User login
New Data on Hospitalist Schedules
With last month’s publication of the 2012 State of Hospital Medicine report (www.hospitalmedicine.org/survey), we have some fascinating new information about the scheduling choices of HM groups—some of which has never been collected by SHM before.
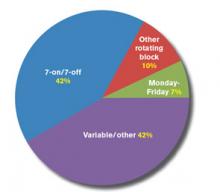
For example, we learned this year that 42% of respondent groups serving adult patients predominantly utilize a schedule of seven days on followed by seven days off (“seven-on, seven-off”), while another 42% use variable/other scheduling patterns. A small minority of groups utilize other types of rotating block schedules (e.g. five-on/five-off) or Monday-Friday schedules. The type of schedule used varies a lot by area of the country, ownership/employment model, and other group characteristics.
Full-time adult medicine hospitalists working shift-based schedules now work a median of 182 shifts, or work periods, annually, down from 188 the last time SHM asked this question in 2005. For doctors working hybrid schedules, including both shifts and on-call duties, the number of shifts declined to 204 from 215 in 2005. During the same period, hospitalists’ annual encounter volume also has declined, though compensation has continued its inexorable rise.
So if the number of shifts worked and patient encounters both have declined since 2005, why do hospitalists feel so much busier today?
Well, for one thing, we learned in this year’s survey that 75% of adult hospitalist groups schedule day shifts of 12 to 13.9 hours in length, while the other 25% use shorter day shifts. About 85% of night shifts are also 12 to 13.9 hours long, while the preponderance of evening/swing shifts fall into either the 10- to 11.9-hour range (45%) or the eight-hours-or-less range (33%). In 2005, the median shift length for all respondents—both adult and pediatric—was 11 hours for groups using shift-based models, and only eight hours for groups using hybrid or other scheduling models. So although this year’s data is not presented in the same way as it was in 2005, it would appear that the typical shift length might have increased some.
In addition, in 2005, only 51% of groups reported having an on-site provider at night. This year, 55% of groups reported having total on-site nighttime coverage, and an additional 28% reported using a combination of on-site and on-call coverage. And the proportion of groups reporting no responsibility for night coverage at all declined to about 1% from 8%. I’m guessing the need to work more nights also contributes to hospitalists’ feelings of increased workload.
Although encounters have decreased, hospitalist wRVUs have risen dramatically. In part, this is due to adjustments in Medicare wRVU values for typical E&M services, but I believe it also is the result of increased patient complexity and/or improved documentation and coding by hospitalists—both of which require more time.
And finally, hospitalists are being asked to do a lot more nonclinical work these days, such as participating in quality-improvement (QI) and patient-flow initiatives, and championing the implementation of electronic health records (EHRs).
All of these factors, and probably others, have combined to make the typical hospitalist’s job much more complex and demanding today than it was in 2005, despite working a few less shifts and have a few less patient encounters annually.
Leslie Flores is SHM senior advisor, practice management.
With last month’s publication of the 2012 State of Hospital Medicine report (www.hospitalmedicine.org/survey), we have some fascinating new information about the scheduling choices of HM groups—some of which has never been collected by SHM before.
For example, we learned this year that 42% of respondent groups serving adult patients predominantly utilize a schedule of seven days on followed by seven days off (“seven-on, seven-off”), while another 42% use variable/other scheduling patterns. A small minority of groups utilize other types of rotating block schedules (e.g. five-on/five-off) or Monday-Friday schedules. The type of schedule used varies a lot by area of the country, ownership/employment model, and other group characteristics.
Full-time adult medicine hospitalists working shift-based schedules now work a median of 182 shifts, or work periods, annually, down from 188 the last time SHM asked this question in 2005. For doctors working hybrid schedules, including both shifts and on-call duties, the number of shifts declined to 204 from 215 in 2005. During the same period, hospitalists’ annual encounter volume also has declined, though compensation has continued its inexorable rise.
So if the number of shifts worked and patient encounters both have declined since 2005, why do hospitalists feel so much busier today?
Well, for one thing, we learned in this year’s survey that 75% of adult hospitalist groups schedule day shifts of 12 to 13.9 hours in length, while the other 25% use shorter day shifts. About 85% of night shifts are also 12 to 13.9 hours long, while the preponderance of evening/swing shifts fall into either the 10- to 11.9-hour range (45%) or the eight-hours-or-less range (33%). In 2005, the median shift length for all respondents—both adult and pediatric—was 11 hours for groups using shift-based models, and only eight hours for groups using hybrid or other scheduling models. So although this year’s data is not presented in the same way as it was in 2005, it would appear that the typical shift length might have increased some.
In addition, in 2005, only 51% of groups reported having an on-site provider at night. This year, 55% of groups reported having total on-site nighttime coverage, and an additional 28% reported using a combination of on-site and on-call coverage. And the proportion of groups reporting no responsibility for night coverage at all declined to about 1% from 8%. I’m guessing the need to work more nights also contributes to hospitalists’ feelings of increased workload.
Although encounters have decreased, hospitalist wRVUs have risen dramatically. In part, this is due to adjustments in Medicare wRVU values for typical E&M services, but I believe it also is the result of increased patient complexity and/or improved documentation and coding by hospitalists—both of which require more time.
And finally, hospitalists are being asked to do a lot more nonclinical work these days, such as participating in quality-improvement (QI) and patient-flow initiatives, and championing the implementation of electronic health records (EHRs).
All of these factors, and probably others, have combined to make the typical hospitalist’s job much more complex and demanding today than it was in 2005, despite working a few less shifts and have a few less patient encounters annually.
Leslie Flores is SHM senior advisor, practice management.
With last month’s publication of the 2012 State of Hospital Medicine report (www.hospitalmedicine.org/survey), we have some fascinating new information about the scheduling choices of HM groups—some of which has never been collected by SHM before.
For example, we learned this year that 42% of respondent groups serving adult patients predominantly utilize a schedule of seven days on followed by seven days off (“seven-on, seven-off”), while another 42% use variable/other scheduling patterns. A small minority of groups utilize other types of rotating block schedules (e.g. five-on/five-off) or Monday-Friday schedules. The type of schedule used varies a lot by area of the country, ownership/employment model, and other group characteristics.
Full-time adult medicine hospitalists working shift-based schedules now work a median of 182 shifts, or work periods, annually, down from 188 the last time SHM asked this question in 2005. For doctors working hybrid schedules, including both shifts and on-call duties, the number of shifts declined to 204 from 215 in 2005. During the same period, hospitalists’ annual encounter volume also has declined, though compensation has continued its inexorable rise.
So if the number of shifts worked and patient encounters both have declined since 2005, why do hospitalists feel so much busier today?
Well, for one thing, we learned in this year’s survey that 75% of adult hospitalist groups schedule day shifts of 12 to 13.9 hours in length, while the other 25% use shorter day shifts. About 85% of night shifts are also 12 to 13.9 hours long, while the preponderance of evening/swing shifts fall into either the 10- to 11.9-hour range (45%) or the eight-hours-or-less range (33%). In 2005, the median shift length for all respondents—both adult and pediatric—was 11 hours for groups using shift-based models, and only eight hours for groups using hybrid or other scheduling models. So although this year’s data is not presented in the same way as it was in 2005, it would appear that the typical shift length might have increased some.
In addition, in 2005, only 51% of groups reported having an on-site provider at night. This year, 55% of groups reported having total on-site nighttime coverage, and an additional 28% reported using a combination of on-site and on-call coverage. And the proportion of groups reporting no responsibility for night coverage at all declined to about 1% from 8%. I’m guessing the need to work more nights also contributes to hospitalists’ feelings of increased workload.
Although encounters have decreased, hospitalist wRVUs have risen dramatically. In part, this is due to adjustments in Medicare wRVU values for typical E&M services, but I believe it also is the result of increased patient complexity and/or improved documentation and coding by hospitalists—both of which require more time.
And finally, hospitalists are being asked to do a lot more nonclinical work these days, such as participating in quality-improvement (QI) and patient-flow initiatives, and championing the implementation of electronic health records (EHRs).
All of these factors, and probably others, have combined to make the typical hospitalist’s job much more complex and demanding today than it was in 2005, despite working a few less shifts and have a few less patient encounters annually.
Leslie Flores is SHM senior advisor, practice management.
Ready to Become a Fellow in Hospital Medicine?
Fellowship has its privileges. For SHM’s Fellows and Senior Fellows in Hospital Medicine, it means demonstrating leadership and critical experience in a rapidly growing medical specialty. It also means receiving recognition among peers at SHM’s annual meeting and access to the SHM Fellows Lounge.
In addition to being able to use the FHM, SFHM, or MHM designations for professional purposes, Fellows receive an official certificate, listing on the SHM website, and even discounts on products in the SHM online store.
The application process can take time, so plan ahead and apply early. The application deadline for the 2013 class of Fellows is January 18.
For more information, visit www.hospitalmedicine.org/fellows.
Fellowship has its privileges. For SHM’s Fellows and Senior Fellows in Hospital Medicine, it means demonstrating leadership and critical experience in a rapidly growing medical specialty. It also means receiving recognition among peers at SHM’s annual meeting and access to the SHM Fellows Lounge.
In addition to being able to use the FHM, SFHM, or MHM designations for professional purposes, Fellows receive an official certificate, listing on the SHM website, and even discounts on products in the SHM online store.
The application process can take time, so plan ahead and apply early. The application deadline for the 2013 class of Fellows is January 18.
For more information, visit www.hospitalmedicine.org/fellows.
Fellowship has its privileges. For SHM’s Fellows and Senior Fellows in Hospital Medicine, it means demonstrating leadership and critical experience in a rapidly growing medical specialty. It also means receiving recognition among peers at SHM’s annual meeting and access to the SHM Fellows Lounge.
In addition to being able to use the FHM, SFHM, or MHM designations for professional purposes, Fellows receive an official certificate, listing on the SHM website, and even discounts on products in the SHM online store.
The application process can take time, so plan ahead and apply early. The application deadline for the 2013 class of Fellows is January 18.
For more information, visit www.hospitalmedicine.org/fellows.
Hospitalists On the Move
Hospitalist John C. Sorg, MD, recently was appointed medical director of the hospitalist program at North Arkansas Regional Medical Center in Harrison, Ark. Dr. Sorg is board-certified in internal medicine and spent nearly 20 years in private practice in Elkhart, Ind.
Chintu Sharma, MD, is the July Physician of the Month at Carroll Hospital Center in Westminster, Md. Dr. Sharma has been a hospitalist at Carroll for more than two years, and his supervisors say that he leads by example in providing excellent patient care.
Karim Godamunne, MD, is the new chief medical officer of North Fulton Hospital in Roswell, Ga. Dr. Godamunne also serves as the HM group’s medical director at North Fulton.
After working with the HM group at Covenant HealthCare in Saginaw, Mich., since 2003, Iris Mangulabnan, MD, FACP, has been named the group’s medical director. The program employs 27 providers, 18 of whom are hospitalists.
Deborah Puckhaber, MD, has been named medical director of the hospitalist service at North Country Hospital in Newport, Vt. Dr. Puckhaber completed her medical training at the State University of New York Buffalo School of Medicine, and practiced adolescent and internal medicine for 14 years before becoming a hospitalist.
Kenric Maynor, MD, has been named HM director of Geisinger Health System in Pennsylvania. In addition to his duties of overseeing the HM programs at six area hospitals, Dr. Maynor will implement a new program at Geisinger Community Medical Center in Scranton.
Adam Fall, MD, SFHM, has joined TeamHealth’s Hospital Medicine Eastern Division as regional medical director for its eastern Tennessee and Georgia regions.
Jeffrey L. Dryden, DO, is the new medical director of the hospitalist team at Ozarks Medical Center in West Plains, Mo. Dr. Dryden has been practicing medicine for more than 20 years, and currently serves as a member of the American Osteopathic Association, the American College of Osteopathic Internists, and the South Central Ozark Association of Osteopathic Physicians.
Hospitalist John C. Sorg, MD, recently was appointed medical director of the hospitalist program at North Arkansas Regional Medical Center in Harrison, Ark. Dr. Sorg is board-certified in internal medicine and spent nearly 20 years in private practice in Elkhart, Ind.
Chintu Sharma, MD, is the July Physician of the Month at Carroll Hospital Center in Westminster, Md. Dr. Sharma has been a hospitalist at Carroll for more than two years, and his supervisors say that he leads by example in providing excellent patient care.
Karim Godamunne, MD, is the new chief medical officer of North Fulton Hospital in Roswell, Ga. Dr. Godamunne also serves as the HM group’s medical director at North Fulton.
After working with the HM group at Covenant HealthCare in Saginaw, Mich., since 2003, Iris Mangulabnan, MD, FACP, has been named the group’s medical director. The program employs 27 providers, 18 of whom are hospitalists.
Deborah Puckhaber, MD, has been named medical director of the hospitalist service at North Country Hospital in Newport, Vt. Dr. Puckhaber completed her medical training at the State University of New York Buffalo School of Medicine, and practiced adolescent and internal medicine for 14 years before becoming a hospitalist.
Kenric Maynor, MD, has been named HM director of Geisinger Health System in Pennsylvania. In addition to his duties of overseeing the HM programs at six area hospitals, Dr. Maynor will implement a new program at Geisinger Community Medical Center in Scranton.
Adam Fall, MD, SFHM, has joined TeamHealth’s Hospital Medicine Eastern Division as regional medical director for its eastern Tennessee and Georgia regions.
Jeffrey L. Dryden, DO, is the new medical director of the hospitalist team at Ozarks Medical Center in West Plains, Mo. Dr. Dryden has been practicing medicine for more than 20 years, and currently serves as a member of the American Osteopathic Association, the American College of Osteopathic Internists, and the South Central Ozark Association of Osteopathic Physicians.
Hospitalist John C. Sorg, MD, recently was appointed medical director of the hospitalist program at North Arkansas Regional Medical Center in Harrison, Ark. Dr. Sorg is board-certified in internal medicine and spent nearly 20 years in private practice in Elkhart, Ind.
Chintu Sharma, MD, is the July Physician of the Month at Carroll Hospital Center in Westminster, Md. Dr. Sharma has been a hospitalist at Carroll for more than two years, and his supervisors say that he leads by example in providing excellent patient care.
Karim Godamunne, MD, is the new chief medical officer of North Fulton Hospital in Roswell, Ga. Dr. Godamunne also serves as the HM group’s medical director at North Fulton.
After working with the HM group at Covenant HealthCare in Saginaw, Mich., since 2003, Iris Mangulabnan, MD, FACP, has been named the group’s medical director. The program employs 27 providers, 18 of whom are hospitalists.
Deborah Puckhaber, MD, has been named medical director of the hospitalist service at North Country Hospital in Newport, Vt. Dr. Puckhaber completed her medical training at the State University of New York Buffalo School of Medicine, and practiced adolescent and internal medicine for 14 years before becoming a hospitalist.
Kenric Maynor, MD, has been named HM director of Geisinger Health System in Pennsylvania. In addition to his duties of overseeing the HM programs at six area hospitals, Dr. Maynor will implement a new program at Geisinger Community Medical Center in Scranton.
Adam Fall, MD, SFHM, has joined TeamHealth’s Hospital Medicine Eastern Division as regional medical director for its eastern Tennessee and Georgia regions.
Jeffrey L. Dryden, DO, is the new medical director of the hospitalist team at Ozarks Medical Center in West Plains, Mo. Dr. Dryden has been practicing medicine for more than 20 years, and currently serves as a member of the American Osteopathic Association, the American College of Osteopathic Internists, and the South Central Ozark Association of Osteopathic Physicians.
SHM Opposes Bill Eliminating Key Federal Agency
SHM recently joined more than 135 organizations in opposing legislation that would eliminate funding for the Agency for Health Care Research and Quality (AHRQ), according to a July 30 letter. Language terminating the agency was part of a fiscal-year 2013 spending bill approved July 18 by the Republican-controlled Senate Subcommittee on Labor, Health and Human Services, Education, and Related Agencies.
Organized by the Friends of AHRQ Coalition, the letter calls on members of Congress to oppose any bill that terminates the agency and its important research.
“To ‘terminate’ AHRQ in the current fiscal environment is penny-wise and pound-foolish,” the letter states. “AHRQ-funded research is being used in hospitals, private practices, health departments, and communities across the nation to fuel innovation and improve quality, identify waste, and enhance efficiency of the healthcare system. … This research helps Americans get their money’s worth when it comes to healthcare. We need more of it, not less.”
A longtime supporter of AHRQ and its efforts to improve quality and patient safety, SHM is deeply concerned about efforts to eliminate this important agency and will fight to preserve its funding. A markup by the full committee has been postponed indefinitely.
The spending bill approved by the subcommittee also prohibits any patient-centered-outcomes research and all economic research within the National Institutes of Health (NIH). It freezes funding for NIH and rescinds the $1 billion available in 2013 under the Prevention and Public Health Fund. It also rescinds $1.6 billion for the Center for Medicare & Medicaid Innovation (CMMI) and blocks other funding for and implementation of the Affordable Care Act.
Laura Allendorf, SHM senior advisor, advocacy and government affairs
SHM recently joined more than 135 organizations in opposing legislation that would eliminate funding for the Agency for Health Care Research and Quality (AHRQ), according to a July 30 letter. Language terminating the agency was part of a fiscal-year 2013 spending bill approved July 18 by the Republican-controlled Senate Subcommittee on Labor, Health and Human Services, Education, and Related Agencies.
Organized by the Friends of AHRQ Coalition, the letter calls on members of Congress to oppose any bill that terminates the agency and its important research.
“To ‘terminate’ AHRQ in the current fiscal environment is penny-wise and pound-foolish,” the letter states. “AHRQ-funded research is being used in hospitals, private practices, health departments, and communities across the nation to fuel innovation and improve quality, identify waste, and enhance efficiency of the healthcare system. … This research helps Americans get their money’s worth when it comes to healthcare. We need more of it, not less.”
A longtime supporter of AHRQ and its efforts to improve quality and patient safety, SHM is deeply concerned about efforts to eliminate this important agency and will fight to preserve its funding. A markup by the full committee has been postponed indefinitely.
The spending bill approved by the subcommittee also prohibits any patient-centered-outcomes research and all economic research within the National Institutes of Health (NIH). It freezes funding for NIH and rescinds the $1 billion available in 2013 under the Prevention and Public Health Fund. It also rescinds $1.6 billion for the Center for Medicare & Medicaid Innovation (CMMI) and blocks other funding for and implementation of the Affordable Care Act.
Laura Allendorf, SHM senior advisor, advocacy and government affairs
SHM recently joined more than 135 organizations in opposing legislation that would eliminate funding for the Agency for Health Care Research and Quality (AHRQ), according to a July 30 letter. Language terminating the agency was part of a fiscal-year 2013 spending bill approved July 18 by the Republican-controlled Senate Subcommittee on Labor, Health and Human Services, Education, and Related Agencies.
Organized by the Friends of AHRQ Coalition, the letter calls on members of Congress to oppose any bill that terminates the agency and its important research.
“To ‘terminate’ AHRQ in the current fiscal environment is penny-wise and pound-foolish,” the letter states. “AHRQ-funded research is being used in hospitals, private practices, health departments, and communities across the nation to fuel innovation and improve quality, identify waste, and enhance efficiency of the healthcare system. … This research helps Americans get their money’s worth when it comes to healthcare. We need more of it, not less.”
A longtime supporter of AHRQ and its efforts to improve quality and patient safety, SHM is deeply concerned about efforts to eliminate this important agency and will fight to preserve its funding. A markup by the full committee has been postponed indefinitely.
The spending bill approved by the subcommittee also prohibits any patient-centered-outcomes research and all economic research within the National Institutes of Health (NIH). It freezes funding for NIH and rescinds the $1 billion available in 2013 under the Prevention and Public Health Fund. It also rescinds $1.6 billion for the Center for Medicare & Medicaid Innovation (CMMI) and blocks other funding for and implementation of the Affordable Care Act.
Laura Allendorf, SHM senior advisor, advocacy and government affairs
SHM Can Help Learn More about Patient Satisfaction
As elements of the Accountable Care Act are being implemented, improving patient satisfaction has become an important priority for the specialty of hospital medicine. Specifically, under the Hospital Value-Based Purchasing (HVBP) program, a portion of a hospital’s Medicare reimbursement dollars (1% in fiscal-year 2013, growing to 2% in fiscal-year 2017) are at risk. The Centers for Medicare & Medicaid Services (CMS) will use weighted domains to calculate this “at risk” reimbursement, with 30% of the total based on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey measuring patient experience, or satisfaction.
One of the goals of SHM’s Practice Management Committee in 2011 was to provide additional support to the HM community with regard to patient satisfaction. To that end, the committee came up with a series of questions that address the following high-level topics about patient satisfaction surveys:
- The questionnaire;
- The methodology;
- Reports;
- Vendor support; and
- Organization.
To learn more about how to access information from your hospital’s patient satisfaction survey vendor, visit www.hospitalmedicine.org/pm.
As elements of the Accountable Care Act are being implemented, improving patient satisfaction has become an important priority for the specialty of hospital medicine. Specifically, under the Hospital Value-Based Purchasing (HVBP) program, a portion of a hospital’s Medicare reimbursement dollars (1% in fiscal-year 2013, growing to 2% in fiscal-year 2017) are at risk. The Centers for Medicare & Medicaid Services (CMS) will use weighted domains to calculate this “at risk” reimbursement, with 30% of the total based on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey measuring patient experience, or satisfaction.
One of the goals of SHM’s Practice Management Committee in 2011 was to provide additional support to the HM community with regard to patient satisfaction. To that end, the committee came up with a series of questions that address the following high-level topics about patient satisfaction surveys:
- The questionnaire;
- The methodology;
- Reports;
- Vendor support; and
- Organization.
To learn more about how to access information from your hospital’s patient satisfaction survey vendor, visit www.hospitalmedicine.org/pm.
As elements of the Accountable Care Act are being implemented, improving patient satisfaction has become an important priority for the specialty of hospital medicine. Specifically, under the Hospital Value-Based Purchasing (HVBP) program, a portion of a hospital’s Medicare reimbursement dollars (1% in fiscal-year 2013, growing to 2% in fiscal-year 2017) are at risk. The Centers for Medicare & Medicaid Services (CMS) will use weighted domains to calculate this “at risk” reimbursement, with 30% of the total based on the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey measuring patient experience, or satisfaction.
One of the goals of SHM’s Practice Management Committee in 2011 was to provide additional support to the HM community with regard to patient satisfaction. To that end, the committee came up with a series of questions that address the following high-level topics about patient satisfaction surveys:
- The questionnaire;
- The methodology;
- Reports;
- Vendor support; and
- Organization.
To learn more about how to access information from your hospital’s patient satisfaction survey vendor, visit www.hospitalmedicine.org/pm.
Code-H: Learn Hospital-Based Coding from National Experts
What’s better than learning from national experts in hospital-based coding? Learning from them, being able to ask them questions, and sharing your own experiences with others, all at the same time.
CODE-H, which will be offered again this fall, is presented via live webinar at SHM’s new online community, Hospital Medicine Exchange, which enables CODE-H users to post messages to other users and the faculty. Using Hospital Medicine Exchange, CODE-H users can also share their own resources and documents.
Each webinar is archived on the CODE-H site, so participants can log in and learn at any time.
Best of all, one subscription is good for up to 10 participants at each hospital or site, so inviting others at your hospital to participate increases the value.
Used first for CODE-H and SHM’s Hospital Value-Based Purchasing toolkit, Hospital Medicine Exchange will soon be available to all hospitalists as a forum for learning and sharing best practices.
To register for CODE-H, visit www.hospitalmedicine.org/codeh.
What’s better than learning from national experts in hospital-based coding? Learning from them, being able to ask them questions, and sharing your own experiences with others, all at the same time.
CODE-H, which will be offered again this fall, is presented via live webinar at SHM’s new online community, Hospital Medicine Exchange, which enables CODE-H users to post messages to other users and the faculty. Using Hospital Medicine Exchange, CODE-H users can also share their own resources and documents.
Each webinar is archived on the CODE-H site, so participants can log in and learn at any time.
Best of all, one subscription is good for up to 10 participants at each hospital or site, so inviting others at your hospital to participate increases the value.
Used first for CODE-H and SHM’s Hospital Value-Based Purchasing toolkit, Hospital Medicine Exchange will soon be available to all hospitalists as a forum for learning and sharing best practices.
To register for CODE-H, visit www.hospitalmedicine.org/codeh.
What’s better than learning from national experts in hospital-based coding? Learning from them, being able to ask them questions, and sharing your own experiences with others, all at the same time.
CODE-H, which will be offered again this fall, is presented via live webinar at SHM’s new online community, Hospital Medicine Exchange, which enables CODE-H users to post messages to other users and the faculty. Using Hospital Medicine Exchange, CODE-H users can also share their own resources and documents.
Each webinar is archived on the CODE-H site, so participants can log in and learn at any time.
Best of all, one subscription is good for up to 10 participants at each hospital or site, so inviting others at your hospital to participate increases the value.
Used first for CODE-H and SHM’s Hospital Value-Based Purchasing toolkit, Hospital Medicine Exchange will soon be available to all hospitalists as a forum for learning and sharing best practices.
To register for CODE-H, visit www.hospitalmedicine.org/codeh.
Is ‘Meaningful Use’ Safe?
Earlier this summer, the Centers for Medicare & Medicaid Services (CMS) announced that more than 100,000 healthcare providers and 48% of all eligible hospitals are using electronic health records (EHRs) that meet federal standards, and they have benefited from federal incentive programs to do so.1
According to CMS acting administrator Marilyn Tavenner, meeting that provider goal makes 2012 the “Year of Meaningful Use.” She also says healthcare providers have recognized the potential of EHRs to cut down on paperwork, eliminate duplicate screenings and tests, and facilitate better, safer, patient-centered care.2
Belying CMS’ celebratory declarations, however, are concerns among experts that health information technology’s (HIT) actual use falls short of its promise—and might even endanger patients—due to shortcomings in system interoperability, safety, accountability, and other issues.
“Federal funding of IT was a step in the right direction, but it has also created a guaranteed customer base for electronic medical records, so vendors have less incentive to improve their products to meet clinicians needs,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, chair of SHsM’s IT Executive Committee and chief of hospital medicine at the University of New Mexico Health Sciences Center School of Medicine in Albuquerque. “We want systems that help us make better clinical decisions and allow us to work more efficiently. Unfortunately, many hospitalists are frustrated with existing HIT systems, knowing how much better they need to be. It can be a dangerous gamble to push rapid adoption of potentially unsafe systems in hospitals.”
Questioning HIT Safety
Health IT experts affirm that potential danger. Jerry Osheroff, MD, FACP, FACMI, principal and founder of TMIT Consulting LLC and former chief clinical informatics officer for Thomson Reuters Healthcare, says HIT “is most effective when it gets the right information to the right people, through the right channels, in the right format, at the right point in the workflow. The danger comes when it gets one of those five ‘rights’ wrong; that can lead to distraction, confusion, wasted time, missed improvement opportunities, and safety concerns.”
Last November, the Institute of Medicine (IOM) released a scathing critique of HIT’s current ability to ensure patient safety.3 As the federal government invests billions of dollars to encourage hospitals and healthcare providers to adopt HIT, the IOM report said, improvements in care and safety are not yet established, and little evidence exists that quantifies the magnitude of the risk associated with HIT problems—partly because many HIT vendors discourage providers from sharing patient-safety concerns with nondisclosure and “hold harmless” provisions in contracts that shift the liability of unsafe HIT features to care providers.3
The report also cautioned that serious errors involving these technologies—including medication dosing errors, failure to detect fatal illnesses, and treatment delays due to complex data interfaces and poor human-computer interactions or loss of data—have led to several reported patient deaths and injuries. Furthermore, there is no way to publicly track adverse outcomes because there is no systematic regulation or authority to collect, analyze, and disseminate such information.
The report concluded that the current state of safety and health IT is not acceptable and that regulation of the industry might be necessary because the private sector to date has not taken sufficient action on its own to improve HIT safety.
SHM applauds the IOM report as an overdue and direly needed call to action, Dr. Rogers says. SHM sent a letter to the U.S. Department of Health and Human Services underscoring the importance of the IOM report.
“In our practices, we have experienced the threats to patient safety outlined in the report: poor user-interface design, poor workflow, complex data interfaces, lack of system interoperability, and lack of sufficient vendor action to build safer products,” Dr. Rogers says.
“Lack of interoperability—preventing access to patient data from previous physician or other hospital visits—makes a mockery of a coordinated, patient-centered healthcare system,” says HIT researcher Ross Koppel, PhD, faculty member of University of Pennsylvania’s Sociology Department and School of Medicine.
Although Dr. Rogers acknowledges that HIT has the potential to revolutionize healthcare systems, boost quality and safety, and lower cost, he maintains that current HIT products fall short of those ambitious goals. “Vendors typically regard usability of their products as a convenience request by clinicians; any errors are regarded as training issues for physicians,” Dr. Rogers says. “But the way that data is presented on a screen matters—if it is difficult to input or retrieve data and leads to cognitive or process errors, that’s a product redesign issue for which vendors should be held accountable.”
Dr. Koppel says many HIT systems originated from billing system applications “and were not initially designed with the clinical perspective in mind. Hospitalists have to be particularly focused on usability of HIT systems when it comes to patient-safety impacts. They’re not the canary in the coal mine, they’re the miners—often the teachers guiding other clinicians on HIT use.”
Improvement Agenda
SHM fully supports many of the IOM’s recommendations to improve the safety and functionality of HIT systems, including these as stated in an email to its members:
- Remove contractual restrictions, promote public reporting of safety issues, and put a system in place for independent investigations that drive patient-safety improvement.
- Establish standards and a common infrastructure for “interoperable” data exchange across systems.
- Create dual accountability between vendors and providers to address safety concerns that might require
- changes in an IT product’s functionality or design.
- Promote research on usability and human-factors design, safer implementation, and sociotechnical systems associated with HIT.
- Promote education of safety, quality, and reliability principles in design and implementation of HIT among all levels of the workforce, including frontline clinicians and staff, hospital IT, and quality teams—as well as IT vendors themselves.
There also are ongoing efforts in the private sector to improve HIT system functionality. For example, the HIMSS CDS Guidebook Series, of which Dr. Osheroff is lead editor and author and Dr. Rogers is a contributing author, is a respected repository of information synthesizing and vetting critical guidance for the effective implementation of clinical decision support (CDS).
“We’re also working with Greg Maynard [senior vice president of SHM’s Center for Hospital Innovation & Improvement] to use the collaborative’s tools to disseminate clinical-decision-support best practices for improving VTE prophylaxis rates,” Dr. Osheroff notes.
Hospitalists, as central players in quality improvement (QI), standardization, and care coordination, are natural choices as HIT champions, with valuable insight into how HIT systems should be customized to accommodate workflows and order sets in an optimal fashion, Dr. Rogers says.
“As critical as we are about the status of current HIT systems, we believe that systems can be designed more effectively to meet our needs,” he says. “By adopting many of the improvements enumerated in the IOM report, hospitalists are uniquely positioned to advance HIT to help achieve the goals of safer, higher-quality, and more efficient care.”
Christopher Guadagnino is a freelance writer based in Philadelphia.
References
- Centers for Medicare & Medicaid Services. More than 100,000 health care providers paid for using electronic health records. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4383&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&sr. Accessed July 31, 2012.
- Centers for Medicare & Medicaid Services. 2012: the year of meaningful use. The CMS Blog website. Available at: http://blog.cms.gov/2012/03/23/2012-the-year-of-meaningful-use. Accessed July 18, 2012.
- Institute of Medicine of the National Academies. Health IT and patient safety: building safer systems for better care. Institute of Medicine of the National Academies website. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed July 14, 2012.
Earlier this summer, the Centers for Medicare & Medicaid Services (CMS) announced that more than 100,000 healthcare providers and 48% of all eligible hospitals are using electronic health records (EHRs) that meet federal standards, and they have benefited from federal incentive programs to do so.1
According to CMS acting administrator Marilyn Tavenner, meeting that provider goal makes 2012 the “Year of Meaningful Use.” She also says healthcare providers have recognized the potential of EHRs to cut down on paperwork, eliminate duplicate screenings and tests, and facilitate better, safer, patient-centered care.2
Belying CMS’ celebratory declarations, however, are concerns among experts that health information technology’s (HIT) actual use falls short of its promise—and might even endanger patients—due to shortcomings in system interoperability, safety, accountability, and other issues.
“Federal funding of IT was a step in the right direction, but it has also created a guaranteed customer base for electronic medical records, so vendors have less incentive to improve their products to meet clinicians needs,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, chair of SHsM’s IT Executive Committee and chief of hospital medicine at the University of New Mexico Health Sciences Center School of Medicine in Albuquerque. “We want systems that help us make better clinical decisions and allow us to work more efficiently. Unfortunately, many hospitalists are frustrated with existing HIT systems, knowing how much better they need to be. It can be a dangerous gamble to push rapid adoption of potentially unsafe systems in hospitals.”
Questioning HIT Safety
Health IT experts affirm that potential danger. Jerry Osheroff, MD, FACP, FACMI, principal and founder of TMIT Consulting LLC and former chief clinical informatics officer for Thomson Reuters Healthcare, says HIT “is most effective when it gets the right information to the right people, through the right channels, in the right format, at the right point in the workflow. The danger comes when it gets one of those five ‘rights’ wrong; that can lead to distraction, confusion, wasted time, missed improvement opportunities, and safety concerns.”
Last November, the Institute of Medicine (IOM) released a scathing critique of HIT’s current ability to ensure patient safety.3 As the federal government invests billions of dollars to encourage hospitals and healthcare providers to adopt HIT, the IOM report said, improvements in care and safety are not yet established, and little evidence exists that quantifies the magnitude of the risk associated with HIT problems—partly because many HIT vendors discourage providers from sharing patient-safety concerns with nondisclosure and “hold harmless” provisions in contracts that shift the liability of unsafe HIT features to care providers.3
The report also cautioned that serious errors involving these technologies—including medication dosing errors, failure to detect fatal illnesses, and treatment delays due to complex data interfaces and poor human-computer interactions or loss of data—have led to several reported patient deaths and injuries. Furthermore, there is no way to publicly track adverse outcomes because there is no systematic regulation or authority to collect, analyze, and disseminate such information.
The report concluded that the current state of safety and health IT is not acceptable and that regulation of the industry might be necessary because the private sector to date has not taken sufficient action on its own to improve HIT safety.
SHM applauds the IOM report as an overdue and direly needed call to action, Dr. Rogers says. SHM sent a letter to the U.S. Department of Health and Human Services underscoring the importance of the IOM report.
“In our practices, we have experienced the threats to patient safety outlined in the report: poor user-interface design, poor workflow, complex data interfaces, lack of system interoperability, and lack of sufficient vendor action to build safer products,” Dr. Rogers says.
“Lack of interoperability—preventing access to patient data from previous physician or other hospital visits—makes a mockery of a coordinated, patient-centered healthcare system,” says HIT researcher Ross Koppel, PhD, faculty member of University of Pennsylvania’s Sociology Department and School of Medicine.
Although Dr. Rogers acknowledges that HIT has the potential to revolutionize healthcare systems, boost quality and safety, and lower cost, he maintains that current HIT products fall short of those ambitious goals. “Vendors typically regard usability of their products as a convenience request by clinicians; any errors are regarded as training issues for physicians,” Dr. Rogers says. “But the way that data is presented on a screen matters—if it is difficult to input or retrieve data and leads to cognitive or process errors, that’s a product redesign issue for which vendors should be held accountable.”
Dr. Koppel says many HIT systems originated from billing system applications “and were not initially designed with the clinical perspective in mind. Hospitalists have to be particularly focused on usability of HIT systems when it comes to patient-safety impacts. They’re not the canary in the coal mine, they’re the miners—often the teachers guiding other clinicians on HIT use.”
Improvement Agenda
SHM fully supports many of the IOM’s recommendations to improve the safety and functionality of HIT systems, including these as stated in an email to its members:
- Remove contractual restrictions, promote public reporting of safety issues, and put a system in place for independent investigations that drive patient-safety improvement.
- Establish standards and a common infrastructure for “interoperable” data exchange across systems.
- Create dual accountability between vendors and providers to address safety concerns that might require
- changes in an IT product’s functionality or design.
- Promote research on usability and human-factors design, safer implementation, and sociotechnical systems associated with HIT.
- Promote education of safety, quality, and reliability principles in design and implementation of HIT among all levels of the workforce, including frontline clinicians and staff, hospital IT, and quality teams—as well as IT vendors themselves.
There also are ongoing efforts in the private sector to improve HIT system functionality. For example, the HIMSS CDS Guidebook Series, of which Dr. Osheroff is lead editor and author and Dr. Rogers is a contributing author, is a respected repository of information synthesizing and vetting critical guidance for the effective implementation of clinical decision support (CDS).
“We’re also working with Greg Maynard [senior vice president of SHM’s Center for Hospital Innovation & Improvement] to use the collaborative’s tools to disseminate clinical-decision-support best practices for improving VTE prophylaxis rates,” Dr. Osheroff notes.
Hospitalists, as central players in quality improvement (QI), standardization, and care coordination, are natural choices as HIT champions, with valuable insight into how HIT systems should be customized to accommodate workflows and order sets in an optimal fashion, Dr. Rogers says.
“As critical as we are about the status of current HIT systems, we believe that systems can be designed more effectively to meet our needs,” he says. “By adopting many of the improvements enumerated in the IOM report, hospitalists are uniquely positioned to advance HIT to help achieve the goals of safer, higher-quality, and more efficient care.”
Christopher Guadagnino is a freelance writer based in Philadelphia.
References
- Centers for Medicare & Medicaid Services. More than 100,000 health care providers paid for using electronic health records. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4383&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&sr. Accessed July 31, 2012.
- Centers for Medicare & Medicaid Services. 2012: the year of meaningful use. The CMS Blog website. Available at: http://blog.cms.gov/2012/03/23/2012-the-year-of-meaningful-use. Accessed July 18, 2012.
- Institute of Medicine of the National Academies. Health IT and patient safety: building safer systems for better care. Institute of Medicine of the National Academies website. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed July 14, 2012.
Earlier this summer, the Centers for Medicare & Medicaid Services (CMS) announced that more than 100,000 healthcare providers and 48% of all eligible hospitals are using electronic health records (EHRs) that meet federal standards, and they have benefited from federal incentive programs to do so.1
According to CMS acting administrator Marilyn Tavenner, meeting that provider goal makes 2012 the “Year of Meaningful Use.” She also says healthcare providers have recognized the potential of EHRs to cut down on paperwork, eliminate duplicate screenings and tests, and facilitate better, safer, patient-centered care.2
Belying CMS’ celebratory declarations, however, are concerns among experts that health information technology’s (HIT) actual use falls short of its promise—and might even endanger patients—due to shortcomings in system interoperability, safety, accountability, and other issues.
“Federal funding of IT was a step in the right direction, but it has also created a guaranteed customer base for electronic medical records, so vendors have less incentive to improve their products to meet clinicians needs,” says Kendall M. Rogers, MD, CPE, FACP, SFHM, chair of SHsM’s IT Executive Committee and chief of hospital medicine at the University of New Mexico Health Sciences Center School of Medicine in Albuquerque. “We want systems that help us make better clinical decisions and allow us to work more efficiently. Unfortunately, many hospitalists are frustrated with existing HIT systems, knowing how much better they need to be. It can be a dangerous gamble to push rapid adoption of potentially unsafe systems in hospitals.”
Questioning HIT Safety
Health IT experts affirm that potential danger. Jerry Osheroff, MD, FACP, FACMI, principal and founder of TMIT Consulting LLC and former chief clinical informatics officer for Thomson Reuters Healthcare, says HIT “is most effective when it gets the right information to the right people, through the right channels, in the right format, at the right point in the workflow. The danger comes when it gets one of those five ‘rights’ wrong; that can lead to distraction, confusion, wasted time, missed improvement opportunities, and safety concerns.”
Last November, the Institute of Medicine (IOM) released a scathing critique of HIT’s current ability to ensure patient safety.3 As the federal government invests billions of dollars to encourage hospitals and healthcare providers to adopt HIT, the IOM report said, improvements in care and safety are not yet established, and little evidence exists that quantifies the magnitude of the risk associated with HIT problems—partly because many HIT vendors discourage providers from sharing patient-safety concerns with nondisclosure and “hold harmless” provisions in contracts that shift the liability of unsafe HIT features to care providers.3
The report also cautioned that serious errors involving these technologies—including medication dosing errors, failure to detect fatal illnesses, and treatment delays due to complex data interfaces and poor human-computer interactions or loss of data—have led to several reported patient deaths and injuries. Furthermore, there is no way to publicly track adverse outcomes because there is no systematic regulation or authority to collect, analyze, and disseminate such information.
The report concluded that the current state of safety and health IT is not acceptable and that regulation of the industry might be necessary because the private sector to date has not taken sufficient action on its own to improve HIT safety.
SHM applauds the IOM report as an overdue and direly needed call to action, Dr. Rogers says. SHM sent a letter to the U.S. Department of Health and Human Services underscoring the importance of the IOM report.
“In our practices, we have experienced the threats to patient safety outlined in the report: poor user-interface design, poor workflow, complex data interfaces, lack of system interoperability, and lack of sufficient vendor action to build safer products,” Dr. Rogers says.
“Lack of interoperability—preventing access to patient data from previous physician or other hospital visits—makes a mockery of a coordinated, patient-centered healthcare system,” says HIT researcher Ross Koppel, PhD, faculty member of University of Pennsylvania’s Sociology Department and School of Medicine.
Although Dr. Rogers acknowledges that HIT has the potential to revolutionize healthcare systems, boost quality and safety, and lower cost, he maintains that current HIT products fall short of those ambitious goals. “Vendors typically regard usability of their products as a convenience request by clinicians; any errors are regarded as training issues for physicians,” Dr. Rogers says. “But the way that data is presented on a screen matters—if it is difficult to input or retrieve data and leads to cognitive or process errors, that’s a product redesign issue for which vendors should be held accountable.”
Dr. Koppel says many HIT systems originated from billing system applications “and were not initially designed with the clinical perspective in mind. Hospitalists have to be particularly focused on usability of HIT systems when it comes to patient-safety impacts. They’re not the canary in the coal mine, they’re the miners—often the teachers guiding other clinicians on HIT use.”
Improvement Agenda
SHM fully supports many of the IOM’s recommendations to improve the safety and functionality of HIT systems, including these as stated in an email to its members:
- Remove contractual restrictions, promote public reporting of safety issues, and put a system in place for independent investigations that drive patient-safety improvement.
- Establish standards and a common infrastructure for “interoperable” data exchange across systems.
- Create dual accountability between vendors and providers to address safety concerns that might require
- changes in an IT product’s functionality or design.
- Promote research on usability and human-factors design, safer implementation, and sociotechnical systems associated with HIT.
- Promote education of safety, quality, and reliability principles in design and implementation of HIT among all levels of the workforce, including frontline clinicians and staff, hospital IT, and quality teams—as well as IT vendors themselves.
There also are ongoing efforts in the private sector to improve HIT system functionality. For example, the HIMSS CDS Guidebook Series, of which Dr. Osheroff is lead editor and author and Dr. Rogers is a contributing author, is a respected repository of information synthesizing and vetting critical guidance for the effective implementation of clinical decision support (CDS).
“We’re also working with Greg Maynard [senior vice president of SHM’s Center for Hospital Innovation & Improvement] to use the collaborative’s tools to disseminate clinical-decision-support best practices for improving VTE prophylaxis rates,” Dr. Osheroff notes.
Hospitalists, as central players in quality improvement (QI), standardization, and care coordination, are natural choices as HIT champions, with valuable insight into how HIT systems should be customized to accommodate workflows and order sets in an optimal fashion, Dr. Rogers says.
“As critical as we are about the status of current HIT systems, we believe that systems can be designed more effectively to meet our needs,” he says. “By adopting many of the improvements enumerated in the IOM report, hospitalists are uniquely positioned to advance HIT to help achieve the goals of safer, higher-quality, and more efficient care.”
Christopher Guadagnino is a freelance writer based in Philadelphia.
References
- Centers for Medicare & Medicaid Services. More than 100,000 health care providers paid for using electronic health records. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/apps/media/press/release.asp?Counter=4383&intNumPerPage=10&checkDate=&checkKey=&srchType=1&numDays=3500&sr. Accessed July 31, 2012.
- Centers for Medicare & Medicaid Services. 2012: the year of meaningful use. The CMS Blog website. Available at: http://blog.cms.gov/2012/03/23/2012-the-year-of-meaningful-use. Accessed July 18, 2012.
- Institute of Medicine of the National Academies. Health IT and patient safety: building safer systems for better care. Institute of Medicine of the National Academies website. Available at: http://www.iom.edu/Reports/2011/Health-IT-and-Patient-Safety-Building-Safer-Systems-for-Better-Care.aspx. Accessed July 14, 2012.
How to Bridge Common Patient-Hospitalist Communication Gaps
Hospitalists coordinate the care of large numbers of very sick, very complicated patients, making patient-hospitalist communication very important. When done effectively, communication can help hospitalists improve their patients’ sense of well-being and reinforce their adherence to medical treatments post-discharge. It also can build trust and help patients better understand their illnesses.
Nonetheless, communication gaps do occur. The main culprits include time pressures, the lack of a pre-existing patient relationship, patient emotions, medical jargon, and physicians’ tendencies to lecture.
The following five examples outline common communication pitfalls, followed by fundamental skills that can be used to solve communication problems.
Tick, Tock Goes the Clock
Scenario: A hospitalist mentions a medication change during a brief patient visit in the midst of a hectic day. The hospitalist pauses for a moment, glances at his watch, and reaches for the room’s door handle. When no question is forthcoming, he excuses himself to visit the next patient.
The patient has questions about the new medication but feels guilty about taking up the hospitalist’s time. The patient decides she can ask about the medication and the reason for the change when the hospitalist isn’t in such a hurry.
Skill: Creating an environment in which patients are encouraged to ask questions need not result in lengthy conversations. The key is having a clear framework for directing conversations, says Cindy Lien, MD, an academic hospitalist at Beth Israel Deaconess Medical Center in Boston. Dr. Lien uses “Ask-Tell-Ask” as a mnemonic when teaching communication skills to internal-medicine trainees.
“We have a tendency to just tell, tell, tell information,” she says. “Ask-Tell-Ask reminds you that one of the most important things to do is to ask the patient to describe what their understanding is of the situation so you have a sense of where they’re coming from.”
Opening questions can include “What is the most important issue on your mind today?” and “What do you understand about your medications?”
After listening to the patient’s response, tell the patient in a few straightforward sentences the information you need to communicate, Dr. Lien says. Then ask the patient if they understand the information conveyed to them, which will give them a chance to ask questions. Additional questions for the patient can include “Do you need further information at this point?” and “How do you feel about what we’ve discussed?”

—Anthony Back, MD, professor of medicine, University of Washington, Seattle
What’s Your Name Again?
Scenario: A hospitalist wearing professional dress with no nametag enters a patient room and introduces herself before informing the patient that she’s ordered additional tests. The hospitalist visits the patient several times during his hospital stay to discuss test results and self-care instructions upon discharge but never reintroduces herself.
The patient was exhausted and in discomfort when the clinician first introduced herself as a hospitalist. She said her name so quickly that the patient didn’t catch it. The patient sees the hospitalist more often than other providers during his admission, but he’s not sure what her role is and he finds it too awkward to ask.
Skill: First impressions are lasting, so make a solid introduction, says David Meltzer, MD, PhD, FHM, associate professor in the department of medicine at the University of Chicago. Because patients are more likely to identify a hospitalist if they understand the hospitalist has a relationship with their primary-care physician (PCP), the initial greeting should be stated clearly, slowly, and include a reference to the PCP.
“After providing your name, you can say something like, ‘I see you’re Dr. Smith’s patient. I’ve worked with Dr. Smith for many years. We’ll make sure we communicate what happens during your hospitalization. I hope to develop a good relationship with you while you’re in the hospital,’” Dr. Meltzer says.
The hospitalist team should also consider providing brochures with photos of the hospitalists and an explanation of what hospitalists do, says Michael Pistoria, DO, FACP, SFHM, associate chief of the division of general internal medicine at Lehigh Valley Health Network in Allentown, Pa.
“Brochures can be handed to patients at the time of admission with the hospitalist explaining, ‘I’m going to be the doctor in charge of coordinating your care,’” he explains.
Mind Over Matter
Scenario: A hospitalist explains to the patient that her illness is getting worse and more aggressive treatment is advised. While reviewing treatment options, the hospitalist notices the patient is staring out the window, her chin quivering. The hospitalist presses on with what she has to say.
The patient can hear the hospitalist talking, but she’s thinking about how this setback will affect her family. She’s doing all she can to keep from crying and nods her head out of politeness to feign understanding of the information being provided.
Skill: Acknowledging patient emotion is imperative, because doctors who ignore these signals do so at their own professional peril, says Anthony Back, MD, professor of medicine at the University of Washington in Seattle.
“The way our brains are built, emotion will trump cognition every time,” he says. “If you as the doctor keep talking when someone is having an emotional moment, they will generally miss all the information you provided.
“If you see the patient has a lot of emotion, you can say, ‘I notice you are really concerned about this. Can you tell me more?’” Dr. Back says. “Just the act of getting it out in the open will often enable a patient to process the emotion enough so that you can go on to medical issues that are important for the patient to know.”
In most cases, respectfully acknowledging the emotion won’t take long. He says most patients recognize they have limited time with the doctor, and they want to get to the important medical information, too.
It’s Gibberish to Me
Scenario: A hospitalist believes a patient has a solid understanding of his diagnosis. The hospitalist sends the patient for several tests and discusses with him the risks and benefits of various medications and interventions, sometimes using complex terminology.
The patient doesn’t know why he’s had to undergo so many tests. He’s tried to follow along as the hospitalist talks about treatment options and has even asked his daughter to look up medical terminology on her smartphone so he can better understand what is going on. He wishes the hospitalist would explain his condition in basic terms.
Skill: Simplify the language used to communicate with patients by speaking in plain English, says Jeff Greenwald, MD, SFHM, associate professor of medicine at Harvard Medical School and a teaching hospitalist at Massachusetts General Hospital in Boston. Hospitalists should be aware that words and terminology they think are commonplace many times are medical jargon and confusing to patients, he adds.
“For example, when I say ‘take this medication orally,’ that doesn’t strike me as technical language. But ‘orally’ is a word that is not understood by a significant percentage of the population,” Dr. Greenwald says.
A good rule of thumb is to continually check in with patients about the words and terms being used, Dr. Meltzer adds.
“Ask patients if they would like you to explain a term,” he says. “You can say something like, ‘I know this is a term many people aren’t familiar with. Would you like me to tell you more about what it means?’”
—Cindy Lien, MD, academic hospitalist, Beth Israel Deaconess Medical Center, Boston
Data-Dumping
Scenario: A hospitalist checks in on a patient with atrial fibrillation and uses the visit to talk about Coumadin. She instructs the patient on how the drug works in the body, how it increases the chance of bleeding, and how the medication should be taken and monitored.
Later that day, the patient tells her daughter about the hospitalist’s instructions regarding her new medication. The patient remembers that she should avoid certain foods and beverages while on Coumadin but can’t immediately recall what they are. The patient also has trouble recounting what danger signs she should look out for when taking Coumadin.
Skill: Teach-back is an effective tool that can—and should—be used anytime a hospitalist is providing important information to a patient, Dr. Greenwald says. The hospitalist asks the patient to explain back the information in his or her own words in order to determine the patient’s understanding. If errors are identified, the hospitalist can explain the information again to ensure the patient’s comprehension.
“You might say, ‘How are you going to explain to your primary-care doctor about why you’re on an antibiotic?’ or ‘What are you going to tell your son about how your diet has to change?’” Dr. Greenwald says.
He outlines three important elements of teach-back:
- Concentrate on the critical information that patients need to know in order to function;
- Provide information in small bites that the patient can digest; and
- Repeat and reinforce the information with the help of all the members of the care team.
Teach-back should be used consistently, he says, so hospitalists can build on the information taught previously by adding layers to the patient’s knowledge.
Lisa Ryan is a freelance writer in New Jersey.
Hospitalists coordinate the care of large numbers of very sick, very complicated patients, making patient-hospitalist communication very important. When done effectively, communication can help hospitalists improve their patients’ sense of well-being and reinforce their adherence to medical treatments post-discharge. It also can build trust and help patients better understand their illnesses.
Nonetheless, communication gaps do occur. The main culprits include time pressures, the lack of a pre-existing patient relationship, patient emotions, medical jargon, and physicians’ tendencies to lecture.
The following five examples outline common communication pitfalls, followed by fundamental skills that can be used to solve communication problems.
Tick, Tock Goes the Clock
Scenario: A hospitalist mentions a medication change during a brief patient visit in the midst of a hectic day. The hospitalist pauses for a moment, glances at his watch, and reaches for the room’s door handle. When no question is forthcoming, he excuses himself to visit the next patient.
The patient has questions about the new medication but feels guilty about taking up the hospitalist’s time. The patient decides she can ask about the medication and the reason for the change when the hospitalist isn’t in such a hurry.
Skill: Creating an environment in which patients are encouraged to ask questions need not result in lengthy conversations. The key is having a clear framework for directing conversations, says Cindy Lien, MD, an academic hospitalist at Beth Israel Deaconess Medical Center in Boston. Dr. Lien uses “Ask-Tell-Ask” as a mnemonic when teaching communication skills to internal-medicine trainees.
“We have a tendency to just tell, tell, tell information,” she says. “Ask-Tell-Ask reminds you that one of the most important things to do is to ask the patient to describe what their understanding is of the situation so you have a sense of where they’re coming from.”
Opening questions can include “What is the most important issue on your mind today?” and “What do you understand about your medications?”
After listening to the patient’s response, tell the patient in a few straightforward sentences the information you need to communicate, Dr. Lien says. Then ask the patient if they understand the information conveyed to them, which will give them a chance to ask questions. Additional questions for the patient can include “Do you need further information at this point?” and “How do you feel about what we’ve discussed?”

—Anthony Back, MD, professor of medicine, University of Washington, Seattle
What’s Your Name Again?
Scenario: A hospitalist wearing professional dress with no nametag enters a patient room and introduces herself before informing the patient that she’s ordered additional tests. The hospitalist visits the patient several times during his hospital stay to discuss test results and self-care instructions upon discharge but never reintroduces herself.
The patient was exhausted and in discomfort when the clinician first introduced herself as a hospitalist. She said her name so quickly that the patient didn’t catch it. The patient sees the hospitalist more often than other providers during his admission, but he’s not sure what her role is and he finds it too awkward to ask.
Skill: First impressions are lasting, so make a solid introduction, says David Meltzer, MD, PhD, FHM, associate professor in the department of medicine at the University of Chicago. Because patients are more likely to identify a hospitalist if they understand the hospitalist has a relationship with their primary-care physician (PCP), the initial greeting should be stated clearly, slowly, and include a reference to the PCP.
“After providing your name, you can say something like, ‘I see you’re Dr. Smith’s patient. I’ve worked with Dr. Smith for many years. We’ll make sure we communicate what happens during your hospitalization. I hope to develop a good relationship with you while you’re in the hospital,’” Dr. Meltzer says.
The hospitalist team should also consider providing brochures with photos of the hospitalists and an explanation of what hospitalists do, says Michael Pistoria, DO, FACP, SFHM, associate chief of the division of general internal medicine at Lehigh Valley Health Network in Allentown, Pa.
“Brochures can be handed to patients at the time of admission with the hospitalist explaining, ‘I’m going to be the doctor in charge of coordinating your care,’” he explains.
Mind Over Matter
Scenario: A hospitalist explains to the patient that her illness is getting worse and more aggressive treatment is advised. While reviewing treatment options, the hospitalist notices the patient is staring out the window, her chin quivering. The hospitalist presses on with what she has to say.
The patient can hear the hospitalist talking, but she’s thinking about how this setback will affect her family. She’s doing all she can to keep from crying and nods her head out of politeness to feign understanding of the information being provided.
Skill: Acknowledging patient emotion is imperative, because doctors who ignore these signals do so at their own professional peril, says Anthony Back, MD, professor of medicine at the University of Washington in Seattle.
“The way our brains are built, emotion will trump cognition every time,” he says. “If you as the doctor keep talking when someone is having an emotional moment, they will generally miss all the information you provided.
“If you see the patient has a lot of emotion, you can say, ‘I notice you are really concerned about this. Can you tell me more?’” Dr. Back says. “Just the act of getting it out in the open will often enable a patient to process the emotion enough so that you can go on to medical issues that are important for the patient to know.”
In most cases, respectfully acknowledging the emotion won’t take long. He says most patients recognize they have limited time with the doctor, and they want to get to the important medical information, too.
It’s Gibberish to Me
Scenario: A hospitalist believes a patient has a solid understanding of his diagnosis. The hospitalist sends the patient for several tests and discusses with him the risks and benefits of various medications and interventions, sometimes using complex terminology.
The patient doesn’t know why he’s had to undergo so many tests. He’s tried to follow along as the hospitalist talks about treatment options and has even asked his daughter to look up medical terminology on her smartphone so he can better understand what is going on. He wishes the hospitalist would explain his condition in basic terms.
Skill: Simplify the language used to communicate with patients by speaking in plain English, says Jeff Greenwald, MD, SFHM, associate professor of medicine at Harvard Medical School and a teaching hospitalist at Massachusetts General Hospital in Boston. Hospitalists should be aware that words and terminology they think are commonplace many times are medical jargon and confusing to patients, he adds.
“For example, when I say ‘take this medication orally,’ that doesn’t strike me as technical language. But ‘orally’ is a word that is not understood by a significant percentage of the population,” Dr. Greenwald says.
A good rule of thumb is to continually check in with patients about the words and terms being used, Dr. Meltzer adds.
“Ask patients if they would like you to explain a term,” he says. “You can say something like, ‘I know this is a term many people aren’t familiar with. Would you like me to tell you more about what it means?’”
—Cindy Lien, MD, academic hospitalist, Beth Israel Deaconess Medical Center, Boston
Data-Dumping
Scenario: A hospitalist checks in on a patient with atrial fibrillation and uses the visit to talk about Coumadin. She instructs the patient on how the drug works in the body, how it increases the chance of bleeding, and how the medication should be taken and monitored.
Later that day, the patient tells her daughter about the hospitalist’s instructions regarding her new medication. The patient remembers that she should avoid certain foods and beverages while on Coumadin but can’t immediately recall what they are. The patient also has trouble recounting what danger signs she should look out for when taking Coumadin.
Skill: Teach-back is an effective tool that can—and should—be used anytime a hospitalist is providing important information to a patient, Dr. Greenwald says. The hospitalist asks the patient to explain back the information in his or her own words in order to determine the patient’s understanding. If errors are identified, the hospitalist can explain the information again to ensure the patient’s comprehension.
“You might say, ‘How are you going to explain to your primary-care doctor about why you’re on an antibiotic?’ or ‘What are you going to tell your son about how your diet has to change?’” Dr. Greenwald says.
He outlines three important elements of teach-back:
- Concentrate on the critical information that patients need to know in order to function;
- Provide information in small bites that the patient can digest; and
- Repeat and reinforce the information with the help of all the members of the care team.
Teach-back should be used consistently, he says, so hospitalists can build on the information taught previously by adding layers to the patient’s knowledge.
Lisa Ryan is a freelance writer in New Jersey.
Hospitalists coordinate the care of large numbers of very sick, very complicated patients, making patient-hospitalist communication very important. When done effectively, communication can help hospitalists improve their patients’ sense of well-being and reinforce their adherence to medical treatments post-discharge. It also can build trust and help patients better understand their illnesses.
Nonetheless, communication gaps do occur. The main culprits include time pressures, the lack of a pre-existing patient relationship, patient emotions, medical jargon, and physicians’ tendencies to lecture.
The following five examples outline common communication pitfalls, followed by fundamental skills that can be used to solve communication problems.
Tick, Tock Goes the Clock
Scenario: A hospitalist mentions a medication change during a brief patient visit in the midst of a hectic day. The hospitalist pauses for a moment, glances at his watch, and reaches for the room’s door handle. When no question is forthcoming, he excuses himself to visit the next patient.
The patient has questions about the new medication but feels guilty about taking up the hospitalist’s time. The patient decides she can ask about the medication and the reason for the change when the hospitalist isn’t in such a hurry.
Skill: Creating an environment in which patients are encouraged to ask questions need not result in lengthy conversations. The key is having a clear framework for directing conversations, says Cindy Lien, MD, an academic hospitalist at Beth Israel Deaconess Medical Center in Boston. Dr. Lien uses “Ask-Tell-Ask” as a mnemonic when teaching communication skills to internal-medicine trainees.
“We have a tendency to just tell, tell, tell information,” she says. “Ask-Tell-Ask reminds you that one of the most important things to do is to ask the patient to describe what their understanding is of the situation so you have a sense of where they’re coming from.”
Opening questions can include “What is the most important issue on your mind today?” and “What do you understand about your medications?”
After listening to the patient’s response, tell the patient in a few straightforward sentences the information you need to communicate, Dr. Lien says. Then ask the patient if they understand the information conveyed to them, which will give them a chance to ask questions. Additional questions for the patient can include “Do you need further information at this point?” and “How do you feel about what we’ve discussed?”

—Anthony Back, MD, professor of medicine, University of Washington, Seattle
What’s Your Name Again?
Scenario: A hospitalist wearing professional dress with no nametag enters a patient room and introduces herself before informing the patient that she’s ordered additional tests. The hospitalist visits the patient several times during his hospital stay to discuss test results and self-care instructions upon discharge but never reintroduces herself.
The patient was exhausted and in discomfort when the clinician first introduced herself as a hospitalist. She said her name so quickly that the patient didn’t catch it. The patient sees the hospitalist more often than other providers during his admission, but he’s not sure what her role is and he finds it too awkward to ask.
Skill: First impressions are lasting, so make a solid introduction, says David Meltzer, MD, PhD, FHM, associate professor in the department of medicine at the University of Chicago. Because patients are more likely to identify a hospitalist if they understand the hospitalist has a relationship with their primary-care physician (PCP), the initial greeting should be stated clearly, slowly, and include a reference to the PCP.
“After providing your name, you can say something like, ‘I see you’re Dr. Smith’s patient. I’ve worked with Dr. Smith for many years. We’ll make sure we communicate what happens during your hospitalization. I hope to develop a good relationship with you while you’re in the hospital,’” Dr. Meltzer says.
The hospitalist team should also consider providing brochures with photos of the hospitalists and an explanation of what hospitalists do, says Michael Pistoria, DO, FACP, SFHM, associate chief of the division of general internal medicine at Lehigh Valley Health Network in Allentown, Pa.
“Brochures can be handed to patients at the time of admission with the hospitalist explaining, ‘I’m going to be the doctor in charge of coordinating your care,’” he explains.
Mind Over Matter
Scenario: A hospitalist explains to the patient that her illness is getting worse and more aggressive treatment is advised. While reviewing treatment options, the hospitalist notices the patient is staring out the window, her chin quivering. The hospitalist presses on with what she has to say.
The patient can hear the hospitalist talking, but she’s thinking about how this setback will affect her family. She’s doing all she can to keep from crying and nods her head out of politeness to feign understanding of the information being provided.
Skill: Acknowledging patient emotion is imperative, because doctors who ignore these signals do so at their own professional peril, says Anthony Back, MD, professor of medicine at the University of Washington in Seattle.
“The way our brains are built, emotion will trump cognition every time,” he says. “If you as the doctor keep talking when someone is having an emotional moment, they will generally miss all the information you provided.
“If you see the patient has a lot of emotion, you can say, ‘I notice you are really concerned about this. Can you tell me more?’” Dr. Back says. “Just the act of getting it out in the open will often enable a patient to process the emotion enough so that you can go on to medical issues that are important for the patient to know.”
In most cases, respectfully acknowledging the emotion won’t take long. He says most patients recognize they have limited time with the doctor, and they want to get to the important medical information, too.
It’s Gibberish to Me
Scenario: A hospitalist believes a patient has a solid understanding of his diagnosis. The hospitalist sends the patient for several tests and discusses with him the risks and benefits of various medications and interventions, sometimes using complex terminology.
The patient doesn’t know why he’s had to undergo so many tests. He’s tried to follow along as the hospitalist talks about treatment options and has even asked his daughter to look up medical terminology on her smartphone so he can better understand what is going on. He wishes the hospitalist would explain his condition in basic terms.
Skill: Simplify the language used to communicate with patients by speaking in plain English, says Jeff Greenwald, MD, SFHM, associate professor of medicine at Harvard Medical School and a teaching hospitalist at Massachusetts General Hospital in Boston. Hospitalists should be aware that words and terminology they think are commonplace many times are medical jargon and confusing to patients, he adds.
“For example, when I say ‘take this medication orally,’ that doesn’t strike me as technical language. But ‘orally’ is a word that is not understood by a significant percentage of the population,” Dr. Greenwald says.
A good rule of thumb is to continually check in with patients about the words and terms being used, Dr. Meltzer adds.
“Ask patients if they would like you to explain a term,” he says. “You can say something like, ‘I know this is a term many people aren’t familiar with. Would you like me to tell you more about what it means?’”
—Cindy Lien, MD, academic hospitalist, Beth Israel Deaconess Medical Center, Boston
Data-Dumping
Scenario: A hospitalist checks in on a patient with atrial fibrillation and uses the visit to talk about Coumadin. She instructs the patient on how the drug works in the body, how it increases the chance of bleeding, and how the medication should be taken and monitored.
Later that day, the patient tells her daughter about the hospitalist’s instructions regarding her new medication. The patient remembers that she should avoid certain foods and beverages while on Coumadin but can’t immediately recall what they are. The patient also has trouble recounting what danger signs she should look out for when taking Coumadin.
Skill: Teach-back is an effective tool that can—and should—be used anytime a hospitalist is providing important information to a patient, Dr. Greenwald says. The hospitalist asks the patient to explain back the information in his or her own words in order to determine the patient’s understanding. If errors are identified, the hospitalist can explain the information again to ensure the patient’s comprehension.
“You might say, ‘How are you going to explain to your primary-care doctor about why you’re on an antibiotic?’ or ‘What are you going to tell your son about how your diet has to change?’” Dr. Greenwald says.
He outlines three important elements of teach-back:
- Concentrate on the critical information that patients need to know in order to function;
- Provide information in small bites that the patient can digest; and
- Repeat and reinforce the information with the help of all the members of the care team.
Teach-back should be used consistently, he says, so hospitalists can build on the information taught previously by adding layers to the patient’s knowledge.
Lisa Ryan is a freelance writer in New Jersey.
Palliative-Care-Focused Hospitalist Appreciates Training the Next Generation
Chithra Perumalswami, MD, knew early on what she wanted to do with her life. As a teenager, she volunteered in an ED and with a hospice group, volunteerism that continued throughout her education. When she graduated from high school, she was tapped for Brown University’s Program in Liberal Medical Education, which calls itself the only baccalaureate-MD program in the Ivy League. And though she eventually turned down the offer, she pursued dual majors in cellular and molecular biology and English at the University of Michigan, where she earned her medical degree in 2004 and completed her residency.
In 2009, she participated in the Palliative Care Education and Practice Program at Harvard Medical School in Boston, a two-week post-graduate course aimed at professional development for physicians dedicated to careers in palliative-care education. “I really found that there were just so many aspects to caring for a patient as a palliative-care specialist and as a hospitalist that really strike at the heart of what being a doctor is,” says Dr. Perumalswami, assistant professor of medicine in the Division of Hospital Medicine at Northwestern Memorial Hospital in Chicago and one of four new members of Team Hospitalist. “I think it’s been an interest I’ve always had. During my residency training, I definitely experienced quite a few patient cases where I felt that we really needed to help patients and their families, and I didn’t necessarily have the best skill set to do that until I had more experience and more training.”
Dr. Perumalswami now wants to get better at her craft.
“As an academic hospitalist, it’s not just about doing research and writing papers and seeing papers,” she says, “but it’s also developing those leadership skills and helping that become an integral part of the educational experience.”
Question: What drew you to a career in HM?
Answer: I chose a career in academic hospital medicine primarily because I enjoy taking care of acutely ill, hospitalized, adult patients. I also really enjoy teaching medical students, residents, and fellows, and I enjoy doing that in the hospital setting. I think that there’s great satisfaction from taking care of a patient from admission to discharge.… I enjoyed every aspect of internal medicine, and when I graduated, I thought I could choose a subspecialty, but I felt that my skills and my expertise was really in taking care of the hospitalized patient.
Q: You have sought out extra training in palliative care and pain management. How has that impacted your career?
A: It’s not something that I necessarily started out thinking that I would specialize in, but the more I took care of hospitalized patients, the more I realized that we actually take care of a fair number of patients who have really complex symptom needs, and also really have a lot of needs with regard to recognizing when their prognosis is poor and understanding what their options are, if they’re even amenable to a palliative approach. I really felt that that was a skill that I needed to fine-tune. So I ended up gaining enough clinical experience and participating with hospice patients to the point where that’s really supplemented my hospitalist career, because what I found is that it’s made me a better hospitalist, and being a hospitalist has made me a better palliative-care doc.
Q: Working in academia, there’s no way to escape talk of the duty-hour rules recently put in place. What’s your view on the issue?
A: My view is that the work hours are here to stay. I think that there are some definite benefits that we’ve gained from having work hours. I’d say first and foremost of those gains is public trust. I think most physicians will tell you that they don’t want a physician who’s in the 36th hour of their day taking care of them when we know that studies actually can demonstrate that when you’ve been awake that long, that your cognitive abilities decline.
Q: But?
A: I think we have a lot of challenges, though, because a lot of things require creative solutions. And I think the first on that list is education, because that’s the first thing that I think has the potential to drop to the bottom of the list.
Q: In terms of HM’s growth, as you see residents coming through your program, how popular do you think the model is going to be with them moving forward?
A: I do, actually, because as an academic hospitalist, I’ve had several medical students and residents tell me, “Watching you, I think that I want to go into this field.” Or they’ll say, “What do you think about doing this for a year or two?” Or, “What do you think about subspecializing, and then being a hospitalist?” And my answer to all of them is it’s a dynamic specialty, and if you’re up for creating change and being a leader, it’s a good field, because we need people in a lot of different buckets, so to speak. We need people who have done other things in their career to contribute to our field.
Q: How do you prepare trainees for all the challenges coming down the pike?
A: A lot of the people who are doing work in medical education are starting to look to other fields to see if there are other models that we can adapt, or that we can somehow absorb into our practice. I think that there are some parts of our education which are not really formalized early on, but I think we have a lot to learn from organizational behavior circles, and systems that actually look at teams and leadership.
Q: What do the next five to 10 years hold for you?
A: All physician leaders have to stay somewhat in the clinical world. I think if you lose sight of that, you can’t be a very effective leader, or a very effective agent for change. Because part of my work is with palliative care, and I really feel that it’s affected my work as a hospitalist in a positive way, I don’t think I ever see myself leaving the clinical world completely. But I do see myself becoming, ideally, more involved with leadership and more involved with helping to train the next set of leaders.
Q: What do you see as SHM’s role specific to academic HM?
A: HM is changing the way healthcare is delivered in the U.S., and I think having an organization to represent us is vital to our success in other arenas of change—including healthcare policy and innovative care models. I see SHM as a large umbrella group, of which academic HM is one part. Academic hospitalists are increasingly involved in the education of future generations of physicians, and are uniquely poised for facilitating cascading leadership. The traditional, hierarchical model of attending-fellow-resident-medical student is shifting, and academic hospitalists are well-suited to study and explore this leadership structure and how it affects patient care, feedback, and mentoring.
Richard Quinn is a freelance writer based in New Jersey.
Chithra Perumalswami, MD, knew early on what she wanted to do with her life. As a teenager, she volunteered in an ED and with a hospice group, volunteerism that continued throughout her education. When she graduated from high school, she was tapped for Brown University’s Program in Liberal Medical Education, which calls itself the only baccalaureate-MD program in the Ivy League. And though she eventually turned down the offer, she pursued dual majors in cellular and molecular biology and English at the University of Michigan, where she earned her medical degree in 2004 and completed her residency.
In 2009, she participated in the Palliative Care Education and Practice Program at Harvard Medical School in Boston, a two-week post-graduate course aimed at professional development for physicians dedicated to careers in palliative-care education. “I really found that there were just so many aspects to caring for a patient as a palliative-care specialist and as a hospitalist that really strike at the heart of what being a doctor is,” says Dr. Perumalswami, assistant professor of medicine in the Division of Hospital Medicine at Northwestern Memorial Hospital in Chicago and one of four new members of Team Hospitalist. “I think it’s been an interest I’ve always had. During my residency training, I definitely experienced quite a few patient cases where I felt that we really needed to help patients and their families, and I didn’t necessarily have the best skill set to do that until I had more experience and more training.”
Dr. Perumalswami now wants to get better at her craft.
“As an academic hospitalist, it’s not just about doing research and writing papers and seeing papers,” she says, “but it’s also developing those leadership skills and helping that become an integral part of the educational experience.”
Question: What drew you to a career in HM?
Answer: I chose a career in academic hospital medicine primarily because I enjoy taking care of acutely ill, hospitalized, adult patients. I also really enjoy teaching medical students, residents, and fellows, and I enjoy doing that in the hospital setting. I think that there’s great satisfaction from taking care of a patient from admission to discharge.… I enjoyed every aspect of internal medicine, and when I graduated, I thought I could choose a subspecialty, but I felt that my skills and my expertise was really in taking care of the hospitalized patient.
Q: You have sought out extra training in palliative care and pain management. How has that impacted your career?
A: It’s not something that I necessarily started out thinking that I would specialize in, but the more I took care of hospitalized patients, the more I realized that we actually take care of a fair number of patients who have really complex symptom needs, and also really have a lot of needs with regard to recognizing when their prognosis is poor and understanding what their options are, if they’re even amenable to a palliative approach. I really felt that that was a skill that I needed to fine-tune. So I ended up gaining enough clinical experience and participating with hospice patients to the point where that’s really supplemented my hospitalist career, because what I found is that it’s made me a better hospitalist, and being a hospitalist has made me a better palliative-care doc.
Q: Working in academia, there’s no way to escape talk of the duty-hour rules recently put in place. What’s your view on the issue?
A: My view is that the work hours are here to stay. I think that there are some definite benefits that we’ve gained from having work hours. I’d say first and foremost of those gains is public trust. I think most physicians will tell you that they don’t want a physician who’s in the 36th hour of their day taking care of them when we know that studies actually can demonstrate that when you’ve been awake that long, that your cognitive abilities decline.
Q: But?
A: I think we have a lot of challenges, though, because a lot of things require creative solutions. And I think the first on that list is education, because that’s the first thing that I think has the potential to drop to the bottom of the list.
Q: In terms of HM’s growth, as you see residents coming through your program, how popular do you think the model is going to be with them moving forward?
A: I do, actually, because as an academic hospitalist, I’ve had several medical students and residents tell me, “Watching you, I think that I want to go into this field.” Or they’ll say, “What do you think about doing this for a year or two?” Or, “What do you think about subspecializing, and then being a hospitalist?” And my answer to all of them is it’s a dynamic specialty, and if you’re up for creating change and being a leader, it’s a good field, because we need people in a lot of different buckets, so to speak. We need people who have done other things in their career to contribute to our field.
Q: How do you prepare trainees for all the challenges coming down the pike?
A: A lot of the people who are doing work in medical education are starting to look to other fields to see if there are other models that we can adapt, or that we can somehow absorb into our practice. I think that there are some parts of our education which are not really formalized early on, but I think we have a lot to learn from organizational behavior circles, and systems that actually look at teams and leadership.
Q: What do the next five to 10 years hold for you?
A: All physician leaders have to stay somewhat in the clinical world. I think if you lose sight of that, you can’t be a very effective leader, or a very effective agent for change. Because part of my work is with palliative care, and I really feel that it’s affected my work as a hospitalist in a positive way, I don’t think I ever see myself leaving the clinical world completely. But I do see myself becoming, ideally, more involved with leadership and more involved with helping to train the next set of leaders.
Q: What do you see as SHM’s role specific to academic HM?
A: HM is changing the way healthcare is delivered in the U.S., and I think having an organization to represent us is vital to our success in other arenas of change—including healthcare policy and innovative care models. I see SHM as a large umbrella group, of which academic HM is one part. Academic hospitalists are increasingly involved in the education of future generations of physicians, and are uniquely poised for facilitating cascading leadership. The traditional, hierarchical model of attending-fellow-resident-medical student is shifting, and academic hospitalists are well-suited to study and explore this leadership structure and how it affects patient care, feedback, and mentoring.
Richard Quinn is a freelance writer based in New Jersey.
Chithra Perumalswami, MD, knew early on what she wanted to do with her life. As a teenager, she volunteered in an ED and with a hospice group, volunteerism that continued throughout her education. When she graduated from high school, she was tapped for Brown University’s Program in Liberal Medical Education, which calls itself the only baccalaureate-MD program in the Ivy League. And though she eventually turned down the offer, she pursued dual majors in cellular and molecular biology and English at the University of Michigan, where she earned her medical degree in 2004 and completed her residency.
In 2009, she participated in the Palliative Care Education and Practice Program at Harvard Medical School in Boston, a two-week post-graduate course aimed at professional development for physicians dedicated to careers in palliative-care education. “I really found that there were just so many aspects to caring for a patient as a palliative-care specialist and as a hospitalist that really strike at the heart of what being a doctor is,” says Dr. Perumalswami, assistant professor of medicine in the Division of Hospital Medicine at Northwestern Memorial Hospital in Chicago and one of four new members of Team Hospitalist. “I think it’s been an interest I’ve always had. During my residency training, I definitely experienced quite a few patient cases where I felt that we really needed to help patients and their families, and I didn’t necessarily have the best skill set to do that until I had more experience and more training.”
Dr. Perumalswami now wants to get better at her craft.
“As an academic hospitalist, it’s not just about doing research and writing papers and seeing papers,” she says, “but it’s also developing those leadership skills and helping that become an integral part of the educational experience.”
Question: What drew you to a career in HM?
Answer: I chose a career in academic hospital medicine primarily because I enjoy taking care of acutely ill, hospitalized, adult patients. I also really enjoy teaching medical students, residents, and fellows, and I enjoy doing that in the hospital setting. I think that there’s great satisfaction from taking care of a patient from admission to discharge.… I enjoyed every aspect of internal medicine, and when I graduated, I thought I could choose a subspecialty, but I felt that my skills and my expertise was really in taking care of the hospitalized patient.
Q: You have sought out extra training in palliative care and pain management. How has that impacted your career?
A: It’s not something that I necessarily started out thinking that I would specialize in, but the more I took care of hospitalized patients, the more I realized that we actually take care of a fair number of patients who have really complex symptom needs, and also really have a lot of needs with regard to recognizing when their prognosis is poor and understanding what their options are, if they’re even amenable to a palliative approach. I really felt that that was a skill that I needed to fine-tune. So I ended up gaining enough clinical experience and participating with hospice patients to the point where that’s really supplemented my hospitalist career, because what I found is that it’s made me a better hospitalist, and being a hospitalist has made me a better palliative-care doc.
Q: Working in academia, there’s no way to escape talk of the duty-hour rules recently put in place. What’s your view on the issue?
A: My view is that the work hours are here to stay. I think that there are some definite benefits that we’ve gained from having work hours. I’d say first and foremost of those gains is public trust. I think most physicians will tell you that they don’t want a physician who’s in the 36th hour of their day taking care of them when we know that studies actually can demonstrate that when you’ve been awake that long, that your cognitive abilities decline.
Q: But?
A: I think we have a lot of challenges, though, because a lot of things require creative solutions. And I think the first on that list is education, because that’s the first thing that I think has the potential to drop to the bottom of the list.
Q: In terms of HM’s growth, as you see residents coming through your program, how popular do you think the model is going to be with them moving forward?
A: I do, actually, because as an academic hospitalist, I’ve had several medical students and residents tell me, “Watching you, I think that I want to go into this field.” Or they’ll say, “What do you think about doing this for a year or two?” Or, “What do you think about subspecializing, and then being a hospitalist?” And my answer to all of them is it’s a dynamic specialty, and if you’re up for creating change and being a leader, it’s a good field, because we need people in a lot of different buckets, so to speak. We need people who have done other things in their career to contribute to our field.
Q: How do you prepare trainees for all the challenges coming down the pike?
A: A lot of the people who are doing work in medical education are starting to look to other fields to see if there are other models that we can adapt, or that we can somehow absorb into our practice. I think that there are some parts of our education which are not really formalized early on, but I think we have a lot to learn from organizational behavior circles, and systems that actually look at teams and leadership.
Q: What do the next five to 10 years hold for you?
A: All physician leaders have to stay somewhat in the clinical world. I think if you lose sight of that, you can’t be a very effective leader, or a very effective agent for change. Because part of my work is with palliative care, and I really feel that it’s affected my work as a hospitalist in a positive way, I don’t think I ever see myself leaving the clinical world completely. But I do see myself becoming, ideally, more involved with leadership and more involved with helping to train the next set of leaders.
Q: What do you see as SHM’s role specific to academic HM?
A: HM is changing the way healthcare is delivered in the U.S., and I think having an organization to represent us is vital to our success in other arenas of change—including healthcare policy and innovative care models. I see SHM as a large umbrella group, of which academic HM is one part. Academic hospitalists are increasingly involved in the education of future generations of physicians, and are uniquely poised for facilitating cascading leadership. The traditional, hierarchical model of attending-fellow-resident-medical student is shifting, and academic hospitalists are well-suited to study and explore this leadership structure and how it affects patient care, feedback, and mentoring.
Richard Quinn is a freelance writer based in New Jersey.
OB/GYN Hospitalists Emerge as a Specialty
The OB/GYN hospitalist field is growing, with at least 164 identified programs and 1,500 to 2,500 practitioners who spend all or part of their workweek in hospital labor and delivery departments. SHM and the American College of Obstetricians and Gynecologists helped birth the 90-member Society of OB/GYN Hospitalists in 2011, but it is now independent, says founding president Rob Olson, MD, an OB/GYN hospitalist practicing in Bellingham, Wash. The fledgling society is planning its second annual conference, Sept. 27-29 in Denver, with obstetric emergency simulation training, clinical lectures, and pearls from the experience of general hospitalist practice by HM pioneer John Nelson, MD, MHM.
Also known as laborists, these board-certified OB/GYN docs’ dedicated presence affords rapid on-site response to changes in patients’ conditions, Dr. Olson says. Laborists might cover nights and weekends, pick up unassigned patients, or cover for private obstetricians who are fully engaged. Laborists do not supplant the private practitioner’s role in delivering babies in the hospital, Dr. Olson says, “unless the private physician asks them to,” which, he adds, is happening more often.
Laborists typically are limited to labor and delivery services, although some also address gynecological cases in the ED. Most of the programs provide coverage 24/7, and invariably they are in facilities with medical hospitalists who might consult on medical complications for expectant mothers. One to two new programs open every month, Dr. Olson says, and his website lists 120 job openings. For information, visit www.ObGynHospitalist.com.
The OB/GYN hospitalist field is growing, with at least 164 identified programs and 1,500 to 2,500 practitioners who spend all or part of their workweek in hospital labor and delivery departments. SHM and the American College of Obstetricians and Gynecologists helped birth the 90-member Society of OB/GYN Hospitalists in 2011, but it is now independent, says founding president Rob Olson, MD, an OB/GYN hospitalist practicing in Bellingham, Wash. The fledgling society is planning its second annual conference, Sept. 27-29 in Denver, with obstetric emergency simulation training, clinical lectures, and pearls from the experience of general hospitalist practice by HM pioneer John Nelson, MD, MHM.
Also known as laborists, these board-certified OB/GYN docs’ dedicated presence affords rapid on-site response to changes in patients’ conditions, Dr. Olson says. Laborists might cover nights and weekends, pick up unassigned patients, or cover for private obstetricians who are fully engaged. Laborists do not supplant the private practitioner’s role in delivering babies in the hospital, Dr. Olson says, “unless the private physician asks them to,” which, he adds, is happening more often.
Laborists typically are limited to labor and delivery services, although some also address gynecological cases in the ED. Most of the programs provide coverage 24/7, and invariably they are in facilities with medical hospitalists who might consult on medical complications for expectant mothers. One to two new programs open every month, Dr. Olson says, and his website lists 120 job openings. For information, visit www.ObGynHospitalist.com.
The OB/GYN hospitalist field is growing, with at least 164 identified programs and 1,500 to 2,500 practitioners who spend all or part of their workweek in hospital labor and delivery departments. SHM and the American College of Obstetricians and Gynecologists helped birth the 90-member Society of OB/GYN Hospitalists in 2011, but it is now independent, says founding president Rob Olson, MD, an OB/GYN hospitalist practicing in Bellingham, Wash. The fledgling society is planning its second annual conference, Sept. 27-29 in Denver, with obstetric emergency simulation training, clinical lectures, and pearls from the experience of general hospitalist practice by HM pioneer John Nelson, MD, MHM.
Also known as laborists, these board-certified OB/GYN docs’ dedicated presence affords rapid on-site response to changes in patients’ conditions, Dr. Olson says. Laborists might cover nights and weekends, pick up unassigned patients, or cover for private obstetricians who are fully engaged. Laborists do not supplant the private practitioner’s role in delivering babies in the hospital, Dr. Olson says, “unless the private physician asks them to,” which, he adds, is happening more often.
Laborists typically are limited to labor and delivery services, although some also address gynecological cases in the ED. Most of the programs provide coverage 24/7, and invariably they are in facilities with medical hospitalists who might consult on medical complications for expectant mothers. One to two new programs open every month, Dr. Olson says, and his website lists 120 job openings. For information, visit www.ObGynHospitalist.com.