User login
What to do when adolescents with ADHD self-medicate with bath salts
Designer drugs are rapidly making inroads with young people, primarily because of easier access, lower overall cost, and nebulous legality. These drugs are made as variants of illicit drugs or new formulations and sold as “research chemicals” and labeled as “not for human consumption,” which allows them to fall outside existing laws. The ingredients typically are not detected in a urine drug screen.
Notoriously addictive, these designer drugs, such as bath salts, are known to incorporate synthetic cathinones—namely, methylone, mephedrone or methylenedioxypyrovalerone (MDPV). The stimulant, amphetamine-like effects of bath salts make the drug attractive to adolescents with attention-deficit/hyperactivity disorder (ADHD).
Why do teens gravitate toward bath salts?
Adolescents with undiagnosed ADHD might self-medicate with drugs that are suited for addressing restlessness, intrapsychic turmoil, and other symptoms of ADHD. In 2 case studies, using the self-medication hypothesis, people with ADHD were more likely to seek cocaine by means of “self-selection.”1 These drug-seeking behaviors often led to cocaine dependence, even when other substances, such as alcohol or Cannabis, were available.
Methylphenidate and other ADHD pharmacotherapies influence the nucleus accumbens in a manner similar to that of cocaine. These findings suggest that adolescents with ADHD and cocaine dependence might respond to therapeutic interventions that substitute cocaine with psychostimulants.1
Bath salts fall within the same spectrum of psychostimulant agents as methylphenidate and cocaine. MDPV approximates the effect of methylphenidate at low doses, and cocaine at higher doses. It often is marketed under the name “Ivory Wave” and could be confused with cocaine. Self-administration of MDPV can induce psychoactive effects that help alleviate ADHD symptoms; adolescents might continue to experience enhanced concentration and overall performance.2 Also, because of the low cost of “legal” bath salts, they are an appealing alternative to cocaine for self-medication.
Managing the sequelae of bath salt intoxication
Bath salts may produce sympathomimetic effects greater than cocaine, which require a proactive approach to symptom management. A medley of unknown ingredients in bath salt preparations makes it difficult for clinicians to gauge the pharmacological impact on individual patients; therefore, therapeutic interventions are on a case-by-case basis. However, emergencies concerning amphetamines and amphetamine analogues and derivatives often have similar presentations.
Cardiovascular effects. MDPV-specific urine and blood tests conducted on patients admitted to the emergency room showed a 10-fold increase in overall dopamine levels compared with those who took cocaine. As a sympathomimetic, high doses of dopamine are responsible for raising blood pressure and could lead to the development of pronounced cardiovascular effects.3,4
Agitation. Clinicians generally are advised to treat agitation before providing a more comprehensive assessment of symptoms. Endotracheal intubation often is a required for adequate control of agitation. Bath salt-induced agitation often is treated with IV benzodiazepines.4,5 Monitor patients for excessive sedation or new-onset “paradoxical agitation” as a function of ongoing benzo-diazepine therapy. Clinicians also may choose to co-administer an antipsychotic with benzodiazepines, although the practice is not universally encouraged for agitation control.
Mephedrone produces a delirious state in conjunction with psychotic symptoms. Antipsychotic therapy has been suggested for addressing ongoing agitation.6
Tachycardia. Symptomatic treatment of tachycardia involves beta blockers, such as labetalol. Nitroglycerine has evidence of efficacy for chest pain associated with cocaine intoxication; however, it is unclear whether it is effective for similar drugs of abuse.4
Multi-organ collapse caused by MDPV necessitates aggressive intervention, including prompt dialysis. Carefully evaluate the patient for the presence of organ-specific insults and initiate supportive measures accordingly. Pronounced agitation with hyperthermia might portend severely compromised renal, hepatic, and/or cardiac function in MDPV users.7 Those who present with MDPV intoxication and concomitant renal injury seem to benefit from hemodialysis.8 Repeat intoxication events may yield a presentation of acute renal injury replete with metabolic derangements, including metabolic acidosis, hyperuricemia, and rhabdomyolysis.9 Thorough patient assessments and interventions are useful in determining long-term outcomes, including issues pertaining to mortality.
Confronting an epidemic
Adolescents are quickly adopting designer drugs as a readily accessible form of recreational “legal highs.”10 Public awareness and educational initiatives can bring to light the dangers of these substances that exert powerful and, sometimes, unpredictable psychoactive effects on the user.
Self-mutilation and suicidal ideation also have been documented among those who ingested bath salts. These reports appear to be escalating across Europe and the United States. On a national level, U.S. poison centers have reported an almost 20-fold increase in calls regarding bath salts between 2010 and 2011.5 It is of utmost importance for clinicians and emergency personnel to familiarize themselves with the sympathomimetic toxidrome and management for bath salt consumption.
1. Mariani JJ, Khantzian EJ, Levin FR. The self-medication hypothesis and psychostimulant treatment of cocaine dependence: an update. Am J Addict. 2014;23(2):189-193.
2. Deluca P, Schifano F, Davey Z, et al. MDPV Report: Psychonaut Web Mapping Research Project. https://catbull.com/alamut/Bibliothek/PsychonautMDPVreport. pdf. Updated June 8, 2010. Accessed October 27, 2015.
3. National Institute on Drug Abuse. What are bath salts? http://teens.drugabuse.gov/drug-facts/bath-salts. Updated October 23, 2015. Accessed October 27, 2015.
4. Richards JR, Derlet RW, Albertson TE, et al. Methamphetamine, “bath salts,” and other amphetamine-related derivatives. Enliven: Toxicology and Allied Clinical Pharmacology. 2014;1(1):1-15.
5. Olives TD, Orozco BS, Stellpflug SJ. Bath salts: the ivory wave of trouble. West J Emerg Med. 2012;13(1):58-62.
6. Kasick DP, McKnight CA, Klisovic E. “Bath salt” ingestion leading to severe intoxication delirium: two cases and a brief review of the emergence of mephedrone use. Am J Drug Alcohol Abuse. 2012;38(2):176-180.
7. Borek HA, Holstege CP. Hyperthermia and multiorgan failure after abuse of “bath salts” containing 3,4-methylenedioxypyrovalerone. Ann Emerg Med. 2012;60(1):103-105.
8. Regunath H, Ariyamuthu VK, Dalal P, et al. Bath salt intoxication causing acute kidney injury requiring hemodialysis. Hemodial Int. 2012;16(suppl 1):S47-S49.
9. Adebamiro A, Perazella MA. Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis. 2012;59(2):273-275.
10. Federation of American Societies for Experimental Biology. New designer drug, ‘bath salts,’ may confer additional risk for adolescents. EurekAlert. http://www.eurekalert.org/ pub_releases/2013-04/foas-ndd041813.php. Published April 23, 2013. Accessed November 10, 2015.
Designer drugs are rapidly making inroads with young people, primarily because of easier access, lower overall cost, and nebulous legality. These drugs are made as variants of illicit drugs or new formulations and sold as “research chemicals” and labeled as “not for human consumption,” which allows them to fall outside existing laws. The ingredients typically are not detected in a urine drug screen.
Notoriously addictive, these designer drugs, such as bath salts, are known to incorporate synthetic cathinones—namely, methylone, mephedrone or methylenedioxypyrovalerone (MDPV). The stimulant, amphetamine-like effects of bath salts make the drug attractive to adolescents with attention-deficit/hyperactivity disorder (ADHD).
Why do teens gravitate toward bath salts?
Adolescents with undiagnosed ADHD might self-medicate with drugs that are suited for addressing restlessness, intrapsychic turmoil, and other symptoms of ADHD. In 2 case studies, using the self-medication hypothesis, people with ADHD were more likely to seek cocaine by means of “self-selection.”1 These drug-seeking behaviors often led to cocaine dependence, even when other substances, such as alcohol or Cannabis, were available.
Methylphenidate and other ADHD pharmacotherapies influence the nucleus accumbens in a manner similar to that of cocaine. These findings suggest that adolescents with ADHD and cocaine dependence might respond to therapeutic interventions that substitute cocaine with psychostimulants.1
Bath salts fall within the same spectrum of psychostimulant agents as methylphenidate and cocaine. MDPV approximates the effect of methylphenidate at low doses, and cocaine at higher doses. It often is marketed under the name “Ivory Wave” and could be confused with cocaine. Self-administration of MDPV can induce psychoactive effects that help alleviate ADHD symptoms; adolescents might continue to experience enhanced concentration and overall performance.2 Also, because of the low cost of “legal” bath salts, they are an appealing alternative to cocaine for self-medication.
Managing the sequelae of bath salt intoxication
Bath salts may produce sympathomimetic effects greater than cocaine, which require a proactive approach to symptom management. A medley of unknown ingredients in bath salt preparations makes it difficult for clinicians to gauge the pharmacological impact on individual patients; therefore, therapeutic interventions are on a case-by-case basis. However, emergencies concerning amphetamines and amphetamine analogues and derivatives often have similar presentations.
Cardiovascular effects. MDPV-specific urine and blood tests conducted on patients admitted to the emergency room showed a 10-fold increase in overall dopamine levels compared with those who took cocaine. As a sympathomimetic, high doses of dopamine are responsible for raising blood pressure and could lead to the development of pronounced cardiovascular effects.3,4
Agitation. Clinicians generally are advised to treat agitation before providing a more comprehensive assessment of symptoms. Endotracheal intubation often is a required for adequate control of agitation. Bath salt-induced agitation often is treated with IV benzodiazepines.4,5 Monitor patients for excessive sedation or new-onset “paradoxical agitation” as a function of ongoing benzo-diazepine therapy. Clinicians also may choose to co-administer an antipsychotic with benzodiazepines, although the practice is not universally encouraged for agitation control.
Mephedrone produces a delirious state in conjunction with psychotic symptoms. Antipsychotic therapy has been suggested for addressing ongoing agitation.6
Tachycardia. Symptomatic treatment of tachycardia involves beta blockers, such as labetalol. Nitroglycerine has evidence of efficacy for chest pain associated with cocaine intoxication; however, it is unclear whether it is effective for similar drugs of abuse.4
Multi-organ collapse caused by MDPV necessitates aggressive intervention, including prompt dialysis. Carefully evaluate the patient for the presence of organ-specific insults and initiate supportive measures accordingly. Pronounced agitation with hyperthermia might portend severely compromised renal, hepatic, and/or cardiac function in MDPV users.7 Those who present with MDPV intoxication and concomitant renal injury seem to benefit from hemodialysis.8 Repeat intoxication events may yield a presentation of acute renal injury replete with metabolic derangements, including metabolic acidosis, hyperuricemia, and rhabdomyolysis.9 Thorough patient assessments and interventions are useful in determining long-term outcomes, including issues pertaining to mortality.
Confronting an epidemic
Adolescents are quickly adopting designer drugs as a readily accessible form of recreational “legal highs.”10 Public awareness and educational initiatives can bring to light the dangers of these substances that exert powerful and, sometimes, unpredictable psychoactive effects on the user.
Self-mutilation and suicidal ideation also have been documented among those who ingested bath salts. These reports appear to be escalating across Europe and the United States. On a national level, U.S. poison centers have reported an almost 20-fold increase in calls regarding bath salts between 2010 and 2011.5 It is of utmost importance for clinicians and emergency personnel to familiarize themselves with the sympathomimetic toxidrome and management for bath salt consumption.
Designer drugs are rapidly making inroads with young people, primarily because of easier access, lower overall cost, and nebulous legality. These drugs are made as variants of illicit drugs or new formulations and sold as “research chemicals” and labeled as “not for human consumption,” which allows them to fall outside existing laws. The ingredients typically are not detected in a urine drug screen.
Notoriously addictive, these designer drugs, such as bath salts, are known to incorporate synthetic cathinones—namely, methylone, mephedrone or methylenedioxypyrovalerone (MDPV). The stimulant, amphetamine-like effects of bath salts make the drug attractive to adolescents with attention-deficit/hyperactivity disorder (ADHD).
Why do teens gravitate toward bath salts?
Adolescents with undiagnosed ADHD might self-medicate with drugs that are suited for addressing restlessness, intrapsychic turmoil, and other symptoms of ADHD. In 2 case studies, using the self-medication hypothesis, people with ADHD were more likely to seek cocaine by means of “self-selection.”1 These drug-seeking behaviors often led to cocaine dependence, even when other substances, such as alcohol or Cannabis, were available.
Methylphenidate and other ADHD pharmacotherapies influence the nucleus accumbens in a manner similar to that of cocaine. These findings suggest that adolescents with ADHD and cocaine dependence might respond to therapeutic interventions that substitute cocaine with psychostimulants.1
Bath salts fall within the same spectrum of psychostimulant agents as methylphenidate and cocaine. MDPV approximates the effect of methylphenidate at low doses, and cocaine at higher doses. It often is marketed under the name “Ivory Wave” and could be confused with cocaine. Self-administration of MDPV can induce psychoactive effects that help alleviate ADHD symptoms; adolescents might continue to experience enhanced concentration and overall performance.2 Also, because of the low cost of “legal” bath salts, they are an appealing alternative to cocaine for self-medication.
Managing the sequelae of bath salt intoxication
Bath salts may produce sympathomimetic effects greater than cocaine, which require a proactive approach to symptom management. A medley of unknown ingredients in bath salt preparations makes it difficult for clinicians to gauge the pharmacological impact on individual patients; therefore, therapeutic interventions are on a case-by-case basis. However, emergencies concerning amphetamines and amphetamine analogues and derivatives often have similar presentations.
Cardiovascular effects. MDPV-specific urine and blood tests conducted on patients admitted to the emergency room showed a 10-fold increase in overall dopamine levels compared with those who took cocaine. As a sympathomimetic, high doses of dopamine are responsible for raising blood pressure and could lead to the development of pronounced cardiovascular effects.3,4
Agitation. Clinicians generally are advised to treat agitation before providing a more comprehensive assessment of symptoms. Endotracheal intubation often is a required for adequate control of agitation. Bath salt-induced agitation often is treated with IV benzodiazepines.4,5 Monitor patients for excessive sedation or new-onset “paradoxical agitation” as a function of ongoing benzo-diazepine therapy. Clinicians also may choose to co-administer an antipsychotic with benzodiazepines, although the practice is not universally encouraged for agitation control.
Mephedrone produces a delirious state in conjunction with psychotic symptoms. Antipsychotic therapy has been suggested for addressing ongoing agitation.6
Tachycardia. Symptomatic treatment of tachycardia involves beta blockers, such as labetalol. Nitroglycerine has evidence of efficacy for chest pain associated with cocaine intoxication; however, it is unclear whether it is effective for similar drugs of abuse.4
Multi-organ collapse caused by MDPV necessitates aggressive intervention, including prompt dialysis. Carefully evaluate the patient for the presence of organ-specific insults and initiate supportive measures accordingly. Pronounced agitation with hyperthermia might portend severely compromised renal, hepatic, and/or cardiac function in MDPV users.7 Those who present with MDPV intoxication and concomitant renal injury seem to benefit from hemodialysis.8 Repeat intoxication events may yield a presentation of acute renal injury replete with metabolic derangements, including metabolic acidosis, hyperuricemia, and rhabdomyolysis.9 Thorough patient assessments and interventions are useful in determining long-term outcomes, including issues pertaining to mortality.
Confronting an epidemic
Adolescents are quickly adopting designer drugs as a readily accessible form of recreational “legal highs.”10 Public awareness and educational initiatives can bring to light the dangers of these substances that exert powerful and, sometimes, unpredictable psychoactive effects on the user.
Self-mutilation and suicidal ideation also have been documented among those who ingested bath salts. These reports appear to be escalating across Europe and the United States. On a national level, U.S. poison centers have reported an almost 20-fold increase in calls regarding bath salts between 2010 and 2011.5 It is of utmost importance for clinicians and emergency personnel to familiarize themselves with the sympathomimetic toxidrome and management for bath salt consumption.
1. Mariani JJ, Khantzian EJ, Levin FR. The self-medication hypothesis and psychostimulant treatment of cocaine dependence: an update. Am J Addict. 2014;23(2):189-193.
2. Deluca P, Schifano F, Davey Z, et al. MDPV Report: Psychonaut Web Mapping Research Project. https://catbull.com/alamut/Bibliothek/PsychonautMDPVreport. pdf. Updated June 8, 2010. Accessed October 27, 2015.
3. National Institute on Drug Abuse. What are bath salts? http://teens.drugabuse.gov/drug-facts/bath-salts. Updated October 23, 2015. Accessed October 27, 2015.
4. Richards JR, Derlet RW, Albertson TE, et al. Methamphetamine, “bath salts,” and other amphetamine-related derivatives. Enliven: Toxicology and Allied Clinical Pharmacology. 2014;1(1):1-15.
5. Olives TD, Orozco BS, Stellpflug SJ. Bath salts: the ivory wave of trouble. West J Emerg Med. 2012;13(1):58-62.
6. Kasick DP, McKnight CA, Klisovic E. “Bath salt” ingestion leading to severe intoxication delirium: two cases and a brief review of the emergence of mephedrone use. Am J Drug Alcohol Abuse. 2012;38(2):176-180.
7. Borek HA, Holstege CP. Hyperthermia and multiorgan failure after abuse of “bath salts” containing 3,4-methylenedioxypyrovalerone. Ann Emerg Med. 2012;60(1):103-105.
8. Regunath H, Ariyamuthu VK, Dalal P, et al. Bath salt intoxication causing acute kidney injury requiring hemodialysis. Hemodial Int. 2012;16(suppl 1):S47-S49.
9. Adebamiro A, Perazella MA. Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis. 2012;59(2):273-275.
10. Federation of American Societies for Experimental Biology. New designer drug, ‘bath salts,’ may confer additional risk for adolescents. EurekAlert. http://www.eurekalert.org/ pub_releases/2013-04/foas-ndd041813.php. Published April 23, 2013. Accessed November 10, 2015.
1. Mariani JJ, Khantzian EJ, Levin FR. The self-medication hypothesis and psychostimulant treatment of cocaine dependence: an update. Am J Addict. 2014;23(2):189-193.
2. Deluca P, Schifano F, Davey Z, et al. MDPV Report: Psychonaut Web Mapping Research Project. https://catbull.com/alamut/Bibliothek/PsychonautMDPVreport. pdf. Updated June 8, 2010. Accessed October 27, 2015.
3. National Institute on Drug Abuse. What are bath salts? http://teens.drugabuse.gov/drug-facts/bath-salts. Updated October 23, 2015. Accessed October 27, 2015.
4. Richards JR, Derlet RW, Albertson TE, et al. Methamphetamine, “bath salts,” and other amphetamine-related derivatives. Enliven: Toxicology and Allied Clinical Pharmacology. 2014;1(1):1-15.
5. Olives TD, Orozco BS, Stellpflug SJ. Bath salts: the ivory wave of trouble. West J Emerg Med. 2012;13(1):58-62.
6. Kasick DP, McKnight CA, Klisovic E. “Bath salt” ingestion leading to severe intoxication delirium: two cases and a brief review of the emergence of mephedrone use. Am J Drug Alcohol Abuse. 2012;38(2):176-180.
7. Borek HA, Holstege CP. Hyperthermia and multiorgan failure after abuse of “bath salts” containing 3,4-methylenedioxypyrovalerone. Ann Emerg Med. 2012;60(1):103-105.
8. Regunath H, Ariyamuthu VK, Dalal P, et al. Bath salt intoxication causing acute kidney injury requiring hemodialysis. Hemodial Int. 2012;16(suppl 1):S47-S49.
9. Adebamiro A, Perazella MA. Recurrent acute kidney injury following bath salts intoxication. Am J Kidney Dis. 2012;59(2):273-275.
10. Federation of American Societies for Experimental Biology. New designer drug, ‘bath salts,’ may confer additional risk for adolescents. EurekAlert. http://www.eurekalert.org/ pub_releases/2013-04/foas-ndd041813.php. Published April 23, 2013. Accessed November 10, 2015.
To blog or not to blog? That is the marketing question
Few methods can build your practice and reputation as well as blogging— nor can they give you as much grief. Your opinions can become known to a wide audience; you might influence public thinking or behavior; and you might become associated with a particular expertise at almost no financial cost. Yet, having regular deadlines to produce creative content can be stressful, and the time required to do it well has its own cost.
What is it?
“Blog” is the collapsed expression of “Web log.” Blogging is posting your thoughts on a Web site for colleagues or consumers, or both, to read. Typically, a blog is written as if you were writing a newspaper column; word count varies, from 250 to 1,000 words. Alternative formats are auditory (podcasts) or visual (vlog) but those media require greater technical proficiency and take more time to produce.
Whether you decide to write or record your blog entry, be guided by this advice:
• The subject matter can be anything you choose, but will be easiest to write when what you write about is based on your expertise.
• The format can be stream of consciousness,essay, or bulleted lists or slides; the latter is the most common and often follows a how-to or list format (eg, “Top [number] strategies to XYZ” or “[Number] of things you didn’t know about ABC”).
• End the blog with a cliffhanger or a call-to-action statement that invites readers to comment (especially if you then comment on their comments), to help drive interest.
• Generate material at a consistent interval (eg, once a week or twice a month), so your readers can look forward to your soliloquies on a regular basis.
Your professional Web site can serve as a venue for your blog. Using a WordPressa-based site, for example, offers a user-friendly way to compose your dispatch, add formatting (headers, bullets, color, images, etc.) as you see fit, and then publish it. It requires little technical expertise and adds no extra expense to your Web site. Alternatively, you might wish to contact editors at magazines or blog aggregators with story ideas, and let them handle the logistics if your content is appealing to them.
aWordPress is a Web site creation and management tool.
Spreading the word
There is much you can do to publicize your blog.
• Take advantage of social media. Build up your contacts on LinkedIn and follow other bloggers and large news sites on Twitter. Often, recipients will respond in-kind. Then, for each new piece, post or tweet it in these accounts.
• Offer an e-mail subscription so that readers can easily follow you (by means of a free WordPress plug-in, for example).
• Be found in search engines, such as Google, by writing high-quality, original content. Don’t force certain keywords into your article in the hopes that search engines find them—doing so tends to make writing more robotic and can lower your page rank.
Successful strategies
Regularly setting time aside so that the process is enjoyable and not onerously deadline-driven lends satisfaction to the experience and comes through in the quality of the composition. To save time, consider dictating your thoughts to your computer or phone, then outsource transcription.
Don’t overlook the bounty of material in your day-to-day life: stories from sessions; discoveries from your own reading or the latest news; and lectures you give. All of these can serve as inspiration and material for posts. Jot down these moments in a notebook as soon as they come up, or else the memory will likely slip away.
Just as with other forms of social media, be mindful of appropriate boundaries. Do not disclose identifying patient information; even revealing facets of your life might not be appropriate for current or future patients to have access to. On the other hand, it might be therapeutic for them to know select personal information, such as how you have handled past dilemmas, that reveals you are a real person (a “whole object” in psychoanalytic terms), and that models meaningful thoughts or deeds.
You’ll find your voice, in time
Getting started with blogging often is the toughest part. Finding the right format, material, and routine will take time. Eventually, you will find your blogging voice, and will value the unique opportunity to brand your practice and yourself, provide valuable content to your readers, and find an outlet for artistic expression.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Few methods can build your practice and reputation as well as blogging— nor can they give you as much grief. Your opinions can become known to a wide audience; you might influence public thinking or behavior; and you might become associated with a particular expertise at almost no financial cost. Yet, having regular deadlines to produce creative content can be stressful, and the time required to do it well has its own cost.
What is it?
“Blog” is the collapsed expression of “Web log.” Blogging is posting your thoughts on a Web site for colleagues or consumers, or both, to read. Typically, a blog is written as if you were writing a newspaper column; word count varies, from 250 to 1,000 words. Alternative formats are auditory (podcasts) or visual (vlog) but those media require greater technical proficiency and take more time to produce.
Whether you decide to write or record your blog entry, be guided by this advice:
• The subject matter can be anything you choose, but will be easiest to write when what you write about is based on your expertise.
• The format can be stream of consciousness,essay, or bulleted lists or slides; the latter is the most common and often follows a how-to or list format (eg, “Top [number] strategies to XYZ” or “[Number] of things you didn’t know about ABC”).
• End the blog with a cliffhanger or a call-to-action statement that invites readers to comment (especially if you then comment on their comments), to help drive interest.
• Generate material at a consistent interval (eg, once a week or twice a month), so your readers can look forward to your soliloquies on a regular basis.
Your professional Web site can serve as a venue for your blog. Using a WordPressa-based site, for example, offers a user-friendly way to compose your dispatch, add formatting (headers, bullets, color, images, etc.) as you see fit, and then publish it. It requires little technical expertise and adds no extra expense to your Web site. Alternatively, you might wish to contact editors at magazines or blog aggregators with story ideas, and let them handle the logistics if your content is appealing to them.
aWordPress is a Web site creation and management tool.
Spreading the word
There is much you can do to publicize your blog.
• Take advantage of social media. Build up your contacts on LinkedIn and follow other bloggers and large news sites on Twitter. Often, recipients will respond in-kind. Then, for each new piece, post or tweet it in these accounts.
• Offer an e-mail subscription so that readers can easily follow you (by means of a free WordPress plug-in, for example).
• Be found in search engines, such as Google, by writing high-quality, original content. Don’t force certain keywords into your article in the hopes that search engines find them—doing so tends to make writing more robotic and can lower your page rank.
Successful strategies
Regularly setting time aside so that the process is enjoyable and not onerously deadline-driven lends satisfaction to the experience and comes through in the quality of the composition. To save time, consider dictating your thoughts to your computer or phone, then outsource transcription.
Don’t overlook the bounty of material in your day-to-day life: stories from sessions; discoveries from your own reading or the latest news; and lectures you give. All of these can serve as inspiration and material for posts. Jot down these moments in a notebook as soon as they come up, or else the memory will likely slip away.
Just as with other forms of social media, be mindful of appropriate boundaries. Do not disclose identifying patient information; even revealing facets of your life might not be appropriate for current or future patients to have access to. On the other hand, it might be therapeutic for them to know select personal information, such as how you have handled past dilemmas, that reveals you are a real person (a “whole object” in psychoanalytic terms), and that models meaningful thoughts or deeds.
You’ll find your voice, in time
Getting started with blogging often is the toughest part. Finding the right format, material, and routine will take time. Eventually, you will find your blogging voice, and will value the unique opportunity to brand your practice and yourself, provide valuable content to your readers, and find an outlet for artistic expression.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Few methods can build your practice and reputation as well as blogging— nor can they give you as much grief. Your opinions can become known to a wide audience; you might influence public thinking or behavior; and you might become associated with a particular expertise at almost no financial cost. Yet, having regular deadlines to produce creative content can be stressful, and the time required to do it well has its own cost.
What is it?
“Blog” is the collapsed expression of “Web log.” Blogging is posting your thoughts on a Web site for colleagues or consumers, or both, to read. Typically, a blog is written as if you were writing a newspaper column; word count varies, from 250 to 1,000 words. Alternative formats are auditory (podcasts) or visual (vlog) but those media require greater technical proficiency and take more time to produce.
Whether you decide to write or record your blog entry, be guided by this advice:
• The subject matter can be anything you choose, but will be easiest to write when what you write about is based on your expertise.
• The format can be stream of consciousness,essay, or bulleted lists or slides; the latter is the most common and often follows a how-to or list format (eg, “Top [number] strategies to XYZ” or “[Number] of things you didn’t know about ABC”).
• End the blog with a cliffhanger or a call-to-action statement that invites readers to comment (especially if you then comment on their comments), to help drive interest.
• Generate material at a consistent interval (eg, once a week or twice a month), so your readers can look forward to your soliloquies on a regular basis.
Your professional Web site can serve as a venue for your blog. Using a WordPressa-based site, for example, offers a user-friendly way to compose your dispatch, add formatting (headers, bullets, color, images, etc.) as you see fit, and then publish it. It requires little technical expertise and adds no extra expense to your Web site. Alternatively, you might wish to contact editors at magazines or blog aggregators with story ideas, and let them handle the logistics if your content is appealing to them.
aWordPress is a Web site creation and management tool.
Spreading the word
There is much you can do to publicize your blog.
• Take advantage of social media. Build up your contacts on LinkedIn and follow other bloggers and large news sites on Twitter. Often, recipients will respond in-kind. Then, for each new piece, post or tweet it in these accounts.
• Offer an e-mail subscription so that readers can easily follow you (by means of a free WordPress plug-in, for example).
• Be found in search engines, such as Google, by writing high-quality, original content. Don’t force certain keywords into your article in the hopes that search engines find them—doing so tends to make writing more robotic and can lower your page rank.
Successful strategies
Regularly setting time aside so that the process is enjoyable and not onerously deadline-driven lends satisfaction to the experience and comes through in the quality of the composition. To save time, consider dictating your thoughts to your computer or phone, then outsource transcription.
Don’t overlook the bounty of material in your day-to-day life: stories from sessions; discoveries from your own reading or the latest news; and lectures you give. All of these can serve as inspiration and material for posts. Jot down these moments in a notebook as soon as they come up, or else the memory will likely slip away.
Just as with other forms of social media, be mindful of appropriate boundaries. Do not disclose identifying patient information; even revealing facets of your life might not be appropriate for current or future patients to have access to. On the other hand, it might be therapeutic for them to know select personal information, such as how you have handled past dilemmas, that reveals you are a real person (a “whole object” in psychoanalytic terms), and that models meaningful thoughts or deeds.
You’ll find your voice, in time
Getting started with blogging often is the toughest part. Finding the right format, material, and routine will take time. Eventually, you will find your blogging voice, and will value the unique opportunity to brand your practice and yourself, provide valuable content to your readers, and find an outlet for artistic expression.
Disclosure
Dr. Braslow is the founder of Luminello.com.
Awareness and management of obstetrical complications of depression
When a patient who has a preexisting medical illness seeks prenatal care, the obstetrician asks herself (himself) 2 questions:
• What impact will the illness have on the pregnancy?
• What impact will the pregnancy have on the illness?
Depression is both a pregnancy-associated and pregnancy-independent illness, which, in the setting of a pregnant woman who has a depressive disorder, makes these questions particularly difficult to answer. In such a case, coordination of care with a mental health provider is essential.
Awareness of the obstetrical complications associated with depression during pregnancy, as well as their implications for the future health of the mother–infant dyad, is important for the entire care team. This article reviews the associations and interconnectedness of depression with complications of pregnancy, childbirth, and the neonatal period.
Diagnosis of depression during prenatal care
The American College of Obstetricians and Gynecologists (ACOG) states that evidence is insufficient to support a recommendation for universal screening for depression among prenatal patients, although such screening should be considered.1 There is considerable variability among obstetrical providers regarding the practice of depression screening; tools to be used if such screening is done; and screening frequency through the pregnancy.
Discernment of depression is difficult. Many somatic symptoms of depression overlap with common prenatal complaints and, consequentially, can be overlooked. Among a sample of 700 pregnant women, for example, 56% complained of lack of energy; 19%, of insomnia; and 19%, of appetite changes.2 Weight change, of course, is universal.
The 10-question self-rating Edinburgh Postnatal Depression Scale has been validated for use during pregnancy and postnatally. This screening instrument can be helpful for differentiating purely physical complaints from mental distress due to depressive symptoms.2,3
When an obstetrical provider suspects a depressive disorder, or one has been diagnosed, she (he) faces the problem of what to do with that information. Women of low socioeconomic status and victims of domestic violence are at increased risk of depression during pregnancy, but barriers to appropriate referral can seem nearly insurmountable because they lack insurance and social support.4-9
In addition, within the setting of numerous tasks that need attending during the relatively short prenatal period, it is common for women newly given a diagnosis of depression to fail to follow up on a referral to a mental health provider.
Although most providers will “check in” with a depressed or at-risk patient at each prenatal visit about her mood, any effort at follow-up can be overshadowed by tangible physical concerns, such as preterm contractions, fetal growth restriction, and coordination of routine testing that has been delayed because of scant prenatal care. All these physical concerns and circumstances of care are associated with maternal depression, as we will discuss.
Preterm labor and birth
Preterm labor is defined as uterine contractions that lead to cervical change before 37 weeks gestational age. Preterm labor increases the risk of preterm birth; preterm labor precedes 50% of preterm births. Preterm birth is the leading cause of neonatal mortality in the United States, and rates of morbidity and mortality increase as gestational age decreases.10 Common neonatal complications related to prematurity are shown in the Figure.11
Women who suffer from depression have an increased risk of preterm labor and preterm birth, as many studies of treated and untreated depressed pregnant women have shown.12-20 The causative mechanism is unknown; it has been proposed that the increase in maternal cortisol production associated with depression and distress triggers overproduction of placental cortisol releasing hormone, which is thought to be involved in initiation of parturition.21,22 Depression also is associated with other risk factors for preterm birth, such as low socioeconomic status, substance use, and smoking.
Intrauterine growth restriction
Women who have depression during pregnancy have an increased risk of intrauterine growth restriction (IUGR), which leads to delivery of an infant who is small for gestational age (SGA) or of low birth weight (LBW) (weighing <2,500 g at birth), or both.23 Again, the basis of the association between depression and IUGR and SGA is unknown; it is theorized that increased levels of cortisol and catecholamines associated with maternal distress might, by increasing blood pressure and inducing vasoconstriction, cause placental hypoperfusion.24,25
It also is possible that the association of depression with other risk factors for IUGR, such as smoking, substance use, obesity, and poor prenatal care, puts the infants of depressed women at risk of growth restriction.26 Several large-scale studies showed that the association between LBW and depression is lost when smoking and substance use are accounted for; other studies, however, found a persistent association in untreated depressed women when smokers, substance users, and drinkers were excluded.17,26,27
IUGR infants are at increased risk of iatrogenic prematurity and stillbirth. Fetuses that weigh <10th percentile for their gestational age are delivered no later than 40 weeks; delivery can be indicated as early as 32 weeks, depending on the results of other antenatal tests. Women who have a growth-restricted infant have a higher risk of cesarean delivery because growth-restricted infants often have less reserve and poorer tolerance of labor.
Preeclampsia and eclampsia
Preeclampsia is defined as blood pressure >140/90 mm HG on at least 2 occasions, with proteinuria, that occurs later than the twentieth week of pregnancy in women who did not have hypertension or renal dysfunction at baseline. Preeclampsia is a progressive disease that can cause severe maternal morbidity, including renal failure, stroke, hepatic rupture, pulmonary edema, and heart failure.
Eclampsia refers to onset of seizures in the setting of preeclampsia. These 2 hypertensive disorders are the third leading world wide cause of maternal mortality.28
Depressed women have an elevated risk of preeclampsia. The association between preeclampsia and depression might be caused by the presence of increased levels of inflammatory mediators29,30; other comorbidities, such as increased body mass index, also might be involved, but the risk for preeclampsia in depressed women still is increased after controlling for obesity.31
The presence of preeclampsia is responsible for a high percentage of iatrogenic preterm births, because the cure for the disorder is delivery—even at early or previable gestational age. Complication rates for mother and infant are high.
The presence of preeclampsia is a significant risk factor for intrauterine fetal demise. Treating the mother after delivery involves administration of IV magnesium for 24 hours; often, the mother is separated from her infant for a day after birth.
Impact on prenatal care
Depression increases odds that women will have fewer prenatal visits.32 During pregnancy, women typically initiate prenatal care during the first trimester, when pregnancy-dating ultrasonography and early screening tests for chromosomal abnormalities are performed. Prenatal visits occur monthly until the third trimester, then every 2 weeks between 32 and 36 weeks’ gestation, increasing to weekly after 36 weeks’ gestation.
The increased number of visits in late pregnancy allows for early detection and treatment of hypertensive disorders; assesses fetal well-being; and decreases the risks of morbidity and mortality for mother and fetus.33 Because women who suffer from depression are at increased risk of an array of adverse pregnancy outcomes, the importance of regular and timely prenatal care cannot be understated.
In addition, the prenatal visit gives the obstetrician the opportunity to connect women with other specialists for management of any unmet medical needs. One study showed that, when women have adequate prenatal care (measured by the number of visits), the association between preterm birth and self-reported maternal depression was eliminated.34
Substance use
Substance use and depression often co-exist.35,36 Unlike screening for depression, screening for substance use is universal during prenatal care. Studies have shown that women who screen positive for depression are at higher risk of a number of comorbidities, including substance use.37,38 Conversely, women who use substances are more likely to screen positive for depression.
Evidence suggests that best practice might be to screen for depression in any woman who has a positive drug screen, if a provider is not routinely screening their general patient population.39 Substance use in pregnancy is associated with a number of poor outcomes, including placental abruption (cocaine use); dysmorphic facies and congenital anomalies (alcohol); and neonatal abstinence syndrome (heroin).
Antidepressants in pregnancy
A full discussion of the risks and benefits associated with pharmacotherapy for depression in pregnancy is beyond the scope of this article. Generally, antidepressant use is fraught with concerns over teratogenicity and adverse fetal outcomes. Although ACOG states that (1) pharmacotherapy for depression should be individualized and (2) most selective serotonin reuptake inhibitors (SSRIs) are not considered major teratogenic agents, many obstetricians and patients feel uncomfortable using these medications in pregnancy.40 Often, pre-pregnancy antidepressants are discontinued in the first trimester; one large population-based study found that only 0.9% of women who had depression filled their antidepressant prescription consistently throughout their pregnancy.41
It is unclear whether antidepressant use in pregnancy contributes to the risk of preterm birth seen in women who have depression. In a large population-based study, use of antidepressants in the second trimester was associated with preterm delivery but severe depression was not.18 A recent meta-analysis revealed an increased risk of preterm birth in women who used an antidepressant, compared with healthy women and untreated depressed women.42
Research limits, unanswered questions. Regrettably, it is difficult to untangle risk factors for preterm birth among depressed women without randomized controlled studies that are not ethically feasible. It cannot be said with certainty whether antidepressant pharmacotherapy is associated with a higher risk of preterm birth than depression alone.
Likewise, it is difficult to clarify the extent to which antidepressants contribute to infant growth restriction, if at all. Two recent meta-analyses concluded that exposure to antidepressants is associated with a statistically significant risk of LBW.42,43 However, increased severity of depressive symptoms generally is associated with exposure to antidepressants during pregnancy, and a randomized controlled trial is, again, impossible to conduct for ethical reasons.
Whereas a plausible biological mechanism associating IUGR, SGA, and LBW with depression exists, the same cannot be said for antidepressants. In one study, exposure to maternal depression altered the expression of certain placental genes but exposure to SSRIs did not cause further changes. This suggests that, on a cellular level, placental function might differ in depressed women.44 Although antidepressants do cross the placenta, it remains to be seen whether fetal growth is impacted as a result. One study found decreased fetal head circumference in infants who had been exposed to antidepressants during pregnancy, but no increased risk for having a SGA or LWB infant.45
Obstetrical management and mental health implications
Treated or not, women who suffer depression are a high-risk group when it comes to preterm birth and a host of other pregnancy comorbidities. Women with serious complications of pregnancy often are hospitalized for observation, and can undergo a prolonged stay when close proximity to medical services or a surgical suite is required.
For example, hospitalization until delivery is the standard of care for women who have preterm premature rupture of membranes or preeclampsia before 34 weeks’ gestation. Prolonged inpatient admissions and associated restriction of activity is profoundly deleterious on mood, with depression and anxiety significantly correlated with length of stay.46,47 Given the associations between depression and preterm birth, it might be reasonable to consider screening antenatal inpatients at risk of preterm birth for depression on a regular basis, so that treatment can be initiated if needed.
Depression during pregnancy is relatively common; an estimated 12.7% of pregnant women are affected at some time between conception and birth.48 Not only does depression appear to have deleterious effects on pregnancy outcomes, it also plays a pivotal role in the qualitative experience of pregnancy for the mother.
Bottom Line
Awareness of obstetrical complications associated with depression in pregnancy is important for the entire care team, including the psychiatrist and obstetrician. Depression not only appears to have deleterious effects on pregnancy outcomes, it also plays a pivotal role in the qualitative experience of pregnancy for the mother. Antidepressant use generally is fraught with concerns over teratogenicity and adverse fetal outcomes.
Related Resources
• Freeman MP. Some SSRIs are better than others for pregnant women (audio interview). Current Psychiatry. 2014;13(7). http://www.currentpsychiatry.com/specialty-focus/practice-trends/article/some-ssris-are-better-thanothers-for-pregnant-women/e3adb4704e25492f3e15331fc1cc058d.html.
• Freeman MP, Joffe H, Cohen LS. Postpartum depression: Help patients find the right treatment. Current Psychiatry. 2012;11(11):14-16,19-21.
Disclosures
Dr. Habecker reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Freeman is a member of the advisory board of JDS Therapeutics, Sunovion Pharmaceuticals, Inc., and Takeda Pharmaceutical Co. She receives research grant support from Takeda Pharmaceutical Co.
1. American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 630. 2015;125:1268-1271.
2. Apter G, Devouche E, Garez V, et al. Pregnancy, somatic complaints and depression: a French population-based study. Eur J Obstet Gynecol Reprod Biol. 2013;171(1):35-39.
3. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EDDS). J Reprod Infant Psychol. 1990;8(2):99-107.
4. Gotlib IH, Whiffen VE, Mount JH, et al. Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269-274.
5. Melville JL, Gavin A, Guo Y, et al. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116(5):1064-1070.
6. Leddy M, Haaga D, Gray J, et al. Postpartum mental health screening and diagnosis by obstetrician-gynecologists. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
7. McFarlane J, Maddoux J, Cesario S, et al. Effect of abuse during pregnancy on maternal and child safety and functioning for 24 months after delivery. Obstet Gynecol. 2014;123(4):839-847.
8. Vesga-López O, Bianco C, Keyes K, et al. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805-815.
9. Farr SL, Bitsko RH, Hayes DK, et al. Mental health and access to services among US women of reproductive age. Am J Obstet Gynecol. 2010;203(6):542.e1-e542.e9. doi: 10.1016/j.ajog.2010.07.007.
10. Committee on Practice Bulletins—Obstetrics; The American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012;120(4):964-973.
11. Stoll BJ, Hansen NI, Bell EF, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443-456.
12. Steer RA, Scholl TO, Hediger ML, et al. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45(10):1093-1099.
13. Goldenberg RL, Cliver SP, Mulvihill FX, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175(5):1317-1324.
14. Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797-802.
15. Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68(6):938-946.
16. Goedhart G, Snijders AC, Hesselink AE, et al. Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a large multiethnic cohort study. Psychosom Med. 2010;72(8):769-776.
17. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
18. Hayes RM, Wu P, Shelton RC, et al. Maternal antidepressant use and adverse outcomes: a cohort study of 228,876 pregnancies [published online April 30, 2012]. Am J Obstet Gynecol. 2012;207(1):49.e1-49.e9. doi: 10.1016/j. ajog.2012.04.028.
19. McDonagh MS, Matthews A, Phillipi C, et al. Depression drug treatment outcomes in pregnancy and the postpartum period: a systematic review and meta-analysis. Obstet Gynecol. 2014;124(3):526-534.
20. Sahingöz M, Yuksel G, Karsidag C, et al. Birth weight and preterm birth in babies of pregnant women with major depression in relation to treatment with antidepressants. J Clin Psychopharmacol. 2014;34(2):226-229.
When a patient who has a preexisting medical illness seeks prenatal care, the obstetrician asks herself (himself) 2 questions:
• What impact will the illness have on the pregnancy?
• What impact will the pregnancy have on the illness?
Depression is both a pregnancy-associated and pregnancy-independent illness, which, in the setting of a pregnant woman who has a depressive disorder, makes these questions particularly difficult to answer. In such a case, coordination of care with a mental health provider is essential.
Awareness of the obstetrical complications associated with depression during pregnancy, as well as their implications for the future health of the mother–infant dyad, is important for the entire care team. This article reviews the associations and interconnectedness of depression with complications of pregnancy, childbirth, and the neonatal period.
Diagnosis of depression during prenatal care
The American College of Obstetricians and Gynecologists (ACOG) states that evidence is insufficient to support a recommendation for universal screening for depression among prenatal patients, although such screening should be considered.1 There is considerable variability among obstetrical providers regarding the practice of depression screening; tools to be used if such screening is done; and screening frequency through the pregnancy.
Discernment of depression is difficult. Many somatic symptoms of depression overlap with common prenatal complaints and, consequentially, can be overlooked. Among a sample of 700 pregnant women, for example, 56% complained of lack of energy; 19%, of insomnia; and 19%, of appetite changes.2 Weight change, of course, is universal.
The 10-question self-rating Edinburgh Postnatal Depression Scale has been validated for use during pregnancy and postnatally. This screening instrument can be helpful for differentiating purely physical complaints from mental distress due to depressive symptoms.2,3
When an obstetrical provider suspects a depressive disorder, or one has been diagnosed, she (he) faces the problem of what to do with that information. Women of low socioeconomic status and victims of domestic violence are at increased risk of depression during pregnancy, but barriers to appropriate referral can seem nearly insurmountable because they lack insurance and social support.4-9
In addition, within the setting of numerous tasks that need attending during the relatively short prenatal period, it is common for women newly given a diagnosis of depression to fail to follow up on a referral to a mental health provider.
Although most providers will “check in” with a depressed or at-risk patient at each prenatal visit about her mood, any effort at follow-up can be overshadowed by tangible physical concerns, such as preterm contractions, fetal growth restriction, and coordination of routine testing that has been delayed because of scant prenatal care. All these physical concerns and circumstances of care are associated with maternal depression, as we will discuss.
Preterm labor and birth
Preterm labor is defined as uterine contractions that lead to cervical change before 37 weeks gestational age. Preterm labor increases the risk of preterm birth; preterm labor precedes 50% of preterm births. Preterm birth is the leading cause of neonatal mortality in the United States, and rates of morbidity and mortality increase as gestational age decreases.10 Common neonatal complications related to prematurity are shown in the Figure.11
Women who suffer from depression have an increased risk of preterm labor and preterm birth, as many studies of treated and untreated depressed pregnant women have shown.12-20 The causative mechanism is unknown; it has been proposed that the increase in maternal cortisol production associated with depression and distress triggers overproduction of placental cortisol releasing hormone, which is thought to be involved in initiation of parturition.21,22 Depression also is associated with other risk factors for preterm birth, such as low socioeconomic status, substance use, and smoking.
Intrauterine growth restriction
Women who have depression during pregnancy have an increased risk of intrauterine growth restriction (IUGR), which leads to delivery of an infant who is small for gestational age (SGA) or of low birth weight (LBW) (weighing <2,500 g at birth), or both.23 Again, the basis of the association between depression and IUGR and SGA is unknown; it is theorized that increased levels of cortisol and catecholamines associated with maternal distress might, by increasing blood pressure and inducing vasoconstriction, cause placental hypoperfusion.24,25
It also is possible that the association of depression with other risk factors for IUGR, such as smoking, substance use, obesity, and poor prenatal care, puts the infants of depressed women at risk of growth restriction.26 Several large-scale studies showed that the association between LBW and depression is lost when smoking and substance use are accounted for; other studies, however, found a persistent association in untreated depressed women when smokers, substance users, and drinkers were excluded.17,26,27
IUGR infants are at increased risk of iatrogenic prematurity and stillbirth. Fetuses that weigh <10th percentile for their gestational age are delivered no later than 40 weeks; delivery can be indicated as early as 32 weeks, depending on the results of other antenatal tests. Women who have a growth-restricted infant have a higher risk of cesarean delivery because growth-restricted infants often have less reserve and poorer tolerance of labor.
Preeclampsia and eclampsia
Preeclampsia is defined as blood pressure >140/90 mm HG on at least 2 occasions, with proteinuria, that occurs later than the twentieth week of pregnancy in women who did not have hypertension or renal dysfunction at baseline. Preeclampsia is a progressive disease that can cause severe maternal morbidity, including renal failure, stroke, hepatic rupture, pulmonary edema, and heart failure.
Eclampsia refers to onset of seizures in the setting of preeclampsia. These 2 hypertensive disorders are the third leading world wide cause of maternal mortality.28
Depressed women have an elevated risk of preeclampsia. The association between preeclampsia and depression might be caused by the presence of increased levels of inflammatory mediators29,30; other comorbidities, such as increased body mass index, also might be involved, but the risk for preeclampsia in depressed women still is increased after controlling for obesity.31
The presence of preeclampsia is responsible for a high percentage of iatrogenic preterm births, because the cure for the disorder is delivery—even at early or previable gestational age. Complication rates for mother and infant are high.
The presence of preeclampsia is a significant risk factor for intrauterine fetal demise. Treating the mother after delivery involves administration of IV magnesium for 24 hours; often, the mother is separated from her infant for a day after birth.
Impact on prenatal care
Depression increases odds that women will have fewer prenatal visits.32 During pregnancy, women typically initiate prenatal care during the first trimester, when pregnancy-dating ultrasonography and early screening tests for chromosomal abnormalities are performed. Prenatal visits occur monthly until the third trimester, then every 2 weeks between 32 and 36 weeks’ gestation, increasing to weekly after 36 weeks’ gestation.
The increased number of visits in late pregnancy allows for early detection and treatment of hypertensive disorders; assesses fetal well-being; and decreases the risks of morbidity and mortality for mother and fetus.33 Because women who suffer from depression are at increased risk of an array of adverse pregnancy outcomes, the importance of regular and timely prenatal care cannot be understated.
In addition, the prenatal visit gives the obstetrician the opportunity to connect women with other specialists for management of any unmet medical needs. One study showed that, when women have adequate prenatal care (measured by the number of visits), the association between preterm birth and self-reported maternal depression was eliminated.34
Substance use
Substance use and depression often co-exist.35,36 Unlike screening for depression, screening for substance use is universal during prenatal care. Studies have shown that women who screen positive for depression are at higher risk of a number of comorbidities, including substance use.37,38 Conversely, women who use substances are more likely to screen positive for depression.
Evidence suggests that best practice might be to screen for depression in any woman who has a positive drug screen, if a provider is not routinely screening their general patient population.39 Substance use in pregnancy is associated with a number of poor outcomes, including placental abruption (cocaine use); dysmorphic facies and congenital anomalies (alcohol); and neonatal abstinence syndrome (heroin).
Antidepressants in pregnancy
A full discussion of the risks and benefits associated with pharmacotherapy for depression in pregnancy is beyond the scope of this article. Generally, antidepressant use is fraught with concerns over teratogenicity and adverse fetal outcomes. Although ACOG states that (1) pharmacotherapy for depression should be individualized and (2) most selective serotonin reuptake inhibitors (SSRIs) are not considered major teratogenic agents, many obstetricians and patients feel uncomfortable using these medications in pregnancy.40 Often, pre-pregnancy antidepressants are discontinued in the first trimester; one large population-based study found that only 0.9% of women who had depression filled their antidepressant prescription consistently throughout their pregnancy.41
It is unclear whether antidepressant use in pregnancy contributes to the risk of preterm birth seen in women who have depression. In a large population-based study, use of antidepressants in the second trimester was associated with preterm delivery but severe depression was not.18 A recent meta-analysis revealed an increased risk of preterm birth in women who used an antidepressant, compared with healthy women and untreated depressed women.42
Research limits, unanswered questions. Regrettably, it is difficult to untangle risk factors for preterm birth among depressed women without randomized controlled studies that are not ethically feasible. It cannot be said with certainty whether antidepressant pharmacotherapy is associated with a higher risk of preterm birth than depression alone.
Likewise, it is difficult to clarify the extent to which antidepressants contribute to infant growth restriction, if at all. Two recent meta-analyses concluded that exposure to antidepressants is associated with a statistically significant risk of LBW.42,43 However, increased severity of depressive symptoms generally is associated with exposure to antidepressants during pregnancy, and a randomized controlled trial is, again, impossible to conduct for ethical reasons.
Whereas a plausible biological mechanism associating IUGR, SGA, and LBW with depression exists, the same cannot be said for antidepressants. In one study, exposure to maternal depression altered the expression of certain placental genes but exposure to SSRIs did not cause further changes. This suggests that, on a cellular level, placental function might differ in depressed women.44 Although antidepressants do cross the placenta, it remains to be seen whether fetal growth is impacted as a result. One study found decreased fetal head circumference in infants who had been exposed to antidepressants during pregnancy, but no increased risk for having a SGA or LWB infant.45
Obstetrical management and mental health implications
Treated or not, women who suffer depression are a high-risk group when it comes to preterm birth and a host of other pregnancy comorbidities. Women with serious complications of pregnancy often are hospitalized for observation, and can undergo a prolonged stay when close proximity to medical services or a surgical suite is required.
For example, hospitalization until delivery is the standard of care for women who have preterm premature rupture of membranes or preeclampsia before 34 weeks’ gestation. Prolonged inpatient admissions and associated restriction of activity is profoundly deleterious on mood, with depression and anxiety significantly correlated with length of stay.46,47 Given the associations between depression and preterm birth, it might be reasonable to consider screening antenatal inpatients at risk of preterm birth for depression on a regular basis, so that treatment can be initiated if needed.
Depression during pregnancy is relatively common; an estimated 12.7% of pregnant women are affected at some time between conception and birth.48 Not only does depression appear to have deleterious effects on pregnancy outcomes, it also plays a pivotal role in the qualitative experience of pregnancy for the mother.
Bottom Line
Awareness of obstetrical complications associated with depression in pregnancy is important for the entire care team, including the psychiatrist and obstetrician. Depression not only appears to have deleterious effects on pregnancy outcomes, it also plays a pivotal role in the qualitative experience of pregnancy for the mother. Antidepressant use generally is fraught with concerns over teratogenicity and adverse fetal outcomes.
Related Resources
• Freeman MP. Some SSRIs are better than others for pregnant women (audio interview). Current Psychiatry. 2014;13(7). http://www.currentpsychiatry.com/specialty-focus/practice-trends/article/some-ssris-are-better-thanothers-for-pregnant-women/e3adb4704e25492f3e15331fc1cc058d.html.
• Freeman MP, Joffe H, Cohen LS. Postpartum depression: Help patients find the right treatment. Current Psychiatry. 2012;11(11):14-16,19-21.
Disclosures
Dr. Habecker reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Freeman is a member of the advisory board of JDS Therapeutics, Sunovion Pharmaceuticals, Inc., and Takeda Pharmaceutical Co. She receives research grant support from Takeda Pharmaceutical Co.
When a patient who has a preexisting medical illness seeks prenatal care, the obstetrician asks herself (himself) 2 questions:
• What impact will the illness have on the pregnancy?
• What impact will the pregnancy have on the illness?
Depression is both a pregnancy-associated and pregnancy-independent illness, which, in the setting of a pregnant woman who has a depressive disorder, makes these questions particularly difficult to answer. In such a case, coordination of care with a mental health provider is essential.
Awareness of the obstetrical complications associated with depression during pregnancy, as well as their implications for the future health of the mother–infant dyad, is important for the entire care team. This article reviews the associations and interconnectedness of depression with complications of pregnancy, childbirth, and the neonatal period.
Diagnosis of depression during prenatal care
The American College of Obstetricians and Gynecologists (ACOG) states that evidence is insufficient to support a recommendation for universal screening for depression among prenatal patients, although such screening should be considered.1 There is considerable variability among obstetrical providers regarding the practice of depression screening; tools to be used if such screening is done; and screening frequency through the pregnancy.
Discernment of depression is difficult. Many somatic symptoms of depression overlap with common prenatal complaints and, consequentially, can be overlooked. Among a sample of 700 pregnant women, for example, 56% complained of lack of energy; 19%, of insomnia; and 19%, of appetite changes.2 Weight change, of course, is universal.
The 10-question self-rating Edinburgh Postnatal Depression Scale has been validated for use during pregnancy and postnatally. This screening instrument can be helpful for differentiating purely physical complaints from mental distress due to depressive symptoms.2,3
When an obstetrical provider suspects a depressive disorder, or one has been diagnosed, she (he) faces the problem of what to do with that information. Women of low socioeconomic status and victims of domestic violence are at increased risk of depression during pregnancy, but barriers to appropriate referral can seem nearly insurmountable because they lack insurance and social support.4-9
In addition, within the setting of numerous tasks that need attending during the relatively short prenatal period, it is common for women newly given a diagnosis of depression to fail to follow up on a referral to a mental health provider.
Although most providers will “check in” with a depressed or at-risk patient at each prenatal visit about her mood, any effort at follow-up can be overshadowed by tangible physical concerns, such as preterm contractions, fetal growth restriction, and coordination of routine testing that has been delayed because of scant prenatal care. All these physical concerns and circumstances of care are associated with maternal depression, as we will discuss.
Preterm labor and birth
Preterm labor is defined as uterine contractions that lead to cervical change before 37 weeks gestational age. Preterm labor increases the risk of preterm birth; preterm labor precedes 50% of preterm births. Preterm birth is the leading cause of neonatal mortality in the United States, and rates of morbidity and mortality increase as gestational age decreases.10 Common neonatal complications related to prematurity are shown in the Figure.11
Women who suffer from depression have an increased risk of preterm labor and preterm birth, as many studies of treated and untreated depressed pregnant women have shown.12-20 The causative mechanism is unknown; it has been proposed that the increase in maternal cortisol production associated with depression and distress triggers overproduction of placental cortisol releasing hormone, which is thought to be involved in initiation of parturition.21,22 Depression also is associated with other risk factors for preterm birth, such as low socioeconomic status, substance use, and smoking.
Intrauterine growth restriction
Women who have depression during pregnancy have an increased risk of intrauterine growth restriction (IUGR), which leads to delivery of an infant who is small for gestational age (SGA) or of low birth weight (LBW) (weighing <2,500 g at birth), or both.23 Again, the basis of the association between depression and IUGR and SGA is unknown; it is theorized that increased levels of cortisol and catecholamines associated with maternal distress might, by increasing blood pressure and inducing vasoconstriction, cause placental hypoperfusion.24,25
It also is possible that the association of depression with other risk factors for IUGR, such as smoking, substance use, obesity, and poor prenatal care, puts the infants of depressed women at risk of growth restriction.26 Several large-scale studies showed that the association between LBW and depression is lost when smoking and substance use are accounted for; other studies, however, found a persistent association in untreated depressed women when smokers, substance users, and drinkers were excluded.17,26,27
IUGR infants are at increased risk of iatrogenic prematurity and stillbirth. Fetuses that weigh <10th percentile for their gestational age are delivered no later than 40 weeks; delivery can be indicated as early as 32 weeks, depending on the results of other antenatal tests. Women who have a growth-restricted infant have a higher risk of cesarean delivery because growth-restricted infants often have less reserve and poorer tolerance of labor.
Preeclampsia and eclampsia
Preeclampsia is defined as blood pressure >140/90 mm HG on at least 2 occasions, with proteinuria, that occurs later than the twentieth week of pregnancy in women who did not have hypertension or renal dysfunction at baseline. Preeclampsia is a progressive disease that can cause severe maternal morbidity, including renal failure, stroke, hepatic rupture, pulmonary edema, and heart failure.
Eclampsia refers to onset of seizures in the setting of preeclampsia. These 2 hypertensive disorders are the third leading world wide cause of maternal mortality.28
Depressed women have an elevated risk of preeclampsia. The association between preeclampsia and depression might be caused by the presence of increased levels of inflammatory mediators29,30; other comorbidities, such as increased body mass index, also might be involved, but the risk for preeclampsia in depressed women still is increased after controlling for obesity.31
The presence of preeclampsia is responsible for a high percentage of iatrogenic preterm births, because the cure for the disorder is delivery—even at early or previable gestational age. Complication rates for mother and infant are high.
The presence of preeclampsia is a significant risk factor for intrauterine fetal demise. Treating the mother after delivery involves administration of IV magnesium for 24 hours; often, the mother is separated from her infant for a day after birth.
Impact on prenatal care
Depression increases odds that women will have fewer prenatal visits.32 During pregnancy, women typically initiate prenatal care during the first trimester, when pregnancy-dating ultrasonography and early screening tests for chromosomal abnormalities are performed. Prenatal visits occur monthly until the third trimester, then every 2 weeks between 32 and 36 weeks’ gestation, increasing to weekly after 36 weeks’ gestation.
The increased number of visits in late pregnancy allows for early detection and treatment of hypertensive disorders; assesses fetal well-being; and decreases the risks of morbidity and mortality for mother and fetus.33 Because women who suffer from depression are at increased risk of an array of adverse pregnancy outcomes, the importance of regular and timely prenatal care cannot be understated.
In addition, the prenatal visit gives the obstetrician the opportunity to connect women with other specialists for management of any unmet medical needs. One study showed that, when women have adequate prenatal care (measured by the number of visits), the association between preterm birth and self-reported maternal depression was eliminated.34
Substance use
Substance use and depression often co-exist.35,36 Unlike screening for depression, screening for substance use is universal during prenatal care. Studies have shown that women who screen positive for depression are at higher risk of a number of comorbidities, including substance use.37,38 Conversely, women who use substances are more likely to screen positive for depression.
Evidence suggests that best practice might be to screen for depression in any woman who has a positive drug screen, if a provider is not routinely screening their general patient population.39 Substance use in pregnancy is associated with a number of poor outcomes, including placental abruption (cocaine use); dysmorphic facies and congenital anomalies (alcohol); and neonatal abstinence syndrome (heroin).
Antidepressants in pregnancy
A full discussion of the risks and benefits associated with pharmacotherapy for depression in pregnancy is beyond the scope of this article. Generally, antidepressant use is fraught with concerns over teratogenicity and adverse fetal outcomes. Although ACOG states that (1) pharmacotherapy for depression should be individualized and (2) most selective serotonin reuptake inhibitors (SSRIs) are not considered major teratogenic agents, many obstetricians and patients feel uncomfortable using these medications in pregnancy.40 Often, pre-pregnancy antidepressants are discontinued in the first trimester; one large population-based study found that only 0.9% of women who had depression filled their antidepressant prescription consistently throughout their pregnancy.41
It is unclear whether antidepressant use in pregnancy contributes to the risk of preterm birth seen in women who have depression. In a large population-based study, use of antidepressants in the second trimester was associated with preterm delivery but severe depression was not.18 A recent meta-analysis revealed an increased risk of preterm birth in women who used an antidepressant, compared with healthy women and untreated depressed women.42
Research limits, unanswered questions. Regrettably, it is difficult to untangle risk factors for preterm birth among depressed women without randomized controlled studies that are not ethically feasible. It cannot be said with certainty whether antidepressant pharmacotherapy is associated with a higher risk of preterm birth than depression alone.
Likewise, it is difficult to clarify the extent to which antidepressants contribute to infant growth restriction, if at all. Two recent meta-analyses concluded that exposure to antidepressants is associated with a statistically significant risk of LBW.42,43 However, increased severity of depressive symptoms generally is associated with exposure to antidepressants during pregnancy, and a randomized controlled trial is, again, impossible to conduct for ethical reasons.
Whereas a plausible biological mechanism associating IUGR, SGA, and LBW with depression exists, the same cannot be said for antidepressants. In one study, exposure to maternal depression altered the expression of certain placental genes but exposure to SSRIs did not cause further changes. This suggests that, on a cellular level, placental function might differ in depressed women.44 Although antidepressants do cross the placenta, it remains to be seen whether fetal growth is impacted as a result. One study found decreased fetal head circumference in infants who had been exposed to antidepressants during pregnancy, but no increased risk for having a SGA or LWB infant.45
Obstetrical management and mental health implications
Treated or not, women who suffer depression are a high-risk group when it comes to preterm birth and a host of other pregnancy comorbidities. Women with serious complications of pregnancy often are hospitalized for observation, and can undergo a prolonged stay when close proximity to medical services or a surgical suite is required.
For example, hospitalization until delivery is the standard of care for women who have preterm premature rupture of membranes or preeclampsia before 34 weeks’ gestation. Prolonged inpatient admissions and associated restriction of activity is profoundly deleterious on mood, with depression and anxiety significantly correlated with length of stay.46,47 Given the associations between depression and preterm birth, it might be reasonable to consider screening antenatal inpatients at risk of preterm birth for depression on a regular basis, so that treatment can be initiated if needed.
Depression during pregnancy is relatively common; an estimated 12.7% of pregnant women are affected at some time between conception and birth.48 Not only does depression appear to have deleterious effects on pregnancy outcomes, it also plays a pivotal role in the qualitative experience of pregnancy for the mother.
Bottom Line
Awareness of obstetrical complications associated with depression in pregnancy is important for the entire care team, including the psychiatrist and obstetrician. Depression not only appears to have deleterious effects on pregnancy outcomes, it also plays a pivotal role in the qualitative experience of pregnancy for the mother. Antidepressant use generally is fraught with concerns over teratogenicity and adverse fetal outcomes.
Related Resources
• Freeman MP. Some SSRIs are better than others for pregnant women (audio interview). Current Psychiatry. 2014;13(7). http://www.currentpsychiatry.com/specialty-focus/practice-trends/article/some-ssris-are-better-thanothers-for-pregnant-women/e3adb4704e25492f3e15331fc1cc058d.html.
• Freeman MP, Joffe H, Cohen LS. Postpartum depression: Help patients find the right treatment. Current Psychiatry. 2012;11(11):14-16,19-21.
Disclosures
Dr. Habecker reports no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Freeman is a member of the advisory board of JDS Therapeutics, Sunovion Pharmaceuticals, Inc., and Takeda Pharmaceutical Co. She receives research grant support from Takeda Pharmaceutical Co.
1. American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 630. 2015;125:1268-1271.
2. Apter G, Devouche E, Garez V, et al. Pregnancy, somatic complaints and depression: a French population-based study. Eur J Obstet Gynecol Reprod Biol. 2013;171(1):35-39.
3. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EDDS). J Reprod Infant Psychol. 1990;8(2):99-107.
4. Gotlib IH, Whiffen VE, Mount JH, et al. Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269-274.
5. Melville JL, Gavin A, Guo Y, et al. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116(5):1064-1070.
6. Leddy M, Haaga D, Gray J, et al. Postpartum mental health screening and diagnosis by obstetrician-gynecologists. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
7. McFarlane J, Maddoux J, Cesario S, et al. Effect of abuse during pregnancy on maternal and child safety and functioning for 24 months after delivery. Obstet Gynecol. 2014;123(4):839-847.
8. Vesga-López O, Bianco C, Keyes K, et al. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805-815.
9. Farr SL, Bitsko RH, Hayes DK, et al. Mental health and access to services among US women of reproductive age. Am J Obstet Gynecol. 2010;203(6):542.e1-e542.e9. doi: 10.1016/j.ajog.2010.07.007.
10. Committee on Practice Bulletins—Obstetrics; The American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012;120(4):964-973.
11. Stoll BJ, Hansen NI, Bell EF, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443-456.
12. Steer RA, Scholl TO, Hediger ML, et al. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45(10):1093-1099.
13. Goldenberg RL, Cliver SP, Mulvihill FX, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175(5):1317-1324.
14. Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797-802.
15. Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68(6):938-946.
16. Goedhart G, Snijders AC, Hesselink AE, et al. Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a large multiethnic cohort study. Psychosom Med. 2010;72(8):769-776.
17. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
18. Hayes RM, Wu P, Shelton RC, et al. Maternal antidepressant use and adverse outcomes: a cohort study of 228,876 pregnancies [published online April 30, 2012]. Am J Obstet Gynecol. 2012;207(1):49.e1-49.e9. doi: 10.1016/j. ajog.2012.04.028.
19. McDonagh MS, Matthews A, Phillipi C, et al. Depression drug treatment outcomes in pregnancy and the postpartum period: a systematic review and meta-analysis. Obstet Gynecol. 2014;124(3):526-534.
20. Sahingöz M, Yuksel G, Karsidag C, et al. Birth weight and preterm birth in babies of pregnant women with major depression in relation to treatment with antidepressants. J Clin Psychopharmacol. 2014;34(2):226-229.
1. American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. Committee opinion no. 630. 2015;125:1268-1271.
2. Apter G, Devouche E, Garez V, et al. Pregnancy, somatic complaints and depression: a French population-based study. Eur J Obstet Gynecol Reprod Biol. 2013;171(1):35-39.
3. Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale (EDDS). J Reprod Infant Psychol. 1990;8(2):99-107.
4. Gotlib IH, Whiffen VE, Mount JH, et al. Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol. 1989;57(2):269-274.
5. Melville JL, Gavin A, Guo Y, et al. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116(5):1064-1070.
6. Leddy M, Haaga D, Gray J, et al. Postpartum mental health screening and diagnosis by obstetrician-gynecologists. J Psychosom Obstet Gynaecol. 2011;32(1):27-34.
7. McFarlane J, Maddoux J, Cesario S, et al. Effect of abuse during pregnancy on maternal and child safety and functioning for 24 months after delivery. Obstet Gynecol. 2014;123(4):839-847.
8. Vesga-López O, Bianco C, Keyes K, et al. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805-815.
9. Farr SL, Bitsko RH, Hayes DK, et al. Mental health and access to services among US women of reproductive age. Am J Obstet Gynecol. 2010;203(6):542.e1-e542.e9. doi: 10.1016/j.ajog.2010.07.007.
10. Committee on Practice Bulletins—Obstetrics; The American College of Obstetricians and Gynecologists. Practice bulletin no. 130: prediction and prevention of preterm birth. Obstet Gynecol. 2012;120(4):964-973.
11. Stoll BJ, Hansen NI, Bell EF, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443-456.
12. Steer RA, Scholl TO, Hediger ML, et al. Self-reported depression and negative pregnancy outcomes. J Clin Epidemiol. 1992;45(10):1093-1099.
13. Goldenberg RL, Cliver SP, Mulvihill FX, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. Am J Obstet Gynecol. 1996;175(5):1317-1324.
14. Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. Am J Epidemiol. 2002;156(9):797-802.
15. Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med. 2006;68(6):938-946.
16. Goedhart G, Snijders AC, Hesselink AE, et al. Maternal depressive symptoms in relation to perinatal mortality and morbidity: results from a large multiethnic cohort study. Psychosom Med. 2010;72(8):769-776.
17. Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010;67(10):1012-1024.
18. Hayes RM, Wu P, Shelton RC, et al. Maternal antidepressant use and adverse outcomes: a cohort study of 228,876 pregnancies [published online April 30, 2012]. Am J Obstet Gynecol. 2012;207(1):49.e1-49.e9. doi: 10.1016/j. ajog.2012.04.028.
19. McDonagh MS, Matthews A, Phillipi C, et al. Depression drug treatment outcomes in pregnancy and the postpartum period: a systematic review and meta-analysis. Obstet Gynecol. 2014;124(3):526-534.
20. Sahingöz M, Yuksel G, Karsidag C, et al. Birth weight and preterm birth in babies of pregnant women with major depression in relation to treatment with antidepressants. J Clin Psychopharmacol. 2014;34(2):226-229.
U.S. flu activity increases slightly
Activity of influenza-like illness (ILI) “increased slightly in the United States” during week 5 of the 2015-2016 influenza season, the Centers for Disease Control and Prevention reported Nov. 20.
Thirteen states were above level-1 activity as of Nov. 14, 2015, compared with seven the week before. South Carolina jumped all the way up to “moderate” activity (level 6) and Missouri and Oklahoma moved into the low-activity category (level 4). Oregon remained at a still-minimal level 3, while Arizona, Georgia, Illinois, Louisiana, Maine, Mississippi, Texas, Utah, and Virginia are at level 2, according to the CDC.
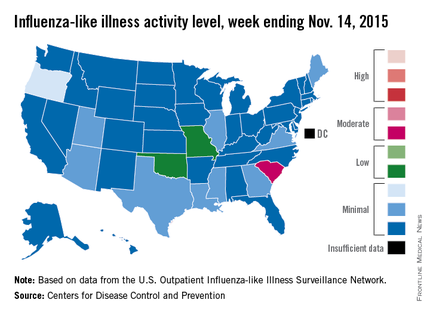
The first influenza-associated pediatric death was reported this week, although it actually occurred during week 4 (the week ending Nov. 7), the CDC said. There has been an average of 143 flu-associated pediatric deaths over the last three flu seasons.
ILI is defined as fever (temperature of 100° F or greater) and cough and/or sore throat. Activity level within a state is the proportion of outpatient visits to health care providers for influenza-like illness.
That proportion for the United States overall was 1.6%, which is up from last week’s 1.4% but still below the national baseline of 2.1%, the CDC said.
Activity of influenza-like illness (ILI) “increased slightly in the United States” during week 5 of the 2015-2016 influenza season, the Centers for Disease Control and Prevention reported Nov. 20.
Thirteen states were above level-1 activity as of Nov. 14, 2015, compared with seven the week before. South Carolina jumped all the way up to “moderate” activity (level 6) and Missouri and Oklahoma moved into the low-activity category (level 4). Oregon remained at a still-minimal level 3, while Arizona, Georgia, Illinois, Louisiana, Maine, Mississippi, Texas, Utah, and Virginia are at level 2, according to the CDC.
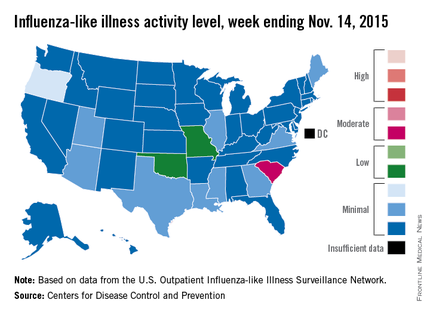
The first influenza-associated pediatric death was reported this week, although it actually occurred during week 4 (the week ending Nov. 7), the CDC said. There has been an average of 143 flu-associated pediatric deaths over the last three flu seasons.
ILI is defined as fever (temperature of 100° F or greater) and cough and/or sore throat. Activity level within a state is the proportion of outpatient visits to health care providers for influenza-like illness.
That proportion for the United States overall was 1.6%, which is up from last week’s 1.4% but still below the national baseline of 2.1%, the CDC said.
Activity of influenza-like illness (ILI) “increased slightly in the United States” during week 5 of the 2015-2016 influenza season, the Centers for Disease Control and Prevention reported Nov. 20.
Thirteen states were above level-1 activity as of Nov. 14, 2015, compared with seven the week before. South Carolina jumped all the way up to “moderate” activity (level 6) and Missouri and Oklahoma moved into the low-activity category (level 4). Oregon remained at a still-minimal level 3, while Arizona, Georgia, Illinois, Louisiana, Maine, Mississippi, Texas, Utah, and Virginia are at level 2, according to the CDC.
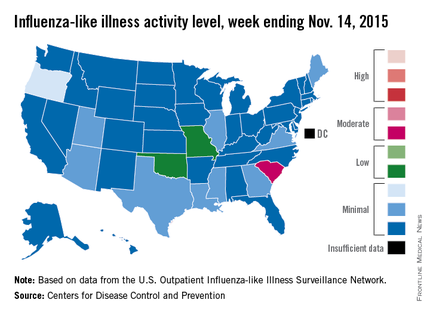
The first influenza-associated pediatric death was reported this week, although it actually occurred during week 4 (the week ending Nov. 7), the CDC said. There has been an average of 143 flu-associated pediatric deaths over the last three flu seasons.
ILI is defined as fever (temperature of 100° F or greater) and cough and/or sore throat. Activity level within a state is the proportion of outpatient visits to health care providers for influenza-like illness.
That proportion for the United States overall was 1.6%, which is up from last week’s 1.4% but still below the national baseline of 2.1%, the CDC said.
Malignant catatonia and aphasia follow multiple-drug overdose
CASE Improvement, then decline
Ms. M, age 37, is brought to the hospital after her husband found her at home, after an unknown duration of impaired consciousness. Her husband reports that Ms. M had normal cognitive functioning before this event, with no difficulty completing activities of daily living. Ms. M’s medical and psychiatric histories are notable for type 2 diabetes mellitus, unspecified bipolar disorder, and opioid, cocaine, and alcohol use disorders. Her medications include paroxetine, 40 mg/d, and gabapentin, 1,200 mg/d.
First admission. Poor inspiratory effort and oxygen saturation of 70% leads to emergent intubation. Serum laboratory studies reveal a white blood cell (WBC) count at 10,900/μL and creatinine phosphokinase level of 25,000 U/L. Urine drug screen is positive for tetrahydrocannabinol, cocaine, and opioids.
Ms. M is admitted to the ICU for management of rhabdomyolysis and multi-organ system failure, including acute hypoxic kidney injury.
By hospital Day 7, the tube is extubated with no recorded physical neurologic deficits. Mental status exam is normal, except for impaired memory of events surrounding the admission. Ms. M is discharged home with a recommendation for outpatient follow-up.
2 Weeks later. Ms. M is brought to the emergency department after a progressive decrease in social interaction, limited oral intake, decline in activities of daily living, and urinary incontinence. Results from laboratory studies are within normal limits; brain MRI is negative; EEG shows generalized moderate slowing.
During psychiatric evaluation, Ms. M is mute and staring continuously. Examination reveals oppositional paratonia (gegenhalten), catalepsy, prominent negativism, and waxy flexibility, all suggestive of catatonia. IV lorazepam is initiated at 1 mg every 8 hours, titrated to 2 mg, 3 times a day.
Ms. M is transferred to a psychiatric hospital for further treatment of catatonia.
Second admission. Evaluation with the Bush-Francis Catatonia Rating Scale supported a diagnosis of catatonia, with the presence of >3 features from the 14-item screen and a score of 16 on the 23-item rating scale.1 After titrating lorazepam to 9 mg/d with minimal therapeutic impact, the psychiatry team consults the electroconvulsive therapy (ECT) service, who deems Ms. M to be an appropriate candidate and petitions for court-ordered ECT.
On hospital Day 8, Ms. M has a fever of 104°F, tachycardia at 180 beats per minute, increased rigidity, and a WBC count of 17,800/μL. She is transferred to the ICU, with a presumptive diagnosis of malignant catatonia.
The medical evaluation, including general laboratory studies, EEG, and spinal fluid analysis, is unremarkable. Because of vital sign instability, 2 ECT treatments are completed in the general hospital before Ms. M resumes psychiatric inpatient care.
By the tenth ECT treatment, Ms. M is no longer febrile and experiences no further autonomic instability or psychomotor features of catatonia. Despite these improvements, she is noted to have persistent word-finding difficulty.
Which test would you order as the next step in your work up?
a) EEG
b) lumbar puncture
c) MRI
d) CT
The authors’ observations
In approximately 25% of cases, catatonia is caused by a general medical condition2; as such, a comprehensive medical workup is vital for assessment and management of catatonic patients. In Ms. M’s case, we considered several medical causes, including nutritional deficiency, infection, a toxin, renal or hepatic impairment, hypothyroidism, seizure, and stroke. Evaluation included measurement of thyroid-stimulating hormone, vitamin B12, and folic acid levels; urinalysis and urine drug screen; chest radiography; lumbar puncture; neuroimaging; and EEG (Table 1).
Several conditions in the differential diagnosis were noteworthy. Ms. M’s severe and sudden neurologic decline, along with a positive urine drug screen for substances of abuse, raised concern about overdose leading to toxic encephalopathy or hypoxic brain injury. Ms. M’s oxygen saturation when she was found was moderately hypoxic at 70%, which is not a level associated with hypoxic brain damage.
We also considered posterior reversible encephalopathy syndrome (PRES), which presents variably with nausea, visual impairment, disturbance in consciousness, seizures, and focal neurologic signs.3 Although 67% to 80% of patients with PRES also have acute hypertension, blood pressure elevation is not necessary for the diagnosis.4 Similar to toxic leukoencephalopathy, PRES is diagnosed by brain MRI, with classic signs of posterior white-matter edema.
Case reports also describe an uncommon demyelinating syndrome, delayed post-hypoxic leukoencephalopathy (DPHL), which develops several weeks or months after a cerebral anoxic insult.5 In Ms. M’s case, brain MRI performed during her second medical hospitalization, 7 days after the initial neuropsychiatric decline, was unremarkable. Using this result to rule out DPHL would have been premature because pathognomonic abnormalities can appear as long as 40 days after the anoxic insult. Given our differential diagnosis, we ordered a repeat MRI.
Etiology and pathophysiology
First described in 1979, DPHL is rare, posing diagnostic challenges for clinical providers.6 Although the exact incidence of DPHL is unknown, the precipitating event typically involves cerebral anoxia, which can occur through carbon monoxide (CO) poisoning, strangulation, cardiac arrest, respiratory failure, and overdose from sedatives and narcotics (Table 2).7 DPHL was first observed in a small percentage (2.75%) of patients suffering from CO poisoning.8,9 Progression of the disease generally includes a period of unconsciousness, then a lucid interval that can last 2 to 40 days, followed by the abrupt onset of neuropsychiatric symptoms.10 The specific pathophysiologic mechanism is unknown, but has been hypothesized to involve inferior compensatory response to decreased oxygenation in the white matter.
Diagnosis and clinical features
DPHL can be divided into 2 clinical variations: parkinsonism and akinetic mutism. The former consists of conventional parkinsonian features along with agitation, apathy, hallucinations, dystonic posturing, and odd behaviors. The latter variant presents with apathy, minimal response to pain, functional bowel and bladder incontinence, mutism, and, at times, inappropriate laughter or tearfulness.5 Both variants share similar features with hypokinetic forms of catatonia.
DPHL is a diagnosis of exclusion. A careful history is critical to establish the possibility of a recent anoxic event. MRI findings, including hyperintensities in the cerebral white matter on T2-based sequencing, are suggestive of the disease. A choline peak on magnetic resonance spectroscopy also might be present in patients with DPHL, although it is not specific to the diagnosis.
Early reports of DPHL suggested an associated deficiency of arylsulfatase A, an enzyme required in the modulation of myelin; however, more recent case reports are conflicting.11 Familial mutations in the gene for arylsulfatase A also result in metachromatic leukodystrophy, and adult onset can present with psychiatric symptoms, including delusions and hallucinations.12
Treatment and prognosis
The treatment of DPHL consists primarily of supportive care and rehabilitation with physical, occupational, and speech therapy.11 With these measures, most patients improve after 3 to 6 months; however, a large percentage sustain some long-term cognitive deficit, the most prevalent symptom being frontal executive dysfunction.5
OUTCOME Supportive care
A second MRI shows diffuse hyperintensities in the white matter that spare the cerebellum and brainstem (Figure). This finding is pathognomonic for DPHL.
ECT is discontinued because there is no evidence to support ECT-associated improvement in DPHL. Moreover, ECT might worsen the clinical course through increased stress and metabolic demand on the brain.13
Because the primary treatment of DPHL is early rehabilitation, we consider that Ms. M would benefit most from increased supportive care and therapy. She is discharged to a brain injury rehabilitation facility, where metoprolol is prescribed for mild tachycardia, along with thiamine and vitamins B12 and D. Physical, occupational, and speech therapy are continued.
Approximately 3 weeks after admission to the rehabilitation program, Ms. M is discharged home. Although she improves in overall activities of daily living, she continues to experience moderate communication deficits and occasional external distractibility.
Bottom Line
Although delayed post-hypoxic leukoencephalopathy is considered rare, consider it in the differential diagnosis when a patient has a recent history of an anoxic event followed by the abrupt onset of neuropsychiatric symptoms. Keep in mind that the condition can be missed if an MRI is obtained too early, and the clinical signs can mimic hypokinetic catatonia.
Related Resources
• Meyer MA. Delayed post-hypoxic leukoencephalopathy: case report with a review of disease pathophysiology. Neurol Int. 2013;5(3):e13. doi: 10.4081/ni.2013.e13.
• Aljarallah S, Al-Hussain F. Acute fatal posthypoxic leukoencephalopathy following benzodiazepine overdose: a case report and review of the literature. BMC Neurol. 2015;15:69.
Drug Brand Names
Gabapentin • Neurontin
Lorazepam • Ativan
Metoprolol • Lopressor
Paroxetine • Paxil
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of com
1. Bush G, Fink M, Petrides G, et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129-136.
2. Azzam PN, Gopalan P. Prototypes of catatonia: diagnostic and therapeutic challenges in the general hospital. Psychosomatics. 2013;54(1):88-93.
3. Tormoehlen LM. Toxic leukoencephalopathies. Neurol Clin. 2011;29(3):591-605
4. Legriel S, Pico F, Azoulay E. Understanding posterior reversible encephalopathy syndrome. In: Vincent JL, ed. Annual update in intensive care and emergency medicine. Heidelberg, Germany: Springer Berlin Heidelberg; 2011:631-653.
5. Schprecher D, Mehta L. The syndrome of delayed post-hypoxic leukoencephalopathy. NeuroRehabilitation. 2010;26(1):65-72.
6. Wallace IR, Dynan C, Esmonde T. One confused patient, many confused physicians: a case of delayed post-hypoxic leucoencephalopathy. QJM. 2010;103(3):193-194.
7. Lou M, Jing CH, Selim MH, et al. Delayed substantia nigra damage and leukoencephalopathy after hypoxic-ischemic injury. J Neurol Sci. 2009;277(1-2):147-149.
8. Choi IS. Delayed neurologic sequelae in carbon monoxide intoxication. Arch Neurol. 1983;40(7):433-435.
9. Molloy S, Soh C, Williams TL. Reversible delayed posthypoxic leukoencephalopathy. AJNR Am J Neuroradiol. 2006;27(8):1763-1765.
10. Shprecher DR, Flanigan KM, Smith AG, et al. Clinical and diagnostic features of delayed hypoxic leukoencephalopathy. J Neuropsychiatry Clin Neurosci. 2008;20(4):473-477.
11. Lee BH, Lyketsos CG. Delayed post-hypoxic leukoencephalopathy. Psychosomatics. 2001;42(6):530-533.
12. Hyde TM, Ziegler JC, Weinberger DR. Psychiatric disturbances in metachromatic leukodystrophy. Insights into the neurobiology of psychosis. Arch Neurol. 1992;49(4):401-406.
13. Quinn DK, Abbott CC. Catatonia after cerebral hypoxia: do the usual treatments apply? Psychosomatics. 2014;55(6):525-535.
CASE Improvement, then decline
Ms. M, age 37, is brought to the hospital after her husband found her at home, after an unknown duration of impaired consciousness. Her husband reports that Ms. M had normal cognitive functioning before this event, with no difficulty completing activities of daily living. Ms. M’s medical and psychiatric histories are notable for type 2 diabetes mellitus, unspecified bipolar disorder, and opioid, cocaine, and alcohol use disorders. Her medications include paroxetine, 40 mg/d, and gabapentin, 1,200 mg/d.
First admission. Poor inspiratory effort and oxygen saturation of 70% leads to emergent intubation. Serum laboratory studies reveal a white blood cell (WBC) count at 10,900/μL and creatinine phosphokinase level of 25,000 U/L. Urine drug screen is positive for tetrahydrocannabinol, cocaine, and opioids.
Ms. M is admitted to the ICU for management of rhabdomyolysis and multi-organ system failure, including acute hypoxic kidney injury.
By hospital Day 7, the tube is extubated with no recorded physical neurologic deficits. Mental status exam is normal, except for impaired memory of events surrounding the admission. Ms. M is discharged home with a recommendation for outpatient follow-up.
2 Weeks later. Ms. M is brought to the emergency department after a progressive decrease in social interaction, limited oral intake, decline in activities of daily living, and urinary incontinence. Results from laboratory studies are within normal limits; brain MRI is negative; EEG shows generalized moderate slowing.
During psychiatric evaluation, Ms. M is mute and staring continuously. Examination reveals oppositional paratonia (gegenhalten), catalepsy, prominent negativism, and waxy flexibility, all suggestive of catatonia. IV lorazepam is initiated at 1 mg every 8 hours, titrated to 2 mg, 3 times a day.
Ms. M is transferred to a psychiatric hospital for further treatment of catatonia.
Second admission. Evaluation with the Bush-Francis Catatonia Rating Scale supported a diagnosis of catatonia, with the presence of >3 features from the 14-item screen and a score of 16 on the 23-item rating scale.1 After titrating lorazepam to 9 mg/d with minimal therapeutic impact, the psychiatry team consults the electroconvulsive therapy (ECT) service, who deems Ms. M to be an appropriate candidate and petitions for court-ordered ECT.
On hospital Day 8, Ms. M has a fever of 104°F, tachycardia at 180 beats per minute, increased rigidity, and a WBC count of 17,800/μL. She is transferred to the ICU, with a presumptive diagnosis of malignant catatonia.
The medical evaluation, including general laboratory studies, EEG, and spinal fluid analysis, is unremarkable. Because of vital sign instability, 2 ECT treatments are completed in the general hospital before Ms. M resumes psychiatric inpatient care.
By the tenth ECT treatment, Ms. M is no longer febrile and experiences no further autonomic instability or psychomotor features of catatonia. Despite these improvements, she is noted to have persistent word-finding difficulty.
Which test would you order as the next step in your work up?
a) EEG
b) lumbar puncture
c) MRI
d) CT
The authors’ observations
In approximately 25% of cases, catatonia is caused by a general medical condition2; as such, a comprehensive medical workup is vital for assessment and management of catatonic patients. In Ms. M’s case, we considered several medical causes, including nutritional deficiency, infection, a toxin, renal or hepatic impairment, hypothyroidism, seizure, and stroke. Evaluation included measurement of thyroid-stimulating hormone, vitamin B12, and folic acid levels; urinalysis and urine drug screen; chest radiography; lumbar puncture; neuroimaging; and EEG (Table 1).
Several conditions in the differential diagnosis were noteworthy. Ms. M’s severe and sudden neurologic decline, along with a positive urine drug screen for substances of abuse, raised concern about overdose leading to toxic encephalopathy or hypoxic brain injury. Ms. M’s oxygen saturation when she was found was moderately hypoxic at 70%, which is not a level associated with hypoxic brain damage.
We also considered posterior reversible encephalopathy syndrome (PRES), which presents variably with nausea, visual impairment, disturbance in consciousness, seizures, and focal neurologic signs.3 Although 67% to 80% of patients with PRES also have acute hypertension, blood pressure elevation is not necessary for the diagnosis.4 Similar to toxic leukoencephalopathy, PRES is diagnosed by brain MRI, with classic signs of posterior white-matter edema.
Case reports also describe an uncommon demyelinating syndrome, delayed post-hypoxic leukoencephalopathy (DPHL), which develops several weeks or months after a cerebral anoxic insult.5 In Ms. M’s case, brain MRI performed during her second medical hospitalization, 7 days after the initial neuropsychiatric decline, was unremarkable. Using this result to rule out DPHL would have been premature because pathognomonic abnormalities can appear as long as 40 days after the anoxic insult. Given our differential diagnosis, we ordered a repeat MRI.
Etiology and pathophysiology
First described in 1979, DPHL is rare, posing diagnostic challenges for clinical providers.6 Although the exact incidence of DPHL is unknown, the precipitating event typically involves cerebral anoxia, which can occur through carbon monoxide (CO) poisoning, strangulation, cardiac arrest, respiratory failure, and overdose from sedatives and narcotics (Table 2).7 DPHL was first observed in a small percentage (2.75%) of patients suffering from CO poisoning.8,9 Progression of the disease generally includes a period of unconsciousness, then a lucid interval that can last 2 to 40 days, followed by the abrupt onset of neuropsychiatric symptoms.10 The specific pathophysiologic mechanism is unknown, but has been hypothesized to involve inferior compensatory response to decreased oxygenation in the white matter.
Diagnosis and clinical features
DPHL can be divided into 2 clinical variations: parkinsonism and akinetic mutism. The former consists of conventional parkinsonian features along with agitation, apathy, hallucinations, dystonic posturing, and odd behaviors. The latter variant presents with apathy, minimal response to pain, functional bowel and bladder incontinence, mutism, and, at times, inappropriate laughter or tearfulness.5 Both variants share similar features with hypokinetic forms of catatonia.
DPHL is a diagnosis of exclusion. A careful history is critical to establish the possibility of a recent anoxic event. MRI findings, including hyperintensities in the cerebral white matter on T2-based sequencing, are suggestive of the disease. A choline peak on magnetic resonance spectroscopy also might be present in patients with DPHL, although it is not specific to the diagnosis.
Early reports of DPHL suggested an associated deficiency of arylsulfatase A, an enzyme required in the modulation of myelin; however, more recent case reports are conflicting.11 Familial mutations in the gene for arylsulfatase A also result in metachromatic leukodystrophy, and adult onset can present with psychiatric symptoms, including delusions and hallucinations.12
Treatment and prognosis
The treatment of DPHL consists primarily of supportive care and rehabilitation with physical, occupational, and speech therapy.11 With these measures, most patients improve after 3 to 6 months; however, a large percentage sustain some long-term cognitive deficit, the most prevalent symptom being frontal executive dysfunction.5
OUTCOME Supportive care
A second MRI shows diffuse hyperintensities in the white matter that spare the cerebellum and brainstem (Figure). This finding is pathognomonic for DPHL.
ECT is discontinued because there is no evidence to support ECT-associated improvement in DPHL. Moreover, ECT might worsen the clinical course through increased stress and metabolic demand on the brain.13
Because the primary treatment of DPHL is early rehabilitation, we consider that Ms. M would benefit most from increased supportive care and therapy. She is discharged to a brain injury rehabilitation facility, where metoprolol is prescribed for mild tachycardia, along with thiamine and vitamins B12 and D. Physical, occupational, and speech therapy are continued.
Approximately 3 weeks after admission to the rehabilitation program, Ms. M is discharged home. Although she improves in overall activities of daily living, she continues to experience moderate communication deficits and occasional external distractibility.
Bottom Line
Although delayed post-hypoxic leukoencephalopathy is considered rare, consider it in the differential diagnosis when a patient has a recent history of an anoxic event followed by the abrupt onset of neuropsychiatric symptoms. Keep in mind that the condition can be missed if an MRI is obtained too early, and the clinical signs can mimic hypokinetic catatonia.
Related Resources
• Meyer MA. Delayed post-hypoxic leukoencephalopathy: case report with a review of disease pathophysiology. Neurol Int. 2013;5(3):e13. doi: 10.4081/ni.2013.e13.
• Aljarallah S, Al-Hussain F. Acute fatal posthypoxic leukoencephalopathy following benzodiazepine overdose: a case report and review of the literature. BMC Neurol. 2015;15:69.
Drug Brand Names
Gabapentin • Neurontin
Lorazepam • Ativan
Metoprolol • Lopressor
Paroxetine • Paxil
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of com
CASE Improvement, then decline
Ms. M, age 37, is brought to the hospital after her husband found her at home, after an unknown duration of impaired consciousness. Her husband reports that Ms. M had normal cognitive functioning before this event, with no difficulty completing activities of daily living. Ms. M’s medical and psychiatric histories are notable for type 2 diabetes mellitus, unspecified bipolar disorder, and opioid, cocaine, and alcohol use disorders. Her medications include paroxetine, 40 mg/d, and gabapentin, 1,200 mg/d.
First admission. Poor inspiratory effort and oxygen saturation of 70% leads to emergent intubation. Serum laboratory studies reveal a white blood cell (WBC) count at 10,900/μL and creatinine phosphokinase level of 25,000 U/L. Urine drug screen is positive for tetrahydrocannabinol, cocaine, and opioids.
Ms. M is admitted to the ICU for management of rhabdomyolysis and multi-organ system failure, including acute hypoxic kidney injury.
By hospital Day 7, the tube is extubated with no recorded physical neurologic deficits. Mental status exam is normal, except for impaired memory of events surrounding the admission. Ms. M is discharged home with a recommendation for outpatient follow-up.
2 Weeks later. Ms. M is brought to the emergency department after a progressive decrease in social interaction, limited oral intake, decline in activities of daily living, and urinary incontinence. Results from laboratory studies are within normal limits; brain MRI is negative; EEG shows generalized moderate slowing.
During psychiatric evaluation, Ms. M is mute and staring continuously. Examination reveals oppositional paratonia (gegenhalten), catalepsy, prominent negativism, and waxy flexibility, all suggestive of catatonia. IV lorazepam is initiated at 1 mg every 8 hours, titrated to 2 mg, 3 times a day.
Ms. M is transferred to a psychiatric hospital for further treatment of catatonia.
Second admission. Evaluation with the Bush-Francis Catatonia Rating Scale supported a diagnosis of catatonia, with the presence of >3 features from the 14-item screen and a score of 16 on the 23-item rating scale.1 After titrating lorazepam to 9 mg/d with minimal therapeutic impact, the psychiatry team consults the electroconvulsive therapy (ECT) service, who deems Ms. M to be an appropriate candidate and petitions for court-ordered ECT.
On hospital Day 8, Ms. M has a fever of 104°F, tachycardia at 180 beats per minute, increased rigidity, and a WBC count of 17,800/μL. She is transferred to the ICU, with a presumptive diagnosis of malignant catatonia.
The medical evaluation, including general laboratory studies, EEG, and spinal fluid analysis, is unremarkable. Because of vital sign instability, 2 ECT treatments are completed in the general hospital before Ms. M resumes psychiatric inpatient care.
By the tenth ECT treatment, Ms. M is no longer febrile and experiences no further autonomic instability or psychomotor features of catatonia. Despite these improvements, she is noted to have persistent word-finding difficulty.
Which test would you order as the next step in your work up?
a) EEG
b) lumbar puncture
c) MRI
d) CT
The authors’ observations
In approximately 25% of cases, catatonia is caused by a general medical condition2; as such, a comprehensive medical workup is vital for assessment and management of catatonic patients. In Ms. M’s case, we considered several medical causes, including nutritional deficiency, infection, a toxin, renal or hepatic impairment, hypothyroidism, seizure, and stroke. Evaluation included measurement of thyroid-stimulating hormone, vitamin B12, and folic acid levels; urinalysis and urine drug screen; chest radiography; lumbar puncture; neuroimaging; and EEG (Table 1).
Several conditions in the differential diagnosis were noteworthy. Ms. M’s severe and sudden neurologic decline, along with a positive urine drug screen for substances of abuse, raised concern about overdose leading to toxic encephalopathy or hypoxic brain injury. Ms. M’s oxygen saturation when she was found was moderately hypoxic at 70%, which is not a level associated with hypoxic brain damage.
We also considered posterior reversible encephalopathy syndrome (PRES), which presents variably with nausea, visual impairment, disturbance in consciousness, seizures, and focal neurologic signs.3 Although 67% to 80% of patients with PRES also have acute hypertension, blood pressure elevation is not necessary for the diagnosis.4 Similar to toxic leukoencephalopathy, PRES is diagnosed by brain MRI, with classic signs of posterior white-matter edema.
Case reports also describe an uncommon demyelinating syndrome, delayed post-hypoxic leukoencephalopathy (DPHL), which develops several weeks or months after a cerebral anoxic insult.5 In Ms. M’s case, brain MRI performed during her second medical hospitalization, 7 days after the initial neuropsychiatric decline, was unremarkable. Using this result to rule out DPHL would have been premature because pathognomonic abnormalities can appear as long as 40 days after the anoxic insult. Given our differential diagnosis, we ordered a repeat MRI.
Etiology and pathophysiology
First described in 1979, DPHL is rare, posing diagnostic challenges for clinical providers.6 Although the exact incidence of DPHL is unknown, the precipitating event typically involves cerebral anoxia, which can occur through carbon monoxide (CO) poisoning, strangulation, cardiac arrest, respiratory failure, and overdose from sedatives and narcotics (Table 2).7 DPHL was first observed in a small percentage (2.75%) of patients suffering from CO poisoning.8,9 Progression of the disease generally includes a period of unconsciousness, then a lucid interval that can last 2 to 40 days, followed by the abrupt onset of neuropsychiatric symptoms.10 The specific pathophysiologic mechanism is unknown, but has been hypothesized to involve inferior compensatory response to decreased oxygenation in the white matter.
Diagnosis and clinical features
DPHL can be divided into 2 clinical variations: parkinsonism and akinetic mutism. The former consists of conventional parkinsonian features along with agitation, apathy, hallucinations, dystonic posturing, and odd behaviors. The latter variant presents with apathy, minimal response to pain, functional bowel and bladder incontinence, mutism, and, at times, inappropriate laughter or tearfulness.5 Both variants share similar features with hypokinetic forms of catatonia.
DPHL is a diagnosis of exclusion. A careful history is critical to establish the possibility of a recent anoxic event. MRI findings, including hyperintensities in the cerebral white matter on T2-based sequencing, are suggestive of the disease. A choline peak on magnetic resonance spectroscopy also might be present in patients with DPHL, although it is not specific to the diagnosis.
Early reports of DPHL suggested an associated deficiency of arylsulfatase A, an enzyme required in the modulation of myelin; however, more recent case reports are conflicting.11 Familial mutations in the gene for arylsulfatase A also result in metachromatic leukodystrophy, and adult onset can present with psychiatric symptoms, including delusions and hallucinations.12
Treatment and prognosis
The treatment of DPHL consists primarily of supportive care and rehabilitation with physical, occupational, and speech therapy.11 With these measures, most patients improve after 3 to 6 months; however, a large percentage sustain some long-term cognitive deficit, the most prevalent symptom being frontal executive dysfunction.5
OUTCOME Supportive care
A second MRI shows diffuse hyperintensities in the white matter that spare the cerebellum and brainstem (Figure). This finding is pathognomonic for DPHL.
ECT is discontinued because there is no evidence to support ECT-associated improvement in DPHL. Moreover, ECT might worsen the clinical course through increased stress and metabolic demand on the brain.13
Because the primary treatment of DPHL is early rehabilitation, we consider that Ms. M would benefit most from increased supportive care and therapy. She is discharged to a brain injury rehabilitation facility, where metoprolol is prescribed for mild tachycardia, along with thiamine and vitamins B12 and D. Physical, occupational, and speech therapy are continued.
Approximately 3 weeks after admission to the rehabilitation program, Ms. M is discharged home. Although she improves in overall activities of daily living, she continues to experience moderate communication deficits and occasional external distractibility.
Bottom Line
Although delayed post-hypoxic leukoencephalopathy is considered rare, consider it in the differential diagnosis when a patient has a recent history of an anoxic event followed by the abrupt onset of neuropsychiatric symptoms. Keep in mind that the condition can be missed if an MRI is obtained too early, and the clinical signs can mimic hypokinetic catatonia.
Related Resources
• Meyer MA. Delayed post-hypoxic leukoencephalopathy: case report with a review of disease pathophysiology. Neurol Int. 2013;5(3):e13. doi: 10.4081/ni.2013.e13.
• Aljarallah S, Al-Hussain F. Acute fatal posthypoxic leukoencephalopathy following benzodiazepine overdose: a case report and review of the literature. BMC Neurol. 2015;15:69.
Drug Brand Names
Gabapentin • Neurontin
Lorazepam • Ativan
Metoprolol • Lopressor
Paroxetine • Paxil
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of com
1. Bush G, Fink M, Petrides G, et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129-136.
2. Azzam PN, Gopalan P. Prototypes of catatonia: diagnostic and therapeutic challenges in the general hospital. Psychosomatics. 2013;54(1):88-93.
3. Tormoehlen LM. Toxic leukoencephalopathies. Neurol Clin. 2011;29(3):591-605
4. Legriel S, Pico F, Azoulay E. Understanding posterior reversible encephalopathy syndrome. In: Vincent JL, ed. Annual update in intensive care and emergency medicine. Heidelberg, Germany: Springer Berlin Heidelberg; 2011:631-653.
5. Schprecher D, Mehta L. The syndrome of delayed post-hypoxic leukoencephalopathy. NeuroRehabilitation. 2010;26(1):65-72.
6. Wallace IR, Dynan C, Esmonde T. One confused patient, many confused physicians: a case of delayed post-hypoxic leucoencephalopathy. QJM. 2010;103(3):193-194.
7. Lou M, Jing CH, Selim MH, et al. Delayed substantia nigra damage and leukoencephalopathy after hypoxic-ischemic injury. J Neurol Sci. 2009;277(1-2):147-149.
8. Choi IS. Delayed neurologic sequelae in carbon monoxide intoxication. Arch Neurol. 1983;40(7):433-435.
9. Molloy S, Soh C, Williams TL. Reversible delayed posthypoxic leukoencephalopathy. AJNR Am J Neuroradiol. 2006;27(8):1763-1765.
10. Shprecher DR, Flanigan KM, Smith AG, et al. Clinical and diagnostic features of delayed hypoxic leukoencephalopathy. J Neuropsychiatry Clin Neurosci. 2008;20(4):473-477.
11. Lee BH, Lyketsos CG. Delayed post-hypoxic leukoencephalopathy. Psychosomatics. 2001;42(6):530-533.
12. Hyde TM, Ziegler JC, Weinberger DR. Psychiatric disturbances in metachromatic leukodystrophy. Insights into the neurobiology of psychosis. Arch Neurol. 1992;49(4):401-406.
13. Quinn DK, Abbott CC. Catatonia after cerebral hypoxia: do the usual treatments apply? Psychosomatics. 2014;55(6):525-535.
1. Bush G, Fink M, Petrides G, et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand. 1996;93(2):129-136.
2. Azzam PN, Gopalan P. Prototypes of catatonia: diagnostic and therapeutic challenges in the general hospital. Psychosomatics. 2013;54(1):88-93.
3. Tormoehlen LM. Toxic leukoencephalopathies. Neurol Clin. 2011;29(3):591-605
4. Legriel S, Pico F, Azoulay E. Understanding posterior reversible encephalopathy syndrome. In: Vincent JL, ed. Annual update in intensive care and emergency medicine. Heidelberg, Germany: Springer Berlin Heidelberg; 2011:631-653.
5. Schprecher D, Mehta L. The syndrome of delayed post-hypoxic leukoencephalopathy. NeuroRehabilitation. 2010;26(1):65-72.
6. Wallace IR, Dynan C, Esmonde T. One confused patient, many confused physicians: a case of delayed post-hypoxic leucoencephalopathy. QJM. 2010;103(3):193-194.
7. Lou M, Jing CH, Selim MH, et al. Delayed substantia nigra damage and leukoencephalopathy after hypoxic-ischemic injury. J Neurol Sci. 2009;277(1-2):147-149.
8. Choi IS. Delayed neurologic sequelae in carbon monoxide intoxication. Arch Neurol. 1983;40(7):433-435.
9. Molloy S, Soh C, Williams TL. Reversible delayed posthypoxic leukoencephalopathy. AJNR Am J Neuroradiol. 2006;27(8):1763-1765.
10. Shprecher DR, Flanigan KM, Smith AG, et al. Clinical and diagnostic features of delayed hypoxic leukoencephalopathy. J Neuropsychiatry Clin Neurosci. 2008;20(4):473-477.
11. Lee BH, Lyketsos CG. Delayed post-hypoxic leukoencephalopathy. Psychosomatics. 2001;42(6):530-533.
12. Hyde TM, Ziegler JC, Weinberger DR. Psychiatric disturbances in metachromatic leukodystrophy. Insights into the neurobiology of psychosis. Arch Neurol. 1992;49(4):401-406.
13. Quinn DK, Abbott CC. Catatonia after cerebral hypoxia: do the usual treatments apply? Psychosomatics. 2014;55(6):525-535.
A decade after the CATIE study, the focus has shifted from effectiveness to neuroprotection
This past September, exactly 10 years after publication of the primary findings of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study1—namely, that effectiveness (defined as all-cause discontinuation) was not different across first-generation antipsychotics (FGAs) and second generation antipsychotics (SGAs)— a new meta-analysis by Vita et al2 of differences in cortical gray-matter change between those 2 classes of antipsychotics offers a reminder: The clinical focus of the CATIE study overlooked important neurobiological and neuroprotective differences between FGAs and SGAs.
How drastically 1 decade can change the scientific perspective! Vita et al’s meta-analysis and meta-regression encompassed all 18 MRI studies of cortical gray matter in patients with schizophrenia.2 Earlier studies (published between 1983 and 2014) had lumped together patients who were receiving an FGA and those receiving an SGA, and authors reported overall reduction in cortical gray matter with prolonged antipsychotic treatment.
Remarkable findings emerge
When Vita et al2 analyzed FGA- and SGA-treated patients separately, however, they found a significant reduction in cortical gray matter in the FGA group but not in the SGA group. In fact, while higher daily dosages of FGAs were associated with greater reduction in cortical gray matter, higher dosages of SGAs were associated with lower cortical gray matter reduction and, in some samples, with an increase in volume of cortical gray matter.
The researchers hypothesized that the differential effects of FGAs and SGAs might be attributable to the neurotoxicity of typical FGAs and the neuroprotective effect of atypical SGAs.
Hindsight
The key neurobiological difference between FGAs and SGAs reported by Vita et al2 was not addressed in the CATIE study, leading, at that time, to a rush to judgment that all antipsychotics are the same. This conclusion emboldened managed-care organizations to mandate use of older (and cheaper) generic FGAs instead of newer (and more expensive) SGAs— most of which have become available as generic equivalents since the CATIE study was completed.
Investigators in the CATIE study— of which I was one—cannot be blamed for not focusing on neurotoxicity and neuroprotection; those data were not on the psychiatry’s radar when the CATIE study was designed in 1998. The major focus was on whether SGAs (new on the scene in the late 1990s) were more efficacious, safe, and tolerable (that is, more effective) than FGAs.
In fact, the first study reporting that SGAs stimulated neurogenesis (in animals) was published in 2002,3 when the CATIE study was more than half complete. Research into the neuroprotective properties of SGAs then grew rapidly. In fact, the principal investigator of the CATIE study conducted a head-to-head comparison of FGA haloperidol and SGA olanzapine in a sample of first-episode schizophrenia patients4; over 1 year of follow-up, it was determined that patients in the haloperidol-treated group exhibited significant brain volume loss on MRI but those in the olanzapine-treated group did not. This study was published in 2005—the same year the CATIE study was published!
SGAs offer neuroprotection
Over the past decade, the neuroprotective effects of SGAs5 and the neurotoxic effects of FGAs6 have been studied intensively, revealing that SGAs have multiple neuroprotective effects. These effects include:
• stimulation of the production of new brain cells (neurons and glia), known as neurogenesis5,7,8
• an increase in neurotrophic factors, such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF),9 which are found at a significantly low level in patients with psychosis10
• reversal of phencyclidine (PCP)-induced changes in gene expression11
• neuroprotection against ischemic stroke12-14
• reversal of PCP-induced loss of dendritic spines in the frontal cortex15
• prevention of oligodendrocyte damage caused by interferon gamma-stimulated microglia16,17
• reversal of loss of dendritic spines in the prefrontal cortex induced by dopamine depletion18
• an anti-inflammatory effect19,20
• protection against β-amyloid and hydrogen peroxide-induced cell death21
• protection against prefrontal cortical neuronal damage caused by dizocilpine (MK-801)22
• reversal of a PCP-induced decrease in the glutathione level and alteration of antioxidant defenses23
• protection of cortical neurons from glutamate neurotoxicity.24
One reason why SGAs are neuroprotective, but FGAs are not, can be attributed to their receptor profiles. FGAs block dopamine D2 receptors far more than serotonin 2A receptors, whereas SGAs do the opposite: They block 5-HT2A receptors 500% to 1,000% more than they block D2 receptors. This difference is associated in turn with a different neurobiological and neuroprotective profiles, such as a decrease or an increase in BDNF.25,26
Neither similar nor interchangeable
Since publication of the findings of the CATIE study, the primary investigator has proposed that neuroprotection can be a therapeutic strategy to prevent neurodegeneration and neurodeterioration associated with schizophrenia.27 Given the preponderance of data showing that SGAs have numerous neuroprotective properties but FGAs have many neurotoxic effects,6 the message to psychiatric practitioners, a decade after the CATIE study, is that the 2 generations of antipsychotic agents are not really similar or interchangeable. They might have similar clinical effectiveness but they exert very different neurobiological effects.
The proof of the pudding is in the eating: Despite the findings of the CATIE study, the vast majority of psychiatrists would prefer to treat their own family members with an SGA, not an FGA, if the need for antipsychotic medication arises.
1. Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223.
2. Vita A, De Peri L, Deste G, et al. The effect of antipsychotic treatment on cortical gray matter changes in schizophrenia: does the class matter? A meta-analysis and meta-regression of longitudinal magnetic resonance imaging studies. Biol Psychiatry. 2015;78(6):403-412.
3. Wakade CG, Mahadik SP, Waller JL, et al. Atypical neuroleptics stimulate neurogenesis in adult rat brain. J Neurosci Res. 2002;69(1):72-79.
4. Lieberman JA, Tollefson GD, Charles C, et al; HGDH Study Group. Antipsychotic drug effects on brain morphology in first-episode psychosis. Arch Gen Psychiatry. 2005;62(4):361-370.
5. Nasrallah HA. Impaired neuroplasticity in schizophrenia and the neuro-regenerative effects of atypical antipsychotics. Medscape Psychiatry. http://www.medscape.org/viewarticle/569521. Published January 31, 2008. Accessed November 10, 2015.
6. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2012;12(7):7-8.
7. Nandra KS, Agius M. The differences between typical and atypical antipsychotics: the effects on neurogenesis. Psychiatr Danub. 2012;24(suppl 1):S95-S99.
8. Nasrallah HA, Hopkins T, Pixley SK, et al. Differential effects of antipsychotic and antidepressant drugs on neurogenic region in rats. Brain Res. 2010;354:23-29.
9. Pillai A, Tery AV, Mahadik SP. Differential effects of long-term treatment with typical and atypical antipsychotics on NGF and BNDF levels in rat striatum and hippocampus. Schizophr Res. 2006;82(1):95-106.
10. Buckley PF, Pillai A, Evans D, et al. Brain derived neurotropic factor in first-episode psychosis. Schizophr Res. 2007;91(1-3):1-5.
11. Martin MV, Mimics K, Nisenbaum LK, et al. Olanzapine reversed brain gene expression changes induced by phencyclidines treatment in non-human primates. Mol Neuropsychiatry. 2015;1(2):82-93.
12. Yan BC, Park JH, Ahn JH, et al. Neuroprotection of posttreatment with risperidone, an atypical antipsychotic drug, in rat and gerbil models of ischemic stroke and the maintenance of antioxidants in a gerbil model of ischemic stroke. J Neurosci Res. 2014;92(6):795-807.
13. Yulug B, Yildiz A, Güzel O, et al. Risperidone attenuates brain damage after focal cerebral ischemia in vivo. Brain Res Bull. 2006;69(6):656-659.
14. Yulug B, Yildiz A, Hüdaoglu O, et al. Olanzapine attenuates brain damage after focal cerebral ischemia in vivo. Brain Res Bull. 2006;71(1-3):296-300.
15. Elsworth JD, Morrow BA. Hajszan T, et al. Phencyclidine-induced loss of asymmetric spine synapses in rodent prefrontal cortex is reversed by acute and chronic treatment with olanzapine. Neuropsychopharmacology. 2001;36(10):2054-2061.
16. Seki Y, Kato TA, Monji A, et al. Pretreatment of aripiprazole and minocycline, but not haloperidol, suppresses oligodendrocyte damage from interferon-y-stimulated microglia in co-culture model. Schizophr Res. 2013;151(1-3):20-28.
17. Bian Q, Kato T, Monji A, et al. The effect of atypical antipsychotics, perospirone, ziprasidone and quetiapine on microglial activation induced by interferon-gamma. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):42-48.
18. Wang HD, Deutch AY. Dopamine depletion of the prefrontal cortex induces dendritic spine loss: reversal by atypical antipsychotic drug treatment. Neuropsychopharmacology. 2008;33(6):1276-1286.
19. Miller BJ, Buckley P, Seabolt W, et al. Meta-analysis of cytokine alternations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70(7):663-671.
20. Nasrallah HA. Beyond dopamine: The ‘other’ effects of antipsychotics. Current Psychiatry. 2013;12(6):8-9.
21. Yang MC, Lung FW. Neuroprotection of paliperidone on SH-SY5Y cells against β-amyloid peptide(25-35), N-methyl-4-phenylpyridinium ion, and hydrogen peroxide-induced cell death. Psychopharmacology (Berl). 2011;217(3):397-410.
22. Peng L, Zhu D, Feng X, et al. Paliperidone protects prefrontal cortical neurons from damages caused by MK-801 via Akt1/GSK3β _signaling pathway. Schizophr Res. 2013;147(1):14-23.23.
Stojkovic´ T, Radonjic´ NV, Velimirovic´ M, et al. Risperidone reverses phencyclidine induced decrease in glutathione levels and alternations of antioxidant defense in rat brain. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39(1):192-199.
24. Koprivica V, Regardie K, Wolff C, et al. Aripiprazole protects cortical neurons from glutamate toxicity. Eur J Pharmacol. 2011;651(1-3):73-76.
25. Vaidya VA, Marek GJ, Aghajanian GK, et al. 5-HT2A receptor-mediated regulation of brain-derived neurotrophic factor mRNA in the hippocampus and the neocortex. J Neurosci. 1997;17(8):2785-2795.
26. Meridith GE, Switzer RC 3rd, Napier TC. Short-term, D2 receptor blockade induces synaptic degeneration, reduces levels of tyrosine hydroxylase and brain-derived neurotrophic factor, and enhances D2-mediated firing in the ventral pallidum. Brain Res. 2004;995(1):14-22.
27. Lieberman JA, Perkins DO, Jarskog LF. Neuroprotection: a therapeutic strategy to prevent deterioration associated with schizophrenia. CNS Spectr. 2007;12(suppl 4):1-13; quiz 14.
This past September, exactly 10 years after publication of the primary findings of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study1—namely, that effectiveness (defined as all-cause discontinuation) was not different across first-generation antipsychotics (FGAs) and second generation antipsychotics (SGAs)— a new meta-analysis by Vita et al2 of differences in cortical gray-matter change between those 2 classes of antipsychotics offers a reminder: The clinical focus of the CATIE study overlooked important neurobiological and neuroprotective differences between FGAs and SGAs.
How drastically 1 decade can change the scientific perspective! Vita et al’s meta-analysis and meta-regression encompassed all 18 MRI studies of cortical gray matter in patients with schizophrenia.2 Earlier studies (published between 1983 and 2014) had lumped together patients who were receiving an FGA and those receiving an SGA, and authors reported overall reduction in cortical gray matter with prolonged antipsychotic treatment.
Remarkable findings emerge
When Vita et al2 analyzed FGA- and SGA-treated patients separately, however, they found a significant reduction in cortical gray matter in the FGA group but not in the SGA group. In fact, while higher daily dosages of FGAs were associated with greater reduction in cortical gray matter, higher dosages of SGAs were associated with lower cortical gray matter reduction and, in some samples, with an increase in volume of cortical gray matter.
The researchers hypothesized that the differential effects of FGAs and SGAs might be attributable to the neurotoxicity of typical FGAs and the neuroprotective effect of atypical SGAs.
Hindsight
The key neurobiological difference between FGAs and SGAs reported by Vita et al2 was not addressed in the CATIE study, leading, at that time, to a rush to judgment that all antipsychotics are the same. This conclusion emboldened managed-care organizations to mandate use of older (and cheaper) generic FGAs instead of newer (and more expensive) SGAs— most of which have become available as generic equivalents since the CATIE study was completed.
Investigators in the CATIE study— of which I was one—cannot be blamed for not focusing on neurotoxicity and neuroprotection; those data were not on the psychiatry’s radar when the CATIE study was designed in 1998. The major focus was on whether SGAs (new on the scene in the late 1990s) were more efficacious, safe, and tolerable (that is, more effective) than FGAs.
In fact, the first study reporting that SGAs stimulated neurogenesis (in animals) was published in 2002,3 when the CATIE study was more than half complete. Research into the neuroprotective properties of SGAs then grew rapidly. In fact, the principal investigator of the CATIE study conducted a head-to-head comparison of FGA haloperidol and SGA olanzapine in a sample of first-episode schizophrenia patients4; over 1 year of follow-up, it was determined that patients in the haloperidol-treated group exhibited significant brain volume loss on MRI but those in the olanzapine-treated group did not. This study was published in 2005—the same year the CATIE study was published!
SGAs offer neuroprotection
Over the past decade, the neuroprotective effects of SGAs5 and the neurotoxic effects of FGAs6 have been studied intensively, revealing that SGAs have multiple neuroprotective effects. These effects include:
• stimulation of the production of new brain cells (neurons and glia), known as neurogenesis5,7,8
• an increase in neurotrophic factors, such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF),9 which are found at a significantly low level in patients with psychosis10
• reversal of phencyclidine (PCP)-induced changes in gene expression11
• neuroprotection against ischemic stroke12-14
• reversal of PCP-induced loss of dendritic spines in the frontal cortex15
• prevention of oligodendrocyte damage caused by interferon gamma-stimulated microglia16,17
• reversal of loss of dendritic spines in the prefrontal cortex induced by dopamine depletion18
• an anti-inflammatory effect19,20
• protection against β-amyloid and hydrogen peroxide-induced cell death21
• protection against prefrontal cortical neuronal damage caused by dizocilpine (MK-801)22
• reversal of a PCP-induced decrease in the glutathione level and alteration of antioxidant defenses23
• protection of cortical neurons from glutamate neurotoxicity.24
One reason why SGAs are neuroprotective, but FGAs are not, can be attributed to their receptor profiles. FGAs block dopamine D2 receptors far more than serotonin 2A receptors, whereas SGAs do the opposite: They block 5-HT2A receptors 500% to 1,000% more than they block D2 receptors. This difference is associated in turn with a different neurobiological and neuroprotective profiles, such as a decrease or an increase in BDNF.25,26
Neither similar nor interchangeable
Since publication of the findings of the CATIE study, the primary investigator has proposed that neuroprotection can be a therapeutic strategy to prevent neurodegeneration and neurodeterioration associated with schizophrenia.27 Given the preponderance of data showing that SGAs have numerous neuroprotective properties but FGAs have many neurotoxic effects,6 the message to psychiatric practitioners, a decade after the CATIE study, is that the 2 generations of antipsychotic agents are not really similar or interchangeable. They might have similar clinical effectiveness but they exert very different neurobiological effects.
The proof of the pudding is in the eating: Despite the findings of the CATIE study, the vast majority of psychiatrists would prefer to treat their own family members with an SGA, not an FGA, if the need for antipsychotic medication arises.
This past September, exactly 10 years after publication of the primary findings of the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study1—namely, that effectiveness (defined as all-cause discontinuation) was not different across first-generation antipsychotics (FGAs) and second generation antipsychotics (SGAs)— a new meta-analysis by Vita et al2 of differences in cortical gray-matter change between those 2 classes of antipsychotics offers a reminder: The clinical focus of the CATIE study overlooked important neurobiological and neuroprotective differences between FGAs and SGAs.
How drastically 1 decade can change the scientific perspective! Vita et al’s meta-analysis and meta-regression encompassed all 18 MRI studies of cortical gray matter in patients with schizophrenia.2 Earlier studies (published between 1983 and 2014) had lumped together patients who were receiving an FGA and those receiving an SGA, and authors reported overall reduction in cortical gray matter with prolonged antipsychotic treatment.
Remarkable findings emerge
When Vita et al2 analyzed FGA- and SGA-treated patients separately, however, they found a significant reduction in cortical gray matter in the FGA group but not in the SGA group. In fact, while higher daily dosages of FGAs were associated with greater reduction in cortical gray matter, higher dosages of SGAs were associated with lower cortical gray matter reduction and, in some samples, with an increase in volume of cortical gray matter.
The researchers hypothesized that the differential effects of FGAs and SGAs might be attributable to the neurotoxicity of typical FGAs and the neuroprotective effect of atypical SGAs.
Hindsight
The key neurobiological difference between FGAs and SGAs reported by Vita et al2 was not addressed in the CATIE study, leading, at that time, to a rush to judgment that all antipsychotics are the same. This conclusion emboldened managed-care organizations to mandate use of older (and cheaper) generic FGAs instead of newer (and more expensive) SGAs— most of which have become available as generic equivalents since the CATIE study was completed.
Investigators in the CATIE study— of which I was one—cannot be blamed for not focusing on neurotoxicity and neuroprotection; those data were not on the psychiatry’s radar when the CATIE study was designed in 1998. The major focus was on whether SGAs (new on the scene in the late 1990s) were more efficacious, safe, and tolerable (that is, more effective) than FGAs.
In fact, the first study reporting that SGAs stimulated neurogenesis (in animals) was published in 2002,3 when the CATIE study was more than half complete. Research into the neuroprotective properties of SGAs then grew rapidly. In fact, the principal investigator of the CATIE study conducted a head-to-head comparison of FGA haloperidol and SGA olanzapine in a sample of first-episode schizophrenia patients4; over 1 year of follow-up, it was determined that patients in the haloperidol-treated group exhibited significant brain volume loss on MRI but those in the olanzapine-treated group did not. This study was published in 2005—the same year the CATIE study was published!
SGAs offer neuroprotection
Over the past decade, the neuroprotective effects of SGAs5 and the neurotoxic effects of FGAs6 have been studied intensively, revealing that SGAs have multiple neuroprotective effects. These effects include:
• stimulation of the production of new brain cells (neurons and glia), known as neurogenesis5,7,8
• an increase in neurotrophic factors, such as nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF),9 which are found at a significantly low level in patients with psychosis10
• reversal of phencyclidine (PCP)-induced changes in gene expression11
• neuroprotection against ischemic stroke12-14
• reversal of PCP-induced loss of dendritic spines in the frontal cortex15
• prevention of oligodendrocyte damage caused by interferon gamma-stimulated microglia16,17
• reversal of loss of dendritic spines in the prefrontal cortex induced by dopamine depletion18
• an anti-inflammatory effect19,20
• protection against β-amyloid and hydrogen peroxide-induced cell death21
• protection against prefrontal cortical neuronal damage caused by dizocilpine (MK-801)22
• reversal of a PCP-induced decrease in the glutathione level and alteration of antioxidant defenses23
• protection of cortical neurons from glutamate neurotoxicity.24
One reason why SGAs are neuroprotective, but FGAs are not, can be attributed to their receptor profiles. FGAs block dopamine D2 receptors far more than serotonin 2A receptors, whereas SGAs do the opposite: They block 5-HT2A receptors 500% to 1,000% more than they block D2 receptors. This difference is associated in turn with a different neurobiological and neuroprotective profiles, such as a decrease or an increase in BDNF.25,26
Neither similar nor interchangeable
Since publication of the findings of the CATIE study, the primary investigator has proposed that neuroprotection can be a therapeutic strategy to prevent neurodegeneration and neurodeterioration associated with schizophrenia.27 Given the preponderance of data showing that SGAs have numerous neuroprotective properties but FGAs have many neurotoxic effects,6 the message to psychiatric practitioners, a decade after the CATIE study, is that the 2 generations of antipsychotic agents are not really similar or interchangeable. They might have similar clinical effectiveness but they exert very different neurobiological effects.
The proof of the pudding is in the eating: Despite the findings of the CATIE study, the vast majority of psychiatrists would prefer to treat their own family members with an SGA, not an FGA, if the need for antipsychotic medication arises.
1. Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223.
2. Vita A, De Peri L, Deste G, et al. The effect of antipsychotic treatment on cortical gray matter changes in schizophrenia: does the class matter? A meta-analysis and meta-regression of longitudinal magnetic resonance imaging studies. Biol Psychiatry. 2015;78(6):403-412.
3. Wakade CG, Mahadik SP, Waller JL, et al. Atypical neuroleptics stimulate neurogenesis in adult rat brain. J Neurosci Res. 2002;69(1):72-79.
4. Lieberman JA, Tollefson GD, Charles C, et al; HGDH Study Group. Antipsychotic drug effects on brain morphology in first-episode psychosis. Arch Gen Psychiatry. 2005;62(4):361-370.
5. Nasrallah HA. Impaired neuroplasticity in schizophrenia and the neuro-regenerative effects of atypical antipsychotics. Medscape Psychiatry. http://www.medscape.org/viewarticle/569521. Published January 31, 2008. Accessed November 10, 2015.
6. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2012;12(7):7-8.
7. Nandra KS, Agius M. The differences between typical and atypical antipsychotics: the effects on neurogenesis. Psychiatr Danub. 2012;24(suppl 1):S95-S99.
8. Nasrallah HA, Hopkins T, Pixley SK, et al. Differential effects of antipsychotic and antidepressant drugs on neurogenic region in rats. Brain Res. 2010;354:23-29.
9. Pillai A, Tery AV, Mahadik SP. Differential effects of long-term treatment with typical and atypical antipsychotics on NGF and BNDF levels in rat striatum and hippocampus. Schizophr Res. 2006;82(1):95-106.
10. Buckley PF, Pillai A, Evans D, et al. Brain derived neurotropic factor in first-episode psychosis. Schizophr Res. 2007;91(1-3):1-5.
11. Martin MV, Mimics K, Nisenbaum LK, et al. Olanzapine reversed brain gene expression changes induced by phencyclidines treatment in non-human primates. Mol Neuropsychiatry. 2015;1(2):82-93.
12. Yan BC, Park JH, Ahn JH, et al. Neuroprotection of posttreatment with risperidone, an atypical antipsychotic drug, in rat and gerbil models of ischemic stroke and the maintenance of antioxidants in a gerbil model of ischemic stroke. J Neurosci Res. 2014;92(6):795-807.
13. Yulug B, Yildiz A, Güzel O, et al. Risperidone attenuates brain damage after focal cerebral ischemia in vivo. Brain Res Bull. 2006;69(6):656-659.
14. Yulug B, Yildiz A, Hüdaoglu O, et al. Olanzapine attenuates brain damage after focal cerebral ischemia in vivo. Brain Res Bull. 2006;71(1-3):296-300.
15. Elsworth JD, Morrow BA. Hajszan T, et al. Phencyclidine-induced loss of asymmetric spine synapses in rodent prefrontal cortex is reversed by acute and chronic treatment with olanzapine. Neuropsychopharmacology. 2001;36(10):2054-2061.
16. Seki Y, Kato TA, Monji A, et al. Pretreatment of aripiprazole and minocycline, but not haloperidol, suppresses oligodendrocyte damage from interferon-y-stimulated microglia in co-culture model. Schizophr Res. 2013;151(1-3):20-28.
17. Bian Q, Kato T, Monji A, et al. The effect of atypical antipsychotics, perospirone, ziprasidone and quetiapine on microglial activation induced by interferon-gamma. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):42-48.
18. Wang HD, Deutch AY. Dopamine depletion of the prefrontal cortex induces dendritic spine loss: reversal by atypical antipsychotic drug treatment. Neuropsychopharmacology. 2008;33(6):1276-1286.
19. Miller BJ, Buckley P, Seabolt W, et al. Meta-analysis of cytokine alternations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70(7):663-671.
20. Nasrallah HA. Beyond dopamine: The ‘other’ effects of antipsychotics. Current Psychiatry. 2013;12(6):8-9.
21. Yang MC, Lung FW. Neuroprotection of paliperidone on SH-SY5Y cells against β-amyloid peptide(25-35), N-methyl-4-phenylpyridinium ion, and hydrogen peroxide-induced cell death. Psychopharmacology (Berl). 2011;217(3):397-410.
22. Peng L, Zhu D, Feng X, et al. Paliperidone protects prefrontal cortical neurons from damages caused by MK-801 via Akt1/GSK3β _signaling pathway. Schizophr Res. 2013;147(1):14-23.23.
Stojkovic´ T, Radonjic´ NV, Velimirovic´ M, et al. Risperidone reverses phencyclidine induced decrease in glutathione levels and alternations of antioxidant defense in rat brain. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39(1):192-199.
24. Koprivica V, Regardie K, Wolff C, et al. Aripiprazole protects cortical neurons from glutamate toxicity. Eur J Pharmacol. 2011;651(1-3):73-76.
25. Vaidya VA, Marek GJ, Aghajanian GK, et al. 5-HT2A receptor-mediated regulation of brain-derived neurotrophic factor mRNA in the hippocampus and the neocortex. J Neurosci. 1997;17(8):2785-2795.
26. Meridith GE, Switzer RC 3rd, Napier TC. Short-term, D2 receptor blockade induces synaptic degeneration, reduces levels of tyrosine hydroxylase and brain-derived neurotrophic factor, and enhances D2-mediated firing in the ventral pallidum. Brain Res. 2004;995(1):14-22.
27. Lieberman JA, Perkins DO, Jarskog LF. Neuroprotection: a therapeutic strategy to prevent deterioration associated with schizophrenia. CNS Spectr. 2007;12(suppl 4):1-13; quiz 14.
1. Lieberman JA, Stroup TS, McEvoy JP, et al; Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) Investigators. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209-1223.
2. Vita A, De Peri L, Deste G, et al. The effect of antipsychotic treatment on cortical gray matter changes in schizophrenia: does the class matter? A meta-analysis and meta-regression of longitudinal magnetic resonance imaging studies. Biol Psychiatry. 2015;78(6):403-412.
3. Wakade CG, Mahadik SP, Waller JL, et al. Atypical neuroleptics stimulate neurogenesis in adult rat brain. J Neurosci Res. 2002;69(1):72-79.
4. Lieberman JA, Tollefson GD, Charles C, et al; HGDH Study Group. Antipsychotic drug effects on brain morphology in first-episode psychosis. Arch Gen Psychiatry. 2005;62(4):361-370.
5. Nasrallah HA. Impaired neuroplasticity in schizophrenia and the neuro-regenerative effects of atypical antipsychotics. Medscape Psychiatry. http://www.medscape.org/viewarticle/569521. Published January 31, 2008. Accessed November 10, 2015.
6. Nasrallah HA. Haloperidol clearly is neurotoxic. Should it be banned? Current Psychiatry. 2012;12(7):7-8.
7. Nandra KS, Agius M. The differences between typical and atypical antipsychotics: the effects on neurogenesis. Psychiatr Danub. 2012;24(suppl 1):S95-S99.
8. Nasrallah HA, Hopkins T, Pixley SK, et al. Differential effects of antipsychotic and antidepressant drugs on neurogenic region in rats. Brain Res. 2010;354:23-29.
9. Pillai A, Tery AV, Mahadik SP. Differential effects of long-term treatment with typical and atypical antipsychotics on NGF and BNDF levels in rat striatum and hippocampus. Schizophr Res. 2006;82(1):95-106.
10. Buckley PF, Pillai A, Evans D, et al. Brain derived neurotropic factor in first-episode psychosis. Schizophr Res. 2007;91(1-3):1-5.
11. Martin MV, Mimics K, Nisenbaum LK, et al. Olanzapine reversed brain gene expression changes induced by phencyclidines treatment in non-human primates. Mol Neuropsychiatry. 2015;1(2):82-93.
12. Yan BC, Park JH, Ahn JH, et al. Neuroprotection of posttreatment with risperidone, an atypical antipsychotic drug, in rat and gerbil models of ischemic stroke and the maintenance of antioxidants in a gerbil model of ischemic stroke. J Neurosci Res. 2014;92(6):795-807.
13. Yulug B, Yildiz A, Güzel O, et al. Risperidone attenuates brain damage after focal cerebral ischemia in vivo. Brain Res Bull. 2006;69(6):656-659.
14. Yulug B, Yildiz A, Hüdaoglu O, et al. Olanzapine attenuates brain damage after focal cerebral ischemia in vivo. Brain Res Bull. 2006;71(1-3):296-300.
15. Elsworth JD, Morrow BA. Hajszan T, et al. Phencyclidine-induced loss of asymmetric spine synapses in rodent prefrontal cortex is reversed by acute and chronic treatment with olanzapine. Neuropsychopharmacology. 2001;36(10):2054-2061.
16. Seki Y, Kato TA, Monji A, et al. Pretreatment of aripiprazole and minocycline, but not haloperidol, suppresses oligodendrocyte damage from interferon-y-stimulated microglia in co-culture model. Schizophr Res. 2013;151(1-3):20-28.
17. Bian Q, Kato T, Monji A, et al. The effect of atypical antipsychotics, perospirone, ziprasidone and quetiapine on microglial activation induced by interferon-gamma. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(1):42-48.
18. Wang HD, Deutch AY. Dopamine depletion of the prefrontal cortex induces dendritic spine loss: reversal by atypical antipsychotic drug treatment. Neuropsychopharmacology. 2008;33(6):1276-1286.
19. Miller BJ, Buckley P, Seabolt W, et al. Meta-analysis of cytokine alternations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry. 2011;70(7):663-671.
20. Nasrallah HA. Beyond dopamine: The ‘other’ effects of antipsychotics. Current Psychiatry. 2013;12(6):8-9.
21. Yang MC, Lung FW. Neuroprotection of paliperidone on SH-SY5Y cells against β-amyloid peptide(25-35), N-methyl-4-phenylpyridinium ion, and hydrogen peroxide-induced cell death. Psychopharmacology (Berl). 2011;217(3):397-410.
22. Peng L, Zhu D, Feng X, et al. Paliperidone protects prefrontal cortical neurons from damages caused by MK-801 via Akt1/GSK3β _signaling pathway. Schizophr Res. 2013;147(1):14-23.23.
Stojkovic´ T, Radonjic´ NV, Velimirovic´ M, et al. Risperidone reverses phencyclidine induced decrease in glutathione levels and alternations of antioxidant defense in rat brain. Prog Neuropsychopharmacol Biol Psychiatry. 2012;39(1):192-199.
24. Koprivica V, Regardie K, Wolff C, et al. Aripiprazole protects cortical neurons from glutamate toxicity. Eur J Pharmacol. 2011;651(1-3):73-76.
25. Vaidya VA, Marek GJ, Aghajanian GK, et al. 5-HT2A receptor-mediated regulation of brain-derived neurotrophic factor mRNA in the hippocampus and the neocortex. J Neurosci. 1997;17(8):2785-2795.
26. Meridith GE, Switzer RC 3rd, Napier TC. Short-term, D2 receptor blockade induces synaptic degeneration, reduces levels of tyrosine hydroxylase and brain-derived neurotrophic factor, and enhances D2-mediated firing in the ventral pallidum. Brain Res. 2004;995(1):14-22.
27. Lieberman JA, Perkins DO, Jarskog LF. Neuroprotection: a therapeutic strategy to prevent deterioration associated with schizophrenia. CNS Spectr. 2007;12(suppl 4):1-13; quiz 14.
Cardiothoracic Surgery Resident Poster Competition
Represent your institution with a scientific poster of your clinical/investigative research at the 2016 AATS Annual Meeting in Baltimore, Maryland, May 14-18, 2016. The Competition is open to senior cardiothoracic surgery residents and/or congenital heart surgery fellows worldwide
North American residents must (1) Be in their last year of either an ACGME-accredited or RCPSC-accredited US or Canadian cardiothoracic surgery residency program or congenital heart surgery fellowship, and (2) Upload a support letter from their Program Director as part of their application.
International residents must (1) Be in their last year of a cardiothoracic training program at an AATS Member’s institution, and (2) Upload a sponsor letter from an AATS member at their institution as part of their application.
Application — Residents/fellows must provide a brief abstract of the research on their posters. Research may include information previously presented and/or published.
Benefits — Participant/institutions will (1) Receive a $500 stipend to offset travel and hotel accommodation to the Annual Meeting, (2) Receive a complimentary Annual Meeting registration, and (3) Have access to a Skills Course (Saturday, May 14) and Postgraduate Course (Sunday, May 15).
The participant’s training program will be responsible for the cost of any additional resident/fellow travel and accommodations.
Deadline: January 22, 2016
Represent your institution with a scientific poster of your clinical/investigative research at the 2016 AATS Annual Meeting in Baltimore, Maryland, May 14-18, 2016. The Competition is open to senior cardiothoracic surgery residents and/or congenital heart surgery fellows worldwide
North American residents must (1) Be in their last year of either an ACGME-accredited or RCPSC-accredited US or Canadian cardiothoracic surgery residency program or congenital heart surgery fellowship, and (2) Upload a support letter from their Program Director as part of their application.
International residents must (1) Be in their last year of a cardiothoracic training program at an AATS Member’s institution, and (2) Upload a sponsor letter from an AATS member at their institution as part of their application.
Application — Residents/fellows must provide a brief abstract of the research on their posters. Research may include information previously presented and/or published.
Benefits — Participant/institutions will (1) Receive a $500 stipend to offset travel and hotel accommodation to the Annual Meeting, (2) Receive a complimentary Annual Meeting registration, and (3) Have access to a Skills Course (Saturday, May 14) and Postgraduate Course (Sunday, May 15).
The participant’s training program will be responsible for the cost of any additional resident/fellow travel and accommodations.
Deadline: January 22, 2016
Represent your institution with a scientific poster of your clinical/investigative research at the 2016 AATS Annual Meeting in Baltimore, Maryland, May 14-18, 2016. The Competition is open to senior cardiothoracic surgery residents and/or congenital heart surgery fellows worldwide
North American residents must (1) Be in their last year of either an ACGME-accredited or RCPSC-accredited US or Canadian cardiothoracic surgery residency program or congenital heart surgery fellowship, and (2) Upload a support letter from their Program Director as part of their application.
International residents must (1) Be in their last year of a cardiothoracic training program at an AATS Member’s institution, and (2) Upload a sponsor letter from an AATS member at their institution as part of their application.
Application — Residents/fellows must provide a brief abstract of the research on their posters. Research may include information previously presented and/or published.
Benefits — Participant/institutions will (1) Receive a $500 stipend to offset travel and hotel accommodation to the Annual Meeting, (2) Receive a complimentary Annual Meeting registration, and (3) Have access to a Skills Course (Saturday, May 14) and Postgraduate Course (Sunday, May 15).
The participant’s training program will be responsible for the cost of any additional resident/fellow travel and accommodations.
Deadline: January 22, 2016
Apply to the AATS Summer Internship Scholarship
Medical students: Submissions are open for the AATS Summer Internship Scholarship giving up to 40 successful candidates the opportunity to spend eight weeks during the summer working in the cardiothoracic surgery department of a North American AATS member.
Program Goal — The program aims to broaden medical students’ educational experiences and to provide insight into cardiothoracic surgery.
Eligibility — (1) Candidates must be a North American first- or second-year medical student (as of January 2, 2016), (2) Host sponsor (an AATS member) must provide a letter of support/approval, and (3) Internships must take place at the institution of the host sponsor.
Application — The application must include no more than a one-page outline that includes what the candidate hopes to accomplish during his/her eight-week scholarship and specifies the proposed intern’s exposure to CT surgery, including both laboratory and clinical experience
Selection — (1) No more than two students from a single institution may receive a scholarship, (2) If two students from the same institution are selected, each must have a different host sponsor, and (3) Award recipients must agree to submit a summary report and evaluation of their experience to AATS within 60 days of internship completion.
Deadline: Friday, January 15, 2016
Medical students: Submissions are open for the AATS Summer Internship Scholarship giving up to 40 successful candidates the opportunity to spend eight weeks during the summer working in the cardiothoracic surgery department of a North American AATS member.
Program Goal — The program aims to broaden medical students’ educational experiences and to provide insight into cardiothoracic surgery.
Eligibility — (1) Candidates must be a North American first- or second-year medical student (as of January 2, 2016), (2) Host sponsor (an AATS member) must provide a letter of support/approval, and (3) Internships must take place at the institution of the host sponsor.
Application — The application must include no more than a one-page outline that includes what the candidate hopes to accomplish during his/her eight-week scholarship and specifies the proposed intern’s exposure to CT surgery, including both laboratory and clinical experience
Selection — (1) No more than two students from a single institution may receive a scholarship, (2) If two students from the same institution are selected, each must have a different host sponsor, and (3) Award recipients must agree to submit a summary report and evaluation of their experience to AATS within 60 days of internship completion.
Deadline: Friday, January 15, 2016
Medical students: Submissions are open for the AATS Summer Internship Scholarship giving up to 40 successful candidates the opportunity to spend eight weeks during the summer working in the cardiothoracic surgery department of a North American AATS member.
Program Goal — The program aims to broaden medical students’ educational experiences and to provide insight into cardiothoracic surgery.
Eligibility — (1) Candidates must be a North American first- or second-year medical student (as of January 2, 2016), (2) Host sponsor (an AATS member) must provide a letter of support/approval, and (3) Internships must take place at the institution of the host sponsor.
Application — The application must include no more than a one-page outline that includes what the candidate hopes to accomplish during his/her eight-week scholarship and specifies the proposed intern’s exposure to CT surgery, including both laboratory and clinical experience
Selection — (1) No more than two students from a single institution may receive a scholarship, (2) If two students from the same institution are selected, each must have a different host sponsor, and (3) Award recipients must agree to submit a summary report and evaluation of their experience to AATS within 60 days of internship completion.
Deadline: Friday, January 15, 2016
Be an AATS Member for a Day
Medical Students, General Surgery Residents and I-6 CT Surgical Residents — Submissions are open for the AATS Member for a Day program. Up to 30 successful candidates will have the opportunity to accompany an AATS Member Mentor for portions of the 2016 AATS Annual Meeting.
Dates/Location: May 14-18, 2016, Baltimore, MD
Eligibility — Applicants must be North American medical students, general surgery residents or I-6 cardiothoracic residents (within their first three years).
Program Goals — Are to (1) offer insight into cardiothoracic surgery, and (2) provide an opportunity to network and build relationships within the cardiothoracic surgical community.
Benefits — (1) Complimentary hotel accommodation for a minimum of three and maximum of four nights at an AATS Annual Meeting hotel, (2) a $500 stipend to help offset travel costs, and (3) an additional $250 stipend to offset the cost of meals.
Deadline: Friday, January 15, 2016
Medical Students, General Surgery Residents and I-6 CT Surgical Residents — Submissions are open for the AATS Member for a Day program. Up to 30 successful candidates will have the opportunity to accompany an AATS Member Mentor for portions of the 2016 AATS Annual Meeting.
Dates/Location: May 14-18, 2016, Baltimore, MD
Eligibility — Applicants must be North American medical students, general surgery residents or I-6 cardiothoracic residents (within their first three years).
Program Goals — Are to (1) offer insight into cardiothoracic surgery, and (2) provide an opportunity to network and build relationships within the cardiothoracic surgical community.
Benefits — (1) Complimentary hotel accommodation for a minimum of three and maximum of four nights at an AATS Annual Meeting hotel, (2) a $500 stipend to help offset travel costs, and (3) an additional $250 stipend to offset the cost of meals.
Deadline: Friday, January 15, 2016
Medical Students, General Surgery Residents and I-6 CT Surgical Residents — Submissions are open for the AATS Member for a Day program. Up to 30 successful candidates will have the opportunity to accompany an AATS Member Mentor for portions of the 2016 AATS Annual Meeting.
Dates/Location: May 14-18, 2016, Baltimore, MD
Eligibility — Applicants must be North American medical students, general surgery residents or I-6 cardiothoracic residents (within their first three years).
Program Goals — Are to (1) offer insight into cardiothoracic surgery, and (2) provide an opportunity to network and build relationships within the cardiothoracic surgical community.
Benefits — (1) Complimentary hotel accommodation for a minimum of three and maximum of four nights at an AATS Annual Meeting hotel, (2) a $500 stipend to help offset travel costs, and (3) an additional $250 stipend to offset the cost of meals.
Deadline: Friday, January 15, 2016
ACR: Years of TNF blockers did not increase risk of lymphoma in RA
SAN FRANCISCO – Rheumatoid arthritis conferred a doubling of the risk of lymphoma when compared against the general population in a large Swedish registry study, regardless of the patients’ experience with biological disease-modifying antirheumatic drugs.
But patients who took biological disease-modifying antirheumatic drugs (bDMARDs) had a sixfold greater risk of natural killer or T-cell lymphoma than did the general population, and that association was about four times stronger than for patients who had never taken biologics, reported Dr. Karin Hellgren, who led the study at the Karolinska Institute in Stockholm. That finding in particular shows the need to keep studying the links between bDMARDs and specific lymphoma subtypes, he said.
Severe rheumatoid arthritis seems to strongly increase the risk of lymphoma (Arthritis Rheum. 2006;54[3]:692-701), but researchers have debated whether the reason relates to bDMARDs or RA itself. Clinical trials have produced conflicting results; observational studies have reported no overall link between bDMARDs and lymphoma, but have raised questions about long-term exposure, the effects of individual agents, and lymphoma subtypes, Dr. Hellgren said at the annual meeting of the American College of Rheumatology.
To delve deeper into these issues, he and his associates compared 15 years of data for 13,240 RA patients on bDMARDs from the Swedish Biologics (ARTIS), Patient, and Cancer Registers and a national cohort of 46,568 bDMARD-naive patients. The researchers also compared both groups with 458,846 age- and gender-matched adults from the Swedish Population Register, following individuals until the end of 2012 or until lymphoma diagnosis, death, emigration, or bDMARD initiation, in the case of the naive patients.
Overall, patients with RA averaged one diagnosis of lymphoma per 1,000 population, compared with 0.5 cases per 1,000 for the overall population of Sweden, Dr. Hellgren said. In terms of absolute numbers, there were 241 cases of lymphoma among bDMARD-naive patients, 1,413 cases in the general population, and 69 cases among patients on bDMARDs, including 68 who were taking TNF inhibitors. The average age of the latter group of patients was 57 years. They had been diagnosed with RA at about age 50, had a mean 28-joint Disease Activity Score score of 5.3, and averaged 5.9 years of exposure to TNF inhibitors. Their risk of any type of malignant lymphoma was about 20% higher than for bDMARD-naive patients, but the difference was insignificant overall and in subgroups stratified by gender, age, and year starting treatment. Likewise, although patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), there was no significant difference in risk compared with bDMARD-naive patients.
“There also were no statistically significant differences between drugs,” including infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira), Dr. Hellgren said. “In terms of the newer TNF inhibitors and other biologics, data are still too scarce to evaluate,” he added. Both exposed and bDMARD-naive patients were at especially high risk of Hodgkin lymphoma and diffuse large B-cell lymphoma, compared with the general population, but the strongest association of all was between bDMARD exposure and natural killer or T-cell lymphoma (HR, 6.0; 95% CI, 2.7-13.3). “The distribution of lymphoma subtypes warrants further assessment,” Dr. Hellgren concluded.
The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.
SAN FRANCISCO – Rheumatoid arthritis conferred a doubling of the risk of lymphoma when compared against the general population in a large Swedish registry study, regardless of the patients’ experience with biological disease-modifying antirheumatic drugs.
But patients who took biological disease-modifying antirheumatic drugs (bDMARDs) had a sixfold greater risk of natural killer or T-cell lymphoma than did the general population, and that association was about four times stronger than for patients who had never taken biologics, reported Dr. Karin Hellgren, who led the study at the Karolinska Institute in Stockholm. That finding in particular shows the need to keep studying the links between bDMARDs and specific lymphoma subtypes, he said.
Severe rheumatoid arthritis seems to strongly increase the risk of lymphoma (Arthritis Rheum. 2006;54[3]:692-701), but researchers have debated whether the reason relates to bDMARDs or RA itself. Clinical trials have produced conflicting results; observational studies have reported no overall link between bDMARDs and lymphoma, but have raised questions about long-term exposure, the effects of individual agents, and lymphoma subtypes, Dr. Hellgren said at the annual meeting of the American College of Rheumatology.
To delve deeper into these issues, he and his associates compared 15 years of data for 13,240 RA patients on bDMARDs from the Swedish Biologics (ARTIS), Patient, and Cancer Registers and a national cohort of 46,568 bDMARD-naive patients. The researchers also compared both groups with 458,846 age- and gender-matched adults from the Swedish Population Register, following individuals until the end of 2012 or until lymphoma diagnosis, death, emigration, or bDMARD initiation, in the case of the naive patients.
Overall, patients with RA averaged one diagnosis of lymphoma per 1,000 population, compared with 0.5 cases per 1,000 for the overall population of Sweden, Dr. Hellgren said. In terms of absolute numbers, there were 241 cases of lymphoma among bDMARD-naive patients, 1,413 cases in the general population, and 69 cases among patients on bDMARDs, including 68 who were taking TNF inhibitors. The average age of the latter group of patients was 57 years. They had been diagnosed with RA at about age 50, had a mean 28-joint Disease Activity Score score of 5.3, and averaged 5.9 years of exposure to TNF inhibitors. Their risk of any type of malignant lymphoma was about 20% higher than for bDMARD-naive patients, but the difference was insignificant overall and in subgroups stratified by gender, age, and year starting treatment. Likewise, although patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), there was no significant difference in risk compared with bDMARD-naive patients.
“There also were no statistically significant differences between drugs,” including infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira), Dr. Hellgren said. “In terms of the newer TNF inhibitors and other biologics, data are still too scarce to evaluate,” he added. Both exposed and bDMARD-naive patients were at especially high risk of Hodgkin lymphoma and diffuse large B-cell lymphoma, compared with the general population, but the strongest association of all was between bDMARD exposure and natural killer or T-cell lymphoma (HR, 6.0; 95% CI, 2.7-13.3). “The distribution of lymphoma subtypes warrants further assessment,” Dr. Hellgren concluded.
The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.
SAN FRANCISCO – Rheumatoid arthritis conferred a doubling of the risk of lymphoma when compared against the general population in a large Swedish registry study, regardless of the patients’ experience with biological disease-modifying antirheumatic drugs.
But patients who took biological disease-modifying antirheumatic drugs (bDMARDs) had a sixfold greater risk of natural killer or T-cell lymphoma than did the general population, and that association was about four times stronger than for patients who had never taken biologics, reported Dr. Karin Hellgren, who led the study at the Karolinska Institute in Stockholm. That finding in particular shows the need to keep studying the links between bDMARDs and specific lymphoma subtypes, he said.
Severe rheumatoid arthritis seems to strongly increase the risk of lymphoma (Arthritis Rheum. 2006;54[3]:692-701), but researchers have debated whether the reason relates to bDMARDs or RA itself. Clinical trials have produced conflicting results; observational studies have reported no overall link between bDMARDs and lymphoma, but have raised questions about long-term exposure, the effects of individual agents, and lymphoma subtypes, Dr. Hellgren said at the annual meeting of the American College of Rheumatology.
To delve deeper into these issues, he and his associates compared 15 years of data for 13,240 RA patients on bDMARDs from the Swedish Biologics (ARTIS), Patient, and Cancer Registers and a national cohort of 46,568 bDMARD-naive patients. The researchers also compared both groups with 458,846 age- and gender-matched adults from the Swedish Population Register, following individuals until the end of 2012 or until lymphoma diagnosis, death, emigration, or bDMARD initiation, in the case of the naive patients.
Overall, patients with RA averaged one diagnosis of lymphoma per 1,000 population, compared with 0.5 cases per 1,000 for the overall population of Sweden, Dr. Hellgren said. In terms of absolute numbers, there were 241 cases of lymphoma among bDMARD-naive patients, 1,413 cases in the general population, and 69 cases among patients on bDMARDs, including 68 who were taking TNF inhibitors. The average age of the latter group of patients was 57 years. They had been diagnosed with RA at about age 50, had a mean 28-joint Disease Activity Score score of 5.3, and averaged 5.9 years of exposure to TNF inhibitors. Their risk of any type of malignant lymphoma was about 20% higher than for bDMARD-naive patients, but the difference was insignificant overall and in subgroups stratified by gender, age, and year starting treatment. Likewise, although patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), there was no significant difference in risk compared with bDMARD-naive patients.
“There also were no statistically significant differences between drugs,” including infliximab (Remicade), etanercept (Enbrel), and adalimumab (Humira), Dr. Hellgren said. “In terms of the newer TNF inhibitors and other biologics, data are still too scarce to evaluate,” he added. Both exposed and bDMARD-naive patients were at especially high risk of Hodgkin lymphoma and diffuse large B-cell lymphoma, compared with the general population, but the strongest association of all was between bDMARD exposure and natural killer or T-cell lymphoma (HR, 6.0; 95% CI, 2.7-13.3). “The distribution of lymphoma subtypes warrants further assessment,” Dr. Hellgren concluded.
The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.
AT THE ACR ANNUAL MEETING
Key clinical point: Exposure to biological disease-modifying antirheumatic drugs did not increase the overall risk of lymphoma among patients with rheumatoid arthritis.
Major finding: Patients were at greater risk of lymphoma if they had been on bDMARDs for 5-15 years (hazard ratio, 1.9) than for less time (HRs, about 1.0), but there was no significant difference in risk compared with bDMARD-naive patients. However, patients on bDMARDs had about a fourfold greater risk of NK/T-cell lymphoma compared with bDMARD-naive patients.
Data source: A matched registry analysis of 13,240 patients from the Swedish Biologics (ARTIS), Patient, and Cancer Registers; 46,568 bio-naive patients; and 458,846 members of the general population.
Disclosures: The ARTIS registry is funded by AbbVie, Bristol-Myers Squibb, Roche, Merck, Pfizer, Sobi, Lilly, and UCB. Dr. Hellgren had no disclosures. One coauthor reported financial relationships with AstraZeneca, Pfizer, UCB, Roche, Merck, Bristol-Myers Squibb, and AbbVie.