User login
Daily Sedation Interruption among Intubated Not Helpful
Clinical question: Does sedation by protocol, in combination with daily sedative interruption, reduce the duration of mechanical ventilation and ICU stay?
Background: Limiting excessive sedation in mechanically ventilated adults is associated with shorter duration of mechanical ventilation and lower risk of delirium. Two strategies to minimize sedation are daily sedation interruptions and protocolized sedation. These strategies have not been evaluated in combination.
Study design: Randomized controlled trial.
Setting: Tertiary-care medical and surgical ICUs in Canada and the U.S.
Synopsis: This randomized controlled trial conducted in 430 critically ill, mechanically ventilated adults at 16 tertiary-care ICUs showed no difference in time to extubation (mean seven days in each group) or ICU length of stay (mean 10 days in each group) in protocolized sedation and sedation interruption compared with protocolized sedation alone. The daily interruption group received higher mean daily doses of midazolam and fentanyl, increased number of boluses of benzodiazepines and opiates, and required increased nurse workload. There was no difference in unintentional endotracheal tube removal or rate of delirium.
A limitation of this study was the use of continuous opioid and/or benzodiazepine infusions instead of bolus dosing. Hospitalists involved in critical care should be careful about changing their practice based on this study alone.
Bottom line: The addition of daily sedation interruptions in mechanically ventilated patients treated with protocolized sedation does not reduce duration of ventilation or ICU stay.
Citation: Mehta S, Burry L, Cook D, et al. Daily sedation interruption in mechanically ventilated critically ill patients cared for with a sedation protocol. JAMA. 2012;308:1985-1992.
Clinical question: Does sedation by protocol, in combination with daily sedative interruption, reduce the duration of mechanical ventilation and ICU stay?
Background: Limiting excessive sedation in mechanically ventilated adults is associated with shorter duration of mechanical ventilation and lower risk of delirium. Two strategies to minimize sedation are daily sedation interruptions and protocolized sedation. These strategies have not been evaluated in combination.
Study design: Randomized controlled trial.
Setting: Tertiary-care medical and surgical ICUs in Canada and the U.S.
Synopsis: This randomized controlled trial conducted in 430 critically ill, mechanically ventilated adults at 16 tertiary-care ICUs showed no difference in time to extubation (mean seven days in each group) or ICU length of stay (mean 10 days in each group) in protocolized sedation and sedation interruption compared with protocolized sedation alone. The daily interruption group received higher mean daily doses of midazolam and fentanyl, increased number of boluses of benzodiazepines and opiates, and required increased nurse workload. There was no difference in unintentional endotracheal tube removal or rate of delirium.
A limitation of this study was the use of continuous opioid and/or benzodiazepine infusions instead of bolus dosing. Hospitalists involved in critical care should be careful about changing their practice based on this study alone.
Bottom line: The addition of daily sedation interruptions in mechanically ventilated patients treated with protocolized sedation does not reduce duration of ventilation or ICU stay.
Citation: Mehta S, Burry L, Cook D, et al. Daily sedation interruption in mechanically ventilated critically ill patients cared for with a sedation protocol. JAMA. 2012;308:1985-1992.
Clinical question: Does sedation by protocol, in combination with daily sedative interruption, reduce the duration of mechanical ventilation and ICU stay?
Background: Limiting excessive sedation in mechanically ventilated adults is associated with shorter duration of mechanical ventilation and lower risk of delirium. Two strategies to minimize sedation are daily sedation interruptions and protocolized sedation. These strategies have not been evaluated in combination.
Study design: Randomized controlled trial.
Setting: Tertiary-care medical and surgical ICUs in Canada and the U.S.
Synopsis: This randomized controlled trial conducted in 430 critically ill, mechanically ventilated adults at 16 tertiary-care ICUs showed no difference in time to extubation (mean seven days in each group) or ICU length of stay (mean 10 days in each group) in protocolized sedation and sedation interruption compared with protocolized sedation alone. The daily interruption group received higher mean daily doses of midazolam and fentanyl, increased number of boluses of benzodiazepines and opiates, and required increased nurse workload. There was no difference in unintentional endotracheal tube removal or rate of delirium.
A limitation of this study was the use of continuous opioid and/or benzodiazepine infusions instead of bolus dosing. Hospitalists involved in critical care should be careful about changing their practice based on this study alone.
Bottom line: The addition of daily sedation interruptions in mechanically ventilated patients treated with protocolized sedation does not reduce duration of ventilation or ICU stay.
Citation: Mehta S, Burry L, Cook D, et al. Daily sedation interruption in mechanically ventilated critically ill patients cared for with a sedation protocol. JAMA. 2012;308:1985-1992.
Risk for Falls Might Not Affect Anticoagulation Decision
Clinical question: Do patients on oral anticoagulation with high fall risk have an increased incidence of major bleeding?
Background: Despite proven efficacy, oral anticoagulation remains underprescribed. The most commonly cited reasons for not providing oral anticoagulation when clinically indicated are risk of falls and concern for major bleeding.
Study design: Prospective cohort study.
Setting: Internal-medicine inpatient and outpatient services of a university hospital in Switzerland.
Synopsis: This study followed 515 patients on oral anticoagulation for 12 months. Patients at high risk for falls were identified using validated questions known to predict fall risk. Overall, 35 patients had a first major bleed. In multivariate analysis, high fall risk was not associated with an increased incidence of major bleeding (hazard ratio 1.09; 95% confidence interval, 0.54-2.21). Only 1 in 3 fall-related bleeds occurred in the high-fall-risk group.
This study was limited significantly by selection bias. The majority of patients studied already were on anticoagulation therapy for at least three months prior to enrolling in the study, presumably without major bleeding. It is probable that some higher-risk patients were not offered anticoagulation at all and would have been ineligible for the study. This study cohort might have had a lower bleeding risk than members of the general population being started on anticoagulation.
Bottom line: This prospective cohort study shows that patients on oral anticoagulation at high risk of falls did not have significantly increased rates of major bleeding; however, selection bias might have led to an underestimation of bleeding risk. Hospitalists should continue to individualize anticoagulation decisions.
Citation: Donzé J, Clair C, Hug B, et al. Risk of falls and major bleeds in patients on oral anticoagulation therapy. Am J Med. 2012;125:773-778.
Clinical question: Do patients on oral anticoagulation with high fall risk have an increased incidence of major bleeding?
Background: Despite proven efficacy, oral anticoagulation remains underprescribed. The most commonly cited reasons for not providing oral anticoagulation when clinically indicated are risk of falls and concern for major bleeding.
Study design: Prospective cohort study.
Setting: Internal-medicine inpatient and outpatient services of a university hospital in Switzerland.
Synopsis: This study followed 515 patients on oral anticoagulation for 12 months. Patients at high risk for falls were identified using validated questions known to predict fall risk. Overall, 35 patients had a first major bleed. In multivariate analysis, high fall risk was not associated with an increased incidence of major bleeding (hazard ratio 1.09; 95% confidence interval, 0.54-2.21). Only 1 in 3 fall-related bleeds occurred in the high-fall-risk group.
This study was limited significantly by selection bias. The majority of patients studied already were on anticoagulation therapy for at least three months prior to enrolling in the study, presumably without major bleeding. It is probable that some higher-risk patients were not offered anticoagulation at all and would have been ineligible for the study. This study cohort might have had a lower bleeding risk than members of the general population being started on anticoagulation.
Bottom line: This prospective cohort study shows that patients on oral anticoagulation at high risk of falls did not have significantly increased rates of major bleeding; however, selection bias might have led to an underestimation of bleeding risk. Hospitalists should continue to individualize anticoagulation decisions.
Citation: Donzé J, Clair C, Hug B, et al. Risk of falls and major bleeds in patients on oral anticoagulation therapy. Am J Med. 2012;125:773-778.
Clinical question: Do patients on oral anticoagulation with high fall risk have an increased incidence of major bleeding?
Background: Despite proven efficacy, oral anticoagulation remains underprescribed. The most commonly cited reasons for not providing oral anticoagulation when clinically indicated are risk of falls and concern for major bleeding.
Study design: Prospective cohort study.
Setting: Internal-medicine inpatient and outpatient services of a university hospital in Switzerland.
Synopsis: This study followed 515 patients on oral anticoagulation for 12 months. Patients at high risk for falls were identified using validated questions known to predict fall risk. Overall, 35 patients had a first major bleed. In multivariate analysis, high fall risk was not associated with an increased incidence of major bleeding (hazard ratio 1.09; 95% confidence interval, 0.54-2.21). Only 1 in 3 fall-related bleeds occurred in the high-fall-risk group.
This study was limited significantly by selection bias. The majority of patients studied already were on anticoagulation therapy for at least three months prior to enrolling in the study, presumably without major bleeding. It is probable that some higher-risk patients were not offered anticoagulation at all and would have been ineligible for the study. This study cohort might have had a lower bleeding risk than members of the general population being started on anticoagulation.
Bottom line: This prospective cohort study shows that patients on oral anticoagulation at high risk of falls did not have significantly increased rates of major bleeding; however, selection bias might have led to an underestimation of bleeding risk. Hospitalists should continue to individualize anticoagulation decisions.
Citation: Donzé J, Clair C, Hug B, et al. Risk of falls and major bleeds in patients on oral anticoagulation therapy. Am J Med. 2012;125:773-778.
Improving Transitions from ED to Inpatient Care
Clinical question: Can a multidisciplinary focus group identify “best practices” for ensuring efficient and effective transitions of care between the ED and the inpatient setting?
Background: In the admission process, communication failures can lead to preventable adverse effects. Little has been done to evaluate or improve the interservice handoff between the ED physician and the HM physician.
Study design: Concept article.
Synopsis: Handoffs between ED physicians and HM physicians are complex due to differing pressures, cultures, and expectations. The authors recommend an interactive handoff conversation that is organized, focuses on key principles, and is accompanied by a mutual understanding of the differences between specialties. ED physicians and hospitalists should work together to develop joint expectations on content, delivery, and timing of patient handoffs.
One proposed method includes the current clinical condition of the patient, a working problem statement with degree of certainty and rationale, essential aspects of the history and physical, a brief summary of the ED course, analysis of key tests, pending data with unambiguous assignment for follow-up, and any unusual circumstances. Further research is required to determine if these suggestions improve patient outcomes.
Bottom line: Joint expectations and standardized handoff methods between emergency physicians and hospitalists are likely to foster improved communication and patient care.
Citation: Beach C, Cheung DS, Apker J, et al. Improving inter-unit transitions of care between emergency physicians and hospital medicine physicians: a conceptual approach. Acad Emerg Med. 2012;19:1188-1195.
Clinical question: Can a multidisciplinary focus group identify “best practices” for ensuring efficient and effective transitions of care between the ED and the inpatient setting?
Background: In the admission process, communication failures can lead to preventable adverse effects. Little has been done to evaluate or improve the interservice handoff between the ED physician and the HM physician.
Study design: Concept article.
Synopsis: Handoffs between ED physicians and HM physicians are complex due to differing pressures, cultures, and expectations. The authors recommend an interactive handoff conversation that is organized, focuses on key principles, and is accompanied by a mutual understanding of the differences between specialties. ED physicians and hospitalists should work together to develop joint expectations on content, delivery, and timing of patient handoffs.
One proposed method includes the current clinical condition of the patient, a working problem statement with degree of certainty and rationale, essential aspects of the history and physical, a brief summary of the ED course, analysis of key tests, pending data with unambiguous assignment for follow-up, and any unusual circumstances. Further research is required to determine if these suggestions improve patient outcomes.
Bottom line: Joint expectations and standardized handoff methods between emergency physicians and hospitalists are likely to foster improved communication and patient care.
Citation: Beach C, Cheung DS, Apker J, et al. Improving inter-unit transitions of care between emergency physicians and hospital medicine physicians: a conceptual approach. Acad Emerg Med. 2012;19:1188-1195.
Clinical question: Can a multidisciplinary focus group identify “best practices” for ensuring efficient and effective transitions of care between the ED and the inpatient setting?
Background: In the admission process, communication failures can lead to preventable adverse effects. Little has been done to evaluate or improve the interservice handoff between the ED physician and the HM physician.
Study design: Concept article.
Synopsis: Handoffs between ED physicians and HM physicians are complex due to differing pressures, cultures, and expectations. The authors recommend an interactive handoff conversation that is organized, focuses on key principles, and is accompanied by a mutual understanding of the differences between specialties. ED physicians and hospitalists should work together to develop joint expectations on content, delivery, and timing of patient handoffs.
One proposed method includes the current clinical condition of the patient, a working problem statement with degree of certainty and rationale, essential aspects of the history and physical, a brief summary of the ED course, analysis of key tests, pending data with unambiguous assignment for follow-up, and any unusual circumstances. Further research is required to determine if these suggestions improve patient outcomes.
Bottom line: Joint expectations and standardized handoff methods between emergency physicians and hospitalists are likely to foster improved communication and patient care.
Citation: Beach C, Cheung DS, Apker J, et al. Improving inter-unit transitions of care between emergency physicians and hospital medicine physicians: a conceptual approach. Acad Emerg Med. 2012;19:1188-1195.
Serious Complications from Opioid Overuse in Hospitalized Patients Prompts Nationwide Alert
Opioid overuse can spell the onset of onerous consequences. The analgesics can slow breathing to dangerous levels and lead to dizziness, nausea, and falls.
Citing these concerns, The Joint Commission issued a Sentinel Event Alert in August 2012 that urged hospitals to take specific measures to help avoid serious complications and even deaths from the use of such opioids as morphine, oxycodone, and methadone.
“The Joint Commission recognizes that there is an opportunity to improve the care of patients on opioids in acute-care settings,” spokeswoman Elizabeth Eaken Zhani says. “Healthcare workers need to be aware of the risks to patients in prescribing opioids.”
Adverse events involving opioids include dosing errors and improper monitoring of patients and drug interactions. Patients who have sleep apnea, are obese, or very ill—with such conditions as pulmonary disease, congestive heart failure, or impaired renal function—might be at higher risk for harm from opioids.
—Beth B. Murinson, MS, MD, PhD, associate professor, director of pain education, department of neurology, The Johns University Hopkins School of Medicine, Baltimore
“The alert was issued in response to concerns that opioid analgesics are among the top three drugs in which medication-related adverse events are reported to The Joint Commission,” Zhani says. “They also rank among the drugs most frequently associated with adverse drug events.”
Opioids are associated with numerous problems—underprescribing, overprescribing, tolerance, dependence, and drug abuse. To prevent accidental overuse, The Joint Commission recommends that healthcare organizations provide ongoing oversight of patients receiving these drugs. Pain-management specialists or pharmacists should review treatment plans and also track incidents involving opioids.
Harnessing available technology also helps improve prescribing safety. In addition to creating alerts for dosing limits, The Joint Commission suggests using “tall man” lettering in electronic ordering systems, conversion support to calculate correct dosages, and patient-controlled analgesia. Education and training in the safe use of opioids should be provided for clinicians, staff, and patients. And standardized tools should be employed to screen patients for risk factors, such as oversedation and respiratory depression.
“Opioids aren’t dangerous in themselves,” says Solomon Liao, MD, FAAHPM, a hospitalist and director of palliative-care services at the University of California at Irvine. “Opioids are dangerous when prescribers don’t know what they’re doing. It’s like the old saying, ‘Guns don’t kill people; people kill people.’”
Overdose deaths from opioid pain relievers have escalated, nearly quadrupling from 1999 to 2008. These deaths now exceed fatalities due to heroin and cocaine combined. In 2008, drug overdoses in the United States caused 36,450 deaths; opioid analgesics were involved in 14,800 (73.8%) of 20,044 prescription drug overdose deaths, according to the Centers for Disease Control and Prevention.1
Vital statistics data suggest that methadone is involved in one-third of opioid pain-reliever-related overdose deaths, even though it accounts for only a small percentage of prescriptions for opioid analgesics. The rate of methadone overdose deaths in the U.S. in 2009 was 5.5 times the rate in 1999, prompting an urgent call for interventions to address misuse and abuse.2
“The greatest safety concern The Joint Commission’s report cites is that sedation precedes respiratory depression in many cases, and clinicians need to pay more attention to that side effect and patients who are inherently at risk for developing respiratory problems related to opioids,” says Paul Arnstein, RN, PhD, FAAN, Connell Nursing Research Scholar and clinical nurse specialist for pain relief at Massachusetts General Hospital in Boston.
A Double-Edged Sword
Opioids deliver good pain control with minimal adverse effects for some patients but not for others, and there is insufficient evidence to foresee who will fare well and who won’t. “What we can predict,” Arnstein says, “is that certain patients—the very old, very young, very ill, and those receiving medicines that interact with opioids—are vulnerable to some of the more dangerous effects.”
The risk of respiratory depression also mounts in those who are opioid-naïve, as well as in an increasingly obese population.
“This does not mean we withhold pain relief,” says Judith A. Paice, PhD, RN, a contributor to The Joint Commission’s alert and director of the cancer pain program in the hematology-oncology division at Northwestern University’s Feinberg School of Medicine. Instead, “we need to determine the most effective monitoring techniques in a setting where hospitals are cutting back on staffing,” she adds.
Other risk factors for respiratory depression include sleep apnea (correlated with obesity but also possible in the absence of excess weight), large thoracic or abdominal incisions, and use of other sedating drugs. Among patients in the chronic cancer pain or palliative-care setting, respiratory depression is highly unusual because dosages are increased gradually, Paice says. Strong consensus supports prescribing opioids for acute episodes of pain, as well as chronic management of cancer and other life-threatening illnesses, including HIV/AIDS and cardiac and neuromuscular conditions.
Considerable variations exist in screening for risk of opioid-induced sedation and hospital monitoring practices. There is also a shortage of information and no consensus on the advantages of costly technology-supported monitoring, such as pulse oximetry (measuring oxygen saturation) and capnography (measuring end-tidal carbon dioxide), in hospitalized patients receiving opioids for pain therapy, according to guidelines from the American Society for Pain Management Nursing.3
Although technological monitoring adds valuable data to patient status, it does not replace frequent assessments—the most important intervention in detecting sedation before respiratory depression. Technological monitoring should be considered for patients at high risk for decline, says the guidelines’ lead author, Donna Jarzyna, MS, RN-BC, CNS-BC, an adult health clinical nurse specialist consulting in an alumna role for the University of Arizona Medical Center in Tucson. “Many organizations are currently making an effort,” she says, “to determine which patients should be monitored with a higher degree of intensity and with greater frequency.”
Patient-controlled analgesia (PCA) also has some limitations. In theory, it offers built-in safety features—if patients become too sedated, they can’t push a button for extra doses—but that isn’t always the case. For instance, some patients may have “stacked” three to four doses before sedation and respiratory depression develop. “When things go wrong with PCA, patients are four times more likely to be seriously harmed than when nurses administer the medications,” says Arnstein, who is a past president of the American Society for Pain Management Nursing. “Thus, vigilant nurse-supervised opioid therapy is vitally important.”

—Paul Arnstein, RN, PhD, FAAN, Connell Nursing Research Scholar, clinical nurse specialist for pain relief, Massachusetts General Hospital, Boston
Simple Steps Save Lives
Most critical events associated with opioids occur during the first 24 hours of post-operative care. Combined with close monitoring, understanding the risk factors for respiratory depression and making adjustments based on an individual’s needs and response helps prevent a precarious situation in which a patient vacillates quickly from a wide-awake status to a sleepy state.
“There’s a very progressive amount of sedation,” says Deb Gordon, RN, DNP, FAAN, a contributor to The Joint Commission’s alert and a teaching associate in the department of anesthesiology and pain medicine at the University of Washington in Seattle.
Developing a pain treatment plan with a reassessment component is essential to exercising caution against potential harm from opioids.
“The Joint Commission’s guidance is wonderfully helpful and will benefit patients,” says Beth B. Murinson, MS, MD, PhD, associate professor and director of pain education in the department of neurology at Johns Hopkins University School of Medicine in Baltimore. “Getting opioid pain relief right is critically important as lives are hanging in the balance on both sides of this problem: Too little pain relief and millions will suffer; too much and lives are at risk.”
Hospitalists should be familiar with a few opioids that they feel comfortable prescribing, Dr. Murinson says. Be prepared to easily identify the major idiosyncratic effects and ordinary side effects of these medications and become well versed in opioid conversion.
“This is a classic problem in the field because, although the opioids are generally similar in their efficacy against pain, they have markedly different potencies against pain,” she explains. “A dose of 2 mg of morphine may need to be ‘converted’ to X mg of another opioid, depending on local practice patterns and preferences.”
Some drugs pose special risks. For example, transdermal fentanyl is “appropriate only for use in people who need opioid-level analgesia for an extended period of time and whose analgesic requirements are stable. This is not the case for folks with acute pain or who are just starting on opioids,” cautions Scott Strassels, PhD, PharmD, BCPS, assistant professor in the College of Pharmacy at the University of Texas in Austin and a board member of the American Pain Society. “Similarly, methadone is a good analgesic, but it requires very careful use due to its pharmacokinetic profile.”
Healthcare professionals from a variety of disciplines should be involved in pain-management efforts within a hospital setting. As for who takes the initiative, “it probably should be the person who is most qualified—be it a physician, nurse, or pharmacist,” Strassels says. “I’ve seen pharmacist-led teams, nurse-led teams, and those with physicians leading the effort.”
Clinicians who prescribe pain medications should be cognizant of nonpharmacologic alternatives to opioids. Multimodal options include physical therapy, acupuncture, manipulation or massage, and non-narcotic analgesics, such as acetaminophen and muscle relaxants. Non-narcotics may lower the dose of opioids needed to effectively manage pain, according to The Joint Commission.
The alert also provides information on suggested actions to avoid unintended consequences of using opioids. Hospitals should fully inform and provide written instructions to the patient and family or caregiver about the potential risks of tolerance, addiction, physical dependency, and withdrawal from opioids. When providing this information at discharge, the hospital also should list phone numbers to call if there are any questions.
In some unfortunate cases, opioids prescribed for pain also are used by patients’ family members, friends, and others. In such instances, says Northwestern’s Paice, usage occurs commonly with polypharmacy and without monitoring, and this contributes to an increased risk of death associated with opioids.
“There is concern that drugs prescribed for legitimate purposes are reaching the wrong hands,” Paice says. “We need to make the public, particularly patients and their family members, aware of safety strategies.”
Susan Kreimer is a freelance writer in New York City.
References
- Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-1492.
- Centers for Disease Control and Prevention. Vital signs: risk for overdose from methadone used for pain relief—United States, 1999-2010. MMWR Morb Mortal Wkly Rep. 2012;61(26):493-497.
- Jarzyna D, Jungquist CR, Pasero C, et al. American Society for Pain Management Nursing guidelines on monitoring for opioid-induced sedation and respiratory depression. Pain Manag Nurs. 2011;12(3):118-145.
Opioid overuse can spell the onset of onerous consequences. The analgesics can slow breathing to dangerous levels and lead to dizziness, nausea, and falls.
Citing these concerns, The Joint Commission issued a Sentinel Event Alert in August 2012 that urged hospitals to take specific measures to help avoid serious complications and even deaths from the use of such opioids as morphine, oxycodone, and methadone.
“The Joint Commission recognizes that there is an opportunity to improve the care of patients on opioids in acute-care settings,” spokeswoman Elizabeth Eaken Zhani says. “Healthcare workers need to be aware of the risks to patients in prescribing opioids.”
Adverse events involving opioids include dosing errors and improper monitoring of patients and drug interactions. Patients who have sleep apnea, are obese, or very ill—with such conditions as pulmonary disease, congestive heart failure, or impaired renal function—might be at higher risk for harm from opioids.
—Beth B. Murinson, MS, MD, PhD, associate professor, director of pain education, department of neurology, The Johns University Hopkins School of Medicine, Baltimore
“The alert was issued in response to concerns that opioid analgesics are among the top three drugs in which medication-related adverse events are reported to The Joint Commission,” Zhani says. “They also rank among the drugs most frequently associated with adverse drug events.”
Opioids are associated with numerous problems—underprescribing, overprescribing, tolerance, dependence, and drug abuse. To prevent accidental overuse, The Joint Commission recommends that healthcare organizations provide ongoing oversight of patients receiving these drugs. Pain-management specialists or pharmacists should review treatment plans and also track incidents involving opioids.
Harnessing available technology also helps improve prescribing safety. In addition to creating alerts for dosing limits, The Joint Commission suggests using “tall man” lettering in electronic ordering systems, conversion support to calculate correct dosages, and patient-controlled analgesia. Education and training in the safe use of opioids should be provided for clinicians, staff, and patients. And standardized tools should be employed to screen patients for risk factors, such as oversedation and respiratory depression.
“Opioids aren’t dangerous in themselves,” says Solomon Liao, MD, FAAHPM, a hospitalist and director of palliative-care services at the University of California at Irvine. “Opioids are dangerous when prescribers don’t know what they’re doing. It’s like the old saying, ‘Guns don’t kill people; people kill people.’”
Overdose deaths from opioid pain relievers have escalated, nearly quadrupling from 1999 to 2008. These deaths now exceed fatalities due to heroin and cocaine combined. In 2008, drug overdoses in the United States caused 36,450 deaths; opioid analgesics were involved in 14,800 (73.8%) of 20,044 prescription drug overdose deaths, according to the Centers for Disease Control and Prevention.1
Vital statistics data suggest that methadone is involved in one-third of opioid pain-reliever-related overdose deaths, even though it accounts for only a small percentage of prescriptions for opioid analgesics. The rate of methadone overdose deaths in the U.S. in 2009 was 5.5 times the rate in 1999, prompting an urgent call for interventions to address misuse and abuse.2
“The greatest safety concern The Joint Commission’s report cites is that sedation precedes respiratory depression in many cases, and clinicians need to pay more attention to that side effect and patients who are inherently at risk for developing respiratory problems related to opioids,” says Paul Arnstein, RN, PhD, FAAN, Connell Nursing Research Scholar and clinical nurse specialist for pain relief at Massachusetts General Hospital in Boston.
A Double-Edged Sword
Opioids deliver good pain control with minimal adverse effects for some patients but not for others, and there is insufficient evidence to foresee who will fare well and who won’t. “What we can predict,” Arnstein says, “is that certain patients—the very old, very young, very ill, and those receiving medicines that interact with opioids—are vulnerable to some of the more dangerous effects.”
The risk of respiratory depression also mounts in those who are opioid-naïve, as well as in an increasingly obese population.
“This does not mean we withhold pain relief,” says Judith A. Paice, PhD, RN, a contributor to The Joint Commission’s alert and director of the cancer pain program in the hematology-oncology division at Northwestern University’s Feinberg School of Medicine. Instead, “we need to determine the most effective monitoring techniques in a setting where hospitals are cutting back on staffing,” she adds.
Other risk factors for respiratory depression include sleep apnea (correlated with obesity but also possible in the absence of excess weight), large thoracic or abdominal incisions, and use of other sedating drugs. Among patients in the chronic cancer pain or palliative-care setting, respiratory depression is highly unusual because dosages are increased gradually, Paice says. Strong consensus supports prescribing opioids for acute episodes of pain, as well as chronic management of cancer and other life-threatening illnesses, including HIV/AIDS and cardiac and neuromuscular conditions.
Considerable variations exist in screening for risk of opioid-induced sedation and hospital monitoring practices. There is also a shortage of information and no consensus on the advantages of costly technology-supported monitoring, such as pulse oximetry (measuring oxygen saturation) and capnography (measuring end-tidal carbon dioxide), in hospitalized patients receiving opioids for pain therapy, according to guidelines from the American Society for Pain Management Nursing.3
Although technological monitoring adds valuable data to patient status, it does not replace frequent assessments—the most important intervention in detecting sedation before respiratory depression. Technological monitoring should be considered for patients at high risk for decline, says the guidelines’ lead author, Donna Jarzyna, MS, RN-BC, CNS-BC, an adult health clinical nurse specialist consulting in an alumna role for the University of Arizona Medical Center in Tucson. “Many organizations are currently making an effort,” she says, “to determine which patients should be monitored with a higher degree of intensity and with greater frequency.”
Patient-controlled analgesia (PCA) also has some limitations. In theory, it offers built-in safety features—if patients become too sedated, they can’t push a button for extra doses—but that isn’t always the case. For instance, some patients may have “stacked” three to four doses before sedation and respiratory depression develop. “When things go wrong with PCA, patients are four times more likely to be seriously harmed than when nurses administer the medications,” says Arnstein, who is a past president of the American Society for Pain Management Nursing. “Thus, vigilant nurse-supervised opioid therapy is vitally important.”

—Paul Arnstein, RN, PhD, FAAN, Connell Nursing Research Scholar, clinical nurse specialist for pain relief, Massachusetts General Hospital, Boston
Simple Steps Save Lives
Most critical events associated with opioids occur during the first 24 hours of post-operative care. Combined with close monitoring, understanding the risk factors for respiratory depression and making adjustments based on an individual’s needs and response helps prevent a precarious situation in which a patient vacillates quickly from a wide-awake status to a sleepy state.
“There’s a very progressive amount of sedation,” says Deb Gordon, RN, DNP, FAAN, a contributor to The Joint Commission’s alert and a teaching associate in the department of anesthesiology and pain medicine at the University of Washington in Seattle.
Developing a pain treatment plan with a reassessment component is essential to exercising caution against potential harm from opioids.
“The Joint Commission’s guidance is wonderfully helpful and will benefit patients,” says Beth B. Murinson, MS, MD, PhD, associate professor and director of pain education in the department of neurology at Johns Hopkins University School of Medicine in Baltimore. “Getting opioid pain relief right is critically important as lives are hanging in the balance on both sides of this problem: Too little pain relief and millions will suffer; too much and lives are at risk.”
Hospitalists should be familiar with a few opioids that they feel comfortable prescribing, Dr. Murinson says. Be prepared to easily identify the major idiosyncratic effects and ordinary side effects of these medications and become well versed in opioid conversion.
“This is a classic problem in the field because, although the opioids are generally similar in their efficacy against pain, they have markedly different potencies against pain,” she explains. “A dose of 2 mg of morphine may need to be ‘converted’ to X mg of another opioid, depending on local practice patterns and preferences.”
Some drugs pose special risks. For example, transdermal fentanyl is “appropriate only for use in people who need opioid-level analgesia for an extended period of time and whose analgesic requirements are stable. This is not the case for folks with acute pain or who are just starting on opioids,” cautions Scott Strassels, PhD, PharmD, BCPS, assistant professor in the College of Pharmacy at the University of Texas in Austin and a board member of the American Pain Society. “Similarly, methadone is a good analgesic, but it requires very careful use due to its pharmacokinetic profile.”
Healthcare professionals from a variety of disciplines should be involved in pain-management efforts within a hospital setting. As for who takes the initiative, “it probably should be the person who is most qualified—be it a physician, nurse, or pharmacist,” Strassels says. “I’ve seen pharmacist-led teams, nurse-led teams, and those with physicians leading the effort.”
Clinicians who prescribe pain medications should be cognizant of nonpharmacologic alternatives to opioids. Multimodal options include physical therapy, acupuncture, manipulation or massage, and non-narcotic analgesics, such as acetaminophen and muscle relaxants. Non-narcotics may lower the dose of opioids needed to effectively manage pain, according to The Joint Commission.
The alert also provides information on suggested actions to avoid unintended consequences of using opioids. Hospitals should fully inform and provide written instructions to the patient and family or caregiver about the potential risks of tolerance, addiction, physical dependency, and withdrawal from opioids. When providing this information at discharge, the hospital also should list phone numbers to call if there are any questions.
In some unfortunate cases, opioids prescribed for pain also are used by patients’ family members, friends, and others. In such instances, says Northwestern’s Paice, usage occurs commonly with polypharmacy and without monitoring, and this contributes to an increased risk of death associated with opioids.
“There is concern that drugs prescribed for legitimate purposes are reaching the wrong hands,” Paice says. “We need to make the public, particularly patients and their family members, aware of safety strategies.”
Susan Kreimer is a freelance writer in New York City.
References
- Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-1492.
- Centers for Disease Control and Prevention. Vital signs: risk for overdose from methadone used for pain relief—United States, 1999-2010. MMWR Morb Mortal Wkly Rep. 2012;61(26):493-497.
- Jarzyna D, Jungquist CR, Pasero C, et al. American Society for Pain Management Nursing guidelines on monitoring for opioid-induced sedation and respiratory depression. Pain Manag Nurs. 2011;12(3):118-145.
Opioid overuse can spell the onset of onerous consequences. The analgesics can slow breathing to dangerous levels and lead to dizziness, nausea, and falls.
Citing these concerns, The Joint Commission issued a Sentinel Event Alert in August 2012 that urged hospitals to take specific measures to help avoid serious complications and even deaths from the use of such opioids as morphine, oxycodone, and methadone.
“The Joint Commission recognizes that there is an opportunity to improve the care of patients on opioids in acute-care settings,” spokeswoman Elizabeth Eaken Zhani says. “Healthcare workers need to be aware of the risks to patients in prescribing opioids.”
Adverse events involving opioids include dosing errors and improper monitoring of patients and drug interactions. Patients who have sleep apnea, are obese, or very ill—with such conditions as pulmonary disease, congestive heart failure, or impaired renal function—might be at higher risk for harm from opioids.
—Beth B. Murinson, MS, MD, PhD, associate professor, director of pain education, department of neurology, The Johns University Hopkins School of Medicine, Baltimore
“The alert was issued in response to concerns that opioid analgesics are among the top three drugs in which medication-related adverse events are reported to The Joint Commission,” Zhani says. “They also rank among the drugs most frequently associated with adverse drug events.”
Opioids are associated with numerous problems—underprescribing, overprescribing, tolerance, dependence, and drug abuse. To prevent accidental overuse, The Joint Commission recommends that healthcare organizations provide ongoing oversight of patients receiving these drugs. Pain-management specialists or pharmacists should review treatment plans and also track incidents involving opioids.
Harnessing available technology also helps improve prescribing safety. In addition to creating alerts for dosing limits, The Joint Commission suggests using “tall man” lettering in electronic ordering systems, conversion support to calculate correct dosages, and patient-controlled analgesia. Education and training in the safe use of opioids should be provided for clinicians, staff, and patients. And standardized tools should be employed to screen patients for risk factors, such as oversedation and respiratory depression.
“Opioids aren’t dangerous in themselves,” says Solomon Liao, MD, FAAHPM, a hospitalist and director of palliative-care services at the University of California at Irvine. “Opioids are dangerous when prescribers don’t know what they’re doing. It’s like the old saying, ‘Guns don’t kill people; people kill people.’”
Overdose deaths from opioid pain relievers have escalated, nearly quadrupling from 1999 to 2008. These deaths now exceed fatalities due to heroin and cocaine combined. In 2008, drug overdoses in the United States caused 36,450 deaths; opioid analgesics were involved in 14,800 (73.8%) of 20,044 prescription drug overdose deaths, according to the Centers for Disease Control and Prevention.1
Vital statistics data suggest that methadone is involved in one-third of opioid pain-reliever-related overdose deaths, even though it accounts for only a small percentage of prescriptions for opioid analgesics. The rate of methadone overdose deaths in the U.S. in 2009 was 5.5 times the rate in 1999, prompting an urgent call for interventions to address misuse and abuse.2
“The greatest safety concern The Joint Commission’s report cites is that sedation precedes respiratory depression in many cases, and clinicians need to pay more attention to that side effect and patients who are inherently at risk for developing respiratory problems related to opioids,” says Paul Arnstein, RN, PhD, FAAN, Connell Nursing Research Scholar and clinical nurse specialist for pain relief at Massachusetts General Hospital in Boston.
A Double-Edged Sword
Opioids deliver good pain control with minimal adverse effects for some patients but not for others, and there is insufficient evidence to foresee who will fare well and who won’t. “What we can predict,” Arnstein says, “is that certain patients—the very old, very young, very ill, and those receiving medicines that interact with opioids—are vulnerable to some of the more dangerous effects.”
The risk of respiratory depression also mounts in those who are opioid-naïve, as well as in an increasingly obese population.
“This does not mean we withhold pain relief,” says Judith A. Paice, PhD, RN, a contributor to The Joint Commission’s alert and director of the cancer pain program in the hematology-oncology division at Northwestern University’s Feinberg School of Medicine. Instead, “we need to determine the most effective monitoring techniques in a setting where hospitals are cutting back on staffing,” she adds.
Other risk factors for respiratory depression include sleep apnea (correlated with obesity but also possible in the absence of excess weight), large thoracic or abdominal incisions, and use of other sedating drugs. Among patients in the chronic cancer pain or palliative-care setting, respiratory depression is highly unusual because dosages are increased gradually, Paice says. Strong consensus supports prescribing opioids for acute episodes of pain, as well as chronic management of cancer and other life-threatening illnesses, including HIV/AIDS and cardiac and neuromuscular conditions.
Considerable variations exist in screening for risk of opioid-induced sedation and hospital monitoring practices. There is also a shortage of information and no consensus on the advantages of costly technology-supported monitoring, such as pulse oximetry (measuring oxygen saturation) and capnography (measuring end-tidal carbon dioxide), in hospitalized patients receiving opioids for pain therapy, according to guidelines from the American Society for Pain Management Nursing.3
Although technological monitoring adds valuable data to patient status, it does not replace frequent assessments—the most important intervention in detecting sedation before respiratory depression. Technological monitoring should be considered for patients at high risk for decline, says the guidelines’ lead author, Donna Jarzyna, MS, RN-BC, CNS-BC, an adult health clinical nurse specialist consulting in an alumna role for the University of Arizona Medical Center in Tucson. “Many organizations are currently making an effort,” she says, “to determine which patients should be monitored with a higher degree of intensity and with greater frequency.”
Patient-controlled analgesia (PCA) also has some limitations. In theory, it offers built-in safety features—if patients become too sedated, they can’t push a button for extra doses—but that isn’t always the case. For instance, some patients may have “stacked” three to four doses before sedation and respiratory depression develop. “When things go wrong with PCA, patients are four times more likely to be seriously harmed than when nurses administer the medications,” says Arnstein, who is a past president of the American Society for Pain Management Nursing. “Thus, vigilant nurse-supervised opioid therapy is vitally important.”

—Paul Arnstein, RN, PhD, FAAN, Connell Nursing Research Scholar, clinical nurse specialist for pain relief, Massachusetts General Hospital, Boston
Simple Steps Save Lives
Most critical events associated with opioids occur during the first 24 hours of post-operative care. Combined with close monitoring, understanding the risk factors for respiratory depression and making adjustments based on an individual’s needs and response helps prevent a precarious situation in which a patient vacillates quickly from a wide-awake status to a sleepy state.
“There’s a very progressive amount of sedation,” says Deb Gordon, RN, DNP, FAAN, a contributor to The Joint Commission’s alert and a teaching associate in the department of anesthesiology and pain medicine at the University of Washington in Seattle.
Developing a pain treatment plan with a reassessment component is essential to exercising caution against potential harm from opioids.
“The Joint Commission’s guidance is wonderfully helpful and will benefit patients,” says Beth B. Murinson, MS, MD, PhD, associate professor and director of pain education in the department of neurology at Johns Hopkins University School of Medicine in Baltimore. “Getting opioid pain relief right is critically important as lives are hanging in the balance on both sides of this problem: Too little pain relief and millions will suffer; too much and lives are at risk.”
Hospitalists should be familiar with a few opioids that they feel comfortable prescribing, Dr. Murinson says. Be prepared to easily identify the major idiosyncratic effects and ordinary side effects of these medications and become well versed in opioid conversion.
“This is a classic problem in the field because, although the opioids are generally similar in their efficacy against pain, they have markedly different potencies against pain,” she explains. “A dose of 2 mg of morphine may need to be ‘converted’ to X mg of another opioid, depending on local practice patterns and preferences.”
Some drugs pose special risks. For example, transdermal fentanyl is “appropriate only for use in people who need opioid-level analgesia for an extended period of time and whose analgesic requirements are stable. This is not the case for folks with acute pain or who are just starting on opioids,” cautions Scott Strassels, PhD, PharmD, BCPS, assistant professor in the College of Pharmacy at the University of Texas in Austin and a board member of the American Pain Society. “Similarly, methadone is a good analgesic, but it requires very careful use due to its pharmacokinetic profile.”
Healthcare professionals from a variety of disciplines should be involved in pain-management efforts within a hospital setting. As for who takes the initiative, “it probably should be the person who is most qualified—be it a physician, nurse, or pharmacist,” Strassels says. “I’ve seen pharmacist-led teams, nurse-led teams, and those with physicians leading the effort.”
Clinicians who prescribe pain medications should be cognizant of nonpharmacologic alternatives to opioids. Multimodal options include physical therapy, acupuncture, manipulation or massage, and non-narcotic analgesics, such as acetaminophen and muscle relaxants. Non-narcotics may lower the dose of opioids needed to effectively manage pain, according to The Joint Commission.
The alert also provides information on suggested actions to avoid unintended consequences of using opioids. Hospitals should fully inform and provide written instructions to the patient and family or caregiver about the potential risks of tolerance, addiction, physical dependency, and withdrawal from opioids. When providing this information at discharge, the hospital also should list phone numbers to call if there are any questions.
In some unfortunate cases, opioids prescribed for pain also are used by patients’ family members, friends, and others. In such instances, says Northwestern’s Paice, usage occurs commonly with polypharmacy and without monitoring, and this contributes to an increased risk of death associated with opioids.
“There is concern that drugs prescribed for legitimate purposes are reaching the wrong hands,” Paice says. “We need to make the public, particularly patients and their family members, aware of safety strategies.”
Susan Kreimer is a freelance writer in New York City.
References
- Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999-2008. MMWR Morb Mortal Wkly Rep. 2011;60(43):1487-1492.
- Centers for Disease Control and Prevention. Vital signs: risk for overdose from methadone used for pain relief—United States, 1999-2010. MMWR Morb Mortal Wkly Rep. 2012;61(26):493-497.
- Jarzyna D, Jungquist CR, Pasero C, et al. American Society for Pain Management Nursing guidelines on monitoring for opioid-induced sedation and respiratory depression. Pain Manag Nurs. 2011;12(3):118-145.
Patient Understanding of ED Discharge Instructions Is Poor
Clinical question: How well do patients understand discharge instructions regarding post-ED care?
Background: Studies have demonstrated that patients discharged from the ED often lack appropriate understanding of their care. Knowledge deficits are particularly common in the area of post-ED care; however, it is not clear in which aspects of post-ED care these knowledge deficits are most pronounced.
Study design: Prospective cohort study.
Setting: Single-center academic urban hospital.
Synopsis: The researchers in this study discharged patients from the ED with five common diagnoses: ankle sprain, back pain, head injury, kidney stone, and laceration. Interviewers used formalized questioning to assess patient comprehension in five specific areas of post-ED care: diagnosis, medication, follow-up care, home care, and return instructions. Rates of severe knowledge deficits were most pronounced in the domains of home care (40.1%) and return instructions (50.7%). Rates of severe knowledge deficits in the domains of diagnosis, medication, and follow-up care were 3.2%, 3.2%, and 18.4%, respectively.
Though performed in the ED, the results of this study could inform the approach to inpatient discharges. However, the exclusion of patients with psychiatric disease, cognitive impairment, and multiple diagnoses suggests that the results might be even worse in a complicated inpatient cohort. The study also indicates that discharge instructions for home care and return precautions merit closer attention.
Bottom line: Patients discharged from the ED demonstrate poor comprehension of discharge instructions regarding post-ED care.
Citation: Engel KG, Buckley BA, Forth VE, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest? Acad Emerg Med. 2012;19:1035-1044.
Clinical question: How well do patients understand discharge instructions regarding post-ED care?
Background: Studies have demonstrated that patients discharged from the ED often lack appropriate understanding of their care. Knowledge deficits are particularly common in the area of post-ED care; however, it is not clear in which aspects of post-ED care these knowledge deficits are most pronounced.
Study design: Prospective cohort study.
Setting: Single-center academic urban hospital.
Synopsis: The researchers in this study discharged patients from the ED with five common diagnoses: ankle sprain, back pain, head injury, kidney stone, and laceration. Interviewers used formalized questioning to assess patient comprehension in five specific areas of post-ED care: diagnosis, medication, follow-up care, home care, and return instructions. Rates of severe knowledge deficits were most pronounced in the domains of home care (40.1%) and return instructions (50.7%). Rates of severe knowledge deficits in the domains of diagnosis, medication, and follow-up care were 3.2%, 3.2%, and 18.4%, respectively.
Though performed in the ED, the results of this study could inform the approach to inpatient discharges. However, the exclusion of patients with psychiatric disease, cognitive impairment, and multiple diagnoses suggests that the results might be even worse in a complicated inpatient cohort. The study also indicates that discharge instructions for home care and return precautions merit closer attention.
Bottom line: Patients discharged from the ED demonstrate poor comprehension of discharge instructions regarding post-ED care.
Citation: Engel KG, Buckley BA, Forth VE, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest? Acad Emerg Med. 2012;19:1035-1044.
Clinical question: How well do patients understand discharge instructions regarding post-ED care?
Background: Studies have demonstrated that patients discharged from the ED often lack appropriate understanding of their care. Knowledge deficits are particularly common in the area of post-ED care; however, it is not clear in which aspects of post-ED care these knowledge deficits are most pronounced.
Study design: Prospective cohort study.
Setting: Single-center academic urban hospital.
Synopsis: The researchers in this study discharged patients from the ED with five common diagnoses: ankle sprain, back pain, head injury, kidney stone, and laceration. Interviewers used formalized questioning to assess patient comprehension in five specific areas of post-ED care: diagnosis, medication, follow-up care, home care, and return instructions. Rates of severe knowledge deficits were most pronounced in the domains of home care (40.1%) and return instructions (50.7%). Rates of severe knowledge deficits in the domains of diagnosis, medication, and follow-up care were 3.2%, 3.2%, and 18.4%, respectively.
Though performed in the ED, the results of this study could inform the approach to inpatient discharges. However, the exclusion of patients with psychiatric disease, cognitive impairment, and multiple diagnoses suggests that the results might be even worse in a complicated inpatient cohort. The study also indicates that discharge instructions for home care and return precautions merit closer attention.
Bottom line: Patients discharged from the ED demonstrate poor comprehension of discharge instructions regarding post-ED care.
Citation: Engel KG, Buckley BA, Forth VE, et al. Patient understanding of emergency department discharge instructions: where are knowledge deficits greatest? Acad Emerg Med. 2012;19:1035-1044.
ACEIs and ARBs Associated with Contrast-Induced AKI
Clinical question: Does the pharmacologic renin-angiotensin-aldosterone (RAAS) system blockade increase the risk for contrast-induced acute kidney injury (CI-AKI) after cardiac catheterization?
Background: Prior prospective studies have demonstrated conflicting results regarding the deleterious versus protective effects of RAAS blockade prior to cardiac catheterization.
Study design: Retrospective, propensity-score-matched cohort study.
Setting: Single-center teaching hospital in South Korea.
Synopsis: Researchers identified patients who had cardiac catheterization and applied propensity-score matching to generate cohorts of periprocedural angiotensin converting enzyme inhibitor (ACEI) and angiotensin receptor blocker (ARB) users versus non-users. CI-AKI occurred more frequently in patients treated with ACEIs/ARBs compared to those who were not (11.4% vs. 6.3%, respectively; P<0.001).
This study was limited by its observational design. Although the propensity-score matching improves the internal validity, it is possible that unaccounted confounders were present. This trial might stimulate interest in re-examining this issue in larger prospective trials, but it should not alter current practice.
Bottom line: RAAS blockade during cardiac catheterization is associated with increased risk for CI-AKI, but further randomized trials are needed to confirm this conclusion.
Citation: Rim MY, Ro H, Kang WC, et al. The effect of renin-angiotensin-aldosterone system blockade on contrast-induced acute kidney injury: a propensity-matched study. Am J Kidney Dis. 2012;60:576-582.
Clinical question: Does the pharmacologic renin-angiotensin-aldosterone (RAAS) system blockade increase the risk for contrast-induced acute kidney injury (CI-AKI) after cardiac catheterization?
Background: Prior prospective studies have demonstrated conflicting results regarding the deleterious versus protective effects of RAAS blockade prior to cardiac catheterization.
Study design: Retrospective, propensity-score-matched cohort study.
Setting: Single-center teaching hospital in South Korea.
Synopsis: Researchers identified patients who had cardiac catheterization and applied propensity-score matching to generate cohorts of periprocedural angiotensin converting enzyme inhibitor (ACEI) and angiotensin receptor blocker (ARB) users versus non-users. CI-AKI occurred more frequently in patients treated with ACEIs/ARBs compared to those who were not (11.4% vs. 6.3%, respectively; P<0.001).
This study was limited by its observational design. Although the propensity-score matching improves the internal validity, it is possible that unaccounted confounders were present. This trial might stimulate interest in re-examining this issue in larger prospective trials, but it should not alter current practice.
Bottom line: RAAS blockade during cardiac catheterization is associated with increased risk for CI-AKI, but further randomized trials are needed to confirm this conclusion.
Citation: Rim MY, Ro H, Kang WC, et al. The effect of renin-angiotensin-aldosterone system blockade on contrast-induced acute kidney injury: a propensity-matched study. Am J Kidney Dis. 2012;60:576-582.
Clinical question: Does the pharmacologic renin-angiotensin-aldosterone (RAAS) system blockade increase the risk for contrast-induced acute kidney injury (CI-AKI) after cardiac catheterization?
Background: Prior prospective studies have demonstrated conflicting results regarding the deleterious versus protective effects of RAAS blockade prior to cardiac catheterization.
Study design: Retrospective, propensity-score-matched cohort study.
Setting: Single-center teaching hospital in South Korea.
Synopsis: Researchers identified patients who had cardiac catheterization and applied propensity-score matching to generate cohorts of periprocedural angiotensin converting enzyme inhibitor (ACEI) and angiotensin receptor blocker (ARB) users versus non-users. CI-AKI occurred more frequently in patients treated with ACEIs/ARBs compared to those who were not (11.4% vs. 6.3%, respectively; P<0.001).
This study was limited by its observational design. Although the propensity-score matching improves the internal validity, it is possible that unaccounted confounders were present. This trial might stimulate interest in re-examining this issue in larger prospective trials, but it should not alter current practice.
Bottom line: RAAS blockade during cardiac catheterization is associated with increased risk for CI-AKI, but further randomized trials are needed to confirm this conclusion.
Citation: Rim MY, Ro H, Kang WC, et al. The effect of renin-angiotensin-aldosterone system blockade on contrast-induced acute kidney injury: a propensity-matched study. Am J Kidney Dis. 2012;60:576-582.
Effect of Nonpayment on Nosocomial Infection Rates in U.S. Hospitals
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Clinical question: Did the 2008 Center for Medicare & Medicaid Services (CMS) policy denying additional payment for hospital-acquired conditions result in decreased rates of nosocomial infections?
Background: In an effort to curtail preventable complications, CMS implemented a policy of nonpayment for certain healthcare-acquired conditions beginning in October 2008. The effect of this policy on rates of nosocomial infections, including central venous catheter-associated bloodstream infections and catheter-associated urinary tract infections, is unknown.
Study design: Quasi-experimental.
Setting: Data collected from 398 hospitals participating in the National Healthcare Safety Network of the Centers for Disease Control and Prevention.
Synopsis: Investigators analyzed rates of nosocomial infections in participating hospitals before and after implementation of the 2008 nonpayment policy. The rates of decline in central venous catheter infections were not significantly different in the pre-implementation and post-implementation periods (4.8% per quarter and 4.7% per quarter, respectively; incidence-rate ratio 1.0; P=0.97). Similar results were found with regard to catheter-associated UTIs before and after policy initiation (3.9% per quarter and 0.9% per quarter, incidence-rate ratio 1.03; P=0.08). Results did not vary between states with and without mandatory reporting of nosocomial infections.
While this study’s broad scope limits the ability to draw firm conclusions, it does highlight the need for careful evaluation and quantification of the outcomes resulting from CMS’ expansion of policies for financial incentives and disincentives.
Bottom line: National rates of decline in nosocomial infections were unchanged before and after implementation of CMS’ nonpayment policy in 2008.
Citation: Lee GM, Kleinman K, Soumerai SB, et al. Effect of nonpayment for preventable infections in U.S. hospitals. N Engl J Med. 2012;367:1428-1437
Radiofrequency Ablation and Antiarrythmics as First-Line Therapy in Atrial Fibrillation
Clinical question: How does radiofrequency ablation compare to antiarrhythmic therapy as first-line treatment for paroxysmal atrial fibrillation (AF)?
Background: Current American College of Cardiology/American Heart Association (ACC/AHA) guidelines support radiofrequency ablation in high-volume centers for select patients with symptomatic, paroxysmal AF who have failed antiarrhythmic therapy (Class I recommendation). Little data exist regarding catheter ablation as a first-line intervention.
Study design: Randomized prospective cohort study.
Setting: Multicenter Danish trial.
Synopsis: Investigators randomized patients with symptomatic paroxysmal AF who were deemed to be good candidates for rhythm control to antiarrhythmic therapy versus radiofrequency catheter ablation. Patients had seven-day Holter monitoring at three, six, 12, 18, and 24 months. There was no significant difference in the cumulative burden of AF between the antiarrhythmic and ablation groups (19% and 13%, respectively; P=0.10). Secondary outcomes including quality of life and cumulative burden of symptomatic AF did not vary significantly between the groups. Crossover was high, with 35% of patients randomized to antiarrhythmic therapy eventually undergoing catheter ablation during the trial. There was no statistically significant difference in adverse events between the two groups.
This trial lends credence to the current ACC/AHA guidelines recommending radiofrequency ablation as second-line therapy for patients with AF after failing antiarrhythmics.
Bottom line: Radiofrequency ablation and antiarrhythmic therapy have similar efficacy as first-line therapy in paroxysmal AF.
Citation: Nielsen JC, Johannessen A, Raatikainen P, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012;367:1587-1595.
Clinical question: How does radiofrequency ablation compare to antiarrhythmic therapy as first-line treatment for paroxysmal atrial fibrillation (AF)?
Background: Current American College of Cardiology/American Heart Association (ACC/AHA) guidelines support radiofrequency ablation in high-volume centers for select patients with symptomatic, paroxysmal AF who have failed antiarrhythmic therapy (Class I recommendation). Little data exist regarding catheter ablation as a first-line intervention.
Study design: Randomized prospective cohort study.
Setting: Multicenter Danish trial.
Synopsis: Investigators randomized patients with symptomatic paroxysmal AF who were deemed to be good candidates for rhythm control to antiarrhythmic therapy versus radiofrequency catheter ablation. Patients had seven-day Holter monitoring at three, six, 12, 18, and 24 months. There was no significant difference in the cumulative burden of AF between the antiarrhythmic and ablation groups (19% and 13%, respectively; P=0.10). Secondary outcomes including quality of life and cumulative burden of symptomatic AF did not vary significantly between the groups. Crossover was high, with 35% of patients randomized to antiarrhythmic therapy eventually undergoing catheter ablation during the trial. There was no statistically significant difference in adverse events between the two groups.
This trial lends credence to the current ACC/AHA guidelines recommending radiofrequency ablation as second-line therapy for patients with AF after failing antiarrhythmics.
Bottom line: Radiofrequency ablation and antiarrhythmic therapy have similar efficacy as first-line therapy in paroxysmal AF.
Citation: Nielsen JC, Johannessen A, Raatikainen P, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012;367:1587-1595.
Clinical question: How does radiofrequency ablation compare to antiarrhythmic therapy as first-line treatment for paroxysmal atrial fibrillation (AF)?
Background: Current American College of Cardiology/American Heart Association (ACC/AHA) guidelines support radiofrequency ablation in high-volume centers for select patients with symptomatic, paroxysmal AF who have failed antiarrhythmic therapy (Class I recommendation). Little data exist regarding catheter ablation as a first-line intervention.
Study design: Randomized prospective cohort study.
Setting: Multicenter Danish trial.
Synopsis: Investigators randomized patients with symptomatic paroxysmal AF who were deemed to be good candidates for rhythm control to antiarrhythmic therapy versus radiofrequency catheter ablation. Patients had seven-day Holter monitoring at three, six, 12, 18, and 24 months. There was no significant difference in the cumulative burden of AF between the antiarrhythmic and ablation groups (19% and 13%, respectively; P=0.10). Secondary outcomes including quality of life and cumulative burden of symptomatic AF did not vary significantly between the groups. Crossover was high, with 35% of patients randomized to antiarrhythmic therapy eventually undergoing catheter ablation during the trial. There was no statistically significant difference in adverse events between the two groups.
This trial lends credence to the current ACC/AHA guidelines recommending radiofrequency ablation as second-line therapy for patients with AF after failing antiarrhythmics.
Bottom line: Radiofrequency ablation and antiarrhythmic therapy have similar efficacy as first-line therapy in paroxysmal AF.
Citation: Nielsen JC, Johannessen A, Raatikainen P, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012;367:1587-1595.
Win Whitcomb: Mortality Rates Become a Measuring Stick for Hospital Performance
—Blue Oyster Cult
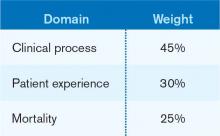
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
—Blue Oyster Cult
The designers of the hospital value-based purchasing (HVBP) program sought to include outcomes measures in 2014, and when they did, mortality was their choice. Specifically, HVBP for fiscal-year 2014 (starting October 2013) will include 30-day mortality rates for myocardial infarction, heart failure, and pneumonia. The weighting for the mortality domain will be 25% (see Table 1).
To review the requirements for the HVBP program in FY2014: All hospitals will have 1.25% of their Medicare inpatient payments withheld. They can earn back none, some, all, or an amount in excess of the 1.25%, depending on performance in the performance domains. To put it in perspective, 1.25% of Medicare inpatient payments for a 320-bed hospital are about $1 million. Such a hospital will have about $250,000 at risk in the mortality domain in FY2014.
Given the role hospitalists play in quality and safety initiatives, and the importance of medical record documentation in defining the risk of mortality and severity of illness, we can be crucial players in how our hospitals perform with regard to mortality.
Focus Areas for Mortality Reduction
Although many hospitalists might think that reducing mortality is like “boiling the ocean,” there are some areas where we can clearly focus our attention. There are four priority areas we should target in the coming years (also see Figure 1):
Reduce harm. This may take the form of reducing hospital-acquired infections, such as catheter-related UTIs, Clostridium difficile, and central-line-associated bloodstream infections, or reducing hospital-acquired VTE, falls, and delirium. Many hospital-acquired conditions have a collection, or bundle, of preventive practices. Hospitalists can work both in an institutional leadership capacity and in the course of daily clinical practice to implement bundles and best practices to reduce patient harm.
Improve teamwork. With hospitalists, “you started to have teams caring for inpatients in a coordinated way. So I regard this as [hospitalists] coming into their own, their vision of the future starting to really take hold,” said Brent James, coauthor of the recent Institute of Medicine report “Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.” Partly, we’ve accomplished this through simply “showing up” and partly we’ve done it through becoming students of the art and science of teamwork. An example of teamwork training, developed by the Defense Department and the Agency for Healthcare Quality and Research (AHRQ), is TeamSTEPPS, which offers a systematic approach to cooperation, coordination, and communication among team members. Optimal patient resuscitation, in-hospital handoffs, rapid-response teams, and early-warning systems are essential pieces of teamwork that may reduce mortality.
Improve evidence-based care. This domain covers process measures aimed at optimizing care, including reducing mortality. For HVBP in particular, myocardial infarction, heart failure, and pneumonia are the focus.
Improve transitions of care. Best practices for care transitions and reducing readmissions, including advance-care planning, involvement of palliative care and hospice, and coordination with post-acute care, can be a key part of reducing 30-day mortality.
Documentation Integrity
Accurately capturing a patient’s condition in the medical record is crucial to assigning severity of illness and risk of mortality. Because mortality rates are severity-adjusted, accurate documentation is another important dimension to potentially improving a hospital’s performance with regard to the mortality domain. This is one more reason to work closely with your hospital’s documentation specialists.
Don’t Be Afraid...
Proponents of mortality as a quality measure point to it as the ultimate reflection of the care provided. While moving the needle might seem like a task too big to undertake, a disciplined approach to the elements of the driver diagram combined with a robust documentation program can provide your institution with a tangible focus on this definitive measure.
Dr. Whitcomb is medical director of healthcare quality at Baystate Medical Center in Springfield, Mass. He is a co-founder and past president of SHM. Email him at wfwhit@comcast.net.
Multidisciplinary Palliative-Care Consults Help Reduce Hospital Readmissions
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.
Research on seriously ill, hospitalized, Medicare-age patients finds that those who received inpatient consultations from a multidisciplinary, palliative-care team (including a physician, nurse, and social worker) had lower 30-day hospital readmission rates.1 Ten percent of discharged patients who received the palliative-care consult were readmitted within 30 days at an urban HMO medical center in Los Angeles County during the same period, even though they were sicker than the overall discharged population.
Receipt of hospice care or home-based palliative-care services following discharge was also associated with significantly lower rates of readmissions, suggesting opportunities for systemic cost savings from earlier access to longitudinal, or ongoing, palliative-care services, says Susan Enguidanos, MPH, PhD, assistant professor of gerontology at the University of Southern California in Los Angeles. Patients discharged from the hospital without any follow-up care in the home had higher odds of readmission.
“Hospitals and medical centers should seriously consider an inpatient palliative care consultation team for many reasons, mostly arising from findings from other studies that have demonstrated improved quality of life, pain and symptom management, satisfaction with medical care, and other promising outcomes,” Dr. Enguidanos says. “Our study suggests that longitudinal palliative care is also associated with the lower readmission rate.”
References
- Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15(12):1356-1361.
- The Advisory Board Company. Mastering the cardiovascular care continuum: strategies for bridging divides among providers and across time. The Advisory Board Company website. Available at: http://www.advisory.com/Research/Cardiovascular-Roundtable/Studies/2012/Mastering-the-Cardiovascular-Care-Continuum. Accessed Jan. 8, 2013.
- Misky G, Carlson T, Klem P, et al. Development and implementation of a clinical care pathway for acute VTE reduces hospital utilization and cost at an urban tertiary care center [abstract]. J Hosp Med. 2012;7 Suppl 2:S66-S67.
- Versel N. Health IT holds key to better care integration. Information Week website. Available at: http://www.informationweek.com/healthcare/interoperability/health-it-holds-key-to-better-care-integ/240012443. Accessed Jan. 8, 2013.
- Office of Inspector General. Early Assessment Finds That CMS Faces Obstacles in Overseeing the Medicare EHR Incentive Program. Office of Inspector General website. Available at: https://oig.hhs.gov/oei/reports/oei-05-11-00250.asp. Accessed Jan. 8, 2013.