User login
Copaxone lipoatrophy far more common than reported
DALLAS – The risk of lipoatrophy with glatiramer acetate is greater than 60%, according to a review of 73 multiple sclerosis patients at one clinic.
The risk is "substantially higher than previously reported and [is] often the sole factor prompting patients to switch to another MS [disease-modifying therapy]. Our data also suggest that a heightened risk of lipoatrophy is an inherent autoimmune problem and is not necessarily mitigated by vigilant injection-site rotation. The psychological consequences may be significant," said investigator Dr. Ronald Bailey, director of the MS clinic at the Riverside (Calif.) Medical Clinic.
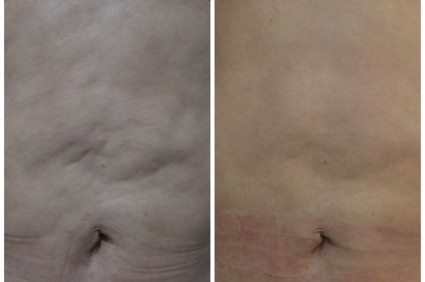
A total of 46 glatiramer acetate (GA, Copaxone) patients (63%) developed lipoatrophy, an injection-site indentation that can be deep and disfiguring; 35 (76%) of them used an autoinjector. Once noted, the dents didn’t improve during a 3-year observation period, which included photographic documentation and instructions on how to inject the drug every 3 months.
In some patients, lipoatrophy developed within the first 3 months of starting the shots and was noted at multiple injection sites, which prompted the team to suspect that an autoimmune reaction was at work. "Upon GA treatment discontinuation, lipoatrophy remained permanent," he noted.
Lipoatrophy "appears to progress, even when you stop the injections. It’s a pretty impressive disfiguration. It’s important to emphasize [with patients] that this isn’t necessarily going to be remedied with plastic surgery. [However,] if patients were stable, most of them thought that this was a small price to pay to be in remission," Dr. Bailey said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
GA labeling reports the risk of lipoatrophy to be 2% with the 20-mg/mL daily formulation, which has been on the market for almost 2 decades, and 0.5% with the 40-mg/mL three times weekly option, which was approved by the Food and Drug Administration in 2014. Lipoatrophy "is thought to be permanent. There is no known therapy. To assist in possibly minimizing these events, the patient should be advised to follow proper injection technique and to rotate injection sites with each injection," according to the GA label, which is in contrast with the Riverside finding that site rotation wasn’t much help.
Most of the patients at the clinic were women, in keeping with MS epidemiology, and 40 (55%) opted for the autoinjector, specifically the Autoject 2; the device’s labeling notes that the autoinjector can "help with hard-to-reach areas on your body." Perhaps, by helping patients reach those difficult areas, the autoinjector makes it easier to miss the proper subcutaneous fat layer. That might have something to do with the problem, Dr. Bailey said, but the team simply reported their observations and didn’t report any statistical analysis of the findings, so it’s impossible to discern causes, he noted.
The findings aren’t new for some. The "prevalence of lipoatrophy [is] much higher than expected," one team noted several years ago (Can. J. Neurol. Sci. 2004;31:58-63).
No one knows why GA seems to cause lipoatrophy. Maybe "an elevation in tumor necrosis factor–alpha ... causes a dedifferentiation of adipocytes in [subcutaneous] tissue," Dr. Bailey said.
He is a paid spokesman for Genzyme, Biogen, and Teva, the maker of GA. There was no outside funding for the project.
autoimmune problem, vigilant injection-site rotation, Dr. Ronald Bailey, glatiramer acetate, GA, Copaxone, lipoatrophy, injection-site indentation, autoinjector, Lipoatrophy, Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Food and Drug Administration, proper injection technique,
DALLAS – The risk of lipoatrophy with glatiramer acetate is greater than 60%, according to a review of 73 multiple sclerosis patients at one clinic.
The risk is "substantially higher than previously reported and [is] often the sole factor prompting patients to switch to another MS [disease-modifying therapy]. Our data also suggest that a heightened risk of lipoatrophy is an inherent autoimmune problem and is not necessarily mitigated by vigilant injection-site rotation. The psychological consequences may be significant," said investigator Dr. Ronald Bailey, director of the MS clinic at the Riverside (Calif.) Medical Clinic.
A total of 46 glatiramer acetate (GA, Copaxone) patients (63%) developed lipoatrophy, an injection-site indentation that can be deep and disfiguring; 35 (76%) of them used an autoinjector. Once noted, the dents didn’t improve during a 3-year observation period, which included photographic documentation and instructions on how to inject the drug every 3 months.
In some patients, lipoatrophy developed within the first 3 months of starting the shots and was noted at multiple injection sites, which prompted the team to suspect that an autoimmune reaction was at work. "Upon GA treatment discontinuation, lipoatrophy remained permanent," he noted.
Lipoatrophy "appears to progress, even when you stop the injections. It’s a pretty impressive disfiguration. It’s important to emphasize [with patients] that this isn’t necessarily going to be remedied with plastic surgery. [However,] if patients were stable, most of them thought that this was a small price to pay to be in remission," Dr. Bailey said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
GA labeling reports the risk of lipoatrophy to be 2% with the 20-mg/mL daily formulation, which has been on the market for almost 2 decades, and 0.5% with the 40-mg/mL three times weekly option, which was approved by the Food and Drug Administration in 2014. Lipoatrophy "is thought to be permanent. There is no known therapy. To assist in possibly minimizing these events, the patient should be advised to follow proper injection technique and to rotate injection sites with each injection," according to the GA label, which is in contrast with the Riverside finding that site rotation wasn’t much help.
Most of the patients at the clinic were women, in keeping with MS epidemiology, and 40 (55%) opted for the autoinjector, specifically the Autoject 2; the device’s labeling notes that the autoinjector can "help with hard-to-reach areas on your body." Perhaps, by helping patients reach those difficult areas, the autoinjector makes it easier to miss the proper subcutaneous fat layer. That might have something to do with the problem, Dr. Bailey said, but the team simply reported their observations and didn’t report any statistical analysis of the findings, so it’s impossible to discern causes, he noted.
The findings aren’t new for some. The "prevalence of lipoatrophy [is] much higher than expected," one team noted several years ago (Can. J. Neurol. Sci. 2004;31:58-63).
No one knows why GA seems to cause lipoatrophy. Maybe "an elevation in tumor necrosis factor–alpha ... causes a dedifferentiation of adipocytes in [subcutaneous] tissue," Dr. Bailey said.
He is a paid spokesman for Genzyme, Biogen, and Teva, the maker of GA. There was no outside funding for the project.
DALLAS – The risk of lipoatrophy with glatiramer acetate is greater than 60%, according to a review of 73 multiple sclerosis patients at one clinic.
The risk is "substantially higher than previously reported and [is] often the sole factor prompting patients to switch to another MS [disease-modifying therapy]. Our data also suggest that a heightened risk of lipoatrophy is an inherent autoimmune problem and is not necessarily mitigated by vigilant injection-site rotation. The psychological consequences may be significant," said investigator Dr. Ronald Bailey, director of the MS clinic at the Riverside (Calif.) Medical Clinic.
A total of 46 glatiramer acetate (GA, Copaxone) patients (63%) developed lipoatrophy, an injection-site indentation that can be deep and disfiguring; 35 (76%) of them used an autoinjector. Once noted, the dents didn’t improve during a 3-year observation period, which included photographic documentation and instructions on how to inject the drug every 3 months.
In some patients, lipoatrophy developed within the first 3 months of starting the shots and was noted at multiple injection sites, which prompted the team to suspect that an autoimmune reaction was at work. "Upon GA treatment discontinuation, lipoatrophy remained permanent," he noted.
Lipoatrophy "appears to progress, even when you stop the injections. It’s a pretty impressive disfiguration. It’s important to emphasize [with patients] that this isn’t necessarily going to be remedied with plastic surgery. [However,] if patients were stable, most of them thought that this was a small price to pay to be in remission," Dr. Bailey said at a meeting of the Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis.
GA labeling reports the risk of lipoatrophy to be 2% with the 20-mg/mL daily formulation, which has been on the market for almost 2 decades, and 0.5% with the 40-mg/mL three times weekly option, which was approved by the Food and Drug Administration in 2014. Lipoatrophy "is thought to be permanent. There is no known therapy. To assist in possibly minimizing these events, the patient should be advised to follow proper injection technique and to rotate injection sites with each injection," according to the GA label, which is in contrast with the Riverside finding that site rotation wasn’t much help.
Most of the patients at the clinic were women, in keeping with MS epidemiology, and 40 (55%) opted for the autoinjector, specifically the Autoject 2; the device’s labeling notes that the autoinjector can "help with hard-to-reach areas on your body." Perhaps, by helping patients reach those difficult areas, the autoinjector makes it easier to miss the proper subcutaneous fat layer. That might have something to do with the problem, Dr. Bailey said, but the team simply reported their observations and didn’t report any statistical analysis of the findings, so it’s impossible to discern causes, he noted.
The findings aren’t new for some. The "prevalence of lipoatrophy [is] much higher than expected," one team noted several years ago (Can. J. Neurol. Sci. 2004;31:58-63).
No one knows why GA seems to cause lipoatrophy. Maybe "an elevation in tumor necrosis factor–alpha ... causes a dedifferentiation of adipocytes in [subcutaneous] tissue," Dr. Bailey said.
He is a paid spokesman for Genzyme, Biogen, and Teva, the maker of GA. There was no outside funding for the project.
autoimmune problem, vigilant injection-site rotation, Dr. Ronald Bailey, glatiramer acetate, GA, Copaxone, lipoatrophy, injection-site indentation, autoinjector, Lipoatrophy, Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Food and Drug Administration, proper injection technique,
autoimmune problem, vigilant injection-site rotation, Dr. Ronald Bailey, glatiramer acetate, GA, Copaxone, lipoatrophy, injection-site indentation, autoinjector, Lipoatrophy, Consortium of Multiple Sclerosis Centers and the Americas Committee for Treatment and Research in Multiple Sclerosis, Food and Drug Administration, proper injection technique,
AT THE CMSC/ACTRIMS ANNUAL MEETING
Key clinical point: The rate of lipoatrophy with glatiramer acetate may be much higher than reported in the drug’s label.
Major finding: Of 73 glatiramer acetate patients, 46 (63%) developed lipoatrophy, sometimes within 3 months of starting the shots.
Data Source: Patient observation every 3 months for 3 years.
Disclosures: The lead investigator is a paid spokesman for Teva, the maker of Copaxone. There was no outside funding for the project.
Acquired Progressive Lymphangioma in the Inguinal Area Mimicking Giant Condyloma Acuminatum
Lymphangioma Circumscriptum of the Vulva in a Patient With Noonan Syndrome
Attacking Medical Errors in Dermatology
Strep infection linked to death after liposuction at ‘spa’
Four confirmed and nine suspected cases of invasive group A Streptococcus infection, including one fatality, developed after liposuction at a chain of "medical spas" in Maryland and Pennsylvania, according to a report published online May 26 in JAMA Internal Medicine.
In addition to the previously healthy woman who died, the three other patients with confirmed infections were hospitalized for up to 77 days for necrotizing fasciitis, as well as streptococcal toxic shock syndrome. Each patient required two to six surgical debridements. "Our findings underscore the importance of improved oversight of the increasingly complex surgical procedures that are performed at outpatient facilities that are not subject to state or federal regulation," said Amanda L. Beaudoin, Ph.D., of the epidemic intelligence service, Centers for Disease Control and Prevention, and her associates.
A public health investigation revealed that 13 infections developed among a possible 55 men and women (mean age, 39 years) interviewed who underwent liposuction during a 2-month period at two facilities that also offered Botox (onabotulinumtoxinA) injections, laser hair removal, and tattoo removal. One physician, who was not board certified in plastic surgery, performed all the procedures in which invasive group A Streptococcus infection developed. This physician and his surgical assistant were later found to be carrying the same strain of the erythromycin-, clindamycin-, and tetracycline-resistant organism when throat and anal cultures were obtained, said Dr. Beaudoin, who is also with the Pennsylvania Department of Health, Harrisburg, and her colleagues.
During the outbreak period, the physician reported that he had self-treated cellulitis of his hands with cephalexin, and the assistant reported having had a sore throat. Both said that they had used surgical masks and gowns during the procedures, but not during surgical marking, preoperative preparation, or postoperative care. However, multiple patients reported that the surgical team didn’t wear masks or gowns during the procedure, and one said that the surgical team consumed food in the procedure room.
A limited site assessment of the involved facilities revealed visibly dirty equipment; no designation of "clean" and "dirty" areas for disinfection and sterilization of equipment; surgical scrub materials left open to the air; no records of the use and maintenance of autoclaves or of performance checks on them; inadequately labeled, multiple-dose, and expired vials of medication; nonsterile surgical dressings stored in high-traffic areas; no written policies regarding infection prevention; and no records of employee training in infection prevention, the investigators said (JAMA Intern. Med. 2014 May 26 [doi:10.1001/jamainternmed.2014.1875]).
When patients ask about cosmetic procedures, physicians should emphasize that they choose a surgeon fully trained in cosmetic surgery who operates out of an accredited surgical center or hospital. All physicians should be alert to the possibility of infection after their patients undergo cosmetic surgery, "including suspicion of necrotizing fasciitis as a possible postoperative complication," Dr. Beaudoin and her associates said.
The investigators reported no financial conflicts of interest.
Tragedies like the one described by Dr. Beaudoin and her colleagues will continue to occur unless all physicians who perform cosmetic procedures are appropriately trained, and all cosmetic surgery adheres to rigorous safety standards, said Dr. Daniel J. Morgan and Dr. Anthony D. Harris.
The number of "medical spas" in the United States rose from fewer than 500 in 2003 to 1,750 in 2011. "Often, the physicians who work at medical spas are not board certified; they may have no special training or may learn the trade with brief course work," the investigators noted.
To better protect patients, "states should urgently enact legislation that establishes the regulation of all outpatient surgical facilities, as well as oversight by state public health officials. Invasive surgical procedures performed at medical spas should have a high level of scrutiny, and [such] facilities ... should adopt the federal standards proposed for ambulatory surgical centers" and should be subject to audits and site visits, they said.
Dr. Morgan and Dr. Harris are in the department of public health and epidemiology at the University of Maryland, Baltimore. Dr. Morgan is also with the Veterans Affairs Maryland Healthcare System, Baltimore. Dr. Harris reported no relevant conflicts of interest. Dr. Morgan reported serving as a consultant for Welch Allyn and Sanogiene regarding planning infection control research. These remarks were taken from their invited commentary accompanying Dr. Beaudoin’s report (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed.2014.441]).
Tragedies like the one described by Dr. Beaudoin and her colleagues will continue to occur unless all physicians who perform cosmetic procedures are appropriately trained, and all cosmetic surgery adheres to rigorous safety standards, said Dr. Daniel J. Morgan and Dr. Anthony D. Harris.
The number of "medical spas" in the United States rose from fewer than 500 in 2003 to 1,750 in 2011. "Often, the physicians who work at medical spas are not board certified; they may have no special training or may learn the trade with brief course work," the investigators noted.
To better protect patients, "states should urgently enact legislation that establishes the regulation of all outpatient surgical facilities, as well as oversight by state public health officials. Invasive surgical procedures performed at medical spas should have a high level of scrutiny, and [such] facilities ... should adopt the federal standards proposed for ambulatory surgical centers" and should be subject to audits and site visits, they said.
Dr. Morgan and Dr. Harris are in the department of public health and epidemiology at the University of Maryland, Baltimore. Dr. Morgan is also with the Veterans Affairs Maryland Healthcare System, Baltimore. Dr. Harris reported no relevant conflicts of interest. Dr. Morgan reported serving as a consultant for Welch Allyn and Sanogiene regarding planning infection control research. These remarks were taken from their invited commentary accompanying Dr. Beaudoin’s report (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed.2014.441]).
Tragedies like the one described by Dr. Beaudoin and her colleagues will continue to occur unless all physicians who perform cosmetic procedures are appropriately trained, and all cosmetic surgery adheres to rigorous safety standards, said Dr. Daniel J. Morgan and Dr. Anthony D. Harris.
The number of "medical spas" in the United States rose from fewer than 500 in 2003 to 1,750 in 2011. "Often, the physicians who work at medical spas are not board certified; they may have no special training or may learn the trade with brief course work," the investigators noted.
To better protect patients, "states should urgently enact legislation that establishes the regulation of all outpatient surgical facilities, as well as oversight by state public health officials. Invasive surgical procedures performed at medical spas should have a high level of scrutiny, and [such] facilities ... should adopt the federal standards proposed for ambulatory surgical centers" and should be subject to audits and site visits, they said.
Dr. Morgan and Dr. Harris are in the department of public health and epidemiology at the University of Maryland, Baltimore. Dr. Morgan is also with the Veterans Affairs Maryland Healthcare System, Baltimore. Dr. Harris reported no relevant conflicts of interest. Dr. Morgan reported serving as a consultant for Welch Allyn and Sanogiene regarding planning infection control research. These remarks were taken from their invited commentary accompanying Dr. Beaudoin’s report (JAMA Intern. Med. 2014 [doi:10.1001/jamainternmed.2014.441]).
Four confirmed and nine suspected cases of invasive group A Streptococcus infection, including one fatality, developed after liposuction at a chain of "medical spas" in Maryland and Pennsylvania, according to a report published online May 26 in JAMA Internal Medicine.
In addition to the previously healthy woman who died, the three other patients with confirmed infections were hospitalized for up to 77 days for necrotizing fasciitis, as well as streptococcal toxic shock syndrome. Each patient required two to six surgical debridements. "Our findings underscore the importance of improved oversight of the increasingly complex surgical procedures that are performed at outpatient facilities that are not subject to state or federal regulation," said Amanda L. Beaudoin, Ph.D., of the epidemic intelligence service, Centers for Disease Control and Prevention, and her associates.
A public health investigation revealed that 13 infections developed among a possible 55 men and women (mean age, 39 years) interviewed who underwent liposuction during a 2-month period at two facilities that also offered Botox (onabotulinumtoxinA) injections, laser hair removal, and tattoo removal. One physician, who was not board certified in plastic surgery, performed all the procedures in which invasive group A Streptococcus infection developed. This physician and his surgical assistant were later found to be carrying the same strain of the erythromycin-, clindamycin-, and tetracycline-resistant organism when throat and anal cultures were obtained, said Dr. Beaudoin, who is also with the Pennsylvania Department of Health, Harrisburg, and her colleagues.
During the outbreak period, the physician reported that he had self-treated cellulitis of his hands with cephalexin, and the assistant reported having had a sore throat. Both said that they had used surgical masks and gowns during the procedures, but not during surgical marking, preoperative preparation, or postoperative care. However, multiple patients reported that the surgical team didn’t wear masks or gowns during the procedure, and one said that the surgical team consumed food in the procedure room.
A limited site assessment of the involved facilities revealed visibly dirty equipment; no designation of "clean" and "dirty" areas for disinfection and sterilization of equipment; surgical scrub materials left open to the air; no records of the use and maintenance of autoclaves or of performance checks on them; inadequately labeled, multiple-dose, and expired vials of medication; nonsterile surgical dressings stored in high-traffic areas; no written policies regarding infection prevention; and no records of employee training in infection prevention, the investigators said (JAMA Intern. Med. 2014 May 26 [doi:10.1001/jamainternmed.2014.1875]).
When patients ask about cosmetic procedures, physicians should emphasize that they choose a surgeon fully trained in cosmetic surgery who operates out of an accredited surgical center or hospital. All physicians should be alert to the possibility of infection after their patients undergo cosmetic surgery, "including suspicion of necrotizing fasciitis as a possible postoperative complication," Dr. Beaudoin and her associates said.
The investigators reported no financial conflicts of interest.
Four confirmed and nine suspected cases of invasive group A Streptococcus infection, including one fatality, developed after liposuction at a chain of "medical spas" in Maryland and Pennsylvania, according to a report published online May 26 in JAMA Internal Medicine.
In addition to the previously healthy woman who died, the three other patients with confirmed infections were hospitalized for up to 77 days for necrotizing fasciitis, as well as streptococcal toxic shock syndrome. Each patient required two to six surgical debridements. "Our findings underscore the importance of improved oversight of the increasingly complex surgical procedures that are performed at outpatient facilities that are not subject to state or federal regulation," said Amanda L. Beaudoin, Ph.D., of the epidemic intelligence service, Centers for Disease Control and Prevention, and her associates.
A public health investigation revealed that 13 infections developed among a possible 55 men and women (mean age, 39 years) interviewed who underwent liposuction during a 2-month period at two facilities that also offered Botox (onabotulinumtoxinA) injections, laser hair removal, and tattoo removal. One physician, who was not board certified in plastic surgery, performed all the procedures in which invasive group A Streptococcus infection developed. This physician and his surgical assistant were later found to be carrying the same strain of the erythromycin-, clindamycin-, and tetracycline-resistant organism when throat and anal cultures were obtained, said Dr. Beaudoin, who is also with the Pennsylvania Department of Health, Harrisburg, and her colleagues.
During the outbreak period, the physician reported that he had self-treated cellulitis of his hands with cephalexin, and the assistant reported having had a sore throat. Both said that they had used surgical masks and gowns during the procedures, but not during surgical marking, preoperative preparation, or postoperative care. However, multiple patients reported that the surgical team didn’t wear masks or gowns during the procedure, and one said that the surgical team consumed food in the procedure room.
A limited site assessment of the involved facilities revealed visibly dirty equipment; no designation of "clean" and "dirty" areas for disinfection and sterilization of equipment; surgical scrub materials left open to the air; no records of the use and maintenance of autoclaves or of performance checks on them; inadequately labeled, multiple-dose, and expired vials of medication; nonsterile surgical dressings stored in high-traffic areas; no written policies regarding infection prevention; and no records of employee training in infection prevention, the investigators said (JAMA Intern. Med. 2014 May 26 [doi:10.1001/jamainternmed.2014.1875]).
When patients ask about cosmetic procedures, physicians should emphasize that they choose a surgeon fully trained in cosmetic surgery who operates out of an accredited surgical center or hospital. All physicians should be alert to the possibility of infection after their patients undergo cosmetic surgery, "including suspicion of necrotizing fasciitis as a possible postoperative complication," Dr. Beaudoin and her associates said.
The investigators reported no financial conflicts of interest.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Infection, including necrotizing fasciitis, can be a possibility after cosmetic surgery.
Major finding: Four confirmed and nine suspected cases of severe invasive group A Streptococcus infection caused one death and required four patients to be hospitalized for up to 77 days and to undergo up to six surgical debridements because of necrotizing fasciitis and toxic shock syndrome.
Data source: An epidemiologic investigation of an outbreak among patients undergoing liposuction at two "health spas" not subject to state or federal regulation.
Disclosures: Dr. Beaudoin and her associates reported no potential financial conflicts of interest.
The springtime eruptions
The spectrum of idiopathic ultraviolet-induced dermatoses includes the most severe variant, polymorphous light eruption (PMLE), in which erythematous papules, papulovesicles, and plaques form from a delayed type IV hypersensitivity reaction to the sun. Its milder cousins, benign summer light eruption and juvenile springtime eruption, are milder, more transient variants.
Patients may experience sudden-onset, pruritic, sometimes painful papules and papulovesicles or cheilitis within 30 minutes to several hours of exposure to UV light in areas normally covered in the winter months. The rash subsides over 1-7 days (or sooner with effective topical steroid administration and strict sun avoidance) and without scarring. Occasionally, patients experience systemic flulike symptoms after sun exposure. Triggers can be UVA, UVB, or UVC. However, because most cases appear in the spring, describing these variants as benign summer light eruption is something of a misnomer.
These seasonal rashes are often underrecognized in skin of color patients, particularly those with Fitzpatrick skin types III-VI, because many practitioners assume a protective role of melanin (Photochem. Photobiol. Sci. 2013;12:65-77). A study by Kerr and Lim identified 280 patients with photodermatoses; 135 (48%) were African American, 110 (40%) were white, and 35 (12%) were other ethnicities. They noted a significantly higher proportion of African Americans with PMLE, compared with whites (J. Am. Acad. Dermatol. 2007;57:638-43). Also, Native Americans have a hereditary form of PMLE with autosomal dominant inheritance that can involve the face and is most common in patients with Fitzpatrick skin types III-VI.
For sun-sensitive patients, and especially skin of color patients, diagnosis and treatment include ruling out other photosensitive diseases such as systemic lupus, and then counseling about the importance of sun avoidance and the use of sunscreens, which include both UVA and UVB protection. Prophylactic phototherapy or photochemotherapy at the beginning of spring for several weeks may prevent flare-ups throughout the summer. PUVA (psoralen and UVA) therapy, as well as UVB phototherapy, have been successful at preventing flares in several studies. Topical steroids, antihistamines, and oral prednisone are mainstays of treatment for severe flares, alone or in combination with phototherapy. For severe cases, or those recalcitrant to first-line treatment, antimalarials, azathioprine, and thalidomide have been used with variable efficacy.
Particularly at this time of year, I always ask patients with photo-distributed rashes about their ethnicities. One can never assume ethnicity, culture, skin type, background, or even photosensitivity based on skin color alone. I have been surprised by the many patients with dark skin who may have Native American origins who present with photosensitive rashes, or the many patients with hereditary photosensitive rashes with fair skin. Our beautiful, multicultural society makes it harder to define or categorize dermatoses by skin type alone, based on the definitions we have set for skin type in our literature today.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif.
The spectrum of idiopathic ultraviolet-induced dermatoses includes the most severe variant, polymorphous light eruption (PMLE), in which erythematous papules, papulovesicles, and plaques form from a delayed type IV hypersensitivity reaction to the sun. Its milder cousins, benign summer light eruption and juvenile springtime eruption, are milder, more transient variants.
Patients may experience sudden-onset, pruritic, sometimes painful papules and papulovesicles or cheilitis within 30 minutes to several hours of exposure to UV light in areas normally covered in the winter months. The rash subsides over 1-7 days (or sooner with effective topical steroid administration and strict sun avoidance) and without scarring. Occasionally, patients experience systemic flulike symptoms after sun exposure. Triggers can be UVA, UVB, or UVC. However, because most cases appear in the spring, describing these variants as benign summer light eruption is something of a misnomer.
These seasonal rashes are often underrecognized in skin of color patients, particularly those with Fitzpatrick skin types III-VI, because many practitioners assume a protective role of melanin (Photochem. Photobiol. Sci. 2013;12:65-77). A study by Kerr and Lim identified 280 patients with photodermatoses; 135 (48%) were African American, 110 (40%) were white, and 35 (12%) were other ethnicities. They noted a significantly higher proportion of African Americans with PMLE, compared with whites (J. Am. Acad. Dermatol. 2007;57:638-43). Also, Native Americans have a hereditary form of PMLE with autosomal dominant inheritance that can involve the face and is most common in patients with Fitzpatrick skin types III-VI.
For sun-sensitive patients, and especially skin of color patients, diagnosis and treatment include ruling out other photosensitive diseases such as systemic lupus, and then counseling about the importance of sun avoidance and the use of sunscreens, which include both UVA and UVB protection. Prophylactic phototherapy or photochemotherapy at the beginning of spring for several weeks may prevent flare-ups throughout the summer. PUVA (psoralen and UVA) therapy, as well as UVB phototherapy, have been successful at preventing flares in several studies. Topical steroids, antihistamines, and oral prednisone are mainstays of treatment for severe flares, alone or in combination with phototherapy. For severe cases, or those recalcitrant to first-line treatment, antimalarials, azathioprine, and thalidomide have been used with variable efficacy.
Particularly at this time of year, I always ask patients with photo-distributed rashes about their ethnicities. One can never assume ethnicity, culture, skin type, background, or even photosensitivity based on skin color alone. I have been surprised by the many patients with dark skin who may have Native American origins who present with photosensitive rashes, or the many patients with hereditary photosensitive rashes with fair skin. Our beautiful, multicultural society makes it harder to define or categorize dermatoses by skin type alone, based on the definitions we have set for skin type in our literature today.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif.
The spectrum of idiopathic ultraviolet-induced dermatoses includes the most severe variant, polymorphous light eruption (PMLE), in which erythematous papules, papulovesicles, and plaques form from a delayed type IV hypersensitivity reaction to the sun. Its milder cousins, benign summer light eruption and juvenile springtime eruption, are milder, more transient variants.
Patients may experience sudden-onset, pruritic, sometimes painful papules and papulovesicles or cheilitis within 30 minutes to several hours of exposure to UV light in areas normally covered in the winter months. The rash subsides over 1-7 days (or sooner with effective topical steroid administration and strict sun avoidance) and without scarring. Occasionally, patients experience systemic flulike symptoms after sun exposure. Triggers can be UVA, UVB, or UVC. However, because most cases appear in the spring, describing these variants as benign summer light eruption is something of a misnomer.
These seasonal rashes are often underrecognized in skin of color patients, particularly those with Fitzpatrick skin types III-VI, because many practitioners assume a protective role of melanin (Photochem. Photobiol. Sci. 2013;12:65-77). A study by Kerr and Lim identified 280 patients with photodermatoses; 135 (48%) were African American, 110 (40%) were white, and 35 (12%) were other ethnicities. They noted a significantly higher proportion of African Americans with PMLE, compared with whites (J. Am. Acad. Dermatol. 2007;57:638-43). Also, Native Americans have a hereditary form of PMLE with autosomal dominant inheritance that can involve the face and is most common in patients with Fitzpatrick skin types III-VI.
For sun-sensitive patients, and especially skin of color patients, diagnosis and treatment include ruling out other photosensitive diseases such as systemic lupus, and then counseling about the importance of sun avoidance and the use of sunscreens, which include both UVA and UVB protection. Prophylactic phototherapy or photochemotherapy at the beginning of spring for several weeks may prevent flare-ups throughout the summer. PUVA (psoralen and UVA) therapy, as well as UVB phototherapy, have been successful at preventing flares in several studies. Topical steroids, antihistamines, and oral prednisone are mainstays of treatment for severe flares, alone or in combination with phototherapy. For severe cases, or those recalcitrant to first-line treatment, antimalarials, azathioprine, and thalidomide have been used with variable efficacy.
Particularly at this time of year, I always ask patients with photo-distributed rashes about their ethnicities. One can never assume ethnicity, culture, skin type, background, or even photosensitivity based on skin color alone. I have been surprised by the many patients with dark skin who may have Native American origins who present with photosensitive rashes, or the many patients with hereditary photosensitive rashes with fair skin. Our beautiful, multicultural society makes it harder to define or categorize dermatoses by skin type alone, based on the definitions we have set for skin type in our literature today.
Dr. Talakoub and Dr. Wesley are co-contributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice at McLean (Va.) Dermatology Center. Dr. Wesley practices dermatology in Beverly Hills, Calif.
VIDEO: Creative cuts make more aesthetic surgical dressings
ORLANDO – A few cuts in the surgical dressing material, a process that Dr. Kristin Smallwood calls ‘pinking,’ can make a big difference for patients.
Dr. Smallwood was inspired by the cutting techniques used in sewing and quickly realized that a few cuts here and there on the wound dressing not only helped with applying appropriate pressure, but also yielded more aesthetically pleasing results.
In an interview at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Smallwood, who practices in Cocoa Beach, Fla., shows exactly how she makes her creative cuts.
On Twitter @naseemsmiller

ORLANDO – A few cuts in the surgical dressing material, a process that Dr. Kristin Smallwood calls ‘pinking,’ can make a big difference for patients.
Dr. Smallwood was inspired by the cutting techniques used in sewing and quickly realized that a few cuts here and there on the wound dressing not only helped with applying appropriate pressure, but also yielded more aesthetically pleasing results.
In an interview at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Smallwood, who practices in Cocoa Beach, Fla., shows exactly how she makes her creative cuts.
On Twitter @naseemsmiller

ORLANDO – A few cuts in the surgical dressing material, a process that Dr. Kristin Smallwood calls ‘pinking,’ can make a big difference for patients.
Dr. Smallwood was inspired by the cutting techniques used in sewing and quickly realized that a few cuts here and there on the wound dressing not only helped with applying appropriate pressure, but also yielded more aesthetically pleasing results.
In an interview at the annual meeting of the Florida Society of Dermatology and Dermatologic Surgery, Dr. Smallwood, who practices in Cocoa Beach, Fla., shows exactly how she makes her creative cuts.
On Twitter @naseemsmiller

AT FSDDS 14
Picosecond laser makes its mark for tattoo removal
PHOENIX – Three small case series reported at the annual meeting of the American Society for Laser Medicine and Surgery reported good results using a picosecond laser for tattoo removal and explored different regimens for treatment.
One study at a single center used a 532-nm Nd-YAG laser with a pulse duration of 450-500 picoseconds (ps) in all 17 patients. Up to 10 treatments spaced every 4-8 weeks used a spot size of 2.5-5 mm, an energy density of 0.3-2.2 J/cm2, and a frequency of 5 Hz in a single pass. Some patients also were treated with a 1,064-nm Nd:YAG laser with a pulse duration of 500-600 ns or a 755-nm alexandrite laser with a pulse duration of 550-750 ns.
A single treatment cleared 75% of red pigment in tattoos on nine patients treated with the 532-nm picosecond laser. Red ink cleared completely in two patients after a second or third session, Dr. Hamad Al-Abdulrazzaq and his associates reported at the meeting.
Difficult-to-remove yellow pigment lightened by 75% in three patients after two to four treatments with the 532-ns picosecond laser.
Black ink cleared by 50%-75% after one or two treatments in four patients using the 1,064-ps laser, reported Dr. Al-Abdulrazzaq, a fellow at the Laser and Skin Surgery Center of New York.
Although there were no signs of scarring or textural skin changes after treatment, one patient developed paradoxical darkening that was removed using the 1,064-nm picosecond laser. Other adverse events were as expected with laser treatment, including erythema, edema, hypopigmentation, pain, mild blistering, and crust formation that healed within a week, Dr. Al-Abdulrazzaq said.
Nearly 90% of patients reported satisfaction with treatment, and nearly 70% said they were extremely satisfied.
A separate study compared single-pass to dual-pass treatments for 26 tattoos on 20 patients using a 755-nm, 750-ps alexandrite laser. Half of each tattoo received a single pass and the other half underwent two passes separated by a 20-minute interval at multiple treatment sessions.
After the first session, the two-pass method produced a 3.4-fold improvement in pigment, significantly better than a 2.1-fold improvement seen after a single-pass treatment, Dr. Trenton Custis and his associates reported. After three treatment sessions, pigment had improved 4.5-fold using the dual-pass method and 3.3-fold using the single-pass method, a statistically significant difference.
Lasers whose pulse durations are in the picosecond range produce a very high peak power that yields more rapid heating and photoacoustic shattering of the ink, which may allow for fewer treatments compared with conventional laser methods, said Dr. Custis, a procedural dermatology fellow at the University of California, Davis.
A separate dose-ranging study applied test spots of 1.3-4.1 J/cm2 over tattoos and adjacent normal skin on 18 patients using a 755-nm alexandrite laser. The best-tolerated fluence based on the test spots was used for half of each tattoo over the course of four treatments, and the other half of each tattoo received escalating doses not to exceed 4.1 J/cm2.
Initial laser treatment using lower fluences (1.3-2.0 J/cm2) were best tolerated, Dr. Emil A. Tanghetti and his associates reported. Higher initial doses were associated with discomfort, blistering, transient hypopigmentation, and postinflammatory hyperpigmentation, said Dr. Tanghetti of the Center for Dermatology and Laser Surgery, Sacramento, Calif.
The 1.3- to 2.0-J/cm2 fluences produced significant clearing of the tattoo, but dose escalation up to 4.1 J/cm2 appeared to better clear the tattoos with minimal side effects. "Dose escalation rather than high-dose treatment is tolerated best by patients with less downtime and blistering," he said. Fluences of 2 J/cm2 seemed to be necessary for consistent clearing of tattoos over four treatments. Blue, green, and light-black ink often disappeared after one treatment.
"Based upon this data and our experience, the picosecond alexandrite is our laser of choice for most of our tattoo patients," Dr. Tanghetti said. It’s important to consider skin type, tanning history, and other variables when choosing a fluence, he added.
An estimated 20% of U.S. residents have a tattoo. Requests for laser tattoo removal increased by 52% from 2012 to 2013, Dr. Al-Abdulrazzaq said.
Dr. Tanghetti reported financial associations with Cynosure. Dr. Al-Abdulrazzaq reported having no disclosures; one of his coinvestigators reported financial associations with Cynosure and four other companies. Dr. Custis reported financial associations with Cynosure and 12 other companies.
On Twitter @sherryboschert
PHOENIX – Three small case series reported at the annual meeting of the American Society for Laser Medicine and Surgery reported good results using a picosecond laser for tattoo removal and explored different regimens for treatment.
One study at a single center used a 532-nm Nd-YAG laser with a pulse duration of 450-500 picoseconds (ps) in all 17 patients. Up to 10 treatments spaced every 4-8 weeks used a spot size of 2.5-5 mm, an energy density of 0.3-2.2 J/cm2, and a frequency of 5 Hz in a single pass. Some patients also were treated with a 1,064-nm Nd:YAG laser with a pulse duration of 500-600 ns or a 755-nm alexandrite laser with a pulse duration of 550-750 ns.
A single treatment cleared 75% of red pigment in tattoos on nine patients treated with the 532-nm picosecond laser. Red ink cleared completely in two patients after a second or third session, Dr. Hamad Al-Abdulrazzaq and his associates reported at the meeting.
Difficult-to-remove yellow pigment lightened by 75% in three patients after two to four treatments with the 532-ns picosecond laser.
Black ink cleared by 50%-75% after one or two treatments in four patients using the 1,064-ps laser, reported Dr. Al-Abdulrazzaq, a fellow at the Laser and Skin Surgery Center of New York.
Although there were no signs of scarring or textural skin changes after treatment, one patient developed paradoxical darkening that was removed using the 1,064-nm picosecond laser. Other adverse events were as expected with laser treatment, including erythema, edema, hypopigmentation, pain, mild blistering, and crust formation that healed within a week, Dr. Al-Abdulrazzaq said.
Nearly 90% of patients reported satisfaction with treatment, and nearly 70% said they were extremely satisfied.
A separate study compared single-pass to dual-pass treatments for 26 tattoos on 20 patients using a 755-nm, 750-ps alexandrite laser. Half of each tattoo received a single pass and the other half underwent two passes separated by a 20-minute interval at multiple treatment sessions.
After the first session, the two-pass method produced a 3.4-fold improvement in pigment, significantly better than a 2.1-fold improvement seen after a single-pass treatment, Dr. Trenton Custis and his associates reported. After three treatment sessions, pigment had improved 4.5-fold using the dual-pass method and 3.3-fold using the single-pass method, a statistically significant difference.
Lasers whose pulse durations are in the picosecond range produce a very high peak power that yields more rapid heating and photoacoustic shattering of the ink, which may allow for fewer treatments compared with conventional laser methods, said Dr. Custis, a procedural dermatology fellow at the University of California, Davis.
A separate dose-ranging study applied test spots of 1.3-4.1 J/cm2 over tattoos and adjacent normal skin on 18 patients using a 755-nm alexandrite laser. The best-tolerated fluence based on the test spots was used for half of each tattoo over the course of four treatments, and the other half of each tattoo received escalating doses not to exceed 4.1 J/cm2.
Initial laser treatment using lower fluences (1.3-2.0 J/cm2) were best tolerated, Dr. Emil A. Tanghetti and his associates reported. Higher initial doses were associated with discomfort, blistering, transient hypopigmentation, and postinflammatory hyperpigmentation, said Dr. Tanghetti of the Center for Dermatology and Laser Surgery, Sacramento, Calif.
The 1.3- to 2.0-J/cm2 fluences produced significant clearing of the tattoo, but dose escalation up to 4.1 J/cm2 appeared to better clear the tattoos with minimal side effects. "Dose escalation rather than high-dose treatment is tolerated best by patients with less downtime and blistering," he said. Fluences of 2 J/cm2 seemed to be necessary for consistent clearing of tattoos over four treatments. Blue, green, and light-black ink often disappeared after one treatment.
"Based upon this data and our experience, the picosecond alexandrite is our laser of choice for most of our tattoo patients," Dr. Tanghetti said. It’s important to consider skin type, tanning history, and other variables when choosing a fluence, he added.
An estimated 20% of U.S. residents have a tattoo. Requests for laser tattoo removal increased by 52% from 2012 to 2013, Dr. Al-Abdulrazzaq said.
Dr. Tanghetti reported financial associations with Cynosure. Dr. Al-Abdulrazzaq reported having no disclosures; one of his coinvestigators reported financial associations with Cynosure and four other companies. Dr. Custis reported financial associations with Cynosure and 12 other companies.
On Twitter @sherryboschert
PHOENIX – Three small case series reported at the annual meeting of the American Society for Laser Medicine and Surgery reported good results using a picosecond laser for tattoo removal and explored different regimens for treatment.
One study at a single center used a 532-nm Nd-YAG laser with a pulse duration of 450-500 picoseconds (ps) in all 17 patients. Up to 10 treatments spaced every 4-8 weeks used a spot size of 2.5-5 mm, an energy density of 0.3-2.2 J/cm2, and a frequency of 5 Hz in a single pass. Some patients also were treated with a 1,064-nm Nd:YAG laser with a pulse duration of 500-600 ns or a 755-nm alexandrite laser with a pulse duration of 550-750 ns.
A single treatment cleared 75% of red pigment in tattoos on nine patients treated with the 532-nm picosecond laser. Red ink cleared completely in two patients after a second or third session, Dr. Hamad Al-Abdulrazzaq and his associates reported at the meeting.
Difficult-to-remove yellow pigment lightened by 75% in three patients after two to four treatments with the 532-ns picosecond laser.
Black ink cleared by 50%-75% after one or two treatments in four patients using the 1,064-ps laser, reported Dr. Al-Abdulrazzaq, a fellow at the Laser and Skin Surgery Center of New York.
Although there were no signs of scarring or textural skin changes after treatment, one patient developed paradoxical darkening that was removed using the 1,064-nm picosecond laser. Other adverse events were as expected with laser treatment, including erythema, edema, hypopigmentation, pain, mild blistering, and crust formation that healed within a week, Dr. Al-Abdulrazzaq said.
Nearly 90% of patients reported satisfaction with treatment, and nearly 70% said they were extremely satisfied.
A separate study compared single-pass to dual-pass treatments for 26 tattoos on 20 patients using a 755-nm, 750-ps alexandrite laser. Half of each tattoo received a single pass and the other half underwent two passes separated by a 20-minute interval at multiple treatment sessions.
After the first session, the two-pass method produced a 3.4-fold improvement in pigment, significantly better than a 2.1-fold improvement seen after a single-pass treatment, Dr. Trenton Custis and his associates reported. After three treatment sessions, pigment had improved 4.5-fold using the dual-pass method and 3.3-fold using the single-pass method, a statistically significant difference.
Lasers whose pulse durations are in the picosecond range produce a very high peak power that yields more rapid heating and photoacoustic shattering of the ink, which may allow for fewer treatments compared with conventional laser methods, said Dr. Custis, a procedural dermatology fellow at the University of California, Davis.
A separate dose-ranging study applied test spots of 1.3-4.1 J/cm2 over tattoos and adjacent normal skin on 18 patients using a 755-nm alexandrite laser. The best-tolerated fluence based on the test spots was used for half of each tattoo over the course of four treatments, and the other half of each tattoo received escalating doses not to exceed 4.1 J/cm2.
Initial laser treatment using lower fluences (1.3-2.0 J/cm2) were best tolerated, Dr. Emil A. Tanghetti and his associates reported. Higher initial doses were associated with discomfort, blistering, transient hypopigmentation, and postinflammatory hyperpigmentation, said Dr. Tanghetti of the Center for Dermatology and Laser Surgery, Sacramento, Calif.
The 1.3- to 2.0-J/cm2 fluences produced significant clearing of the tattoo, but dose escalation up to 4.1 J/cm2 appeared to better clear the tattoos with minimal side effects. "Dose escalation rather than high-dose treatment is tolerated best by patients with less downtime and blistering," he said. Fluences of 2 J/cm2 seemed to be necessary for consistent clearing of tattoos over four treatments. Blue, green, and light-black ink often disappeared after one treatment.
"Based upon this data and our experience, the picosecond alexandrite is our laser of choice for most of our tattoo patients," Dr. Tanghetti said. It’s important to consider skin type, tanning history, and other variables when choosing a fluence, he added.
An estimated 20% of U.S. residents have a tattoo. Requests for laser tattoo removal increased by 52% from 2012 to 2013, Dr. Al-Abdulrazzaq said.
Dr. Tanghetti reported financial associations with Cynosure. Dr. Al-Abdulrazzaq reported having no disclosures; one of his coinvestigators reported financial associations with Cynosure and four other companies. Dr. Custis reported financial associations with Cynosure and 12 other companies.
On Twitter @sherryboschert
AT LASER 2014
Brazilian patients favor noninvasive body contouring technique
PHOENIX – Patient satisfaction was 100% after treatment with a device combining multipolar radiofrequency and magnetic pulse fields for body contouring, based on data from a series of 260 adults in Brazil.
A total of 60% of patients reported "excellent" satisfaction and 40% reported "good" satisfaction when surveyed shortly after the treatment, Dr. Rafael Nunes said at the annual meeting of the American Society for Laser Medicine and Surgery.
Patients underwent up to six weekly treatments for laxity, wrinkles, or lipodystrophy on the abdomen, flanks, and/or leg areas using the Venus Freeze (MP)2system. The device heats collagen fibers in the skin to produce skin tightening. "The goal is not to reduce volume, but to reshape," said Dr. Nunes, a plastic surgeon in Rio de Janeiro, Brazil.
It’s important to recognize that "if the patient stops the treatments or changes diet habits, probably the results would be totally lost," he said. "Body contouring is challenging."
However, patients who don’t want more invasive body shaping procedures, such as implants, hyaluronic acid, or liposuction, may be pleased with the simplicity of radiofrequency and magnetic pulse, he noted. "The question in our country is, what do patients want? They don’t want to go to the hospital, they don’t like invasive procedures or recovery periods."
The patients in this study had a mean age of 43 years and a mean weight of 66 kg. Ninety percent were female.
After pretreatment with glycerine solution, the 15-minute treatments aimed for a temperature of 41-42° C and uniform erythema on the surface of a 20-cm x 20-cm area.
Side effects immediately after treatment included bruising in 2% of patients, local heat in 78%, edema in 54%, and erythema in 56%. There were no burns. No side effects were seen 5 days later, or at a 3-month follow-up visit.
"In this small study, it [the combination regimen] was a safe and effective treatment for body contouring with no pain, no down time, and high subject satisfaction," Dr. Nunes said
Dr. Nunes reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Patient satisfaction was 100% after treatment with a device combining multipolar radiofrequency and magnetic pulse fields for body contouring, based on data from a series of 260 adults in Brazil.
A total of 60% of patients reported "excellent" satisfaction and 40% reported "good" satisfaction when surveyed shortly after the treatment, Dr. Rafael Nunes said at the annual meeting of the American Society for Laser Medicine and Surgery.
Patients underwent up to six weekly treatments for laxity, wrinkles, or lipodystrophy on the abdomen, flanks, and/or leg areas using the Venus Freeze (MP)2system. The device heats collagen fibers in the skin to produce skin tightening. "The goal is not to reduce volume, but to reshape," said Dr. Nunes, a plastic surgeon in Rio de Janeiro, Brazil.
It’s important to recognize that "if the patient stops the treatments or changes diet habits, probably the results would be totally lost," he said. "Body contouring is challenging."
However, patients who don’t want more invasive body shaping procedures, such as implants, hyaluronic acid, or liposuction, may be pleased with the simplicity of radiofrequency and magnetic pulse, he noted. "The question in our country is, what do patients want? They don’t want to go to the hospital, they don’t like invasive procedures or recovery periods."
The patients in this study had a mean age of 43 years and a mean weight of 66 kg. Ninety percent were female.
After pretreatment with glycerine solution, the 15-minute treatments aimed for a temperature of 41-42° C and uniform erythema on the surface of a 20-cm x 20-cm area.
Side effects immediately after treatment included bruising in 2% of patients, local heat in 78%, edema in 54%, and erythema in 56%. There were no burns. No side effects were seen 5 days later, or at a 3-month follow-up visit.
"In this small study, it [the combination regimen] was a safe and effective treatment for body contouring with no pain, no down time, and high subject satisfaction," Dr. Nunes said
Dr. Nunes reported having no disclosures.
On Twitter @sherryboschert
PHOENIX – Patient satisfaction was 100% after treatment with a device combining multipolar radiofrequency and magnetic pulse fields for body contouring, based on data from a series of 260 adults in Brazil.
A total of 60% of patients reported "excellent" satisfaction and 40% reported "good" satisfaction when surveyed shortly after the treatment, Dr. Rafael Nunes said at the annual meeting of the American Society for Laser Medicine and Surgery.
Patients underwent up to six weekly treatments for laxity, wrinkles, or lipodystrophy on the abdomen, flanks, and/or leg areas using the Venus Freeze (MP)2system. The device heats collagen fibers in the skin to produce skin tightening. "The goal is not to reduce volume, but to reshape," said Dr. Nunes, a plastic surgeon in Rio de Janeiro, Brazil.
It’s important to recognize that "if the patient stops the treatments or changes diet habits, probably the results would be totally lost," he said. "Body contouring is challenging."
However, patients who don’t want more invasive body shaping procedures, such as implants, hyaluronic acid, or liposuction, may be pleased with the simplicity of radiofrequency and magnetic pulse, he noted. "The question in our country is, what do patients want? They don’t want to go to the hospital, they don’t like invasive procedures or recovery periods."
The patients in this study had a mean age of 43 years and a mean weight of 66 kg. Ninety percent were female.
After pretreatment with glycerine solution, the 15-minute treatments aimed for a temperature of 41-42° C and uniform erythema on the surface of a 20-cm x 20-cm area.
Side effects immediately after treatment included bruising in 2% of patients, local heat in 78%, edema in 54%, and erythema in 56%. There were no burns. No side effects were seen 5 days later, or at a 3-month follow-up visit.
"In this small study, it [the combination regimen] was a safe and effective treatment for body contouring with no pain, no down time, and high subject satisfaction," Dr. Nunes said
Dr. Nunes reported having no disclosures.
On Twitter @sherryboschert
AT LASER 2014
Key clinical point: The findings highlight the importance of understanding patients’ preferences while managing their expectations.
Major finding: Satisfaction after treatment was "excellent" in 60% of patients and "good" in 40%.
Data source: A case series of body contouring using radiofrequency and magnetic pulse in 260 patients at five Brazilian centers.
Disclosures: Dr. Nunes reported having no disclosures.
RealSelf
If you have patients who express interest in cosmetic procedures, and especially if you are a cosmetic dermatologist or a plastic surgeon, you might want to familiarize yourself with RealSelf.com. Founded in 2006, RealSelf is an online community for learning and sharing information about cosmetic surgery, dermatology, dentistry, and other elective treatments. In 2013, the site had 36 million unique visitors, and it is expected to grow.
Why might RealSelf be relevant for you? Simply put, it’s another channel to market you and your practice. It works by allowing physicians to answer users’ questions about cosmetic procedures ranging from rhinoplasty and liposuction to tattoo removal and Botox. Over time, your participation can lead to new consultations at your practice.
To ensure credibility, physicians must be board-certified in order to join RealSelf’s physician community. There is an element of game mechanics: The more active the physician, the more exposure his or her profile and practice receives. Similarly, paid subscriptions lead to more exposure than free subscriptions (more on this later.) Although this model does not appeal to some physicians, many of them do like the platform, and see it as a way to build a reputation as an expert and to market their practices.
Unlike doctor review sites that focus on the physician, RealSelf focuses on the procedure. For each procedure, users will find actual patient reviews and before and after photos, as well as Q&A’s with board-certified physicians. Users will also find licensed physicians in their area as well as the average cost for the procedure. RealSelf believes that patients value transparency, and including prices creates transparency.
Since most patients genuinely want to help other patients make informed medical decisions, the reviews tend to be thoughtful and thorough, and many of them contain multiple before-and-after photos. As a physician perusing the patient reviews, you’ll start to notice that most of them are reasonable. For example, customer satisfaction with laser treatment for melasma was 51%, whereas satisfaction for laser treatment for rosacea was 80%.
Patients and prospective patients are flocking to the site because it allows them to share their experiences, interact with other patients, and gain access to physician experts in the field. Many patients have difficulty making decisions about cosmetic procedures; RealSelf aims to alleviate their fears and help them "make confident health and beauty decisions." If a prospective patient wants to see a video of tattoo removal or Botox injections, he or she can. If a patient wants to ask physicians their opinions, he or she can. According to RealSelf, physicians have answered over 500,000 questions on the site.
Of course, all this isn’t free for physicians. RealSelf is a business. They have a tiered membership – free, pro, and spotlight. To obtain free membership, you simply visit the site and follow the prompts to "claim your profile." Once your profile is completed, you will have access to a "doctor advisor" who can help you "optimize your visibility on the site." Both "pro" and "spotlight" offer additional benefits, such as integrating patient reviews on your practice website, promotions on Facebook and Twitter, extended directory listings, and exposure in your local area. RealSelf does not discuss costs of membership until you have claimed your profile.
Only you can determine if RealSelf is beneficial to you and your practice. If, for example, you’re not looking for new patients, then you might find it unnecessary. But at the very least, you’ll know what RealSelf is the next time a fellow cosmetic physician brings it up at a conference. And it’s never a bad idea to be familiar with current social technologies that may affect your livelihood.
If you’ve used RealSelf, let us know what you think. For more information, visit RealSelf.com.
Disclaimer: I have no financial interest in RealSelf and am not an active member.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @Dermdoc on Twitter.
If you have patients who express interest in cosmetic procedures, and especially if you are a cosmetic dermatologist or a plastic surgeon, you might want to familiarize yourself with RealSelf.com. Founded in 2006, RealSelf is an online community for learning and sharing information about cosmetic surgery, dermatology, dentistry, and other elective treatments. In 2013, the site had 36 million unique visitors, and it is expected to grow.
Why might RealSelf be relevant for you? Simply put, it’s another channel to market you and your practice. It works by allowing physicians to answer users’ questions about cosmetic procedures ranging from rhinoplasty and liposuction to tattoo removal and Botox. Over time, your participation can lead to new consultations at your practice.
To ensure credibility, physicians must be board-certified in order to join RealSelf’s physician community. There is an element of game mechanics: The more active the physician, the more exposure his or her profile and practice receives. Similarly, paid subscriptions lead to more exposure than free subscriptions (more on this later.) Although this model does not appeal to some physicians, many of them do like the platform, and see it as a way to build a reputation as an expert and to market their practices.
Unlike doctor review sites that focus on the physician, RealSelf focuses on the procedure. For each procedure, users will find actual patient reviews and before and after photos, as well as Q&A’s with board-certified physicians. Users will also find licensed physicians in their area as well as the average cost for the procedure. RealSelf believes that patients value transparency, and including prices creates transparency.
Since most patients genuinely want to help other patients make informed medical decisions, the reviews tend to be thoughtful and thorough, and many of them contain multiple before-and-after photos. As a physician perusing the patient reviews, you’ll start to notice that most of them are reasonable. For example, customer satisfaction with laser treatment for melasma was 51%, whereas satisfaction for laser treatment for rosacea was 80%.
Patients and prospective patients are flocking to the site because it allows them to share their experiences, interact with other patients, and gain access to physician experts in the field. Many patients have difficulty making decisions about cosmetic procedures; RealSelf aims to alleviate their fears and help them "make confident health and beauty decisions." If a prospective patient wants to see a video of tattoo removal or Botox injections, he or she can. If a patient wants to ask physicians their opinions, he or she can. According to RealSelf, physicians have answered over 500,000 questions on the site.
Of course, all this isn’t free for physicians. RealSelf is a business. They have a tiered membership – free, pro, and spotlight. To obtain free membership, you simply visit the site and follow the prompts to "claim your profile." Once your profile is completed, you will have access to a "doctor advisor" who can help you "optimize your visibility on the site." Both "pro" and "spotlight" offer additional benefits, such as integrating patient reviews on your practice website, promotions on Facebook and Twitter, extended directory listings, and exposure in your local area. RealSelf does not discuss costs of membership until you have claimed your profile.
Only you can determine if RealSelf is beneficial to you and your practice. If, for example, you’re not looking for new patients, then you might find it unnecessary. But at the very least, you’ll know what RealSelf is the next time a fellow cosmetic physician brings it up at a conference. And it’s never a bad idea to be familiar with current social technologies that may affect your livelihood.
If you’ve used RealSelf, let us know what you think. For more information, visit RealSelf.com.
Disclaimer: I have no financial interest in RealSelf and am not an active member.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @Dermdoc on Twitter.
If you have patients who express interest in cosmetic procedures, and especially if you are a cosmetic dermatologist or a plastic surgeon, you might want to familiarize yourself with RealSelf.com. Founded in 2006, RealSelf is an online community for learning and sharing information about cosmetic surgery, dermatology, dentistry, and other elective treatments. In 2013, the site had 36 million unique visitors, and it is expected to grow.
Why might RealSelf be relevant for you? Simply put, it’s another channel to market you and your practice. It works by allowing physicians to answer users’ questions about cosmetic procedures ranging from rhinoplasty and liposuction to tattoo removal and Botox. Over time, your participation can lead to new consultations at your practice.
To ensure credibility, physicians must be board-certified in order to join RealSelf’s physician community. There is an element of game mechanics: The more active the physician, the more exposure his or her profile and practice receives. Similarly, paid subscriptions lead to more exposure than free subscriptions (more on this later.) Although this model does not appeal to some physicians, many of them do like the platform, and see it as a way to build a reputation as an expert and to market their practices.
Unlike doctor review sites that focus on the physician, RealSelf focuses on the procedure. For each procedure, users will find actual patient reviews and before and after photos, as well as Q&A’s with board-certified physicians. Users will also find licensed physicians in their area as well as the average cost for the procedure. RealSelf believes that patients value transparency, and including prices creates transparency.
Since most patients genuinely want to help other patients make informed medical decisions, the reviews tend to be thoughtful and thorough, and many of them contain multiple before-and-after photos. As a physician perusing the patient reviews, you’ll start to notice that most of them are reasonable. For example, customer satisfaction with laser treatment for melasma was 51%, whereas satisfaction for laser treatment for rosacea was 80%.
Patients and prospective patients are flocking to the site because it allows them to share their experiences, interact with other patients, and gain access to physician experts in the field. Many patients have difficulty making decisions about cosmetic procedures; RealSelf aims to alleviate their fears and help them "make confident health and beauty decisions." If a prospective patient wants to see a video of tattoo removal or Botox injections, he or she can. If a patient wants to ask physicians their opinions, he or she can. According to RealSelf, physicians have answered over 500,000 questions on the site.
Of course, all this isn’t free for physicians. RealSelf is a business. They have a tiered membership – free, pro, and spotlight. To obtain free membership, you simply visit the site and follow the prompts to "claim your profile." Once your profile is completed, you will have access to a "doctor advisor" who can help you "optimize your visibility on the site." Both "pro" and "spotlight" offer additional benefits, such as integrating patient reviews on your practice website, promotions on Facebook and Twitter, extended directory listings, and exposure in your local area. RealSelf does not discuss costs of membership until you have claimed your profile.
Only you can determine if RealSelf is beneficial to you and your practice. If, for example, you’re not looking for new patients, then you might find it unnecessary. But at the very least, you’ll know what RealSelf is the next time a fellow cosmetic physician brings it up at a conference. And it’s never a bad idea to be familiar with current social technologies that may affect your livelihood.
If you’ve used RealSelf, let us know what you think. For more information, visit RealSelf.com.
Disclaimer: I have no financial interest in RealSelf and am not an active member.
Dr. Benabio is a partner physician in the department of dermatology of the Southern California Permanente Group in San Diego and a volunteer clinical assistant professor at the University of California, San Diego. Dr. Benabio is @Dermdoc on Twitter.