User login
‘Meaningful’ antitumor activity with lenalidomide monotherapy in ATL
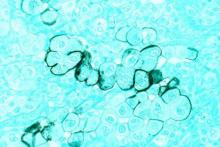
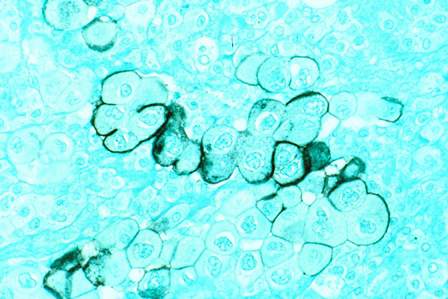
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Lenalidomide monotherapy demonstrated “meaningful” antitumor activity in patients with relapsed or recurrent aggressive adult T-cell leukemia/lymphoma (ATL), according to new findings.
Among 26 patients enrolled in the study, 11 responses were observed, for an overall response rate of 42% (95% CI, 23%-63%). This included four complete responses and one unconfirmed complete response.
The tumor control rate was 73%, achieved in 19 patients, and the toxicity profile was manageable. Overall, these findings hint at the potential of lenalidomide to “become a treatment option in this patient population,” wrote Takashi Ishida, MD, of Nagoya City University Graduate School of Medical Sciences, Aichi, Japan, and his colleagues (J Clin Oncol. 2016 Sep 12. doi: 10.1200/JCO.2016.67.7732).
ATL is a difficult disease to treat, and it has a poor prognosis, as it is resistant to conventional chemotherapeutic agents and treatment options are currently limited. Lenalidomide, an oral immunomodulatory agent, has demonstrated both antiproliferative and antineoplastic activity in B-cell lymphomas in preclinical studies, and a previous phase I trial established a maximum tolerated dosage (25 mg/d) in a small cohort of Japanese patients with relapsed ATL or other peripheral T-cell lymphomas (PTCL).
Based on these preliminary results, Dr. Ishida and his coauthors designed the current multicenter phase II study, to evaluate the efficacy and safety of lenalidomide monotherapy in 26 patients with relapsed or recurrent ATL.
At a median follow-up of 3.9 months, responses were observed in 33% of patients (5 of 15) with acute disease, 57% (4 of 7) with lymphoma, and 50% (2 of 4) for unfavorable chronic ATL. Patient responses according to disease site were 31% for target (nodal and extranodal) lesions, 75% for cutaneous lesions, and 60% for peripheral blood.
The median time to relapse was 1.9 months (range, 1.8-3.7 months), while the median time to progression was 3.8 months (95% CI, 1.9 to not estimable [NE]). The median and mean duration of response for the entire cohort were NE (95% CI, 0.5 months to NE) and 5.2 months (range, 0 to 16.6 months), respectively.
Progression-free survival was 3.8 months (95% CI, 1.9 months to NE) and for overall survival, it was 20.3 months (95% CI, 9.1 months to NE).
Adverse events occurred in more than 20% of patients and the most common hematologic event was thrombocytopenia (77%). The most common nonhematologic event was increased C-reactive protein (42%), and hypoalbuminemia and hypoproteinemia were observed in about a third of patients, as were constipation, hyponatremia, and hypocalcemia (all 31%).
Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Lenalidomide demonstrated clinical activity with acceptable toxicity in recurrent or relapsed ATL.
Major finding: The overall response rate was 42%, and this included four complete responses and one unconfirmed complete response.
Data source: Multicenter phase II trial comprising 26 patients with relapsed or recurrent ATL.
Disclosures: Dr. Ishida and several coauthors reported multiple relationships with industry, including Celgene K.K. (Tokyo), the study’s sponsor.
Worry may attenuate link between psychiatric symptoms, poorer cognitive performance
SAN FRANCISCO – Unexpectedly, worry predicted better cognitive performance among older adults with mild symptoms of anxiety and depression, according to a cross-sectional, community-based study.
“This just flies in the face of everything that we know about worry in the adult literature,” said Sherry A. Beaudreau, PhD, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University. The findings suggest that older worriers might score lower on some cognitive measures if their worry declines through treatment, she said at the 2016 congress of the International Psychogeriatric Association.
Old age often is marked by mild symptoms of anxiety and depression that do not meet criteria for a psychiatric diagnosis, but nonetheless predict poorer cognitive performance and mild dementia, Dr. Beaudreau said. Recent work has linked anxiety to decreased attentional control, and late life depression, to slow information processing, delayed verbal memory, and other cognitive deficits. Emerging evidence also suggests that worry leads to worse performance on tests of inhibitory ability and delayed memory, Dr. Beaudreau added.
To further test these relationships, she and her associates studied 119 older adults who were living in the San Francisco Bay area between 2010 and 2012. They averaged 74 years of age (range, 65-91 years), 92% were non-Hispanic white, and 56% were women.
Most of the cohort performed well on the Rey Auditory Verbal Learning test, which assesses word recall after a delay of 20-30 minutes, and also scored above average on condition 3 of the Delis-Kaplan Executive Function System, which is a color word assessment of inhibitory control, Dr. Beaudreau reported. Individuals also tended to score low on the Beck Anxiety Inventory and the Beck Depressive Inventory II, with average scores of 3.7 (range, 0-29) and 5.6 (0-41), respectively. The mean score on the Penn State Worry Questionnaire was 37.7, with a range of 16-76.
Regardless of whether their anxiety score was low or high, those who worried more had significantly better inhibitory control than those who worried less (P = .003), Dr. Beaudreau said. “So folks with high worry actually seemed to be doing better in terms of their inhibitory ability,” she added. “This is intriguing to me, because we assume that anxiety is affecting cognition, but worry seems to be doing something different.”
High worry also predicted significantly better inhibitory control among individuals with both low and high depression scores (P = .03), she reported. For the word recall test, worry did not seem to affect performance in the absence of depression, but high worry predicted significantly better word recall among individuals with high depression scores (P = .009).
“These results suggest that psychiatric symptoms of anxiety and depression are modulated by worry severity, and it’s interesting that this finding was so consistent throughout the analyses,” Dr. Beaudreau said. Future studies should examine these relationships in groups of older psychiatric patients stratified by symptom severity rather than diagnosis, she added.
The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
SAN FRANCISCO – Unexpectedly, worry predicted better cognitive performance among older adults with mild symptoms of anxiety and depression, according to a cross-sectional, community-based study.
“This just flies in the face of everything that we know about worry in the adult literature,” said Sherry A. Beaudreau, PhD, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University. The findings suggest that older worriers might score lower on some cognitive measures if their worry declines through treatment, she said at the 2016 congress of the International Psychogeriatric Association.
Old age often is marked by mild symptoms of anxiety and depression that do not meet criteria for a psychiatric diagnosis, but nonetheless predict poorer cognitive performance and mild dementia, Dr. Beaudreau said. Recent work has linked anxiety to decreased attentional control, and late life depression, to slow information processing, delayed verbal memory, and other cognitive deficits. Emerging evidence also suggests that worry leads to worse performance on tests of inhibitory ability and delayed memory, Dr. Beaudreau added.
To further test these relationships, she and her associates studied 119 older adults who were living in the San Francisco Bay area between 2010 and 2012. They averaged 74 years of age (range, 65-91 years), 92% were non-Hispanic white, and 56% were women.
Most of the cohort performed well on the Rey Auditory Verbal Learning test, which assesses word recall after a delay of 20-30 minutes, and also scored above average on condition 3 of the Delis-Kaplan Executive Function System, which is a color word assessment of inhibitory control, Dr. Beaudreau reported. Individuals also tended to score low on the Beck Anxiety Inventory and the Beck Depressive Inventory II, with average scores of 3.7 (range, 0-29) and 5.6 (0-41), respectively. The mean score on the Penn State Worry Questionnaire was 37.7, with a range of 16-76.
Regardless of whether their anxiety score was low or high, those who worried more had significantly better inhibitory control than those who worried less (P = .003), Dr. Beaudreau said. “So folks with high worry actually seemed to be doing better in terms of their inhibitory ability,” she added. “This is intriguing to me, because we assume that anxiety is affecting cognition, but worry seems to be doing something different.”
High worry also predicted significantly better inhibitory control among individuals with both low and high depression scores (P = .03), she reported. For the word recall test, worry did not seem to affect performance in the absence of depression, but high worry predicted significantly better word recall among individuals with high depression scores (P = .009).
“These results suggest that psychiatric symptoms of anxiety and depression are modulated by worry severity, and it’s interesting that this finding was so consistent throughout the analyses,” Dr. Beaudreau said. Future studies should examine these relationships in groups of older psychiatric patients stratified by symptom severity rather than diagnosis, she added.
The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
SAN FRANCISCO – Unexpectedly, worry predicted better cognitive performance among older adults with mild symptoms of anxiety and depression, according to a cross-sectional, community-based study.
“This just flies in the face of everything that we know about worry in the adult literature,” said Sherry A. Beaudreau, PhD, of the department of psychiatry and behavioral sciences at Stanford (Calif.) University. The findings suggest that older worriers might score lower on some cognitive measures if their worry declines through treatment, she said at the 2016 congress of the International Psychogeriatric Association.
Old age often is marked by mild symptoms of anxiety and depression that do not meet criteria for a psychiatric diagnosis, but nonetheless predict poorer cognitive performance and mild dementia, Dr. Beaudreau said. Recent work has linked anxiety to decreased attentional control, and late life depression, to slow information processing, delayed verbal memory, and other cognitive deficits. Emerging evidence also suggests that worry leads to worse performance on tests of inhibitory ability and delayed memory, Dr. Beaudreau added.
To further test these relationships, she and her associates studied 119 older adults who were living in the San Francisco Bay area between 2010 and 2012. They averaged 74 years of age (range, 65-91 years), 92% were non-Hispanic white, and 56% were women.
Most of the cohort performed well on the Rey Auditory Verbal Learning test, which assesses word recall after a delay of 20-30 minutes, and also scored above average on condition 3 of the Delis-Kaplan Executive Function System, which is a color word assessment of inhibitory control, Dr. Beaudreau reported. Individuals also tended to score low on the Beck Anxiety Inventory and the Beck Depressive Inventory II, with average scores of 3.7 (range, 0-29) and 5.6 (0-41), respectively. The mean score on the Penn State Worry Questionnaire was 37.7, with a range of 16-76.
Regardless of whether their anxiety score was low or high, those who worried more had significantly better inhibitory control than those who worried less (P = .003), Dr. Beaudreau said. “So folks with high worry actually seemed to be doing better in terms of their inhibitory ability,” she added. “This is intriguing to me, because we assume that anxiety is affecting cognition, but worry seems to be doing something different.”
High worry also predicted significantly better inhibitory control among individuals with both low and high depression scores (P = .03), she reported. For the word recall test, worry did not seem to affect performance in the absence of depression, but high worry predicted significantly better word recall among individuals with high depression scores (P = .009).
“These results suggest that psychiatric symptoms of anxiety and depression are modulated by worry severity, and it’s interesting that this finding was so consistent throughout the analyses,” Dr. Beaudreau said. Future studies should examine these relationships in groups of older psychiatric patients stratified by symptom severity rather than diagnosis, she added.
The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
AT IPA 2016
Key clinical point: In older adults, worry seems to attenuate the relationship between anxiety and depression and poorer cognitive performance.
Major finding: High worry predicted significantly better inhibitory control and delayed word recall, even in the presence of high anxiety and depression symptoms.
Data source: A cross-sectional study of 119 community-dwelling adults who averaged 74 years old.
Disclosures: The work was supported by the Alzheimer’s Association and the Stanford/VA Alzheimer’s Center. Dr. Beaudreau had no relevant financial disclosures.
Neoadjuvant therapy improves survival in pancreatic cancer
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Pancreatic cancer patients who received neoadjuvant therapy (NAT) followed by resection had better outcomes than did those who underwent upfront resection, investigators report.
Among patients with clinical stage I or II resected pancreatic head adenocarcinoma, the median survival was higher among those who had received NAT, compared with those who had upfront resection (26 months vs. 21 months; P less than .01).
The survival benefit remained consistent for both clinical stage I (29 months vs. 23 months; P less than .01) and clinical stage II (24 months vs. 20 months; P less than .01).
“This study lends further support for the use of NAT as a favorable patient selection strategy in the management of resectable, early-stage pancreatic adenocarcinoma,” wrote Ali A. Mokdad, MD, of the University of Texas Southwestern Medical Center, Dallas, and his colleagues (J Clin Oncol. 2016 Sep 19. doi: 10.1200/JCO.2016.68.5081).
The researchers compared overall survival between patients who received NAT with subsequent resection with those who received upfront resection, and they also looked at the patient subset of those who received adjuvant therapy.
The cohort included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma who were identified from the National Cancer Database (2006-2012). The patients who received NAT followed by curative-intent resection were matched with patients whose tumors were resected upfront, and the researchers evaluated early postoperative and oncologic outcomes.
Overall survival at 1, 3, and 5 years was 83%, 35%, and 21% in the NAT arm, compared to 71%, 29%, and 18% among patients who underwent upfront surgery, respectively. In the NAT arm, overall mortality was reduced, with an estimated hazard ratio (HR) of 0.72 (95% CI, 0.68-0.76).
In comparison with the subset of patients who received adjuvant therapy, median survival was statistically significantly longer in the NAT group (26 months vs. 23 months; stratified log-rank P less than .01). Overall survival for the adjuvant therapy group at 1, 3, and 5 years was 78%, 31%, and 18%, respectively.
Upon multivariable analysis, the overall survival difference continued to favor the NAT group vs. the adjuvant therapy arm (adjusted HR, 0.83; 95% CI, 0.78-0.89).
Early postoperative morbidity and mortality did not differ between groups. Compared with patients who received NAT, the upfront surgery group had a higher pathologic T stage (pT3 and T4: 86% vs. 73%; P less than .01) and were more likely to have positive lymph nodes (73% vs. 48%; P less than .01) and positive resection margin (24% vs. 17%; P less than .01).
The data “will hopefully provide support and encouragement for participation in the currently open clinical trials evaluating the role of NAT for clinically staged patients with resectable pancreatic cancer,” the authors concluded.
No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Neoadjuvant therapy improves outcomes in pancreatic cancer.
Major finding: Neoadjuvant therapy was associated with improved survival compared with surgery alone, with a median survival of 26 months vs. 21 months.
Data source: Retrospective database study that included 15,237 patients with clinical stage I or II resected pancreatic head adenocarcinoma.
Disclosures: No outside funding source was disclosed. Coauthor Sam C. Wang, MD, declared a relationship with patent/intellectual panel for a prognostic gene panel for gastric cancer. All other authors declared no disclosures.
Try non-TNF biologics for RA if anti-TNF fails
Rheumatoid arthritis patients who were unsuccessfully treated with anti–tumor necrosis factor drugs fared significantly better when treated with a non-TNF biologic than with a second anti-TNF drug in a 52-week, randomized, clinical trial of 300 adults.
Overall, 69% of patients who received a non-TNF biologic achieved clinical response, defined as a good or moderate EULAR response at 24 weeks, compared with 52% of patients who received a second anti-TNF drug, wrote Jacques-Eric Gottenberg, MD, PhD, of Strasbourg (France) University Hospital and his colleagues.
Patients were randomized to a non-TNF biologic or a second anti-TNF drug, with the choice of biologic left to the clinician. Patients were assessed at 12, 24, and 52 weeks.
“In addition to the superiority of the non-TNF treatment for the primary outcome at week 24, the non-TNF treatment was associated with a better EULAR response than a second anti-TNF drug at weeks 12 and 52,” the researchers noted. Significantly more patients in the non-TNF group reported low disease activity at 6 months and 12 months, compared with the second anti-TNF group, they added.
A total of 18 patients in the non-TNF group and 13 patients in the second anti-TNF group experienced serious adverse events; the most common were serious infections (in 33% and 77% of the non-TNF and anti-TNF groups, respectively) and cardiovascular events (33% vs. 8%, respectively).
The study was supported by the French Ministry of Health and promoted by Strasbourg University Hospital. Dr. Gottenberg disclosed financial support from AbbVie, Pfizer, and Roche, and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, UCB, GlaxoSmithKline, and Novartis.
The findings were published online Sept. 20 (JAMA 2016;316[11]:1172-80).
Rheumatoid arthritis patients who were unsuccessfully treated with anti–tumor necrosis factor drugs fared significantly better when treated with a non-TNF biologic than with a second anti-TNF drug in a 52-week, randomized, clinical trial of 300 adults.
Overall, 69% of patients who received a non-TNF biologic achieved clinical response, defined as a good or moderate EULAR response at 24 weeks, compared with 52% of patients who received a second anti-TNF drug, wrote Jacques-Eric Gottenberg, MD, PhD, of Strasbourg (France) University Hospital and his colleagues.
Patients were randomized to a non-TNF biologic or a second anti-TNF drug, with the choice of biologic left to the clinician. Patients were assessed at 12, 24, and 52 weeks.
“In addition to the superiority of the non-TNF treatment for the primary outcome at week 24, the non-TNF treatment was associated with a better EULAR response than a second anti-TNF drug at weeks 12 and 52,” the researchers noted. Significantly more patients in the non-TNF group reported low disease activity at 6 months and 12 months, compared with the second anti-TNF group, they added.
A total of 18 patients in the non-TNF group and 13 patients in the second anti-TNF group experienced serious adverse events; the most common were serious infections (in 33% and 77% of the non-TNF and anti-TNF groups, respectively) and cardiovascular events (33% vs. 8%, respectively).
The study was supported by the French Ministry of Health and promoted by Strasbourg University Hospital. Dr. Gottenberg disclosed financial support from AbbVie, Pfizer, and Roche, and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, UCB, GlaxoSmithKline, and Novartis.
The findings were published online Sept. 20 (JAMA 2016;316[11]:1172-80).
Rheumatoid arthritis patients who were unsuccessfully treated with anti–tumor necrosis factor drugs fared significantly better when treated with a non-TNF biologic than with a second anti-TNF drug in a 52-week, randomized, clinical trial of 300 adults.
Overall, 69% of patients who received a non-TNF biologic achieved clinical response, defined as a good or moderate EULAR response at 24 weeks, compared with 52% of patients who received a second anti-TNF drug, wrote Jacques-Eric Gottenberg, MD, PhD, of Strasbourg (France) University Hospital and his colleagues.
Patients were randomized to a non-TNF biologic or a second anti-TNF drug, with the choice of biologic left to the clinician. Patients were assessed at 12, 24, and 52 weeks.
“In addition to the superiority of the non-TNF treatment for the primary outcome at week 24, the non-TNF treatment was associated with a better EULAR response than a second anti-TNF drug at weeks 12 and 52,” the researchers noted. Significantly more patients in the non-TNF group reported low disease activity at 6 months and 12 months, compared with the second anti-TNF group, they added.
A total of 18 patients in the non-TNF group and 13 patients in the second anti-TNF group experienced serious adverse events; the most common were serious infections (in 33% and 77% of the non-TNF and anti-TNF groups, respectively) and cardiovascular events (33% vs. 8%, respectively).
The study was supported by the French Ministry of Health and promoted by Strasbourg University Hospital. Dr. Gottenberg disclosed financial support from AbbVie, Pfizer, and Roche, and personal fees from Bristol-Myers Squibb, Merck Sharp & Dohme, UCB, GlaxoSmithKline, and Novartis.
The findings were published online Sept. 20 (JAMA 2016;316[11]:1172-80).
FROM JAMA
Buprenorphine restrictions don’t hinder addiction therapy
Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment, as some had feared, according to a Research Letter published online Sept. 20 in JAMA.
Physicians who wish to treat opioid use disorders using buprenorphine are allowed to prescribe the drug to up to 30 patients during the first year they offer the treatment, and after that, they may request that the limit be increased to 100 patients. Some experts have expressed concern that this requirement may pose a barrier to buprenorphine therapy. To examine this possibility, researchers analyzed information in a database of prescriptions filled at retail pharmacies across the United States.
The investigators focused on buprenorphine prescriptions filled during a 3-year period in seven states with the highest rates of addiction therapy: California, Florida, Massachusetts, Michigan, New York, Pennsylvania, and Texas. They identified 3,234 physician prescribers and 245,016 patients receiving a new buprenorphine prescription during the study period, said Bradley D. Stein, MD, PhD, of the RAND Corporation, Pittsburgh, and his associates.
A substantial proportion of the physician prescribers – 20% – treated only 1-3 patients, and an additional 49% treated fewer than the 30-patient limit. Only 9% of physician prescribers treated more than 75 patients. So the restrictions on the number of concurrent prescriptions do not appear to pose a barrier to buprenorphine therapy, Dr. Stein and his associates said (JAMA. 2016 Sep 20;316[11]:1211-2).
An unexpected finding was that the median duration of buprenorphine therapy was only 53 days, even though clinical recommendations specify that up to 12 months of treatment is beneficial, and longer duration of therapy is associated with better outcomes.
These findings indicate that strategies for improving access to addiction therapy may not need to target prescription limits, the investigators said.
Dr. Stein and his associates said their research was supported by the National Institute on Drug Abuse. He reported having served on the advisory board of Otsuka Pharmaceuticals, and the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment, as some had feared, according to a Research Letter published online Sept. 20 in JAMA.
Physicians who wish to treat opioid use disorders using buprenorphine are allowed to prescribe the drug to up to 30 patients during the first year they offer the treatment, and after that, they may request that the limit be increased to 100 patients. Some experts have expressed concern that this requirement may pose a barrier to buprenorphine therapy. To examine this possibility, researchers analyzed information in a database of prescriptions filled at retail pharmacies across the United States.
The investigators focused on buprenorphine prescriptions filled during a 3-year period in seven states with the highest rates of addiction therapy: California, Florida, Massachusetts, Michigan, New York, Pennsylvania, and Texas. They identified 3,234 physician prescribers and 245,016 patients receiving a new buprenorphine prescription during the study period, said Bradley D. Stein, MD, PhD, of the RAND Corporation, Pittsburgh, and his associates.
A substantial proportion of the physician prescribers – 20% – treated only 1-3 patients, and an additional 49% treated fewer than the 30-patient limit. Only 9% of physician prescribers treated more than 75 patients. So the restrictions on the number of concurrent prescriptions do not appear to pose a barrier to buprenorphine therapy, Dr. Stein and his associates said (JAMA. 2016 Sep 20;316[11]:1211-2).
An unexpected finding was that the median duration of buprenorphine therapy was only 53 days, even though clinical recommendations specify that up to 12 months of treatment is beneficial, and longer duration of therapy is associated with better outcomes.
These findings indicate that strategies for improving access to addiction therapy may not need to target prescription limits, the investigators said.
Dr. Stein and his associates said their research was supported by the National Institute on Drug Abuse. He reported having served on the advisory board of Otsuka Pharmaceuticals, and the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment, as some had feared, according to a Research Letter published online Sept. 20 in JAMA.
Physicians who wish to treat opioid use disorders using buprenorphine are allowed to prescribe the drug to up to 30 patients during the first year they offer the treatment, and after that, they may request that the limit be increased to 100 patients. Some experts have expressed concern that this requirement may pose a barrier to buprenorphine therapy. To examine this possibility, researchers analyzed information in a database of prescriptions filled at retail pharmacies across the United States.
The investigators focused on buprenorphine prescriptions filled during a 3-year period in seven states with the highest rates of addiction therapy: California, Florida, Massachusetts, Michigan, New York, Pennsylvania, and Texas. They identified 3,234 physician prescribers and 245,016 patients receiving a new buprenorphine prescription during the study period, said Bradley D. Stein, MD, PhD, of the RAND Corporation, Pittsburgh, and his associates.
A substantial proportion of the physician prescribers – 20% – treated only 1-3 patients, and an additional 49% treated fewer than the 30-patient limit. Only 9% of physician prescribers treated more than 75 patients. So the restrictions on the number of concurrent prescriptions do not appear to pose a barrier to buprenorphine therapy, Dr. Stein and his associates said (JAMA. 2016 Sep 20;316[11]:1211-2).
An unexpected finding was that the median duration of buprenorphine therapy was only 53 days, even though clinical recommendations specify that up to 12 months of treatment is beneficial, and longer duration of therapy is associated with better outcomes.
These findings indicate that strategies for improving access to addiction therapy may not need to target prescription limits, the investigators said.
Dr. Stein and his associates said their research was supported by the National Institute on Drug Abuse. He reported having served on the advisory board of Otsuka Pharmaceuticals, and the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
FROM JAMA
Key clinical point: Restrictions on the number of buprenorphine prescriptions a physician can write in a given year do not hinder addiction treatment.
Major finding: Most (69%) of physician prescribers treated fewer than the 30-patient limit for buprenorphine prescriptions in a given year
Data source: An analysis of pharmacy data regarding 3,234 buprenorphine prescribers in seven states during a 3-year period.
Disclosures: This work was supported by the National Institute on Drug Abuse. Dr. Stein reported having served on an advisory board of Otsuka Pharmaceuticals; the other investigators reported receiving royalties from Cambridge University Press and UpToDate.
Analyses strengthen FLAME’s findings
LONDON – In chronic obstructive pulmonary disease (COPD), the advantage of a long-acting beta agonist (LABA) plus a long-acting muscarinic antagonist (LAMA) over a LABA plus an inhaled corticosteroid (ICS) was observed in every subgroup in the FLAME trial evaluated, according to post hoc analyses presented at the annual congress of the European Respiratory Society.
“We thought that we might not see the difference in the COPD patients with more severe disease, but the advantage was consistent even among those who entered the trial on triple therapy,” reported Jadwiga A. Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute, Imperial College, London.
FLAME, the recently published study that compared LABA/LAMA to LABA/ICS, was planned as a noninferiority study with the underlying hypothesis that LABA/LAMA would perform as well as LABA/ICS for the primary outcome of annual rate of COPD exacerbations (N Engl J Med. 2016;374:2222-34). Instead, the 11% lower rate of exacerbations for LABA/LAMA proved statistically significant (P = .003).
Six post hoc FLAME analyses were presented at the 2016 ERS Congress to further explore this result. All supported the main result. In addition to evaluating those who entered the trial on a LABA/LAMA/ICS triple-therapy combination, the analyses covered a broad array of subgroups defined by age, smoking history, and COPD severity as defined by Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications.
In FLAME, 3,362 COPD patients who had at least one exacerbation in the preceding year were randomized to the LABA indacaterol (110 mcg) plus the LAMA glycopyrronium (50 mcg) once daily or the combination of the LABA salmeterol (50 mcg) and the ICS fluticasone (500 mcg) twice daily. In addition to the relative advantage on the primary outcome of any exacerbation, the LABA/LAMA combination also significantly reduced the rate of moderate to severe exacerbations (P less than .001), and it extended the times to the first moderate to severe exacerbation (P less than .001) and the first severe exacerbation (P = .046), according to the published data.
In the post hoc analyses, the advantage of LABA/LAMA relative to LAMA/ICS was remarkably consistent. For example, in stratifications made for age (less than 55 years, 55 to less than 65 years, 65-75 years, and greater than or equal to 75 years) at least a numerical advantage of LABA/LAMA was seen in all age groups for prevention of any exacerbation, and the difference reached statistical significance for those in the age group 55 to greater than 65 years. For prevention of moderate to severe exacerbations, the treatments were found to be equivalent for individuals younger than 55 years, but LABA/LAMA was statistically superior for the other three age categories.
For ex-smokers, unlike current smokers, the numerical advantage of LABA/LAMA over LABA/ICS for reduction in the rate ratio of all exacerbations did not reach statistical significance, but the LABA/LAMA combination did provide a statistically significant advantage for both ex-smokers and current smokers for moderate to severe exacerbations.
For patients with two or more exacerbations in the year prior to enrollment in FLAME, the relative degree of protection was of magnitude similar to that of patients with only one exacerbation even though the relative advantage in those with multiple prior exacerbations did not reach statistical significance. However, the lack of significance was likely due to the relatively small number of patients in this subpopulation, according to Dr. Wedzicha.
Similarly, the LABA/LAMA combination was at least numerically superior to LABA/ICS for all exacerbations and for moderate to severe exacerbations across GOLD classifications with one exception. When compared for relative protection against moderate to severe exacerbations, there was a slight and nonsignificant disadvantage for LABA/LAMA, but, again, Dr. Wedzicha reported, “the number of patients in this subgroup was quite small.”
In another FLAME post hoc analysis, the odds ratio (OR) for exacerbations among the 1,893 patients (56.3%) who were on ICS at study entry was found to be almost identical to the OR among those who were not. Specifically, the ORs for all exacerbations and moderate to severe exacerbations were 0.88 (P = .008) and 0.86 (P = .018), respectively, for those previously treated with ICS and 0.88 (P = .021) and 0.78 (P = .002), respectively, for those who had not been treated with ICS.
The LABA/LAMA combination was also superior to LABA/ICS for improvements in quality of life, which was measured via the St. George’s Respiratory Questionnaire. With an improvement of at least four units on the St. George’s Respiratory Questionnaire defined as clinically meaningful, 49.5% of LABA/LAMA patients versus 43.8% of LABA/ICS patients (P less than .024) benefited on this measure.
Overall, the results from the FLAME post hoc analyses have demonstrated “remarkable consistency,” Dr. Wedzicha reported. Taken together, she said the data “imply that LABA/LAMA is the first choice of treatment for COPD patients at risk of exacerbation.”
LONDON – In chronic obstructive pulmonary disease (COPD), the advantage of a long-acting beta agonist (LABA) plus a long-acting muscarinic antagonist (LAMA) over a LABA plus an inhaled corticosteroid (ICS) was observed in every subgroup in the FLAME trial evaluated, according to post hoc analyses presented at the annual congress of the European Respiratory Society.
“We thought that we might not see the difference in the COPD patients with more severe disease, but the advantage was consistent even among those who entered the trial on triple therapy,” reported Jadwiga A. Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute, Imperial College, London.
FLAME, the recently published study that compared LABA/LAMA to LABA/ICS, was planned as a noninferiority study with the underlying hypothesis that LABA/LAMA would perform as well as LABA/ICS for the primary outcome of annual rate of COPD exacerbations (N Engl J Med. 2016;374:2222-34). Instead, the 11% lower rate of exacerbations for LABA/LAMA proved statistically significant (P = .003).
Six post hoc FLAME analyses were presented at the 2016 ERS Congress to further explore this result. All supported the main result. In addition to evaluating those who entered the trial on a LABA/LAMA/ICS triple-therapy combination, the analyses covered a broad array of subgroups defined by age, smoking history, and COPD severity as defined by Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications.
In FLAME, 3,362 COPD patients who had at least one exacerbation in the preceding year were randomized to the LABA indacaterol (110 mcg) plus the LAMA glycopyrronium (50 mcg) once daily or the combination of the LABA salmeterol (50 mcg) and the ICS fluticasone (500 mcg) twice daily. In addition to the relative advantage on the primary outcome of any exacerbation, the LABA/LAMA combination also significantly reduced the rate of moderate to severe exacerbations (P less than .001), and it extended the times to the first moderate to severe exacerbation (P less than .001) and the first severe exacerbation (P = .046), according to the published data.
In the post hoc analyses, the advantage of LABA/LAMA relative to LAMA/ICS was remarkably consistent. For example, in stratifications made for age (less than 55 years, 55 to less than 65 years, 65-75 years, and greater than or equal to 75 years) at least a numerical advantage of LABA/LAMA was seen in all age groups for prevention of any exacerbation, and the difference reached statistical significance for those in the age group 55 to greater than 65 years. For prevention of moderate to severe exacerbations, the treatments were found to be equivalent for individuals younger than 55 years, but LABA/LAMA was statistically superior for the other three age categories.
For ex-smokers, unlike current smokers, the numerical advantage of LABA/LAMA over LABA/ICS for reduction in the rate ratio of all exacerbations did not reach statistical significance, but the LABA/LAMA combination did provide a statistically significant advantage for both ex-smokers and current smokers for moderate to severe exacerbations.
For patients with two or more exacerbations in the year prior to enrollment in FLAME, the relative degree of protection was of magnitude similar to that of patients with only one exacerbation even though the relative advantage in those with multiple prior exacerbations did not reach statistical significance. However, the lack of significance was likely due to the relatively small number of patients in this subpopulation, according to Dr. Wedzicha.
Similarly, the LABA/LAMA combination was at least numerically superior to LABA/ICS for all exacerbations and for moderate to severe exacerbations across GOLD classifications with one exception. When compared for relative protection against moderate to severe exacerbations, there was a slight and nonsignificant disadvantage for LABA/LAMA, but, again, Dr. Wedzicha reported, “the number of patients in this subgroup was quite small.”
In another FLAME post hoc analysis, the odds ratio (OR) for exacerbations among the 1,893 patients (56.3%) who were on ICS at study entry was found to be almost identical to the OR among those who were not. Specifically, the ORs for all exacerbations and moderate to severe exacerbations were 0.88 (P = .008) and 0.86 (P = .018), respectively, for those previously treated with ICS and 0.88 (P = .021) and 0.78 (P = .002), respectively, for those who had not been treated with ICS.
The LABA/LAMA combination was also superior to LABA/ICS for improvements in quality of life, which was measured via the St. George’s Respiratory Questionnaire. With an improvement of at least four units on the St. George’s Respiratory Questionnaire defined as clinically meaningful, 49.5% of LABA/LAMA patients versus 43.8% of LABA/ICS patients (P less than .024) benefited on this measure.
Overall, the results from the FLAME post hoc analyses have demonstrated “remarkable consistency,” Dr. Wedzicha reported. Taken together, she said the data “imply that LABA/LAMA is the first choice of treatment for COPD patients at risk of exacerbation.”
LONDON – In chronic obstructive pulmonary disease (COPD), the advantage of a long-acting beta agonist (LABA) plus a long-acting muscarinic antagonist (LAMA) over a LABA plus an inhaled corticosteroid (ICS) was observed in every subgroup in the FLAME trial evaluated, according to post hoc analyses presented at the annual congress of the European Respiratory Society.
“We thought that we might not see the difference in the COPD patients with more severe disease, but the advantage was consistent even among those who entered the trial on triple therapy,” reported Jadwiga A. Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute, Imperial College, London.
FLAME, the recently published study that compared LABA/LAMA to LABA/ICS, was planned as a noninferiority study with the underlying hypothesis that LABA/LAMA would perform as well as LABA/ICS for the primary outcome of annual rate of COPD exacerbations (N Engl J Med. 2016;374:2222-34). Instead, the 11% lower rate of exacerbations for LABA/LAMA proved statistically significant (P = .003).
Six post hoc FLAME analyses were presented at the 2016 ERS Congress to further explore this result. All supported the main result. In addition to evaluating those who entered the trial on a LABA/LAMA/ICS triple-therapy combination, the analyses covered a broad array of subgroups defined by age, smoking history, and COPD severity as defined by Global Initiative for Chronic Obstructive Lung Disease (GOLD) classifications.
In FLAME, 3,362 COPD patients who had at least one exacerbation in the preceding year were randomized to the LABA indacaterol (110 mcg) plus the LAMA glycopyrronium (50 mcg) once daily or the combination of the LABA salmeterol (50 mcg) and the ICS fluticasone (500 mcg) twice daily. In addition to the relative advantage on the primary outcome of any exacerbation, the LABA/LAMA combination also significantly reduced the rate of moderate to severe exacerbations (P less than .001), and it extended the times to the first moderate to severe exacerbation (P less than .001) and the first severe exacerbation (P = .046), according to the published data.
In the post hoc analyses, the advantage of LABA/LAMA relative to LAMA/ICS was remarkably consistent. For example, in stratifications made for age (less than 55 years, 55 to less than 65 years, 65-75 years, and greater than or equal to 75 years) at least a numerical advantage of LABA/LAMA was seen in all age groups for prevention of any exacerbation, and the difference reached statistical significance for those in the age group 55 to greater than 65 years. For prevention of moderate to severe exacerbations, the treatments were found to be equivalent for individuals younger than 55 years, but LABA/LAMA was statistically superior for the other three age categories.
For ex-smokers, unlike current smokers, the numerical advantage of LABA/LAMA over LABA/ICS for reduction in the rate ratio of all exacerbations did not reach statistical significance, but the LABA/LAMA combination did provide a statistically significant advantage for both ex-smokers and current smokers for moderate to severe exacerbations.
For patients with two or more exacerbations in the year prior to enrollment in FLAME, the relative degree of protection was of magnitude similar to that of patients with only one exacerbation even though the relative advantage in those with multiple prior exacerbations did not reach statistical significance. However, the lack of significance was likely due to the relatively small number of patients in this subpopulation, according to Dr. Wedzicha.
Similarly, the LABA/LAMA combination was at least numerically superior to LABA/ICS for all exacerbations and for moderate to severe exacerbations across GOLD classifications with one exception. When compared for relative protection against moderate to severe exacerbations, there was a slight and nonsignificant disadvantage for LABA/LAMA, but, again, Dr. Wedzicha reported, “the number of patients in this subgroup was quite small.”
In another FLAME post hoc analysis, the odds ratio (OR) for exacerbations among the 1,893 patients (56.3%) who were on ICS at study entry was found to be almost identical to the OR among those who were not. Specifically, the ORs for all exacerbations and moderate to severe exacerbations were 0.88 (P = .008) and 0.86 (P = .018), respectively, for those previously treated with ICS and 0.88 (P = .021) and 0.78 (P = .002), respectively, for those who had not been treated with ICS.
The LABA/LAMA combination was also superior to LABA/ICS for improvements in quality of life, which was measured via the St. George’s Respiratory Questionnaire. With an improvement of at least four units on the St. George’s Respiratory Questionnaire defined as clinically meaningful, 49.5% of LABA/LAMA patients versus 43.8% of LABA/ICS patients (P less than .024) benefited on this measure.
Overall, the results from the FLAME post hoc analyses have demonstrated “remarkable consistency,” Dr. Wedzicha reported. Taken together, she said the data “imply that LABA/LAMA is the first choice of treatment for COPD patients at risk of exacerbation.”
At THE ERS CONGRESS 2016
Key clinical point: The advantage of a LABA/LAMA combination over LABA/ICS in COPD patients persists regardless of patient subgroup.
Major finding: In a series of post hoc analyses from the FLAME trial, the advantage of LABA/LAMA was observed in every subgroup evaluated.
Data source: Post hoc analyses of phase III trial.
Disclosures: Dr Wedzicha reported financial relationships with Bayer, Chiesi, Boehringer Ingelheim, GlaxoSmithKline, Johnson & Johnson, Novartis, Pfizer, Takeda, and Vifor Pharma
EPO improves cognitive impairment in depression
VIENNA – Recombinant human erythropoietin appears to be a cognitive enhancer in patients with unipolar or bipolar depression accompanied by cognitive impairment, Kamilla W. Miskowiak, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
She presented a pooled analysis of her two pilot randomized, placebo-controlled clinical trials totaling 79 patients with treatment-resistant unipolar or partly remitted bipolar depression associated with baseline cognitive impairment. She found that 8 weeks of once-weekly intravenous infusions of high-dose human recombinant erythropoetin (Epogen), also known as epoetin alfa (EPO), resulted in clinically meaningful improvement in cognition 1 week post treatment, as measured on neuropsychological tests assessing the speed of complex cognitive processing, verbal memory, attention span, concentration, working memory, and strategic planning ability. Saline infusions had no effect.
Moreover, follow-up testing conducted 6 weeks after the final treatment session showed continued full maintenance of the initial cognitive gains, which averaged an 11% improvement over baseline. The full duration of effect will be determined in the next round of studies, which will feature 12 weeks of EPO and 6 months of off-treatment follow-up, added Dr. Miskowiak, a senior research psychologist at the University of Copenhagen.
In an interview, she emphasized that the mechanism of benefit doesn’t appear to be related to EPO’s signature ability to boost red blood cell (RBC) production and raise hemoglobin levels. After all, she noted, RBCs were back to normal within 2 weeks after treatment ended, yet the objective cognitive improvements continued. Instead, the mechanism involves EPO’s capacity to enhance brain neuroplasticity, an effect that was demonstrated first in animal studies and subsequently in Dr. Miskowiak’s clinical trials.
“We did MRI functional and structural brain scans at baseline and after completion of treatment, and we saw that EPO increased left hippocampal volume. In fact, it was the structural change in hippocampal volume in response to EPO that was the single strongest predictor of cognitive improvement in multivariate analyses adjusted for age, illness chronicity, depressive symptom severity, gender, and other factors,” according to Dr. Miskowiak.
Physicians who use EPO to treat anemia might blanch at the doses of EPO administered to improve cognitive impairments in patients with affective disorders. Instead of giving 50-100 U/kg of body weight several times per week, as is common in treating anemia, the patients in her studies typically received 40,000 U/wk.
“We used much, much higher doses than are given to affect the bone marrow in patients with anemia, because only about 1% of the IV dose passes across the blood/brain barrier,” she explained.
Because EPO, even in conventional doses, is associated with an increased risk of blood clots, patients were ineligible for the cognition-improvement trials if they had a history of venous thromboembolism, coronary disease, or cancer. Moreover, their RBC and platelet activity levels were monitored on a weekly basis. No untoward effects were seen, Dr. Miskowiak continued.
“Patients really liked coming in for this therapy. Many of them were quite chronic, with years of illness, yet adherence was excellent,” she said.
Early in the developmental pipeline are an intranasal variant of EPO and a carbamylated EPO designed to cross the blood/brain barrier efficiently in order to achieve direct brain neuroplasticity-stimulating effects with minimal impact on RBC production.
Dr. Miskowiak stressed that EPO as a treatment for cognitive dysfunction associated with affective disorders is not ready for prime time use in clinical practice. The next round of randomized, placebo-controlled clinical trials, due to start early in 2017, will attempt to replicate her pilot study findings while pinning down the optimal dosing regimen. The new trials will feature longer off-treatment follow-up as well as quality-of-life measures and an economic analysis that includes assessment of the ability to return to work.
“This therapy may be attractive from an economic perspective,” according to the psychologist. “I don’t see this as first-line therapy in clinical practice, though,” she added. “It will be reserved for the more severely cognitively impaired patients.”
Eduard Vieta, MD, professor and chair of the department of psychiatry and psychology at the University of Barcelona, commented that cognitive impairment is now recognized as a core aspect of affective disorders. There is a huge unmet need for treatments that address this disease aspect. The drugs now available for treatment of bipolar disorder and unipolar depression don’t improve the associated cognitive impairments. Indeed, up to 40% of patients in remission from major depressive disorder and 70% in remission from bipolar disorder continue to experience neurocognitive symptoms.
Dr. Miskowiak’s work was funded by the Danish Ministry of Science, Innovation, and Higher Education. She reported having no relevant financial conflicts of interest.
VIENNA – Recombinant human erythropoietin appears to be a cognitive enhancer in patients with unipolar or bipolar depression accompanied by cognitive impairment, Kamilla W. Miskowiak, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
She presented a pooled analysis of her two pilot randomized, placebo-controlled clinical trials totaling 79 patients with treatment-resistant unipolar or partly remitted bipolar depression associated with baseline cognitive impairment. She found that 8 weeks of once-weekly intravenous infusions of high-dose human recombinant erythropoetin (Epogen), also known as epoetin alfa (EPO), resulted in clinically meaningful improvement in cognition 1 week post treatment, as measured on neuropsychological tests assessing the speed of complex cognitive processing, verbal memory, attention span, concentration, working memory, and strategic planning ability. Saline infusions had no effect.
Moreover, follow-up testing conducted 6 weeks after the final treatment session showed continued full maintenance of the initial cognitive gains, which averaged an 11% improvement over baseline. The full duration of effect will be determined in the next round of studies, which will feature 12 weeks of EPO and 6 months of off-treatment follow-up, added Dr. Miskowiak, a senior research psychologist at the University of Copenhagen.
In an interview, she emphasized that the mechanism of benefit doesn’t appear to be related to EPO’s signature ability to boost red blood cell (RBC) production and raise hemoglobin levels. After all, she noted, RBCs were back to normal within 2 weeks after treatment ended, yet the objective cognitive improvements continued. Instead, the mechanism involves EPO’s capacity to enhance brain neuroplasticity, an effect that was demonstrated first in animal studies and subsequently in Dr. Miskowiak’s clinical trials.
“We did MRI functional and structural brain scans at baseline and after completion of treatment, and we saw that EPO increased left hippocampal volume. In fact, it was the structural change in hippocampal volume in response to EPO that was the single strongest predictor of cognitive improvement in multivariate analyses adjusted for age, illness chronicity, depressive symptom severity, gender, and other factors,” according to Dr. Miskowiak.
Physicians who use EPO to treat anemia might blanch at the doses of EPO administered to improve cognitive impairments in patients with affective disorders. Instead of giving 50-100 U/kg of body weight several times per week, as is common in treating anemia, the patients in her studies typically received 40,000 U/wk.
“We used much, much higher doses than are given to affect the bone marrow in patients with anemia, because only about 1% of the IV dose passes across the blood/brain barrier,” she explained.
Because EPO, even in conventional doses, is associated with an increased risk of blood clots, patients were ineligible for the cognition-improvement trials if they had a history of venous thromboembolism, coronary disease, or cancer. Moreover, their RBC and platelet activity levels were monitored on a weekly basis. No untoward effects were seen, Dr. Miskowiak continued.
“Patients really liked coming in for this therapy. Many of them were quite chronic, with years of illness, yet adherence was excellent,” she said.
Early in the developmental pipeline are an intranasal variant of EPO and a carbamylated EPO designed to cross the blood/brain barrier efficiently in order to achieve direct brain neuroplasticity-stimulating effects with minimal impact on RBC production.
Dr. Miskowiak stressed that EPO as a treatment for cognitive dysfunction associated with affective disorders is not ready for prime time use in clinical practice. The next round of randomized, placebo-controlled clinical trials, due to start early in 2017, will attempt to replicate her pilot study findings while pinning down the optimal dosing regimen. The new trials will feature longer off-treatment follow-up as well as quality-of-life measures and an economic analysis that includes assessment of the ability to return to work.
“This therapy may be attractive from an economic perspective,” according to the psychologist. “I don’t see this as first-line therapy in clinical practice, though,” she added. “It will be reserved for the more severely cognitively impaired patients.”
Eduard Vieta, MD, professor and chair of the department of psychiatry and psychology at the University of Barcelona, commented that cognitive impairment is now recognized as a core aspect of affective disorders. There is a huge unmet need for treatments that address this disease aspect. The drugs now available for treatment of bipolar disorder and unipolar depression don’t improve the associated cognitive impairments. Indeed, up to 40% of patients in remission from major depressive disorder and 70% in remission from bipolar disorder continue to experience neurocognitive symptoms.
Dr. Miskowiak’s work was funded by the Danish Ministry of Science, Innovation, and Higher Education. She reported having no relevant financial conflicts of interest.
VIENNA – Recombinant human erythropoietin appears to be a cognitive enhancer in patients with unipolar or bipolar depression accompanied by cognitive impairment, Kamilla W. Miskowiak, PhD, reported at the annual congress of the European College of Neuropsychopharmacology.
She presented a pooled analysis of her two pilot randomized, placebo-controlled clinical trials totaling 79 patients with treatment-resistant unipolar or partly remitted bipolar depression associated with baseline cognitive impairment. She found that 8 weeks of once-weekly intravenous infusions of high-dose human recombinant erythropoetin (Epogen), also known as epoetin alfa (EPO), resulted in clinically meaningful improvement in cognition 1 week post treatment, as measured on neuropsychological tests assessing the speed of complex cognitive processing, verbal memory, attention span, concentration, working memory, and strategic planning ability. Saline infusions had no effect.
Moreover, follow-up testing conducted 6 weeks after the final treatment session showed continued full maintenance of the initial cognitive gains, which averaged an 11% improvement over baseline. The full duration of effect will be determined in the next round of studies, which will feature 12 weeks of EPO and 6 months of off-treatment follow-up, added Dr. Miskowiak, a senior research psychologist at the University of Copenhagen.
In an interview, she emphasized that the mechanism of benefit doesn’t appear to be related to EPO’s signature ability to boost red blood cell (RBC) production and raise hemoglobin levels. After all, she noted, RBCs were back to normal within 2 weeks after treatment ended, yet the objective cognitive improvements continued. Instead, the mechanism involves EPO’s capacity to enhance brain neuroplasticity, an effect that was demonstrated first in animal studies and subsequently in Dr. Miskowiak’s clinical trials.
“We did MRI functional and structural brain scans at baseline and after completion of treatment, and we saw that EPO increased left hippocampal volume. In fact, it was the structural change in hippocampal volume in response to EPO that was the single strongest predictor of cognitive improvement in multivariate analyses adjusted for age, illness chronicity, depressive symptom severity, gender, and other factors,” according to Dr. Miskowiak.
Physicians who use EPO to treat anemia might blanch at the doses of EPO administered to improve cognitive impairments in patients with affective disorders. Instead of giving 50-100 U/kg of body weight several times per week, as is common in treating anemia, the patients in her studies typically received 40,000 U/wk.
“We used much, much higher doses than are given to affect the bone marrow in patients with anemia, because only about 1% of the IV dose passes across the blood/brain barrier,” she explained.
Because EPO, even in conventional doses, is associated with an increased risk of blood clots, patients were ineligible for the cognition-improvement trials if they had a history of venous thromboembolism, coronary disease, or cancer. Moreover, their RBC and platelet activity levels were monitored on a weekly basis. No untoward effects were seen, Dr. Miskowiak continued.
“Patients really liked coming in for this therapy. Many of them were quite chronic, with years of illness, yet adherence was excellent,” she said.
Early in the developmental pipeline are an intranasal variant of EPO and a carbamylated EPO designed to cross the blood/brain barrier efficiently in order to achieve direct brain neuroplasticity-stimulating effects with minimal impact on RBC production.
Dr. Miskowiak stressed that EPO as a treatment for cognitive dysfunction associated with affective disorders is not ready for prime time use in clinical practice. The next round of randomized, placebo-controlled clinical trials, due to start early in 2017, will attempt to replicate her pilot study findings while pinning down the optimal dosing regimen. The new trials will feature longer off-treatment follow-up as well as quality-of-life measures and an economic analysis that includes assessment of the ability to return to work.
“This therapy may be attractive from an economic perspective,” according to the psychologist. “I don’t see this as first-line therapy in clinical practice, though,” she added. “It will be reserved for the more severely cognitively impaired patients.”
Eduard Vieta, MD, professor and chair of the department of psychiatry and psychology at the University of Barcelona, commented that cognitive impairment is now recognized as a core aspect of affective disorders. There is a huge unmet need for treatments that address this disease aspect. The drugs now available for treatment of bipolar disorder and unipolar depression don’t improve the associated cognitive impairments. Indeed, up to 40% of patients in remission from major depressive disorder and 70% in remission from bipolar disorder continue to experience neurocognitive symptoms.
Dr. Miskowiak’s work was funded by the Danish Ministry of Science, Innovation, and Higher Education. She reported having no relevant financial conflicts of interest.
AT THE ECNP CONGRESS
Key clinical point: Recombinant human erythropoietin enhances brain neuroplasticity and achieves measurable improvements in cognitive impairment associated with unipolar or bipolar depression.
Major finding: Patients with cognitive impairment related to unipolar or bipolar depression responded to a series of infusions of recombinant human erythropoietin with a significant improvement in neuropsychological test scores that was maintained unabated 6 weeks after their final infusion.
Data source: A retrospective analysis of pooled data from two randomized, placebo-controlled trials totaling 79 patients with unipolar or bipolar depression.
Disclosures: This work was funded by the Danish Ministry of Science, Innovation, and Higher Education. The presenter reported having no relevant financial conflicts of interest.
Siponimod curbs disability in secondary progressive multiple sclerosis
LONDON – Siponimod delayed disability progression in patients with secondary progressive multiple sclerosis, according to top-line findings from the phase III EXPAND study.
Siponimod reduced the primary endpoint of the time to 3-month confirmed disease progression (CDP) assessed via the Expanded Disability Status Scale (EDSS) by 21%, compared with placebo (P = .013).
“It is reassuring that this primary outcome is supported by an important secondary outcome of the time to CDP at 6 months,” presenting author Ludwig Kappos, MD, of University Hospital Basel (Switzerland), said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
He reported that a 26% reduction in the 6-month CDP was also observed comparing the active and placebo treatments (P = .006) in the multicenter, randomized, double-blind trial that involved 1,646 patients “with the whole spectrum” of secondary progressive multiple sclerosis (SPMS).
The findings build on those of the phase II BOLD study in patients with relapsing-remitting MS (RRMS) (Lancet Neurol. 2013;12[8]:756-67) and showed a reduction in relapse rates and a reduction in the number of brain lesions seen on MRI scans for siponimod, compared with placebo.
Recently reported data from the 24-month extension of the BOLD phase II trial (JAMA Neurol. 2016;73[9]:1089-98) also showed that disease activity was low in patients treated with siponimod, and that there were no new safety signals. Dose reduction during initiation mitigated cardiac adverse effects, an approach that was also used successfully in the phase III study.
Siponimod is a once-daily oral treatment being developed by Novartis for the treatment of MS. Like fingolimod (Gilenya), which is licensed for the treatment of RRMS, siponimod is a selective sphingosine 1-phosphate receptor (S1P) modulator. Unlike fingolimod, which targets S1P subtypes 1, 3, 4, and 5, siponimod only targets the S1P 1 and 5 subtypes.
Fingolimod is also known to cause temporary changes in heart rate, heartbeat, and blood pressure, which necessitates early electrocardiographic monitoring during the first 6 hours when the drug is first given. At the present time, it doesn’t seem that siponimod will have unwanted cardiac effects, but longer-term follow-up data are needed.
“Adverse events were as you would expect with an S1P receptor modulator,” Dr. Kappos said, noting that there was nothing new. Overall, any adverse event occurred in 88% of actively-treated and 81% of placebo-treated patients. The rate of serious adverse events was similar in the siponimod (3.8%) and placebo (3.7%) arms, and a similar percentage of patients were reported to have infections (48% and 49%, respectively).
Analysis of all the various secondary endpoints is still ongoing; Dr. Kappos noted that the primary endpoint data had just recently become available. Some initial findings, however, show benefit for siponimod over placebo.
The change in T2 lesion volume from baseline to both 12 and 24 months was significantly less with siponimod than with placebo, at a 79.1% lower average change (P less than .0001).
The annualized relapse rate was reduced by 55% with the active treatment versus placebo, and there was less percent change in brain volume with active therapy versus placebo from baseline to 12 and 24 months’ follow-up (23.4% lower average change, P = .0002).
The time to 3-month confirmed worsening by 20% or more from baseline in the timed 25-foot walk test was reduced by 6.2%. Although not significant, the trend was “in the right direction,” Dr. Kappos said.
The mean age of recruited patients was 48 years, with an average duration of MS of 16-17 years, and just under 4 years since their conversion to SPMS. Baseline EDSS was a mean of 5.4, around 35%-37% had one or more relapses in the 2 years before screening, and 20% had gadolinium-enhancing lesions at baseline.
A variety of predefined subgroup analyses showed a benefit for siponimod over placebo. These included analyses looking at the effect by the number of gadolinium-enhancing lesions at baseline, previous disease-modifying treatment, whether patients’ MS was rapidly progressing, whether patients’ disease was moderate or severe, the baseline EDSS, and the duration of MS since the first recognition of symptoms.
“What is the optimal patient population?” an audience member asked Dr. Kappos during the Q&A period following his presentation at the ECTRIMS meeting. He responded: “I think younger patients with the more active disease will certainly be the best candidates.” But, he added, it was reassuring to note that the drug seems to work equally well in all patient subtypes.
Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from multiple MS drug manufacturers – including Novartis – and charitable organizations.
LONDON – Siponimod delayed disability progression in patients with secondary progressive multiple sclerosis, according to top-line findings from the phase III EXPAND study.
Siponimod reduced the primary endpoint of the time to 3-month confirmed disease progression (CDP) assessed via the Expanded Disability Status Scale (EDSS) by 21%, compared with placebo (P = .013).
“It is reassuring that this primary outcome is supported by an important secondary outcome of the time to CDP at 6 months,” presenting author Ludwig Kappos, MD, of University Hospital Basel (Switzerland), said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
He reported that a 26% reduction in the 6-month CDP was also observed comparing the active and placebo treatments (P = .006) in the multicenter, randomized, double-blind trial that involved 1,646 patients “with the whole spectrum” of secondary progressive multiple sclerosis (SPMS).
The findings build on those of the phase II BOLD study in patients with relapsing-remitting MS (RRMS) (Lancet Neurol. 2013;12[8]:756-67) and showed a reduction in relapse rates and a reduction in the number of brain lesions seen on MRI scans for siponimod, compared with placebo.
Recently reported data from the 24-month extension of the BOLD phase II trial (JAMA Neurol. 2016;73[9]:1089-98) also showed that disease activity was low in patients treated with siponimod, and that there were no new safety signals. Dose reduction during initiation mitigated cardiac adverse effects, an approach that was also used successfully in the phase III study.
Siponimod is a once-daily oral treatment being developed by Novartis for the treatment of MS. Like fingolimod (Gilenya), which is licensed for the treatment of RRMS, siponimod is a selective sphingosine 1-phosphate receptor (S1P) modulator. Unlike fingolimod, which targets S1P subtypes 1, 3, 4, and 5, siponimod only targets the S1P 1 and 5 subtypes.
Fingolimod is also known to cause temporary changes in heart rate, heartbeat, and blood pressure, which necessitates early electrocardiographic monitoring during the first 6 hours when the drug is first given. At the present time, it doesn’t seem that siponimod will have unwanted cardiac effects, but longer-term follow-up data are needed.
“Adverse events were as you would expect with an S1P receptor modulator,” Dr. Kappos said, noting that there was nothing new. Overall, any adverse event occurred in 88% of actively-treated and 81% of placebo-treated patients. The rate of serious adverse events was similar in the siponimod (3.8%) and placebo (3.7%) arms, and a similar percentage of patients were reported to have infections (48% and 49%, respectively).
Analysis of all the various secondary endpoints is still ongoing; Dr. Kappos noted that the primary endpoint data had just recently become available. Some initial findings, however, show benefit for siponimod over placebo.
The change in T2 lesion volume from baseline to both 12 and 24 months was significantly less with siponimod than with placebo, at a 79.1% lower average change (P less than .0001).
The annualized relapse rate was reduced by 55% with the active treatment versus placebo, and there was less percent change in brain volume with active therapy versus placebo from baseline to 12 and 24 months’ follow-up (23.4% lower average change, P = .0002).
The time to 3-month confirmed worsening by 20% or more from baseline in the timed 25-foot walk test was reduced by 6.2%. Although not significant, the trend was “in the right direction,” Dr. Kappos said.
The mean age of recruited patients was 48 years, with an average duration of MS of 16-17 years, and just under 4 years since their conversion to SPMS. Baseline EDSS was a mean of 5.4, around 35%-37% had one or more relapses in the 2 years before screening, and 20% had gadolinium-enhancing lesions at baseline.
A variety of predefined subgroup analyses showed a benefit for siponimod over placebo. These included analyses looking at the effect by the number of gadolinium-enhancing lesions at baseline, previous disease-modifying treatment, whether patients’ MS was rapidly progressing, whether patients’ disease was moderate or severe, the baseline EDSS, and the duration of MS since the first recognition of symptoms.
“What is the optimal patient population?” an audience member asked Dr. Kappos during the Q&A period following his presentation at the ECTRIMS meeting. He responded: “I think younger patients with the more active disease will certainly be the best candidates.” But, he added, it was reassuring to note that the drug seems to work equally well in all patient subtypes.
Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from multiple MS drug manufacturers – including Novartis – and charitable organizations.
LONDON – Siponimod delayed disability progression in patients with secondary progressive multiple sclerosis, according to top-line findings from the phase III EXPAND study.
Siponimod reduced the primary endpoint of the time to 3-month confirmed disease progression (CDP) assessed via the Expanded Disability Status Scale (EDSS) by 21%, compared with placebo (P = .013).
“It is reassuring that this primary outcome is supported by an important secondary outcome of the time to CDP at 6 months,” presenting author Ludwig Kappos, MD, of University Hospital Basel (Switzerland), said at the annual congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
He reported that a 26% reduction in the 6-month CDP was also observed comparing the active and placebo treatments (P = .006) in the multicenter, randomized, double-blind trial that involved 1,646 patients “with the whole spectrum” of secondary progressive multiple sclerosis (SPMS).
The findings build on those of the phase II BOLD study in patients with relapsing-remitting MS (RRMS) (Lancet Neurol. 2013;12[8]:756-67) and showed a reduction in relapse rates and a reduction in the number of brain lesions seen on MRI scans for siponimod, compared with placebo.
Recently reported data from the 24-month extension of the BOLD phase II trial (JAMA Neurol. 2016;73[9]:1089-98) also showed that disease activity was low in patients treated with siponimod, and that there were no new safety signals. Dose reduction during initiation mitigated cardiac adverse effects, an approach that was also used successfully in the phase III study.
Siponimod is a once-daily oral treatment being developed by Novartis for the treatment of MS. Like fingolimod (Gilenya), which is licensed for the treatment of RRMS, siponimod is a selective sphingosine 1-phosphate receptor (S1P) modulator. Unlike fingolimod, which targets S1P subtypes 1, 3, 4, and 5, siponimod only targets the S1P 1 and 5 subtypes.
Fingolimod is also known to cause temporary changes in heart rate, heartbeat, and blood pressure, which necessitates early electrocardiographic monitoring during the first 6 hours when the drug is first given. At the present time, it doesn’t seem that siponimod will have unwanted cardiac effects, but longer-term follow-up data are needed.
“Adverse events were as you would expect with an S1P receptor modulator,” Dr. Kappos said, noting that there was nothing new. Overall, any adverse event occurred in 88% of actively-treated and 81% of placebo-treated patients. The rate of serious adverse events was similar in the siponimod (3.8%) and placebo (3.7%) arms, and a similar percentage of patients were reported to have infections (48% and 49%, respectively).
Analysis of all the various secondary endpoints is still ongoing; Dr. Kappos noted that the primary endpoint data had just recently become available. Some initial findings, however, show benefit for siponimod over placebo.
The change in T2 lesion volume from baseline to both 12 and 24 months was significantly less with siponimod than with placebo, at a 79.1% lower average change (P less than .0001).
The annualized relapse rate was reduced by 55% with the active treatment versus placebo, and there was less percent change in brain volume with active therapy versus placebo from baseline to 12 and 24 months’ follow-up (23.4% lower average change, P = .0002).
The time to 3-month confirmed worsening by 20% or more from baseline in the timed 25-foot walk test was reduced by 6.2%. Although not significant, the trend was “in the right direction,” Dr. Kappos said.
The mean age of recruited patients was 48 years, with an average duration of MS of 16-17 years, and just under 4 years since their conversion to SPMS. Baseline EDSS was a mean of 5.4, around 35%-37% had one or more relapses in the 2 years before screening, and 20% had gadolinium-enhancing lesions at baseline.
A variety of predefined subgroup analyses showed a benefit for siponimod over placebo. These included analyses looking at the effect by the number of gadolinium-enhancing lesions at baseline, previous disease-modifying treatment, whether patients’ MS was rapidly progressing, whether patients’ disease was moderate or severe, the baseline EDSS, and the duration of MS since the first recognition of symptoms.
“What is the optimal patient population?” an audience member asked Dr. Kappos during the Q&A period following his presentation at the ECTRIMS meeting. He responded: “I think younger patients with the more active disease will certainly be the best candidates.” But, he added, it was reassuring to note that the drug seems to work equally well in all patient subtypes.
Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from multiple MS drug manufacturers – including Novartis – and charitable organizations.
AT ECTRIMS 2016
Key clinical point: Siponimod is an investigational treatment that could help patients with secondary progressive multiple sclerosis.
Major finding: Siponimod reduced the 3-month confirmed disability progression by 21%, compared with placebo (hazard ratio, 0.79; P = .013).
Data source: Phase III, multicenter, randomized, double-blind, placebo-controlled trial of siponimod versus placebo in the treatment of 1,646 patients with SPMS.
Disclosures: Novartis funded the study. Dr. Kappos disclosed that his institution has received financial support for research purposes from many MS drug manufacturers – including Novartis – and charitable organizations.
New members welcomed to Consultant Board
We are pleased to welcome Laura Searcy and Cathy Haut to the Pediatric News Consultant Board.
Laura Searcy, MN, APRN, PPCNP-BC, is a pediatric nurse practitioner with more than 25 years’ experience in clinical practice, health policy, and advocacy with a focus on pediatric primary care, child and adolescent injury prevention, substance abuse prevention, and government affairs. Receiving her bachelor’s degree in nursing from the University of Florida in Gainesville, she earned her master’s degree in child health and pediatric nurse practitioner degrees from Emory University in Atlanta. Currently on the medical staff at WellStar Kennestone Regional Medical Center in Marietta, Ga., delivering care to newborns, Ms. Searcy has served as a preceptor and clinical instructor for all levels of nursing students at many institutions.
President of the National Association of Pediatric Nurse Practitioners (NAPNAP), Ms. Searcy previously served on the NAPNAP executive board as president-elect and health policy committee chair. She is a past Georgia NAPNAP chapter president and legislative chair as well as a cofounder of the Georgia Coalition of Advanced Practice Registered Nurses. A member of the American Association of Nurse Practitioners (AANP), Ms. Searcy received the 2014 AANP Nurse Practitioner State Award for Excellence from Georgia.
Widely recognized for her leadership skills, Ms. Searcy gained much of her governance experience serving three terms, including chair and vice chair, on the Cobb County Georgia Board of Education. The U.S. Secretary of Education appointed her to the Southeast Regional Advisement Committee, and the Georgia School Board Association appointed her to the National School Board Association Federal Relations Network. Ms. Searcy also has more than 12 years of nonprofit board experience, working with children’s advocacy centers and youth alcohol and drug-abuse prevention organizations.
Cathy Haut, DNP, CPNP-AC, CPNP-PC, CCRN, is a pediatric nurse practitioner who is the immediate past president of NAPNAP. She received her Master of Science degree as a neonatal clinical nurse specialist at the University of Maryland in the early 1990s and a post–master’s certificate as a pediatric nurse practitioner in 1997. Dr. Haut completed the Doctor of Nursing Practice program in 2010, focusing on pediatric nurses’ knowledge and attitudes toward palliative care. Board-certified in both primary and acute care, she has worked in pediatrics for more than 30 years, the past 19 years as a pediatric nurse practitioner. A fellow in the American Association of Colleges of Nurse’s Leadership for Academic Nursing Program, she holds a certificate in teaching in nursing education.
Dr. Haut works at Beacon Pediatrics, a large primary care practice in Rehoboth Beach, Del. She also works part time for Pediatrix Medical Group, serving the Pediatric Intensive Care Unit medical team at the Herman & Walter Samuelson Children’s Hospital at Sinai in Baltimore and serves as adjunct faculty at the University of Maryland School of Nursing, also in Baltimore.
The coeditor of a textbook, Lippincott Certification Review: Pediatric Acute Care Nurse Practitioner, Dr. Haut has published and presented on many clinical and professional topics. She has volunteered for different nursing organizations in a variety of positions, and has been an active member and leader of NAPNAP’s Maryland Chesapeake Chapter since 1996, serving as president in 2006-2007.
We are pleased to welcome Laura Searcy and Cathy Haut to the Pediatric News Consultant Board.
Laura Searcy, MN, APRN, PPCNP-BC, is a pediatric nurse practitioner with more than 25 years’ experience in clinical practice, health policy, and advocacy with a focus on pediatric primary care, child and adolescent injury prevention, substance abuse prevention, and government affairs. Receiving her bachelor’s degree in nursing from the University of Florida in Gainesville, she earned her master’s degree in child health and pediatric nurse practitioner degrees from Emory University in Atlanta. Currently on the medical staff at WellStar Kennestone Regional Medical Center in Marietta, Ga., delivering care to newborns, Ms. Searcy has served as a preceptor and clinical instructor for all levels of nursing students at many institutions.
President of the National Association of Pediatric Nurse Practitioners (NAPNAP), Ms. Searcy previously served on the NAPNAP executive board as president-elect and health policy committee chair. She is a past Georgia NAPNAP chapter president and legislative chair as well as a cofounder of the Georgia Coalition of Advanced Practice Registered Nurses. A member of the American Association of Nurse Practitioners (AANP), Ms. Searcy received the 2014 AANP Nurse Practitioner State Award for Excellence from Georgia.
Widely recognized for her leadership skills, Ms. Searcy gained much of her governance experience serving three terms, including chair and vice chair, on the Cobb County Georgia Board of Education. The U.S. Secretary of Education appointed her to the Southeast Regional Advisement Committee, and the Georgia School Board Association appointed her to the National School Board Association Federal Relations Network. Ms. Searcy also has more than 12 years of nonprofit board experience, working with children’s advocacy centers and youth alcohol and drug-abuse prevention organizations.
Cathy Haut, DNP, CPNP-AC, CPNP-PC, CCRN, is a pediatric nurse practitioner who is the immediate past president of NAPNAP. She received her Master of Science degree as a neonatal clinical nurse specialist at the University of Maryland in the early 1990s and a post–master’s certificate as a pediatric nurse practitioner in 1997. Dr. Haut completed the Doctor of Nursing Practice program in 2010, focusing on pediatric nurses’ knowledge and attitudes toward palliative care. Board-certified in both primary and acute care, she has worked in pediatrics for more than 30 years, the past 19 years as a pediatric nurse practitioner. A fellow in the American Association of Colleges of Nurse’s Leadership for Academic Nursing Program, she holds a certificate in teaching in nursing education.
Dr. Haut works at Beacon Pediatrics, a large primary care practice in Rehoboth Beach, Del. She also works part time for Pediatrix Medical Group, serving the Pediatric Intensive Care Unit medical team at the Herman & Walter Samuelson Children’s Hospital at Sinai in Baltimore and serves as adjunct faculty at the University of Maryland School of Nursing, also in Baltimore.
The coeditor of a textbook, Lippincott Certification Review: Pediatric Acute Care Nurse Practitioner, Dr. Haut has published and presented on many clinical and professional topics. She has volunteered for different nursing organizations in a variety of positions, and has been an active member and leader of NAPNAP’s Maryland Chesapeake Chapter since 1996, serving as president in 2006-2007.
We are pleased to welcome Laura Searcy and Cathy Haut to the Pediatric News Consultant Board.
Laura Searcy, MN, APRN, PPCNP-BC, is a pediatric nurse practitioner with more than 25 years’ experience in clinical practice, health policy, and advocacy with a focus on pediatric primary care, child and adolescent injury prevention, substance abuse prevention, and government affairs. Receiving her bachelor’s degree in nursing from the University of Florida in Gainesville, she earned her master’s degree in child health and pediatric nurse practitioner degrees from Emory University in Atlanta. Currently on the medical staff at WellStar Kennestone Regional Medical Center in Marietta, Ga., delivering care to newborns, Ms. Searcy has served as a preceptor and clinical instructor for all levels of nursing students at many institutions.
President of the National Association of Pediatric Nurse Practitioners (NAPNAP), Ms. Searcy previously served on the NAPNAP executive board as president-elect and health policy committee chair. She is a past Georgia NAPNAP chapter president and legislative chair as well as a cofounder of the Georgia Coalition of Advanced Practice Registered Nurses. A member of the American Association of Nurse Practitioners (AANP), Ms. Searcy received the 2014 AANP Nurse Practitioner State Award for Excellence from Georgia.
Widely recognized for her leadership skills, Ms. Searcy gained much of her governance experience serving three terms, including chair and vice chair, on the Cobb County Georgia Board of Education. The U.S. Secretary of Education appointed her to the Southeast Regional Advisement Committee, and the Georgia School Board Association appointed her to the National School Board Association Federal Relations Network. Ms. Searcy also has more than 12 years of nonprofit board experience, working with children’s advocacy centers and youth alcohol and drug-abuse prevention organizations.
Cathy Haut, DNP, CPNP-AC, CPNP-PC, CCRN, is a pediatric nurse practitioner who is the immediate past president of NAPNAP. She received her Master of Science degree as a neonatal clinical nurse specialist at the University of Maryland in the early 1990s and a post–master’s certificate as a pediatric nurse practitioner in 1997. Dr. Haut completed the Doctor of Nursing Practice program in 2010, focusing on pediatric nurses’ knowledge and attitudes toward palliative care. Board-certified in both primary and acute care, she has worked in pediatrics for more than 30 years, the past 19 years as a pediatric nurse practitioner. A fellow in the American Association of Colleges of Nurse’s Leadership for Academic Nursing Program, she holds a certificate in teaching in nursing education.
Dr. Haut works at Beacon Pediatrics, a large primary care practice in Rehoboth Beach, Del. She also works part time for Pediatrix Medical Group, serving the Pediatric Intensive Care Unit medical team at the Herman & Walter Samuelson Children’s Hospital at Sinai in Baltimore and serves as adjunct faculty at the University of Maryland School of Nursing, also in Baltimore.
The coeditor of a textbook, Lippincott Certification Review: Pediatric Acute Care Nurse Practitioner, Dr. Haut has published and presented on many clinical and professional topics. She has volunteered for different nursing organizations in a variety of positions, and has been an active member and leader of NAPNAP’s Maryland Chesapeake Chapter since 1996, serving as president in 2006-2007.
Optimal medical therapy doesn’t affect DAPT efficacy
ROME – Continued dual-antiplatelet therapy beyond 12 months after coronary stenting is neither helped nor hindered by concomitant background optimal medical therapy, according to a secondary analysis of the landmark DAPT trial.
Numerous studies have shown that only 46%-66% of patients with stable ischemic heart disease are adherent to guideline-directed optimal medical therapy (OMT) with statins, beta-blockers, and ACE inhibitors or angiotensin receptor blockers. Yet until this new analysis from DAPT (the Dual Antiplatelet Therapy Study), the impact of OMT on the treatment effect of prolonged DAPT was unstudied, Charles D. Resor, MD, said at the annual congress of the European Society of Cardiology.
It was plausible that the treatment benefit of continued DAPT beyond 12 months after coronary stenting might be stunted by concomitant OMT, or alternatively that OMT and DAPT might exert synergistic effects in reducing the risk of ischemic events. As it turned out, neither of these possibilities turned out to be the case, according to Dr. Resor of Brigham and Women’s Hospital, Boston.
“I think OMT is underutilized, but while we would like physicians to emphasize OMT use in more cases, the decision to use DAPT beyond 12 months should be made irrespective of OMT use,” he said.
“That’s an important message for clinicians,” commented session cochair Keith A.A. Fox, MD, of the University of Edinburgh.
The landmark DAPT trial established that there is a significant benefit of continued dual-antiplatelet therapy beyond 12 months from coronary stenting in patients with stable ischemic heart disease (N Engl J Med. 2014 Dec 4;371:2155-66). Dr. Resor presented a secondary analysis of clinical outcomes in 11,643 study participants stratified by their OMT status as well as by whether they were randomized to dual-antiplatelet therapy or aspirin plus placebo.
Sixty-three percent of subjects were on OMT at enrollment. Adherence to OMT was high: At 30 months post stenting, 62% of participants remained on OMT.
Between 12 and 30 months after percutaneous coronary intervention, continued dual-antiplatelet therapy in patients also on OMT was associated with a 2.1% incidence of acute MI, a 36% reduction in risk, compared with the 3.3% rate in subjects on placebo plus OMT. In patients not on OMT, the MI rate was 2.2% in those on dual-antiplatelet therapy versus 5.2% with placebo, for a 59% relative risk reduction in the active treatment arm.
The rate of the composite endpoint of major adverse cardiovascular and cerebrovascular events in patients on dual-antiplatelet therapy and OMT was 4.2%, compared with a 5.0% rate in patients on placebo and OMT.
Moderate or severe bleeding, as measured by the Global Use of Strategies to Open Occluded Arteries (GUSTO) criteria occurred in 2.2% of patients on dual-antiplatelet therapy and OMT, compared with 1.0% in those on placebo plus OMT. In patients not on OMT, the bleeding rate was 2.8% in the dual-antiplatelet therapy group and 2.2% with placebo, a nonsignificant difference.
Overall, patients on OMT had significantly lower rates of acute MI than those not on OMT (2.7%, compared with 3.7%), as well as fewer major adverse cardiovascular and cerebrovascular events (4.6% versus 5.7%), and less moderate or severe bleeding (1.6%, compared with 2.5% in patients not on OMT). However, rates of stroke, stent thrombosis, and death didn’t differ between patients on OMT and those who were not.
“While the associations between OMT use and lower rates of MI and MACCE [major adverse cardiovascular and cerebrovascular events] were expected, the association with lower rates of moderate or severe bleeding was not; we suspect the lower bleeding risk is mostly due to some residual confounding,” according to Dr. Resor.
He reported having no financial conflicts of interest regarding the new secondary analysis of DAPT, which was sponsored by the Harvard Clinical Research Institute.
Simultaneously with Dr. Resor’s presentation, the new DAPT study analysis was published online (Circulation. 2016 Aug 30. doi: 10.1161/CIRCULATIONAHA.116.024531.)
ROME – Continued dual-antiplatelet therapy beyond 12 months after coronary stenting is neither helped nor hindered by concomitant background optimal medical therapy, according to a secondary analysis of the landmark DAPT trial.
Numerous studies have shown that only 46%-66% of patients with stable ischemic heart disease are adherent to guideline-directed optimal medical therapy (OMT) with statins, beta-blockers, and ACE inhibitors or angiotensin receptor blockers. Yet until this new analysis from DAPT (the Dual Antiplatelet Therapy Study), the impact of OMT on the treatment effect of prolonged DAPT was unstudied, Charles D. Resor, MD, said at the annual congress of the European Society of Cardiology.
It was plausible that the treatment benefit of continued DAPT beyond 12 months after coronary stenting might be stunted by concomitant OMT, or alternatively that OMT and DAPT might exert synergistic effects in reducing the risk of ischemic events. As it turned out, neither of these possibilities turned out to be the case, according to Dr. Resor of Brigham and Women’s Hospital, Boston.
“I think OMT is underutilized, but while we would like physicians to emphasize OMT use in more cases, the decision to use DAPT beyond 12 months should be made irrespective of OMT use,” he said.
“That’s an important message for clinicians,” commented session cochair Keith A.A. Fox, MD, of the University of Edinburgh.
The landmark DAPT trial established that there is a significant benefit of continued dual-antiplatelet therapy beyond 12 months from coronary stenting in patients with stable ischemic heart disease (N Engl J Med. 2014 Dec 4;371:2155-66). Dr. Resor presented a secondary analysis of clinical outcomes in 11,643 study participants stratified by their OMT status as well as by whether they were randomized to dual-antiplatelet therapy or aspirin plus placebo.
Sixty-three percent of subjects were on OMT at enrollment. Adherence to OMT was high: At 30 months post stenting, 62% of participants remained on OMT.
Between 12 and 30 months after percutaneous coronary intervention, continued dual-antiplatelet therapy in patients also on OMT was associated with a 2.1% incidence of acute MI, a 36% reduction in risk, compared with the 3.3% rate in subjects on placebo plus OMT. In patients not on OMT, the MI rate was 2.2% in those on dual-antiplatelet therapy versus 5.2% with placebo, for a 59% relative risk reduction in the active treatment arm.
The rate of the composite endpoint of major adverse cardiovascular and cerebrovascular events in patients on dual-antiplatelet therapy and OMT was 4.2%, compared with a 5.0% rate in patients on placebo and OMT.
Moderate or severe bleeding, as measured by the Global Use of Strategies to Open Occluded Arteries (GUSTO) criteria occurred in 2.2% of patients on dual-antiplatelet therapy and OMT, compared with 1.0% in those on placebo plus OMT. In patients not on OMT, the bleeding rate was 2.8% in the dual-antiplatelet therapy group and 2.2% with placebo, a nonsignificant difference.
Overall, patients on OMT had significantly lower rates of acute MI than those not on OMT (2.7%, compared with 3.7%), as well as fewer major adverse cardiovascular and cerebrovascular events (4.6% versus 5.7%), and less moderate or severe bleeding (1.6%, compared with 2.5% in patients not on OMT). However, rates of stroke, stent thrombosis, and death didn’t differ between patients on OMT and those who were not.
“While the associations between OMT use and lower rates of MI and MACCE [major adverse cardiovascular and cerebrovascular events] were expected, the association with lower rates of moderate or severe bleeding was not; we suspect the lower bleeding risk is mostly due to some residual confounding,” according to Dr. Resor.
He reported having no financial conflicts of interest regarding the new secondary analysis of DAPT, which was sponsored by the Harvard Clinical Research Institute.
Simultaneously with Dr. Resor’s presentation, the new DAPT study analysis was published online (Circulation. 2016 Aug 30. doi: 10.1161/CIRCULATIONAHA.116.024531.)
ROME – Continued dual-antiplatelet therapy beyond 12 months after coronary stenting is neither helped nor hindered by concomitant background optimal medical therapy, according to a secondary analysis of the landmark DAPT trial.
Numerous studies have shown that only 46%-66% of patients with stable ischemic heart disease are adherent to guideline-directed optimal medical therapy (OMT) with statins, beta-blockers, and ACE inhibitors or angiotensin receptor blockers. Yet until this new analysis from DAPT (the Dual Antiplatelet Therapy Study), the impact of OMT on the treatment effect of prolonged DAPT was unstudied, Charles D. Resor, MD, said at the annual congress of the European Society of Cardiology.
It was plausible that the treatment benefit of continued DAPT beyond 12 months after coronary stenting might be stunted by concomitant OMT, or alternatively that OMT and DAPT might exert synergistic effects in reducing the risk of ischemic events. As it turned out, neither of these possibilities turned out to be the case, according to Dr. Resor of Brigham and Women’s Hospital, Boston.
“I think OMT is underutilized, but while we would like physicians to emphasize OMT use in more cases, the decision to use DAPT beyond 12 months should be made irrespective of OMT use,” he said.
“That’s an important message for clinicians,” commented session cochair Keith A.A. Fox, MD, of the University of Edinburgh.
The landmark DAPT trial established that there is a significant benefit of continued dual-antiplatelet therapy beyond 12 months from coronary stenting in patients with stable ischemic heart disease (N Engl J Med. 2014 Dec 4;371:2155-66). Dr. Resor presented a secondary analysis of clinical outcomes in 11,643 study participants stratified by their OMT status as well as by whether they were randomized to dual-antiplatelet therapy or aspirin plus placebo.
Sixty-three percent of subjects were on OMT at enrollment. Adherence to OMT was high: At 30 months post stenting, 62% of participants remained on OMT.
Between 12 and 30 months after percutaneous coronary intervention, continued dual-antiplatelet therapy in patients also on OMT was associated with a 2.1% incidence of acute MI, a 36% reduction in risk, compared with the 3.3% rate in subjects on placebo plus OMT. In patients not on OMT, the MI rate was 2.2% in those on dual-antiplatelet therapy versus 5.2% with placebo, for a 59% relative risk reduction in the active treatment arm.
The rate of the composite endpoint of major adverse cardiovascular and cerebrovascular events in patients on dual-antiplatelet therapy and OMT was 4.2%, compared with a 5.0% rate in patients on placebo and OMT.
Moderate or severe bleeding, as measured by the Global Use of Strategies to Open Occluded Arteries (GUSTO) criteria occurred in 2.2% of patients on dual-antiplatelet therapy and OMT, compared with 1.0% in those on placebo plus OMT. In patients not on OMT, the bleeding rate was 2.8% in the dual-antiplatelet therapy group and 2.2% with placebo, a nonsignificant difference.
Overall, patients on OMT had significantly lower rates of acute MI than those not on OMT (2.7%, compared with 3.7%), as well as fewer major adverse cardiovascular and cerebrovascular events (4.6% versus 5.7%), and less moderate or severe bleeding (1.6%, compared with 2.5% in patients not on OMT). However, rates of stroke, stent thrombosis, and death didn’t differ between patients on OMT and those who were not.
“While the associations between OMT use and lower rates of MI and MACCE [major adverse cardiovascular and cerebrovascular events] were expected, the association with lower rates of moderate or severe bleeding was not; we suspect the lower bleeding risk is mostly due to some residual confounding,” according to Dr. Resor.
He reported having no financial conflicts of interest regarding the new secondary analysis of DAPT, which was sponsored by the Harvard Clinical Research Institute.
Simultaneously with Dr. Resor’s presentation, the new DAPT study analysis was published online (Circulation. 2016 Aug 30. doi: 10.1161/CIRCULATIONAHA.116.024531.)
AT THE ESC CONGRESS 2016
Key clinical point: The decision to use DAPT beyond 12 months should be made irrespective of optimal medical therapy use.
Major finding: Between 12 and 30 months after coronary stenting, continued dual-antiplatelet therapy was associated with a 2.1% rate of acute MI in patients on optimal medical therapy and a 2.2% rate in those not on optimal medical therapy.
Data source: A secondary analysis of 11,648 participants in the double-blind, randomized Dual Antiplatelet Therapy Study who were followed prospectively for the period of 12-30 months post PCI.
Disclosures: The study presenter reported having no financial conflicts regarding the new secondary analysis of DAPT, which was sponsored by the Harvard Clinical Research Institute.