User login
Concurrent Atopic Dermatitis and Psoriasis Successfully Treated With Dual Biologic Therapy
Atopic dermatitis (AD) and psoriasis are common skin diseases in which dysfunction of the epidermal barrier leads to skin inflammation and altered expression of proinflammatory cytokines.1 There often is overlap in the clinical and histopathologic features of AD and psoriasis, which can make diagnosis a challenge. Persistent late-stage AD can present with psoriasiform lichenified changes, and psoriasis lesions in the acute stage can have an eczematous appearance.2 Histologically, chronic psoriasis lesions share many overlapping features with AD, and some subsets of AD with IL-17 predominance (ie, intrinsic, pediatric, presentation in Asian patients) exhibit a psoriasiform appearance.3,4
Atopic dermatitis and psoriasis are considered 2 distinct conditions because AD is a helper T cell (TH2)–driven disease with subsequent overproduction of IL-4 and IL-13 and psoriasis is a TH17 cell–driven disease with overproduction of IL-173; however, the shared features of AD and psoriasis represent an underlying immunopathological spectrum2,5,6 in which one condition can develop following treatment of the other condition (immunological shift in pathways), both conditions can occur at different times in a patient’s life with alternating cycles of disease flares, or both conditions can coexist as an overlapping syndrome.1,2 A retrospective study from 2012 to 2019 estimated the prevalence of concomitant AD and psoriasis in the United States at 1.3%, with AD following the diagnosis of psoriasis in 67% of cases.1 Concurrent AD and psoriasis—when both diseases flaresimultaneously—is the rarest scenario.2,5
Treatment modalities for AD include topical corticosteroids, which act on immune cells to suppress the release of proinflammatory cytokines, as well as dupilumab, which offers targeted blockade of involved cytokines IL-4 and IL-13. Psoriasis can be treated with multiple immune modulators, including topical corticosteroids and vitamin D analogs, as well as systemic medications that reduce T-cell activation and inflammatory cytokines through targeting of IFN-γ, IL-2, tumor necrosis factor α, IL-17, and IL-23.7,8
We present the case of a patient with long-standing concurrent, treatment-resistant AD and psoriasis who was successfully treated with dual biologic therapy with guselkumab and dupilumab.
Case Report
A 62-year-old woman presented to our dermatology clinic with red itchy scales and painful fissures on the palms, hands, and soles of more than 12 years’ duration. Her medical history included an allergy to amoxicillin-clavulanate as well as an allergy to both dog and cat dander on prick testing. Her family history included dyshidrotic eczema in her mother. A complete blood cell count with differential was within reference range. A shave biopsy of the right dorsal hand performed at the onset of symptoms at an outside facility revealed hyperkeratotic acanthotic epidermis with a mild perivascular lymphocytic infiltrate.
Results of patch testing indicated contact hypersensitivity to the botanical rosin colophonium (or colophony); carba mix (1, 3-diphenylguanidine, zinc dibutyldithiocarbamate, and zinc diethydithiocarbamate); thiuram mix (tetramethylthiuram disulfide, tetramethylthiuram monosulfide, and tetraethylthiuram disulfide); n,n-diphenylguanidine; and tixocortol-21-pivalate. Our patient was given guidance on avoiding these agents, as it was suspected that exposure may be exacerbating the psoriasis. The psoriasis was treated with topical corticosteroids, keratolytics, and calcineurin inhibitors, all of which offered minimal or no relief. Trials of systemic agents, including methotrexate (discontinued because transaminitis developed), etanercept, adalimumab, and apremilast for 6 to 10 months did not provide improvement.

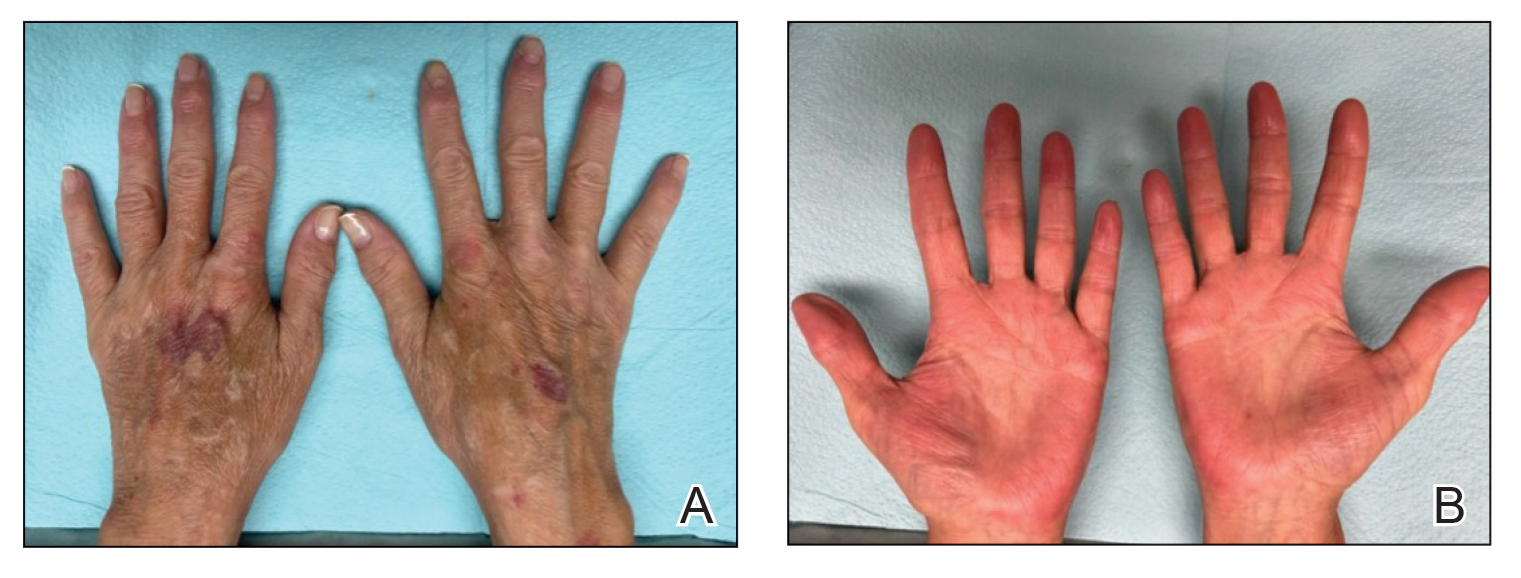
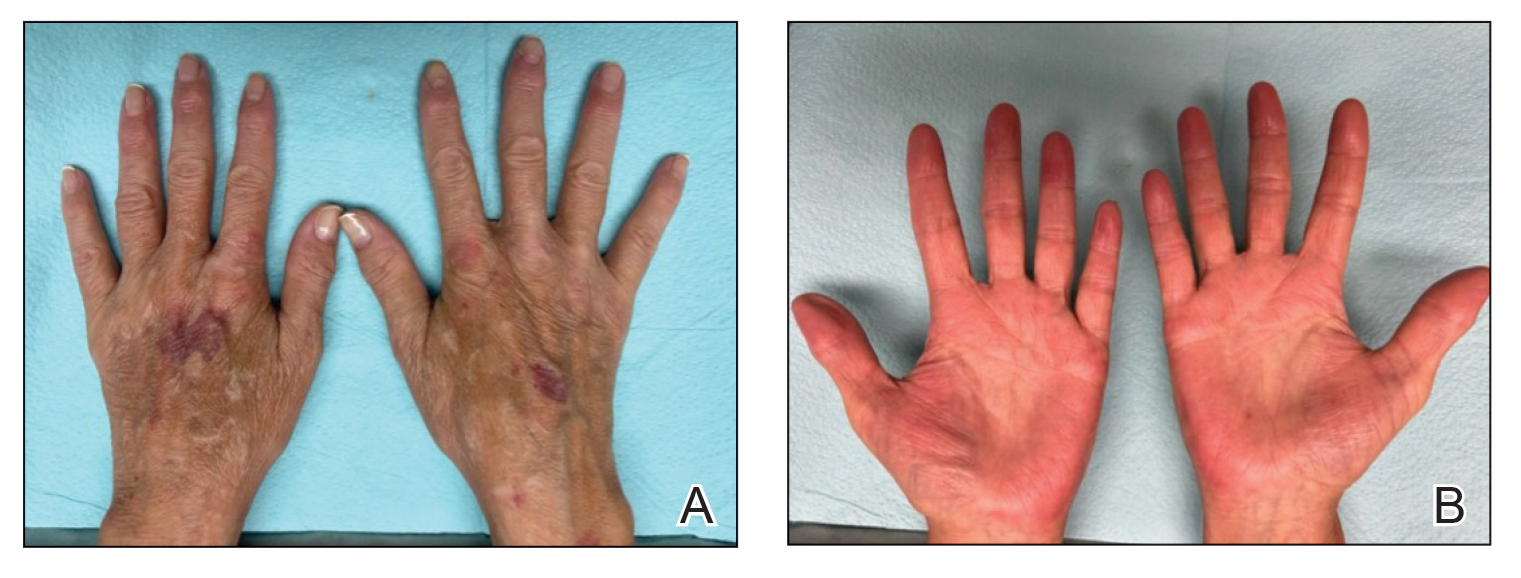
Two years prior to the current presentation, our patient had been treated with the IL-23 inhibitor guselkumab, which provided moderate improvement. When she presented to our clinic, physical examination while she was taking guselkumab demonstrated prurigo with excoriations of the extremities, hyperkeratosis with scaling and fissures of the soles, erythematous scaly plaques on the palms and dorsal surface of the hands, and mild onycholysis of the nails (Figures 1 and 2). Because we were concerned about concomitant intrinsic AD, dupilumab was initiated in conjunction with guselkumab. A second biopsy was considered but deferred in favor of clinical monitoring.
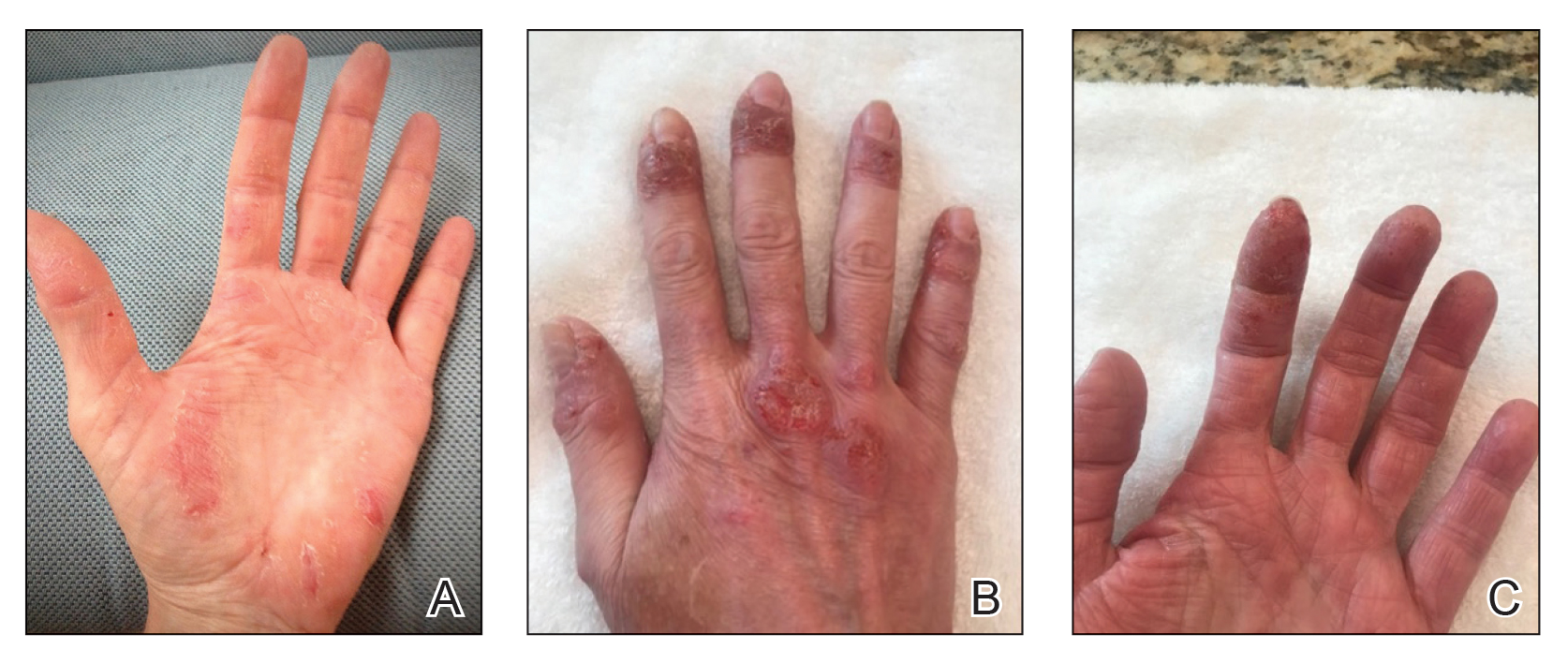
After 1 year of dual biologic therapy, the patient experienced near-complete resolution of symptoms. The psoriasis completely resolved from an initial body surface area of 5%, and the AD body surface area decreased from 30% to 2% (Figure 3). The patient reported no adverse effects from treatment.
Comment
Atopic dermatitis and psoriasis involve complex immunopathology and a spectrum of cytokines that might explain the overlap in their clinical and histopathologic presentations.
Atopic dermatitis—Atopic dermatitis involves TH1, TH2, TH9, TH17, and TH22 cells; TH2 cells release IL-4, IL-5, and IL-13, all of which are key cytokines in the inflammatory pathway of AD.9,10 Activation of the helper T-cell subset and the release of cytokines differ slightly based on the subcategory of AD and the stage of exacerbation. In addition to TH2-cell activation, TH1 cells and TH22 cells—which release IL-12 and IL-22, respectively—are active in both intrinsic and extrinsic AD. TH17 cells and TH9 cells—which release IL-17 and IL-9, respectively—are more prominent in the intrinsic pathway than in the extrinsic pathway.9 Intrinsic AD is recognized by a lack of eosinophilia, female predominance, and delayed onset compared to extrinsic AD; there also is a lack of history of atopy.1 Extrinsic AD is characterized by eosinophilia as well as a personal and family history of atopy.11 Our patient—a female with onset in older adulthood, lack of eosinophilia, and a family history of atopy—displayed features of both intrinsic and extrinsic AD.
Psoriasis—The immunopathology of psoriasis involves stimulation of dendritic cells, which activate TH17 cells through IL-23. TH17 cells then release IL-17 and IL-22. Therefore, both AD and psoriasis involve activation of TH22 and TH1 cells, with increased IL-17 and IL-22 production.3,10,12 IL-17 and IL-22 induce epidermal hyperplasia; IL-22 also contributes to skin barrier dysfunction.12 Therefore, it might be reasonable to consider psoriasis and AD as diseases that exist across a T-cell axis spectrum, thereby accounting for some overlap in disease characteristics.3
Dual Biologic Therapy—Dupilumab blocks the IL-4 receptor α subunit, a receptor for IL-4 and IL-13, which are key cytokines in the pathogenesis of AD.10 Guselkumab inhibits IL-23, thus blocking the inflammatory cascade of TH17 cell activation and release of IL-17 and IL-22 in the psoriasis pathway.13 Although an immunopathological spectrum exists between the 2 diseases, the continued presence of AD symptoms after blocking the IL-23 cascade suggests that additional blockade of TH2 cells is required to control AD in patients with true concurrent disease.
Accurate diagnosis of AD and/or psoriasis is important when considering targeted treatment of these conditions with biologics. The use of dual biologics is limited by a paucity of data regarding the safety of these agents when given in combination. A recent meta-analysis of dual biologic therapy in patients with inflammatory bowel disease demonstrated acceptable safety results with a pooled adverse reaction rate of 31%.14
Anchoring Bias—Anchoring bias can occur when a clinician’s decisions are influenced by a particular event or reference point, which might cause them to disregard subsequent evidence. Our case illustrates the importance of critically assessing the response to treatment and being mindful of the potential influence of anchoring bias on the differential diagnosis. Although overcoming biases in conditions with clinical overlap can be challenging, it is important to consider coexisting AD and psoriasis in patients with extensive hand involvement when multiple treatments have failed and only a partial response to targeted pathways has been achieved. In our case, the patient also had contact hypersensitivity to tixocortol-21-pivalate, which indicates hypersensitivity to many prescription topical corticosteroids, oral prednisone, and over-the-counter hydrocortisone; however, topical corticosteroids continued to be prescribed for her, which might have contributed to the lack of improvement and even exacerbated the rash.
Future Considerations—A consideration for the future in this case is discontinuing guselkumab to observe whether symptoms recur. We discussed this option with the patient, but she opted to continue treatment with dupilumab and guselkumab because of the symptom resolution.
Conclusion
Concomitant disease can present as an overlapping pattern in the same area, whereas other regions might have geographically isolated disease. Our patient’s overlap of symptoms, the failure of multiple treatments, and the partial improvement she experienced on guselkumab made diagnosis and management challenging; however, dual biologic therapy was successful.
- Barry K, Zancanaro P, Casseres R, et al. Concomitant atopic dermatitis and psoriasis—a retrospective review. J Dermatolog Treat. 2021;32:716-720. doi:10.1080/09546634.2019.1702147
- Bozek A, Zajac M, Krupka M. Atopic dermatitis and psoriasis as overlapping syndromes. Mediators Inflamm. 2020;2020:7527859. doi:10.1155/2020/7527859
- Guttman-Yassky E, Krueger JG. Atopic dermatitis and psoriasis: two different immune diseases or one spectrum? Curr Opin Immunol. 2017;48:68-73. doi:10.1016/j.coi.2017.08.008
- De Rosa G, Mignogna C. The histopathology of psoriasis. Reumatismo. 2007;59(suppl 1):46-48. doi:10.4081/reumatismo.2007.1s.46
- Docampo A, MJ, I, et al. Response to letter to the editor: ‘psoriasis dermatitis: an overlap condition of psoriasis and atopic dermatitis in children.’ J Eur Acad Dermatol Venereol. 2019;33:E410-E412. doi:10.1111/jdv.15716
- Johnson MC, Bowers NL, Strowd LC. Concurrent atopic dermatitis and psoriasis vulgaris: implications for targeted biologic therapy. Cutis. 2022;109:110-112. doi:10.12788/cutis.0453
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445-1486. doi:10.1016/j.jaad.2020.02.044
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351. doi:10.1016/j.jaad.2013.10.010
- Klonowska J, Glen J, Nowicki RJ, et al. New cytokines in the pathogenesis of atopic dermatitis—new therapeutic targets. Int J Mol Sci. 2018;19:3086. doi:10.3390/ijms19103086
- Ratchataswan T, Banzon TM, Thyssen JP, et al. Biologics for treatment of atopic dermatitis: current status and future prospect. J Allergy Clin Immunol Pract. 2021;9:1053-1065. doi:10.1016/j.jaip.2020.11.034
- Czarnowicki T, He H, Krueger JG, et al. Atopic dermatitis endotypes and implications for targeted therapeutics. J Allergy Clin Immunol. 2019;143:1-11. doi:10.1016/j.jaci.2018.10.032
- Tokuyama M, Mabuchi T. New treatment addressing the pathogenesis of psoriasis. Int J Mol Sci. 2020;21:7488. doi:10.3390/ijms21207488
- Gordon KB, Armstrong AW, Foley P, et al. Guselkumab efficacy after withdrawal is associated with suppression of serum IL-23-regulated IL-17 and IL-22 in psoriasis: VOYAGE 2 study. J Invest Dermatol. 2019;139:2437-2446.e1. doi:10.1016/j.jid.2019.05.016
- Gold SL, Steinlauf AF. Efficacy and safety of dual biologic therapy in patients with inflammatory bowel disease: a review of the literature. Gastroenterol Hepatol (N Y). 2021;17:406-414.
Atopic dermatitis (AD) and psoriasis are common skin diseases in which dysfunction of the epidermal barrier leads to skin inflammation and altered expression of proinflammatory cytokines.1 There often is overlap in the clinical and histopathologic features of AD and psoriasis, which can make diagnosis a challenge. Persistent late-stage AD can present with psoriasiform lichenified changes, and psoriasis lesions in the acute stage can have an eczematous appearance.2 Histologically, chronic psoriasis lesions share many overlapping features with AD, and some subsets of AD with IL-17 predominance (ie, intrinsic, pediatric, presentation in Asian patients) exhibit a psoriasiform appearance.3,4
Atopic dermatitis and psoriasis are considered 2 distinct conditions because AD is a helper T cell (TH2)–driven disease with subsequent overproduction of IL-4 and IL-13 and psoriasis is a TH17 cell–driven disease with overproduction of IL-173; however, the shared features of AD and psoriasis represent an underlying immunopathological spectrum2,5,6 in which one condition can develop following treatment of the other condition (immunological shift in pathways), both conditions can occur at different times in a patient’s life with alternating cycles of disease flares, or both conditions can coexist as an overlapping syndrome.1,2 A retrospective study from 2012 to 2019 estimated the prevalence of concomitant AD and psoriasis in the United States at 1.3%, with AD following the diagnosis of psoriasis in 67% of cases.1 Concurrent AD and psoriasis—when both diseases flaresimultaneously—is the rarest scenario.2,5
Treatment modalities for AD include topical corticosteroids, which act on immune cells to suppress the release of proinflammatory cytokines, as well as dupilumab, which offers targeted blockade of involved cytokines IL-4 and IL-13. Psoriasis can be treated with multiple immune modulators, including topical corticosteroids and vitamin D analogs, as well as systemic medications that reduce T-cell activation and inflammatory cytokines through targeting of IFN-γ, IL-2, tumor necrosis factor α, IL-17, and IL-23.7,8
We present the case of a patient with long-standing concurrent, treatment-resistant AD and psoriasis who was successfully treated with dual biologic therapy with guselkumab and dupilumab.
Case Report
A 62-year-old woman presented to our dermatology clinic with red itchy scales and painful fissures on the palms, hands, and soles of more than 12 years’ duration. Her medical history included an allergy to amoxicillin-clavulanate as well as an allergy to both dog and cat dander on prick testing. Her family history included dyshidrotic eczema in her mother. A complete blood cell count with differential was within reference range. A shave biopsy of the right dorsal hand performed at the onset of symptoms at an outside facility revealed hyperkeratotic acanthotic epidermis with a mild perivascular lymphocytic infiltrate.
Results of patch testing indicated contact hypersensitivity to the botanical rosin colophonium (or colophony); carba mix (1, 3-diphenylguanidine, zinc dibutyldithiocarbamate, and zinc diethydithiocarbamate); thiuram mix (tetramethylthiuram disulfide, tetramethylthiuram monosulfide, and tetraethylthiuram disulfide); n,n-diphenylguanidine; and tixocortol-21-pivalate. Our patient was given guidance on avoiding these agents, as it was suspected that exposure may be exacerbating the psoriasis. The psoriasis was treated with topical corticosteroids, keratolytics, and calcineurin inhibitors, all of which offered minimal or no relief. Trials of systemic agents, including methotrexate (discontinued because transaminitis developed), etanercept, adalimumab, and apremilast for 6 to 10 months did not provide improvement.

Two years prior to the current presentation, our patient had been treated with the IL-23 inhibitor guselkumab, which provided moderate improvement. When she presented to our clinic, physical examination while she was taking guselkumab demonstrated prurigo with excoriations of the extremities, hyperkeratosis with scaling and fissures of the soles, erythematous scaly plaques on the palms and dorsal surface of the hands, and mild onycholysis of the nails (Figures 1 and 2). Because we were concerned about concomitant intrinsic AD, dupilumab was initiated in conjunction with guselkumab. A second biopsy was considered but deferred in favor of clinical monitoring.
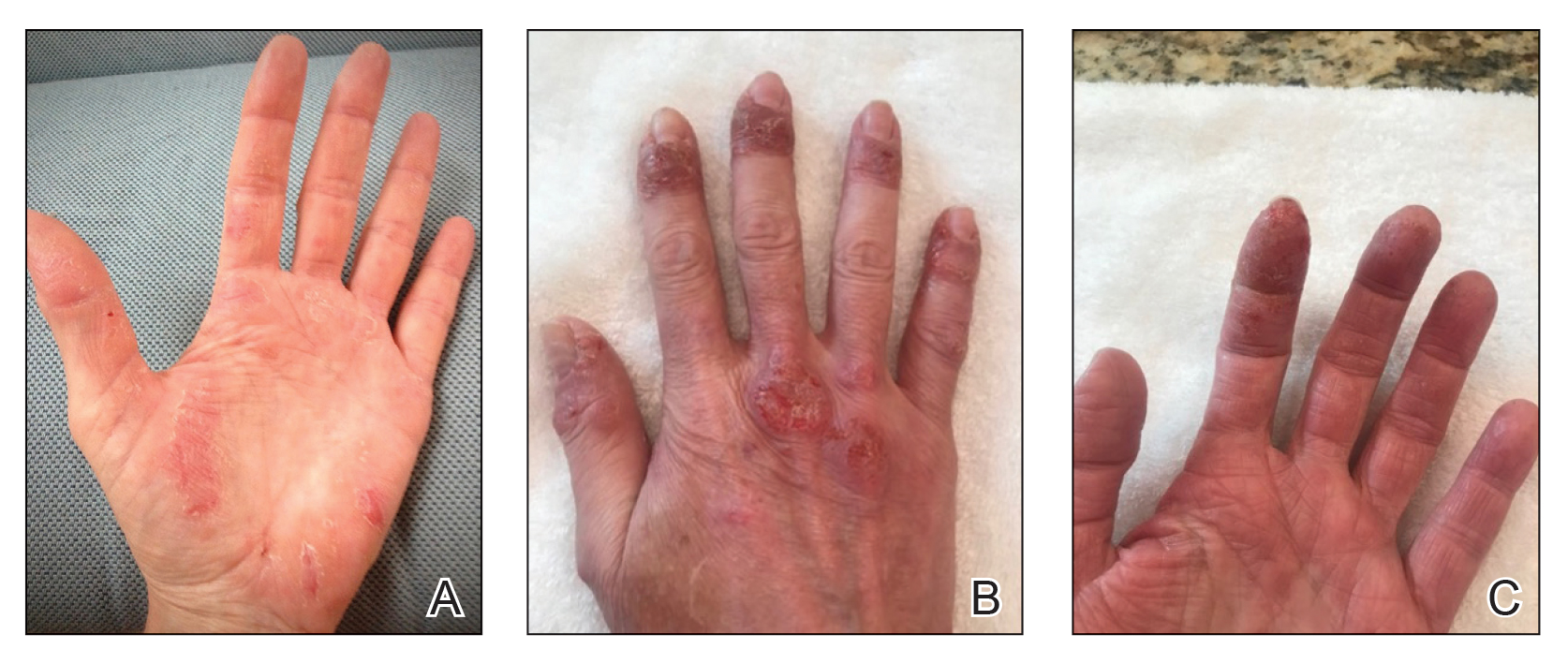
After 1 year of dual biologic therapy, the patient experienced near-complete resolution of symptoms. The psoriasis completely resolved from an initial body surface area of 5%, and the AD body surface area decreased from 30% to 2% (Figure 3). The patient reported no adverse effects from treatment.
Comment
Atopic dermatitis and psoriasis involve complex immunopathology and a spectrum of cytokines that might explain the overlap in their clinical and histopathologic presentations.
Atopic dermatitis—Atopic dermatitis involves TH1, TH2, TH9, TH17, and TH22 cells; TH2 cells release IL-4, IL-5, and IL-13, all of which are key cytokines in the inflammatory pathway of AD.9,10 Activation of the helper T-cell subset and the release of cytokines differ slightly based on the subcategory of AD and the stage of exacerbation. In addition to TH2-cell activation, TH1 cells and TH22 cells—which release IL-12 and IL-22, respectively—are active in both intrinsic and extrinsic AD. TH17 cells and TH9 cells—which release IL-17 and IL-9, respectively—are more prominent in the intrinsic pathway than in the extrinsic pathway.9 Intrinsic AD is recognized by a lack of eosinophilia, female predominance, and delayed onset compared to extrinsic AD; there also is a lack of history of atopy.1 Extrinsic AD is characterized by eosinophilia as well as a personal and family history of atopy.11 Our patient—a female with onset in older adulthood, lack of eosinophilia, and a family history of atopy—displayed features of both intrinsic and extrinsic AD.
Psoriasis—The immunopathology of psoriasis involves stimulation of dendritic cells, which activate TH17 cells through IL-23. TH17 cells then release IL-17 and IL-22. Therefore, both AD and psoriasis involve activation of TH22 and TH1 cells, with increased IL-17 and IL-22 production.3,10,12 IL-17 and IL-22 induce epidermal hyperplasia; IL-22 also contributes to skin barrier dysfunction.12 Therefore, it might be reasonable to consider psoriasis and AD as diseases that exist across a T-cell axis spectrum, thereby accounting for some overlap in disease characteristics.3
Dual Biologic Therapy—Dupilumab blocks the IL-4 receptor α subunit, a receptor for IL-4 and IL-13, which are key cytokines in the pathogenesis of AD.10 Guselkumab inhibits IL-23, thus blocking the inflammatory cascade of TH17 cell activation and release of IL-17 and IL-22 in the psoriasis pathway.13 Although an immunopathological spectrum exists between the 2 diseases, the continued presence of AD symptoms after blocking the IL-23 cascade suggests that additional blockade of TH2 cells is required to control AD in patients with true concurrent disease.
Accurate diagnosis of AD and/or psoriasis is important when considering targeted treatment of these conditions with biologics. The use of dual biologics is limited by a paucity of data regarding the safety of these agents when given in combination. A recent meta-analysis of dual biologic therapy in patients with inflammatory bowel disease demonstrated acceptable safety results with a pooled adverse reaction rate of 31%.14
Anchoring Bias—Anchoring bias can occur when a clinician’s decisions are influenced by a particular event or reference point, which might cause them to disregard subsequent evidence. Our case illustrates the importance of critically assessing the response to treatment and being mindful of the potential influence of anchoring bias on the differential diagnosis. Although overcoming biases in conditions with clinical overlap can be challenging, it is important to consider coexisting AD and psoriasis in patients with extensive hand involvement when multiple treatments have failed and only a partial response to targeted pathways has been achieved. In our case, the patient also had contact hypersensitivity to tixocortol-21-pivalate, which indicates hypersensitivity to many prescription topical corticosteroids, oral prednisone, and over-the-counter hydrocortisone; however, topical corticosteroids continued to be prescribed for her, which might have contributed to the lack of improvement and even exacerbated the rash.
Future Considerations—A consideration for the future in this case is discontinuing guselkumab to observe whether symptoms recur. We discussed this option with the patient, but she opted to continue treatment with dupilumab and guselkumab because of the symptom resolution.
Conclusion
Concomitant disease can present as an overlapping pattern in the same area, whereas other regions might have geographically isolated disease. Our patient’s overlap of symptoms, the failure of multiple treatments, and the partial improvement she experienced on guselkumab made diagnosis and management challenging; however, dual biologic therapy was successful.
Atopic dermatitis (AD) and psoriasis are common skin diseases in which dysfunction of the epidermal barrier leads to skin inflammation and altered expression of proinflammatory cytokines.1 There often is overlap in the clinical and histopathologic features of AD and psoriasis, which can make diagnosis a challenge. Persistent late-stage AD can present with psoriasiform lichenified changes, and psoriasis lesions in the acute stage can have an eczematous appearance.2 Histologically, chronic psoriasis lesions share many overlapping features with AD, and some subsets of AD with IL-17 predominance (ie, intrinsic, pediatric, presentation in Asian patients) exhibit a psoriasiform appearance.3,4
Atopic dermatitis and psoriasis are considered 2 distinct conditions because AD is a helper T cell (TH2)–driven disease with subsequent overproduction of IL-4 and IL-13 and psoriasis is a TH17 cell–driven disease with overproduction of IL-173; however, the shared features of AD and psoriasis represent an underlying immunopathological spectrum2,5,6 in which one condition can develop following treatment of the other condition (immunological shift in pathways), both conditions can occur at different times in a patient’s life with alternating cycles of disease flares, or both conditions can coexist as an overlapping syndrome.1,2 A retrospective study from 2012 to 2019 estimated the prevalence of concomitant AD and psoriasis in the United States at 1.3%, with AD following the diagnosis of psoriasis in 67% of cases.1 Concurrent AD and psoriasis—when both diseases flaresimultaneously—is the rarest scenario.2,5
Treatment modalities for AD include topical corticosteroids, which act on immune cells to suppress the release of proinflammatory cytokines, as well as dupilumab, which offers targeted blockade of involved cytokines IL-4 and IL-13. Psoriasis can be treated with multiple immune modulators, including topical corticosteroids and vitamin D analogs, as well as systemic medications that reduce T-cell activation and inflammatory cytokines through targeting of IFN-γ, IL-2, tumor necrosis factor α, IL-17, and IL-23.7,8
We present the case of a patient with long-standing concurrent, treatment-resistant AD and psoriasis who was successfully treated with dual biologic therapy with guselkumab and dupilumab.
Case Report
A 62-year-old woman presented to our dermatology clinic with red itchy scales and painful fissures on the palms, hands, and soles of more than 12 years’ duration. Her medical history included an allergy to amoxicillin-clavulanate as well as an allergy to both dog and cat dander on prick testing. Her family history included dyshidrotic eczema in her mother. A complete blood cell count with differential was within reference range. A shave biopsy of the right dorsal hand performed at the onset of symptoms at an outside facility revealed hyperkeratotic acanthotic epidermis with a mild perivascular lymphocytic infiltrate.
Results of patch testing indicated contact hypersensitivity to the botanical rosin colophonium (or colophony); carba mix (1, 3-diphenylguanidine, zinc dibutyldithiocarbamate, and zinc diethydithiocarbamate); thiuram mix (tetramethylthiuram disulfide, tetramethylthiuram monosulfide, and tetraethylthiuram disulfide); n,n-diphenylguanidine; and tixocortol-21-pivalate. Our patient was given guidance on avoiding these agents, as it was suspected that exposure may be exacerbating the psoriasis. The psoriasis was treated with topical corticosteroids, keratolytics, and calcineurin inhibitors, all of which offered minimal or no relief. Trials of systemic agents, including methotrexate (discontinued because transaminitis developed), etanercept, adalimumab, and apremilast for 6 to 10 months did not provide improvement.

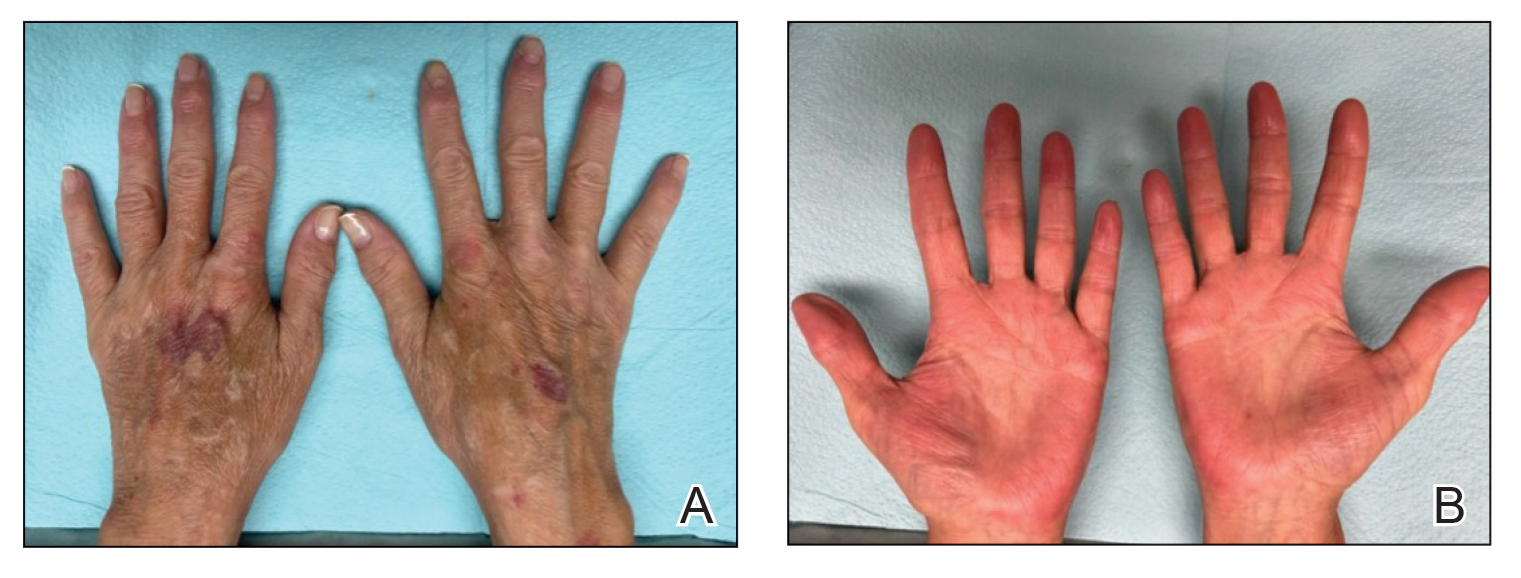
Two years prior to the current presentation, our patient had been treated with the IL-23 inhibitor guselkumab, which provided moderate improvement. When she presented to our clinic, physical examination while she was taking guselkumab demonstrated prurigo with excoriations of the extremities, hyperkeratosis with scaling and fissures of the soles, erythematous scaly plaques on the palms and dorsal surface of the hands, and mild onycholysis of the nails (Figures 1 and 2). Because we were concerned about concomitant intrinsic AD, dupilumab was initiated in conjunction with guselkumab. A second biopsy was considered but deferred in favor of clinical monitoring.
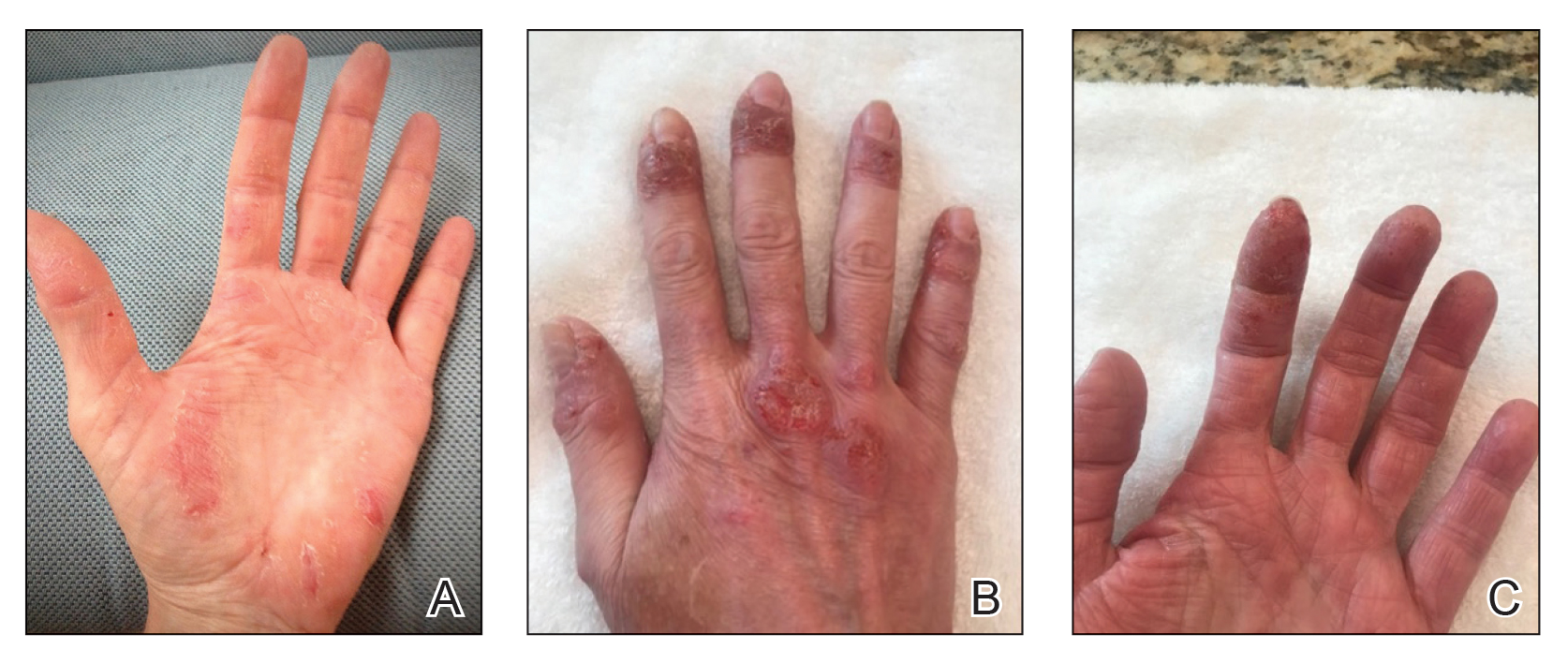
After 1 year of dual biologic therapy, the patient experienced near-complete resolution of symptoms. The psoriasis completely resolved from an initial body surface area of 5%, and the AD body surface area decreased from 30% to 2% (Figure 3). The patient reported no adverse effects from treatment.
Comment
Atopic dermatitis and psoriasis involve complex immunopathology and a spectrum of cytokines that might explain the overlap in their clinical and histopathologic presentations.
Atopic dermatitis—Atopic dermatitis involves TH1, TH2, TH9, TH17, and TH22 cells; TH2 cells release IL-4, IL-5, and IL-13, all of which are key cytokines in the inflammatory pathway of AD.9,10 Activation of the helper T-cell subset and the release of cytokines differ slightly based on the subcategory of AD and the stage of exacerbation. In addition to TH2-cell activation, TH1 cells and TH22 cells—which release IL-12 and IL-22, respectively—are active in both intrinsic and extrinsic AD. TH17 cells and TH9 cells—which release IL-17 and IL-9, respectively—are more prominent in the intrinsic pathway than in the extrinsic pathway.9 Intrinsic AD is recognized by a lack of eosinophilia, female predominance, and delayed onset compared to extrinsic AD; there also is a lack of history of atopy.1 Extrinsic AD is characterized by eosinophilia as well as a personal and family history of atopy.11 Our patient—a female with onset in older adulthood, lack of eosinophilia, and a family history of atopy—displayed features of both intrinsic and extrinsic AD.
Psoriasis—The immunopathology of psoriasis involves stimulation of dendritic cells, which activate TH17 cells through IL-23. TH17 cells then release IL-17 and IL-22. Therefore, both AD and psoriasis involve activation of TH22 and TH1 cells, with increased IL-17 and IL-22 production.3,10,12 IL-17 and IL-22 induce epidermal hyperplasia; IL-22 also contributes to skin barrier dysfunction.12 Therefore, it might be reasonable to consider psoriasis and AD as diseases that exist across a T-cell axis spectrum, thereby accounting for some overlap in disease characteristics.3
Dual Biologic Therapy—Dupilumab blocks the IL-4 receptor α subunit, a receptor for IL-4 and IL-13, which are key cytokines in the pathogenesis of AD.10 Guselkumab inhibits IL-23, thus blocking the inflammatory cascade of TH17 cell activation and release of IL-17 and IL-22 in the psoriasis pathway.13 Although an immunopathological spectrum exists between the 2 diseases, the continued presence of AD symptoms after blocking the IL-23 cascade suggests that additional blockade of TH2 cells is required to control AD in patients with true concurrent disease.
Accurate diagnosis of AD and/or psoriasis is important when considering targeted treatment of these conditions with biologics. The use of dual biologics is limited by a paucity of data regarding the safety of these agents when given in combination. A recent meta-analysis of dual biologic therapy in patients with inflammatory bowel disease demonstrated acceptable safety results with a pooled adverse reaction rate of 31%.14
Anchoring Bias—Anchoring bias can occur when a clinician’s decisions are influenced by a particular event or reference point, which might cause them to disregard subsequent evidence. Our case illustrates the importance of critically assessing the response to treatment and being mindful of the potential influence of anchoring bias on the differential diagnosis. Although overcoming biases in conditions with clinical overlap can be challenging, it is important to consider coexisting AD and psoriasis in patients with extensive hand involvement when multiple treatments have failed and only a partial response to targeted pathways has been achieved. In our case, the patient also had contact hypersensitivity to tixocortol-21-pivalate, which indicates hypersensitivity to many prescription topical corticosteroids, oral prednisone, and over-the-counter hydrocortisone; however, topical corticosteroids continued to be prescribed for her, which might have contributed to the lack of improvement and even exacerbated the rash.
Future Considerations—A consideration for the future in this case is discontinuing guselkumab to observe whether symptoms recur. We discussed this option with the patient, but she opted to continue treatment with dupilumab and guselkumab because of the symptom resolution.
Conclusion
Concomitant disease can present as an overlapping pattern in the same area, whereas other regions might have geographically isolated disease. Our patient’s overlap of symptoms, the failure of multiple treatments, and the partial improvement she experienced on guselkumab made diagnosis and management challenging; however, dual biologic therapy was successful.
- Barry K, Zancanaro P, Casseres R, et al. Concomitant atopic dermatitis and psoriasis—a retrospective review. J Dermatolog Treat. 2021;32:716-720. doi:10.1080/09546634.2019.1702147
- Bozek A, Zajac M, Krupka M. Atopic dermatitis and psoriasis as overlapping syndromes. Mediators Inflamm. 2020;2020:7527859. doi:10.1155/2020/7527859
- Guttman-Yassky E, Krueger JG. Atopic dermatitis and psoriasis: two different immune diseases or one spectrum? Curr Opin Immunol. 2017;48:68-73. doi:10.1016/j.coi.2017.08.008
- De Rosa G, Mignogna C. The histopathology of psoriasis. Reumatismo. 2007;59(suppl 1):46-48. doi:10.4081/reumatismo.2007.1s.46
- Docampo A, MJ, I, et al. Response to letter to the editor: ‘psoriasis dermatitis: an overlap condition of psoriasis and atopic dermatitis in children.’ J Eur Acad Dermatol Venereol. 2019;33:E410-E412. doi:10.1111/jdv.15716
- Johnson MC, Bowers NL, Strowd LC. Concurrent atopic dermatitis and psoriasis vulgaris: implications for targeted biologic therapy. Cutis. 2022;109:110-112. doi:10.12788/cutis.0453
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445-1486. doi:10.1016/j.jaad.2020.02.044
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351. doi:10.1016/j.jaad.2013.10.010
- Klonowska J, Glen J, Nowicki RJ, et al. New cytokines in the pathogenesis of atopic dermatitis—new therapeutic targets. Int J Mol Sci. 2018;19:3086. doi:10.3390/ijms19103086
- Ratchataswan T, Banzon TM, Thyssen JP, et al. Biologics for treatment of atopic dermatitis: current status and future prospect. J Allergy Clin Immunol Pract. 2021;9:1053-1065. doi:10.1016/j.jaip.2020.11.034
- Czarnowicki T, He H, Krueger JG, et al. Atopic dermatitis endotypes and implications for targeted therapeutics. J Allergy Clin Immunol. 2019;143:1-11. doi:10.1016/j.jaci.2018.10.032
- Tokuyama M, Mabuchi T. New treatment addressing the pathogenesis of psoriasis. Int J Mol Sci. 2020;21:7488. doi:10.3390/ijms21207488
- Gordon KB, Armstrong AW, Foley P, et al. Guselkumab efficacy after withdrawal is associated with suppression of serum IL-23-regulated IL-17 and IL-22 in psoriasis: VOYAGE 2 study. J Invest Dermatol. 2019;139:2437-2446.e1. doi:10.1016/j.jid.2019.05.016
- Gold SL, Steinlauf AF. Efficacy and safety of dual biologic therapy in patients with inflammatory bowel disease: a review of the literature. Gastroenterol Hepatol (N Y). 2021;17:406-414.
- Barry K, Zancanaro P, Casseres R, et al. Concomitant atopic dermatitis and psoriasis—a retrospective review. J Dermatolog Treat. 2021;32:716-720. doi:10.1080/09546634.2019.1702147
- Bozek A, Zajac M, Krupka M. Atopic dermatitis and psoriasis as overlapping syndromes. Mediators Inflamm. 2020;2020:7527859. doi:10.1155/2020/7527859
- Guttman-Yassky E, Krueger JG. Atopic dermatitis and psoriasis: two different immune diseases or one spectrum? Curr Opin Immunol. 2017;48:68-73. doi:10.1016/j.coi.2017.08.008
- De Rosa G, Mignogna C. The histopathology of psoriasis. Reumatismo. 2007;59(suppl 1):46-48. doi:10.4081/reumatismo.2007.1s.46
- Docampo A, MJ, I, et al. Response to letter to the editor: ‘psoriasis dermatitis: an overlap condition of psoriasis and atopic dermatitis in children.’ J Eur Acad Dermatol Venereol. 2019;33:E410-E412. doi:10.1111/jdv.15716
- Johnson MC, Bowers NL, Strowd LC. Concurrent atopic dermatitis and psoriasis vulgaris: implications for targeted biologic therapy. Cutis. 2022;109:110-112. doi:10.12788/cutis.0453
- Menter A, Gelfand JM, Connor C, et al. Joint American Academy of Dermatology–National Psoriasis Foundation guidelines of care for the management of psoriasis with systemic nonbiologic therapies. J Am Acad Dermatol. 2020;82:1445-1486. doi:10.1016/j.jaad.2020.02.044
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351. doi:10.1016/j.jaad.2013.10.010
- Klonowska J, Glen J, Nowicki RJ, et al. New cytokines in the pathogenesis of atopic dermatitis—new therapeutic targets. Int J Mol Sci. 2018;19:3086. doi:10.3390/ijms19103086
- Ratchataswan T, Banzon TM, Thyssen JP, et al. Biologics for treatment of atopic dermatitis: current status and future prospect. J Allergy Clin Immunol Pract. 2021;9:1053-1065. doi:10.1016/j.jaip.2020.11.034
- Czarnowicki T, He H, Krueger JG, et al. Atopic dermatitis endotypes and implications for targeted therapeutics. J Allergy Clin Immunol. 2019;143:1-11. doi:10.1016/j.jaci.2018.10.032
- Tokuyama M, Mabuchi T. New treatment addressing the pathogenesis of psoriasis. Int J Mol Sci. 2020;21:7488. doi:10.3390/ijms21207488
- Gordon KB, Armstrong AW, Foley P, et al. Guselkumab efficacy after withdrawal is associated with suppression of serum IL-23-regulated IL-17 and IL-22 in psoriasis: VOYAGE 2 study. J Invest Dermatol. 2019;139:2437-2446.e1. doi:10.1016/j.jid.2019.05.016
- Gold SL, Steinlauf AF. Efficacy and safety of dual biologic therapy in patients with inflammatory bowel disease: a review of the literature. Gastroenterol Hepatol (N Y). 2021;17:406-414.
Practice Points
- Atopic dermatitis and psoriasis can share clinical and histopathologic features, which represents their underlying immunopathologic spectrum.
- Atopic dermatitis and psoriasis can coexist in a single patient, which may be suspected from a clinical picture of treatment-resistant disease, a partial response to targeted therapies, or extensive hand involvement.
Idiopathic Granulomatous Lobular Mastitis: A Mimicker of Inflammatory Breast Cancer
Idiopathic granulomatous lobular mastitis (IGLM) is a rare, chronic inflammatory breast disease first described in 1972.1 IGLM usually affects women during reproductive years and has similar clinical features to breast cancer.2 Ultrasonography and mammography yield nonspecific results and cannot adequately differentiate between malignancy and inflammation.3 Magnetic resonance imaging (MRI) is known to be more sensitive in detecting lesions in dense breasts; however, it does not differentiate between granulomatous lesions and other disorders.4,5 Histopathology is the gold standard for diagnosis.1-12
Infectious and autoimmune causes of granulomatous mastitis must be excluded before establishing an IGLM diagnosis. The clinical quandary that remains is how to adequately manage the disease. Although there are no defined treatment guidelines, current literature has proposed a multimodal strategy.6,9 In this report, we describe a case of IGLM successfully treated with surgical excision after failed medical therapy.
Case Presentation
A 43-year-old gravida 5, para 4 White woman presented with a 2-week history of right breast tenderness, heaviness, warmth, and redness that was refractory to cephalexin and dicloxacillin. She had no personal or family history of breast cancer; never had breast surgery and breastfed all 4 children.
An examination of the right breast demonstrated erythema and an 8-cm tender mass in the right lower outer quadrant but no skin retraction or dimpling (Figure 1). The mammography, concerning for inflammatory breast cancer, was category BI-RADS 4 and demonstrated a suspicious right axillary lymph node (Figure 2).
A core needle breast biopsy revealed granulomatous mastitis (Figure 3A), without evidence of malignancy. Rheumatology and endocrinology excluded secondary causes of granulomatous mastitis (ie, sarcoidosis, tuberculosis, granulomatosis with polyangiitis, and other autoimmune conditions). A pituitary MRI to assess an elevated serum prolactin level showed no evidence of microadenoma.
After a prolonged course of 8 months of unsuccessful therapy with prednisone and methotrexate, the patient was referred for surgical excision. Culture and special stains (Gram stain, periodic acid-Schiff stain, acid-fast Bacillus culture, Fite stain, and Brown and Benn stain) of the breast tissue were negative for organisms (Figure 3B). Seven months after excision the patient was doing well and had no evidence of recurrence.
Discussion
IGLM is a rare, chronic benign inflammatory breast disease of unknown etiology and more commonly reported in individuals of Mediterranean descent.13 It is believed that hyperprolactinemia causing extravasation of fat and protein during milk letdown leads to lymphocyte and macrophage migration, resulting in a localized autoimmune response in the breast ducts.10,14
There are 2 types of granulomatous mastitis: idiopathic and specific. Infectious, autoimmune, and malignant causes of granulomatous mastitis (ie, tuberculosis, sarcoidosis, Corynebacterium spp, granulomatosis with polyangiitis, systemic lupus erythematosus, Behçet disease, ductal ectasia, or granulomatous reaction in a carcinoma) must be excluded prior to establishing an IGLM diagnosis, as these can be fatal if left untreated.15 The most frequent findings on ultrasound and mammography are hypoechoic masses and focal asymmetric densities, respectively.3,5 MRI has been proposed more for surveillance in patients with chronic IGLM.4,5 Histopathology—featuring lobular noncaseating granulomas with epithelioid histiocytes; and multinucleated giant cells in a background of neutrophils, lymphocytes, plasma cells, and eosinophils—is the gold standard for diagnosing IGLM.1-12
There are currently no universal treatment guidelines and management usually consists of observation, systemic and topical steroids, or surgery.3,13 Topical and injectable steroids have been effective in treating both initial and recurrent IGLM in patients who are unable to be treated with systemic steroids.16-18 Due to reported high recurrence rates with steroid tapers, adjunctive therapy with methotrexate, azathioprine, colchicine, and hydroxychloroquine have been proposed.1,3-6,10-12
Additionally, antibiotics are recommended only in the management of IGLM when microbial co-infection is concerning, such as with Corynebacterium spp.9,11,19-22 Histologically, this bacterium is distinct from IGLM and demonstrates granulomatous, neutrophilic inflammation within cystic spaces.19-21 Wide surgical excision with negative margins is the only definitive treatment to reduce recurrence and expedite recovery time.2,3,7-10 Notably, surgical excision has been associated with poor wound healing and occasional recurrence compared with medication alone.5,11
Although IGLM is normally a benign process, chronic disease has been related (without causality) to infiltrating breast carcinoma.4 A proposed theory for the development of malignancy suggests that chronic inflammation leading to free radical formation can result in cellular dysplasia and cancer.23
Conclusions
Fifty years after its first description, IGLM is still a poorly understood disease. There remains no consensus behind its etiology or management. In our case, we demonstrated a stepwise treatment progression, beginning with medical therapy before proceeding to surgical cure. Given concerns for poor wound healing and postsurgical infections, monitoring the response and recurrence to an initial trial of conservative medical treatment is not unreasonable. Because of possible risk for malignancy with chronic IGLM, patients should not delay surgical excision if their condition remains refractory to medical therapy alone.
1. Garcia-Rodiguez JA, Pattullo A. Idiopathic granulomatous mastitis: a mimicking disease in a pregnant woman: a case report. BMC Res Notes. 2013;6:95. doi.10.1186/1756-0500-6-95
2. Gurleyik G, Aktekin A, Aker F, Karagulle H, Saglamc A. Medical and surgical treatment of idiopathic granulomatous lobular mastitis: a benign inflammatory disease mimicking invasive carcinoma. J Breast Cancer. 2012;15(1):119-123. doi:10.4048/jbc.2012.15.1.119
3. Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G. Granulomatous lobular mastitis: imaging, diagnosis, and treatment. AJR Am J Roentgenol. 2009;193(2):574-581. doi:10.2214/AJR.08.1528
4. Mazlan L, Suhaimi SN, Jasmin SJ, Latar NH, Adzman S, Muhammad R. Breast carcinoma occurring from chronic granulomatous mastitis. Malays J Med Sci. 2012;19(2):82-85.
5. Patel RA, Strickland P, Sankara IR, Pinkston G, Many W Jr, Rodriguez M. Idiopathic granulomatous mastitis: case reports and review of literature. J Gen Intern Med. 2010;25(3):270-273. doi:10.1007/s11606-009-1207-2
6. Akbulut S, Yilmaz D, Bakir S. Methotrexate in the management of idiopathic granulomatous mastitis: review of 108 published cases and report of four cases. Breast J. 2011;17(6):661-668. doi:10.1111/j.1524-4741.2011.01162.x
7. Ergin AB, Cristofanilli M, Daw H, Tahan G, Gong Y. Recurrent granulomatous mastitis mimicking inflammatory breast cancer. BMJ Case Rep. 2011;2011:bcr0720103156. doi:10.1136/bcr.07.2010.3156
8. Hladik M, Schoeller T, Ensat F, Wechselberger G. Idiopathic granulomatous mastitis: successful treatment by mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2011;64(12):1604-1607. doi:10.1016/j.bjps.2011.07.01
9. Hur SM, Cho DH, Lee SK, et al. Experience of treatment of patients with granulomatous lobular mastitis. J Korean Surg Soc. 2013;85(1):1-6. doi:10.4174/jkss.2013.85.1.
10. Kayahan M, Kadioglu H, Muslumanoglu M. Management of patients with granulomatous mastitis: analysis of 31 cases. Breast Care (Basel). 2012;7(3):226-230. doi:10.1159/000337758
11. Neel A, Hello M, Cottereau A, et al. Long-term outcome in idiopathic granulomatous mastitis: a western multicentre study. QJM. 2013;106(5):433-441. doi:10.1093/qjmed/hct040
12. Seo HR, Na KY, Yim HE, et al. Differential diagnosis in idiopathic granulomatous mastitis and tuberculous mastitis. J Breast Cancer. 2012;15(1):111-118. doi:10.4048/jbc.2012.15.1.111
13. Martinez-Ramos D, Simon-Monterde L, Suelves-Piqueres C, et al. Idiopathic granulomatous mastitis: a systematic review of 3060 patients. Breast J. 2019;25(6):1245-1250. doi:10.1111/tbj.13446
14. Lin CH, Hsu CW, Tsao TY, Chou J. Idiopathic granulomatous mastitis associated with risperidone-induced hyperprolactinemia. Diagn Pathol. 2012;7:2. doi:10.1186/1746-1596-7-2
15. Goulabchand R, Hafidi A, Van de Perre P, et al. Mastitis in autoimmune diseases: review of the literature, diagnostic pathway, and pathophysiological key players. J Clin Med. 2020;9(4):958. doi:10.3390/jcm9040958
16. Altintoprak F. Topical steroids to treat granulomatous mastitis: a case report. Korean J Intern Med. 2011;26(3):356-359. doi:10.3904/kjim.2011.26.3.356
17. Tang A, Dominguez DA, Edquilang JK, et al. Granulomatous mastitis: comparison of novel treatment of steroid injection and current management. J Surg Res. 2020;254:300-305. doi:10.1016/j.jss.2020.04.018
18. Toktas O, Toprak N. Treatment results of intralesional steroid injection and topical steroid administration in pregnant women with idiopathic granulomatous mastitis. Eur J Breast Health. 2021;17(3):283-287. doi:10.4274/ejbh.galenos.2021.2021-2-4
19. Bercot B, Kannengiesser C, Oudin C, et al. First description of NOD2 variant associated with defective neutrophil responses in a woman with granulomatous mastitis related to corynebacteria. J Clin Microbiol. 2009;47(9):3034-3037. doi:10.1128/JCM.00561-09
20. Renshaw AA, Derhagopian RP, Gould EW. Cystic neutrophilic granulomatous mastitis: an underappreciated pattern strongly associated with gram-positive bacilli. Am J Clin Pathol. 2011;136(3):424-427. doi:10.1309/AJCP1W9JBRYOQSNZ
21. Stary CM, Lee YS, Balfour J. Idiopathic granulomatous mastitis associated with corynebacterium sp. Infection. Hawaii Med J. 2011;70(5):99-101.
22. Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology. 2003;35(2):109-119.
23. Rakoff-Nahoum S. Why cancer and inflammation? Yale J Biol Med. 2006;79(3-4):123-130.
Idiopathic granulomatous lobular mastitis (IGLM) is a rare, chronic inflammatory breast disease first described in 1972.1 IGLM usually affects women during reproductive years and has similar clinical features to breast cancer.2 Ultrasonography and mammography yield nonspecific results and cannot adequately differentiate between malignancy and inflammation.3 Magnetic resonance imaging (MRI) is known to be more sensitive in detecting lesions in dense breasts; however, it does not differentiate between granulomatous lesions and other disorders.4,5 Histopathology is the gold standard for diagnosis.1-12
Infectious and autoimmune causes of granulomatous mastitis must be excluded before establishing an IGLM diagnosis. The clinical quandary that remains is how to adequately manage the disease. Although there are no defined treatment guidelines, current literature has proposed a multimodal strategy.6,9 In this report, we describe a case of IGLM successfully treated with surgical excision after failed medical therapy.
Case Presentation
A 43-year-old gravida 5, para 4 White woman presented with a 2-week history of right breast tenderness, heaviness, warmth, and redness that was refractory to cephalexin and dicloxacillin. She had no personal or family history of breast cancer; never had breast surgery and breastfed all 4 children.
An examination of the right breast demonstrated erythema and an 8-cm tender mass in the right lower outer quadrant but no skin retraction or dimpling (Figure 1). The mammography, concerning for inflammatory breast cancer, was category BI-RADS 4 and demonstrated a suspicious right axillary lymph node (Figure 2).
A core needle breast biopsy revealed granulomatous mastitis (Figure 3A), without evidence of malignancy. Rheumatology and endocrinology excluded secondary causes of granulomatous mastitis (ie, sarcoidosis, tuberculosis, granulomatosis with polyangiitis, and other autoimmune conditions). A pituitary MRI to assess an elevated serum prolactin level showed no evidence of microadenoma.
After a prolonged course of 8 months of unsuccessful therapy with prednisone and methotrexate, the patient was referred for surgical excision. Culture and special stains (Gram stain, periodic acid-Schiff stain, acid-fast Bacillus culture, Fite stain, and Brown and Benn stain) of the breast tissue were negative for organisms (Figure 3B). Seven months after excision the patient was doing well and had no evidence of recurrence.
Discussion
IGLM is a rare, chronic benign inflammatory breast disease of unknown etiology and more commonly reported in individuals of Mediterranean descent.13 It is believed that hyperprolactinemia causing extravasation of fat and protein during milk letdown leads to lymphocyte and macrophage migration, resulting in a localized autoimmune response in the breast ducts.10,14
There are 2 types of granulomatous mastitis: idiopathic and specific. Infectious, autoimmune, and malignant causes of granulomatous mastitis (ie, tuberculosis, sarcoidosis, Corynebacterium spp, granulomatosis with polyangiitis, systemic lupus erythematosus, Behçet disease, ductal ectasia, or granulomatous reaction in a carcinoma) must be excluded prior to establishing an IGLM diagnosis, as these can be fatal if left untreated.15 The most frequent findings on ultrasound and mammography are hypoechoic masses and focal asymmetric densities, respectively.3,5 MRI has been proposed more for surveillance in patients with chronic IGLM.4,5 Histopathology—featuring lobular noncaseating granulomas with epithelioid histiocytes; and multinucleated giant cells in a background of neutrophils, lymphocytes, plasma cells, and eosinophils—is the gold standard for diagnosing IGLM.1-12
There are currently no universal treatment guidelines and management usually consists of observation, systemic and topical steroids, or surgery.3,13 Topical and injectable steroids have been effective in treating both initial and recurrent IGLM in patients who are unable to be treated with systemic steroids.16-18 Due to reported high recurrence rates with steroid tapers, adjunctive therapy with methotrexate, azathioprine, colchicine, and hydroxychloroquine have been proposed.1,3-6,10-12
Additionally, antibiotics are recommended only in the management of IGLM when microbial co-infection is concerning, such as with Corynebacterium spp.9,11,19-22 Histologically, this bacterium is distinct from IGLM and demonstrates granulomatous, neutrophilic inflammation within cystic spaces.19-21 Wide surgical excision with negative margins is the only definitive treatment to reduce recurrence and expedite recovery time.2,3,7-10 Notably, surgical excision has been associated with poor wound healing and occasional recurrence compared with medication alone.5,11
Although IGLM is normally a benign process, chronic disease has been related (without causality) to infiltrating breast carcinoma.4 A proposed theory for the development of malignancy suggests that chronic inflammation leading to free radical formation can result in cellular dysplasia and cancer.23
Conclusions
Fifty years after its first description, IGLM is still a poorly understood disease. There remains no consensus behind its etiology or management. In our case, we demonstrated a stepwise treatment progression, beginning with medical therapy before proceeding to surgical cure. Given concerns for poor wound healing and postsurgical infections, monitoring the response and recurrence to an initial trial of conservative medical treatment is not unreasonable. Because of possible risk for malignancy with chronic IGLM, patients should not delay surgical excision if their condition remains refractory to medical therapy alone.
Idiopathic granulomatous lobular mastitis (IGLM) is a rare, chronic inflammatory breast disease first described in 1972.1 IGLM usually affects women during reproductive years and has similar clinical features to breast cancer.2 Ultrasonography and mammography yield nonspecific results and cannot adequately differentiate between malignancy and inflammation.3 Magnetic resonance imaging (MRI) is known to be more sensitive in detecting lesions in dense breasts; however, it does not differentiate between granulomatous lesions and other disorders.4,5 Histopathology is the gold standard for diagnosis.1-12
Infectious and autoimmune causes of granulomatous mastitis must be excluded before establishing an IGLM diagnosis. The clinical quandary that remains is how to adequately manage the disease. Although there are no defined treatment guidelines, current literature has proposed a multimodal strategy.6,9 In this report, we describe a case of IGLM successfully treated with surgical excision after failed medical therapy.
Case Presentation
A 43-year-old gravida 5, para 4 White woman presented with a 2-week history of right breast tenderness, heaviness, warmth, and redness that was refractory to cephalexin and dicloxacillin. She had no personal or family history of breast cancer; never had breast surgery and breastfed all 4 children.
An examination of the right breast demonstrated erythema and an 8-cm tender mass in the right lower outer quadrant but no skin retraction or dimpling (Figure 1). The mammography, concerning for inflammatory breast cancer, was category BI-RADS 4 and demonstrated a suspicious right axillary lymph node (Figure 2).
A core needle breast biopsy revealed granulomatous mastitis (Figure 3A), without evidence of malignancy. Rheumatology and endocrinology excluded secondary causes of granulomatous mastitis (ie, sarcoidosis, tuberculosis, granulomatosis with polyangiitis, and other autoimmune conditions). A pituitary MRI to assess an elevated serum prolactin level showed no evidence of microadenoma.
After a prolonged course of 8 months of unsuccessful therapy with prednisone and methotrexate, the patient was referred for surgical excision. Culture and special stains (Gram stain, periodic acid-Schiff stain, acid-fast Bacillus culture, Fite stain, and Brown and Benn stain) of the breast tissue were negative for organisms (Figure 3B). Seven months after excision the patient was doing well and had no evidence of recurrence.
Discussion
IGLM is a rare, chronic benign inflammatory breast disease of unknown etiology and more commonly reported in individuals of Mediterranean descent.13 It is believed that hyperprolactinemia causing extravasation of fat and protein during milk letdown leads to lymphocyte and macrophage migration, resulting in a localized autoimmune response in the breast ducts.10,14
There are 2 types of granulomatous mastitis: idiopathic and specific. Infectious, autoimmune, and malignant causes of granulomatous mastitis (ie, tuberculosis, sarcoidosis, Corynebacterium spp, granulomatosis with polyangiitis, systemic lupus erythematosus, Behçet disease, ductal ectasia, or granulomatous reaction in a carcinoma) must be excluded prior to establishing an IGLM diagnosis, as these can be fatal if left untreated.15 The most frequent findings on ultrasound and mammography are hypoechoic masses and focal asymmetric densities, respectively.3,5 MRI has been proposed more for surveillance in patients with chronic IGLM.4,5 Histopathology—featuring lobular noncaseating granulomas with epithelioid histiocytes; and multinucleated giant cells in a background of neutrophils, lymphocytes, plasma cells, and eosinophils—is the gold standard for diagnosing IGLM.1-12
There are currently no universal treatment guidelines and management usually consists of observation, systemic and topical steroids, or surgery.3,13 Topical and injectable steroids have been effective in treating both initial and recurrent IGLM in patients who are unable to be treated with systemic steroids.16-18 Due to reported high recurrence rates with steroid tapers, adjunctive therapy with methotrexate, azathioprine, colchicine, and hydroxychloroquine have been proposed.1,3-6,10-12
Additionally, antibiotics are recommended only in the management of IGLM when microbial co-infection is concerning, such as with Corynebacterium spp.9,11,19-22 Histologically, this bacterium is distinct from IGLM and demonstrates granulomatous, neutrophilic inflammation within cystic spaces.19-21 Wide surgical excision with negative margins is the only definitive treatment to reduce recurrence and expedite recovery time.2,3,7-10 Notably, surgical excision has been associated with poor wound healing and occasional recurrence compared with medication alone.5,11
Although IGLM is normally a benign process, chronic disease has been related (without causality) to infiltrating breast carcinoma.4 A proposed theory for the development of malignancy suggests that chronic inflammation leading to free radical formation can result in cellular dysplasia and cancer.23
Conclusions
Fifty years after its first description, IGLM is still a poorly understood disease. There remains no consensus behind its etiology or management. In our case, we demonstrated a stepwise treatment progression, beginning with medical therapy before proceeding to surgical cure. Given concerns for poor wound healing and postsurgical infections, monitoring the response and recurrence to an initial trial of conservative medical treatment is not unreasonable. Because of possible risk for malignancy with chronic IGLM, patients should not delay surgical excision if their condition remains refractory to medical therapy alone.
1. Garcia-Rodiguez JA, Pattullo A. Idiopathic granulomatous mastitis: a mimicking disease in a pregnant woman: a case report. BMC Res Notes. 2013;6:95. doi.10.1186/1756-0500-6-95
2. Gurleyik G, Aktekin A, Aker F, Karagulle H, Saglamc A. Medical and surgical treatment of idiopathic granulomatous lobular mastitis: a benign inflammatory disease mimicking invasive carcinoma. J Breast Cancer. 2012;15(1):119-123. doi:10.4048/jbc.2012.15.1.119
3. Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G. Granulomatous lobular mastitis: imaging, diagnosis, and treatment. AJR Am J Roentgenol. 2009;193(2):574-581. doi:10.2214/AJR.08.1528
4. Mazlan L, Suhaimi SN, Jasmin SJ, Latar NH, Adzman S, Muhammad R. Breast carcinoma occurring from chronic granulomatous mastitis. Malays J Med Sci. 2012;19(2):82-85.
5. Patel RA, Strickland P, Sankara IR, Pinkston G, Many W Jr, Rodriguez M. Idiopathic granulomatous mastitis: case reports and review of literature. J Gen Intern Med. 2010;25(3):270-273. doi:10.1007/s11606-009-1207-2
6. Akbulut S, Yilmaz D, Bakir S. Methotrexate in the management of idiopathic granulomatous mastitis: review of 108 published cases and report of four cases. Breast J. 2011;17(6):661-668. doi:10.1111/j.1524-4741.2011.01162.x
7. Ergin AB, Cristofanilli M, Daw H, Tahan G, Gong Y. Recurrent granulomatous mastitis mimicking inflammatory breast cancer. BMJ Case Rep. 2011;2011:bcr0720103156. doi:10.1136/bcr.07.2010.3156
8. Hladik M, Schoeller T, Ensat F, Wechselberger G. Idiopathic granulomatous mastitis: successful treatment by mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2011;64(12):1604-1607. doi:10.1016/j.bjps.2011.07.01
9. Hur SM, Cho DH, Lee SK, et al. Experience of treatment of patients with granulomatous lobular mastitis. J Korean Surg Soc. 2013;85(1):1-6. doi:10.4174/jkss.2013.85.1.
10. Kayahan M, Kadioglu H, Muslumanoglu M. Management of patients with granulomatous mastitis: analysis of 31 cases. Breast Care (Basel). 2012;7(3):226-230. doi:10.1159/000337758
11. Neel A, Hello M, Cottereau A, et al. Long-term outcome in idiopathic granulomatous mastitis: a western multicentre study. QJM. 2013;106(5):433-441. doi:10.1093/qjmed/hct040
12. Seo HR, Na KY, Yim HE, et al. Differential diagnosis in idiopathic granulomatous mastitis and tuberculous mastitis. J Breast Cancer. 2012;15(1):111-118. doi:10.4048/jbc.2012.15.1.111
13. Martinez-Ramos D, Simon-Monterde L, Suelves-Piqueres C, et al. Idiopathic granulomatous mastitis: a systematic review of 3060 patients. Breast J. 2019;25(6):1245-1250. doi:10.1111/tbj.13446
14. Lin CH, Hsu CW, Tsao TY, Chou J. Idiopathic granulomatous mastitis associated with risperidone-induced hyperprolactinemia. Diagn Pathol. 2012;7:2. doi:10.1186/1746-1596-7-2
15. Goulabchand R, Hafidi A, Van de Perre P, et al. Mastitis in autoimmune diseases: review of the literature, diagnostic pathway, and pathophysiological key players. J Clin Med. 2020;9(4):958. doi:10.3390/jcm9040958
16. Altintoprak F. Topical steroids to treat granulomatous mastitis: a case report. Korean J Intern Med. 2011;26(3):356-359. doi:10.3904/kjim.2011.26.3.356
17. Tang A, Dominguez DA, Edquilang JK, et al. Granulomatous mastitis: comparison of novel treatment of steroid injection and current management. J Surg Res. 2020;254:300-305. doi:10.1016/j.jss.2020.04.018
18. Toktas O, Toprak N. Treatment results of intralesional steroid injection and topical steroid administration in pregnant women with idiopathic granulomatous mastitis. Eur J Breast Health. 2021;17(3):283-287. doi:10.4274/ejbh.galenos.2021.2021-2-4
19. Bercot B, Kannengiesser C, Oudin C, et al. First description of NOD2 variant associated with defective neutrophil responses in a woman with granulomatous mastitis related to corynebacteria. J Clin Microbiol. 2009;47(9):3034-3037. doi:10.1128/JCM.00561-09
20. Renshaw AA, Derhagopian RP, Gould EW. Cystic neutrophilic granulomatous mastitis: an underappreciated pattern strongly associated with gram-positive bacilli. Am J Clin Pathol. 2011;136(3):424-427. doi:10.1309/AJCP1W9JBRYOQSNZ
21. Stary CM, Lee YS, Balfour J. Idiopathic granulomatous mastitis associated with corynebacterium sp. Infection. Hawaii Med J. 2011;70(5):99-101.
22. Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology. 2003;35(2):109-119.
23. Rakoff-Nahoum S. Why cancer and inflammation? Yale J Biol Med. 2006;79(3-4):123-130.
1. Garcia-Rodiguez JA, Pattullo A. Idiopathic granulomatous mastitis: a mimicking disease in a pregnant woman: a case report. BMC Res Notes. 2013;6:95. doi.10.1186/1756-0500-6-95
2. Gurleyik G, Aktekin A, Aker F, Karagulle H, Saglamc A. Medical and surgical treatment of idiopathic granulomatous lobular mastitis: a benign inflammatory disease mimicking invasive carcinoma. J Breast Cancer. 2012;15(1):119-123. doi:10.4048/jbc.2012.15.1.119
3. Hovanessian Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G. Granulomatous lobular mastitis: imaging, diagnosis, and treatment. AJR Am J Roentgenol. 2009;193(2):574-581. doi:10.2214/AJR.08.1528
4. Mazlan L, Suhaimi SN, Jasmin SJ, Latar NH, Adzman S, Muhammad R. Breast carcinoma occurring from chronic granulomatous mastitis. Malays J Med Sci. 2012;19(2):82-85.
5. Patel RA, Strickland P, Sankara IR, Pinkston G, Many W Jr, Rodriguez M. Idiopathic granulomatous mastitis: case reports and review of literature. J Gen Intern Med. 2010;25(3):270-273. doi:10.1007/s11606-009-1207-2
6. Akbulut S, Yilmaz D, Bakir S. Methotrexate in the management of idiopathic granulomatous mastitis: review of 108 published cases and report of four cases. Breast J. 2011;17(6):661-668. doi:10.1111/j.1524-4741.2011.01162.x
7. Ergin AB, Cristofanilli M, Daw H, Tahan G, Gong Y. Recurrent granulomatous mastitis mimicking inflammatory breast cancer. BMJ Case Rep. 2011;2011:bcr0720103156. doi:10.1136/bcr.07.2010.3156
8. Hladik M, Schoeller T, Ensat F, Wechselberger G. Idiopathic granulomatous mastitis: successful treatment by mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg. 2011;64(12):1604-1607. doi:10.1016/j.bjps.2011.07.01
9. Hur SM, Cho DH, Lee SK, et al. Experience of treatment of patients with granulomatous lobular mastitis. J Korean Surg Soc. 2013;85(1):1-6. doi:10.4174/jkss.2013.85.1.
10. Kayahan M, Kadioglu H, Muslumanoglu M. Management of patients with granulomatous mastitis: analysis of 31 cases. Breast Care (Basel). 2012;7(3):226-230. doi:10.1159/000337758
11. Neel A, Hello M, Cottereau A, et al. Long-term outcome in idiopathic granulomatous mastitis: a western multicentre study. QJM. 2013;106(5):433-441. doi:10.1093/qjmed/hct040
12. Seo HR, Na KY, Yim HE, et al. Differential diagnosis in idiopathic granulomatous mastitis and tuberculous mastitis. J Breast Cancer. 2012;15(1):111-118. doi:10.4048/jbc.2012.15.1.111
13. Martinez-Ramos D, Simon-Monterde L, Suelves-Piqueres C, et al. Idiopathic granulomatous mastitis: a systematic review of 3060 patients. Breast J. 2019;25(6):1245-1250. doi:10.1111/tbj.13446
14. Lin CH, Hsu CW, Tsao TY, Chou J. Idiopathic granulomatous mastitis associated with risperidone-induced hyperprolactinemia. Diagn Pathol. 2012;7:2. doi:10.1186/1746-1596-7-2
15. Goulabchand R, Hafidi A, Van de Perre P, et al. Mastitis in autoimmune diseases: review of the literature, diagnostic pathway, and pathophysiological key players. J Clin Med. 2020;9(4):958. doi:10.3390/jcm9040958
16. Altintoprak F. Topical steroids to treat granulomatous mastitis: a case report. Korean J Intern Med. 2011;26(3):356-359. doi:10.3904/kjim.2011.26.3.356
17. Tang A, Dominguez DA, Edquilang JK, et al. Granulomatous mastitis: comparison of novel treatment of steroid injection and current management. J Surg Res. 2020;254:300-305. doi:10.1016/j.jss.2020.04.018
18. Toktas O, Toprak N. Treatment results of intralesional steroid injection and topical steroid administration in pregnant women with idiopathic granulomatous mastitis. Eur J Breast Health. 2021;17(3):283-287. doi:10.4274/ejbh.galenos.2021.2021-2-4
19. Bercot B, Kannengiesser C, Oudin C, et al. First description of NOD2 variant associated with defective neutrophil responses in a woman with granulomatous mastitis related to corynebacteria. J Clin Microbiol. 2009;47(9):3034-3037. doi:10.1128/JCM.00561-09
20. Renshaw AA, Derhagopian RP, Gould EW. Cystic neutrophilic granulomatous mastitis: an underappreciated pattern strongly associated with gram-positive bacilli. Am J Clin Pathol. 2011;136(3):424-427. doi:10.1309/AJCP1W9JBRYOQSNZ
21. Stary CM, Lee YS, Balfour J. Idiopathic granulomatous mastitis associated with corynebacterium sp. Infection. Hawaii Med J. 2011;70(5):99-101.
22. Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology. 2003;35(2):109-119.
23. Rakoff-Nahoum S. Why cancer and inflammation? Yale J Biol Med. 2006;79(3-4):123-130.
Supplements Are Not a Synonym for Safe: Suspected Liver Injury From Ashwagandha
Many patients take herbals as alternative supplements to boost energy and mood. There are increasing reports of unintended adverse effects related to these supplements, particularly to the liver.1-3 A study by the Drug-Induced Liver Injury Network found that liver injury caused by herbals and dietary supplements has increased from 7% in 2004 to 20% in 2013.4
The supplement ashwagandha has become increasingly popular. Ashwagandha is extracted from the root of Withania somnifera (
To date, the factors defining the population at risk for ashwagandha toxicity are unclear, and an understanding of how to diagnose drug-induced liver injury is still immature in clinical practice. The regulation and study of the herbal and dietary supplement industry remain challenging. While many so-called natural substances are well tolerated, others can have unanticipated and harmful adverse effects and drug interactions. Future research should not only identify potentially harmful substances, but also which patients may be at greatest risk.
Case Presentation
A 48-year-old man with a history of severe alcohol use disorder (AUD) complicated by fatty liver and withdrawal seizures and delirium tremens, hypertension, depression, and anxiety presented to the emergency department (ED) after 4 days of having jaundice, epigastric abdominal pain, dark urine, and pale stools. In the preceding months, he had increased his alcohol use to as many as 12 drinks daily due to depression. After experiencing a blackout, he stopped drinking 7 days before presenting to the ED. He felt withdrawal symptoms, including tremors, diaphoresis, abdominal pain, nausea, and vomiting. On the third day of withdrawals, he reported that he had started taking an over-the-counter testosterone-boosting supplement to increase his energy, which he referred to as TestBoost—a mix of 8 ingredients, including ashwagandha, eleuthero root, Hawthorn berry, longjack, ginseng root, mushroom extract, bindii, and horny goat weed. After taking the supplement for 2 days, he noticed that his urine darkened, his stools became paler, his abdominal pain worsened, and he became jaundiced. After 2 additional days without improvement, and still taking the supplement, he presented to the ED. He reported having no fever, chills, recent illness, chest pain, shortness of breath, melena, lower extremity swelling, recent travel, or any changes in medications.
The patient had a 100.1 °F temperature, 102 beats per minute pulse; 129/94 mm Hg blood pressure, 18 beats per minute respiratory rate, and 97% oxygen saturation on room air on admission. He was in no acute distress, though his examination was notable for generalized jaundice and scleral icterus. He was mildly tender to palpation in the epigastric and right upper quadrant region. He was alert and oriented without confusion. He did not have any asterixis or spider angiomas, though he had scattered bruises on his left flank and left calf. His laboratory results were notable for mildly elevated aspartate aminotransferase (AST), 58 U/L (reference range, 13-35); alanine transaminase (ALT), 49 U/L (reference range, 7-45); and alkaline phosphatase (ALP), 98 U/L (reference range 33-94); total bilirubin, 13.6 mg/dL (reference range, 0.2-1.0); direct bilirubin, 8.4 mg/dL (reference range, 0.2-1); and international normalized ratio (INR), 1.11 (reference range, 2-3). His white blood cell and platelet counts were not remarkable at 9790/μL (reference range, 4500-11,000) and 337,000/μL (reference range, 150,000-440,000), respectively. Abdominal ultrasound and computed tomography (CT) revealed fatty liver with contracted gallbladder and no biliary dilatation. Urine ethanol levels were negative. The gastrointestinal (GI) service was consulted and agreed that his cholestatic injury was nonobstructive and likely related to the ashwagandha component of his supplement. The recommendation was cessation with close outpatient follow-up.
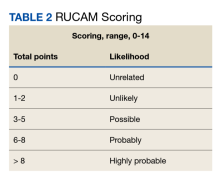
The patient was not prescribed any additional medications, such as steroids or ursodiol. He ceased supplement use following hospitalization; but relapsed into alcohol use 1 month after his discharge. Within 3 weeks, his total bilirubin had improved to 2.87 mg/dL, though AST, ALT, and ALP worsened to 127 U/L, 152 U/L, and 140 U/L, respectively. According to the notes of his psychiatrist who saw him at the time the laboratory tests were drawn, he had remained sober since discharge. His acute hepatitis panel drawn on admission was negative, and he demonstrated immunity to hepatitis A and B. Urine toxicology was negative. Antinuclear antibody (ANA) test was negative 1 year prior to discharge. Epstein-Barr virus (EBV), cytomegalovirus (CMV), ANA, antismooth muscle antibody, and immunoglobulins were not checked as suspicion for these etiologies was low. The Roussel Uclaf Causality Assessment Method (RUCAM) score was calculated as 6 (+1 for timing, +2 for drop in total bilirubin, +1 for ethanol risk factor, 0 for no other drugs, 0 for rule out of other diseases, +2 for known hepatotoxicity, 0 no repeat administration) for this patient indicating probable adverse drug reaction liver injury (Tables 1 and 2). However, we acknowledge that CMV, EBV, and herpes simplex virus status were not tested.
The 8 ingredients contained in TestBoost aside from ashwagandha did not have any major known liver adverse effects per a major database of medications. The other ingredients include eleuthero root, Hawthorn berry (crataegus laevigata), longjack (eurycoma longifolla) root, American ginseng root (American panax ginseng—panax quinquefolius), and Cordyceps mycelium (mushroom) extract, bindii (Tribulus terrestris), and epimedium grandiflorum (horny goat weed).6 No assays were performed to confirm purity of the ingredients in the patient’s supplement container.
Alcoholic hepatitis is an important consideration in this patient with AUD, though the timing of symptoms with supplement use and the cholestatic injury pattern with normal INR seems more consistent with drug-induced injury. Viral, infectious, and obstructive etiologies also were investigated. Acute viral hepatitis was ruled out based on bloodwork. The normal hepatobiliary tree on both ultrasound and CT effectively ruled out acute cholecystitis, cholangitis, and choledocholithiasis and there was no further indication for magnetic resonance cholangiopancreatography. There was no hepatic vein clot suggestive of Budd-Chiari syndrome. Autoimmune hepatitis was thought to be unlikely given that the etiology of injury seemed cholestatic in nature. Given the timing of the liver injury relative to supplement use it is likely that ashwagandha was a causative factor of this patient’s liver injury overlaid on an already strained liver from increased alcohol abuse.
The patient did not follow up with the GI service as an outpatient. There are no reports that the patient continued using the testosterone booster. His bilirubin improved dramatically within 1.5 months while his liver enzymes peaked 3 weeks later, with ALT ≥ AST. During his next admission 3 months later, he had relapsed, and his liver enzymes had the classic 2:1 AST to ALT ratio.
Discussion
Generally, ashwagandha has been thought to be well tolerated and possibly hepatoprotective.7-10 However, recent studies suggest potential for hepatotoxicity, though without clear guidance about which patients are most at risk.5,11,12 A study by Inagaki and colleagues suggests the potential for dose-dependent mechanism of liver injury, and this is supported by in vitro CYP450 inhibition with high doses of W Somnifera extract.11,13 We hypothesize that there may be a multihit process that makes some patients more susceptible to supplement harm, particularly those with repeated exposures and with ongoing exposure to hepatic toxins, such as AUD.14 Supplements should be used with more caution in these individuals.
Additionally, although there are no validated guidelines to confirm the diagnosis of drug-induced liver injury (DILI) from a manufactured medication or herbal remedy, the Council for International Organizations of Medical Sciences (CIOMS) developed RUCAM, a set of diagnostic criteria for DILI, which can be used to determine the probability of DILI based on pattern of injury.15 Although not widely used in clinical practice, RUCAM can help identify the possibility of DILI outside of expert consensus.16 It seems to have better discriminative ability than the Maria and Victorino scale, also used to identify DILI.16,17 While there is no replacement for clinical judgment, these scales may aid in identifying potential causes of DILI. The National Institutes of Health also has a LiverTox online tool that can assist health care professionals in identifying potentially hepatotoxic substances.6
Conclusions
We present a patient with AUD who developed cholestatic liver injury after ashwagandha use. Crucial to the diagnostic process is quantifying the amount ingested before presentation and the presence of contaminants, which is currently difficult to quantify given the lack of mechanisms to test supplements expediently in this manner in the clinical setting, which also requires the patient to bring in the supplements directly. There is also a lack of regulation and uniformity in these products. A clinician may be inclined to measure ashwagandha serum levels; however, such a test is not available to our knowledge. Nonetheless, using clinical tools such as RUCAM and utilizing databases, such as LiverTox, may help clinicians identify and remove potentially unsafe supplements. While there are many possible synergies between current medical practice and herbal remedies, practitioners must take care to first do no harm, as outlined in our Hippocratic Oath.
1. Navarro VJ. Herbal and dietary supplement hepatotoxicity. Semin Liver Dis. 2009;29(4):373-382. doi:10.1055/s-0029-1240006
2. Suk KT, Kim DJ, Kim CH, et al. A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol. 2012;107(9):1380-1387. doi:10.1038/ajg.2012.138
3. Shen T, Liu Y, Shang J, et al. Incidence and etiology of drug-induced liver injury in mainland China. Gastroenterology. 2019;156(8):2230-2241.e11. doi:10.1053/j.gastro.2019.02.002
4. Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology. 2014;60(4):1399-1408. doi:10.1002/hep.27317
5. Björnsson HK, Björnsson, Avula B, et al. (2020). Ashwagandha‐induced liver injury: a case series from Iceland and the US Drug‐Induced Liver Injury Network. Liver Int. 2020;40(4):825-829. doi:10.1111/liv.14393
6. National Institute of Diabetes and Digestive and Kidney Diseases. LiverTox: clinical and research information on drug-induced liver injury [internet]. Ashwagandha. Updated May 2, 2019. Accessed August 7, 2023. https://www.ncbi.nlm.nih.gov/books/NBK548536
7. Kumar G, Srivastava A, Sharma SK, Rao TD, Gupta YK. Efficacy and safety evaluation of Ayurvedic treatment (ashwagandha powder & Sidh Makardhwaj) in rheumatoid arthritis patients: a pilot prospective study. Indian J Med Res. 2015;141(1):100-106. doi:10.4103/0971-5916.154510
8. Kumar G, Srivastava A, Sharma SK, Gupta YK. Safety and efficacy evaluation of Ayurvedic treatment (arjuna powder and Arogyavardhini Vati) in dyslipidemia patients: a pilot prospective cohort clinical study. 2012;33(2):197-201. doi:10.4103/0974-8520.105238
9. Sultana N, Shimmi S, Parash MT, Akhtar J. Effects of ashwagandha (Withania somnifera) root extract on some serum liver marker enzymes (AST, ALT) in gentamicin intoxicated rats. J Bangladesh Soc Physiologist. 2012;7(1): 1-7. doi:10.3329/JBSP.V7I1.11152
10. Patel DP, Yan T, Kim D, et al. Withaferin A improves nonalcoholic steatohepatitis in mice. J Pharmacol Exp Ther. 2019;371(2):360-374. doi:10.1124/jpet.119.256792
11. Inagaki K, Mori N, Honda Y, Takaki S, Tsuji K, Chayama K. A case of drug-induced liver injury with prolonged severe intrahepatic cholestasis induced by ashwagandha. Kanzo. 2017;58(8):448-454. doi:10.2957/kanzo.58.448
12. Alali F, Hermez K, Ullah N. Acute hepatitis induced by a unique combination of herbal supplements. Am J Gastroenterol. 2018;113:S1661.
13. Sava J, Varghese A, Pandita N. Lack of the cytochrome P450 3A interaction of methanolic extract of Withania somnifera, Withaferin A, Withanolide A and Withanoside IV. J Pharm Negative Results. 2013;4(1):26.
14. Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349(5):474-485. doi:10.1056/NEJMra021844.
15. Danan G, Benichou C. Causality assessment of adverse reactions to drugs-I. A novel method based on the conclusions of International Consensus Meeting: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46:1323–1333. doi:10.1016/0895-4356(93)90101-6
16. Hayashi PH. Causality assessment in drug-induced liver injury. Semin Liver Dis. 2009;29(4):348-356. doi.10.1002/cld.615
17. Lucena MI, Camargo R, Andrade RJ, Perez-Sanchez CJ, Sanchez De La Cuesta F. Comparison of two clinical scales for causality assessment in hepatotoxicity. Hepatology. 2001;33(1):123-130. doi:10.1053/jhep.2001.20645
Many patients take herbals as alternative supplements to boost energy and mood. There are increasing reports of unintended adverse effects related to these supplements, particularly to the liver.1-3 A study by the Drug-Induced Liver Injury Network found that liver injury caused by herbals and dietary supplements has increased from 7% in 2004 to 20% in 2013.4
The supplement ashwagandha has become increasingly popular. Ashwagandha is extracted from the root of Withania somnifera (
To date, the factors defining the population at risk for ashwagandha toxicity are unclear, and an understanding of how to diagnose drug-induced liver injury is still immature in clinical practice. The regulation and study of the herbal and dietary supplement industry remain challenging. While many so-called natural substances are well tolerated, others can have unanticipated and harmful adverse effects and drug interactions. Future research should not only identify potentially harmful substances, but also which patients may be at greatest risk.
Case Presentation
A 48-year-old man with a history of severe alcohol use disorder (AUD) complicated by fatty liver and withdrawal seizures and delirium tremens, hypertension, depression, and anxiety presented to the emergency department (ED) after 4 days of having jaundice, epigastric abdominal pain, dark urine, and pale stools. In the preceding months, he had increased his alcohol use to as many as 12 drinks daily due to depression. After experiencing a blackout, he stopped drinking 7 days before presenting to the ED. He felt withdrawal symptoms, including tremors, diaphoresis, abdominal pain, nausea, and vomiting. On the third day of withdrawals, he reported that he had started taking an over-the-counter testosterone-boosting supplement to increase his energy, which he referred to as TestBoost—a mix of 8 ingredients, including ashwagandha, eleuthero root, Hawthorn berry, longjack, ginseng root, mushroom extract, bindii, and horny goat weed. After taking the supplement for 2 days, he noticed that his urine darkened, his stools became paler, his abdominal pain worsened, and he became jaundiced. After 2 additional days without improvement, and still taking the supplement, he presented to the ED. He reported having no fever, chills, recent illness, chest pain, shortness of breath, melena, lower extremity swelling, recent travel, or any changes in medications.
The patient had a 100.1 °F temperature, 102 beats per minute pulse; 129/94 mm Hg blood pressure, 18 beats per minute respiratory rate, and 97% oxygen saturation on room air on admission. He was in no acute distress, though his examination was notable for generalized jaundice and scleral icterus. He was mildly tender to palpation in the epigastric and right upper quadrant region. He was alert and oriented without confusion. He did not have any asterixis or spider angiomas, though he had scattered bruises on his left flank and left calf. His laboratory results were notable for mildly elevated aspartate aminotransferase (AST), 58 U/L (reference range, 13-35); alanine transaminase (ALT), 49 U/L (reference range, 7-45); and alkaline phosphatase (ALP), 98 U/L (reference range 33-94); total bilirubin, 13.6 mg/dL (reference range, 0.2-1.0); direct bilirubin, 8.4 mg/dL (reference range, 0.2-1); and international normalized ratio (INR), 1.11 (reference range, 2-3). His white blood cell and platelet counts were not remarkable at 9790/μL (reference range, 4500-11,000) and 337,000/μL (reference range, 150,000-440,000), respectively. Abdominal ultrasound and computed tomography (CT) revealed fatty liver with contracted gallbladder and no biliary dilatation. Urine ethanol levels were negative. The gastrointestinal (GI) service was consulted and agreed that his cholestatic injury was nonobstructive and likely related to the ashwagandha component of his supplement. The recommendation was cessation with close outpatient follow-up.
The patient was not prescribed any additional medications, such as steroids or ursodiol. He ceased supplement use following hospitalization; but relapsed into alcohol use 1 month after his discharge. Within 3 weeks, his total bilirubin had improved to 2.87 mg/dL, though AST, ALT, and ALP worsened to 127 U/L, 152 U/L, and 140 U/L, respectively. According to the notes of his psychiatrist who saw him at the time the laboratory tests were drawn, he had remained sober since discharge. His acute hepatitis panel drawn on admission was negative, and he demonstrated immunity to hepatitis A and B. Urine toxicology was negative. Antinuclear antibody (ANA) test was negative 1 year prior to discharge. Epstein-Barr virus (EBV), cytomegalovirus (CMV), ANA, antismooth muscle antibody, and immunoglobulins were not checked as suspicion for these etiologies was low. The Roussel Uclaf Causality Assessment Method (RUCAM) score was calculated as 6 (+1 for timing, +2 for drop in total bilirubin, +1 for ethanol risk factor, 0 for no other drugs, 0 for rule out of other diseases, +2 for known hepatotoxicity, 0 no repeat administration) for this patient indicating probable adverse drug reaction liver injury (Tables 1 and 2). However, we acknowledge that CMV, EBV, and herpes simplex virus status were not tested.
The 8 ingredients contained in TestBoost aside from ashwagandha did not have any major known liver adverse effects per a major database of medications. The other ingredients include eleuthero root, Hawthorn berry (crataegus laevigata), longjack (eurycoma longifolla) root, American ginseng root (American panax ginseng—panax quinquefolius), and Cordyceps mycelium (mushroom) extract, bindii (Tribulus terrestris), and epimedium grandiflorum (horny goat weed).6 No assays were performed to confirm purity of the ingredients in the patient’s supplement container.
Alcoholic hepatitis is an important consideration in this patient with AUD, though the timing of symptoms with supplement use and the cholestatic injury pattern with normal INR seems more consistent with drug-induced injury. Viral, infectious, and obstructive etiologies also were investigated. Acute viral hepatitis was ruled out based on bloodwork. The normal hepatobiliary tree on both ultrasound and CT effectively ruled out acute cholecystitis, cholangitis, and choledocholithiasis and there was no further indication for magnetic resonance cholangiopancreatography. There was no hepatic vein clot suggestive of Budd-Chiari syndrome. Autoimmune hepatitis was thought to be unlikely given that the etiology of injury seemed cholestatic in nature. Given the timing of the liver injury relative to supplement use it is likely that ashwagandha was a causative factor of this patient’s liver injury overlaid on an already strained liver from increased alcohol abuse.
The patient did not follow up with the GI service as an outpatient. There are no reports that the patient continued using the testosterone booster. His bilirubin improved dramatically within 1.5 months while his liver enzymes peaked 3 weeks later, with ALT ≥ AST. During his next admission 3 months later, he had relapsed, and his liver enzymes had the classic 2:1 AST to ALT ratio.
Discussion
Generally, ashwagandha has been thought to be well tolerated and possibly hepatoprotective.7-10 However, recent studies suggest potential for hepatotoxicity, though without clear guidance about which patients are most at risk.5,11,12 A study by Inagaki and colleagues suggests the potential for dose-dependent mechanism of liver injury, and this is supported by in vitro CYP450 inhibition with high doses of W Somnifera extract.11,13 We hypothesize that there may be a multihit process that makes some patients more susceptible to supplement harm, particularly those with repeated exposures and with ongoing exposure to hepatic toxins, such as AUD.14 Supplements should be used with more caution in these individuals.
Additionally, although there are no validated guidelines to confirm the diagnosis of drug-induced liver injury (DILI) from a manufactured medication or herbal remedy, the Council for International Organizations of Medical Sciences (CIOMS) developed RUCAM, a set of diagnostic criteria for DILI, which can be used to determine the probability of DILI based on pattern of injury.15 Although not widely used in clinical practice, RUCAM can help identify the possibility of DILI outside of expert consensus.16 It seems to have better discriminative ability than the Maria and Victorino scale, also used to identify DILI.16,17 While there is no replacement for clinical judgment, these scales may aid in identifying potential causes of DILI. The National Institutes of Health also has a LiverTox online tool that can assist health care professionals in identifying potentially hepatotoxic substances.6
Conclusions
We present a patient with AUD who developed cholestatic liver injury after ashwagandha use. Crucial to the diagnostic process is quantifying the amount ingested before presentation and the presence of contaminants, which is currently difficult to quantify given the lack of mechanisms to test supplements expediently in this manner in the clinical setting, which also requires the patient to bring in the supplements directly. There is also a lack of regulation and uniformity in these products. A clinician may be inclined to measure ashwagandha serum levels; however, such a test is not available to our knowledge. Nonetheless, using clinical tools such as RUCAM and utilizing databases, such as LiverTox, may help clinicians identify and remove potentially unsafe supplements. While there are many possible synergies between current medical practice and herbal remedies, practitioners must take care to first do no harm, as outlined in our Hippocratic Oath.
Many patients take herbals as alternative supplements to boost energy and mood. There are increasing reports of unintended adverse effects related to these supplements, particularly to the liver.1-3 A study by the Drug-Induced Liver Injury Network found that liver injury caused by herbals and dietary supplements has increased from 7% in 2004 to 20% in 2013.4
The supplement ashwagandha has become increasingly popular. Ashwagandha is extracted from the root of Withania somnifera (
To date, the factors defining the population at risk for ashwagandha toxicity are unclear, and an understanding of how to diagnose drug-induced liver injury is still immature in clinical practice. The regulation and study of the herbal and dietary supplement industry remain challenging. While many so-called natural substances are well tolerated, others can have unanticipated and harmful adverse effects and drug interactions. Future research should not only identify potentially harmful substances, but also which patients may be at greatest risk.
Case Presentation
A 48-year-old man with a history of severe alcohol use disorder (AUD) complicated by fatty liver and withdrawal seizures and delirium tremens, hypertension, depression, and anxiety presented to the emergency department (ED) after 4 days of having jaundice, epigastric abdominal pain, dark urine, and pale stools. In the preceding months, he had increased his alcohol use to as many as 12 drinks daily due to depression. After experiencing a blackout, he stopped drinking 7 days before presenting to the ED. He felt withdrawal symptoms, including tremors, diaphoresis, abdominal pain, nausea, and vomiting. On the third day of withdrawals, he reported that he had started taking an over-the-counter testosterone-boosting supplement to increase his energy, which he referred to as TestBoost—a mix of 8 ingredients, including ashwagandha, eleuthero root, Hawthorn berry, longjack, ginseng root, mushroom extract, bindii, and horny goat weed. After taking the supplement for 2 days, he noticed that his urine darkened, his stools became paler, his abdominal pain worsened, and he became jaundiced. After 2 additional days without improvement, and still taking the supplement, he presented to the ED. He reported having no fever, chills, recent illness, chest pain, shortness of breath, melena, lower extremity swelling, recent travel, or any changes in medications.
The patient had a 100.1 °F temperature, 102 beats per minute pulse; 129/94 mm Hg blood pressure, 18 beats per minute respiratory rate, and 97% oxygen saturation on room air on admission. He was in no acute distress, though his examination was notable for generalized jaundice and scleral icterus. He was mildly tender to palpation in the epigastric and right upper quadrant region. He was alert and oriented without confusion. He did not have any asterixis or spider angiomas, though he had scattered bruises on his left flank and left calf. His laboratory results were notable for mildly elevated aspartate aminotransferase (AST), 58 U/L (reference range, 13-35); alanine transaminase (ALT), 49 U/L (reference range, 7-45); and alkaline phosphatase (ALP), 98 U/L (reference range 33-94); total bilirubin, 13.6 mg/dL (reference range, 0.2-1.0); direct bilirubin, 8.4 mg/dL (reference range, 0.2-1); and international normalized ratio (INR), 1.11 (reference range, 2-3). His white blood cell and platelet counts were not remarkable at 9790/μL (reference range, 4500-11,000) and 337,000/μL (reference range, 150,000-440,000), respectively. Abdominal ultrasound and computed tomography (CT) revealed fatty liver with contracted gallbladder and no biliary dilatation. Urine ethanol levels were negative. The gastrointestinal (GI) service was consulted and agreed that his cholestatic injury was nonobstructive and likely related to the ashwagandha component of his supplement. The recommendation was cessation with close outpatient follow-up.
The patient was not prescribed any additional medications, such as steroids or ursodiol. He ceased supplement use following hospitalization; but relapsed into alcohol use 1 month after his discharge. Within 3 weeks, his total bilirubin had improved to 2.87 mg/dL, though AST, ALT, and ALP worsened to 127 U/L, 152 U/L, and 140 U/L, respectively. According to the notes of his psychiatrist who saw him at the time the laboratory tests were drawn, he had remained sober since discharge. His acute hepatitis panel drawn on admission was negative, and he demonstrated immunity to hepatitis A and B. Urine toxicology was negative. Antinuclear antibody (ANA) test was negative 1 year prior to discharge. Epstein-Barr virus (EBV), cytomegalovirus (CMV), ANA, antismooth muscle antibody, and immunoglobulins were not checked as suspicion for these etiologies was low. The Roussel Uclaf Causality Assessment Method (RUCAM) score was calculated as 6 (+1 for timing, +2 for drop in total bilirubin, +1 for ethanol risk factor, 0 for no other drugs, 0 for rule out of other diseases, +2 for known hepatotoxicity, 0 no repeat administration) for this patient indicating probable adverse drug reaction liver injury (Tables 1 and 2). However, we acknowledge that CMV, EBV, and herpes simplex virus status were not tested.
The 8 ingredients contained in TestBoost aside from ashwagandha did not have any major known liver adverse effects per a major database of medications. The other ingredients include eleuthero root, Hawthorn berry (crataegus laevigata), longjack (eurycoma longifolla) root, American ginseng root (American panax ginseng—panax quinquefolius), and Cordyceps mycelium (mushroom) extract, bindii (Tribulus terrestris), and epimedium grandiflorum (horny goat weed).6 No assays were performed to confirm purity of the ingredients in the patient’s supplement container.
Alcoholic hepatitis is an important consideration in this patient with AUD, though the timing of symptoms with supplement use and the cholestatic injury pattern with normal INR seems more consistent with drug-induced injury. Viral, infectious, and obstructive etiologies also were investigated. Acute viral hepatitis was ruled out based on bloodwork. The normal hepatobiliary tree on both ultrasound and CT effectively ruled out acute cholecystitis, cholangitis, and choledocholithiasis and there was no further indication for magnetic resonance cholangiopancreatography. There was no hepatic vein clot suggestive of Budd-Chiari syndrome. Autoimmune hepatitis was thought to be unlikely given that the etiology of injury seemed cholestatic in nature. Given the timing of the liver injury relative to supplement use it is likely that ashwagandha was a causative factor of this patient’s liver injury overlaid on an already strained liver from increased alcohol abuse.
The patient did not follow up with the GI service as an outpatient. There are no reports that the patient continued using the testosterone booster. His bilirubin improved dramatically within 1.5 months while his liver enzymes peaked 3 weeks later, with ALT ≥ AST. During his next admission 3 months later, he had relapsed, and his liver enzymes had the classic 2:1 AST to ALT ratio.
Discussion
Generally, ashwagandha has been thought to be well tolerated and possibly hepatoprotective.7-10 However, recent studies suggest potential for hepatotoxicity, though without clear guidance about which patients are most at risk.5,11,12 A study by Inagaki and colleagues suggests the potential for dose-dependent mechanism of liver injury, and this is supported by in vitro CYP450 inhibition with high doses of W Somnifera extract.11,13 We hypothesize that there may be a multihit process that makes some patients more susceptible to supplement harm, particularly those with repeated exposures and with ongoing exposure to hepatic toxins, such as AUD.14 Supplements should be used with more caution in these individuals.
Additionally, although there are no validated guidelines to confirm the diagnosis of drug-induced liver injury (DILI) from a manufactured medication or herbal remedy, the Council for International Organizations of Medical Sciences (CIOMS) developed RUCAM, a set of diagnostic criteria for DILI, which can be used to determine the probability of DILI based on pattern of injury.15 Although not widely used in clinical practice, RUCAM can help identify the possibility of DILI outside of expert consensus.16 It seems to have better discriminative ability than the Maria and Victorino scale, also used to identify DILI.16,17 While there is no replacement for clinical judgment, these scales may aid in identifying potential causes of DILI. The National Institutes of Health also has a LiverTox online tool that can assist health care professionals in identifying potentially hepatotoxic substances.6
Conclusions
We present a patient with AUD who developed cholestatic liver injury after ashwagandha use. Crucial to the diagnostic process is quantifying the amount ingested before presentation and the presence of contaminants, which is currently difficult to quantify given the lack of mechanisms to test supplements expediently in this manner in the clinical setting, which also requires the patient to bring in the supplements directly. There is also a lack of regulation and uniformity in these products. A clinician may be inclined to measure ashwagandha serum levels; however, such a test is not available to our knowledge. Nonetheless, using clinical tools such as RUCAM and utilizing databases, such as LiverTox, may help clinicians identify and remove potentially unsafe supplements. While there are many possible synergies between current medical practice and herbal remedies, practitioners must take care to first do no harm, as outlined in our Hippocratic Oath.
1. Navarro VJ. Herbal and dietary supplement hepatotoxicity. Semin Liver Dis. 2009;29(4):373-382. doi:10.1055/s-0029-1240006
2. Suk KT, Kim DJ, Kim CH, et al. A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol. 2012;107(9):1380-1387. doi:10.1038/ajg.2012.138
3. Shen T, Liu Y, Shang J, et al. Incidence and etiology of drug-induced liver injury in mainland China. Gastroenterology. 2019;156(8):2230-2241.e11. doi:10.1053/j.gastro.2019.02.002
4. Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology. 2014;60(4):1399-1408. doi:10.1002/hep.27317
5. Björnsson HK, Björnsson, Avula B, et al. (2020). Ashwagandha‐induced liver injury: a case series from Iceland and the US Drug‐Induced Liver Injury Network. Liver Int. 2020;40(4):825-829. doi:10.1111/liv.14393
6. National Institute of Diabetes and Digestive and Kidney Diseases. LiverTox: clinical and research information on drug-induced liver injury [internet]. Ashwagandha. Updated May 2, 2019. Accessed August 7, 2023. https://www.ncbi.nlm.nih.gov/books/NBK548536
7. Kumar G, Srivastava A, Sharma SK, Rao TD, Gupta YK. Efficacy and safety evaluation of Ayurvedic treatment (ashwagandha powder & Sidh Makardhwaj) in rheumatoid arthritis patients: a pilot prospective study. Indian J Med Res. 2015;141(1):100-106. doi:10.4103/0971-5916.154510
8. Kumar G, Srivastava A, Sharma SK, Gupta YK. Safety and efficacy evaluation of Ayurvedic treatment (arjuna powder and Arogyavardhini Vati) in dyslipidemia patients: a pilot prospective cohort clinical study. 2012;33(2):197-201. doi:10.4103/0974-8520.105238
9. Sultana N, Shimmi S, Parash MT, Akhtar J. Effects of ashwagandha (Withania somnifera) root extract on some serum liver marker enzymes (AST, ALT) in gentamicin intoxicated rats. J Bangladesh Soc Physiologist. 2012;7(1): 1-7. doi:10.3329/JBSP.V7I1.11152
10. Patel DP, Yan T, Kim D, et al. Withaferin A improves nonalcoholic steatohepatitis in mice. J Pharmacol Exp Ther. 2019;371(2):360-374. doi:10.1124/jpet.119.256792
11. Inagaki K, Mori N, Honda Y, Takaki S, Tsuji K, Chayama K. A case of drug-induced liver injury with prolonged severe intrahepatic cholestasis induced by ashwagandha. Kanzo. 2017;58(8):448-454. doi:10.2957/kanzo.58.448
12. Alali F, Hermez K, Ullah N. Acute hepatitis induced by a unique combination of herbal supplements. Am J Gastroenterol. 2018;113:S1661.
13. Sava J, Varghese A, Pandita N. Lack of the cytochrome P450 3A interaction of methanolic extract of Withania somnifera, Withaferin A, Withanolide A and Withanoside IV. J Pharm Negative Results. 2013;4(1):26.
14. Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349(5):474-485. doi:10.1056/NEJMra021844.
15. Danan G, Benichou C. Causality assessment of adverse reactions to drugs-I. A novel method based on the conclusions of International Consensus Meeting: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46:1323–1333. doi:10.1016/0895-4356(93)90101-6
16. Hayashi PH. Causality assessment in drug-induced liver injury. Semin Liver Dis. 2009;29(4):348-356. doi.10.1002/cld.615
17. Lucena MI, Camargo R, Andrade RJ, Perez-Sanchez CJ, Sanchez De La Cuesta F. Comparison of two clinical scales for causality assessment in hepatotoxicity. Hepatology. 2001;33(1):123-130. doi:10.1053/jhep.2001.20645
1. Navarro VJ. Herbal and dietary supplement hepatotoxicity. Semin Liver Dis. 2009;29(4):373-382. doi:10.1055/s-0029-1240006
2. Suk KT, Kim DJ, Kim CH, et al. A prospective nationwide study of drug-induced liver injury in Korea. Am J Gastroenterol. 2012;107(9):1380-1387. doi:10.1038/ajg.2012.138
3. Shen T, Liu Y, Shang J, et al. Incidence and etiology of drug-induced liver injury in mainland China. Gastroenterology. 2019;156(8):2230-2241.e11. doi:10.1053/j.gastro.2019.02.002
4. Navarro VJ, Barnhart H, Bonkovsky HL, et al. Liver injury from herbals and dietary supplements in the U.S. Drug-Induced Liver Injury Network. Hepatology. 2014;60(4):1399-1408. doi:10.1002/hep.27317
5. Björnsson HK, Björnsson, Avula B, et al. (2020). Ashwagandha‐induced liver injury: a case series from Iceland and the US Drug‐Induced Liver Injury Network. Liver Int. 2020;40(4):825-829. doi:10.1111/liv.14393
6. National Institute of Diabetes and Digestive and Kidney Diseases. LiverTox: clinical and research information on drug-induced liver injury [internet]. Ashwagandha. Updated May 2, 2019. Accessed August 7, 2023. https://www.ncbi.nlm.nih.gov/books/NBK548536
7. Kumar G, Srivastava A, Sharma SK, Rao TD, Gupta YK. Efficacy and safety evaluation of Ayurvedic treatment (ashwagandha powder & Sidh Makardhwaj) in rheumatoid arthritis patients: a pilot prospective study. Indian J Med Res. 2015;141(1):100-106. doi:10.4103/0971-5916.154510
8. Kumar G, Srivastava A, Sharma SK, Gupta YK. Safety and efficacy evaluation of Ayurvedic treatment (arjuna powder and Arogyavardhini Vati) in dyslipidemia patients: a pilot prospective cohort clinical study. 2012;33(2):197-201. doi:10.4103/0974-8520.105238
9. Sultana N, Shimmi S, Parash MT, Akhtar J. Effects of ashwagandha (Withania somnifera) root extract on some serum liver marker enzymes (AST, ALT) in gentamicin intoxicated rats. J Bangladesh Soc Physiologist. 2012;7(1): 1-7. doi:10.3329/JBSP.V7I1.11152
10. Patel DP, Yan T, Kim D, et al. Withaferin A improves nonalcoholic steatohepatitis in mice. J Pharmacol Exp Ther. 2019;371(2):360-374. doi:10.1124/jpet.119.256792
11. Inagaki K, Mori N, Honda Y, Takaki S, Tsuji K, Chayama K. A case of drug-induced liver injury with prolonged severe intrahepatic cholestasis induced by ashwagandha. Kanzo. 2017;58(8):448-454. doi:10.2957/kanzo.58.448
12. Alali F, Hermez K, Ullah N. Acute hepatitis induced by a unique combination of herbal supplements. Am J Gastroenterol. 2018;113:S1661.
13. Sava J, Varghese A, Pandita N. Lack of the cytochrome P450 3A interaction of methanolic extract of Withania somnifera, Withaferin A, Withanolide A and Withanoside IV. J Pharm Negative Results. 2013;4(1):26.
14. Lee WM. Drug-induced hepatotoxicity. N Engl J Med. 2003;349(5):474-485. doi:10.1056/NEJMra021844.
15. Danan G, Benichou C. Causality assessment of adverse reactions to drugs-I. A novel method based on the conclusions of International Consensus Meeting: application to drug-induced liver injuries. J Clin Epidemiol. 1993;46:1323–1333. doi:10.1016/0895-4356(93)90101-6
16. Hayashi PH. Causality assessment in drug-induced liver injury. Semin Liver Dis. 2009;29(4):348-356. doi.10.1002/cld.615
17. Lucena MI, Camargo R, Andrade RJ, Perez-Sanchez CJ, Sanchez De La Cuesta F. Comparison of two clinical scales for causality assessment in hepatotoxicity. Hepatology. 2001;33(1):123-130. doi:10.1053/jhep.2001.20645
Role of Prophylactic Cranial Irradiation in Small Cell Carcinoma of Urinary Bladder: Case Report and Literature Review
INTRODUCTION
Urinary bladder is an extremely rare site of extrapulmonary small cell cancer (EPSCC). Unlike small cell lung cancer (SCLC), there is no clear guideline for prophylactic cranial irradiation (PCI) for EPSCC. In this case report and literature review, we discuss small cell cancer of urinary bladder (SCCUB) and the role of PCI in SCCUB.
CASE PRESENTATION
A 74-year-old male presented with gross hematuria and an unremarkable physical examination. CT showed 1.7 cm right anterolateral bladder wall thickening. Cystoscopy revealed a 2-3 cm high-grade bladder lesion. Pathology from transurethral resection of the tumor was consistent with T1N0M0 small cell carcinoma. MRI brain and FDG-PET showed no extravesical disease. Patient received four cycles of neoadjuvant carboplatin/etoposide per his preference as he wanted to protect his hearing due to his profession followed by radical cystoprostatectomy. Post-op pathology showed clear margins. We decided to forego PCI in favor of interval surveillance with MRI and follow- up images remain negative for distant metastases.
DISCUSSION
EPSCC accounts for 2.5-5% of all SCC, very rare in male genitourinary tract. Treatment approach is derived from SCLC, guided by extent of disease and patient’s functional status. Role of PCI in EPSCC has not been clearly described, and even less evidence is available for SCCUB. From a review of eleven studies in PubMed for the role of PCI in SCCUB or EPSCC, we found that SCCUB has lower incidence of brain metastases than SCLC. One study suggested that SCCUB arises from totipotent cells in the submucosa, unlike Kulchitsky cell origin of SCLC. This difference might explain the difference in their metastatic behavior. With this background, PCI is not routinely recommended for limited- stage SCCUB. There might still be a role for PCI in extensive SCCUB with high metastatic burden. More studies are needed to update the guidelines for the role of PCI for these tumors.
CONCLUSIONS
Per this literature review, PCI is not routinely recommended for SCCUB, likely due to different cells of origin compared to SCLC. Future studies should focus on characterizing differences in their metastatic behavior and updating guidelines for PCI for SCCUB.
INTRODUCTION
Urinary bladder is an extremely rare site of extrapulmonary small cell cancer (EPSCC). Unlike small cell lung cancer (SCLC), there is no clear guideline for prophylactic cranial irradiation (PCI) for EPSCC. In this case report and literature review, we discuss small cell cancer of urinary bladder (SCCUB) and the role of PCI in SCCUB.
CASE PRESENTATION
A 74-year-old male presented with gross hematuria and an unremarkable physical examination. CT showed 1.7 cm right anterolateral bladder wall thickening. Cystoscopy revealed a 2-3 cm high-grade bladder lesion. Pathology from transurethral resection of the tumor was consistent with T1N0M0 small cell carcinoma. MRI brain and FDG-PET showed no extravesical disease. Patient received four cycles of neoadjuvant carboplatin/etoposide per his preference as he wanted to protect his hearing due to his profession followed by radical cystoprostatectomy. Post-op pathology showed clear margins. We decided to forego PCI in favor of interval surveillance with MRI and follow- up images remain negative for distant metastases.
DISCUSSION
EPSCC accounts for 2.5-5% of all SCC, very rare in male genitourinary tract. Treatment approach is derived from SCLC, guided by extent of disease and patient’s functional status. Role of PCI in EPSCC has not been clearly described, and even less evidence is available for SCCUB. From a review of eleven studies in PubMed for the role of PCI in SCCUB or EPSCC, we found that SCCUB has lower incidence of brain metastases than SCLC. One study suggested that SCCUB arises from totipotent cells in the submucosa, unlike Kulchitsky cell origin of SCLC. This difference might explain the difference in their metastatic behavior. With this background, PCI is not routinely recommended for limited- stage SCCUB. There might still be a role for PCI in extensive SCCUB with high metastatic burden. More studies are needed to update the guidelines for the role of PCI for these tumors.
CONCLUSIONS
Per this literature review, PCI is not routinely recommended for SCCUB, likely due to different cells of origin compared to SCLC. Future studies should focus on characterizing differences in their metastatic behavior and updating guidelines for PCI for SCCUB.
INTRODUCTION
Urinary bladder is an extremely rare site of extrapulmonary small cell cancer (EPSCC). Unlike small cell lung cancer (SCLC), there is no clear guideline for prophylactic cranial irradiation (PCI) for EPSCC. In this case report and literature review, we discuss small cell cancer of urinary bladder (SCCUB) and the role of PCI in SCCUB.
CASE PRESENTATION
A 74-year-old male presented with gross hematuria and an unremarkable physical examination. CT showed 1.7 cm right anterolateral bladder wall thickening. Cystoscopy revealed a 2-3 cm high-grade bladder lesion. Pathology from transurethral resection of the tumor was consistent with T1N0M0 small cell carcinoma. MRI brain and FDG-PET showed no extravesical disease. Patient received four cycles of neoadjuvant carboplatin/etoposide per his preference as he wanted to protect his hearing due to his profession followed by radical cystoprostatectomy. Post-op pathology showed clear margins. We decided to forego PCI in favor of interval surveillance with MRI and follow- up images remain negative for distant metastases.
DISCUSSION
EPSCC accounts for 2.5-5% of all SCC, very rare in male genitourinary tract. Treatment approach is derived from SCLC, guided by extent of disease and patient’s functional status. Role of PCI in EPSCC has not been clearly described, and even less evidence is available for SCCUB. From a review of eleven studies in PubMed for the role of PCI in SCCUB or EPSCC, we found that SCCUB has lower incidence of brain metastases than SCLC. One study suggested that SCCUB arises from totipotent cells in the submucosa, unlike Kulchitsky cell origin of SCLC. This difference might explain the difference in their metastatic behavior. With this background, PCI is not routinely recommended for limited- stage SCCUB. There might still be a role for PCI in extensive SCCUB with high metastatic burden. More studies are needed to update the guidelines for the role of PCI for these tumors.
CONCLUSIONS
Per this literature review, PCI is not routinely recommended for SCCUB, likely due to different cells of origin compared to SCLC. Future studies should focus on characterizing differences in their metastatic behavior and updating guidelines for PCI for SCCUB.
Metastatic Urothelial Carcinoma Presenting as Mediastinal Lymphadenopathy Without Appreciable Bladder Mass in a Patient With Chronic Lymphocytic Leukemia
INTRODUCTION
Lymphadenopathy in Chronic Lymphocytic Leukemia (CLL) is a very common feature. However, sudden increase in lymphadenopathy or other symptoms like weight loss should be evaluated for possible metastatic malignancy. We describe a CLL patient with diffuse mediastinal lymphadenopathy who was diagnosed with metastatic bladder cancer without a primary bladder tumor mass on imaging.
CASE DESCRIPTION
A 60-year-old man with a 60 pack-year smoking history, alcoholic cirrhosis, and a 5-year history of stage 1 CLL presented with 3 months of progressive shortness of breath; persistent cough; chills; hemoptysis; and a steady weight loss of 35 lbs. Notably, he had no bladder symptoms. Initial labs showed leukocytosis of 35.8k with a lymphocytic predominance. Screening low-dose chest CT was positive for diffuse mediastinal lymphadenopathy. Subsequent PET/CT revealed numerous hypermetabolic lymph nodes in the neck, mediastinum, left hilum, and right periaortic abdominal region. CT Chest, Abdomen, Pelvis revealed progressive lymphadenopathy as seen in prior imaging, stable pulmonary nodules up to 4 mm in size, and splenomegaly. No distant primary sites, including of the bladder, were identified. Mediastinal lymph node biopsy confirmed metastatic poorly differentiated carcinoma with immunohistochemical staining negative for p40, p63, CK20, TTF-1, Napsin A, CDX2, CA19- 9, Calretinin, and D2-40 and positive for CK7, GATA3, Ber-EP4, and Uroplakin, supporting bladder as primary origin. Urology deferred a cystoscopy given his lack of urinary symptoms and positive biopsy and was started on Carboplatin/Gemcitabine for his metastatic disease. He was ineligible for Cisplatin given his cirrhosis and hearing impairment.
DISCUSSION
In patients with CLL, new onset mediastinal lymphadenopathy is concerning for disease progression and possible transformation to a diffuse b-cell lymphoma. However, this symptom has a broad differential, including primary lung carcinomas, sarcomas, and metastatic disease. While our patient’s PET/CT and pan-CT failed to identify a distant primary site, maintaining a low clinical suspicion for metastatic disease and doing a thorough work-up was paramount. Only through immunohistochemical staining were we able to diagnosis this patient with urothelial carcinoma.
CONCLUSIONS
Biopsy with immunohistochemical staining and maintaining a low suspicion for worsening lymphadenopathy can identify unusually presenting urothelial carcinomas in CLL patients.
INTRODUCTION
Lymphadenopathy in Chronic Lymphocytic Leukemia (CLL) is a very common feature. However, sudden increase in lymphadenopathy or other symptoms like weight loss should be evaluated for possible metastatic malignancy. We describe a CLL patient with diffuse mediastinal lymphadenopathy who was diagnosed with metastatic bladder cancer without a primary bladder tumor mass on imaging.
CASE DESCRIPTION
A 60-year-old man with a 60 pack-year smoking history, alcoholic cirrhosis, and a 5-year history of stage 1 CLL presented with 3 months of progressive shortness of breath; persistent cough; chills; hemoptysis; and a steady weight loss of 35 lbs. Notably, he had no bladder symptoms. Initial labs showed leukocytosis of 35.8k with a lymphocytic predominance. Screening low-dose chest CT was positive for diffuse mediastinal lymphadenopathy. Subsequent PET/CT revealed numerous hypermetabolic lymph nodes in the neck, mediastinum, left hilum, and right periaortic abdominal region. CT Chest, Abdomen, Pelvis revealed progressive lymphadenopathy as seen in prior imaging, stable pulmonary nodules up to 4 mm in size, and splenomegaly. No distant primary sites, including of the bladder, were identified. Mediastinal lymph node biopsy confirmed metastatic poorly differentiated carcinoma with immunohistochemical staining negative for p40, p63, CK20, TTF-1, Napsin A, CDX2, CA19- 9, Calretinin, and D2-40 and positive for CK7, GATA3, Ber-EP4, and Uroplakin, supporting bladder as primary origin. Urology deferred a cystoscopy given his lack of urinary symptoms and positive biopsy and was started on Carboplatin/Gemcitabine for his metastatic disease. He was ineligible for Cisplatin given his cirrhosis and hearing impairment.
DISCUSSION
In patients with CLL, new onset mediastinal lymphadenopathy is concerning for disease progression and possible transformation to a diffuse b-cell lymphoma. However, this symptom has a broad differential, including primary lung carcinomas, sarcomas, and metastatic disease. While our patient’s PET/CT and pan-CT failed to identify a distant primary site, maintaining a low clinical suspicion for metastatic disease and doing a thorough work-up was paramount. Only through immunohistochemical staining were we able to diagnosis this patient with urothelial carcinoma.
CONCLUSIONS
Biopsy with immunohistochemical staining and maintaining a low suspicion for worsening lymphadenopathy can identify unusually presenting urothelial carcinomas in CLL patients.
INTRODUCTION
Lymphadenopathy in Chronic Lymphocytic Leukemia (CLL) is a very common feature. However, sudden increase in lymphadenopathy or other symptoms like weight loss should be evaluated for possible metastatic malignancy. We describe a CLL patient with diffuse mediastinal lymphadenopathy who was diagnosed with metastatic bladder cancer without a primary bladder tumor mass on imaging.
CASE DESCRIPTION
A 60-year-old man with a 60 pack-year smoking history, alcoholic cirrhosis, and a 5-year history of stage 1 CLL presented with 3 months of progressive shortness of breath; persistent cough; chills; hemoptysis; and a steady weight loss of 35 lbs. Notably, he had no bladder symptoms. Initial labs showed leukocytosis of 35.8k with a lymphocytic predominance. Screening low-dose chest CT was positive for diffuse mediastinal lymphadenopathy. Subsequent PET/CT revealed numerous hypermetabolic lymph nodes in the neck, mediastinum, left hilum, and right periaortic abdominal region. CT Chest, Abdomen, Pelvis revealed progressive lymphadenopathy as seen in prior imaging, stable pulmonary nodules up to 4 mm in size, and splenomegaly. No distant primary sites, including of the bladder, were identified. Mediastinal lymph node biopsy confirmed metastatic poorly differentiated carcinoma with immunohistochemical staining negative for p40, p63, CK20, TTF-1, Napsin A, CDX2, CA19- 9, Calretinin, and D2-40 and positive for CK7, GATA3, Ber-EP4, and Uroplakin, supporting bladder as primary origin. Urology deferred a cystoscopy given his lack of urinary symptoms and positive biopsy and was started on Carboplatin/Gemcitabine for his metastatic disease. He was ineligible for Cisplatin given his cirrhosis and hearing impairment.
DISCUSSION
In patients with CLL, new onset mediastinal lymphadenopathy is concerning for disease progression and possible transformation to a diffuse b-cell lymphoma. However, this symptom has a broad differential, including primary lung carcinomas, sarcomas, and metastatic disease. While our patient’s PET/CT and pan-CT failed to identify a distant primary site, maintaining a low clinical suspicion for metastatic disease and doing a thorough work-up was paramount. Only through immunohistochemical staining were we able to diagnosis this patient with urothelial carcinoma.
CONCLUSIONS
Biopsy with immunohistochemical staining and maintaining a low suspicion for worsening lymphadenopathy can identify unusually presenting urothelial carcinomas in CLL patients.
24-year-old woman • large joint arthralgias • history of type 1 diabetes, seizures, migraines • Dx?
THE CASE
A 24-year-old woman with a history of type 1 diabetes, seizure disorder, and migraines presented to a rural Federally Qualified Health Center (FQHC) with progressive and severe symmetric large joint arthralgias of several weeks’ duration. The patient’s existing medications included etonogestrel 68 mg subdermal implant, levetiracetam 1500 mg bid, insulin glargine 26 units subcutaneously nightly, and insulin lispro 20 units subcutaneously tid (before meals).
An examination revealed symmetrically edematous elbows, wrists, and fingers. Subsequent serologic analyses and a telemedicine consultation with a rheumatologist confirmed a diagnosis of rheumatoid arthritis (RA). The patient’s lab work was positive for antinuclear antibody titers (1:40), rheumatoid factor (513 IU/mL), and anticyclic citrullinated peptide antibodies (248 units/mL). Treatment was started with prednisone 60 mg PO daily, methotrexate 20 mg PO weekly, and hydroxychloroquine 400 mg PO daily. (The benefits of prednisone in treating this patient’s severe arthralgias outweighed concerns over its use in a patient with diabetes.)
After 2 months of receiving RA therapy, the patient underwent further work-up to assess its effectiveness
Upon receiving a diagnosis of active hepatitis C, the patient acknowledged that she’d had unprotected heterosexual intercourse and shared used insulin syringes with friends.
THE DIAGNOSIS
Consideration was given to a diagnosis of HCV arthropathy, which can present as an RA-like arthritis in HCV-infected individuals, in the differential diagnosis.1 A cohort study found HCV-associated arthropathy occurred in 6.8% of those with chronic HCV infection.2
However, the symmetrical involvement of shoulders and knees as the patient’s primary arthralgias, and a rheumatologic work-up showing the presence of anticyclic citrullinated peptide antibody levels, confirmed the diagnosis of RA with coexisting HCV.
DISCUSSION
Delivering interdisciplinary care in a rural area
Although evidence-based guidelines and online HCV Treatment Path programs guided the initial evaluation of potential treatments for this patient, her multiple comorbidities prompted us to seek out additional, interdisciplinary advice through a resource for underserved communities called Project Extension for Community Healthcare Outcomes (ECHO; see “What is Project ECHO?3,4”). The patient’s case was presented virtually, without identifying information, to a multidisciplinary HCV team. Two treatment options were suggested:
- sofosbuvir/velpatasvir (400 mg/100 mg) for 12 weeks or
- glecaprevir/pibrentasvir (100 mg/40 mg) for 8 weeks.
SIDEBAR
What is Project ECHO?
Project Extension for Community Healthcare Outcomes (ECHO) began as an avenue to connect hepatitis C virus (HCV) treatment experts to providers in underserved communities within New Mexico. Specialists can offer their clinical guidance to community clinicians without seeing the patient themselves.3 Project ECHO now has expanded to connect community clinicians across the United States and globally to specialists who treat other chronic conditions.4 More information about Project ECHO can be found at hsc.unm.edu/echo.
Both are evidence-based and recommended treatment options according to the HCV treatment guidelines issued jointly by the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America.5
In most patients with HCV, treatment is guided by a number of factors, including pill burden, access to care, duration of therapy, drug interactions, and patient-specific needs. After analyzing all aspects of this patient’s case, 2 major concerns guided our shared decision-making process on treatment.
The best treatment is what works for the patient
Owing to the patient’s multiple comorbidities and prescribed medications for chronic diseases, concerns about possible medication interactions with the HCV treatment options were a factor in her HCV treatment plan. Additionally, the patient had significant social determinants of health barriers that made continued treatment and follow-up challenging.
The potential interaction of HCV infection treatment with the patient’s current methotrexate therapy for her RA was a primary concern. To determine the risk for interactions, the team used the University of Liverpool HEP/HIV Drug Interactions Checker, which helps identify possible interactions with these disease-specific medication therapies.6
Both sofosbuvir/velpatasvir and glecaprevir/pibrentasvir have a potential interaction with methotrexate and are driven by a similar mechanism. Methotrexate is a substrate of the Breast Cancer Resistance Protein efflux transporter (BCRP), and the components of both sofosbuvir/velpatasvir and glecaprevir/pibrentasvir are inhibitors of BCRP.7 The inhibition of this efflux transporter can lead to an increased concentration of methotrexate, increasing the risk for methotrexate toxicity.7
Since no quantitative data exist regarding the degree of inhibition that these HCV drugs exert on BCRP, the team considered sofosbuvir/velpatasvir and glecaprevir/pibrentasvir to have equal risk with regard to potential for drug interactions.
The patient’s barriers to treatment were another area of concern that directed our therapy decision. The patient had multiple barriers, including poor access to health care because of transportation issues, multiple children requiring care, a variety of chronic diseases, and other life stressors. Shared decision-making ensured our patient’s autonomy in choosing a specific treatment.
The patient’s social situation and preference narrowed the team’s basis for medication choice primarily down to the duration of therapy: 8 weeks of glecaprevir/pibrentasvir vs 12 weeks of sofosbuvir/velpatasvir. The patient mentioned multiple transportation challenges for follow-up visits to the clinic and therefore wanted to utilize the shorter treatment duration. Follow-up is needed every 4 weeks, so the patient was able to go from 3 to 2 visits.
For problems, there are solutions. Following careful consideration of these patient-specific factors and preferences, the team decided to begin therapy with glecaprevir/pibrentasvir. The patient worked with an outreach specialist at the FQHC to coordinate care and complete paperwork for the Project ECHO consultation. The outreach specialist also assisted the patient in completing paperwork for the Patient Assistance Program for HCV treatment. Because the patient is being cared for at an FQHC, the clinic’s in-house pharmacy was able to utilize the 340B Federal Drug Pricing Program, which makes otherwise out-of-reach medicines affordable for patients such as ours.
Our patient has had no issues with treatment adherence, adverse effects, or follow-up appointments. The patient’s RA symptoms have improved significantly without any discernable worsening of her HCV infection.
THE TAKEAWAY
This case shines a light on the multiple challenges (clinical, geographic, and financial) that could have come between our patient and proper treatment—but ultimately, did not. The Project ECHO model of care remains a viable way to provide patients who live in rural and underserved communities and who have active HCV and other underlying chronic conditions with interdisciplinary care that can improve health outcomes.
1. Kemmer NM, Sherman KE. Hepatitis C-related arthropathy: diagnostic and treatment considerations. J Musculoskelet Med. 2010;27:351-354.
2. Ferucci ED, Choromanski TL, Varney DT, et al. Prevalence and correlates of hepatitis C virus-associated inflammatory arthritis in a population-based cohort. Semin Arthritis Rheum. 2017;47:445-450. doi: 10.1016/j.semarthrit.2017.04.004
3. Arora S, Kalishman S, Thornton K, et al. Expanding access to hepatitis C virus treatment--Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52:1124-1133. doi: 10.1002/hep.23802
4. Blecker S, Paul MM, Jones S, et al. A Project ECHO and community health worker intervention for patients with diabetes. Am J Med. 2021;S0002-9343(21)00811-1. doi: 10.1016/j.amjmed.2021.12.002
5. AASLD-IDSA. Recommendations for testing, managing, and treating hepatitis C. Accessed June 16, 2023. www.hcvguidelines.org
6. HEP/HIV Drug Interactions Checker University of Liverpool. Interaction Report. Published 2022. Accessed June 26, 2023. www.hep-druginteractions.org/downloads/ajd45jg-4er5-67oy-ur43- 009ert.pdf?interaction_ids%5B%5D=88015&interaction_ids%5B%5D=91366
7. Hong J, Wright RC, Partovi N, et al. Review of clinically relevant drug interactions with next generation hepatitis C direct-acting antiviral agents. J Clin Transl Hepatol. 2020;8:322-335. doi: 10.14218/JCTH.2020.00034
THE CASE
A 24-year-old woman with a history of type 1 diabetes, seizure disorder, and migraines presented to a rural Federally Qualified Health Center (FQHC) with progressive and severe symmetric large joint arthralgias of several weeks’ duration. The patient’s existing medications included etonogestrel 68 mg subdermal implant, levetiracetam 1500 mg bid, insulin glargine 26 units subcutaneously nightly, and insulin lispro 20 units subcutaneously tid (before meals).
An examination revealed symmetrically edematous elbows, wrists, and fingers. Subsequent serologic analyses and a telemedicine consultation with a rheumatologist confirmed a diagnosis of rheumatoid arthritis (RA). The patient’s lab work was positive for antinuclear antibody titers (1:40), rheumatoid factor (513 IU/mL), and anticyclic citrullinated peptide antibodies (248 units/mL). Treatment was started with prednisone 60 mg PO daily, methotrexate 20 mg PO weekly, and hydroxychloroquine 400 mg PO daily. (The benefits of prednisone in treating this patient’s severe arthralgias outweighed concerns over its use in a patient with diabetes.)
After 2 months of receiving RA therapy, the patient underwent further work-up to assess its effectiveness
Upon receiving a diagnosis of active hepatitis C, the patient acknowledged that she’d had unprotected heterosexual intercourse and shared used insulin syringes with friends.
THE DIAGNOSIS
Consideration was given to a diagnosis of HCV arthropathy, which can present as an RA-like arthritis in HCV-infected individuals, in the differential diagnosis.1 A cohort study found HCV-associated arthropathy occurred in 6.8% of those with chronic HCV infection.2
However, the symmetrical involvement of shoulders and knees as the patient’s primary arthralgias, and a rheumatologic work-up showing the presence of anticyclic citrullinated peptide antibody levels, confirmed the diagnosis of RA with coexisting HCV.
DISCUSSION
Delivering interdisciplinary care in a rural area
Although evidence-based guidelines and online HCV Treatment Path programs guided the initial evaluation of potential treatments for this patient, her multiple comorbidities prompted us to seek out additional, interdisciplinary advice through a resource for underserved communities called Project Extension for Community Healthcare Outcomes (ECHO; see “What is Project ECHO?3,4”). The patient’s case was presented virtually, without identifying information, to a multidisciplinary HCV team. Two treatment options were suggested:
- sofosbuvir/velpatasvir (400 mg/100 mg) for 12 weeks or
- glecaprevir/pibrentasvir (100 mg/40 mg) for 8 weeks.
SIDEBAR
What is Project ECHO?
Project Extension for Community Healthcare Outcomes (ECHO) began as an avenue to connect hepatitis C virus (HCV) treatment experts to providers in underserved communities within New Mexico. Specialists can offer their clinical guidance to community clinicians without seeing the patient themselves.3 Project ECHO now has expanded to connect community clinicians across the United States and globally to specialists who treat other chronic conditions.4 More information about Project ECHO can be found at hsc.unm.edu/echo.
Both are evidence-based and recommended treatment options according to the HCV treatment guidelines issued jointly by the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America.5
In most patients with HCV, treatment is guided by a number of factors, including pill burden, access to care, duration of therapy, drug interactions, and patient-specific needs. After analyzing all aspects of this patient’s case, 2 major concerns guided our shared decision-making process on treatment.
The best treatment is what works for the patient
Owing to the patient’s multiple comorbidities and prescribed medications for chronic diseases, concerns about possible medication interactions with the HCV treatment options were a factor in her HCV treatment plan. Additionally, the patient had significant social determinants of health barriers that made continued treatment and follow-up challenging.
The potential interaction of HCV infection treatment with the patient’s current methotrexate therapy for her RA was a primary concern. To determine the risk for interactions, the team used the University of Liverpool HEP/HIV Drug Interactions Checker, which helps identify possible interactions with these disease-specific medication therapies.6
Both sofosbuvir/velpatasvir and glecaprevir/pibrentasvir have a potential interaction with methotrexate and are driven by a similar mechanism. Methotrexate is a substrate of the Breast Cancer Resistance Protein efflux transporter (BCRP), and the components of both sofosbuvir/velpatasvir and glecaprevir/pibrentasvir are inhibitors of BCRP.7 The inhibition of this efflux transporter can lead to an increased concentration of methotrexate, increasing the risk for methotrexate toxicity.7
Since no quantitative data exist regarding the degree of inhibition that these HCV drugs exert on BCRP, the team considered sofosbuvir/velpatasvir and glecaprevir/pibrentasvir to have equal risk with regard to potential for drug interactions.
The patient’s barriers to treatment were another area of concern that directed our therapy decision. The patient had multiple barriers, including poor access to health care because of transportation issues, multiple children requiring care, a variety of chronic diseases, and other life stressors. Shared decision-making ensured our patient’s autonomy in choosing a specific treatment.
The patient’s social situation and preference narrowed the team’s basis for medication choice primarily down to the duration of therapy: 8 weeks of glecaprevir/pibrentasvir vs 12 weeks of sofosbuvir/velpatasvir. The patient mentioned multiple transportation challenges for follow-up visits to the clinic and therefore wanted to utilize the shorter treatment duration. Follow-up is needed every 4 weeks, so the patient was able to go from 3 to 2 visits.
For problems, there are solutions. Following careful consideration of these patient-specific factors and preferences, the team decided to begin therapy with glecaprevir/pibrentasvir. The patient worked with an outreach specialist at the FQHC to coordinate care and complete paperwork for the Project ECHO consultation. The outreach specialist also assisted the patient in completing paperwork for the Patient Assistance Program for HCV treatment. Because the patient is being cared for at an FQHC, the clinic’s in-house pharmacy was able to utilize the 340B Federal Drug Pricing Program, which makes otherwise out-of-reach medicines affordable for patients such as ours.
Our patient has had no issues with treatment adherence, adverse effects, or follow-up appointments. The patient’s RA symptoms have improved significantly without any discernable worsening of her HCV infection.
THE TAKEAWAY
This case shines a light on the multiple challenges (clinical, geographic, and financial) that could have come between our patient and proper treatment—but ultimately, did not. The Project ECHO model of care remains a viable way to provide patients who live in rural and underserved communities and who have active HCV and other underlying chronic conditions with interdisciplinary care that can improve health outcomes.
THE CASE
A 24-year-old woman with a history of type 1 diabetes, seizure disorder, and migraines presented to a rural Federally Qualified Health Center (FQHC) with progressive and severe symmetric large joint arthralgias of several weeks’ duration. The patient’s existing medications included etonogestrel 68 mg subdermal implant, levetiracetam 1500 mg bid, insulin glargine 26 units subcutaneously nightly, and insulin lispro 20 units subcutaneously tid (before meals).
An examination revealed symmetrically edematous elbows, wrists, and fingers. Subsequent serologic analyses and a telemedicine consultation with a rheumatologist confirmed a diagnosis of rheumatoid arthritis (RA). The patient’s lab work was positive for antinuclear antibody titers (1:40), rheumatoid factor (513 IU/mL), and anticyclic citrullinated peptide antibodies (248 units/mL). Treatment was started with prednisone 60 mg PO daily, methotrexate 20 mg PO weekly, and hydroxychloroquine 400 mg PO daily. (The benefits of prednisone in treating this patient’s severe arthralgias outweighed concerns over its use in a patient with diabetes.)
After 2 months of receiving RA therapy, the patient underwent further work-up to assess its effectiveness
Upon receiving a diagnosis of active hepatitis C, the patient acknowledged that she’d had unprotected heterosexual intercourse and shared used insulin syringes with friends.
THE DIAGNOSIS
Consideration was given to a diagnosis of HCV arthropathy, which can present as an RA-like arthritis in HCV-infected individuals, in the differential diagnosis.1 A cohort study found HCV-associated arthropathy occurred in 6.8% of those with chronic HCV infection.2
However, the symmetrical involvement of shoulders and knees as the patient’s primary arthralgias, and a rheumatologic work-up showing the presence of anticyclic citrullinated peptide antibody levels, confirmed the diagnosis of RA with coexisting HCV.
DISCUSSION
Delivering interdisciplinary care in a rural area
Although evidence-based guidelines and online HCV Treatment Path programs guided the initial evaluation of potential treatments for this patient, her multiple comorbidities prompted us to seek out additional, interdisciplinary advice through a resource for underserved communities called Project Extension for Community Healthcare Outcomes (ECHO; see “What is Project ECHO?3,4”). The patient’s case was presented virtually, without identifying information, to a multidisciplinary HCV team. Two treatment options were suggested:
- sofosbuvir/velpatasvir (400 mg/100 mg) for 12 weeks or
- glecaprevir/pibrentasvir (100 mg/40 mg) for 8 weeks.
SIDEBAR
What is Project ECHO?
Project Extension for Community Healthcare Outcomes (ECHO) began as an avenue to connect hepatitis C virus (HCV) treatment experts to providers in underserved communities within New Mexico. Specialists can offer their clinical guidance to community clinicians without seeing the patient themselves.3 Project ECHO now has expanded to connect community clinicians across the United States and globally to specialists who treat other chronic conditions.4 More information about Project ECHO can be found at hsc.unm.edu/echo.
Both are evidence-based and recommended treatment options according to the HCV treatment guidelines issued jointly by the American Association for the Study of Liver Diseases and the Infectious Diseases Society of America.5
In most patients with HCV, treatment is guided by a number of factors, including pill burden, access to care, duration of therapy, drug interactions, and patient-specific needs. After analyzing all aspects of this patient’s case, 2 major concerns guided our shared decision-making process on treatment.
The best treatment is what works for the patient
Owing to the patient’s multiple comorbidities and prescribed medications for chronic diseases, concerns about possible medication interactions with the HCV treatment options were a factor in her HCV treatment plan. Additionally, the patient had significant social determinants of health barriers that made continued treatment and follow-up challenging.
The potential interaction of HCV infection treatment with the patient’s current methotrexate therapy for her RA was a primary concern. To determine the risk for interactions, the team used the University of Liverpool HEP/HIV Drug Interactions Checker, which helps identify possible interactions with these disease-specific medication therapies.6
Both sofosbuvir/velpatasvir and glecaprevir/pibrentasvir have a potential interaction with methotrexate and are driven by a similar mechanism. Methotrexate is a substrate of the Breast Cancer Resistance Protein efflux transporter (BCRP), and the components of both sofosbuvir/velpatasvir and glecaprevir/pibrentasvir are inhibitors of BCRP.7 The inhibition of this efflux transporter can lead to an increased concentration of methotrexate, increasing the risk for methotrexate toxicity.7
Since no quantitative data exist regarding the degree of inhibition that these HCV drugs exert on BCRP, the team considered sofosbuvir/velpatasvir and glecaprevir/pibrentasvir to have equal risk with regard to potential for drug interactions.
The patient’s barriers to treatment were another area of concern that directed our therapy decision. The patient had multiple barriers, including poor access to health care because of transportation issues, multiple children requiring care, a variety of chronic diseases, and other life stressors. Shared decision-making ensured our patient’s autonomy in choosing a specific treatment.
The patient’s social situation and preference narrowed the team’s basis for medication choice primarily down to the duration of therapy: 8 weeks of glecaprevir/pibrentasvir vs 12 weeks of sofosbuvir/velpatasvir. The patient mentioned multiple transportation challenges for follow-up visits to the clinic and therefore wanted to utilize the shorter treatment duration. Follow-up is needed every 4 weeks, so the patient was able to go from 3 to 2 visits.
For problems, there are solutions. Following careful consideration of these patient-specific factors and preferences, the team decided to begin therapy with glecaprevir/pibrentasvir. The patient worked with an outreach specialist at the FQHC to coordinate care and complete paperwork for the Project ECHO consultation. The outreach specialist also assisted the patient in completing paperwork for the Patient Assistance Program for HCV treatment. Because the patient is being cared for at an FQHC, the clinic’s in-house pharmacy was able to utilize the 340B Federal Drug Pricing Program, which makes otherwise out-of-reach medicines affordable for patients such as ours.
Our patient has had no issues with treatment adherence, adverse effects, or follow-up appointments. The patient’s RA symptoms have improved significantly without any discernable worsening of her HCV infection.
THE TAKEAWAY
This case shines a light on the multiple challenges (clinical, geographic, and financial) that could have come between our patient and proper treatment—but ultimately, did not. The Project ECHO model of care remains a viable way to provide patients who live in rural and underserved communities and who have active HCV and other underlying chronic conditions with interdisciplinary care that can improve health outcomes.
1. Kemmer NM, Sherman KE. Hepatitis C-related arthropathy: diagnostic and treatment considerations. J Musculoskelet Med. 2010;27:351-354.
2. Ferucci ED, Choromanski TL, Varney DT, et al. Prevalence and correlates of hepatitis C virus-associated inflammatory arthritis in a population-based cohort. Semin Arthritis Rheum. 2017;47:445-450. doi: 10.1016/j.semarthrit.2017.04.004
3. Arora S, Kalishman S, Thornton K, et al. Expanding access to hepatitis C virus treatment--Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52:1124-1133. doi: 10.1002/hep.23802
4. Blecker S, Paul MM, Jones S, et al. A Project ECHO and community health worker intervention for patients with diabetes. Am J Med. 2021;S0002-9343(21)00811-1. doi: 10.1016/j.amjmed.2021.12.002
5. AASLD-IDSA. Recommendations for testing, managing, and treating hepatitis C. Accessed June 16, 2023. www.hcvguidelines.org
6. HEP/HIV Drug Interactions Checker University of Liverpool. Interaction Report. Published 2022. Accessed June 26, 2023. www.hep-druginteractions.org/downloads/ajd45jg-4er5-67oy-ur43- 009ert.pdf?interaction_ids%5B%5D=88015&interaction_ids%5B%5D=91366
7. Hong J, Wright RC, Partovi N, et al. Review of clinically relevant drug interactions with next generation hepatitis C direct-acting antiviral agents. J Clin Transl Hepatol. 2020;8:322-335. doi: 10.14218/JCTH.2020.00034
1. Kemmer NM, Sherman KE. Hepatitis C-related arthropathy: diagnostic and treatment considerations. J Musculoskelet Med. 2010;27:351-354.
2. Ferucci ED, Choromanski TL, Varney DT, et al. Prevalence and correlates of hepatitis C virus-associated inflammatory arthritis in a population-based cohort. Semin Arthritis Rheum. 2017;47:445-450. doi: 10.1016/j.semarthrit.2017.04.004
3. Arora S, Kalishman S, Thornton K, et al. Expanding access to hepatitis C virus treatment--Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology. 2010;52:1124-1133. doi: 10.1002/hep.23802
4. Blecker S, Paul MM, Jones S, et al. A Project ECHO and community health worker intervention for patients with diabetes. Am J Med. 2021;S0002-9343(21)00811-1. doi: 10.1016/j.amjmed.2021.12.002
5. AASLD-IDSA. Recommendations for testing, managing, and treating hepatitis C. Accessed June 16, 2023. www.hcvguidelines.org
6. HEP/HIV Drug Interactions Checker University of Liverpool. Interaction Report. Published 2022. Accessed June 26, 2023. www.hep-druginteractions.org/downloads/ajd45jg-4er5-67oy-ur43- 009ert.pdf?interaction_ids%5B%5D=88015&interaction_ids%5B%5D=91366
7. Hong J, Wright RC, Partovi N, et al. Review of clinically relevant drug interactions with next generation hepatitis C direct-acting antiviral agents. J Clin Transl Hepatol. 2020;8:322-335. doi: 10.14218/JCTH.2020.00034
► Large joint arthralgias
► History of type 1 diabetes, seizures, migraines
49-year-old woman • headache and neck pain radiating to ears and eyes • severe hypertension • Dx?
THE CASE
A 49-year-old woman was hospitalized with a headache and neck pain that radiated to her ears and eyes in the context of severe hypertension (270/150 mm Hg). Her medical history was significant for heterozygous factor V Leiden mutation, longstanding untreated hypertension, and multiple severe episodes of HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome during pregnancy.
After receiving antihypertensive treatment at a community hospital, her blood pressure gradually improved to 160/100 mm Hg with the addition of a third medication. However, on Day 3 of her stay, her systolic blood pressure rose to more than 200 mm Hg and was accompanied by somnolence, emesis, and paleness. She was transferred to a tertiary care center.
THE DIAGNOSIS
On admission, the patient had left-side hemiparesis and facial droop with dysarthria, resulting in a National Institutes of Health Stroke Scale (NIHSS) score of 7 (out of 42) and a Glasgow Coma Scale (GCS) score of 13 (out of 15). Noncontrast computed tomography (CT) and CT angiography of the head and neck were ordered and showed occlusion of both intracranial vertebral arteries. There were also signs of multifocal infarction in her occipital lobes, thus systemic recombinant human-tissue plasminogen activator (tPA) could not be administered.
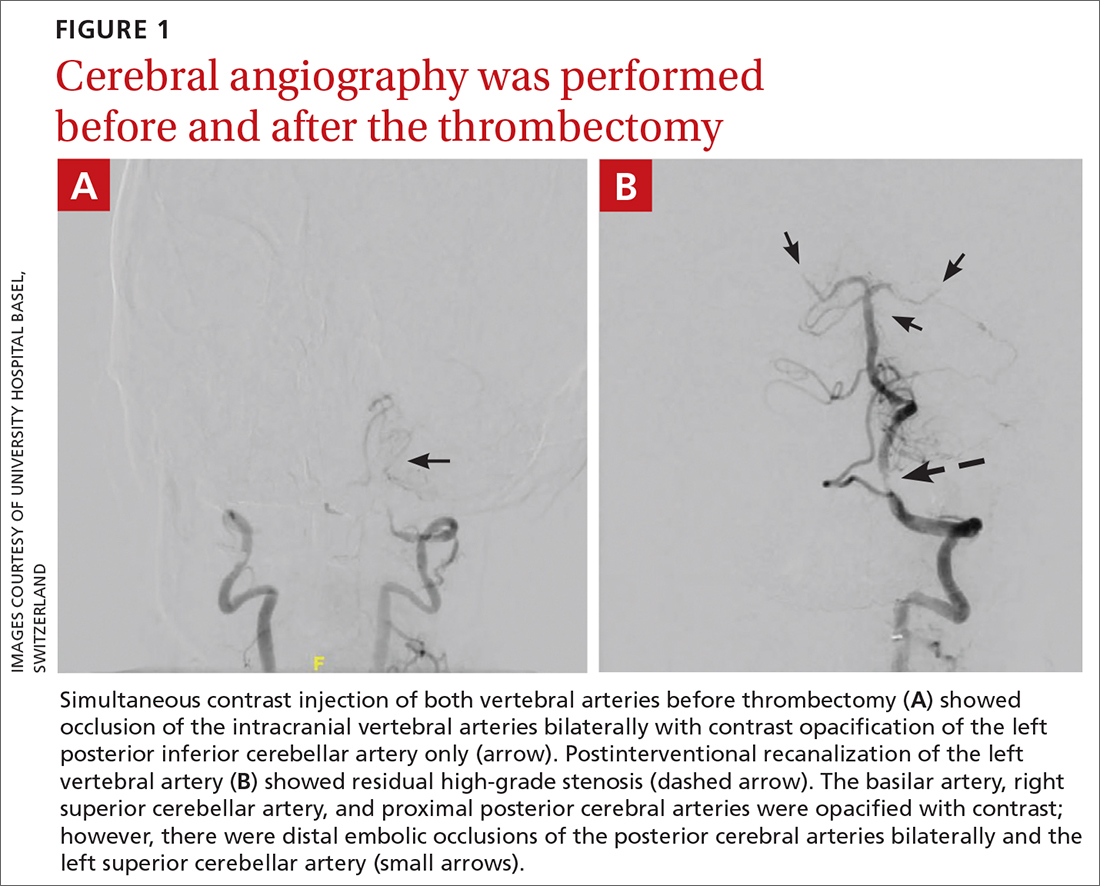
The patient was next taken to the angiography suite, where a digital subtraction angiography confirmed the presence of bilateral vertebral artery occlusions (FIGURE 1A). A thrombectomy was performed to open the left occluded segment, resulting in recanalization; however, a high-grade stenosis remained in the intracranial left vertebral artery (FIGURE 1B). The right vertebral artery had a severe extracranial origin stenosis, and balloon angioplasty was performed in order to reach the intracranial circulation; however, the occlusion of the intracranial right vertebral artery segment could not be catheterized. Subsequent magnetic resonance imaging (MRI) with a time-of-flight magnetic resonance angiography showed that the intracranial left vertebral artery with high-grade stenosis had closed down again; thus, there was occlusion of both intracranial vertebral arteries and absent flow signal in the basilar artery (FIGURE 2). There were scattered small acute strokes within the cerebellum, brainstem, and occipital lobes.
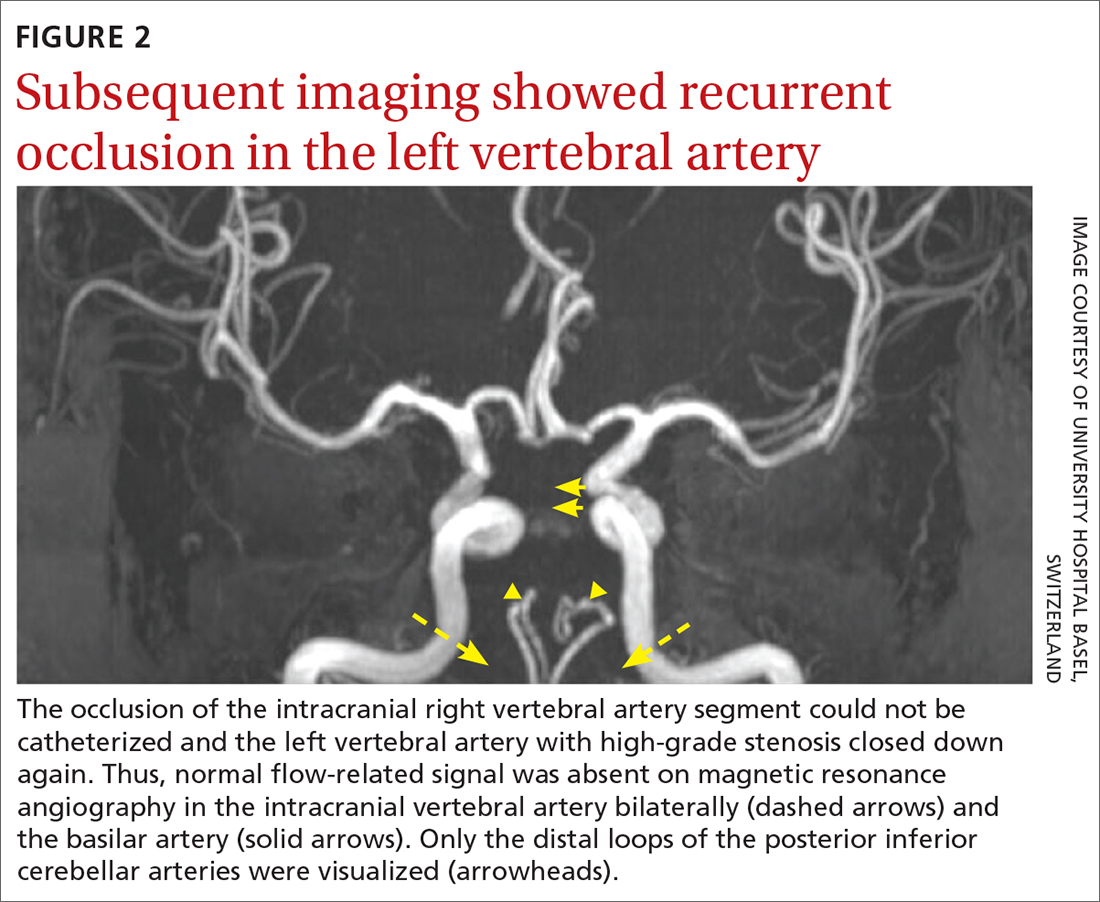
Unfortunately, within 48 hours, the patient’s NIHSS score increased from 7 to 29. She developed tetraplegia, was significantly less responsive (GCS score, 3/15), and required intubation and mechanical ventilation. Reopening the stenosis and keeping it open with a stent would be an aggressive procedure with poor odds for success and would require antithrombotic medications with the associated risk for intracranial hemorrhage in the setting of demarcated strokes. Thus, no further intervention was pursued.
Further standard stroke work-up (echocardiography, extracranial ultrasound of the cerebral circulation, and vasculitis screening) was unremarkable. In the intensive care unit, intravenous therapeutic heparin was initiated because of the potential prothrombotic effect of the factor V Leiden mutation but was subsequently switched to dual anti-aggregation therapy (aspirin 100 mg/d and clopidogrel 75 mg/d) as secondary stroke prevention given the final diagnosis of severe atherosclerosis. Nevertheless, the patient remained tetraplegic with a partial locked-in syndrome when she was discharged, after 2 weeks in the tertiary care center, to a rehabilitation center.
DISCUSSION
Posterior circulation strokes account for 20% to 25% of all ischemic strokes1,2 and are associated with infarction within the vertebrobasilar arterial system. Common etiologies of these infarctions include atherosclerosis (as seen in our patient), embolism, small-artery penetrating disease, and arterial dissection.2 Although the estimated overall mortality of these strokes is low (3.6% to 11%),2 basilar occlusion syndrome, in particular, is a life-threatening condition with a high mortality rate of 80% to 90%.3
Continue to: Diagnosis can be particularly challenging...
Diagnosis can be particularly challenging due to the anatomic variations of posterior arterial circulation, as well as the fluctuating nonfocal or multifocal symptoms.2 Specific symptoms include vertigo, ataxia, unilateral motor weakness, dysarthria, and oculomotor dysfunction. However, nonspecific symptoms such as headache, nausea, dizziness, hoarseness, falls, and Horner syndrome may be the only presenting signs of a posterior circulation stroke—as was the case with our patient.2 Her radiating neck pain could have been interpreted as a pointer to vertebral artery dissection within the context of severe hypertension.4 Unfortunately, the diagnosis was delayed and head imaging was obtained only after her mental status deteriorated.
Immediate neuroimaging is necessary to guide treatment in patients with suspected acute posterior circulation stroke,1,5,6 although it is not always definitive. While CT is pivotal in stroke work-up and may reliably exclude intracranial hemorrhage, its ability to detect acute posterior circulation ischemic strokes is limited given its poor visualization of the posterior fossa (as low as 16% sensitivity).5 Fortunately, CT angiography has a high sensitivity (nearing 100%) for large-vessel occlusion and high predictive values for dissection (65%-100% positive predictive value and 70%-98% negative predictive value).5,7 Diffusion-weighted MRI (when available in the emergency setting) has the highest sensitivity for detecting acute infarcts, although posterior circulation infarcts still can be missed (19% false-negative rate).5,8 Thus, correlative vessel imaging with magnetic resonance or CT angiography is very important, along with a high index of suspicion. In some instances, repeat MRI may be necessary to detect small strokes.
A patient-specific approach to management is key for individuals with suspected posterior circulation stroke.5 Because specific data for the appropriate management of posterior circulation ischemic stroke are lacking, current American Heart Association/American Stroke Association (AHA/ASA) guidelines apply to anterior and posterior circulation strokes.6 For eligible patients without multifocal disease, intravenous tPA is the first-line therapy and should be initiated according to guidelines within 4.5 hours of stroke onset9; it is important to note that these guidelines are based on studies that focused more on anterior circulation strokes than posterior circulation strokes.6,9-13 This can be done in combination with endovascular therapy, which consists of mechanical thrombectomy, intra-arterial thrombolysis, or a combination of revascularization techniques.3,5,6
Mechanical thrombectomy specifically has high proven recanalization rates for all target vessels.3-6 The latest AHA/ASA guidelines recommend mechanical thrombectomy be performed within 6 hours of stroke onset.6 However, there is emerging evidence that suggests this timeframe should be extended—even beyond 24 hours—given the poor prognosis of posterior circulation strokes.5,6,14 More data on the management of posterior circulation strokes are urgently needed to better understand which therapeutic approach is most efficient.
In patients such as ours, who have evidence of multifocal disease, treatment may be limited to endovascular therapy. Intracranial stenting of symptomatic lesions in particular has been controversial since the publication of the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis trial, which found that aggressive medical management was superior to stenting in patients who recently had a transient ischemic attack or stroke attributed to stenosis.15 Although additional studies have been performed, there are no definitive data on the topic—and certainly no data in the emergency setting.16 Further challenges are raised in patients with bilateral disease, as was the case with this patient.
When our patient was admitted to the rehabilitation clinic, she had a GCS score of 10 to 11/15. After 9 months of rehabilitation, she was discharged home with a GCS score of 15/15 and persistent left-side hemiparesis.
THE TAKEAWAY
Posterior circulation stroke is a life-threatening disease that may manifest with a variety of symptoms and be difficult to identify on emergent imaging. Thus, a high degree of clinical suspicion and additional follow-up are paramount to ensure prompt diagnosis and a patient-tailored treatment strategy.
CORRESPONDENCE
Kristine A. Blackham, MD, Associate Professor, University Hospital Basel, Petersgraben 4, 4031 Basel, Switzerland; kristine.blackham@gmail.com Orcid no: 0000-0002-1620-1144 (Dr. Blackham); 0000-0002- 5225-5414 (Dr. Saleh)
1. Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM. 2003;96:27-54. doi: 10.1093/qjmed/hcg003
2. Sparaco M, Ciolli L, Zini A. Posterior circulation ischaemic stroke–a review part I: anatomy, aetiology and clinical presentations. Neurol Sci. 2019;40:1995-2006. doi: 10.1007/s10072-019-03977-2
3. Lin DDM, Gailloud P, Beauchamp NJ, et al. Combined stent placement and thrombolysis in acute vertebrobasilar ischemic stroke. AJNR Am J Neuroradiol. 2003;24:1827-1833.
4. Pezzini A, Caso V, Zanferrari C, et al. Arterial hypertension as risk factor for spontaneous cervical artery dissection. A case-control study. J Neurol Neurosurg Psychiatry. 2006;77:95-97. doi:10.1136/jnnp.2005.063107
5. Merwick Á, Werring D. Posterior circulation ischaemic stroke. BMJ. 2014;348:g3175. doi: 10.1136/bmj.g3175
6. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46-e110. doi: 10.1161/STR.0000000000000158
7. Provenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR angiography, and CT angiography in the diagnosis of carotid and vertebral artery dissection: a review of the medical literature. AJR Am J Roentgenol. 2009;193:1167-1174. doi: 10.2214/AJR.08.1688
8. Husnoo Q. A case of missed diagnosis of posterior circulation stroke. Clin Med (Lond). 2019;19(suppl 2):63. doi: 10.7861/clinmedicine.19-2-s63
9. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-1329. doi: 10.1056/NEJMoa0804656
10. Schneider AM, Neuhaus AA, Hadley G, et al. Posterior circulation ischaemic stroke diagnosis and management. Clin Med (Lond). 2023;23:219-227. doi: 10.7861/clinmed.2022-0499
11. Dorňák T, Král M, Šaňák D, et al. Intravenous thrombolysis in posterior circulation stroke. Front Neurol. 2019;10:417. doi: 10.3389/fneur.2019.00417
12. van der Hoeven EJ, Schonewille WJ, Vos JA, et al. The Basilar Artery International Cooperation Study (BASICS): study protocol for a randomised controlled trial. Trials. 2013;14:200. doi: 10.1186/1745-6215-14-200
13. Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30. doi: 10.3389/fneur.2014.00030
14. Purrucker JC, Ringleb PA, Seker F, et al. Leaving the day behind: endovascular therapy beyond 24 h in acute stroke of the anterior and posterior circulation. Ther Adv Neurol Disord. 2022;15:17562864221101083. doi: 10.1177/17562864221101083
15. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003. doi: 10.1056/NEJMoa1105335
16. Markus HS, Michel P. Treatment of posterior circulation stroke: acute management and secondary prevention. Int J Stroke. 2022;17:723-732. doi: 10.1177/17474930221107500
THE CASE
A 49-year-old woman was hospitalized with a headache and neck pain that radiated to her ears and eyes in the context of severe hypertension (270/150 mm Hg). Her medical history was significant for heterozygous factor V Leiden mutation, longstanding untreated hypertension, and multiple severe episodes of HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome during pregnancy.
After receiving antihypertensive treatment at a community hospital, her blood pressure gradually improved to 160/100 mm Hg with the addition of a third medication. However, on Day 3 of her stay, her systolic blood pressure rose to more than 200 mm Hg and was accompanied by somnolence, emesis, and paleness. She was transferred to a tertiary care center.
THE DIAGNOSIS
On admission, the patient had left-side hemiparesis and facial droop with dysarthria, resulting in a National Institutes of Health Stroke Scale (NIHSS) score of 7 (out of 42) and a Glasgow Coma Scale (GCS) score of 13 (out of 15). Noncontrast computed tomography (CT) and CT angiography of the head and neck were ordered and showed occlusion of both intracranial vertebral arteries. There were also signs of multifocal infarction in her occipital lobes, thus systemic recombinant human-tissue plasminogen activator (tPA) could not be administered.
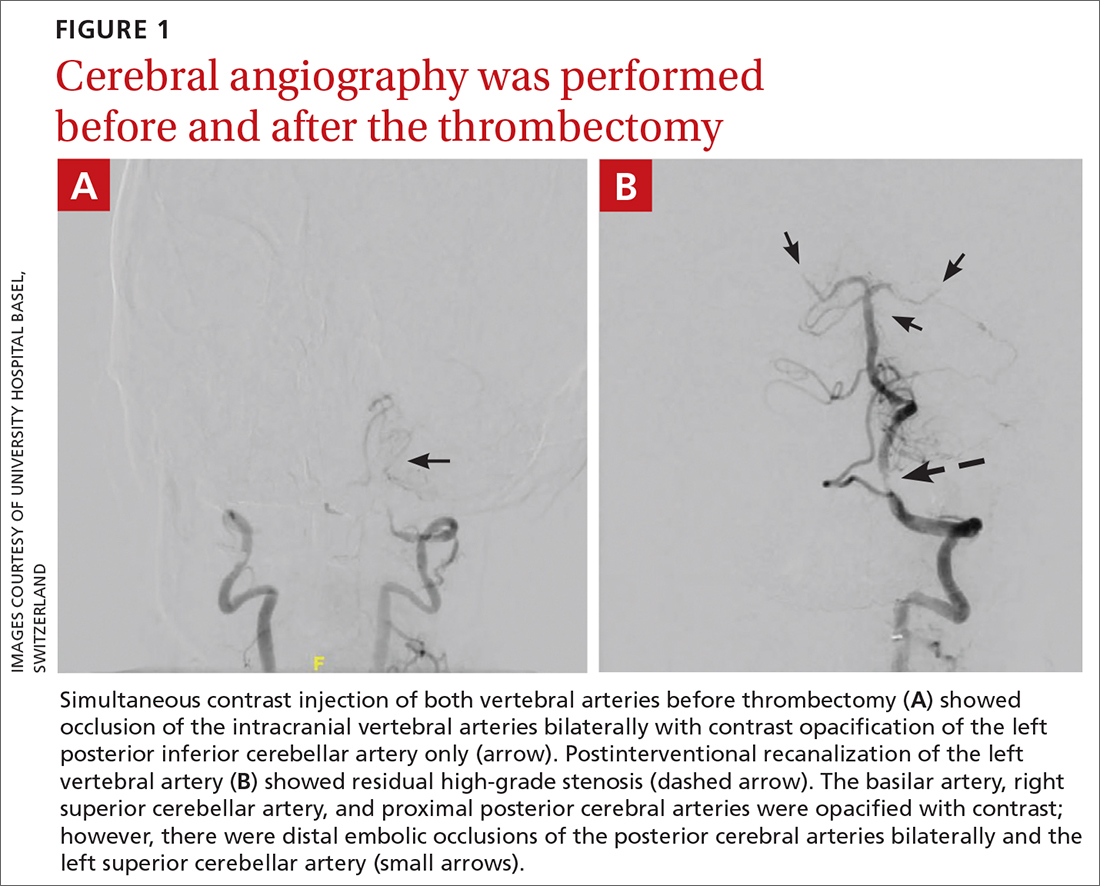
The patient was next taken to the angiography suite, where a digital subtraction angiography confirmed the presence of bilateral vertebral artery occlusions (FIGURE 1A). A thrombectomy was performed to open the left occluded segment, resulting in recanalization; however, a high-grade stenosis remained in the intracranial left vertebral artery (FIGURE 1B). The right vertebral artery had a severe extracranial origin stenosis, and balloon angioplasty was performed in order to reach the intracranial circulation; however, the occlusion of the intracranial right vertebral artery segment could not be catheterized. Subsequent magnetic resonance imaging (MRI) with a time-of-flight magnetic resonance angiography showed that the intracranial left vertebral artery with high-grade stenosis had closed down again; thus, there was occlusion of both intracranial vertebral arteries and absent flow signal in the basilar artery (FIGURE 2). There were scattered small acute strokes within the cerebellum, brainstem, and occipital lobes.
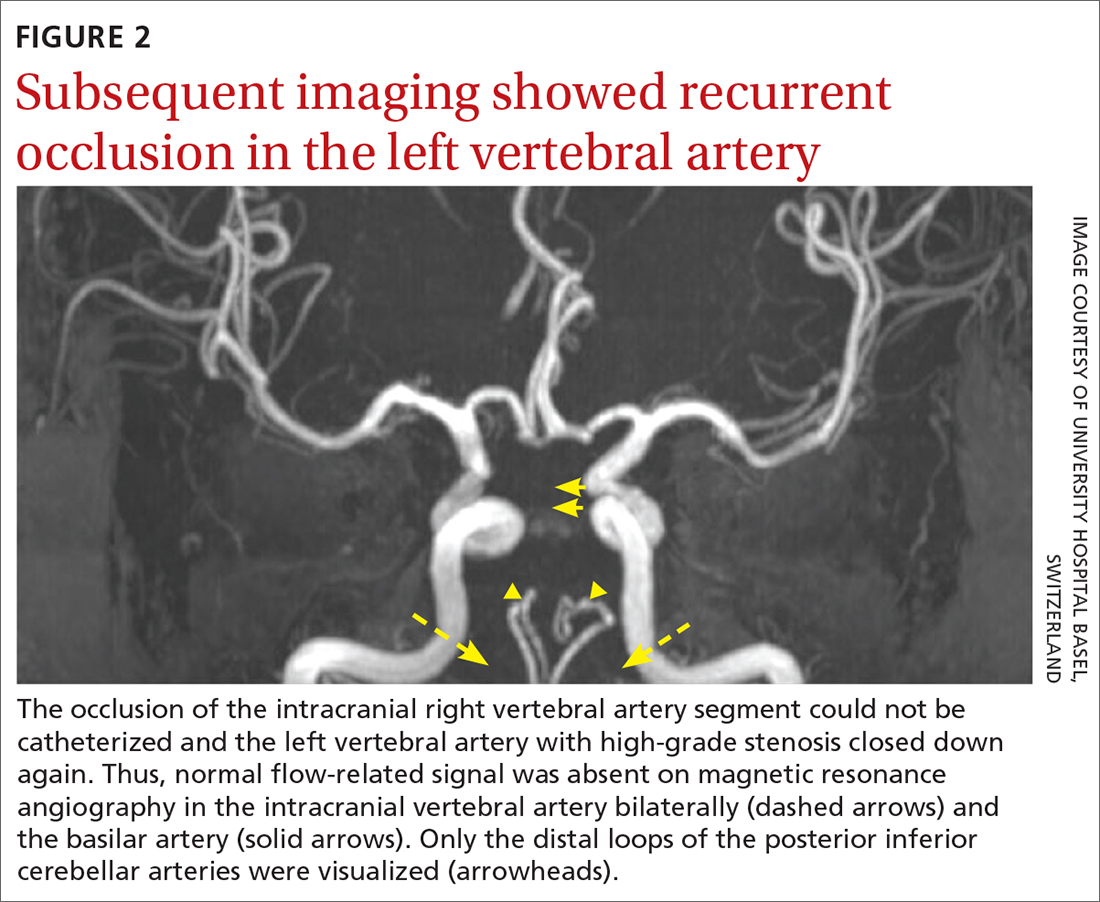
Unfortunately, within 48 hours, the patient’s NIHSS score increased from 7 to 29. She developed tetraplegia, was significantly less responsive (GCS score, 3/15), and required intubation and mechanical ventilation. Reopening the stenosis and keeping it open with a stent would be an aggressive procedure with poor odds for success and would require antithrombotic medications with the associated risk for intracranial hemorrhage in the setting of demarcated strokes. Thus, no further intervention was pursued.
Further standard stroke work-up (echocardiography, extracranial ultrasound of the cerebral circulation, and vasculitis screening) was unremarkable. In the intensive care unit, intravenous therapeutic heparin was initiated because of the potential prothrombotic effect of the factor V Leiden mutation but was subsequently switched to dual anti-aggregation therapy (aspirin 100 mg/d and clopidogrel 75 mg/d) as secondary stroke prevention given the final diagnosis of severe atherosclerosis. Nevertheless, the patient remained tetraplegic with a partial locked-in syndrome when she was discharged, after 2 weeks in the tertiary care center, to a rehabilitation center.
DISCUSSION
Posterior circulation strokes account for 20% to 25% of all ischemic strokes1,2 and are associated with infarction within the vertebrobasilar arterial system. Common etiologies of these infarctions include atherosclerosis (as seen in our patient), embolism, small-artery penetrating disease, and arterial dissection.2 Although the estimated overall mortality of these strokes is low (3.6% to 11%),2 basilar occlusion syndrome, in particular, is a life-threatening condition with a high mortality rate of 80% to 90%.3
Continue to: Diagnosis can be particularly challenging...
Diagnosis can be particularly challenging due to the anatomic variations of posterior arterial circulation, as well as the fluctuating nonfocal or multifocal symptoms.2 Specific symptoms include vertigo, ataxia, unilateral motor weakness, dysarthria, and oculomotor dysfunction. However, nonspecific symptoms such as headache, nausea, dizziness, hoarseness, falls, and Horner syndrome may be the only presenting signs of a posterior circulation stroke—as was the case with our patient.2 Her radiating neck pain could have been interpreted as a pointer to vertebral artery dissection within the context of severe hypertension.4 Unfortunately, the diagnosis was delayed and head imaging was obtained only after her mental status deteriorated.
Immediate neuroimaging is necessary to guide treatment in patients with suspected acute posterior circulation stroke,1,5,6 although it is not always definitive. While CT is pivotal in stroke work-up and may reliably exclude intracranial hemorrhage, its ability to detect acute posterior circulation ischemic strokes is limited given its poor visualization of the posterior fossa (as low as 16% sensitivity).5 Fortunately, CT angiography has a high sensitivity (nearing 100%) for large-vessel occlusion and high predictive values for dissection (65%-100% positive predictive value and 70%-98% negative predictive value).5,7 Diffusion-weighted MRI (when available in the emergency setting) has the highest sensitivity for detecting acute infarcts, although posterior circulation infarcts still can be missed (19% false-negative rate).5,8 Thus, correlative vessel imaging with magnetic resonance or CT angiography is very important, along with a high index of suspicion. In some instances, repeat MRI may be necessary to detect small strokes.
A patient-specific approach to management is key for individuals with suspected posterior circulation stroke.5 Because specific data for the appropriate management of posterior circulation ischemic stroke are lacking, current American Heart Association/American Stroke Association (AHA/ASA) guidelines apply to anterior and posterior circulation strokes.6 For eligible patients without multifocal disease, intravenous tPA is the first-line therapy and should be initiated according to guidelines within 4.5 hours of stroke onset9; it is important to note that these guidelines are based on studies that focused more on anterior circulation strokes than posterior circulation strokes.6,9-13 This can be done in combination with endovascular therapy, which consists of mechanical thrombectomy, intra-arterial thrombolysis, or a combination of revascularization techniques.3,5,6
Mechanical thrombectomy specifically has high proven recanalization rates for all target vessels.3-6 The latest AHA/ASA guidelines recommend mechanical thrombectomy be performed within 6 hours of stroke onset.6 However, there is emerging evidence that suggests this timeframe should be extended—even beyond 24 hours—given the poor prognosis of posterior circulation strokes.5,6,14 More data on the management of posterior circulation strokes are urgently needed to better understand which therapeutic approach is most efficient.
In patients such as ours, who have evidence of multifocal disease, treatment may be limited to endovascular therapy. Intracranial stenting of symptomatic lesions in particular has been controversial since the publication of the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis trial, which found that aggressive medical management was superior to stenting in patients who recently had a transient ischemic attack or stroke attributed to stenosis.15 Although additional studies have been performed, there are no definitive data on the topic—and certainly no data in the emergency setting.16 Further challenges are raised in patients with bilateral disease, as was the case with this patient.
When our patient was admitted to the rehabilitation clinic, she had a GCS score of 10 to 11/15. After 9 months of rehabilitation, she was discharged home with a GCS score of 15/15 and persistent left-side hemiparesis.
THE TAKEAWAY
Posterior circulation stroke is a life-threatening disease that may manifest with a variety of symptoms and be difficult to identify on emergent imaging. Thus, a high degree of clinical suspicion and additional follow-up are paramount to ensure prompt diagnosis and a patient-tailored treatment strategy.
CORRESPONDENCE
Kristine A. Blackham, MD, Associate Professor, University Hospital Basel, Petersgraben 4, 4031 Basel, Switzerland; kristine.blackham@gmail.com Orcid no: 0000-0002-1620-1144 (Dr. Blackham); 0000-0002- 5225-5414 (Dr. Saleh)
THE CASE
A 49-year-old woman was hospitalized with a headache and neck pain that radiated to her ears and eyes in the context of severe hypertension (270/150 mm Hg). Her medical history was significant for heterozygous factor V Leiden mutation, longstanding untreated hypertension, and multiple severe episodes of HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome during pregnancy.
After receiving antihypertensive treatment at a community hospital, her blood pressure gradually improved to 160/100 mm Hg with the addition of a third medication. However, on Day 3 of her stay, her systolic blood pressure rose to more than 200 mm Hg and was accompanied by somnolence, emesis, and paleness. She was transferred to a tertiary care center.
THE DIAGNOSIS
On admission, the patient had left-side hemiparesis and facial droop with dysarthria, resulting in a National Institutes of Health Stroke Scale (NIHSS) score of 7 (out of 42) and a Glasgow Coma Scale (GCS) score of 13 (out of 15). Noncontrast computed tomography (CT) and CT angiography of the head and neck were ordered and showed occlusion of both intracranial vertebral arteries. There were also signs of multifocal infarction in her occipital lobes, thus systemic recombinant human-tissue plasminogen activator (tPA) could not be administered.
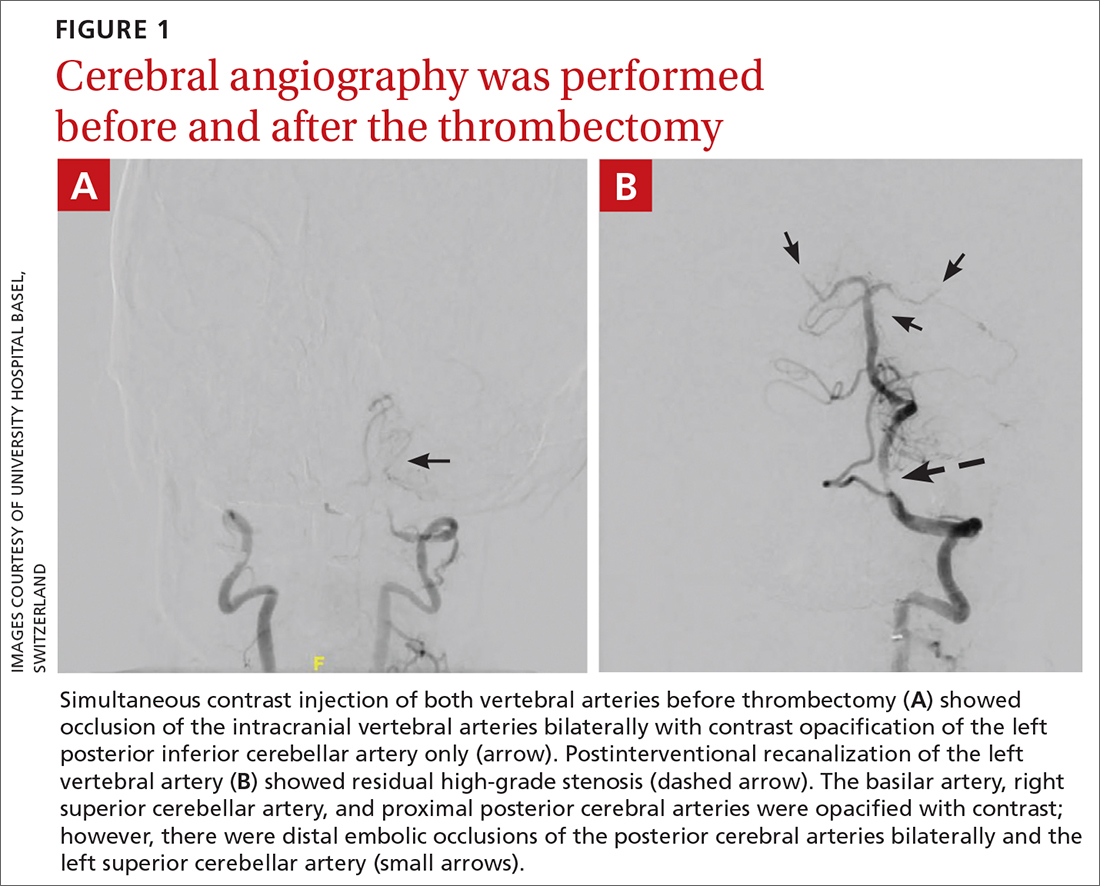
The patient was next taken to the angiography suite, where a digital subtraction angiography confirmed the presence of bilateral vertebral artery occlusions (FIGURE 1A). A thrombectomy was performed to open the left occluded segment, resulting in recanalization; however, a high-grade stenosis remained in the intracranial left vertebral artery (FIGURE 1B). The right vertebral artery had a severe extracranial origin stenosis, and balloon angioplasty was performed in order to reach the intracranial circulation; however, the occlusion of the intracranial right vertebral artery segment could not be catheterized. Subsequent magnetic resonance imaging (MRI) with a time-of-flight magnetic resonance angiography showed that the intracranial left vertebral artery with high-grade stenosis had closed down again; thus, there was occlusion of both intracranial vertebral arteries and absent flow signal in the basilar artery (FIGURE 2). There were scattered small acute strokes within the cerebellum, brainstem, and occipital lobes.
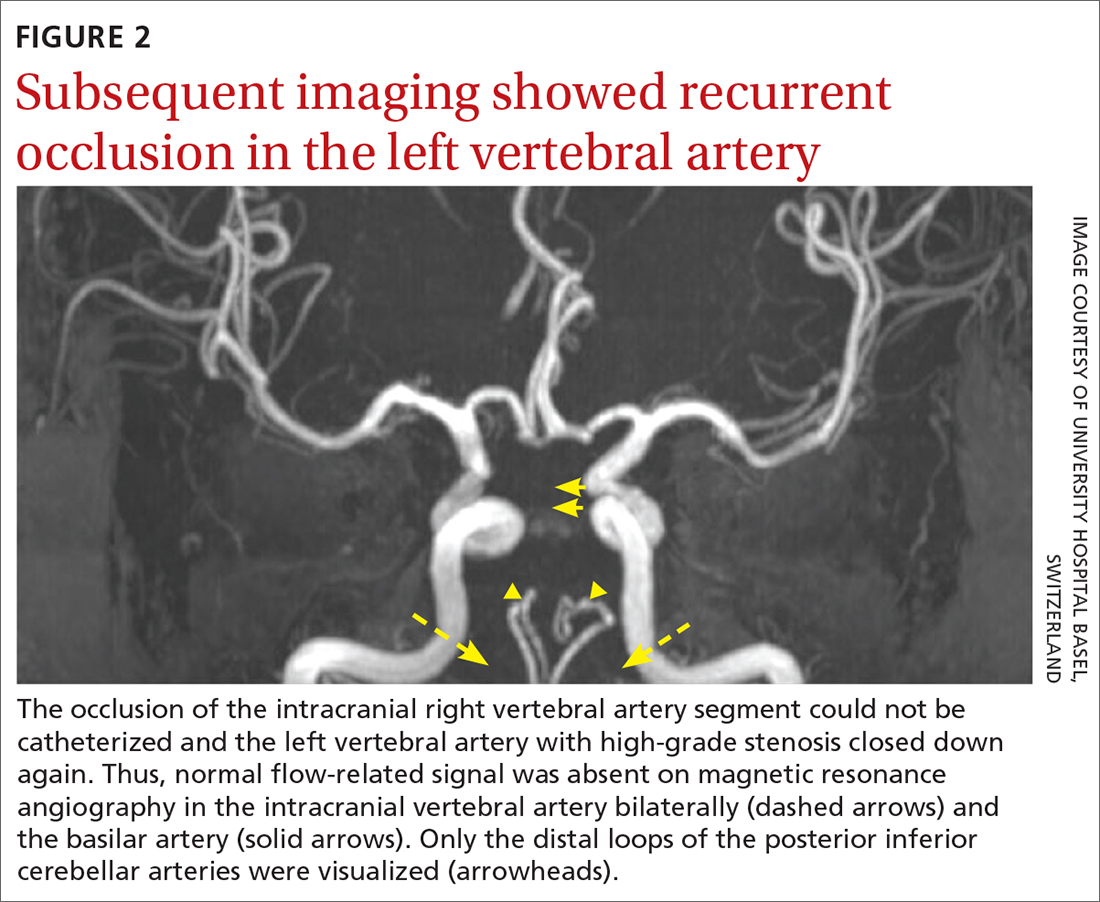
Unfortunately, within 48 hours, the patient’s NIHSS score increased from 7 to 29. She developed tetraplegia, was significantly less responsive (GCS score, 3/15), and required intubation and mechanical ventilation. Reopening the stenosis and keeping it open with a stent would be an aggressive procedure with poor odds for success and would require antithrombotic medications with the associated risk for intracranial hemorrhage in the setting of demarcated strokes. Thus, no further intervention was pursued.
Further standard stroke work-up (echocardiography, extracranial ultrasound of the cerebral circulation, and vasculitis screening) was unremarkable. In the intensive care unit, intravenous therapeutic heparin was initiated because of the potential prothrombotic effect of the factor V Leiden mutation but was subsequently switched to dual anti-aggregation therapy (aspirin 100 mg/d and clopidogrel 75 mg/d) as secondary stroke prevention given the final diagnosis of severe atherosclerosis. Nevertheless, the patient remained tetraplegic with a partial locked-in syndrome when she was discharged, after 2 weeks in the tertiary care center, to a rehabilitation center.
DISCUSSION
Posterior circulation strokes account for 20% to 25% of all ischemic strokes1,2 and are associated with infarction within the vertebrobasilar arterial system. Common etiologies of these infarctions include atherosclerosis (as seen in our patient), embolism, small-artery penetrating disease, and arterial dissection.2 Although the estimated overall mortality of these strokes is low (3.6% to 11%),2 basilar occlusion syndrome, in particular, is a life-threatening condition with a high mortality rate of 80% to 90%.3
Continue to: Diagnosis can be particularly challenging...
Diagnosis can be particularly challenging due to the anatomic variations of posterior arterial circulation, as well as the fluctuating nonfocal or multifocal symptoms.2 Specific symptoms include vertigo, ataxia, unilateral motor weakness, dysarthria, and oculomotor dysfunction. However, nonspecific symptoms such as headache, nausea, dizziness, hoarseness, falls, and Horner syndrome may be the only presenting signs of a posterior circulation stroke—as was the case with our patient.2 Her radiating neck pain could have been interpreted as a pointer to vertebral artery dissection within the context of severe hypertension.4 Unfortunately, the diagnosis was delayed and head imaging was obtained only after her mental status deteriorated.
Immediate neuroimaging is necessary to guide treatment in patients with suspected acute posterior circulation stroke,1,5,6 although it is not always definitive. While CT is pivotal in stroke work-up and may reliably exclude intracranial hemorrhage, its ability to detect acute posterior circulation ischemic strokes is limited given its poor visualization of the posterior fossa (as low as 16% sensitivity).5 Fortunately, CT angiography has a high sensitivity (nearing 100%) for large-vessel occlusion and high predictive values for dissection (65%-100% positive predictive value and 70%-98% negative predictive value).5,7 Diffusion-weighted MRI (when available in the emergency setting) has the highest sensitivity for detecting acute infarcts, although posterior circulation infarcts still can be missed (19% false-negative rate).5,8 Thus, correlative vessel imaging with magnetic resonance or CT angiography is very important, along with a high index of suspicion. In some instances, repeat MRI may be necessary to detect small strokes.
A patient-specific approach to management is key for individuals with suspected posterior circulation stroke.5 Because specific data for the appropriate management of posterior circulation ischemic stroke are lacking, current American Heart Association/American Stroke Association (AHA/ASA) guidelines apply to anterior and posterior circulation strokes.6 For eligible patients without multifocal disease, intravenous tPA is the first-line therapy and should be initiated according to guidelines within 4.5 hours of stroke onset9; it is important to note that these guidelines are based on studies that focused more on anterior circulation strokes than posterior circulation strokes.6,9-13 This can be done in combination with endovascular therapy, which consists of mechanical thrombectomy, intra-arterial thrombolysis, or a combination of revascularization techniques.3,5,6
Mechanical thrombectomy specifically has high proven recanalization rates for all target vessels.3-6 The latest AHA/ASA guidelines recommend mechanical thrombectomy be performed within 6 hours of stroke onset.6 However, there is emerging evidence that suggests this timeframe should be extended—even beyond 24 hours—given the poor prognosis of posterior circulation strokes.5,6,14 More data on the management of posterior circulation strokes are urgently needed to better understand which therapeutic approach is most efficient.
In patients such as ours, who have evidence of multifocal disease, treatment may be limited to endovascular therapy. Intracranial stenting of symptomatic lesions in particular has been controversial since the publication of the Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis trial, which found that aggressive medical management was superior to stenting in patients who recently had a transient ischemic attack or stroke attributed to stenosis.15 Although additional studies have been performed, there are no definitive data on the topic—and certainly no data in the emergency setting.16 Further challenges are raised in patients with bilateral disease, as was the case with this patient.
When our patient was admitted to the rehabilitation clinic, she had a GCS score of 10 to 11/15. After 9 months of rehabilitation, she was discharged home with a GCS score of 15/15 and persistent left-side hemiparesis.
THE TAKEAWAY
Posterior circulation stroke is a life-threatening disease that may manifest with a variety of symptoms and be difficult to identify on emergent imaging. Thus, a high degree of clinical suspicion and additional follow-up are paramount to ensure prompt diagnosis and a patient-tailored treatment strategy.
CORRESPONDENCE
Kristine A. Blackham, MD, Associate Professor, University Hospital Basel, Petersgraben 4, 4031 Basel, Switzerland; kristine.blackham@gmail.com Orcid no: 0000-0002-1620-1144 (Dr. Blackham); 0000-0002- 5225-5414 (Dr. Saleh)
1. Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM. 2003;96:27-54. doi: 10.1093/qjmed/hcg003
2. Sparaco M, Ciolli L, Zini A. Posterior circulation ischaemic stroke–a review part I: anatomy, aetiology and clinical presentations. Neurol Sci. 2019;40:1995-2006. doi: 10.1007/s10072-019-03977-2
3. Lin DDM, Gailloud P, Beauchamp NJ, et al. Combined stent placement and thrombolysis in acute vertebrobasilar ischemic stroke. AJNR Am J Neuroradiol. 2003;24:1827-1833.
4. Pezzini A, Caso V, Zanferrari C, et al. Arterial hypertension as risk factor for spontaneous cervical artery dissection. A case-control study. J Neurol Neurosurg Psychiatry. 2006;77:95-97. doi:10.1136/jnnp.2005.063107
5. Merwick Á, Werring D. Posterior circulation ischaemic stroke. BMJ. 2014;348:g3175. doi: 10.1136/bmj.g3175
6. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46-e110. doi: 10.1161/STR.0000000000000158
7. Provenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR angiography, and CT angiography in the diagnosis of carotid and vertebral artery dissection: a review of the medical literature. AJR Am J Roentgenol. 2009;193:1167-1174. doi: 10.2214/AJR.08.1688
8. Husnoo Q. A case of missed diagnosis of posterior circulation stroke. Clin Med (Lond). 2019;19(suppl 2):63. doi: 10.7861/clinmedicine.19-2-s63
9. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-1329. doi: 10.1056/NEJMoa0804656
10. Schneider AM, Neuhaus AA, Hadley G, et al. Posterior circulation ischaemic stroke diagnosis and management. Clin Med (Lond). 2023;23:219-227. doi: 10.7861/clinmed.2022-0499
11. Dorňák T, Král M, Šaňák D, et al. Intravenous thrombolysis in posterior circulation stroke. Front Neurol. 2019;10:417. doi: 10.3389/fneur.2019.00417
12. van der Hoeven EJ, Schonewille WJ, Vos JA, et al. The Basilar Artery International Cooperation Study (BASICS): study protocol for a randomised controlled trial. Trials. 2013;14:200. doi: 10.1186/1745-6215-14-200
13. Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30. doi: 10.3389/fneur.2014.00030
14. Purrucker JC, Ringleb PA, Seker F, et al. Leaving the day behind: endovascular therapy beyond 24 h in acute stroke of the anterior and posterior circulation. Ther Adv Neurol Disord. 2022;15:17562864221101083. doi: 10.1177/17562864221101083
15. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003. doi: 10.1056/NEJMoa1105335
16. Markus HS, Michel P. Treatment of posterior circulation stroke: acute management and secondary prevention. Int J Stroke. 2022;17:723-732. doi: 10.1177/17474930221107500
1. Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM. 2003;96:27-54. doi: 10.1093/qjmed/hcg003
2. Sparaco M, Ciolli L, Zini A. Posterior circulation ischaemic stroke–a review part I: anatomy, aetiology and clinical presentations. Neurol Sci. 2019;40:1995-2006. doi: 10.1007/s10072-019-03977-2
3. Lin DDM, Gailloud P, Beauchamp NJ, et al. Combined stent placement and thrombolysis in acute vertebrobasilar ischemic stroke. AJNR Am J Neuroradiol. 2003;24:1827-1833.
4. Pezzini A, Caso V, Zanferrari C, et al. Arterial hypertension as risk factor for spontaneous cervical artery dissection. A case-control study. J Neurol Neurosurg Psychiatry. 2006;77:95-97. doi:10.1136/jnnp.2005.063107
5. Merwick Á, Werring D. Posterior circulation ischaemic stroke. BMJ. 2014;348:g3175. doi: 10.1136/bmj.g3175
6. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46-e110. doi: 10.1161/STR.0000000000000158
7. Provenzale JM, Sarikaya B. Comparison of test performance characteristics of MRI, MR angiography, and CT angiography in the diagnosis of carotid and vertebral artery dissection: a review of the medical literature. AJR Am J Roentgenol. 2009;193:1167-1174. doi: 10.2214/AJR.08.1688
8. Husnoo Q. A case of missed diagnosis of posterior circulation stroke. Clin Med (Lond). 2019;19(suppl 2):63. doi: 10.7861/clinmedicine.19-2-s63
9. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317-1329. doi: 10.1056/NEJMoa0804656
10. Schneider AM, Neuhaus AA, Hadley G, et al. Posterior circulation ischaemic stroke diagnosis and management. Clin Med (Lond). 2023;23:219-227. doi: 10.7861/clinmed.2022-0499
11. Dorňák T, Král M, Šaňák D, et al. Intravenous thrombolysis in posterior circulation stroke. Front Neurol. 2019;10:417. doi: 10.3389/fneur.2019.00417
12. van der Hoeven EJ, Schonewille WJ, Vos JA, et al. The Basilar Artery International Cooperation Study (BASICS): study protocol for a randomised controlled trial. Trials. 2013;14:200. doi: 10.1186/1745-6215-14-200
13. Nouh A, Remke J, Ruland S. Ischemic posterior circulation stroke: a review of anatomy, clinical presentations, diagnosis, and current management. Front Neurol. 2014;5:30. doi: 10.3389/fneur.2014.00030
14. Purrucker JC, Ringleb PA, Seker F, et al. Leaving the day behind: endovascular therapy beyond 24 h in acute stroke of the anterior and posterior circulation. Ther Adv Neurol Disord. 2022;15:17562864221101083. doi: 10.1177/17562864221101083
15. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011;365:993-1003. doi: 10.1056/NEJMoa1105335
16. Markus HS, Michel P. Treatment of posterior circulation stroke: acute management and secondary prevention. Int J Stroke. 2022;17:723-732. doi: 10.1177/17474930221107500
► Headache and neck pain radiating to ears and eyes
► Severe hypertension
A Case of Compound Heterozygous Factor V Leiden and Prothrombin G20210A Mutations With Recurrent Arterial Thromboembolism
BACKGROUND
There are 5 germline mutations that lead to hypercoagulability in the general population including: Factor V Leiden (FVL), Prothrombin G20210A (F2A), Protein C Deficiency (PCD), Protein S Deficiency (PSD), and Antithrombin Deficiency (ATD). Typical guidance is to defer testing, as it is thought not to change management.
CASE REPORT
We present a case of a patient who was found to be compound heterozygous mutations for FVL and F2A, who presented with two episodes of arterial thromboembolism resulting in cerebrovascular accident (CVA). A 63-year-old male with past medical history of hypertension, a CVA four years prior, and medication non-compliance presents with new onset left sided hemiparesis after an episode of convulsions. MRI and CT imaging of the head revealed ischemic CVA secondary to thromboembolism in the right posterior cerebral artery’s (PCA), P1 branch. Following administration of tissue plasminogen activator (tPA) he had rapid symptom improvement. This second ischemic CVA prompted a workup which was notable for: negative echocardiogram, negative 30-day cardiac monitor, CT chest negative for malignancy, no significant vascular findings, negative for antiphospholipid syndrome, but genetic testing revealed the patient to be heterozygous for FVL and F2A mutations. He was started on apixaban 5 mg twice daily for ongoing secondary prevention. Though medication compliance continues to be difficult, after being placed on direct anticoagulant (DOAC), he has not had recurrent venous or arterial thrombotic events. A small case series found double heterozygosity for FVL and F2A further increases the risk of venous thromboembolism up to 17% or more in a lifetime.
CONCLUSIONS
Although current recommendations advocate against testing for specific mutations in most cases as it is likely not to change management1, this case suggests that it may be of some benefit in patients that have a workup that does not yield a clear etiology, especially in cryptogenic stroke which is typically managed with aspirin rather than direct oral anticoagulant.
BACKGROUND
There are 5 germline mutations that lead to hypercoagulability in the general population including: Factor V Leiden (FVL), Prothrombin G20210A (F2A), Protein C Deficiency (PCD), Protein S Deficiency (PSD), and Antithrombin Deficiency (ATD). Typical guidance is to defer testing, as it is thought not to change management.
CASE REPORT
We present a case of a patient who was found to be compound heterozygous mutations for FVL and F2A, who presented with two episodes of arterial thromboembolism resulting in cerebrovascular accident (CVA). A 63-year-old male with past medical history of hypertension, a CVA four years prior, and medication non-compliance presents with new onset left sided hemiparesis after an episode of convulsions. MRI and CT imaging of the head revealed ischemic CVA secondary to thromboembolism in the right posterior cerebral artery’s (PCA), P1 branch. Following administration of tissue plasminogen activator (tPA) he had rapid symptom improvement. This second ischemic CVA prompted a workup which was notable for: negative echocardiogram, negative 30-day cardiac monitor, CT chest negative for malignancy, no significant vascular findings, negative for antiphospholipid syndrome, but genetic testing revealed the patient to be heterozygous for FVL and F2A mutations. He was started on apixaban 5 mg twice daily for ongoing secondary prevention. Though medication compliance continues to be difficult, after being placed on direct anticoagulant (DOAC), he has not had recurrent venous or arterial thrombotic events. A small case series found double heterozygosity for FVL and F2A further increases the risk of venous thromboembolism up to 17% or more in a lifetime.
CONCLUSIONS
Although current recommendations advocate against testing for specific mutations in most cases as it is likely not to change management1, this case suggests that it may be of some benefit in patients that have a workup that does not yield a clear etiology, especially in cryptogenic stroke which is typically managed with aspirin rather than direct oral anticoagulant.
BACKGROUND
There are 5 germline mutations that lead to hypercoagulability in the general population including: Factor V Leiden (FVL), Prothrombin G20210A (F2A), Protein C Deficiency (PCD), Protein S Deficiency (PSD), and Antithrombin Deficiency (ATD). Typical guidance is to defer testing, as it is thought not to change management.
CASE REPORT
We present a case of a patient who was found to be compound heterozygous mutations for FVL and F2A, who presented with two episodes of arterial thromboembolism resulting in cerebrovascular accident (CVA). A 63-year-old male with past medical history of hypertension, a CVA four years prior, and medication non-compliance presents with new onset left sided hemiparesis after an episode of convulsions. MRI and CT imaging of the head revealed ischemic CVA secondary to thromboembolism in the right posterior cerebral artery’s (PCA), P1 branch. Following administration of tissue plasminogen activator (tPA) he had rapid symptom improvement. This second ischemic CVA prompted a workup which was notable for: negative echocardiogram, negative 30-day cardiac monitor, CT chest negative for malignancy, no significant vascular findings, negative for antiphospholipid syndrome, but genetic testing revealed the patient to be heterozygous for FVL and F2A mutations. He was started on apixaban 5 mg twice daily for ongoing secondary prevention. Though medication compliance continues to be difficult, after being placed on direct anticoagulant (DOAC), he has not had recurrent venous or arterial thrombotic events. A small case series found double heterozygosity for FVL and F2A further increases the risk of venous thromboembolism up to 17% or more in a lifetime.
CONCLUSIONS
Although current recommendations advocate against testing for specific mutations in most cases as it is likely not to change management1, this case suggests that it may be of some benefit in patients that have a workup that does not yield a clear etiology, especially in cryptogenic stroke which is typically managed with aspirin rather than direct oral anticoagulant.
Successful Treatment With Oral Steroids of Autoimmune Hemolytic Anemia Associated With Kikuchi-Fujimoto Disease and Systemic Lupus Erythematosus
INTRODUCTION
We present an unusual case of autoimmune hemolytic anemia (AIHA) associated with Kikuchi-Fujimoto Disease (KFD) and systemic lupus erythematosus (SLE) that resolved with steroid therapy.
CASE PRESENTATION
A 25-year-old female with no medical history presented with 6 weeks of high fevers, syncope, and 10-lb weight loss. Exam revealed generalized lymphadenopathy (LAD) and tiny malar papules. Labs showed IgG and IgM Coombs-positivity, hemoglobin of 5 g/dL, hyperbilirubinemia, low haptoglobin, LDH >2000 IU/L, thrombocytopenia, and leukopenia. Cryoglobulins were absent. Hemophagocytic lymphohistiocytosis (HLH) markers showed ferritin of 18,000 ng/mL, moderately elevated soluble IL-2 receptor, negative CD107, minimally elevated CXCL9, borderline transaminitis, and high-normal triglycerides. ANA was 1:1280, speckled, with high anti-RNP, high anti-Smith, and negative anti-dsDNA antibodies. CT confirmed LAD without organomegaly. A 4cm excised node reviewed at 2 institutions showed necrotizing lymphadenitis without granulomas, consistent with KFD. Flow cytometry and gene rearrangement assay showed no monoclonality. Bone marrow biopsy demonstrated erythroid hyperplasia, normal flow cytometry, and no hemophagocytosis. Infectious workup was unremarkable. Treatment was initiated with 50mg prednisone daily, weaned off over 5 months. 2 months post-initiation, the fevers resolved, hemoglobin increased, and LDH normalized. 3 months later, rheumatology service diagnosed SLE based on 2019 ACR/EULAR Criteria and initiated hydroxychloroquine. 9 months later, patient remains without recurrence.
DISCUSSION
KFD presents subacutely with LAD, fever, weight loss, and varying skin findings, often self-resolving. Diagnosis requires lymph node biopsy. Etiology is unclear, with infectious, neoplastic, and autoimmune mechanisms implicated. Studies suggest up to 15% of patients have SLE.
CONCLUSIONS
This case is a rare combination of AIHA, KFD, and SLE successfully treated with steroids and, later, hydroxychloroquine. It calls for vigilance for KFD in patients with LAD and AIHA. A successful treatment strategy could include highdose steroids. The presentation may mimic lymphoma and HLH, which must be ruled out with careful pathologic and lab evaluation. To our knowledge, this is the 3rd reported case of KFD with AIHA, and 2nd case of concomitant SLE, KFD, and AIHA. The only similar patient was treated with methylprednisolone and cyclophosphamide and did not have longer-term follow-up.
INTRODUCTION
We present an unusual case of autoimmune hemolytic anemia (AIHA) associated with Kikuchi-Fujimoto Disease (KFD) and systemic lupus erythematosus (SLE) that resolved with steroid therapy.
CASE PRESENTATION
A 25-year-old female with no medical history presented with 6 weeks of high fevers, syncope, and 10-lb weight loss. Exam revealed generalized lymphadenopathy (LAD) and tiny malar papules. Labs showed IgG and IgM Coombs-positivity, hemoglobin of 5 g/dL, hyperbilirubinemia, low haptoglobin, LDH >2000 IU/L, thrombocytopenia, and leukopenia. Cryoglobulins were absent. Hemophagocytic lymphohistiocytosis (HLH) markers showed ferritin of 18,000 ng/mL, moderately elevated soluble IL-2 receptor, negative CD107, minimally elevated CXCL9, borderline transaminitis, and high-normal triglycerides. ANA was 1:1280, speckled, with high anti-RNP, high anti-Smith, and negative anti-dsDNA antibodies. CT confirmed LAD without organomegaly. A 4cm excised node reviewed at 2 institutions showed necrotizing lymphadenitis without granulomas, consistent with KFD. Flow cytometry and gene rearrangement assay showed no monoclonality. Bone marrow biopsy demonstrated erythroid hyperplasia, normal flow cytometry, and no hemophagocytosis. Infectious workup was unremarkable. Treatment was initiated with 50mg prednisone daily, weaned off over 5 months. 2 months post-initiation, the fevers resolved, hemoglobin increased, and LDH normalized. 3 months later, rheumatology service diagnosed SLE based on 2019 ACR/EULAR Criteria and initiated hydroxychloroquine. 9 months later, patient remains without recurrence.
DISCUSSION
KFD presents subacutely with LAD, fever, weight loss, and varying skin findings, often self-resolving. Diagnosis requires lymph node biopsy. Etiology is unclear, with infectious, neoplastic, and autoimmune mechanisms implicated. Studies suggest up to 15% of patients have SLE.
CONCLUSIONS
This case is a rare combination of AIHA, KFD, and SLE successfully treated with steroids and, later, hydroxychloroquine. It calls for vigilance for KFD in patients with LAD and AIHA. A successful treatment strategy could include highdose steroids. The presentation may mimic lymphoma and HLH, which must be ruled out with careful pathologic and lab evaluation. To our knowledge, this is the 3rd reported case of KFD with AIHA, and 2nd case of concomitant SLE, KFD, and AIHA. The only similar patient was treated with methylprednisolone and cyclophosphamide and did not have longer-term follow-up.
INTRODUCTION
We present an unusual case of autoimmune hemolytic anemia (AIHA) associated with Kikuchi-Fujimoto Disease (KFD) and systemic lupus erythematosus (SLE) that resolved with steroid therapy.
CASE PRESENTATION
A 25-year-old female with no medical history presented with 6 weeks of high fevers, syncope, and 10-lb weight loss. Exam revealed generalized lymphadenopathy (LAD) and tiny malar papules. Labs showed IgG and IgM Coombs-positivity, hemoglobin of 5 g/dL, hyperbilirubinemia, low haptoglobin, LDH >2000 IU/L, thrombocytopenia, and leukopenia. Cryoglobulins were absent. Hemophagocytic lymphohistiocytosis (HLH) markers showed ferritin of 18,000 ng/mL, moderately elevated soluble IL-2 receptor, negative CD107, minimally elevated CXCL9, borderline transaminitis, and high-normal triglycerides. ANA was 1:1280, speckled, with high anti-RNP, high anti-Smith, and negative anti-dsDNA antibodies. CT confirmed LAD without organomegaly. A 4cm excised node reviewed at 2 institutions showed necrotizing lymphadenitis without granulomas, consistent with KFD. Flow cytometry and gene rearrangement assay showed no monoclonality. Bone marrow biopsy demonstrated erythroid hyperplasia, normal flow cytometry, and no hemophagocytosis. Infectious workup was unremarkable. Treatment was initiated with 50mg prednisone daily, weaned off over 5 months. 2 months post-initiation, the fevers resolved, hemoglobin increased, and LDH normalized. 3 months later, rheumatology service diagnosed SLE based on 2019 ACR/EULAR Criteria and initiated hydroxychloroquine. 9 months later, patient remains without recurrence.
DISCUSSION
KFD presents subacutely with LAD, fever, weight loss, and varying skin findings, often self-resolving. Diagnosis requires lymph node biopsy. Etiology is unclear, with infectious, neoplastic, and autoimmune mechanisms implicated. Studies suggest up to 15% of patients have SLE.
CONCLUSIONS
This case is a rare combination of AIHA, KFD, and SLE successfully treated with steroids and, later, hydroxychloroquine. It calls for vigilance for KFD in patients with LAD and AIHA. A successful treatment strategy could include highdose steroids. The presentation may mimic lymphoma and HLH, which must be ruled out with careful pathologic and lab evaluation. To our knowledge, this is the 3rd reported case of KFD with AIHA, and 2nd case of concomitant SLE, KFD, and AIHA. The only similar patient was treated with methylprednisolone and cyclophosphamide and did not have longer-term follow-up.