User login
Domestic violence amid COVID-19: Helping your patients from afar
Roger R., MD, a primary care physician from Philadelphia, set up a telemedicine appointment with a 24-year-old female patient who was experiencing headaches and was worried she might have COVID-19.
During the televisit, Dr. R. noticed that “Tonya” (not her real name) had a purplish bruise under her right eye. When asked how she got the bruise, Tonya said she had bumped into a dresser. The physician suspected abuse. He then heard a man’s voice in the background and thought it might belong to the abuser. “Is this a good time for you to talk?” he asked Tonya.
Tonya hesitated.
“When might be a better time?”
Tonya suggested an alternate time, and the physician called her then. During the visit, she shared that her fiancé, a car salesman who was also sheltering at home, was punching her.
“He always had a bad temper. Once he shoved me, but he’s never hit me before. And when he was upset, we used to go out to eat and he calmed down. Now, we’re stuck inside, we can’t even get away from each other to go to work, and he’s getting scary,” she told the doctor.
The physician asked if she would like to be connected with a domestic violence counselor. When Tonya agreed, he called Jessica DuBois Palardy, a licensed social worker and the program supervisor at STOP Intimate Partner Violence, a Philadelphia-based collaborative project of the Children’s Hospital of Philadelphia and the Lutheran Settlement House’s Bilingual Domestic Violence Program.
A ‘horrifying’ trend
Tonya’s story is not unique. A United Nations report shows that there has been a “horrifying global surge in domestic violence” linked to “lockdowns imposed by the governments responding to the COVID-19 pandemic.” The United States is no exception – 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
Carole Warshaw, MD, director of the National Center on Domestic Violence, Trauma, and Mental Health in Chicago, said, “We know that intimate partner violence is increasing among people sheltering at home, and that abuse has become more severe.”
Even in nonabusive situations, being confined together at close quarters, often amid family stress and financial hardship, can be wearing, and tempers can flare. In an abusive relationship, “the main contributor to violence during shelter-in-place restrictions is that the isolation gives abusers more opportunities for controlling their partners, who have fewer options for accessing safety and support,” Dr. Warshaw said.
It is critical to “approach every clinical encounter knowing that domestic violence may be at play,” she emphasized.
Physicians might be the most important lifeline
Physicians are already facing myriad COVID-19–related challenges, and having another concern to keep in mind may be daunting.
“We’re in uncharted territory and we’re all trying to figure out how to navigate this time, how to practice medicine via phone and video conferences, and how to deal with the financial repercussions of the pandemic – not to mention concern for the health of our families,” said Peter F. Cronholm, MD, associate professor of family medicine and community health at the Hospital of the University of Pennsylvania, Philadelphia. “So maintaining vigilance is often difficult. Nevertheless, it’s important not to let this critical issue fall to the wayside.”
Marcella Nyachogo, MSW, a licensed social worker and assistant director of the Bilingual Domestic Violence Program, noted that physicians and other health care providers “may be the only people the patient interacts with, since the abuser may cut the survivor off from family and friends. And because the survivor isn’t leaving the house, he or she doesn’t have an opportunity to interact with coworkers or others – which makes health care providers the most important lifeline.”
COVID-19 as a weapon of abuse
Carey Watson, MD, regional medical director of the Family Violence Prevention Program at Kaiser Permanente in northern California, points to a disturbing trend in COVID-19–related abuse.
“Unfortunately, I’m hearing more and more accounts of how the illness itself can be one more weapon in the abuser’s arsenal,” she said.
Experts say that increasingly, abusers are claiming that their partner, who is employed in an “essential” job outside the home, is carrying the virus, and they are using this as a means of control and manipulation.
This is especially true of abusive partners of health care providers, Dr. Watson noted. She recounted the story of a divorced nurse whose husband did not allow her to have contact with their children, allegedly out of concern that she might have COVID-19, and would threaten her with a gun when she protested.
“It is important to keep this abusive tactic in mind, not only when dealing with patients but also with fellow physicians and health care professionals, and check in to see if everything is okay – especially if they seem particularly stressed out or distant,” Dr. Watson recommended.
Trust your clinical gut
How can you tell if your patients might be experiencing abuse when you’re not seeing them in person?
Pay attention to subtle signals and “trust your clinical gut when something doesn’t feel right,” Ms. Nyachogo advised.
If a patient’s demeanor is jittery or anxious or if someone next to him or her is answering all the questions or interrupting the visit, these could be red flags.
Dr. Cronholm added that telemedicine visits offer a “rare window into a patient’s home life that would not be available in an office visit.” For example, a house in disarray, the presence of broken objects, or the presence of another person hovering in the background suggests the need for further exploration.
“The main thing for all providers to keep in mind is ‘first, do no harm,’ ” Ms. Nyachogo emphasized.
“Our agency has been working for years with medical professionals in how to screen and connect folks with help most effectively and safely, and – although the specific situations posed by COVID are new – the overall approach is the same, which is to proceed with caution in how you approach the subject and how you make referrals,” she said.
Begin by asking if it is a convenient time to talk.
“This question takes the onus off the patient, who may not know how to communicate that she has no privacy or is in the middle of an argument,” explained Elsa Swenson, program manager of Home Free community program, which serves individuals experiencing domestic violence. The program is part of Minnesota-based Missions Inc. Programs, which serves those experiencing domestic abuse and chemical dependency.
If the patient indicates that it isn’t a convenient time to talk, find out when would be a better time. “This might be difficult for busy physicians and may not be what they’re accustomed to when calling a patient at home, but the patient’s circumstances are unknown to you, so it’s essential to organize around their ability to talk,” Ms. Swenson noted.
‘Are you alone?’
Another important piece of information is whether the patient has privacy – which can be tricky if the abuser is standing right there.
“You don’t want to tip the abuser off to your concerns, so you need to frame the question in a neutral way,” Dr. Watson advised.
For example, you might say that HIPAA laws require that you conduct the consultation with no one else present, and find out if there is a location in the house where the patient can have privacy.
It might be easier to talk on the phone than via video, suggests Florence Remes, a New Jersey–based licensed social worker who specializes in domestic violence. Going into another room and playing music or turning on the television might make it less obvious that a call is taking place, and the abuser would be less likely to overhear the caller’s conversation.
Dr. Watson suggested that questions about abuse might be included with other questions and asked in a simple yes/no format. “I’d like to ask you some standard questions I’m asking everyone during the pandemic. Do you have a cough or fever? Do you have any other physical symptoms? Do you have access to hand sanitizer? How is your sleep? Are you experiencing stress? Do you feel safe at home?”
The abuser, if present, will only hear the patient’s “yes” or “no” without knowing the question. If the patient indicates that she is being abused but is unable to talk, a later time can be arranged to further explore the issue.
Technology is a double-edged sword
Modern technologies have been a great boon to patients and physicians during this time of social distancing, allowing ongoing contact and health care when it would not otherwise have been possible. On the other hand, technology is fraught with potential dangers that can jeopardize the patient’s safety and compromise privacy.
Ms. Remes recounted the story of “Susan,” a client with whom she had been conducting teletherapy visits using an approved HIPAA-compliant telemedicine forum. Susan was working from home because of shelter-in-place restrictions. Her husband had been abusive, and Susan was concerned he might be “sabotaging” the household’s WiFi to isolate her from outside sources of support.
At the recommendation of Ms. Remes, Susan continued sessions either via phone calls or by using the WhatsApp program on her cellphone. Many of the requirements governing HIPAA privacy regulations have been temporarily relaxed, and clinicians can use non–encrypted forms of transmission, such as FaceTime, WhatsApp, or Skype, if no other platform is available.
But even cellphones have risks, Dr. Warshaw noted. The patient’s abuser might track texts or look at call logs – especially on unsecured platforms. It’s advisable to ask patients about who has access to their phone and computer and discuss ways to increase security.
Follow the patient’s lead
Proceed slowly and start with nonthreatening questions, Ms. Palardy advised. “I notice you have some injuries; can you tell me how you got them? Did someone hurt you? What does your relationship look like when you argue? Is there anything that makes you feel uncomfortable or unsafe?”
Emphasizing that you are asking these questions because of care and concern is reassuring and helps patients to feel they are not alone, Ms. Nyachogo pointed out.
“As your doctor, I’m worried about your health and (if relevant) your children’s safety. I can help connect you with counseling and support, legal resources, and a shelter, and everything is free and confidential. Would you be interested?” she said.
If the client acknowledges abuse, “follow their lead, but don’t push too hard,” Ms. Nyachogo warned.
“It is the client’s choice whether or not to take action,” she noted. “I’ve met survivors who said that it wasn’t until a doctor or nurse expressed concern about bruises that it even occurred to them that they were being abused. Some lied to the doctor about how they got hurt – but the question planted a seed, even though it might have taken years to follow up on the referral,” she said.
What if the patient doesn’t want to get help?
If a patient is not ready to seek help, you can create a home-safety plan. This might include setting follow-up times. If you don’t hear from him or her, you should then call the police. Or you might create a “code word,” such as “apple pie.” If the patient uses that word during a session, you know her life is in danger, Ms. Remes suggested.
Providing written information about how to get help is important but can be problematic if the abuser finds it.
Ms. Nyachogo recommends e-mailing follow-up materials that cover a variety of topics, such as keeping safe during the COVID-19 pandemic, relaxation, healthy eating, getting exercise while homebound, activities for children, and suggestions for hotlines and other resources if one is feeling suicidal or unsafe.
“If you present these as your ‘standard’ follow-up materials, the abuser is less likely to become suspicious,” Ms. Nyachogo noted.
Resources are available during COVID-19
All of the experts emphasize that resources for victims of domestic violence remain available during the COVID-19 pandemic, although some shelters may be operating at reduced capacity. Some agencies are finding alternatives to group shelters, such as hotels or Airbnb, which carry less risk of catching COVID-19.
Referring a patient to domestic violence resources is a delicate process. “You don’t want referring the patient for help to further endanger their life,” Ms. Nyachogo said.
The more you can take the burden off the patient, the better. If she is interested in getting help, you can call a domestic violence counselor or advocate while she is on the phone.
“This type of ‘warm handoff’ is what Tonya’s physician did,” Ms. Palardy recounted.
A warm handoff requires that physicians be familiar with domestic violence resources, Dr. Warshaw emphasized.
“Don’t wait until you are working with someone who needs help to find out where to refer them. Take the time to proactively research local agencies specializing in domestic violence and have their phone numbers on hand, so you can offer resources immediately if the person is interested,” she advised. The National Domestic Violence Hotline can also assist with safety planning and access to local resources.
‘Thinking on your feet’ critical for physicians
Addressing domestic violence during this unprecedented time requires “thinking on your feet” about novel forms of detection and intervention, Dr. Watson said. This involves a combination of clinical acumen, creativity, and finely honed intuition.
Ms. Nyachogo added, “Keeping an eye on domestic violence can feel like an extra burden, but don’t forget that it is lifesaving work.”
Resources
National Domestic Violence Hotline
- 800-799-SAFE (7233)
- The patient can also text LOVEIS to 22522.
National Center on Domestic Violence, Trauma, and Mental Health
- Provides resources for health care, mental health, and substance use treatment and recovery support providers on responding to domestic violence and other trauma.
- Provides resources for professionals and patients regarding access to substance use and mental health care during the COVID-1 pandemic.
- Provides support for parents, caregivers, and children during the pandemic.
- Provides resources for advocates serving families affected by domestic violence.
- A state-by-state guide to local resources
Children’s Hospital of Philadelphia Research Institute
STOP Intimate Partner Violence (IPV)
New Jersey Coalition for Domestic Violence
American Bar Association COVID-19 resources for communities
- Text HOME to 741741.
National Network to End Domestic Violence (NNEDV) COVID-19 Technology Safety
A version of this article originally appeared on Medscape.com.
Roger R., MD, a primary care physician from Philadelphia, set up a telemedicine appointment with a 24-year-old female patient who was experiencing headaches and was worried she might have COVID-19.
During the televisit, Dr. R. noticed that “Tonya” (not her real name) had a purplish bruise under her right eye. When asked how she got the bruise, Tonya said she had bumped into a dresser. The physician suspected abuse. He then heard a man’s voice in the background and thought it might belong to the abuser. “Is this a good time for you to talk?” he asked Tonya.
Tonya hesitated.
“When might be a better time?”
Tonya suggested an alternate time, and the physician called her then. During the visit, she shared that her fiancé, a car salesman who was also sheltering at home, was punching her.
“He always had a bad temper. Once he shoved me, but he’s never hit me before. And when he was upset, we used to go out to eat and he calmed down. Now, we’re stuck inside, we can’t even get away from each other to go to work, and he’s getting scary,” she told the doctor.
The physician asked if she would like to be connected with a domestic violence counselor. When Tonya agreed, he called Jessica DuBois Palardy, a licensed social worker and the program supervisor at STOP Intimate Partner Violence, a Philadelphia-based collaborative project of the Children’s Hospital of Philadelphia and the Lutheran Settlement House’s Bilingual Domestic Violence Program.
A ‘horrifying’ trend
Tonya’s story is not unique. A United Nations report shows that there has been a “horrifying global surge in domestic violence” linked to “lockdowns imposed by the governments responding to the COVID-19 pandemic.” The United States is no exception – 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
Carole Warshaw, MD, director of the National Center on Domestic Violence, Trauma, and Mental Health in Chicago, said, “We know that intimate partner violence is increasing among people sheltering at home, and that abuse has become more severe.”
Even in nonabusive situations, being confined together at close quarters, often amid family stress and financial hardship, can be wearing, and tempers can flare. In an abusive relationship, “the main contributor to violence during shelter-in-place restrictions is that the isolation gives abusers more opportunities for controlling their partners, who have fewer options for accessing safety and support,” Dr. Warshaw said.
It is critical to “approach every clinical encounter knowing that domestic violence may be at play,” she emphasized.
Physicians might be the most important lifeline
Physicians are already facing myriad COVID-19–related challenges, and having another concern to keep in mind may be daunting.
“We’re in uncharted territory and we’re all trying to figure out how to navigate this time, how to practice medicine via phone and video conferences, and how to deal with the financial repercussions of the pandemic – not to mention concern for the health of our families,” said Peter F. Cronholm, MD, associate professor of family medicine and community health at the Hospital of the University of Pennsylvania, Philadelphia. “So maintaining vigilance is often difficult. Nevertheless, it’s important not to let this critical issue fall to the wayside.”
Marcella Nyachogo, MSW, a licensed social worker and assistant director of the Bilingual Domestic Violence Program, noted that physicians and other health care providers “may be the only people the patient interacts with, since the abuser may cut the survivor off from family and friends. And because the survivor isn’t leaving the house, he or she doesn’t have an opportunity to interact with coworkers or others – which makes health care providers the most important lifeline.”
COVID-19 as a weapon of abuse
Carey Watson, MD, regional medical director of the Family Violence Prevention Program at Kaiser Permanente in northern California, points to a disturbing trend in COVID-19–related abuse.
“Unfortunately, I’m hearing more and more accounts of how the illness itself can be one more weapon in the abuser’s arsenal,” she said.
Experts say that increasingly, abusers are claiming that their partner, who is employed in an “essential” job outside the home, is carrying the virus, and they are using this as a means of control and manipulation.
This is especially true of abusive partners of health care providers, Dr. Watson noted. She recounted the story of a divorced nurse whose husband did not allow her to have contact with their children, allegedly out of concern that she might have COVID-19, and would threaten her with a gun when she protested.
“It is important to keep this abusive tactic in mind, not only when dealing with patients but also with fellow physicians and health care professionals, and check in to see if everything is okay – especially if they seem particularly stressed out or distant,” Dr. Watson recommended.
Trust your clinical gut
How can you tell if your patients might be experiencing abuse when you’re not seeing them in person?
Pay attention to subtle signals and “trust your clinical gut when something doesn’t feel right,” Ms. Nyachogo advised.
If a patient’s demeanor is jittery or anxious or if someone next to him or her is answering all the questions or interrupting the visit, these could be red flags.
Dr. Cronholm added that telemedicine visits offer a “rare window into a patient’s home life that would not be available in an office visit.” For example, a house in disarray, the presence of broken objects, or the presence of another person hovering in the background suggests the need for further exploration.
“The main thing for all providers to keep in mind is ‘first, do no harm,’ ” Ms. Nyachogo emphasized.
“Our agency has been working for years with medical professionals in how to screen and connect folks with help most effectively and safely, and – although the specific situations posed by COVID are new – the overall approach is the same, which is to proceed with caution in how you approach the subject and how you make referrals,” she said.
Begin by asking if it is a convenient time to talk.
“This question takes the onus off the patient, who may not know how to communicate that she has no privacy or is in the middle of an argument,” explained Elsa Swenson, program manager of Home Free community program, which serves individuals experiencing domestic violence. The program is part of Minnesota-based Missions Inc. Programs, which serves those experiencing domestic abuse and chemical dependency.
If the patient indicates that it isn’t a convenient time to talk, find out when would be a better time. “This might be difficult for busy physicians and may not be what they’re accustomed to when calling a patient at home, but the patient’s circumstances are unknown to you, so it’s essential to organize around their ability to talk,” Ms. Swenson noted.
‘Are you alone?’
Another important piece of information is whether the patient has privacy – which can be tricky if the abuser is standing right there.
“You don’t want to tip the abuser off to your concerns, so you need to frame the question in a neutral way,” Dr. Watson advised.
For example, you might say that HIPAA laws require that you conduct the consultation with no one else present, and find out if there is a location in the house where the patient can have privacy.
It might be easier to talk on the phone than via video, suggests Florence Remes, a New Jersey–based licensed social worker who specializes in domestic violence. Going into another room and playing music or turning on the television might make it less obvious that a call is taking place, and the abuser would be less likely to overhear the caller’s conversation.
Dr. Watson suggested that questions about abuse might be included with other questions and asked in a simple yes/no format. “I’d like to ask you some standard questions I’m asking everyone during the pandemic. Do you have a cough or fever? Do you have any other physical symptoms? Do you have access to hand sanitizer? How is your sleep? Are you experiencing stress? Do you feel safe at home?”
The abuser, if present, will only hear the patient’s “yes” or “no” without knowing the question. If the patient indicates that she is being abused but is unable to talk, a later time can be arranged to further explore the issue.
Technology is a double-edged sword
Modern technologies have been a great boon to patients and physicians during this time of social distancing, allowing ongoing contact and health care when it would not otherwise have been possible. On the other hand, technology is fraught with potential dangers that can jeopardize the patient’s safety and compromise privacy.
Ms. Remes recounted the story of “Susan,” a client with whom she had been conducting teletherapy visits using an approved HIPAA-compliant telemedicine forum. Susan was working from home because of shelter-in-place restrictions. Her husband had been abusive, and Susan was concerned he might be “sabotaging” the household’s WiFi to isolate her from outside sources of support.
At the recommendation of Ms. Remes, Susan continued sessions either via phone calls or by using the WhatsApp program on her cellphone. Many of the requirements governing HIPAA privacy regulations have been temporarily relaxed, and clinicians can use non–encrypted forms of transmission, such as FaceTime, WhatsApp, or Skype, if no other platform is available.
But even cellphones have risks, Dr. Warshaw noted. The patient’s abuser might track texts or look at call logs – especially on unsecured platforms. It’s advisable to ask patients about who has access to their phone and computer and discuss ways to increase security.
Follow the patient’s lead
Proceed slowly and start with nonthreatening questions, Ms. Palardy advised. “I notice you have some injuries; can you tell me how you got them? Did someone hurt you? What does your relationship look like when you argue? Is there anything that makes you feel uncomfortable or unsafe?”
Emphasizing that you are asking these questions because of care and concern is reassuring and helps patients to feel they are not alone, Ms. Nyachogo pointed out.
“As your doctor, I’m worried about your health and (if relevant) your children’s safety. I can help connect you with counseling and support, legal resources, and a shelter, and everything is free and confidential. Would you be interested?” she said.
If the client acknowledges abuse, “follow their lead, but don’t push too hard,” Ms. Nyachogo warned.
“It is the client’s choice whether or not to take action,” she noted. “I’ve met survivors who said that it wasn’t until a doctor or nurse expressed concern about bruises that it even occurred to them that they were being abused. Some lied to the doctor about how they got hurt – but the question planted a seed, even though it might have taken years to follow up on the referral,” she said.
What if the patient doesn’t want to get help?
If a patient is not ready to seek help, you can create a home-safety plan. This might include setting follow-up times. If you don’t hear from him or her, you should then call the police. Or you might create a “code word,” such as “apple pie.” If the patient uses that word during a session, you know her life is in danger, Ms. Remes suggested.
Providing written information about how to get help is important but can be problematic if the abuser finds it.
Ms. Nyachogo recommends e-mailing follow-up materials that cover a variety of topics, such as keeping safe during the COVID-19 pandemic, relaxation, healthy eating, getting exercise while homebound, activities for children, and suggestions for hotlines and other resources if one is feeling suicidal or unsafe.
“If you present these as your ‘standard’ follow-up materials, the abuser is less likely to become suspicious,” Ms. Nyachogo noted.
Resources are available during COVID-19
All of the experts emphasize that resources for victims of domestic violence remain available during the COVID-19 pandemic, although some shelters may be operating at reduced capacity. Some agencies are finding alternatives to group shelters, such as hotels or Airbnb, which carry less risk of catching COVID-19.
Referring a patient to domestic violence resources is a delicate process. “You don’t want referring the patient for help to further endanger their life,” Ms. Nyachogo said.
The more you can take the burden off the patient, the better. If she is interested in getting help, you can call a domestic violence counselor or advocate while she is on the phone.
“This type of ‘warm handoff’ is what Tonya’s physician did,” Ms. Palardy recounted.
A warm handoff requires that physicians be familiar with domestic violence resources, Dr. Warshaw emphasized.
“Don’t wait until you are working with someone who needs help to find out where to refer them. Take the time to proactively research local agencies specializing in domestic violence and have their phone numbers on hand, so you can offer resources immediately if the person is interested,” she advised. The National Domestic Violence Hotline can also assist with safety planning and access to local resources.
‘Thinking on your feet’ critical for physicians
Addressing domestic violence during this unprecedented time requires “thinking on your feet” about novel forms of detection and intervention, Dr. Watson said. This involves a combination of clinical acumen, creativity, and finely honed intuition.
Ms. Nyachogo added, “Keeping an eye on domestic violence can feel like an extra burden, but don’t forget that it is lifesaving work.”
Resources
National Domestic Violence Hotline
- 800-799-SAFE (7233)
- The patient can also text LOVEIS to 22522.
National Center on Domestic Violence, Trauma, and Mental Health
- Provides resources for health care, mental health, and substance use treatment and recovery support providers on responding to domestic violence and other trauma.
- Provides resources for professionals and patients regarding access to substance use and mental health care during the COVID-1 pandemic.
- Provides support for parents, caregivers, and children during the pandemic.
- Provides resources for advocates serving families affected by domestic violence.
- A state-by-state guide to local resources
Children’s Hospital of Philadelphia Research Institute
STOP Intimate Partner Violence (IPV)
New Jersey Coalition for Domestic Violence
American Bar Association COVID-19 resources for communities
- Text HOME to 741741.
National Network to End Domestic Violence (NNEDV) COVID-19 Technology Safety
A version of this article originally appeared on Medscape.com.
Roger R., MD, a primary care physician from Philadelphia, set up a telemedicine appointment with a 24-year-old female patient who was experiencing headaches and was worried she might have COVID-19.
During the televisit, Dr. R. noticed that “Tonya” (not her real name) had a purplish bruise under her right eye. When asked how she got the bruise, Tonya said she had bumped into a dresser. The physician suspected abuse. He then heard a man’s voice in the background and thought it might belong to the abuser. “Is this a good time for you to talk?” he asked Tonya.
Tonya hesitated.
“When might be a better time?”
Tonya suggested an alternate time, and the physician called her then. During the visit, she shared that her fiancé, a car salesman who was also sheltering at home, was punching her.
“He always had a bad temper. Once he shoved me, but he’s never hit me before. And when he was upset, we used to go out to eat and he calmed down. Now, we’re stuck inside, we can’t even get away from each other to go to work, and he’s getting scary,” she told the doctor.
The physician asked if she would like to be connected with a domestic violence counselor. When Tonya agreed, he called Jessica DuBois Palardy, a licensed social worker and the program supervisor at STOP Intimate Partner Violence, a Philadelphia-based collaborative project of the Children’s Hospital of Philadelphia and the Lutheran Settlement House’s Bilingual Domestic Violence Program.
A ‘horrifying’ trend
Tonya’s story is not unique. A United Nations report shows that there has been a “horrifying global surge in domestic violence” linked to “lockdowns imposed by the governments responding to the COVID-19 pandemic.” The United States is no exception – 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
Carole Warshaw, MD, director of the National Center on Domestic Violence, Trauma, and Mental Health in Chicago, said, “We know that intimate partner violence is increasing among people sheltering at home, and that abuse has become more severe.”
Even in nonabusive situations, being confined together at close quarters, often amid family stress and financial hardship, can be wearing, and tempers can flare. In an abusive relationship, “the main contributor to violence during shelter-in-place restrictions is that the isolation gives abusers more opportunities for controlling their partners, who have fewer options for accessing safety and support,” Dr. Warshaw said.
It is critical to “approach every clinical encounter knowing that domestic violence may be at play,” she emphasized.
Physicians might be the most important lifeline
Physicians are already facing myriad COVID-19–related challenges, and having another concern to keep in mind may be daunting.
“We’re in uncharted territory and we’re all trying to figure out how to navigate this time, how to practice medicine via phone and video conferences, and how to deal with the financial repercussions of the pandemic – not to mention concern for the health of our families,” said Peter F. Cronholm, MD, associate professor of family medicine and community health at the Hospital of the University of Pennsylvania, Philadelphia. “So maintaining vigilance is often difficult. Nevertheless, it’s important not to let this critical issue fall to the wayside.”
Marcella Nyachogo, MSW, a licensed social worker and assistant director of the Bilingual Domestic Violence Program, noted that physicians and other health care providers “may be the only people the patient interacts with, since the abuser may cut the survivor off from family and friends. And because the survivor isn’t leaving the house, he or she doesn’t have an opportunity to interact with coworkers or others – which makes health care providers the most important lifeline.”
COVID-19 as a weapon of abuse
Carey Watson, MD, regional medical director of the Family Violence Prevention Program at Kaiser Permanente in northern California, points to a disturbing trend in COVID-19–related abuse.
“Unfortunately, I’m hearing more and more accounts of how the illness itself can be one more weapon in the abuser’s arsenal,” she said.
Experts say that increasingly, abusers are claiming that their partner, who is employed in an “essential” job outside the home, is carrying the virus, and they are using this as a means of control and manipulation.
This is especially true of abusive partners of health care providers, Dr. Watson noted. She recounted the story of a divorced nurse whose husband did not allow her to have contact with their children, allegedly out of concern that she might have COVID-19, and would threaten her with a gun when she protested.
“It is important to keep this abusive tactic in mind, not only when dealing with patients but also with fellow physicians and health care professionals, and check in to see if everything is okay – especially if they seem particularly stressed out or distant,” Dr. Watson recommended.
Trust your clinical gut
How can you tell if your patients might be experiencing abuse when you’re not seeing them in person?
Pay attention to subtle signals and “trust your clinical gut when something doesn’t feel right,” Ms. Nyachogo advised.
If a patient’s demeanor is jittery or anxious or if someone next to him or her is answering all the questions or interrupting the visit, these could be red flags.
Dr. Cronholm added that telemedicine visits offer a “rare window into a patient’s home life that would not be available in an office visit.” For example, a house in disarray, the presence of broken objects, or the presence of another person hovering in the background suggests the need for further exploration.
“The main thing for all providers to keep in mind is ‘first, do no harm,’ ” Ms. Nyachogo emphasized.
“Our agency has been working for years with medical professionals in how to screen and connect folks with help most effectively and safely, and – although the specific situations posed by COVID are new – the overall approach is the same, which is to proceed with caution in how you approach the subject and how you make referrals,” she said.
Begin by asking if it is a convenient time to talk.
“This question takes the onus off the patient, who may not know how to communicate that she has no privacy or is in the middle of an argument,” explained Elsa Swenson, program manager of Home Free community program, which serves individuals experiencing domestic violence. The program is part of Minnesota-based Missions Inc. Programs, which serves those experiencing domestic abuse and chemical dependency.
If the patient indicates that it isn’t a convenient time to talk, find out when would be a better time. “This might be difficult for busy physicians and may not be what they’re accustomed to when calling a patient at home, but the patient’s circumstances are unknown to you, so it’s essential to organize around their ability to talk,” Ms. Swenson noted.
‘Are you alone?’
Another important piece of information is whether the patient has privacy – which can be tricky if the abuser is standing right there.
“You don’t want to tip the abuser off to your concerns, so you need to frame the question in a neutral way,” Dr. Watson advised.
For example, you might say that HIPAA laws require that you conduct the consultation with no one else present, and find out if there is a location in the house where the patient can have privacy.
It might be easier to talk on the phone than via video, suggests Florence Remes, a New Jersey–based licensed social worker who specializes in domestic violence. Going into another room and playing music or turning on the television might make it less obvious that a call is taking place, and the abuser would be less likely to overhear the caller’s conversation.
Dr. Watson suggested that questions about abuse might be included with other questions and asked in a simple yes/no format. “I’d like to ask you some standard questions I’m asking everyone during the pandemic. Do you have a cough or fever? Do you have any other physical symptoms? Do you have access to hand sanitizer? How is your sleep? Are you experiencing stress? Do you feel safe at home?”
The abuser, if present, will only hear the patient’s “yes” or “no” without knowing the question. If the patient indicates that she is being abused but is unable to talk, a later time can be arranged to further explore the issue.
Technology is a double-edged sword
Modern technologies have been a great boon to patients and physicians during this time of social distancing, allowing ongoing contact and health care when it would not otherwise have been possible. On the other hand, technology is fraught with potential dangers that can jeopardize the patient’s safety and compromise privacy.
Ms. Remes recounted the story of “Susan,” a client with whom she had been conducting teletherapy visits using an approved HIPAA-compliant telemedicine forum. Susan was working from home because of shelter-in-place restrictions. Her husband had been abusive, and Susan was concerned he might be “sabotaging” the household’s WiFi to isolate her from outside sources of support.
At the recommendation of Ms. Remes, Susan continued sessions either via phone calls or by using the WhatsApp program on her cellphone. Many of the requirements governing HIPAA privacy regulations have been temporarily relaxed, and clinicians can use non–encrypted forms of transmission, such as FaceTime, WhatsApp, or Skype, if no other platform is available.
But even cellphones have risks, Dr. Warshaw noted. The patient’s abuser might track texts or look at call logs – especially on unsecured platforms. It’s advisable to ask patients about who has access to their phone and computer and discuss ways to increase security.
Follow the patient’s lead
Proceed slowly and start with nonthreatening questions, Ms. Palardy advised. “I notice you have some injuries; can you tell me how you got them? Did someone hurt you? What does your relationship look like when you argue? Is there anything that makes you feel uncomfortable or unsafe?”
Emphasizing that you are asking these questions because of care and concern is reassuring and helps patients to feel they are not alone, Ms. Nyachogo pointed out.
“As your doctor, I’m worried about your health and (if relevant) your children’s safety. I can help connect you with counseling and support, legal resources, and a shelter, and everything is free and confidential. Would you be interested?” she said.
If the client acknowledges abuse, “follow their lead, but don’t push too hard,” Ms. Nyachogo warned.
“It is the client’s choice whether or not to take action,” she noted. “I’ve met survivors who said that it wasn’t until a doctor or nurse expressed concern about bruises that it even occurred to them that they were being abused. Some lied to the doctor about how they got hurt – but the question planted a seed, even though it might have taken years to follow up on the referral,” she said.
What if the patient doesn’t want to get help?
If a patient is not ready to seek help, you can create a home-safety plan. This might include setting follow-up times. If you don’t hear from him or her, you should then call the police. Or you might create a “code word,” such as “apple pie.” If the patient uses that word during a session, you know her life is in danger, Ms. Remes suggested.
Providing written information about how to get help is important but can be problematic if the abuser finds it.
Ms. Nyachogo recommends e-mailing follow-up materials that cover a variety of topics, such as keeping safe during the COVID-19 pandemic, relaxation, healthy eating, getting exercise while homebound, activities for children, and suggestions for hotlines and other resources if one is feeling suicidal or unsafe.
“If you present these as your ‘standard’ follow-up materials, the abuser is less likely to become suspicious,” Ms. Nyachogo noted.
Resources are available during COVID-19
All of the experts emphasize that resources for victims of domestic violence remain available during the COVID-19 pandemic, although some shelters may be operating at reduced capacity. Some agencies are finding alternatives to group shelters, such as hotels or Airbnb, which carry less risk of catching COVID-19.
Referring a patient to domestic violence resources is a delicate process. “You don’t want referring the patient for help to further endanger their life,” Ms. Nyachogo said.
The more you can take the burden off the patient, the better. If she is interested in getting help, you can call a domestic violence counselor or advocate while she is on the phone.
“This type of ‘warm handoff’ is what Tonya’s physician did,” Ms. Palardy recounted.
A warm handoff requires that physicians be familiar with domestic violence resources, Dr. Warshaw emphasized.
“Don’t wait until you are working with someone who needs help to find out where to refer them. Take the time to proactively research local agencies specializing in domestic violence and have their phone numbers on hand, so you can offer resources immediately if the person is interested,” she advised. The National Domestic Violence Hotline can also assist with safety planning and access to local resources.
‘Thinking on your feet’ critical for physicians
Addressing domestic violence during this unprecedented time requires “thinking on your feet” about novel forms of detection and intervention, Dr. Watson said. This involves a combination of clinical acumen, creativity, and finely honed intuition.
Ms. Nyachogo added, “Keeping an eye on domestic violence can feel like an extra burden, but don’t forget that it is lifesaving work.”
Resources
National Domestic Violence Hotline
- 800-799-SAFE (7233)
- The patient can also text LOVEIS to 22522.
National Center on Domestic Violence, Trauma, and Mental Health
- Provides resources for health care, mental health, and substance use treatment and recovery support providers on responding to domestic violence and other trauma.
- Provides resources for professionals and patients regarding access to substance use and mental health care during the COVID-1 pandemic.
- Provides support for parents, caregivers, and children during the pandemic.
- Provides resources for advocates serving families affected by domestic violence.
- A state-by-state guide to local resources
Children’s Hospital of Philadelphia Research Institute
STOP Intimate Partner Violence (IPV)
New Jersey Coalition for Domestic Violence
American Bar Association COVID-19 resources for communities
- Text HOME to 741741.
National Network to End Domestic Violence (NNEDV) COVID-19 Technology Safety
A version of this article originally appeared on Medscape.com.
Domestic abuse linked to cardiac disease, mortality in women
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
Adult female survivors of domestic abuse were at least one-third more likely to develop cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality over a short follow-up period, although they did not face a higher risk of hypertension, a new British study finds.
The study, published in the Journal of the American Heart Association, provides more evidence of a link between domestic abuse and poor health, even in younger women.
“The prevalence of domestic abuse is vast, so any increased risk in cardiometabolic disease may translate into a large burden of potentially preventable illness in society,” said study lead author Joht Singh Chandan, PhD, MBBS, of the University of Birmingham (England) and University of Warwick in Coventry, England, in an interview.
The researchers retrospectively tracked primary care patients in the United Kingdom from 1995-2017. They compared 18,547 adult female survivors of domestic abuse with a group of 72,231 other women who were matched to them at baseline by age, body mass index, smoking status, and a measure known as the Townsend deprivation score.
The average age of women in the groups was 37 years plus or minus 13 in the domestic abuse group and 37 years plus or minus 12 in the unexposed group. In both groups, 45% of women smoked; women in the domestic abuse group were more likely to drink excessively (10%), compared with those in the unexposed group (4%).
Researchers followed the women in the domestic abuse group for an average of 2 years and the unexposed group for 3 years. Those in the domestic abuse group were more likely to fall out of the study because they transferred to other medical practices.
Over the study period, 181 women in the domestic abuse group and 644 women in the unexposed group developed cardiovascular disease outcomes (adjusted incidence rate ratio, 1.31; 95% confidence interval, 1.11-1.55; P = .001). They were also more likely to develop type 2 diabetes (adjusted IRR, 1.51; 95% CI, 1.30-1.76; P less than .001) and all-cause mortality (adjusted IRR, 1.44; 95% CI, 1.24-1.67; P less than.001). But there was no increased risk of hypertension (adjusted IRR, 0.99; 95% CI, 0.88-1.12; P = 0.873).
Why might exposure to domestic abuse boost cardiovascular risk? “Although our study was not able to answer exactly why this relationship exists, Dr. Chandan said. “These can be broadly put into three categories: adoption of poor lifestyle behaviors due to difficult circumstances (physical inactivity, poor diet, disrupted sleep, substance misuse and smoking); associated development of mental ill health; and the alteration of the immune, metabolic, neuroendocrine, and autonomic nervous system due to the impact of stress on the body.”
It’s not clear why the risk of hypertension may be an outlier among cardiovascular outcomes, Dr. Chandan said. However, he pointed to a similar study whose results hinted that survivors of emotional abuse may be more susceptible to a negative impact on hypertension (Ann Epidemiol. 2012 Aug;22[8]:562-7). The new study does not provide information about the type of abuse suffered by subjects.
Adrienne O’Neil, PhD, a family violence practitioner and cardiovascular epidemiologist at Deakin University in Geelong, Australia, said in an interview that the study is “a very useful contribution to the literature.” However, she cautioned that the study might have missed cases of domestic abuse because it relies on reports from primary care practitioners.
As for the findings, she said they’re surprising because of the divergence of major cardiovascular outcomes such as ischemic heart disease and stroke in groups of women with an average age of 37. “These differential health outcomes were observed over a 2-3 period. You probably wouldn’t expect to see a divergence in cardiovascular outcomes for 5-10 years in this age group.”
Dr. O’Neil said that, moving forward, the research can be helpful to understanding the rise of cardiovascular disease in women aged 35-54, especially in the United States. “The way we assess an individual’s risk of having a heart attack in the future is largely guided by evidence based on men. For a long time, this has neglected female-specific risk factors like polycystic ovary syndrome and hypertensive disorders of pregnancy but also conditions and exposures to which young women are especially vulnerable like depression, anxiety and [domestic abuse],” she said.
“This research is important as it gives us clues about who may be at elevated risk to help us guide prevention efforts. Equally, there is some evidence that chest pain presentation may be a useful predictor of domestic abuse victimization so there could be multiple lines of further inquiry.”
Dr. Chandan, the other study authors, and Dr. O’Neil reported no relevant disclosures.
SOURCE: Chandan JS et al. J Am Heart Assoc. 2020. doi: 10.1161/JAHA.119.014580.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Movement-based yoga ‘viable’ for depression in many mental disorders
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Movement-based yoga appears to ease depressive symptoms in a wide range of mental health disorders, a new systematic review and meta-analysis suggest.
Results of the research, which included 19 studies and more than 1,000 patients with a variety of mental health diagnoses, showed that those who practiced yoga experienced greater reductions in depressive symptoms versus those undergoing no treatment, usual treatment, or attention-control exercises. In addition, there was a dose-dependent effect such that more weekly yoga sessions were associated with the greatest reduction in depressive symptoms.
“Once we reviewed all the existing science about the mental health benefits of movement-based yoga, we found that movement-based yoga – which is the same thing as postural yoga or asana – helped reduce symptoms of depression,” study investigator Jacinta Brinsley, BClinExPhys, of the University of South Australia, Adelaide, said in an interview.
“We also found those who practiced more frequently had bigger reductions. However, it didn’t matter how long the individual sessions were; what mattered was how many times per week people practiced,” she added.
The researchers noted that the study is the first to focus specifically on movement-based yoga.
“We excluded meditative forms of yoga, which have often been included in previous reviews, yielding mixed findings. The other thing we’ve done a bit differently is pool all the different diagnoses together and then look at depressive symptoms across them,” said Ms. Brinsley.
The study was published online May 18 in the British Journal of Sports Medicine.
Getting clarity
Depressive disorders are currently the world’s leading cause of disability, affecting more than 340 million people.
Most individuals who suffer from depressive disorders also experience a host of physical comorbidities including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular disease.
Perhaps not surprisingly, physical inactivity is also associated with higher levels of depressive symptoms, which may be the reason some international organizations now recommend that physical activity be included as part of routine psychiatric care.
One potential form of exercise is yoga, which has become popular in Western culture, including among psychiatric patients. Although previous systematic reviews and meta-analyses have examined the effects of various yoga interventions on mental health, none has investigated the benefits of yoga across a range of psychiatric diagnoses.
What’s more, the authors of these reviews all urge caution when interpreting their results because of potential heterogeneity of the various yoga interventions, as well as poor methodological reporting.
“As an exercise physiologist, I prescribe evidence-based treatment,” said Ms. Brinsley. “I was interested in seeing if there’s evidence to support movement-based yoga in people who were struggling with mental health or who had a diagnosed mental illness.
“The [previous] findings are quite contradictory and there’s not a clear outcome in terms of intervention results, so we pooled the data and ran the meta-analysis, thinking it would be a great way to add some important evidence to the science,” she added.
To allow for a more comprehensive assessment of yoga’s potential mental health benefits, the investigators included a range of mental health diagnoses.
Dose-dependent effect
Studies were only included in the analysis if they were randomized, controlled trials with a yoga intervention that had a minimum of 50% physical activity during each session in adults with a recognized diagnosed mental disorder. Control conditions were defined as treatment as usual, wait list, or attention controls.
Two investigators independently scanned article titles and abstracts, and a final list of articles for the study was decided by consensus. Study quality was reported using the PEDro checklist; a random-effects meta-analysis was conducted using Comprehensive Meta-Analysis software.
A total of 3,880 records were identified and screened. The investigators assessed full-text versions of 80 articles, 19 of which (1,080 patients) were eligible for inclusion in the review.
Of these, nine studies included patients with a depressive disorder; five trials were in patients with a diagnosis of schizophrenia, three studies included patients with a diagnosis of PTSD, one study included patients diagnosed with alcohol dependence, and one study included patients with a range of psychiatric disorders.
Of the 1,080 patients included in the review, 578 were assigned to yoga and 502 to control conditions. Yoga practice involved a mixture of movement, breathing exercises, and/or mindfulness, but the movement component took up more than half of each session.
The yoga interventions lasted an average of 2.4 months (range, 1.5-2.5 months), with an average of 1.6 sessions per week (range, 1-3 sessions) that lasted an average of 60 minutes (range, 20-90 minutes).
Of the 19 studies (632 patients), 13 reported changes in depressive symptoms and were therefore included in the meta-analysis. The six studies excluded from the quantitative analysis did not report depression symptom scores.
With respect to primary outcomes, individuals who performed yoga showed a greater reduction in depressive symptoms, compared with the three control groups (standardized mean difference, –0.41; 95% CI, –0.65 to –0.17; P < .001).
Specific subgroup analyses showed a moderate effect of yoga on depressive symptoms, compared with wait-list controls (SMD, –0.58; P < .05), treatment as usual (SMD, –0.39; P = .31), and attention controls (SMD, –0.21; P = .22).
Subgroup analyses were also performed with respect to diagnostic category. These data showed a moderate effect of yoga on depressive symptoms in depressive disorders (SMD, –0.40; P < .01), no effect in PTSD (SMD, –0.01; P = .95), a nominal effect in alcohol use disorders (SMD, –0.24; P = .69), and a marked effect in schizophrenia (SMD, –0.90; P < .01).
Movement may be key
Researchers also performed a series of meta-regression analyses, which showed that the number of yoga sessions performed each week had a significant effect on depressive symptoms. Indeed, individuals with higher session frequencies demonstrated a greater improvement in symptoms (beta, –0.44; P < .001).
These findings, said Ms. Brinsley, suggest yoga may be a viable intervention for managing depressive symptoms in patients with a variety of mental disorders.
Based on these findings, along with other conventional forms of exercise.
Equally important was the finding that the number of weekly yoga sessions moderated the effect of depressive symptoms, as it may inform the future design of yoga interventions in patients with mental disorders.
With this in mind, the researchers recommended that such interventions should aim to increase the frequency or weekly sessions rather than the duration of each individual session or the overall duration of the intervention.
However, said Ms. Brinsley, these findings suggest it is the physical aspect of the yoga practice that may be key.
“Yoga comprises several different components, including the movement postures, the breathing component, and the mindfulness or meditative component, but in this meta-analysis we looked specifically at yoga that was at least 50% movement based. So it might have also included mindfulness and breathing, but it had to have the movement,” she said.
Don’t discount meditation
Commenting on the findings, Holger Cramer, MSc, PhD, DSc, who was not involved in the study, noted that the systematic review and meta-analysis builds on a number of previous reviews regarding the benefits of yoga for mental disorders.
“Surprisingly, the largest effect in this analysis was found in schizophrenia, even higher than in patients with depressive disorders,” said Dr. Cramer of the University of Duisburg-Essen (Germany). “This is in strong contradiction to what would otherwise be expected. As the authors point out, only about a quarter of all schizophrenia patients suffer from depression, so there should not be so much room for improvement.”
Dr. Cramer also advised against reducing yoga to simply a physical undertaking. “We have shown in our meta-analysis that those interventions focusing on meditation and/or breathing techniques are the most effective ones,” he added.
As such, he urged that breathing techniques be a part of yoga for treating depression in psychiatric disorders, though care should be taken in patients with PTSD, “since breath control might be perceived as unpleasant.”
For Ms. Brinsley, the findings help solidify yoga’s potential as a genuine treatment option for a variety of mental health patients suffering depressive symptoms.
“It’s about acknowledging that yoga can be a helpful part of treatment and can have a significant effect on mental health,” she noted.
At the same time, practitioners also need to acknowledge that patients suffering from mental health disorders may struggle with motivation when it comes to activities such as yoga.
“Engaging in a new activity can be particularly challenging if you’re struggling with mental health. Nevertheless, it’s important for people to have a choice and do something they enjoy. And yoga can be another tool in their toolbox for managing their mental health,” she said.
The study was funded by the U.K. National Institute for Health Research and Health Education England. Ms. Brinsley and Dr. Cramer have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19: Psychiatrists assess geriatric harm from social distancing
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
One of the greatest tragedies of the first wave of the COVID-19 pandemic has been the failure of health policy makers to anticipate and mitigate the enormous havoc the policy of social distancing would wreak on mental health and cognitive function in older persons, speakers agreed at a webinar on COVID-19, social distancing, and its impact on social and mental health in the elderly hosted by the International Psychogeriatric Association in collaboration with INTERDEM.
“Social distancing” is a two-edged sword: It is for now and the foreseeable future the only available effective strategy for protecting against infection in the older population most vulnerable to severe forms of COVID-19. Yet social distancing also has caused many elderly – particularly those in nursing homes and other long-term care facilities – to plunge into a profound experience of loneliness, isolation, distress, feelings of abandonment, anxiety, depression, and accelerated cognitive deterioration. And this needn’t have happened, the mental health professionals asserted.
“When are we going to get rid of the term ‘social distancing?’ ” asked IPA President William E. Reichman, MD. “Many have appreciated – including the World Health Organization – that the real issue is physical distancing to prevent contagion. And physical distancing doesn’t have to mean social distancing.”
Social connectedness between elderly persons and their peers and family members can be maintained and should be emphatically encouraged during the physical distancing required by the pandemic, said Myrra Vernooij-Dassen, PhD, of Radboud University in Nigmegen, the Netherlands, and chair of INTERDEM, a pan-European network of dementia researchers.
This can be achieved using readily available technologies, including the telephone and videoconferencing, as well as by creating opportunities for supervised masked visits between a family member and an elderly loved one in outdoor courtyards or gardens within long-term care facilities. And yet, as the pandemic seized hold in many parts of the world, family members were blocked from entry to these facilities, she observed.
Impact on mental health, cognition
Dr. Vernooij-Dassen noted that studies of previous quarantine periods as well as preliminary findings during the COVID-19 pandemic demonstrate an inverse relationship between social isolation measures and cognitive functioning in the elderly.
“ Conversely, epidemiologic data indicate that a socially integrated lifestyle had a favorable influence on cognitive functioning and could even delay onset of dementia,” she said.
INTERDEM is backing two ongoing studies evaluating the hypothesis that interventions fostering increased social interaction among elderly individuals can delay onset of dementia or favorably affect its course. The proposed mechanism of benefit is stimulation of brain plasticity to enhance cognitive reserve.
“This is a hypothesis of hope. We know that social interaction for humans is like water to plants – we really, really need it,” she explained.
Diego de Leo, MD, PhD, emeritus professor of psychiatry and former director of the Australian Institute for Suicide Research and Prevention at Griffith University in Brisbane, was living in hard-hit Padua, Italy, during the first surge of COVID-19. He described his anecdotal experience.
“What I hear from many Italian colleagues and friends and directors of mental health services is that emergency admissions related to mental disorders declined during the first wave of the COVID pandemic. For example, not many people attended emergency departments due to suicide attempts; there was a very marked decrease in the number of suicide attempts during the worst days of the pandemic,” he said.
People with psychiatric conditions were afraid to go to the hospital because they thought they would contract the infection and die there. That’s changing now, however.
“Now there is an increased number of admissions to mental health units. A new wave. It has been a U-shaped curve. And we’re now witnessing an increasing number of fatal suicides due to persistent fears, due to people imagining that there is no more room for them, and no more future for them from a financial point of view – which is the major negative outcome of this crisis. It will be a disaster for many families,” the psychiatrist continued.
A noteworthy phenomenon in northern Italy was that, when tablets were made available to nursing home residents in an effort to enhance their connectedness to the outside world, those with dementia often became so frustrated and confused by their difficulty in using the devices that they developed a hypokinetic delirium marked by refusal to eat or leave their bed, he reported.
It’s far too early to have reliable data on suicide trends in response to the pandemic, according to Dr. de Leo. But one thing is for sure: The strategy of social distancing employed to curb COVID-19 has increased the prevalence of known risk factors for suicide in older individuals, including loneliness, anxiety, and depression; increased alcohol use; and a perception of being a burden on society. Dr. de Leo directs a foundation dedicated to helping people experiencing traumatic bereavement, and in one recent week, the foundation was contacted by eight families in the province of Padua with a recent death by suicide apparently related to fallout from the COVID-19 pandemic. That’s an unusually high spike in suicide in a province with a population of 1 million.
“People probably preferred to end the agitation, the fear, the extreme anxiety about their destiny by deciding to prematurely truncate their life. That has been reported by nursing staff,” he said.
The Italian government has determined that, to date, 36% of all COVID-related deaths have occurred in people aged 85 years or older, and 84% of deaths were in individuals aged at least 70 years. And in Milan and the surrounding province of Lombardy, it’s estimated that COVID-19 has taken the lives of 25% of all nursing home residents. The North American experience has been uncomfortably similar.
“Almost 80% of COVID deaths in Canada have occurred in congregate settings,” observed Dr. Reichman, professor of psychiatry at the University of Toronto, and president and CEO of Baycrest Health Sciences, a geriatric research center.
“Certainly, the appalling number of deaths in nursing homes is the No. 1 horror of the pandemic,” declared Carmelle Peisah, MBBS, MD, a psychiatrist at the University of New South Wales in Kensington, Australia.
The fire next time
The conventional wisdom holds that COVID-19 has caused all sorts of mayhem in the delivery of elder care. Not so, in Dr. Reichman’s view.
“I would suggest that the pandemic has not caused many of the problems we talk about, it’s actually revealed problems that have always been there under the surface. For example, many older people, even before COVID-19, were socially isolated, socially distant. They had difficulty connecting with their relatives, difficulty accessing transportation to get to the store to buy food and see their doctors, and to interact with other older people,” the psychiatrist said.
“I would say as well that the pandemic didn’t cause the problems we’ve seen in long-term congregate senior care. The pandemic revealed them. We’ve had facilities where older people were severely crowded together, which compromises their quality of life, even when there’s not a pandemic. We’ve had difficulty staffing these kinds of environments with people that are paid an honest wage for the very hard work that they do. In many of these settings they’re inadequately trained, not only in infection prevention and control but in all other aspects of care. And the pandemic has revealed that many of these organizations are not properly funded. The government doesn’t support them well enough across jurisdictions, and they can’t raise enough philanthropic funds to provide the kind of quality of life that residents demand,” Dr. Reichman continued.
Could the pandemic spur improved elder care? His hope is that health care professionals, politicians, and society at large will learn from the devastation left by the first surge of the pandemic and will lobby for the resources necessary for much-needed improvements in geriatric care.
“We need to be better prepared should there be not only a second wave of this pandemic, but for other pandemics to come,” Dr. Reichman concluded.
The speakers indicated they had no financial conflicts regarding their presentations.
Suicide often associated with bullying in LGBTQ youth
based on analysis of a national database.
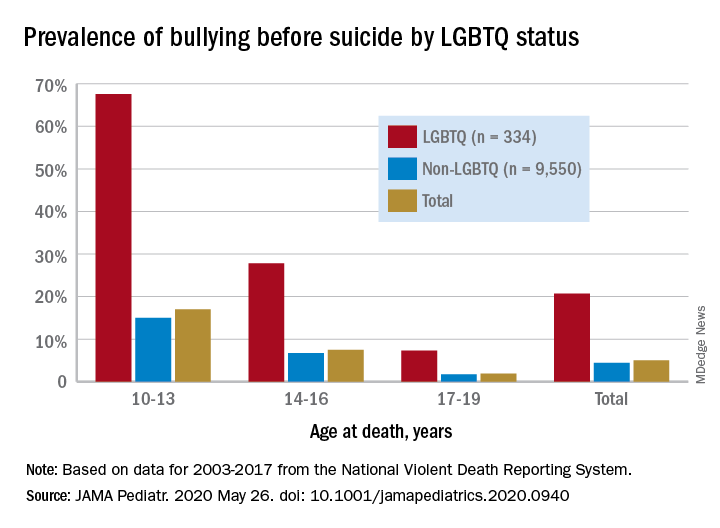
Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.
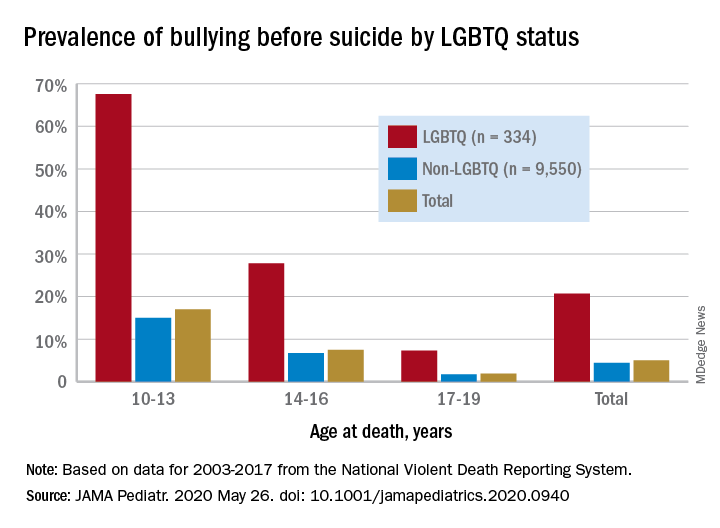
Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.
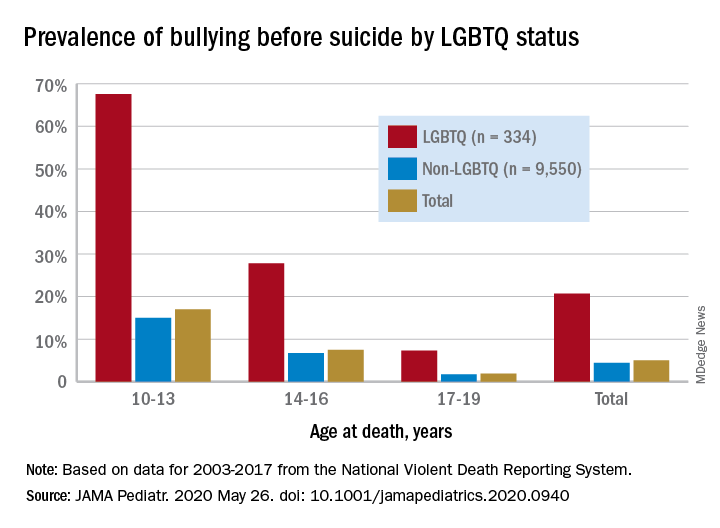
Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
FROM JAMA PEDIATRICS
Consider ketamine and psychotherapy combo
Preliminary data show intervention helps patients with SUDs
As an addiction psychiatrist specializing in the use of ketamine-assisted psychotherapy, both in patients with mood disorders and substance use disorders, I would like to offer some perspective about limits and possibilities of ketamine and esketamine.
Single infusions of ketamine targeting unipolar mood symptoms indeed yield initial 24-hour response rates of about 60%-70%, though those rates fall precipitously with time.1 Where single treatments fall short in terms of durability of benefit, a series of multiple treatments – modeled around electroconvulsive therapy and pending a noninferiority study to compare the two2 – provide for more robust and durable results.3
Esketamine nasal spray, recently approved by the Food and Drug Administration for treatment-resistant major depressive disorder, consists of one of the component stereoisomers of ketamine and is administered at first twice weekly and then less frequently with time. It now, like off-label ketamine,4 sees clinical use as monotherapy for MDD, as an alternative for patients who have intolerance or lack of response to first-line treatments such as SSRIs.
Ketamine, while perhaps less directly validated and more stigmatized for psychiatric use, recently has been demonstrated in a rigorous trial as noninferior in terms of antidepressant benefit at 24 hours,5 and a multitude of published case studies document maintenance of benefit with repeat doses over a period of months.6 Ketamine notably enjoys several advantages over esketamine as a treatment option: a cost one to two orders of magnitude lower7 (esketamine nasal spray sees a wholesale price of $600-$900 per dose), greater versatility in dose, and lack of a restrictive REMS program.8 The $1-$2 cost of a dose of ketamine means that the clinical barrier of prior authorizations is largely a nonissue and may in and of itself vastly improve access to this novel and efficacious treatment.
My clinical experience involves providing ketamine as an intramuscular bolus along with contemporaneous psychotherapy; such combination of medication and psychotherapy intervention may be more effective than ketamine alone9 and has seen impressive initial results in the treatment of alcohol use disorder, termed ketamine psychedelic therapy.10 I can affirm these hopeful initial findings in the treatment of both mood and substance use disorders, and have observed maintained response from mood symptoms for a period of 1-4 years in several patients, with such sessions provided approximately monthly.11
I hope these preliminary data inform more rigorous study of long-term ketamine as a treatment for psychiatric indications.
Dr. Ryan is a board-certified psychiatrist and addiction psychiatrist who practices in Los Angeles. He has written several articles and a book chapter on ketamine. Dr. Ryan has no disclosures.
References
1. Murrough JW et al. Am J Psychiatry. 2013;170(10):1134-42.
2. Mathew SJ et al. Contemp Clin Trials. 2019;77:19-26.
3. Singh JB et al. Am J Psychiatry. 2016;173(8):816-26.
4. Calabrese L. Int J Psychiatr Res. 2019; 2(5):1-12.
5. Correia-Melo FS et al. J Affect Disord. 2020;264:527-34.
6. Ryan WC, Marta CJ, Koek RJ. Ketamine and depression, in “The Ketamine Papers: Science, Therapy, and Transformation.” Santa Cruz, Calif.: Multidisciplinary Association for Psychedelic Studies, 2016.
7. Institute for Clinical and Economic Review. “Esketamine for the Treatment of Treatment-Resistant Depression: Effectiveness and Value.” Final report. 2019 Jun 20.
8. Spravato package insert. Titusville, N.J.: Janssen Pharmaceuticals.
9. Dore J et al. J Psychoactive Drugs. 2019;51(2):189-98.
10. Krupitsky EM and Grinenko AY. J Psychoactive Drugs. 1997;29(2):165-83.
11. Ryan WC. Ketamine-assisted psychotherapy: Theory and chart review. KRIYA Ketamine Research Institute Conference. Hillsborough, Calif. 2019. Nov 9.
Preliminary data show intervention helps patients with SUDs
Preliminary data show intervention helps patients with SUDs
As an addiction psychiatrist specializing in the use of ketamine-assisted psychotherapy, both in patients with mood disorders and substance use disorders, I would like to offer some perspective about limits and possibilities of ketamine and esketamine.
Single infusions of ketamine targeting unipolar mood symptoms indeed yield initial 24-hour response rates of about 60%-70%, though those rates fall precipitously with time.1 Where single treatments fall short in terms of durability of benefit, a series of multiple treatments – modeled around electroconvulsive therapy and pending a noninferiority study to compare the two2 – provide for more robust and durable results.3
Esketamine nasal spray, recently approved by the Food and Drug Administration for treatment-resistant major depressive disorder, consists of one of the component stereoisomers of ketamine and is administered at first twice weekly and then less frequently with time. It now, like off-label ketamine,4 sees clinical use as monotherapy for MDD, as an alternative for patients who have intolerance or lack of response to first-line treatments such as SSRIs.
Ketamine, while perhaps less directly validated and more stigmatized for psychiatric use, recently has been demonstrated in a rigorous trial as noninferior in terms of antidepressant benefit at 24 hours,5 and a multitude of published case studies document maintenance of benefit with repeat doses over a period of months.6 Ketamine notably enjoys several advantages over esketamine as a treatment option: a cost one to two orders of magnitude lower7 (esketamine nasal spray sees a wholesale price of $600-$900 per dose), greater versatility in dose, and lack of a restrictive REMS program.8 The $1-$2 cost of a dose of ketamine means that the clinical barrier of prior authorizations is largely a nonissue and may in and of itself vastly improve access to this novel and efficacious treatment.
My clinical experience involves providing ketamine as an intramuscular bolus along with contemporaneous psychotherapy; such combination of medication and psychotherapy intervention may be more effective than ketamine alone9 and has seen impressive initial results in the treatment of alcohol use disorder, termed ketamine psychedelic therapy.10 I can affirm these hopeful initial findings in the treatment of both mood and substance use disorders, and have observed maintained response from mood symptoms for a period of 1-4 years in several patients, with such sessions provided approximately monthly.11
I hope these preliminary data inform more rigorous study of long-term ketamine as a treatment for psychiatric indications.
Dr. Ryan is a board-certified psychiatrist and addiction psychiatrist who practices in Los Angeles. He has written several articles and a book chapter on ketamine. Dr. Ryan has no disclosures.
References
1. Murrough JW et al. Am J Psychiatry. 2013;170(10):1134-42.
2. Mathew SJ et al. Contemp Clin Trials. 2019;77:19-26.
3. Singh JB et al. Am J Psychiatry. 2016;173(8):816-26.
4. Calabrese L. Int J Psychiatr Res. 2019; 2(5):1-12.
5. Correia-Melo FS et al. J Affect Disord. 2020;264:527-34.
6. Ryan WC, Marta CJ, Koek RJ. Ketamine and depression, in “The Ketamine Papers: Science, Therapy, and Transformation.” Santa Cruz, Calif.: Multidisciplinary Association for Psychedelic Studies, 2016.
7. Institute for Clinical and Economic Review. “Esketamine for the Treatment of Treatment-Resistant Depression: Effectiveness and Value.” Final report. 2019 Jun 20.
8. Spravato package insert. Titusville, N.J.: Janssen Pharmaceuticals.
9. Dore J et al. J Psychoactive Drugs. 2019;51(2):189-98.
10. Krupitsky EM and Grinenko AY. J Psychoactive Drugs. 1997;29(2):165-83.
11. Ryan WC. Ketamine-assisted psychotherapy: Theory and chart review. KRIYA Ketamine Research Institute Conference. Hillsborough, Calif. 2019. Nov 9.
As an addiction psychiatrist specializing in the use of ketamine-assisted psychotherapy, both in patients with mood disorders and substance use disorders, I would like to offer some perspective about limits and possibilities of ketamine and esketamine.
Single infusions of ketamine targeting unipolar mood symptoms indeed yield initial 24-hour response rates of about 60%-70%, though those rates fall precipitously with time.1 Where single treatments fall short in terms of durability of benefit, a series of multiple treatments – modeled around electroconvulsive therapy and pending a noninferiority study to compare the two2 – provide for more robust and durable results.3
Esketamine nasal spray, recently approved by the Food and Drug Administration for treatment-resistant major depressive disorder, consists of one of the component stereoisomers of ketamine and is administered at first twice weekly and then less frequently with time. It now, like off-label ketamine,4 sees clinical use as monotherapy for MDD, as an alternative for patients who have intolerance or lack of response to first-line treatments such as SSRIs.
Ketamine, while perhaps less directly validated and more stigmatized for psychiatric use, recently has been demonstrated in a rigorous trial as noninferior in terms of antidepressant benefit at 24 hours,5 and a multitude of published case studies document maintenance of benefit with repeat doses over a period of months.6 Ketamine notably enjoys several advantages over esketamine as a treatment option: a cost one to two orders of magnitude lower7 (esketamine nasal spray sees a wholesale price of $600-$900 per dose), greater versatility in dose, and lack of a restrictive REMS program.8 The $1-$2 cost of a dose of ketamine means that the clinical barrier of prior authorizations is largely a nonissue and may in and of itself vastly improve access to this novel and efficacious treatment.
My clinical experience involves providing ketamine as an intramuscular bolus along with contemporaneous psychotherapy; such combination of medication and psychotherapy intervention may be more effective than ketamine alone9 and has seen impressive initial results in the treatment of alcohol use disorder, termed ketamine psychedelic therapy.10 I can affirm these hopeful initial findings in the treatment of both mood and substance use disorders, and have observed maintained response from mood symptoms for a period of 1-4 years in several patients, with such sessions provided approximately monthly.11
I hope these preliminary data inform more rigorous study of long-term ketamine as a treatment for psychiatric indications.
Dr. Ryan is a board-certified psychiatrist and addiction psychiatrist who practices in Los Angeles. He has written several articles and a book chapter on ketamine. Dr. Ryan has no disclosures.
References
1. Murrough JW et al. Am J Psychiatry. 2013;170(10):1134-42.
2. Mathew SJ et al. Contemp Clin Trials. 2019;77:19-26.
3. Singh JB et al. Am J Psychiatry. 2016;173(8):816-26.
4. Calabrese L. Int J Psychiatr Res. 2019; 2(5):1-12.
5. Correia-Melo FS et al. J Affect Disord. 2020;264:527-34.
6. Ryan WC, Marta CJ, Koek RJ. Ketamine and depression, in “The Ketamine Papers: Science, Therapy, and Transformation.” Santa Cruz, Calif.: Multidisciplinary Association for Psychedelic Studies, 2016.
7. Institute for Clinical and Economic Review. “Esketamine for the Treatment of Treatment-Resistant Depression: Effectiveness and Value.” Final report. 2019 Jun 20.
8. Spravato package insert. Titusville, N.J.: Janssen Pharmaceuticals.
9. Dore J et al. J Psychoactive Drugs. 2019;51(2):189-98.
10. Krupitsky EM and Grinenko AY. J Psychoactive Drugs. 1997;29(2):165-83.
11. Ryan WC. Ketamine-assisted psychotherapy: Theory and chart review. KRIYA Ketamine Research Institute Conference. Hillsborough, Calif. 2019. Nov 9.
ARBs didn't raise suicide risk in large VA study
Angiotensin receptor blocker therapy was not associated with any hint of increased risk of suicide, compared with treatment with an ACE inhibitor, in a large national Veterans Affairs study, Kallisse R. Dent, MPH, reported at the virtual annual meeting of the American Association of Suicidology.
The VA study thus fails to confirm the results of an earlier Canadian, population-based, nested case-control study, which concluded that exposure to an angiotensin receptor blocker (ARB) was independently associated with an adjusted 63% increase risk of death by suicide, compared with ACE inhibitor users. The Canadian study drew considerable attention, noted Ms. Dent, of the VA Office of Mental Health and Suicide Prevention.
The Canadian study included 964 Ontario residents who died by suicide within 100 days of receiving an ACE inhibitor or ARB. They were matched by age, sex, and the presence of hypertension and diabetes to 3,856 controls, all of whom were on an ACE inhibitor or ARB for the 100 days prior to the patient’s suicide. All subjects were aged at least 66 years.
The Canadian investigators recommended that ACE inhibitors should be used instead of ARBs whenever possible, particularly in patients with major mental illness (JAMA Netw Open. 2019 Oct 2;2[10]:e1913304). This was a study that demanded replication because of the enormous potential impact that recommendation could have upon clinical care. ACE inhibitors and ARBs are among the most widely prescribed of all medications, with approved indications for treatment of hypertension, chronic kidney disease, diabetes, and heart failure, Ms. Dent observed.
The Canadian investigators noted that a differential effect on suicide risk for the two drug classes was mechanistically plausible. Those drugs can cross the blood-brain barrier to varying extents, where they could conceivably interfere with central angiotensin II activity, which in turn could result in increased activity of substance P, as well as anxiety and stress secondary to increased activity of the hypothalamic-pituitary-adrenal axis.
Ms. Dent and coinvestigators harnessed VA suicide surveillance resources to conduct a nested case-control study that included all 1,311 deaths by suicide during 2015-2017 among patients in the VA system who had an active prescription for an ACE inhibitor or ARB during the 100 days immediately prior to death. As in the Canadian study, these individuals were matched 4:1 to 5,243 controls who did not die by suicide and had an active prescription for an ARB or ACE inhibitor during the 100 days prior to the date of suicide.
Those rates were not significantly different from the rates found in controls, 21.6% of whom were on an ARB and 78.4% were on an ACE inhibitor. In a multivariate analysis adjusted for the same potential confounders included in the Canadian study – including Charlson Comorbidity Index score; drug use; and diagnosis of alcohol use disorder, coronary artery disease, stroke, and chronic liver or kidney disease – being on an ARB was associated with a 9% lower risk of suicide than being on an ACE inhibitor, a nonsignificant difference.
A point of pride for the investigators was that, because of the VA’s sophisticated patient care database and comprehensive suicide analytics, the VA researchers were able to very quickly determine the lack of generalizability of the Canadian findings to a different patient population. Indeed, the entire VA case-control study was completed in less than 2 months.
Ms. Dent reported having no financial conflicts regarding the study, which was sponsored by the Department of Veterans Affairs.
Angiotensin receptor blocker therapy was not associated with any hint of increased risk of suicide, compared with treatment with an ACE inhibitor, in a large national Veterans Affairs study, Kallisse R. Dent, MPH, reported at the virtual annual meeting of the American Association of Suicidology.
The VA study thus fails to confirm the results of an earlier Canadian, population-based, nested case-control study, which concluded that exposure to an angiotensin receptor blocker (ARB) was independently associated with an adjusted 63% increase risk of death by suicide, compared with ACE inhibitor users. The Canadian study drew considerable attention, noted Ms. Dent, of the VA Office of Mental Health and Suicide Prevention.
The Canadian study included 964 Ontario residents who died by suicide within 100 days of receiving an ACE inhibitor or ARB. They were matched by age, sex, and the presence of hypertension and diabetes to 3,856 controls, all of whom were on an ACE inhibitor or ARB for the 100 days prior to the patient’s suicide. All subjects were aged at least 66 years.
The Canadian investigators recommended that ACE inhibitors should be used instead of ARBs whenever possible, particularly in patients with major mental illness (JAMA Netw Open. 2019 Oct 2;2[10]:e1913304). This was a study that demanded replication because of the enormous potential impact that recommendation could have upon clinical care. ACE inhibitors and ARBs are among the most widely prescribed of all medications, with approved indications for treatment of hypertension, chronic kidney disease, diabetes, and heart failure, Ms. Dent observed.
The Canadian investigators noted that a differential effect on suicide risk for the two drug classes was mechanistically plausible. Those drugs can cross the blood-brain barrier to varying extents, where they could conceivably interfere with central angiotensin II activity, which in turn could result in increased activity of substance P, as well as anxiety and stress secondary to increased activity of the hypothalamic-pituitary-adrenal axis.
Ms. Dent and coinvestigators harnessed VA suicide surveillance resources to conduct a nested case-control study that included all 1,311 deaths by suicide during 2015-2017 among patients in the VA system who had an active prescription for an ACE inhibitor or ARB during the 100 days immediately prior to death. As in the Canadian study, these individuals were matched 4:1 to 5,243 controls who did not die by suicide and had an active prescription for an ARB or ACE inhibitor during the 100 days prior to the date of suicide.
Those rates were not significantly different from the rates found in controls, 21.6% of whom were on an ARB and 78.4% were on an ACE inhibitor. In a multivariate analysis adjusted for the same potential confounders included in the Canadian study – including Charlson Comorbidity Index score; drug use; and diagnosis of alcohol use disorder, coronary artery disease, stroke, and chronic liver or kidney disease – being on an ARB was associated with a 9% lower risk of suicide than being on an ACE inhibitor, a nonsignificant difference.
A point of pride for the investigators was that, because of the VA’s sophisticated patient care database and comprehensive suicide analytics, the VA researchers were able to very quickly determine the lack of generalizability of the Canadian findings to a different patient population. Indeed, the entire VA case-control study was completed in less than 2 months.
Ms. Dent reported having no financial conflicts regarding the study, which was sponsored by the Department of Veterans Affairs.
Angiotensin receptor blocker therapy was not associated with any hint of increased risk of suicide, compared with treatment with an ACE inhibitor, in a large national Veterans Affairs study, Kallisse R. Dent, MPH, reported at the virtual annual meeting of the American Association of Suicidology.
The VA study thus fails to confirm the results of an earlier Canadian, population-based, nested case-control study, which concluded that exposure to an angiotensin receptor blocker (ARB) was independently associated with an adjusted 63% increase risk of death by suicide, compared with ACE inhibitor users. The Canadian study drew considerable attention, noted Ms. Dent, of the VA Office of Mental Health and Suicide Prevention.
The Canadian study included 964 Ontario residents who died by suicide within 100 days of receiving an ACE inhibitor or ARB. They were matched by age, sex, and the presence of hypertension and diabetes to 3,856 controls, all of whom were on an ACE inhibitor or ARB for the 100 days prior to the patient’s suicide. All subjects were aged at least 66 years.
The Canadian investigators recommended that ACE inhibitors should be used instead of ARBs whenever possible, particularly in patients with major mental illness (JAMA Netw Open. 2019 Oct 2;2[10]:e1913304). This was a study that demanded replication because of the enormous potential impact that recommendation could have upon clinical care. ACE inhibitors and ARBs are among the most widely prescribed of all medications, with approved indications for treatment of hypertension, chronic kidney disease, diabetes, and heart failure, Ms. Dent observed.
The Canadian investigators noted that a differential effect on suicide risk for the two drug classes was mechanistically plausible. Those drugs can cross the blood-brain barrier to varying extents, where they could conceivably interfere with central angiotensin II activity, which in turn could result in increased activity of substance P, as well as anxiety and stress secondary to increased activity of the hypothalamic-pituitary-adrenal axis.
Ms. Dent and coinvestigators harnessed VA suicide surveillance resources to conduct a nested case-control study that included all 1,311 deaths by suicide during 2015-2017 among patients in the VA system who had an active prescription for an ACE inhibitor or ARB during the 100 days immediately prior to death. As in the Canadian study, these individuals were matched 4:1 to 5,243 controls who did not die by suicide and had an active prescription for an ARB or ACE inhibitor during the 100 days prior to the date of suicide.
Those rates were not significantly different from the rates found in controls, 21.6% of whom were on an ARB and 78.4% were on an ACE inhibitor. In a multivariate analysis adjusted for the same potential confounders included in the Canadian study – including Charlson Comorbidity Index score; drug use; and diagnosis of alcohol use disorder, coronary artery disease, stroke, and chronic liver or kidney disease – being on an ARB was associated with a 9% lower risk of suicide than being on an ACE inhibitor, a nonsignificant difference.
A point of pride for the investigators was that, because of the VA’s sophisticated patient care database and comprehensive suicide analytics, the VA researchers were able to very quickly determine the lack of generalizability of the Canadian findings to a different patient population. Indeed, the entire VA case-control study was completed in less than 2 months.
Ms. Dent reported having no financial conflicts regarding the study, which was sponsored by the Department of Veterans Affairs.
FROM AAS20
An unexplained exacerbation of depression, anxiety, and panic
CASE Depression, anxiety, and panic attacks
At the urging of his parents Mr. P, age 33, presents to the partial hospitalization program (PHP) for worsening depression and anxiety, daily panic attacks with accompanying diaphoresis and headache, and the possibility that he may have taken an overdose of zolpidem. Mr. P denies taking an intentional overdose of zolpidem, claiming instead that he was having a sleep-walking episode and did not realize how many pills he took.
In addition to daily panic attacks, Mr. P reports having trouble falling asleep, overwhelming sadness, and daily passive suicidal ideation without a plan or active intent.
Mr. P cannot identify a specific trigger to this most recent exacerbation of depressed/anxious mood, but instead describes it as slowly building over the past 6 to 8 months. Mr. P says the panic attacks occur without warning and states, “I feel like my heart is going to jump out of my chest; I get a terrible headache, and I sweat like crazy. Sometimes I just feel like I’m about to pass out or die.” Although these episodes had been present for approximately 2 years, they now occur almost daily.
HISTORY Inconsistent adherence
For the last year, Mr. P had been taking alprazolam, 0.5 mg twice daily, and paroxetine, 20 mg/d, and these medications provided moderate relief of his depressive/anxious symptoms. However, he stopped taking both medications approximately 3 or 4 weeks ago when he ran out. He also takes propranolol, 20 mg/d, sporadically, for hypertension. In the past, he had been prescribed carvedilol, clonidine, and lisinopril—all with varying degrees of relief of his hypertension. He denies a family history of hypertension or any other chronic or acute health problems. He reports that he has been sober from alcohol for 19 months but smokes 1 to 2 marijuana cigarettes a day.
EVALUATION Elevated blood pressure and pulse
Mr. P’s physical examination and medical review of systems are unremarkable, except for an elevated blood pressure (190/110 mm Hg) and pulse (92 beats per minute); he also has a headache. A repeat blood pressure test later in the day is 172/94 mm Hg, with a pulse of 100 beats per minute. His urine drug screen is positive only for delta-9-tetrahydrocannabinol (THC).
[polldaddy:10558304]
The author’s observations
A CBC with differential is helpful for ruling out infection and anemia as causes of anxiety and depression.1 In Mr. P’s case, there were no concerning symptoms that pointed to anemia or infection as likely causes of his anxiety, depression, or panic attacks. A TSH level also would be reasonable, because hyperthyroidism can present as anxiety, while hyperthyroidism or hypothyroidism each can present as depression.1 However, both Mr. P’s medical history and physical examination were not concerning for thyroid disease, making it unlikely that he had either of those conditions. A review of Mr. P’s medical records indicated that within the past 6 months, his primary care physician (PCP) had ordered a CBC and TSH test; the results of both were within normal limits.
Serum porphyrin tests can exclude porphyria as a contributor to Mr. P’s anxiety and depression. Porphyrias are a group of 8 inherited disorders that involve accumulation of heme precursors (porphyrins) in the CNS and subcutaneous tissue.2 Collectively, porphyrias affect approximately 1 in 200,000 people.2 Anxiety and depression are strongly associated with porphyria, but do not occur secondary to the illness; depression and anxiety appear to be intrinsic personality features in people with porphyria.3 Skin lesions and abdominal pain are the most common symptoms,3 and there is a higher incidence of hypertension in people with porphyria than in the general population.4 Mr. P does not report any heritable disorders, nor does he appear to have any CNS disturbance or unusual cutaneous lesions, which makes it unlikely that this disorder is related to his psychiatric symptoms.
Continue to: A serum metanephrines test measures...
A serum metanephrines test measures the metabolites of epinephrine and norepinephrine. These catecholamines are produced in excess by an adrenal or extra-adrenal tumor seen in pheochromocytoma. The classic triad of symptoms of pheochromocytoma are hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic (Table 15-7). This type of tumor is rare, with an annual incidence of only 2 to 8 cases per 1 million individuals. Among people with hypertension, the annual incidence is 0.1% to 1.0%, and for those with an adrenal mass, the annual incidence is 5% (Table 26,8). Autopsy studies suggest that up to 50% of pheochromocytomas are undiagnosed.8 Left untreated, pheochromocytoma can result in hypertensive crisis, arrhythmia, myocardial infarction, multisystem organ failure, and premature death.7Table 36,7 highlights some causes of false-positive serum on metanephrines testing.
EVALUATION Metanephrines testing
Mr. P has what appears to be treatment-resistant hypertension, accompanied by the classic symptoms observed in most patients with pheochromocytoma. Because Mr. P is participating in the PHP 6 days per week for 6 hours each day, visiting his PCP would be inconvenient, so the treatment team orders the serum metanephrines test. If a positive result is found, Mr. P will be referred to his PCP for further assessment and follow-up care with endocrinology.
TREATMENT Pharmacotherapy to target anxiety and panic
Next, the treatment team establishes a safety plan for Mr. P, and restarts paroxetine, 20 mg/d, to target his depressed and anxious mood. Alprazolam, 0.5 mg twice daily, is started to target anxious mood and panic symptoms, and to allow time for the anxiolytic properties of the paroxetine to become fully effective. The alprazolam will be tapered and stopped after 2 weeks. Mr. P is started on hydroxyzine, 1 to 2 25-mg tablets 2 to 3 times daily as needed for anxious mood and panic symptoms.
The serum metanephrines test results are equivocal, with a slight elevation of both epinephrine and norepinephrine that is too low to confirm a diagnosis of pheochromocytoma but too elevated to exclude it (Table 49). With Mr. P’s consent, the treatment team contacts his PCP and convey the results of this test. Mr. P schedules an appointment with his PCP for the following week for further assessment and confirmatory pheochromocytoma testing.
After 1 week, Mr. P remains anxious, with a slight reduction in panic attacks from multiple attacks each day to 3 or 4 attacks per week. The team considers adding an additional anxiolytic agent.
[polldaddy:10558305]
Continue to: The author's observations
The author’s observations
The triad of symptoms in pheochromocytoma results directly from the intermittent release of catecholamines into systemic circulation. Surges of epinephrine and norepinephrine lead to headaches, palpitations, diaphoresis, and (less commonly) gastrointestinal symptoms such as nausea, vomiting, and constipation. Persistent or episodic hypertension may be present, with 13% of patients maintaining a normal blood pressure.5-7 Patients with pheochromocytoma-related anxiety typically have substantial or complete resolution of anxiety and panic attacks after tumor resection.6,8,10
Because of their ability to raise catecholamine levels, several medications, including some psychotropics, can lead to false-positive results on serum and urine metanephrines testing. Tricyclic antidepressants and beta-blockers can cause false-positive results on plasma assays, while buspirone can cause false-positives on urinalysis assays.5 Trazodone, on the other hand, exhibits no catecholaminergic activity and its alpha-1 adrenergic antagonism may actually have some benefit in pheochromocytoma.11 Alpha-1 adrenergic antagonism with doxazosin, prazosin, or terazosin is the first-line of treatment in reducing pheochromocytoma-related hypertension.7 Treatment with a beta-blocker is safe only after alpha-adrenergic blockade occurs. While beta-blockers are useful for reducing the palpitations and anxiety observed in patients with pheochromocytoma, they must not be used alone due to the risk of hypertensive crisis resulting from unopposed alpha-adrenergic agonist activated vasoconstriction.5,7
TREATMENT CBT provides benefit
Mr. P decides against receiving an additional agent for anxiety and instead decides to wait for the outcome of the confirmatory pheochromocytoma testing. He continues to take alprazolam, and both his depressed mood and anxiety improve. His panic attacks continue to lessen, and he appears to benefit from cognitive-behavioral therapy provided during group therapy. Mr. P is advised by his PCP to taper and stop the alprazolam 3 to 5 days before his 24-hour urine metanephrines test because benzodiazepines can lead to false-positive results on a urinalysis assay.7
OUTCOME Remission of anxiety and depression
Mr. P has a repeat serum metanephrines test and a 24-hour urinalysis assay. Both are negative for pheochromocytoma. His PCP refers him to cardiology for management of treatment-resistant hypertension. He is discharged from the PHP and continues psychotherapy for depression and anxiety in an intensive outpatient program (IOP). Throughout his PHP and IOP treatments, he continues to take paroxetine and hydroxyzine. He achieves a successful remission of his anxiety and depression, with partial but significant remission of his panic attacks.
The author’s observations
Although Mr. P did not have pheochromocytoma, it is important to rule out this rare condition in patients who present with treatment-resistant hypertension and/or treatment-resistant anxiety.
Continue to: Bottom Line
Bottom Line
Pheochromocytoma is a tumor of the adrenal gland. The classic triad of symptoms of this rare condition is hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic. Several medications, including tricyclic antidepressants, beta-blockers, and buspirone, can lead to false-positive results on the serum and urine metanephrines testing used to diagnose pheochromocytoma.
Related Resources
- National Organization for Rare Disorders. Rare Disease Database: pheochromocytoma. www.rarediseases.org/rare-diseases/pheochromocytoma/.
- Young WF Jr. Clinical presentation and diagnosis of pheochromocytoma. UpToDate. www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-pheochromocytoma. Published January 2020.
Drug Brand Names
Alprazolam • Xanax
Amitriptyline • Elavil
Buspirone • Buspar
Carvedilol • Coreg
Clonidine • Catapres
Doxazosin • Cardura
Hydroxyzine • Vistaril
Lisinopril • Prinivil, Zestril
Paroxetine • Paxil
Prazosin • Minipress
Propranolol • Inderal
Terazosin • Hytrin
Trazodone • Desyrel
Zolpidem • Ambien
1. Morrison J. When psychological problems mask medical disorders: a guide for psychotherapists. 2nd ed. New York, NY: The Guilford Press; 2015.
2. American Porphyria Foundation. About porphyria. https://porphyriafoundation.org/patients/about-porphyria. Accessed May 13, 2020.
3. Millward L, Kelly P, King A, et al. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis. 2005;28(6):1099-1107.
4. Bonkovsky H, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyria consortium. Am J Med. 2014;127(12):1233-1241.
5. Tsirlin A, Oo Y, Sharma R, et al. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-238.
6. Leung A, Zun L, Nordstrom K, et al. Psychiatric emergencies for physicians: clinical management and approach to distinguishing pheochromocytoma from psychiatric and thyrotoxic diseases in the emergency room. J Emerg Med. 2017;53(5):712-716.
7. Garg M, Kharb S, Brar KS, et al. Medical management of pheochromocytoma: role of the endocrinologist. Indian J Endocrinol and Metab. 2011;15(suppl 4):S329-S336. doi: 10.4103/2230-8210.86976.
8. Zardawi I. Phaeochromocytoma masquerading as anxiety and depression. Am J Case Rep. 2013;14:161-163.
9. ARUP Laboratories. Test directory. https://www.aruplab.com. Accessed February 11, 2020.
10. Sriram P, Raghavan V. Pheochromocytoma presenting as anxiety disorder: a case report. Asian J Psychiatr. 2017;29:83-84.
11. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge, UK: Cambridge University Press; 2013.
CASE Depression, anxiety, and panic attacks
At the urging of his parents Mr. P, age 33, presents to the partial hospitalization program (PHP) for worsening depression and anxiety, daily panic attacks with accompanying diaphoresis and headache, and the possibility that he may have taken an overdose of zolpidem. Mr. P denies taking an intentional overdose of zolpidem, claiming instead that he was having a sleep-walking episode and did not realize how many pills he took.
In addition to daily panic attacks, Mr. P reports having trouble falling asleep, overwhelming sadness, and daily passive suicidal ideation without a plan or active intent.
Mr. P cannot identify a specific trigger to this most recent exacerbation of depressed/anxious mood, but instead describes it as slowly building over the past 6 to 8 months. Mr. P says the panic attacks occur without warning and states, “I feel like my heart is going to jump out of my chest; I get a terrible headache, and I sweat like crazy. Sometimes I just feel like I’m about to pass out or die.” Although these episodes had been present for approximately 2 years, they now occur almost daily.
HISTORY Inconsistent adherence
For the last year, Mr. P had been taking alprazolam, 0.5 mg twice daily, and paroxetine, 20 mg/d, and these medications provided moderate relief of his depressive/anxious symptoms. However, he stopped taking both medications approximately 3 or 4 weeks ago when he ran out. He also takes propranolol, 20 mg/d, sporadically, for hypertension. In the past, he had been prescribed carvedilol, clonidine, and lisinopril—all with varying degrees of relief of his hypertension. He denies a family history of hypertension or any other chronic or acute health problems. He reports that he has been sober from alcohol for 19 months but smokes 1 to 2 marijuana cigarettes a day.
EVALUATION Elevated blood pressure and pulse
Mr. P’s physical examination and medical review of systems are unremarkable, except for an elevated blood pressure (190/110 mm Hg) and pulse (92 beats per minute); he also has a headache. A repeat blood pressure test later in the day is 172/94 mm Hg, with a pulse of 100 beats per minute. His urine drug screen is positive only for delta-9-tetrahydrocannabinol (THC).
[polldaddy:10558304]
The author’s observations
A CBC with differential is helpful for ruling out infection and anemia as causes of anxiety and depression.1 In Mr. P’s case, there were no concerning symptoms that pointed to anemia or infection as likely causes of his anxiety, depression, or panic attacks. A TSH level also would be reasonable, because hyperthyroidism can present as anxiety, while hyperthyroidism or hypothyroidism each can present as depression.1 However, both Mr. P’s medical history and physical examination were not concerning for thyroid disease, making it unlikely that he had either of those conditions. A review of Mr. P’s medical records indicated that within the past 6 months, his primary care physician (PCP) had ordered a CBC and TSH test; the results of both were within normal limits.
Serum porphyrin tests can exclude porphyria as a contributor to Mr. P’s anxiety and depression. Porphyrias are a group of 8 inherited disorders that involve accumulation of heme precursors (porphyrins) in the CNS and subcutaneous tissue.2 Collectively, porphyrias affect approximately 1 in 200,000 people.2 Anxiety and depression are strongly associated with porphyria, but do not occur secondary to the illness; depression and anxiety appear to be intrinsic personality features in people with porphyria.3 Skin lesions and abdominal pain are the most common symptoms,3 and there is a higher incidence of hypertension in people with porphyria than in the general population.4 Mr. P does not report any heritable disorders, nor does he appear to have any CNS disturbance or unusual cutaneous lesions, which makes it unlikely that this disorder is related to his psychiatric symptoms.
Continue to: A serum metanephrines test measures...
A serum metanephrines test measures the metabolites of epinephrine and norepinephrine. These catecholamines are produced in excess by an adrenal or extra-adrenal tumor seen in pheochromocytoma. The classic triad of symptoms of pheochromocytoma are hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic (Table 15-7). This type of tumor is rare, with an annual incidence of only 2 to 8 cases per 1 million individuals. Among people with hypertension, the annual incidence is 0.1% to 1.0%, and for those with an adrenal mass, the annual incidence is 5% (Table 26,8). Autopsy studies suggest that up to 50% of pheochromocytomas are undiagnosed.8 Left untreated, pheochromocytoma can result in hypertensive crisis, arrhythmia, myocardial infarction, multisystem organ failure, and premature death.7Table 36,7 highlights some causes of false-positive serum on metanephrines testing.
EVALUATION Metanephrines testing
Mr. P has what appears to be treatment-resistant hypertension, accompanied by the classic symptoms observed in most patients with pheochromocytoma. Because Mr. P is participating in the PHP 6 days per week for 6 hours each day, visiting his PCP would be inconvenient, so the treatment team orders the serum metanephrines test. If a positive result is found, Mr. P will be referred to his PCP for further assessment and follow-up care with endocrinology.
TREATMENT Pharmacotherapy to target anxiety and panic
Next, the treatment team establishes a safety plan for Mr. P, and restarts paroxetine, 20 mg/d, to target his depressed and anxious mood. Alprazolam, 0.5 mg twice daily, is started to target anxious mood and panic symptoms, and to allow time for the anxiolytic properties of the paroxetine to become fully effective. The alprazolam will be tapered and stopped after 2 weeks. Mr. P is started on hydroxyzine, 1 to 2 25-mg tablets 2 to 3 times daily as needed for anxious mood and panic symptoms.
The serum metanephrines test results are equivocal, with a slight elevation of both epinephrine and norepinephrine that is too low to confirm a diagnosis of pheochromocytoma but too elevated to exclude it (Table 49). With Mr. P’s consent, the treatment team contacts his PCP and convey the results of this test. Mr. P schedules an appointment with his PCP for the following week for further assessment and confirmatory pheochromocytoma testing.
After 1 week, Mr. P remains anxious, with a slight reduction in panic attacks from multiple attacks each day to 3 or 4 attacks per week. The team considers adding an additional anxiolytic agent.
[polldaddy:10558305]
Continue to: The author's observations
The author’s observations
The triad of symptoms in pheochromocytoma results directly from the intermittent release of catecholamines into systemic circulation. Surges of epinephrine and norepinephrine lead to headaches, palpitations, diaphoresis, and (less commonly) gastrointestinal symptoms such as nausea, vomiting, and constipation. Persistent or episodic hypertension may be present, with 13% of patients maintaining a normal blood pressure.5-7 Patients with pheochromocytoma-related anxiety typically have substantial or complete resolution of anxiety and panic attacks after tumor resection.6,8,10
Because of their ability to raise catecholamine levels, several medications, including some psychotropics, can lead to false-positive results on serum and urine metanephrines testing. Tricyclic antidepressants and beta-blockers can cause false-positive results on plasma assays, while buspirone can cause false-positives on urinalysis assays.5 Trazodone, on the other hand, exhibits no catecholaminergic activity and its alpha-1 adrenergic antagonism may actually have some benefit in pheochromocytoma.11 Alpha-1 adrenergic antagonism with doxazosin, prazosin, or terazosin is the first-line of treatment in reducing pheochromocytoma-related hypertension.7 Treatment with a beta-blocker is safe only after alpha-adrenergic blockade occurs. While beta-blockers are useful for reducing the palpitations and anxiety observed in patients with pheochromocytoma, they must not be used alone due to the risk of hypertensive crisis resulting from unopposed alpha-adrenergic agonist activated vasoconstriction.5,7
TREATMENT CBT provides benefit
Mr. P decides against receiving an additional agent for anxiety and instead decides to wait for the outcome of the confirmatory pheochromocytoma testing. He continues to take alprazolam, and both his depressed mood and anxiety improve. His panic attacks continue to lessen, and he appears to benefit from cognitive-behavioral therapy provided during group therapy. Mr. P is advised by his PCP to taper and stop the alprazolam 3 to 5 days before his 24-hour urine metanephrines test because benzodiazepines can lead to false-positive results on a urinalysis assay.7
OUTCOME Remission of anxiety and depression
Mr. P has a repeat serum metanephrines test and a 24-hour urinalysis assay. Both are negative for pheochromocytoma. His PCP refers him to cardiology for management of treatment-resistant hypertension. He is discharged from the PHP and continues psychotherapy for depression and anxiety in an intensive outpatient program (IOP). Throughout his PHP and IOP treatments, he continues to take paroxetine and hydroxyzine. He achieves a successful remission of his anxiety and depression, with partial but significant remission of his panic attacks.
The author’s observations
Although Mr. P did not have pheochromocytoma, it is important to rule out this rare condition in patients who present with treatment-resistant hypertension and/or treatment-resistant anxiety.
Continue to: Bottom Line
Bottom Line
Pheochromocytoma is a tumor of the adrenal gland. The classic triad of symptoms of this rare condition is hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic. Several medications, including tricyclic antidepressants, beta-blockers, and buspirone, can lead to false-positive results on the serum and urine metanephrines testing used to diagnose pheochromocytoma.
Related Resources
- National Organization for Rare Disorders. Rare Disease Database: pheochromocytoma. www.rarediseases.org/rare-diseases/pheochromocytoma/.
- Young WF Jr. Clinical presentation and diagnosis of pheochromocytoma. UpToDate. www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-pheochromocytoma. Published January 2020.
Drug Brand Names
Alprazolam • Xanax
Amitriptyline • Elavil
Buspirone • Buspar
Carvedilol • Coreg
Clonidine • Catapres
Doxazosin • Cardura
Hydroxyzine • Vistaril
Lisinopril • Prinivil, Zestril
Paroxetine • Paxil
Prazosin • Minipress
Propranolol • Inderal
Terazosin • Hytrin
Trazodone • Desyrel
Zolpidem • Ambien
CASE Depression, anxiety, and panic attacks
At the urging of his parents Mr. P, age 33, presents to the partial hospitalization program (PHP) for worsening depression and anxiety, daily panic attacks with accompanying diaphoresis and headache, and the possibility that he may have taken an overdose of zolpidem. Mr. P denies taking an intentional overdose of zolpidem, claiming instead that he was having a sleep-walking episode and did not realize how many pills he took.
In addition to daily panic attacks, Mr. P reports having trouble falling asleep, overwhelming sadness, and daily passive suicidal ideation without a plan or active intent.
Mr. P cannot identify a specific trigger to this most recent exacerbation of depressed/anxious mood, but instead describes it as slowly building over the past 6 to 8 months. Mr. P says the panic attacks occur without warning and states, “I feel like my heart is going to jump out of my chest; I get a terrible headache, and I sweat like crazy. Sometimes I just feel like I’m about to pass out or die.” Although these episodes had been present for approximately 2 years, they now occur almost daily.
HISTORY Inconsistent adherence
For the last year, Mr. P had been taking alprazolam, 0.5 mg twice daily, and paroxetine, 20 mg/d, and these medications provided moderate relief of his depressive/anxious symptoms. However, he stopped taking both medications approximately 3 or 4 weeks ago when he ran out. He also takes propranolol, 20 mg/d, sporadically, for hypertension. In the past, he had been prescribed carvedilol, clonidine, and lisinopril—all with varying degrees of relief of his hypertension. He denies a family history of hypertension or any other chronic or acute health problems. He reports that he has been sober from alcohol for 19 months but smokes 1 to 2 marijuana cigarettes a day.
EVALUATION Elevated blood pressure and pulse
Mr. P’s physical examination and medical review of systems are unremarkable, except for an elevated blood pressure (190/110 mm Hg) and pulse (92 beats per minute); he also has a headache. A repeat blood pressure test later in the day is 172/94 mm Hg, with a pulse of 100 beats per minute. His urine drug screen is positive only for delta-9-tetrahydrocannabinol (THC).
[polldaddy:10558304]
The author’s observations
A CBC with differential is helpful for ruling out infection and anemia as causes of anxiety and depression.1 In Mr. P’s case, there were no concerning symptoms that pointed to anemia or infection as likely causes of his anxiety, depression, or panic attacks. A TSH level also would be reasonable, because hyperthyroidism can present as anxiety, while hyperthyroidism or hypothyroidism each can present as depression.1 However, both Mr. P’s medical history and physical examination were not concerning for thyroid disease, making it unlikely that he had either of those conditions. A review of Mr. P’s medical records indicated that within the past 6 months, his primary care physician (PCP) had ordered a CBC and TSH test; the results of both were within normal limits.
Serum porphyrin tests can exclude porphyria as a contributor to Mr. P’s anxiety and depression. Porphyrias are a group of 8 inherited disorders that involve accumulation of heme precursors (porphyrins) in the CNS and subcutaneous tissue.2 Collectively, porphyrias affect approximately 1 in 200,000 people.2 Anxiety and depression are strongly associated with porphyria, but do not occur secondary to the illness; depression and anxiety appear to be intrinsic personality features in people with porphyria.3 Skin lesions and abdominal pain are the most common symptoms,3 and there is a higher incidence of hypertension in people with porphyria than in the general population.4 Mr. P does not report any heritable disorders, nor does he appear to have any CNS disturbance or unusual cutaneous lesions, which makes it unlikely that this disorder is related to his psychiatric symptoms.
Continue to: A serum metanephrines test measures...
A serum metanephrines test measures the metabolites of epinephrine and norepinephrine. These catecholamines are produced in excess by an adrenal or extra-adrenal tumor seen in pheochromocytoma. The classic triad of symptoms of pheochromocytoma are hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic (Table 15-7). This type of tumor is rare, with an annual incidence of only 2 to 8 cases per 1 million individuals. Among people with hypertension, the annual incidence is 0.1% to 1.0%, and for those with an adrenal mass, the annual incidence is 5% (Table 26,8). Autopsy studies suggest that up to 50% of pheochromocytomas are undiagnosed.8 Left untreated, pheochromocytoma can result in hypertensive crisis, arrhythmia, myocardial infarction, multisystem organ failure, and premature death.7Table 36,7 highlights some causes of false-positive serum on metanephrines testing.
EVALUATION Metanephrines testing
Mr. P has what appears to be treatment-resistant hypertension, accompanied by the classic symptoms observed in most patients with pheochromocytoma. Because Mr. P is participating in the PHP 6 days per week for 6 hours each day, visiting his PCP would be inconvenient, so the treatment team orders the serum metanephrines test. If a positive result is found, Mr. P will be referred to his PCP for further assessment and follow-up care with endocrinology.
TREATMENT Pharmacotherapy to target anxiety and panic
Next, the treatment team establishes a safety plan for Mr. P, and restarts paroxetine, 20 mg/d, to target his depressed and anxious mood. Alprazolam, 0.5 mg twice daily, is started to target anxious mood and panic symptoms, and to allow time for the anxiolytic properties of the paroxetine to become fully effective. The alprazolam will be tapered and stopped after 2 weeks. Mr. P is started on hydroxyzine, 1 to 2 25-mg tablets 2 to 3 times daily as needed for anxious mood and panic symptoms.
The serum metanephrines test results are equivocal, with a slight elevation of both epinephrine and norepinephrine that is too low to confirm a diagnosis of pheochromocytoma but too elevated to exclude it (Table 49). With Mr. P’s consent, the treatment team contacts his PCP and convey the results of this test. Mr. P schedules an appointment with his PCP for the following week for further assessment and confirmatory pheochromocytoma testing.
After 1 week, Mr. P remains anxious, with a slight reduction in panic attacks from multiple attacks each day to 3 or 4 attacks per week. The team considers adding an additional anxiolytic agent.
[polldaddy:10558305]
Continue to: The author's observations
The author’s observations
The triad of symptoms in pheochromocytoma results directly from the intermittent release of catecholamines into systemic circulation. Surges of epinephrine and norepinephrine lead to headaches, palpitations, diaphoresis, and (less commonly) gastrointestinal symptoms such as nausea, vomiting, and constipation. Persistent or episodic hypertension may be present, with 13% of patients maintaining a normal blood pressure.5-7 Patients with pheochromocytoma-related anxiety typically have substantial or complete resolution of anxiety and panic attacks after tumor resection.6,8,10
Because of their ability to raise catecholamine levels, several medications, including some psychotropics, can lead to false-positive results on serum and urine metanephrines testing. Tricyclic antidepressants and beta-blockers can cause false-positive results on plasma assays, while buspirone can cause false-positives on urinalysis assays.5 Trazodone, on the other hand, exhibits no catecholaminergic activity and its alpha-1 adrenergic antagonism may actually have some benefit in pheochromocytoma.11 Alpha-1 adrenergic antagonism with doxazosin, prazosin, or terazosin is the first-line of treatment in reducing pheochromocytoma-related hypertension.7 Treatment with a beta-blocker is safe only after alpha-adrenergic blockade occurs. While beta-blockers are useful for reducing the palpitations and anxiety observed in patients with pheochromocytoma, they must not be used alone due to the risk of hypertensive crisis resulting from unopposed alpha-adrenergic agonist activated vasoconstriction.5,7
TREATMENT CBT provides benefit
Mr. P decides against receiving an additional agent for anxiety and instead decides to wait for the outcome of the confirmatory pheochromocytoma testing. He continues to take alprazolam, and both his depressed mood and anxiety improve. His panic attacks continue to lessen, and he appears to benefit from cognitive-behavioral therapy provided during group therapy. Mr. P is advised by his PCP to taper and stop the alprazolam 3 to 5 days before his 24-hour urine metanephrines test because benzodiazepines can lead to false-positive results on a urinalysis assay.7
OUTCOME Remission of anxiety and depression
Mr. P has a repeat serum metanephrines test and a 24-hour urinalysis assay. Both are negative for pheochromocytoma. His PCP refers him to cardiology for management of treatment-resistant hypertension. He is discharged from the PHP and continues psychotherapy for depression and anxiety in an intensive outpatient program (IOP). Throughout his PHP and IOP treatments, he continues to take paroxetine and hydroxyzine. He achieves a successful remission of his anxiety and depression, with partial but significant remission of his panic attacks.
The author’s observations
Although Mr. P did not have pheochromocytoma, it is important to rule out this rare condition in patients who present with treatment-resistant hypertension and/or treatment-resistant anxiety.
Continue to: Bottom Line
Bottom Line
Pheochromocytoma is a tumor of the adrenal gland. The classic triad of symptoms of this rare condition is hypertension, sweating, and headache; approximately 30% of patients report significant anxiety and panic. Several medications, including tricyclic antidepressants, beta-blockers, and buspirone, can lead to false-positive results on the serum and urine metanephrines testing used to diagnose pheochromocytoma.
Related Resources
- National Organization for Rare Disorders. Rare Disease Database: pheochromocytoma. www.rarediseases.org/rare-diseases/pheochromocytoma/.
- Young WF Jr. Clinical presentation and diagnosis of pheochromocytoma. UpToDate. www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-pheochromocytoma. Published January 2020.
Drug Brand Names
Alprazolam • Xanax
Amitriptyline • Elavil
Buspirone • Buspar
Carvedilol • Coreg
Clonidine • Catapres
Doxazosin • Cardura
Hydroxyzine • Vistaril
Lisinopril • Prinivil, Zestril
Paroxetine • Paxil
Prazosin • Minipress
Propranolol • Inderal
Terazosin • Hytrin
Trazodone • Desyrel
Zolpidem • Ambien
1. Morrison J. When psychological problems mask medical disorders: a guide for psychotherapists. 2nd ed. New York, NY: The Guilford Press; 2015.
2. American Porphyria Foundation. About porphyria. https://porphyriafoundation.org/patients/about-porphyria. Accessed May 13, 2020.
3. Millward L, Kelly P, King A, et al. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis. 2005;28(6):1099-1107.
4. Bonkovsky H, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyria consortium. Am J Med. 2014;127(12):1233-1241.
5. Tsirlin A, Oo Y, Sharma R, et al. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-238.
6. Leung A, Zun L, Nordstrom K, et al. Psychiatric emergencies for physicians: clinical management and approach to distinguishing pheochromocytoma from psychiatric and thyrotoxic diseases in the emergency room. J Emerg Med. 2017;53(5):712-716.
7. Garg M, Kharb S, Brar KS, et al. Medical management of pheochromocytoma: role of the endocrinologist. Indian J Endocrinol and Metab. 2011;15(suppl 4):S329-S336. doi: 10.4103/2230-8210.86976.
8. Zardawi I. Phaeochromocytoma masquerading as anxiety and depression. Am J Case Rep. 2013;14:161-163.
9. ARUP Laboratories. Test directory. https://www.aruplab.com. Accessed February 11, 2020.
10. Sriram P, Raghavan V. Pheochromocytoma presenting as anxiety disorder: a case report. Asian J Psychiatr. 2017;29:83-84.
11. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge, UK: Cambridge University Press; 2013.
1. Morrison J. When psychological problems mask medical disorders: a guide for psychotherapists. 2nd ed. New York, NY: The Guilford Press; 2015.
2. American Porphyria Foundation. About porphyria. https://porphyriafoundation.org/patients/about-porphyria. Accessed May 13, 2020.
3. Millward L, Kelly P, King A, et al. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis. 2005;28(6):1099-1107.
4. Bonkovsky H, Maddukuri VC, Yazici C, et al. Acute porphyrias in the USA: features of 108 subjects from porphyria consortium. Am J Med. 2014;127(12):1233-1241.
5. Tsirlin A, Oo Y, Sharma R, et al. Pheochromocytoma: a review. Maturitas. 2014;77(3):229-238.
6. Leung A, Zun L, Nordstrom K, et al. Psychiatric emergencies for physicians: clinical management and approach to distinguishing pheochromocytoma from psychiatric and thyrotoxic diseases in the emergency room. J Emerg Med. 2017;53(5):712-716.
7. Garg M, Kharb S, Brar KS, et al. Medical management of pheochromocytoma: role of the endocrinologist. Indian J Endocrinol and Metab. 2011;15(suppl 4):S329-S336. doi: 10.4103/2230-8210.86976.
8. Zardawi I. Phaeochromocytoma masquerading as anxiety and depression. Am J Case Rep. 2013;14:161-163.
9. ARUP Laboratories. Test directory. https://www.aruplab.com. Accessed February 11, 2020.
10. Sriram P, Raghavan V. Pheochromocytoma presenting as anxiety disorder: a case report. Asian J Psychiatr. 2017;29:83-84.
11. Stahl SM. Stahl’s essential psychopharmacology: neuroscientific basis and practical applications. Cambridge, UK: Cambridge University Press; 2013.
The resident’s role in combating burnout among medical students
Burnout among health care professionals has been increasingly recognized by the medical community over the past several years. The concern for burnout among medical students is equally serious. In this article, I review the prevalence of burnout among medical students, and the personal and clinical effects they experience. I also discuss how as psychiatry residents we can be more effective in preventing and identifying medical student burnout.
An underappreciated problem
Burnout has been defined as long-term unresolvable job stress that leads to exhaustion and feeling overwhelmed, cynical, and detached from work, and lacking a sense of personal accomplishment. It can lead to depression, anxiety, and suicidal ideation—one survey found that 5.8% of medical students had experienced suicidal ideation at some point in the previous 12 months.1 Burnout affects not only the individual, but also his/her team and patients. One study found that compared to medical students who didn’t report burnout, medical students who did had lower scores on measures of empathy and professionalism.2
While burnout among physicians and residents has received increasing attention, it often may go unrecognized and unreported in medical students. A literature review that included 51 studies found 28% to 45% of medical students report burnout.3 In a survey at one institution, 60% of medical students reported burnout.4 It is evident that medical schools have an important role in helping to minimize burnout rates in their students, and many schools are working toward this goal. However, what happens when students leave the classroom setting for clinical rotations?
A recent study found burnout among medical students peaks during the third year of medical school.5 This is when students are on their clinical rotations, new to the hospital environment, and without the inherent structure and support of being at school.
How residents can help
Like most medical students, while on my clinical rotations, I spent most of my day with residents, and I believe residents can help to both recognize burnout in medical students and prevent it.
The first step in addressing this problem is to understand why it occurs. A survey of medical students showed that inadequate sleep and decreased exercise play a significant role in burnout rates.6 Another study found a correlation between burnout and feeling emotionally exhausted and a decreased perceived quality of life.7 A medical student I recently worked with stated, “How can you not feel burnt out? Juggling work hours, studying, debt, health, and trying to have a life… something always gets dropped.”
So as residents, what can we do to identify and assist medical students who are experiencing burnout, or are at risk of getting there? When needed, we can utilize our psychiatry training to assess our students for depression and substance use disorders, and connect them with appropriate resources. When identifying a medical student with burnout, I believe it can become necessary to notify the attending, the site director responsible for the student, and often the school, so that the student has access to all available resources.
Continue to: It's as important to be proactive...
It’s as important to be proactive as it is to be reactive. Engaging in regular check-ins with our students about self-care and workload, as well as asking about how they are feeling, can offer them opportunities to talk about issues that they might not be getting anywhere else. One medical student I worked with told me, “It’s easy to fade into the background as the student, or to feel like I can’t complain because this is just how medical school is supposed to be.” We have the ability to change this notion with each student we work with.
It is likely that as residents we have worked with a student struggling with burnout without even realizing it. I believe we can play an important role in helping to prevent burnout by identifying at-risk students, offering assistance, and encouraging them to seek professional help. Someone’s life may depend on it.
1. Dyrbye L, Thomas M, Massie F, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341.
2. Brazeau C, Schroeder R, Rovi S. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(suppl 10):S33-S36. doi: 10.1097/ACM.0b013e3181ed4c47.
3. IsHak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242.
4. Chang E, Eddins-Folensbee F, Coverdale J. Survey of the prevalence of burnout, stress, depression, and the use of supports by medical students at one school. Acad Psychiatry. 2012;36(3):177-182.
5. Hansell MW, Ungerleider RM, Brooks CA, et al. Temporal trends in medical student burnout. Fam Med. 2019;51(5):399-404.
6. Wolf M, Rosenstock J. Inadequate sleep and exercise associated with burnout and depression among medical students. Acad Psychiatry. 2017;41(2):174-179.
7. Colby L, Mareka M, Pillay S, et al. The association between the levels of burnout and quality of life among fourth-year medical students at the University of the Free State. S Afr J Psychiatr. 2018;24:1101.
Burnout among health care professionals has been increasingly recognized by the medical community over the past several years. The concern for burnout among medical students is equally serious. In this article, I review the prevalence of burnout among medical students, and the personal and clinical effects they experience. I also discuss how as psychiatry residents we can be more effective in preventing and identifying medical student burnout.
An underappreciated problem
Burnout has been defined as long-term unresolvable job stress that leads to exhaustion and feeling overwhelmed, cynical, and detached from work, and lacking a sense of personal accomplishment. It can lead to depression, anxiety, and suicidal ideation—one survey found that 5.8% of medical students had experienced suicidal ideation at some point in the previous 12 months.1 Burnout affects not only the individual, but also his/her team and patients. One study found that compared to medical students who didn’t report burnout, medical students who did had lower scores on measures of empathy and professionalism.2
While burnout among physicians and residents has received increasing attention, it often may go unrecognized and unreported in medical students. A literature review that included 51 studies found 28% to 45% of medical students report burnout.3 In a survey at one institution, 60% of medical students reported burnout.4 It is evident that medical schools have an important role in helping to minimize burnout rates in their students, and many schools are working toward this goal. However, what happens when students leave the classroom setting for clinical rotations?
A recent study found burnout among medical students peaks during the third year of medical school.5 This is when students are on their clinical rotations, new to the hospital environment, and without the inherent structure and support of being at school.
How residents can help
Like most medical students, while on my clinical rotations, I spent most of my day with residents, and I believe residents can help to both recognize burnout in medical students and prevent it.
The first step in addressing this problem is to understand why it occurs. A survey of medical students showed that inadequate sleep and decreased exercise play a significant role in burnout rates.6 Another study found a correlation between burnout and feeling emotionally exhausted and a decreased perceived quality of life.7 A medical student I recently worked with stated, “How can you not feel burnt out? Juggling work hours, studying, debt, health, and trying to have a life… something always gets dropped.”
So as residents, what can we do to identify and assist medical students who are experiencing burnout, or are at risk of getting there? When needed, we can utilize our psychiatry training to assess our students for depression and substance use disorders, and connect them with appropriate resources. When identifying a medical student with burnout, I believe it can become necessary to notify the attending, the site director responsible for the student, and often the school, so that the student has access to all available resources.
Continue to: It's as important to be proactive...
It’s as important to be proactive as it is to be reactive. Engaging in regular check-ins with our students about self-care and workload, as well as asking about how they are feeling, can offer them opportunities to talk about issues that they might not be getting anywhere else. One medical student I worked with told me, “It’s easy to fade into the background as the student, or to feel like I can’t complain because this is just how medical school is supposed to be.” We have the ability to change this notion with each student we work with.
It is likely that as residents we have worked with a student struggling with burnout without even realizing it. I believe we can play an important role in helping to prevent burnout by identifying at-risk students, offering assistance, and encouraging them to seek professional help. Someone’s life may depend on it.
Burnout among health care professionals has been increasingly recognized by the medical community over the past several years. The concern for burnout among medical students is equally serious. In this article, I review the prevalence of burnout among medical students, and the personal and clinical effects they experience. I also discuss how as psychiatry residents we can be more effective in preventing and identifying medical student burnout.
An underappreciated problem
Burnout has been defined as long-term unresolvable job stress that leads to exhaustion and feeling overwhelmed, cynical, and detached from work, and lacking a sense of personal accomplishment. It can lead to depression, anxiety, and suicidal ideation—one survey found that 5.8% of medical students had experienced suicidal ideation at some point in the previous 12 months.1 Burnout affects not only the individual, but also his/her team and patients. One study found that compared to medical students who didn’t report burnout, medical students who did had lower scores on measures of empathy and professionalism.2
While burnout among physicians and residents has received increasing attention, it often may go unrecognized and unreported in medical students. A literature review that included 51 studies found 28% to 45% of medical students report burnout.3 In a survey at one institution, 60% of medical students reported burnout.4 It is evident that medical schools have an important role in helping to minimize burnout rates in their students, and many schools are working toward this goal. However, what happens when students leave the classroom setting for clinical rotations?
A recent study found burnout among medical students peaks during the third year of medical school.5 This is when students are on their clinical rotations, new to the hospital environment, and without the inherent structure and support of being at school.
How residents can help
Like most medical students, while on my clinical rotations, I spent most of my day with residents, and I believe residents can help to both recognize burnout in medical students and prevent it.
The first step in addressing this problem is to understand why it occurs. A survey of medical students showed that inadequate sleep and decreased exercise play a significant role in burnout rates.6 Another study found a correlation between burnout and feeling emotionally exhausted and a decreased perceived quality of life.7 A medical student I recently worked with stated, “How can you not feel burnt out? Juggling work hours, studying, debt, health, and trying to have a life… something always gets dropped.”
So as residents, what can we do to identify and assist medical students who are experiencing burnout, or are at risk of getting there? When needed, we can utilize our psychiatry training to assess our students for depression and substance use disorders, and connect them with appropriate resources. When identifying a medical student with burnout, I believe it can become necessary to notify the attending, the site director responsible for the student, and often the school, so that the student has access to all available resources.
Continue to: It's as important to be proactive...
It’s as important to be proactive as it is to be reactive. Engaging in regular check-ins with our students about self-care and workload, as well as asking about how they are feeling, can offer them opportunities to talk about issues that they might not be getting anywhere else. One medical student I worked with told me, “It’s easy to fade into the background as the student, or to feel like I can’t complain because this is just how medical school is supposed to be.” We have the ability to change this notion with each student we work with.
It is likely that as residents we have worked with a student struggling with burnout without even realizing it. I believe we can play an important role in helping to prevent burnout by identifying at-risk students, offering assistance, and encouraging them to seek professional help. Someone’s life may depend on it.
1. Dyrbye L, Thomas M, Massie F, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341.
2. Brazeau C, Schroeder R, Rovi S. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(suppl 10):S33-S36. doi: 10.1097/ACM.0b013e3181ed4c47.
3. IsHak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242.
4. Chang E, Eddins-Folensbee F, Coverdale J. Survey of the prevalence of burnout, stress, depression, and the use of supports by medical students at one school. Acad Psychiatry. 2012;36(3):177-182.
5. Hansell MW, Ungerleider RM, Brooks CA, et al. Temporal trends in medical student burnout. Fam Med. 2019;51(5):399-404.
6. Wolf M, Rosenstock J. Inadequate sleep and exercise associated with burnout and depression among medical students. Acad Psychiatry. 2017;41(2):174-179.
7. Colby L, Mareka M, Pillay S, et al. The association between the levels of burnout and quality of life among fourth-year medical students at the University of the Free State. S Afr J Psychiatr. 2018;24:1101.
1. Dyrbye L, Thomas M, Massie F, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341.
2. Brazeau C, Schroeder R, Rovi S. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(suppl 10):S33-S36. doi: 10.1097/ACM.0b013e3181ed4c47.
3. IsHak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242.
4. Chang E, Eddins-Folensbee F, Coverdale J. Survey of the prevalence of burnout, stress, depression, and the use of supports by medical students at one school. Acad Psychiatry. 2012;36(3):177-182.
5. Hansell MW, Ungerleider RM, Brooks CA, et al. Temporal trends in medical student burnout. Fam Med. 2019;51(5):399-404.
6. Wolf M, Rosenstock J. Inadequate sleep and exercise associated with burnout and depression among medical students. Acad Psychiatry. 2017;41(2):174-179.
7. Colby L, Mareka M, Pillay S, et al. The association between the levels of burnout and quality of life among fourth-year medical students at the University of the Free State. S Afr J Psychiatr. 2018;24:1101.
Many clinicians still not asking about postpartum depression
Health care providers fail to ask one in five prenatal patients and one in eight postpartum patients about depression, according to the Centers for Disease Control and Prevention. Although the prevalence of screening has risen in recent years, many women could be suffering in silence.
“[U]ndetected and untreated perinatal depression can have negative health consequences for the mothers and their babies,” said coauthor Jean Y. Ko, PhD, from the division of reproductive health at the National Center for Chronic Disease Prevention and Health Promotion.
Dr. Ko and colleagues reported their findings in an article published in Morbidity and Mortality Weekly Report.
The researchers analyzed self-reported data on postpartum depressive symptoms (PDS) collected in 2018 by the Pregnancy Risk Assessment Monitoring System (PRAMS). Participants were stratified on the basis of location and maternal and infant characteristics, including age, race/ethnicity, and education level. Women who had recently given birth to one or more live infants answered questions about whether they had been screened by health care providers for depression during perinatal visits.
The prevalence of PDS among women from 31 PRAMS sites was 13.2%. States with lower prevalences included Illinois (9.7%), Massachusetts (10.3%), and Wisconsin (10.5%); states with higher prevalences included Mississippi (23.5%), West Virginia (19.4%), and Michigan (16.4%).
Some groups were at higher risk for PDS than others. The prevalence was greater than 20% among women who were aged 19 years or younger, were of American Indian or Alaska Native ethnicity, smoked during the perinatal period, experienced perinatal depression, or whose infant died after birth.
Depressive symptoms were also more common among women who received assistance from the Women, Infants, and Children program; were Medicaid beneficiaries at the time of delivery; smoked cigarettes during the last trimester of pregnancy; breastfed their infants for fewer than 8 weeks; or had experienced intimate partner violence while pregnant or before.
Small rise in screening
Overall, 79.1% of women said a health care provider had inquired about depression during the prenatal period. Prenatal screening for depression was lowest in Puerto Rico (50.7%), Mississippi (69.4%), Utah (69.5%), and Kentucky (69.5%) and was highest in Alaska (90.7%), Minnesota (90.6%), and Maine (90.5%).
Among 22 continuously reporting sites, the prevalence of prenatal depression screening rose significantly from 76.2% in 2016 to 79.3% in 2018 (P < .05) .
“It is unclear what might account for this small increase,” Dr. Ko said. “There may be additional factors, such as women may be becoming more comfortable reporting symptoms of depression. With continued awareness about the need to screen every pregnant and postpartum woman for depression, we can expect things to continue to improve.”
Overall, 90.1% of respondents reported a postpartum visit; of those, 87.4% said a health care provider had asked about depression during that visit.
Screening during the postpartum period was highest in Vermont (96.2%), Minnesota (95.9%), and Maine (95.5%) and was lowest in Puerto Rico (50.7%), New York City (73.1%), and Louisiana (75.0%).
Among the 22 sites that reported continuously, the prevalence of screening for postpartum depression rose significantly from 84.1% to 88.0% (P < .05), “with an average annual percentage point increase of 1.8%,” the authors wrote.
‘Missed opportunities’
“PRAMS responses are reported an average of 4 months postpartum, which suggests persistence of [depressive] symptoms,” the authors wrote.
Dr. Ko said that mental health conditions play a role in approximately 9% of pregnancy-related deaths and that not asking about depression represents “missed opportunities to potentially identify and treat women with depression.” The United States Preventive Services Task Force recommends screening all adults for depression, including women during pregnancy and the postpartum period, she added.
When asked what can be done to improve screening that has not already been tried, Dr. Ko said the CDC is currently evaluating a study called the Program in Support of Moms (PRISM), which “is designed to help obstetrics and gynecology practices address the significant public health issue of depression during and after pregnancy. PRISM aims to close gaps in health care delivery to ensure that women with depression during and after pregnancy receive the best treatment, which can result in improvement in their symptoms.”
Dr. Ko added that the Health Resources and Services Administration has funded seven states to begin “programs to support providers to screen, assess, refer, and treat pregnant and postpartum women for depression and other behavioral health conditions. States can use initiatives like Healthy Start, home visiting, and Title V Maternal and Child Health Services Block Grant programs as levers to improve screening and address maternal depression.
“Screening is just one part of addressing perinatal depression. Health care providers need to refer women to appropriate resources in order to get the proper diagnosis, treatment, and follow-up care for management of depression,” Dr. Ko concluded.
The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Health care providers fail to ask one in five prenatal patients and one in eight postpartum patients about depression, according to the Centers for Disease Control and Prevention. Although the prevalence of screening has risen in recent years, many women could be suffering in silence.
“[U]ndetected and untreated perinatal depression can have negative health consequences for the mothers and their babies,” said coauthor Jean Y. Ko, PhD, from the division of reproductive health at the National Center for Chronic Disease Prevention and Health Promotion.
Dr. Ko and colleagues reported their findings in an article published in Morbidity and Mortality Weekly Report.
The researchers analyzed self-reported data on postpartum depressive symptoms (PDS) collected in 2018 by the Pregnancy Risk Assessment Monitoring System (PRAMS). Participants were stratified on the basis of location and maternal and infant characteristics, including age, race/ethnicity, and education level. Women who had recently given birth to one or more live infants answered questions about whether they had been screened by health care providers for depression during perinatal visits.
The prevalence of PDS among women from 31 PRAMS sites was 13.2%. States with lower prevalences included Illinois (9.7%), Massachusetts (10.3%), and Wisconsin (10.5%); states with higher prevalences included Mississippi (23.5%), West Virginia (19.4%), and Michigan (16.4%).
Some groups were at higher risk for PDS than others. The prevalence was greater than 20% among women who were aged 19 years or younger, were of American Indian or Alaska Native ethnicity, smoked during the perinatal period, experienced perinatal depression, or whose infant died after birth.
Depressive symptoms were also more common among women who received assistance from the Women, Infants, and Children program; were Medicaid beneficiaries at the time of delivery; smoked cigarettes during the last trimester of pregnancy; breastfed their infants for fewer than 8 weeks; or had experienced intimate partner violence while pregnant or before.
Small rise in screening
Overall, 79.1% of women said a health care provider had inquired about depression during the prenatal period. Prenatal screening for depression was lowest in Puerto Rico (50.7%), Mississippi (69.4%), Utah (69.5%), and Kentucky (69.5%) and was highest in Alaska (90.7%), Minnesota (90.6%), and Maine (90.5%).
Among 22 continuously reporting sites, the prevalence of prenatal depression screening rose significantly from 76.2% in 2016 to 79.3% in 2018 (P < .05) .
“It is unclear what might account for this small increase,” Dr. Ko said. “There may be additional factors, such as women may be becoming more comfortable reporting symptoms of depression. With continued awareness about the need to screen every pregnant and postpartum woman for depression, we can expect things to continue to improve.”
Overall, 90.1% of respondents reported a postpartum visit; of those, 87.4% said a health care provider had asked about depression during that visit.
Screening during the postpartum period was highest in Vermont (96.2%), Minnesota (95.9%), and Maine (95.5%) and was lowest in Puerto Rico (50.7%), New York City (73.1%), and Louisiana (75.0%).
Among the 22 sites that reported continuously, the prevalence of screening for postpartum depression rose significantly from 84.1% to 88.0% (P < .05), “with an average annual percentage point increase of 1.8%,” the authors wrote.
‘Missed opportunities’
“PRAMS responses are reported an average of 4 months postpartum, which suggests persistence of [depressive] symptoms,” the authors wrote.
Dr. Ko said that mental health conditions play a role in approximately 9% of pregnancy-related deaths and that not asking about depression represents “missed opportunities to potentially identify and treat women with depression.” The United States Preventive Services Task Force recommends screening all adults for depression, including women during pregnancy and the postpartum period, she added.
When asked what can be done to improve screening that has not already been tried, Dr. Ko said the CDC is currently evaluating a study called the Program in Support of Moms (PRISM), which “is designed to help obstetrics and gynecology practices address the significant public health issue of depression during and after pregnancy. PRISM aims to close gaps in health care delivery to ensure that women with depression during and after pregnancy receive the best treatment, which can result in improvement in their symptoms.”
Dr. Ko added that the Health Resources and Services Administration has funded seven states to begin “programs to support providers to screen, assess, refer, and treat pregnant and postpartum women for depression and other behavioral health conditions. States can use initiatives like Healthy Start, home visiting, and Title V Maternal and Child Health Services Block Grant programs as levers to improve screening and address maternal depression.
“Screening is just one part of addressing perinatal depression. Health care providers need to refer women to appropriate resources in order to get the proper diagnosis, treatment, and follow-up care for management of depression,” Dr. Ko concluded.
The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Health care providers fail to ask one in five prenatal patients and one in eight postpartum patients about depression, according to the Centers for Disease Control and Prevention. Although the prevalence of screening has risen in recent years, many women could be suffering in silence.
“[U]ndetected and untreated perinatal depression can have negative health consequences for the mothers and their babies,” said coauthor Jean Y. Ko, PhD, from the division of reproductive health at the National Center for Chronic Disease Prevention and Health Promotion.
Dr. Ko and colleagues reported their findings in an article published in Morbidity and Mortality Weekly Report.
The researchers analyzed self-reported data on postpartum depressive symptoms (PDS) collected in 2018 by the Pregnancy Risk Assessment Monitoring System (PRAMS). Participants were stratified on the basis of location and maternal and infant characteristics, including age, race/ethnicity, and education level. Women who had recently given birth to one or more live infants answered questions about whether they had been screened by health care providers for depression during perinatal visits.
The prevalence of PDS among women from 31 PRAMS sites was 13.2%. States with lower prevalences included Illinois (9.7%), Massachusetts (10.3%), and Wisconsin (10.5%); states with higher prevalences included Mississippi (23.5%), West Virginia (19.4%), and Michigan (16.4%).
Some groups were at higher risk for PDS than others. The prevalence was greater than 20% among women who were aged 19 years or younger, were of American Indian or Alaska Native ethnicity, smoked during the perinatal period, experienced perinatal depression, or whose infant died after birth.
Depressive symptoms were also more common among women who received assistance from the Women, Infants, and Children program; were Medicaid beneficiaries at the time of delivery; smoked cigarettes during the last trimester of pregnancy; breastfed their infants for fewer than 8 weeks; or had experienced intimate partner violence while pregnant or before.
Small rise in screening
Overall, 79.1% of women said a health care provider had inquired about depression during the prenatal period. Prenatal screening for depression was lowest in Puerto Rico (50.7%), Mississippi (69.4%), Utah (69.5%), and Kentucky (69.5%) and was highest in Alaska (90.7%), Minnesota (90.6%), and Maine (90.5%).
Among 22 continuously reporting sites, the prevalence of prenatal depression screening rose significantly from 76.2% in 2016 to 79.3% in 2018 (P < .05) .
“It is unclear what might account for this small increase,” Dr. Ko said. “There may be additional factors, such as women may be becoming more comfortable reporting symptoms of depression. With continued awareness about the need to screen every pregnant and postpartum woman for depression, we can expect things to continue to improve.”
Overall, 90.1% of respondents reported a postpartum visit; of those, 87.4% said a health care provider had asked about depression during that visit.
Screening during the postpartum period was highest in Vermont (96.2%), Minnesota (95.9%), and Maine (95.5%) and was lowest in Puerto Rico (50.7%), New York City (73.1%), and Louisiana (75.0%).
Among the 22 sites that reported continuously, the prevalence of screening for postpartum depression rose significantly from 84.1% to 88.0% (P < .05), “with an average annual percentage point increase of 1.8%,” the authors wrote.
‘Missed opportunities’
“PRAMS responses are reported an average of 4 months postpartum, which suggests persistence of [depressive] symptoms,” the authors wrote.
Dr. Ko said that mental health conditions play a role in approximately 9% of pregnancy-related deaths and that not asking about depression represents “missed opportunities to potentially identify and treat women with depression.” The United States Preventive Services Task Force recommends screening all adults for depression, including women during pregnancy and the postpartum period, she added.
When asked what can be done to improve screening that has not already been tried, Dr. Ko said the CDC is currently evaluating a study called the Program in Support of Moms (PRISM), which “is designed to help obstetrics and gynecology practices address the significant public health issue of depression during and after pregnancy. PRISM aims to close gaps in health care delivery to ensure that women with depression during and after pregnancy receive the best treatment, which can result in improvement in their symptoms.”
Dr. Ko added that the Health Resources and Services Administration has funded seven states to begin “programs to support providers to screen, assess, refer, and treat pregnant and postpartum women for depression and other behavioral health conditions. States can use initiatives like Healthy Start, home visiting, and Title V Maternal and Child Health Services Block Grant programs as levers to improve screening and address maternal depression.
“Screening is just one part of addressing perinatal depression. Health care providers need to refer women to appropriate resources in order to get the proper diagnosis, treatment, and follow-up care for management of depression,” Dr. Ko concluded.
The authors disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.