User login
Strong Leadership Evident at HM13
After wrapping up the SHM annual meeting, I was left with a sense of security about hospital medicine’s future. This security I can summarize in a single word: leadership. SHM has long had a strong set of leaders, which are needed now more than ever. With explosive expansion in volume and scope, hospitalist practice is going to require tireless leadership in the coming years and decades to ensure our trajectory is strategic and viable.
The Science
Wikipedia describes leadership as “a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task.” Notice a few key words in that definition? “Process,” which implies that it takes time, patience, and tenacity. It is not something that automatically happens without any time or effort. Also notice the word “influence,” which does not include “power” or “authority” or “pay grade”—all terms that are entirely overused and misused in the medical industry.
There is a wealth of literature describing what leadership is and what it takes to be a leader. There are an abundance of theories on what traits and characteristics make up a good leader, and an equal abundance of theories on how great leaders evolve. Some subscribe to the inherited theory, in which genetic makeup will at least partially dictate whether you will be a “natural-born” a leader. Others subscribe to the belief that leadership is more situational, whereby leaders are effective in some situations but ineffective in others. Still others believe leaders emerge as a mixture of nature and nurture, that most good leaders can lead in a variety of climates and situations, but that a perfect leadership situation might not emerge for any one leader. For other leaders, a perfect situational opportunity might emerge that suits their leadership style, and transformational change can occur under their direction.
The science of leadership has found that some personal traits are more commonly associated with leaders than nonleaders, including extraversion, self-efficacy, conscientiousness, intelligence, and openness to experience. However, absence of these characteristics does not guarantee a hopeless leadership void; equally true, the presence of them does not guarantee good leadership.
The Art
So one can go on for the length of an encyclopedia about the science of leadership, but what about the art of leadership? The ability of a leader to “read the audience,” to “take the pulse” of their staff, to strategize their next foray into new territory, or to say no to a new (seemingly exciting) opportunity. It is the art of leadership that is much more intriguing. I have had the good fortune of seeing a variety of incredible leaders at work, both within and outside of SHM, including their artful mastery of difficult situations.
There were plenty of these artful masters exemplified over the course of the three-day meeting worthy of mention. Three outgoing board members have long led the society down many strategic pathways with brilliance and ease. Lakshmi Halasyamani is wise, kind, and even-keeled. Eric Siegal is sharp-minded, sharp-witted, and sharp-tongued. Joe Li is authentic, energetic, and conscientious. Three oncoming members will bring vast experience and collective wisdom to the SHM board—Brad Sharpe, Patrick Torcson, and Howard Epstein.
In the brief session celebrating the past presidents, I was struck by the number of impressive names and faces who all have gone on to do an array of other jobs. Together, they represent a collective footprint of impressive magnitude. As past president Shaun Frost gave his thoughtful exit speech, and new president Eric Howell gave his lively, energetic, and humorous entry speech, I was reassured that we indeed are in good hands, with a foothold of grounded past leaders, and a wealth of talent on the launching board. Moreover, the introduction of three new Masters in Hospital Medicine—Scott Flanders, Jeff Wiese, and David Meltzer—adds to the collective wisdom and talent of SHM.
We were blessed at the meeting by the presence of other incredible leaders in health care, including Patrick Conway and David Feinberg. Dr. Conway, the CMO of Medicare, is a service-minded colleague determined to make CMS more transparent, easier to traverse, and more aligned with what its recipients really need. Dr. Feinberg is a genuinely compassionate physician who has transformed UCLA medical center from a Motel 6 to a Ritz-Carlton in customer service. I have seen him speak before and had quite a bit of respect for him to begin with, but to watch how he handled a flock of unwieldy and uninvited guests on the stage was more than what anyone could expect from a great leader.
The Art of the Science
As we continue this unwieldy and unpredictable journey that we call health care and hospital medicine, the need for effective leadership within the industry will continue to increase. And there is little need to argue about whether leaders are naturally born, because there are more leaders needed than there are natural-born. So either way, many of us have to figure out how to be leaders, whether of a small program, a newly formed group, or a large conglomerate. And whether your contribution is large or small, it will be a contribution nonetheless.
Just as Mother Teresa was once presented with a statement from a reporter about how her care for the poor and neglected was just a “drop in the bucket” on combating poverty and dispassion. She paused and agreed: “Yes, it is just a drop in the bucket but it’s my drop.”
Just as Dr. Feinberg recounted when he was first offered the CEO position at UCLA, as an interim and unlikely candidate, he didn’t know what to do, so he just started doing what he knew how to do best. He just started walking around the hospital seeing patients, listening, visiting, saying “hello,” and giving out his business cards (his drop in the bucket). He wasn’t trying to do anything terribly innovative or strategic at the time—at least, not that he admits to. And anyone who watches Larry Wellikson work a boardroom or a ballroom can learn something about the art of leadership.
So think of leadership not as a secret sauce, or set of skills that can only be relegated to those enshrined with the DNA of a Kennedy or an MBA from an Ivy League school. It is a willingness to try to get some drops in some buckets, and lead people in a common direction. It is about being unambiguously committed and completely authentic, with a little science, and a lot of art.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
After wrapping up the SHM annual meeting, I was left with a sense of security about hospital medicine’s future. This security I can summarize in a single word: leadership. SHM has long had a strong set of leaders, which are needed now more than ever. With explosive expansion in volume and scope, hospitalist practice is going to require tireless leadership in the coming years and decades to ensure our trajectory is strategic and viable.
The Science
Wikipedia describes leadership as “a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task.” Notice a few key words in that definition? “Process,” which implies that it takes time, patience, and tenacity. It is not something that automatically happens without any time or effort. Also notice the word “influence,” which does not include “power” or “authority” or “pay grade”—all terms that are entirely overused and misused in the medical industry.
There is a wealth of literature describing what leadership is and what it takes to be a leader. There are an abundance of theories on what traits and characteristics make up a good leader, and an equal abundance of theories on how great leaders evolve. Some subscribe to the inherited theory, in which genetic makeup will at least partially dictate whether you will be a “natural-born” a leader. Others subscribe to the belief that leadership is more situational, whereby leaders are effective in some situations but ineffective in others. Still others believe leaders emerge as a mixture of nature and nurture, that most good leaders can lead in a variety of climates and situations, but that a perfect leadership situation might not emerge for any one leader. For other leaders, a perfect situational opportunity might emerge that suits their leadership style, and transformational change can occur under their direction.
The science of leadership has found that some personal traits are more commonly associated with leaders than nonleaders, including extraversion, self-efficacy, conscientiousness, intelligence, and openness to experience. However, absence of these characteristics does not guarantee a hopeless leadership void; equally true, the presence of them does not guarantee good leadership.
The Art
So one can go on for the length of an encyclopedia about the science of leadership, but what about the art of leadership? The ability of a leader to “read the audience,” to “take the pulse” of their staff, to strategize their next foray into new territory, or to say no to a new (seemingly exciting) opportunity. It is the art of leadership that is much more intriguing. I have had the good fortune of seeing a variety of incredible leaders at work, both within and outside of SHM, including their artful mastery of difficult situations.
There were plenty of these artful masters exemplified over the course of the three-day meeting worthy of mention. Three outgoing board members have long led the society down many strategic pathways with brilliance and ease. Lakshmi Halasyamani is wise, kind, and even-keeled. Eric Siegal is sharp-minded, sharp-witted, and sharp-tongued. Joe Li is authentic, energetic, and conscientious. Three oncoming members will bring vast experience and collective wisdom to the SHM board—Brad Sharpe, Patrick Torcson, and Howard Epstein.
In the brief session celebrating the past presidents, I was struck by the number of impressive names and faces who all have gone on to do an array of other jobs. Together, they represent a collective footprint of impressive magnitude. As past president Shaun Frost gave his thoughtful exit speech, and new president Eric Howell gave his lively, energetic, and humorous entry speech, I was reassured that we indeed are in good hands, with a foothold of grounded past leaders, and a wealth of talent on the launching board. Moreover, the introduction of three new Masters in Hospital Medicine—Scott Flanders, Jeff Wiese, and David Meltzer—adds to the collective wisdom and talent of SHM.
We were blessed at the meeting by the presence of other incredible leaders in health care, including Patrick Conway and David Feinberg. Dr. Conway, the CMO of Medicare, is a service-minded colleague determined to make CMS more transparent, easier to traverse, and more aligned with what its recipients really need. Dr. Feinberg is a genuinely compassionate physician who has transformed UCLA medical center from a Motel 6 to a Ritz-Carlton in customer service. I have seen him speak before and had quite a bit of respect for him to begin with, but to watch how he handled a flock of unwieldy and uninvited guests on the stage was more than what anyone could expect from a great leader.
The Art of the Science
As we continue this unwieldy and unpredictable journey that we call health care and hospital medicine, the need for effective leadership within the industry will continue to increase. And there is little need to argue about whether leaders are naturally born, because there are more leaders needed than there are natural-born. So either way, many of us have to figure out how to be leaders, whether of a small program, a newly formed group, or a large conglomerate. And whether your contribution is large or small, it will be a contribution nonetheless.
Just as Mother Teresa was once presented with a statement from a reporter about how her care for the poor and neglected was just a “drop in the bucket” on combating poverty and dispassion. She paused and agreed: “Yes, it is just a drop in the bucket but it’s my drop.”
Just as Dr. Feinberg recounted when he was first offered the CEO position at UCLA, as an interim and unlikely candidate, he didn’t know what to do, so he just started doing what he knew how to do best. He just started walking around the hospital seeing patients, listening, visiting, saying “hello,” and giving out his business cards (his drop in the bucket). He wasn’t trying to do anything terribly innovative or strategic at the time—at least, not that he admits to. And anyone who watches Larry Wellikson work a boardroom or a ballroom can learn something about the art of leadership.
So think of leadership not as a secret sauce, or set of skills that can only be relegated to those enshrined with the DNA of a Kennedy or an MBA from an Ivy League school. It is a willingness to try to get some drops in some buckets, and lead people in a common direction. It is about being unambiguously committed and completely authentic, with a little science, and a lot of art.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
After wrapping up the SHM annual meeting, I was left with a sense of security about hospital medicine’s future. This security I can summarize in a single word: leadership. SHM has long had a strong set of leaders, which are needed now more than ever. With explosive expansion in volume and scope, hospitalist practice is going to require tireless leadership in the coming years and decades to ensure our trajectory is strategic and viable.
The Science
Wikipedia describes leadership as “a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task.” Notice a few key words in that definition? “Process,” which implies that it takes time, patience, and tenacity. It is not something that automatically happens without any time or effort. Also notice the word “influence,” which does not include “power” or “authority” or “pay grade”—all terms that are entirely overused and misused in the medical industry.
There is a wealth of literature describing what leadership is and what it takes to be a leader. There are an abundance of theories on what traits and characteristics make up a good leader, and an equal abundance of theories on how great leaders evolve. Some subscribe to the inherited theory, in which genetic makeup will at least partially dictate whether you will be a “natural-born” a leader. Others subscribe to the belief that leadership is more situational, whereby leaders are effective in some situations but ineffective in others. Still others believe leaders emerge as a mixture of nature and nurture, that most good leaders can lead in a variety of climates and situations, but that a perfect leadership situation might not emerge for any one leader. For other leaders, a perfect situational opportunity might emerge that suits their leadership style, and transformational change can occur under their direction.
The science of leadership has found that some personal traits are more commonly associated with leaders than nonleaders, including extraversion, self-efficacy, conscientiousness, intelligence, and openness to experience. However, absence of these characteristics does not guarantee a hopeless leadership void; equally true, the presence of them does not guarantee good leadership.
The Art
So one can go on for the length of an encyclopedia about the science of leadership, but what about the art of leadership? The ability of a leader to “read the audience,” to “take the pulse” of their staff, to strategize their next foray into new territory, or to say no to a new (seemingly exciting) opportunity. It is the art of leadership that is much more intriguing. I have had the good fortune of seeing a variety of incredible leaders at work, both within and outside of SHM, including their artful mastery of difficult situations.
There were plenty of these artful masters exemplified over the course of the three-day meeting worthy of mention. Three outgoing board members have long led the society down many strategic pathways with brilliance and ease. Lakshmi Halasyamani is wise, kind, and even-keeled. Eric Siegal is sharp-minded, sharp-witted, and sharp-tongued. Joe Li is authentic, energetic, and conscientious. Three oncoming members will bring vast experience and collective wisdom to the SHM board—Brad Sharpe, Patrick Torcson, and Howard Epstein.
In the brief session celebrating the past presidents, I was struck by the number of impressive names and faces who all have gone on to do an array of other jobs. Together, they represent a collective footprint of impressive magnitude. As past president Shaun Frost gave his thoughtful exit speech, and new president Eric Howell gave his lively, energetic, and humorous entry speech, I was reassured that we indeed are in good hands, with a foothold of grounded past leaders, and a wealth of talent on the launching board. Moreover, the introduction of three new Masters in Hospital Medicine—Scott Flanders, Jeff Wiese, and David Meltzer—adds to the collective wisdom and talent of SHM.
We were blessed at the meeting by the presence of other incredible leaders in health care, including Patrick Conway and David Feinberg. Dr. Conway, the CMO of Medicare, is a service-minded colleague determined to make CMS more transparent, easier to traverse, and more aligned with what its recipients really need. Dr. Feinberg is a genuinely compassionate physician who has transformed UCLA medical center from a Motel 6 to a Ritz-Carlton in customer service. I have seen him speak before and had quite a bit of respect for him to begin with, but to watch how he handled a flock of unwieldy and uninvited guests on the stage was more than what anyone could expect from a great leader.
The Art of the Science
As we continue this unwieldy and unpredictable journey that we call health care and hospital medicine, the need for effective leadership within the industry will continue to increase. And there is little need to argue about whether leaders are naturally born, because there are more leaders needed than there are natural-born. So either way, many of us have to figure out how to be leaders, whether of a small program, a newly formed group, or a large conglomerate. And whether your contribution is large or small, it will be a contribution nonetheless.
Just as Mother Teresa was once presented with a statement from a reporter about how her care for the poor and neglected was just a “drop in the bucket” on combating poverty and dispassion. She paused and agreed: “Yes, it is just a drop in the bucket but it’s my drop.”
Just as Dr. Feinberg recounted when he was first offered the CEO position at UCLA, as an interim and unlikely candidate, he didn’t know what to do, so he just started doing what he knew how to do best. He just started walking around the hospital seeing patients, listening, visiting, saying “hello,” and giving out his business cards (his drop in the bucket). He wasn’t trying to do anything terribly innovative or strategic at the time—at least, not that he admits to. And anyone who watches Larry Wellikson work a boardroom or a ballroom can learn something about the art of leadership.
So think of leadership not as a secret sauce, or set of skills that can only be relegated to those enshrined with the DNA of a Kennedy or an MBA from an Ivy League school. It is a willingness to try to get some drops in some buckets, and lead people in a common direction. It is about being unambiguously committed and completely authentic, with a little science, and a lot of art.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Letters: Medicare Official Says 'Physician Compare' Website Does Not Provide Performance Data on Individual Doctors
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
I read the article “Call for Transparency in Health-Care Performance Results to Impact Hospitalists” (January 2013, p. 47) by Shaun Frost, MD, SFHM, president of the Society of Hospital Medicine, with interest. I’d like to clarify a key point about Physician Compare. In the article, the statement that the Physician Compare website (www.medicare.gov/find-a-doctor) provides performance information on individual doctors is inaccurate.
The Affordable Care Act (ACA) states that the Centers for Medicare & Medicaid Services (CMS) must have a plan in place by Jan. 1, 2013, to include quality-of-care information on the site. To meet that requirement, CMS has established a plan that initiates a phased approach to public reporting. The 2012 Physician Fee Schedule (PFS) Final Rule was the first step in that phased approach. This rule established that the first measures to be reported on the site would be group-level measures for data collected no sooner than program year 2012. A second critical step is the 2013 PFS Proposed Rule, which outlines a longer-term public reporting plan. According to this plan, we expect the first set of group-level quality measure data to be included on the site in calendar year 2014. We are targeting publishing individual-level quality measures no sooner than 2015 reflecting data collected in program year 2014, if technically feasible.
As you may be aware, Physician Compare is undergoing a redesign to significantly improve the underlying database and thus the information on Physician Compare, as well as the ease of use and functionality of the site. We’ll be unveiling the redesigned site soon. We welcome your feedback and look forward to maintaining a dialogue with you as Physician Compare continues to evolve.
Rashaan Byers, MPH, social science research analyst, Centers forMedicare & Medicaid Services, Center for Clinical Standards & Quality, Quality Measurement & Health Assessment Group
Dr. Frost responds:
I thank Mr. Byers for his clarification regarding the current content on the CMS Physician Compare website, and agree that at the present time the website does not report individual physician clinical performance data.
Physician Compare, however, does currently report if an individual physician participated in the CMS Physician Quality Reporting System (PQRS) by stating “this professional chose to take part in Medicare’s PQRS, and reported quality information satisfactorily for the year 2010.” For those physicians who did not participate in PQRS, their personal website pages do not make reference to the PQRS program.
As the intent of transparency is to educate consumers to make informed choices about where to seek health care, care providers should know that their participation in PQRS is currently publically reported. It is, therefore, possible that patient decisions about whom to seek care from may be influenced by this.
As acknowledged in my January 2013 column in The Hospitalist, Physician Compare currently reports very little information. We should expect this to change, however, as Medicare moves forward with developing a plan to publically report valid and reliable individual physician performance metrics. CMS’ clarification of the timeline by which we can expect to see more detailed information is thus greatly appreciated.
The take-home message for hospitalists is that public reporting of care provider performance will become increasingly comprehensive and transparent in the future. As pointed out, CMS’ present plan targets the publication of individual, physician-level quality measures as soon as 2015, which will reflect actual performance during program year 2014. The measurement period is thus less than one year away, so it behooves us all to focus ever more intently on delivering high-value healthcare.
Shaun Frost, MD, SFHM, past president, SHM
Cough and Back Pain in a Man With COPD
ANSWER
The radiograph shows some evidence of hyperinflated lungs, consistent with COPD. There is a small right effusion evident.
Of note is a superior mediastinal mass, which is causing right-sided and anterior displacement of the intrathoracic trachea. The differential includes possible adenopathy related to a carcinoma or a substernal goiter. Further diagnostic studies and surgical evaluation are warranted.
In this particular case, review of the patient’s imaging history showed he had a chest radiograph two years ago, at which time these findings were present. This favors substernal goiter as the diagnosis. Multinodular goiter was later confirmed with a thyroid ultrasound, and referral to general surgery was made.
ANSWER
The radiograph shows some evidence of hyperinflated lungs, consistent with COPD. There is a small right effusion evident.
Of note is a superior mediastinal mass, which is causing right-sided and anterior displacement of the intrathoracic trachea. The differential includes possible adenopathy related to a carcinoma or a substernal goiter. Further diagnostic studies and surgical evaluation are warranted.
In this particular case, review of the patient’s imaging history showed he had a chest radiograph two years ago, at which time these findings were present. This favors substernal goiter as the diagnosis. Multinodular goiter was later confirmed with a thyroid ultrasound, and referral to general surgery was made.
ANSWER
The radiograph shows some evidence of hyperinflated lungs, consistent with COPD. There is a small right effusion evident.
Of note is a superior mediastinal mass, which is causing right-sided and anterior displacement of the intrathoracic trachea. The differential includes possible adenopathy related to a carcinoma or a substernal goiter. Further diagnostic studies and surgical evaluation are warranted.
In this particular case, review of the patient’s imaging history showed he had a chest radiograph two years ago, at which time these findings were present. This favors substernal goiter as the diagnosis. Multinodular goiter was later confirmed with a thyroid ultrasound, and referral to general surgery was made.

A 60-year-old man presents for evaluation of fever, cough, and back pain. His symptoms have been intermittent but have worsened over the past month or so. He has had no treatment prior to today’s visit. His medical history is significant for hypertension, COPD, and chronic renal insufficiency. He denies any history of tobacco use. On physical exam, you see an older man in no obvious distress. His vital signs are stable. He is afe-brile, with a blood pressure of 150/90 mm Hg, a heart rate of 66 beats/min, and a respiratory rate of 18 breaths/min. His O2 saturation is 98% on room air. His neck is supple, with no evidence of ade-nopathy. Lung sounds are slightly decreased bilaterally, with a few crackles heard. The rest of his physical exam, overall, is normal. You order preliminary lab work as well as a chest radiograph (shown). What is your impression?
Integrating Incretin-Based Therapy into Type 2 Diabetes Management
The glucagon-like peptide-1 receptor (GLP-1R) agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors have quickly become important treatment options for persons with type 2 diabetes. This article reviews the differences among the 3 GLP-1R agonists and 4 DPP-4 inhibitors currently available and how these differences impact treatment individualization. Emphasis is placed on strategies to improve patient self-management with the GLP-1R agonists, particularly those related to nausea and vomiting and medication adherence.
Physicians and Physician Assistants – Click Here to Take the Test
The glucagon-like peptide-1 receptor (GLP-1R) agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors have quickly become important treatment options for persons with type 2 diabetes. This article reviews the differences among the 3 GLP-1R agonists and 4 DPP-4 inhibitors currently available and how these differences impact treatment individualization. Emphasis is placed on strategies to improve patient self-management with the GLP-1R agonists, particularly those related to nausea and vomiting and medication adherence.
Physicians and Physician Assistants – Click Here to Take the Test
The glucagon-like peptide-1 receptor (GLP-1R) agonists and dipeptidyl peptidase-4 (DPP-4) inhibitors have quickly become important treatment options for persons with type 2 diabetes. This article reviews the differences among the 3 GLP-1R agonists and 4 DPP-4 inhibitors currently available and how these differences impact treatment individualization. Emphasis is placed on strategies to improve patient self-management with the GLP-1R agonists, particularly those related to nausea and vomiting and medication adherence.
Physicians and Physician Assistants – Click Here to Take the Test
Hospitalists on the Move
Patrick Torcson, MD, MMM, FACP, SFHM, has been named vice president and chief integration officer at St. Tammany Parish Hospital (STPH) in Covington, La.
Dr. Torcson's new duties will revolve around quality improvement through health information technology. Dr. Torcson will continue to work as director of STPH's hospital medicine program, which he helped establish in 2005.
Kathleen McGraw, MD, FHM, has been named 2013 Community Clinician of the Year by the Franklin District Medical Society. Dr. McGraw is chief medical officer at Brattleboro (Vt.) Memorial Hospital. She previously served as hospitalist medical director at Baystate Franklin Medical Center in Greenfield, Mass.
Hospitalist R. Wayne Cooper, MD, received the 2013 Physician of the Year Award from Lake Regional Health System in Osage Beach, Mo. Dr. Cooper was chosen by a panel of hospital staff doctors and administrators for his kindness, dedication, and positive attitude. Dr. Cooper has been a hospitalist at Lake Regional since 2010.
Steve Beerman, MD, is the new hospitalist medical director at Good Samaritan Hospital in Cincinnati. Dr. Beerman has been a hospitalist at the 650-bed acute-care hospital since 2003.
Bryan Strader, MD, is the new hospitalist medical director at 420-bed Bethesda North Hospital (BNH) in Cincinnati. Dr. Strader joined the BNH hospitalist team in 2006.
Bradley Lembcke, MD, recently received EmCare's Summit Award for 2013 Hospitalist of the Year. Dr. Lembcke is a hospitalist at Baylor University Medical Center (BUMC) in Dallas, the country's largest and oldest hospitalist group. BUMC is a 1,065-bed, nonprofit teaching hospital.
Chintu Sharma, MD, has been awarded the 2013 Physician of the Year award at Carroll Hospital Center in Westminster, Md. Dr. Sharma has been a practicing hospitalist at Carroll since 2010.
Business Moves
Brentwood, Tenn.-based Cogent HMG began providing hospitalist services to inpatients at 275-bed Western Maryland Regional Medical Center in Cumberland, Md., on April 1 as part of a new contract. Cogent supplies contracted hospitalist services to more than 100 U.S. hospitals.
Sound Physicians, based in Tacoma, Wash., has announced plans to begin managing hospitalist services at Sentara Obici Hospital in Suffolk, Va. The 168-bed facility is one of 10 Sentara Medical Group acute-care hospitals throughout Virginia. Sound Physicians manages more than 650 hospitalists at more than 70 facilities across the U.S.
IPC: The Hospitalist Company, based in North Hollywood, Calif., recently announced its acquisition of two Wichita, Kan.-area hospitalist practices. Kansas Inpatient Services LLC and Kansas Long Term Care Physicians LLC both provide hospitalists in and around the greater Wichita area. Together they encounter an estimated 90,000 inpatients per year. IPC serves hospitals and practices in 28 states.
Mauldin, S.C.-based OB Hospitalist Group (OBHG) is now providing OBGYN services to the new obstetrics emergency department at 350-bed Athens (Ga.) Regional Medical Center. OBHG provides OBGYN hospitalist services in 45 programs throughout the country.
Patrick Torcson, MD, MMM, FACP, SFHM, has been named vice president and chief integration officer at St. Tammany Parish Hospital (STPH) in Covington, La.
Dr. Torcson's new duties will revolve around quality improvement through health information technology. Dr. Torcson will continue to work as director of STPH's hospital medicine program, which he helped establish in 2005.
Kathleen McGraw, MD, FHM, has been named 2013 Community Clinician of the Year by the Franklin District Medical Society. Dr. McGraw is chief medical officer at Brattleboro (Vt.) Memorial Hospital. She previously served as hospitalist medical director at Baystate Franklin Medical Center in Greenfield, Mass.
Hospitalist R. Wayne Cooper, MD, received the 2013 Physician of the Year Award from Lake Regional Health System in Osage Beach, Mo. Dr. Cooper was chosen by a panel of hospital staff doctors and administrators for his kindness, dedication, and positive attitude. Dr. Cooper has been a hospitalist at Lake Regional since 2010.
Steve Beerman, MD, is the new hospitalist medical director at Good Samaritan Hospital in Cincinnati. Dr. Beerman has been a hospitalist at the 650-bed acute-care hospital since 2003.
Bryan Strader, MD, is the new hospitalist medical director at 420-bed Bethesda North Hospital (BNH) in Cincinnati. Dr. Strader joined the BNH hospitalist team in 2006.
Bradley Lembcke, MD, recently received EmCare's Summit Award for 2013 Hospitalist of the Year. Dr. Lembcke is a hospitalist at Baylor University Medical Center (BUMC) in Dallas, the country's largest and oldest hospitalist group. BUMC is a 1,065-bed, nonprofit teaching hospital.
Chintu Sharma, MD, has been awarded the 2013 Physician of the Year award at Carroll Hospital Center in Westminster, Md. Dr. Sharma has been a practicing hospitalist at Carroll since 2010.
Business Moves
Brentwood, Tenn.-based Cogent HMG began providing hospitalist services to inpatients at 275-bed Western Maryland Regional Medical Center in Cumberland, Md., on April 1 as part of a new contract. Cogent supplies contracted hospitalist services to more than 100 U.S. hospitals.
Sound Physicians, based in Tacoma, Wash., has announced plans to begin managing hospitalist services at Sentara Obici Hospital in Suffolk, Va. The 168-bed facility is one of 10 Sentara Medical Group acute-care hospitals throughout Virginia. Sound Physicians manages more than 650 hospitalists at more than 70 facilities across the U.S.
IPC: The Hospitalist Company, based in North Hollywood, Calif., recently announced its acquisition of two Wichita, Kan.-area hospitalist practices. Kansas Inpatient Services LLC and Kansas Long Term Care Physicians LLC both provide hospitalists in and around the greater Wichita area. Together they encounter an estimated 90,000 inpatients per year. IPC serves hospitals and practices in 28 states.
Mauldin, S.C.-based OB Hospitalist Group (OBHG) is now providing OBGYN services to the new obstetrics emergency department at 350-bed Athens (Ga.) Regional Medical Center. OBHG provides OBGYN hospitalist services in 45 programs throughout the country.
Patrick Torcson, MD, MMM, FACP, SFHM, has been named vice president and chief integration officer at St. Tammany Parish Hospital (STPH) in Covington, La.
Dr. Torcson's new duties will revolve around quality improvement through health information technology. Dr. Torcson will continue to work as director of STPH's hospital medicine program, which he helped establish in 2005.
Kathleen McGraw, MD, FHM, has been named 2013 Community Clinician of the Year by the Franklin District Medical Society. Dr. McGraw is chief medical officer at Brattleboro (Vt.) Memorial Hospital. She previously served as hospitalist medical director at Baystate Franklin Medical Center in Greenfield, Mass.
Hospitalist R. Wayne Cooper, MD, received the 2013 Physician of the Year Award from Lake Regional Health System in Osage Beach, Mo. Dr. Cooper was chosen by a panel of hospital staff doctors and administrators for his kindness, dedication, and positive attitude. Dr. Cooper has been a hospitalist at Lake Regional since 2010.
Steve Beerman, MD, is the new hospitalist medical director at Good Samaritan Hospital in Cincinnati. Dr. Beerman has been a hospitalist at the 650-bed acute-care hospital since 2003.
Bryan Strader, MD, is the new hospitalist medical director at 420-bed Bethesda North Hospital (BNH) in Cincinnati. Dr. Strader joined the BNH hospitalist team in 2006.
Bradley Lembcke, MD, recently received EmCare's Summit Award for 2013 Hospitalist of the Year. Dr. Lembcke is a hospitalist at Baylor University Medical Center (BUMC) in Dallas, the country's largest and oldest hospitalist group. BUMC is a 1,065-bed, nonprofit teaching hospital.
Chintu Sharma, MD, has been awarded the 2013 Physician of the Year award at Carroll Hospital Center in Westminster, Md. Dr. Sharma has been a practicing hospitalist at Carroll since 2010.
Business Moves
Brentwood, Tenn.-based Cogent HMG began providing hospitalist services to inpatients at 275-bed Western Maryland Regional Medical Center in Cumberland, Md., on April 1 as part of a new contract. Cogent supplies contracted hospitalist services to more than 100 U.S. hospitals.
Sound Physicians, based in Tacoma, Wash., has announced plans to begin managing hospitalist services at Sentara Obici Hospital in Suffolk, Va. The 168-bed facility is one of 10 Sentara Medical Group acute-care hospitals throughout Virginia. Sound Physicians manages more than 650 hospitalists at more than 70 facilities across the U.S.
IPC: The Hospitalist Company, based in North Hollywood, Calif., recently announced its acquisition of two Wichita, Kan.-area hospitalist practices. Kansas Inpatient Services LLC and Kansas Long Term Care Physicians LLC both provide hospitalists in and around the greater Wichita area. Together they encounter an estimated 90,000 inpatients per year. IPC serves hospitals and practices in 28 states.
Mauldin, S.C.-based OB Hospitalist Group (OBHG) is now providing OBGYN services to the new obstetrics emergency department at 350-bed Athens (Ga.) Regional Medical Center. OBHG provides OBGYN hospitalist services in 45 programs throughout the country.
Behavioral Economics Can Accelerate Adoption of Choosing Wisely Campaign
SHM has gotten behind the Choosing Wisely campaign in a big way. Earlier this year, SHM announced lists of suggested practices for adult and pediatric hospital medicine (see Table 1). To keep it on the front burner, hospitalists John Bulger and Ian Jenkins held a pre-course at HM13 devoted entirely to quality-improvement (QI) approaches to implementing and sustaining the practices outlined in the campaign. During the main meeting, they did an encore presentation, with Doug Carlson and Ricardo Quinonez presenting the elements of Choosing Wisely for pediatric hospital medicine.
The widely publicized campaign arose from an American Board of Internal Medicine (ABIM) Foundation grant program to “facilitate the development of innovative, emerging strategies to advance appropriate health-care decision-making and stewardship of health-care resources.” (For more information, visit www.abimfoundation.org.)
Adoption of many of the suggested Choosing Wisely practices will require a change in deeply ingrained, habitual behaviors. We assert that rational, reflective, cognitive processes might not be enough to overturn these behaviors, and that we must look to other mental systems to achieve the consistent adoption of the campaign’s suggested practices. An analogy exists in economics, where theories behind classical economics are challenged by behavioral economics.
What is behavioral economics? Classical economics asserts the individual as “homo economicus”: a person making rational, predictable decisions to advance their interests. However, due to social or professional influence, behavior often does not comport to expected ends. We succumb, sympathize, or follow the pack, diverging from the rulebook. Behavioral economics attempts to understand and compensate for these deviations.
In medicine, we often yield to cognitive biases. To simplify decision-making, we generalize our observations to arrive at decisions quickly. Daniel Kahneman, winner of the Nobel Memorial Prize in Economic Sciences, describes Type I thinking as fast and automatic, and Type II thinking as slow and effortful. Using Kahneman’s framework, we attempt to understand where reasoning may stray and, in turn, introduce environmental changes to achieve better outcomes.
How does this relate to Choosing Wisely? Embracing and embedding the practices of the Choosing Wisely campaign in day-to-day practice will require change in how we approach the clinical decisions we make each day. How can we create the conditions so as not to yield to the status quo?
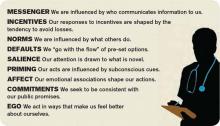
The MINDSPACE framework
King et al in a recent Health Affairs article describe the MINDSPACE framework (see Table 2), which captures nine effects on behavior—messenger, incentives, norms, defaults, salience, priming, affect, commitments, and ego—that mostly involve automatic systems (Kahneman’s Type I), and how we can leverage them to minimize ineffective health care.1 Below, we describe Choosing Wisely’s HM components and how MINDSPACE can help promote better practice.
Messenger refers to the importance we place on the source of information conveyed to us. In the campaign, the ABIM Foundation engaged professional societies to come up with a list of specialty-specific practices. We know physicians pay more attention to messages from professional societies than, for example, insurance companies. Having the chair of medicine, the chief of hospital medicine, or the vice president of quality officially sanction the campaign’s practices at your organization leverages messengers.
Incentives, while widely used in health care, have had mixed results in terms of their utility in improving outcomes. People are loss-averse, and behavioral economics leverages that finding, which means incentives structured as penalties seem to have more powerful effects than bonuses. While the familiar pay-for-performance programs might not yield desired results, the evidence base continues to grow, and we have lots to learn. Does a 2% bonus change culture? What would really facilitate modifications in your test ordering patterns?
Norms, or what we perceive as the views of the majority, shape our behavior. How do we establish new ones? We all know the axiom “culture eats strategy for breakfast,” and, like patterned antibiotic administration, redirecting behavior requires examination of why we order items. Often, we order not because the drug combination conforms to standards, but because our training programs imbue us with less-than-ideal habits. These habits become standards, and their root causes require layered examination.
Defaults suggest that we are more likely to embrace a certain behavior if we otherwise need to “opt out” to avoid the behavior. We know that, for example, automatic enrollment in retirement savings plans has dramatically increased participation in such programs. For the Choosing Wisely campaign, the suggested practices should be set up as the default option. Examples include appropriate auto-stop orders for urinary catheters, telemetry, oximetry, or the requirement for added clicks to order daily CBCs. Think about ED orders and how they become substitute defaults once patients arrive on the wards. How do you disrupt the inertia?
Salience is when an individual makes a decision based on what is novel or what their attention is drawn to. Anticipating what subspecialists might expect, what your CMO demands, or what trainees envisage in their supervising attendings all may subconsciously override best judgment and deter best practice.
Priming describes how simple cues—often detected by our subconscious—influence decisions we make. When a physician, perhaps out of concern but often due to poorly reasoned or cavalier messaging, scribes “consider test X,” we involuntarily complete the act. We assume, because of the prime, that we need to act accordingly.
Affect is when we rely on gut feelings to make decisions. Emotions guide our ordering a urinary catheter for incontinence or transfusing to a HGB of 10, even when evidence contradicts what we might know as correct. Countering these actions requires credible stops to convert our emotions to reason (think clinical decision support with teeth).
Commitments are made in advance of an undertaking, behavioral economics suggests, as a way to combat the moment when willpower fails and desired behaviors go by the wayside. By publically signing a contract, in front of your group, chair, or medical director, and going on record as having pledged something, chances of success increase.
Ego, which underpins the need for a positive self-image, can drive the kind of automatic behavior that enables one to compare favorably to others. This effect has driven much of the motivation to perform well on public reporting of hospital quality measures. But ideal reporting of results must be valid; otherwise, attribution of subpar outcomes justifies the usual refrains of “not my responsibility” or the “system needs fixing, not me.”
Conclusions
Choosing Wisely is an ambitious undertaking made up of more than 90 suggested best practices put forth by 25 medical societies. In their book “Nudge,” authors Richard Thaler and Cass Sunstein describe how automatic behaviors arise from the environment or context in which choices to engage in such behaviors are presented.2 For the Choosing Wisely campaign to have staying power, we submit that institutional leaders and front-line clinicians will need to create a context where the safest, most cost-effective choices are the automatic, or nearly automatic, ones.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at wfwhit@comcast.net. Dr. Flansbaum is director of hospitalist services at Lenox Hill Hospital in New York City and an SHM Public Policy Committee member.
References
- King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff (Millwood). 2013;32(4):661-668.
- Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth and happiness. New Haven, Conn: Yale University Press; 2008.
SHM has gotten behind the Choosing Wisely campaign in a big way. Earlier this year, SHM announced lists of suggested practices for adult and pediatric hospital medicine (see Table 1). To keep it on the front burner, hospitalists John Bulger and Ian Jenkins held a pre-course at HM13 devoted entirely to quality-improvement (QI) approaches to implementing and sustaining the practices outlined in the campaign. During the main meeting, they did an encore presentation, with Doug Carlson and Ricardo Quinonez presenting the elements of Choosing Wisely for pediatric hospital medicine.
The widely publicized campaign arose from an American Board of Internal Medicine (ABIM) Foundation grant program to “facilitate the development of innovative, emerging strategies to advance appropriate health-care decision-making and stewardship of health-care resources.” (For more information, visit www.abimfoundation.org.)
Adoption of many of the suggested Choosing Wisely practices will require a change in deeply ingrained, habitual behaviors. We assert that rational, reflective, cognitive processes might not be enough to overturn these behaviors, and that we must look to other mental systems to achieve the consistent adoption of the campaign’s suggested practices. An analogy exists in economics, where theories behind classical economics are challenged by behavioral economics.
What is behavioral economics? Classical economics asserts the individual as “homo economicus”: a person making rational, predictable decisions to advance their interests. However, due to social or professional influence, behavior often does not comport to expected ends. We succumb, sympathize, or follow the pack, diverging from the rulebook. Behavioral economics attempts to understand and compensate for these deviations.
In medicine, we often yield to cognitive biases. To simplify decision-making, we generalize our observations to arrive at decisions quickly. Daniel Kahneman, winner of the Nobel Memorial Prize in Economic Sciences, describes Type I thinking as fast and automatic, and Type II thinking as slow and effortful. Using Kahneman’s framework, we attempt to understand where reasoning may stray and, in turn, introduce environmental changes to achieve better outcomes.
How does this relate to Choosing Wisely? Embracing and embedding the practices of the Choosing Wisely campaign in day-to-day practice will require change in how we approach the clinical decisions we make each day. How can we create the conditions so as not to yield to the status quo?
The MINDSPACE framework
King et al in a recent Health Affairs article describe the MINDSPACE framework (see Table 2), which captures nine effects on behavior—messenger, incentives, norms, defaults, salience, priming, affect, commitments, and ego—that mostly involve automatic systems (Kahneman’s Type I), and how we can leverage them to minimize ineffective health care.1 Below, we describe Choosing Wisely’s HM components and how MINDSPACE can help promote better practice.
Messenger refers to the importance we place on the source of information conveyed to us. In the campaign, the ABIM Foundation engaged professional societies to come up with a list of specialty-specific practices. We know physicians pay more attention to messages from professional societies than, for example, insurance companies. Having the chair of medicine, the chief of hospital medicine, or the vice president of quality officially sanction the campaign’s practices at your organization leverages messengers.
Incentives, while widely used in health care, have had mixed results in terms of their utility in improving outcomes. People are loss-averse, and behavioral economics leverages that finding, which means incentives structured as penalties seem to have more powerful effects than bonuses. While the familiar pay-for-performance programs might not yield desired results, the evidence base continues to grow, and we have lots to learn. Does a 2% bonus change culture? What would really facilitate modifications in your test ordering patterns?
Norms, or what we perceive as the views of the majority, shape our behavior. How do we establish new ones? We all know the axiom “culture eats strategy for breakfast,” and, like patterned antibiotic administration, redirecting behavior requires examination of why we order items. Often, we order not because the drug combination conforms to standards, but because our training programs imbue us with less-than-ideal habits. These habits become standards, and their root causes require layered examination.
Defaults suggest that we are more likely to embrace a certain behavior if we otherwise need to “opt out” to avoid the behavior. We know that, for example, automatic enrollment in retirement savings plans has dramatically increased participation in such programs. For the Choosing Wisely campaign, the suggested practices should be set up as the default option. Examples include appropriate auto-stop orders for urinary catheters, telemetry, oximetry, or the requirement for added clicks to order daily CBCs. Think about ED orders and how they become substitute defaults once patients arrive on the wards. How do you disrupt the inertia?
Salience is when an individual makes a decision based on what is novel or what their attention is drawn to. Anticipating what subspecialists might expect, what your CMO demands, or what trainees envisage in their supervising attendings all may subconsciously override best judgment and deter best practice.
Priming describes how simple cues—often detected by our subconscious—influence decisions we make. When a physician, perhaps out of concern but often due to poorly reasoned or cavalier messaging, scribes “consider test X,” we involuntarily complete the act. We assume, because of the prime, that we need to act accordingly.
Affect is when we rely on gut feelings to make decisions. Emotions guide our ordering a urinary catheter for incontinence or transfusing to a HGB of 10, even when evidence contradicts what we might know as correct. Countering these actions requires credible stops to convert our emotions to reason (think clinical decision support with teeth).
Commitments are made in advance of an undertaking, behavioral economics suggests, as a way to combat the moment when willpower fails and desired behaviors go by the wayside. By publically signing a contract, in front of your group, chair, or medical director, and going on record as having pledged something, chances of success increase.
Ego, which underpins the need for a positive self-image, can drive the kind of automatic behavior that enables one to compare favorably to others. This effect has driven much of the motivation to perform well on public reporting of hospital quality measures. But ideal reporting of results must be valid; otherwise, attribution of subpar outcomes justifies the usual refrains of “not my responsibility” or the “system needs fixing, not me.”
Conclusions
Choosing Wisely is an ambitious undertaking made up of more than 90 suggested best practices put forth by 25 medical societies. In their book “Nudge,” authors Richard Thaler and Cass Sunstein describe how automatic behaviors arise from the environment or context in which choices to engage in such behaviors are presented.2 For the Choosing Wisely campaign to have staying power, we submit that institutional leaders and front-line clinicians will need to create a context where the safest, most cost-effective choices are the automatic, or nearly automatic, ones.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at wfwhit@comcast.net. Dr. Flansbaum is director of hospitalist services at Lenox Hill Hospital in New York City and an SHM Public Policy Committee member.
References
- King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff (Millwood). 2013;32(4):661-668.
- Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth and happiness. New Haven, Conn: Yale University Press; 2008.
SHM has gotten behind the Choosing Wisely campaign in a big way. Earlier this year, SHM announced lists of suggested practices for adult and pediatric hospital medicine (see Table 1). To keep it on the front burner, hospitalists John Bulger and Ian Jenkins held a pre-course at HM13 devoted entirely to quality-improvement (QI) approaches to implementing and sustaining the practices outlined in the campaign. During the main meeting, they did an encore presentation, with Doug Carlson and Ricardo Quinonez presenting the elements of Choosing Wisely for pediatric hospital medicine.
The widely publicized campaign arose from an American Board of Internal Medicine (ABIM) Foundation grant program to “facilitate the development of innovative, emerging strategies to advance appropriate health-care decision-making and stewardship of health-care resources.” (For more information, visit www.abimfoundation.org.)
Adoption of many of the suggested Choosing Wisely practices will require a change in deeply ingrained, habitual behaviors. We assert that rational, reflective, cognitive processes might not be enough to overturn these behaviors, and that we must look to other mental systems to achieve the consistent adoption of the campaign’s suggested practices. An analogy exists in economics, where theories behind classical economics are challenged by behavioral economics.
What is behavioral economics? Classical economics asserts the individual as “homo economicus”: a person making rational, predictable decisions to advance their interests. However, due to social or professional influence, behavior often does not comport to expected ends. We succumb, sympathize, or follow the pack, diverging from the rulebook. Behavioral economics attempts to understand and compensate for these deviations.
In medicine, we often yield to cognitive biases. To simplify decision-making, we generalize our observations to arrive at decisions quickly. Daniel Kahneman, winner of the Nobel Memorial Prize in Economic Sciences, describes Type I thinking as fast and automatic, and Type II thinking as slow and effortful. Using Kahneman’s framework, we attempt to understand where reasoning may stray and, in turn, introduce environmental changes to achieve better outcomes.
How does this relate to Choosing Wisely? Embracing and embedding the practices of the Choosing Wisely campaign in day-to-day practice will require change in how we approach the clinical decisions we make each day. How can we create the conditions so as not to yield to the status quo?
The MINDSPACE framework
King et al in a recent Health Affairs article describe the MINDSPACE framework (see Table 2), which captures nine effects on behavior—messenger, incentives, norms, defaults, salience, priming, affect, commitments, and ego—that mostly involve automatic systems (Kahneman’s Type I), and how we can leverage them to minimize ineffective health care.1 Below, we describe Choosing Wisely’s HM components and how MINDSPACE can help promote better practice.
Messenger refers to the importance we place on the source of information conveyed to us. In the campaign, the ABIM Foundation engaged professional societies to come up with a list of specialty-specific practices. We know physicians pay more attention to messages from professional societies than, for example, insurance companies. Having the chair of medicine, the chief of hospital medicine, or the vice president of quality officially sanction the campaign’s practices at your organization leverages messengers.
Incentives, while widely used in health care, have had mixed results in terms of their utility in improving outcomes. People are loss-averse, and behavioral economics leverages that finding, which means incentives structured as penalties seem to have more powerful effects than bonuses. While the familiar pay-for-performance programs might not yield desired results, the evidence base continues to grow, and we have lots to learn. Does a 2% bonus change culture? What would really facilitate modifications in your test ordering patterns?
Norms, or what we perceive as the views of the majority, shape our behavior. How do we establish new ones? We all know the axiom “culture eats strategy for breakfast,” and, like patterned antibiotic administration, redirecting behavior requires examination of why we order items. Often, we order not because the drug combination conforms to standards, but because our training programs imbue us with less-than-ideal habits. These habits become standards, and their root causes require layered examination.
Defaults suggest that we are more likely to embrace a certain behavior if we otherwise need to “opt out” to avoid the behavior. We know that, for example, automatic enrollment in retirement savings plans has dramatically increased participation in such programs. For the Choosing Wisely campaign, the suggested practices should be set up as the default option. Examples include appropriate auto-stop orders for urinary catheters, telemetry, oximetry, or the requirement for added clicks to order daily CBCs. Think about ED orders and how they become substitute defaults once patients arrive on the wards. How do you disrupt the inertia?
Salience is when an individual makes a decision based on what is novel or what their attention is drawn to. Anticipating what subspecialists might expect, what your CMO demands, or what trainees envisage in their supervising attendings all may subconsciously override best judgment and deter best practice.
Priming describes how simple cues—often detected by our subconscious—influence decisions we make. When a physician, perhaps out of concern but often due to poorly reasoned or cavalier messaging, scribes “consider test X,” we involuntarily complete the act. We assume, because of the prime, that we need to act accordingly.
Affect is when we rely on gut feelings to make decisions. Emotions guide our ordering a urinary catheter for incontinence or transfusing to a HGB of 10, even when evidence contradicts what we might know as correct. Countering these actions requires credible stops to convert our emotions to reason (think clinical decision support with teeth).
Commitments are made in advance of an undertaking, behavioral economics suggests, as a way to combat the moment when willpower fails and desired behaviors go by the wayside. By publically signing a contract, in front of your group, chair, or medical director, and going on record as having pledged something, chances of success increase.
Ego, which underpins the need for a positive self-image, can drive the kind of automatic behavior that enables one to compare favorably to others. This effect has driven much of the motivation to perform well on public reporting of hospital quality measures. But ideal reporting of results must be valid; otherwise, attribution of subpar outcomes justifies the usual refrains of “not my responsibility” or the “system needs fixing, not me.”
Conclusions
Choosing Wisely is an ambitious undertaking made up of more than 90 suggested best practices put forth by 25 medical societies. In their book “Nudge,” authors Richard Thaler and Cass Sunstein describe how automatic behaviors arise from the environment or context in which choices to engage in such behaviors are presented.2 For the Choosing Wisely campaign to have staying power, we submit that institutional leaders and front-line clinicians will need to create a context where the safest, most cost-effective choices are the automatic, or nearly automatic, ones.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is co-founder and past president of SHM. Email him at wfwhit@comcast.net. Dr. Flansbaum is director of hospitalist services at Lenox Hill Hospital in New York City and an SHM Public Policy Committee member.
References
- King D, Greaves F, Vlaev I, Darzi A. Approaches based on behavioral economics could help nudge patients and providers toward lower health spending growth. Health Aff (Millwood). 2013;32(4):661-668.
- Thaler RH, Sunstein CR. Nudge: improving decisions about health, wealth and happiness. New Haven, Conn: Yale University Press; 2008.
Effective Clinical Documentation Can Influence Medicare Reimbursement
Back in the 1980s, I would go by medical records every day or two and find, on the front of the charts of my recently discharged patients, a form listing the diagnoses the hospital was billing to Medicare. Before the hospital could submit a patient’s bill, the attending physician was required to review the form and, by signing it, indicate agreement.
The requirement for this signature by the physician went away a long time ago and in my memory is one of the very few examples of reducing a doctor’s paperwork.
For my first few months in practice, I regularly would seek out the people who completed the form and explain they had misunderstood the patient’s clinical situation. “The main issue was a urinary tract infection,” I would say, “but you listed diabetes as the principal diagnosis.”
I don’t ever remember them changing anything based on my feedback. Instead, they explained to me that, for billing purposes, it was legitimate to list diabetes as the principal diagnosis because it had the additional benefit of resulting in a higher payment to the hospital than having “urinary tract infection” listed first.
Such was my introduction to the world of documentation and coding for hospital billing purposes and how it can sometimes differ significantly from the way a doctor sees the clinical picture. Things have evolved a lot since then, but the way doctors document medical conditions still has a huge influence on hospital reimbursement.
Hospital CDI Programs
About 80% of hospitals have formal clinical documentation improvement (CDI) programs to help ensure all clinical conditions are captured and described in the medical record in ways that are valuable for billing and other recordkeeping purposes. These programs might lead to you receive queries about your documentation. For example, you might be asked to clarify whether your patient’s pneumonia might be on the basis of aspiration.
Within SHM’s Code-H program, Dr. Richard Pinson, a former ED physician who now works with Houston-based HCQ Consulting, has a good presentation explaining these documentation issues. In it, he makes the point that, in addition to influencing how hospitals are paid, the way various conditions are documented also influences quality ratings.
Novel Approach
The most common approach to engaging hospitalists in CDI initiatives is to have them attend a presentation on the topic, then put in place documentation specialists who generate queries asking the doctor to clarify diagnoses when it might influence payment, severity of illness determination, etc. Dr. Kenji Asakura, a Seattle hospitalist, and Erik Ordal, MBA, have a company called ClinIntell that analyzes each hospitalist (or other specialty) group’s historical patient mix and trains them on the documentation issues that they see most often. The idea of this focused approach is to make “documentation queries” unnecessary, or at least much less necessary. The benefits of this approach are many, including reducing or eliminating the risk of “leading queries”—that is, queries that seem to encourage the doctor to document a diagnosis because it is an advantage to the hospital rather than a well-considered medical opinion. Leading queries can be regarded as fraudulent and can get a lot of people in trouble.
I asked Kenji and Erik if they could provide me with a list of common documentation issues that most hospitalists need to know more about. Table 1 is what they came up with. I hope it helps you and your practice.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
Back in the 1980s, I would go by medical records every day or two and find, on the front of the charts of my recently discharged patients, a form listing the diagnoses the hospital was billing to Medicare. Before the hospital could submit a patient’s bill, the attending physician was required to review the form and, by signing it, indicate agreement.
The requirement for this signature by the physician went away a long time ago and in my memory is one of the very few examples of reducing a doctor’s paperwork.
For my first few months in practice, I regularly would seek out the people who completed the form and explain they had misunderstood the patient’s clinical situation. “The main issue was a urinary tract infection,” I would say, “but you listed diabetes as the principal diagnosis.”
I don’t ever remember them changing anything based on my feedback. Instead, they explained to me that, for billing purposes, it was legitimate to list diabetes as the principal diagnosis because it had the additional benefit of resulting in a higher payment to the hospital than having “urinary tract infection” listed first.
Such was my introduction to the world of documentation and coding for hospital billing purposes and how it can sometimes differ significantly from the way a doctor sees the clinical picture. Things have evolved a lot since then, but the way doctors document medical conditions still has a huge influence on hospital reimbursement.
Hospital CDI Programs
About 80% of hospitals have formal clinical documentation improvement (CDI) programs to help ensure all clinical conditions are captured and described in the medical record in ways that are valuable for billing and other recordkeeping purposes. These programs might lead to you receive queries about your documentation. For example, you might be asked to clarify whether your patient’s pneumonia might be on the basis of aspiration.
Within SHM’s Code-H program, Dr. Richard Pinson, a former ED physician who now works with Houston-based HCQ Consulting, has a good presentation explaining these documentation issues. In it, he makes the point that, in addition to influencing how hospitals are paid, the way various conditions are documented also influences quality ratings.
Novel Approach
The most common approach to engaging hospitalists in CDI initiatives is to have them attend a presentation on the topic, then put in place documentation specialists who generate queries asking the doctor to clarify diagnoses when it might influence payment, severity of illness determination, etc. Dr. Kenji Asakura, a Seattle hospitalist, and Erik Ordal, MBA, have a company called ClinIntell that analyzes each hospitalist (or other specialty) group’s historical patient mix and trains them on the documentation issues that they see most often. The idea of this focused approach is to make “documentation queries” unnecessary, or at least much less necessary. The benefits of this approach are many, including reducing or eliminating the risk of “leading queries”—that is, queries that seem to encourage the doctor to document a diagnosis because it is an advantage to the hospital rather than a well-considered medical opinion. Leading queries can be regarded as fraudulent and can get a lot of people in trouble.
I asked Kenji and Erik if they could provide me with a list of common documentation issues that most hospitalists need to know more about. Table 1 is what they came up with. I hope it helps you and your practice.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
Back in the 1980s, I would go by medical records every day or two and find, on the front of the charts of my recently discharged patients, a form listing the diagnoses the hospital was billing to Medicare. Before the hospital could submit a patient’s bill, the attending physician was required to review the form and, by signing it, indicate agreement.
The requirement for this signature by the physician went away a long time ago and in my memory is one of the very few examples of reducing a doctor’s paperwork.
For my first few months in practice, I regularly would seek out the people who completed the form and explain they had misunderstood the patient’s clinical situation. “The main issue was a urinary tract infection,” I would say, “but you listed diabetes as the principal diagnosis.”
I don’t ever remember them changing anything based on my feedback. Instead, they explained to me that, for billing purposes, it was legitimate to list diabetes as the principal diagnosis because it had the additional benefit of resulting in a higher payment to the hospital than having “urinary tract infection” listed first.
Such was my introduction to the world of documentation and coding for hospital billing purposes and how it can sometimes differ significantly from the way a doctor sees the clinical picture. Things have evolved a lot since then, but the way doctors document medical conditions still has a huge influence on hospital reimbursement.
Hospital CDI Programs
About 80% of hospitals have formal clinical documentation improvement (CDI) programs to help ensure all clinical conditions are captured and described in the medical record in ways that are valuable for billing and other recordkeeping purposes. These programs might lead to you receive queries about your documentation. For example, you might be asked to clarify whether your patient’s pneumonia might be on the basis of aspiration.
Within SHM’s Code-H program, Dr. Richard Pinson, a former ED physician who now works with Houston-based HCQ Consulting, has a good presentation explaining these documentation issues. In it, he makes the point that, in addition to influencing how hospitals are paid, the way various conditions are documented also influences quality ratings.
Novel Approach
The most common approach to engaging hospitalists in CDI initiatives is to have them attend a presentation on the topic, then put in place documentation specialists who generate queries asking the doctor to clarify diagnoses when it might influence payment, severity of illness determination, etc. Dr. Kenji Asakura, a Seattle hospitalist, and Erik Ordal, MBA, have a company called ClinIntell that analyzes each hospitalist (or other specialty) group’s historical patient mix and trains them on the documentation issues that they see most often. The idea of this focused approach is to make “documentation queries” unnecessary, or at least much less necessary. The benefits of this approach are many, including reducing or eliminating the risk of “leading queries”—that is, queries that seem to encourage the doctor to document a diagnosis because it is an advantage to the hospital rather than a well-considered medical opinion. Leading queries can be regarded as fraudulent and can get a lot of people in trouble.
I asked Kenji and Erik if they could provide me with a list of common documentation issues that most hospitalists need to know more about. Table 1 is what they came up with. I hope it helps you and your practice.
Dr. Nelson has been a practicing hospitalist since 1988. He is co-founder and past president of SHM, and principal in Nelson Flores Hospital Medicine Consultants. He is co-director for SHM's "Best Practices in Managing a Hospital Medicine Program" course. Write to him at john.nelson@nelsonflores.com.
Hospitalists Should Refrain from Texting Patient Information
Refrain from Texting about Your Patients
Can I text my partners patient information?
–Stephen Henry, San Luis Obispo, Calif.
Dr. Hospitalist responds:
Can you? Sure. Do you? Probably. Should you? No.
Texting any patient information falls under the category of ePHI (Electronic Protected Health Information) as part of HIPAA. Technically, such patient-specific information must be protected at all times. Once you send a text, at least three copies are known to exist: one on each of the devices, plus one copy on the network it went through, adding for each network it has to cross. Sure, your phone may be password-protected, but is your partner’s? What about the carrier? How protected is their data?
HIPAA goes into excruciating technical detail about all the safeguards that must be present. You are more than welcome to read it (www.hhs.gov/ocr/privacy/hipaa/administrative/securityrule) to see if you meet all the standards. Or you can take my word for it: You don’t.
So you can see why most health organizations expressly prohibit the texting of patient information. If you rang up your local health-care or hospital lawyer, I’m sure they would tell you to never text patient information. Is that reasonable advice? In 2013, I doubt it.
So what’s the practical advice to follow? For starters, password-protect your phone, if you haven’t already. Nothing worse than losing your phone and having patient information on it. A lot of the OCR (Office for Civil Rights, a branch of Health and Human Services) fines for HIPAA violations stem from folks misplacing unencrypted devices with patient information on them.
Just as important, don’t text anything that you wouldn’t want to see blown up on a lawyer’s display board in court. I’ve seen some really egregious examples of communication between doctors that have no business being preserved electronically. Texting “Mr. X in Room 2101 is a meth-using, narcotic-seeking, half-naked, lunatic troll” is an absolutely stupid thing to do. For that matter, so are remarks that seem less offensive: “And his son is completely unreasonable.” Save your commentary and stick to the facts, because you just generated three copies forever.
If you receive an insensitive text, don’t reply. Simply call the sending physician to discuss any issues. Even being on a “secure” texting network won’t protect you from errors of commission.
If I were to text about a patient (purely hypothetically, mind you), I would limit the information as much as possible. Keep it simple and generic (what HIPAA likes to call “de-identified information”)—for example, “Room 428 is ready for discharge.”
Please, hold the subjective commentary. There is no good reason to have an extended text exchange about a patient; you are creating an electronic trail that has no good reason to exist and never really goes away. It’s just the same as writing in the chart, except that it has the illusion of privacy. And that’s all it is: an illusion.
At the end of the day, I’d probably worry more about the discoverable aspect of your text messages in a lawsuit than the possibility of a HIPAA fine, but neither one sounds like much fun to me.
Refrain from Texting about Your Patients
Can I text my partners patient information?
–Stephen Henry, San Luis Obispo, Calif.
Dr. Hospitalist responds:
Can you? Sure. Do you? Probably. Should you? No.
Texting any patient information falls under the category of ePHI (Electronic Protected Health Information) as part of HIPAA. Technically, such patient-specific information must be protected at all times. Once you send a text, at least three copies are known to exist: one on each of the devices, plus one copy on the network it went through, adding for each network it has to cross. Sure, your phone may be password-protected, but is your partner’s? What about the carrier? How protected is their data?
HIPAA goes into excruciating technical detail about all the safeguards that must be present. You are more than welcome to read it (www.hhs.gov/ocr/privacy/hipaa/administrative/securityrule) to see if you meet all the standards. Or you can take my word for it: You don’t.
So you can see why most health organizations expressly prohibit the texting of patient information. If you rang up your local health-care or hospital lawyer, I’m sure they would tell you to never text patient information. Is that reasonable advice? In 2013, I doubt it.
So what’s the practical advice to follow? For starters, password-protect your phone, if you haven’t already. Nothing worse than losing your phone and having patient information on it. A lot of the OCR (Office for Civil Rights, a branch of Health and Human Services) fines for HIPAA violations stem from folks misplacing unencrypted devices with patient information on them.
Just as important, don’t text anything that you wouldn’t want to see blown up on a lawyer’s display board in court. I’ve seen some really egregious examples of communication between doctors that have no business being preserved electronically. Texting “Mr. X in Room 2101 is a meth-using, narcotic-seeking, half-naked, lunatic troll” is an absolutely stupid thing to do. For that matter, so are remarks that seem less offensive: “And his son is completely unreasonable.” Save your commentary and stick to the facts, because you just generated three copies forever.
If you receive an insensitive text, don’t reply. Simply call the sending physician to discuss any issues. Even being on a “secure” texting network won’t protect you from errors of commission.
If I were to text about a patient (purely hypothetically, mind you), I would limit the information as much as possible. Keep it simple and generic (what HIPAA likes to call “de-identified information”)—for example, “Room 428 is ready for discharge.”
Please, hold the subjective commentary. There is no good reason to have an extended text exchange about a patient; you are creating an electronic trail that has no good reason to exist and never really goes away. It’s just the same as writing in the chart, except that it has the illusion of privacy. And that’s all it is: an illusion.
At the end of the day, I’d probably worry more about the discoverable aspect of your text messages in a lawsuit than the possibility of a HIPAA fine, but neither one sounds like much fun to me.
Refrain from Texting about Your Patients
Can I text my partners patient information?
–Stephen Henry, San Luis Obispo, Calif.
Dr. Hospitalist responds:
Can you? Sure. Do you? Probably. Should you? No.
Texting any patient information falls under the category of ePHI (Electronic Protected Health Information) as part of HIPAA. Technically, such patient-specific information must be protected at all times. Once you send a text, at least three copies are known to exist: one on each of the devices, plus one copy on the network it went through, adding for each network it has to cross. Sure, your phone may be password-protected, but is your partner’s? What about the carrier? How protected is their data?
HIPAA goes into excruciating technical detail about all the safeguards that must be present. You are more than welcome to read it (www.hhs.gov/ocr/privacy/hipaa/administrative/securityrule) to see if you meet all the standards. Or you can take my word for it: You don’t.
So you can see why most health organizations expressly prohibit the texting of patient information. If you rang up your local health-care or hospital lawyer, I’m sure they would tell you to never text patient information. Is that reasonable advice? In 2013, I doubt it.
So what’s the practical advice to follow? For starters, password-protect your phone, if you haven’t already. Nothing worse than losing your phone and having patient information on it. A lot of the OCR (Office for Civil Rights, a branch of Health and Human Services) fines for HIPAA violations stem from folks misplacing unencrypted devices with patient information on them.
Just as important, don’t text anything that you wouldn’t want to see blown up on a lawyer’s display board in court. I’ve seen some really egregious examples of communication between doctors that have no business being preserved electronically. Texting “Mr. X in Room 2101 is a meth-using, narcotic-seeking, half-naked, lunatic troll” is an absolutely stupid thing to do. For that matter, so are remarks that seem less offensive: “And his son is completely unreasonable.” Save your commentary and stick to the facts, because you just generated three copies forever.
If you receive an insensitive text, don’t reply. Simply call the sending physician to discuss any issues. Even being on a “secure” texting network won’t protect you from errors of commission.
If I were to text about a patient (purely hypothetically, mind you), I would limit the information as much as possible. Keep it simple and generic (what HIPAA likes to call “de-identified information”)—for example, “Room 428 is ready for discharge.”
Please, hold the subjective commentary. There is no good reason to have an extended text exchange about a patient; you are creating an electronic trail that has no good reason to exist and never really goes away. It’s just the same as writing in the chart, except that it has the illusion of privacy. And that’s all it is: an illusion.
At the end of the day, I’d probably worry more about the discoverable aspect of your text messages in a lawsuit than the possibility of a HIPAA fine, but neither one sounds like much fun to me.
What Is the Best Management of Hereditary Angioedema?
Case
A 36-year-old man with a known history of hereditary angioedema (HAE) presents with severe orofacial swelling and laryngeal angioedema, requiring expectant management, including endotracheal intubation. His previous angioedema (AE) episodes involved his hands, feet, and genitalia; episodes generally occurred after physical trauma. Ten years prior to admission, he had an episode of secondary small bowel obstruction. The patient had been prescribed prophylactic danazol (Danacrine) 100 mg BID but he had gradually been reducing the dosage due to mood changes; at the time of presentation, he had already tapered to 100 mg danazol three times per week (Monday, Wednesday, and Friday).
Overview
HAE is an autosomal dominant condition characterized by localized, episodic swelling of the deeper dermal layers and/or mucosal tissue. Its acute presentation can vary in severity; presentations can be lethal.
HAE is generally unresponsive to conventional treatments used for other causes of AE (e.g. food or drug reactions) including glucocorticoids, antihistamines, and epinephrine. The pharmacologic treatment of acute attacks, as well as for short- and long-term prophylaxis of HAE, has evolved significantly in recent years and now includes several forms of C1 inhibitor (C1INH) protein replacement, as well as a bradykinin antagonist, and a kallikrein inhibitor.
Review of the Data
Epidemiology. HAE is an autosomal dominant disease with prevalence in the U.S. of 1 in 10,000 to 1 in 50,000 patients. All ethnic groups are equally affected, with no gender predilection. In most cases, a positive family history is present; however, in 25% of cases, spontaneous mutations occur such that an unremarkable family history does not rule out the diagnosis.1
Pathophysiology. In the past decade, there has been substantial advancement in our understanding of HAE pathophysiology. HAE occurs as a result of functional or quantitative C1 esterase inhibitor (C1INH) deficiency.
C1INH belongs to a group of proteins known as serpins (serine protease inhibitors). The C1INH gene is located on chromosome 11, and has several polymorphic sites, which predispose to spontaneous mutations.1
Bradykinin is the core bioactive mediator, which causes vasodilation, smooth muscle contraction, and subsequent edema.1 C1INH regulates bradykinin production by blocking kallikrein’s conversion of factor XII into XIIa, prekallikrein to kallikrein, and cleavage of high-molecular-weight kininogen by activated kallikrein to form bradykinin (see Figure 1).1,2
Clinical Manifestations
HAE is characterized by recurrent episodes of swelling, the frequency and severity of which are quite variable. Virtually all HAE patients have abdominal- and extremity-swelling episodes, and 50% will have episodes of laryngeal swelling; other involved areas might include the face, oropharynx, and genitalia.4 These episodes are usually unilateral; edema is nonpruritic, nonpitting, and often painless. Episodes involving the oropharynx, larynx, and abdomen can be associated with potentially serious morbidity and mortality.1, 3
HAE episodes usually commence during late childhood and early puberty (on average at age 11). Approximately half of HAE patients will have oropharyngeal involvement that might occur many years, even decades, after the initial onset of the disease. The annual rate of severe, life-threatening laryngeal edema was 0.9% in a recent retrospective study.4
Severity of the disease is variable. Attacks are episodic, and occur on average every 10 to 20 days in untreated patients. These attacks typically peak over 24 hours, then usually resolve after 48 to 72 hours. However, the complete resolution of signs and symptoms can last for up to one week after the attacks.5
There is no concomitant pruritus or urticaria that accompanies the AE. However, erythema marginatum, an evanescent nonpruritic rash with serpiginous borders involving the trunk and inner surface of extremities but sparing the face, might herald the onset of an episode. This rash usually has central pallor that blanches with pressure and worsens with heat.
HAE can be triggered by stressful events, including trauma, surgery, menstruation, and viral infections. However, in many instances, HAE attacks occur without an identifiable cause.5
Differential Diagnosis from Other Causes of Angioedema
Type I HAE is characterized by a quantitative C1INH deficiency (which is functionally abnormal as well), and occurs in 85% of patients. Type II HAE occurs in 15% of patients, and results from a functionally abnormal C1INH.
In patients with Type I and II HAE, as well as acquired C1 inhibitor deficiency (ACID), C4 levels are low during and between attacks. C2 levels are also low during acute attacks. In ACID, levels of C1q are also reduced; these patients require further workup to rule out an undiagnosed malignancy or an autoimmune process. In contrast, patients with ACE-induced, idiopathic, and allergic AE have normal complement profiles.3,6
Type III is a more recently described type of HAE that is rare, not well understood, and generally affects women.3,6 Clinically, it resembles Type I and Type II HAE but complement levels, including C1 inhibitor, are normal (see Table 1).
Treatment
HAE types I, II, III, and ACID are generally unresponsive to glucocorticoids, antihistamines, and epinephrine. These forms of AE may be exacerbated by exogenous estrogen.1,8 For this reason, HAE patients should avoid oral hormonal contraception and estrogen replacement therapy. In addition, ACE inhibitors should also be avoided based on their effect on bradykinin degradation.
Until the introduction of newer therapeutic choices, as noted in our case, the treatment of acute attacks of AE was essentially supportive. Patients with impending laryngeal obstruction were managed with intubation prior to progression of the AE to limit airway patency. Prior to the modern era, a substantial proportion of HAE patients died of asphyxiation.
Fresh frozen plasma (FFP) has been used to treat acute HAE attacks, but given its content of contact system proteins (in addition to C1INH), FFP might also pose a risk for worsening of HAE; for this reason, it must be given cautiously to patients who are symptomatic.9
In the past decade, there has been significant progress in the available treatments for HAE. Currently in the U.S., there are several agents recently approved by, or have pending approvals from, the FDA, including several forms of C1INH replacement, a bradykinin antagonist, and a kallikrein inhibitor.
The C1 esterase inhibitor (human) drugs are administered intravenously; both have been shown to be efficacious and safe. Nanofiltered C1 inhibitor provided relief in a median time of two hours when used acutely; when used as prophylaxis, it decreased the number of attacks in a three-month period by 50% (six vs. 12 with placebo, P<0.001).11
The other C1INH is rhucin, still not approved in U.S. This drug is characterized by a short half-life (approximately two to four hours) compared with the plasma-derived C1INH agents (24 to 48 hours). It is contraindicated in patients with rabbit hypersensitivity, as it is purified from rabbit breast milk.10
Ecallantide is a kallikrein inhibitor for acute therapy that is administered via three subcutaneous injections. This agent has been linked to allergic/anaphylactic reactions in a minority of patients (approximately 4%); therefore, it should be administered cautiously, by a health-care provider, and in a setting where anaphylaxis can be successfully managed.12 Icatibant is a bradykinin antagonist recently approved in the U.S. and administered SC via a single injection.10
In light of the development of these new agents, there is a need for updated guidelines for the long- and short-term prophylaxis and acute management of HAE. A recent guideline focused on the management of HAE in gynecologic and obstetric patients recommended the use of plasma-derived C1INH C1 esterase inhibitor (human) (Cinryze) for short- and long-term prophylaxis and acute treatment of HAE.13 The effect of pregnancy on HAE is variable: Some women worsen and other women have less swelling during their pregnancy. Swelling at the time of parturition is rare; however, the risk rises during the post-partum period.
Type III HAE. An additional form of HAE has been recognized with a pattern of AE episodes that mimics Type I or Type II HAE but with unremarkable laboratory studies of the complement cascade, including C1 inhibitor level and function. At this time, there is no laboratory test with which a diagnosis of Type III HAE can be confirmed. The diagnosis should be suspected in patients with a strong family history of AE reflecting autosomal dominant inheritance. In some, but not all, cases, the condition is manifest in association with high estrogen levels (e.g. pregnancy or administration of oral contraceptives). Type III HAE patients have a salutary response to the same agents that are efficacious for Type I and II HAE.
Acquired C1 inhibitor deficiency (ACID). ACID generally occurs in adults and is clinically indistinguishable from HAE. ACID is not associated with a remarkable family history of AE. In contrast to HAE, this is a consumptive deficiency of C1 inhibitor and results from enhanced catabolism that exceeds the capacity for regenerating C1 inhibitor protein. It is often associated with neoplastic (usually lymphoproliferative) or autoimmune disorders; treatment of the underlying condition frequently leads to improvement in ACID. Although its management is similar to HAE, it tends to be more responsive to anti-fibrinolytics. A salutary response to C1INH replacement therapy might not occur in patients with autoantibodies to C1 inhibitor, but efficacy of ecallantide and icatibant for the treatment of acquired AE has been reported.14, 15
ACEI angioedema. Treatment with angiotensin-converting enzyme inhibitors (ACE-I) has been associated with recurrent AE without urticaria in 0.1 to 0.7% of patients exposed to these drugs.16 Angioedema from ACE-I more frequently occurs within the first few months of therapy, but it might occur even after years of continuous therapy. ACEI-induced AE is secondary to impaired degradation of bradykinin. The main treatment is to discontinue the offending agent and avoid all other ACE-I, as this is a class-specific reaction.17
Angiotensin receptor blockers (ARBs) have been associated less commonly with AE. The mechanism for ARB-associated AE has not been elucidated. A meta-analysis showed that in 2% to 17% of patients who were switched to ARBs, recurrence of AE was observed.18 From the pooling of these data with two randomized controlled trials, it is estimated that approximately 10% or less of patients with ACEI-associated AE who switched to ARBs will develop AE.19 In the majority of cases, patients can be switched to ARBs with no recurrence of AE; however, the decision to prescribe an ARB to a patient who has had AE while receiving ACEI should be made carefully on an individualized risk/benefit basis.19
Preventive Treatment
The 17 α-alkylated androgens that can be used for treatment of HAE are danazol (Danacrine), stanozolol (Winstrol), oxandralone (Oxandrine) and methyltestosterone (Android). In patients with HAE, attenuated androgens can significantly reduce the frequency and severity of attacks; however, their use is limited by risk for untoward effects (virilization, abnormal liver function tests, change in libido, anxiety, etc.).21 There is also a risk for hepatotoxicity, including development of hepatic adenomas and hepatic carcinoma.
Antifibrinolytics also may have efficacy for HAE, but these agents have been associated with a variety of adverse effects, including nausea and diarrhea, postural hypotension, fatigue, enhanced thrombosis, retinal changes, and teratogenicity.8, 22, 23
In 2009, long-term prophylaxis with C1-INH concentrate was recommended for patients with HAE with frequent or disabling attacks, a history of laryngeal attacks, and poor quality of life. The 2007 International Consensus Algorithm for the Diagnosis, Therapy, and Management of HAE recommended long-term prophylaxis in patients with more than one monthly severe HAE attack, more than five days of disability per month, or any history of airway compromise.24, 25
The decision to prescribe long-term prophylaxis, and the dose/frequency of medication required, should be individualized based on clinical parameters, such as frequency and severity of attacks, and not on C1 INH or C4 levels.
Perioperative Considerations
It is well established that any trauma, including dental procedures or surgery, can precipitate HAE attacks. For this reason, short-term prophylactic treatment in HAE patients undergoing procedures is recommended. Ideally, avoiding endotracheal intubation is the best approach; however, if intubation cannot be avoided, then adequate prophylaxis should be administered.2
Attenuated androgens can be given up to seven days before a procedure, or C1 INH can be administered 24 hours in advance. If C1 INH is unavailable, FFP can be given six to 12 hours in advance in patients who are not symptomatic; in case of endotracheal intubation, either FFP or C1 INH should be administered immediately before.2
Several case reports in multiple specialty surgical patients (abdominal surgery, cardiopulmonary bypass, orthopedic surgery, etc.) have confirmed the successful use of C1 INH in the prevention of acute attacks with favorable outcomes.2
There is no need to follow C1 INH levels, as it has no clinical relevance.
Back to the Case
The patient was admitted to the ICU and received a total of eight units of FFP. He was transferred to our institution and was able to be extubated three days after initial presentation. Laboratory studies revealed C4 10mg/dL and C1 esterase inhibitor 10mg/dL (both low).
Danazol was resumed. However, within several months after discharge, Cinryze became available in the U.S. market and was eventually prescribed. The patient has not had further significant attacks requiring inpatient management.
Dr. Auron is an assistant professor of medicine and pediatrics at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University. Dr. Lang is co-director of the Asthma Center and director of the Allergy/Immunology Fellowship Training Program at the Cleveland Clinic.
References
- Bernstein, JA. Update on angioedema: evaluation, diagnosis, and treatment. Allergy Asthma Proc. 2011;32(6):408-412.
- Levy JH, Freiberger DJ, Roback J. Hereditary angioedema: current and emerging treatment options. Anesth Analg. 2010;110(5):1271-1280.
- Busse PJ. Angioedema: Differential diagnosis and treatment. Allergy Asthma Proc. 2011;32:Suppl 1:S3-S11.
- Khan DA. Hereditary angioedema: historical aspects, classification, pathophysiology, clinical presentation, and laboratory diagnosis. Allergy Asthma Proc. 2011;32(1):1-10.
- Bork K, Meng G, Staubach P, Hardt, J. Hereditary angioedema: new findings concerning symptoms, affected organs, and course. Am J Med. 2006;119(3):267-274.
- Zuraw BL, Christiansen SC. Pathogenesis and laboratory diagnosis of hereditary angioedema. Allergy Asthma Proc. 2009;30:487-492.
- Frazer-Abel A, Giclas PC. Update on laboratory tests for the diagnosis and differentiation of hereditary angioedema and acquired angioedema. Allergy Asthma Proc. 2011;32:Suppl 1:S17-S21.
- Banerjee A. Current treatment of hereditary angioedema: an update on clinical studies. Allergy Asthma Proc. 2010;31:398-406.
- Donaldson VH. Therapy of "the neurotic edema." N Engl J Med. 1972;286(15):835-836.
- Riedl MA. Update on the acute treatment of hereditary angioedema. Allergy Asthma Proc. 2011;32:11-16.
- Zuraw BL, Busse PJ, White M, et al. Nanofiltered C1 inhibitor concentrate for treatment of hereditary angioedema. N Engl J Med. 2010;363:513-522.
- Cicardi M, Levy RJ, McNeil DL. Ecallantide for the treatment of acute attacks in hereditary angioedema. N Engl J Med. 2010;363:523-531.
- Caballero T, Farkas H, Bouillet L, et al. International consensus and practical guidelines on the gynecologic and obstetric management of female patients with hereditary angioedema caused by C1 inhibitor deficiency. J Allergy Clin Immunol. 2012;129(2):308-320.
- Cicardi M, Zanichelli A. Acquired angioedema. J Allergy Clin Immunol. 2010;6(1):14.
- Zanichelli A, Badini M, Nataloni I, Montano N, Cicardi M. Treatment of acquired angioedema with icatibant: a case report. Intern Emerg Med. 2011;6(3):279-280.
- Byrd JB, Adam A, Brown NJ. Angiotensin-converting enzyme inhibitor-associated angioedema. Immunol Allergy Clin North Am. 2006;26(4):725-737.
- Haymore BR, Yoon J, Mikita CP, Klote MM, DeZee KJ. Risk of angioedema with angiotensin receptor blockers in patients with prior angioedema associated with angiotensin-converting enzyme inhibitors: a meta-analysis. Ann Allergy Asthma Immunol. 2008;101(5):495-499.
- Beavers CJ, Dunn SP, Macaulay TE. The role of angiotensin receptor blockers in patients with angiotensin-converting enzyme inhibitor-induced angioedema. Ann Pharmacother. 2011;45(4):520-524.
- Nzeako UC. Diagnosis and management of angioedema with abdominal involvement: a gastroenterology perspective. World J Gastroenterol. 2010; 16(39):4913-4921.
- Banerji A, Sloane DE, Sheffer AL. Hereditary angioedema: a current state-of-the-art review, V: attenuated androgens for the treatment of hereditary angioedema. Ann Allergy Asthma Immunol. 2008;100(1) (Suppl 2):S19-22.
- Zuraw BL. Clinical practice. Hereditary angioedema. N Engl J Med. 2008; 359(10):1027-1036.
- Zuraw BL. Hereditary angioedema: a current state-of-the-art review, IV: short- and long-term treatment of hereditary angioedema: out with the old and in with the new? Ann Allergy Asthma Immunol. 2008;100(1) (Suppl 2):S13-S18.
- Bowen T, Cicardi M, Bork K, et al. Hereditary angioedema: a current state-of-the-art review, VII: Canadian Hungarian 2007 International Consensus Algorithm for the Diagnosis, Therapy, and Management of Hereditary Angioedema. Ann Allergy Asthma Immunol. 2008;100(1)(Suppl 2):S30-40.
- Craig T, Riedl M, Dykewicz M, et al. When is prophylaxis for hereditary angioedema necessary? Ann Allergy Asthma Immunol. 2009.102(5):366-372.
- Frank MM. Update on preventive therapy (prophylaxis) of hereditary angioedema. Allergy Asthma Proc. 2011;32(1):17-21.
Case
A 36-year-old man with a known history of hereditary angioedema (HAE) presents with severe orofacial swelling and laryngeal angioedema, requiring expectant management, including endotracheal intubation. His previous angioedema (AE) episodes involved his hands, feet, and genitalia; episodes generally occurred after physical trauma. Ten years prior to admission, he had an episode of secondary small bowel obstruction. The patient had been prescribed prophylactic danazol (Danacrine) 100 mg BID but he had gradually been reducing the dosage due to mood changes; at the time of presentation, he had already tapered to 100 mg danazol three times per week (Monday, Wednesday, and Friday).
Overview
HAE is an autosomal dominant condition characterized by localized, episodic swelling of the deeper dermal layers and/or mucosal tissue. Its acute presentation can vary in severity; presentations can be lethal.
HAE is generally unresponsive to conventional treatments used for other causes of AE (e.g. food or drug reactions) including glucocorticoids, antihistamines, and epinephrine. The pharmacologic treatment of acute attacks, as well as for short- and long-term prophylaxis of HAE, has evolved significantly in recent years and now includes several forms of C1 inhibitor (C1INH) protein replacement, as well as a bradykinin antagonist, and a kallikrein inhibitor.
Review of the Data
Epidemiology. HAE is an autosomal dominant disease with prevalence in the U.S. of 1 in 10,000 to 1 in 50,000 patients. All ethnic groups are equally affected, with no gender predilection. In most cases, a positive family history is present; however, in 25% of cases, spontaneous mutations occur such that an unremarkable family history does not rule out the diagnosis.1
Pathophysiology. In the past decade, there has been substantial advancement in our understanding of HAE pathophysiology. HAE occurs as a result of functional or quantitative C1 esterase inhibitor (C1INH) deficiency.
C1INH belongs to a group of proteins known as serpins (serine protease inhibitors). The C1INH gene is located on chromosome 11, and has several polymorphic sites, which predispose to spontaneous mutations.1
Bradykinin is the core bioactive mediator, which causes vasodilation, smooth muscle contraction, and subsequent edema.1 C1INH regulates bradykinin production by blocking kallikrein’s conversion of factor XII into XIIa, prekallikrein to kallikrein, and cleavage of high-molecular-weight kininogen by activated kallikrein to form bradykinin (see Figure 1).1,2
Clinical Manifestations
HAE is characterized by recurrent episodes of swelling, the frequency and severity of which are quite variable. Virtually all HAE patients have abdominal- and extremity-swelling episodes, and 50% will have episodes of laryngeal swelling; other involved areas might include the face, oropharynx, and genitalia.4 These episodes are usually unilateral; edema is nonpruritic, nonpitting, and often painless. Episodes involving the oropharynx, larynx, and abdomen can be associated with potentially serious morbidity and mortality.1, 3
HAE episodes usually commence during late childhood and early puberty (on average at age 11). Approximately half of HAE patients will have oropharyngeal involvement that might occur many years, even decades, after the initial onset of the disease. The annual rate of severe, life-threatening laryngeal edema was 0.9% in a recent retrospective study.4
Severity of the disease is variable. Attacks are episodic, and occur on average every 10 to 20 days in untreated patients. These attacks typically peak over 24 hours, then usually resolve after 48 to 72 hours. However, the complete resolution of signs and symptoms can last for up to one week after the attacks.5
There is no concomitant pruritus or urticaria that accompanies the AE. However, erythema marginatum, an evanescent nonpruritic rash with serpiginous borders involving the trunk and inner surface of extremities but sparing the face, might herald the onset of an episode. This rash usually has central pallor that blanches with pressure and worsens with heat.
HAE can be triggered by stressful events, including trauma, surgery, menstruation, and viral infections. However, in many instances, HAE attacks occur without an identifiable cause.5
Differential Diagnosis from Other Causes of Angioedema
Type I HAE is characterized by a quantitative C1INH deficiency (which is functionally abnormal as well), and occurs in 85% of patients. Type II HAE occurs in 15% of patients, and results from a functionally abnormal C1INH.
In patients with Type I and II HAE, as well as acquired C1 inhibitor deficiency (ACID), C4 levels are low during and between attacks. C2 levels are also low during acute attacks. In ACID, levels of C1q are also reduced; these patients require further workup to rule out an undiagnosed malignancy or an autoimmune process. In contrast, patients with ACE-induced, idiopathic, and allergic AE have normal complement profiles.3,6
Type III is a more recently described type of HAE that is rare, not well understood, and generally affects women.3,6 Clinically, it resembles Type I and Type II HAE but complement levels, including C1 inhibitor, are normal (see Table 1).
Treatment
HAE types I, II, III, and ACID are generally unresponsive to glucocorticoids, antihistamines, and epinephrine. These forms of AE may be exacerbated by exogenous estrogen.1,8 For this reason, HAE patients should avoid oral hormonal contraception and estrogen replacement therapy. In addition, ACE inhibitors should also be avoided based on their effect on bradykinin degradation.
Until the introduction of newer therapeutic choices, as noted in our case, the treatment of acute attacks of AE was essentially supportive. Patients with impending laryngeal obstruction were managed with intubation prior to progression of the AE to limit airway patency. Prior to the modern era, a substantial proportion of HAE patients died of asphyxiation.
Fresh frozen plasma (FFP) has been used to treat acute HAE attacks, but given its content of contact system proteins (in addition to C1INH), FFP might also pose a risk for worsening of HAE; for this reason, it must be given cautiously to patients who are symptomatic.9
In the past decade, there has been significant progress in the available treatments for HAE. Currently in the U.S., there are several agents recently approved by, or have pending approvals from, the FDA, including several forms of C1INH replacement, a bradykinin antagonist, and a kallikrein inhibitor.
The C1 esterase inhibitor (human) drugs are administered intravenously; both have been shown to be efficacious and safe. Nanofiltered C1 inhibitor provided relief in a median time of two hours when used acutely; when used as prophylaxis, it decreased the number of attacks in a three-month period by 50% (six vs. 12 with placebo, P<0.001).11
The other C1INH is rhucin, still not approved in U.S. This drug is characterized by a short half-life (approximately two to four hours) compared with the plasma-derived C1INH agents (24 to 48 hours). It is contraindicated in patients with rabbit hypersensitivity, as it is purified from rabbit breast milk.10
Ecallantide is a kallikrein inhibitor for acute therapy that is administered via three subcutaneous injections. This agent has been linked to allergic/anaphylactic reactions in a minority of patients (approximately 4%); therefore, it should be administered cautiously, by a health-care provider, and in a setting where anaphylaxis can be successfully managed.12 Icatibant is a bradykinin antagonist recently approved in the U.S. and administered SC via a single injection.10
In light of the development of these new agents, there is a need for updated guidelines for the long- and short-term prophylaxis and acute management of HAE. A recent guideline focused on the management of HAE in gynecologic and obstetric patients recommended the use of plasma-derived C1INH C1 esterase inhibitor (human) (Cinryze) for short- and long-term prophylaxis and acute treatment of HAE.13 The effect of pregnancy on HAE is variable: Some women worsen and other women have less swelling during their pregnancy. Swelling at the time of parturition is rare; however, the risk rises during the post-partum period.
Type III HAE. An additional form of HAE has been recognized with a pattern of AE episodes that mimics Type I or Type II HAE but with unremarkable laboratory studies of the complement cascade, including C1 inhibitor level and function. At this time, there is no laboratory test with which a diagnosis of Type III HAE can be confirmed. The diagnosis should be suspected in patients with a strong family history of AE reflecting autosomal dominant inheritance. In some, but not all, cases, the condition is manifest in association with high estrogen levels (e.g. pregnancy or administration of oral contraceptives). Type III HAE patients have a salutary response to the same agents that are efficacious for Type I and II HAE.
Acquired C1 inhibitor deficiency (ACID). ACID generally occurs in adults and is clinically indistinguishable from HAE. ACID is not associated with a remarkable family history of AE. In contrast to HAE, this is a consumptive deficiency of C1 inhibitor and results from enhanced catabolism that exceeds the capacity for regenerating C1 inhibitor protein. It is often associated with neoplastic (usually lymphoproliferative) or autoimmune disorders; treatment of the underlying condition frequently leads to improvement in ACID. Although its management is similar to HAE, it tends to be more responsive to anti-fibrinolytics. A salutary response to C1INH replacement therapy might not occur in patients with autoantibodies to C1 inhibitor, but efficacy of ecallantide and icatibant for the treatment of acquired AE has been reported.14, 15
ACEI angioedema. Treatment with angiotensin-converting enzyme inhibitors (ACE-I) has been associated with recurrent AE without urticaria in 0.1 to 0.7% of patients exposed to these drugs.16 Angioedema from ACE-I more frequently occurs within the first few months of therapy, but it might occur even after years of continuous therapy. ACEI-induced AE is secondary to impaired degradation of bradykinin. The main treatment is to discontinue the offending agent and avoid all other ACE-I, as this is a class-specific reaction.17
Angiotensin receptor blockers (ARBs) have been associated less commonly with AE. The mechanism for ARB-associated AE has not been elucidated. A meta-analysis showed that in 2% to 17% of patients who were switched to ARBs, recurrence of AE was observed.18 From the pooling of these data with two randomized controlled trials, it is estimated that approximately 10% or less of patients with ACEI-associated AE who switched to ARBs will develop AE.19 In the majority of cases, patients can be switched to ARBs with no recurrence of AE; however, the decision to prescribe an ARB to a patient who has had AE while receiving ACEI should be made carefully on an individualized risk/benefit basis.19
Preventive Treatment
The 17 α-alkylated androgens that can be used for treatment of HAE are danazol (Danacrine), stanozolol (Winstrol), oxandralone (Oxandrine) and methyltestosterone (Android). In patients with HAE, attenuated androgens can significantly reduce the frequency and severity of attacks; however, their use is limited by risk for untoward effects (virilization, abnormal liver function tests, change in libido, anxiety, etc.).21 There is also a risk for hepatotoxicity, including development of hepatic adenomas and hepatic carcinoma.
Antifibrinolytics also may have efficacy for HAE, but these agents have been associated with a variety of adverse effects, including nausea and diarrhea, postural hypotension, fatigue, enhanced thrombosis, retinal changes, and teratogenicity.8, 22, 23
In 2009, long-term prophylaxis with C1-INH concentrate was recommended for patients with HAE with frequent or disabling attacks, a history of laryngeal attacks, and poor quality of life. The 2007 International Consensus Algorithm for the Diagnosis, Therapy, and Management of HAE recommended long-term prophylaxis in patients with more than one monthly severe HAE attack, more than five days of disability per month, or any history of airway compromise.24, 25
The decision to prescribe long-term prophylaxis, and the dose/frequency of medication required, should be individualized based on clinical parameters, such as frequency and severity of attacks, and not on C1 INH or C4 levels.
Perioperative Considerations
It is well established that any trauma, including dental procedures or surgery, can precipitate HAE attacks. For this reason, short-term prophylactic treatment in HAE patients undergoing procedures is recommended. Ideally, avoiding endotracheal intubation is the best approach; however, if intubation cannot be avoided, then adequate prophylaxis should be administered.2
Attenuated androgens can be given up to seven days before a procedure, or C1 INH can be administered 24 hours in advance. If C1 INH is unavailable, FFP can be given six to 12 hours in advance in patients who are not symptomatic; in case of endotracheal intubation, either FFP or C1 INH should be administered immediately before.2
Several case reports in multiple specialty surgical patients (abdominal surgery, cardiopulmonary bypass, orthopedic surgery, etc.) have confirmed the successful use of C1 INH in the prevention of acute attacks with favorable outcomes.2
There is no need to follow C1 INH levels, as it has no clinical relevance.
Back to the Case
The patient was admitted to the ICU and received a total of eight units of FFP. He was transferred to our institution and was able to be extubated three days after initial presentation. Laboratory studies revealed C4 10mg/dL and C1 esterase inhibitor 10mg/dL (both low).
Danazol was resumed. However, within several months after discharge, Cinryze became available in the U.S. market and was eventually prescribed. The patient has not had further significant attacks requiring inpatient management.
Dr. Auron is an assistant professor of medicine and pediatrics at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University. Dr. Lang is co-director of the Asthma Center and director of the Allergy/Immunology Fellowship Training Program at the Cleveland Clinic.
References
- Bernstein, JA. Update on angioedema: evaluation, diagnosis, and treatment. Allergy Asthma Proc. 2011;32(6):408-412.
- Levy JH, Freiberger DJ, Roback J. Hereditary angioedema: current and emerging treatment options. Anesth Analg. 2010;110(5):1271-1280.
- Busse PJ. Angioedema: Differential diagnosis and treatment. Allergy Asthma Proc. 2011;32:Suppl 1:S3-S11.
- Khan DA. Hereditary angioedema: historical aspects, classification, pathophysiology, clinical presentation, and laboratory diagnosis. Allergy Asthma Proc. 2011;32(1):1-10.
- Bork K, Meng G, Staubach P, Hardt, J. Hereditary angioedema: new findings concerning symptoms, affected organs, and course. Am J Med. 2006;119(3):267-274.
- Zuraw BL, Christiansen SC. Pathogenesis and laboratory diagnosis of hereditary angioedema. Allergy Asthma Proc. 2009;30:487-492.
- Frazer-Abel A, Giclas PC. Update on laboratory tests for the diagnosis and differentiation of hereditary angioedema and acquired angioedema. Allergy Asthma Proc. 2011;32:Suppl 1:S17-S21.
- Banerjee A. Current treatment of hereditary angioedema: an update on clinical studies. Allergy Asthma Proc. 2010;31:398-406.
- Donaldson VH. Therapy of "the neurotic edema." N Engl J Med. 1972;286(15):835-836.
- Riedl MA. Update on the acute treatment of hereditary angioedema. Allergy Asthma Proc. 2011;32:11-16.
- Zuraw BL, Busse PJ, White M, et al. Nanofiltered C1 inhibitor concentrate for treatment of hereditary angioedema. N Engl J Med. 2010;363:513-522.
- Cicardi M, Levy RJ, McNeil DL. Ecallantide for the treatment of acute attacks in hereditary angioedema. N Engl J Med. 2010;363:523-531.
- Caballero T, Farkas H, Bouillet L, et al. International consensus and practical guidelines on the gynecologic and obstetric management of female patients with hereditary angioedema caused by C1 inhibitor deficiency. J Allergy Clin Immunol. 2012;129(2):308-320.
- Cicardi M, Zanichelli A. Acquired angioedema. J Allergy Clin Immunol. 2010;6(1):14.
- Zanichelli A, Badini M, Nataloni I, Montano N, Cicardi M. Treatment of acquired angioedema with icatibant: a case report. Intern Emerg Med. 2011;6(3):279-280.
- Byrd JB, Adam A, Brown NJ. Angiotensin-converting enzyme inhibitor-associated angioedema. Immunol Allergy Clin North Am. 2006;26(4):725-737.
- Haymore BR, Yoon J, Mikita CP, Klote MM, DeZee KJ. Risk of angioedema with angiotensin receptor blockers in patients with prior angioedema associated with angiotensin-converting enzyme inhibitors: a meta-analysis. Ann Allergy Asthma Immunol. 2008;101(5):495-499.
- Beavers CJ, Dunn SP, Macaulay TE. The role of angiotensin receptor blockers in patients with angiotensin-converting enzyme inhibitor-induced angioedema. Ann Pharmacother. 2011;45(4):520-524.
- Nzeako UC. Diagnosis and management of angioedema with abdominal involvement: a gastroenterology perspective. World J Gastroenterol. 2010; 16(39):4913-4921.
- Banerji A, Sloane DE, Sheffer AL. Hereditary angioedema: a current state-of-the-art review, V: attenuated androgens for the treatment of hereditary angioedema. Ann Allergy Asthma Immunol. 2008;100(1) (Suppl 2):S19-22.
- Zuraw BL. Clinical practice. Hereditary angioedema. N Engl J Med. 2008; 359(10):1027-1036.
- Zuraw BL. Hereditary angioedema: a current state-of-the-art review, IV: short- and long-term treatment of hereditary angioedema: out with the old and in with the new? Ann Allergy Asthma Immunol. 2008;100(1) (Suppl 2):S13-S18.
- Bowen T, Cicardi M, Bork K, et al. Hereditary angioedema: a current state-of-the-art review, VII: Canadian Hungarian 2007 International Consensus Algorithm for the Diagnosis, Therapy, and Management of Hereditary Angioedema. Ann Allergy Asthma Immunol. 2008;100(1)(Suppl 2):S30-40.
- Craig T, Riedl M, Dykewicz M, et al. When is prophylaxis for hereditary angioedema necessary? Ann Allergy Asthma Immunol. 2009.102(5):366-372.
- Frank MM. Update on preventive therapy (prophylaxis) of hereditary angioedema. Allergy Asthma Proc. 2011;32(1):17-21.
Case
A 36-year-old man with a known history of hereditary angioedema (HAE) presents with severe orofacial swelling and laryngeal angioedema, requiring expectant management, including endotracheal intubation. His previous angioedema (AE) episodes involved his hands, feet, and genitalia; episodes generally occurred after physical trauma. Ten years prior to admission, he had an episode of secondary small bowel obstruction. The patient had been prescribed prophylactic danazol (Danacrine) 100 mg BID but he had gradually been reducing the dosage due to mood changes; at the time of presentation, he had already tapered to 100 mg danazol three times per week (Monday, Wednesday, and Friday).
Overview
HAE is an autosomal dominant condition characterized by localized, episodic swelling of the deeper dermal layers and/or mucosal tissue. Its acute presentation can vary in severity; presentations can be lethal.
HAE is generally unresponsive to conventional treatments used for other causes of AE (e.g. food or drug reactions) including glucocorticoids, antihistamines, and epinephrine. The pharmacologic treatment of acute attacks, as well as for short- and long-term prophylaxis of HAE, has evolved significantly in recent years and now includes several forms of C1 inhibitor (C1INH) protein replacement, as well as a bradykinin antagonist, and a kallikrein inhibitor.
Review of the Data
Epidemiology. HAE is an autosomal dominant disease with prevalence in the U.S. of 1 in 10,000 to 1 in 50,000 patients. All ethnic groups are equally affected, with no gender predilection. In most cases, a positive family history is present; however, in 25% of cases, spontaneous mutations occur such that an unremarkable family history does not rule out the diagnosis.1
Pathophysiology. In the past decade, there has been substantial advancement in our understanding of HAE pathophysiology. HAE occurs as a result of functional or quantitative C1 esterase inhibitor (C1INH) deficiency.
C1INH belongs to a group of proteins known as serpins (serine protease inhibitors). The C1INH gene is located on chromosome 11, and has several polymorphic sites, which predispose to spontaneous mutations.1
Bradykinin is the core bioactive mediator, which causes vasodilation, smooth muscle contraction, and subsequent edema.1 C1INH regulates bradykinin production by blocking kallikrein’s conversion of factor XII into XIIa, prekallikrein to kallikrein, and cleavage of high-molecular-weight kininogen by activated kallikrein to form bradykinin (see Figure 1).1,2
Clinical Manifestations
HAE is characterized by recurrent episodes of swelling, the frequency and severity of which are quite variable. Virtually all HAE patients have abdominal- and extremity-swelling episodes, and 50% will have episodes of laryngeal swelling; other involved areas might include the face, oropharynx, and genitalia.4 These episodes are usually unilateral; edema is nonpruritic, nonpitting, and often painless. Episodes involving the oropharynx, larynx, and abdomen can be associated with potentially serious morbidity and mortality.1, 3
HAE episodes usually commence during late childhood and early puberty (on average at age 11). Approximately half of HAE patients will have oropharyngeal involvement that might occur many years, even decades, after the initial onset of the disease. The annual rate of severe, life-threatening laryngeal edema was 0.9% in a recent retrospective study.4
Severity of the disease is variable. Attacks are episodic, and occur on average every 10 to 20 days in untreated patients. These attacks typically peak over 24 hours, then usually resolve after 48 to 72 hours. However, the complete resolution of signs and symptoms can last for up to one week after the attacks.5
There is no concomitant pruritus or urticaria that accompanies the AE. However, erythema marginatum, an evanescent nonpruritic rash with serpiginous borders involving the trunk and inner surface of extremities but sparing the face, might herald the onset of an episode. This rash usually has central pallor that blanches with pressure and worsens with heat.
HAE can be triggered by stressful events, including trauma, surgery, menstruation, and viral infections. However, in many instances, HAE attacks occur without an identifiable cause.5
Differential Diagnosis from Other Causes of Angioedema
Type I HAE is characterized by a quantitative C1INH deficiency (which is functionally abnormal as well), and occurs in 85% of patients. Type II HAE occurs in 15% of patients, and results from a functionally abnormal C1INH.
In patients with Type I and II HAE, as well as acquired C1 inhibitor deficiency (ACID), C4 levels are low during and between attacks. C2 levels are also low during acute attacks. In ACID, levels of C1q are also reduced; these patients require further workup to rule out an undiagnosed malignancy or an autoimmune process. In contrast, patients with ACE-induced, idiopathic, and allergic AE have normal complement profiles.3,6
Type III is a more recently described type of HAE that is rare, not well understood, and generally affects women.3,6 Clinically, it resembles Type I and Type II HAE but complement levels, including C1 inhibitor, are normal (see Table 1).
Treatment
HAE types I, II, III, and ACID are generally unresponsive to glucocorticoids, antihistamines, and epinephrine. These forms of AE may be exacerbated by exogenous estrogen.1,8 For this reason, HAE patients should avoid oral hormonal contraception and estrogen replacement therapy. In addition, ACE inhibitors should also be avoided based on their effect on bradykinin degradation.
Until the introduction of newer therapeutic choices, as noted in our case, the treatment of acute attacks of AE was essentially supportive. Patients with impending laryngeal obstruction were managed with intubation prior to progression of the AE to limit airway patency. Prior to the modern era, a substantial proportion of HAE patients died of asphyxiation.
Fresh frozen plasma (FFP) has been used to treat acute HAE attacks, but given its content of contact system proteins (in addition to C1INH), FFP might also pose a risk for worsening of HAE; for this reason, it must be given cautiously to patients who are symptomatic.9
In the past decade, there has been significant progress in the available treatments for HAE. Currently in the U.S., there are several agents recently approved by, or have pending approvals from, the FDA, including several forms of C1INH replacement, a bradykinin antagonist, and a kallikrein inhibitor.
The C1 esterase inhibitor (human) drugs are administered intravenously; both have been shown to be efficacious and safe. Nanofiltered C1 inhibitor provided relief in a median time of two hours when used acutely; when used as prophylaxis, it decreased the number of attacks in a three-month period by 50% (six vs. 12 with placebo, P<0.001).11
The other C1INH is rhucin, still not approved in U.S. This drug is characterized by a short half-life (approximately two to four hours) compared with the plasma-derived C1INH agents (24 to 48 hours). It is contraindicated in patients with rabbit hypersensitivity, as it is purified from rabbit breast milk.10
Ecallantide is a kallikrein inhibitor for acute therapy that is administered via three subcutaneous injections. This agent has been linked to allergic/anaphylactic reactions in a minority of patients (approximately 4%); therefore, it should be administered cautiously, by a health-care provider, and in a setting where anaphylaxis can be successfully managed.12 Icatibant is a bradykinin antagonist recently approved in the U.S. and administered SC via a single injection.10
In light of the development of these new agents, there is a need for updated guidelines for the long- and short-term prophylaxis and acute management of HAE. A recent guideline focused on the management of HAE in gynecologic and obstetric patients recommended the use of plasma-derived C1INH C1 esterase inhibitor (human) (Cinryze) for short- and long-term prophylaxis and acute treatment of HAE.13 The effect of pregnancy on HAE is variable: Some women worsen and other women have less swelling during their pregnancy. Swelling at the time of parturition is rare; however, the risk rises during the post-partum period.
Type III HAE. An additional form of HAE has been recognized with a pattern of AE episodes that mimics Type I or Type II HAE but with unremarkable laboratory studies of the complement cascade, including C1 inhibitor level and function. At this time, there is no laboratory test with which a diagnosis of Type III HAE can be confirmed. The diagnosis should be suspected in patients with a strong family history of AE reflecting autosomal dominant inheritance. In some, but not all, cases, the condition is manifest in association with high estrogen levels (e.g. pregnancy or administration of oral contraceptives). Type III HAE patients have a salutary response to the same agents that are efficacious for Type I and II HAE.
Acquired C1 inhibitor deficiency (ACID). ACID generally occurs in adults and is clinically indistinguishable from HAE. ACID is not associated with a remarkable family history of AE. In contrast to HAE, this is a consumptive deficiency of C1 inhibitor and results from enhanced catabolism that exceeds the capacity for regenerating C1 inhibitor protein. It is often associated with neoplastic (usually lymphoproliferative) or autoimmune disorders; treatment of the underlying condition frequently leads to improvement in ACID. Although its management is similar to HAE, it tends to be more responsive to anti-fibrinolytics. A salutary response to C1INH replacement therapy might not occur in patients with autoantibodies to C1 inhibitor, but efficacy of ecallantide and icatibant for the treatment of acquired AE has been reported.14, 15
ACEI angioedema. Treatment with angiotensin-converting enzyme inhibitors (ACE-I) has been associated with recurrent AE without urticaria in 0.1 to 0.7% of patients exposed to these drugs.16 Angioedema from ACE-I more frequently occurs within the first few months of therapy, but it might occur even after years of continuous therapy. ACEI-induced AE is secondary to impaired degradation of bradykinin. The main treatment is to discontinue the offending agent and avoid all other ACE-I, as this is a class-specific reaction.17
Angiotensin receptor blockers (ARBs) have been associated less commonly with AE. The mechanism for ARB-associated AE has not been elucidated. A meta-analysis showed that in 2% to 17% of patients who were switched to ARBs, recurrence of AE was observed.18 From the pooling of these data with two randomized controlled trials, it is estimated that approximately 10% or less of patients with ACEI-associated AE who switched to ARBs will develop AE.19 In the majority of cases, patients can be switched to ARBs with no recurrence of AE; however, the decision to prescribe an ARB to a patient who has had AE while receiving ACEI should be made carefully on an individualized risk/benefit basis.19
Preventive Treatment
The 17 α-alkylated androgens that can be used for treatment of HAE are danazol (Danacrine), stanozolol (Winstrol), oxandralone (Oxandrine) and methyltestosterone (Android). In patients with HAE, attenuated androgens can significantly reduce the frequency and severity of attacks; however, their use is limited by risk for untoward effects (virilization, abnormal liver function tests, change in libido, anxiety, etc.).21 There is also a risk for hepatotoxicity, including development of hepatic adenomas and hepatic carcinoma.
Antifibrinolytics also may have efficacy for HAE, but these agents have been associated with a variety of adverse effects, including nausea and diarrhea, postural hypotension, fatigue, enhanced thrombosis, retinal changes, and teratogenicity.8, 22, 23
In 2009, long-term prophylaxis with C1-INH concentrate was recommended for patients with HAE with frequent or disabling attacks, a history of laryngeal attacks, and poor quality of life. The 2007 International Consensus Algorithm for the Diagnosis, Therapy, and Management of HAE recommended long-term prophylaxis in patients with more than one monthly severe HAE attack, more than five days of disability per month, or any history of airway compromise.24, 25
The decision to prescribe long-term prophylaxis, and the dose/frequency of medication required, should be individualized based on clinical parameters, such as frequency and severity of attacks, and not on C1 INH or C4 levels.
Perioperative Considerations
It is well established that any trauma, including dental procedures or surgery, can precipitate HAE attacks. For this reason, short-term prophylactic treatment in HAE patients undergoing procedures is recommended. Ideally, avoiding endotracheal intubation is the best approach; however, if intubation cannot be avoided, then adequate prophylaxis should be administered.2
Attenuated androgens can be given up to seven days before a procedure, or C1 INH can be administered 24 hours in advance. If C1 INH is unavailable, FFP can be given six to 12 hours in advance in patients who are not symptomatic; in case of endotracheal intubation, either FFP or C1 INH should be administered immediately before.2
Several case reports in multiple specialty surgical patients (abdominal surgery, cardiopulmonary bypass, orthopedic surgery, etc.) have confirmed the successful use of C1 INH in the prevention of acute attacks with favorable outcomes.2
There is no need to follow C1 INH levels, as it has no clinical relevance.
Back to the Case
The patient was admitted to the ICU and received a total of eight units of FFP. He was transferred to our institution and was able to be extubated three days after initial presentation. Laboratory studies revealed C4 10mg/dL and C1 esterase inhibitor 10mg/dL (both low).
Danazol was resumed. However, within several months after discharge, Cinryze became available in the U.S. market and was eventually prescribed. The patient has not had further significant attacks requiring inpatient management.
Dr. Auron is an assistant professor of medicine and pediatrics at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University. Dr. Lang is co-director of the Asthma Center and director of the Allergy/Immunology Fellowship Training Program at the Cleveland Clinic.
References
- Bernstein, JA. Update on angioedema: evaluation, diagnosis, and treatment. Allergy Asthma Proc. 2011;32(6):408-412.
- Levy JH, Freiberger DJ, Roback J. Hereditary angioedema: current and emerging treatment options. Anesth Analg. 2010;110(5):1271-1280.
- Busse PJ. Angioedema: Differential diagnosis and treatment. Allergy Asthma Proc. 2011;32:Suppl 1:S3-S11.
- Khan DA. Hereditary angioedema: historical aspects, classification, pathophysiology, clinical presentation, and laboratory diagnosis. Allergy Asthma Proc. 2011;32(1):1-10.
- Bork K, Meng G, Staubach P, Hardt, J. Hereditary angioedema: new findings concerning symptoms, affected organs, and course. Am J Med. 2006;119(3):267-274.
- Zuraw BL, Christiansen SC. Pathogenesis and laboratory diagnosis of hereditary angioedema. Allergy Asthma Proc. 2009;30:487-492.
- Frazer-Abel A, Giclas PC. Update on laboratory tests for the diagnosis and differentiation of hereditary angioedema and acquired angioedema. Allergy Asthma Proc. 2011;32:Suppl 1:S17-S21.
- Banerjee A. Current treatment of hereditary angioedema: an update on clinical studies. Allergy Asthma Proc. 2010;31:398-406.
- Donaldson VH. Therapy of "the neurotic edema." N Engl J Med. 1972;286(15):835-836.
- Riedl MA. Update on the acute treatment of hereditary angioedema. Allergy Asthma Proc. 2011;32:11-16.
- Zuraw BL, Busse PJ, White M, et al. Nanofiltered C1 inhibitor concentrate for treatment of hereditary angioedema. N Engl J Med. 2010;363:513-522.
- Cicardi M, Levy RJ, McNeil DL. Ecallantide for the treatment of acute attacks in hereditary angioedema. N Engl J Med. 2010;363:523-531.
- Caballero T, Farkas H, Bouillet L, et al. International consensus and practical guidelines on the gynecologic and obstetric management of female patients with hereditary angioedema caused by C1 inhibitor deficiency. J Allergy Clin Immunol. 2012;129(2):308-320.
- Cicardi M, Zanichelli A. Acquired angioedema. J Allergy Clin Immunol. 2010;6(1):14.
- Zanichelli A, Badini M, Nataloni I, Montano N, Cicardi M. Treatment of acquired angioedema with icatibant: a case report. Intern Emerg Med. 2011;6(3):279-280.
- Byrd JB, Adam A, Brown NJ. Angiotensin-converting enzyme inhibitor-associated angioedema. Immunol Allergy Clin North Am. 2006;26(4):725-737.
- Haymore BR, Yoon J, Mikita CP, Klote MM, DeZee KJ. Risk of angioedema with angiotensin receptor blockers in patients with prior angioedema associated with angiotensin-converting enzyme inhibitors: a meta-analysis. Ann Allergy Asthma Immunol. 2008;101(5):495-499.
- Beavers CJ, Dunn SP, Macaulay TE. The role of angiotensin receptor blockers in patients with angiotensin-converting enzyme inhibitor-induced angioedema. Ann Pharmacother. 2011;45(4):520-524.
- Nzeako UC. Diagnosis and management of angioedema with abdominal involvement: a gastroenterology perspective. World J Gastroenterol. 2010; 16(39):4913-4921.
- Banerji A, Sloane DE, Sheffer AL. Hereditary angioedema: a current state-of-the-art review, V: attenuated androgens for the treatment of hereditary angioedema. Ann Allergy Asthma Immunol. 2008;100(1) (Suppl 2):S19-22.
- Zuraw BL. Clinical practice. Hereditary angioedema. N Engl J Med. 2008; 359(10):1027-1036.
- Zuraw BL. Hereditary angioedema: a current state-of-the-art review, IV: short- and long-term treatment of hereditary angioedema: out with the old and in with the new? Ann Allergy Asthma Immunol. 2008;100(1) (Suppl 2):S13-S18.
- Bowen T, Cicardi M, Bork K, et al. Hereditary angioedema: a current state-of-the-art review, VII: Canadian Hungarian 2007 International Consensus Algorithm for the Diagnosis, Therapy, and Management of Hereditary Angioedema. Ann Allergy Asthma Immunol. 2008;100(1)(Suppl 2):S30-40.
- Craig T, Riedl M, Dykewicz M, et al. When is prophylaxis for hereditary angioedema necessary? Ann Allergy Asthma Immunol. 2009.102(5):366-372.
- Frank MM. Update on preventive therapy (prophylaxis) of hereditary angioedema. Allergy Asthma Proc. 2011;32(1):17-21.
Nonurgent Pediatric Admissions on Weekends Bump Up Hospital Costs
Clinical question: Do weekend admissions for failure to thrive (FTT) result in higher costs and length of stay (LOS)?
Background: FTT accounts for up to 5% of all admissions for children younger than 2 years of age. The optimal approach to inpatient or outpatient care is not well defined. Hospitalizations sometimes are used to facilitate costly and intense workups for organic disease. Given the nonurgent nature of this condition and expected barriers to efficient workup on weekends, it is likely that weekend admissions for FTT might not add much value.
Study design: Retrospective cohort study.
Setting: Forty-two tertiary-care pediatric hospitals.
Synopsis: A total of 23,332 children younger than 2 were studied over an eight-year period. Saturday and Sunday admissions resulted in an average increase in LOS by 1.93 days and an increase in cost by $2,785 when compared with weekday admissions. Patients admitted on weekends were more likely to have imaging studies and lab tests performed, but were less likely to have a discharge diagnosis of FTT. The authors estimate that if one-half of the weekend admissions from 2010 with a consistent FTT diagnosis at admission and discharge were converted to a Monday admission, $534,145 in savings to the health-care system would result.
One notable limitation of the authors’ conclusions is that patients admitted on weekends appeared to have more organic diagnoses documented and might in fact have been more acutely ill, requiring more workup and intervention. Researchers were not able to further explore this using the administrative data. Nonetheless, a subset of weekend admissions with a consistent FTT diagnosis appeared to represent no value added to the system, and potentially could have resulted in a $3.5 million cost savings had they simply been admitted instead on a weekday.
Bottom line: Nonurgent weekend admissions for FTT are inefficient.
Citation: Thompson RT, Bennett WE, Finnell SME, Downs SM. Increased length of stay and costs associated with weekend admissions for failure to thrive. Pediatrics. 2012;131:e805-e810.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: Do weekend admissions for failure to thrive (FTT) result in higher costs and length of stay (LOS)?
Background: FTT accounts for up to 5% of all admissions for children younger than 2 years of age. The optimal approach to inpatient or outpatient care is not well defined. Hospitalizations sometimes are used to facilitate costly and intense workups for organic disease. Given the nonurgent nature of this condition and expected barriers to efficient workup on weekends, it is likely that weekend admissions for FTT might not add much value.
Study design: Retrospective cohort study.
Setting: Forty-two tertiary-care pediatric hospitals.
Synopsis: A total of 23,332 children younger than 2 were studied over an eight-year period. Saturday and Sunday admissions resulted in an average increase in LOS by 1.93 days and an increase in cost by $2,785 when compared with weekday admissions. Patients admitted on weekends were more likely to have imaging studies and lab tests performed, but were less likely to have a discharge diagnosis of FTT. The authors estimate that if one-half of the weekend admissions from 2010 with a consistent FTT diagnosis at admission and discharge were converted to a Monday admission, $534,145 in savings to the health-care system would result.
One notable limitation of the authors’ conclusions is that patients admitted on weekends appeared to have more organic diagnoses documented and might in fact have been more acutely ill, requiring more workup and intervention. Researchers were not able to further explore this using the administrative data. Nonetheless, a subset of weekend admissions with a consistent FTT diagnosis appeared to represent no value added to the system, and potentially could have resulted in a $3.5 million cost savings had they simply been admitted instead on a weekday.
Bottom line: Nonurgent weekend admissions for FTT are inefficient.
Citation: Thompson RT, Bennett WE, Finnell SME, Downs SM. Increased length of stay and costs associated with weekend admissions for failure to thrive. Pediatrics. 2012;131:e805-e810.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.
Clinical question: Do weekend admissions for failure to thrive (FTT) result in higher costs and length of stay (LOS)?
Background: FTT accounts for up to 5% of all admissions for children younger than 2 years of age. The optimal approach to inpatient or outpatient care is not well defined. Hospitalizations sometimes are used to facilitate costly and intense workups for organic disease. Given the nonurgent nature of this condition and expected barriers to efficient workup on weekends, it is likely that weekend admissions for FTT might not add much value.
Study design: Retrospective cohort study.
Setting: Forty-two tertiary-care pediatric hospitals.
Synopsis: A total of 23,332 children younger than 2 were studied over an eight-year period. Saturday and Sunday admissions resulted in an average increase in LOS by 1.93 days and an increase in cost by $2,785 when compared with weekday admissions. Patients admitted on weekends were more likely to have imaging studies and lab tests performed, but were less likely to have a discharge diagnosis of FTT. The authors estimate that if one-half of the weekend admissions from 2010 with a consistent FTT diagnosis at admission and discharge were converted to a Monday admission, $534,145 in savings to the health-care system would result.
One notable limitation of the authors’ conclusions is that patients admitted on weekends appeared to have more organic diagnoses documented and might in fact have been more acutely ill, requiring more workup and intervention. Researchers were not able to further explore this using the administrative data. Nonetheless, a subset of weekend admissions with a consistent FTT diagnosis appeared to represent no value added to the system, and potentially could have resulted in a $3.5 million cost savings had they simply been admitted instead on a weekday.
Bottom line: Nonurgent weekend admissions for FTT are inefficient.
Citation: Thompson RT, Bennett WE, Finnell SME, Downs SM. Increased length of stay and costs associated with weekend admissions for failure to thrive. Pediatrics. 2012;131:e805-e810.
Reviewed by Pediatric Editor Mark Shen, MD, SFHM, medical director of hospital medicine at Dell Children's Medical Center, Austin, Texas.