User login
Does maternal sleep position affect risk of stillbirth?
WHAT DOES THIS MEAN FOR PRACTICE?
Encourage pregnant patients to not go to sleep in the supine position, especially those who:
- are obese
- have medical complications of pregnancy
- have a history of prior stillbirth
- smoke
- are of advanced maternal age
Normal prepregnancy weight becoming less normal
according to the Centers for Disease Control and Prevention.
The overall prevalence of normal prepregnancy weight declined from 47.3% to 45.1% over that period in 36 states, the District of Columbia, and New York City, which reports natality data separately from New York state. The decreases were statistically significant in 26 states and New York City, the CDC investigators reported (MMWR. 2018 Jan 5;66[51-2]:1402-7).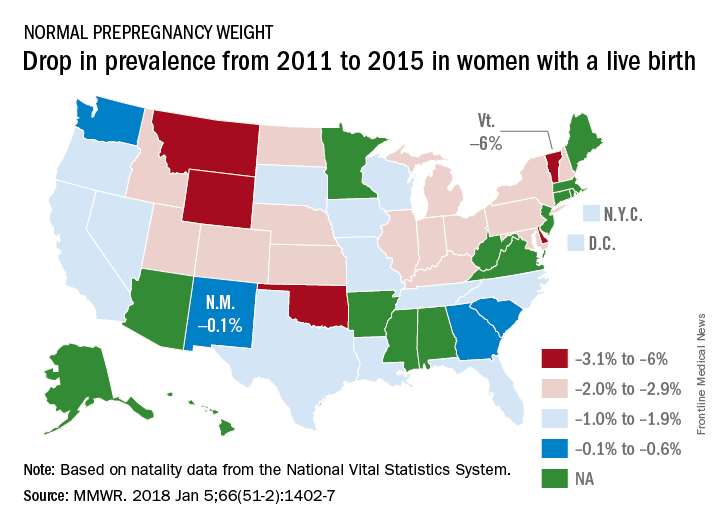
Based on data from 48 states, D.C., and New York City, the distribution of prevalence for the BMI categories in 2015 was 3.6% underweight, 45% normal weight, 25.8% overweight, and 25.6% obese, the investigators said.
The CDC analysis was based on natality data from the National Vital Statistics System. The standard birth certificate was revised in 2003 to include maternal height and prepregnancy weight, but only 38 jurisdictions were using it by 2011. By 2015, all states except Connecticut and New Jersey had adopted its use.
according to the Centers for Disease Control and Prevention.
The overall prevalence of normal prepregnancy weight declined from 47.3% to 45.1% over that period in 36 states, the District of Columbia, and New York City, which reports natality data separately from New York state. The decreases were statistically significant in 26 states and New York City, the CDC investigators reported (MMWR. 2018 Jan 5;66[51-2]:1402-7).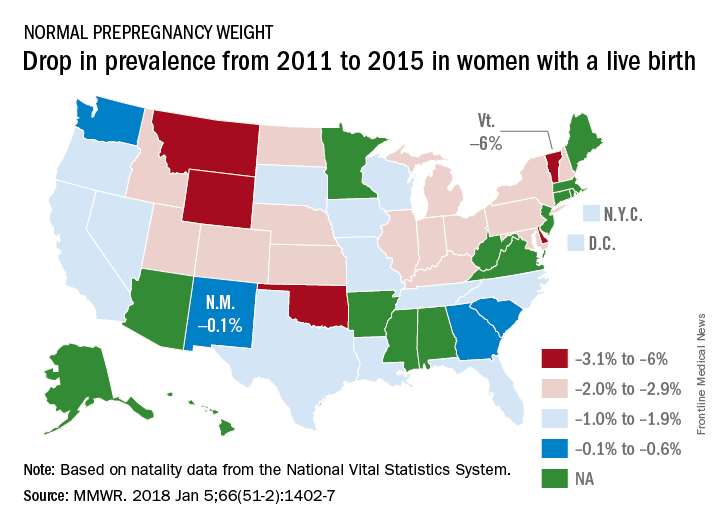
Based on data from 48 states, D.C., and New York City, the distribution of prevalence for the BMI categories in 2015 was 3.6% underweight, 45% normal weight, 25.8% overweight, and 25.6% obese, the investigators said.
The CDC analysis was based on natality data from the National Vital Statistics System. The standard birth certificate was revised in 2003 to include maternal height and prepregnancy weight, but only 38 jurisdictions were using it by 2011. By 2015, all states except Connecticut and New Jersey had adopted its use.
according to the Centers for Disease Control and Prevention.
The overall prevalence of normal prepregnancy weight declined from 47.3% to 45.1% over that period in 36 states, the District of Columbia, and New York City, which reports natality data separately from New York state. The decreases were statistically significant in 26 states and New York City, the CDC investigators reported (MMWR. 2018 Jan 5;66[51-2]:1402-7).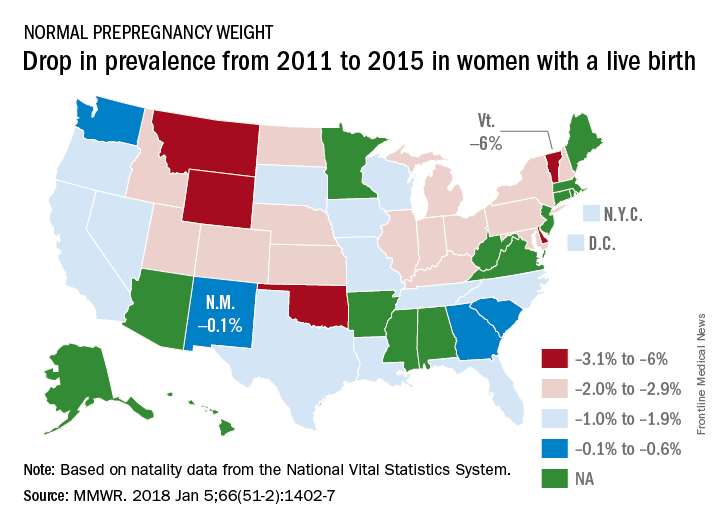
Based on data from 48 states, D.C., and New York City, the distribution of prevalence for the BMI categories in 2015 was 3.6% underweight, 45% normal weight, 25.8% overweight, and 25.6% obese, the investigators said.
The CDC analysis was based on natality data from the National Vital Statistics System. The standard birth certificate was revised in 2003 to include maternal height and prepregnancy weight, but only 38 jurisdictions were using it by 2011. By 2015, all states except Connecticut and New Jersey had adopted its use.
FROM MMWR
Role of Obstructive Sleep Apnea in HTN
Heart disease and stroke are leading causes of death and disability. High blood pressure (BP) is a major risk factor for both.
The 2017 guidelines regarding “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure” (JNC 7) were recently published, which is an update incorporating new information from studies regarding BP-related risk of cardiovascular disease (CVD) and strategies to improve hypertension (HTN) treatment and control.
Screening for secondary causes of HTN is necessary for new-onset or uncontrolled HTN in adults, including drug-resistant HTN. Screening includes testing for obstructive sleep apnea, which is highly prevalent in this population.
Obstructive sleep apnea is a common chronic condition characterized by recurrent collapse of upper airways during sleep, inducing intermittent episodes of apnea/hypopnea, hypoxemia, and sleep disruption (Pedrosa RP, et al. Chest. 2013;144[5]:1487).
It is estimated to affect 17% of US adults but is overwhelmingly underrecognized and untreated (JAMA. 2012;307[20]:2169). The prevalence is higher in men than women. The major risk factors for OSA are obesity, male sex, and advancing age. Since these conditions oftentimes predispose to and are concomitant with HTN, it can be challenging to determine the independent effects of OSA on the development of HTN.
The relationship between obstructive sleep apnea (OSA) and HTN has been a point of interest for decades, with untreated OSA being associated with an increased risk for developing new-onset HTN (JAMA. 2012;307[20]:2169).
There have been several landmark trials that have sought to determine the extent of a causal relationship between OSAS and HTN. Sleep Heart Health Study (Sleep. 2006;29;1009) was one such study, which was limited by the inability to prove that OSA preceded the onset of HTN.
Wisconsin Sleep Cohort (N Engl J Med. 2000;342:1378) was another landmark prospective longitudinal study that implicates OSA as a possible causal factor in HTN. The notable limitation of the study was the presence of HTN after initial assessment was found to be dependent upon the severity of OSA at baseline.
While these two cohort studies found an association between OSA and HTN, the Vitoria Sleep Cohort out of Spain (Am J Respir Crit Care Med. 2011;184[11]:1299), the third and most recent longitudinal cohort study, looked at younger and thinner patients than the SHHS and the Wisconsin Sleep Cohort, failed to show a significant association between OSA and incident HTN. Methodologic differences may help to explain the disparity in results.
NREM sleep has normal circadian variation of BP, causing “dipping” of both systolic and diastolic BP at night due to decreased sympathetic and increased parasympathetic activity. REM sleep has predominant sympathetic activity and transient nocturnal BP surges.
OSA results in hypoxemia, which causes nocturnal catecholamine surges, resulting in nocturnal increase in heart rate and BP that is most prominent during post-apneic hyperventilation.
Reduced nocturnal BP (nondipping) or even higher nocturnal BP than daytime BP is an undoubted risk factor for hypertensive patients due to the end-organ damage and subsequent cardiovascular events. With sleep apnea, sleep quality is decreased due to frequent arousal from sleep (Hypertension. 2006;47[5]:833).
Sleep duration of less than or equal to 5 hours per night was shown to significantly increase risk for HTN in patients less than or equal to 60 years of age, even after controlling for obesity and diabetes.
Sleep Heart Health Study suggests that sleep duration above or below a median of 7 to 8 hours per night is associated with a higher prevalence of HTN (Sleep. 2006;29:1009). Thus, improving duration and quality of sleep in sleep apnea patients may help decrease the risk of developing HTN.
Key question: Will treatment of OSA appreciably alter BP?
Continuous positive airway pressure (CPAP) is an efficacious treatment of choice for OSA. Interventional trials, though limited by issues related to compliance, have shown CPAP to acutely reduce sympathetic drive and BP during sleep. However, this improvement in BP control is not entirely consistent in all patients with the data being less clear-cut regarding nighttime CPAP therapy and impact on daytime BP.
A randomized controlled trial from Barbe et al suggests that normotensive subjects with severe OSA but without demonstrable daytime sleepiness are immune to the BP-reducing effects of CPAP (Ann Intern Med. 2001;134:1015); those who were objectively sleepy had a more robust response to the BP lowering effects of CPAP with better cardiovascular outcomes among patients who were adherent to CPAP therapy (≥4 hours per night).
Sleep Apnea Cardiovascular Endpoints (SAVE) study looked at CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea (N Engl J Med. 2016;375:919). CPAP significantly reduced snoring and daytime sleepiness and improved health-related quality of life and mood, but the risk of serious cardiovascular events was not lower among patients who received treatment with CPAP in addition to usual care compared with usual care alone. This study was not powered to provide definitive answers regarding the effects of CPAP on secondary cardiovascular end points, and the use of PAP was less than 4 hours.
A recent systematic review and meta-analysis looked at “Association of Positive Airway Pressure with Cardiovascular Events and Death in Adults with Sleep Apnea” (JAMA. 2017;318(2):156). No significant associations between PAP treatment and a range of cardiovascular events were noted in this meta-analysis.
It is possible that the limited adherence to therapy in many trials was insufficient to drive protection, along with short follow-up duration of most trials that may have given insufficient time for PAP to have affected vascular outcomes.
In a cross-over study of valsartan and CPAP, combining drug treatment with CPAP appeared to have a more synergistic effect in reducing BP than either agent alone (Am J Respir Crit Care Med. 2010;182:954).
The beneficial effect of CPAP remains an open question. Considering the multifactorial pathophysiology of OSA-associated HTN, proven therapies, such as BP lowering, lipid lowering, and antiplatelet therapy, along with PAP therapy, should be utilized. This combination strategy is likely to be more effective in improving both nocturnal and daytime BP control in OSA.
Dr. Singh is Director, Sleep Disorder and Research Center, Michael E. DeBakey VA Medical Center; and Dr. Singh is Assistant Professor and Dr. Velamuri is Associate Professor, Pulmonary, Critical Care and Sleep Medicine, Baylor College of Medicine. Houston, Texas.
Heart disease and stroke are leading causes of death and disability. High blood pressure (BP) is a major risk factor for both.
The 2017 guidelines regarding “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure” (JNC 7) were recently published, which is an update incorporating new information from studies regarding BP-related risk of cardiovascular disease (CVD) and strategies to improve hypertension (HTN) treatment and control.
Screening for secondary causes of HTN is necessary for new-onset or uncontrolled HTN in adults, including drug-resistant HTN. Screening includes testing for obstructive sleep apnea, which is highly prevalent in this population.
Obstructive sleep apnea is a common chronic condition characterized by recurrent collapse of upper airways during sleep, inducing intermittent episodes of apnea/hypopnea, hypoxemia, and sleep disruption (Pedrosa RP, et al. Chest. 2013;144[5]:1487).
It is estimated to affect 17% of US adults but is overwhelmingly underrecognized and untreated (JAMA. 2012;307[20]:2169). The prevalence is higher in men than women. The major risk factors for OSA are obesity, male sex, and advancing age. Since these conditions oftentimes predispose to and are concomitant with HTN, it can be challenging to determine the independent effects of OSA on the development of HTN.
The relationship between obstructive sleep apnea (OSA) and HTN has been a point of interest for decades, with untreated OSA being associated with an increased risk for developing new-onset HTN (JAMA. 2012;307[20]:2169).
There have been several landmark trials that have sought to determine the extent of a causal relationship between OSAS and HTN. Sleep Heart Health Study (Sleep. 2006;29;1009) was one such study, which was limited by the inability to prove that OSA preceded the onset of HTN.
Wisconsin Sleep Cohort (N Engl J Med. 2000;342:1378) was another landmark prospective longitudinal study that implicates OSA as a possible causal factor in HTN. The notable limitation of the study was the presence of HTN after initial assessment was found to be dependent upon the severity of OSA at baseline.
While these two cohort studies found an association between OSA and HTN, the Vitoria Sleep Cohort out of Spain (Am J Respir Crit Care Med. 2011;184[11]:1299), the third and most recent longitudinal cohort study, looked at younger and thinner patients than the SHHS and the Wisconsin Sleep Cohort, failed to show a significant association between OSA and incident HTN. Methodologic differences may help to explain the disparity in results.
NREM sleep has normal circadian variation of BP, causing “dipping” of both systolic and diastolic BP at night due to decreased sympathetic and increased parasympathetic activity. REM sleep has predominant sympathetic activity and transient nocturnal BP surges.
OSA results in hypoxemia, which causes nocturnal catecholamine surges, resulting in nocturnal increase in heart rate and BP that is most prominent during post-apneic hyperventilation.
Reduced nocturnal BP (nondipping) or even higher nocturnal BP than daytime BP is an undoubted risk factor for hypertensive patients due to the end-organ damage and subsequent cardiovascular events. With sleep apnea, sleep quality is decreased due to frequent arousal from sleep (Hypertension. 2006;47[5]:833).
Sleep duration of less than or equal to 5 hours per night was shown to significantly increase risk for HTN in patients less than or equal to 60 years of age, even after controlling for obesity and diabetes.
Sleep Heart Health Study suggests that sleep duration above or below a median of 7 to 8 hours per night is associated with a higher prevalence of HTN (Sleep. 2006;29:1009). Thus, improving duration and quality of sleep in sleep apnea patients may help decrease the risk of developing HTN.
Key question: Will treatment of OSA appreciably alter BP?
Continuous positive airway pressure (CPAP) is an efficacious treatment of choice for OSA. Interventional trials, though limited by issues related to compliance, have shown CPAP to acutely reduce sympathetic drive and BP during sleep. However, this improvement in BP control is not entirely consistent in all patients with the data being less clear-cut regarding nighttime CPAP therapy and impact on daytime BP.
A randomized controlled trial from Barbe et al suggests that normotensive subjects with severe OSA but without demonstrable daytime sleepiness are immune to the BP-reducing effects of CPAP (Ann Intern Med. 2001;134:1015); those who were objectively sleepy had a more robust response to the BP lowering effects of CPAP with better cardiovascular outcomes among patients who were adherent to CPAP therapy (≥4 hours per night).
Sleep Apnea Cardiovascular Endpoints (SAVE) study looked at CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea (N Engl J Med. 2016;375:919). CPAP significantly reduced snoring and daytime sleepiness and improved health-related quality of life and mood, but the risk of serious cardiovascular events was not lower among patients who received treatment with CPAP in addition to usual care compared with usual care alone. This study was not powered to provide definitive answers regarding the effects of CPAP on secondary cardiovascular end points, and the use of PAP was less than 4 hours.
A recent systematic review and meta-analysis looked at “Association of Positive Airway Pressure with Cardiovascular Events and Death in Adults with Sleep Apnea” (JAMA. 2017;318(2):156). No significant associations between PAP treatment and a range of cardiovascular events were noted in this meta-analysis.
It is possible that the limited adherence to therapy in many trials was insufficient to drive protection, along with short follow-up duration of most trials that may have given insufficient time for PAP to have affected vascular outcomes.
In a cross-over study of valsartan and CPAP, combining drug treatment with CPAP appeared to have a more synergistic effect in reducing BP than either agent alone (Am J Respir Crit Care Med. 2010;182:954).
The beneficial effect of CPAP remains an open question. Considering the multifactorial pathophysiology of OSA-associated HTN, proven therapies, such as BP lowering, lipid lowering, and antiplatelet therapy, along with PAP therapy, should be utilized. This combination strategy is likely to be more effective in improving both nocturnal and daytime BP control in OSA.
Dr. Singh is Director, Sleep Disorder and Research Center, Michael E. DeBakey VA Medical Center; and Dr. Singh is Assistant Professor and Dr. Velamuri is Associate Professor, Pulmonary, Critical Care and Sleep Medicine, Baylor College of Medicine. Houston, Texas.
Heart disease and stroke are leading causes of death and disability. High blood pressure (BP) is a major risk factor for both.
The 2017 guidelines regarding “Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure” (JNC 7) were recently published, which is an update incorporating new information from studies regarding BP-related risk of cardiovascular disease (CVD) and strategies to improve hypertension (HTN) treatment and control.
Screening for secondary causes of HTN is necessary for new-onset or uncontrolled HTN in adults, including drug-resistant HTN. Screening includes testing for obstructive sleep apnea, which is highly prevalent in this population.
Obstructive sleep apnea is a common chronic condition characterized by recurrent collapse of upper airways during sleep, inducing intermittent episodes of apnea/hypopnea, hypoxemia, and sleep disruption (Pedrosa RP, et al. Chest. 2013;144[5]:1487).
It is estimated to affect 17% of US adults but is overwhelmingly underrecognized and untreated (JAMA. 2012;307[20]:2169). The prevalence is higher in men than women. The major risk factors for OSA are obesity, male sex, and advancing age. Since these conditions oftentimes predispose to and are concomitant with HTN, it can be challenging to determine the independent effects of OSA on the development of HTN.
The relationship between obstructive sleep apnea (OSA) and HTN has been a point of interest for decades, with untreated OSA being associated with an increased risk for developing new-onset HTN (JAMA. 2012;307[20]:2169).
There have been several landmark trials that have sought to determine the extent of a causal relationship between OSAS and HTN. Sleep Heart Health Study (Sleep. 2006;29;1009) was one such study, which was limited by the inability to prove that OSA preceded the onset of HTN.
Wisconsin Sleep Cohort (N Engl J Med. 2000;342:1378) was another landmark prospective longitudinal study that implicates OSA as a possible causal factor in HTN. The notable limitation of the study was the presence of HTN after initial assessment was found to be dependent upon the severity of OSA at baseline.
While these two cohort studies found an association between OSA and HTN, the Vitoria Sleep Cohort out of Spain (Am J Respir Crit Care Med. 2011;184[11]:1299), the third and most recent longitudinal cohort study, looked at younger and thinner patients than the SHHS and the Wisconsin Sleep Cohort, failed to show a significant association between OSA and incident HTN. Methodologic differences may help to explain the disparity in results.
NREM sleep has normal circadian variation of BP, causing “dipping” of both systolic and diastolic BP at night due to decreased sympathetic and increased parasympathetic activity. REM sleep has predominant sympathetic activity and transient nocturnal BP surges.
OSA results in hypoxemia, which causes nocturnal catecholamine surges, resulting in nocturnal increase in heart rate and BP that is most prominent during post-apneic hyperventilation.
Reduced nocturnal BP (nondipping) or even higher nocturnal BP than daytime BP is an undoubted risk factor for hypertensive patients due to the end-organ damage and subsequent cardiovascular events. With sleep apnea, sleep quality is decreased due to frequent arousal from sleep (Hypertension. 2006;47[5]:833).
Sleep duration of less than or equal to 5 hours per night was shown to significantly increase risk for HTN in patients less than or equal to 60 years of age, even after controlling for obesity and diabetes.
Sleep Heart Health Study suggests that sleep duration above or below a median of 7 to 8 hours per night is associated with a higher prevalence of HTN (Sleep. 2006;29:1009). Thus, improving duration and quality of sleep in sleep apnea patients may help decrease the risk of developing HTN.
Key question: Will treatment of OSA appreciably alter BP?
Continuous positive airway pressure (CPAP) is an efficacious treatment of choice for OSA. Interventional trials, though limited by issues related to compliance, have shown CPAP to acutely reduce sympathetic drive and BP during sleep. However, this improvement in BP control is not entirely consistent in all patients with the data being less clear-cut regarding nighttime CPAP therapy and impact on daytime BP.
A randomized controlled trial from Barbe et al suggests that normotensive subjects with severe OSA but without demonstrable daytime sleepiness are immune to the BP-reducing effects of CPAP (Ann Intern Med. 2001;134:1015); those who were objectively sleepy had a more robust response to the BP lowering effects of CPAP with better cardiovascular outcomes among patients who were adherent to CPAP therapy (≥4 hours per night).
Sleep Apnea Cardiovascular Endpoints (SAVE) study looked at CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea (N Engl J Med. 2016;375:919). CPAP significantly reduced snoring and daytime sleepiness and improved health-related quality of life and mood, but the risk of serious cardiovascular events was not lower among patients who received treatment with CPAP in addition to usual care compared with usual care alone. This study was not powered to provide definitive answers regarding the effects of CPAP on secondary cardiovascular end points, and the use of PAP was less than 4 hours.
A recent systematic review and meta-analysis looked at “Association of Positive Airway Pressure with Cardiovascular Events and Death in Adults with Sleep Apnea” (JAMA. 2017;318(2):156). No significant associations between PAP treatment and a range of cardiovascular events were noted in this meta-analysis.
It is possible that the limited adherence to therapy in many trials was insufficient to drive protection, along with short follow-up duration of most trials that may have given insufficient time for PAP to have affected vascular outcomes.
In a cross-over study of valsartan and CPAP, combining drug treatment with CPAP appeared to have a more synergistic effect in reducing BP than either agent alone (Am J Respir Crit Care Med. 2010;182:954).
The beneficial effect of CPAP remains an open question. Considering the multifactorial pathophysiology of OSA-associated HTN, proven therapies, such as BP lowering, lipid lowering, and antiplatelet therapy, along with PAP therapy, should be utilized. This combination strategy is likely to be more effective in improving both nocturnal and daytime BP control in OSA.
Dr. Singh is Director, Sleep Disorder and Research Center, Michael E. DeBakey VA Medical Center; and Dr. Singh is Assistant Professor and Dr. Velamuri is Associate Professor, Pulmonary, Critical Care and Sleep Medicine, Baylor College of Medicine. Houston, Texas.
Check orthostatic vital signs within 1 minute
Clinical question: What is the relationship between timing of measurement of postural blood pressure (BP) and adverse clinical outcomes?
Background: Guidelines recommend measuring postural BP after 3 minutes of standing to avoid potentially false-positive readings obtained before that interval. In SPRINT, orthostatic hypotension (OH) determined at 1 minute was associated with higher risk of emergency department visits for OH and syncope. Whether that finding was because of the shortened interval of measurement is uncertain.
Setting: Four U.S. communities over 2 decades.
Synopsis: In a cohort of 11,429 middle-aged patients, upright BP was measured every 25 seconds over a 5-minute interval after participants had been supine for 20 minutes. About 2-3 seconds elapsed between the end of one BP measurement and the initiation of the next. OH was defined as a 20–mm Hg drop in systolic BP. After researchers adjusted for covariates, OH at 30 seconds and 1 minute were associated with higher odds of dizziness, fracture, syncope, death, and motor vehicle crashes recorded over a median follow-up of 23 years. Measurements after 1 minute were not reliably associated with any adverse outcomes.
Bottom line: Measuring OH at 30 seconds and 1 minute reliably identifies patients at risk for associated adverse clinical outcomes.
Citation: Juraschek SP et al. Association of history of dizziness and long-term adverse outcomes with early vs. later orthostatic hypotension times in middle-aged adults. JAMA Intern Med. 2017 Sep 1;177(9):1316-23.
Dr. Anderson is an associate program director in the internal medicine residency training program at the University of Colorado School of Medicine and a hospitalist at the VA Eastern Colorado Health Care System in Denver.
Clinical question: What is the relationship between timing of measurement of postural blood pressure (BP) and adverse clinical outcomes?
Background: Guidelines recommend measuring postural BP after 3 minutes of standing to avoid potentially false-positive readings obtained before that interval. In SPRINT, orthostatic hypotension (OH) determined at 1 minute was associated with higher risk of emergency department visits for OH and syncope. Whether that finding was because of the shortened interval of measurement is uncertain.
Setting: Four U.S. communities over 2 decades.
Synopsis: In a cohort of 11,429 middle-aged patients, upright BP was measured every 25 seconds over a 5-minute interval after participants had been supine for 20 minutes. About 2-3 seconds elapsed between the end of one BP measurement and the initiation of the next. OH was defined as a 20–mm Hg drop in systolic BP. After researchers adjusted for covariates, OH at 30 seconds and 1 minute were associated with higher odds of dizziness, fracture, syncope, death, and motor vehicle crashes recorded over a median follow-up of 23 years. Measurements after 1 minute were not reliably associated with any adverse outcomes.
Bottom line: Measuring OH at 30 seconds and 1 minute reliably identifies patients at risk for associated adverse clinical outcomes.
Citation: Juraschek SP et al. Association of history of dizziness and long-term adverse outcomes with early vs. later orthostatic hypotension times in middle-aged adults. JAMA Intern Med. 2017 Sep 1;177(9):1316-23.
Dr. Anderson is an associate program director in the internal medicine residency training program at the University of Colorado School of Medicine and a hospitalist at the VA Eastern Colorado Health Care System in Denver.
Clinical question: What is the relationship between timing of measurement of postural blood pressure (BP) and adverse clinical outcomes?
Background: Guidelines recommend measuring postural BP after 3 minutes of standing to avoid potentially false-positive readings obtained before that interval. In SPRINT, orthostatic hypotension (OH) determined at 1 minute was associated with higher risk of emergency department visits for OH and syncope. Whether that finding was because of the shortened interval of measurement is uncertain.
Setting: Four U.S. communities over 2 decades.
Synopsis: In a cohort of 11,429 middle-aged patients, upright BP was measured every 25 seconds over a 5-minute interval after participants had been supine for 20 minutes. About 2-3 seconds elapsed between the end of one BP measurement and the initiation of the next. OH was defined as a 20–mm Hg drop in systolic BP. After researchers adjusted for covariates, OH at 30 seconds and 1 minute were associated with higher odds of dizziness, fracture, syncope, death, and motor vehicle crashes recorded over a median follow-up of 23 years. Measurements after 1 minute were not reliably associated with any adverse outcomes.
Bottom line: Measuring OH at 30 seconds and 1 minute reliably identifies patients at risk for associated adverse clinical outcomes.
Citation: Juraschek SP et al. Association of history of dizziness and long-term adverse outcomes with early vs. later orthostatic hypotension times in middle-aged adults. JAMA Intern Med. 2017 Sep 1;177(9):1316-23.
Dr. Anderson is an associate program director in the internal medicine residency training program at the University of Colorado School of Medicine and a hospitalist at the VA Eastern Colorado Health Care System in Denver.
Smart Ways to Give More Now
Your gift today truly has an immediate impact that makes a difference now.
We also want you to benefit as much as possible from your generosity.
Gifts of Appreciated Securities, Mutual Funds, and Investments
If you have owned any of these longer than 1 year and they have appreciated in value, they provide a smart option for gifting. You will avoid the capital gains tax, and you also receive a charitable income tax deduction if you itemize your tax return.
The Charitable Individual Retirement Plan Option
If you are 70 1/2, you may distribute funds from your IRA directly to the CHEST Foundation.
You will not pay any income taxes, and it will also qualify for your required minimum withdrawal. You may distribute up to $100,000 per person per year ($200,000 if you are married and both own an IRA).
Retirement Plan Beneficiary Designation
You may also designate a charity as a beneficiary of your IRA, 401K, or 403B.
This will avoid any income tax, so 100% will be directed to the charity of your choice.
For more information on these and other ways to support the CHEST Foundation, confidentially and with no obligation, contact Angela Perillo, CHEST Director of Development & Foundation Operations, at aperillo@chestnet.org.
Your gift today truly has an immediate impact that makes a difference now.
We also want you to benefit as much as possible from your generosity.
Gifts of Appreciated Securities, Mutual Funds, and Investments
If you have owned any of these longer than 1 year and they have appreciated in value, they provide a smart option for gifting. You will avoid the capital gains tax, and you also receive a charitable income tax deduction if you itemize your tax return.
The Charitable Individual Retirement Plan Option
If you are 70 1/2, you may distribute funds from your IRA directly to the CHEST Foundation.
You will not pay any income taxes, and it will also qualify for your required minimum withdrawal. You may distribute up to $100,000 per person per year ($200,000 if you are married and both own an IRA).
Retirement Plan Beneficiary Designation
You may also designate a charity as a beneficiary of your IRA, 401K, or 403B.
This will avoid any income tax, so 100% will be directed to the charity of your choice.
For more information on these and other ways to support the CHEST Foundation, confidentially and with no obligation, contact Angela Perillo, CHEST Director of Development & Foundation Operations, at aperillo@chestnet.org.
Your gift today truly has an immediate impact that makes a difference now.
We also want you to benefit as much as possible from your generosity.
Gifts of Appreciated Securities, Mutual Funds, and Investments
If you have owned any of these longer than 1 year and they have appreciated in value, they provide a smart option for gifting. You will avoid the capital gains tax, and you also receive a charitable income tax deduction if you itemize your tax return.
The Charitable Individual Retirement Plan Option
If you are 70 1/2, you may distribute funds from your IRA directly to the CHEST Foundation.
You will not pay any income taxes, and it will also qualify for your required minimum withdrawal. You may distribute up to $100,000 per person per year ($200,000 if you are married and both own an IRA).
Retirement Plan Beneficiary Designation
You may also designate a charity as a beneficiary of your IRA, 401K, or 403B.
This will avoid any income tax, so 100% will be directed to the charity of your choice.
For more information on these and other ways to support the CHEST Foundation, confidentially and with no obligation, contact Angela Perillo, CHEST Director of Development & Foundation Operations, at aperillo@chestnet.org.
Congratulations, CHEST! 2017 Accreditation With Commendation
On December 2, CHEST received Accreditation with Commendation from the Accreditation Council for Continuing Medical Education (ACCME). This achievement grants CHEST accreditation through November 2023, and places the organization in the highest tier of continuing medical education (CME) providers.
“It is a true privilege to serve as a member of our outstanding CHEST Education team. We are very proud of our education program and have worked very hard to provide CHEST members and their health-care team with state-of-the-art learning opportunities,” said Alex Niven, MD, FCCP, current Chair of CHEST’s Education Committee, “ACCME Accreditation with Commendation is an important benchmark of this success, and we look forward to further advancing CHEST’s leadership role in medical education through its simulation, active learning, and other innovative educational offerings.”
To receive accreditation from the ACCME, CHEST met all of the requirements of the ACCME, has transitioned clinician knowledge into action, and has enhanced procedural performance to improve patient outcomes. Accreditation with Commendation is “a reward for going above and beyond requirements--having the absolute best practices and for striving to meet the aspirational goals of medical education,” said William Kelly, MD, FCCP, previous Chair of CHEST’s Education Committee.
In achieving Accreditation with Commendation, CHEST demonstrated compliance with the following:
• Improving the professional practice by consistently integrating CME into CHEST processes.
• Utilization of noneducation strategies such as the CHEST Foundation’s grant programs and disease awareness campaigns, to enhance change as an adjunct to CHEST’s activities/educational interventions.
• Identification of factors that effect patient outcomes and are outside of the provider’s control.
• Implementation of educational strategies, including the offering of additional training to improve procedural capabilities, so as to remove, overcome, or address barriers to physician change.
• Building of bridges with stakeholders such as The France Foundation, National Comprehensive Cancer Network (NCCN), and the American Society for Clinical Pathology (ASCP), through collaboration and cooperation.
• Participation within an institutional framework for health-care quality improvement.
• Positioned to influence the scope and content of activities/educational interventions.
On December 2, CHEST received Accreditation with Commendation from the Accreditation Council for Continuing Medical Education (ACCME). This achievement grants CHEST accreditation through November 2023, and places the organization in the highest tier of continuing medical education (CME) providers.
“It is a true privilege to serve as a member of our outstanding CHEST Education team. We are very proud of our education program and have worked very hard to provide CHEST members and their health-care team with state-of-the-art learning opportunities,” said Alex Niven, MD, FCCP, current Chair of CHEST’s Education Committee, “ACCME Accreditation with Commendation is an important benchmark of this success, and we look forward to further advancing CHEST’s leadership role in medical education through its simulation, active learning, and other innovative educational offerings.”
To receive accreditation from the ACCME, CHEST met all of the requirements of the ACCME, has transitioned clinician knowledge into action, and has enhanced procedural performance to improve patient outcomes. Accreditation with Commendation is “a reward for going above and beyond requirements--having the absolute best practices and for striving to meet the aspirational goals of medical education,” said William Kelly, MD, FCCP, previous Chair of CHEST’s Education Committee.
In achieving Accreditation with Commendation, CHEST demonstrated compliance with the following:
• Improving the professional practice by consistently integrating CME into CHEST processes.
• Utilization of noneducation strategies such as the CHEST Foundation’s grant programs and disease awareness campaigns, to enhance change as an adjunct to CHEST’s activities/educational interventions.
• Identification of factors that effect patient outcomes and are outside of the provider’s control.
• Implementation of educational strategies, including the offering of additional training to improve procedural capabilities, so as to remove, overcome, or address barriers to physician change.
• Building of bridges with stakeholders such as The France Foundation, National Comprehensive Cancer Network (NCCN), and the American Society for Clinical Pathology (ASCP), through collaboration and cooperation.
• Participation within an institutional framework for health-care quality improvement.
• Positioned to influence the scope and content of activities/educational interventions.
On December 2, CHEST received Accreditation with Commendation from the Accreditation Council for Continuing Medical Education (ACCME). This achievement grants CHEST accreditation through November 2023, and places the organization in the highest tier of continuing medical education (CME) providers.
“It is a true privilege to serve as a member of our outstanding CHEST Education team. We are very proud of our education program and have worked very hard to provide CHEST members and their health-care team with state-of-the-art learning opportunities,” said Alex Niven, MD, FCCP, current Chair of CHEST’s Education Committee, “ACCME Accreditation with Commendation is an important benchmark of this success, and we look forward to further advancing CHEST’s leadership role in medical education through its simulation, active learning, and other innovative educational offerings.”
To receive accreditation from the ACCME, CHEST met all of the requirements of the ACCME, has transitioned clinician knowledge into action, and has enhanced procedural performance to improve patient outcomes. Accreditation with Commendation is “a reward for going above and beyond requirements--having the absolute best practices and for striving to meet the aspirational goals of medical education,” said William Kelly, MD, FCCP, previous Chair of CHEST’s Education Committee.
In achieving Accreditation with Commendation, CHEST demonstrated compliance with the following:
• Improving the professional practice by consistently integrating CME into CHEST processes.
• Utilization of noneducation strategies such as the CHEST Foundation’s grant programs and disease awareness campaigns, to enhance change as an adjunct to CHEST’s activities/educational interventions.
• Identification of factors that effect patient outcomes and are outside of the provider’s control.
• Implementation of educational strategies, including the offering of additional training to improve procedural capabilities, so as to remove, overcome, or address barriers to physician change.
• Building of bridges with stakeholders such as The France Foundation, National Comprehensive Cancer Network (NCCN), and the American Society for Clinical Pathology (ASCP), through collaboration and cooperation.
• Participation within an institutional framework for health-care quality improvement.
• Positioned to influence the scope and content of activities/educational interventions.
Live Streaming at CHEST 2017
In April 2016, Facebook launched Facebook Live, a tool for live streaming to a Facebook page to share live video with their followers on Facebook. At CHEST 2016, the CHEST New Media team began to experiment with live video with some early success. The CHEST 2017 team made the decision, based on the organization’s goal to help educate clinicians to improve patient care, to live stream complete sessions from CHEST 2017. With the help of the CHEST 2017 Education Committee and the Social Media Work Group, more than 25 sessions were selected and live streamed.
CHEST’s efforts on Facebook Live resulted in the following:
- Total people reached: 133,737
- Total video views: 34,449
- Total minutes watched: 30,786 (or 513 hours, or 21 days)
- Total interactions: 1,050 (eg, likes, loves, hahas, etc)
- Total shares: 302
The content concept was well received, and comments ranged from followers chiming in with their location, appreciation for live streaming, and even comments from patients.
- “Thank you for sharing this live presentation.”
- “Here from Mexico !!”
- “Here from Natal/RN, Brazil”
- “Here from Milan, Italy.”
- “Appreciate this live streaming on important sessions, big service for those who couldn’t attend!!”
- “My brother survived after six days on ECMO. I am so glad to have him.”
- “It’s a great chance for physicians working in pulmonology and general practice to get the pearls of guidelines from American College to improve clinical practice. Now distance doesn’t matter”
Plans are underway for live streaming from CHEST 2018 in San Antonio. To view the CHEST 2017 live stream videos, visit CHEST’s Facebook page, facebook.com/accpchest.
In April 2016, Facebook launched Facebook Live, a tool for live streaming to a Facebook page to share live video with their followers on Facebook. At CHEST 2016, the CHEST New Media team began to experiment with live video with some early success. The CHEST 2017 team made the decision, based on the organization’s goal to help educate clinicians to improve patient care, to live stream complete sessions from CHEST 2017. With the help of the CHEST 2017 Education Committee and the Social Media Work Group, more than 25 sessions were selected and live streamed.
CHEST’s efforts on Facebook Live resulted in the following:
- Total people reached: 133,737
- Total video views: 34,449
- Total minutes watched: 30,786 (or 513 hours, or 21 days)
- Total interactions: 1,050 (eg, likes, loves, hahas, etc)
- Total shares: 302
The content concept was well received, and comments ranged from followers chiming in with their location, appreciation for live streaming, and even comments from patients.
- “Thank you for sharing this live presentation.”
- “Here from Mexico !!”
- “Here from Natal/RN, Brazil”
- “Here from Milan, Italy.”
- “Appreciate this live streaming on important sessions, big service for those who couldn’t attend!!”
- “My brother survived after six days on ECMO. I am so glad to have him.”
- “It’s a great chance for physicians working in pulmonology and general practice to get the pearls of guidelines from American College to improve clinical practice. Now distance doesn’t matter”
Plans are underway for live streaming from CHEST 2018 in San Antonio. To view the CHEST 2017 live stream videos, visit CHEST’s Facebook page, facebook.com/accpchest.
In April 2016, Facebook launched Facebook Live, a tool for live streaming to a Facebook page to share live video with their followers on Facebook. At CHEST 2016, the CHEST New Media team began to experiment with live video with some early success. The CHEST 2017 team made the decision, based on the organization’s goal to help educate clinicians to improve patient care, to live stream complete sessions from CHEST 2017. With the help of the CHEST 2017 Education Committee and the Social Media Work Group, more than 25 sessions were selected and live streamed.
CHEST’s efforts on Facebook Live resulted in the following:
- Total people reached: 133,737
- Total video views: 34,449
- Total minutes watched: 30,786 (or 513 hours, or 21 days)
- Total interactions: 1,050 (eg, likes, loves, hahas, etc)
- Total shares: 302
The content concept was well received, and comments ranged from followers chiming in with their location, appreciation for live streaming, and even comments from patients.
- “Thank you for sharing this live presentation.”
- “Here from Mexico !!”
- “Here from Natal/RN, Brazil”
- “Here from Milan, Italy.”
- “Appreciate this live streaming on important sessions, big service for those who couldn’t attend!!”
- “My brother survived after six days on ECMO. I am so glad to have him.”
- “It’s a great chance for physicians working in pulmonology and general practice to get the pearls of guidelines from American College to improve clinical practice. Now distance doesn’t matter”
Plans are underway for live streaming from CHEST 2018 in San Antonio. To view the CHEST 2017 live stream videos, visit CHEST’s Facebook page, facebook.com/accpchest.
This Month in CHEST® Editor’s Picks
Editorial
Introducing the CHEST Teaching, Education, and Career Hub
Dr. G. T. Bosslet and Dr. M. Miles
Training, Education, and Career Hub - TEaCH
Dr. R. W. Ashton, et al.
Commentary
Higher Priced Older Pharmaceuticals: How Should We Respond?
Dr. R. S. Irwin, et al.
Giants in Chest Medicine
Jeffrey M. Drazen, MD, FCCP
Dr. A. S. Slutsky
Dr. R. S. Irwin, et al.
Original Research
Three-Hour Bundle Compliance and Outcomes in Patients With Undiagnosed Severe Sepsis
Dr. A. S. Deis, et al.
A Phase II Clinical Trial of Low-Dose Inhaled Carbon Monoxide in Idiopathic Pulmonary Fibrosis
Dr. I. O. Rosas, et al.
Editorial
Introducing the CHEST Teaching, Education, and Career Hub
Dr. G. T. Bosslet and Dr. M. Miles
Training, Education, and Career Hub - TEaCH
Dr. R. W. Ashton, et al.
Commentary
Higher Priced Older Pharmaceuticals: How Should We Respond?
Dr. R. S. Irwin, et al.
Giants in Chest Medicine
Jeffrey M. Drazen, MD, FCCP
Dr. A. S. Slutsky
Dr. R. S. Irwin, et al.
Original Research
Three-Hour Bundle Compliance and Outcomes in Patients With Undiagnosed Severe Sepsis
Dr. A. S. Deis, et al.
A Phase II Clinical Trial of Low-Dose Inhaled Carbon Monoxide in Idiopathic Pulmonary Fibrosis
Dr. I. O. Rosas, et al.
Editorial
Introducing the CHEST Teaching, Education, and Career Hub
Dr. G. T. Bosslet and Dr. M. Miles
Training, Education, and Career Hub - TEaCH
Dr. R. W. Ashton, et al.
Commentary
Higher Priced Older Pharmaceuticals: How Should We Respond?
Dr. R. S. Irwin, et al.
Giants in Chest Medicine
Jeffrey M. Drazen, MD, FCCP
Dr. A. S. Slutsky
Dr. R. S. Irwin, et al.
Original Research
Three-Hour Bundle Compliance and Outcomes in Patients With Undiagnosed Severe Sepsis
Dr. A. S. Deis, et al.
A Phase II Clinical Trial of Low-Dose Inhaled Carbon Monoxide in Idiopathic Pulmonary Fibrosis
Dr. I. O. Rosas, et al.
Another Small Win to Raise the Tobacco Purchasing Age to 21
The Elk Grove Village, Illinois, Board of Trustees passed the “Tobacco 21” ordinance that will raise the tobacco purchasing age to 21, which includes nicotine vaping. The policy, which will go into effect January 1, 2018, will protect young people from beginning a lifetime of addiction and, ultimately, save their lives.
Kevin L Kovitz MD, MBA, FCCP, attended the Village Board meeting to advocate for “Tobacco 21.” He is a Sustaining Member of the CHEST Foundation, continually exemplifying what it is to be a lung health champion.
Dr. Kovitz noted, “This policy will protect our kids from the scourge of Big Tobacco and save funding for health-care costs and, most importantly, will ultimately save lives. The ordinance will protect the most vulnerable parts of our population, our children. Raising the legal age puts tobacco products on par with alcohol and protects young adults from developing a dangerous lifelong habit.”
Five US states have also passed Tobacco 21; they include California, Hawaii, Maine, New Jersey, and Oregon. There are many local ordinances around the country but more are needed.
Advocating for this ordinance demonstrates the effectiveness of grassroots advocacy in our local communities.
The Elk Grove Village, Illinois, Board of Trustees passed the “Tobacco 21” ordinance that will raise the tobacco purchasing age to 21, which includes nicotine vaping. The policy, which will go into effect January 1, 2018, will protect young people from beginning a lifetime of addiction and, ultimately, save their lives.
Kevin L Kovitz MD, MBA, FCCP, attended the Village Board meeting to advocate for “Tobacco 21.” He is a Sustaining Member of the CHEST Foundation, continually exemplifying what it is to be a lung health champion.
Dr. Kovitz noted, “This policy will protect our kids from the scourge of Big Tobacco and save funding for health-care costs and, most importantly, will ultimately save lives. The ordinance will protect the most vulnerable parts of our population, our children. Raising the legal age puts tobacco products on par with alcohol and protects young adults from developing a dangerous lifelong habit.”
Five US states have also passed Tobacco 21; they include California, Hawaii, Maine, New Jersey, and Oregon. There are many local ordinances around the country but more are needed.
Advocating for this ordinance demonstrates the effectiveness of grassroots advocacy in our local communities.
The Elk Grove Village, Illinois, Board of Trustees passed the “Tobacco 21” ordinance that will raise the tobacco purchasing age to 21, which includes nicotine vaping. The policy, which will go into effect January 1, 2018, will protect young people from beginning a lifetime of addiction and, ultimately, save their lives.
Kevin L Kovitz MD, MBA, FCCP, attended the Village Board meeting to advocate for “Tobacco 21.” He is a Sustaining Member of the CHEST Foundation, continually exemplifying what it is to be a lung health champion.
Dr. Kovitz noted, “This policy will protect our kids from the scourge of Big Tobacco and save funding for health-care costs and, most importantly, will ultimately save lives. The ordinance will protect the most vulnerable parts of our population, our children. Raising the legal age puts tobacco products on par with alcohol and protects young adults from developing a dangerous lifelong habit.”
Five US states have also passed Tobacco 21; they include California, Hawaii, Maine, New Jersey, and Oregon. There are many local ordinances around the country but more are needed.
Advocating for this ordinance demonstrates the effectiveness of grassroots advocacy in our local communities.
BP targets questioned, Candida auris infections
Cardiovascular Medicine and Surgery
The Holy Grail of Blood Pressure Management?
Blood pressure treatment recommendations have been confusing over the past few years. The Joint National Committee (JNC) 8 stirred up controversy in 2014 because they raised the recommended tolerating systolic blood pressures, in certain people aged 60 and above, up to 150 mm Hg [James, et al. JAMA. 2014;311(5):507-520]. The new AHA/ACC hypertension guidelines cosponsored by 11 societies generated controversy because they changed the definition of hypertension (normal <120/80 mm Hg, elevated 120-129/80-89, stage 1 130-139/80-89, or stage 2 >140/90) [Whelton et al. J Am Coll Cardiol. 2017 pii:S0735-1097(17)41519-1]. The SPRINT trial [Wright, et al. N Engl J Med. 2015;373:2103-2116] largely influenced these recommendations. SPRINT demonstrated a 25% relative risk reduction of heart attack, stroke, cardiovascular death, or decompensated heart failure with more aggressive blood pressure management (BP goal <120/90 vs <140/90).
This new classification would label 46% of Americans, or 103.3 million people, as hypertensive. However, there is uncertainty in how broadly applicable the SPRINT results are, particularly in those under the age of 45. The majority of large clinical trials, including SPRINT, have limited numbers of patients who were less than 50 years old and, therefore, it is unknown if younger patients benefit to the same degree. The absolute improvement is also questionable because as an editorial points out [Welch, “Don’t Let New Blood Pressure Guidelines Raise Yours” NY Times. Nov. 15, 2017], the primary endpoint in SPRINT only occurred in less than or equal to 8% of patients.
These guidelines reinforce the need to measure ambulatory blood pressures, perform proper in-office blood pressure measurements, and emphasize lifestyle modifications. Whether aggressive blood pressure management is worth the potential risks and the degree to which ideal blood pressure measurement can be applied to real world practices, remains uncertain.
David J. Nagel, MD, PhD Steering Committee Member
Chest Infections
Candida auris
Invasive fungal infections are frequently managed by ICU physicians and are a leading cause of mortality among critically ill patients. Invasive candidiasis is associated with an attributable mortality rate of up to 49%. Historically, the majority of these infections has been caused by Candida albicans, but this may be changing.
The first outbreak of Candida auris in the Americas (18 patients) occurred in the ICU of a hospital in Venezuela. Resistance to common azoles was documented, and half of the isolates showed decreased susceptibility to amphotericin B. As of August 2017, a total 153 clinical cases of C auris infection have been reported to CDC from 10 US states; most have occurred in New York and New Jersey.
What has been learned from these cases is that close contacts can be colonized, colonization can be persistent (approximately 9 months), the yeast can survive in the hospital environment, bleach or sporicide is needed for elimination, isolation precautions are recommended as for MDRO bacteria, and serial resistance to echinocandins has been observed.
Principal takeaways:
1Candida auris isolates are often MDR, with some strains having elevated MICs to drugs in all the three major classes of antifungal medications.
2The isolates are difficult to identify and require specialized methods, such as MALDI-TOF or molecular identification based on sequencing.
3Misidentification may lead to inappropriate treatment.
4C auris has the propensity to cause outbreaks in health-care settings, as has been reported in several countries, and resistance may result in treatment failure.
Richard Winn, MD, MS, FCCPImmediate Past Chair
References
1. Sarma S. Current perspective on emergence, diagnosis and drug resistance in Candida auris. Infect Drug Resistance. 2017;10:155–165.
2. Pan American Health Organization/World Health Organization. Epidemiological Alert: Candida auris outbreaks in health care services. October 3, Washington, DC: PAHO/WHO; 2016.
3. Centers for Disease Control and Prevention. Global emergence of invasive infections caused by the multidrug-resistant yeast Candida auris. CDC; 2016 [updated June 24, 2016]
Cardiovascular Medicine and Surgery
The Holy Grail of Blood Pressure Management?
Blood pressure treatment recommendations have been confusing over the past few years. The Joint National Committee (JNC) 8 stirred up controversy in 2014 because they raised the recommended tolerating systolic blood pressures, in certain people aged 60 and above, up to 150 mm Hg [James, et al. JAMA. 2014;311(5):507-520]. The new AHA/ACC hypertension guidelines cosponsored by 11 societies generated controversy because they changed the definition of hypertension (normal <120/80 mm Hg, elevated 120-129/80-89, stage 1 130-139/80-89, or stage 2 >140/90) [Whelton et al. J Am Coll Cardiol. 2017 pii:S0735-1097(17)41519-1]. The SPRINT trial [Wright, et al. N Engl J Med. 2015;373:2103-2116] largely influenced these recommendations. SPRINT demonstrated a 25% relative risk reduction of heart attack, stroke, cardiovascular death, or decompensated heart failure with more aggressive blood pressure management (BP goal <120/90 vs <140/90).
This new classification would label 46% of Americans, or 103.3 million people, as hypertensive. However, there is uncertainty in how broadly applicable the SPRINT results are, particularly in those under the age of 45. The majority of large clinical trials, including SPRINT, have limited numbers of patients who were less than 50 years old and, therefore, it is unknown if younger patients benefit to the same degree. The absolute improvement is also questionable because as an editorial points out [Welch, “Don’t Let New Blood Pressure Guidelines Raise Yours” NY Times. Nov. 15, 2017], the primary endpoint in SPRINT only occurred in less than or equal to 8% of patients.
These guidelines reinforce the need to measure ambulatory blood pressures, perform proper in-office blood pressure measurements, and emphasize lifestyle modifications. Whether aggressive blood pressure management is worth the potential risks and the degree to which ideal blood pressure measurement can be applied to real world practices, remains uncertain.
David J. Nagel, MD, PhD Steering Committee Member
Chest Infections
Candida auris
Invasive fungal infections are frequently managed by ICU physicians and are a leading cause of mortality among critically ill patients. Invasive candidiasis is associated with an attributable mortality rate of up to 49%. Historically, the majority of these infections has been caused by Candida albicans, but this may be changing.
The first outbreak of Candida auris in the Americas (18 patients) occurred in the ICU of a hospital in Venezuela. Resistance to common azoles was documented, and half of the isolates showed decreased susceptibility to amphotericin B. As of August 2017, a total 153 clinical cases of C auris infection have been reported to CDC from 10 US states; most have occurred in New York and New Jersey.
What has been learned from these cases is that close contacts can be colonized, colonization can be persistent (approximately 9 months), the yeast can survive in the hospital environment, bleach or sporicide is needed for elimination, isolation precautions are recommended as for MDRO bacteria, and serial resistance to echinocandins has been observed.
Principal takeaways:
1Candida auris isolates are often MDR, with some strains having elevated MICs to drugs in all the three major classes of antifungal medications.
2The isolates are difficult to identify and require specialized methods, such as MALDI-TOF or molecular identification based on sequencing.
3Misidentification may lead to inappropriate treatment.
4C auris has the propensity to cause outbreaks in health-care settings, as has been reported in several countries, and resistance may result in treatment failure.
Richard Winn, MD, MS, FCCPImmediate Past Chair
References
1. Sarma S. Current perspective on emergence, diagnosis and drug resistance in Candida auris. Infect Drug Resistance. 2017;10:155–165.
2. Pan American Health Organization/World Health Organization. Epidemiological Alert: Candida auris outbreaks in health care services. October 3, Washington, DC: PAHO/WHO; 2016.
3. Centers for Disease Control and Prevention. Global emergence of invasive infections caused by the multidrug-resistant yeast Candida auris. CDC; 2016 [updated June 24, 2016]
Cardiovascular Medicine and Surgery
The Holy Grail of Blood Pressure Management?
Blood pressure treatment recommendations have been confusing over the past few years. The Joint National Committee (JNC) 8 stirred up controversy in 2014 because they raised the recommended tolerating systolic blood pressures, in certain people aged 60 and above, up to 150 mm Hg [James, et al. JAMA. 2014;311(5):507-520]. The new AHA/ACC hypertension guidelines cosponsored by 11 societies generated controversy because they changed the definition of hypertension (normal <120/80 mm Hg, elevated 120-129/80-89, stage 1 130-139/80-89, or stage 2 >140/90) [Whelton et al. J Am Coll Cardiol. 2017 pii:S0735-1097(17)41519-1]. The SPRINT trial [Wright, et al. N Engl J Med. 2015;373:2103-2116] largely influenced these recommendations. SPRINT demonstrated a 25% relative risk reduction of heart attack, stroke, cardiovascular death, or decompensated heart failure with more aggressive blood pressure management (BP goal <120/90 vs <140/90).
This new classification would label 46% of Americans, or 103.3 million people, as hypertensive. However, there is uncertainty in how broadly applicable the SPRINT results are, particularly in those under the age of 45. The majority of large clinical trials, including SPRINT, have limited numbers of patients who were less than 50 years old and, therefore, it is unknown if younger patients benefit to the same degree. The absolute improvement is also questionable because as an editorial points out [Welch, “Don’t Let New Blood Pressure Guidelines Raise Yours” NY Times. Nov. 15, 2017], the primary endpoint in SPRINT only occurred in less than or equal to 8% of patients.
These guidelines reinforce the need to measure ambulatory blood pressures, perform proper in-office blood pressure measurements, and emphasize lifestyle modifications. Whether aggressive blood pressure management is worth the potential risks and the degree to which ideal blood pressure measurement can be applied to real world practices, remains uncertain.
David J. Nagel, MD, PhD Steering Committee Member
Chest Infections
Candida auris
Invasive fungal infections are frequently managed by ICU physicians and are a leading cause of mortality among critically ill patients. Invasive candidiasis is associated with an attributable mortality rate of up to 49%. Historically, the majority of these infections has been caused by Candida albicans, but this may be changing.
The first outbreak of Candida auris in the Americas (18 patients) occurred in the ICU of a hospital in Venezuela. Resistance to common azoles was documented, and half of the isolates showed decreased susceptibility to amphotericin B. As of August 2017, a total 153 clinical cases of C auris infection have been reported to CDC from 10 US states; most have occurred in New York and New Jersey.
What has been learned from these cases is that close contacts can be colonized, colonization can be persistent (approximately 9 months), the yeast can survive in the hospital environment, bleach or sporicide is needed for elimination, isolation precautions are recommended as for MDRO bacteria, and serial resistance to echinocandins has been observed.
Principal takeaways:
1Candida auris isolates are often MDR, with some strains having elevated MICs to drugs in all the three major classes of antifungal medications.
2The isolates are difficult to identify and require specialized methods, such as MALDI-TOF or molecular identification based on sequencing.
3Misidentification may lead to inappropriate treatment.
4C auris has the propensity to cause outbreaks in health-care settings, as has been reported in several countries, and resistance may result in treatment failure.
Richard Winn, MD, MS, FCCPImmediate Past Chair
References
1. Sarma S. Current perspective on emergence, diagnosis and drug resistance in Candida auris. Infect Drug Resistance. 2017;10:155–165.
2. Pan American Health Organization/World Health Organization. Epidemiological Alert: Candida auris outbreaks in health care services. October 3, Washington, DC: PAHO/WHO; 2016.
3. Centers for Disease Control and Prevention. Global emergence of invasive infections caused by the multidrug-resistant yeast Candida auris. CDC; 2016 [updated June 24, 2016]





