User login
Various adjuncts to IVIg help treat coronary artery abnormalities in pediatric Kawasaki disease
Two studies published in Pediatrics add new information on potential therapies as adjuncts to intravenous immunoglobulin to treat coronary artery abnormalities in pediatric Kawasaki disease patients.
In the phase 3, randomized, placebo-controlled EATAK (Etanercept as Adjunctive Treatment for Acute Kawasaki Disease) trial, Michael A. Portman, MD, and his colleagues examine the effects of adding etanercept to intravenous immunoglobulin (IVIg) to study IVIg resistance in children with Kawasaki disease.
The researchers enrolled 201 participants from eight pediatric centers who received an IVIg infusion followed immediately by either subcutaneous etanercept (0.8 mg/kg; n = 100) or placebo (n = 101) and then received two more weekly doses. They performed a subgroup analysis based on age, gender, and race. The participants were between 2 months and 18 years old with incomplete (10 etanercept, 12 placebo) or complete Kawasaki disease as determined by American Heart Association criteria and American Academy of Pediatrics 2004 criteria.
Of the 35 patients who showed IVIg resistance and received a second dose, the IVIg resistance rate for participants receiving etanercept was 13%, compared with 22% in the placebo group. The overall odds ratio for IVIg resistance was 0.54. While etanercept did not lower the rate of IVIg resistance in participants younger than 1 year old, it significantly reduced IVIg resistance in those older than 1 year.
IVIg fever response significantly differed by race, which ranged from Asian participants having a 7% resistance rate to African Americans having a resistance rate of 57%.
Forty-five of all participants had greater than 2.5 baseline coronary z scores, 23 in the etanercept group and 22 in the placebo group. While etanercept reduced change in coronary z score among participants with baseline dilation (P = .04) and without baseline dilation (P = .001), there was no improvement among participants in the placebo group. Etanercept additionally reduced progression of dilation, compared with the placebo group (P = .03). The researchers noted etanercept had a good safety profile, and there were no differences between the groups receiving the intervention or placebo.
“With these considerations, EATAK results reveal a reasonable risk/benefit profile for etanercept,” Dr. Portman of Seattle Children’s Research Institute, and his colleagues concluded. “Future clinical trials, conducted in these subgroups or stratified according to patient demographics or genotypes, will be necessary to validate our findings before wide clinical adoption.”
In a second study, Audrey Dionne, MD, of Boston Children’s Hospital, and her colleagues explored how corticosteroids or infliximab together with IVIg can reduce the progression of coronary artery aneurysms (CAA). They performed a retrospective study of 121 children (73% boys; median age, 3 years) with Kawasaki disease and CAA at three different centers who received corticosteroid and IVIg therapy (n = 30), infliximab and IVIg therapy (n = 58), or IVIg alone (n = 33). The children had a coronary z score greater than or equal to 2.5 and less than 10, and there were no significant differences between median z scores among the treatment groups (P = .39).
The researchers found that patients who received corticosteroids with IVIg therapy were protected against coronary size progression (coefficient, −1.31); in addition, those patients who received infliximab and IVIg therapy were protected against coronary size progression at follow-up (coefficient, −1.07), the researchers said. Those on placebo were not.
“Our data suggest that adjunctive treatment at the time of diagnosis may be beneficial in patients with CAA,” Dr. Dionne and colleagues concluded. “Future adequately powered, prospective randomized trials are needed to determine the best adjunctive treatment of patients with KD [Kawasaki disease] who present with coronary changes.”
The EATAK trial was funded by the Food and Drug Administration Office of Orphan Product Development, Amgen, and the National Institutes of Health. Dr. Portman and colleagues reported no relevant financial disclosures. The study from Dionne et al. received funding from the McCance Family Foundation and the Vella Fund. One of the authors reported being a paid expert witness for missed diagnoses of Kawasaki disease, which was unrelated to the study. The other authors said they had no conflicts of interest.
SOURCES: Portman MA et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3675; Dionne A et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3341.
Two studies published in Pediatrics add new information on potential therapies as adjuncts to intravenous immunoglobulin to treat coronary artery abnormalities in pediatric Kawasaki disease patients.
In the phase 3, randomized, placebo-controlled EATAK (Etanercept as Adjunctive Treatment for Acute Kawasaki Disease) trial, Michael A. Portman, MD, and his colleagues examine the effects of adding etanercept to intravenous immunoglobulin (IVIg) to study IVIg resistance in children with Kawasaki disease.
The researchers enrolled 201 participants from eight pediatric centers who received an IVIg infusion followed immediately by either subcutaneous etanercept (0.8 mg/kg; n = 100) or placebo (n = 101) and then received two more weekly doses. They performed a subgroup analysis based on age, gender, and race. The participants were between 2 months and 18 years old with incomplete (10 etanercept, 12 placebo) or complete Kawasaki disease as determined by American Heart Association criteria and American Academy of Pediatrics 2004 criteria.
Of the 35 patients who showed IVIg resistance and received a second dose, the IVIg resistance rate for participants receiving etanercept was 13%, compared with 22% in the placebo group. The overall odds ratio for IVIg resistance was 0.54. While etanercept did not lower the rate of IVIg resistance in participants younger than 1 year old, it significantly reduced IVIg resistance in those older than 1 year.
IVIg fever response significantly differed by race, which ranged from Asian participants having a 7% resistance rate to African Americans having a resistance rate of 57%.
Forty-five of all participants had greater than 2.5 baseline coronary z scores, 23 in the etanercept group and 22 in the placebo group. While etanercept reduced change in coronary z score among participants with baseline dilation (P = .04) and without baseline dilation (P = .001), there was no improvement among participants in the placebo group. Etanercept additionally reduced progression of dilation, compared with the placebo group (P = .03). The researchers noted etanercept had a good safety profile, and there were no differences between the groups receiving the intervention or placebo.
“With these considerations, EATAK results reveal a reasonable risk/benefit profile for etanercept,” Dr. Portman of Seattle Children’s Research Institute, and his colleagues concluded. “Future clinical trials, conducted in these subgroups or stratified according to patient demographics or genotypes, will be necessary to validate our findings before wide clinical adoption.”
In a second study, Audrey Dionne, MD, of Boston Children’s Hospital, and her colleagues explored how corticosteroids or infliximab together with IVIg can reduce the progression of coronary artery aneurysms (CAA). They performed a retrospective study of 121 children (73% boys; median age, 3 years) with Kawasaki disease and CAA at three different centers who received corticosteroid and IVIg therapy (n = 30), infliximab and IVIg therapy (n = 58), or IVIg alone (n = 33). The children had a coronary z score greater than or equal to 2.5 and less than 10, and there were no significant differences between median z scores among the treatment groups (P = .39).
The researchers found that patients who received corticosteroids with IVIg therapy were protected against coronary size progression (coefficient, −1.31); in addition, those patients who received infliximab and IVIg therapy were protected against coronary size progression at follow-up (coefficient, −1.07), the researchers said. Those on placebo were not.
“Our data suggest that adjunctive treatment at the time of diagnosis may be beneficial in patients with CAA,” Dr. Dionne and colleagues concluded. “Future adequately powered, prospective randomized trials are needed to determine the best adjunctive treatment of patients with KD [Kawasaki disease] who present with coronary changes.”
The EATAK trial was funded by the Food and Drug Administration Office of Orphan Product Development, Amgen, and the National Institutes of Health. Dr. Portman and colleagues reported no relevant financial disclosures. The study from Dionne et al. received funding from the McCance Family Foundation and the Vella Fund. One of the authors reported being a paid expert witness for missed diagnoses of Kawasaki disease, which was unrelated to the study. The other authors said they had no conflicts of interest.
SOURCES: Portman MA et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3675; Dionne A et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3341.
Two studies published in Pediatrics add new information on potential therapies as adjuncts to intravenous immunoglobulin to treat coronary artery abnormalities in pediatric Kawasaki disease patients.
In the phase 3, randomized, placebo-controlled EATAK (Etanercept as Adjunctive Treatment for Acute Kawasaki Disease) trial, Michael A. Portman, MD, and his colleagues examine the effects of adding etanercept to intravenous immunoglobulin (IVIg) to study IVIg resistance in children with Kawasaki disease.
The researchers enrolled 201 participants from eight pediatric centers who received an IVIg infusion followed immediately by either subcutaneous etanercept (0.8 mg/kg; n = 100) or placebo (n = 101) and then received two more weekly doses. They performed a subgroup analysis based on age, gender, and race. The participants were between 2 months and 18 years old with incomplete (10 etanercept, 12 placebo) or complete Kawasaki disease as determined by American Heart Association criteria and American Academy of Pediatrics 2004 criteria.
Of the 35 patients who showed IVIg resistance and received a second dose, the IVIg resistance rate for participants receiving etanercept was 13%, compared with 22% in the placebo group. The overall odds ratio for IVIg resistance was 0.54. While etanercept did not lower the rate of IVIg resistance in participants younger than 1 year old, it significantly reduced IVIg resistance in those older than 1 year.
IVIg fever response significantly differed by race, which ranged from Asian participants having a 7% resistance rate to African Americans having a resistance rate of 57%.
Forty-five of all participants had greater than 2.5 baseline coronary z scores, 23 in the etanercept group and 22 in the placebo group. While etanercept reduced change in coronary z score among participants with baseline dilation (P = .04) and without baseline dilation (P = .001), there was no improvement among participants in the placebo group. Etanercept additionally reduced progression of dilation, compared with the placebo group (P = .03). The researchers noted etanercept had a good safety profile, and there were no differences between the groups receiving the intervention or placebo.
“With these considerations, EATAK results reveal a reasonable risk/benefit profile for etanercept,” Dr. Portman of Seattle Children’s Research Institute, and his colleagues concluded. “Future clinical trials, conducted in these subgroups or stratified according to patient demographics or genotypes, will be necessary to validate our findings before wide clinical adoption.”
In a second study, Audrey Dionne, MD, of Boston Children’s Hospital, and her colleagues explored how corticosteroids or infliximab together with IVIg can reduce the progression of coronary artery aneurysms (CAA). They performed a retrospective study of 121 children (73% boys; median age, 3 years) with Kawasaki disease and CAA at three different centers who received corticosteroid and IVIg therapy (n = 30), infliximab and IVIg therapy (n = 58), or IVIg alone (n = 33). The children had a coronary z score greater than or equal to 2.5 and less than 10, and there were no significant differences between median z scores among the treatment groups (P = .39).
The researchers found that patients who received corticosteroids with IVIg therapy were protected against coronary size progression (coefficient, −1.31); in addition, those patients who received infliximab and IVIg therapy were protected against coronary size progression at follow-up (coefficient, −1.07), the researchers said. Those on placebo were not.
“Our data suggest that adjunctive treatment at the time of diagnosis may be beneficial in patients with CAA,” Dr. Dionne and colleagues concluded. “Future adequately powered, prospective randomized trials are needed to determine the best adjunctive treatment of patients with KD [Kawasaki disease] who present with coronary changes.”
The EATAK trial was funded by the Food and Drug Administration Office of Orphan Product Development, Amgen, and the National Institutes of Health. Dr. Portman and colleagues reported no relevant financial disclosures. The study from Dionne et al. received funding from the McCance Family Foundation and the Vella Fund. One of the authors reported being a paid expert witness for missed diagnoses of Kawasaki disease, which was unrelated to the study. The other authors said they had no conflicts of interest.
SOURCES: Portman MA et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3675; Dionne A et al. Pediatrics. 2019. doi: 10.1542/peds.2018-3341.
FROM PEDIATRICS
CardioMEMS cuts heart failure hospitalizations in post-approval study
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
NEW ORLEANS – Frequent, noninvasive measurement of pulmonary artery pressure in patients with advanced heart failure and an implanted CardioMEMS device that allows this measurement led to management that produced a substantial reduction in heart failure hospitalizations, compared with each patient’s history, in a real-world study.
The Food and Drug Administration–mandated CardioMEMS Post-Approval Study included 1,200 patients who received CardioMEMS implants after it received U.S. marketing approval. The study showed that when clinicians and patients used the device in routine practice, presumably as part of a structured management system designed to take advantage of the pulmonary artery (PA) pressures the device provides, the result safely produced a 58% cut in heart failure hospitalizations during the year following device placement when compared to each patient’s own hospitalization history during the year before they got the CardioMEMS device, David M. Shavelle, MD, said at the at the annual meeting of the American College of Cardiology. This statistically significant result for the study’s primary endpoint showed an absolute reduction in the average rate of heart failure hospitalizations from 1.24 per patient during the year before the CardioMEMS placement to 0.52 hospitalizations per patient during the 12 months after placement, an average reduction of 0.72 hospitalizations/patient, said Dr. Shavelle, an interventional cardiologist at the University of Southern California in Los Angeles.
Another notable finding was that this benefit from CardioMEMS placement and use occurred at roughly similar rates in patients with New York Heart Association class III heart failure regardless of whether they had a reduced ejection fraction (40% or less), a mid-range ejection fraction (41%-50%), or preserved ejection fraction (greater than 50%), making CardioMEMS use one of the few treatments to produce any proven benefit in patients with heart failure with preserved ejection fraction. In that subgroup, 30% of the 1,200 enrolled patients had an average cut of 0.68 hospitalizations in the year after CardioMEMS implantation, a 61% drop, relative to the year before they received the device.
The results also fulfilled the study’s two prespecified safety measures. Among the 1,214 patients in the study assessed for safety, which included the 1,200 patients who received the device and 4 patients in whom placement failed, 4 patients had a device or system related complication during the study, a 0.3% rate, compared with a prespecified objective performance criteria of less than 20%. Among the 1,200 patients with a functioning CardioMEMS sensor, one patient (0.1%) had a device failure, compared with the study’s objective performance criteria of less than 10%.
The performance of the CardioMEMS device and the benefit it provided to patients in the post-approval study closely tracked its performance during the published pivotal trial (Lancet. 2011 Feb 19;377[9766]:658-66). On the basis of the pivotal trial results, the FDA approved CardioMEMS for U.S. marketing in 2014. Since then, the company has reported that about 10,000 U.S. heart failure patients have received these devices, Dr. Shavelle said.
“The benefit was seen across the range of ejection fractions; that’s very important,” commented Gurusher Panjrath, MD, director of advanced heart failure at George Washington University in Washington and a designated discussant for Dr. Shavelle’s report. “The safety seemed very good, and the efficacy was consistent” with prior reports. “There also was high compliance. The key to success is the structure” of patient management, Dr. Pangroth said. “The data are limited by who is monitoring patients and their data and how much of that contact influences patient outcomes.”
That final comment by Dr. Panjrath highlighted the biggest caveat that heart failure clinicians have raised about judging the efficacy of CardioMEMS. To achieve clinical efficacy, the implanted device requires diligent, virtually daily interrogation and data transmission by the patient, assessment of a large amount of data for each patient by the patient’s clinical team, and responsiveness by the patient to medication adjustments directed by the clinical team to deal with episodes of rising PA pressure.
“The device itself has no benefit. It’s the actions prompted by the device that have benefit,” noted Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern University in Chicago and a second designated discussant for the report.
Dr. Shavelle agreed that for the CardioMEMS device to have an impact, one basic requirement is to identify patients who will cooperate with data collection and transmission and also with changes in their medications that are sent to them in response to PA pressure changes. This means selecting patients who appear to have problems with volume overload, including prior hospitalizations for decompensation, and patients who are comfortable interacting with their clinical-care providers. It also means excluding patients who are too sick to benefit from this intervention. He estimated that at his center more than 95% of class III heart failure patients who qualified for inclusion in the post-approval study by clinical criteria were also judged reasonable recipients of the device based on their willingness to cooperate with this system. He also estimated that at the University of Southern California the heart failure clinical team is now caring for about 150 patients with a CardioMEMS device implanted.
Another concern is teasing apart the specific benefit of collecting and using PA pressure data from the contact that the clinical team maintains with CardioMEMS patients.
“If nurses are contacting patients more often, is it the device or the communication? We need to look at that very carefully in a study that had no control group,” Dr. Yancy said in an interview. Contact with a nurse “is the best thing you can do for heart failure patients.”
Dr. Shavelle countered that several reports from past studies that assessed case management and regular monitoring of and contact with heart failure patients but without PA pressure data failed to showed any consistent benefit to patients.
“If you pick the right patients, CardioMEMS works. There is no question in my mind that the device works,” Dr. Shavelle said in an interview. “If you pick the wrong patient, who will not send the data or follow dose changes, then it won’t work.”
The study was sponsored by Abbott, the company that markets the CardioMEMS HF System. Dr. Shavelle has been a consultant to and speaker on behalf of Abbott Vascular and he has received research funding from Abbott Vascular, Abiomed, Biocardia, and V-Wave. Dr. Yancy had an unspecified financial relationship with Abbott Laboratories. Dr. Panjrath had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Shavelle DM et al. American College of Cardiology annual meeting, abstract 405-16.
REPORTING FROM ACC 2019
AFib screening cuts hospitalizations and ED visits
NEW ORLEANS – People diagnosed with atrial fibrillation by screening with a wearable ECG patch had significantly fewer emergency department visits or hospital admissions, compared with similar people diagnosed with atrial fibrillation by usual-care surveillance in an observational study with 5,109 total participants.
People diagnosed with atrial fibrillation (AFib) through screening had a statistically significant 80% relative cut in hospitalizations and a 65% cut in emergency department visits during 12 months of follow-up, compared with controls in the study who had their AFib identified and diagnosed as part of routine practice, Steven R. Steinhubl, MD, said at the annual meeting of the American College of Cardiology.
The data also showed no difference between the screened and control patients identified with AFib in the average number of cardiologist consultations during a year of follow-up, and a trend that missed statistical significance for 16% fewer primary care physician visits in Afib patients diagnosed by screening rather than by routine surveillance.
These findings provided some insight into the potential clinical impact of AFib screening in at-risk people. Dr. Steinhubl and his associates plan to report on the incidence of strokes and MIs in the two study subgroups after 3 years of follow-up, but he noted that preliminary findings for these two outcomes after 1 year indicated that active screening for AFib also had reduced these rates, compared with waiting for the arrhythmia to become apparent by emergence of symptoms.
The data came from the mSToPS (mHealth Screening to Prevent Strokes) study, which randomized 2,659 U.S. residents enrolled in a large health plan who had risk factors for AFib to either immediate or delayed arrhythmia assessment by ECG patches. Half the participants used a patch for about 14 days immediately and then a second time 3 months later, while the other half waited 4 months and then wore an ECG patch for 2 weeks and again 3 months later. The primary endpoint, first reported at the ACC annual meeting a year before and subsequently published, was the incidence of newly diagnosed AFib during the first 4 months in the actively monitored cohort, compared with a cohort followed by usual care. The results showed that screening identified AFib in 3.9% of people, while no screening and usual-practice follow-up identified a 0.9% incidence of AFib, showing that screening worked better for AFib case identification (JAMA. 2018 Jul 10;320[2]:146-55).
To examine the clinical impact of screening and an increased incidence of diagnosed AFib cases, Dr. Steinhubl and his associates focused on 1,725 of the original 2,659 patients who underwent ECG patch assessment, either immediate or delayed, and continued through 12 months of follow-up, and compared them with 3,384 matched controls who never underwent ECG patch screening but were also followed for 12 months for incident AFib identified during routine care and surveillance. This resulted in a cumulative incidence of newly diagnosed AFib of 6.3% in those who had worn two ECG patches and 2.3% among the matched controls.
During follow-up, use of various interventions was more common among the screened people than the controls. Initiation of anticoagulation treatment started in 4.0% of the entire screened group, compared with 1.9% of the controls, The screened people also had a 0.9% rate of receiving a pacemaker or defibrillator, a 0.8% rate of starting on treatment with an antiarrhythmic drug, and a 0.3% rate of undergoing catheter ablation, compared with none, 0.3%, and one of the controls, respectively, said Dr. Steinhubl, director of digital medicine at the Scripps Research Translational Institute in La Jolla, Calif.
The mSToPS study was funded by Janssen. Dr. Steinhubl has received research funding from DynoSense, EasyG, Janssen, the Qualcomm Foundation, and Striv.
SOURCE: Steinhubl SR et al. J Am Coll Cardiol. 2019 Mar 12;73(9)suppl 1:296.
NEW ORLEANS – People diagnosed with atrial fibrillation by screening with a wearable ECG patch had significantly fewer emergency department visits or hospital admissions, compared with similar people diagnosed with atrial fibrillation by usual-care surveillance in an observational study with 5,109 total participants.
People diagnosed with atrial fibrillation (AFib) through screening had a statistically significant 80% relative cut in hospitalizations and a 65% cut in emergency department visits during 12 months of follow-up, compared with controls in the study who had their AFib identified and diagnosed as part of routine practice, Steven R. Steinhubl, MD, said at the annual meeting of the American College of Cardiology.
The data also showed no difference between the screened and control patients identified with AFib in the average number of cardiologist consultations during a year of follow-up, and a trend that missed statistical significance for 16% fewer primary care physician visits in Afib patients diagnosed by screening rather than by routine surveillance.
These findings provided some insight into the potential clinical impact of AFib screening in at-risk people. Dr. Steinhubl and his associates plan to report on the incidence of strokes and MIs in the two study subgroups after 3 years of follow-up, but he noted that preliminary findings for these two outcomes after 1 year indicated that active screening for AFib also had reduced these rates, compared with waiting for the arrhythmia to become apparent by emergence of symptoms.
The data came from the mSToPS (mHealth Screening to Prevent Strokes) study, which randomized 2,659 U.S. residents enrolled in a large health plan who had risk factors for AFib to either immediate or delayed arrhythmia assessment by ECG patches. Half the participants used a patch for about 14 days immediately and then a second time 3 months later, while the other half waited 4 months and then wore an ECG patch for 2 weeks and again 3 months later. The primary endpoint, first reported at the ACC annual meeting a year before and subsequently published, was the incidence of newly diagnosed AFib during the first 4 months in the actively monitored cohort, compared with a cohort followed by usual care. The results showed that screening identified AFib in 3.9% of people, while no screening and usual-practice follow-up identified a 0.9% incidence of AFib, showing that screening worked better for AFib case identification (JAMA. 2018 Jul 10;320[2]:146-55).
To examine the clinical impact of screening and an increased incidence of diagnosed AFib cases, Dr. Steinhubl and his associates focused on 1,725 of the original 2,659 patients who underwent ECG patch assessment, either immediate or delayed, and continued through 12 months of follow-up, and compared them with 3,384 matched controls who never underwent ECG patch screening but were also followed for 12 months for incident AFib identified during routine care and surveillance. This resulted in a cumulative incidence of newly diagnosed AFib of 6.3% in those who had worn two ECG patches and 2.3% among the matched controls.
During follow-up, use of various interventions was more common among the screened people than the controls. Initiation of anticoagulation treatment started in 4.0% of the entire screened group, compared with 1.9% of the controls, The screened people also had a 0.9% rate of receiving a pacemaker or defibrillator, a 0.8% rate of starting on treatment with an antiarrhythmic drug, and a 0.3% rate of undergoing catheter ablation, compared with none, 0.3%, and one of the controls, respectively, said Dr. Steinhubl, director of digital medicine at the Scripps Research Translational Institute in La Jolla, Calif.
The mSToPS study was funded by Janssen. Dr. Steinhubl has received research funding from DynoSense, EasyG, Janssen, the Qualcomm Foundation, and Striv.
SOURCE: Steinhubl SR et al. J Am Coll Cardiol. 2019 Mar 12;73(9)suppl 1:296.
NEW ORLEANS – People diagnosed with atrial fibrillation by screening with a wearable ECG patch had significantly fewer emergency department visits or hospital admissions, compared with similar people diagnosed with atrial fibrillation by usual-care surveillance in an observational study with 5,109 total participants.
People diagnosed with atrial fibrillation (AFib) through screening had a statistically significant 80% relative cut in hospitalizations and a 65% cut in emergency department visits during 12 months of follow-up, compared with controls in the study who had their AFib identified and diagnosed as part of routine practice, Steven R. Steinhubl, MD, said at the annual meeting of the American College of Cardiology.
The data also showed no difference between the screened and control patients identified with AFib in the average number of cardiologist consultations during a year of follow-up, and a trend that missed statistical significance for 16% fewer primary care physician visits in Afib patients diagnosed by screening rather than by routine surveillance.
These findings provided some insight into the potential clinical impact of AFib screening in at-risk people. Dr. Steinhubl and his associates plan to report on the incidence of strokes and MIs in the two study subgroups after 3 years of follow-up, but he noted that preliminary findings for these two outcomes after 1 year indicated that active screening for AFib also had reduced these rates, compared with waiting for the arrhythmia to become apparent by emergence of symptoms.
The data came from the mSToPS (mHealth Screening to Prevent Strokes) study, which randomized 2,659 U.S. residents enrolled in a large health plan who had risk factors for AFib to either immediate or delayed arrhythmia assessment by ECG patches. Half the participants used a patch for about 14 days immediately and then a second time 3 months later, while the other half waited 4 months and then wore an ECG patch for 2 weeks and again 3 months later. The primary endpoint, first reported at the ACC annual meeting a year before and subsequently published, was the incidence of newly diagnosed AFib during the first 4 months in the actively monitored cohort, compared with a cohort followed by usual care. The results showed that screening identified AFib in 3.9% of people, while no screening and usual-practice follow-up identified a 0.9% incidence of AFib, showing that screening worked better for AFib case identification (JAMA. 2018 Jul 10;320[2]:146-55).
To examine the clinical impact of screening and an increased incidence of diagnosed AFib cases, Dr. Steinhubl and his associates focused on 1,725 of the original 2,659 patients who underwent ECG patch assessment, either immediate or delayed, and continued through 12 months of follow-up, and compared them with 3,384 matched controls who never underwent ECG patch screening but were also followed for 12 months for incident AFib identified during routine care and surveillance. This resulted in a cumulative incidence of newly diagnosed AFib of 6.3% in those who had worn two ECG patches and 2.3% among the matched controls.
During follow-up, use of various interventions was more common among the screened people than the controls. Initiation of anticoagulation treatment started in 4.0% of the entire screened group, compared with 1.9% of the controls, The screened people also had a 0.9% rate of receiving a pacemaker or defibrillator, a 0.8% rate of starting on treatment with an antiarrhythmic drug, and a 0.3% rate of undergoing catheter ablation, compared with none, 0.3%, and one of the controls, respectively, said Dr. Steinhubl, director of digital medicine at the Scripps Research Translational Institute in La Jolla, Calif.
The mSToPS study was funded by Janssen. Dr. Steinhubl has received research funding from DynoSense, EasyG, Janssen, the Qualcomm Foundation, and Striv.
SOURCE: Steinhubl SR et al. J Am Coll Cardiol. 2019 Mar 12;73(9)suppl 1:296.
REPORTING FROM ACC 2019
WISE sheds light on angina in INOCA
NEW ORLEANS – A higher baseline average coronary peak flow velocity is an independent predictor of angina in women with symptomatic ischemia and nonobstructive coronary artery disease (INOCA), according to a new report from the WISE-CVD study.
WISE-CVD (the Women’s Ischemia Syndrome Evaluation: Coronary Vascular Dysfunction) project is a National Institutes of Health–sponsored series of studies. WISE investigators have previously shown that higher baseline average peak flow velocity (BAPV) is correlated with volumetric flow and is an independent predictor of major adverse cardiovascular events. However, until now the relationship between BAPV and anginal symptoms hadn’t been investigated, Nissi S. Suppogu, MD, observed at the annual meeting of the American College of Cardiology.
She reported on 260 women with angiographically evaluated symptomatic INOCA who participated in WISE-CVD. They were divided into two groups based upon their BAPV: 123 had a BAPV of 22 cm/sec or more, and 137 had a BAPV of less than 22 cm/sec.
Women in the high BAPV group had more frequent angina as shown by their average score of 50 on that domain of the Seattle Angina Questionnaire, compared with 60 in the low-BAPV group. The high-BAPV group also had significantly worse angina-related quality of life as reflected in their lower score on that dimension of a related instrument, the Seattle Angina Questionnaire–7.
Further support for the notion that high-BAPV women with INOCA have more severe angina than those with low BAPV comes from the finding that they were significantly more likely to use nitrates (37.6% of them did so, compared with 22.6% of low-BAPV women) and ranolazine, or Ranexa (7.9% versus 1.7%). In addition, the high-BAPV patients had numerically greater usage of other antianginal agents – beta-blockers, calcium channel blockers, and ACE inhibitors or angiotensin receptor blockers – although these differences didn’t reach statistical significance, reported Dr. Suppogu of Cedars-Sinai Medical Center in Los Angeles.
She reported having no financial conflicts regarding her presentation.
NEW ORLEANS – A higher baseline average coronary peak flow velocity is an independent predictor of angina in women with symptomatic ischemia and nonobstructive coronary artery disease (INOCA), according to a new report from the WISE-CVD study.
WISE-CVD (the Women’s Ischemia Syndrome Evaluation: Coronary Vascular Dysfunction) project is a National Institutes of Health–sponsored series of studies. WISE investigators have previously shown that higher baseline average peak flow velocity (BAPV) is correlated with volumetric flow and is an independent predictor of major adverse cardiovascular events. However, until now the relationship between BAPV and anginal symptoms hadn’t been investigated, Nissi S. Suppogu, MD, observed at the annual meeting of the American College of Cardiology.
She reported on 260 women with angiographically evaluated symptomatic INOCA who participated in WISE-CVD. They were divided into two groups based upon their BAPV: 123 had a BAPV of 22 cm/sec or more, and 137 had a BAPV of less than 22 cm/sec.
Women in the high BAPV group had more frequent angina as shown by their average score of 50 on that domain of the Seattle Angina Questionnaire, compared with 60 in the low-BAPV group. The high-BAPV group also had significantly worse angina-related quality of life as reflected in their lower score on that dimension of a related instrument, the Seattle Angina Questionnaire–7.
Further support for the notion that high-BAPV women with INOCA have more severe angina than those with low BAPV comes from the finding that they were significantly more likely to use nitrates (37.6% of them did so, compared with 22.6% of low-BAPV women) and ranolazine, or Ranexa (7.9% versus 1.7%). In addition, the high-BAPV patients had numerically greater usage of other antianginal agents – beta-blockers, calcium channel blockers, and ACE inhibitors or angiotensin receptor blockers – although these differences didn’t reach statistical significance, reported Dr. Suppogu of Cedars-Sinai Medical Center in Los Angeles.
She reported having no financial conflicts regarding her presentation.
NEW ORLEANS – A higher baseline average coronary peak flow velocity is an independent predictor of angina in women with symptomatic ischemia and nonobstructive coronary artery disease (INOCA), according to a new report from the WISE-CVD study.
WISE-CVD (the Women’s Ischemia Syndrome Evaluation: Coronary Vascular Dysfunction) project is a National Institutes of Health–sponsored series of studies. WISE investigators have previously shown that higher baseline average peak flow velocity (BAPV) is correlated with volumetric flow and is an independent predictor of major adverse cardiovascular events. However, until now the relationship between BAPV and anginal symptoms hadn’t been investigated, Nissi S. Suppogu, MD, observed at the annual meeting of the American College of Cardiology.
She reported on 260 women with angiographically evaluated symptomatic INOCA who participated in WISE-CVD. They were divided into two groups based upon their BAPV: 123 had a BAPV of 22 cm/sec or more, and 137 had a BAPV of less than 22 cm/sec.
Women in the high BAPV group had more frequent angina as shown by their average score of 50 on that domain of the Seattle Angina Questionnaire, compared with 60 in the low-BAPV group. The high-BAPV group also had significantly worse angina-related quality of life as reflected in their lower score on that dimension of a related instrument, the Seattle Angina Questionnaire–7.
Further support for the notion that high-BAPV women with INOCA have more severe angina than those with low BAPV comes from the finding that they were significantly more likely to use nitrates (37.6% of them did so, compared with 22.6% of low-BAPV women) and ranolazine, or Ranexa (7.9% versus 1.7%). In addition, the high-BAPV patients had numerically greater usage of other antianginal agents – beta-blockers, calcium channel blockers, and ACE inhibitors or angiotensin receptor blockers – although these differences didn’t reach statistical significance, reported Dr. Suppogu of Cedars-Sinai Medical Center in Los Angeles.
She reported having no financial conflicts regarding her presentation.
REPORTING FROM ACC 19
SGLT2 inhibitors prevent HF hospitalization regardless of baseline LVEF
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.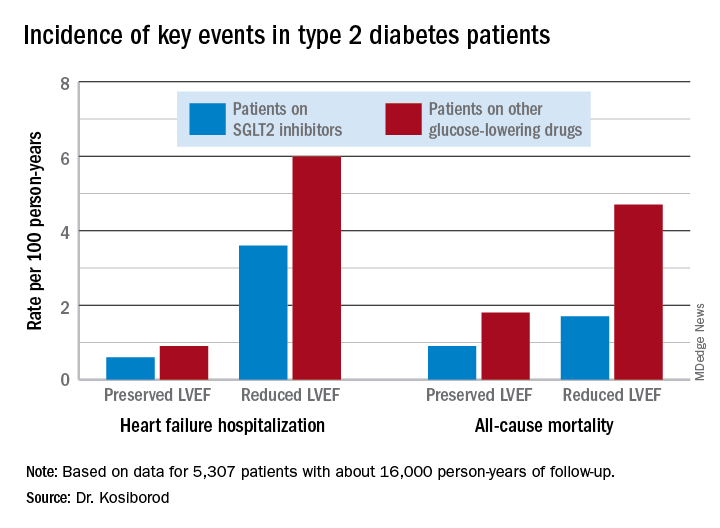
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.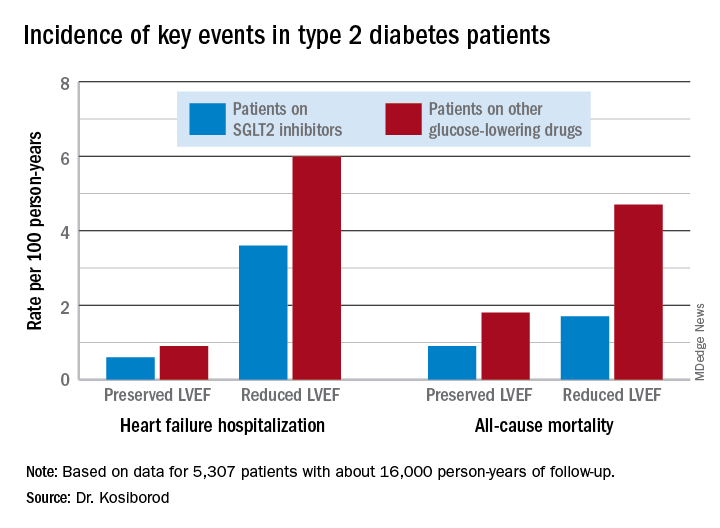
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
NEW ORLEANS – based on data from a large real-world patient registry.
“The observed beneficial effects of SGLT2 inhibitors on heart failure may extend across the range of baseline ejection fractions,” Mikhail Kosiborod, MD, observed at the annual meeting of the American College of Cardiology.
This is an important new insight. The major randomized cardiovascular outcome trials that showed lower risks of heart failure hospitalization and all-cause mortality in type 2 diabetic patients on an SGLT2 inhibitor, such as EMPA-REG OUTCOME for empagliflozin (Jardiance) and CANVAS for canagliflozin (Invokana), didn’t include information on baseline LVEF. So until now it has been unclear whether the beneficial effects of the SGLT2 inhibitors preventing heart failure hospitalization vary depending upon LVEF, explained Dr. Kosiborod, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
He presented an analysis drawn from the patient database kept by Maccabi Healthcare Services in Israel. The study included 5,307 patients with type 2 diabetes and an LVEF measurement recorded in their chart at the time they started on either empagliflozin or dapagliflozin (Farxiga) and an equal number of propensity-matched type 2 diabetic controls who started on other glucose-lowering drugs, most commonly an oral dipeptidyl peptidase-4 inhibitor.
During roughly 16,000 person-years of follow-up, 239 deaths occurred. Compared with patients on another glucose-lowering drug, the risk of death from all causes was reduced by 47% among patients who were on an SGLT2 inhibitor and had a baseline LVEF of 50% or greater and by 62% among the 9% of subjects who had a baseline LVEF less than 50%.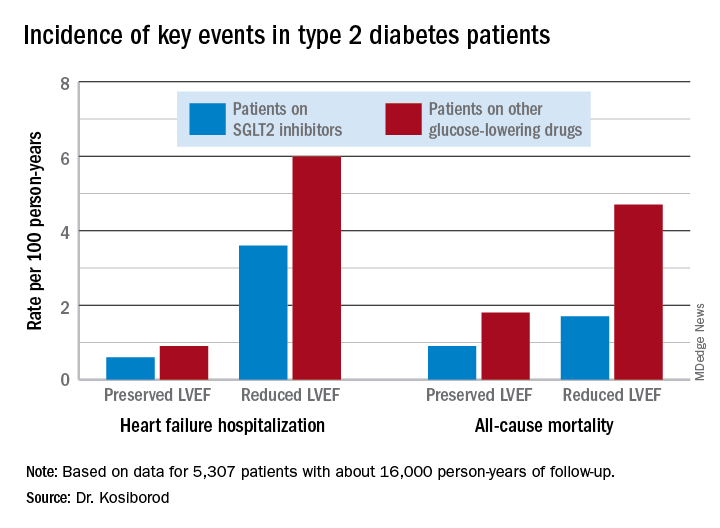
Similarly, the risk of heart failure hospitalization was reduced by 29% in SGLT2 inhibitor users with a preserved LVEF and by 27% if they had a reduced LVEF.
For the composite endpoint of heart failure hospitalization or all-cause mortality, the risk reductions associated with SGLT2 inhibitor therapy were 45% with preserved and 39% with reduced LVEF.
Session comoderator Prakash C. Deedwania, MD, noted that there are ongoing major randomized trials of various SGLT2 inhibitors in patients with known heart failure, with cardiovascular death and heart failure hospitalization as primary endpoints. He asked Dr. Kosiborod whether, given that the results of these studies aren’t in yet, he thinks clinicians should be prescribing SGLT2 inhibitors to diabetic or prediabetic patients who don’t have clinical symptoms of heart failure but may have a marker of increased risk, such as an elevated B-type natriuretic peptide.
“At least in my mind, we have more than enough evidence at this point to say that SGLT2 inhibitors are effective in preventing heart failure,” Dr. Kosiborod replied.
“Obviously, if your risk for developing a condition is higher at baseline, then the absolute benefit that you’re going to get from using an agent that’s effective in preventing that event is going to be higher and the number needed to treat is going to be lower. So if you have a patient at high risk for heart failure by whatever risk predictor you’re using and the patient doesn’t yet have heart failure but does have diabetes, which is already a risk factor for heart failure, I think we have pretty solid data now that SGLT2 inhibitors will likely be effective in preventing heart failure in that kind of patient population. But I don’t think we have definitive data at this point to say that the drugs are effective in treating heart failure in people who already have a manifest clinical syndrome of heart failure, which is why we’re doing all these clinical trials now,” he continued.
Dr. Deedwania urged audience members to make the effort to become comfortable in prescribing SGLT2 inhibitors for their patients with type 2 diabetes.
“Many different surveys show that these drugs are not being utilized effectively by cardiologists,” noted Dr. Deedwania, professor of medicine at the University of California, San Francisco, and director of the heart failure program at the university’s Fresno campus.
“As cardiologists, we may not want to own diabetes, but we at least have to feel that we have the ownership of treating the diabetic patient with cardiovascular disease with appropriate drugs. We don’t need to depend on endocrinologists because if we do these patients may become lost,” he said.
Dr. Kosiborod concurred, citing evidence that diabetic patients with cardiovascular disease are much more likely to see a cardiologist than an endocrinologist in the course of usual care.
“There’s definitely a golden opportunity here to intervene to reduce risk,” he said.
Dr. Kosiborod reported serving as a consultant to roughly a dozen pharmaceutical companies.
SOURCE: Kosiborod M. ACC 19, Abstract #1024-07.
REPORTING FROM ACC 19
Quick Byte: Hope for HF patients
A new device shows promise for heart failure patients, according to a recent study.
In a trial, 614 patients with severe heart failure were randomly assigned to receive standard medical treatment and a MitraClip, which helps repair the damaged mitral valve, or to receive medical treatment alone.
Among those who received only medical treatment, 151 were hospitalized for heart failure in the ensuing 2 years and 61 died. Among those who got the device, 92 were hospitalized for heart failure during the same period and 28 died.
Reference
1. Kolata G. Tiny Device is a ‘Huge Advance’ for Treatment of Severe Heart Failure. New York Times. Sept 23, 2018. https://www.nytimes.com/2018/09/23/health/heart-failure-valve-repair-microclip.html. Accessed Oct 10, 2018.
A new device shows promise for heart failure patients, according to a recent study.
In a trial, 614 patients with severe heart failure were randomly assigned to receive standard medical treatment and a MitraClip, which helps repair the damaged mitral valve, or to receive medical treatment alone.
Among those who received only medical treatment, 151 were hospitalized for heart failure in the ensuing 2 years and 61 died. Among those who got the device, 92 were hospitalized for heart failure during the same period and 28 died.
Reference
1. Kolata G. Tiny Device is a ‘Huge Advance’ for Treatment of Severe Heart Failure. New York Times. Sept 23, 2018. https://www.nytimes.com/2018/09/23/health/heart-failure-valve-repair-microclip.html. Accessed Oct 10, 2018.
A new device shows promise for heart failure patients, according to a recent study.
In a trial, 614 patients with severe heart failure were randomly assigned to receive standard medical treatment and a MitraClip, which helps repair the damaged mitral valve, or to receive medical treatment alone.
Among those who received only medical treatment, 151 were hospitalized for heart failure in the ensuing 2 years and 61 died. Among those who got the device, 92 were hospitalized for heart failure during the same period and 28 died.
Reference
1. Kolata G. Tiny Device is a ‘Huge Advance’ for Treatment of Severe Heart Failure. New York Times. Sept 23, 2018. https://www.nytimes.com/2018/09/23/health/heart-failure-valve-repair-microclip.html. Accessed Oct 10, 2018.
Does withholding an ACE inhibitor or ARB before surgery improve outcomes?
EVIDENCE SUMMARY
An international prospective cohort study analyzed data from 14,687 patients, 4802 of whom were on an ACEI or ARB, to study the effect on 30-day morbidity and mortality of withholding the medications 24 hours before a noncardiac surgery.1 Of the ACEI or ARB users, 26% (1245) withheld their medication and 3557 continued it 24 hours before surgery.
Large study shows benefit in withholding meds
Patients who withheld the ACEI or ARB were less likely to experience the primary composite outcome of all-cause death, stroke, or myocardial injury (150/1245 [12%] vs 459/3557 [12.9%]; adjusted relative risk [RR] = 0.82; 95% confidence interval [CI], 0.70-0.96; P = .01; number needed to treat [NNT] = 116) and intraoperative hypotension (adjusted RR = 0.80; 95% CI, 0.72-0.93; P < .001; NNT = 18). For the NNT calculation, which the investigators didn’t perform, the treatment is the number needed to withhold an ACEI or ARB to show benefit.
Smaller, weaker studies yield different results
A retrospective cohort analysis of propensity-matched ACEI users with ACEI nonusers (9028 in each group) undergoing noncardiac surgery compared intra- and postoperative respiratory complications or mortality.2 The study found no association with either 30-day mortality (odds ratio [OR] = 0.93; 95% CI, 0.73-1.19) or the composite of in-hospital morbidity and mortality (OR = 1.06; 95% CI, 0.97-1.15). Limitations included comparison of users with nonusers as opposed to an intention-to-withhold study, the retrospective nature of the study, and the fact that outcomes were gathered from ICD-9 billing codes rather than obtained prospectively.
A Cochrane review assessed the benefits and harms of perioperative ACEIs or ARBs on mortality and morbidity in adults undergoing any type of surgery.3 Seven RCTs with a total of 571 participants were included in the review. Overall, the review didn’t find evidence to support prevention of mortality, morbidity, and complications by perioperative ACEIs or ARBs because the included studies were of low and very low methodological quality, had a high risk for bias, and lacked power. Moreover, the review didn’t assess the effect of withholding ACEIs or ARBs before surgery.
A random-effects meta-analysis of 5 studies (3 randomized trials and 2 observational studies) totaling 434 patients suggested that patients receiving ACEIs or ARBs immediately before surgery were more likely to develop hypotension requiring vasopressors (RR = 1.50; 95% CI, 1.15-1.96).4 Sufficient data weren’t available to assess other outcomes, and the included studies were relatively small and generally not powered to observe clinically significant consequences nor designed to measure the incidence of patient-important outcomes.
Continue to: RECOMMENDATIONS
RECOMMENDATIONS
The 2014 American College of Cardiology/American Heart Association Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery states that continuing ACEIs or ARBs perioperatively is reasonable (class IIa recommendation [moderate benefit of treatment relative to risk]; level of evidence [LOE], B [data from limited populations and single randomized or nonrandomized trials]). 5
The guideline also recommends that if ACEIs or ARBs are held before surgery, it is reasonable to restart them as soon as clinically feasible postoperatively (class IIa recommendation; LOE, C [data from very limited populations and consensus opinion or case studies]).
Editor’s Takeaway
The results of the large prospective cohort contradict those of previous smaller, methodologically weaker studies, and the new findings should be taken seriously.1 Nevertheless, selection bias (why did investigators stop the ACEI?) remains. Until we have a large RCT, the preop question to ask may be why not stop the ACEI?
1. Roshanov PS, Rochwerg B, Patel A, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the Vascular Events in Noncardiac Surgery Patients Cohort Evaluation prospective cohort. Anesthesiology. 2017;126:16-27.
2. Turan A, You J, Shiba A, et al. Angiotensin converting enzyme inhibitors are not associated with respiratory complications or mortality after noncardiac surgery. Anesth Analg. 2012;114:552-560.
3. Zou Z, Yuan HB, Yang B, et al. Perioperative angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers for preventing mortality and morbidity in adults. Cochrane Database Syst Rev. 2016;(1):CD009210.
4. Rosenman DJ, McDonald FS, Ebbert JO, et al. Clinical consequences of withholding versus administering renin-angiotensin-aldosterone system antagonists in the preoperative period. J Hosp Med. 2008;3:319-325.
5. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 2014;130:e278-e333.
EVIDENCE SUMMARY
An international prospective cohort study analyzed data from 14,687 patients, 4802 of whom were on an ACEI or ARB, to study the effect on 30-day morbidity and mortality of withholding the medications 24 hours before a noncardiac surgery.1 Of the ACEI or ARB users, 26% (1245) withheld their medication and 3557 continued it 24 hours before surgery.
Large study shows benefit in withholding meds
Patients who withheld the ACEI or ARB were less likely to experience the primary composite outcome of all-cause death, stroke, or myocardial injury (150/1245 [12%] vs 459/3557 [12.9%]; adjusted relative risk [RR] = 0.82; 95% confidence interval [CI], 0.70-0.96; P = .01; number needed to treat [NNT] = 116) and intraoperative hypotension (adjusted RR = 0.80; 95% CI, 0.72-0.93; P < .001; NNT = 18). For the NNT calculation, which the investigators didn’t perform, the treatment is the number needed to withhold an ACEI or ARB to show benefit.
Smaller, weaker studies yield different results
A retrospective cohort analysis of propensity-matched ACEI users with ACEI nonusers (9028 in each group) undergoing noncardiac surgery compared intra- and postoperative respiratory complications or mortality.2 The study found no association with either 30-day mortality (odds ratio [OR] = 0.93; 95% CI, 0.73-1.19) or the composite of in-hospital morbidity and mortality (OR = 1.06; 95% CI, 0.97-1.15). Limitations included comparison of users with nonusers as opposed to an intention-to-withhold study, the retrospective nature of the study, and the fact that outcomes were gathered from ICD-9 billing codes rather than obtained prospectively.
A Cochrane review assessed the benefits and harms of perioperative ACEIs or ARBs on mortality and morbidity in adults undergoing any type of surgery.3 Seven RCTs with a total of 571 participants were included in the review. Overall, the review didn’t find evidence to support prevention of mortality, morbidity, and complications by perioperative ACEIs or ARBs because the included studies were of low and very low methodological quality, had a high risk for bias, and lacked power. Moreover, the review didn’t assess the effect of withholding ACEIs or ARBs before surgery.
A random-effects meta-analysis of 5 studies (3 randomized trials and 2 observational studies) totaling 434 patients suggested that patients receiving ACEIs or ARBs immediately before surgery were more likely to develop hypotension requiring vasopressors (RR = 1.50; 95% CI, 1.15-1.96).4 Sufficient data weren’t available to assess other outcomes, and the included studies were relatively small and generally not powered to observe clinically significant consequences nor designed to measure the incidence of patient-important outcomes.
Continue to: RECOMMENDATIONS
RECOMMENDATIONS
The 2014 American College of Cardiology/American Heart Association Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery states that continuing ACEIs or ARBs perioperatively is reasonable (class IIa recommendation [moderate benefit of treatment relative to risk]; level of evidence [LOE], B [data from limited populations and single randomized or nonrandomized trials]). 5
The guideline also recommends that if ACEIs or ARBs are held before surgery, it is reasonable to restart them as soon as clinically feasible postoperatively (class IIa recommendation; LOE, C [data from very limited populations and consensus opinion or case studies]).
Editor’s Takeaway
The results of the large prospective cohort contradict those of previous smaller, methodologically weaker studies, and the new findings should be taken seriously.1 Nevertheless, selection bias (why did investigators stop the ACEI?) remains. Until we have a large RCT, the preop question to ask may be why not stop the ACEI?
EVIDENCE SUMMARY
An international prospective cohort study analyzed data from 14,687 patients, 4802 of whom were on an ACEI or ARB, to study the effect on 30-day morbidity and mortality of withholding the medications 24 hours before a noncardiac surgery.1 Of the ACEI or ARB users, 26% (1245) withheld their medication and 3557 continued it 24 hours before surgery.
Large study shows benefit in withholding meds
Patients who withheld the ACEI or ARB were less likely to experience the primary composite outcome of all-cause death, stroke, or myocardial injury (150/1245 [12%] vs 459/3557 [12.9%]; adjusted relative risk [RR] = 0.82; 95% confidence interval [CI], 0.70-0.96; P = .01; number needed to treat [NNT] = 116) and intraoperative hypotension (adjusted RR = 0.80; 95% CI, 0.72-0.93; P < .001; NNT = 18). For the NNT calculation, which the investigators didn’t perform, the treatment is the number needed to withhold an ACEI or ARB to show benefit.
Smaller, weaker studies yield different results
A retrospective cohort analysis of propensity-matched ACEI users with ACEI nonusers (9028 in each group) undergoing noncardiac surgery compared intra- and postoperative respiratory complications or mortality.2 The study found no association with either 30-day mortality (odds ratio [OR] = 0.93; 95% CI, 0.73-1.19) or the composite of in-hospital morbidity and mortality (OR = 1.06; 95% CI, 0.97-1.15). Limitations included comparison of users with nonusers as opposed to an intention-to-withhold study, the retrospective nature of the study, and the fact that outcomes were gathered from ICD-9 billing codes rather than obtained prospectively.
A Cochrane review assessed the benefits and harms of perioperative ACEIs or ARBs on mortality and morbidity in adults undergoing any type of surgery.3 Seven RCTs with a total of 571 participants were included in the review. Overall, the review didn’t find evidence to support prevention of mortality, morbidity, and complications by perioperative ACEIs or ARBs because the included studies were of low and very low methodological quality, had a high risk for bias, and lacked power. Moreover, the review didn’t assess the effect of withholding ACEIs or ARBs before surgery.
A random-effects meta-analysis of 5 studies (3 randomized trials and 2 observational studies) totaling 434 patients suggested that patients receiving ACEIs or ARBs immediately before surgery were more likely to develop hypotension requiring vasopressors (RR = 1.50; 95% CI, 1.15-1.96).4 Sufficient data weren’t available to assess other outcomes, and the included studies were relatively small and generally not powered to observe clinically significant consequences nor designed to measure the incidence of patient-important outcomes.
Continue to: RECOMMENDATIONS
RECOMMENDATIONS
The 2014 American College of Cardiology/American Heart Association Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery states that continuing ACEIs or ARBs perioperatively is reasonable (class IIa recommendation [moderate benefit of treatment relative to risk]; level of evidence [LOE], B [data from limited populations and single randomized or nonrandomized trials]). 5
The guideline also recommends that if ACEIs or ARBs are held before surgery, it is reasonable to restart them as soon as clinically feasible postoperatively (class IIa recommendation; LOE, C [data from very limited populations and consensus opinion or case studies]).
Editor’s Takeaway
The results of the large prospective cohort contradict those of previous smaller, methodologically weaker studies, and the new findings should be taken seriously.1 Nevertheless, selection bias (why did investigators stop the ACEI?) remains. Until we have a large RCT, the preop question to ask may be why not stop the ACEI?
1. Roshanov PS, Rochwerg B, Patel A, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the Vascular Events in Noncardiac Surgery Patients Cohort Evaluation prospective cohort. Anesthesiology. 2017;126:16-27.
2. Turan A, You J, Shiba A, et al. Angiotensin converting enzyme inhibitors are not associated with respiratory complications or mortality after noncardiac surgery. Anesth Analg. 2012;114:552-560.
3. Zou Z, Yuan HB, Yang B, et al. Perioperative angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers for preventing mortality and morbidity in adults. Cochrane Database Syst Rev. 2016;(1):CD009210.
4. Rosenman DJ, McDonald FS, Ebbert JO, et al. Clinical consequences of withholding versus administering renin-angiotensin-aldosterone system antagonists in the preoperative period. J Hosp Med. 2008;3:319-325.
5. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 2014;130:e278-e333.
1. Roshanov PS, Rochwerg B, Patel A, et al. Withholding versus continuing angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers before noncardiac surgery: an analysis of the Vascular Events in Noncardiac Surgery Patients Cohort Evaluation prospective cohort. Anesthesiology. 2017;126:16-27.
2. Turan A, You J, Shiba A, et al. Angiotensin converting enzyme inhibitors are not associated with respiratory complications or mortality after noncardiac surgery. Anesth Analg. 2012;114:552-560.
3. Zou Z, Yuan HB, Yang B, et al. Perioperative angiotensin-converting enzyme inhibitors or angiotensin II type 1 receptor blockers for preventing mortality and morbidity in adults. Cochrane Database Syst Rev. 2016;(1):CD009210.
4. Rosenman DJ, McDonald FS, Ebbert JO, et al. Clinical consequences of withholding versus administering renin-angiotensin-aldosterone system antagonists in the preoperative period. J Hosp Med. 2008;3:319-325.
5. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 2014;130:e278-e333.
EVIDENCE-BASED ANSWER:
A guarded yes, because the evidence of benefit is from observational studies and applies to noncardiac surgery. Withholding angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) 24 hours before noncardiac surgery has been associated with a 30-day lower risk for all-cause death, stroke, myocardial injury, and intraoperative hypotension (18% adjusted relative risk reduction).
The finding is based on 1 international prospective cohort study and, of note, is an association and a likelihood of benefit. Confirmation would require a large randomized trial (RCT; strength of recommendation [SOR]: B, good-quality international prospective cohort study).
Guidelines are not mandates
Just like the 2018 hypertension treatment guidelines, the 2018 Guidelines on the Management of Blood Cholesterol developed by the American College of Cardiology and the American Heart Association (ACC/AHA) have made treatment decisions much more complicated. In this issue of JFP, Wójcik and Shapiro summarize the 70-page document to help family physicians and other primary health care professionals use these complex guidelines in everyday practice.
The good news is that not much has changed from the 2013 ACC/AHA cholesterol guidelines regarding the treatment of patients with established cardiovascular disease and diabetes mellitus, and those with familial hyperlipidemia—the groups at highest risk for major cardiovascular events. Most of these patients should be treated aggressively, and a target low-density lipoprotein of 70 mg/dL is recommended.
The new guidelines recommend using ezetimibe or a PCSK9 inhibitor if the goal of 70 mg/dL cannot be achieved with a statin alone. There is randomized trial evidence to support the benefit of this aggressive approach. Generic ezetimibe costs about $20 per month,1 but the PCSK9 inhibitors are about $500 per month,2,3 so cost may be a treatment barrier for the 2 monoclonal antibodies approved for cardiovascular prevention: evolocumab and alirocumab.
For primary prevention, the new guidelines are much more complicated. They divide cardiovascular risk into 4 tiers depending on the 10-year risk for atherosclerotic cardiovascular disease calculated using the “pooled cohort equation.” Treatment recommendations are more aggressive for those at higher risk. Although it intuitively makes sense to treat those at higher risk more aggressively, there is no clinical trial evidence to support this approach’s superiority over the simpler approach recommended in the 2013 guidelines.
I find the recommendations for screening and primary prevention in adults ages 75 and older and for children and teens to be problematic. A meta-analysis of 28 studies found no statin treatment benefit for primary prevention in those older than 70.4 And there are no randomized trials showing benefit of screening and treating children and teens for hyperlipidemia.
On a positive note, most patients do not need to fast prior to having their lipids measured.
Read the 2018 cholesterol treatment guideline summary in this issue of JFP. But as you do so, remember that guidelines are guidelines; they are not mandates for treatment. You may need to customize these guidelines for your practice and your patients. In my opinion, the simpler 2013 cholesterol guidelines remain good guidelines.
1. Ezetimibe prices. GoodRx. www.goodrx.com/ezetimibe. Accessed April 24, 2019.
2. Dangi-Garimella S. Amgen announces 60% reduction in list price of PCSK9 inhibitor evolocumab. AJMC. October 24, 2018. https://www.ajmc.com/newsroom/amgen-announces-60-reduction-in-list-price-of-pcsk9-inhibitor-evolocumab. Accessed May 1, 2019.
3. Kuchler H. Sanofi and Regeneron cut price of Praluent by 60%. Financial Times. February 11, 2019. https://www.ft.com/content/d1b34cca-2e18-11e9-8744-e7016697f225. Accessed May 1, 2019.
4. Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomized controlled trials. Lancet. 2019;393:407-415.
Just like the 2018 hypertension treatment guidelines, the 2018 Guidelines on the Management of Blood Cholesterol developed by the American College of Cardiology and the American Heart Association (ACC/AHA) have made treatment decisions much more complicated. In this issue of JFP, Wójcik and Shapiro summarize the 70-page document to help family physicians and other primary health care professionals use these complex guidelines in everyday practice.
The good news is that not much has changed from the 2013 ACC/AHA cholesterol guidelines regarding the treatment of patients with established cardiovascular disease and diabetes mellitus, and those with familial hyperlipidemia—the groups at highest risk for major cardiovascular events. Most of these patients should be treated aggressively, and a target low-density lipoprotein of 70 mg/dL is recommended.
The new guidelines recommend using ezetimibe or a PCSK9 inhibitor if the goal of 70 mg/dL cannot be achieved with a statin alone. There is randomized trial evidence to support the benefit of this aggressive approach. Generic ezetimibe costs about $20 per month,1 but the PCSK9 inhibitors are about $500 per month,2,3 so cost may be a treatment barrier for the 2 monoclonal antibodies approved for cardiovascular prevention: evolocumab and alirocumab.
For primary prevention, the new guidelines are much more complicated. They divide cardiovascular risk into 4 tiers depending on the 10-year risk for atherosclerotic cardiovascular disease calculated using the “pooled cohort equation.” Treatment recommendations are more aggressive for those at higher risk. Although it intuitively makes sense to treat those at higher risk more aggressively, there is no clinical trial evidence to support this approach’s superiority over the simpler approach recommended in the 2013 guidelines.
I find the recommendations for screening and primary prevention in adults ages 75 and older and for children and teens to be problematic. A meta-analysis of 28 studies found no statin treatment benefit for primary prevention in those older than 70.4 And there are no randomized trials showing benefit of screening and treating children and teens for hyperlipidemia.
On a positive note, most patients do not need to fast prior to having their lipids measured.
Read the 2018 cholesterol treatment guideline summary in this issue of JFP. But as you do so, remember that guidelines are guidelines; they are not mandates for treatment. You may need to customize these guidelines for your practice and your patients. In my opinion, the simpler 2013 cholesterol guidelines remain good guidelines.
Just like the 2018 hypertension treatment guidelines, the 2018 Guidelines on the Management of Blood Cholesterol developed by the American College of Cardiology and the American Heart Association (ACC/AHA) have made treatment decisions much more complicated. In this issue of JFP, Wójcik and Shapiro summarize the 70-page document to help family physicians and other primary health care professionals use these complex guidelines in everyday practice.
The good news is that not much has changed from the 2013 ACC/AHA cholesterol guidelines regarding the treatment of patients with established cardiovascular disease and diabetes mellitus, and those with familial hyperlipidemia—the groups at highest risk for major cardiovascular events. Most of these patients should be treated aggressively, and a target low-density lipoprotein of 70 mg/dL is recommended.
The new guidelines recommend using ezetimibe or a PCSK9 inhibitor if the goal of 70 mg/dL cannot be achieved with a statin alone. There is randomized trial evidence to support the benefit of this aggressive approach. Generic ezetimibe costs about $20 per month,1 but the PCSK9 inhibitors are about $500 per month,2,3 so cost may be a treatment barrier for the 2 monoclonal antibodies approved for cardiovascular prevention: evolocumab and alirocumab.
For primary prevention, the new guidelines are much more complicated. They divide cardiovascular risk into 4 tiers depending on the 10-year risk for atherosclerotic cardiovascular disease calculated using the “pooled cohort equation.” Treatment recommendations are more aggressive for those at higher risk. Although it intuitively makes sense to treat those at higher risk more aggressively, there is no clinical trial evidence to support this approach’s superiority over the simpler approach recommended in the 2013 guidelines.
I find the recommendations for screening and primary prevention in adults ages 75 and older and for children and teens to be problematic. A meta-analysis of 28 studies found no statin treatment benefit for primary prevention in those older than 70.4 And there are no randomized trials showing benefit of screening and treating children and teens for hyperlipidemia.
On a positive note, most patients do not need to fast prior to having their lipids measured.
Read the 2018 cholesterol treatment guideline summary in this issue of JFP. But as you do so, remember that guidelines are guidelines; they are not mandates for treatment. You may need to customize these guidelines for your practice and your patients. In my opinion, the simpler 2013 cholesterol guidelines remain good guidelines.
1. Ezetimibe prices. GoodRx. www.goodrx.com/ezetimibe. Accessed April 24, 2019.
2. Dangi-Garimella S. Amgen announces 60% reduction in list price of PCSK9 inhibitor evolocumab. AJMC. October 24, 2018. https://www.ajmc.com/newsroom/amgen-announces-60-reduction-in-list-price-of-pcsk9-inhibitor-evolocumab. Accessed May 1, 2019.
3. Kuchler H. Sanofi and Regeneron cut price of Praluent by 60%. Financial Times. February 11, 2019. https://www.ft.com/content/d1b34cca-2e18-11e9-8744-e7016697f225. Accessed May 1, 2019.
4. Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomized controlled trials. Lancet. 2019;393:407-415.
1. Ezetimibe prices. GoodRx. www.goodrx.com/ezetimibe. Accessed April 24, 2019.
2. Dangi-Garimella S. Amgen announces 60% reduction in list price of PCSK9 inhibitor evolocumab. AJMC. October 24, 2018. https://www.ajmc.com/newsroom/amgen-announces-60-reduction-in-list-price-of-pcsk9-inhibitor-evolocumab. Accessed May 1, 2019.
3. Kuchler H. Sanofi and Regeneron cut price of Praluent by 60%. Financial Times. February 11, 2019. https://www.ft.com/content/d1b34cca-2e18-11e9-8744-e7016697f225. Accessed May 1, 2019.
4. Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of statin therapy in older people: a meta-analysis of individual participant data from 28 randomized controlled trials. Lancet. 2019;393:407-415.
2019 USPSTF update
Over the past year through early 2019, the US Preventive Services Task Force made 34 recommendations on 19 different topics. Twenty-six were reaffirmations of recommendations made in previous years (TABLE 11); the Task Force attempts to reassess topics every 7 years. Two new topics were addressed with 2 new recommendations, and 6 previous recommendations were revised or reversed (TABLE 22-9).
This Practice Alert discusses the new and the changed recommendations. (In 2018, the Practice Alert podcast series covered screening for ovarian cancer [April], prostate cancer [June], and cervical cancer [October], and EKG screening for cardiovascular disease [November].) All current Task Force recommendations are available on the USPSTF Web site.1
New topics
Perinatal depression prevention
The Task Force recommends that clinicians counsel pregnant women and women in the first year postpartum who are at increased risk for perinatal depression, or refer for such services. The recommendation applies to those who are not diagnosed with depression but are at increased risk.
Perinatal depression can negatively affect both mother and child in several ways and occurs at a rate close to 9% during pregnancy and 37% during the first year postpartum.2 The interventions studied by the Task Force included cognitive behavioral therapy and interpersonal therapy; most sessions were initiated in the second trimester of pregnancy and varied in number of sessions and intensity. The Task Force includes the following in the list of risks that should prompt a referral: a history of depression, current depressive symptoms that fall short of that needed for a depression diagnosis, low income, adolescent or single parenthood, recent intimate partner violence, elevated anxiety symptoms, physical or sexual abuse, or a history of significant negative life events. (See “Postpartum anxiety: More common than you think,” in the April issue.)
Atrial fibrillation
The Task Force found insufficient evidence to recommend for or against the use of electrocardiography (EKG) to screen for atrial fibrillation (AF).3
Revisions of previous recommendations
Cervical cancer screening
Skin cancer prevention
The Task Force made 2 revisions to the 2012 recommendation on preventing skin cancer through behavioral counseling to avoid ultraviolet (UV) radiation.6 These recommendations continue to focus on those with fair skin. The first revision: The earliest age at which children (through their guardians) can benefit from counseling on UV avoidance has been lowered from age 10 years to 6 months. The second revision: Some adults older than age 24 can also benefit from such counseling if they have fair skin and other skin cancer risks such as using tanning beds, having a history of sunburns or previous skin cancer, having an increased number of nevi (moles) and atypical nevi, having human immunodeficiency virus (HIV) infection, having received an organ transplant, or having a family history of skin cancer.
Continue to: Those at risk...
Those at risk can reduce their chances of skin cancer by using broad-spectrum sunscreens and sun-protective clothing, and by avoiding sun exposure and indoor tanning beds.
Fall prevention
In a reversal of its 2012 recommendation, the Task Force now recommends against the use of vitamin D supplementation to prevent falls in community-dwelling adults 65 years or older.7 In a reanalysis of previous studies on this topic, along with new evidence, the Task Force concluded that vitamin D supplementation offers no benefit for preventing falls in adults who are not vitamin D deficient.
Screening for scoliosis in adolescents
In 2004 the USPSTF recommended against screening for idiopathic scoliosis in children and adolescents 10 to 18 years of age. In its most recent review, the Task Force continued to find no direct evidence of the benefit of screening and inadequate evidence on the long-term benefits of reduction in spinal curvature through exercise, surgery, and bracing. However, following a reanalysis of the potential harms of these treatments and the use of a new analytic framework, the Task Force concluded it is not possible at this time to assess the balance of benefits and harms of screening.8
Prostate cancer screening
In its most controversial action, the Task Force reversed its 2012 recommendation against routine prostate-specific antigen–based screening for prostate cancer in men ages 55 to 69 years and now lists this as a “C” recommendation.9 The potential benefits of screening include preventing 1.3 deaths from prostate cancer per 1000 men screened over 13 years and approximately 3 cases of metastatic prostate cancer. However, no trials have found a reduction in all-cause mortality from screening. Contrast that with the known harms of screening: 15% false positive results over 10 years; 1% hospitalization rate among those undergoing a prostate biopsy; over-diagnosis and resultant treatment of 20% to 50% of men diagnosed with prostate cancer through screening; and incontinence and erectile dysfunction in 20% and 67%, respectively, of men following prostatectomy.9
Based on these outcomes, the Task Force “does not recommend screening for prostate cancer unless men express a preference for screening after being informed of and understanding the benefits and risks.”9 The Task Force continues to recommend against screening men ages 70 years and older.
Continue to: The change in this recommendation...
The change in this recommendation and its wording present dilemmas for family physicians: whether to discuss potential screening with all men ages 55 to 69; to selectively discuss it with those at high risk (principally African Americans and those with a strong family history of prostate cancer); or to address the issue only if a patient asks about it. In addition, if a man requests screening, how often should it be performed? Most clinical trials have found equal benefit from testing less frequently than every year, with fewer harms. The Task Force provided little or no guidance on these issues.
Final advice: D recommendations
The Task Force reaffirmed that 7 services have either no benefit or cause more harm than benefit (TABLE 11). Family physicians should be familiar with these services, as well as all Task Force D recommendations, and avoid recommending them or providing them. High quality preventive care involves both providing services of proven benefit and avoiding those that do not.
1. USPSTF. Published recommendations. https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations. Accessed March 25, 2019.
2. USPSTF. Final recommendation statement. Perinatal depression: preventive interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/perinatal-depression-preventive-interventions. Accessed March 25, 2019.
3. USPSTF. Atrial fibrillation: screening with electrocardiography. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/atrial-fibrillation-screening-with-electrocardiography. Accessed March 25, 2019.
4. USPSTF. Screening for atrial fibrillation with electrocardiography. JAMA. 2018;320:478-484.
5. USPSTF. Cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening2. Accessed March 25, 2019.
6. USPSTF. Skin cancer prevention: behavioral counseling. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/skin-cancer-counseling2. Accessed March 25, 2019.
7. USPSTF. Falls prevention in community-dwelling older adults: interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/falls-prevention-in-older-adults-interventions1. Accessed March 25, 2019.
8. USPSTF. Adolescent idiopathic scoliosis: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/adolescent-idiopathic-scoliosis-screening1. Accessed March 25, 2019.
9. USPSTF. Prostate cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prostate-cancer-screening1#consider. Accessed March 25, 2019.
Over the past year through early 2019, the US Preventive Services Task Force made 34 recommendations on 19 different topics. Twenty-six were reaffirmations of recommendations made in previous years (TABLE 11); the Task Force attempts to reassess topics every 7 years. Two new topics were addressed with 2 new recommendations, and 6 previous recommendations were revised or reversed (TABLE 22-9).
This Practice Alert discusses the new and the changed recommendations. (In 2018, the Practice Alert podcast series covered screening for ovarian cancer [April], prostate cancer [June], and cervical cancer [October], and EKG screening for cardiovascular disease [November].) All current Task Force recommendations are available on the USPSTF Web site.1
New topics
Perinatal depression prevention
The Task Force recommends that clinicians counsel pregnant women and women in the first year postpartum who are at increased risk for perinatal depression, or refer for such services. The recommendation applies to those who are not diagnosed with depression but are at increased risk.
Perinatal depression can negatively affect both mother and child in several ways and occurs at a rate close to 9% during pregnancy and 37% during the first year postpartum.2 The interventions studied by the Task Force included cognitive behavioral therapy and interpersonal therapy; most sessions were initiated in the second trimester of pregnancy and varied in number of sessions and intensity. The Task Force includes the following in the list of risks that should prompt a referral: a history of depression, current depressive symptoms that fall short of that needed for a depression diagnosis, low income, adolescent or single parenthood, recent intimate partner violence, elevated anxiety symptoms, physical or sexual abuse, or a history of significant negative life events. (See “Postpartum anxiety: More common than you think,” in the April issue.)
Atrial fibrillation
The Task Force found insufficient evidence to recommend for or against the use of electrocardiography (EKG) to screen for atrial fibrillation (AF).3
Revisions of previous recommendations
Cervical cancer screening
Skin cancer prevention
The Task Force made 2 revisions to the 2012 recommendation on preventing skin cancer through behavioral counseling to avoid ultraviolet (UV) radiation.6 These recommendations continue to focus on those with fair skin. The first revision: The earliest age at which children (through their guardians) can benefit from counseling on UV avoidance has been lowered from age 10 years to 6 months. The second revision: Some adults older than age 24 can also benefit from such counseling if they have fair skin and other skin cancer risks such as using tanning beds, having a history of sunburns or previous skin cancer, having an increased number of nevi (moles) and atypical nevi, having human immunodeficiency virus (HIV) infection, having received an organ transplant, or having a family history of skin cancer.
Continue to: Those at risk...
Those at risk can reduce their chances of skin cancer by using broad-spectrum sunscreens and sun-protective clothing, and by avoiding sun exposure and indoor tanning beds.
Fall prevention
In a reversal of its 2012 recommendation, the Task Force now recommends against the use of vitamin D supplementation to prevent falls in community-dwelling adults 65 years or older.7 In a reanalysis of previous studies on this topic, along with new evidence, the Task Force concluded that vitamin D supplementation offers no benefit for preventing falls in adults who are not vitamin D deficient.
Screening for scoliosis in adolescents
In 2004 the USPSTF recommended against screening for idiopathic scoliosis in children and adolescents 10 to 18 years of age. In its most recent review, the Task Force continued to find no direct evidence of the benefit of screening and inadequate evidence on the long-term benefits of reduction in spinal curvature through exercise, surgery, and bracing. However, following a reanalysis of the potential harms of these treatments and the use of a new analytic framework, the Task Force concluded it is not possible at this time to assess the balance of benefits and harms of screening.8
Prostate cancer screening
In its most controversial action, the Task Force reversed its 2012 recommendation against routine prostate-specific antigen–based screening for prostate cancer in men ages 55 to 69 years and now lists this as a “C” recommendation.9 The potential benefits of screening include preventing 1.3 deaths from prostate cancer per 1000 men screened over 13 years and approximately 3 cases of metastatic prostate cancer. However, no trials have found a reduction in all-cause mortality from screening. Contrast that with the known harms of screening: 15% false positive results over 10 years; 1% hospitalization rate among those undergoing a prostate biopsy; over-diagnosis and resultant treatment of 20% to 50% of men diagnosed with prostate cancer through screening; and incontinence and erectile dysfunction in 20% and 67%, respectively, of men following prostatectomy.9
Based on these outcomes, the Task Force “does not recommend screening for prostate cancer unless men express a preference for screening after being informed of and understanding the benefits and risks.”9 The Task Force continues to recommend against screening men ages 70 years and older.
Continue to: The change in this recommendation...
The change in this recommendation and its wording present dilemmas for family physicians: whether to discuss potential screening with all men ages 55 to 69; to selectively discuss it with those at high risk (principally African Americans and those with a strong family history of prostate cancer); or to address the issue only if a patient asks about it. In addition, if a man requests screening, how often should it be performed? Most clinical trials have found equal benefit from testing less frequently than every year, with fewer harms. The Task Force provided little or no guidance on these issues.
Final advice: D recommendations
The Task Force reaffirmed that 7 services have either no benefit or cause more harm than benefit (TABLE 11). Family physicians should be familiar with these services, as well as all Task Force D recommendations, and avoid recommending them or providing them. High quality preventive care involves both providing services of proven benefit and avoiding those that do not.
Over the past year through early 2019, the US Preventive Services Task Force made 34 recommendations on 19 different topics. Twenty-six were reaffirmations of recommendations made in previous years (TABLE 11); the Task Force attempts to reassess topics every 7 years. Two new topics were addressed with 2 new recommendations, and 6 previous recommendations were revised or reversed (TABLE 22-9).
This Practice Alert discusses the new and the changed recommendations. (In 2018, the Practice Alert podcast series covered screening for ovarian cancer [April], prostate cancer [June], and cervical cancer [October], and EKG screening for cardiovascular disease [November].) All current Task Force recommendations are available on the USPSTF Web site.1
New topics
Perinatal depression prevention
The Task Force recommends that clinicians counsel pregnant women and women in the first year postpartum who are at increased risk for perinatal depression, or refer for such services. The recommendation applies to those who are not diagnosed with depression but are at increased risk.
Perinatal depression can negatively affect both mother and child in several ways and occurs at a rate close to 9% during pregnancy and 37% during the first year postpartum.2 The interventions studied by the Task Force included cognitive behavioral therapy and interpersonal therapy; most sessions were initiated in the second trimester of pregnancy and varied in number of sessions and intensity. The Task Force includes the following in the list of risks that should prompt a referral: a history of depression, current depressive symptoms that fall short of that needed for a depression diagnosis, low income, adolescent or single parenthood, recent intimate partner violence, elevated anxiety symptoms, physical or sexual abuse, or a history of significant negative life events. (See “Postpartum anxiety: More common than you think,” in the April issue.)
Atrial fibrillation
The Task Force found insufficient evidence to recommend for or against the use of electrocardiography (EKG) to screen for atrial fibrillation (AF).3
Revisions of previous recommendations
Cervical cancer screening
Skin cancer prevention
The Task Force made 2 revisions to the 2012 recommendation on preventing skin cancer through behavioral counseling to avoid ultraviolet (UV) radiation.6 These recommendations continue to focus on those with fair skin. The first revision: The earliest age at which children (through their guardians) can benefit from counseling on UV avoidance has been lowered from age 10 years to 6 months. The second revision: Some adults older than age 24 can also benefit from such counseling if they have fair skin and other skin cancer risks such as using tanning beds, having a history of sunburns or previous skin cancer, having an increased number of nevi (moles) and atypical nevi, having human immunodeficiency virus (HIV) infection, having received an organ transplant, or having a family history of skin cancer.
Continue to: Those at risk...
Those at risk can reduce their chances of skin cancer by using broad-spectrum sunscreens and sun-protective clothing, and by avoiding sun exposure and indoor tanning beds.
Fall prevention
In a reversal of its 2012 recommendation, the Task Force now recommends against the use of vitamin D supplementation to prevent falls in community-dwelling adults 65 years or older.7 In a reanalysis of previous studies on this topic, along with new evidence, the Task Force concluded that vitamin D supplementation offers no benefit for preventing falls in adults who are not vitamin D deficient.
Screening for scoliosis in adolescents
In 2004 the USPSTF recommended against screening for idiopathic scoliosis in children and adolescents 10 to 18 years of age. In its most recent review, the Task Force continued to find no direct evidence of the benefit of screening and inadequate evidence on the long-term benefits of reduction in spinal curvature through exercise, surgery, and bracing. However, following a reanalysis of the potential harms of these treatments and the use of a new analytic framework, the Task Force concluded it is not possible at this time to assess the balance of benefits and harms of screening.8
Prostate cancer screening
In its most controversial action, the Task Force reversed its 2012 recommendation against routine prostate-specific antigen–based screening for prostate cancer in men ages 55 to 69 years and now lists this as a “C” recommendation.9 The potential benefits of screening include preventing 1.3 deaths from prostate cancer per 1000 men screened over 13 years and approximately 3 cases of metastatic prostate cancer. However, no trials have found a reduction in all-cause mortality from screening. Contrast that with the known harms of screening: 15% false positive results over 10 years; 1% hospitalization rate among those undergoing a prostate biopsy; over-diagnosis and resultant treatment of 20% to 50% of men diagnosed with prostate cancer through screening; and incontinence and erectile dysfunction in 20% and 67%, respectively, of men following prostatectomy.9
Based on these outcomes, the Task Force “does not recommend screening for prostate cancer unless men express a preference for screening after being informed of and understanding the benefits and risks.”9 The Task Force continues to recommend against screening men ages 70 years and older.
Continue to: The change in this recommendation...
The change in this recommendation and its wording present dilemmas for family physicians: whether to discuss potential screening with all men ages 55 to 69; to selectively discuss it with those at high risk (principally African Americans and those with a strong family history of prostate cancer); or to address the issue only if a patient asks about it. In addition, if a man requests screening, how often should it be performed? Most clinical trials have found equal benefit from testing less frequently than every year, with fewer harms. The Task Force provided little or no guidance on these issues.
Final advice: D recommendations
The Task Force reaffirmed that 7 services have either no benefit or cause more harm than benefit (TABLE 11). Family physicians should be familiar with these services, as well as all Task Force D recommendations, and avoid recommending them or providing them. High quality preventive care involves both providing services of proven benefit and avoiding those that do not.
1. USPSTF. Published recommendations. https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations. Accessed March 25, 2019.
2. USPSTF. Final recommendation statement. Perinatal depression: preventive interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/perinatal-depression-preventive-interventions. Accessed March 25, 2019.
3. USPSTF. Atrial fibrillation: screening with electrocardiography. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/atrial-fibrillation-screening-with-electrocardiography. Accessed March 25, 2019.
4. USPSTF. Screening for atrial fibrillation with electrocardiography. JAMA. 2018;320:478-484.
5. USPSTF. Cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening2. Accessed March 25, 2019.
6. USPSTF. Skin cancer prevention: behavioral counseling. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/skin-cancer-counseling2. Accessed March 25, 2019.
7. USPSTF. Falls prevention in community-dwelling older adults: interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/falls-prevention-in-older-adults-interventions1. Accessed March 25, 2019.
8. USPSTF. Adolescent idiopathic scoliosis: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/adolescent-idiopathic-scoliosis-screening1. Accessed March 25, 2019.
9. USPSTF. Prostate cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prostate-cancer-screening1#consider. Accessed March 25, 2019.
1. USPSTF. Published recommendations. https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations. Accessed March 25, 2019.
2. USPSTF. Final recommendation statement. Perinatal depression: preventive interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/perinatal-depression-preventive-interventions. Accessed March 25, 2019.
3. USPSTF. Atrial fibrillation: screening with electrocardiography. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/atrial-fibrillation-screening-with-electrocardiography. Accessed March 25, 2019.
4. USPSTF. Screening for atrial fibrillation with electrocardiography. JAMA. 2018;320:478-484.
5. USPSTF. Cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening2. Accessed March 25, 2019.
6. USPSTF. Skin cancer prevention: behavioral counseling. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/skin-cancer-counseling2. Accessed March 25, 2019.
7. USPSTF. Falls prevention in community-dwelling older adults: interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/falls-prevention-in-older-adults-interventions1. Accessed March 25, 2019.
8. USPSTF. Adolescent idiopathic scoliosis: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/adolescent-idiopathic-scoliosis-screening1. Accessed March 25, 2019.
9. USPSTF. Prostate cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/prostate-cancer-screening1#consider. Accessed March 25, 2019.
Translating AHA/ACC cholesterol guidelines into meaningful risk reduction
A new cholesterol guideline1 builds on the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guidelines,2 which were a major paradigm shift in the evaluation and management of blood cholesterol levels and risk for atherosclerotic cardiovascular disease (ASCVD). The work was presented (and simultaneously published) on November 10, 2018, at the annual AHA Scientific Sessions in Chicago. Full text,1 an executive summary,3 and accompanying systematic review of evidence4 are available online.
The 2018 AHA/ACC cholesterol guideline represents a step forward in ASCVD prevention—especially in primary prevention, where it provides guidance for risk refinement and personalization. In this article, we mine the details of what has changed and what is new in this guideline so that you can prepare to adopt the recommendations in your practice.
2013 and 2018 guidelines: Similarities, differences
As in earlier iterations, the 2018 guideline emphasizes healthy lifestyle across the life-course as the basis of ASCVD prevention—as elaborated in the 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk.5 In contrast to the 2013 guidelines,2 the 2018 guideline is more comprehensive and more personalized, focusing on risk assessment for individual patients, rather than simply providing population-based approaches. Moreover, the guideline isn’t limited to adults: It makes recommendations pertaining to children and adolescents.1
TABLE 11,2 compares the most important differences between the 2013 and 2018 guidelines.
The 2013 ACC/AHA guidelines eliminated low-density lipoprotein cholesterol (LDL-C) and non-high-density lipoprotein cholesterol (non-HDL-C)a goals of therapy and replaced them with the concept of 4 “statin benefit groups”—that is, patient populations for which clear evidence supports the role of statin therapy.4 In the 2018 guideline, statin benefit groups have been maintained, although without explicit use of this term.1
Primary prevention. Although no major changes in statin indications are made for patients with (1) established ASCVD (ie, for secondary prevention), (2) diabetes mellitus (DM) and who are 40 to 75 years of age, or (3) a primary LDL-C elevation ≥ 190 mg/dL, significant changes were made for primary prevention patients ages 40 to 75 years.1 ASCVD risk calculation using the 2013 pooled cohort equations (PCE) is still recommended4; however, risk estimation is refined by the use of specific so-called risk-enhancing factors (TABLE 21). In cases in which the risk decision remains uncertain, obtaining the coronary artery calcium (CAC) score (which we’ll describe shortly) using specialized computed tomography (CT) is advised to facilitate the shared physician–patient decision-making process.1
LDL-C and non-HDL-C thresholds. Although LDL-C and non-HDL-C goals are not overtly brought back from the 2002 National Cholesterol Education Program/Adult Treatment Panel guidelines,6 the new guideline does introduce LDL-C and non-HDL-C thresholds—levels at which adding nonstatin therapy can be considered, in contrast to previous goals to which therapy was titrated. Definitions of statin intensity remain the same: Moderate-intensity statin therapy is expected to reduce the LDL-C level by 30% to 50%; high-intensity statin therapy, by ≥ 50%.1 The intensity of statin therapy has been de-escalated in the intermediate-risk group, where previous guidelines advised high-intensity statin therapy,4 and replaced with moderate-intensity statin therapy (similar to 2016 US Preventive Services Task Force [USPSTF] recommendations7).
[polldaddy:10312157]
Continue to: Fasting vs nonfasting lipid profiles
Fasting vs nonfasting lipid profiles. In contrast to previous guidelines,2,8 which used fasting lipid profiles, nonfasting lipid profiles are now recommended for establishing a baseline LDL-C level and for ASCVD risk estimation for most patients—as long as the triglycerides (TG) level is < 400 mg/dL. When the calculated LDL-C level is < 70 mg/dL using the standard Friedewald formula, obtaining a direct LDL-C or a modified LDL-C estimate9 is deemed reasonable to improve accuracy. (The modified LDL-C can be estimated using The Johns Hopkins Hospital’s free “LDL Cholesterol Calculator” [www.hopkinsmedicine.org/apps/all-apps/ldl-cholesterol-calculator]).
A fasting lipid profile is still preferred for patients who have a family history of a lipid disorder. The definition of hypertriglyceridemia has been revised from a fasting TG level ≥ 150 mg/dL to a nonfasting or fasting TG level ≥ 175 mg/dL.1
Nonstatin add-on therapy. The new guideline supports the addition of nonstatin therapies to maximally tolerated statin therapy in patients who have established ASCVD or a primary LDL-C elevation ≥ 190 mg/dL when (1) the LDL-C level has not been reduced by the expected percentage (≥ 50% for high-intensity statin therapy) or (2) explicit LDL-C level thresholds have been met.1
The principal 2 groups of recommended nonstatins for which there is randomized, controlled trial evidence of cardiovascular benefit are (1) the cholesterol-absorbing agent ezetimibe10 and (2) the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors evolocumab11 and alirocumab.12
AAFP’s guarded positions on the 2013 and 2018 guidelines
The American Academy of Family Physicians (AAFP) welcomed the patient-centered and outcome-oriented aspects of the 2013 ACC/AHA guidelines, endorsing them with 3 qualifications.13
- Many of the recommendations were based on expert opinion, not rigorous research results—in particular, not on the findings of randomized controlled trials (although key points are based on high-quality evidence).
- There were conflicts of interest disclosed for 15 members of the guidelines panel, including a vice chair.
- Validation of the PCE risk estimation tool was lacking.
Continue to: AAFP announced...
AAFP announced in March that it does not endorse the 2018 AHA/ACC guideline, asserting that (1) only a small portion of the recommendations, primarily focused on the addition of nonstatin therapy, were addressed by an independent systematic review and (2) many of the guideline recommendations are based on low-quality or insufficient evidence. AAFP nevertheless bestowed an “affirmation of value” designation on the guideline—meaning that it provides some benefit for family physicians’ practice without fulfilling all criteria for full endorsement.14
Detailed recommendations from the 2018 guideline
Lifestyle modification
When talking about ASCVD risk with patients, it is important to review current lifestyle habits (eg, diet, physical activity, weight or body mass index, and tobacco use). Subsequent to that conversation, a healthy lifestyle should be endorsed and relevant advice provided. In addition, patient-directed materials (eg, ACC’s CardioSmart [www.cardiosmart.org]; AHA’s Life’s Simple 7 [www.heart.org/en/professional/workplace-health/lifes-simple-7]; and the National Lipid Association’s Patient Tear Sheets [www.lipid.org/practicetools/tools/tearsheets] and Clinicians’ Lifestyle Modification Toolbox [www.lipid.org/CLMT]) and referrals (eg, to cardiac rehabilitation, a dietitian, a smoking-cessation program) should be provided.1
Primary prevention of ASCVD
Risk assessment for primary prevention is now approached as a process, rather than the simple risk calculation used in the 2013 ACC/AHA guidelines.2 Assessment involves risk estimation followed by risk personalization, which, in some cases, is followed by risk reclassification using CAC scoring.1
Patients are classified into 1 of 4 risk groups, based on the PCE1:
- low (< 5%)
- borderline (5%-7.5%)
- intermediate (7.5%-19.9%)
- high (≥ 20%).
However, the PCE-based risk score is a population-based tool, which might not reflect the actual risk of individual patients. In some populations, PCE underestimates ASCVD risk; in others, it overestimates risk. A central tenet of the new guideline is personalization of risk, taking into account the unique circumstances of each patient. Moreover, the new guideline provides guidance on how to interpret the PCE risk score for several different ethnic and racial groups.1
Continue to: Medical therapy
Medical therapy. The decision to start lipid-lowering therapy should be made after a physician–patient discussion that considers costs of therapy as well as patient preferences and values in the context of shared decision-making. Discussion should include a review of major risk factors (eg, cigarette smoking, elevated blood pressure, and the LDL-C level), the PCE risk score, the presence of risk-enhancing factors (TABLE 21), potential benefits of lifestyle changes and statin therapy, and the potential for adverse drug effects and drug–drug interactions.1
If the estimated ASCVD risk is 7.5%-19.9%, starting moderate-intensity statin therapy is recommended. Risk-enhancing factors favor initiation of statin therapy, even in patients at borderline risk (5%-7.5%). If risk is uncertain, the CAC score can be used to facilitate shared decision-making.1 The use of CAC is in agreement with the USPSTF statement that CAC can moderately improve discrimination and reclassification, but has an unclear effect on downstream health care utilization.15 Importantly, CAC should not be measured routinely in patients already taking a statin because its primary role is to facilitate shared decision-making regarding initiation of statin therapy.16
If the 10-year ASCVD risk is ≥ 20%, high-intensity statin therapy is advised, without need to obtain the CAC score. If high-intensity statin therapy is advisable but not acceptable to, or tolerated by, the patient, it might be reasonable to add a nonstatin drug (ezetimibe or a bile-acid sequestrant) to moderate-intensity statin therapy.1
Risk-enhancing factors (TABLE 21) apply to intermediate- and borderline-risk patients. Importantly, these factors include membership in specific ethnic groups, conditions specific to females, and male–female distinctions in risk. Risk-enhancing factors also incorporate biomarkers that are often measured by lipid specialists, such as lipoprotein(a) (Lp[a]) and apolipoprotein B (ApoB).1
Lp(a) is an atherogenic particle, akin to an LDL particle, that consists of a molecule of apolipoprotein (a) (a nonfunctional mimic of a portion of plasminogen) covalently bound to ApoB, like the one found on the LDL particle. Lp(a) is proportionally associated with an increased risk for ASCVD and aortic stenosis at a level > 50 mg/dL.17 A family history of premature ASCVD is a relative indication for measuring Lp(a).1
Continue to: When and why to measure CAC
When and why to measure CAC
If the decision to initiate statin therapy is still uncertain after risk estimation and personalization, or when a patient is undecided about committing to lifelong lipid-lowering therapy, the new guideline recommends obtaining a CAC score to inform the shared decision-making process.1,18 Measurement of CAC is obtained by noncontrast, electrocardiographic-gated CT that can be performed in 10 to 15 minutes, requiring approximately 1 millisievert of radiation (equivalent of the approximate dose absorbed during 2 mammograms). Although measurement of the CAC score is generally not covered by insurance, its cost ($50-$450) nationwide makes it accessible.19
CAC measures the presence (or absence) of subclinical atherosclerosis by detecting calcified plaque in coronary arteries. The absolute CAC score is expressed in Agatston units; an age–gender population percentile is also provided. Keep in mind that the presence of any CAC (ie, a score > 0) is abnormal and demonstrates the presence of subclinical coronary artery disease. The prevalence of CAC > 0 increases with age, but a significant percentage of older people have a CAC score = 0. When CAC > 0, additional information is provided by the distribution of plaque burden among the different coronary arteries.20
Among intermediate-risk patients, 50% have CAC = 0 and, therefore, a very low event rate over the ensuing 10 years, which allows statin therapy to be safely deferred unless certain risk factors are present (eg, family history, smoking, DM).1,18 It is reasonable to repeat CAC testing in 5 to 10 years to assess whether subclinical atherosclerosis has developed. The 2018 guideline emphasizes that, when the CAC score is > 0 but < 100 Agatston units, statin therapy is favored, especially in patients > 55 years of age; when the CAC score is ≥ 100 Agatston units or at the ≥ 75th percentile, statin therapy is indicated regardless of age.1
Patients who might benefit from knowing their CAC score include those who are:
- reluctant to initiate statin therapy but who want to understand their risk and potential for benefit more precisely
- concerned about the need to reinstitute statin therapy after discontinuing it because of statin-associated adverse effects
- older (men, 55-80 years; women, 60-80 years) who have a low burden of risk factors and who question whether they would benefit from statin therapy
- middle-aged (40-55 years) and who have a PCE-calculated risk of 5% to < 7.5% for ASCVD and factors that increase their risk for ASCVD, even though they are in a borderline-risk group.1
Primary prevention in special populations
Older patients. In adults ≥ 75 years who have an LDL-C level 70 to 189 mg/dL, initiating a moderate-intensity statin might be reasonable; however, it might also be reasonable to stop treatment in this population when physical or cognitive decline, multiple morbidities, frailty, or reduced life expectancy limits the potential benefit of statin therapy. It might be reasonable to use the CAC score in adults 76 to 80 years of age who have an LDL-C level of 70 to 189 mg/dL to reclassify those whose CAC score = 0, so that they can avoid statin therapy.1
Continue to: Children and adolescents
Children and adolescents. In alignment with current pediatric guidelines,21 but in contrast to USPSTF reccomendations,22 the 2018 ACC/AHA guideline endorses universal lipid screening for pediatric patients (see TABLE W11,21,22). It is reasonable to obtain a fasting lipid profile or nonfasting non-HDL-C in all children and adolescents who have neither cardiovascular risk factors nor a family history of early cardiovascular disease to detect moderate-to-severe lipid abnormalities. Screening should be done once at 9 to 11 years of age and again at 17 to 21 years.1
A screening test as early as 2 years of age to detect familial hypercholesterolemia (FH) is reasonable when a family history of either early CVD or significant hypercholesterolemia is present. The guideline endorses reverse cascade screening for detection of FH in family members of children and adolescents who have severe hypercholesterolemia.1
In children and adolescents with a lipid abnormality, especially when associated with the metabolic syndrome, lifestyle counseling is beneficial for lowering the LDL-C level. In children and adolescents ≥ 10 years of age with (1) an LDL-C level persistently ≥ 190 mg/dL or (2) an LDL level ≥ 160 mg/dL plus a clinical presentation consistent with FH, it is reasonable to initiate statin therapy if they do not respond adequately to 3 to 6 months of lifestyle therapy.1
Ethnicity as a risk-modifying factor. The PCE distinguishes between US adults of European ancestry and African ancestry, but no other ethnic groups are distinguished.4 The new guideline advocates for the use of PCE in other populations; however, it states that, for clinical decision-making purposes, it is reasonable, in adults of different races and ethnicities, for the physician to review racial and ethnic features that can influence ASCVD risk to allow adjustment of the choice of statin or intensity of treatment. Specifically, South Asian ancestry is now treated as a risk-enhancing factor, given the high prevalence of premature and extensive ASCVD in this patient population.1
Concerns specific to women. Considering conditions specific to women as potential risk-enhancing factors is advised when discussing lifestyle intervention and the potential for benefit from statin therapy—in particular, (1) in the setting of premature menopause (< 40 years) and (2) when there is a history of a pregnancy-associated disorder (eg, hypertension, preeclampsia, gestational DM, a small-for-gestational-age infant, and preterm delivery). If the decision is made to initiate statin therapy in women of childbearing age who are sexually active, there is a guideline mandate to counsel patients on using reliable contraception. When pregnancy is planned, statin therapy should be discontinued 1 to 2 months before pregnancy is attempted; when pregnancy occurs while a patient is taking a statin, therapy should be stopped as soon as the pregnancy is discovered.1
Continue to: Adults with chronic kidney disease
Adults with chronic kidney disease. Chronic kidney disease that is not treated with dialysis or kidney transplantation is considered a risk-enhancing factor; initiation of a moderate-intensity statin or a moderate-intensity statin plus ezetimibe can be useful in patients with chronic kidney disease who are 40 to 75 years of age and have an LDL-C level of 70 to 189 mg/dL and a PCE-calculated risk ≥ 7.5%. In adults with advanced kidney disease that requires dialysis who are already taking a statin, it may be reasonable to continue the statin; however, initiation of a statin in adults with advanced kidney disease who require dialysis is not recommended because of an apparent lack of benefit.1
Adults with a chronic inflammatory disorder or human immunodeficiency virus infection. Any of these conditions are treated as risk-enhancing factors; in a risk discussion with affected patients, therefore, moderate-intensity statin therapy or high-intensity statin therapy is favored for those 40 to 75 years of age who have an LDL-C level of 70 to 189 mg/dL and PCE-calculated risk ≥ 7.5%. A fasting lipid profile and assessment of ASCVD risk factors for these patients can be useful (1) as a guide to the potential benefit of statin therapy and (2) for monitoring or adjusting lipid-lowering drug therapy before, and 4 to 12 weeks after, starting inflammatory disease-modifying therapy or antiretroviral therapy.
In adults with rheumatoid arthritis who undergo ASCVD risk assessment with a lipid profile, it can be useful to recheck lipid values and other major ASCVD risk factors 2 to 4 months after the inflammatory disease has been controlled.1
Primary hypercholesterolemia
The diagnosis and management of heterozygous or homozygous familial hypercholesterolemia (HeFH or HoFH) is beyond the scope of the 2018 ACC/AHA cholesterol guidelines; instead, the 2015 AHA Scientific Statement, “The Agenda for Familial Hypercholesterolemia,” provides a contemporary review of these topics.23 However, the 2018 cholesterol guideline does acknowledge that an LDL-C level ≥ 190 mg/dL often corresponds to primary (ie, genetic) hypercholesterolemia.
In patients 20 to 75 years of age who have a primary elevation of LDL-C level ≥ 190 mg/dL, the guideline recommends initiation of high-intensity statin therapy without calculating ASCVD risk using the PCE. If a > 50% LDL-C reduction is not achieved, or if the LDL-C level on maximally tolerated statin therapy remains ≥ 100 mg/dL, adding ezetimibe is considered reasonable. If there is < 50% reduction in the LDL-C level while taking maximally tolerated statin and ezetimibe therapy, adding a bile-acid sequestrant can be considered, as long as the TG level is not > 300 mg/dL (ie, bile-acid sequestrants can elevate the TG level significantly).
Continue to: In patients 30 to 75 years of age...
In patients 30 to 75 years of age who have a diagnosis of HeFH and an LDL-C level ≥ 100 mg/dL while taking maximally tolerated statin and ezetimibe therapy, the addition of a PCSK9 inhibitor can be considered. Regardless of whether there is a diagnosis of HeFH, addition of a PCSK9 inhibitor can be considered in patients 40 to 75 years of age who have a baseline LDL-C level ≥ 220 mg/dL and who achieve an on-treatment LDL-C level ≥ 130 mg/dL while receiving maximally tolerated statin therapy and ezetimibe.1
Diabetes mellitus
In patients with DM who are 40 to 75 years of age, moderate-intensity statin therapy is recommended without calculating the 10-year ASCVD risk. When the LDL-C level is 70 to 189 mg/dL, however, it is reasonable to use the PCE to assess 10-year ASCVD risk to facilitate risk stratification.
In patients with DM who are at higher risk, especially those who have multiple risk factors or are 50 to 75 years of age, it is reasonable to use a high-intensity statin to reduce the LDL-C level by ≥ 50 %. In adults > 75 years of age with DM who are already on statin therapy, it is reasonable to continue statin therapy; for those that age who are not on statin therapy, it might be reasonable to initiate statin therapy after a physician–patient discussion of potential benefits and risks.
In adults with DM and PCE-calculated risk ≥ 20%, it might be reasonable to add ezetimibe to maximally tolerated statin therapy to reduce the LDL-C level by ≥ 50%. In adults 20 to 39 years of age with DM of long duration (≥ 10 years of type 2 DM, ≥ 20 years of type 1 DM), albuminuria (≥ 30 μg of albumin/mg creatinine), estimated glomerular filtration rate < 60 mL/min/1.73 m2, retinopathy, neuropathy, or ankle-brachial index < 0.9, it might be reasonable to initiate statin therapy.1
Secondary prevention
Presence of clinical ASCVD. In patients with clinical ASCVD who are ≤ 75 years of age, high-intensity statin therapy should be initiated or continued, with the aim of achieving ≥ 50% reduction in the LDL-C level. When high-intensity statin therapy is contraindicated or if a patient experiences statin-associated adverse effects, moderate-intensity statin therapy should be initiated or continued with the aim of achieving a 30% to 49% reduction in the LDL-C level.
Continue to: In patients...
In patients > 75 years of age with clinical ASCVD, it is reasonable to initiate or continue moderate- or high-intensity statin therapy after evaluation of the potential for ASCVD risk reduction, adverse effects, and drug–drug interactions, as well as patient frailty and patient preference.1
Very high risk. In patients at very high risk (this includes a history of multiple major ASCVD events or 1 major ASCVD event plus multiple high-risk conditions), maximally tolerated LDL-C-lowering therapy should include maximally tolerated statin therapy and ezetimibe before considering a PCSK9 inhibitor. An LDL-C level ≥ 70 mg/dL or a non-HDL-C level ≥ 100 mg/dL is considered a reasonable threshold for adding a PCSK9 inhibitor to background lipid-lowering therapy1 (TABLE 31).
Heart failure. In patients with heart failure who have (1) a reduced ejection fraction attributable to ischemic heart disease, (2) a reasonable life expectancy (3-5 years), and (3) are not already on a statin because of ASCVD, consider initiating moderate-intensity statin therapy to reduce the risk for an ASCVD event.1
Reduction of elevated triglycerides
The guideline defines moderate hypertriglyceridemia as a nonfasting or fasting TG level of 175 to 499 mg/dL. Such a finding is considered a risk-enhancing factor and is 1 of 5 components of the metabolic syndrome. Three independent measurements are advised to diagnose primary moderate hypertriglyceridemia. Severe hypertriglyceridemia is diagnosed when the fasting TG level is ≥ 500 mg/dL.1
In moderate hypertriglyceridemia, most TGs are carried in very-low-density lipoprotein particles; in severe hypertriglyceridemia, on the other hand, chylomicrons predominate, raising the risk for pancreatitis. In adults with severe hypertriglyceridemia, therefore—especially when the fasting TG level is ≥ 1000 mg/dL—it is reasonable to identify and address other causes of hypertriglyceridemia. If TGs are persistently elevated or increasing, levels should be reduced to prevent acute pancreatitis with a very low-fat diet and by avoiding refined carbohydrates and alcohol; consuming omega-3 fatty acids; and, if necessary, taking a fibrate.1
Continue to: In adults...
In adults ≥ 20 years of age with moderate hypertriglyceridemia, lifestyle factors (eg, obesity, metabolic syndrome), secondary factors (eg, DM, chronic liver or kidney disease, nephrotic syndrome, hypothyroidism), and medications that increase the TG level need to be addressed first. In adults 40 to 75 years of age with moderate or severe hypertriglyceridemia and a PCE-calculated ASCVD risk ≥ 7.5%, it is reasonable to reevaluate risk after lifestyle and secondary factors are addressed and to consider a persistently elevated TG level as a factor favoring initiation or intensification of statin therapy. In adults 40 to 75 years of age with severe hypertriglyceridemia and ASCVD risk ≥ 7.5%, it is reasonable to address reversible causes of a high TG level and to initiate statin therapy.1
Other considerations in cholesterol management
Tools to assess adherence
The response to lifestyle and statin therapy should be evaluated by the percentage reduction in the LDL-C level compared with baseline, not by assessment of the absolute LDL-C level. When seeing a patient whose treatment is ongoing, a baseline level can be estimated using a desktop LDL-calculator app.
Adherence and percentage response to LDL-C–lowering medications and lifestyle changes should be evaluated with repeat lipid measurement 4 to 12 weeks after either a statin is initiated or the dosage is adjusted, and repeated every 3 to 12 months as needed. In patients with established ASCVD who are at very high risk, triggers for adding nonstatin therapy are defined by a threshold LDL-C level ≥ 70 mg/dL on maximal statin therapy.1
Interventions focused on improving adherence to prescribed therapy are recommended for management of adults with an elevated cholesterol level. These interventions include telephone reminders, calendar reminders, integrated multidisciplinary educational activities, and pharmacist-led interventions, such as simplification of the medication regimen to once-daily dosing.1
Statin safety and associated adverse effects
A physician–patient risk discussion is recommended before initiating statin therapy to review net clinical benefit, during which the 2 parties weigh the potential for ASCVD risk reduction against the potential for statin-associated adverse effects, statin–drug interactions, and safety, with the physician emphasizing that adverse effects can be addressed successfully.
Continue to: Statins are one of...
Statins are one of the safest classes of medication, with an excellent risk-benefit ratio. However, there are myriad confusing media reports regarding potential adverse effects and safety of the statin class—reports that often lead patients to discontinue or refuse statins.
Statin-associated adverse effects include the common statin-associated muscle symptoms (SAMS), new-onset DM, cognitive effects, and hepatic injury. The frequency of new-onset DM depends on the population exposed to statins, with a higher incidence of new-onset DM found in patients who are already predisposed, such as those with obesity, prediabetes, and metabolic syndrome. Cognitive effects are rare and difficult to interpret; they were not reported in the large statin mega-trials but have been described in case reports. Significant transaminase elevations > 3 times the upper limit of normal are infrequent; hepatic failure with statins is extremely rare and found at the same incidence in the general population.1
SAMS include (in order of decreasing prevalence)24:
- myalgias with a normal creatine kinase (CK) level
- conditions such as myositis or myopathy (elevated CK level)
- rhabdomyolysis (CK level > 10 times the upper limit of normal, plus renal injury)
- extremely rare statin-associated autoimmune myopathy, with detectable 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase antibodies.
In patients with SAMS, thorough assessment of symptoms is recommended, in addition to evaluation for nonstatin causes and predisposing factors. Identification of potential SAMS-predisposing factors is recommended before initiation of treatment, including demographics (eg, East-Asian ancestry), comorbid conditions (eg, hypothyroidism and vitamin D deficiency), and use of medications adversely affecting statin metabolism (eg, cyclosporine).
In patients with statin-associated adverse effects that are not severe, it is recommended to reassess and rechallenge to achieve a maximal lowering of the LDL-C level by a modified dosing regimen or an alternate statin or by combining a statin with nonstatin therapy. In patients with increased risk for DM or new-onset DM, it is recommended to continue statin therapy.
Continue to: Routine CK and liver function testing...
Routine CK and liver function testing is not useful in patients treated with statins; however, it is recommended that CK be measured in patients with severe SAMS or objective muscle weakness, or both, and to measure liver function if symptoms suggest hepatotoxicity. In patients at increased risk for ASCVD who have chronic, stable liver disease (including non-alcoholic fatty liver disease), it is reasonable, when appropriately indicated, to use statins after obtaining baseline measurements and determining a schedule of monitoring and safety checks.
In patients at increased risk for ASCVD who have severe or recurrent SAMS after appropriate statin rechallenge, it is reasonable to use nonstatin therapy that is likely to provide net clinical benefit. The guideline does not recommend routine use of coenzyme Q10 supplementation for the treatment or prevention of SAMS.1
Guideline criticism
Guideline development is challenging on multiple levels, including balancing perspectives from multiple stakeholders. Nevertheless, the 2018 AHA/ACC cholesterol guideline builds nicely on progress made since its 2013 predecessor was released.4 This document was developed with the participation of representatives from 10 professional societies in addition to the ACC and AHA—notably, the National Lipid Association and American Society for Preventive Cardiology.1
To refine risk estimation and facilitate shared decision-making, the new guideline introduced so-called risk-enhancing factors and use of the CAC.1 However, some potential risk-enhancing factors were left out: erectile dysfunction, for example, often a marker of increased cardiovascular risk in men < 50 years of age.25 In addition, although pretreatment ApoB was introduced as a risk-enhancing factor,1 no recommendation is given to measure ApoB after initiation of therapy for evaluation of residual cardiovascular risk, as endorsed in other guidelines.26,27
Moreover, the guideline does not include the “extreme risk” category in the guideline developed by the American Association of Clinical Endocrinologists (AACE).28 Although the 2018 AHA/ACC guideline introduces < 70 mg/dL and < 100 mg/dL LDL-C thresholds,1 the < 55 mg/dL LDL-C threshold used for patients in the AACE/American College of Endocrinology extreme-risk category is not mentioned.26 This omission might leave patients who are at extreme ASCVD risk without optimal lipid-lowering therapy. Similarly, the guideline does not elaborate on the diagnosis and treatment of HoFH and HeFH.1 The age cutoff of 30 years for the recommendation to consider PCSK9 inhibitors in patients with HeFH appears arbitrary and excludes younger FH patients who have an extreme LDL-C elevation from potentially important therapy.23
Continue to: Guidelines are dynamic instruments...
Guidelines are dynamic instruments that require constant updating, given the production of new evidence. In fact, the results of the Reduction of Cardiovascular Events With Icosapent Ethyl-Intervention Trial (REDUCE-IT) were presented at the same meeting at which this guideline was unveiled.29 REDUCE-IT demonstrated an astonishing highly significant 25% reduction in the composite primary major adverse cardiovascular event outcome in patients with an LDL-C level of 44 to 100 mg/dL on statin therapy, who had a TG level of 135 to 499 mg/dL and had been treated for a median of 4.9 years with 4 g of pure eicosapentaenoic acid.
In addition, the guideline’s value statements, which address the need to consider the cost of drugs in determining most appropriate treatment, are no longer accurate because the price of PCSK9 inhibitors has dropped by more than half since the guideline was issued.30
An upward climb to clinical payoff
Even after close study of the 2018 AHA/ACC cholesterol guideline, implementing it in practice might remain a challenge to clinicians who are inexperienced in ordering lipid markers such as Lp(a) and interpreting the CAC score. Moreover, initiating and monitoring nonstatin therapies will be a demanding task—especially with PCSK9 inhibitors, which present access difficulties because they are relatively expensive (even after the recent price cut). That’s why, when there is doubt in the mind of the physician or other provider, we will likely see more referrals to specialists in lipid management and ASCVD risk estimation to optimize preventive therapy.31
CORRESPONDENCE
Cezary Wójcik, MD, PhD, FNLA, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR 97239; cezarywojcik2000@gmail.com
1. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 8. pii: S0735-1097(18)39034-X. [Epub ahead of print]
2. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1-S45.
3. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 3. pii: S0735-1097(18)39033-8. [Epub ahead of print]
4. Wilson PWF, Polonsky TS, Miedema MD, et al. Systematic review for the 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 3. pii: S0735-1097(18)39035-1. [Epub ahead of print]
5. Eckel RH, Jakicic JM, Ard JD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960-2984.
6. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel III): final report. Circulation. 2002;106:3143-3421.
7. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:1997-2007.
8. National Cholesterol Education Program. Second report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel II). Circulation. 1994;89:1333-1445.
9. Martin SS, Giugliano RP, Murphy SA, et al. Comparison of low-density lipoprotein cholesterol assessment by Martin/Hopkins estimation, Friedewald estimation, and preparative ultracentrifugation: insights from the FOURIER trial. JAMA Cardiol. 2018;3:749-753.
10. Cannon CP, Blazing MA, Giugliano RP, et al; IMPROVE-IT Investigators. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387-2397.
11. Sabatine MS, Giugliano RP, Keech AC, et al; FOURIER Steering Committee and Investigators. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713-1722.
12. Szarek M, White HD, Schwartz GG, et al; ODYSSEY OUTCOMES Committees and Investigators. Alirocumab reduces total nonfatal cardiovascular and fatal events in the ODYSSEY OUTCOMES trial. J Am Coll Cardiol. 2019;73:387-396.
13. Crawford C. AAFP endorses ACC/AHA cholesterol management guidelines with qualifications. Leawood, KS: American Academy of Family Physicians; 2014 June 18. www.aafp.org/news/health-of-the-public/20140618cholesterolgdlnendorse.html. Accessed March 20, 2019.
14. Crawford C. AAFP News. AAFP affirms value of new cholesterol management guideline. March 20, 2019. www.aafp.org/news/health-of-the-public/20190320acc-ahacholguidln.html?cmpid=em_AP_20190320. Accessed April 1, 2019.
15. Lin JS, Evans CV, Johnson E, et al. Nontraditional Risk Factors in Cardiovascular Disease Risk Assessment: A Systematic Evidence Report for the U.S. Preventive Services Task Force. Evidence Synthesis, No. 166. Rockville, MD: Agency for Healthcare Research and Quality (US); 2018 Jul. Report No.: 17-05225-EF-1.
16. Puri R, Nicholls SJ, Shao M, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am Coll Cardiol. 2015;65:1273-1282.
17. Gencer B, Kronenberg F, Stroes ES, et al. Lipoprotein(a): the revenant. Eur Heart J. 2017;38:1553-1560.
18. Michos ED, Blaha MJ, Blumenthal RS. Use of the coronary artery calcium score in discussion of initiation of statin therapy in primary prevention. Mayo Clin Proc. 2017;92:1831-1841.
19. MDsave. Cardiac CT calcium scoring. www.mdsave.com/procedures/cardiac-ct-calcium-scoring/d785f4cf. Accessed Aprl 1, 2019.
20. Blaha MJ, Budoff MJ, Tota-Maharaj R, et al. Improving the CAC score by addition of regional measures of calcium distribution: multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging. 2016;9:1407-1416.
21. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213-S256.
22. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for lipid disorders in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:625-633.
23. Gidding SS, Champagne MA, de Ferranti SD, et al; American Heart Association Atherosclerosis, Hypertension, and Obesity in Young Committee of Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and Council on Lifestyle and Cardiometabolic Health. The agenda for familial hypercholesterolemia: a scientific statement from the American Heart Association. Circulation. 2015;132:2167-2192.
24. Newman CB, Preiss D, Tobert JA, et al; American Heart Association Clinical Lipidology, Lipoprotein, Metabolism and Thrombosis Committee, a Joint Committee of the Council on Atherosclerosis, Thrombosis and Vascular Biology and Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke Council. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39:e38-e81.
25. Miner M, Parish SJ, Billups KL, et al. Erectile dysfunction and subclinical cardiovascular disease. Sex Med Rev. 2018 Jan 27. pii: S2050-0521(18)30009-X. [Epub ahead of print]
26. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87.
27. Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263-1282.
28. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87.
29. Bhatt DL, Steg PG, Miller M, et al; REDUCE-IT Investigators. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380:11-22.
30. Dangi-Garimella S. Amgen announces 60% reduction in list price of PCSK9 inhibitor evolocumab. AJMC Managed Markets Network. October 24, 2018. https://www.ajmc.com/newsroom/amgen-announces-60-reduction-in-list-price-of-pcsk9-inhibitor-evolocumab. Accessed April 12, 2019.
31. Kaufman TM, Duell PB, Purnell JQ, et al. Application of PCSK9 inhibitors in practice: challenges and opportunities. Circ Res. 2017;121:499-501.
A new cholesterol guideline1 builds on the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guidelines,2 which were a major paradigm shift in the evaluation and management of blood cholesterol levels and risk for atherosclerotic cardiovascular disease (ASCVD). The work was presented (and simultaneously published) on November 10, 2018, at the annual AHA Scientific Sessions in Chicago. Full text,1 an executive summary,3 and accompanying systematic review of evidence4 are available online.
The 2018 AHA/ACC cholesterol guideline represents a step forward in ASCVD prevention—especially in primary prevention, where it provides guidance for risk refinement and personalization. In this article, we mine the details of what has changed and what is new in this guideline so that you can prepare to adopt the recommendations in your practice.
2013 and 2018 guidelines: Similarities, differences
As in earlier iterations, the 2018 guideline emphasizes healthy lifestyle across the life-course as the basis of ASCVD prevention—as elaborated in the 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk.5 In contrast to the 2013 guidelines,2 the 2018 guideline is more comprehensive and more personalized, focusing on risk assessment for individual patients, rather than simply providing population-based approaches. Moreover, the guideline isn’t limited to adults: It makes recommendations pertaining to children and adolescents.1
TABLE 11,2 compares the most important differences between the 2013 and 2018 guidelines.
The 2013 ACC/AHA guidelines eliminated low-density lipoprotein cholesterol (LDL-C) and non-high-density lipoprotein cholesterol (non-HDL-C)a goals of therapy and replaced them with the concept of 4 “statin benefit groups”—that is, patient populations for which clear evidence supports the role of statin therapy.4 In the 2018 guideline, statin benefit groups have been maintained, although without explicit use of this term.1
Primary prevention. Although no major changes in statin indications are made for patients with (1) established ASCVD (ie, for secondary prevention), (2) diabetes mellitus (DM) and who are 40 to 75 years of age, or (3) a primary LDL-C elevation ≥ 190 mg/dL, significant changes were made for primary prevention patients ages 40 to 75 years.1 ASCVD risk calculation using the 2013 pooled cohort equations (PCE) is still recommended4; however, risk estimation is refined by the use of specific so-called risk-enhancing factors (TABLE 21). In cases in which the risk decision remains uncertain, obtaining the coronary artery calcium (CAC) score (which we’ll describe shortly) using specialized computed tomography (CT) is advised to facilitate the shared physician–patient decision-making process.1
LDL-C and non-HDL-C thresholds. Although LDL-C and non-HDL-C goals are not overtly brought back from the 2002 National Cholesterol Education Program/Adult Treatment Panel guidelines,6 the new guideline does introduce LDL-C and non-HDL-C thresholds—levels at which adding nonstatin therapy can be considered, in contrast to previous goals to which therapy was titrated. Definitions of statin intensity remain the same: Moderate-intensity statin therapy is expected to reduce the LDL-C level by 30% to 50%; high-intensity statin therapy, by ≥ 50%.1 The intensity of statin therapy has been de-escalated in the intermediate-risk group, where previous guidelines advised high-intensity statin therapy,4 and replaced with moderate-intensity statin therapy (similar to 2016 US Preventive Services Task Force [USPSTF] recommendations7).
[polldaddy:10312157]
Continue to: Fasting vs nonfasting lipid profiles
Fasting vs nonfasting lipid profiles. In contrast to previous guidelines,2,8 which used fasting lipid profiles, nonfasting lipid profiles are now recommended for establishing a baseline LDL-C level and for ASCVD risk estimation for most patients—as long as the triglycerides (TG) level is < 400 mg/dL. When the calculated LDL-C level is < 70 mg/dL using the standard Friedewald formula, obtaining a direct LDL-C or a modified LDL-C estimate9 is deemed reasonable to improve accuracy. (The modified LDL-C can be estimated using The Johns Hopkins Hospital’s free “LDL Cholesterol Calculator” [www.hopkinsmedicine.org/apps/all-apps/ldl-cholesterol-calculator]).
A fasting lipid profile is still preferred for patients who have a family history of a lipid disorder. The definition of hypertriglyceridemia has been revised from a fasting TG level ≥ 150 mg/dL to a nonfasting or fasting TG level ≥ 175 mg/dL.1
Nonstatin add-on therapy. The new guideline supports the addition of nonstatin therapies to maximally tolerated statin therapy in patients who have established ASCVD or a primary LDL-C elevation ≥ 190 mg/dL when (1) the LDL-C level has not been reduced by the expected percentage (≥ 50% for high-intensity statin therapy) or (2) explicit LDL-C level thresholds have been met.1
The principal 2 groups of recommended nonstatins for which there is randomized, controlled trial evidence of cardiovascular benefit are (1) the cholesterol-absorbing agent ezetimibe10 and (2) the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors evolocumab11 and alirocumab.12
AAFP’s guarded positions on the 2013 and 2018 guidelines
The American Academy of Family Physicians (AAFP) welcomed the patient-centered and outcome-oriented aspects of the 2013 ACC/AHA guidelines, endorsing them with 3 qualifications.13
- Many of the recommendations were based on expert opinion, not rigorous research results—in particular, not on the findings of randomized controlled trials (although key points are based on high-quality evidence).
- There were conflicts of interest disclosed for 15 members of the guidelines panel, including a vice chair.
- Validation of the PCE risk estimation tool was lacking.
Continue to: AAFP announced...
AAFP announced in March that it does not endorse the 2018 AHA/ACC guideline, asserting that (1) only a small portion of the recommendations, primarily focused on the addition of nonstatin therapy, were addressed by an independent systematic review and (2) many of the guideline recommendations are based on low-quality or insufficient evidence. AAFP nevertheless bestowed an “affirmation of value” designation on the guideline—meaning that it provides some benefit for family physicians’ practice without fulfilling all criteria for full endorsement.14
Detailed recommendations from the 2018 guideline
Lifestyle modification
When talking about ASCVD risk with patients, it is important to review current lifestyle habits (eg, diet, physical activity, weight or body mass index, and tobacco use). Subsequent to that conversation, a healthy lifestyle should be endorsed and relevant advice provided. In addition, patient-directed materials (eg, ACC’s CardioSmart [www.cardiosmart.org]; AHA’s Life’s Simple 7 [www.heart.org/en/professional/workplace-health/lifes-simple-7]; and the National Lipid Association’s Patient Tear Sheets [www.lipid.org/practicetools/tools/tearsheets] and Clinicians’ Lifestyle Modification Toolbox [www.lipid.org/CLMT]) and referrals (eg, to cardiac rehabilitation, a dietitian, a smoking-cessation program) should be provided.1
Primary prevention of ASCVD
Risk assessment for primary prevention is now approached as a process, rather than the simple risk calculation used in the 2013 ACC/AHA guidelines.2 Assessment involves risk estimation followed by risk personalization, which, in some cases, is followed by risk reclassification using CAC scoring.1
Patients are classified into 1 of 4 risk groups, based on the PCE1:
- low (< 5%)
- borderline (5%-7.5%)
- intermediate (7.5%-19.9%)
- high (≥ 20%).
However, the PCE-based risk score is a population-based tool, which might not reflect the actual risk of individual patients. In some populations, PCE underestimates ASCVD risk; in others, it overestimates risk. A central tenet of the new guideline is personalization of risk, taking into account the unique circumstances of each patient. Moreover, the new guideline provides guidance on how to interpret the PCE risk score for several different ethnic and racial groups.1
Continue to: Medical therapy
Medical therapy. The decision to start lipid-lowering therapy should be made after a physician–patient discussion that considers costs of therapy as well as patient preferences and values in the context of shared decision-making. Discussion should include a review of major risk factors (eg, cigarette smoking, elevated blood pressure, and the LDL-C level), the PCE risk score, the presence of risk-enhancing factors (TABLE 21), potential benefits of lifestyle changes and statin therapy, and the potential for adverse drug effects and drug–drug interactions.1
If the estimated ASCVD risk is 7.5%-19.9%, starting moderate-intensity statin therapy is recommended. Risk-enhancing factors favor initiation of statin therapy, even in patients at borderline risk (5%-7.5%). If risk is uncertain, the CAC score can be used to facilitate shared decision-making.1 The use of CAC is in agreement with the USPSTF statement that CAC can moderately improve discrimination and reclassification, but has an unclear effect on downstream health care utilization.15 Importantly, CAC should not be measured routinely in patients already taking a statin because its primary role is to facilitate shared decision-making regarding initiation of statin therapy.16
If the 10-year ASCVD risk is ≥ 20%, high-intensity statin therapy is advised, without need to obtain the CAC score. If high-intensity statin therapy is advisable but not acceptable to, or tolerated by, the patient, it might be reasonable to add a nonstatin drug (ezetimibe or a bile-acid sequestrant) to moderate-intensity statin therapy.1
Risk-enhancing factors (TABLE 21) apply to intermediate- and borderline-risk patients. Importantly, these factors include membership in specific ethnic groups, conditions specific to females, and male–female distinctions in risk. Risk-enhancing factors also incorporate biomarkers that are often measured by lipid specialists, such as lipoprotein(a) (Lp[a]) and apolipoprotein B (ApoB).1
Lp(a) is an atherogenic particle, akin to an LDL particle, that consists of a molecule of apolipoprotein (a) (a nonfunctional mimic of a portion of plasminogen) covalently bound to ApoB, like the one found on the LDL particle. Lp(a) is proportionally associated with an increased risk for ASCVD and aortic stenosis at a level > 50 mg/dL.17 A family history of premature ASCVD is a relative indication for measuring Lp(a).1
Continue to: When and why to measure CAC
When and why to measure CAC
If the decision to initiate statin therapy is still uncertain after risk estimation and personalization, or when a patient is undecided about committing to lifelong lipid-lowering therapy, the new guideline recommends obtaining a CAC score to inform the shared decision-making process.1,18 Measurement of CAC is obtained by noncontrast, electrocardiographic-gated CT that can be performed in 10 to 15 minutes, requiring approximately 1 millisievert of radiation (equivalent of the approximate dose absorbed during 2 mammograms). Although measurement of the CAC score is generally not covered by insurance, its cost ($50-$450) nationwide makes it accessible.19
CAC measures the presence (or absence) of subclinical atherosclerosis by detecting calcified plaque in coronary arteries. The absolute CAC score is expressed in Agatston units; an age–gender population percentile is also provided. Keep in mind that the presence of any CAC (ie, a score > 0) is abnormal and demonstrates the presence of subclinical coronary artery disease. The prevalence of CAC > 0 increases with age, but a significant percentage of older people have a CAC score = 0. When CAC > 0, additional information is provided by the distribution of plaque burden among the different coronary arteries.20
Among intermediate-risk patients, 50% have CAC = 0 and, therefore, a very low event rate over the ensuing 10 years, which allows statin therapy to be safely deferred unless certain risk factors are present (eg, family history, smoking, DM).1,18 It is reasonable to repeat CAC testing in 5 to 10 years to assess whether subclinical atherosclerosis has developed. The 2018 guideline emphasizes that, when the CAC score is > 0 but < 100 Agatston units, statin therapy is favored, especially in patients > 55 years of age; when the CAC score is ≥ 100 Agatston units or at the ≥ 75th percentile, statin therapy is indicated regardless of age.1
Patients who might benefit from knowing their CAC score include those who are:
- reluctant to initiate statin therapy but who want to understand their risk and potential for benefit more precisely
- concerned about the need to reinstitute statin therapy after discontinuing it because of statin-associated adverse effects
- older (men, 55-80 years; women, 60-80 years) who have a low burden of risk factors and who question whether they would benefit from statin therapy
- middle-aged (40-55 years) and who have a PCE-calculated risk of 5% to < 7.5% for ASCVD and factors that increase their risk for ASCVD, even though they are in a borderline-risk group.1
Primary prevention in special populations
Older patients. In adults ≥ 75 years who have an LDL-C level 70 to 189 mg/dL, initiating a moderate-intensity statin might be reasonable; however, it might also be reasonable to stop treatment in this population when physical or cognitive decline, multiple morbidities, frailty, or reduced life expectancy limits the potential benefit of statin therapy. It might be reasonable to use the CAC score in adults 76 to 80 years of age who have an LDL-C level of 70 to 189 mg/dL to reclassify those whose CAC score = 0, so that they can avoid statin therapy.1
Continue to: Children and adolescents
Children and adolescents. In alignment with current pediatric guidelines,21 but in contrast to USPSTF reccomendations,22 the 2018 ACC/AHA guideline endorses universal lipid screening for pediatric patients (see TABLE W11,21,22). It is reasonable to obtain a fasting lipid profile or nonfasting non-HDL-C in all children and adolescents who have neither cardiovascular risk factors nor a family history of early cardiovascular disease to detect moderate-to-severe lipid abnormalities. Screening should be done once at 9 to 11 years of age and again at 17 to 21 years.1
A screening test as early as 2 years of age to detect familial hypercholesterolemia (FH) is reasonable when a family history of either early CVD or significant hypercholesterolemia is present. The guideline endorses reverse cascade screening for detection of FH in family members of children and adolescents who have severe hypercholesterolemia.1
In children and adolescents with a lipid abnormality, especially when associated with the metabolic syndrome, lifestyle counseling is beneficial for lowering the LDL-C level. In children and adolescents ≥ 10 years of age with (1) an LDL-C level persistently ≥ 190 mg/dL or (2) an LDL level ≥ 160 mg/dL plus a clinical presentation consistent with FH, it is reasonable to initiate statin therapy if they do not respond adequately to 3 to 6 months of lifestyle therapy.1
Ethnicity as a risk-modifying factor. The PCE distinguishes between US adults of European ancestry and African ancestry, but no other ethnic groups are distinguished.4 The new guideline advocates for the use of PCE in other populations; however, it states that, for clinical decision-making purposes, it is reasonable, in adults of different races and ethnicities, for the physician to review racial and ethnic features that can influence ASCVD risk to allow adjustment of the choice of statin or intensity of treatment. Specifically, South Asian ancestry is now treated as a risk-enhancing factor, given the high prevalence of premature and extensive ASCVD in this patient population.1
Concerns specific to women. Considering conditions specific to women as potential risk-enhancing factors is advised when discussing lifestyle intervention and the potential for benefit from statin therapy—in particular, (1) in the setting of premature menopause (< 40 years) and (2) when there is a history of a pregnancy-associated disorder (eg, hypertension, preeclampsia, gestational DM, a small-for-gestational-age infant, and preterm delivery). If the decision is made to initiate statin therapy in women of childbearing age who are sexually active, there is a guideline mandate to counsel patients on using reliable contraception. When pregnancy is planned, statin therapy should be discontinued 1 to 2 months before pregnancy is attempted; when pregnancy occurs while a patient is taking a statin, therapy should be stopped as soon as the pregnancy is discovered.1
Continue to: Adults with chronic kidney disease
Adults with chronic kidney disease. Chronic kidney disease that is not treated with dialysis or kidney transplantation is considered a risk-enhancing factor; initiation of a moderate-intensity statin or a moderate-intensity statin plus ezetimibe can be useful in patients with chronic kidney disease who are 40 to 75 years of age and have an LDL-C level of 70 to 189 mg/dL and a PCE-calculated risk ≥ 7.5%. In adults with advanced kidney disease that requires dialysis who are already taking a statin, it may be reasonable to continue the statin; however, initiation of a statin in adults with advanced kidney disease who require dialysis is not recommended because of an apparent lack of benefit.1
Adults with a chronic inflammatory disorder or human immunodeficiency virus infection. Any of these conditions are treated as risk-enhancing factors; in a risk discussion with affected patients, therefore, moderate-intensity statin therapy or high-intensity statin therapy is favored for those 40 to 75 years of age who have an LDL-C level of 70 to 189 mg/dL and PCE-calculated risk ≥ 7.5%. A fasting lipid profile and assessment of ASCVD risk factors for these patients can be useful (1) as a guide to the potential benefit of statin therapy and (2) for monitoring or adjusting lipid-lowering drug therapy before, and 4 to 12 weeks after, starting inflammatory disease-modifying therapy or antiretroviral therapy.
In adults with rheumatoid arthritis who undergo ASCVD risk assessment with a lipid profile, it can be useful to recheck lipid values and other major ASCVD risk factors 2 to 4 months after the inflammatory disease has been controlled.1
Primary hypercholesterolemia
The diagnosis and management of heterozygous or homozygous familial hypercholesterolemia (HeFH or HoFH) is beyond the scope of the 2018 ACC/AHA cholesterol guidelines; instead, the 2015 AHA Scientific Statement, “The Agenda for Familial Hypercholesterolemia,” provides a contemporary review of these topics.23 However, the 2018 cholesterol guideline does acknowledge that an LDL-C level ≥ 190 mg/dL often corresponds to primary (ie, genetic) hypercholesterolemia.
In patients 20 to 75 years of age who have a primary elevation of LDL-C level ≥ 190 mg/dL, the guideline recommends initiation of high-intensity statin therapy without calculating ASCVD risk using the PCE. If a > 50% LDL-C reduction is not achieved, or if the LDL-C level on maximally tolerated statin therapy remains ≥ 100 mg/dL, adding ezetimibe is considered reasonable. If there is < 50% reduction in the LDL-C level while taking maximally tolerated statin and ezetimibe therapy, adding a bile-acid sequestrant can be considered, as long as the TG level is not > 300 mg/dL (ie, bile-acid sequestrants can elevate the TG level significantly).
Continue to: In patients 30 to 75 years of age...
In patients 30 to 75 years of age who have a diagnosis of HeFH and an LDL-C level ≥ 100 mg/dL while taking maximally tolerated statin and ezetimibe therapy, the addition of a PCSK9 inhibitor can be considered. Regardless of whether there is a diagnosis of HeFH, addition of a PCSK9 inhibitor can be considered in patients 40 to 75 years of age who have a baseline LDL-C level ≥ 220 mg/dL and who achieve an on-treatment LDL-C level ≥ 130 mg/dL while receiving maximally tolerated statin therapy and ezetimibe.1
Diabetes mellitus
In patients with DM who are 40 to 75 years of age, moderate-intensity statin therapy is recommended without calculating the 10-year ASCVD risk. When the LDL-C level is 70 to 189 mg/dL, however, it is reasonable to use the PCE to assess 10-year ASCVD risk to facilitate risk stratification.
In patients with DM who are at higher risk, especially those who have multiple risk factors or are 50 to 75 years of age, it is reasonable to use a high-intensity statin to reduce the LDL-C level by ≥ 50 %. In adults > 75 years of age with DM who are already on statin therapy, it is reasonable to continue statin therapy; for those that age who are not on statin therapy, it might be reasonable to initiate statin therapy after a physician–patient discussion of potential benefits and risks.
In adults with DM and PCE-calculated risk ≥ 20%, it might be reasonable to add ezetimibe to maximally tolerated statin therapy to reduce the LDL-C level by ≥ 50%. In adults 20 to 39 years of age with DM of long duration (≥ 10 years of type 2 DM, ≥ 20 years of type 1 DM), albuminuria (≥ 30 μg of albumin/mg creatinine), estimated glomerular filtration rate < 60 mL/min/1.73 m2, retinopathy, neuropathy, or ankle-brachial index < 0.9, it might be reasonable to initiate statin therapy.1
Secondary prevention
Presence of clinical ASCVD. In patients with clinical ASCVD who are ≤ 75 years of age, high-intensity statin therapy should be initiated or continued, with the aim of achieving ≥ 50% reduction in the LDL-C level. When high-intensity statin therapy is contraindicated or if a patient experiences statin-associated adverse effects, moderate-intensity statin therapy should be initiated or continued with the aim of achieving a 30% to 49% reduction in the LDL-C level.
Continue to: In patients...
In patients > 75 years of age with clinical ASCVD, it is reasonable to initiate or continue moderate- or high-intensity statin therapy after evaluation of the potential for ASCVD risk reduction, adverse effects, and drug–drug interactions, as well as patient frailty and patient preference.1
Very high risk. In patients at very high risk (this includes a history of multiple major ASCVD events or 1 major ASCVD event plus multiple high-risk conditions), maximally tolerated LDL-C-lowering therapy should include maximally tolerated statin therapy and ezetimibe before considering a PCSK9 inhibitor. An LDL-C level ≥ 70 mg/dL or a non-HDL-C level ≥ 100 mg/dL is considered a reasonable threshold for adding a PCSK9 inhibitor to background lipid-lowering therapy1 (TABLE 31).
Heart failure. In patients with heart failure who have (1) a reduced ejection fraction attributable to ischemic heart disease, (2) a reasonable life expectancy (3-5 years), and (3) are not already on a statin because of ASCVD, consider initiating moderate-intensity statin therapy to reduce the risk for an ASCVD event.1
Reduction of elevated triglycerides
The guideline defines moderate hypertriglyceridemia as a nonfasting or fasting TG level of 175 to 499 mg/dL. Such a finding is considered a risk-enhancing factor and is 1 of 5 components of the metabolic syndrome. Three independent measurements are advised to diagnose primary moderate hypertriglyceridemia. Severe hypertriglyceridemia is diagnosed when the fasting TG level is ≥ 500 mg/dL.1
In moderate hypertriglyceridemia, most TGs are carried in very-low-density lipoprotein particles; in severe hypertriglyceridemia, on the other hand, chylomicrons predominate, raising the risk for pancreatitis. In adults with severe hypertriglyceridemia, therefore—especially when the fasting TG level is ≥ 1000 mg/dL—it is reasonable to identify and address other causes of hypertriglyceridemia. If TGs are persistently elevated or increasing, levels should be reduced to prevent acute pancreatitis with a very low-fat diet and by avoiding refined carbohydrates and alcohol; consuming omega-3 fatty acids; and, if necessary, taking a fibrate.1
Continue to: In adults...
In adults ≥ 20 years of age with moderate hypertriglyceridemia, lifestyle factors (eg, obesity, metabolic syndrome), secondary factors (eg, DM, chronic liver or kidney disease, nephrotic syndrome, hypothyroidism), and medications that increase the TG level need to be addressed first. In adults 40 to 75 years of age with moderate or severe hypertriglyceridemia and a PCE-calculated ASCVD risk ≥ 7.5%, it is reasonable to reevaluate risk after lifestyle and secondary factors are addressed and to consider a persistently elevated TG level as a factor favoring initiation or intensification of statin therapy. In adults 40 to 75 years of age with severe hypertriglyceridemia and ASCVD risk ≥ 7.5%, it is reasonable to address reversible causes of a high TG level and to initiate statin therapy.1
Other considerations in cholesterol management
Tools to assess adherence
The response to lifestyle and statin therapy should be evaluated by the percentage reduction in the LDL-C level compared with baseline, not by assessment of the absolute LDL-C level. When seeing a patient whose treatment is ongoing, a baseline level can be estimated using a desktop LDL-calculator app.
Adherence and percentage response to LDL-C–lowering medications and lifestyle changes should be evaluated with repeat lipid measurement 4 to 12 weeks after either a statin is initiated or the dosage is adjusted, and repeated every 3 to 12 months as needed. In patients with established ASCVD who are at very high risk, triggers for adding nonstatin therapy are defined by a threshold LDL-C level ≥ 70 mg/dL on maximal statin therapy.1
Interventions focused on improving adherence to prescribed therapy are recommended for management of adults with an elevated cholesterol level. These interventions include telephone reminders, calendar reminders, integrated multidisciplinary educational activities, and pharmacist-led interventions, such as simplification of the medication regimen to once-daily dosing.1
Statin safety and associated adverse effects
A physician–patient risk discussion is recommended before initiating statin therapy to review net clinical benefit, during which the 2 parties weigh the potential for ASCVD risk reduction against the potential for statin-associated adverse effects, statin–drug interactions, and safety, with the physician emphasizing that adverse effects can be addressed successfully.
Continue to: Statins are one of...
Statins are one of the safest classes of medication, with an excellent risk-benefit ratio. However, there are myriad confusing media reports regarding potential adverse effects and safety of the statin class—reports that often lead patients to discontinue or refuse statins.
Statin-associated adverse effects include the common statin-associated muscle symptoms (SAMS), new-onset DM, cognitive effects, and hepatic injury. The frequency of new-onset DM depends on the population exposed to statins, with a higher incidence of new-onset DM found in patients who are already predisposed, such as those with obesity, prediabetes, and metabolic syndrome. Cognitive effects are rare and difficult to interpret; they were not reported in the large statin mega-trials but have been described in case reports. Significant transaminase elevations > 3 times the upper limit of normal are infrequent; hepatic failure with statins is extremely rare and found at the same incidence in the general population.1
SAMS include (in order of decreasing prevalence)24:
- myalgias with a normal creatine kinase (CK) level
- conditions such as myositis or myopathy (elevated CK level)
- rhabdomyolysis (CK level > 10 times the upper limit of normal, plus renal injury)
- extremely rare statin-associated autoimmune myopathy, with detectable 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase antibodies.
In patients with SAMS, thorough assessment of symptoms is recommended, in addition to evaluation for nonstatin causes and predisposing factors. Identification of potential SAMS-predisposing factors is recommended before initiation of treatment, including demographics (eg, East-Asian ancestry), comorbid conditions (eg, hypothyroidism and vitamin D deficiency), and use of medications adversely affecting statin metabolism (eg, cyclosporine).
In patients with statin-associated adverse effects that are not severe, it is recommended to reassess and rechallenge to achieve a maximal lowering of the LDL-C level by a modified dosing regimen or an alternate statin or by combining a statin with nonstatin therapy. In patients with increased risk for DM or new-onset DM, it is recommended to continue statin therapy.
Continue to: Routine CK and liver function testing...
Routine CK and liver function testing is not useful in patients treated with statins; however, it is recommended that CK be measured in patients with severe SAMS or objective muscle weakness, or both, and to measure liver function if symptoms suggest hepatotoxicity. In patients at increased risk for ASCVD who have chronic, stable liver disease (including non-alcoholic fatty liver disease), it is reasonable, when appropriately indicated, to use statins after obtaining baseline measurements and determining a schedule of monitoring and safety checks.
In patients at increased risk for ASCVD who have severe or recurrent SAMS after appropriate statin rechallenge, it is reasonable to use nonstatin therapy that is likely to provide net clinical benefit. The guideline does not recommend routine use of coenzyme Q10 supplementation for the treatment or prevention of SAMS.1
Guideline criticism
Guideline development is challenging on multiple levels, including balancing perspectives from multiple stakeholders. Nevertheless, the 2018 AHA/ACC cholesterol guideline builds nicely on progress made since its 2013 predecessor was released.4 This document was developed with the participation of representatives from 10 professional societies in addition to the ACC and AHA—notably, the National Lipid Association and American Society for Preventive Cardiology.1
To refine risk estimation and facilitate shared decision-making, the new guideline introduced so-called risk-enhancing factors and use of the CAC.1 However, some potential risk-enhancing factors were left out: erectile dysfunction, for example, often a marker of increased cardiovascular risk in men < 50 years of age.25 In addition, although pretreatment ApoB was introduced as a risk-enhancing factor,1 no recommendation is given to measure ApoB after initiation of therapy for evaluation of residual cardiovascular risk, as endorsed in other guidelines.26,27
Moreover, the guideline does not include the “extreme risk” category in the guideline developed by the American Association of Clinical Endocrinologists (AACE).28 Although the 2018 AHA/ACC guideline introduces < 70 mg/dL and < 100 mg/dL LDL-C thresholds,1 the < 55 mg/dL LDL-C threshold used for patients in the AACE/American College of Endocrinology extreme-risk category is not mentioned.26 This omission might leave patients who are at extreme ASCVD risk without optimal lipid-lowering therapy. Similarly, the guideline does not elaborate on the diagnosis and treatment of HoFH and HeFH.1 The age cutoff of 30 years for the recommendation to consider PCSK9 inhibitors in patients with HeFH appears arbitrary and excludes younger FH patients who have an extreme LDL-C elevation from potentially important therapy.23
Continue to: Guidelines are dynamic instruments...
Guidelines are dynamic instruments that require constant updating, given the production of new evidence. In fact, the results of the Reduction of Cardiovascular Events With Icosapent Ethyl-Intervention Trial (REDUCE-IT) were presented at the same meeting at which this guideline was unveiled.29 REDUCE-IT demonstrated an astonishing highly significant 25% reduction in the composite primary major adverse cardiovascular event outcome in patients with an LDL-C level of 44 to 100 mg/dL on statin therapy, who had a TG level of 135 to 499 mg/dL and had been treated for a median of 4.9 years with 4 g of pure eicosapentaenoic acid.
In addition, the guideline’s value statements, which address the need to consider the cost of drugs in determining most appropriate treatment, are no longer accurate because the price of PCSK9 inhibitors has dropped by more than half since the guideline was issued.30
An upward climb to clinical payoff
Even after close study of the 2018 AHA/ACC cholesterol guideline, implementing it in practice might remain a challenge to clinicians who are inexperienced in ordering lipid markers such as Lp(a) and interpreting the CAC score. Moreover, initiating and monitoring nonstatin therapies will be a demanding task—especially with PCSK9 inhibitors, which present access difficulties because they are relatively expensive (even after the recent price cut). That’s why, when there is doubt in the mind of the physician or other provider, we will likely see more referrals to specialists in lipid management and ASCVD risk estimation to optimize preventive therapy.31
CORRESPONDENCE
Cezary Wójcik, MD, PhD, FNLA, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR 97239; cezarywojcik2000@gmail.com
A new cholesterol guideline1 builds on the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guidelines,2 which were a major paradigm shift in the evaluation and management of blood cholesterol levels and risk for atherosclerotic cardiovascular disease (ASCVD). The work was presented (and simultaneously published) on November 10, 2018, at the annual AHA Scientific Sessions in Chicago. Full text,1 an executive summary,3 and accompanying systematic review of evidence4 are available online.
The 2018 AHA/ACC cholesterol guideline represents a step forward in ASCVD prevention—especially in primary prevention, where it provides guidance for risk refinement and personalization. In this article, we mine the details of what has changed and what is new in this guideline so that you can prepare to adopt the recommendations in your practice.
2013 and 2018 guidelines: Similarities, differences
As in earlier iterations, the 2018 guideline emphasizes healthy lifestyle across the life-course as the basis of ASCVD prevention—as elaborated in the 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk.5 In contrast to the 2013 guidelines,2 the 2018 guideline is more comprehensive and more personalized, focusing on risk assessment for individual patients, rather than simply providing population-based approaches. Moreover, the guideline isn’t limited to adults: It makes recommendations pertaining to children and adolescents.1
TABLE 11,2 compares the most important differences between the 2013 and 2018 guidelines.
The 2013 ACC/AHA guidelines eliminated low-density lipoprotein cholesterol (LDL-C) and non-high-density lipoprotein cholesterol (non-HDL-C)a goals of therapy and replaced them with the concept of 4 “statin benefit groups”—that is, patient populations for which clear evidence supports the role of statin therapy.4 In the 2018 guideline, statin benefit groups have been maintained, although without explicit use of this term.1
Primary prevention. Although no major changes in statin indications are made for patients with (1) established ASCVD (ie, for secondary prevention), (2) diabetes mellitus (DM) and who are 40 to 75 years of age, or (3) a primary LDL-C elevation ≥ 190 mg/dL, significant changes were made for primary prevention patients ages 40 to 75 years.1 ASCVD risk calculation using the 2013 pooled cohort equations (PCE) is still recommended4; however, risk estimation is refined by the use of specific so-called risk-enhancing factors (TABLE 21). In cases in which the risk decision remains uncertain, obtaining the coronary artery calcium (CAC) score (which we’ll describe shortly) using specialized computed tomography (CT) is advised to facilitate the shared physician–patient decision-making process.1
LDL-C and non-HDL-C thresholds. Although LDL-C and non-HDL-C goals are not overtly brought back from the 2002 National Cholesterol Education Program/Adult Treatment Panel guidelines,6 the new guideline does introduce LDL-C and non-HDL-C thresholds—levels at which adding nonstatin therapy can be considered, in contrast to previous goals to which therapy was titrated. Definitions of statin intensity remain the same: Moderate-intensity statin therapy is expected to reduce the LDL-C level by 30% to 50%; high-intensity statin therapy, by ≥ 50%.1 The intensity of statin therapy has been de-escalated in the intermediate-risk group, where previous guidelines advised high-intensity statin therapy,4 and replaced with moderate-intensity statin therapy (similar to 2016 US Preventive Services Task Force [USPSTF] recommendations7).
[polldaddy:10312157]
Continue to: Fasting vs nonfasting lipid profiles
Fasting vs nonfasting lipid profiles. In contrast to previous guidelines,2,8 which used fasting lipid profiles, nonfasting lipid profiles are now recommended for establishing a baseline LDL-C level and for ASCVD risk estimation for most patients—as long as the triglycerides (TG) level is < 400 mg/dL. When the calculated LDL-C level is < 70 mg/dL using the standard Friedewald formula, obtaining a direct LDL-C or a modified LDL-C estimate9 is deemed reasonable to improve accuracy. (The modified LDL-C can be estimated using The Johns Hopkins Hospital’s free “LDL Cholesterol Calculator” [www.hopkinsmedicine.org/apps/all-apps/ldl-cholesterol-calculator]).
A fasting lipid profile is still preferred for patients who have a family history of a lipid disorder. The definition of hypertriglyceridemia has been revised from a fasting TG level ≥ 150 mg/dL to a nonfasting or fasting TG level ≥ 175 mg/dL.1
Nonstatin add-on therapy. The new guideline supports the addition of nonstatin therapies to maximally tolerated statin therapy in patients who have established ASCVD or a primary LDL-C elevation ≥ 190 mg/dL when (1) the LDL-C level has not been reduced by the expected percentage (≥ 50% for high-intensity statin therapy) or (2) explicit LDL-C level thresholds have been met.1
The principal 2 groups of recommended nonstatins for which there is randomized, controlled trial evidence of cardiovascular benefit are (1) the cholesterol-absorbing agent ezetimibe10 and (2) the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors evolocumab11 and alirocumab.12
AAFP’s guarded positions on the 2013 and 2018 guidelines
The American Academy of Family Physicians (AAFP) welcomed the patient-centered and outcome-oriented aspects of the 2013 ACC/AHA guidelines, endorsing them with 3 qualifications.13
- Many of the recommendations were based on expert opinion, not rigorous research results—in particular, not on the findings of randomized controlled trials (although key points are based on high-quality evidence).
- There were conflicts of interest disclosed for 15 members of the guidelines panel, including a vice chair.
- Validation of the PCE risk estimation tool was lacking.
Continue to: AAFP announced...
AAFP announced in March that it does not endorse the 2018 AHA/ACC guideline, asserting that (1) only a small portion of the recommendations, primarily focused on the addition of nonstatin therapy, were addressed by an independent systematic review and (2) many of the guideline recommendations are based on low-quality or insufficient evidence. AAFP nevertheless bestowed an “affirmation of value” designation on the guideline—meaning that it provides some benefit for family physicians’ practice without fulfilling all criteria for full endorsement.14
Detailed recommendations from the 2018 guideline
Lifestyle modification
When talking about ASCVD risk with patients, it is important to review current lifestyle habits (eg, diet, physical activity, weight or body mass index, and tobacco use). Subsequent to that conversation, a healthy lifestyle should be endorsed and relevant advice provided. In addition, patient-directed materials (eg, ACC’s CardioSmart [www.cardiosmart.org]; AHA’s Life’s Simple 7 [www.heart.org/en/professional/workplace-health/lifes-simple-7]; and the National Lipid Association’s Patient Tear Sheets [www.lipid.org/practicetools/tools/tearsheets] and Clinicians’ Lifestyle Modification Toolbox [www.lipid.org/CLMT]) and referrals (eg, to cardiac rehabilitation, a dietitian, a smoking-cessation program) should be provided.1
Primary prevention of ASCVD
Risk assessment for primary prevention is now approached as a process, rather than the simple risk calculation used in the 2013 ACC/AHA guidelines.2 Assessment involves risk estimation followed by risk personalization, which, in some cases, is followed by risk reclassification using CAC scoring.1
Patients are classified into 1 of 4 risk groups, based on the PCE1:
- low (< 5%)
- borderline (5%-7.5%)
- intermediate (7.5%-19.9%)
- high (≥ 20%).
However, the PCE-based risk score is a population-based tool, which might not reflect the actual risk of individual patients. In some populations, PCE underestimates ASCVD risk; in others, it overestimates risk. A central tenet of the new guideline is personalization of risk, taking into account the unique circumstances of each patient. Moreover, the new guideline provides guidance on how to interpret the PCE risk score for several different ethnic and racial groups.1
Continue to: Medical therapy
Medical therapy. The decision to start lipid-lowering therapy should be made after a physician–patient discussion that considers costs of therapy as well as patient preferences and values in the context of shared decision-making. Discussion should include a review of major risk factors (eg, cigarette smoking, elevated blood pressure, and the LDL-C level), the PCE risk score, the presence of risk-enhancing factors (TABLE 21), potential benefits of lifestyle changes and statin therapy, and the potential for adverse drug effects and drug–drug interactions.1
If the estimated ASCVD risk is 7.5%-19.9%, starting moderate-intensity statin therapy is recommended. Risk-enhancing factors favor initiation of statin therapy, even in patients at borderline risk (5%-7.5%). If risk is uncertain, the CAC score can be used to facilitate shared decision-making.1 The use of CAC is in agreement with the USPSTF statement that CAC can moderately improve discrimination and reclassification, but has an unclear effect on downstream health care utilization.15 Importantly, CAC should not be measured routinely in patients already taking a statin because its primary role is to facilitate shared decision-making regarding initiation of statin therapy.16
If the 10-year ASCVD risk is ≥ 20%, high-intensity statin therapy is advised, without need to obtain the CAC score. If high-intensity statin therapy is advisable but not acceptable to, or tolerated by, the patient, it might be reasonable to add a nonstatin drug (ezetimibe or a bile-acid sequestrant) to moderate-intensity statin therapy.1
Risk-enhancing factors (TABLE 21) apply to intermediate- and borderline-risk patients. Importantly, these factors include membership in specific ethnic groups, conditions specific to females, and male–female distinctions in risk. Risk-enhancing factors also incorporate biomarkers that are often measured by lipid specialists, such as lipoprotein(a) (Lp[a]) and apolipoprotein B (ApoB).1
Lp(a) is an atherogenic particle, akin to an LDL particle, that consists of a molecule of apolipoprotein (a) (a nonfunctional mimic of a portion of plasminogen) covalently bound to ApoB, like the one found on the LDL particle. Lp(a) is proportionally associated with an increased risk for ASCVD and aortic stenosis at a level > 50 mg/dL.17 A family history of premature ASCVD is a relative indication for measuring Lp(a).1
Continue to: When and why to measure CAC
When and why to measure CAC
If the decision to initiate statin therapy is still uncertain after risk estimation and personalization, or when a patient is undecided about committing to lifelong lipid-lowering therapy, the new guideline recommends obtaining a CAC score to inform the shared decision-making process.1,18 Measurement of CAC is obtained by noncontrast, electrocardiographic-gated CT that can be performed in 10 to 15 minutes, requiring approximately 1 millisievert of radiation (equivalent of the approximate dose absorbed during 2 mammograms). Although measurement of the CAC score is generally not covered by insurance, its cost ($50-$450) nationwide makes it accessible.19
CAC measures the presence (or absence) of subclinical atherosclerosis by detecting calcified plaque in coronary arteries. The absolute CAC score is expressed in Agatston units; an age–gender population percentile is also provided. Keep in mind that the presence of any CAC (ie, a score > 0) is abnormal and demonstrates the presence of subclinical coronary artery disease. The prevalence of CAC > 0 increases with age, but a significant percentage of older people have a CAC score = 0. When CAC > 0, additional information is provided by the distribution of plaque burden among the different coronary arteries.20
Among intermediate-risk patients, 50% have CAC = 0 and, therefore, a very low event rate over the ensuing 10 years, which allows statin therapy to be safely deferred unless certain risk factors are present (eg, family history, smoking, DM).1,18 It is reasonable to repeat CAC testing in 5 to 10 years to assess whether subclinical atherosclerosis has developed. The 2018 guideline emphasizes that, when the CAC score is > 0 but < 100 Agatston units, statin therapy is favored, especially in patients > 55 years of age; when the CAC score is ≥ 100 Agatston units or at the ≥ 75th percentile, statin therapy is indicated regardless of age.1
Patients who might benefit from knowing their CAC score include those who are:
- reluctant to initiate statin therapy but who want to understand their risk and potential for benefit more precisely
- concerned about the need to reinstitute statin therapy after discontinuing it because of statin-associated adverse effects
- older (men, 55-80 years; women, 60-80 years) who have a low burden of risk factors and who question whether they would benefit from statin therapy
- middle-aged (40-55 years) and who have a PCE-calculated risk of 5% to < 7.5% for ASCVD and factors that increase their risk for ASCVD, even though they are in a borderline-risk group.1
Primary prevention in special populations
Older patients. In adults ≥ 75 years who have an LDL-C level 70 to 189 mg/dL, initiating a moderate-intensity statin might be reasonable; however, it might also be reasonable to stop treatment in this population when physical or cognitive decline, multiple morbidities, frailty, or reduced life expectancy limits the potential benefit of statin therapy. It might be reasonable to use the CAC score in adults 76 to 80 years of age who have an LDL-C level of 70 to 189 mg/dL to reclassify those whose CAC score = 0, so that they can avoid statin therapy.1
Continue to: Children and adolescents
Children and adolescents. In alignment with current pediatric guidelines,21 but in contrast to USPSTF reccomendations,22 the 2018 ACC/AHA guideline endorses universal lipid screening for pediatric patients (see TABLE W11,21,22). It is reasonable to obtain a fasting lipid profile or nonfasting non-HDL-C in all children and adolescents who have neither cardiovascular risk factors nor a family history of early cardiovascular disease to detect moderate-to-severe lipid abnormalities. Screening should be done once at 9 to 11 years of age and again at 17 to 21 years.1
A screening test as early as 2 years of age to detect familial hypercholesterolemia (FH) is reasonable when a family history of either early CVD or significant hypercholesterolemia is present. The guideline endorses reverse cascade screening for detection of FH in family members of children and adolescents who have severe hypercholesterolemia.1
In children and adolescents with a lipid abnormality, especially when associated with the metabolic syndrome, lifestyle counseling is beneficial for lowering the LDL-C level. In children and adolescents ≥ 10 years of age with (1) an LDL-C level persistently ≥ 190 mg/dL or (2) an LDL level ≥ 160 mg/dL plus a clinical presentation consistent with FH, it is reasonable to initiate statin therapy if they do not respond adequately to 3 to 6 months of lifestyle therapy.1
Ethnicity as a risk-modifying factor. The PCE distinguishes between US adults of European ancestry and African ancestry, but no other ethnic groups are distinguished.4 The new guideline advocates for the use of PCE in other populations; however, it states that, for clinical decision-making purposes, it is reasonable, in adults of different races and ethnicities, for the physician to review racial and ethnic features that can influence ASCVD risk to allow adjustment of the choice of statin or intensity of treatment. Specifically, South Asian ancestry is now treated as a risk-enhancing factor, given the high prevalence of premature and extensive ASCVD in this patient population.1
Concerns specific to women. Considering conditions specific to women as potential risk-enhancing factors is advised when discussing lifestyle intervention and the potential for benefit from statin therapy—in particular, (1) in the setting of premature menopause (< 40 years) and (2) when there is a history of a pregnancy-associated disorder (eg, hypertension, preeclampsia, gestational DM, a small-for-gestational-age infant, and preterm delivery). If the decision is made to initiate statin therapy in women of childbearing age who are sexually active, there is a guideline mandate to counsel patients on using reliable contraception. When pregnancy is planned, statin therapy should be discontinued 1 to 2 months before pregnancy is attempted; when pregnancy occurs while a patient is taking a statin, therapy should be stopped as soon as the pregnancy is discovered.1
Continue to: Adults with chronic kidney disease
Adults with chronic kidney disease. Chronic kidney disease that is not treated with dialysis or kidney transplantation is considered a risk-enhancing factor; initiation of a moderate-intensity statin or a moderate-intensity statin plus ezetimibe can be useful in patients with chronic kidney disease who are 40 to 75 years of age and have an LDL-C level of 70 to 189 mg/dL and a PCE-calculated risk ≥ 7.5%. In adults with advanced kidney disease that requires dialysis who are already taking a statin, it may be reasonable to continue the statin; however, initiation of a statin in adults with advanced kidney disease who require dialysis is not recommended because of an apparent lack of benefit.1
Adults with a chronic inflammatory disorder or human immunodeficiency virus infection. Any of these conditions are treated as risk-enhancing factors; in a risk discussion with affected patients, therefore, moderate-intensity statin therapy or high-intensity statin therapy is favored for those 40 to 75 years of age who have an LDL-C level of 70 to 189 mg/dL and PCE-calculated risk ≥ 7.5%. A fasting lipid profile and assessment of ASCVD risk factors for these patients can be useful (1) as a guide to the potential benefit of statin therapy and (2) for monitoring or adjusting lipid-lowering drug therapy before, and 4 to 12 weeks after, starting inflammatory disease-modifying therapy or antiretroviral therapy.
In adults with rheumatoid arthritis who undergo ASCVD risk assessment with a lipid profile, it can be useful to recheck lipid values and other major ASCVD risk factors 2 to 4 months after the inflammatory disease has been controlled.1
Primary hypercholesterolemia
The diagnosis and management of heterozygous or homozygous familial hypercholesterolemia (HeFH or HoFH) is beyond the scope of the 2018 ACC/AHA cholesterol guidelines; instead, the 2015 AHA Scientific Statement, “The Agenda for Familial Hypercholesterolemia,” provides a contemporary review of these topics.23 However, the 2018 cholesterol guideline does acknowledge that an LDL-C level ≥ 190 mg/dL often corresponds to primary (ie, genetic) hypercholesterolemia.
In patients 20 to 75 years of age who have a primary elevation of LDL-C level ≥ 190 mg/dL, the guideline recommends initiation of high-intensity statin therapy without calculating ASCVD risk using the PCE. If a > 50% LDL-C reduction is not achieved, or if the LDL-C level on maximally tolerated statin therapy remains ≥ 100 mg/dL, adding ezetimibe is considered reasonable. If there is < 50% reduction in the LDL-C level while taking maximally tolerated statin and ezetimibe therapy, adding a bile-acid sequestrant can be considered, as long as the TG level is not > 300 mg/dL (ie, bile-acid sequestrants can elevate the TG level significantly).
Continue to: In patients 30 to 75 years of age...
In patients 30 to 75 years of age who have a diagnosis of HeFH and an LDL-C level ≥ 100 mg/dL while taking maximally tolerated statin and ezetimibe therapy, the addition of a PCSK9 inhibitor can be considered. Regardless of whether there is a diagnosis of HeFH, addition of a PCSK9 inhibitor can be considered in patients 40 to 75 years of age who have a baseline LDL-C level ≥ 220 mg/dL and who achieve an on-treatment LDL-C level ≥ 130 mg/dL while receiving maximally tolerated statin therapy and ezetimibe.1
Diabetes mellitus
In patients with DM who are 40 to 75 years of age, moderate-intensity statin therapy is recommended without calculating the 10-year ASCVD risk. When the LDL-C level is 70 to 189 mg/dL, however, it is reasonable to use the PCE to assess 10-year ASCVD risk to facilitate risk stratification.
In patients with DM who are at higher risk, especially those who have multiple risk factors or are 50 to 75 years of age, it is reasonable to use a high-intensity statin to reduce the LDL-C level by ≥ 50 %. In adults > 75 years of age with DM who are already on statin therapy, it is reasonable to continue statin therapy; for those that age who are not on statin therapy, it might be reasonable to initiate statin therapy after a physician–patient discussion of potential benefits and risks.
In adults with DM and PCE-calculated risk ≥ 20%, it might be reasonable to add ezetimibe to maximally tolerated statin therapy to reduce the LDL-C level by ≥ 50%. In adults 20 to 39 years of age with DM of long duration (≥ 10 years of type 2 DM, ≥ 20 years of type 1 DM), albuminuria (≥ 30 μg of albumin/mg creatinine), estimated glomerular filtration rate < 60 mL/min/1.73 m2, retinopathy, neuropathy, or ankle-brachial index < 0.9, it might be reasonable to initiate statin therapy.1
Secondary prevention
Presence of clinical ASCVD. In patients with clinical ASCVD who are ≤ 75 years of age, high-intensity statin therapy should be initiated or continued, with the aim of achieving ≥ 50% reduction in the LDL-C level. When high-intensity statin therapy is contraindicated or if a patient experiences statin-associated adverse effects, moderate-intensity statin therapy should be initiated or continued with the aim of achieving a 30% to 49% reduction in the LDL-C level.
Continue to: In patients...
In patients > 75 years of age with clinical ASCVD, it is reasonable to initiate or continue moderate- or high-intensity statin therapy after evaluation of the potential for ASCVD risk reduction, adverse effects, and drug–drug interactions, as well as patient frailty and patient preference.1
Very high risk. In patients at very high risk (this includes a history of multiple major ASCVD events or 1 major ASCVD event plus multiple high-risk conditions), maximally tolerated LDL-C-lowering therapy should include maximally tolerated statin therapy and ezetimibe before considering a PCSK9 inhibitor. An LDL-C level ≥ 70 mg/dL or a non-HDL-C level ≥ 100 mg/dL is considered a reasonable threshold for adding a PCSK9 inhibitor to background lipid-lowering therapy1 (TABLE 31).
Heart failure. In patients with heart failure who have (1) a reduced ejection fraction attributable to ischemic heart disease, (2) a reasonable life expectancy (3-5 years), and (3) are not already on a statin because of ASCVD, consider initiating moderate-intensity statin therapy to reduce the risk for an ASCVD event.1
Reduction of elevated triglycerides
The guideline defines moderate hypertriglyceridemia as a nonfasting or fasting TG level of 175 to 499 mg/dL. Such a finding is considered a risk-enhancing factor and is 1 of 5 components of the metabolic syndrome. Three independent measurements are advised to diagnose primary moderate hypertriglyceridemia. Severe hypertriglyceridemia is diagnosed when the fasting TG level is ≥ 500 mg/dL.1
In moderate hypertriglyceridemia, most TGs are carried in very-low-density lipoprotein particles; in severe hypertriglyceridemia, on the other hand, chylomicrons predominate, raising the risk for pancreatitis. In adults with severe hypertriglyceridemia, therefore—especially when the fasting TG level is ≥ 1000 mg/dL—it is reasonable to identify and address other causes of hypertriglyceridemia. If TGs are persistently elevated or increasing, levels should be reduced to prevent acute pancreatitis with a very low-fat diet and by avoiding refined carbohydrates and alcohol; consuming omega-3 fatty acids; and, if necessary, taking a fibrate.1
Continue to: In adults...
In adults ≥ 20 years of age with moderate hypertriglyceridemia, lifestyle factors (eg, obesity, metabolic syndrome), secondary factors (eg, DM, chronic liver or kidney disease, nephrotic syndrome, hypothyroidism), and medications that increase the TG level need to be addressed first. In adults 40 to 75 years of age with moderate or severe hypertriglyceridemia and a PCE-calculated ASCVD risk ≥ 7.5%, it is reasonable to reevaluate risk after lifestyle and secondary factors are addressed and to consider a persistently elevated TG level as a factor favoring initiation or intensification of statin therapy. In adults 40 to 75 years of age with severe hypertriglyceridemia and ASCVD risk ≥ 7.5%, it is reasonable to address reversible causes of a high TG level and to initiate statin therapy.1
Other considerations in cholesterol management
Tools to assess adherence
The response to lifestyle and statin therapy should be evaluated by the percentage reduction in the LDL-C level compared with baseline, not by assessment of the absolute LDL-C level. When seeing a patient whose treatment is ongoing, a baseline level can be estimated using a desktop LDL-calculator app.
Adherence and percentage response to LDL-C–lowering medications and lifestyle changes should be evaluated with repeat lipid measurement 4 to 12 weeks after either a statin is initiated or the dosage is adjusted, and repeated every 3 to 12 months as needed. In patients with established ASCVD who are at very high risk, triggers for adding nonstatin therapy are defined by a threshold LDL-C level ≥ 70 mg/dL on maximal statin therapy.1
Interventions focused on improving adherence to prescribed therapy are recommended for management of adults with an elevated cholesterol level. These interventions include telephone reminders, calendar reminders, integrated multidisciplinary educational activities, and pharmacist-led interventions, such as simplification of the medication regimen to once-daily dosing.1
Statin safety and associated adverse effects
A physician–patient risk discussion is recommended before initiating statin therapy to review net clinical benefit, during which the 2 parties weigh the potential for ASCVD risk reduction against the potential for statin-associated adverse effects, statin–drug interactions, and safety, with the physician emphasizing that adverse effects can be addressed successfully.
Continue to: Statins are one of...
Statins are one of the safest classes of medication, with an excellent risk-benefit ratio. However, there are myriad confusing media reports regarding potential adverse effects and safety of the statin class—reports that often lead patients to discontinue or refuse statins.
Statin-associated adverse effects include the common statin-associated muscle symptoms (SAMS), new-onset DM, cognitive effects, and hepatic injury. The frequency of new-onset DM depends on the population exposed to statins, with a higher incidence of new-onset DM found in patients who are already predisposed, such as those with obesity, prediabetes, and metabolic syndrome. Cognitive effects are rare and difficult to interpret; they were not reported in the large statin mega-trials but have been described in case reports. Significant transaminase elevations > 3 times the upper limit of normal are infrequent; hepatic failure with statins is extremely rare and found at the same incidence in the general population.1
SAMS include (in order of decreasing prevalence)24:
- myalgias with a normal creatine kinase (CK) level
- conditions such as myositis or myopathy (elevated CK level)
- rhabdomyolysis (CK level > 10 times the upper limit of normal, plus renal injury)
- extremely rare statin-associated autoimmune myopathy, with detectable 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase antibodies.
In patients with SAMS, thorough assessment of symptoms is recommended, in addition to evaluation for nonstatin causes and predisposing factors. Identification of potential SAMS-predisposing factors is recommended before initiation of treatment, including demographics (eg, East-Asian ancestry), comorbid conditions (eg, hypothyroidism and vitamin D deficiency), and use of medications adversely affecting statin metabolism (eg, cyclosporine).
In patients with statin-associated adverse effects that are not severe, it is recommended to reassess and rechallenge to achieve a maximal lowering of the LDL-C level by a modified dosing regimen or an alternate statin or by combining a statin with nonstatin therapy. In patients with increased risk for DM or new-onset DM, it is recommended to continue statin therapy.
Continue to: Routine CK and liver function testing...
Routine CK and liver function testing is not useful in patients treated with statins; however, it is recommended that CK be measured in patients with severe SAMS or objective muscle weakness, or both, and to measure liver function if symptoms suggest hepatotoxicity. In patients at increased risk for ASCVD who have chronic, stable liver disease (including non-alcoholic fatty liver disease), it is reasonable, when appropriately indicated, to use statins after obtaining baseline measurements and determining a schedule of monitoring and safety checks.
In patients at increased risk for ASCVD who have severe or recurrent SAMS after appropriate statin rechallenge, it is reasonable to use nonstatin therapy that is likely to provide net clinical benefit. The guideline does not recommend routine use of coenzyme Q10 supplementation for the treatment or prevention of SAMS.1
Guideline criticism
Guideline development is challenging on multiple levels, including balancing perspectives from multiple stakeholders. Nevertheless, the 2018 AHA/ACC cholesterol guideline builds nicely on progress made since its 2013 predecessor was released.4 This document was developed with the participation of representatives from 10 professional societies in addition to the ACC and AHA—notably, the National Lipid Association and American Society for Preventive Cardiology.1
To refine risk estimation and facilitate shared decision-making, the new guideline introduced so-called risk-enhancing factors and use of the CAC.1 However, some potential risk-enhancing factors were left out: erectile dysfunction, for example, often a marker of increased cardiovascular risk in men < 50 years of age.25 In addition, although pretreatment ApoB was introduced as a risk-enhancing factor,1 no recommendation is given to measure ApoB after initiation of therapy for evaluation of residual cardiovascular risk, as endorsed in other guidelines.26,27
Moreover, the guideline does not include the “extreme risk” category in the guideline developed by the American Association of Clinical Endocrinologists (AACE).28 Although the 2018 AHA/ACC guideline introduces < 70 mg/dL and < 100 mg/dL LDL-C thresholds,1 the < 55 mg/dL LDL-C threshold used for patients in the AACE/American College of Endocrinology extreme-risk category is not mentioned.26 This omission might leave patients who are at extreme ASCVD risk without optimal lipid-lowering therapy. Similarly, the guideline does not elaborate on the diagnosis and treatment of HoFH and HeFH.1 The age cutoff of 30 years for the recommendation to consider PCSK9 inhibitors in patients with HeFH appears arbitrary and excludes younger FH patients who have an extreme LDL-C elevation from potentially important therapy.23
Continue to: Guidelines are dynamic instruments...
Guidelines are dynamic instruments that require constant updating, given the production of new evidence. In fact, the results of the Reduction of Cardiovascular Events With Icosapent Ethyl-Intervention Trial (REDUCE-IT) were presented at the same meeting at which this guideline was unveiled.29 REDUCE-IT demonstrated an astonishing highly significant 25% reduction in the composite primary major adverse cardiovascular event outcome in patients with an LDL-C level of 44 to 100 mg/dL on statin therapy, who had a TG level of 135 to 499 mg/dL and had been treated for a median of 4.9 years with 4 g of pure eicosapentaenoic acid.
In addition, the guideline’s value statements, which address the need to consider the cost of drugs in determining most appropriate treatment, are no longer accurate because the price of PCSK9 inhibitors has dropped by more than half since the guideline was issued.30
An upward climb to clinical payoff
Even after close study of the 2018 AHA/ACC cholesterol guideline, implementing it in practice might remain a challenge to clinicians who are inexperienced in ordering lipid markers such as Lp(a) and interpreting the CAC score. Moreover, initiating and monitoring nonstatin therapies will be a demanding task—especially with PCSK9 inhibitors, which present access difficulties because they are relatively expensive (even after the recent price cut). That’s why, when there is doubt in the mind of the physician or other provider, we will likely see more referrals to specialists in lipid management and ASCVD risk estimation to optimize preventive therapy.31
CORRESPONDENCE
Cezary Wójcik, MD, PhD, FNLA, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR 97239; cezarywojcik2000@gmail.com
1. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 8. pii: S0735-1097(18)39034-X. [Epub ahead of print]
2. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1-S45.
3. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 3. pii: S0735-1097(18)39033-8. [Epub ahead of print]
4. Wilson PWF, Polonsky TS, Miedema MD, et al. Systematic review for the 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 3. pii: S0735-1097(18)39035-1. [Epub ahead of print]
5. Eckel RH, Jakicic JM, Ard JD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960-2984.
6. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel III): final report. Circulation. 2002;106:3143-3421.
7. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:1997-2007.
8. National Cholesterol Education Program. Second report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel II). Circulation. 1994;89:1333-1445.
9. Martin SS, Giugliano RP, Murphy SA, et al. Comparison of low-density lipoprotein cholesterol assessment by Martin/Hopkins estimation, Friedewald estimation, and preparative ultracentrifugation: insights from the FOURIER trial. JAMA Cardiol. 2018;3:749-753.
10. Cannon CP, Blazing MA, Giugliano RP, et al; IMPROVE-IT Investigators. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387-2397.
11. Sabatine MS, Giugliano RP, Keech AC, et al; FOURIER Steering Committee and Investigators. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713-1722.
12. Szarek M, White HD, Schwartz GG, et al; ODYSSEY OUTCOMES Committees and Investigators. Alirocumab reduces total nonfatal cardiovascular and fatal events in the ODYSSEY OUTCOMES trial. J Am Coll Cardiol. 2019;73:387-396.
13. Crawford C. AAFP endorses ACC/AHA cholesterol management guidelines with qualifications. Leawood, KS: American Academy of Family Physicians; 2014 June 18. www.aafp.org/news/health-of-the-public/20140618cholesterolgdlnendorse.html. Accessed March 20, 2019.
14. Crawford C. AAFP News. AAFP affirms value of new cholesterol management guideline. March 20, 2019. www.aafp.org/news/health-of-the-public/20190320acc-ahacholguidln.html?cmpid=em_AP_20190320. Accessed April 1, 2019.
15. Lin JS, Evans CV, Johnson E, et al. Nontraditional Risk Factors in Cardiovascular Disease Risk Assessment: A Systematic Evidence Report for the U.S. Preventive Services Task Force. Evidence Synthesis, No. 166. Rockville, MD: Agency for Healthcare Research and Quality (US); 2018 Jul. Report No.: 17-05225-EF-1.
16. Puri R, Nicholls SJ, Shao M, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am Coll Cardiol. 2015;65:1273-1282.
17. Gencer B, Kronenberg F, Stroes ES, et al. Lipoprotein(a): the revenant. Eur Heart J. 2017;38:1553-1560.
18. Michos ED, Blaha MJ, Blumenthal RS. Use of the coronary artery calcium score in discussion of initiation of statin therapy in primary prevention. Mayo Clin Proc. 2017;92:1831-1841.
19. MDsave. Cardiac CT calcium scoring. www.mdsave.com/procedures/cardiac-ct-calcium-scoring/d785f4cf. Accessed Aprl 1, 2019.
20. Blaha MJ, Budoff MJ, Tota-Maharaj R, et al. Improving the CAC score by addition of regional measures of calcium distribution: multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging. 2016;9:1407-1416.
21. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213-S256.
22. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for lipid disorders in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:625-633.
23. Gidding SS, Champagne MA, de Ferranti SD, et al; American Heart Association Atherosclerosis, Hypertension, and Obesity in Young Committee of Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and Council on Lifestyle and Cardiometabolic Health. The agenda for familial hypercholesterolemia: a scientific statement from the American Heart Association. Circulation. 2015;132:2167-2192.
24. Newman CB, Preiss D, Tobert JA, et al; American Heart Association Clinical Lipidology, Lipoprotein, Metabolism and Thrombosis Committee, a Joint Committee of the Council on Atherosclerosis, Thrombosis and Vascular Biology and Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke Council. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39:e38-e81.
25. Miner M, Parish SJ, Billups KL, et al. Erectile dysfunction and subclinical cardiovascular disease. Sex Med Rev. 2018 Jan 27. pii: S2050-0521(18)30009-X. [Epub ahead of print]
26. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87.
27. Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263-1282.
28. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87.
29. Bhatt DL, Steg PG, Miller M, et al; REDUCE-IT Investigators. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380:11-22.
30. Dangi-Garimella S. Amgen announces 60% reduction in list price of PCSK9 inhibitor evolocumab. AJMC Managed Markets Network. October 24, 2018. https://www.ajmc.com/newsroom/amgen-announces-60-reduction-in-list-price-of-pcsk9-inhibitor-evolocumab. Accessed April 12, 2019.
31. Kaufman TM, Duell PB, Purnell JQ, et al. Application of PCSK9 inhibitors in practice: challenges and opportunities. Circ Res. 2017;121:499-501.
1. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 8. pii: S0735-1097(18)39034-X. [Epub ahead of print]
2. Stone NJ, Robinson JG, Lichtenstein AH, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S1-S45.
3. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 3. pii: S0735-1097(18)39033-8. [Epub ahead of print]
4. Wilson PWF, Polonsky TS, Miedema MD, et al. Systematic review for the 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018 Nov 3. pii: S0735-1097(18)39035-1. [Epub ahead of print]
5. Eckel RH, Jakicic JM, Ard JD, et al; American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2960-2984.
6. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel III): final report. Circulation. 2002;106:3143-3421.
7. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:1997-2007.
8. National Cholesterol Education Program. Second report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (adult treatment panel II). Circulation. 1994;89:1333-1445.
9. Martin SS, Giugliano RP, Murphy SA, et al. Comparison of low-density lipoprotein cholesterol assessment by Martin/Hopkins estimation, Friedewald estimation, and preparative ultracentrifugation: insights from the FOURIER trial. JAMA Cardiol. 2018;3:749-753.
10. Cannon CP, Blazing MA, Giugliano RP, et al; IMPROVE-IT Investigators. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387-2397.
11. Sabatine MS, Giugliano RP, Keech AC, et al; FOURIER Steering Committee and Investigators. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713-1722.
12. Szarek M, White HD, Schwartz GG, et al; ODYSSEY OUTCOMES Committees and Investigators. Alirocumab reduces total nonfatal cardiovascular and fatal events in the ODYSSEY OUTCOMES trial. J Am Coll Cardiol. 2019;73:387-396.
13. Crawford C. AAFP endorses ACC/AHA cholesterol management guidelines with qualifications. Leawood, KS: American Academy of Family Physicians; 2014 June 18. www.aafp.org/news/health-of-the-public/20140618cholesterolgdlnendorse.html. Accessed March 20, 2019.
14. Crawford C. AAFP News. AAFP affirms value of new cholesterol management guideline. March 20, 2019. www.aafp.org/news/health-of-the-public/20190320acc-ahacholguidln.html?cmpid=em_AP_20190320. Accessed April 1, 2019.
15. Lin JS, Evans CV, Johnson E, et al. Nontraditional Risk Factors in Cardiovascular Disease Risk Assessment: A Systematic Evidence Report for the U.S. Preventive Services Task Force. Evidence Synthesis, No. 166. Rockville, MD: Agency for Healthcare Research and Quality (US); 2018 Jul. Report No.: 17-05225-EF-1.
16. Puri R, Nicholls SJ, Shao M, et al. Impact of statins on serial coronary calcification during atheroma progression and regression. J Am Coll Cardiol. 2015;65:1273-1282.
17. Gencer B, Kronenberg F, Stroes ES, et al. Lipoprotein(a): the revenant. Eur Heart J. 2017;38:1553-1560.
18. Michos ED, Blaha MJ, Blumenthal RS. Use of the coronary artery calcium score in discussion of initiation of statin therapy in primary prevention. Mayo Clin Proc. 2017;92:1831-1841.
19. MDsave. Cardiac CT calcium scoring. www.mdsave.com/procedures/cardiac-ct-calcium-scoring/d785f4cf. Accessed Aprl 1, 2019.
20. Blaha MJ, Budoff MJ, Tota-Maharaj R, et al. Improving the CAC score by addition of regional measures of calcium distribution: multi-ethnic study of atherosclerosis. JACC Cardiovasc Imaging. 2016;9:1407-1416.
21. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: summary report. Pediatrics. 2011;128(Suppl 5):S213-S256.
22. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Screening for lipid disorders in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:625-633.
23. Gidding SS, Champagne MA, de Ferranti SD, et al; American Heart Association Atherosclerosis, Hypertension, and Obesity in Young Committee of Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and Council on Lifestyle and Cardiometabolic Health. The agenda for familial hypercholesterolemia: a scientific statement from the American Heart Association. Circulation. 2015;132:2167-2192.
24. Newman CB, Preiss D, Tobert JA, et al; American Heart Association Clinical Lipidology, Lipoprotein, Metabolism and Thrombosis Committee, a Joint Committee of the Council on Atherosclerosis, Thrombosis and Vascular Biology and Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; and Stroke Council. Statin safety and associated adverse events: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39:e38-e81.
25. Miner M, Parish SJ, Billups KL, et al. Erectile dysfunction and subclinical cardiovascular disease. Sex Med Rev. 2018 Jan 27. pii: S2050-0521(18)30009-X. [Epub ahead of print]
26. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87.
27. Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263-1282.
28. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1-87.
29. Bhatt DL, Steg PG, Miller M, et al; REDUCE-IT Investigators. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380:11-22.
30. Dangi-Garimella S. Amgen announces 60% reduction in list price of PCSK9 inhibitor evolocumab. AJMC Managed Markets Network. October 24, 2018. https://www.ajmc.com/newsroom/amgen-announces-60-reduction-in-list-price-of-pcsk9-inhibitor-evolocumab. Accessed April 12, 2019.
31. Kaufman TM, Duell PB, Purnell JQ, et al. Application of PCSK9 inhibitors in practice: challenges and opportunities. Circ Res. 2017;121:499-501.
PRACTICE RECOMMENDATIONS
› Reduce the low-density lipoprotein cholesterol (LDL-C) level in patients with clinical atherosclerotic cardiovascular disease (ASCVD) using high-intensity statin therapy or maximally tolerated statin therapy. A
› Use an LDL-C threshold of 70 mg/dL to prompt consideration of adding nonstatin therapy in patients who have very high-risk ASCVD. A
› Start high-intensity statin therapy in patients who have primary hypercholesterolemia (LDL-C level ≥ 190 mg/dL) without calculating the 10-year ASCVD risk. A
› Begin moderate-intensity statin therapy in patients 40 to 75 years of age who have diabetes mellitus and an LDL-C level ≥ 70 mg/dL without calculating 10-year ASCVD risk. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series