User login
Understanding Focal Cortical Dysplasia-Induced Epilepsy
The epilepsy associated with focal cortical dysplasia remains a major challenge, but early recognition of the disorder will allow clinicians to consider the possibility of resective surgery, which has been shown to eliminate seizures in some patients.
- A recent review of the medical literature found that most children with focal cortical dysplasia have intractable focal epilepsy.
- The epilepsy observed in patients with focal cortical dysplasia is related to activation of the mTOR pathway and altered receptor neurotransmission.
- The literature review discusses the epidemiology, natural history, and mechanisms that precipitate seizures in children with focal cortical dysplasia.
- Between 25% and 29% of children in a surgical series had focal cortical dysplasia.
Challenges in managing epilepsy associated with focal cortical dysplasia in children. Epilepsy Res. 2018;145:1-17.
The epilepsy associated with focal cortical dysplasia remains a major challenge, but early recognition of the disorder will allow clinicians to consider the possibility of resective surgery, which has been shown to eliminate seizures in some patients.
- A recent review of the medical literature found that most children with focal cortical dysplasia have intractable focal epilepsy.
- The epilepsy observed in patients with focal cortical dysplasia is related to activation of the mTOR pathway and altered receptor neurotransmission.
- The literature review discusses the epidemiology, natural history, and mechanisms that precipitate seizures in children with focal cortical dysplasia.
- Between 25% and 29% of children in a surgical series had focal cortical dysplasia.
Challenges in managing epilepsy associated with focal cortical dysplasia in children. Epilepsy Res. 2018;145:1-17.
The epilepsy associated with focal cortical dysplasia remains a major challenge, but early recognition of the disorder will allow clinicians to consider the possibility of resective surgery, which has been shown to eliminate seizures in some patients.
- A recent review of the medical literature found that most children with focal cortical dysplasia have intractable focal epilepsy.
- The epilepsy observed in patients with focal cortical dysplasia is related to activation of the mTOR pathway and altered receptor neurotransmission.
- The literature review discusses the epidemiology, natural history, and mechanisms that precipitate seizures in children with focal cortical dysplasia.
- Between 25% and 29% of children in a surgical series had focal cortical dysplasia.
Challenges in managing epilepsy associated with focal cortical dysplasia in children. Epilepsy Res. 2018;145:1-17.
Medication Patterns Changing for Pregnant Women with Epilepsy
Drug therapy for pregnant women with epilepsy has changed markedly in recent years according to analysis of data from the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study.
- MONEAD, an NIH-funded, observational, multicenter study that looked at pregnancy outcomes in mothers and their children, included women ages 14-45 years and up to 20 weeks pregnant.
- Among 351 pregnant women with epilepsy enrolled in the study, 73.8% (259) were on monotherapy and 21.9% (77) on polytherapy; 4% were not taking an antiepileptic drug.
- Lamotrigine was the most popular drug in women on monotherapy, followed by levetiracetam, carbamazepine, zonisamide, oxcarbazepine, and topiramate.
- The most common polypharmacy regimen included lamotrigine and levetiracetam.
The researchers point out that these percentages only reflect drug usage in US tertiary epilepsy centers and may not indicate usage in community practice.
MONEAD Investigator Group. Changes in antiepileptic drug-prescribing patterns in pregnant women with epilepsy. Epilepsy Behav. 2018;84:10-14.
Drug therapy for pregnant women with epilepsy has changed markedly in recent years according to analysis of data from the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study.
- MONEAD, an NIH-funded, observational, multicenter study that looked at pregnancy outcomes in mothers and their children, included women ages 14-45 years and up to 20 weeks pregnant.
- Among 351 pregnant women with epilepsy enrolled in the study, 73.8% (259) were on monotherapy and 21.9% (77) on polytherapy; 4% were not taking an antiepileptic drug.
- Lamotrigine was the most popular drug in women on monotherapy, followed by levetiracetam, carbamazepine, zonisamide, oxcarbazepine, and topiramate.
- The most common polypharmacy regimen included lamotrigine and levetiracetam.
The researchers point out that these percentages only reflect drug usage in US tertiary epilepsy centers and may not indicate usage in community practice.
MONEAD Investigator Group. Changes in antiepileptic drug-prescribing patterns in pregnant women with epilepsy. Epilepsy Behav. 2018;84:10-14.
Drug therapy for pregnant women with epilepsy has changed markedly in recent years according to analysis of data from the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study.
- MONEAD, an NIH-funded, observational, multicenter study that looked at pregnancy outcomes in mothers and their children, included women ages 14-45 years and up to 20 weeks pregnant.
- Among 351 pregnant women with epilepsy enrolled in the study, 73.8% (259) were on monotherapy and 21.9% (77) on polytherapy; 4% were not taking an antiepileptic drug.
- Lamotrigine was the most popular drug in women on monotherapy, followed by levetiracetam, carbamazepine, zonisamide, oxcarbazepine, and topiramate.
- The most common polypharmacy regimen included lamotrigine and levetiracetam.
The researchers point out that these percentages only reflect drug usage in US tertiary epilepsy centers and may not indicate usage in community practice.
MONEAD Investigator Group. Changes in antiepileptic drug-prescribing patterns in pregnant women with epilepsy. Epilepsy Behav. 2018;84:10-14.
A call for ‘changing the social norms’ on naloxone
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
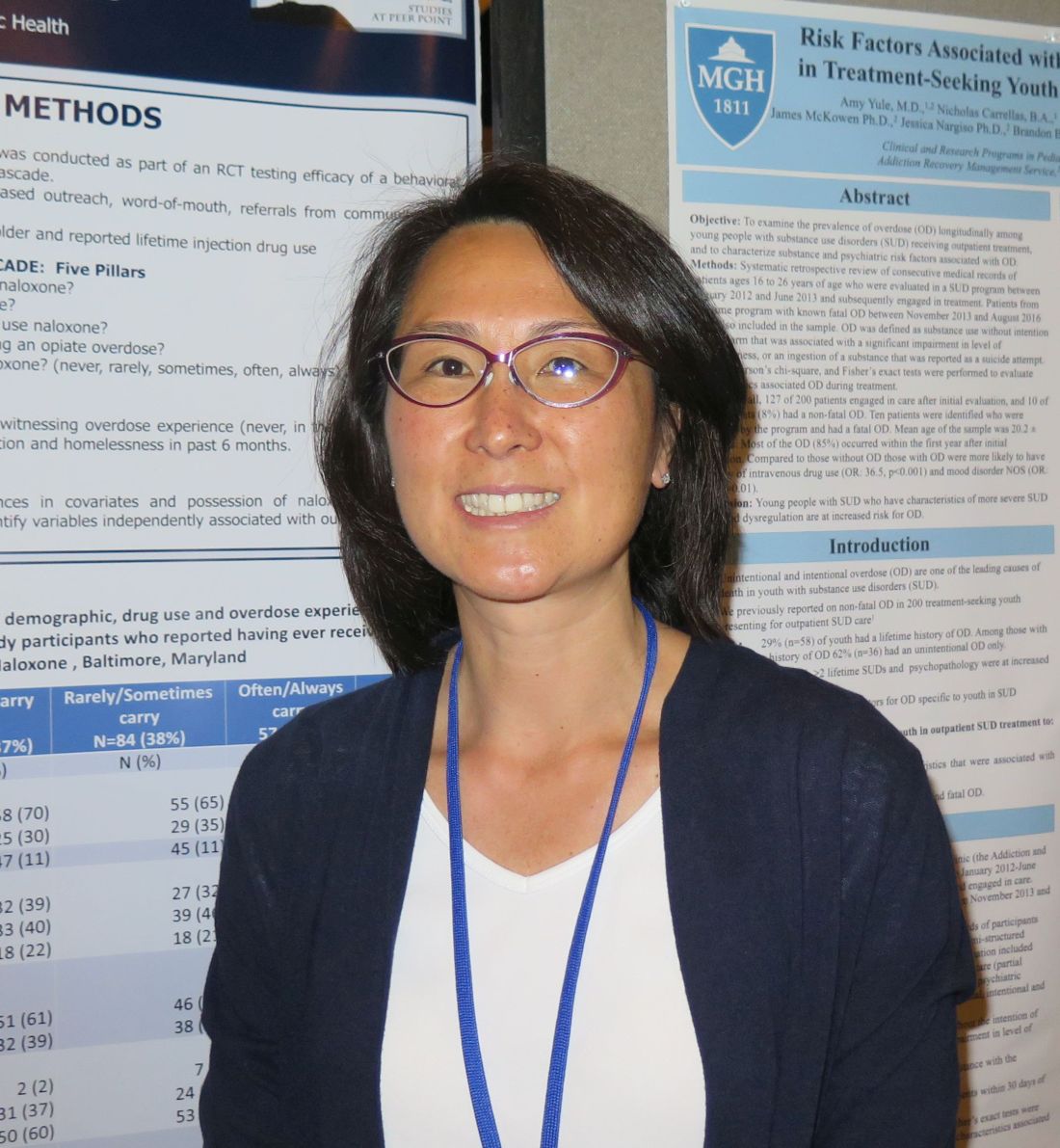
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
SAN DIEGO – Among individuals with a history of injection drug use, more than one-third reported never or sometimes carrying naloxone, while just one in four reported carrying with it them at all times.
Those are key findings from a survey that set out to examine gaps in the naloxone cascade in a sample of people who inject drugs.
“In order to save a life, you have to have the naloxone with you at all times,” lead study author Karin E. Tobin, PhD, said in an interview at the annual meeting of the College on Problems of Drug Dependence.
While emerging research demonstrates the positive impact of opioid overdose education and community naloxone distribution programs to reduce opioid-related overdose deaths, opiate overdose continues to be a major cause of mortality, said Dr. Tobin, who is affiliated with the department of health behavior and society at Johns Hopkins University, Baltimore. “We’ve made a lot of progress in convincing people that naloxone is not addictive, and that it’s not going to cause any harm,” she said. “Now, drug users aren’t afraid to ask for it. Still, we wondered: If everyone knows about naloxone and no one is embarrassed to talk about it, why are people still dying [from opioid overdoses] in Baltimore?”
She and her associates conducted a cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use. The data came from a baseline survey that was conducted as part of a randomized, controlled trial testing the efficacy of a behavioral intervention focused on the Hepatitis C cascade. Individuals were asked to answer questions related to the five steps of the naloxone cascade: awareness (have you ever heard about naloxone?), access (have you ever received naloxone?), training (have you ever been trained to use naloxone?), use (have you ever used naloxone during an opiate overdose?), and possession (how often do you carry naloxone?)
More than half of the survey respondents (65%) were male; mean age was 47 years. For the previous 6 months, more than half of the sample reported the use of crack (64%), heroin (74%), and other injectable drugs (57%), while 90% reported having ever witnessed an overdose – 59% in the prior year alone. Dr. Tobin and her associates found that 90% of respondents had heard about naloxone, 69% had received it, and 60% had been trained to use it. In addition, 37% reported never carrying naloxone, 38% sometimes carried it, 33% said they had used naloxone at some point, and 25% said they always carried it with them.
On multinomial regression analysis, the researchers found that carrying naloxone often or always was significantly associated with the following variables: female sex (odds ratio, 2.77), having ever witnessed an overdose (OR, 1.84), having injected in the past 12 months (OR, 1.75), and having ever used naloxone during an overdose (OR, 4.33). The latter finding is especially important, “because it means that we just have to let people practice using it,” said Dr. Tobin, who noted that more research is needed to understand reasons why injection drug users do not always carry naloxone. “We need to start changing the social norms about carrying naloxone. You never know when it will be useful.”
The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
AT CPDD 2018
Key clinical point: Increasing possession of naloxone among people who use opiates is essential.
Major finding:. Carrying naloxone often or always was significantly associated with several variables, including female sex (odds ratio, 2.77) and having ever used naloxone during an overdose (OR, 4.33).
Study details: A cross-sectional survey of 353 individuals aged 18 and older in Baltimore who self-reported a lifetime history of injection drug use.
Disclosures: The National Institute on Drug Abuse supported the study. Dr. Tobin reported having no financial disclosures.
Do free meals to physicians affect opioid prescribing?
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
SAN DIEGO – Physicians who receive gifts and free meals from opioid manufacturers prescribe more opioids than do their counterparts, a new study suggests.
A sampling of doctors who reported marketing payments or gifts prescribed more of the drugs the following year even as their colleagues prescribed fewer. Researchers also found signs of a dose-effect relationship between more free meals received and more opioid medications prescribed.
The findings, presented at the annual meeting of the College on Problems of Drug Dependence and recently published, do not prove a link between free meals and the massive, deadly opioid epidemic. And the purpose of pharmaceutical marketing, of course, is to persuade physicians to prescribe medications, the researchers noted. The report was published in JAMA Internal Medicine.
Still, in light of the opioid epidemic, “there’s a national effort to reduce overprescribing. Our database suggests that the pharmaceutical industry may be a counterforce,” lead author and pediatrician Scott E. Hadland, MD, MPH, of Boston University, said in an interview.
The findings suggest “it doesn’t take much money to get doctors to potentially prescribe more opioids,” he added.
According to data from the Centers for Disease Control and Prevention, a record number of people – 52,404 – died from drug overdoses in 2015, and nearly 13,000 of the deaths were attributable to prescription drugs (natural or semi-synthetic). An estimated 12.5 million people aged 12 and older in 2015, meanwhile, recently had misused prescription pain relievers.
For the new study, Dr. Hadland and his colleagues sought to understand whether opioid marketing in 2014 influenced prescribing in 2015.
The researchers retrospectively tracked 369,139 physicians in a Medicare Part D database who prescribed opioids in 2015 and found that 7% reported receiving opioid marketing – speaking fees ($6.2 million), meals ($1.8 million), travel ($731,000), consulting fees ($290,000), and education ($80,000).
Overall, received marketing.
“The effect is very subtle,” said Dr. Hadland, an addiction medicine specialist at the university. “Nine percent does not seem like a large number, but when you’re talking about hundreds of thousands of physicians, that’s a large number of opioids being prescribed.”
The study takes only Medicare Part D opioid prescriptions into account, and includes only about 42% of the active national physician workforce, he noted.
The researchers linked rising numbers of meals received in 2014 per physician – from 1 to more than 10 – to a steady increase in the number of opioid claims per physician. For example, physicians who received 1 meal made about 150 opioid claims, while those who received more than 10 made more than 700 claims.
As for physician motivations, Dr. Hadland said, he doesn’t believe “this is intentional for most physicians. If you asked the vast majority of physicians in our study, ‘Do you believe marketing is influencing your prescribing?’ most would say no.”
But the findings, he said, still raise questions.
Going forward, researchers plan to study the effect of opioid marketing on public health, he added.
Dr. Hadland reports funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reports funding from NIDA. No additional relevant disclosures were reported.
SOURCE: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
REPORTING FROM CPDD 2018
Key clinical point: Opioid marketing appears to affect physician prescribing practices.
Major finding: Physicians who received opioid marketing payments and meals in 2014 prescribed an adjusted 9% more opioids in 2015 than did their opioid-prescribing colleagues.
Study details: Retrospective 2014-2015 analysis of 369,139 opioid-prescribing physicians in a Medicare Part D database.
Disclosures: Dr. Hadland reported funding from the National Institute on Drug Abuse, Society for Adolescent Health and Medicine, Thrasher Research Fund, and Academic Pediatric Association. Another author reported funding from NIDA. No additional relevant disclosures were reported.
Source: Hadland SE et al. JAMA Intern Med. 2018 Jun 1;178(6):861-3.
Gene signature might identify patients at risk of CAR T-associated neurotoxicity
CHICAGO—A specific gene signature might be able to identify patients at risk of CD19 CAR T-cell associated neurotoxicity, according to results of an exploratory analysis presented at the 2018 ASCO Annual Meeting.
The analysis, based on bone marrow samples from patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) treated with JCAR015 in the ROCKET trial, helped identify a set of neurotoxicity-associated genes that separated patients based on molecular subtype.
“These findings suggest that patient risk stratification by molecular subtype of disease or gene expression signature may play a role in identifying patients at elevated risk of neurotoxicity,” said Jae Park, MD, of Memorial Sloan Kettering Cancer Center, New York, New York, in a presentation of the findings (abstract 7007).
The phase 2 ROCKET study included adult patients with relapsed or refractory morphological (>5% blasts in bone marrow) CD-19 positive disease in first salvage or greater, including post allogeneic hematopoietic stem cell transplantation (HSCT). Prior blinatumomab was allowed.
The tumor gene expression study presented at ASCO was based on sequenced RNA from pre-apheresis bone marrow samples available for 31 patients in the ROCKET study.
Investigators identified a set of 10 genes expressed more frequently in bone marrow samples from patients in ROCKET with low (grade 0-1) neurotoxicity, and 7 that were more frequent in those who had severe (grade 4-5) neurotoxicity.
Looking at B-cell ALL samples in public datasets by molecular subtype, they found genes highly expressed in the low neurotoxicity ROCKET patients were also highly expressed in Philadelphia chromosome-positive (Ph+) and Ph-like subtypes.
Conversely, the genes highly expressed in the severe neurotoxicity patients were also highly expressed in non-Ph-like samples.
A total of 16 ROCKET patients were classified as having Ph-like gene expression and 15 as having non-Ph-like expression.
There were no grade 4-5 neurotoxicity events in the Ph-like patients, while both grade 3+ and grade 4+ neurotoxicity were significantly more prevalent in the non-Ph-like patients, investigators reported.
One of the most differentially expressed genes in the set was CCL17, which was higher in the low-neurotoxicity tumor samples, and likewise highly expressed in Ph-like B-cell ALL, according to the report.
“[CCL17] may serve as an early biomarker for differentiating severe neurotoxicity,” Dr Park said.
These findings are now being validated in the previously mentioned data set, as well as other studies to see if the findings can be replicated, according to Dr Park.
Juno Therapeutics, a Celgene company, shut down the phase 2 ROCKET trial of JCAR015 in 2017 after 2 clinical holds in 2016 and 5 patient deaths.
CHICAGO—A specific gene signature might be able to identify patients at risk of CD19 CAR T-cell associated neurotoxicity, according to results of an exploratory analysis presented at the 2018 ASCO Annual Meeting.
The analysis, based on bone marrow samples from patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) treated with JCAR015 in the ROCKET trial, helped identify a set of neurotoxicity-associated genes that separated patients based on molecular subtype.
“These findings suggest that patient risk stratification by molecular subtype of disease or gene expression signature may play a role in identifying patients at elevated risk of neurotoxicity,” said Jae Park, MD, of Memorial Sloan Kettering Cancer Center, New York, New York, in a presentation of the findings (abstract 7007).
The phase 2 ROCKET study included adult patients with relapsed or refractory morphological (>5% blasts in bone marrow) CD-19 positive disease in first salvage or greater, including post allogeneic hematopoietic stem cell transplantation (HSCT). Prior blinatumomab was allowed.
The tumor gene expression study presented at ASCO was based on sequenced RNA from pre-apheresis bone marrow samples available for 31 patients in the ROCKET study.
Investigators identified a set of 10 genes expressed more frequently in bone marrow samples from patients in ROCKET with low (grade 0-1) neurotoxicity, and 7 that were more frequent in those who had severe (grade 4-5) neurotoxicity.
Looking at B-cell ALL samples in public datasets by molecular subtype, they found genes highly expressed in the low neurotoxicity ROCKET patients were also highly expressed in Philadelphia chromosome-positive (Ph+) and Ph-like subtypes.
Conversely, the genes highly expressed in the severe neurotoxicity patients were also highly expressed in non-Ph-like samples.
A total of 16 ROCKET patients were classified as having Ph-like gene expression and 15 as having non-Ph-like expression.
There were no grade 4-5 neurotoxicity events in the Ph-like patients, while both grade 3+ and grade 4+ neurotoxicity were significantly more prevalent in the non-Ph-like patients, investigators reported.
One of the most differentially expressed genes in the set was CCL17, which was higher in the low-neurotoxicity tumor samples, and likewise highly expressed in Ph-like B-cell ALL, according to the report.
“[CCL17] may serve as an early biomarker for differentiating severe neurotoxicity,” Dr Park said.
These findings are now being validated in the previously mentioned data set, as well as other studies to see if the findings can be replicated, according to Dr Park.
Juno Therapeutics, a Celgene company, shut down the phase 2 ROCKET trial of JCAR015 in 2017 after 2 clinical holds in 2016 and 5 patient deaths.
CHICAGO—A specific gene signature might be able to identify patients at risk of CD19 CAR T-cell associated neurotoxicity, according to results of an exploratory analysis presented at the 2018 ASCO Annual Meeting.
The analysis, based on bone marrow samples from patients with relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) treated with JCAR015 in the ROCKET trial, helped identify a set of neurotoxicity-associated genes that separated patients based on molecular subtype.
“These findings suggest that patient risk stratification by molecular subtype of disease or gene expression signature may play a role in identifying patients at elevated risk of neurotoxicity,” said Jae Park, MD, of Memorial Sloan Kettering Cancer Center, New York, New York, in a presentation of the findings (abstract 7007).
The phase 2 ROCKET study included adult patients with relapsed or refractory morphological (>5% blasts in bone marrow) CD-19 positive disease in first salvage or greater, including post allogeneic hematopoietic stem cell transplantation (HSCT). Prior blinatumomab was allowed.
The tumor gene expression study presented at ASCO was based on sequenced RNA from pre-apheresis bone marrow samples available for 31 patients in the ROCKET study.
Investigators identified a set of 10 genes expressed more frequently in bone marrow samples from patients in ROCKET with low (grade 0-1) neurotoxicity, and 7 that were more frequent in those who had severe (grade 4-5) neurotoxicity.
Looking at B-cell ALL samples in public datasets by molecular subtype, they found genes highly expressed in the low neurotoxicity ROCKET patients were also highly expressed in Philadelphia chromosome-positive (Ph+) and Ph-like subtypes.
Conversely, the genes highly expressed in the severe neurotoxicity patients were also highly expressed in non-Ph-like samples.
A total of 16 ROCKET patients were classified as having Ph-like gene expression and 15 as having non-Ph-like expression.
There were no grade 4-5 neurotoxicity events in the Ph-like patients, while both grade 3+ and grade 4+ neurotoxicity were significantly more prevalent in the non-Ph-like patients, investigators reported.
One of the most differentially expressed genes in the set was CCL17, which was higher in the low-neurotoxicity tumor samples, and likewise highly expressed in Ph-like B-cell ALL, according to the report.
“[CCL17] may serve as an early biomarker for differentiating severe neurotoxicity,” Dr Park said.
These findings are now being validated in the previously mentioned data set, as well as other studies to see if the findings can be replicated, according to Dr Park.
Juno Therapeutics, a Celgene company, shut down the phase 2 ROCKET trial of JCAR015 in 2017 after 2 clinical holds in 2016 and 5 patient deaths.
FDA places SB-generated CAR T-cell therapy on clinical hold
The US Food and Drug Administrated (FDA) placed a clinical hold on the phase 1 trial of the Sleeping Beauty (SB)-generated CAR T-cell therapy in relapsed or refractory leukemia and lymphoma patients.
The Sleeping Beauty platform was designed to very rapidly manufacture CD19-specific CAR T cells at the point of care.
All SB-CAR T-cell processing is planned to take place within 2 days at the healthcare facility, thus eliminating shipping cells from hospitals to production sites and back again.
The FDA is requesting more chemistry, manufacturing, and control (CMC) information before allowing the trial to proceed.
The Sleeping Beauty technology, a non-viral transposon/transposase system, has the potential to reduce the costs and complexity associated with recombinant viral vector-based immunotherapy, according to developers.
Ziopharm Oncology, Precigen, Inc, a wholly owned subsidiary of Intrexon Corporation, and the University of Texas MD Anderson Cancer Center, are developing the Sleeping Beauty CAR T cell therapy.
“We know what is needed to address the hold issues and are looking forward to responding to the agency in a timely manner,” said Laurence Cooper, MD, PhD, chief executive officer of Ziopharm, in a corporate release.
“We are undertaking cutting-edge science and are on the verge of a paradigm shift based on our approach to very rapidly manufacture CD19-specific T cells within 2 days using our non-viral approach to CAR-T therapy based on the Sleeping Beauty platform.”
The phase 1 trial in question is a third-generation trial in which the CAR T cells are designed to co-express CD19-specific CAR, membrane-bound interleukin 15, and a safety switch.
The findings from earlier generation phase 1 trials have been previously reported in The Journal of Clinical Investigation.
The US Food and Drug Administrated (FDA) placed a clinical hold on the phase 1 trial of the Sleeping Beauty (SB)-generated CAR T-cell therapy in relapsed or refractory leukemia and lymphoma patients.
The Sleeping Beauty platform was designed to very rapidly manufacture CD19-specific CAR T cells at the point of care.
All SB-CAR T-cell processing is planned to take place within 2 days at the healthcare facility, thus eliminating shipping cells from hospitals to production sites and back again.
The FDA is requesting more chemistry, manufacturing, and control (CMC) information before allowing the trial to proceed.
The Sleeping Beauty technology, a non-viral transposon/transposase system, has the potential to reduce the costs and complexity associated with recombinant viral vector-based immunotherapy, according to developers.
Ziopharm Oncology, Precigen, Inc, a wholly owned subsidiary of Intrexon Corporation, and the University of Texas MD Anderson Cancer Center, are developing the Sleeping Beauty CAR T cell therapy.
“We know what is needed to address the hold issues and are looking forward to responding to the agency in a timely manner,” said Laurence Cooper, MD, PhD, chief executive officer of Ziopharm, in a corporate release.
“We are undertaking cutting-edge science and are on the verge of a paradigm shift based on our approach to very rapidly manufacture CD19-specific T cells within 2 days using our non-viral approach to CAR-T therapy based on the Sleeping Beauty platform.”
The phase 1 trial in question is a third-generation trial in which the CAR T cells are designed to co-express CD19-specific CAR, membrane-bound interleukin 15, and a safety switch.
The findings from earlier generation phase 1 trials have been previously reported in The Journal of Clinical Investigation.
The US Food and Drug Administrated (FDA) placed a clinical hold on the phase 1 trial of the Sleeping Beauty (SB)-generated CAR T-cell therapy in relapsed or refractory leukemia and lymphoma patients.
The Sleeping Beauty platform was designed to very rapidly manufacture CD19-specific CAR T cells at the point of care.
All SB-CAR T-cell processing is planned to take place within 2 days at the healthcare facility, thus eliminating shipping cells from hospitals to production sites and back again.
The FDA is requesting more chemistry, manufacturing, and control (CMC) information before allowing the trial to proceed.
The Sleeping Beauty technology, a non-viral transposon/transposase system, has the potential to reduce the costs and complexity associated with recombinant viral vector-based immunotherapy, according to developers.
Ziopharm Oncology, Precigen, Inc, a wholly owned subsidiary of Intrexon Corporation, and the University of Texas MD Anderson Cancer Center, are developing the Sleeping Beauty CAR T cell therapy.
“We know what is needed to address the hold issues and are looking forward to responding to the agency in a timely manner,” said Laurence Cooper, MD, PhD, chief executive officer of Ziopharm, in a corporate release.
“We are undertaking cutting-edge science and are on the verge of a paradigm shift based on our approach to very rapidly manufacture CD19-specific T cells within 2 days using our non-viral approach to CAR-T therapy based on the Sleeping Beauty platform.”
The phase 1 trial in question is a third-generation trial in which the CAR T cells are designed to co-express CD19-specific CAR, membrane-bound interleukin 15, and a safety switch.
The findings from earlier generation phase 1 trials have been previously reported in The Journal of Clinical Investigation.
Inflammatory myopathy following tattoo reported in an immunocompromised patient
A case of inflammatory .
Writing in the June 18 online edition of BMJ Case Reports, clinicians described a 31-year-old woman who was on long-term immunosuppressive therapy after bilateral lung transplants for cystic fibrosis.
The woman received a large, colored tattoo on her upper leg, with no immediate complications beyond the usual mild skin irritation. However, 9 days later, she developed pain in her left thigh and knee that was severe enough to require analgesic treatment that included tramadol and paracetamol.
The pain settled over the following few months, but the woman continued to experience a sense of fullness from her hip to knee along the medial side of her thigh. She presented to a rheumatology clinic 10 months after she was tattooed, with pain that was still constant and disturbing her sleep, but with no apparent aggravating factors and, otherwise, she was in good health.
Work-up included an MRI that showed focal inflammation of the vastus medialis muscle, particularly in the distal third, but a biopsy found no bacterial growth, nor was there any bacterial or fungal infection found in fluid drawn from the knee. However, histopathology revealed scattered internal nuclei, atrophic fibers, a mild perivascular inflammatory infiltrate, and upregulation of human leukocyte antigen.
In the report, William T. Wilson, MD, and his colleagues from the department of trauma and orthopedics, NHS Greater Glasgow and Clyde, Glasgow, said that these findings gave the impression of an inflammatory myopathy in which the pathologic response may have been influenced by the immunosuppression.
“To our knowledge, there have been no previously reported cases of tattoo-associated reactions causing an inflammatory myopathy,” they wrote. “This could be a rare occurrence or represent an underdiagnosis for patients presenting with similar symptoms having had tattoos.”
The authors suggested there was a chance that the myopathy may have been stimulated by a toxin or pathogen introduced during tattoo procedure. However, they pointed out that they could not identify a causative pathogen, although the timing of onset and location of symptoms correlated with the tattoo application.
“This case serves as a reminder to consider tattoo-related complications as part of the differential diagnosis when patients, especially the immune-suppressed, present with unusual atraumatic musculoskeletal symptoms,” they wrote.
After the biopsy, the woman received physiotherapy in the form of basic quadriceps-strengthening exercises. Her condition did not start to improve until about 1 year after the onset of symptoms, and by 3 years, she had no more pain and had resumed normal activities.
No funding or conflicts of interest were declared.
SOURCE: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi: 10.1136/bcr-2018-224968.
A case of inflammatory .
Writing in the June 18 online edition of BMJ Case Reports, clinicians described a 31-year-old woman who was on long-term immunosuppressive therapy after bilateral lung transplants for cystic fibrosis.
The woman received a large, colored tattoo on her upper leg, with no immediate complications beyond the usual mild skin irritation. However, 9 days later, she developed pain in her left thigh and knee that was severe enough to require analgesic treatment that included tramadol and paracetamol.
The pain settled over the following few months, but the woman continued to experience a sense of fullness from her hip to knee along the medial side of her thigh. She presented to a rheumatology clinic 10 months after she was tattooed, with pain that was still constant and disturbing her sleep, but with no apparent aggravating factors and, otherwise, she was in good health.
Work-up included an MRI that showed focal inflammation of the vastus medialis muscle, particularly in the distal third, but a biopsy found no bacterial growth, nor was there any bacterial or fungal infection found in fluid drawn from the knee. However, histopathology revealed scattered internal nuclei, atrophic fibers, a mild perivascular inflammatory infiltrate, and upregulation of human leukocyte antigen.
In the report, William T. Wilson, MD, and his colleagues from the department of trauma and orthopedics, NHS Greater Glasgow and Clyde, Glasgow, said that these findings gave the impression of an inflammatory myopathy in which the pathologic response may have been influenced by the immunosuppression.
“To our knowledge, there have been no previously reported cases of tattoo-associated reactions causing an inflammatory myopathy,” they wrote. “This could be a rare occurrence or represent an underdiagnosis for patients presenting with similar symptoms having had tattoos.”
The authors suggested there was a chance that the myopathy may have been stimulated by a toxin or pathogen introduced during tattoo procedure. However, they pointed out that they could not identify a causative pathogen, although the timing of onset and location of symptoms correlated with the tattoo application.
“This case serves as a reminder to consider tattoo-related complications as part of the differential diagnosis when patients, especially the immune-suppressed, present with unusual atraumatic musculoskeletal symptoms,” they wrote.
After the biopsy, the woman received physiotherapy in the form of basic quadriceps-strengthening exercises. Her condition did not start to improve until about 1 year after the onset of symptoms, and by 3 years, she had no more pain and had resumed normal activities.
No funding or conflicts of interest were declared.
SOURCE: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi: 10.1136/bcr-2018-224968.
A case of inflammatory .
Writing in the June 18 online edition of BMJ Case Reports, clinicians described a 31-year-old woman who was on long-term immunosuppressive therapy after bilateral lung transplants for cystic fibrosis.
The woman received a large, colored tattoo on her upper leg, with no immediate complications beyond the usual mild skin irritation. However, 9 days later, she developed pain in her left thigh and knee that was severe enough to require analgesic treatment that included tramadol and paracetamol.
The pain settled over the following few months, but the woman continued to experience a sense of fullness from her hip to knee along the medial side of her thigh. She presented to a rheumatology clinic 10 months after she was tattooed, with pain that was still constant and disturbing her sleep, but with no apparent aggravating factors and, otherwise, she was in good health.
Work-up included an MRI that showed focal inflammation of the vastus medialis muscle, particularly in the distal third, but a biopsy found no bacterial growth, nor was there any bacterial or fungal infection found in fluid drawn from the knee. However, histopathology revealed scattered internal nuclei, atrophic fibers, a mild perivascular inflammatory infiltrate, and upregulation of human leukocyte antigen.
In the report, William T. Wilson, MD, and his colleagues from the department of trauma and orthopedics, NHS Greater Glasgow and Clyde, Glasgow, said that these findings gave the impression of an inflammatory myopathy in which the pathologic response may have been influenced by the immunosuppression.
“To our knowledge, there have been no previously reported cases of tattoo-associated reactions causing an inflammatory myopathy,” they wrote. “This could be a rare occurrence or represent an underdiagnosis for patients presenting with similar symptoms having had tattoos.”
The authors suggested there was a chance that the myopathy may have been stimulated by a toxin or pathogen introduced during tattoo procedure. However, they pointed out that they could not identify a causative pathogen, although the timing of onset and location of symptoms correlated with the tattoo application.
“This case serves as a reminder to consider tattoo-related complications as part of the differential diagnosis when patients, especially the immune-suppressed, present with unusual atraumatic musculoskeletal symptoms,” they wrote.
After the biopsy, the woman received physiotherapy in the form of basic quadriceps-strengthening exercises. Her condition did not start to improve until about 1 year after the onset of symptoms, and by 3 years, she had no more pain and had resumed normal activities.
No funding or conflicts of interest were declared.
SOURCE: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi: 10.1136/bcr-2018-224968.
FROM BMJ CASE REPORTS
Key clinical point: Consider tattoo-induced myopathy in immunosuppressed individuals.
Major finding: Tattooing has been linked to inflammatory myopathy in an immunosuppressed woman.
Study details: A report of a 31-year-old double lung transplant recipient who developed inflammatory myopathy after receiving a tattoo.
Disclosures: No funding or conflicts of interest were declared.
Source: Wilson W et al. BMJ Case Rep. 2018. Jun 18. doi:10.1136/bcr-2018-224968.
Rural cancer patients report faster care than urban counterparts
in a survey of 6,826 Medicare beneficiaries.
Taken as a whole, a similar quality of care was reported between the two groups, but the picture changed when racial/ethnic subgroups were considered. Non-Hispanic black and Hispanic patients in rural locations reported inferior care to their urban counterparts, investigators wrote in Cancer.
“Cancer patients living in rural areas are vulnerable and have unique health care needs,” wrote lead author Michelle A. Mollica, PhD, of the National Cancer Institute, and her colleagues. “To our knowledge, this is the first study to explore the patient’s perception of the timeliness of care in such a large, multiregion sample of cancer patients.”
In 2003, the National Academy of Medicine concluded that living in a rural environment was associated with poorer health. Existing research surrounding cancer has echoed this concern, showing that rural patients have higher rates of cancer and mortality, longer delays in diagnosis, and limited access to care.
The current, retrospective study involved 6,140 urban and 686 rural Medicare beneficiaries who were aged at least 65 years when diagnosed with either breast, lung, colorectal, or prostate cancer. Consumer Assessment of Healthcare Providers and Systems surveys were conducted between 1998 and 2013, then linked with data from the Surveillance, Epidemiology, and End Results registry program.
Surveys were conducted within 12 months of diagnosis, during which time patients were asked about their access to care as defined by two composites: “Getting Needed Care” and “Getting Care Quickly.” Getting Needed Care included ease of making appointments and receiving treatments and Getting Care Quickly questions asked about appointment delays and time spent waiting at the doctor’s office. Answers were converted to a numerical score from 0 to 100, with 0 being the worst and 100 being the best.
For both composites, mean scores for urban and rural locations were greater than 85 out of 100.
In contrast to previous studies, urban patients reported longer delays in care, scoring Getting Care Quickly 2.27 points lower than rural patients (P = .02). Pacific Islanders and non-Hispanic Asian patients from rural places reported even faster care, ranking about 8 points higher than urban patients of the same race/ethnicity.
Locality did not have a significant impact on Getting Needed Care unless race/ethnicity was also considered (P = .04). Non-Hispanic white patients from rural locations scored Getting Needed Care about 2 points higher than urban white patients, while Hispanic and non-Hispanic black patients had an opposite trend, with this rural cohort ranking Getting Needed Care lower than urban patients of the same race/ethnicity.
“Geographic residence is but one important factor in cancer care delivery,” the authors noted. “There is a need for fine-grained research looking at specific barriers for urban residents, experiences of racial/ethnic minority survivors residing in rural areas, and rural-urban differences in the clinic settings in which medical care is delivered.”
The authors had no disclosures to report.
SOURCE: Mollica MA et al. Cancer. 2018 Jun 7. doi: 10.1002/cncr.31541.
in a survey of 6,826 Medicare beneficiaries.
Taken as a whole, a similar quality of care was reported between the two groups, but the picture changed when racial/ethnic subgroups were considered. Non-Hispanic black and Hispanic patients in rural locations reported inferior care to their urban counterparts, investigators wrote in Cancer.
“Cancer patients living in rural areas are vulnerable and have unique health care needs,” wrote lead author Michelle A. Mollica, PhD, of the National Cancer Institute, and her colleagues. “To our knowledge, this is the first study to explore the patient’s perception of the timeliness of care in such a large, multiregion sample of cancer patients.”
In 2003, the National Academy of Medicine concluded that living in a rural environment was associated with poorer health. Existing research surrounding cancer has echoed this concern, showing that rural patients have higher rates of cancer and mortality, longer delays in diagnosis, and limited access to care.
The current, retrospective study involved 6,140 urban and 686 rural Medicare beneficiaries who were aged at least 65 years when diagnosed with either breast, lung, colorectal, or prostate cancer. Consumer Assessment of Healthcare Providers and Systems surveys were conducted between 1998 and 2013, then linked with data from the Surveillance, Epidemiology, and End Results registry program.
Surveys were conducted within 12 months of diagnosis, during which time patients were asked about their access to care as defined by two composites: “Getting Needed Care” and “Getting Care Quickly.” Getting Needed Care included ease of making appointments and receiving treatments and Getting Care Quickly questions asked about appointment delays and time spent waiting at the doctor’s office. Answers were converted to a numerical score from 0 to 100, with 0 being the worst and 100 being the best.
For both composites, mean scores for urban and rural locations were greater than 85 out of 100.
In contrast to previous studies, urban patients reported longer delays in care, scoring Getting Care Quickly 2.27 points lower than rural patients (P = .02). Pacific Islanders and non-Hispanic Asian patients from rural places reported even faster care, ranking about 8 points higher than urban patients of the same race/ethnicity.
Locality did not have a significant impact on Getting Needed Care unless race/ethnicity was also considered (P = .04). Non-Hispanic white patients from rural locations scored Getting Needed Care about 2 points higher than urban white patients, while Hispanic and non-Hispanic black patients had an opposite trend, with this rural cohort ranking Getting Needed Care lower than urban patients of the same race/ethnicity.
“Geographic residence is but one important factor in cancer care delivery,” the authors noted. “There is a need for fine-grained research looking at specific barriers for urban residents, experiences of racial/ethnic minority survivors residing in rural areas, and rural-urban differences in the clinic settings in which medical care is delivered.”
The authors had no disclosures to report.
SOURCE: Mollica MA et al. Cancer. 2018 Jun 7. doi: 10.1002/cncr.31541.
in a survey of 6,826 Medicare beneficiaries.
Taken as a whole, a similar quality of care was reported between the two groups, but the picture changed when racial/ethnic subgroups were considered. Non-Hispanic black and Hispanic patients in rural locations reported inferior care to their urban counterparts, investigators wrote in Cancer.
“Cancer patients living in rural areas are vulnerable and have unique health care needs,” wrote lead author Michelle A. Mollica, PhD, of the National Cancer Institute, and her colleagues. “To our knowledge, this is the first study to explore the patient’s perception of the timeliness of care in such a large, multiregion sample of cancer patients.”
In 2003, the National Academy of Medicine concluded that living in a rural environment was associated with poorer health. Existing research surrounding cancer has echoed this concern, showing that rural patients have higher rates of cancer and mortality, longer delays in diagnosis, and limited access to care.
The current, retrospective study involved 6,140 urban and 686 rural Medicare beneficiaries who were aged at least 65 years when diagnosed with either breast, lung, colorectal, or prostate cancer. Consumer Assessment of Healthcare Providers and Systems surveys were conducted between 1998 and 2013, then linked with data from the Surveillance, Epidemiology, and End Results registry program.
Surveys were conducted within 12 months of diagnosis, during which time patients were asked about their access to care as defined by two composites: “Getting Needed Care” and “Getting Care Quickly.” Getting Needed Care included ease of making appointments and receiving treatments and Getting Care Quickly questions asked about appointment delays and time spent waiting at the doctor’s office. Answers were converted to a numerical score from 0 to 100, with 0 being the worst and 100 being the best.
For both composites, mean scores for urban and rural locations were greater than 85 out of 100.
In contrast to previous studies, urban patients reported longer delays in care, scoring Getting Care Quickly 2.27 points lower than rural patients (P = .02). Pacific Islanders and non-Hispanic Asian patients from rural places reported even faster care, ranking about 8 points higher than urban patients of the same race/ethnicity.
Locality did not have a significant impact on Getting Needed Care unless race/ethnicity was also considered (P = .04). Non-Hispanic white patients from rural locations scored Getting Needed Care about 2 points higher than urban white patients, while Hispanic and non-Hispanic black patients had an opposite trend, with this rural cohort ranking Getting Needed Care lower than urban patients of the same race/ethnicity.
“Geographic residence is but one important factor in cancer care delivery,” the authors noted. “There is a need for fine-grained research looking at specific barriers for urban residents, experiences of racial/ethnic minority survivors residing in rural areas, and rural-urban differences in the clinic settings in which medical care is delivered.”
The authors had no disclosures to report.
SOURCE: Mollica MA et al. Cancer. 2018 Jun 7. doi: 10.1002/cncr.31541.
FROM CANCER
Key clinical point: Cancer patients living in rural areas reported more timely care than urban patients.
Major finding: In a Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey, urban patients rated “Getting Care Quickly” 2.27 points lower than rural patients (P = .02).
Study details: A retrospective study of 6,140 urban and 686 rural Medicare beneficiaries who were aged at least 65 years when diagnosed with either breast, lung, colorectal, or prostate cancer. CAHPS patient experience surveys were conducted between 1998 and 2013, then linked with Surveillance, Epidemiology, and End Results data.
Disclosures: The authors had no disclosures to report.
Source: Mollica MA et al. Cancer. 2018 Jun 7. doi: 10.1002/cncr.31541.
Type 2 Diabetes Increases the Risk of Parkinson’s Disease
The risk is particularly high among younger patients and those with complications from diabetes.
Patients with type 2 diabetes mellitus have an increased risk of developing Parkinson’s disease later in life, according to an investigation published online ahead of print June 13 in Neurology. The magnitude of risk is greater in younger patients and in patients with complications from diabetes.
Investigators have hypothesized an association between diabetes and the risk of Parkinson’s disease, but studies of the potential link have had conflicting results. Thomas T. Warner, MD, PhD, Professor of Clinical Neurology at University College London (UCL), and colleagues conducted a retrospective cohort study to examine this question anew.
Analyzing a Nationwide Hospital Database
The researchers reviewed English national Hospital Episode Statistics and mortality data collected between 1999 and 2011 and created a cohort of 2,017,115 patients who had been admitted for hospital care with a diagnosis of type 2 diabetes. They created a reference cohort of 6,173,208 patients without diabetes who were admitted for minor medical and surgical procedures. Conditions in this cohort included sprains, inguinal hernia, bruising, and hip replacement. People with Parkinson’s disease, ischemic cerebral infarction, vascular parkinsonism, drug-induced secondary parkinsonism, and normal pressure hydrocephalus were excluded from the study. Dr. Warner and colleagues created multivariable Cox proportional hazard regression models to estimate the risk of subsequent Parkinson’s disease.
Participants with diabetes had a greater risk of a subsequent diagnosis of Parkinson’s disease than patients in the reference cohort (adjusted hazard ratio [HR], 1.32). In subgroup analyses, the researchers found that the risk was substantially higher among patients between ages 25 and 44 (adjusted HR, 3.81) and those with complicated diabetes (adjusted HR, 1.49). Genetic factors may exert a relatively greater effect on younger people, and this difference may account for the increased risk among younger participants with diabetes, said the authors.
The adjusted HR of Parkinson’s disease was 1.40 in patients with diabetes between ages 65 and 74 and 1.18 in those age 75 or older. “The association in elderly patients may be the consequence of disrupted insulin signaling secondary to additional lifestyle and environmental factors causing cumulative pathogenic brain changes,” said Dr. Warner and colleagues.
No Adjustment for Potential Confounders
The large size of the database and the ability to exclude people with cerebrovascular disease and drug-induced and vascular parkinsonisms were among the study’s main strengths, according to the authors. Its weaknesses included an inability to adjust for potential confounders and the lack of clinical information about Parkinson’s disease ascertainment beyond routinely collected data.
The results could help researchers identify “new ways to treat or prevent the development of Parkinson’s disease, such as use of antidiabetes drugs to restore the brain’s insulin signaling,” said Dr. Warner. “A UCL-led study published last year found that a drug commonly used to treat diabetes shows promise in not only relieving Parkinson’s disease symptoms, but potentially altering the course of the disease itself. What we do not know is whether trying to treat people with type 2 diabetes better would reduce the risk of developing Parkinson’s disease.”
—Erik Greb
Suggested Reading
De Pablo-Fernandez E, Goldacre R, Pakpoor J, et al. Association between diabetes and subsequent Parkinson disease: a record-linkage cohort study. Neurology. 2018 Jun 13 [Epub ahead of print].
The risk is particularly high among younger patients and those with complications from diabetes.
The risk is particularly high among younger patients and those with complications from diabetes.
Patients with type 2 diabetes mellitus have an increased risk of developing Parkinson’s disease later in life, according to an investigation published online ahead of print June 13 in Neurology. The magnitude of risk is greater in younger patients and in patients with complications from diabetes.
Investigators have hypothesized an association between diabetes and the risk of Parkinson’s disease, but studies of the potential link have had conflicting results. Thomas T. Warner, MD, PhD, Professor of Clinical Neurology at University College London (UCL), and colleagues conducted a retrospective cohort study to examine this question anew.
Analyzing a Nationwide Hospital Database
The researchers reviewed English national Hospital Episode Statistics and mortality data collected between 1999 and 2011 and created a cohort of 2,017,115 patients who had been admitted for hospital care with a diagnosis of type 2 diabetes. They created a reference cohort of 6,173,208 patients without diabetes who were admitted for minor medical and surgical procedures. Conditions in this cohort included sprains, inguinal hernia, bruising, and hip replacement. People with Parkinson’s disease, ischemic cerebral infarction, vascular parkinsonism, drug-induced secondary parkinsonism, and normal pressure hydrocephalus were excluded from the study. Dr. Warner and colleagues created multivariable Cox proportional hazard regression models to estimate the risk of subsequent Parkinson’s disease.
Participants with diabetes had a greater risk of a subsequent diagnosis of Parkinson’s disease than patients in the reference cohort (adjusted hazard ratio [HR], 1.32). In subgroup analyses, the researchers found that the risk was substantially higher among patients between ages 25 and 44 (adjusted HR, 3.81) and those with complicated diabetes (adjusted HR, 1.49). Genetic factors may exert a relatively greater effect on younger people, and this difference may account for the increased risk among younger participants with diabetes, said the authors.
The adjusted HR of Parkinson’s disease was 1.40 in patients with diabetes between ages 65 and 74 and 1.18 in those age 75 or older. “The association in elderly patients may be the consequence of disrupted insulin signaling secondary to additional lifestyle and environmental factors causing cumulative pathogenic brain changes,” said Dr. Warner and colleagues.
No Adjustment for Potential Confounders
The large size of the database and the ability to exclude people with cerebrovascular disease and drug-induced and vascular parkinsonisms were among the study’s main strengths, according to the authors. Its weaknesses included an inability to adjust for potential confounders and the lack of clinical information about Parkinson’s disease ascertainment beyond routinely collected data.
The results could help researchers identify “new ways to treat or prevent the development of Parkinson’s disease, such as use of antidiabetes drugs to restore the brain’s insulin signaling,” said Dr. Warner. “A UCL-led study published last year found that a drug commonly used to treat diabetes shows promise in not only relieving Parkinson’s disease symptoms, but potentially altering the course of the disease itself. What we do not know is whether trying to treat people with type 2 diabetes better would reduce the risk of developing Parkinson’s disease.”
—Erik Greb
Suggested Reading
De Pablo-Fernandez E, Goldacre R, Pakpoor J, et al. Association between diabetes and subsequent Parkinson disease: a record-linkage cohort study. Neurology. 2018 Jun 13 [Epub ahead of print].
Patients with type 2 diabetes mellitus have an increased risk of developing Parkinson’s disease later in life, according to an investigation published online ahead of print June 13 in Neurology. The magnitude of risk is greater in younger patients and in patients with complications from diabetes.
Investigators have hypothesized an association between diabetes and the risk of Parkinson’s disease, but studies of the potential link have had conflicting results. Thomas T. Warner, MD, PhD, Professor of Clinical Neurology at University College London (UCL), and colleagues conducted a retrospective cohort study to examine this question anew.
Analyzing a Nationwide Hospital Database
The researchers reviewed English national Hospital Episode Statistics and mortality data collected between 1999 and 2011 and created a cohort of 2,017,115 patients who had been admitted for hospital care with a diagnosis of type 2 diabetes. They created a reference cohort of 6,173,208 patients without diabetes who were admitted for minor medical and surgical procedures. Conditions in this cohort included sprains, inguinal hernia, bruising, and hip replacement. People with Parkinson’s disease, ischemic cerebral infarction, vascular parkinsonism, drug-induced secondary parkinsonism, and normal pressure hydrocephalus were excluded from the study. Dr. Warner and colleagues created multivariable Cox proportional hazard regression models to estimate the risk of subsequent Parkinson’s disease.
Participants with diabetes had a greater risk of a subsequent diagnosis of Parkinson’s disease than patients in the reference cohort (adjusted hazard ratio [HR], 1.32). In subgroup analyses, the researchers found that the risk was substantially higher among patients between ages 25 and 44 (adjusted HR, 3.81) and those with complicated diabetes (adjusted HR, 1.49). Genetic factors may exert a relatively greater effect on younger people, and this difference may account for the increased risk among younger participants with diabetes, said the authors.
The adjusted HR of Parkinson’s disease was 1.40 in patients with diabetes between ages 65 and 74 and 1.18 in those age 75 or older. “The association in elderly patients may be the consequence of disrupted insulin signaling secondary to additional lifestyle and environmental factors causing cumulative pathogenic brain changes,” said Dr. Warner and colleagues.
No Adjustment for Potential Confounders
The large size of the database and the ability to exclude people with cerebrovascular disease and drug-induced and vascular parkinsonisms were among the study’s main strengths, according to the authors. Its weaknesses included an inability to adjust for potential confounders and the lack of clinical information about Parkinson’s disease ascertainment beyond routinely collected data.
The results could help researchers identify “new ways to treat or prevent the development of Parkinson’s disease, such as use of antidiabetes drugs to restore the brain’s insulin signaling,” said Dr. Warner. “A UCL-led study published last year found that a drug commonly used to treat diabetes shows promise in not only relieving Parkinson’s disease symptoms, but potentially altering the course of the disease itself. What we do not know is whether trying to treat people with type 2 diabetes better would reduce the risk of developing Parkinson’s disease.”
—Erik Greb
Suggested Reading
De Pablo-Fernandez E, Goldacre R, Pakpoor J, et al. Association between diabetes and subsequent Parkinson disease: a record-linkage cohort study. Neurology. 2018 Jun 13 [Epub ahead of print].
In T2DM, healthy lifestyle lowers CVD risk, mortality
, according to the results of a pooled analysis of two large observational cohort studies.
Relevant criteria included following a high-quality diet, not smoking, exercising moderately to vigorously for at least 2.5 hours per week, and limiting alcohol intake to 5-15 g of alcohol per day for women or 5-30 g/day for men. After the researchers controlled for possible confounders, individuals who met at least three of these criteria had about a 52% lower risk of new-onset CVD (adjusted hazard ratio, 0.48; 95% confidence interval, 0.40-0.59) and a 68% lower risk of CVD-related mortality (HR, 0.32; 95% CI, 0.22-0.47), said Gang Liu, PhD, of Harvard T.H. Chan School of Public Health, Boston, and his associates. “Further research is needed to identify the most effective strategies to encourage patients with diabetes to adopt and maintain a healthy lifestyle,” they wrote. The report was published online June 18 in the Journal of the American College of Cardiology.
Cardiovascular disease is common in type 2 diabetes (T2DM), but few studies have examined the possible mitigating effects of healthy lifestyle. For this study, the researchers analyzed questionnaire data for 11,527 participants with T2DM diagnosed after enrollment in either the Nurses’ Health Study or the Health Professionals Follow-Up Study. Over an average follow-up time of 13.3 years, there were 2,311 incident cases of CVD, including 498 cases of stroke, and 858 deaths from CVD. The reduced risk of cardiovascular events remained significant even after the researchers controlled for factors such as body mass index, hypertension, hypercholesterolemia, use of antihypertensive agents, cholesterol lowering drugs, diabetes medication, and hemoglobin A1c.
Healthy lifestyle also was associated with significant reductions in the individual risk of coronary heart disease (HR, 0.53) and stroke (HR, 0.33), the investigators said. In this population, 40% of the risk of CVD mortality could be attributed to poor adherence to a healthy lifestyle, they added. Importantly, individuals who improved their lifestyle after a T2DM diagnosis had a significantly lower risk of CVD and CVD mortality than those who did not. The findings, they concluded, “support the tremendous benefits of adopting a healthy lifestyle in reducing the subsequent burden of cardiovascular complications in patients with T2DM.”
The National Institutes of Health provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Liu G et al. J Am Coll Cardiol. 2018;71:2867-76. doi: 10.1016/j.jacc.2018.04.027.
The findings send “a clear message” that health care promotion, advocacy, and research should keep focusing on healthy lifestyle factors, not only to improve glycemic control, but also to cut overall cardiovascular risk, experts wrote in an accompanying editorial.
The study supported a healthy lifestyle across the board, from overall CVD risk reduction to reduced risk of coronary heart disease or stroke, even after the researchers controlled for important potential confounders, wrote Kim Connelly, MBBS, PhD, Sumeet Gandhi, MD, and Edward Horton, MD. Their comments were published in Journal of the American College of Cardiology.
“Encouragingly, patients who increased the number of low-risk lifestyle factors from the time of initial diagnosis were also shown to have a lower incidence of cardiovascular disease,” they added.
But many questions persist, they noted. These include which diets are best, how much alcohol really is safe, whether there are minimum or maximum exercises thresholds, which type of exercise (if any) is best, how to monitor compliance, which health care professional should prescribe diet and exercise, and whether the findings are generalizable to groups of other ethnicities or socioeconomic levels.
Dr. Connelly and Dr. Gandhi are with University of Toronto. Dr. Horton is with Harvard University, Boston. Dr. Connelly disclosed ties to Servier, Boehringer Ingelheim, Janssen, Merck, AstraZeneca, and Novartis. Dr. Gandhi and Dr. Horton reported having no conflicts. These comments summarize their editorial (J Am Coll Cardiol. 2018;71:2877-79).
The findings send “a clear message” that health care promotion, advocacy, and research should keep focusing on healthy lifestyle factors, not only to improve glycemic control, but also to cut overall cardiovascular risk, experts wrote in an accompanying editorial.
The study supported a healthy lifestyle across the board, from overall CVD risk reduction to reduced risk of coronary heart disease or stroke, even after the researchers controlled for important potential confounders, wrote Kim Connelly, MBBS, PhD, Sumeet Gandhi, MD, and Edward Horton, MD. Their comments were published in Journal of the American College of Cardiology.
“Encouragingly, patients who increased the number of low-risk lifestyle factors from the time of initial diagnosis were also shown to have a lower incidence of cardiovascular disease,” they added.
But many questions persist, they noted. These include which diets are best, how much alcohol really is safe, whether there are minimum or maximum exercises thresholds, which type of exercise (if any) is best, how to monitor compliance, which health care professional should prescribe diet and exercise, and whether the findings are generalizable to groups of other ethnicities or socioeconomic levels.
Dr. Connelly and Dr. Gandhi are with University of Toronto. Dr. Horton is with Harvard University, Boston. Dr. Connelly disclosed ties to Servier, Boehringer Ingelheim, Janssen, Merck, AstraZeneca, and Novartis. Dr. Gandhi and Dr. Horton reported having no conflicts. These comments summarize their editorial (J Am Coll Cardiol. 2018;71:2877-79).
The findings send “a clear message” that health care promotion, advocacy, and research should keep focusing on healthy lifestyle factors, not only to improve glycemic control, but also to cut overall cardiovascular risk, experts wrote in an accompanying editorial.
The study supported a healthy lifestyle across the board, from overall CVD risk reduction to reduced risk of coronary heart disease or stroke, even after the researchers controlled for important potential confounders, wrote Kim Connelly, MBBS, PhD, Sumeet Gandhi, MD, and Edward Horton, MD. Their comments were published in Journal of the American College of Cardiology.
“Encouragingly, patients who increased the number of low-risk lifestyle factors from the time of initial diagnosis were also shown to have a lower incidence of cardiovascular disease,” they added.
But many questions persist, they noted. These include which diets are best, how much alcohol really is safe, whether there are minimum or maximum exercises thresholds, which type of exercise (if any) is best, how to monitor compliance, which health care professional should prescribe diet and exercise, and whether the findings are generalizable to groups of other ethnicities or socioeconomic levels.
Dr. Connelly and Dr. Gandhi are with University of Toronto. Dr. Horton is with Harvard University, Boston. Dr. Connelly disclosed ties to Servier, Boehringer Ingelheim, Janssen, Merck, AstraZeneca, and Novartis. Dr. Gandhi and Dr. Horton reported having no conflicts. These comments summarize their editorial (J Am Coll Cardiol. 2018;71:2877-79).
, according to the results of a pooled analysis of two large observational cohort studies.
Relevant criteria included following a high-quality diet, not smoking, exercising moderately to vigorously for at least 2.5 hours per week, and limiting alcohol intake to 5-15 g of alcohol per day for women or 5-30 g/day for men. After the researchers controlled for possible confounders, individuals who met at least three of these criteria had about a 52% lower risk of new-onset CVD (adjusted hazard ratio, 0.48; 95% confidence interval, 0.40-0.59) and a 68% lower risk of CVD-related mortality (HR, 0.32; 95% CI, 0.22-0.47), said Gang Liu, PhD, of Harvard T.H. Chan School of Public Health, Boston, and his associates. “Further research is needed to identify the most effective strategies to encourage patients with diabetes to adopt and maintain a healthy lifestyle,” they wrote. The report was published online June 18 in the Journal of the American College of Cardiology.
Cardiovascular disease is common in type 2 diabetes (T2DM), but few studies have examined the possible mitigating effects of healthy lifestyle. For this study, the researchers analyzed questionnaire data for 11,527 participants with T2DM diagnosed after enrollment in either the Nurses’ Health Study or the Health Professionals Follow-Up Study. Over an average follow-up time of 13.3 years, there were 2,311 incident cases of CVD, including 498 cases of stroke, and 858 deaths from CVD. The reduced risk of cardiovascular events remained significant even after the researchers controlled for factors such as body mass index, hypertension, hypercholesterolemia, use of antihypertensive agents, cholesterol lowering drugs, diabetes medication, and hemoglobin A1c.
Healthy lifestyle also was associated with significant reductions in the individual risk of coronary heart disease (HR, 0.53) and stroke (HR, 0.33), the investigators said. In this population, 40% of the risk of CVD mortality could be attributed to poor adherence to a healthy lifestyle, they added. Importantly, individuals who improved their lifestyle after a T2DM diagnosis had a significantly lower risk of CVD and CVD mortality than those who did not. The findings, they concluded, “support the tremendous benefits of adopting a healthy lifestyle in reducing the subsequent burden of cardiovascular complications in patients with T2DM.”
The National Institutes of Health provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Liu G et al. J Am Coll Cardiol. 2018;71:2867-76. doi: 10.1016/j.jacc.2018.04.027.
, according to the results of a pooled analysis of two large observational cohort studies.
Relevant criteria included following a high-quality diet, not smoking, exercising moderately to vigorously for at least 2.5 hours per week, and limiting alcohol intake to 5-15 g of alcohol per day for women or 5-30 g/day for men. After the researchers controlled for possible confounders, individuals who met at least three of these criteria had about a 52% lower risk of new-onset CVD (adjusted hazard ratio, 0.48; 95% confidence interval, 0.40-0.59) and a 68% lower risk of CVD-related mortality (HR, 0.32; 95% CI, 0.22-0.47), said Gang Liu, PhD, of Harvard T.H. Chan School of Public Health, Boston, and his associates. “Further research is needed to identify the most effective strategies to encourage patients with diabetes to adopt and maintain a healthy lifestyle,” they wrote. The report was published online June 18 in the Journal of the American College of Cardiology.
Cardiovascular disease is common in type 2 diabetes (T2DM), but few studies have examined the possible mitigating effects of healthy lifestyle. For this study, the researchers analyzed questionnaire data for 11,527 participants with T2DM diagnosed after enrollment in either the Nurses’ Health Study or the Health Professionals Follow-Up Study. Over an average follow-up time of 13.3 years, there were 2,311 incident cases of CVD, including 498 cases of stroke, and 858 deaths from CVD. The reduced risk of cardiovascular events remained significant even after the researchers controlled for factors such as body mass index, hypertension, hypercholesterolemia, use of antihypertensive agents, cholesterol lowering drugs, diabetes medication, and hemoglobin A1c.
Healthy lifestyle also was associated with significant reductions in the individual risk of coronary heart disease (HR, 0.53) and stroke (HR, 0.33), the investigators said. In this population, 40% of the risk of CVD mortality could be attributed to poor adherence to a healthy lifestyle, they added. Importantly, individuals who improved their lifestyle after a T2DM diagnosis had a significantly lower risk of CVD and CVD mortality than those who did not. The findings, they concluded, “support the tremendous benefits of adopting a healthy lifestyle in reducing the subsequent burden of cardiovascular complications in patients with T2DM.”
The National Institutes of Health provided funding. The investigators reported having no relevant conflicts of interest.
SOURCE: Liu G et al. J Am Coll Cardiol. 2018;71:2867-76. doi: 10.1016/j.jacc.2018.04.027.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Eating a high-quality diet, not smoking, exercising for at least 150 minutes weekly, and drinking only moderate amounts of alcohol led to a statistically significant decrease in risk of cardiovascular disease among persons with type 2 diabetes mellitus.
Major finding: Over an average of 13.3 years of follow-up, the adjusted risk of CVD was 52% lower in participants with at least three of these healthy lifestyle factors compared with those with none (multivariate-adjusted HR, 0.48; 95% CI, 0.40-0.59).
Study details: Pooled analysis of data from 11,527 patients from the Nurses’ Health Study and the Health Professionals Follow-Up Study.
Disclosures: The National Institutes of Health provided funding. The investigators reported having no relevant conflicts of interest.
Source: Liu G et al. J Am Coll Cardiol. 2018;71:2867-76.