User login
Numb Toes and Other Woes: Diabetic Peripheral and Autonomic Neuropathies
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This video was filmed at Metabolic & Endocrine Disease Summit (MEDS). Click here to learn more.
Study identifies characteristics that may constitute the MS prodrome
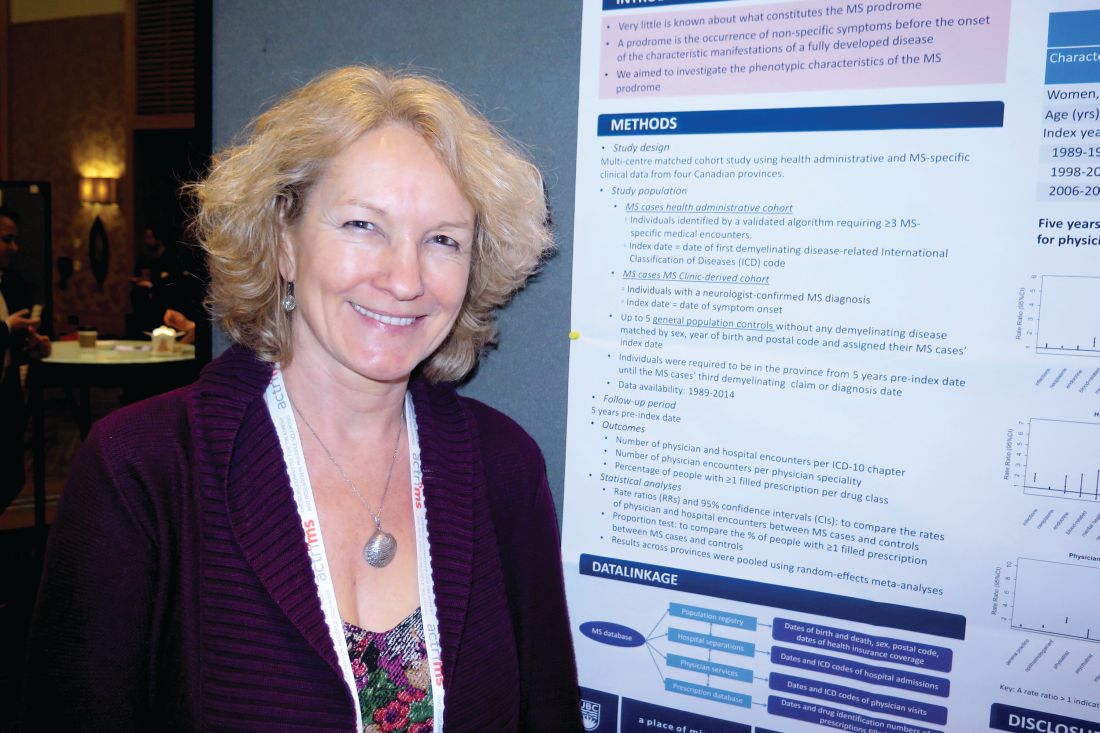
SAN DIEGO – Compared with controls, patients who developed MS were more frequently admitted to the hospital or visited a physician for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system in the 5 years prior to MS onset, a multicenter matched cohort study found.
“People are seeking help for different conditions that are most likely related to their MS,” one of the study authors, Elaine Kingwell, PhD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “It suggests there could be opportunity to recognize and possibly diagnose and treat MS earlier.”
In a previously published study (Lancet Neurol. 2017;16[6]:445-51) led by Helen Tremlett, PhD, and first author Jose Wijnands, PhD, the team found increased health care utilization in people with MS across all health sectors – physician, hospital, and pharmacy (prescriptions filled).
For the current study, the team set out to identify early signs and symptoms that could define the MS prodrome. “We wanted to know why people went to the hospital, why people went to their physician, what kind of drugs they were prescribed, and what kind of specialists they saw,” explained Dr. Kingwell, an epidemiologist in the department of neurology at the University of British Columbia, Vancouver.
The researchers used health administrative and MS-specific data from four Canadian provinces to conduct a multicenter matched cohort study. Individuals were required to be in the province from 5 years pre-index date, measured as either the first demyelinating event in health administrative data or MS onset as determined by the treating neurologist, until the MS cases’ third demyelinating claim or diagnosis date. The potential for a prodromal period was examined in the 5 years pre-index date, and outcomes of interest were number of physician and hospital encounters per ICD-10 chapter, number of physician encounters per physician specialty, and percentage of people with one or more filled prescription per drug class.
The researchers used rate ratios and 95% confidence intervals to compare the rates of physician and hospital encounters between MS cases and controls and the proportion test to compare the percentage of people with one or more filled prescriptions between MS cases and controls. They used random-effects meta-analyses to pool results across Canadian provinces.
The population consisted of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics. Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), musculoskeletal system (RR = 1.19-1.70), and genitourinary system (RR = 1.17-1.59), Dr. Kingwell and her associates reported.
Cases also had more encounters with psychiatrists (RR = 1.48-1.66) and urologists (RR = 1.49-1.80), and a higher proportion of filled prescriptions for hormonal preparations and drugs related to the musculoskeletal or genitourinary systems (ranging from 1.1 to 1.5 times higher; P less than .02 for all associations). “While we did not examine each individual drug, we did group drugs by their therapeutic class,” Dr. Wijnands noted in an interview after the meeting. “As for the increased number of visits to psychiatrists, it is intriguing. We don’t necessarily know all the reasons why. It opens up a lot of questions for people to follow up on.”
In contrast, MS cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78-0.88).
Dr. Wijnands acknowledged certain limitations of the study, including its reliance on administrative data to measure the prodromal period. “When we described the prodrome itself, we relied on ICD codes from the physician and hospital data as well as prescriptions filled. Issues or problems for which individuals do not seek medical attention, for instance, would not be captured in our study,” she said.
The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SOURCE: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
SAN DIEGO – Compared with controls, patients who developed MS were more frequently admitted to the hospital or visited a physician for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system in the 5 years prior to MS onset, a multicenter matched cohort study found.
“People are seeking help for different conditions that are most likely related to their MS,” one of the study authors, Elaine Kingwell, PhD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “It suggests there could be opportunity to recognize and possibly diagnose and treat MS earlier.”
In a previously published study (Lancet Neurol. 2017;16[6]:445-51) led by Helen Tremlett, PhD, and first author Jose Wijnands, PhD, the team found increased health care utilization in people with MS across all health sectors – physician, hospital, and pharmacy (prescriptions filled).
For the current study, the team set out to identify early signs and symptoms that could define the MS prodrome. “We wanted to know why people went to the hospital, why people went to their physician, what kind of drugs they were prescribed, and what kind of specialists they saw,” explained Dr. Kingwell, an epidemiologist in the department of neurology at the University of British Columbia, Vancouver.
The researchers used health administrative and MS-specific data from four Canadian provinces to conduct a multicenter matched cohort study. Individuals were required to be in the province from 5 years pre-index date, measured as either the first demyelinating event in health administrative data or MS onset as determined by the treating neurologist, until the MS cases’ third demyelinating claim or diagnosis date. The potential for a prodromal period was examined in the 5 years pre-index date, and outcomes of interest were number of physician and hospital encounters per ICD-10 chapter, number of physician encounters per physician specialty, and percentage of people with one or more filled prescription per drug class.
The researchers used rate ratios and 95% confidence intervals to compare the rates of physician and hospital encounters between MS cases and controls and the proportion test to compare the percentage of people with one or more filled prescriptions between MS cases and controls. They used random-effects meta-analyses to pool results across Canadian provinces.
The population consisted of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics. Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), musculoskeletal system (RR = 1.19-1.70), and genitourinary system (RR = 1.17-1.59), Dr. Kingwell and her associates reported.
Cases also had more encounters with psychiatrists (RR = 1.48-1.66) and urologists (RR = 1.49-1.80), and a higher proportion of filled prescriptions for hormonal preparations and drugs related to the musculoskeletal or genitourinary systems (ranging from 1.1 to 1.5 times higher; P less than .02 for all associations). “While we did not examine each individual drug, we did group drugs by their therapeutic class,” Dr. Wijnands noted in an interview after the meeting. “As for the increased number of visits to psychiatrists, it is intriguing. We don’t necessarily know all the reasons why. It opens up a lot of questions for people to follow up on.”
In contrast, MS cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78-0.88).
Dr. Wijnands acknowledged certain limitations of the study, including its reliance on administrative data to measure the prodromal period. “When we described the prodrome itself, we relied on ICD codes from the physician and hospital data as well as prescriptions filled. Issues or problems for which individuals do not seek medical attention, for instance, would not be captured in our study,” she said.
The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SOURCE: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
SAN DIEGO – Compared with controls, patients who developed MS were more frequently admitted to the hospital or visited a physician for problems related to the nervous system, sensory organs, musculoskeletal system, and genitourinary system in the 5 years prior to MS onset, a multicenter matched cohort study found.
“People are seeking help for different conditions that are most likely related to their MS,” one of the study authors, Elaine Kingwell, PhD, said in an interview at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. “It suggests there could be opportunity to recognize and possibly diagnose and treat MS earlier.”
In a previously published study (Lancet Neurol. 2017;16[6]:445-51) led by Helen Tremlett, PhD, and first author Jose Wijnands, PhD, the team found increased health care utilization in people with MS across all health sectors – physician, hospital, and pharmacy (prescriptions filled).
For the current study, the team set out to identify early signs and symptoms that could define the MS prodrome. “We wanted to know why people went to the hospital, why people went to their physician, what kind of drugs they were prescribed, and what kind of specialists they saw,” explained Dr. Kingwell, an epidemiologist in the department of neurology at the University of British Columbia, Vancouver.
The researchers used health administrative and MS-specific data from four Canadian provinces to conduct a multicenter matched cohort study. Individuals were required to be in the province from 5 years pre-index date, measured as either the first demyelinating event in health administrative data or MS onset as determined by the treating neurologist, until the MS cases’ third demyelinating claim or diagnosis date. The potential for a prodromal period was examined in the 5 years pre-index date, and outcomes of interest were number of physician and hospital encounters per ICD-10 chapter, number of physician encounters per physician specialty, and percentage of people with one or more filled prescription per drug class.
The researchers used rate ratios and 95% confidence intervals to compare the rates of physician and hospital encounters between MS cases and controls and the proportion test to compare the percentage of people with one or more filled prescriptions between MS cases and controls. They used random-effects meta-analyses to pool results across Canadian provinces.
The population consisted of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics. Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), musculoskeletal system (RR = 1.19-1.70), and genitourinary system (RR = 1.17-1.59), Dr. Kingwell and her associates reported.
Cases also had more encounters with psychiatrists (RR = 1.48-1.66) and urologists (RR = 1.49-1.80), and a higher proportion of filled prescriptions for hormonal preparations and drugs related to the musculoskeletal or genitourinary systems (ranging from 1.1 to 1.5 times higher; P less than .02 for all associations). “While we did not examine each individual drug, we did group drugs by their therapeutic class,” Dr. Wijnands noted in an interview after the meeting. “As for the increased number of visits to psychiatrists, it is intriguing. We don’t necessarily know all the reasons why. It opens up a lot of questions for people to follow up on.”
In contrast, MS cases had fewer pregnancy-related encounters, compared with controls (RR = 0.78-0.88).
Dr. Wijnands acknowledged certain limitations of the study, including its reliance on administrative data to measure the prodromal period. “When we described the prodrome itself, we relied on ICD codes from the physician and hospital data as well as prescriptions filled. Issues or problems for which individuals do not seek medical attention, for instance, would not be captured in our study,” she said.
The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
dbrunk@frontlinemedcom.com
SOURCE: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
REPORTING FROM ACTRIMS FORUM 2018
Key clinical point: Several phenotypic characteristics may constitute the MS prodrome.
Major finding: Compared with controls, in the 5 years before the first demyelinating claim or symptom onset, MS cases had more physician and hospital encounters for the nervous system (rate ratio = 1.70-4.75), sensory organs (RR = 1.40-2.28), and musculoskeletal system (RR = 1.19-1.70).
Study details: A multicenter matched cohort study of 13,951 MS patients and 66,940 controls derived from a health administration cohort and 3,202 MS patients and 16,006 controls derived from MS clinics.
Disclosures: The study was funded by the National MS Society. Dr. Wijnands receives salary support from the Michael Smith Foundation for Health Research /The Koehle Family Foundation, coauthor Ruth Ann Marrie, MD, PhD, holds the Waugh Family Chair in Multiple Sclerosis, and Dr. Tremlett is funded by the Canada Research Chair Program. Dr. Kingwell reported having no financial disclosures.
Source: Kingwell E et al. ACTRIMS Forum 2018, late-breaking poster 254.
Physicians often bypass cognition, depression screening in MS
SAN DIEGO – A new study finds that physicians at two . Physicians who did perform screening hardly ever used validated tools and often didn’t refer appropriate patients for higher-level care.
In addition, researchers interviewed 13 leading MS specialists from coast to coast and “found that about half reported not using formal screening tools to assess cognitive impairment and depression,” said study coauthor Tamar Sapir, PhD, chief scientific officer with Prime Education, a firm based in Fort Lauderdale, Fla., that provides a variety of health-related services such as training and research.
The study findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Three of the study authors spoke in interviews.
The researchers sought to understand how frequently MS patients are screened for cognitive problems and depression.
“Cognitive impairment is experienced by approximately half of patients with multiple sclerosis, yet many are never screened or treated, which can impact their daily activities, their ability to work, and overall quality of life,” Dr. Sapir said.
Depression, meanwhile, is believed to be much more common in patients with MS than in the general population, with one recent meta-analysis of 58 studies finding that the average prevalence was 31%. Other research suggests depression is underdiagnosed and undertreated in this population (J Neurol Sci. 2017 Jan 15;372:331-41; ISRN Neurology. 2012, Article ID 427102. doi: 10.5402/2012/427102).
For the current study, researchers tracked 300 patients at two unidentified MS clinics via their charts over a 2-year period from 2014 to 2016. Their median age was 52 years, 76% were women, and 15 had experienced at least one relapse within the previous 24 months.
“Screening for cognitive impairment and depression was documented for only 52% and 63% of MS patients, respectively, and only about a quarter of patients diagnosed with these conditions were referred to a higher level of care,” said lead author Guy J. Buckle, MD, MPH, of the Andrew C. Carlos MS Institute at Shepherd Center in Atlanta.
Among all 300 patients, just 2% and 4% were screened using a validated tool for cognitive impairment and depression, respectively.
The screening often turned up evidence of the conditions: Physicians saw signs of cognitive impairment in 69% and 78% of those screened aged under 65 years and aged 65 and older, respectively, and they detected depression in 71% and 54% of those screened in those two age groups, respectively.
Researchers also noted several disparities. “Cognitive screening was conducted more frequently in older, employed, or white patients, while the presence of cognitive impairment was documented more often in black, nonworking, and those on Medicare or Medicaid,” Dr. Buckle said. “Depression screening was performed most frequently in older or white patients, yet depression was more common in younger, nonworking patients and those on Medicare/Medicaid.”
In another part of their study, researchers surveyed 13 unidentified “national leaders” in MS research and treatment. Just seven said they used validated tools to screen for cognitive impairment and six said they used them to screen for depression.
“We hear from MS specialists that they want to be measuring for cognition but don’t know how to efficiently work it into their routine, how to approach the patient, and what tools to use,” said study coauthor Derrick S. Robertson, MD, of the University of South Florida, Tampa. “In addition, there is no one tool that is accepted in the MS treatment community.”
MS specialists who didn’t use the screening tests also pointed to factors like lack of reimbursement and lack of integration into electronic medical records. “Doubt very much that neurologists have time to use any of these tests,” one respondent said, referring to cognitive impairment screening.
What’s next? “There are several new exciting developments in clinical trials demonstrating efficacy of disease-modifying therapies in maintaining or improving cognition in patients with relapsing MS,” Dr. Robertson said. “This highlights the urgent need to overcome barriers to use of formal cognitive screening tools in clinical practice to identify patients who need a higher level of care, and perhaps even a change in treatment with the ultimate goal to improve quality of life and overall outcomes.”
Genentech funded the study through an educational grant. Dr. Sapir and three other study authors reported no relevant disclosures. Dr. Buckle and Dr. Robertson reported multiple disclosures, including principle investigator and advisory board/panel member work.
SOURCE: Buckle GJ et al. ACTRIMS Forum 2018, abstract No. P161.
SAN DIEGO – A new study finds that physicians at two . Physicians who did perform screening hardly ever used validated tools and often didn’t refer appropriate patients for higher-level care.
In addition, researchers interviewed 13 leading MS specialists from coast to coast and “found that about half reported not using formal screening tools to assess cognitive impairment and depression,” said study coauthor Tamar Sapir, PhD, chief scientific officer with Prime Education, a firm based in Fort Lauderdale, Fla., that provides a variety of health-related services such as training and research.
The study findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Three of the study authors spoke in interviews.
The researchers sought to understand how frequently MS patients are screened for cognitive problems and depression.
“Cognitive impairment is experienced by approximately half of patients with multiple sclerosis, yet many are never screened or treated, which can impact their daily activities, their ability to work, and overall quality of life,” Dr. Sapir said.
Depression, meanwhile, is believed to be much more common in patients with MS than in the general population, with one recent meta-analysis of 58 studies finding that the average prevalence was 31%. Other research suggests depression is underdiagnosed and undertreated in this population (J Neurol Sci. 2017 Jan 15;372:331-41; ISRN Neurology. 2012, Article ID 427102. doi: 10.5402/2012/427102).
For the current study, researchers tracked 300 patients at two unidentified MS clinics via their charts over a 2-year period from 2014 to 2016. Their median age was 52 years, 76% were women, and 15 had experienced at least one relapse within the previous 24 months.
“Screening for cognitive impairment and depression was documented for only 52% and 63% of MS patients, respectively, and only about a quarter of patients diagnosed with these conditions were referred to a higher level of care,” said lead author Guy J. Buckle, MD, MPH, of the Andrew C. Carlos MS Institute at Shepherd Center in Atlanta.
Among all 300 patients, just 2% and 4% were screened using a validated tool for cognitive impairment and depression, respectively.
The screening often turned up evidence of the conditions: Physicians saw signs of cognitive impairment in 69% and 78% of those screened aged under 65 years and aged 65 and older, respectively, and they detected depression in 71% and 54% of those screened in those two age groups, respectively.
Researchers also noted several disparities. “Cognitive screening was conducted more frequently in older, employed, or white patients, while the presence of cognitive impairment was documented more often in black, nonworking, and those on Medicare or Medicaid,” Dr. Buckle said. “Depression screening was performed most frequently in older or white patients, yet depression was more common in younger, nonworking patients and those on Medicare/Medicaid.”
In another part of their study, researchers surveyed 13 unidentified “national leaders” in MS research and treatment. Just seven said they used validated tools to screen for cognitive impairment and six said they used them to screen for depression.
“We hear from MS specialists that they want to be measuring for cognition but don’t know how to efficiently work it into their routine, how to approach the patient, and what tools to use,” said study coauthor Derrick S. Robertson, MD, of the University of South Florida, Tampa. “In addition, there is no one tool that is accepted in the MS treatment community.”
MS specialists who didn’t use the screening tests also pointed to factors like lack of reimbursement and lack of integration into electronic medical records. “Doubt very much that neurologists have time to use any of these tests,” one respondent said, referring to cognitive impairment screening.
What’s next? “There are several new exciting developments in clinical trials demonstrating efficacy of disease-modifying therapies in maintaining or improving cognition in patients with relapsing MS,” Dr. Robertson said. “This highlights the urgent need to overcome barriers to use of formal cognitive screening tools in clinical practice to identify patients who need a higher level of care, and perhaps even a change in treatment with the ultimate goal to improve quality of life and overall outcomes.”
Genentech funded the study through an educational grant. Dr. Sapir and three other study authors reported no relevant disclosures. Dr. Buckle and Dr. Robertson reported multiple disclosures, including principle investigator and advisory board/panel member work.
SOURCE: Buckle GJ et al. ACTRIMS Forum 2018, abstract No. P161.
SAN DIEGO – A new study finds that physicians at two . Physicians who did perform screening hardly ever used validated tools and often didn’t refer appropriate patients for higher-level care.
In addition, researchers interviewed 13 leading MS specialists from coast to coast and “found that about half reported not using formal screening tools to assess cognitive impairment and depression,” said study coauthor Tamar Sapir, PhD, chief scientific officer with Prime Education, a firm based in Fort Lauderdale, Fla., that provides a variety of health-related services such as training and research.
The study findings were presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis. Three of the study authors spoke in interviews.
The researchers sought to understand how frequently MS patients are screened for cognitive problems and depression.
“Cognitive impairment is experienced by approximately half of patients with multiple sclerosis, yet many are never screened or treated, which can impact their daily activities, their ability to work, and overall quality of life,” Dr. Sapir said.
Depression, meanwhile, is believed to be much more common in patients with MS than in the general population, with one recent meta-analysis of 58 studies finding that the average prevalence was 31%. Other research suggests depression is underdiagnosed and undertreated in this population (J Neurol Sci. 2017 Jan 15;372:331-41; ISRN Neurology. 2012, Article ID 427102. doi: 10.5402/2012/427102).
For the current study, researchers tracked 300 patients at two unidentified MS clinics via their charts over a 2-year period from 2014 to 2016. Their median age was 52 years, 76% were women, and 15 had experienced at least one relapse within the previous 24 months.
“Screening for cognitive impairment and depression was documented for only 52% and 63% of MS patients, respectively, and only about a quarter of patients diagnosed with these conditions were referred to a higher level of care,” said lead author Guy J. Buckle, MD, MPH, of the Andrew C. Carlos MS Institute at Shepherd Center in Atlanta.
Among all 300 patients, just 2% and 4% were screened using a validated tool for cognitive impairment and depression, respectively.
The screening often turned up evidence of the conditions: Physicians saw signs of cognitive impairment in 69% and 78% of those screened aged under 65 years and aged 65 and older, respectively, and they detected depression in 71% and 54% of those screened in those two age groups, respectively.
Researchers also noted several disparities. “Cognitive screening was conducted more frequently in older, employed, or white patients, while the presence of cognitive impairment was documented more often in black, nonworking, and those on Medicare or Medicaid,” Dr. Buckle said. “Depression screening was performed most frequently in older or white patients, yet depression was more common in younger, nonworking patients and those on Medicare/Medicaid.”
In another part of their study, researchers surveyed 13 unidentified “national leaders” in MS research and treatment. Just seven said they used validated tools to screen for cognitive impairment and six said they used them to screen for depression.
“We hear from MS specialists that they want to be measuring for cognition but don’t know how to efficiently work it into their routine, how to approach the patient, and what tools to use,” said study coauthor Derrick S. Robertson, MD, of the University of South Florida, Tampa. “In addition, there is no one tool that is accepted in the MS treatment community.”
MS specialists who didn’t use the screening tests also pointed to factors like lack of reimbursement and lack of integration into electronic medical records. “Doubt very much that neurologists have time to use any of these tests,” one respondent said, referring to cognitive impairment screening.
What’s next? “There are several new exciting developments in clinical trials demonstrating efficacy of disease-modifying therapies in maintaining or improving cognition in patients with relapsing MS,” Dr. Robertson said. “This highlights the urgent need to overcome barriers to use of formal cognitive screening tools in clinical practice to identify patients who need a higher level of care, and perhaps even a change in treatment with the ultimate goal to improve quality of life and overall outcomes.”
Genentech funded the study through an educational grant. Dr. Sapir and three other study authors reported no relevant disclosures. Dr. Buckle and Dr. Robertson reported multiple disclosures, including principle investigator and advisory board/panel member work.
SOURCE: Buckle GJ et al. ACTRIMS Forum 2018, abstract No. P161.
REPORTING FROM ACTRIMS FORUM 2018
Key clinical point: Screening often turns up signs of trouble, but many MS patients are not screened annually for depression and cognitive impairment.
Major finding: 52% and 63% of patients with MS were screened for cognitive impairment and depression, respectively, over a 1-year period. Study details: 2-year analysis of medical records from two MS clinics in the Southeast.
Disclosures: Genentech funded the study through an educational grant. Some of the study authors reported various disclosures.
Source: Buckle GJ et al. ACTRIMS Forum 2018, abstract No. P161.
Patients want information on religious hospitals’ restrictions
A majority of women want to know about restrictions on care imposed by some religious hospitals, based on data from a survey of 1,430 women.
The survey results, published in the American Journal of Obstetrics and Gynecology, showed that 35% of women thought knowing a hospital’s religion was important when choosing care, but many more – 81% – said that knowing a hospital’s religious restrictions on care was important.
The discrepancy between respondents’ desire to know a hospital’s religious orientation and to know any religious restrictions suggests that many women may have been unaware of restrictions before taking the survey, wrote Lori R. Freedman, PhD, of the University of California, San Francisco, and her colleagues.
Religious hospitals in the United States, 70% of which are Catholic, are a growing part of the health care system, but “no prior studies have asked women from across the United States what information they have and want to have before deciding where to seek care for a miscarriage or other reproductive condition that may be affected by the hospital’s religion,” the researchers said.
The researchers conducted an online survey of women aged 18-45 years who were part of the AmeriSpeak panel, a national database that includes civilian, noninstitutionalized adults. Approximately one-quarter (24%) of the women reported attending a weekly religious service.
Overall, Catholic women were no more likely than non-Catholic women to state that knowing a hospital’s religion or religious-based care restrictions was important. For example, 71% of the participants overall said an acceptable option was to admit a patient, inform her of all treatment options for miscarriage, and refer her elsewhere if she chose an option not available on religious grounds.
“ACOG recommends that institutions make information about all reproductive options available to patients and safeguard patients’ rights to access care consistent with the patient’s own values; however, Catholic hospitals may lack financial, legal, and ideological incentives to voluntarily comply with ACOG’s recommendations,” the researchers noted.
The study findings were limited by several factors, including the use of a panel-based sample and a response rate of approximately 50%. The results, however, suggest that patients need more complete information before choosing a hospital, the researchers said.
The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
SOURCE: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
A majority of women want to know about restrictions on care imposed by some religious hospitals, based on data from a survey of 1,430 women.
The survey results, published in the American Journal of Obstetrics and Gynecology, showed that 35% of women thought knowing a hospital’s religion was important when choosing care, but many more – 81% – said that knowing a hospital’s religious restrictions on care was important.
The discrepancy between respondents’ desire to know a hospital’s religious orientation and to know any religious restrictions suggests that many women may have been unaware of restrictions before taking the survey, wrote Lori R. Freedman, PhD, of the University of California, San Francisco, and her colleagues.
Religious hospitals in the United States, 70% of which are Catholic, are a growing part of the health care system, but “no prior studies have asked women from across the United States what information they have and want to have before deciding where to seek care for a miscarriage or other reproductive condition that may be affected by the hospital’s religion,” the researchers said.
The researchers conducted an online survey of women aged 18-45 years who were part of the AmeriSpeak panel, a national database that includes civilian, noninstitutionalized adults. Approximately one-quarter (24%) of the women reported attending a weekly religious service.
Overall, Catholic women were no more likely than non-Catholic women to state that knowing a hospital’s religion or religious-based care restrictions was important. For example, 71% of the participants overall said an acceptable option was to admit a patient, inform her of all treatment options for miscarriage, and refer her elsewhere if she chose an option not available on religious grounds.
“ACOG recommends that institutions make information about all reproductive options available to patients and safeguard patients’ rights to access care consistent with the patient’s own values; however, Catholic hospitals may lack financial, legal, and ideological incentives to voluntarily comply with ACOG’s recommendations,” the researchers noted.
The study findings were limited by several factors, including the use of a panel-based sample and a response rate of approximately 50%. The results, however, suggest that patients need more complete information before choosing a hospital, the researchers said.
The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
SOURCE: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
A majority of women want to know about restrictions on care imposed by some religious hospitals, based on data from a survey of 1,430 women.
The survey results, published in the American Journal of Obstetrics and Gynecology, showed that 35% of women thought knowing a hospital’s religion was important when choosing care, but many more – 81% – said that knowing a hospital’s religious restrictions on care was important.
The discrepancy between respondents’ desire to know a hospital’s religious orientation and to know any religious restrictions suggests that many women may have been unaware of restrictions before taking the survey, wrote Lori R. Freedman, PhD, of the University of California, San Francisco, and her colleagues.
Religious hospitals in the United States, 70% of which are Catholic, are a growing part of the health care system, but “no prior studies have asked women from across the United States what information they have and want to have before deciding where to seek care for a miscarriage or other reproductive condition that may be affected by the hospital’s religion,” the researchers said.
The researchers conducted an online survey of women aged 18-45 years who were part of the AmeriSpeak panel, a national database that includes civilian, noninstitutionalized adults. Approximately one-quarter (24%) of the women reported attending a weekly religious service.
Overall, Catholic women were no more likely than non-Catholic women to state that knowing a hospital’s religion or religious-based care restrictions was important. For example, 71% of the participants overall said an acceptable option was to admit a patient, inform her of all treatment options for miscarriage, and refer her elsewhere if she chose an option not available on religious grounds.
“ACOG recommends that institutions make information about all reproductive options available to patients and safeguard patients’ rights to access care consistent with the patient’s own values; however, Catholic hospitals may lack financial, legal, and ideological incentives to voluntarily comply with ACOG’s recommendations,” the researchers noted.
The study findings were limited by several factors, including the use of a panel-based sample and a response rate of approximately 50%. The results, however, suggest that patients need more complete information before choosing a hospital, the researchers said.
The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
SOURCE: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
FROM AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Key clinical point: Many patients receiving care at religious hospitals are unaware of restrictions on treatment.
Major finding: Approximately 81% of women said it was important to know a hospital’s religious restrictions on care.
Study details: Survey of 1,430 women aged 18-45 years.
Disclosures: The researchers had no financial conflicts to disclose. Dr. Freedman was supported by the Greenwall Foundation. The study was supported by the Society for Family Planning.
Source: Freedman LR et al. Am J Obstet Gynecol. 2018;218:251.e1-9.
Dermatology practice gaps: Missed diagnoses
KAUAI, HAWAII – Up to 130,000 patients hospitalized for treatment of lower extremity cellulitis annually in the United States turn out to have been misdiagnosed – and therein lies an opportunity for dermatologists to make a difference, according to Erik J. Stratman, MD, chairman of the department of dermatology at the Marshfield (Wisc.) Clinic.
As a section editor for UptoDate, he monitors the medical literature to identify , which he defines as things he and, he suspects, many other dermatologists are “either doing or not doing in practice that we shouldn’t or should be doing,” he explained at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
At the Hawaii meeting, he zeroed in on two such practice gaps pertaining to missed diagnoses.
Lower extremity cellulitis
A 2017 American Academy of Dermatology report on the national burden of skin disease contained eye-popping figures on the heavy toll of cellulitis. Cellulitis is the most common form of skin and soft tissue infection (SSTI). To put that into perspective, the annual incidence of SSTIs is 10-fold greater than that of pneumonia. Indeed, SSTIs account for 10% of all infectious disease–related hospitalizations across the country. There are 2.3 million emergency department visits per year for cellulitis, 14%-17% of which result in hospitalization (J Am Acad Dermatol. 2017 May;76[5]:958-972.e2).
Dr. Stratman, who is on the board of directors of the American Board of Dermatology, was favorably impressed with the work of a multicenter group of investigators who scrutinized 259 consecutive patients admitted with a diagnosis of lower extremity cellulitis through the emergency department at Massachusetts General Hospital in Boston. Seventy-nine of them (30.5%), were found to be misdiagnosed. Fifty-two of the 79 misdiagnosed patients had been admitted primarily for treatment of their supposed cellulitis: 44 of these 52, or 85%, didn’t require hospitalization, and 48 of the 52, or 92%, received unnecessary antibiotics.
Extrapolating from this experience, with application of cost data provided by the U.S. Agency for Healthcare Research and Quality, the investigators estimated that misdiagnosis of cellulitis results in 50,000 to 130,000 unnecessary hospitalizations annually. These hospitalizations for what the investigators termed “pseudocellulitis,” the majority of which is stasis dermatitis, resulted in inpatient costs estimated at up to $515 million per year. The unnecessary hospitalizations also led to an estimated 9,000 nosocomial infections, up to 5,000 Clostridium difficile infections, and a projected two to six cases of anaphylaxis resulting from exposure to the unnecessary antibiotics (JAMA Dermatol. 2017;153[2]:141-6).
Dr. Stratman said that the large Massachusetts General Hospital study mirrors his own experience when called upon to do a hospital consultation, as well as that of other dermatologists he has spoken with: “The number-one reason we get consulted is for stuff that is wrongfully admitted, mainly cellulitis.”
The investigators then went on to develop a simple prediction model for lower extremity cellulitis based upon their data. It’s called the ALT-70 score, an acronym for Asymmetric, Leukocytosis, Tachycardia, and Age greater than 70. A patient gets 3 points if one leg is affected, zero if both are. Age 70 or more is worth 2 points. A heart rate of 90 beats per minute or higher gets 1 point, as does a WBC of at least 10,000 per uL. A score of 0-2 spells at least an 83% likelihood that the patient has pseudocellulitis, while a score of 5 or points indicates at least an 82% likelihood of true cellulitis (J Am Acad Dermatol. 2017 Apr;76[4]:618-625.e2).
“If you don’t reach a score of 3, you’d better think a little bit harder before you hang that bag of vancomycin,” Dr. Stratman observed.
He ascribed the huge problem of misdiagnosed lower extremity cellulitis to several causes: emergency medicine physicians, hospitalists, and primary care physicians receive minimal dermatology training. In addition, there are no reliable diagnostic studies for the infection, and dermatologists are seldom consulted on patients with red legs, either because there are no dermatologists in a particular community or they don’t want to be consulted.
“It’s not all the dermatologists’ fault. Have you tried to get credentialed at a hospital lately? It’s a 1½-inch stack of papers and 8½ hours of electronic medical record training, if you’re lucky. So there are definitely barriers to overcoming this gap,” Dr. Stratman pointed out.
The best solution, he continued, is for dermatologists to take the initiative in educating hospitalists, emergency medicine specialists, and primary care physicians on the common mimickers of cellulitis, especially stasis dermatitis and contact dermatitis. This can happen through grand rounds presentations and feedback to consulting physicians.
“I think dermatologists have to take the lead on this,” Dr. Stratman said.
Underscreening for autoimmune thyroid disease in vitiligo patients
The international Vitiligo Working Group, citing evidence that 19% of patients with vitiligo have concomitant autoimmune thyroid disease and that the risk of developing this endocrine disease doubles every 5 years that a patient has vitiligo, has issued a call to action for dermatologists to ensure that their patients with vitiligo undergo periodic screening (J Am Acad Dermatol. 2017 Jul;77[1]:1-13).
This recommendation was based upon insights provided by a French prospective, observational study of 626 patients with vitiligo. The French investigators found that the risk of autoimmune thyroid disease doubled every 5 years and was associated with female sex, younger age at vitiligo onset, vitiligo on the trunk, and a personal history of autoimmune disease. They recommended screening every 2 years for thyroid-stimulating hormone and free thyroxine levels, as well as checking for serum antithyroperoxidase antibodies (Br J Dermatol. 2013 Apr;168[4]:756-61).
Dr. Stratman noted that some dermatologists may feel that ordering thyroid screening tests is outside their scope of practice. In that case, it’s important to engage with their vitiligo patient’s primary care physician to make sure the screening gets done.
He reported having no financial conflicts of interest regarding his presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – Up to 130,000 patients hospitalized for treatment of lower extremity cellulitis annually in the United States turn out to have been misdiagnosed – and therein lies an opportunity for dermatologists to make a difference, according to Erik J. Stratman, MD, chairman of the department of dermatology at the Marshfield (Wisc.) Clinic.
As a section editor for UptoDate, he monitors the medical literature to identify , which he defines as things he and, he suspects, many other dermatologists are “either doing or not doing in practice that we shouldn’t or should be doing,” he explained at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
At the Hawaii meeting, he zeroed in on two such practice gaps pertaining to missed diagnoses.
Lower extremity cellulitis
A 2017 American Academy of Dermatology report on the national burden of skin disease contained eye-popping figures on the heavy toll of cellulitis. Cellulitis is the most common form of skin and soft tissue infection (SSTI). To put that into perspective, the annual incidence of SSTIs is 10-fold greater than that of pneumonia. Indeed, SSTIs account for 10% of all infectious disease–related hospitalizations across the country. There are 2.3 million emergency department visits per year for cellulitis, 14%-17% of which result in hospitalization (J Am Acad Dermatol. 2017 May;76[5]:958-972.e2).
Dr. Stratman, who is on the board of directors of the American Board of Dermatology, was favorably impressed with the work of a multicenter group of investigators who scrutinized 259 consecutive patients admitted with a diagnosis of lower extremity cellulitis through the emergency department at Massachusetts General Hospital in Boston. Seventy-nine of them (30.5%), were found to be misdiagnosed. Fifty-two of the 79 misdiagnosed patients had been admitted primarily for treatment of their supposed cellulitis: 44 of these 52, or 85%, didn’t require hospitalization, and 48 of the 52, or 92%, received unnecessary antibiotics.
Extrapolating from this experience, with application of cost data provided by the U.S. Agency for Healthcare Research and Quality, the investigators estimated that misdiagnosis of cellulitis results in 50,000 to 130,000 unnecessary hospitalizations annually. These hospitalizations for what the investigators termed “pseudocellulitis,” the majority of which is stasis dermatitis, resulted in inpatient costs estimated at up to $515 million per year. The unnecessary hospitalizations also led to an estimated 9,000 nosocomial infections, up to 5,000 Clostridium difficile infections, and a projected two to six cases of anaphylaxis resulting from exposure to the unnecessary antibiotics (JAMA Dermatol. 2017;153[2]:141-6).
Dr. Stratman said that the large Massachusetts General Hospital study mirrors his own experience when called upon to do a hospital consultation, as well as that of other dermatologists he has spoken with: “The number-one reason we get consulted is for stuff that is wrongfully admitted, mainly cellulitis.”
The investigators then went on to develop a simple prediction model for lower extremity cellulitis based upon their data. It’s called the ALT-70 score, an acronym for Asymmetric, Leukocytosis, Tachycardia, and Age greater than 70. A patient gets 3 points if one leg is affected, zero if both are. Age 70 or more is worth 2 points. A heart rate of 90 beats per minute or higher gets 1 point, as does a WBC of at least 10,000 per uL. A score of 0-2 spells at least an 83% likelihood that the patient has pseudocellulitis, while a score of 5 or points indicates at least an 82% likelihood of true cellulitis (J Am Acad Dermatol. 2017 Apr;76[4]:618-625.e2).
“If you don’t reach a score of 3, you’d better think a little bit harder before you hang that bag of vancomycin,” Dr. Stratman observed.
He ascribed the huge problem of misdiagnosed lower extremity cellulitis to several causes: emergency medicine physicians, hospitalists, and primary care physicians receive minimal dermatology training. In addition, there are no reliable diagnostic studies for the infection, and dermatologists are seldom consulted on patients with red legs, either because there are no dermatologists in a particular community or they don’t want to be consulted.
“It’s not all the dermatologists’ fault. Have you tried to get credentialed at a hospital lately? It’s a 1½-inch stack of papers and 8½ hours of electronic medical record training, if you’re lucky. So there are definitely barriers to overcoming this gap,” Dr. Stratman pointed out.
The best solution, he continued, is for dermatologists to take the initiative in educating hospitalists, emergency medicine specialists, and primary care physicians on the common mimickers of cellulitis, especially stasis dermatitis and contact dermatitis. This can happen through grand rounds presentations and feedback to consulting physicians.
“I think dermatologists have to take the lead on this,” Dr. Stratman said.
Underscreening for autoimmune thyroid disease in vitiligo patients
The international Vitiligo Working Group, citing evidence that 19% of patients with vitiligo have concomitant autoimmune thyroid disease and that the risk of developing this endocrine disease doubles every 5 years that a patient has vitiligo, has issued a call to action for dermatologists to ensure that their patients with vitiligo undergo periodic screening (J Am Acad Dermatol. 2017 Jul;77[1]:1-13).
This recommendation was based upon insights provided by a French prospective, observational study of 626 patients with vitiligo. The French investigators found that the risk of autoimmune thyroid disease doubled every 5 years and was associated with female sex, younger age at vitiligo onset, vitiligo on the trunk, and a personal history of autoimmune disease. They recommended screening every 2 years for thyroid-stimulating hormone and free thyroxine levels, as well as checking for serum antithyroperoxidase antibodies (Br J Dermatol. 2013 Apr;168[4]:756-61).
Dr. Stratman noted that some dermatologists may feel that ordering thyroid screening tests is outside their scope of practice. In that case, it’s important to engage with their vitiligo patient’s primary care physician to make sure the screening gets done.
He reported having no financial conflicts of interest regarding his presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – Up to 130,000 patients hospitalized for treatment of lower extremity cellulitis annually in the United States turn out to have been misdiagnosed – and therein lies an opportunity for dermatologists to make a difference, according to Erik J. Stratman, MD, chairman of the department of dermatology at the Marshfield (Wisc.) Clinic.
As a section editor for UptoDate, he monitors the medical literature to identify , which he defines as things he and, he suspects, many other dermatologists are “either doing or not doing in practice that we shouldn’t or should be doing,” he explained at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation.
At the Hawaii meeting, he zeroed in on two such practice gaps pertaining to missed diagnoses.
Lower extremity cellulitis
A 2017 American Academy of Dermatology report on the national burden of skin disease contained eye-popping figures on the heavy toll of cellulitis. Cellulitis is the most common form of skin and soft tissue infection (SSTI). To put that into perspective, the annual incidence of SSTIs is 10-fold greater than that of pneumonia. Indeed, SSTIs account for 10% of all infectious disease–related hospitalizations across the country. There are 2.3 million emergency department visits per year for cellulitis, 14%-17% of which result in hospitalization (J Am Acad Dermatol. 2017 May;76[5]:958-972.e2).
Dr. Stratman, who is on the board of directors of the American Board of Dermatology, was favorably impressed with the work of a multicenter group of investigators who scrutinized 259 consecutive patients admitted with a diagnosis of lower extremity cellulitis through the emergency department at Massachusetts General Hospital in Boston. Seventy-nine of them (30.5%), were found to be misdiagnosed. Fifty-two of the 79 misdiagnosed patients had been admitted primarily for treatment of their supposed cellulitis: 44 of these 52, or 85%, didn’t require hospitalization, and 48 of the 52, or 92%, received unnecessary antibiotics.
Extrapolating from this experience, with application of cost data provided by the U.S. Agency for Healthcare Research and Quality, the investigators estimated that misdiagnosis of cellulitis results in 50,000 to 130,000 unnecessary hospitalizations annually. These hospitalizations for what the investigators termed “pseudocellulitis,” the majority of which is stasis dermatitis, resulted in inpatient costs estimated at up to $515 million per year. The unnecessary hospitalizations also led to an estimated 9,000 nosocomial infections, up to 5,000 Clostridium difficile infections, and a projected two to six cases of anaphylaxis resulting from exposure to the unnecessary antibiotics (JAMA Dermatol. 2017;153[2]:141-6).
Dr. Stratman said that the large Massachusetts General Hospital study mirrors his own experience when called upon to do a hospital consultation, as well as that of other dermatologists he has spoken with: “The number-one reason we get consulted is for stuff that is wrongfully admitted, mainly cellulitis.”
The investigators then went on to develop a simple prediction model for lower extremity cellulitis based upon their data. It’s called the ALT-70 score, an acronym for Asymmetric, Leukocytosis, Tachycardia, and Age greater than 70. A patient gets 3 points if one leg is affected, zero if both are. Age 70 or more is worth 2 points. A heart rate of 90 beats per minute or higher gets 1 point, as does a WBC of at least 10,000 per uL. A score of 0-2 spells at least an 83% likelihood that the patient has pseudocellulitis, while a score of 5 or points indicates at least an 82% likelihood of true cellulitis (J Am Acad Dermatol. 2017 Apr;76[4]:618-625.e2).
“If you don’t reach a score of 3, you’d better think a little bit harder before you hang that bag of vancomycin,” Dr. Stratman observed.
He ascribed the huge problem of misdiagnosed lower extremity cellulitis to several causes: emergency medicine physicians, hospitalists, and primary care physicians receive minimal dermatology training. In addition, there are no reliable diagnostic studies for the infection, and dermatologists are seldom consulted on patients with red legs, either because there are no dermatologists in a particular community or they don’t want to be consulted.
“It’s not all the dermatologists’ fault. Have you tried to get credentialed at a hospital lately? It’s a 1½-inch stack of papers and 8½ hours of electronic medical record training, if you’re lucky. So there are definitely barriers to overcoming this gap,” Dr. Stratman pointed out.
The best solution, he continued, is for dermatologists to take the initiative in educating hospitalists, emergency medicine specialists, and primary care physicians on the common mimickers of cellulitis, especially stasis dermatitis and contact dermatitis. This can happen through grand rounds presentations and feedback to consulting physicians.
“I think dermatologists have to take the lead on this,” Dr. Stratman said.
Underscreening for autoimmune thyroid disease in vitiligo patients
The international Vitiligo Working Group, citing evidence that 19% of patients with vitiligo have concomitant autoimmune thyroid disease and that the risk of developing this endocrine disease doubles every 5 years that a patient has vitiligo, has issued a call to action for dermatologists to ensure that their patients with vitiligo undergo periodic screening (J Am Acad Dermatol. 2017 Jul;77[1]:1-13).
This recommendation was based upon insights provided by a French prospective, observational study of 626 patients with vitiligo. The French investigators found that the risk of autoimmune thyroid disease doubled every 5 years and was associated with female sex, younger age at vitiligo onset, vitiligo on the trunk, and a personal history of autoimmune disease. They recommended screening every 2 years for thyroid-stimulating hormone and free thyroxine levels, as well as checking for serum antithyroperoxidase antibodies (Br J Dermatol. 2013 Apr;168[4]:756-61).
Dr. Stratman noted that some dermatologists may feel that ordering thyroid screening tests is outside their scope of practice. In that case, it’s important to engage with their vitiligo patient’s primary care physician to make sure the screening gets done.
He reported having no financial conflicts of interest regarding his presentation.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
No link found between OR skullcaps and infection
JACKSONVILLE, FLA. – Surgeons who choose to wear a skullcap in the OR can point to yet another study with evidence to bolster their preference.
Two major hospital and nursing credentialing organizations have recommended that hospitals ban skullcaps from the operating room as a practice to control surgical site infections, but a study of almost 2,000 operations at an academic medical center has found that strictly enforcing the ban had no impact on infection rates, according to results of a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study, conducted at Thomas Jefferson University in Philadelphia, showed that rates of surgical site infections (SSIs) were almost identical in the year before and the year after the institution implemented the skullcap ban. “The overall surgical site infection rate was 5.4%, and there were no differences in surgical site infections before or after the headwear policy was adopted,” said Arturo J. Rios-Diaz, MD. The Joint Commission and the Association of periOperative Registered Nurses recommend against the use of skullcaps.
The study reviewed American College of Surgeons National Surgical Quality Improvement Program data on 1,901 patients who had 1,950 clean or clean-contaminated general surgery procedures in 2015, the year before the ban was implemented, and in 2016 (767 in 2015 and 1,183 in 2016). The most common procedures were colectomy (18.2%), pancreatectomy (13.5%), and ventral hernia repair (9.9%). The study excluded orthopedic and vascular operations and any cases with sepsis or an active infection at the time of surgery.
There were some differences between the pre- and postban patient groups. The preban group was younger (median age, 57.91 years vs. 59.75, P = .01) but had more patients who were obese, measured as body mass index above 30 kg/m2 (42.37% vs. 35.23%, P less than .01), and smokers (16.18% vs. 12.27%, P = .02). Wound classification also differed: clean, 38.55% before vs. 43.91% after; and clean-contaminated, 61.45% vs. 56.09% (P = .02). All other demographic and clinical characteristics were similar between the two groups.
“In multivariate logistic regression models controlling for these confounders, there was no association of the banning of skullcaps with decreased surgical site infection rates,” Dr. Rios-Diaz said.
“The adoption of guidelines targeted to optimize patient care should always be welcomed by surgeons,” he said. “However, if they’re going to be implemented on a national level, these policies must be based on higher levels of evidence, so further studies are warranted to assess the validity of the [Joint Commission] headwear guidelines.” According to Dr. Rios-Diaz, the recommendations from the Association of periOperative Registered Nurses are based on two case series from the 1960s and 1970s.
Thomas Jefferson University once again allows skullcaps in the OR, he said.
Dr. Rios-Diaz and his coauthors had no financial relationships to disclose.
SOURCE: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
JACKSONVILLE, FLA. – Surgeons who choose to wear a skullcap in the OR can point to yet another study with evidence to bolster their preference.
Two major hospital and nursing credentialing organizations have recommended that hospitals ban skullcaps from the operating room as a practice to control surgical site infections, but a study of almost 2,000 operations at an academic medical center has found that strictly enforcing the ban had no impact on infection rates, according to results of a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study, conducted at Thomas Jefferson University in Philadelphia, showed that rates of surgical site infections (SSIs) were almost identical in the year before and the year after the institution implemented the skullcap ban. “The overall surgical site infection rate was 5.4%, and there were no differences in surgical site infections before or after the headwear policy was adopted,” said Arturo J. Rios-Diaz, MD. The Joint Commission and the Association of periOperative Registered Nurses recommend against the use of skullcaps.
The study reviewed American College of Surgeons National Surgical Quality Improvement Program data on 1,901 patients who had 1,950 clean or clean-contaminated general surgery procedures in 2015, the year before the ban was implemented, and in 2016 (767 in 2015 and 1,183 in 2016). The most common procedures were colectomy (18.2%), pancreatectomy (13.5%), and ventral hernia repair (9.9%). The study excluded orthopedic and vascular operations and any cases with sepsis or an active infection at the time of surgery.
There were some differences between the pre- and postban patient groups. The preban group was younger (median age, 57.91 years vs. 59.75, P = .01) but had more patients who were obese, measured as body mass index above 30 kg/m2 (42.37% vs. 35.23%, P less than .01), and smokers (16.18% vs. 12.27%, P = .02). Wound classification also differed: clean, 38.55% before vs. 43.91% after; and clean-contaminated, 61.45% vs. 56.09% (P = .02). All other demographic and clinical characteristics were similar between the two groups.
“In multivariate logistic regression models controlling for these confounders, there was no association of the banning of skullcaps with decreased surgical site infection rates,” Dr. Rios-Diaz said.
“The adoption of guidelines targeted to optimize patient care should always be welcomed by surgeons,” he said. “However, if they’re going to be implemented on a national level, these policies must be based on higher levels of evidence, so further studies are warranted to assess the validity of the [Joint Commission] headwear guidelines.” According to Dr. Rios-Diaz, the recommendations from the Association of periOperative Registered Nurses are based on two case series from the 1960s and 1970s.
Thomas Jefferson University once again allows skullcaps in the OR, he said.
Dr. Rios-Diaz and his coauthors had no financial relationships to disclose.
SOURCE: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
JACKSONVILLE, FLA. – Surgeons who choose to wear a skullcap in the OR can point to yet another study with evidence to bolster their preference.
Two major hospital and nursing credentialing organizations have recommended that hospitals ban skullcaps from the operating room as a practice to control surgical site infections, but a study of almost 2,000 operations at an academic medical center has found that strictly enforcing the ban had no impact on infection rates, according to results of a study presented at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
The study, conducted at Thomas Jefferson University in Philadelphia, showed that rates of surgical site infections (SSIs) were almost identical in the year before and the year after the institution implemented the skullcap ban. “The overall surgical site infection rate was 5.4%, and there were no differences in surgical site infections before or after the headwear policy was adopted,” said Arturo J. Rios-Diaz, MD. The Joint Commission and the Association of periOperative Registered Nurses recommend against the use of skullcaps.
The study reviewed American College of Surgeons National Surgical Quality Improvement Program data on 1,901 patients who had 1,950 clean or clean-contaminated general surgery procedures in 2015, the year before the ban was implemented, and in 2016 (767 in 2015 and 1,183 in 2016). The most common procedures were colectomy (18.2%), pancreatectomy (13.5%), and ventral hernia repair (9.9%). The study excluded orthopedic and vascular operations and any cases with sepsis or an active infection at the time of surgery.
There were some differences between the pre- and postban patient groups. The preban group was younger (median age, 57.91 years vs. 59.75, P = .01) but had more patients who were obese, measured as body mass index above 30 kg/m2 (42.37% vs. 35.23%, P less than .01), and smokers (16.18% vs. 12.27%, P = .02). Wound classification also differed: clean, 38.55% before vs. 43.91% after; and clean-contaminated, 61.45% vs. 56.09% (P = .02). All other demographic and clinical characteristics were similar between the two groups.
“In multivariate logistic regression models controlling for these confounders, there was no association of the banning of skullcaps with decreased surgical site infection rates,” Dr. Rios-Diaz said.
“The adoption of guidelines targeted to optimize patient care should always be welcomed by surgeons,” he said. “However, if they’re going to be implemented on a national level, these policies must be based on higher levels of evidence, so further studies are warranted to assess the validity of the [Joint Commission] headwear guidelines.” According to Dr. Rios-Diaz, the recommendations from the Association of periOperative Registered Nurses are based on two case series from the 1960s and 1970s.
Thomas Jefferson University once again allows skullcaps in the OR, he said.
Dr. Rios-Diaz and his coauthors had no financial relationships to disclose.
SOURCE: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
REPORTING FROM THE ACADEMIC SURGICAL CONGRESS
Key clinical point: Findings of this study do not support the ban on surgical skullcaps.
Major finding: No association was found between the skullcap ban and decreased surgical site infection.
Study details: Analysis of ACS NSQIP data on 1,950 surgical cases from before and after the skullcap ban.
Disclosures: The investigators had no financial relationships to disclose.
Source: Rios-Diaz AJ et al. Annual Academic Surgical Congress. Abstract 09.11.
Dermoscopy will help diagnose pediatric melanomas
Adding dermoscopy to the classic and modified melanoma ABCD criteria will help speed detection of melanoma in children, said Cristina Carrera, MD, of the University of Barcelona, and her associates.
Pediatric melanomas make up less than 3% of pediatric cancers and 1%-4% of all melanomas, occurring more commonly in adolescents than in children aged 5-9 years. These cancers often are thicker when first seen because of delay in diagnosis and/or differences in growth dynamics. Delay in diagnosis may occur because of the low incidence of pediatric melanoma and because classic melanoma criteria – ABCD: asymmetry, border irregularity, multiple colors, diameter (6 mm) – don’t always apply, they said.
A modified clinical ABCD rule of ‘‘amelanotic, bleeding bump, color uniformity, and de novo lesion of any diameter’’ was proposed to improve early detection of pediatric melanoma. And because dermoscopy improves melanoma diagnosis in adults, researchers decided to examine clinical and dermascopic findings in a group of pediatric melanoma cases.
Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across nine countries (Australia, Belgium, Brazil, France, Israel, Italy, Serbia, Spain, and the United States), and clinical and dermoscopic specimens were examined by two experienced reviewers.
The mean age of the patients was 15 years, and 26 of the patients were female. Histopathologically, 28% of the pediatric melanomas were classified as spitzoid and 72% as nonspitzoid. Patients with a spitzoid melanoma were significantly younger than those with nonspitzoid melanoma (12.5 vs. 16 years, P = .004). All of the spitzoid tumors were invasive, and they were significantly thicker than the nonspitzoid melanomas (2.6 vs. 1.2 mm, P = .004). Also, these lesions more frequently were ulcerated than nonspitzoid melanomas (29% vs. 8%, P = .06). Melanomas associated with a nevus more often were among nonspitzoid than spitzoid melanomas (62% vs. 27% P = .02), and the congenital type of nevus was linked most often with nonspitzoid melanomas (25 of 27 [92.6%]), Dr. Carrera and her associates reported.
The pediatric melanomas in this study appeared most frequently on the lower extremities (31%), followed by the back (27%). Spitzoid melanomas most often appeared on the limbs (73%); nonspitzoid melanomas were likely to occur on the torso (52%).
In the majority of cases (52%), the overall clinical morphology was considered to fulfill the classic melanoma ABCD criteria. The remaining lesions that did not fulfill the conventional ABCD criteria were called benign-appearing tumors or nodular/polypoid tumors. Spitzoid melanomas most often were nodular/ polypoid (47%), while most nonspitzoid melanomas (59%) were melanoma-like. Only 21% of the pediatric melanomas fulfilled the modified melanoma ABCD criteria, they noted.
On dermoscopy, which was available in 49 cases, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03); a nevus-like pattern in 9 cases was seen only among nonspitzoid melanomas. A vascular pink Spitz-like pattern in seven cases mostly was associated with spitzoid melanomas (86%, P less than .002). A pigmented Reed-like pattern seen in seven cases occurred more often among spitzoid melanomas, but this did not reach statistical significance, the investigators wrote.
In terms of appearance, “red and white colors, milky red areas, polymorphous vessels, and shiny white structures were associated with spitzoid melanoma. Dark brown color, atypical network, and structureless areas were associated with nonspitzoid melanomas,” Dr. Carrera and her associates said.
Dermoscopic patterns that were pink spitzoid or Reed-like were more likely to be histopathologically classified as spitzoid. These pediatric melanomas were linked with younger age, occurrence on the limbs, and de novo development. On the other hand, dermoscopic patterns that were multicomponent or nevus-like were likely to be histopathologically classified as nonspitzoid. These lesions were linked with older age, fair skin phenotype, family history of melanoma, and a preexisting nevus, the researchers said.
“In contrast to previous reports, the present study highlights the fact that the majority of melanomas diagnosed in patients younger than 20 years look similar to melanomas found in adults. Nonspitzoid melanomas were associated with adolescence and with the presence of melanoma risk factors. All nonspitzoid melanomas displayed dermoscopic features associated with melanoma. Spitzoid melanomas were associated with younger age, location on the extremities, and nodular/polypoid clinical morphology. Dermoscopy of spitzoid melanomas revealed atypical vessels and shiny white lines (if amelanotic) or an asymmetric starburst pattern (if pigmented),” Dr. Carrera and her associates concluded.
The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was confinanced by numerous other grants.
SOURCE: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88. doi: 10.1016/j.jaad.2017.09.065.
Adding dermoscopy to the classic and modified melanoma ABCD criteria will help speed detection of melanoma in children, said Cristina Carrera, MD, of the University of Barcelona, and her associates.
Pediatric melanomas make up less than 3% of pediatric cancers and 1%-4% of all melanomas, occurring more commonly in adolescents than in children aged 5-9 years. These cancers often are thicker when first seen because of delay in diagnosis and/or differences in growth dynamics. Delay in diagnosis may occur because of the low incidence of pediatric melanoma and because classic melanoma criteria – ABCD: asymmetry, border irregularity, multiple colors, diameter (6 mm) – don’t always apply, they said.
A modified clinical ABCD rule of ‘‘amelanotic, bleeding bump, color uniformity, and de novo lesion of any diameter’’ was proposed to improve early detection of pediatric melanoma. And because dermoscopy improves melanoma diagnosis in adults, researchers decided to examine clinical and dermascopic findings in a group of pediatric melanoma cases.
Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across nine countries (Australia, Belgium, Brazil, France, Israel, Italy, Serbia, Spain, and the United States), and clinical and dermoscopic specimens were examined by two experienced reviewers.
The mean age of the patients was 15 years, and 26 of the patients were female. Histopathologically, 28% of the pediatric melanomas were classified as spitzoid and 72% as nonspitzoid. Patients with a spitzoid melanoma were significantly younger than those with nonspitzoid melanoma (12.5 vs. 16 years, P = .004). All of the spitzoid tumors were invasive, and they were significantly thicker than the nonspitzoid melanomas (2.6 vs. 1.2 mm, P = .004). Also, these lesions more frequently were ulcerated than nonspitzoid melanomas (29% vs. 8%, P = .06). Melanomas associated with a nevus more often were among nonspitzoid than spitzoid melanomas (62% vs. 27% P = .02), and the congenital type of nevus was linked most often with nonspitzoid melanomas (25 of 27 [92.6%]), Dr. Carrera and her associates reported.
The pediatric melanomas in this study appeared most frequently on the lower extremities (31%), followed by the back (27%). Spitzoid melanomas most often appeared on the limbs (73%); nonspitzoid melanomas were likely to occur on the torso (52%).
In the majority of cases (52%), the overall clinical morphology was considered to fulfill the classic melanoma ABCD criteria. The remaining lesions that did not fulfill the conventional ABCD criteria were called benign-appearing tumors or nodular/polypoid tumors. Spitzoid melanomas most often were nodular/ polypoid (47%), while most nonspitzoid melanomas (59%) were melanoma-like. Only 21% of the pediatric melanomas fulfilled the modified melanoma ABCD criteria, they noted.
On dermoscopy, which was available in 49 cases, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03); a nevus-like pattern in 9 cases was seen only among nonspitzoid melanomas. A vascular pink Spitz-like pattern in seven cases mostly was associated with spitzoid melanomas (86%, P less than .002). A pigmented Reed-like pattern seen in seven cases occurred more often among spitzoid melanomas, but this did not reach statistical significance, the investigators wrote.
In terms of appearance, “red and white colors, milky red areas, polymorphous vessels, and shiny white structures were associated with spitzoid melanoma. Dark brown color, atypical network, and structureless areas were associated with nonspitzoid melanomas,” Dr. Carrera and her associates said.
Dermoscopic patterns that were pink spitzoid or Reed-like were more likely to be histopathologically classified as spitzoid. These pediatric melanomas were linked with younger age, occurrence on the limbs, and de novo development. On the other hand, dermoscopic patterns that were multicomponent or nevus-like were likely to be histopathologically classified as nonspitzoid. These lesions were linked with older age, fair skin phenotype, family history of melanoma, and a preexisting nevus, the researchers said.
“In contrast to previous reports, the present study highlights the fact that the majority of melanomas diagnosed in patients younger than 20 years look similar to melanomas found in adults. Nonspitzoid melanomas were associated with adolescence and with the presence of melanoma risk factors. All nonspitzoid melanomas displayed dermoscopic features associated with melanoma. Spitzoid melanomas were associated with younger age, location on the extremities, and nodular/polypoid clinical morphology. Dermoscopy of spitzoid melanomas revealed atypical vessels and shiny white lines (if amelanotic) or an asymmetric starburst pattern (if pigmented),” Dr. Carrera and her associates concluded.
The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was confinanced by numerous other grants.
SOURCE: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88. doi: 10.1016/j.jaad.2017.09.065.
Adding dermoscopy to the classic and modified melanoma ABCD criteria will help speed detection of melanoma in children, said Cristina Carrera, MD, of the University of Barcelona, and her associates.
Pediatric melanomas make up less than 3% of pediatric cancers and 1%-4% of all melanomas, occurring more commonly in adolescents than in children aged 5-9 years. These cancers often are thicker when first seen because of delay in diagnosis and/or differences in growth dynamics. Delay in diagnosis may occur because of the low incidence of pediatric melanoma and because classic melanoma criteria – ABCD: asymmetry, border irregularity, multiple colors, diameter (6 mm) – don’t always apply, they said.
A modified clinical ABCD rule of ‘‘amelanotic, bleeding bump, color uniformity, and de novo lesion of any diameter’’ was proposed to improve early detection of pediatric melanoma. And because dermoscopy improves melanoma diagnosis in adults, researchers decided to examine clinical and dermascopic findings in a group of pediatric melanoma cases.
Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across nine countries (Australia, Belgium, Brazil, France, Israel, Italy, Serbia, Spain, and the United States), and clinical and dermoscopic specimens were examined by two experienced reviewers.
The mean age of the patients was 15 years, and 26 of the patients were female. Histopathologically, 28% of the pediatric melanomas were classified as spitzoid and 72% as nonspitzoid. Patients with a spitzoid melanoma were significantly younger than those with nonspitzoid melanoma (12.5 vs. 16 years, P = .004). All of the spitzoid tumors were invasive, and they were significantly thicker than the nonspitzoid melanomas (2.6 vs. 1.2 mm, P = .004). Also, these lesions more frequently were ulcerated than nonspitzoid melanomas (29% vs. 8%, P = .06). Melanomas associated with a nevus more often were among nonspitzoid than spitzoid melanomas (62% vs. 27% P = .02), and the congenital type of nevus was linked most often with nonspitzoid melanomas (25 of 27 [92.6%]), Dr. Carrera and her associates reported.
The pediatric melanomas in this study appeared most frequently on the lower extremities (31%), followed by the back (27%). Spitzoid melanomas most often appeared on the limbs (73%); nonspitzoid melanomas were likely to occur on the torso (52%).
In the majority of cases (52%), the overall clinical morphology was considered to fulfill the classic melanoma ABCD criteria. The remaining lesions that did not fulfill the conventional ABCD criteria were called benign-appearing tumors or nodular/polypoid tumors. Spitzoid melanomas most often were nodular/ polypoid (47%), while most nonspitzoid melanomas (59%) were melanoma-like. Only 21% of the pediatric melanomas fulfilled the modified melanoma ABCD criteria, they noted.
On dermoscopy, which was available in 49 cases, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03); a nevus-like pattern in 9 cases was seen only among nonspitzoid melanomas. A vascular pink Spitz-like pattern in seven cases mostly was associated with spitzoid melanomas (86%, P less than .002). A pigmented Reed-like pattern seen in seven cases occurred more often among spitzoid melanomas, but this did not reach statistical significance, the investigators wrote.
In terms of appearance, “red and white colors, milky red areas, polymorphous vessels, and shiny white structures were associated with spitzoid melanoma. Dark brown color, atypical network, and structureless areas were associated with nonspitzoid melanomas,” Dr. Carrera and her associates said.
Dermoscopic patterns that were pink spitzoid or Reed-like were more likely to be histopathologically classified as spitzoid. These pediatric melanomas were linked with younger age, occurrence on the limbs, and de novo development. On the other hand, dermoscopic patterns that were multicomponent or nevus-like were likely to be histopathologically classified as nonspitzoid. These lesions were linked with older age, fair skin phenotype, family history of melanoma, and a preexisting nevus, the researchers said.
“In contrast to previous reports, the present study highlights the fact that the majority of melanomas diagnosed in patients younger than 20 years look similar to melanomas found in adults. Nonspitzoid melanomas were associated with adolescence and with the presence of melanoma risk factors. All nonspitzoid melanomas displayed dermoscopic features associated with melanoma. Spitzoid melanomas were associated with younger age, location on the extremities, and nodular/polypoid clinical morphology. Dermoscopy of spitzoid melanomas revealed atypical vessels and shiny white lines (if amelanotic) or an asymmetric starburst pattern (if pigmented),” Dr. Carrera and her associates concluded.
The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was confinanced by numerous other grants.
SOURCE: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88. doi: 10.1016/j.jaad.2017.09.065.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Key clinical point:
Major finding: On dermoscopy, a multicomponent pattern seen in 24 cases mostly was associated with nonspitzoid melanoma (88%, P less than.03).
Data source: Fifty-two pediatric melanoma cases from 51 patients were collected from pigmented lesion clinics across 9 countries.
Disclosures: The investigators had no relevant financial disclosures. The study was supported in part through a grant from the National Institutes of Health/ National Cancer Institute. The research at the melanoma unit in Barcelona was partially funded by grants from the Spanish Fondo de Investigaciones Sanitarias and CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; it was cofinanced by numerous other grants.
Source: Carrera C et al. J Am Acad Dermatol. 2018;78(2):278-88.
Study spotlights body image dissatisfaction in pediatric IBD
LAS VEGAS – Among current steroid use, higher body mass index percentile, and comorbid mood disorder.
The findings come from a cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort, presented by Jennifer Claytor, MS, at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Ms. Claytor, a fourth-year medical student at the University of North Carolina at Chapel Hill, and her associates asked study participants aged 5-18 years to complete surveys on demographics, disease characteristics, and the IMPACT-35 questionnaire and Patient-Reported Outcomes Measurement Information System (PROMIS) tools for assessment of psychological patient-reported outcomes. The pediatric ulcerative colitis activity index and the short Crohn’s disease activity index were used to measure disease activity.
The researchers classified body image dissatisfaction as being present if the patients selected “I look awful” or “I look bad” from the list of possible responses to the question, “How do you feel about the way you look?” Next, they performed bivariate analyses to assess associations between body image dissatisfaction and demographic, disease-related, and psychosocial factors and created logistic regression models to evaluate independent associations between selected risk factors and body image dissatisfaction. “There has been some literature which suggests that for boys, weight and not body image dissatisfaction predicts worse psychosocial outcomes,” Ms. Claytor said. “But for girls it’s body image dissatisfaction, irrespective of weight.”
Of the 664 patients, 74 (3.3%) met criteria for body image dissatisfaction. Compared with patients who did not meet criteria for body image dissatisfaction, those who did were significantly more likely to be female (69% vs. 44%, respectively; P less than .001), older (mean age of 15 vs. 13 years; P less than .001), and diagnosed with IBD an older age (median of 12 vs. 10 years; P less than .001). Ms. Claytor and her associates also found that individuals with body image dissatisfaction had a higher median BMI percentile (P = .02), higher rates of active disease (57% vs. 26%; P less than .001), higher rates of current steroid use (18% vs. 8%; P = .004), and higher rates of depression and anxiety (P less than .001).
After adjusting for age, body mass index, remission, steroid use, and other factors, the odds for developing body image dissatisfaction was highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73), female gender (OR, 2.31), and current steroid use (OR, 1.59). “I think this points to the need for enhanced counseling services and being aware of these characteristics,” Ms. Claytor said. She reported having no financial disclosures.
SOURCE: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
*This story was updated on 3/26.
LAS VEGAS – Among current steroid use, higher body mass index percentile, and comorbid mood disorder.
The findings come from a cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort, presented by Jennifer Claytor, MS, at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Ms. Claytor, a fourth-year medical student at the University of North Carolina at Chapel Hill, and her associates asked study participants aged 5-18 years to complete surveys on demographics, disease characteristics, and the IMPACT-35 questionnaire and Patient-Reported Outcomes Measurement Information System (PROMIS) tools for assessment of psychological patient-reported outcomes. The pediatric ulcerative colitis activity index and the short Crohn’s disease activity index were used to measure disease activity.
The researchers classified body image dissatisfaction as being present if the patients selected “I look awful” or “I look bad” from the list of possible responses to the question, “How do you feel about the way you look?” Next, they performed bivariate analyses to assess associations between body image dissatisfaction and demographic, disease-related, and psychosocial factors and created logistic regression models to evaluate independent associations between selected risk factors and body image dissatisfaction. “There has been some literature which suggests that for boys, weight and not body image dissatisfaction predicts worse psychosocial outcomes,” Ms. Claytor said. “But for girls it’s body image dissatisfaction, irrespective of weight.”
Of the 664 patients, 74 (3.3%) met criteria for body image dissatisfaction. Compared with patients who did not meet criteria for body image dissatisfaction, those who did were significantly more likely to be female (69% vs. 44%, respectively; P less than .001), older (mean age of 15 vs. 13 years; P less than .001), and diagnosed with IBD an older age (median of 12 vs. 10 years; P less than .001). Ms. Claytor and her associates also found that individuals with body image dissatisfaction had a higher median BMI percentile (P = .02), higher rates of active disease (57% vs. 26%; P less than .001), higher rates of current steroid use (18% vs. 8%; P = .004), and higher rates of depression and anxiety (P less than .001).
After adjusting for age, body mass index, remission, steroid use, and other factors, the odds for developing body image dissatisfaction was highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73), female gender (OR, 2.31), and current steroid use (OR, 1.59). “I think this points to the need for enhanced counseling services and being aware of these characteristics,” Ms. Claytor said. She reported having no financial disclosures.
SOURCE: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
*This story was updated on 3/26.
LAS VEGAS – Among current steroid use, higher body mass index percentile, and comorbid mood disorder.
The findings come from a cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort, presented by Jennifer Claytor, MS, at the Crohn’s & Colitis Congress, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
Ms. Claytor, a fourth-year medical student at the University of North Carolina at Chapel Hill, and her associates asked study participants aged 5-18 years to complete surveys on demographics, disease characteristics, and the IMPACT-35 questionnaire and Patient-Reported Outcomes Measurement Information System (PROMIS) tools for assessment of psychological patient-reported outcomes. The pediatric ulcerative colitis activity index and the short Crohn’s disease activity index were used to measure disease activity.
The researchers classified body image dissatisfaction as being present if the patients selected “I look awful” or “I look bad” from the list of possible responses to the question, “How do you feel about the way you look?” Next, they performed bivariate analyses to assess associations between body image dissatisfaction and demographic, disease-related, and psychosocial factors and created logistic regression models to evaluate independent associations between selected risk factors and body image dissatisfaction. “There has been some literature which suggests that for boys, weight and not body image dissatisfaction predicts worse psychosocial outcomes,” Ms. Claytor said. “But for girls it’s body image dissatisfaction, irrespective of weight.”
Of the 664 patients, 74 (3.3%) met criteria for body image dissatisfaction. Compared with patients who did not meet criteria for body image dissatisfaction, those who did were significantly more likely to be female (69% vs. 44%, respectively; P less than .001), older (mean age of 15 vs. 13 years; P less than .001), and diagnosed with IBD an older age (median of 12 vs. 10 years; P less than .001). Ms. Claytor and her associates also found that individuals with body image dissatisfaction had a higher median BMI percentile (P = .02), higher rates of active disease (57% vs. 26%; P less than .001), higher rates of current steroid use (18% vs. 8%; P = .004), and higher rates of depression and anxiety (P less than .001).
After adjusting for age, body mass index, remission, steroid use, and other factors, the odds for developing body image dissatisfaction was highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73), female gender (OR, 2.31), and current steroid use (OR, 1.59). “I think this points to the need for enhanced counseling services and being aware of these characteristics,” Ms. Claytor said. She reported having no financial disclosures.
SOURCE: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
*This story was updated on 3/26.
REPORTING FROM CROHN’S & COLITIS CONGRESS
Key clinical point: Interventions to target modifiable risk factors for body image dissatisfaction may improve quality of life in pediatric IBD patients.
Major finding: The odds for developing body image dissatisfaction were highest among those with anxiety (odds ratio, 5.42), followed by depression (OR, 4.73) and female gender (OR, 2.31).
Study details: A cross-sectional study of 664 patients enrolled in the Crohn’s & Colitis Foundation’s Partners Kids & Teens cohort.
Disclosures: Ms. Claytor reported having no financial disclosures.
Source: Claytor J et al. Crohn’s & Colitis Congress, Poster 15.
Bladder cancer: Two chemoradiation therapy regimens on par for muscle-invasive disease
SAN FRANCISCO – Two concurrent chemoradiation induction regimens had similar safety and efficacy when used as part of a bladder-sparing strategy in patients with muscle-invasive bladder cancer, suggest primary results of the NRG/RTOG 0712 trial. But one offers better patient convenience.
The selective bladder-preservation paradigm entails maximal transurethral resection of the bladder tumor (TURBT) followed by induction radiation and concomitant chemotherapy, lead author John J. Coen, MD, a radiation oncologist with 21st Century Oncology, Providence, Rhode Island, noted at the 2018 Genitourinary Cancers Symposium. Patients then undergo cystoscopy to assess their response.
“A key component of this therapy is close urologic surveillance,” he noted. “This is trimodality therapy with close urologic surveillance, and cystectomy is prompted at the earliest time it’s indicated.”
The 70 patients enrolled in the multicenter randomized phase 2 trial had undergone TURBT and were randomized evenly to twice-daily radiation plus 5-flourouracil-cisplatin (the RTOG standard at the time of trial planning) or to daily radiation plus gemcitabine (a modification of a successful regimen developed at the University of Michigan). All were offered adjuvant chemotherapy regardless of whether they responded and whether they underwent consolidation therapy or cystectomy.
At a median follow-up of 5.1 years among the 52 evaluable patients, the 3-year rate of freedom from distant metastasis, the trial’s primary endpoint, was 78% with twice-daily radiation plus 5-flourouracil-cisplatin and 84% with daily radiation plus gemcitabine, according to results reported at the symposium, which was sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Both values were higher than the trial’s predefined benchmark of 75% for defining the regimen as promising. “This trial wasn’t necessarily powered to compare arms, so the conclusion would be that both arms exceeded the benchmark and it would be appropriate to evaluate both arms further in subsequent trials,” Dr. Coen commented.
In each trial arm, more than three-fourths of patients had a complete response, and about two-thirds of patients were alive and free of distant metastasis with their bladder intact at 3 years.
Toxicity, which was supposed to be the tie-breaker if efficacy was similar, was also essentially the same for the two regimens. Both were fairly well tolerated in the acute period; the primary grade 3 and 4 toxicities were hematologic ones.
“So where do we go from here? I think this trial does demonstrate concurrent gemcitabine is a reasonable alternative to cisplatin for patients undergoing selective bladder preservation,” Dr. Coen summarized. “This is especially important in patients with poor renal function or hearing loss. And bladder cancer is often a disease in the elderly, so tolerance of various regimens is a very important aspect to planning further trials.”
“This trial also demonstrates that daily radiation is a reasonable alternative to twice-a-day radiation, which had become the standard through the RTOG on more contemporary trials,” he added. “Daily radiation would allow wider adoption of selective bladder preservation by trimodality therapy.”
Clinical implications
“I would have to see more details about the toxicity data for the chemotherapy, the radiosensitizers,” session co-chair Yair Lotan, MD, a professor of urology at the UT Southwestern Medical Center, Dallas, Texas, commented in an interview. “But in general, if you have two equivalent protocols in terms of effectiveness, and one is less toxic or more convenient, that’s always preferable. From the standpoint of coming once a day rather than twice a day to get radiation, if I were a patient, I would prefer that regimen”
Current practice in this patient population likely hinges on where a patient is treated, he said. “Based on the new nonmetastatic muscle-invasive guidelines, many of them would be recommended surgery or possibly chemoradiation protocols, and then there are a lot of factors such as patient preference and outcomes that would probably impact the decision making.”
“Certainly, this study won’t prove standard of care because standard of care in the global picture for a patient with muscle-invasive disease really will depend on a randomized trial of surgery versus radiation or chemoradiation, multimodal therapies,” Dr. Lotan maintained. “Not every patient is even eligible; some patients with hydronephrosis or unresectable disease may not be the best candidates for multimodal therapy. But more information from these types of trials may help clinicians decide which multimodal therapy approach to use.”
Study details
Patients enrolled in NRG/RTOG 0712, a multicenter randomized phase 2 trial supported by the National Cancer Institute, had clinical T2 or T3-4a bladder cancer. Hydronephrosis and obvious lymph node involvement were exclusion criteria.
Like the rate of freedom from metastasis, the rate of complete response after induction therapy was similar for the two arms: 87.9% with twice-daily radiation plus 5-flourouracil-cisplatin and 75.8% with daily radiation plus gemcitabine.
“These rates exceed historical complete response rates, and this is likely a result of improved selection over time and more thorough TURBTs performed over time,” Dr. Coen proposed. “Over the course of multiple successive RTOG trials, our selection criteria have been refined. One excellent example would be that hydronephrosis has been excluded on more contemporary trials, but if you look at older trials, those patients were included.”
The 3-year rate of bladder-intact distant metastasis–free survival was 66.7% and 69%, respectively. “This is a very important endpoint. These results are excellent,” he commented. “And there is really no appreciable difference between the two arms on the actuarial analysis.”
As far as specific treatment failure events in the trial overall, three patients died, eight underwent cystectomy, and eight developed distant metastases. Although numbers were small, these events appeared fairly evenly distributed across arms.
The rate of grade 3 or 4 acute toxicity was 57.6% with twice-daily radiation plus 5-flourouracil-cisplatin and 54.6% with daily radiation plus gemcitabine. The large majority of events were blood and bone marrow toxicity. “It’s quite notable that the rates of GU and GI toxicity were very low,” commented Dr. Coen, who disclosed that he had no relevant conflicts of interest.
SOURCE: Coen, J. et al, 2018 Genitourinary Cancers Symposium, Abstract 408
SAN FRANCISCO – Two concurrent chemoradiation induction regimens had similar safety and efficacy when used as part of a bladder-sparing strategy in patients with muscle-invasive bladder cancer, suggest primary results of the NRG/RTOG 0712 trial. But one offers better patient convenience.
The selective bladder-preservation paradigm entails maximal transurethral resection of the bladder tumor (TURBT) followed by induction radiation and concomitant chemotherapy, lead author John J. Coen, MD, a radiation oncologist with 21st Century Oncology, Providence, Rhode Island, noted at the 2018 Genitourinary Cancers Symposium. Patients then undergo cystoscopy to assess their response.
“A key component of this therapy is close urologic surveillance,” he noted. “This is trimodality therapy with close urologic surveillance, and cystectomy is prompted at the earliest time it’s indicated.”
The 70 patients enrolled in the multicenter randomized phase 2 trial had undergone TURBT and were randomized evenly to twice-daily radiation plus 5-flourouracil-cisplatin (the RTOG standard at the time of trial planning) or to daily radiation plus gemcitabine (a modification of a successful regimen developed at the University of Michigan). All were offered adjuvant chemotherapy regardless of whether they responded and whether they underwent consolidation therapy or cystectomy.
At a median follow-up of 5.1 years among the 52 evaluable patients, the 3-year rate of freedom from distant metastasis, the trial’s primary endpoint, was 78% with twice-daily radiation plus 5-flourouracil-cisplatin and 84% with daily radiation plus gemcitabine, according to results reported at the symposium, which was sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Both values were higher than the trial’s predefined benchmark of 75% for defining the regimen as promising. “This trial wasn’t necessarily powered to compare arms, so the conclusion would be that both arms exceeded the benchmark and it would be appropriate to evaluate both arms further in subsequent trials,” Dr. Coen commented.
In each trial arm, more than three-fourths of patients had a complete response, and about two-thirds of patients were alive and free of distant metastasis with their bladder intact at 3 years.
Toxicity, which was supposed to be the tie-breaker if efficacy was similar, was also essentially the same for the two regimens. Both were fairly well tolerated in the acute period; the primary grade 3 and 4 toxicities were hematologic ones.
“So where do we go from here? I think this trial does demonstrate concurrent gemcitabine is a reasonable alternative to cisplatin for patients undergoing selective bladder preservation,” Dr. Coen summarized. “This is especially important in patients with poor renal function or hearing loss. And bladder cancer is often a disease in the elderly, so tolerance of various regimens is a very important aspect to planning further trials.”
“This trial also demonstrates that daily radiation is a reasonable alternative to twice-a-day radiation, which had become the standard through the RTOG on more contemporary trials,” he added. “Daily radiation would allow wider adoption of selective bladder preservation by trimodality therapy.”
Clinical implications
“I would have to see more details about the toxicity data for the chemotherapy, the radiosensitizers,” session co-chair Yair Lotan, MD, a professor of urology at the UT Southwestern Medical Center, Dallas, Texas, commented in an interview. “But in general, if you have two equivalent protocols in terms of effectiveness, and one is less toxic or more convenient, that’s always preferable. From the standpoint of coming once a day rather than twice a day to get radiation, if I were a patient, I would prefer that regimen”
Current practice in this patient population likely hinges on where a patient is treated, he said. “Based on the new nonmetastatic muscle-invasive guidelines, many of them would be recommended surgery or possibly chemoradiation protocols, and then there are a lot of factors such as patient preference and outcomes that would probably impact the decision making.”
“Certainly, this study won’t prove standard of care because standard of care in the global picture for a patient with muscle-invasive disease really will depend on a randomized trial of surgery versus radiation or chemoradiation, multimodal therapies,” Dr. Lotan maintained. “Not every patient is even eligible; some patients with hydronephrosis or unresectable disease may not be the best candidates for multimodal therapy. But more information from these types of trials may help clinicians decide which multimodal therapy approach to use.”
Study details
Patients enrolled in NRG/RTOG 0712, a multicenter randomized phase 2 trial supported by the National Cancer Institute, had clinical T2 or T3-4a bladder cancer. Hydronephrosis and obvious lymph node involvement were exclusion criteria.
Like the rate of freedom from metastasis, the rate of complete response after induction therapy was similar for the two arms: 87.9% with twice-daily radiation plus 5-flourouracil-cisplatin and 75.8% with daily radiation plus gemcitabine.
“These rates exceed historical complete response rates, and this is likely a result of improved selection over time and more thorough TURBTs performed over time,” Dr. Coen proposed. “Over the course of multiple successive RTOG trials, our selection criteria have been refined. One excellent example would be that hydronephrosis has been excluded on more contemporary trials, but if you look at older trials, those patients were included.”
The 3-year rate of bladder-intact distant metastasis–free survival was 66.7% and 69%, respectively. “This is a very important endpoint. These results are excellent,” he commented. “And there is really no appreciable difference between the two arms on the actuarial analysis.”
As far as specific treatment failure events in the trial overall, three patients died, eight underwent cystectomy, and eight developed distant metastases. Although numbers were small, these events appeared fairly evenly distributed across arms.
The rate of grade 3 or 4 acute toxicity was 57.6% with twice-daily radiation plus 5-flourouracil-cisplatin and 54.6% with daily radiation plus gemcitabine. The large majority of events were blood and bone marrow toxicity. “It’s quite notable that the rates of GU and GI toxicity were very low,” commented Dr. Coen, who disclosed that he had no relevant conflicts of interest.
SOURCE: Coen, J. et al, 2018 Genitourinary Cancers Symposium, Abstract 408
SAN FRANCISCO – Two concurrent chemoradiation induction regimens had similar safety and efficacy when used as part of a bladder-sparing strategy in patients with muscle-invasive bladder cancer, suggest primary results of the NRG/RTOG 0712 trial. But one offers better patient convenience.
The selective bladder-preservation paradigm entails maximal transurethral resection of the bladder tumor (TURBT) followed by induction radiation and concomitant chemotherapy, lead author John J. Coen, MD, a radiation oncologist with 21st Century Oncology, Providence, Rhode Island, noted at the 2018 Genitourinary Cancers Symposium. Patients then undergo cystoscopy to assess their response.
“A key component of this therapy is close urologic surveillance,” he noted. “This is trimodality therapy with close urologic surveillance, and cystectomy is prompted at the earliest time it’s indicated.”
The 70 patients enrolled in the multicenter randomized phase 2 trial had undergone TURBT and were randomized evenly to twice-daily radiation plus 5-flourouracil-cisplatin (the RTOG standard at the time of trial planning) or to daily radiation plus gemcitabine (a modification of a successful regimen developed at the University of Michigan). All were offered adjuvant chemotherapy regardless of whether they responded and whether they underwent consolidation therapy or cystectomy.
At a median follow-up of 5.1 years among the 52 evaluable patients, the 3-year rate of freedom from distant metastasis, the trial’s primary endpoint, was 78% with twice-daily radiation plus 5-flourouracil-cisplatin and 84% with daily radiation plus gemcitabine, according to results reported at the symposium, which was sponsored by the American Society of Clinical Oncology, ASTRO, and the Society of Urologic Oncology.
Both values were higher than the trial’s predefined benchmark of 75% for defining the regimen as promising. “This trial wasn’t necessarily powered to compare arms, so the conclusion would be that both arms exceeded the benchmark and it would be appropriate to evaluate both arms further in subsequent trials,” Dr. Coen commented.
In each trial arm, more than three-fourths of patients had a complete response, and about two-thirds of patients were alive and free of distant metastasis with their bladder intact at 3 years.
Toxicity, which was supposed to be the tie-breaker if efficacy was similar, was also essentially the same for the two regimens. Both were fairly well tolerated in the acute period; the primary grade 3 and 4 toxicities were hematologic ones.
“So where do we go from here? I think this trial does demonstrate concurrent gemcitabine is a reasonable alternative to cisplatin for patients undergoing selective bladder preservation,” Dr. Coen summarized. “This is especially important in patients with poor renal function or hearing loss. And bladder cancer is often a disease in the elderly, so tolerance of various regimens is a very important aspect to planning further trials.”
“This trial also demonstrates that daily radiation is a reasonable alternative to twice-a-day radiation, which had become the standard through the RTOG on more contemporary trials,” he added. “Daily radiation would allow wider adoption of selective bladder preservation by trimodality therapy.”
Clinical implications
“I would have to see more details about the toxicity data for the chemotherapy, the radiosensitizers,” session co-chair Yair Lotan, MD, a professor of urology at the UT Southwestern Medical Center, Dallas, Texas, commented in an interview. “But in general, if you have two equivalent protocols in terms of effectiveness, and one is less toxic or more convenient, that’s always preferable. From the standpoint of coming once a day rather than twice a day to get radiation, if I were a patient, I would prefer that regimen”
Current practice in this patient population likely hinges on where a patient is treated, he said. “Based on the new nonmetastatic muscle-invasive guidelines, many of them would be recommended surgery or possibly chemoradiation protocols, and then there are a lot of factors such as patient preference and outcomes that would probably impact the decision making.”
“Certainly, this study won’t prove standard of care because standard of care in the global picture for a patient with muscle-invasive disease really will depend on a randomized trial of surgery versus radiation or chemoradiation, multimodal therapies,” Dr. Lotan maintained. “Not every patient is even eligible; some patients with hydronephrosis or unresectable disease may not be the best candidates for multimodal therapy. But more information from these types of trials may help clinicians decide which multimodal therapy approach to use.”
Study details
Patients enrolled in NRG/RTOG 0712, a multicenter randomized phase 2 trial supported by the National Cancer Institute, had clinical T2 or T3-4a bladder cancer. Hydronephrosis and obvious lymph node involvement were exclusion criteria.
Like the rate of freedom from metastasis, the rate of complete response after induction therapy was similar for the two arms: 87.9% with twice-daily radiation plus 5-flourouracil-cisplatin and 75.8% with daily radiation plus gemcitabine.
“These rates exceed historical complete response rates, and this is likely a result of improved selection over time and more thorough TURBTs performed over time,” Dr. Coen proposed. “Over the course of multiple successive RTOG trials, our selection criteria have been refined. One excellent example would be that hydronephrosis has been excluded on more contemporary trials, but if you look at older trials, those patients were included.”
The 3-year rate of bladder-intact distant metastasis–free survival was 66.7% and 69%, respectively. “This is a very important endpoint. These results are excellent,” he commented. “And there is really no appreciable difference between the two arms on the actuarial analysis.”
As far as specific treatment failure events in the trial overall, three patients died, eight underwent cystectomy, and eight developed distant metastases. Although numbers were small, these events appeared fairly evenly distributed across arms.
The rate of grade 3 or 4 acute toxicity was 57.6% with twice-daily radiation plus 5-flourouracil-cisplatin and 54.6% with daily radiation plus gemcitabine. The large majority of events were blood and bone marrow toxicity. “It’s quite notable that the rates of GU and GI toxicity were very low,” commented Dr. Coen, who disclosed that he had no relevant conflicts of interest.
SOURCE: Coen, J. et al, 2018 Genitourinary Cancers Symposium, Abstract 408
AT THE GENITOURINARY CANCERS SYMPOSIUM
Key clinical point:
Major finding: The rate of freedom from distant metastasis at 3 years was 77.8% with twice-daily radiation plus 5-flourouracil-cisplatin and 84.0% with daily radiation plus gemcitabine.
Data source: A multicenter randomized phase 2 trial among 70 patients with muscle-invasive (cT2-4a) bladder cancer who had undergone TURBT (NRG/RTOG 0712 trial).
Disclosures: Dr. Coen disclosed that he had no relevant conflicts of interest. The trial was supported by the National Cancer Institute.
Source: Coen, J. et al, 2018 Genitourinary Cancers Symposium, Abstract 408.
Minority of dermatologists prescribe majority of opioids
Opioid prescribing among dermatologists is concentrated among a relative few, with surgeons and those in Southern states overrepresented, according to a study of Medicare Part D data for 2014.
“A small number of dermatologists account for a large percentage of the prescriptions. And it’s concentrated among dermatology surgeons, who are likely giving a standard prescription for a 4-day course of opioids after surgery,” senior author Arash Mostaghimi, MD, the director of inpatient services in the dermatology department at Brigham and Women’s Hospital, Boston, said in a press release issued by the hospital.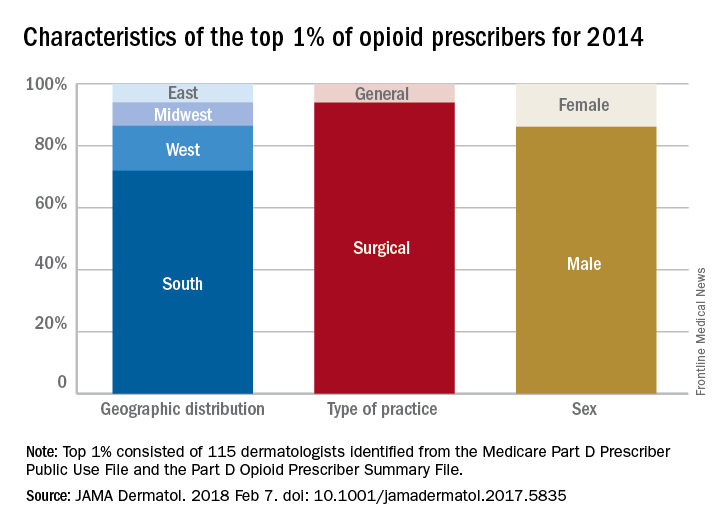
A closer look at those 115 top prescribers shows that 108, or 94%, worked in a surgical practice, 72% were located in Southern states, and 86% were male. Among all the dermatologists in the study, those in the South also had an opioid prescribing rate (2.77 claims/1,000 Medicare beneficiaries) that was more than triple the rate in the Northeast (0.83 claims/1,000 beneficiaries), the investigators said.
they noted, and may have created, based on consumption habits after Mohs microsurgery, a reservoir of more than 490,000 unused pills “that poses a substantial risk for future misuse.”
The study was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences. The investigators did not report any conflicts of interest.
SOURCE: Cao S et al. JAMA Dermatol. 2018 Feb 7. doi: 10.1001/jamadermatol.2017.5835.
Opioid prescribing among dermatologists is concentrated among a relative few, with surgeons and those in Southern states overrepresented, according to a study of Medicare Part D data for 2014.
“A small number of dermatologists account for a large percentage of the prescriptions. And it’s concentrated among dermatology surgeons, who are likely giving a standard prescription for a 4-day course of opioids after surgery,” senior author Arash Mostaghimi, MD, the director of inpatient services in the dermatology department at Brigham and Women’s Hospital, Boston, said in a press release issued by the hospital.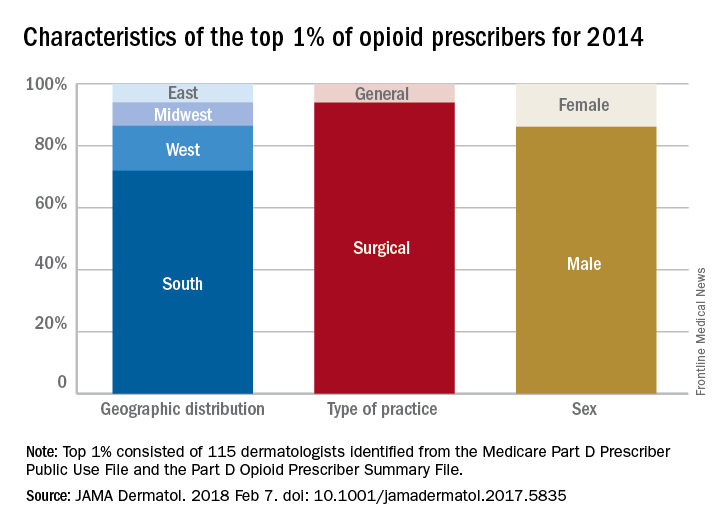
A closer look at those 115 top prescribers shows that 108, or 94%, worked in a surgical practice, 72% were located in Southern states, and 86% were male. Among all the dermatologists in the study, those in the South also had an opioid prescribing rate (2.77 claims/1,000 Medicare beneficiaries) that was more than triple the rate in the Northeast (0.83 claims/1,000 beneficiaries), the investigators said.
they noted, and may have created, based on consumption habits after Mohs microsurgery, a reservoir of more than 490,000 unused pills “that poses a substantial risk for future misuse.”
The study was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences. The investigators did not report any conflicts of interest.
SOURCE: Cao S et al. JAMA Dermatol. 2018 Feb 7. doi: 10.1001/jamadermatol.2017.5835.
Opioid prescribing among dermatologists is concentrated among a relative few, with surgeons and those in Southern states overrepresented, according to a study of Medicare Part D data for 2014.
“A small number of dermatologists account for a large percentage of the prescriptions. And it’s concentrated among dermatology surgeons, who are likely giving a standard prescription for a 4-day course of opioids after surgery,” senior author Arash Mostaghimi, MD, the director of inpatient services in the dermatology department at Brigham and Women’s Hospital, Boston, said in a press release issued by the hospital.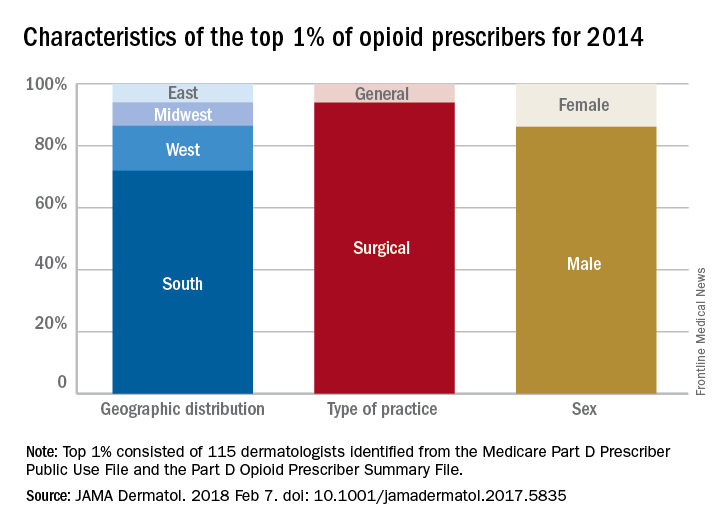
A closer look at those 115 top prescribers shows that 108, or 94%, worked in a surgical practice, 72% were located in Southern states, and 86% were male. Among all the dermatologists in the study, those in the South also had an opioid prescribing rate (2.77 claims/1,000 Medicare beneficiaries) that was more than triple the rate in the Northeast (0.83 claims/1,000 beneficiaries), the investigators said.
they noted, and may have created, based on consumption habits after Mohs microsurgery, a reservoir of more than 490,000 unused pills “that poses a substantial risk for future misuse.”
The study was supported by the National Institutes of Health’s National Center for Advancing Translational Sciences. The investigators did not report any conflicts of interest.
SOURCE: Cao S et al. JAMA Dermatol. 2018 Feb 7. doi: 10.1001/jamadermatol.2017.5835.
FROM JAMA DERMATOLOGY