User login
Should you sell your practice to a private equity firm?
More and more physicians are being wooed by private equity firms that want to buy their practices. The total value of private equity deals in health care in 2019 is estimated at about $120 billion, and it’s expected to grow over the coming years.
While the potential profit may seem alluring, physicians have mixed feelings as to whether this will be a boon or a disappointment.
Angelo Falcone, MD, a former emergency physician in Rockville, Md., found that a private equity investment transformed his career path.
For 19 years, Dr. Falcone was CEO of an emergency medicine group with 35 partners that staffed 10 emergency departments, mostly in Maryland. “We were a pretty small operation looking to get bigger, but to do that would require a substantial investment,” he said.
In 2015, after checking out all their options, the partners decided to sell to US Acute Care Solutions (USACS), a new private equity company founded by Welsh, Carson, Anderson & Stowe, an investment firm in New York. Private equity can be used to expand practices and pay for new equipment. Dr. Falcone, serving as a USACS board member and its operational president, helped spur the company’s astounding growth. Today, USACS has about 5,000 physicians and other clinicians operating in 30 states.
In 2019, Dr. Falcone stepped down from his management post at USACS, took training in integrative medicine, and 2 years later opened a solo integrative medicine practice in Rockville. The new practice, which operates on a concierge model, is not connected with USACS, but Dr, Falcone still sits on the USACS board.
“I had a great experience at USACS. I believe in the power of private equity to support our patients and physicians,” Dr. Falcone said. “Now, at age 58, I have a second career in integrative medicine.”
Private equity is still controversial
David Fleeger, MD, has a different opinion of private equity. “I get offers from private equity firms fairly often, but I’m not seriously interested,” said Dr. Fleeger, a surgeon with Central Texas Colon and Rectal Surgeons in Austin.
“We don’t want to sell to anybody; we want to control our destiny,” he said. “We don’t have to borrow money or repay loans, and we don’t expect to get a windfall for the practice. The profits in medicine are too narrow for that to be realistic. There is no free lunch.”
Some of the doctors who sign up for private equity deals become dissatisfied and want to end the arrangement, according to John Pinto, an ophthalmic practice management consultant in San Diego.
“I get calls about once a month from doctors who want to get out of a private equity deal or revise the terms,” he said. “Some complaints are that the PE firm was too tight with the budget, wouldn’t hire needed staff, mismanaged operations, or otherwise mishandled their investment in the practice.”
It’s difficult for disgruntled physicians to exit a private equity deal, Mr. Pinto said. They commonly have to give up part of the payment they had received for their practice if they leave prematurely, and depending on the jurisdiction, stiff noncompete clauses in their contract won’t allow them to practice nearby.
Disillusioned physicians – and even many physicians who had good experiences with private equity – usually don’t want to air their complaints in public. One reason most of these doctors keep silent is that they have signed nondisclosure and nondisparagement agreements that are part of most private equity deals.
The private equity proposition
Private equity firms typically pay a great deal more for practices than hospitals or even many large private practices, according to James D. Wall, an attorney in Winston-Salem, N.C., who has handled many private equity deals. Mr. Wall said private equity often organizes physicians around one specialty. One advantage these physicians have over hospital-employed physicians is that they aren’t under pressure to refer within a network.
Private equity companies set values for practices on the basis of their earnings before interest, taxes, depreciation, and amortization (EBITDA), said Howard Bogard, an attorney with Burr & Forman in Raleigh, N.C., who has handled many deals. Mr. Bogard said the amount physicians are paid is usually between 4 and 12 times’ EBITDA, so if your practice is earning $1 million a year in EBITDA, you would get $4 million to $12 million for it.
Of the total price tag, “Doctors get a hefty immediate payment when they sell,” Mr. Bogard said. “It might be 70% of the purchase price up front, and the 30% left over is equity in the buyer. The private equity firm then sells the practice 5-7 years later, and at that time, the physician’s equity is converted to cash and equity in the new buyer, often at the same 70/30 ratio. The idea is to keep the doctor interested in staying.”
Private equity firms expand practices to receive more favorable reimbursements and achieve economies of scale, according to Jane Zhu, MD, an assistant professor of medicine at Oregon Health & Science University, Portland, who has studied the phenomenon. Dr. Zhu said these firms may enhance profits by contracting with Medicare Advantage plans, joining accountable care organizations (ACOs), having their physicians work longer hours, and using advanced-practice clinicians instead of physicians.
“They want to make a large return in the order of 20% per year over several years, but they don’t want to strip the practice of value, because they’ll need to sell it to a new investor,” Dr. Zhu said.
When doctors sell to a private equity firm, they become employees and often have to take a pay cut, but their pay may rise again as new efficiencies are instituted. This occurred for partners in Minnesota Eye Consultants (MEC), an 11-member ophthalmology practice in Bloomington, Minn., that helped found Unifeye Vision Partners (UVP), a private equity company financed by Chicago-based Waud Capital Partners.
“When we sold the practice in 2017, we expected to see a 30% cut in the partners’ personal income,” said Richard L. Lindstrom, MD, who headed MEC until he retired last year. “Now, coming into the 6th year, all of the former partners who are still working are earning 10% above presale levels, except for one doctor who wanted to work fewer hours.” These doctors aren’t working longer hours but rather are benefiting from efficiencies, such as adding scribes and improving scheduling, he said.
Private equity brought discipline to the practice, said Dr. Lindstrom, who still sits on the Unifeye board. “In an independent practice, the partners may decide on a new piece of equipment because it would be fun to have, not because they’ve done a financial analysis,” he said. “We don’t wing it anymore.”
On the other hand, according to Dr. Zhu, some private equity firms may use draconian methods to improve efficiency. “Doctors may be expected to order or perform more services or work faster or longer to reach a certain threshold,” she said.
Can private equity uphold your interests?
To win over doctors, a private equity firm may agree to finance projects that the doctors want. For example, Dr. Lindstrom said after his group joined Unifeye, Waud Capital agreed to finance the doctors’ plan to open a new $6 million office. Before the deal, the partners would have had to take out a $6 million loan and personally guarantee it, he said.
A private equity firm may even agree to support the selling doctors’ practice philosophy, such as serving low-income patients – as long as it has a revenue stream. Luis Benavides, MD, is part of a seven-physician family medicine practice that treats many low-income patients in Laredo, Tex. “There is a lot of poverty here,” he said. This March, the group sold to a large private equity company, whose name Dr. Benavides preferred not to reveal.
One reason they made the new arrangement, Dr. Benavides said, was to qualify for ACO REACH, a new Medicare payment program that is mostly used in underserved areas and that allows more distribution of shared savings payments. “Our goal has always been better care,” he said. “We want to know how we can best serve our community.”
Dr. Benavides acknowledges that he has less independence in the new arrangement, but “I already lost my independence when I went from solo practice to a group,” he said. “The upside of a larger organization is that other people may have better ideas than you have.”
Private equity firms often set up governance structures to give physicians some measure of control. Dr. Lindstrom said the governing board of his former practice is solely made up of physicians and deals with local issues such as what office doctors will work in and how many patients they will see. Waud Capital has control of the Unifeye board of directors, but it mainly deals with larger issues, such as acquisition of more practices, he said.
In rare instances, private equity gives doctors control. Dr. Falcone said that from the start of USACS, doctors owned 65% of the company, and in 2020, the physician partners bought out Welsh Carson. “Then we engaged the private equity firm Apollo Global Management, which lent us money for the buyout and became our capital partner, with the doctors now owning 98% of the company,” he said.
On the other hand, some private equity arrangements reportedly have little regard for doctors’ well-being, especially if they are new doctors who didn’t participate in the deal and don’t have equity in it. Dr. Zhu recalled that a new physician was recruited by a practice and was promised a partnership track, but she wasn’t told that the partners were negotiating a private equity deal. “She didn’t find out until the practice was sold months later,” Dr. Zhu said. “The chances of her getting any equity now are unclear.”
Making sure that you pick a company that has your interests at heart requires a lot of digging. Dr. Lindstrom said he and his partners took 3 years to make a decision. They hired a broker to pick the 10 best private equity firms. Then they met with those companies and hired a law firm and an accounting firm to assess them. As the partners inched toward a deal, they voted on each of five critical steps in the decision-making process, he said. He noted that each vote was unanimous.
Impact of private equity
“Private equity deals are changing the health care landscape,” Mr. Wall said. “They are creating large, independent practices that help physicians remain independent from hospital systems and potentially have the clout to get more favorable reimbursements.”
“There is a lot of misunderstanding and mistrust among physicians about private equity,” Dr. Benavides said. “I imagine it will take a while for it to be accepted.”
Until the COVID pandemic, the annual number of private equity deals for doctors had been rising. Will it recover that pace? Mr. Pinto said rising interest rates may dampen activity in the near future.
“The private equity firm often performs a leveraged buyout using borrowed money,” he explained. “This works better when interest rates are low, but interest rates are trending higher. Private equity firms aren’t going away, but they may have to be less generous as the cost of money rises.”
A version of this article first appeared on Medscape.com.
More and more physicians are being wooed by private equity firms that want to buy their practices. The total value of private equity deals in health care in 2019 is estimated at about $120 billion, and it’s expected to grow over the coming years.
While the potential profit may seem alluring, physicians have mixed feelings as to whether this will be a boon or a disappointment.
Angelo Falcone, MD, a former emergency physician in Rockville, Md., found that a private equity investment transformed his career path.
For 19 years, Dr. Falcone was CEO of an emergency medicine group with 35 partners that staffed 10 emergency departments, mostly in Maryland. “We were a pretty small operation looking to get bigger, but to do that would require a substantial investment,” he said.
In 2015, after checking out all their options, the partners decided to sell to US Acute Care Solutions (USACS), a new private equity company founded by Welsh, Carson, Anderson & Stowe, an investment firm in New York. Private equity can be used to expand practices and pay for new equipment. Dr. Falcone, serving as a USACS board member and its operational president, helped spur the company’s astounding growth. Today, USACS has about 5,000 physicians and other clinicians operating in 30 states.
In 2019, Dr. Falcone stepped down from his management post at USACS, took training in integrative medicine, and 2 years later opened a solo integrative medicine practice in Rockville. The new practice, which operates on a concierge model, is not connected with USACS, but Dr, Falcone still sits on the USACS board.
“I had a great experience at USACS. I believe in the power of private equity to support our patients and physicians,” Dr. Falcone said. “Now, at age 58, I have a second career in integrative medicine.”
Private equity is still controversial
David Fleeger, MD, has a different opinion of private equity. “I get offers from private equity firms fairly often, but I’m not seriously interested,” said Dr. Fleeger, a surgeon with Central Texas Colon and Rectal Surgeons in Austin.
“We don’t want to sell to anybody; we want to control our destiny,” he said. “We don’t have to borrow money or repay loans, and we don’t expect to get a windfall for the practice. The profits in medicine are too narrow for that to be realistic. There is no free lunch.”
Some of the doctors who sign up for private equity deals become dissatisfied and want to end the arrangement, according to John Pinto, an ophthalmic practice management consultant in San Diego.
“I get calls about once a month from doctors who want to get out of a private equity deal or revise the terms,” he said. “Some complaints are that the PE firm was too tight with the budget, wouldn’t hire needed staff, mismanaged operations, or otherwise mishandled their investment in the practice.”
It’s difficult for disgruntled physicians to exit a private equity deal, Mr. Pinto said. They commonly have to give up part of the payment they had received for their practice if they leave prematurely, and depending on the jurisdiction, stiff noncompete clauses in their contract won’t allow them to practice nearby.
Disillusioned physicians – and even many physicians who had good experiences with private equity – usually don’t want to air their complaints in public. One reason most of these doctors keep silent is that they have signed nondisclosure and nondisparagement agreements that are part of most private equity deals.
The private equity proposition
Private equity firms typically pay a great deal more for practices than hospitals or even many large private practices, according to James D. Wall, an attorney in Winston-Salem, N.C., who has handled many private equity deals. Mr. Wall said private equity often organizes physicians around one specialty. One advantage these physicians have over hospital-employed physicians is that they aren’t under pressure to refer within a network.
Private equity companies set values for practices on the basis of their earnings before interest, taxes, depreciation, and amortization (EBITDA), said Howard Bogard, an attorney with Burr & Forman in Raleigh, N.C., who has handled many deals. Mr. Bogard said the amount physicians are paid is usually between 4 and 12 times’ EBITDA, so if your practice is earning $1 million a year in EBITDA, you would get $4 million to $12 million for it.
Of the total price tag, “Doctors get a hefty immediate payment when they sell,” Mr. Bogard said. “It might be 70% of the purchase price up front, and the 30% left over is equity in the buyer. The private equity firm then sells the practice 5-7 years later, and at that time, the physician’s equity is converted to cash and equity in the new buyer, often at the same 70/30 ratio. The idea is to keep the doctor interested in staying.”
Private equity firms expand practices to receive more favorable reimbursements and achieve economies of scale, according to Jane Zhu, MD, an assistant professor of medicine at Oregon Health & Science University, Portland, who has studied the phenomenon. Dr. Zhu said these firms may enhance profits by contracting with Medicare Advantage plans, joining accountable care organizations (ACOs), having their physicians work longer hours, and using advanced-practice clinicians instead of physicians.
“They want to make a large return in the order of 20% per year over several years, but they don’t want to strip the practice of value, because they’ll need to sell it to a new investor,” Dr. Zhu said.
When doctors sell to a private equity firm, they become employees and often have to take a pay cut, but their pay may rise again as new efficiencies are instituted. This occurred for partners in Minnesota Eye Consultants (MEC), an 11-member ophthalmology practice in Bloomington, Minn., that helped found Unifeye Vision Partners (UVP), a private equity company financed by Chicago-based Waud Capital Partners.
“When we sold the practice in 2017, we expected to see a 30% cut in the partners’ personal income,” said Richard L. Lindstrom, MD, who headed MEC until he retired last year. “Now, coming into the 6th year, all of the former partners who are still working are earning 10% above presale levels, except for one doctor who wanted to work fewer hours.” These doctors aren’t working longer hours but rather are benefiting from efficiencies, such as adding scribes and improving scheduling, he said.
Private equity brought discipline to the practice, said Dr. Lindstrom, who still sits on the Unifeye board. “In an independent practice, the partners may decide on a new piece of equipment because it would be fun to have, not because they’ve done a financial analysis,” he said. “We don’t wing it anymore.”
On the other hand, according to Dr. Zhu, some private equity firms may use draconian methods to improve efficiency. “Doctors may be expected to order or perform more services or work faster or longer to reach a certain threshold,” she said.
Can private equity uphold your interests?
To win over doctors, a private equity firm may agree to finance projects that the doctors want. For example, Dr. Lindstrom said after his group joined Unifeye, Waud Capital agreed to finance the doctors’ plan to open a new $6 million office. Before the deal, the partners would have had to take out a $6 million loan and personally guarantee it, he said.
A private equity firm may even agree to support the selling doctors’ practice philosophy, such as serving low-income patients – as long as it has a revenue stream. Luis Benavides, MD, is part of a seven-physician family medicine practice that treats many low-income patients in Laredo, Tex. “There is a lot of poverty here,” he said. This March, the group sold to a large private equity company, whose name Dr. Benavides preferred not to reveal.
One reason they made the new arrangement, Dr. Benavides said, was to qualify for ACO REACH, a new Medicare payment program that is mostly used in underserved areas and that allows more distribution of shared savings payments. “Our goal has always been better care,” he said. “We want to know how we can best serve our community.”
Dr. Benavides acknowledges that he has less independence in the new arrangement, but “I already lost my independence when I went from solo practice to a group,” he said. “The upside of a larger organization is that other people may have better ideas than you have.”
Private equity firms often set up governance structures to give physicians some measure of control. Dr. Lindstrom said the governing board of his former practice is solely made up of physicians and deals with local issues such as what office doctors will work in and how many patients they will see. Waud Capital has control of the Unifeye board of directors, but it mainly deals with larger issues, such as acquisition of more practices, he said.
In rare instances, private equity gives doctors control. Dr. Falcone said that from the start of USACS, doctors owned 65% of the company, and in 2020, the physician partners bought out Welsh Carson. “Then we engaged the private equity firm Apollo Global Management, which lent us money for the buyout and became our capital partner, with the doctors now owning 98% of the company,” he said.
On the other hand, some private equity arrangements reportedly have little regard for doctors’ well-being, especially if they are new doctors who didn’t participate in the deal and don’t have equity in it. Dr. Zhu recalled that a new physician was recruited by a practice and was promised a partnership track, but she wasn’t told that the partners were negotiating a private equity deal. “She didn’t find out until the practice was sold months later,” Dr. Zhu said. “The chances of her getting any equity now are unclear.”
Making sure that you pick a company that has your interests at heart requires a lot of digging. Dr. Lindstrom said he and his partners took 3 years to make a decision. They hired a broker to pick the 10 best private equity firms. Then they met with those companies and hired a law firm and an accounting firm to assess them. As the partners inched toward a deal, they voted on each of five critical steps in the decision-making process, he said. He noted that each vote was unanimous.
Impact of private equity
“Private equity deals are changing the health care landscape,” Mr. Wall said. “They are creating large, independent practices that help physicians remain independent from hospital systems and potentially have the clout to get more favorable reimbursements.”
“There is a lot of misunderstanding and mistrust among physicians about private equity,” Dr. Benavides said. “I imagine it will take a while for it to be accepted.”
Until the COVID pandemic, the annual number of private equity deals for doctors had been rising. Will it recover that pace? Mr. Pinto said rising interest rates may dampen activity in the near future.
“The private equity firm often performs a leveraged buyout using borrowed money,” he explained. “This works better when interest rates are low, but interest rates are trending higher. Private equity firms aren’t going away, but they may have to be less generous as the cost of money rises.”
A version of this article first appeared on Medscape.com.
More and more physicians are being wooed by private equity firms that want to buy their practices. The total value of private equity deals in health care in 2019 is estimated at about $120 billion, and it’s expected to grow over the coming years.
While the potential profit may seem alluring, physicians have mixed feelings as to whether this will be a boon or a disappointment.
Angelo Falcone, MD, a former emergency physician in Rockville, Md., found that a private equity investment transformed his career path.
For 19 years, Dr. Falcone was CEO of an emergency medicine group with 35 partners that staffed 10 emergency departments, mostly in Maryland. “We were a pretty small operation looking to get bigger, but to do that would require a substantial investment,” he said.
In 2015, after checking out all their options, the partners decided to sell to US Acute Care Solutions (USACS), a new private equity company founded by Welsh, Carson, Anderson & Stowe, an investment firm in New York. Private equity can be used to expand practices and pay for new equipment. Dr. Falcone, serving as a USACS board member and its operational president, helped spur the company’s astounding growth. Today, USACS has about 5,000 physicians and other clinicians operating in 30 states.
In 2019, Dr. Falcone stepped down from his management post at USACS, took training in integrative medicine, and 2 years later opened a solo integrative medicine practice in Rockville. The new practice, which operates on a concierge model, is not connected with USACS, but Dr, Falcone still sits on the USACS board.
“I had a great experience at USACS. I believe in the power of private equity to support our patients and physicians,” Dr. Falcone said. “Now, at age 58, I have a second career in integrative medicine.”
Private equity is still controversial
David Fleeger, MD, has a different opinion of private equity. “I get offers from private equity firms fairly often, but I’m not seriously interested,” said Dr. Fleeger, a surgeon with Central Texas Colon and Rectal Surgeons in Austin.
“We don’t want to sell to anybody; we want to control our destiny,” he said. “We don’t have to borrow money or repay loans, and we don’t expect to get a windfall for the practice. The profits in medicine are too narrow for that to be realistic. There is no free lunch.”
Some of the doctors who sign up for private equity deals become dissatisfied and want to end the arrangement, according to John Pinto, an ophthalmic practice management consultant in San Diego.
“I get calls about once a month from doctors who want to get out of a private equity deal or revise the terms,” he said. “Some complaints are that the PE firm was too tight with the budget, wouldn’t hire needed staff, mismanaged operations, or otherwise mishandled their investment in the practice.”
It’s difficult for disgruntled physicians to exit a private equity deal, Mr. Pinto said. They commonly have to give up part of the payment they had received for their practice if they leave prematurely, and depending on the jurisdiction, stiff noncompete clauses in their contract won’t allow them to practice nearby.
Disillusioned physicians – and even many physicians who had good experiences with private equity – usually don’t want to air their complaints in public. One reason most of these doctors keep silent is that they have signed nondisclosure and nondisparagement agreements that are part of most private equity deals.
The private equity proposition
Private equity firms typically pay a great deal more for practices than hospitals or even many large private practices, according to James D. Wall, an attorney in Winston-Salem, N.C., who has handled many private equity deals. Mr. Wall said private equity often organizes physicians around one specialty. One advantage these physicians have over hospital-employed physicians is that they aren’t under pressure to refer within a network.
Private equity companies set values for practices on the basis of their earnings before interest, taxes, depreciation, and amortization (EBITDA), said Howard Bogard, an attorney with Burr & Forman in Raleigh, N.C., who has handled many deals. Mr. Bogard said the amount physicians are paid is usually between 4 and 12 times’ EBITDA, so if your practice is earning $1 million a year in EBITDA, you would get $4 million to $12 million for it.
Of the total price tag, “Doctors get a hefty immediate payment when they sell,” Mr. Bogard said. “It might be 70% of the purchase price up front, and the 30% left over is equity in the buyer. The private equity firm then sells the practice 5-7 years later, and at that time, the physician’s equity is converted to cash and equity in the new buyer, often at the same 70/30 ratio. The idea is to keep the doctor interested in staying.”
Private equity firms expand practices to receive more favorable reimbursements and achieve economies of scale, according to Jane Zhu, MD, an assistant professor of medicine at Oregon Health & Science University, Portland, who has studied the phenomenon. Dr. Zhu said these firms may enhance profits by contracting with Medicare Advantage plans, joining accountable care organizations (ACOs), having their physicians work longer hours, and using advanced-practice clinicians instead of physicians.
“They want to make a large return in the order of 20% per year over several years, but they don’t want to strip the practice of value, because they’ll need to sell it to a new investor,” Dr. Zhu said.
When doctors sell to a private equity firm, they become employees and often have to take a pay cut, but their pay may rise again as new efficiencies are instituted. This occurred for partners in Minnesota Eye Consultants (MEC), an 11-member ophthalmology practice in Bloomington, Minn., that helped found Unifeye Vision Partners (UVP), a private equity company financed by Chicago-based Waud Capital Partners.
“When we sold the practice in 2017, we expected to see a 30% cut in the partners’ personal income,” said Richard L. Lindstrom, MD, who headed MEC until he retired last year. “Now, coming into the 6th year, all of the former partners who are still working are earning 10% above presale levels, except for one doctor who wanted to work fewer hours.” These doctors aren’t working longer hours but rather are benefiting from efficiencies, such as adding scribes and improving scheduling, he said.
Private equity brought discipline to the practice, said Dr. Lindstrom, who still sits on the Unifeye board. “In an independent practice, the partners may decide on a new piece of equipment because it would be fun to have, not because they’ve done a financial analysis,” he said. “We don’t wing it anymore.”
On the other hand, according to Dr. Zhu, some private equity firms may use draconian methods to improve efficiency. “Doctors may be expected to order or perform more services or work faster or longer to reach a certain threshold,” she said.
Can private equity uphold your interests?
To win over doctors, a private equity firm may agree to finance projects that the doctors want. For example, Dr. Lindstrom said after his group joined Unifeye, Waud Capital agreed to finance the doctors’ plan to open a new $6 million office. Before the deal, the partners would have had to take out a $6 million loan and personally guarantee it, he said.
A private equity firm may even agree to support the selling doctors’ practice philosophy, such as serving low-income patients – as long as it has a revenue stream. Luis Benavides, MD, is part of a seven-physician family medicine practice that treats many low-income patients in Laredo, Tex. “There is a lot of poverty here,” he said. This March, the group sold to a large private equity company, whose name Dr. Benavides preferred not to reveal.
One reason they made the new arrangement, Dr. Benavides said, was to qualify for ACO REACH, a new Medicare payment program that is mostly used in underserved areas and that allows more distribution of shared savings payments. “Our goal has always been better care,” he said. “We want to know how we can best serve our community.”
Dr. Benavides acknowledges that he has less independence in the new arrangement, but “I already lost my independence when I went from solo practice to a group,” he said. “The upside of a larger organization is that other people may have better ideas than you have.”
Private equity firms often set up governance structures to give physicians some measure of control. Dr. Lindstrom said the governing board of his former practice is solely made up of physicians and deals with local issues such as what office doctors will work in and how many patients they will see. Waud Capital has control of the Unifeye board of directors, but it mainly deals with larger issues, such as acquisition of more practices, he said.
In rare instances, private equity gives doctors control. Dr. Falcone said that from the start of USACS, doctors owned 65% of the company, and in 2020, the physician partners bought out Welsh Carson. “Then we engaged the private equity firm Apollo Global Management, which lent us money for the buyout and became our capital partner, with the doctors now owning 98% of the company,” he said.
On the other hand, some private equity arrangements reportedly have little regard for doctors’ well-being, especially if they are new doctors who didn’t participate in the deal and don’t have equity in it. Dr. Zhu recalled that a new physician was recruited by a practice and was promised a partnership track, but she wasn’t told that the partners were negotiating a private equity deal. “She didn’t find out until the practice was sold months later,” Dr. Zhu said. “The chances of her getting any equity now are unclear.”
Making sure that you pick a company that has your interests at heart requires a lot of digging. Dr. Lindstrom said he and his partners took 3 years to make a decision. They hired a broker to pick the 10 best private equity firms. Then they met with those companies and hired a law firm and an accounting firm to assess them. As the partners inched toward a deal, they voted on each of five critical steps in the decision-making process, he said. He noted that each vote was unanimous.
Impact of private equity
“Private equity deals are changing the health care landscape,” Mr. Wall said. “They are creating large, independent practices that help physicians remain independent from hospital systems and potentially have the clout to get more favorable reimbursements.”
“There is a lot of misunderstanding and mistrust among physicians about private equity,” Dr. Benavides said. “I imagine it will take a while for it to be accepted.”
Until the COVID pandemic, the annual number of private equity deals for doctors had been rising. Will it recover that pace? Mr. Pinto said rising interest rates may dampen activity in the near future.
“The private equity firm often performs a leveraged buyout using borrowed money,” he explained. “This works better when interest rates are low, but interest rates are trending higher. Private equity firms aren’t going away, but they may have to be less generous as the cost of money rises.”
A version of this article first appeared on Medscape.com.
Saddled with med school debt, yet left out of loan forgiveness plans
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.
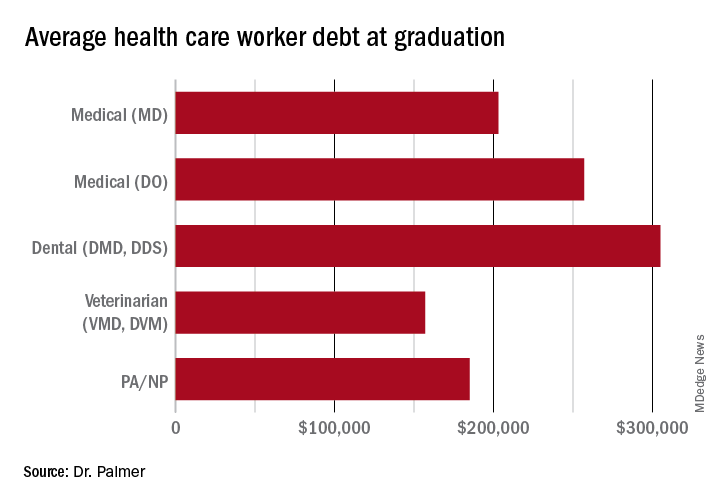
The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.
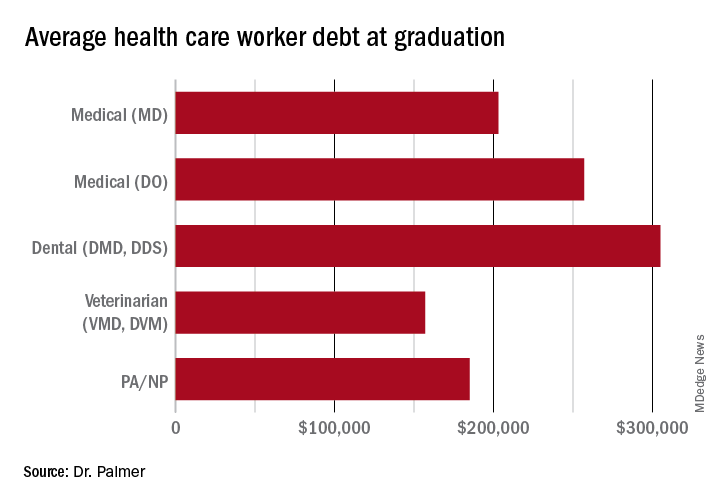
The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.
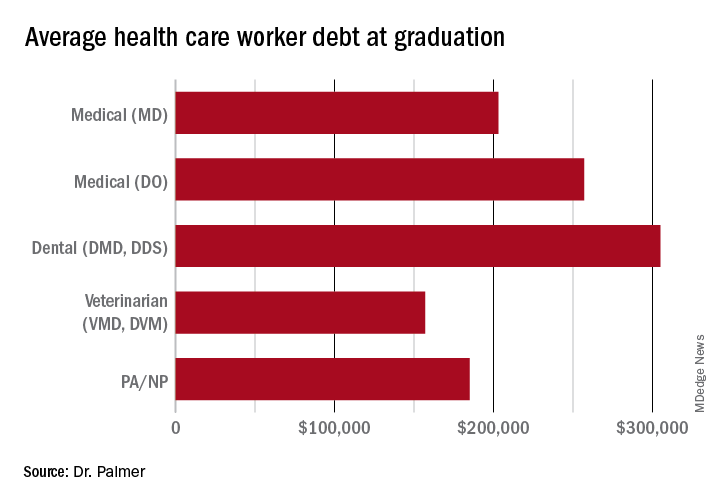
The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
Dermatologist arrested for allegedly poisoning radiologist husband
It is a story that has quickly gone viral around the world:
Yue Yu, MD, aged 45, was booked into the Orange County Jail on Aug. 4, after Irvine Police had been called to her residence that day by her husband, Jack Chen, MD, 53, a radiologist. Dr. Chen provided the police with video evidence that he said showed Dr. Yu pouring a drain-opening chemical into his hot lemonade drink.
“The victim sustained significant internal injuries but is expected to recover,” the Irvine police department said in a statement.
Dr. Yu was released after paying a $30,000 bond and has not been formally charged, according to the New York Post.
In a statement to the court on Aug. 5, Dr. Chen said he and the couple’s two children had long suffered verbal abuse from his wife and her mother, according to the Post. Multiple news organizations reported that Dr. Chen filed for divorce and also for a restraining order against Dr. Yu on that day.
After feeling ill for months – and being diagnosed with ulcers and esophageal inflammation – Dr. Chen reportedly set up video cameras in the couple’s house. He said he caught Dr. Yu on camera pouring something into his drink on several occasions in July.
According to NBC News, Dr. Yu’s attorney, David E. Wohl, said that Dr. Yu “vehemently and unequivocally denies ever attempting to poison her husband or anyone else.”
Dr. Yu received her medical degree from Washington University in St. Louis in 2006 and has no disciplinary actions against her, according to the Medical Board of California. She was head of dermatology at Mission Heritage Medical Group, but her name and information have been scrubbed from that group’s website. Mission Heritage is affiliated with Providence Mission Hospital. A spokesperson for the hospital told NBC News that it is cooperating with the police investigation and that no patients are in danger.
The dermatologist is due to report back to court in November, NBC News said.
A version of this article first appeared on Medscape.com.
It is a story that has quickly gone viral around the world:
Yue Yu, MD, aged 45, was booked into the Orange County Jail on Aug. 4, after Irvine Police had been called to her residence that day by her husband, Jack Chen, MD, 53, a radiologist. Dr. Chen provided the police with video evidence that he said showed Dr. Yu pouring a drain-opening chemical into his hot lemonade drink.
“The victim sustained significant internal injuries but is expected to recover,” the Irvine police department said in a statement.
Dr. Yu was released after paying a $30,000 bond and has not been formally charged, according to the New York Post.
In a statement to the court on Aug. 5, Dr. Chen said he and the couple’s two children had long suffered verbal abuse from his wife and her mother, according to the Post. Multiple news organizations reported that Dr. Chen filed for divorce and also for a restraining order against Dr. Yu on that day.
After feeling ill for months – and being diagnosed with ulcers and esophageal inflammation – Dr. Chen reportedly set up video cameras in the couple’s house. He said he caught Dr. Yu on camera pouring something into his drink on several occasions in July.
According to NBC News, Dr. Yu’s attorney, David E. Wohl, said that Dr. Yu “vehemently and unequivocally denies ever attempting to poison her husband or anyone else.”
Dr. Yu received her medical degree from Washington University in St. Louis in 2006 and has no disciplinary actions against her, according to the Medical Board of California. She was head of dermatology at Mission Heritage Medical Group, but her name and information have been scrubbed from that group’s website. Mission Heritage is affiliated with Providence Mission Hospital. A spokesperson for the hospital told NBC News that it is cooperating with the police investigation and that no patients are in danger.
The dermatologist is due to report back to court in November, NBC News said.
A version of this article first appeared on Medscape.com.
It is a story that has quickly gone viral around the world:
Yue Yu, MD, aged 45, was booked into the Orange County Jail on Aug. 4, after Irvine Police had been called to her residence that day by her husband, Jack Chen, MD, 53, a radiologist. Dr. Chen provided the police with video evidence that he said showed Dr. Yu pouring a drain-opening chemical into his hot lemonade drink.
“The victim sustained significant internal injuries but is expected to recover,” the Irvine police department said in a statement.
Dr. Yu was released after paying a $30,000 bond and has not been formally charged, according to the New York Post.
In a statement to the court on Aug. 5, Dr. Chen said he and the couple’s two children had long suffered verbal abuse from his wife and her mother, according to the Post. Multiple news organizations reported that Dr. Chen filed for divorce and also for a restraining order against Dr. Yu on that day.
After feeling ill for months – and being diagnosed with ulcers and esophageal inflammation – Dr. Chen reportedly set up video cameras in the couple’s house. He said he caught Dr. Yu on camera pouring something into his drink on several occasions in July.
According to NBC News, Dr. Yu’s attorney, David E. Wohl, said that Dr. Yu “vehemently and unequivocally denies ever attempting to poison her husband or anyone else.”
Dr. Yu received her medical degree from Washington University in St. Louis in 2006 and has no disciplinary actions against her, according to the Medical Board of California. She was head of dermatology at Mission Heritage Medical Group, but her name and information have been scrubbed from that group’s website. Mission Heritage is affiliated with Providence Mission Hospital. A spokesperson for the hospital told NBC News that it is cooperating with the police investigation and that no patients are in danger.
The dermatologist is due to report back to court in November, NBC News said.
A version of this article first appeared on Medscape.com.
Pro-life ob.gyns. say Dobbs not end of abortion struggle
After 49 years of labor, abortion foes received the ultimate victory in June when the United States Supreme Court struck down a federal right to terminate pregnancy. Among those most heartened by the ruling was a small organization of doctors who specialize in women’s reproductive health. The group’s leader, while grateful for the win, isn’t ready for a curtain call. Instead, she sees her task as moving from a national stage to 50 regional ones.
The decision in Dobbs v. Jackson, which overturned a woman’s constitutional right to obtain an abortion, was the biggest but not final quarry for the American Association of Pro-Life Obstetricians and Gynecologists (AAPLOG). “It actually doesn’t change anything except to turn the whole discussion on abortion back to the states, which in our opinion is where it should have been 50 years ago,” Donna Harrison, MD, the group’s chief executive officer, said in a recent interview.
Dr. Harrison, an obstetrician-gynecologist and adjunct professor of bioethics at Trinity International University in Deerfield, Ind., said she was proud of “our small role in bringing science” to the top court’s attention, noting that the ruling incorporated some of AAPLOG’s medical arguments in reversing Roe v. Wade, the 1973 decision that created a right to abortion – and prompted her group’s founding. The ruling, for instance, agreed – in a departure from the generally accepted science – that a fetus is viable at 15 weeks, and the procedure is risky for mothers thereafter. “You could congratulate us for perseverance and for bringing that information, which has been in the peer-reviewed literature for a long time, to the justices’ attention,” she said.
Dr. Harrison said she was pleased that the Supreme Court agreed with the “science” that guided its decision to overturn Roe. That the court was willing to embrace that evidence troubles the American College of Obstetricians and Gynecologists (ACOG), the nation’s leading professional group for reproductive health experts.
Defending the ‘second patient’
AAPLOG operates under the belief that life begins at the moment of fertilization, at which point “we defend the life of our second patient, the human being in the womb,” Dr. Harrison said. “For a very long time, ob.gyns. who valued both patients were not given a voice, and I think now we’re finding our voice.” The group will continue supporting abortion restrictions at the state level.
AAPLOG, with 6,000 members, was considered a “special interest” group within ACOG until the college discontinued such subgroups in 2013. ACOG, numbering 60,000 members, calls the Dobbs ruling “a huge step back for women and everyone who is seeking access to ob.gyn. care,” said Molly Meegan, JD, ACOG’s chief legal officer. Ms. Meegan expressed concern over the newfound influence of AAPLOG, which she called “a single-issue, single-topic, single-advocacy organization.”
Pro-choice groups, including ACOG, worry that the reversal of Roe has provided AAPLOG with an undeserved veneer of medical expertise. The decision also allowed judges and legislators to “insert themselves into nuanced and complex situations” they know little about and will rely on groups like AAPLOG to exert influence, Ms. Meegan said.
In turn, Dr. Harrison described ACOG as engaging in “rabid, pro-abortion activism.”
The number of abortions in the United States had steadily declined from a peak of 1.4 million per year in 1990 until 2017, after which it has risen slightly. In 2019, according to the U.S. Centers for Disease Control and Prevention, 625,000 abortions occurred nationally. Of those, 42.3% were medication abortions performed in the first 9 weeks, using a combination of the drugs mifepristone and misoprostol. Medication abortions now account for more than half of all pregnancy terminations in the United States, according to the Guttmacher Institute.
Dr. Harrison said that medication abortions put women at an elevated risk of serious, sometimes deadly bleeding, while ACOG points to evidence that the risk of childbirth to women is significantly higher. She also is no fan of Plan B, the “morning after” pill, which is available to women without having to consult a doctor. She described abortifacients as “a huge danger to women being harmed” by medications available over the counter.
In Dr. Harrison’s view, the 10-year-old Ohio girl who traveled to Indiana to obtain an abortion after she became pregnant as the result of rape should have continued her pregnancy. So, too, should young girls who are the victims of incest. “Incest is a horrific crime,” she said, “but aborting a girl because of incest doesn’t make her un-raped. It just adds another trauma.”
When told of Dr. Harrison’s comment, Ms. Meegan paused for 5 seconds before saying, “I think that statement speaks for itself.”
Louise Perkins King, MD, JD, an ob.gyn. and director of reproductive bioethics at Harvard Medical School, Boston, said she had the “horrific” experience of delivering a baby to an 11-year-old girl.
“Children are not fully developed, and they should not be having children,” Dr. King said.
Anne-Marie E. Amies Oelschlager, MD, vice chair of ACOG’s Clinical Consensus Committee and an ob.gyn. at Seattle Children’s in Washington, said in a statement that adolescents who are sexually assaulted are at extremely high risk of depression and posttraumatic stress disorder. “Do we expect a fourth-grader to carry a pregnancy to term, deliver, and expect that child to carry on after this horror?,” she asked.
Dr. Harrison dismissed such concerns. “Somehow abortion is a mental health treatment? Abortion doesn’t treat mental health problems,” she said. “Is there any proof that aborting in those circumstances improves their mental health? I would tell you there is very little research about it. …There are human beings involved, and this child who was raped, who also had a child, who was a human being, who is no longer.”
Dr. Harrison said the Dobbs decision would have no effect on up to 93% of ob.gyns. who don’t perform abortions. Dr. King said the reason that most don’t perform the procedure is the “stigma” attached to abortion. “It’s still frowned upon,” she said. “We don’t talk about it as health care.”
Ms. Meegan added that ob.gyns. are fearful in the wake of the Dobbs decision because “they might find themselves subject to civil and criminal penalties.”
Dr. Harrison said that Roe was always a political decision and the science was always behind AAPLOG – something both Ms. Meegan and Dr. King dispute. Ms. Meegan and Dr. King said they are concerned about the chilling effects on both women and their clinicians, especially with laws that prevent referrals and travel to other states.
“You can’t compel me to give blood or bone marrow,” Dr. King said. “You can’t even compel me to give my hair for somebody, and you can’t compel me to give an organ. And all of a sudden when I’m pregnant, all my rights are out the window?”
A version of this article first appeared on Medscape.com.
After 49 years of labor, abortion foes received the ultimate victory in June when the United States Supreme Court struck down a federal right to terminate pregnancy. Among those most heartened by the ruling was a small organization of doctors who specialize in women’s reproductive health. The group’s leader, while grateful for the win, isn’t ready for a curtain call. Instead, she sees her task as moving from a national stage to 50 regional ones.
The decision in Dobbs v. Jackson, which overturned a woman’s constitutional right to obtain an abortion, was the biggest but not final quarry for the American Association of Pro-Life Obstetricians and Gynecologists (AAPLOG). “It actually doesn’t change anything except to turn the whole discussion on abortion back to the states, which in our opinion is where it should have been 50 years ago,” Donna Harrison, MD, the group’s chief executive officer, said in a recent interview.
Dr. Harrison, an obstetrician-gynecologist and adjunct professor of bioethics at Trinity International University in Deerfield, Ind., said she was proud of “our small role in bringing science” to the top court’s attention, noting that the ruling incorporated some of AAPLOG’s medical arguments in reversing Roe v. Wade, the 1973 decision that created a right to abortion – and prompted her group’s founding. The ruling, for instance, agreed – in a departure from the generally accepted science – that a fetus is viable at 15 weeks, and the procedure is risky for mothers thereafter. “You could congratulate us for perseverance and for bringing that information, which has been in the peer-reviewed literature for a long time, to the justices’ attention,” she said.
Dr. Harrison said she was pleased that the Supreme Court agreed with the “science” that guided its decision to overturn Roe. That the court was willing to embrace that evidence troubles the American College of Obstetricians and Gynecologists (ACOG), the nation’s leading professional group for reproductive health experts.
Defending the ‘second patient’
AAPLOG operates under the belief that life begins at the moment of fertilization, at which point “we defend the life of our second patient, the human being in the womb,” Dr. Harrison said. “For a very long time, ob.gyns. who valued both patients were not given a voice, and I think now we’re finding our voice.” The group will continue supporting abortion restrictions at the state level.
AAPLOG, with 6,000 members, was considered a “special interest” group within ACOG until the college discontinued such subgroups in 2013. ACOG, numbering 60,000 members, calls the Dobbs ruling “a huge step back for women and everyone who is seeking access to ob.gyn. care,” said Molly Meegan, JD, ACOG’s chief legal officer. Ms. Meegan expressed concern over the newfound influence of AAPLOG, which she called “a single-issue, single-topic, single-advocacy organization.”
Pro-choice groups, including ACOG, worry that the reversal of Roe has provided AAPLOG with an undeserved veneer of medical expertise. The decision also allowed judges and legislators to “insert themselves into nuanced and complex situations” they know little about and will rely on groups like AAPLOG to exert influence, Ms. Meegan said.
In turn, Dr. Harrison described ACOG as engaging in “rabid, pro-abortion activism.”
The number of abortions in the United States had steadily declined from a peak of 1.4 million per year in 1990 until 2017, after which it has risen slightly. In 2019, according to the U.S. Centers for Disease Control and Prevention, 625,000 abortions occurred nationally. Of those, 42.3% were medication abortions performed in the first 9 weeks, using a combination of the drugs mifepristone and misoprostol. Medication abortions now account for more than half of all pregnancy terminations in the United States, according to the Guttmacher Institute.
Dr. Harrison said that medication abortions put women at an elevated risk of serious, sometimes deadly bleeding, while ACOG points to evidence that the risk of childbirth to women is significantly higher. She also is no fan of Plan B, the “morning after” pill, which is available to women without having to consult a doctor. She described abortifacients as “a huge danger to women being harmed” by medications available over the counter.
In Dr. Harrison’s view, the 10-year-old Ohio girl who traveled to Indiana to obtain an abortion after she became pregnant as the result of rape should have continued her pregnancy. So, too, should young girls who are the victims of incest. “Incest is a horrific crime,” she said, “but aborting a girl because of incest doesn’t make her un-raped. It just adds another trauma.”
When told of Dr. Harrison’s comment, Ms. Meegan paused for 5 seconds before saying, “I think that statement speaks for itself.”
Louise Perkins King, MD, JD, an ob.gyn. and director of reproductive bioethics at Harvard Medical School, Boston, said she had the “horrific” experience of delivering a baby to an 11-year-old girl.
“Children are not fully developed, and they should not be having children,” Dr. King said.
Anne-Marie E. Amies Oelschlager, MD, vice chair of ACOG’s Clinical Consensus Committee and an ob.gyn. at Seattle Children’s in Washington, said in a statement that adolescents who are sexually assaulted are at extremely high risk of depression and posttraumatic stress disorder. “Do we expect a fourth-grader to carry a pregnancy to term, deliver, and expect that child to carry on after this horror?,” she asked.
Dr. Harrison dismissed such concerns. “Somehow abortion is a mental health treatment? Abortion doesn’t treat mental health problems,” she said. “Is there any proof that aborting in those circumstances improves their mental health? I would tell you there is very little research about it. …There are human beings involved, and this child who was raped, who also had a child, who was a human being, who is no longer.”
Dr. Harrison said the Dobbs decision would have no effect on up to 93% of ob.gyns. who don’t perform abortions. Dr. King said the reason that most don’t perform the procedure is the “stigma” attached to abortion. “It’s still frowned upon,” she said. “We don’t talk about it as health care.”
Ms. Meegan added that ob.gyns. are fearful in the wake of the Dobbs decision because “they might find themselves subject to civil and criminal penalties.”
Dr. Harrison said that Roe was always a political decision and the science was always behind AAPLOG – something both Ms. Meegan and Dr. King dispute. Ms. Meegan and Dr. King said they are concerned about the chilling effects on both women and their clinicians, especially with laws that prevent referrals and travel to other states.
“You can’t compel me to give blood or bone marrow,” Dr. King said. “You can’t even compel me to give my hair for somebody, and you can’t compel me to give an organ. And all of a sudden when I’m pregnant, all my rights are out the window?”
A version of this article first appeared on Medscape.com.
After 49 years of labor, abortion foes received the ultimate victory in June when the United States Supreme Court struck down a federal right to terminate pregnancy. Among those most heartened by the ruling was a small organization of doctors who specialize in women’s reproductive health. The group’s leader, while grateful for the win, isn’t ready for a curtain call. Instead, she sees her task as moving from a national stage to 50 regional ones.
The decision in Dobbs v. Jackson, which overturned a woman’s constitutional right to obtain an abortion, was the biggest but not final quarry for the American Association of Pro-Life Obstetricians and Gynecologists (AAPLOG). “It actually doesn’t change anything except to turn the whole discussion on abortion back to the states, which in our opinion is where it should have been 50 years ago,” Donna Harrison, MD, the group’s chief executive officer, said in a recent interview.
Dr. Harrison, an obstetrician-gynecologist and adjunct professor of bioethics at Trinity International University in Deerfield, Ind., said she was proud of “our small role in bringing science” to the top court’s attention, noting that the ruling incorporated some of AAPLOG’s medical arguments in reversing Roe v. Wade, the 1973 decision that created a right to abortion – and prompted her group’s founding. The ruling, for instance, agreed – in a departure from the generally accepted science – that a fetus is viable at 15 weeks, and the procedure is risky for mothers thereafter. “You could congratulate us for perseverance and for bringing that information, which has been in the peer-reviewed literature for a long time, to the justices’ attention,” she said.
Dr. Harrison said she was pleased that the Supreme Court agreed with the “science” that guided its decision to overturn Roe. That the court was willing to embrace that evidence troubles the American College of Obstetricians and Gynecologists (ACOG), the nation’s leading professional group for reproductive health experts.
Defending the ‘second patient’
AAPLOG operates under the belief that life begins at the moment of fertilization, at which point “we defend the life of our second patient, the human being in the womb,” Dr. Harrison said. “For a very long time, ob.gyns. who valued both patients were not given a voice, and I think now we’re finding our voice.” The group will continue supporting abortion restrictions at the state level.
AAPLOG, with 6,000 members, was considered a “special interest” group within ACOG until the college discontinued such subgroups in 2013. ACOG, numbering 60,000 members, calls the Dobbs ruling “a huge step back for women and everyone who is seeking access to ob.gyn. care,” said Molly Meegan, JD, ACOG’s chief legal officer. Ms. Meegan expressed concern over the newfound influence of AAPLOG, which she called “a single-issue, single-topic, single-advocacy organization.”
Pro-choice groups, including ACOG, worry that the reversal of Roe has provided AAPLOG with an undeserved veneer of medical expertise. The decision also allowed judges and legislators to “insert themselves into nuanced and complex situations” they know little about and will rely on groups like AAPLOG to exert influence, Ms. Meegan said.
In turn, Dr. Harrison described ACOG as engaging in “rabid, pro-abortion activism.”
The number of abortions in the United States had steadily declined from a peak of 1.4 million per year in 1990 until 2017, after which it has risen slightly. In 2019, according to the U.S. Centers for Disease Control and Prevention, 625,000 abortions occurred nationally. Of those, 42.3% were medication abortions performed in the first 9 weeks, using a combination of the drugs mifepristone and misoprostol. Medication abortions now account for more than half of all pregnancy terminations in the United States, according to the Guttmacher Institute.
Dr. Harrison said that medication abortions put women at an elevated risk of serious, sometimes deadly bleeding, while ACOG points to evidence that the risk of childbirth to women is significantly higher. She also is no fan of Plan B, the “morning after” pill, which is available to women without having to consult a doctor. She described abortifacients as “a huge danger to women being harmed” by medications available over the counter.
In Dr. Harrison’s view, the 10-year-old Ohio girl who traveled to Indiana to obtain an abortion after she became pregnant as the result of rape should have continued her pregnancy. So, too, should young girls who are the victims of incest. “Incest is a horrific crime,” she said, “but aborting a girl because of incest doesn’t make her un-raped. It just adds another trauma.”
When told of Dr. Harrison’s comment, Ms. Meegan paused for 5 seconds before saying, “I think that statement speaks for itself.”
Louise Perkins King, MD, JD, an ob.gyn. and director of reproductive bioethics at Harvard Medical School, Boston, said she had the “horrific” experience of delivering a baby to an 11-year-old girl.
“Children are not fully developed, and they should not be having children,” Dr. King said.
Anne-Marie E. Amies Oelschlager, MD, vice chair of ACOG’s Clinical Consensus Committee and an ob.gyn. at Seattle Children’s in Washington, said in a statement that adolescents who are sexually assaulted are at extremely high risk of depression and posttraumatic stress disorder. “Do we expect a fourth-grader to carry a pregnancy to term, deliver, and expect that child to carry on after this horror?,” she asked.
Dr. Harrison dismissed such concerns. “Somehow abortion is a mental health treatment? Abortion doesn’t treat mental health problems,” she said. “Is there any proof that aborting in those circumstances improves their mental health? I would tell you there is very little research about it. …There are human beings involved, and this child who was raped, who also had a child, who was a human being, who is no longer.”
Dr. Harrison said the Dobbs decision would have no effect on up to 93% of ob.gyns. who don’t perform abortions. Dr. King said the reason that most don’t perform the procedure is the “stigma” attached to abortion. “It’s still frowned upon,” she said. “We don’t talk about it as health care.”
Ms. Meegan added that ob.gyns. are fearful in the wake of the Dobbs decision because “they might find themselves subject to civil and criminal penalties.”
Dr. Harrison said that Roe was always a political decision and the science was always behind AAPLOG – something both Ms. Meegan and Dr. King dispute. Ms. Meegan and Dr. King said they are concerned about the chilling effects on both women and their clinicians, especially with laws that prevent referrals and travel to other states.
“You can’t compel me to give blood or bone marrow,” Dr. King said. “You can’t even compel me to give my hair for somebody, and you can’t compel me to give an organ. And all of a sudden when I’m pregnant, all my rights are out the window?”
A version of this article first appeared on Medscape.com.
No guarantees
Recently Sermo had an interesting case report. A young woman, a few hours after undergoing cupping and acupuncture to her upper back, developed dyspnea and presented to the emergency department. There she was found to have a pneumothorax requiring chest tube placement.
I’m certainly not an expert on pneumothoraces, cupping, or acupuncture. Maybe the occurrence is coincidental, though it certainly is temporally concerning.
If I were to cause a pneumothorax doing an electromyography and nerve conduction velocity of the chest wall or upper back, I’m sure I’d have a lot to answer for. Beyond just arranging care for the patient and explaining things to her and her family members, I’d probably have to deal with a board investigation and/or malpractice claim.
Yet, in my experience, people who provide such services rarely face legal accountability, whereas their counterparts in allopathic medicine regularly do so. How many late-night TV attorney ads have you seen that say “have you been injured by an acupuncturist?”
Me, neither.
I’m not going to go into the questions of whether acupuncture, or even cupping, do anything at all. But this case also raises the point that people tend to think of “alternative” medical treatments as things that, while of unclear benefit, are generally harmless.
The fact is that There probably never will be. No matter how well trained and intentioned the person doing it is, there is always the chance of something going wrong. Human error, mechanical failure, bad luck. As they say, dung happens.
In medicine we think about the risk-benefit ratio and proceed accordingly. But the risk, no matter how low, is never zero. People need to understand this applies to pretty much everything health-related. Even over-the-counter supplements, no matter how great their claims may sound (also unproven) have their issues.
Caveat emptor.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently Sermo had an interesting case report. A young woman, a few hours after undergoing cupping and acupuncture to her upper back, developed dyspnea and presented to the emergency department. There she was found to have a pneumothorax requiring chest tube placement.
I’m certainly not an expert on pneumothoraces, cupping, or acupuncture. Maybe the occurrence is coincidental, though it certainly is temporally concerning.
If I were to cause a pneumothorax doing an electromyography and nerve conduction velocity of the chest wall or upper back, I’m sure I’d have a lot to answer for. Beyond just arranging care for the patient and explaining things to her and her family members, I’d probably have to deal with a board investigation and/or malpractice claim.
Yet, in my experience, people who provide such services rarely face legal accountability, whereas their counterparts in allopathic medicine regularly do so. How many late-night TV attorney ads have you seen that say “have you been injured by an acupuncturist?”
Me, neither.
I’m not going to go into the questions of whether acupuncture, or even cupping, do anything at all. But this case also raises the point that people tend to think of “alternative” medical treatments as things that, while of unclear benefit, are generally harmless.
The fact is that There probably never will be. No matter how well trained and intentioned the person doing it is, there is always the chance of something going wrong. Human error, mechanical failure, bad luck. As they say, dung happens.
In medicine we think about the risk-benefit ratio and proceed accordingly. But the risk, no matter how low, is never zero. People need to understand this applies to pretty much everything health-related. Even over-the-counter supplements, no matter how great their claims may sound (also unproven) have their issues.
Caveat emptor.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Recently Sermo had an interesting case report. A young woman, a few hours after undergoing cupping and acupuncture to her upper back, developed dyspnea and presented to the emergency department. There she was found to have a pneumothorax requiring chest tube placement.
I’m certainly not an expert on pneumothoraces, cupping, or acupuncture. Maybe the occurrence is coincidental, though it certainly is temporally concerning.
If I were to cause a pneumothorax doing an electromyography and nerve conduction velocity of the chest wall or upper back, I’m sure I’d have a lot to answer for. Beyond just arranging care for the patient and explaining things to her and her family members, I’d probably have to deal with a board investigation and/or malpractice claim.
Yet, in my experience, people who provide such services rarely face legal accountability, whereas their counterparts in allopathic medicine regularly do so. How many late-night TV attorney ads have you seen that say “have you been injured by an acupuncturist?”
Me, neither.
I’m not going to go into the questions of whether acupuncture, or even cupping, do anything at all. But this case also raises the point that people tend to think of “alternative” medical treatments as things that, while of unclear benefit, are generally harmless.
The fact is that There probably never will be. No matter how well trained and intentioned the person doing it is, there is always the chance of something going wrong. Human error, mechanical failure, bad luck. As they say, dung happens.
In medicine we think about the risk-benefit ratio and proceed accordingly. But the risk, no matter how low, is never zero. People need to understand this applies to pretty much everything health-related. Even over-the-counter supplements, no matter how great their claims may sound (also unproven) have their issues.
Caveat emptor.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Power-morcellation hysterectomies declined and most performed with no containment bag
The use of laparoscopic power morcellators for minimally invasive hysterectomy has significantly decreased, and while the use of containment bags increased after the U.S. Food and Drug Administration’s 2014 safety warning about power morcellators, most procedures employing them are still performed without bags, according to a large database study in Obstetrics & Gynecology.
Containment bags are thought to limit the dissemination of potentially pathologic tissue, including unsuspected cancerous cells.
Rates of uterine cancer in women having morcellation were similar before and after the 2014 FDA guidance, and containment bags were used in only a small proportion of women with uterine cancer, according to findings from a research group led by Jason D. Wright, MD, of the division of gynecologic oncology at Columbia University, New York.
“Despite warnings from professional societies and regulatory agencies, as well as intense public scrutiny after the FDA warnings, the majority of morcellated uterine cancers occurred with uncontained laparoscopic power morcellation,” Dr. Wright and associates wrote, adding that the findings have important policy implications. First, efforts are needed to ensure morcellation is avoided in women with pathologic abnormalities. Second, despite regulatory approval, the safety and efficacy of containment bags remain uncertain, and the use and outcomes of these devices should be monitored closely.
The authors noted that laparoscopic power morcellation with a containment bag actually carries a small but significant increase in the risk of complications, compared with uncontained morcellation.
The study
Drawing on the Premier Healthcare Database, the researchers looked at deidentified patients aged 18 years or older who underwent laparoscopic supracervical hysterectomy from 2010 to 2018. The largest age group having the procedure consisted of women aged 40-49.
Patients were stratified based on use of laparoscopic power morcellators.
The cohort was further stratified as either pre–FDA guidance (2010 quarter 1 to 2014 quarter 1) or post–FDA guidance (2014 quarter 2 to 2018 quarter 2).
In the final cohort of 67,115 patients, laparoscopic power morcellator use decreased from 66.7% in 2013 quarter 4 to 13.3% by 2018 quarter 2. The likelihood of using this device decreased by 9.5% for each quarter elapsed in the post–FDA warning period (risk ratio, 0.91; 95% confidence interval, 0.90-0.91).
In other findings, containment bag use rose from 5.2% in 2013 quarter 4 to 15.2% by 2018 quarter 2. The likelihood of containment bag use rose by 3% for each quarter elapsed in the post–FDA warning period (RR, 1.03; 95% CI, 1.02-1.05).
Among women who underwent surgery with laparoscopic power morcellator use, uterine cancers or sarcomas were identified in 54 (0.17%) before the FDA guidance, compared with 7 (0.12%) after the guidance (P = .45).
Containment bags were used in 11.1% of women with uterine cancers or sarcomas before the FDA guidance, compared with 14.3% after the guidance (P = .12). The perioperative complication rate was 3.3% among women who had laparoscopic power morcellator use without a containment bag, compared with 4.5% (P = .001) in those with a containment bag (adjusted RR, 1.35; 95% CI, 1.12-1.64).
A related editorial argued that the backlash against power morcellation was unwarranted and an example of “reactionary medicine.”
Ben A. Abdu, MD, and Cameron Lowry, MD, of the department of obstetrics and gynecology at the University of Tennessee Health Science Center in Memphis, noted that with the known advantages of laparoscopy over laparotomy – decreased blood loss, decreased pain, and fewer wound complications and infections – it is of paramount importance to continue to offer minimally invasive surgery whenever possible. After the FDA raised safety concerns, there was a rise in the rate of open abdominal hysterectomy, which was accompanied by an increase in surgical morbidity. “Perhaps for now we should avoid throwing the baby out with the bath water,” they wrote.
The editorialists pointed out that any surgery may entail unintended complications. “It is also important to remember that there is a risk of dissemination of malignant tissue whether or not power morcellation is used, and it has even been observed in laparotomy,” they stated, noting that bag rupture and tissue spillage can occur even when the containment bag remains intact.
The downward trend in the use of power morcellators observed by Dr. Wright’s group is of serious concern, the commentators added, especially because the FDA communication was made in response to a rare occurrence and possibly resting on an overestimation of risk. “Based on their review of the medical literature at the time, the FDA cited prevalence estimates of 1 in 352 for any uterine sarcoma and 1 in 498 for leiomyosarcoma,” they wrote. “Many authors have expressed concern that the FDA data review was overestimated.” For example, they cite a meta-analysis using prospective data in which the prevalence of occult leiomyosarcoma was estimated at 1 in 8,300. Despite this extremely low prevalence, there has been an almost total nationwide hospital moratorium on the use of power morcellation, which will likely continue. Some manufacturers have ceased or limited production, distribution, and sales of these devices, they noted.
According to Dr. Michael L. Nimaroff, MD, however, chief of minimally invasive gynecologic surgery at Northwell Health in New Hyde Park, N.Y., the general post–FDA-guidance backlash did not have much effect on expert practitioners in this surgical field. “Those of us who specialize in minimally invasive gynecologic surgery, which has many benefits for the patients, never pivoted,” he told this news organization. “We continued to perform it but more conscientiously and with more concern for safety.”
As for morcellator use, added Dr. Nimaroff, specialists were so accustomed to doing these surgeries before the containment systems were made available that they don’t miss the power morcellator. “We actually retrieve tissue manually, and most of our morcellations, if they’re not contained manually, are retrieved vaginally or through a slightly bigger incision. So patients still benefit from minimally invasive surgery, and in some cases these techniques actually shorten the operation.”
This study received no external funding. Dr. Wright is editor in chief of Obstetrics & Gynecology. He reported royalties from UpToDate and has received research support from Merck. Coauthor Dr. Hou has served as a consultant for Foundation Medicine and Natera. Dr. Abdu and Dr. Lowry disclosed no competing interests, as did Dr. Nimaroff.
The use of laparoscopic power morcellators for minimally invasive hysterectomy has significantly decreased, and while the use of containment bags increased after the U.S. Food and Drug Administration’s 2014 safety warning about power morcellators, most procedures employing them are still performed without bags, according to a large database study in Obstetrics & Gynecology.
Containment bags are thought to limit the dissemination of potentially pathologic tissue, including unsuspected cancerous cells.
Rates of uterine cancer in women having morcellation were similar before and after the 2014 FDA guidance, and containment bags were used in only a small proportion of women with uterine cancer, according to findings from a research group led by Jason D. Wright, MD, of the division of gynecologic oncology at Columbia University, New York.
“Despite warnings from professional societies and regulatory agencies, as well as intense public scrutiny after the FDA warnings, the majority of morcellated uterine cancers occurred with uncontained laparoscopic power morcellation,” Dr. Wright and associates wrote, adding that the findings have important policy implications. First, efforts are needed to ensure morcellation is avoided in women with pathologic abnormalities. Second, despite regulatory approval, the safety and efficacy of containment bags remain uncertain, and the use and outcomes of these devices should be monitored closely.
The authors noted that laparoscopic power morcellation with a containment bag actually carries a small but significant increase in the risk of complications, compared with uncontained morcellation.
The study
Drawing on the Premier Healthcare Database, the researchers looked at deidentified patients aged 18 years or older who underwent laparoscopic supracervical hysterectomy from 2010 to 2018. The largest age group having the procedure consisted of women aged 40-49.
Patients were stratified based on use of laparoscopic power morcellators.
The cohort was further stratified as either pre–FDA guidance (2010 quarter 1 to 2014 quarter 1) or post–FDA guidance (2014 quarter 2 to 2018 quarter 2).
In the final cohort of 67,115 patients, laparoscopic power morcellator use decreased from 66.7% in 2013 quarter 4 to 13.3% by 2018 quarter 2. The likelihood of using this device decreased by 9.5% for each quarter elapsed in the post–FDA warning period (risk ratio, 0.91; 95% confidence interval, 0.90-0.91).
In other findings, containment bag use rose from 5.2% in 2013 quarter 4 to 15.2% by 2018 quarter 2. The likelihood of containment bag use rose by 3% for each quarter elapsed in the post–FDA warning period (RR, 1.03; 95% CI, 1.02-1.05).
Among women who underwent surgery with laparoscopic power morcellator use, uterine cancers or sarcomas were identified in 54 (0.17%) before the FDA guidance, compared with 7 (0.12%) after the guidance (P = .45).
Containment bags were used in 11.1% of women with uterine cancers or sarcomas before the FDA guidance, compared with 14.3% after the guidance (P = .12). The perioperative complication rate was 3.3% among women who had laparoscopic power morcellator use without a containment bag, compared with 4.5% (P = .001) in those with a containment bag (adjusted RR, 1.35; 95% CI, 1.12-1.64).
A related editorial argued that the backlash against power morcellation was unwarranted and an example of “reactionary medicine.”
Ben A. Abdu, MD, and Cameron Lowry, MD, of the department of obstetrics and gynecology at the University of Tennessee Health Science Center in Memphis, noted that with the known advantages of laparoscopy over laparotomy – decreased blood loss, decreased pain, and fewer wound complications and infections – it is of paramount importance to continue to offer minimally invasive surgery whenever possible. After the FDA raised safety concerns, there was a rise in the rate of open abdominal hysterectomy, which was accompanied by an increase in surgical morbidity. “Perhaps for now we should avoid throwing the baby out with the bath water,” they wrote.
The editorialists pointed out that any surgery may entail unintended complications. “It is also important to remember that there is a risk of dissemination of malignant tissue whether or not power morcellation is used, and it has even been observed in laparotomy,” they stated, noting that bag rupture and tissue spillage can occur even when the containment bag remains intact.
The downward trend in the use of power morcellators observed by Dr. Wright’s group is of serious concern, the commentators added, especially because the FDA communication was made in response to a rare occurrence and possibly resting on an overestimation of risk. “Based on their review of the medical literature at the time, the FDA cited prevalence estimates of 1 in 352 for any uterine sarcoma and 1 in 498 for leiomyosarcoma,” they wrote. “Many authors have expressed concern that the FDA data review was overestimated.” For example, they cite a meta-analysis using prospective data in which the prevalence of occult leiomyosarcoma was estimated at 1 in 8,300. Despite this extremely low prevalence, there has been an almost total nationwide hospital moratorium on the use of power morcellation, which will likely continue. Some manufacturers have ceased or limited production, distribution, and sales of these devices, they noted.
According to Dr. Michael L. Nimaroff, MD, however, chief of minimally invasive gynecologic surgery at Northwell Health in New Hyde Park, N.Y., the general post–FDA-guidance backlash did not have much effect on expert practitioners in this surgical field. “Those of us who specialize in minimally invasive gynecologic surgery, which has many benefits for the patients, never pivoted,” he told this news organization. “We continued to perform it but more conscientiously and with more concern for safety.”
As for morcellator use, added Dr. Nimaroff, specialists were so accustomed to doing these surgeries before the containment systems were made available that they don’t miss the power morcellator. “We actually retrieve tissue manually, and most of our morcellations, if they’re not contained manually, are retrieved vaginally or through a slightly bigger incision. So patients still benefit from minimally invasive surgery, and in some cases these techniques actually shorten the operation.”
This study received no external funding. Dr. Wright is editor in chief of Obstetrics & Gynecology. He reported royalties from UpToDate and has received research support from Merck. Coauthor Dr. Hou has served as a consultant for Foundation Medicine and Natera. Dr. Abdu and Dr. Lowry disclosed no competing interests, as did Dr. Nimaroff.
The use of laparoscopic power morcellators for minimally invasive hysterectomy has significantly decreased, and while the use of containment bags increased after the U.S. Food and Drug Administration’s 2014 safety warning about power morcellators, most procedures employing them are still performed without bags, according to a large database study in Obstetrics & Gynecology.
Containment bags are thought to limit the dissemination of potentially pathologic tissue, including unsuspected cancerous cells.
Rates of uterine cancer in women having morcellation were similar before and after the 2014 FDA guidance, and containment bags were used in only a small proportion of women with uterine cancer, according to findings from a research group led by Jason D. Wright, MD, of the division of gynecologic oncology at Columbia University, New York.
“Despite warnings from professional societies and regulatory agencies, as well as intense public scrutiny after the FDA warnings, the majority of morcellated uterine cancers occurred with uncontained laparoscopic power morcellation,” Dr. Wright and associates wrote, adding that the findings have important policy implications. First, efforts are needed to ensure morcellation is avoided in women with pathologic abnormalities. Second, despite regulatory approval, the safety and efficacy of containment bags remain uncertain, and the use and outcomes of these devices should be monitored closely.
The authors noted that laparoscopic power morcellation with a containment bag actually carries a small but significant increase in the risk of complications, compared with uncontained morcellation.
The study
Drawing on the Premier Healthcare Database, the researchers looked at deidentified patients aged 18 years or older who underwent laparoscopic supracervical hysterectomy from 2010 to 2018. The largest age group having the procedure consisted of women aged 40-49.
Patients were stratified based on use of laparoscopic power morcellators.
The cohort was further stratified as either pre–FDA guidance (2010 quarter 1 to 2014 quarter 1) or post–FDA guidance (2014 quarter 2 to 2018 quarter 2).
In the final cohort of 67,115 patients, laparoscopic power morcellator use decreased from 66.7% in 2013 quarter 4 to 13.3% by 2018 quarter 2. The likelihood of using this device decreased by 9.5% for each quarter elapsed in the post–FDA warning period (risk ratio, 0.91; 95% confidence interval, 0.90-0.91).
In other findings, containment bag use rose from 5.2% in 2013 quarter 4 to 15.2% by 2018 quarter 2. The likelihood of containment bag use rose by 3% for each quarter elapsed in the post–FDA warning period (RR, 1.03; 95% CI, 1.02-1.05).
Among women who underwent surgery with laparoscopic power morcellator use, uterine cancers or sarcomas were identified in 54 (0.17%) before the FDA guidance, compared with 7 (0.12%) after the guidance (P = .45).
Containment bags were used in 11.1% of women with uterine cancers or sarcomas before the FDA guidance, compared with 14.3% after the guidance (P = .12). The perioperative complication rate was 3.3% among women who had laparoscopic power morcellator use without a containment bag, compared with 4.5% (P = .001) in those with a containment bag (adjusted RR, 1.35; 95% CI, 1.12-1.64).
A related editorial argued that the backlash against power morcellation was unwarranted and an example of “reactionary medicine.”
Ben A. Abdu, MD, and Cameron Lowry, MD, of the department of obstetrics and gynecology at the University of Tennessee Health Science Center in Memphis, noted that with the known advantages of laparoscopy over laparotomy – decreased blood loss, decreased pain, and fewer wound complications and infections – it is of paramount importance to continue to offer minimally invasive surgery whenever possible. After the FDA raised safety concerns, there was a rise in the rate of open abdominal hysterectomy, which was accompanied by an increase in surgical morbidity. “Perhaps for now we should avoid throwing the baby out with the bath water,” they wrote.
The editorialists pointed out that any surgery may entail unintended complications. “It is also important to remember that there is a risk of dissemination of malignant tissue whether or not power morcellation is used, and it has even been observed in laparotomy,” they stated, noting that bag rupture and tissue spillage can occur even when the containment bag remains intact.
The downward trend in the use of power morcellators observed by Dr. Wright’s group is of serious concern, the commentators added, especially because the FDA communication was made in response to a rare occurrence and possibly resting on an overestimation of risk. “Based on their review of the medical literature at the time, the FDA cited prevalence estimates of 1 in 352 for any uterine sarcoma and 1 in 498 for leiomyosarcoma,” they wrote. “Many authors have expressed concern that the FDA data review was overestimated.” For example, they cite a meta-analysis using prospective data in which the prevalence of occult leiomyosarcoma was estimated at 1 in 8,300. Despite this extremely low prevalence, there has been an almost total nationwide hospital moratorium on the use of power morcellation, which will likely continue. Some manufacturers have ceased or limited production, distribution, and sales of these devices, they noted.
According to Dr. Michael L. Nimaroff, MD, however, chief of minimally invasive gynecologic surgery at Northwell Health in New Hyde Park, N.Y., the general post–FDA-guidance backlash did not have much effect on expert practitioners in this surgical field. “Those of us who specialize in minimally invasive gynecologic surgery, which has many benefits for the patients, never pivoted,” he told this news organization. “We continued to perform it but more conscientiously and with more concern for safety.”
As for morcellator use, added Dr. Nimaroff, specialists were so accustomed to doing these surgeries before the containment systems were made available that they don’t miss the power morcellator. “We actually retrieve tissue manually, and most of our morcellations, if they’re not contained manually, are retrieved vaginally or through a slightly bigger incision. So patients still benefit from minimally invasive surgery, and in some cases these techniques actually shorten the operation.”
This study received no external funding. Dr. Wright is editor in chief of Obstetrics & Gynecology. He reported royalties from UpToDate and has received research support from Merck. Coauthor Dr. Hou has served as a consultant for Foundation Medicine and Natera. Dr. Abdu and Dr. Lowry disclosed no competing interests, as did Dr. Nimaroff.
FROM OBSTETRICS & GYNECOLOGY
James Roberts, MD, trailblazer in EM, dies at age 76
at the age of 76 years. Dr. Roberts was coauthor of the foundational EM text, Clinical Procedures in Emergency Medicine and Acute Care , and was among the first physicians in the world to be board certified in EM. He was a prominent member of the American College of Emergency Physicians, a long-time contributor and editorial board chair for Emergency Medicine News, and a founding member of the American College of Medical Toxicology. He previously served as chairman of the Mercy Catholic Medical Center emergency department in Philadelphia, and vice chairman of the department of emergency medicine at Drexel University, Philadelphia.
“Dr. Roberts was a prominent EM physician and a pioneer in emergency medicine,” said Robert Glatter, MD, assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y.. “He is a revered and respected figure in emergency medicine.” This sentiment was echoed by his colleagues and former students across the EM world.
“How does one describe a unicorn?” Leslie Dye, MD, past president of the ACMT wrote in a tribute to Dr. Roberts on the ACMT website. “There are existing words, but he should have words that belong solely to him. Compassionate, irreverent, brilliant, funny, sarcastic, HUMBLE, modest, kind, inquisitive, and one of the best doctors I have ever met.”
By all accounts, Dr. Roberts lived his life according to words he wrote in a 2018 column for Emergency Medicine News, “How to Be a Good EP.” “Emergency medicine is not just a job, it’s a lifestyle, but there is more to life than medicine. You can never make up a missed championship soccer game, anniversary, birthday, or chance to take your son or daughter fishing. In a heartbeat your children will be on their own and will likely have trouble finding time for you. Remember that you might need a shift off someday, so be ready to help a colleague with a similar request.”
He is survived by a large extended family, including his daughter Martha, son Matthew, and spouse of more than 40 years, Lydia Forte Roberts.
A version of this article first appeared on Medscape.com.
at the age of 76 years. Dr. Roberts was coauthor of the foundational EM text, Clinical Procedures in Emergency Medicine and Acute Care , and was among the first physicians in the world to be board certified in EM. He was a prominent member of the American College of Emergency Physicians, a long-time contributor and editorial board chair for Emergency Medicine News, and a founding member of the American College of Medical Toxicology. He previously served as chairman of the Mercy Catholic Medical Center emergency department in Philadelphia, and vice chairman of the department of emergency medicine at Drexel University, Philadelphia.
“Dr. Roberts was a prominent EM physician and a pioneer in emergency medicine,” said Robert Glatter, MD, assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y.. “He is a revered and respected figure in emergency medicine.” This sentiment was echoed by his colleagues and former students across the EM world.
“How does one describe a unicorn?” Leslie Dye, MD, past president of the ACMT wrote in a tribute to Dr. Roberts on the ACMT website. “There are existing words, but he should have words that belong solely to him. Compassionate, irreverent, brilliant, funny, sarcastic, HUMBLE, modest, kind, inquisitive, and one of the best doctors I have ever met.”
By all accounts, Dr. Roberts lived his life according to words he wrote in a 2018 column for Emergency Medicine News, “How to Be a Good EP.” “Emergency medicine is not just a job, it’s a lifestyle, but there is more to life than medicine. You can never make up a missed championship soccer game, anniversary, birthday, or chance to take your son or daughter fishing. In a heartbeat your children will be on their own and will likely have trouble finding time for you. Remember that you might need a shift off someday, so be ready to help a colleague with a similar request.”
He is survived by a large extended family, including his daughter Martha, son Matthew, and spouse of more than 40 years, Lydia Forte Roberts.
A version of this article first appeared on Medscape.com.
at the age of 76 years. Dr. Roberts was coauthor of the foundational EM text, Clinical Procedures in Emergency Medicine and Acute Care , and was among the first physicians in the world to be board certified in EM. He was a prominent member of the American College of Emergency Physicians, a long-time contributor and editorial board chair for Emergency Medicine News, and a founding member of the American College of Medical Toxicology. He previously served as chairman of the Mercy Catholic Medical Center emergency department in Philadelphia, and vice chairman of the department of emergency medicine at Drexel University, Philadelphia.
“Dr. Roberts was a prominent EM physician and a pioneer in emergency medicine,” said Robert Glatter, MD, assistant professor of emergency medicine at Hofstra University, Hempstead, N.Y.. “He is a revered and respected figure in emergency medicine.” This sentiment was echoed by his colleagues and former students across the EM world.
“How does one describe a unicorn?” Leslie Dye, MD, past president of the ACMT wrote in a tribute to Dr. Roberts on the ACMT website. “There are existing words, but he should have words that belong solely to him. Compassionate, irreverent, brilliant, funny, sarcastic, HUMBLE, modest, kind, inquisitive, and one of the best doctors I have ever met.”
By all accounts, Dr. Roberts lived his life according to words he wrote in a 2018 column for Emergency Medicine News, “How to Be a Good EP.” “Emergency medicine is not just a job, it’s a lifestyle, but there is more to life than medicine. You can never make up a missed championship soccer game, anniversary, birthday, or chance to take your son or daughter fishing. In a heartbeat your children will be on their own and will likely have trouble finding time for you. Remember that you might need a shift off someday, so be ready to help a colleague with a similar request.”
He is survived by a large extended family, including his daughter Martha, son Matthew, and spouse of more than 40 years, Lydia Forte Roberts.
A version of this article first appeared on Medscape.com.
Patients and doctors trapped in a gray zone when abortion laws and emergency care mandate conflict
Each week, Kim Puterbaugh, MD, sees several pregnant patients at a Cleveland hospital who are experiencing complications involving bleeding or infection. The ob.gyn. has to make quick decisions about how to treat them, including whether to remove the dead or dying fetus to protect the health and life of the mother. Leaving in place a fetus that has no chance of survival dramatically increases the chance of maternal infection and permanent injury.
But now her medical decisions are complicated by Ohio’s new abortion law, which generally prohibits abortions after 6 weeks of pregnancy if cardiac activity is detected in the embryo or fetus – which can persist for hours or days even if a pregnancy has no chance of progressing. Given the new law, University Hospitals Cleveland Medical Center has streamlined its system of having an administrator and legal team on call for Dr. Puterbaugh and other physicians if anyone questions whether the planned treatment is allowed under the law.
Since the Supreme Court erased the constitutional right to abortion in June, Dr. Puterbaugh said these cases put her and doctors like her in an impossible position – squeezing doctors between antiabortion laws in Ohio and other states and the federal Emergency Medical Treatment & Labor Act. That 1986 law requires hospitals and physicians to provide screening and stabilizing treatment – including abortion, if necessary – in emergency situations.
“It’s a challenge to balance both those two things,” said Dr. Puterbaugh, president of the Society of OB/GYN Hospitalists. “But it’s not really a challenge to me because, in my mind, the life and health of the mother always comes first.”
The Biden administration argues that EMTALA trumps state abortion bans in emergency situations. On Aug. 2, the Department of Justice filed a federal lawsuit challenging an Idaho law that bans abortion in nearly all circumstances. The suit claims the law would make it a criminal offense for medical providers to comply with EMTALA’s requirement to provide abortion, if needed, for women experiencing emergency pregnancy complications.
In a July policy guidance and letter, the Department of Health & Human Services reaffirmed that EMTALA requires hospitals and physicians to offer life- or health-saving medical services, including abortion, in emergency situations. The letter refers to situations such as ectopic pregnancies, severe blood pressure spikes known as preeclampsia, and premature ruptures of the membrane causing a woman’s water to break before her pregnancy is viable.
The guidance stressed that this federal requirement supersedes any state laws that bar abortion, and that hospitals and physicians who don’t comply with the federal mandate could face civil fines and termination from the Medicare and Medicaid programs.
There are no known reports so far of EMTALA investigations arising from denial of emergency care in pregnancy situations.
But elected officials in states that have sharply restricted abortion disagree with the federal judgment. Texas Attorney General Ken Paxton sued the Biden administration in July to prevent the federal government from using the EMTALA law to require abortions in emergency cases. The suit claims that EMTALA doesn’t specifically mandate particular medical procedures such as abortion.
Abortion foes argue that state antiabortion laws already include adequate exceptions when a pregnant woman’s life or health is in danger. John Seago, president of Texas Right to Life, said one of Texas’ laws specifies that treatment for ectopic pregnancies or miscarriages is not prohibited. In addition, the law defines a medical emergency allowing abortion as a condition in which a woman is at serious risk of a “substantial impairment of a major bodily function.”
Mr. Seago blamed the news media and medical associations for deliberately sowing confusion about the laws. “The law is very clear,” he said.
Legal wrangling aside, in practice, physicians and hospital lawyers say much depends on the interpretation of vaguely worded exceptions in state abortion bans, and that’s further complicated by the existence of contradictory laws, such as those banning abortion based on cardiac activity. And medical providers don’t want to risk criminal prosecution, fines, and loss of licensure if someone accuses them of violating these confusing laws.
Louise Joy, an attorney in Austin, Tex., who represents hospitals and other health care providers, said her clients perhaps are being overly cautious, but that’s not surprising. “I try to encourage them to do the right thing, but I can’t assure them they’ll be risk free.”
A lot hinges on when a pregnancy-ending complication is deemed an emergency, a moment that is hard to define. Some Missouri women have come to the hospital ED with mild cramping and bleeding and were found to have an ectopic pregnancy that hadn’t ruptured yet, colleagues have told Alison Haddock, MD, a Houston emergency physician who chairs the board of the American College of Emergency Physicians. The standard treatment is to provide the drug methotrexate, which can terminate a pregnancy.
“You’re stable until it ruptures, then it becomes unstable,” she said. “But how unstable do you need to be? The woman’s life is not clearly at risk yet. It’s not clear if EMTALA applies. There will be a lot of gray areas that make it really tough for emergency physicians who want to do what’s right for patients without violating any laws.”
Physicians and hospital attorneys are hoping for clearer federal guidance and guarantees of protection from state prosecutors who might oppose their medical judgment on political grounds.
“This is when we need the federal government to step up and say: ‘Doctors, you must provide the standard of care, and we will prevent the prosecution of anyone who is following appropriate medical practices and doing the right thing for patients,” Ms. Joy said.
They are also hoping that the federal government will proactively investigate without waiting for complaints from individuals whenever appropriate emergency medical care might have been withheld because of the new laws. The New York Times reported in July that a 35-year-old woman in the Dallas–Fort Worth area was denied a dilation and evacuation procedure for her first-trimester miscarriage, despite severe pain and bleeding. The hospital reportedly sent her home with advice to return if she was bleeding heavily. The hospital did not respond to a request for comment for this article.
“If a hospital has a policy saying that when the correct medical procedure for a woman in the emergency department is abortion but physicians can’t do that, that’s a violation of EMTALA that CMS should find actionable,” said Thomas Barker, a former general counsel for the Centers for Medicare & Medicaid Services who advises hospitals on EMTALA compliance issues.
In another potential EMTALA case, Valerie Williams, MD, reported that, after Louisiana implemented its near-total ban on abortion with criminal penalties, her hospital in the New Orleans area blocked her from performing a dilation and evacuation procedure on a pregnant patient whose water broke at 16 weeks. The patient was forced to go through a painful, hours-long labor to deliver a nonviable fetus, with heavy loss of blood.
“This was the first time in my 15-year career that I could not give a patient the care they needed,” Dr. Williams wrote in a court affidavit as part of a case seeking to block the state’s abortion law. “This is a travesty.”
But CMS often relies on state agencies to investigate alleged EMTALA violations. That raises questions about how seriously those investigations will be conducted in states where officials have embraced strict limits on any medical services they deem abortion related.
In July, the Texas Medical Association warned that hospitals are pressing doctors to send pregnant patients with complications home, to wait until they expel the fetus – known as expectant management – rather than treating them at the hospital to remove the fetal remains, according to The Dallas Morning News. In a letter to the Texas Medical Board, the medical association said delayed or denied care risks patients’ future reproductive ability and poses a serious risk to their immediate health.
A study published in the American Journal of Obstetrics and Gynecology found that, after Texas implemented its tight abortion restrictions in September, patients with pregnancy complications experienced much worse outcomes than similar patients in states without abortion bans. Of those treated with expectant management at two major Dallas hospitals, 57% suffered serious complications such as bleeding and infection, compared with 33% who chose immediate pregnancy termination in other states.
Ob.gyns. and emergency physicians say they expect to be on the phone frequently with lawyers to get advice on complying with state antiabortion laws while they are seeing pregnant patients with emergency and near-emergency complications.
“This will endanger women’s lives, no question about it,” Dr. Puterbaugh said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Each week, Kim Puterbaugh, MD, sees several pregnant patients at a Cleveland hospital who are experiencing complications involving bleeding or infection. The ob.gyn. has to make quick decisions about how to treat them, including whether to remove the dead or dying fetus to protect the health and life of the mother. Leaving in place a fetus that has no chance of survival dramatically increases the chance of maternal infection and permanent injury.
But now her medical decisions are complicated by Ohio’s new abortion law, which generally prohibits abortions after 6 weeks of pregnancy if cardiac activity is detected in the embryo or fetus – which can persist for hours or days even if a pregnancy has no chance of progressing. Given the new law, University Hospitals Cleveland Medical Center has streamlined its system of having an administrator and legal team on call for Dr. Puterbaugh and other physicians if anyone questions whether the planned treatment is allowed under the law.
Since the Supreme Court erased the constitutional right to abortion in June, Dr. Puterbaugh said these cases put her and doctors like her in an impossible position – squeezing doctors between antiabortion laws in Ohio and other states and the federal Emergency Medical Treatment & Labor Act. That 1986 law requires hospitals and physicians to provide screening and stabilizing treatment – including abortion, if necessary – in emergency situations.
“It’s a challenge to balance both those two things,” said Dr. Puterbaugh, president of the Society of OB/GYN Hospitalists. “But it’s not really a challenge to me because, in my mind, the life and health of the mother always comes first.”
The Biden administration argues that EMTALA trumps state abortion bans in emergency situations. On Aug. 2, the Department of Justice filed a federal lawsuit challenging an Idaho law that bans abortion in nearly all circumstances. The suit claims the law would make it a criminal offense for medical providers to comply with EMTALA’s requirement to provide abortion, if needed, for women experiencing emergency pregnancy complications.
In a July policy guidance and letter, the Department of Health & Human Services reaffirmed that EMTALA requires hospitals and physicians to offer life- or health-saving medical services, including abortion, in emergency situations. The letter refers to situations such as ectopic pregnancies, severe blood pressure spikes known as preeclampsia, and premature ruptures of the membrane causing a woman’s water to break before her pregnancy is viable.
The guidance stressed that this federal requirement supersedes any state laws that bar abortion, and that hospitals and physicians who don’t comply with the federal mandate could face civil fines and termination from the Medicare and Medicaid programs.
There are no known reports so far of EMTALA investigations arising from denial of emergency care in pregnancy situations.
But elected officials in states that have sharply restricted abortion disagree with the federal judgment. Texas Attorney General Ken Paxton sued the Biden administration in July to prevent the federal government from using the EMTALA law to require abortions in emergency cases. The suit claims that EMTALA doesn’t specifically mandate particular medical procedures such as abortion.
Abortion foes argue that state antiabortion laws already include adequate exceptions when a pregnant woman’s life or health is in danger. John Seago, president of Texas Right to Life, said one of Texas’ laws specifies that treatment for ectopic pregnancies or miscarriages is not prohibited. In addition, the law defines a medical emergency allowing abortion as a condition in which a woman is at serious risk of a “substantial impairment of a major bodily function.”
Mr. Seago blamed the news media and medical associations for deliberately sowing confusion about the laws. “The law is very clear,” he said.
Legal wrangling aside, in practice, physicians and hospital lawyers say much depends on the interpretation of vaguely worded exceptions in state abortion bans, and that’s further complicated by the existence of contradictory laws, such as those banning abortion based on cardiac activity. And medical providers don’t want to risk criminal prosecution, fines, and loss of licensure if someone accuses them of violating these confusing laws.
Louise Joy, an attorney in Austin, Tex., who represents hospitals and other health care providers, said her clients perhaps are being overly cautious, but that’s not surprising. “I try to encourage them to do the right thing, but I can’t assure them they’ll be risk free.”
A lot hinges on when a pregnancy-ending complication is deemed an emergency, a moment that is hard to define. Some Missouri women have come to the hospital ED with mild cramping and bleeding and were found to have an ectopic pregnancy that hadn’t ruptured yet, colleagues have told Alison Haddock, MD, a Houston emergency physician who chairs the board of the American College of Emergency Physicians. The standard treatment is to provide the drug methotrexate, which can terminate a pregnancy.
“You’re stable until it ruptures, then it becomes unstable,” she said. “But how unstable do you need to be? The woman’s life is not clearly at risk yet. It’s not clear if EMTALA applies. There will be a lot of gray areas that make it really tough for emergency physicians who want to do what’s right for patients without violating any laws.”
Physicians and hospital attorneys are hoping for clearer federal guidance and guarantees of protection from state prosecutors who might oppose their medical judgment on political grounds.
“This is when we need the federal government to step up and say: ‘Doctors, you must provide the standard of care, and we will prevent the prosecution of anyone who is following appropriate medical practices and doing the right thing for patients,” Ms. Joy said.
They are also hoping that the federal government will proactively investigate without waiting for complaints from individuals whenever appropriate emergency medical care might have been withheld because of the new laws. The New York Times reported in July that a 35-year-old woman in the Dallas–Fort Worth area was denied a dilation and evacuation procedure for her first-trimester miscarriage, despite severe pain and bleeding. The hospital reportedly sent her home with advice to return if she was bleeding heavily. The hospital did not respond to a request for comment for this article.
“If a hospital has a policy saying that when the correct medical procedure for a woman in the emergency department is abortion but physicians can’t do that, that’s a violation of EMTALA that CMS should find actionable,” said Thomas Barker, a former general counsel for the Centers for Medicare & Medicaid Services who advises hospitals on EMTALA compliance issues.
In another potential EMTALA case, Valerie Williams, MD, reported that, after Louisiana implemented its near-total ban on abortion with criminal penalties, her hospital in the New Orleans area blocked her from performing a dilation and evacuation procedure on a pregnant patient whose water broke at 16 weeks. The patient was forced to go through a painful, hours-long labor to deliver a nonviable fetus, with heavy loss of blood.
“This was the first time in my 15-year career that I could not give a patient the care they needed,” Dr. Williams wrote in a court affidavit as part of a case seeking to block the state’s abortion law. “This is a travesty.”
But CMS often relies on state agencies to investigate alleged EMTALA violations. That raises questions about how seriously those investigations will be conducted in states where officials have embraced strict limits on any medical services they deem abortion related.
In July, the Texas Medical Association warned that hospitals are pressing doctors to send pregnant patients with complications home, to wait until they expel the fetus – known as expectant management – rather than treating them at the hospital to remove the fetal remains, according to The Dallas Morning News. In a letter to the Texas Medical Board, the medical association said delayed or denied care risks patients’ future reproductive ability and poses a serious risk to their immediate health.
A study published in the American Journal of Obstetrics and Gynecology found that, after Texas implemented its tight abortion restrictions in September, patients with pregnancy complications experienced much worse outcomes than similar patients in states without abortion bans. Of those treated with expectant management at two major Dallas hospitals, 57% suffered serious complications such as bleeding and infection, compared with 33% who chose immediate pregnancy termination in other states.
Ob.gyns. and emergency physicians say they expect to be on the phone frequently with lawyers to get advice on complying with state antiabortion laws while they are seeing pregnant patients with emergency and near-emergency complications.
“This will endanger women’s lives, no question about it,” Dr. Puterbaugh said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Each week, Kim Puterbaugh, MD, sees several pregnant patients at a Cleveland hospital who are experiencing complications involving bleeding or infection. The ob.gyn. has to make quick decisions about how to treat them, including whether to remove the dead or dying fetus to protect the health and life of the mother. Leaving in place a fetus that has no chance of survival dramatically increases the chance of maternal infection and permanent injury.
But now her medical decisions are complicated by Ohio’s new abortion law, which generally prohibits abortions after 6 weeks of pregnancy if cardiac activity is detected in the embryo or fetus – which can persist for hours or days even if a pregnancy has no chance of progressing. Given the new law, University Hospitals Cleveland Medical Center has streamlined its system of having an administrator and legal team on call for Dr. Puterbaugh and other physicians if anyone questions whether the planned treatment is allowed under the law.
Since the Supreme Court erased the constitutional right to abortion in June, Dr. Puterbaugh said these cases put her and doctors like her in an impossible position – squeezing doctors between antiabortion laws in Ohio and other states and the federal Emergency Medical Treatment & Labor Act. That 1986 law requires hospitals and physicians to provide screening and stabilizing treatment – including abortion, if necessary – in emergency situations.
“It’s a challenge to balance both those two things,” said Dr. Puterbaugh, president of the Society of OB/GYN Hospitalists. “But it’s not really a challenge to me because, in my mind, the life and health of the mother always comes first.”
The Biden administration argues that EMTALA trumps state abortion bans in emergency situations. On Aug. 2, the Department of Justice filed a federal lawsuit challenging an Idaho law that bans abortion in nearly all circumstances. The suit claims the law would make it a criminal offense for medical providers to comply with EMTALA’s requirement to provide abortion, if needed, for women experiencing emergency pregnancy complications.
In a July policy guidance and letter, the Department of Health & Human Services reaffirmed that EMTALA requires hospitals and physicians to offer life- or health-saving medical services, including abortion, in emergency situations. The letter refers to situations such as ectopic pregnancies, severe blood pressure spikes known as preeclampsia, and premature ruptures of the membrane causing a woman’s water to break before her pregnancy is viable.
The guidance stressed that this federal requirement supersedes any state laws that bar abortion, and that hospitals and physicians who don’t comply with the federal mandate could face civil fines and termination from the Medicare and Medicaid programs.
There are no known reports so far of EMTALA investigations arising from denial of emergency care in pregnancy situations.
But elected officials in states that have sharply restricted abortion disagree with the federal judgment. Texas Attorney General Ken Paxton sued the Biden administration in July to prevent the federal government from using the EMTALA law to require abortions in emergency cases. The suit claims that EMTALA doesn’t specifically mandate particular medical procedures such as abortion.
Abortion foes argue that state antiabortion laws already include adequate exceptions when a pregnant woman’s life or health is in danger. John Seago, president of Texas Right to Life, said one of Texas’ laws specifies that treatment for ectopic pregnancies or miscarriages is not prohibited. In addition, the law defines a medical emergency allowing abortion as a condition in which a woman is at serious risk of a “substantial impairment of a major bodily function.”
Mr. Seago blamed the news media and medical associations for deliberately sowing confusion about the laws. “The law is very clear,” he said.
Legal wrangling aside, in practice, physicians and hospital lawyers say much depends on the interpretation of vaguely worded exceptions in state abortion bans, and that’s further complicated by the existence of contradictory laws, such as those banning abortion based on cardiac activity. And medical providers don’t want to risk criminal prosecution, fines, and loss of licensure if someone accuses them of violating these confusing laws.
Louise Joy, an attorney in Austin, Tex., who represents hospitals and other health care providers, said her clients perhaps are being overly cautious, but that’s not surprising. “I try to encourage them to do the right thing, but I can’t assure them they’ll be risk free.”
A lot hinges on when a pregnancy-ending complication is deemed an emergency, a moment that is hard to define. Some Missouri women have come to the hospital ED with mild cramping and bleeding and were found to have an ectopic pregnancy that hadn’t ruptured yet, colleagues have told Alison Haddock, MD, a Houston emergency physician who chairs the board of the American College of Emergency Physicians. The standard treatment is to provide the drug methotrexate, which can terminate a pregnancy.
“You’re stable until it ruptures, then it becomes unstable,” she said. “But how unstable do you need to be? The woman’s life is not clearly at risk yet. It’s not clear if EMTALA applies. There will be a lot of gray areas that make it really tough for emergency physicians who want to do what’s right for patients without violating any laws.”
Physicians and hospital attorneys are hoping for clearer federal guidance and guarantees of protection from state prosecutors who might oppose their medical judgment on political grounds.
“This is when we need the federal government to step up and say: ‘Doctors, you must provide the standard of care, and we will prevent the prosecution of anyone who is following appropriate medical practices and doing the right thing for patients,” Ms. Joy said.
They are also hoping that the federal government will proactively investigate without waiting for complaints from individuals whenever appropriate emergency medical care might have been withheld because of the new laws. The New York Times reported in July that a 35-year-old woman in the Dallas–Fort Worth area was denied a dilation and evacuation procedure for her first-trimester miscarriage, despite severe pain and bleeding. The hospital reportedly sent her home with advice to return if she was bleeding heavily. The hospital did not respond to a request for comment for this article.
“If a hospital has a policy saying that when the correct medical procedure for a woman in the emergency department is abortion but physicians can’t do that, that’s a violation of EMTALA that CMS should find actionable,” said Thomas Barker, a former general counsel for the Centers for Medicare & Medicaid Services who advises hospitals on EMTALA compliance issues.
In another potential EMTALA case, Valerie Williams, MD, reported that, after Louisiana implemented its near-total ban on abortion with criminal penalties, her hospital in the New Orleans area blocked her from performing a dilation and evacuation procedure on a pregnant patient whose water broke at 16 weeks. The patient was forced to go through a painful, hours-long labor to deliver a nonviable fetus, with heavy loss of blood.
“This was the first time in my 15-year career that I could not give a patient the care they needed,” Dr. Williams wrote in a court affidavit as part of a case seeking to block the state’s abortion law. “This is a travesty.”
But CMS often relies on state agencies to investigate alleged EMTALA violations. That raises questions about how seriously those investigations will be conducted in states where officials have embraced strict limits on any medical services they deem abortion related.
In July, the Texas Medical Association warned that hospitals are pressing doctors to send pregnant patients with complications home, to wait until they expel the fetus – known as expectant management – rather than treating them at the hospital to remove the fetal remains, according to The Dallas Morning News. In a letter to the Texas Medical Board, the medical association said delayed or denied care risks patients’ future reproductive ability and poses a serious risk to their immediate health.
A study published in the American Journal of Obstetrics and Gynecology found that, after Texas implemented its tight abortion restrictions in September, patients with pregnancy complications experienced much worse outcomes than similar patients in states without abortion bans. Of those treated with expectant management at two major Dallas hospitals, 57% suffered serious complications such as bleeding and infection, compared with 33% who chose immediate pregnancy termination in other states.
Ob.gyns. and emergency physicians say they expect to be on the phone frequently with lawyers to get advice on complying with state antiabortion laws while they are seeing pregnant patients with emergency and near-emergency complications.
“This will endanger women’s lives, no question about it,” Dr. Puterbaugh said.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
My patient planned to murder me
San Diego internist David B. Bittleman, MD, was finishing an appointment with a patient when the man’s caregiver slipped Dr. Bittleman a note as the patient walked out of the room.
“Call me tomorrow,” the mysterious message read.
Dr. Bittleman phoned the caregiver, who was the patient’s ex-wife, the next day. He assumed she wanted to discuss a routine issue, such as the patient’s treatment. But the reason she wanted to talk privately was far more ominous.
“He wants to kill you,” she said.
Dr. Bittleman was shocked. The caregiver told Dr. Bittleman she believed her ex-husband was serious.
“The ex-wife and two adult sons were very alarmed by his erratic behavior,” Dr. Bittleman recalled. “She made it very clear that he said he planned to kill me. I feared for my life because I took his threat at face value.”
Patient sends alarming message, makes threats
When he went into medicine, Dr. Bittleman never imagined that he’d have to worry about being attacked or killed by a patient.
After spending 20 years in private practice, Dr. Bittleman was excited to accept a position at the Veterans Affairs San Diego health system. His extended family lived in the area, and he looked forward to helping veterans and to working with students, he said.
Dr. Bittleman had practiced primary care at the VA for about 5 years when he encountered the threatening patient, a veteran in his 60’s. The man was suffering from musculoskeletal pain and mental illness.
The patient had taken opioids on and off for many years. Dr. Bittleman felt that to continue the medication would not be safe, considering the man’s lifestyle.
“He had been maintained on oxycodone for chronic pain by previous providers, but I thought that was dangerous, given that he was mixing it with alcohol and marijuana,” he said. “I met with him and a substance use disorder physician for a conference call, and we explained we would need to taper the medication and eventually stop the opioids.”
Dr. Bittleman pleaded with the patient to enter drug rehab, and he offered him inpatient care for treatment of withdrawal. The man refused.
A few weeks later, Dr. Bittleman was checking the health center’s electronic messaging system. He found a disturbing message from the patient.
“You better learn jiu jitsu and hand-to-hand combat if you ever take my opioids away,” the message read. “You better learn how to defend yourself!”
Dr. Bittleman contacted the VA police and reported the message. The patient was interviewed by mental health professionals, but they did not believe he was dangerous, according to Dr. Bittleman.
“They are pretty limited to what they can do,” he said. “At a private practice, the patient might be fired or no longer allowed to come into the building, but the VA is a safety net institution. I’m not sure if he was even reprimanded.”
Two months later, the patient’s ex-wife shared the alarming news that the patient wanted to kill the doctor.
Dr. Bittleman went back to the police. They suggested he file a restraining order, which he sought that afternoon. By the end of the day, the judge had issued the restraining order, according to Dr. Bittleman and court records. The patient could not come within 100 yards of the physician, his clinic, car, or home.
But there was one frightening caveat. The order was temporary. It would last for only 2 weeks. To make the order permanent, Dr. Bittleman would have to go before the judge and argue why it was needed.
He wouldn’t be alone at the hearing. Someone else would be just paces away – the patient who wanted to murder him.
Doctor and patient face off before judge
As the hearing neared, Dr. Bittleman felt anxious, outraged, and fearful. He wondered whether the patient might make good on his threat.
Some colleagues suggested that Bittleman buy a gun, while others recommended he carry pepper spray. Dr. Bittleman had no interest in learning how to use a gun, he said. He took comfort in the fact that there were armed guards and metal detectors in his building, and there was a panic button under his desk.
“I was not sure I wanted to take care of patients anymore, especially chronic pain patients,” he said. “However, I went for some counseling with the Employee Assistance Program, and the therapist was helpful in normalizing my anxiety and acknowledging my fear.”
On the day of the hearing, Dr. Bittleman sat in the back of the courtroom. The patient, who sat near the front, glanced at Dr. Bittleman with a slight smile.
When his case was called, the judge explained that as the plaintiff, the burden was on Dr. Bittleman to prove the patient was a threat to his safety. He provided the judge a copy of the threatening message and a copy of the ex-wife’s note.
After reading the documents, the judge asked the patient to explain his side. The patient complained that the VA had denied him certain benefits and that he was forced to receive mental health treatment rehab that he “didn’t need.” The judge eventually interrupted the man to ask if he had threatened to kill Dr. Bittleman.
“Oh yes, your honor, I did say that, but I was only joking,” he told the judge.
The admission was enough. The judge issued a restraining order against the patient that would last 1 year. He could not have firearms, and if he violated the order, he would be arrested.
The terrifying saga was finally over.
“I never heard from the patient again,” Dr. Bittleman said. “His [care] location was changed, and police were required to come to all his visits with his new provider. I was relieved that if he ever came near me, he was going to jail.”
To raise awareness about such ordeals and the hassles that can follow, Dr. Bittleman wrote an article about his experience, which was published in the Annals of Family Medicine. He continues to treat patients at the VA, including those with chronic pain, but the memory of the menacing patient resurfaces from time to time.
“I do still think about it,” he said. “I know how to use my panic button, and I test it every 90 days. If there is a patient who concerns me, I will have the VA police wait nearby. I am very aware and upset by violence. When I hear about a doctor getting killed, I feel a clutch in my chest. How could I not relate? Here is a doctor who worked hard, who dedicated their life to help patients, and it comes to this? It’s so revolting. It makes me sick.”
Can you identify a violent patient?
Concern over threatening patients has grown across the country after recent violent attacks against physicians in Oklahoma and California. Two physicians were shot to death in June 2022 when a patient opened fire inside a Tulsa medical building. The primary target of the shooting was a surgeon who had performed surgery on the patient. Also in June, two nurses and an emergency physician were stabbed by a patient inside the Encino Hospital Medical Center. They survived.
The attacks raise questions about how to identify potentially violent patients and how to mitigate possible violence.
Threats and violence against health care professionals are nothing new, but they’re finally getting the attention they deserve, says Derek Schaller, MD, an emergency physician and assistant professor of emergency medicine at Central Michigan University in Mount Pleasant.
“Violence against personnel in medicine has been an issue for a long time; it’s just finally making headlines,” he said. “Way back when, it almost seemed like it was part of the job, part of the gig. But it shouldn’t be part of the gig. It’s not something we should be dealing with.”
It’s common for health care professionals and health centers to take a reactive approach to violent patients, but Dr. Schaller encourages a more proactive strategy. Central Michigan University Health, for example, recently studied its past violent encounters and analyzed the characteristics of violent patients. The analysis came after an increase in violent patient episodes at the health center in the past year, Dr. Schaller said.
The study yielded some interesting results, including that a large percentage of patients who became violent in the emergency department did so within the first hour they were in the hospital, he said.
“You would have thought it’s the patients who have been there and have been stuck in the emergency department for a while and who became disgruntled, but that was not the case,” Dr. Schaller said.
He recommends that physicians, medical practices, and hospitals carry out similar assessments of their patient populations and of past violent encounters to determine trends. His institution will be implementing a screening tool in triage to identify patients more likely to become violent so that health care professionals can intervene earlier, he said.
Such a screening tool is already demonstrating success in a variety of medical settings.
About 10 years ago, a research team led by Son Chae Kim, PhD, RN, found that the 10-item Aggressive Behavior Risk Assessment Tool (ABRAT) was able to identify potentially violent patients with reasonable sensitivity and specificity in hospital medical-surgical units.
Subsequently, the tool was modified for long-term care facilities, and again, researchers found that ABRAT was able to identify potentially violent residents with reasonable sensitivity and specificity, said Dr. Kim, ABRAT developer and a professor at Point Loma Nazarene University, San Diego.
In 2021, researchers embedded the checklist into an electronic health record (EHR) system and tested ABRAT in emergency departments.
“Currently, we are working with computer programmers to build an app that would make the ABRAT very easy to use in conjunction with EHR,” Dr. Kim said. “Instead of a nurse searching the EHR to find out if the patient has history of mental illness or aggressive behavior in the past, the app would automatically search the EHR and combine the nurse’s quick observation whether the patient is confused, agitated, staring, or threatening, to automatically calculate the violence risk.”
Dr. Kim and her team also developed a tool called VEST (Violent Event Severity Tool), a standardized objective workplace violence severity assessment. They are working with programmers to incorporate VEST into the app as well.
Dr. Kim’s hope is that the ABRAT tool can be modified for use in a range of health care settings.
A version of this article first appeared on Medscape.com.
San Diego internist David B. Bittleman, MD, was finishing an appointment with a patient when the man’s caregiver slipped Dr. Bittleman a note as the patient walked out of the room.
“Call me tomorrow,” the mysterious message read.
Dr. Bittleman phoned the caregiver, who was the patient’s ex-wife, the next day. He assumed she wanted to discuss a routine issue, such as the patient’s treatment. But the reason she wanted to talk privately was far more ominous.
“He wants to kill you,” she said.
Dr. Bittleman was shocked. The caregiver told Dr. Bittleman she believed her ex-husband was serious.
“The ex-wife and two adult sons were very alarmed by his erratic behavior,” Dr. Bittleman recalled. “She made it very clear that he said he planned to kill me. I feared for my life because I took his threat at face value.”
Patient sends alarming message, makes threats
When he went into medicine, Dr. Bittleman never imagined that he’d have to worry about being attacked or killed by a patient.
After spending 20 years in private practice, Dr. Bittleman was excited to accept a position at the Veterans Affairs San Diego health system. His extended family lived in the area, and he looked forward to helping veterans and to working with students, he said.
Dr. Bittleman had practiced primary care at the VA for about 5 years when he encountered the threatening patient, a veteran in his 60’s. The man was suffering from musculoskeletal pain and mental illness.
The patient had taken opioids on and off for many years. Dr. Bittleman felt that to continue the medication would not be safe, considering the man’s lifestyle.
“He had been maintained on oxycodone for chronic pain by previous providers, but I thought that was dangerous, given that he was mixing it with alcohol and marijuana,” he said. “I met with him and a substance use disorder physician for a conference call, and we explained we would need to taper the medication and eventually stop the opioids.”
Dr. Bittleman pleaded with the patient to enter drug rehab, and he offered him inpatient care for treatment of withdrawal. The man refused.
A few weeks later, Dr. Bittleman was checking the health center’s electronic messaging system. He found a disturbing message from the patient.
“You better learn jiu jitsu and hand-to-hand combat if you ever take my opioids away,” the message read. “You better learn how to defend yourself!”
Dr. Bittleman contacted the VA police and reported the message. The patient was interviewed by mental health professionals, but they did not believe he was dangerous, according to Dr. Bittleman.
“They are pretty limited to what they can do,” he said. “At a private practice, the patient might be fired or no longer allowed to come into the building, but the VA is a safety net institution. I’m not sure if he was even reprimanded.”
Two months later, the patient’s ex-wife shared the alarming news that the patient wanted to kill the doctor.
Dr. Bittleman went back to the police. They suggested he file a restraining order, which he sought that afternoon. By the end of the day, the judge had issued the restraining order, according to Dr. Bittleman and court records. The patient could not come within 100 yards of the physician, his clinic, car, or home.
But there was one frightening caveat. The order was temporary. It would last for only 2 weeks. To make the order permanent, Dr. Bittleman would have to go before the judge and argue why it was needed.
He wouldn’t be alone at the hearing. Someone else would be just paces away – the patient who wanted to murder him.
Doctor and patient face off before judge
As the hearing neared, Dr. Bittleman felt anxious, outraged, and fearful. He wondered whether the patient might make good on his threat.
Some colleagues suggested that Bittleman buy a gun, while others recommended he carry pepper spray. Dr. Bittleman had no interest in learning how to use a gun, he said. He took comfort in the fact that there were armed guards and metal detectors in his building, and there was a panic button under his desk.
“I was not sure I wanted to take care of patients anymore, especially chronic pain patients,” he said. “However, I went for some counseling with the Employee Assistance Program, and the therapist was helpful in normalizing my anxiety and acknowledging my fear.”
On the day of the hearing, Dr. Bittleman sat in the back of the courtroom. The patient, who sat near the front, glanced at Dr. Bittleman with a slight smile.
When his case was called, the judge explained that as the plaintiff, the burden was on Dr. Bittleman to prove the patient was a threat to his safety. He provided the judge a copy of the threatening message and a copy of the ex-wife’s note.
After reading the documents, the judge asked the patient to explain his side. The patient complained that the VA had denied him certain benefits and that he was forced to receive mental health treatment rehab that he “didn’t need.” The judge eventually interrupted the man to ask if he had threatened to kill Dr. Bittleman.
“Oh yes, your honor, I did say that, but I was only joking,” he told the judge.
The admission was enough. The judge issued a restraining order against the patient that would last 1 year. He could not have firearms, and if he violated the order, he would be arrested.
The terrifying saga was finally over.
“I never heard from the patient again,” Dr. Bittleman said. “His [care] location was changed, and police were required to come to all his visits with his new provider. I was relieved that if he ever came near me, he was going to jail.”
To raise awareness about such ordeals and the hassles that can follow, Dr. Bittleman wrote an article about his experience, which was published in the Annals of Family Medicine. He continues to treat patients at the VA, including those with chronic pain, but the memory of the menacing patient resurfaces from time to time.
“I do still think about it,” he said. “I know how to use my panic button, and I test it every 90 days. If there is a patient who concerns me, I will have the VA police wait nearby. I am very aware and upset by violence. When I hear about a doctor getting killed, I feel a clutch in my chest. How could I not relate? Here is a doctor who worked hard, who dedicated their life to help patients, and it comes to this? It’s so revolting. It makes me sick.”
Can you identify a violent patient?
Concern over threatening patients has grown across the country after recent violent attacks against physicians in Oklahoma and California. Two physicians were shot to death in June 2022 when a patient opened fire inside a Tulsa medical building. The primary target of the shooting was a surgeon who had performed surgery on the patient. Also in June, two nurses and an emergency physician were stabbed by a patient inside the Encino Hospital Medical Center. They survived.
The attacks raise questions about how to identify potentially violent patients and how to mitigate possible violence.
Threats and violence against health care professionals are nothing new, but they’re finally getting the attention they deserve, says Derek Schaller, MD, an emergency physician and assistant professor of emergency medicine at Central Michigan University in Mount Pleasant.
“Violence against personnel in medicine has been an issue for a long time; it’s just finally making headlines,” he said. “Way back when, it almost seemed like it was part of the job, part of the gig. But it shouldn’t be part of the gig. It’s not something we should be dealing with.”
It’s common for health care professionals and health centers to take a reactive approach to violent patients, but Dr. Schaller encourages a more proactive strategy. Central Michigan University Health, for example, recently studied its past violent encounters and analyzed the characteristics of violent patients. The analysis came after an increase in violent patient episodes at the health center in the past year, Dr. Schaller said.
The study yielded some interesting results, including that a large percentage of patients who became violent in the emergency department did so within the first hour they were in the hospital, he said.
“You would have thought it’s the patients who have been there and have been stuck in the emergency department for a while and who became disgruntled, but that was not the case,” Dr. Schaller said.
He recommends that physicians, medical practices, and hospitals carry out similar assessments of their patient populations and of past violent encounters to determine trends. His institution will be implementing a screening tool in triage to identify patients more likely to become violent so that health care professionals can intervene earlier, he said.
Such a screening tool is already demonstrating success in a variety of medical settings.
About 10 years ago, a research team led by Son Chae Kim, PhD, RN, found that the 10-item Aggressive Behavior Risk Assessment Tool (ABRAT) was able to identify potentially violent patients with reasonable sensitivity and specificity in hospital medical-surgical units.
Subsequently, the tool was modified for long-term care facilities, and again, researchers found that ABRAT was able to identify potentially violent residents with reasonable sensitivity and specificity, said Dr. Kim, ABRAT developer and a professor at Point Loma Nazarene University, San Diego.
In 2021, researchers embedded the checklist into an electronic health record (EHR) system and tested ABRAT in emergency departments.
“Currently, we are working with computer programmers to build an app that would make the ABRAT very easy to use in conjunction with EHR,” Dr. Kim said. “Instead of a nurse searching the EHR to find out if the patient has history of mental illness or aggressive behavior in the past, the app would automatically search the EHR and combine the nurse’s quick observation whether the patient is confused, agitated, staring, or threatening, to automatically calculate the violence risk.”
Dr. Kim and her team also developed a tool called VEST (Violent Event Severity Tool), a standardized objective workplace violence severity assessment. They are working with programmers to incorporate VEST into the app as well.
Dr. Kim’s hope is that the ABRAT tool can be modified for use in a range of health care settings.
A version of this article first appeared on Medscape.com.
San Diego internist David B. Bittleman, MD, was finishing an appointment with a patient when the man’s caregiver slipped Dr. Bittleman a note as the patient walked out of the room.
“Call me tomorrow,” the mysterious message read.
Dr. Bittleman phoned the caregiver, who was the patient’s ex-wife, the next day. He assumed she wanted to discuss a routine issue, such as the patient’s treatment. But the reason she wanted to talk privately was far more ominous.
“He wants to kill you,” she said.
Dr. Bittleman was shocked. The caregiver told Dr. Bittleman she believed her ex-husband was serious.
“The ex-wife and two adult sons were very alarmed by his erratic behavior,” Dr. Bittleman recalled. “She made it very clear that he said he planned to kill me. I feared for my life because I took his threat at face value.”
Patient sends alarming message, makes threats
When he went into medicine, Dr. Bittleman never imagined that he’d have to worry about being attacked or killed by a patient.
After spending 20 years in private practice, Dr. Bittleman was excited to accept a position at the Veterans Affairs San Diego health system. His extended family lived in the area, and he looked forward to helping veterans and to working with students, he said.
Dr. Bittleman had practiced primary care at the VA for about 5 years when he encountered the threatening patient, a veteran in his 60’s. The man was suffering from musculoskeletal pain and mental illness.
The patient had taken opioids on and off for many years. Dr. Bittleman felt that to continue the medication would not be safe, considering the man’s lifestyle.
“He had been maintained on oxycodone for chronic pain by previous providers, but I thought that was dangerous, given that he was mixing it with alcohol and marijuana,” he said. “I met with him and a substance use disorder physician for a conference call, and we explained we would need to taper the medication and eventually stop the opioids.”
Dr. Bittleman pleaded with the patient to enter drug rehab, and he offered him inpatient care for treatment of withdrawal. The man refused.
A few weeks later, Dr. Bittleman was checking the health center’s electronic messaging system. He found a disturbing message from the patient.
“You better learn jiu jitsu and hand-to-hand combat if you ever take my opioids away,” the message read. “You better learn how to defend yourself!”
Dr. Bittleman contacted the VA police and reported the message. The patient was interviewed by mental health professionals, but they did not believe he was dangerous, according to Dr. Bittleman.
“They are pretty limited to what they can do,” he said. “At a private practice, the patient might be fired or no longer allowed to come into the building, but the VA is a safety net institution. I’m not sure if he was even reprimanded.”
Two months later, the patient’s ex-wife shared the alarming news that the patient wanted to kill the doctor.
Dr. Bittleman went back to the police. They suggested he file a restraining order, which he sought that afternoon. By the end of the day, the judge had issued the restraining order, according to Dr. Bittleman and court records. The patient could not come within 100 yards of the physician, his clinic, car, or home.
But there was one frightening caveat. The order was temporary. It would last for only 2 weeks. To make the order permanent, Dr. Bittleman would have to go before the judge and argue why it was needed.
He wouldn’t be alone at the hearing. Someone else would be just paces away – the patient who wanted to murder him.
Doctor and patient face off before judge
As the hearing neared, Dr. Bittleman felt anxious, outraged, and fearful. He wondered whether the patient might make good on his threat.
Some colleagues suggested that Bittleman buy a gun, while others recommended he carry pepper spray. Dr. Bittleman had no interest in learning how to use a gun, he said. He took comfort in the fact that there were armed guards and metal detectors in his building, and there was a panic button under his desk.
“I was not sure I wanted to take care of patients anymore, especially chronic pain patients,” he said. “However, I went for some counseling with the Employee Assistance Program, and the therapist was helpful in normalizing my anxiety and acknowledging my fear.”
On the day of the hearing, Dr. Bittleman sat in the back of the courtroom. The patient, who sat near the front, glanced at Dr. Bittleman with a slight smile.
When his case was called, the judge explained that as the plaintiff, the burden was on Dr. Bittleman to prove the patient was a threat to his safety. He provided the judge a copy of the threatening message and a copy of the ex-wife’s note.
After reading the documents, the judge asked the patient to explain his side. The patient complained that the VA had denied him certain benefits and that he was forced to receive mental health treatment rehab that he “didn’t need.” The judge eventually interrupted the man to ask if he had threatened to kill Dr. Bittleman.
“Oh yes, your honor, I did say that, but I was only joking,” he told the judge.
The admission was enough. The judge issued a restraining order against the patient that would last 1 year. He could not have firearms, and if he violated the order, he would be arrested.
The terrifying saga was finally over.
“I never heard from the patient again,” Dr. Bittleman said. “His [care] location was changed, and police were required to come to all his visits with his new provider. I was relieved that if he ever came near me, he was going to jail.”
To raise awareness about such ordeals and the hassles that can follow, Dr. Bittleman wrote an article about his experience, which was published in the Annals of Family Medicine. He continues to treat patients at the VA, including those with chronic pain, but the memory of the menacing patient resurfaces from time to time.
“I do still think about it,” he said. “I know how to use my panic button, and I test it every 90 days. If there is a patient who concerns me, I will have the VA police wait nearby. I am very aware and upset by violence. When I hear about a doctor getting killed, I feel a clutch in my chest. How could I not relate? Here is a doctor who worked hard, who dedicated their life to help patients, and it comes to this? It’s so revolting. It makes me sick.”
Can you identify a violent patient?
Concern over threatening patients has grown across the country after recent violent attacks against physicians in Oklahoma and California. Two physicians were shot to death in June 2022 when a patient opened fire inside a Tulsa medical building. The primary target of the shooting was a surgeon who had performed surgery on the patient. Also in June, two nurses and an emergency physician were stabbed by a patient inside the Encino Hospital Medical Center. They survived.
The attacks raise questions about how to identify potentially violent patients and how to mitigate possible violence.
Threats and violence against health care professionals are nothing new, but they’re finally getting the attention they deserve, says Derek Schaller, MD, an emergency physician and assistant professor of emergency medicine at Central Michigan University in Mount Pleasant.
“Violence against personnel in medicine has been an issue for a long time; it’s just finally making headlines,” he said. “Way back when, it almost seemed like it was part of the job, part of the gig. But it shouldn’t be part of the gig. It’s not something we should be dealing with.”
It’s common for health care professionals and health centers to take a reactive approach to violent patients, but Dr. Schaller encourages a more proactive strategy. Central Michigan University Health, for example, recently studied its past violent encounters and analyzed the characteristics of violent patients. The analysis came after an increase in violent patient episodes at the health center in the past year, Dr. Schaller said.
The study yielded some interesting results, including that a large percentage of patients who became violent in the emergency department did so within the first hour they were in the hospital, he said.
“You would have thought it’s the patients who have been there and have been stuck in the emergency department for a while and who became disgruntled, but that was not the case,” Dr. Schaller said.
He recommends that physicians, medical practices, and hospitals carry out similar assessments of their patient populations and of past violent encounters to determine trends. His institution will be implementing a screening tool in triage to identify patients more likely to become violent so that health care professionals can intervene earlier, he said.
Such a screening tool is already demonstrating success in a variety of medical settings.
About 10 years ago, a research team led by Son Chae Kim, PhD, RN, found that the 10-item Aggressive Behavior Risk Assessment Tool (ABRAT) was able to identify potentially violent patients with reasonable sensitivity and specificity in hospital medical-surgical units.
Subsequently, the tool was modified for long-term care facilities, and again, researchers found that ABRAT was able to identify potentially violent residents with reasonable sensitivity and specificity, said Dr. Kim, ABRAT developer and a professor at Point Loma Nazarene University, San Diego.
In 2021, researchers embedded the checklist into an electronic health record (EHR) system and tested ABRAT in emergency departments.
“Currently, we are working with computer programmers to build an app that would make the ABRAT very easy to use in conjunction with EHR,” Dr. Kim said. “Instead of a nurse searching the EHR to find out if the patient has history of mental illness or aggressive behavior in the past, the app would automatically search the EHR and combine the nurse’s quick observation whether the patient is confused, agitated, staring, or threatening, to automatically calculate the violence risk.”
Dr. Kim and her team also developed a tool called VEST (Violent Event Severity Tool), a standardized objective workplace violence severity assessment. They are working with programmers to incorporate VEST into the app as well.
Dr. Kim’s hope is that the ABRAT tool can be modified for use in a range of health care settings.
A version of this article first appeared on Medscape.com.
10 new ways docs could face legal troubles post Roe
Doctors in states where abortion is legal are likely to be the next target for antiabortion activists who want to deter residents from seeking abortions across state lines, say legal experts.
Antiabortion legislators in several states are mounting efforts to clamp down on out-of-state abortions, which they view as a legal loophole.
Nineteen states have already banned the use of telemedicine to prescribe medication abortion by requiring the clinician to be physically present when the medication is administered. These states include Arizona, Louisiana, Tennessee, and Texas, which also recently criminalized sending abortion pills through the mail.
Some state legislators plan to introduce legislation based on a Texas abortion ban enacted last year in which private citizens can sue anyone who assists state residents in obtaining an out-of-state abortion.
Meanwhile, legislators in states including New York where abortion is legal have introduced bills to shield doctors involved in reproductive care from possible negative actions by medical malpractice companies and professional misconduct charges.
This news organization asked legal experts for advice on how doctors can protect themselves and still provide appropriate medical care in this rapidly changing legal landscape. Here’s what they had to say.
1. What if patients from states where abortion is banned want to come to my practice in a legal state? What should I be aware of?
“Doctors should do what they think is medically necessary, but they should be aware of potential criminal and/or civil consequences in a patient’s home state, especially if those states have staked out more extreme positions on abortion such as Texas, Oklahoma, and Louisiana,” says Katherine Florey, JD, a professor at the University of California, Davis, School of Law.
The patient’s home state would need to have criminal laws in place that would explicitly ban residents from obtaining out-of-state abortions. “Probably the greater risk on the criminal front is that many states have existing laws that don’t specify their geographical reach but that could be construed to allow for criminal jurisdiction over out-of-state providers who help residents in obtaining an abortion,” she says.
However, criminal laws would be harder to enforce because of constitutional obstacles that would require the U.S. Supreme Court to resolve in a court case. Another barrier is that criminal law typically requires that a significant element of the offense take place in the prosecuting state, says Ms. Florey.
2. Am I likely to be sued by a patient from a state with an abortion ban?
“It’s more likely that states with abortion bans will pursue civil liability cases, particularly in states such as Texas and Oklahoma that allow private individuals to pursue lawsuits against individuals providing or assisting with abortions.”
Such liability is particularly appealing to antiabortion states because it allows them to target abortion care providers rather than the women seeking abortions, an approach that might be both more politically palatable and more effective in achieving abortion-restriction goals, says Ms. Florey.
“It’s not just the threat of jail time that can deter physicians from providing abortions. They can face significant career consequences from civil liability, including being reported to their medical licensing boards and having their malpractice insurance premiums increase,” says Ms. Florey.
3. What if I provide ‘abortion pill’ prescriptions by telemedicine to a patient in another state?
Doctors need to know what the rules are in the patient’s home state because states generally regard where the patient is located as where telemedicine is legally conducted, says Ms. Florey. “It’s more problematic to conduct telemedicine in states where it’s illegal. It could be viewed legally as if the doctor were prescribing a medication abortion in the patient’s state.”
Ms. Florey also advises doctors to find out whether the patient’s home state bans medication abortions. “The courts or states could decide that the physician is practicing in the jurisdiction where the patient is located even if care is provided remotely. In that case, the doctor would have to comply with all the laws of that state.”
She recommends that doctors counsel patients seeking medication abortions to come to the state where abortion is legal and get on their computers there.
“It’s not a perfect solution, but it provides more legal protection than providing medication abortion across state lines,” says Ms. Florey.
4. Can doctors be sued by patients for not informing them of the full range of treatment options, including abortion, when their health is at risk?
If the doctor is in a state that has banned abortion and the procedure is illegal, they can’t recommend something that the law doesn’t allow, says Ms. Florey.
It’s a tough call for doctors in states where abortion is illegal because they could get into legal trouble if they counsel a woman to get an abortion and the court later deems it was not medically necessary, says Ms. Florey.
But doctors could also get into legal trouble if they don’t counsel a woman to get an abortion if her life is in danger and she meets the exception in the abortion ban.
“Ultimately, I think doctors have to follow their conscience and best medical judgment but recognize the legal hazards that exist. If a physician is seeing a lot of out-of-state patients from a single jurisdiction (such as a neighboring state), it would be best to consult with an attorney from that state,” advises Ms. Florey.
5. If a patient from another state comes to me (in a legal state) for abortion care, am I required to provide them with any warnings, information, and so on?
Doctors may be required by some antiabortion states to mention certain risks, especially to the mother’s mental health, that could arise from abortions even if they are not well-supported by evidence, says Ms. Florey.
If a warning is required in a patient’s home state and there were complications from the procedure or the patient became depressed, it could be grounds for a civil lawsuit, says Ms. Florey.
“There is a Montana case, for example, where the plaintiff sued for malpractice after having an abortion. She alleged that she was given medically inaccurate information about the fetus’s HIV status, but she also claimed that she wasn’t informed that she might become depressed as a result of the abortion,” says Ms. Florey. (The case was ultimately decided on a different ground.)
6. What about complications from abortion care that I provided to a patient from another state? What are my responsibilities and risks? Can I be sued for malpractice when the patient returns to her home state?
If physicians can’t monitor the patients after their visit and something goes wrong, the doctors are at greater risk of negligence and being sued for malpractice in the patient’s home state, says Ms. Florey.
She recommends that doctors ask patients to stay for monitoring after the procedure. “I realize that may not be possible for all patients, but it’s a much safer alternative,” says Ms. Florey.
Otherwise, if the doctor communicates with the patient about the complications in her antiabortion state, the state’s courts could view the doctor as having ties to the state and claim they have jurisdiction in the case and apply the state’s laws, says Ms. Florey.
“Criminal jurisdiction would be more of stretch because the central conduct happened out of state, but states could still try to prosecute a case,” she says.
7. If a patient comes to me from another state, are there any residency requirements, or does the person need to find residence in my state for a period of time? Am I responsible for knowing their arrangements?
Generally, as a constitutional principle, a person can go to another state and have the services that a resident is entitled to, says Ms. Florey.
“States can’t normally discriminate against patients from out of state, so it’s not a residency requirement unless a state imposes one. If a state did that, it would probably be unconstitutional,” she says.
It would be less risky legally, though, if a patient remains in the state where she received abortion care for a significant period of time, says Ms. Florey.
8. How can I protect the privacy of patients’ medical records if they received an abortion or other reproductive care in the state?
To some extent, HIPAA accommodates state laws that mandate reporting of patient information, says Lisa C. Ikemoto, JD, also a professor at the UC Davis School of Law.
The Privacy Rule doesn’t require doctors to disclose protected health information about a patient when state laws require reporting. But the rule allows them to disclose private health information when there’s a court order such as a warrant or subpoena, says Ms. Ikemoto.
“Providers should make sure that patient information remains in records that are HIPAA protected. Some states, including California, have enacted privacy laws that are more protective of patient information,” she says.
The Department of Health & Human Services issued new guidance in June for health care professionals to clarify what the Privacy Rule requires them to report in light of the restrictive abortion laws.
9. I practice in a state where abortion is legal. Can I be extradited to another state if I’m prosecuted for crimes relating to reproductive health services?
Yes, generally, if your state allows it, says Ms. Florey. States have a constitutional obligation to extradite citizens of a different state if that person’s home state asks for that, but states do not have to extradite their own citizens.
However, traditionally, states have cooperated with extradition requests and most states have laws in place providing for extradition in those circumstances, which they could change to exempt abortion providers.
A handful of states – Connecticut, New York, Delaware, and New Jersey – have passed laws specifically shielding medical providers from being prosecuted under abortion restrictions passed in other states.
Governors in Massachusetts, Minnesota, New Mexico, and Nevada have issued executive orders saying they will not extradite abortion providers to states that have banned abortion provision, and that state employees will generally not comply with those out-of-state investigations.
10. Should I increase my malpractice insurance in anticipation of more potential legal problems from patients coming to me from antiabortion states?
Yes, I would recommend that doctors increase their malpractice coverage because of the increased legal risks they could face.
“It’s possible that a state might file a lawsuit against out-of-state abortion providers. Criminal prosecution is also a possibility, but the obstacles to prosecuting a case against an out-of-state provider would be considerable, especially if their home state has passed laws shielding abortion providers,” says Ms. Florey.
Individual malpractice claims or some sort of private enforcement action in a state that has established one would be more likely, she adds.
Ms. Florey advises doctors to monitor this rapidly evolving area of law. “Everything I am saying today could change with a single Supreme Court case. There will also be this kind of push/pull as antiabortion states try to crack down on out-of-state residents who provide or assist in abortion and physicians’ home states that try to protect them from legal consequences.”
A version of this article first appeared on Medscape.com.
Doctors in states where abortion is legal are likely to be the next target for antiabortion activists who want to deter residents from seeking abortions across state lines, say legal experts.
Antiabortion legislators in several states are mounting efforts to clamp down on out-of-state abortions, which they view as a legal loophole.
Nineteen states have already banned the use of telemedicine to prescribe medication abortion by requiring the clinician to be physically present when the medication is administered. These states include Arizona, Louisiana, Tennessee, and Texas, which also recently criminalized sending abortion pills through the mail.
Some state legislators plan to introduce legislation based on a Texas abortion ban enacted last year in which private citizens can sue anyone who assists state residents in obtaining an out-of-state abortion.
Meanwhile, legislators in states including New York where abortion is legal have introduced bills to shield doctors involved in reproductive care from possible negative actions by medical malpractice companies and professional misconduct charges.
This news organization asked legal experts for advice on how doctors can protect themselves and still provide appropriate medical care in this rapidly changing legal landscape. Here’s what they had to say.
1. What if patients from states where abortion is banned want to come to my practice in a legal state? What should I be aware of?
“Doctors should do what they think is medically necessary, but they should be aware of potential criminal and/or civil consequences in a patient’s home state, especially if those states have staked out more extreme positions on abortion such as Texas, Oklahoma, and Louisiana,” says Katherine Florey, JD, a professor at the University of California, Davis, School of Law.
The patient’s home state would need to have criminal laws in place that would explicitly ban residents from obtaining out-of-state abortions. “Probably the greater risk on the criminal front is that many states have existing laws that don’t specify their geographical reach but that could be construed to allow for criminal jurisdiction over out-of-state providers who help residents in obtaining an abortion,” she says.
However, criminal laws would be harder to enforce because of constitutional obstacles that would require the U.S. Supreme Court to resolve in a court case. Another barrier is that criminal law typically requires that a significant element of the offense take place in the prosecuting state, says Ms. Florey.
2. Am I likely to be sued by a patient from a state with an abortion ban?
“It’s more likely that states with abortion bans will pursue civil liability cases, particularly in states such as Texas and Oklahoma that allow private individuals to pursue lawsuits against individuals providing or assisting with abortions.”
Such liability is particularly appealing to antiabortion states because it allows them to target abortion care providers rather than the women seeking abortions, an approach that might be both more politically palatable and more effective in achieving abortion-restriction goals, says Ms. Florey.
“It’s not just the threat of jail time that can deter physicians from providing abortions. They can face significant career consequences from civil liability, including being reported to their medical licensing boards and having their malpractice insurance premiums increase,” says Ms. Florey.
3. What if I provide ‘abortion pill’ prescriptions by telemedicine to a patient in another state?
Doctors need to know what the rules are in the patient’s home state because states generally regard where the patient is located as where telemedicine is legally conducted, says Ms. Florey. “It’s more problematic to conduct telemedicine in states where it’s illegal. It could be viewed legally as if the doctor were prescribing a medication abortion in the patient’s state.”
Ms. Florey also advises doctors to find out whether the patient’s home state bans medication abortions. “The courts or states could decide that the physician is practicing in the jurisdiction where the patient is located even if care is provided remotely. In that case, the doctor would have to comply with all the laws of that state.”
She recommends that doctors counsel patients seeking medication abortions to come to the state where abortion is legal and get on their computers there.
“It’s not a perfect solution, but it provides more legal protection than providing medication abortion across state lines,” says Ms. Florey.
4. Can doctors be sued by patients for not informing them of the full range of treatment options, including abortion, when their health is at risk?
If the doctor is in a state that has banned abortion and the procedure is illegal, they can’t recommend something that the law doesn’t allow, says Ms. Florey.
It’s a tough call for doctors in states where abortion is illegal because they could get into legal trouble if they counsel a woman to get an abortion and the court later deems it was not medically necessary, says Ms. Florey.
But doctors could also get into legal trouble if they don’t counsel a woman to get an abortion if her life is in danger and she meets the exception in the abortion ban.
“Ultimately, I think doctors have to follow their conscience and best medical judgment but recognize the legal hazards that exist. If a physician is seeing a lot of out-of-state patients from a single jurisdiction (such as a neighboring state), it would be best to consult with an attorney from that state,” advises Ms. Florey.
5. If a patient from another state comes to me (in a legal state) for abortion care, am I required to provide them with any warnings, information, and so on?
Doctors may be required by some antiabortion states to mention certain risks, especially to the mother’s mental health, that could arise from abortions even if they are not well-supported by evidence, says Ms. Florey.
If a warning is required in a patient’s home state and there were complications from the procedure or the patient became depressed, it could be grounds for a civil lawsuit, says Ms. Florey.
“There is a Montana case, for example, where the plaintiff sued for malpractice after having an abortion. She alleged that she was given medically inaccurate information about the fetus’s HIV status, but she also claimed that she wasn’t informed that she might become depressed as a result of the abortion,” says Ms. Florey. (The case was ultimately decided on a different ground.)
6. What about complications from abortion care that I provided to a patient from another state? What are my responsibilities and risks? Can I be sued for malpractice when the patient returns to her home state?
If physicians can’t monitor the patients after their visit and something goes wrong, the doctors are at greater risk of negligence and being sued for malpractice in the patient’s home state, says Ms. Florey.
She recommends that doctors ask patients to stay for monitoring after the procedure. “I realize that may not be possible for all patients, but it’s a much safer alternative,” says Ms. Florey.
Otherwise, if the doctor communicates with the patient about the complications in her antiabortion state, the state’s courts could view the doctor as having ties to the state and claim they have jurisdiction in the case and apply the state’s laws, says Ms. Florey.
“Criminal jurisdiction would be more of stretch because the central conduct happened out of state, but states could still try to prosecute a case,” she says.
7. If a patient comes to me from another state, are there any residency requirements, or does the person need to find residence in my state for a period of time? Am I responsible for knowing their arrangements?
Generally, as a constitutional principle, a person can go to another state and have the services that a resident is entitled to, says Ms. Florey.
“States can’t normally discriminate against patients from out of state, so it’s not a residency requirement unless a state imposes one. If a state did that, it would probably be unconstitutional,” she says.
It would be less risky legally, though, if a patient remains in the state where she received abortion care for a significant period of time, says Ms. Florey.
8. How can I protect the privacy of patients’ medical records if they received an abortion or other reproductive care in the state?
To some extent, HIPAA accommodates state laws that mandate reporting of patient information, says Lisa C. Ikemoto, JD, also a professor at the UC Davis School of Law.
The Privacy Rule doesn’t require doctors to disclose protected health information about a patient when state laws require reporting. But the rule allows them to disclose private health information when there’s a court order such as a warrant or subpoena, says Ms. Ikemoto.
“Providers should make sure that patient information remains in records that are HIPAA protected. Some states, including California, have enacted privacy laws that are more protective of patient information,” she says.
The Department of Health & Human Services issued new guidance in June for health care professionals to clarify what the Privacy Rule requires them to report in light of the restrictive abortion laws.
9. I practice in a state where abortion is legal. Can I be extradited to another state if I’m prosecuted for crimes relating to reproductive health services?
Yes, generally, if your state allows it, says Ms. Florey. States have a constitutional obligation to extradite citizens of a different state if that person’s home state asks for that, but states do not have to extradite their own citizens.
However, traditionally, states have cooperated with extradition requests and most states have laws in place providing for extradition in those circumstances, which they could change to exempt abortion providers.
A handful of states – Connecticut, New York, Delaware, and New Jersey – have passed laws specifically shielding medical providers from being prosecuted under abortion restrictions passed in other states.
Governors in Massachusetts, Minnesota, New Mexico, and Nevada have issued executive orders saying they will not extradite abortion providers to states that have banned abortion provision, and that state employees will generally not comply with those out-of-state investigations.
10. Should I increase my malpractice insurance in anticipation of more potential legal problems from patients coming to me from antiabortion states?
Yes, I would recommend that doctors increase their malpractice coverage because of the increased legal risks they could face.
“It’s possible that a state might file a lawsuit against out-of-state abortion providers. Criminal prosecution is also a possibility, but the obstacles to prosecuting a case against an out-of-state provider would be considerable, especially if their home state has passed laws shielding abortion providers,” says Ms. Florey.
Individual malpractice claims or some sort of private enforcement action in a state that has established one would be more likely, she adds.
Ms. Florey advises doctors to monitor this rapidly evolving area of law. “Everything I am saying today could change with a single Supreme Court case. There will also be this kind of push/pull as antiabortion states try to crack down on out-of-state residents who provide or assist in abortion and physicians’ home states that try to protect them from legal consequences.”
A version of this article first appeared on Medscape.com.
Doctors in states where abortion is legal are likely to be the next target for antiabortion activists who want to deter residents from seeking abortions across state lines, say legal experts.
Antiabortion legislators in several states are mounting efforts to clamp down on out-of-state abortions, which they view as a legal loophole.
Nineteen states have already banned the use of telemedicine to prescribe medication abortion by requiring the clinician to be physically present when the medication is administered. These states include Arizona, Louisiana, Tennessee, and Texas, which also recently criminalized sending abortion pills through the mail.
Some state legislators plan to introduce legislation based on a Texas abortion ban enacted last year in which private citizens can sue anyone who assists state residents in obtaining an out-of-state abortion.
Meanwhile, legislators in states including New York where abortion is legal have introduced bills to shield doctors involved in reproductive care from possible negative actions by medical malpractice companies and professional misconduct charges.
This news organization asked legal experts for advice on how doctors can protect themselves and still provide appropriate medical care in this rapidly changing legal landscape. Here’s what they had to say.
1. What if patients from states where abortion is banned want to come to my practice in a legal state? What should I be aware of?
“Doctors should do what they think is medically necessary, but they should be aware of potential criminal and/or civil consequences in a patient’s home state, especially if those states have staked out more extreme positions on abortion such as Texas, Oklahoma, and Louisiana,” says Katherine Florey, JD, a professor at the University of California, Davis, School of Law.
The patient’s home state would need to have criminal laws in place that would explicitly ban residents from obtaining out-of-state abortions. “Probably the greater risk on the criminal front is that many states have existing laws that don’t specify their geographical reach but that could be construed to allow for criminal jurisdiction over out-of-state providers who help residents in obtaining an abortion,” she says.
However, criminal laws would be harder to enforce because of constitutional obstacles that would require the U.S. Supreme Court to resolve in a court case. Another barrier is that criminal law typically requires that a significant element of the offense take place in the prosecuting state, says Ms. Florey.
2. Am I likely to be sued by a patient from a state with an abortion ban?
“It’s more likely that states with abortion bans will pursue civil liability cases, particularly in states such as Texas and Oklahoma that allow private individuals to pursue lawsuits against individuals providing or assisting with abortions.”
Such liability is particularly appealing to antiabortion states because it allows them to target abortion care providers rather than the women seeking abortions, an approach that might be both more politically palatable and more effective in achieving abortion-restriction goals, says Ms. Florey.
“It’s not just the threat of jail time that can deter physicians from providing abortions. They can face significant career consequences from civil liability, including being reported to their medical licensing boards and having their malpractice insurance premiums increase,” says Ms. Florey.
3. What if I provide ‘abortion pill’ prescriptions by telemedicine to a patient in another state?
Doctors need to know what the rules are in the patient’s home state because states generally regard where the patient is located as where telemedicine is legally conducted, says Ms. Florey. “It’s more problematic to conduct telemedicine in states where it’s illegal. It could be viewed legally as if the doctor were prescribing a medication abortion in the patient’s state.”
Ms. Florey also advises doctors to find out whether the patient’s home state bans medication abortions. “The courts or states could decide that the physician is practicing in the jurisdiction where the patient is located even if care is provided remotely. In that case, the doctor would have to comply with all the laws of that state.”
She recommends that doctors counsel patients seeking medication abortions to come to the state where abortion is legal and get on their computers there.
“It’s not a perfect solution, but it provides more legal protection than providing medication abortion across state lines,” says Ms. Florey.
4. Can doctors be sued by patients for not informing them of the full range of treatment options, including abortion, when their health is at risk?
If the doctor is in a state that has banned abortion and the procedure is illegal, they can’t recommend something that the law doesn’t allow, says Ms. Florey.
It’s a tough call for doctors in states where abortion is illegal because they could get into legal trouble if they counsel a woman to get an abortion and the court later deems it was not medically necessary, says Ms. Florey.
But doctors could also get into legal trouble if they don’t counsel a woman to get an abortion if her life is in danger and she meets the exception in the abortion ban.
“Ultimately, I think doctors have to follow their conscience and best medical judgment but recognize the legal hazards that exist. If a physician is seeing a lot of out-of-state patients from a single jurisdiction (such as a neighboring state), it would be best to consult with an attorney from that state,” advises Ms. Florey.
5. If a patient from another state comes to me (in a legal state) for abortion care, am I required to provide them with any warnings, information, and so on?
Doctors may be required by some antiabortion states to mention certain risks, especially to the mother’s mental health, that could arise from abortions even if they are not well-supported by evidence, says Ms. Florey.
If a warning is required in a patient’s home state and there were complications from the procedure or the patient became depressed, it could be grounds for a civil lawsuit, says Ms. Florey.
“There is a Montana case, for example, where the plaintiff sued for malpractice after having an abortion. She alleged that she was given medically inaccurate information about the fetus’s HIV status, but she also claimed that she wasn’t informed that she might become depressed as a result of the abortion,” says Ms. Florey. (The case was ultimately decided on a different ground.)
6. What about complications from abortion care that I provided to a patient from another state? What are my responsibilities and risks? Can I be sued for malpractice when the patient returns to her home state?
If physicians can’t monitor the patients after their visit and something goes wrong, the doctors are at greater risk of negligence and being sued for malpractice in the patient’s home state, says Ms. Florey.
She recommends that doctors ask patients to stay for monitoring after the procedure. “I realize that may not be possible for all patients, but it’s a much safer alternative,” says Ms. Florey.
Otherwise, if the doctor communicates with the patient about the complications in her antiabortion state, the state’s courts could view the doctor as having ties to the state and claim they have jurisdiction in the case and apply the state’s laws, says Ms. Florey.
“Criminal jurisdiction would be more of stretch because the central conduct happened out of state, but states could still try to prosecute a case,” she says.
7. If a patient comes to me from another state, are there any residency requirements, or does the person need to find residence in my state for a period of time? Am I responsible for knowing their arrangements?
Generally, as a constitutional principle, a person can go to another state and have the services that a resident is entitled to, says Ms. Florey.
“States can’t normally discriminate against patients from out of state, so it’s not a residency requirement unless a state imposes one. If a state did that, it would probably be unconstitutional,” she says.
It would be less risky legally, though, if a patient remains in the state where she received abortion care for a significant period of time, says Ms. Florey.
8. How can I protect the privacy of patients’ medical records if they received an abortion or other reproductive care in the state?
To some extent, HIPAA accommodates state laws that mandate reporting of patient information, says Lisa C. Ikemoto, JD, also a professor at the UC Davis School of Law.
The Privacy Rule doesn’t require doctors to disclose protected health information about a patient when state laws require reporting. But the rule allows them to disclose private health information when there’s a court order such as a warrant or subpoena, says Ms. Ikemoto.
“Providers should make sure that patient information remains in records that are HIPAA protected. Some states, including California, have enacted privacy laws that are more protective of patient information,” she says.
The Department of Health & Human Services issued new guidance in June for health care professionals to clarify what the Privacy Rule requires them to report in light of the restrictive abortion laws.
9. I practice in a state where abortion is legal. Can I be extradited to another state if I’m prosecuted for crimes relating to reproductive health services?
Yes, generally, if your state allows it, says Ms. Florey. States have a constitutional obligation to extradite citizens of a different state if that person’s home state asks for that, but states do not have to extradite their own citizens.
However, traditionally, states have cooperated with extradition requests and most states have laws in place providing for extradition in those circumstances, which they could change to exempt abortion providers.
A handful of states – Connecticut, New York, Delaware, and New Jersey – have passed laws specifically shielding medical providers from being prosecuted under abortion restrictions passed in other states.
Governors in Massachusetts, Minnesota, New Mexico, and Nevada have issued executive orders saying they will not extradite abortion providers to states that have banned abortion provision, and that state employees will generally not comply with those out-of-state investigations.
10. Should I increase my malpractice insurance in anticipation of more potential legal problems from patients coming to me from antiabortion states?
Yes, I would recommend that doctors increase their malpractice coverage because of the increased legal risks they could face.
“It’s possible that a state might file a lawsuit against out-of-state abortion providers. Criminal prosecution is also a possibility, but the obstacles to prosecuting a case against an out-of-state provider would be considerable, especially if their home state has passed laws shielding abortion providers,” says Ms. Florey.
Individual malpractice claims or some sort of private enforcement action in a state that has established one would be more likely, she adds.
Ms. Florey advises doctors to monitor this rapidly evolving area of law. “Everything I am saying today could change with a single Supreme Court case. There will also be this kind of push/pull as antiabortion states try to crack down on out-of-state residents who provide or assist in abortion and physicians’ home states that try to protect them from legal consequences.”
A version of this article first appeared on Medscape.com.




