User login
Autism Spectrum Disorders Are on the Rise
The estimated prevalence of autism spectrum disorder (ASD) is higher than previously recorded, according to the Autism and Developmental Disabilities Monitoring (ADDM) Network. Between 2000- 2014, the prevalence increased from 6.7 to 16.8 per 1,000 children, a jump of about 150%.
Autism and Developmental Disabilities Monitoring is a surveillance system that estimates the prevalence of autism spectrum disorder among children aged 8 years who live within 11 sites (Arizona, Arkansas, Colorado, Georgia, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Tennessee, and Wisconsin). Autism and Developmental Disabilities Monitoring does not depend on family or practitioner reporting to determine ASD case status. Instead, staff conduct surveillance in a 2-phase process: reviewing children’s evaluation records from data sources in the community (including “developmental assessments completed by a wide range of health and education providers”), and compiling them into a comprehensive record that is then reviewed by ≤ 1 experienced clinicians.
Certain characteristics remained similar in 2014 compared with earlier surveillance years, ADDM researchers say. For instance, the median age of earliest known ASD diagnosis was 52 months in 2014, compared with close to 53 months in previous years.
However, male-to-female prevalence changed slightly, from 4.5:1 to 4:1, driven by a greater relative increase in ASD prevalence among girls since 2012. Autism and Developmental Disabilities Monitoring also points to a trend that begun in 2002 of a decrease in the ratios of white to black children and white to Hispanic children. Historically, ADDM researchers say, estimates have been 20% to 30% higher among white children compared with black children and 50% to 70% higher compared with Hispanic children. In 2014, those numbers dropped to 7% (the lowest difference ever observed by ADDM) and 22%, respectively.
Implementation of the new DSM-5 case definition had little effect on the overall number of children identified with ASD in 2014, ADDM researchers say.
The estimated prevalence of autism spectrum disorder (ASD) is higher than previously recorded, according to the Autism and Developmental Disabilities Monitoring (ADDM) Network. Between 2000- 2014, the prevalence increased from 6.7 to 16.8 per 1,000 children, a jump of about 150%.
Autism and Developmental Disabilities Monitoring is a surveillance system that estimates the prevalence of autism spectrum disorder among children aged 8 years who live within 11 sites (Arizona, Arkansas, Colorado, Georgia, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Tennessee, and Wisconsin). Autism and Developmental Disabilities Monitoring does not depend on family or practitioner reporting to determine ASD case status. Instead, staff conduct surveillance in a 2-phase process: reviewing children’s evaluation records from data sources in the community (including “developmental assessments completed by a wide range of health and education providers”), and compiling them into a comprehensive record that is then reviewed by ≤ 1 experienced clinicians.
Certain characteristics remained similar in 2014 compared with earlier surveillance years, ADDM researchers say. For instance, the median age of earliest known ASD diagnosis was 52 months in 2014, compared with close to 53 months in previous years.
However, male-to-female prevalence changed slightly, from 4.5:1 to 4:1, driven by a greater relative increase in ASD prevalence among girls since 2012. Autism and Developmental Disabilities Monitoring also points to a trend that begun in 2002 of a decrease in the ratios of white to black children and white to Hispanic children. Historically, ADDM researchers say, estimates have been 20% to 30% higher among white children compared with black children and 50% to 70% higher compared with Hispanic children. In 2014, those numbers dropped to 7% (the lowest difference ever observed by ADDM) and 22%, respectively.
Implementation of the new DSM-5 case definition had little effect on the overall number of children identified with ASD in 2014, ADDM researchers say.
The estimated prevalence of autism spectrum disorder (ASD) is higher than previously recorded, according to the Autism and Developmental Disabilities Monitoring (ADDM) Network. Between 2000- 2014, the prevalence increased from 6.7 to 16.8 per 1,000 children, a jump of about 150%.
Autism and Developmental Disabilities Monitoring is a surveillance system that estimates the prevalence of autism spectrum disorder among children aged 8 years who live within 11 sites (Arizona, Arkansas, Colorado, Georgia, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Tennessee, and Wisconsin). Autism and Developmental Disabilities Monitoring does not depend on family or practitioner reporting to determine ASD case status. Instead, staff conduct surveillance in a 2-phase process: reviewing children’s evaluation records from data sources in the community (including “developmental assessments completed by a wide range of health and education providers”), and compiling them into a comprehensive record that is then reviewed by ≤ 1 experienced clinicians.
Certain characteristics remained similar in 2014 compared with earlier surveillance years, ADDM researchers say. For instance, the median age of earliest known ASD diagnosis was 52 months in 2014, compared with close to 53 months in previous years.
However, male-to-female prevalence changed slightly, from 4.5:1 to 4:1, driven by a greater relative increase in ASD prevalence among girls since 2012. Autism and Developmental Disabilities Monitoring also points to a trend that begun in 2002 of a decrease in the ratios of white to black children and white to Hispanic children. Historically, ADDM researchers say, estimates have been 20% to 30% higher among white children compared with black children and 50% to 70% higher compared with Hispanic children. In 2014, those numbers dropped to 7% (the lowest difference ever observed by ADDM) and 22%, respectively.
Implementation of the new DSM-5 case definition had little effect on the overall number of children identified with ASD in 2014, ADDM researchers say.
VA Care Matches—or Bests—Non-VA Care
Researchers from RAND Corp. compared performance between each VA facility and 3 corresponding non-VA settings with similar geographic settings, size, and complexity of care, using recent data on patient safety, mortality and readmission, inpatient and outpatient effectiveness, and patient-centered care.
VA hospitals performed on average the same as or significantly better than the non-VA hospitals on all 6 measures of inpatient safety, all 3 inpatient mortality measures, and 12 inpatient effectiveness measures. VA facilities also performed significantly better than commercial HMOs and Medicaid HMOs for all 16 outpatient effectiveness measures. Compared with Medicare HMOs, the VA did significantly better on 14 measures and did not differ on 2.
However, the VA performance was worse than the non-VA hospitals on 3 readmission measures and 2 effectiveness measures. For example, VA inpatient performance was significantly lower on the patient experience measure for pain management.
The researchers saw “high variation” across VA facilities in performance on some quality measures, although they note that variation was even greater among non-VA hospitals. “The variation among VA health facilities shows that veterans in some areas are not receiving the same high-quality care that other VA facilities are able to provide,” said Carrie Farmer, a co-author of the study.
Researchers from RAND Corp. compared performance between each VA facility and 3 corresponding non-VA settings with similar geographic settings, size, and complexity of care, using recent data on patient safety, mortality and readmission, inpatient and outpatient effectiveness, and patient-centered care.
VA hospitals performed on average the same as or significantly better than the non-VA hospitals on all 6 measures of inpatient safety, all 3 inpatient mortality measures, and 12 inpatient effectiveness measures. VA facilities also performed significantly better than commercial HMOs and Medicaid HMOs for all 16 outpatient effectiveness measures. Compared with Medicare HMOs, the VA did significantly better on 14 measures and did not differ on 2.
However, the VA performance was worse than the non-VA hospitals on 3 readmission measures and 2 effectiveness measures. For example, VA inpatient performance was significantly lower on the patient experience measure for pain management.
The researchers saw “high variation” across VA facilities in performance on some quality measures, although they note that variation was even greater among non-VA hospitals. “The variation among VA health facilities shows that veterans in some areas are not receiving the same high-quality care that other VA facilities are able to provide,” said Carrie Farmer, a co-author of the study.
Researchers from RAND Corp. compared performance between each VA facility and 3 corresponding non-VA settings with similar geographic settings, size, and complexity of care, using recent data on patient safety, mortality and readmission, inpatient and outpatient effectiveness, and patient-centered care.
VA hospitals performed on average the same as or significantly better than the non-VA hospitals on all 6 measures of inpatient safety, all 3 inpatient mortality measures, and 12 inpatient effectiveness measures. VA facilities also performed significantly better than commercial HMOs and Medicaid HMOs for all 16 outpatient effectiveness measures. Compared with Medicare HMOs, the VA did significantly better on 14 measures and did not differ on 2.
However, the VA performance was worse than the non-VA hospitals on 3 readmission measures and 2 effectiveness measures. For example, VA inpatient performance was significantly lower on the patient experience measure for pain management.
The researchers saw “high variation” across VA facilities in performance on some quality measures, although they note that variation was even greater among non-VA hospitals. “The variation among VA health facilities shows that veterans in some areas are not receiving the same high-quality care that other VA facilities are able to provide,” said Carrie Farmer, a co-author of the study.
Umbralisib can revitalize ruxolitinib in MF
STOCKHOLM—The PI3K delta inhibitor umbralisib can “augment or resurrect” responses to ruxolitinib in patients with myelofibrosis (MF), according to a speaker at the 23rd Congress of the European Hematology Association (EHA).
Results of a phase 1 study showed that adding umbralisib to treatment with ruxolitinib could induce responses in MF patients who had a suboptimal or lost response to ruxolitinib.
Of the 23 patients who received the combination, 2 achieved a complete remission (CR), 11 had clinical improvement, and 8 had stable disease.
In addition, umbralisib plus ruxolitinib was considered well-tolerated. The most common adverse event (AE) was anemia.
Tamara K. Moyo, MD, PhD, of Vanderbilt University Medical Center in Nashville, Tennessee, presented these results at the EHA Congress as abstract S133. The research was sponsored by TG Therapeutics.
Patients
Dr Moyo reported results in 23 MF patients who had a suboptimal response, lost a response, or had no response while on a stable dose of ruxolitinib for at least 8 weeks. Their median age was 67 (range, 49-83), and 61% were male.
Patients had primary MF (30%), post-essential thrombocythemia (ET) MF (43%), or post-polycythemia vera (PV) MF (26%). Forty-three percent of patients had JAK2 V617F, 30% had CALR mutations, 17% had MPL mutations, and 13% were triple-negative. One patient had co-occurring CALR and MPL mutations.
Most patients had an ECOG performance score of 0 (39%) or 1 (52%). All had intermediate-1 (35%), intermediate-2 (35%), or high-risk disease (30%) according to DIPSS Plus.
Sixty-one percent of patients had splenomegaly.
Treatment
In stage 1, the patients received stable ruxolitinib and escalating umbralisib. In stage 2, patients received escalating ruxolitinib and umbralisib at the maximum tolerated dose (MTD) established from stage 1.
Patients could then proceed to expansion cohorts in which they would receive any dose of ruxolitinib and umbralisib at the MTD. The expansion cohorts include patients with treatment-naïve MF, PV, chronic myelomonocytic leukemia, and myelodysplastic syndromes/myeloproliferative neoplasms.
However, Dr Moyo reported only on the 23 ruxolitinib-experienced MF patients.
Safety
There were 2 dose-limiting toxicities of asymptomatic, grade 3 amylase/lipase elevations. One occurred in a patient receiving 800 mg of umbralisib daily and 10 mg of ruxolitinib twice daily. The other occurred in a patient receiving 800 mg of umbralisib daily and 15 mg of ruxolitinib twice daily.
Therefore, 600 mg daily was deemed the MTD of umbralisib.
Seventeen patients had at least 1 AE. There were 17 grade 3 or higher AEs in 13 patients.
AEs of any grade included anemia (n=10), neutrophil decrease (n=2), platelet decrease (n=5), AST increase (n=6), ALT increase (n=3), amylase increase (n=3), lipase increase (n=3), diarrhea (n=2), colitis (n=1), dyspnea (n=1), upper respiratory infection (n=2), pneumonia (n=4), other infections (n=6), and sepsis (n=1).
Grade 3 AEs included anemia (n=3), neutrophil decrease (n=2), amylase increase (n=2), lipase increase (n=2), diarrhea (n=2), colitis (n=1), dyspnea (n=1), pneumonia (n=1), and other infections (n=2). The case of sepsis was the only grade 4 AE.
Dr Moyo noted that anemia—the most common AE—was commonly attributed to disease rather than study treatment.
The case of colitis, which was grade 3, was deemed possibly related to treatment, so the patient was removed from the study.
Thirteen patients had discontinued study treatment at the time of analysis. Aside from the patient who discontinued due to colitis, 2 patients went off study due to dose-limiting toxicities, 3 due to progressive disease, 6 due to physician or patient decision, and 1 due to transplant.
Efficacy
Two patients could not be assessed for efficacy, and 8 had stable disease on umbralisib and ruxolitinib.
The combination produced clinical improvement—reduction in spleen volume, increase in hemoglobin, and improvement in MF-related symptoms—in 11 patients (48%).
And 2 patients (9%) achieved a CR. Dr Moyo said there were “few commonalities” between these 2 patients.
Both had intermediate-1-risk disease as well as persistent or progressive MF-related symptoms and thrombocytosis at baseline. However, 1 patient had post-ET MF, and 1 had post-PV MF.
The post-ET MF patient had an MPL driver mutation. She received ruxolitinib at 20 mg twice daily and umbralisib at 400 mg daily. The patient achieved a CR at cycle 15 and remained on study 2 years before proceeding to transplant. The patient is now about 1 year from her transplant with no evidence of disease.
The post-PV patient had a JAK2 V617F driver mutation. She received ruxolitinib at 15 mg twice daily and umbralisib at 600 mg daily. The patient achieved a CR at cycle 5 and remains on study, currently receiving cycle 12 of treatment.
Dr Moyo said these results suggest “the addition of umbralisib to ruxolitinib can augment or resurrect a response in MF patients who have had suboptimal or lost response to ruxolitinib alone, and this treatment combination warrants further investigation.”
STOCKHOLM—The PI3K delta inhibitor umbralisib can “augment or resurrect” responses to ruxolitinib in patients with myelofibrosis (MF), according to a speaker at the 23rd Congress of the European Hematology Association (EHA).
Results of a phase 1 study showed that adding umbralisib to treatment with ruxolitinib could induce responses in MF patients who had a suboptimal or lost response to ruxolitinib.
Of the 23 patients who received the combination, 2 achieved a complete remission (CR), 11 had clinical improvement, and 8 had stable disease.
In addition, umbralisib plus ruxolitinib was considered well-tolerated. The most common adverse event (AE) was anemia.
Tamara K. Moyo, MD, PhD, of Vanderbilt University Medical Center in Nashville, Tennessee, presented these results at the EHA Congress as abstract S133. The research was sponsored by TG Therapeutics.
Patients
Dr Moyo reported results in 23 MF patients who had a suboptimal response, lost a response, or had no response while on a stable dose of ruxolitinib for at least 8 weeks. Their median age was 67 (range, 49-83), and 61% were male.
Patients had primary MF (30%), post-essential thrombocythemia (ET) MF (43%), or post-polycythemia vera (PV) MF (26%). Forty-three percent of patients had JAK2 V617F, 30% had CALR mutations, 17% had MPL mutations, and 13% were triple-negative. One patient had co-occurring CALR and MPL mutations.
Most patients had an ECOG performance score of 0 (39%) or 1 (52%). All had intermediate-1 (35%), intermediate-2 (35%), or high-risk disease (30%) according to DIPSS Plus.
Sixty-one percent of patients had splenomegaly.
Treatment
In stage 1, the patients received stable ruxolitinib and escalating umbralisib. In stage 2, patients received escalating ruxolitinib and umbralisib at the maximum tolerated dose (MTD) established from stage 1.
Patients could then proceed to expansion cohorts in which they would receive any dose of ruxolitinib and umbralisib at the MTD. The expansion cohorts include patients with treatment-naïve MF, PV, chronic myelomonocytic leukemia, and myelodysplastic syndromes/myeloproliferative neoplasms.
However, Dr Moyo reported only on the 23 ruxolitinib-experienced MF patients.
Safety
There were 2 dose-limiting toxicities of asymptomatic, grade 3 amylase/lipase elevations. One occurred in a patient receiving 800 mg of umbralisib daily and 10 mg of ruxolitinib twice daily. The other occurred in a patient receiving 800 mg of umbralisib daily and 15 mg of ruxolitinib twice daily.
Therefore, 600 mg daily was deemed the MTD of umbralisib.
Seventeen patients had at least 1 AE. There were 17 grade 3 or higher AEs in 13 patients.
AEs of any grade included anemia (n=10), neutrophil decrease (n=2), platelet decrease (n=5), AST increase (n=6), ALT increase (n=3), amylase increase (n=3), lipase increase (n=3), diarrhea (n=2), colitis (n=1), dyspnea (n=1), upper respiratory infection (n=2), pneumonia (n=4), other infections (n=6), and sepsis (n=1).
Grade 3 AEs included anemia (n=3), neutrophil decrease (n=2), amylase increase (n=2), lipase increase (n=2), diarrhea (n=2), colitis (n=1), dyspnea (n=1), pneumonia (n=1), and other infections (n=2). The case of sepsis was the only grade 4 AE.
Dr Moyo noted that anemia—the most common AE—was commonly attributed to disease rather than study treatment.
The case of colitis, which was grade 3, was deemed possibly related to treatment, so the patient was removed from the study.
Thirteen patients had discontinued study treatment at the time of analysis. Aside from the patient who discontinued due to colitis, 2 patients went off study due to dose-limiting toxicities, 3 due to progressive disease, 6 due to physician or patient decision, and 1 due to transplant.
Efficacy
Two patients could not be assessed for efficacy, and 8 had stable disease on umbralisib and ruxolitinib.
The combination produced clinical improvement—reduction in spleen volume, increase in hemoglobin, and improvement in MF-related symptoms—in 11 patients (48%).
And 2 patients (9%) achieved a CR. Dr Moyo said there were “few commonalities” between these 2 patients.
Both had intermediate-1-risk disease as well as persistent or progressive MF-related symptoms and thrombocytosis at baseline. However, 1 patient had post-ET MF, and 1 had post-PV MF.
The post-ET MF patient had an MPL driver mutation. She received ruxolitinib at 20 mg twice daily and umbralisib at 400 mg daily. The patient achieved a CR at cycle 15 and remained on study 2 years before proceeding to transplant. The patient is now about 1 year from her transplant with no evidence of disease.
The post-PV patient had a JAK2 V617F driver mutation. She received ruxolitinib at 15 mg twice daily and umbralisib at 600 mg daily. The patient achieved a CR at cycle 5 and remains on study, currently receiving cycle 12 of treatment.
Dr Moyo said these results suggest “the addition of umbralisib to ruxolitinib can augment or resurrect a response in MF patients who have had suboptimal or lost response to ruxolitinib alone, and this treatment combination warrants further investigation.”
STOCKHOLM—The PI3K delta inhibitor umbralisib can “augment or resurrect” responses to ruxolitinib in patients with myelofibrosis (MF), according to a speaker at the 23rd Congress of the European Hematology Association (EHA).
Results of a phase 1 study showed that adding umbralisib to treatment with ruxolitinib could induce responses in MF patients who had a suboptimal or lost response to ruxolitinib.
Of the 23 patients who received the combination, 2 achieved a complete remission (CR), 11 had clinical improvement, and 8 had stable disease.
In addition, umbralisib plus ruxolitinib was considered well-tolerated. The most common adverse event (AE) was anemia.
Tamara K. Moyo, MD, PhD, of Vanderbilt University Medical Center in Nashville, Tennessee, presented these results at the EHA Congress as abstract S133. The research was sponsored by TG Therapeutics.
Patients
Dr Moyo reported results in 23 MF patients who had a suboptimal response, lost a response, or had no response while on a stable dose of ruxolitinib for at least 8 weeks. Their median age was 67 (range, 49-83), and 61% were male.
Patients had primary MF (30%), post-essential thrombocythemia (ET) MF (43%), or post-polycythemia vera (PV) MF (26%). Forty-three percent of patients had JAK2 V617F, 30% had CALR mutations, 17% had MPL mutations, and 13% were triple-negative. One patient had co-occurring CALR and MPL mutations.
Most patients had an ECOG performance score of 0 (39%) or 1 (52%). All had intermediate-1 (35%), intermediate-2 (35%), or high-risk disease (30%) according to DIPSS Plus.
Sixty-one percent of patients had splenomegaly.
Treatment
In stage 1, the patients received stable ruxolitinib and escalating umbralisib. In stage 2, patients received escalating ruxolitinib and umbralisib at the maximum tolerated dose (MTD) established from stage 1.
Patients could then proceed to expansion cohorts in which they would receive any dose of ruxolitinib and umbralisib at the MTD. The expansion cohorts include patients with treatment-naïve MF, PV, chronic myelomonocytic leukemia, and myelodysplastic syndromes/myeloproliferative neoplasms.
However, Dr Moyo reported only on the 23 ruxolitinib-experienced MF patients.
Safety
There were 2 dose-limiting toxicities of asymptomatic, grade 3 amylase/lipase elevations. One occurred in a patient receiving 800 mg of umbralisib daily and 10 mg of ruxolitinib twice daily. The other occurred in a patient receiving 800 mg of umbralisib daily and 15 mg of ruxolitinib twice daily.
Therefore, 600 mg daily was deemed the MTD of umbralisib.
Seventeen patients had at least 1 AE. There were 17 grade 3 or higher AEs in 13 patients.
AEs of any grade included anemia (n=10), neutrophil decrease (n=2), platelet decrease (n=5), AST increase (n=6), ALT increase (n=3), amylase increase (n=3), lipase increase (n=3), diarrhea (n=2), colitis (n=1), dyspnea (n=1), upper respiratory infection (n=2), pneumonia (n=4), other infections (n=6), and sepsis (n=1).
Grade 3 AEs included anemia (n=3), neutrophil decrease (n=2), amylase increase (n=2), lipase increase (n=2), diarrhea (n=2), colitis (n=1), dyspnea (n=1), pneumonia (n=1), and other infections (n=2). The case of sepsis was the only grade 4 AE.
Dr Moyo noted that anemia—the most common AE—was commonly attributed to disease rather than study treatment.
The case of colitis, which was grade 3, was deemed possibly related to treatment, so the patient was removed from the study.
Thirteen patients had discontinued study treatment at the time of analysis. Aside from the patient who discontinued due to colitis, 2 patients went off study due to dose-limiting toxicities, 3 due to progressive disease, 6 due to physician or patient decision, and 1 due to transplant.
Efficacy
Two patients could not be assessed for efficacy, and 8 had stable disease on umbralisib and ruxolitinib.
The combination produced clinical improvement—reduction in spleen volume, increase in hemoglobin, and improvement in MF-related symptoms—in 11 patients (48%).
And 2 patients (9%) achieved a CR. Dr Moyo said there were “few commonalities” between these 2 patients.
Both had intermediate-1-risk disease as well as persistent or progressive MF-related symptoms and thrombocytosis at baseline. However, 1 patient had post-ET MF, and 1 had post-PV MF.
The post-ET MF patient had an MPL driver mutation. She received ruxolitinib at 20 mg twice daily and umbralisib at 400 mg daily. The patient achieved a CR at cycle 15 and remained on study 2 years before proceeding to transplant. The patient is now about 1 year from her transplant with no evidence of disease.
The post-PV patient had a JAK2 V617F driver mutation. She received ruxolitinib at 15 mg twice daily and umbralisib at 600 mg daily. The patient achieved a CR at cycle 5 and remains on study, currently receiving cycle 12 of treatment.
Dr Moyo said these results suggest “the addition of umbralisib to ruxolitinib can augment or resurrect a response in MF patients who have had suboptimal or lost response to ruxolitinib alone, and this treatment combination warrants further investigation.”
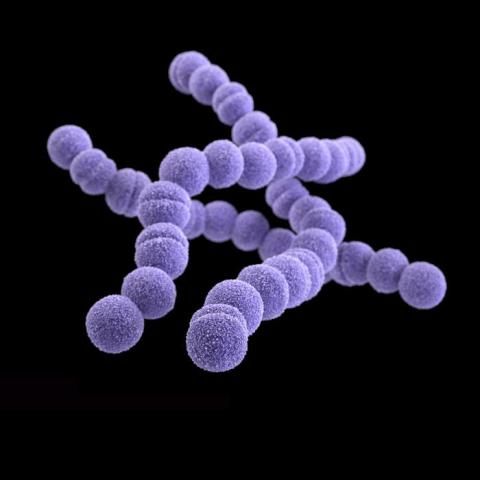
Quality improvement initiative reduced unnecessary GAS pharyngitis testing, report says
Unnecessary testing for group A streptococcal (GAS) pharyngitis was less common in one ambulatory pediatrics practice after a collaborative interprofessional quality improvement (QI) initiative, results of a study found.
The average monthly frequency of unnecessary testing in that practice fell from 64% before the intervention to 41% afterward. Although the initiative did not appear to improve appropriate antibiotic use for GAS pharyngitis, most of the providers (88%) perceived an improvement in their ability to communicate with families about appropriate antibiotic use and the need for testing, Laura E. Norton, MD, of the University of Minnesota, Minneapolis, and her associates wrote.
The QI project was implemented at a pediatrics practice with two locations in Kansas City, Mo., with 12 board-certified pediatricians, 19 nurses, and 4 certified nurse practitioners who provide care for more than 40,000 children annually. Interventions that were part of this project included education for providers, patients, and families; office procedure modifications;and discussions with providers about communicating with families, along with periodic feedback to providers on improvement in outcomes measures.
Dr. Norton and her colleagues defined unnecessary GAS pharyngitis testing as testing in a patient with two or more viral symptoms (conjunctivitis, coryza, cough, diarrhea, hoarse voice, and viral exanthema), aged less than 3 years with no documentation of a household contact with GAS pharyngitis, absence of sore throat, or absence of examination findings expected in GAS pharyngitis cases.
The investigators illustrated a reduction in frequency of unnecessary testing from the monthly average of 64% to 41% using a P-chart, a type of graph used in statistical quality control to illustrate the proportion of defective or nonconforming values. They reported a significant reduction in unnecessary testing in children younger than 3 years from the pre- to postintervention period (P = .017).
Dr. Norton and her coauthors said they were aiming for a larger magnitude of improvement, which may have been in part because of cognitive bias. “Some providers reported fear of complications that could result from missed GAS pharyngitis diagnosis as a driver of their decision to perform GAS pharyngitis testing.”
There was no significant improvement in appropriate use of antibiotics for GAS pharyngitis from pre- to postintervention period, which Dr. Norton and her associates said points to a need for further research in other pediatric practices. “Adherence to guideline-based, first-line antibiotic selection was higher in this practice than reported in published national data, leaving little room for improvement.”
Dr. Norton and her coauthors had no relevant financial disclosures.
SOURCE: Norton LE, et al. Pediatrics. 2018;142(1):e20172033.
Unnecessary testing for group A streptococcal (GAS) pharyngitis was less common in one ambulatory pediatrics practice after a collaborative interprofessional quality improvement (QI) initiative, results of a study found.
The average monthly frequency of unnecessary testing in that practice fell from 64% before the intervention to 41% afterward. Although the initiative did not appear to improve appropriate antibiotic use for GAS pharyngitis, most of the providers (88%) perceived an improvement in their ability to communicate with families about appropriate antibiotic use and the need for testing, Laura E. Norton, MD, of the University of Minnesota, Minneapolis, and her associates wrote.
The QI project was implemented at a pediatrics practice with two locations in Kansas City, Mo., with 12 board-certified pediatricians, 19 nurses, and 4 certified nurse practitioners who provide care for more than 40,000 children annually. Interventions that were part of this project included education for providers, patients, and families; office procedure modifications;and discussions with providers about communicating with families, along with periodic feedback to providers on improvement in outcomes measures.
Dr. Norton and her colleagues defined unnecessary GAS pharyngitis testing as testing in a patient with two or more viral symptoms (conjunctivitis, coryza, cough, diarrhea, hoarse voice, and viral exanthema), aged less than 3 years with no documentation of a household contact with GAS pharyngitis, absence of sore throat, or absence of examination findings expected in GAS pharyngitis cases.
The investigators illustrated a reduction in frequency of unnecessary testing from the monthly average of 64% to 41% using a P-chart, a type of graph used in statistical quality control to illustrate the proportion of defective or nonconforming values. They reported a significant reduction in unnecessary testing in children younger than 3 years from the pre- to postintervention period (P = .017).
Dr. Norton and her coauthors said they were aiming for a larger magnitude of improvement, which may have been in part because of cognitive bias. “Some providers reported fear of complications that could result from missed GAS pharyngitis diagnosis as a driver of their decision to perform GAS pharyngitis testing.”
There was no significant improvement in appropriate use of antibiotics for GAS pharyngitis from pre- to postintervention period, which Dr. Norton and her associates said points to a need for further research in other pediatric practices. “Adherence to guideline-based, first-line antibiotic selection was higher in this practice than reported in published national data, leaving little room for improvement.”
Dr. Norton and her coauthors had no relevant financial disclosures.
SOURCE: Norton LE, et al. Pediatrics. 2018;142(1):e20172033.
Unnecessary testing for group A streptococcal (GAS) pharyngitis was less common in one ambulatory pediatrics practice after a collaborative interprofessional quality improvement (QI) initiative, results of a study found.
The average monthly frequency of unnecessary testing in that practice fell from 64% before the intervention to 41% afterward. Although the initiative did not appear to improve appropriate antibiotic use for GAS pharyngitis, most of the providers (88%) perceived an improvement in their ability to communicate with families about appropriate antibiotic use and the need for testing, Laura E. Norton, MD, of the University of Minnesota, Minneapolis, and her associates wrote.
The QI project was implemented at a pediatrics practice with two locations in Kansas City, Mo., with 12 board-certified pediatricians, 19 nurses, and 4 certified nurse practitioners who provide care for more than 40,000 children annually. Interventions that were part of this project included education for providers, patients, and families; office procedure modifications;and discussions with providers about communicating with families, along with periodic feedback to providers on improvement in outcomes measures.
Dr. Norton and her colleagues defined unnecessary GAS pharyngitis testing as testing in a patient with two or more viral symptoms (conjunctivitis, coryza, cough, diarrhea, hoarse voice, and viral exanthema), aged less than 3 years with no documentation of a household contact with GAS pharyngitis, absence of sore throat, or absence of examination findings expected in GAS pharyngitis cases.
The investigators illustrated a reduction in frequency of unnecessary testing from the monthly average of 64% to 41% using a P-chart, a type of graph used in statistical quality control to illustrate the proportion of defective or nonconforming values. They reported a significant reduction in unnecessary testing in children younger than 3 years from the pre- to postintervention period (P = .017).
Dr. Norton and her coauthors said they were aiming for a larger magnitude of improvement, which may have been in part because of cognitive bias. “Some providers reported fear of complications that could result from missed GAS pharyngitis diagnosis as a driver of their decision to perform GAS pharyngitis testing.”
There was no significant improvement in appropriate use of antibiotics for GAS pharyngitis from pre- to postintervention period, which Dr. Norton and her associates said points to a need for further research in other pediatric practices. “Adherence to guideline-based, first-line antibiotic selection was higher in this practice than reported in published national data, leaving little room for improvement.”
Dr. Norton and her coauthors had no relevant financial disclosures.
SOURCE: Norton LE, et al. Pediatrics. 2018;142(1):e20172033.
FROM PEDIATRICS
Key clinical point: An interprofessional collaboration using quality improvement methods may improve adherence to guideline-based GAS pharyngitis testing.
Major finding:
Study details: A quality improvement initiative implemented at one two-location pediatrics practice providing care for more than 40,000 children annually.
Disclosures: The authors had no financial disclosures or potential conflicts of interest.
Source: Norton LE et al. Pediatrics. 2018;142(1):e20172033.
Treat Acute PE With a Team Approach
Current advancements and care of acute pulmonary embolism (PE) patients will be the focus of Wednesday morning’s session, “Treating Acute PE and Developing a Pulmonary Embolism Response Team.”
“PE is a silent killer and its incidence is only increasing,” said session co-moderator Linda Le, MD, an assistant professor of cardiovascular surgery at Houston Methodist Hospital in Texas. “In recent years, there has been more evidence to support a streamlined approach with a collaborative PE response team to not only improve patient outcomes but also to decrease the incidence and long-term morbidity of this disease.”Populations at highest risk for PE include those who have had surgery or trauma, or women around the time of childbirth, said session co-moderator Ellen Dillavou, MD, an associate professor of surgery at Duke University Medical Center in Durham, N.C. “We have a variety of new devices that can treat patients safely and effectively with lower lytic doses and smaller profiles. We are also gaining knowledge regarding the incidence of post-PE pulmonary hypertension. We are figuring out who is at risk and what treatments are needed.”
The session will cover the morbidity of severe PE, practical noninvasive diagnostic imaging techniques, risk stratification, and appropriate treatment options. Two talks will address how to develop a PE response team (PERT) collaboration and go over the role of the PERT in massive and submassive PE. These teams – a cooperation of multiple specialties that can include cardiologists, intensivists, vascular surgeons, cardiac surgeons, ER physicians, pulmonologists, and interventional radiologists – are becoming more common in large academic centers and some community hospitals. “The goals of a PERT team are to respond rapidly when a diagnosis of massive or submassive PE is made, as well as to individualize and coordinate care for these complex patients,” Dr. Le said. “A fundamental component of the team is the collaboration of multiple specialties in which all experts involved have the same goals in mind – to improve patient outcomes.”
PERT teams are effective and a good way to establish intra-institutional collaboration, Dr. Dillavou said. When creating a PERT, she said, “It is really important to see what people are qualified and enthusiastic in your area. All politics are local, so partnering with other specialists is key. I like to start these projects by coming in with an outline and plans, but then inviting others to contribute so everyone feels they have a voice and so the best practices can be derived.”
“These presentations will give current PERT users up-to-the-minute information that attendees can take back to their home institutions to make sure best practices are being used,” said Dr. Dillavou. “For those starting out, there will be a lot of practical advice. The lecturers also will be available for questions and tips.”
Wednesday
10:15 a.m.-1:15 p.m.
HCC, Room 304
P4: Treating Acute PE and Developing a Pulmonary Embolism Response Team (PERT)
Current advancements and care of acute pulmonary embolism (PE) patients will be the focus of Wednesday morning’s session, “Treating Acute PE and Developing a Pulmonary Embolism Response Team.”
“PE is a silent killer and its incidence is only increasing,” said session co-moderator Linda Le, MD, an assistant professor of cardiovascular surgery at Houston Methodist Hospital in Texas. “In recent years, there has been more evidence to support a streamlined approach with a collaborative PE response team to not only improve patient outcomes but also to decrease the incidence and long-term morbidity of this disease.”Populations at highest risk for PE include those who have had surgery or trauma, or women around the time of childbirth, said session co-moderator Ellen Dillavou, MD, an associate professor of surgery at Duke University Medical Center in Durham, N.C. “We have a variety of new devices that can treat patients safely and effectively with lower lytic doses and smaller profiles. We are also gaining knowledge regarding the incidence of post-PE pulmonary hypertension. We are figuring out who is at risk and what treatments are needed.”
The session will cover the morbidity of severe PE, practical noninvasive diagnostic imaging techniques, risk stratification, and appropriate treatment options. Two talks will address how to develop a PE response team (PERT) collaboration and go over the role of the PERT in massive and submassive PE. These teams – a cooperation of multiple specialties that can include cardiologists, intensivists, vascular surgeons, cardiac surgeons, ER physicians, pulmonologists, and interventional radiologists – are becoming more common in large academic centers and some community hospitals. “The goals of a PERT team are to respond rapidly when a diagnosis of massive or submassive PE is made, as well as to individualize and coordinate care for these complex patients,” Dr. Le said. “A fundamental component of the team is the collaboration of multiple specialties in which all experts involved have the same goals in mind – to improve patient outcomes.”
PERT teams are effective and a good way to establish intra-institutional collaboration, Dr. Dillavou said. When creating a PERT, she said, “It is really important to see what people are qualified and enthusiastic in your area. All politics are local, so partnering with other specialists is key. I like to start these projects by coming in with an outline and plans, but then inviting others to contribute so everyone feels they have a voice and so the best practices can be derived.”
“These presentations will give current PERT users up-to-the-minute information that attendees can take back to their home institutions to make sure best practices are being used,” said Dr. Dillavou. “For those starting out, there will be a lot of practical advice. The lecturers also will be available for questions and tips.”
Wednesday
10:15 a.m.-1:15 p.m.
HCC, Room 304
P4: Treating Acute PE and Developing a Pulmonary Embolism Response Team (PERT)
Current advancements and care of acute pulmonary embolism (PE) patients will be the focus of Wednesday morning’s session, “Treating Acute PE and Developing a Pulmonary Embolism Response Team.”
“PE is a silent killer and its incidence is only increasing,” said session co-moderator Linda Le, MD, an assistant professor of cardiovascular surgery at Houston Methodist Hospital in Texas. “In recent years, there has been more evidence to support a streamlined approach with a collaborative PE response team to not only improve patient outcomes but also to decrease the incidence and long-term morbidity of this disease.”Populations at highest risk for PE include those who have had surgery or trauma, or women around the time of childbirth, said session co-moderator Ellen Dillavou, MD, an associate professor of surgery at Duke University Medical Center in Durham, N.C. “We have a variety of new devices that can treat patients safely and effectively with lower lytic doses and smaller profiles. We are also gaining knowledge regarding the incidence of post-PE pulmonary hypertension. We are figuring out who is at risk and what treatments are needed.”
The session will cover the morbidity of severe PE, practical noninvasive diagnostic imaging techniques, risk stratification, and appropriate treatment options. Two talks will address how to develop a PE response team (PERT) collaboration and go over the role of the PERT in massive and submassive PE. These teams – a cooperation of multiple specialties that can include cardiologists, intensivists, vascular surgeons, cardiac surgeons, ER physicians, pulmonologists, and interventional radiologists – are becoming more common in large academic centers and some community hospitals. “The goals of a PERT team are to respond rapidly when a diagnosis of massive or submassive PE is made, as well as to individualize and coordinate care for these complex patients,” Dr. Le said. “A fundamental component of the team is the collaboration of multiple specialties in which all experts involved have the same goals in mind – to improve patient outcomes.”
PERT teams are effective and a good way to establish intra-institutional collaboration, Dr. Dillavou said. When creating a PERT, she said, “It is really important to see what people are qualified and enthusiastic in your area. All politics are local, so partnering with other specialists is key. I like to start these projects by coming in with an outline and plans, but then inviting others to contribute so everyone feels they have a voice and so the best practices can be derived.”
“These presentations will give current PERT users up-to-the-minute information that attendees can take back to their home institutions to make sure best practices are being used,” said Dr. Dillavou. “For those starting out, there will be a lot of practical advice. The lecturers also will be available for questions and tips.”
Wednesday
10:15 a.m.-1:15 p.m.
HCC, Room 304
P4: Treating Acute PE and Developing a Pulmonary Embolism Response Team (PERT)
VESS: Exploring the Surgical Management of Aberrant Subclavian Artery Associated With Aortic Arch Anomalies
Tiziano Tallarita, MD, of the Mayo Clinic, Rochester, Minn., and his colleagues performed a study to examine the surgical management of aberrant subclavian artery (aSCA) associated with aortic arch anomalies at their institution over a 24-year period. “This study represents one of the largest surgical series on aSCA,” according to Dr. Tallarita.
He will present their data on this rare condition at the first of two sessions sponsored by the Vascular and Endovascular Surgery Society (VESS) on Wednesday at the Vascular Annual Meeting. They identified 39 consecutive patients who underwent surgery for aSCA from 1994 to 2017. Clinical presentation, surgical treatment, 30-day morbidity and mortality, and follow-up were assessed.
The median patient age was 46 years and 56% were women. Right aSCA with a left-sided arch was present in 30 patients (77%) with a Kommerell’s diverticulum (KD) in 20, and an aortic aneurysm or dissection in 14. Left aSCA was present in 9 patients (23%), all of whom had a right-sided aortic arch; aortic dissection was present in 6 patients.
Across all patients, one or more symptoms included dysphagia in 25 (65%), dyspnea in 16 (41%), chest pain in 11 (28%), and upper extremity ischemia in 7 (18%). Six of the patients (15%) required emergency surgery, two each for contained rupture and aortic dissection, and one each for rapid aneurysm growth and severe respiratory distress. The aberrant artery was treated by transposition in 23 patients, carotid subclavian bypass in 10 and ascending aorta to subclavian bypass in 6. Two patients with transposition of the left aSCA also had transposition of the vertebral artery. Primary repair of the KD was done in 14 patients, with the distal arch and/or proximal descending thoracic aorta being replaced in 10.
TEVAR was used to exclude the KD in the remaining 6 patients, all of whom had a left sided aortic arch. Nine patients did not need aortic repair.
Dr. Tallarita and colleagues found that one patient died from pulmonary embolism within 30 days of operation (2.6%). “Perioperative morbidity was 18%, with 7 patients developing one or more complications,” added Dr. Tallarita.
Over a median follow-up of 22.5 months (range 0-193), two patients died (5%), neither procedure-or aortic-related. Three-year survival was 84%, and no one needed re-intervention.
“The presence of KD or aortic disease increased the complexity of the repair. Right-sided aortic arch was always associated with KD and frequently with aortic disease,” according to Dr. Tallarita and his colleagues. “Treatment of aSCA with and without associated aortic disease can be accomplished with low morbidity and mortality, and excellent mid-term patency,” they concluded.
Tiziano Tallarita, MD, of the Mayo Clinic, Rochester, Minn., and his colleagues performed a study to examine the surgical management of aberrant subclavian artery (aSCA) associated with aortic arch anomalies at their institution over a 24-year period. “This study represents one of the largest surgical series on aSCA,” according to Dr. Tallarita.
He will present their data on this rare condition at the first of two sessions sponsored by the Vascular and Endovascular Surgery Society (VESS) on Wednesday at the Vascular Annual Meeting. They identified 39 consecutive patients who underwent surgery for aSCA from 1994 to 2017. Clinical presentation, surgical treatment, 30-day morbidity and mortality, and follow-up were assessed.
The median patient age was 46 years and 56% were women. Right aSCA with a left-sided arch was present in 30 patients (77%) with a Kommerell’s diverticulum (KD) in 20, and an aortic aneurysm or dissection in 14. Left aSCA was present in 9 patients (23%), all of whom had a right-sided aortic arch; aortic dissection was present in 6 patients.
Across all patients, one or more symptoms included dysphagia in 25 (65%), dyspnea in 16 (41%), chest pain in 11 (28%), and upper extremity ischemia in 7 (18%). Six of the patients (15%) required emergency surgery, two each for contained rupture and aortic dissection, and one each for rapid aneurysm growth and severe respiratory distress. The aberrant artery was treated by transposition in 23 patients, carotid subclavian bypass in 10 and ascending aorta to subclavian bypass in 6. Two patients with transposition of the left aSCA also had transposition of the vertebral artery. Primary repair of the KD was done in 14 patients, with the distal arch and/or proximal descending thoracic aorta being replaced in 10.
TEVAR was used to exclude the KD in the remaining 6 patients, all of whom had a left sided aortic arch. Nine patients did not need aortic repair.
Dr. Tallarita and colleagues found that one patient died from pulmonary embolism within 30 days of operation (2.6%). “Perioperative morbidity was 18%, with 7 patients developing one or more complications,” added Dr. Tallarita.
Over a median follow-up of 22.5 months (range 0-193), two patients died (5%), neither procedure-or aortic-related. Three-year survival was 84%, and no one needed re-intervention.
“The presence of KD or aortic disease increased the complexity of the repair. Right-sided aortic arch was always associated with KD and frequently with aortic disease,” according to Dr. Tallarita and his colleagues. “Treatment of aSCA with and without associated aortic disease can be accomplished with low morbidity and mortality, and excellent mid-term patency,” they concluded.
Tiziano Tallarita, MD, of the Mayo Clinic, Rochester, Minn., and his colleagues performed a study to examine the surgical management of aberrant subclavian artery (aSCA) associated with aortic arch anomalies at their institution over a 24-year period. “This study represents one of the largest surgical series on aSCA,” according to Dr. Tallarita.
He will present their data on this rare condition at the first of two sessions sponsored by the Vascular and Endovascular Surgery Society (VESS) on Wednesday at the Vascular Annual Meeting. They identified 39 consecutive patients who underwent surgery for aSCA from 1994 to 2017. Clinical presentation, surgical treatment, 30-day morbidity and mortality, and follow-up were assessed.
The median patient age was 46 years and 56% were women. Right aSCA with a left-sided arch was present in 30 patients (77%) with a Kommerell’s diverticulum (KD) in 20, and an aortic aneurysm or dissection in 14. Left aSCA was present in 9 patients (23%), all of whom had a right-sided aortic arch; aortic dissection was present in 6 patients.
Across all patients, one or more symptoms included dysphagia in 25 (65%), dyspnea in 16 (41%), chest pain in 11 (28%), and upper extremity ischemia in 7 (18%). Six of the patients (15%) required emergency surgery, two each for contained rupture and aortic dissection, and one each for rapid aneurysm growth and severe respiratory distress. The aberrant artery was treated by transposition in 23 patients, carotid subclavian bypass in 10 and ascending aorta to subclavian bypass in 6. Two patients with transposition of the left aSCA also had transposition of the vertebral artery. Primary repair of the KD was done in 14 patients, with the distal arch and/or proximal descending thoracic aorta being replaced in 10.
TEVAR was used to exclude the KD in the remaining 6 patients, all of whom had a left sided aortic arch. Nine patients did not need aortic repair.
Dr. Tallarita and colleagues found that one patient died from pulmonary embolism within 30 days of operation (2.6%). “Perioperative morbidity was 18%, with 7 patients developing one or more complications,” added Dr. Tallarita.
Over a median follow-up of 22.5 months (range 0-193), two patients died (5%), neither procedure-or aortic-related. Three-year survival was 84%, and no one needed re-intervention.
“The presence of KD or aortic disease increased the complexity of the repair. Right-sided aortic arch was always associated with KD and frequently with aortic disease,” according to Dr. Tallarita and his colleagues. “Treatment of aSCA with and without associated aortic disease can be accomplished with low morbidity and mortality, and excellent mid-term patency,” they concluded.
VESS: Hospital Volume Is Tied to the Outcomes of Thoracoabdominal Aortic Aneurysm Repair
Contemporary data on outcomes in open thoracoabdominal aortic aneurysm (TAAA) repair is limited to reports from major aortic reference centers showing excellent outcomes, rather than broad-based, real-world observations. In order to deal with this deficiency, Virendra I. Patel, MD, and his colleagues at the Columbia University Medical Center, New York, performed a study to characterize the national experience of open TAAA repair using national outcomes data.
In Wednesday’s Vascular and Endovascular Surgery Society (VESS) session, Dr. Patel will discuss their results, with a primary focus on the influence of operative volume on mortality and morbidity.
He and his colleagues queried the Nationwide Inpatient Sample data from 1998 to 2011, including all patients with a diagnosis of TAAA who underwent open operative repair. Patients with a concomitant procedure code for cardioplegia, coronary bypass, heart valve surgery, and endovascular aortic repair were excluded, leaving 14,263 patients included in this analysis.
These patients were further stratified into tertiles based on the operative volume of the institution that performed their operation: low volume (LV, less than 3 cases/year), medium volume (MV, 3-11 cases/year), high volume (HV, greater than 11 cases/year), according to Dr. Patel.
Baseline demographics as well as perioperative outcomes were compared between the three groups and multivariable logistic regression was performed to determine predictors of operative mortality and morbidity. They also performed subgroup analyses of patients presenting for elective surgery and those presenting for urgent/emergent surgery.
The overall operative mortality was 21% for the entire cohort, with operative mortality being significantly higher at LV (26%) and MV (21%) centers compared to HV centers (15%, P less than .05). This difference was similar in both the elective (18% and 14% vs. 12%, respectively) as well as the urgent/emergent (34% and 30% vs. 19%) surgery groups.
They also found that rates of blood transfusion as well as acute renal failure were significantly lower in the HV group. Multivariable analysis revealed that when compared to the HV group, patients operated on at LV (OR 1.9, P less than .05) and MV (OR 1.5, P less than .05) had at least 1.5 times the odds of in-hospital mortality.
The HV group also showed significantly lower odds of dying in the subgroup analyses of both the elective and the urgent/emergent groups. Similarly, patients operated on at LV (OR 1.3) centers had significantly higher odds of having major morbidity when compared to HV centers.
“Our results show that national mortality for TAAA is much higher than the operative mortality quoted by national reference centers. Patients operated on at high volume centers have a significant reduction in mortality and morbidity compared to other lower volume centers. This relationship is true in the elective as well the urgent/emergent population suggesting referral to higher volume centers or centers of excellence,” Dr. Patel concluded. VC
Contemporary data on outcomes in open thoracoabdominal aortic aneurysm (TAAA) repair is limited to reports from major aortic reference centers showing excellent outcomes, rather than broad-based, real-world observations. In order to deal with this deficiency, Virendra I. Patel, MD, and his colleagues at the Columbia University Medical Center, New York, performed a study to characterize the national experience of open TAAA repair using national outcomes data.
In Wednesday’s Vascular and Endovascular Surgery Society (VESS) session, Dr. Patel will discuss their results, with a primary focus on the influence of operative volume on mortality and morbidity.
He and his colleagues queried the Nationwide Inpatient Sample data from 1998 to 2011, including all patients with a diagnosis of TAAA who underwent open operative repair. Patients with a concomitant procedure code for cardioplegia, coronary bypass, heart valve surgery, and endovascular aortic repair were excluded, leaving 14,263 patients included in this analysis.
These patients were further stratified into tertiles based on the operative volume of the institution that performed their operation: low volume (LV, less than 3 cases/year), medium volume (MV, 3-11 cases/year), high volume (HV, greater than 11 cases/year), according to Dr. Patel.
Baseline demographics as well as perioperative outcomes were compared between the three groups and multivariable logistic regression was performed to determine predictors of operative mortality and morbidity. They also performed subgroup analyses of patients presenting for elective surgery and those presenting for urgent/emergent surgery.
The overall operative mortality was 21% for the entire cohort, with operative mortality being significantly higher at LV (26%) and MV (21%) centers compared to HV centers (15%, P less than .05). This difference was similar in both the elective (18% and 14% vs. 12%, respectively) as well as the urgent/emergent (34% and 30% vs. 19%) surgery groups.
They also found that rates of blood transfusion as well as acute renal failure were significantly lower in the HV group. Multivariable analysis revealed that when compared to the HV group, patients operated on at LV (OR 1.9, P less than .05) and MV (OR 1.5, P less than .05) had at least 1.5 times the odds of in-hospital mortality.
The HV group also showed significantly lower odds of dying in the subgroup analyses of both the elective and the urgent/emergent groups. Similarly, patients operated on at LV (OR 1.3) centers had significantly higher odds of having major morbidity when compared to HV centers.
“Our results show that national mortality for TAAA is much higher than the operative mortality quoted by national reference centers. Patients operated on at high volume centers have a significant reduction in mortality and morbidity compared to other lower volume centers. This relationship is true in the elective as well the urgent/emergent population suggesting referral to higher volume centers or centers of excellence,” Dr. Patel concluded. VC
Contemporary data on outcomes in open thoracoabdominal aortic aneurysm (TAAA) repair is limited to reports from major aortic reference centers showing excellent outcomes, rather than broad-based, real-world observations. In order to deal with this deficiency, Virendra I. Patel, MD, and his colleagues at the Columbia University Medical Center, New York, performed a study to characterize the national experience of open TAAA repair using national outcomes data.
In Wednesday’s Vascular and Endovascular Surgery Society (VESS) session, Dr. Patel will discuss their results, with a primary focus on the influence of operative volume on mortality and morbidity.
He and his colleagues queried the Nationwide Inpatient Sample data from 1998 to 2011, including all patients with a diagnosis of TAAA who underwent open operative repair. Patients with a concomitant procedure code for cardioplegia, coronary bypass, heart valve surgery, and endovascular aortic repair were excluded, leaving 14,263 patients included in this analysis.
These patients were further stratified into tertiles based on the operative volume of the institution that performed their operation: low volume (LV, less than 3 cases/year), medium volume (MV, 3-11 cases/year), high volume (HV, greater than 11 cases/year), according to Dr. Patel.
Baseline demographics as well as perioperative outcomes were compared between the three groups and multivariable logistic regression was performed to determine predictors of operative mortality and morbidity. They also performed subgroup analyses of patients presenting for elective surgery and those presenting for urgent/emergent surgery.
The overall operative mortality was 21% for the entire cohort, with operative mortality being significantly higher at LV (26%) and MV (21%) centers compared to HV centers (15%, P less than .05). This difference was similar in both the elective (18% and 14% vs. 12%, respectively) as well as the urgent/emergent (34% and 30% vs. 19%) surgery groups.
They also found that rates of blood transfusion as well as acute renal failure were significantly lower in the HV group. Multivariable analysis revealed that when compared to the HV group, patients operated on at LV (OR 1.9, P less than .05) and MV (OR 1.5, P less than .05) had at least 1.5 times the odds of in-hospital mortality.
The HV group also showed significantly lower odds of dying in the subgroup analyses of both the elective and the urgent/emergent groups. Similarly, patients operated on at LV (OR 1.3) centers had significantly higher odds of having major morbidity when compared to HV centers.
“Our results show that national mortality for TAAA is much higher than the operative mortality quoted by national reference centers. Patients operated on at high volume centers have a significant reduction in mortality and morbidity compared to other lower volume centers. This relationship is true in the elective as well the urgent/emergent population suggesting referral to higher volume centers or centers of excellence,” Dr. Patel concluded. VC
VAM Session: Physician, Heal Thyself
Between billing, coding, keeping electronic medical records up to date and … oh yes, … actual surgery, vascular surgeons increasingly report feeling overwhelmed and burned out.
In fact, vascular surgeons and trauma surgeons occupy some of the top rungs among the surgical subspecialties at risk for burnout, according to a 2009 study on the topic.
The Society for Vascular Surgery has created a Wellness Task Force to address causes, concerns, and possible solutions to the issue. The group, co-led by Drs. Dawn Coleman and Malachi Sheahan, has already distributed one detailed survey (to which approximately 800 people responded) and is in the process of readying another.
Burnout also will be addressed at a breakfast session at the Vascular Annual Meeting. “Promoting Physician Wellness: Achieving Quadruple Aim” will be held from 6:30 – 8 a.m. Friday in Room 304/306 of HCC. Tickets are required and may be obtained at a registration counter.
The first survey, preliminary results of which may be presented during the session, sought data on symptoms, if burnout were affecting work and contributing factors that are creating burnout. It also included questions on work schedules, including on-call shifts, how much work respondents were bringing home and electronic medical records.
The second survey, said Dr. Sheahan, hopes to delve deeper into other factors, such as physical stressors and wear and tear on a vascular surgeon’s body.
He noted that he wrote his first column on burnout for “Vascular Specialist” more than a year ago, when he did not yet know the issue’s prevalence. “The articles I’d seen were more than 10 years old,” he said. “I got a lot of feedback which told me there was something definitely there.” Together, he and Dr. Coleman wrote a series of three articles on burnout. Positive reaction led to creation of the Task Force and then to the upcoming VAM presentation.
Topics include changes in medical and surgical practice in the 21st century, the hidden costs of burnout for both physician and patient, interventions to enhance surgeons’ personal well-being, what burnout is and why it occurs, strategies to combat it, and a “Societal Call to Action: Can We Improve Physician Wellness?”
Dr. Sheahan said he hopes to uncover more facts and feedback. For example, do researchers report the same level of burnout as surgeons in private practice? Do surgeons in rural settings have different, or more, stressors than those in urban environments?
He — and others who have written about physician burnout — believes electronic medical records play a big part. “I’m almost positive it’s going to prove a major factor,” he said. “It takes so much more time – time we don’t have.” At least five different medical record systems that don’t talk to each other exist, he said. “How did we develop that?” he asked. “It’s a very aggravating problem.”
Possible solutions also will be explored. Dr. Sheahan advocates that these solutions focus less on personal resilience and more on institutional change. “I believe that if we, on a large scale, tie the problem into our own productivity, health, and our own patient safety, they’ll have no choice but to change,” he said. One example would be to hold software engineers and hospital administrators accountable and get them to fix the lack of integration in EMR systems.
A “rewards program” has possibilities as well. Credits, such as meals delivered for a week, are given for tasks over and above the norm. Stanford University has used this and it shows promise, Dr. Sheahan said.
Some experts have suggested resilience training. Dr. Sheahan disagrees. “Doctors are resilient by nature. Those who aren’t got weeded out a long time ago.” And teaching people to “deal with” stress isn’t the answer, he added. “We have to try to remove the stressors.
“Just let us do what we’re good at. Physicians are happiest, safest, and most productive when doing what we were trained to do,” he said. “We now have so many things that take us away from patient care. It is these distractors that I believe lead to burnout.”
B5: Promoting Physician Wellness: Achieving Quadruple Aim
Friday, 6:30 – 8:00 a.m.
HCC, Room 304/306
Between billing, coding, keeping electronic medical records up to date and … oh yes, … actual surgery, vascular surgeons increasingly report feeling overwhelmed and burned out.
In fact, vascular surgeons and trauma surgeons occupy some of the top rungs among the surgical subspecialties at risk for burnout, according to a 2009 study on the topic.
The Society for Vascular Surgery has created a Wellness Task Force to address causes, concerns, and possible solutions to the issue. The group, co-led by Drs. Dawn Coleman and Malachi Sheahan, has already distributed one detailed survey (to which approximately 800 people responded) and is in the process of readying another.
Burnout also will be addressed at a breakfast session at the Vascular Annual Meeting. “Promoting Physician Wellness: Achieving Quadruple Aim” will be held from 6:30 – 8 a.m. Friday in Room 304/306 of HCC. Tickets are required and may be obtained at a registration counter.
The first survey, preliminary results of which may be presented during the session, sought data on symptoms, if burnout were affecting work and contributing factors that are creating burnout. It also included questions on work schedules, including on-call shifts, how much work respondents were bringing home and electronic medical records.
The second survey, said Dr. Sheahan, hopes to delve deeper into other factors, such as physical stressors and wear and tear on a vascular surgeon’s body.
He noted that he wrote his first column on burnout for “Vascular Specialist” more than a year ago, when he did not yet know the issue’s prevalence. “The articles I’d seen were more than 10 years old,” he said. “I got a lot of feedback which told me there was something definitely there.” Together, he and Dr. Coleman wrote a series of three articles on burnout. Positive reaction led to creation of the Task Force and then to the upcoming VAM presentation.
Topics include changes in medical and surgical practice in the 21st century, the hidden costs of burnout for both physician and patient, interventions to enhance surgeons’ personal well-being, what burnout is and why it occurs, strategies to combat it, and a “Societal Call to Action: Can We Improve Physician Wellness?”
Dr. Sheahan said he hopes to uncover more facts and feedback. For example, do researchers report the same level of burnout as surgeons in private practice? Do surgeons in rural settings have different, or more, stressors than those in urban environments?
He — and others who have written about physician burnout — believes electronic medical records play a big part. “I’m almost positive it’s going to prove a major factor,” he said. “It takes so much more time – time we don’t have.” At least five different medical record systems that don’t talk to each other exist, he said. “How did we develop that?” he asked. “It’s a very aggravating problem.”
Possible solutions also will be explored. Dr. Sheahan advocates that these solutions focus less on personal resilience and more on institutional change. “I believe that if we, on a large scale, tie the problem into our own productivity, health, and our own patient safety, they’ll have no choice but to change,” he said. One example would be to hold software engineers and hospital administrators accountable and get them to fix the lack of integration in EMR systems.
A “rewards program” has possibilities as well. Credits, such as meals delivered for a week, are given for tasks over and above the norm. Stanford University has used this and it shows promise, Dr. Sheahan said.
Some experts have suggested resilience training. Dr. Sheahan disagrees. “Doctors are resilient by nature. Those who aren’t got weeded out a long time ago.” And teaching people to “deal with” stress isn’t the answer, he added. “We have to try to remove the stressors.
“Just let us do what we’re good at. Physicians are happiest, safest, and most productive when doing what we were trained to do,” he said. “We now have so many things that take us away from patient care. It is these distractors that I believe lead to burnout.”
B5: Promoting Physician Wellness: Achieving Quadruple Aim
Friday, 6:30 – 8:00 a.m.
HCC, Room 304/306
Between billing, coding, keeping electronic medical records up to date and … oh yes, … actual surgery, vascular surgeons increasingly report feeling overwhelmed and burned out.
In fact, vascular surgeons and trauma surgeons occupy some of the top rungs among the surgical subspecialties at risk for burnout, according to a 2009 study on the topic.
The Society for Vascular Surgery has created a Wellness Task Force to address causes, concerns, and possible solutions to the issue. The group, co-led by Drs. Dawn Coleman and Malachi Sheahan, has already distributed one detailed survey (to which approximately 800 people responded) and is in the process of readying another.
Burnout also will be addressed at a breakfast session at the Vascular Annual Meeting. “Promoting Physician Wellness: Achieving Quadruple Aim” will be held from 6:30 – 8 a.m. Friday in Room 304/306 of HCC. Tickets are required and may be obtained at a registration counter.
The first survey, preliminary results of which may be presented during the session, sought data on symptoms, if burnout were affecting work and contributing factors that are creating burnout. It also included questions on work schedules, including on-call shifts, how much work respondents were bringing home and electronic medical records.
The second survey, said Dr. Sheahan, hopes to delve deeper into other factors, such as physical stressors and wear and tear on a vascular surgeon’s body.
He noted that he wrote his first column on burnout for “Vascular Specialist” more than a year ago, when he did not yet know the issue’s prevalence. “The articles I’d seen were more than 10 years old,” he said. “I got a lot of feedback which told me there was something definitely there.” Together, he and Dr. Coleman wrote a series of three articles on burnout. Positive reaction led to creation of the Task Force and then to the upcoming VAM presentation.
Topics include changes in medical and surgical practice in the 21st century, the hidden costs of burnout for both physician and patient, interventions to enhance surgeons’ personal well-being, what burnout is and why it occurs, strategies to combat it, and a “Societal Call to Action: Can We Improve Physician Wellness?”
Dr. Sheahan said he hopes to uncover more facts and feedback. For example, do researchers report the same level of burnout as surgeons in private practice? Do surgeons in rural settings have different, or more, stressors than those in urban environments?
He — and others who have written about physician burnout — believes electronic medical records play a big part. “I’m almost positive it’s going to prove a major factor,” he said. “It takes so much more time – time we don’t have.” At least five different medical record systems that don’t talk to each other exist, he said. “How did we develop that?” he asked. “It’s a very aggravating problem.”
Possible solutions also will be explored. Dr. Sheahan advocates that these solutions focus less on personal resilience and more on institutional change. “I believe that if we, on a large scale, tie the problem into our own productivity, health, and our own patient safety, they’ll have no choice but to change,” he said. One example would be to hold software engineers and hospital administrators accountable and get them to fix the lack of integration in EMR systems.
A “rewards program” has possibilities as well. Credits, such as meals delivered for a week, are given for tasks over and above the norm. Stanford University has used this and it shows promise, Dr. Sheahan said.
Some experts have suggested resilience training. Dr. Sheahan disagrees. “Doctors are resilient by nature. Those who aren’t got weeded out a long time ago.” And teaching people to “deal with” stress isn’t the answer, he added. “We have to try to remove the stressors.
“Just let us do what we’re good at. Physicians are happiest, safest, and most productive when doing what we were trained to do,” he said. “We now have so many things that take us away from patient care. It is these distractors that I believe lead to burnout.”
B5: Promoting Physician Wellness: Achieving Quadruple Aim
Friday, 6:30 – 8:00 a.m.
HCC, Room 304/306
SVS Booth will be in the Exhibit Hall
SVS members who are attending the Vascular Annual Meeting can get in-person help with any application issues, or, indeed any membership services concerns. The SVS Booth, #1015, in the Exhibit Hall will be staffed both Thursday and Friday, June 21-22. SVS staff members will be able to provide information on a wide range of topics, including:
• Member services, including
- The benefits of belonging
- Dues
- Membership applications
- Log-in issues
- Contact information updates – don’t fall off the contacts list!
• The Affinity Program of expanded benefits
• Educational products, including the fourth edition of the Vascular Education Self-Assessment Program (VESAP), the SVS coding Class, the SVS Vascular Research Initiatives Conference and the Rutherford’s Vascular Surgery book.
• The Journal of Vascular Surgery publications (offering JVS socks!)
• The SVS Patient Safety Organization Vascular Quality Initiative
• Quality and clinical practice guideline initiatives (including printed copies of four of the latest SVS guidelines)
• The Mobile App or VAM Planner
• The SVS Foundation and the SVS Political Action Committee; members can make a donation to either or both
• Scan the QR code as part of the Exhibit Hall Scavenger Hunt
Enter to win a prize: Those who drop by can be entered into a drawing for three prizes: an SVS Membership waiver for next year, free VAM 2019 registration and VAM on Demand from the ’18 meeting. In addition, while supplies last, visitors also can pick up a memento of their visit.
SVS members who are attending the Vascular Annual Meeting can get in-person help with any application issues, or, indeed any membership services concerns. The SVS Booth, #1015, in the Exhibit Hall will be staffed both Thursday and Friday, June 21-22. SVS staff members will be able to provide information on a wide range of topics, including:
• Member services, including
- The benefits of belonging
- Dues
- Membership applications
- Log-in issues
- Contact information updates – don’t fall off the contacts list!
• The Affinity Program of expanded benefits
• Educational products, including the fourth edition of the Vascular Education Self-Assessment Program (VESAP), the SVS coding Class, the SVS Vascular Research Initiatives Conference and the Rutherford’s Vascular Surgery book.
• The Journal of Vascular Surgery publications (offering JVS socks!)
• The SVS Patient Safety Organization Vascular Quality Initiative
• Quality and clinical practice guideline initiatives (including printed copies of four of the latest SVS guidelines)
• The Mobile App or VAM Planner
• The SVS Foundation and the SVS Political Action Committee; members can make a donation to either or both
• Scan the QR code as part of the Exhibit Hall Scavenger Hunt
Enter to win a prize: Those who drop by can be entered into a drawing for three prizes: an SVS Membership waiver for next year, free VAM 2019 registration and VAM on Demand from the ’18 meeting. In addition, while supplies last, visitors also can pick up a memento of their visit.
SVS members who are attending the Vascular Annual Meeting can get in-person help with any application issues, or, indeed any membership services concerns. The SVS Booth, #1015, in the Exhibit Hall will be staffed both Thursday and Friday, June 21-22. SVS staff members will be able to provide information on a wide range of topics, including:
• Member services, including
- The benefits of belonging
- Dues
- Membership applications
- Log-in issues
- Contact information updates – don’t fall off the contacts list!
• The Affinity Program of expanded benefits
• Educational products, including the fourth edition of the Vascular Education Self-Assessment Program (VESAP), the SVS coding Class, the SVS Vascular Research Initiatives Conference and the Rutherford’s Vascular Surgery book.
• The Journal of Vascular Surgery publications (offering JVS socks!)
• The SVS Patient Safety Organization Vascular Quality Initiative
• Quality and clinical practice guideline initiatives (including printed copies of four of the latest SVS guidelines)
• The Mobile App or VAM Planner
• The SVS Foundation and the SVS Political Action Committee; members can make a donation to either or both
• Scan the QR code as part of the Exhibit Hall Scavenger Hunt
Enter to win a prize: Those who drop by can be entered into a drawing for three prizes: an SVS Membership waiver for next year, free VAM 2019 registration and VAM on Demand from the ’18 meeting. In addition, while supplies last, visitors also can pick up a memento of their visit.
A Look into the Future at the Crawford Forum
Will the demand be sufficient for the supply of the vascular surgery work force in the United States? That topic, along with potential solutions, will be front and center at the E. Stanley Crawford Critical Issues Forum from 10:30 a.m. to 12 p.m. See HCC, Ballroom A/B.
Will the demand be sufficient for the supply of the vascular surgery work force in the United States? That topic, along with potential solutions, will be front and center at the E. Stanley Crawford Critical Issues Forum from 10:30 a.m. to 12 p.m. See HCC, Ballroom A/B.
Will the demand be sufficient for the supply of the vascular surgery work force in the United States? That topic, along with potential solutions, will be front and center at the E. Stanley Crawford Critical Issues Forum from 10:30 a.m. to 12 p.m. See HCC, Ballroom A/B.