User login
Omega-3 fatty acids for psychiatric illness
Discuss this article at www.facebook.com/CurrentPsychiatry
Epidemiologic data suggest that people who consume diets rich in omega-3 fatty acids (FAs)—long-chain polyunsaturated FAs such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)—have a decreased risk of major depressive disorder (MDD), postpartum depression, and bipolar disorder (BD).1-5 Omega-3 FA concentration may impact serotonin and dopamine transmission via effects on cell membrane fluidity.6 Therefore, decreased intake may increase the risk of several psychiatric disorders. As the average Western diet has changed over the last 2 centuries, omega-3 FA consumption has decreased.7 Omega-3 FAs cannot be synthesized by the body and must come from exogenous sources, such as fish and nuts. For a discussion of different types of dietary fats, see Box 1.8
Should we advise our patients to increase their omega-3 FA consumption? The American Psychiatric Association (APA) and the American Heart Association (AHA) recommend omega-3 FA consumption for the general population and in some cases, supplementation for specific disorders (Box 2).9-12 New data has been published since Current Psychiatry last reviewed the evidence for using omega-3 FAs for psychiatric conditions in 2004.8 This article looks at the latest evidence on the use of omega-3 FAs to treat mood disorders, schizophrenia, dementia, and other psychiatric conditions.
Dietary fat is saturated or unsaturated. Unsaturated fats are further categorized as monounsaturated or polyunsaturated (PUFA). PUFAs contain a hydrocarbon chain with ≥2 double bonds.8 The position of this double bond relative to the methyl end carbon—or “omega” carbon—groups the PUFAs into 2 categories:8
- omega-6 fatty acids, including arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids, including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). ALA is a metabolic precursor to EPA and DHA.
PUFAs—in particular AA and DHA—are thought to contribute to cell membrane fluidity, modulation of neurotransmitters, and signal transduction pathways. As precursors to eicosanoids and cytokines, PUFAs may affect anti-inflammatory response systems.
Consumption of omega-3 fatty acids (FAs) reduces risk for arrhythmia, thrombosis, and atherosclerotic plaque, according to American Heart Association (AHA) guidelines. Omega-3 FA intake also may improve endothelial function, slightly lower blood pressure, and reduce inflammatory response. Replacing dietary saturated fat with polyunsaturated fat reduces coronary heart disease risk by 19%.9 The AHA recommends that all adults eat fish, particularly oily fish such as salmon or tuna, ≥2 times per week. Patients with documented coronary heart disease should consume 1 g/d eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) combined10 either via oily fish or omega-3 FA capsules. Side effects of omega-3 FA supplements are minor and include mild gastrointestinal discomfort, mostly burping or an unpleasant aftertaste; no cases of bleeding have been reported.11
For patients with hypertriglyceridemia, 2 to 4 g/d may be useful. Because of a theoretical risk of bleeding, doses >3 g/d should be supervised by a physician.
Because psychiatric illnesses and cardiovascular disease may be comorbid, the Omega-3 FA Subcommittee of the American Psychiatric Association supports the AHA’s guidelines regarding fish consumption, and further recommends that patients with mood, impulse control, or psychotic disorders consume ≥1 g/d of combined EPA and DHA.12
Limitations of the data
Reviewing the literature on omega-3 FAs to treat psychiatric disorders is hampered by several difficulties:13
- studies may evaluate the use of EPA alone, EPA combined with DHA, or DHA alone
- the doses of EPA and DHA and ratio of EPA to DHA of the supplements used in clinical trials varies greatly
- patients’ dietary consumption of omega-3 FAs is difficult to control
- DSM diagnostic criteria, as well as severity of illness, differ within studies.
In addition, studies may use omega-3 FAs as monotherapy or as adjuncts. All of these factors lead to difficulty interpreting the literature, as well as trouble in extracting data for meta-analysis.
Omega-3 FAs for mood disorders
MDD and other depressive diagnoses. Several meta-analyses examining the use of omega-3 FAs for treating depressive disorders have had equivocal findings. Variability in results might be partially explained by differences in the severity of baseline depression among diverse study populations, diagnostic variation, differing omega-3 supplementation protocols, or other issues.13 In addition, publication bias also may affect results.
In a 2011 literature review and meta-analysis of omega-3 FAs as monotherapy or an adjunct to antidepressants to treat MDD, Bloch and Hannestad6 concluded that omega-3 FAs offer a small but nonsignificant benefit in treating MDD. This review suggested that omega-3 FAs may be more effective in patients with more severe depression. The effects of varying levels of EPA vs DHA were not examined.
In a systematic review and meta-analysis, Appleton et al14 concluded that omega-3 FA supplements have little beneficial effect on depressed mood in individuals who do not have a depressive illness diagnosis (eg, MDD). However, this study did not consider the differential effects of EPA vs DHA on treatment response. Patients diagnosed with a depressive illness received greater benefits from omega-3 FA supplementation, although the patients in this study were heterogeneous. Similar to Bloch and Hannestad, Appleton et al14 found that omega-3 FA supplementation may be most beneficial for depressed patients with more severe symptoms, but is unlikely to help those with mild-to-moderate symptoms or individuals without symptoms who aim to prevent depression.
A meta-analysis by Martins15 looked at EPA vs DHA to treat depressive illness and found that only supplements that were mostly or completely EPA effectively treated depressive symptoms. Martins also found that severity of illness is key for positive treatment outcomes; there was a significant relationship between higher baseline depression levels and efficacy.15 Martins noted that omega-3 FA therapy was more effective as a treatment than a preventive strategy, and that adding omega-3 FAs to antidepressants was more efficacious than omega-3 FAs alone.15
A meta-analysis of clinical trials of omega-3 FAs for depressive illness suggested EPA should be ≥60% of total EPA + DHA.16
BD. A recent meta-analysis of 6 randomized controlled trials (RCTs) found that adding omega-3 supplements to mood stabilizers in patients with BD was associated with a statistically significant reduction of depressive symptoms, but was not effective for treating mania.17 The authors suggested patients with BD—especially those with comorbid cardiovascular or metabolic conditions— increase their dietary consumption of foods containing omega-3 FAs (Table)18 and, if necessary, take a supplement of 1 to 1.5 g/d of mixed EPA and DHA, with a higher ratio of EPA.19 See Box 3 for a box on how to read omega-3 supplement labels.
In a small RCT of 51 children and adolescents (age 6 to 17) with symptomatic bipolar I or bipolar II disorder, supplementation with flax oil (alpha-linolenic acid, a polyunsaturated omega-3 FA that is a precursor to EPA and DHA) did not affect symptoms as measured by several rating scales.20
Perinatal and postpartum depression. Omega-3 FAs are considered a safe treatment for depressive disorders during pregnancy because they provide neurodevelopmental benefits for neonates and have few contraindications during pregnancy.21 RCTs of omega-3 FA monotherapy for perinatal depression have been small (≤51 patients) and produced mixed findings.21 A pilot study (N = 16) of patients with postpartum depression found a significant decrease in depressive symptoms with EPA treatment.22 More research is needed before omega-3 FA supplementation can be recommended during pregnancy.
Table
Foods with healthy fats: From best to worst
| Polyunsaturated fats | Omega-3 | Fish-based: oily fish, including salmon, tuna, mackerel, lake trout, herring, and sardines Plant-based: tofu and other forms of soybeans; walnuts and flaxseed and their oils, and canola oil |
| Omega-6 | Only available in plant-based form: corn, soy, and safflower oil | |
| Monosaturated fats | Olive and peanut oil | |
| Saturated fats | Red meats, high-fat dairy, and partially hydrogenated oils | |
| Source: Reference 18 | ||
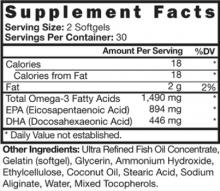
Because nutritional supplements vary, advise patients to look at the supplement facts on the back of a bottle of omega-3 fatty acids. The American Psychiatric Association recommends patients take a total eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) of 1 g/d; EPA should be ≥60% of total EPA + DHA.
This image is an example of a label that would meet the appropriate criteria. Total EPA + DHA = 1,490 mg and EPA is 60% of this combined total.
Source: Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584
Schizophrenia
In a Cochrane review of 8 studies of patients with schizophrenia, adjunctive treatment with omega-3 FAs led to >25% reduction in the Positive and Negative Syndrome Scale, but this improvement was not statistically significant.23 Omega-3 FAs did not decrease tardive dyskinesia symptoms as measured by the Abnormal Involuntary Movement Scale. The authors stated that results were inconclusive, and use of omega-3 FAs in patients with schizophrenia remains experimental. In a separate meta-analysis that included 335 patients with schizophrenia, EPA augmentation had no beneficial effect on psychotic symptoms.24
In a double-blind RCT of 81 adolescents and young adults (age 13 to 25) at ultra-high risk of psychotic illness, 5% of patients who received 1.2 g/d of omega-3 FAs developed a psychotic disorder compared with 28% of patients receiving placebo.25 The authors concluded that supplementation with omega-3 FAs may be a safe and effective strategy for young patients with subthreshold psychotic symptoms.
Dementia
Studies evaluating the relationship between omega-3 FAs and dementia risk have revealed mixed findings.26,27 In a pilot study of 10 geriatric patients with moderately severe dementia related to thrombotic cerebrovascular disorder, DHA supplementation led to improved Hamilton Depression Rating Scale and Mini-Mental State Examination (MMSE) scores compared with controls.28 In another study, administering EPA to 64 patients with Alzheimer’s disease significantly improved MMSE scores, with maximum improvement at 3 months, but this benefit dissipated after 6 months of treatment.29 In a study of 22 patients with various types of dementia, Suzuki et al30 found that DHA supplementation improved scores on a Japanese dementia scale. These studies show promise, but more evidence is necessary before recommendations can be made.
Other psychiatric disorders
Omega-3 FAs as monotherapy or an adjunct to psychostimulants does not seem to improve symptoms in children who meet DSM-IV-TR criteria for attention-deficit/hyperactivity disorder (ADHD).31-33 Studies of omega-3 FAs as treatment for anxiety and personality disorders are limited. To date, omega-3 FAs as adjunctive treatment in obsessive-compulsive disorder (OCD) and monotherapy in borderline personality disorder have not shown efficacy.34,35
Using omega-3 FAs in practice
Based on new data and several recent meta-analyses, clinical recommendations have emerged. Sarris et al17 suggested patients with BD increase dietary intake of omega-3 FAs or take a supplement with 1 to 1.5 g/d of mixed EPA and DHA (with a higher ratio of EPA). In MDD, the type of omega-3 FA supplementation seems to be important; EPA seems to be the primary component for efficacy.15,19 Additionally, the more severe the depression, the more likely symptoms will respond to omega-3 FAs.6,14,15 Omega-3 FAs are not effective at preventing depression14,15 and evidence is equivocal for treating perinatal depression.21 Omega-3 FA supplementation has not shown efficacy for patients with schizophrenia,23,24 although it may prevent transition to psychosis in adolescents and young adults at ultra-high risk for a psychotic disorder.25 Data examining omega-3 FA supplementation in postpartum depression22 and dementia28,29 are limited but show promise. Omega-3 FAs appear to lack efficacy in ADHD,31-33 OCD,34 and borderline personality disorder.35
Related Resources
- National Center for Complementary and Alternative Medicine. Omega-3 fatty acids. http://nccam.nih.gov/health/omega3.
- National Institutes of Health. Office of Dietary Supplements. Working group report: Omega-3 fatty acids and cardiovascular disease. http://ods.od.nih.gov/Health_Information/omega_3_fatty_acids.aspx.
Disclosure
Dr. Morreale reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv. 2001;52(4):529-531.
3. Silvers KM, Scott KM. Fish consumption and self-reported physical and mental health status. Public Health Nutr. 2002;5(3):427-431.
4. Timonen M, Horrobin DF, Jokelaienen J, et al. Fish consumption and depression: the northern Finland 1966 birth cohort study. J Affect Disord. 2004;82(3):447-452.
5. Freeman MP, Rapaport MH. Omega-3 fatty acids and depression: from cellular mechanisms to clinical care. J Clin Psychiatry. 2011;72(2):258-259.
6. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis [published online ahead of print September 20 2011]. Mol Psychiatry. doi: 10.1038/mp.2011.100.
7. Parker G, Gibson NA, Brotchie H, et al. Omega-3 fatty acids and mood disorders. Am J Psychiatry. 2006;163(6):969-978.
8. Martinez JM, Marangell LB. Omega-3 fatty acids: do ‘fish oils’ have a therapeutic role in psychiatry? Current Psychiatry. 2004;3(1):25-52.
9. Mozaffarian D, Micha R, Wallace S. Effects of coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252.-
10. Kris-Etherton PM, Harris WS, Appel LJ. AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151-152.
11. Freeman MP, Fava M, Lake J, et al. Complementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin Psychiatry. 2010;71(6):669-681.
12. Freeman MP, Hibbeln J, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006;67(12):1954-1967.
13. Mischoulon D. The impact of omega-3 fatty acids on depressive disorders and suicidality: can we reconcile 2 studies with seemingly contradictory results? J Clin Psychiatry. 2011;72(12):1574-1576.
14. Appleton KM, Rogers PJ, Andrew RN. Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Am J Clin Nutr. 2010;91(31):757-770.
15. Martins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525-542.
16. Young G, Conquer J. Omega-3 fatty acids and neuropsychiatric disorders. Reprod Nutr Dev. 2005;45(1):1-28.
17. Sarris J, Mischoulon D, Schweitzer I. Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry. 2012;73(1):81-86.
18. Sacks F. Ask the expert: omega-3 fatty acids. The Nutrition Source.http://www.hsph.harvard.edu/nutritionsource/questions/omega-3/index.html. Accessed July 23 2012.
19. Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584.
20. Gracious BL, Chirieac MC, Costescu S, et al. Randomized, placebo-controlled trial of flax oil in pediatric bipolar disorder. Bipolar Disord. 2010;12(2):142-154.
21. Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(suppl 5):7-11.
22. Freeman MP, Hibbeln JR, Wisner KL, et al. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta Psychiatr Scand. 2006;113(1):31-35.
23. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid supplementation for schizophrenia. Cochrane Database Syst Rev. 2006;(3):CD001257.-
24. Fusar-Poli P, Berger G. Eicosapentaenoic acid interventions in schizophrenia: meta-analysis of randomized placebo-controlled studies. J Clin Psychopharmacol. 2012;32(2):179-185.
25. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
26. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940-946.
27. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915-1921.
28. Terano T, Fujishiro S, Ban T, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids. 1999;34 suppl:S345-S346.
29. Otsuka M. Analysis of dietary factors in Alzheimer’s disease: clinical use of nutritional intervention for prevention and treatment of dementia [in Japanese]. Nihon Ronen Igakkai Zasshi. 2000;37(12):970-973.
30. Suzuki H, Morikawa Y, Takahashi H. Effect of DHA oil supplementation in intelligence and visual acuity in the elderly. World Rev Nutr Diet. 2001;88:68-71.
31. Joshi K, Lad S, Kale M, et al. Supplementation with flax oil and vitamin C improves the outcome of attention deficit hyperactivity disorder (ADHD). Prostaglandins Leukot Essent Fatty Acids. 2006;74(1):17-21.
32. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr. 2001;139(2):189-196.
33. Hirayama S, Hamazaki T, Terasawa K. Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder - a placebo-controlled double-blind study. Eur J Clin Nutr. 2004;58(3):467-473.
34. Fux M, Benjamin J, Nemets B. A placebo-controlled cross-over trial of adjunctive EPA in OCD. J Psychiatr Res. 2004;38(3):323-325.
35. Zanarini MC, Frankenburg FR. Omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
Discuss this article at www.facebook.com/CurrentPsychiatry
Epidemiologic data suggest that people who consume diets rich in omega-3 fatty acids (FAs)—long-chain polyunsaturated FAs such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)—have a decreased risk of major depressive disorder (MDD), postpartum depression, and bipolar disorder (BD).1-5 Omega-3 FA concentration may impact serotonin and dopamine transmission via effects on cell membrane fluidity.6 Therefore, decreased intake may increase the risk of several psychiatric disorders. As the average Western diet has changed over the last 2 centuries, omega-3 FA consumption has decreased.7 Omega-3 FAs cannot be synthesized by the body and must come from exogenous sources, such as fish and nuts. For a discussion of different types of dietary fats, see Box 1.8
Should we advise our patients to increase their omega-3 FA consumption? The American Psychiatric Association (APA) and the American Heart Association (AHA) recommend omega-3 FA consumption for the general population and in some cases, supplementation for specific disorders (Box 2).9-12 New data has been published since Current Psychiatry last reviewed the evidence for using omega-3 FAs for psychiatric conditions in 2004.8 This article looks at the latest evidence on the use of omega-3 FAs to treat mood disorders, schizophrenia, dementia, and other psychiatric conditions.
Dietary fat is saturated or unsaturated. Unsaturated fats are further categorized as monounsaturated or polyunsaturated (PUFA). PUFAs contain a hydrocarbon chain with ≥2 double bonds.8 The position of this double bond relative to the methyl end carbon—or “omega” carbon—groups the PUFAs into 2 categories:8
- omega-6 fatty acids, including arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids, including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). ALA is a metabolic precursor to EPA and DHA.
PUFAs—in particular AA and DHA—are thought to contribute to cell membrane fluidity, modulation of neurotransmitters, and signal transduction pathways. As precursors to eicosanoids and cytokines, PUFAs may affect anti-inflammatory response systems.
Consumption of omega-3 fatty acids (FAs) reduces risk for arrhythmia, thrombosis, and atherosclerotic plaque, according to American Heart Association (AHA) guidelines. Omega-3 FA intake also may improve endothelial function, slightly lower blood pressure, and reduce inflammatory response. Replacing dietary saturated fat with polyunsaturated fat reduces coronary heart disease risk by 19%.9 The AHA recommends that all adults eat fish, particularly oily fish such as salmon or tuna, ≥2 times per week. Patients with documented coronary heart disease should consume 1 g/d eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) combined10 either via oily fish or omega-3 FA capsules. Side effects of omega-3 FA supplements are minor and include mild gastrointestinal discomfort, mostly burping or an unpleasant aftertaste; no cases of bleeding have been reported.11
For patients with hypertriglyceridemia, 2 to 4 g/d may be useful. Because of a theoretical risk of bleeding, doses >3 g/d should be supervised by a physician.
Because psychiatric illnesses and cardiovascular disease may be comorbid, the Omega-3 FA Subcommittee of the American Psychiatric Association supports the AHA’s guidelines regarding fish consumption, and further recommends that patients with mood, impulse control, or psychotic disorders consume ≥1 g/d of combined EPA and DHA.12
Limitations of the data
Reviewing the literature on omega-3 FAs to treat psychiatric disorders is hampered by several difficulties:13
- studies may evaluate the use of EPA alone, EPA combined with DHA, or DHA alone
- the doses of EPA and DHA and ratio of EPA to DHA of the supplements used in clinical trials varies greatly
- patients’ dietary consumption of omega-3 FAs is difficult to control
- DSM diagnostic criteria, as well as severity of illness, differ within studies.
In addition, studies may use omega-3 FAs as monotherapy or as adjuncts. All of these factors lead to difficulty interpreting the literature, as well as trouble in extracting data for meta-analysis.
Omega-3 FAs for mood disorders
MDD and other depressive diagnoses. Several meta-analyses examining the use of omega-3 FAs for treating depressive disorders have had equivocal findings. Variability in results might be partially explained by differences in the severity of baseline depression among diverse study populations, diagnostic variation, differing omega-3 supplementation protocols, or other issues.13 In addition, publication bias also may affect results.
In a 2011 literature review and meta-analysis of omega-3 FAs as monotherapy or an adjunct to antidepressants to treat MDD, Bloch and Hannestad6 concluded that omega-3 FAs offer a small but nonsignificant benefit in treating MDD. This review suggested that omega-3 FAs may be more effective in patients with more severe depression. The effects of varying levels of EPA vs DHA were not examined.
In a systematic review and meta-analysis, Appleton et al14 concluded that omega-3 FA supplements have little beneficial effect on depressed mood in individuals who do not have a depressive illness diagnosis (eg, MDD). However, this study did not consider the differential effects of EPA vs DHA on treatment response. Patients diagnosed with a depressive illness received greater benefits from omega-3 FA supplementation, although the patients in this study were heterogeneous. Similar to Bloch and Hannestad, Appleton et al14 found that omega-3 FA supplementation may be most beneficial for depressed patients with more severe symptoms, but is unlikely to help those with mild-to-moderate symptoms or individuals without symptoms who aim to prevent depression.
A meta-analysis by Martins15 looked at EPA vs DHA to treat depressive illness and found that only supplements that were mostly or completely EPA effectively treated depressive symptoms. Martins also found that severity of illness is key for positive treatment outcomes; there was a significant relationship between higher baseline depression levels and efficacy.15 Martins noted that omega-3 FA therapy was more effective as a treatment than a preventive strategy, and that adding omega-3 FAs to antidepressants was more efficacious than omega-3 FAs alone.15
A meta-analysis of clinical trials of omega-3 FAs for depressive illness suggested EPA should be ≥60% of total EPA + DHA.16
BD. A recent meta-analysis of 6 randomized controlled trials (RCTs) found that adding omega-3 supplements to mood stabilizers in patients with BD was associated with a statistically significant reduction of depressive symptoms, but was not effective for treating mania.17 The authors suggested patients with BD—especially those with comorbid cardiovascular or metabolic conditions— increase their dietary consumption of foods containing omega-3 FAs (Table)18 and, if necessary, take a supplement of 1 to 1.5 g/d of mixed EPA and DHA, with a higher ratio of EPA.19 See Box 3 for a box on how to read omega-3 supplement labels.
In a small RCT of 51 children and adolescents (age 6 to 17) with symptomatic bipolar I or bipolar II disorder, supplementation with flax oil (alpha-linolenic acid, a polyunsaturated omega-3 FA that is a precursor to EPA and DHA) did not affect symptoms as measured by several rating scales.20
Perinatal and postpartum depression. Omega-3 FAs are considered a safe treatment for depressive disorders during pregnancy because they provide neurodevelopmental benefits for neonates and have few contraindications during pregnancy.21 RCTs of omega-3 FA monotherapy for perinatal depression have been small (≤51 patients) and produced mixed findings.21 A pilot study (N = 16) of patients with postpartum depression found a significant decrease in depressive symptoms with EPA treatment.22 More research is needed before omega-3 FA supplementation can be recommended during pregnancy.
Table
Foods with healthy fats: From best to worst
| Polyunsaturated fats | Omega-3 | Fish-based: oily fish, including salmon, tuna, mackerel, lake trout, herring, and sardines Plant-based: tofu and other forms of soybeans; walnuts and flaxseed and their oils, and canola oil |
| Omega-6 | Only available in plant-based form: corn, soy, and safflower oil | |
| Monosaturated fats | Olive and peanut oil | |
| Saturated fats | Red meats, high-fat dairy, and partially hydrogenated oils | |
| Source: Reference 18 | ||
Because nutritional supplements vary, advise patients to look at the supplement facts on the back of a bottle of omega-3 fatty acids. The American Psychiatric Association recommends patients take a total eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) of 1 g/d; EPA should be ≥60% of total EPA + DHA.
This image is an example of a label that would meet the appropriate criteria. Total EPA + DHA = 1,490 mg and EPA is 60% of this combined total.
Source: Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584
Schizophrenia
In a Cochrane review of 8 studies of patients with schizophrenia, adjunctive treatment with omega-3 FAs led to >25% reduction in the Positive and Negative Syndrome Scale, but this improvement was not statistically significant.23 Omega-3 FAs did not decrease tardive dyskinesia symptoms as measured by the Abnormal Involuntary Movement Scale. The authors stated that results were inconclusive, and use of omega-3 FAs in patients with schizophrenia remains experimental. In a separate meta-analysis that included 335 patients with schizophrenia, EPA augmentation had no beneficial effect on psychotic symptoms.24
In a double-blind RCT of 81 adolescents and young adults (age 13 to 25) at ultra-high risk of psychotic illness, 5% of patients who received 1.2 g/d of omega-3 FAs developed a psychotic disorder compared with 28% of patients receiving placebo.25 The authors concluded that supplementation with omega-3 FAs may be a safe and effective strategy for young patients with subthreshold psychotic symptoms.
Dementia
Studies evaluating the relationship between omega-3 FAs and dementia risk have revealed mixed findings.26,27 In a pilot study of 10 geriatric patients with moderately severe dementia related to thrombotic cerebrovascular disorder, DHA supplementation led to improved Hamilton Depression Rating Scale and Mini-Mental State Examination (MMSE) scores compared with controls.28 In another study, administering EPA to 64 patients with Alzheimer’s disease significantly improved MMSE scores, with maximum improvement at 3 months, but this benefit dissipated after 6 months of treatment.29 In a study of 22 patients with various types of dementia, Suzuki et al30 found that DHA supplementation improved scores on a Japanese dementia scale. These studies show promise, but more evidence is necessary before recommendations can be made.
Other psychiatric disorders
Omega-3 FAs as monotherapy or an adjunct to psychostimulants does not seem to improve symptoms in children who meet DSM-IV-TR criteria for attention-deficit/hyperactivity disorder (ADHD).31-33 Studies of omega-3 FAs as treatment for anxiety and personality disorders are limited. To date, omega-3 FAs as adjunctive treatment in obsessive-compulsive disorder (OCD) and monotherapy in borderline personality disorder have not shown efficacy.34,35
Using omega-3 FAs in practice
Based on new data and several recent meta-analyses, clinical recommendations have emerged. Sarris et al17 suggested patients with BD increase dietary intake of omega-3 FAs or take a supplement with 1 to 1.5 g/d of mixed EPA and DHA (with a higher ratio of EPA). In MDD, the type of omega-3 FA supplementation seems to be important; EPA seems to be the primary component for efficacy.15,19 Additionally, the more severe the depression, the more likely symptoms will respond to omega-3 FAs.6,14,15 Omega-3 FAs are not effective at preventing depression14,15 and evidence is equivocal for treating perinatal depression.21 Omega-3 FA supplementation has not shown efficacy for patients with schizophrenia,23,24 although it may prevent transition to psychosis in adolescents and young adults at ultra-high risk for a psychotic disorder.25 Data examining omega-3 FA supplementation in postpartum depression22 and dementia28,29 are limited but show promise. Omega-3 FAs appear to lack efficacy in ADHD,31-33 OCD,34 and borderline personality disorder.35
Related Resources
- National Center for Complementary and Alternative Medicine. Omega-3 fatty acids. http://nccam.nih.gov/health/omega3.
- National Institutes of Health. Office of Dietary Supplements. Working group report: Omega-3 fatty acids and cardiovascular disease. http://ods.od.nih.gov/Health_Information/omega_3_fatty_acids.aspx.
Disclosure
Dr. Morreale reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Epidemiologic data suggest that people who consume diets rich in omega-3 fatty acids (FAs)—long-chain polyunsaturated FAs such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA)—have a decreased risk of major depressive disorder (MDD), postpartum depression, and bipolar disorder (BD).1-5 Omega-3 FA concentration may impact serotonin and dopamine transmission via effects on cell membrane fluidity.6 Therefore, decreased intake may increase the risk of several psychiatric disorders. As the average Western diet has changed over the last 2 centuries, omega-3 FA consumption has decreased.7 Omega-3 FAs cannot be synthesized by the body and must come from exogenous sources, such as fish and nuts. For a discussion of different types of dietary fats, see Box 1.8
Should we advise our patients to increase their omega-3 FA consumption? The American Psychiatric Association (APA) and the American Heart Association (AHA) recommend omega-3 FA consumption for the general population and in some cases, supplementation for specific disorders (Box 2).9-12 New data has been published since Current Psychiatry last reviewed the evidence for using omega-3 FAs for psychiatric conditions in 2004.8 This article looks at the latest evidence on the use of omega-3 FAs to treat mood disorders, schizophrenia, dementia, and other psychiatric conditions.
Dietary fat is saturated or unsaturated. Unsaturated fats are further categorized as monounsaturated or polyunsaturated (PUFA). PUFAs contain a hydrocarbon chain with ≥2 double bonds.8 The position of this double bond relative to the methyl end carbon—or “omega” carbon—groups the PUFAs into 2 categories:8
- omega-6 fatty acids, including arachidonic acid (AA) and linoleic acid (LA)
- omega-3 fatty acids, including eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and alpha-linolenic acid (ALA). ALA is a metabolic precursor to EPA and DHA.
PUFAs—in particular AA and DHA—are thought to contribute to cell membrane fluidity, modulation of neurotransmitters, and signal transduction pathways. As precursors to eicosanoids and cytokines, PUFAs may affect anti-inflammatory response systems.
Consumption of omega-3 fatty acids (FAs) reduces risk for arrhythmia, thrombosis, and atherosclerotic plaque, according to American Heart Association (AHA) guidelines. Omega-3 FA intake also may improve endothelial function, slightly lower blood pressure, and reduce inflammatory response. Replacing dietary saturated fat with polyunsaturated fat reduces coronary heart disease risk by 19%.9 The AHA recommends that all adults eat fish, particularly oily fish such as salmon or tuna, ≥2 times per week. Patients with documented coronary heart disease should consume 1 g/d eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) combined10 either via oily fish or omega-3 FA capsules. Side effects of omega-3 FA supplements are minor and include mild gastrointestinal discomfort, mostly burping or an unpleasant aftertaste; no cases of bleeding have been reported.11
For patients with hypertriglyceridemia, 2 to 4 g/d may be useful. Because of a theoretical risk of bleeding, doses >3 g/d should be supervised by a physician.
Because psychiatric illnesses and cardiovascular disease may be comorbid, the Omega-3 FA Subcommittee of the American Psychiatric Association supports the AHA’s guidelines regarding fish consumption, and further recommends that patients with mood, impulse control, or psychotic disorders consume ≥1 g/d of combined EPA and DHA.12
Limitations of the data
Reviewing the literature on omega-3 FAs to treat psychiatric disorders is hampered by several difficulties:13
- studies may evaluate the use of EPA alone, EPA combined with DHA, or DHA alone
- the doses of EPA and DHA and ratio of EPA to DHA of the supplements used in clinical trials varies greatly
- patients’ dietary consumption of omega-3 FAs is difficult to control
- DSM diagnostic criteria, as well as severity of illness, differ within studies.
In addition, studies may use omega-3 FAs as monotherapy or as adjuncts. All of these factors lead to difficulty interpreting the literature, as well as trouble in extracting data for meta-analysis.
Omega-3 FAs for mood disorders
MDD and other depressive diagnoses. Several meta-analyses examining the use of omega-3 FAs for treating depressive disorders have had equivocal findings. Variability in results might be partially explained by differences in the severity of baseline depression among diverse study populations, diagnostic variation, differing omega-3 supplementation protocols, or other issues.13 In addition, publication bias also may affect results.
In a 2011 literature review and meta-analysis of omega-3 FAs as monotherapy or an adjunct to antidepressants to treat MDD, Bloch and Hannestad6 concluded that omega-3 FAs offer a small but nonsignificant benefit in treating MDD. This review suggested that omega-3 FAs may be more effective in patients with more severe depression. The effects of varying levels of EPA vs DHA were not examined.
In a systematic review and meta-analysis, Appleton et al14 concluded that omega-3 FA supplements have little beneficial effect on depressed mood in individuals who do not have a depressive illness diagnosis (eg, MDD). However, this study did not consider the differential effects of EPA vs DHA on treatment response. Patients diagnosed with a depressive illness received greater benefits from omega-3 FA supplementation, although the patients in this study were heterogeneous. Similar to Bloch and Hannestad, Appleton et al14 found that omega-3 FA supplementation may be most beneficial for depressed patients with more severe symptoms, but is unlikely to help those with mild-to-moderate symptoms or individuals without symptoms who aim to prevent depression.
A meta-analysis by Martins15 looked at EPA vs DHA to treat depressive illness and found that only supplements that were mostly or completely EPA effectively treated depressive symptoms. Martins also found that severity of illness is key for positive treatment outcomes; there was a significant relationship between higher baseline depression levels and efficacy.15 Martins noted that omega-3 FA therapy was more effective as a treatment than a preventive strategy, and that adding omega-3 FAs to antidepressants was more efficacious than omega-3 FAs alone.15
A meta-analysis of clinical trials of omega-3 FAs for depressive illness suggested EPA should be ≥60% of total EPA + DHA.16
BD. A recent meta-analysis of 6 randomized controlled trials (RCTs) found that adding omega-3 supplements to mood stabilizers in patients with BD was associated with a statistically significant reduction of depressive symptoms, but was not effective for treating mania.17 The authors suggested patients with BD—especially those with comorbid cardiovascular or metabolic conditions— increase their dietary consumption of foods containing omega-3 FAs (Table)18 and, if necessary, take a supplement of 1 to 1.5 g/d of mixed EPA and DHA, with a higher ratio of EPA.19 See Box 3 for a box on how to read omega-3 supplement labels.
In a small RCT of 51 children and adolescents (age 6 to 17) with symptomatic bipolar I or bipolar II disorder, supplementation with flax oil (alpha-linolenic acid, a polyunsaturated omega-3 FA that is a precursor to EPA and DHA) did not affect symptoms as measured by several rating scales.20
Perinatal and postpartum depression. Omega-3 FAs are considered a safe treatment for depressive disorders during pregnancy because they provide neurodevelopmental benefits for neonates and have few contraindications during pregnancy.21 RCTs of omega-3 FA monotherapy for perinatal depression have been small (≤51 patients) and produced mixed findings.21 A pilot study (N = 16) of patients with postpartum depression found a significant decrease in depressive symptoms with EPA treatment.22 More research is needed before omega-3 FA supplementation can be recommended during pregnancy.
Table
Foods with healthy fats: From best to worst
| Polyunsaturated fats | Omega-3 | Fish-based: oily fish, including salmon, tuna, mackerel, lake trout, herring, and sardines Plant-based: tofu and other forms of soybeans; walnuts and flaxseed and their oils, and canola oil |
| Omega-6 | Only available in plant-based form: corn, soy, and safflower oil | |
| Monosaturated fats | Olive and peanut oil | |
| Saturated fats | Red meats, high-fat dairy, and partially hydrogenated oils | |
| Source: Reference 18 | ||
Because nutritional supplements vary, advise patients to look at the supplement facts on the back of a bottle of omega-3 fatty acids. The American Psychiatric Association recommends patients take a total eicosapentaenoic acid (EPA) + docosahexaenoic acid (DHA) of 1 g/d; EPA should be ≥60% of total EPA + DHA.
This image is an example of a label that would meet the appropriate criteria. Total EPA + DHA = 1,490 mg and EPA is 60% of this combined total.
Source: Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584
Schizophrenia
In a Cochrane review of 8 studies of patients with schizophrenia, adjunctive treatment with omega-3 FAs led to >25% reduction in the Positive and Negative Syndrome Scale, but this improvement was not statistically significant.23 Omega-3 FAs did not decrease tardive dyskinesia symptoms as measured by the Abnormal Involuntary Movement Scale. The authors stated that results were inconclusive, and use of omega-3 FAs in patients with schizophrenia remains experimental. In a separate meta-analysis that included 335 patients with schizophrenia, EPA augmentation had no beneficial effect on psychotic symptoms.24
In a double-blind RCT of 81 adolescents and young adults (age 13 to 25) at ultra-high risk of psychotic illness, 5% of patients who received 1.2 g/d of omega-3 FAs developed a psychotic disorder compared with 28% of patients receiving placebo.25 The authors concluded that supplementation with omega-3 FAs may be a safe and effective strategy for young patients with subthreshold psychotic symptoms.
Dementia
Studies evaluating the relationship between omega-3 FAs and dementia risk have revealed mixed findings.26,27 In a pilot study of 10 geriatric patients with moderately severe dementia related to thrombotic cerebrovascular disorder, DHA supplementation led to improved Hamilton Depression Rating Scale and Mini-Mental State Examination (MMSE) scores compared with controls.28 In another study, administering EPA to 64 patients with Alzheimer’s disease significantly improved MMSE scores, with maximum improvement at 3 months, but this benefit dissipated after 6 months of treatment.29 In a study of 22 patients with various types of dementia, Suzuki et al30 found that DHA supplementation improved scores on a Japanese dementia scale. These studies show promise, but more evidence is necessary before recommendations can be made.
Other psychiatric disorders
Omega-3 FAs as monotherapy or an adjunct to psychostimulants does not seem to improve symptoms in children who meet DSM-IV-TR criteria for attention-deficit/hyperactivity disorder (ADHD).31-33 Studies of omega-3 FAs as treatment for anxiety and personality disorders are limited. To date, omega-3 FAs as adjunctive treatment in obsessive-compulsive disorder (OCD) and monotherapy in borderline personality disorder have not shown efficacy.34,35
Using omega-3 FAs in practice
Based on new data and several recent meta-analyses, clinical recommendations have emerged. Sarris et al17 suggested patients with BD increase dietary intake of omega-3 FAs or take a supplement with 1 to 1.5 g/d of mixed EPA and DHA (with a higher ratio of EPA). In MDD, the type of omega-3 FA supplementation seems to be important; EPA seems to be the primary component for efficacy.15,19 Additionally, the more severe the depression, the more likely symptoms will respond to omega-3 FAs.6,14,15 Omega-3 FAs are not effective at preventing depression14,15 and evidence is equivocal for treating perinatal depression.21 Omega-3 FA supplementation has not shown efficacy for patients with schizophrenia,23,24 although it may prevent transition to psychosis in adolescents and young adults at ultra-high risk for a psychotic disorder.25 Data examining omega-3 FA supplementation in postpartum depression22 and dementia28,29 are limited but show promise. Omega-3 FAs appear to lack efficacy in ADHD,31-33 OCD,34 and borderline personality disorder.35
Related Resources
- National Center for Complementary and Alternative Medicine. Omega-3 fatty acids. http://nccam.nih.gov/health/omega3.
- National Institutes of Health. Office of Dietary Supplements. Working group report: Omega-3 fatty acids and cardiovascular disease. http://ods.od.nih.gov/Health_Information/omega_3_fatty_acids.aspx.
Disclosure
Dr. Morreale reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv. 2001;52(4):529-531.
3. Silvers KM, Scott KM. Fish consumption and self-reported physical and mental health status. Public Health Nutr. 2002;5(3):427-431.
4. Timonen M, Horrobin DF, Jokelaienen J, et al. Fish consumption and depression: the northern Finland 1966 birth cohort study. J Affect Disord. 2004;82(3):447-452.
5. Freeman MP, Rapaport MH. Omega-3 fatty acids and depression: from cellular mechanisms to clinical care. J Clin Psychiatry. 2011;72(2):258-259.
6. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis [published online ahead of print September 20 2011]. Mol Psychiatry. doi: 10.1038/mp.2011.100.
7. Parker G, Gibson NA, Brotchie H, et al. Omega-3 fatty acids and mood disorders. Am J Psychiatry. 2006;163(6):969-978.
8. Martinez JM, Marangell LB. Omega-3 fatty acids: do ‘fish oils’ have a therapeutic role in psychiatry? Current Psychiatry. 2004;3(1):25-52.
9. Mozaffarian D, Micha R, Wallace S. Effects of coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252.-
10. Kris-Etherton PM, Harris WS, Appel LJ. AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151-152.
11. Freeman MP, Fava M, Lake J, et al. Complementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin Psychiatry. 2010;71(6):669-681.
12. Freeman MP, Hibbeln J, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006;67(12):1954-1967.
13. Mischoulon D. The impact of omega-3 fatty acids on depressive disorders and suicidality: can we reconcile 2 studies with seemingly contradictory results? J Clin Psychiatry. 2011;72(12):1574-1576.
14. Appleton KM, Rogers PJ, Andrew RN. Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Am J Clin Nutr. 2010;91(31):757-770.
15. Martins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525-542.
16. Young G, Conquer J. Omega-3 fatty acids and neuropsychiatric disorders. Reprod Nutr Dev. 2005;45(1):1-28.
17. Sarris J, Mischoulon D, Schweitzer I. Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry. 2012;73(1):81-86.
18. Sacks F. Ask the expert: omega-3 fatty acids. The Nutrition Source.http://www.hsph.harvard.edu/nutritionsource/questions/omega-3/index.html. Accessed July 23 2012.
19. Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584.
20. Gracious BL, Chirieac MC, Costescu S, et al. Randomized, placebo-controlled trial of flax oil in pediatric bipolar disorder. Bipolar Disord. 2010;12(2):142-154.
21. Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(suppl 5):7-11.
22. Freeman MP, Hibbeln JR, Wisner KL, et al. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta Psychiatr Scand. 2006;113(1):31-35.
23. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid supplementation for schizophrenia. Cochrane Database Syst Rev. 2006;(3):CD001257.-
24. Fusar-Poli P, Berger G. Eicosapentaenoic acid interventions in schizophrenia: meta-analysis of randomized placebo-controlled studies. J Clin Psychopharmacol. 2012;32(2):179-185.
25. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
26. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940-946.
27. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915-1921.
28. Terano T, Fujishiro S, Ban T, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids. 1999;34 suppl:S345-S346.
29. Otsuka M. Analysis of dietary factors in Alzheimer’s disease: clinical use of nutritional intervention for prevention and treatment of dementia [in Japanese]. Nihon Ronen Igakkai Zasshi. 2000;37(12):970-973.
30. Suzuki H, Morikawa Y, Takahashi H. Effect of DHA oil supplementation in intelligence and visual acuity in the elderly. World Rev Nutr Diet. 2001;88:68-71.
31. Joshi K, Lad S, Kale M, et al. Supplementation with flax oil and vitamin C improves the outcome of attention deficit hyperactivity disorder (ADHD). Prostaglandins Leukot Essent Fatty Acids. 2006;74(1):17-21.
32. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr. 2001;139(2):189-196.
33. Hirayama S, Hamazaki T, Terasawa K. Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder - a placebo-controlled double-blind study. Eur J Clin Nutr. 2004;58(3):467-473.
34. Fux M, Benjamin J, Nemets B. A placebo-controlled cross-over trial of adjunctive EPA in OCD. J Psychiatr Res. 2004;38(3):323-325.
35. Zanarini MC, Frankenburg FR. Omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
1. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213.-
2. Tanskanen A, Hibbeln JR, Tuomilehto J, et al. Fish consumption and depressive symptoms in the general population in Finland. Psychiatr Serv. 2001;52(4):529-531.
3. Silvers KM, Scott KM. Fish consumption and self-reported physical and mental health status. Public Health Nutr. 2002;5(3):427-431.
4. Timonen M, Horrobin DF, Jokelaienen J, et al. Fish consumption and depression: the northern Finland 1966 birth cohort study. J Affect Disord. 2004;82(3):447-452.
5. Freeman MP, Rapaport MH. Omega-3 fatty acids and depression: from cellular mechanisms to clinical care. J Clin Psychiatry. 2011;72(2):258-259.
6. Bloch MH, Hannestad J. Omega-3 fatty acids for the treatment of depression: systematic review and meta-analysis [published online ahead of print September 20 2011]. Mol Psychiatry. doi: 10.1038/mp.2011.100.
7. Parker G, Gibson NA, Brotchie H, et al. Omega-3 fatty acids and mood disorders. Am J Psychiatry. 2006;163(6):969-978.
8. Martinez JM, Marangell LB. Omega-3 fatty acids: do ‘fish oils’ have a therapeutic role in psychiatry? Current Psychiatry. 2004;3(1):25-52.
9. Mozaffarian D, Micha R, Wallace S. Effects of coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. 2010;7(3):e1000252.-
10. Kris-Etherton PM, Harris WS, Appel LJ. AHA Nutrition Committee. American Heart Association. Omega-3 fatty acids and cardiovascular disease: new recommendations from the American Heart Association. Arterioscler Thromb Vasc Biol. 2003;23(2):151-152.
11. Freeman MP, Fava M, Lake J, et al. Complementary and alternative medicine in major depressive disorder: the American Psychiatric Association Task Force report. J Clin Psychiatry. 2010;71(6):669-681.
12. Freeman MP, Hibbeln J, Wisner KL, et al. Omega-3 fatty acids: evidence basis for treatment and future research in psychiatry. J Clin Psychiatry. 2006;67(12):1954-1967.
13. Mischoulon D. The impact of omega-3 fatty acids on depressive disorders and suicidality: can we reconcile 2 studies with seemingly contradictory results? J Clin Psychiatry. 2011;72(12):1574-1576.
14. Appleton KM, Rogers PJ, Andrew RN. Updated systematic review and meta-analysis of the effects of n-3 long-chain polyunsaturated fatty acids on depressed mood. Am J Clin Nutr. 2010;91(31):757-770.
15. Martins JG. EPA but not DHA appears to be responsible for the efficacy of omega-3 long chain polyunsaturated fatty acid supplementation in depression: evidence from a meta-analysis of randomized controlled trials. J Am Coll Nutr. 2009;28(5):525-542.
16. Young G, Conquer J. Omega-3 fatty acids and neuropsychiatric disorders. Reprod Nutr Dev. 2005;45(1):1-28.
17. Sarris J, Mischoulon D, Schweitzer I. Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression. J Clin Psychiatry. 2012;73(1):81-86.
18. Sacks F. Ask the expert: omega-3 fatty acids. The Nutrition Source.http://www.hsph.harvard.edu/nutritionsource/questions/omega-3/index.html. Accessed July 23 2012.
19. Sublette ME, Ellis SP, Geant AL, et al. Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. J Clin Psychiatry. 2011;72(12):1577-1584.
20. Gracious BL, Chirieac MC, Costescu S, et al. Randomized, placebo-controlled trial of flax oil in pediatric bipolar disorder. Bipolar Disord. 2010;12(2):142-154.
21. Freeman MP. Omega-3 fatty acids in major depressive disorder. J Clin Psychiatry. 2009;70(suppl 5):7-11.
22. Freeman MP, Hibbeln JR, Wisner KL, et al. Randomized dose-ranging pilot trial of omega-3 fatty acids for postpartum depression. Acta Psychiatr Scand. 2006;113(1):31-35.
23. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty acid supplementation for schizophrenia. Cochrane Database Syst Rev. 2006;(3):CD001257.-
24. Fusar-Poli P, Berger G. Eicosapentaenoic acid interventions in schizophrenia: meta-analysis of randomized placebo-controlled studies. J Clin Psychopharmacol. 2012;32(2):179-185.
25. Amminger GP, Schäfer MR, Papageorgiou K, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67(2):146-154.
26. Morris MC, Evans DA, Bienias JL, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940-946.
27. Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915-1921.
28. Terano T, Fujishiro S, Ban T, et al. Docosahexaenoic acid supplementation improves the moderately severe dementia from thrombotic cerebrovascular diseases. Lipids. 1999;34 suppl:S345-S346.
29. Otsuka M. Analysis of dietary factors in Alzheimer’s disease: clinical use of nutritional intervention for prevention and treatment of dementia [in Japanese]. Nihon Ronen Igakkai Zasshi. 2000;37(12):970-973.
30. Suzuki H, Morikawa Y, Takahashi H. Effect of DHA oil supplementation in intelligence and visual acuity in the elderly. World Rev Nutr Diet. 2001;88:68-71.
31. Joshi K, Lad S, Kale M, et al. Supplementation with flax oil and vitamin C improves the outcome of attention deficit hyperactivity disorder (ADHD). Prostaglandins Leukot Essent Fatty Acids. 2006;74(1):17-21.
32. Voigt RG, Llorente AM, Jensen CL, et al. A randomized, double-blind, placebo-controlled trial of docosahexaenoic acid supplementation in children with attention-deficit/hyperactivity disorder. J Pediatr. 2001;139(2):189-196.
33. Hirayama S, Hamazaki T, Terasawa K. Effect of docosahexaenoic acid-containing food administration on symptoms of attention-deficit/hyperactivity disorder - a placebo-controlled double-blind study. Eur J Clin Nutr. 2004;58(3):467-473.
34. Fux M, Benjamin J, Nemets B. A placebo-controlled cross-over trial of adjunctive EPA in OCD. J Psychiatr Res. 2004;38(3):323-325.
35. Zanarini MC, Frankenburg FR. Omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind placebo-controlled pilot study. Am J Psychiatry. 2003;160(1):167-169.
How to target psychiatric symptoms of Huntington’s disease
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatric symptoms are a common and debilitating manifestation of Huntington’s disease (HD), a progressive, inherited neurodegenerative disorder also characterized by chorea (involuntary, nonrepetitive movements) and cognitive decline. The prevalence of HD is 4 to 8 patients per 100,000 persons in most populations of European descent, with lower prevalence among non-Europeans.1 HD is caused by an abnormal expansion of a trinucleotide (CAG) repeat sequence on chromosome 4, and is inherited in an autosomal dominant fashion, meaning a HD patient’s child has a 50% chance of inheriting the mutation. The expansion is located in the gene that encodes the “huntingtin” protein, the normal function of which is not well understood.
There’s no cure for HD, and treatments primarily are directed at symptom control. Psychiatric symptoms include depression, apathy, anxiety, and psychosis (Table).2-4 Treating patients with HD can be challenging because most psychiatrists will see only a handful of patients with this multifaceted illness during their careers. See Box 1 for a case study of a patient with HD.
Table
Psychiatric symptoms of HD
| Anxiety |
| Apathy |
| Delusions |
| Disinhibitions, impulsivity, aggressive behavior |
| Dysphoria |
| Euphoria |
| Hallucinations |
| Irritability |
| Obsessions and compulsions |
| HD: Huntington’s disease Source: References 2-4 |
Mr. M, age 50, was diagnosed with Huntington’s disease (HD) 1 year ago. He returns to our psychiatric clinic for treatment of depressive symptoms and temper. Previously, he was prescribed citalopram, 40 mg/d; eventually low-dose olanzapine, 2.5 mg at night, was added. Mr. M reported better temper control, but his low mood, irritability, hopelessness, and amotivation were not significantly improved.
Mr. M left his job at a software company because he had difficulty completing tasks as the result of mood and cognitive changes. He wants to return to work, but feels that he would be unable to complete his job duties.
He begins a trial of bupropion, 150 mg/d, to improve the vegetative component of his mood symptoms to help him return to work. Mr. M now complains of worsening chorea, irritability, and insomnia, with continued difficulty completing tasks. He is intermittently tearful throughout the interview.
Mr. M continues to struggle with mood symptoms that likely are related to the stressful experience of declining function and the intrinsic evolution of HD. His chorea worsens on bupropion; this agent is discontinued and replaced with mirtazapine, 15 mg at night, for his depressive symptoms and insomnia. Citalopram and olanzapine are unchanged. Mr. M is advised to follow up with our HD psychiatry team in 1 month, and is referred for brief psychotherapy. We remind him—as we do for all of our HD patients—to call the HD clinic or 911 if he becomes suicidal. Ongoing treatment efforts likely will be complex, given the multifaceted and progressive nature of his disease.
Psychiatric sequelae
In general, psychiatric symptoms of HD become increasingly prevalent over time (Box 2).3,5 In a 2001 study of 52 HD patients by Paulsen et al,2 51 patients had ≥1 psychiatric symptom, such as dysphoria (69.2%), agitation (67.3%), irritability (65.4%), apathy (55.8%), and anxiety (51.9%); delusions (11.5%) and hallucinations (1.9%) were less prevalent.2 Similarly, Thompson et al3 followed 111 HD patients for ≥3 years and all experienced psychiatric symptoms.
According to Thompson et al,3 the presence and severity of apathy, irritability, and depression trend differently across the course of Huntington’s disease (HD). Apathy worsens with disease progression, closely following cognitive and motor symptoms. Irritability increases significantly, but this effect seems confined to early stages of HD. Depressive symptoms appear to decline slightly as HD advances, although it is unclear if this is because of antidepressants’ effects, increasing emotional blunting, and waning insight in later stages of HD, or another unknown factor.3 This study did not examine psychotic symptoms over time because few patients were experiencing delusions or hallucinations.
Similar to Thompson et al, Naarding et al5 found that apathy and depression in HD follow distinct time courses. Depression is a feature of early HD and apathy worsens with overall disease progression.
Depressed mood and functional ability—not cognitive or motor symptoms6—are the 2 most critical factors linked to health-related quality of life in HD. Hamilton et al7 found that apathy or executive dysfunction in HD patients is strongly related to decline in ability to complete activities of daily living, and may be severely debilitating.
Apathy. Often mistaken for a symptom of depression, apathy’s presentation may resemble anhedonia or fatigue; however, research suggests that depression and apathy are distinct conditions. Naarding et al
5 noted that apathy is more common than depressive symptoms in HD patients and may be a hallmark symptom of HD.
Depression affects most HD patients, and often is most severe early in the disease course. Hubers et al8 found that 20% of 100 HD patients had suicidal ideation. The strongest predictor was depressed mood.
Sleep disturbances and daytime somnolence are common among HD patients, and patients with comorbid depression report more disturbed sleep. Managing disturbed sleep and daytime somnolence in HD, with emphasis on comorbid depression, may improve the quality of life of patients and their caregivers.9
Anxiety was present in >50% of HD patients in a study by Paulsen et al2 and 37% evaluated by Craufurd et al.10 Craufurd et al10 also reported that 61% of patients were “physically tense and unable to relax.”
Among HD patients, 5% report obsessions and 10% report compulsive behaviors; these symptoms appear to become increasingly common as HD progresses.4,10
Impulsivity and disinhibition. Craufurd et al10 found that 71% of HD patients experienced poor judgment and self-monitoring, 40% had poor temper control and verbal outbursts, 22% exhibited threatening behavior or violence, and 6% had disinhibited or inappropriate sexual behavior.10
Recent studies have shown higher rates of disinhibition in “presymptomatic” gene-positive subjects vs gene-negative controls, suggesting that these symptoms may arise early in HD.11 Further, researchers demonstrated that patients lack symptom awareness and rate themselves as less impaired than their caregivers do.11
In our clinical experience, impulsivity frequently is encountered and creates significant conflict between patients and their caregivers. We speculate that when coupled with depressive symptoms of HD, impulsivity and disinhibition may play an important role in the high rates of suicidality seen in these patients.
Psychosis. Delusions and hallucinations are less common in HD than other psychiatric symptoms. Craufurd et al10 reported 3% of HD patients had delusions, 3% had auditory hallucinations, 2% had tactile hallucinations, and no patients had visual hallucinations.
A few case reports and a small study by Tsuang et al12 suggested that psychotic features in HD may be similar to those seen in paranoid schizophrenia. Tsuang et al12 also noted that more severe HD-related psychosis tends to cluster in families, which suggests that susceptibility to HD psychosis may be heritable.
Treating psychiatric symptoms
High-quality randomized controlled trials of pharmacotherapies for psychiatric symptoms in HD patients are lacking. Decisions regarding which agents to use often are based on case reports or clinical experience. The suggestions below are based on available evidence and our clinical experience.
Depression. Depressive symptoms in HD seem to respond to conventional pharmacologic treatments for major depressive disorder (MDD). A small trial of venlafaxine extended-release (XR) in 26 HD patients with MDD showed statistically significant improvements in depressive symptoms; however, this trial was not blinded and did not have a placebo group.13 In addition, 1 in 5 patients developed significant side effects—nausea, irritability, or worsening chorea.13
Evidence for selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs) is lacking. Antidepressant choice should be based on patient response, side effect profile, and the need for secondary therapeutic effects.14
We often prescribe sertraline, citalopram, or escitalopram for our HD patients because of the relative absence of drug-drug interactions and favorable safety profile in medically and surgically ill patients. However, it’s important to tailor the treatment approach to your patient’s needs—eg, patients prone to forgetting their medicine may benefit from a drug with a longer half-life, such as fluoxetine. We avoid TCAs because of their anticholinergic effects, which may worsen dementia symptoms. Because HD patients have high rates of suicidality, agents that are highly toxic when taken in overdose should be used with caution.
One small study of HD patients with MDD or bipolar disorder showed clinical improvement in depressive symptoms after electroconvulsive therapy (ECT).15 Patients who suffered from comorbid delusions had the best improvements in mood.15 ECT likely is a good choice for HD patients who have failed several antidepressants, are suicidal, or who have depression with psychotic features.16
Apathy. A 2011 review concluded that no evidence-based recommendations regarding pharmacologic treatment for apathy in HD can be made because of lack of research.7 The Huntington’s Disease Society of America’s (HDSA) A Physician’s Guide to Managing Huntington’s Disease includes recommendations for treating apathy based on clinical experience.16 It suggests a nonsedating SSRI, followed by a trial of methylphenidate, pemoline, or dextroamphetamine if SSRIs were unsuccessful.
16 The HDSA guide notes psychostimulants may worsen irritability in HD and have a high potential for abuse. ECT appears to have little effect on apathy.15
Anxiety. A small, open-label study of 11 patients found that olanzapine, 5 mg/d, significantly improved depression, anxiety, irritability, and obsessive behavior in HD patients.17
The HDSA guide suggests treating anxiety and obsessive-compulsive symptoms as you would in patients without HD. For anxiety, SSRIs and possibly a short-term trial of a low-dose benzodiazepine (ie, lorazepam, clonazepam) are suggested.16 Benzodiazepines may increase the risk of falls and delirium in this population. Anecdotally, buspirone is helpful in some patients, with a starting dose of 5 mg 2 to 3 times per day and increased to 20 to 30 mg/d in divided doses.16 For obsessive-compulsive symptoms, SSRIs are recommended; atypical antipsychotics are reserved for severe or refractory symptoms.16
Disinhibition and impulsivity. There’s no research on treating disinhibition and impulsivity in HD. In our clinical experience, atypical antipsychotics are the most helpful. Factors regarding choosing an agent and dosing levels are similar to those for psychotic symptoms.
Psychotic symptoms. Most studies of typical and atypical antipsychotics for HD psychosis have shown beneficial effects.14,16-21 Neurologists frequently use these agents for managing chorea. Both neurologic and psychiatric features of the patient’s presentation must be considered when selecting a drug because treatment directed at 1 component of the disease may inadvertently exacerbate another. Specifically, higher potency antipsychotics (eg, haloperidol) are effective for chorea but can dramatically worsen bradykinesia; lower potency agents (eg, quetiapine) are less helpful for chorea but do not significantly worsen rigidity symptoms.
Olanzapine has been shown to improve chorea, anxiety, irritability, depression, sleep dysfunction, and weight loss in addition to psychotic symptoms.14,17 We find that olanzapine treats a constellation of symptoms common among HD patients, and we prescribe it frequently. Because olanzapine is considered a mid-potency agent, we find it’s best suited for concurrent control of psychotic symptoms and mild to moderate chorea in patients with minimal bradykinesia. Start olanzapine at 2.5 mg/d and gradually increase to 5 to 10 mg/d as tolerated.14
Risperidone is effective for treating psychosis and chorea. It can be started at 0.5 to 1 mg/d, and gradually increased to 6 to 8 mg/d.14 The depot formulation of risperidone has been shown to be effective in HD, which may help patients adhere to their medication.18 Risperidone is a mid-high potency antipsychotic, and in our experience is best used to control psychotic symptoms in patients with moderate chorea and few or no symptoms of bradykinesia or rigidity.
Quetiapine reduces psychotic symptoms, agitation, irritability, and insomnia without worsening bradykinesia or rigidity,19 but it is not beneficial for chorea. It can be started at 12.5 mg/d and gradually increased for effect as tolerated, up to 600 mg/d (depending on indication), in 2 or 3 divided doses.14
Haloperidol is a high-potency typical antipsychotic and may help psychotic patients with severe chorea; it should not be used in patients with bradykinesia. Start haloperidol at 0.5 to 1 mg/d and gradually increase to 6 to 8 mg/d as tolerated.14 Because of higher likelihood of side effects with typical antipsychotics, we often reserve its use for patients whose psychosis does not respond to atypical agents.
Other antipsychotics. Aripiprazole in HD has been examined in only 2 single- patient case reports20,21; the drug appeared to reduce psychosis and possibly chorea. Clozapine’s effectiveness for HD psychosis is not well known. It does not appear to be helpful for chorea and can cause agranulocytosis.22
Because one of the hallmarks of HD is dementia, it is worth noting that the FDA has issued a “black-box” warning on the use of antipsychotic drugs in patients with dementia because of concerns regarding increased mortality. However, drawing specific conclusions is difficult because the FDA warning is based on studies that looked primarily at Alzheimer’s disease and vascular dementia, not HD.
Other pharmacotherapies
Tetrabenazine is the only FDA-approved drug for treating HD. However, it carries a “black-box” warning for increased risk of depression and suicidal ideation and is contraindicated in suicidal patients and those with untreated or inadequately treated depression.
Although several small trials have had conflicting results regarding its benefit, amantadine sometimes is used to treat chorea.23-25 For more information about tetrabenazine and amantadine, see Box 3.
Tetrabenazine, the only FDA-approved drug for treating Huntington’s disease (HD), is a dopamine-depleting agent given to control chorea. In a 12-week, randomized, double-blind, placebo-controlled clinical trial, tetrabenazine was shown to be effective in HD patients.a Treatment with tetrabenazine results in symptomatic improvement of chorea, but does not slow or alter the course of the disease. Tetrabenazine can provide relief from choreiform movements, but these benefits should be balanced with the risks of depression and suicidality.a Tetrabenazine is known to prolong QTc interval, and should be used with caution in combination with other drugs that have the potential to do the same (eg, antipsychotics).a
Several case reports have found an association between tetrabenazine and development of neuroleptic malignant syndrome (NMS).b-d Be aware of the clinical characteristics of NMS—mental status change, rigidity, fever, and dysautonomia—and use caution when starting patients taking tetrabenazine on antipsychotics or other agents known to cause NMS.
Amantadine also has been used to treat chorea in HD patients who are unable to tolerate tetrabenazine or antipsychotics. Our neurologists sometimes have found it to be beneficial in patients with juvenile-onset HD because these patients often have debilitating dystonia. Be aware that amantadine is known to precipitate or worsen psychosis.e
References
- Food and Drug Administration. NDA 21-894 Xenazine® (tetrabenazine). Risk evaluation and mitigation strategy (REMS). Click here. Published August 15, 2008. Updated April 2011. Accessed June 20, 2012.
- Stevens E, Roman A, Houa M, et al. Severe hyperthermia during tetrabenazine therapy for tardive dyskinesia. Intensive Care Med. 1998;24(4):369-371.
- Petzinger GM, Bressman SB. A case of tetrabenazine-induced neuroleptic malignant syndrome after prolonged treatment. Mov Disord. 1997;12(2):246-248.
- Ossemann M, Sindic CJ, Laterre C. Tetrabenazine as a cause of neuroleptic malignant syndrome. Mov Disord. 1996;11(1):95.
- Wolters EC. Dopaminomimetic psychosis in Parkinson’s disease patients: diagnosis and treatment. Neurology. 1999;52 (7 suppl 3):S10-S13.
Related Resources
- Huntington’s Disease Society of America. www.hdsa.org.
- Family Caregiver Alliance. Huntington’s disease. www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=574.
- Huntington Study Group. www.huntington-study-group.org.
- Huntington’s Disease Advocacy Center. www.hdac.org.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Wellbutrin XL, others
- Buspirone • BuSpar
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Dextroamphetamine • Dexedrine
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
- Methylphenidate • Concerta, Ritalin, others
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Tetrabenazine • Xenazine
- Venlafaxine XR • Effexor XR
Disclosures
Dr. Scher is a consultant to the advisory board for Lundbeck.
Ms. Kocsis reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89(4):365-376.
2. Paulsen JS, Ready RE, Hamilton JM, et al. Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310-314.
3. Thompson JC, Harris J, Sollom AC, et al. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2012;24(1):53-60.
4. Beglinger LJ, Langbehn DR, Duff K, et al. Probability of obsessive and compulsive symptoms in Huntington’s disease. Biol Psychiatry. 2007;61(3):415-418.
5. Naarding P, Janzing JG, Eling P, et al. Apathy is not depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2009;21(3):266-270.
6. Ho AK, Gilbert AS, Mason SL, et al. Health-related quality of life in Huntington’s disease: which factors matter most? Mov Disord. 2009;24(4):574-578.
7. Hamilton JM, Salmon DP, Corey-Bloom J, et al. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2003;74(1):120-122.
8. Hubers AA, Reedeker N, Giltay EJ, et al. Suicidality in Huntington’s disease. J Affect Disord. 2012;136(3):550-557.
9. Videnovic A, Leurgans S, Fan W, et al. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15(6):471-474.
10. Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219-226.
11. Duff K, Paulsen JS, Beglinger LJ, et al. “Frontal” behaviors before the diagnosis of Huntington’s disease and their relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22(2):196-207.
12. Tsuang D, Almqvist EW, Lipe H, et al. Familial aggregation of psychotic symptoms in Huntington’s disease. Am J Psychiatry. 2000;157(12):1955-1959.
13. Holl AK, Wilkinson L, Painold A, et al. Combating depression in Huntington’s disease: effective antidepressive treatment with venlafaxine XR. Int Clin Psychopharmacol. 2010;25(1):46-50.
14. Killoran A, Biglan KM. Therapeutics in Huntington’s disease. Curr Treat Options Neurol. 2012;14(2):137-149.
15. Ranen NG, Peyser CE, Folstein SE. ECT as a treatment for depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 1994;6(2):154-159.
16. Rosenblatt A, Ranen NG, Nance MA, et al. A physician’s guide to the management of Huntington’s disease. 2nd edition. http://www.hdsa.org/images/content/1/1/11289.pdf. Published 1999. Accessed July 27, 2012.
17. Squitieri F, Cannella M, Piorcellini A, et al. Short-term effects of olanzapine in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(1):69-72.
18. Johnston TG. Risperidone long-acting injection and Huntington’s disease: case series with significant psychiatric and behavioural symptoms. Int Clin Psychopharmacol. 2011;26(2):114-119.
19. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
20. Lin WC, Chou YH. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
21. Oulis P, Mourikis I, Konstantakopoulos G, et al. Aripiprazole in the treatment of olanzapine-resistant psychotic and motor symptoms of Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2010;22(3):352c.e4-352c.e5.
22. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomised comparative study. J Neurol Neurosurg Psychiatry. 1997;63(1):35-39.
23. Verhagen Metman L, Morris MJ, Farmer C, et al. Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology. 2002;59(5):694-699.
24. Lucetti C, Del Dotto P, Gambaccini G, et al. IV amantadine improves chorea in Huntington’s disease: an acute randomized, controlled study. Neurology. 2003;60(12):1995-1997.
25. O’Suilleabhain P, Dewey RB, Jr. A randomized trial of amantadine in Huntington disease. Arch Neurol. 2003;60(7):996-998.
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatric symptoms are a common and debilitating manifestation of Huntington’s disease (HD), a progressive, inherited neurodegenerative disorder also characterized by chorea (involuntary, nonrepetitive movements) and cognitive decline. The prevalence of HD is 4 to 8 patients per 100,000 persons in most populations of European descent, with lower prevalence among non-Europeans.1 HD is caused by an abnormal expansion of a trinucleotide (CAG) repeat sequence on chromosome 4, and is inherited in an autosomal dominant fashion, meaning a HD patient’s child has a 50% chance of inheriting the mutation. The expansion is located in the gene that encodes the “huntingtin” protein, the normal function of which is not well understood.
There’s no cure for HD, and treatments primarily are directed at symptom control. Psychiatric symptoms include depression, apathy, anxiety, and psychosis (Table).2-4 Treating patients with HD can be challenging because most psychiatrists will see only a handful of patients with this multifaceted illness during their careers. See Box 1 for a case study of a patient with HD.
Table
Psychiatric symptoms of HD
| Anxiety |
| Apathy |
| Delusions |
| Disinhibitions, impulsivity, aggressive behavior |
| Dysphoria |
| Euphoria |
| Hallucinations |
| Irritability |
| Obsessions and compulsions |
| HD: Huntington’s disease Source: References 2-4 |
Mr. M, age 50, was diagnosed with Huntington’s disease (HD) 1 year ago. He returns to our psychiatric clinic for treatment of depressive symptoms and temper. Previously, he was prescribed citalopram, 40 mg/d; eventually low-dose olanzapine, 2.5 mg at night, was added. Mr. M reported better temper control, but his low mood, irritability, hopelessness, and amotivation were not significantly improved.
Mr. M left his job at a software company because he had difficulty completing tasks as the result of mood and cognitive changes. He wants to return to work, but feels that he would be unable to complete his job duties.
He begins a trial of bupropion, 150 mg/d, to improve the vegetative component of his mood symptoms to help him return to work. Mr. M now complains of worsening chorea, irritability, and insomnia, with continued difficulty completing tasks. He is intermittently tearful throughout the interview.
Mr. M continues to struggle with mood symptoms that likely are related to the stressful experience of declining function and the intrinsic evolution of HD. His chorea worsens on bupropion; this agent is discontinued and replaced with mirtazapine, 15 mg at night, for his depressive symptoms and insomnia. Citalopram and olanzapine are unchanged. Mr. M is advised to follow up with our HD psychiatry team in 1 month, and is referred for brief psychotherapy. We remind him—as we do for all of our HD patients—to call the HD clinic or 911 if he becomes suicidal. Ongoing treatment efforts likely will be complex, given the multifaceted and progressive nature of his disease.
Psychiatric sequelae
In general, psychiatric symptoms of HD become increasingly prevalent over time (Box 2).3,5 In a 2001 study of 52 HD patients by Paulsen et al,2 51 patients had ≥1 psychiatric symptom, such as dysphoria (69.2%), agitation (67.3%), irritability (65.4%), apathy (55.8%), and anxiety (51.9%); delusions (11.5%) and hallucinations (1.9%) were less prevalent.2 Similarly, Thompson et al3 followed 111 HD patients for ≥3 years and all experienced psychiatric symptoms.
According to Thompson et al,3 the presence and severity of apathy, irritability, and depression trend differently across the course of Huntington’s disease (HD). Apathy worsens with disease progression, closely following cognitive and motor symptoms. Irritability increases significantly, but this effect seems confined to early stages of HD. Depressive symptoms appear to decline slightly as HD advances, although it is unclear if this is because of antidepressants’ effects, increasing emotional blunting, and waning insight in later stages of HD, or another unknown factor.3 This study did not examine psychotic symptoms over time because few patients were experiencing delusions or hallucinations.
Similar to Thompson et al, Naarding et al5 found that apathy and depression in HD follow distinct time courses. Depression is a feature of early HD and apathy worsens with overall disease progression.
Depressed mood and functional ability—not cognitive or motor symptoms6—are the 2 most critical factors linked to health-related quality of life in HD. Hamilton et al7 found that apathy or executive dysfunction in HD patients is strongly related to decline in ability to complete activities of daily living, and may be severely debilitating.
Apathy. Often mistaken for a symptom of depression, apathy’s presentation may resemble anhedonia or fatigue; however, research suggests that depression and apathy are distinct conditions. Naarding et al
5 noted that apathy is more common than depressive symptoms in HD patients and may be a hallmark symptom of HD.
Depression affects most HD patients, and often is most severe early in the disease course. Hubers et al8 found that 20% of 100 HD patients had suicidal ideation. The strongest predictor was depressed mood.
Sleep disturbances and daytime somnolence are common among HD patients, and patients with comorbid depression report more disturbed sleep. Managing disturbed sleep and daytime somnolence in HD, with emphasis on comorbid depression, may improve the quality of life of patients and their caregivers.9
Anxiety was present in >50% of HD patients in a study by Paulsen et al2 and 37% evaluated by Craufurd et al.10 Craufurd et al10 also reported that 61% of patients were “physically tense and unable to relax.”
Among HD patients, 5% report obsessions and 10% report compulsive behaviors; these symptoms appear to become increasingly common as HD progresses.4,10
Impulsivity and disinhibition. Craufurd et al10 found that 71% of HD patients experienced poor judgment and self-monitoring, 40% had poor temper control and verbal outbursts, 22% exhibited threatening behavior or violence, and 6% had disinhibited or inappropriate sexual behavior.10
Recent studies have shown higher rates of disinhibition in “presymptomatic” gene-positive subjects vs gene-negative controls, suggesting that these symptoms may arise early in HD.11 Further, researchers demonstrated that patients lack symptom awareness and rate themselves as less impaired than their caregivers do.11
In our clinical experience, impulsivity frequently is encountered and creates significant conflict between patients and their caregivers. We speculate that when coupled with depressive symptoms of HD, impulsivity and disinhibition may play an important role in the high rates of suicidality seen in these patients.
Psychosis. Delusions and hallucinations are less common in HD than other psychiatric symptoms. Craufurd et al10 reported 3% of HD patients had delusions, 3% had auditory hallucinations, 2% had tactile hallucinations, and no patients had visual hallucinations.
A few case reports and a small study by Tsuang et al12 suggested that psychotic features in HD may be similar to those seen in paranoid schizophrenia. Tsuang et al12 also noted that more severe HD-related psychosis tends to cluster in families, which suggests that susceptibility to HD psychosis may be heritable.
Treating psychiatric symptoms
High-quality randomized controlled trials of pharmacotherapies for psychiatric symptoms in HD patients are lacking. Decisions regarding which agents to use often are based on case reports or clinical experience. The suggestions below are based on available evidence and our clinical experience.
Depression. Depressive symptoms in HD seem to respond to conventional pharmacologic treatments for major depressive disorder (MDD). A small trial of venlafaxine extended-release (XR) in 26 HD patients with MDD showed statistically significant improvements in depressive symptoms; however, this trial was not blinded and did not have a placebo group.13 In addition, 1 in 5 patients developed significant side effects—nausea, irritability, or worsening chorea.13
Evidence for selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs) is lacking. Antidepressant choice should be based on patient response, side effect profile, and the need for secondary therapeutic effects.14
We often prescribe sertraline, citalopram, or escitalopram for our HD patients because of the relative absence of drug-drug interactions and favorable safety profile in medically and surgically ill patients. However, it’s important to tailor the treatment approach to your patient’s needs—eg, patients prone to forgetting their medicine may benefit from a drug with a longer half-life, such as fluoxetine. We avoid TCAs because of their anticholinergic effects, which may worsen dementia symptoms. Because HD patients have high rates of suicidality, agents that are highly toxic when taken in overdose should be used with caution.
One small study of HD patients with MDD or bipolar disorder showed clinical improvement in depressive symptoms after electroconvulsive therapy (ECT).15 Patients who suffered from comorbid delusions had the best improvements in mood.15 ECT likely is a good choice for HD patients who have failed several antidepressants, are suicidal, or who have depression with psychotic features.16
Apathy. A 2011 review concluded that no evidence-based recommendations regarding pharmacologic treatment for apathy in HD can be made because of lack of research.7 The Huntington’s Disease Society of America’s (HDSA) A Physician’s Guide to Managing Huntington’s Disease includes recommendations for treating apathy based on clinical experience.16 It suggests a nonsedating SSRI, followed by a trial of methylphenidate, pemoline, or dextroamphetamine if SSRIs were unsuccessful.
16 The HDSA guide notes psychostimulants may worsen irritability in HD and have a high potential for abuse. ECT appears to have little effect on apathy.15
Anxiety. A small, open-label study of 11 patients found that olanzapine, 5 mg/d, significantly improved depression, anxiety, irritability, and obsessive behavior in HD patients.17
The HDSA guide suggests treating anxiety and obsessive-compulsive symptoms as you would in patients without HD. For anxiety, SSRIs and possibly a short-term trial of a low-dose benzodiazepine (ie, lorazepam, clonazepam) are suggested.16 Benzodiazepines may increase the risk of falls and delirium in this population. Anecdotally, buspirone is helpful in some patients, with a starting dose of 5 mg 2 to 3 times per day and increased to 20 to 30 mg/d in divided doses.16 For obsessive-compulsive symptoms, SSRIs are recommended; atypical antipsychotics are reserved for severe or refractory symptoms.16
Disinhibition and impulsivity. There’s no research on treating disinhibition and impulsivity in HD. In our clinical experience, atypical antipsychotics are the most helpful. Factors regarding choosing an agent and dosing levels are similar to those for psychotic symptoms.
Psychotic symptoms. Most studies of typical and atypical antipsychotics for HD psychosis have shown beneficial effects.14,16-21 Neurologists frequently use these agents for managing chorea. Both neurologic and psychiatric features of the patient’s presentation must be considered when selecting a drug because treatment directed at 1 component of the disease may inadvertently exacerbate another. Specifically, higher potency antipsychotics (eg, haloperidol) are effective for chorea but can dramatically worsen bradykinesia; lower potency agents (eg, quetiapine) are less helpful for chorea but do not significantly worsen rigidity symptoms.
Olanzapine has been shown to improve chorea, anxiety, irritability, depression, sleep dysfunction, and weight loss in addition to psychotic symptoms.14,17 We find that olanzapine treats a constellation of symptoms common among HD patients, and we prescribe it frequently. Because olanzapine is considered a mid-potency agent, we find it’s best suited for concurrent control of psychotic symptoms and mild to moderate chorea in patients with minimal bradykinesia. Start olanzapine at 2.5 mg/d and gradually increase to 5 to 10 mg/d as tolerated.14
Risperidone is effective for treating psychosis and chorea. It can be started at 0.5 to 1 mg/d, and gradually increased to 6 to 8 mg/d.14 The depot formulation of risperidone has been shown to be effective in HD, which may help patients adhere to their medication.18 Risperidone is a mid-high potency antipsychotic, and in our experience is best used to control psychotic symptoms in patients with moderate chorea and few or no symptoms of bradykinesia or rigidity.
Quetiapine reduces psychotic symptoms, agitation, irritability, and insomnia without worsening bradykinesia or rigidity,19 but it is not beneficial for chorea. It can be started at 12.5 mg/d and gradually increased for effect as tolerated, up to 600 mg/d (depending on indication), in 2 or 3 divided doses.14
Haloperidol is a high-potency typical antipsychotic and may help psychotic patients with severe chorea; it should not be used in patients with bradykinesia. Start haloperidol at 0.5 to 1 mg/d and gradually increase to 6 to 8 mg/d as tolerated.14 Because of higher likelihood of side effects with typical antipsychotics, we often reserve its use for patients whose psychosis does not respond to atypical agents.
Other antipsychotics. Aripiprazole in HD has been examined in only 2 single- patient case reports20,21; the drug appeared to reduce psychosis and possibly chorea. Clozapine’s effectiveness for HD psychosis is not well known. It does not appear to be helpful for chorea and can cause agranulocytosis.22
Because one of the hallmarks of HD is dementia, it is worth noting that the FDA has issued a “black-box” warning on the use of antipsychotic drugs in patients with dementia because of concerns regarding increased mortality. However, drawing specific conclusions is difficult because the FDA warning is based on studies that looked primarily at Alzheimer’s disease and vascular dementia, not HD.
Other pharmacotherapies
Tetrabenazine is the only FDA-approved drug for treating HD. However, it carries a “black-box” warning for increased risk of depression and suicidal ideation and is contraindicated in suicidal patients and those with untreated or inadequately treated depression.
Although several small trials have had conflicting results regarding its benefit, amantadine sometimes is used to treat chorea.23-25 For more information about tetrabenazine and amantadine, see Box 3.
Tetrabenazine, the only FDA-approved drug for treating Huntington’s disease (HD), is a dopamine-depleting agent given to control chorea. In a 12-week, randomized, double-blind, placebo-controlled clinical trial, tetrabenazine was shown to be effective in HD patients.a Treatment with tetrabenazine results in symptomatic improvement of chorea, but does not slow or alter the course of the disease. Tetrabenazine can provide relief from choreiform movements, but these benefits should be balanced with the risks of depression and suicidality.a Tetrabenazine is known to prolong QTc interval, and should be used with caution in combination with other drugs that have the potential to do the same (eg, antipsychotics).a
Several case reports have found an association between tetrabenazine and development of neuroleptic malignant syndrome (NMS).b-d Be aware of the clinical characteristics of NMS—mental status change, rigidity, fever, and dysautonomia—and use caution when starting patients taking tetrabenazine on antipsychotics or other agents known to cause NMS.
Amantadine also has been used to treat chorea in HD patients who are unable to tolerate tetrabenazine or antipsychotics. Our neurologists sometimes have found it to be beneficial in patients with juvenile-onset HD because these patients often have debilitating dystonia. Be aware that amantadine is known to precipitate or worsen psychosis.e
References
- Food and Drug Administration. NDA 21-894 Xenazine® (tetrabenazine). Risk evaluation and mitigation strategy (REMS). Click here. Published August 15, 2008. Updated April 2011. Accessed June 20, 2012.
- Stevens E, Roman A, Houa M, et al. Severe hyperthermia during tetrabenazine therapy for tardive dyskinesia. Intensive Care Med. 1998;24(4):369-371.
- Petzinger GM, Bressman SB. A case of tetrabenazine-induced neuroleptic malignant syndrome after prolonged treatment. Mov Disord. 1997;12(2):246-248.
- Ossemann M, Sindic CJ, Laterre C. Tetrabenazine as a cause of neuroleptic malignant syndrome. Mov Disord. 1996;11(1):95.
- Wolters EC. Dopaminomimetic psychosis in Parkinson’s disease patients: diagnosis and treatment. Neurology. 1999;52 (7 suppl 3):S10-S13.
Related Resources
- Huntington’s Disease Society of America. www.hdsa.org.
- Family Caregiver Alliance. Huntington’s disease. www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=574.
- Huntington Study Group. www.huntington-study-group.org.
- Huntington’s Disease Advocacy Center. www.hdac.org.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Wellbutrin XL, others
- Buspirone • BuSpar
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Dextroamphetamine • Dexedrine
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
- Methylphenidate • Concerta, Ritalin, others
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Tetrabenazine • Xenazine
- Venlafaxine XR • Effexor XR
Disclosures
Dr. Scher is a consultant to the advisory board for Lundbeck.
Ms. Kocsis reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Psychiatric symptoms are a common and debilitating manifestation of Huntington’s disease (HD), a progressive, inherited neurodegenerative disorder also characterized by chorea (involuntary, nonrepetitive movements) and cognitive decline. The prevalence of HD is 4 to 8 patients per 100,000 persons in most populations of European descent, with lower prevalence among non-Europeans.1 HD is caused by an abnormal expansion of a trinucleotide (CAG) repeat sequence on chromosome 4, and is inherited in an autosomal dominant fashion, meaning a HD patient’s child has a 50% chance of inheriting the mutation. The expansion is located in the gene that encodes the “huntingtin” protein, the normal function of which is not well understood.
There’s no cure for HD, and treatments primarily are directed at symptom control. Psychiatric symptoms include depression, apathy, anxiety, and psychosis (Table).2-4 Treating patients with HD can be challenging because most psychiatrists will see only a handful of patients with this multifaceted illness during their careers. See Box 1 for a case study of a patient with HD.
Table
Psychiatric symptoms of HD
| Anxiety |
| Apathy |
| Delusions |
| Disinhibitions, impulsivity, aggressive behavior |
| Dysphoria |
| Euphoria |
| Hallucinations |
| Irritability |
| Obsessions and compulsions |
| HD: Huntington’s disease Source: References 2-4 |
Mr. M, age 50, was diagnosed with Huntington’s disease (HD) 1 year ago. He returns to our psychiatric clinic for treatment of depressive symptoms and temper. Previously, he was prescribed citalopram, 40 mg/d; eventually low-dose olanzapine, 2.5 mg at night, was added. Mr. M reported better temper control, but his low mood, irritability, hopelessness, and amotivation were not significantly improved.
Mr. M left his job at a software company because he had difficulty completing tasks as the result of mood and cognitive changes. He wants to return to work, but feels that he would be unable to complete his job duties.
He begins a trial of bupropion, 150 mg/d, to improve the vegetative component of his mood symptoms to help him return to work. Mr. M now complains of worsening chorea, irritability, and insomnia, with continued difficulty completing tasks. He is intermittently tearful throughout the interview.
Mr. M continues to struggle with mood symptoms that likely are related to the stressful experience of declining function and the intrinsic evolution of HD. His chorea worsens on bupropion; this agent is discontinued and replaced with mirtazapine, 15 mg at night, for his depressive symptoms and insomnia. Citalopram and olanzapine are unchanged. Mr. M is advised to follow up with our HD psychiatry team in 1 month, and is referred for brief psychotherapy. We remind him—as we do for all of our HD patients—to call the HD clinic or 911 if he becomes suicidal. Ongoing treatment efforts likely will be complex, given the multifaceted and progressive nature of his disease.
Psychiatric sequelae
In general, psychiatric symptoms of HD become increasingly prevalent over time (Box 2).3,5 In a 2001 study of 52 HD patients by Paulsen et al,2 51 patients had ≥1 psychiatric symptom, such as dysphoria (69.2%), agitation (67.3%), irritability (65.4%), apathy (55.8%), and anxiety (51.9%); delusions (11.5%) and hallucinations (1.9%) were less prevalent.2 Similarly, Thompson et al3 followed 111 HD patients for ≥3 years and all experienced psychiatric symptoms.
According to Thompson et al,3 the presence and severity of apathy, irritability, and depression trend differently across the course of Huntington’s disease (HD). Apathy worsens with disease progression, closely following cognitive and motor symptoms. Irritability increases significantly, but this effect seems confined to early stages of HD. Depressive symptoms appear to decline slightly as HD advances, although it is unclear if this is because of antidepressants’ effects, increasing emotional blunting, and waning insight in later stages of HD, or another unknown factor.3 This study did not examine psychotic symptoms over time because few patients were experiencing delusions or hallucinations.
Similar to Thompson et al, Naarding et al5 found that apathy and depression in HD follow distinct time courses. Depression is a feature of early HD and apathy worsens with overall disease progression.
Depressed mood and functional ability—not cognitive or motor symptoms6—are the 2 most critical factors linked to health-related quality of life in HD. Hamilton et al7 found that apathy or executive dysfunction in HD patients is strongly related to decline in ability to complete activities of daily living, and may be severely debilitating.
Apathy. Often mistaken for a symptom of depression, apathy’s presentation may resemble anhedonia or fatigue; however, research suggests that depression and apathy are distinct conditions. Naarding et al
5 noted that apathy is more common than depressive symptoms in HD patients and may be a hallmark symptom of HD.
Depression affects most HD patients, and often is most severe early in the disease course. Hubers et al8 found that 20% of 100 HD patients had suicidal ideation. The strongest predictor was depressed mood.
Sleep disturbances and daytime somnolence are common among HD patients, and patients with comorbid depression report more disturbed sleep. Managing disturbed sleep and daytime somnolence in HD, with emphasis on comorbid depression, may improve the quality of life of patients and their caregivers.9
Anxiety was present in >50% of HD patients in a study by Paulsen et al2 and 37% evaluated by Craufurd et al.10 Craufurd et al10 also reported that 61% of patients were “physically tense and unable to relax.”
Among HD patients, 5% report obsessions and 10% report compulsive behaviors; these symptoms appear to become increasingly common as HD progresses.4,10
Impulsivity and disinhibition. Craufurd et al10 found that 71% of HD patients experienced poor judgment and self-monitoring, 40% had poor temper control and verbal outbursts, 22% exhibited threatening behavior or violence, and 6% had disinhibited or inappropriate sexual behavior.10
Recent studies have shown higher rates of disinhibition in “presymptomatic” gene-positive subjects vs gene-negative controls, suggesting that these symptoms may arise early in HD.11 Further, researchers demonstrated that patients lack symptom awareness and rate themselves as less impaired than their caregivers do.11
In our clinical experience, impulsivity frequently is encountered and creates significant conflict between patients and their caregivers. We speculate that when coupled with depressive symptoms of HD, impulsivity and disinhibition may play an important role in the high rates of suicidality seen in these patients.
Psychosis. Delusions and hallucinations are less common in HD than other psychiatric symptoms. Craufurd et al10 reported 3% of HD patients had delusions, 3% had auditory hallucinations, 2% had tactile hallucinations, and no patients had visual hallucinations.
A few case reports and a small study by Tsuang et al12 suggested that psychotic features in HD may be similar to those seen in paranoid schizophrenia. Tsuang et al12 also noted that more severe HD-related psychosis tends to cluster in families, which suggests that susceptibility to HD psychosis may be heritable.
Treating psychiatric symptoms
High-quality randomized controlled trials of pharmacotherapies for psychiatric symptoms in HD patients are lacking. Decisions regarding which agents to use often are based on case reports or clinical experience. The suggestions below are based on available evidence and our clinical experience.
Depression. Depressive symptoms in HD seem to respond to conventional pharmacologic treatments for major depressive disorder (MDD). A small trial of venlafaxine extended-release (XR) in 26 HD patients with MDD showed statistically significant improvements in depressive symptoms; however, this trial was not blinded and did not have a placebo group.13 In addition, 1 in 5 patients developed significant side effects—nausea, irritability, or worsening chorea.13
Evidence for selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors, and tricyclic antidepressants (TCAs) is lacking. Antidepressant choice should be based on patient response, side effect profile, and the need for secondary therapeutic effects.14
We often prescribe sertraline, citalopram, or escitalopram for our HD patients because of the relative absence of drug-drug interactions and favorable safety profile in medically and surgically ill patients. However, it’s important to tailor the treatment approach to your patient’s needs—eg, patients prone to forgetting their medicine may benefit from a drug with a longer half-life, such as fluoxetine. We avoid TCAs because of their anticholinergic effects, which may worsen dementia symptoms. Because HD patients have high rates of suicidality, agents that are highly toxic when taken in overdose should be used with caution.
One small study of HD patients with MDD or bipolar disorder showed clinical improvement in depressive symptoms after electroconvulsive therapy (ECT).15 Patients who suffered from comorbid delusions had the best improvements in mood.15 ECT likely is a good choice for HD patients who have failed several antidepressants, are suicidal, or who have depression with psychotic features.16
Apathy. A 2011 review concluded that no evidence-based recommendations regarding pharmacologic treatment for apathy in HD can be made because of lack of research.7 The Huntington’s Disease Society of America’s (HDSA) A Physician’s Guide to Managing Huntington’s Disease includes recommendations for treating apathy based on clinical experience.16 It suggests a nonsedating SSRI, followed by a trial of methylphenidate, pemoline, or dextroamphetamine if SSRIs were unsuccessful.
16 The HDSA guide notes psychostimulants may worsen irritability in HD and have a high potential for abuse. ECT appears to have little effect on apathy.15
Anxiety. A small, open-label study of 11 patients found that olanzapine, 5 mg/d, significantly improved depression, anxiety, irritability, and obsessive behavior in HD patients.17
The HDSA guide suggests treating anxiety and obsessive-compulsive symptoms as you would in patients without HD. For anxiety, SSRIs and possibly a short-term trial of a low-dose benzodiazepine (ie, lorazepam, clonazepam) are suggested.16 Benzodiazepines may increase the risk of falls and delirium in this population. Anecdotally, buspirone is helpful in some patients, with a starting dose of 5 mg 2 to 3 times per day and increased to 20 to 30 mg/d in divided doses.16 For obsessive-compulsive symptoms, SSRIs are recommended; atypical antipsychotics are reserved for severe or refractory symptoms.16
Disinhibition and impulsivity. There’s no research on treating disinhibition and impulsivity in HD. In our clinical experience, atypical antipsychotics are the most helpful. Factors regarding choosing an agent and dosing levels are similar to those for psychotic symptoms.
Psychotic symptoms. Most studies of typical and atypical antipsychotics for HD psychosis have shown beneficial effects.14,16-21 Neurologists frequently use these agents for managing chorea. Both neurologic and psychiatric features of the patient’s presentation must be considered when selecting a drug because treatment directed at 1 component of the disease may inadvertently exacerbate another. Specifically, higher potency antipsychotics (eg, haloperidol) are effective for chorea but can dramatically worsen bradykinesia; lower potency agents (eg, quetiapine) are less helpful for chorea but do not significantly worsen rigidity symptoms.
Olanzapine has been shown to improve chorea, anxiety, irritability, depression, sleep dysfunction, and weight loss in addition to psychotic symptoms.14,17 We find that olanzapine treats a constellation of symptoms common among HD patients, and we prescribe it frequently. Because olanzapine is considered a mid-potency agent, we find it’s best suited for concurrent control of psychotic symptoms and mild to moderate chorea in patients with minimal bradykinesia. Start olanzapine at 2.5 mg/d and gradually increase to 5 to 10 mg/d as tolerated.14
Risperidone is effective for treating psychosis and chorea. It can be started at 0.5 to 1 mg/d, and gradually increased to 6 to 8 mg/d.14 The depot formulation of risperidone has been shown to be effective in HD, which may help patients adhere to their medication.18 Risperidone is a mid-high potency antipsychotic, and in our experience is best used to control psychotic symptoms in patients with moderate chorea and few or no symptoms of bradykinesia or rigidity.
Quetiapine reduces psychotic symptoms, agitation, irritability, and insomnia without worsening bradykinesia or rigidity,19 but it is not beneficial for chorea. It can be started at 12.5 mg/d and gradually increased for effect as tolerated, up to 600 mg/d (depending on indication), in 2 or 3 divided doses.14
Haloperidol is a high-potency typical antipsychotic and may help psychotic patients with severe chorea; it should not be used in patients with bradykinesia. Start haloperidol at 0.5 to 1 mg/d and gradually increase to 6 to 8 mg/d as tolerated.14 Because of higher likelihood of side effects with typical antipsychotics, we often reserve its use for patients whose psychosis does not respond to atypical agents.
Other antipsychotics. Aripiprazole in HD has been examined in only 2 single- patient case reports20,21; the drug appeared to reduce psychosis and possibly chorea. Clozapine’s effectiveness for HD psychosis is not well known. It does not appear to be helpful for chorea and can cause agranulocytosis.22
Because one of the hallmarks of HD is dementia, it is worth noting that the FDA has issued a “black-box” warning on the use of antipsychotic drugs in patients with dementia because of concerns regarding increased mortality. However, drawing specific conclusions is difficult because the FDA warning is based on studies that looked primarily at Alzheimer’s disease and vascular dementia, not HD.
Other pharmacotherapies
Tetrabenazine is the only FDA-approved drug for treating HD. However, it carries a “black-box” warning for increased risk of depression and suicidal ideation and is contraindicated in suicidal patients and those with untreated or inadequately treated depression.
Although several small trials have had conflicting results regarding its benefit, amantadine sometimes is used to treat chorea.23-25 For more information about tetrabenazine and amantadine, see Box 3.
Tetrabenazine, the only FDA-approved drug for treating Huntington’s disease (HD), is a dopamine-depleting agent given to control chorea. In a 12-week, randomized, double-blind, placebo-controlled clinical trial, tetrabenazine was shown to be effective in HD patients.a Treatment with tetrabenazine results in symptomatic improvement of chorea, but does not slow or alter the course of the disease. Tetrabenazine can provide relief from choreiform movements, but these benefits should be balanced with the risks of depression and suicidality.a Tetrabenazine is known to prolong QTc interval, and should be used with caution in combination with other drugs that have the potential to do the same (eg, antipsychotics).a
Several case reports have found an association between tetrabenazine and development of neuroleptic malignant syndrome (NMS).b-d Be aware of the clinical characteristics of NMS—mental status change, rigidity, fever, and dysautonomia—and use caution when starting patients taking tetrabenazine on antipsychotics or other agents known to cause NMS.
Amantadine also has been used to treat chorea in HD patients who are unable to tolerate tetrabenazine or antipsychotics. Our neurologists sometimes have found it to be beneficial in patients with juvenile-onset HD because these patients often have debilitating dystonia. Be aware that amantadine is known to precipitate or worsen psychosis.e
References
- Food and Drug Administration. NDA 21-894 Xenazine® (tetrabenazine). Risk evaluation and mitigation strategy (REMS). Click here. Published August 15, 2008. Updated April 2011. Accessed June 20, 2012.
- Stevens E, Roman A, Houa M, et al. Severe hyperthermia during tetrabenazine therapy for tardive dyskinesia. Intensive Care Med. 1998;24(4):369-371.
- Petzinger GM, Bressman SB. A case of tetrabenazine-induced neuroleptic malignant syndrome after prolonged treatment. Mov Disord. 1997;12(2):246-248.
- Ossemann M, Sindic CJ, Laterre C. Tetrabenazine as a cause of neuroleptic malignant syndrome. Mov Disord. 1996;11(1):95.
- Wolters EC. Dopaminomimetic psychosis in Parkinson’s disease patients: diagnosis and treatment. Neurology. 1999;52 (7 suppl 3):S10-S13.
Related Resources
- Huntington’s Disease Society of America. www.hdsa.org.
- Family Caregiver Alliance. Huntington’s disease. www.caregiver.org/caregiver/jsp/content_node.jsp?nodeid=574.
- Huntington Study Group. www.huntington-study-group.org.
- Huntington’s Disease Advocacy Center. www.hdac.org.
Drug Brand Names
- Amantadine • Symmetrel
- Aripiprazole • Abilify
- Bupropion • Wellbutrin, Wellbutrin XL, others
- Buspirone • BuSpar
- Citalopram • Celexa
- Clonazepam • Klonopin
- Clozapine • Clozaril
- Dextroamphetamine • Dexedrine
- Escitalopram • Lexapro
- Fluoxetine • Prozac
- Haloperidol • Haldol
- Lorazepam • Ativan
- Methylphenidate • Concerta, Ritalin, others
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Pemoline • Cylert
- Quetiapine • Seroquel
- Risperidone • Risperdal
- Sertraline • Zoloft
- Tetrabenazine • Xenazine
- Venlafaxine XR • Effexor XR
Disclosures
Dr. Scher is a consultant to the advisory board for Lundbeck.
Ms. Kocsis reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89(4):365-376.
2. Paulsen JS, Ready RE, Hamilton JM, et al. Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310-314.
3. Thompson JC, Harris J, Sollom AC, et al. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2012;24(1):53-60.
4. Beglinger LJ, Langbehn DR, Duff K, et al. Probability of obsessive and compulsive symptoms in Huntington’s disease. Biol Psychiatry. 2007;61(3):415-418.
5. Naarding P, Janzing JG, Eling P, et al. Apathy is not depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2009;21(3):266-270.
6. Ho AK, Gilbert AS, Mason SL, et al. Health-related quality of life in Huntington’s disease: which factors matter most? Mov Disord. 2009;24(4):574-578.
7. Hamilton JM, Salmon DP, Corey-Bloom J, et al. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2003;74(1):120-122.
8. Hubers AA, Reedeker N, Giltay EJ, et al. Suicidality in Huntington’s disease. J Affect Disord. 2012;136(3):550-557.
9. Videnovic A, Leurgans S, Fan W, et al. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15(6):471-474.
10. Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219-226.
11. Duff K, Paulsen JS, Beglinger LJ, et al. “Frontal” behaviors before the diagnosis of Huntington’s disease and their relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22(2):196-207.
12. Tsuang D, Almqvist EW, Lipe H, et al. Familial aggregation of psychotic symptoms in Huntington’s disease. Am J Psychiatry. 2000;157(12):1955-1959.
13. Holl AK, Wilkinson L, Painold A, et al. Combating depression in Huntington’s disease: effective antidepressive treatment with venlafaxine XR. Int Clin Psychopharmacol. 2010;25(1):46-50.
14. Killoran A, Biglan KM. Therapeutics in Huntington’s disease. Curr Treat Options Neurol. 2012;14(2):137-149.
15. Ranen NG, Peyser CE, Folstein SE. ECT as a treatment for depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 1994;6(2):154-159.
16. Rosenblatt A, Ranen NG, Nance MA, et al. A physician’s guide to the management of Huntington’s disease. 2nd edition. http://www.hdsa.org/images/content/1/1/11289.pdf. Published 1999. Accessed July 27, 2012.
17. Squitieri F, Cannella M, Piorcellini A, et al. Short-term effects of olanzapine in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(1):69-72.
18. Johnston TG. Risperidone long-acting injection and Huntington’s disease: case series with significant psychiatric and behavioural symptoms. Int Clin Psychopharmacol. 2011;26(2):114-119.
19. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
20. Lin WC, Chou YH. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
21. Oulis P, Mourikis I, Konstantakopoulos G, et al. Aripiprazole in the treatment of olanzapine-resistant psychotic and motor symptoms of Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2010;22(3):352c.e4-352c.e5.
22. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomised comparative study. J Neurol Neurosurg Psychiatry. 1997;63(1):35-39.
23. Verhagen Metman L, Morris MJ, Farmer C, et al. Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology. 2002;59(5):694-699.
24. Lucetti C, Del Dotto P, Gambaccini G, et al. IV amantadine improves chorea in Huntington’s disease: an acute randomized, controlled study. Neurology. 2003;60(12):1995-1997.
25. O’Suilleabhain P, Dewey RB, Jr. A randomized trial of amantadine in Huntington disease. Arch Neurol. 2003;60(7):996-998.
1. Harper PS. The epidemiology of Huntington’s disease. Hum Genet. 1992;89(4):365-376.
2. Paulsen JS, Ready RE, Hamilton JM, et al. Neuropsychiatric aspects of Huntington’s disease. J Neurol Neurosurg Psychiatry. 2001;71(3):310-314.
3. Thompson JC, Harris J, Sollom AC, et al. Longitudinal evaluation of neuropsychiatric symptoms in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2012;24(1):53-60.
4. Beglinger LJ, Langbehn DR, Duff K, et al. Probability of obsessive and compulsive symptoms in Huntington’s disease. Biol Psychiatry. 2007;61(3):415-418.
5. Naarding P, Janzing JG, Eling P, et al. Apathy is not depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2009;21(3):266-270.
6. Ho AK, Gilbert AS, Mason SL, et al. Health-related quality of life in Huntington’s disease: which factors matter most? Mov Disord. 2009;24(4):574-578.
7. Hamilton JM, Salmon DP, Corey-Bloom J, et al. Behavioural abnormalities contribute to functional decline in Huntington’s disease. J Neurol Neurosurg Psychiatry. 2003;74(1):120-122.
8. Hubers AA, Reedeker N, Giltay EJ, et al. Suicidality in Huntington’s disease. J Affect Disord. 2012;136(3):550-557.
9. Videnovic A, Leurgans S, Fan W, et al. Daytime somnolence and nocturnal sleep disturbances in Huntington disease. Parkinsonism Relat Disord. 2009;15(6):471-474.
10. Craufurd D, Thompson JC, Snowden JS. Behavioral changes in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(4):219-226.
11. Duff K, Paulsen JS, Beglinger LJ, et al. “Frontal” behaviors before the diagnosis of Huntington’s disease and their relationship to markers of disease progression: evidence of early lack of awareness. J Neuropsychiatry Clin Neurosci. 2010;22(2):196-207.
12. Tsuang D, Almqvist EW, Lipe H, et al. Familial aggregation of psychotic symptoms in Huntington’s disease. Am J Psychiatry. 2000;157(12):1955-1959.
13. Holl AK, Wilkinson L, Painold A, et al. Combating depression in Huntington’s disease: effective antidepressive treatment with venlafaxine XR. Int Clin Psychopharmacol. 2010;25(1):46-50.
14. Killoran A, Biglan KM. Therapeutics in Huntington’s disease. Curr Treat Options Neurol. 2012;14(2):137-149.
15. Ranen NG, Peyser CE, Folstein SE. ECT as a treatment for depression in Huntington’s disease. J Neuropsychiatry Clin Neurosci. 1994;6(2):154-159.
16. Rosenblatt A, Ranen NG, Nance MA, et al. A physician’s guide to the management of Huntington’s disease. 2nd edition. http://www.hdsa.org/images/content/1/1/11289.pdf. Published 1999. Accessed July 27, 2012.
17. Squitieri F, Cannella M, Piorcellini A, et al. Short-term effects of olanzapine in Huntington disease. Neuropsychiatry Neuropsychol Behav Neurol. 2001;14(1):69-72.
18. Johnston TG. Risperidone long-acting injection and Huntington’s disease: case series with significant psychiatric and behavioural symptoms. Int Clin Psychopharmacol. 2011;26(2):114-119.
19. Alpay M, Koroshetz WJ. Quetiapine in the treatment of behavioral disturbances in patients with Huntington’s disease. Psychosomatics. 2006;47(1):70-72.
20. Lin WC, Chou YH. Aripiprazole effects on psychosis and chorea in a patient with Huntington’s disease. Am J Psychiatry. 2008;165(9):1207-1208.
21. Oulis P, Mourikis I, Konstantakopoulos G, et al. Aripiprazole in the treatment of olanzapine-resistant psychotic and motor symptoms of Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2010;22(3):352c.e4-352c.e5.
22. van Vugt JP, Siesling S, Vergeer M, et al. Clozapine versus placebo in Huntington’s disease: a double blind randomised comparative study. J Neurol Neurosurg Psychiatry. 1997;63(1):35-39.
23. Verhagen Metman L, Morris MJ, Farmer C, et al. Huntington’s disease: a randomized, controlled trial using the NMDA-antagonist amantadine. Neurology. 2002;59(5):694-699.
24. Lucetti C, Del Dotto P, Gambaccini G, et al. IV amantadine improves chorea in Huntington’s disease: an acute randomized, controlled study. Neurology. 2003;60(12):1995-1997.
25. O’Suilleabhain P, Dewey RB, Jr. A randomized trial of amantadine in Huntington disease. Arch Neurol. 2003;60(7):996-998.
Psychiatric advance directives: May you disregard them?
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient stopped antipsychotic medication, experienced a recurrence of paranoid schizophrenia, and now is involuntarily hospitalized. During her admission assessment, she said she had a “psychiatric advance directive.” I obtained the document, which says she refuses psychopharmacologic treatment under any circumstances. Without medication, she might take years to recover. How should I proceed?
Submitted by “Dr. Y”
Most psychiatrists who regularly practice hospital-based care know their state’s legal procedures for forcing psychotic, civilly committed patients to take medication to relieve their acute symptoms. In most jurisdictions, courts will order medication over a patient’s objection after finding that the patient lacks competence to refuse antipsychotic therapy and that the proposed treatment is in the patient’s best interest.1
But if a patient has a psychiatric advance directive (PAD) that opposes psychotropic medication, things may become complicated. To decide what to do if a patient’s PAD precludes administering a treatment you think is necessary, you should understand:
- what PADs do
- what courts have said about PADs
- what your state’s laws say about PADs
- where and when to seek legal advice.
What are advance directives?
An advance directive (or “declaration”) for health care (ADHC) is a legal document executed by a competent individual that states preferences regarding medical treatment should that individual become incapable of making or expressing decisions.2-4 An ADHC may be a “living will” that lays out instructions for specific health care situations or a “durable power of attorney” (DPOA) that designates a proxy decision maker, or it may include elements of both. In 1990, the U.S. Congress passed the Patient Self-Determination Act,5 which required health care institutions that receive Medicare or Medicaid to ask patients whether they have ADHCs and to give patients information about state laws governing ADHCs.
Modeled after medical advance directives, PADs let competent individuals declare their wishes should they need psychiatric treatment during a period of decision-making incapacity.3,4 At least 25 states have advance directive statutes specific to psychiatry.6 Depending on the state, PADs may allow individuals to assert their preferences regarding psychotropic medication, electroconvulsive therapy (ECT), alternatives to hospitalization, location and length of voluntary hospitalization, the treating psychiatrist, seclusion and restraint, emergency medications, and visitors.
Prevalence and praise
The prevalence of PADs is unknown. A 2006 survey of 1,011 psychiatric outpatients in California, Florida, Illinois, Massachusetts, and North Carolina by Swanson et al7 found only 4% to 13% of patients previously executed a PAD. However, most participants said that if given the opportunity and assistance, they would create a PAD.7
Psychiatric advocacy groups have lauded the development of PADs. For example, the National Alliance on Mental Illness’ position is that “PADs should be considered as a way to empower consumers to take a more active role in their treatment, and as a way to avoid conflicts over treatment and medication issues.”8 Proponents suggest that PADs:
- promote autonomy
- foster communication between patients and treatment providers
- increase compliance with medication
- reduce involuntary treatment and judicial involvement.4,8
Mental Health America launched My Plan, My Life: My Psychiatric Advance Directive in September 2011 to increase public awareness of the availability of PADs.9 Therefore, it is safe to assume that most psychiatrists will encounter patients with PADs.
What if a PAD blocks treatment?
What happens when an adult such as Dr. Y’s patient has a PAD that precludes effective treatment? A similar situation led to Hargrave v Vermont.10
Nancy Hargrave, a Vermont woman with schizophrenia and a history of psychiatric hospitalizations, executed a DPOA—Vermont does not have a separate statute for PADs—in which she explicitly refused “any and all anti-psychotic, neuroleptic, psychotropic, or psychoactive medications,” and ECT.10
In anticipation of situations like this, Vermont’s legislature passed Act 114, a 1998 state law that required caregivers to abide by the DPOAs of civilly committed individuals and mentally ill prisoners for 45 days.10 After this time, a court may override the advance directive and allow involuntary medication administration if a patient “ha[d] not experienced a significant clinical improvement in his or her mental state, and remain[ed] incompetent.”10
In 1999, Hargrave sued the state of Vermont and other parties in federal court, alleging that Act 114 constituted discrimination under Title II of the Americans with Disabilities Act11 because Act 114 excluded her from participating in the “services, programs, or activities of a public entity,” namely, the use of her DPOA under Vermont state law.10 The federal district court sided with Hargrave, concluding that “Act 114 was facially discriminatory against mentally disabled individuals.” One year later, the U.S. Court of Appeals for the Second Circuit affirmed the district court’s ruling.
Surprisingly, no other court has adjudicated this issue. However, in Second Circuit states—Vermont, New York, and Connecticut—DPOAs of mentally ill patients cannot be abrogated. This is an unsettling notion for many psychiatrists, because, as Paul Appelbaum, MD, explains, “Advance directives may now constitute an ironclad bulwark against future involuntary treatment with medication—except in emergencies—even for incompetent, committed patients and even when the alternative is long-term institutional care.”12 Other scholars have pointed out that giving physicians an avenue to override or disregard patients’ directives would negate their intended purpose, which is to have one’s competently expressed wishes followed when one’s decision-making capacity is compromised.6,13
Doctors’ duties
How you should respond to an involuntary patient’s PAD depends on which state you practice in. A physician’s obligation to comply with a patient’s PAD depends on state law, and most states with PAD laws provide some latitude or options if physicians believe they should not comply with a patient’s wishes.6,13Table 114-18 cites examples of statutory language regarding a physician’s duty to comply with a PAD.
A survey of 164 psychiatrists in North Carolina provides some insight into psychiatrists’ perceptions of PADs.19 After reading a hypothetical scenario about a mentally ill individual whose PAD expressed refusal of hospitalization or treatment with antipsychotics, 47% of the psychiatrists chose to override the PAD. The authors found that “PAD override was more likely among psychiatrists who worked in hospital emergency departments; those who were concerned about patients’ violence risk and lack of insight; and those who were legally defensive.”
In addition to addressing conflicts between patients’ PADs and doctors’ views about proper treatment, some state laws also contain clauses that spell out the limits of physician liability in cases of physician compliance or noncompliance with PADs. Excerpts from 2 such laws appear in Table 2.16-17
Table 1
Examples of state laws on compliance with psychiatric advance directives
| State | Provider compliance |
|---|---|
| Kentucky14 | Providers must provide mental health treatment that complies with the instructions in an advance directive to the fullest extent possible when the instructions are within standards for mental and physical health care and permitted by state and federal law. Providers may override expressed refusals of treatment only if a court order contradicts the advance directive or an emergency endangers a patient’s life or poses a serious risk to physical health |
| Ohio15 | A provider who does not wish to comply with a patient’s declaration must notify the patient and any proxy and document the notification. The provider may not interfere with the patient’s transfer to another provider who is willing to follow the patient’s declaration. Providers may subject a patient to treatment contrary to a declaration only if:
|
| Oklahoma16 | Physicians and psychologists must follow as closely as possible the terms of a patient’s declaration. A provider who cannot comply with the terms of the patient’s declaration must make arrangements to transfer the patient and the appropriate medical records without delay to another physician or psychologist |
| Pennsylvania17 | If a provider cannot in good conscience comply with a patient’s declaration because the instructions are contrary to accepted clinical practice and medical standards, the provider must make every reasonable effort to help transfer care to another provider who will comply with the declaration. While the transfer is pending, the provider must provide treatment in a way that is consistent with the declaration. If reasonable efforts to transfer fail, the patient may be discharged |
| Utah18 | A physician must comply with a declaration to the fullest extent possible, consistent with reasonable medical practice, the availability of treatments requested, and applicable law. A physician may subject a patient to treatment contrary to wishes expressed in a declaration if:
|
Table 2
Excerpts from state laws on PAD-related liability
| State | Liability or immunity |
|---|---|
| Oklahoma16 | A provider who transfers the patient without unreasonable delay to another provider or who makes a good faith attempt to do so may not be subject to criminal prosecution or civil liability. The provider may not be found to have committed an act of unprofessional conduct for refusal to comply with the terms of the declaration, and transfer under such circumstances shall not constitute abandonment. However, the failure of a provider to transfer in accordance with this subsection shall constitute professional misconduct |
| Pennsylvania17 | A provider who acts in good faith and consistent with the statute may not be subject to criminal or civil liability, discipline for unprofessional conduct, or administrative sanctions. A provider may not be found to have committed an act of unprofessional conduct by the relevant state professional board because the provider refused to comply with:
|
| PAD: psychiatric advance directive | |
Related Resources
- National Resource Center on Psychiatric Advance Directives. www.nrc-pad.org.
- Duke University Program on Psychiatric Advance Directives. http://pad.duhs.duke.edu.
- Hung EK, McNiel DE, Binder RL. Covert medication in psychiatric emergencies: is it ever ethically permissible? J Am Acad Psychiatry Law. 2012;40(2):239-245.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Eclavea RP, Martin LD. State-created right to refuse medication. 53 Am. Jur. 2d Mentally Impaired Persons § 111 (West 2012).
2. Aitken PV, Jr. Incorporating advance care planning into family practice. Am Fam Physician. 1999;59(3):605-614, 617–620.
3. Gallagher EM. Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychol Public Policy Law. 1998;4(3):746-787.
4. DeWolf Bosek MS, Ring ME, Cady RF. Do psychiatric advance directives protect autonomy? JONAS Healthc Law Ethics Regul. 2008;10(1):17-24.
5. Patient Self Determination Act 42 USC § 1395cc 1396a (1994)
6. Swanson JW, McCrary SV, Swartz MS, et al. Superseding psychiatric advance directives: ethical and legal considerations. J Am Acad Psychiatry Law. 2006;34(3):385-394.
7. Swanson J, Swartz M, Ferron J, et al. Psychiatric advance directives among public mental health consumers in five U.S. cities: prevalence, demand, and correlates. J Am Acad Psychiatry Law. 2006;34(1):43-57.
8. National Alliance on Mental Illness. Psychiatric advance directives. http://www.nami.org/Template.cfm?Section=Issue_Spotlights&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=5&ContentID=8217. Accessed July 11, 2012.
9. Mental Health America. My plan, my life: my psychiatric advance directive. http://www.myplanmylife.com. Accessed July 23, 2012.
10. Hargrave v Vermont 340 F3d 27 (2d Cir Vt 2003).
11. Americans with Disabilities Act, 42 USCA § 12132
12. Appelbaum PS. Law & psychiatry: psychiatric advance directives and the treatment of committed patients. Psychiatr Serv. 2004;55(7):751-752, 763.
13. Appelbaum PS. Commentary: psychiatric advance directives at a crossroads—when can PADs be overridden? J Am Acad Psychiatry Law. 2006;34(3):395-397.
14. Ky Rev State § 202A.426 (Michie 2012).
15. Ohio Rev Code § 2135.07 (Page 2012).
16. 43A Okla. St.§ 11-110 (Lexis 2012).
17. 20 Pa. Cons. Stat. §5804.
18. Utah Code Ann. § 62A-15-1003 (Lexis, 2012).
19. Swanson JW, Van McCrary S, Swartz MS, et al. Overriding psychiatric advance directives: factors associated with psychiatrists’ decisions to preempt patients’ advance refusal of hospitalization and medication. Law Hum Behav. 2007;31(1):77-90.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient stopped antipsychotic medication, experienced a recurrence of paranoid schizophrenia, and now is involuntarily hospitalized. During her admission assessment, she said she had a “psychiatric advance directive.” I obtained the document, which says she refuses psychopharmacologic treatment under any circumstances. Without medication, she might take years to recover. How should I proceed?
Submitted by “Dr. Y”
Most psychiatrists who regularly practice hospital-based care know their state’s legal procedures for forcing psychotic, civilly committed patients to take medication to relieve their acute symptoms. In most jurisdictions, courts will order medication over a patient’s objection after finding that the patient lacks competence to refuse antipsychotic therapy and that the proposed treatment is in the patient’s best interest.1
But if a patient has a psychiatric advance directive (PAD) that opposes psychotropic medication, things may become complicated. To decide what to do if a patient’s PAD precludes administering a treatment you think is necessary, you should understand:
- what PADs do
- what courts have said about PADs
- what your state’s laws say about PADs
- where and when to seek legal advice.
What are advance directives?
An advance directive (or “declaration”) for health care (ADHC) is a legal document executed by a competent individual that states preferences regarding medical treatment should that individual become incapable of making or expressing decisions.2-4 An ADHC may be a “living will” that lays out instructions for specific health care situations or a “durable power of attorney” (DPOA) that designates a proxy decision maker, or it may include elements of both. In 1990, the U.S. Congress passed the Patient Self-Determination Act,5 which required health care institutions that receive Medicare or Medicaid to ask patients whether they have ADHCs and to give patients information about state laws governing ADHCs.
Modeled after medical advance directives, PADs let competent individuals declare their wishes should they need psychiatric treatment during a period of decision-making incapacity.3,4 At least 25 states have advance directive statutes specific to psychiatry.6 Depending on the state, PADs may allow individuals to assert their preferences regarding psychotropic medication, electroconvulsive therapy (ECT), alternatives to hospitalization, location and length of voluntary hospitalization, the treating psychiatrist, seclusion and restraint, emergency medications, and visitors.
Prevalence and praise
The prevalence of PADs is unknown. A 2006 survey of 1,011 psychiatric outpatients in California, Florida, Illinois, Massachusetts, and North Carolina by Swanson et al7 found only 4% to 13% of patients previously executed a PAD. However, most participants said that if given the opportunity and assistance, they would create a PAD.7
Psychiatric advocacy groups have lauded the development of PADs. For example, the National Alliance on Mental Illness’ position is that “PADs should be considered as a way to empower consumers to take a more active role in their treatment, and as a way to avoid conflicts over treatment and medication issues.”8 Proponents suggest that PADs:
- promote autonomy
- foster communication between patients and treatment providers
- increase compliance with medication
- reduce involuntary treatment and judicial involvement.4,8
Mental Health America launched My Plan, My Life: My Psychiatric Advance Directive in September 2011 to increase public awareness of the availability of PADs.9 Therefore, it is safe to assume that most psychiatrists will encounter patients with PADs.
What if a PAD blocks treatment?
What happens when an adult such as Dr. Y’s patient has a PAD that precludes effective treatment? A similar situation led to Hargrave v Vermont.10
Nancy Hargrave, a Vermont woman with schizophrenia and a history of psychiatric hospitalizations, executed a DPOA—Vermont does not have a separate statute for PADs—in which she explicitly refused “any and all anti-psychotic, neuroleptic, psychotropic, or psychoactive medications,” and ECT.10
In anticipation of situations like this, Vermont’s legislature passed Act 114, a 1998 state law that required caregivers to abide by the DPOAs of civilly committed individuals and mentally ill prisoners for 45 days.10 After this time, a court may override the advance directive and allow involuntary medication administration if a patient “ha[d] not experienced a significant clinical improvement in his or her mental state, and remain[ed] incompetent.”10
In 1999, Hargrave sued the state of Vermont and other parties in federal court, alleging that Act 114 constituted discrimination under Title II of the Americans with Disabilities Act11 because Act 114 excluded her from participating in the “services, programs, or activities of a public entity,” namely, the use of her DPOA under Vermont state law.10 The federal district court sided with Hargrave, concluding that “Act 114 was facially discriminatory against mentally disabled individuals.” One year later, the U.S. Court of Appeals for the Second Circuit affirmed the district court’s ruling.
Surprisingly, no other court has adjudicated this issue. However, in Second Circuit states—Vermont, New York, and Connecticut—DPOAs of mentally ill patients cannot be abrogated. This is an unsettling notion for many psychiatrists, because, as Paul Appelbaum, MD, explains, “Advance directives may now constitute an ironclad bulwark against future involuntary treatment with medication—except in emergencies—even for incompetent, committed patients and even when the alternative is long-term institutional care.”12 Other scholars have pointed out that giving physicians an avenue to override or disregard patients’ directives would negate their intended purpose, which is to have one’s competently expressed wishes followed when one’s decision-making capacity is compromised.6,13
Doctors’ duties
How you should respond to an involuntary patient’s PAD depends on which state you practice in. A physician’s obligation to comply with a patient’s PAD depends on state law, and most states with PAD laws provide some latitude or options if physicians believe they should not comply with a patient’s wishes.6,13Table 114-18 cites examples of statutory language regarding a physician’s duty to comply with a PAD.
A survey of 164 psychiatrists in North Carolina provides some insight into psychiatrists’ perceptions of PADs.19 After reading a hypothetical scenario about a mentally ill individual whose PAD expressed refusal of hospitalization or treatment with antipsychotics, 47% of the psychiatrists chose to override the PAD. The authors found that “PAD override was more likely among psychiatrists who worked in hospital emergency departments; those who were concerned about patients’ violence risk and lack of insight; and those who were legally defensive.”
In addition to addressing conflicts between patients’ PADs and doctors’ views about proper treatment, some state laws also contain clauses that spell out the limits of physician liability in cases of physician compliance or noncompliance with PADs. Excerpts from 2 such laws appear in Table 2.16-17
Table 1
Examples of state laws on compliance with psychiatric advance directives
| State | Provider compliance |
|---|---|
| Kentucky14 | Providers must provide mental health treatment that complies with the instructions in an advance directive to the fullest extent possible when the instructions are within standards for mental and physical health care and permitted by state and federal law. Providers may override expressed refusals of treatment only if a court order contradicts the advance directive or an emergency endangers a patient’s life or poses a serious risk to physical health |
| Ohio15 | A provider who does not wish to comply with a patient’s declaration must notify the patient and any proxy and document the notification. The provider may not interfere with the patient’s transfer to another provider who is willing to follow the patient’s declaration. Providers may subject a patient to treatment contrary to a declaration only if:
|
| Oklahoma16 | Physicians and psychologists must follow as closely as possible the terms of a patient’s declaration. A provider who cannot comply with the terms of the patient’s declaration must make arrangements to transfer the patient and the appropriate medical records without delay to another physician or psychologist |
| Pennsylvania17 | If a provider cannot in good conscience comply with a patient’s declaration because the instructions are contrary to accepted clinical practice and medical standards, the provider must make every reasonable effort to help transfer care to another provider who will comply with the declaration. While the transfer is pending, the provider must provide treatment in a way that is consistent with the declaration. If reasonable efforts to transfer fail, the patient may be discharged |
| Utah18 | A physician must comply with a declaration to the fullest extent possible, consistent with reasonable medical practice, the availability of treatments requested, and applicable law. A physician may subject a patient to treatment contrary to wishes expressed in a declaration if:
|
Table 2
Excerpts from state laws on PAD-related liability
| State | Liability or immunity |
|---|---|
| Oklahoma16 | A provider who transfers the patient without unreasonable delay to another provider or who makes a good faith attempt to do so may not be subject to criminal prosecution or civil liability. The provider may not be found to have committed an act of unprofessional conduct for refusal to comply with the terms of the declaration, and transfer under such circumstances shall not constitute abandonment. However, the failure of a provider to transfer in accordance with this subsection shall constitute professional misconduct |
| Pennsylvania17 | A provider who acts in good faith and consistent with the statute may not be subject to criminal or civil liability, discipline for unprofessional conduct, or administrative sanctions. A provider may not be found to have committed an act of unprofessional conduct by the relevant state professional board because the provider refused to comply with:
|
| PAD: psychiatric advance directive | |
Related Resources
- National Resource Center on Psychiatric Advance Directives. www.nrc-pad.org.
- Duke University Program on Psychiatric Advance Directives. http://pad.duhs.duke.edu.
- Hung EK, McNiel DE, Binder RL. Covert medication in psychiatric emergencies: is it ever ethically permissible? J Am Acad Psychiatry Law. 2012;40(2):239-245.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient stopped antipsychotic medication, experienced a recurrence of paranoid schizophrenia, and now is involuntarily hospitalized. During her admission assessment, she said she had a “psychiatric advance directive.” I obtained the document, which says she refuses psychopharmacologic treatment under any circumstances. Without medication, she might take years to recover. How should I proceed?
Submitted by “Dr. Y”
Most psychiatrists who regularly practice hospital-based care know their state’s legal procedures for forcing psychotic, civilly committed patients to take medication to relieve their acute symptoms. In most jurisdictions, courts will order medication over a patient’s objection after finding that the patient lacks competence to refuse antipsychotic therapy and that the proposed treatment is in the patient’s best interest.1
But if a patient has a psychiatric advance directive (PAD) that opposes psychotropic medication, things may become complicated. To decide what to do if a patient’s PAD precludes administering a treatment you think is necessary, you should understand:
- what PADs do
- what courts have said about PADs
- what your state’s laws say about PADs
- where and when to seek legal advice.
What are advance directives?
An advance directive (or “declaration”) for health care (ADHC) is a legal document executed by a competent individual that states preferences regarding medical treatment should that individual become incapable of making or expressing decisions.2-4 An ADHC may be a “living will” that lays out instructions for specific health care situations or a “durable power of attorney” (DPOA) that designates a proxy decision maker, or it may include elements of both. In 1990, the U.S. Congress passed the Patient Self-Determination Act,5 which required health care institutions that receive Medicare or Medicaid to ask patients whether they have ADHCs and to give patients information about state laws governing ADHCs.
Modeled after medical advance directives, PADs let competent individuals declare their wishes should they need psychiatric treatment during a period of decision-making incapacity.3,4 At least 25 states have advance directive statutes specific to psychiatry.6 Depending on the state, PADs may allow individuals to assert their preferences regarding psychotropic medication, electroconvulsive therapy (ECT), alternatives to hospitalization, location and length of voluntary hospitalization, the treating psychiatrist, seclusion and restraint, emergency medications, and visitors.
Prevalence and praise
The prevalence of PADs is unknown. A 2006 survey of 1,011 psychiatric outpatients in California, Florida, Illinois, Massachusetts, and North Carolina by Swanson et al7 found only 4% to 13% of patients previously executed a PAD. However, most participants said that if given the opportunity and assistance, they would create a PAD.7
Psychiatric advocacy groups have lauded the development of PADs. For example, the National Alliance on Mental Illness’ position is that “PADs should be considered as a way to empower consumers to take a more active role in their treatment, and as a way to avoid conflicts over treatment and medication issues.”8 Proponents suggest that PADs:
- promote autonomy
- foster communication between patients and treatment providers
- increase compliance with medication
- reduce involuntary treatment and judicial involvement.4,8
Mental Health America launched My Plan, My Life: My Psychiatric Advance Directive in September 2011 to increase public awareness of the availability of PADs.9 Therefore, it is safe to assume that most psychiatrists will encounter patients with PADs.
What if a PAD blocks treatment?
What happens when an adult such as Dr. Y’s patient has a PAD that precludes effective treatment? A similar situation led to Hargrave v Vermont.10
Nancy Hargrave, a Vermont woman with schizophrenia and a history of psychiatric hospitalizations, executed a DPOA—Vermont does not have a separate statute for PADs—in which she explicitly refused “any and all anti-psychotic, neuroleptic, psychotropic, or psychoactive medications,” and ECT.10
In anticipation of situations like this, Vermont’s legislature passed Act 114, a 1998 state law that required caregivers to abide by the DPOAs of civilly committed individuals and mentally ill prisoners for 45 days.10 After this time, a court may override the advance directive and allow involuntary medication administration if a patient “ha[d] not experienced a significant clinical improvement in his or her mental state, and remain[ed] incompetent.”10
In 1999, Hargrave sued the state of Vermont and other parties in federal court, alleging that Act 114 constituted discrimination under Title II of the Americans with Disabilities Act11 because Act 114 excluded her from participating in the “services, programs, or activities of a public entity,” namely, the use of her DPOA under Vermont state law.10 The federal district court sided with Hargrave, concluding that “Act 114 was facially discriminatory against mentally disabled individuals.” One year later, the U.S. Court of Appeals for the Second Circuit affirmed the district court’s ruling.
Surprisingly, no other court has adjudicated this issue. However, in Second Circuit states—Vermont, New York, and Connecticut—DPOAs of mentally ill patients cannot be abrogated. This is an unsettling notion for many psychiatrists, because, as Paul Appelbaum, MD, explains, “Advance directives may now constitute an ironclad bulwark against future involuntary treatment with medication—except in emergencies—even for incompetent, committed patients and even when the alternative is long-term institutional care.”12 Other scholars have pointed out that giving physicians an avenue to override or disregard patients’ directives would negate their intended purpose, which is to have one’s competently expressed wishes followed when one’s decision-making capacity is compromised.6,13
Doctors’ duties
How you should respond to an involuntary patient’s PAD depends on which state you practice in. A physician’s obligation to comply with a patient’s PAD depends on state law, and most states with PAD laws provide some latitude or options if physicians believe they should not comply with a patient’s wishes.6,13Table 114-18 cites examples of statutory language regarding a physician’s duty to comply with a PAD.
A survey of 164 psychiatrists in North Carolina provides some insight into psychiatrists’ perceptions of PADs.19 After reading a hypothetical scenario about a mentally ill individual whose PAD expressed refusal of hospitalization or treatment with antipsychotics, 47% of the psychiatrists chose to override the PAD. The authors found that “PAD override was more likely among psychiatrists who worked in hospital emergency departments; those who were concerned about patients’ violence risk and lack of insight; and those who were legally defensive.”
In addition to addressing conflicts between patients’ PADs and doctors’ views about proper treatment, some state laws also contain clauses that spell out the limits of physician liability in cases of physician compliance or noncompliance with PADs. Excerpts from 2 such laws appear in Table 2.16-17
Table 1
Examples of state laws on compliance with psychiatric advance directives
| State | Provider compliance |
|---|---|
| Kentucky14 | Providers must provide mental health treatment that complies with the instructions in an advance directive to the fullest extent possible when the instructions are within standards for mental and physical health care and permitted by state and federal law. Providers may override expressed refusals of treatment only if a court order contradicts the advance directive or an emergency endangers a patient’s life or poses a serious risk to physical health |
| Ohio15 | A provider who does not wish to comply with a patient’s declaration must notify the patient and any proxy and document the notification. The provider may not interfere with the patient’s transfer to another provider who is willing to follow the patient’s declaration. Providers may subject a patient to treatment contrary to a declaration only if:
|
| Oklahoma16 | Physicians and psychologists must follow as closely as possible the terms of a patient’s declaration. A provider who cannot comply with the terms of the patient’s declaration must make arrangements to transfer the patient and the appropriate medical records without delay to another physician or psychologist |
| Pennsylvania17 | If a provider cannot in good conscience comply with a patient’s declaration because the instructions are contrary to accepted clinical practice and medical standards, the provider must make every reasonable effort to help transfer care to another provider who will comply with the declaration. While the transfer is pending, the provider must provide treatment in a way that is consistent with the declaration. If reasonable efforts to transfer fail, the patient may be discharged |
| Utah18 | A physician must comply with a declaration to the fullest extent possible, consistent with reasonable medical practice, the availability of treatments requested, and applicable law. A physician may subject a patient to treatment contrary to wishes expressed in a declaration if:
|
Table 2
Excerpts from state laws on PAD-related liability
| State | Liability or immunity |
|---|---|
| Oklahoma16 | A provider who transfers the patient without unreasonable delay to another provider or who makes a good faith attempt to do so may not be subject to criminal prosecution or civil liability. The provider may not be found to have committed an act of unprofessional conduct for refusal to comply with the terms of the declaration, and transfer under such circumstances shall not constitute abandonment. However, the failure of a provider to transfer in accordance with this subsection shall constitute professional misconduct |
| Pennsylvania17 | A provider who acts in good faith and consistent with the statute may not be subject to criminal or civil liability, discipline for unprofessional conduct, or administrative sanctions. A provider may not be found to have committed an act of unprofessional conduct by the relevant state professional board because the provider refused to comply with:
|
| PAD: psychiatric advance directive | |
Related Resources
- National Resource Center on Psychiatric Advance Directives. www.nrc-pad.org.
- Duke University Program on Psychiatric Advance Directives. http://pad.duhs.duke.edu.
- Hung EK, McNiel DE, Binder RL. Covert medication in psychiatric emergencies: is it ever ethically permissible? J Am Acad Psychiatry Law. 2012;40(2):239-245.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Eclavea RP, Martin LD. State-created right to refuse medication. 53 Am. Jur. 2d Mentally Impaired Persons § 111 (West 2012).
2. Aitken PV, Jr. Incorporating advance care planning into family practice. Am Fam Physician. 1999;59(3):605-614, 617–620.
3. Gallagher EM. Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychol Public Policy Law. 1998;4(3):746-787.
4. DeWolf Bosek MS, Ring ME, Cady RF. Do psychiatric advance directives protect autonomy? JONAS Healthc Law Ethics Regul. 2008;10(1):17-24.
5. Patient Self Determination Act 42 USC § 1395cc 1396a (1994)
6. Swanson JW, McCrary SV, Swartz MS, et al. Superseding psychiatric advance directives: ethical and legal considerations. J Am Acad Psychiatry Law. 2006;34(3):385-394.
7. Swanson J, Swartz M, Ferron J, et al. Psychiatric advance directives among public mental health consumers in five U.S. cities: prevalence, demand, and correlates. J Am Acad Psychiatry Law. 2006;34(1):43-57.
8. National Alliance on Mental Illness. Psychiatric advance directives. http://www.nami.org/Template.cfm?Section=Issue_Spotlights&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=5&ContentID=8217. Accessed July 11, 2012.
9. Mental Health America. My plan, my life: my psychiatric advance directive. http://www.myplanmylife.com. Accessed July 23, 2012.
10. Hargrave v Vermont 340 F3d 27 (2d Cir Vt 2003).
11. Americans with Disabilities Act, 42 USCA § 12132
12. Appelbaum PS. Law & psychiatry: psychiatric advance directives and the treatment of committed patients. Psychiatr Serv. 2004;55(7):751-752, 763.
13. Appelbaum PS. Commentary: psychiatric advance directives at a crossroads—when can PADs be overridden? J Am Acad Psychiatry Law. 2006;34(3):395-397.
14. Ky Rev State § 202A.426 (Michie 2012).
15. Ohio Rev Code § 2135.07 (Page 2012).
16. 43A Okla. St.§ 11-110 (Lexis 2012).
17. 20 Pa. Cons. Stat. §5804.
18. Utah Code Ann. § 62A-15-1003 (Lexis, 2012).
19. Swanson JW, Van McCrary S, Swartz MS, et al. Overriding psychiatric advance directives: factors associated with psychiatrists’ decisions to preempt patients’ advance refusal of hospitalization and medication. Law Hum Behav. 2007;31(1):77-90.
1. Eclavea RP, Martin LD. State-created right to refuse medication. 53 Am. Jur. 2d Mentally Impaired Persons § 111 (West 2012).
2. Aitken PV, Jr. Incorporating advance care planning into family practice. Am Fam Physician. 1999;59(3):605-614, 617–620.
3. Gallagher EM. Advance directives for psychiatric care: a theoretical and practical overview for legal professionals. Psychol Public Policy Law. 1998;4(3):746-787.
4. DeWolf Bosek MS, Ring ME, Cady RF. Do psychiatric advance directives protect autonomy? JONAS Healthc Law Ethics Regul. 2008;10(1):17-24.
5. Patient Self Determination Act 42 USC § 1395cc 1396a (1994)
6. Swanson JW, McCrary SV, Swartz MS, et al. Superseding psychiatric advance directives: ethical and legal considerations. J Am Acad Psychiatry Law. 2006;34(3):385-394.
7. Swanson J, Swartz M, Ferron J, et al. Psychiatric advance directives among public mental health consumers in five U.S. cities: prevalence, demand, and correlates. J Am Acad Psychiatry Law. 2006;34(1):43-57.
8. National Alliance on Mental Illness. Psychiatric advance directives. http://www.nami.org/Template.cfm?Section=Issue_Spotlights&Template=/TaggedPage/TaggedPageDisplay.cfm&TPLID=5&ContentID=8217. Accessed July 11, 2012.
9. Mental Health America. My plan, my life: my psychiatric advance directive. http://www.myplanmylife.com. Accessed July 23, 2012.
10. Hargrave v Vermont 340 F3d 27 (2d Cir Vt 2003).
11. Americans with Disabilities Act, 42 USCA § 12132
12. Appelbaum PS. Law & psychiatry: psychiatric advance directives and the treatment of committed patients. Psychiatr Serv. 2004;55(7):751-752, 763.
13. Appelbaum PS. Commentary: psychiatric advance directives at a crossroads—when can PADs be overridden? J Am Acad Psychiatry Law. 2006;34(3):395-397.
14. Ky Rev State § 202A.426 (Michie 2012).
15. Ohio Rev Code § 2135.07 (Page 2012).
16. 43A Okla. St.§ 11-110 (Lexis 2012).
17. 20 Pa. Cons. Stat. §5804.
18. Utah Code Ann. § 62A-15-1003 (Lexis, 2012).
19. Swanson JW, Van McCrary S, Swartz MS, et al. Overriding psychiatric advance directives: factors associated with psychiatrists’ decisions to preempt patients’ advance refusal of hospitalization and medication. Law Hum Behav. 2007;31(1):77-90.
Diagnostic puzzler: Hypertension in teen
A review of the patient’s blood pressure since admission indicated consistently elevated systolic and diastolic pressures, on average, of 170/105 mm Hg. Additionally, his serum potassium levels ranged from 2.4 to 3.1 mmol/L (normal 3.5-5.1 mmol/L).
A detailed medical history and review of previous records revealed that an initial diagnosis of hypertension had been made during a routine sports physical at age 14, although the patient was cleared for full activity. Over the previous year, the patient said he had gained weight—much of it in the abdomen—and experienced sleep disturbances, increasing fatigability, muscle weakness, hair loss, and declining performance in his high school sports. In addition, he had noticed increased facial flushing and sweating.
On physical exam, we noted an obese male (height 5’5’’, weight 191.5 lb, BMI 30.86 kg/m2) with the following vital signs: temperature 97.9°F, pulse 105 bpm, and blood pressure 177/111 mm Hg. Pertinent physical exam findings outside of his surgical site included diffusely thinning hair, moon facies, facial plethora, increased supraclavicular and dorsocervical fat pads, thoracic and abdominal striae, thinned skin overlying his upper and lower extremities, and lower extremity edema ( FIGURE 1 ). All other exam findings were within normal limits.
Initial blood chemistry lab results revealed hyperglycemia (290 mg/dL; random normal, <200 mg/dL), hypokalemia (3.0 mmol/L; normal, 3.5-5.4 mmol/L), hypochloremia (96 mmol/L; normal, 98-107 mmol/L), and a mean corpuscular volume of 101.2 fL (normal, 80-100 fL). The patient also had a white blood cell (WBC) count of 14,400/mcL with a predominance of neutrophils and 6 bands, and a high sensitivity C-reactive protein level of 7.5 mg/dL (normal, <0.748 mg/dL).
FIGURE 1
The signs were all there
Our patient exhibited thinning hair (A), moon facies (B), dorsocervical fat pads (“buffalo hump”) (C), and abdominal striae (D).
WHAT ADDITIONAL TESTING WOULD YOU ORDER?
WHAT IS YOUR PRESUMPTIVE DIAGNOSIS?
Suspecting Cushing’s syndrome, we ordered cortisol and ACTH
Based on our initial findings, we ordered a 24-hour urinary free cortisol and plasma adrenocorticotropic hormone (ACTH) level—both of which had to be sent to outside laboratories. We also ordered a computed tomography (CT) scan of the patient’s adrenal glands and magnetic resonance imaging (MRI) of his pituitary gland.
The CT scan revealed mild hyperplasia of the adrenal glands bilaterally; the MRI demonstrated a 7 × 6 × 6 mm pituitary microadenoma ( FIGURE 2 ) in the anterior portion of the gland. In addition, a 6 × 6 × 1 mm lesion was noted—thought to be a Rathke’s cleft (Pars intermedia) cyst by the reviewing radiologist.
The patient’s initial cortisol and ACTH lab work revealed a urinary cortisol level of 5089.2 mcg/24 h (normal, 3-55 mcg/24 h) and an ACTH level of 216 pg/mL (normal, 9-57 pg/mL for ages 3-17 years).
We diagnosed Cushing’s syndrome in this patient.
FIGURE 2
MRI reveals pituitary microadenoma
The patient had a microadenoma in the anterior portion of the pituitary gland (yellow arrow), and a lesion believed to be a Rathke’s cleft cyst (white arrow).
Differentiating between ACTH-dependent and -independent Cushing’s syndrome
Cushing’s syndrome is a constellation of signs and symptoms caused by an overproduction of cortisol, which results in a variety of abnormalities in the hypothalamic-pituitary-adrenal axis. In general, the syndrome is differentiated as either ACTH-dependent or ACTH-independent, based on the underlying cause.1 Examples of ACTH-dependent Cushing’s syndrome include pituitary adenoma (formally classified as Cushing’s disease) and ectopic ACTH or corticotrophin-releasing hormone-producing tumors. Examples of ACTH-independent Cushing’s syndrome include adrenal adenoma or carcinoma and exogenous glucocorticoid therapy.2
Clinical manifestations include obesity, hypertension (usually with some degree of concurrent hypokalemia), skin abnormalities (eg, plethora, hirsutism, violaceous striae), musculoskeletal weakness, neuropsychiatric symptoms (eg, depression), gonadal dysfunction, and metabolic derangements, including glucose intolerance, diabetes, and hyperlipidemia. In children, a near universal decrease in linear growth secondary to hypercortisolism is seen.3
Investigating a suspected case of Cushing’s syndrome can be divided into 2 stages: confirming the diagnosis and establishing the etiology. The following tests can be used to make the diagnosis: 24-hour urinary free cortisol, low-dose dexamethasone suppression, and late-night salivary cortisol. Several of these tests require late-night administration that necessitates hospital admission. These tests are typically followed by a CT scan of the patient’s adrenal glands and/or an MRI of the patient’s pituitary gland to evaluate the etiology. Additionally, as demonstrated by the patient described here, ongoing issues with hypertension, metabolic abnormalities, and hyperglycemia may require intensive intervention and management.4
Don't be fooled
Potential complications in diagnosing the syndrome, however, can cloud an accurate diagnosis—especially early in the disease process. In addition to biochemical similarities between Cushing’s syndrome and obesity, depression, and alcoholism, ACTH-dependent Cushing’s syndrome can undergo cyclical or intermittent activity and can remain in remission for years.1 Also, ectopic ACTH-secreting tumors may, by virtue of their small size and location, go undetected.
Don’t try to lower BP through usual means
Hypertension, a hallmark finding in approximately 80% of adults and 47% of children with Cushing’s syndrome,5 stems from hypercortisol-driven pathologic changes in the mechanisms controlling plasma volume, peripheral vascular resistance, and cardiac output. In addition, these cortisol-driven changes have a direct effect on mineralocorticoid and glucocorticoid receptors within the central nervous system. Secondary effects such as insulin resistance and the development of sleep apnea further complicate the management of this generally treatment-resistant hypertension. Lastly, specific mechanisms such as the cross-reactivity of excess glucocorticoids with mineralocorticoid receptors acting on targets within the kidney, can also lead to metabolic derangements, such as profound hypokalemia and metabolic alkalosis.
Thus, controlling hypertension and the metabolic changes seen in Cushing’s syndrome often requires addressing the underlying hypercortisolism rather than achieving normotension and normal serum electrolytes through the usual means.5
Treatment puts our patient back on track
Our patient was transferred to a tertiary care hospital for further management and consultation with endocrinology and neurosurgery. He was started on high-dose ketoconazole, an imidazole-derivative antifungal medication that acts to inhibit adrenal steroidogenesis and has been used successfully in patients with Cushing’s syndrome.6,7 (Ketoconazole is typically dosed at 400-1200 mg/d7 and can be used for >6 months to 1 year, or temporarily in advance of surgery.)
Our patient underwent successful transsphenoidal adenectomy by neurosurgery, and his blood pressure, serum electrolytes, and serum glucose returned to normal levels. He is about to begin his senior year in high school.
CORRESPONDENCE Michael Barna, MD, Department of Family Medicine, Naval Hospital Camp Pendleton, Box 555191, Camp Pendleton, CA 92055; michael.barna@med.navy.mil
1. Carroll TB, Aron DC, Findling JW, et al. Glucocorticoids and adrenal androgens. In: Gardner D, Shoback D, eds. Greenspan’s Basic & Clinical Endocrinology. 9th ed. New York: McGraw-Hill; 2011:285–327.
2. Trainer PJ, Grossman A. The diagnosis and differential diagnosis of Cushing’s syndrome. Clin Endocrinol (Oxf). 1991;34:317-330.
3. Voutilainen R, Leisti S, Perheentupa J. Growth in Cushing syndrome. Eur J Pediatr. 1985;144:141-145.
4. Giordano R, Picu A, Marinazzo E, et al. Metabolic and cardiovascular outcomes in patients with Cushing’s syndrome of different aetiologies during active disease and 1 year after remission. Clin Endocrinol (Oxf). 2011;75:354-360.
5. Cicala MV, Mantero F. Hypertension in Cushing’s syndrome: from pathogenesis to treatment. Neuroendocrinology. 2010;92(suppl 1):44-49.
6. Atkinson A. The treatment of Cushing’s syndrome. Clin Endocrinol (Oxf). 1991;34:507-513.
7. Tabarin A, Navarranne A, Guerin J, et al. Use of ketoconazole in the treatment of Cushing’s disease and ectopic ACTH syndrome. Clin Endocrinol (Oxf). 1991;34:63-69.
A review of the patient’s blood pressure since admission indicated consistently elevated systolic and diastolic pressures, on average, of 170/105 mm Hg. Additionally, his serum potassium levels ranged from 2.4 to 3.1 mmol/L (normal 3.5-5.1 mmol/L).
A detailed medical history and review of previous records revealed that an initial diagnosis of hypertension had been made during a routine sports physical at age 14, although the patient was cleared for full activity. Over the previous year, the patient said he had gained weight—much of it in the abdomen—and experienced sleep disturbances, increasing fatigability, muscle weakness, hair loss, and declining performance in his high school sports. In addition, he had noticed increased facial flushing and sweating.
On physical exam, we noted an obese male (height 5’5’’, weight 191.5 lb, BMI 30.86 kg/m2) with the following vital signs: temperature 97.9°F, pulse 105 bpm, and blood pressure 177/111 mm Hg. Pertinent physical exam findings outside of his surgical site included diffusely thinning hair, moon facies, facial plethora, increased supraclavicular and dorsocervical fat pads, thoracic and abdominal striae, thinned skin overlying his upper and lower extremities, and lower extremity edema ( FIGURE 1 ). All other exam findings were within normal limits.
Initial blood chemistry lab results revealed hyperglycemia (290 mg/dL; random normal, <200 mg/dL), hypokalemia (3.0 mmol/L; normal, 3.5-5.4 mmol/L), hypochloremia (96 mmol/L; normal, 98-107 mmol/L), and a mean corpuscular volume of 101.2 fL (normal, 80-100 fL). The patient also had a white blood cell (WBC) count of 14,400/mcL with a predominance of neutrophils and 6 bands, and a high sensitivity C-reactive protein level of 7.5 mg/dL (normal, <0.748 mg/dL).
FIGURE 1
The signs were all there
Our patient exhibited thinning hair (A), moon facies (B), dorsocervical fat pads (“buffalo hump”) (C), and abdominal striae (D).
WHAT ADDITIONAL TESTING WOULD YOU ORDER?
WHAT IS YOUR PRESUMPTIVE DIAGNOSIS?
Suspecting Cushing’s syndrome, we ordered cortisol and ACTH
Based on our initial findings, we ordered a 24-hour urinary free cortisol and plasma adrenocorticotropic hormone (ACTH) level—both of which had to be sent to outside laboratories. We also ordered a computed tomography (CT) scan of the patient’s adrenal glands and magnetic resonance imaging (MRI) of his pituitary gland.
The CT scan revealed mild hyperplasia of the adrenal glands bilaterally; the MRI demonstrated a 7 × 6 × 6 mm pituitary microadenoma ( FIGURE 2 ) in the anterior portion of the gland. In addition, a 6 × 6 × 1 mm lesion was noted—thought to be a Rathke’s cleft (Pars intermedia) cyst by the reviewing radiologist.
The patient’s initial cortisol and ACTH lab work revealed a urinary cortisol level of 5089.2 mcg/24 h (normal, 3-55 mcg/24 h) and an ACTH level of 216 pg/mL (normal, 9-57 pg/mL for ages 3-17 years).
We diagnosed Cushing’s syndrome in this patient.
FIGURE 2
MRI reveals pituitary microadenoma
The patient had a microadenoma in the anterior portion of the pituitary gland (yellow arrow), and a lesion believed to be a Rathke’s cleft cyst (white arrow).
Differentiating between ACTH-dependent and -independent Cushing’s syndrome
Cushing’s syndrome is a constellation of signs and symptoms caused by an overproduction of cortisol, which results in a variety of abnormalities in the hypothalamic-pituitary-adrenal axis. In general, the syndrome is differentiated as either ACTH-dependent or ACTH-independent, based on the underlying cause.1 Examples of ACTH-dependent Cushing’s syndrome include pituitary adenoma (formally classified as Cushing’s disease) and ectopic ACTH or corticotrophin-releasing hormone-producing tumors. Examples of ACTH-independent Cushing’s syndrome include adrenal adenoma or carcinoma and exogenous glucocorticoid therapy.2
Clinical manifestations include obesity, hypertension (usually with some degree of concurrent hypokalemia), skin abnormalities (eg, plethora, hirsutism, violaceous striae), musculoskeletal weakness, neuropsychiatric symptoms (eg, depression), gonadal dysfunction, and metabolic derangements, including glucose intolerance, diabetes, and hyperlipidemia. In children, a near universal decrease in linear growth secondary to hypercortisolism is seen.3
Investigating a suspected case of Cushing’s syndrome can be divided into 2 stages: confirming the diagnosis and establishing the etiology. The following tests can be used to make the diagnosis: 24-hour urinary free cortisol, low-dose dexamethasone suppression, and late-night salivary cortisol. Several of these tests require late-night administration that necessitates hospital admission. These tests are typically followed by a CT scan of the patient’s adrenal glands and/or an MRI of the patient’s pituitary gland to evaluate the etiology. Additionally, as demonstrated by the patient described here, ongoing issues with hypertension, metabolic abnormalities, and hyperglycemia may require intensive intervention and management.4
Don't be fooled
Potential complications in diagnosing the syndrome, however, can cloud an accurate diagnosis—especially early in the disease process. In addition to biochemical similarities between Cushing’s syndrome and obesity, depression, and alcoholism, ACTH-dependent Cushing’s syndrome can undergo cyclical or intermittent activity and can remain in remission for years.1 Also, ectopic ACTH-secreting tumors may, by virtue of their small size and location, go undetected.
Don’t try to lower BP through usual means
Hypertension, a hallmark finding in approximately 80% of adults and 47% of children with Cushing’s syndrome,5 stems from hypercortisol-driven pathologic changes in the mechanisms controlling plasma volume, peripheral vascular resistance, and cardiac output. In addition, these cortisol-driven changes have a direct effect on mineralocorticoid and glucocorticoid receptors within the central nervous system. Secondary effects such as insulin resistance and the development of sleep apnea further complicate the management of this generally treatment-resistant hypertension. Lastly, specific mechanisms such as the cross-reactivity of excess glucocorticoids with mineralocorticoid receptors acting on targets within the kidney, can also lead to metabolic derangements, such as profound hypokalemia and metabolic alkalosis.
Thus, controlling hypertension and the metabolic changes seen in Cushing’s syndrome often requires addressing the underlying hypercortisolism rather than achieving normotension and normal serum electrolytes through the usual means.5
Treatment puts our patient back on track
Our patient was transferred to a tertiary care hospital for further management and consultation with endocrinology and neurosurgery. He was started on high-dose ketoconazole, an imidazole-derivative antifungal medication that acts to inhibit adrenal steroidogenesis and has been used successfully in patients with Cushing’s syndrome.6,7 (Ketoconazole is typically dosed at 400-1200 mg/d7 and can be used for >6 months to 1 year, or temporarily in advance of surgery.)
Our patient underwent successful transsphenoidal adenectomy by neurosurgery, and his blood pressure, serum electrolytes, and serum glucose returned to normal levels. He is about to begin his senior year in high school.
CORRESPONDENCE Michael Barna, MD, Department of Family Medicine, Naval Hospital Camp Pendleton, Box 555191, Camp Pendleton, CA 92055; michael.barna@med.navy.mil
A review of the patient’s blood pressure since admission indicated consistently elevated systolic and diastolic pressures, on average, of 170/105 mm Hg. Additionally, his serum potassium levels ranged from 2.4 to 3.1 mmol/L (normal 3.5-5.1 mmol/L).
A detailed medical history and review of previous records revealed that an initial diagnosis of hypertension had been made during a routine sports physical at age 14, although the patient was cleared for full activity. Over the previous year, the patient said he had gained weight—much of it in the abdomen—and experienced sleep disturbances, increasing fatigability, muscle weakness, hair loss, and declining performance in his high school sports. In addition, he had noticed increased facial flushing and sweating.
On physical exam, we noted an obese male (height 5’5’’, weight 191.5 lb, BMI 30.86 kg/m2) with the following vital signs: temperature 97.9°F, pulse 105 bpm, and blood pressure 177/111 mm Hg. Pertinent physical exam findings outside of his surgical site included diffusely thinning hair, moon facies, facial plethora, increased supraclavicular and dorsocervical fat pads, thoracic and abdominal striae, thinned skin overlying his upper and lower extremities, and lower extremity edema ( FIGURE 1 ). All other exam findings were within normal limits.
Initial blood chemistry lab results revealed hyperglycemia (290 mg/dL; random normal, <200 mg/dL), hypokalemia (3.0 mmol/L; normal, 3.5-5.4 mmol/L), hypochloremia (96 mmol/L; normal, 98-107 mmol/L), and a mean corpuscular volume of 101.2 fL (normal, 80-100 fL). The patient also had a white blood cell (WBC) count of 14,400/mcL with a predominance of neutrophils and 6 bands, and a high sensitivity C-reactive protein level of 7.5 mg/dL (normal, <0.748 mg/dL).
FIGURE 1
The signs were all there
Our patient exhibited thinning hair (A), moon facies (B), dorsocervical fat pads (“buffalo hump”) (C), and abdominal striae (D).
WHAT ADDITIONAL TESTING WOULD YOU ORDER?
WHAT IS YOUR PRESUMPTIVE DIAGNOSIS?
Suspecting Cushing’s syndrome, we ordered cortisol and ACTH
Based on our initial findings, we ordered a 24-hour urinary free cortisol and plasma adrenocorticotropic hormone (ACTH) level—both of which had to be sent to outside laboratories. We also ordered a computed tomography (CT) scan of the patient’s adrenal glands and magnetic resonance imaging (MRI) of his pituitary gland.
The CT scan revealed mild hyperplasia of the adrenal glands bilaterally; the MRI demonstrated a 7 × 6 × 6 mm pituitary microadenoma ( FIGURE 2 ) in the anterior portion of the gland. In addition, a 6 × 6 × 1 mm lesion was noted—thought to be a Rathke’s cleft (Pars intermedia) cyst by the reviewing radiologist.
The patient’s initial cortisol and ACTH lab work revealed a urinary cortisol level of 5089.2 mcg/24 h (normal, 3-55 mcg/24 h) and an ACTH level of 216 pg/mL (normal, 9-57 pg/mL for ages 3-17 years).
We diagnosed Cushing’s syndrome in this patient.
FIGURE 2
MRI reveals pituitary microadenoma
The patient had a microadenoma in the anterior portion of the pituitary gland (yellow arrow), and a lesion believed to be a Rathke’s cleft cyst (white arrow).
Differentiating between ACTH-dependent and -independent Cushing’s syndrome
Cushing’s syndrome is a constellation of signs and symptoms caused by an overproduction of cortisol, which results in a variety of abnormalities in the hypothalamic-pituitary-adrenal axis. In general, the syndrome is differentiated as either ACTH-dependent or ACTH-independent, based on the underlying cause.1 Examples of ACTH-dependent Cushing’s syndrome include pituitary adenoma (formally classified as Cushing’s disease) and ectopic ACTH or corticotrophin-releasing hormone-producing tumors. Examples of ACTH-independent Cushing’s syndrome include adrenal adenoma or carcinoma and exogenous glucocorticoid therapy.2
Clinical manifestations include obesity, hypertension (usually with some degree of concurrent hypokalemia), skin abnormalities (eg, plethora, hirsutism, violaceous striae), musculoskeletal weakness, neuropsychiatric symptoms (eg, depression), gonadal dysfunction, and metabolic derangements, including glucose intolerance, diabetes, and hyperlipidemia. In children, a near universal decrease in linear growth secondary to hypercortisolism is seen.3
Investigating a suspected case of Cushing’s syndrome can be divided into 2 stages: confirming the diagnosis and establishing the etiology. The following tests can be used to make the diagnosis: 24-hour urinary free cortisol, low-dose dexamethasone suppression, and late-night salivary cortisol. Several of these tests require late-night administration that necessitates hospital admission. These tests are typically followed by a CT scan of the patient’s adrenal glands and/or an MRI of the patient’s pituitary gland to evaluate the etiology. Additionally, as demonstrated by the patient described here, ongoing issues with hypertension, metabolic abnormalities, and hyperglycemia may require intensive intervention and management.4
Don't be fooled
Potential complications in diagnosing the syndrome, however, can cloud an accurate diagnosis—especially early in the disease process. In addition to biochemical similarities between Cushing’s syndrome and obesity, depression, and alcoholism, ACTH-dependent Cushing’s syndrome can undergo cyclical or intermittent activity and can remain in remission for years.1 Also, ectopic ACTH-secreting tumors may, by virtue of their small size and location, go undetected.
Don’t try to lower BP through usual means
Hypertension, a hallmark finding in approximately 80% of adults and 47% of children with Cushing’s syndrome,5 stems from hypercortisol-driven pathologic changes in the mechanisms controlling plasma volume, peripheral vascular resistance, and cardiac output. In addition, these cortisol-driven changes have a direct effect on mineralocorticoid and glucocorticoid receptors within the central nervous system. Secondary effects such as insulin resistance and the development of sleep apnea further complicate the management of this generally treatment-resistant hypertension. Lastly, specific mechanisms such as the cross-reactivity of excess glucocorticoids with mineralocorticoid receptors acting on targets within the kidney, can also lead to metabolic derangements, such as profound hypokalemia and metabolic alkalosis.
Thus, controlling hypertension and the metabolic changes seen in Cushing’s syndrome often requires addressing the underlying hypercortisolism rather than achieving normotension and normal serum electrolytes through the usual means.5
Treatment puts our patient back on track
Our patient was transferred to a tertiary care hospital for further management and consultation with endocrinology and neurosurgery. He was started on high-dose ketoconazole, an imidazole-derivative antifungal medication that acts to inhibit adrenal steroidogenesis and has been used successfully in patients with Cushing’s syndrome.6,7 (Ketoconazole is typically dosed at 400-1200 mg/d7 and can be used for >6 months to 1 year, or temporarily in advance of surgery.)
Our patient underwent successful transsphenoidal adenectomy by neurosurgery, and his blood pressure, serum electrolytes, and serum glucose returned to normal levels. He is about to begin his senior year in high school.
CORRESPONDENCE Michael Barna, MD, Department of Family Medicine, Naval Hospital Camp Pendleton, Box 555191, Camp Pendleton, CA 92055; michael.barna@med.navy.mil
1. Carroll TB, Aron DC, Findling JW, et al. Glucocorticoids and adrenal androgens. In: Gardner D, Shoback D, eds. Greenspan’s Basic & Clinical Endocrinology. 9th ed. New York: McGraw-Hill; 2011:285–327.
2. Trainer PJ, Grossman A. The diagnosis and differential diagnosis of Cushing’s syndrome. Clin Endocrinol (Oxf). 1991;34:317-330.
3. Voutilainen R, Leisti S, Perheentupa J. Growth in Cushing syndrome. Eur J Pediatr. 1985;144:141-145.
4. Giordano R, Picu A, Marinazzo E, et al. Metabolic and cardiovascular outcomes in patients with Cushing’s syndrome of different aetiologies during active disease and 1 year after remission. Clin Endocrinol (Oxf). 2011;75:354-360.
5. Cicala MV, Mantero F. Hypertension in Cushing’s syndrome: from pathogenesis to treatment. Neuroendocrinology. 2010;92(suppl 1):44-49.
6. Atkinson A. The treatment of Cushing’s syndrome. Clin Endocrinol (Oxf). 1991;34:507-513.
7. Tabarin A, Navarranne A, Guerin J, et al. Use of ketoconazole in the treatment of Cushing’s disease and ectopic ACTH syndrome. Clin Endocrinol (Oxf). 1991;34:63-69.
1. Carroll TB, Aron DC, Findling JW, et al. Glucocorticoids and adrenal androgens. In: Gardner D, Shoback D, eds. Greenspan’s Basic & Clinical Endocrinology. 9th ed. New York: McGraw-Hill; 2011:285–327.
2. Trainer PJ, Grossman A. The diagnosis and differential diagnosis of Cushing’s syndrome. Clin Endocrinol (Oxf). 1991;34:317-330.
3. Voutilainen R, Leisti S, Perheentupa J. Growth in Cushing syndrome. Eur J Pediatr. 1985;144:141-145.
4. Giordano R, Picu A, Marinazzo E, et al. Metabolic and cardiovascular outcomes in patients with Cushing’s syndrome of different aetiologies during active disease and 1 year after remission. Clin Endocrinol (Oxf). 2011;75:354-360.
5. Cicala MV, Mantero F. Hypertension in Cushing’s syndrome: from pathogenesis to treatment. Neuroendocrinology. 2010;92(suppl 1):44-49.
6. Atkinson A. The treatment of Cushing’s syndrome. Clin Endocrinol (Oxf). 1991;34:507-513.
7. Tabarin A, Navarranne A, Guerin J, et al. Use of ketoconazole in the treatment of Cushing’s disease and ectopic ACTH syndrome. Clin Endocrinol (Oxf). 1991;34:63-69.
Onychomycosis: A simpler in-office technique for sampling specimens
Background In onychomycosis, proper specimen collection is essential for an accurate diagnosis and initiation of appropriate therapy. Several techniques and locations have been suggested for specimen collection.
Objective To investigate the optimal technique of fungal sampling in onychomycosis.
Methods We reexamined 106 patients with distal and lateral subungual onychomycosis (DLSO) of the toenails. (The diagnosis had previously been confirmed by a laboratory mycological examination—both potassium hydroxide [KOH] test and fungal culture—of samples obtained by the proximal sampling approach.) We collected fungal specimens from the distal nail bed first, and later from the distal underside of the nail plate. The collected specimens underwent laboratory mycological examination.
Results KOH testing was positive in 84 (79.2%) specimens from the distal nail bed and only in 60 (56.6%) from the distal underside of the nail plate (P=.0007); cultures were positive in 93 (87.7%) and 76 (71.7%) specimens, respectively (P=.0063). Combining results from both locations showed positive KOH test results in 92 (86.8%) of the 106 patients and positive cultures in 100 (94.3%) patients.
Conclusions Based on our study, we suggest that in cases of suspected DLSO, material should be obtained by scraping nail material from the distal underside of the nail and then collecting all the material from the distal part of the nail bed.
When assessing possible onychomycosis, conventional practice is to take samples from the most proximal infected area. But this approach is usually technically difficult and may cause discomfort to patients.1-6 We therefore sought to determine the optimal location for fungal sampling from the distal part of the affected nail.
Methods
To assess the accuracy of distal sampling in diagnosing distal and lateral subungual onychomycosis (DLSO) of the toenails, we reevaluated 106 patients with DLSO previously confirmed by microscopic visualization of fungi in potassium hydroxide (KOH) solution and by fungal culture of specimens obtained using the proximal sampling approach.
Before we obtained our samples, we cleaned the nails with alcohol and pared the most distal part of the nails in an effort to eliminate contaminant molds and bacteria. Using a 1- or 2-mm curette, we took specimens first from the distal nail bed and, second, from the distal underside of the nail plate ( FIGURE ). We separated specimens for use in either direct KOH visualization or in fungal culture using Sabouraud’s Dextrose agar (Novamed; Jerusalem, Israel), which contains chloramphenicol or streptomycin and penicillin to prevent contamination.
FIGURE
Distal sampling for distal and lateral subungual onychomycosis
Using a 2-mm curette, we collected specimens from the distal nail bed first (A), and then from the distal underside of the nail plate (B). However, our recommendation for clinical practice is to reverse this order of sampling to collect all possible material.
Statistical analyses
We recorded sociodemographic characteristics and fungal culture results in basic descriptive (prevalence) tables. In univariate analysis, we used t-tests to compare the means of continuous variables (eg, age, duration of fungal infection). To assess the distribution of categorical parameters (eg, sex) and to gauge the efficacy of the different probing techniques, we used chi-square (χ2) tests. We analyzed coded data using SPSS (Chicago, IL) for Windows software, version 12.
We conducted the study according to the rules of the local Helsinki Committee.
Results
We examined 106 patients with DLSO, of which 65 (61.3%) were male and 41 (38.7%) were female, ages 23 to 72 years (mean age, 44.6). The duration of fungal infection ranged from 3 to 30 years, with a mean of 14.9 years. In 70.8% of cases, the infection involved the first toenail. Duration of the fungal disease did not differ significantly between the sexes.
KOH test results were positive for 84 (79.2%) specimens from the distal nail bed, and for only 60 (56.6%) specimens from the distal underside of the nail plate (P=.0007); culture results were positive for 93 (87.7%) and 76 (71.7%) specimens, respectively (P=.0063). Combining results from both locations (all positive samples from the nail bed, plus positive samples from the nail underside when results from the nail bed were negative) yielded confirmation with KOH testing in 92 (86.8%) patients and with culture in 100 (94.3%) patients. There were no statistically significant differences between the combined results of both locations and the results from the distal nail bed alone (KOH, P=.143; culture, P=.149) ( TABLE ).
TABLE
Accuracy of distal sampling in 106 patients with confirmed DLSO
| Nail bed | Underside of nail plate | P value | Combined results | P value* | |
|---|---|---|---|---|---|
| Positive KOH | 84 (79.2%) | 60 (56.65%) | .0007 | 92 (86.8%) | .143 |
| Positive culture | 93 (87.7%) | 76 (71.7%) | .0063 | 100 (94.3%) | .149 |
| *Differences between results from sampling the nail bed alone and results from combined nail bed and nail plate sampling were not statistically significant. DLSO, distal and lateral subungual onychomycosis; KOH, potassium hydroxide. | |||||
Discussion
In DLSO, most dermatophyte species invade the middle and ventral layers of the nail plate adjacent to the nail bed, where the keratin is soft and close to the living cells below. In fact, the nail bed is probably the primary invasion site of dermatophytes, and it acts as a reservoir for continual reinfection of the growing nail.7 Obtaining confirmation of fungal infection before initiating antifungal treatment is the gold standard in clinical practice, given that antifungal agents have potentially serious adverse effects, that treatment is expensive, and that medicolegal issues exist.8
The standard methods used to detect a fungal nail infection are direct microscopy with KOH preparation and fungal culture. The KOH test is the simplest, least expensive method used in the detection of fungi, but it cannot identify the specific pathogen. Fungal speciation is done by culture. More accurate histopathologic evaluation is possible with periodic acid-Schiff stain, immunofluorescent microscopy with calcofluor stain, or polymerase chain reaction, but these techniques are more expensive and less feasible in outpatient clinics.9
The diagnostic accuracy of the KOH test and fungal culture ranges from 50% to 70%, depending on the experience of the laboratory technician and the methods used to collect and prepare the sample.8-10 It is better to take samples from the most proximal infected area by curettage or drilling, but this technique is usually more difficult than a distal approach, should be performed by skilled personnel, and may cause discomfort to patients.3,5,6
Our recommendation for practice. Earlier studies suggested that nail specimens should be taken from the nail bed.11-13 We sampled the nail bed first in our study because, in trying to determine an optimal location for sampling, we wanted to avoid contaminating nail-bed specimens with debris from the underside of the nail. In practice, however, we suggest that, in cases of suspected DLSO, clinicians first obtain specimens from the distal underside of the nail, and then collect all remaining material from the distal part of the nail bed. This technique is simple and can easily be performed in an office setting. If test results are negative but DLSO remains clinically likely, test a second sample after a week or 2.
CORRESPONDENCE Boaz Amichai, MD, Department of Dermatology, Sheba Medical Center, Tel-Hashomer, Israel; boazam@clalit.org.il
1. Lawry MA, Haneke E, Strobeck K, et al. Methods for diagnosing onychomycosis: a comparative study and review of the literature. Arch Dermatol. 2000;136:1112-1116.
2. Elewski BE. Diagnostic techniques for confirming onychomycosis. J Am Acad Dermatol. 1996;35(3 pt 2):S6-S9.
3. Heikkila H. Isolation of fungi from onychomycosis-suspected nails by two methods: clipping and drilling. Mycoses. 1996;39:479-482.
4. Mochizuki T, Kawasaki M, Tanabe H, et al. A nail drilling method suitable for the diagnosis of onychomycosis. J Dermatol. 2005;32:108-113.
5. Shemer A, Trau H, Davidovici B, et al. Nail sampling in onychomycosis: comparative study of curettage from three sites of the infected nail. J Dtsch Dermatol Ges. 2007;5:1108-1111.
6. Shemer A, Trau H, Davidovici B, et al. Collection of fungi samples from nails: comparative study of curettage and drilling techniques. J Eur Acad Dermatol Venereol. 2008;22:182-185.
7. Hay RJ, Baran R, Haneke E. Fungal (onychomycosis) and other infections involving the nail apparatus. In: Baran R, Dawber RPR, eds. Disease of the Nails and Their Management. 2nd ed. Oxford, England: Blackwell Sciences Ltd; 1994: 97–134.
8. Daniel CR, 3rd, Elewski BE. The diagnosis of nail fungus infection revisited. Arch Dermatol. 2000;136:1162-1164.
9. Weinberg JM, Koestenblatt EK, Tutrone WD, et al. Comparison of diagnostic methods in the evaluation of onychomycosis. J Am Acad Dermatol. 2003;49:193-197.
10. Arnold B, Kianifrad F, Tavakkol A. A comparison of KOH and culture results from two mycology laboratories for the diagnosis of onychomycosis during a randomized, multicenter clinical trial: a subset study. J Am Podiatr Med Assoc. 2005;95:421-423.
11. English MP. Nails and fungi. Br J Dermatol. 1976;94:697-701.
12. Elewski BE. Clinical pearl: diagnosis of onychomycosis. J Am Acad Dermatol. 1995;32:500-501.
13. Rodgers P, Bassler M. Treating onychomycosis. Am Fam Physician. 2001;63:663-672, 677–678.
Background In onychomycosis, proper specimen collection is essential for an accurate diagnosis and initiation of appropriate therapy. Several techniques and locations have been suggested for specimen collection.
Objective To investigate the optimal technique of fungal sampling in onychomycosis.
Methods We reexamined 106 patients with distal and lateral subungual onychomycosis (DLSO) of the toenails. (The diagnosis had previously been confirmed by a laboratory mycological examination—both potassium hydroxide [KOH] test and fungal culture—of samples obtained by the proximal sampling approach.) We collected fungal specimens from the distal nail bed first, and later from the distal underside of the nail plate. The collected specimens underwent laboratory mycological examination.
Results KOH testing was positive in 84 (79.2%) specimens from the distal nail bed and only in 60 (56.6%) from the distal underside of the nail plate (P=.0007); cultures were positive in 93 (87.7%) and 76 (71.7%) specimens, respectively (P=.0063). Combining results from both locations showed positive KOH test results in 92 (86.8%) of the 106 patients and positive cultures in 100 (94.3%) patients.
Conclusions Based on our study, we suggest that in cases of suspected DLSO, material should be obtained by scraping nail material from the distal underside of the nail and then collecting all the material from the distal part of the nail bed.
When assessing possible onychomycosis, conventional practice is to take samples from the most proximal infected area. But this approach is usually technically difficult and may cause discomfort to patients.1-6 We therefore sought to determine the optimal location for fungal sampling from the distal part of the affected nail.
Methods
To assess the accuracy of distal sampling in diagnosing distal and lateral subungual onychomycosis (DLSO) of the toenails, we reevaluated 106 patients with DLSO previously confirmed by microscopic visualization of fungi in potassium hydroxide (KOH) solution and by fungal culture of specimens obtained using the proximal sampling approach.
Before we obtained our samples, we cleaned the nails with alcohol and pared the most distal part of the nails in an effort to eliminate contaminant molds and bacteria. Using a 1- or 2-mm curette, we took specimens first from the distal nail bed and, second, from the distal underside of the nail plate ( FIGURE ). We separated specimens for use in either direct KOH visualization or in fungal culture using Sabouraud’s Dextrose agar (Novamed; Jerusalem, Israel), which contains chloramphenicol or streptomycin and penicillin to prevent contamination.
FIGURE
Distal sampling for distal and lateral subungual onychomycosis
Using a 2-mm curette, we collected specimens from the distal nail bed first (A), and then from the distal underside of the nail plate (B). However, our recommendation for clinical practice is to reverse this order of sampling to collect all possible material.
Statistical analyses
We recorded sociodemographic characteristics and fungal culture results in basic descriptive (prevalence) tables. In univariate analysis, we used t-tests to compare the means of continuous variables (eg, age, duration of fungal infection). To assess the distribution of categorical parameters (eg, sex) and to gauge the efficacy of the different probing techniques, we used chi-square (χ2) tests. We analyzed coded data using SPSS (Chicago, IL) for Windows software, version 12.
We conducted the study according to the rules of the local Helsinki Committee.
Results
We examined 106 patients with DLSO, of which 65 (61.3%) were male and 41 (38.7%) were female, ages 23 to 72 years (mean age, 44.6). The duration of fungal infection ranged from 3 to 30 years, with a mean of 14.9 years. In 70.8% of cases, the infection involved the first toenail. Duration of the fungal disease did not differ significantly between the sexes.
KOH test results were positive for 84 (79.2%) specimens from the distal nail bed, and for only 60 (56.6%) specimens from the distal underside of the nail plate (P=.0007); culture results were positive for 93 (87.7%) and 76 (71.7%) specimens, respectively (P=.0063). Combining results from both locations (all positive samples from the nail bed, plus positive samples from the nail underside when results from the nail bed were negative) yielded confirmation with KOH testing in 92 (86.8%) patients and with culture in 100 (94.3%) patients. There were no statistically significant differences between the combined results of both locations and the results from the distal nail bed alone (KOH, P=.143; culture, P=.149) ( TABLE ).
TABLE
Accuracy of distal sampling in 106 patients with confirmed DLSO
| Nail bed | Underside of nail plate | P value | Combined results | P value* | |
|---|---|---|---|---|---|
| Positive KOH | 84 (79.2%) | 60 (56.65%) | .0007 | 92 (86.8%) | .143 |
| Positive culture | 93 (87.7%) | 76 (71.7%) | .0063 | 100 (94.3%) | .149 |
| *Differences between results from sampling the nail bed alone and results from combined nail bed and nail plate sampling were not statistically significant. DLSO, distal and lateral subungual onychomycosis; KOH, potassium hydroxide. | |||||
Discussion
In DLSO, most dermatophyte species invade the middle and ventral layers of the nail plate adjacent to the nail bed, where the keratin is soft and close to the living cells below. In fact, the nail bed is probably the primary invasion site of dermatophytes, and it acts as a reservoir for continual reinfection of the growing nail.7 Obtaining confirmation of fungal infection before initiating antifungal treatment is the gold standard in clinical practice, given that antifungal agents have potentially serious adverse effects, that treatment is expensive, and that medicolegal issues exist.8
The standard methods used to detect a fungal nail infection are direct microscopy with KOH preparation and fungal culture. The KOH test is the simplest, least expensive method used in the detection of fungi, but it cannot identify the specific pathogen. Fungal speciation is done by culture. More accurate histopathologic evaluation is possible with periodic acid-Schiff stain, immunofluorescent microscopy with calcofluor stain, or polymerase chain reaction, but these techniques are more expensive and less feasible in outpatient clinics.9
The diagnostic accuracy of the KOH test and fungal culture ranges from 50% to 70%, depending on the experience of the laboratory technician and the methods used to collect and prepare the sample.8-10 It is better to take samples from the most proximal infected area by curettage or drilling, but this technique is usually more difficult than a distal approach, should be performed by skilled personnel, and may cause discomfort to patients.3,5,6
Our recommendation for practice. Earlier studies suggested that nail specimens should be taken from the nail bed.11-13 We sampled the nail bed first in our study because, in trying to determine an optimal location for sampling, we wanted to avoid contaminating nail-bed specimens with debris from the underside of the nail. In practice, however, we suggest that, in cases of suspected DLSO, clinicians first obtain specimens from the distal underside of the nail, and then collect all remaining material from the distal part of the nail bed. This technique is simple and can easily be performed in an office setting. If test results are negative but DLSO remains clinically likely, test a second sample after a week or 2.
CORRESPONDENCE Boaz Amichai, MD, Department of Dermatology, Sheba Medical Center, Tel-Hashomer, Israel; boazam@clalit.org.il
Background In onychomycosis, proper specimen collection is essential for an accurate diagnosis and initiation of appropriate therapy. Several techniques and locations have been suggested for specimen collection.
Objective To investigate the optimal technique of fungal sampling in onychomycosis.
Methods We reexamined 106 patients with distal and lateral subungual onychomycosis (DLSO) of the toenails. (The diagnosis had previously been confirmed by a laboratory mycological examination—both potassium hydroxide [KOH] test and fungal culture—of samples obtained by the proximal sampling approach.) We collected fungal specimens from the distal nail bed first, and later from the distal underside of the nail plate. The collected specimens underwent laboratory mycological examination.
Results KOH testing was positive in 84 (79.2%) specimens from the distal nail bed and only in 60 (56.6%) from the distal underside of the nail plate (P=.0007); cultures were positive in 93 (87.7%) and 76 (71.7%) specimens, respectively (P=.0063). Combining results from both locations showed positive KOH test results in 92 (86.8%) of the 106 patients and positive cultures in 100 (94.3%) patients.
Conclusions Based on our study, we suggest that in cases of suspected DLSO, material should be obtained by scraping nail material from the distal underside of the nail and then collecting all the material from the distal part of the nail bed.
When assessing possible onychomycosis, conventional practice is to take samples from the most proximal infected area. But this approach is usually technically difficult and may cause discomfort to patients.1-6 We therefore sought to determine the optimal location for fungal sampling from the distal part of the affected nail.
Methods
To assess the accuracy of distal sampling in diagnosing distal and lateral subungual onychomycosis (DLSO) of the toenails, we reevaluated 106 patients with DLSO previously confirmed by microscopic visualization of fungi in potassium hydroxide (KOH) solution and by fungal culture of specimens obtained using the proximal sampling approach.
Before we obtained our samples, we cleaned the nails with alcohol and pared the most distal part of the nails in an effort to eliminate contaminant molds and bacteria. Using a 1- or 2-mm curette, we took specimens first from the distal nail bed and, second, from the distal underside of the nail plate ( FIGURE ). We separated specimens for use in either direct KOH visualization or in fungal culture using Sabouraud’s Dextrose agar (Novamed; Jerusalem, Israel), which contains chloramphenicol or streptomycin and penicillin to prevent contamination.
FIGURE
Distal sampling for distal and lateral subungual onychomycosis
Using a 2-mm curette, we collected specimens from the distal nail bed first (A), and then from the distal underside of the nail plate (B). However, our recommendation for clinical practice is to reverse this order of sampling to collect all possible material.
Statistical analyses
We recorded sociodemographic characteristics and fungal culture results in basic descriptive (prevalence) tables. In univariate analysis, we used t-tests to compare the means of continuous variables (eg, age, duration of fungal infection). To assess the distribution of categorical parameters (eg, sex) and to gauge the efficacy of the different probing techniques, we used chi-square (χ2) tests. We analyzed coded data using SPSS (Chicago, IL) for Windows software, version 12.
We conducted the study according to the rules of the local Helsinki Committee.
Results
We examined 106 patients with DLSO, of which 65 (61.3%) were male and 41 (38.7%) were female, ages 23 to 72 years (mean age, 44.6). The duration of fungal infection ranged from 3 to 30 years, with a mean of 14.9 years. In 70.8% of cases, the infection involved the first toenail. Duration of the fungal disease did not differ significantly between the sexes.
KOH test results were positive for 84 (79.2%) specimens from the distal nail bed, and for only 60 (56.6%) specimens from the distal underside of the nail plate (P=.0007); culture results were positive for 93 (87.7%) and 76 (71.7%) specimens, respectively (P=.0063). Combining results from both locations (all positive samples from the nail bed, plus positive samples from the nail underside when results from the nail bed were negative) yielded confirmation with KOH testing in 92 (86.8%) patients and with culture in 100 (94.3%) patients. There were no statistically significant differences between the combined results of both locations and the results from the distal nail bed alone (KOH, P=.143; culture, P=.149) ( TABLE ).
TABLE
Accuracy of distal sampling in 106 patients with confirmed DLSO
| Nail bed | Underside of nail plate | P value | Combined results | P value* | |
|---|---|---|---|---|---|
| Positive KOH | 84 (79.2%) | 60 (56.65%) | .0007 | 92 (86.8%) | .143 |
| Positive culture | 93 (87.7%) | 76 (71.7%) | .0063 | 100 (94.3%) | .149 |
| *Differences between results from sampling the nail bed alone and results from combined nail bed and nail plate sampling were not statistically significant. DLSO, distal and lateral subungual onychomycosis; KOH, potassium hydroxide. | |||||
Discussion
In DLSO, most dermatophyte species invade the middle and ventral layers of the nail plate adjacent to the nail bed, where the keratin is soft and close to the living cells below. In fact, the nail bed is probably the primary invasion site of dermatophytes, and it acts as a reservoir for continual reinfection of the growing nail.7 Obtaining confirmation of fungal infection before initiating antifungal treatment is the gold standard in clinical practice, given that antifungal agents have potentially serious adverse effects, that treatment is expensive, and that medicolegal issues exist.8
The standard methods used to detect a fungal nail infection are direct microscopy with KOH preparation and fungal culture. The KOH test is the simplest, least expensive method used in the detection of fungi, but it cannot identify the specific pathogen. Fungal speciation is done by culture. More accurate histopathologic evaluation is possible with periodic acid-Schiff stain, immunofluorescent microscopy with calcofluor stain, or polymerase chain reaction, but these techniques are more expensive and less feasible in outpatient clinics.9
The diagnostic accuracy of the KOH test and fungal culture ranges from 50% to 70%, depending on the experience of the laboratory technician and the methods used to collect and prepare the sample.8-10 It is better to take samples from the most proximal infected area by curettage or drilling, but this technique is usually more difficult than a distal approach, should be performed by skilled personnel, and may cause discomfort to patients.3,5,6
Our recommendation for practice. Earlier studies suggested that nail specimens should be taken from the nail bed.11-13 We sampled the nail bed first in our study because, in trying to determine an optimal location for sampling, we wanted to avoid contaminating nail-bed specimens with debris from the underside of the nail. In practice, however, we suggest that, in cases of suspected DLSO, clinicians first obtain specimens from the distal underside of the nail, and then collect all remaining material from the distal part of the nail bed. This technique is simple and can easily be performed in an office setting. If test results are negative but DLSO remains clinically likely, test a second sample after a week or 2.
CORRESPONDENCE Boaz Amichai, MD, Department of Dermatology, Sheba Medical Center, Tel-Hashomer, Israel; boazam@clalit.org.il
1. Lawry MA, Haneke E, Strobeck K, et al. Methods for diagnosing onychomycosis: a comparative study and review of the literature. Arch Dermatol. 2000;136:1112-1116.
2. Elewski BE. Diagnostic techniques for confirming onychomycosis. J Am Acad Dermatol. 1996;35(3 pt 2):S6-S9.
3. Heikkila H. Isolation of fungi from onychomycosis-suspected nails by two methods: clipping and drilling. Mycoses. 1996;39:479-482.
4. Mochizuki T, Kawasaki M, Tanabe H, et al. A nail drilling method suitable for the diagnosis of onychomycosis. J Dermatol. 2005;32:108-113.
5. Shemer A, Trau H, Davidovici B, et al. Nail sampling in onychomycosis: comparative study of curettage from three sites of the infected nail. J Dtsch Dermatol Ges. 2007;5:1108-1111.
6. Shemer A, Trau H, Davidovici B, et al. Collection of fungi samples from nails: comparative study of curettage and drilling techniques. J Eur Acad Dermatol Venereol. 2008;22:182-185.
7. Hay RJ, Baran R, Haneke E. Fungal (onychomycosis) and other infections involving the nail apparatus. In: Baran R, Dawber RPR, eds. Disease of the Nails and Their Management. 2nd ed. Oxford, England: Blackwell Sciences Ltd; 1994: 97–134.
8. Daniel CR, 3rd, Elewski BE. The diagnosis of nail fungus infection revisited. Arch Dermatol. 2000;136:1162-1164.
9. Weinberg JM, Koestenblatt EK, Tutrone WD, et al. Comparison of diagnostic methods in the evaluation of onychomycosis. J Am Acad Dermatol. 2003;49:193-197.
10. Arnold B, Kianifrad F, Tavakkol A. A comparison of KOH and culture results from two mycology laboratories for the diagnosis of onychomycosis during a randomized, multicenter clinical trial: a subset study. J Am Podiatr Med Assoc. 2005;95:421-423.
11. English MP. Nails and fungi. Br J Dermatol. 1976;94:697-701.
12. Elewski BE. Clinical pearl: diagnosis of onychomycosis. J Am Acad Dermatol. 1995;32:500-501.
13. Rodgers P, Bassler M. Treating onychomycosis. Am Fam Physician. 2001;63:663-672, 677–678.
1. Lawry MA, Haneke E, Strobeck K, et al. Methods for diagnosing onychomycosis: a comparative study and review of the literature. Arch Dermatol. 2000;136:1112-1116.
2. Elewski BE. Diagnostic techniques for confirming onychomycosis. J Am Acad Dermatol. 1996;35(3 pt 2):S6-S9.
3. Heikkila H. Isolation of fungi from onychomycosis-suspected nails by two methods: clipping and drilling. Mycoses. 1996;39:479-482.
4. Mochizuki T, Kawasaki M, Tanabe H, et al. A nail drilling method suitable for the diagnosis of onychomycosis. J Dermatol. 2005;32:108-113.
5. Shemer A, Trau H, Davidovici B, et al. Nail sampling in onychomycosis: comparative study of curettage from three sites of the infected nail. J Dtsch Dermatol Ges. 2007;5:1108-1111.
6. Shemer A, Trau H, Davidovici B, et al. Collection of fungi samples from nails: comparative study of curettage and drilling techniques. J Eur Acad Dermatol Venereol. 2008;22:182-185.
7. Hay RJ, Baran R, Haneke E. Fungal (onychomycosis) and other infections involving the nail apparatus. In: Baran R, Dawber RPR, eds. Disease of the Nails and Their Management. 2nd ed. Oxford, England: Blackwell Sciences Ltd; 1994: 97–134.
8. Daniel CR, 3rd, Elewski BE. The diagnosis of nail fungus infection revisited. Arch Dermatol. 2000;136:1162-1164.
9. Weinberg JM, Koestenblatt EK, Tutrone WD, et al. Comparison of diagnostic methods in the evaluation of onychomycosis. J Am Acad Dermatol. 2003;49:193-197.
10. Arnold B, Kianifrad F, Tavakkol A. A comparison of KOH and culture results from two mycology laboratories for the diagnosis of onychomycosis during a randomized, multicenter clinical trial: a subset study. J Am Podiatr Med Assoc. 2005;95:421-423.
11. English MP. Nails and fungi. Br J Dermatol. 1976;94:697-701.
12. Elewski BE. Clinical pearl: diagnosis of onychomycosis. J Am Acad Dermatol. 1995;32:500-501.
13. Rodgers P, Bassler M. Treating onychomycosis. Am Fam Physician. 2001;63:663-672, 677–678.
Aspirin for primary prevention of CVD: Are the right people using it?
Purpose Aspirin is recommended for the primary prevention of cardiovascular disease (CVD) in adults at high risk, but little is known about sociodemographic disparities in prophylactic aspirin use. This study examined the association between sociodemographic characteristics and regular aspirin use among adults in Wisconsin who are free of CVD.
Methods A cross-sectional design was used, and data collected from 2008 to 2010. Regular aspirin use (aspirin therapy) was defined as taking aspirin most days of the week. We found 831 individuals for whom complete data were available for regression analyses and stratified the sample into 2 groups: those for whom aspirin therapy was indicated and those for whom it was not indicated, based on national guidelines.
Results Of the 268 patients for whom aspirin therapy was indicated, only 83 (31%) were using it regularly, and 102 (18%) of the 563 participants who did not have an aspirin indication were taking it regularly. In the group with an aspirin indication, participants who were older had higher rates of regular aspirin use than younger patients (odds ratio [OR]=1.07; P<.001), and women had significantly higher adjusted odds of regular aspirin use than men (OR=3.49; P=.021). Among those for whom aspirin therapy was not indicated, the adjusted odds of regular aspirin use were significantly higher among older participants (OR=1.07; P<.001) vs their younger counterparts, and significantly lower among Hispanic or nonwhite participants (OR=0.32; P=.063) relative to non-Hispanic whites.
Conclusions Aspirin therapy is underused by those at high risk for CVD—individuals who could gain cardioprotection from regular use—and overused by those at low risk for CVD, for whom the risk of major bleeding outweighs the potential benefit. Stronger primary care initiatives may be needed to ensure that patients undergo regular screening for aspirin use, particularly middle-aged men at high CVD risk. Patient education may be needed, as well, to better inform people (particularly older, non-Hispanic whites) about the risks of regular aspirin use that is not medically indicated.
Cardiovascular disease (CVD) is the principal cause of death in the United States.1 As the population grows older and obesity and diabetes become increasingly prevalent, the prevalence of CVD is also expected to rise.2,3 Fortunately, many CVD events can be prevented or delayed by modifying risk factors such as hyperlipidemia, hypertension, and smoking. Interventions associated with a reduction in risk have led to a reduction in CVD events4,5 and contributed to a steady decline in cardiac deaths.6
Control of platelet aggregation is a cornerstone of primary CVD prevention.7 In an outpatient setting, this usually translates into identifying patients who are at high risk for a CVD event and advising them to take low-dose aspirin daily or every other day. Although not without controversy,8,9 the US Preventive Services Task Force (USPSTF) recommends regular aspirin use for primary CVD prevention for middle-aged to older men at high risk for myocardial infarction (MI) and women at high risk for ischemic stroke.10
The efficacy of this intervention is proven: In primary prevention trials, regular aspirin use is associated with a 14% reduction in the likelihood of CVD events over 7 years.11 What’s more, aspirin therapy, as recommended by the USPSTF, is among the most cost-effective clinic-based preventive measures.12
In 2004, 41% of US adults age 40 or older reported taking aspirin regularly13 —an increase of approximately 20% since 1999.14 More recent data from a national population-based cohort study found that 41% of adults ages 45 to 90 years who did not have CVD but were at moderate to high risk for a CVD event reported taking aspirin ≥3 days per week.15 In the same study, almost one-fourth of those at low CVD risk also reported regular aspirin use.
While regular aspirin use for primary CVD prevention has been on the rise,13,14 the extent to which this intervention has penetrated various segments of the population is unclear. Several studies have found that aspirin use is consistently highest among those who are older, male, and white.15-17 Other socioeconomic variables (eg, education level, employment, marital status) have received little attention. And no previous study has used national guidelines for aspirin therapy to stratify samples.
A look at overuse and underuse. To ensure that aspirin therapy for primary CVD prevention is directed at those who are most likely to benefit from it, a better understanding of variables associated with both aspirin overuse and underuse is needed. This area of research is important, in part because direct-to-consumer aspirin marketing may be particularly influential among groups at low risk for CVD—for whom the risk of excess bleeding outweighs the potential for disease prevention.13,18
This study was undertaken to examine the association between specific sociodemographic variables and aspirin use among a representative sample of Wisconsin adults without CVD, looking both at those for whom aspirin therapy is indicated and those for whom it is not indicated based on national guidelines.
Methods
Design
We used a cross-sectional design, with data from the Survey of the Health of Wisconsin (SHOW),19 an annual survey of Wisconsin residents ages 21 to 74 years. SHOW uses a 2-stage stratified cluster sampling design to select households, with all age-eligible household members invited to participate. Recruitment for the annual survey consists of general community-wide announcements, as well as an initial letter and up to 6 visits to the randomly selected households to encourage participation.
By the end of 2010, SHOW had 1572 enrollees—about 53% of all eligible invitees. The demographic profile of SHOW enrollees was similar to US census data for all Wisconsin adults during the same time frame.19 All SHOW procedures were approved by the University of Wisconsin Institutional Review Board, and all participants provided informed consent.
Study sample
Our analyses were based on data provided by SHOW participants who were screened and enrolled between 2008 and 2010. To be included in our study, participants had to be between the ages of 35 and 74 years; not pregnant, on active military duty, or institutionalized; and have no personal history of CVD (myocardial infarction, angina, stroke, or transient ischemic attack) or CVD risk equivalent (type 1 or type 2 diabetes) at the time of recruitment. Data on key study variables had to be available, as well. (We used 35 years as the lower age limit because of the very low likelihood of CVD in younger individuals.)
We stratified the analytical sample (N=831) into 2 groups—participants for whom aspirin therapy was indicated and those for whom it was not indicated—in order to examine aspirin’s appropriate (recommended) and inappropriate use.
Measures
Outcome. The outcome variable was aspirin use. SHOW had asked participants how often they took aspirin. Similar to the methods used by Sanchez et al,15 we classified those who reported taking aspirin most (≥4) days of the week as regular aspirin users. All others were classified as nonregular aspirin users. Participants were not asked about the daily dose or weekly volume of aspirin.
Variables
Sociodemographic variables considered in our analysis were age, sex, race/ethnicity, education level, marital/partner status, employment status, health insurance, and region of residence within Wisconsin.
All participants underwent physical examinations, conducted as part of SHOW, at either a permanent or mobile exam center. Blood pressure was measured after a 5-minute rest period in a seated position, and the average of the last 2 out of 3 consecutive measurements was reported. Body mass index (BMI) was calculated, and blood samples were obtained by venipuncture, processed immediately, and sent to the Marshfield Clinic laboratory for measuring total and high-density lipoprotein (HDL) cholesterol.
Indications for aspirin therapy. We stratified the sample by those who were and those who were not candidates for aspirin therapy for primary CVD prevention based on the latest guidelines from the USPSTF ( FIGURE ).10 The Task Force recommends aspirin therapy for men ages 45 to 74 years with a moderate or greater 10-year risk of a coronary heart disease (CHD) event and women ages 55 to 74 years with a moderate or greater 10-year risk of stroke. We used the global CVD risk equation derived from the Framingham Heart Study (based on age, sex, smoking status, systolic blood pressure, and total and HDL cholesterol) to calculate each participant’s 10-year risk and, thus, determine whether aspirin therapy was or was not indicated.20 Total and HDL cholesterol values were missing for 94 participants in the analytical sample; their 10-year CVD risk was estimated using BMI, a reasonable alternative to more conventional CVD risk prediction when laboratory values are unavailable.21
FIGURE
Study (SHOW) sample, stratified based on aspirin indication10
*US Preventive Services Task Force guidelines were slightly modified for this analysis: The upper age bound was reduced from 79 to 74 years because the Survey of the Health of Wisconsin did not enroll participants >74 years.
CHD, coronary heart disease; CVD, cardiovascular disease; DM, diabetes mellitus; N/A, not applicable; SHOW, Survey of the Health of Wisconsin.
Statistical analyses
All analytical procedures were conducted using Statistical Analysis Software (SAS Version 9.2; Cary, NC). A complete-case framework was used.
We used multivariate logistic regression for survey data (PROC SURVEYLOGISTIC; SAS Institute, Cary, NC) to examine the association between aspirin use and sociodemographic variables. Two separate analyses were conducted, one of participants for whom aspirin therapy was indicated and the other for participants for whom it was not. The outcomes were modeled dichotomously, as regular vs nonregular aspirin users, and a collinearity check was done. 21
Initially, we created univariate models to gauge the crude relationship between each variable and aspirin use. Any variable with P<.20 in its univariate association with regular aspirin use was considered for inclusion in the final multivariate regression model. In the multivariate analyses, we sequentially eliminated variables with the weakest association with aspirin use until only significant (P<.10) independent predictors remained. Appropriate weighting was applied based on survey strata and cluster structure.19
Results
Of the 831 participants who met the eligibility criteria for our analysis, 268 (32%) had an aspirin indication. TABLE 1 shows the key characteristics of the analytical sample, stratified by those for whom aspirin was indicated and those for whom it was not. The sample was primarily middle-aged (mean age 52.4±0.36) and non-Hispanic white (93%). Compared with those for whom aspirin therapy was not indicated, the group with an aspirin indication was significantly older (56.9 vs 50.3) and had a significantly higher proportion of males (97% vs 19%). As expected, those for whom aspirin was indicated were also at higher risk for CHD and stroke, most notably as a result of significantly higher systolic BP (131.9 vs 121.5 mm Hg) and lower HDL cholesterol (42.5 vs 52.6 mg/dL) compared with participants without an aspirin indication.
TABLE 1
Study sample, by sociodemographic variable and aspirin indication
| Variable | Full sample (N=831) | Aspirin indicated (n=268) | Aspirin not indicated (n=563) |
|---|---|---|---|
| Mean age, y | 52.4 | 56.9 | 50.3 |
| Sex, n Male Female | 367 464 | 259 9 | 108 455 |
| Race/ethnicity, n White, non-Hispanic Nonwhite/Hispanic | 776 55 | 252 16 | 524 39 |
| Marital status, n Married/partnered Not married or partnered | 637 194 | 215 53 | 422 141 |
| Health insurance, n Uninsured Insured | 76 755 | 26 242 | 50 513 |
| Education, n ≤High school Associate’s degree ≥Bachelor’s degree | 217 312 302 | 77 107 84 | 140 205 218 |
| Employment, n Unemployed Student/retiree/home Employed | 98 147 586 | 33 52 183 | 65 95 403 |
When aspirin was indicated, use was linked to age and sex
In the group with an aspirin indication (n=268), 83 (31%) reported taking aspirin most days of the week. The initial examination of sociodemographic variables showed that age, sex, and employment status demonstrated significant univariate associations with regular aspirin use ( TABLE 2 ). In the multivariate model, however, the odds of regular aspirin use were significantly greater among participants who were older (odds ratio [OR], 1.07; P<.001) or female (OR, 3.49; P=.021) compared with participants who were younger or male, respectively.
TABLE 2
Participants who have an aspirin indication: Association between sociodemographic variables and regular aspirin use
| Variable | Regular aspirin use, OR (95% CI) | P value* |
|---|---|---|
| Age Older vs younger | 1.07 (1.04-1.11) | .001 |
| Sex Female vs male | 3.89 (1.42-10.67)† | .008 |
| Race/ethnicity Nonwhite/Hispanic vs white non-Hispanic | 0.55 (0.09-3.47) | .526 |
| Marital status Not married/partnered vs married/partner | 0.83 (0.36-1.95) | .678 |
| Health insurance Uninsured vs insured | 0.86 (0.50-1.47) | .579 |
| Education ≥Bachelor’s degree vs ≤high school Associate’s degree/some college vs ≤high school | 1.58 (0.75-3.34) 1.36 (0.74-2.49) | .234 .325 |
| Employment Student or retired vs employed Unemployed vs employed | 2.96 (1.74-5.03) 0.62 (0.25-1.56) | .001 .314 |
| *Significance was defined as P<.10. †Multivariate adjusted model: 3.49 (95% CI, 1.21-10.07; P=.021). CI, confidence interval; OR, odds ratio. | ||
When aspirin was not indicated, age and sex still affected use
Among the 563 participants for whom aspirin therapy was not indicated, 102 (18%) reported taking aspirin regularly. Age, sex, race/ethnicity, health insurance, and employment ( TABLE 3 ), as well as region of residence and study enrollment year, had significant univariate associations with regular aspirin use; these variables were tested for potential inclusion in the multivariate model. In the final multivariate regression model, the odds of regular aspirin use were significantly greater among participants who were older (OR, 1.07; P<.001) and significantly lower among participants who were Hispanic or nonwhite (OR, 0.32; P=.063).
TABLE 3
Participants who do not have an aspirin indication: Association between sociodemographic variables and regular aspirin use
| Variable | Regular aspirin use, OR (95% CI) | P value* |
|---|---|---|
| Age Older vs younger | 1.07 (1.04-1.10) | .001 |
| Sex Female vs male | 1.60 (0.84-3.04) | .152 |
| Race/ethnicity Nonwhite or Hispanic vs white non-Hispanic | 0.23 (0.07- 0.73)† | .013 |
| Marital status Not married/partnered vs married/partnered | 1.00 (0.63-1.59) | .992 |
| Health insurance Uninsured vs insured | 0.36 (0.11- 1.15) | .086 |
| Education Bachelor’s or higher vs high school or less Associate’s/some college vs high school or less | 0.74 (0.35-1.57) 0.67 (0.38-1.17) | .431 .158 |
| Employment Student/retired vs employed Unemployed vs employed | 2.35 (1.32-4.20) 0.78 (0.26- 2.34) | .004 .652 |
| *Significance was defined as P<.10. †Multivariate adjusted model: 0.32 (95% CI, 0.10-1.06; P=.063). CI, confidence interval; OR, odds ratio. | ||
Discussion
Aspirin was generally underutilized in the group with significant CVD risk (n=268) in our study, with slightly less than a third of participants for whom aspirin therapy was indicated taking it most days of the week. Despite trends of increased aspirin use among US adults in recent years,15 aspirin therapy in the 2008-2010 SHOW sample was lower than in 2005 to 2008. It was also lower than national estimates of aspirin use for primary CVD prevention15,22 —but about 20% higher than estimates of overall aspirin use in Wisconsin 20 years ago.23 Consistent with previous research, the final adjusted model and sensitivity analysis indicated that older individuals were more likely to take aspirin regularly.
Contrary to the findings in some previous studies,15-17 however, our analysis suggested that women had a higher adjusted odds of regular aspirin use compared with men. This result should be interpreted with extreme caution, however, because so few females (9 of 464 [3%]) met the current USPSTF criteria for aspirin therapy for primary CVD prevention. The previous USPSTF guidelines24,25 were less conservative, with a lower minimum age and threshold for CVD risk for women. The revision is the likely result of recent primary prevention trials10 that found regular aspirin use provided less cardioprotection for younger women.
The sample without an aspirin indication—roughly twice the size of the group with an aspirin indication (563 vs 268), which is reflective of the general population of Wisconsin—was useful in highlighting inappropriate use. There were clear indications of aspirin overuse in this group, with 18% of the sample reporting that they took aspirin regularly. The finding that inappropriate aspirin use was more likely in non-Hispanic whites vs minorities is similar to the result of an earlier study in which blacks, Hispanics, and Chinese Americans with low CVD risk were much less likely to report regular aspirin use compared with whites at low risk.15
The main concern with regular aspirin use in those for whom it is not indicated for primary CVD prevention is the risk of upper gastrointestinal bleeding and, less commonly, hemorrhagic stroke.26 To illustrate this point, consider the following: About 10% of SHOW participants ages 35 to 74 years had no history of CVD and no indication for aspirin therapy based on the latest USPSTF guidelines, but took aspirin regularly nonetheless. Extrapolating those numbers to the entire state of Wisconsin would suggest that approximately 270,000 state residents have a similar profile. Assuming an extra 1.3 major bleeding events per 1000 person-years of regular aspirin use (as a meta-analysis of studies of adverse events associated with antiplatelet therapy found),27 that would translate into an estimated 350 major bleeding events per year in Wisconsin that are attributable to aspirin overuse.
In view of the current USPSTF recommendations,10 aspirin is not optimally utilized by Wisconsin residents for the primary prevention of CVD. Aspirin therapy is not used enough by those with a high CVD risk, who could derive substantial vascular disease protection from it. Conversely, aspirin therapy is overused by those with a low CVD risk, for whom the risk of major bleeding is significantly higher than the potential for vascular disease protection. Furthermore, younger individuals at high CVD risk appear to be least likely to take aspirin regularly.
Recommendations
The strongest modifiable predictor of regular aspirin use is a recommendation from a clinician.13 Therefore, we recommend stronger primary care initiatives to ensure that patients are screened for aspirin use more frequently, particularly middle-aged men at high CVD risk. This clinic-based initiative could reach a larger proportion of the general population when combined with broader, community-oriented CVD preventive services.28
More precise marketing and education are also needed. Because aspirin is a low-cost over-the-counter product that leads the consumer market for analgesics,29 the general public (and older, non-Hispanic whites, in particular) needs to be better informed about the risks of medically inappropriate aspirin use for primary CVD prevention.
Study limitations
Selection and measurement biases were among the chief study limitations.
Study (SHOW) enrollment rate was slightly above 50%, with steady increases in enrollment each year (from 46% in 2008-2009 to 56% in 2010) due to expanded recruitment and consolidation of field operations.
Aspirin use was self-reported, and SHOW did not capture the reason for taking it (eg, CVD prevention or pain management). Some evidence of overreporting of aspirin use among older individuals exists,30 suggesting that a more objective measure of aspirin use (eg, pill bottle verification or blood platelet aggregation test) could yield different results.
Certain confounders were not measured, most notably contraindications to aspirin (eg, genetic platelet abnormalities). Such findings could explain some patterns of aspirin use in both strata, as up to 10% of any given population has a contraindication to aspirin due to allergy, intolerance, gastrointestinal ulcer, concomitant anticoagulant medication, or other high bleeding risk.18,31 Few of these variables were known about our sample.
TABLE 4W (available below) provides a breakdown of some possible aspirin contraindications, as well as possible reasons other than primary CVD prevention for regular aspirin use. Because clinical judgment is often required to assess the degree of severity of a given health condition in order to deem it an aspirin contraindication, these findings could not reliably be used to reclassify participants. We present them simply for hypothesis generation.
Some data collection predates the current USPSTF guidelines,10 which could have resulted in a misclassification of participants’ aspirin indication. However, sensitivity analyses restricted to the 2010 sample alone—the only one with data collection after the newer guidelines were released—did not reveal any meaningful differences.
Other methodological limitations include the less racially diverse population of Wisconsin compared with other parts of the country and the sample size, which did not permit testing for statistical interactions and perhaps resulted in larger confidence intervals for some associations (eg, race/ethnicity) relative to the population as a whole.
TABLE 4W
Possible reasons for aspirin use—or contraindication— by aspirin indication*
| Has a doctor or other health professional ever told you that you had … | Aspirin indicated (n=268) | Aspirin not indicated (n=563) | ||
|---|---|---|---|---|
| Regular aspirin user (n=83) | Nonregular aspirin user (n=185) | Regular aspirin user (n=102) | Nonregular aspirin user (n=461) | |
| Migraine headache Yes No | 20 (24%) 63 (76%) | 28 (15%) 157 (85%) | 24 (24%) 78 (76%) | 76 (16%) 385 (84%) |
| Arthritis† Yes No | 2 (2%) 81 (98%) | 1 (1%) 184 (99%) | 12 (12%) 90 (88%) | 26 (6%) 435 (94%) |
| Stomach or intestinal ulcer Yes No | 5 (6%) 78 (94%) | 6 (3%) 179 (97%) | 7 (7%) 95 (93%) | 10 (2%) 451 (98%) |
| Reflux or GERD Yes No | 8 (10%) 75 (90%) | 14 (8%) 171 (92%) | 11 (11%) 91 (89%) | 32 (7%) 429 (93%) |
| Values presented as n (%). *Data not included in study analysis. †Osteoarthritis or rheumatoid arthritis. GERD, gastric esophageal reflux disease. | ||||
Acknowledgement
The authors thank Matt Walsh, PhD, for his assistance in creating the analytical dataset, as well as Sally Steward-Townsend, Susan Wright, Bri Deyo, Bethany Varley, and the rest of the Survey of the Health of Wisconsin staff.
CORRESPONDENCE Jeffrey J. VanWormer, PhD, Epidemiology Research Center, Marshfield Clinic Research Foundation, 1000 North Oak Avenue, Marshfield, WI 54449; vanwormer.jeffrey@mcrf.mfldclin.edu
1. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18-e209.
2. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-944.
3. Sullivan PW, Ghushchyan V, Wyatt HR. The medical cost of cardiometabolic risk factor clusters in the United States. Obesity. 2007;15:3150-3158.
4. Pearson TA, Blair SN, Daniels SR, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388-391.
5. Kriekard P, Gharacholou SM, Peterson ED. Primary and secondary prevention of cardiovascular disease in older adults: a status report. Clin Geriatr Med. 2009;25:745-755.
6. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388-2398.
7. Hennekens CH, Schneider WR. The need for wider and appropriate utilization of aspirin and statins in the treatment and prevention of cardiovascular disease. Expert Rev Cardiovasc Ther. 2008;6:95-107.
8. Barnett H, Burrill P, Iheanacho I. Don’t use aspirin for primary prevention of cardiovascular disease. BMJ. 2010;340:c1805.-
9. Sanchez-Ross M, Waller AH, Maher J, et al. Aspirin for the prevention of cardiovascular morbidity. Minerva Med. 2010;101:205-214.
10. S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US preventive services task force recommendation statement. Ann Intern Med. 2009;150:396-404.
11. Bartolucci AA, Tendera M, Howard G. Meta-analysis of multiple primary prevention trials of cardiovascular events using aspirin. Am J Cardiol. 2011;107:1796-1801.
12. Maciosek MV, Coffield AB, Edwards NM, et al. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52-61.
13. Pignone M, Anderson GK, Binns K, et al. Aspirin use among adults aged 40 and older in the United States results of a national survey. Am J Prev Med. 2007;32:403-407.
14. Ajani UA, Ford ES, Greenland KJ, et al. Aspirin use among US adults: behavioral risk factor surveillance system. Am J Prev Med. 2006;30:74-77.
15. Sanchez DR, Diez Roux AV, Michos ED, et al. Comparison of the racial/ethnic prevalence of regular aspirin use for the primary prevention of coronary heart disease from the multi-ethnic study of atherosclerosis. Am J Cardiol. 2011;107:41-46.
16. Stafford RS, Monti V, Ma J. Underutilization of aspirin persists in US ambulatory care for the secondary and primary prevention of cardiovascular disease. PLoS Med. 2005;2:e353.-
17. Rodondi N, Vittinghoff E, Cornuz J, et al. Aspirin use for the primary prevention of coronary heart disease in older adults. Am J Med. 2005;118(suppl):1288e1-1288e9.
18. Rodondi N, Cornuz J, Marques-Vidal P, et al. Aspirin use for the primary prevention of coronary heart disease: a population-based study in Switzerland. Prev Med. 2008;46:137-144.
19. Nieto FJ, Peppard PE, Engelman CD, et al. The Survey of the Health of Wisconsin (SHOW), a novel infrastructure for population health research: rationale and methods. BMC Public Health. 2010;10:785.-
20. D’Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743-753.
21. Cody RP, Smith JK. Applied Statistics and the SAS Programming Language. New York, NY: Prentice Hall; 2005.
22. Mallonee S, Daniels CG, Mold JW, et al. Increasing aspirin use among persons at risk for cardiovascular events in Oklahoma. J Okla State Med Assoc. 2010;103:254-260.
23. Centers for Disease Control and Prevention (CDC). Prevalence of aspirin use to prevent heart disease—Wisconsin, 1991, and Michigan, 1994. MMWR Morb Mortal Wkly Rep. 1997;46:498-502.
24. US Preventive Services Task Force. Aspirin for the primary prevention of cardiovascular events: recommendation and rationale. Ann Intern Med. 2002;136:157-160.
25. Werner M, Kelsberg G, Weismantel AM. Which healthy adults should take aspirin? J Fam Pract. 2004;53:146-150.
26. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
27. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006;119:624-638.
28. VanWormer JJ, Johnson PJ, Pereira RF, et al. The Heart of New Ulm project: using community-based cardiometabolic risk factor screenings in a rural population health improvement initiative. Popul Health Manag. 2012;15:135-143.
29. Jeffreys D. Aspirin: The Remarkable Story of a Wonder Drug. New York, NY: Bloomsbury Publishing; 2005.
30. Smith NL, Psaty BM, Heckbert SR, et al. The reliability of medication inventory methods compared to serum levels of cardiovascular drugs in the elderly. J Clin Epidemiol. 1999;52:143-146.
31. Hedman J, Kaprio J, Poussa T, et al. Prevalence of asthma, aspirin intolerance, nasal polyposis and chronic obstructive pulmonary disease in a population-based study. Int J Epidemiol. 1999;28:717-722.
Purpose Aspirin is recommended for the primary prevention of cardiovascular disease (CVD) in adults at high risk, but little is known about sociodemographic disparities in prophylactic aspirin use. This study examined the association between sociodemographic characteristics and regular aspirin use among adults in Wisconsin who are free of CVD.
Methods A cross-sectional design was used, and data collected from 2008 to 2010. Regular aspirin use (aspirin therapy) was defined as taking aspirin most days of the week. We found 831 individuals for whom complete data were available for regression analyses and stratified the sample into 2 groups: those for whom aspirin therapy was indicated and those for whom it was not indicated, based on national guidelines.
Results Of the 268 patients for whom aspirin therapy was indicated, only 83 (31%) were using it regularly, and 102 (18%) of the 563 participants who did not have an aspirin indication were taking it regularly. In the group with an aspirin indication, participants who were older had higher rates of regular aspirin use than younger patients (odds ratio [OR]=1.07; P<.001), and women had significantly higher adjusted odds of regular aspirin use than men (OR=3.49; P=.021). Among those for whom aspirin therapy was not indicated, the adjusted odds of regular aspirin use were significantly higher among older participants (OR=1.07; P<.001) vs their younger counterparts, and significantly lower among Hispanic or nonwhite participants (OR=0.32; P=.063) relative to non-Hispanic whites.
Conclusions Aspirin therapy is underused by those at high risk for CVD—individuals who could gain cardioprotection from regular use—and overused by those at low risk for CVD, for whom the risk of major bleeding outweighs the potential benefit. Stronger primary care initiatives may be needed to ensure that patients undergo regular screening for aspirin use, particularly middle-aged men at high CVD risk. Patient education may be needed, as well, to better inform people (particularly older, non-Hispanic whites) about the risks of regular aspirin use that is not medically indicated.
Cardiovascular disease (CVD) is the principal cause of death in the United States.1 As the population grows older and obesity and diabetes become increasingly prevalent, the prevalence of CVD is also expected to rise.2,3 Fortunately, many CVD events can be prevented or delayed by modifying risk factors such as hyperlipidemia, hypertension, and smoking. Interventions associated with a reduction in risk have led to a reduction in CVD events4,5 and contributed to a steady decline in cardiac deaths.6
Control of platelet aggregation is a cornerstone of primary CVD prevention.7 In an outpatient setting, this usually translates into identifying patients who are at high risk for a CVD event and advising them to take low-dose aspirin daily or every other day. Although not without controversy,8,9 the US Preventive Services Task Force (USPSTF) recommends regular aspirin use for primary CVD prevention for middle-aged to older men at high risk for myocardial infarction (MI) and women at high risk for ischemic stroke.10
The efficacy of this intervention is proven: In primary prevention trials, regular aspirin use is associated with a 14% reduction in the likelihood of CVD events over 7 years.11 What’s more, aspirin therapy, as recommended by the USPSTF, is among the most cost-effective clinic-based preventive measures.12
In 2004, 41% of US adults age 40 or older reported taking aspirin regularly13 —an increase of approximately 20% since 1999.14 More recent data from a national population-based cohort study found that 41% of adults ages 45 to 90 years who did not have CVD but were at moderate to high risk for a CVD event reported taking aspirin ≥3 days per week.15 In the same study, almost one-fourth of those at low CVD risk also reported regular aspirin use.
While regular aspirin use for primary CVD prevention has been on the rise,13,14 the extent to which this intervention has penetrated various segments of the population is unclear. Several studies have found that aspirin use is consistently highest among those who are older, male, and white.15-17 Other socioeconomic variables (eg, education level, employment, marital status) have received little attention. And no previous study has used national guidelines for aspirin therapy to stratify samples.
A look at overuse and underuse. To ensure that aspirin therapy for primary CVD prevention is directed at those who are most likely to benefit from it, a better understanding of variables associated with both aspirin overuse and underuse is needed. This area of research is important, in part because direct-to-consumer aspirin marketing may be particularly influential among groups at low risk for CVD—for whom the risk of excess bleeding outweighs the potential for disease prevention.13,18
This study was undertaken to examine the association between specific sociodemographic variables and aspirin use among a representative sample of Wisconsin adults without CVD, looking both at those for whom aspirin therapy is indicated and those for whom it is not indicated based on national guidelines.
Methods
Design
We used a cross-sectional design, with data from the Survey of the Health of Wisconsin (SHOW),19 an annual survey of Wisconsin residents ages 21 to 74 years. SHOW uses a 2-stage stratified cluster sampling design to select households, with all age-eligible household members invited to participate. Recruitment for the annual survey consists of general community-wide announcements, as well as an initial letter and up to 6 visits to the randomly selected households to encourage participation.
By the end of 2010, SHOW had 1572 enrollees—about 53% of all eligible invitees. The demographic profile of SHOW enrollees was similar to US census data for all Wisconsin adults during the same time frame.19 All SHOW procedures were approved by the University of Wisconsin Institutional Review Board, and all participants provided informed consent.
Study sample
Our analyses were based on data provided by SHOW participants who were screened and enrolled between 2008 and 2010. To be included in our study, participants had to be between the ages of 35 and 74 years; not pregnant, on active military duty, or institutionalized; and have no personal history of CVD (myocardial infarction, angina, stroke, or transient ischemic attack) or CVD risk equivalent (type 1 or type 2 diabetes) at the time of recruitment. Data on key study variables had to be available, as well. (We used 35 years as the lower age limit because of the very low likelihood of CVD in younger individuals.)
We stratified the analytical sample (N=831) into 2 groups—participants for whom aspirin therapy was indicated and those for whom it was not indicated—in order to examine aspirin’s appropriate (recommended) and inappropriate use.
Measures
Outcome. The outcome variable was aspirin use. SHOW had asked participants how often they took aspirin. Similar to the methods used by Sanchez et al,15 we classified those who reported taking aspirin most (≥4) days of the week as regular aspirin users. All others were classified as nonregular aspirin users. Participants were not asked about the daily dose or weekly volume of aspirin.
Variables
Sociodemographic variables considered in our analysis were age, sex, race/ethnicity, education level, marital/partner status, employment status, health insurance, and region of residence within Wisconsin.
All participants underwent physical examinations, conducted as part of SHOW, at either a permanent or mobile exam center. Blood pressure was measured after a 5-minute rest period in a seated position, and the average of the last 2 out of 3 consecutive measurements was reported. Body mass index (BMI) was calculated, and blood samples were obtained by venipuncture, processed immediately, and sent to the Marshfield Clinic laboratory for measuring total and high-density lipoprotein (HDL) cholesterol.
Indications for aspirin therapy. We stratified the sample by those who were and those who were not candidates for aspirin therapy for primary CVD prevention based on the latest guidelines from the USPSTF ( FIGURE ).10 The Task Force recommends aspirin therapy for men ages 45 to 74 years with a moderate or greater 10-year risk of a coronary heart disease (CHD) event and women ages 55 to 74 years with a moderate or greater 10-year risk of stroke. We used the global CVD risk equation derived from the Framingham Heart Study (based on age, sex, smoking status, systolic blood pressure, and total and HDL cholesterol) to calculate each participant’s 10-year risk and, thus, determine whether aspirin therapy was or was not indicated.20 Total and HDL cholesterol values were missing for 94 participants in the analytical sample; their 10-year CVD risk was estimated using BMI, a reasonable alternative to more conventional CVD risk prediction when laboratory values are unavailable.21
FIGURE
Study (SHOW) sample, stratified based on aspirin indication10
*US Preventive Services Task Force guidelines were slightly modified for this analysis: The upper age bound was reduced from 79 to 74 years because the Survey of the Health of Wisconsin did not enroll participants >74 years.
CHD, coronary heart disease; CVD, cardiovascular disease; DM, diabetes mellitus; N/A, not applicable; SHOW, Survey of the Health of Wisconsin.
Statistical analyses
All analytical procedures were conducted using Statistical Analysis Software (SAS Version 9.2; Cary, NC). A complete-case framework was used.
We used multivariate logistic regression for survey data (PROC SURVEYLOGISTIC; SAS Institute, Cary, NC) to examine the association between aspirin use and sociodemographic variables. Two separate analyses were conducted, one of participants for whom aspirin therapy was indicated and the other for participants for whom it was not. The outcomes were modeled dichotomously, as regular vs nonregular aspirin users, and a collinearity check was done. 21
Initially, we created univariate models to gauge the crude relationship between each variable and aspirin use. Any variable with P<.20 in its univariate association with regular aspirin use was considered for inclusion in the final multivariate regression model. In the multivariate analyses, we sequentially eliminated variables with the weakest association with aspirin use until only significant (P<.10) independent predictors remained. Appropriate weighting was applied based on survey strata and cluster structure.19
Results
Of the 831 participants who met the eligibility criteria for our analysis, 268 (32%) had an aspirin indication. TABLE 1 shows the key characteristics of the analytical sample, stratified by those for whom aspirin was indicated and those for whom it was not. The sample was primarily middle-aged (mean age 52.4±0.36) and non-Hispanic white (93%). Compared with those for whom aspirin therapy was not indicated, the group with an aspirin indication was significantly older (56.9 vs 50.3) and had a significantly higher proportion of males (97% vs 19%). As expected, those for whom aspirin was indicated were also at higher risk for CHD and stroke, most notably as a result of significantly higher systolic BP (131.9 vs 121.5 mm Hg) and lower HDL cholesterol (42.5 vs 52.6 mg/dL) compared with participants without an aspirin indication.
TABLE 1
Study sample, by sociodemographic variable and aspirin indication
| Variable | Full sample (N=831) | Aspirin indicated (n=268) | Aspirin not indicated (n=563) |
|---|---|---|---|
| Mean age, y | 52.4 | 56.9 | 50.3 |
| Sex, n Male Female | 367 464 | 259 9 | 108 455 |
| Race/ethnicity, n White, non-Hispanic Nonwhite/Hispanic | 776 55 | 252 16 | 524 39 |
| Marital status, n Married/partnered Not married or partnered | 637 194 | 215 53 | 422 141 |
| Health insurance, n Uninsured Insured | 76 755 | 26 242 | 50 513 |
| Education, n ≤High school Associate’s degree ≥Bachelor’s degree | 217 312 302 | 77 107 84 | 140 205 218 |
| Employment, n Unemployed Student/retiree/home Employed | 98 147 586 | 33 52 183 | 65 95 403 |
When aspirin was indicated, use was linked to age and sex
In the group with an aspirin indication (n=268), 83 (31%) reported taking aspirin most days of the week. The initial examination of sociodemographic variables showed that age, sex, and employment status demonstrated significant univariate associations with regular aspirin use ( TABLE 2 ). In the multivariate model, however, the odds of regular aspirin use were significantly greater among participants who were older (odds ratio [OR], 1.07; P<.001) or female (OR, 3.49; P=.021) compared with participants who were younger or male, respectively.
TABLE 2
Participants who have an aspirin indication: Association between sociodemographic variables and regular aspirin use
| Variable | Regular aspirin use, OR (95% CI) | P value* |
|---|---|---|
| Age Older vs younger | 1.07 (1.04-1.11) | .001 |
| Sex Female vs male | 3.89 (1.42-10.67)† | .008 |
| Race/ethnicity Nonwhite/Hispanic vs white non-Hispanic | 0.55 (0.09-3.47) | .526 |
| Marital status Not married/partnered vs married/partner | 0.83 (0.36-1.95) | .678 |
| Health insurance Uninsured vs insured | 0.86 (0.50-1.47) | .579 |
| Education ≥Bachelor’s degree vs ≤high school Associate’s degree/some college vs ≤high school | 1.58 (0.75-3.34) 1.36 (0.74-2.49) | .234 .325 |
| Employment Student or retired vs employed Unemployed vs employed | 2.96 (1.74-5.03) 0.62 (0.25-1.56) | .001 .314 |
| *Significance was defined as P<.10. †Multivariate adjusted model: 3.49 (95% CI, 1.21-10.07; P=.021). CI, confidence interval; OR, odds ratio. | ||
When aspirin was not indicated, age and sex still affected use
Among the 563 participants for whom aspirin therapy was not indicated, 102 (18%) reported taking aspirin regularly. Age, sex, race/ethnicity, health insurance, and employment ( TABLE 3 ), as well as region of residence and study enrollment year, had significant univariate associations with regular aspirin use; these variables were tested for potential inclusion in the multivariate model. In the final multivariate regression model, the odds of regular aspirin use were significantly greater among participants who were older (OR, 1.07; P<.001) and significantly lower among participants who were Hispanic or nonwhite (OR, 0.32; P=.063).
TABLE 3
Participants who do not have an aspirin indication: Association between sociodemographic variables and regular aspirin use
| Variable | Regular aspirin use, OR (95% CI) | P value* |
|---|---|---|
| Age Older vs younger | 1.07 (1.04-1.10) | .001 |
| Sex Female vs male | 1.60 (0.84-3.04) | .152 |
| Race/ethnicity Nonwhite or Hispanic vs white non-Hispanic | 0.23 (0.07- 0.73)† | .013 |
| Marital status Not married/partnered vs married/partnered | 1.00 (0.63-1.59) | .992 |
| Health insurance Uninsured vs insured | 0.36 (0.11- 1.15) | .086 |
| Education Bachelor’s or higher vs high school or less Associate’s/some college vs high school or less | 0.74 (0.35-1.57) 0.67 (0.38-1.17) | .431 .158 |
| Employment Student/retired vs employed Unemployed vs employed | 2.35 (1.32-4.20) 0.78 (0.26- 2.34) | .004 .652 |
| *Significance was defined as P<.10. †Multivariate adjusted model: 0.32 (95% CI, 0.10-1.06; P=.063). CI, confidence interval; OR, odds ratio. | ||
Discussion
Aspirin was generally underutilized in the group with significant CVD risk (n=268) in our study, with slightly less than a third of participants for whom aspirin therapy was indicated taking it most days of the week. Despite trends of increased aspirin use among US adults in recent years,15 aspirin therapy in the 2008-2010 SHOW sample was lower than in 2005 to 2008. It was also lower than national estimates of aspirin use for primary CVD prevention15,22 —but about 20% higher than estimates of overall aspirin use in Wisconsin 20 years ago.23 Consistent with previous research, the final adjusted model and sensitivity analysis indicated that older individuals were more likely to take aspirin regularly.
Contrary to the findings in some previous studies,15-17 however, our analysis suggested that women had a higher adjusted odds of regular aspirin use compared with men. This result should be interpreted with extreme caution, however, because so few females (9 of 464 [3%]) met the current USPSTF criteria for aspirin therapy for primary CVD prevention. The previous USPSTF guidelines24,25 were less conservative, with a lower minimum age and threshold for CVD risk for women. The revision is the likely result of recent primary prevention trials10 that found regular aspirin use provided less cardioprotection for younger women.
The sample without an aspirin indication—roughly twice the size of the group with an aspirin indication (563 vs 268), which is reflective of the general population of Wisconsin—was useful in highlighting inappropriate use. There were clear indications of aspirin overuse in this group, with 18% of the sample reporting that they took aspirin regularly. The finding that inappropriate aspirin use was more likely in non-Hispanic whites vs minorities is similar to the result of an earlier study in which blacks, Hispanics, and Chinese Americans with low CVD risk were much less likely to report regular aspirin use compared with whites at low risk.15
The main concern with regular aspirin use in those for whom it is not indicated for primary CVD prevention is the risk of upper gastrointestinal bleeding and, less commonly, hemorrhagic stroke.26 To illustrate this point, consider the following: About 10% of SHOW participants ages 35 to 74 years had no history of CVD and no indication for aspirin therapy based on the latest USPSTF guidelines, but took aspirin regularly nonetheless. Extrapolating those numbers to the entire state of Wisconsin would suggest that approximately 270,000 state residents have a similar profile. Assuming an extra 1.3 major bleeding events per 1000 person-years of regular aspirin use (as a meta-analysis of studies of adverse events associated with antiplatelet therapy found),27 that would translate into an estimated 350 major bleeding events per year in Wisconsin that are attributable to aspirin overuse.
In view of the current USPSTF recommendations,10 aspirin is not optimally utilized by Wisconsin residents for the primary prevention of CVD. Aspirin therapy is not used enough by those with a high CVD risk, who could derive substantial vascular disease protection from it. Conversely, aspirin therapy is overused by those with a low CVD risk, for whom the risk of major bleeding is significantly higher than the potential for vascular disease protection. Furthermore, younger individuals at high CVD risk appear to be least likely to take aspirin regularly.
Recommendations
The strongest modifiable predictor of regular aspirin use is a recommendation from a clinician.13 Therefore, we recommend stronger primary care initiatives to ensure that patients are screened for aspirin use more frequently, particularly middle-aged men at high CVD risk. This clinic-based initiative could reach a larger proportion of the general population when combined with broader, community-oriented CVD preventive services.28
More precise marketing and education are also needed. Because aspirin is a low-cost over-the-counter product that leads the consumer market for analgesics,29 the general public (and older, non-Hispanic whites, in particular) needs to be better informed about the risks of medically inappropriate aspirin use for primary CVD prevention.
Study limitations
Selection and measurement biases were among the chief study limitations.
Study (SHOW) enrollment rate was slightly above 50%, with steady increases in enrollment each year (from 46% in 2008-2009 to 56% in 2010) due to expanded recruitment and consolidation of field operations.
Aspirin use was self-reported, and SHOW did not capture the reason for taking it (eg, CVD prevention or pain management). Some evidence of overreporting of aspirin use among older individuals exists,30 suggesting that a more objective measure of aspirin use (eg, pill bottle verification or blood platelet aggregation test) could yield different results.
Certain confounders were not measured, most notably contraindications to aspirin (eg, genetic platelet abnormalities). Such findings could explain some patterns of aspirin use in both strata, as up to 10% of any given population has a contraindication to aspirin due to allergy, intolerance, gastrointestinal ulcer, concomitant anticoagulant medication, or other high bleeding risk.18,31 Few of these variables were known about our sample.
TABLE 4W (available below) provides a breakdown of some possible aspirin contraindications, as well as possible reasons other than primary CVD prevention for regular aspirin use. Because clinical judgment is often required to assess the degree of severity of a given health condition in order to deem it an aspirin contraindication, these findings could not reliably be used to reclassify participants. We present them simply for hypothesis generation.
Some data collection predates the current USPSTF guidelines,10 which could have resulted in a misclassification of participants’ aspirin indication. However, sensitivity analyses restricted to the 2010 sample alone—the only one with data collection after the newer guidelines were released—did not reveal any meaningful differences.
Other methodological limitations include the less racially diverse population of Wisconsin compared with other parts of the country and the sample size, which did not permit testing for statistical interactions and perhaps resulted in larger confidence intervals for some associations (eg, race/ethnicity) relative to the population as a whole.
TABLE 4W
Possible reasons for aspirin use—or contraindication— by aspirin indication*
| Has a doctor or other health professional ever told you that you had … | Aspirin indicated (n=268) | Aspirin not indicated (n=563) | ||
|---|---|---|---|---|
| Regular aspirin user (n=83) | Nonregular aspirin user (n=185) | Regular aspirin user (n=102) | Nonregular aspirin user (n=461) | |
| Migraine headache Yes No | 20 (24%) 63 (76%) | 28 (15%) 157 (85%) | 24 (24%) 78 (76%) | 76 (16%) 385 (84%) |
| Arthritis† Yes No | 2 (2%) 81 (98%) | 1 (1%) 184 (99%) | 12 (12%) 90 (88%) | 26 (6%) 435 (94%) |
| Stomach or intestinal ulcer Yes No | 5 (6%) 78 (94%) | 6 (3%) 179 (97%) | 7 (7%) 95 (93%) | 10 (2%) 451 (98%) |
| Reflux or GERD Yes No | 8 (10%) 75 (90%) | 14 (8%) 171 (92%) | 11 (11%) 91 (89%) | 32 (7%) 429 (93%) |
| Values presented as n (%). *Data not included in study analysis. †Osteoarthritis or rheumatoid arthritis. GERD, gastric esophageal reflux disease. | ||||
Acknowledgement
The authors thank Matt Walsh, PhD, for his assistance in creating the analytical dataset, as well as Sally Steward-Townsend, Susan Wright, Bri Deyo, Bethany Varley, and the rest of the Survey of the Health of Wisconsin staff.
CORRESPONDENCE Jeffrey J. VanWormer, PhD, Epidemiology Research Center, Marshfield Clinic Research Foundation, 1000 North Oak Avenue, Marshfield, WI 54449; vanwormer.jeffrey@mcrf.mfldclin.edu
Purpose Aspirin is recommended for the primary prevention of cardiovascular disease (CVD) in adults at high risk, but little is known about sociodemographic disparities in prophylactic aspirin use. This study examined the association between sociodemographic characteristics and regular aspirin use among adults in Wisconsin who are free of CVD.
Methods A cross-sectional design was used, and data collected from 2008 to 2010. Regular aspirin use (aspirin therapy) was defined as taking aspirin most days of the week. We found 831 individuals for whom complete data were available for regression analyses and stratified the sample into 2 groups: those for whom aspirin therapy was indicated and those for whom it was not indicated, based on national guidelines.
Results Of the 268 patients for whom aspirin therapy was indicated, only 83 (31%) were using it regularly, and 102 (18%) of the 563 participants who did not have an aspirin indication were taking it regularly. In the group with an aspirin indication, participants who were older had higher rates of regular aspirin use than younger patients (odds ratio [OR]=1.07; P<.001), and women had significantly higher adjusted odds of regular aspirin use than men (OR=3.49; P=.021). Among those for whom aspirin therapy was not indicated, the adjusted odds of regular aspirin use were significantly higher among older participants (OR=1.07; P<.001) vs their younger counterparts, and significantly lower among Hispanic or nonwhite participants (OR=0.32; P=.063) relative to non-Hispanic whites.
Conclusions Aspirin therapy is underused by those at high risk for CVD—individuals who could gain cardioprotection from regular use—and overused by those at low risk for CVD, for whom the risk of major bleeding outweighs the potential benefit. Stronger primary care initiatives may be needed to ensure that patients undergo regular screening for aspirin use, particularly middle-aged men at high CVD risk. Patient education may be needed, as well, to better inform people (particularly older, non-Hispanic whites) about the risks of regular aspirin use that is not medically indicated.
Cardiovascular disease (CVD) is the principal cause of death in the United States.1 As the population grows older and obesity and diabetes become increasingly prevalent, the prevalence of CVD is also expected to rise.2,3 Fortunately, many CVD events can be prevented or delayed by modifying risk factors such as hyperlipidemia, hypertension, and smoking. Interventions associated with a reduction in risk have led to a reduction in CVD events4,5 and contributed to a steady decline in cardiac deaths.6
Control of platelet aggregation is a cornerstone of primary CVD prevention.7 In an outpatient setting, this usually translates into identifying patients who are at high risk for a CVD event and advising them to take low-dose aspirin daily or every other day. Although not without controversy,8,9 the US Preventive Services Task Force (USPSTF) recommends regular aspirin use for primary CVD prevention for middle-aged to older men at high risk for myocardial infarction (MI) and women at high risk for ischemic stroke.10
The efficacy of this intervention is proven: In primary prevention trials, regular aspirin use is associated with a 14% reduction in the likelihood of CVD events over 7 years.11 What’s more, aspirin therapy, as recommended by the USPSTF, is among the most cost-effective clinic-based preventive measures.12
In 2004, 41% of US adults age 40 or older reported taking aspirin regularly13 —an increase of approximately 20% since 1999.14 More recent data from a national population-based cohort study found that 41% of adults ages 45 to 90 years who did not have CVD but were at moderate to high risk for a CVD event reported taking aspirin ≥3 days per week.15 In the same study, almost one-fourth of those at low CVD risk also reported regular aspirin use.
While regular aspirin use for primary CVD prevention has been on the rise,13,14 the extent to which this intervention has penetrated various segments of the population is unclear. Several studies have found that aspirin use is consistently highest among those who are older, male, and white.15-17 Other socioeconomic variables (eg, education level, employment, marital status) have received little attention. And no previous study has used national guidelines for aspirin therapy to stratify samples.
A look at overuse and underuse. To ensure that aspirin therapy for primary CVD prevention is directed at those who are most likely to benefit from it, a better understanding of variables associated with both aspirin overuse and underuse is needed. This area of research is important, in part because direct-to-consumer aspirin marketing may be particularly influential among groups at low risk for CVD—for whom the risk of excess bleeding outweighs the potential for disease prevention.13,18
This study was undertaken to examine the association between specific sociodemographic variables and aspirin use among a representative sample of Wisconsin adults without CVD, looking both at those for whom aspirin therapy is indicated and those for whom it is not indicated based on national guidelines.
Methods
Design
We used a cross-sectional design, with data from the Survey of the Health of Wisconsin (SHOW),19 an annual survey of Wisconsin residents ages 21 to 74 years. SHOW uses a 2-stage stratified cluster sampling design to select households, with all age-eligible household members invited to participate. Recruitment for the annual survey consists of general community-wide announcements, as well as an initial letter and up to 6 visits to the randomly selected households to encourage participation.
By the end of 2010, SHOW had 1572 enrollees—about 53% of all eligible invitees. The demographic profile of SHOW enrollees was similar to US census data for all Wisconsin adults during the same time frame.19 All SHOW procedures were approved by the University of Wisconsin Institutional Review Board, and all participants provided informed consent.
Study sample
Our analyses were based on data provided by SHOW participants who were screened and enrolled between 2008 and 2010. To be included in our study, participants had to be between the ages of 35 and 74 years; not pregnant, on active military duty, or institutionalized; and have no personal history of CVD (myocardial infarction, angina, stroke, or transient ischemic attack) or CVD risk equivalent (type 1 or type 2 diabetes) at the time of recruitment. Data on key study variables had to be available, as well. (We used 35 years as the lower age limit because of the very low likelihood of CVD in younger individuals.)
We stratified the analytical sample (N=831) into 2 groups—participants for whom aspirin therapy was indicated and those for whom it was not indicated—in order to examine aspirin’s appropriate (recommended) and inappropriate use.
Measures
Outcome. The outcome variable was aspirin use. SHOW had asked participants how often they took aspirin. Similar to the methods used by Sanchez et al,15 we classified those who reported taking aspirin most (≥4) days of the week as regular aspirin users. All others were classified as nonregular aspirin users. Participants were not asked about the daily dose or weekly volume of aspirin.
Variables
Sociodemographic variables considered in our analysis were age, sex, race/ethnicity, education level, marital/partner status, employment status, health insurance, and region of residence within Wisconsin.
All participants underwent physical examinations, conducted as part of SHOW, at either a permanent or mobile exam center. Blood pressure was measured after a 5-minute rest period in a seated position, and the average of the last 2 out of 3 consecutive measurements was reported. Body mass index (BMI) was calculated, and blood samples were obtained by venipuncture, processed immediately, and sent to the Marshfield Clinic laboratory for measuring total and high-density lipoprotein (HDL) cholesterol.
Indications for aspirin therapy. We stratified the sample by those who were and those who were not candidates for aspirin therapy for primary CVD prevention based on the latest guidelines from the USPSTF ( FIGURE ).10 The Task Force recommends aspirin therapy for men ages 45 to 74 years with a moderate or greater 10-year risk of a coronary heart disease (CHD) event and women ages 55 to 74 years with a moderate or greater 10-year risk of stroke. We used the global CVD risk equation derived from the Framingham Heart Study (based on age, sex, smoking status, systolic blood pressure, and total and HDL cholesterol) to calculate each participant’s 10-year risk and, thus, determine whether aspirin therapy was or was not indicated.20 Total and HDL cholesterol values were missing for 94 participants in the analytical sample; their 10-year CVD risk was estimated using BMI, a reasonable alternative to more conventional CVD risk prediction when laboratory values are unavailable.21
FIGURE
Study (SHOW) sample, stratified based on aspirin indication10
*US Preventive Services Task Force guidelines were slightly modified for this analysis: The upper age bound was reduced from 79 to 74 years because the Survey of the Health of Wisconsin did not enroll participants >74 years.
CHD, coronary heart disease; CVD, cardiovascular disease; DM, diabetes mellitus; N/A, not applicable; SHOW, Survey of the Health of Wisconsin.
Statistical analyses
All analytical procedures were conducted using Statistical Analysis Software (SAS Version 9.2; Cary, NC). A complete-case framework was used.
We used multivariate logistic regression for survey data (PROC SURVEYLOGISTIC; SAS Institute, Cary, NC) to examine the association between aspirin use and sociodemographic variables. Two separate analyses were conducted, one of participants for whom aspirin therapy was indicated and the other for participants for whom it was not. The outcomes were modeled dichotomously, as regular vs nonregular aspirin users, and a collinearity check was done. 21
Initially, we created univariate models to gauge the crude relationship between each variable and aspirin use. Any variable with P<.20 in its univariate association with regular aspirin use was considered for inclusion in the final multivariate regression model. In the multivariate analyses, we sequentially eliminated variables with the weakest association with aspirin use until only significant (P<.10) independent predictors remained. Appropriate weighting was applied based on survey strata and cluster structure.19
Results
Of the 831 participants who met the eligibility criteria for our analysis, 268 (32%) had an aspirin indication. TABLE 1 shows the key characteristics of the analytical sample, stratified by those for whom aspirin was indicated and those for whom it was not. The sample was primarily middle-aged (mean age 52.4±0.36) and non-Hispanic white (93%). Compared with those for whom aspirin therapy was not indicated, the group with an aspirin indication was significantly older (56.9 vs 50.3) and had a significantly higher proportion of males (97% vs 19%). As expected, those for whom aspirin was indicated were also at higher risk for CHD and stroke, most notably as a result of significantly higher systolic BP (131.9 vs 121.5 mm Hg) and lower HDL cholesterol (42.5 vs 52.6 mg/dL) compared with participants without an aspirin indication.
TABLE 1
Study sample, by sociodemographic variable and aspirin indication
| Variable | Full sample (N=831) | Aspirin indicated (n=268) | Aspirin not indicated (n=563) |
|---|---|---|---|
| Mean age, y | 52.4 | 56.9 | 50.3 |
| Sex, n Male Female | 367 464 | 259 9 | 108 455 |
| Race/ethnicity, n White, non-Hispanic Nonwhite/Hispanic | 776 55 | 252 16 | 524 39 |
| Marital status, n Married/partnered Not married or partnered | 637 194 | 215 53 | 422 141 |
| Health insurance, n Uninsured Insured | 76 755 | 26 242 | 50 513 |
| Education, n ≤High school Associate’s degree ≥Bachelor’s degree | 217 312 302 | 77 107 84 | 140 205 218 |
| Employment, n Unemployed Student/retiree/home Employed | 98 147 586 | 33 52 183 | 65 95 403 |
When aspirin was indicated, use was linked to age and sex
In the group with an aspirin indication (n=268), 83 (31%) reported taking aspirin most days of the week. The initial examination of sociodemographic variables showed that age, sex, and employment status demonstrated significant univariate associations with regular aspirin use ( TABLE 2 ). In the multivariate model, however, the odds of regular aspirin use were significantly greater among participants who were older (odds ratio [OR], 1.07; P<.001) or female (OR, 3.49; P=.021) compared with participants who were younger or male, respectively.
TABLE 2
Participants who have an aspirin indication: Association between sociodemographic variables and regular aspirin use
| Variable | Regular aspirin use, OR (95% CI) | P value* |
|---|---|---|
| Age Older vs younger | 1.07 (1.04-1.11) | .001 |
| Sex Female vs male | 3.89 (1.42-10.67)† | .008 |
| Race/ethnicity Nonwhite/Hispanic vs white non-Hispanic | 0.55 (0.09-3.47) | .526 |
| Marital status Not married/partnered vs married/partner | 0.83 (0.36-1.95) | .678 |
| Health insurance Uninsured vs insured | 0.86 (0.50-1.47) | .579 |
| Education ≥Bachelor’s degree vs ≤high school Associate’s degree/some college vs ≤high school | 1.58 (0.75-3.34) 1.36 (0.74-2.49) | .234 .325 |
| Employment Student or retired vs employed Unemployed vs employed | 2.96 (1.74-5.03) 0.62 (0.25-1.56) | .001 .314 |
| *Significance was defined as P<.10. †Multivariate adjusted model: 3.49 (95% CI, 1.21-10.07; P=.021). CI, confidence interval; OR, odds ratio. | ||
When aspirin was not indicated, age and sex still affected use
Among the 563 participants for whom aspirin therapy was not indicated, 102 (18%) reported taking aspirin regularly. Age, sex, race/ethnicity, health insurance, and employment ( TABLE 3 ), as well as region of residence and study enrollment year, had significant univariate associations with regular aspirin use; these variables were tested for potential inclusion in the multivariate model. In the final multivariate regression model, the odds of regular aspirin use were significantly greater among participants who were older (OR, 1.07; P<.001) and significantly lower among participants who were Hispanic or nonwhite (OR, 0.32; P=.063).
TABLE 3
Participants who do not have an aspirin indication: Association between sociodemographic variables and regular aspirin use
| Variable | Regular aspirin use, OR (95% CI) | P value* |
|---|---|---|
| Age Older vs younger | 1.07 (1.04-1.10) | .001 |
| Sex Female vs male | 1.60 (0.84-3.04) | .152 |
| Race/ethnicity Nonwhite or Hispanic vs white non-Hispanic | 0.23 (0.07- 0.73)† | .013 |
| Marital status Not married/partnered vs married/partnered | 1.00 (0.63-1.59) | .992 |
| Health insurance Uninsured vs insured | 0.36 (0.11- 1.15) | .086 |
| Education Bachelor’s or higher vs high school or less Associate’s/some college vs high school or less | 0.74 (0.35-1.57) 0.67 (0.38-1.17) | .431 .158 |
| Employment Student/retired vs employed Unemployed vs employed | 2.35 (1.32-4.20) 0.78 (0.26- 2.34) | .004 .652 |
| *Significance was defined as P<.10. †Multivariate adjusted model: 0.32 (95% CI, 0.10-1.06; P=.063). CI, confidence interval; OR, odds ratio. | ||
Discussion
Aspirin was generally underutilized in the group with significant CVD risk (n=268) in our study, with slightly less than a third of participants for whom aspirin therapy was indicated taking it most days of the week. Despite trends of increased aspirin use among US adults in recent years,15 aspirin therapy in the 2008-2010 SHOW sample was lower than in 2005 to 2008. It was also lower than national estimates of aspirin use for primary CVD prevention15,22 —but about 20% higher than estimates of overall aspirin use in Wisconsin 20 years ago.23 Consistent with previous research, the final adjusted model and sensitivity analysis indicated that older individuals were more likely to take aspirin regularly.
Contrary to the findings in some previous studies,15-17 however, our analysis suggested that women had a higher adjusted odds of regular aspirin use compared with men. This result should be interpreted with extreme caution, however, because so few females (9 of 464 [3%]) met the current USPSTF criteria for aspirin therapy for primary CVD prevention. The previous USPSTF guidelines24,25 were less conservative, with a lower minimum age and threshold for CVD risk for women. The revision is the likely result of recent primary prevention trials10 that found regular aspirin use provided less cardioprotection for younger women.
The sample without an aspirin indication—roughly twice the size of the group with an aspirin indication (563 vs 268), which is reflective of the general population of Wisconsin—was useful in highlighting inappropriate use. There were clear indications of aspirin overuse in this group, with 18% of the sample reporting that they took aspirin regularly. The finding that inappropriate aspirin use was more likely in non-Hispanic whites vs minorities is similar to the result of an earlier study in which blacks, Hispanics, and Chinese Americans with low CVD risk were much less likely to report regular aspirin use compared with whites at low risk.15
The main concern with regular aspirin use in those for whom it is not indicated for primary CVD prevention is the risk of upper gastrointestinal bleeding and, less commonly, hemorrhagic stroke.26 To illustrate this point, consider the following: About 10% of SHOW participants ages 35 to 74 years had no history of CVD and no indication for aspirin therapy based on the latest USPSTF guidelines, but took aspirin regularly nonetheless. Extrapolating those numbers to the entire state of Wisconsin would suggest that approximately 270,000 state residents have a similar profile. Assuming an extra 1.3 major bleeding events per 1000 person-years of regular aspirin use (as a meta-analysis of studies of adverse events associated with antiplatelet therapy found),27 that would translate into an estimated 350 major bleeding events per year in Wisconsin that are attributable to aspirin overuse.
In view of the current USPSTF recommendations,10 aspirin is not optimally utilized by Wisconsin residents for the primary prevention of CVD. Aspirin therapy is not used enough by those with a high CVD risk, who could derive substantial vascular disease protection from it. Conversely, aspirin therapy is overused by those with a low CVD risk, for whom the risk of major bleeding is significantly higher than the potential for vascular disease protection. Furthermore, younger individuals at high CVD risk appear to be least likely to take aspirin regularly.
Recommendations
The strongest modifiable predictor of regular aspirin use is a recommendation from a clinician.13 Therefore, we recommend stronger primary care initiatives to ensure that patients are screened for aspirin use more frequently, particularly middle-aged men at high CVD risk. This clinic-based initiative could reach a larger proportion of the general population when combined with broader, community-oriented CVD preventive services.28
More precise marketing and education are also needed. Because aspirin is a low-cost over-the-counter product that leads the consumer market for analgesics,29 the general public (and older, non-Hispanic whites, in particular) needs to be better informed about the risks of medically inappropriate aspirin use for primary CVD prevention.
Study limitations
Selection and measurement biases were among the chief study limitations.
Study (SHOW) enrollment rate was slightly above 50%, with steady increases in enrollment each year (from 46% in 2008-2009 to 56% in 2010) due to expanded recruitment and consolidation of field operations.
Aspirin use was self-reported, and SHOW did not capture the reason for taking it (eg, CVD prevention or pain management). Some evidence of overreporting of aspirin use among older individuals exists,30 suggesting that a more objective measure of aspirin use (eg, pill bottle verification or blood platelet aggregation test) could yield different results.
Certain confounders were not measured, most notably contraindications to aspirin (eg, genetic platelet abnormalities). Such findings could explain some patterns of aspirin use in both strata, as up to 10% of any given population has a contraindication to aspirin due to allergy, intolerance, gastrointestinal ulcer, concomitant anticoagulant medication, or other high bleeding risk.18,31 Few of these variables were known about our sample.
TABLE 4W (available below) provides a breakdown of some possible aspirin contraindications, as well as possible reasons other than primary CVD prevention for regular aspirin use. Because clinical judgment is often required to assess the degree of severity of a given health condition in order to deem it an aspirin contraindication, these findings could not reliably be used to reclassify participants. We present them simply for hypothesis generation.
Some data collection predates the current USPSTF guidelines,10 which could have resulted in a misclassification of participants’ aspirin indication. However, sensitivity analyses restricted to the 2010 sample alone—the only one with data collection after the newer guidelines were released—did not reveal any meaningful differences.
Other methodological limitations include the less racially diverse population of Wisconsin compared with other parts of the country and the sample size, which did not permit testing for statistical interactions and perhaps resulted in larger confidence intervals for some associations (eg, race/ethnicity) relative to the population as a whole.
TABLE 4W
Possible reasons for aspirin use—or contraindication— by aspirin indication*
| Has a doctor or other health professional ever told you that you had … | Aspirin indicated (n=268) | Aspirin not indicated (n=563) | ||
|---|---|---|---|---|
| Regular aspirin user (n=83) | Nonregular aspirin user (n=185) | Regular aspirin user (n=102) | Nonregular aspirin user (n=461) | |
| Migraine headache Yes No | 20 (24%) 63 (76%) | 28 (15%) 157 (85%) | 24 (24%) 78 (76%) | 76 (16%) 385 (84%) |
| Arthritis† Yes No | 2 (2%) 81 (98%) | 1 (1%) 184 (99%) | 12 (12%) 90 (88%) | 26 (6%) 435 (94%) |
| Stomach or intestinal ulcer Yes No | 5 (6%) 78 (94%) | 6 (3%) 179 (97%) | 7 (7%) 95 (93%) | 10 (2%) 451 (98%) |
| Reflux or GERD Yes No | 8 (10%) 75 (90%) | 14 (8%) 171 (92%) | 11 (11%) 91 (89%) | 32 (7%) 429 (93%) |
| Values presented as n (%). *Data not included in study analysis. †Osteoarthritis or rheumatoid arthritis. GERD, gastric esophageal reflux disease. | ||||
Acknowledgement
The authors thank Matt Walsh, PhD, for his assistance in creating the analytical dataset, as well as Sally Steward-Townsend, Susan Wright, Bri Deyo, Bethany Varley, and the rest of the Survey of the Health of Wisconsin staff.
CORRESPONDENCE Jeffrey J. VanWormer, PhD, Epidemiology Research Center, Marshfield Clinic Research Foundation, 1000 North Oak Avenue, Marshfield, WI 54449; vanwormer.jeffrey@mcrf.mfldclin.edu
1. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18-e209.
2. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-944.
3. Sullivan PW, Ghushchyan V, Wyatt HR. The medical cost of cardiometabolic risk factor clusters in the United States. Obesity. 2007;15:3150-3158.
4. Pearson TA, Blair SN, Daniels SR, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388-391.
5. Kriekard P, Gharacholou SM, Peterson ED. Primary and secondary prevention of cardiovascular disease in older adults: a status report. Clin Geriatr Med. 2009;25:745-755.
6. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388-2398.
7. Hennekens CH, Schneider WR. The need for wider and appropriate utilization of aspirin and statins in the treatment and prevention of cardiovascular disease. Expert Rev Cardiovasc Ther. 2008;6:95-107.
8. Barnett H, Burrill P, Iheanacho I. Don’t use aspirin for primary prevention of cardiovascular disease. BMJ. 2010;340:c1805.-
9. Sanchez-Ross M, Waller AH, Maher J, et al. Aspirin for the prevention of cardiovascular morbidity. Minerva Med. 2010;101:205-214.
10. S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US preventive services task force recommendation statement. Ann Intern Med. 2009;150:396-404.
11. Bartolucci AA, Tendera M, Howard G. Meta-analysis of multiple primary prevention trials of cardiovascular events using aspirin. Am J Cardiol. 2011;107:1796-1801.
12. Maciosek MV, Coffield AB, Edwards NM, et al. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52-61.
13. Pignone M, Anderson GK, Binns K, et al. Aspirin use among adults aged 40 and older in the United States results of a national survey. Am J Prev Med. 2007;32:403-407.
14. Ajani UA, Ford ES, Greenland KJ, et al. Aspirin use among US adults: behavioral risk factor surveillance system. Am J Prev Med. 2006;30:74-77.
15. Sanchez DR, Diez Roux AV, Michos ED, et al. Comparison of the racial/ethnic prevalence of regular aspirin use for the primary prevention of coronary heart disease from the multi-ethnic study of atherosclerosis. Am J Cardiol. 2011;107:41-46.
16. Stafford RS, Monti V, Ma J. Underutilization of aspirin persists in US ambulatory care for the secondary and primary prevention of cardiovascular disease. PLoS Med. 2005;2:e353.-
17. Rodondi N, Vittinghoff E, Cornuz J, et al. Aspirin use for the primary prevention of coronary heart disease in older adults. Am J Med. 2005;118(suppl):1288e1-1288e9.
18. Rodondi N, Cornuz J, Marques-Vidal P, et al. Aspirin use for the primary prevention of coronary heart disease: a population-based study in Switzerland. Prev Med. 2008;46:137-144.
19. Nieto FJ, Peppard PE, Engelman CD, et al. The Survey of the Health of Wisconsin (SHOW), a novel infrastructure for population health research: rationale and methods. BMC Public Health. 2010;10:785.-
20. D’Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743-753.
21. Cody RP, Smith JK. Applied Statistics and the SAS Programming Language. New York, NY: Prentice Hall; 2005.
22. Mallonee S, Daniels CG, Mold JW, et al. Increasing aspirin use among persons at risk for cardiovascular events in Oklahoma. J Okla State Med Assoc. 2010;103:254-260.
23. Centers for Disease Control and Prevention (CDC). Prevalence of aspirin use to prevent heart disease—Wisconsin, 1991, and Michigan, 1994. MMWR Morb Mortal Wkly Rep. 1997;46:498-502.
24. US Preventive Services Task Force. Aspirin for the primary prevention of cardiovascular events: recommendation and rationale. Ann Intern Med. 2002;136:157-160.
25. Werner M, Kelsberg G, Weismantel AM. Which healthy adults should take aspirin? J Fam Pract. 2004;53:146-150.
26. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
27. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006;119:624-638.
28. VanWormer JJ, Johnson PJ, Pereira RF, et al. The Heart of New Ulm project: using community-based cardiometabolic risk factor screenings in a rural population health improvement initiative. Popul Health Manag. 2012;15:135-143.
29. Jeffreys D. Aspirin: The Remarkable Story of a Wonder Drug. New York, NY: Bloomsbury Publishing; 2005.
30. Smith NL, Psaty BM, Heckbert SR, et al. The reliability of medication inventory methods compared to serum levels of cardiovascular drugs in the elderly. J Clin Epidemiol. 1999;52:143-146.
31. Hedman J, Kaprio J, Poussa T, et al. Prevalence of asthma, aspirin intolerance, nasal polyposis and chronic obstructive pulmonary disease in a population-based study. Int J Epidemiol. 1999;28:717-722.
1. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18-e209.
2. Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933-944.
3. Sullivan PW, Ghushchyan V, Wyatt HR. The medical cost of cardiometabolic risk factor clusters in the United States. Obesity. 2007;15:3150-3158.
4. Pearson TA, Blair SN, Daniels SR, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update. American Heart Association Science Advisory and Coordinating Committee. Circulation. 2002;106:388-391.
5. Kriekard P, Gharacholou SM, Peterson ED. Primary and secondary prevention of cardiovascular disease in older adults: a status report. Clin Geriatr Med. 2009;25:745-755.
6. Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388-2398.
7. Hennekens CH, Schneider WR. The need for wider and appropriate utilization of aspirin and statins in the treatment and prevention of cardiovascular disease. Expert Rev Cardiovasc Ther. 2008;6:95-107.
8. Barnett H, Burrill P, Iheanacho I. Don’t use aspirin for primary prevention of cardiovascular disease. BMJ. 2010;340:c1805.-
9. Sanchez-Ross M, Waller AH, Maher J, et al. Aspirin for the prevention of cardiovascular morbidity. Minerva Med. 2010;101:205-214.
10. S. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US preventive services task force recommendation statement. Ann Intern Med. 2009;150:396-404.
11. Bartolucci AA, Tendera M, Howard G. Meta-analysis of multiple primary prevention trials of cardiovascular events using aspirin. Am J Cardiol. 2011;107:1796-1801.
12. Maciosek MV, Coffield AB, Edwards NM, et al. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31:52-61.
13. Pignone M, Anderson GK, Binns K, et al. Aspirin use among adults aged 40 and older in the United States results of a national survey. Am J Prev Med. 2007;32:403-407.
14. Ajani UA, Ford ES, Greenland KJ, et al. Aspirin use among US adults: behavioral risk factor surveillance system. Am J Prev Med. 2006;30:74-77.
15. Sanchez DR, Diez Roux AV, Michos ED, et al. Comparison of the racial/ethnic prevalence of regular aspirin use for the primary prevention of coronary heart disease from the multi-ethnic study of atherosclerosis. Am J Cardiol. 2011;107:41-46.
16. Stafford RS, Monti V, Ma J. Underutilization of aspirin persists in US ambulatory care for the secondary and primary prevention of cardiovascular disease. PLoS Med. 2005;2:e353.-
17. Rodondi N, Vittinghoff E, Cornuz J, et al. Aspirin use for the primary prevention of coronary heart disease in older adults. Am J Med. 2005;118(suppl):1288e1-1288e9.
18. Rodondi N, Cornuz J, Marques-Vidal P, et al. Aspirin use for the primary prevention of coronary heart disease: a population-based study in Switzerland. Prev Med. 2008;46:137-144.
19. Nieto FJ, Peppard PE, Engelman CD, et al. The Survey of the Health of Wisconsin (SHOW), a novel infrastructure for population health research: rationale and methods. BMC Public Health. 2010;10:785.-
20. D’Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743-753.
21. Cody RP, Smith JK. Applied Statistics and the SAS Programming Language. New York, NY: Prentice Hall; 2005.
22. Mallonee S, Daniels CG, Mold JW, et al. Increasing aspirin use among persons at risk for cardiovascular events in Oklahoma. J Okla State Med Assoc. 2010;103:254-260.
23. Centers for Disease Control and Prevention (CDC). Prevalence of aspirin use to prevent heart disease—Wisconsin, 1991, and Michigan, 1994. MMWR Morb Mortal Wkly Rep. 1997;46:498-502.
24. US Preventive Services Task Force. Aspirin for the primary prevention of cardiovascular events: recommendation and rationale. Ann Intern Med. 2002;136:157-160.
25. Werner M, Kelsberg G, Weismantel AM. Which healthy adults should take aspirin? J Fam Pract. 2004;53:146-150.
26. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary prevention of cardiovascular events in women and men: a sex-specific meta-analysis of randomized controlled trials. JAMA. 2006;295:306-313.
27. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006;119:624-638.
28. VanWormer JJ, Johnson PJ, Pereira RF, et al. The Heart of New Ulm project: using community-based cardiometabolic risk factor screenings in a rural population health improvement initiative. Popul Health Manag. 2012;15:135-143.
29. Jeffreys D. Aspirin: The Remarkable Story of a Wonder Drug. New York, NY: Bloomsbury Publishing; 2005.
30. Smith NL, Psaty BM, Heckbert SR, et al. The reliability of medication inventory methods compared to serum levels of cardiovascular drugs in the elderly. J Clin Epidemiol. 1999;52:143-146.
31. Hedman J, Kaprio J, Poussa T, et al. Prevalence of asthma, aspirin intolerance, nasal polyposis and chronic obstructive pulmonary disease in a population-based study. Int J Epidemiol. 1999;28:717-722.
Access to specialized treatment by adult Hispanic brain tumor patients: findings from a single-institution retrospective study
Background: The Hispanic population accounts for 15% of the population of the United States, and for as much as 75% in cities throughout California. Racial disparities that are reflected by limited access to health care and worse disease outcomes are well documented for adult Hispanic cancer patients.
Objective: To determine whether there are similar disparities—including delays in accessing surgery, radiation, and oncologic care—for adult Hispanic non English-speaking (HNES) neuro-oncology patients and white English-only–speaking (WES) patients in an academic, tertiary care center with a multidisciplinary neuro-oncology team.
Methods: This retrospective study was conducted at the Chao Family Comprehensive Cancer Center of the University of California, Irvine. All patients who were diagnosed with a primary brain tumor during January 1, 2003, to December 31, 2008, were identified and data were collected on their age, sex, ethnicity, languages spoken, diagnosis, and insurance status. The times from the date of diagnosis to the date of surgery, from the date of surgery to the date of starting radiation (if indicated), and from the date of finishing radiation to the date of starting chemotherapy (if indicated) were also recorded.
Results: Most of the HNES patients (56.4%) had state insurance for the indigent, whereas most of the WES patients (41.8%) had private insurance from a health maintenance organization. Moreover, 12.8% of HNES patients were uninsured, compared with 4.5% of WES patients. There were no significant delays in the time from diagnosis to surgery, but there was a significant delay in access to radiation treatment (P .023). There were no differences on overall survival between the 2 groups of patients.
Limitations: This is a retrospective study of a relatively small number of patients. Larger studies are needed to corroborate these findings
Conclusions: The findings demonstrate that there are disparities in insurance status and access to radiation therapy between HNES and WES neuro-oncology patients.
*To read the the full article, click on the link at the top of this introduction.
Background: The Hispanic population accounts for 15% of the population of the United States, and for as much as 75% in cities throughout California. Racial disparities that are reflected by limited access to health care and worse disease outcomes are well documented for adult Hispanic cancer patients.
Objective: To determine whether there are similar disparities—including delays in accessing surgery, radiation, and oncologic care—for adult Hispanic non English-speaking (HNES) neuro-oncology patients and white English-only–speaking (WES) patients in an academic, tertiary care center with a multidisciplinary neuro-oncology team.
Methods: This retrospective study was conducted at the Chao Family Comprehensive Cancer Center of the University of California, Irvine. All patients who were diagnosed with a primary brain tumor during January 1, 2003, to December 31, 2008, were identified and data were collected on their age, sex, ethnicity, languages spoken, diagnosis, and insurance status. The times from the date of diagnosis to the date of surgery, from the date of surgery to the date of starting radiation (if indicated), and from the date of finishing radiation to the date of starting chemotherapy (if indicated) were also recorded.
Results: Most of the HNES patients (56.4%) had state insurance for the indigent, whereas most of the WES patients (41.8%) had private insurance from a health maintenance organization. Moreover, 12.8% of HNES patients were uninsured, compared with 4.5% of WES patients. There were no significant delays in the time from diagnosis to surgery, but there was a significant delay in access to radiation treatment (P .023). There were no differences on overall survival between the 2 groups of patients.
Limitations: This is a retrospective study of a relatively small number of patients. Larger studies are needed to corroborate these findings
Conclusions: The findings demonstrate that there are disparities in insurance status and access to radiation therapy between HNES and WES neuro-oncology patients.
*To read the the full article, click on the link at the top of this introduction.
Background: The Hispanic population accounts for 15% of the population of the United States, and for as much as 75% in cities throughout California. Racial disparities that are reflected by limited access to health care and worse disease outcomes are well documented for adult Hispanic cancer patients.
Objective: To determine whether there are similar disparities—including delays in accessing surgery, radiation, and oncologic care—for adult Hispanic non English-speaking (HNES) neuro-oncology patients and white English-only–speaking (WES) patients in an academic, tertiary care center with a multidisciplinary neuro-oncology team.
Methods: This retrospective study was conducted at the Chao Family Comprehensive Cancer Center of the University of California, Irvine. All patients who were diagnosed with a primary brain tumor during January 1, 2003, to December 31, 2008, were identified and data were collected on their age, sex, ethnicity, languages spoken, diagnosis, and insurance status. The times from the date of diagnosis to the date of surgery, from the date of surgery to the date of starting radiation (if indicated), and from the date of finishing radiation to the date of starting chemotherapy (if indicated) were also recorded.
Results: Most of the HNES patients (56.4%) had state insurance for the indigent, whereas most of the WES patients (41.8%) had private insurance from a health maintenance organization. Moreover, 12.8% of HNES patients were uninsured, compared with 4.5% of WES patients. There were no significant delays in the time from diagnosis to surgery, but there was a significant delay in access to radiation treatment (P .023). There were no differences on overall survival between the 2 groups of patients.
Limitations: This is a retrospective study of a relatively small number of patients. Larger studies are needed to corroborate these findings
Conclusions: The findings demonstrate that there are disparities in insurance status and access to radiation therapy between HNES and WES neuro-oncology patients.
*To read the the full article, click on the link at the top of this introduction.
Intravenous iron in chemotherapy and cancer-related anemia
Recent guidance from the Centers for Medicare and Medicaid Services restricting erythropoiesis-stimulating agents (ESAs) in chemotherapy and cancer-related anemias has resulted in an increase in transfusions. Nine studies, without published contradictory evidence, have shown optimization of the response to ESAs by intravenous (IV) iron when the iron was added to the treatment of chemotherapy-induced anemia. The synergy observed, although greater in iron deficiency, was independent of pretreatment iron parameters. Three studies demonstrated decreased transfusions when IV iron is administered without ESAs. Discordant recommendations regarding IV iron currently exist among the American Society of Hematology/American Society of Clinical Oncology guidelines, the National Comprehensive Cancer Network, and the European Society of Medical Oncology. This discordance is at least partly the result of misconceptions about the clinical nature and incidence of adverse effects with IV iron. Other reasons for this discordance are presented in this review. Based on thousands of studied patients, we conclude that IV iron is safe and probably safer than most physicians realize. Education is needed relating to the interpretation of minor, subclinical infusion reactions that resolve without therapy. IV iron without ESAs may be an effective treatment for chemotherapy-induced anemia and warrants further study. We present evidence supporting the conclusion that baseline serum hepcidin levels may predict responses to IV iron, and we examine the published evidence supporting the conclusion that IV iron should be a standard addition to the management of chemotherapy and cancer-related anemia.
Click on the PDF icon at the top of this introduction to read the full article.
Recent guidance from the Centers for Medicare and Medicaid Services restricting erythropoiesis-stimulating agents (ESAs) in chemotherapy and cancer-related anemias has resulted in an increase in transfusions. Nine studies, without published contradictory evidence, have shown optimization of the response to ESAs by intravenous (IV) iron when the iron was added to the treatment of chemotherapy-induced anemia. The synergy observed, although greater in iron deficiency, was independent of pretreatment iron parameters. Three studies demonstrated decreased transfusions when IV iron is administered without ESAs. Discordant recommendations regarding IV iron currently exist among the American Society of Hematology/American Society of Clinical Oncology guidelines, the National Comprehensive Cancer Network, and the European Society of Medical Oncology. This discordance is at least partly the result of misconceptions about the clinical nature and incidence of adverse effects with IV iron. Other reasons for this discordance are presented in this review. Based on thousands of studied patients, we conclude that IV iron is safe and probably safer than most physicians realize. Education is needed relating to the interpretation of minor, subclinical infusion reactions that resolve without therapy. IV iron without ESAs may be an effective treatment for chemotherapy-induced anemia and warrants further study. We present evidence supporting the conclusion that baseline serum hepcidin levels may predict responses to IV iron, and we examine the published evidence supporting the conclusion that IV iron should be a standard addition to the management of chemotherapy and cancer-related anemia.
Click on the PDF icon at the top of this introduction to read the full article.
Recent guidance from the Centers for Medicare and Medicaid Services restricting erythropoiesis-stimulating agents (ESAs) in chemotherapy and cancer-related anemias has resulted in an increase in transfusions. Nine studies, without published contradictory evidence, have shown optimization of the response to ESAs by intravenous (IV) iron when the iron was added to the treatment of chemotherapy-induced anemia. The synergy observed, although greater in iron deficiency, was independent of pretreatment iron parameters. Three studies demonstrated decreased transfusions when IV iron is administered without ESAs. Discordant recommendations regarding IV iron currently exist among the American Society of Hematology/American Society of Clinical Oncology guidelines, the National Comprehensive Cancer Network, and the European Society of Medical Oncology. This discordance is at least partly the result of misconceptions about the clinical nature and incidence of adverse effects with IV iron. Other reasons for this discordance are presented in this review. Based on thousands of studied patients, we conclude that IV iron is safe and probably safer than most physicians realize. Education is needed relating to the interpretation of minor, subclinical infusion reactions that resolve without therapy. IV iron without ESAs may be an effective treatment for chemotherapy-induced anemia and warrants further study. We present evidence supporting the conclusion that baseline serum hepcidin levels may predict responses to IV iron, and we examine the published evidence supporting the conclusion that IV iron should be a standard addition to the management of chemotherapy and cancer-related anemia.
Click on the PDF icon at the top of this introduction to read the full article.
Warn Parents to Beware of Button Batteries
Counsel parents in your practice that young children can be seriously injured or die from playing with or ingesting button batteries.
Injuries from these coin-sized batteries are on the rise, with 2.5 times as many children under age 13 showing up at an emergency department in 2010 compared with 1998, according to a study in the Aug. 31 issue of Morbidity and Mortality Weekly Report (2012:61:661-6). This increase from 1,900 cases in 1998 to 4,800 in 2010 aligns with the growing popularity of these batteries in remote controls, toys, light-up jewelry, and other devices.
"As the use of these batteries expands, so do the estimated number of ED-treated battery exposures in children, with the vast majority of these involving ingestions," Jacqueline Ferrante, Ph.D., of the U.S. Consumer Product Safety Commission (CPSC) Division of Health Sciences, and her colleagues stated in the report.
Injuries from batteries placed in a child’s nose or acid burns from ruptured batteries also are included in the report.
"Ensure that parents are aware of the problem so that batteries are kept away from young children," Dr. Ferrante said in an interview. Advise them to check remote controls and other electronic devices for easily accessible battery compartments, especially those that can be opened without a screwdriver, she advised.
An estimated 40,400 children younger than 13 years were treated at U.S. emergency departments for battery-related injuries between 1997 and 2010.
Additional CPSC databases covering 1995-2010 were searched for battery-related deaths in children under age 13. Of the 14 reported deaths, 12 children had confirmed exposure to button cell batteries. All children who died were aged 4 years and younger.
Diagnosis can be a challenge. Not all children can or are willing to report swallowing a battery or giving one to a sibling, the authors noted. In addition, the typical vomiting, abdominal pain, fever, diarrhea, respiratory distress, and dysphagia associated with battery ingestion are nonspecific symptoms (Pediatr. Emerg. Care 2008;24:313-6).
"Consider battery ingestion in the differential diagnosis of any child presenting with nonspecific GI symptoms or unexplained respiratory distress because of the serious consequences associated with a delayed or missed diagnosis," Dr. Ferrante said.
Complicating matters is the timing of injury, which can vary from 2 hours after ingestion for serious esophageal burns to more than 2 weeks for fatal hemorrhage following endoscopic removal of a button battery. The growing recognition of these injuries drove pediatric gastroenterologists at the University of Colorado Denver to develop guidelines for the management of button battery–induced hemorrhage (J. Pediatr. Gastroenterol. Nutr. 2011;52:585-9).
Nickle-sized, 3-V lithium button batteries can easily lodge in a child’s esophagus, and were most frequently associated with serious complications and death, according to the report.
Although outside the scope of the report, Dr. Ferrante also suggested pediatricians warn parents about ingestion of strong powerful magnets. This is another often-overlooked injury with similar issues and consequences, she said. "There are even cases where injury resulted from co-ingestion of a button battery and a strong magnet."
For the current study, Dr. Ferrante and her colleagues analyzed the National Electronic Injury Surveillance System (NEISS) database to quantify nonfatal, battery-related ED visits. They assessed other CPSC data to identify the battery-related deaths.
The NEISS data only comprise emergency department visits, so any child treated for battery ingestion in a doctor’s office or as an outpatient is not included in the study, a potential limitation. In addition, the number of fatal incidents involving batteries and children younger than 13 years is likely underrepresented because of the type of data collected, the authors noted.
The authors had no relevant financial disclosures. Click here for more information on battery hazards provided by the U.S. Consumer Product Safety Commission.
Counsel parents in your practice that young children can be seriously injured or die from playing with or ingesting button batteries.
Injuries from these coin-sized batteries are on the rise, with 2.5 times as many children under age 13 showing up at an emergency department in 2010 compared with 1998, according to a study in the Aug. 31 issue of Morbidity and Mortality Weekly Report (2012:61:661-6). This increase from 1,900 cases in 1998 to 4,800 in 2010 aligns with the growing popularity of these batteries in remote controls, toys, light-up jewelry, and other devices.
"As the use of these batteries expands, so do the estimated number of ED-treated battery exposures in children, with the vast majority of these involving ingestions," Jacqueline Ferrante, Ph.D., of the U.S. Consumer Product Safety Commission (CPSC) Division of Health Sciences, and her colleagues stated in the report.
Injuries from batteries placed in a child’s nose or acid burns from ruptured batteries also are included in the report.
"Ensure that parents are aware of the problem so that batteries are kept away from young children," Dr. Ferrante said in an interview. Advise them to check remote controls and other electronic devices for easily accessible battery compartments, especially those that can be opened without a screwdriver, she advised.
An estimated 40,400 children younger than 13 years were treated at U.S. emergency departments for battery-related injuries between 1997 and 2010.
Additional CPSC databases covering 1995-2010 were searched for battery-related deaths in children under age 13. Of the 14 reported deaths, 12 children had confirmed exposure to button cell batteries. All children who died were aged 4 years and younger.
Diagnosis can be a challenge. Not all children can or are willing to report swallowing a battery or giving one to a sibling, the authors noted. In addition, the typical vomiting, abdominal pain, fever, diarrhea, respiratory distress, and dysphagia associated with battery ingestion are nonspecific symptoms (Pediatr. Emerg. Care 2008;24:313-6).
"Consider battery ingestion in the differential diagnosis of any child presenting with nonspecific GI symptoms or unexplained respiratory distress because of the serious consequences associated with a delayed or missed diagnosis," Dr. Ferrante said.
Complicating matters is the timing of injury, which can vary from 2 hours after ingestion for serious esophageal burns to more than 2 weeks for fatal hemorrhage following endoscopic removal of a button battery. The growing recognition of these injuries drove pediatric gastroenterologists at the University of Colorado Denver to develop guidelines for the management of button battery–induced hemorrhage (J. Pediatr. Gastroenterol. Nutr. 2011;52:585-9).
Nickle-sized, 3-V lithium button batteries can easily lodge in a child’s esophagus, and were most frequently associated with serious complications and death, according to the report.
Although outside the scope of the report, Dr. Ferrante also suggested pediatricians warn parents about ingestion of strong powerful magnets. This is another often-overlooked injury with similar issues and consequences, she said. "There are even cases where injury resulted from co-ingestion of a button battery and a strong magnet."
For the current study, Dr. Ferrante and her colleagues analyzed the National Electronic Injury Surveillance System (NEISS) database to quantify nonfatal, battery-related ED visits. They assessed other CPSC data to identify the battery-related deaths.
The NEISS data only comprise emergency department visits, so any child treated for battery ingestion in a doctor’s office or as an outpatient is not included in the study, a potential limitation. In addition, the number of fatal incidents involving batteries and children younger than 13 years is likely underrepresented because of the type of data collected, the authors noted.
The authors had no relevant financial disclosures. Click here for more information on battery hazards provided by the U.S. Consumer Product Safety Commission.
Counsel parents in your practice that young children can be seriously injured or die from playing with or ingesting button batteries.
Injuries from these coin-sized batteries are on the rise, with 2.5 times as many children under age 13 showing up at an emergency department in 2010 compared with 1998, according to a study in the Aug. 31 issue of Morbidity and Mortality Weekly Report (2012:61:661-6). This increase from 1,900 cases in 1998 to 4,800 in 2010 aligns with the growing popularity of these batteries in remote controls, toys, light-up jewelry, and other devices.
"As the use of these batteries expands, so do the estimated number of ED-treated battery exposures in children, with the vast majority of these involving ingestions," Jacqueline Ferrante, Ph.D., of the U.S. Consumer Product Safety Commission (CPSC) Division of Health Sciences, and her colleagues stated in the report.
Injuries from batteries placed in a child’s nose or acid burns from ruptured batteries also are included in the report.
"Ensure that parents are aware of the problem so that batteries are kept away from young children," Dr. Ferrante said in an interview. Advise them to check remote controls and other electronic devices for easily accessible battery compartments, especially those that can be opened without a screwdriver, she advised.
An estimated 40,400 children younger than 13 years were treated at U.S. emergency departments for battery-related injuries between 1997 and 2010.
Additional CPSC databases covering 1995-2010 were searched for battery-related deaths in children under age 13. Of the 14 reported deaths, 12 children had confirmed exposure to button cell batteries. All children who died were aged 4 years and younger.
Diagnosis can be a challenge. Not all children can or are willing to report swallowing a battery or giving one to a sibling, the authors noted. In addition, the typical vomiting, abdominal pain, fever, diarrhea, respiratory distress, and dysphagia associated with battery ingestion are nonspecific symptoms (Pediatr. Emerg. Care 2008;24:313-6).
"Consider battery ingestion in the differential diagnosis of any child presenting with nonspecific GI symptoms or unexplained respiratory distress because of the serious consequences associated with a delayed or missed diagnosis," Dr. Ferrante said.
Complicating matters is the timing of injury, which can vary from 2 hours after ingestion for serious esophageal burns to more than 2 weeks for fatal hemorrhage following endoscopic removal of a button battery. The growing recognition of these injuries drove pediatric gastroenterologists at the University of Colorado Denver to develop guidelines for the management of button battery–induced hemorrhage (J. Pediatr. Gastroenterol. Nutr. 2011;52:585-9).
Nickle-sized, 3-V lithium button batteries can easily lodge in a child’s esophagus, and were most frequently associated with serious complications and death, according to the report.
Although outside the scope of the report, Dr. Ferrante also suggested pediatricians warn parents about ingestion of strong powerful magnets. This is another often-overlooked injury with similar issues and consequences, she said. "There are even cases where injury resulted from co-ingestion of a button battery and a strong magnet."
For the current study, Dr. Ferrante and her colleagues analyzed the National Electronic Injury Surveillance System (NEISS) database to quantify nonfatal, battery-related ED visits. They assessed other CPSC data to identify the battery-related deaths.
The NEISS data only comprise emergency department visits, so any child treated for battery ingestion in a doctor’s office or as an outpatient is not included in the study, a potential limitation. In addition, the number of fatal incidents involving batteries and children younger than 13 years is likely underrepresented because of the type of data collected, the authors noted.
The authors had no relevant financial disclosures. Click here for more information on battery hazards provided by the U.S. Consumer Product Safety Commission.
FROM MORBIDITY AND MORTALITY WEEKLY REPORT
Major Finding: An estimated 40,400 children were treated at U.S. emergency departments between 1997 and 2010 for battery-related injuries. Twelve of the 14 reported deaths involved button batteries.
Data Source: This is a study of fatal and nonfatal injuries related to battery exposure in children 13 years and younger from U.S. Consumer Product Safety Commission databases.
Disclosures: The authors had no relevant financial disclosures.
FDA Approves Linaclotide for Constipation Conditions
The Food and Drug Administration approved linaclotide on Aug. 30 to treat two conditions: chronic idiopathic constipation and irritable bowel syndrome with constipation in adults.
Linaclotide (Linzess) is administered as a capsule taken once daily on an empty stomach, at least 30 minutes before the first meal of the day. This agent helps relieve constipation by increasing the frequency of bowel movements. In irritable bowel syndrome with constipation (IBS-C), linaclotide has been shown to reduce abdominal pain, according to a statement from the FDA.
The drug is approved with a boxed warning to alert patients and health care professionals that linaclotide should not be used in patients 16 years of age and younger. The most common side effect reported during the clinical studies was diarrhea, the statement said.
According to the FDA, the safety and effectiveness of linaclotide for the management of IBS-C were established in two double-blind studies (Gastroenterology 2011;140:S138 and Gastroenterology 2011;140:S135). A total of 1,604 patients were randomly assigned to take 290 mcg of linaclotide or a placebo for at least 12 weeks. Linaclotide was more effective in reducing abdominal pain and increasing the number of complete spontaneous bowel movements, compared with placebo, in both trials.
The safety and effectiveness of linaclotide for the management of chronic idiopathic constipation also were established in two double-blind studies (N. Engl. J. Med. 2011;365:527-36). A total of 1,272 patients were randomly assigned to take 145 mcg or 290 mcg linaclotide or a placebo for 12 weeks. Patients on linaclotide had more complete spontaneous bowel movements than did those taking the placebo. The 290-mcg dose is not approved for chronic constipation because the data showed that it was no more effective than the 145-mcg dose.
Linzess is marketed by Ironwood Pharmaceuticals Inc.
Linaclotide is currently the only FDA-approved medication indicated for increasing bowel movements and decreasing abdominal pain in men and women with irritable bowel syndrome with constipation (IBS-C). It has been shown to be efficacious in relieving abdominal pain and constipation in patients with IBS-C, and constipation in those with chronic idiopathic constipation (CIC). The drug is a peripherally-acting agent that activates guanylate cyclase-C (GC-C) on intestinal epithelial cells resulting in increased intracellular and extracellular concentrations of cyclic guanosine monophosphate (cGMP).
Relief of constipation symptoms in IBS-C and CIC is believed to be due to an increase in intracellular cGMP resulting in chloride and fluid secretion through the cystic fibrosis transmembrane conductance regulator (CFTR) ion channel and acceleration of colonic transit. Linaclotide’s effect on reducing abdominal pain in IBS-C is thought to be due to increased extracellular cGMP, which has been shown to decrease firing of sensory nerves within the bowel wall in preclinical animal studies.
Patients with CIC who responded to linaclotide had at least three complete spontaneous bowel movements (CSBMs) per week and an increase in one CSBM for at least 9 out of 12 weeks. The 145 mcg and 290 mcg daily doses showed a statistically significant benefit over placebo; the FDA has approved only the lower dose for CIC. The efficacy of linaclotide was sustained throughout the 12 weeks of the trials.
The dose of 290 mcg per day was approved for the treatment of IBS-C, which is usually differentiated from CIC by the presence of predominant abdominal pain associated with constipation. The significant improvement in CSBMs occurred within the first week of treatment. The decrease in abdominal pain was more gradual and appeared to reach its maximum effect at 8 weeks. The significant effect of linaclotide on abdominal pain may be due to an additional independent effect beyond relief of constipation, but further studies are needed to better understand linaclotide’s effect on abdominal pain.
LIN CHANG, M.D., is co-director of the Oppenheimer Family Center for Neurobiology of Stress and director of the Digestive Health and Nutrition Clinic at the University of California, Los Angeles. She is a consultant for Ironwood Pharmaceuticals and Forest Laboratories and has received grant support from Ironwood Pharmaceuticals.
Linaclotide is currently the only FDA-approved medication indicated for increasing bowel movements and decreasing abdominal pain in men and women with irritable bowel syndrome with constipation (IBS-C). It has been shown to be efficacious in relieving abdominal pain and constipation in patients with IBS-C, and constipation in those with chronic idiopathic constipation (CIC). The drug is a peripherally-acting agent that activates guanylate cyclase-C (GC-C) on intestinal epithelial cells resulting in increased intracellular and extracellular concentrations of cyclic guanosine monophosphate (cGMP).
Relief of constipation symptoms in IBS-C and CIC is believed to be due to an increase in intracellular cGMP resulting in chloride and fluid secretion through the cystic fibrosis transmembrane conductance regulator (CFTR) ion channel and acceleration of colonic transit. Linaclotide’s effect on reducing abdominal pain in IBS-C is thought to be due to increased extracellular cGMP, which has been shown to decrease firing of sensory nerves within the bowel wall in preclinical animal studies.
Patients with CIC who responded to linaclotide had at least three complete spontaneous bowel movements (CSBMs) per week and an increase in one CSBM for at least 9 out of 12 weeks. The 145 mcg and 290 mcg daily doses showed a statistically significant benefit over placebo; the FDA has approved only the lower dose for CIC. The efficacy of linaclotide was sustained throughout the 12 weeks of the trials.
The dose of 290 mcg per day was approved for the treatment of IBS-C, which is usually differentiated from CIC by the presence of predominant abdominal pain associated with constipation. The significant improvement in CSBMs occurred within the first week of treatment. The decrease in abdominal pain was more gradual and appeared to reach its maximum effect at 8 weeks. The significant effect of linaclotide on abdominal pain may be due to an additional independent effect beyond relief of constipation, but further studies are needed to better understand linaclotide’s effect on abdominal pain.
LIN CHANG, M.D., is co-director of the Oppenheimer Family Center for Neurobiology of Stress and director of the Digestive Health and Nutrition Clinic at the University of California, Los Angeles. She is a consultant for Ironwood Pharmaceuticals and Forest Laboratories and has received grant support from Ironwood Pharmaceuticals.
Linaclotide is currently the only FDA-approved medication indicated for increasing bowel movements and decreasing abdominal pain in men and women with irritable bowel syndrome with constipation (IBS-C). It has been shown to be efficacious in relieving abdominal pain and constipation in patients with IBS-C, and constipation in those with chronic idiopathic constipation (CIC). The drug is a peripherally-acting agent that activates guanylate cyclase-C (GC-C) on intestinal epithelial cells resulting in increased intracellular and extracellular concentrations of cyclic guanosine monophosphate (cGMP).
Relief of constipation symptoms in IBS-C and CIC is believed to be due to an increase in intracellular cGMP resulting in chloride and fluid secretion through the cystic fibrosis transmembrane conductance regulator (CFTR) ion channel and acceleration of colonic transit. Linaclotide’s effect on reducing abdominal pain in IBS-C is thought to be due to increased extracellular cGMP, which has been shown to decrease firing of sensory nerves within the bowel wall in preclinical animal studies.
Patients with CIC who responded to linaclotide had at least three complete spontaneous bowel movements (CSBMs) per week and an increase in one CSBM for at least 9 out of 12 weeks. The 145 mcg and 290 mcg daily doses showed a statistically significant benefit over placebo; the FDA has approved only the lower dose for CIC. The efficacy of linaclotide was sustained throughout the 12 weeks of the trials.
The dose of 290 mcg per day was approved for the treatment of IBS-C, which is usually differentiated from CIC by the presence of predominant abdominal pain associated with constipation. The significant improvement in CSBMs occurred within the first week of treatment. The decrease in abdominal pain was more gradual and appeared to reach its maximum effect at 8 weeks. The significant effect of linaclotide on abdominal pain may be due to an additional independent effect beyond relief of constipation, but further studies are needed to better understand linaclotide’s effect on abdominal pain.
LIN CHANG, M.D., is co-director of the Oppenheimer Family Center for Neurobiology of Stress and director of the Digestive Health and Nutrition Clinic at the University of California, Los Angeles. She is a consultant for Ironwood Pharmaceuticals and Forest Laboratories and has received grant support from Ironwood Pharmaceuticals.
The Food and Drug Administration approved linaclotide on Aug. 30 to treat two conditions: chronic idiopathic constipation and irritable bowel syndrome with constipation in adults.
Linaclotide (Linzess) is administered as a capsule taken once daily on an empty stomach, at least 30 minutes before the first meal of the day. This agent helps relieve constipation by increasing the frequency of bowel movements. In irritable bowel syndrome with constipation (IBS-C), linaclotide has been shown to reduce abdominal pain, according to a statement from the FDA.
The drug is approved with a boxed warning to alert patients and health care professionals that linaclotide should not be used in patients 16 years of age and younger. The most common side effect reported during the clinical studies was diarrhea, the statement said.
According to the FDA, the safety and effectiveness of linaclotide for the management of IBS-C were established in two double-blind studies (Gastroenterology 2011;140:S138 and Gastroenterology 2011;140:S135). A total of 1,604 patients were randomly assigned to take 290 mcg of linaclotide or a placebo for at least 12 weeks. Linaclotide was more effective in reducing abdominal pain and increasing the number of complete spontaneous bowel movements, compared with placebo, in both trials.
The safety and effectiveness of linaclotide for the management of chronic idiopathic constipation also were established in two double-blind studies (N. Engl. J. Med. 2011;365:527-36). A total of 1,272 patients were randomly assigned to take 145 mcg or 290 mcg linaclotide or a placebo for 12 weeks. Patients on linaclotide had more complete spontaneous bowel movements than did those taking the placebo. The 290-mcg dose is not approved for chronic constipation because the data showed that it was no more effective than the 145-mcg dose.
Linzess is marketed by Ironwood Pharmaceuticals Inc.
The Food and Drug Administration approved linaclotide on Aug. 30 to treat two conditions: chronic idiopathic constipation and irritable bowel syndrome with constipation in adults.
Linaclotide (Linzess) is administered as a capsule taken once daily on an empty stomach, at least 30 minutes before the first meal of the day. This agent helps relieve constipation by increasing the frequency of bowel movements. In irritable bowel syndrome with constipation (IBS-C), linaclotide has been shown to reduce abdominal pain, according to a statement from the FDA.
The drug is approved with a boxed warning to alert patients and health care professionals that linaclotide should not be used in patients 16 years of age and younger. The most common side effect reported during the clinical studies was diarrhea, the statement said.
According to the FDA, the safety and effectiveness of linaclotide for the management of IBS-C were established in two double-blind studies (Gastroenterology 2011;140:S138 and Gastroenterology 2011;140:S135). A total of 1,604 patients were randomly assigned to take 290 mcg of linaclotide or a placebo for at least 12 weeks. Linaclotide was more effective in reducing abdominal pain and increasing the number of complete spontaneous bowel movements, compared with placebo, in both trials.
The safety and effectiveness of linaclotide for the management of chronic idiopathic constipation also were established in two double-blind studies (N. Engl. J. Med. 2011;365:527-36). A total of 1,272 patients were randomly assigned to take 145 mcg or 290 mcg linaclotide or a placebo for 12 weeks. Patients on linaclotide had more complete spontaneous bowel movements than did those taking the placebo. The 290-mcg dose is not approved for chronic constipation because the data showed that it was no more effective than the 145-mcg dose.
Linzess is marketed by Ironwood Pharmaceuticals Inc.