User login
ACC, AHA release first cardiovascular disease primary prevention guideline
that takes into account each person’s social determinants of health. The guideline substantially dialed down prior recommendations on aspirin for primary prevention by calling for no use in people older than 70 years and infrequent use in those 40-70 years old.
The American College of Cardiology and the American Heart Association released their 2019 guideline on the primary prevention of cardiovascular disease on March 17, during the annual meeting of the American College of Cardiology (J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.). The guideline is a “one-stop shop” that pulls together existing recommendations from the two organizations and combines it with some new recommendations that address issues such as aspirin prophylaxis, and the social setting of each person, said Donna K. Arnett, Ph.D., professor of epidemiology at the University of Kentucky, dean of the university’s College of Public Health, and co-chair of the guideline writing panel.
“We made the social determinants of health front and center. With many people, clinicians don’t ask whether they have access to healthy foods or a way to get to the pharmacy. Asking about these issues is step one,” toward helping people address their social situation, Dr. Arnett said while introducing the new guideline in a press briefing. The guideline recommends that clinicians assess the social determinants for each person treated for cardiovascular disease prevention using a screening tool developed by the U.S. Centers for Medicare & Medicaid Services and made available by the National Academy of Medicine (NAM Perspectives. 2017; doi:10.31478/201705b).
“No other guideline has highlighted the social determinants of health,” noted Erin D. Michos, MD, associate director of preventive cardiology at Johns Hopkins Medicine in Baltimore, and a member of the guideline-writing panel. Other overarching themes of the guideline are its emphasis on the need for a team of clinicians to deliver all the disparate and time-consuming facets of care needed for comprehensive primary prevention of cardiovascular disease, and its call for a healthy lifestyle throughout life as foundations for prevention, Dr. Michos said in an interview.
With 48 recommendations, the guideline also deals with prevention issues such as a healthy diet and body mass, appropriate control of diabetes, smoking cessation, and control of blood pressure and cholesterol (see chart). The writing committee took the cholesterol and blood pressure recommendations directly from recent guidelines from the ACC and AHA in 2017 (blood pressure:J Amer Coll Cardiol. 2018 May;71[19]:e177-e248) and 2018 (cholesterol:Circulation. 2018 Nov 10;doi: 10.1161/CIR.0000000000000625).
The other major, new recommendations in the guideline deal with aspirin use for primary prevention, which recently underwent a shake up with publication of results from several studies that showed less cardiovascular benefit and more potential bleeding harm from routine aspirin prophylaxis than previously appreciated. Among the most notable of these reports, which led to a class III recommendation – do not use – for aspirin in people more than 70 years old came from the ASPREE (Aspirin in Reducing Events in the Elderly) study (New Engl J Med. 2018 Oct 18;379[16]:1519-28). For those 40-70 years old, the recommendation is class IIb, worded as “might be considered for select adults.”

“Generally no, occasionally yes,” is aspirin appropriate for people in this age group, notably those at high risk for cardiovascular disease and also at low risk for bleeding, explained Amit Khera, MD, a guideline-panel member, and professor of medicine and director of preventive cardiology at the University of Texas Southwestern Medical Center in Dallas.
As a guideline for primary prevention, a prime target audience is primary care physicians, who would need to be instrumental in applying the guideline. But the guideline recommendations released by the ACC and AHA for blood pressure management in 2017 were not accepted by U.S. groups that represent primary care physicians, the American College of Physicians, and the American Academy of Family Physicians.
John J. Warner, MD, an interventional cardiologist, executive vice president for health system affairs at UT Southwestern, and president of the AHA when the blood pressure guideline came out said that the ACC and AHA “learned some lessons” from the blood pressure experience. The societies responded this time around by “trying to view the document through as many lenses as possible” during the peer review process, Dr. Warner said during the press conference.
“I don’t think the new guideline will be seen as anything except positive,” commented Martha Gulati, MD, professor of medicine and chief of cardiology at the University of Arizona in Phoenix. Collecting all the cardiovascular disease recommendations for primary prevention in one document “helps clinicians access the information easily and helps patients see the big picture,” said Dr. Gulati, who was not involved in the guideline’s writing or review.
She especially applauded the recommendations to assess each person’s social determinants of health, the team-care approach, and the recommendations dealing with diet and other aspects of a healthy lifestyle. “This was a perfect time” to bring together the existing blood pressure and cholesterol guidelines, the new guidance on aspirin use, and the other recommendation in a single document, she said in an interview.
Dr. Arnett, Dr. Michos, Dr. Khera, Dr. Warner, and Dr. Gulati had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Arnett DK et al. J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.
that takes into account each person’s social determinants of health. The guideline substantially dialed down prior recommendations on aspirin for primary prevention by calling for no use in people older than 70 years and infrequent use in those 40-70 years old.
The American College of Cardiology and the American Heart Association released their 2019 guideline on the primary prevention of cardiovascular disease on March 17, during the annual meeting of the American College of Cardiology (J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.). The guideline is a “one-stop shop” that pulls together existing recommendations from the two organizations and combines it with some new recommendations that address issues such as aspirin prophylaxis, and the social setting of each person, said Donna K. Arnett, Ph.D., professor of epidemiology at the University of Kentucky, dean of the university’s College of Public Health, and co-chair of the guideline writing panel.
“We made the social determinants of health front and center. With many people, clinicians don’t ask whether they have access to healthy foods or a way to get to the pharmacy. Asking about these issues is step one,” toward helping people address their social situation, Dr. Arnett said while introducing the new guideline in a press briefing. The guideline recommends that clinicians assess the social determinants for each person treated for cardiovascular disease prevention using a screening tool developed by the U.S. Centers for Medicare & Medicaid Services and made available by the National Academy of Medicine (NAM Perspectives. 2017; doi:10.31478/201705b).
“No other guideline has highlighted the social determinants of health,” noted Erin D. Michos, MD, associate director of preventive cardiology at Johns Hopkins Medicine in Baltimore, and a member of the guideline-writing panel. Other overarching themes of the guideline are its emphasis on the need for a team of clinicians to deliver all the disparate and time-consuming facets of care needed for comprehensive primary prevention of cardiovascular disease, and its call for a healthy lifestyle throughout life as foundations for prevention, Dr. Michos said in an interview.
With 48 recommendations, the guideline also deals with prevention issues such as a healthy diet and body mass, appropriate control of diabetes, smoking cessation, and control of blood pressure and cholesterol (see chart). The writing committee took the cholesterol and blood pressure recommendations directly from recent guidelines from the ACC and AHA in 2017 (blood pressure:J Amer Coll Cardiol. 2018 May;71[19]:e177-e248) and 2018 (cholesterol:Circulation. 2018 Nov 10;doi: 10.1161/CIR.0000000000000625).
The other major, new recommendations in the guideline deal with aspirin use for primary prevention, which recently underwent a shake up with publication of results from several studies that showed less cardiovascular benefit and more potential bleeding harm from routine aspirin prophylaxis than previously appreciated. Among the most notable of these reports, which led to a class III recommendation – do not use – for aspirin in people more than 70 years old came from the ASPREE (Aspirin in Reducing Events in the Elderly) study (New Engl J Med. 2018 Oct 18;379[16]:1519-28). For those 40-70 years old, the recommendation is class IIb, worded as “might be considered for select adults.”

“Generally no, occasionally yes,” is aspirin appropriate for people in this age group, notably those at high risk for cardiovascular disease and also at low risk for bleeding, explained Amit Khera, MD, a guideline-panel member, and professor of medicine and director of preventive cardiology at the University of Texas Southwestern Medical Center in Dallas.
As a guideline for primary prevention, a prime target audience is primary care physicians, who would need to be instrumental in applying the guideline. But the guideline recommendations released by the ACC and AHA for blood pressure management in 2017 were not accepted by U.S. groups that represent primary care physicians, the American College of Physicians, and the American Academy of Family Physicians.
John J. Warner, MD, an interventional cardiologist, executive vice president for health system affairs at UT Southwestern, and president of the AHA when the blood pressure guideline came out said that the ACC and AHA “learned some lessons” from the blood pressure experience. The societies responded this time around by “trying to view the document through as many lenses as possible” during the peer review process, Dr. Warner said during the press conference.
“I don’t think the new guideline will be seen as anything except positive,” commented Martha Gulati, MD, professor of medicine and chief of cardiology at the University of Arizona in Phoenix. Collecting all the cardiovascular disease recommendations for primary prevention in one document “helps clinicians access the information easily and helps patients see the big picture,” said Dr. Gulati, who was not involved in the guideline’s writing or review.
She especially applauded the recommendations to assess each person’s social determinants of health, the team-care approach, and the recommendations dealing with diet and other aspects of a healthy lifestyle. “This was a perfect time” to bring together the existing blood pressure and cholesterol guidelines, the new guidance on aspirin use, and the other recommendation in a single document, she said in an interview.
Dr. Arnett, Dr. Michos, Dr. Khera, Dr. Warner, and Dr. Gulati had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Arnett DK et al. J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.
that takes into account each person’s social determinants of health. The guideline substantially dialed down prior recommendations on aspirin for primary prevention by calling for no use in people older than 70 years and infrequent use in those 40-70 years old.
The American College of Cardiology and the American Heart Association released their 2019 guideline on the primary prevention of cardiovascular disease on March 17, during the annual meeting of the American College of Cardiology (J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.). The guideline is a “one-stop shop” that pulls together existing recommendations from the two organizations and combines it with some new recommendations that address issues such as aspirin prophylaxis, and the social setting of each person, said Donna K. Arnett, Ph.D., professor of epidemiology at the University of Kentucky, dean of the university’s College of Public Health, and co-chair of the guideline writing panel.
“We made the social determinants of health front and center. With many people, clinicians don’t ask whether they have access to healthy foods or a way to get to the pharmacy. Asking about these issues is step one,” toward helping people address their social situation, Dr. Arnett said while introducing the new guideline in a press briefing. The guideline recommends that clinicians assess the social determinants for each person treated for cardiovascular disease prevention using a screening tool developed by the U.S. Centers for Medicare & Medicaid Services and made available by the National Academy of Medicine (NAM Perspectives. 2017; doi:10.31478/201705b).
“No other guideline has highlighted the social determinants of health,” noted Erin D. Michos, MD, associate director of preventive cardiology at Johns Hopkins Medicine in Baltimore, and a member of the guideline-writing panel. Other overarching themes of the guideline are its emphasis on the need for a team of clinicians to deliver all the disparate and time-consuming facets of care needed for comprehensive primary prevention of cardiovascular disease, and its call for a healthy lifestyle throughout life as foundations for prevention, Dr. Michos said in an interview.
With 48 recommendations, the guideline also deals with prevention issues such as a healthy diet and body mass, appropriate control of diabetes, smoking cessation, and control of blood pressure and cholesterol (see chart). The writing committee took the cholesterol and blood pressure recommendations directly from recent guidelines from the ACC and AHA in 2017 (blood pressure:J Amer Coll Cardiol. 2018 May;71[19]:e177-e248) and 2018 (cholesterol:Circulation. 2018 Nov 10;doi: 10.1161/CIR.0000000000000625).
The other major, new recommendations in the guideline deal with aspirin use for primary prevention, which recently underwent a shake up with publication of results from several studies that showed less cardiovascular benefit and more potential bleeding harm from routine aspirin prophylaxis than previously appreciated. Among the most notable of these reports, which led to a class III recommendation – do not use – for aspirin in people more than 70 years old came from the ASPREE (Aspirin in Reducing Events in the Elderly) study (New Engl J Med. 2018 Oct 18;379[16]:1519-28). For those 40-70 years old, the recommendation is class IIb, worded as “might be considered for select adults.”

“Generally no, occasionally yes,” is aspirin appropriate for people in this age group, notably those at high risk for cardiovascular disease and also at low risk for bleeding, explained Amit Khera, MD, a guideline-panel member, and professor of medicine and director of preventive cardiology at the University of Texas Southwestern Medical Center in Dallas.
As a guideline for primary prevention, a prime target audience is primary care physicians, who would need to be instrumental in applying the guideline. But the guideline recommendations released by the ACC and AHA for blood pressure management in 2017 were not accepted by U.S. groups that represent primary care physicians, the American College of Physicians, and the American Academy of Family Physicians.
John J. Warner, MD, an interventional cardiologist, executive vice president for health system affairs at UT Southwestern, and president of the AHA when the blood pressure guideline came out said that the ACC and AHA “learned some lessons” from the blood pressure experience. The societies responded this time around by “trying to view the document through as many lenses as possible” during the peer review process, Dr. Warner said during the press conference.
“I don’t think the new guideline will be seen as anything except positive,” commented Martha Gulati, MD, professor of medicine and chief of cardiology at the University of Arizona in Phoenix. Collecting all the cardiovascular disease recommendations for primary prevention in one document “helps clinicians access the information easily and helps patients see the big picture,” said Dr. Gulati, who was not involved in the guideline’s writing or review.
She especially applauded the recommendations to assess each person’s social determinants of health, the team-care approach, and the recommendations dealing with diet and other aspects of a healthy lifestyle. “This was a perfect time” to bring together the existing blood pressure and cholesterol guidelines, the new guidance on aspirin use, and the other recommendation in a single document, she said in an interview.
Dr. Arnett, Dr. Michos, Dr. Khera, Dr. Warner, and Dr. Gulati had no disclosures.
mzoler@mdedge.com
On Twitter @mitchelzoler
SOURCE: Arnett DK et al. J Amer Coll Cardiol. 2019 March 17;doi: 10.1016/j.jacc.2019.03.010.
REPORTING FROM ACC 2019
Antibiotic-eluting envelope reduces CIED infections
An absorbable, antibiotic-eluting envelope around cardiac implantable electronic devices could significantly reduce the incidence of infection, according to a presentation at the annual meeting of the American College of Cardiology.
The WRAP-IT trial, which was simultaneously published online March 17 in the New England Journal of Medicine, involved 6,983 patients undergoing cardiac implantable electronic device (CIED) implantation, replacement, revision, or upgrade. Patients were randomized either to receive the TYRX Absorbable Antibacterial Envelope or not.
After a mean follow-up of 20.7 months, there was a significant 40% lower rate of major infections in the envelope group compared to the control group, which met the efficacy objective of the study. Researchers saw 30 major infections in 25 patients in the envelope group; in the control group, there were 45 major infections in 42 patients (P = 0.04). The trial excluded patients at high risk of systemic infection due to other sources and patients with existing infection.
“CIED infection is a rare but serious event, and its management requires prolonged hospitalization, which involves device and lead extraction with adjunctive antibiotic therapy,” wrote Dr. Khaldoun G. Tarakji, from The Cleveland Clinic, and co-authors. “Despite proper management of CIED infection, both short- and long-term mortality remains high.”
One previous randomized study had shown that intravenous administration of antibiotics during CIED procedures can reduce the risk of infection, while a different study failed to find a benefit. The vast majority of patients in this study (98.7%) received periprocedural antibiotics, 74.5% received pocket wash and 29.6% received post-procedural antibiotics. These strategies were not controlled, but there is no clear evidence that any particular strategy influenced the infection rate, the authors wrote.
Patients in the envelope group experienced numerically fewer pocket infections but more endocarditis or bacteremia compared to those in the control group, a finding that the authors could not explain.
The most common pathogen responsible was staphylococcus, but data on antibiotic susceptibility was not collected. The authors stressed that this limited their ability to assess the risk of antibiotic resistance developing.
In this study, the researchers noted that the reduction in the risk of infection was greater among individuals who were implanted with higher-power devices, compared to those implanted with low-power devices or an initial cardiac resynchronization therapy device.
However, they said, the rate of infections was generally lower among those receiving low-power devices.
There was no increase in complications related to use of the envelope. The rate of complications occurring within 12 months of the procedure and relating to the CIED procedure or envelope was 6% in the envelope group and 6.9% in the control group.
When major infections were excluded, the rate of complications in each group was 5.7% and 5/9% respectively. There was also no significant difference in mortality rates between the two groups (17.4% and 17.8% respectively).
The authors wrote that while use of the envelope can require a slightly larger CIED dissection pocket, this was not associated with increased procedural time or complications. The envelope was successfully implanted in 99.7% of procedure attempts.
“There were fewer system revisions in the envelope group than in the control group and no complications due to allergy to the envelope mesh, polymer, or antibiotics,” they wrote.
The study was supported by Medtronic, the maker of the TYRX Absorbable Antibacterial Envelope. Twenty-four authors declared institutional funding or research grants from Medtronic, thirteen declared fees, consultancies and other support from private industry outside the submitted work. Three authors were employees of Medtronic.
SOURCE: Tarakji K et al. NEJM, 2019, March 17. DOI: 10.1056/NEJMoa1901111
An absorbable, antibiotic-eluting envelope around cardiac implantable electronic devices could significantly reduce the incidence of infection, according to a presentation at the annual meeting of the American College of Cardiology.
The WRAP-IT trial, which was simultaneously published online March 17 in the New England Journal of Medicine, involved 6,983 patients undergoing cardiac implantable electronic device (CIED) implantation, replacement, revision, or upgrade. Patients were randomized either to receive the TYRX Absorbable Antibacterial Envelope or not.
After a mean follow-up of 20.7 months, there was a significant 40% lower rate of major infections in the envelope group compared to the control group, which met the efficacy objective of the study. Researchers saw 30 major infections in 25 patients in the envelope group; in the control group, there were 45 major infections in 42 patients (P = 0.04). The trial excluded patients at high risk of systemic infection due to other sources and patients with existing infection.
“CIED infection is a rare but serious event, and its management requires prolonged hospitalization, which involves device and lead extraction with adjunctive antibiotic therapy,” wrote Dr. Khaldoun G. Tarakji, from The Cleveland Clinic, and co-authors. “Despite proper management of CIED infection, both short- and long-term mortality remains high.”
One previous randomized study had shown that intravenous administration of antibiotics during CIED procedures can reduce the risk of infection, while a different study failed to find a benefit. The vast majority of patients in this study (98.7%) received periprocedural antibiotics, 74.5% received pocket wash and 29.6% received post-procedural antibiotics. These strategies were not controlled, but there is no clear evidence that any particular strategy influenced the infection rate, the authors wrote.
Patients in the envelope group experienced numerically fewer pocket infections but more endocarditis or bacteremia compared to those in the control group, a finding that the authors could not explain.
The most common pathogen responsible was staphylococcus, but data on antibiotic susceptibility was not collected. The authors stressed that this limited their ability to assess the risk of antibiotic resistance developing.
In this study, the researchers noted that the reduction in the risk of infection was greater among individuals who were implanted with higher-power devices, compared to those implanted with low-power devices or an initial cardiac resynchronization therapy device.
However, they said, the rate of infections was generally lower among those receiving low-power devices.
There was no increase in complications related to use of the envelope. The rate of complications occurring within 12 months of the procedure and relating to the CIED procedure or envelope was 6% in the envelope group and 6.9% in the control group.
When major infections were excluded, the rate of complications in each group was 5.7% and 5/9% respectively. There was also no significant difference in mortality rates between the two groups (17.4% and 17.8% respectively).
The authors wrote that while use of the envelope can require a slightly larger CIED dissection pocket, this was not associated with increased procedural time or complications. The envelope was successfully implanted in 99.7% of procedure attempts.
“There were fewer system revisions in the envelope group than in the control group and no complications due to allergy to the envelope mesh, polymer, or antibiotics,” they wrote.
The study was supported by Medtronic, the maker of the TYRX Absorbable Antibacterial Envelope. Twenty-four authors declared institutional funding or research grants from Medtronic, thirteen declared fees, consultancies and other support from private industry outside the submitted work. Three authors were employees of Medtronic.
SOURCE: Tarakji K et al. NEJM, 2019, March 17. DOI: 10.1056/NEJMoa1901111
An absorbable, antibiotic-eluting envelope around cardiac implantable electronic devices could significantly reduce the incidence of infection, according to a presentation at the annual meeting of the American College of Cardiology.
The WRAP-IT trial, which was simultaneously published online March 17 in the New England Journal of Medicine, involved 6,983 patients undergoing cardiac implantable electronic device (CIED) implantation, replacement, revision, or upgrade. Patients were randomized either to receive the TYRX Absorbable Antibacterial Envelope or not.
After a mean follow-up of 20.7 months, there was a significant 40% lower rate of major infections in the envelope group compared to the control group, which met the efficacy objective of the study. Researchers saw 30 major infections in 25 patients in the envelope group; in the control group, there were 45 major infections in 42 patients (P = 0.04). The trial excluded patients at high risk of systemic infection due to other sources and patients with existing infection.
“CIED infection is a rare but serious event, and its management requires prolonged hospitalization, which involves device and lead extraction with adjunctive antibiotic therapy,” wrote Dr. Khaldoun G. Tarakji, from The Cleveland Clinic, and co-authors. “Despite proper management of CIED infection, both short- and long-term mortality remains high.”
One previous randomized study had shown that intravenous administration of antibiotics during CIED procedures can reduce the risk of infection, while a different study failed to find a benefit. The vast majority of patients in this study (98.7%) received periprocedural antibiotics, 74.5% received pocket wash and 29.6% received post-procedural antibiotics. These strategies were not controlled, but there is no clear evidence that any particular strategy influenced the infection rate, the authors wrote.
Patients in the envelope group experienced numerically fewer pocket infections but more endocarditis or bacteremia compared to those in the control group, a finding that the authors could not explain.
The most common pathogen responsible was staphylococcus, but data on antibiotic susceptibility was not collected. The authors stressed that this limited their ability to assess the risk of antibiotic resistance developing.
In this study, the researchers noted that the reduction in the risk of infection was greater among individuals who were implanted with higher-power devices, compared to those implanted with low-power devices or an initial cardiac resynchronization therapy device.
However, they said, the rate of infections was generally lower among those receiving low-power devices.
There was no increase in complications related to use of the envelope. The rate of complications occurring within 12 months of the procedure and relating to the CIED procedure or envelope was 6% in the envelope group and 6.9% in the control group.
When major infections were excluded, the rate of complications in each group was 5.7% and 5/9% respectively. There was also no significant difference in mortality rates between the two groups (17.4% and 17.8% respectively).
The authors wrote that while use of the envelope can require a slightly larger CIED dissection pocket, this was not associated with increased procedural time or complications. The envelope was successfully implanted in 99.7% of procedure attempts.
“There were fewer system revisions in the envelope group than in the control group and no complications due to allergy to the envelope mesh, polymer, or antibiotics,” they wrote.
The study was supported by Medtronic, the maker of the TYRX Absorbable Antibacterial Envelope. Twenty-four authors declared institutional funding or research grants from Medtronic, thirteen declared fees, consultancies and other support from private industry outside the submitted work. Three authors were employees of Medtronic.
SOURCE: Tarakji K et al. NEJM, 2019, March 17. DOI: 10.1056/NEJMoa1901111
FROM ACC 19
Apple Watch algorithm showed 84% positive predictive value for Afib
, investigators reported at the annual meeting of the American College of Cardiology.
This was a single-arm, prospective, open-label, observational study of unprecedented size and speediness of completion. It included nearly 420,000 self-enrolled adults living in the U.S., with 8 months of monitoring. But despite the study’s flashy size and trendy digital health theme, the researchers were careful not to oversell the findings.
“This study was just meant to be a very, very first step in trying to learn if this kind of technology can help us to prevent stroke. It was not a randomized trial of a public health intervention for screening. This is the first half of the first inning. Rigorous investigation of this technology and its potential use in clinical settings will need to happen. But we do think from a trial and operational standpoint the Apple Heart Study provides a solid foundation upon which further research in digital health can be conducted,” according to Mintu Turakhia, MD, co-principal investigator and an electrophysiologist as well as executive director of the Center for Digital Health at Stanford (Calif.) University, which conducted the study.
The study was conducted virtually. Screening, consent, and data gathering were performed electronically by smartphone. Participants had to have an Apple Watch Series 1, 2, or 3, and an Apple iPhone 5 or more recent model in order to join. The majority of subjects were under age 40, and just 6% were age 65 or older, when the risks of atrial fibrillation (AFib) and stroke are higher. All participants self-reported having no history of AFib nor currently being on anticoagulation.
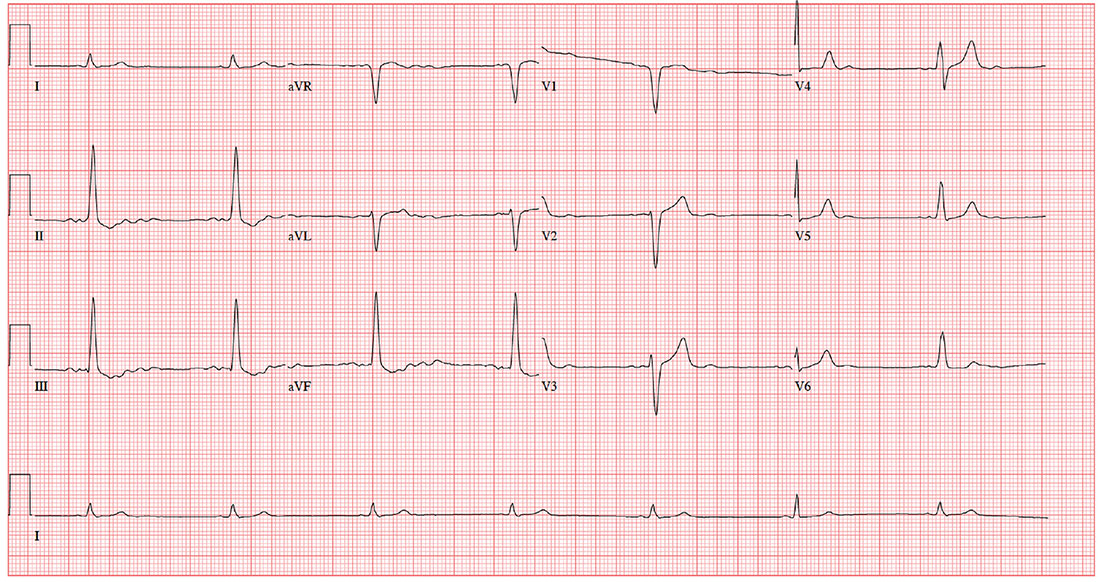
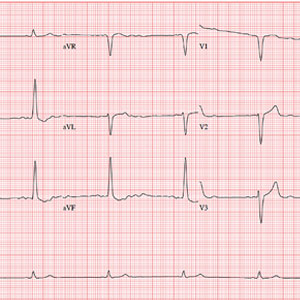
The study algorithm utilized the Apple Watch’s built-in light sensor technology to opportunistically sample the time interval between pulses when the wearer was still. An irregular time interval triggered a cascade of more frequent sampling. If 5 of 6 samples were irregular within a 48-hour period, the wearer received an irregular rhythm notification along with a prompt to contact a participating physician via telemedicine. The physician could then arrange for an ECG patch to be mailed to the participant, who wore it for up to 7 days before mailing it back for analysis.
Among the key findings in the Apple Heart Study: the irregular pulse notification rate was low overall, at 0.5%, ranging from 0.16% in the under-40 group to 3.2% in subjects age 65 or older. As a result, the study population of particular interest nosedived from an initial 419,297 to the less than 2,100 who received an irregular pulse notification. Of the 658 participants who were subsequently sent an ECG patch, 450 returned it for analysis.
An average of 13 days went by between an irregular pulse notification and ECG patch receipt and activation, so it wasn’t particularly surprising that only 34% of the patches were positive for AFib, since early-stage paroxysmal AFib comes and goes. However, of the 86 subjects who received a new notification of an irregular rhythm while they were wearing a patch, 72 simultaneously showed AFib on their patch. That translates to an 84% positive predictive value for an irregular rhythm notification as an indicator of AFib.
Of the 153 subjects with evidence of AFib on their ECG patch, 20% proved to be in AFib for the full week they wore it. Of those with AFib, 89% had a longest episode of at least 1 hour in duration.
Several discussants expressed reservations about this approach to finding individuals with previously undetected AFib. Jeanne E. Poole, MD, an electrophysiologist and professor of medicine at the University of Washington in Seattle, observed that the question of whether patients with asymptomatic AFib should receive oral anticoagulation therapy is as-yet unanswered and is the focus of ongoing randomized trials. The Apple Heart Study approach, she said, “might lead a lot of patients into being treated unnecessarily or prematurely, or flooding doctors’ offices with a lot of young people.”
Co-principal investigator Marco Perez, MD, an electrophysiologist at Stanford, replied, “Stroke is important, and we all worry about it. But it’s also important that there are other things atrial fibrillation is associated with, like cardiomyopathy and heart failure. So finding atrial fibrillation in a young population might be important. Maybe they don’t need anticoagulation, but maybe there’s something else going on.”
Patrick T. O’Gara, MD, professor of medicine at Harvard University, Boston, was concerned about what he called “the signal-to-noise ratio – the noise that will come in when there is an irregularity detected on the watch that could range from anything from ventricular premature beats to atrial fibrillation.” He is also leery of what he considers to be at this point the excessive hype surrounding direct-to-consumer wearable digital health technology.
“I applaud your circumspection,” he told Dr. Turakhia and Dr. Perez. “I understand very directly from you that these are limited observations. But it’s a good step forward.”
Dr. Perez reported receiving research funding from and serving as a consultant to Apple. Dr. Turakhia reported serving as a consultant to AliveCor and Cardiva Medical.
Their presentation was immediately followed by a related panel discussion titled, “Digital Disruption at Our Doorstep – Implications for Clinicians and Patients.” Session moderator John Rumsfeld, MD, chief innovation officer at the ACC and professor of medicine at the University of Colorado, Denver, kicked things off by observing, “Digital health technology certainly exists. There’ve been billions of dollars invested in digital health. Outside of health care there’s been successful digital transformation of almost every other sector of the economy except for health care. But we deliver care pretty much the same as we have for the past 50 or more years.”
Paul Stoeffels, MD, chief scientific officer at Johnson & Johnson, said physicians and payers want to see evidence of benefit before adopting change. Towards that end, he announced that Johnson & Johnson and Apple are collaborating on a randomized controlled trial called the HEARTLINE study. The active intervention arm in the study involves utilization of the Apple Watch’s irregular pulse notification algorithm, with confirmation of AFib to be achieved using the ECG app incorporated in the latest version of the watch, coupled with a medication adherence app developed by Johnson & Johnson. Enrollment of 150,000 U.S. adults age 65 and older is planned to begin this summer. The study, conducted on a digital platform akin to the Apple Heart Study, will look at the intervention’s impact on rates of stroke, MI, and death as well as AF detection.
Maulik Majmudar, MD, a cardiologist and chief health officer for health and wellness at Amazon, declared, “There’s no doubt in my mind that digital solutions will become a mainstay in our care delivery going forward. The question is really not if, but when.”
He predicted that just as the past two decades have seen the birth of new medical specialties, including hospitalists and cardiovascular intensivists, the next 10 years or so will see the creation of a new field within cardiovascular medicine, whose skilled practitioners might be called ‘digitalists’ – experts in collecting, moving, and safeguarding massive quantities of digital health data.
Robert Califf, MD, vice chancellor for health data science at Duke Health in Durham, N.C., addressed the issue of how society is going to pay for a shift to digital health: “It’s very simple. I don’t see any way that fee-for-service medicine can deal with this. It’s just not possible. If you think we’re going to add on more cost to the system by doing virtual visits, I just do not see that happening. Our solution to the payment system is to get rid of fee-for-service medicine and go to pay-for-value. The minute you’re in pay-for-value, virtual visits and digital information will become the way to do it – to move the treatment and the interaction more to home and less of having people wait in doctors’ offices and spending time in hospitals.”
SOURCE: Turakhia M, ACC 19 NCT03335800
, investigators reported at the annual meeting of the American College of Cardiology.
This was a single-arm, prospective, open-label, observational study of unprecedented size and speediness of completion. It included nearly 420,000 self-enrolled adults living in the U.S., with 8 months of monitoring. But despite the study’s flashy size and trendy digital health theme, the researchers were careful not to oversell the findings.
“This study was just meant to be a very, very first step in trying to learn if this kind of technology can help us to prevent stroke. It was not a randomized trial of a public health intervention for screening. This is the first half of the first inning. Rigorous investigation of this technology and its potential use in clinical settings will need to happen. But we do think from a trial and operational standpoint the Apple Heart Study provides a solid foundation upon which further research in digital health can be conducted,” according to Mintu Turakhia, MD, co-principal investigator and an electrophysiologist as well as executive director of the Center for Digital Health at Stanford (Calif.) University, which conducted the study.
The study was conducted virtually. Screening, consent, and data gathering were performed electronically by smartphone. Participants had to have an Apple Watch Series 1, 2, or 3, and an Apple iPhone 5 or more recent model in order to join. The majority of subjects were under age 40, and just 6% were age 65 or older, when the risks of atrial fibrillation (AFib) and stroke are higher. All participants self-reported having no history of AFib nor currently being on anticoagulation.
The study algorithm utilized the Apple Watch’s built-in light sensor technology to opportunistically sample the time interval between pulses when the wearer was still. An irregular time interval triggered a cascade of more frequent sampling. If 5 of 6 samples were irregular within a 48-hour period, the wearer received an irregular rhythm notification along with a prompt to contact a participating physician via telemedicine. The physician could then arrange for an ECG patch to be mailed to the participant, who wore it for up to 7 days before mailing it back for analysis.
Among the key findings in the Apple Heart Study: the irregular pulse notification rate was low overall, at 0.5%, ranging from 0.16% in the under-40 group to 3.2% in subjects age 65 or older. As a result, the study population of particular interest nosedived from an initial 419,297 to the less than 2,100 who received an irregular pulse notification. Of the 658 participants who were subsequently sent an ECG patch, 450 returned it for analysis.
An average of 13 days went by between an irregular pulse notification and ECG patch receipt and activation, so it wasn’t particularly surprising that only 34% of the patches were positive for AFib, since early-stage paroxysmal AFib comes and goes. However, of the 86 subjects who received a new notification of an irregular rhythm while they were wearing a patch, 72 simultaneously showed AFib on their patch. That translates to an 84% positive predictive value for an irregular rhythm notification as an indicator of AFib.
Of the 153 subjects with evidence of AFib on their ECG patch, 20% proved to be in AFib for the full week they wore it. Of those with AFib, 89% had a longest episode of at least 1 hour in duration.
Several discussants expressed reservations about this approach to finding individuals with previously undetected AFib. Jeanne E. Poole, MD, an electrophysiologist and professor of medicine at the University of Washington in Seattle, observed that the question of whether patients with asymptomatic AFib should receive oral anticoagulation therapy is as-yet unanswered and is the focus of ongoing randomized trials. The Apple Heart Study approach, she said, “might lead a lot of patients into being treated unnecessarily or prematurely, or flooding doctors’ offices with a lot of young people.”
Co-principal investigator Marco Perez, MD, an electrophysiologist at Stanford, replied, “Stroke is important, and we all worry about it. But it’s also important that there are other things atrial fibrillation is associated with, like cardiomyopathy and heart failure. So finding atrial fibrillation in a young population might be important. Maybe they don’t need anticoagulation, but maybe there’s something else going on.”
Patrick T. O’Gara, MD, professor of medicine at Harvard University, Boston, was concerned about what he called “the signal-to-noise ratio – the noise that will come in when there is an irregularity detected on the watch that could range from anything from ventricular premature beats to atrial fibrillation.” He is also leery of what he considers to be at this point the excessive hype surrounding direct-to-consumer wearable digital health technology.
“I applaud your circumspection,” he told Dr. Turakhia and Dr. Perez. “I understand very directly from you that these are limited observations. But it’s a good step forward.”
Dr. Perez reported receiving research funding from and serving as a consultant to Apple. Dr. Turakhia reported serving as a consultant to AliveCor and Cardiva Medical.
Their presentation was immediately followed by a related panel discussion titled, “Digital Disruption at Our Doorstep – Implications for Clinicians and Patients.” Session moderator John Rumsfeld, MD, chief innovation officer at the ACC and professor of medicine at the University of Colorado, Denver, kicked things off by observing, “Digital health technology certainly exists. There’ve been billions of dollars invested in digital health. Outside of health care there’s been successful digital transformation of almost every other sector of the economy except for health care. But we deliver care pretty much the same as we have for the past 50 or more years.”
Paul Stoeffels, MD, chief scientific officer at Johnson & Johnson, said physicians and payers want to see evidence of benefit before adopting change. Towards that end, he announced that Johnson & Johnson and Apple are collaborating on a randomized controlled trial called the HEARTLINE study. The active intervention arm in the study involves utilization of the Apple Watch’s irregular pulse notification algorithm, with confirmation of AFib to be achieved using the ECG app incorporated in the latest version of the watch, coupled with a medication adherence app developed by Johnson & Johnson. Enrollment of 150,000 U.S. adults age 65 and older is planned to begin this summer. The study, conducted on a digital platform akin to the Apple Heart Study, will look at the intervention’s impact on rates of stroke, MI, and death as well as AF detection.
Maulik Majmudar, MD, a cardiologist and chief health officer for health and wellness at Amazon, declared, “There’s no doubt in my mind that digital solutions will become a mainstay in our care delivery going forward. The question is really not if, but when.”
He predicted that just as the past two decades have seen the birth of new medical specialties, including hospitalists and cardiovascular intensivists, the next 10 years or so will see the creation of a new field within cardiovascular medicine, whose skilled practitioners might be called ‘digitalists’ – experts in collecting, moving, and safeguarding massive quantities of digital health data.
Robert Califf, MD, vice chancellor for health data science at Duke Health in Durham, N.C., addressed the issue of how society is going to pay for a shift to digital health: “It’s very simple. I don’t see any way that fee-for-service medicine can deal with this. It’s just not possible. If you think we’re going to add on more cost to the system by doing virtual visits, I just do not see that happening. Our solution to the payment system is to get rid of fee-for-service medicine and go to pay-for-value. The minute you’re in pay-for-value, virtual visits and digital information will become the way to do it – to move the treatment and the interaction more to home and less of having people wait in doctors’ offices and spending time in hospitals.”
SOURCE: Turakhia M, ACC 19 NCT03335800
, investigators reported at the annual meeting of the American College of Cardiology.
This was a single-arm, prospective, open-label, observational study of unprecedented size and speediness of completion. It included nearly 420,000 self-enrolled adults living in the U.S., with 8 months of monitoring. But despite the study’s flashy size and trendy digital health theme, the researchers were careful not to oversell the findings.
“This study was just meant to be a very, very first step in trying to learn if this kind of technology can help us to prevent stroke. It was not a randomized trial of a public health intervention for screening. This is the first half of the first inning. Rigorous investigation of this technology and its potential use in clinical settings will need to happen. But we do think from a trial and operational standpoint the Apple Heart Study provides a solid foundation upon which further research in digital health can be conducted,” according to Mintu Turakhia, MD, co-principal investigator and an electrophysiologist as well as executive director of the Center for Digital Health at Stanford (Calif.) University, which conducted the study.
The study was conducted virtually. Screening, consent, and data gathering were performed electronically by smartphone. Participants had to have an Apple Watch Series 1, 2, or 3, and an Apple iPhone 5 or more recent model in order to join. The majority of subjects were under age 40, and just 6% were age 65 or older, when the risks of atrial fibrillation (AFib) and stroke are higher. All participants self-reported having no history of AFib nor currently being on anticoagulation.
The study algorithm utilized the Apple Watch’s built-in light sensor technology to opportunistically sample the time interval between pulses when the wearer was still. An irregular time interval triggered a cascade of more frequent sampling. If 5 of 6 samples were irregular within a 48-hour period, the wearer received an irregular rhythm notification along with a prompt to contact a participating physician via telemedicine. The physician could then arrange for an ECG patch to be mailed to the participant, who wore it for up to 7 days before mailing it back for analysis.
Among the key findings in the Apple Heart Study: the irregular pulse notification rate was low overall, at 0.5%, ranging from 0.16% in the under-40 group to 3.2% in subjects age 65 or older. As a result, the study population of particular interest nosedived from an initial 419,297 to the less than 2,100 who received an irregular pulse notification. Of the 658 participants who were subsequently sent an ECG patch, 450 returned it for analysis.
An average of 13 days went by between an irregular pulse notification and ECG patch receipt and activation, so it wasn’t particularly surprising that only 34% of the patches were positive for AFib, since early-stage paroxysmal AFib comes and goes. However, of the 86 subjects who received a new notification of an irregular rhythm while they were wearing a patch, 72 simultaneously showed AFib on their patch. That translates to an 84% positive predictive value for an irregular rhythm notification as an indicator of AFib.
Of the 153 subjects with evidence of AFib on their ECG patch, 20% proved to be in AFib for the full week they wore it. Of those with AFib, 89% had a longest episode of at least 1 hour in duration.
Several discussants expressed reservations about this approach to finding individuals with previously undetected AFib. Jeanne E. Poole, MD, an electrophysiologist and professor of medicine at the University of Washington in Seattle, observed that the question of whether patients with asymptomatic AFib should receive oral anticoagulation therapy is as-yet unanswered and is the focus of ongoing randomized trials. The Apple Heart Study approach, she said, “might lead a lot of patients into being treated unnecessarily or prematurely, or flooding doctors’ offices with a lot of young people.”
Co-principal investigator Marco Perez, MD, an electrophysiologist at Stanford, replied, “Stroke is important, and we all worry about it. But it’s also important that there are other things atrial fibrillation is associated with, like cardiomyopathy and heart failure. So finding atrial fibrillation in a young population might be important. Maybe they don’t need anticoagulation, but maybe there’s something else going on.”
Patrick T. O’Gara, MD, professor of medicine at Harvard University, Boston, was concerned about what he called “the signal-to-noise ratio – the noise that will come in when there is an irregularity detected on the watch that could range from anything from ventricular premature beats to atrial fibrillation.” He is also leery of what he considers to be at this point the excessive hype surrounding direct-to-consumer wearable digital health technology.
“I applaud your circumspection,” he told Dr. Turakhia and Dr. Perez. “I understand very directly from you that these are limited observations. But it’s a good step forward.”
Dr. Perez reported receiving research funding from and serving as a consultant to Apple. Dr. Turakhia reported serving as a consultant to AliveCor and Cardiva Medical.
Their presentation was immediately followed by a related panel discussion titled, “Digital Disruption at Our Doorstep – Implications for Clinicians and Patients.” Session moderator John Rumsfeld, MD, chief innovation officer at the ACC and professor of medicine at the University of Colorado, Denver, kicked things off by observing, “Digital health technology certainly exists. There’ve been billions of dollars invested in digital health. Outside of health care there’s been successful digital transformation of almost every other sector of the economy except for health care. But we deliver care pretty much the same as we have for the past 50 or more years.”
Paul Stoeffels, MD, chief scientific officer at Johnson & Johnson, said physicians and payers want to see evidence of benefit before adopting change. Towards that end, he announced that Johnson & Johnson and Apple are collaborating on a randomized controlled trial called the HEARTLINE study. The active intervention arm in the study involves utilization of the Apple Watch’s irregular pulse notification algorithm, with confirmation of AFib to be achieved using the ECG app incorporated in the latest version of the watch, coupled with a medication adherence app developed by Johnson & Johnson. Enrollment of 150,000 U.S. adults age 65 and older is planned to begin this summer. The study, conducted on a digital platform akin to the Apple Heart Study, will look at the intervention’s impact on rates of stroke, MI, and death as well as AF detection.
Maulik Majmudar, MD, a cardiologist and chief health officer for health and wellness at Amazon, declared, “There’s no doubt in my mind that digital solutions will become a mainstay in our care delivery going forward. The question is really not if, but when.”
He predicted that just as the past two decades have seen the birth of new medical specialties, including hospitalists and cardiovascular intensivists, the next 10 years or so will see the creation of a new field within cardiovascular medicine, whose skilled practitioners might be called ‘digitalists’ – experts in collecting, moving, and safeguarding massive quantities of digital health data.
Robert Califf, MD, vice chancellor for health data science at Duke Health in Durham, N.C., addressed the issue of how society is going to pay for a shift to digital health: “It’s very simple. I don’t see any way that fee-for-service medicine can deal with this. It’s just not possible. If you think we’re going to add on more cost to the system by doing virtual visits, I just do not see that happening. Our solution to the payment system is to get rid of fee-for-service medicine and go to pay-for-value. The minute you’re in pay-for-value, virtual visits and digital information will become the way to do it – to move the treatment and the interaction more to home and less of having people wait in doctors’ offices and spending time in hospitals.”
SOURCE: Turakhia M, ACC 19 NCT03335800
REPORTING FROM ACC 19
Apple Watch algorithm brings wearables closer to clinical practice
NEW ORLEANS – , Matthew W. Martinez, MD, medical director of the Sports Cardiology and Hypertrophic Cardiomyopathy Center at the Lehigh Valley Health Network in Allentown, Pa., said in a video interview.
The Apple Heart Study, presented at the annual meeting of the American College of Cardiology, evaluated a mobile app that uses the watch’s existing light sensor technology to detect subtle changes that might indicate an arrhythmia.
The Apple Watch generates a tachogram, which is a plot of time between heart beats. If an abnormal tachogram occurs five out of six times, they are analyzed by an algorithm and sent to the Apple Watch.
The positive predictive value for the tachogram was 71%, and the positive predictive value for the notification was 84%.
Dr. Martinez, who is lead cardiologist for U.S. Major League Soccer and is also heavily involved with the National Football League, said that the study helps clinicians understand the utility of wearable technology.
His take home from the study is that, when people are notified by their watch, they should notify their health care provider, and the provider should take it seriously.
Dr. Martinez was not involved in the Apple Heart Study, and had no relevant disclosures.
bjancin@mdedge.com
NEW ORLEANS – , Matthew W. Martinez, MD, medical director of the Sports Cardiology and Hypertrophic Cardiomyopathy Center at the Lehigh Valley Health Network in Allentown, Pa., said in a video interview.
The Apple Heart Study, presented at the annual meeting of the American College of Cardiology, evaluated a mobile app that uses the watch’s existing light sensor technology to detect subtle changes that might indicate an arrhythmia.
The Apple Watch generates a tachogram, which is a plot of time between heart beats. If an abnormal tachogram occurs five out of six times, they are analyzed by an algorithm and sent to the Apple Watch.
The positive predictive value for the tachogram was 71%, and the positive predictive value for the notification was 84%.
Dr. Martinez, who is lead cardiologist for U.S. Major League Soccer and is also heavily involved with the National Football League, said that the study helps clinicians understand the utility of wearable technology.
His take home from the study is that, when people are notified by their watch, they should notify their health care provider, and the provider should take it seriously.
Dr. Martinez was not involved in the Apple Heart Study, and had no relevant disclosures.
bjancin@mdedge.com
NEW ORLEANS – , Matthew W. Martinez, MD, medical director of the Sports Cardiology and Hypertrophic Cardiomyopathy Center at the Lehigh Valley Health Network in Allentown, Pa., said in a video interview.
The Apple Heart Study, presented at the annual meeting of the American College of Cardiology, evaluated a mobile app that uses the watch’s existing light sensor technology to detect subtle changes that might indicate an arrhythmia.
The Apple Watch generates a tachogram, which is a plot of time between heart beats. If an abnormal tachogram occurs five out of six times, they are analyzed by an algorithm and sent to the Apple Watch.
The positive predictive value for the tachogram was 71%, and the positive predictive value for the notification was 84%.
Dr. Martinez, who is lead cardiologist for U.S. Major League Soccer and is also heavily involved with the National Football League, said that the study helps clinicians understand the utility of wearable technology.
His take home from the study is that, when people are notified by their watch, they should notify their health care provider, and the provider should take it seriously.
Dr. Martinez was not involved in the Apple Heart Study, and had no relevant disclosures.
bjancin@mdedge.com
REPORTING FROM ACC 19
CAC score over 1,000 carries higher risks
, based on data from a large retrospective study presented by Allison W. Peng at the annual meeting of the American College of Cardiology.
“Our data argues for consideration of CAC 1000 (or more) as a distinct group with CVD mortality greater than that of contemporary secondary prevention trials ... We showed that those with CAC 1000 (or more) have both a higher area and density of calcification, a more dispersed pattern of calcification in their coronary artery tree (the majority with 4-vessel disease), with a markedly more diffuse distribution of extra-coronary calcification compared to the other CAC groups,” Ms. Peng and her colleagues wrote in the study, which was published online in the Journal of the American College of Cardiology.
Future guidelines should address these patients as a distinct risk group that might gain the most benefit from targeted, aggressive preventive therapy, the researchers said.
Current guidelines identify individuals with CAC scores over 400 as the highest risk group. With a mean follow-up time of 12.3 years, the results from 66,636 asymptomatic individuals in the CAC consortium study, which included over 2,800 patients with CAC (Agatston) scores of 1,000 or more, indicate patients with CAC scores of 1000 or more have nearly a 2-fold higher risk of CVD mortality compared to those with CAC scores of 400-999. While the mortality risk levels off slightly in those with scores exceeding 1000, all-cause and cause-specific mortality risk still increases with no apparent upper CAC threshold.
Patients with a CAC score of at least 1000 were 66.3 years old, on average; 86.3% were male, 52.4% had 4-vessel CAC, and they had a larger total CAC area.
Compared to patients with CAC scores of 400-999, those with a CAC score of 1000 or more had a greater risk of cardiovascular disease (HR, 1.71; 95% CI, 1.41-2.08), coronary heart disease (HR, 1.84; 95% CI, 1.43-2.36), cancer (HR, 1.36; 95% CI, 1.07-1.73), and all-cause mortality (HR, 1.51; 95% CI, 1.33-1.70).
Those with CAC scores of 400-999 had a 2.1, 3.6, 2.7, and 9.8 mortality rate per 1000 person-years for CHD, CVD, cancer, and all-cause mortality, respectively. But those with CAC scores of 1000 of more had a 5.1, 8.0, 4.6, and 18.8 mortality rate per 1000 person-years for CHD, CVD, cancer, and all-cause mortality, respectively.
The leading cause of death was CVD; 36.5% in the CAC 400-999 group and 42.6% in the CAC 1000 or more group. CHD mortality, as a subset of CVD mortality, constituted 21.1% of deaths in the CAC 400-999 group and 27.1% of deaths in the CAC 1000 or more group.
“Future randomized controlled trials of aggressive preventative therapies, for example PCSK9-inhibitors and anti-inflammatory drugs, in patients with CAC ≥ 1000, may prove helpful to evaluate the benefits of such treatment in this unique group,” the authors wrote. They also urged updating current guidelines to reflect best practices for these patients.
The study was funded by The National Institutes of Health. The authors have no relevant financial disclosures.
SOURCE: Peng A et al. Journal of the American College of Cardiology.
, based on data from a large retrospective study presented by Allison W. Peng at the annual meeting of the American College of Cardiology.
“Our data argues for consideration of CAC 1000 (or more) as a distinct group with CVD mortality greater than that of contemporary secondary prevention trials ... We showed that those with CAC 1000 (or more) have both a higher area and density of calcification, a more dispersed pattern of calcification in their coronary artery tree (the majority with 4-vessel disease), with a markedly more diffuse distribution of extra-coronary calcification compared to the other CAC groups,” Ms. Peng and her colleagues wrote in the study, which was published online in the Journal of the American College of Cardiology.
Future guidelines should address these patients as a distinct risk group that might gain the most benefit from targeted, aggressive preventive therapy, the researchers said.
Current guidelines identify individuals with CAC scores over 400 as the highest risk group. With a mean follow-up time of 12.3 years, the results from 66,636 asymptomatic individuals in the CAC consortium study, which included over 2,800 patients with CAC (Agatston) scores of 1,000 or more, indicate patients with CAC scores of 1000 or more have nearly a 2-fold higher risk of CVD mortality compared to those with CAC scores of 400-999. While the mortality risk levels off slightly in those with scores exceeding 1000, all-cause and cause-specific mortality risk still increases with no apparent upper CAC threshold.
Patients with a CAC score of at least 1000 were 66.3 years old, on average; 86.3% were male, 52.4% had 4-vessel CAC, and they had a larger total CAC area.
Compared to patients with CAC scores of 400-999, those with a CAC score of 1000 or more had a greater risk of cardiovascular disease (HR, 1.71; 95% CI, 1.41-2.08), coronary heart disease (HR, 1.84; 95% CI, 1.43-2.36), cancer (HR, 1.36; 95% CI, 1.07-1.73), and all-cause mortality (HR, 1.51; 95% CI, 1.33-1.70).
Those with CAC scores of 400-999 had a 2.1, 3.6, 2.7, and 9.8 mortality rate per 1000 person-years for CHD, CVD, cancer, and all-cause mortality, respectively. But those with CAC scores of 1000 of more had a 5.1, 8.0, 4.6, and 18.8 mortality rate per 1000 person-years for CHD, CVD, cancer, and all-cause mortality, respectively.
The leading cause of death was CVD; 36.5% in the CAC 400-999 group and 42.6% in the CAC 1000 or more group. CHD mortality, as a subset of CVD mortality, constituted 21.1% of deaths in the CAC 400-999 group and 27.1% of deaths in the CAC 1000 or more group.
“Future randomized controlled trials of aggressive preventative therapies, for example PCSK9-inhibitors and anti-inflammatory drugs, in patients with CAC ≥ 1000, may prove helpful to evaluate the benefits of such treatment in this unique group,” the authors wrote. They also urged updating current guidelines to reflect best practices for these patients.
The study was funded by The National Institutes of Health. The authors have no relevant financial disclosures.
SOURCE: Peng A et al. Journal of the American College of Cardiology.
, based on data from a large retrospective study presented by Allison W. Peng at the annual meeting of the American College of Cardiology.
“Our data argues for consideration of CAC 1000 (or more) as a distinct group with CVD mortality greater than that of contemporary secondary prevention trials ... We showed that those with CAC 1000 (or more) have both a higher area and density of calcification, a more dispersed pattern of calcification in their coronary artery tree (the majority with 4-vessel disease), with a markedly more diffuse distribution of extra-coronary calcification compared to the other CAC groups,” Ms. Peng and her colleagues wrote in the study, which was published online in the Journal of the American College of Cardiology.
Future guidelines should address these patients as a distinct risk group that might gain the most benefit from targeted, aggressive preventive therapy, the researchers said.
Current guidelines identify individuals with CAC scores over 400 as the highest risk group. With a mean follow-up time of 12.3 years, the results from 66,636 asymptomatic individuals in the CAC consortium study, which included over 2,800 patients with CAC (Agatston) scores of 1,000 or more, indicate patients with CAC scores of 1000 or more have nearly a 2-fold higher risk of CVD mortality compared to those with CAC scores of 400-999. While the mortality risk levels off slightly in those with scores exceeding 1000, all-cause and cause-specific mortality risk still increases with no apparent upper CAC threshold.
Patients with a CAC score of at least 1000 were 66.3 years old, on average; 86.3% were male, 52.4% had 4-vessel CAC, and they had a larger total CAC area.
Compared to patients with CAC scores of 400-999, those with a CAC score of 1000 or more had a greater risk of cardiovascular disease (HR, 1.71; 95% CI, 1.41-2.08), coronary heart disease (HR, 1.84; 95% CI, 1.43-2.36), cancer (HR, 1.36; 95% CI, 1.07-1.73), and all-cause mortality (HR, 1.51; 95% CI, 1.33-1.70).
Those with CAC scores of 400-999 had a 2.1, 3.6, 2.7, and 9.8 mortality rate per 1000 person-years for CHD, CVD, cancer, and all-cause mortality, respectively. But those with CAC scores of 1000 of more had a 5.1, 8.0, 4.6, and 18.8 mortality rate per 1000 person-years for CHD, CVD, cancer, and all-cause mortality, respectively.
The leading cause of death was CVD; 36.5% in the CAC 400-999 group and 42.6% in the CAC 1000 or more group. CHD mortality, as a subset of CVD mortality, constituted 21.1% of deaths in the CAC 400-999 group and 27.1% of deaths in the CAC 1000 or more group.
“Future randomized controlled trials of aggressive preventative therapies, for example PCSK9-inhibitors and anti-inflammatory drugs, in patients with CAC ≥ 1000, may prove helpful to evaluate the benefits of such treatment in this unique group,” the authors wrote. They also urged updating current guidelines to reflect best practices for these patients.
The study was funded by The National Institutes of Health. The authors have no relevant financial disclosures.
SOURCE: Peng A et al. Journal of the American College of Cardiology.
FROM ACC 2019
FDA advises alternatives to paclitaxel-coated devices for PAD, pending review
“Alternative treatment options should generally be used for most patients,” rather than paclitaxel-coated balloons and stents for peripheral arterial disease (PAD), pending an ongoing safety review, according to the Food and Drug Administration.
The FDA conducted a preliminary analysis of long-term follow-up data (up to 5 years in some studies) of the pivotal premarket randomized trials for paclitaxel-coated products indicated for peripheral arterial disease (PAD). In a Letter to Healthcare providers issued March 15, the FDA reported that their preliminary review of these data found “a potentially concerning signal of increased long-term mortality in study subjects treated with paclitaxel-coated products, compared to patients treated with uncoated devices.”
The three trials (totaling 975 patients) that had 5-year follow-up data demonstrated an approximately 50% increased risk of mortality in subjects treated with paclitaxel-coated devices vs. those treated with control devices (20.1% vs. 13.4% crude risk of death at 5 years), according to the agency.
The FDA indicated that these data “should be interpreted with caution for several reasons.” They cited a large variability in the risk estimate of mortality because of the limited amount of long-term data and pointed out that the studies were not designed to be pooled. In addition, the specific cause and mechanism of the increased mortality was unknown.
The FDA also announced that they are planning on convening an Advisory Committee meeting of the Circulatory System Devices Panel to address this issue, including plausible mechanisms for this mortality effect, a re-examination of the benefit-risk profile, modifications of current and future clinical trials regarding these devices, and guidance to any regulatory action, as needed. The timing of this meeting is to be announced within the upcoming weeks.
The FDA letter further stated that the agency intends to conduct additional analyses “to determine whether the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”
mlesney@mdedge.com
SOURCE: Food and Drug Administration Letter to Healthcare Providers. 2019 Mar 15.
“Alternative treatment options should generally be used for most patients,” rather than paclitaxel-coated balloons and stents for peripheral arterial disease (PAD), pending an ongoing safety review, according to the Food and Drug Administration.
The FDA conducted a preliminary analysis of long-term follow-up data (up to 5 years in some studies) of the pivotal premarket randomized trials for paclitaxel-coated products indicated for peripheral arterial disease (PAD). In a Letter to Healthcare providers issued March 15, the FDA reported that their preliminary review of these data found “a potentially concerning signal of increased long-term mortality in study subjects treated with paclitaxel-coated products, compared to patients treated with uncoated devices.”
The three trials (totaling 975 patients) that had 5-year follow-up data demonstrated an approximately 50% increased risk of mortality in subjects treated with paclitaxel-coated devices vs. those treated with control devices (20.1% vs. 13.4% crude risk of death at 5 years), according to the agency.
The FDA indicated that these data “should be interpreted with caution for several reasons.” They cited a large variability in the risk estimate of mortality because of the limited amount of long-term data and pointed out that the studies were not designed to be pooled. In addition, the specific cause and mechanism of the increased mortality was unknown.
The FDA also announced that they are planning on convening an Advisory Committee meeting of the Circulatory System Devices Panel to address this issue, including plausible mechanisms for this mortality effect, a re-examination of the benefit-risk profile, modifications of current and future clinical trials regarding these devices, and guidance to any regulatory action, as needed. The timing of this meeting is to be announced within the upcoming weeks.
The FDA letter further stated that the agency intends to conduct additional analyses “to determine whether the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”
mlesney@mdedge.com
SOURCE: Food and Drug Administration Letter to Healthcare Providers. 2019 Mar 15.
“Alternative treatment options should generally be used for most patients,” rather than paclitaxel-coated balloons and stents for peripheral arterial disease (PAD), pending an ongoing safety review, according to the Food and Drug Administration.
The FDA conducted a preliminary analysis of long-term follow-up data (up to 5 years in some studies) of the pivotal premarket randomized trials for paclitaxel-coated products indicated for peripheral arterial disease (PAD). In a Letter to Healthcare providers issued March 15, the FDA reported that their preliminary review of these data found “a potentially concerning signal of increased long-term mortality in study subjects treated with paclitaxel-coated products, compared to patients treated with uncoated devices.”
The three trials (totaling 975 patients) that had 5-year follow-up data demonstrated an approximately 50% increased risk of mortality in subjects treated with paclitaxel-coated devices vs. those treated with control devices (20.1% vs. 13.4% crude risk of death at 5 years), according to the agency.
The FDA indicated that these data “should be interpreted with caution for several reasons.” They cited a large variability in the risk estimate of mortality because of the limited amount of long-term data and pointed out that the studies were not designed to be pooled. In addition, the specific cause and mechanism of the increased mortality was unknown.
The FDA also announced that they are planning on convening an Advisory Committee meeting of the Circulatory System Devices Panel to address this issue, including plausible mechanisms for this mortality effect, a re-examination of the benefit-risk profile, modifications of current and future clinical trials regarding these devices, and guidance to any regulatory action, as needed. The timing of this meeting is to be announced within the upcoming weeks.
The FDA letter further stated that the agency intends to conduct additional analyses “to determine whether the benefits continue to outweigh the risks for approved paclitaxel-coated balloons and paclitaxel-eluting stents when used in accordance with their indications for use.”
mlesney@mdedge.com
SOURCE: Food and Drug Administration Letter to Healthcare Providers. 2019 Mar 15.
Key clinical point: FDA advises that alternatives to paclitaxel-coated devices for PAD should be used for most patients.
Major finding: Five-year data demonstrated an approximately 50% increased risk of mortality in patients with paclitaxel-coated devices, compared with uncoated ones.
Study details: Preliminary FDA review of three trials with 975 patients.
Disclosures: Study is funded and performed by the FDA.
Source: Food and Drug Administration. Letter to Healthcare Providers. 2019 Mar 15.
Light physical activity lowers CVD risk in older women
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Older women do not get enough physical activity, so this finding that light physical activity is associated with improved coronary heart disease and cardiovascular disease outcomes supports the recent scientific report by the 2018 Physical Activity Guidelines Advisory Committee. It is also helpful in extending the evidence about the benefits of physical activity in reducing incident coronary heart disease to older women, as previous studies on this topic showed such benefits in men.
These findings should remind health care professionals, systems, and agencies to promote the 2018 Physical Activity Guidelines for Americans to all patients. Otherwise, the future health and well-being of older women is likely to suffer from the consequences of sedentary behavior and inadequate physical activity.
Gregory W. Heath, DHSc, MPH, is from the department of health and human performance at the University of Tennessee, Chattanooga. These comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0405). No conflicts of interest were reported.
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
Even light physical activity can significantly reduce the risks of acquiring coronary heart disease specifically and the broad range of cardiovascular diseases in older women, new data suggests.
A paper published in JAMA Network Open reported the outcome of a prospective cohort study in 5,861 women, with a mean age of 78.5 years, who wore accelerometers for 7 days to measure physical activity.
than those in the lowest quartile of activity, who engaged in less than 3.9 hours per day, after adjusting for factors such as comorbidities, lifestyle, and cardiovascular risk.
Similarly, those in the highest quartile had an 18% lower risk of cardiovascular disease than those in the lowest quartile, after adjusting for potential confounders.
Researchers saw a significant dose-dependent decrease in the risk for incident coronary heart disease and cardiovascular disease with increasing light physical activity, such that each 1-hour increment of activity was associated with a 20% decrease in coronary heart disease risk and 10% decrease in cardiovascular disease risk.
Andrea Z. LaCroix, PhD, from the University of California, San Diego, and her coauthors noted that physical activity guidelines for aerobic activity suggest 75 minutes of vigorous physical activity or 150 minutes of moderate activity each day, but only around 25% of U.S. women aged over 75 years are estimated to meet this requirement.
“These guidelines may have discouraged PA [physical activity] when perceived to be unattainable by large segments of the population,” they wrote.
While the majority of active time in older adults is spent doing light physical activity, little is known about the cardiovascular effects of participating in this level of activity. “A major barrier has been that self-reported questionnaires measuring leisure-time PA do not adequately capture light PA that is acquired throughout the day in activities of daily living,” they wrote.
The study also looked at the impact of moderate to vigorous physical activity, finding a significant 46% reduction between the highest to lowest quartiles of activity in coronary heart disease risk and a 31% reduction in cardiovascular disease risk.
Even after adjusting for the use of lipid-lowering medication, antihypertensive medication or healthy eating scores, the results remained unchanged. The researchers also saw no change when women with angina and heart failure at baseline were excluded or when they excluded cardiovascular events that occurred during the first 6 months of follow-up.
The study was supported by the National Heart, Lung, and Blood Institute; the National Institutes of Health; and the Department of Health & Human Services. Six authors reported receiving funding from the study supporters and other research institutions, and one reported membership on the advisory committee for physical activity guidelines. No other conflicts of interest were reported.
SOURCE: LaCroix AZ et al. JAMA Netw Open. 2019 Mar 15. doi: 10.1001/jamanetworkopen.2019.0419.
FROM JAMA NETWORK OPEN
New LDL-lowering drug under FDA review
This week in MDedge Cardiocast: A novel drug lowers LDL in on top of maximums statins, invasive cardiology is a top money maker for hospitals, a meta-analysis parses the heart and kidney benefits of new diabetes drugs, and the AHA warns that heart-harming toxins may hurt hookah smokers.
Amazon Alexa
Apple Podcasts
Google Podcasts
TuneIn
This week in MDedge Cardiocast: A novel drug lowers LDL in on top of maximums statins, invasive cardiology is a top money maker for hospitals, a meta-analysis parses the heart and kidney benefits of new diabetes drugs, and the AHA warns that heart-harming toxins may hurt hookah smokers.
Amazon Alexa
Apple Podcasts
Google Podcasts
TuneIn
This week in MDedge Cardiocast: A novel drug lowers LDL in on top of maximums statins, invasive cardiology is a top money maker for hospitals, a meta-analysis parses the heart and kidney benefits of new diabetes drugs, and the AHA warns that heart-harming toxins may hurt hookah smokers.
Amazon Alexa
Apple Podcasts
Google Podcasts
TuneIn
A Vital Clue to the Problem
ANSWER
The correct interpretation is a bit challenging. You’ve confirmed the electrodes were placed correctly; however, the P waves are unusual (best seen in lead II) and are suggestive of an ectopic atrial rhythm. In lead II, there are two P waves for each QRS complex, consistent with second-degree atrioventricular (AV) block with 2:1 AV conduction. The QRS complex is wide at 130 ms without a right or left bundle branch pattern, consistent with a nonspecific intraventricular conduction block, and there is evidence of nonspecific ST-T wave abnormality.
These changes were new compared with the patient’s preoperative ECG, which showed sinus rhythm and no evidence of heart block.
ANSWER
The correct interpretation is a bit challenging. You’ve confirmed the electrodes were placed correctly; however, the P waves are unusual (best seen in lead II) and are suggestive of an ectopic atrial rhythm. In lead II, there are two P waves for each QRS complex, consistent with second-degree atrioventricular (AV) block with 2:1 AV conduction. The QRS complex is wide at 130 ms without a right or left bundle branch pattern, consistent with a nonspecific intraventricular conduction block, and there is evidence of nonspecific ST-T wave abnormality.
These changes were new compared with the patient’s preoperative ECG, which showed sinus rhythm and no evidence of heart block.
ANSWER
The correct interpretation is a bit challenging. You’ve confirmed the electrodes were placed correctly; however, the P waves are unusual (best seen in lead II) and are suggestive of an ectopic atrial rhythm. In lead II, there are two P waves for each QRS complex, consistent with second-degree atrioventricular (AV) block with 2:1 AV conduction. The QRS complex is wide at 130 ms without a right or left bundle branch pattern, consistent with a nonspecific intraventricular conduction block, and there is evidence of nonspecific ST-T wave abnormality.
These changes were new compared with the patient’s preoperative ECG, which showed sinus rhythm and no evidence of heart block.
Two days ago, a 76-year-old man underwent surgical repair of a left femoral fracture sustained in an automobile accident. Last night, his vital signs were concerning for asymptomatic bradycardia, prompting an order for ECG prior to morning rounds. His postoperative surgical course has been otherwise uneventful, and he is using minimal narcotic analgesia.
The patient has a long history of mild hypertension, which is well controlled with hydrochlorothiazide (50 mg/d). Otherwise, his medical history shows no angina, dyspnea, shortness of breath, or palpitations. There is no history of thyroid dysfunction or renal disease.
A pack-a-day smoker since age 15, the patient has been using a nicotine patch during his hospital stay. In the past 36 hours, he has taken 4 acetaminophen/oxycodone tablets (325/5 mg).
The patient works on a 400-acre ranch with about 100 head of cattle. His alcohol consumption was heavy until about 12 years ago, when he “blacked out” and gave up drinking altogether. He attends Alcoholics Anonymous meetings and leads sessions at his church. He denies recreational or illicit drug use.
Family history is positive for prostate cancer in his father and lung cancer in two brothers. His mother died of a hemorrhagic stroke at age 84.
The review of systems is remarkable only for discomfort due to an indwelling Foley catheter placed at the time of the surgery. He has no other specific complaints.
This morning, his vital signs include a blood pressure of 108/60 mm Hg; pulse, 42 beats/min; and O2 saturation, 100% on 2L of oxygen via nasal prongs.
When you arrive at the patient’s room, the ECG is in progress. The technician expresses concern about the tracing and shows you that the electrodes are placed properly. Looking at the ECG, you see a ventricular rate of 42 beats/min; PR interval, unmeasured; QRS duration, 130 ms; QT/QTc interval, 514/429 ms; P axis, +83°; R axis, +84°; and T axis, –43°. What is your interpretation?
Bempedoic acid safely dropped LDL, now seeks FDA approval
Based on its performance, bempedoic acid seems on track for agency approval.
Aside from demonstrating safety, the efficacy goal of the CLEAR Harmony (Evaluation of Long-Term Safety and Tolerability of ETC-1002 in High-Risk Patients With Hyperlipidemia and High CV Risk) trial was to cut LDL cholesterol as an add-on to maximally tolerated statin treatment, as well as discretionary use of other lipid-lowering agents in patients with atherosclerotic cardiovascular disease.
That goal appeared to be met by the CLEAR Harmony results, as well as the results from four other studies that contributed data to the approval application filed for bempedoic acid. A clinical outcomes study is underway with more than 12,000 patients aimed at showing incremental clinical benefit from bempedoic acid on top of approved treatments for lowering LDL cholesterol, but those results are not expected until 2022. Until then, the application’s data focus on the evidence that the new drug safely lowers LDL cholesterol when used on top of existing treatments.
“Bempedoic acid provides an additional therapeutic option to safely lower LDL cholesterol in patients with high risk for atherosclerotic cardiovascular disease already treated with a statin,” Kausik K. Ray, MD, said when he first reported these findings during the annual meeting of the European Society of Cardiology last August in Munich. The same results appeared in a newly released article (N Engl J Med. 2019 Mar 14;380[11]:1022-32).
Maximum recommended statin dosages exist because, for every doubling of the statin dosage, LDL cholesterol levels drop by about another 6%, but adverse events grow more common. Because bempedoic acid and other ATP citrate lyase inhibitors work via the same metabolic pathway as that of statins – HMG CoA reductase inhibitors – “we did not know whether squeezing another 20% of LDL cholesterol lowering would be tolerated. What we have clearly and reassuringly shown is it is well tolerated,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
The CLEAR Harmony results showed in 2,230 randomized patients that treatment with bempedoic acid cut LDL cholesterol levels by an average of 18% more compared with placebo in the intention-to-treat analysis, and by 20% in an on-treatment analysis.
By seeking U.S. marketing approval for bempedoic acid based on LDL-lowering and safety only, but without data on clinical endpoints, the company developing the drug is following a path already established by several other lipid-lowering drug classes.
“Statins, ezetimibe and the PCSK9 inhibitors were all approved based on clinical trial results that showed LDL-cholesterol reductions with what the FDA judged to be acceptable safety, but without results from completed outcomes trials,” Christie M. Ballantyne, MD, a coauthor of the CLEAR Harmony study and professor and chief of cardiology at Baylor College of Medicine in Houston, said in an interview.
Stephen Nicholls, MD, professor of cardiology at Monash University in Melbourne, added in an interview that “the precedent has been to conditionally approve LDL cholesterol–lowering drugs at this stage of development, based on the large body of evidence demonstrating that LDL cholesterol–lowering consistently produces clinical benefit.”
To gain more confidence that treatment with bempedoic acid exerts a benefit to patients prior to availability of clinical-outcome results, the developing company sponsored a genetic and epidemiologic study that looked at the association between naturally occurring mutations that dampen the activity of ATP citrate lyase, an enzyme that metabolically sits just upstream from HMG CoA reductase, the enzyme that statins target. Dr. Nicholls, Dr. Ray, and several other collaborators devised “genetic scores” that took into account variants of the gene that codes for ATP citrate lyase, and a separate score for HMG CoA reductase variants. Each score estimated a person’s activity for each of these enzymes. The researchers then used the scores to classify enzymatic activity in more than 650,000 people in several different databases, including more than 100,000 people with a history of major cardiovascular events.
The results showed that “genetic variants that mimic the effect of ATP citrate lyase inhibitors and statins appeared to lower plasma LDL cholesterol levels by the same mechanism of action. They were associated with nearly identical effects on the risk of cardiovascular disease and cancer per unit decrease in the LDL cholesterol level,” the investigators said in an article published concurrently with the CLEAR Harmony results (N Engl J Med. 2019 March 14;380[11]:1033-42).
This finding “strengthens the likelihood that an outcome trial will show benefits,” Steven E. Nissen, MD, chairman of cardiovascular medicine at the Cleveland Clinic Foundation, and a lead investigator in the bempedoic acid outcomes trial, CLEAR Outcomes, said in an interview.
Dr. Nicholls noted that, on the basis of the genetic study’s results “it would seem very reasonable to extrapolate and expect that bempedoic acid should reduce cardiovascular events.”
The data reported by Dr. Ray and his associates from the CLEAR Harmony trial showed that overall, the adverse-event rates associated with bempedoic acid treatment were similar to the rates seen in patients who received placebo. But Michael V. Holmes, MD, who wrote an editorial that accompanied both reports, highlighted a few differences in the adverse event rates that concerned him. These were a statistically significant higher rate of gout and blood uric acid levels on bempedoic acid treatment compared with controls, a significantly higher rate of discontinuations because of adverse events, and nominally higher rates of death, cardiovascular death, and heart failure hospitalization, said Dr. Holmes, an epidemiologist at the University of Oxford, England.
But Dr. Nissen said that “the safety ‘signals’ involve very small numbers of patients and do not raise major concerns. The increases in gout and uric acid are worth noting, but are less weighty than the disease the drug is intended to treat: major cardiovascular events.”
Dr. Nichols added that “the large cardiovascular outcome trial will provide the opportunity to further study safety and potential side effects. I’m hesitant to overinterpret event data from a relatively small clinical trial that primarily focused on the lipid effects.”
Despite recent success of the PCSK9 inhibitors as an add-on or substitute for statin treatment of elevated LDL cholesterol, the cost of the drugs in this class has made the cardiovascular disease community eager for another alternative to statins.
“The PCSK9 inhibitors are extremely effective, but uptake has been slow due to their cost and formulary restrictions,” said Dr. Ballantyne. “Many high-risk patients continue to have persistently elevated levels of LDL cholesterol.” Bempedoic acid is “a new therapy that can help people who continue to have elevations of LDL cholesterol despite current therapies.”
CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
SOURCEs: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
The primary endpoint of bempedoic acid’s safety, assessed by means of the incidence of adverse events and changes in safety laboratory variables during the CLEAR Harmony trial, did not differ meaningfully between the bempedoic acid group and the placebo group. However, patients in the bempedoic acid group had an excess risk of adverse events leading to discontinuation of the blinded trial regimen, an excess risk of gout, and higher blood concentrations of uric acid than those in the placebo group.
In further analyses of nonprimary and secondary endpoints, there were additional potentially troubling signals, although the 95% confidence intervals were wide: 0.9% of the patients treated with bempedoic acid died, compared with 0.3% of those in the placebo group; 0.4% and 0.1%, respectively, died from adjudicated cardiovascular disease; and 0.6% and 0.1%, respectively, were hospitalized for heart failure. Although the findings are potentially alarming, the imprecision that is reflected in the 95% confidence intervals renders the relative risk values virtually meaningless, but can these effect estimates be unseen?
The cumulative data from randomized treatment trials and from studies of human genetics say that, for a given reduction in the LDL cholesterol level, drugs that inhibit ATP citrate lyase and do not have off-target effects ought to yield reductions in the risk of cardiovascular disease that are similar to those achieved with statins. However, analysis of endpoints in treatment trials for which there is marginal statistical power is best avoided. Fortunately for bempedoic acid, an ongoing phase 3, cardiovascular outcome trial will provide additional information.
More broadly, the genetic characterization of drug targets is set to revolutionize how we develop medicines.
Michael V. Holmes, MD, is an epidemiologist at the University of Oxford, England. He made these comments in a published editorial (N Engl J Med. 2019 Mar 14;380[11]:1076-9). He had no disclosures.
The primary endpoint of bempedoic acid’s safety, assessed by means of the incidence of adverse events and changes in safety laboratory variables during the CLEAR Harmony trial, did not differ meaningfully between the bempedoic acid group and the placebo group. However, patients in the bempedoic acid group had an excess risk of adverse events leading to discontinuation of the blinded trial regimen, an excess risk of gout, and higher blood concentrations of uric acid than those in the placebo group.
In further analyses of nonprimary and secondary endpoints, there were additional potentially troubling signals, although the 95% confidence intervals were wide: 0.9% of the patients treated with bempedoic acid died, compared with 0.3% of those in the placebo group; 0.4% and 0.1%, respectively, died from adjudicated cardiovascular disease; and 0.6% and 0.1%, respectively, were hospitalized for heart failure. Although the findings are potentially alarming, the imprecision that is reflected in the 95% confidence intervals renders the relative risk values virtually meaningless, but can these effect estimates be unseen?
The cumulative data from randomized treatment trials and from studies of human genetics say that, for a given reduction in the LDL cholesterol level, drugs that inhibit ATP citrate lyase and do not have off-target effects ought to yield reductions in the risk of cardiovascular disease that are similar to those achieved with statins. However, analysis of endpoints in treatment trials for which there is marginal statistical power is best avoided. Fortunately for bempedoic acid, an ongoing phase 3, cardiovascular outcome trial will provide additional information.
More broadly, the genetic characterization of drug targets is set to revolutionize how we develop medicines.
Michael V. Holmes, MD, is an epidemiologist at the University of Oxford, England. He made these comments in a published editorial (N Engl J Med. 2019 Mar 14;380[11]:1076-9). He had no disclosures.
The primary endpoint of bempedoic acid’s safety, assessed by means of the incidence of adverse events and changes in safety laboratory variables during the CLEAR Harmony trial, did not differ meaningfully between the bempedoic acid group and the placebo group. However, patients in the bempedoic acid group had an excess risk of adverse events leading to discontinuation of the blinded trial regimen, an excess risk of gout, and higher blood concentrations of uric acid than those in the placebo group.
In further analyses of nonprimary and secondary endpoints, there were additional potentially troubling signals, although the 95% confidence intervals were wide: 0.9% of the patients treated with bempedoic acid died, compared with 0.3% of those in the placebo group; 0.4% and 0.1%, respectively, died from adjudicated cardiovascular disease; and 0.6% and 0.1%, respectively, were hospitalized for heart failure. Although the findings are potentially alarming, the imprecision that is reflected in the 95% confidence intervals renders the relative risk values virtually meaningless, but can these effect estimates be unseen?
The cumulative data from randomized treatment trials and from studies of human genetics say that, for a given reduction in the LDL cholesterol level, drugs that inhibit ATP citrate lyase and do not have off-target effects ought to yield reductions in the risk of cardiovascular disease that are similar to those achieved with statins. However, analysis of endpoints in treatment trials for which there is marginal statistical power is best avoided. Fortunately for bempedoic acid, an ongoing phase 3, cardiovascular outcome trial will provide additional information.
More broadly, the genetic characterization of drug targets is set to revolutionize how we develop medicines.
Michael V. Holmes, MD, is an epidemiologist at the University of Oxford, England. He made these comments in a published editorial (N Engl J Med. 2019 Mar 14;380[11]:1076-9). He had no disclosures.
Based on its performance, bempedoic acid seems on track for agency approval.
Aside from demonstrating safety, the efficacy goal of the CLEAR Harmony (Evaluation of Long-Term Safety and Tolerability of ETC-1002 in High-Risk Patients With Hyperlipidemia and High CV Risk) trial was to cut LDL cholesterol as an add-on to maximally tolerated statin treatment, as well as discretionary use of other lipid-lowering agents in patients with atherosclerotic cardiovascular disease.
That goal appeared to be met by the CLEAR Harmony results, as well as the results from four other studies that contributed data to the approval application filed for bempedoic acid. A clinical outcomes study is underway with more than 12,000 patients aimed at showing incremental clinical benefit from bempedoic acid on top of approved treatments for lowering LDL cholesterol, but those results are not expected until 2022. Until then, the application’s data focus on the evidence that the new drug safely lowers LDL cholesterol when used on top of existing treatments.
“Bempedoic acid provides an additional therapeutic option to safely lower LDL cholesterol in patients with high risk for atherosclerotic cardiovascular disease already treated with a statin,” Kausik K. Ray, MD, said when he first reported these findings during the annual meeting of the European Society of Cardiology last August in Munich. The same results appeared in a newly released article (N Engl J Med. 2019 Mar 14;380[11]:1022-32).
Maximum recommended statin dosages exist because, for every doubling of the statin dosage, LDL cholesterol levels drop by about another 6%, but adverse events grow more common. Because bempedoic acid and other ATP citrate lyase inhibitors work via the same metabolic pathway as that of statins – HMG CoA reductase inhibitors – “we did not know whether squeezing another 20% of LDL cholesterol lowering would be tolerated. What we have clearly and reassuringly shown is it is well tolerated,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
The CLEAR Harmony results showed in 2,230 randomized patients that treatment with bempedoic acid cut LDL cholesterol levels by an average of 18% more compared with placebo in the intention-to-treat analysis, and by 20% in an on-treatment analysis.
By seeking U.S. marketing approval for bempedoic acid based on LDL-lowering and safety only, but without data on clinical endpoints, the company developing the drug is following a path already established by several other lipid-lowering drug classes.
“Statins, ezetimibe and the PCSK9 inhibitors were all approved based on clinical trial results that showed LDL-cholesterol reductions with what the FDA judged to be acceptable safety, but without results from completed outcomes trials,” Christie M. Ballantyne, MD, a coauthor of the CLEAR Harmony study and professor and chief of cardiology at Baylor College of Medicine in Houston, said in an interview.
Stephen Nicholls, MD, professor of cardiology at Monash University in Melbourne, added in an interview that “the precedent has been to conditionally approve LDL cholesterol–lowering drugs at this stage of development, based on the large body of evidence demonstrating that LDL cholesterol–lowering consistently produces clinical benefit.”
To gain more confidence that treatment with bempedoic acid exerts a benefit to patients prior to availability of clinical-outcome results, the developing company sponsored a genetic and epidemiologic study that looked at the association between naturally occurring mutations that dampen the activity of ATP citrate lyase, an enzyme that metabolically sits just upstream from HMG CoA reductase, the enzyme that statins target. Dr. Nicholls, Dr. Ray, and several other collaborators devised “genetic scores” that took into account variants of the gene that codes for ATP citrate lyase, and a separate score for HMG CoA reductase variants. Each score estimated a person’s activity for each of these enzymes. The researchers then used the scores to classify enzymatic activity in more than 650,000 people in several different databases, including more than 100,000 people with a history of major cardiovascular events.
The results showed that “genetic variants that mimic the effect of ATP citrate lyase inhibitors and statins appeared to lower plasma LDL cholesterol levels by the same mechanism of action. They were associated with nearly identical effects on the risk of cardiovascular disease and cancer per unit decrease in the LDL cholesterol level,” the investigators said in an article published concurrently with the CLEAR Harmony results (N Engl J Med. 2019 March 14;380[11]:1033-42).
This finding “strengthens the likelihood that an outcome trial will show benefits,” Steven E. Nissen, MD, chairman of cardiovascular medicine at the Cleveland Clinic Foundation, and a lead investigator in the bempedoic acid outcomes trial, CLEAR Outcomes, said in an interview.
Dr. Nicholls noted that, on the basis of the genetic study’s results “it would seem very reasonable to extrapolate and expect that bempedoic acid should reduce cardiovascular events.”
The data reported by Dr. Ray and his associates from the CLEAR Harmony trial showed that overall, the adverse-event rates associated with bempedoic acid treatment were similar to the rates seen in patients who received placebo. But Michael V. Holmes, MD, who wrote an editorial that accompanied both reports, highlighted a few differences in the adverse event rates that concerned him. These were a statistically significant higher rate of gout and blood uric acid levels on bempedoic acid treatment compared with controls, a significantly higher rate of discontinuations because of adverse events, and nominally higher rates of death, cardiovascular death, and heart failure hospitalization, said Dr. Holmes, an epidemiologist at the University of Oxford, England.
But Dr. Nissen said that “the safety ‘signals’ involve very small numbers of patients and do not raise major concerns. The increases in gout and uric acid are worth noting, but are less weighty than the disease the drug is intended to treat: major cardiovascular events.”
Dr. Nichols added that “the large cardiovascular outcome trial will provide the opportunity to further study safety and potential side effects. I’m hesitant to overinterpret event data from a relatively small clinical trial that primarily focused on the lipid effects.”
Despite recent success of the PCSK9 inhibitors as an add-on or substitute for statin treatment of elevated LDL cholesterol, the cost of the drugs in this class has made the cardiovascular disease community eager for another alternative to statins.
“The PCSK9 inhibitors are extremely effective, but uptake has been slow due to their cost and formulary restrictions,” said Dr. Ballantyne. “Many high-risk patients continue to have persistently elevated levels of LDL cholesterol.” Bempedoic acid is “a new therapy that can help people who continue to have elevations of LDL cholesterol despite current therapies.”
CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
SOURCEs: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
Based on its performance, bempedoic acid seems on track for agency approval.
Aside from demonstrating safety, the efficacy goal of the CLEAR Harmony (Evaluation of Long-Term Safety and Tolerability of ETC-1002 in High-Risk Patients With Hyperlipidemia and High CV Risk) trial was to cut LDL cholesterol as an add-on to maximally tolerated statin treatment, as well as discretionary use of other lipid-lowering agents in patients with atherosclerotic cardiovascular disease.
That goal appeared to be met by the CLEAR Harmony results, as well as the results from four other studies that contributed data to the approval application filed for bempedoic acid. A clinical outcomes study is underway with more than 12,000 patients aimed at showing incremental clinical benefit from bempedoic acid on top of approved treatments for lowering LDL cholesterol, but those results are not expected until 2022. Until then, the application’s data focus on the evidence that the new drug safely lowers LDL cholesterol when used on top of existing treatments.
“Bempedoic acid provides an additional therapeutic option to safely lower LDL cholesterol in patients with high risk for atherosclerotic cardiovascular disease already treated with a statin,” Kausik K. Ray, MD, said when he first reported these findings during the annual meeting of the European Society of Cardiology last August in Munich. The same results appeared in a newly released article (N Engl J Med. 2019 Mar 14;380[11]:1022-32).
Maximum recommended statin dosages exist because, for every doubling of the statin dosage, LDL cholesterol levels drop by about another 6%, but adverse events grow more common. Because bempedoic acid and other ATP citrate lyase inhibitors work via the same metabolic pathway as that of statins – HMG CoA reductase inhibitors – “we did not know whether squeezing another 20% of LDL cholesterol lowering would be tolerated. What we have clearly and reassuringly shown is it is well tolerated,” said Dr. Ray, a cardiologist and professor of public health at Imperial College, London.
The CLEAR Harmony results showed in 2,230 randomized patients that treatment with bempedoic acid cut LDL cholesterol levels by an average of 18% more compared with placebo in the intention-to-treat analysis, and by 20% in an on-treatment analysis.
By seeking U.S. marketing approval for bempedoic acid based on LDL-lowering and safety only, but without data on clinical endpoints, the company developing the drug is following a path already established by several other lipid-lowering drug classes.
“Statins, ezetimibe and the PCSK9 inhibitors were all approved based on clinical trial results that showed LDL-cholesterol reductions with what the FDA judged to be acceptable safety, but without results from completed outcomes trials,” Christie M. Ballantyne, MD, a coauthor of the CLEAR Harmony study and professor and chief of cardiology at Baylor College of Medicine in Houston, said in an interview.
Stephen Nicholls, MD, professor of cardiology at Monash University in Melbourne, added in an interview that “the precedent has been to conditionally approve LDL cholesterol–lowering drugs at this stage of development, based on the large body of evidence demonstrating that LDL cholesterol–lowering consistently produces clinical benefit.”
To gain more confidence that treatment with bempedoic acid exerts a benefit to patients prior to availability of clinical-outcome results, the developing company sponsored a genetic and epidemiologic study that looked at the association between naturally occurring mutations that dampen the activity of ATP citrate lyase, an enzyme that metabolically sits just upstream from HMG CoA reductase, the enzyme that statins target. Dr. Nicholls, Dr. Ray, and several other collaborators devised “genetic scores” that took into account variants of the gene that codes for ATP citrate lyase, and a separate score for HMG CoA reductase variants. Each score estimated a person’s activity for each of these enzymes. The researchers then used the scores to classify enzymatic activity in more than 650,000 people in several different databases, including more than 100,000 people with a history of major cardiovascular events.
The results showed that “genetic variants that mimic the effect of ATP citrate lyase inhibitors and statins appeared to lower plasma LDL cholesterol levels by the same mechanism of action. They were associated with nearly identical effects on the risk of cardiovascular disease and cancer per unit decrease in the LDL cholesterol level,” the investigators said in an article published concurrently with the CLEAR Harmony results (N Engl J Med. 2019 March 14;380[11]:1033-42).
This finding “strengthens the likelihood that an outcome trial will show benefits,” Steven E. Nissen, MD, chairman of cardiovascular medicine at the Cleveland Clinic Foundation, and a lead investigator in the bempedoic acid outcomes trial, CLEAR Outcomes, said in an interview.
Dr. Nicholls noted that, on the basis of the genetic study’s results “it would seem very reasonable to extrapolate and expect that bempedoic acid should reduce cardiovascular events.”
The data reported by Dr. Ray and his associates from the CLEAR Harmony trial showed that overall, the adverse-event rates associated with bempedoic acid treatment were similar to the rates seen in patients who received placebo. But Michael V. Holmes, MD, who wrote an editorial that accompanied both reports, highlighted a few differences in the adverse event rates that concerned him. These were a statistically significant higher rate of gout and blood uric acid levels on bempedoic acid treatment compared with controls, a significantly higher rate of discontinuations because of adverse events, and nominally higher rates of death, cardiovascular death, and heart failure hospitalization, said Dr. Holmes, an epidemiologist at the University of Oxford, England.
But Dr. Nissen said that “the safety ‘signals’ involve very small numbers of patients and do not raise major concerns. The increases in gout and uric acid are worth noting, but are less weighty than the disease the drug is intended to treat: major cardiovascular events.”
Dr. Nichols added that “the large cardiovascular outcome trial will provide the opportunity to further study safety and potential side effects. I’m hesitant to overinterpret event data from a relatively small clinical trial that primarily focused on the lipid effects.”
Despite recent success of the PCSK9 inhibitors as an add-on or substitute for statin treatment of elevated LDL cholesterol, the cost of the drugs in this class has made the cardiovascular disease community eager for another alternative to statins.
“The PCSK9 inhibitors are extremely effective, but uptake has been slow due to their cost and formulary restrictions,” said Dr. Ballantyne. “Many high-risk patients continue to have persistently elevated levels of LDL cholesterol.” Bempedoic acid is “a new therapy that can help people who continue to have elevations of LDL cholesterol despite current therapies.”
CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
SOURCEs: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.
Key clinical point: Bempedoic acid safely lowed LDL cholesterol levels in a pivotal trial.
Major finding: In the intention-to-treat analysis, bempedoic acid cut LDL cholesterol by 18%; by 20% in an on-treatment analysis.
Study details: CLEAR Harmony, a multicenter, randomized trial with 2,230 patients.
Disclosures: CLEAR Harmony and the genetic study were sponsored by Esperion, the company developing bempedoic acid. Dr. Ray has been a consultant to several drug companies but had no other financial relationship to Esperion. Dr. Ballantyne and Dr. Nicholls have been consultants to and have received research funding from Esperion and from several other companies. Dr. Nissen is leading an Esperion-sponsored study but has no financial relationships with the company or with other companies.
Sources: N Engl J Med. 2019 Mar 14;380[11]:1022-32 and 1033-42.