurring in at least 10% of the previously treated patients included nausea/vomiting (31%), myalgia/arthralgia (17%), fatigue (14%), rash (14%), diarrhea (14%), hemorrhage (10%), bone growth and development events (10%), and shortness of breath (10%).
Dasatinib-related AEs occurring in at least 10% of the newly diagnosed patients included nausea/vomiting (20%), myalgia/arthralgia (10%), fatigue (11%), rash (19%), diarrhea (18%), and hemorrhage (10%).
Transplant strategy not viable for aggressive B-NHL
Transplant with radioimmunotherapy (RIT)-based conditioning is a viable treatment option for patients with indolent—but not aggressive—B-cell non-Hodgkin lymphomas (NHLs), according to researchers.
Long-term follow-up data showed “excellent” outcomes in patients with indolent B-NHL who received conditioning with 90Y-ibritumomab tiuxetan plus fludarabine and low-dose total body irradiation (TBI) prior to HLA-matched hematopoietic stem cell transplant (HSCT).
However, long-term outcomes were inferior in patients with diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma (MCL).
Camille E. Puronen, MD, of the University of Washington in Seattle, and her colleagues reported these results in Biology of Blood and Marrow Transplantation.
The study enrolled 40 patients with high-risk B-NHL. This included DLBCL (n=14), chronic lymphocytic leukemia (CLL; n=10), MCL (n=8), follicular lymphoma (FL; n=6); hairy cell leukemia (HCL; n=1), and marginal zone lymphoma (MZL; n=1).
Patients were treated with 0.4 mCi/kg 90Y-ibritumomab tiuxetan, given 2 weeks prior to HSCT, to a maximum dose of 32 mCi.
Patients also received fludarabine at 30 mg/m2 on day 5, 6, and 7 prior to HSCT and 2 Gy TBI given on the day of transplant.
In an earlier report, the objective response rate (ORR) was 60%, and 35% of patients had a complete response (CR) or unconfirmed CR.
The researchers said early responses were not associated with disease bulk or chemoresistance, as the ORR was 59% in patients with bulky or chemoresistant disease.
However, responses were associated with histology, as the ORR was 38% in patients with DLBCL, 50% in those with MCL, 83% in those with FL, and 90% in those with CLL.
Long-term survival
In the current report, 11 of 40 patients were still alive at a median follow up of 9 years (range, 5.3 to 10.2). Fourteen patients died of disease progression, and 14 died from complications of HSCT.
The 5-year overall survival (OS) was 40%, and the 5-year progression-free survival (PFS) was 28%.
The best survival rates were in patients with indolent histology. The 5-year PFS was 44% in these patients, and the 5-year OS was 67%.
The researchers said early CR was not associated with long-term survival. However, patients who had at least stable disease (SD) at earlier time points did have the opportunity to achieve long-term survival. All patients who progressed before day 84 were dead by the 1-year mark.
Of the 11 patients who were still alive at a median follow up of 9 years, 4 had a CR or unconfirmed CR at day 84 (FL: 1; CLL: 2; MCL: 1); 6 were in partial response (CLL: 3; FL: 1; MCL: 1; MZL: 1); and 1 patient with FL had SD.
Among the 18 patients with indolent NHL, long-term PFS was observed in 5 of the 7 patients who achieved early CR and 8 of the 11 patients who did not achieve early CR.
Two of the 4 MCL patients who achieved an early CR had long-term PFS, but none of the MCL patients without an early CR had long-term PFS.
Among DLBCL patients, 1 of the 4 who achieved early CR had long-term PFS, but none of the patients without an early CR had long-term PFS. Only 1 DLBCL patient survived beyond 5 years. None survived beyond 8 years.
The researchers said the favorable outcomes in patients with indolent B-NHL are consistent with the known efficacy of RIT and the graft-versus-leukemia effect in these patients.
The team also noted that, since this trial began, several novel agents have been approved for the treatment of indolent B-NHL, which means allogeneic HSCT is often moved to later in the disease course.
The researchers concluded that 90Y-ibritumomab tiuxetan-based conditioning could “continue to play an important role in these settings,” but “improved strategies are needed” for patients with MCL and DLBCL.
Transplant with radioimmunotherapy (RIT)-based conditioning is a viable treatment option for patients with indolent—but not aggressive—B-cell non-Hodgkin lymphomas (NHLs), according to researchers.
Long-term follow-up data showed “excellent” outcomes in patients with indolent B-NHL who received conditioning with 90Y-ibritumomab tiuxetan plus fludarabine and low-dose total body irradiation (TBI) prior to HLA-matched hematopoietic stem cell transplant (HSCT).
However, long-term outcomes were inferior in patients with diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma (MCL).
Camille E. Puronen, MD, of the University of Washington in Seattle, and her colleagues reported these results in Biology of Blood and Marrow Transplantation.
The study enrolled 40 patients with high-risk B-NHL. This included DLBCL (n=14), chronic lymphocytic leukemia (CLL; n=10), MCL (n=8), follicular lymphoma (FL; n=6); hairy cell leukemia (HCL; n=1), and marginal zone lymphoma (MZL; n=1).
Patients were treated with 0.4 mCi/kg 90Y-ibritumomab tiuxetan, given 2 weeks prior to HSCT, to a maximum dose of 32 mCi.
Patients also received fludarabine at 30 mg/m2 on day 5, 6, and 7 prior to HSCT and 2 Gy TBI given on the day of transplant.
In an earlier report, the objective response rate (ORR) was 60%, and 35% of patients had a complete response (CR) or unconfirmed CR.
The researchers said early responses were not associated with disease bulk or chemoresistance, as the ORR was 59% in patients with bulky or chemoresistant disease.
However, responses were associated with histology, as the ORR was 38% in patients with DLBCL, 50% in those with MCL, 83% in those with FL, and 90% in those with CLL.
Long-term survival
In the current report, 11 of 40 patients were still alive at a median follow up of 9 years (range, 5.3 to 10.2). Fourteen patients died of disease progression, and 14 died from complications of HSCT.
The 5-year overall survival (OS) was 40%, and the 5-year progression-free survival (PFS) was 28%.
The best survival rates were in patients with indolent histology. The 5-year PFS was 44% in these patients, and the 5-year OS was 67%.
The researchers said early CR was not associated with long-term survival. However, patients who had at least stable disease (SD) at earlier time points did have the opportunity to achieve long-term survival. All patients who progressed before day 84 were dead by the 1-year mark.
Of the 11 patients who were still alive at a median follow up of 9 years, 4 had a CR or unconfirmed CR at day 84 (FL: 1; CLL: 2; MCL: 1); 6 were in partial response (CLL: 3; FL: 1; MCL: 1; MZL: 1); and 1 patient with FL had SD.
Among the 18 patients with indolent NHL, long-term PFS was observed in 5 of the 7 patients who achieved early CR and 8 of the 11 patients who did not achieve early CR.
Two of the 4 MCL patients who achieved an early CR had long-term PFS, but none of the MCL patients without an early CR had long-term PFS.
Among DLBCL patients, 1 of the 4 who achieved early CR had long-term PFS, but none of the patients without an early CR had long-term PFS. Only 1 DLBCL patient survived beyond 5 years. None survived beyond 8 years.
The researchers said the favorable outcomes in patients with indolent B-NHL are consistent with the known efficacy of RIT and the graft-versus-leukemia effect in these patients.
The team also noted that, since this trial began, several novel agents have been approved for the treatment of indolent B-NHL, which means allogeneic HSCT is often moved to later in the disease course.
The researchers concluded that 90Y-ibritumomab tiuxetan-based conditioning could “continue to play an important role in these settings,” but “improved strategies are needed” for patients with MCL and DLBCL.
Transplant with radioimmunotherapy (RIT)-based conditioning is a viable treatment option for patients with indolent—but not aggressive—B-cell non-Hodgkin lymphomas (NHLs), according to researchers.
Long-term follow-up data showed “excellent” outcomes in patients with indolent B-NHL who received conditioning with 90Y-ibritumomab tiuxetan plus fludarabine and low-dose total body irradiation (TBI) prior to HLA-matched hematopoietic stem cell transplant (HSCT).
However, long-term outcomes were inferior in patients with diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma (MCL).
Camille E. Puronen, MD, of the University of Washington in Seattle, and her colleagues reported these results in Biology of Blood and Marrow Transplantation.
The study enrolled 40 patients with high-risk B-NHL. This included DLBCL (n=14), chronic lymphocytic leukemia (CLL; n=10), MCL (n=8), follicular lymphoma (FL; n=6); hairy cell leukemia (HCL; n=1), and marginal zone lymphoma (MZL; n=1).
Patients were treated with 0.4 mCi/kg 90Y-ibritumomab tiuxetan, given 2 weeks prior to HSCT, to a maximum dose of 32 mCi.
Patients also received fludarabine at 30 mg/m2 on day 5, 6, and 7 prior to HSCT and 2 Gy TBI given on the day of transplant.
In an earlier report, the objective response rate (ORR) was 60%, and 35% of patients had a complete response (CR) or unconfirmed CR.
The researchers said early responses were not associated with disease bulk or chemoresistance, as the ORR was 59% in patients with bulky or chemoresistant disease.
However, responses were associated with histology, as the ORR was 38% in patients with DLBCL, 50% in those with MCL, 83% in those with FL, and 90% in those with CLL.
Long-term survival
In the current report, 11 of 40 patients were still alive at a median follow up of 9 years (range, 5.3 to 10.2). Fourteen patients died of disease progression, and 14 died from complications of HSCT.
The 5-year overall survival (OS) was 40%, and the 5-year progression-free survival (PFS) was 28%.
The best survival rates were in patients with indolent histology. The 5-year PFS was 44% in these patients, and the 5-year OS was 67%.
The researchers said early CR was not associated with long-term survival. However, patients who had at least stable disease (SD) at earlier time points did have the opportunity to achieve long-term survival. All patients who progressed before day 84 were dead by the 1-year mark.
Of the 11 patients who were still alive at a median follow up of 9 years, 4 had a CR or unconfirmed CR at day 84 (FL: 1; CLL: 2; MCL: 1); 6 were in partial response (CLL: 3; FL: 1; MCL: 1; MZL: 1); and 1 patient with FL had SD.
Among the 18 patients with indolent NHL, long-term PFS was observed in 5 of the 7 patients who achieved early CR and 8 of the 11 patients who did not achieve early CR.
Two of the 4 MCL patients who achieved an early CR had long-term PFS, but none of the MCL patients without an early CR had long-term PFS.
Among DLBCL patients, 1 of the 4 who achieved early CR had long-term PFS, but none of the patients without an early CR had long-term PFS. Only 1 DLBCL patient survived beyond 5 years. None survived beyond 8 years.
The researchers said the favorable outcomes in patients with indolent B-NHL are consistent with the known efficacy of RIT and the graft-versus-leukemia effect in these patients.
The team also noted that, since this trial began, several novel agents have been approved for the treatment of indolent B-NHL, which means allogeneic HSCT is often moved to later in the disease course.
The researchers concluded that 90Y-ibritumomab tiuxetan-based conditioning could “continue to play an important role in these settings,” but “improved strategies are needed” for patients with MCL and DLBCL.
Drug proves active in resistant MM
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
STOCKHOLM—The alkylating peptide melflufen has demonstrated activity in patients with treatment-resistant multiple myeloma (MM).
In a phase 2 trial, melflufen plus dexamethasone produced an overall response rate (ORR) of 32.1% in MM patients who were refractory to pomalidomide and/or daratumumab and had failed treatment with immunomodulatory drugs (IMiDs) and proteasome inhibitors (PIs).
Nearly all patients experienced an adverse event (AE) related to study treatment, and most of these were hematologic events.
These results, from the ongoing HORIZON trial, were presented at the 23rd Congress of the European Hematology Association (EHA) as abstract PF581.
The research was sponsored by Oncopeptides AB, the company developing melflufen.
“With an increasing number of patients with highly resistant myeloma, there is a real need for additional treatment options based on new mechanisms of action,” said study investigator Paul Richardson, MD, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“[Melflufen], a peptidase-enhanced compound, with its potent activity, manageable tolerability, and lack of shared resistance mechanisms with other modalities, is a promising molecule that is making encouraging progress in clinical development.”
Patients and treatment
The data presented at EHA include 62 patients. The data cut-off was May 10, 2018.
The patients had a median age of 62.5 (range, 41-82), 54% had high-risk cytogenetics, and 46% were ISS stage III. The patients had a median of 5.5 prior lines of therapy, and their median time since initial diagnosis was 6.1 years.
All patients were refractory to pomalidomide or daratumumab, 56% were refractory to both drugs, and 89% were double-refractory to IMiDs and PIs. Ninety-eight percent of patients had disease progression on or within 60 days of completing their last therapy.
Patients received melflufen at 40 mg (intravenously over 30 minutes) on day 1 of each 28-day cycle. They also received dexamethasone at 40 mg weekly. Patients were treated until disease progression, unacceptable toxicity, or withdrawal of consent.
At the data cutoff, 49 patients (79%) had completed at least 2 cycles of melflufen. The median number of cycles was 2 (range, 1-11).
Twenty-one patients (34%) were still receiving study treatment at the data cutoff. Reasons for discontinuation included disease progression (47%), AEs (15%), and physician decision (3%). One discontinuation was due to patient request.
Results
Fifty-six patients received at least 1 dose of melflufen and were evaluable for response.
The ORR was 32.1%, and the clinical benefit rate was 39.3%. ORR was defined as partial response (PR) or better, and clinical benefit rate was defined as minor response or better.
Two percent of patients had a complete response, 9% had a very good PR, 21% had a PR, and 7% had a minor response. Forty-five percent of patients had stable disease, and 16% progressed.
Subgroup analyses showed that response didn’t vary across refractory subsets, but it did vary according to the underlying disease and health status of the patient.
Treatment-related AEs occurred in 97% of all patients (60/62), and grade 3/4 treatment-related AEs occurred in 77% (n=48).
Grade 3/4 treatment-related AEs included neutropenia (60%), thrombocytopenia (60%), anemia (31%), leukopenia (6%), lymphopenia (6%), febrile neutropenia (6%), and infections (6%).
Twenty-one percent of patients had at least 1 treatment-related serious AE. The most frequent were febrile neutropenia (6%) and pneumonia (3%).
There were no treatment-related deaths.
How the IHS Reduced Kidney Disease in the Highest-risk Population
Alaska is a vast state—larger than Texas, Montana, and California combined. It is also home to the highest percentage of American Indian (AI) and Alaska Native (AN) persons in the United States. These two populations—collectively referred to as Native Americans—have been served by the Indian Health Services (IHS) since it was established through the Snyder Act of 1921, in response to the dismal health conditions of the indigenous tribes in this country.1 Across the US (not only in Alaska), the IHS has partnered with AI/AN peoples to decrease health disparities in a culturally acceptable manner that honors and protects their traditions and values.
The IHS—which in 2016 comprised 2,500 nurses, 750 physicians, 700 pharmacists, 200 PAs and NPs, and 280 dentists, as well as nutritionists, diabetes educators, administrators, and other professionals—has made huge advances in decreasing health disparities in their populations. Among them: decreased rates of tuberculosis and of maternal and infant deaths.
However, life expectancy among Native Americans remains four years shorter than that of the rest of the US population. This disparity can be traced to three recalcitrant factors: unintentional injuries, liver disease, and diabetes.
The IHS practitioners decided to tackle diabetes with a multipronged approach. And what they achieved is astonishing.
WHAT THEY DID
Worldwide, diabetes is the most common cause of kidney failure; identifying patients with diabetes and early-stage chronic kidney disease allows for aggressive treatment that can slow progression to kidney failure and dialysis.
The IHS providers knew when they decided to tackle the problem of diabetes in the AI/AN population that the incidence was 16%—and the rate of diabetes leading to kidney failure in this population was the highest for any ethnic group in the US.2,3 And yet …
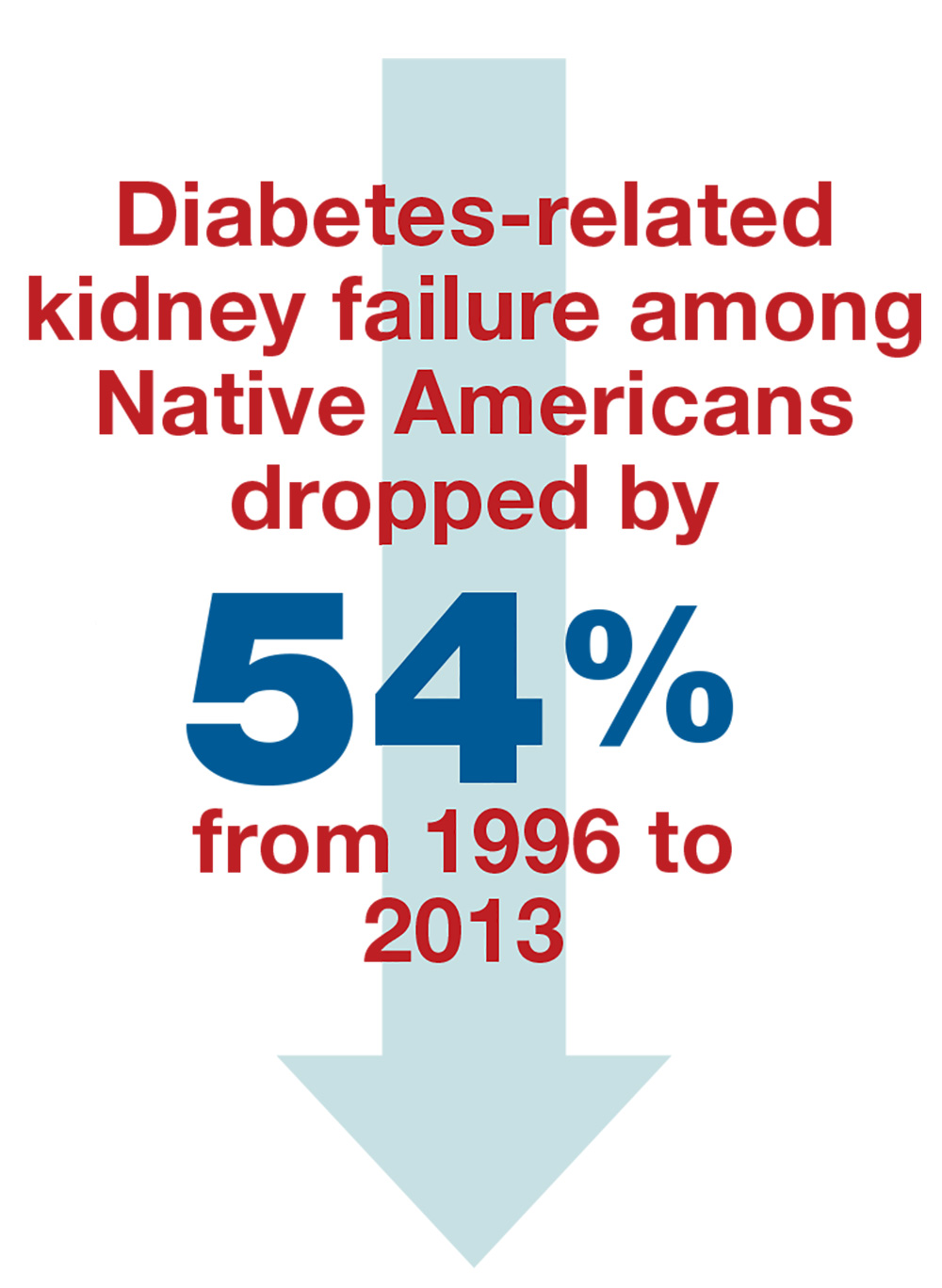
From 1996 to 2013, the rate of diabetes-related kidney failure among Native Americans dropped by 54%.3 Yes—the group of patients with the highest percentage of diabetes diagnoses has had the greatest improvement in prevention of kidney failure.4
Continue to: Some of the clinical achievements that contributed to...
Some of the clinical achievements that contributed to this significant change include
- Increased use of ACE inhibitors or angiotensin receptor blockers (ARBs) (from 42% to 74% over a five-year period)
- Reduced average blood pressure among hypertensive patients (to 133/76 mm Hg)
- Improved blood glucose control (by 10%)
- Increased testing for kidney disease among older patients (50% higher than the rest of the Medicare diabetes population).3
HOW THEY DID IT
This is not rocket science. The IHS staff integrated both population- and team-based approaches to achieve a more impressive decrease than ever could have been expected. In retrospect, perhaps this success should not come as such a surprise—many religious beliefs held by Native Americans focus around society, communal harmony, kinship, and cooperation.
The population health approach focused on promoting the wellness of the entire community and connecting people to local resources, including healthy food, transportation, housing, and mental health care. In the team approach, IHS medical experts implemented strategies to improve patient education, community outreach, care coordination, health outcome tracking, and access to a wide variety of health care providers.3,5
In a place like Alaska—where the northernmost city, Barrow, is more than 700 miles (two hours by plane) from Anchorage, and the southeastern Annette Island is more than 1,000 miles (six hours by plane) from the capital—this can be an especially challenging prospect. To reduce travel burden for rural patients, the IHS sponsors a diabetes team that travels from village to village. Nephrology services are not included in these field visits, however, so the kidney team relies heavily on telehealth. This requires extensive clinic staff coordination, as well as equipment and knowledgeable information systems support teams.
Other challenges require educational and logistical solutions. As noted, the use of ACE inhibitors and ARBs increased through the IHS’s efforts—and contributed to the delayed progression of diabetic kidney disease—but those additional prescriptions necessitate patient education. Understanding of these medications can be limited; many rural patients trust that when the bottle is empty, their practitioner has treated and cured their disease—mistakenly believing that no refills are needed. And even when the need to continue the prescription is understood, rural clinics may have difficulty tracking appointments and prescriptions written by providers at specialty clinics in Anchorage, making ongoing refills an issue.
Continue to: The necessary dietary changes can also be...
The necessary dietary changes can also be difficult for AI/AN populations. For example, in rural Alaska, tap water may not be safe to drink, and soda costs less than bottled water. Fresh produce is expensive and has often begun to spoil by the time it reaches local stores. The Native villagers often prefer their usual diets of gathered berries, fish, and red meat from subsistence hunting, making implementation of dietary changes difficult.
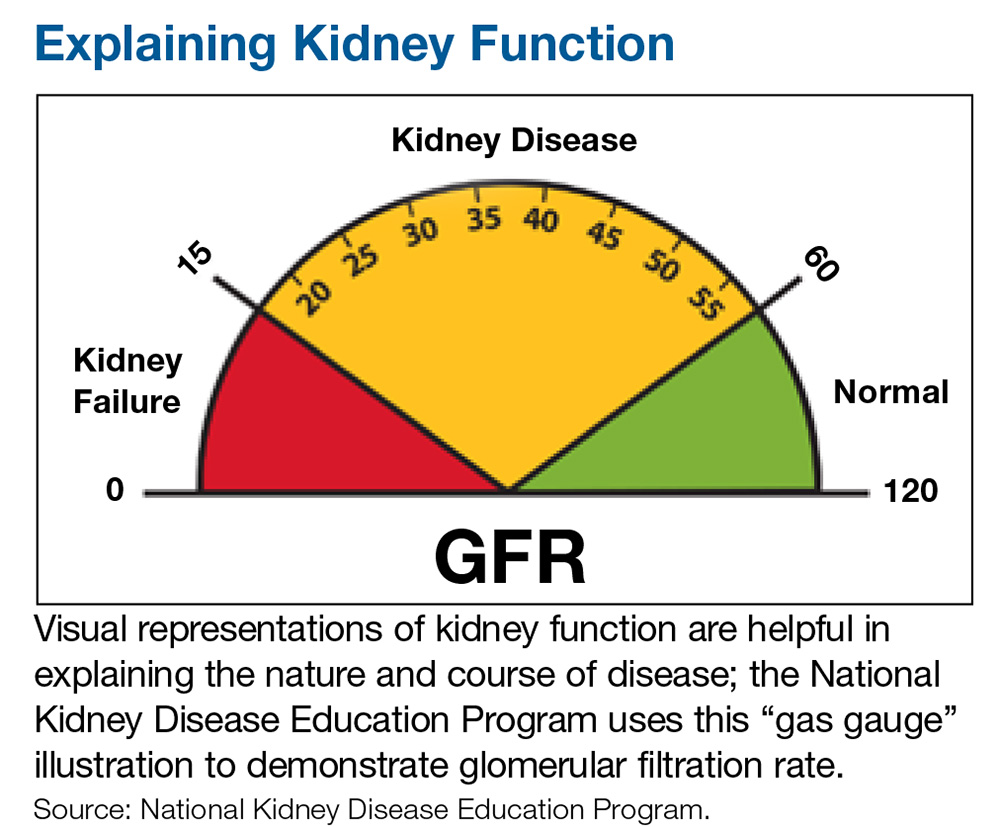
However, as the success of the IHS initiative shows, challenges can be met and overcome by practitioners who see a need, formulate a solution individualized to the circumstance, and think outside the box. One of the keys is developing a trusting relationship with patients. Another is to recognize informational needs and utilize available resources to educate patients. For example, visual representations of kidney function tend to be helpful in explaining the nature and course of disease; the National Kidney Disease Education Program uses an illustration similar to a gas gauge to demonstrate glomerular filtration rate (which would otherwise seem abstract and hard to understand for some patients; see below).6 When you understand your patient population and their needs, it makes addressing the challenging aspects of health care and prevention easier.
CONCLUSION
The results that the IHS achieved should serve as an example for all Americans with diabetes and their health care providers. We must be open to delivery of care via different approaches and practitioners in order to successfully help patients of different backgrounds and circumstances. This is the individualization of care that we hear so much about.
In 2016, the costs of caring for the kidney failure population were greater than the entire budget of the NIH. By aggressively identifying and treating patients at risk for kidney failure, we can slow disease progression—saving society money, but more importantly allowing our patients many more years of life free from the constraints of dialysis. —MET, RB
Mandy E. Thompson, PA-C
Kidney Center of Denver Health
Robin Bassett, DNP
Nephrology and Hypertension Associates, Anchorage
Adjunct Professor, NP program, University of Alaska, Anchorage
1. Indian Health Service. Legislation. www.ihs.gov/aboutihs/legislation. Accessed June 13, 2018.
2. National Health Interview Survey and Indian Health Service, 2010-2012.
3. CDC. Native Americans with diabetes. www.cdc.gov/vitalsigns/aian-diabetes/. Accessed June 13, 2018.
4. United States Renal Data System. Figure 1.5: Trends in adjusted* ESRD incidence rate (per million/year), by race, in the U.S. population, 1996-2014. In: 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
5. Indian Health Service. Special diabetes program for Indians. www.ihs.gov/newsroom/factsheets/diabetes. Accessed June 13, 2018.
6. National Kidney Disease Education Program. How well are your kidneys working? Explaining your kidney test results. www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/explain-kidney-test-results. Accessed June 13, 2018.
Alaska is a vast state—larger than Texas, Montana, and California combined. It is also home to the highest percentage of American Indian (AI) and Alaska Native (AN) persons in the United States. These two populations—collectively referred to as Native Americans—have been served by the Indian Health Services (IHS) since it was established through the Snyder Act of 1921, in response to the dismal health conditions of the indigenous tribes in this country.1 Across the US (not only in Alaska), the IHS has partnered with AI/AN peoples to decrease health disparities in a culturally acceptable manner that honors and protects their traditions and values.
The IHS—which in 2016 comprised 2,500 nurses, 750 physicians, 700 pharmacists, 200 PAs and NPs, and 280 dentists, as well as nutritionists, diabetes educators, administrators, and other professionals—has made huge advances in decreasing health disparities in their populations. Among them: decreased rates of tuberculosis and of maternal and infant deaths.
However, life expectancy among Native Americans remains four years shorter than that of the rest of the US population. This disparity can be traced to three recalcitrant factors: unintentional injuries, liver disease, and diabetes.
The IHS practitioners decided to tackle diabetes with a multipronged approach. And what they achieved is astonishing.
WHAT THEY DID
Worldwide, diabetes is the most common cause of kidney failure; identifying patients with diabetes and early-stage chronic kidney disease allows for aggressive treatment that can slow progression to kidney failure and dialysis.
The IHS providers knew when they decided to tackle the problem of diabetes in the AI/AN population that the incidence was 16%—and the rate of diabetes leading to kidney failure in this population was the highest for any ethnic group in the US.2,3 And yet …
From 1996 to 2013, the rate of diabetes-related kidney failure among Native Americans dropped by 54%.3 Yes—the group of patients with the highest percentage of diabetes diagnoses has had the greatest improvement in prevention of kidney failure.4
Continue to: Some of the clinical achievements that contributed to...
Some of the clinical achievements that contributed to this significant change include
- Increased use of ACE inhibitors or angiotensin receptor blockers (ARBs) (from 42% to 74% over a five-year period)
- Reduced average blood pressure among hypertensive patients (to 133/76 mm Hg)
- Improved blood glucose control (by 10%)
- Increased testing for kidney disease among older patients (50% higher than the rest of the Medicare diabetes population).3
HOW THEY DID IT
This is not rocket science. The IHS staff integrated both population- and team-based approaches to achieve a more impressive decrease than ever could have been expected. In retrospect, perhaps this success should not come as such a surprise—many religious beliefs held by Native Americans focus around society, communal harmony, kinship, and cooperation.
The population health approach focused on promoting the wellness of the entire community and connecting people to local resources, including healthy food, transportation, housing, and mental health care. In the team approach, IHS medical experts implemented strategies to improve patient education, community outreach, care coordination, health outcome tracking, and access to a wide variety of health care providers.3,5
In a place like Alaska—where the northernmost city, Barrow, is more than 700 miles (two hours by plane) from Anchorage, and the southeastern Annette Island is more than 1,000 miles (six hours by plane) from the capital—this can be an especially challenging prospect. To reduce travel burden for rural patients, the IHS sponsors a diabetes team that travels from village to village. Nephrology services are not included in these field visits, however, so the kidney team relies heavily on telehealth. This requires extensive clinic staff coordination, as well as equipment and knowledgeable information systems support teams.
Other challenges require educational and logistical solutions. As noted, the use of ACE inhibitors and ARBs increased through the IHS’s efforts—and contributed to the delayed progression of diabetic kidney disease—but those additional prescriptions necessitate patient education. Understanding of these medications can be limited; many rural patients trust that when the bottle is empty, their practitioner has treated and cured their disease—mistakenly believing that no refills are needed. And even when the need to continue the prescription is understood, rural clinics may have difficulty tracking appointments and prescriptions written by providers at specialty clinics in Anchorage, making ongoing refills an issue.
Continue to: The necessary dietary changes can also be...
The necessary dietary changes can also be difficult for AI/AN populations. For example, in rural Alaska, tap water may not be safe to drink, and soda costs less than bottled water. Fresh produce is expensive and has often begun to spoil by the time it reaches local stores. The Native villagers often prefer their usual diets of gathered berries, fish, and red meat from subsistence hunting, making implementation of dietary changes difficult.
However, as the success of the IHS initiative shows, challenges can be met and overcome by practitioners who see a need, formulate a solution individualized to the circumstance, and think outside the box. One of the keys is developing a trusting relationship with patients. Another is to recognize informational needs and utilize available resources to educate patients. For example, visual representations of kidney function tend to be helpful in explaining the nature and course of disease; the National Kidney Disease Education Program uses an illustration similar to a gas gauge to demonstrate glomerular filtration rate (which would otherwise seem abstract and hard to understand for some patients; see below).6 When you understand your patient population and their needs, it makes addressing the challenging aspects of health care and prevention easier.
CONCLUSION
The results that the IHS achieved should serve as an example for all Americans with diabetes and their health care providers. We must be open to delivery of care via different approaches and practitioners in order to successfully help patients of different backgrounds and circumstances. This is the individualization of care that we hear so much about.
In 2016, the costs of caring for the kidney failure population were greater than the entire budget of the NIH. By aggressively identifying and treating patients at risk for kidney failure, we can slow disease progression—saving society money, but more importantly allowing our patients many more years of life free from the constraints of dialysis. —MET, RB
Mandy E. Thompson, PA-C
Kidney Center of Denver Health
Robin Bassett, DNP
Nephrology and Hypertension Associates, Anchorage
Adjunct Professor, NP program, University of Alaska, Anchorage
Alaska is a vast state—larger than Texas, Montana, and California combined. It is also home to the highest percentage of American Indian (AI) and Alaska Native (AN) persons in the United States. These two populations—collectively referred to as Native Americans—have been served by the Indian Health Services (IHS) since it was established through the Snyder Act of 1921, in response to the dismal health conditions of the indigenous tribes in this country.1 Across the US (not only in Alaska), the IHS has partnered with AI/AN peoples to decrease health disparities in a culturally acceptable manner that honors and protects their traditions and values.
The IHS—which in 2016 comprised 2,500 nurses, 750 physicians, 700 pharmacists, 200 PAs and NPs, and 280 dentists, as well as nutritionists, diabetes educators, administrators, and other professionals—has made huge advances in decreasing health disparities in their populations. Among them: decreased rates of tuberculosis and of maternal and infant deaths.
However, life expectancy among Native Americans remains four years shorter than that of the rest of the US population. This disparity can be traced to three recalcitrant factors: unintentional injuries, liver disease, and diabetes.
The IHS practitioners decided to tackle diabetes with a multipronged approach. And what they achieved is astonishing.
WHAT THEY DID
Worldwide, diabetes is the most common cause of kidney failure; identifying patients with diabetes and early-stage chronic kidney disease allows for aggressive treatment that can slow progression to kidney failure and dialysis.
The IHS providers knew when they decided to tackle the problem of diabetes in the AI/AN population that the incidence was 16%—and the rate of diabetes leading to kidney failure in this population was the highest for any ethnic group in the US.2,3 And yet …
From 1996 to 2013, the rate of diabetes-related kidney failure among Native Americans dropped by 54%.3 Yes—the group of patients with the highest percentage of diabetes diagnoses has had the greatest improvement in prevention of kidney failure.4
Continue to: Some of the clinical achievements that contributed to...
Some of the clinical achievements that contributed to this significant change include
- Increased use of ACE inhibitors or angiotensin receptor blockers (ARBs) (from 42% to 74% over a five-year period)
- Reduced average blood pressure among hypertensive patients (to 133/76 mm Hg)
- Improved blood glucose control (by 10%)
- Increased testing for kidney disease among older patients (50% higher than the rest of the Medicare diabetes population).3
HOW THEY DID IT
This is not rocket science. The IHS staff integrated both population- and team-based approaches to achieve a more impressive decrease than ever could have been expected. In retrospect, perhaps this success should not come as such a surprise—many religious beliefs held by Native Americans focus around society, communal harmony, kinship, and cooperation.
The population health approach focused on promoting the wellness of the entire community and connecting people to local resources, including healthy food, transportation, housing, and mental health care. In the team approach, IHS medical experts implemented strategies to improve patient education, community outreach, care coordination, health outcome tracking, and access to a wide variety of health care providers.3,5
In a place like Alaska—where the northernmost city, Barrow, is more than 700 miles (two hours by plane) from Anchorage, and the southeastern Annette Island is more than 1,000 miles (six hours by plane) from the capital—this can be an especially challenging prospect. To reduce travel burden for rural patients, the IHS sponsors a diabetes team that travels from village to village. Nephrology services are not included in these field visits, however, so the kidney team relies heavily on telehealth. This requires extensive clinic staff coordination, as well as equipment and knowledgeable information systems support teams.
Other challenges require educational and logistical solutions. As noted, the use of ACE inhibitors and ARBs increased through the IHS’s efforts—and contributed to the delayed progression of diabetic kidney disease—but those additional prescriptions necessitate patient education. Understanding of these medications can be limited; many rural patients trust that when the bottle is empty, their practitioner has treated and cured their disease—mistakenly believing that no refills are needed. And even when the need to continue the prescription is understood, rural clinics may have difficulty tracking appointments and prescriptions written by providers at specialty clinics in Anchorage, making ongoing refills an issue.
Continue to: The necessary dietary changes can also be...
The necessary dietary changes can also be difficult for AI/AN populations. For example, in rural Alaska, tap water may not be safe to drink, and soda costs less than bottled water. Fresh produce is expensive and has often begun to spoil by the time it reaches local stores. The Native villagers often prefer their usual diets of gathered berries, fish, and red meat from subsistence hunting, making implementation of dietary changes difficult.
However, as the success of the IHS initiative shows, challenges can be met and overcome by practitioners who see a need, formulate a solution individualized to the circumstance, and think outside the box. One of the keys is developing a trusting relationship with patients. Another is to recognize informational needs and utilize available resources to educate patients. For example, visual representations of kidney function tend to be helpful in explaining the nature and course of disease; the National Kidney Disease Education Program uses an illustration similar to a gas gauge to demonstrate glomerular filtration rate (which would otherwise seem abstract and hard to understand for some patients; see below).6 When you understand your patient population and their needs, it makes addressing the challenging aspects of health care and prevention easier.
CONCLUSION
The results that the IHS achieved should serve as an example for all Americans with diabetes and their health care providers. We must be open to delivery of care via different approaches and practitioners in order to successfully help patients of different backgrounds and circumstances. This is the individualization of care that we hear so much about.
In 2016, the costs of caring for the kidney failure population were greater than the entire budget of the NIH. By aggressively identifying and treating patients at risk for kidney failure, we can slow disease progression—saving society money, but more importantly allowing our patients many more years of life free from the constraints of dialysis. —MET, RB
Mandy E. Thompson, PA-C
Kidney Center of Denver Health
Robin Bassett, DNP
Nephrology and Hypertension Associates, Anchorage
Adjunct Professor, NP program, University of Alaska, Anchorage
1. Indian Health Service. Legislation. www.ihs.gov/aboutihs/legislation. Accessed June 13, 2018.
2. National Health Interview Survey and Indian Health Service, 2010-2012.
3. CDC. Native Americans with diabetes. www.cdc.gov/vitalsigns/aian-diabetes/. Accessed June 13, 2018.
4. United States Renal Data System. Figure 1.5: Trends in adjusted* ESRD incidence rate (per million/year), by race, in the U.S. population, 1996-2014. In: 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
5. Indian Health Service. Special diabetes program for Indians. www.ihs.gov/newsroom/factsheets/diabetes. Accessed June 13, 2018.
6. National Kidney Disease Education Program. How well are your kidneys working? Explaining your kidney test results. www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/explain-kidney-test-results. Accessed June 13, 2018.
1. Indian Health Service. Legislation. www.ihs.gov/aboutihs/legislation. Accessed June 13, 2018.
2. National Health Interview Survey and Indian Health Service, 2010-2012.
3. CDC. Native Americans with diabetes. www.cdc.gov/vitalsigns/aian-diabetes/. Accessed June 13, 2018.
4. United States Renal Data System. Figure 1.5: Trends in adjusted* ESRD incidence rate (per million/year), by race, in the U.S. population, 1996-2014. In: 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2016.
5. Indian Health Service. Special diabetes program for Indians. www.ihs.gov/newsroom/factsheets/diabetes. Accessed June 13, 2018.
6. National Kidney Disease Education Program. How well are your kidneys working? Explaining your kidney test results. www.niddk.nih.gov/health-information/professionals/clinical-tools-patient-education-outreach/explain-kidney-test-results. Accessed June 13, 2018.
Study busts three migraine trigger myths
SAN FRANCISCO – Half of migraineurs suspect chocolate can trigger their migraine attacks, but new evidence from a large prospective study suggests almost 99% of them are mistaken.
Additional analyses of this same dataset of 774 individuals with migraine threw cold water on two other widely accepted putative migraine triggers: neck pain/tension and dietary nitrate intake, Stephen Donoghue, PhD, reported at the annual meeting of the American Headache Society.
He presented a series of statistical analyses of often-cited migraine attack triggers conducted in 774 migraineurs who registered to use N1–Headache, a sophisticated proprietary digital headache diary. At the outset, participants rated on a 0-10 scale how strongly they suspected chocolate, neck pain or tension, and other factors acted as triggers for migraine attacks in their own personal experience. They then spent 2-3 minutes daily tracking more than 70 migraine-related elements for at least 90 days, recording the data using an iPhone or iPad rather than using a traditional, more hit-or-miss conventional paper diary.
The N1–Headache software, developed by Curelator of Cambridge, Mass., then tackled the key issue of what proportion of individuals who suspected a given trigger actually showed a statistically significant association prospectively between an individual’s day-to-day variations in experiencing that trigger and their headache risk, explained Dr. Donoghue, vice president for clinical development for Curelator.
Chocolate
The Curelator concept involves bringing personalized medicine to headache patients by identifying their true migraine attack triggers, which can enable individuals to deal with those triggers without the disruption involved in unnecessarily avoiding numerous nontriggers or missing real triggers.
The study results punctured some widely held beliefs. For example, at baseline 51% of migraineurs indicated they suspected chocolate served to some degree as a trigger for their own migraine attacks; the majority of them rated their suspicion as moderate or strong. However, in individually determined correlations, chocolate was indeed associated with migraine attacks in only 1.3% of those who suspected it to be a trigger. Moreover, in an another 3.9% of chocolate suspecters, chocolate consumption was actually associated with decreased risk; in other words, for them, chocolate appeared to serve as a protector against migraine, despite their preconceptions.
Also, among the 49% of participants who didn’t consider chocolate to be a personal migraine attack trigger, the Curelator analysis demonstrated that chocolate consumption was associated with a significantly increased risk of migraine attack in 2.2%, and a significantly lower risk of migraine in another 1.5%.
Neck pain/tension
Eighty percent of migraineurs who registered to use N1–Headache via the company’s website or the App Store indicated they believed neck pain/tension to be a migraine trigger for them; 46% rated it as a strong trigger. The detailed analysis of 90 days’ worth of data showed that 32% of participants with adequate data showed a statistically significant association between neck pain/tension and migraine headache.
The strength of an individual’s suspicion of neck paint/tension as a trigger was associated with the frequency of a statistically confirmed association. However, unlike for chocolate, there were zero instances where neck pain/tension was associated with protection against migraine.
In a twist, when the investigators reanalyzed their data after eliminating those instances where neck pain/tension occurred 1 day before the start of the headache, the association disappeared.
“The temporal association that we find using the lag-day analysis strongly suggests that neck pain/tension is part of the symptomatology of migraine attacks rather than acting as a trigger,” Dr. Donoghue observed.
This concept is strongly supported by a recent German study that used neck muscle electromyography to establish the same point (J Headache Pain. 2018 Mar 20;19[1]:26), he added.
Dr. Donoghue offered one caveat regarding the Curelator analyses: “We can’t say whether or not neck pain/tension and these other factors are actually triggers. What we’re looking at is associations. We’re not showing causality.”
Nitrates in food
Of the participants in this Curelator study, 45% suspected nitrate intake was a trigger for their migraine attacks, including 24% who rated the strength of their suspicion as moderate or severe. Of those who suspected nitrates, Cox proportional hazards modeling identified 2.2% in whom a significant association between nitrate consumption and increased migraine attack risk was present and another 1.1% in whom nitrates were associated with decreased risk, which suggests that they act as a possible protector in some cases. An individual’s strength of suspicion regarding nitrates proved unrelated to the actual risk of an association.
In subjects who did not suspect nitrates as a migraine trigger, Dr. Donoghue and colleagues identified 3.5% in whom nitrate intake was actually statistically associated with increased risk and 1.7% in whom it was linked to decreased risk.
The study was funded by Curelator, where Dr. Donoghue is employed.
SOURCE: Donoghue S et al. Headache. 2018 Jun;58(52):104,109,110.
SAN FRANCISCO – Half of migraineurs suspect chocolate can trigger their migraine attacks, but new evidence from a large prospective study suggests almost 99% of them are mistaken.
Additional analyses of this same dataset of 774 individuals with migraine threw cold water on two other widely accepted putative migraine triggers: neck pain/tension and dietary nitrate intake, Stephen Donoghue, PhD, reported at the annual meeting of the American Headache Society.
He presented a series of statistical analyses of often-cited migraine attack triggers conducted in 774 migraineurs who registered to use N1–Headache, a sophisticated proprietary digital headache diary. At the outset, participants rated on a 0-10 scale how strongly they suspected chocolate, neck pain or tension, and other factors acted as triggers for migraine attacks in their own personal experience. They then spent 2-3 minutes daily tracking more than 70 migraine-related elements for at least 90 days, recording the data using an iPhone or iPad rather than using a traditional, more hit-or-miss conventional paper diary.
The N1–Headache software, developed by Curelator of Cambridge, Mass., then tackled the key issue of what proportion of individuals who suspected a given trigger actually showed a statistically significant association prospectively between an individual’s day-to-day variations in experiencing that trigger and their headache risk, explained Dr. Donoghue, vice president for clinical development for Curelator.
Chocolate
The Curelator concept involves bringing personalized medicine to headache patients by identifying their true migraine attack triggers, which can enable individuals to deal with those triggers without the disruption involved in unnecessarily avoiding numerous nontriggers or missing real triggers.
The study results punctured some widely held beliefs. For example, at baseline 51% of migraineurs indicated they suspected chocolate served to some degree as a trigger for their own migraine attacks; the majority of them rated their suspicion as moderate or strong. However, in individually determined correlations, chocolate was indeed associated with migraine attacks in only 1.3% of those who suspected it to be a trigger. Moreover, in an another 3.9% of chocolate suspecters, chocolate consumption was actually associated with decreased risk; in other words, for them, chocolate appeared to serve as a protector against migraine, despite their preconceptions.
Also, among the 49% of participants who didn’t consider chocolate to be a personal migraine attack trigger, the Curelator analysis demonstrated that chocolate consumption was associated with a significantly increased risk of migraine attack in 2.2%, and a significantly lower risk of migraine in another 1.5%.
Neck pain/tension
Eighty percent of migraineurs who registered to use N1–Headache via the company’s website or the App Store indicated they believed neck pain/tension to be a migraine trigger for them; 46% rated it as a strong trigger. The detailed analysis of 90 days’ worth of data showed that 32% of participants with adequate data showed a statistically significant association between neck pain/tension and migraine headache.
The strength of an individual’s suspicion of neck paint/tension as a trigger was associated with the frequency of a statistically confirmed association. However, unlike for chocolate, there were zero instances where neck pain/tension was associated with protection against migraine.
In a twist, when the investigators reanalyzed their data after eliminating those instances where neck pain/tension occurred 1 day before the start of the headache, the association disappeared.
“The temporal association that we find using the lag-day analysis strongly suggests that neck pain/tension is part of the symptomatology of migraine attacks rather than acting as a trigger,” Dr. Donoghue observed.
This concept is strongly supported by a recent German study that used neck muscle electromyography to establish the same point (J Headache Pain. 2018 Mar 20;19[1]:26), he added.
Dr. Donoghue offered one caveat regarding the Curelator analyses: “We can’t say whether or not neck pain/tension and these other factors are actually triggers. What we’re looking at is associations. We’re not showing causality.”
Nitrates in food
Of the participants in this Curelator study, 45% suspected nitrate intake was a trigger for their migraine attacks, including 24% who rated the strength of their suspicion as moderate or severe. Of those who suspected nitrates, Cox proportional hazards modeling identified 2.2% in whom a significant association between nitrate consumption and increased migraine attack risk was present and another 1.1% in whom nitrates were associated with decreased risk, which suggests that they act as a possible protector in some cases. An individual’s strength of suspicion regarding nitrates proved unrelated to the actual risk of an association.
In subjects who did not suspect nitrates as a migraine trigger, Dr. Donoghue and colleagues identified 3.5% in whom nitrate intake was actually statistically associated with increased risk and 1.7% in whom it was linked to decreased risk.
The study was funded by Curelator, where Dr. Donoghue is employed.
SOURCE: Donoghue S et al. Headache. 2018 Jun;58(52):104,109,110.
SAN FRANCISCO – Half of migraineurs suspect chocolate can trigger their migraine attacks, but new evidence from a large prospective study suggests almost 99% of them are mistaken.
Additional analyses of this same dataset of 774 individuals with migraine threw cold water on two other widely accepted putative migraine triggers: neck pain/tension and dietary nitrate intake, Stephen Donoghue, PhD, reported at the annual meeting of the American Headache Society.
He presented a series of statistical analyses of often-cited migraine attack triggers conducted in 774 migraineurs who registered to use N1–Headache, a sophisticated proprietary digital headache diary. At the outset, participants rated on a 0-10 scale how strongly they suspected chocolate, neck pain or tension, and other factors acted as triggers for migraine attacks in their own personal experience. They then spent 2-3 minutes daily tracking more than 70 migraine-related elements for at least 90 days, recording the data using an iPhone or iPad rather than using a traditional, more hit-or-miss conventional paper diary.
The N1–Headache software, developed by Curelator of Cambridge, Mass., then tackled the key issue of what proportion of individuals who suspected a given trigger actually showed a statistically significant association prospectively between an individual’s day-to-day variations in experiencing that trigger and their headache risk, explained Dr. Donoghue, vice president for clinical development for Curelator.
Chocolate
The Curelator concept involves bringing personalized medicine to headache patients by identifying their true migraine attack triggers, which can enable individuals to deal with those triggers without the disruption involved in unnecessarily avoiding numerous nontriggers or missing real triggers.
The study results punctured some widely held beliefs. For example, at baseline 51% of migraineurs indicated they suspected chocolate served to some degree as a trigger for their own migraine attacks; the majority of them rated their suspicion as moderate or strong. However, in individually determined correlations, chocolate was indeed associated with migraine attacks in only 1.3% of those who suspected it to be a trigger. Moreover, in an another 3.9% of chocolate suspecters, chocolate consumption was actually associated with decreased risk; in other words, for them, chocolate appeared to serve as a protector against migraine, despite their preconceptions.
Also, among the 49% of participants who didn’t consider chocolate to be a personal migraine attack trigger, the Curelator analysis demonstrated that chocolate consumption was associated with a significantly increased risk of migraine attack in 2.2%, and a significantly lower risk of migraine in another 1.5%.
Neck pain/tension
Eighty percent of migraineurs who registered to use N1–Headache via the company’s website or the App Store indicated they believed neck pain/tension to be a migraine trigger for them; 46% rated it as a strong trigger. The detailed analysis of 90 days’ worth of data showed that 32% of participants with adequate data showed a statistically significant association between neck pain/tension and migraine headache.
The strength of an individual’s suspicion of neck paint/tension as a trigger was associated with the frequency of a statistically confirmed association. However, unlike for chocolate, there were zero instances where neck pain/tension was associated with protection against migraine.
In a twist, when the investigators reanalyzed their data after eliminating those instances where neck pain/tension occurred 1 day before the start of the headache, the association disappeared.
“The temporal association that we find using the lag-day analysis strongly suggests that neck pain/tension is part of the symptomatology of migraine attacks rather than acting as a trigger,” Dr. Donoghue observed.
This concept is strongly supported by a recent German study that used neck muscle electromyography to establish the same point (J Headache Pain. 2018 Mar 20;19[1]:26), he added.
Dr. Donoghue offered one caveat regarding the Curelator analyses: “We can’t say whether or not neck pain/tension and these other factors are actually triggers. What we’re looking at is associations. We’re not showing causality.”
Nitrates in food
Of the participants in this Curelator study, 45% suspected nitrate intake was a trigger for their migraine attacks, including 24% who rated the strength of their suspicion as moderate or severe. Of those who suspected nitrates, Cox proportional hazards modeling identified 2.2% in whom a significant association between nitrate consumption and increased migraine attack risk was present and another 1.1% in whom nitrates were associated with decreased risk, which suggests that they act as a possible protector in some cases. An individual’s strength of suspicion regarding nitrates proved unrelated to the actual risk of an association.
In subjects who did not suspect nitrates as a migraine trigger, Dr. Donoghue and colleagues identified 3.5% in whom nitrate intake was actually statistically associated with increased risk and 1.7% in whom it was linked to decreased risk.
The study was funded by Curelator, where Dr. Donoghue is employed.
SOURCE: Donoghue S et al. Headache. 2018 Jun;58(52):104,109,110.
REPORTING FROM the AHS Annual MEETING
Key clinical point: Migraine patients are most often way off base regarding their suspected attack triggers.
Major finding: Half of migraineurs suspect chocolate triggers their headache attacks, and almost 99% of them are wrong.
Study details: This prospective study included 774 migraineurs who completed a detailed electronic headache diary for at least 90 consecutive days, with correlations between migraine attacks and putative triggers being analyzed by proprietary software.
Disclosures: The study was sponsored by Curelator and presented by a company executive.
Source: Donoghue S et al. Headache. 2018 Jun;58(52):104,109,110.
Study profiles sleep disruption in depression
Waking theta reduced in depression
BALTIMORE – Disruption of slow-wave activity may potentially explain the positive influence that sleep deprivation may have on major depressive disorder, according to results of a study presented at the annual meeting of the Associated Professional Sleep Societies.
Jennifer Goldschmied, PhD, of the University of Pennsylvania, Philadelphia, reported preliminary results of a study of slow-wave activity (SWA) disruption in 26 subjects – 12 healthy controls and 14 people diagnosed with major depressive disorder – that found a significant decrease of about 20% in waking theta activity, as measured with EEG, in the MDD group. In the 3-night sleep study, conducted at the University of Michigan, Ann Arbor, an adaptation night was followed by baseline and SWA disruption nights with EEGs performed each night. After the baseline night, patients also had a morning and afternoon EEG.
Across the baseline day, patients with depression showed “no modulation of theta activity whatsoever,” Dr. Goldschmied said. “And then we see, following slow-wave disruption, a significant decrease in theta activity,” whereas, healthy controls showed no change in waking theta following slow-wave disruption. “So what this means is that the presence of SWA may actually be facilitating the reduction of theta or sleep propensity during typical sleep in healthy individuals,” she added. In MDD patients, the decline in theta power following slow-wave disruption was from around 5.4 to 4.3.
Dr. Goldschmied noted that this finding somewhat supports what is known as the synaptic homeostasis hypothesis that University of Wisconsin researchers Giulio Tononi, MD, PhD, and Chiara Cirelli, MD, PhD, reported (Brain Res Bull. 2003;62:143-50). This hypothesis holds that SWA is a marker of synaptic strength and promotes the downscaling of synaptic strength during sleep. No method for measuring synaptic strength in humans exists, Dr. Goldschmied added, but waking theta can be considered a proxy for net synaptic strength across the cortex.
Dr. Goldschmied noted other research that has found SWA disruption improves mood (Psychiatry Res. 2015;228:715-8; J Psychiatr Res. 2011;45:1019-26), but the study she reported on found no role of decreased theta activity in that change. “To go even further,” she said, “we looked at the entire data set and found no relationship between the decrease in theta and any of the measures of sleep architecture – so there’s really no way to predict this decrease in our sample of people with depression.”
SWA plays a significant role in depression and merits more study, Dr. Goldschmied said. She noted that future research should examine the effects of SWA disruption in a larger sample, investigate theta findings with other proxy measures of synaptic strength such as brain-derived neurotrophic factor and transcranial magnetic stimulation, explore differences in SWA between sexes, and explore how SWA enhancement influences mood and theta activity.
Dr. Goldschmied reported having no financial relationships.
SOURCE: Goldschmied J et al. Sleep 2018, Abstract 0245.
Waking theta reduced in depression
Waking theta reduced in depression
BALTIMORE – Disruption of slow-wave activity may potentially explain the positive influence that sleep deprivation may have on major depressive disorder, according to results of a study presented at the annual meeting of the Associated Professional Sleep Societies.
Jennifer Goldschmied, PhD, of the University of Pennsylvania, Philadelphia, reported preliminary results of a study of slow-wave activity (SWA) disruption in 26 subjects – 12 healthy controls and 14 people diagnosed with major depressive disorder – that found a significant decrease of about 20% in waking theta activity, as measured with EEG, in the MDD group. In the 3-night sleep study, conducted at the University of Michigan, Ann Arbor, an adaptation night was followed by baseline and SWA disruption nights with EEGs performed each night. After the baseline night, patients also had a morning and afternoon EEG.
Across the baseline day, patients with depression showed “no modulation of theta activity whatsoever,” Dr. Goldschmied said. “And then we see, following slow-wave disruption, a significant decrease in theta activity,” whereas, healthy controls showed no change in waking theta following slow-wave disruption. “So what this means is that the presence of SWA may actually be facilitating the reduction of theta or sleep propensity during typical sleep in healthy individuals,” she added. In MDD patients, the decline in theta power following slow-wave disruption was from around 5.4 to 4.3.
Dr. Goldschmied noted that this finding somewhat supports what is known as the synaptic homeostasis hypothesis that University of Wisconsin researchers Giulio Tononi, MD, PhD, and Chiara Cirelli, MD, PhD, reported (Brain Res Bull. 2003;62:143-50). This hypothesis holds that SWA is a marker of synaptic strength and promotes the downscaling of synaptic strength during sleep. No method for measuring synaptic strength in humans exists, Dr. Goldschmied added, but waking theta can be considered a proxy for net synaptic strength across the cortex.
Dr. Goldschmied noted other research that has found SWA disruption improves mood (Psychiatry Res. 2015;228:715-8; J Psychiatr Res. 2011;45:1019-26), but the study she reported on found no role of decreased theta activity in that change. “To go even further,” she said, “we looked at the entire data set and found no relationship between the decrease in theta and any of the measures of sleep architecture – so there’s really no way to predict this decrease in our sample of people with depression.”
SWA plays a significant role in depression and merits more study, Dr. Goldschmied said. She noted that future research should examine the effects of SWA disruption in a larger sample, investigate theta findings with other proxy measures of synaptic strength such as brain-derived neurotrophic factor and transcranial magnetic stimulation, explore differences in SWA between sexes, and explore how SWA enhancement influences mood and theta activity.
Dr. Goldschmied reported having no financial relationships.
SOURCE: Goldschmied J et al. Sleep 2018, Abstract 0245.
BALTIMORE – Disruption of slow-wave activity may potentially explain the positive influence that sleep deprivation may have on major depressive disorder, according to results of a study presented at the annual meeting of the Associated Professional Sleep Societies.
Jennifer Goldschmied, PhD, of the University of Pennsylvania, Philadelphia, reported preliminary results of a study of slow-wave activity (SWA) disruption in 26 subjects – 12 healthy controls and 14 people diagnosed with major depressive disorder – that found a significant decrease of about 20% in waking theta activity, as measured with EEG, in the MDD group. In the 3-night sleep study, conducted at the University of Michigan, Ann Arbor, an adaptation night was followed by baseline and SWA disruption nights with EEGs performed each night. After the baseline night, patients also had a morning and afternoon EEG.
Across the baseline day, patients with depression showed “no modulation of theta activity whatsoever,” Dr. Goldschmied said. “And then we see, following slow-wave disruption, a significant decrease in theta activity,” whereas, healthy controls showed no change in waking theta following slow-wave disruption. “So what this means is that the presence of SWA may actually be facilitating the reduction of theta or sleep propensity during typical sleep in healthy individuals,” she added. In MDD patients, the decline in theta power following slow-wave disruption was from around 5.4 to 4.3.
Dr. Goldschmied noted that this finding somewhat supports what is known as the synaptic homeostasis hypothesis that University of Wisconsin researchers Giulio Tononi, MD, PhD, and Chiara Cirelli, MD, PhD, reported (Brain Res Bull. 2003;62:143-50). This hypothesis holds that SWA is a marker of synaptic strength and promotes the downscaling of synaptic strength during sleep. No method for measuring synaptic strength in humans exists, Dr. Goldschmied added, but waking theta can be considered a proxy for net synaptic strength across the cortex.
Dr. Goldschmied noted other research that has found SWA disruption improves mood (Psychiatry Res. 2015;228:715-8; J Psychiatr Res. 2011;45:1019-26), but the study she reported on found no role of decreased theta activity in that change. “To go even further,” she said, “we looked at the entire data set and found no relationship between the decrease in theta and any of the measures of sleep architecture – so there’s really no way to predict this decrease in our sample of people with depression.”
SWA plays a significant role in depression and merits more study, Dr. Goldschmied said. She noted that future research should examine the effects of SWA disruption in a larger sample, investigate theta findings with other proxy measures of synaptic strength such as brain-derived neurotrophic factor and transcranial magnetic stimulation, explore differences in SWA between sexes, and explore how SWA enhancement influences mood and theta activity.
Dr. Goldschmied reported having no financial relationships.
SOURCE: Goldschmied J et al. Sleep 2018, Abstract 0245.
REPORTING FROM SLEEP 2018
Key clinical point: Patients with major depression have reduced brain activity after sleep disruption.
Major finding: Morning theta activity was 20% lower following slow-wave disruption in patients with major depressive disorder than in healthy controls.
Data source: EEG measures of 14 individuals with major depressive disorder and 12 healthy controls in the evening before sleep and the morning following sleep after 1 night of baseline and 1 night of selective slow-wave disrupted sleep.
Disclosure: Dr. Goldschmied had no financial relationships to disclose.
Source: Goldschmied J et al. Sleep 2018, Abstract 0245.
Patient Satisfaction and Quality of Care: A Prospective Study at Outpatient Dermatology Clinics
The Patient Protection and Affordable Care Act has increased the number of insured Americans by more than 20 million individuals.1 Approximately half of the newly insured have an income at or below 138% of the poverty level and are on average younger, sicker, and more likely to report poor to fair health compared to those individuals who already had health care coverage.2 Specialties such as dermatology are faced with the challenge of expanding access to these newly insured individuals while also improving quality of care.
Because of the complexity of defining quality in medicine, patient satisfaction is being used as a proxy for quality, with physicians evaluated and reimbursed based on patient satisfaction scores. Little research has been conducted to validate the relationship between patient satisfaction and quality; however, one study showed online reviews from patients on Yelp correlated with traditional markers of quality, such as mortality and readmission rates, lending credibility to the notion that patient satisfaction equates quality of care.3 Moreover, prospective studies have found positive correlations between patient satisfaction and compliance to therapy4,5; however, these studies may not give a complete picture of the relationship between patient satisfaction and quality of care, as other studies also have illustrated that, more often than not, factors extrinsic to actual medical care (eg, time spent in the waiting room) play a considerable role in patient satisfaction scores.6-9
When judging the quality of care that is provided, one study found that patients rate physicians based on interpersonal skills and not care delivered.8 Another important factor related to patient satisfaction is the anonymity of the surveys. Patients who have negative experiences are more likely to respond to online surveys than those who have positive experiences, skewing overall ratings.6 Additionally, because of Health Insurance Portability and Accountability Act regulations, physicians often are unable to respond directly to public patient reviews, resulting in an incomplete picture of the quality of care provided.
Ultimately, even if physicians do not agree that patient satisfaction correlates with quality of care, it is increasingly being used as a marker of such. Leading health care systems are embracing this new weight on patient satisfaction by increasing transparency and publishing patient satisfaction results online, allowing patients more access to physician reviews.
In dermatology, patient satisfaction serves an even more important role, as traditional markers of quality such as mortality and hospital readmission rates are not reasonable measures of patient care in this specialty, leaving patient satisfaction as one of the most accessible markers insurance companies and prospective patients can use to evaluate dermatologists. Furthermore, treatment modalities in dermatology often aim to improve quality of life, of which patient satisfaction arguably serves as an indicator. Ideally, patient satisfaction would allow physicians to identify areas where they may be better able to meet patients’ needs. However, patient satisfaction scores rarely are used as outcome measures in studies and are notoriously difficult to ascertain, as they tend to be inaccurate and may be unreliable in correlation with physician skill and training or may be skewed by patients’ desires to please their physicians.10 There also is a lack of standardized tools and scales to quantitatively judge outcomes in procedural surgeries.
Although patient satisfaction is being used as a measure of quality of care and is particularly necessary in a field such as dermatology that has outcome measures that are subjective in nature, there is a gap in the current literature regarding patient satisfaction and dermatology. To fill this gap, we conducted a prospective study of targeted interventions administered at outpatient dermatology clinics to determine if they resulted in statistically significant increases in patient satisfaction measures, particularly among Spanish-speaking patients.
Methods
We conducted a prospective study evaluating patient satisfaction in the outpatient dermatology clinics of LAC+USC Medical Center in Los Angeles, California, spanning over 1 year. During this time period, patients were randomly selected to participate and were asked to complete the Short-Form Patient Satisfaction Questionnaire (PSQ-18), which asked patients to rate their care experience on a 5-point Likert scale (1=strongly agree; 5=strongly disagree). The survey was separated into the following 7 subscales or categories looking at different aspects of care: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with physician, and accessibility and convenience. Patients were given this survey both before and after targeted interventions to improve patient satisfaction were implemented. The targeted interventions were created based on literature review in the factors affecting patient satisfaction. The change in relative satisfaction was then determined using statistical analysis. The study was approved by the University of Southern California Health Science institutional review board.
Results
Of 470 patients surveyed, the average age was 49 years. Fifty percent of respondents were male, 70% self-identified as Hispanic, 45% spoke Spanish as their native language, and 69% reported a mean annual household income of less than $15,000. When scores were stratified, English-speaking patients were significantly more satisfied than Spanish-speaking patients in the categories of technical quality (P.0340), financial aspects (P.0301), interpersonal manner (P.0037), and time spent with physician (P.0059). Specifically, in the time spent with physician category, the lowest scores were found in females, patients aged 18 to 29 years, and patients with a mean annual household income less than $15,000. These demographics correlate well with many of the newly insured and intimate the need for improved patient satisfaction, particularly in this subset of patients.
After analyzing baseline patient satisfaction scores, we implemented targeted interventions such as creating a call tree, developing multilingual disease-specific patient handouts, instituting quarterly nursing in-services, which judged interpersonal and occupational nursing skills, and recruiting bilingual staff. These interventions were implemented simultaneously and were selected with the goal of reducing the impact of the language barrier between physicians and patients and increasing accessibility to clinics. Following approximately 3 months of these interventions, performance on many categories increased in our demographics that were lowest performing when we collected baseline data. In Spanish-speaking respondents, improvement in several categories approached statistical significance, including general satisfaction (P.110), interpersonal skills (P.080), and time spent with physician (P.096). When stratifying by income and age, patients with a mean annual household income less than $15,000 demonstrated an improved technical quality (P.066) subscale score, and participants aged 18 to 29 years showed improvement in both accessibility and convenience (P.053) and financial aspects (P.056) subscales.
Comment
The categories where improvements were found are noteworthy and suggest that certain aspects of care are more important than others. Although it seems intuitive that clinical acumen and training should be important contributors to patient satisfaction, one study that analyzed 1000 online comments regarding patient satisfaction with dermatologists on the website DrScore.com found that most comments concerned physician personality and interpersonal skills rather than medical judgment and acumen,4 suggesting that a patient’s perception of the character of the physician directly affects patient satisfaction scores. This notion was reiterated by other studies, including one that found that a patient’s perception of the physician’s kindness and empathy skills, is the most important measure of quality of care scores.8 Although this perception can be intimidating to some physicians, as certain interpersonal skills are difficult to change, it is reassuring to note that external environment and cues, such as the clinic building and staff, also seem to affect interpersonal ratings. As seen in our study, patient ratings of a physician’s interpersonal skills increased after educational materials for staff and patients were created and more bilingual staff was recruited. Other environmental changes, such as spending a few more minutes with patients and sitting down when talking to patients, are relatively easy to administer and can improve patient satisfaction scores.8
Although some of the scores in our study approached but did not reach statistical significance, likely because of a small sample size, they suggest that targeted interventions can improve patient satisfaction. They also suggested that targeted interventions are particularly useful in Spanish-speaking patients, younger patients, and patients from lower socioeconomic backgrounds, which are all characteristics of the newly insured under the Patient Protection and Affordable Health Care Act.
Our study also is unique in that dermatology as a specialty is lagging in quality improvement studies. In the few studies evaluating patient satisfaction in the literature, the care provided by dermatologists was painted in a positive light.6,11 One study evaluated 45 dermatology practices and reported average patient satisfaction scores of 3.46 and 4.72 of 5 on Yelp and ZocDoc, respectively.11 Another study looking at dermatologist ratings on DrScore.com found that the majority of patients were satisfied with the care they received.6
Although these studies seem encouraging, they have several limitations. First, their results were not stratified by patient demographics and therefore may not be generalizable to low-income populations that constitute much of the newly insured. Secondly, the observational nature and limited number of studies prohibit meaningful conclusions from being drawn and leave many questions unanswered. Additionally, although the raw patient satisfaction scores seem good, dermatology is lacking compared to the patient satisfaction scores within other specialties. A study of more than 28,000 Yelp reviews of 23 specialties found that dermatology ranked second to last, ahead of only psychiatry.7 Of course, given the observational nature of this study, it is impossible to generalize, as many confounders (eg, medical comorbidities, patient age) may have skewed the dermatology ranking. Regardless, there is always room for improvement, and luckily improving patient satisfaction is not an elusive goal.
Conclusion
As dermatologists, our interventions often improve quality of life; therefore, we are positioned to be leaders in the quality improvement field. Despite the numerous limitations of using patient satisfaction as a measure for quality of care, it is used by payers to determine reimbursement and patients to select providers. Encouraging initial data from our prospective study demonstrate that small interventions can increase patient satisfaction. Continued work to maximize patient satisfaction is needed to improve outcomes for our patients, help validate the quality of care being provided, and further solidify the importance of having insurers maintain sufficient dermatologists in their networks.
- Uberoi N, Finegold K, Gee E. Health insurance coverage and the Affordable Care Act, 2010-2016. US Department of Health & Human Services website. https://aspe.hhs.gov/system/files/pdf/187551/ACA2010-2016.pdf. Published March 3, 2016. Accessed May 18, 2018.
- Shatzer A, Long SK, Zuckerman S. Who are the newly insured as of early March 2014? Urban Institute Health Policy Center website. http://hrms.urban.org/briefs/Who-Are-the-Newly-Insured.html. Published May 22, 2014. Accessed May 18, 2018.
- Bardach NS, Asteria-Peñaloza R, Boscardin WJ, et al. The relationship between commercial website ratings and traditional hospital performance measures in the USA. BMJ Qual Saf. 2013;22:194-202.
- Kincey J, Bradshaw P, Ley P. Patient satisfaction and reported acceptance of medical advice in general practice. J R Coll Gen Pract. 1975;25:558-566.
- Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication. patients’ response to medical advice. N Engl J Med. 1969;280:535-540.
- Ali ST, Feldman SR. Patient satisfaction in dermatology: a qualitative assessment. Dermatol Online J. 2014;20. pii:doj_21534.
- Internet study: highest educated & trained doctors get poorest online reviews. Vanguard Communications website. https://vanguard communications.net/best-online-doctor-reviews/. Published April 22, 2015. Accessed May 18, 2018.
- Uhas AA, Camacho FT, Feldman SR, et al. The relationship between physician friendliness and caring, and patient satisfaction: findings from an internet-based survey. Patient. 2008;1:91-96.
- Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007;7:31.
- Maibach HI, Gorouhi F. Evidence-Based Dermatology. 2nd ed. Shelton, CT: People’s Medical Publishing House-USA; 2011.
- Smith R, Lipoff J. Evaluation of dermatology practice online reviews. JAMA Dermatol. 2016;152:153-157.
The Patient Protection and Affordable Care Act has increased the number of insured Americans by more than 20 million individuals.1 Approximately half of the newly insured have an income at or below 138% of the poverty level and are on average younger, sicker, and more likely to report poor to fair health compared to those individuals who already had health care coverage.2 Specialties such as dermatology are faced with the challenge of expanding access to these newly insured individuals while also improving quality of care.
Because of the complexity of defining quality in medicine, patient satisfaction is being used as a proxy for quality, with physicians evaluated and reimbursed based on patient satisfaction scores. Little research has been conducted to validate the relationship between patient satisfaction and quality; however, one study showed online reviews from patients on Yelp correlated with traditional markers of quality, such as mortality and readmission rates, lending credibility to the notion that patient satisfaction equates quality of care.3 Moreover, prospective studies have found positive correlations between patient satisfaction and compliance to therapy4,5; however, these studies may not give a complete picture of the relationship between patient satisfaction and quality of care, as other studies also have illustrated that, more often than not, factors extrinsic to actual medical care (eg, time spent in the waiting room) play a considerable role in patient satisfaction scores.6-9
When judging the quality of care that is provided, one study found that patients rate physicians based on interpersonal skills and not care delivered.8 Another important factor related to patient satisfaction is the anonymity of the surveys. Patients who have negative experiences are more likely to respond to online surveys than those who have positive experiences, skewing overall ratings.6 Additionally, because of Health Insurance Portability and Accountability Act regulations, physicians often are unable to respond directly to public patient reviews, resulting in an incomplete picture of the quality of care provided.
Ultimately, even if physicians do not agree that patient satisfaction correlates with quality of care, it is increasingly being used as a marker of such. Leading health care systems are embracing this new weight on patient satisfaction by increasing transparency and publishing patient satisfaction results online, allowing patients more access to physician reviews.
In dermatology, patient satisfaction serves an even more important role, as traditional markers of quality such as mortality and hospital readmission rates are not reasonable measures of patient care in this specialty, leaving patient satisfaction as one of the most accessible markers insurance companies and prospective patients can use to evaluate dermatologists. Furthermore, treatment modalities in dermatology often aim to improve quality of life, of which patient satisfaction arguably serves as an indicator. Ideally, patient satisfaction would allow physicians to identify areas where they may be better able to meet patients’ needs. However, patient satisfaction scores rarely are used as outcome measures in studies and are notoriously difficult to ascertain, as they tend to be inaccurate and may be unreliable in correlation with physician skill and training or may be skewed by patients’ desires to please their physicians.10 There also is a lack of standardized tools and scales to quantitatively judge outcomes in procedural surgeries.
Although patient satisfaction is being used as a measure of quality of care and is particularly necessary in a field such as dermatology that has outcome measures that are subjective in nature, there is a gap in the current literature regarding patient satisfaction and dermatology. To fill this gap, we conducted a prospective study of targeted interventions administered at outpatient dermatology clinics to determine if they resulted in statistically significant increases in patient satisfaction measures, particularly among Spanish-speaking patients.
Methods
We conducted a prospective study evaluating patient satisfaction in the outpatient dermatology clinics of LAC+USC Medical Center in Los Angeles, California, spanning over 1 year. During this time period, patients were randomly selected to participate and were asked to complete the Short-Form Patient Satisfaction Questionnaire (PSQ-18), which asked patients to rate their care experience on a 5-point Likert scale (1=strongly agree; 5=strongly disagree). The survey was separated into the following 7 subscales or categories looking at different aspects of care: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with physician, and accessibility and convenience. Patients were given this survey both before and after targeted interventions to improve patient satisfaction were implemented. The targeted interventions were created based on literature review in the factors affecting patient satisfaction. The change in relative satisfaction was then determined using statistical analysis. The study was approved by the University of Southern California Health Science institutional review board.
Results
Of 470 patients surveyed, the average age was 49 years. Fifty percent of respondents were male, 70% self-identified as Hispanic, 45% spoke Spanish as their native language, and 69% reported a mean annual household income of less than $15,000. When scores were stratified, English-speaking patients were significantly more satisfied than Spanish-speaking patients in the categories of technical quality (P.0340), financial aspects (P.0301), interpersonal manner (P.0037), and time spent with physician (P.0059). Specifically, in the time spent with physician category, the lowest scores were found in females, patients aged 18 to 29 years, and patients with a mean annual household income less than $15,000. These demographics correlate well with many of the newly insured and intimate the need for improved patient satisfaction, particularly in this subset of patients.
After analyzing baseline patient satisfaction scores, we implemented targeted interventions such as creating a call tree, developing multilingual disease-specific patient handouts, instituting quarterly nursing in-services, which judged interpersonal and occupational nursing skills, and recruiting bilingual staff. These interventions were implemented simultaneously and were selected with the goal of reducing the impact of the language barrier between physicians and patients and increasing accessibility to clinics. Following approximately 3 months of these interventions, performance on many categories increased in our demographics that were lowest performing when we collected baseline data. In Spanish-speaking respondents, improvement in several categories approached statistical significance, including general satisfaction (P.110), interpersonal skills (P.080), and time spent with physician (P.096). When stratifying by income and age, patients with a mean annual household income less than $15,000 demonstrated an improved technical quality (P.066) subscale score, and participants aged 18 to 29 years showed improvement in both accessibility and convenience (P.053) and financial aspects (P.056) subscales.
Comment
The categories where improvements were found are noteworthy and suggest that certain aspects of care are more important than others. Although it seems intuitive that clinical acumen and training should be important contributors to patient satisfaction, one study that analyzed 1000 online comments regarding patient satisfaction with dermatologists on the website DrScore.com found that most comments concerned physician personality and interpersonal skills rather than medical judgment and acumen,4 suggesting that a patient’s perception of the character of the physician directly affects patient satisfaction scores. This notion was reiterated by other studies, including one that found that a patient’s perception of the physician’s kindness and empathy skills, is the most important measure of quality of care scores.8 Although this perception can be intimidating to some physicians, as certain interpersonal skills are difficult to change, it is reassuring to note that external environment and cues, such as the clinic building and staff, also seem to affect interpersonal ratings. As seen in our study, patient ratings of a physician’s interpersonal skills increased after educational materials for staff and patients were created and more bilingual staff was recruited. Other environmental changes, such as spending a few more minutes with patients and sitting down when talking to patients, are relatively easy to administer and can improve patient satisfaction scores.8
Although some of the scores in our study approached but did not reach statistical significance, likely because of a small sample size, they suggest that targeted interventions can improve patient satisfaction. They also suggested that targeted interventions are particularly useful in Spanish-speaking patients, younger patients, and patients from lower socioeconomic backgrounds, which are all characteristics of the newly insured under the Patient Protection and Affordable Health Care Act.
Our study also is unique in that dermatology as a specialty is lagging in quality improvement studies. In the few studies evaluating patient satisfaction in the literature, the care provided by dermatologists was painted in a positive light.6,11 One study evaluated 45 dermatology practices and reported average patient satisfaction scores of 3.46 and 4.72 of 5 on Yelp and ZocDoc, respectively.11 Another study looking at dermatologist ratings on DrScore.com found that the majority of patients were satisfied with the care they received.6
Although these studies seem encouraging, they have several limitations. First, their results were not stratified by patient demographics and therefore may not be generalizable to low-income populations that constitute much of the newly insured. Secondly, the observational nature and limited number of studies prohibit meaningful conclusions from being drawn and leave many questions unanswered. Additionally, although the raw patient satisfaction scores seem good, dermatology is lacking compared to the patient satisfaction scores within other specialties. A study of more than 28,000 Yelp reviews of 23 specialties found that dermatology ranked second to last, ahead of only psychiatry.7 Of course, given the observational nature of this study, it is impossible to generalize, as many confounders (eg, medical comorbidities, patient age) may have skewed the dermatology ranking. Regardless, there is always room for improvement, and luckily improving patient satisfaction is not an elusive goal.
Conclusion
As dermatologists, our interventions often improve quality of life; therefore, we are positioned to be leaders in the quality improvement field. Despite the numerous limitations of using patient satisfaction as a measure for quality of care, it is used by payers to determine reimbursement and patients to select providers. Encouraging initial data from our prospective study demonstrate that small interventions can increase patient satisfaction. Continued work to maximize patient satisfaction is needed to improve outcomes for our patients, help validate the quality of care being provided, and further solidify the importance of having insurers maintain sufficient dermatologists in their networks.
The Patient Protection and Affordable Care Act has increased the number of insured Americans by more than 20 million individuals.1 Approximately half of the newly insured have an income at or below 138% of the poverty level and are on average younger, sicker, and more likely to report poor to fair health compared to those individuals who already had health care coverage.2 Specialties such as dermatology are faced with the challenge of expanding access to these newly insured individuals while also improving quality of care.
Because of the complexity of defining quality in medicine, patient satisfaction is being used as a proxy for quality, with physicians evaluated and reimbursed based on patient satisfaction scores. Little research has been conducted to validate the relationship between patient satisfaction and quality; however, one study showed online reviews from patients on Yelp correlated with traditional markers of quality, such as mortality and readmission rates, lending credibility to the notion that patient satisfaction equates quality of care.3 Moreover, prospective studies have found positive correlations between patient satisfaction and compliance to therapy4,5; however, these studies may not give a complete picture of the relationship between patient satisfaction and quality of care, as other studies also have illustrated that, more often than not, factors extrinsic to actual medical care (eg, time spent in the waiting room) play a considerable role in patient satisfaction scores.6-9
When judging the quality of care that is provided, one study found that patients rate physicians based on interpersonal skills and not care delivered.8 Another important factor related to patient satisfaction is the anonymity of the surveys. Patients who have negative experiences are more likely to respond to online surveys than those who have positive experiences, skewing overall ratings.6 Additionally, because of Health Insurance Portability and Accountability Act regulations, physicians often are unable to respond directly to public patient reviews, resulting in an incomplete picture of the quality of care provided.
Ultimately, even if physicians do not agree that patient satisfaction correlates with quality of care, it is increasingly being used as a marker of such. Leading health care systems are embracing this new weight on patient satisfaction by increasing transparency and publishing patient satisfaction results online, allowing patients more access to physician reviews.
In dermatology, patient satisfaction serves an even more important role, as traditional markers of quality such as mortality and hospital readmission rates are not reasonable measures of patient care in this specialty, leaving patient satisfaction as one of the most accessible markers insurance companies and prospective patients can use to evaluate dermatologists. Furthermore, treatment modalities in dermatology often aim to improve quality of life, of which patient satisfaction arguably serves as an indicator. Ideally, patient satisfaction would allow physicians to identify areas where they may be better able to meet patients’ needs. However, patient satisfaction scores rarely are used as outcome measures in studies and are notoriously difficult to ascertain, as they tend to be inaccurate and may be unreliable in correlation with physician skill and training or may be skewed by patients’ desires to please their physicians.10 There also is a lack of standardized tools and scales to quantitatively judge outcomes in procedural surgeries.
Although patient satisfaction is being used as a measure of quality of care and is particularly necessary in a field such as dermatology that has outcome measures that are subjective in nature, there is a gap in the current literature regarding patient satisfaction and dermatology. To fill this gap, we conducted a prospective study of targeted interventions administered at outpatient dermatology clinics to determine if they resulted in statistically significant increases in patient satisfaction measures, particularly among Spanish-speaking patients.
Methods
We conducted a prospective study evaluating patient satisfaction in the outpatient dermatology clinics of LAC+USC Medical Center in Los Angeles, California, spanning over 1 year. During this time period, patients were randomly selected to participate and were asked to complete the Short-Form Patient Satisfaction Questionnaire (PSQ-18), which asked patients to rate their care experience on a 5-point Likert scale (1=strongly agree; 5=strongly disagree). The survey was separated into the following 7 subscales or categories looking at different aspects of care: general satisfaction, technical quality, interpersonal manner, communication, financial aspects, time spent with physician, and accessibility and convenience. Patients were given this survey both before and after targeted interventions to improve patient satisfaction were implemented. The targeted interventions were created based on literature review in the factors affecting patient satisfaction. The change in relative satisfaction was then determined using statistical analysis. The study was approved by the University of Southern California Health Science institutional review board.
Results
Of 470 patients surveyed, the average age was 49 years. Fifty percent of respondents were male, 70% self-identified as Hispanic, 45% spoke Spanish as their native language, and 69% reported a mean annual household income of less than $15,000. When scores were stratified, English-speaking patients were significantly more satisfied than Spanish-speaking patients in the categories of technical quality (P.0340), financial aspects (P.0301), interpersonal manner (P.0037), and time spent with physician (P.0059). Specifically, in the time spent with physician category, the lowest scores were found in females, patients aged 18 to 29 years, and patients with a mean annual household income less than $15,000. These demographics correlate well with many of the newly insured and intimate the need for improved patient satisfaction, particularly in this subset of patients.
After analyzing baseline patient satisfaction scores, we implemented targeted interventions such as creating a call tree, developing multilingual disease-specific patient handouts, instituting quarterly nursing in-services, which judged interpersonal and occupational nursing skills, and recruiting bilingual staff. These interventions were implemented simultaneously and were selected with the goal of reducing the impact of the language barrier between physicians and patients and increasing accessibility to clinics. Following approximately 3 months of these interventions, performance on many categories increased in our demographics that were lowest performing when we collected baseline data. In Spanish-speaking respondents, improvement in several categories approached statistical significance, including general satisfaction (P.110), interpersonal skills (P.080), and time spent with physician (P.096). When stratifying by income and age, patients with a mean annual household income less than $15,000 demonstrated an improved technical quality (P.066) subscale score, and participants aged 18 to 29 years showed improvement in both accessibility and convenience (P.053) and financial aspects (P.056) subscales.
Comment
The categories where improvements were found are noteworthy and suggest that certain aspects of care are more important than others. Although it seems intuitive that clinical acumen and training should be important contributors to patient satisfaction, one study that analyzed 1000 online comments regarding patient satisfaction with dermatologists on the website DrScore.com found that most comments concerned physician personality and interpersonal skills rather than medical judgment and acumen,4 suggesting that a patient’s perception of the character of the physician directly affects patient satisfaction scores. This notion was reiterated by other studies, including one that found that a patient’s perception of the physician’s kindness and empathy skills, is the most important measure of quality of care scores.8 Although this perception can be intimidating to some physicians, as certain interpersonal skills are difficult to change, it is reassuring to note that external environment and cues, such as the clinic building and staff, also seem to affect interpersonal ratings. As seen in our study, patient ratings of a physician’s interpersonal skills increased after educational materials for staff and patients were created and more bilingual staff was recruited. Other environmental changes, such as spending a few more minutes with patients and sitting down when talking to patients, are relatively easy to administer and can improve patient satisfaction scores.8
Although some of the scores in our study approached but did not reach statistical significance, likely because of a small sample size, they suggest that targeted interventions can improve patient satisfaction. They also suggested that targeted interventions are particularly useful in Spanish-speaking patients, younger patients, and patients from lower socioeconomic backgrounds, which are all characteristics of the newly insured under the Patient Protection and Affordable Health Care Act.
Our study also is unique in that dermatology as a specialty is lagging in quality improvement studies. In the few studies evaluating patient satisfaction in the literature, the care provided by dermatologists was painted in a positive light.6,11 One study evaluated 45 dermatology practices and reported average patient satisfaction scores of 3.46 and 4.72 of 5 on Yelp and ZocDoc, respectively.11 Another study looking at dermatologist ratings on DrScore.com found that the majority of patients were satisfied with the care they received.6
Although these studies seem encouraging, they have several limitations. First, their results were not stratified by patient demographics and therefore may not be generalizable to low-income populations that constitute much of the newly insured. Secondly, the observational nature and limited number of studies prohibit meaningful conclusions from being drawn and leave many questions unanswered. Additionally, although the raw patient satisfaction scores seem good, dermatology is lacking compared to the patient satisfaction scores within other specialties. A study of more than 28,000 Yelp reviews of 23 specialties found that dermatology ranked second to last, ahead of only psychiatry.7 Of course, given the observational nature of this study, it is impossible to generalize, as many confounders (eg, medical comorbidities, patient age) may have skewed the dermatology ranking. Regardless, there is always room for improvement, and luckily improving patient satisfaction is not an elusive goal.
Conclusion
As dermatologists, our interventions often improve quality of life; therefore, we are positioned to be leaders in the quality improvement field. Despite the numerous limitations of using patient satisfaction as a measure for quality of care, it is used by payers to determine reimbursement and patients to select providers. Encouraging initial data from our prospective study demonstrate that small interventions can increase patient satisfaction. Continued work to maximize patient satisfaction is needed to improve outcomes for our patients, help validate the quality of care being provided, and further solidify the importance of having insurers maintain sufficient dermatologists in their networks.
- Uberoi N, Finegold K, Gee E. Health insurance coverage and the Affordable Care Act, 2010-2016. US Department of Health & Human Services website. https://aspe.hhs.gov/system/files/pdf/187551/ACA2010-2016.pdf. Published March 3, 2016. Accessed May 18, 2018.
- Shatzer A, Long SK, Zuckerman S. Who are the newly insured as of early March 2014? Urban Institute Health Policy Center website. http://hrms.urban.org/briefs/Who-Are-the-Newly-Insured.html. Published May 22, 2014. Accessed May 18, 2018.
- Bardach NS, Asteria-Peñaloza R, Boscardin WJ, et al. The relationship between commercial website ratings and traditional hospital performance measures in the USA. BMJ Qual Saf. 2013;22:194-202.
- Kincey J, Bradshaw P, Ley P. Patient satisfaction and reported acceptance of medical advice in general practice. J R Coll Gen Pract. 1975;25:558-566.
- Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication. patients’ response to medical advice. N Engl J Med. 1969;280:535-540.
- Ali ST, Feldman SR. Patient satisfaction in dermatology: a qualitative assessment. Dermatol Online J. 2014;20. pii:doj_21534.
- Internet study: highest educated & trained doctors get poorest online reviews. Vanguard Communications website. https://vanguard communications.net/best-online-doctor-reviews/. Published April 22, 2015. Accessed May 18, 2018.
- Uhas AA, Camacho FT, Feldman SR, et al. The relationship between physician friendliness and caring, and patient satisfaction: findings from an internet-based survey. Patient. 2008;1:91-96.
- Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007;7:31.
- Maibach HI, Gorouhi F. Evidence-Based Dermatology. 2nd ed. Shelton, CT: People’s Medical Publishing House-USA; 2011.
- Smith R, Lipoff J. Evaluation of dermatology practice online reviews. JAMA Dermatol. 2016;152:153-157.
- Uberoi N, Finegold K, Gee E. Health insurance coverage and the Affordable Care Act, 2010-2016. US Department of Health & Human Services website. https://aspe.hhs.gov/system/files/pdf/187551/ACA2010-2016.pdf. Published March 3, 2016. Accessed May 18, 2018.
- Shatzer A, Long SK, Zuckerman S. Who are the newly insured as of early March 2014? Urban Institute Health Policy Center website. http://hrms.urban.org/briefs/Who-Are-the-Newly-Insured.html. Published May 22, 2014. Accessed May 18, 2018.
- Bardach NS, Asteria-Peñaloza R, Boscardin WJ, et al. The relationship between commercial website ratings and traditional hospital performance measures in the USA. BMJ Qual Saf. 2013;22:194-202.
- Kincey J, Bradshaw P, Ley P. Patient satisfaction and reported acceptance of medical advice in general practice. J R Coll Gen Pract. 1975;25:558-566.
- Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication. patients’ response to medical advice. N Engl J Med. 1969;280:535-540.
- Ali ST, Feldman SR. Patient satisfaction in dermatology: a qualitative assessment. Dermatol Online J. 2014;20. pii:doj_21534.
- Internet study: highest educated & trained doctors get poorest online reviews. Vanguard Communications website. https://vanguard communications.net/best-online-doctor-reviews/. Published April 22, 2015. Accessed May 18, 2018.
- Uhas AA, Camacho FT, Feldman SR, et al. The relationship between physician friendliness and caring, and patient satisfaction: findings from an internet-based survey. Patient. 2008;1:91-96.
- Anderson RT, Camacho FT, Balkrishnan R. Willing to wait?: the influence of patient wait time on satisfaction with primary care. BMC Health Serv Res. 2007;7:31.
- Maibach HI, Gorouhi F. Evidence-Based Dermatology. 2nd ed. Shelton, CT: People’s Medical Publishing House-USA; 2011.
- Smith R, Lipoff J. Evaluation of dermatology practice online reviews. JAMA Dermatol. 2016;152:153-157.
Practice Points
- It is becoming increasingly important, particularly in the field of dermatology, to both measure and work to improve patient satisfaction scores.
- Preliminary research has found that simple interventions, such as providing disease-specific handouts and interpreter services, can improve satisfaction scores, making patient satisfaction an achievable goal.