User login
How EBV causes lymphoma, other cancers

among uninfected cells (blue)
Image courtesy of
Benjamin Chaigne-Delalande
New research published in Nature Communications appears to explain how Epstein-Barr virus (EBV) reprograms cells into cancer cells.
Investigators said they discovered a mechanism by which EBV particles induce chromosomal instability without establishing a chronic infection, thereby conferring a risk for the development of tumors that do not necessarily carry the viral genome.
“The contribution of the viral infection to cancer development in patients with a weakened immune system is well understood,” said study author Henri-Jacques Delecluse, MD, PhD, of the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) in Heidelberg.
“But in the majority of cases, it remains unclear how an EBV infection leads to cancer development.”
With their research, Dr Delecluse and his colleagues found that BNRF1, a protein component of EBV, promotes the development of cancer. They said BNRF1 induces centrosome amplification, which is associated with chromosomal instability.
When a dividing cell comes in contact with EBV, BNRF1 frequently prompts the formation of an excessive number of centrosomes. As a result, chromosomes are no longer divided equally and accurately between daughter cells—a known cancer risk factor.
In contrast, when the investigators studied EBV deficient of BNRF1, they found the virus did not interfere with chromosome distribution to daughter cells.
The team noted that EBV normally remains silent in a few infected cells, but, occasionally, it reactivates to produce viral offspring that infects nearby cells. As a consequence, these cells come in close contact with BNRF1, thus increasing their risk of transforming into cancer cells.
“The novelty of our work is that we have uncovered a component of the viral particle as a cancer driver,” Dr Delecluse said. “All human-tumors viruses that have been studied so far cause cancer in a completely different manner.”
“Usually, the genetic material of the viruses needs to be permanently present in the infected cell, thus causing the activation of one or several viral genes that cause cancer development. However, these gene products are not present in the infectious particle itself.”
Dr Delecluse and his colleagues therefore suspect that EBV could cause cancers other than those that have already been linked to EBV. Certain cancers might not have been linked to the virus because they do not carry the viral genetic material.
“We must push forward with the development of a vaccine against EBV infection,” Dr Delecluse said. “This would be the most direct strategy to prevent an infection with the virus.”
“Our latest results show that the first infection could already be a cancer risk, and this fits with earlier work that showed an increase in the incidence of Hodgkin’s lymphoma in people who underwent an episode of infectious mononucleosis.” ![]()

among uninfected cells (blue)
Image courtesy of
Benjamin Chaigne-Delalande
New research published in Nature Communications appears to explain how Epstein-Barr virus (EBV) reprograms cells into cancer cells.
Investigators said they discovered a mechanism by which EBV particles induce chromosomal instability without establishing a chronic infection, thereby conferring a risk for the development of tumors that do not necessarily carry the viral genome.
“The contribution of the viral infection to cancer development in patients with a weakened immune system is well understood,” said study author Henri-Jacques Delecluse, MD, PhD, of the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) in Heidelberg.
“But in the majority of cases, it remains unclear how an EBV infection leads to cancer development.”
With their research, Dr Delecluse and his colleagues found that BNRF1, a protein component of EBV, promotes the development of cancer. They said BNRF1 induces centrosome amplification, which is associated with chromosomal instability.
When a dividing cell comes in contact with EBV, BNRF1 frequently prompts the formation of an excessive number of centrosomes. As a result, chromosomes are no longer divided equally and accurately between daughter cells—a known cancer risk factor.
In contrast, when the investigators studied EBV deficient of BNRF1, they found the virus did not interfere with chromosome distribution to daughter cells.
The team noted that EBV normally remains silent in a few infected cells, but, occasionally, it reactivates to produce viral offspring that infects nearby cells. As a consequence, these cells come in close contact with BNRF1, thus increasing their risk of transforming into cancer cells.
“The novelty of our work is that we have uncovered a component of the viral particle as a cancer driver,” Dr Delecluse said. “All human-tumors viruses that have been studied so far cause cancer in a completely different manner.”
“Usually, the genetic material of the viruses needs to be permanently present in the infected cell, thus causing the activation of one or several viral genes that cause cancer development. However, these gene products are not present in the infectious particle itself.”
Dr Delecluse and his colleagues therefore suspect that EBV could cause cancers other than those that have already been linked to EBV. Certain cancers might not have been linked to the virus because they do not carry the viral genetic material.
“We must push forward with the development of a vaccine against EBV infection,” Dr Delecluse said. “This would be the most direct strategy to prevent an infection with the virus.”
“Our latest results show that the first infection could already be a cancer risk, and this fits with earlier work that showed an increase in the incidence of Hodgkin’s lymphoma in people who underwent an episode of infectious mononucleosis.” ![]()

among uninfected cells (blue)
Image courtesy of
Benjamin Chaigne-Delalande
New research published in Nature Communications appears to explain how Epstein-Barr virus (EBV) reprograms cells into cancer cells.
Investigators said they discovered a mechanism by which EBV particles induce chromosomal instability without establishing a chronic infection, thereby conferring a risk for the development of tumors that do not necessarily carry the viral genome.
“The contribution of the viral infection to cancer development in patients with a weakened immune system is well understood,” said study author Henri-Jacques Delecluse, MD, PhD, of the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) in Heidelberg.
“But in the majority of cases, it remains unclear how an EBV infection leads to cancer development.”
With their research, Dr Delecluse and his colleagues found that BNRF1, a protein component of EBV, promotes the development of cancer. They said BNRF1 induces centrosome amplification, which is associated with chromosomal instability.
When a dividing cell comes in contact with EBV, BNRF1 frequently prompts the formation of an excessive number of centrosomes. As a result, chromosomes are no longer divided equally and accurately between daughter cells—a known cancer risk factor.
In contrast, when the investigators studied EBV deficient of BNRF1, they found the virus did not interfere with chromosome distribution to daughter cells.
The team noted that EBV normally remains silent in a few infected cells, but, occasionally, it reactivates to produce viral offspring that infects nearby cells. As a consequence, these cells come in close contact with BNRF1, thus increasing their risk of transforming into cancer cells.
“The novelty of our work is that we have uncovered a component of the viral particle as a cancer driver,” Dr Delecluse said. “All human-tumors viruses that have been studied so far cause cancer in a completely different manner.”
“Usually, the genetic material of the viruses needs to be permanently present in the infected cell, thus causing the activation of one or several viral genes that cause cancer development. However, these gene products are not present in the infectious particle itself.”
Dr Delecluse and his colleagues therefore suspect that EBV could cause cancers other than those that have already been linked to EBV. Certain cancers might not have been linked to the virus because they do not carry the viral genetic material.
“We must push forward with the development of a vaccine against EBV infection,” Dr Delecluse said. “This would be the most direct strategy to prevent an infection with the virus.”
“Our latest results show that the first infection could already be a cancer risk, and this fits with earlier work that showed an increase in the incidence of Hodgkin’s lymphoma in people who underwent an episode of infectious mononucleosis.” ![]()
G-CSF could prevent infertility in cancer patients

Granulocyte colony-stimulating factor (G-CSF) could prevent infertility in male cancer patients, according to preclinical research published in Reproductive Biology and Endocrinology.
Researchers said they found that G-CSF protects spermatogenesis after alkylating chemotherapy by stimulating the proliferation of surviving spermatogonia.
The team also found evidence to suggest that G-CSF may be useful as a fertility-restoring treatment.
The researchers have been pursuing initiatives to restore fertility in men who have lost their ability to have children as a result of cancer treatments they received as children.
While working on methods to restart sperm production, the team discovered a link between G-CSF and the absence of normal damage to reproductive ability.
“We were using G-CSF to prevent infections in our research experiments,” said study author Brian Hermann, PhD, of The University of Texas at San Antonio.
“It turned out that the drug also had the unexpected impact of guarding against male infertility.”
To test the fertility-related impact of G-CSF, the researchers treated male mice with G-CSF before and/or after treatment with busulfan.
The team then evaluated effects on spermatogenesis in these mice and control mice that only received busulfan.
G-CSF had a protective effect on spermatogenesis that was stable for at least 19 weeks after chemotherapy.
And mice treated with G-CSF for 4 days after busulfan showed modestly enhanced spermatogenic recovery compared to controls.
The researchers said these results suggest G-CSF promotes spermatogonial proliferation, leading to enhanced spermatogenic regeneration from surviving spermatogonial stem cells. ![]()

Granulocyte colony-stimulating factor (G-CSF) could prevent infertility in male cancer patients, according to preclinical research published in Reproductive Biology and Endocrinology.
Researchers said they found that G-CSF protects spermatogenesis after alkylating chemotherapy by stimulating the proliferation of surviving spermatogonia.
The team also found evidence to suggest that G-CSF may be useful as a fertility-restoring treatment.
The researchers have been pursuing initiatives to restore fertility in men who have lost their ability to have children as a result of cancer treatments they received as children.
While working on methods to restart sperm production, the team discovered a link between G-CSF and the absence of normal damage to reproductive ability.
“We were using G-CSF to prevent infections in our research experiments,” said study author Brian Hermann, PhD, of The University of Texas at San Antonio.
“It turned out that the drug also had the unexpected impact of guarding against male infertility.”
To test the fertility-related impact of G-CSF, the researchers treated male mice with G-CSF before and/or after treatment with busulfan.
The team then evaluated effects on spermatogenesis in these mice and control mice that only received busulfan.
G-CSF had a protective effect on spermatogenesis that was stable for at least 19 weeks after chemotherapy.
And mice treated with G-CSF for 4 days after busulfan showed modestly enhanced spermatogenic recovery compared to controls.
The researchers said these results suggest G-CSF promotes spermatogonial proliferation, leading to enhanced spermatogenic regeneration from surviving spermatogonial stem cells. ![]()

Granulocyte colony-stimulating factor (G-CSF) could prevent infertility in male cancer patients, according to preclinical research published in Reproductive Biology and Endocrinology.
Researchers said they found that G-CSF protects spermatogenesis after alkylating chemotherapy by stimulating the proliferation of surviving spermatogonia.
The team also found evidence to suggest that G-CSF may be useful as a fertility-restoring treatment.
The researchers have been pursuing initiatives to restore fertility in men who have lost their ability to have children as a result of cancer treatments they received as children.
While working on methods to restart sperm production, the team discovered a link between G-CSF and the absence of normal damage to reproductive ability.
“We were using G-CSF to prevent infections in our research experiments,” said study author Brian Hermann, PhD, of The University of Texas at San Antonio.
“It turned out that the drug also had the unexpected impact of guarding against male infertility.”
To test the fertility-related impact of G-CSF, the researchers treated male mice with G-CSF before and/or after treatment with busulfan.
The team then evaluated effects on spermatogenesis in these mice and control mice that only received busulfan.
G-CSF had a protective effect on spermatogenesis that was stable for at least 19 weeks after chemotherapy.
And mice treated with G-CSF for 4 days after busulfan showed modestly enhanced spermatogenic recovery compared to controls.
The researchers said these results suggest G-CSF promotes spermatogonial proliferation, leading to enhanced spermatogenic regeneration from surviving spermatogonial stem cells. ![]()
Therapy shows promise for treating hemophilia B

that can develop hemophilia B
A plant-made therapy has demonstrated safety and efficacy in dogs with hemophilia B, according to research published in Molecular Therapy.
Previously, researchers found they could produce freeze-dried lettuce cells expressing human coagulation factor IX (FIX) fused with cholera toxin B subunit (CTB).
These cells were able to prevent inhibitor formation and allergic reactions to intravenous FIX therapy in mice with hemophilia B.
With the current study, the researchers showed that lettuce cells expressing CTB-FIX were safe and could prevent anaphylaxis and inhibitor formation in dogs receiving intravenous FIX to treat hemophilia B.
“The results were quite dramatic,” said study author Henry Daniell, PhD, of the University of Pennsylvania in Philadelphia.
“We corrected blood clotting time in each of the dogs and were able to suppress antibody formation as well. All signs point to this material being ready for the clinic.”
This study made use of Dr Daniell’s patented plant-based drug-production platform, in which genetic modifications enable the growth of plants that have specified human proteins in their leaves.
The researchers grew lettuce that had been modified to produce a fusion protein of human FIX and CTB. CTB helps the fused protein cross the intestinal lining as the lettuce cells are digested by gut microbes, while the plant cell walls protect FIX from digestion.
The researchers said they were able to achieve commercial-scale production of CTB-FIX fusions expressed in lettuce chloroplasts by growing the plants in a hydroponic facility.
The team first tested their product in 2 dogs with hemophilia B. Twice a week for 10 months, the dogs consumed the freeze-dried lettuce material, which was spiked with bacon flavor and sprinkled on their food.
Observing no negative effects of the treatment, the researchers went on to a more robust study, including 4 dogs that were fed the lettuce material and 4 that served as controls.
The 4 dogs in the experimental group were fed the lettuce material for 4 weeks. At that point, they also began receiving weekly injections of FIX, which continued for 8 weeks. The control dogs only received the FIX injections.
All 4 dogs in the control group developed significant levels of antibodies against FIX, and 2 had visible anaphylactic reactions that required the administration of antihistamine.
In contrast, 3 of the 4 dogs in the experimental group had only minimal levels of one type of antibody, IgG2, and no detectable levels of IgG1 or IgE.
The fourth dog in the experimental group had only a partial response to the lettuce cells expressing CTB-FIX. The researchers believe this was due to a pre-existing antibody to human FIX.
Overall, levels of IgG2 were 32 times lower in the experimental group than in the controls.
In addition, the dogs showed no negative side effects from ingesting the lettuce material, and blood samples taken throughout the experiment revealed no signs of toxicity.
“Looking at the dogs that were fed the lettuce material, you can see it’s quite effective,” Dr Daniell said. “They either developed no antibodies to factor IX, or their antibodies went up just a little bit and then came down.”
The next steps for the researchers include additional toxicology and pharmacokinetics studies before applying for an investigational new drug application with the US Food and Drug Administration, a step they hope to take before the end of the year. ![]()

that can develop hemophilia B
A plant-made therapy has demonstrated safety and efficacy in dogs with hemophilia B, according to research published in Molecular Therapy.
Previously, researchers found they could produce freeze-dried lettuce cells expressing human coagulation factor IX (FIX) fused with cholera toxin B subunit (CTB).
These cells were able to prevent inhibitor formation and allergic reactions to intravenous FIX therapy in mice with hemophilia B.
With the current study, the researchers showed that lettuce cells expressing CTB-FIX were safe and could prevent anaphylaxis and inhibitor formation in dogs receiving intravenous FIX to treat hemophilia B.
“The results were quite dramatic,” said study author Henry Daniell, PhD, of the University of Pennsylvania in Philadelphia.
“We corrected blood clotting time in each of the dogs and were able to suppress antibody formation as well. All signs point to this material being ready for the clinic.”
This study made use of Dr Daniell’s patented plant-based drug-production platform, in which genetic modifications enable the growth of plants that have specified human proteins in their leaves.
The researchers grew lettuce that had been modified to produce a fusion protein of human FIX and CTB. CTB helps the fused protein cross the intestinal lining as the lettuce cells are digested by gut microbes, while the plant cell walls protect FIX from digestion.
The researchers said they were able to achieve commercial-scale production of CTB-FIX fusions expressed in lettuce chloroplasts by growing the plants in a hydroponic facility.
The team first tested their product in 2 dogs with hemophilia B. Twice a week for 10 months, the dogs consumed the freeze-dried lettuce material, which was spiked with bacon flavor and sprinkled on their food.
Observing no negative effects of the treatment, the researchers went on to a more robust study, including 4 dogs that were fed the lettuce material and 4 that served as controls.
The 4 dogs in the experimental group were fed the lettuce material for 4 weeks. At that point, they also began receiving weekly injections of FIX, which continued for 8 weeks. The control dogs only received the FIX injections.
All 4 dogs in the control group developed significant levels of antibodies against FIX, and 2 had visible anaphylactic reactions that required the administration of antihistamine.
In contrast, 3 of the 4 dogs in the experimental group had only minimal levels of one type of antibody, IgG2, and no detectable levels of IgG1 or IgE.
The fourth dog in the experimental group had only a partial response to the lettuce cells expressing CTB-FIX. The researchers believe this was due to a pre-existing antibody to human FIX.
Overall, levels of IgG2 were 32 times lower in the experimental group than in the controls.
In addition, the dogs showed no negative side effects from ingesting the lettuce material, and blood samples taken throughout the experiment revealed no signs of toxicity.
“Looking at the dogs that were fed the lettuce material, you can see it’s quite effective,” Dr Daniell said. “They either developed no antibodies to factor IX, or their antibodies went up just a little bit and then came down.”
The next steps for the researchers include additional toxicology and pharmacokinetics studies before applying for an investigational new drug application with the US Food and Drug Administration, a step they hope to take before the end of the year. ![]()

that can develop hemophilia B
A plant-made therapy has demonstrated safety and efficacy in dogs with hemophilia B, according to research published in Molecular Therapy.
Previously, researchers found they could produce freeze-dried lettuce cells expressing human coagulation factor IX (FIX) fused with cholera toxin B subunit (CTB).
These cells were able to prevent inhibitor formation and allergic reactions to intravenous FIX therapy in mice with hemophilia B.
With the current study, the researchers showed that lettuce cells expressing CTB-FIX were safe and could prevent anaphylaxis and inhibitor formation in dogs receiving intravenous FIX to treat hemophilia B.
“The results were quite dramatic,” said study author Henry Daniell, PhD, of the University of Pennsylvania in Philadelphia.
“We corrected blood clotting time in each of the dogs and were able to suppress antibody formation as well. All signs point to this material being ready for the clinic.”
This study made use of Dr Daniell’s patented plant-based drug-production platform, in which genetic modifications enable the growth of plants that have specified human proteins in their leaves.
The researchers grew lettuce that had been modified to produce a fusion protein of human FIX and CTB. CTB helps the fused protein cross the intestinal lining as the lettuce cells are digested by gut microbes, while the plant cell walls protect FIX from digestion.
The researchers said they were able to achieve commercial-scale production of CTB-FIX fusions expressed in lettuce chloroplasts by growing the plants in a hydroponic facility.
The team first tested their product in 2 dogs with hemophilia B. Twice a week for 10 months, the dogs consumed the freeze-dried lettuce material, which was spiked with bacon flavor and sprinkled on their food.
Observing no negative effects of the treatment, the researchers went on to a more robust study, including 4 dogs that were fed the lettuce material and 4 that served as controls.
The 4 dogs in the experimental group were fed the lettuce material for 4 weeks. At that point, they also began receiving weekly injections of FIX, which continued for 8 weeks. The control dogs only received the FIX injections.
All 4 dogs in the control group developed significant levels of antibodies against FIX, and 2 had visible anaphylactic reactions that required the administration of antihistamine.
In contrast, 3 of the 4 dogs in the experimental group had only minimal levels of one type of antibody, IgG2, and no detectable levels of IgG1 or IgE.
The fourth dog in the experimental group had only a partial response to the lettuce cells expressing CTB-FIX. The researchers believe this was due to a pre-existing antibody to human FIX.
Overall, levels of IgG2 were 32 times lower in the experimental group than in the controls.
In addition, the dogs showed no negative side effects from ingesting the lettuce material, and blood samples taken throughout the experiment revealed no signs of toxicity.
“Looking at the dogs that were fed the lettuce material, you can see it’s quite effective,” Dr Daniell said. “They either developed no antibodies to factor IX, or their antibodies went up just a little bit and then came down.”
The next steps for the researchers include additional toxicology and pharmacokinetics studies before applying for an investigational new drug application with the US Food and Drug Administration, a step they hope to take before the end of the year. ![]()
New NCI Formulary May Help Streamline Cancer Clinical Trials
Normally, negotiations to use drugs in preclinical studies and clinical trials can take as long as 18 months. But the National Cancer Institute’s (NCI) new drug formulary will allow investigators at NCI-designated cancer centers quicker access to approved and investigational agents, helping make more effective treatments available sooner.
The NCI Formulary, a public-private partnership between NCI and pharmaceutical and biotechnology companies, is one of NCI’s efforts in support of the Cancer Moonshot (ex-Vice President Biden’s call for greater collaboration and faster development of new therapies). The formulary enables NCI to act as an intermediary between investigators at cancer centers and participating pharmaceutical companies, streamlining arrangements for access to and use of drugs.
The formulary launched with 15 targeted agents from 6 pharmaceutical companies: Bristol-Myers Squibb, Eli Lilly and Company, Genentech, Kyowa Hakko Kirin, Loxo Oncology, and Xcovery Holding Company LLC.
Normally, negotiations to use drugs in preclinical studies and clinical trials can take as long as 18 months. But the National Cancer Institute’s (NCI) new drug formulary will allow investigators at NCI-designated cancer centers quicker access to approved and investigational agents, helping make more effective treatments available sooner.
The NCI Formulary, a public-private partnership between NCI and pharmaceutical and biotechnology companies, is one of NCI’s efforts in support of the Cancer Moonshot (ex-Vice President Biden’s call for greater collaboration and faster development of new therapies). The formulary enables NCI to act as an intermediary between investigators at cancer centers and participating pharmaceutical companies, streamlining arrangements for access to and use of drugs.
The formulary launched with 15 targeted agents from 6 pharmaceutical companies: Bristol-Myers Squibb, Eli Lilly and Company, Genentech, Kyowa Hakko Kirin, Loxo Oncology, and Xcovery Holding Company LLC.
Normally, negotiations to use drugs in preclinical studies and clinical trials can take as long as 18 months. But the National Cancer Institute’s (NCI) new drug formulary will allow investigators at NCI-designated cancer centers quicker access to approved and investigational agents, helping make more effective treatments available sooner.
The NCI Formulary, a public-private partnership between NCI and pharmaceutical and biotechnology companies, is one of NCI’s efforts in support of the Cancer Moonshot (ex-Vice President Biden’s call for greater collaboration and faster development of new therapies). The formulary enables NCI to act as an intermediary between investigators at cancer centers and participating pharmaceutical companies, streamlining arrangements for access to and use of drugs.
The formulary launched with 15 targeted agents from 6 pharmaceutical companies: Bristol-Myers Squibb, Eli Lilly and Company, Genentech, Kyowa Hakko Kirin, Loxo Oncology, and Xcovery Holding Company LLC.
Ginseng Derivatives May Protect Against Flu
Ginsenosides are pharmacologically active components of ginseng, which often is used to relieve coughs and colds. They also have been found to have antineoplastic, antioxidant, antimicrobial, and antifungal properties; other studies suggest neuroprotective properties as well. Ginsenosides may act against coxsackievirus B3, enterovirus 71, human rhinovirus 3, and hemagglutinating virus of Japan (HVJ) infection. But do they have an antiviral effect on influenza?
Related: A New Kind of Flu Drug
Researchers from University Health Network & Shantou University Medical College and Guangdong Provincial Key Laboratory of Infectious Diseases and Molecular Immunopathology, both in China, and University of Toronto in Canada conducted a study in mice of the anti-influenza properties of ginseng and ginseng-derived compounds both in vitro and in vivo. They found that ginsenosides exerted “strong antiviral activity” to 2009 pandemic H1N1 virus. Ginsenoside protected the animals from infection and lowered viral titers in their lungs.
Sugars were the key to the effectiveness of the ginsenosides, which are composed of a steroid skeleton with various sugar groups attached. The researchers note that previous studies have shown that ginsenosides’ anticancer activity and antioxidant activity are related to the type and position of sugar moieties.
Related: How Common is Flu Without Fever?
The pilot experiment did not have negative or toxic effects on the animals or in cell proliferation in vitro, thus “defining the nontoxic nature and therapeutic value of these compounds,” the researchers say. They also point out that in phase 2 randomized clinical trials in children, oral consumption of ginseng extract as an alternative influenza treatment did not result in severe adverse effects. They suggest that their findings could spur other research into a novel antiviral drug for influenza.
Source:
Dong W, Farooqui A, Leon AJ, Kelvin DJ. PloS One. 2017;12(2):e0171936.
doi: 10.1371/journal.pone.0171936.
Ginsenosides are pharmacologically active components of ginseng, which often is used to relieve coughs and colds. They also have been found to have antineoplastic, antioxidant, antimicrobial, and antifungal properties; other studies suggest neuroprotective properties as well. Ginsenosides may act against coxsackievirus B3, enterovirus 71, human rhinovirus 3, and hemagglutinating virus of Japan (HVJ) infection. But do they have an antiviral effect on influenza?
Related: A New Kind of Flu Drug
Researchers from University Health Network & Shantou University Medical College and Guangdong Provincial Key Laboratory of Infectious Diseases and Molecular Immunopathology, both in China, and University of Toronto in Canada conducted a study in mice of the anti-influenza properties of ginseng and ginseng-derived compounds both in vitro and in vivo. They found that ginsenosides exerted “strong antiviral activity” to 2009 pandemic H1N1 virus. Ginsenoside protected the animals from infection and lowered viral titers in their lungs.
Sugars were the key to the effectiveness of the ginsenosides, which are composed of a steroid skeleton with various sugar groups attached. The researchers note that previous studies have shown that ginsenosides’ anticancer activity and antioxidant activity are related to the type and position of sugar moieties.
Related: How Common is Flu Without Fever?
The pilot experiment did not have negative or toxic effects on the animals or in cell proliferation in vitro, thus “defining the nontoxic nature and therapeutic value of these compounds,” the researchers say. They also point out that in phase 2 randomized clinical trials in children, oral consumption of ginseng extract as an alternative influenza treatment did not result in severe adverse effects. They suggest that their findings could spur other research into a novel antiviral drug for influenza.
Source:
Dong W, Farooqui A, Leon AJ, Kelvin DJ. PloS One. 2017;12(2):e0171936.
doi: 10.1371/journal.pone.0171936.
Ginsenosides are pharmacologically active components of ginseng, which often is used to relieve coughs and colds. They also have been found to have antineoplastic, antioxidant, antimicrobial, and antifungal properties; other studies suggest neuroprotective properties as well. Ginsenosides may act against coxsackievirus B3, enterovirus 71, human rhinovirus 3, and hemagglutinating virus of Japan (HVJ) infection. But do they have an antiviral effect on influenza?
Related: A New Kind of Flu Drug
Researchers from University Health Network & Shantou University Medical College and Guangdong Provincial Key Laboratory of Infectious Diseases and Molecular Immunopathology, both in China, and University of Toronto in Canada conducted a study in mice of the anti-influenza properties of ginseng and ginseng-derived compounds both in vitro and in vivo. They found that ginsenosides exerted “strong antiviral activity” to 2009 pandemic H1N1 virus. Ginsenoside protected the animals from infection and lowered viral titers in their lungs.
Sugars were the key to the effectiveness of the ginsenosides, which are composed of a steroid skeleton with various sugar groups attached. The researchers note that previous studies have shown that ginsenosides’ anticancer activity and antioxidant activity are related to the type and position of sugar moieties.
Related: How Common is Flu Without Fever?
The pilot experiment did not have negative or toxic effects on the animals or in cell proliferation in vitro, thus “defining the nontoxic nature and therapeutic value of these compounds,” the researchers say. They also point out that in phase 2 randomized clinical trials in children, oral consumption of ginseng extract as an alternative influenza treatment did not result in severe adverse effects. They suggest that their findings could spur other research into a novel antiviral drug for influenza.
Source:
Dong W, Farooqui A, Leon AJ, Kelvin DJ. PloS One. 2017;12(2):e0171936.
doi: 10.1371/journal.pone.0171936.
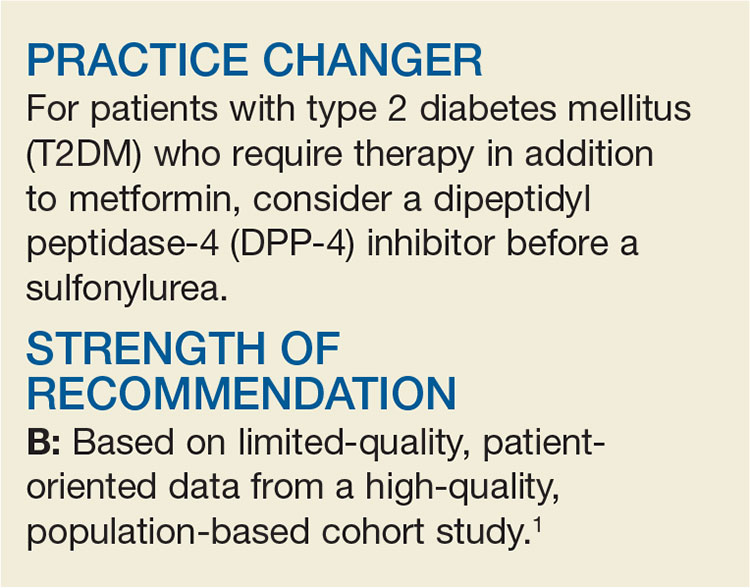
Need an Add-on to Metformin? Consider This
A 58-year-old woman with T2DM and heart failure returns to your office for follow-up. She has been on the maximum dose of metformin alone for the past six months, but her A1C is now 7.8%. She wants to avoid injections. What do you recommend?
There is surprisingly little consensus about what to add to metformin for patients with T2DM who require a second agent to achieve their glycemic goal. Attaining glycemic control earlier in the course of the disease may lead to reduced overall cardiovascular (CV) risk, so the choice of a second drug is an important one.2 While the proven mortality benefit, wide availability, and low cost of metformin make it well-established as initial pharmacotherapy, no second-choice drug has amassed enough evidence of benefit to become the add-on therapy of choice.
The professional societies are of little assistance; dual-therapy recommendations from the American Diabetes Association and the European Association for the Study of Diabetes do not specify a preference.3 Although the American Association of Clinical Endocrinologists/American College of Endocrinology suggest a hierarchy of choices, it is based on expert consensus recommendations.4
A look at the options
Options for add-on therapy include sulfonylureas, thiazolidines, DPP-4 inhibitors, sodium glucose cotransporter 2 inhibitors, glucagon-like peptide 1 (GLP-1) agonists, and insulin. Providers frequently prescribe sulfonylureas after metformin because they are low in cost, have long-term safety data, and are effective at lowering A1C. They work by directly stimulating insulin secretion via pancreatic ß-cells in a glucose-independent manner. But as a 2010 meta-analysis revealed, sulfonylureas carry significant risk for hypoglycemia (relative risk [RR], 4.57) and weight gain (average, 2.06 kg), compared to placebo.5
DPP-4 inhibitors, on the other hand, induce insulin secretion in a glucose-dependent manner through an incretin mechanism. Combined with metformin, they provide glucose control similar to that achieved with the combination of a sulfonylurea and metformin.6 DPP-4 inhibitors were initially found to be associated with fewer CV events and less hypoglycemia than sulfonylureas but were subsequently linked to an increased risk for heart failure–related hospitalization.7
A recent study provides more data on the effects of DPP-4s added to metformin.1
STUDY SUMMARY
DPP-4s as effective, less risky
This observational cohort study compared DPP-4 inhibitors and sulfonylureas when combined with metformin for the treatment of T2DM.1 Outcomes were all-cause mortality, major adverse CV events (defined as hospitalization for ischemic stroke or myocardial infarction [MI]), and hospitalizations for either heart failure or hypoglycemia. The study included data from the National Health Insurance Research Database in Taiwan on more than 70,000 patients (ages 20 and older) with diagnosed T2DM. Individuals adherent to metformin were considered to be enrolled in the cohort on the day they began using either a DPP-4 inhibitor or a sulfonylurea, in addition to metformin.
The researchers collected additional data on socioeconomic factors, urbanization, robustness of the local health care system, Charlson Comorbidity Index, adapted Diabetes Complications Severity Index, and other comorbidities and medications that could affect the outcomes of interest. Participants were then matched by propensity score into 10,089 pairs, each consisting of one DPP-4 inhibitor user and one sulfonylurea user.
After mean follow-up of 2.8 years, the investigators used Cox regression analysis to evaluate the relative hazards of the outcomes. Subgroup analysis stratified by age, sex, Charlson Comorbidity Index, hypertension, chronic kidney disease, hospitalization for heart failure, MI, and cerebrovascular disease yielded results similar to those of the primary analysis for each outcome. Similar results were also obtained when the data were analyzed without propensity-score matching.
The researchers found that users of DPP-4 inhibitors—compared with those who used sulfonylureas—had a lower risk for all-cause mortality (366 vs 488 deaths; hazard ratio [HR], 0.63; number needed to treat [NNT], 117), major cardiac events (209 vs 282 events; HR, 0.68; NNT, 191), ischemic stroke (144 vs 203 strokes; HR, 0.64; NNT, 246), and hypoglycemia (89 vs 170 events; HR, 0.43; NNT, 201). There were no significant differences in the occurrence of MIs (69 vs 88 MIs; HR, 0.75) or the number of hospitalizations for heart failure (100 vs 100 events; HR, 0.78) between the two groups.
WHAT’S NEW
Lower risks for death, CV events, and hypoglycemia
This study found that when added to metformin, DPP-4 inhibitors were associated with lower risks for all-cause mortality, CV events, and hypoglycemia when compared to sulfonylureas. Additionally, DPP-4 inhibitors did not increase the risk for heart failure hospitalization. A recent multicenter observational study of nearly 1.5 million patients on the effects of incretin-based treatments (including DPP-4 inhibitors and GLP-1 agonists) found no increased risk for heart failure hospitalization with DPP-4 inhibitors, compared to other combinations of oral T2DM agents.8
CAVEATS
Did unmeasured confounders play a role?
Unmeasured confounders potentially bias all observational population cohort results. In this particular study, there may have been unmeasured but significant patient factors that providers used to choose diabetes medications. Also, the study did not evaluate diabetes control, although previous studies have shown similar glucose control between sulfonylureas and DPP-4 inhibitors when added to metformin.6
Another caveat is that the results from this study group may not be generalizable to other populations due to physiologic differences. People of Asian ancestry are at risk for T2DM at a lower BMI than people of European ancestry, which could affect the outcomes of interest.9
Furthermore, the study did not evaluate outcomes based on whether patients were taking first-, second-, or third-generation sulfonylureas. Some sulfonylureas (eg, glyburide) carry a higher risk for hypoglycemia, which could bias the results.10
Lastly, the study only provides guidance when choosing between a sulfonylurea and a DPP-4 inhibitor for secondline pharmacotherapy. The GRADE trial, due to be completed in 2023, is comparing sulfonylureas, DPP-4 inhibitors, GLP-1 agonists, and insulin as add-on medications to metformin; it may provide more data on which to base treatment decisions.11
CHALLENGES TO IMPLEMENTATION
DPP-4s are more expensive
Sulfonylureas and DPP-4 inhibitors are both available as generic medications, but the cost of DPP-4 inhibitors remains significantly higher.12 Higher copays and deductibles could affect patient preference. For patients without health insurance, sulfonylureas are available on the discounted drug lists of many major retailers, while DPP-4 inhibitors are not.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2017;66(1):42-44.
1. Ou SM, Shih CJ, Chao PW, et al. Effects of clinical outcomes of adding dipeptidyl peptidase-4 inhibitors versus sulfonylureas to metformin therapy in patients with type 2 diabetes mellitus. Ann Intern Med. 2015;163:663-672.
2. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372:2197-2206.
3. American Diabetes Association. Standards of Medical Care in Diabetes—2016. Diabetes Care. 2016;39(suppl 1).
4. Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm—2016 Executive Summary. Endocr Pract. 2016;22: 84-113.
5. Phung OJ, Scholle JM, Talwar M, et al. Effect of noninsulin antidiabetic drugs added to metformin therapy on glycemic control, weight gain, and hypoglycemia in type 2 diabetes. JAMA. 2010;303:1410-1418.
6. Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. 2012;380:475-483.
7. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317-1326.
8. Filion KB, Azoulay L, Platt RW, et al. A multicenter observational study of incretin-based drugs and heart failure. N Engl J Med. 2016;374:1145-1154.
9. Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, pathophysiology. JAMA. 2009;301:2129-2140.
10. Gangji AS, Cukierman T, Gerstein HC, et al. A systematic review and meta-analysis of hypoglycemia and cardiovascular events: a comparison of glyburide with other secretagogues and with insulin. Diabetes Care. 2007;30:389-394.
11. Nathan DM, Buse JB, Kahn SE, et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care. 2013;36:2254-2261.
12. GoodRx. Gliptins. www.goodrx.com/gliptins. Accessed January 4, 2017.
A 58-year-old woman with T2DM and heart failure returns to your office for follow-up. She has been on the maximum dose of metformin alone for the past six months, but her A1C is now 7.8%. She wants to avoid injections. What do you recommend?
There is surprisingly little consensus about what to add to metformin for patients with T2DM who require a second agent to achieve their glycemic goal. Attaining glycemic control earlier in the course of the disease may lead to reduced overall cardiovascular (CV) risk, so the choice of a second drug is an important one.2 While the proven mortality benefit, wide availability, and low cost of metformin make it well-established as initial pharmacotherapy, no second-choice drug has amassed enough evidence of benefit to become the add-on therapy of choice.
The professional societies are of little assistance; dual-therapy recommendations from the American Diabetes Association and the European Association for the Study of Diabetes do not specify a preference.3 Although the American Association of Clinical Endocrinologists/American College of Endocrinology suggest a hierarchy of choices, it is based on expert consensus recommendations.4
A look at the options
Options for add-on therapy include sulfonylureas, thiazolidines, DPP-4 inhibitors, sodium glucose cotransporter 2 inhibitors, glucagon-like peptide 1 (GLP-1) agonists, and insulin. Providers frequently prescribe sulfonylureas after metformin because they are low in cost, have long-term safety data, and are effective at lowering A1C. They work by directly stimulating insulin secretion via pancreatic ß-cells in a glucose-independent manner. But as a 2010 meta-analysis revealed, sulfonylureas carry significant risk for hypoglycemia (relative risk [RR], 4.57) and weight gain (average, 2.06 kg), compared to placebo.5
DPP-4 inhibitors, on the other hand, induce insulin secretion in a glucose-dependent manner through an incretin mechanism. Combined with metformin, they provide glucose control similar to that achieved with the combination of a sulfonylurea and metformin.6 DPP-4 inhibitors were initially found to be associated with fewer CV events and less hypoglycemia than sulfonylureas but were subsequently linked to an increased risk for heart failure–related hospitalization.7
A recent study provides more data on the effects of DPP-4s added to metformin.1
STUDY SUMMARY
DPP-4s as effective, less risky
This observational cohort study compared DPP-4 inhibitors and sulfonylureas when combined with metformin for the treatment of T2DM.1 Outcomes were all-cause mortality, major adverse CV events (defined as hospitalization for ischemic stroke or myocardial infarction [MI]), and hospitalizations for either heart failure or hypoglycemia. The study included data from the National Health Insurance Research Database in Taiwan on more than 70,000 patients (ages 20 and older) with diagnosed T2DM. Individuals adherent to metformin were considered to be enrolled in the cohort on the day they began using either a DPP-4 inhibitor or a sulfonylurea, in addition to metformin.
The researchers collected additional data on socioeconomic factors, urbanization, robustness of the local health care system, Charlson Comorbidity Index, adapted Diabetes Complications Severity Index, and other comorbidities and medications that could affect the outcomes of interest. Participants were then matched by propensity score into 10,089 pairs, each consisting of one DPP-4 inhibitor user and one sulfonylurea user.
After mean follow-up of 2.8 years, the investigators used Cox regression analysis to evaluate the relative hazards of the outcomes. Subgroup analysis stratified by age, sex, Charlson Comorbidity Index, hypertension, chronic kidney disease, hospitalization for heart failure, MI, and cerebrovascular disease yielded results similar to those of the primary analysis for each outcome. Similar results were also obtained when the data were analyzed without propensity-score matching.
The researchers found that users of DPP-4 inhibitors—compared with those who used sulfonylureas—had a lower risk for all-cause mortality (366 vs 488 deaths; hazard ratio [HR], 0.63; number needed to treat [NNT], 117), major cardiac events (209 vs 282 events; HR, 0.68; NNT, 191), ischemic stroke (144 vs 203 strokes; HR, 0.64; NNT, 246), and hypoglycemia (89 vs 170 events; HR, 0.43; NNT, 201). There were no significant differences in the occurrence of MIs (69 vs 88 MIs; HR, 0.75) or the number of hospitalizations for heart failure (100 vs 100 events; HR, 0.78) between the two groups.
WHAT’S NEW
Lower risks for death, CV events, and hypoglycemia
This study found that when added to metformin, DPP-4 inhibitors were associated with lower risks for all-cause mortality, CV events, and hypoglycemia when compared to sulfonylureas. Additionally, DPP-4 inhibitors did not increase the risk for heart failure hospitalization. A recent multicenter observational study of nearly 1.5 million patients on the effects of incretin-based treatments (including DPP-4 inhibitors and GLP-1 agonists) found no increased risk for heart failure hospitalization with DPP-4 inhibitors, compared to other combinations of oral T2DM agents.8
CAVEATS
Did unmeasured confounders play a role?
Unmeasured confounders potentially bias all observational population cohort results. In this particular study, there may have been unmeasured but significant patient factors that providers used to choose diabetes medications. Also, the study did not evaluate diabetes control, although previous studies have shown similar glucose control between sulfonylureas and DPP-4 inhibitors when added to metformin.6
Another caveat is that the results from this study group may not be generalizable to other populations due to physiologic differences. People of Asian ancestry are at risk for T2DM at a lower BMI than people of European ancestry, which could affect the outcomes of interest.9
Furthermore, the study did not evaluate outcomes based on whether patients were taking first-, second-, or third-generation sulfonylureas. Some sulfonylureas (eg, glyburide) carry a higher risk for hypoglycemia, which could bias the results.10
Lastly, the study only provides guidance when choosing between a sulfonylurea and a DPP-4 inhibitor for secondline pharmacotherapy. The GRADE trial, due to be completed in 2023, is comparing sulfonylureas, DPP-4 inhibitors, GLP-1 agonists, and insulin as add-on medications to metformin; it may provide more data on which to base treatment decisions.11
CHALLENGES TO IMPLEMENTATION
DPP-4s are more expensive
Sulfonylureas and DPP-4 inhibitors are both available as generic medications, but the cost of DPP-4 inhibitors remains significantly higher.12 Higher copays and deductibles could affect patient preference. For patients without health insurance, sulfonylureas are available on the discounted drug lists of many major retailers, while DPP-4 inhibitors are not.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2017;66(1):42-44.
A 58-year-old woman with T2DM and heart failure returns to your office for follow-up. She has been on the maximum dose of metformin alone for the past six months, but her A1C is now 7.8%. She wants to avoid injections. What do you recommend?
There is surprisingly little consensus about what to add to metformin for patients with T2DM who require a second agent to achieve their glycemic goal. Attaining glycemic control earlier in the course of the disease may lead to reduced overall cardiovascular (CV) risk, so the choice of a second drug is an important one.2 While the proven mortality benefit, wide availability, and low cost of metformin make it well-established as initial pharmacotherapy, no second-choice drug has amassed enough evidence of benefit to become the add-on therapy of choice.
The professional societies are of little assistance; dual-therapy recommendations from the American Diabetes Association and the European Association for the Study of Diabetes do not specify a preference.3 Although the American Association of Clinical Endocrinologists/American College of Endocrinology suggest a hierarchy of choices, it is based on expert consensus recommendations.4
A look at the options
Options for add-on therapy include sulfonylureas, thiazolidines, DPP-4 inhibitors, sodium glucose cotransporter 2 inhibitors, glucagon-like peptide 1 (GLP-1) agonists, and insulin. Providers frequently prescribe sulfonylureas after metformin because they are low in cost, have long-term safety data, and are effective at lowering A1C. They work by directly stimulating insulin secretion via pancreatic ß-cells in a glucose-independent manner. But as a 2010 meta-analysis revealed, sulfonylureas carry significant risk for hypoglycemia (relative risk [RR], 4.57) and weight gain (average, 2.06 kg), compared to placebo.5
DPP-4 inhibitors, on the other hand, induce insulin secretion in a glucose-dependent manner through an incretin mechanism. Combined with metformin, they provide glucose control similar to that achieved with the combination of a sulfonylurea and metformin.6 DPP-4 inhibitors were initially found to be associated with fewer CV events and less hypoglycemia than sulfonylureas but were subsequently linked to an increased risk for heart failure–related hospitalization.7
A recent study provides more data on the effects of DPP-4s added to metformin.1
STUDY SUMMARY
DPP-4s as effective, less risky
This observational cohort study compared DPP-4 inhibitors and sulfonylureas when combined with metformin for the treatment of T2DM.1 Outcomes were all-cause mortality, major adverse CV events (defined as hospitalization for ischemic stroke or myocardial infarction [MI]), and hospitalizations for either heart failure or hypoglycemia. The study included data from the National Health Insurance Research Database in Taiwan on more than 70,000 patients (ages 20 and older) with diagnosed T2DM. Individuals adherent to metformin were considered to be enrolled in the cohort on the day they began using either a DPP-4 inhibitor or a sulfonylurea, in addition to metformin.
The researchers collected additional data on socioeconomic factors, urbanization, robustness of the local health care system, Charlson Comorbidity Index, adapted Diabetes Complications Severity Index, and other comorbidities and medications that could affect the outcomes of interest. Participants were then matched by propensity score into 10,089 pairs, each consisting of one DPP-4 inhibitor user and one sulfonylurea user.
After mean follow-up of 2.8 years, the investigators used Cox regression analysis to evaluate the relative hazards of the outcomes. Subgroup analysis stratified by age, sex, Charlson Comorbidity Index, hypertension, chronic kidney disease, hospitalization for heart failure, MI, and cerebrovascular disease yielded results similar to those of the primary analysis for each outcome. Similar results were also obtained when the data were analyzed without propensity-score matching.
The researchers found that users of DPP-4 inhibitors—compared with those who used sulfonylureas—had a lower risk for all-cause mortality (366 vs 488 deaths; hazard ratio [HR], 0.63; number needed to treat [NNT], 117), major cardiac events (209 vs 282 events; HR, 0.68; NNT, 191), ischemic stroke (144 vs 203 strokes; HR, 0.64; NNT, 246), and hypoglycemia (89 vs 170 events; HR, 0.43; NNT, 201). There were no significant differences in the occurrence of MIs (69 vs 88 MIs; HR, 0.75) or the number of hospitalizations for heart failure (100 vs 100 events; HR, 0.78) between the two groups.
WHAT’S NEW
Lower risks for death, CV events, and hypoglycemia
This study found that when added to metformin, DPP-4 inhibitors were associated with lower risks for all-cause mortality, CV events, and hypoglycemia when compared to sulfonylureas. Additionally, DPP-4 inhibitors did not increase the risk for heart failure hospitalization. A recent multicenter observational study of nearly 1.5 million patients on the effects of incretin-based treatments (including DPP-4 inhibitors and GLP-1 agonists) found no increased risk for heart failure hospitalization with DPP-4 inhibitors, compared to other combinations of oral T2DM agents.8
CAVEATS
Did unmeasured confounders play a role?
Unmeasured confounders potentially bias all observational population cohort results. In this particular study, there may have been unmeasured but significant patient factors that providers used to choose diabetes medications. Also, the study did not evaluate diabetes control, although previous studies have shown similar glucose control between sulfonylureas and DPP-4 inhibitors when added to metformin.6
Another caveat is that the results from this study group may not be generalizable to other populations due to physiologic differences. People of Asian ancestry are at risk for T2DM at a lower BMI than people of European ancestry, which could affect the outcomes of interest.9
Furthermore, the study did not evaluate outcomes based on whether patients were taking first-, second-, or third-generation sulfonylureas. Some sulfonylureas (eg, glyburide) carry a higher risk for hypoglycemia, which could bias the results.10
Lastly, the study only provides guidance when choosing between a sulfonylurea and a DPP-4 inhibitor for secondline pharmacotherapy. The GRADE trial, due to be completed in 2023, is comparing sulfonylureas, DPP-4 inhibitors, GLP-1 agonists, and insulin as add-on medications to metformin; it may provide more data on which to base treatment decisions.11
CHALLENGES TO IMPLEMENTATION
DPP-4s are more expensive
Sulfonylureas and DPP-4 inhibitors are both available as generic medications, but the cost of DPP-4 inhibitors remains significantly higher.12 Higher copays and deductibles could affect patient preference. For patients without health insurance, sulfonylureas are available on the discounted drug lists of many major retailers, while DPP-4 inhibitors are not.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice. 2017;66(1):42-44.
1. Ou SM, Shih CJ, Chao PW, et al. Effects of clinical outcomes of adding dipeptidyl peptidase-4 inhibitors versus sulfonylureas to metformin therapy in patients with type 2 diabetes mellitus. Ann Intern Med. 2015;163:663-672.
2. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372:2197-2206.
3. American Diabetes Association. Standards of Medical Care in Diabetes—2016. Diabetes Care. 2016;39(suppl 1).
4. Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm—2016 Executive Summary. Endocr Pract. 2016;22: 84-113.
5. Phung OJ, Scholle JM, Talwar M, et al. Effect of noninsulin antidiabetic drugs added to metformin therapy on glycemic control, weight gain, and hypoglycemia in type 2 diabetes. JAMA. 2010;303:1410-1418.
6. Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. 2012;380:475-483.
7. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317-1326.
8. Filion KB, Azoulay L, Platt RW, et al. A multicenter observational study of incretin-based drugs and heart failure. N Engl J Med. 2016;374:1145-1154.
9. Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, pathophysiology. JAMA. 2009;301:2129-2140.
10. Gangji AS, Cukierman T, Gerstein HC, et al. A systematic review and meta-analysis of hypoglycemia and cardiovascular events: a comparison of glyburide with other secretagogues and with insulin. Diabetes Care. 2007;30:389-394.
11. Nathan DM, Buse JB, Kahn SE, et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care. 2013;36:2254-2261.
12. GoodRx. Gliptins. www.goodrx.com/gliptins. Accessed January 4, 2017.
1. Ou SM, Shih CJ, Chao PW, et al. Effects of clinical outcomes of adding dipeptidyl peptidase-4 inhibitors versus sulfonylureas to metformin therapy in patients with type 2 diabetes mellitus. Ann Intern Med. 2015;163:663-672.
2. Hayward RA, Reaven PD, Wiitala WL, et al. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372:2197-2206.
3. American Diabetes Association. Standards of Medical Care in Diabetes—2016. Diabetes Care. 2016;39(suppl 1).
4. Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm—2016 Executive Summary. Endocr Pract. 2016;22: 84-113.
5. Phung OJ, Scholle JM, Talwar M, et al. Effect of noninsulin antidiabetic drugs added to metformin therapy on glycemic control, weight gain, and hypoglycemia in type 2 diabetes. JAMA. 2010;303:1410-1418.
6. Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. 2012;380:475-483.
7. Scirica BM, Bhatt DL, Braunwald E, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317-1326.
8. Filion KB, Azoulay L, Platt RW, et al. A multicenter observational study of incretin-based drugs and heart failure. N Engl J Med. 2016;374:1145-1154.
9. Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, pathophysiology. JAMA. 2009;301:2129-2140.
10. Gangji AS, Cukierman T, Gerstein HC, et al. A systematic review and meta-analysis of hypoglycemia and cardiovascular events: a comparison of glyburide with other secretagogues and with insulin. Diabetes Care. 2007;30:389-394.
11. Nathan DM, Buse JB, Kahn SE, et al. Rationale and design of the glycemia reduction approaches in diabetes: a comparative effectiveness study (GRADE). Diabetes Care. 2013;36:2254-2261.
12. GoodRx. Gliptins. www.goodrx.com/gliptins. Accessed January 4, 2017.
More readmissions with delays in discharge summaries
Clinical question: Is there an association between time to completion of discharge summary and hospital readmission?
Background: Thirty-day hospital readmission is one of the quality indicators for inpatient care and a higher rate can result in monetary penalties. Several interventions aimed at reducing this occurrence have been studied in different settings with variable success. Timely completion of discharge summary can possibly affect readmissions by providing crucial information to outpatient providers caring for patients across the care continuum.
Study design: Retrospective cohort study.
Setting: Johns Hopkins University, Baltimore.
Bottom line: Delays in completion of discharge summaries was significantly associated with higher rates of hospital readmission. It’s unclear however whether timely completion is a surrogate indicator of other important causative factors.
Citations: Hoyer EH, Odonkor CA, Bhatia SN, et al. Association between days to complete inpatient discharge summaries with all-payer hospital readmissions in Maryland. J Hosp Med. 2016; 11(6):393-400.
Dr. Rachoin is an assistant professor of clinical medicine and associate division head, Hospital Medicine, at Cooper Medical School at Rowan University. He works as a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: Is there an association between time to completion of discharge summary and hospital readmission?
Background: Thirty-day hospital readmission is one of the quality indicators for inpatient care and a higher rate can result in monetary penalties. Several interventions aimed at reducing this occurrence have been studied in different settings with variable success. Timely completion of discharge summary can possibly affect readmissions by providing crucial information to outpatient providers caring for patients across the care continuum.
Study design: Retrospective cohort study.
Setting: Johns Hopkins University, Baltimore.
Bottom line: Delays in completion of discharge summaries was significantly associated with higher rates of hospital readmission. It’s unclear however whether timely completion is a surrogate indicator of other important causative factors.
Citations: Hoyer EH, Odonkor CA, Bhatia SN, et al. Association between days to complete inpatient discharge summaries with all-payer hospital readmissions in Maryland. J Hosp Med. 2016; 11(6):393-400.
Dr. Rachoin is an assistant professor of clinical medicine and associate division head, Hospital Medicine, at Cooper Medical School at Rowan University. He works as a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: Is there an association between time to completion of discharge summary and hospital readmission?
Background: Thirty-day hospital readmission is one of the quality indicators for inpatient care and a higher rate can result in monetary penalties. Several interventions aimed at reducing this occurrence have been studied in different settings with variable success. Timely completion of discharge summary can possibly affect readmissions by providing crucial information to outpatient providers caring for patients across the care continuum.
Study design: Retrospective cohort study.
Setting: Johns Hopkins University, Baltimore.
Bottom line: Delays in completion of discharge summaries was significantly associated with higher rates of hospital readmission. It’s unclear however whether timely completion is a surrogate indicator of other important causative factors.
Citations: Hoyer EH, Odonkor CA, Bhatia SN, et al. Association between days to complete inpatient discharge summaries with all-payer hospital readmissions in Maryland. J Hosp Med. 2016; 11(6):393-400.
Dr. Rachoin is an assistant professor of clinical medicine and associate division head, Hospital Medicine, at Cooper Medical School at Rowan University. He works as a hospitalist at Cooper University Hospital in Camden, N.J.
AKI is common in young, critically ill adults
Clinical question: What are the epidemiology, risk factors, and associated morbidity and mortality of acute kidney injury (AKI) in critically ill children and young adults?
Background: Adult studies on acute kidney injury have shown increasing mortality and morbidity when both plasma creatinine and urine output were used to diagnose AKI than when used alone. Studies of AKI in children have also been limited.
Setting: International (32 pediatric intensive care units across Asia, Australia, Europe, and North America).
Synopsis: 4,984 patients aged 3 months to 25 years with a predicted ICU stay of at least 48 hours were considered for enrollment, of which 4,683 were included in the final analysis. The primary outcome was 28-day mortality. Secondary outcomes were length of stay in the ICU, receipt and duration of mechanical ventilation, receipt of extracorporeal membrane oxygenation, and renal-replacement therapy. A total of 26.9% of patients developed AKI in the first 7 days of an ICU admission. Severe AKI increased mortality by day 28 (adjusted odds ratio, 1.77; 95% confidence interval, 1.17-2.68) and was associated with increased use of renal-replacement therapy and mechanical ventilation and longer stays in the ICU. Urine output predicted mortality more accurately than did plasma creatinine, and using plasma creatinine alone failed to identify two-thirds of patients with low urine output.
Bottom line: In critically ill young patients, AKI is a common occurrence and is associated with both an increased morbidity and mortality. In a majority of patients with low urine output, plasma creatinine was a poor discriminant of renal function.
Citations: Kaddourah A, Basu RK, Bagshaw SM, et al. Epidemiology of acute kidney injury in critically ill children and young adults. N Eng J Med. 2017; 376 (1):11-20.
Dr. Rachoin is an assistant professor of clinical medicine and associate division head, Hospital Medicine, at Cooper Medical School at Rowan University. He works as a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: What are the epidemiology, risk factors, and associated morbidity and mortality of acute kidney injury (AKI) in critically ill children and young adults?
Background: Adult studies on acute kidney injury have shown increasing mortality and morbidity when both plasma creatinine and urine output were used to diagnose AKI than when used alone. Studies of AKI in children have also been limited.
Setting: International (32 pediatric intensive care units across Asia, Australia, Europe, and North America).
Synopsis: 4,984 patients aged 3 months to 25 years with a predicted ICU stay of at least 48 hours were considered for enrollment, of which 4,683 were included in the final analysis. The primary outcome was 28-day mortality. Secondary outcomes were length of stay in the ICU, receipt and duration of mechanical ventilation, receipt of extracorporeal membrane oxygenation, and renal-replacement therapy. A total of 26.9% of patients developed AKI in the first 7 days of an ICU admission. Severe AKI increased mortality by day 28 (adjusted odds ratio, 1.77; 95% confidence interval, 1.17-2.68) and was associated with increased use of renal-replacement therapy and mechanical ventilation and longer stays in the ICU. Urine output predicted mortality more accurately than did plasma creatinine, and using plasma creatinine alone failed to identify two-thirds of patients with low urine output.
Bottom line: In critically ill young patients, AKI is a common occurrence and is associated with both an increased morbidity and mortality. In a majority of patients with low urine output, plasma creatinine was a poor discriminant of renal function.
Citations: Kaddourah A, Basu RK, Bagshaw SM, et al. Epidemiology of acute kidney injury in critically ill children and young adults. N Eng J Med. 2017; 376 (1):11-20.
Dr. Rachoin is an assistant professor of clinical medicine and associate division head, Hospital Medicine, at Cooper Medical School at Rowan University. He works as a hospitalist at Cooper University Hospital in Camden, N.J.
Clinical question: What are the epidemiology, risk factors, and associated morbidity and mortality of acute kidney injury (AKI) in critically ill children and young adults?
Background: Adult studies on acute kidney injury have shown increasing mortality and morbidity when both plasma creatinine and urine output were used to diagnose AKI than when used alone. Studies of AKI in children have also been limited.
Setting: International (32 pediatric intensive care units across Asia, Australia, Europe, and North America).
Synopsis: 4,984 patients aged 3 months to 25 years with a predicted ICU stay of at least 48 hours were considered for enrollment, of which 4,683 were included in the final analysis. The primary outcome was 28-day mortality. Secondary outcomes were length of stay in the ICU, receipt and duration of mechanical ventilation, receipt of extracorporeal membrane oxygenation, and renal-replacement therapy. A total of 26.9% of patients developed AKI in the first 7 days of an ICU admission. Severe AKI increased mortality by day 28 (adjusted odds ratio, 1.77; 95% confidence interval, 1.17-2.68) and was associated with increased use of renal-replacement therapy and mechanical ventilation and longer stays in the ICU. Urine output predicted mortality more accurately than did plasma creatinine, and using plasma creatinine alone failed to identify two-thirds of patients with low urine output.
Bottom line: In critically ill young patients, AKI is a common occurrence and is associated with both an increased morbidity and mortality. In a majority of patients with low urine output, plasma creatinine was a poor discriminant of renal function.
Citations: Kaddourah A, Basu RK, Bagshaw SM, et al. Epidemiology of acute kidney injury in critically ill children and young adults. N Eng J Med. 2017; 376 (1):11-20.
Dr. Rachoin is an assistant professor of clinical medicine and associate division head, Hospital Medicine, at Cooper Medical School at Rowan University. He works as a hospitalist at Cooper University Hospital in Camden, N.J.
In CLL, specific mutation is key to ibrutinib resistance
Acquired BTKC481S and PLCG2 mutations led to ibrutinib resistance in chronic lymphocytic leukemia (CLL), investigators reported online in the Journal of Clinical Oncology.
These mutations preceded 85% of clinical relapses, appearing a median of 9.3 months beforehand, Jennifer A. Woyach, MD, and her associates from the Ohio State University, Columbus, concluded from a retrospective study of 308 patients. In a separate prospective study of 112 patients, acquired BTKC481S mutation and clonal expansion preceded all eight cases of relapse, they said. “Relapse of CLL after ibrutinib is an issue of increasing clinical significance,” they concluded. “We show that mutations in Bruton tyrosine kinase (BTK) and PLCG2 appear early and have the potential to be used as a biomarker for future relapse, suggesting an opportunity for intervention.”
Ibrutinib has transformed the CLL treatment landscape, but patients face poor outcomes if they relapse with Richter transformation or develop progressive disease. Past work has linked ibrutinib resistance to acquired mutations in BTK at the binding site of ibrutinib and in PLCG2 located just downstream. But the scope of ibrutinib resistance in CLL and key mutational players were unknown (J Clin Oncol. 2017. doi: 10.1200/JCO.2016.70.2282).
To fill that gap, the researchers retrospectively analyzed data from four sequential ibrutinib CLL trials at the Ohio State University. The separate prospective analysis involved analyzing the entire BTK and PLCG2 coding regions every 3 months.
In the retrospective study, patients had received a median of 3 and up to 16 prior therapies. Given the median follow-up period of 3.4 years, about 19% of patients experienced clinical relapse within 4 years of starting ibrutinib, the researchers estimated (95% confidence interval, 14%-24%). Deep sequencing by Ion Torrent (Life Technologies) identified mutations in BTKC481S and/or PLCG2, in 40 of 47 (85%) relapses. In 31 cases, BTKC481S was the sole mutation. Mutational burdens varied among patients, but generally correlated with CLL progression in peripheral blood versus primarily nodal relapse.
At baseline, 172 (58%) of retrospective study participants had complex cytogenetics, 52% had del(13q), 40% had del(17p), and 21% had MYC abnormality. Median age was 65 years (range, 26-91 years) and 70% of patients were female. Multivariable analyses linked transformation to complex karyotype (hazard ratio, 5.0; 95% CI, 1.5-16.5) and MYC abnormality (HR, 2.5; 95% CI, 1.0-4.7), and linked progressive CLL to age younger than 65 years, complex karyotype, and del(17)(p13.1).
Richter transformation usually occurred within 2 years of starting ibrutinib and had a cumulative 4-year incidence of 10%, the investigators also reported. Patients survived a median of only 3.9 months after stopping ibrutinib because of transformation. The cumulative rate of progressive CLL was higher (19.1%), but early progression was rare, and patients who stopped ibrutinib because of progression survived longer (median, 22.7 months).
In the prospective study, all eight patients with BTKC481S who had not yet clinically relapsed nonetheless had increasing frequency of this mutation over time, the investigators reported. Together, the findings confirm BTK and PLCG2 mutations as the key players in CLL resistance to ibrutinib, they stated. Perhaps most importantly, they reveal “a prolonged period of asymptomatic clonal expression” in CLL that precedes clinical relapse and provides a window of opportunity to target these cells with novel therapies in clinical trials, they wrote.
Given that ibrutinib was approved for use in relapsed CLL only 2 years ago, “We are likely just starting to see the first emergence of relapse in the community setting,” the researchers concluded. “Enhanced knowledge of both the molecular and clinical mechanisms of relapse may allow for strategic alterations in monitoring and management that could change the natural history of ibrutinib resistance.”
Funding sources included the D. Warren Brown Foundation, Mr. and Mrs. Michael Thomas, the Four Winds Foundation, the Leukemia and Lymphoma Society, Pelotonia, and the National Cancer Institute. Pharmacyclics also provided partial support. Dr. Woyach disclosed ties to Janssen, Acerta Pharma, Karyopharm Therapeutics, and MorphoSys, and a provisional patent related to C481S detection.
Acquired BTKC481S and PLCG2 mutations led to ibrutinib resistance in chronic lymphocytic leukemia (CLL), investigators reported online in the Journal of Clinical Oncology.
These mutations preceded 85% of clinical relapses, appearing a median of 9.3 months beforehand, Jennifer A. Woyach, MD, and her associates from the Ohio State University, Columbus, concluded from a retrospective study of 308 patients. In a separate prospective study of 112 patients, acquired BTKC481S mutation and clonal expansion preceded all eight cases of relapse, they said. “Relapse of CLL after ibrutinib is an issue of increasing clinical significance,” they concluded. “We show that mutations in Bruton tyrosine kinase (BTK) and PLCG2 appear early and have the potential to be used as a biomarker for future relapse, suggesting an opportunity for intervention.”
Ibrutinib has transformed the CLL treatment landscape, but patients face poor outcomes if they relapse with Richter transformation or develop progressive disease. Past work has linked ibrutinib resistance to acquired mutations in BTK at the binding site of ibrutinib and in PLCG2 located just downstream. But the scope of ibrutinib resistance in CLL and key mutational players were unknown (J Clin Oncol. 2017. doi: 10.1200/JCO.2016.70.2282).
To fill that gap, the researchers retrospectively analyzed data from four sequential ibrutinib CLL trials at the Ohio State University. The separate prospective analysis involved analyzing the entire BTK and PLCG2 coding regions every 3 months.
In the retrospective study, patients had received a median of 3 and up to 16 prior therapies. Given the median follow-up period of 3.4 years, about 19% of patients experienced clinical relapse within 4 years of starting ibrutinib, the researchers estimated (95% confidence interval, 14%-24%). Deep sequencing by Ion Torrent (Life Technologies) identified mutations in BTKC481S and/or PLCG2, in 40 of 47 (85%) relapses. In 31 cases, BTKC481S was the sole mutation. Mutational burdens varied among patients, but generally correlated with CLL progression in peripheral blood versus primarily nodal relapse.
At baseline, 172 (58%) of retrospective study participants had complex cytogenetics, 52% had del(13q), 40% had del(17p), and 21% had MYC abnormality. Median age was 65 years (range, 26-91 years) and 70% of patients were female. Multivariable analyses linked transformation to complex karyotype (hazard ratio, 5.0; 95% CI, 1.5-16.5) and MYC abnormality (HR, 2.5; 95% CI, 1.0-4.7), and linked progressive CLL to age younger than 65 years, complex karyotype, and del(17)(p13.1).
Richter transformation usually occurred within 2 years of starting ibrutinib and had a cumulative 4-year incidence of 10%, the investigators also reported. Patients survived a median of only 3.9 months after stopping ibrutinib because of transformation. The cumulative rate of progressive CLL was higher (19.1%), but early progression was rare, and patients who stopped ibrutinib because of progression survived longer (median, 22.7 months).
In the prospective study, all eight patients with BTKC481S who had not yet clinically relapsed nonetheless had increasing frequency of this mutation over time, the investigators reported. Together, the findings confirm BTK and PLCG2 mutations as the key players in CLL resistance to ibrutinib, they stated. Perhaps most importantly, they reveal “a prolonged period of asymptomatic clonal expression” in CLL that precedes clinical relapse and provides a window of opportunity to target these cells with novel therapies in clinical trials, they wrote.
Given that ibrutinib was approved for use in relapsed CLL only 2 years ago, “We are likely just starting to see the first emergence of relapse in the community setting,” the researchers concluded. “Enhanced knowledge of both the molecular and clinical mechanisms of relapse may allow for strategic alterations in monitoring and management that could change the natural history of ibrutinib resistance.”
Funding sources included the D. Warren Brown Foundation, Mr. and Mrs. Michael Thomas, the Four Winds Foundation, the Leukemia and Lymphoma Society, Pelotonia, and the National Cancer Institute. Pharmacyclics also provided partial support. Dr. Woyach disclosed ties to Janssen, Acerta Pharma, Karyopharm Therapeutics, and MorphoSys, and a provisional patent related to C481S detection.
Acquired BTKC481S and PLCG2 mutations led to ibrutinib resistance in chronic lymphocytic leukemia (CLL), investigators reported online in the Journal of Clinical Oncology.
These mutations preceded 85% of clinical relapses, appearing a median of 9.3 months beforehand, Jennifer A. Woyach, MD, and her associates from the Ohio State University, Columbus, concluded from a retrospective study of 308 patients. In a separate prospective study of 112 patients, acquired BTKC481S mutation and clonal expansion preceded all eight cases of relapse, they said. “Relapse of CLL after ibrutinib is an issue of increasing clinical significance,” they concluded. “We show that mutations in Bruton tyrosine kinase (BTK) and PLCG2 appear early and have the potential to be used as a biomarker for future relapse, suggesting an opportunity for intervention.”
Ibrutinib has transformed the CLL treatment landscape, but patients face poor outcomes if they relapse with Richter transformation or develop progressive disease. Past work has linked ibrutinib resistance to acquired mutations in BTK at the binding site of ibrutinib and in PLCG2 located just downstream. But the scope of ibrutinib resistance in CLL and key mutational players were unknown (J Clin Oncol. 2017. doi: 10.1200/JCO.2016.70.2282).
To fill that gap, the researchers retrospectively analyzed data from four sequential ibrutinib CLL trials at the Ohio State University. The separate prospective analysis involved analyzing the entire BTK and PLCG2 coding regions every 3 months.
In the retrospective study, patients had received a median of 3 and up to 16 prior therapies. Given the median follow-up period of 3.4 years, about 19% of patients experienced clinical relapse within 4 years of starting ibrutinib, the researchers estimated (95% confidence interval, 14%-24%). Deep sequencing by Ion Torrent (Life Technologies) identified mutations in BTKC481S and/or PLCG2, in 40 of 47 (85%) relapses. In 31 cases, BTKC481S was the sole mutation. Mutational burdens varied among patients, but generally correlated with CLL progression in peripheral blood versus primarily nodal relapse.
At baseline, 172 (58%) of retrospective study participants had complex cytogenetics, 52% had del(13q), 40% had del(17p), and 21% had MYC abnormality. Median age was 65 years (range, 26-91 years) and 70% of patients were female. Multivariable analyses linked transformation to complex karyotype (hazard ratio, 5.0; 95% CI, 1.5-16.5) and MYC abnormality (HR, 2.5; 95% CI, 1.0-4.7), and linked progressive CLL to age younger than 65 years, complex karyotype, and del(17)(p13.1).
Richter transformation usually occurred within 2 years of starting ibrutinib and had a cumulative 4-year incidence of 10%, the investigators also reported. Patients survived a median of only 3.9 months after stopping ibrutinib because of transformation. The cumulative rate of progressive CLL was higher (19.1%), but early progression was rare, and patients who stopped ibrutinib because of progression survived longer (median, 22.7 months).
In the prospective study, all eight patients with BTKC481S who had not yet clinically relapsed nonetheless had increasing frequency of this mutation over time, the investigators reported. Together, the findings confirm BTK and PLCG2 mutations as the key players in CLL resistance to ibrutinib, they stated. Perhaps most importantly, they reveal “a prolonged period of asymptomatic clonal expression” in CLL that precedes clinical relapse and provides a window of opportunity to target these cells with novel therapies in clinical trials, they wrote.
Given that ibrutinib was approved for use in relapsed CLL only 2 years ago, “We are likely just starting to see the first emergence of relapse in the community setting,” the researchers concluded. “Enhanced knowledge of both the molecular and clinical mechanisms of relapse may allow for strategic alterations in monitoring and management that could change the natural history of ibrutinib resistance.”
Funding sources included the D. Warren Brown Foundation, Mr. and Mrs. Michael Thomas, the Four Winds Foundation, the Leukemia and Lymphoma Society, Pelotonia, and the National Cancer Institute. Pharmacyclics also provided partial support. Dr. Woyach disclosed ties to Janssen, Acerta Pharma, Karyopharm Therapeutics, and MorphoSys, and a provisional patent related to C481S detection.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Acquired mutations in BTKC481S and PLCG2 predict ibrutinib resistance in chronic lymphocytic leukemia.
Major finding: These mutations appeared a median of 9.3 months before clinical relapse in 85% of cases. In a separate study, all eight CLL patients who relapsed on ibrutinib had previously developed the BTKC481S mutation with clonal expansion.
Data source: A retrospective analysis of 308 CLL patients from four ibrutinib trials, and a separate prospective study of 118 CLL patients.
Disclosures: Funding sources included the D. Warren Brown Foundation, Mr. and Mrs. Michael Thomas, the Four Winds Foundation, the Leukemia and Lymphoma Society, Pelotonia, and the National Cancer Institute. Pharmacyclics also provided partial support. Dr. Woyach disclosed ties to Janssen, Acerta Pharma, Karyopharm Therapeutics, and MorphoSys, and a provisional patent related to C481S detection.
Outpatient visits for CNS polypharmacy rising among elderly
The number of outpatient visits for CNS polypharmacy by adults aged 65 and older more than doubled between 2004 and 2013, especially among those who reside in rural areas, results from a large analysis of national data showed.
“With each new revision of the Beers Criteria, the list of psychotropic medications considered potentially inappropriate in the elderly has grown,” researchers led by Donovan T. Maust, MD, wrote in a research letter published online Feb. 13, 2017, in JAMA Internal Medicine. “Opioids have recently been included in a Beers measure of central nervous system polypharmacy. Prescribing related drug combinations also received increased regulatory attention when the U.S. Food and Drug Administration recently ordered a black box warning to alert patients of serious risks, including death, caused by opioids coprescribed with CNS depressants.”
Dr. Maust and his associates found that annual CNS polypharmacy visits by adults 65 years or older increased from 1.50 million in 2004 to 3.68 million in 2013, or 0.6% of visits in 2004 to 1.4% in 2013 (adjusted odds ratio of 3.12; P less than .001). The largest increases were observed among rural visits and those for visits with no mental health or pain diagnoses (aOR of 4.99 and 2.65, respectively.)
More than two-thirds of polypharmacy visits (68%) were by women, and 17% were by those who lived in rural areas. In addition, nearly half of polypharmacy visits studied (46%) included neither mental health nor pain diagnoses. No significant demographic differences were observed between polypharmacy visits with and without opioids. “Older adults have become more open to mental health treatment,” the researchers concluded. “Because of limited access to specialty care and a preference to receive treatment in primary care settings, it is unsurprising that mental health treatment has expanded in nonpsychiatric settings.”
Dr. Maust was supported by the Beeson Career Development Award Program. The other researchers reported having no financial disclosures.
The number of outpatient visits for CNS polypharmacy by adults aged 65 and older more than doubled between 2004 and 2013, especially among those who reside in rural areas, results from a large analysis of national data showed.
“With each new revision of the Beers Criteria, the list of psychotropic medications considered potentially inappropriate in the elderly has grown,” researchers led by Donovan T. Maust, MD, wrote in a research letter published online Feb. 13, 2017, in JAMA Internal Medicine. “Opioids have recently been included in a Beers measure of central nervous system polypharmacy. Prescribing related drug combinations also received increased regulatory attention when the U.S. Food and Drug Administration recently ordered a black box warning to alert patients of serious risks, including death, caused by opioids coprescribed with CNS depressants.”
Dr. Maust and his associates found that annual CNS polypharmacy visits by adults 65 years or older increased from 1.50 million in 2004 to 3.68 million in 2013, or 0.6% of visits in 2004 to 1.4% in 2013 (adjusted odds ratio of 3.12; P less than .001). The largest increases were observed among rural visits and those for visits with no mental health or pain diagnoses (aOR of 4.99 and 2.65, respectively.)
More than two-thirds of polypharmacy visits (68%) were by women, and 17% were by those who lived in rural areas. In addition, nearly half of polypharmacy visits studied (46%) included neither mental health nor pain diagnoses. No significant demographic differences were observed between polypharmacy visits with and without opioids. “Older adults have become more open to mental health treatment,” the researchers concluded. “Because of limited access to specialty care and a preference to receive treatment in primary care settings, it is unsurprising that mental health treatment has expanded in nonpsychiatric settings.”
Dr. Maust was supported by the Beeson Career Development Award Program. The other researchers reported having no financial disclosures.
The number of outpatient visits for CNS polypharmacy by adults aged 65 and older more than doubled between 2004 and 2013, especially among those who reside in rural areas, results from a large analysis of national data showed.
“With each new revision of the Beers Criteria, the list of psychotropic medications considered potentially inappropriate in the elderly has grown,” researchers led by Donovan T. Maust, MD, wrote in a research letter published online Feb. 13, 2017, in JAMA Internal Medicine. “Opioids have recently been included in a Beers measure of central nervous system polypharmacy. Prescribing related drug combinations also received increased regulatory attention when the U.S. Food and Drug Administration recently ordered a black box warning to alert patients of serious risks, including death, caused by opioids coprescribed with CNS depressants.”
Dr. Maust and his associates found that annual CNS polypharmacy visits by adults 65 years or older increased from 1.50 million in 2004 to 3.68 million in 2013, or 0.6% of visits in 2004 to 1.4% in 2013 (adjusted odds ratio of 3.12; P less than .001). The largest increases were observed among rural visits and those for visits with no mental health or pain diagnoses (aOR of 4.99 and 2.65, respectively.)
More than two-thirds of polypharmacy visits (68%) were by women, and 17% were by those who lived in rural areas. In addition, nearly half of polypharmacy visits studied (46%) included neither mental health nor pain diagnoses. No significant demographic differences were observed between polypharmacy visits with and without opioids. “Older adults have become more open to mental health treatment,” the researchers concluded. “Because of limited access to specialty care and a preference to receive treatment in primary care settings, it is unsurprising that mental health treatment has expanded in nonpsychiatric settings.”
Dr. Maust was supported by the Beeson Career Development Award Program. The other researchers reported having no financial disclosures.
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Annual CNS polypharmacy visits by adults 65 years or older increased from 1.50 million in 2004 to 3.68 million in 2013.
Data source: An analysis of 97,910 outpatients aged 65 and older from the National Ambulatory Medical Care Survey (NAMCS) from 2004 through 2013.
Disclosures: Dr. Maust was supported by the Beeson Career Development Award Program. The other researchers reported having no financial disclosures.