User login
Site of morphea lesions predicts risk of extracutaneous manifestations
LAKE TAHOE, CALIF. – Morphea lesions on the extensor extremities, face, and superior head are associated with higher rates of extracutaneous involvement, results from a multicenter retrospective study showed.
“We know that risk is highest with linear morphea,” lead study author Yvonne E. Chiu, MD, said at the annual meeting of the Society for Pediatric Dermatology. “Specifically, . However, risk stratification within each of those sites has never really been studied before.”
Dr. Chiu, who is a pediatric dermatologist at the Medical College of Wisconsin and Children’s Hospital of Wisconsin in Milwaukee, and her associates carried out a 14-site retrospective study in an effort to characterize morphea lesional distribution and to determine which sites had the highest risk for extracutaneous manifestations. They limited the analysis to patients with pediatric-onset morphea before the age of 18 and adequate lesional photographs in their clinical record. Patients with extragenital lichen sclerosis and atrophoderma were included in the analysis, but those with pansclerotic morphea and eosinophilic fasciitis were excluded. The researchers used custom web-based software to map the morphea lesions, and linked those data to a REDCap database where demographic and clinical information was stored. From this, the researchers tracked neurologic symptoms such as seizures, migraine headaches, other headaches, or any other neurologic signs or symptoms; neurologic testing results from those who underwent MRI, CT, and EEG; musculoskeletal symptoms such as arthritis, arthralgias, joint contracture, leg length discrepancy, and other musculoskeletal issues, as well as ophthalmologic manifestations including uveitis and other ophthalmologic symptoms. Logistic regression was used to analyze association of body sites with extracutaneous involvement.
Dr. Chiu, who also directs the dermatology residency program at the Medical College of Wisconsin, reported findings from 826 patients with 2,467 skin lesions of morphea, or an average of about 1.92 lesions per patient. Consistent with prior reports, most patients were female (73%), and the most prevalent subtype was linear morphea (56%), followed by plaque (29%), generalized (8%), and mixed (7%).
The trunk was the single most commonly affected body site, seen in 36% of cases. “However, if you lumped all body sites together, the extremities were the most commonly affected site (44%), while 16% of lesions involved the head and 4% involved the neck,” Dr. Chiu said. Patients with linear morphea had the highest rate of extracutaneous involvement. Specifically, 34% had musculoskeletal involvement, 24% had neurologic involvement, and 10% had ophthalmologic involvement. There were small rates of extracutaneous manifestations in the other types of morphea as well.
The most common musculoskeletal complications among patients with linear morphea were arthralgias (20%) and joint contractures (17%), followed by other musculoskeletal complications (15%), leg length discrepancy (5%), and arthritis (2%). Contrary to previously published reports, nonmigraine headaches were more common than seizures among patients with linear morphea (17% vs. 4%, respectively), while 4% of subjects had migraine headaches. Of the 134 subjects who underwent neuroimaging, 19% had abnormal results. Ophthalmologic complications were rare among patients overall, with the exception of those who had linear morphea. Of these cases, 1% had uveitis, and 9% had some other ophthalmologic condition.
Among all patients, the researchers found that left-extremity and extensor-extremity lesions had a stronger association with musculoskeletal involvement (odds ratios of 1.26 and 1.94, respectively). “The reasons for this are unclear,” Dr. Chiu said. “We didn’t assess handedness in our study, but that perhaps could explain it; 90% of the general population is right-hand dominant, so perhaps there’s some sort of protective effect if you’re using an extremity more. Joint contractures showed the greatest discrepancy between left and right extremity. So perhaps if you’re using that one side more, you’re less likely to have a joint contracture.”
When the researchers limited the analysis to head lesions, they observed no significant difference in the lesions between the left and right head (OR, 0.72), but anterior head lesions had a stronger association with neurologic signs or symptoms, compared with posterior head lesions (OR, 2.56), as did superior head lesions, compared with inferior head lesions (OR, 2.23). The association between head lesion location and ophthalmologic involvement was not significant.
“The odds of extracutaneous manifestations vary by site of morphea lesions, with higher odds seen on the left extremity, extensor extremity, the anterior head, and the superior head,” Dr. Chiu concluded. “Further research can be done to perhaps help us decide whether this necessitates difference in management or screening.”
The project was funded by the Pediatric Dermatology Research Alliance and the SPD. Dr. Chiu reported having no relevant financial disclosures.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – Morphea lesions on the extensor extremities, face, and superior head are associated with higher rates of extracutaneous involvement, results from a multicenter retrospective study showed.
“We know that risk is highest with linear morphea,” lead study author Yvonne E. Chiu, MD, said at the annual meeting of the Society for Pediatric Dermatology. “Specifically, . However, risk stratification within each of those sites has never really been studied before.”
Dr. Chiu, who is a pediatric dermatologist at the Medical College of Wisconsin and Children’s Hospital of Wisconsin in Milwaukee, and her associates carried out a 14-site retrospective study in an effort to characterize morphea lesional distribution and to determine which sites had the highest risk for extracutaneous manifestations. They limited the analysis to patients with pediatric-onset morphea before the age of 18 and adequate lesional photographs in their clinical record. Patients with extragenital lichen sclerosis and atrophoderma were included in the analysis, but those with pansclerotic morphea and eosinophilic fasciitis were excluded. The researchers used custom web-based software to map the morphea lesions, and linked those data to a REDCap database where demographic and clinical information was stored. From this, the researchers tracked neurologic symptoms such as seizures, migraine headaches, other headaches, or any other neurologic signs or symptoms; neurologic testing results from those who underwent MRI, CT, and EEG; musculoskeletal symptoms such as arthritis, arthralgias, joint contracture, leg length discrepancy, and other musculoskeletal issues, as well as ophthalmologic manifestations including uveitis and other ophthalmologic symptoms. Logistic regression was used to analyze association of body sites with extracutaneous involvement.
Dr. Chiu, who also directs the dermatology residency program at the Medical College of Wisconsin, reported findings from 826 patients with 2,467 skin lesions of morphea, or an average of about 1.92 lesions per patient. Consistent with prior reports, most patients were female (73%), and the most prevalent subtype was linear morphea (56%), followed by plaque (29%), generalized (8%), and mixed (7%).
The trunk was the single most commonly affected body site, seen in 36% of cases. “However, if you lumped all body sites together, the extremities were the most commonly affected site (44%), while 16% of lesions involved the head and 4% involved the neck,” Dr. Chiu said. Patients with linear morphea had the highest rate of extracutaneous involvement. Specifically, 34% had musculoskeletal involvement, 24% had neurologic involvement, and 10% had ophthalmologic involvement. There were small rates of extracutaneous manifestations in the other types of morphea as well.
The most common musculoskeletal complications among patients with linear morphea were arthralgias (20%) and joint contractures (17%), followed by other musculoskeletal complications (15%), leg length discrepancy (5%), and arthritis (2%). Contrary to previously published reports, nonmigraine headaches were more common than seizures among patients with linear morphea (17% vs. 4%, respectively), while 4% of subjects had migraine headaches. Of the 134 subjects who underwent neuroimaging, 19% had abnormal results. Ophthalmologic complications were rare among patients overall, with the exception of those who had linear morphea. Of these cases, 1% had uveitis, and 9% had some other ophthalmologic condition.
Among all patients, the researchers found that left-extremity and extensor-extremity lesions had a stronger association with musculoskeletal involvement (odds ratios of 1.26 and 1.94, respectively). “The reasons for this are unclear,” Dr. Chiu said. “We didn’t assess handedness in our study, but that perhaps could explain it; 90% of the general population is right-hand dominant, so perhaps there’s some sort of protective effect if you’re using an extremity more. Joint contractures showed the greatest discrepancy between left and right extremity. So perhaps if you’re using that one side more, you’re less likely to have a joint contracture.”
When the researchers limited the analysis to head lesions, they observed no significant difference in the lesions between the left and right head (OR, 0.72), but anterior head lesions had a stronger association with neurologic signs or symptoms, compared with posterior head lesions (OR, 2.56), as did superior head lesions, compared with inferior head lesions (OR, 2.23). The association between head lesion location and ophthalmologic involvement was not significant.
“The odds of extracutaneous manifestations vary by site of morphea lesions, with higher odds seen on the left extremity, extensor extremity, the anterior head, and the superior head,” Dr. Chiu concluded. “Further research can be done to perhaps help us decide whether this necessitates difference in management or screening.”
The project was funded by the Pediatric Dermatology Research Alliance and the SPD. Dr. Chiu reported having no relevant financial disclosures.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – Morphea lesions on the extensor extremities, face, and superior head are associated with higher rates of extracutaneous involvement, results from a multicenter retrospective study showed.
“We know that risk is highest with linear morphea,” lead study author Yvonne E. Chiu, MD, said at the annual meeting of the Society for Pediatric Dermatology. “Specifically, . However, risk stratification within each of those sites has never really been studied before.”
Dr. Chiu, who is a pediatric dermatologist at the Medical College of Wisconsin and Children’s Hospital of Wisconsin in Milwaukee, and her associates carried out a 14-site retrospective study in an effort to characterize morphea lesional distribution and to determine which sites had the highest risk for extracutaneous manifestations. They limited the analysis to patients with pediatric-onset morphea before the age of 18 and adequate lesional photographs in their clinical record. Patients with extragenital lichen sclerosis and atrophoderma were included in the analysis, but those with pansclerotic morphea and eosinophilic fasciitis were excluded. The researchers used custom web-based software to map the morphea lesions, and linked those data to a REDCap database where demographic and clinical information was stored. From this, the researchers tracked neurologic symptoms such as seizures, migraine headaches, other headaches, or any other neurologic signs or symptoms; neurologic testing results from those who underwent MRI, CT, and EEG; musculoskeletal symptoms such as arthritis, arthralgias, joint contracture, leg length discrepancy, and other musculoskeletal issues, as well as ophthalmologic manifestations including uveitis and other ophthalmologic symptoms. Logistic regression was used to analyze association of body sites with extracutaneous involvement.
Dr. Chiu, who also directs the dermatology residency program at the Medical College of Wisconsin, reported findings from 826 patients with 2,467 skin lesions of morphea, or an average of about 1.92 lesions per patient. Consistent with prior reports, most patients were female (73%), and the most prevalent subtype was linear morphea (56%), followed by plaque (29%), generalized (8%), and mixed (7%).
The trunk was the single most commonly affected body site, seen in 36% of cases. “However, if you lumped all body sites together, the extremities were the most commonly affected site (44%), while 16% of lesions involved the head and 4% involved the neck,” Dr. Chiu said. Patients with linear morphea had the highest rate of extracutaneous involvement. Specifically, 34% had musculoskeletal involvement, 24% had neurologic involvement, and 10% had ophthalmologic involvement. There were small rates of extracutaneous manifestations in the other types of morphea as well.
The most common musculoskeletal complications among patients with linear morphea were arthralgias (20%) and joint contractures (17%), followed by other musculoskeletal complications (15%), leg length discrepancy (5%), and arthritis (2%). Contrary to previously published reports, nonmigraine headaches were more common than seizures among patients with linear morphea (17% vs. 4%, respectively), while 4% of subjects had migraine headaches. Of the 134 subjects who underwent neuroimaging, 19% had abnormal results. Ophthalmologic complications were rare among patients overall, with the exception of those who had linear morphea. Of these cases, 1% had uveitis, and 9% had some other ophthalmologic condition.
Among all patients, the researchers found that left-extremity and extensor-extremity lesions had a stronger association with musculoskeletal involvement (odds ratios of 1.26 and 1.94, respectively). “The reasons for this are unclear,” Dr. Chiu said. “We didn’t assess handedness in our study, but that perhaps could explain it; 90% of the general population is right-hand dominant, so perhaps there’s some sort of protective effect if you’re using an extremity more. Joint contractures showed the greatest discrepancy between left and right extremity. So perhaps if you’re using that one side more, you’re less likely to have a joint contracture.”
When the researchers limited the analysis to head lesions, they observed no significant difference in the lesions between the left and right head (OR, 0.72), but anterior head lesions had a stronger association with neurologic signs or symptoms, compared with posterior head lesions (OR, 2.56), as did superior head lesions, compared with inferior head lesions (OR, 2.23). The association between head lesion location and ophthalmologic involvement was not significant.
“The odds of extracutaneous manifestations vary by site of morphea lesions, with higher odds seen on the left extremity, extensor extremity, the anterior head, and the superior head,” Dr. Chiu concluded. “Further research can be done to perhaps help us decide whether this necessitates difference in management or screening.”
The project was funded by the Pediatric Dermatology Research Alliance and the SPD. Dr. Chiu reported having no relevant financial disclosures.
dbrunk@mdedge.com
REPORTING FROM SPD 2018
Key clinical point: Extracutaneous involvement is more likely when morphea lesions are present on the extensor extremities, face, and superior head.
Major finding: Patients with linear morphea had the highest rate of extracutaneous involvement. Specifically, 34% had musculoskeletal involvement, 24% had neurologic involvement, and 10% had ophthalmologic involvement.
Study details: A multicenter retrospective study of 826 patients with 2,467 skin lesions of morphea.
Disclosures: The study was funded by the Pediatric Dermatology Research Alliance and the SPD. Dr. Chiu reported having no relevant financial disclosures.
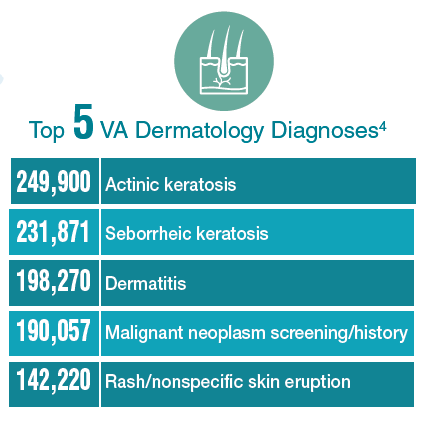
Federal Health Care Data Trends: Dermatology
There is significant variation among the civilian, active-duty, and veteran populations in regard to dermatologic conditions. Civilians most frequently visit a specialist with complaints of eczema, dermatitis, acne, and other benign conditions. Among active-duty service members, infections and allergic bite reactions are the most common reasons for a trip to a health care facility. In contrast, veterans are more likely to be diagnosed with precancerous skin conditions or to receive a screening for malignant skin cancers.
Click here to continue reading.
There is significant variation among the civilian, active-duty, and veteran populations in regard to dermatologic conditions. Civilians most frequently visit a specialist with complaints of eczema, dermatitis, acne, and other benign conditions. Among active-duty service members, infections and allergic bite reactions are the most common reasons for a trip to a health care facility. In contrast, veterans are more likely to be diagnosed with precancerous skin conditions or to receive a screening for malignant skin cancers.
Click here to continue reading.
There is significant variation among the civilian, active-duty, and veteran populations in regard to dermatologic conditions. Civilians most frequently visit a specialist with complaints of eczema, dermatitis, acne, and other benign conditions. Among active-duty service members, infections and allergic bite reactions are the most common reasons for a trip to a health care facility. In contrast, veterans are more likely to be diagnosed with precancerous skin conditions or to receive a screening for malignant skin cancers.
Click here to continue reading.
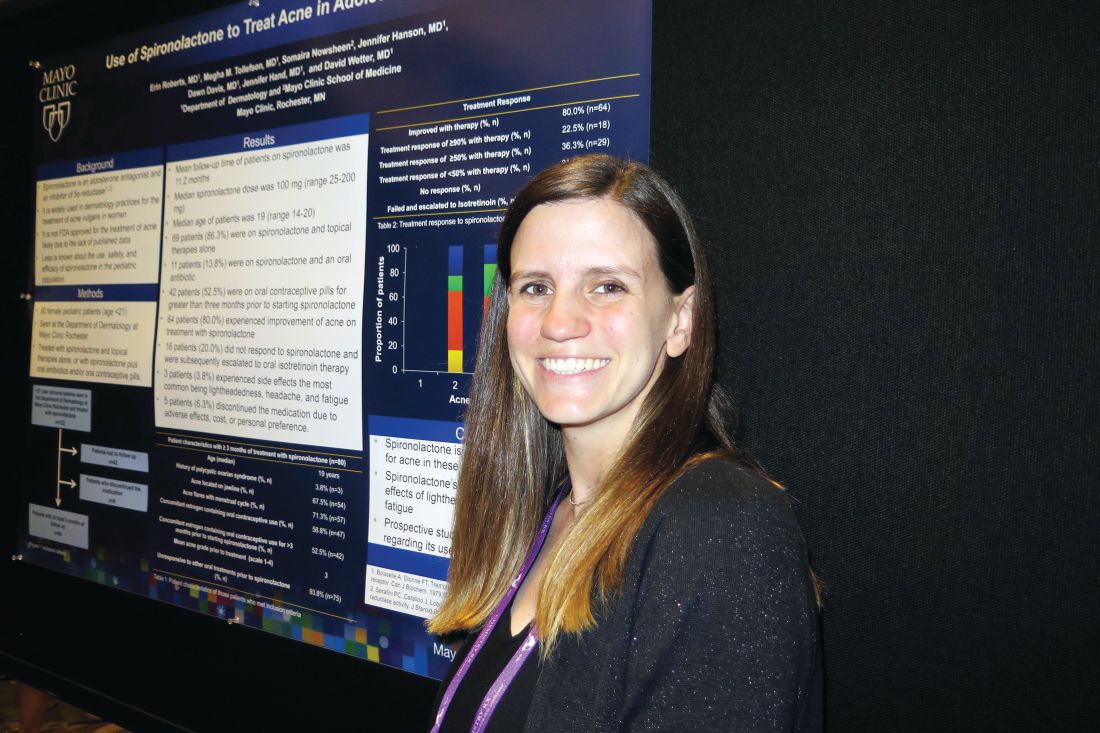
Spironolactone effectively treats acne in adolescent females
LAKE TAHOE, CALIF. –
In an interview at the annual meeting of the Society for Pediatric Dermatology, study author Erin Roberts, MD, said that while spironolactone is widely used in dermatology for treating acne vulgaris in women, it is not approved by the Food and Drug Administration for the treatment of acne, likely because published data are lacking. In addition, she said, less is known about its use, safety, and efficacy in the pediatric population.
Dr. Roberts, a resident in the department of dermatology at the Mayo Clinic, Rochester, Minn., and her associates retrospectively reviewed 80 female patients younger than 21 years of age who were treated with spironolactone and topical therapies alone, or with spironolactone plus oral antibiotics and/or contraceptive pills. All patients were seen by clinicians at the Mayo department of dermatology and were followed for a mean of 11.2 months.
The mean age of patients was 19 years and 71.3% had acne flares with their menstrual cycles, 67.5% had acne located on the jawline, 58.8% had concomitant use of an estrogen-containing oral contraceptive, and 93.8% were unresponsive to other oral treatments prior to using spironolactone.
The median spironolactone daily dose was 100 mg, and ranged between 25 mg and 200 mg. Following acne score assessments, the researchers observed that 64 of the 80 patients (80%) experienced improvement of acne on treatment with spironolactone, while 16 (20%) did not respond and were subsequently escalated to oral isotretinoin therapy. Three patients (3.8%) experienced side effects, most commonly lightheadedness, headache, and fatigue, while five patients stopped taking the medication because of adverse effects, cost, or personal preference.
“It was nice to see that spironolactone did improve acne,” Dr. Roberts said. “We think of it as something to use for patients in their 20s, but not as much for patients in their teens. I think it could be a good option for them.” She also recommended starting patients on a dose of 100 mg daily. “We saw that it does have a dose response,” Dr. Roberts said. “It wasn’t until patients got to 100 mg daily that we started to see significant improvement.”
She reported having no financial disclosures.
LAKE TAHOE, CALIF. –
In an interview at the annual meeting of the Society for Pediatric Dermatology, study author Erin Roberts, MD, said that while spironolactone is widely used in dermatology for treating acne vulgaris in women, it is not approved by the Food and Drug Administration for the treatment of acne, likely because published data are lacking. In addition, she said, less is known about its use, safety, and efficacy in the pediatric population.
Dr. Roberts, a resident in the department of dermatology at the Mayo Clinic, Rochester, Minn., and her associates retrospectively reviewed 80 female patients younger than 21 years of age who were treated with spironolactone and topical therapies alone, or with spironolactone plus oral antibiotics and/or contraceptive pills. All patients were seen by clinicians at the Mayo department of dermatology and were followed for a mean of 11.2 months.
The mean age of patients was 19 years and 71.3% had acne flares with their menstrual cycles, 67.5% had acne located on the jawline, 58.8% had concomitant use of an estrogen-containing oral contraceptive, and 93.8% were unresponsive to other oral treatments prior to using spironolactone.
The median spironolactone daily dose was 100 mg, and ranged between 25 mg and 200 mg. Following acne score assessments, the researchers observed that 64 of the 80 patients (80%) experienced improvement of acne on treatment with spironolactone, while 16 (20%) did not respond and were subsequently escalated to oral isotretinoin therapy. Three patients (3.8%) experienced side effects, most commonly lightheadedness, headache, and fatigue, while five patients stopped taking the medication because of adverse effects, cost, or personal preference.
“It was nice to see that spironolactone did improve acne,” Dr. Roberts said. “We think of it as something to use for patients in their 20s, but not as much for patients in their teens. I think it could be a good option for them.” She also recommended starting patients on a dose of 100 mg daily. “We saw that it does have a dose response,” Dr. Roberts said. “It wasn’t until patients got to 100 mg daily that we started to see significant improvement.”
She reported having no financial disclosures.
LAKE TAHOE, CALIF. –
In an interview at the annual meeting of the Society for Pediatric Dermatology, study author Erin Roberts, MD, said that while spironolactone is widely used in dermatology for treating acne vulgaris in women, it is not approved by the Food and Drug Administration for the treatment of acne, likely because published data are lacking. In addition, she said, less is known about its use, safety, and efficacy in the pediatric population.
Dr. Roberts, a resident in the department of dermatology at the Mayo Clinic, Rochester, Minn., and her associates retrospectively reviewed 80 female patients younger than 21 years of age who were treated with spironolactone and topical therapies alone, or with spironolactone plus oral antibiotics and/or contraceptive pills. All patients were seen by clinicians at the Mayo department of dermatology and were followed for a mean of 11.2 months.
The mean age of patients was 19 years and 71.3% had acne flares with their menstrual cycles, 67.5% had acne located on the jawline, 58.8% had concomitant use of an estrogen-containing oral contraceptive, and 93.8% were unresponsive to other oral treatments prior to using spironolactone.
The median spironolactone daily dose was 100 mg, and ranged between 25 mg and 200 mg. Following acne score assessments, the researchers observed that 64 of the 80 patients (80%) experienced improvement of acne on treatment with spironolactone, while 16 (20%) did not respond and were subsequently escalated to oral isotretinoin therapy. Three patients (3.8%) experienced side effects, most commonly lightheadedness, headache, and fatigue, while five patients stopped taking the medication because of adverse effects, cost, or personal preference.
“It was nice to see that spironolactone did improve acne,” Dr. Roberts said. “We think of it as something to use for patients in their 20s, but not as much for patients in their teens. I think it could be a good option for them.” She also recommended starting patients on a dose of 100 mg daily. “We saw that it does have a dose response,” Dr. Roberts said. “It wasn’t until patients got to 100 mg daily that we started to see significant improvement.”
She reported having no financial disclosures.
AT SPD 2018
Key clinical point: Use of spironolactone for acne may be limited by side effects of lightheadedness, headache, and fatigue.
Major finding: Following acne score assessments, the researchers observed that 64 of the 80 patients (80%) experienced improvement of acne on treatment with spironolactone.
Study details: A retrospective review of 80 adolescent females who were treated with spironolactone and topical therapies alone, or with spironolactone plus oral antibiotics and/or contraceptive pills.
Disclosures: Dr. Roberts reported having no financial disclosures.
New analysis improves understanding of PHACE syndrome
LAKE TAHOE, CALIF. –
In addition, children with isolated S2 or parotid hemangiomas should be recognized as having lower risk for PHACE, and specifics of evaluation should be discussed with parents on a case-by-case basis.
Those are key findings from a retrospective cohort study presented by Colleen Cotton, MD, at the annual meeting of the Society for Pediatric Dermatology.
An association between large facial hemangiomas and multiple abnormalities was described as early as 1978, but it wasn’t until 1996 that researchers first proposed the term PHACE to describe the association (Arch Dermatol. 1996;132[3]:307-11). As the National Institutes of Health explain, “PHACE is an acronym for a neurocutaneous syndrome encompassing the following features: posterior fossa brain malformations, hemangiomas of the face, arterial anomalies, cardiac anomalies, and eye abnormalities.” Official diagnostic criteria for PHACE were not established until 2009 (Pediatrics. 2009;124[5]:1447-56) and were updated in 2016 (J Pediatr. 2016;178:24-33.e2).
“A multicenter, prospective, cohort study published in 2010 estimated the incidence of PHACE to be 31% in patients with large facial hemangiomas, while a retrospective study published in 2017 estimated the incidence to be as high as 58%,” Dr. Cotton, chief dermatology resident at the University of Arizona, Tucson, said in an interview in advance of the meeting. “With the current understanding of risk for PHACE, any child with a facial hemangioma of greater than or equal to 5 cm in diameter receives a full work-up for the syndrome. However, there has been anecdotal evidence that patients with certain subtypes of hemangiomas (such as parotid hemangiomas) may not carry this same risk.”
In what is believed to be the largest study of its kind, Dr. Cotton and her associates retrospectively analyzed data from 244 patients from 13 pediatric dermatology centers who were fully evaluated for PHACE between August 2009 and December 2014. The investigators also performed subgroup analyses on different hemangioma characteristics, including parotid hemangiomas and specific facial segments of involvement. All patients underwent magnetic resonance imaging/magnetic resonance angiography of the head and neck, and the researchers collected data on age at diagnosis; gender; patterns of hemangioma presentation, including location, size, and depth; diagnostic procedures and results; and type and number of associated anomalies. An expert reviewed photographs or diagrams to confirm facial segment locations.
Of the 244 patients, 34.7% met criteria for PHACE syndrome. On multivariate analysis, the following factors were found to be independently and significantly associated with a risk for PHACE: bilateral location (positive predictive value, 54.9%), S1 involvement (PPV, 49.5%), S3 involvement (PPV, 39.5%), and area greater than 25cm2 (PPV, 44.8%), with a P value less than .05 for all associations.
Risk of PHACE also increased with the number of locations involved, with a sharp increase observed at three or more locations (PPV, 65.5%; P less than .001). In patients with one unilateral segment involved, S2 and S3 carried a significantly lower risk (P less than .03). Parotid hemangiomas had a negative predictive value of 80.4% (P = .035).
“While we found that patients with parotid hemangiomas had a lower risk of PHACE, 10 patients with parotid hemangiomas did have PHACE, and 90% of those patients had cerebral arterial anomalies,” Dr. Cotton said. “However, only one of these patients had an isolated unilateral parotid hemangioma without other facial segment involvement. Additionally, two patients with isolated involvement of the midcheek below the eye [the S2 location, which was another low risk segment] also had PHACE, both of whom would have been missed without MRI/MRA [magnetic resonance angiography].”
She acknowledged certain limitations of the study, including its retrospective design. “Additionally, many of the very large hemangiomas were not measured in size, and so, estimated sizes needed to be used in calculating relationship of hemangioma size with risk of PHACE,” she said.
The study was funded in part by a grant from the Pediatric Dermatology Research Alliance.* Dr. Cotton reported having no relevant financial disclosures.
Correction, 7/20/18: An earlier version of this article misstated the name of the Pediatric Dermatology Research Alliance.
LAKE TAHOE, CALIF. –
In addition, children with isolated S2 or parotid hemangiomas should be recognized as having lower risk for PHACE, and specifics of evaluation should be discussed with parents on a case-by-case basis.
Those are key findings from a retrospective cohort study presented by Colleen Cotton, MD, at the annual meeting of the Society for Pediatric Dermatology.
An association between large facial hemangiomas and multiple abnormalities was described as early as 1978, but it wasn’t until 1996 that researchers first proposed the term PHACE to describe the association (Arch Dermatol. 1996;132[3]:307-11). As the National Institutes of Health explain, “PHACE is an acronym for a neurocutaneous syndrome encompassing the following features: posterior fossa brain malformations, hemangiomas of the face, arterial anomalies, cardiac anomalies, and eye abnormalities.” Official diagnostic criteria for PHACE were not established until 2009 (Pediatrics. 2009;124[5]:1447-56) and were updated in 2016 (J Pediatr. 2016;178:24-33.e2).
“A multicenter, prospective, cohort study published in 2010 estimated the incidence of PHACE to be 31% in patients with large facial hemangiomas, while a retrospective study published in 2017 estimated the incidence to be as high as 58%,” Dr. Cotton, chief dermatology resident at the University of Arizona, Tucson, said in an interview in advance of the meeting. “With the current understanding of risk for PHACE, any child with a facial hemangioma of greater than or equal to 5 cm in diameter receives a full work-up for the syndrome. However, there has been anecdotal evidence that patients with certain subtypes of hemangiomas (such as parotid hemangiomas) may not carry this same risk.”
In what is believed to be the largest study of its kind, Dr. Cotton and her associates retrospectively analyzed data from 244 patients from 13 pediatric dermatology centers who were fully evaluated for PHACE between August 2009 and December 2014. The investigators also performed subgroup analyses on different hemangioma characteristics, including parotid hemangiomas and specific facial segments of involvement. All patients underwent magnetic resonance imaging/magnetic resonance angiography of the head and neck, and the researchers collected data on age at diagnosis; gender; patterns of hemangioma presentation, including location, size, and depth; diagnostic procedures and results; and type and number of associated anomalies. An expert reviewed photographs or diagrams to confirm facial segment locations.
Of the 244 patients, 34.7% met criteria for PHACE syndrome. On multivariate analysis, the following factors were found to be independently and significantly associated with a risk for PHACE: bilateral location (positive predictive value, 54.9%), S1 involvement (PPV, 49.5%), S3 involvement (PPV, 39.5%), and area greater than 25cm2 (PPV, 44.8%), with a P value less than .05 for all associations.
Risk of PHACE also increased with the number of locations involved, with a sharp increase observed at three or more locations (PPV, 65.5%; P less than .001). In patients with one unilateral segment involved, S2 and S3 carried a significantly lower risk (P less than .03). Parotid hemangiomas had a negative predictive value of 80.4% (P = .035).
“While we found that patients with parotid hemangiomas had a lower risk of PHACE, 10 patients with parotid hemangiomas did have PHACE, and 90% of those patients had cerebral arterial anomalies,” Dr. Cotton said. “However, only one of these patients had an isolated unilateral parotid hemangioma without other facial segment involvement. Additionally, two patients with isolated involvement of the midcheek below the eye [the S2 location, which was another low risk segment] also had PHACE, both of whom would have been missed without MRI/MRA [magnetic resonance angiography].”
She acknowledged certain limitations of the study, including its retrospective design. “Additionally, many of the very large hemangiomas were not measured in size, and so, estimated sizes needed to be used in calculating relationship of hemangioma size with risk of PHACE,” she said.
The study was funded in part by a grant from the Pediatric Dermatology Research Alliance.* Dr. Cotton reported having no relevant financial disclosures.
Correction, 7/20/18: An earlier version of this article misstated the name of the Pediatric Dermatology Research Alliance.
LAKE TAHOE, CALIF. –
In addition, children with isolated S2 or parotid hemangiomas should be recognized as having lower risk for PHACE, and specifics of evaluation should be discussed with parents on a case-by-case basis.
Those are key findings from a retrospective cohort study presented by Colleen Cotton, MD, at the annual meeting of the Society for Pediatric Dermatology.
An association between large facial hemangiomas and multiple abnormalities was described as early as 1978, but it wasn’t until 1996 that researchers first proposed the term PHACE to describe the association (Arch Dermatol. 1996;132[3]:307-11). As the National Institutes of Health explain, “PHACE is an acronym for a neurocutaneous syndrome encompassing the following features: posterior fossa brain malformations, hemangiomas of the face, arterial anomalies, cardiac anomalies, and eye abnormalities.” Official diagnostic criteria for PHACE were not established until 2009 (Pediatrics. 2009;124[5]:1447-56) and were updated in 2016 (J Pediatr. 2016;178:24-33.e2).
“A multicenter, prospective, cohort study published in 2010 estimated the incidence of PHACE to be 31% in patients with large facial hemangiomas, while a retrospective study published in 2017 estimated the incidence to be as high as 58%,” Dr. Cotton, chief dermatology resident at the University of Arizona, Tucson, said in an interview in advance of the meeting. “With the current understanding of risk for PHACE, any child with a facial hemangioma of greater than or equal to 5 cm in diameter receives a full work-up for the syndrome. However, there has been anecdotal evidence that patients with certain subtypes of hemangiomas (such as parotid hemangiomas) may not carry this same risk.”
In what is believed to be the largest study of its kind, Dr. Cotton and her associates retrospectively analyzed data from 244 patients from 13 pediatric dermatology centers who were fully evaluated for PHACE between August 2009 and December 2014. The investigators also performed subgroup analyses on different hemangioma characteristics, including parotid hemangiomas and specific facial segments of involvement. All patients underwent magnetic resonance imaging/magnetic resonance angiography of the head and neck, and the researchers collected data on age at diagnosis; gender; patterns of hemangioma presentation, including location, size, and depth; diagnostic procedures and results; and type and number of associated anomalies. An expert reviewed photographs or diagrams to confirm facial segment locations.
Of the 244 patients, 34.7% met criteria for PHACE syndrome. On multivariate analysis, the following factors were found to be independently and significantly associated with a risk for PHACE: bilateral location (positive predictive value, 54.9%), S1 involvement (PPV, 49.5%), S3 involvement (PPV, 39.5%), and area greater than 25cm2 (PPV, 44.8%), with a P value less than .05 for all associations.
Risk of PHACE also increased with the number of locations involved, with a sharp increase observed at three or more locations (PPV, 65.5%; P less than .001). In patients with one unilateral segment involved, S2 and S3 carried a significantly lower risk (P less than .03). Parotid hemangiomas had a negative predictive value of 80.4% (P = .035).
“While we found that patients with parotid hemangiomas had a lower risk of PHACE, 10 patients with parotid hemangiomas did have PHACE, and 90% of those patients had cerebral arterial anomalies,” Dr. Cotton said. “However, only one of these patients had an isolated unilateral parotid hemangioma without other facial segment involvement. Additionally, two patients with isolated involvement of the midcheek below the eye [the S2 location, which was another low risk segment] also had PHACE, both of whom would have been missed without MRI/MRA [magnetic resonance angiography].”
She acknowledged certain limitations of the study, including its retrospective design. “Additionally, many of the very large hemangiomas were not measured in size, and so, estimated sizes needed to be used in calculating relationship of hemangioma size with risk of PHACE,” she said.
The study was funded in part by a grant from the Pediatric Dermatology Research Alliance.* Dr. Cotton reported having no relevant financial disclosures.
Correction, 7/20/18: An earlier version of this article misstated the name of the Pediatric Dermatology Research Alliance.
FROM SPD 2018
Key clinical point: Children with large, high-risk facial hemangiomas should be prioritized for PHACE syndrome work-up.
Major finding: On multivariate analysis, the following factors were found to be independently and significantly associated with a risk for PHACE: bilateral location (positive predictive value, 54.9%), S1 involvement (PPV, 49.5%), S3 involvement (PPV, 39.5%), and area greater than 25 cm2 (PPV, 44.8%; P less than .05 for all associations).
Study details: A retrospective evaluation of 244 patients from 13 pediatric dermatology who were fully evaluated for PHACE between August 2009 and December 2014.
Disclosures: The study was funded in part by a grant from the Pediatric Dermatology Research Association. Dr. Cotton reported having no financial disclosures.
Rash on forearm
The FP did not recognize the rash, so she decided to do a Google search. She typed the following terms into the search box: linear hypopigmented papules on the arm of a child. Almost every result described lichen striatus.
The photographs were very similar, and the description was a great fit for the patient’s condition. Clearly, this was not poison ivy and was unrelated to the camping trip. The physician learned that lichen striatus is a benign idiopathic condition that often affects children on a single extremity. The flat-topped papules tend to run parallel to the long axis of the extremity following Blaschko lines (lines related to embryogenesis). In darker-skinned patients, the papules are often hypopigmented. The papules are usually asymptomatic and resolve on their own, over time.
The mother was reassured and happy to hear that this would go away without any treatment. The physician was delighted to have been able to make a diagnosis by using her ability to describe the rash and the “intelligence” of the search engine.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
The FP did not recognize the rash, so she decided to do a Google search. She typed the following terms into the search box: linear hypopigmented papules on the arm of a child. Almost every result described lichen striatus.
The photographs were very similar, and the description was a great fit for the patient’s condition. Clearly, this was not poison ivy and was unrelated to the camping trip. The physician learned that lichen striatus is a benign idiopathic condition that often affects children on a single extremity. The flat-topped papules tend to run parallel to the long axis of the extremity following Blaschko lines (lines related to embryogenesis). In darker-skinned patients, the papules are often hypopigmented. The papules are usually asymptomatic and resolve on their own, over time.
The mother was reassured and happy to hear that this would go away without any treatment. The physician was delighted to have been able to make a diagnosis by using her ability to describe the rash and the “intelligence” of the search engine.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
The FP did not recognize the rash, so she decided to do a Google search. She typed the following terms into the search box: linear hypopigmented papules on the arm of a child. Almost every result described lichen striatus.
The photographs were very similar, and the description was a great fit for the patient’s condition. Clearly, this was not poison ivy and was unrelated to the camping trip. The physician learned that lichen striatus is a benign idiopathic condition that often affects children on a single extremity. The flat-topped papules tend to run parallel to the long axis of the extremity following Blaschko lines (lines related to embryogenesis). In darker-skinned patients, the papules are often hypopigmented. The papules are usually asymptomatic and resolve on their own, over time.
The mother was reassured and happy to hear that this would go away without any treatment. The physician was delighted to have been able to make a diagnosis by using her ability to describe the rash and the “intelligence” of the search engine.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
Early BCC seen in teen kidney transplant patient
A 17-year-old girl seen in a Portuguese dermatology clinic was found to have a nodular basal cell carcinoma on the parietal region of her scalp. The nodule appeared 6 years after she had received a kidney transplant, according to João Borges-Costa, MD, PhD, who submitted the case report.
Since the transplant, the girl had been maintained on immunosuppressive medication of tacrolimus 1 mg twice daily, mycophenolate sodium 360 mg twice daily, and prednisolone 10 mg every other day. The 1-cm nodule was pigmented; dermatoscopy did not yield clarity about whether the lesion was melanocytic. An excisional biopsy with 0.5-cm margins was performed, and histology confirmed that the lesion was a nodular pigmented basal cell carcinoma that had been excised completely.
The case, said Dr. Borges-Costa, shows that skin cancers can develop earlier than the typical 12-18 years after pediatric transplantation. Most reported cases have been squamous cell cancers and melanomas, and often are associated with lack of appropriate sun protection behavior.
The patient, a Caucasian, was a sailor who used sunscreen but did not typically wear a hat while sailing, reported Dr. Borges-Costa, a dermatologist at the University of Lisbon. Her family history was significant for a grandparent with melanoma.
Dr. Borges noted that the parents and patient were given advice regarding the importance of the lifelong use of sun-protective clothing and headgear. “Education of pediatric organ recipients and their parents about sun protection is important because, as occurred with our patient, protective clothing and hats are frequently forgotten.”
Because of the ongoing potential for skin malignancies, early referral “after transplantation to specialized dermatology outpatient clinics, similar to what is now advocated for transplanted adults, could help in surveillance and improve adherence to sun-protective measures,” he added.
SOURCE: Borges-Costa J et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13537..
A 17-year-old girl seen in a Portuguese dermatology clinic was found to have a nodular basal cell carcinoma on the parietal region of her scalp. The nodule appeared 6 years after she had received a kidney transplant, according to João Borges-Costa, MD, PhD, who submitted the case report.
Since the transplant, the girl had been maintained on immunosuppressive medication of tacrolimus 1 mg twice daily, mycophenolate sodium 360 mg twice daily, and prednisolone 10 mg every other day. The 1-cm nodule was pigmented; dermatoscopy did not yield clarity about whether the lesion was melanocytic. An excisional biopsy with 0.5-cm margins was performed, and histology confirmed that the lesion was a nodular pigmented basal cell carcinoma that had been excised completely.
The case, said Dr. Borges-Costa, shows that skin cancers can develop earlier than the typical 12-18 years after pediatric transplantation. Most reported cases have been squamous cell cancers and melanomas, and often are associated with lack of appropriate sun protection behavior.
The patient, a Caucasian, was a sailor who used sunscreen but did not typically wear a hat while sailing, reported Dr. Borges-Costa, a dermatologist at the University of Lisbon. Her family history was significant for a grandparent with melanoma.
Dr. Borges noted that the parents and patient were given advice regarding the importance of the lifelong use of sun-protective clothing and headgear. “Education of pediatric organ recipients and their parents about sun protection is important because, as occurred with our patient, protective clothing and hats are frequently forgotten.”
Because of the ongoing potential for skin malignancies, early referral “after transplantation to specialized dermatology outpatient clinics, similar to what is now advocated for transplanted adults, could help in surveillance and improve adherence to sun-protective measures,” he added.
SOURCE: Borges-Costa J et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13537..
A 17-year-old girl seen in a Portuguese dermatology clinic was found to have a nodular basal cell carcinoma on the parietal region of her scalp. The nodule appeared 6 years after she had received a kidney transplant, according to João Borges-Costa, MD, PhD, who submitted the case report.
Since the transplant, the girl had been maintained on immunosuppressive medication of tacrolimus 1 mg twice daily, mycophenolate sodium 360 mg twice daily, and prednisolone 10 mg every other day. The 1-cm nodule was pigmented; dermatoscopy did not yield clarity about whether the lesion was melanocytic. An excisional biopsy with 0.5-cm margins was performed, and histology confirmed that the lesion was a nodular pigmented basal cell carcinoma that had been excised completely.
The case, said Dr. Borges-Costa, shows that skin cancers can develop earlier than the typical 12-18 years after pediatric transplantation. Most reported cases have been squamous cell cancers and melanomas, and often are associated with lack of appropriate sun protection behavior.
The patient, a Caucasian, was a sailor who used sunscreen but did not typically wear a hat while sailing, reported Dr. Borges-Costa, a dermatologist at the University of Lisbon. Her family history was significant for a grandparent with melanoma.
Dr. Borges noted that the parents and patient were given advice regarding the importance of the lifelong use of sun-protective clothing and headgear. “Education of pediatric organ recipients and their parents about sun protection is important because, as occurred with our patient, protective clothing and hats are frequently forgotten.”
Because of the ongoing potential for skin malignancies, early referral “after transplantation to specialized dermatology outpatient clinics, similar to what is now advocated for transplanted adults, could help in surveillance and improve adherence to sun-protective measures,” he added.
SOURCE: Borges-Costa J et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13537..
FROM PEDIATRIC DERMATOLOGY
Sunscreen use in grade schoolers: Wide racial, ethnic disparities seen
and the figures were much lower for non-Hispanic black children.
Just 23% of fifth graders almost always used sunscreen, according to data drawn from the Healthy Passages study, which surveyed the parents or caregivers of 5,119 fifth graders. That figure was similar in the 1,802 Hispanic respondents, but fell to just 6% of the 1,748 non-Hispanic black respondents.
Some other factors that were associated with less chance of adherence to sunscreen use included being male and having lower socioeconomic status, wrote Christina M. Correnti, MD, and her study coauthors. The report was published in in Pediatric Dermatology. Perhaps surprisingly, they said, “School-based sun-safety education and involvement in team sports were not significant factors.”
Healthy Passages is a prospective multisite cohort study of child and adolescent health. Dr. Correnti, a dermatology resident at the University of Maryland, Baltimore, and her colleagues used baseline Healthy Passages data collected from the period of 2004-2006. Children enrolled in fifth grade at public schools in Birmingham, Ala., Houston, and Los Angeles, together with their caregivers, participated in the survey. Deidentified demographic data were collected, and participants were asked about four preventive health behaviors in addition to sunscreen use and flossing teeth: brushing teeth, helmet use, seatbelt use, and well-child examinations.
Dr. Correnti and her colleagues used multivariable analysis to calculate odds ratios for the association between the various demographic factors and other preventive behaviors and sunscreen use. They found that sunscreen adherence was correlated with all other preventive behaviors (P less than .001), but that the interrelationship with helmet use was confounded by racial and ethnic variables. Seatbelt use was not significantly correlated with sunscreen use for non-Hispanic black or Hispanic respondents.
“Children from more-educated and affluent households were more likely to use sun protection. Perhaps they had greater parental awareness and practice of sun safe habits,” wrote Dr. Correnti and her colleagues, noting that other work has shown that even low-income parents generally don’t see the cost of sunscreen as a barrier to use.
Although overall use of sunscreen among non-Hispanic black children was low, both non-Hispanic black and Hispanic children were more likely to use sunscreen if they had three or more sunburns within the prior 12 months. “Although darker skin tones may afford some sun protection, melanoma incidence is growing in Hispanic populations,” the researchers wrote.
To address these overall low rates of sunscreen use, the investigators discussed the utility of a variety of education options. The well-child visit affords an opportunity to reinforce the importance of preventive behaviors, but physicians may run into a time crunch and forgo thorough sun safety education, they said. Written materials can be a useful adjunct for clinicians in this setting.
“Health care practitioners may use absence of other preventive behaviors as potential markers for inadequate sunscreen use, prompting a point-of-care sun-safety intervention,” they suggested.
A school-based public health approach offers another route for education. “School sun-safety programs may alleviate the primary care burden,” wrote Dr. Correnti and her coinvestigators. The opportunity to deliver repeated, age-tailored messages as children progress through school may be effective in promoting healthy sun behaviors. Messaging that focuses on the negative effects of sun exposure on appearance such as age spots and wrinkles have been more effective than those warning of the risk of skin cancer for teens; investigating appearance-based content for this age group might be a good idea, the authors said.
The fact that the survey sites were in southern cities may mean that national rates of consistent sunscreen use for elementary schoolers may be even lower, said Dr. Correnti and her coauthors. Many other real-world factors, such as frequency and amount of sunscreen applied and the use of sun-protective clothing, couldn’t be captured by the survey, they acknowledged.
“Even in the most adherent group, non-Hispanic whites, only 44.8% always used sunscreen,” the researchers wrote. The study’s findings leave plenty of room for implementation of broad-based programs, especially in low-resource communities.
The National Institutes of Health funded the research. Dr. Correnti was supported by NIH awards.
SOURCE: Correnti CM et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13550.
and the figures were much lower for non-Hispanic black children.
Just 23% of fifth graders almost always used sunscreen, according to data drawn from the Healthy Passages study, which surveyed the parents or caregivers of 5,119 fifth graders. That figure was similar in the 1,802 Hispanic respondents, but fell to just 6% of the 1,748 non-Hispanic black respondents.
Some other factors that were associated with less chance of adherence to sunscreen use included being male and having lower socioeconomic status, wrote Christina M. Correnti, MD, and her study coauthors. The report was published in in Pediatric Dermatology. Perhaps surprisingly, they said, “School-based sun-safety education and involvement in team sports were not significant factors.”
Healthy Passages is a prospective multisite cohort study of child and adolescent health. Dr. Correnti, a dermatology resident at the University of Maryland, Baltimore, and her colleagues used baseline Healthy Passages data collected from the period of 2004-2006. Children enrolled in fifth grade at public schools in Birmingham, Ala., Houston, and Los Angeles, together with their caregivers, participated in the survey. Deidentified demographic data were collected, and participants were asked about four preventive health behaviors in addition to sunscreen use and flossing teeth: brushing teeth, helmet use, seatbelt use, and well-child examinations.
Dr. Correnti and her colleagues used multivariable analysis to calculate odds ratios for the association between the various demographic factors and other preventive behaviors and sunscreen use. They found that sunscreen adherence was correlated with all other preventive behaviors (P less than .001), but that the interrelationship with helmet use was confounded by racial and ethnic variables. Seatbelt use was not significantly correlated with sunscreen use for non-Hispanic black or Hispanic respondents.
“Children from more-educated and affluent households were more likely to use sun protection. Perhaps they had greater parental awareness and practice of sun safe habits,” wrote Dr. Correnti and her colleagues, noting that other work has shown that even low-income parents generally don’t see the cost of sunscreen as a barrier to use.
Although overall use of sunscreen among non-Hispanic black children was low, both non-Hispanic black and Hispanic children were more likely to use sunscreen if they had three or more sunburns within the prior 12 months. “Although darker skin tones may afford some sun protection, melanoma incidence is growing in Hispanic populations,” the researchers wrote.
To address these overall low rates of sunscreen use, the investigators discussed the utility of a variety of education options. The well-child visit affords an opportunity to reinforce the importance of preventive behaviors, but physicians may run into a time crunch and forgo thorough sun safety education, they said. Written materials can be a useful adjunct for clinicians in this setting.
“Health care practitioners may use absence of other preventive behaviors as potential markers for inadequate sunscreen use, prompting a point-of-care sun-safety intervention,” they suggested.
A school-based public health approach offers another route for education. “School sun-safety programs may alleviate the primary care burden,” wrote Dr. Correnti and her coinvestigators. The opportunity to deliver repeated, age-tailored messages as children progress through school may be effective in promoting healthy sun behaviors. Messaging that focuses on the negative effects of sun exposure on appearance such as age spots and wrinkles have been more effective than those warning of the risk of skin cancer for teens; investigating appearance-based content for this age group might be a good idea, the authors said.
The fact that the survey sites were in southern cities may mean that national rates of consistent sunscreen use for elementary schoolers may be even lower, said Dr. Correnti and her coauthors. Many other real-world factors, such as frequency and amount of sunscreen applied and the use of sun-protective clothing, couldn’t be captured by the survey, they acknowledged.
“Even in the most adherent group, non-Hispanic whites, only 44.8% always used sunscreen,” the researchers wrote. The study’s findings leave plenty of room for implementation of broad-based programs, especially in low-resource communities.
The National Institutes of Health funded the research. Dr. Correnti was supported by NIH awards.
SOURCE: Correnti CM et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13550.
and the figures were much lower for non-Hispanic black children.
Just 23% of fifth graders almost always used sunscreen, according to data drawn from the Healthy Passages study, which surveyed the parents or caregivers of 5,119 fifth graders. That figure was similar in the 1,802 Hispanic respondents, but fell to just 6% of the 1,748 non-Hispanic black respondents.
Some other factors that were associated with less chance of adherence to sunscreen use included being male and having lower socioeconomic status, wrote Christina M. Correnti, MD, and her study coauthors. The report was published in in Pediatric Dermatology. Perhaps surprisingly, they said, “School-based sun-safety education and involvement in team sports were not significant factors.”
Healthy Passages is a prospective multisite cohort study of child and adolescent health. Dr. Correnti, a dermatology resident at the University of Maryland, Baltimore, and her colleagues used baseline Healthy Passages data collected from the period of 2004-2006. Children enrolled in fifth grade at public schools in Birmingham, Ala., Houston, and Los Angeles, together with their caregivers, participated in the survey. Deidentified demographic data were collected, and participants were asked about four preventive health behaviors in addition to sunscreen use and flossing teeth: brushing teeth, helmet use, seatbelt use, and well-child examinations.
Dr. Correnti and her colleagues used multivariable analysis to calculate odds ratios for the association between the various demographic factors and other preventive behaviors and sunscreen use. They found that sunscreen adherence was correlated with all other preventive behaviors (P less than .001), but that the interrelationship with helmet use was confounded by racial and ethnic variables. Seatbelt use was not significantly correlated with sunscreen use for non-Hispanic black or Hispanic respondents.
“Children from more-educated and affluent households were more likely to use sun protection. Perhaps they had greater parental awareness and practice of sun safe habits,” wrote Dr. Correnti and her colleagues, noting that other work has shown that even low-income parents generally don’t see the cost of sunscreen as a barrier to use.
Although overall use of sunscreen among non-Hispanic black children was low, both non-Hispanic black and Hispanic children were more likely to use sunscreen if they had three or more sunburns within the prior 12 months. “Although darker skin tones may afford some sun protection, melanoma incidence is growing in Hispanic populations,” the researchers wrote.
To address these overall low rates of sunscreen use, the investigators discussed the utility of a variety of education options. The well-child visit affords an opportunity to reinforce the importance of preventive behaviors, but physicians may run into a time crunch and forgo thorough sun safety education, they said. Written materials can be a useful adjunct for clinicians in this setting.
“Health care practitioners may use absence of other preventive behaviors as potential markers for inadequate sunscreen use, prompting a point-of-care sun-safety intervention,” they suggested.
A school-based public health approach offers another route for education. “School sun-safety programs may alleviate the primary care burden,” wrote Dr. Correnti and her coinvestigators. The opportunity to deliver repeated, age-tailored messages as children progress through school may be effective in promoting healthy sun behaviors. Messaging that focuses on the negative effects of sun exposure on appearance such as age spots and wrinkles have been more effective than those warning of the risk of skin cancer for teens; investigating appearance-based content for this age group might be a good idea, the authors said.
The fact that the survey sites were in southern cities may mean that national rates of consistent sunscreen use for elementary schoolers may be even lower, said Dr. Correnti and her coauthors. Many other real-world factors, such as frequency and amount of sunscreen applied and the use of sun-protective clothing, couldn’t be captured by the survey, they acknowledged.
“Even in the most adherent group, non-Hispanic whites, only 44.8% always used sunscreen,” the researchers wrote. The study’s findings leave plenty of room for implementation of broad-based programs, especially in low-resource communities.
The National Institutes of Health funded the research. Dr. Correnti was supported by NIH awards.
SOURCE: Correnti CM et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13550.
FROM PEDIATRIC DERMATOLOGY
Key clinical point: Most parents surveyed said their children didn’t use sunscreen consistently.
Major finding: Of non-Hispanic black children, 6% almost always used sunscreen.
Study details: Data drawn from Healthy Passages, a prospective cohort study of 5,119 fifth-graders and their parents or caregivers.
Disclosures: The National Institutes of Health funded the research. Dr. Correnti was supported by NIH awards.
Source: Correnti C et al. Pediatr Dermatol. 2018. doi: 10.1111/pde.13550.
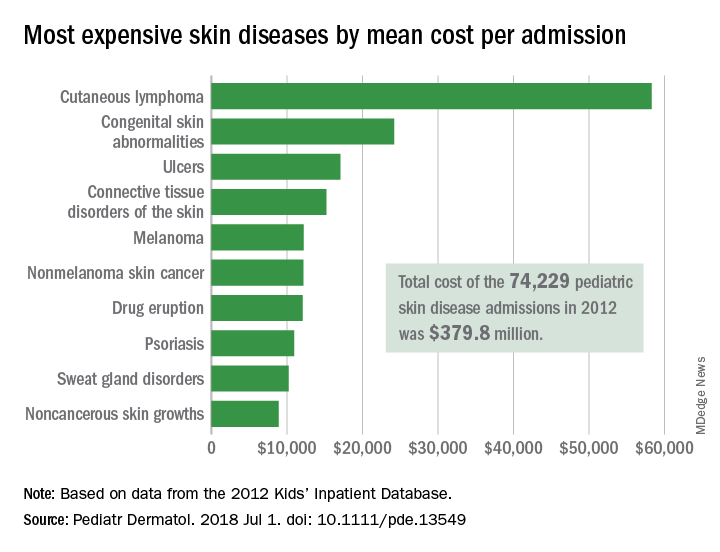
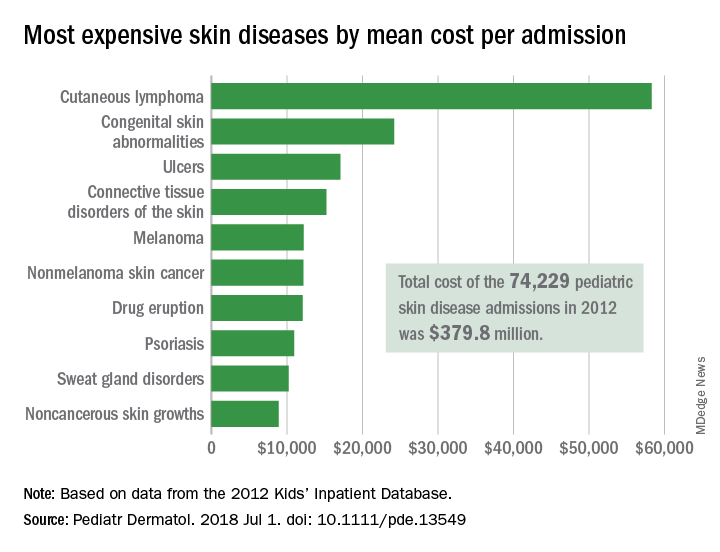
Pediatric dermatology admissions: Crunching the numbers
according to data from the Agency for Healthcare Research and Quality.
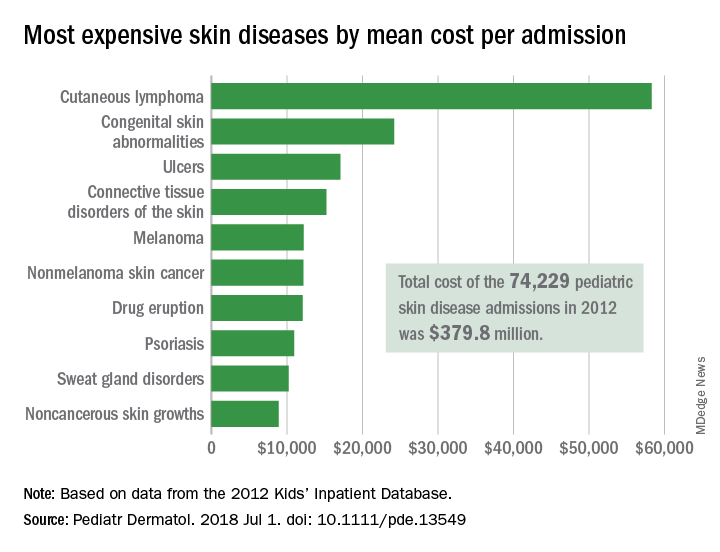
There were 74,229 such admissions in the United States that year – all others totaled 1.77 million – and the children at the highest risk for dermatology hospitalization were those living in communities with the lowest household incomes, the uninsured and those on Medicaid, and those living in the South, Justin D. Arnold of George Washington University, Washington, and his associates said in Pediatric Dermatology.
“Individuals from communities of low socioeconomic status may be more likely to be hospitalized because of gaps in insurance coverage, difficulty with transportation, or inconsistent access to preventative medical care, which for skin disease, would include access to an outpatient pediatric dermatologist,” they wrote.
All those admissions for skin diseases cost the health care system $379.8 million in 2012, or 1.9% of the $20.3 billion spent on all pediatric hospitalizations, excluding those related to pregnancy or childbirth. The mean cost of a skin disease admission was $5,211 for a child aged less than 18 years, compared with $11,409 for nondermatology admissions, according to data from the 2012 Kids’ Inpatient Database, which includes records of pediatric discharges from 44 states.
Cutaneous lymphoma was the most expensive skin disease per admission at a mean cost of $58,294, with congenital skin abnormalities second at $24,186, and ulcers third at $17,064. Bacterial skin infections and infestations were only the 19th most expensive admission at $4,135, but it was by far the most common (59,115 admissions) and the most expensive overall, with a total cost of $240 million. The second most common condition was viral diseases with 3,812 admissions and the next most expensive total was $33.5 million for connective tissue disorders, Mr. Arnold and his associates said.
Multivariate models that adjusted for such factors as age, sex, and race revealed that “the risk of hospitalization for skin disease increased as the median income of one’s zip code declined,” the investigators noted. The adjusted odds ratio for hospitalization in the lowest-income quartile (less than $39,000) was 1.22, compared with the highest-income quartile.
Insurance status also affected hospitalization, putting children from families with no insurance (aOR, 1.35) and those on Medicaid (aOR, 1.17) at a disadvantage, compared with those who had private insurance. “Policy makers should consider increasing Medicaid reimbursement rates to outpatient dermatologists, which might encourage more clinicians to accept this form of insurance and thereby expand access to preventative skin care,” they said.
Regional differences also were observed, which put children from the southern states at the highest risk (aOR, 1.32), compared with those in the West, which could be related to access issues. “In 2016, 4 of the 10 communities in the United States with the lowest density of dermatologists were in the South, suggesting that the high rate of hospitalizations there may also be partially attributed to lack of access to dermatologists,” Mr. Arnold and his associates wrote.
The investigators did not report funding or disclose conflicts of interest.
SOURCE: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
according to data from the Agency for Healthcare Research and Quality.
There were 74,229 such admissions in the United States that year – all others totaled 1.77 million – and the children at the highest risk for dermatology hospitalization were those living in communities with the lowest household incomes, the uninsured and those on Medicaid, and those living in the South, Justin D. Arnold of George Washington University, Washington, and his associates said in Pediatric Dermatology.
“Individuals from communities of low socioeconomic status may be more likely to be hospitalized because of gaps in insurance coverage, difficulty with transportation, or inconsistent access to preventative medical care, which for skin disease, would include access to an outpatient pediatric dermatologist,” they wrote.
All those admissions for skin diseases cost the health care system $379.8 million in 2012, or 1.9% of the $20.3 billion spent on all pediatric hospitalizations, excluding those related to pregnancy or childbirth. The mean cost of a skin disease admission was $5,211 for a child aged less than 18 years, compared with $11,409 for nondermatology admissions, according to data from the 2012 Kids’ Inpatient Database, which includes records of pediatric discharges from 44 states.
Cutaneous lymphoma was the most expensive skin disease per admission at a mean cost of $58,294, with congenital skin abnormalities second at $24,186, and ulcers third at $17,064. Bacterial skin infections and infestations were only the 19th most expensive admission at $4,135, but it was by far the most common (59,115 admissions) and the most expensive overall, with a total cost of $240 million. The second most common condition was viral diseases with 3,812 admissions and the next most expensive total was $33.5 million for connective tissue disorders, Mr. Arnold and his associates said.
Multivariate models that adjusted for such factors as age, sex, and race revealed that “the risk of hospitalization for skin disease increased as the median income of one’s zip code declined,” the investigators noted. The adjusted odds ratio for hospitalization in the lowest-income quartile (less than $39,000) was 1.22, compared with the highest-income quartile.
Insurance status also affected hospitalization, putting children from families with no insurance (aOR, 1.35) and those on Medicaid (aOR, 1.17) at a disadvantage, compared with those who had private insurance. “Policy makers should consider increasing Medicaid reimbursement rates to outpatient dermatologists, which might encourage more clinicians to accept this form of insurance and thereby expand access to preventative skin care,” they said.
Regional differences also were observed, which put children from the southern states at the highest risk (aOR, 1.32), compared with those in the West, which could be related to access issues. “In 2016, 4 of the 10 communities in the United States with the lowest density of dermatologists were in the South, suggesting that the high rate of hospitalizations there may also be partially attributed to lack of access to dermatologists,” Mr. Arnold and his associates wrote.
The investigators did not report funding or disclose conflicts of interest.
SOURCE: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
according to data from the Agency for Healthcare Research and Quality.
There were 74,229 such admissions in the United States that year – all others totaled 1.77 million – and the children at the highest risk for dermatology hospitalization were those living in communities with the lowest household incomes, the uninsured and those on Medicaid, and those living in the South, Justin D. Arnold of George Washington University, Washington, and his associates said in Pediatric Dermatology.
“Individuals from communities of low socioeconomic status may be more likely to be hospitalized because of gaps in insurance coverage, difficulty with transportation, or inconsistent access to preventative medical care, which for skin disease, would include access to an outpatient pediatric dermatologist,” they wrote.
All those admissions for skin diseases cost the health care system $379.8 million in 2012, or 1.9% of the $20.3 billion spent on all pediatric hospitalizations, excluding those related to pregnancy or childbirth. The mean cost of a skin disease admission was $5,211 for a child aged less than 18 years, compared with $11,409 for nondermatology admissions, according to data from the 2012 Kids’ Inpatient Database, which includes records of pediatric discharges from 44 states.
Cutaneous lymphoma was the most expensive skin disease per admission at a mean cost of $58,294, with congenital skin abnormalities second at $24,186, and ulcers third at $17,064. Bacterial skin infections and infestations were only the 19th most expensive admission at $4,135, but it was by far the most common (59,115 admissions) and the most expensive overall, with a total cost of $240 million. The second most common condition was viral diseases with 3,812 admissions and the next most expensive total was $33.5 million for connective tissue disorders, Mr. Arnold and his associates said.
Multivariate models that adjusted for such factors as age, sex, and race revealed that “the risk of hospitalization for skin disease increased as the median income of one’s zip code declined,” the investigators noted. The adjusted odds ratio for hospitalization in the lowest-income quartile (less than $39,000) was 1.22, compared with the highest-income quartile.
Insurance status also affected hospitalization, putting children from families with no insurance (aOR, 1.35) and those on Medicaid (aOR, 1.17) at a disadvantage, compared with those who had private insurance. “Policy makers should consider increasing Medicaid reimbursement rates to outpatient dermatologists, which might encourage more clinicians to accept this form of insurance and thereby expand access to preventative skin care,” they said.
Regional differences also were observed, which put children from the southern states at the highest risk (aOR, 1.32), compared with those in the West, which could be related to access issues. “In 2016, 4 of the 10 communities in the United States with the lowest density of dermatologists were in the South, suggesting that the high rate of hospitalizations there may also be partially attributed to lack of access to dermatologists,” Mr. Arnold and his associates wrote.
The investigators did not report funding or disclose conflicts of interest.
SOURCE: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
FROM PEDIATRIC DERMATOLOGY
Key clinical point: Children at the highest risk for dermatology hospitalization lived in communities with the lowest household incomes, were uninsured or on Medicaid, or lived in the South.
Major finding: Admissions for skin diseases cost $379.8 million in 2012, or 1.9% of all spending on pediatric hospitalizations.
Study details: A statistical analysis of the 2012 Kids’ Inpatient Database.
Disclosures: The investigators did not report funding or disclose conflicts of interest.
Source: Arnold JD et al. Pediatr Dermatol. 2018 Jul 1. doi: 10.1111/pde.13549.
Under the Cover of Darkness
When he was about 12, a now 41-year-old man noticed that the skin on his left chest was darkening. For several years afterward, the darkness spread and deepened, and the area became hairy. In young adulthood, he experienced occasional outbreaks of what looked like acne on the lesion; this eventually cleared.
He now finds the hairiness increasingly bothersome, so he shaves the worst parts of it. Upon consulting his primary care provider, he was assured that the lesion is “a birthmark.” Unsatisfied with this answer, the patient took the advice of a friend and decided to consult dermatology.
EXAMINATION
A polygonal, hyperpigmented, hypertrichotic patch covers most of the patient’s left pectoral area. The lateral margin is irregular but well-defined. There is obvious partial regrowth of the shaved hair on the lateral margin, but it stops abruptly at that point.

The breast and surrounding tissue appear normal. No areas of hyperpigmentation or hypertrichosis are seen elsewhere.
What is the diagnosis?
DISCUSSION
First described by William Becker in 1948 (and subsequently named for him), the Becker nevus (BN) received little research attention until a French study of 20,000 young men showed a prevalence of 0.5%. Nearly half of the subjects had first noticed the lesion before the age of 10—a somewhat surprising finding, since abundant evidence implicates androgens in its genesis. (This is supported by the condition’s predominance in males, the increased numbers of androgen receptors and melanocytes in the affected skin, and the prevalence of hypertrichosis.)
The researchers were also surprised to find that only 30% of the reported lesions occurred above the nipple, because the first descriptions of BN gave the impression that the shoulder and chest were most commonly affected. We now know that BN can also be found on arms and legs.
Usually a benign condition, BN can be associated with skeletal or soft-tissue deformities in the affected area (eg, ipsilateral breast hypoplasia). Malignancies—most notably melanoma—have also been reported with BN but are especially uncommon.
The differential includes the café-au-lait macules of neurofibromatosis, Albright disease, and congenital melanocytic nevus. The history of BN (ie, presentation, hypertrichosis, gender of patient, and distribution) usually allow a clinical diagnosis.
Treatment is limited to laser hair removal or laser removal or reduction of pigment.
TAKE-HOME LEARNING POINTS
- Becker nevus (BN) is far more common in males than females.
- BN typically manifests during puberty, which aligns with the suspected androgenic etiology.
- Though the shoulders and chest are the most commonly affected areas, BNs can also appear on the flank, arms, or legs.
- The lesions are rarely associated with serious pathology; hypoplasia of the ipsilateral breast is the most common of these complications.
When he was about 12, a now 41-year-old man noticed that the skin on his left chest was darkening. For several years afterward, the darkness spread and deepened, and the area became hairy. In young adulthood, he experienced occasional outbreaks of what looked like acne on the lesion; this eventually cleared.
He now finds the hairiness increasingly bothersome, so he shaves the worst parts of it. Upon consulting his primary care provider, he was assured that the lesion is “a birthmark.” Unsatisfied with this answer, the patient took the advice of a friend and decided to consult dermatology.
EXAMINATION
A polygonal, hyperpigmented, hypertrichotic patch covers most of the patient’s left pectoral area. The lateral margin is irregular but well-defined. There is obvious partial regrowth of the shaved hair on the lateral margin, but it stops abruptly at that point.

The breast and surrounding tissue appear normal. No areas of hyperpigmentation or hypertrichosis are seen elsewhere.
What is the diagnosis?
DISCUSSION
First described by William Becker in 1948 (and subsequently named for him), the Becker nevus (BN) received little research attention until a French study of 20,000 young men showed a prevalence of 0.5%. Nearly half of the subjects had first noticed the lesion before the age of 10—a somewhat surprising finding, since abundant evidence implicates androgens in its genesis. (This is supported by the condition’s predominance in males, the increased numbers of androgen receptors and melanocytes in the affected skin, and the prevalence of hypertrichosis.)
The researchers were also surprised to find that only 30% of the reported lesions occurred above the nipple, because the first descriptions of BN gave the impression that the shoulder and chest were most commonly affected. We now know that BN can also be found on arms and legs.
Usually a benign condition, BN can be associated with skeletal or soft-tissue deformities in the affected area (eg, ipsilateral breast hypoplasia). Malignancies—most notably melanoma—have also been reported with BN but are especially uncommon.
The differential includes the café-au-lait macules of neurofibromatosis, Albright disease, and congenital melanocytic nevus. The history of BN (ie, presentation, hypertrichosis, gender of patient, and distribution) usually allow a clinical diagnosis.
Treatment is limited to laser hair removal or laser removal or reduction of pigment.
TAKE-HOME LEARNING POINTS
- Becker nevus (BN) is far more common in males than females.
- BN typically manifests during puberty, which aligns with the suspected androgenic etiology.
- Though the shoulders and chest are the most commonly affected areas, BNs can also appear on the flank, arms, or legs.
- The lesions are rarely associated with serious pathology; hypoplasia of the ipsilateral breast is the most common of these complications.
When he was about 12, a now 41-year-old man noticed that the skin on his left chest was darkening. For several years afterward, the darkness spread and deepened, and the area became hairy. In young adulthood, he experienced occasional outbreaks of what looked like acne on the lesion; this eventually cleared.
He now finds the hairiness increasingly bothersome, so he shaves the worst parts of it. Upon consulting his primary care provider, he was assured that the lesion is “a birthmark.” Unsatisfied with this answer, the patient took the advice of a friend and decided to consult dermatology.
EXAMINATION
A polygonal, hyperpigmented, hypertrichotic patch covers most of the patient’s left pectoral area. The lateral margin is irregular but well-defined. There is obvious partial regrowth of the shaved hair on the lateral margin, but it stops abruptly at that point.

The breast and surrounding tissue appear normal. No areas of hyperpigmentation or hypertrichosis are seen elsewhere.
What is the diagnosis?
DISCUSSION
First described by William Becker in 1948 (and subsequently named for him), the Becker nevus (BN) received little research attention until a French study of 20,000 young men showed a prevalence of 0.5%. Nearly half of the subjects had first noticed the lesion before the age of 10—a somewhat surprising finding, since abundant evidence implicates androgens in its genesis. (This is supported by the condition’s predominance in males, the increased numbers of androgen receptors and melanocytes in the affected skin, and the prevalence of hypertrichosis.)
The researchers were also surprised to find that only 30% of the reported lesions occurred above the nipple, because the first descriptions of BN gave the impression that the shoulder and chest were most commonly affected. We now know that BN can also be found on arms and legs.
Usually a benign condition, BN can be associated with skeletal or soft-tissue deformities in the affected area (eg, ipsilateral breast hypoplasia). Malignancies—most notably melanoma—have also been reported with BN but are especially uncommon.
The differential includes the café-au-lait macules of neurofibromatosis, Albright disease, and congenital melanocytic nevus. The history of BN (ie, presentation, hypertrichosis, gender of patient, and distribution) usually allow a clinical diagnosis.
Treatment is limited to laser hair removal or laser removal or reduction of pigment.
TAKE-HOME LEARNING POINTS
- Becker nevus (BN) is far more common in males than females.
- BN typically manifests during puberty, which aligns with the suspected androgenic etiology.
- Though the shoulders and chest are the most commonly affected areas, BNs can also appear on the flank, arms, or legs.
- The lesions are rarely associated with serious pathology; hypoplasia of the ipsilateral breast is the most common of these complications.
Bumps under eyes

The FP diagnosed syringomas in this patient.
He explained that the bumps are benign tumors that occur frequently on the lower eyelids and upper cheeks. They are completely unrelated to the birth control pill and can develop in men, and run in families, too. While syringomas appear to occur more often in women than men, there are no known causative agents. These are benign growths of the eccrine sweat glands.
Treatment options include cryosurgery, electrosurgery, or chemical destruction with trichloroacetic acid. All of these approaches need to be performed carefully, as the syringomas are so close to the eye. Also, these treatments are only modestly effective; new syringomas can form. And there are no preventive treatments.
In this case, the patient had light brown skin, so there was a risk of causing permanent hypopigmentation with any of these destructive methods. The patient was reassured about the benign nature of the condition; she decided not to seek therapy.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.

The FP diagnosed syringomas in this patient.
He explained that the bumps are benign tumors that occur frequently on the lower eyelids and upper cheeks. They are completely unrelated to the birth control pill and can develop in men, and run in families, too. While syringomas appear to occur more often in women than men, there are no known causative agents. These are benign growths of the eccrine sweat glands.
Treatment options include cryosurgery, electrosurgery, or chemical destruction with trichloroacetic acid. All of these approaches need to be performed carefully, as the syringomas are so close to the eye. Also, these treatments are only modestly effective; new syringomas can form. And there are no preventive treatments.
In this case, the patient had light brown skin, so there was a risk of causing permanent hypopigmentation with any of these destructive methods. The patient was reassured about the benign nature of the condition; she decided not to seek therapy.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.

The FP diagnosed syringomas in this patient.
He explained that the bumps are benign tumors that occur frequently on the lower eyelids and upper cheeks. They are completely unrelated to the birth control pill and can develop in men, and run in families, too. While syringomas appear to occur more often in women than men, there are no known causative agents. These are benign growths of the eccrine sweat glands.
Treatment options include cryosurgery, electrosurgery, or chemical destruction with trichloroacetic acid. All of these approaches need to be performed carefully, as the syringomas are so close to the eye. Also, these treatments are only modestly effective; new syringomas can form. And there are no preventive treatments.
In this case, the patient had light brown skin, so there was a risk of causing permanent hypopigmentation with any of these destructive methods. The patient was reassured about the benign nature of the condition; she decided not to seek therapy.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.