User login
Obesity: When to consider medication
Modest weight loss of 5% to 10% among patients who are overweight or obese can result in a clinically relevant reduction in cardiovascular (CV) disease risk.1 This amount of weight loss can increase insulin sensitivity in adipose tissue, liver, and muscle, and have a positive impact on blood sugar, blood pressure, triglycerides, and high-density lipoprotein cholesterol.1,2
All patients who are obese or overweight with increased CV risk should be counseled on diet, exercise, and other behavioral interventions.3 Weight loss secondary to lifestyle modification alone, however, leads to adaptive physiologic responses, which increase appetite and reduce energy expenditure.4-6
Pharmacotherapy can counteract this metabolic adaptation and lead to sustained weight loss. Antiobesity medication can be considered if a patient has a body mass index (BMI) ≥30 kg/m2 or ≥27 kg/m2 with obesity-related comorbidities such as hypertension, type 2 diabetes, dyslipidemia, or obstructive sleep apnea.3,7
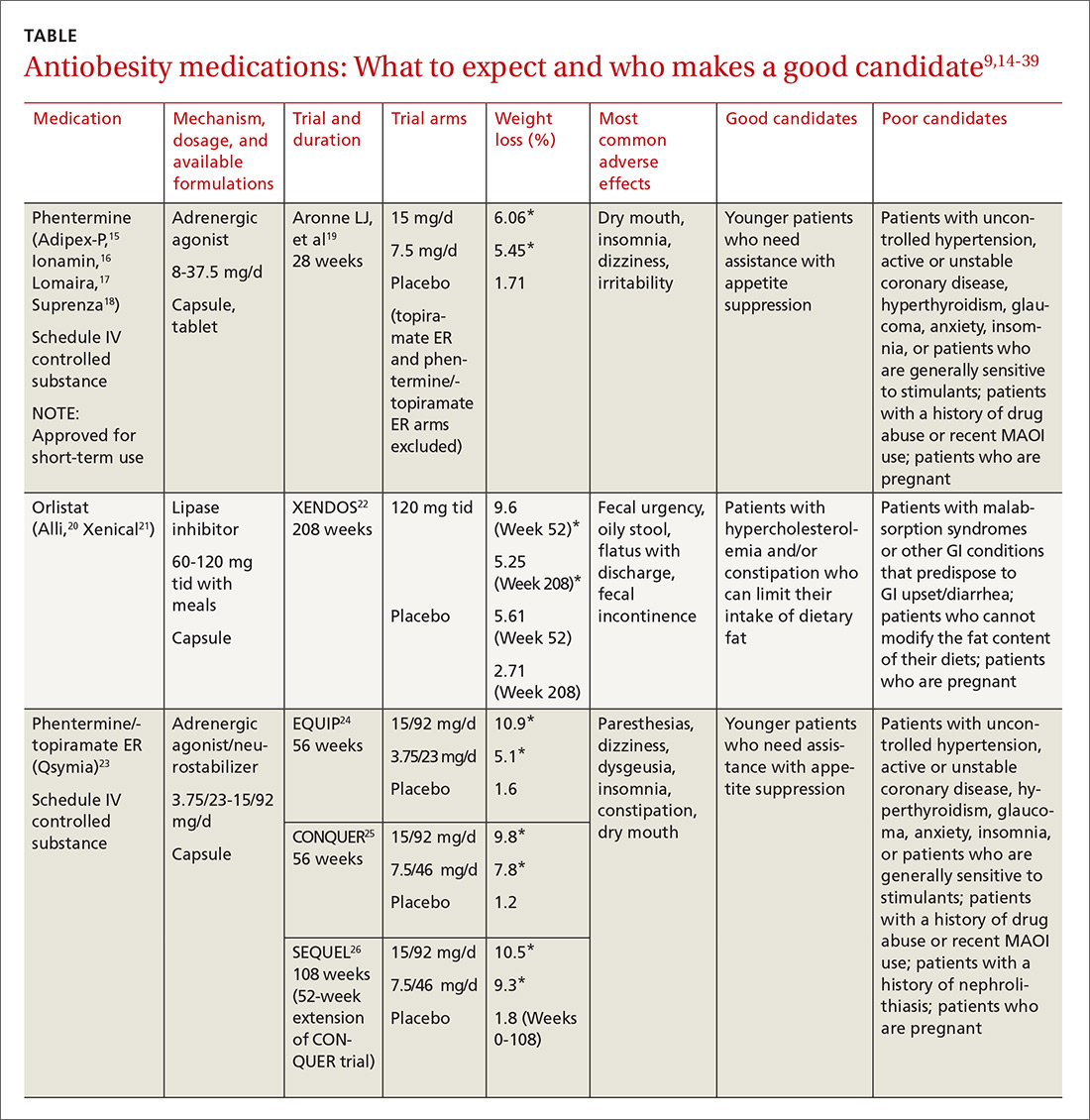
Until recently, there were few pharmacologic options approved by the US Food and Drug Administration (FDA) for the management of obesity. The mainstays of treatment were phentermine (Adipex-P, Ionamin, Suprenza) and orlistat (Alli, Xenical). Since 2012, however, 4 agents have been approved as adjuncts to a reduced-calorie diet and increased physical activity for long-term weight management.8,9 Phentermine/topiramate extended-release (ER) (Qsymia) and lorcaserin (Belviq) were approved in 2012,10,11 and naltrexone sustained release (SR)/bupropion SR (Contrave) and liraglutide 3 mg (Saxenda) were approved in 201412,13 (TABLE9,14-39). These medications have the potential to not only limit weight gain, but also promote weight loss and, thus, improve blood pressure, cholesterol, glucose, and insulin.40
Despite the growing obesity epidemic and the availability of several additional medications for chronic weight management, use of antiobesity pharmacotherapy has been limited. Barriers to use include inadequate training of health care professionals, poor insurance coverage for new agents, and low reimbursement for office visits to address weight.41
In addition, the number of obesity medicine specialists, while increasing, is still not sufficient. Therefore, it is imperative for other health care professionals—namely family practitioners—to be aware of the treatment options available to patients who are overweight or obese and to be adept at using them.
In this review, we present 4 cases that depict patients who could benefit from the addition of antiobesity pharmacotherapy to a comprehensive treatment plan that includes diet, physical activity, and behavioral modification.
[polldaddy:9840472]
CASE 1 Melissa C, a 27-year-old woman with obesity (BMI 33 kg/m2), hyperlipidemia, and migraine headaches, presents for weight management. Despite a calorie-reduced diet and 200 minutes per week of exercise for the past 6 months, she has been unable to lose weight. The only medications she’s taking are oral contraceptive pills and sumatriptan, as needed. She suffers from migraines 3 times a month and has no anxiety. Laboratory test results are normal with the exception of an elevated low-density lipoprotein (LDL) level.
Which medication is an appropriate next step for Ms. C?
Discussion
When considering an antiobesity agent for any patient, there are 2 important questions to ask:
- Are there contraindications, drug-drug interactions, or undesirable adverse effects associated with this medication that could be problematic for the patient?
- Can this medication improve other symptoms or conditions the patient has?
In addition, see “Before prescribing antiobesity medication . . .”
SIDEBAR
Before prescribing antiobesity medication . . .Have a frank discussion with the patient and be sure to cover the following points:
- The rationale for pharmacologic treatment is to counteract adaptive physiologic responses, which increase appetite and reduce energy expenditure, in response to diet-induced weight loss.
- Antiobesity medication is only one component of a comprehensive treatment plan, which also includes diet, physical activity, and behavior modification.
- Antiobesity agents are intended for long-term use, as obesity is a chronic disease. If/when you stop the medication, there may be some weight regain, similar to an increase in blood pressure after discontinuing an antihypertensive agent.
- Because antiobesity medications improve many parameters including glucose/hemoglobin A1c, lipids, blood pressure, and waist circumference, it is possible that the addition of one antiobesity medication can reduce, or even eliminate, the need for several other medications.
Remember that many patients who present for obesity management have experienced weight bias. It is important to not be judgmental, but rather explain why obesity is a chronic disease. If patients understand the physiology of their condition, they will understand that their limited success with weight loss in the past is not just a matter of willpower. Lifestyle change and weight loss are extremely difficult, so it is important to provide encouragement and support for ongoing behavioral modification.
Phentermine/topiramate ER is a good first choice for this young patient with class I (BMI 30-34.9 kg/m2) obesity and migraines, as she can likely tolerate a stimulant and her migraines might improve with topiramate. Before starting the medication, ask about insomnia and nephrolithiasis in addition to anxiety and other contraindications (ie, glaucoma, hyperthyroidism, recent monoamine oxidase inhibitor use, or a known hypersensitivity or idiosyncrasy to sympathomimetic amines).23 The most common adverse events reported in phase III trials were dry mouth, paresthesia, and constipation.24-26
Not for pregnant women. Women of childbearing age must have a negative pregnancy test before starting phentermine/topiramate ER and every month while taking the medication. The FDA requires a Risk Evaluation and Mitigation Strategy (REMS) to inform prescribers and patients about the increased risk of congenital malformation, specifically orofacial clefts, in infants exposed to topiramate during the first trimester of pregnancy.42 REMS focuses on the importance of pregnancy prevention, the consistent use of birth control, and the need to discontinue phentermine/topiramate ER immediately if pregnancy occurs.
Flexible dosing. Phentermine/topiramate ER is available in 4 dosages: phentermine 3.75 mg/topiramate 23 mg ER; phentermine 7.5 mg/topiramate 46 mg ER; phentermine 11.25 mg/topiramate 69 mg ER; and phentermine 15 mg/topiramate 92 mg ER. Gradual dose escalation minimizes risks and adverse events.23
Monitor patients frequently to evaluate for adverse effects and ensure adherence to diet, exercise, and lifestyle modifications. If weight loss is slower or less robust than expected, check for dietary indiscretion, as medications have limited efficacy without appropriate behavioral changes.
Discontinue phentermine/topiramate ER if the patient does not achieve 5% weight loss after 12 weeks on the maximum dose, as it is unlikely that she will achieve and sustain clinically meaningful weight loss with continued treatment.23 In this case, consider another agent with a different mechanism of action. Any of the other antiobesity medications could be appropriate for this patient.
CASE 2 Norman S, a 52-year-old overweight man (BMI 29 kg/m2) with type 2 diabetes, hyperlipidemia, osteoarthritis, and glaucoma, has recently hit a plateau with his weight loss. He lost 45 pounds secondary to diet and exercise, but hasn’t been able to lose any more. He also struggles with constant hunger. His medications include metformin 1000 mg bid, atorvastatin 10 mg/d, and occasional acetaminophen/oxycodone for knee pain until he undergoes a left knee replacement. Laboratory values are normal except for a hemoglobin A1c of 7.2%.
Mr. S is afraid of needles and cannot tolerate stimulants due to anxiety. Which medication is an appropriate next step for this patient?
Discussion
Lorcaserin is a good choice for this patient who is overweight and has several weight-related comorbidities. He has worked hard to lose a significant number of pounds, and is now at high risk of regaining them. That’s because his appetite has increased with his new exercise regimen, but his energy expenditure has decreased secondary to metabolic adaptation.
Narrowing the field. Naltrexone SR/bupropion SR cannot be used because of his opioid use. Phentermine/topiramate ER is contraindicated for patients with glaucoma, and liraglutide 3 mg is not appropriate given the patient’s fear of needles.
He could try orlistat, especially if he struggles with constipation, but the gastrointestinal adverse effects are difficult for many patients to tolerate. While not an antiobesity medication, a sodium-glucose co-transporter 2 (SGLT2) inhibitor could be prescribed for his diabetes and may also promote weight loss.43
An appealing choice. The glucose-lowering effect of lorcaserin could provide an added benefit for the patient. The BLOOM-DM (Behavioral modification and lorcaserin for overweight and obesity management in diabetes mellitus) study reported a mean reduction in hemoglobin A1c of 0.9% in the treatment group compared with a 0.4% reduction in the placebo group,30 and the effect of lorcaserin on A1c appeared to be independent of weight loss.
Mechanism of action: Cause for concern? Although lorcaserin selectively binds to serotonin 5-HT2C receptors, the theoretical risk of cardiac valvulopathy was evaluated in phase III studies, as fenfluramine, a 5-HT2B-receptor agonist, was withdrawn from the US market in 1997 for this reason.44 Both the BLOOM (Behavioral modification and lorcaserin for overweight and obesity management) and BLOSSOM (Behavioral modification and lorcaserin second study for obesity management) studies found that lorcaserin did not increase the incidence of FDA-defined cardiac valvulopathy.28,29
Formulations/adverse effects. Lorcaserin is available in 2 formulations: 10-mg tablets, which are taken twice daily, or 20-mg XR tablets, which are taken once daily. Both are generally well tolerated.27,45 The most common adverse event reported in phase III trials was headache.28,30,43 Discontinue lorcaserin if the patient does not lose 5% of his initial weight after 12 weeks, as weight loss at this stage is a good predictor of longer-term success.46
Some patients don’t respond. Interestingly, a subset of patients do not respond to lorcaserin. The most likely explanation for different responses to the medication is that there are many causes of obesity, only some of which respond to 5-HT2C agonism. Currently, we do not perform pharmacogenomic testing before prescribing lorcaserin, but perhaps an inexpensive test to identify responders will be available in the future.
CASE 3 Kathryn M, a 38-year-old woman with obesity (BMI 42 kg/m2), obstructive sleep apnea, gastroesophageal reflux disease, and depression, is eager to get better control over her weight. Her medications include lansoprazole 30 mg/d and a multivitamin. She reports constantly thinking about food and not being able to control her impulses to buy large quantities of unhealthy snacks. She is so preoccupied by thoughts of food that she has difficulty concentrating at work.
Ms. M smokes a quarter of a pack of cigarettes daily, but she is ready to quit. She views bariatric surgery as a “last resort” and has no anxiety, pain, or history of seizures. Which medication is appropriate for this patient?
Discussion
This patient with class III obesity (BMI ≥40 kg/m2) is eligible for bariatric surgery; however, she is not interested in pursuing it at this time. It is important to discuss all of her options before deciding on a treatment plan. For patients like Ms. M, who would benefit from more than modest weight loss, consider a multidisciplinary approach including lifestyle modifications, pharmacotherapy, devices (eg, an intragastric balloon), and/or surgery. You would need to make clear to Ms. M that she may still be eligible for insurance coverage for surgery if she changes her mind after pursuing other treatments as long as her BMI remains ≥35 kg/m2 with obesity-related comorbidities.
Naltrexone SR/bupropion SR is a good choice for Ms. M because she describes debilitating cravings and addictive behavior surrounding food. Patients taking naltrexone SR/bupropion SR in the Contrave Obesity Research (COR)-I and COR-II phase III trials experienced a reduced frequency of food cravings, reduced difficulty in resisting food cravings, and an increased ability to control eating compared with those assigned to placebo.32,33
Added benefits. Bupropion could also help Ms. M quit smoking and improve her mood, as it is FDA-approved for smoking cessation and depression. She denies anxiety and seizures, so bupropion is not contraindicated. Even if a patient denies a history of seizure, ask about any conditions that predispose to seizures, such as anorexia nervosa or bulimia or the abrupt discontinuation of alcohol, benzodiazepines, barbiturates, or antiepileptic drugs.
Opioid use. Although the patient denies pain, ask about potential opioid use, as naltrexone is an opioid receptor antagonist. Patients should be informed that opioids may be ineffective if they are required unexpectedly (eg, for trauma) and that naltrexone SR/bupropion SR should be withheld for any planned surgical procedure potentially requiring opioid use.
Other options. While naltrexone SR/bupropion SR is the most appropriate choice for this patient because it addresses Ms. M’s problematic eating behaviors while potentially improving mood and assisting with smoking cessation, phentermine/topiramate ER, lorcaserin, and liraglutide 3 mg could also be used and should certainly be tried if naltrexone SR/bupropion SR does not produce the desired weight loss.
Adverse effects. Titrate naltrexone SR/bupropion SR slowly to the treatment dose to minimize risks and adverse events.31 The most common adverse effects reported in phase III trials were nausea, constipation, and headache.34,35,45,46 Discontinue naltrexone SR/bupropion SR if the patient does not achieve 5% weight loss at 16 weeks (after 12 weeks at the maintenance dose).31
CASE 4 William P, a 65-year-old man with obesity (BMI 39 kg/m2) who underwent Roux-en-Y gastric bypass surgery and who has type 2 diabetes, congestive heart failure, coronary artery disease, hypertension, and hyperlipidemia, remains concerned about his weight. He lost 100 lbs following surgery and maintained his weight for 3 years, but then regained 30 lbs. He comes in for an office visit because he’s concerned about his increasing blood sugar and wants to prevent further weight gain. His medications include metformin 1000 mg bid, lisinopril 5 mg/d, carvedilol 12.5 mg bid, simvastatin 20 mg/d, and aspirin 81 mg/d. Laboratory test results are normal except for a hemoglobin A1c of 8%. He denies pancreatitis and a personal or family history of thyroid cancer.
Which medication is an appropriate next step for Mr. P?
Discussion
Pharmacotherapy is a great option for this patient, who is regaining weight following bariatric surgery. Phentermine/topiramate ER is the only medication that would be contraindicated because of his heart disease. Lorcaserin and naltrexone SR/bupropion SR could be considered, but liraglutide 3 mg is the most appropriate option, given his need for further glucose control.
Furthermore, the recent LEADER (Liraglutide effect and action in diabetes: evaluation of CV outcome results) trial reported a significant mortality benefit with liraglutide 1.8 mg/d among patients with type 2 diabetes and high CV risk.47 The study found that liraglutide was superior to placebo in reducing CV events.
Contraindications. Ask patients about a history of pancreatitis before starting liraglutide 3 mg given the possible increased risk. In addition, liraglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with multiple endocrine neoplasia syndrome type 2. Thyroid C-cell tumors have been found in rodents given supratherapeutic doses of liraglutide;48 however, there is no evidence of liraglutide causing C-cell tumors in humans.
For patients taking a medication that can cause hypoglycemia, such as insulin or a sulfonylurea, monitor blood sugar and consider reducing the dose of that medication when starting liraglutide.
Administration and titration. Liraglutide is injected subcutaneously once daily. The dose is titrated up weekly to reduce gastrointestinal symptoms.36 The most common adverse effects reported in phase III trials were nausea, diarrhea, and constipation.37-39 Discontinue liraglutide 3 mg if the patient does not lose at least 4% of baseline body weight after 16 weeks.49
CORRESPONDENCE
Katherine H. Saunders, MD, DABOM, Comprehensive Weight Control Center, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell Medicine, 1165 York Avenue, New York, NY 10065; kph2001@med.cornell.edu.
1. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481-1486.
2. Magkos F, Fraterrigo G, Yoshino J. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016;23:591-601.
3. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985-3023.
4. Sumithran P, Predergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597-1604.
5. Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes (Lond). 2015;39:1188-1196.
6. Fothergill E, Guo J, Howard L, et al. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity (Silver Spring). 2016;24:1612-1619.
7. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100:342-362.
8. Saunders KH, Shukla AP, Igel LI, et al. Pharmacotherapy for obesity. Endocrinol Metab Clin North Am. 2016;45:521-538.
9. Saunders KH, Kumar RB, Igel LI, et al. Pharmacologic approaches to weight management: recent gains and shortfalls in combating obesity. Curr Atheroscler Rep. 2016;18:36.
10. US Food and Drug Administration. Drug approval package. Qsymia. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/022580Orig1s000_qsymia_toc.cfm. Accessed August 28, 2017.
11. Arena Pharmaceuticals. Arena Pharmaceuticals and Eisai announce FDA approval of BELVIQ® (lorcaserin HCl) for chronic weight management in adults who are overweight with a comorbidity or obese. Available at: http://invest.arenapharm.com/releasedetail.cfm?ReleaseID=687182. Accessed August 28, 2017.
12. Drugs.com. Contrave approval history. Available at: https://www.drugs.com/history/contrave.html. Accessed August 28, 2017.
13. US Food and Drug Administration. Drugs@FDA: FDA approved drug products. Available at: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=206321. Accessed August 28, 2017.
14. Igel LI, Kumar RB, Saunders KH, et al. Practical use of pharmacotherapy for obesity. Gastroenterology. 2017;152:1765-1779.
15. Adipex-P package insert. Available at: http://www.iodine.com/drug/phentermine/fda-package-insert. Accessed August 28, 2017.
16. Ionamin package insert. Available at: http://druginserts.com/lib/rx/meds/ionamin/. Accessed August 28, 2017.
17. Lomaira package insert. Available at: https://www.lomaira.com/Prescribing_Information.pdf. Accessed August 28, 2017.
18. Suprenza package insert. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/202088s001lbl.pdf. Accessed August 28, 2017.
19. Aronne LJ, Wadden TA, Peterson C, et al. Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity (Silver Spring). 2013;21:2163-2171.
20. Alli package labeling. Available at: http://druginserts.com/lib/otc/meds/alli-1/. Accessed August 28, 2017.
21. Xenical package insert. Available at: https://www.gene.com/download/pdf/xenical_prescribing.pdf. Accessed August 28, 2017.
22. Torgerson JS, Hauptman J, Boldrin MN, et al. XENical in the prevention of Diabetes in Obese Subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155-161.
23. Qsymia package insert. Available at: https://www.qsymia.com/pdf/prescribing-information.pdf. Accessed August 28, 2017.
24. Allison DB, Gadde KM, Garvey WT, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity (Silver Spring). 2012;20:330-342.
25. Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomized, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341-1352.
26. Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95:297-308.
27. Belviq package insert. Available at: https://www.belviq.com/-/media/Files/BelviqConsolidation/PDF/Belviq_Prescribing_information-pdf.PDF?la=en. Accessed August 28, 2017.
28. Smith SR, Weissman NJ, Anderson CM, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010;363:245-256.
29. Fidler MC, Sanchez M, Raether B, et al. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. J Clin Endocrinol Metab. 2011;96:3067-3077.
30. O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. Obesity (Silver Spring). 2012;20:1426-1436.
31. Contrave package insert. Available at: https://contrave.com/wp-content/uploads/2017/05/Contrave_PI.pdf. Accessed August 28, 2017.
32. Greenway FL, Fujioka K, Plodkowski RA, et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2010;376:595-605.
33. Apovian CM, Aronne L, Rubino D, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring). 2013;21:935-943.
34. Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity (Silver Spring). 2011;19:110-120.
35. Hollander P, Gupta AK, Plodkowski R, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36:4022-4029.
36. Saxenda package insert. Available at: http://www.novo-pi.com/saxenda.pdf. Accessed August 28, 2017.
37. Pi-Sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373:11-22.
38. Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE Diabetes randomized clinical trial. JAMA. 2015;314:687-699.
39. Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet induced weight loss: the SCALE Maintenance randomized study. Int J Obes (Lond). 2013;37:1443-1451.
40. Saunders KH, Igel LI, Aronne LJ. An update on naltrexone/bupropion extended-release in the treatment of obesity. Expert Opin Pharmacother. 2016. [Epub ahead of print]
41. Thomas CE, Mauer EA, Shukla AP, et al. Low adoption of weight loss medications: a comparison of prescribing patterns of antiobesity pharmacotherapies and SGLT2s. Obesity (Silver Spring). 2016;24:1955-1961.
42. Qsymia Risk Evaluation and Mitigation Strategy (REMS). VIVUS, Inc. Available at: http://www.qsymiarems.com. Accessed January 16, 2017.
43. Zinman B, Wanner C, Lachin JM, et al. Empaglifozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117-2128.
44. US Food and Drug Administration. FDA announces withdrawal fenfluramine and dexfenfluramine (Fen-Phen). Available at: https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm179871.htm. Accessed August 28, 2017.
45. Belviq XR package insert. Available at: https://www.belviq.com/-/media/Files/BelviqConsolidation/PDF/belviqxr_prescribing_information-pdf.PDF?la=en. Accessed January 16, 2017.
46. Smith SR, O’Neil PM, Astrup A. Early weight loss while on lorcaserin, diet and exercise as a predictor of week 52 weight-loss outcomes. Obesity (Silver Spring). 2014;22:2137-2146.
47. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311-322.
48. Madsen LW, Knauf JA, Gotfredsen C, et al. GLP-1 receptor agonists and the thyroid: C-cell effects in mice are mediated via the GLP-1 receptor and not associated with RET activation. Endocrinology. 2012;153:1538-1547.
49. Fujioka K, O’Neil PM, Davies M, et al. Early weight loss with liraglutide 3.0 mg predicts 1-year weight loss and is associated with improvements in clinical markers. Obesity (Silver Spring). 2016;24:2278-2288.
Modest weight loss of 5% to 10% among patients who are overweight or obese can result in a clinically relevant reduction in cardiovascular (CV) disease risk.1 This amount of weight loss can increase insulin sensitivity in adipose tissue, liver, and muscle, and have a positive impact on blood sugar, blood pressure, triglycerides, and high-density lipoprotein cholesterol.1,2
All patients who are obese or overweight with increased CV risk should be counseled on diet, exercise, and other behavioral interventions.3 Weight loss secondary to lifestyle modification alone, however, leads to adaptive physiologic responses, which increase appetite and reduce energy expenditure.4-6
Pharmacotherapy can counteract this metabolic adaptation and lead to sustained weight loss. Antiobesity medication can be considered if a patient has a body mass index (BMI) ≥30 kg/m2 or ≥27 kg/m2 with obesity-related comorbidities such as hypertension, type 2 diabetes, dyslipidemia, or obstructive sleep apnea.3,7
Until recently, there were few pharmacologic options approved by the US Food and Drug Administration (FDA) for the management of obesity. The mainstays of treatment were phentermine (Adipex-P, Ionamin, Suprenza) and orlistat (Alli, Xenical). Since 2012, however, 4 agents have been approved as adjuncts to a reduced-calorie diet and increased physical activity for long-term weight management.8,9 Phentermine/topiramate extended-release (ER) (Qsymia) and lorcaserin (Belviq) were approved in 2012,10,11 and naltrexone sustained release (SR)/bupropion SR (Contrave) and liraglutide 3 mg (Saxenda) were approved in 201412,13 (TABLE9,14-39). These medications have the potential to not only limit weight gain, but also promote weight loss and, thus, improve blood pressure, cholesterol, glucose, and insulin.40
Despite the growing obesity epidemic and the availability of several additional medications for chronic weight management, use of antiobesity pharmacotherapy has been limited. Barriers to use include inadequate training of health care professionals, poor insurance coverage for new agents, and low reimbursement for office visits to address weight.41
In addition, the number of obesity medicine specialists, while increasing, is still not sufficient. Therefore, it is imperative for other health care professionals—namely family practitioners—to be aware of the treatment options available to patients who are overweight or obese and to be adept at using them.
In this review, we present 4 cases that depict patients who could benefit from the addition of antiobesity pharmacotherapy to a comprehensive treatment plan that includes diet, physical activity, and behavioral modification.
[polldaddy:9840472]
CASE 1 Melissa C, a 27-year-old woman with obesity (BMI 33 kg/m2), hyperlipidemia, and migraine headaches, presents for weight management. Despite a calorie-reduced diet and 200 minutes per week of exercise for the past 6 months, she has been unable to lose weight. The only medications she’s taking are oral contraceptive pills and sumatriptan, as needed. She suffers from migraines 3 times a month and has no anxiety. Laboratory test results are normal with the exception of an elevated low-density lipoprotein (LDL) level.
Which medication is an appropriate next step for Ms. C?
Discussion
When considering an antiobesity agent for any patient, there are 2 important questions to ask:
- Are there contraindications, drug-drug interactions, or undesirable adverse effects associated with this medication that could be problematic for the patient?
- Can this medication improve other symptoms or conditions the patient has?
In addition, see “Before prescribing antiobesity medication . . .”
SIDEBAR
Before prescribing antiobesity medication . . .Have a frank discussion with the patient and be sure to cover the following points:
- The rationale for pharmacologic treatment is to counteract adaptive physiologic responses, which increase appetite and reduce energy expenditure, in response to diet-induced weight loss.
- Antiobesity medication is only one component of a comprehensive treatment plan, which also includes diet, physical activity, and behavior modification.
- Antiobesity agents are intended for long-term use, as obesity is a chronic disease. If/when you stop the medication, there may be some weight regain, similar to an increase in blood pressure after discontinuing an antihypertensive agent.
- Because antiobesity medications improve many parameters including glucose/hemoglobin A1c, lipids, blood pressure, and waist circumference, it is possible that the addition of one antiobesity medication can reduce, or even eliminate, the need for several other medications.
Remember that many patients who present for obesity management have experienced weight bias. It is important to not be judgmental, but rather explain why obesity is a chronic disease. If patients understand the physiology of their condition, they will understand that their limited success with weight loss in the past is not just a matter of willpower. Lifestyle change and weight loss are extremely difficult, so it is important to provide encouragement and support for ongoing behavioral modification.
Phentermine/topiramate ER is a good first choice for this young patient with class I (BMI 30-34.9 kg/m2) obesity and migraines, as she can likely tolerate a stimulant and her migraines might improve with topiramate. Before starting the medication, ask about insomnia and nephrolithiasis in addition to anxiety and other contraindications (ie, glaucoma, hyperthyroidism, recent monoamine oxidase inhibitor use, or a known hypersensitivity or idiosyncrasy to sympathomimetic amines).23 The most common adverse events reported in phase III trials were dry mouth, paresthesia, and constipation.24-26
Not for pregnant women. Women of childbearing age must have a negative pregnancy test before starting phentermine/topiramate ER and every month while taking the medication. The FDA requires a Risk Evaluation and Mitigation Strategy (REMS) to inform prescribers and patients about the increased risk of congenital malformation, specifically orofacial clefts, in infants exposed to topiramate during the first trimester of pregnancy.42 REMS focuses on the importance of pregnancy prevention, the consistent use of birth control, and the need to discontinue phentermine/topiramate ER immediately if pregnancy occurs.
Flexible dosing. Phentermine/topiramate ER is available in 4 dosages: phentermine 3.75 mg/topiramate 23 mg ER; phentermine 7.5 mg/topiramate 46 mg ER; phentermine 11.25 mg/topiramate 69 mg ER; and phentermine 15 mg/topiramate 92 mg ER. Gradual dose escalation minimizes risks and adverse events.23
Monitor patients frequently to evaluate for adverse effects and ensure adherence to diet, exercise, and lifestyle modifications. If weight loss is slower or less robust than expected, check for dietary indiscretion, as medications have limited efficacy without appropriate behavioral changes.
Discontinue phentermine/topiramate ER if the patient does not achieve 5% weight loss after 12 weeks on the maximum dose, as it is unlikely that she will achieve and sustain clinically meaningful weight loss with continued treatment.23 In this case, consider another agent with a different mechanism of action. Any of the other antiobesity medications could be appropriate for this patient.
CASE 2 Norman S, a 52-year-old overweight man (BMI 29 kg/m2) with type 2 diabetes, hyperlipidemia, osteoarthritis, and glaucoma, has recently hit a plateau with his weight loss. He lost 45 pounds secondary to diet and exercise, but hasn’t been able to lose any more. He also struggles with constant hunger. His medications include metformin 1000 mg bid, atorvastatin 10 mg/d, and occasional acetaminophen/oxycodone for knee pain until he undergoes a left knee replacement. Laboratory values are normal except for a hemoglobin A1c of 7.2%.
Mr. S is afraid of needles and cannot tolerate stimulants due to anxiety. Which medication is an appropriate next step for this patient?
Discussion
Lorcaserin is a good choice for this patient who is overweight and has several weight-related comorbidities. He has worked hard to lose a significant number of pounds, and is now at high risk of regaining them. That’s because his appetite has increased with his new exercise regimen, but his energy expenditure has decreased secondary to metabolic adaptation.
Narrowing the field. Naltrexone SR/bupropion SR cannot be used because of his opioid use. Phentermine/topiramate ER is contraindicated for patients with glaucoma, and liraglutide 3 mg is not appropriate given the patient’s fear of needles.
He could try orlistat, especially if he struggles with constipation, but the gastrointestinal adverse effects are difficult for many patients to tolerate. While not an antiobesity medication, a sodium-glucose co-transporter 2 (SGLT2) inhibitor could be prescribed for his diabetes and may also promote weight loss.43
An appealing choice. The glucose-lowering effect of lorcaserin could provide an added benefit for the patient. The BLOOM-DM (Behavioral modification and lorcaserin for overweight and obesity management in diabetes mellitus) study reported a mean reduction in hemoglobin A1c of 0.9% in the treatment group compared with a 0.4% reduction in the placebo group,30 and the effect of lorcaserin on A1c appeared to be independent of weight loss.
Mechanism of action: Cause for concern? Although lorcaserin selectively binds to serotonin 5-HT2C receptors, the theoretical risk of cardiac valvulopathy was evaluated in phase III studies, as fenfluramine, a 5-HT2B-receptor agonist, was withdrawn from the US market in 1997 for this reason.44 Both the BLOOM (Behavioral modification and lorcaserin for overweight and obesity management) and BLOSSOM (Behavioral modification and lorcaserin second study for obesity management) studies found that lorcaserin did not increase the incidence of FDA-defined cardiac valvulopathy.28,29
Formulations/adverse effects. Lorcaserin is available in 2 formulations: 10-mg tablets, which are taken twice daily, or 20-mg XR tablets, which are taken once daily. Both are generally well tolerated.27,45 The most common adverse event reported in phase III trials was headache.28,30,43 Discontinue lorcaserin if the patient does not lose 5% of his initial weight after 12 weeks, as weight loss at this stage is a good predictor of longer-term success.46
Some patients don’t respond. Interestingly, a subset of patients do not respond to lorcaserin. The most likely explanation for different responses to the medication is that there are many causes of obesity, only some of which respond to 5-HT2C agonism. Currently, we do not perform pharmacogenomic testing before prescribing lorcaserin, but perhaps an inexpensive test to identify responders will be available in the future.
CASE 3 Kathryn M, a 38-year-old woman with obesity (BMI 42 kg/m2), obstructive sleep apnea, gastroesophageal reflux disease, and depression, is eager to get better control over her weight. Her medications include lansoprazole 30 mg/d and a multivitamin. She reports constantly thinking about food and not being able to control her impulses to buy large quantities of unhealthy snacks. She is so preoccupied by thoughts of food that she has difficulty concentrating at work.
Ms. M smokes a quarter of a pack of cigarettes daily, but she is ready to quit. She views bariatric surgery as a “last resort” and has no anxiety, pain, or history of seizures. Which medication is appropriate for this patient?
Discussion
This patient with class III obesity (BMI ≥40 kg/m2) is eligible for bariatric surgery; however, she is not interested in pursuing it at this time. It is important to discuss all of her options before deciding on a treatment plan. For patients like Ms. M, who would benefit from more than modest weight loss, consider a multidisciplinary approach including lifestyle modifications, pharmacotherapy, devices (eg, an intragastric balloon), and/or surgery. You would need to make clear to Ms. M that she may still be eligible for insurance coverage for surgery if she changes her mind after pursuing other treatments as long as her BMI remains ≥35 kg/m2 with obesity-related comorbidities.
Naltrexone SR/bupropion SR is a good choice for Ms. M because she describes debilitating cravings and addictive behavior surrounding food. Patients taking naltrexone SR/bupropion SR in the Contrave Obesity Research (COR)-I and COR-II phase III trials experienced a reduced frequency of food cravings, reduced difficulty in resisting food cravings, and an increased ability to control eating compared with those assigned to placebo.32,33
Added benefits. Bupropion could also help Ms. M quit smoking and improve her mood, as it is FDA-approved for smoking cessation and depression. She denies anxiety and seizures, so bupropion is not contraindicated. Even if a patient denies a history of seizure, ask about any conditions that predispose to seizures, such as anorexia nervosa or bulimia or the abrupt discontinuation of alcohol, benzodiazepines, barbiturates, or antiepileptic drugs.
Opioid use. Although the patient denies pain, ask about potential opioid use, as naltrexone is an opioid receptor antagonist. Patients should be informed that opioids may be ineffective if they are required unexpectedly (eg, for trauma) and that naltrexone SR/bupropion SR should be withheld for any planned surgical procedure potentially requiring opioid use.
Other options. While naltrexone SR/bupropion SR is the most appropriate choice for this patient because it addresses Ms. M’s problematic eating behaviors while potentially improving mood and assisting with smoking cessation, phentermine/topiramate ER, lorcaserin, and liraglutide 3 mg could also be used and should certainly be tried if naltrexone SR/bupropion SR does not produce the desired weight loss.
Adverse effects. Titrate naltrexone SR/bupropion SR slowly to the treatment dose to minimize risks and adverse events.31 The most common adverse effects reported in phase III trials were nausea, constipation, and headache.34,35,45,46 Discontinue naltrexone SR/bupropion SR if the patient does not achieve 5% weight loss at 16 weeks (after 12 weeks at the maintenance dose).31
CASE 4 William P, a 65-year-old man with obesity (BMI 39 kg/m2) who underwent Roux-en-Y gastric bypass surgery and who has type 2 diabetes, congestive heart failure, coronary artery disease, hypertension, and hyperlipidemia, remains concerned about his weight. He lost 100 lbs following surgery and maintained his weight for 3 years, but then regained 30 lbs. He comes in for an office visit because he’s concerned about his increasing blood sugar and wants to prevent further weight gain. His medications include metformin 1000 mg bid, lisinopril 5 mg/d, carvedilol 12.5 mg bid, simvastatin 20 mg/d, and aspirin 81 mg/d. Laboratory test results are normal except for a hemoglobin A1c of 8%. He denies pancreatitis and a personal or family history of thyroid cancer.
Which medication is an appropriate next step for Mr. P?
Discussion
Pharmacotherapy is a great option for this patient, who is regaining weight following bariatric surgery. Phentermine/topiramate ER is the only medication that would be contraindicated because of his heart disease. Lorcaserin and naltrexone SR/bupropion SR could be considered, but liraglutide 3 mg is the most appropriate option, given his need for further glucose control.
Furthermore, the recent LEADER (Liraglutide effect and action in diabetes: evaluation of CV outcome results) trial reported a significant mortality benefit with liraglutide 1.8 mg/d among patients with type 2 diabetes and high CV risk.47 The study found that liraglutide was superior to placebo in reducing CV events.
Contraindications. Ask patients about a history of pancreatitis before starting liraglutide 3 mg given the possible increased risk. In addition, liraglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with multiple endocrine neoplasia syndrome type 2. Thyroid C-cell tumors have been found in rodents given supratherapeutic doses of liraglutide;48 however, there is no evidence of liraglutide causing C-cell tumors in humans.
For patients taking a medication that can cause hypoglycemia, such as insulin or a sulfonylurea, monitor blood sugar and consider reducing the dose of that medication when starting liraglutide.
Administration and titration. Liraglutide is injected subcutaneously once daily. The dose is titrated up weekly to reduce gastrointestinal symptoms.36 The most common adverse effects reported in phase III trials were nausea, diarrhea, and constipation.37-39 Discontinue liraglutide 3 mg if the patient does not lose at least 4% of baseline body weight after 16 weeks.49
CORRESPONDENCE
Katherine H. Saunders, MD, DABOM, Comprehensive Weight Control Center, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell Medicine, 1165 York Avenue, New York, NY 10065; kph2001@med.cornell.edu.
Modest weight loss of 5% to 10% among patients who are overweight or obese can result in a clinically relevant reduction in cardiovascular (CV) disease risk.1 This amount of weight loss can increase insulin sensitivity in adipose tissue, liver, and muscle, and have a positive impact on blood sugar, blood pressure, triglycerides, and high-density lipoprotein cholesterol.1,2
All patients who are obese or overweight with increased CV risk should be counseled on diet, exercise, and other behavioral interventions.3 Weight loss secondary to lifestyle modification alone, however, leads to adaptive physiologic responses, which increase appetite and reduce energy expenditure.4-6
Pharmacotherapy can counteract this metabolic adaptation and lead to sustained weight loss. Antiobesity medication can be considered if a patient has a body mass index (BMI) ≥30 kg/m2 or ≥27 kg/m2 with obesity-related comorbidities such as hypertension, type 2 diabetes, dyslipidemia, or obstructive sleep apnea.3,7
Until recently, there were few pharmacologic options approved by the US Food and Drug Administration (FDA) for the management of obesity. The mainstays of treatment were phentermine (Adipex-P, Ionamin, Suprenza) and orlistat (Alli, Xenical). Since 2012, however, 4 agents have been approved as adjuncts to a reduced-calorie diet and increased physical activity for long-term weight management.8,9 Phentermine/topiramate extended-release (ER) (Qsymia) and lorcaserin (Belviq) were approved in 2012,10,11 and naltrexone sustained release (SR)/bupropion SR (Contrave) and liraglutide 3 mg (Saxenda) were approved in 201412,13 (TABLE9,14-39). These medications have the potential to not only limit weight gain, but also promote weight loss and, thus, improve blood pressure, cholesterol, glucose, and insulin.40
Despite the growing obesity epidemic and the availability of several additional medications for chronic weight management, use of antiobesity pharmacotherapy has been limited. Barriers to use include inadequate training of health care professionals, poor insurance coverage for new agents, and low reimbursement for office visits to address weight.41
In addition, the number of obesity medicine specialists, while increasing, is still not sufficient. Therefore, it is imperative for other health care professionals—namely family practitioners—to be aware of the treatment options available to patients who are overweight or obese and to be adept at using them.
In this review, we present 4 cases that depict patients who could benefit from the addition of antiobesity pharmacotherapy to a comprehensive treatment plan that includes diet, physical activity, and behavioral modification.
[polldaddy:9840472]
CASE 1 Melissa C, a 27-year-old woman with obesity (BMI 33 kg/m2), hyperlipidemia, and migraine headaches, presents for weight management. Despite a calorie-reduced diet and 200 minutes per week of exercise for the past 6 months, she has been unable to lose weight. The only medications she’s taking are oral contraceptive pills and sumatriptan, as needed. She suffers from migraines 3 times a month and has no anxiety. Laboratory test results are normal with the exception of an elevated low-density lipoprotein (LDL) level.
Which medication is an appropriate next step for Ms. C?
Discussion
When considering an antiobesity agent for any patient, there are 2 important questions to ask:
- Are there contraindications, drug-drug interactions, or undesirable adverse effects associated with this medication that could be problematic for the patient?
- Can this medication improve other symptoms or conditions the patient has?
In addition, see “Before prescribing antiobesity medication . . .”
SIDEBAR
Before prescribing antiobesity medication . . .Have a frank discussion with the patient and be sure to cover the following points:
- The rationale for pharmacologic treatment is to counteract adaptive physiologic responses, which increase appetite and reduce energy expenditure, in response to diet-induced weight loss.
- Antiobesity medication is only one component of a comprehensive treatment plan, which also includes diet, physical activity, and behavior modification.
- Antiobesity agents are intended for long-term use, as obesity is a chronic disease. If/when you stop the medication, there may be some weight regain, similar to an increase in blood pressure after discontinuing an antihypertensive agent.
- Because antiobesity medications improve many parameters including glucose/hemoglobin A1c, lipids, blood pressure, and waist circumference, it is possible that the addition of one antiobesity medication can reduce, or even eliminate, the need for several other medications.
Remember that many patients who present for obesity management have experienced weight bias. It is important to not be judgmental, but rather explain why obesity is a chronic disease. If patients understand the physiology of their condition, they will understand that their limited success with weight loss in the past is not just a matter of willpower. Lifestyle change and weight loss are extremely difficult, so it is important to provide encouragement and support for ongoing behavioral modification.
Phentermine/topiramate ER is a good first choice for this young patient with class I (BMI 30-34.9 kg/m2) obesity and migraines, as she can likely tolerate a stimulant and her migraines might improve with topiramate. Before starting the medication, ask about insomnia and nephrolithiasis in addition to anxiety and other contraindications (ie, glaucoma, hyperthyroidism, recent monoamine oxidase inhibitor use, or a known hypersensitivity or idiosyncrasy to sympathomimetic amines).23 The most common adverse events reported in phase III trials were dry mouth, paresthesia, and constipation.24-26
Not for pregnant women. Women of childbearing age must have a negative pregnancy test before starting phentermine/topiramate ER and every month while taking the medication. The FDA requires a Risk Evaluation and Mitigation Strategy (REMS) to inform prescribers and patients about the increased risk of congenital malformation, specifically orofacial clefts, in infants exposed to topiramate during the first trimester of pregnancy.42 REMS focuses on the importance of pregnancy prevention, the consistent use of birth control, and the need to discontinue phentermine/topiramate ER immediately if pregnancy occurs.
Flexible dosing. Phentermine/topiramate ER is available in 4 dosages: phentermine 3.75 mg/topiramate 23 mg ER; phentermine 7.5 mg/topiramate 46 mg ER; phentermine 11.25 mg/topiramate 69 mg ER; and phentermine 15 mg/topiramate 92 mg ER. Gradual dose escalation minimizes risks and adverse events.23
Monitor patients frequently to evaluate for adverse effects and ensure adherence to diet, exercise, and lifestyle modifications. If weight loss is slower or less robust than expected, check for dietary indiscretion, as medications have limited efficacy without appropriate behavioral changes.
Discontinue phentermine/topiramate ER if the patient does not achieve 5% weight loss after 12 weeks on the maximum dose, as it is unlikely that she will achieve and sustain clinically meaningful weight loss with continued treatment.23 In this case, consider another agent with a different mechanism of action. Any of the other antiobesity medications could be appropriate for this patient.
CASE 2 Norman S, a 52-year-old overweight man (BMI 29 kg/m2) with type 2 diabetes, hyperlipidemia, osteoarthritis, and glaucoma, has recently hit a plateau with his weight loss. He lost 45 pounds secondary to diet and exercise, but hasn’t been able to lose any more. He also struggles with constant hunger. His medications include metformin 1000 mg bid, atorvastatin 10 mg/d, and occasional acetaminophen/oxycodone for knee pain until he undergoes a left knee replacement. Laboratory values are normal except for a hemoglobin A1c of 7.2%.
Mr. S is afraid of needles and cannot tolerate stimulants due to anxiety. Which medication is an appropriate next step for this patient?
Discussion
Lorcaserin is a good choice for this patient who is overweight and has several weight-related comorbidities. He has worked hard to lose a significant number of pounds, and is now at high risk of regaining them. That’s because his appetite has increased with his new exercise regimen, but his energy expenditure has decreased secondary to metabolic adaptation.
Narrowing the field. Naltrexone SR/bupropion SR cannot be used because of his opioid use. Phentermine/topiramate ER is contraindicated for patients with glaucoma, and liraglutide 3 mg is not appropriate given the patient’s fear of needles.
He could try orlistat, especially if he struggles with constipation, but the gastrointestinal adverse effects are difficult for many patients to tolerate. While not an antiobesity medication, a sodium-glucose co-transporter 2 (SGLT2) inhibitor could be prescribed for his diabetes and may also promote weight loss.43
An appealing choice. The glucose-lowering effect of lorcaserin could provide an added benefit for the patient. The BLOOM-DM (Behavioral modification and lorcaserin for overweight and obesity management in diabetes mellitus) study reported a mean reduction in hemoglobin A1c of 0.9% in the treatment group compared with a 0.4% reduction in the placebo group,30 and the effect of lorcaserin on A1c appeared to be independent of weight loss.
Mechanism of action: Cause for concern? Although lorcaserin selectively binds to serotonin 5-HT2C receptors, the theoretical risk of cardiac valvulopathy was evaluated in phase III studies, as fenfluramine, a 5-HT2B-receptor agonist, was withdrawn from the US market in 1997 for this reason.44 Both the BLOOM (Behavioral modification and lorcaserin for overweight and obesity management) and BLOSSOM (Behavioral modification and lorcaserin second study for obesity management) studies found that lorcaserin did not increase the incidence of FDA-defined cardiac valvulopathy.28,29
Formulations/adverse effects. Lorcaserin is available in 2 formulations: 10-mg tablets, which are taken twice daily, or 20-mg XR tablets, which are taken once daily. Both are generally well tolerated.27,45 The most common adverse event reported in phase III trials was headache.28,30,43 Discontinue lorcaserin if the patient does not lose 5% of his initial weight after 12 weeks, as weight loss at this stage is a good predictor of longer-term success.46
Some patients don’t respond. Interestingly, a subset of patients do not respond to lorcaserin. The most likely explanation for different responses to the medication is that there are many causes of obesity, only some of which respond to 5-HT2C agonism. Currently, we do not perform pharmacogenomic testing before prescribing lorcaserin, but perhaps an inexpensive test to identify responders will be available in the future.
CASE 3 Kathryn M, a 38-year-old woman with obesity (BMI 42 kg/m2), obstructive sleep apnea, gastroesophageal reflux disease, and depression, is eager to get better control over her weight. Her medications include lansoprazole 30 mg/d and a multivitamin. She reports constantly thinking about food and not being able to control her impulses to buy large quantities of unhealthy snacks. She is so preoccupied by thoughts of food that she has difficulty concentrating at work.
Ms. M smokes a quarter of a pack of cigarettes daily, but she is ready to quit. She views bariatric surgery as a “last resort” and has no anxiety, pain, or history of seizures. Which medication is appropriate for this patient?
Discussion
This patient with class III obesity (BMI ≥40 kg/m2) is eligible for bariatric surgery; however, she is not interested in pursuing it at this time. It is important to discuss all of her options before deciding on a treatment plan. For patients like Ms. M, who would benefit from more than modest weight loss, consider a multidisciplinary approach including lifestyle modifications, pharmacotherapy, devices (eg, an intragastric balloon), and/or surgery. You would need to make clear to Ms. M that she may still be eligible for insurance coverage for surgery if she changes her mind after pursuing other treatments as long as her BMI remains ≥35 kg/m2 with obesity-related comorbidities.
Naltrexone SR/bupropion SR is a good choice for Ms. M because she describes debilitating cravings and addictive behavior surrounding food. Patients taking naltrexone SR/bupropion SR in the Contrave Obesity Research (COR)-I and COR-II phase III trials experienced a reduced frequency of food cravings, reduced difficulty in resisting food cravings, and an increased ability to control eating compared with those assigned to placebo.32,33
Added benefits. Bupropion could also help Ms. M quit smoking and improve her mood, as it is FDA-approved for smoking cessation and depression. She denies anxiety and seizures, so bupropion is not contraindicated. Even if a patient denies a history of seizure, ask about any conditions that predispose to seizures, such as anorexia nervosa or bulimia or the abrupt discontinuation of alcohol, benzodiazepines, barbiturates, or antiepileptic drugs.
Opioid use. Although the patient denies pain, ask about potential opioid use, as naltrexone is an opioid receptor antagonist. Patients should be informed that opioids may be ineffective if they are required unexpectedly (eg, for trauma) and that naltrexone SR/bupropion SR should be withheld for any planned surgical procedure potentially requiring opioid use.
Other options. While naltrexone SR/bupropion SR is the most appropriate choice for this patient because it addresses Ms. M’s problematic eating behaviors while potentially improving mood and assisting with smoking cessation, phentermine/topiramate ER, lorcaserin, and liraglutide 3 mg could also be used and should certainly be tried if naltrexone SR/bupropion SR does not produce the desired weight loss.
Adverse effects. Titrate naltrexone SR/bupropion SR slowly to the treatment dose to minimize risks and adverse events.31 The most common adverse effects reported in phase III trials were nausea, constipation, and headache.34,35,45,46 Discontinue naltrexone SR/bupropion SR if the patient does not achieve 5% weight loss at 16 weeks (after 12 weeks at the maintenance dose).31
CASE 4 William P, a 65-year-old man with obesity (BMI 39 kg/m2) who underwent Roux-en-Y gastric bypass surgery and who has type 2 diabetes, congestive heart failure, coronary artery disease, hypertension, and hyperlipidemia, remains concerned about his weight. He lost 100 lbs following surgery and maintained his weight for 3 years, but then regained 30 lbs. He comes in for an office visit because he’s concerned about his increasing blood sugar and wants to prevent further weight gain. His medications include metformin 1000 mg bid, lisinopril 5 mg/d, carvedilol 12.5 mg bid, simvastatin 20 mg/d, and aspirin 81 mg/d. Laboratory test results are normal except for a hemoglobin A1c of 8%. He denies pancreatitis and a personal or family history of thyroid cancer.
Which medication is an appropriate next step for Mr. P?
Discussion
Pharmacotherapy is a great option for this patient, who is regaining weight following bariatric surgery. Phentermine/topiramate ER is the only medication that would be contraindicated because of his heart disease. Lorcaserin and naltrexone SR/bupropion SR could be considered, but liraglutide 3 mg is the most appropriate option, given his need for further glucose control.
Furthermore, the recent LEADER (Liraglutide effect and action in diabetes: evaluation of CV outcome results) trial reported a significant mortality benefit with liraglutide 1.8 mg/d among patients with type 2 diabetes and high CV risk.47 The study found that liraglutide was superior to placebo in reducing CV events.
Contraindications. Ask patients about a history of pancreatitis before starting liraglutide 3 mg given the possible increased risk. In addition, liraglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with multiple endocrine neoplasia syndrome type 2. Thyroid C-cell tumors have been found in rodents given supratherapeutic doses of liraglutide;48 however, there is no evidence of liraglutide causing C-cell tumors in humans.
For patients taking a medication that can cause hypoglycemia, such as insulin or a sulfonylurea, monitor blood sugar and consider reducing the dose of that medication when starting liraglutide.
Administration and titration. Liraglutide is injected subcutaneously once daily. The dose is titrated up weekly to reduce gastrointestinal symptoms.36 The most common adverse effects reported in phase III trials were nausea, diarrhea, and constipation.37-39 Discontinue liraglutide 3 mg if the patient does not lose at least 4% of baseline body weight after 16 weeks.49
CORRESPONDENCE
Katherine H. Saunders, MD, DABOM, Comprehensive Weight Control Center, Division of Endocrinology, Diabetes and Metabolism, Weill Cornell Medicine, 1165 York Avenue, New York, NY 10065; kph2001@med.cornell.edu.
1. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481-1486.
2. Magkos F, Fraterrigo G, Yoshino J. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016;23:591-601.
3. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985-3023.
4. Sumithran P, Predergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597-1604.
5. Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes (Lond). 2015;39:1188-1196.
6. Fothergill E, Guo J, Howard L, et al. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity (Silver Spring). 2016;24:1612-1619.
7. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100:342-362.
8. Saunders KH, Shukla AP, Igel LI, et al. Pharmacotherapy for obesity. Endocrinol Metab Clin North Am. 2016;45:521-538.
9. Saunders KH, Kumar RB, Igel LI, et al. Pharmacologic approaches to weight management: recent gains and shortfalls in combating obesity. Curr Atheroscler Rep. 2016;18:36.
10. US Food and Drug Administration. Drug approval package. Qsymia. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/022580Orig1s000_qsymia_toc.cfm. Accessed August 28, 2017.
11. Arena Pharmaceuticals. Arena Pharmaceuticals and Eisai announce FDA approval of BELVIQ® (lorcaserin HCl) for chronic weight management in adults who are overweight with a comorbidity or obese. Available at: http://invest.arenapharm.com/releasedetail.cfm?ReleaseID=687182. Accessed August 28, 2017.
12. Drugs.com. Contrave approval history. Available at: https://www.drugs.com/history/contrave.html. Accessed August 28, 2017.
13. US Food and Drug Administration. Drugs@FDA: FDA approved drug products. Available at: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=206321. Accessed August 28, 2017.
14. Igel LI, Kumar RB, Saunders KH, et al. Practical use of pharmacotherapy for obesity. Gastroenterology. 2017;152:1765-1779.
15. Adipex-P package insert. Available at: http://www.iodine.com/drug/phentermine/fda-package-insert. Accessed August 28, 2017.
16. Ionamin package insert. Available at: http://druginserts.com/lib/rx/meds/ionamin/. Accessed August 28, 2017.
17. Lomaira package insert. Available at: https://www.lomaira.com/Prescribing_Information.pdf. Accessed August 28, 2017.
18. Suprenza package insert. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/202088s001lbl.pdf. Accessed August 28, 2017.
19. Aronne LJ, Wadden TA, Peterson C, et al. Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity (Silver Spring). 2013;21:2163-2171.
20. Alli package labeling. Available at: http://druginserts.com/lib/otc/meds/alli-1/. Accessed August 28, 2017.
21. Xenical package insert. Available at: https://www.gene.com/download/pdf/xenical_prescribing.pdf. Accessed August 28, 2017.
22. Torgerson JS, Hauptman J, Boldrin MN, et al. XENical in the prevention of Diabetes in Obese Subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155-161.
23. Qsymia package insert. Available at: https://www.qsymia.com/pdf/prescribing-information.pdf. Accessed August 28, 2017.
24. Allison DB, Gadde KM, Garvey WT, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity (Silver Spring). 2012;20:330-342.
25. Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomized, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341-1352.
26. Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95:297-308.
27. Belviq package insert. Available at: https://www.belviq.com/-/media/Files/BelviqConsolidation/PDF/Belviq_Prescribing_information-pdf.PDF?la=en. Accessed August 28, 2017.
28. Smith SR, Weissman NJ, Anderson CM, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010;363:245-256.
29. Fidler MC, Sanchez M, Raether B, et al. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. J Clin Endocrinol Metab. 2011;96:3067-3077.
30. O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. Obesity (Silver Spring). 2012;20:1426-1436.
31. Contrave package insert. Available at: https://contrave.com/wp-content/uploads/2017/05/Contrave_PI.pdf. Accessed August 28, 2017.
32. Greenway FL, Fujioka K, Plodkowski RA, et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2010;376:595-605.
33. Apovian CM, Aronne L, Rubino D, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring). 2013;21:935-943.
34. Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity (Silver Spring). 2011;19:110-120.
35. Hollander P, Gupta AK, Plodkowski R, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36:4022-4029.
36. Saxenda package insert. Available at: http://www.novo-pi.com/saxenda.pdf. Accessed August 28, 2017.
37. Pi-Sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373:11-22.
38. Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE Diabetes randomized clinical trial. JAMA. 2015;314:687-699.
39. Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet induced weight loss: the SCALE Maintenance randomized study. Int J Obes (Lond). 2013;37:1443-1451.
40. Saunders KH, Igel LI, Aronne LJ. An update on naltrexone/bupropion extended-release in the treatment of obesity. Expert Opin Pharmacother. 2016. [Epub ahead of print]
41. Thomas CE, Mauer EA, Shukla AP, et al. Low adoption of weight loss medications: a comparison of prescribing patterns of antiobesity pharmacotherapies and SGLT2s. Obesity (Silver Spring). 2016;24:1955-1961.
42. Qsymia Risk Evaluation and Mitigation Strategy (REMS). VIVUS, Inc. Available at: http://www.qsymiarems.com. Accessed January 16, 2017.
43. Zinman B, Wanner C, Lachin JM, et al. Empaglifozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117-2128.
44. US Food and Drug Administration. FDA announces withdrawal fenfluramine and dexfenfluramine (Fen-Phen). Available at: https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm179871.htm. Accessed August 28, 2017.
45. Belviq XR package insert. Available at: https://www.belviq.com/-/media/Files/BelviqConsolidation/PDF/belviqxr_prescribing_information-pdf.PDF?la=en. Accessed January 16, 2017.
46. Smith SR, O’Neil PM, Astrup A. Early weight loss while on lorcaserin, diet and exercise as a predictor of week 52 weight-loss outcomes. Obesity (Silver Spring). 2014;22:2137-2146.
47. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311-322.
48. Madsen LW, Knauf JA, Gotfredsen C, et al. GLP-1 receptor agonists and the thyroid: C-cell effects in mice are mediated via the GLP-1 receptor and not associated with RET activation. Endocrinology. 2012;153:1538-1547.
49. Fujioka K, O’Neil PM, Davies M, et al. Early weight loss with liraglutide 3.0 mg predicts 1-year weight loss and is associated with improvements in clinical markers. Obesity (Silver Spring). 2016;24:2278-2288.
1. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481-1486.
2. Magkos F, Fraterrigo G, Yoshino J. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016;23:591-601.
3. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985-3023.
4. Sumithran P, Predergast LA, Delbridge E, et al. Long-term persistence of hormonal adaptations to weight loss. N Engl J Med. 2011;365:1597-1604.
5. Greenway FL. Physiological adaptations to weight loss and factors favouring weight regain. Int J Obes (Lond). 2015;39:1188-1196.
6. Fothergill E, Guo J, Howard L, et al. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity (Silver Spring). 2016;24:1612-1619.
7. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100:342-362.
8. Saunders KH, Shukla AP, Igel LI, et al. Pharmacotherapy for obesity. Endocrinol Metab Clin North Am. 2016;45:521-538.
9. Saunders KH, Kumar RB, Igel LI, et al. Pharmacologic approaches to weight management: recent gains and shortfalls in combating obesity. Curr Atheroscler Rep. 2016;18:36.
10. US Food and Drug Administration. Drug approval package. Qsymia. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/022580Orig1s000_qsymia_toc.cfm. Accessed August 28, 2017.
11. Arena Pharmaceuticals. Arena Pharmaceuticals and Eisai announce FDA approval of BELVIQ® (lorcaserin HCl) for chronic weight management in adults who are overweight with a comorbidity or obese. Available at: http://invest.arenapharm.com/releasedetail.cfm?ReleaseID=687182. Accessed August 28, 2017.
12. Drugs.com. Contrave approval history. Available at: https://www.drugs.com/history/contrave.html. Accessed August 28, 2017.
13. US Food and Drug Administration. Drugs@FDA: FDA approved drug products. Available at: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=206321. Accessed August 28, 2017.
14. Igel LI, Kumar RB, Saunders KH, et al. Practical use of pharmacotherapy for obesity. Gastroenterology. 2017;152:1765-1779.
15. Adipex-P package insert. Available at: http://www.iodine.com/drug/phentermine/fda-package-insert. Accessed August 28, 2017.
16. Ionamin package insert. Available at: http://druginserts.com/lib/rx/meds/ionamin/. Accessed August 28, 2017.
17. Lomaira package insert. Available at: https://www.lomaira.com/Prescribing_Information.pdf. Accessed August 28, 2017.
18. Suprenza package insert. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/202088s001lbl.pdf. Accessed August 28, 2017.
19. Aronne LJ, Wadden TA, Peterson C, et al. Evaluation of phentermine and topiramate versus phentermine/topiramate extended-release in obese adults. Obesity (Silver Spring). 2013;21:2163-2171.
20. Alli package labeling. Available at: http://druginserts.com/lib/otc/meds/alli-1/. Accessed August 28, 2017.
21. Xenical package insert. Available at: https://www.gene.com/download/pdf/xenical_prescribing.pdf. Accessed August 28, 2017.
22. Torgerson JS, Hauptman J, Boldrin MN, et al. XENical in the prevention of Diabetes in Obese Subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155-161.
23. Qsymia package insert. Available at: https://www.qsymia.com/pdf/prescribing-information.pdf. Accessed August 28, 2017.
24. Allison DB, Gadde KM, Garvey WT, et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled trial (EQUIP). Obesity (Silver Spring). 2012;20:330-342.
25. Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomized, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341-1352.
26. Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95:297-308.
27. Belviq package insert. Available at: https://www.belviq.com/-/media/Files/BelviqConsolidation/PDF/Belviq_Prescribing_information-pdf.PDF?la=en. Accessed August 28, 2017.
28. Smith SR, Weissman NJ, Anderson CM, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N Engl J Med. 2010;363:245-256.
29. Fidler MC, Sanchez M, Raether B, et al. A one-year randomized trial of lorcaserin for weight loss in obese and overweight adults: the BLOSSOM trial. J Clin Endocrinol Metab. 2011;96:3067-3077.
30. O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. Obesity (Silver Spring). 2012;20:1426-1436.
31. Contrave package insert. Available at: https://contrave.com/wp-content/uploads/2017/05/Contrave_PI.pdf. Accessed August 28, 2017.
32. Greenway FL, Fujioka K, Plodkowski RA, et al. Effect of naltrexone plus bupropion on weight loss in overweight and obese adults (COR-I): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2010;376:595-605.
33. Apovian CM, Aronne L, Rubino D, et al. A randomized, phase 3 trial of naltrexone SR/bupropion SR on weight and obesity-related risk factors (COR-II). Obesity (Silver Spring). 2013;21:935-943.
34. Wadden TA, Foreyt JP, Foster GD, et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the COR-BMOD trial. Obesity (Silver Spring). 2011;19:110-120.
35. Hollander P, Gupta AK, Plodkowski R, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36:4022-4029.
36. Saxenda package insert. Available at: http://www.novo-pi.com/saxenda.pdf. Accessed August 28, 2017.
37. Pi-Sunyer X, Astrup A, Fujioka K, et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med. 2015;373:11-22.
38. Davies MJ, Bergenstal R, Bode B, et al. Efficacy of liraglutide for weight loss among patients with type 2 diabetes: the SCALE Diabetes randomized clinical trial. JAMA. 2015;314:687-699.
39. Wadden TA, Hollander P, Klein S, et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet induced weight loss: the SCALE Maintenance randomized study. Int J Obes (Lond). 2013;37:1443-1451.
40. Saunders KH, Igel LI, Aronne LJ. An update on naltrexone/bupropion extended-release in the treatment of obesity. Expert Opin Pharmacother. 2016. [Epub ahead of print]
41. Thomas CE, Mauer EA, Shukla AP, et al. Low adoption of weight loss medications: a comparison of prescribing patterns of antiobesity pharmacotherapies and SGLT2s. Obesity (Silver Spring). 2016;24:1955-1961.
42. Qsymia Risk Evaluation and Mitigation Strategy (REMS). VIVUS, Inc. Available at: http://www.qsymiarems.com. Accessed January 16, 2017.
43. Zinman B, Wanner C, Lachin JM, et al. Empaglifozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117-2128.
44. US Food and Drug Administration. FDA announces withdrawal fenfluramine and dexfenfluramine (Fen-Phen). Available at: https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm179871.htm. Accessed August 28, 2017.
45. Belviq XR package insert. Available at: https://www.belviq.com/-/media/Files/BelviqConsolidation/PDF/belviqxr_prescribing_information-pdf.PDF?la=en. Accessed January 16, 2017.
46. Smith SR, O’Neil PM, Astrup A. Early weight loss while on lorcaserin, diet and exercise as a predictor of week 52 weight-loss outcomes. Obesity (Silver Spring). 2014;22:2137-2146.
47. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311-322.
48. Madsen LW, Knauf JA, Gotfredsen C, et al. GLP-1 receptor agonists and the thyroid: C-cell effects in mice are mediated via the GLP-1 receptor and not associated with RET activation. Endocrinology. 2012;153:1538-1547.
49. Fujioka K, O’Neil PM, Davies M, et al. Early weight loss with liraglutide 3.0 mg predicts 1-year weight loss and is associated with improvements in clinical markers. Obesity (Silver Spring). 2016;24:2278-2288.
From The Journal of Family Practice | 2017;66(10):608-616.
PRACTICE RECOMMENDATIONS
For patients with a body mass index (BMI) ≥30 kg/m2 or BMI ≥27 kg/m2 with weight-related comorbidities:
› Consider antiobesity pharmacotherapy when diet, exercise, and behavior modification do not produce sufficient weight loss. A
› Continue an antiobesity medication if it is deemed effective and well tolerated. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
As cord blood inventory increases, use declines
Recently, the US has seen a decline in the use of cord blood in transplants, according to a study by the RAND Corporation.
The research revealed a significant increase in the national cord blood inventory but also suggested many cord blood units may go unused because they have a total nucleated cell (TNC) count of less than 1.25 billion cells per unit.
RAND researchers conducted this study by examining past research about cord blood banks, analyzing data on public cord blood bank collection and use, and interviewing stakeholders such as blood bank leaders and transplant center physicians.
The data showed the number of hematopoietic stem cell transplants (HSCTs) performed in the US has increased in recent years.
However, the percentage of HSCTs in which cord blood is used has declined, from about 12% (n=822) of all HSCTs in 2010 to about 8% (n=718) of all HSCTs in 2015.
At the same time, public cord blood banks in the US have greatly increased their inventory. This is, at least in part, because the federal government began offering subsidies to public contractor banks with the goal of helping them obtain 150,000 new units of high-quality cord blood.
The numeric goal has been met, as the inventory currently exceeds 200,000 units. However, many of the units cannot be considered high-quality because they have a TNC count of less than 1.25 billion cells.
The researchers noted that the government subsidies are not structured to discourage the processing and banking of cord blood units with lower TNC counts.
In fact, the team found that about half of the national inventory is made up of cord blood units with TNC counts of less than 1.25 billion cells. They said the probability that such a unit will be used in a given year is about 0.1%, and there’s an 11% chance it will ever be used.
On the other hand, there is a 1% to 3% chance a cord blood unit with a TNC count of more than 1.5 billion will be used in a given year, and there’s a 61% chance it will ever be used.
Therefore, the researchers recommend the federal government find ways to encourage public cord blood banks to collect samples with higher TNC counts, as they will help expand the utility of the national inventory.
Support for this research was provided by the US Department of Health and Human Services, Office of the Assistant Secretary of Health. ![]()
Recently, the US has seen a decline in the use of cord blood in transplants, according to a study by the RAND Corporation.
The research revealed a significant increase in the national cord blood inventory but also suggested many cord blood units may go unused because they have a total nucleated cell (TNC) count of less than 1.25 billion cells per unit.
RAND researchers conducted this study by examining past research about cord blood banks, analyzing data on public cord blood bank collection and use, and interviewing stakeholders such as blood bank leaders and transplant center physicians.
The data showed the number of hematopoietic stem cell transplants (HSCTs) performed in the US has increased in recent years.
However, the percentage of HSCTs in which cord blood is used has declined, from about 12% (n=822) of all HSCTs in 2010 to about 8% (n=718) of all HSCTs in 2015.
At the same time, public cord blood banks in the US have greatly increased their inventory. This is, at least in part, because the federal government began offering subsidies to public contractor banks with the goal of helping them obtain 150,000 new units of high-quality cord blood.
The numeric goal has been met, as the inventory currently exceeds 200,000 units. However, many of the units cannot be considered high-quality because they have a TNC count of less than 1.25 billion cells.
The researchers noted that the government subsidies are not structured to discourage the processing and banking of cord blood units with lower TNC counts.
In fact, the team found that about half of the national inventory is made up of cord blood units with TNC counts of less than 1.25 billion cells. They said the probability that such a unit will be used in a given year is about 0.1%, and there’s an 11% chance it will ever be used.
On the other hand, there is a 1% to 3% chance a cord blood unit with a TNC count of more than 1.5 billion will be used in a given year, and there’s a 61% chance it will ever be used.
Therefore, the researchers recommend the federal government find ways to encourage public cord blood banks to collect samples with higher TNC counts, as they will help expand the utility of the national inventory.
Support for this research was provided by the US Department of Health and Human Services, Office of the Assistant Secretary of Health. ![]()
Recently, the US has seen a decline in the use of cord blood in transplants, according to a study by the RAND Corporation.
The research revealed a significant increase in the national cord blood inventory but also suggested many cord blood units may go unused because they have a total nucleated cell (TNC) count of less than 1.25 billion cells per unit.
RAND researchers conducted this study by examining past research about cord blood banks, analyzing data on public cord blood bank collection and use, and interviewing stakeholders such as blood bank leaders and transplant center physicians.
The data showed the number of hematopoietic stem cell transplants (HSCTs) performed in the US has increased in recent years.
However, the percentage of HSCTs in which cord blood is used has declined, from about 12% (n=822) of all HSCTs in 2010 to about 8% (n=718) of all HSCTs in 2015.
At the same time, public cord blood banks in the US have greatly increased their inventory. This is, at least in part, because the federal government began offering subsidies to public contractor banks with the goal of helping them obtain 150,000 new units of high-quality cord blood.
The numeric goal has been met, as the inventory currently exceeds 200,000 units. However, many of the units cannot be considered high-quality because they have a TNC count of less than 1.25 billion cells.
The researchers noted that the government subsidies are not structured to discourage the processing and banking of cord blood units with lower TNC counts.
In fact, the team found that about half of the national inventory is made up of cord blood units with TNC counts of less than 1.25 billion cells. They said the probability that such a unit will be used in a given year is about 0.1%, and there’s an 11% chance it will ever be used.
On the other hand, there is a 1% to 3% chance a cord blood unit with a TNC count of more than 1.5 billion will be used in a given year, and there’s a 61% chance it will ever be used.
Therefore, the researchers recommend the federal government find ways to encourage public cord blood banks to collect samples with higher TNC counts, as they will help expand the utility of the national inventory.
Support for this research was provided by the US Department of Health and Human Services, Office of the Assistant Secretary of Health. ![]()
Confusion recurs 2 weeks after fall
A 77-year-old woman presented to the emergency department complaining of a headache following a syncopal episode (while standing) earlier that day. She said that she’d lost consciousness for several minutes, and then experienced several minutes of mild confusion that resolved spontaneously.
On physical exam, she was oriented to person and place, but not time. She had a contusion in her left occipitoparietal region without extensive bruising or deformity. The patient had normal cardiopulmonary, abdominal, and neurologic exams. Her past medical history included hypertension and normal pressure hydrocephalus, and her vital signs were within normal limits. She was taking aspirin once daily.The patient’s initial head and neck computerized tomography (CT) scans were normal (FIGURE 1), but she was hospitalized because of her confusion. During her hospitalization, the patient had mild episodic headaches that resolved with acetaminophen. The next day, her confusion resolved, and repeat CT scans were unchanged. She was discharged within 24 hours.
Two weeks later, the patient returned to the hospital after her daughter found her on the toilet, unable to stand up from the sitting position. She was confused and experienced a worsening of headache during transport to the hospital. No recurrent falls or additional episodes of trauma were reported. A CT scan was performed.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Delayed acute subdural hematoma
The CT scan (FIGURE 2) revealed an acute on chronic large left frontotemporoparietal and a right frontoparietal subdural hematoma (SDH) with resultant left to right subfalcine herniation. The patient was given a diagnosis of a delayed acute subdural hematoma (DASH)—an acute subdural hematoma that is not apparent on an initial CT scan, but is detected on follow-up CT imaging days or weeks after the injury.1 The incidence of DASH is approximately 0.5% among acute SDH patients who require operative treatment.1
Because DASH is rare, there is a lot of uncertainty surrounding its presentation, pathophysiology, and outcomes. In the few cases that have been described, patients have varied from those who were healthy, and had no coagulation abnormalities, to those who were elderly and taking anticoagulants.2,3 In addition, the period between the head injury and the development of SDH is variable.3
While not much is known about DASH, the mechanism of acute SDH has been widely studied and researched. Acute SDH, which typically follows a head trauma, results from the tearing of bridging veins that lack supporting structures and are most vulnerable to injury when crossing the subdural space.4 The potential pathophysiology for DASH is not completely understood, but is likely to involve subtle damage to the bridging veins of the brain that continue to leak over a matter of hours and days.1,5
Two risk factors to consider. Increasing age and use of oral anticoagulants can increase the risk of developing an intracranial lesion after head injury.3 Due to the infrequency of DASH, the same risk factors for SDH should be considered for DASH. These factors make it increasingly important to establish guidelines on how to approach mild traumatic brain injury (TBI) in both DASH and SDH, especially for those who are elderly or have been on anticoagulation therapy.
Differential Dx
The differential diagnosis for our patient’s decline and altered mentation weeks after the initial event included worsening normal pressure hydrocephalus, cerebrovascular accident, and seizure.
Normal pressure hydrocephalus typically has a more chronic onset than DASH. It manifests with the classic triad of dementia, incontinence, and magnetic or festinating gait (“wild, wet, and wobbly”).
Cerebrovascular accidents are most often associated with focal neurologic deficits, which can be ischemic or hemorrhagic. If hemorrhagic, the hemorrhage is typically parenchymal and not subdural.
Seizure, especially partial complex seizure, can arise after trauma and may not involve obvious motor movements. Symptoms generally abate over a few minutes to hours with treatment. Electroencephalogram and CT scan can differentiate seizure from a subdural hematoma.
Keep DASH on your radar screen
The American College of Emergency Physicians states that a non-contrast head CT scan is indicated in head trauma patients with loss of consciousness if one or more of the following is present: age >60 years, vomiting, headache, drug or alcohol intoxication, short-term memory deficits, posttraumatic seizure, Glasgow Coma Scale score of <15, focal neurologic deficits, and coagulopathy.6
Some have suggested that the initial head CT scan be delayed by up to 8 hours to prevent missing a slowly developing intracranial hemorrhage. Others suggest that the CT scan be repeated at 24 hours. Still others have suggested that patients with even mild TBI be admitted for a period of observation if any risk factors, such as age or history of anticoagulation therapy, are noted.
Because there is no evidence to support delaying the initial head CT scan, physicians should be thorough in their evaluation of head trauma patients with loss of consciousness and consider a repeat CT scan of the head if worsening of any symptoms occurs. Physicians should also consider a repeat CT scan of the head for patients at high risk, including the elderly and those who have taken anticoagulants.
In addition, patients with traumatic head injuries must be properly counseled to return if they experience repeated vomiting, worsening headache, memory loss, confusion, focal neurologic deficit, abnormal behavior, increased sleepiness, or seizures.6 An extra precaution for high-risk patients includes suggesting adequate follow-up with a primary care physician to help monitor recovery and prevent any occurrences of DASH from going unnoticed.
Our patient underwent a mini-craniotomy. Postoperatively, she was discharged to a skilled nursing facility and ultimately made a complete recovery.
CORRESPONDENCE
Andrew Muck, MD, Department of Emergency Medicine, University of Texas Health San Antonio, 7703 Floyd Curl Drive, MSC 7736, San Antonio, TX 78229; muck@uthscsa.edu.
1. Cohen T, Gudeman S. In: Narayan RK, ed. Delayed Traumatic Intracranial Hematoma. Neurotrauma. New York, NY: McGraw-Hill;1995:689-701.
2. Matsuda W, Sugimoto K, Sato N, et al. Delayed onset of posttraumatic acute subdural hematoma after mild head injury with normal computed tomography: a case report and brief review. J Trauma. 2008;65:461-463.
3. Itshayek E, Rosenthal G, Fraifeld S, et al. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58:E851-E856.
4. Culotta VP, Sermentilli ME, Gerold K, et al. Clinicopathological heterogeneity in the classification of mild head injury. Neurosurgery. 1996;38:245-250.
5. Shabani S, Nguyen HS, Doan N, et al. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016;96:66-71.
6. Jagoda AS, Bazarian JJ, Bruns Jr JJ, et al. Clinical Policy: Neuroimaging and Decisionmaking in Adult Mild Traumatic Brain Injury in the Acute Setting. Ann Emerg Med. 2008;52:714-748.
A 77-year-old woman presented to the emergency department complaining of a headache following a syncopal episode (while standing) earlier that day. She said that she’d lost consciousness for several minutes, and then experienced several minutes of mild confusion that resolved spontaneously.
On physical exam, she was oriented to person and place, but not time. She had a contusion in her left occipitoparietal region without extensive bruising or deformity. The patient had normal cardiopulmonary, abdominal, and neurologic exams. Her past medical history included hypertension and normal pressure hydrocephalus, and her vital signs were within normal limits. She was taking aspirin once daily.The patient’s initial head and neck computerized tomography (CT) scans were normal (FIGURE 1), but she was hospitalized because of her confusion. During her hospitalization, the patient had mild episodic headaches that resolved with acetaminophen. The next day, her confusion resolved, and repeat CT scans were unchanged. She was discharged within 24 hours.
Two weeks later, the patient returned to the hospital after her daughter found her on the toilet, unable to stand up from the sitting position. She was confused and experienced a worsening of headache during transport to the hospital. No recurrent falls or additional episodes of trauma were reported. A CT scan was performed.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Delayed acute subdural hematoma
The CT scan (FIGURE 2) revealed an acute on chronic large left frontotemporoparietal and a right frontoparietal subdural hematoma (SDH) with resultant left to right subfalcine herniation. The patient was given a diagnosis of a delayed acute subdural hematoma (DASH)—an acute subdural hematoma that is not apparent on an initial CT scan, but is detected on follow-up CT imaging days or weeks after the injury.1 The incidence of DASH is approximately 0.5% among acute SDH patients who require operative treatment.1
Because DASH is rare, there is a lot of uncertainty surrounding its presentation, pathophysiology, and outcomes. In the few cases that have been described, patients have varied from those who were healthy, and had no coagulation abnormalities, to those who were elderly and taking anticoagulants.2,3 In addition, the period between the head injury and the development of SDH is variable.3
While not much is known about DASH, the mechanism of acute SDH has been widely studied and researched. Acute SDH, which typically follows a head trauma, results from the tearing of bridging veins that lack supporting structures and are most vulnerable to injury when crossing the subdural space.4 The potential pathophysiology for DASH is not completely understood, but is likely to involve subtle damage to the bridging veins of the brain that continue to leak over a matter of hours and days.1,5
Two risk factors to consider. Increasing age and use of oral anticoagulants can increase the risk of developing an intracranial lesion after head injury.3 Due to the infrequency of DASH, the same risk factors for SDH should be considered for DASH. These factors make it increasingly important to establish guidelines on how to approach mild traumatic brain injury (TBI) in both DASH and SDH, especially for those who are elderly or have been on anticoagulation therapy.
Differential Dx
The differential diagnosis for our patient’s decline and altered mentation weeks after the initial event included worsening normal pressure hydrocephalus, cerebrovascular accident, and seizure.
Normal pressure hydrocephalus typically has a more chronic onset than DASH. It manifests with the classic triad of dementia, incontinence, and magnetic or festinating gait (“wild, wet, and wobbly”).
Cerebrovascular accidents are most often associated with focal neurologic deficits, which can be ischemic or hemorrhagic. If hemorrhagic, the hemorrhage is typically parenchymal and not subdural.
Seizure, especially partial complex seizure, can arise after trauma and may not involve obvious motor movements. Symptoms generally abate over a few minutes to hours with treatment. Electroencephalogram and CT scan can differentiate seizure from a subdural hematoma.
Keep DASH on your radar screen
The American College of Emergency Physicians states that a non-contrast head CT scan is indicated in head trauma patients with loss of consciousness if one or more of the following is present: age >60 years, vomiting, headache, drug or alcohol intoxication, short-term memory deficits, posttraumatic seizure, Glasgow Coma Scale score of <15, focal neurologic deficits, and coagulopathy.6
Some have suggested that the initial head CT scan be delayed by up to 8 hours to prevent missing a slowly developing intracranial hemorrhage. Others suggest that the CT scan be repeated at 24 hours. Still others have suggested that patients with even mild TBI be admitted for a period of observation if any risk factors, such as age or history of anticoagulation therapy, are noted.
Because there is no evidence to support delaying the initial head CT scan, physicians should be thorough in their evaluation of head trauma patients with loss of consciousness and consider a repeat CT scan of the head if worsening of any symptoms occurs. Physicians should also consider a repeat CT scan of the head for patients at high risk, including the elderly and those who have taken anticoagulants.
In addition, patients with traumatic head injuries must be properly counseled to return if they experience repeated vomiting, worsening headache, memory loss, confusion, focal neurologic deficit, abnormal behavior, increased sleepiness, or seizures.6 An extra precaution for high-risk patients includes suggesting adequate follow-up with a primary care physician to help monitor recovery and prevent any occurrences of DASH from going unnoticed.
Our patient underwent a mini-craniotomy. Postoperatively, she was discharged to a skilled nursing facility and ultimately made a complete recovery.
CORRESPONDENCE
Andrew Muck, MD, Department of Emergency Medicine, University of Texas Health San Antonio, 7703 Floyd Curl Drive, MSC 7736, San Antonio, TX 78229; muck@uthscsa.edu.
A 77-year-old woman presented to the emergency department complaining of a headache following a syncopal episode (while standing) earlier that day. She said that she’d lost consciousness for several minutes, and then experienced several minutes of mild confusion that resolved spontaneously.
On physical exam, she was oriented to person and place, but not time. She had a contusion in her left occipitoparietal region without extensive bruising or deformity. The patient had normal cardiopulmonary, abdominal, and neurologic exams. Her past medical history included hypertension and normal pressure hydrocephalus, and her vital signs were within normal limits. She was taking aspirin once daily.The patient’s initial head and neck computerized tomography (CT) scans were normal (FIGURE 1), but she was hospitalized because of her confusion. During her hospitalization, the patient had mild episodic headaches that resolved with acetaminophen. The next day, her confusion resolved, and repeat CT scans were unchanged. She was discharged within 24 hours.
Two weeks later, the patient returned to the hospital after her daughter found her on the toilet, unable to stand up from the sitting position. She was confused and experienced a worsening of headache during transport to the hospital. No recurrent falls or additional episodes of trauma were reported. A CT scan was performed.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Delayed acute subdural hematoma
The CT scan (FIGURE 2) revealed an acute on chronic large left frontotemporoparietal and a right frontoparietal subdural hematoma (SDH) with resultant left to right subfalcine herniation. The patient was given a diagnosis of a delayed acute subdural hematoma (DASH)—an acute subdural hematoma that is not apparent on an initial CT scan, but is detected on follow-up CT imaging days or weeks after the injury.1 The incidence of DASH is approximately 0.5% among acute SDH patients who require operative treatment.1
Because DASH is rare, there is a lot of uncertainty surrounding its presentation, pathophysiology, and outcomes. In the few cases that have been described, patients have varied from those who were healthy, and had no coagulation abnormalities, to those who were elderly and taking anticoagulants.2,3 In addition, the period between the head injury and the development of SDH is variable.3
While not much is known about DASH, the mechanism of acute SDH has been widely studied and researched. Acute SDH, which typically follows a head trauma, results from the tearing of bridging veins that lack supporting structures and are most vulnerable to injury when crossing the subdural space.4 The potential pathophysiology for DASH is not completely understood, but is likely to involve subtle damage to the bridging veins of the brain that continue to leak over a matter of hours and days.1,5
Two risk factors to consider. Increasing age and use of oral anticoagulants can increase the risk of developing an intracranial lesion after head injury.3 Due to the infrequency of DASH, the same risk factors for SDH should be considered for DASH. These factors make it increasingly important to establish guidelines on how to approach mild traumatic brain injury (TBI) in both DASH and SDH, especially for those who are elderly or have been on anticoagulation therapy.
Differential Dx
The differential diagnosis for our patient’s decline and altered mentation weeks after the initial event included worsening normal pressure hydrocephalus, cerebrovascular accident, and seizure.
Normal pressure hydrocephalus typically has a more chronic onset than DASH. It manifests with the classic triad of dementia, incontinence, and magnetic or festinating gait (“wild, wet, and wobbly”).
Cerebrovascular accidents are most often associated with focal neurologic deficits, which can be ischemic or hemorrhagic. If hemorrhagic, the hemorrhage is typically parenchymal and not subdural.
Seizure, especially partial complex seizure, can arise after trauma and may not involve obvious motor movements. Symptoms generally abate over a few minutes to hours with treatment. Electroencephalogram and CT scan can differentiate seizure from a subdural hematoma.
Keep DASH on your radar screen
The American College of Emergency Physicians states that a non-contrast head CT scan is indicated in head trauma patients with loss of consciousness if one or more of the following is present: age >60 years, vomiting, headache, drug or alcohol intoxication, short-term memory deficits, posttraumatic seizure, Glasgow Coma Scale score of <15, focal neurologic deficits, and coagulopathy.6
Some have suggested that the initial head CT scan be delayed by up to 8 hours to prevent missing a slowly developing intracranial hemorrhage. Others suggest that the CT scan be repeated at 24 hours. Still others have suggested that patients with even mild TBI be admitted for a period of observation if any risk factors, such as age or history of anticoagulation therapy, are noted.
Because there is no evidence to support delaying the initial head CT scan, physicians should be thorough in their evaluation of head trauma patients with loss of consciousness and consider a repeat CT scan of the head if worsening of any symptoms occurs. Physicians should also consider a repeat CT scan of the head for patients at high risk, including the elderly and those who have taken anticoagulants.
In addition, patients with traumatic head injuries must be properly counseled to return if they experience repeated vomiting, worsening headache, memory loss, confusion, focal neurologic deficit, abnormal behavior, increased sleepiness, or seizures.6 An extra precaution for high-risk patients includes suggesting adequate follow-up with a primary care physician to help monitor recovery and prevent any occurrences of DASH from going unnoticed.
Our patient underwent a mini-craniotomy. Postoperatively, she was discharged to a skilled nursing facility and ultimately made a complete recovery.
CORRESPONDENCE
Andrew Muck, MD, Department of Emergency Medicine, University of Texas Health San Antonio, 7703 Floyd Curl Drive, MSC 7736, San Antonio, TX 78229; muck@uthscsa.edu.
1. Cohen T, Gudeman S. In: Narayan RK, ed. Delayed Traumatic Intracranial Hematoma. Neurotrauma. New York, NY: McGraw-Hill;1995:689-701.
2. Matsuda W, Sugimoto K, Sato N, et al. Delayed onset of posttraumatic acute subdural hematoma after mild head injury with normal computed tomography: a case report and brief review. J Trauma. 2008;65:461-463.
3. Itshayek E, Rosenthal G, Fraifeld S, et al. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58:E851-E856.
4. Culotta VP, Sermentilli ME, Gerold K, et al. Clinicopathological heterogeneity in the classification of mild head injury. Neurosurgery. 1996;38:245-250.
5. Shabani S, Nguyen HS, Doan N, et al. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016;96:66-71.
6. Jagoda AS, Bazarian JJ, Bruns Jr JJ, et al. Clinical Policy: Neuroimaging and Decisionmaking in Adult Mild Traumatic Brain Injury in the Acute Setting. Ann Emerg Med. 2008;52:714-748.
1. Cohen T, Gudeman S. In: Narayan RK, ed. Delayed Traumatic Intracranial Hematoma. Neurotrauma. New York, NY: McGraw-Hill;1995:689-701.
2. Matsuda W, Sugimoto K, Sato N, et al. Delayed onset of posttraumatic acute subdural hematoma after mild head injury with normal computed tomography: a case report and brief review. J Trauma. 2008;65:461-463.
3. Itshayek E, Rosenthal G, Fraifeld S, et al. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58:E851-E856.
4. Culotta VP, Sermentilli ME, Gerold K, et al. Clinicopathological heterogeneity in the classification of mild head injury. Neurosurgery. 1996;38:245-250.
5. Shabani S, Nguyen HS, Doan N, et al. Case Report and Review of Literature of Delayed Acute Subdural Hematoma. World Neurosurg. 2016;96:66-71.
6. Jagoda AS, Bazarian JJ, Bruns Jr JJ, et al. Clinical Policy: Neuroimaging and Decisionmaking in Adult Mild Traumatic Brain Injury in the Acute Setting. Ann Emerg Med. 2008;52:714-748.
Fever, rash, and leukopenia in a 32-year-old man • Dx?
THE CASE
A 32-year-old man was admitted to our hospital with fever, chills, malaise, leukopenia, and a rash. About 3 weeks earlier, he’d had oral maxillofacial surgery and started a 10-day course of prophylactic amoxicillin/clavulanic acid. Fifteen days after the surgery, he developed a fever (temperature, 103˚ F), chills, arthralgia, myalgia, cough, diarrhea, and malaise. He was seen by his physician, who obtained a chest x-ray showing a lingular infiltrate. The physician diagnosed influenza and pneumonia in this patient, and prescribed oseltamivir, azithromycin, and an additional course of amoxicillin/clavulanic acid.
Upon admission to the hospital, laboratory tests revealed a white blood cell count (WBC) of 3.1 k/mcL (normal: 3.2-10.8 k/mcL). The patient’s physical examination was notable for lip edema, white mucous membrane plaques, submandibular and inguinal lymphadenopathy, and a morbilliform rash across his chest (FIGURE 1). Broad-spectrum antibiotics were initiated for presumed sepsis.
On hospital day (HD) 1, tests revealed a WBC count of 1.8 k/mcL, an erythrocyte sedimentation rate of 53 mm/hr (normal: 20-30 mm/hr for women, 15-20 mm/hr for men), and a C-reactive protein level of 6.7 mg/dL (normal: <0.5 mg/dL). A repeat chest x-ray and orofacial computerized tomography scan were normal.
By HD 3, all bacterial cultures were negative, but the patient was positive for human herpesvirus (HHV)-6 on viral cultures. His leukopenia persisted and he had elevated levels of alanine transaminase ranging from 40 to 73 U/L (normal: 6-43 U/L) and aspartate aminotransferase ranging from 66 to 108 U/L (normal range: 10-40 U/L), both downtrending during his hospitalization. He also had elevated levels of antinuclear antibodies (ANAs) and anti-Smith (Sm) antibody titers.
A posterior-auricular biopsy was consistent with lymphocytic perivasculitis. The rash continued to progress, involving his chest, abdomen, and face (FIGURE 2). Bacterial and viral cultures remained negative and on HD 4, broad-spectrum antibiotics were discontinued.
THE DIAGNOSIS
We diagnosed the patient with DRESS (drug reaction with eosinophilia and systemic symptoms) based on persistent fever, onset of cutaneous manifestations (facial edema and morbilliform eruption), lymphadenopathy, increased liver function tests, and recent exposure to an offending drug. The patient did not have eosinophilia; however, atypical lymphocytes were present on his peripheral smear.
DISCUSSION
DRESS is typically characterized by fever, rash, eosinophilia, atypical lymphocytes, lymphadenopathy, and organ involvement (primarily liver, but multiple organ systems can be affected).1 Patients with severe symptoms have renal involvement, anemia, respiratory and cardiac symptoms (chest pain, tachycardia, and myocarditis), and transaminase levels up to 5 times greater than normal.1-3 Anticonvulsants and antibiotics are the most common offending classes among the medications that are associated with DRESS (TABLE 1).2,4
The reported incidence of DRESS is between one in 1000 and one in 10,000 drug exposures.1 Due to the broad presentation and a lack of established diagnostic criteria associated with DRESS, this number may be even higher. DRESS has a 10% mortality rate,1 and hepatic necrosis is the most common cause of death.2
Certain people may be more prone to DRESS. People with certain gene mutations that code for drug detoxification enzymes have shown a greater incidence of DRESS.5 Viral reactivation, commonly of HHV-6, has also been shown to have an effect on the pathogenesis of DRESS. Additionally, genetic predisposition involving specific human leukocyte antigens (HLAs) makes certain people more prone to the development of DRESS (TABLE 2).2,5
Case reports have demonstrated a link between certain autoimmune syndromes and DRESS, specifically Grave’s disease and type 1 diabetes mellitus.2
A unique finding of this case was the presence of elevated ANA and anti-Sm antibody titers at initial presentation, with spontaneous negative seroconversion 2 months later. Because of these 2 findings, as well as the patient’s leukopenia and rash, he briefly met 4 of the 11 criteria set forth by the American College of Rheumatology for a diagnosis of systemic lupus erythematosus (SLE).6 It is unclear whether the transiently elevated anti-Sm antibody titers were an acute phase reactant due to DRESS, a viral illness, or an evolving autoimmune process.
The false-positive rate for anti-Sm antibodies in association with DRESS has not been previously reported.
MAKING THE DIAGNOSIS
Distinguishing DRESS from other life-threatening cutaneous drug reactions, particularly Stevens-Johnson syndrome and toxic epidermal necrolysis, can be difficult. Likewise, acute bacterial/viral infections, autoimmune syndromes, vasculitis, and hematologic diseases can mimic DRESS.7 Exposure to an offending drug 2 to 6 weeks prior to the onset of symptoms is supportive of DRESS.
This scoring system can help. The RegiSCAR (Registry of Severe Cutaneous Adverse Reaction) has developed a scoring system to aid in the accurate diagnosis of DRESS.1,8 The scoring consists of 8 categories: fever, eosinophilia, enlarged lymph nodes, atypical lymphocytes, skin involvement, organ involvement, time of resolution, and the evaluation of other potential causes.1 Each category is graded a number from -1 (not supportive of DRESS) to 2 (highly supportive of DRESS) based on the patient’s presentation. The total score grades potential cases as “no,” “possible,” “probable,” or “definite.”1,8 In one review, cases classified as “probable” or “definite” by the RegiSCAR scoring system constituted 88% of the cases reported in the literature.1
Two tests that can also aid in the diagnosis of DRESS include patch testing (exposing the skin to a diluted version of the suspected offending drug and observing for a local reaction) and lymphocyte transformation tests. The latter are a better method of diagnosing drug-induced DRESS, with a sensitivity of 60% to 70%, and a specificity of 85%.9 However, this testing is not readily available.
Once DRESS is diagnosed, the offending drug should be immediately discontinued. For mild cases, supportive treatment is recommended. For more severe cases, the use of corticosteroids tapered over several months is the treatment of choice.10 Further studies are needed to determine the optimal type of corticosteroids, as well as the dose, route, and duration of therapy. Immunotherapy, plasmapheresis, and antivirals have been used with mixed results.10,11
Our patient was started on topical and systemic oral corticosteroids. Within 24 hours, his fever resolved and his rash improved. By HD 7, his laboratory values were normal and he was discharged.
The patient was advised that in the future, he should avoid exposure to the penicillin class of medication.
THE TAKEAWAY
The presence of rash, fever, lymphadenopathy, eosinophilia, atypical lymphocytes, liver involvement, and HHV-6 reactivation in the absence of sepsis should raise suspicion for DRESS. Early diagnosis, discontinuation of the culprit drug, and timely treatment are imperative in the management of the condition. Due to a potential genetic predisposition to DRESS, clinicians should use caution when treating first-degree family members with the same class of medication that was problematic for their relative. Long-term sequelae, such as Grave’s disease and diabetes mellitus, have been reported following DRESS. Therefore, long-term monitoring with appropriate testing is recommended.
1. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124:588-597.
2. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68:693.e1-e14.
3. Bourgeois GP, Cafardi JA, Groysman V, et al. Fulminant myocarditis as a late sequelae of DRESS-2 cases. J Am Acad Dermatol. 2011;65:889-890.
4. Cho YT, Yang CW, Chu CY. Drug reaction with eosinophilia and systemic symptoms (DRESS): an interplay among drugs, viruses, and immune system. Int J Mol Sci. 2017;18:1-21.
5. Alfirevic A, Pirmohamed M. Drug-induced hypersensitivity and the HLA complex. Pharmaceuticals (Basel). 2011;4:69-90.
6. American College of Rheumatology. 1997 Update of the 1982 American College of Rheumatology Revised Criteria for Classification of Systemic Lupus Erythematosus. Available at: https://www.rheumatology.org/Portals/0/Files/1982%20SLE%20Classification_Excerpt.pdf. Accessed August 30, 2017.
7. Descamps V, Ben Saïd B, Sassolas B, et al. Management of drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010;137:703-708.
8. Peyrière H, Dereure O, Breton H, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155:422-428.
9. Pichler WJ, Tilch J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy. 2004;59:809-820.
10. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome part II: management and therapeutics. J Am Acad Dermatol. 2013;68:709.e1-e9.
11. Funck-Brentano E, Duong TA, Bouvresses S, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72:246-252.
THE CASE
A 32-year-old man was admitted to our hospital with fever, chills, malaise, leukopenia, and a rash. About 3 weeks earlier, he’d had oral maxillofacial surgery and started a 10-day course of prophylactic amoxicillin/clavulanic acid. Fifteen days after the surgery, he developed a fever (temperature, 103˚ F), chills, arthralgia, myalgia, cough, diarrhea, and malaise. He was seen by his physician, who obtained a chest x-ray showing a lingular infiltrate. The physician diagnosed influenza and pneumonia in this patient, and prescribed oseltamivir, azithromycin, and an additional course of amoxicillin/clavulanic acid.
Upon admission to the hospital, laboratory tests revealed a white blood cell count (WBC) of 3.1 k/mcL (normal: 3.2-10.8 k/mcL). The patient’s physical examination was notable for lip edema, white mucous membrane plaques, submandibular and inguinal lymphadenopathy, and a morbilliform rash across his chest (FIGURE 1). Broad-spectrum antibiotics were initiated for presumed sepsis.
On hospital day (HD) 1, tests revealed a WBC count of 1.8 k/mcL, an erythrocyte sedimentation rate of 53 mm/hr (normal: 20-30 mm/hr for women, 15-20 mm/hr for men), and a C-reactive protein level of 6.7 mg/dL (normal: <0.5 mg/dL). A repeat chest x-ray and orofacial computerized tomography scan were normal.
By HD 3, all bacterial cultures were negative, but the patient was positive for human herpesvirus (HHV)-6 on viral cultures. His leukopenia persisted and he had elevated levels of alanine transaminase ranging from 40 to 73 U/L (normal: 6-43 U/L) and aspartate aminotransferase ranging from 66 to 108 U/L (normal range: 10-40 U/L), both downtrending during his hospitalization. He also had elevated levels of antinuclear antibodies (ANAs) and anti-Smith (Sm) antibody titers.
A posterior-auricular biopsy was consistent with lymphocytic perivasculitis. The rash continued to progress, involving his chest, abdomen, and face (FIGURE 2). Bacterial and viral cultures remained negative and on HD 4, broad-spectrum antibiotics were discontinued.
THE DIAGNOSIS
We diagnosed the patient with DRESS (drug reaction with eosinophilia and systemic symptoms) based on persistent fever, onset of cutaneous manifestations (facial edema and morbilliform eruption), lymphadenopathy, increased liver function tests, and recent exposure to an offending drug. The patient did not have eosinophilia; however, atypical lymphocytes were present on his peripheral smear.
DISCUSSION
DRESS is typically characterized by fever, rash, eosinophilia, atypical lymphocytes, lymphadenopathy, and organ involvement (primarily liver, but multiple organ systems can be affected).1 Patients with severe symptoms have renal involvement, anemia, respiratory and cardiac symptoms (chest pain, tachycardia, and myocarditis), and transaminase levels up to 5 times greater than normal.1-3 Anticonvulsants and antibiotics are the most common offending classes among the medications that are associated with DRESS (TABLE 1).2,4
The reported incidence of DRESS is between one in 1000 and one in 10,000 drug exposures.1 Due to the broad presentation and a lack of established diagnostic criteria associated with DRESS, this number may be even higher. DRESS has a 10% mortality rate,1 and hepatic necrosis is the most common cause of death.2
Certain people may be more prone to DRESS. People with certain gene mutations that code for drug detoxification enzymes have shown a greater incidence of DRESS.5 Viral reactivation, commonly of HHV-6, has also been shown to have an effect on the pathogenesis of DRESS. Additionally, genetic predisposition involving specific human leukocyte antigens (HLAs) makes certain people more prone to the development of DRESS (TABLE 2).2,5
Case reports have demonstrated a link between certain autoimmune syndromes and DRESS, specifically Grave’s disease and type 1 diabetes mellitus.2
A unique finding of this case was the presence of elevated ANA and anti-Sm antibody titers at initial presentation, with spontaneous negative seroconversion 2 months later. Because of these 2 findings, as well as the patient’s leukopenia and rash, he briefly met 4 of the 11 criteria set forth by the American College of Rheumatology for a diagnosis of systemic lupus erythematosus (SLE).6 It is unclear whether the transiently elevated anti-Sm antibody titers were an acute phase reactant due to DRESS, a viral illness, or an evolving autoimmune process.
The false-positive rate for anti-Sm antibodies in association with DRESS has not been previously reported.
MAKING THE DIAGNOSIS
Distinguishing DRESS from other life-threatening cutaneous drug reactions, particularly Stevens-Johnson syndrome and toxic epidermal necrolysis, can be difficult. Likewise, acute bacterial/viral infections, autoimmune syndromes, vasculitis, and hematologic diseases can mimic DRESS.7 Exposure to an offending drug 2 to 6 weeks prior to the onset of symptoms is supportive of DRESS.
This scoring system can help. The RegiSCAR (Registry of Severe Cutaneous Adverse Reaction) has developed a scoring system to aid in the accurate diagnosis of DRESS.1,8 The scoring consists of 8 categories: fever, eosinophilia, enlarged lymph nodes, atypical lymphocytes, skin involvement, organ involvement, time of resolution, and the evaluation of other potential causes.1 Each category is graded a number from -1 (not supportive of DRESS) to 2 (highly supportive of DRESS) based on the patient’s presentation. The total score grades potential cases as “no,” “possible,” “probable,” or “definite.”1,8 In one review, cases classified as “probable” or “definite” by the RegiSCAR scoring system constituted 88% of the cases reported in the literature.1
Two tests that can also aid in the diagnosis of DRESS include patch testing (exposing the skin to a diluted version of the suspected offending drug and observing for a local reaction) and lymphocyte transformation tests. The latter are a better method of diagnosing drug-induced DRESS, with a sensitivity of 60% to 70%, and a specificity of 85%.9 However, this testing is not readily available.
Once DRESS is diagnosed, the offending drug should be immediately discontinued. For mild cases, supportive treatment is recommended. For more severe cases, the use of corticosteroids tapered over several months is the treatment of choice.10 Further studies are needed to determine the optimal type of corticosteroids, as well as the dose, route, and duration of therapy. Immunotherapy, plasmapheresis, and antivirals have been used with mixed results.10,11
Our patient was started on topical and systemic oral corticosteroids. Within 24 hours, his fever resolved and his rash improved. By HD 7, his laboratory values were normal and he was discharged.
The patient was advised that in the future, he should avoid exposure to the penicillin class of medication.
THE TAKEAWAY
The presence of rash, fever, lymphadenopathy, eosinophilia, atypical lymphocytes, liver involvement, and HHV-6 reactivation in the absence of sepsis should raise suspicion for DRESS. Early diagnosis, discontinuation of the culprit drug, and timely treatment are imperative in the management of the condition. Due to a potential genetic predisposition to DRESS, clinicians should use caution when treating first-degree family members with the same class of medication that was problematic for their relative. Long-term sequelae, such as Grave’s disease and diabetes mellitus, have been reported following DRESS. Therefore, long-term monitoring with appropriate testing is recommended.
THE CASE
A 32-year-old man was admitted to our hospital with fever, chills, malaise, leukopenia, and a rash. About 3 weeks earlier, he’d had oral maxillofacial surgery and started a 10-day course of prophylactic amoxicillin/clavulanic acid. Fifteen days after the surgery, he developed a fever (temperature, 103˚ F), chills, arthralgia, myalgia, cough, diarrhea, and malaise. He was seen by his physician, who obtained a chest x-ray showing a lingular infiltrate. The physician diagnosed influenza and pneumonia in this patient, and prescribed oseltamivir, azithromycin, and an additional course of amoxicillin/clavulanic acid.
Upon admission to the hospital, laboratory tests revealed a white blood cell count (WBC) of 3.1 k/mcL (normal: 3.2-10.8 k/mcL). The patient’s physical examination was notable for lip edema, white mucous membrane plaques, submandibular and inguinal lymphadenopathy, and a morbilliform rash across his chest (FIGURE 1). Broad-spectrum antibiotics were initiated for presumed sepsis.
On hospital day (HD) 1, tests revealed a WBC count of 1.8 k/mcL, an erythrocyte sedimentation rate of 53 mm/hr (normal: 20-30 mm/hr for women, 15-20 mm/hr for men), and a C-reactive protein level of 6.7 mg/dL (normal: <0.5 mg/dL). A repeat chest x-ray and orofacial computerized tomography scan were normal.
By HD 3, all bacterial cultures were negative, but the patient was positive for human herpesvirus (HHV)-6 on viral cultures. His leukopenia persisted and he had elevated levels of alanine transaminase ranging from 40 to 73 U/L (normal: 6-43 U/L) and aspartate aminotransferase ranging from 66 to 108 U/L (normal range: 10-40 U/L), both downtrending during his hospitalization. He also had elevated levels of antinuclear antibodies (ANAs) and anti-Smith (Sm) antibody titers.
A posterior-auricular biopsy was consistent with lymphocytic perivasculitis. The rash continued to progress, involving his chest, abdomen, and face (FIGURE 2). Bacterial and viral cultures remained negative and on HD 4, broad-spectrum antibiotics were discontinued.
THE DIAGNOSIS
We diagnosed the patient with DRESS (drug reaction with eosinophilia and systemic symptoms) based on persistent fever, onset of cutaneous manifestations (facial edema and morbilliform eruption), lymphadenopathy, increased liver function tests, and recent exposure to an offending drug. The patient did not have eosinophilia; however, atypical lymphocytes were present on his peripheral smear.
DISCUSSION
DRESS is typically characterized by fever, rash, eosinophilia, atypical lymphocytes, lymphadenopathy, and organ involvement (primarily liver, but multiple organ systems can be affected).1 Patients with severe symptoms have renal involvement, anemia, respiratory and cardiac symptoms (chest pain, tachycardia, and myocarditis), and transaminase levels up to 5 times greater than normal.1-3 Anticonvulsants and antibiotics are the most common offending classes among the medications that are associated with DRESS (TABLE 1).2,4
The reported incidence of DRESS is between one in 1000 and one in 10,000 drug exposures.1 Due to the broad presentation and a lack of established diagnostic criteria associated with DRESS, this number may be even higher. DRESS has a 10% mortality rate,1 and hepatic necrosis is the most common cause of death.2
Certain people may be more prone to DRESS. People with certain gene mutations that code for drug detoxification enzymes have shown a greater incidence of DRESS.5 Viral reactivation, commonly of HHV-6, has also been shown to have an effect on the pathogenesis of DRESS. Additionally, genetic predisposition involving specific human leukocyte antigens (HLAs) makes certain people more prone to the development of DRESS (TABLE 2).2,5
Case reports have demonstrated a link between certain autoimmune syndromes and DRESS, specifically Grave’s disease and type 1 diabetes mellitus.2
A unique finding of this case was the presence of elevated ANA and anti-Sm antibody titers at initial presentation, with spontaneous negative seroconversion 2 months later. Because of these 2 findings, as well as the patient’s leukopenia and rash, he briefly met 4 of the 11 criteria set forth by the American College of Rheumatology for a diagnosis of systemic lupus erythematosus (SLE).6 It is unclear whether the transiently elevated anti-Sm antibody titers were an acute phase reactant due to DRESS, a viral illness, or an evolving autoimmune process.
The false-positive rate for anti-Sm antibodies in association with DRESS has not been previously reported.
MAKING THE DIAGNOSIS
Distinguishing DRESS from other life-threatening cutaneous drug reactions, particularly Stevens-Johnson syndrome and toxic epidermal necrolysis, can be difficult. Likewise, acute bacterial/viral infections, autoimmune syndromes, vasculitis, and hematologic diseases can mimic DRESS.7 Exposure to an offending drug 2 to 6 weeks prior to the onset of symptoms is supportive of DRESS.
This scoring system can help. The RegiSCAR (Registry of Severe Cutaneous Adverse Reaction) has developed a scoring system to aid in the accurate diagnosis of DRESS.1,8 The scoring consists of 8 categories: fever, eosinophilia, enlarged lymph nodes, atypical lymphocytes, skin involvement, organ involvement, time of resolution, and the evaluation of other potential causes.1 Each category is graded a number from -1 (not supportive of DRESS) to 2 (highly supportive of DRESS) based on the patient’s presentation. The total score grades potential cases as “no,” “possible,” “probable,” or “definite.”1,8 In one review, cases classified as “probable” or “definite” by the RegiSCAR scoring system constituted 88% of the cases reported in the literature.1
Two tests that can also aid in the diagnosis of DRESS include patch testing (exposing the skin to a diluted version of the suspected offending drug and observing for a local reaction) and lymphocyte transformation tests. The latter are a better method of diagnosing drug-induced DRESS, with a sensitivity of 60% to 70%, and a specificity of 85%.9 However, this testing is not readily available.
Once DRESS is diagnosed, the offending drug should be immediately discontinued. For mild cases, supportive treatment is recommended. For more severe cases, the use of corticosteroids tapered over several months is the treatment of choice.10 Further studies are needed to determine the optimal type of corticosteroids, as well as the dose, route, and duration of therapy. Immunotherapy, plasmapheresis, and antivirals have been used with mixed results.10,11
Our patient was started on topical and systemic oral corticosteroids. Within 24 hours, his fever resolved and his rash improved. By HD 7, his laboratory values were normal and he was discharged.
The patient was advised that in the future, he should avoid exposure to the penicillin class of medication.
THE TAKEAWAY
The presence of rash, fever, lymphadenopathy, eosinophilia, atypical lymphocytes, liver involvement, and HHV-6 reactivation in the absence of sepsis should raise suspicion for DRESS. Early diagnosis, discontinuation of the culprit drug, and timely treatment are imperative in the management of the condition. Due to a potential genetic predisposition to DRESS, clinicians should use caution when treating first-degree family members with the same class of medication that was problematic for their relative. Long-term sequelae, such as Grave’s disease and diabetes mellitus, have been reported following DRESS. Therefore, long-term monitoring with appropriate testing is recommended.
1. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124:588-597.
2. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68:693.e1-e14.
3. Bourgeois GP, Cafardi JA, Groysman V, et al. Fulminant myocarditis as a late sequelae of DRESS-2 cases. J Am Acad Dermatol. 2011;65:889-890.
4. Cho YT, Yang CW, Chu CY. Drug reaction with eosinophilia and systemic symptoms (DRESS): an interplay among drugs, viruses, and immune system. Int J Mol Sci. 2017;18:1-21.
5. Alfirevic A, Pirmohamed M. Drug-induced hypersensitivity and the HLA complex. Pharmaceuticals (Basel). 2011;4:69-90.
6. American College of Rheumatology. 1997 Update of the 1982 American College of Rheumatology Revised Criteria for Classification of Systemic Lupus Erythematosus. Available at: https://www.rheumatology.org/Portals/0/Files/1982%20SLE%20Classification_Excerpt.pdf. Accessed August 30, 2017.
7. Descamps V, Ben Saïd B, Sassolas B, et al. Management of drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010;137:703-708.
8. Peyrière H, Dereure O, Breton H, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155:422-428.
9. Pichler WJ, Tilch J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy. 2004;59:809-820.
10. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome part II: management and therapeutics. J Am Acad Dermatol. 2013;68:709.e1-e9.
11. Funck-Brentano E, Duong TA, Bouvresses S, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72:246-252.
1. Cacoub P, Musette P, Descamps V, et al. The DRESS syndrome: a literature review. Am J Med. 2011;124:588-597.
2. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome: Part I. Clinical perspectives. J Am Acad Dermatol. 2013;68:693.e1-e14.
3. Bourgeois GP, Cafardi JA, Groysman V, et al. Fulminant myocarditis as a late sequelae of DRESS-2 cases. J Am Acad Dermatol. 2011;65:889-890.
4. Cho YT, Yang CW, Chu CY. Drug reaction with eosinophilia and systemic symptoms (DRESS): an interplay among drugs, viruses, and immune system. Int J Mol Sci. 2017;18:1-21.
5. Alfirevic A, Pirmohamed M. Drug-induced hypersensitivity and the HLA complex. Pharmaceuticals (Basel). 2011;4:69-90.
6. American College of Rheumatology. 1997 Update of the 1982 American College of Rheumatology Revised Criteria for Classification of Systemic Lupus Erythematosus. Available at: https://www.rheumatology.org/Portals/0/Files/1982%20SLE%20Classification_Excerpt.pdf. Accessed August 30, 2017.
7. Descamps V, Ben Saïd B, Sassolas B, et al. Management of drug reaction with eosinophilia and systemic symptoms (DRESS). Ann Dermatol Venereol. 2010;137:703-708.
8. Peyrière H, Dereure O, Breton H, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155:422-428.
9. Pichler WJ, Tilch J. The lymphocyte transformation test in the diagnosis of drug hypersensitivity. Allergy. 2004;59:809-820.
10. Husain Z, Reddy BY, Schwartz RA. DRESS syndrome part II: management and therapeutics. J Am Acad Dermatol. 2013;68:709.e1-e9.
11. Funck-Brentano E, Duong TA, Bouvresses S, et al. Therapeutic management of DRESS: a retrospective study of 38 cases. J Am Acad Dermatol. 2015;72:246-252.
Are oral emergency contraceptives a safe & effective form of long-term birth control?
EVIDENCE SUMMARY
A systematic review of 22 trials (13 case series, 8 prospective, nonrandomized studies, and one randomized controlled trial; 12,407 patients) conducted in Europe, Asia, and the Americas evaluated the likelihood of pregnancy with repeated use of precoital and postcoital hormonal contraception.1 Some trials used more than one dose or medication. Many had inadequate reporting of research methods. Results were reported using the Pearl Index (PI)—the number of pregnancies per 100 woman-years.
In 11 studies (2700 patients), women took 750 mcg of levonorgestrel from 24 hours before to 24 hours after intercourse for an average duration of 5 cycles or months. Coital frequency varied from 1 to 15 times per month. The PI ranged from 0 to 18.6, with a pooled PI of 5.4 (95% confidence interval [CI], 4.1-7.0). Three of the trials (915 patients), with research methods reported as good, had a pooled PI of 8.9 (95% CI, 5.1-14.4). No serious adverse effects were reported in 10 of the 11 studies, but menstrual irregularity was commonly observed. In one of the largest studies (1315 patients), only 3% of women discontinued treatment because of adverse effects.
Six other trials (5785 patients) of levonorgestrel taken at doses ranging from 150 mcg to 1 mg for a mean duration of 9.2 cycles reported PIs of 0 to 9. Breakthrough bleeding was the most common adverse event. When all 17 studies of levonorgestrel were combined, the PI was 4.9 (95% CI, 4.3-5.5). The remaining studies in the systematic review described medicines not commonly used for emergency contraception or not available in the United States.
Other reported adverse effects: Headache, nausea, abdominal pain
A prospective, open-label study enrolled 321 women 18 to 45 years of age from Asia, Europe, and South America to evaluate the safety and efficacy of levonorgestrel 1.5 mg taken before or within 24 hours of intercourse as the exclusive means of contraception.2 Women who were lactating or recently postpartum were excluded; condoms were permitted for women who had concerns about risk of sexually transmitted illness. Data analysis included estimates of perfect use (consistent and correct use of levonorgestrel only) and typical use (use of other contraceptive methods in addition to levonorgestrel).
At baseline, weight, blood pressure, and hemoglobin were documented, and follow-up visits occurred at 2.5, 4.5, and 6.5 months. Pregnancy tests, blood pressure, and adverse effects were assessed at each visit; weight and hemoglobin were evaluated at the final visit. The primary outcome measure was the PI in women younger than 35 years who used only levonorgestrel for contraception.
In women younger than 35 years (208 patients), the PI was 11 (95% CI, 5.7-13.1) with perfect use and 10.3 (95% CI, 5.4-19.9) with typical use. In all ages 18 to 45 years, the PI was 7.1 (95% CI, 3.8-13.1) for typical use and 7.5 (95% CI, 4-13.9) for perfect use. Most women took 4 to 6 doses per month.
The most commonly reported adverse effects were headache (29%), nausea or abdominal pain (16%), influenza (11%), and acne or candidiasis (8%). Bleeding patterns varied with a tendency toward longer bleeding initially and lighter menstrual periods and less anemia in some patients at the end of the study.
RECOMMENDATIONS
The Office of Population Research at Princeton University suggests that moderate repeat use of emergency contraceptives is unlikely to cause serious harm, but estimates that women using progestin-only emergency contraception on a regular basis would have a 20% chance of pregnancy in a year.3
The American College of Obstetricians and Gynecologists states that long-term use of emergency contraception is less effective than other methods and may result in higher hormone levels and more adverse effects than other established means.4
The International Consortium for Emergency Contraception concluded that there is no basis for limiting the number of times that emergency contraceptives may be used in a menstrual cycle, that emergency contraceptives are safe, and that, although they are less effective than other forms of long-term contraception, using them repeatedly is more effective than using no method.5
The Society of Obstetricians and Gynecologists of Canada states that emergency contraception is intended for occasional use as a backup method.6 The Society also notes that repeat use isn’t as effective as regular use of other forms of contraception.
The Faculty of Sexual & Reproductive Healthcare of the (British) Royal College of Obstetricians and Gynaecologists says that use of levonorgestrel can be considered even if previously used one or more times in a menstrual cycle (SOR: D, based on non-analytical studies and expert opinion).7 The organization also recommends that emergency contraceptive providers share with patients that oral emergency contraceptive methods should not be used for long-term contraception (SOR: Good Practice Point, based on clinical experience of the guideline development group).
The Guttmacher Institute reports that without contraception, approximately 85% of sexually active women become pregnant each year.8 Long-acting reversible methods, such as implants and intrauterine devices, have annual pregnancy rates of 0.05% to 0.8%. With perfect (consistent and correct) use, combined oral contraceptives have a 0.3% annual pregnancy rate, but the rate rises to 9% with typical use. Condoms, when used perfectly, are associated with a 2% annual rate of pregnancy compared with an 18% rate with typical use.
1. Halpern V, Raymond EG, Lopez LM. Repeated use of pre-and postcoital hormonal contraception for the prevention of pregnancy. Cochrane Database Syst Rev. 2014 Sep 26;(9):CD007595.
2. Festin MPR, Bahamondes L, Nguyen TMH, et al. A prospective, open-label, single arm, multicentre study to evaluate efficacy, safety and acceptability of pericoital oral contraception using levonorgestrel 1.5mg. Hum Reprod. 2016;31:530-540.
3. Trussell J, Raymond EG, Cleland K. Emergency Contraception: A Last Chance to Prevent Unintended Pregnancy. Princeton, NJ: Office of Population Research & Association of Reproductive Health Professionals, June 2017. Available at: http://ec.princeton.edu/questions/ec-review.pdf. Accessed June 28, 2017.
4. American College of Obstetricians and Gynecologists. Emergency contraception. Obstet Gynecol. 2015;126:e1-e11.
5. International Consortium for Emergency Contraception. Repeated Use of Emergency Contraceptive Pills: The Facts. New York, NY: ICEC, October 2015. Available at: www.cecinfo.org/custom-content/uploads/2015/10/ICEC_Repeat-Use_Oct-2015.pdf. Accessed June 28, 2017.
6. Dunn S, Guilbert E, Burnett M, et al. Emergency contraception. J Obstet Can. 2012;34:870–878.
7. Faculty of Sexual & Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists. FSRH Guideline: Emergency Contraception. March 2017 (Updated May 29, 2017). Available at: https://www.fsrh.org/standards-and-guidance/documents/ceu-clinical-guidance-emergency-contraception-march-2017/. Accessed June 28, 2017.
8. Guttmacher Institute. Contraceptive Use in the United States. New York, NY: Guttmacher Institute, September 2016. Available at: www.guttmacher.org/fact-sheet/contraceptive-use-united-states. Accessed June 28, 2017.
EVIDENCE SUMMARY
A systematic review of 22 trials (13 case series, 8 prospective, nonrandomized studies, and one randomized controlled trial; 12,407 patients) conducted in Europe, Asia, and the Americas evaluated the likelihood of pregnancy with repeated use of precoital and postcoital hormonal contraception.1 Some trials used more than one dose or medication. Many had inadequate reporting of research methods. Results were reported using the Pearl Index (PI)—the number of pregnancies per 100 woman-years.
In 11 studies (2700 patients), women took 750 mcg of levonorgestrel from 24 hours before to 24 hours after intercourse for an average duration of 5 cycles or months. Coital frequency varied from 1 to 15 times per month. The PI ranged from 0 to 18.6, with a pooled PI of 5.4 (95% confidence interval [CI], 4.1-7.0). Three of the trials (915 patients), with research methods reported as good, had a pooled PI of 8.9 (95% CI, 5.1-14.4). No serious adverse effects were reported in 10 of the 11 studies, but menstrual irregularity was commonly observed. In one of the largest studies (1315 patients), only 3% of women discontinued treatment because of adverse effects.
Six other trials (5785 patients) of levonorgestrel taken at doses ranging from 150 mcg to 1 mg for a mean duration of 9.2 cycles reported PIs of 0 to 9. Breakthrough bleeding was the most common adverse event. When all 17 studies of levonorgestrel were combined, the PI was 4.9 (95% CI, 4.3-5.5). The remaining studies in the systematic review described medicines not commonly used for emergency contraception or not available in the United States.
Other reported adverse effects: Headache, nausea, abdominal pain
A prospective, open-label study enrolled 321 women 18 to 45 years of age from Asia, Europe, and South America to evaluate the safety and efficacy of levonorgestrel 1.5 mg taken before or within 24 hours of intercourse as the exclusive means of contraception.2 Women who were lactating or recently postpartum were excluded; condoms were permitted for women who had concerns about risk of sexually transmitted illness. Data analysis included estimates of perfect use (consistent and correct use of levonorgestrel only) and typical use (use of other contraceptive methods in addition to levonorgestrel).
At baseline, weight, blood pressure, and hemoglobin were documented, and follow-up visits occurred at 2.5, 4.5, and 6.5 months. Pregnancy tests, blood pressure, and adverse effects were assessed at each visit; weight and hemoglobin were evaluated at the final visit. The primary outcome measure was the PI in women younger than 35 years who used only levonorgestrel for contraception.
In women younger than 35 years (208 patients), the PI was 11 (95% CI, 5.7-13.1) with perfect use and 10.3 (95% CI, 5.4-19.9) with typical use. In all ages 18 to 45 years, the PI was 7.1 (95% CI, 3.8-13.1) for typical use and 7.5 (95% CI, 4-13.9) for perfect use. Most women took 4 to 6 doses per month.
The most commonly reported adverse effects were headache (29%), nausea or abdominal pain (16%), influenza (11%), and acne or candidiasis (8%). Bleeding patterns varied with a tendency toward longer bleeding initially and lighter menstrual periods and less anemia in some patients at the end of the study.
RECOMMENDATIONS
The Office of Population Research at Princeton University suggests that moderate repeat use of emergency contraceptives is unlikely to cause serious harm, but estimates that women using progestin-only emergency contraception on a regular basis would have a 20% chance of pregnancy in a year.3
The American College of Obstetricians and Gynecologists states that long-term use of emergency contraception is less effective than other methods and may result in higher hormone levels and more adverse effects than other established means.4
The International Consortium for Emergency Contraception concluded that there is no basis for limiting the number of times that emergency contraceptives may be used in a menstrual cycle, that emergency contraceptives are safe, and that, although they are less effective than other forms of long-term contraception, using them repeatedly is more effective than using no method.5
The Society of Obstetricians and Gynecologists of Canada states that emergency contraception is intended for occasional use as a backup method.6 The Society also notes that repeat use isn’t as effective as regular use of other forms of contraception.
The Faculty of Sexual & Reproductive Healthcare of the (British) Royal College of Obstetricians and Gynaecologists says that use of levonorgestrel can be considered even if previously used one or more times in a menstrual cycle (SOR: D, based on non-analytical studies and expert opinion).7 The organization also recommends that emergency contraceptive providers share with patients that oral emergency contraceptive methods should not be used for long-term contraception (SOR: Good Practice Point, based on clinical experience of the guideline development group).
The Guttmacher Institute reports that without contraception, approximately 85% of sexually active women become pregnant each year.8 Long-acting reversible methods, such as implants and intrauterine devices, have annual pregnancy rates of 0.05% to 0.8%. With perfect (consistent and correct) use, combined oral contraceptives have a 0.3% annual pregnancy rate, but the rate rises to 9% with typical use. Condoms, when used perfectly, are associated with a 2% annual rate of pregnancy compared with an 18% rate with typical use.
EVIDENCE SUMMARY
A systematic review of 22 trials (13 case series, 8 prospective, nonrandomized studies, and one randomized controlled trial; 12,407 patients) conducted in Europe, Asia, and the Americas evaluated the likelihood of pregnancy with repeated use of precoital and postcoital hormonal contraception.1 Some trials used more than one dose or medication. Many had inadequate reporting of research methods. Results were reported using the Pearl Index (PI)—the number of pregnancies per 100 woman-years.
In 11 studies (2700 patients), women took 750 mcg of levonorgestrel from 24 hours before to 24 hours after intercourse for an average duration of 5 cycles or months. Coital frequency varied from 1 to 15 times per month. The PI ranged from 0 to 18.6, with a pooled PI of 5.4 (95% confidence interval [CI], 4.1-7.0). Three of the trials (915 patients), with research methods reported as good, had a pooled PI of 8.9 (95% CI, 5.1-14.4). No serious adverse effects were reported in 10 of the 11 studies, but menstrual irregularity was commonly observed. In one of the largest studies (1315 patients), only 3% of women discontinued treatment because of adverse effects.
Six other trials (5785 patients) of levonorgestrel taken at doses ranging from 150 mcg to 1 mg for a mean duration of 9.2 cycles reported PIs of 0 to 9. Breakthrough bleeding was the most common adverse event. When all 17 studies of levonorgestrel were combined, the PI was 4.9 (95% CI, 4.3-5.5). The remaining studies in the systematic review described medicines not commonly used for emergency contraception or not available in the United States.
Other reported adverse effects: Headache, nausea, abdominal pain
A prospective, open-label study enrolled 321 women 18 to 45 years of age from Asia, Europe, and South America to evaluate the safety and efficacy of levonorgestrel 1.5 mg taken before or within 24 hours of intercourse as the exclusive means of contraception.2 Women who were lactating or recently postpartum were excluded; condoms were permitted for women who had concerns about risk of sexually transmitted illness. Data analysis included estimates of perfect use (consistent and correct use of levonorgestrel only) and typical use (use of other contraceptive methods in addition to levonorgestrel).
At baseline, weight, blood pressure, and hemoglobin were documented, and follow-up visits occurred at 2.5, 4.5, and 6.5 months. Pregnancy tests, blood pressure, and adverse effects were assessed at each visit; weight and hemoglobin were evaluated at the final visit. The primary outcome measure was the PI in women younger than 35 years who used only levonorgestrel for contraception.
In women younger than 35 years (208 patients), the PI was 11 (95% CI, 5.7-13.1) with perfect use and 10.3 (95% CI, 5.4-19.9) with typical use. In all ages 18 to 45 years, the PI was 7.1 (95% CI, 3.8-13.1) for typical use and 7.5 (95% CI, 4-13.9) for perfect use. Most women took 4 to 6 doses per month.
The most commonly reported adverse effects were headache (29%), nausea or abdominal pain (16%), influenza (11%), and acne or candidiasis (8%). Bleeding patterns varied with a tendency toward longer bleeding initially and lighter menstrual periods and less anemia in some patients at the end of the study.
RECOMMENDATIONS
The Office of Population Research at Princeton University suggests that moderate repeat use of emergency contraceptives is unlikely to cause serious harm, but estimates that women using progestin-only emergency contraception on a regular basis would have a 20% chance of pregnancy in a year.3
The American College of Obstetricians and Gynecologists states that long-term use of emergency contraception is less effective than other methods and may result in higher hormone levels and more adverse effects than other established means.4
The International Consortium for Emergency Contraception concluded that there is no basis for limiting the number of times that emergency contraceptives may be used in a menstrual cycle, that emergency contraceptives are safe, and that, although they are less effective than other forms of long-term contraception, using them repeatedly is more effective than using no method.5
The Society of Obstetricians and Gynecologists of Canada states that emergency contraception is intended for occasional use as a backup method.6 The Society also notes that repeat use isn’t as effective as regular use of other forms of contraception.
The Faculty of Sexual & Reproductive Healthcare of the (British) Royal College of Obstetricians and Gynaecologists says that use of levonorgestrel can be considered even if previously used one or more times in a menstrual cycle (SOR: D, based on non-analytical studies and expert opinion).7 The organization also recommends that emergency contraceptive providers share with patients that oral emergency contraceptive methods should not be used for long-term contraception (SOR: Good Practice Point, based on clinical experience of the guideline development group).
The Guttmacher Institute reports that without contraception, approximately 85% of sexually active women become pregnant each year.8 Long-acting reversible methods, such as implants and intrauterine devices, have annual pregnancy rates of 0.05% to 0.8%. With perfect (consistent and correct) use, combined oral contraceptives have a 0.3% annual pregnancy rate, but the rate rises to 9% with typical use. Condoms, when used perfectly, are associated with a 2% annual rate of pregnancy compared with an 18% rate with typical use.
1. Halpern V, Raymond EG, Lopez LM. Repeated use of pre-and postcoital hormonal contraception for the prevention of pregnancy. Cochrane Database Syst Rev. 2014 Sep 26;(9):CD007595.
2. Festin MPR, Bahamondes L, Nguyen TMH, et al. A prospective, open-label, single arm, multicentre study to evaluate efficacy, safety and acceptability of pericoital oral contraception using levonorgestrel 1.5mg. Hum Reprod. 2016;31:530-540.
3. Trussell J, Raymond EG, Cleland K. Emergency Contraception: A Last Chance to Prevent Unintended Pregnancy. Princeton, NJ: Office of Population Research & Association of Reproductive Health Professionals, June 2017. Available at: http://ec.princeton.edu/questions/ec-review.pdf. Accessed June 28, 2017.
4. American College of Obstetricians and Gynecologists. Emergency contraception. Obstet Gynecol. 2015;126:e1-e11.
5. International Consortium for Emergency Contraception. Repeated Use of Emergency Contraceptive Pills: The Facts. New York, NY: ICEC, October 2015. Available at: www.cecinfo.org/custom-content/uploads/2015/10/ICEC_Repeat-Use_Oct-2015.pdf. Accessed June 28, 2017.
6. Dunn S, Guilbert E, Burnett M, et al. Emergency contraception. J Obstet Can. 2012;34:870–878.
7. Faculty of Sexual & Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists. FSRH Guideline: Emergency Contraception. March 2017 (Updated May 29, 2017). Available at: https://www.fsrh.org/standards-and-guidance/documents/ceu-clinical-guidance-emergency-contraception-march-2017/. Accessed June 28, 2017.
8. Guttmacher Institute. Contraceptive Use in the United States. New York, NY: Guttmacher Institute, September 2016. Available at: www.guttmacher.org/fact-sheet/contraceptive-use-united-states. Accessed June 28, 2017.
1. Halpern V, Raymond EG, Lopez LM. Repeated use of pre-and postcoital hormonal contraception for the prevention of pregnancy. Cochrane Database Syst Rev. 2014 Sep 26;(9):CD007595.
2. Festin MPR, Bahamondes L, Nguyen TMH, et al. A prospective, open-label, single arm, multicentre study to evaluate efficacy, safety and acceptability of pericoital oral contraception using levonorgestrel 1.5mg. Hum Reprod. 2016;31:530-540.
3. Trussell J, Raymond EG, Cleland K. Emergency Contraception: A Last Chance to Prevent Unintended Pregnancy. Princeton, NJ: Office of Population Research & Association of Reproductive Health Professionals, June 2017. Available at: http://ec.princeton.edu/questions/ec-review.pdf. Accessed June 28, 2017.
4. American College of Obstetricians and Gynecologists. Emergency contraception. Obstet Gynecol. 2015;126:e1-e11.
5. International Consortium for Emergency Contraception. Repeated Use of Emergency Contraceptive Pills: The Facts. New York, NY: ICEC, October 2015. Available at: www.cecinfo.org/custom-content/uploads/2015/10/ICEC_Repeat-Use_Oct-2015.pdf. Accessed June 28, 2017.
6. Dunn S, Guilbert E, Burnett M, et al. Emergency contraception. J Obstet Can. 2012;34:870–878.
7. Faculty of Sexual & Reproductive Healthcare of the Royal College of Obstetricians and Gynaecologists. FSRH Guideline: Emergency Contraception. March 2017 (Updated May 29, 2017). Available at: https://www.fsrh.org/standards-and-guidance/documents/ceu-clinical-guidance-emergency-contraception-march-2017/. Accessed June 28, 2017.
8. Guttmacher Institute. Contraceptive Use in the United States. New York, NY: Guttmacher Institute, September 2016. Available at: www.guttmacher.org/fact-sheet/contraceptive-use-united-states. Accessed June 28, 2017.
Evidence-based answers from the Family Physicians Inquiries Network
EVIDENCE-BASED ANSWER:
Yes, but not as effective as some other methods. Annual pregnancy rates in women using pericoital levonorgestrel 150 mcg to 1 mg range from 4.9% to 8.9%; menstrual irregularity is the most common adverse effect (strength of recommendation [SOR]: B, Cochrane review of lower-quality trials).
In women younger than 35 years who have sexual intercourse 6 or fewer times per month, correct and consistent use of pericoital levonorgestrel 1.5 mg results in an annual pregnancy rate of 11% (SOR: B, one large prospective, open-label trial).
Pericoital contraception is less effective than long-acting reversible contraceptives (annual pregnancy rates of 0.05%-0.8%) or perfect use of combined oral contraceptives (0.3% annual pregnancy rate), but similar to, or better than, typical use of combined oral contraception (9%) and condoms (18%).
When to “CAP” off treatment for pneumonia
ILLUSTRATIVE CASE
A 65-year-old woman is admitted to your inpatient service from your family health center. She is diagnosed with community-acquired pneumonia (CAP) based on a 5-day history of cough and fever and a positive chest x-ray. She now requires oxygen at rest. She has a past medical history of hypertension and diabetes, both of which have been controlled on oral medications. Antibiotic therapy is initiated for the treatment of the pneumonia, but what treatment duration is ideal?
The World Health Organization estimates that pneumonia is the third most common cause of mortality worldwide, causing 3.2 million deaths per year.2 Appropriate prescribing of antibiotics is critical for the successful treatment of CAP.
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) created consensus guidelines, published in 2007, for the treatment of CAP.3 These guidelines recommend a minimum 5-day course of antibiotics if the patient is clinically stable, which is defined as: afebrile for 48 hours, heart rate ≤100 beats/minute, respiratory rate ≤24 respirations/minute, systolic blood pressure ≥90 mm Hg, oxygen saturation ≥90%, normal mental status, and able to tolerate oral intake. Longer antibiotic treatment durations are recommended on an individualized basis, if, for example, the isolated pathogen is not susceptible to the initial antibiotic or if the infection was caused by an extrapulmonary source.
However, these recommendations are not routinely followed. Practitioners often make it their custom to prescribe longer courses of antibiotics.4 And yet we know that there are several reasons to consider shorter courses of antibiotics, including lower health care costs, fewer adverse effects, and lower rates of bacterial resistance.5-7
Two meta-analyses were performed to compare the safety and efficacy of short- (≤7 days) vs long-course (>7 days) antibiotic therapy in CAP.8,9 Both meta-analyses found no difference in efficacy or safety between shorter and longer courses of antibiotic treatment regimens for CAP. Secondary outcomes noted a trend toward decreased antibiotic-associated adverse events with shorter courses of therapy.8,9
While these meta-analyses supported shorter courses of antibiotics for CAP, there are limitations to the broad implementation of their findings. Studies included in these analyses utilized a variety of antibiotic treatment regimens and longer courses (7 days vs 5 days) that are not recommended by the IDSA/ATS guidelines. Additionally, studies included both inpatient and outpatient treatment groups, so findings may not apply to an exclusively inpatient CAP population.8,9
This study sought to validate the IDSA/ATS guidelines recommending a 5-day course of antibiotics for hospitalized patients with CAP.1
STUDY SUMMARY
No differences in clinical outcomes between 5 days of Tx—and longer
This multicenter, double-blind, noninferiority randomized trial compared short-term antibiotic treatment duration (5 days) to physician-discretion antibiotic treatment duration among 312 patients ≥18 years of age admitted for CAP to one of 4 teaching hospitals in Spain.1 Pneumonia was diagnosed on chest radiograph with at least one symptom: cough, fever, dyspnea, or chest pain. Patients were excluded if, among other things, they had an immunocompromising condition, lived in a nursing home, had a recent hospital stay, used antibiotics within the previous 30 days, or had an uncommon pathogen, such as Pseudomonas aeruginosa or Staphylococcus aureus.1
Patients were randomized after receiving a minimum of 5 days of antibiotics to an intervention group (where, if clinically stable, no further antibiotics were given) or a control group (where physicians determined antibiotic duration).1 Primary outcomes were clinical success rate at Days 10 and 30 from admission, defined as resolution of signs and symptoms of CAP without further antibiotics, and improvement of CAP-related symptoms as determined by an 18-item CAP symptom questionnaire. This questionnaire was scored 0 to 90, where higher scores indicated greater severity. Secondary outcomes included: duration of antibiotic use, time to clinical improvement, mortality, hospital readmission, hospital length of stay, and CAP recurrence.1A total of 312 patients were randomized with 162 patients in the intervention group and 150 patients in the control group. The mean age of patients in the intervention and control groups was 66.2 and 64.7 years, respectively. Other baseline demographics were similar between the groups. Nearly 80% of patients received quinolone treatment; <10% received a beta-lactam plus a macrolide.1
Clinical success rates were similar for the control and intervention groups, respectively, at Day 10 (49% vs 56%; P=.18) and Day 30 (89% vs 92%; P=.33). There was shorter median treatment duration with antibiotics in the intervention group compared with the control group (5 days vs 10 days; P<.001) and fewer 30-day hospital readmissions (1.4% vs 6.6%; P=.02). There were no differences for other secondary outcomes.1
WHAT’S NEW
Clinical support for 2007 guidelines
This is the first study to clinically support the IDSA/ATS guidelines, which state that a 5-day course of antibiotic therapy for hospitalized adults with CAP is effective and without increased risk of adverse events.
CAVEATS
Generaliz
This study focused on antibiotic duration for the treatment of CAP in hospitalized patients and mainly used quinolone antibiotics. It remains unclear if duration of therapy is as effective in the outpatient setting or when using alternative antibiotic regimens.
If patients continued to have symptoms (such as fever or low oxygen saturation on room air) after 5 days of antibiotic treatment, antibiotic treatment was continued in the study. Thus, patients in real life who continue to have symptoms may need individualized therapy and may require more than 5 days of antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotics end before clinical improvement occurs
This study noted an average of 12 days in both groups for patients to achieve clinical improvement, with upwards of 15 to 18 days for patients to return to normal activity. Patients and providers may be dissatisfied if the treatment course ends days before clinical improvement of symptoms. This may cause prescribers to lengthen the duration of antibiotic therapy inappropriately.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.
2. World Health Organization. The top 10 causes of death. Available at: http://www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed September 5, 2017.
3. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Aliberti S, Blasi F, Zanaboni AM, et al. Duration of antibiotic therapy in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2010;36:128-134.
5. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of ß-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365-370.
6. Opmeer BC, el Moussaoui R, Bossuyt PM, et al. Costs associated with shorter duration of antibiotic therapy in hospitalized patients with mild-to-moderate severe community-acquired pneumonia. J Antimicrob Chemother. 2007;60:1131-1136.
7. File TM Jr. Clinical efficacy of newer agents in short-duration therapy for community-acquired pneumonia. Clin Infect Dis. 2004;39(suppl 3):S159-S164.
8. Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
9. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841-1854.
ILLUSTRATIVE CASE
A 65-year-old woman is admitted to your inpatient service from your family health center. She is diagnosed with community-acquired pneumonia (CAP) based on a 5-day history of cough and fever and a positive chest x-ray. She now requires oxygen at rest. She has a past medical history of hypertension and diabetes, both of which have been controlled on oral medications. Antibiotic therapy is initiated for the treatment of the pneumonia, but what treatment duration is ideal?
The World Health Organization estimates that pneumonia is the third most common cause of mortality worldwide, causing 3.2 million deaths per year.2 Appropriate prescribing of antibiotics is critical for the successful treatment of CAP.
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) created consensus guidelines, published in 2007, for the treatment of CAP.3 These guidelines recommend a minimum 5-day course of antibiotics if the patient is clinically stable, which is defined as: afebrile for 48 hours, heart rate ≤100 beats/minute, respiratory rate ≤24 respirations/minute, systolic blood pressure ≥90 mm Hg, oxygen saturation ≥90%, normal mental status, and able to tolerate oral intake. Longer antibiotic treatment durations are recommended on an individualized basis, if, for example, the isolated pathogen is not susceptible to the initial antibiotic or if the infection was caused by an extrapulmonary source.
However, these recommendations are not routinely followed. Practitioners often make it their custom to prescribe longer courses of antibiotics.4 And yet we know that there are several reasons to consider shorter courses of antibiotics, including lower health care costs, fewer adverse effects, and lower rates of bacterial resistance.5-7
Two meta-analyses were performed to compare the safety and efficacy of short- (≤7 days) vs long-course (>7 days) antibiotic therapy in CAP.8,9 Both meta-analyses found no difference in efficacy or safety between shorter and longer courses of antibiotic treatment regimens for CAP. Secondary outcomes noted a trend toward decreased antibiotic-associated adverse events with shorter courses of therapy.8,9
While these meta-analyses supported shorter courses of antibiotics for CAP, there are limitations to the broad implementation of their findings. Studies included in these analyses utilized a variety of antibiotic treatment regimens and longer courses (7 days vs 5 days) that are not recommended by the IDSA/ATS guidelines. Additionally, studies included both inpatient and outpatient treatment groups, so findings may not apply to an exclusively inpatient CAP population.8,9
This study sought to validate the IDSA/ATS guidelines recommending a 5-day course of antibiotics for hospitalized patients with CAP.1
STUDY SUMMARY
No differences in clinical outcomes between 5 days of Tx—and longer
This multicenter, double-blind, noninferiority randomized trial compared short-term antibiotic treatment duration (5 days) to physician-discretion antibiotic treatment duration among 312 patients ≥18 years of age admitted for CAP to one of 4 teaching hospitals in Spain.1 Pneumonia was diagnosed on chest radiograph with at least one symptom: cough, fever, dyspnea, or chest pain. Patients were excluded if, among other things, they had an immunocompromising condition, lived in a nursing home, had a recent hospital stay, used antibiotics within the previous 30 days, or had an uncommon pathogen, such as Pseudomonas aeruginosa or Staphylococcus aureus.1
Patients were randomized after receiving a minimum of 5 days of antibiotics to an intervention group (where, if clinically stable, no further antibiotics were given) or a control group (where physicians determined antibiotic duration).1 Primary outcomes were clinical success rate at Days 10 and 30 from admission, defined as resolution of signs and symptoms of CAP without further antibiotics, and improvement of CAP-related symptoms as determined by an 18-item CAP symptom questionnaire. This questionnaire was scored 0 to 90, where higher scores indicated greater severity. Secondary outcomes included: duration of antibiotic use, time to clinical improvement, mortality, hospital readmission, hospital length of stay, and CAP recurrence.1A total of 312 patients were randomized with 162 patients in the intervention group and 150 patients in the control group. The mean age of patients in the intervention and control groups was 66.2 and 64.7 years, respectively. Other baseline demographics were similar between the groups. Nearly 80% of patients received quinolone treatment; <10% received a beta-lactam plus a macrolide.1
Clinical success rates were similar for the control and intervention groups, respectively, at Day 10 (49% vs 56%; P=.18) and Day 30 (89% vs 92%; P=.33). There was shorter median treatment duration with antibiotics in the intervention group compared with the control group (5 days vs 10 days; P<.001) and fewer 30-day hospital readmissions (1.4% vs 6.6%; P=.02). There were no differences for other secondary outcomes.1
WHAT’S NEW
Clinical support for 2007 guidelines
This is the first study to clinically support the IDSA/ATS guidelines, which state that a 5-day course of antibiotic therapy for hospitalized adults with CAP is effective and without increased risk of adverse events.
CAVEATS
Generaliz
This study focused on antibiotic duration for the treatment of CAP in hospitalized patients and mainly used quinolone antibiotics. It remains unclear if duration of therapy is as effective in the outpatient setting or when using alternative antibiotic regimens.
If patients continued to have symptoms (such as fever or low oxygen saturation on room air) after 5 days of antibiotic treatment, antibiotic treatment was continued in the study. Thus, patients in real life who continue to have symptoms may need individualized therapy and may require more than 5 days of antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotics end before clinical improvement occurs
This study noted an average of 12 days in both groups for patients to achieve clinical improvement, with upwards of 15 to 18 days for patients to return to normal activity. Patients and providers may be dissatisfied if the treatment course ends days before clinical improvement of symptoms. This may cause prescribers to lengthen the duration of antibiotic therapy inappropriately.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 65-year-old woman is admitted to your inpatient service from your family health center. She is diagnosed with community-acquired pneumonia (CAP) based on a 5-day history of cough and fever and a positive chest x-ray. She now requires oxygen at rest. She has a past medical history of hypertension and diabetes, both of which have been controlled on oral medications. Antibiotic therapy is initiated for the treatment of the pneumonia, but what treatment duration is ideal?
The World Health Organization estimates that pneumonia is the third most common cause of mortality worldwide, causing 3.2 million deaths per year.2 Appropriate prescribing of antibiotics is critical for the successful treatment of CAP.
The Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) created consensus guidelines, published in 2007, for the treatment of CAP.3 These guidelines recommend a minimum 5-day course of antibiotics if the patient is clinically stable, which is defined as: afebrile for 48 hours, heart rate ≤100 beats/minute, respiratory rate ≤24 respirations/minute, systolic blood pressure ≥90 mm Hg, oxygen saturation ≥90%, normal mental status, and able to tolerate oral intake. Longer antibiotic treatment durations are recommended on an individualized basis, if, for example, the isolated pathogen is not susceptible to the initial antibiotic or if the infection was caused by an extrapulmonary source.
However, these recommendations are not routinely followed. Practitioners often make it their custom to prescribe longer courses of antibiotics.4 And yet we know that there are several reasons to consider shorter courses of antibiotics, including lower health care costs, fewer adverse effects, and lower rates of bacterial resistance.5-7
Two meta-analyses were performed to compare the safety and efficacy of short- (≤7 days) vs long-course (>7 days) antibiotic therapy in CAP.8,9 Both meta-analyses found no difference in efficacy or safety between shorter and longer courses of antibiotic treatment regimens for CAP. Secondary outcomes noted a trend toward decreased antibiotic-associated adverse events with shorter courses of therapy.8,9
While these meta-analyses supported shorter courses of antibiotics for CAP, there are limitations to the broad implementation of their findings. Studies included in these analyses utilized a variety of antibiotic treatment regimens and longer courses (7 days vs 5 days) that are not recommended by the IDSA/ATS guidelines. Additionally, studies included both inpatient and outpatient treatment groups, so findings may not apply to an exclusively inpatient CAP population.8,9
This study sought to validate the IDSA/ATS guidelines recommending a 5-day course of antibiotics for hospitalized patients with CAP.1
STUDY SUMMARY
No differences in clinical outcomes between 5 days of Tx—and longer
This multicenter, double-blind, noninferiority randomized trial compared short-term antibiotic treatment duration (5 days) to physician-discretion antibiotic treatment duration among 312 patients ≥18 years of age admitted for CAP to one of 4 teaching hospitals in Spain.1 Pneumonia was diagnosed on chest radiograph with at least one symptom: cough, fever, dyspnea, or chest pain. Patients were excluded if, among other things, they had an immunocompromising condition, lived in a nursing home, had a recent hospital stay, used antibiotics within the previous 30 days, or had an uncommon pathogen, such as Pseudomonas aeruginosa or Staphylococcus aureus.1
Patients were randomized after receiving a minimum of 5 days of antibiotics to an intervention group (where, if clinically stable, no further antibiotics were given) or a control group (where physicians determined antibiotic duration).1 Primary outcomes were clinical success rate at Days 10 and 30 from admission, defined as resolution of signs and symptoms of CAP without further antibiotics, and improvement of CAP-related symptoms as determined by an 18-item CAP symptom questionnaire. This questionnaire was scored 0 to 90, where higher scores indicated greater severity. Secondary outcomes included: duration of antibiotic use, time to clinical improvement, mortality, hospital readmission, hospital length of stay, and CAP recurrence.1A total of 312 patients were randomized with 162 patients in the intervention group and 150 patients in the control group. The mean age of patients in the intervention and control groups was 66.2 and 64.7 years, respectively. Other baseline demographics were similar between the groups. Nearly 80% of patients received quinolone treatment; <10% received a beta-lactam plus a macrolide.1
Clinical success rates were similar for the control and intervention groups, respectively, at Day 10 (49% vs 56%; P=.18) and Day 30 (89% vs 92%; P=.33). There was shorter median treatment duration with antibiotics in the intervention group compared with the control group (5 days vs 10 days; P<.001) and fewer 30-day hospital readmissions (1.4% vs 6.6%; P=.02). There were no differences for other secondary outcomes.1
WHAT’S NEW
Clinical support for 2007 guidelines
This is the first study to clinically support the IDSA/ATS guidelines, which state that a 5-day course of antibiotic therapy for hospitalized adults with CAP is effective and without increased risk of adverse events.
CAVEATS
Generaliz
This study focused on antibiotic duration for the treatment of CAP in hospitalized patients and mainly used quinolone antibiotics. It remains unclear if duration of therapy is as effective in the outpatient setting or when using alternative antibiotic regimens.
If patients continued to have symptoms (such as fever or low oxygen saturation on room air) after 5 days of antibiotic treatment, antibiotic treatment was continued in the study. Thus, patients in real life who continue to have symptoms may need individualized therapy and may require more than 5 days of antibiotics.
CHALLENGES TO IMPLEMENTATION
Antibiotics end before clinical improvement occurs
This study noted an average of 12 days in both groups for patients to achieve clinical improvement, with upwards of 15 to 18 days for patients to return to normal activity. Patients and providers may be dissatisfied if the treatment course ends days before clinical improvement of symptoms. This may cause prescribers to lengthen the duration of antibiotic therapy inappropriately.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.
2. World Health Organization. The top 10 causes of death. Available at: http://www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed September 5, 2017.
3. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Aliberti S, Blasi F, Zanaboni AM, et al. Duration of antibiotic therapy in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2010;36:128-134.
5. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of ß-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365-370.
6. Opmeer BC, el Moussaoui R, Bossuyt PM, et al. Costs associated with shorter duration of antibiotic therapy in hospitalized patients with mild-to-moderate severe community-acquired pneumonia. J Antimicrob Chemother. 2007;60:1131-1136.
7. File TM Jr. Clinical efficacy of newer agents in short-duration therapy for community-acquired pneumonia. Clin Infect Dis. 2004;39(suppl 3):S159-S164.
8. Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
9. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841-1854.
1. Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.
2. World Health Organization. The top 10 causes of death. Available at: http://www.who.int/mediacentre/factsheets/fs310/en/index.html. Accessed September 5, 2017.
3. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27-S72.
4. Aliberti S, Blasi F, Zanaboni AM, et al. Duration of antibiotic therapy in hospitalised patients with community-acquired pneumonia. Eur Respir J. 2010;36:128-134.
5. Guillemot D, Carbon C, Balkau B, et al. Low dosage and long treatment duration of ß-lactam: risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA. 1998;279:365-370.
6. Opmeer BC, el Moussaoui R, Bossuyt PM, et al. Costs associated with shorter duration of antibiotic therapy in hospitalized patients with mild-to-moderate severe community-acquired pneumonia. J Antimicrob Chemother. 2007;60:1131-1136.
7. File TM Jr. Clinical efficacy of newer agents in short-duration therapy for community-acquired pneumonia. Clin Infect Dis. 2004;39(suppl 3):S159-S164.
8. Li JZ, Winston LG, Moore DH, et al. Efficacy of short-course antibiotic regimens for community-acquired pneumonia: a meta-analysis. Am J Med. 2007;120:783-790.
9. Dimopoulos G, Matthaiou DK, Karageorgopoulos DE, et al. Short- versus long-course antibacterial therapy for community-acquired pneumonia: a meta-analysis. Drugs. 2008;68:1841-1854.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
PRACTICE CHANGER
Prescribe 5 days of antibiotic treatment for inpatients with community-acquired pneumonia because it produces the same clinical success rates as longer treatment regimens, but is associated with fewer negative patient outcomes.1
STRENGTH OF RECOMMENDATION
B: Based on a single, good-quality randomized control trial.
Uranga A, España PP, Bilbao A, et al. Duration of antibiotic treatment in community-acquired pneumonia: a multicenter randomized clinical trial. JAMA Intern Med. 2016;176:1257-1265.1
Intraoral lesion • history of cirrhosis and smoking • Dx?
THE CASE
A 56-year-old white man presented at our dental clinic for routine care. The intraoral examination revealed an asymptomatic red lesion with white vesicle-like areas on the right side of the soft palate (FIGURE). The extraoral examination was normal, and regional lymph nodes were nonpalpable. The patient’s medical history included liver cirrhosis and pancreatitis. He also had a 30-year history of alcohol misuse (1-5 drinks per day) and a 30-pack-year smoking history. (The patient had stopped drinking at the time of presentation, and had quit smoking 2 years earlier.) We instructed him to gargle with warm salt water at home and return in 2 weeks. At follow-up, the lesion was unresolved, so a biopsy was performed.
THE DIAGNOSIS
The clinical diagnosis was erythroplakia. Trauma from food burn and inflammation of the salivary gland were both considered, but ultimately ruled out due to lack of symptoms and persistence of the lesion after 14 days. The pathology report confirmed a diagnosis of squamous cell carcinoma (SCC) in situ. Based on the pathology report, we referred the patient to an oral surgeon for wide surgical excision with evaluation of the margins.
Because of its location and subtle presentation, the lesion could have been easily overlooked, underscoring the importance of routinely going beyond dentition to examine the soft tissues of the mouth.
DISCUSSION
SCC is the most common cancer found in the oral cavity, accounting for 90% of all oral malignancies.1,2 Other malignancies include lymphomas, sarcomas, melanomas, salivary gland neoplasms, and metastasis from other sites.3,4 Predisposing factors include tobacco use (namely inhaled methods and chewing tobacco), alcohol misuse, human papillomavirus infection, and chewing betel nut.1,5 (Betel nuts grow on a species of palm tree mainly found in India, Pakistan, and Bangladesh. They are commonly chewed for their caffeine-like effect and are known to be carcinogenic.)
Presentation. SCC of the oral cavity can have various presentations. The lesion can appear as white, red, a mix of white and red, as a mass, or as a nonhealing ulcer. While some patients may be asymptomatic (as was ours), some may have signs and symptoms such as pain, bleeding, difficulty swallowing, difficulty wearing dentures, or a neck mass.6 A history of smoking and alcohol misuse, which was present in this case, should heighten suspicion and prompt further investigation of oral lesions.
Location. The most common intraoral site for oral cancer is the tongue (on the posterolateral border) followed by the floor of the mouth. Other common sites in descending order are the soft palate, gingiva, buccal mucosa, labial mucosa, and hard palate.1 (Our patient’s lesion was on the border of the hard and soft palate).
Treatment of oral cancer is surgical. In some cases, depending on the stage and size of the tumor, radiation and chemotherapy may be considered.3,5 Approximately two-thirds of oral cancers are detected in the later stages.7 The 5-year survival rate for people with oral SCC found at stages III or IV ranges from 32% to 45%, while the rate for those with SCC detected at stages I or II is 58% to 72%.1 Patients with a history of oral cancer have a 20-fold increased risk of a recurrence in the oral cavity or of developing cancer in the surrounding areas, such as the larynx, esophagus, and lungs, underscoring the necessity of adequate follow-up in these patients.2,3,5
Who is at risk?
In 2015, there were an estimated 45,780 new cases of oral cavity and pharyngeal cancer and 8650 deaths from these causes.8 Although oral cancer accounts for only 3% of all cancers in the United States, it is the eighth most common cancer in males and the 15th most common in females.1 Prevalence differs tremendously by location, however. In India, for example, oral cancer accounts for 30% of all cancers.9 Regardless of location, incidence increases with age; 62 is the average age at diagnosis.2 Oral cancers are also more common among African Americans than among Caucasians.1,3,5
Smokers are 2 to 3 times more likely to develop oral cancer than nonsmokers.1 This risk increases with amount and duration of smoking.1 The combination of smoking and alcohol use has a synergistic effect, increasing the likelihood of developing oral cancer 15 fold.1,3
Alcohol use. Among male patients with oral cancer, one-third are heavy alcohol users.1 In fact, one study found that 20% of these patients have cirrhosis of the liver.1 Thus, it makes good clinical sense to routinely examine the soft tissue of the oral cavity for abnormalities in patients with alcohol-induced cirrhosis of the liver.
Our patient. We placed our patient on a 3-month recall and stressed the importance of not smoking. The patient had surgery and a good outcome was documented. The patient indicated at follow-up that he’d started drinking again and was referred for counseling.
TAKEAWAY
It’s important to pay attention to color differences in the oral cavity on routine visits, particularly in patients with known risk factors for SCC. Patients with a lesion in the oral cavity should be seen again within 2 weeks. If the lesion is unresolved, the patient should be referred for further examination and/or biopsy. The possibility of recurrent oral cancer or cancer in the surrounding areas makes these patients good candidates for frequent follow-up examinations.
We strongly suggest that primary care physicians encourage their patients with the known predisposing risk factors of tobacco use and chronic alcohol misuse to quit these habits, visit their dentists for annual oral cancer screenings, and report any oral symptoms promptly to their medical and/or dental care providers. The asymptomatic nature of many of these lesions underscores the importance of following this advice. As is the case with most other cancers, survival rate is dependent on the stage of the disease at diagnosis.
1. Neville BW, Damm DD, Allen CM, et al. Oral and Maxillofacial Pathology. 4th ed. Philadelphia, PA: Elsevier, Inc; 2016:374-388.
2. American Cancer Society. What are the key statistics about oral cavity and oropharyngeal cancer? Available at: https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html. Accessed August 28, 2017.
3. The Oral Cancer Foundation. Oral cancer facts. Available at: http://oralcancerfoundation.org/facts/. Accessed August 28, 2017.
4. Zini A, Czerninski R, Sqan-Cohen HD. Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. 2010;39:299-305.
5. National Institute of Health. National Cancer Institute. Oral Cavity and Oropharyngeal Cancer Screening (PDQ®)–Patient Version. Available at: https://www.cancer.gov/types/head-and-neck/patient/oral-screening-pdq. Accessed August 28, 2017.
6. Groome PA, Rohland SL, Hall SF, et al. A population-based study of factors associated with early versus late stage oral cavity cancer diagnoses. Oral Oncol. 2011;47:642-647.
7. Dodd VJ, Schenck DP, Chaney EH, et al. Assessing oral cancer awareness among rural Latino migrant workers. J Immigr Minor Health. 2016;18:552-560.
8. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29.
9. Coelho KR. Challenges of the oral cancer burden in India. J Cancer Epidemiol. 2012;2012:701932.
THE CASE
A 56-year-old white man presented at our dental clinic for routine care. The intraoral examination revealed an asymptomatic red lesion with white vesicle-like areas on the right side of the soft palate (FIGURE). The extraoral examination was normal, and regional lymph nodes were nonpalpable. The patient’s medical history included liver cirrhosis and pancreatitis. He also had a 30-year history of alcohol misuse (1-5 drinks per day) and a 30-pack-year smoking history. (The patient had stopped drinking at the time of presentation, and had quit smoking 2 years earlier.) We instructed him to gargle with warm salt water at home and return in 2 weeks. At follow-up, the lesion was unresolved, so a biopsy was performed.
THE DIAGNOSIS
The clinical diagnosis was erythroplakia. Trauma from food burn and inflammation of the salivary gland were both considered, but ultimately ruled out due to lack of symptoms and persistence of the lesion after 14 days. The pathology report confirmed a diagnosis of squamous cell carcinoma (SCC) in situ. Based on the pathology report, we referred the patient to an oral surgeon for wide surgical excision with evaluation of the margins.
Because of its location and subtle presentation, the lesion could have been easily overlooked, underscoring the importance of routinely going beyond dentition to examine the soft tissues of the mouth.
DISCUSSION
SCC is the most common cancer found in the oral cavity, accounting for 90% of all oral malignancies.1,2 Other malignancies include lymphomas, sarcomas, melanomas, salivary gland neoplasms, and metastasis from other sites.3,4 Predisposing factors include tobacco use (namely inhaled methods and chewing tobacco), alcohol misuse, human papillomavirus infection, and chewing betel nut.1,5 (Betel nuts grow on a species of palm tree mainly found in India, Pakistan, and Bangladesh. They are commonly chewed for their caffeine-like effect and are known to be carcinogenic.)
Presentation. SCC of the oral cavity can have various presentations. The lesion can appear as white, red, a mix of white and red, as a mass, or as a nonhealing ulcer. While some patients may be asymptomatic (as was ours), some may have signs and symptoms such as pain, bleeding, difficulty swallowing, difficulty wearing dentures, or a neck mass.6 A history of smoking and alcohol misuse, which was present in this case, should heighten suspicion and prompt further investigation of oral lesions.
Location. The most common intraoral site for oral cancer is the tongue (on the posterolateral border) followed by the floor of the mouth. Other common sites in descending order are the soft palate, gingiva, buccal mucosa, labial mucosa, and hard palate.1 (Our patient’s lesion was on the border of the hard and soft palate).
Treatment of oral cancer is surgical. In some cases, depending on the stage and size of the tumor, radiation and chemotherapy may be considered.3,5 Approximately two-thirds of oral cancers are detected in the later stages.7 The 5-year survival rate for people with oral SCC found at stages III or IV ranges from 32% to 45%, while the rate for those with SCC detected at stages I or II is 58% to 72%.1 Patients with a history of oral cancer have a 20-fold increased risk of a recurrence in the oral cavity or of developing cancer in the surrounding areas, such as the larynx, esophagus, and lungs, underscoring the necessity of adequate follow-up in these patients.2,3,5
Who is at risk?
In 2015, there were an estimated 45,780 new cases of oral cavity and pharyngeal cancer and 8650 deaths from these causes.8 Although oral cancer accounts for only 3% of all cancers in the United States, it is the eighth most common cancer in males and the 15th most common in females.1 Prevalence differs tremendously by location, however. In India, for example, oral cancer accounts for 30% of all cancers.9 Regardless of location, incidence increases with age; 62 is the average age at diagnosis.2 Oral cancers are also more common among African Americans than among Caucasians.1,3,5
Smokers are 2 to 3 times more likely to develop oral cancer than nonsmokers.1 This risk increases with amount and duration of smoking.1 The combination of smoking and alcohol use has a synergistic effect, increasing the likelihood of developing oral cancer 15 fold.1,3
Alcohol use. Among male patients with oral cancer, one-third are heavy alcohol users.1 In fact, one study found that 20% of these patients have cirrhosis of the liver.1 Thus, it makes good clinical sense to routinely examine the soft tissue of the oral cavity for abnormalities in patients with alcohol-induced cirrhosis of the liver.
Our patient. We placed our patient on a 3-month recall and stressed the importance of not smoking. The patient had surgery and a good outcome was documented. The patient indicated at follow-up that he’d started drinking again and was referred for counseling.
TAKEAWAY
It’s important to pay attention to color differences in the oral cavity on routine visits, particularly in patients with known risk factors for SCC. Patients with a lesion in the oral cavity should be seen again within 2 weeks. If the lesion is unresolved, the patient should be referred for further examination and/or biopsy. The possibility of recurrent oral cancer or cancer in the surrounding areas makes these patients good candidates for frequent follow-up examinations.
We strongly suggest that primary care physicians encourage their patients with the known predisposing risk factors of tobacco use and chronic alcohol misuse to quit these habits, visit their dentists for annual oral cancer screenings, and report any oral symptoms promptly to their medical and/or dental care providers. The asymptomatic nature of many of these lesions underscores the importance of following this advice. As is the case with most other cancers, survival rate is dependent on the stage of the disease at diagnosis.
THE CASE
A 56-year-old white man presented at our dental clinic for routine care. The intraoral examination revealed an asymptomatic red lesion with white vesicle-like areas on the right side of the soft palate (FIGURE). The extraoral examination was normal, and regional lymph nodes were nonpalpable. The patient’s medical history included liver cirrhosis and pancreatitis. He also had a 30-year history of alcohol misuse (1-5 drinks per day) and a 30-pack-year smoking history. (The patient had stopped drinking at the time of presentation, and had quit smoking 2 years earlier.) We instructed him to gargle with warm salt water at home and return in 2 weeks. At follow-up, the lesion was unresolved, so a biopsy was performed.
THE DIAGNOSIS
The clinical diagnosis was erythroplakia. Trauma from food burn and inflammation of the salivary gland were both considered, but ultimately ruled out due to lack of symptoms and persistence of the lesion after 14 days. The pathology report confirmed a diagnosis of squamous cell carcinoma (SCC) in situ. Based on the pathology report, we referred the patient to an oral surgeon for wide surgical excision with evaluation of the margins.
Because of its location and subtle presentation, the lesion could have been easily overlooked, underscoring the importance of routinely going beyond dentition to examine the soft tissues of the mouth.
DISCUSSION
SCC is the most common cancer found in the oral cavity, accounting for 90% of all oral malignancies.1,2 Other malignancies include lymphomas, sarcomas, melanomas, salivary gland neoplasms, and metastasis from other sites.3,4 Predisposing factors include tobacco use (namely inhaled methods and chewing tobacco), alcohol misuse, human papillomavirus infection, and chewing betel nut.1,5 (Betel nuts grow on a species of palm tree mainly found in India, Pakistan, and Bangladesh. They are commonly chewed for their caffeine-like effect and are known to be carcinogenic.)
Presentation. SCC of the oral cavity can have various presentations. The lesion can appear as white, red, a mix of white and red, as a mass, or as a nonhealing ulcer. While some patients may be asymptomatic (as was ours), some may have signs and symptoms such as pain, bleeding, difficulty swallowing, difficulty wearing dentures, or a neck mass.6 A history of smoking and alcohol misuse, which was present in this case, should heighten suspicion and prompt further investigation of oral lesions.
Location. The most common intraoral site for oral cancer is the tongue (on the posterolateral border) followed by the floor of the mouth. Other common sites in descending order are the soft palate, gingiva, buccal mucosa, labial mucosa, and hard palate.1 (Our patient’s lesion was on the border of the hard and soft palate).
Treatment of oral cancer is surgical. In some cases, depending on the stage and size of the tumor, radiation and chemotherapy may be considered.3,5 Approximately two-thirds of oral cancers are detected in the later stages.7 The 5-year survival rate for people with oral SCC found at stages III or IV ranges from 32% to 45%, while the rate for those with SCC detected at stages I or II is 58% to 72%.1 Patients with a history of oral cancer have a 20-fold increased risk of a recurrence in the oral cavity or of developing cancer in the surrounding areas, such as the larynx, esophagus, and lungs, underscoring the necessity of adequate follow-up in these patients.2,3,5
Who is at risk?
In 2015, there were an estimated 45,780 new cases of oral cavity and pharyngeal cancer and 8650 deaths from these causes.8 Although oral cancer accounts for only 3% of all cancers in the United States, it is the eighth most common cancer in males and the 15th most common in females.1 Prevalence differs tremendously by location, however. In India, for example, oral cancer accounts for 30% of all cancers.9 Regardless of location, incidence increases with age; 62 is the average age at diagnosis.2 Oral cancers are also more common among African Americans than among Caucasians.1,3,5
Smokers are 2 to 3 times more likely to develop oral cancer than nonsmokers.1 This risk increases with amount and duration of smoking.1 The combination of smoking and alcohol use has a synergistic effect, increasing the likelihood of developing oral cancer 15 fold.1,3
Alcohol use. Among male patients with oral cancer, one-third are heavy alcohol users.1 In fact, one study found that 20% of these patients have cirrhosis of the liver.1 Thus, it makes good clinical sense to routinely examine the soft tissue of the oral cavity for abnormalities in patients with alcohol-induced cirrhosis of the liver.
Our patient. We placed our patient on a 3-month recall and stressed the importance of not smoking. The patient had surgery and a good outcome was documented. The patient indicated at follow-up that he’d started drinking again and was referred for counseling.
TAKEAWAY
It’s important to pay attention to color differences in the oral cavity on routine visits, particularly in patients with known risk factors for SCC. Patients with a lesion in the oral cavity should be seen again within 2 weeks. If the lesion is unresolved, the patient should be referred for further examination and/or biopsy. The possibility of recurrent oral cancer or cancer in the surrounding areas makes these patients good candidates for frequent follow-up examinations.
We strongly suggest that primary care physicians encourage their patients with the known predisposing risk factors of tobacco use and chronic alcohol misuse to quit these habits, visit their dentists for annual oral cancer screenings, and report any oral symptoms promptly to their medical and/or dental care providers. The asymptomatic nature of many of these lesions underscores the importance of following this advice. As is the case with most other cancers, survival rate is dependent on the stage of the disease at diagnosis.
1. Neville BW, Damm DD, Allen CM, et al. Oral and Maxillofacial Pathology. 4th ed. Philadelphia, PA: Elsevier, Inc; 2016:374-388.
2. American Cancer Society. What are the key statistics about oral cavity and oropharyngeal cancer? Available at: https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html. Accessed August 28, 2017.
3. The Oral Cancer Foundation. Oral cancer facts. Available at: http://oralcancerfoundation.org/facts/. Accessed August 28, 2017.
4. Zini A, Czerninski R, Sqan-Cohen HD. Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. 2010;39:299-305.
5. National Institute of Health. National Cancer Institute. Oral Cavity and Oropharyngeal Cancer Screening (PDQ®)–Patient Version. Available at: https://www.cancer.gov/types/head-and-neck/patient/oral-screening-pdq. Accessed August 28, 2017.
6. Groome PA, Rohland SL, Hall SF, et al. A population-based study of factors associated with early versus late stage oral cavity cancer diagnoses. Oral Oncol. 2011;47:642-647.
7. Dodd VJ, Schenck DP, Chaney EH, et al. Assessing oral cancer awareness among rural Latino migrant workers. J Immigr Minor Health. 2016;18:552-560.
8. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29.
9. Coelho KR. Challenges of the oral cancer burden in India. J Cancer Epidemiol. 2012;2012:701932.
1. Neville BW, Damm DD, Allen CM, et al. Oral and Maxillofacial Pathology. 4th ed. Philadelphia, PA: Elsevier, Inc; 2016:374-388.
2. American Cancer Society. What are the key statistics about oral cavity and oropharyngeal cancer? Available at: https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html. Accessed August 28, 2017.
3. The Oral Cancer Foundation. Oral cancer facts. Available at: http://oralcancerfoundation.org/facts/. Accessed August 28, 2017.
4. Zini A, Czerninski R, Sqan-Cohen HD. Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. 2010;39:299-305.
5. National Institute of Health. National Cancer Institute. Oral Cavity and Oropharyngeal Cancer Screening (PDQ®)–Patient Version. Available at: https://www.cancer.gov/types/head-and-neck/patient/oral-screening-pdq. Accessed August 28, 2017.
6. Groome PA, Rohland SL, Hall SF, et al. A population-based study of factors associated with early versus late stage oral cavity cancer diagnoses. Oral Oncol. 2011;47:642-647.
7. Dodd VJ, Schenck DP, Chaney EH, et al. Assessing oral cancer awareness among rural Latino migrant workers. J Immigr Minor Health. 2016;18:552-560.
8. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5-29.
9. Coelho KR. Challenges of the oral cancer burden in India. J Cancer Epidemiol. 2012;2012:701932.
Is obesity a disease?
It depends on whom you ask. But if you ask me, obesity should not be labeled a disease.
I understand the rationale for calling obesity a disease—it helps legitimize the time we spend treating obesity and aids in getting paid for that time. Some people have distinct diseases, such as Prader-Willi syndrome, hypothyroidism, and Cushing’s syndrome that can cause obesity, and perhaps massive obesity is best categorized and treated as a disease. But the “garden variety” obesity that affects nearly 40% of the US adult population1 behaves more like a risk factor than a disease. Think of other continuous variables like blood pressure and cholesterol—the higher the measurement, the higher the risk of a plethora of medical problems.
Obesity is a global public health problem that is due largely—at least in this country—to the widespread availability of inexpensive, calorie-packed foods, as well as a desire by a screen-addicted society to stay home and “play” online rather than outdoors. Obesity is a health risk factor produced by our current social milieu and modified by genetics and personal health habits.
So what can we do? We need to recognize our limited, but important, role and remain nonjudgmental with our overweight and obese patients when they are unsuccessful at losing weight. It is easy to play the blame game, even in subtle ways. Recognizing that obesity is more of a social issue than a personal behavioral issue is a great place to start. Asking patients what they want to do and helping them set goals and find the resources to reach their goals can be helpful. Celebrating even small decreases in weight or increases in physical activity is always good medicine. Remember that a 5% to 10% weight loss has medically beneficial effects, especially for patients with diabetes.2
In addition to recommendations (and referrals) to help patients reduce calories and increase exercise, we have other weight-loss tools to draw upon. Gastric bypass surgery is certainly effective—especially for obese patients with diabetes. And
So whether you consider obesity a disease, or not, we now have even more ways with which to combat it.
1. Ogden CL, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;219:1-8.
2. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481-1486.
It depends on whom you ask. But if you ask me, obesity should not be labeled a disease.
I understand the rationale for calling obesity a disease—it helps legitimize the time we spend treating obesity and aids in getting paid for that time. Some people have distinct diseases, such as Prader-Willi syndrome, hypothyroidism, and Cushing’s syndrome that can cause obesity, and perhaps massive obesity is best categorized and treated as a disease. But the “garden variety” obesity that affects nearly 40% of the US adult population1 behaves more like a risk factor than a disease. Think of other continuous variables like blood pressure and cholesterol—the higher the measurement, the higher the risk of a plethora of medical problems.
Obesity is a global public health problem that is due largely—at least in this country—to the widespread availability of inexpensive, calorie-packed foods, as well as a desire by a screen-addicted society to stay home and “play” online rather than outdoors. Obesity is a health risk factor produced by our current social milieu and modified by genetics and personal health habits.
So what can we do? We need to recognize our limited, but important, role and remain nonjudgmental with our overweight and obese patients when they are unsuccessful at losing weight. It is easy to play the blame game, even in subtle ways. Recognizing that obesity is more of a social issue than a personal behavioral issue is a great place to start. Asking patients what they want to do and helping them set goals and find the resources to reach their goals can be helpful. Celebrating even small decreases in weight or increases in physical activity is always good medicine. Remember that a 5% to 10% weight loss has medically beneficial effects, especially for patients with diabetes.2
In addition to recommendations (and referrals) to help patients reduce calories and increase exercise, we have other weight-loss tools to draw upon. Gastric bypass surgery is certainly effective—especially for obese patients with diabetes. And
So whether you consider obesity a disease, or not, we now have even more ways with which to combat it.
It depends on whom you ask. But if you ask me, obesity should not be labeled a disease.
I understand the rationale for calling obesity a disease—it helps legitimize the time we spend treating obesity and aids in getting paid for that time. Some people have distinct diseases, such as Prader-Willi syndrome, hypothyroidism, and Cushing’s syndrome that can cause obesity, and perhaps massive obesity is best categorized and treated as a disease. But the “garden variety” obesity that affects nearly 40% of the US adult population1 behaves more like a risk factor than a disease. Think of other continuous variables like blood pressure and cholesterol—the higher the measurement, the higher the risk of a plethora of medical problems.
Obesity is a global public health problem that is due largely—at least in this country—to the widespread availability of inexpensive, calorie-packed foods, as well as a desire by a screen-addicted society to stay home and “play” online rather than outdoors. Obesity is a health risk factor produced by our current social milieu and modified by genetics and personal health habits.
So what can we do? We need to recognize our limited, but important, role and remain nonjudgmental with our overweight and obese patients when they are unsuccessful at losing weight. It is easy to play the blame game, even in subtle ways. Recognizing that obesity is more of a social issue than a personal behavioral issue is a great place to start. Asking patients what they want to do and helping them set goals and find the resources to reach their goals can be helpful. Celebrating even small decreases in weight or increases in physical activity is always good medicine. Remember that a 5% to 10% weight loss has medically beneficial effects, especially for patients with diabetes.2
In addition to recommendations (and referrals) to help patients reduce calories and increase exercise, we have other weight-loss tools to draw upon. Gastric bypass surgery is certainly effective—especially for obese patients with diabetes. And
So whether you consider obesity a disease, or not, we now have even more ways with which to combat it.
1. Ogden CL, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;219:1-8.
2. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481-1486.
1. Ogden CL, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2011-2014. NCHS Data Brief. 2015;219:1-8.
2. Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481-1486.
Posttraumatic stress disorder: Often missed in primary care
THE CASE
DeSean W,* a 47-year-old man, returned to his primary care clinic with a new complaint of epigastric burning that had been bothering him for the past 4 months. He had tried several over-the-counter remedies, which provided no relief. He also remained concerned—despite assurances to the contrary at previous clinic visits—that he had contracted a sexually-transmitted disease (STD) after going to a bar one night 4 to 5 months ago. At 2 other clinic visits since that time, STD test results were negative. At this current visit, symptoms and details of sexual history were unchanged since the last visit, with the exception of the epigastric pain.
When asked if he thought he had contracted an STD through a sexual encounter the night he went to the bar, he emphatically said he would not cheat on his wife. Surprisingly, given his concern, he avoided further discussion on modes of contracting an STD.
The physician prescribed ranitidine 150 mg bid for the epigastric burning and explained, once more, the significance of the STD test results. However, he also decided to further examine Mr. W’s concern about STDs and the night he may have contracted one.
HOW WOULD YOU PROCEED WITH THIS PATIENT?
*The patient’s name has been changed to protect his privacy.
SCOPE OF THE PROBLEM
Despite being as common as asthma, posttraumatic stress disorder (PTSD) often remains undiagnosed and untreated in primary care.1 In brief, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines PTSD as persistent and long-term changes in thoughts or mood following actual or threatened exposure to death, serious injury, or sexual assault that leads to re-experiencing, functional impairment, physiologic stress reactions, and avoidance of thoughts or situations associated with the original trauma.2 More than one in 10 women and one in 20 men experience PTSD in their lifetime.2,3 Population-based studies have not yet determined the prevalence among children.3 Almost 40% of US adults report having experienced a trauma before age 13, and about one-third of these go on to develop PTSD.4
Individuals with PTSD have higher rates of somatic complaints, overall medical utilization, prescription use, physical and social disability, attempted suicide, and all-cause mortality.3,5-7 PTSD is associated with increased risk for cardiac, gastrointestinal, metabolic, and immunologic illnesses, other psychiatric illnesses, risky health behaviors, and decreased medical adherence.4,6 Additionally, prevention and treatment efforts for STDs and obesity are less effective among those with trauma histories.4 Thus, detection and treatment of PTSD improves the likelihood of successfully treating other health concerns.
THE ESSENTIALS OF A PTSD DIAGNOSIS
DSM-5 diagnosis of PTSD requires the experience of a trauma and resultant symptoms from each of 4 symptom-clusters:2
- one or more re-experiencing symptoms (eg, intrusive memories or recurrent distressing dreams, psychological distress or physiologic reactions to reminders of the trauma)
- one or more avoidance symptoms (eg, avoidance of trauma memories or of people and places that trigger a reminder of the trauma)
- two or more changes in thoughts or mood (eg, negative beliefs about self or others, social detachment, anhedonia)
- two or more changes in arousal activity (eg, sleep problems, hypervigilance, inability to concentrate).
Since many people experiencing traumas do not develop PTSD,5,8 symptoms must last at least one month to meet the criteria for diagnosis.2 Sexual trauma, experiencing multiple traumas, and lack of social support increase the risk that an individual will develop PTSD.9-11 Notably, symptom onset will be delayed 6 months or more in some individuals,2,8 making it more difficult for those patients and clinicians to connect symptoms to the trauma.12
Differential diagnosis
PTSD must be differentiated from other mental health conditions with overlapping symptoms (TABLE 12,8,13), but it may also be comorbid with one or more of these other conditions. When patients with PTSD do report mental health symptoms, providers often focus on the depressive symptoms that overlap with PTSD, and on substance use, which often accompanies PTSD, leaving PTSD undetected.9
Given that depressed/irritable mood, decreased participation in pleasurable activities, negative views of the world, attention difficulties, sleep difficulties, feelings of guilt, and agitation/restlessness are symptoms of both depression and PTSD,2 it is particularly important to screen patients with depressive symptoms for trauma history.
Why PTSD is often missed
Due to the impact of PTSD on overall health, the rates of PTSD in primary care clinics may be higher than in the general population.14 Thus, primary care clinicians are likely seeing PTSD more often than they realize. In fact, a systematic review showed that clinicians detected 0% to 52% of their patients with PTSD, missing at least half of all PTSD diagnoses.9
Detecting PTSD can be challenging for several reasons. Symptoms can span the emotional, social, physical, and behavioral aspects of an individual’s life, so patients and clinicians alike may regard symptoms as unrelated to PTSD.8 Primary symptom presentation may vary, with some people reporting anxiety symptoms, others mostly depressive symptoms, and others arousal, dissociative, or—as in our patient’s case—somatic symptoms.2 In affected children, parents may report emotional or behavioral problems without mentioning the trauma.2 Additionally, for traumas that were not a single event, such as long-term child abuse, patients may have difficulty identifying symptom onset.2
CASE
The physician screened Mr. W for trauma exposure as part of the differential. Mr. W revealed that he had blacked out at the bar, despite drinking only moderately, and that he awoke with anal pain. He believed he had been drugged and sexually assaulted. Further screening for PTSD symptoms related to this event confirmed multiple associated symptoms. He acknowledged that his epigastric pain had started soon after the trauma and, after further discussion, began to link his stomach pain and other new symptoms revealed by the PTSD screen (hypervigilance, avoidance, change in mood) to the trauma.
As happened in this case, most PTSD patients present with somatic complaints rather than reporting a traumatic experience and having associated effects. This in turn usually leads clinicians to consider only non-PTSD diagnoses.6,9,15 Core avoidance symptoms are a major reason for such a presentation in PTSD patients.14 Patients avoid thoughts, feelings, and conversations that remind them of the trauma.13 As a result, they are less likely to voluntarily report trauma. They avoid thinking about how their current symptoms may be associated with their trauma and are reluctant to talk about their trauma with clinicians.5,9,8,12
Another barrier to diagnosis is a belief that PTSD is primarily experienced by combat veterans1 (TABLE 22,4-6,8,9,12,14-18). While PTSD is detected more often among veterans due to regular screening through the Department of Veterans Affairs,14 the vast majority of PTSD cases are related to civilian traumas such as sexual assault, child abuse, and car accidents.5,9 In fact, the estimated
SCREENING: WHAT TO LOOK FOR
Since individuals with PTSD mainly seek treatment for associated physical symptoms,14 primary care is particularly important for identification of PTSD and treatment access. The US Preventative Services Task Force does not yet have any recommendations for screening for PTSD. The American Psychiatric Association recommends that a trauma history be included in all initial psychiatric evaluations of adults.19 Screens can target high-risk populations and can be repeated across the lifespan,9 as traumas can occur at any age and symptoms may not emerge until years after the trauma.2,4 Factors in a patient’s history associated with high risk of PTSD include the following:
- known trauma exposure (eg, treatment at the emergency department following motor vehicle collision, natural disaster, assault),6
- frequent medical visits or unexplained physical symptoms,5,8
- family members who are trauma victims,8
- involvement in juvenile justice system,4,12
- sensitive or invasive exams (eg, pelvic exams) that trigger symptoms or contribute to retraumatization,12,20 and
- any medical condition (eg, hypertension, chronic pain, sleep disorder), self-destructive behavior (eg, drug or alcohol abuse, low impulse control), or social/occupational issues (eg, unemployment, social isolation, fighting) with a known link to PTSD.2,4,6,8
The first step in screening. Given a patient’s reported symptoms, assess for trauma exposure to determine whether PTSD should be included in the differential diagnosis. Overlooking PTSD as a possible source of symptoms can result in misattributing them to other causes.4,8 Listing common traumas, or using a standardized list such as the Life Events Checklist, can help identify patients with trauma exposure.8,21 However, do not make the patient provide details of the traumatic event(s), as that can exacerbate symptoms if PTSD is present.6 It is sufficient to know the category of the trauma (eg, sexual assault) without making the patient describe who was involved and what happened.6
The second step in screening. If a patient reveals trauma exposure, consider using an instrument such as the Primary Care PTSD Screen (PC-PTSD) or the PTSD Checklist, both available online, to screen for PTSD symptoms related to the identified trauma.6,9,21-23 Since these measures screen for symptoms but do not ask about trauma exposure, false positives can occur if a trauma is not first identified (such as through the Life Events Checklist) due to symptom overlap with other conditions (TABLE 12,8,13).21
Treatment is effective, even decades after a traumatic event
Provide anyone who has been traumatized with information about common after effects, symptoms of PTSD, and available treatments.8 Keep in mind that initial symptom severity after trauma exposure does not correlate with long-term symptoms,8 and about half of adults will recover without treatment within 3 months.1,2,5 The first month of symptoms may be addressed with patient education and watchful waiting. But if symptoms don’t subside after a month, consider offering treatment1 with the understanding that, for some individuals, symptoms may yet resolve on their own.
Detecting and treating PTSD early can decrease its deleterious effects on health and cut down on years of functional impairment.1 Even decades after an initial traumatic event, PTSD treatments can be effective.8 Children may experience functional impairment without meeting full criteria for PTSD, and can also benefit from treatment.7
INTEGRATING EXPOSURE AND COGNITIVE THERAPIES IS KEY
Offer any patient who meets criteria for PTSD a referral for exposure therapy and trauma-focused cognitive behavioral therapy (TF-CBT), the first-line treatments for PTSD.1,4,8,24,25
Exposure therapies for PTSD are supported by strong evidence and help patients to become desensitized to distressful memories through gradual, repeated exposures in a relaxed or safe space.8,26
Cognitive methods, such as cognitive processing therapy, cognitive behavioral therapy, and cognitive reprocessing have moderate strength of evidence, and may be combined with exposure therapy.26 Cognitive therapies help patients change thoughts, beliefs, and behaviors that contribute to PTSD symptoms.8,26
Exposure and TF-CBT have the most empirical evidence for child, adolescent, and adult PTSD, and are effective for the range of PTSD symptoms,4,8,25 including avoidance—a fundamental component of PTSD that drives other PTSD symptoms27—comorbid depression, and other emotions associated with trauma (eg, shame, guilt, and anger).8,25 Family involvement is recommended for children and adolescents.4
For patients with comorbid substance abuse, offer integrated PTSD/substance abuse treatment, which is more effective than isolated treatment of each.4 Relaxation training can be helpful as an adjunct to TF-CBT, but is not sufficient as a stand-alone treatment.13 Other psychotherapies, such as supportive, psychodynamic, systemic, and hypnotherapy, have not proved effective.14
Eye Movement Desensitization and Reprocessing (EMDR), a much publicized but controversial treatment, integrates components of exposure and cognitive therapies with therapist-directed eye movements.28-30 Patients imagine their trauma while the therapist directs their eye movements, which is thought to provide exposure to trauma images and memories, thereby reducing symptoms. EMDR has been found to reduce PTSD symptoms with a low to moderate strength-of-evidence rating.26 However, it has not proved more effective than other exposure and cognitive therapies, and its unique component (eg, eye movements) has not added any effect to outcomes.28-31
Other newer therapies, such as Acceptance and Commitment Therapy7,24,27 and online and computer-assisted treatments, are being evaluated.14
Medications take on an adjunct role to therapy
Drug treatment of PTSD has not been effective in children or adolescents.4,8 In adults, medications have helped relieve some symptoms of PTSD. However, given their low effect sizes, medications are not recommended as first-line treatments over exposure and TF-CBT. Their usefulness lies chiefly in an adjunct role to exposure and cognitive therapies or for patients who refuse psychotherapy.4,8,25
Selective serotonin reuptake inhibitors such as fluoxetine, paroxetine, and sertraline, have been effective for such PTSD symptoms as intrusive thoughts, negative or irritable mood, anxiety, restlessness, attention difficulties, and hyperarousal.1,8
While benzodiazepines have been used to control anxiety, hyperarousal, and insomnia, they have not been effective for most other PTSD symptoms, including avoidance, re-experiencing, and cognitive symptoms. Furthermore, they are not recommended given their augmentative effect on other related symptoms and associated conditions (eg, dissociation, disinhibition, substance abuse) and possible interference with desensitization that occurs in exposure therapy.1,5
If a patient has significant insomnia and PTSD-related nightmares, consider starting prazosin at 1 mg/d and titrating up to an effective dose, which typically ranges from 5 to 20 mg per day.1,5 Additionally, trazodone or antihistamines may be used to enhance sleep.1
COORDINATION OF CARE
Upon identifying PTSD and offering treatment, introduce the patient to a mental health provider as part of the referral process, which strongly encourages patient engagement in treatment.14 Collaborate with the psychotherapist throughout treatment to facilitate a biopsychosocial approach to the patient’s care, and coordinate the monitoring and treatment of any comorbid physical conditions.
The Substance Abuse and Mental Health Services Administration has proposed a framework for multisystem Trauma-Informed Care (TIC), in which the primary care physician has many roles, including:12,20
- recording or communicating sensitive private information to other providers through the electronic medical record in a manner that does not interfere with a patient’s development of trust or lead to exposure and retraumatization,
- performing invasive physical exams in a sensitive and patient-centered manner, and
- using support and shared decision-making in clinical encounters.
Physicians can also connect patients with PTSD to programs or groups that aid in developing resilience, such as physical exercise classes, social support networks, and community involvement opportunities.4
CASE
The physician referred Mr. W to an onsite psychologist. At a subsequent clinic visit in which he was seen by a different primary care physician, Mr. W expressed new concerns about shoulder pain and changes in a mole. During this visit, Mr. W was asked whether he had followed up on the earlier referral for counseling. He replied that he had attended an intake appointment with the psychologist, but that he had not wanted to talk about what had happened to him and therefore avoided future appointments.*
He remained concerned that he might have an STD, but declined medication for PTSD because he felt he was “moving on” with his life.
*Author’s note: Getting patients to open up about their trauma exposure can be difficult. If the patient isn’t ready, simply bringing up the experience can trigger avoidance. It’s often helpful to encourage patients to first develop a relationship with their therapist, then later discuss the details of their trauma when they are ready. This encourages patients to engage in the counseling process.
CORRESPONDENCE
Adrienne A. Williams, PhD, Department of Family Medicine, University of Illinois at Chicago College of Medicine, 1919 W Taylor Street, MC663, Chicago, IL 60612; awms@uic.edu.
1. Bobo WV, Warner CH, Warner CM. The management of post traumatic stress disorder (PTSD) in the primary care setting. South Med J. 2007;100:797-802.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
3. Gradus JL. Epidemiology of PTSD. National Center for PTSD. Available at: http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Updated 2017. Accessed August 16, 2017.
4. Gerson R, Rappaport N. Traumatic stress and posttraumatic stress disorder in youth: recent research findings on clinical impact, assessment, and treatment. J Adolesc Health. 2013;52:137-143.
5. Zohar J, Juven-Wetzler A, Myers V, et al. Post-traumatic stress disorder: facts and fiction. Curr Opin Psychiatry. 2008;21:74-77.
6. Spoont MR, Williams JW Jr, Kehle-Forbes S, et al. Does this patient have posttraumatic stress disorder? Rational clinical examination systematic review. JAMA. 2015;314:501-510.
7. Woidneck MR, Morrison KL, Twohig MP. Acceptance and commitment therapy for the treatment of posttraumatic stress among adolescents. Behav Modif. 2014;38:451-476.
8. National Collaborating Centre for Mental Health (UK). Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. Available at: https://www.ncbi.nlm.nih.gov/books/NBK56494. Accessed August 16, 2017.
9. Greene T, Neria Y, Gross R. Prevalence, detection and correlates of PTSD in the primary care setting: a systematic review. J Clin Psychol Med Settings. 2016;23:160-180.
10. Gavranidou M, Rosner R. The weaker sex? Gender and post-traumatic stress disorder. Depress Anxiety. 2003;17:130-139.
11. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748-766.
12. SAMHSA’s Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. Available at: http://store.samhsa.gov/shin/content/SMA14-4884/SMA14-4884.pdf. Accessed September 13, 2017.
13. Mulick PS, Landes SJ, Kanter JW. Contextual behavior therapies in the treatment of PTSD: a review. Int J Behav Consult Ther. 2005;1:223-238.
14. Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268-280.
15. Forneris CA, Gartlehner G, Brownley KA, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med. 2013;44:635-650.
16. Trivedi RB, Post EP, Sun H, et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health. 2015;105:2564-2569.
17. United States Census Bureau. Facts for features: Veteran’s day 2016: Nov. 11. Available at: https://www.census.gov/newsroom/facts-for-features/2016/cb16-ff21.html. Accessed August 16, 2017.
18. United States Census Bureau. U.S. and World Population Clock. Available at: https://www.census.gov/popclock/. Accessed August 16, 2017.
19. American Psychiatric Association. Guidelines and implementation. In: Practice Guidelines for the Psychiatric Evaluation of Adults. 3rd ed. Arlington, Va: American Psychiatric Association; 2015:9-45.
20. Williams AA, Williams M. A guide to performing pelvic speculum exams: a patient-centered approach to reducing iatrogenic effects. Teach Learn Med. 2013;25:383-391.
21. U.S. Department of Veterans Affairs. Life events checklist for DSM-5 (LEC-5). Available at: http://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp. Accessed September 13, 2017.
22. U.S. Department of Veterans Affairs. Primary care PTSD screen for DSM-5 (PC-PTSD). Available at: http://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp. Accessed September 13, 2017.
23. Spoont M, Arbisi P, Fu S, et al. Screening for Post-Traumatic Stress Disorder (PTSD) in Primary Care: A Systematic Review. Available at: https://www.ncbi.nlm.nih.gov/books/NBK126691/. Accessed Sept 13, 2017
24. Gallagher MW, Thompson-Hollands J, Bourgeois ML, et al. Cognitive behavioral treatments for adult posttraumatic stress disorder: current status and future directions. J Contemp Psychother. 2015;45:235-243.
25. Kar N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: a review. Neuropsychiatr Dis Treat. 2011;7:167-181.
26. Cusack K, Jonas DE, Forneris CA, et al. Psychological treatments for adults with posttraumatic stress disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2016;43:128-141.
27. Thompson BL, Luoma JB, LeJeune JT. Using acceptance and commitment therapy to guide exposure-based interventions for posttraumatic stress disorder. J Contemp Psychother. 2013;43:133-140.
28. Lohr JM, Hooke W, Gist R, et al. Novel and controversial treatments for trauma-related stress disorders. In: Lilienfeld SO, Lynn SJ, Lohr JM, eds. Science and Pseudoscience in Clinical Psychology. New York, NY: Guilford Press; 2003:243-272.
29. Sikes C, Sikes V. EMDR: Why the controversy? Traumatol. 2003;9:169-182.
30. Davidson PR, Parker KCH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol. 2001;69:305-316.
31. Devilly GJ. Power therapies and possible threats to the science of psychology and psychiatry. Aust N Z J Psychiatry. 2005;39:437-445.
THE CASE
DeSean W,* a 47-year-old man, returned to his primary care clinic with a new complaint of epigastric burning that had been bothering him for the past 4 months. He had tried several over-the-counter remedies, which provided no relief. He also remained concerned—despite assurances to the contrary at previous clinic visits—that he had contracted a sexually-transmitted disease (STD) after going to a bar one night 4 to 5 months ago. At 2 other clinic visits since that time, STD test results were negative. At this current visit, symptoms and details of sexual history were unchanged since the last visit, with the exception of the epigastric pain.
When asked if he thought he had contracted an STD through a sexual encounter the night he went to the bar, he emphatically said he would not cheat on his wife. Surprisingly, given his concern, he avoided further discussion on modes of contracting an STD.
The physician prescribed ranitidine 150 mg bid for the epigastric burning and explained, once more, the significance of the STD test results. However, he also decided to further examine Mr. W’s concern about STDs and the night he may have contracted one.
HOW WOULD YOU PROCEED WITH THIS PATIENT?
*The patient’s name has been changed to protect his privacy.
SCOPE OF THE PROBLEM
Despite being as common as asthma, posttraumatic stress disorder (PTSD) often remains undiagnosed and untreated in primary care.1 In brief, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines PTSD as persistent and long-term changes in thoughts or mood following actual or threatened exposure to death, serious injury, or sexual assault that leads to re-experiencing, functional impairment, physiologic stress reactions, and avoidance of thoughts or situations associated with the original trauma.2 More than one in 10 women and one in 20 men experience PTSD in their lifetime.2,3 Population-based studies have not yet determined the prevalence among children.3 Almost 40% of US adults report having experienced a trauma before age 13, and about one-third of these go on to develop PTSD.4
Individuals with PTSD have higher rates of somatic complaints, overall medical utilization, prescription use, physical and social disability, attempted suicide, and all-cause mortality.3,5-7 PTSD is associated with increased risk for cardiac, gastrointestinal, metabolic, and immunologic illnesses, other psychiatric illnesses, risky health behaviors, and decreased medical adherence.4,6 Additionally, prevention and treatment efforts for STDs and obesity are less effective among those with trauma histories.4 Thus, detection and treatment of PTSD improves the likelihood of successfully treating other health concerns.
THE ESSENTIALS OF A PTSD DIAGNOSIS
DSM-5 diagnosis of PTSD requires the experience of a trauma and resultant symptoms from each of 4 symptom-clusters:2
- one or more re-experiencing symptoms (eg, intrusive memories or recurrent distressing dreams, psychological distress or physiologic reactions to reminders of the trauma)
- one or more avoidance symptoms (eg, avoidance of trauma memories or of people and places that trigger a reminder of the trauma)
- two or more changes in thoughts or mood (eg, negative beliefs about self or others, social detachment, anhedonia)
- two or more changes in arousal activity (eg, sleep problems, hypervigilance, inability to concentrate).
Since many people experiencing traumas do not develop PTSD,5,8 symptoms must last at least one month to meet the criteria for diagnosis.2 Sexual trauma, experiencing multiple traumas, and lack of social support increase the risk that an individual will develop PTSD.9-11 Notably, symptom onset will be delayed 6 months or more in some individuals,2,8 making it more difficult for those patients and clinicians to connect symptoms to the trauma.12
Differential diagnosis
PTSD must be differentiated from other mental health conditions with overlapping symptoms (TABLE 12,8,13), but it may also be comorbid with one or more of these other conditions. When patients with PTSD do report mental health symptoms, providers often focus on the depressive symptoms that overlap with PTSD, and on substance use, which often accompanies PTSD, leaving PTSD undetected.9
Given that depressed/irritable mood, decreased participation in pleasurable activities, negative views of the world, attention difficulties, sleep difficulties, feelings of guilt, and agitation/restlessness are symptoms of both depression and PTSD,2 it is particularly important to screen patients with depressive symptoms for trauma history.
Why PTSD is often missed
Due to the impact of PTSD on overall health, the rates of PTSD in primary care clinics may be higher than in the general population.14 Thus, primary care clinicians are likely seeing PTSD more often than they realize. In fact, a systematic review showed that clinicians detected 0% to 52% of their patients with PTSD, missing at least half of all PTSD diagnoses.9
Detecting PTSD can be challenging for several reasons. Symptoms can span the emotional, social, physical, and behavioral aspects of an individual’s life, so patients and clinicians alike may regard symptoms as unrelated to PTSD.8 Primary symptom presentation may vary, with some people reporting anxiety symptoms, others mostly depressive symptoms, and others arousal, dissociative, or—as in our patient’s case—somatic symptoms.2 In affected children, parents may report emotional or behavioral problems without mentioning the trauma.2 Additionally, for traumas that were not a single event, such as long-term child abuse, patients may have difficulty identifying symptom onset.2
CASE
The physician screened Mr. W for trauma exposure as part of the differential. Mr. W revealed that he had blacked out at the bar, despite drinking only moderately, and that he awoke with anal pain. He believed he had been drugged and sexually assaulted. Further screening for PTSD symptoms related to this event confirmed multiple associated symptoms. He acknowledged that his epigastric pain had started soon after the trauma and, after further discussion, began to link his stomach pain and other new symptoms revealed by the PTSD screen (hypervigilance, avoidance, change in mood) to the trauma.
As happened in this case, most PTSD patients present with somatic complaints rather than reporting a traumatic experience and having associated effects. This in turn usually leads clinicians to consider only non-PTSD diagnoses.6,9,15 Core avoidance symptoms are a major reason for such a presentation in PTSD patients.14 Patients avoid thoughts, feelings, and conversations that remind them of the trauma.13 As a result, they are less likely to voluntarily report trauma. They avoid thinking about how their current symptoms may be associated with their trauma and are reluctant to talk about their trauma with clinicians.5,9,8,12
Another barrier to diagnosis is a belief that PTSD is primarily experienced by combat veterans1 (TABLE 22,4-6,8,9,12,14-18). While PTSD is detected more often among veterans due to regular screening through the Department of Veterans Affairs,14 the vast majority of PTSD cases are related to civilian traumas such as sexual assault, child abuse, and car accidents.5,9 In fact, the estimated
SCREENING: WHAT TO LOOK FOR
Since individuals with PTSD mainly seek treatment for associated physical symptoms,14 primary care is particularly important for identification of PTSD and treatment access. The US Preventative Services Task Force does not yet have any recommendations for screening for PTSD. The American Psychiatric Association recommends that a trauma history be included in all initial psychiatric evaluations of adults.19 Screens can target high-risk populations and can be repeated across the lifespan,9 as traumas can occur at any age and symptoms may not emerge until years after the trauma.2,4 Factors in a patient’s history associated with high risk of PTSD include the following:
- known trauma exposure (eg, treatment at the emergency department following motor vehicle collision, natural disaster, assault),6
- frequent medical visits or unexplained physical symptoms,5,8
- family members who are trauma victims,8
- involvement in juvenile justice system,4,12
- sensitive or invasive exams (eg, pelvic exams) that trigger symptoms or contribute to retraumatization,12,20 and
- any medical condition (eg, hypertension, chronic pain, sleep disorder), self-destructive behavior (eg, drug or alcohol abuse, low impulse control), or social/occupational issues (eg, unemployment, social isolation, fighting) with a known link to PTSD.2,4,6,8
The first step in screening. Given a patient’s reported symptoms, assess for trauma exposure to determine whether PTSD should be included in the differential diagnosis. Overlooking PTSD as a possible source of symptoms can result in misattributing them to other causes.4,8 Listing common traumas, or using a standardized list such as the Life Events Checklist, can help identify patients with trauma exposure.8,21 However, do not make the patient provide details of the traumatic event(s), as that can exacerbate symptoms if PTSD is present.6 It is sufficient to know the category of the trauma (eg, sexual assault) without making the patient describe who was involved and what happened.6
The second step in screening. If a patient reveals trauma exposure, consider using an instrument such as the Primary Care PTSD Screen (PC-PTSD) or the PTSD Checklist, both available online, to screen for PTSD symptoms related to the identified trauma.6,9,21-23 Since these measures screen for symptoms but do not ask about trauma exposure, false positives can occur if a trauma is not first identified (such as through the Life Events Checklist) due to symptom overlap with other conditions (TABLE 12,8,13).21
Treatment is effective, even decades after a traumatic event
Provide anyone who has been traumatized with information about common after effects, symptoms of PTSD, and available treatments.8 Keep in mind that initial symptom severity after trauma exposure does not correlate with long-term symptoms,8 and about half of adults will recover without treatment within 3 months.1,2,5 The first month of symptoms may be addressed with patient education and watchful waiting. But if symptoms don’t subside after a month, consider offering treatment1 with the understanding that, for some individuals, symptoms may yet resolve on their own.
Detecting and treating PTSD early can decrease its deleterious effects on health and cut down on years of functional impairment.1 Even decades after an initial traumatic event, PTSD treatments can be effective.8 Children may experience functional impairment without meeting full criteria for PTSD, and can also benefit from treatment.7
INTEGRATING EXPOSURE AND COGNITIVE THERAPIES IS KEY
Offer any patient who meets criteria for PTSD a referral for exposure therapy and trauma-focused cognitive behavioral therapy (TF-CBT), the first-line treatments for PTSD.1,4,8,24,25
Exposure therapies for PTSD are supported by strong evidence and help patients to become desensitized to distressful memories through gradual, repeated exposures in a relaxed or safe space.8,26
Cognitive methods, such as cognitive processing therapy, cognitive behavioral therapy, and cognitive reprocessing have moderate strength of evidence, and may be combined with exposure therapy.26 Cognitive therapies help patients change thoughts, beliefs, and behaviors that contribute to PTSD symptoms.8,26
Exposure and TF-CBT have the most empirical evidence for child, adolescent, and adult PTSD, and are effective for the range of PTSD symptoms,4,8,25 including avoidance—a fundamental component of PTSD that drives other PTSD symptoms27—comorbid depression, and other emotions associated with trauma (eg, shame, guilt, and anger).8,25 Family involvement is recommended for children and adolescents.4
For patients with comorbid substance abuse, offer integrated PTSD/substance abuse treatment, which is more effective than isolated treatment of each.4 Relaxation training can be helpful as an adjunct to TF-CBT, but is not sufficient as a stand-alone treatment.13 Other psychotherapies, such as supportive, psychodynamic, systemic, and hypnotherapy, have not proved effective.14
Eye Movement Desensitization and Reprocessing (EMDR), a much publicized but controversial treatment, integrates components of exposure and cognitive therapies with therapist-directed eye movements.28-30 Patients imagine their trauma while the therapist directs their eye movements, which is thought to provide exposure to trauma images and memories, thereby reducing symptoms. EMDR has been found to reduce PTSD symptoms with a low to moderate strength-of-evidence rating.26 However, it has not proved more effective than other exposure and cognitive therapies, and its unique component (eg, eye movements) has not added any effect to outcomes.28-31
Other newer therapies, such as Acceptance and Commitment Therapy7,24,27 and online and computer-assisted treatments, are being evaluated.14
Medications take on an adjunct role to therapy
Drug treatment of PTSD has not been effective in children or adolescents.4,8 In adults, medications have helped relieve some symptoms of PTSD. However, given their low effect sizes, medications are not recommended as first-line treatments over exposure and TF-CBT. Their usefulness lies chiefly in an adjunct role to exposure and cognitive therapies or for patients who refuse psychotherapy.4,8,25
Selective serotonin reuptake inhibitors such as fluoxetine, paroxetine, and sertraline, have been effective for such PTSD symptoms as intrusive thoughts, negative or irritable mood, anxiety, restlessness, attention difficulties, and hyperarousal.1,8
While benzodiazepines have been used to control anxiety, hyperarousal, and insomnia, they have not been effective for most other PTSD symptoms, including avoidance, re-experiencing, and cognitive symptoms. Furthermore, they are not recommended given their augmentative effect on other related symptoms and associated conditions (eg, dissociation, disinhibition, substance abuse) and possible interference with desensitization that occurs in exposure therapy.1,5
If a patient has significant insomnia and PTSD-related nightmares, consider starting prazosin at 1 mg/d and titrating up to an effective dose, which typically ranges from 5 to 20 mg per day.1,5 Additionally, trazodone or antihistamines may be used to enhance sleep.1
COORDINATION OF CARE
Upon identifying PTSD and offering treatment, introduce the patient to a mental health provider as part of the referral process, which strongly encourages patient engagement in treatment.14 Collaborate with the psychotherapist throughout treatment to facilitate a biopsychosocial approach to the patient’s care, and coordinate the monitoring and treatment of any comorbid physical conditions.
The Substance Abuse and Mental Health Services Administration has proposed a framework for multisystem Trauma-Informed Care (TIC), in which the primary care physician has many roles, including:12,20
- recording or communicating sensitive private information to other providers through the electronic medical record in a manner that does not interfere with a patient’s development of trust or lead to exposure and retraumatization,
- performing invasive physical exams in a sensitive and patient-centered manner, and
- using support and shared decision-making in clinical encounters.
Physicians can also connect patients with PTSD to programs or groups that aid in developing resilience, such as physical exercise classes, social support networks, and community involvement opportunities.4
CASE
The physician referred Mr. W to an onsite psychologist. At a subsequent clinic visit in which he was seen by a different primary care physician, Mr. W expressed new concerns about shoulder pain and changes in a mole. During this visit, Mr. W was asked whether he had followed up on the earlier referral for counseling. He replied that he had attended an intake appointment with the psychologist, but that he had not wanted to talk about what had happened to him and therefore avoided future appointments.*
He remained concerned that he might have an STD, but declined medication for PTSD because he felt he was “moving on” with his life.
*Author’s note: Getting patients to open up about their trauma exposure can be difficult. If the patient isn’t ready, simply bringing up the experience can trigger avoidance. It’s often helpful to encourage patients to first develop a relationship with their therapist, then later discuss the details of their trauma when they are ready. This encourages patients to engage in the counseling process.
CORRESPONDENCE
Adrienne A. Williams, PhD, Department of Family Medicine, University of Illinois at Chicago College of Medicine, 1919 W Taylor Street, MC663, Chicago, IL 60612; awms@uic.edu.
THE CASE
DeSean W,* a 47-year-old man, returned to his primary care clinic with a new complaint of epigastric burning that had been bothering him for the past 4 months. He had tried several over-the-counter remedies, which provided no relief. He also remained concerned—despite assurances to the contrary at previous clinic visits—that he had contracted a sexually-transmitted disease (STD) after going to a bar one night 4 to 5 months ago. At 2 other clinic visits since that time, STD test results were negative. At this current visit, symptoms and details of sexual history were unchanged since the last visit, with the exception of the epigastric pain.
When asked if he thought he had contracted an STD through a sexual encounter the night he went to the bar, he emphatically said he would not cheat on his wife. Surprisingly, given his concern, he avoided further discussion on modes of contracting an STD.
The physician prescribed ranitidine 150 mg bid for the epigastric burning and explained, once more, the significance of the STD test results. However, he also decided to further examine Mr. W’s concern about STDs and the night he may have contracted one.
HOW WOULD YOU PROCEED WITH THIS PATIENT?
*The patient’s name has been changed to protect his privacy.
SCOPE OF THE PROBLEM
Despite being as common as asthma, posttraumatic stress disorder (PTSD) often remains undiagnosed and untreated in primary care.1 In brief, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines PTSD as persistent and long-term changes in thoughts or mood following actual or threatened exposure to death, serious injury, or sexual assault that leads to re-experiencing, functional impairment, physiologic stress reactions, and avoidance of thoughts or situations associated with the original trauma.2 More than one in 10 women and one in 20 men experience PTSD in their lifetime.2,3 Population-based studies have not yet determined the prevalence among children.3 Almost 40% of US adults report having experienced a trauma before age 13, and about one-third of these go on to develop PTSD.4
Individuals with PTSD have higher rates of somatic complaints, overall medical utilization, prescription use, physical and social disability, attempted suicide, and all-cause mortality.3,5-7 PTSD is associated with increased risk for cardiac, gastrointestinal, metabolic, and immunologic illnesses, other psychiatric illnesses, risky health behaviors, and decreased medical adherence.4,6 Additionally, prevention and treatment efforts for STDs and obesity are less effective among those with trauma histories.4 Thus, detection and treatment of PTSD improves the likelihood of successfully treating other health concerns.
THE ESSENTIALS OF A PTSD DIAGNOSIS
DSM-5 diagnosis of PTSD requires the experience of a trauma and resultant symptoms from each of 4 symptom-clusters:2
- one or more re-experiencing symptoms (eg, intrusive memories or recurrent distressing dreams, psychological distress or physiologic reactions to reminders of the trauma)
- one or more avoidance symptoms (eg, avoidance of trauma memories or of people and places that trigger a reminder of the trauma)
- two or more changes in thoughts or mood (eg, negative beliefs about self or others, social detachment, anhedonia)
- two or more changes in arousal activity (eg, sleep problems, hypervigilance, inability to concentrate).
Since many people experiencing traumas do not develop PTSD,5,8 symptoms must last at least one month to meet the criteria for diagnosis.2 Sexual trauma, experiencing multiple traumas, and lack of social support increase the risk that an individual will develop PTSD.9-11 Notably, symptom onset will be delayed 6 months or more in some individuals,2,8 making it more difficult for those patients and clinicians to connect symptoms to the trauma.12
Differential diagnosis
PTSD must be differentiated from other mental health conditions with overlapping symptoms (TABLE 12,8,13), but it may also be comorbid with one or more of these other conditions. When patients with PTSD do report mental health symptoms, providers often focus on the depressive symptoms that overlap with PTSD, and on substance use, which often accompanies PTSD, leaving PTSD undetected.9
Given that depressed/irritable mood, decreased participation in pleasurable activities, negative views of the world, attention difficulties, sleep difficulties, feelings of guilt, and agitation/restlessness are symptoms of both depression and PTSD,2 it is particularly important to screen patients with depressive symptoms for trauma history.
Why PTSD is often missed
Due to the impact of PTSD on overall health, the rates of PTSD in primary care clinics may be higher than in the general population.14 Thus, primary care clinicians are likely seeing PTSD more often than they realize. In fact, a systematic review showed that clinicians detected 0% to 52% of their patients with PTSD, missing at least half of all PTSD diagnoses.9
Detecting PTSD can be challenging for several reasons. Symptoms can span the emotional, social, physical, and behavioral aspects of an individual’s life, so patients and clinicians alike may regard symptoms as unrelated to PTSD.8 Primary symptom presentation may vary, with some people reporting anxiety symptoms, others mostly depressive symptoms, and others arousal, dissociative, or—as in our patient’s case—somatic symptoms.2 In affected children, parents may report emotional or behavioral problems without mentioning the trauma.2 Additionally, for traumas that were not a single event, such as long-term child abuse, patients may have difficulty identifying symptom onset.2
CASE
The physician screened Mr. W for trauma exposure as part of the differential. Mr. W revealed that he had blacked out at the bar, despite drinking only moderately, and that he awoke with anal pain. He believed he had been drugged and sexually assaulted. Further screening for PTSD symptoms related to this event confirmed multiple associated symptoms. He acknowledged that his epigastric pain had started soon after the trauma and, after further discussion, began to link his stomach pain and other new symptoms revealed by the PTSD screen (hypervigilance, avoidance, change in mood) to the trauma.
As happened in this case, most PTSD patients present with somatic complaints rather than reporting a traumatic experience and having associated effects. This in turn usually leads clinicians to consider only non-PTSD diagnoses.6,9,15 Core avoidance symptoms are a major reason for such a presentation in PTSD patients.14 Patients avoid thoughts, feelings, and conversations that remind them of the trauma.13 As a result, they are less likely to voluntarily report trauma. They avoid thinking about how their current symptoms may be associated with their trauma and are reluctant to talk about their trauma with clinicians.5,9,8,12
Another barrier to diagnosis is a belief that PTSD is primarily experienced by combat veterans1 (TABLE 22,4-6,8,9,12,14-18). While PTSD is detected more often among veterans due to regular screening through the Department of Veterans Affairs,14 the vast majority of PTSD cases are related to civilian traumas such as sexual assault, child abuse, and car accidents.5,9 In fact, the estimated
SCREENING: WHAT TO LOOK FOR
Since individuals with PTSD mainly seek treatment for associated physical symptoms,14 primary care is particularly important for identification of PTSD and treatment access. The US Preventative Services Task Force does not yet have any recommendations for screening for PTSD. The American Psychiatric Association recommends that a trauma history be included in all initial psychiatric evaluations of adults.19 Screens can target high-risk populations and can be repeated across the lifespan,9 as traumas can occur at any age and symptoms may not emerge until years after the trauma.2,4 Factors in a patient’s history associated with high risk of PTSD include the following:
- known trauma exposure (eg, treatment at the emergency department following motor vehicle collision, natural disaster, assault),6
- frequent medical visits or unexplained physical symptoms,5,8
- family members who are trauma victims,8
- involvement in juvenile justice system,4,12
- sensitive or invasive exams (eg, pelvic exams) that trigger symptoms or contribute to retraumatization,12,20 and
- any medical condition (eg, hypertension, chronic pain, sleep disorder), self-destructive behavior (eg, drug or alcohol abuse, low impulse control), or social/occupational issues (eg, unemployment, social isolation, fighting) with a known link to PTSD.2,4,6,8
The first step in screening. Given a patient’s reported symptoms, assess for trauma exposure to determine whether PTSD should be included in the differential diagnosis. Overlooking PTSD as a possible source of symptoms can result in misattributing them to other causes.4,8 Listing common traumas, or using a standardized list such as the Life Events Checklist, can help identify patients with trauma exposure.8,21 However, do not make the patient provide details of the traumatic event(s), as that can exacerbate symptoms if PTSD is present.6 It is sufficient to know the category of the trauma (eg, sexual assault) without making the patient describe who was involved and what happened.6
The second step in screening. If a patient reveals trauma exposure, consider using an instrument such as the Primary Care PTSD Screen (PC-PTSD) or the PTSD Checklist, both available online, to screen for PTSD symptoms related to the identified trauma.6,9,21-23 Since these measures screen for symptoms but do not ask about trauma exposure, false positives can occur if a trauma is not first identified (such as through the Life Events Checklist) due to symptom overlap with other conditions (TABLE 12,8,13).21
Treatment is effective, even decades after a traumatic event
Provide anyone who has been traumatized with information about common after effects, symptoms of PTSD, and available treatments.8 Keep in mind that initial symptom severity after trauma exposure does not correlate with long-term symptoms,8 and about half of adults will recover without treatment within 3 months.1,2,5 The first month of symptoms may be addressed with patient education and watchful waiting. But if symptoms don’t subside after a month, consider offering treatment1 with the understanding that, for some individuals, symptoms may yet resolve on their own.
Detecting and treating PTSD early can decrease its deleterious effects on health and cut down on years of functional impairment.1 Even decades after an initial traumatic event, PTSD treatments can be effective.8 Children may experience functional impairment without meeting full criteria for PTSD, and can also benefit from treatment.7
INTEGRATING EXPOSURE AND COGNITIVE THERAPIES IS KEY
Offer any patient who meets criteria for PTSD a referral for exposure therapy and trauma-focused cognitive behavioral therapy (TF-CBT), the first-line treatments for PTSD.1,4,8,24,25
Exposure therapies for PTSD are supported by strong evidence and help patients to become desensitized to distressful memories through gradual, repeated exposures in a relaxed or safe space.8,26
Cognitive methods, such as cognitive processing therapy, cognitive behavioral therapy, and cognitive reprocessing have moderate strength of evidence, and may be combined with exposure therapy.26 Cognitive therapies help patients change thoughts, beliefs, and behaviors that contribute to PTSD symptoms.8,26
Exposure and TF-CBT have the most empirical evidence for child, adolescent, and adult PTSD, and are effective for the range of PTSD symptoms,4,8,25 including avoidance—a fundamental component of PTSD that drives other PTSD symptoms27—comorbid depression, and other emotions associated with trauma (eg, shame, guilt, and anger).8,25 Family involvement is recommended for children and adolescents.4
For patients with comorbid substance abuse, offer integrated PTSD/substance abuse treatment, which is more effective than isolated treatment of each.4 Relaxation training can be helpful as an adjunct to TF-CBT, but is not sufficient as a stand-alone treatment.13 Other psychotherapies, such as supportive, psychodynamic, systemic, and hypnotherapy, have not proved effective.14
Eye Movement Desensitization and Reprocessing (EMDR), a much publicized but controversial treatment, integrates components of exposure and cognitive therapies with therapist-directed eye movements.28-30 Patients imagine their trauma while the therapist directs their eye movements, which is thought to provide exposure to trauma images and memories, thereby reducing symptoms. EMDR has been found to reduce PTSD symptoms with a low to moderate strength-of-evidence rating.26 However, it has not proved more effective than other exposure and cognitive therapies, and its unique component (eg, eye movements) has not added any effect to outcomes.28-31
Other newer therapies, such as Acceptance and Commitment Therapy7,24,27 and online and computer-assisted treatments, are being evaluated.14
Medications take on an adjunct role to therapy
Drug treatment of PTSD has not been effective in children or adolescents.4,8 In adults, medications have helped relieve some symptoms of PTSD. However, given their low effect sizes, medications are not recommended as first-line treatments over exposure and TF-CBT. Their usefulness lies chiefly in an adjunct role to exposure and cognitive therapies or for patients who refuse psychotherapy.4,8,25
Selective serotonin reuptake inhibitors such as fluoxetine, paroxetine, and sertraline, have been effective for such PTSD symptoms as intrusive thoughts, negative or irritable mood, anxiety, restlessness, attention difficulties, and hyperarousal.1,8
While benzodiazepines have been used to control anxiety, hyperarousal, and insomnia, they have not been effective for most other PTSD symptoms, including avoidance, re-experiencing, and cognitive symptoms. Furthermore, they are not recommended given their augmentative effect on other related symptoms and associated conditions (eg, dissociation, disinhibition, substance abuse) and possible interference with desensitization that occurs in exposure therapy.1,5
If a patient has significant insomnia and PTSD-related nightmares, consider starting prazosin at 1 mg/d and titrating up to an effective dose, which typically ranges from 5 to 20 mg per day.1,5 Additionally, trazodone or antihistamines may be used to enhance sleep.1
COORDINATION OF CARE
Upon identifying PTSD and offering treatment, introduce the patient to a mental health provider as part of the referral process, which strongly encourages patient engagement in treatment.14 Collaborate with the psychotherapist throughout treatment to facilitate a biopsychosocial approach to the patient’s care, and coordinate the monitoring and treatment of any comorbid physical conditions.
The Substance Abuse and Mental Health Services Administration has proposed a framework for multisystem Trauma-Informed Care (TIC), in which the primary care physician has many roles, including:12,20
- recording or communicating sensitive private information to other providers through the electronic medical record in a manner that does not interfere with a patient’s development of trust or lead to exposure and retraumatization,
- performing invasive physical exams in a sensitive and patient-centered manner, and
- using support and shared decision-making in clinical encounters.
Physicians can also connect patients with PTSD to programs or groups that aid in developing resilience, such as physical exercise classes, social support networks, and community involvement opportunities.4
CASE
The physician referred Mr. W to an onsite psychologist. At a subsequent clinic visit in which he was seen by a different primary care physician, Mr. W expressed new concerns about shoulder pain and changes in a mole. During this visit, Mr. W was asked whether he had followed up on the earlier referral for counseling. He replied that he had attended an intake appointment with the psychologist, but that he had not wanted to talk about what had happened to him and therefore avoided future appointments.*
He remained concerned that he might have an STD, but declined medication for PTSD because he felt he was “moving on” with his life.
*Author’s note: Getting patients to open up about their trauma exposure can be difficult. If the patient isn’t ready, simply bringing up the experience can trigger avoidance. It’s often helpful to encourage patients to first develop a relationship with their therapist, then later discuss the details of their trauma when they are ready. This encourages patients to engage in the counseling process.
CORRESPONDENCE
Adrienne A. Williams, PhD, Department of Family Medicine, University of Illinois at Chicago College of Medicine, 1919 W Taylor Street, MC663, Chicago, IL 60612; awms@uic.edu.
1. Bobo WV, Warner CH, Warner CM. The management of post traumatic stress disorder (PTSD) in the primary care setting. South Med J. 2007;100:797-802.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
3. Gradus JL. Epidemiology of PTSD. National Center for PTSD. Available at: http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Updated 2017. Accessed August 16, 2017.
4. Gerson R, Rappaport N. Traumatic stress and posttraumatic stress disorder in youth: recent research findings on clinical impact, assessment, and treatment. J Adolesc Health. 2013;52:137-143.
5. Zohar J, Juven-Wetzler A, Myers V, et al. Post-traumatic stress disorder: facts and fiction. Curr Opin Psychiatry. 2008;21:74-77.
6. Spoont MR, Williams JW Jr, Kehle-Forbes S, et al. Does this patient have posttraumatic stress disorder? Rational clinical examination systematic review. JAMA. 2015;314:501-510.
7. Woidneck MR, Morrison KL, Twohig MP. Acceptance and commitment therapy for the treatment of posttraumatic stress among adolescents. Behav Modif. 2014;38:451-476.
8. National Collaborating Centre for Mental Health (UK). Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. Available at: https://www.ncbi.nlm.nih.gov/books/NBK56494. Accessed August 16, 2017.
9. Greene T, Neria Y, Gross R. Prevalence, detection and correlates of PTSD in the primary care setting: a systematic review. J Clin Psychol Med Settings. 2016;23:160-180.
10. Gavranidou M, Rosner R. The weaker sex? Gender and post-traumatic stress disorder. Depress Anxiety. 2003;17:130-139.
11. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748-766.
12. SAMHSA’s Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. Available at: http://store.samhsa.gov/shin/content/SMA14-4884/SMA14-4884.pdf. Accessed September 13, 2017.
13. Mulick PS, Landes SJ, Kanter JW. Contextual behavior therapies in the treatment of PTSD: a review. Int J Behav Consult Ther. 2005;1:223-238.
14. Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268-280.
15. Forneris CA, Gartlehner G, Brownley KA, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med. 2013;44:635-650.
16. Trivedi RB, Post EP, Sun H, et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health. 2015;105:2564-2569.
17. United States Census Bureau. Facts for features: Veteran’s day 2016: Nov. 11. Available at: https://www.census.gov/newsroom/facts-for-features/2016/cb16-ff21.html. Accessed August 16, 2017.
18. United States Census Bureau. U.S. and World Population Clock. Available at: https://www.census.gov/popclock/. Accessed August 16, 2017.
19. American Psychiatric Association. Guidelines and implementation. In: Practice Guidelines for the Psychiatric Evaluation of Adults. 3rd ed. Arlington, Va: American Psychiatric Association; 2015:9-45.
20. Williams AA, Williams M. A guide to performing pelvic speculum exams: a patient-centered approach to reducing iatrogenic effects. Teach Learn Med. 2013;25:383-391.
21. U.S. Department of Veterans Affairs. Life events checklist for DSM-5 (LEC-5). Available at: http://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp. Accessed September 13, 2017.
22. U.S. Department of Veterans Affairs. Primary care PTSD screen for DSM-5 (PC-PTSD). Available at: http://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp. Accessed September 13, 2017.
23. Spoont M, Arbisi P, Fu S, et al. Screening for Post-Traumatic Stress Disorder (PTSD) in Primary Care: A Systematic Review. Available at: https://www.ncbi.nlm.nih.gov/books/NBK126691/. Accessed Sept 13, 2017
24. Gallagher MW, Thompson-Hollands J, Bourgeois ML, et al. Cognitive behavioral treatments for adult posttraumatic stress disorder: current status and future directions. J Contemp Psychother. 2015;45:235-243.
25. Kar N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: a review. Neuropsychiatr Dis Treat. 2011;7:167-181.
26. Cusack K, Jonas DE, Forneris CA, et al. Psychological treatments for adults with posttraumatic stress disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2016;43:128-141.
27. Thompson BL, Luoma JB, LeJeune JT. Using acceptance and commitment therapy to guide exposure-based interventions for posttraumatic stress disorder. J Contemp Psychother. 2013;43:133-140.
28. Lohr JM, Hooke W, Gist R, et al. Novel and controversial treatments for trauma-related stress disorders. In: Lilienfeld SO, Lynn SJ, Lohr JM, eds. Science and Pseudoscience in Clinical Psychology. New York, NY: Guilford Press; 2003:243-272.
29. Sikes C, Sikes V. EMDR: Why the controversy? Traumatol. 2003;9:169-182.
30. Davidson PR, Parker KCH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol. 2001;69:305-316.
31. Devilly GJ. Power therapies and possible threats to the science of psychology and psychiatry. Aust N Z J Psychiatry. 2005;39:437-445.
1. Bobo WV, Warner CH, Warner CM. The management of post traumatic stress disorder (PTSD) in the primary care setting. South Med J. 2007;100:797-802.
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
3. Gradus JL. Epidemiology of PTSD. National Center for PTSD. Available at: http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp. Updated 2017. Accessed August 16, 2017.
4. Gerson R, Rappaport N. Traumatic stress and posttraumatic stress disorder in youth: recent research findings on clinical impact, assessment, and treatment. J Adolesc Health. 2013;52:137-143.
5. Zohar J, Juven-Wetzler A, Myers V, et al. Post-traumatic stress disorder: facts and fiction. Curr Opin Psychiatry. 2008;21:74-77.
6. Spoont MR, Williams JW Jr, Kehle-Forbes S, et al. Does this patient have posttraumatic stress disorder? Rational clinical examination systematic review. JAMA. 2015;314:501-510.
7. Woidneck MR, Morrison KL, Twohig MP. Acceptance and commitment therapy for the treatment of posttraumatic stress among adolescents. Behav Modif. 2014;38:451-476.
8. National Collaborating Centre for Mental Health (UK). Post-traumatic stress disorder: the management of PTSD in adults and children in primary and secondary care. Available at: https://www.ncbi.nlm.nih.gov/books/NBK56494. Accessed August 16, 2017.
9. Greene T, Neria Y, Gross R. Prevalence, detection and correlates of PTSD in the primary care setting: a systematic review. J Clin Psychol Med Settings. 2016;23:160-180.
10. Gavranidou M, Rosner R. The weaker sex? Gender and post-traumatic stress disorder. Depress Anxiety. 2003;17:130-139.
11. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748-766.
12. SAMHSA’s Trauma and Justice Strategic Initiative. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. Available at: http://store.samhsa.gov/shin/content/SMA14-4884/SMA14-4884.pdf. Accessed September 13, 2017.
13. Mulick PS, Landes SJ, Kanter JW. Contextual behavior therapies in the treatment of PTSD: a review. Int J Behav Consult Ther. 2005;1:223-238.
14. Possemato K. The current state of intervention research for posttraumatic stress disorder within the primary care setting. J Clin Psychol Med Settings. 2011;18:268-280.
15. Forneris CA, Gartlehner G, Brownley KA, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med. 2013;44:635-650.
16. Trivedi RB, Post EP, Sun H, et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health. 2015;105:2564-2569.
17. United States Census Bureau. Facts for features: Veteran’s day 2016: Nov. 11. Available at: https://www.census.gov/newsroom/facts-for-features/2016/cb16-ff21.html. Accessed August 16, 2017.
18. United States Census Bureau. U.S. and World Population Clock. Available at: https://www.census.gov/popclock/. Accessed August 16, 2017.
19. American Psychiatric Association. Guidelines and implementation. In: Practice Guidelines for the Psychiatric Evaluation of Adults. 3rd ed. Arlington, Va: American Psychiatric Association; 2015:9-45.
20. Williams AA, Williams M. A guide to performing pelvic speculum exams: a patient-centered approach to reducing iatrogenic effects. Teach Learn Med. 2013;25:383-391.
21. U.S. Department of Veterans Affairs. Life events checklist for DSM-5 (LEC-5). Available at: http://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp. Accessed September 13, 2017.
22. U.S. Department of Veterans Affairs. Primary care PTSD screen for DSM-5 (PC-PTSD). Available at: http://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp. Accessed September 13, 2017.
23. Spoont M, Arbisi P, Fu S, et al. Screening for Post-Traumatic Stress Disorder (PTSD) in Primary Care: A Systematic Review. Available at: https://www.ncbi.nlm.nih.gov/books/NBK126691/. Accessed Sept 13, 2017
24. Gallagher MW, Thompson-Hollands J, Bourgeois ML, et al. Cognitive behavioral treatments for adult posttraumatic stress disorder: current status and future directions. J Contemp Psychother. 2015;45:235-243.
25. Kar N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: a review. Neuropsychiatr Dis Treat. 2011;7:167-181.
26. Cusack K, Jonas DE, Forneris CA, et al. Psychological treatments for adults with posttraumatic stress disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2016;43:128-141.
27. Thompson BL, Luoma JB, LeJeune JT. Using acceptance and commitment therapy to guide exposure-based interventions for posttraumatic stress disorder. J Contemp Psychother. 2013;43:133-140.
28. Lohr JM, Hooke W, Gist R, et al. Novel and controversial treatments for trauma-related stress disorders. In: Lilienfeld SO, Lynn SJ, Lohr JM, eds. Science and Pseudoscience in Clinical Psychology. New York, NY: Guilford Press; 2003:243-272.
29. Sikes C, Sikes V. EMDR: Why the controversy? Traumatol. 2003;9:169-182.
30. Davidson PR, Parker KCH. Eye movement desensitization and reprocessing (EMDR): a meta-analysis. J Consult Clin Psychol. 2001;69:305-316.
31. Devilly GJ. Power therapies and possible threats to the science of psychology and psychiatry. Aust N Z J Psychiatry. 2005;39:437-445.
Effectively engaging patients in everyday health-care decisions
The discipline of family medicine is committed to providing patient-centered care through recommendations that are grounded both in evidence and in patients’ personal values.1,2 The current health care environment, however, often demands heavy reliance on outcome-based performance metrics that can be insensitive to patient preferences.3 This tension necessitates models of decision-making that maximize reliance on measured performance, yet fulfill the clinician’s fiduciary responsibility to prioritize patients’ interests. The philosophy and practice of shared decision-making (SDM) can facilitate these aims.
The 3 elements of shared decision-making
SDM provides a framework for offering everyday medical advice and facilitating informed consent.4 Its 3 elements are:
- discussing with patients relevant information about their health conditions, possible treatments, and likely outcomes,
- clarifying and understanding a patient’s unique values and priorities and how they relate to the treatment options, and
- enabling a patient to select a care plan that is in keeping with his or her personal goals.5
This model is significant not only from a theoretical perspective, but also from a practical one. Studies have shown that both health outcomes and patient satisfaction improve when patients participate more actively in health care decision-making.6,7
Unfortunately, there is evidence that some decision-making practices in primary care settings remain inadequate. For example, unlike the standard disclosure of procedure risks in surgical settings, the burdens of cancer screening are frequently omitted from primary care discussions.8 Moreover, agreement about what should be disclosed, as well as how to disclose it, is still not sufficient. The following 3 recommendations, one for each element of SDM, aim to help clinicians effectively engage patients in everyday decision-making.
1. Provide patients with relevant information
The first element of SDM requires discussing the health-related information that is relevant to the patient’s decision-making process. The literature about informed consent supports explaining the risks that are common, as well as those that are particularly dangerous, and the likely benefits of recommended treatment, nontreatment, and alternative treatments.9 Moreover, adequate informed consent requires identifying what a reasonable person in a particular patient’s position would want to know.10
Accounting for “a patient’s position” is significant because it signals that personal factors (eg, the individual’s beliefs, goals, and familial responsibilities) are as important as the patient’s external clinical situation and what can be known by reviewing medical evidence. Incorporating a patient’s particular circumstances distinguishes patient-centered care from the mechanical application of generic best practices. This is the standard for what information should be provided.
When evidence is lacking. Clinicians facilitating decisions for which data is lacking should convey the best available evidence, including the inherent uncertainties. Like evidence-based medicine (EBM), the principles of SDM should be at work in most clinical encounters. The extent to which one engages in SDM depends upon the seriousness of the proposed interventions, the degree to which the decision is preference-sensitive, and the availability of evidence.
Statistics: Explain absolute and baseline risk
It is generally better to provide absolute risk rather than relative risk, because people perceive absolute risk reductions more accurately.11 Presentation of risks, in terms of relative risk or relative risk reduction, typically exaggerates the benefits of treatment, especially when the risk is small. This exaggeration makes it more likely that patients will accept interventions they might otherwise have rejected after reviewing the data more fully. Furthermore, relative risk statistics can impact clinicians’ perceptions, leading them to recommend an intervention more often than they might when absolute risk statistics are discussed.12
But even absolute risk, if presented on its own, can be misleading. A reasonable person trying to determine the value of an intervention needs to know his or her baseline risk of an event, in addition to his or her absolute risk with the intervention. For example, a hypothetical absolute risk reduction associated with a breast cancer treatment of 10% has different meanings, depending upon whether the baseline risk is 10% or 80%. A reduction from 10% to 0% would be a miraculous cure, while going from 80% to 70% may be viewed as only a slight improvement. Try as we might to present a single neat statistic, presenting both baseline risk and absolute risk with intervention is often necessary.13
How to effectively communicate medical information
Many patients struggle with processing information that is expressed as a probability.14 Patients process frequencies (eg, 10 in 100) better than probabilities (eg, 10%), and there is evidence that they understand best when decision aids are used.15 Decision aids, such as pictographs (FIGURE16), are supplementary, evidence-based tools for effectively communicating with patients and their families in a way that facilitates comparison between available options. Such aids are readily available online for many conditions or can be created using various software tools.16,17
Pictographs reveal that there is a values-sensitive decision to be made and visually demonstrate the outcomes associated with each option. Both pictographs and bar graphs have been shown to improve patient understanding and satisfaction.11 The benefit of pictographs is their ability to effectively, and simultaneously, convey both the numerator and the denominator in frequency statistics.12,18
There is high-quality evidence demonstrating that decision aids enhance an individual’s knowledge about the treatment and screening options available to them. A 2014 Cochrane review of the effects of decision aids found that they increased average knowledge scores when compared to usual care.15 Decision aids also improved accurate perception of risk.15 It is our belief that one of the reasons pictographs work so well is that they combine the salience of absolute risks with and without intervention.12,13
Beyond increased understanding, the Cochrane review also found high-quality evidence indicating that people who make decisions using decision aids feel less decisional conflict when compared to usual care.15 Moreover, in the context of SDM, decisional conflict may contribute to patients passing the decision-making responsibility to their clinician.19 And finally, there is moderate-quality evidence that patients are more likely to participate in decision-making when given tools such as pictographs.15
A potential barrier to putting pictographs into practice concerns perceptions that decision aids increase the length of office visits. Indeed, previous studies have identified perceived time constraints as one of the major barriers to enacting SDM in clinical settings.20 On this topic, the Cochrane review offers variable yet potentially promising results: Studies of the effects on appointment length ranged from a decrease of 8 minutes to an increase of 23 minutes.15 These results suggest that, under the right circumstances, pictographs can be used to facilitate SDM within the constraints of current clinical practice. More research is needed to determine the optimal circumstances that promote efficient SDM.
2. Elicit the patient’s unique values and priorities
Formalized approaches to building rapport with patients have been popular for more than 2 decades,21,22 and they are now routinely part of medical training. Nevertheless, there is always room for improvement when it comes to aligning treatment and screening recommendations with patient values. Some decision aids are designed to offer the added benefit of clarifying individual values and, thus, increase the likelihood that patients will make decisions that are more in line with their goals.15
When decision aids are not available to elicit patient values, clinicians can integrate preference-clarifying questions as part of the standard patient encounter.23 These questions are aimed at surfacing the values underlying what the patient wants, what the patient does not want, and most importantly, why.
“Why” matters because it ultimately helps the clinician understand the patient’s mindset, enabling the clinician to help the patient make choices that serve his or her values.24 Eliciting values not only promotes patient well-being and self-determination, but also facilitates the development of empathic patient-clinician partnerships.
Categorizing decisions. Regardless of the particular method chosen to elicit patient values, the underlying questions faced by many patients often fit into one of 2 categories: 1) Do I prefer quality of life over length of life? or 2) Am I willing to be inconvenienced now to prevent more severe illness later? Clarifying the category into which a decision falls may open the conversation and help to explore patients’ values and priorities. Alternatively, asking questions such as, “Thinking about this decision, what is the most important aspect for you to consider?”25 may facilitate the conversation.
Much of the research on techniques geared to elicit values comes from the palliative care and oncology literature.26 Although this research generally focuses on decisions about serious illness or end-of-life preferences, preference-sensitive decisions in primary care settings create a need for clinicians who are effective in eliciting patient values.
The more serious and preference-sensitive the decision, the deeper the clinician needs to explore the patient’s personal goals. Despite scant literature about seemingly innocuous decisions, we recommend that clinicians elicit from their patients a brief, but overt, acknowledgement of the values guiding their choice for most preference-sensitive decisions.
3. Offer a professional recommendation
Once clinicians have a sense of an individual’s values and priorities, they are positioned to make a professional recommendation that aligns with these values and priorities, and leaves room for the patient to reach a decision. Historically, one of the clinician’s major roles was to provide advice and recommendations to patients. For a long time, this was done without the patient’s involvement in the decision-making.27
With an increasing emphasis on patient self-determination over the last 50 years, there has been some concern that the pendulum is swinging too far in the opposite direction, with clinicians shying away from providing specific recommendations.28 Although this line of thinking acknowledges the power of the clinician to influence patients, it falls short of distinguishing between a personal recommendation and a professional one. While personal recommendations have no place in medical decision-making, clinicians should offer patients a professional recommendation, along with their rationale.
How do personal and professional recommendations differ?
Personal recommendations arise from clinicians considering what they themselves might decide if they were in the patient’s position. Such recommendations are inappropriate because every person has unique values and priorities.
In contrast, professional recommendations stem from the clinician’s knowledge of the best available evidence, his or her understanding of the patient’s values, and his or her weaving of these pieces together in the context of the patient’s specific clinical presentation. Experienced clinicians bring all 3 elements of SDM to bear in making professional recommendations, even if these recommendations are at odds with what they might choose for themselves.
EBM and SDM: Not so different after all?
Another way to understand the legitimacy of a professional recommendation is to view the parallels between SDM and EBM. From the outset, EBM positioned itself as arising from the best available evidence, the patient’s values, and clinical expertise29—elements that are strikingly similar to the components of SDM.
Although commonly overlooked, the concept of EBM recognizes that established evidence alone is not sufficient for decision-making.30 Additionally, EBM allows for making a recommendation that may not appear to be guideline-based, because guidelines typically do not take into account individual patient preferences.30-32 What’s more, both EBM and SDM highlight the essential contribution of the clinician’s judgment about his or her patient’s unique presentation.
Thus, both EBM and SDM are dependent on the professional communicating a recommendation to the patient. This communication involves not only making clear what one recommends, but also why one recommends it. For example, a clinician might say the following to a patient with worsening asthma symptoms:
“The asthma guidelines give us 2 treatment options. We can either double the dose of your inhaled corticosteroid, or start a 5-day course of corticosteroid pills. Given your concerns about the adverse effects of the pills, and the moderate severity of this exacerbation, I recommend doubling the dose of your inhaled corticosteroid. We can reconsider the pills if your symptoms worsen or if you don’t improve within the next week. How does that sound to you?”
An informed choice. Explaining the evidence, articulating the patient’s values, and summarizing the clinical elements that went into the clinician’s recommendation clarifies and signals to the patient that this is a professional recommendation. Ultimately, the process of SDM concludes with the patient considering the clinician’s recommendation and making an informed choice from the available options.
CORRESPONDENCE
David J. Satin, MD, 2020 E 28th St., Minneapolis, MN 55407; sati0003@umn.edu.
1. Medalie JH. Family Medicine: Principles and Applications. Baltimore, MD: Williams and Wilkins; 1978.
2. Philips RL Jr, Brundgardt S, Lesko SE, et al. The future role of the family physician in the United States: a rigorous exercise in definition. Ann Fam Med. 2014;12:250-255.
3. Berwick DM. Era 3 for medicine and health care. JAMA. 2016;315:1329-1330.
4. Edwards A, Elwyn G. Shared decision making in health care: achieving evidence-based patient choice. 2nd ed. Oxford, United Kingdom: Oxford University Press; 2009.
5. American Medical Association. Shared decision making H-373.997. Available at: https://policysearch.ama-assn.org/policyfinder/detail/H-373.997%20?uri=%2FAMADoc%2FHOD.xml-0-3162.xml. Accessed September 6, 2017.
6. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32:207-214.
7. Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8:410-417.
8. Fowler FJ Jr, Gerstein BS, Barry MJ. How patient centered are medical decisions? Results of a national survey. JAMA Intern Med. 2013;173:1215-1221.
9. Spatz ES, Krumhoiz HM, Moulton BW. The new era of informed consent: getting to a reasonable-patient standard through shared decision making. JAMA. 2016;315:2063-2064.
10. Faden RR, Becker C, Lewis C, et al. Disclosure of information to patients in medical care. Med Care. 1981;19:718-733.
11. Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161:270-280.
12. Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst. 2011;103:1436-1443.
13. Stovitz SD, Shrier I. Medical decision making and the importance of baseline risk. Br J Gen Pract. 2013;63:e795-e797.
14. Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37-44.
15. Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011:CD001431.
16. Mayo Clinic. Statin choice decision aid. Available at: https://statindecisionaid.mayoclinic.org/index.php/statin/index. Accessed September 6, 2017.
17. Risk Science Center and Center for Bioethics and Social Sciences in Medicine, University of Michigan. Icon Array. Available at: http://www.iconarray.com/. Accessed September 6, 2017.
18. Price M, Cameron R, Butow P. Communicating risk information: the influence of graphical display format on quantitative information perception–accuracy, comprehension and preferences. Patient Educ Couns. 2007;69:121-128.
19. Kon AA. The shared decision making continuum. JAMA. 2010;304:903-904.
20. Légaré F1, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526-535.
21. Haidet P, Paterniti DA. “Building” a history rather than “taking” one: a perspective on information sharing during the medical interview. Arch Intern Med. 2003;163:1134-1140.
22. Frankel RM, Stein R. Getting the most out of the clinical encounter: the four habits model. J Med Pract Manage. 2001;16:184-194.
23. Delbanco TL. Enriching the doctor-patient relationship by inviting the patient’s perspective. Ann Intern Med. 1992;116:414-418.
24. Doukas DJ, McCullough LB. The values history: the evaluation of the patient’s values and advance directives. J Fam Pract. 1991;32:145-153.
25. Stiggelbout AM, Van der Weijden T, De Wit MP, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256.
26. Bernacki RE, Block SD, American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174:1994-2003.
27. Katz J. The Silent World of Doctor and Patient. Baltimore, MD, and London, England: The Johns Hopkins University Press; 1984.
28. Baylis F, Downie J. Professional recommendations: disclosing facts and values. J Med Ethics. 2001;27:20-24.
29. Sackett DL, Rosenburg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72.
30. Montori VM, Brito JP, Murad MH. The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. JAMA. 2013;310:2053-2054.
31. Mora S, Ames JM, Manson JE. Low-dose aspirin in the primary prevention of cardiovascular disease: shared decision making in clinical practice. JAMA. 2016;316:709-710.
32. Stovitz SD, Satin D, Shrier I. Shared decision making regarding aspirin in primary prevention of cardiovascular disease. JAMA. 2016;316:2276.
The discipline of family medicine is committed to providing patient-centered care through recommendations that are grounded both in evidence and in patients’ personal values.1,2 The current health care environment, however, often demands heavy reliance on outcome-based performance metrics that can be insensitive to patient preferences.3 This tension necessitates models of decision-making that maximize reliance on measured performance, yet fulfill the clinician’s fiduciary responsibility to prioritize patients’ interests. The philosophy and practice of shared decision-making (SDM) can facilitate these aims.
The 3 elements of shared decision-making
SDM provides a framework for offering everyday medical advice and facilitating informed consent.4 Its 3 elements are:
- discussing with patients relevant information about their health conditions, possible treatments, and likely outcomes,
- clarifying and understanding a patient’s unique values and priorities and how they relate to the treatment options, and
- enabling a patient to select a care plan that is in keeping with his or her personal goals.5
This model is significant not only from a theoretical perspective, but also from a practical one. Studies have shown that both health outcomes and patient satisfaction improve when patients participate more actively in health care decision-making.6,7
Unfortunately, there is evidence that some decision-making practices in primary care settings remain inadequate. For example, unlike the standard disclosure of procedure risks in surgical settings, the burdens of cancer screening are frequently omitted from primary care discussions.8 Moreover, agreement about what should be disclosed, as well as how to disclose it, is still not sufficient. The following 3 recommendations, one for each element of SDM, aim to help clinicians effectively engage patients in everyday decision-making.
1. Provide patients with relevant information
The first element of SDM requires discussing the health-related information that is relevant to the patient’s decision-making process. The literature about informed consent supports explaining the risks that are common, as well as those that are particularly dangerous, and the likely benefits of recommended treatment, nontreatment, and alternative treatments.9 Moreover, adequate informed consent requires identifying what a reasonable person in a particular patient’s position would want to know.10
Accounting for “a patient’s position” is significant because it signals that personal factors (eg, the individual’s beliefs, goals, and familial responsibilities) are as important as the patient’s external clinical situation and what can be known by reviewing medical evidence. Incorporating a patient’s particular circumstances distinguishes patient-centered care from the mechanical application of generic best practices. This is the standard for what information should be provided.
When evidence is lacking. Clinicians facilitating decisions for which data is lacking should convey the best available evidence, including the inherent uncertainties. Like evidence-based medicine (EBM), the principles of SDM should be at work in most clinical encounters. The extent to which one engages in SDM depends upon the seriousness of the proposed interventions, the degree to which the decision is preference-sensitive, and the availability of evidence.
Statistics: Explain absolute and baseline risk
It is generally better to provide absolute risk rather than relative risk, because people perceive absolute risk reductions more accurately.11 Presentation of risks, in terms of relative risk or relative risk reduction, typically exaggerates the benefits of treatment, especially when the risk is small. This exaggeration makes it more likely that patients will accept interventions they might otherwise have rejected after reviewing the data more fully. Furthermore, relative risk statistics can impact clinicians’ perceptions, leading them to recommend an intervention more often than they might when absolute risk statistics are discussed.12
But even absolute risk, if presented on its own, can be misleading. A reasonable person trying to determine the value of an intervention needs to know his or her baseline risk of an event, in addition to his or her absolute risk with the intervention. For example, a hypothetical absolute risk reduction associated with a breast cancer treatment of 10% has different meanings, depending upon whether the baseline risk is 10% or 80%. A reduction from 10% to 0% would be a miraculous cure, while going from 80% to 70% may be viewed as only a slight improvement. Try as we might to present a single neat statistic, presenting both baseline risk and absolute risk with intervention is often necessary.13
How to effectively communicate medical information
Many patients struggle with processing information that is expressed as a probability.14 Patients process frequencies (eg, 10 in 100) better than probabilities (eg, 10%), and there is evidence that they understand best when decision aids are used.15 Decision aids, such as pictographs (FIGURE16), are supplementary, evidence-based tools for effectively communicating with patients and their families in a way that facilitates comparison between available options. Such aids are readily available online for many conditions or can be created using various software tools.16,17
Pictographs reveal that there is a values-sensitive decision to be made and visually demonstrate the outcomes associated with each option. Both pictographs and bar graphs have been shown to improve patient understanding and satisfaction.11 The benefit of pictographs is their ability to effectively, and simultaneously, convey both the numerator and the denominator in frequency statistics.12,18
There is high-quality evidence demonstrating that decision aids enhance an individual’s knowledge about the treatment and screening options available to them. A 2014 Cochrane review of the effects of decision aids found that they increased average knowledge scores when compared to usual care.15 Decision aids also improved accurate perception of risk.15 It is our belief that one of the reasons pictographs work so well is that they combine the salience of absolute risks with and without intervention.12,13
Beyond increased understanding, the Cochrane review also found high-quality evidence indicating that people who make decisions using decision aids feel less decisional conflict when compared to usual care.15 Moreover, in the context of SDM, decisional conflict may contribute to patients passing the decision-making responsibility to their clinician.19 And finally, there is moderate-quality evidence that patients are more likely to participate in decision-making when given tools such as pictographs.15
A potential barrier to putting pictographs into practice concerns perceptions that decision aids increase the length of office visits. Indeed, previous studies have identified perceived time constraints as one of the major barriers to enacting SDM in clinical settings.20 On this topic, the Cochrane review offers variable yet potentially promising results: Studies of the effects on appointment length ranged from a decrease of 8 minutes to an increase of 23 minutes.15 These results suggest that, under the right circumstances, pictographs can be used to facilitate SDM within the constraints of current clinical practice. More research is needed to determine the optimal circumstances that promote efficient SDM.
2. Elicit the patient’s unique values and priorities
Formalized approaches to building rapport with patients have been popular for more than 2 decades,21,22 and they are now routinely part of medical training. Nevertheless, there is always room for improvement when it comes to aligning treatment and screening recommendations with patient values. Some decision aids are designed to offer the added benefit of clarifying individual values and, thus, increase the likelihood that patients will make decisions that are more in line with their goals.15
When decision aids are not available to elicit patient values, clinicians can integrate preference-clarifying questions as part of the standard patient encounter.23 These questions are aimed at surfacing the values underlying what the patient wants, what the patient does not want, and most importantly, why.
“Why” matters because it ultimately helps the clinician understand the patient’s mindset, enabling the clinician to help the patient make choices that serve his or her values.24 Eliciting values not only promotes patient well-being and self-determination, but also facilitates the development of empathic patient-clinician partnerships.
Categorizing decisions. Regardless of the particular method chosen to elicit patient values, the underlying questions faced by many patients often fit into one of 2 categories: 1) Do I prefer quality of life over length of life? or 2) Am I willing to be inconvenienced now to prevent more severe illness later? Clarifying the category into which a decision falls may open the conversation and help to explore patients’ values and priorities. Alternatively, asking questions such as, “Thinking about this decision, what is the most important aspect for you to consider?”25 may facilitate the conversation.
Much of the research on techniques geared to elicit values comes from the palliative care and oncology literature.26 Although this research generally focuses on decisions about serious illness or end-of-life preferences, preference-sensitive decisions in primary care settings create a need for clinicians who are effective in eliciting patient values.
The more serious and preference-sensitive the decision, the deeper the clinician needs to explore the patient’s personal goals. Despite scant literature about seemingly innocuous decisions, we recommend that clinicians elicit from their patients a brief, but overt, acknowledgement of the values guiding their choice for most preference-sensitive decisions.
3. Offer a professional recommendation
Once clinicians have a sense of an individual’s values and priorities, they are positioned to make a professional recommendation that aligns with these values and priorities, and leaves room for the patient to reach a decision. Historically, one of the clinician’s major roles was to provide advice and recommendations to patients. For a long time, this was done without the patient’s involvement in the decision-making.27
With an increasing emphasis on patient self-determination over the last 50 years, there has been some concern that the pendulum is swinging too far in the opposite direction, with clinicians shying away from providing specific recommendations.28 Although this line of thinking acknowledges the power of the clinician to influence patients, it falls short of distinguishing between a personal recommendation and a professional one. While personal recommendations have no place in medical decision-making, clinicians should offer patients a professional recommendation, along with their rationale.
How do personal and professional recommendations differ?
Personal recommendations arise from clinicians considering what they themselves might decide if they were in the patient’s position. Such recommendations are inappropriate because every person has unique values and priorities.
In contrast, professional recommendations stem from the clinician’s knowledge of the best available evidence, his or her understanding of the patient’s values, and his or her weaving of these pieces together in the context of the patient’s specific clinical presentation. Experienced clinicians bring all 3 elements of SDM to bear in making professional recommendations, even if these recommendations are at odds with what they might choose for themselves.
EBM and SDM: Not so different after all?
Another way to understand the legitimacy of a professional recommendation is to view the parallels between SDM and EBM. From the outset, EBM positioned itself as arising from the best available evidence, the patient’s values, and clinical expertise29—elements that are strikingly similar to the components of SDM.
Although commonly overlooked, the concept of EBM recognizes that established evidence alone is not sufficient for decision-making.30 Additionally, EBM allows for making a recommendation that may not appear to be guideline-based, because guidelines typically do not take into account individual patient preferences.30-32 What’s more, both EBM and SDM highlight the essential contribution of the clinician’s judgment about his or her patient’s unique presentation.
Thus, both EBM and SDM are dependent on the professional communicating a recommendation to the patient. This communication involves not only making clear what one recommends, but also why one recommends it. For example, a clinician might say the following to a patient with worsening asthma symptoms:
“The asthma guidelines give us 2 treatment options. We can either double the dose of your inhaled corticosteroid, or start a 5-day course of corticosteroid pills. Given your concerns about the adverse effects of the pills, and the moderate severity of this exacerbation, I recommend doubling the dose of your inhaled corticosteroid. We can reconsider the pills if your symptoms worsen or if you don’t improve within the next week. How does that sound to you?”
An informed choice. Explaining the evidence, articulating the patient’s values, and summarizing the clinical elements that went into the clinician’s recommendation clarifies and signals to the patient that this is a professional recommendation. Ultimately, the process of SDM concludes with the patient considering the clinician’s recommendation and making an informed choice from the available options.
CORRESPONDENCE
David J. Satin, MD, 2020 E 28th St., Minneapolis, MN 55407; sati0003@umn.edu.
The discipline of family medicine is committed to providing patient-centered care through recommendations that are grounded both in evidence and in patients’ personal values.1,2 The current health care environment, however, often demands heavy reliance on outcome-based performance metrics that can be insensitive to patient preferences.3 This tension necessitates models of decision-making that maximize reliance on measured performance, yet fulfill the clinician’s fiduciary responsibility to prioritize patients’ interests. The philosophy and practice of shared decision-making (SDM) can facilitate these aims.
The 3 elements of shared decision-making
SDM provides a framework for offering everyday medical advice and facilitating informed consent.4 Its 3 elements are:
- discussing with patients relevant information about their health conditions, possible treatments, and likely outcomes,
- clarifying and understanding a patient’s unique values and priorities and how they relate to the treatment options, and
- enabling a patient to select a care plan that is in keeping with his or her personal goals.5
This model is significant not only from a theoretical perspective, but also from a practical one. Studies have shown that both health outcomes and patient satisfaction improve when patients participate more actively in health care decision-making.6,7
Unfortunately, there is evidence that some decision-making practices in primary care settings remain inadequate. For example, unlike the standard disclosure of procedure risks in surgical settings, the burdens of cancer screening are frequently omitted from primary care discussions.8 Moreover, agreement about what should be disclosed, as well as how to disclose it, is still not sufficient. The following 3 recommendations, one for each element of SDM, aim to help clinicians effectively engage patients in everyday decision-making.
1. Provide patients with relevant information
The first element of SDM requires discussing the health-related information that is relevant to the patient’s decision-making process. The literature about informed consent supports explaining the risks that are common, as well as those that are particularly dangerous, and the likely benefits of recommended treatment, nontreatment, and alternative treatments.9 Moreover, adequate informed consent requires identifying what a reasonable person in a particular patient’s position would want to know.10
Accounting for “a patient’s position” is significant because it signals that personal factors (eg, the individual’s beliefs, goals, and familial responsibilities) are as important as the patient’s external clinical situation and what can be known by reviewing medical evidence. Incorporating a patient’s particular circumstances distinguishes patient-centered care from the mechanical application of generic best practices. This is the standard for what information should be provided.
When evidence is lacking. Clinicians facilitating decisions for which data is lacking should convey the best available evidence, including the inherent uncertainties. Like evidence-based medicine (EBM), the principles of SDM should be at work in most clinical encounters. The extent to which one engages in SDM depends upon the seriousness of the proposed interventions, the degree to which the decision is preference-sensitive, and the availability of evidence.
Statistics: Explain absolute and baseline risk
It is generally better to provide absolute risk rather than relative risk, because people perceive absolute risk reductions more accurately.11 Presentation of risks, in terms of relative risk or relative risk reduction, typically exaggerates the benefits of treatment, especially when the risk is small. This exaggeration makes it more likely that patients will accept interventions they might otherwise have rejected after reviewing the data more fully. Furthermore, relative risk statistics can impact clinicians’ perceptions, leading them to recommend an intervention more often than they might when absolute risk statistics are discussed.12
But even absolute risk, if presented on its own, can be misleading. A reasonable person trying to determine the value of an intervention needs to know his or her baseline risk of an event, in addition to his or her absolute risk with the intervention. For example, a hypothetical absolute risk reduction associated with a breast cancer treatment of 10% has different meanings, depending upon whether the baseline risk is 10% or 80%. A reduction from 10% to 0% would be a miraculous cure, while going from 80% to 70% may be viewed as only a slight improvement. Try as we might to present a single neat statistic, presenting both baseline risk and absolute risk with intervention is often necessary.13
How to effectively communicate medical information
Many patients struggle with processing information that is expressed as a probability.14 Patients process frequencies (eg, 10 in 100) better than probabilities (eg, 10%), and there is evidence that they understand best when decision aids are used.15 Decision aids, such as pictographs (FIGURE16), are supplementary, evidence-based tools for effectively communicating with patients and their families in a way that facilitates comparison between available options. Such aids are readily available online for many conditions or can be created using various software tools.16,17
Pictographs reveal that there is a values-sensitive decision to be made and visually demonstrate the outcomes associated with each option. Both pictographs and bar graphs have been shown to improve patient understanding and satisfaction.11 The benefit of pictographs is their ability to effectively, and simultaneously, convey both the numerator and the denominator in frequency statistics.12,18
There is high-quality evidence demonstrating that decision aids enhance an individual’s knowledge about the treatment and screening options available to them. A 2014 Cochrane review of the effects of decision aids found that they increased average knowledge scores when compared to usual care.15 Decision aids also improved accurate perception of risk.15 It is our belief that one of the reasons pictographs work so well is that they combine the salience of absolute risks with and without intervention.12,13
Beyond increased understanding, the Cochrane review also found high-quality evidence indicating that people who make decisions using decision aids feel less decisional conflict when compared to usual care.15 Moreover, in the context of SDM, decisional conflict may contribute to patients passing the decision-making responsibility to their clinician.19 And finally, there is moderate-quality evidence that patients are more likely to participate in decision-making when given tools such as pictographs.15
A potential barrier to putting pictographs into practice concerns perceptions that decision aids increase the length of office visits. Indeed, previous studies have identified perceived time constraints as one of the major barriers to enacting SDM in clinical settings.20 On this topic, the Cochrane review offers variable yet potentially promising results: Studies of the effects on appointment length ranged from a decrease of 8 minutes to an increase of 23 minutes.15 These results suggest that, under the right circumstances, pictographs can be used to facilitate SDM within the constraints of current clinical practice. More research is needed to determine the optimal circumstances that promote efficient SDM.
2. Elicit the patient’s unique values and priorities
Formalized approaches to building rapport with patients have been popular for more than 2 decades,21,22 and they are now routinely part of medical training. Nevertheless, there is always room for improvement when it comes to aligning treatment and screening recommendations with patient values. Some decision aids are designed to offer the added benefit of clarifying individual values and, thus, increase the likelihood that patients will make decisions that are more in line with their goals.15
When decision aids are not available to elicit patient values, clinicians can integrate preference-clarifying questions as part of the standard patient encounter.23 These questions are aimed at surfacing the values underlying what the patient wants, what the patient does not want, and most importantly, why.
“Why” matters because it ultimately helps the clinician understand the patient’s mindset, enabling the clinician to help the patient make choices that serve his or her values.24 Eliciting values not only promotes patient well-being and self-determination, but also facilitates the development of empathic patient-clinician partnerships.
Categorizing decisions. Regardless of the particular method chosen to elicit patient values, the underlying questions faced by many patients often fit into one of 2 categories: 1) Do I prefer quality of life over length of life? or 2) Am I willing to be inconvenienced now to prevent more severe illness later? Clarifying the category into which a decision falls may open the conversation and help to explore patients’ values and priorities. Alternatively, asking questions such as, “Thinking about this decision, what is the most important aspect for you to consider?”25 may facilitate the conversation.
Much of the research on techniques geared to elicit values comes from the palliative care and oncology literature.26 Although this research generally focuses on decisions about serious illness or end-of-life preferences, preference-sensitive decisions in primary care settings create a need for clinicians who are effective in eliciting patient values.
The more serious and preference-sensitive the decision, the deeper the clinician needs to explore the patient’s personal goals. Despite scant literature about seemingly innocuous decisions, we recommend that clinicians elicit from their patients a brief, but overt, acknowledgement of the values guiding their choice for most preference-sensitive decisions.
3. Offer a professional recommendation
Once clinicians have a sense of an individual’s values and priorities, they are positioned to make a professional recommendation that aligns with these values and priorities, and leaves room for the patient to reach a decision. Historically, one of the clinician’s major roles was to provide advice and recommendations to patients. For a long time, this was done without the patient’s involvement in the decision-making.27
With an increasing emphasis on patient self-determination over the last 50 years, there has been some concern that the pendulum is swinging too far in the opposite direction, with clinicians shying away from providing specific recommendations.28 Although this line of thinking acknowledges the power of the clinician to influence patients, it falls short of distinguishing between a personal recommendation and a professional one. While personal recommendations have no place in medical decision-making, clinicians should offer patients a professional recommendation, along with their rationale.
How do personal and professional recommendations differ?
Personal recommendations arise from clinicians considering what they themselves might decide if they were in the patient’s position. Such recommendations are inappropriate because every person has unique values and priorities.
In contrast, professional recommendations stem from the clinician’s knowledge of the best available evidence, his or her understanding of the patient’s values, and his or her weaving of these pieces together in the context of the patient’s specific clinical presentation. Experienced clinicians bring all 3 elements of SDM to bear in making professional recommendations, even if these recommendations are at odds with what they might choose for themselves.
EBM and SDM: Not so different after all?
Another way to understand the legitimacy of a professional recommendation is to view the parallels between SDM and EBM. From the outset, EBM positioned itself as arising from the best available evidence, the patient’s values, and clinical expertise29—elements that are strikingly similar to the components of SDM.
Although commonly overlooked, the concept of EBM recognizes that established evidence alone is not sufficient for decision-making.30 Additionally, EBM allows for making a recommendation that may not appear to be guideline-based, because guidelines typically do not take into account individual patient preferences.30-32 What’s more, both EBM and SDM highlight the essential contribution of the clinician’s judgment about his or her patient’s unique presentation.
Thus, both EBM and SDM are dependent on the professional communicating a recommendation to the patient. This communication involves not only making clear what one recommends, but also why one recommends it. For example, a clinician might say the following to a patient with worsening asthma symptoms:
“The asthma guidelines give us 2 treatment options. We can either double the dose of your inhaled corticosteroid, or start a 5-day course of corticosteroid pills. Given your concerns about the adverse effects of the pills, and the moderate severity of this exacerbation, I recommend doubling the dose of your inhaled corticosteroid. We can reconsider the pills if your symptoms worsen or if you don’t improve within the next week. How does that sound to you?”
An informed choice. Explaining the evidence, articulating the patient’s values, and summarizing the clinical elements that went into the clinician’s recommendation clarifies and signals to the patient that this is a professional recommendation. Ultimately, the process of SDM concludes with the patient considering the clinician’s recommendation and making an informed choice from the available options.
CORRESPONDENCE
David J. Satin, MD, 2020 E 28th St., Minneapolis, MN 55407; sati0003@umn.edu.
1. Medalie JH. Family Medicine: Principles and Applications. Baltimore, MD: Williams and Wilkins; 1978.
2. Philips RL Jr, Brundgardt S, Lesko SE, et al. The future role of the family physician in the United States: a rigorous exercise in definition. Ann Fam Med. 2014;12:250-255.
3. Berwick DM. Era 3 for medicine and health care. JAMA. 2016;315:1329-1330.
4. Edwards A, Elwyn G. Shared decision making in health care: achieving evidence-based patient choice. 2nd ed. Oxford, United Kingdom: Oxford University Press; 2009.
5. American Medical Association. Shared decision making H-373.997. Available at: https://policysearch.ama-assn.org/policyfinder/detail/H-373.997%20?uri=%2FAMADoc%2FHOD.xml-0-3162.xml. Accessed September 6, 2017.
6. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32:207-214.
7. Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8:410-417.
8. Fowler FJ Jr, Gerstein BS, Barry MJ. How patient centered are medical decisions? Results of a national survey. JAMA Intern Med. 2013;173:1215-1221.
9. Spatz ES, Krumhoiz HM, Moulton BW. The new era of informed consent: getting to a reasonable-patient standard through shared decision making. JAMA. 2016;315:2063-2064.
10. Faden RR, Becker C, Lewis C, et al. Disclosure of information to patients in medical care. Med Care. 1981;19:718-733.
11. Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161:270-280.
12. Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst. 2011;103:1436-1443.
13. Stovitz SD, Shrier I. Medical decision making and the importance of baseline risk. Br J Gen Pract. 2013;63:e795-e797.
14. Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37-44.
15. Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011:CD001431.
16. Mayo Clinic. Statin choice decision aid. Available at: https://statindecisionaid.mayoclinic.org/index.php/statin/index. Accessed September 6, 2017.
17. Risk Science Center and Center for Bioethics and Social Sciences in Medicine, University of Michigan. Icon Array. Available at: http://www.iconarray.com/. Accessed September 6, 2017.
18. Price M, Cameron R, Butow P. Communicating risk information: the influence of graphical display format on quantitative information perception–accuracy, comprehension and preferences. Patient Educ Couns. 2007;69:121-128.
19. Kon AA. The shared decision making continuum. JAMA. 2010;304:903-904.
20. Légaré F1, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526-535.
21. Haidet P, Paterniti DA. “Building” a history rather than “taking” one: a perspective on information sharing during the medical interview. Arch Intern Med. 2003;163:1134-1140.
22. Frankel RM, Stein R. Getting the most out of the clinical encounter: the four habits model. J Med Pract Manage. 2001;16:184-194.
23. Delbanco TL. Enriching the doctor-patient relationship by inviting the patient’s perspective. Ann Intern Med. 1992;116:414-418.
24. Doukas DJ, McCullough LB. The values history: the evaluation of the patient’s values and advance directives. J Fam Pract. 1991;32:145-153.
25. Stiggelbout AM, Van der Weijden T, De Wit MP, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256.
26. Bernacki RE, Block SD, American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174:1994-2003.
27. Katz J. The Silent World of Doctor and Patient. Baltimore, MD, and London, England: The Johns Hopkins University Press; 1984.
28. Baylis F, Downie J. Professional recommendations: disclosing facts and values. J Med Ethics. 2001;27:20-24.
29. Sackett DL, Rosenburg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72.
30. Montori VM, Brito JP, Murad MH. The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. JAMA. 2013;310:2053-2054.
31. Mora S, Ames JM, Manson JE. Low-dose aspirin in the primary prevention of cardiovascular disease: shared decision making in clinical practice. JAMA. 2016;316:709-710.
32. Stovitz SD, Satin D, Shrier I. Shared decision making regarding aspirin in primary prevention of cardiovascular disease. JAMA. 2016;316:2276.
1. Medalie JH. Family Medicine: Principles and Applications. Baltimore, MD: Williams and Wilkins; 1978.
2. Philips RL Jr, Brundgardt S, Lesko SE, et al. The future role of the family physician in the United States: a rigorous exercise in definition. Ann Fam Med. 2014;12:250-255.
3. Berwick DM. Era 3 for medicine and health care. JAMA. 2016;315:1329-1330.
4. Edwards A, Elwyn G. Shared decision making in health care: achieving evidence-based patient choice. 2nd ed. Oxford, United Kingdom: Oxford University Press; 2009.
5. American Medical Association. Shared decision making H-373.997. Available at: https://policysearch.ama-assn.org/policyfinder/detail/H-373.997%20?uri=%2FAMADoc%2FHOD.xml-0-3162.xml. Accessed September 6, 2017.
6. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32:207-214.
7. Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8:410-417.
8. Fowler FJ Jr, Gerstein BS, Barry MJ. How patient centered are medical decisions? Results of a national survey. JAMA Intern Med. 2013;173:1215-1221.
9. Spatz ES, Krumhoiz HM, Moulton BW. The new era of informed consent: getting to a reasonable-patient standard through shared decision making. JAMA. 2016;315:2063-2064.
10. Faden RR, Becker C, Lewis C, et al. Disclosure of information to patients in medical care. Med Care. 1981;19:718-733.
11. Zipkin DA, Umscheid CA, Keating NL, et al. Evidence-based risk communication: a systematic review. Ann Intern Med. 2014;161:270-280.
12. Fagerlin A, Zikmund-Fisher BJ, Ubel PA. Helping patients decide: ten steps to better risk communication. J Natl Cancer Inst. 2011;103:1436-1443.
13. Stovitz SD, Shrier I. Medical decision making and the importance of baseline risk. Br J Gen Pract. 2013;63:e795-e797.
14. Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37-44.
15. Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011:CD001431.
16. Mayo Clinic. Statin choice decision aid. Available at: https://statindecisionaid.mayoclinic.org/index.php/statin/index. Accessed September 6, 2017.
17. Risk Science Center and Center for Bioethics and Social Sciences in Medicine, University of Michigan. Icon Array. Available at: http://www.iconarray.com/. Accessed September 6, 2017.
18. Price M, Cameron R, Butow P. Communicating risk information: the influence of graphical display format on quantitative information perception–accuracy, comprehension and preferences. Patient Educ Couns. 2007;69:121-128.
19. Kon AA. The shared decision making continuum. JAMA. 2010;304:903-904.
20. Légaré F1, Ratté S, Gravel K, et al. Barriers and facilitators to implementing shared decision making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526-535.
21. Haidet P, Paterniti DA. “Building” a history rather than “taking” one: a perspective on information sharing during the medical interview. Arch Intern Med. 2003;163:1134-1140.
22. Frankel RM, Stein R. Getting the most out of the clinical encounter: the four habits model. J Med Pract Manage. 2001;16:184-194.
23. Delbanco TL. Enriching the doctor-patient relationship by inviting the patient’s perspective. Ann Intern Med. 1992;116:414-418.
24. Doukas DJ, McCullough LB. The values history: the evaluation of the patient’s values and advance directives. J Fam Pract. 1991;32:145-153.
25. Stiggelbout AM, Van der Weijden T, De Wit MP, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256.
26. Bernacki RE, Block SD, American College of Physicians High Value Care Task Force. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174:1994-2003.
27. Katz J. The Silent World of Doctor and Patient. Baltimore, MD, and London, England: The Johns Hopkins University Press; 1984.
28. Baylis F, Downie J. Professional recommendations: disclosing facts and values. J Med Ethics. 2001;27:20-24.
29. Sackett DL, Rosenburg WM, Gray JA, et al. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71-72.
30. Montori VM, Brito JP, Murad MH. The optimal practice of evidence-based medicine: incorporating patient preferences in practice guidelines. JAMA. 2013;310:2053-2054.
31. Mora S, Ames JM, Manson JE. Low-dose aspirin in the primary prevention of cardiovascular disease: shared decision making in clinical practice. JAMA. 2016;316:709-710.
32. Stovitz SD, Satin D, Shrier I. Shared decision making regarding aspirin in primary prevention of cardiovascular disease. JAMA. 2016;316:2276.
PRACTICE RECOMMENDATIONS
› Provide patients with information in terms of absolute and baseline risks, ideally using pictograph decision aids. A
› Elicit the patient’s values and priorities by categorizing decisions and asking broad open-ended questions. C
› Offer patients a professional (not a personal) recommendation, including your rationale. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series