User login
New insights into sleep, pregnancy weight gain
BALTIMORE – Pregnant women who are overweight and obese are like the general population in that the less they sleep, the more weight they gain, particularly in the first half of pregnancy. However, unlike in the larger adult population, prolonged daily total eating time was not associated with gestational weight gain in these women, particularly early in pregnancy, according to findings from a small study presented at the Associated Professional Sleep Societies annual meeting.
Those findings point to a need to further study the , said Rachel P. Kolko, PhD, a postdoctoral scholar at the University of Pittsburgh, Western Psychiatric Institute and Clinic.
“The association with total sleep time was found to be significant, such that if you had less sleep, you had higher amounts of weight gain; we did not find a significant relation with our eating window variable,” Dr. Kolko said.
She reported on research involving 62 pregnant women, 53% of whom were overweight with a body mass index of 25-29.9 kg/m2 and 47% of whom were obese with BMI greater than 30. Forty-seven percent of the study population was nonwhite.
The research grew out of a need to identify potentially modifiable factors to curtail excessive gestational weight gain during pregnancy, she said. The study hypotheses were that both shorter total sleep time and longer total eating time would lead to higher gestational weight gain, but the study confirmed only the former as a contributing factor.
The women in the study were at 12-20 weeks of pregnancy. Gestational weight gain was calculated as the difference between self-reported prepregnancy weight and current weight. Total sleep time was based on the Pittsburgh Sleep Quality Index, and total eating time was calculated as the time difference between the day’s first meal or snack of more than 50 calories and the last, as self-reported.
Average total sleep time was 7.8 hours, with total eating time spanning 10.8 hours. On average, study participants gained 9.7 pounds through the first half of pregnancy, Dr. Kolko said. She noted that the Institute of Medicine, now known as the National Academy of Medicine, recommends that women who are overweight women gain 15-25 pounds during pregnancy and women who are obese gain 11-20 pounds (JAMA. 2017;317:2207-25). “Already about 20% of our sample has gained that amount of weight within the first half of pregnancy,” she said.
“Total sleep time was related to a higher early gestational weight in women with overweight and obesity, and it’s possible that addressing this may affect and hopefully improve women’s weight gain during early pregnancy to fit within those guidelines,” she said.
Future research should look at the entire gestational period – possibly targeting sleep patterns during pregnancy – and should expand to include women who are not overweight or obese, Dr. Kolko noted.
Dr. Kolko reported having no financial relationships to disclose.
SOURCE: Kolko RP, et al., SLEEP 2018, Abstract 0692.
BALTIMORE – Pregnant women who are overweight and obese are like the general population in that the less they sleep, the more weight they gain, particularly in the first half of pregnancy. However, unlike in the larger adult population, prolonged daily total eating time was not associated with gestational weight gain in these women, particularly early in pregnancy, according to findings from a small study presented at the Associated Professional Sleep Societies annual meeting.
Those findings point to a need to further study the , said Rachel P. Kolko, PhD, a postdoctoral scholar at the University of Pittsburgh, Western Psychiatric Institute and Clinic.
“The association with total sleep time was found to be significant, such that if you had less sleep, you had higher amounts of weight gain; we did not find a significant relation with our eating window variable,” Dr. Kolko said.
She reported on research involving 62 pregnant women, 53% of whom were overweight with a body mass index of 25-29.9 kg/m2 and 47% of whom were obese with BMI greater than 30. Forty-seven percent of the study population was nonwhite.
The research grew out of a need to identify potentially modifiable factors to curtail excessive gestational weight gain during pregnancy, she said. The study hypotheses were that both shorter total sleep time and longer total eating time would lead to higher gestational weight gain, but the study confirmed only the former as a contributing factor.
The women in the study were at 12-20 weeks of pregnancy. Gestational weight gain was calculated as the difference between self-reported prepregnancy weight and current weight. Total sleep time was based on the Pittsburgh Sleep Quality Index, and total eating time was calculated as the time difference between the day’s first meal or snack of more than 50 calories and the last, as self-reported.
Average total sleep time was 7.8 hours, with total eating time spanning 10.8 hours. On average, study participants gained 9.7 pounds through the first half of pregnancy, Dr. Kolko said. She noted that the Institute of Medicine, now known as the National Academy of Medicine, recommends that women who are overweight women gain 15-25 pounds during pregnancy and women who are obese gain 11-20 pounds (JAMA. 2017;317:2207-25). “Already about 20% of our sample has gained that amount of weight within the first half of pregnancy,” she said.
“Total sleep time was related to a higher early gestational weight in women with overweight and obesity, and it’s possible that addressing this may affect and hopefully improve women’s weight gain during early pregnancy to fit within those guidelines,” she said.
Future research should look at the entire gestational period – possibly targeting sleep patterns during pregnancy – and should expand to include women who are not overweight or obese, Dr. Kolko noted.
Dr. Kolko reported having no financial relationships to disclose.
SOURCE: Kolko RP, et al., SLEEP 2018, Abstract 0692.
BALTIMORE – Pregnant women who are overweight and obese are like the general population in that the less they sleep, the more weight they gain, particularly in the first half of pregnancy. However, unlike in the larger adult population, prolonged daily total eating time was not associated with gestational weight gain in these women, particularly early in pregnancy, according to findings from a small study presented at the Associated Professional Sleep Societies annual meeting.
Those findings point to a need to further study the , said Rachel P. Kolko, PhD, a postdoctoral scholar at the University of Pittsburgh, Western Psychiatric Institute and Clinic.
“The association with total sleep time was found to be significant, such that if you had less sleep, you had higher amounts of weight gain; we did not find a significant relation with our eating window variable,” Dr. Kolko said.
She reported on research involving 62 pregnant women, 53% of whom were overweight with a body mass index of 25-29.9 kg/m2 and 47% of whom were obese with BMI greater than 30. Forty-seven percent of the study population was nonwhite.
The research grew out of a need to identify potentially modifiable factors to curtail excessive gestational weight gain during pregnancy, she said. The study hypotheses were that both shorter total sleep time and longer total eating time would lead to higher gestational weight gain, but the study confirmed only the former as a contributing factor.
The women in the study were at 12-20 weeks of pregnancy. Gestational weight gain was calculated as the difference between self-reported prepregnancy weight and current weight. Total sleep time was based on the Pittsburgh Sleep Quality Index, and total eating time was calculated as the time difference between the day’s first meal or snack of more than 50 calories and the last, as self-reported.
Average total sleep time was 7.8 hours, with total eating time spanning 10.8 hours. On average, study participants gained 9.7 pounds through the first half of pregnancy, Dr. Kolko said. She noted that the Institute of Medicine, now known as the National Academy of Medicine, recommends that women who are overweight women gain 15-25 pounds during pregnancy and women who are obese gain 11-20 pounds (JAMA. 2017;317:2207-25). “Already about 20% of our sample has gained that amount of weight within the first half of pregnancy,” she said.
“Total sleep time was related to a higher early gestational weight in women with overweight and obesity, and it’s possible that addressing this may affect and hopefully improve women’s weight gain during early pregnancy to fit within those guidelines,” she said.
Future research should look at the entire gestational period – possibly targeting sleep patterns during pregnancy – and should expand to include women who are not overweight or obese, Dr. Kolko noted.
Dr. Kolko reported having no financial relationships to disclose.
SOURCE: Kolko RP, et al., SLEEP 2018, Abstract 0692.
REPORTING FROM SLEEP 2018
Key clinical point: In overweight/obese women, shorter sleep times are linked to early gestational weight gain.
Major finding: Overweight/obese women slept 30% less and had higher gestational weight gain in early pregnancy.
Study details: Study of 62 women between 12 and 20 weeks’ gestation with prepregnancy BMI greater than 25 kg/m2.
Disclosures: Dr. Kolko reported having no financial relationships.
Source: Kolko RP et al. SLEEP 2018, Abstract 0692.
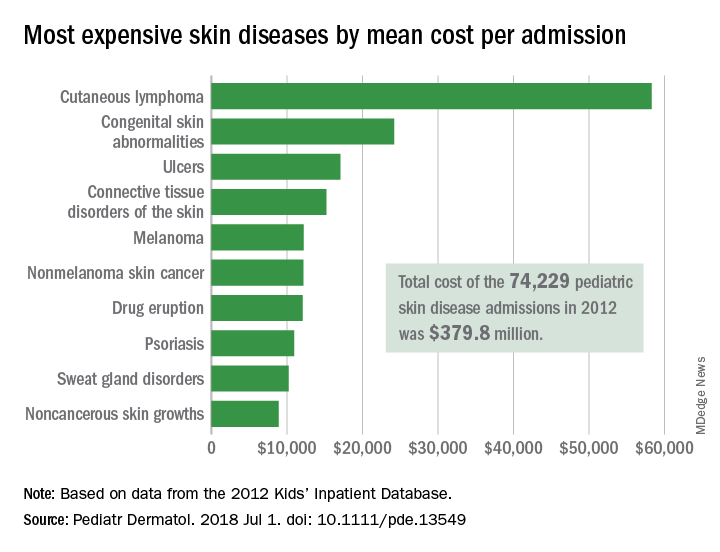
Pediatric dermatology admissions: Crunching the numbers
according to data from the Agency for Healthcare Research and Quality.
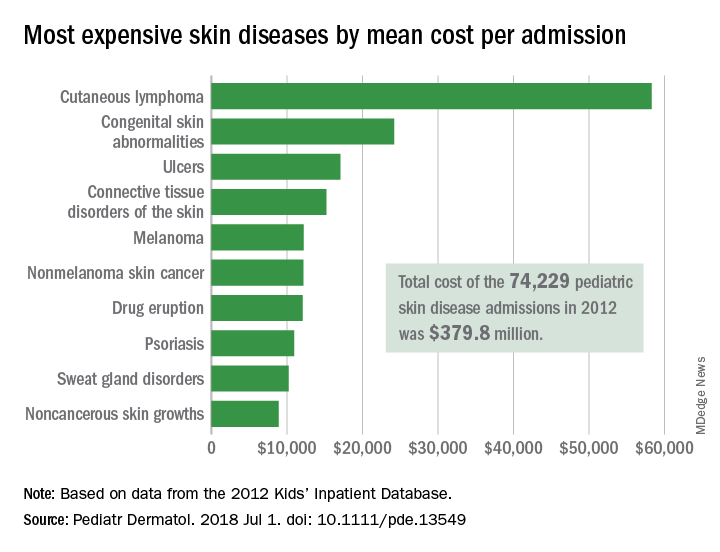
There were 74,229 such admissions in the United States that year – all others totaled 1.77 million – and the children at the highest risk for dermatology hospitalization were those living in communities with the lowest household incomes, the uninsured and those on Medicaid, and those living in the South, Justin D. Arnold of George Washington University, Washington, and his associates said in Pediatric Dermatology.
“Individuals from communities of low socioeconomic status may be more likely to be hospitalized because of gaps in insurance coverage, difficulty with transportation, or inconsistent access to preventative medical care, which for skin disease, would include access to an outpatient pediatric dermatologist,” they wrote.
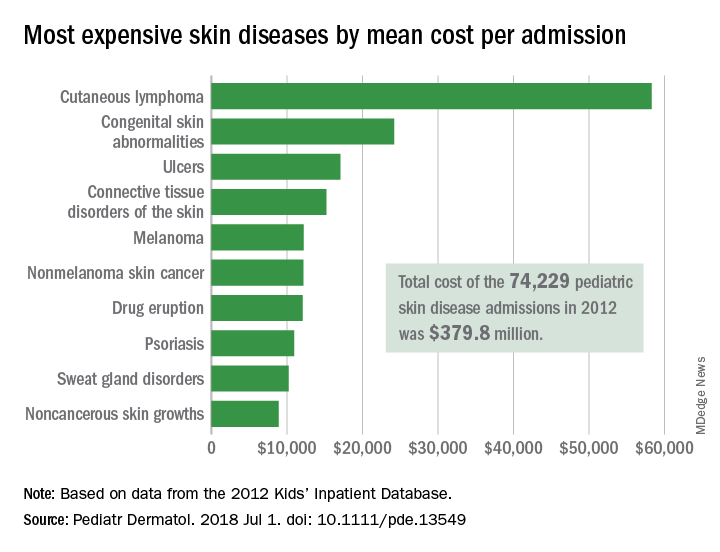
All those admissions for skin diseases cost the health care system $379.8 million in 2012, or 1.9% of the $20.3 billion spent on all pediatric hospitalizations, excluding those related to pregnancy or childbirth. The mean cost of a skin disease admission was $5,211 for a child aged less than 18 years, compared with $11,409 for nondermatology admissions, according to data from the 2012 Kids’ Inpatient Database, which includes records of pediatric discharges from 44 states.
Cutaneous lymphoma was the most expensive skin disease per admission at a mean cost of $58,294, with congenital skin abnormalities second at $24,186, and ulcers third at $17,064. Bacterial skin infections and infestations were only the 19th most expensive admission at $4,135, but it was by far the most common (59,115 admissions) and the most expensive overall, with a total cost of $240 million. The second most common condition was viral diseases with 3,812 admissions and the next most expensive total was $33.5 million for connective tissue disorders, Mr. Arnold and his associates said.
Multivariate models that adjusted for such factors as age, sex, and race revealed that “the risk of hospitalization for skin disease increased as the median income of one’s zip code declined,” the investigators noted. The adjusted odds ratio for hospitalization in the lowest-income quartile (less than $39,000) was 1.22, compared with the highest-income quartile.
Insurance status also affected hospitalization, putting children from families with no insurance (aOR, 1.35) and those on Medicaid (aOR, 1.17) at a disadvantage, compared with those who had private insurance. “Policy makers should consider increasing Medicaid reimbursement rates to outpatient dermatologists, which might encourage more clinicians to accept this form of insurance and thereby expand access to preventative skin care,” they said.
Regional differences also were observed, which put children from the southern states at the highest risk (aOR, 1.32), compared with those in the West, which could be related to access issues. “In 2016, 4 of the 10 communities in the United States with the lowest density of dermatologists were in the South, suggesting that the high rate of hospitalizations there may also be partially attributed to lack of access to dermatologists,” Mr. Arnold and his associates wrote.
The investigators did not report funding or disclose conflicts of interest.
SOURCE: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
according to data from the Agency for Healthcare Research and Quality.
There were 74,229 such admissions in the United States that year – all others totaled 1.77 million – and the children at the highest risk for dermatology hospitalization were those living in communities with the lowest household incomes, the uninsured and those on Medicaid, and those living in the South, Justin D. Arnold of George Washington University, Washington, and his associates said in Pediatric Dermatology.
“Individuals from communities of low socioeconomic status may be more likely to be hospitalized because of gaps in insurance coverage, difficulty with transportation, or inconsistent access to preventative medical care, which for skin disease, would include access to an outpatient pediatric dermatologist,” they wrote.
All those admissions for skin diseases cost the health care system $379.8 million in 2012, or 1.9% of the $20.3 billion spent on all pediatric hospitalizations, excluding those related to pregnancy or childbirth. The mean cost of a skin disease admission was $5,211 for a child aged less than 18 years, compared with $11,409 for nondermatology admissions, according to data from the 2012 Kids’ Inpatient Database, which includes records of pediatric discharges from 44 states.
Cutaneous lymphoma was the most expensive skin disease per admission at a mean cost of $58,294, with congenital skin abnormalities second at $24,186, and ulcers third at $17,064. Bacterial skin infections and infestations were only the 19th most expensive admission at $4,135, but it was by far the most common (59,115 admissions) and the most expensive overall, with a total cost of $240 million. The second most common condition was viral diseases with 3,812 admissions and the next most expensive total was $33.5 million for connective tissue disorders, Mr. Arnold and his associates said.
Multivariate models that adjusted for such factors as age, sex, and race revealed that “the risk of hospitalization for skin disease increased as the median income of one’s zip code declined,” the investigators noted. The adjusted odds ratio for hospitalization in the lowest-income quartile (less than $39,000) was 1.22, compared with the highest-income quartile.
Insurance status also affected hospitalization, putting children from families with no insurance (aOR, 1.35) and those on Medicaid (aOR, 1.17) at a disadvantage, compared with those who had private insurance. “Policy makers should consider increasing Medicaid reimbursement rates to outpatient dermatologists, which might encourage more clinicians to accept this form of insurance and thereby expand access to preventative skin care,” they said.
Regional differences also were observed, which put children from the southern states at the highest risk (aOR, 1.32), compared with those in the West, which could be related to access issues. “In 2016, 4 of the 10 communities in the United States with the lowest density of dermatologists were in the South, suggesting that the high rate of hospitalizations there may also be partially attributed to lack of access to dermatologists,” Mr. Arnold and his associates wrote.
The investigators did not report funding or disclose conflicts of interest.
SOURCE: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
according to data from the Agency for Healthcare Research and Quality.
There were 74,229 such admissions in the United States that year – all others totaled 1.77 million – and the children at the highest risk for dermatology hospitalization were those living in communities with the lowest household incomes, the uninsured and those on Medicaid, and those living in the South, Justin D. Arnold of George Washington University, Washington, and his associates said in Pediatric Dermatology.
“Individuals from communities of low socioeconomic status may be more likely to be hospitalized because of gaps in insurance coverage, difficulty with transportation, or inconsistent access to preventative medical care, which for skin disease, would include access to an outpatient pediatric dermatologist,” they wrote.
All those admissions for skin diseases cost the health care system $379.8 million in 2012, or 1.9% of the $20.3 billion spent on all pediatric hospitalizations, excluding those related to pregnancy or childbirth. The mean cost of a skin disease admission was $5,211 for a child aged less than 18 years, compared with $11,409 for nondermatology admissions, according to data from the 2012 Kids’ Inpatient Database, which includes records of pediatric discharges from 44 states.
Cutaneous lymphoma was the most expensive skin disease per admission at a mean cost of $58,294, with congenital skin abnormalities second at $24,186, and ulcers third at $17,064. Bacterial skin infections and infestations were only the 19th most expensive admission at $4,135, but it was by far the most common (59,115 admissions) and the most expensive overall, with a total cost of $240 million. The second most common condition was viral diseases with 3,812 admissions and the next most expensive total was $33.5 million for connective tissue disorders, Mr. Arnold and his associates said.
Multivariate models that adjusted for such factors as age, sex, and race revealed that “the risk of hospitalization for skin disease increased as the median income of one’s zip code declined,” the investigators noted. The adjusted odds ratio for hospitalization in the lowest-income quartile (less than $39,000) was 1.22, compared with the highest-income quartile.
Insurance status also affected hospitalization, putting children from families with no insurance (aOR, 1.35) and those on Medicaid (aOR, 1.17) at a disadvantage, compared with those who had private insurance. “Policy makers should consider increasing Medicaid reimbursement rates to outpatient dermatologists, which might encourage more clinicians to accept this form of insurance and thereby expand access to preventative skin care,” they said.
Regional differences also were observed, which put children from the southern states at the highest risk (aOR, 1.32), compared with those in the West, which could be related to access issues. “In 2016, 4 of the 10 communities in the United States with the lowest density of dermatologists were in the South, suggesting that the high rate of hospitalizations there may also be partially attributed to lack of access to dermatologists,” Mr. Arnold and his associates wrote.
The investigators did not report funding or disclose conflicts of interest.
SOURCE: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
FROM PEDIATRIC DERMATOLOGY
Key clinical point: Children at the highest risk for dermatology hospitalization lived in communities with the lowest household incomes, were uninsured or on Medicaid, or lived in the South.
Major finding: Admissions for skin diseases cost $379.8 million in 2012, or 1.9% of all spending on pediatric hospitalizations.
Study details: A statistical analysis of the 2012 Kids’ Inpatient Database.
Disclosures: The investigators did not report funding or disclose conflicts of interest.
Source: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
Family separations and the intergenerational transmission of trauma
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Growing up, I was always intrigued by the strong emotions that even the mildest separation evoked within me. As a psychiatrist, I now believe that these emotions were related to my family’s difficulty with separation, a concept likely transmitted from my grandmother’s sudden separation as a child.
The political circumstances of the “Kindertransport” and the recent family separation at the southern U.S. border differ, but the Kindertransport is a model for studying the effects of forced parent-child separation and its intergenerational transmission. As a rescue operation that took place immediately before World War II, the Kindertransport was the emigration of approximately 10,000 German Jewish children from Germany and Nazi-occupied countries to England. Even though they were not literally forced, the parents involved were compelled to separate from their children to give their children a chance to survive.
In a recent letter1 published in The New York Times, Eva Yachnes, herself a Kindertransport participant, reflected on the current situation at the southern U.S. border. She alluded to the lifelong effects of her own separation at the age of 6 when emigrating from Vienna to Germany. Personally, as a granddaughter of a Kindertransport participant, I am particularly concerned about the intergenerational transmission of the trauma of family separation.
Since early May 2018, more than 2,000 children have been forcibly separated from their parents after illegally crossing the border. As part of a “zero tolerance policy,” the separation was characterized by the Trump administration as a deterrent to illegal border crossings. Although many Americans are horrified by the news reports about family separation, psychiatrists in particular have expressed concern about this trauma. The American Psychiatric Association issued a statement2 warning that “any forced separation is highly stressful for children and can cause lifelong trauma.” Several weeks later, the APA joined several other mental health organizations in a letter3 calling for the immediate end of enforcement of those policies. In that letter, the organizations said forced separations can cause “an increased risk of ... mental illnesses such as depression, anxiety, and posttraumatic stress disorder.”
What must psychiatrists understand about the impact of childhood trauma? How can psychiatrists approach treatment of children separated from their parents? Are there ways to minimize the risk for intergenerational impact of this trauma?
What do we know?
Childhood trauma is influenced by multiple factors and can be expressed in several ways. According to research,4 the age of the child at the time of traumatic event, the frequency of traumatic experiences, and the degree to which the child’s caretakers were involved in the trauma are factors that influence the extent of psychological damage. This research also suggests that childhood trauma is associated with emotional dysregulation, aggression against self and others, difficulties in attention and dissociation, medical problems, and difficulty with navigating adult interpersonal relationships.
When viewed through the lens of attachment theory, the forced separation of a child from its caretakers is a potent form of childhood trauma. Joanna E. Chambers, MD, summarizes and explains John Bowlby’s attachment theory as a neurobiological system originating from an infant’s connection to the primary caretaker. This connection becomes a lifelong model for all subsequent relationships.
Any traumatic disruptions in the development of this system puts the child at risk of developing “insecure attachment.” This insecure attachment can lead to lifelong emotional problems for the child, affecting the quality of subsequent marital relationships, relationships to children, and the development of personality disorders.
In addition, it correlates to the development of psychiatric illnesses, specifically depression and anxiety. There is also a plausible biological basis for attachment theory. Both oxytocin, a hormone released in human bonding, and social interaction itself have been shown to decrease cortisol levels. Elevated cortisol has been found to negatively affect infant brain development, Dr. Chambers argued.5
Given those significant effects of childhood trauma, it is understandable that there exists a concept of “intergenerational transmission of trauma.” Originating from studies of Holocaust survivors and their descendants, researchers Amy Lehrner, PhD, and Rachel Yehuda, PhD, conceptualize intergenerational transmission of trauma as the intergenerational impact of prenatal PTSD.6 This impact is expressed as a predisposition in the offspring of Holocaust survivors to developing PTSD, difficulties in individuation and separation, higher rates of mood and anxiety disorders, and higher rates of physical health issues.
Although they are complex and clearly multidetermined, Dr. Yehuda and Dr. Lehrner also summarize plausible biological theories for the intergenerational transmission of trauma. Epigenetic differences in the hypothalamic-pituitary-adrenal axis, circadian rhythm, urinary and plasma cortisol levels, glucocorticoid sensitivity, and regulation of the glucocorticoid receptor gene all have been found in Holocaust offspring with parental PTSD, in contrast to offspring without parental PTSD.6
What can we as psychiatrists do?
We are uniquely equipped to take several concrete steps to help mitigate the effects of these traumatic events. Among them, we can:
- Provide opportunities for the child and the family to process their experience. This can be profoundly healing and can help minimize the devastating psychological effects of this separation.
- Become acquainted with the concept of intergenerational transmission of resilience.
- Work with trauma survivors to develop their own personal narratives and cultural rituals surrounding the trauma.6
- Encourage second- and third-generation descendants to engage in artistic expression of the trauma, visit places of importance to their parents, and engage in social and political activism. These are all expressions of resilience in the offspring of trauma victims.6
In summary, recent U.S. political events have caused thousands of children to be forcibly separated from their parents. Those separations are traumatic and can have lifelong psychological implications for the children and their offspring. It is important to provide quality mental health treatment to these children with a specific focus on treating PTSD and processing the traumatic experience. Psychological treatment can help mitigate the effects of the traumatic separation and create a sense of resiliency.
References
1. New York Times. June 20, 2018. “My separation trauma.”
2. American Psychiatric Association statement, May 30, 2018.
3. Letter to the departments of Justice, Health & Human Services, and Homeland Security, June 20, 2018.
4. Child Adolesc Psychiatric Clin N Am. 2003;(12.2):293-318.
5. Psychodynamic Psychiatry. 2017 Dec;45(4):542-63.
6. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Jan;10(1):22-9.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital of the Northwell Health System, Glen Oaks, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine after graduating from the Albert Einstein College of Medicine and Yeshiva University with a B.A. in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Growing up, I was always intrigued by the strong emotions that even the mildest separation evoked within me. As a psychiatrist, I now believe that these emotions were related to my family’s difficulty with separation, a concept likely transmitted from my grandmother’s sudden separation as a child.
The political circumstances of the “Kindertransport” and the recent family separation at the southern U.S. border differ, but the Kindertransport is a model for studying the effects of forced parent-child separation and its intergenerational transmission. As a rescue operation that took place immediately before World War II, the Kindertransport was the emigration of approximately 10,000 German Jewish children from Germany and Nazi-occupied countries to England. Even though they were not literally forced, the parents involved were compelled to separate from their children to give their children a chance to survive.
In a recent letter1 published in The New York Times, Eva Yachnes, herself a Kindertransport participant, reflected on the current situation at the southern U.S. border. She alluded to the lifelong effects of her own separation at the age of 6 when emigrating from Vienna to Germany. Personally, as a granddaughter of a Kindertransport participant, I am particularly concerned about the intergenerational transmission of the trauma of family separation.
Since early May 2018, more than 2,000 children have been forcibly separated from their parents after illegally crossing the border. As part of a “zero tolerance policy,” the separation was characterized by the Trump administration as a deterrent to illegal border crossings. Although many Americans are horrified by the news reports about family separation, psychiatrists in particular have expressed concern about this trauma. The American Psychiatric Association issued a statement2 warning that “any forced separation is highly stressful for children and can cause lifelong trauma.” Several weeks later, the APA joined several other mental health organizations in a letter3 calling for the immediate end of enforcement of those policies. In that letter, the organizations said forced separations can cause “an increased risk of ... mental illnesses such as depression, anxiety, and posttraumatic stress disorder.”
What must psychiatrists understand about the impact of childhood trauma? How can psychiatrists approach treatment of children separated from their parents? Are there ways to minimize the risk for intergenerational impact of this trauma?
What do we know?
Childhood trauma is influenced by multiple factors and can be expressed in several ways. According to research,4 the age of the child at the time of traumatic event, the frequency of traumatic experiences, and the degree to which the child’s caretakers were involved in the trauma are factors that influence the extent of psychological damage. This research also suggests that childhood trauma is associated with emotional dysregulation, aggression against self and others, difficulties in attention and dissociation, medical problems, and difficulty with navigating adult interpersonal relationships.
When viewed through the lens of attachment theory, the forced separation of a child from its caretakers is a potent form of childhood trauma. Joanna E. Chambers, MD, summarizes and explains John Bowlby’s attachment theory as a neurobiological system originating from an infant’s connection to the primary caretaker. This connection becomes a lifelong model for all subsequent relationships.
Any traumatic disruptions in the development of this system puts the child at risk of developing “insecure attachment.” This insecure attachment can lead to lifelong emotional problems for the child, affecting the quality of subsequent marital relationships, relationships to children, and the development of personality disorders.
In addition, it correlates to the development of psychiatric illnesses, specifically depression and anxiety. There is also a plausible biological basis for attachment theory. Both oxytocin, a hormone released in human bonding, and social interaction itself have been shown to decrease cortisol levels. Elevated cortisol has been found to negatively affect infant brain development, Dr. Chambers argued.5
Given those significant effects of childhood trauma, it is understandable that there exists a concept of “intergenerational transmission of trauma.” Originating from studies of Holocaust survivors and their descendants, researchers Amy Lehrner, PhD, and Rachel Yehuda, PhD, conceptualize intergenerational transmission of trauma as the intergenerational impact of prenatal PTSD.6 This impact is expressed as a predisposition in the offspring of Holocaust survivors to developing PTSD, difficulties in individuation and separation, higher rates of mood and anxiety disorders, and higher rates of physical health issues.
Although they are complex and clearly multidetermined, Dr. Yehuda and Dr. Lehrner also summarize plausible biological theories for the intergenerational transmission of trauma. Epigenetic differences in the hypothalamic-pituitary-adrenal axis, circadian rhythm, urinary and plasma cortisol levels, glucocorticoid sensitivity, and regulation of the glucocorticoid receptor gene all have been found in Holocaust offspring with parental PTSD, in contrast to offspring without parental PTSD.6
What can we as psychiatrists do?
We are uniquely equipped to take several concrete steps to help mitigate the effects of these traumatic events. Among them, we can:
- Provide opportunities for the child and the family to process their experience. This can be profoundly healing and can help minimize the devastating psychological effects of this separation.
- Become acquainted with the concept of intergenerational transmission of resilience.
- Work with trauma survivors to develop their own personal narratives and cultural rituals surrounding the trauma.6
- Encourage second- and third-generation descendants to engage in artistic expression of the trauma, visit places of importance to their parents, and engage in social and political activism. These are all expressions of resilience in the offspring of trauma victims.6
In summary, recent U.S. political events have caused thousands of children to be forcibly separated from their parents. Those separations are traumatic and can have lifelong psychological implications for the children and their offspring. It is important to provide quality mental health treatment to these children with a specific focus on treating PTSD and processing the traumatic experience. Psychological treatment can help mitigate the effects of the traumatic separation and create a sense of resiliency.
References
1. New York Times. June 20, 2018. “My separation trauma.”
2. American Psychiatric Association statement, May 30, 2018.
3. Letter to the departments of Justice, Health & Human Services, and Homeland Security, June 20, 2018.
4. Child Adolesc Psychiatric Clin N Am. 2003;(12.2):293-318.
5. Psychodynamic Psychiatry. 2017 Dec;45(4):542-63.
6. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Jan;10(1):22-9.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital of the Northwell Health System, Glen Oaks, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine after graduating from the Albert Einstein College of Medicine and Yeshiva University with a B.A. in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
Editor’s Note: Alison M. Heru, MD, the Families in Psychiatry columnist, invited Dr. Reinstein to address this topic.
Growing up, I was always intrigued by the strong emotions that even the mildest separation evoked within me. As a psychiatrist, I now believe that these emotions were related to my family’s difficulty with separation, a concept likely transmitted from my grandmother’s sudden separation as a child.
The political circumstances of the “Kindertransport” and the recent family separation at the southern U.S. border differ, but the Kindertransport is a model for studying the effects of forced parent-child separation and its intergenerational transmission. As a rescue operation that took place immediately before World War II, the Kindertransport was the emigration of approximately 10,000 German Jewish children from Germany and Nazi-occupied countries to England. Even though they were not literally forced, the parents involved were compelled to separate from their children to give their children a chance to survive.
In a recent letter1 published in The New York Times, Eva Yachnes, herself a Kindertransport participant, reflected on the current situation at the southern U.S. border. She alluded to the lifelong effects of her own separation at the age of 6 when emigrating from Vienna to Germany. Personally, as a granddaughter of a Kindertransport participant, I am particularly concerned about the intergenerational transmission of the trauma of family separation.
Since early May 2018, more than 2,000 children have been forcibly separated from their parents after illegally crossing the border. As part of a “zero tolerance policy,” the separation was characterized by the Trump administration as a deterrent to illegal border crossings. Although many Americans are horrified by the news reports about family separation, psychiatrists in particular have expressed concern about this trauma. The American Psychiatric Association issued a statement2 warning that “any forced separation is highly stressful for children and can cause lifelong trauma.” Several weeks later, the APA joined several other mental health organizations in a letter3 calling for the immediate end of enforcement of those policies. In that letter, the organizations said forced separations can cause “an increased risk of ... mental illnesses such as depression, anxiety, and posttraumatic stress disorder.”
What must psychiatrists understand about the impact of childhood trauma? How can psychiatrists approach treatment of children separated from their parents? Are there ways to minimize the risk for intergenerational impact of this trauma?
What do we know?
Childhood trauma is influenced by multiple factors and can be expressed in several ways. According to research,4 the age of the child at the time of traumatic event, the frequency of traumatic experiences, and the degree to which the child’s caretakers were involved in the trauma are factors that influence the extent of psychological damage. This research also suggests that childhood trauma is associated with emotional dysregulation, aggression against self and others, difficulties in attention and dissociation, medical problems, and difficulty with navigating adult interpersonal relationships.
When viewed through the lens of attachment theory, the forced separation of a child from its caretakers is a potent form of childhood trauma. Joanna E. Chambers, MD, summarizes and explains John Bowlby’s attachment theory as a neurobiological system originating from an infant’s connection to the primary caretaker. This connection becomes a lifelong model for all subsequent relationships.
Any traumatic disruptions in the development of this system puts the child at risk of developing “insecure attachment.” This insecure attachment can lead to lifelong emotional problems for the child, affecting the quality of subsequent marital relationships, relationships to children, and the development of personality disorders.
In addition, it correlates to the development of psychiatric illnesses, specifically depression and anxiety. There is also a plausible biological basis for attachment theory. Both oxytocin, a hormone released in human bonding, and social interaction itself have been shown to decrease cortisol levels. Elevated cortisol has been found to negatively affect infant brain development, Dr. Chambers argued.5
Given those significant effects of childhood trauma, it is understandable that there exists a concept of “intergenerational transmission of trauma.” Originating from studies of Holocaust survivors and their descendants, researchers Amy Lehrner, PhD, and Rachel Yehuda, PhD, conceptualize intergenerational transmission of trauma as the intergenerational impact of prenatal PTSD.6 This impact is expressed as a predisposition in the offspring of Holocaust survivors to developing PTSD, difficulties in individuation and separation, higher rates of mood and anxiety disorders, and higher rates of physical health issues.
Although they are complex and clearly multidetermined, Dr. Yehuda and Dr. Lehrner also summarize plausible biological theories for the intergenerational transmission of trauma. Epigenetic differences in the hypothalamic-pituitary-adrenal axis, circadian rhythm, urinary and plasma cortisol levels, glucocorticoid sensitivity, and regulation of the glucocorticoid receptor gene all have been found in Holocaust offspring with parental PTSD, in contrast to offspring without parental PTSD.6
What can we as psychiatrists do?
We are uniquely equipped to take several concrete steps to help mitigate the effects of these traumatic events. Among them, we can:
- Provide opportunities for the child and the family to process their experience. This can be profoundly healing and can help minimize the devastating psychological effects of this separation.
- Become acquainted with the concept of intergenerational transmission of resilience.
- Work with trauma survivors to develop their own personal narratives and cultural rituals surrounding the trauma.6
- Encourage second- and third-generation descendants to engage in artistic expression of the trauma, visit places of importance to their parents, and engage in social and political activism. These are all expressions of resilience in the offspring of trauma victims.6
In summary, recent U.S. political events have caused thousands of children to be forcibly separated from their parents. Those separations are traumatic and can have lifelong psychological implications for the children and their offspring. It is important to provide quality mental health treatment to these children with a specific focus on treating PTSD and processing the traumatic experience. Psychological treatment can help mitigate the effects of the traumatic separation and create a sense of resiliency.
References
1. New York Times. June 20, 2018. “My separation trauma.”
2. American Psychiatric Association statement, May 30, 2018.
3. Letter to the departments of Justice, Health & Human Services, and Homeland Security, June 20, 2018.
4. Child Adolesc Psychiatric Clin N Am. 2003;(12.2):293-318.
5. Psychodynamic Psychiatry. 2017 Dec;45(4):542-63.
6. Psychological Trauma: Theory, Research, Practice, and Policy. 2018 Jan;10(1):22-9.
Dr. Reinstein is a psychiatry attending at Zucker Hillside Hospital of the Northwell Health System, Glen Oaks, New York. Her clinical interests include reproductive psychiatry and family therapy, with a specific focus on maternal mental health. Dr. Reinstein completed her adult psychiatry residency training at Montefiore Hospital/Albert Einstein College of Medicine after graduating from the Albert Einstein College of Medicine and Yeshiva University with a B.A. in biology. She is one of the recipients of the 4th Annual Resident Recognition Award for Excellence in Family Oriented Care.
ICH: Recent NOAC use associated with lower risk of in-hospital mortality, compared with warfarin
Background: Previous studies comparing NOACs with warfarin have demonstrated a lower incidence of ICH in patients receiving NOACs. Data have been limited, though, regarding ICH with recent anticoagulant use and in-hospital mortality.
Study design: Retrospective cohort study.
Setting: More than 1,600 U.S. hospitals that participate in the Get With The Guidelines–Stroke national registry.
Synopsis: Of 141,311 patients admitted with ICH, 10.6% were receiving warfarin and 3.5% were receiving NOACs prior to hospitalization. Prior use of warfarin or NOACs, compared with no anticoagulant use, was associated with higher in-hospital mortality. However, use of NOACs, compared with use of warfarin, was associated with lower in-hospital mortality risk (adjusted risk difference, –5.7%; adjusted odds ratio, 0.75). Among patients with prior NOAC use, 54% of them were using rivaroxaban.
A limitation to this study is that reversal strategies, such as the use of vitamin K, fresh frozen plasma, or intravenous factor concentrates, were not available in the database. In addition, since rivaroxaban accounted for more than half the NOACs used, it may be difficult to apply the overall findings to all other available NOACs.
Bottom line: In patients admitted for ICH, prior use of NOACs, compared with warfarin, was associated with lower risk of in-hospital mortality.
Citation: Inohara T et al. Association of intracerebral hemorrhage among patients taking non–vitamin K antagonist vs. vitamin K antagonist oral anticoagulants with in-hospital mortality. JAMA. 2018 Feb 6;319(5):463-73.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Background: Previous studies comparing NOACs with warfarin have demonstrated a lower incidence of ICH in patients receiving NOACs. Data have been limited, though, regarding ICH with recent anticoagulant use and in-hospital mortality.
Study design: Retrospective cohort study.
Setting: More than 1,600 U.S. hospitals that participate in the Get With The Guidelines–Stroke national registry.
Synopsis: Of 141,311 patients admitted with ICH, 10.6% were receiving warfarin and 3.5% were receiving NOACs prior to hospitalization. Prior use of warfarin or NOACs, compared with no anticoagulant use, was associated with higher in-hospital mortality. However, use of NOACs, compared with use of warfarin, was associated with lower in-hospital mortality risk (adjusted risk difference, –5.7%; adjusted odds ratio, 0.75). Among patients with prior NOAC use, 54% of them were using rivaroxaban.
A limitation to this study is that reversal strategies, such as the use of vitamin K, fresh frozen plasma, or intravenous factor concentrates, were not available in the database. In addition, since rivaroxaban accounted for more than half the NOACs used, it may be difficult to apply the overall findings to all other available NOACs.
Bottom line: In patients admitted for ICH, prior use of NOACs, compared with warfarin, was associated with lower risk of in-hospital mortality.
Citation: Inohara T et al. Association of intracerebral hemorrhage among patients taking non–vitamin K antagonist vs. vitamin K antagonist oral anticoagulants with in-hospital mortality. JAMA. 2018 Feb 6;319(5):463-73.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Background: Previous studies comparing NOACs with warfarin have demonstrated a lower incidence of ICH in patients receiving NOACs. Data have been limited, though, regarding ICH with recent anticoagulant use and in-hospital mortality.
Study design: Retrospective cohort study.
Setting: More than 1,600 U.S. hospitals that participate in the Get With The Guidelines–Stroke national registry.
Synopsis: Of 141,311 patients admitted with ICH, 10.6% were receiving warfarin and 3.5% were receiving NOACs prior to hospitalization. Prior use of warfarin or NOACs, compared with no anticoagulant use, was associated with higher in-hospital mortality. However, use of NOACs, compared with use of warfarin, was associated with lower in-hospital mortality risk (adjusted risk difference, –5.7%; adjusted odds ratio, 0.75). Among patients with prior NOAC use, 54% of them were using rivaroxaban.
A limitation to this study is that reversal strategies, such as the use of vitamin K, fresh frozen plasma, or intravenous factor concentrates, were not available in the database. In addition, since rivaroxaban accounted for more than half the NOACs used, it may be difficult to apply the overall findings to all other available NOACs.
Bottom line: In patients admitted for ICH, prior use of NOACs, compared with warfarin, was associated with lower risk of in-hospital mortality.
Citation: Inohara T et al. Association of intracerebral hemorrhage among patients taking non–vitamin K antagonist vs. vitamin K antagonist oral anticoagulants with in-hospital mortality. JAMA. 2018 Feb 6;319(5):463-73.
Dr. Farkhondehpour is a hospitalist at UC San Diego Health and an assistant clinical professor at the University of California, San Diego.
Trial finds link between OSA, aortic diameter
BALTIMORE – Individuals with moderate to severe and thus may be at a heightened risk of cardiovascular events, according to an analysis of a national, multisite research study presented at the annual meeting of the Associated Professional Sleep Societies.
The study evaluated a subgroup of 708 patients with no history of cardiovascular disease (CVD) from the Multi-Ethnic Study of Atherosclerosis (MESA).
Dr. Kwon noted that previous studies have shown that patients with thoracic aortopathy have a high rate of obstructive sleep apnea (OSA) (Am J Respir Crit Care Med. 2003;168:1528-31), and those with OSA tend to have higher thoracic aortic size (J Am Coll Cardiol. 2008;52:885-6). “There’s also a degree of evidence suggesting that OSA is associated with high arterial stiffness, which is a marker of primary organ damage and a major cardiovascular risk that is predictive of cardiovascular disease,” Dr. Kwon said (J Intl Med Res. 2011;39:228-38). However, he also noted that some studies have found no relationship between OSA and aortic disease (Respiration. 2006;73:741-50). “The question can be raised as to whether sleep apnea may have implications” in thoracic aortic disease, he said.
Dr. Kwon’s study evaluated three groups: patients with no OSA (apnea hypopnea index [AHI] less than 5, n = 87); mild OSA (AHI 5-15, n = 215); and severe OSA (AHI greater than 15, n = 406). All patients had polysomnography as part of an ancillary study. Cardiac MRI measured these three features of aortic function and physiology (unadjusted results):
Diameter at the pulmonary artery bifurcation, which ranged from 3.13 cm in patients with no OSA to 3.37 cm in those with severe OSA (P = .0017).
Pulse wave velocity, which averaged 8.07 m/s in the no-OSA group and 9.11 m/s in the severe group (P less than .0001).
Distensibility, or aortic stiffness, which was 1.73%/mm Hg in the no-OSA group, 1.54%/mm Hg in the mild group and 1.68%/mm Hg in the severe group (P = .0141).
“There was maybe some higher pulse wave velocity across the significant OSA group,” Dr. Kwon said. “However, with aortic distensibility, there did not seem to be any significant trend.”
In the adjusted analysis of aortic diameter, “there did appear to be a small but significant difference in the significant OSA group, compared with the reference group,” Dr. Kwon said. He also noted that women with OSA typically had significantly larger aortic diameters than did non-OSA counterparts, whereas that trend was not as pronounced in men.
“Thoracic aorta size does seem to increase with OSA severity, but this has a sex-interaction component; it’s more pronounced in women,” Dr. Kwon said. He also noted a discrepancy in the results: “The functional properties of the aorta did not seem to bear a significant association with OSA severity.”
In explaining why these results differed from previous studies, Dr. Kwon said the study populations or their characteristics may be the cause, or that MRI-based measures of aortic properties have not been extensively studied before. “This is probably the first study to look at an unselected population, use a large sample size that was ethnically diverse, and use cardiac MRI technology,” he said.
Limitations he noted were the study’s cross-sectional nature and its small population of patients with enlarged thoracic aorta size, which left it underpowered to evaluate that population.
Dr. Kwon reported having no financial relationships.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0465.
BALTIMORE – Individuals with moderate to severe and thus may be at a heightened risk of cardiovascular events, according to an analysis of a national, multisite research study presented at the annual meeting of the Associated Professional Sleep Societies.
The study evaluated a subgroup of 708 patients with no history of cardiovascular disease (CVD) from the Multi-Ethnic Study of Atherosclerosis (MESA).
Dr. Kwon noted that previous studies have shown that patients with thoracic aortopathy have a high rate of obstructive sleep apnea (OSA) (Am J Respir Crit Care Med. 2003;168:1528-31), and those with OSA tend to have higher thoracic aortic size (J Am Coll Cardiol. 2008;52:885-6). “There’s also a degree of evidence suggesting that OSA is associated with high arterial stiffness, which is a marker of primary organ damage and a major cardiovascular risk that is predictive of cardiovascular disease,” Dr. Kwon said (J Intl Med Res. 2011;39:228-38). However, he also noted that some studies have found no relationship between OSA and aortic disease (Respiration. 2006;73:741-50). “The question can be raised as to whether sleep apnea may have implications” in thoracic aortic disease, he said.
Dr. Kwon’s study evaluated three groups: patients with no OSA (apnea hypopnea index [AHI] less than 5, n = 87); mild OSA (AHI 5-15, n = 215); and severe OSA (AHI greater than 15, n = 406). All patients had polysomnography as part of an ancillary study. Cardiac MRI measured these three features of aortic function and physiology (unadjusted results):
Diameter at the pulmonary artery bifurcation, which ranged from 3.13 cm in patients with no OSA to 3.37 cm in those with severe OSA (P = .0017).
Pulse wave velocity, which averaged 8.07 m/s in the no-OSA group and 9.11 m/s in the severe group (P less than .0001).
Distensibility, or aortic stiffness, which was 1.73%/mm Hg in the no-OSA group, 1.54%/mm Hg in the mild group and 1.68%/mm Hg in the severe group (P = .0141).
“There was maybe some higher pulse wave velocity across the significant OSA group,” Dr. Kwon said. “However, with aortic distensibility, there did not seem to be any significant trend.”
In the adjusted analysis of aortic diameter, “there did appear to be a small but significant difference in the significant OSA group, compared with the reference group,” Dr. Kwon said. He also noted that women with OSA typically had significantly larger aortic diameters than did non-OSA counterparts, whereas that trend was not as pronounced in men.
“Thoracic aorta size does seem to increase with OSA severity, but this has a sex-interaction component; it’s more pronounced in women,” Dr. Kwon said. He also noted a discrepancy in the results: “The functional properties of the aorta did not seem to bear a significant association with OSA severity.”
In explaining why these results differed from previous studies, Dr. Kwon said the study populations or their characteristics may be the cause, or that MRI-based measures of aortic properties have not been extensively studied before. “This is probably the first study to look at an unselected population, use a large sample size that was ethnically diverse, and use cardiac MRI technology,” he said.
Limitations he noted were the study’s cross-sectional nature and its small population of patients with enlarged thoracic aorta size, which left it underpowered to evaluate that population.
Dr. Kwon reported having no financial relationships.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0465.
BALTIMORE – Individuals with moderate to severe and thus may be at a heightened risk of cardiovascular events, according to an analysis of a national, multisite research study presented at the annual meeting of the Associated Professional Sleep Societies.
The study evaluated a subgroup of 708 patients with no history of cardiovascular disease (CVD) from the Multi-Ethnic Study of Atherosclerosis (MESA).
Dr. Kwon noted that previous studies have shown that patients with thoracic aortopathy have a high rate of obstructive sleep apnea (OSA) (Am J Respir Crit Care Med. 2003;168:1528-31), and those with OSA tend to have higher thoracic aortic size (J Am Coll Cardiol. 2008;52:885-6). “There’s also a degree of evidence suggesting that OSA is associated with high arterial stiffness, which is a marker of primary organ damage and a major cardiovascular risk that is predictive of cardiovascular disease,” Dr. Kwon said (J Intl Med Res. 2011;39:228-38). However, he also noted that some studies have found no relationship between OSA and aortic disease (Respiration. 2006;73:741-50). “The question can be raised as to whether sleep apnea may have implications” in thoracic aortic disease, he said.
Dr. Kwon’s study evaluated three groups: patients with no OSA (apnea hypopnea index [AHI] less than 5, n = 87); mild OSA (AHI 5-15, n = 215); and severe OSA (AHI greater than 15, n = 406). All patients had polysomnography as part of an ancillary study. Cardiac MRI measured these three features of aortic function and physiology (unadjusted results):
Diameter at the pulmonary artery bifurcation, which ranged from 3.13 cm in patients with no OSA to 3.37 cm in those with severe OSA (P = .0017).
Pulse wave velocity, which averaged 8.07 m/s in the no-OSA group and 9.11 m/s in the severe group (P less than .0001).
Distensibility, or aortic stiffness, which was 1.73%/mm Hg in the no-OSA group, 1.54%/mm Hg in the mild group and 1.68%/mm Hg in the severe group (P = .0141).
“There was maybe some higher pulse wave velocity across the significant OSA group,” Dr. Kwon said. “However, with aortic distensibility, there did not seem to be any significant trend.”
In the adjusted analysis of aortic diameter, “there did appear to be a small but significant difference in the significant OSA group, compared with the reference group,” Dr. Kwon said. He also noted that women with OSA typically had significantly larger aortic diameters than did non-OSA counterparts, whereas that trend was not as pronounced in men.
“Thoracic aorta size does seem to increase with OSA severity, but this has a sex-interaction component; it’s more pronounced in women,” Dr. Kwon said. He also noted a discrepancy in the results: “The functional properties of the aorta did not seem to bear a significant association with OSA severity.”
In explaining why these results differed from previous studies, Dr. Kwon said the study populations or their characteristics may be the cause, or that MRI-based measures of aortic properties have not been extensively studied before. “This is probably the first study to look at an unselected population, use a large sample size that was ethnically diverse, and use cardiac MRI technology,” he said.
Limitations he noted were the study’s cross-sectional nature and its small population of patients with enlarged thoracic aorta size, which left it underpowered to evaluate that population.
Dr. Kwon reported having no financial relationships.
SOURCE: Kwon Y et al. SLEEP 2018, Abstract #0465.
REPORTING FROM SLEEP 2018
Key clinical point: Obstructive sleep apnea severity is related to increased aortic artery size.
Major finding: Ascending aortic diameter measured 3.37 cm in patients with severe OSA vs. 3.13 cm with no OSA.
Study details: Subgroup of 708 patients with OSA but no history of cardiovascular disease from the Multi-Ethnic Study of Atherosclerosis.
Disclosures: Dr. Kwon reported having no financial relationships.
Source: Kwon Y et al. SLEEP 2018, Abstract #0465.
Register Today for UCLA / SVS Review Course
The Third Annual UCLA / SVS Symposium on “What’s New in Vascular and Endovascular Surgery" is less than seven weeks away. Register today for this comprehensive course that includes a survey of basic science, pathogenesis, diagnosis and management of the broad spectrum of vascular disorders, plus important new developments. The course will be Aug. 25 to 27 at the Beverly Hilton, Beverly Hills, Calif.
The course registration includes the new (9th) edition of the textbook, “Vascular and Endovascular Surgery: A Comprehensive Review,” edited by Drs. Wesley S. Moore, Peter F. Lawrence and Gustavo S. Oderich. Learn more and register here.
The Third Annual UCLA / SVS Symposium on “What’s New in Vascular and Endovascular Surgery" is less than seven weeks away. Register today for this comprehensive course that includes a survey of basic science, pathogenesis, diagnosis and management of the broad spectrum of vascular disorders, plus important new developments. The course will be Aug. 25 to 27 at the Beverly Hilton, Beverly Hills, Calif.
The course registration includes the new (9th) edition of the textbook, “Vascular and Endovascular Surgery: A Comprehensive Review,” edited by Drs. Wesley S. Moore, Peter F. Lawrence and Gustavo S. Oderich. Learn more and register here.
The Third Annual UCLA / SVS Symposium on “What’s New in Vascular and Endovascular Surgery" is less than seven weeks away. Register today for this comprehensive course that includes a survey of basic science, pathogenesis, diagnosis and management of the broad spectrum of vascular disorders, plus important new developments. The course will be Aug. 25 to 27 at the Beverly Hilton, Beverly Hills, Calif.
The course registration includes the new (9th) edition of the textbook, “Vascular and Endovascular Surgery: A Comprehensive Review,” edited by Drs. Wesley S. Moore, Peter F. Lawrence and Gustavo S. Oderich. Learn more and register here.
Deep Soft Tissue Mass of the Knee
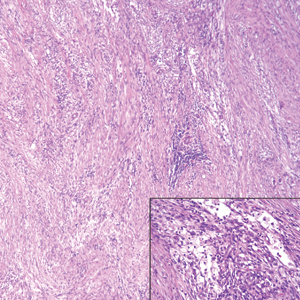
The Diagnosis: Nodular Fasciitis
The diagnosis of spindle cell tumors can be challenging; however, by using a variety of immunoperoxidase stains and fluorescent in situ hybridization (FISH) testing in conjunction with histology, it often is possible to arrive at a definitive diagnosis. For this case, the histologic features in conjunction with the immunoperoxidase stains and FISH were consistent with a diagnosis of nodular fasciitis.
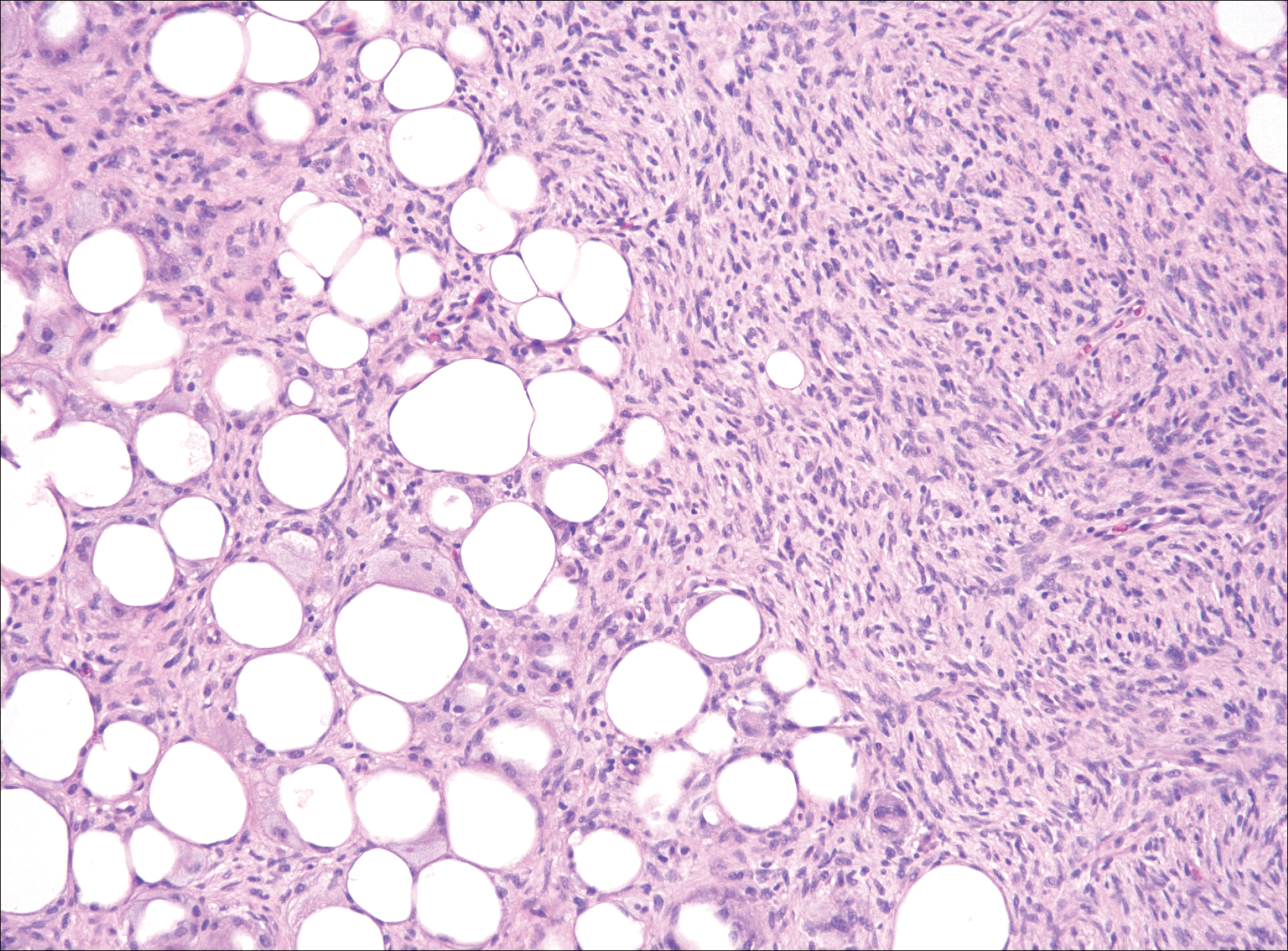
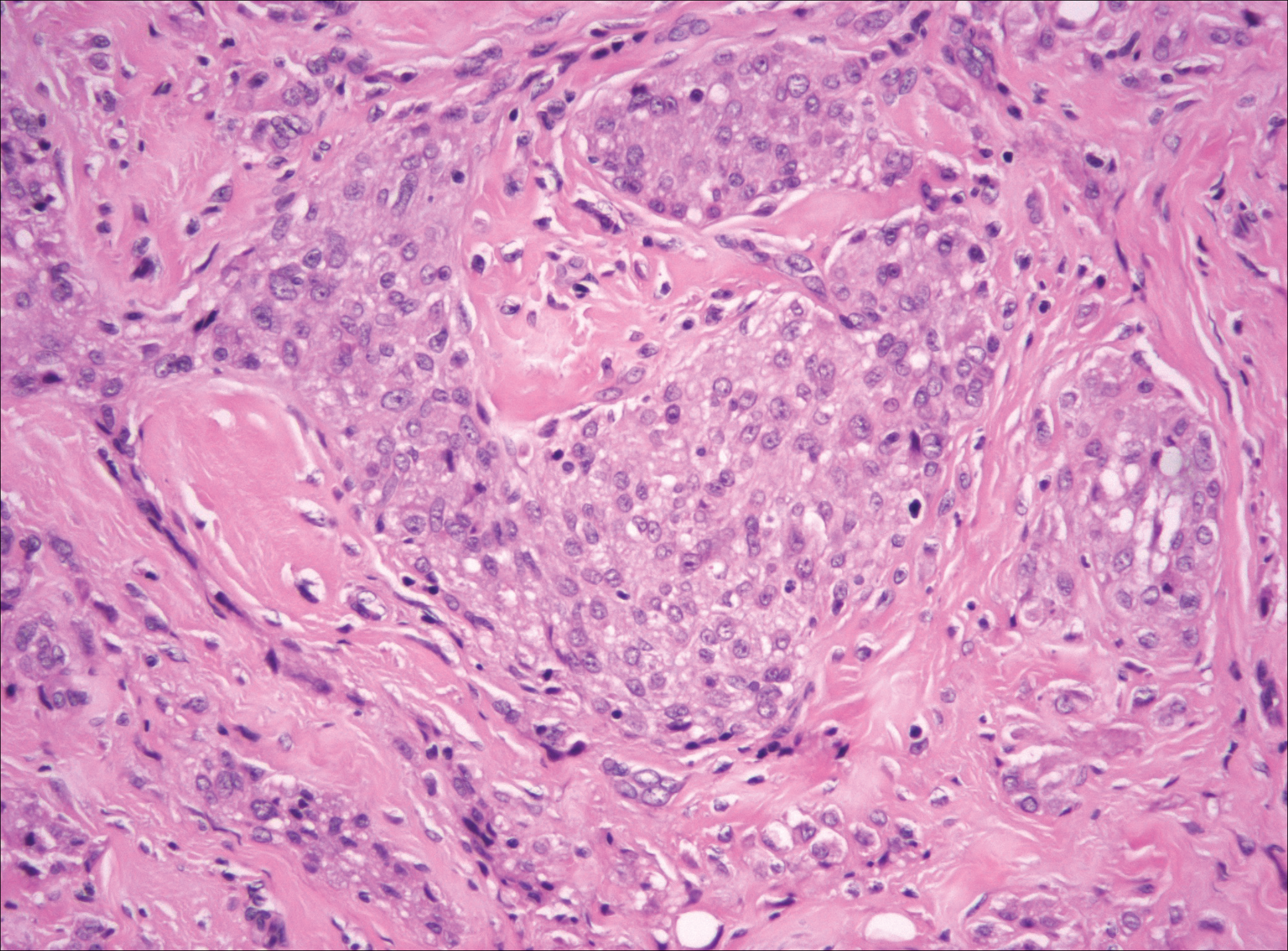
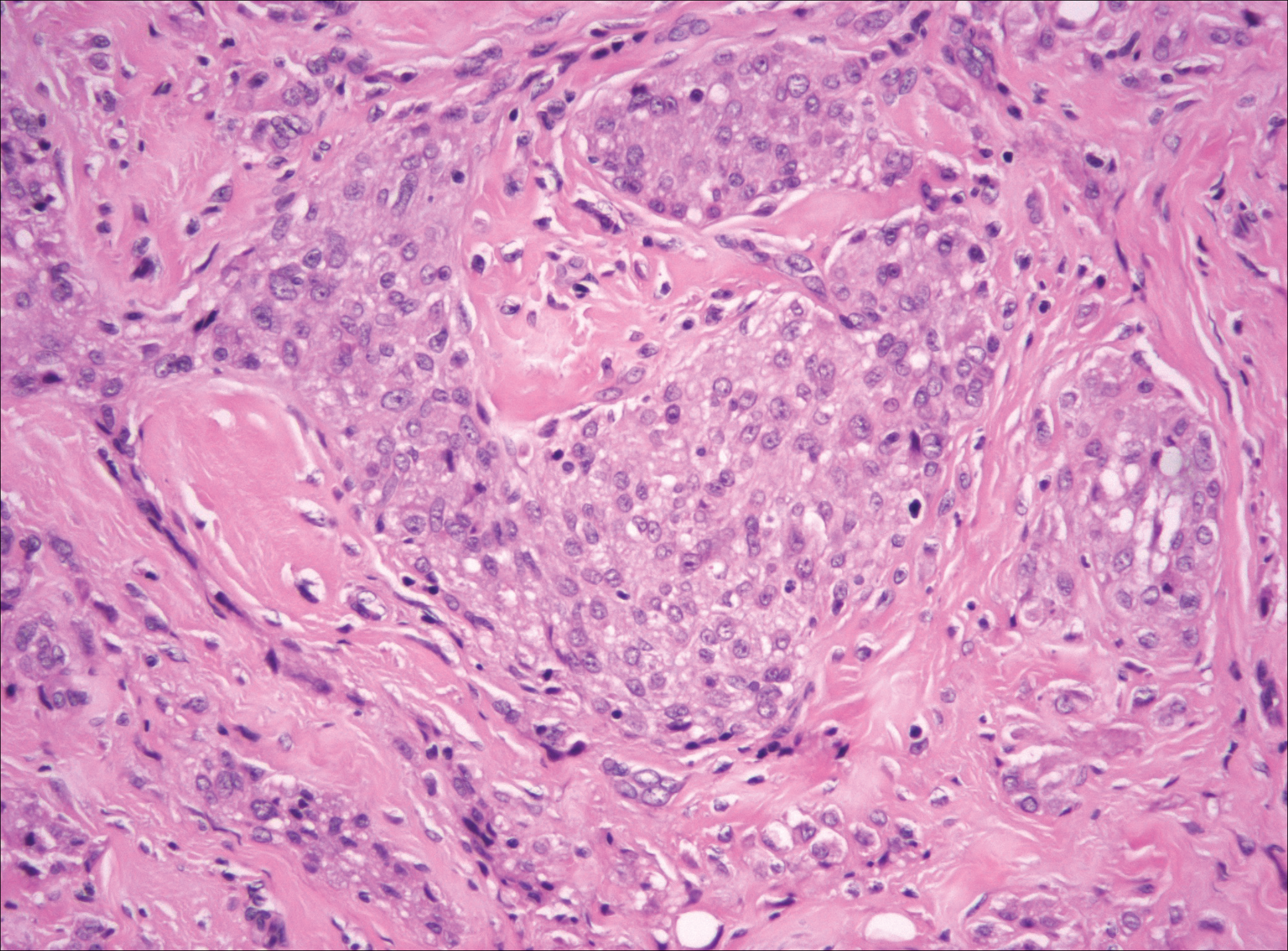
Nodular fasciitis is a benign, self-limiting, myofibroblastic, soft-tissue proliferation typically found in the subcutaneous tissue.1 It can be found anywhere on the body but most commonly on the upper arms and trunk. It most often is seen in young adults, and many cases have been reported in association with a history of trauma to the area.1,2 It typically measures less than 2 cm in diameter.3 The diagnosis of nodular fasciitis is particularly challenging because it mimics sarcoma, both in presentation and in histologic findings with rapid growth, high mitotic activity, and increased cellularity.1,4-7 In contrast to malignancy, nodular fasciitis has no atypical mitoses and little cytologic atypia.8,9 Rather, it contains plump myofibroblasts loosely arranged in a myxoid or fibrous stroma that also may contain lymphocytes, extravasated erythrocytes, and osteoclastlike giant cells distributed throughout.5,10,11 In this case, lymphocytes, extravasated red blood cells, and myxoid change are present, suggesting the diagnosis of nodular fasciitis. In other cases, however, these features may be much more limited, making the diagnosis more challenging. The spindle cells are arranged in poorly defined short fascicles. The tumor cells do not infiltrate between individual adipocytes. There is no notable cytologic atypia.
Because of the difficulty in making the diagnosis, overtreatment of this benign condition can be a problem, causing increased morbidity.1 Erickson-Johnson et al12 identified the role of an ubiquitin-specific peptidase 6, USP6, gene rearrangement on chromosome 17p13 in 92% (44/48) of cases of nodular fasciitis. The USP6 gene most often is rearranged with the myosin heavy chain 9 gene, MYH9, on chromosome 22q12.3. With this rearrangement, the MYH9 promoter leads to the overexpression of USP6, causing tumor formation.2,13 The use of multiple immunoperoxidase stains can be important in the identification of nodular fasciitis. Nodular fasciitis stains negative for S-100, epithelial membrane antigen, CD34, β-catenin, and cytokeratin, but typically stains positive for smooth muscle actin.9
Although dermatofibrosarcoma protuberans (DFSP) was in the differential diagnosis, these tumors tend to have greater cellularity than nodular fasciitis. In addition, the spindle cells of DFSP typically are arranged in a storiform pattern. Another characteristic feature of DFSP is that the tumor cells will infiltrate between adipose cells creating a lacelike or honeycomblike appearance within the subcutaneous tissue (Figure 1). Immunohistochemistry staining and FISH testing may be useful in making a diagnosis of DFSP. These tumors typically are positive for CD34 by immunoperoxidase staining and demonstrate a translocation t(17;22)(q21;q13) between platelet-derived growth factor subunit B gene, PDGFB, and collagen type I alpha 1 chain gene, COL1A1, by FISH.
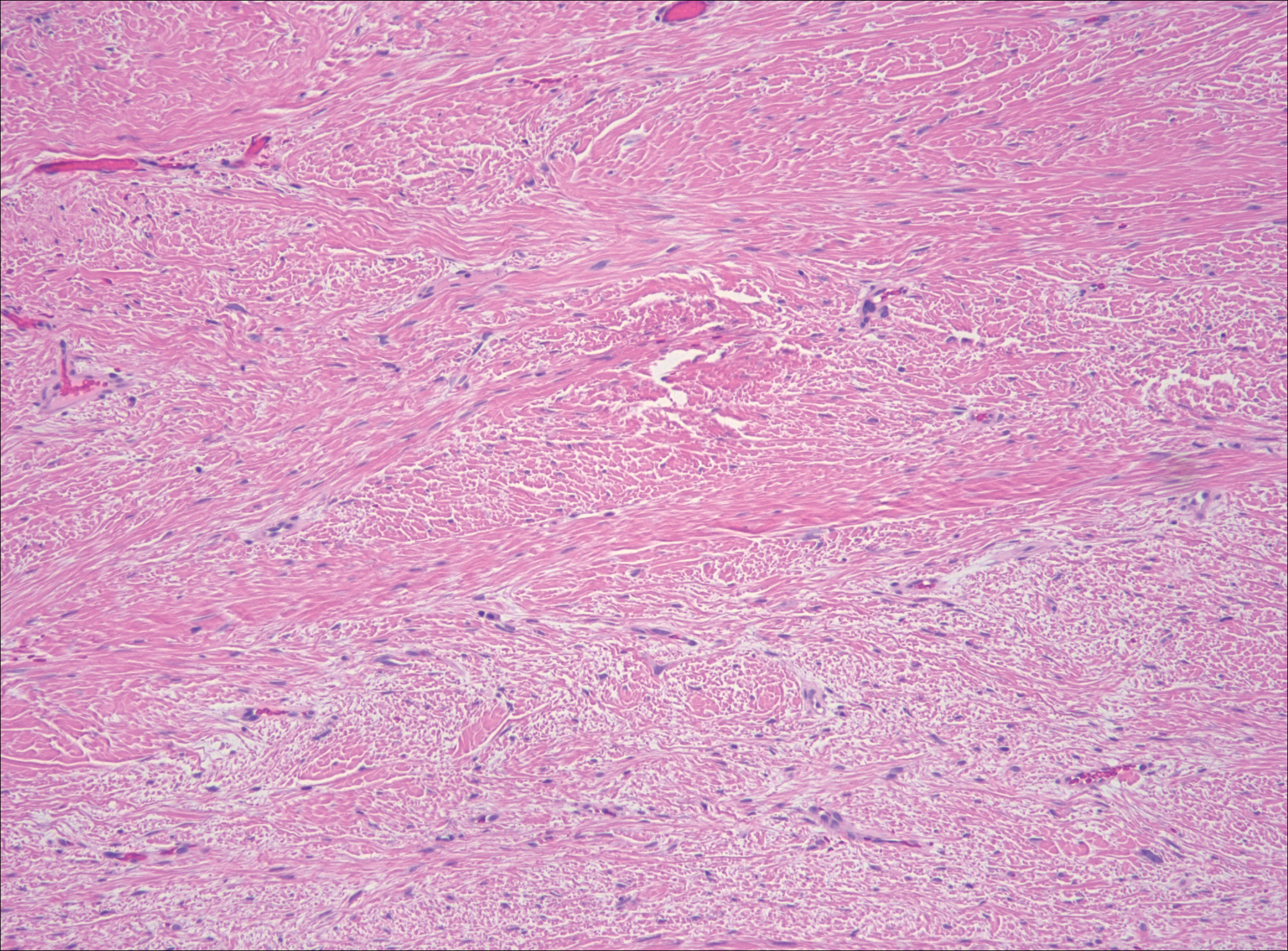
The distinction between the fibrous phase of nodular fasciitis and fibromatosis can be challenging. The size of the lesion may be helpful, with most lesions of nodular fasciitis being less than 3 cm, while lesions of fibromatosis have a mean diameter of 7 cm.5,14 Microscopically, both tumors demonstrate a fascicular growth pattern; however, the fascicles in nodular fasciitis tend to be short and irregular compared to the longer fascicles seen in fibromatosis (Figure 2). Immunohistochemistry staining has limited utility with only 56% (14/25) of superficial fibromatoses having positive nuclear staining for β-catenin.15
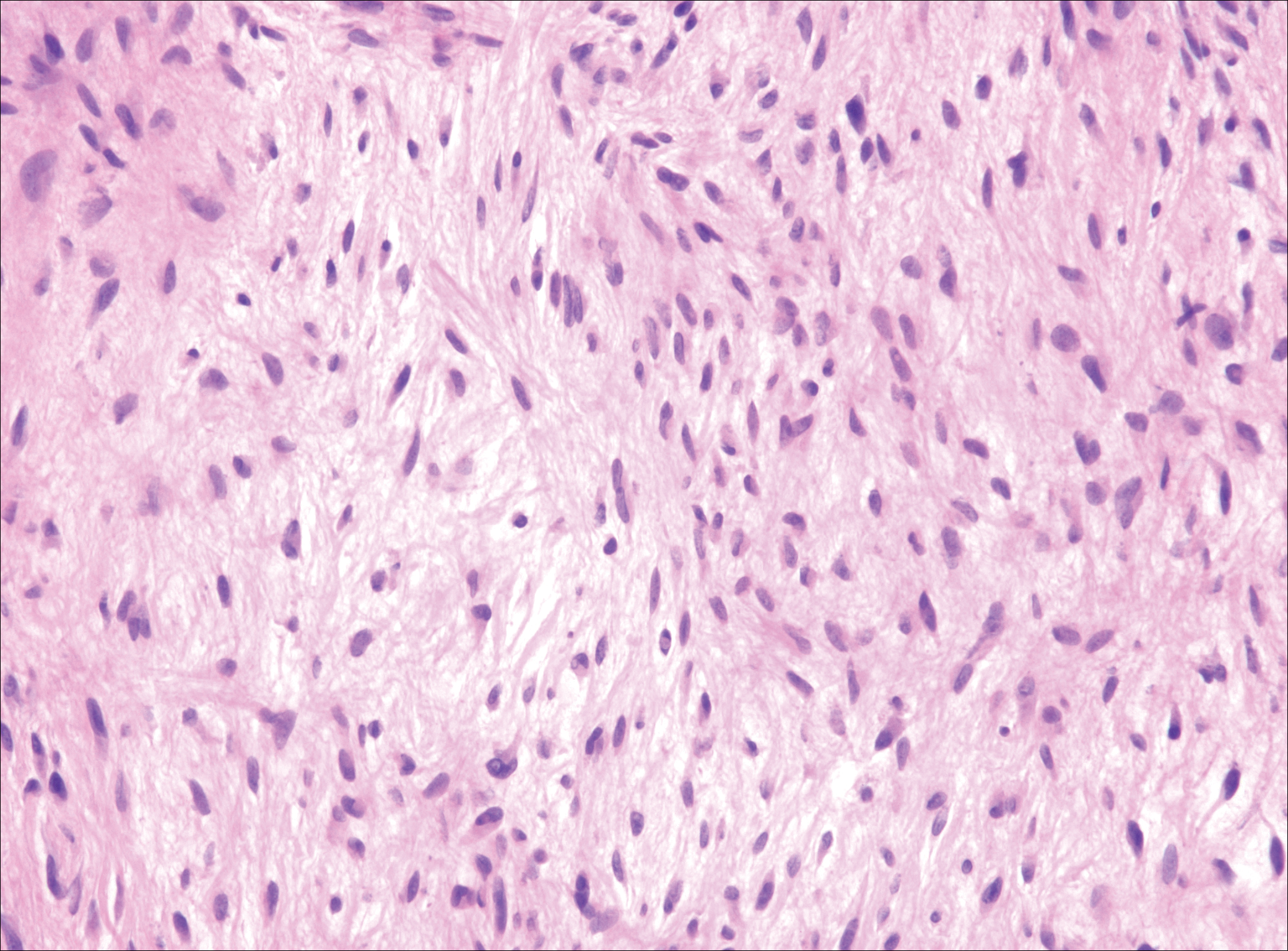
Low-grade fibromyxoid sarcoma (LGFMS) would be unusual in this clinical scenario. Only 13% to 19% of cases present in patients younger than 18 years (mean age, 33 years).16 In LGFMS there are cytologically bland spindle cells that are typically arranged in a patternless or whorled pattern (Figure 3), though fascicular architecture may be seen. There are alternating areas of fibrous and myxoid stroma. A curvilinear vasculature network and lack of lymphocytes and extravasated red blood cells are histologic features favoring LGFMS over nodular fasciitis. Immunohistochemistry staining and FISH testing can be useful in making the diagnosis of LGFMS. These tumors are characterized by a translocation t(7;16)(q34;p11) involving the fusion in sarcoma, FUS, and cAMP responsive element binding protein 3 like 2, CREB3L2, genes.16 Positive immunohistochemistry staining for MUC4 can be seen in up to 100% of LGFMS and is absent in many other spindle cell tumors.16
Plexiform fibrohistiocytic tumor (PFT) is least likely to be confused with nodular fasciitis. Histologically these tumors are characterized by multiple small nodules arranged in a plexiform pattern (Figure 4). Within the nodules, 3 cell types may be noted: spindle fibroblast-like cells, mononuclear histiocyte-like cells, and osteoclastlike cells.17 Either the spindle cells or the mononuclear cells may predominate in cases of PFT. Immunohistochemistry staining of PFT is nonspecific and there are no molecular/FISH studies that can be used to help confirm the diagnosis.
- Shin C, Low I, Ng D, et al. USP6 gene rearrangement in nodular fasciitis and histological mimics. Histopathology. 2016;69:784-791.
- Kumar E, Patel NR, Demicco EG, et al. Cutaneous nodular fasciitis with genetic analysis: a case series. J Cutan Pathol. 2016;43:1143-1149.
- Nishio J. Updates on the cytogenetics and molecular cytogenetics of benign and intermediate soft tissue tumors. Oncol Lett. 2013;5:12-18.
- Lin X, Wang L, Zhang Y, et al. Variable Ki67 proliferative index in 65 cases of nodular fasciitis, compared with fibrosarcoma and fibromatosis. Diagn Pathol. 2013;8:50.
- Goldstein J, Cates J. Differential diagnostic considerations of desmoid-type fibromatosis. Adv Anat Pathol. 2015;22:260-266.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, et al, eds. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyons, France: IARC Press; 2013.
- Bridge JA, Cushman-Vokoun AM. Molecular diagnostics of soft tissue tumors. Arch Pathol Lab Med. 2011;135:588-601.
- Anzeljc AJ, Oliveira AM, Grossniklaus HE, et al. Nodular fasciitis of the orbit: a case report confirmed by molecular cytogenetic analysis. Ophthalmic Plast Reconstr Surg. 2017;33(3S suppl 1):S152-S155.
- de Paula SA, Cruz AA, de Alencar VM, et al. Nodular fasciitis presenting as a large mass in the upper eyelid. Ophthalmic Plast Reconstr Surg. 2006;22:494-495.
- Bernstein KE, Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49:1668-1678.
- Shimizu S, Hashimoto H, Enjoji M. Nodular fasciitis: an analysis of 250 patients. Pathology. 1984;16:161-166.
- Erickson-Johnson MR, Chou MM, Evers BR, et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91:1427-1433.
- Amary MF, Ye H, Berisha F, et al. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013;463:97-98.
- Wirth L, Klein A, Baur-Melnyk A. Desmoid tumors of the extremity and trunk. a retrospective study of 44 patients. BMC Musculoskelet Disord. 2018;19:2.
- Carlson JW, Fletcher CD. Immunohistochemistry for beta-catenin in the differential diagnosis of spindle cells lesions: analysis of a series and review of the literature. Histopathology. 2007;51:509-514.
- Mohamed M, Fisher C, Thway K. Low-grade fibromyxoid sarcoma: clinical, morphologic and genetic features. Ann Diagn Pathol. 2017;28:60-67.
- Taher A, Pushpanathan C. Plexiform fibrohistiocytic tumor: a brief review. Arch Pathol Lab Med. 2007;131:1135-1138.
The Diagnosis: Nodular Fasciitis
The diagnosis of spindle cell tumors can be challenging; however, by using a variety of immunoperoxidase stains and fluorescent in situ hybridization (FISH) testing in conjunction with histology, it often is possible to arrive at a definitive diagnosis. For this case, the histologic features in conjunction with the immunoperoxidase stains and FISH were consistent with a diagnosis of nodular fasciitis.
Nodular fasciitis is a benign, self-limiting, myofibroblastic, soft-tissue proliferation typically found in the subcutaneous tissue.1 It can be found anywhere on the body but most commonly on the upper arms and trunk. It most often is seen in young adults, and many cases have been reported in association with a history of trauma to the area.1,2 It typically measures less than 2 cm in diameter.3 The diagnosis of nodular fasciitis is particularly challenging because it mimics sarcoma, both in presentation and in histologic findings with rapid growth, high mitotic activity, and increased cellularity.1,4-7 In contrast to malignancy, nodular fasciitis has no atypical mitoses and little cytologic atypia.8,9 Rather, it contains plump myofibroblasts loosely arranged in a myxoid or fibrous stroma that also may contain lymphocytes, extravasated erythrocytes, and osteoclastlike giant cells distributed throughout.5,10,11 In this case, lymphocytes, extravasated red blood cells, and myxoid change are present, suggesting the diagnosis of nodular fasciitis. In other cases, however, these features may be much more limited, making the diagnosis more challenging. The spindle cells are arranged in poorly defined short fascicles. The tumor cells do not infiltrate between individual adipocytes. There is no notable cytologic atypia.
Because of the difficulty in making the diagnosis, overtreatment of this benign condition can be a problem, causing increased morbidity.1 Erickson-Johnson et al12 identified the role of an ubiquitin-specific peptidase 6, USP6, gene rearrangement on chromosome 17p13 in 92% (44/48) of cases of nodular fasciitis. The USP6 gene most often is rearranged with the myosin heavy chain 9 gene, MYH9, on chromosome 22q12.3. With this rearrangement, the MYH9 promoter leads to the overexpression of USP6, causing tumor formation.2,13 The use of multiple immunoperoxidase stains can be important in the identification of nodular fasciitis. Nodular fasciitis stains negative for S-100, epithelial membrane antigen, CD34, β-catenin, and cytokeratin, but typically stains positive for smooth muscle actin.9
Although dermatofibrosarcoma protuberans (DFSP) was in the differential diagnosis, these tumors tend to have greater cellularity than nodular fasciitis. In addition, the spindle cells of DFSP typically are arranged in a storiform pattern. Another characteristic feature of DFSP is that the tumor cells will infiltrate between adipose cells creating a lacelike or honeycomblike appearance within the subcutaneous tissue (Figure 1). Immunohistochemistry staining and FISH testing may be useful in making a diagnosis of DFSP. These tumors typically are positive for CD34 by immunoperoxidase staining and demonstrate a translocation t(17;22)(q21;q13) between platelet-derived growth factor subunit B gene, PDGFB, and collagen type I alpha 1 chain gene, COL1A1, by FISH.
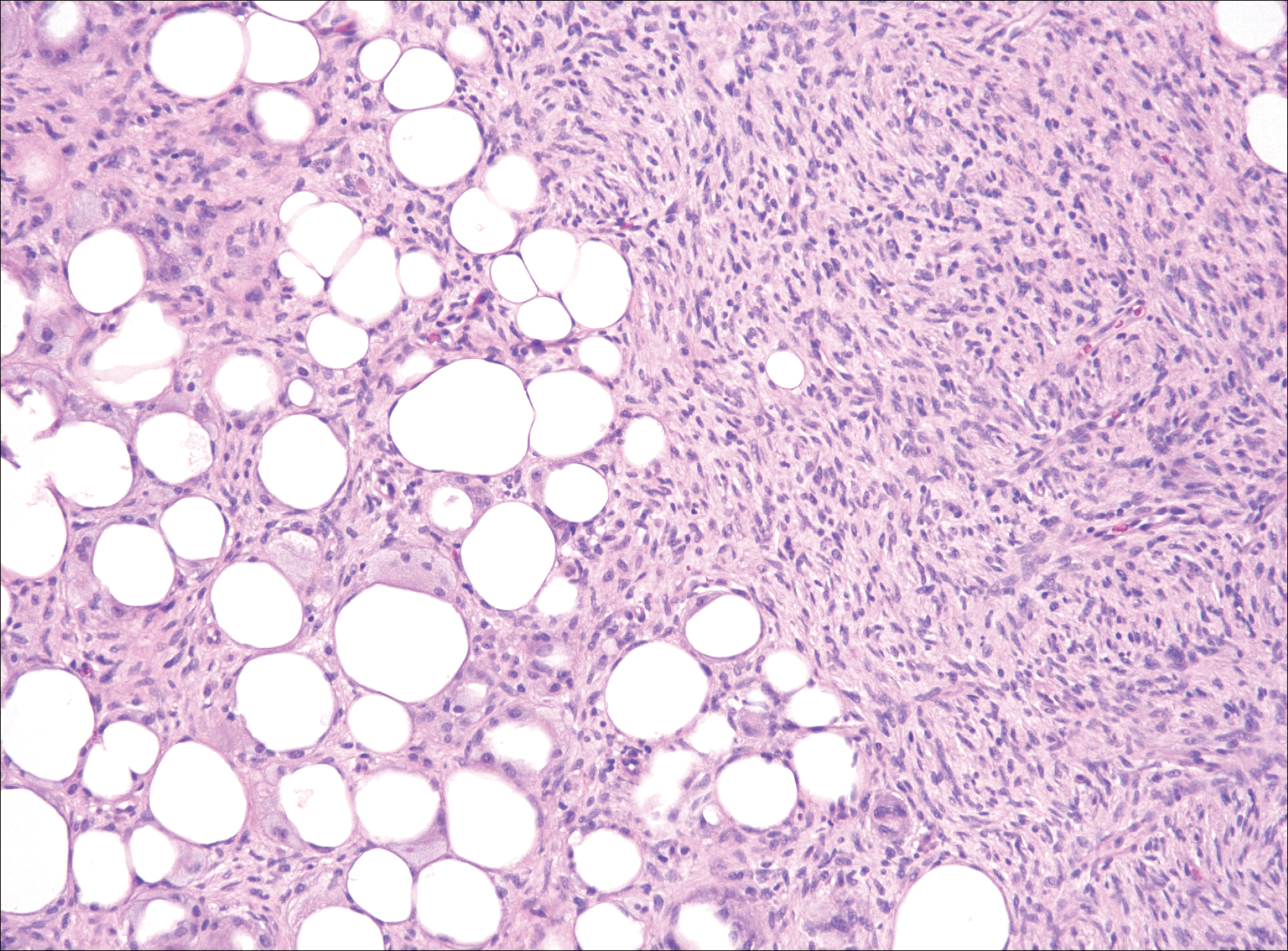
The distinction between the fibrous phase of nodular fasciitis and fibromatosis can be challenging. The size of the lesion may be helpful, with most lesions of nodular fasciitis being less than 3 cm, while lesions of fibromatosis have a mean diameter of 7 cm.5,14 Microscopically, both tumors demonstrate a fascicular growth pattern; however, the fascicles in nodular fasciitis tend to be short and irregular compared to the longer fascicles seen in fibromatosis (Figure 2). Immunohistochemistry staining has limited utility with only 56% (14/25) of superficial fibromatoses having positive nuclear staining for β-catenin.15
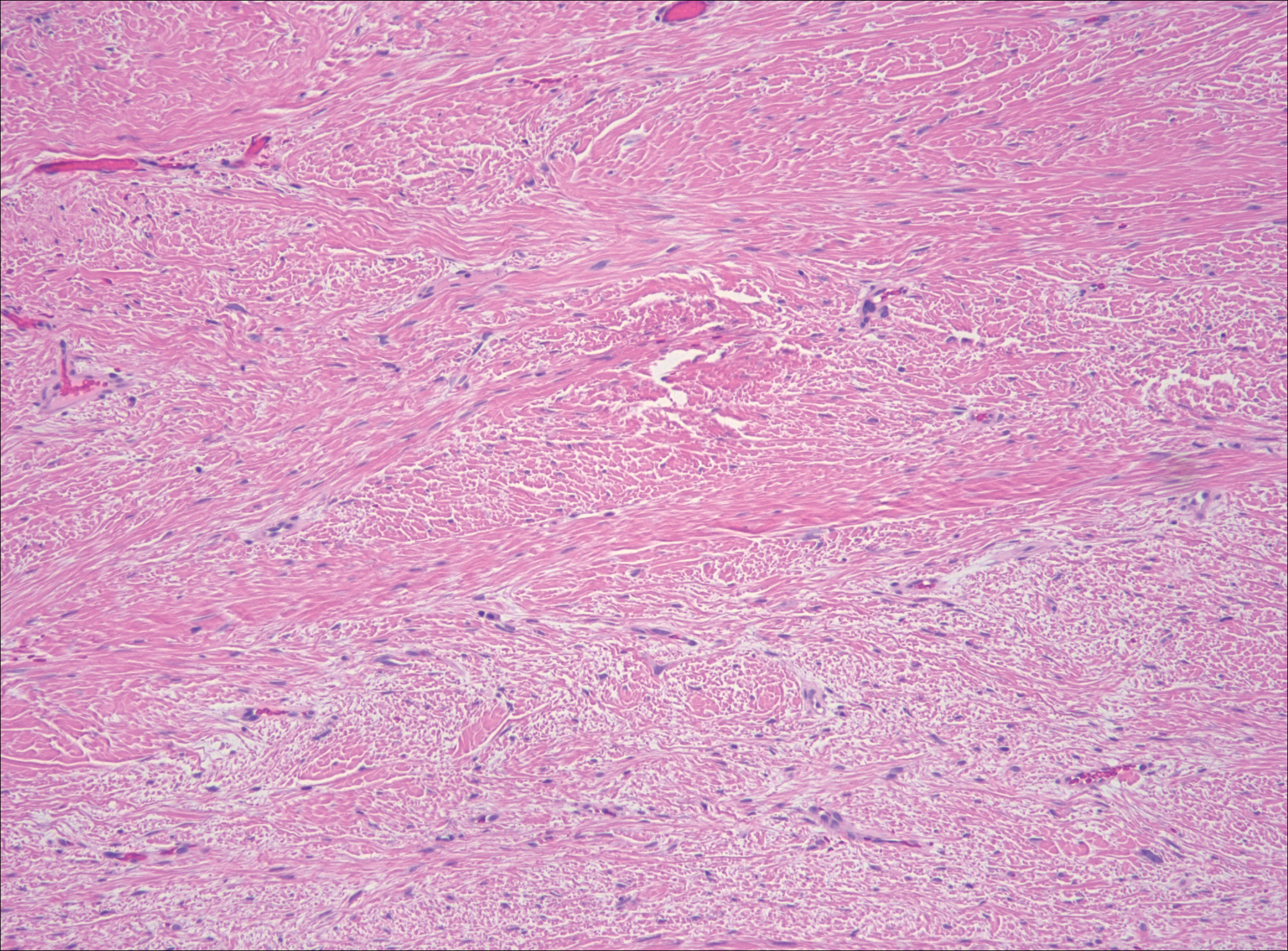
Low-grade fibromyxoid sarcoma (LGFMS) would be unusual in this clinical scenario. Only 13% to 19% of cases present in patients younger than 18 years (mean age, 33 years).16 In LGFMS there are cytologically bland spindle cells that are typically arranged in a patternless or whorled pattern (Figure 3), though fascicular architecture may be seen. There are alternating areas of fibrous and myxoid stroma. A curvilinear vasculature network and lack of lymphocytes and extravasated red blood cells are histologic features favoring LGFMS over nodular fasciitis. Immunohistochemistry staining and FISH testing can be useful in making the diagnosis of LGFMS. These tumors are characterized by a translocation t(7;16)(q34;p11) involving the fusion in sarcoma, FUS, and cAMP responsive element binding protein 3 like 2, CREB3L2, genes.16 Positive immunohistochemistry staining for MUC4 can be seen in up to 100% of LGFMS and is absent in many other spindle cell tumors.16
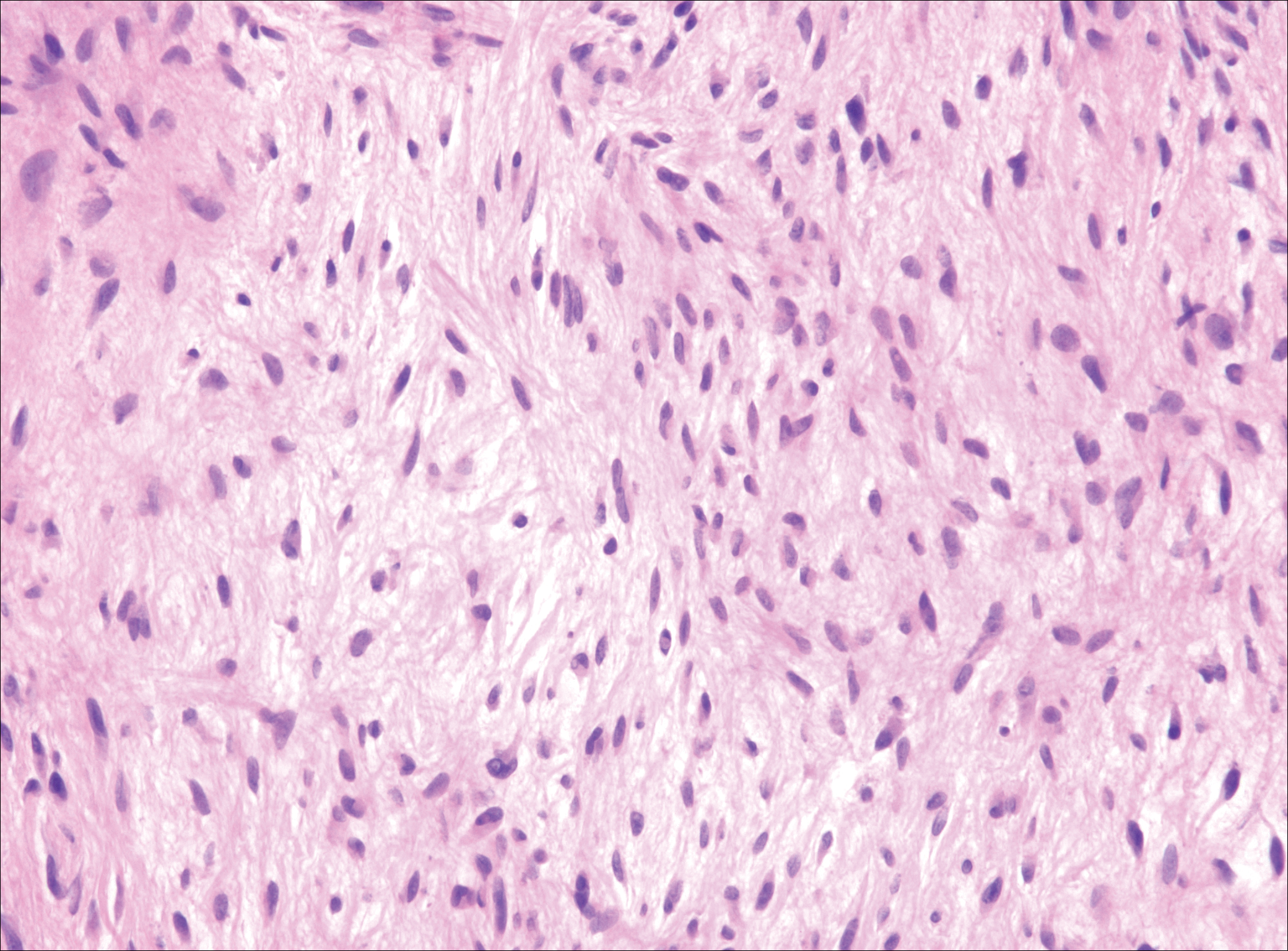
Plexiform fibrohistiocytic tumor (PFT) is least likely to be confused with nodular fasciitis. Histologically these tumors are characterized by multiple small nodules arranged in a plexiform pattern (Figure 4). Within the nodules, 3 cell types may be noted: spindle fibroblast-like cells, mononuclear histiocyte-like cells, and osteoclastlike cells.17 Either the spindle cells or the mononuclear cells may predominate in cases of PFT. Immunohistochemistry staining of PFT is nonspecific and there are no molecular/FISH studies that can be used to help confirm the diagnosis.
The Diagnosis: Nodular Fasciitis
The diagnosis of spindle cell tumors can be challenging; however, by using a variety of immunoperoxidase stains and fluorescent in situ hybridization (FISH) testing in conjunction with histology, it often is possible to arrive at a definitive diagnosis. For this case, the histologic features in conjunction with the immunoperoxidase stains and FISH were consistent with a diagnosis of nodular fasciitis.
Nodular fasciitis is a benign, self-limiting, myofibroblastic, soft-tissue proliferation typically found in the subcutaneous tissue.1 It can be found anywhere on the body but most commonly on the upper arms and trunk. It most often is seen in young adults, and many cases have been reported in association with a history of trauma to the area.1,2 It typically measures less than 2 cm in diameter.3 The diagnosis of nodular fasciitis is particularly challenging because it mimics sarcoma, both in presentation and in histologic findings with rapid growth, high mitotic activity, and increased cellularity.1,4-7 In contrast to malignancy, nodular fasciitis has no atypical mitoses and little cytologic atypia.8,9 Rather, it contains plump myofibroblasts loosely arranged in a myxoid or fibrous stroma that also may contain lymphocytes, extravasated erythrocytes, and osteoclastlike giant cells distributed throughout.5,10,11 In this case, lymphocytes, extravasated red blood cells, and myxoid change are present, suggesting the diagnosis of nodular fasciitis. In other cases, however, these features may be much more limited, making the diagnosis more challenging. The spindle cells are arranged in poorly defined short fascicles. The tumor cells do not infiltrate between individual adipocytes. There is no notable cytologic atypia.
Because of the difficulty in making the diagnosis, overtreatment of this benign condition can be a problem, causing increased morbidity.1 Erickson-Johnson et al12 identified the role of an ubiquitin-specific peptidase 6, USP6, gene rearrangement on chromosome 17p13 in 92% (44/48) of cases of nodular fasciitis. The USP6 gene most often is rearranged with the myosin heavy chain 9 gene, MYH9, on chromosome 22q12.3. With this rearrangement, the MYH9 promoter leads to the overexpression of USP6, causing tumor formation.2,13 The use of multiple immunoperoxidase stains can be important in the identification of nodular fasciitis. Nodular fasciitis stains negative for S-100, epithelial membrane antigen, CD34, β-catenin, and cytokeratin, but typically stains positive for smooth muscle actin.9
Although dermatofibrosarcoma protuberans (DFSP) was in the differential diagnosis, these tumors tend to have greater cellularity than nodular fasciitis. In addition, the spindle cells of DFSP typically are arranged in a storiform pattern. Another characteristic feature of DFSP is that the tumor cells will infiltrate between adipose cells creating a lacelike or honeycomblike appearance within the subcutaneous tissue (Figure 1). Immunohistochemistry staining and FISH testing may be useful in making a diagnosis of DFSP. These tumors typically are positive for CD34 by immunoperoxidase staining and demonstrate a translocation t(17;22)(q21;q13) between platelet-derived growth factor subunit B gene, PDGFB, and collagen type I alpha 1 chain gene, COL1A1, by FISH.
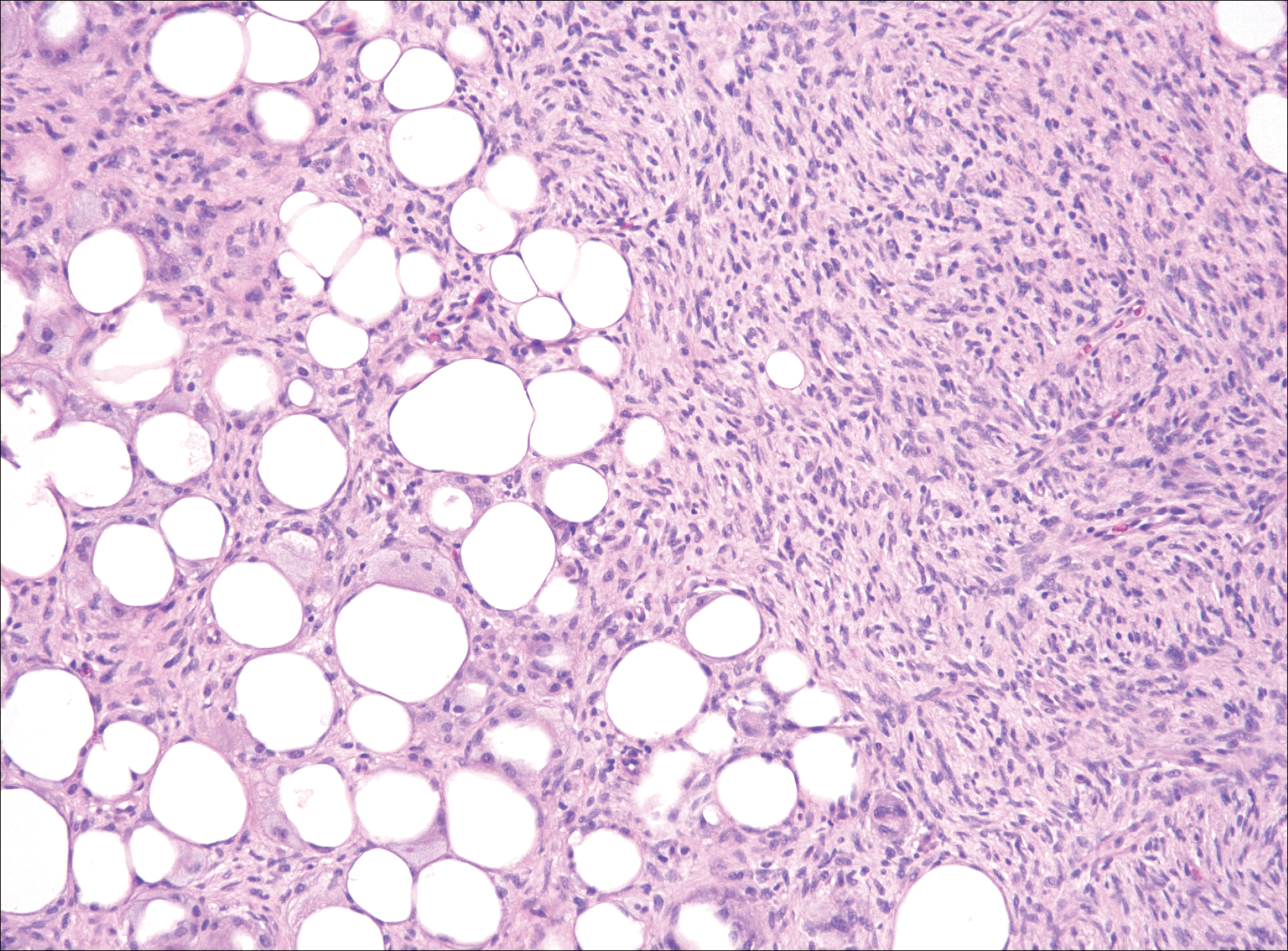
The distinction between the fibrous phase of nodular fasciitis and fibromatosis can be challenging. The size of the lesion may be helpful, with most lesions of nodular fasciitis being less than 3 cm, while lesions of fibromatosis have a mean diameter of 7 cm.5,14 Microscopically, both tumors demonstrate a fascicular growth pattern; however, the fascicles in nodular fasciitis tend to be short and irregular compared to the longer fascicles seen in fibromatosis (Figure 2). Immunohistochemistry staining has limited utility with only 56% (14/25) of superficial fibromatoses having positive nuclear staining for β-catenin.15
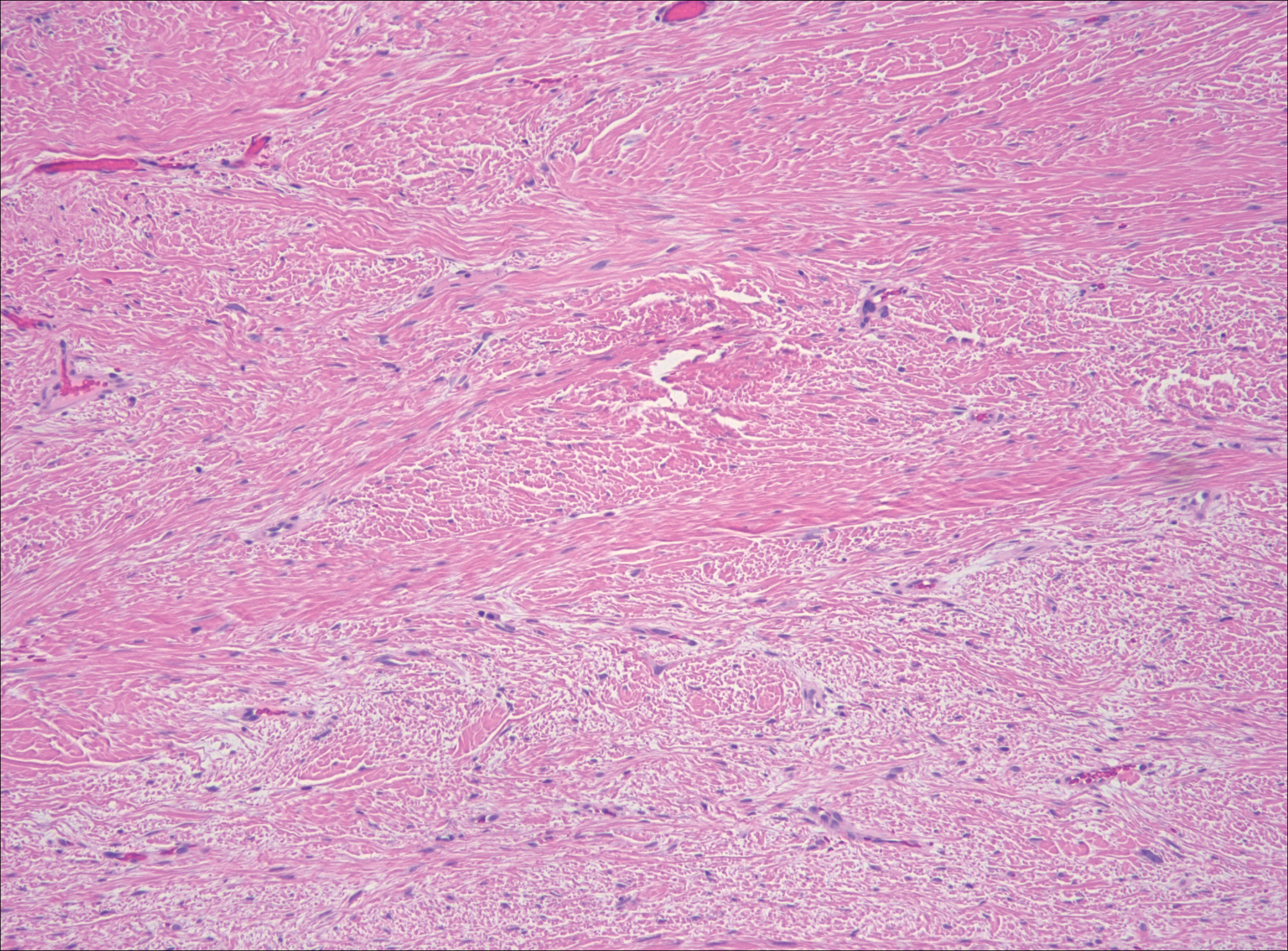
Low-grade fibromyxoid sarcoma (LGFMS) would be unusual in this clinical scenario. Only 13% to 19% of cases present in patients younger than 18 years (mean age, 33 years).16 In LGFMS there are cytologically bland spindle cells that are typically arranged in a patternless or whorled pattern (Figure 3), though fascicular architecture may be seen. There are alternating areas of fibrous and myxoid stroma. A curvilinear vasculature network and lack of lymphocytes and extravasated red blood cells are histologic features favoring LGFMS over nodular fasciitis. Immunohistochemistry staining and FISH testing can be useful in making the diagnosis of LGFMS. These tumors are characterized by a translocation t(7;16)(q34;p11) involving the fusion in sarcoma, FUS, and cAMP responsive element binding protein 3 like 2, CREB3L2, genes.16 Positive immunohistochemistry staining for MUC4 can be seen in up to 100% of LGFMS and is absent in many other spindle cell tumors.16
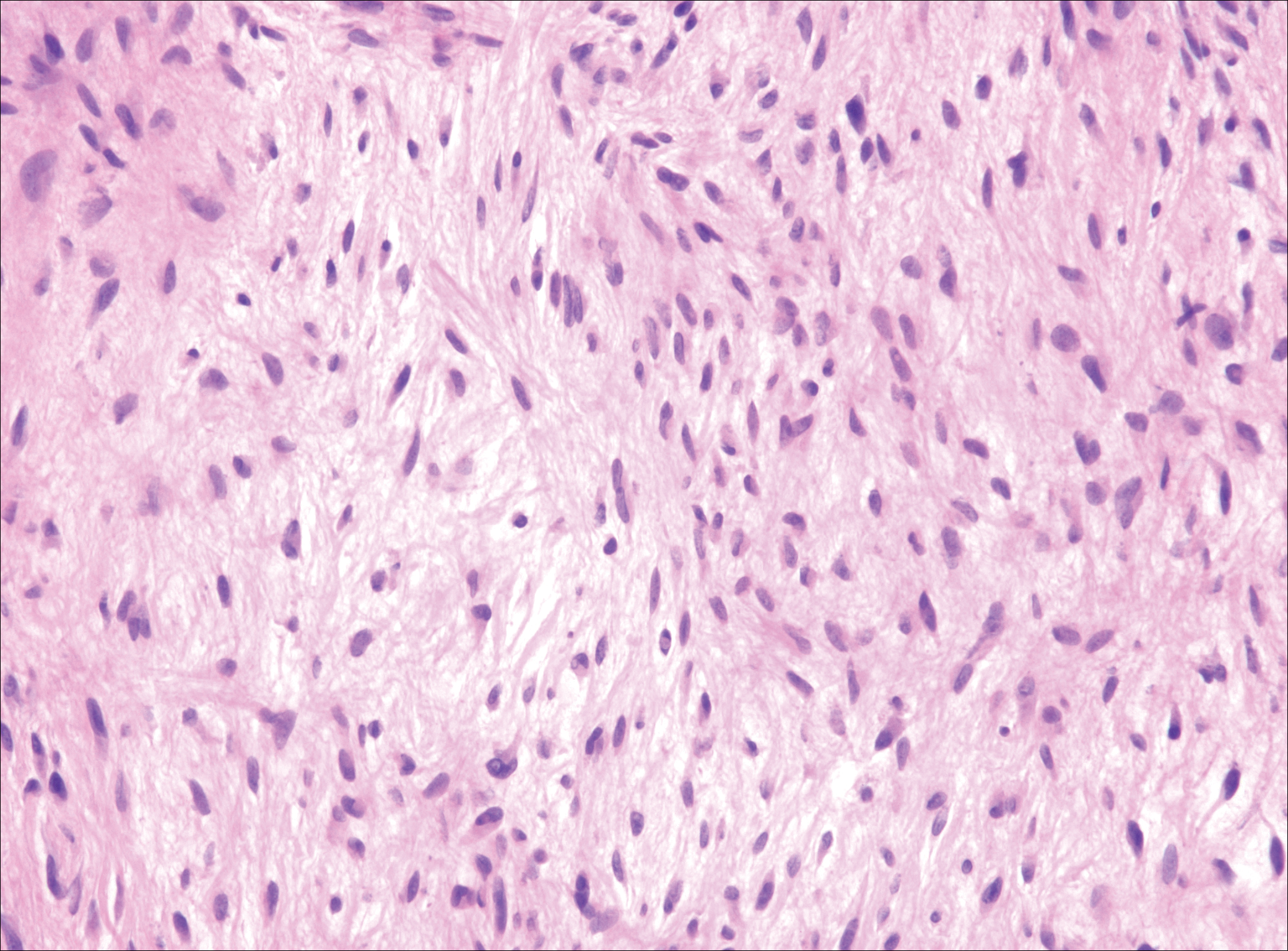
Plexiform fibrohistiocytic tumor (PFT) is least likely to be confused with nodular fasciitis. Histologically these tumors are characterized by multiple small nodules arranged in a plexiform pattern (Figure 4). Within the nodules, 3 cell types may be noted: spindle fibroblast-like cells, mononuclear histiocyte-like cells, and osteoclastlike cells.17 Either the spindle cells or the mononuclear cells may predominate in cases of PFT. Immunohistochemistry staining of PFT is nonspecific and there are no molecular/FISH studies that can be used to help confirm the diagnosis.
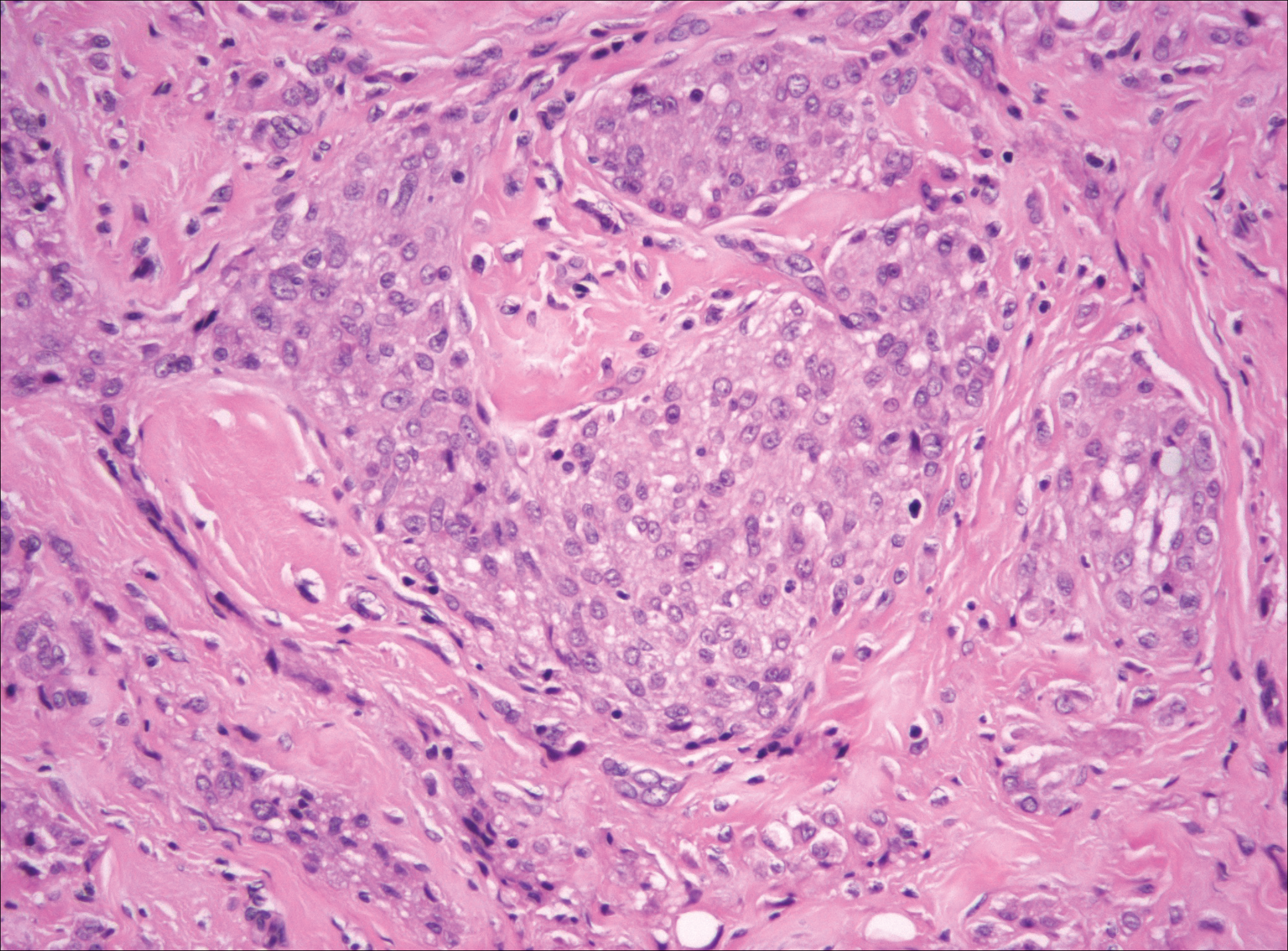
- Shin C, Low I, Ng D, et al. USP6 gene rearrangement in nodular fasciitis and histological mimics. Histopathology. 2016;69:784-791.
- Kumar E, Patel NR, Demicco EG, et al. Cutaneous nodular fasciitis with genetic analysis: a case series. J Cutan Pathol. 2016;43:1143-1149.
- Nishio J. Updates on the cytogenetics and molecular cytogenetics of benign and intermediate soft tissue tumors. Oncol Lett. 2013;5:12-18.
- Lin X, Wang L, Zhang Y, et al. Variable Ki67 proliferative index in 65 cases of nodular fasciitis, compared with fibrosarcoma and fibromatosis. Diagn Pathol. 2013;8:50.
- Goldstein J, Cates J. Differential diagnostic considerations of desmoid-type fibromatosis. Adv Anat Pathol. 2015;22:260-266.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, et al, eds. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyons, France: IARC Press; 2013.
- Bridge JA, Cushman-Vokoun AM. Molecular diagnostics of soft tissue tumors. Arch Pathol Lab Med. 2011;135:588-601.
- Anzeljc AJ, Oliveira AM, Grossniklaus HE, et al. Nodular fasciitis of the orbit: a case report confirmed by molecular cytogenetic analysis. Ophthalmic Plast Reconstr Surg. 2017;33(3S suppl 1):S152-S155.
- de Paula SA, Cruz AA, de Alencar VM, et al. Nodular fasciitis presenting as a large mass in the upper eyelid. Ophthalmic Plast Reconstr Surg. 2006;22:494-495.
- Bernstein KE, Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49:1668-1678.
- Shimizu S, Hashimoto H, Enjoji M. Nodular fasciitis: an analysis of 250 patients. Pathology. 1984;16:161-166.
- Erickson-Johnson MR, Chou MM, Evers BR, et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91:1427-1433.
- Amary MF, Ye H, Berisha F, et al. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013;463:97-98.
- Wirth L, Klein A, Baur-Melnyk A. Desmoid tumors of the extremity and trunk. a retrospective study of 44 patients. BMC Musculoskelet Disord. 2018;19:2.
- Carlson JW, Fletcher CD. Immunohistochemistry for beta-catenin in the differential diagnosis of spindle cells lesions: analysis of a series and review of the literature. Histopathology. 2007;51:509-514.
- Mohamed M, Fisher C, Thway K. Low-grade fibromyxoid sarcoma: clinical, morphologic and genetic features. Ann Diagn Pathol. 2017;28:60-67.
- Taher A, Pushpanathan C. Plexiform fibrohistiocytic tumor: a brief review. Arch Pathol Lab Med. 2007;131:1135-1138.
- Shin C, Low I, Ng D, et al. USP6 gene rearrangement in nodular fasciitis and histological mimics. Histopathology. 2016;69:784-791.
- Kumar E, Patel NR, Demicco EG, et al. Cutaneous nodular fasciitis with genetic analysis: a case series. J Cutan Pathol. 2016;43:1143-1149.
- Nishio J. Updates on the cytogenetics and molecular cytogenetics of benign and intermediate soft tissue tumors. Oncol Lett. 2013;5:12-18.
- Lin X, Wang L, Zhang Y, et al. Variable Ki67 proliferative index in 65 cases of nodular fasciitis, compared with fibrosarcoma and fibromatosis. Diagn Pathol. 2013;8:50.
- Goldstein J, Cates J. Differential diagnostic considerations of desmoid-type fibromatosis. Adv Anat Pathol. 2015;22:260-266.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, et al, eds. WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyons, France: IARC Press; 2013.
- Bridge JA, Cushman-Vokoun AM. Molecular diagnostics of soft tissue tumors. Arch Pathol Lab Med. 2011;135:588-601.
- Anzeljc AJ, Oliveira AM, Grossniklaus HE, et al. Nodular fasciitis of the orbit: a case report confirmed by molecular cytogenetic analysis. Ophthalmic Plast Reconstr Surg. 2017;33(3S suppl 1):S152-S155.
- de Paula SA, Cruz AA, de Alencar VM, et al. Nodular fasciitis presenting as a large mass in the upper eyelid. Ophthalmic Plast Reconstr Surg. 2006;22:494-495.
- Bernstein KE, Lattes R. Nodular (pseudosarcomatous) fasciitis, a nonrecurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49:1668-1678.
- Shimizu S, Hashimoto H, Enjoji M. Nodular fasciitis: an analysis of 250 patients. Pathology. 1984;16:161-166.
- Erickson-Johnson MR, Chou MM, Evers BR, et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab Invest. 2011;91:1427-1433.
- Amary MF, Ye H, Berisha F, et al. Detection of USP6 gene rearrangement in nodular fasciitis: an important diagnostic tool. Virchows Arch. 2013;463:97-98.
- Wirth L, Klein A, Baur-Melnyk A. Desmoid tumors of the extremity and trunk. a retrospective study of 44 patients. BMC Musculoskelet Disord. 2018;19:2.
- Carlson JW, Fletcher CD. Immunohistochemistry for beta-catenin in the differential diagnosis of spindle cells lesions: analysis of a series and review of the literature. Histopathology. 2007;51:509-514.
- Mohamed M, Fisher C, Thway K. Low-grade fibromyxoid sarcoma: clinical, morphologic and genetic features. Ann Diagn Pathol. 2017;28:60-67.
- Taher A, Pushpanathan C. Plexiform fibrohistiocytic tumor: a brief review. Arch Pathol Lab Med. 2007;131:1135-1138.
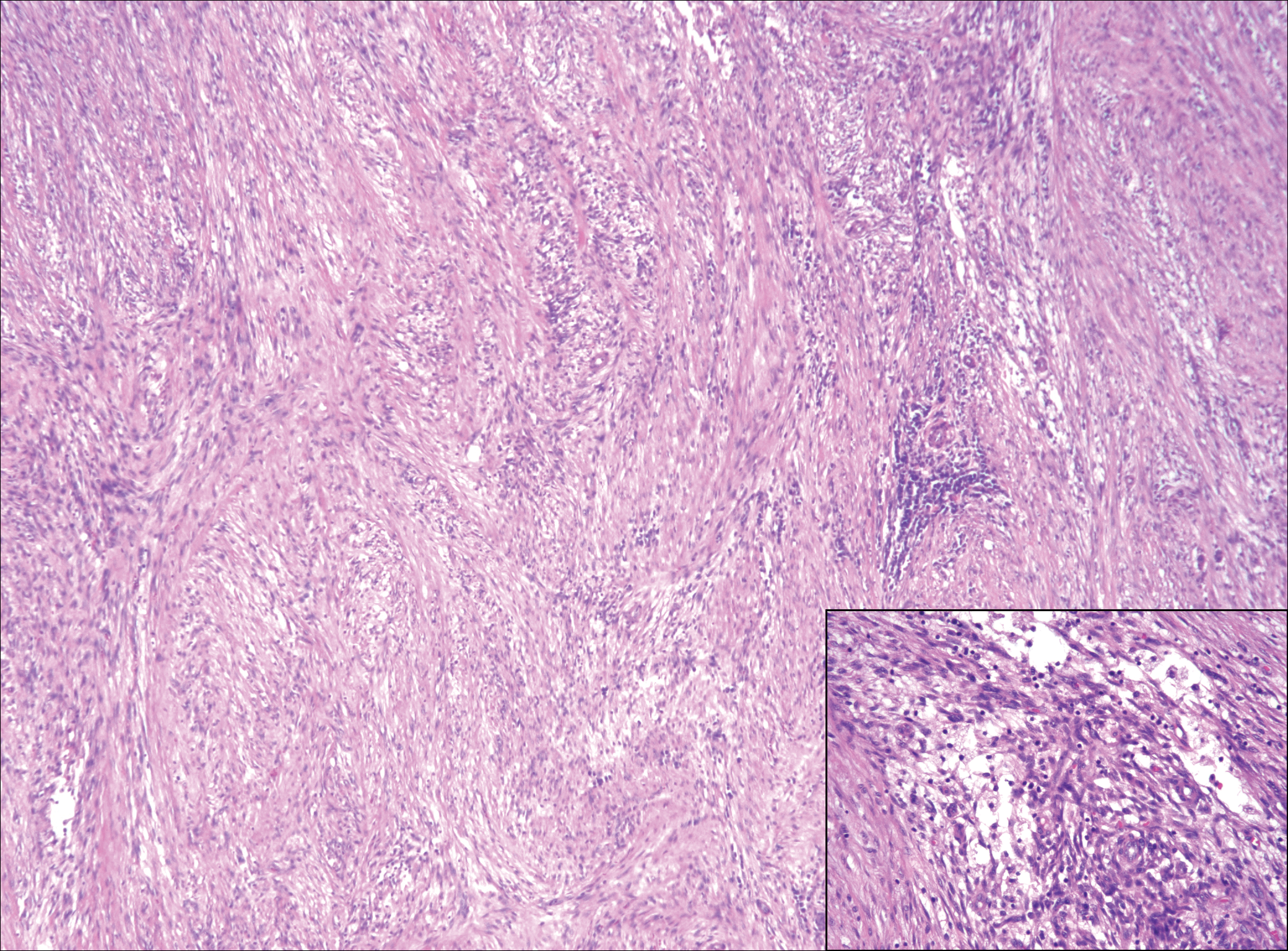
A 16-year-old adolescent girl presented with a bump over the left posterior knee of 1 month's duration. Her medical history was unremarkable. She denied recent trauma or injury to the area. On physical examination there was a visible and palpable tense nontender mass the size of an egg over the left posterior knee. Magnetic resonance imaging showed a lobulated mass-like focus of T2 hyperintensity centered at the subcutaneous tissues and superficial myofascial plane of the gastrocnemius on the posterior knee. Complete excision of the lesion was performed and demonstrated a 2.6.2 ×2.9.2 ×2.1-cm mass within subcutaneous adipose tissue. There was no microscopic involvement of skeletal muscle. Immunohistochemistry staining of the tumor was performed that was positive for smooth muscle actin and negative for desmin, S-100, CD34, pan-cytokeratin, and β-catenin. Fluorescent in situ hybridization testing demonstrated rearrangement of the ubiquitin-specific peptidase 6 gene, USP6, locus (17p13).
Submit Comments on VTE Guidelines by July 25
The American Society of Hematology (ASH) seeks comments by July 25 on draft clinical practice guidelines on venous thromboembolism: VTE Prevention in Surgical Hospitalized Patients.
The draft recommendations and a link to the online survey where comments are collected are available here.
The American Society of Hematology (ASH) seeks comments by July 25 on draft clinical practice guidelines on venous thromboembolism: VTE Prevention in Surgical Hospitalized Patients.
The draft recommendations and a link to the online survey where comments are collected are available here.
The American Society of Hematology (ASH) seeks comments by July 25 on draft clinical practice guidelines on venous thromboembolism: VTE Prevention in Surgical Hospitalized Patients.
The draft recommendations and a link to the online survey where comments are collected are available here.
New and Noteworthy Information—July 2018
Adequate Sleep Associated With Lower Dementia Risk
Short and long daily sleep duration are risk factors for dementia and death in adults age 60 and older, according to a study published online ahead of print June 6 in the Journal of the American Geriatrics Society. In a prospective cohort study, researchers followed 1,517 adults without dementia for 10 years. Self-reported daily sleep durations were grouped into five categories. The association between daily sleep duration and risk of dementia and death was determined using Cox proportional hazards models. During follow-up, 294 participants developed dementia, and 282 died. Age- and sex-adjusted incidence rates of dementia and all-cause mortality were significantly greater in subjects who slept less than 5.0 hours/day or 10.0 or more hours/day than in people who slept from 5.0 to 6.9 hours/day.
Ohara T, Honda T, Hata J, et al. Association between daily sleep duration and risk of dementia and mortality in a Japanese community. J Am Geriatr Soc. 2018 Jun 6 [Epub ahead of print].
Rivaroxaban Not Superior to Aspirin for Stroke Prevention
Rivaroxaban is not superior to aspirin in the prevention of recurrent stroke, according to a study published June 7 in the New England Journal of Medicine. Researchers compared the efficacy and safety of rivaroxaban at a daily dose of 15 mg with aspirin at a daily dose of 100 mg for the prevention of recurrent stroke in patients with recent ischemic stroke that was presumed to be from cerebral embolism. The primary outcome was the first recurrence of ischemic or hemorrhagic stroke or systemic embolism in a time-to-event analysis. At 459 sites, 3,609 patients were randomly assigned to receive rivaroxaban, and 3,604 were randomized to aspirin. Recurrent ischemic stroke occurred in 172 patients in the rivaroxaban group and in 160 in the aspirin group.
Hart RG, Sharma M, Mundl H, et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med. 2018;378(23):2191-2201.
Disintegrating Brain Lesions May Indicate Worsening MS
Atrophied lesion volume may indicate increasing disability in patients with multiple sclerosis (MS), according to a study published online ahead of print June 1 in the Journal of Neuroimaging. A total of 192 patients with clinically isolated syndrome or MS received 3T MRI at baseline and at five years. Investigators quantified lesions at baseline and calculated new and enlarging lesion volumes during the study interval. Atrophied lesion volume was calculated by combining baseline lesion masks with follow-up SIENAX-derived CSF partial volume maps. The researchers evaluated correlations between these measures and disability, as measured by the Expanded Disability Status Scale (EDSS). Atrophied lesion volume was different between MS subtypes and exceeded new lesion volume accumulation in progressive MS. Atrophied lesion volume was the only significant correlate of EDSS change.
Dwyer MG, Bergsland N, Ramasamy DP, et al. Atrophied brain lesion volume: a new imaging biomarker in multiple sclerosis. J Neuroimaging. 2018 Jun 1 [Epub ahead of print].
Do Migraineurs Seek Behavioral Treatment After a Referral?
A significant number of migraineurs are not using effective behavioral treatments for migraine, according to a study published online ahead of print June 5 in Pain Medicine. In a prospective cohort study, researchers tracked 234 patients with migraine who presented to an academic headache center and referred 69 of them for behavioral treatment with an appropriately trained therapist. Fifty-three of the referred patients completed a follow-up interview within three months of their initial appointment and were included in the analysis. Of the patients referred for behavioral treatment, 30 made an appointment. Investigators found no differences between people who started behavioral therapy and people who did not. Study authors did find that people who had previously seen a psychologist for migraine were more likely to initiate therapy.
Minen MT, Azarchi S, Sobolev R, et al. Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: a prospective observational study. Pain Med. 2018 Jun 5 [Epub ahead of print].
TIA Associated With Increased Five-Year Risk of Stroke
People with transient ischemic attack (TIA) are at risk for a cardiovascular event in the following five years, according to a study published June 7 in the New England Journal of Medicine. Researchers evaluated patients who had had a TIA within seven days before enrollment in a registry of TIA clinics. Of 61 sites, 42 had follow-up data on more than 50% of their enrolled patients at five years. The study’s primary outcome was a composite of stroke, acute coronary syndrome, or death from cardiovascular causes, with an emphasis on events that occurred in the second through fifth years. At five years, stroke had occurred in 345 of the 3,847 patients included in the follow-up study, and 149 of them had a stroke during the second through fifth years of follow-up.
Amarenco P, Lavallée PC, Monteiro Tavares L, et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378(23):2182-2190.
Follow-Up Care for TBI Is Not Delivered Adequately
Follow-up care for patients with traumatic brain injury (TBI) is not delivered optimally, according to a study published May 25 in JAMA Network Open. In a cohort study, researchers surveyed 831 participants in the Transforming Research and Clinical Knowledge in TBI initiative about their care after hospital discharge. Follow-up care was defined as providing TBI-related educational materials at discharge, calling patients within two weeks after release, seeing a healthcare provider within two weeks, and seeing a healthcare provider within three months. Approximately 42% of participants reported receiving TBI-related educational material at discharge, and 44% reported seeing a physician or other medical practitioner within three months after injury. Of patients with a positive finding on CT, 39% had not seen a medical practitioner at three months after injury.
Seabury SA, Gaudette E, Goldman DP, et al. Assessment of follow-up care after emergency department presentation for mild traumatic brain injury and concussion: results from the TRACK-TBI study. JAMA Network Open. 2018;1(1):e180210.
Researchers Examine Mortality Rate of Pediatric Stroke
In-hospital mortality occurs in 2.6% of children with arterial ischemic stroke, according to a study published in the May issue of Pediatrics. The retrospective study included 915 infants younger than 1 month and 2,273 children age 1 month to 18 years with stroke at 87 hospitals in 24 countries. Death during hospitalization and cause of death were ascertained from medical records. A total of 14 neonates and 70 children died during hospitalization. Of 48 cases with reported causes of death, 31 were stroke-related. Remaining deaths were attributed to medical disease. In multivariable analysis, congenital heart disease, posterior plus anterior circulation stroke, and stroke presentation without seizures were associated with in-hospital mortality for neonates. Hispanic ethnicity, congenital heart disease, and posterior plus anterior circulation stroke were associated with in-hospital mortality for children.
Beslow LA, Dowling MM, Hassanein SMA, et al. Mortality after pediatric arterial ischemic stroke. Pediatrics. 2018;141(5).
FDA Approves zEEG Dry Electrode Headset
The FDA has approved the zEEG dry electrode EEG headset for clinical use. The zEEG headset is backed by a cloud platform that allows users to upload data instantly, provides tools for analysis, and enables remote interpretation by neurologists. A clinical study found that the zEEG headset provided EEG signal quality that was comparable to that of an approved, traditional EEG system. In two study cohorts, a total of 30 patients were studied for time periods of as long as two hours, and the zEEG device performed at least as well as the reference device, based on predefined acceptance criteria. Study results will be published in the coming months. Zeto, headquartered in Santa Clara, California, markets the device.
South Asian Americans Have High Cardiovascular Mortality
South Asians living in the United States have higher mortality from heart conditions caused by atherosclerosis, such as heart attack and stroke, according to a study published online ahead of print May 24 in Circulation. Investigators reviewed the literature relevant to South Asian populations’ demographics and risk factors, health behaviors, and interventions, including physical activity, diet, medications, and community strategies. South Asians have higher proportional mortality rates from atherosclerotic cardiovascular disease, compared with other Asian groups, largely because of the lower risk observed in East Asian populations. A majority of the risk in South Asians can be explained by the increased prevalence of known risk factors, especially factors related to insulin resistance. The authors found no unique risk factors in this population.
Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018 May 24 [Epub ahead of print].
How Much Exercise Improves Cognition in Older Adults?
Exercising for at least 52 hours over six months is associated with improved cognitive performance in older adults with and without cognitive impairment, according to a study published online ahead of print May 30 in Neurology. Researchers reviewed data for 98 randomized, controlled exercise trials including 11,061 participants with an average age of 73. About 59% of the participants were healthy adults, 26% had mild cognitive impairment, and 15% had dementia. Researchers collected data on exercise session length, intensity, weekly frequency, and amount of exercise over time. Aerobic exercise was the most common form of exercise. In healthy people and people with cognitive impairment, longer term exposure to exercise, at least 52 hours conducted over an average of about six months, improved the brain’s processing speed.
Gomes-Osman J, Cabral DF, Morris TP, et al. Exercise for cognitive brain health in aging. Neurology. 2018 May 30 [Epub ahead of print].
Blood Biomarkers Detect Subconcussive Head Trauma
Blood biomarkers can detect the neurologic injury associated with repetitive subconcussive head trauma, according to a study published online ahead of print May 29 in the Journal of Neurosurgery. A total of 35 National Collegiate Athletic Association football players underwent blood sampling throughout the 2016 football season. Samples were analyzed for plasma concentrations of tau and serum concentrations of neurofilament light. Athletes were categorized as starters or nonstarters, and the investigators assessed between-group differences and time-course differences. In nonstarters, plasma concentrations of tau decreased over the season. Starters had lower plasma concentrations of tau. Plasma concentrations of tau could not be used to distinguish between starters and nonstarters. Serum concentrations of neurofilament light increased as head impacts increased, specifically in starters. Serum neurofilament light distinguished starters from nonstarters.
Oliver JM, Anzalone AJ, Stone JD, et al. Fluctuations in blood biomarkers of head trauma in NCAA football athletes over the course of a season. J Neurosurg. 2018 May 29 [Epub ahead of print].
Model Estimates Risk of Alzheimer’s Disease Dementia
Most people with preclinical Alzheimer’s disease will not develop dementia during their lifetimes, according to a study published online ahead of print May 7 in Alzheimer’s & Dementia. Researchers used a multistate model for Alzheimer’s disease along with US death rates to estimate lifetime and 10-year risks of Alzheimer’s disease dementia. Lifetime risks of Alzheimer’s disease dementia vary by age, gender, and preclinical or clinical disease state. A 70-year-old male with amyloid but no signs of neurodegeneration and no memory loss has a lifetime risk of 19.9%. The lifetime risks for a female with amyloidosis are 8.4% at age 90 and 29.3% at age 65. People younger than 85 with mild cognitive impairment, amyloidosis, and neurodegeneration have lifetime risks of Alzheimer’s disease dementia greater than 50%.
Brookmeyer R, Abdalla N. Estimation of lifetime risks of Alzheimer’s disease dementia using biomarkers for preclinical disease. Alzheimers Dement. 2018 May 7 [Epub ahead of print].
Depression Is Associated With Brain and Memory Outcomes
In a sample of mostly Caribbean Hispanic, stroke-free older adults, greater depressive symptoms were associated with worse episodic memory, smaller cerebral volume, and silent infarcts, according to a study published online ahead of print May 9 in Neurology. Researchers analyzed data from the Northern Manhattan Study. A total of 1,111 participants underwent baseline evaluations of depressive symptoms, MRI markers, and cognitive function. At baseline, 22% of participants had greater depressive symptoms. Greater depressive symptoms were significantly associated with worse baseline episodic memory in models adjusted for sociodemographics, vascular risk factors, behavioral factors, and antidepressant medications. Furthermore, greater depressive symptoms were associated with smaller cerebral parenchymal fraction and increased odds of subclinical brain infarcts, after adjustment for sociodemographics, behavioral factors, and vascular risk factors.
Al Hazzouri AZ, Caunca MR, Nobrega JC. Greater depressive symptoms, cognition, and markers of brain aging. Neurology. 2018 May 9 [Epub ahead of print].
—Kimberly Williams
Adequate Sleep Associated With Lower Dementia Risk
Short and long daily sleep duration are risk factors for dementia and death in adults age 60 and older, according to a study published online ahead of print June 6 in the Journal of the American Geriatrics Society. In a prospective cohort study, researchers followed 1,517 adults without dementia for 10 years. Self-reported daily sleep durations were grouped into five categories. The association between daily sleep duration and risk of dementia and death was determined using Cox proportional hazards models. During follow-up, 294 participants developed dementia, and 282 died. Age- and sex-adjusted incidence rates of dementia and all-cause mortality were significantly greater in subjects who slept less than 5.0 hours/day or 10.0 or more hours/day than in people who slept from 5.0 to 6.9 hours/day.
Ohara T, Honda T, Hata J, et al. Association between daily sleep duration and risk of dementia and mortality in a Japanese community. J Am Geriatr Soc. 2018 Jun 6 [Epub ahead of print].
Rivaroxaban Not Superior to Aspirin for Stroke Prevention
Rivaroxaban is not superior to aspirin in the prevention of recurrent stroke, according to a study published June 7 in the New England Journal of Medicine. Researchers compared the efficacy and safety of rivaroxaban at a daily dose of 15 mg with aspirin at a daily dose of 100 mg for the prevention of recurrent stroke in patients with recent ischemic stroke that was presumed to be from cerebral embolism. The primary outcome was the first recurrence of ischemic or hemorrhagic stroke or systemic embolism in a time-to-event analysis. At 459 sites, 3,609 patients were randomly assigned to receive rivaroxaban, and 3,604 were randomized to aspirin. Recurrent ischemic stroke occurred in 172 patients in the rivaroxaban group and in 160 in the aspirin group.
Hart RG, Sharma M, Mundl H, et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med. 2018;378(23):2191-2201.
Disintegrating Brain Lesions May Indicate Worsening MS
Atrophied lesion volume may indicate increasing disability in patients with multiple sclerosis (MS), according to a study published online ahead of print June 1 in the Journal of Neuroimaging. A total of 192 patients with clinically isolated syndrome or MS received 3T MRI at baseline and at five years. Investigators quantified lesions at baseline and calculated new and enlarging lesion volumes during the study interval. Atrophied lesion volume was calculated by combining baseline lesion masks with follow-up SIENAX-derived CSF partial volume maps. The researchers evaluated correlations between these measures and disability, as measured by the Expanded Disability Status Scale (EDSS). Atrophied lesion volume was different between MS subtypes and exceeded new lesion volume accumulation in progressive MS. Atrophied lesion volume was the only significant correlate of EDSS change.
Dwyer MG, Bergsland N, Ramasamy DP, et al. Atrophied brain lesion volume: a new imaging biomarker in multiple sclerosis. J Neuroimaging. 2018 Jun 1 [Epub ahead of print].
Do Migraineurs Seek Behavioral Treatment After a Referral?
A significant number of migraineurs are not using effective behavioral treatments for migraine, according to a study published online ahead of print June 5 in Pain Medicine. In a prospective cohort study, researchers tracked 234 patients with migraine who presented to an academic headache center and referred 69 of them for behavioral treatment with an appropriately trained therapist. Fifty-three of the referred patients completed a follow-up interview within three months of their initial appointment and were included in the analysis. Of the patients referred for behavioral treatment, 30 made an appointment. Investigators found no differences between people who started behavioral therapy and people who did not. Study authors did find that people who had previously seen a psychologist for migraine were more likely to initiate therapy.
Minen MT, Azarchi S, Sobolev R, et al. Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: a prospective observational study. Pain Med. 2018 Jun 5 [Epub ahead of print].
TIA Associated With Increased Five-Year Risk of Stroke
People with transient ischemic attack (TIA) are at risk for a cardiovascular event in the following five years, according to a study published June 7 in the New England Journal of Medicine. Researchers evaluated patients who had had a TIA within seven days before enrollment in a registry of TIA clinics. Of 61 sites, 42 had follow-up data on more than 50% of their enrolled patients at five years. The study’s primary outcome was a composite of stroke, acute coronary syndrome, or death from cardiovascular causes, with an emphasis on events that occurred in the second through fifth years. At five years, stroke had occurred in 345 of the 3,847 patients included in the follow-up study, and 149 of them had a stroke during the second through fifth years of follow-up.
Amarenco P, Lavallée PC, Monteiro Tavares L, et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378(23):2182-2190.
Follow-Up Care for TBI Is Not Delivered Adequately
Follow-up care for patients with traumatic brain injury (TBI) is not delivered optimally, according to a study published May 25 in JAMA Network Open. In a cohort study, researchers surveyed 831 participants in the Transforming Research and Clinical Knowledge in TBI initiative about their care after hospital discharge. Follow-up care was defined as providing TBI-related educational materials at discharge, calling patients within two weeks after release, seeing a healthcare provider within two weeks, and seeing a healthcare provider within three months. Approximately 42% of participants reported receiving TBI-related educational material at discharge, and 44% reported seeing a physician or other medical practitioner within three months after injury. Of patients with a positive finding on CT, 39% had not seen a medical practitioner at three months after injury.
Seabury SA, Gaudette E, Goldman DP, et al. Assessment of follow-up care after emergency department presentation for mild traumatic brain injury and concussion: results from the TRACK-TBI study. JAMA Network Open. 2018;1(1):e180210.
Researchers Examine Mortality Rate of Pediatric Stroke
In-hospital mortality occurs in 2.6% of children with arterial ischemic stroke, according to a study published in the May issue of Pediatrics. The retrospective study included 915 infants younger than 1 month and 2,273 children age 1 month to 18 years with stroke at 87 hospitals in 24 countries. Death during hospitalization and cause of death were ascertained from medical records. A total of 14 neonates and 70 children died during hospitalization. Of 48 cases with reported causes of death, 31 were stroke-related. Remaining deaths were attributed to medical disease. In multivariable analysis, congenital heart disease, posterior plus anterior circulation stroke, and stroke presentation without seizures were associated with in-hospital mortality for neonates. Hispanic ethnicity, congenital heart disease, and posterior plus anterior circulation stroke were associated with in-hospital mortality for children.
Beslow LA, Dowling MM, Hassanein SMA, et al. Mortality after pediatric arterial ischemic stroke. Pediatrics. 2018;141(5).
FDA Approves zEEG Dry Electrode Headset
The FDA has approved the zEEG dry electrode EEG headset for clinical use. The zEEG headset is backed by a cloud platform that allows users to upload data instantly, provides tools for analysis, and enables remote interpretation by neurologists. A clinical study found that the zEEG headset provided EEG signal quality that was comparable to that of an approved, traditional EEG system. In two study cohorts, a total of 30 patients were studied for time periods of as long as two hours, and the zEEG device performed at least as well as the reference device, based on predefined acceptance criteria. Study results will be published in the coming months. Zeto, headquartered in Santa Clara, California, markets the device.
South Asian Americans Have High Cardiovascular Mortality
South Asians living in the United States have higher mortality from heart conditions caused by atherosclerosis, such as heart attack and stroke, according to a study published online ahead of print May 24 in Circulation. Investigators reviewed the literature relevant to South Asian populations’ demographics and risk factors, health behaviors, and interventions, including physical activity, diet, medications, and community strategies. South Asians have higher proportional mortality rates from atherosclerotic cardiovascular disease, compared with other Asian groups, largely because of the lower risk observed in East Asian populations. A majority of the risk in South Asians can be explained by the increased prevalence of known risk factors, especially factors related to insulin resistance. The authors found no unique risk factors in this population.
Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018 May 24 [Epub ahead of print].
How Much Exercise Improves Cognition in Older Adults?
Exercising for at least 52 hours over six months is associated with improved cognitive performance in older adults with and without cognitive impairment, according to a study published online ahead of print May 30 in Neurology. Researchers reviewed data for 98 randomized, controlled exercise trials including 11,061 participants with an average age of 73. About 59% of the participants were healthy adults, 26% had mild cognitive impairment, and 15% had dementia. Researchers collected data on exercise session length, intensity, weekly frequency, and amount of exercise over time. Aerobic exercise was the most common form of exercise. In healthy people and people with cognitive impairment, longer term exposure to exercise, at least 52 hours conducted over an average of about six months, improved the brain’s processing speed.
Gomes-Osman J, Cabral DF, Morris TP, et al. Exercise for cognitive brain health in aging. Neurology. 2018 May 30 [Epub ahead of print].
Blood Biomarkers Detect Subconcussive Head Trauma
Blood biomarkers can detect the neurologic injury associated with repetitive subconcussive head trauma, according to a study published online ahead of print May 29 in the Journal of Neurosurgery. A total of 35 National Collegiate Athletic Association football players underwent blood sampling throughout the 2016 football season. Samples were analyzed for plasma concentrations of tau and serum concentrations of neurofilament light. Athletes were categorized as starters or nonstarters, and the investigators assessed between-group differences and time-course differences. In nonstarters, plasma concentrations of tau decreased over the season. Starters had lower plasma concentrations of tau. Plasma concentrations of tau could not be used to distinguish between starters and nonstarters. Serum concentrations of neurofilament light increased as head impacts increased, specifically in starters. Serum neurofilament light distinguished starters from nonstarters.
Oliver JM, Anzalone AJ, Stone JD, et al. Fluctuations in blood biomarkers of head trauma in NCAA football athletes over the course of a season. J Neurosurg. 2018 May 29 [Epub ahead of print].
Model Estimates Risk of Alzheimer’s Disease Dementia
Most people with preclinical Alzheimer’s disease will not develop dementia during their lifetimes, according to a study published online ahead of print May 7 in Alzheimer’s & Dementia. Researchers used a multistate model for Alzheimer’s disease along with US death rates to estimate lifetime and 10-year risks of Alzheimer’s disease dementia. Lifetime risks of Alzheimer’s disease dementia vary by age, gender, and preclinical or clinical disease state. A 70-year-old male with amyloid but no signs of neurodegeneration and no memory loss has a lifetime risk of 19.9%. The lifetime risks for a female with amyloidosis are 8.4% at age 90 and 29.3% at age 65. People younger than 85 with mild cognitive impairment, amyloidosis, and neurodegeneration have lifetime risks of Alzheimer’s disease dementia greater than 50%.
Brookmeyer R, Abdalla N. Estimation of lifetime risks of Alzheimer’s disease dementia using biomarkers for preclinical disease. Alzheimers Dement. 2018 May 7 [Epub ahead of print].
Depression Is Associated With Brain and Memory Outcomes
In a sample of mostly Caribbean Hispanic, stroke-free older adults, greater depressive symptoms were associated with worse episodic memory, smaller cerebral volume, and silent infarcts, according to a study published online ahead of print May 9 in Neurology. Researchers analyzed data from the Northern Manhattan Study. A total of 1,111 participants underwent baseline evaluations of depressive symptoms, MRI markers, and cognitive function. At baseline, 22% of participants had greater depressive symptoms. Greater depressive symptoms were significantly associated with worse baseline episodic memory in models adjusted for sociodemographics, vascular risk factors, behavioral factors, and antidepressant medications. Furthermore, greater depressive symptoms were associated with smaller cerebral parenchymal fraction and increased odds of subclinical brain infarcts, after adjustment for sociodemographics, behavioral factors, and vascular risk factors.
Al Hazzouri AZ, Caunca MR, Nobrega JC. Greater depressive symptoms, cognition, and markers of brain aging. Neurology. 2018 May 9 [Epub ahead of print].
—Kimberly Williams
Adequate Sleep Associated With Lower Dementia Risk
Short and long daily sleep duration are risk factors for dementia and death in adults age 60 and older, according to a study published online ahead of print June 6 in the Journal of the American Geriatrics Society. In a prospective cohort study, researchers followed 1,517 adults without dementia for 10 years. Self-reported daily sleep durations were grouped into five categories. The association between daily sleep duration and risk of dementia and death was determined using Cox proportional hazards models. During follow-up, 294 participants developed dementia, and 282 died. Age- and sex-adjusted incidence rates of dementia and all-cause mortality were significantly greater in subjects who slept less than 5.0 hours/day or 10.0 or more hours/day than in people who slept from 5.0 to 6.9 hours/day.
Ohara T, Honda T, Hata J, et al. Association between daily sleep duration and risk of dementia and mortality in a Japanese community. J Am Geriatr Soc. 2018 Jun 6 [Epub ahead of print].
Rivaroxaban Not Superior to Aspirin for Stroke Prevention
Rivaroxaban is not superior to aspirin in the prevention of recurrent stroke, according to a study published June 7 in the New England Journal of Medicine. Researchers compared the efficacy and safety of rivaroxaban at a daily dose of 15 mg with aspirin at a daily dose of 100 mg for the prevention of recurrent stroke in patients with recent ischemic stroke that was presumed to be from cerebral embolism. The primary outcome was the first recurrence of ischemic or hemorrhagic stroke or systemic embolism in a time-to-event analysis. At 459 sites, 3,609 patients were randomly assigned to receive rivaroxaban, and 3,604 were randomized to aspirin. Recurrent ischemic stroke occurred in 172 patients in the rivaroxaban group and in 160 in the aspirin group.
Hart RG, Sharma M, Mundl H, et al. Rivaroxaban for stroke prevention after embolic stroke of undetermined source. N Engl J Med. 2018;378(23):2191-2201.
Disintegrating Brain Lesions May Indicate Worsening MS
Atrophied lesion volume may indicate increasing disability in patients with multiple sclerosis (MS), according to a study published online ahead of print June 1 in the Journal of Neuroimaging. A total of 192 patients with clinically isolated syndrome or MS received 3T MRI at baseline and at five years. Investigators quantified lesions at baseline and calculated new and enlarging lesion volumes during the study interval. Atrophied lesion volume was calculated by combining baseline lesion masks with follow-up SIENAX-derived CSF partial volume maps. The researchers evaluated correlations between these measures and disability, as measured by the Expanded Disability Status Scale (EDSS). Atrophied lesion volume was different between MS subtypes and exceeded new lesion volume accumulation in progressive MS. Atrophied lesion volume was the only significant correlate of EDSS change.
Dwyer MG, Bergsland N, Ramasamy DP, et al. Atrophied brain lesion volume: a new imaging biomarker in multiple sclerosis. J Neuroimaging. 2018 Jun 1 [Epub ahead of print].
Do Migraineurs Seek Behavioral Treatment After a Referral?
A significant number of migraineurs are not using effective behavioral treatments for migraine, according to a study published online ahead of print June 5 in Pain Medicine. In a prospective cohort study, researchers tracked 234 patients with migraine who presented to an academic headache center and referred 69 of them for behavioral treatment with an appropriately trained therapist. Fifty-three of the referred patients completed a follow-up interview within three months of their initial appointment and were included in the analysis. Of the patients referred for behavioral treatment, 30 made an appointment. Investigators found no differences between people who started behavioral therapy and people who did not. Study authors did find that people who had previously seen a psychologist for migraine were more likely to initiate therapy.
Minen MT, Azarchi S, Sobolev R, et al. Factors related to migraine patients’ decisions to initiate behavioral migraine treatment following a headache specialist’s recommendation: a prospective observational study. Pain Med. 2018 Jun 5 [Epub ahead of print].
TIA Associated With Increased Five-Year Risk of Stroke
People with transient ischemic attack (TIA) are at risk for a cardiovascular event in the following five years, according to a study published June 7 in the New England Journal of Medicine. Researchers evaluated patients who had had a TIA within seven days before enrollment in a registry of TIA clinics. Of 61 sites, 42 had follow-up data on more than 50% of their enrolled patients at five years. The study’s primary outcome was a composite of stroke, acute coronary syndrome, or death from cardiovascular causes, with an emphasis on events that occurred in the second through fifth years. At five years, stroke had occurred in 345 of the 3,847 patients included in the follow-up study, and 149 of them had a stroke during the second through fifth years of follow-up.
Amarenco P, Lavallée PC, Monteiro Tavares L, et al. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018;378(23):2182-2190.
Follow-Up Care for TBI Is Not Delivered Adequately
Follow-up care for patients with traumatic brain injury (TBI) is not delivered optimally, according to a study published May 25 in JAMA Network Open. In a cohort study, researchers surveyed 831 participants in the Transforming Research and Clinical Knowledge in TBI initiative about their care after hospital discharge. Follow-up care was defined as providing TBI-related educational materials at discharge, calling patients within two weeks after release, seeing a healthcare provider within two weeks, and seeing a healthcare provider within three months. Approximately 42% of participants reported receiving TBI-related educational material at discharge, and 44% reported seeing a physician or other medical practitioner within three months after injury. Of patients with a positive finding on CT, 39% had not seen a medical practitioner at three months after injury.
Seabury SA, Gaudette E, Goldman DP, et al. Assessment of follow-up care after emergency department presentation for mild traumatic brain injury and concussion: results from the TRACK-TBI study. JAMA Network Open. 2018;1(1):e180210.
Researchers Examine Mortality Rate of Pediatric Stroke
In-hospital mortality occurs in 2.6% of children with arterial ischemic stroke, according to a study published in the May issue of Pediatrics. The retrospective study included 915 infants younger than 1 month and 2,273 children age 1 month to 18 years with stroke at 87 hospitals in 24 countries. Death during hospitalization and cause of death were ascertained from medical records. A total of 14 neonates and 70 children died during hospitalization. Of 48 cases with reported causes of death, 31 were stroke-related. Remaining deaths were attributed to medical disease. In multivariable analysis, congenital heart disease, posterior plus anterior circulation stroke, and stroke presentation without seizures were associated with in-hospital mortality for neonates. Hispanic ethnicity, congenital heart disease, and posterior plus anterior circulation stroke were associated with in-hospital mortality for children.
Beslow LA, Dowling MM, Hassanein SMA, et al. Mortality after pediatric arterial ischemic stroke. Pediatrics. 2018;141(5).
FDA Approves zEEG Dry Electrode Headset
The FDA has approved the zEEG dry electrode EEG headset for clinical use. The zEEG headset is backed by a cloud platform that allows users to upload data instantly, provides tools for analysis, and enables remote interpretation by neurologists. A clinical study found that the zEEG headset provided EEG signal quality that was comparable to that of an approved, traditional EEG system. In two study cohorts, a total of 30 patients were studied for time periods of as long as two hours, and the zEEG device performed at least as well as the reference device, based on predefined acceptance criteria. Study results will be published in the coming months. Zeto, headquartered in Santa Clara, California, markets the device.
South Asian Americans Have High Cardiovascular Mortality
South Asians living in the United States have higher mortality from heart conditions caused by atherosclerosis, such as heart attack and stroke, according to a study published online ahead of print May 24 in Circulation. Investigators reviewed the literature relevant to South Asian populations’ demographics and risk factors, health behaviors, and interventions, including physical activity, diet, medications, and community strategies. South Asians have higher proportional mortality rates from atherosclerotic cardiovascular disease, compared with other Asian groups, largely because of the lower risk observed in East Asian populations. A majority of the risk in South Asians can be explained by the increased prevalence of known risk factors, especially factors related to insulin resistance. The authors found no unique risk factors in this population.
Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018 May 24 [Epub ahead of print].
How Much Exercise Improves Cognition in Older Adults?
Exercising for at least 52 hours over six months is associated with improved cognitive performance in older adults with and without cognitive impairment, according to a study published online ahead of print May 30 in Neurology. Researchers reviewed data for 98 randomized, controlled exercise trials including 11,061 participants with an average age of 73. About 59% of the participants were healthy adults, 26% had mild cognitive impairment, and 15% had dementia. Researchers collected data on exercise session length, intensity, weekly frequency, and amount of exercise over time. Aerobic exercise was the most common form of exercise. In healthy people and people with cognitive impairment, longer term exposure to exercise, at least 52 hours conducted over an average of about six months, improved the brain’s processing speed.
Gomes-Osman J, Cabral DF, Morris TP, et al. Exercise for cognitive brain health in aging. Neurology. 2018 May 30 [Epub ahead of print].
Blood Biomarkers Detect Subconcussive Head Trauma
Blood biomarkers can detect the neurologic injury associated with repetitive subconcussive head trauma, according to a study published online ahead of print May 29 in the Journal of Neurosurgery. A total of 35 National Collegiate Athletic Association football players underwent blood sampling throughout the 2016 football season. Samples were analyzed for plasma concentrations of tau and serum concentrations of neurofilament light. Athletes were categorized as starters or nonstarters, and the investigators assessed between-group differences and time-course differences. In nonstarters, plasma concentrations of tau decreased over the season. Starters had lower plasma concentrations of tau. Plasma concentrations of tau could not be used to distinguish between starters and nonstarters. Serum concentrations of neurofilament light increased as head impacts increased, specifically in starters. Serum neurofilament light distinguished starters from nonstarters.
Oliver JM, Anzalone AJ, Stone JD, et al. Fluctuations in blood biomarkers of head trauma in NCAA football athletes over the course of a season. J Neurosurg. 2018 May 29 [Epub ahead of print].
Model Estimates Risk of Alzheimer’s Disease Dementia
Most people with preclinical Alzheimer’s disease will not develop dementia during their lifetimes, according to a study published online ahead of print May 7 in Alzheimer’s & Dementia. Researchers used a multistate model for Alzheimer’s disease along with US death rates to estimate lifetime and 10-year risks of Alzheimer’s disease dementia. Lifetime risks of Alzheimer’s disease dementia vary by age, gender, and preclinical or clinical disease state. A 70-year-old male with amyloid but no signs of neurodegeneration and no memory loss has a lifetime risk of 19.9%. The lifetime risks for a female with amyloidosis are 8.4% at age 90 and 29.3% at age 65. People younger than 85 with mild cognitive impairment, amyloidosis, and neurodegeneration have lifetime risks of Alzheimer’s disease dementia greater than 50%.
Brookmeyer R, Abdalla N. Estimation of lifetime risks of Alzheimer’s disease dementia using biomarkers for preclinical disease. Alzheimers Dement. 2018 May 7 [Epub ahead of print].
Depression Is Associated With Brain and Memory Outcomes
In a sample of mostly Caribbean Hispanic, stroke-free older adults, greater depressive symptoms were associated with worse episodic memory, smaller cerebral volume, and silent infarcts, according to a study published online ahead of print May 9 in Neurology. Researchers analyzed data from the Northern Manhattan Study. A total of 1,111 participants underwent baseline evaluations of depressive symptoms, MRI markers, and cognitive function. At baseline, 22% of participants had greater depressive symptoms. Greater depressive symptoms were significantly associated with worse baseline episodic memory in models adjusted for sociodemographics, vascular risk factors, behavioral factors, and antidepressant medications. Furthermore, greater depressive symptoms were associated with smaller cerebral parenchymal fraction and increased odds of subclinical brain infarcts, after adjustment for sociodemographics, behavioral factors, and vascular risk factors.
Al Hazzouri AZ, Caunca MR, Nobrega JC. Greater depressive symptoms, cognition, and markers of brain aging. Neurology. 2018 May 9 [Epub ahead of print].
—Kimberly Williams