User login
Respect is key when treating dermatologic conditions in transgender youth
LAKE TAHOE, CALIF. – The way Stanley Vance Jr., MD, sees it, the No. 1 priority in the care of transgender youth is respecting their gender identity.
“This can really help with rapport and also help them continue to engage with your care,” he said at the annual meeting of the Society for Pediatric Dermatology.
One of the first steps is to establish the patient’s chosen name and pronouns. “Ask, use, and be consistent,” said Dr. Vance, an adolescent medicine specialist at the University of California, San Francisco. “Taking it to another level, you can implement system-level tools to ensure that all of your staff consistently use the chosen name and pronouns. and working with the IT department to have a place in our electronic medical record to put the chosen name and preferred pronouns.”
In a study published in the Journal of Adolescent Health, researchers found that the use of chosen names and pronouns for transgender use was associated with reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth.
Dr. Vance, who also holds a staff position at the UCSF Child and Adolescent Clinic, went on to discuss dermatologic considerations for gender diverse youth. In transgender females, estrogens can reduce the quantity and density of body and facial hair, “but it doesn’t necessarily get rid of the hair, so we may refer to dermatology for hair removal or hair reduction. There can also be a decrease in sebum production, which can lead to dry skin for those who are at risk.”
Transgender females often seek laser hair removal or electrolysis to aid in “blendability,” or how they perceive as being female or feminine. “We know that this can help in psychosocial outcomes for these young people,” Dr. Vance said. “Another reason why hair reduction and removal may be important is preoperatively for vaginoplasty.”
In transgender males, testosterone increases male pattern hair growth and can increase male pattern hair loss. “Minoxidil does not interact with gender-affirming hormone treatment. If finasteride needs to be considered, it may interfere with the development of secondary sex characteristics.” Testosterone also increases sebum production and can increase acne, particularly in the first 6 months to 1 year after initiation, and with increased titration. “Some transmasculine youth may need oral isotretinoin, as stopping testosterone can be psychologically damaging,” Dr. Vance said.
“Unfortunately, the iPLEDGE program requirements can be perceived as gender nonaffirming, because patients must register by the sex assigned to them at birth, they must take pregnancy tests, and there can be provider assumptions about sexuality which does not equate with gender identity.”
He recommended having “open and honest” conversations with patients about the requirements and limitations of dispensing oral isotretinoin. “Assure the patient that you will be respectful and affirming of their gender identity while they’re in your office,” Dr. Vance advised. “If the patient has a mental health provider, you can strategize with them to reduce gender dysphoria around this process. Finally, advocating to change the system can not only be helpful for the patient in front of you, but for other patients who are in the same situation.”
He concluded his presentation by describing transgender youth as “some of the most resilient young people I’ve had the pleasure of working with.
“I think that we can all work to make sure they feel supported in who they are,” he said.
Dr. Vance reported having no relevant financial disclosures.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – The way Stanley Vance Jr., MD, sees it, the No. 1 priority in the care of transgender youth is respecting their gender identity.
“This can really help with rapport and also help them continue to engage with your care,” he said at the annual meeting of the Society for Pediatric Dermatology.
One of the first steps is to establish the patient’s chosen name and pronouns. “Ask, use, and be consistent,” said Dr. Vance, an adolescent medicine specialist at the University of California, San Francisco. “Taking it to another level, you can implement system-level tools to ensure that all of your staff consistently use the chosen name and pronouns. and working with the IT department to have a place in our electronic medical record to put the chosen name and preferred pronouns.”
In a study published in the Journal of Adolescent Health, researchers found that the use of chosen names and pronouns for transgender use was associated with reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth.
Dr. Vance, who also holds a staff position at the UCSF Child and Adolescent Clinic, went on to discuss dermatologic considerations for gender diverse youth. In transgender females, estrogens can reduce the quantity and density of body and facial hair, “but it doesn’t necessarily get rid of the hair, so we may refer to dermatology for hair removal or hair reduction. There can also be a decrease in sebum production, which can lead to dry skin for those who are at risk.”
Transgender females often seek laser hair removal or electrolysis to aid in “blendability,” or how they perceive as being female or feminine. “We know that this can help in psychosocial outcomes for these young people,” Dr. Vance said. “Another reason why hair reduction and removal may be important is preoperatively for vaginoplasty.”
In transgender males, testosterone increases male pattern hair growth and can increase male pattern hair loss. “Minoxidil does not interact with gender-affirming hormone treatment. If finasteride needs to be considered, it may interfere with the development of secondary sex characteristics.” Testosterone also increases sebum production and can increase acne, particularly in the first 6 months to 1 year after initiation, and with increased titration. “Some transmasculine youth may need oral isotretinoin, as stopping testosterone can be psychologically damaging,” Dr. Vance said.
“Unfortunately, the iPLEDGE program requirements can be perceived as gender nonaffirming, because patients must register by the sex assigned to them at birth, they must take pregnancy tests, and there can be provider assumptions about sexuality which does not equate with gender identity.”
He recommended having “open and honest” conversations with patients about the requirements and limitations of dispensing oral isotretinoin. “Assure the patient that you will be respectful and affirming of their gender identity while they’re in your office,” Dr. Vance advised. “If the patient has a mental health provider, you can strategize with them to reduce gender dysphoria around this process. Finally, advocating to change the system can not only be helpful for the patient in front of you, but for other patients who are in the same situation.”
He concluded his presentation by describing transgender youth as “some of the most resilient young people I’ve had the pleasure of working with.
“I think that we can all work to make sure they feel supported in who they are,” he said.
Dr. Vance reported having no relevant financial disclosures.
dbrunk@mdedge.com
LAKE TAHOE, CALIF. – The way Stanley Vance Jr., MD, sees it, the No. 1 priority in the care of transgender youth is respecting their gender identity.
“This can really help with rapport and also help them continue to engage with your care,” he said at the annual meeting of the Society for Pediatric Dermatology.
One of the first steps is to establish the patient’s chosen name and pronouns. “Ask, use, and be consistent,” said Dr. Vance, an adolescent medicine specialist at the University of California, San Francisco. “Taking it to another level, you can implement system-level tools to ensure that all of your staff consistently use the chosen name and pronouns. and working with the IT department to have a place in our electronic medical record to put the chosen name and preferred pronouns.”
In a study published in the Journal of Adolescent Health, researchers found that the use of chosen names and pronouns for transgender use was associated with reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth.
Dr. Vance, who also holds a staff position at the UCSF Child and Adolescent Clinic, went on to discuss dermatologic considerations for gender diverse youth. In transgender females, estrogens can reduce the quantity and density of body and facial hair, “but it doesn’t necessarily get rid of the hair, so we may refer to dermatology for hair removal or hair reduction. There can also be a decrease in sebum production, which can lead to dry skin for those who are at risk.”
Transgender females often seek laser hair removal or electrolysis to aid in “blendability,” or how they perceive as being female or feminine. “We know that this can help in psychosocial outcomes for these young people,” Dr. Vance said. “Another reason why hair reduction and removal may be important is preoperatively for vaginoplasty.”
In transgender males, testosterone increases male pattern hair growth and can increase male pattern hair loss. “Minoxidil does not interact with gender-affirming hormone treatment. If finasteride needs to be considered, it may interfere with the development of secondary sex characteristics.” Testosterone also increases sebum production and can increase acne, particularly in the first 6 months to 1 year after initiation, and with increased titration. “Some transmasculine youth may need oral isotretinoin, as stopping testosterone can be psychologically damaging,” Dr. Vance said.
“Unfortunately, the iPLEDGE program requirements can be perceived as gender nonaffirming, because patients must register by the sex assigned to them at birth, they must take pregnancy tests, and there can be provider assumptions about sexuality which does not equate with gender identity.”
He recommended having “open and honest” conversations with patients about the requirements and limitations of dispensing oral isotretinoin. “Assure the patient that you will be respectful and affirming of their gender identity while they’re in your office,” Dr. Vance advised. “If the patient has a mental health provider, you can strategize with them to reduce gender dysphoria around this process. Finally, advocating to change the system can not only be helpful for the patient in front of you, but for other patients who are in the same situation.”
He concluded his presentation by describing transgender youth as “some of the most resilient young people I’ve had the pleasure of working with.
“I think that we can all work to make sure they feel supported in who they are,” he said.
Dr. Vance reported having no relevant financial disclosures.
dbrunk@mdedge.com
EXPERT ANALYSIS FROM SPD 2018
Pediatric vitiligo primarily affects those aged 10-17
LAKE TAHOE, CALIF. – Among children and adolescents, vitiligo appears to predominately affect nonwhite boys and girls between the ages of 10 and 17 years, results from a large cross-sectional analysis demonstrated.
During an interview at the annual meeting of the Society for Pediatric Dermatology, lead study author Jessica Haber, MD, said that, while it’s known vitiligo can have its onset in childhood, there have been no population-based analyses in the United States specific to children and adolescents with the condition.
“We wanted to examine disease burden in the U.S. specifically, because we have such a diverse population,” said Dr. Haber, a second-year resident in the department of dermatology at Northwell Health, New York.
For the study, she and her associates used IBM’s Explorys research analytics platform to conduct a cross-sectional analysis of more than 55 million unique patients across all census regions of the United States. There were 1,630 vitiligo cases identified from a total of 4,242,400 pediatric patients, for an overall standard prevalence of 0.04%, or 40.1 per 100,000 children and adolescents. The proportion of female and male patients with vitiligo was similar (49.1% and 50.9%, respectively), and nearly three-fourths (72.3%) were 10 years of age or older.
The researchers observed no significant difference in the prevalence of vitiligo between males and females (40.2 per 100,000 vs. 40 per 100,000, respectively). The standardized prevalence of vitiligo was greatest in pediatric patients who were of “other” races and ethnicities (including Asian, Hispanic, multiracial, and other; 69.1 per 100,000), followed by African Americans (51.5 per 100,000) and whites (37.9 per 100,000). There were too few vitiligo cases among biracial patients to determine standardized estimates, but the crude prevalence was greatest in this group (68.7 per 100,000).
Two factors could contribute to the increased prevalence of vitiligo observed in nonwhite children and adolescents, Dr. Haber said. One is selection bias.
“It has been reported that both children and adults with higher Fitzpatrick skin types tend to have increased morbidity of their vitiligo, so it may be a selection bias that these patients are seeking out treatment for their disease,” she said. (J Am Acad Dermatol. 2017;77[1]:1-13). That might explain some of our findings, as well.”
While the study findings “don’t necessarily change clinical practice, it is good for us to have a sense of the burden of disease in the pediatric patient population of vitiligo, and to be aware that this is a disease that predominately affects non-Caucasian children and adolescents,” Dr. Haber concluded.
She reported having no financial disclosures.
LAKE TAHOE, CALIF. – Among children and adolescents, vitiligo appears to predominately affect nonwhite boys and girls between the ages of 10 and 17 years, results from a large cross-sectional analysis demonstrated.
During an interview at the annual meeting of the Society for Pediatric Dermatology, lead study author Jessica Haber, MD, said that, while it’s known vitiligo can have its onset in childhood, there have been no population-based analyses in the United States specific to children and adolescents with the condition.
“We wanted to examine disease burden in the U.S. specifically, because we have such a diverse population,” said Dr. Haber, a second-year resident in the department of dermatology at Northwell Health, New York.
For the study, she and her associates used IBM’s Explorys research analytics platform to conduct a cross-sectional analysis of more than 55 million unique patients across all census regions of the United States. There were 1,630 vitiligo cases identified from a total of 4,242,400 pediatric patients, for an overall standard prevalence of 0.04%, or 40.1 per 100,000 children and adolescents. The proportion of female and male patients with vitiligo was similar (49.1% and 50.9%, respectively), and nearly three-fourths (72.3%) were 10 years of age or older.
The researchers observed no significant difference in the prevalence of vitiligo between males and females (40.2 per 100,000 vs. 40 per 100,000, respectively). The standardized prevalence of vitiligo was greatest in pediatric patients who were of “other” races and ethnicities (including Asian, Hispanic, multiracial, and other; 69.1 per 100,000), followed by African Americans (51.5 per 100,000) and whites (37.9 per 100,000). There were too few vitiligo cases among biracial patients to determine standardized estimates, but the crude prevalence was greatest in this group (68.7 per 100,000).
Two factors could contribute to the increased prevalence of vitiligo observed in nonwhite children and adolescents, Dr. Haber said. One is selection bias.
“It has been reported that both children and adults with higher Fitzpatrick skin types tend to have increased morbidity of their vitiligo, so it may be a selection bias that these patients are seeking out treatment for their disease,” she said. (J Am Acad Dermatol. 2017;77[1]:1-13). That might explain some of our findings, as well.”
While the study findings “don’t necessarily change clinical practice, it is good for us to have a sense of the burden of disease in the pediatric patient population of vitiligo, and to be aware that this is a disease that predominately affects non-Caucasian children and adolescents,” Dr. Haber concluded.
She reported having no financial disclosures.
LAKE TAHOE, CALIF. – Among children and adolescents, vitiligo appears to predominately affect nonwhite boys and girls between the ages of 10 and 17 years, results from a large cross-sectional analysis demonstrated.
During an interview at the annual meeting of the Society for Pediatric Dermatology, lead study author Jessica Haber, MD, said that, while it’s known vitiligo can have its onset in childhood, there have been no population-based analyses in the United States specific to children and adolescents with the condition.
“We wanted to examine disease burden in the U.S. specifically, because we have such a diverse population,” said Dr. Haber, a second-year resident in the department of dermatology at Northwell Health, New York.
For the study, she and her associates used IBM’s Explorys research analytics platform to conduct a cross-sectional analysis of more than 55 million unique patients across all census regions of the United States. There were 1,630 vitiligo cases identified from a total of 4,242,400 pediatric patients, for an overall standard prevalence of 0.04%, or 40.1 per 100,000 children and adolescents. The proportion of female and male patients with vitiligo was similar (49.1% and 50.9%, respectively), and nearly three-fourths (72.3%) were 10 years of age or older.
The researchers observed no significant difference in the prevalence of vitiligo between males and females (40.2 per 100,000 vs. 40 per 100,000, respectively). The standardized prevalence of vitiligo was greatest in pediatric patients who were of “other” races and ethnicities (including Asian, Hispanic, multiracial, and other; 69.1 per 100,000), followed by African Americans (51.5 per 100,000) and whites (37.9 per 100,000). There were too few vitiligo cases among biracial patients to determine standardized estimates, but the crude prevalence was greatest in this group (68.7 per 100,000).
Two factors could contribute to the increased prevalence of vitiligo observed in nonwhite children and adolescents, Dr. Haber said. One is selection bias.
“It has been reported that both children and adults with higher Fitzpatrick skin types tend to have increased morbidity of their vitiligo, so it may be a selection bias that these patients are seeking out treatment for their disease,” she said. (J Am Acad Dermatol. 2017;77[1]:1-13). That might explain some of our findings, as well.”
While the study findings “don’t necessarily change clinical practice, it is good for us to have a sense of the burden of disease in the pediatric patient population of vitiligo, and to be aware that this is a disease that predominately affects non-Caucasian children and adolescents,” Dr. Haber concluded.
She reported having no financial disclosures.
REPORTING FROM SPD 2018
Key clinical point: Vitiligo appears to predominately affect nonwhite boys and girls 10 years of age and older in the pediatric population.
Major finding: Of pediatric patients with vitiligo, 72.3% were 10 years of age or older.
Study details: A cross-sectional analysis of 1,630 vitiligo cases identified from a total of 4,242,400 pediatric patients.
Disclosures: Dr. Haber reported having no relevant financial disclosures.
When fingernails are the clue to a bigger problem
CHICAGO – When a child or adolescent comes to the dermatologist’s office with a concern about fingernails or toenails, physician antennae may go up. “The world is different in the world of pediatrics – and even in the world of adolescents,” said Sheila Fallon Friedlander, MD.
In adults, the most common cause of nail dystrophy is tinea, but for younger pediatric patients, less than 1% of nail problems are attributable to fungus, so dermatologists may need to look further.
“It’s so important in kids to do a good history and physical exam,” said Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego. History-taking should include determining whether the condition has been present since birth and how nail appearance has changed over time.
For Dr. Friedlander, the approach to nail abnormalities includes a full head and skin exam. “I always look at the teeth, the hair, the skin,” she said; underlying bony anomalies also may surface. A complete exam often will turn up important clues if a syndrome underpins the nail abnormalities, she said, speaking at the American Academy of Dermatology summer meeting.
Her exemplar patient, she said, is a 19-year-old male who comes in with a parent because he’s bothered by his fingernails, which are dystrophic and small. A head-to-toe exam shows micronychia of both toes and fingers, with lunulae that are triangularly shaped. The hair, skin, and teeth of the patient all were normal in appearance. However, “The knees and elbows were odd,” Dr. Friedlander said.
This patient has nail-patella syndrome. “Even though it’s rare, I want you to think about it,” Dr. Friedlander said. The autosomal dominant condition is seen in about 1 in 50,000 patients. It’s thought to be caused by heterozygous loss-of-function mutations in gene LMX1B, she said, that codes for a LIM homeobox transcription factor 1 beta.
Though the small nails and triangular lunulae may be what brings the patient to the dermatologist’s office, a careful exam and one radiograph can pick up a tetrad of anomalies, Dr. Friedlander said. Abnormalities can be seen in both the knees and elbows; the patellae are often small, and may even be absent. In addition, a hip radiograph will show characteristic “horns” on the posterior iliac crests.
Coming back to the dermatologic exam, Dr. Friedlander said nails may be absent, hypoplastic, and dystrophic – but those are features that can be shared with other nail disorders, inherited and acquired. The pathognomonic finding for nail-patella syndrome is the presence of the triangular lunula, she said.
Now that the diagnosis has been made, Dr. Friedlander asked about this young man: “Where will you refer him?” Knowing the diagnosis means that there are a lot of calls for your staff to make, she said.
The patient with knee patella syndrome should be referred to an orthopedist to assess knees and elbows; radial head subluxation also is common in these patients, she said.
An ophthalmologic referral is important as well; hyperpigmentation of the pupillary margin – a “Lester iris” – can be seen, and increased rates of cataracts and glaucoma also are associated with nail-patella syndrome.
“,” Dr. Friedlander said. Up to half of nail-patella syndrome patients will have kidney involvement that initially presents with hematuria and proteinuria. Because the LMX1B mutation impairs how podocytes and glomerular filtration slits develop and function, up to 10% can develop end-stage renal failure, she said.
Parents also should be on the lookout for associated behavioral issues: “The other thing that’s interesting is that these kids have an increased risk of [attention-deficit/hyperactivity disorder] and major depression,” Dr. Friedlander said.
Dr. Friedlander reported that she had no relevant conflicts of interest.
SOURCE: Friedlander, S. Summer AAD 2018. Session F004.
CHICAGO – When a child or adolescent comes to the dermatologist’s office with a concern about fingernails or toenails, physician antennae may go up. “The world is different in the world of pediatrics – and even in the world of adolescents,” said Sheila Fallon Friedlander, MD.
In adults, the most common cause of nail dystrophy is tinea, but for younger pediatric patients, less than 1% of nail problems are attributable to fungus, so dermatologists may need to look further.
“It’s so important in kids to do a good history and physical exam,” said Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego. History-taking should include determining whether the condition has been present since birth and how nail appearance has changed over time.
For Dr. Friedlander, the approach to nail abnormalities includes a full head and skin exam. “I always look at the teeth, the hair, the skin,” she said; underlying bony anomalies also may surface. A complete exam often will turn up important clues if a syndrome underpins the nail abnormalities, she said, speaking at the American Academy of Dermatology summer meeting.
Her exemplar patient, she said, is a 19-year-old male who comes in with a parent because he’s bothered by his fingernails, which are dystrophic and small. A head-to-toe exam shows micronychia of both toes and fingers, with lunulae that are triangularly shaped. The hair, skin, and teeth of the patient all were normal in appearance. However, “The knees and elbows were odd,” Dr. Friedlander said.
This patient has nail-patella syndrome. “Even though it’s rare, I want you to think about it,” Dr. Friedlander said. The autosomal dominant condition is seen in about 1 in 50,000 patients. It’s thought to be caused by heterozygous loss-of-function mutations in gene LMX1B, she said, that codes for a LIM homeobox transcription factor 1 beta.
Though the small nails and triangular lunulae may be what brings the patient to the dermatologist’s office, a careful exam and one radiograph can pick up a tetrad of anomalies, Dr. Friedlander said. Abnormalities can be seen in both the knees and elbows; the patellae are often small, and may even be absent. In addition, a hip radiograph will show characteristic “horns” on the posterior iliac crests.
Coming back to the dermatologic exam, Dr. Friedlander said nails may be absent, hypoplastic, and dystrophic – but those are features that can be shared with other nail disorders, inherited and acquired. The pathognomonic finding for nail-patella syndrome is the presence of the triangular lunula, she said.
Now that the diagnosis has been made, Dr. Friedlander asked about this young man: “Where will you refer him?” Knowing the diagnosis means that there are a lot of calls for your staff to make, she said.
The patient with knee patella syndrome should be referred to an orthopedist to assess knees and elbows; radial head subluxation also is common in these patients, she said.
An ophthalmologic referral is important as well; hyperpigmentation of the pupillary margin – a “Lester iris” – can be seen, and increased rates of cataracts and glaucoma also are associated with nail-patella syndrome.
“,” Dr. Friedlander said. Up to half of nail-patella syndrome patients will have kidney involvement that initially presents with hematuria and proteinuria. Because the LMX1B mutation impairs how podocytes and glomerular filtration slits develop and function, up to 10% can develop end-stage renal failure, she said.
Parents also should be on the lookout for associated behavioral issues: “The other thing that’s interesting is that these kids have an increased risk of [attention-deficit/hyperactivity disorder] and major depression,” Dr. Friedlander said.
Dr. Friedlander reported that she had no relevant conflicts of interest.
SOURCE: Friedlander, S. Summer AAD 2018. Session F004.
CHICAGO – When a child or adolescent comes to the dermatologist’s office with a concern about fingernails or toenails, physician antennae may go up. “The world is different in the world of pediatrics – and even in the world of adolescents,” said Sheila Fallon Friedlander, MD.
In adults, the most common cause of nail dystrophy is tinea, but for younger pediatric patients, less than 1% of nail problems are attributable to fungus, so dermatologists may need to look further.
“It’s so important in kids to do a good history and physical exam,” said Dr. Friedlander, professor of dermatology and pediatrics at the University of California, San Diego. History-taking should include determining whether the condition has been present since birth and how nail appearance has changed over time.
For Dr. Friedlander, the approach to nail abnormalities includes a full head and skin exam. “I always look at the teeth, the hair, the skin,” she said; underlying bony anomalies also may surface. A complete exam often will turn up important clues if a syndrome underpins the nail abnormalities, she said, speaking at the American Academy of Dermatology summer meeting.
Her exemplar patient, she said, is a 19-year-old male who comes in with a parent because he’s bothered by his fingernails, which are dystrophic and small. A head-to-toe exam shows micronychia of both toes and fingers, with lunulae that are triangularly shaped. The hair, skin, and teeth of the patient all were normal in appearance. However, “The knees and elbows were odd,” Dr. Friedlander said.
This patient has nail-patella syndrome. “Even though it’s rare, I want you to think about it,” Dr. Friedlander said. The autosomal dominant condition is seen in about 1 in 50,000 patients. It’s thought to be caused by heterozygous loss-of-function mutations in gene LMX1B, she said, that codes for a LIM homeobox transcription factor 1 beta.
Though the small nails and triangular lunulae may be what brings the patient to the dermatologist’s office, a careful exam and one radiograph can pick up a tetrad of anomalies, Dr. Friedlander said. Abnormalities can be seen in both the knees and elbows; the patellae are often small, and may even be absent. In addition, a hip radiograph will show characteristic “horns” on the posterior iliac crests.
Coming back to the dermatologic exam, Dr. Friedlander said nails may be absent, hypoplastic, and dystrophic – but those are features that can be shared with other nail disorders, inherited and acquired. The pathognomonic finding for nail-patella syndrome is the presence of the triangular lunula, she said.
Now that the diagnosis has been made, Dr. Friedlander asked about this young man: “Where will you refer him?” Knowing the diagnosis means that there are a lot of calls for your staff to make, she said.
The patient with knee patella syndrome should be referred to an orthopedist to assess knees and elbows; radial head subluxation also is common in these patients, she said.
An ophthalmologic referral is important as well; hyperpigmentation of the pupillary margin – a “Lester iris” – can be seen, and increased rates of cataracts and glaucoma also are associated with nail-patella syndrome.
“,” Dr. Friedlander said. Up to half of nail-patella syndrome patients will have kidney involvement that initially presents with hematuria and proteinuria. Because the LMX1B mutation impairs how podocytes and glomerular filtration slits develop and function, up to 10% can develop end-stage renal failure, she said.
Parents also should be on the lookout for associated behavioral issues: “The other thing that’s interesting is that these kids have an increased risk of [attention-deficit/hyperactivity disorder] and major depression,” Dr. Friedlander said.
Dr. Friedlander reported that she had no relevant conflicts of interest.
SOURCE: Friedlander, S. Summer AAD 2018. Session F004.
REPORTING FROM SUMMER AAD 2018
Oral drug seen preventing angioedema attacks
An experimental agent reduced swelling episodes markedly in patients with hereditary angioedema, according to results from a phase 2 randomized, dose-ranging, placebo-controlled trial.
The drug BCX7353, developed by BioCryst Pharmaceuticals, is taken orally and works by inhibiting plasma kallikrein, an enzyme overexpressed in hereditary angioedema, a rare genetic disease that causes severe tissue swelling. In research published July 26 in the New England Journal of Medicine (N Engl J Med. 2018;379:352-62), Emel Aygören-Pürsün, MD, of Goethe University in Frankfurt, Germany, and colleagues, randomized 77 patients with type 1 or II hereditary angioedema and a pattern of frequent attacks to one of four doses of daily BCX7353, or placebo, for 28 days.
Dr. Aygören-Pürsün’s group found significant reductions in the number of monthly attacks for the three doses used in the study, with the best response seen in the group receiving the second-lowest dose of 125 mg. These patients saw a reduction of 73.8% (P less than .001) in monthly attacks from baseline, and 43% of patients receiving that dose had no attacks during the study period. The higher-dose groups saw more adverse events and apparently less efficacy, with the 250-mg dose associated with a reduction in attacks of 44.6% (P = .01), and for the 350-mg group, a 45.5% reduction (P = .006).
Patients receiving the lowest dose in the study, 62.5 mg, saw a small (about 10%) reduction in attacks that did not reach statistical significance. Gastrointestinal adverse events were reported in the two highest dose groups, and three patients in the 350-mg group dropped out after reporting serious adverse events, including one liver disorder considered likely related to the trial regimen.
The efficacy of the highest doses “was probably masked by gastrointestinal adverse events that may have been misattributed as early symptoms of abdominal angioedema attacks,” the investigators wrote in their analysis. Improvements in angioedema-related quality of life scores, a secondary trial endpoint, reached statistical significance for the 125- and 250-mg doses.
The authors cautioned that the safety of long-term dosing would need to be studied in longer-term trials.
The study was sponsored by the drug manufacturer, BioCryst Pharmaceuticals. All of the study’s authors, including the lead author, disclosed financial relationships in the form of grant support, fees, or employment with the study sponsor.
SOURCE: Aygören-Pürsün et al. N Engl J Med. 2018;379:352-62.
An experimental agent reduced swelling episodes markedly in patients with hereditary angioedema, according to results from a phase 2 randomized, dose-ranging, placebo-controlled trial.
The drug BCX7353, developed by BioCryst Pharmaceuticals, is taken orally and works by inhibiting plasma kallikrein, an enzyme overexpressed in hereditary angioedema, a rare genetic disease that causes severe tissue swelling. In research published July 26 in the New England Journal of Medicine (N Engl J Med. 2018;379:352-62), Emel Aygören-Pürsün, MD, of Goethe University in Frankfurt, Germany, and colleagues, randomized 77 patients with type 1 or II hereditary angioedema and a pattern of frequent attacks to one of four doses of daily BCX7353, or placebo, for 28 days.
Dr. Aygören-Pürsün’s group found significant reductions in the number of monthly attacks for the three doses used in the study, with the best response seen in the group receiving the second-lowest dose of 125 mg. These patients saw a reduction of 73.8% (P less than .001) in monthly attacks from baseline, and 43% of patients receiving that dose had no attacks during the study period. The higher-dose groups saw more adverse events and apparently less efficacy, with the 250-mg dose associated with a reduction in attacks of 44.6% (P = .01), and for the 350-mg group, a 45.5% reduction (P = .006).
Patients receiving the lowest dose in the study, 62.5 mg, saw a small (about 10%) reduction in attacks that did not reach statistical significance. Gastrointestinal adverse events were reported in the two highest dose groups, and three patients in the 350-mg group dropped out after reporting serious adverse events, including one liver disorder considered likely related to the trial regimen.
The efficacy of the highest doses “was probably masked by gastrointestinal adverse events that may have been misattributed as early symptoms of abdominal angioedema attacks,” the investigators wrote in their analysis. Improvements in angioedema-related quality of life scores, a secondary trial endpoint, reached statistical significance for the 125- and 250-mg doses.
The authors cautioned that the safety of long-term dosing would need to be studied in longer-term trials.
The study was sponsored by the drug manufacturer, BioCryst Pharmaceuticals. All of the study’s authors, including the lead author, disclosed financial relationships in the form of grant support, fees, or employment with the study sponsor.
SOURCE: Aygören-Pürsün et al. N Engl J Med. 2018;379:352-62.
An experimental agent reduced swelling episodes markedly in patients with hereditary angioedema, according to results from a phase 2 randomized, dose-ranging, placebo-controlled trial.
The drug BCX7353, developed by BioCryst Pharmaceuticals, is taken orally and works by inhibiting plasma kallikrein, an enzyme overexpressed in hereditary angioedema, a rare genetic disease that causes severe tissue swelling. In research published July 26 in the New England Journal of Medicine (N Engl J Med. 2018;379:352-62), Emel Aygören-Pürsün, MD, of Goethe University in Frankfurt, Germany, and colleagues, randomized 77 patients with type 1 or II hereditary angioedema and a pattern of frequent attacks to one of four doses of daily BCX7353, or placebo, for 28 days.
Dr. Aygören-Pürsün’s group found significant reductions in the number of monthly attacks for the three doses used in the study, with the best response seen in the group receiving the second-lowest dose of 125 mg. These patients saw a reduction of 73.8% (P less than .001) in monthly attacks from baseline, and 43% of patients receiving that dose had no attacks during the study period. The higher-dose groups saw more adverse events and apparently less efficacy, with the 250-mg dose associated with a reduction in attacks of 44.6% (P = .01), and for the 350-mg group, a 45.5% reduction (P = .006).
Patients receiving the lowest dose in the study, 62.5 mg, saw a small (about 10%) reduction in attacks that did not reach statistical significance. Gastrointestinal adverse events were reported in the two highest dose groups, and three patients in the 350-mg group dropped out after reporting serious adverse events, including one liver disorder considered likely related to the trial regimen.
The efficacy of the highest doses “was probably masked by gastrointestinal adverse events that may have been misattributed as early symptoms of abdominal angioedema attacks,” the investigators wrote in their analysis. Improvements in angioedema-related quality of life scores, a secondary trial endpoint, reached statistical significance for the 125- and 250-mg doses.
The authors cautioned that the safety of long-term dosing would need to be studied in longer-term trials.
The study was sponsored by the drug manufacturer, BioCryst Pharmaceuticals. All of the study’s authors, including the lead author, disclosed financial relationships in the form of grant support, fees, or employment with the study sponsor.
SOURCE: Aygören-Pürsün et al. N Engl J Med. 2018;379:352-62.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: An experimental kallikrein inhibitor, taken daily, prevented swelling attacks in people with hereditary angioedema.
Major finding: Patients in a moderate-dose group saw a 73.8% reduction in monthly swelling attacks from baseline, and 43% of saw no attacks.
Study details: A phase 2 study randomizing 77 patients with hereditary angioedema in three countries to one of four escalating doses or placebo.
Disclosures: All authors disclosed some relationship (current or past grant or fee support, or employment) with sponsor, BioCryst Pharmaceuticals.
Source: Aygören-Pürsün et. al. N Engl J Med. 2018;379:352-62.
Study explores adolescents’ views on their skin tone, pressure to tan
LAKE TAHOE, CALIF. –
During an interview at the annual meeting of the Society for Pediatric Dermatology, lead study author Shivani Patel, MD, said that prior research on skin color had focused mainly on adults and its impact on self-esteem and perceived attractiveness, yet little data are available on perceptions of skin color among adolescents.
“During puberty, adolescents receive pressure from friends, family, and social media to conform to a certain acceptable standard of skin tone,” said Dr. Patel, a chief resident in the department of dermatology at Johns Hopkins University, Baltimore. “They will often engage in risky behaviors such as tanning bed use, suntanning, and use of skin lightening creams.”
In an effort to characterize the attitudes of adolescents about their skin tone, she and her associates recruited 50 patients aged 12-19 years who were seen at the Johns Hopkins dermatology clinics. Slightly more than half (56%) were female. They were asked to complete surveys on their use of sunscreen, tanning beds, and skin-lightening creams, as well as to report any family or friends who have used these interventions.
Next, the researchers used Pantone’s Capsure device to record each subject’s skin tone according to a palate of 110 skin colors available from Pantone’s SkinTone Guide, which is intended to match and reproduce lifelike skin tones in a variety of industries. The adolescents were then given the palette and asked which skin tone they felt best represented their skin and which skin tone they wished they had. These differences were compared with their objective measurement by the study team.
Of all respondents, 20% indicated that they felt pressure to have tan skin and were likely to engage in suntanning (P less than .001), a feeling they said started around the age of 12 years and stemmed from perceived pressure from friends and celebrity figures. Those who suntanned were more likely to wear sunscreen (P less than .01), a finding “that was reassuring and showed that they are aware of sunscreen and sun safety,” Dr. Patel said. However, about half of the respondents reported never wearing sunscreen and only two reported wearing sunscreen daily. No one reported using tanning beds, but 8% reported that a family member used them. One adolescent reported using skin lightening creams, and three reported that their mothers used them.
The researchers also found that black and Asian study participants were significantly more likely to desire a skin tone lighter than what they perceived their skin tone to be, while white participants were significantly more likely to desire a darker skin tone (P less than .011 for both associations).
The findings suggest that sun safety initiatives should target prepubertal patients before they engage in risky behaviors, Dr. Patel said. She acknowledged that the small sample size is a limitation of the study, but said that she and her associates hope to conduct a larger-scale analysis.
She reported having no financial disclosures.
LAKE TAHOE, CALIF. –
During an interview at the annual meeting of the Society for Pediatric Dermatology, lead study author Shivani Patel, MD, said that prior research on skin color had focused mainly on adults and its impact on self-esteem and perceived attractiveness, yet little data are available on perceptions of skin color among adolescents.
“During puberty, adolescents receive pressure from friends, family, and social media to conform to a certain acceptable standard of skin tone,” said Dr. Patel, a chief resident in the department of dermatology at Johns Hopkins University, Baltimore. “They will often engage in risky behaviors such as tanning bed use, suntanning, and use of skin lightening creams.”
In an effort to characterize the attitudes of adolescents about their skin tone, she and her associates recruited 50 patients aged 12-19 years who were seen at the Johns Hopkins dermatology clinics. Slightly more than half (56%) were female. They were asked to complete surveys on their use of sunscreen, tanning beds, and skin-lightening creams, as well as to report any family or friends who have used these interventions.
Next, the researchers used Pantone’s Capsure device to record each subject’s skin tone according to a palate of 110 skin colors available from Pantone’s SkinTone Guide, which is intended to match and reproduce lifelike skin tones in a variety of industries. The adolescents were then given the palette and asked which skin tone they felt best represented their skin and which skin tone they wished they had. These differences were compared with their objective measurement by the study team.
Of all respondents, 20% indicated that they felt pressure to have tan skin and were likely to engage in suntanning (P less than .001), a feeling they said started around the age of 12 years and stemmed from perceived pressure from friends and celebrity figures. Those who suntanned were more likely to wear sunscreen (P less than .01), a finding “that was reassuring and showed that they are aware of sunscreen and sun safety,” Dr. Patel said. However, about half of the respondents reported never wearing sunscreen and only two reported wearing sunscreen daily. No one reported using tanning beds, but 8% reported that a family member used them. One adolescent reported using skin lightening creams, and three reported that their mothers used them.
The researchers also found that black and Asian study participants were significantly more likely to desire a skin tone lighter than what they perceived their skin tone to be, while white participants were significantly more likely to desire a darker skin tone (P less than .011 for both associations).
The findings suggest that sun safety initiatives should target prepubertal patients before they engage in risky behaviors, Dr. Patel said. She acknowledged that the small sample size is a limitation of the study, but said that she and her associates hope to conduct a larger-scale analysis.
She reported having no financial disclosures.
LAKE TAHOE, CALIF. –
During an interview at the annual meeting of the Society for Pediatric Dermatology, lead study author Shivani Patel, MD, said that prior research on skin color had focused mainly on adults and its impact on self-esteem and perceived attractiveness, yet little data are available on perceptions of skin color among adolescents.
“During puberty, adolescents receive pressure from friends, family, and social media to conform to a certain acceptable standard of skin tone,” said Dr. Patel, a chief resident in the department of dermatology at Johns Hopkins University, Baltimore. “They will often engage in risky behaviors such as tanning bed use, suntanning, and use of skin lightening creams.”
In an effort to characterize the attitudes of adolescents about their skin tone, she and her associates recruited 50 patients aged 12-19 years who were seen at the Johns Hopkins dermatology clinics. Slightly more than half (56%) were female. They were asked to complete surveys on their use of sunscreen, tanning beds, and skin-lightening creams, as well as to report any family or friends who have used these interventions.
Next, the researchers used Pantone’s Capsure device to record each subject’s skin tone according to a palate of 110 skin colors available from Pantone’s SkinTone Guide, which is intended to match and reproduce lifelike skin tones in a variety of industries. The adolescents were then given the palette and asked which skin tone they felt best represented their skin and which skin tone they wished they had. These differences were compared with their objective measurement by the study team.
Of all respondents, 20% indicated that they felt pressure to have tan skin and were likely to engage in suntanning (P less than .001), a feeling they said started around the age of 12 years and stemmed from perceived pressure from friends and celebrity figures. Those who suntanned were more likely to wear sunscreen (P less than .01), a finding “that was reassuring and showed that they are aware of sunscreen and sun safety,” Dr. Patel said. However, about half of the respondents reported never wearing sunscreen and only two reported wearing sunscreen daily. No one reported using tanning beds, but 8% reported that a family member used them. One adolescent reported using skin lightening creams, and three reported that their mothers used them.
The researchers also found that black and Asian study participants were significantly more likely to desire a skin tone lighter than what they perceived their skin tone to be, while white participants were significantly more likely to desire a darker skin tone (P less than .011 for both associations).
The findings suggest that sun safety initiatives should target prepubertal patients before they engage in risky behaviors, Dr. Patel said. She acknowledged that the small sample size is a limitation of the study, but said that she and her associates hope to conduct a larger-scale analysis.
She reported having no financial disclosures.
REPORTING FROM SPD 2018
Key clinical point: Sun safety initiatives should target prepubertal patients before they engage in risky behaviors.
Major finding: One in five adolescents indicated that they felt pressure to have tan skin and were likely to engage in suntanning (P less than .001).
Study details: A survey of 50 patients aged 12-19 years.
Disclosures: Dr. Patel reported having no financial disclosures.
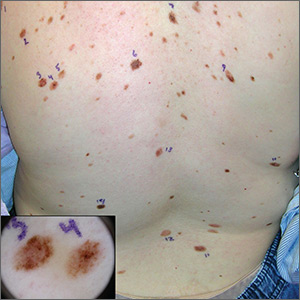
Atypical pigmented lesions on back
The FP recognized that this patient had multiple dysplastic nevi (DN) and was concerned about a possible melanoma.
Although this patient did not have the familial atypical mole and melanoma (FAMM) syndrome, she was at higher risk of developing a melanoma based on the numerous DN that were so visibly apparent on her trunk. (A diagnosis of FAMM requires the occurrence of melanoma in one or more first- or second-degree relatives.)
Total body photography is the current state-of-the-art technology for monitoring patients with multiple atypical moles at higher risk for skin cancer. Small changes in DN and new nevi can be seen best with this technology. Individual flat lesions also can be monitored with dermoscopy over 3 to 4 months.
It is not recommended, however, to follow a suspicious raised lesion over time with dermoscopy and/or photography because a raised lesion might be a nodular melanoma and a delay of diagnosis of over 3 months may worsen the prognosis.
In this case, the patient was happy to be referred to a dermatologist with total body photography. Fortunately, the patient reported back to her FP that the dermatologist did not detect any melanomas, and 2 biopsies that were performed came back as DN only.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
The FP recognized that this patient had multiple dysplastic nevi (DN) and was concerned about a possible melanoma.
Although this patient did not have the familial atypical mole and melanoma (FAMM) syndrome, she was at higher risk of developing a melanoma based on the numerous DN that were so visibly apparent on her trunk. (A diagnosis of FAMM requires the occurrence of melanoma in one or more first- or second-degree relatives.)
Total body photography is the current state-of-the-art technology for monitoring patients with multiple atypical moles at higher risk for skin cancer. Small changes in DN and new nevi can be seen best with this technology. Individual flat lesions also can be monitored with dermoscopy over 3 to 4 months.
It is not recommended, however, to follow a suspicious raised lesion over time with dermoscopy and/or photography because a raised lesion might be a nodular melanoma and a delay of diagnosis of over 3 months may worsen the prognosis.
In this case, the patient was happy to be referred to a dermatologist with total body photography. Fortunately, the patient reported back to her FP that the dermatologist did not detect any melanomas, and 2 biopsies that were performed came back as DN only.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
The FP recognized that this patient had multiple dysplastic nevi (DN) and was concerned about a possible melanoma.
Although this patient did not have the familial atypical mole and melanoma (FAMM) syndrome, she was at higher risk of developing a melanoma based on the numerous DN that were so visibly apparent on her trunk. (A diagnosis of FAMM requires the occurrence of melanoma in one or more first- or second-degree relatives.)
Total body photography is the current state-of-the-art technology for monitoring patients with multiple atypical moles at higher risk for skin cancer. Small changes in DN and new nevi can be seen best with this technology. Individual flat lesions also can be monitored with dermoscopy over 3 to 4 months.
It is not recommended, however, to follow a suspicious raised lesion over time with dermoscopy and/or photography because a raised lesion might be a nodular melanoma and a delay of diagnosis of over 3 months may worsen the prognosis.
In this case, the patient was happy to be referred to a dermatologist with total body photography. Fortunately, the patient reported back to her FP that the dermatologist did not detect any melanomas, and 2 biopsies that were performed came back as DN only.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
Early-onset atopic dermatitis linked to elevated risk for seasonal allergies and asthma
LAKE TAHOE, CALIF. – results from a large, retrospective cohort study demonstrated.
“The atopic march is characterized by a progression from atopic dermatitis, usually early in childhood, to subsequent development of allergic rhinitis and asthma, lead study author Joy Wan, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is thought that the skin acts as the site of primary sensitization through a defective epithelial barrier, which then allows for allergic sensitization to occur in the airways. It is estimated that 30%-60% of AD patients go on to develop asthma and/or allergic rhinitis. However, not all patients complete the so-called atopic march, and this variation in the risk of asthma and allergic rhinitis among AD patients is not very well understood. Better ways to risk stratify these patients are needed.”
One possible explanation for this variation in the risk of atopy in AD patients could be the timing of their dermatitis onset. “We know that atopic dermatitis begins in infancy, but it can start at any age,” said Dr. Wan, who is a fellow in the section of pediatric dermatology at the Children’s Hospital of Philadelphia. “There has been a distinction between early-onset versus late-onset AD. Some past studies have also suggested that there is an increased risk of asthma and allergic rhinitis in children who have early-onset AD before the age of 1 or 2. This suggests that perhaps the model of the atopic march varies between early- and late-onset AD. However, past studies have had several limitations. They’ve often had short durations of follow-up, they’ve only examined narrow ranges of age of onset for AD, and most of them have been designed to primarily evaluate other exposures and outcomes, rather than looking at the timing of AD onset itself.”
For the current study, Dr. Wan and her associates set out to examine the risk of seasonal allergies and asthma among children with AD with respect to the age of AD onset. They used data from the Pediatric Eczema Elective Registry (PEER), an ongoing, prospective U.S. cohort of more than 7,700 children with physician-confirmed AD (JAMA Dermatol. 2014 Jun;150:593-600). All registry participants had used pimecrolimus cream in the past, but children with lymphoproliferative disease were excluded from the registry, as were those with malignancy or those who required the use of systemic immunosuppression.
The researchers evaluated 3,966 subjects in PEER with at least 3 years of follow-up. The exposure of interest was age of AD onset, and they divided patients into three broad age categories: early onset (age 2 years or younger), mid onset (3-7 years), and late onset (8-17 years). Primary outcomes were prevalent seasonal allergies and asthma at the time of registry enrollment, and incident seasonal allergies and asthma during follow-up, assessed via patient surveys every 3 years.
The study population included high proportions of white and black children, and there was a slight predominance of females. The median age at PEER enrollment increased with advancing age of AD onset (5.2 years in the early-onset group vs. 8.2 years in the mid-onset group and 13.1 years in the late-onset group), while the duration of follow-up was fairly similar across the three groups (a median of about 8.3 months). Family history of AD was common across all three groups, while patients in the late-onset group tended to have better control of their AD, compared with their younger counterparts.
At baseline, the prevalence of seasonal allergies was highest among the early-onset group at 74.6%, compared with 69.9% among the mid-onset group and 70.1% among the late-onset group. After adjusting for sex, race, and age at registry enrollment, the relative risk for prevalent seasonal allergies was 9% lower in the mid-onset group (0.91) and 18% lower in the late-onset group (0.82), compared with those in the early-onset group. Next, Dr. Wan and her associates calculated the incidence of seasonal allergies among 1,054 patients who did not have allergies at baseline. The cumulative incidence was highest among the early-onset group (56.1%), followed by the mid-onset group (46.8%), and the late-onset group (30.6%). On adjusted analysis, the relative risk for seasonal allergies among patients who had no allergies at baseline was 18% lower in the mid-onset group (0.82) and 36% lower in the late-onset group (0.64), compared with those in the early-onset group.
In the analysis of asthma risk by age of AD onset, prevalence was highest among patients in the early-onset group at 51.5%, compared with 44.7% among the mid-onset age group and 43% among the late-onset age group. On adjusted analysis, the relative risk for asthma was 15% lower in the mid-onset group (0.85) and 29% lower in the late-onset group (0.71), compared with those in the early-onset group. Meanwhile, the cumulative incidence of asthma among patients without asthma at baseline was also highest in the early-onset group (39.2%), compared with 31.9% in the mid-onset group and 29.9% in the late-onset group.
On adjusted analysis, the relative risk for asthma among this subset of patients was 4% lower in the mid-onset group (0.96) and 8% lower in the late-onset group (0.92), compared with those in the early-onset group, a difference that was not statistically significant. “One possible explanation for this is that asthma tends to develop soon after AD does, and the rates of developing asthma later on, as detected by our study, are nondifferential,” Dr. Wan said. “Another possibility is that the impact of early-onset versus late-onset AD is just different for asthma than it is for seasonal allergies.”
She acknowledged certain limitations of the study, including the risk of misclassification bias and limitations in recall with self-reported data, and the fact that the findings may not be generalizable to all patients with AD.
“Future studies with longer follow-up and studies of adult-onset AD will help extend our findings,” she concluded. “Nevertheless, our findings may inform how we risk stratify patients for AD treatment or atopic march prevention efforts in the future.”
PEER is funded by a grant from Valeant Pharmaceuticals, but Valeant had no role in this study. Dr. Wan reported having no financial disclosures. The study won an award at the meeting for best research presented by a dermatology resident or fellow.
LAKE TAHOE, CALIF. – results from a large, retrospective cohort study demonstrated.
“The atopic march is characterized by a progression from atopic dermatitis, usually early in childhood, to subsequent development of allergic rhinitis and asthma, lead study author Joy Wan, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is thought that the skin acts as the site of primary sensitization through a defective epithelial barrier, which then allows for allergic sensitization to occur in the airways. It is estimated that 30%-60% of AD patients go on to develop asthma and/or allergic rhinitis. However, not all patients complete the so-called atopic march, and this variation in the risk of asthma and allergic rhinitis among AD patients is not very well understood. Better ways to risk stratify these patients are needed.”
One possible explanation for this variation in the risk of atopy in AD patients could be the timing of their dermatitis onset. “We know that atopic dermatitis begins in infancy, but it can start at any age,” said Dr. Wan, who is a fellow in the section of pediatric dermatology at the Children’s Hospital of Philadelphia. “There has been a distinction between early-onset versus late-onset AD. Some past studies have also suggested that there is an increased risk of asthma and allergic rhinitis in children who have early-onset AD before the age of 1 or 2. This suggests that perhaps the model of the atopic march varies between early- and late-onset AD. However, past studies have had several limitations. They’ve often had short durations of follow-up, they’ve only examined narrow ranges of age of onset for AD, and most of them have been designed to primarily evaluate other exposures and outcomes, rather than looking at the timing of AD onset itself.”
For the current study, Dr. Wan and her associates set out to examine the risk of seasonal allergies and asthma among children with AD with respect to the age of AD onset. They used data from the Pediatric Eczema Elective Registry (PEER), an ongoing, prospective U.S. cohort of more than 7,700 children with physician-confirmed AD (JAMA Dermatol. 2014 Jun;150:593-600). All registry participants had used pimecrolimus cream in the past, but children with lymphoproliferative disease were excluded from the registry, as were those with malignancy or those who required the use of systemic immunosuppression.
The researchers evaluated 3,966 subjects in PEER with at least 3 years of follow-up. The exposure of interest was age of AD onset, and they divided patients into three broad age categories: early onset (age 2 years or younger), mid onset (3-7 years), and late onset (8-17 years). Primary outcomes were prevalent seasonal allergies and asthma at the time of registry enrollment, and incident seasonal allergies and asthma during follow-up, assessed via patient surveys every 3 years.
The study population included high proportions of white and black children, and there was a slight predominance of females. The median age at PEER enrollment increased with advancing age of AD onset (5.2 years in the early-onset group vs. 8.2 years in the mid-onset group and 13.1 years in the late-onset group), while the duration of follow-up was fairly similar across the three groups (a median of about 8.3 months). Family history of AD was common across all three groups, while patients in the late-onset group tended to have better control of their AD, compared with their younger counterparts.
At baseline, the prevalence of seasonal allergies was highest among the early-onset group at 74.6%, compared with 69.9% among the mid-onset group and 70.1% among the late-onset group. After adjusting for sex, race, and age at registry enrollment, the relative risk for prevalent seasonal allergies was 9% lower in the mid-onset group (0.91) and 18% lower in the late-onset group (0.82), compared with those in the early-onset group. Next, Dr. Wan and her associates calculated the incidence of seasonal allergies among 1,054 patients who did not have allergies at baseline. The cumulative incidence was highest among the early-onset group (56.1%), followed by the mid-onset group (46.8%), and the late-onset group (30.6%). On adjusted analysis, the relative risk for seasonal allergies among patients who had no allergies at baseline was 18% lower in the mid-onset group (0.82) and 36% lower in the late-onset group (0.64), compared with those in the early-onset group.
In the analysis of asthma risk by age of AD onset, prevalence was highest among patients in the early-onset group at 51.5%, compared with 44.7% among the mid-onset age group and 43% among the late-onset age group. On adjusted analysis, the relative risk for asthma was 15% lower in the mid-onset group (0.85) and 29% lower in the late-onset group (0.71), compared with those in the early-onset group. Meanwhile, the cumulative incidence of asthma among patients without asthma at baseline was also highest in the early-onset group (39.2%), compared with 31.9% in the mid-onset group and 29.9% in the late-onset group.
On adjusted analysis, the relative risk for asthma among this subset of patients was 4% lower in the mid-onset group (0.96) and 8% lower in the late-onset group (0.92), compared with those in the early-onset group, a difference that was not statistically significant. “One possible explanation for this is that asthma tends to develop soon after AD does, and the rates of developing asthma later on, as detected by our study, are nondifferential,” Dr. Wan said. “Another possibility is that the impact of early-onset versus late-onset AD is just different for asthma than it is for seasonal allergies.”
She acknowledged certain limitations of the study, including the risk of misclassification bias and limitations in recall with self-reported data, and the fact that the findings may not be generalizable to all patients with AD.
“Future studies with longer follow-up and studies of adult-onset AD will help extend our findings,” she concluded. “Nevertheless, our findings may inform how we risk stratify patients for AD treatment or atopic march prevention efforts in the future.”
PEER is funded by a grant from Valeant Pharmaceuticals, but Valeant had no role in this study. Dr. Wan reported having no financial disclosures. The study won an award at the meeting for best research presented by a dermatology resident or fellow.
LAKE TAHOE, CALIF. – results from a large, retrospective cohort study demonstrated.
“The atopic march is characterized by a progression from atopic dermatitis, usually early in childhood, to subsequent development of allergic rhinitis and asthma, lead study author Joy Wan, MD, said at the annual meeting of the Society for Pediatric Dermatology. “It is thought that the skin acts as the site of primary sensitization through a defective epithelial barrier, which then allows for allergic sensitization to occur in the airways. It is estimated that 30%-60% of AD patients go on to develop asthma and/or allergic rhinitis. However, not all patients complete the so-called atopic march, and this variation in the risk of asthma and allergic rhinitis among AD patients is not very well understood. Better ways to risk stratify these patients are needed.”
One possible explanation for this variation in the risk of atopy in AD patients could be the timing of their dermatitis onset. “We know that atopic dermatitis begins in infancy, but it can start at any age,” said Dr. Wan, who is a fellow in the section of pediatric dermatology at the Children’s Hospital of Philadelphia. “There has been a distinction between early-onset versus late-onset AD. Some past studies have also suggested that there is an increased risk of asthma and allergic rhinitis in children who have early-onset AD before the age of 1 or 2. This suggests that perhaps the model of the atopic march varies between early- and late-onset AD. However, past studies have had several limitations. They’ve often had short durations of follow-up, they’ve only examined narrow ranges of age of onset for AD, and most of them have been designed to primarily evaluate other exposures and outcomes, rather than looking at the timing of AD onset itself.”
For the current study, Dr. Wan and her associates set out to examine the risk of seasonal allergies and asthma among children with AD with respect to the age of AD onset. They used data from the Pediatric Eczema Elective Registry (PEER), an ongoing, prospective U.S. cohort of more than 7,700 children with physician-confirmed AD (JAMA Dermatol. 2014 Jun;150:593-600). All registry participants had used pimecrolimus cream in the past, but children with lymphoproliferative disease were excluded from the registry, as were those with malignancy or those who required the use of systemic immunosuppression.
The researchers evaluated 3,966 subjects in PEER with at least 3 years of follow-up. The exposure of interest was age of AD onset, and they divided patients into three broad age categories: early onset (age 2 years or younger), mid onset (3-7 years), and late onset (8-17 years). Primary outcomes were prevalent seasonal allergies and asthma at the time of registry enrollment, and incident seasonal allergies and asthma during follow-up, assessed via patient surveys every 3 years.
The study population included high proportions of white and black children, and there was a slight predominance of females. The median age at PEER enrollment increased with advancing age of AD onset (5.2 years in the early-onset group vs. 8.2 years in the mid-onset group and 13.1 years in the late-onset group), while the duration of follow-up was fairly similar across the three groups (a median of about 8.3 months). Family history of AD was common across all three groups, while patients in the late-onset group tended to have better control of their AD, compared with their younger counterparts.
At baseline, the prevalence of seasonal allergies was highest among the early-onset group at 74.6%, compared with 69.9% among the mid-onset group and 70.1% among the late-onset group. After adjusting for sex, race, and age at registry enrollment, the relative risk for prevalent seasonal allergies was 9% lower in the mid-onset group (0.91) and 18% lower in the late-onset group (0.82), compared with those in the early-onset group. Next, Dr. Wan and her associates calculated the incidence of seasonal allergies among 1,054 patients who did not have allergies at baseline. The cumulative incidence was highest among the early-onset group (56.1%), followed by the mid-onset group (46.8%), and the late-onset group (30.6%). On adjusted analysis, the relative risk for seasonal allergies among patients who had no allergies at baseline was 18% lower in the mid-onset group (0.82) and 36% lower in the late-onset group (0.64), compared with those in the early-onset group.
In the analysis of asthma risk by age of AD onset, prevalence was highest among patients in the early-onset group at 51.5%, compared with 44.7% among the mid-onset age group and 43% among the late-onset age group. On adjusted analysis, the relative risk for asthma was 15% lower in the mid-onset group (0.85) and 29% lower in the late-onset group (0.71), compared with those in the early-onset group. Meanwhile, the cumulative incidence of asthma among patients without asthma at baseline was also highest in the early-onset group (39.2%), compared with 31.9% in the mid-onset group and 29.9% in the late-onset group.
On adjusted analysis, the relative risk for asthma among this subset of patients was 4% lower in the mid-onset group (0.96) and 8% lower in the late-onset group (0.92), compared with those in the early-onset group, a difference that was not statistically significant. “One possible explanation for this is that asthma tends to develop soon after AD does, and the rates of developing asthma later on, as detected by our study, are nondifferential,” Dr. Wan said. “Another possibility is that the impact of early-onset versus late-onset AD is just different for asthma than it is for seasonal allergies.”
She acknowledged certain limitations of the study, including the risk of misclassification bias and limitations in recall with self-reported data, and the fact that the findings may not be generalizable to all patients with AD.
“Future studies with longer follow-up and studies of adult-onset AD will help extend our findings,” she concluded. “Nevertheless, our findings may inform how we risk stratify patients for AD treatment or atopic march prevention efforts in the future.”
PEER is funded by a grant from Valeant Pharmaceuticals, but Valeant had no role in this study. Dr. Wan reported having no financial disclosures. The study won an award at the meeting for best research presented by a dermatology resident or fellow.
AT SPD 2018
Birthmark-ipelago
At birth, this now 18-year-old man had what he was told was “only a birthmark.” In the years since, the lesion has darkened and become increasingly well-defined and raised. It is occasionally irritated.
His parents deny any history of seizures, skeletal problems, vision problems, or developmental disabilities in the patient or the family. All parties want the lesion removed.
EXAMINATION
A contiguous linear collection of brown-to-tan papules and nodules runs entirely across the left upper chest, ending on the left shoulder. It measures about 1 cm in width. On closer examination, many of the marks appear to be a mix of milia and comedones.

No similar lesions are seen elsewhere, and the patient’s type IV skin appears normal in all other respects.
What is the diagnosis?
DISCUSSION
Linear epidermal nevi (LEN) are congenital hamartomatous lesions of embryonal ectodermal origin. They are classified based on their main components, which can be
- Sebaceous
- Apocrine
- Eccrine
- Follicular
- Keratinocytic.
The significance of the linear configuration is that in up to one-third of patients another organ system (eg, brain, eyes, bone) will be affected. Associated neurologic problems include seizures and intellectual disability, which are caused by a variety of neuropathologic lesions.
Other forms of epidermal nevi include nevus comedonicus (associated with cataracts) and inflammatory linear verrucous epidermal nevus (ILVEN). Most often seen in early childhood on the limbs, ILVEN accounts for about 5% of all epidermal nevi.
The case patient appeared to have a mixed form, composed of epidermal and comedonal elements. Fortunately, he did not have any other associated abnormalities.
Other items in the differential include lichen striatus, wart, and koebnerized psoriasis.
Treatment for LEN is problematic, due to not only pain and scarring but also the loss of normal pigment. Options include laser, dermabrasion, and surgery. Smaller lesions can simply be excised.
TAKE-HOME LEARNING POINTS
- Linear epidermal nevi (LEN) are benign, unusual, congenital, hamartomatous tumors of embryonal ectodermal origin, which mostly manifest above the waist (ie, shoulders, trunk) in a linear configuration.
- LEN are classified according to their predominant structural element (sebaceous, eccrine, apocrine, follicular, keratinocytic).
- About one-third of all cases involve other organs, including the brain, eyes, or skeleton.
- The differential for LEN includes wart, koebnerized psoriasis, and lichen striatus.
- Treatment can be problematic, but options include laser, dermabrasion, and surgery.
At birth, this now 18-year-old man had what he was told was “only a birthmark.” In the years since, the lesion has darkened and become increasingly well-defined and raised. It is occasionally irritated.
His parents deny any history of seizures, skeletal problems, vision problems, or developmental disabilities in the patient or the family. All parties want the lesion removed.
EXAMINATION
A contiguous linear collection of brown-to-tan papules and nodules runs entirely across the left upper chest, ending on the left shoulder. It measures about 1 cm in width. On closer examination, many of the marks appear to be a mix of milia and comedones.

No similar lesions are seen elsewhere, and the patient’s type IV skin appears normal in all other respects.
What is the diagnosis?
DISCUSSION
Linear epidermal nevi (LEN) are congenital hamartomatous lesions of embryonal ectodermal origin. They are classified based on their main components, which can be
- Sebaceous
- Apocrine
- Eccrine
- Follicular
- Keratinocytic.
The significance of the linear configuration is that in up to one-third of patients another organ system (eg, brain, eyes, bone) will be affected. Associated neurologic problems include seizures and intellectual disability, which are caused by a variety of neuropathologic lesions.
Other forms of epidermal nevi include nevus comedonicus (associated with cataracts) and inflammatory linear verrucous epidermal nevus (ILVEN). Most often seen in early childhood on the limbs, ILVEN accounts for about 5% of all epidermal nevi.
The case patient appeared to have a mixed form, composed of epidermal and comedonal elements. Fortunately, he did not have any other associated abnormalities.
Other items in the differential include lichen striatus, wart, and koebnerized psoriasis.
Treatment for LEN is problematic, due to not only pain and scarring but also the loss of normal pigment. Options include laser, dermabrasion, and surgery. Smaller lesions can simply be excised.
TAKE-HOME LEARNING POINTS
- Linear epidermal nevi (LEN) are benign, unusual, congenital, hamartomatous tumors of embryonal ectodermal origin, which mostly manifest above the waist (ie, shoulders, trunk) in a linear configuration.
- LEN are classified according to their predominant structural element (sebaceous, eccrine, apocrine, follicular, keratinocytic).
- About one-third of all cases involve other organs, including the brain, eyes, or skeleton.
- The differential for LEN includes wart, koebnerized psoriasis, and lichen striatus.
- Treatment can be problematic, but options include laser, dermabrasion, and surgery.
At birth, this now 18-year-old man had what he was told was “only a birthmark.” In the years since, the lesion has darkened and become increasingly well-defined and raised. It is occasionally irritated.
His parents deny any history of seizures, skeletal problems, vision problems, or developmental disabilities in the patient or the family. All parties want the lesion removed.
EXAMINATION
A contiguous linear collection of brown-to-tan papules and nodules runs entirely across the left upper chest, ending on the left shoulder. It measures about 1 cm in width. On closer examination, many of the marks appear to be a mix of milia and comedones.

No similar lesions are seen elsewhere, and the patient’s type IV skin appears normal in all other respects.
What is the diagnosis?
DISCUSSION
Linear epidermal nevi (LEN) are congenital hamartomatous lesions of embryonal ectodermal origin. They are classified based on their main components, which can be
- Sebaceous
- Apocrine
- Eccrine
- Follicular
- Keratinocytic.
The significance of the linear configuration is that in up to one-third of patients another organ system (eg, brain, eyes, bone) will be affected. Associated neurologic problems include seizures and intellectual disability, which are caused by a variety of neuropathologic lesions.
Other forms of epidermal nevi include nevus comedonicus (associated with cataracts) and inflammatory linear verrucous epidermal nevus (ILVEN). Most often seen in early childhood on the limbs, ILVEN accounts for about 5% of all epidermal nevi.
The case patient appeared to have a mixed form, composed of epidermal and comedonal elements. Fortunately, he did not have any other associated abnormalities.
Other items in the differential include lichen striatus, wart, and koebnerized psoriasis.
Treatment for LEN is problematic, due to not only pain and scarring but also the loss of normal pigment. Options include laser, dermabrasion, and surgery. Smaller lesions can simply be excised.
TAKE-HOME LEARNING POINTS
- Linear epidermal nevi (LEN) are benign, unusual, congenital, hamartomatous tumors of embryonal ectodermal origin, which mostly manifest above the waist (ie, shoulders, trunk) in a linear configuration.
- LEN are classified according to their predominant structural element (sebaceous, eccrine, apocrine, follicular, keratinocytic).
- About one-third of all cases involve other organs, including the brain, eyes, or skeleton.
- The differential for LEN includes wart, koebnerized psoriasis, and lichen striatus.
- Treatment can be problematic, but options include laser, dermabrasion, and surgery.
Dark spot on back
A biopsy revealed a compound dysplastic nevus (DN) with no signs of malignancy. There was only mild atypia (if severe atypia is reported, then the lesion often is treated as a melanoma in-situ).
The FP was initially concerned about melanoma, given the size, growth, and other characteristics of the lesion. He performed dermoscopy and noted an irregular network with multiple asymmetrically placed dots off the network. His differential diagnosis included melanoma, melanoma in-situ, and dysplastic nevus. After informed consent, he performed a saucerization (deep shave) with a DermaBlade, taking 2-mm margins of clinically normal skin, which revealed the DN. (See the Watch & Learn video on “Shave biopsy.”)
Dysplastic nevi (with mild to moderate atypia) are benign acquired melanocytic lesions of the skin. Most are compound nevi possessing a junctional and intradermal component. While dysplastic nevi are not premalignant lesions, they do have some (small) potential for malignant transformation and patients with multiple DN have an increased risk for melanoma. Cutting out all the DN does not change that risk of melanoma.
The FP explained that no further treatment was needed and offered yearly skin exams to monitor for melanoma.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
A biopsy revealed a compound dysplastic nevus (DN) with no signs of malignancy. There was only mild atypia (if severe atypia is reported, then the lesion often is treated as a melanoma in-situ).
The FP was initially concerned about melanoma, given the size, growth, and other characteristics of the lesion. He performed dermoscopy and noted an irregular network with multiple asymmetrically placed dots off the network. His differential diagnosis included melanoma, melanoma in-situ, and dysplastic nevus. After informed consent, he performed a saucerization (deep shave) with a DermaBlade, taking 2-mm margins of clinically normal skin, which revealed the DN. (See the Watch & Learn video on “Shave biopsy.”)
Dysplastic nevi (with mild to moderate atypia) are benign acquired melanocytic lesions of the skin. Most are compound nevi possessing a junctional and intradermal component. While dysplastic nevi are not premalignant lesions, they do have some (small) potential for malignant transformation and patients with multiple DN have an increased risk for melanoma. Cutting out all the DN does not change that risk of melanoma.
The FP explained that no further treatment was needed and offered yearly skin exams to monitor for melanoma.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
A biopsy revealed a compound dysplastic nevus (DN) with no signs of malignancy. There was only mild atypia (if severe atypia is reported, then the lesion often is treated as a melanoma in-situ).
The FP was initially concerned about melanoma, given the size, growth, and other characteristics of the lesion. He performed dermoscopy and noted an irregular network with multiple asymmetrically placed dots off the network. His differential diagnosis included melanoma, melanoma in-situ, and dysplastic nevus. After informed consent, he performed a saucerization (deep shave) with a DermaBlade, taking 2-mm margins of clinically normal skin, which revealed the DN. (See the Watch & Learn video on “Shave biopsy.”)
Dysplastic nevi (with mild to moderate atypia) are benign acquired melanocytic lesions of the skin. Most are compound nevi possessing a junctional and intradermal component. While dysplastic nevi are not premalignant lesions, they do have some (small) potential for malignant transformation and patients with multiple DN have an increased risk for melanoma. Cutting out all the DN does not change that risk of melanoma.
The FP explained that no further treatment was needed and offered yearly skin exams to monitor for melanoma.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
Fish pedicures
A letter published in JAMA Dermatology describes an otherwise healthy woman in her 20s who experienced nail abnormalities some months after having a fish pedicure. Onychomadesis, or transverse splitting of the nail plate, occurs when the nail matrix has arrested in producing the nail plate. It can be thought of as more severe form of Beau’s lines, in which the nail itself actually breaks and separates from the proximal nail plate and eventually sheds.
Fish pedicures have a long-standing history in Mediterranean and Middle Eastern cultures for aiding such skin conditions as psoriasis and helping to remove scaly skin. The Garra rufa fish are nonmigratory freshwater fish native to the Persian Gulf and Eastern Mediterranean. Suction allows them to attach to rocks and eat plankton. These “doctor fish,” as they are nicknamed, when placed in a warm bath of 25°C to 30°C, will also eat human skin when starved of their natural food source. As the JAMA Dermatology letter mentions, this was demonstrated in a study in Kangal, Turkey, where Garra rufa fish were used to improve psoriasis by feeding on psoriasis plaques but not normal skin. After 3 weeks of therapy with Garra rufa in 67 patients, there was a 72% reduction in the Psoriasis Area and Severity Index (PASI) score from baseline (Evid Based Complement Alternat Med. 2006 Dec;3[4]:483-8).
Popular in the United States and Europe about a decade ago, fish pedicures have now been banned in 10 U.S. states and in some parts of Europe. While the trend in the United States has waned, fish pedicures have recently become more popular in vacation destinations, such as the Caribbean. The inherent concern of fish pedicures is risk of infection as the same fish are used successively and cannot be adequately sanitized between people.
Two cases of staphylococcus infections and one of Mycobacterium marinum have been reported after fish pedicures. Whether these infections were caused by the fish or the water source, however, remains to be determined. If the fish were transmitting infections, it seems that more infections would likely have been reported, considering the widespread popularity in the past. I, like Antonella Tosti, MD, who commented in a CNN report on the JAMA Dermatology case, also doubt that the fish pedicure alone caused onychomadesis in this woman. In order for onychomadesis to occur, there would have had to have been significant trauma to all 10 nails at the matrix. Would the fish been able to have caused the same amount of trauma to all 10 nails in one setting? While it is possible, I believe a more likely explanation would be an alternate endogenous or exogenous source.
Traditional medicine has been used to enhance beauty and cure ailments for thousands of years before the advent of modern medicine as demonstrated by the Kangal study. Before discounting fish pedicures completely, perhaps some thought should also be given to how this practice affects wildlife and the fish. The CNN report refers to a 2011 investigation by the U.K.’s Fish Health Inspectorate, which “found a bacterial outbreak among thousands of these fish, which had been transported from Indonesia to the United Kingdom pedicure spas. Fish were found with bulging eyes, many hemorrhaging around the gills and mouth. The culprit was found to be a streptococcal bacteria, a strain that is associated with fish like tilapia, according to David Verner-Jeffreys, a senior microbiologist at the Centre for Environment, Fisheries and Aquaculture Science in the U.K.”
Whether or not these fish would pose any risk to humans is unknown, but certainly, this practice adversely affects the welfare of the fish and their environment. The overharvesting of these fish has led the Turkish government to introduce legal protections for the country’s Garra rufa in an attempt to combat overfishing and exploitation.
Perhaps fish pedicures solely for aesthetic reasons should not be practiced because of the potential infection risk – as well as the harm (to both humans and fish) and overharvesting of the fish. If used properly, these fish, however, could be an aid in treating certain skin pathologies.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
A letter published in JAMA Dermatology describes an otherwise healthy woman in her 20s who experienced nail abnormalities some months after having a fish pedicure. Onychomadesis, or transverse splitting of the nail plate, occurs when the nail matrix has arrested in producing the nail plate. It can be thought of as more severe form of Beau’s lines, in which the nail itself actually breaks and separates from the proximal nail plate and eventually sheds.
Fish pedicures have a long-standing history in Mediterranean and Middle Eastern cultures for aiding such skin conditions as psoriasis and helping to remove scaly skin. The Garra rufa fish are nonmigratory freshwater fish native to the Persian Gulf and Eastern Mediterranean. Suction allows them to attach to rocks and eat plankton. These “doctor fish,” as they are nicknamed, when placed in a warm bath of 25°C to 30°C, will also eat human skin when starved of their natural food source. As the JAMA Dermatology letter mentions, this was demonstrated in a study in Kangal, Turkey, where Garra rufa fish were used to improve psoriasis by feeding on psoriasis plaques but not normal skin. After 3 weeks of therapy with Garra rufa in 67 patients, there was a 72% reduction in the Psoriasis Area and Severity Index (PASI) score from baseline (Evid Based Complement Alternat Med. 2006 Dec;3[4]:483-8).
Popular in the United States and Europe about a decade ago, fish pedicures have now been banned in 10 U.S. states and in some parts of Europe. While the trend in the United States has waned, fish pedicures have recently become more popular in vacation destinations, such as the Caribbean. The inherent concern of fish pedicures is risk of infection as the same fish are used successively and cannot be adequately sanitized between people.
Two cases of staphylococcus infections and one of Mycobacterium marinum have been reported after fish pedicures. Whether these infections were caused by the fish or the water source, however, remains to be determined. If the fish were transmitting infections, it seems that more infections would likely have been reported, considering the widespread popularity in the past. I, like Antonella Tosti, MD, who commented in a CNN report on the JAMA Dermatology case, also doubt that the fish pedicure alone caused onychomadesis in this woman. In order for onychomadesis to occur, there would have had to have been significant trauma to all 10 nails at the matrix. Would the fish been able to have caused the same amount of trauma to all 10 nails in one setting? While it is possible, I believe a more likely explanation would be an alternate endogenous or exogenous source.
Traditional medicine has been used to enhance beauty and cure ailments for thousands of years before the advent of modern medicine as demonstrated by the Kangal study. Before discounting fish pedicures completely, perhaps some thought should also be given to how this practice affects wildlife and the fish. The CNN report refers to a 2011 investigation by the U.K.’s Fish Health Inspectorate, which “found a bacterial outbreak among thousands of these fish, which had been transported from Indonesia to the United Kingdom pedicure spas. Fish were found with bulging eyes, many hemorrhaging around the gills and mouth. The culprit was found to be a streptococcal bacteria, a strain that is associated with fish like tilapia, according to David Verner-Jeffreys, a senior microbiologist at the Centre for Environment, Fisheries and Aquaculture Science in the U.K.”
Whether or not these fish would pose any risk to humans is unknown, but certainly, this practice adversely affects the welfare of the fish and their environment. The overharvesting of these fish has led the Turkish government to introduce legal protections for the country’s Garra rufa in an attempt to combat overfishing and exploitation.
Perhaps fish pedicures solely for aesthetic reasons should not be practiced because of the potential infection risk – as well as the harm (to both humans and fish) and overharvesting of the fish. If used properly, these fish, however, could be an aid in treating certain skin pathologies.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.
A letter published in JAMA Dermatology describes an otherwise healthy woman in her 20s who experienced nail abnormalities some months after having a fish pedicure. Onychomadesis, or transverse splitting of the nail plate, occurs when the nail matrix has arrested in producing the nail plate. It can be thought of as more severe form of Beau’s lines, in which the nail itself actually breaks and separates from the proximal nail plate and eventually sheds.
Fish pedicures have a long-standing history in Mediterranean and Middle Eastern cultures for aiding such skin conditions as psoriasis and helping to remove scaly skin. The Garra rufa fish are nonmigratory freshwater fish native to the Persian Gulf and Eastern Mediterranean. Suction allows them to attach to rocks and eat plankton. These “doctor fish,” as they are nicknamed, when placed in a warm bath of 25°C to 30°C, will also eat human skin when starved of their natural food source. As the JAMA Dermatology letter mentions, this was demonstrated in a study in Kangal, Turkey, where Garra rufa fish were used to improve psoriasis by feeding on psoriasis plaques but not normal skin. After 3 weeks of therapy with Garra rufa in 67 patients, there was a 72% reduction in the Psoriasis Area and Severity Index (PASI) score from baseline (Evid Based Complement Alternat Med. 2006 Dec;3[4]:483-8).
Popular in the United States and Europe about a decade ago, fish pedicures have now been banned in 10 U.S. states and in some parts of Europe. While the trend in the United States has waned, fish pedicures have recently become more popular in vacation destinations, such as the Caribbean. The inherent concern of fish pedicures is risk of infection as the same fish are used successively and cannot be adequately sanitized between people.
Two cases of staphylococcus infections and one of Mycobacterium marinum have been reported after fish pedicures. Whether these infections were caused by the fish or the water source, however, remains to be determined. If the fish were transmitting infections, it seems that more infections would likely have been reported, considering the widespread popularity in the past. I, like Antonella Tosti, MD, who commented in a CNN report on the JAMA Dermatology case, also doubt that the fish pedicure alone caused onychomadesis in this woman. In order for onychomadesis to occur, there would have had to have been significant trauma to all 10 nails at the matrix. Would the fish been able to have caused the same amount of trauma to all 10 nails in one setting? While it is possible, I believe a more likely explanation would be an alternate endogenous or exogenous source.
Traditional medicine has been used to enhance beauty and cure ailments for thousands of years before the advent of modern medicine as demonstrated by the Kangal study. Before discounting fish pedicures completely, perhaps some thought should also be given to how this practice affects wildlife and the fish. The CNN report refers to a 2011 investigation by the U.K.’s Fish Health Inspectorate, which “found a bacterial outbreak among thousands of these fish, which had been transported from Indonesia to the United Kingdom pedicure spas. Fish were found with bulging eyes, many hemorrhaging around the gills and mouth. The culprit was found to be a streptococcal bacteria, a strain that is associated with fish like tilapia, according to David Verner-Jeffreys, a senior microbiologist at the Centre for Environment, Fisheries and Aquaculture Science in the U.K.”
Whether or not these fish would pose any risk to humans is unknown, but certainly, this practice adversely affects the welfare of the fish and their environment. The overharvesting of these fish has led the Turkish government to introduce legal protections for the country’s Garra rufa in an attempt to combat overfishing and exploitation.
Perhaps fish pedicures solely for aesthetic reasons should not be practiced because of the potential infection risk – as well as the harm (to both humans and fish) and overharvesting of the fish. If used properly, these fish, however, could be an aid in treating certain skin pathologies.
Dr. Wesley and Dr. Talakoub are co-contributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at dermnews@mdedge.com. They had no relevant disclosures.