User login
These Patients May Be Less Adherent to nAMD Treatment
TOPLINE:
BARCELONA, SPAIN — Patients who receive a diagnosis of neovascular age-related macular degeneration (nAMD) from their primary care clinician may be less likely to adhere to treatment than those who receive the diagnosis from a specialist who provides anti–vascular endothelial growth factor (anti-VEGF) therapy, according to global survey results presented at the European Society of Retina Specialists (EURETINA) 2024. Likewise, patients who self-pay for the medication or who have bilateral nAMD may be less adherent to therapy, researchers found.
METHODOLOGY:
- Researchers analyzed data from 4558 patients with nAMD who participated in the Barometer Global Survey, which involved 77 clinics in 24 countries, including Canada, Mexico, Brazil, Germany, and France.
- The survey included multiple-choice questions on personal characteristics, disease awareness, experiences with treatment, and logistical challenges with getting to appointments.
- An exploratory statistical analysis identified 19 variables that influenced patient adherence to anti-VEGF therapy.
- The researchers classified 670 patients who missed two or more appointments during a 12-month period as nonadherent.
TAKEAWAY:
- Patients with nAMD diagnosed by their family doctor or general practitioner had a threefold higher risk for nonadherence than those diagnosed by the physician treating their nAMD.
- Self-pay was associated with more than twice the odds of nonadherence compared with having insurance coverage (odds ratio [OR], 2.5).
- Compared with unilateral nAMD, bilateral nAMD was associated with higher odds of multiple missed appointments (OR, 1.7).
- Nonadherence increased with the number of anti-VEGF injections, which may show that “longer treatment durations could permit more opportunities for absenteeism,” the investigators noted.
IN PRACTICE:
“Identifying patient characteristics and challenges that may be associated with nonadherence allows clinicians to recognize patients at risk for nonadherence and provide further support before these patients begin to miss appointments,” the study authors wrote.
SOURCE:
This study was led by Laurent Kodjikian, MD, PhD, with Croix-Rousse University Hospital and the University of Lyon in France. The findings were presented in a poster at EURETINA 2024 (September 19-22).
LIMITATIONS:
The survey relied on participant responses using Likert scales and single-choice questions. Patients from the United States were not included in the study.
DISCLOSURES:
The survey and medical writing support for the study were funded by Bayer Consumer Care. Kodjikian and co-authors disclosed consulting work for Bayer and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
BARCELONA, SPAIN — Patients who receive a diagnosis of neovascular age-related macular degeneration (nAMD) from their primary care clinician may be less likely to adhere to treatment than those who receive the diagnosis from a specialist who provides anti–vascular endothelial growth factor (anti-VEGF) therapy, according to global survey results presented at the European Society of Retina Specialists (EURETINA) 2024. Likewise, patients who self-pay for the medication or who have bilateral nAMD may be less adherent to therapy, researchers found.
METHODOLOGY:
- Researchers analyzed data from 4558 patients with nAMD who participated in the Barometer Global Survey, which involved 77 clinics in 24 countries, including Canada, Mexico, Brazil, Germany, and France.
- The survey included multiple-choice questions on personal characteristics, disease awareness, experiences with treatment, and logistical challenges with getting to appointments.
- An exploratory statistical analysis identified 19 variables that influenced patient adherence to anti-VEGF therapy.
- The researchers classified 670 patients who missed two or more appointments during a 12-month period as nonadherent.
TAKEAWAY:
- Patients with nAMD diagnosed by their family doctor or general practitioner had a threefold higher risk for nonadherence than those diagnosed by the physician treating their nAMD.
- Self-pay was associated with more than twice the odds of nonadherence compared with having insurance coverage (odds ratio [OR], 2.5).
- Compared with unilateral nAMD, bilateral nAMD was associated with higher odds of multiple missed appointments (OR, 1.7).
- Nonadherence increased with the number of anti-VEGF injections, which may show that “longer treatment durations could permit more opportunities for absenteeism,” the investigators noted.
IN PRACTICE:
“Identifying patient characteristics and challenges that may be associated with nonadherence allows clinicians to recognize patients at risk for nonadherence and provide further support before these patients begin to miss appointments,” the study authors wrote.
SOURCE:
This study was led by Laurent Kodjikian, MD, PhD, with Croix-Rousse University Hospital and the University of Lyon in France. The findings were presented in a poster at EURETINA 2024 (September 19-22).
LIMITATIONS:
The survey relied on participant responses using Likert scales and single-choice questions. Patients from the United States were not included in the study.
DISCLOSURES:
The survey and medical writing support for the study were funded by Bayer Consumer Care. Kodjikian and co-authors disclosed consulting work for Bayer and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
BARCELONA, SPAIN — Patients who receive a diagnosis of neovascular age-related macular degeneration (nAMD) from their primary care clinician may be less likely to adhere to treatment than those who receive the diagnosis from a specialist who provides anti–vascular endothelial growth factor (anti-VEGF) therapy, according to global survey results presented at the European Society of Retina Specialists (EURETINA) 2024. Likewise, patients who self-pay for the medication or who have bilateral nAMD may be less adherent to therapy, researchers found.
METHODOLOGY:
- Researchers analyzed data from 4558 patients with nAMD who participated in the Barometer Global Survey, which involved 77 clinics in 24 countries, including Canada, Mexico, Brazil, Germany, and France.
- The survey included multiple-choice questions on personal characteristics, disease awareness, experiences with treatment, and logistical challenges with getting to appointments.
- An exploratory statistical analysis identified 19 variables that influenced patient adherence to anti-VEGF therapy.
- The researchers classified 670 patients who missed two or more appointments during a 12-month period as nonadherent.
TAKEAWAY:
- Patients with nAMD diagnosed by their family doctor or general practitioner had a threefold higher risk for nonadherence than those diagnosed by the physician treating their nAMD.
- Self-pay was associated with more than twice the odds of nonadherence compared with having insurance coverage (odds ratio [OR], 2.5).
- Compared with unilateral nAMD, bilateral nAMD was associated with higher odds of multiple missed appointments (OR, 1.7).
- Nonadherence increased with the number of anti-VEGF injections, which may show that “longer treatment durations could permit more opportunities for absenteeism,” the investigators noted.
IN PRACTICE:
“Identifying patient characteristics and challenges that may be associated with nonadherence allows clinicians to recognize patients at risk for nonadherence and provide further support before these patients begin to miss appointments,” the study authors wrote.
SOURCE:
This study was led by Laurent Kodjikian, MD, PhD, with Croix-Rousse University Hospital and the University of Lyon in France. The findings were presented in a poster at EURETINA 2024 (September 19-22).
LIMITATIONS:
The survey relied on participant responses using Likert scales and single-choice questions. Patients from the United States were not included in the study.
DISCLOSURES:
The survey and medical writing support for the study were funded by Bayer Consumer Care. Kodjikian and co-authors disclosed consulting work for Bayer and other pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Is BMI Underestimating Breast Cancer Risk in Postmenopausal Women?
TOPLINE:
Accurate body fat measures are crucial for effective cancer prevention.
METHODOLOGY:
- Researchers conducted a case-control study including 1033 breast cancer cases and 1143 postmenopausal population controls from the MCC-Spain study.
- Participants were aged 20-85 years. BMI was calculated as the ratio of weight to height squared and categorized using World Health Organization standards: < 25, 25-29.9, 30-34.9, and ≥ 35.
- CUN-BAE was calculated using a specific equation and categorized according to the estimated percentage of body fat: < 35%, 35%-39.9%, 40%-44.9%, and ≥ 45%.
- Odds ratios (ORs) were estimated with 95% CIs for both measures (BMI and CUN-BAE) for breast cancer cases using unconditional logistic regression.
TAKEAWAY:
- Excess body weight attributable to the risk for breast cancer was 23% when assessed using a BMI value > 30 and 38% when assessed using a CUN-BAE value > 40% body fat.
- Hormone receptor stratification showed that these differences in population-attributable fractions were only observed in hormone receptor–positive cases, with an estimated burden of 19.9% for BMI and 41.9% for CUN-BAE.
- The highest categories of CUN-BAE showed an increase in the risk for postmenopausal breast cancer (OR, 2.13 for body fat ≥ 45% compared with the reference category < 35%).
- No similar trend was observed for BMI, as the gradient declined after a BMI ≥ 35.
IN PRACTICE:
“The results of our study indicate that excess body fat is a significant risk factor for hormone receptor–positive breast cancer in postmenopausal women. Our findings suggest that the population impact could be underestimated when using traditional BMI estimates, and that more accurate measures of body fat, such as CUN-BAE, should be considered,” the authors of the study wrote.
SOURCE:
This study was led by Verónica Dávila-Batista, University of Las Palmas de Gran Canaria in Las Palmas de Gran Canaria, Spain. It was published online in Journal of Epidemiology and Community Health.
LIMITATIONS:
The case-control design of the study may have limited the ability to establish causal relationships. BMI was self-reported at the time of the interview for controls and 1 year before diagnosis for cancer cases, which may have introduced recall bias. The formula for CUN-BAE was calculated from a sedentary convenience sample, which may not have been representative of the general population. The small sample size of cases that did not express hormone receptors was another limitation. The study’s findings may not be generalizable to non-White populations as non-White participants were excluded.
DISCLOSURES:
Dávila-Batista disclosed receiving grants from the Carlos III Health Institute. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Accurate body fat measures are crucial for effective cancer prevention.
METHODOLOGY:
- Researchers conducted a case-control study including 1033 breast cancer cases and 1143 postmenopausal population controls from the MCC-Spain study.
- Participants were aged 20-85 years. BMI was calculated as the ratio of weight to height squared and categorized using World Health Organization standards: < 25, 25-29.9, 30-34.9, and ≥ 35.
- CUN-BAE was calculated using a specific equation and categorized according to the estimated percentage of body fat: < 35%, 35%-39.9%, 40%-44.9%, and ≥ 45%.
- Odds ratios (ORs) were estimated with 95% CIs for both measures (BMI and CUN-BAE) for breast cancer cases using unconditional logistic regression.
TAKEAWAY:
- Excess body weight attributable to the risk for breast cancer was 23% when assessed using a BMI value > 30 and 38% when assessed using a CUN-BAE value > 40% body fat.
- Hormone receptor stratification showed that these differences in population-attributable fractions were only observed in hormone receptor–positive cases, with an estimated burden of 19.9% for BMI and 41.9% for CUN-BAE.
- The highest categories of CUN-BAE showed an increase in the risk for postmenopausal breast cancer (OR, 2.13 for body fat ≥ 45% compared with the reference category < 35%).
- No similar trend was observed for BMI, as the gradient declined after a BMI ≥ 35.
IN PRACTICE:
“The results of our study indicate that excess body fat is a significant risk factor for hormone receptor–positive breast cancer in postmenopausal women. Our findings suggest that the population impact could be underestimated when using traditional BMI estimates, and that more accurate measures of body fat, such as CUN-BAE, should be considered,” the authors of the study wrote.
SOURCE:
This study was led by Verónica Dávila-Batista, University of Las Palmas de Gran Canaria in Las Palmas de Gran Canaria, Spain. It was published online in Journal of Epidemiology and Community Health.
LIMITATIONS:
The case-control design of the study may have limited the ability to establish causal relationships. BMI was self-reported at the time of the interview for controls and 1 year before diagnosis for cancer cases, which may have introduced recall bias. The formula for CUN-BAE was calculated from a sedentary convenience sample, which may not have been representative of the general population. The small sample size of cases that did not express hormone receptors was another limitation. The study’s findings may not be generalizable to non-White populations as non-White participants were excluded.
DISCLOSURES:
Dávila-Batista disclosed receiving grants from the Carlos III Health Institute. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Accurate body fat measures are crucial for effective cancer prevention.
METHODOLOGY:
- Researchers conducted a case-control study including 1033 breast cancer cases and 1143 postmenopausal population controls from the MCC-Spain study.
- Participants were aged 20-85 years. BMI was calculated as the ratio of weight to height squared and categorized using World Health Organization standards: < 25, 25-29.9, 30-34.9, and ≥ 35.
- CUN-BAE was calculated using a specific equation and categorized according to the estimated percentage of body fat: < 35%, 35%-39.9%, 40%-44.9%, and ≥ 45%.
- Odds ratios (ORs) were estimated with 95% CIs for both measures (BMI and CUN-BAE) for breast cancer cases using unconditional logistic regression.
TAKEAWAY:
- Excess body weight attributable to the risk for breast cancer was 23% when assessed using a BMI value > 30 and 38% when assessed using a CUN-BAE value > 40% body fat.
- Hormone receptor stratification showed that these differences in population-attributable fractions were only observed in hormone receptor–positive cases, with an estimated burden of 19.9% for BMI and 41.9% for CUN-BAE.
- The highest categories of CUN-BAE showed an increase in the risk for postmenopausal breast cancer (OR, 2.13 for body fat ≥ 45% compared with the reference category < 35%).
- No similar trend was observed for BMI, as the gradient declined after a BMI ≥ 35.
IN PRACTICE:
“The results of our study indicate that excess body fat is a significant risk factor for hormone receptor–positive breast cancer in postmenopausal women. Our findings suggest that the population impact could be underestimated when using traditional BMI estimates, and that more accurate measures of body fat, such as CUN-BAE, should be considered,” the authors of the study wrote.
SOURCE:
This study was led by Verónica Dávila-Batista, University of Las Palmas de Gran Canaria in Las Palmas de Gran Canaria, Spain. It was published online in Journal of Epidemiology and Community Health.
LIMITATIONS:
The case-control design of the study may have limited the ability to establish causal relationships. BMI was self-reported at the time of the interview for controls and 1 year before diagnosis for cancer cases, which may have introduced recall bias. The formula for CUN-BAE was calculated from a sedentary convenience sample, which may not have been representative of the general population. The small sample size of cases that did not express hormone receptors was another limitation. The study’s findings may not be generalizable to non-White populations as non-White participants were excluded.
DISCLOSURES:
Dávila-Batista disclosed receiving grants from the Carlos III Health Institute. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Unseen Cost of Weight Loss and Aging: Tackling Sarcopenia
Losses of muscle and strength are inescapable effects of the aging process. Left unchecked, these progressive losses will start to impair physical function.
Once a certain level of impairment occurs, an individual can be diagnosed with sarcopenia, which comes from the Greek words “sarco” (flesh) and “penia” (poverty).
Muscle mass losses generally occur with weight loss, and the increasing use of glucagon-like peptide 1 (GLP-1) medications may lead to greater incidence and prevalence of sarcopenia in the years to come.
A recent meta-analysis of 56 studies (mean participant age, 50 years) found a twofold greater risk for mortality in those with sarcopenia vs those without. Despite its health consequences, sarcopenia tends to be underdiagnosed and, consequently, undertreated at a population and individual level. Part of the reason probably stems from the lack of health insurance reimbursement for individual clinicians and hospital systems to perform sarcopenia screening assessments.
In aging and obesity, it appears justified to include and emphasize a recommendation for sarcopenia screening in medical society guidelines; however, individual patients and clinicians do not need to wait for updated guidelines to implement sarcopenia screening, treatment, and prevention strategies in their own lives and/or clinical practice.
Simple Prevention and Treatment Strategy
Much can be done to help prevent sarcopenia. The primary strategy, unsurprisingly, is engaging in frequent strength training. But that doesn’t mean hours in the gym every week.
With just one session per week over 10 weeks, lean body mass (LBM), a common proxy for muscle mass, increased by 0.33 kg, according to a study which evaluated LBM improvements across different strength training frequencies. Adding a second weekly session was significantly better. In the twice-weekly group, LBM increased by 1.4 kg over 10 weeks, resulting in an increase in LBM more than four times greater than the once-a-week group. (There was no greater improvement in LBM by adding a third weekly session vs two weekly sessions.)
Although that particular study didn’t identify greater benefit at three times a week, compared with twice a week, the specific training routines and lack of a protein consumption assessment may have played a role in that finding.
Underlying the diminishing benefits, a different study found a marginally greater benefit in favor of performing ≥ five sets per major muscle group per week, compared with < five sets per week for increasing muscle in the legs, arms, back, chest, and shoulders.
Expensive gym memberships and fancy equipment are not necessary. While the use of strength training machines and free weights have been viewed by many as the optimal approach, a recent systematic review and meta-analysis found that comparable improvements to strength can be achieved with workouts using resistance bands. For those who struggle to find the time to go to a gym, or for whom gym fees are not financially affordable, resistance bands are a cheaper and more convenient alternative.
Lucas, Assistant Professor of Clinical Medicine, Comprehensive Weight Control Center, Weill Cornell Medicine, New York City, disclosed ties with Measured (Better Health Labs).
A version of this article appeared on Medscape.com.
Losses of muscle and strength are inescapable effects of the aging process. Left unchecked, these progressive losses will start to impair physical function.
Once a certain level of impairment occurs, an individual can be diagnosed with sarcopenia, which comes from the Greek words “sarco” (flesh) and “penia” (poverty).
Muscle mass losses generally occur with weight loss, and the increasing use of glucagon-like peptide 1 (GLP-1) medications may lead to greater incidence and prevalence of sarcopenia in the years to come.
A recent meta-analysis of 56 studies (mean participant age, 50 years) found a twofold greater risk for mortality in those with sarcopenia vs those without. Despite its health consequences, sarcopenia tends to be underdiagnosed and, consequently, undertreated at a population and individual level. Part of the reason probably stems from the lack of health insurance reimbursement for individual clinicians and hospital systems to perform sarcopenia screening assessments.
In aging and obesity, it appears justified to include and emphasize a recommendation for sarcopenia screening in medical society guidelines; however, individual patients and clinicians do not need to wait for updated guidelines to implement sarcopenia screening, treatment, and prevention strategies in their own lives and/or clinical practice.
Simple Prevention and Treatment Strategy
Much can be done to help prevent sarcopenia. The primary strategy, unsurprisingly, is engaging in frequent strength training. But that doesn’t mean hours in the gym every week.
With just one session per week over 10 weeks, lean body mass (LBM), a common proxy for muscle mass, increased by 0.33 kg, according to a study which evaluated LBM improvements across different strength training frequencies. Adding a second weekly session was significantly better. In the twice-weekly group, LBM increased by 1.4 kg over 10 weeks, resulting in an increase in LBM more than four times greater than the once-a-week group. (There was no greater improvement in LBM by adding a third weekly session vs two weekly sessions.)
Although that particular study didn’t identify greater benefit at three times a week, compared with twice a week, the specific training routines and lack of a protein consumption assessment may have played a role in that finding.
Underlying the diminishing benefits, a different study found a marginally greater benefit in favor of performing ≥ five sets per major muscle group per week, compared with < five sets per week for increasing muscle in the legs, arms, back, chest, and shoulders.
Expensive gym memberships and fancy equipment are not necessary. While the use of strength training machines and free weights have been viewed by many as the optimal approach, a recent systematic review and meta-analysis found that comparable improvements to strength can be achieved with workouts using resistance bands. For those who struggle to find the time to go to a gym, or for whom gym fees are not financially affordable, resistance bands are a cheaper and more convenient alternative.
Lucas, Assistant Professor of Clinical Medicine, Comprehensive Weight Control Center, Weill Cornell Medicine, New York City, disclosed ties with Measured (Better Health Labs).
A version of this article appeared on Medscape.com.
Losses of muscle and strength are inescapable effects of the aging process. Left unchecked, these progressive losses will start to impair physical function.
Once a certain level of impairment occurs, an individual can be diagnosed with sarcopenia, which comes from the Greek words “sarco” (flesh) and “penia” (poverty).
Muscle mass losses generally occur with weight loss, and the increasing use of glucagon-like peptide 1 (GLP-1) medications may lead to greater incidence and prevalence of sarcopenia in the years to come.
A recent meta-analysis of 56 studies (mean participant age, 50 years) found a twofold greater risk for mortality in those with sarcopenia vs those without. Despite its health consequences, sarcopenia tends to be underdiagnosed and, consequently, undertreated at a population and individual level. Part of the reason probably stems from the lack of health insurance reimbursement for individual clinicians and hospital systems to perform sarcopenia screening assessments.
In aging and obesity, it appears justified to include and emphasize a recommendation for sarcopenia screening in medical society guidelines; however, individual patients and clinicians do not need to wait for updated guidelines to implement sarcopenia screening, treatment, and prevention strategies in their own lives and/or clinical practice.
Simple Prevention and Treatment Strategy
Much can be done to help prevent sarcopenia. The primary strategy, unsurprisingly, is engaging in frequent strength training. But that doesn’t mean hours in the gym every week.
With just one session per week over 10 weeks, lean body mass (LBM), a common proxy for muscle mass, increased by 0.33 kg, according to a study which evaluated LBM improvements across different strength training frequencies. Adding a second weekly session was significantly better. In the twice-weekly group, LBM increased by 1.4 kg over 10 weeks, resulting in an increase in LBM more than four times greater than the once-a-week group. (There was no greater improvement in LBM by adding a third weekly session vs two weekly sessions.)
Although that particular study didn’t identify greater benefit at three times a week, compared with twice a week, the specific training routines and lack of a protein consumption assessment may have played a role in that finding.
Underlying the diminishing benefits, a different study found a marginally greater benefit in favor of performing ≥ five sets per major muscle group per week, compared with < five sets per week for increasing muscle in the legs, arms, back, chest, and shoulders.
Expensive gym memberships and fancy equipment are not necessary. While the use of strength training machines and free weights have been viewed by many as the optimal approach, a recent systematic review and meta-analysis found that comparable improvements to strength can be achieved with workouts using resistance bands. For those who struggle to find the time to go to a gym, or for whom gym fees are not financially affordable, resistance bands are a cheaper and more convenient alternative.
Lucas, Assistant Professor of Clinical Medicine, Comprehensive Weight Control Center, Weill Cornell Medicine, New York City, disclosed ties with Measured (Better Health Labs).
A version of this article appeared on Medscape.com.
Smartphone Data Flag Early Dementia Risk in Older Adults
a novel real-world study suggested.
During a smartphone-assisted scavenger hunt on a university campus, researchers observed that older adults with subjective cognitive decline (SCD) paused more frequently, likely to reorient themselves, than those without SCD. This behavior served as an identifier of individuals with SCD.
“Deficits in spatial navigation are one of the first signs of Alzheimer’s disease,” said study investigator Nadine Diersch, PhD, guest researcher with the German Center for Neurodegenerative Diseases (DZNE), Tübingen.
This study, said Diersch, provides “first evidence of how a digital footprint for early dementia-related cognitive decline might look like in real-world settings during a short (less than 30 minutes) and remotely performed wayfinding task.”
The study was published online in PLOS Digital Health.
Trouble With Orientation
A total of 72 men and women in their mid-20s to mid-60s participated in the study; 23 of the 48 older adults had SCD but still scored normally on neuropsychological assessments.
All study participants were instructed to independently find five buildings on the medical campus of the Otto-von-Guericke-University Magdeburg in Germany, guided by a smartphone app developed by the study team. Their patterns of movement were tracked by GPS.
All participants had similar knowledge of the campus, and all were experienced in using smartphones. They also practiced using the app beforehand.
In most cases, participants reached the five destinations in less than half an hour. The younger participants performed better than the older ones; on average, the younger adults walked shorter distances and generally did not use the help function on the app as often as the older ones.
In the older adults, the number of orientation stops was predictive of SCD status. The adults with SCD tended to hesitate more at intersections. A decline in executive functioning might explain this finding, Diersch said.
“Intact executive functioning is an important component of efficient navigation, for example, when switching between different navigation strategies or planning a route. However, since this was the first study on that subject, more research is needed to determine the precise contribution of different cognitive processes on digital wayfinding data,” said Diersch.
With more study, “we think that such a smartphone-assisted wayfinding task, performed in the immediate surroundings, could be used as a low-threshold screening tool — for example, to stratify subjects with regard to the need of extended cognitive and clinical diagnostics in specialized care,” she added.
‘A Game Changer’
Commenting on the research, Shaheen Lakhan, MD, PhD, neurologist and researcher based in Miami, Florida, who wasn’t involved in the research, said the findings have the potential to “revolutionize” dementia care.
“We’ve seen smartphones transform everything from banking to dating — now they’re set to reshape brain health monitoring. This ingenious digital scavenger hunt detects cognitive decline in real-world scenarios, bypassing costly, complex tests. It’s a game changer,” said Lakhan.
“Just as we track our steps and calories, we could soon track our cognitive health with a tap. This isn’t just innovation; it’s the future of dementia prevention and care unfolding on our smartphone screens. We’re not just talking about convenience. We’re talking about catching Alzheimer’s before it catches us,” he added.
The next phase, Lakhan noted, would be to develop smartphone apps as digital therapeutics, not just to detect cognitive decline but to treat or even prevent it.
“Imagine your phone not only flagging potential issues but also providing personalized brain training exercises to keep your mind sharp and resilient against dementia,” Lakhan said.
This work was funded by the Deutsche Forschungsgemeinschaft (German Research Foundation) within the Collaborative Research Center “Neural Resources of Cognition” and a DZNE Innovation-2-Application Award. Diersch is now a full-time employee of neotiv. Lakhan had no relevant disclosures.
A version of this article first appeared on Medscape.com.
a novel real-world study suggested.
During a smartphone-assisted scavenger hunt on a university campus, researchers observed that older adults with subjective cognitive decline (SCD) paused more frequently, likely to reorient themselves, than those without SCD. This behavior served as an identifier of individuals with SCD.
“Deficits in spatial navigation are one of the first signs of Alzheimer’s disease,” said study investigator Nadine Diersch, PhD, guest researcher with the German Center for Neurodegenerative Diseases (DZNE), Tübingen.
This study, said Diersch, provides “first evidence of how a digital footprint for early dementia-related cognitive decline might look like in real-world settings during a short (less than 30 minutes) and remotely performed wayfinding task.”
The study was published online in PLOS Digital Health.
Trouble With Orientation
A total of 72 men and women in their mid-20s to mid-60s participated in the study; 23 of the 48 older adults had SCD but still scored normally on neuropsychological assessments.
All study participants were instructed to independently find five buildings on the medical campus of the Otto-von-Guericke-University Magdeburg in Germany, guided by a smartphone app developed by the study team. Their patterns of movement were tracked by GPS.
All participants had similar knowledge of the campus, and all were experienced in using smartphones. They also practiced using the app beforehand.
In most cases, participants reached the five destinations in less than half an hour. The younger participants performed better than the older ones; on average, the younger adults walked shorter distances and generally did not use the help function on the app as often as the older ones.
In the older adults, the number of orientation stops was predictive of SCD status. The adults with SCD tended to hesitate more at intersections. A decline in executive functioning might explain this finding, Diersch said.
“Intact executive functioning is an important component of efficient navigation, for example, when switching between different navigation strategies or planning a route. However, since this was the first study on that subject, more research is needed to determine the precise contribution of different cognitive processes on digital wayfinding data,” said Diersch.
With more study, “we think that such a smartphone-assisted wayfinding task, performed in the immediate surroundings, could be used as a low-threshold screening tool — for example, to stratify subjects with regard to the need of extended cognitive and clinical diagnostics in specialized care,” she added.
‘A Game Changer’
Commenting on the research, Shaheen Lakhan, MD, PhD, neurologist and researcher based in Miami, Florida, who wasn’t involved in the research, said the findings have the potential to “revolutionize” dementia care.
“We’ve seen smartphones transform everything from banking to dating — now they’re set to reshape brain health monitoring. This ingenious digital scavenger hunt detects cognitive decline in real-world scenarios, bypassing costly, complex tests. It’s a game changer,” said Lakhan.
“Just as we track our steps and calories, we could soon track our cognitive health with a tap. This isn’t just innovation; it’s the future of dementia prevention and care unfolding on our smartphone screens. We’re not just talking about convenience. We’re talking about catching Alzheimer’s before it catches us,” he added.
The next phase, Lakhan noted, would be to develop smartphone apps as digital therapeutics, not just to detect cognitive decline but to treat or even prevent it.
“Imagine your phone not only flagging potential issues but also providing personalized brain training exercises to keep your mind sharp and resilient against dementia,” Lakhan said.
This work was funded by the Deutsche Forschungsgemeinschaft (German Research Foundation) within the Collaborative Research Center “Neural Resources of Cognition” and a DZNE Innovation-2-Application Award. Diersch is now a full-time employee of neotiv. Lakhan had no relevant disclosures.
A version of this article first appeared on Medscape.com.
a novel real-world study suggested.
During a smartphone-assisted scavenger hunt on a university campus, researchers observed that older adults with subjective cognitive decline (SCD) paused more frequently, likely to reorient themselves, than those without SCD. This behavior served as an identifier of individuals with SCD.
“Deficits in spatial navigation are one of the first signs of Alzheimer’s disease,” said study investigator Nadine Diersch, PhD, guest researcher with the German Center for Neurodegenerative Diseases (DZNE), Tübingen.
This study, said Diersch, provides “first evidence of how a digital footprint for early dementia-related cognitive decline might look like in real-world settings during a short (less than 30 minutes) and remotely performed wayfinding task.”
The study was published online in PLOS Digital Health.
Trouble With Orientation
A total of 72 men and women in their mid-20s to mid-60s participated in the study; 23 of the 48 older adults had SCD but still scored normally on neuropsychological assessments.
All study participants were instructed to independently find five buildings on the medical campus of the Otto-von-Guericke-University Magdeburg in Germany, guided by a smartphone app developed by the study team. Their patterns of movement were tracked by GPS.
All participants had similar knowledge of the campus, and all were experienced in using smartphones. They also practiced using the app beforehand.
In most cases, participants reached the five destinations in less than half an hour. The younger participants performed better than the older ones; on average, the younger adults walked shorter distances and generally did not use the help function on the app as often as the older ones.
In the older adults, the number of orientation stops was predictive of SCD status. The adults with SCD tended to hesitate more at intersections. A decline in executive functioning might explain this finding, Diersch said.
“Intact executive functioning is an important component of efficient navigation, for example, when switching between different navigation strategies or planning a route. However, since this was the first study on that subject, more research is needed to determine the precise contribution of different cognitive processes on digital wayfinding data,” said Diersch.
With more study, “we think that such a smartphone-assisted wayfinding task, performed in the immediate surroundings, could be used as a low-threshold screening tool — for example, to stratify subjects with regard to the need of extended cognitive and clinical diagnostics in specialized care,” she added.
‘A Game Changer’
Commenting on the research, Shaheen Lakhan, MD, PhD, neurologist and researcher based in Miami, Florida, who wasn’t involved in the research, said the findings have the potential to “revolutionize” dementia care.
“We’ve seen smartphones transform everything from banking to dating — now they’re set to reshape brain health monitoring. This ingenious digital scavenger hunt detects cognitive decline in real-world scenarios, bypassing costly, complex tests. It’s a game changer,” said Lakhan.
“Just as we track our steps and calories, we could soon track our cognitive health with a tap. This isn’t just innovation; it’s the future of dementia prevention and care unfolding on our smartphone screens. We’re not just talking about convenience. We’re talking about catching Alzheimer’s before it catches us,” he added.
The next phase, Lakhan noted, would be to develop smartphone apps as digital therapeutics, not just to detect cognitive decline but to treat or even prevent it.
“Imagine your phone not only flagging potential issues but also providing personalized brain training exercises to keep your mind sharp and resilient against dementia,” Lakhan said.
This work was funded by the Deutsche Forschungsgemeinschaft (German Research Foundation) within the Collaborative Research Center “Neural Resources of Cognition” and a DZNE Innovation-2-Application Award. Diersch is now a full-time employee of neotiv. Lakhan had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM PLOS DIGITAL HEALTH
Long-Term Cognitive Monitoring Warranted After First Stroke
A first stroke in older adults is associated with substantial immediate and accelerated long-term cognitive decline, suggested a new study that underscores the need for continuous cognitive monitoring in this patient population.
Results from the study, which included 14 international cohorts of older adults, showed that stroke was associated with a significant acute decline in global cognition and a small, but significant, acceleration in the rate of cognitive decline over time.
Cognitive assessments in primary care are “crucial, especially since cognitive impairment is frequently missed or undiagnosed in hospitals,” lead author Jessica Lo, MSc, biostatistician and research associate with the Center for Healthy Brain Aging, University of New South Wales, Sydney, Australia, told this news organization.
She suggested clinicians incorporate long-term cognitive assessments into care plans, using more sensitive neuropsychological tests in primary care to detect early signs of cognitive impairment. “Early detection would enable timely interventions to improve outcomes,” Lo said.
She also noted that poststroke care typically includes physical rehabilitation but not cognitive rehabilitation, which many rehabilitation centers aren’t equipped to provide.
The study was published online in JAMA Network Open.
Mapping Cognitive Decline Trajectory
Cognitive impairment after stroke is common, but the trajectory of cognitive decline following a first stroke, relative to prestroke cognitive function, remains unclear.
The investigators leveraged data from 14 population-based cohort studies of 20,860 adults (mean age, 73 years; 59% women) to map the trajectory of cognitive function before and after a first stroke.
The primary outcome was global cognition, defined as the standardized average of four cognitive domains (language, memory, processing speed, and executive function).
During a mean follow-up of 7.5 years, 1041 (5%) adults (mean age, 79 years) experienced a first stroke, a mean of 4.5 years after study entry.
In adjusted analyses, stroke was associated with a significant acute decline of 0.25 SD in global cognition and a “small but significant” acceleration in the rate of decline of −0.038 SD per year, the authors reported.
Stroke was also associated with acute decline in all individual cognitive domains except for memory, with effect sizes ranging from −0.17 to −0.22 SD. Poststroke declines in Mini-Mental State Examination scores (−0.36 SD) were also noted.
In terms of cognitive trajectory, the rate of decline before stroke in survivors was similar to that seen in peers who didn’t have a stroke (−0.048 and −0.049 SD per year in global cognition, respectively).
The researchers did not identify any vascular risk factors moderating cognitive decline following a stroke, consistent with prior research. However, cognitive decline was significantly more rapid in individuals without stroke, regardless of any future stroke, who had a history of diabetes, hypertension, high cholesterol, cardiovascular disease, depression, smoking, or were APOE4 carriers.
“Targeting modifiable vascular risk factors at an early stage may reduce the risk of stroke but also subsequent risk of stroke-related cognitive decline and cognitive impairment,” the researchers noted.
A ‘Major Step’ in the Right Direction
As previously reported by this news organization, in 2023 the American Heart Association (AHA) issued a statement noting that screening for cognitive impairment should be part of multidisciplinary care for stroke survivors.
Commenting for this news organization, Mitchell Elkind, MD, MS, AHA chief clinical science officer, said these new data are consistent with current AHA guidelines and statements that “support screening for cognitive and functional decline in patients both acutely and over the long term after stroke.”
Elkind noted that the 2022 guideline for intracerebral hemorrhage states that cognitive screening should occur “across the continuum of inpatient care and at intervals in the outpatient setting” and provides recommendations for cognitive therapy.
“Our 2021 scientific statement on the primary care of patients after stroke also recommends screening for both depression and cognitive impairment over both the short- and long-term,” said Elkind, professor of neurology and epidemiology at Columbia University Irving Medical Center in New York City.
“These documents recognize the fact that function and cognition can continue to decline years after stroke and that patients’ rehabilitation and support needs may therefore change over time after stroke,” Elkind added.
The authors of an accompanying commentary called it a “major step” in the right direction for the future of long-term stroke outcome assessment.
“As we develop new devices, indications, and time windows for stroke treatment, it may perhaps be wise to ensure trials steer away from simpler outcomes to more complex, granular ones,” wrote Yasmin Sadigh, MSc, and Victor Volovici, MD, PhD, with Erasmus University Medical Center, Rotterdam, the Netherlands.
The study had no commercial funding. The authors and commentary writers and Elkind have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
A first stroke in older adults is associated with substantial immediate and accelerated long-term cognitive decline, suggested a new study that underscores the need for continuous cognitive monitoring in this patient population.
Results from the study, which included 14 international cohorts of older adults, showed that stroke was associated with a significant acute decline in global cognition and a small, but significant, acceleration in the rate of cognitive decline over time.
Cognitive assessments in primary care are “crucial, especially since cognitive impairment is frequently missed or undiagnosed in hospitals,” lead author Jessica Lo, MSc, biostatistician and research associate with the Center for Healthy Brain Aging, University of New South Wales, Sydney, Australia, told this news organization.
She suggested clinicians incorporate long-term cognitive assessments into care plans, using more sensitive neuropsychological tests in primary care to detect early signs of cognitive impairment. “Early detection would enable timely interventions to improve outcomes,” Lo said.
She also noted that poststroke care typically includes physical rehabilitation but not cognitive rehabilitation, which many rehabilitation centers aren’t equipped to provide.
The study was published online in JAMA Network Open.
Mapping Cognitive Decline Trajectory
Cognitive impairment after stroke is common, but the trajectory of cognitive decline following a first stroke, relative to prestroke cognitive function, remains unclear.
The investigators leveraged data from 14 population-based cohort studies of 20,860 adults (mean age, 73 years; 59% women) to map the trajectory of cognitive function before and after a first stroke.
The primary outcome was global cognition, defined as the standardized average of four cognitive domains (language, memory, processing speed, and executive function).
During a mean follow-up of 7.5 years, 1041 (5%) adults (mean age, 79 years) experienced a first stroke, a mean of 4.5 years after study entry.
In adjusted analyses, stroke was associated with a significant acute decline of 0.25 SD in global cognition and a “small but significant” acceleration in the rate of decline of −0.038 SD per year, the authors reported.
Stroke was also associated with acute decline in all individual cognitive domains except for memory, with effect sizes ranging from −0.17 to −0.22 SD. Poststroke declines in Mini-Mental State Examination scores (−0.36 SD) were also noted.
In terms of cognitive trajectory, the rate of decline before stroke in survivors was similar to that seen in peers who didn’t have a stroke (−0.048 and −0.049 SD per year in global cognition, respectively).
The researchers did not identify any vascular risk factors moderating cognitive decline following a stroke, consistent with prior research. However, cognitive decline was significantly more rapid in individuals without stroke, regardless of any future stroke, who had a history of diabetes, hypertension, high cholesterol, cardiovascular disease, depression, smoking, or were APOE4 carriers.
“Targeting modifiable vascular risk factors at an early stage may reduce the risk of stroke but also subsequent risk of stroke-related cognitive decline and cognitive impairment,” the researchers noted.
A ‘Major Step’ in the Right Direction
As previously reported by this news organization, in 2023 the American Heart Association (AHA) issued a statement noting that screening for cognitive impairment should be part of multidisciplinary care for stroke survivors.
Commenting for this news organization, Mitchell Elkind, MD, MS, AHA chief clinical science officer, said these new data are consistent with current AHA guidelines and statements that “support screening for cognitive and functional decline in patients both acutely and over the long term after stroke.”
Elkind noted that the 2022 guideline for intracerebral hemorrhage states that cognitive screening should occur “across the continuum of inpatient care and at intervals in the outpatient setting” and provides recommendations for cognitive therapy.
“Our 2021 scientific statement on the primary care of patients after stroke also recommends screening for both depression and cognitive impairment over both the short- and long-term,” said Elkind, professor of neurology and epidemiology at Columbia University Irving Medical Center in New York City.
“These documents recognize the fact that function and cognition can continue to decline years after stroke and that patients’ rehabilitation and support needs may therefore change over time after stroke,” Elkind added.
The authors of an accompanying commentary called it a “major step” in the right direction for the future of long-term stroke outcome assessment.
“As we develop new devices, indications, and time windows for stroke treatment, it may perhaps be wise to ensure trials steer away from simpler outcomes to more complex, granular ones,” wrote Yasmin Sadigh, MSc, and Victor Volovici, MD, PhD, with Erasmus University Medical Center, Rotterdam, the Netherlands.
The study had no commercial funding. The authors and commentary writers and Elkind have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
A first stroke in older adults is associated with substantial immediate and accelerated long-term cognitive decline, suggested a new study that underscores the need for continuous cognitive monitoring in this patient population.
Results from the study, which included 14 international cohorts of older adults, showed that stroke was associated with a significant acute decline in global cognition and a small, but significant, acceleration in the rate of cognitive decline over time.
Cognitive assessments in primary care are “crucial, especially since cognitive impairment is frequently missed or undiagnosed in hospitals,” lead author Jessica Lo, MSc, biostatistician and research associate with the Center for Healthy Brain Aging, University of New South Wales, Sydney, Australia, told this news organization.
She suggested clinicians incorporate long-term cognitive assessments into care plans, using more sensitive neuropsychological tests in primary care to detect early signs of cognitive impairment. “Early detection would enable timely interventions to improve outcomes,” Lo said.
She also noted that poststroke care typically includes physical rehabilitation but not cognitive rehabilitation, which many rehabilitation centers aren’t equipped to provide.
The study was published online in JAMA Network Open.
Mapping Cognitive Decline Trajectory
Cognitive impairment after stroke is common, but the trajectory of cognitive decline following a first stroke, relative to prestroke cognitive function, remains unclear.
The investigators leveraged data from 14 population-based cohort studies of 20,860 adults (mean age, 73 years; 59% women) to map the trajectory of cognitive function before and after a first stroke.
The primary outcome was global cognition, defined as the standardized average of four cognitive domains (language, memory, processing speed, and executive function).
During a mean follow-up of 7.5 years, 1041 (5%) adults (mean age, 79 years) experienced a first stroke, a mean of 4.5 years after study entry.
In adjusted analyses, stroke was associated with a significant acute decline of 0.25 SD in global cognition and a “small but significant” acceleration in the rate of decline of −0.038 SD per year, the authors reported.
Stroke was also associated with acute decline in all individual cognitive domains except for memory, with effect sizes ranging from −0.17 to −0.22 SD. Poststroke declines in Mini-Mental State Examination scores (−0.36 SD) were also noted.
In terms of cognitive trajectory, the rate of decline before stroke in survivors was similar to that seen in peers who didn’t have a stroke (−0.048 and −0.049 SD per year in global cognition, respectively).
The researchers did not identify any vascular risk factors moderating cognitive decline following a stroke, consistent with prior research. However, cognitive decline was significantly more rapid in individuals without stroke, regardless of any future stroke, who had a history of diabetes, hypertension, high cholesterol, cardiovascular disease, depression, smoking, or were APOE4 carriers.
“Targeting modifiable vascular risk factors at an early stage may reduce the risk of stroke but also subsequent risk of stroke-related cognitive decline and cognitive impairment,” the researchers noted.
A ‘Major Step’ in the Right Direction
As previously reported by this news organization, in 2023 the American Heart Association (AHA) issued a statement noting that screening for cognitive impairment should be part of multidisciplinary care for stroke survivors.
Commenting for this news organization, Mitchell Elkind, MD, MS, AHA chief clinical science officer, said these new data are consistent with current AHA guidelines and statements that “support screening for cognitive and functional decline in patients both acutely and over the long term after stroke.”
Elkind noted that the 2022 guideline for intracerebral hemorrhage states that cognitive screening should occur “across the continuum of inpatient care and at intervals in the outpatient setting” and provides recommendations for cognitive therapy.
“Our 2021 scientific statement on the primary care of patients after stroke also recommends screening for both depression and cognitive impairment over both the short- and long-term,” said Elkind, professor of neurology and epidemiology at Columbia University Irving Medical Center in New York City.
“These documents recognize the fact that function and cognition can continue to decline years after stroke and that patients’ rehabilitation and support needs may therefore change over time after stroke,” Elkind added.
The authors of an accompanying commentary called it a “major step” in the right direction for the future of long-term stroke outcome assessment.
“As we develop new devices, indications, and time windows for stroke treatment, it may perhaps be wise to ensure trials steer away from simpler outcomes to more complex, granular ones,” wrote Yasmin Sadigh, MSc, and Victor Volovici, MD, PhD, with Erasmus University Medical Center, Rotterdam, the Netherlands.
The study had no commercial funding. The authors and commentary writers and Elkind have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
CGM With Geriatric Care Simplifies T1D Management in Seniors
TOPLINE:
METHODOLOGY:
- Researchers evaluated the effectiveness of CGM use enhanced by geriatric principles in adults aged ≥ 65 years with T1D and at least two episodes of hypoglycemia (blood glucose level, < 70 mg/dL for ≥ 20 minutes over 2 weeks), who were either CGM-naive or CGM users prior to the study.
- Participants were randomly assigned to an intervention group using CGM with geriatric principles (ie, adjusting goals based on overall health and simplifying regimens based on CGM patterns and clinical characteristics) or a control group receiving usual care by their endocrinologist.
- The primary outcome was the change in duration of hypoglycemia from baseline to 6 months.
- A cost-effectiveness analysis was also performed for the intervention using a healthcare sector perspective, considering the cost of CGM devices and the cost of medical staff time.
TAKEAWAY:
- Researchers included 131 participants (mean age, 71 years), of whom 68 were in the intervention group (35 CGM-naive) and 63 in the control group (23 CGM-naive).
- The intervention group showed a median reduction of 2.6% in the duration of hypoglycemia vs a 0.3% reduction in the control group (median difference, −2.3%; P < .001).
- This reduction was observed in both CGM users (median difference, −1.2%) and CGM-naive participants (median difference, −2.8%) in the intervention group.
- No significant difference in A1c levels was observed between the intervention and control groups, indicating that CGM enhanced with geriatric principles did not worsen glycemic control.
- The intervention was associated with an incremental cost-effectiveness ratio of $71,623 per quality-adjusted life-year and was cost-effective for CGM-naive participants but at a lower level owing to the high cost of the CGM device.
IN PRACTICE:
“Personalization of goals and simplification of complex regimens can be combined with CGM use to improve management of type 1 diabetes in older adults,” the study authors wrote.
SOURCE:
The study was led by Medha N. Munshi, MD, Joslin Diabetes Center, Boston. It was published online in Diabetes Care.
LIMITATIONS:
The study included a relatively small sample size and an ethnically homogeneous and highly educated cohort, which may have limited the generalizability of its findings. Additionally, the study did not measure adherence to individual simplification strategies, which may have hindered the quantification of behavioral changes.
DISCLOSURES:
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. Two authors declared serving as consultants for pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated the effectiveness of CGM use enhanced by geriatric principles in adults aged ≥ 65 years with T1D and at least two episodes of hypoglycemia (blood glucose level, < 70 mg/dL for ≥ 20 minutes over 2 weeks), who were either CGM-naive or CGM users prior to the study.
- Participants were randomly assigned to an intervention group using CGM with geriatric principles (ie, adjusting goals based on overall health and simplifying regimens based on CGM patterns and clinical characteristics) or a control group receiving usual care by their endocrinologist.
- The primary outcome was the change in duration of hypoglycemia from baseline to 6 months.
- A cost-effectiveness analysis was also performed for the intervention using a healthcare sector perspective, considering the cost of CGM devices and the cost of medical staff time.
TAKEAWAY:
- Researchers included 131 participants (mean age, 71 years), of whom 68 were in the intervention group (35 CGM-naive) and 63 in the control group (23 CGM-naive).
- The intervention group showed a median reduction of 2.6% in the duration of hypoglycemia vs a 0.3% reduction in the control group (median difference, −2.3%; P < .001).
- This reduction was observed in both CGM users (median difference, −1.2%) and CGM-naive participants (median difference, −2.8%) in the intervention group.
- No significant difference in A1c levels was observed between the intervention and control groups, indicating that CGM enhanced with geriatric principles did not worsen glycemic control.
- The intervention was associated with an incremental cost-effectiveness ratio of $71,623 per quality-adjusted life-year and was cost-effective for CGM-naive participants but at a lower level owing to the high cost of the CGM device.
IN PRACTICE:
“Personalization of goals and simplification of complex regimens can be combined with CGM use to improve management of type 1 diabetes in older adults,” the study authors wrote.
SOURCE:
The study was led by Medha N. Munshi, MD, Joslin Diabetes Center, Boston. It was published online in Diabetes Care.
LIMITATIONS:
The study included a relatively small sample size and an ethnically homogeneous and highly educated cohort, which may have limited the generalizability of its findings. Additionally, the study did not measure adherence to individual simplification strategies, which may have hindered the quantification of behavioral changes.
DISCLOSURES:
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. Two authors declared serving as consultants for pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers evaluated the effectiveness of CGM use enhanced by geriatric principles in adults aged ≥ 65 years with T1D and at least two episodes of hypoglycemia (blood glucose level, < 70 mg/dL for ≥ 20 minutes over 2 weeks), who were either CGM-naive or CGM users prior to the study.
- Participants were randomly assigned to an intervention group using CGM with geriatric principles (ie, adjusting goals based on overall health and simplifying regimens based on CGM patterns and clinical characteristics) or a control group receiving usual care by their endocrinologist.
- The primary outcome was the change in duration of hypoglycemia from baseline to 6 months.
- A cost-effectiveness analysis was also performed for the intervention using a healthcare sector perspective, considering the cost of CGM devices and the cost of medical staff time.
TAKEAWAY:
- Researchers included 131 participants (mean age, 71 years), of whom 68 were in the intervention group (35 CGM-naive) and 63 in the control group (23 CGM-naive).
- The intervention group showed a median reduction of 2.6% in the duration of hypoglycemia vs a 0.3% reduction in the control group (median difference, −2.3%; P < .001).
- This reduction was observed in both CGM users (median difference, −1.2%) and CGM-naive participants (median difference, −2.8%) in the intervention group.
- No significant difference in A1c levels was observed between the intervention and control groups, indicating that CGM enhanced with geriatric principles did not worsen glycemic control.
- The intervention was associated with an incremental cost-effectiveness ratio of $71,623 per quality-adjusted life-year and was cost-effective for CGM-naive participants but at a lower level owing to the high cost of the CGM device.
IN PRACTICE:
“Personalization of goals and simplification of complex regimens can be combined with CGM use to improve management of type 1 diabetes in older adults,” the study authors wrote.
SOURCE:
The study was led by Medha N. Munshi, MD, Joslin Diabetes Center, Boston. It was published online in Diabetes Care.
LIMITATIONS:
The study included a relatively small sample size and an ethnically homogeneous and highly educated cohort, which may have limited the generalizability of its findings. Additionally, the study did not measure adherence to individual simplification strategies, which may have hindered the quantification of behavioral changes.
DISCLOSURES:
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health. Two authors declared serving as consultants for pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
CBTI Strategy Reduces Sleeping Pill Use in Canadian Seniors
A strategy developed by Canadian researchers for encouraging older patients with insomnia to wean themselves from sleeping pills and improve their sleep through behavioral techniques is effective, data suggest. If proven helpful for the millions of older Canadians who currently rely on nightly benzodiazepines (BZDs) and non-BZDs (colloquially known as Z drugs) for their sleep, it might yield an additional benefit: Reducing resource utilization.
“We know that cognitive behavioral therapy for insomnia (CBTI) works. It’s recommended as first-line therapy because it works,” study author David Gardner, PharmD, professor of psychiatry at Dalhousie University in Halifax, Nova Scotia, Canada, told this news organization.
“We’re sharing information about sleeping pills, information that has been embedded with behavior-change techniques that lead people to second-guess or rethink their long-term use of sedative hypnotics and then bring that information to their provider or pharmacist to discuss it,” he said.
The results were published in JAMA Psychiatry.
Better Sleep, Fewer Pills
Dr. Gardner and his team created a direct-to-patient, patient-directed, multicomponent knowledge mobilization intervention called Sleepwell. It incorporates best practice– and guideline-based evidence and multiple behavioral change techniques with content and graphics. Dr. Gardner emphasized that it represents a directional shift in care that alleviates providers’ burden without removing it entirely.
To test the intervention’s effectiveness, Dr. Gardner and his team chose New Brunswick as a location for a 6-month, three-arm, open-label, randomized controlled trial; the province has one of the highest rates of sedative use and an older adult population that is vulnerable to the serious side effects of these drugs (eg, cognitive impairment, falls, and frailty). The study was called Your Answers When Needing Sleep in New Brunswick (YAWNS NB).
Eligible participants were aged ≥ 65 years, lived in the community, and had taken benzodiazepine receptor agonists (BZRAs) for ≥ 3 nights per week for 3 or more months. Participants were randomly assigned to a control group or one of the two intervention groups. The YAWNS-1 intervention group (n = 195) received a mailed package containing a cover letter, a booklet outlining how to stop sleeping pills, a booklet on how to “get your sleep back,” and a companion website. The YAWNS-2 group (n = 193) received updated versions of the booklets used in a prior trial. The control group (n = 192) was assigned treatment as usual (TAU).
A greater proportion of YAWNS-1 participants discontinued BZRAs at 6 months (26.2%) and had dose reductions (20.4%), compared with YAWNS-2 participants (20.3% and 14.4%, respectively) and TAU participants (7.5% and 12.8%, respectively). The corresponding numbers needed to mail to achieve an additional discontinuation was 5.3 YAWNS-1 packages and 7.8 YAWNS-2 packages.
At 6 months, BZRA cessation was sustained a mean 13.6 weeks for YAWNS-1, 14.3 weeks for YAWNS-2, and 16.9 weeks for TAU.
Sleep measures also improved with YAWNS-1, compared with YAWNs-2 and TAU. Sleep onset latency was reduced by 26.1 minutes among YAWNS-1 participants, compared with YAWNS-2 (P < .001), and by 27.7 minutes, compared with TAU (P < .001). Wake after sleep onset increased by 4.1 minutes in YAWNS-1, 11.1 minutes in YAWNS-2, and 7.5 minutes in TAU.
Although all participants underwent rigorous assessment before inclusion, less than half of participants receiving either intervention (36% in YAWNS-1 and 43% in YAWNS-2) contacted their provider or pharmacist to discuss BZD dose reductions. This finding may have resulted partly from limited access because of the COVID-19 pandemic, according to the authors.
A Stepped-Care Model
The intervention is intended to help patients “change their approach from sleeping pills to a short-term CBTI course for long-term sleep benefits, and then speak to their provider,” said Dr. Gardner.
He pointed to a post-study follow-up of the study participants’ health providers, most of whom had moderate to extensive experience deprescribing BZRAs, which showed that 87.5%-100% fully or nearly fully agreed with or supported using the Sleepwell strategy and its content with older patients who rely on sedatives.
“Providers said that deprescribing is difficult, time-consuming, and often not a productive use of their time,” said Dr. Gardner. “I see insomnia as a health issue well set up for a stepped-care model. Self-help approaches are at the very bottom of that model and can help shift the initial burden to patients and out of the healthcare system.”
Poor uptake has prevented CBTI from demonstrating its potential, which is a challenge that Charles M. Morin, PhD, professor of psychology at Laval University in Quebec City, Quebec, Canada, attributes to two factors. “Clearly, there aren’t enough providers with this kind of expertise, and it’s not always covered by public health insurance, so people have to pay out of pocket to treat their insomnia,” he said.
“Overall, I think that this was a very nice study, well conducted, with an impressive sample size,” said Dr. Morin, who was not involved in the study. “The results are quite encouraging, telling us that even when older adults have used sleep medications for an average of 10 years, it’s still possible to reduce the medication. But this doesn’t happen alone. People need to be guided in doing that, not only to decrease medication use, but they also need an alternative,” he said.
Dr. Morin questioned how many patients agree to start with a low intensity. “Ideally, it should be a shared decision paradigm, where the physician or whoever sees the patient first presents the available options and explains the pluses and minuses of each. Some patients might choose medication because it’s a quick fix,” he said. “But some might want to do CBTI, even if it takes more work. The results are sustainable over time,” he added.
The study was jointly funded by the Public Health Agency of Canada and the government of New Brunswick as a Healthy Seniors Pilot Project. Dr. Gardner and Dr. Morin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A strategy developed by Canadian researchers for encouraging older patients with insomnia to wean themselves from sleeping pills and improve their sleep through behavioral techniques is effective, data suggest. If proven helpful for the millions of older Canadians who currently rely on nightly benzodiazepines (BZDs) and non-BZDs (colloquially known as Z drugs) for their sleep, it might yield an additional benefit: Reducing resource utilization.
“We know that cognitive behavioral therapy for insomnia (CBTI) works. It’s recommended as first-line therapy because it works,” study author David Gardner, PharmD, professor of psychiatry at Dalhousie University in Halifax, Nova Scotia, Canada, told this news organization.
“We’re sharing information about sleeping pills, information that has been embedded with behavior-change techniques that lead people to second-guess or rethink their long-term use of sedative hypnotics and then bring that information to their provider or pharmacist to discuss it,” he said.
The results were published in JAMA Psychiatry.
Better Sleep, Fewer Pills
Dr. Gardner and his team created a direct-to-patient, patient-directed, multicomponent knowledge mobilization intervention called Sleepwell. It incorporates best practice– and guideline-based evidence and multiple behavioral change techniques with content and graphics. Dr. Gardner emphasized that it represents a directional shift in care that alleviates providers’ burden without removing it entirely.
To test the intervention’s effectiveness, Dr. Gardner and his team chose New Brunswick as a location for a 6-month, three-arm, open-label, randomized controlled trial; the province has one of the highest rates of sedative use and an older adult population that is vulnerable to the serious side effects of these drugs (eg, cognitive impairment, falls, and frailty). The study was called Your Answers When Needing Sleep in New Brunswick (YAWNS NB).
Eligible participants were aged ≥ 65 years, lived in the community, and had taken benzodiazepine receptor agonists (BZRAs) for ≥ 3 nights per week for 3 or more months. Participants were randomly assigned to a control group or one of the two intervention groups. The YAWNS-1 intervention group (n = 195) received a mailed package containing a cover letter, a booklet outlining how to stop sleeping pills, a booklet on how to “get your sleep back,” and a companion website. The YAWNS-2 group (n = 193) received updated versions of the booklets used in a prior trial. The control group (n = 192) was assigned treatment as usual (TAU).
A greater proportion of YAWNS-1 participants discontinued BZRAs at 6 months (26.2%) and had dose reductions (20.4%), compared with YAWNS-2 participants (20.3% and 14.4%, respectively) and TAU participants (7.5% and 12.8%, respectively). The corresponding numbers needed to mail to achieve an additional discontinuation was 5.3 YAWNS-1 packages and 7.8 YAWNS-2 packages.
At 6 months, BZRA cessation was sustained a mean 13.6 weeks for YAWNS-1, 14.3 weeks for YAWNS-2, and 16.9 weeks for TAU.
Sleep measures also improved with YAWNS-1, compared with YAWNs-2 and TAU. Sleep onset latency was reduced by 26.1 minutes among YAWNS-1 participants, compared with YAWNS-2 (P < .001), and by 27.7 minutes, compared with TAU (P < .001). Wake after sleep onset increased by 4.1 minutes in YAWNS-1, 11.1 minutes in YAWNS-2, and 7.5 minutes in TAU.
Although all participants underwent rigorous assessment before inclusion, less than half of participants receiving either intervention (36% in YAWNS-1 and 43% in YAWNS-2) contacted their provider or pharmacist to discuss BZD dose reductions. This finding may have resulted partly from limited access because of the COVID-19 pandemic, according to the authors.
A Stepped-Care Model
The intervention is intended to help patients “change their approach from sleeping pills to a short-term CBTI course for long-term sleep benefits, and then speak to their provider,” said Dr. Gardner.
He pointed to a post-study follow-up of the study participants’ health providers, most of whom had moderate to extensive experience deprescribing BZRAs, which showed that 87.5%-100% fully or nearly fully agreed with or supported using the Sleepwell strategy and its content with older patients who rely on sedatives.
“Providers said that deprescribing is difficult, time-consuming, and often not a productive use of their time,” said Dr. Gardner. “I see insomnia as a health issue well set up for a stepped-care model. Self-help approaches are at the very bottom of that model and can help shift the initial burden to patients and out of the healthcare system.”
Poor uptake has prevented CBTI from demonstrating its potential, which is a challenge that Charles M. Morin, PhD, professor of psychology at Laval University in Quebec City, Quebec, Canada, attributes to two factors. “Clearly, there aren’t enough providers with this kind of expertise, and it’s not always covered by public health insurance, so people have to pay out of pocket to treat their insomnia,” he said.
“Overall, I think that this was a very nice study, well conducted, with an impressive sample size,” said Dr. Morin, who was not involved in the study. “The results are quite encouraging, telling us that even when older adults have used sleep medications for an average of 10 years, it’s still possible to reduce the medication. But this doesn’t happen alone. People need to be guided in doing that, not only to decrease medication use, but they also need an alternative,” he said.
Dr. Morin questioned how many patients agree to start with a low intensity. “Ideally, it should be a shared decision paradigm, where the physician or whoever sees the patient first presents the available options and explains the pluses and minuses of each. Some patients might choose medication because it’s a quick fix,” he said. “But some might want to do CBTI, even if it takes more work. The results are sustainable over time,” he added.
The study was jointly funded by the Public Health Agency of Canada and the government of New Brunswick as a Healthy Seniors Pilot Project. Dr. Gardner and Dr. Morin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A strategy developed by Canadian researchers for encouraging older patients with insomnia to wean themselves from sleeping pills and improve their sleep through behavioral techniques is effective, data suggest. If proven helpful for the millions of older Canadians who currently rely on nightly benzodiazepines (BZDs) and non-BZDs (colloquially known as Z drugs) for their sleep, it might yield an additional benefit: Reducing resource utilization.
“We know that cognitive behavioral therapy for insomnia (CBTI) works. It’s recommended as first-line therapy because it works,” study author David Gardner, PharmD, professor of psychiatry at Dalhousie University in Halifax, Nova Scotia, Canada, told this news organization.
“We’re sharing information about sleeping pills, information that has been embedded with behavior-change techniques that lead people to second-guess or rethink their long-term use of sedative hypnotics and then bring that information to their provider or pharmacist to discuss it,” he said.
The results were published in JAMA Psychiatry.
Better Sleep, Fewer Pills
Dr. Gardner and his team created a direct-to-patient, patient-directed, multicomponent knowledge mobilization intervention called Sleepwell. It incorporates best practice– and guideline-based evidence and multiple behavioral change techniques with content and graphics. Dr. Gardner emphasized that it represents a directional shift in care that alleviates providers’ burden without removing it entirely.
To test the intervention’s effectiveness, Dr. Gardner and his team chose New Brunswick as a location for a 6-month, three-arm, open-label, randomized controlled trial; the province has one of the highest rates of sedative use and an older adult population that is vulnerable to the serious side effects of these drugs (eg, cognitive impairment, falls, and frailty). The study was called Your Answers When Needing Sleep in New Brunswick (YAWNS NB).
Eligible participants were aged ≥ 65 years, lived in the community, and had taken benzodiazepine receptor agonists (BZRAs) for ≥ 3 nights per week for 3 or more months. Participants were randomly assigned to a control group or one of the two intervention groups. The YAWNS-1 intervention group (n = 195) received a mailed package containing a cover letter, a booklet outlining how to stop sleeping pills, a booklet on how to “get your sleep back,” and a companion website. The YAWNS-2 group (n = 193) received updated versions of the booklets used in a prior trial. The control group (n = 192) was assigned treatment as usual (TAU).
A greater proportion of YAWNS-1 participants discontinued BZRAs at 6 months (26.2%) and had dose reductions (20.4%), compared with YAWNS-2 participants (20.3% and 14.4%, respectively) and TAU participants (7.5% and 12.8%, respectively). The corresponding numbers needed to mail to achieve an additional discontinuation was 5.3 YAWNS-1 packages and 7.8 YAWNS-2 packages.
At 6 months, BZRA cessation was sustained a mean 13.6 weeks for YAWNS-1, 14.3 weeks for YAWNS-2, and 16.9 weeks for TAU.
Sleep measures also improved with YAWNS-1, compared with YAWNs-2 and TAU. Sleep onset latency was reduced by 26.1 minutes among YAWNS-1 participants, compared with YAWNS-2 (P < .001), and by 27.7 minutes, compared with TAU (P < .001). Wake after sleep onset increased by 4.1 minutes in YAWNS-1, 11.1 minutes in YAWNS-2, and 7.5 minutes in TAU.
Although all participants underwent rigorous assessment before inclusion, less than half of participants receiving either intervention (36% in YAWNS-1 and 43% in YAWNS-2) contacted their provider or pharmacist to discuss BZD dose reductions. This finding may have resulted partly from limited access because of the COVID-19 pandemic, according to the authors.
A Stepped-Care Model
The intervention is intended to help patients “change their approach from sleeping pills to a short-term CBTI course for long-term sleep benefits, and then speak to their provider,” said Dr. Gardner.
He pointed to a post-study follow-up of the study participants’ health providers, most of whom had moderate to extensive experience deprescribing BZRAs, which showed that 87.5%-100% fully or nearly fully agreed with or supported using the Sleepwell strategy and its content with older patients who rely on sedatives.
“Providers said that deprescribing is difficult, time-consuming, and often not a productive use of their time,” said Dr. Gardner. “I see insomnia as a health issue well set up for a stepped-care model. Self-help approaches are at the very bottom of that model and can help shift the initial burden to patients and out of the healthcare system.”
Poor uptake has prevented CBTI from demonstrating its potential, which is a challenge that Charles M. Morin, PhD, professor of psychology at Laval University in Quebec City, Quebec, Canada, attributes to two factors. “Clearly, there aren’t enough providers with this kind of expertise, and it’s not always covered by public health insurance, so people have to pay out of pocket to treat their insomnia,” he said.
“Overall, I think that this was a very nice study, well conducted, with an impressive sample size,” said Dr. Morin, who was not involved in the study. “The results are quite encouraging, telling us that even when older adults have used sleep medications for an average of 10 years, it’s still possible to reduce the medication. But this doesn’t happen alone. People need to be guided in doing that, not only to decrease medication use, but they also need an alternative,” he said.
Dr. Morin questioned how many patients agree to start with a low intensity. “Ideally, it should be a shared decision paradigm, where the physician or whoever sees the patient first presents the available options and explains the pluses and minuses of each. Some patients might choose medication because it’s a quick fix,” he said. “But some might want to do CBTI, even if it takes more work. The results are sustainable over time,” he added.
The study was jointly funded by the Public Health Agency of Canada and the government of New Brunswick as a Healthy Seniors Pilot Project. Dr. Gardner and Dr. Morin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Age-Friendly Health Systems Transformation: A Whole Person Approach to Support the Well-Being of Older Adults
The COVID-19 pandemic established a new normal for health care delivery, with leaders rethinking core practices to survive and thrive in a changing environment and improve the health and well-being of patients. The Veterans Health Administration (VHA) is embracing a shift in focus from “what is the matter” to “what really matters” to address pre- and postpandemic challenges through a whole health approach.1 Initially conceptualized by the VHA in 2011, whole health “is an approach to health care that empowers and equips people to take charge of their health and well-being so that they can live their life to the fullest.”1 Whole health integrates evidence-based complementary and integrative health (CIH) therapies to manage pain; this includes acupuncture, meditation, tai chi, yoga, massage therapy, guided imagery, biofeedback, and clinical hypnosis.1 The VHA now recognizes well-being as a core value, helping clinicians respond to emerging challenges related to the social determinants of health (eg, access to health care, physical activity, and healthy foods) and guiding health care decision making.1,2
Well-being through empowerment—elements of whole health and Age-Friendly Health Systems (AFHS)—encourages health care institutions to work with employees, patients, and other stakeholders to address global challenges, clinician burnout, and social issues faced by their communities. This approach focuses on life’s purpose and meaning for individuals and inspires leaders to engage with patients, staff, and communities in new, impactful ways by focusing on wellbeing and wholeness rather than illness and disease. Having a higher sense of purpose is associated with lower all-cause mortality, reduced risk of specific diseases, better health behaviors, greater use of preventive services, and fewer hospital days of care.3
This article describes how AFHS supports the well-being of older adults and aligns with the whole health model of care. It also outlines the VHA investment to transform health care to be more person-centered by documenting what matters in the electronic health record (EHR).
AGE-FRIENDLY CARE
Given that nearly half of veterans enrolled in the VHA are aged ≥ 65 years, there is an increased need to identify models of care to support this aging population.4 This is especially critical because older veterans often have multiple chronic conditions and complex care needs that benefit from a whole person approach. The AFHS movement aims to provide evidence-based care aligned with what matters to older adults and provides a mechanism for transforming care to meet the needs of older veterans. This includes addressing age-related health concerns while promoting optimal health outcomes and quality of life. AFHS follows the 4Ms framework: what matters, medication, mentation, and mobility.5 The 4Ms serve as a guide for the health care of older adults in any setting, where each “M” is assessed and acted on to support what matters.5 Since 2020, > 390 teams have developed a plan to implement the 4Ms at 156 VHA facilities, demonstrating the VHA commitment to transforming health care for veterans.6
When VHA teams join the AFHS movement, they may also engage older veterans in a whole health system (WHS) (Figure). While AFHS is designed to improve care for patients aged ≥ 65 years, it also complements whole health, a person-centered approach available to all veterans enrolled in the VHA. Through the WHS and AFHS, veterans are empowered and equipped to take charge of their health and well-being through conversations about their unique goals, preferences, and health priorities.4 Clinicians are challenged to assess what matters by asking questions like, “What brings you joy?” and, “How can we help you meet your health goals?”1,5 These questions shift the conversation from disease-based treatment and enable clinicians to better understand the veteran as a person.1,5
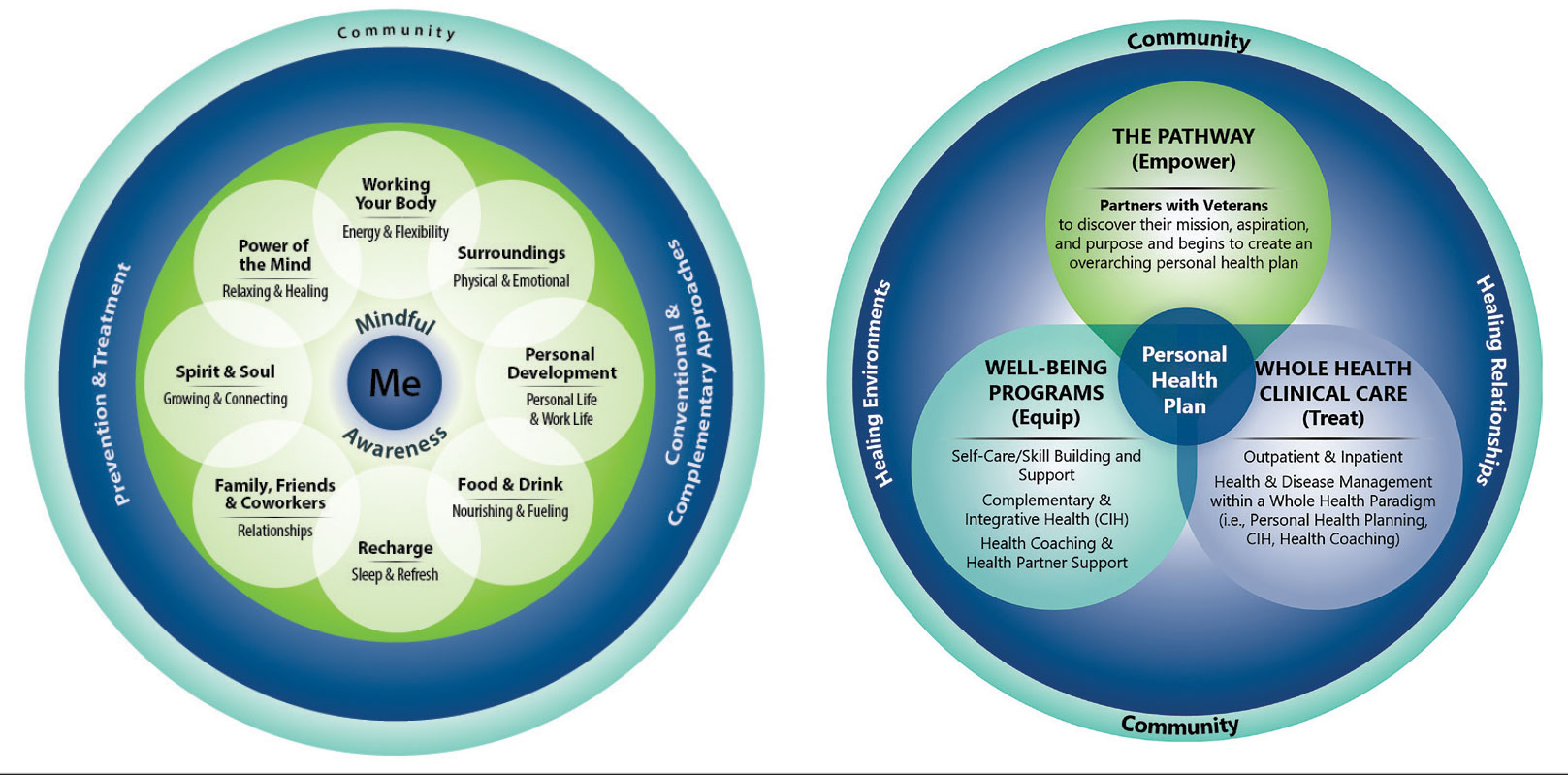
For whole health and AFHS, conversations about what matters are anchored in the veteran’s goals and preferences, especially those facing a significant health change (ie, a new diagnosis or treatment decision).5,7 Together, the veteran’s goals and priorities serve as the foundation for developing person-centered care plans that often go beyond conventional medical treatments to address the physical, mental, emotional, and social aspects of health.
SYSTEM-WIDE DIRECTIVE
The WHS enhances AFHS discussions about what matters to veterans by adding a system-level lens for conceptualizing health care delivery by leveraging the 3 components of WHS: the “pathway,” well-being programs, and whole health clinical care.
The Pathway
Discovering what matters, or the veteran’s “mission, aspiration, and purpose,” begins with the WHS pathway. When stepping into the pathway, veterans begin completing a personal health inventory, or “walking the circle of health,” which encourages self-reflection that focuses on components of their life that can influence health and well-being.1,8 The circle of health offers a visual representation of the 4 most important aspects of health and well-being: First, “Me” at the center as an individual who is the expert on their life, values, goals, and priorities. Only the individual can know what really matters through mindful awareness and what works for their life. Second, self-care consists of 8 areas that impact health and wellbeing: working your body; surroundings; personal development; food and drink; recharge; family, friends, and coworkers; spirit and soul; and power of the mind. Third, professional care consists of prevention, conventional care, and complementary care. Finally, the community that supports the individual.
Well-Being Programs
VHA provides WHS programs that support veterans in building self-care skills and improving their quality of life, often through integrative care clinics that offer coaching and CIH therapies. For example, a veteran who prioritizes mobility when seeking care at an integrative care clinic will not only receive conventional medical treatment for their physical symptoms but may also be offered CIH therapies depending on their goals. The veteran may set a daily mobility goal with their care team that supports what matters, incorporating CIH approaches, such as yoga and tai chi into the care plan.5 These holistic approaches for moving the body can help alleviate physical symptoms, reduce stress, improve mindful awareness, and provide opportunities for self-discovery and growth, thus promote overall well-being
Whole Health Clinical Care
AFHS and the 4Ms embody the clinical care component of the WHS. Because what matters is the driver of the 4Ms, every action taken by the care team supports wellbeing and quality of life by promoting independence, connection, and support, and addressing external factors, such as social determinants of health. At a minimum, well-being includes “functioning well: the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships.”9 From a system perspective, the VHA has begun to normalize focusing on what matters to veterans, using an interprofessional approach, one of the first steps to implementing AFHS.
As the programs expand, AFHS teams can learn from whole health well-being programs and increase the capacity for self-care in older veterans. Learning about the key elements included in the circle of health helps clinicians understand each veteran’s perceived strengths and weaknesses to support their self-care. From there, teams can act on the 4Ms and connect older veterans with the most appropriate programs and services at their facility, ensuring continuum of care.
DOCUMENTATION
The VHA leverages several tools and evidence-based practices to assess and act on what matters for veterans of all ages (Table).5,10-16 The VHA EHR and associated dashboards contain a wealth of information about whole health and AFHS implementation, scale up, and spread. A national AFHS 4Ms note template contains standardized data elements called health factors, which provide a mechanism for monitoring 4Ms care via its related dashboard. This template was developed by an interprofessional workgroup of VHA staff and underwent a thorough human factors engineering review and testing process prior to its release. Although teams continue to personalize care based on what matters to the veteran, data from the standardized 4Ms note template and dashboard provide a way to establish consistent, equitable care across multiple care settings.17
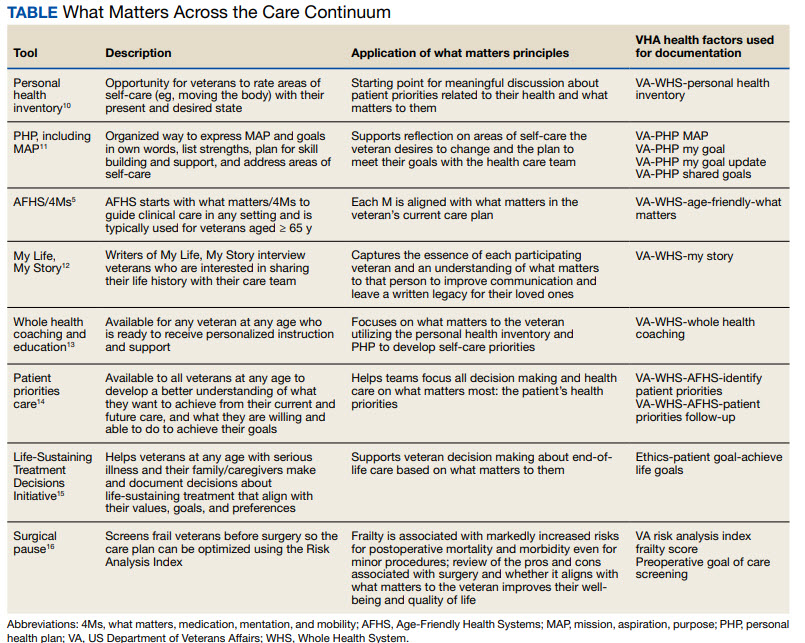
Between January 2022 and December 2023, > 612,000 participants aged ≥ 65 years identified what matters to them through 1.35 million assessments. During that period, > 36,000 veterans aged ≥ 65 years participated in AFHS and had what matters conversations documented. A personalized health plan was completed by 585,270 veterans for a total of 1.1 million assessments.11 Whole health coaching has been documented for > 57,000 veterans with > 200,000 assessments completed.13 In fiscal year 2023, a total of 1,802,131 veterans participated in whole health.
When teams share information about what matters to the veteran in a clinicianfacing format in the EHR, this helps ensure that the VHA honors veteran preferences throughout transitions of care and across all phases of health care. Although the EHR captures data on what matters, measurement of the overall impact on veteran and health system outcomes is essential. Further evaluation and ongoing education are needed to ensure clinicians are accurately and efficiently capturing the care provided by completing the appropriate EHR. Additional challenges include identifying ways to balance the documentation burden, while ensuring notes include valuable patient-centered information to guide care. EHR tools and templates have helped to unlock important insights on health care delivery in the VHA; however, health systems must consider how these clinical practices support the overall well-being of patients. How leaders empower frontline clinicians in any care setting to use these data to drive meaningful change is also important.
TRANSFORMING VHA CARE DELIVERY
In Achieving Whole Health: A New Approach for Veterans and the Nation, the National Academy of Science proposes a framework for the transformation of health care institutions to provide better whole health to veterans.3 Transformation requires change in entire systems and leaders who mobilize people “for participation in the process of change, encouraging a sense of collective identity and collective efficacy, which in turn brings stronger feelings of self-worth and self-efficacy,” and an enhanced sense of meaningfulness in their work and lives.18
Shifting health care approaches to equipping and empowering veterans and employees with whole health and AFHS resources is transformational and requires radically different assumptions and approaches that cannot be realized through traditional approaches. This change requires robust and multifaceted cultural transformation spanning all levels of the organization. Whole health and AFHS are facilitating this transformation by supporting documentation and data needs, tracking outcomes across settings, and accelerating spread to new facilities and care settings nationwide to support older veterans in improving their health and well-being.
Whole health and AFHS are complementary approaches to care that can work to empower veterans (as well as caregivers and clinicians) to align services with what matters most to veterans. Lessons such as standardizing person-centered assessments of what matters, creating supportive structures to better align care with veterans’ priorities, and identifying meaningful veteran and system-level outcomes to help sustain transformational change can be applied from whole health to AFHS. Together these programs have the potential to enhance overall health outcomes and quality of life for veterans.
- Kligler B, Hyde J, Gantt C, Bokhour B. The Whole Health transformation at the Veterans Health Administration: moving from “what’s the matter with you?” to “what matters to you?” Med Care. 2022;60(5):387-391. doi:10.1097/MLR.0000000000001706
- Centers for Disease Control and Prevention. Social determinants of health (SDOH) at CDC. January 17, 2024. Accessed September 12, 2024. https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html
- National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. The National Academies Press; 2023. Accessed September 9, 2024. doi:10.17226/26854
- Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58 Suppl 1(Suppl 1):5-8. doi:10.1111/1475-6773.14110
- Laderman M, Jackson C, Little K, Duong T, Pelton L. “What Matters” to older adults? A toolkit for health systems to design better care with older adults. Institute for Healthcare Improvement; 2019. Accessed September 9, 2024. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Age_Friendly_What_Matters_to_Older_Adults_Toolkit.pdf
- U.S. Department of Veterans Affairs. Age-Friendly Health Systems. Updated September 4, 2024. Accessed September 9, 2024. https://marketplace.va.gov/innovations/age-friendly-health-systems
- Brown TT, Hurley VB, Rodriguez HP, et al. Shared dec i s i o n - m a k i n g l o w e r s m e d i c a l e x p e n d i t u re s a n d the effect is amplified in racially-ethnically concordant relationships. Med Care. 2023;61(8):528-535. doi:10.1097/MLR.0000000000001881
- Kligler B. Whole Health in the Veterans Health Administration. Glob Adv Health Med. 2022;11:2164957X221077214.
- Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y
- U.S. Department of Veterans Affairs. Personal Health Inventory. Updated May 2022. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/docs/PHI-long-May22-fillable-508.pdf doi:10.1177/2164957X221077214
- Veterans Health Administration. Personal Health Plan. Updated March 2019. Accessed September 9, 2024. https:// www.va.gov/WHOLEHEALTH/docs/PersonalHealthPlan_508_03-2019.pdf
- Veterans Health Administration. Whole Health: My Life, My Story. Updated March 20, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/mylifemystory/index.asp
- U.S. Department of Veterans Affairs. Whole Health Library: Whole Health for Skill Building. Updated April 17, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- U.S. Department of Veterans Affairs. Making Decisions: Current Care Planning. Updated May 21, 2024. Accessed September 9, 2024. https://www.va.gov/geriatrics/pages/making_decisions.asp
- U.S. Department of Veterans Affairs. Life-Sustaining Treatment Decisions Initiative (LSTDI). Updated March 2024. Accessed September 12, 2024. https://marketplace.va.gov/innovations/life-sustaining-treatment-decisions-initiative
- U.S. Department of Veterans Affairs. Center for Health Equity Research and Promotion: Surgical Pause Saving Veterans Lives. Updated September 22, 2021. Accessed September 9, 2024. https://www.cherp.research.va.gov/features/Surgical_Pause_Saving_Veterans_Lives.asp
- Munro S, Church K, Berner C, et al. Implementation of an agefriendly template in the Veterans Health Administration electronic health record. J Inform Nurs. 2023;8(3):6-11.
- Burns JM. Transforming Leadership: A New Pursuit of Happiness. Grove Press; 2003.
- US Department of Veterans Affairs, Veterans Health Administration. Whole Health: Circle of Health Overview. Updated May 20, 2024. Accessed September 12, 2024. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
The COVID-19 pandemic established a new normal for health care delivery, with leaders rethinking core practices to survive and thrive in a changing environment and improve the health and well-being of patients. The Veterans Health Administration (VHA) is embracing a shift in focus from “what is the matter” to “what really matters” to address pre- and postpandemic challenges through a whole health approach.1 Initially conceptualized by the VHA in 2011, whole health “is an approach to health care that empowers and equips people to take charge of their health and well-being so that they can live their life to the fullest.”1 Whole health integrates evidence-based complementary and integrative health (CIH) therapies to manage pain; this includes acupuncture, meditation, tai chi, yoga, massage therapy, guided imagery, biofeedback, and clinical hypnosis.1 The VHA now recognizes well-being as a core value, helping clinicians respond to emerging challenges related to the social determinants of health (eg, access to health care, physical activity, and healthy foods) and guiding health care decision making.1,2
Well-being through empowerment—elements of whole health and Age-Friendly Health Systems (AFHS)—encourages health care institutions to work with employees, patients, and other stakeholders to address global challenges, clinician burnout, and social issues faced by their communities. This approach focuses on life’s purpose and meaning for individuals and inspires leaders to engage with patients, staff, and communities in new, impactful ways by focusing on wellbeing and wholeness rather than illness and disease. Having a higher sense of purpose is associated with lower all-cause mortality, reduced risk of specific diseases, better health behaviors, greater use of preventive services, and fewer hospital days of care.3
This article describes how AFHS supports the well-being of older adults and aligns with the whole health model of care. It also outlines the VHA investment to transform health care to be more person-centered by documenting what matters in the electronic health record (EHR).
AGE-FRIENDLY CARE
Given that nearly half of veterans enrolled in the VHA are aged ≥ 65 years, there is an increased need to identify models of care to support this aging population.4 This is especially critical because older veterans often have multiple chronic conditions and complex care needs that benefit from a whole person approach. The AFHS movement aims to provide evidence-based care aligned with what matters to older adults and provides a mechanism for transforming care to meet the needs of older veterans. This includes addressing age-related health concerns while promoting optimal health outcomes and quality of life. AFHS follows the 4Ms framework: what matters, medication, mentation, and mobility.5 The 4Ms serve as a guide for the health care of older adults in any setting, where each “M” is assessed and acted on to support what matters.5 Since 2020, > 390 teams have developed a plan to implement the 4Ms at 156 VHA facilities, demonstrating the VHA commitment to transforming health care for veterans.6
When VHA teams join the AFHS movement, they may also engage older veterans in a whole health system (WHS) (Figure). While AFHS is designed to improve care for patients aged ≥ 65 years, it also complements whole health, a person-centered approach available to all veterans enrolled in the VHA. Through the WHS and AFHS, veterans are empowered and equipped to take charge of their health and well-being through conversations about their unique goals, preferences, and health priorities.4 Clinicians are challenged to assess what matters by asking questions like, “What brings you joy?” and, “How can we help you meet your health goals?”1,5 These questions shift the conversation from disease-based treatment and enable clinicians to better understand the veteran as a person.1,5
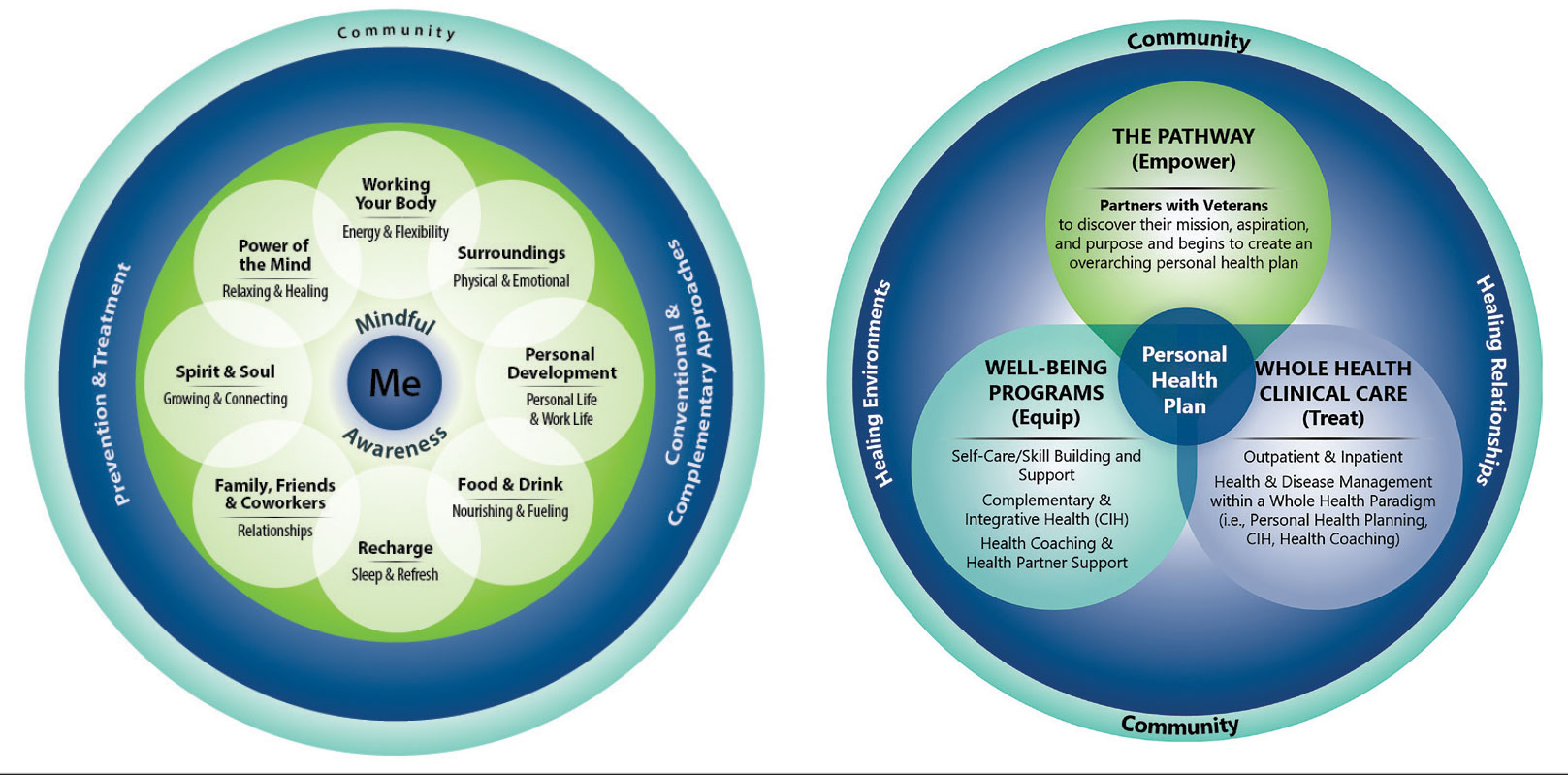
For whole health and AFHS, conversations about what matters are anchored in the veteran’s goals and preferences, especially those facing a significant health change (ie, a new diagnosis or treatment decision).5,7 Together, the veteran’s goals and priorities serve as the foundation for developing person-centered care plans that often go beyond conventional medical treatments to address the physical, mental, emotional, and social aspects of health.
SYSTEM-WIDE DIRECTIVE
The WHS enhances AFHS discussions about what matters to veterans by adding a system-level lens for conceptualizing health care delivery by leveraging the 3 components of WHS: the “pathway,” well-being programs, and whole health clinical care.
The Pathway
Discovering what matters, or the veteran’s “mission, aspiration, and purpose,” begins with the WHS pathway. When stepping into the pathway, veterans begin completing a personal health inventory, or “walking the circle of health,” which encourages self-reflection that focuses on components of their life that can influence health and well-being.1,8 The circle of health offers a visual representation of the 4 most important aspects of health and well-being: First, “Me” at the center as an individual who is the expert on their life, values, goals, and priorities. Only the individual can know what really matters through mindful awareness and what works for their life. Second, self-care consists of 8 areas that impact health and wellbeing: working your body; surroundings; personal development; food and drink; recharge; family, friends, and coworkers; spirit and soul; and power of the mind. Third, professional care consists of prevention, conventional care, and complementary care. Finally, the community that supports the individual.
Well-Being Programs
VHA provides WHS programs that support veterans in building self-care skills and improving their quality of life, often through integrative care clinics that offer coaching and CIH therapies. For example, a veteran who prioritizes mobility when seeking care at an integrative care clinic will not only receive conventional medical treatment for their physical symptoms but may also be offered CIH therapies depending on their goals. The veteran may set a daily mobility goal with their care team that supports what matters, incorporating CIH approaches, such as yoga and tai chi into the care plan.5 These holistic approaches for moving the body can help alleviate physical symptoms, reduce stress, improve mindful awareness, and provide opportunities for self-discovery and growth, thus promote overall well-being
Whole Health Clinical Care
AFHS and the 4Ms embody the clinical care component of the WHS. Because what matters is the driver of the 4Ms, every action taken by the care team supports wellbeing and quality of life by promoting independence, connection, and support, and addressing external factors, such as social determinants of health. At a minimum, well-being includes “functioning well: the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships.”9 From a system perspective, the VHA has begun to normalize focusing on what matters to veterans, using an interprofessional approach, one of the first steps to implementing AFHS.
As the programs expand, AFHS teams can learn from whole health well-being programs and increase the capacity for self-care in older veterans. Learning about the key elements included in the circle of health helps clinicians understand each veteran’s perceived strengths and weaknesses to support their self-care. From there, teams can act on the 4Ms and connect older veterans with the most appropriate programs and services at their facility, ensuring continuum of care.
DOCUMENTATION
The VHA leverages several tools and evidence-based practices to assess and act on what matters for veterans of all ages (Table).5,10-16 The VHA EHR and associated dashboards contain a wealth of information about whole health and AFHS implementation, scale up, and spread. A national AFHS 4Ms note template contains standardized data elements called health factors, which provide a mechanism for monitoring 4Ms care via its related dashboard. This template was developed by an interprofessional workgroup of VHA staff and underwent a thorough human factors engineering review and testing process prior to its release. Although teams continue to personalize care based on what matters to the veteran, data from the standardized 4Ms note template and dashboard provide a way to establish consistent, equitable care across multiple care settings.17
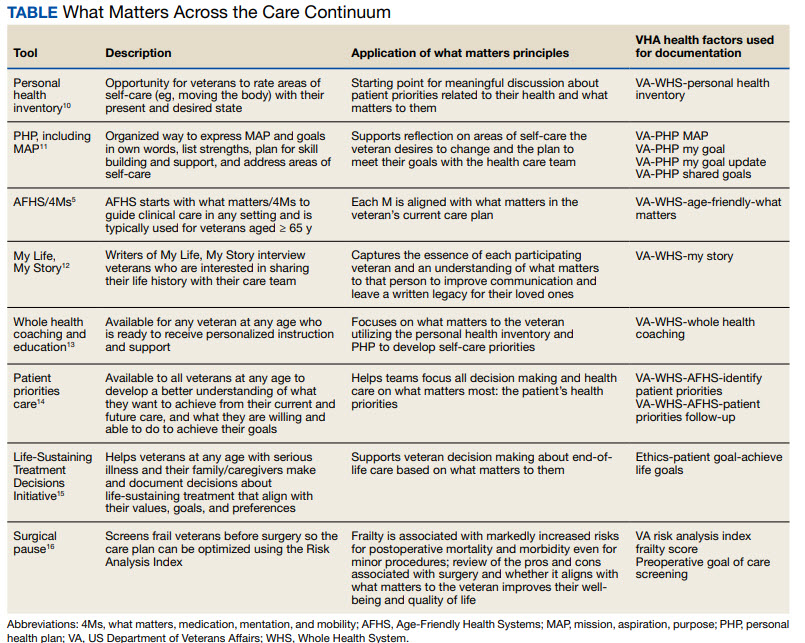
Between January 2022 and December 2023, > 612,000 participants aged ≥ 65 years identified what matters to them through 1.35 million assessments. During that period, > 36,000 veterans aged ≥ 65 years participated in AFHS and had what matters conversations documented. A personalized health plan was completed by 585,270 veterans for a total of 1.1 million assessments.11 Whole health coaching has been documented for > 57,000 veterans with > 200,000 assessments completed.13 In fiscal year 2023, a total of 1,802,131 veterans participated in whole health.
When teams share information about what matters to the veteran in a clinicianfacing format in the EHR, this helps ensure that the VHA honors veteran preferences throughout transitions of care and across all phases of health care. Although the EHR captures data on what matters, measurement of the overall impact on veteran and health system outcomes is essential. Further evaluation and ongoing education are needed to ensure clinicians are accurately and efficiently capturing the care provided by completing the appropriate EHR. Additional challenges include identifying ways to balance the documentation burden, while ensuring notes include valuable patient-centered information to guide care. EHR tools and templates have helped to unlock important insights on health care delivery in the VHA; however, health systems must consider how these clinical practices support the overall well-being of patients. How leaders empower frontline clinicians in any care setting to use these data to drive meaningful change is also important.
TRANSFORMING VHA CARE DELIVERY
In Achieving Whole Health: A New Approach for Veterans and the Nation, the National Academy of Science proposes a framework for the transformation of health care institutions to provide better whole health to veterans.3 Transformation requires change in entire systems and leaders who mobilize people “for participation in the process of change, encouraging a sense of collective identity and collective efficacy, which in turn brings stronger feelings of self-worth and self-efficacy,” and an enhanced sense of meaningfulness in their work and lives.18
Shifting health care approaches to equipping and empowering veterans and employees with whole health and AFHS resources is transformational and requires radically different assumptions and approaches that cannot be realized through traditional approaches. This change requires robust and multifaceted cultural transformation spanning all levels of the organization. Whole health and AFHS are facilitating this transformation by supporting documentation and data needs, tracking outcomes across settings, and accelerating spread to new facilities and care settings nationwide to support older veterans in improving their health and well-being.
Whole health and AFHS are complementary approaches to care that can work to empower veterans (as well as caregivers and clinicians) to align services with what matters most to veterans. Lessons such as standardizing person-centered assessments of what matters, creating supportive structures to better align care with veterans’ priorities, and identifying meaningful veteran and system-level outcomes to help sustain transformational change can be applied from whole health to AFHS. Together these programs have the potential to enhance overall health outcomes and quality of life for veterans.
The COVID-19 pandemic established a new normal for health care delivery, with leaders rethinking core practices to survive and thrive in a changing environment and improve the health and well-being of patients. The Veterans Health Administration (VHA) is embracing a shift in focus from “what is the matter” to “what really matters” to address pre- and postpandemic challenges through a whole health approach.1 Initially conceptualized by the VHA in 2011, whole health “is an approach to health care that empowers and equips people to take charge of their health and well-being so that they can live their life to the fullest.”1 Whole health integrates evidence-based complementary and integrative health (CIH) therapies to manage pain; this includes acupuncture, meditation, tai chi, yoga, massage therapy, guided imagery, biofeedback, and clinical hypnosis.1 The VHA now recognizes well-being as a core value, helping clinicians respond to emerging challenges related to the social determinants of health (eg, access to health care, physical activity, and healthy foods) and guiding health care decision making.1,2
Well-being through empowerment—elements of whole health and Age-Friendly Health Systems (AFHS)—encourages health care institutions to work with employees, patients, and other stakeholders to address global challenges, clinician burnout, and social issues faced by their communities. This approach focuses on life’s purpose and meaning for individuals and inspires leaders to engage with patients, staff, and communities in new, impactful ways by focusing on wellbeing and wholeness rather than illness and disease. Having a higher sense of purpose is associated with lower all-cause mortality, reduced risk of specific diseases, better health behaviors, greater use of preventive services, and fewer hospital days of care.3
This article describes how AFHS supports the well-being of older adults and aligns with the whole health model of care. It also outlines the VHA investment to transform health care to be more person-centered by documenting what matters in the electronic health record (EHR).
AGE-FRIENDLY CARE
Given that nearly half of veterans enrolled in the VHA are aged ≥ 65 years, there is an increased need to identify models of care to support this aging population.4 This is especially critical because older veterans often have multiple chronic conditions and complex care needs that benefit from a whole person approach. The AFHS movement aims to provide evidence-based care aligned with what matters to older adults and provides a mechanism for transforming care to meet the needs of older veterans. This includes addressing age-related health concerns while promoting optimal health outcomes and quality of life. AFHS follows the 4Ms framework: what matters, medication, mentation, and mobility.5 The 4Ms serve as a guide for the health care of older adults in any setting, where each “M” is assessed and acted on to support what matters.5 Since 2020, > 390 teams have developed a plan to implement the 4Ms at 156 VHA facilities, demonstrating the VHA commitment to transforming health care for veterans.6
When VHA teams join the AFHS movement, they may also engage older veterans in a whole health system (WHS) (Figure). While AFHS is designed to improve care for patients aged ≥ 65 years, it also complements whole health, a person-centered approach available to all veterans enrolled in the VHA. Through the WHS and AFHS, veterans are empowered and equipped to take charge of their health and well-being through conversations about their unique goals, preferences, and health priorities.4 Clinicians are challenged to assess what matters by asking questions like, “What brings you joy?” and, “How can we help you meet your health goals?”1,5 These questions shift the conversation from disease-based treatment and enable clinicians to better understand the veteran as a person.1,5
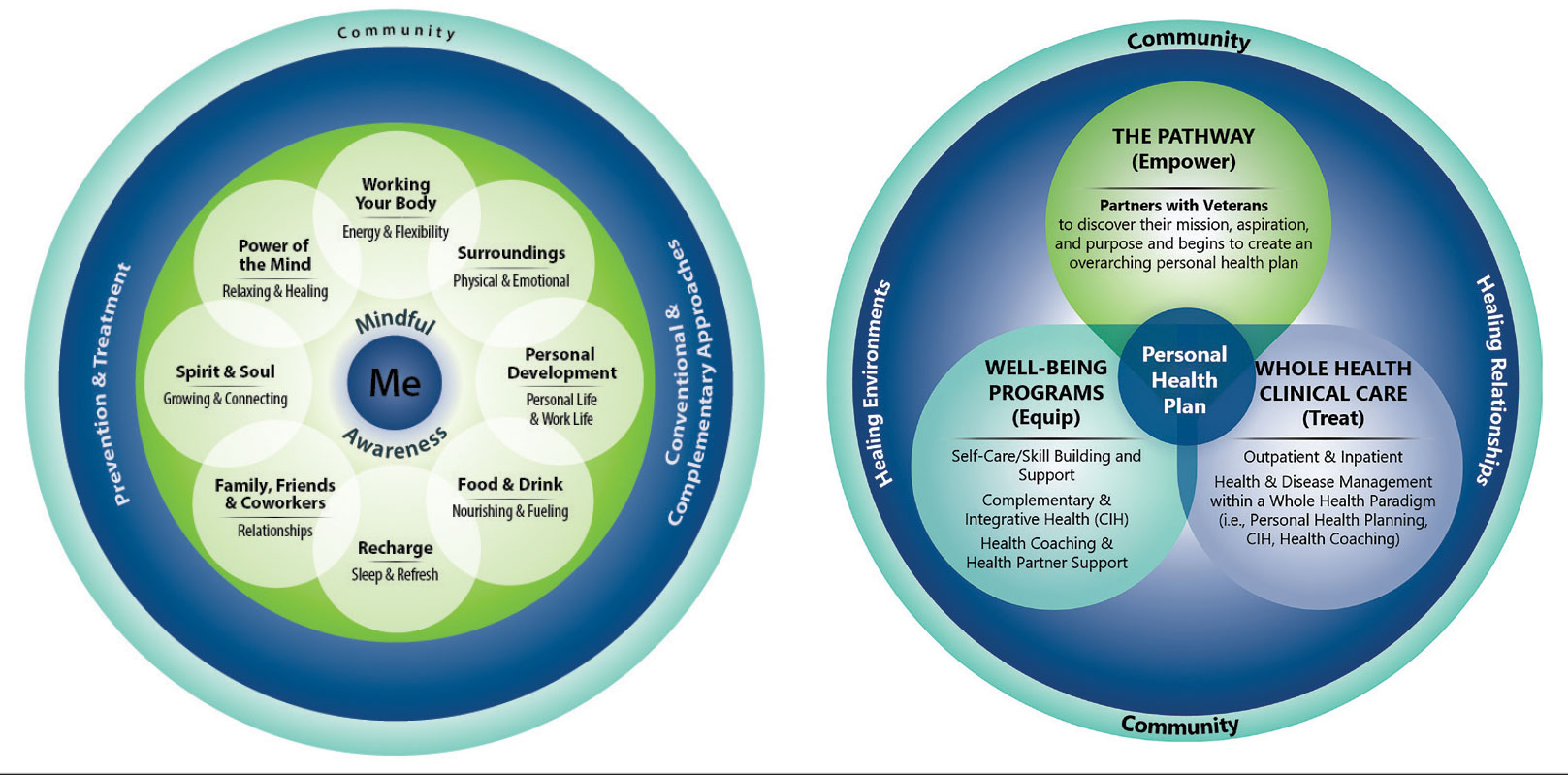
For whole health and AFHS, conversations about what matters are anchored in the veteran’s goals and preferences, especially those facing a significant health change (ie, a new diagnosis or treatment decision).5,7 Together, the veteran’s goals and priorities serve as the foundation for developing person-centered care plans that often go beyond conventional medical treatments to address the physical, mental, emotional, and social aspects of health.
SYSTEM-WIDE DIRECTIVE
The WHS enhances AFHS discussions about what matters to veterans by adding a system-level lens for conceptualizing health care delivery by leveraging the 3 components of WHS: the “pathway,” well-being programs, and whole health clinical care.
The Pathway
Discovering what matters, or the veteran’s “mission, aspiration, and purpose,” begins with the WHS pathway. When stepping into the pathway, veterans begin completing a personal health inventory, or “walking the circle of health,” which encourages self-reflection that focuses on components of their life that can influence health and well-being.1,8 The circle of health offers a visual representation of the 4 most important aspects of health and well-being: First, “Me” at the center as an individual who is the expert on their life, values, goals, and priorities. Only the individual can know what really matters through mindful awareness and what works for their life. Second, self-care consists of 8 areas that impact health and wellbeing: working your body; surroundings; personal development; food and drink; recharge; family, friends, and coworkers; spirit and soul; and power of the mind. Third, professional care consists of prevention, conventional care, and complementary care. Finally, the community that supports the individual.
Well-Being Programs
VHA provides WHS programs that support veterans in building self-care skills and improving their quality of life, often through integrative care clinics that offer coaching and CIH therapies. For example, a veteran who prioritizes mobility when seeking care at an integrative care clinic will not only receive conventional medical treatment for their physical symptoms but may also be offered CIH therapies depending on their goals. The veteran may set a daily mobility goal with their care team that supports what matters, incorporating CIH approaches, such as yoga and tai chi into the care plan.5 These holistic approaches for moving the body can help alleviate physical symptoms, reduce stress, improve mindful awareness, and provide opportunities for self-discovery and growth, thus promote overall well-being
Whole Health Clinical Care
AFHS and the 4Ms embody the clinical care component of the WHS. Because what matters is the driver of the 4Ms, every action taken by the care team supports wellbeing and quality of life by promoting independence, connection, and support, and addressing external factors, such as social determinants of health. At a minimum, well-being includes “functioning well: the experience of positive emotions such as happiness and contentment as well as the development of one’s potential, having some control over one’s life, having a sense of purpose, and experiencing positive relationships.”9 From a system perspective, the VHA has begun to normalize focusing on what matters to veterans, using an interprofessional approach, one of the first steps to implementing AFHS.
As the programs expand, AFHS teams can learn from whole health well-being programs and increase the capacity for self-care in older veterans. Learning about the key elements included in the circle of health helps clinicians understand each veteran’s perceived strengths and weaknesses to support their self-care. From there, teams can act on the 4Ms and connect older veterans with the most appropriate programs and services at their facility, ensuring continuum of care.
DOCUMENTATION
The VHA leverages several tools and evidence-based practices to assess and act on what matters for veterans of all ages (Table).5,10-16 The VHA EHR and associated dashboards contain a wealth of information about whole health and AFHS implementation, scale up, and spread. A national AFHS 4Ms note template contains standardized data elements called health factors, which provide a mechanism for monitoring 4Ms care via its related dashboard. This template was developed by an interprofessional workgroup of VHA staff and underwent a thorough human factors engineering review and testing process prior to its release. Although teams continue to personalize care based on what matters to the veteran, data from the standardized 4Ms note template and dashboard provide a way to establish consistent, equitable care across multiple care settings.17
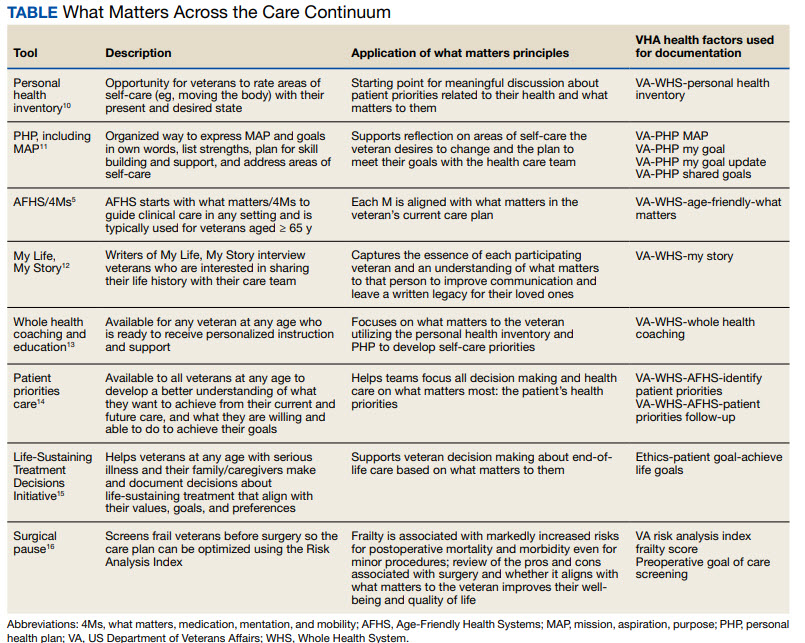
Between January 2022 and December 2023, > 612,000 participants aged ≥ 65 years identified what matters to them through 1.35 million assessments. During that period, > 36,000 veterans aged ≥ 65 years participated in AFHS and had what matters conversations documented. A personalized health plan was completed by 585,270 veterans for a total of 1.1 million assessments.11 Whole health coaching has been documented for > 57,000 veterans with > 200,000 assessments completed.13 In fiscal year 2023, a total of 1,802,131 veterans participated in whole health.
When teams share information about what matters to the veteran in a clinicianfacing format in the EHR, this helps ensure that the VHA honors veteran preferences throughout transitions of care and across all phases of health care. Although the EHR captures data on what matters, measurement of the overall impact on veteran and health system outcomes is essential. Further evaluation and ongoing education are needed to ensure clinicians are accurately and efficiently capturing the care provided by completing the appropriate EHR. Additional challenges include identifying ways to balance the documentation burden, while ensuring notes include valuable patient-centered information to guide care. EHR tools and templates have helped to unlock important insights on health care delivery in the VHA; however, health systems must consider how these clinical practices support the overall well-being of patients. How leaders empower frontline clinicians in any care setting to use these data to drive meaningful change is also important.
TRANSFORMING VHA CARE DELIVERY
In Achieving Whole Health: A New Approach for Veterans and the Nation, the National Academy of Science proposes a framework for the transformation of health care institutions to provide better whole health to veterans.3 Transformation requires change in entire systems and leaders who mobilize people “for participation in the process of change, encouraging a sense of collective identity and collective efficacy, which in turn brings stronger feelings of self-worth and self-efficacy,” and an enhanced sense of meaningfulness in their work and lives.18
Shifting health care approaches to equipping and empowering veterans and employees with whole health and AFHS resources is transformational and requires radically different assumptions and approaches that cannot be realized through traditional approaches. This change requires robust and multifaceted cultural transformation spanning all levels of the organization. Whole health and AFHS are facilitating this transformation by supporting documentation and data needs, tracking outcomes across settings, and accelerating spread to new facilities and care settings nationwide to support older veterans in improving their health and well-being.
Whole health and AFHS are complementary approaches to care that can work to empower veterans (as well as caregivers and clinicians) to align services with what matters most to veterans. Lessons such as standardizing person-centered assessments of what matters, creating supportive structures to better align care with veterans’ priorities, and identifying meaningful veteran and system-level outcomes to help sustain transformational change can be applied from whole health to AFHS. Together these programs have the potential to enhance overall health outcomes and quality of life for veterans.
- Kligler B, Hyde J, Gantt C, Bokhour B. The Whole Health transformation at the Veterans Health Administration: moving from “what’s the matter with you?” to “what matters to you?” Med Care. 2022;60(5):387-391. doi:10.1097/MLR.0000000000001706
- Centers for Disease Control and Prevention. Social determinants of health (SDOH) at CDC. January 17, 2024. Accessed September 12, 2024. https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html
- National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. The National Academies Press; 2023. Accessed September 9, 2024. doi:10.17226/26854
- Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58 Suppl 1(Suppl 1):5-8. doi:10.1111/1475-6773.14110
- Laderman M, Jackson C, Little K, Duong T, Pelton L. “What Matters” to older adults? A toolkit for health systems to design better care with older adults. Institute for Healthcare Improvement; 2019. Accessed September 9, 2024. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Age_Friendly_What_Matters_to_Older_Adults_Toolkit.pdf
- U.S. Department of Veterans Affairs. Age-Friendly Health Systems. Updated September 4, 2024. Accessed September 9, 2024. https://marketplace.va.gov/innovations/age-friendly-health-systems
- Brown TT, Hurley VB, Rodriguez HP, et al. Shared dec i s i o n - m a k i n g l o w e r s m e d i c a l e x p e n d i t u re s a n d the effect is amplified in racially-ethnically concordant relationships. Med Care. 2023;61(8):528-535. doi:10.1097/MLR.0000000000001881
- Kligler B. Whole Health in the Veterans Health Administration. Glob Adv Health Med. 2022;11:2164957X221077214.
- Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y
- U.S. Department of Veterans Affairs. Personal Health Inventory. Updated May 2022. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/docs/PHI-long-May22-fillable-508.pdf doi:10.1177/2164957X221077214
- Veterans Health Administration. Personal Health Plan. Updated March 2019. Accessed September 9, 2024. https:// www.va.gov/WHOLEHEALTH/docs/PersonalHealthPlan_508_03-2019.pdf
- Veterans Health Administration. Whole Health: My Life, My Story. Updated March 20, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/mylifemystory/index.asp
- U.S. Department of Veterans Affairs. Whole Health Library: Whole Health for Skill Building. Updated April 17, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- U.S. Department of Veterans Affairs. Making Decisions: Current Care Planning. Updated May 21, 2024. Accessed September 9, 2024. https://www.va.gov/geriatrics/pages/making_decisions.asp
- U.S. Department of Veterans Affairs. Life-Sustaining Treatment Decisions Initiative (LSTDI). Updated March 2024. Accessed September 12, 2024. https://marketplace.va.gov/innovations/life-sustaining-treatment-decisions-initiative
- U.S. Department of Veterans Affairs. Center for Health Equity Research and Promotion: Surgical Pause Saving Veterans Lives. Updated September 22, 2021. Accessed September 9, 2024. https://www.cherp.research.va.gov/features/Surgical_Pause_Saving_Veterans_Lives.asp
- Munro S, Church K, Berner C, et al. Implementation of an agefriendly template in the Veterans Health Administration electronic health record. J Inform Nurs. 2023;8(3):6-11.
- Burns JM. Transforming Leadership: A New Pursuit of Happiness. Grove Press; 2003.
- US Department of Veterans Affairs, Veterans Health Administration. Whole Health: Circle of Health Overview. Updated May 20, 2024. Accessed September 12, 2024. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
- Kligler B, Hyde J, Gantt C, Bokhour B. The Whole Health transformation at the Veterans Health Administration: moving from “what’s the matter with you?” to “what matters to you?” Med Care. 2022;60(5):387-391. doi:10.1097/MLR.0000000000001706
- Centers for Disease Control and Prevention. Social determinants of health (SDOH) at CDC. January 17, 2024. Accessed September 12, 2024. https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html
- National Academies of Sciences, Engineering, and Medicine. Achieving Whole Health: A New Approach for Veterans and the Nation. The National Academies Press; 2023. Accessed September 9, 2024. doi:10.17226/26854
- Church K, Munro S, Shaughnessy M, Clancy C. Age-friendly health systems: improving care for older adults in the Veterans Health Administration. Health Serv Res. 2023;58 Suppl 1(Suppl 1):5-8. doi:10.1111/1475-6773.14110
- Laderman M, Jackson C, Little K, Duong T, Pelton L. “What Matters” to older adults? A toolkit for health systems to design better care with older adults. Institute for Healthcare Improvement; 2019. Accessed September 9, 2024. https://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHI_Age_Friendly_What_Matters_to_Older_Adults_Toolkit.pdf
- U.S. Department of Veterans Affairs. Age-Friendly Health Systems. Updated September 4, 2024. Accessed September 9, 2024. https://marketplace.va.gov/innovations/age-friendly-health-systems
- Brown TT, Hurley VB, Rodriguez HP, et al. Shared dec i s i o n - m a k i n g l o w e r s m e d i c a l e x p e n d i t u re s a n d the effect is amplified in racially-ethnically concordant relationships. Med Care. 2023;61(8):528-535. doi:10.1097/MLR.0000000000001881
- Kligler B. Whole Health in the Veterans Health Administration. Glob Adv Health Med. 2022;11:2164957X221077214.
- Ruggeri K, Garcia-Garzon E, Maguire Á, Matz S, Huppert FA. Well-being is more than happiness and life satisfaction: a multidimensional analysis of 21 countries. Health Qual Life Outcomes. 2020;18(1):192. doi:10.1186/s12955-020-01423-y
- U.S. Department of Veterans Affairs. Personal Health Inventory. Updated May 2022. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/docs/PHI-long-May22-fillable-508.pdf doi:10.1177/2164957X221077214
- Veterans Health Administration. Personal Health Plan. Updated March 2019. Accessed September 9, 2024. https:// www.va.gov/WHOLEHEALTH/docs/PersonalHealthPlan_508_03-2019.pdf
- Veterans Health Administration. Whole Health: My Life, My Story. Updated March 20, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTH/mylifemystory/index.asp
- U.S. Department of Veterans Affairs. Whole Health Library: Whole Health for Skill Building. Updated April 17, 2024. Accessed September 9, 2024. https://www.va.gov/WHOLEHEALTHLIBRARY/courses/whole-health-skill-building.asp
- U.S. Department of Veterans Affairs. Making Decisions: Current Care Planning. Updated May 21, 2024. Accessed September 9, 2024. https://www.va.gov/geriatrics/pages/making_decisions.asp
- U.S. Department of Veterans Affairs. Life-Sustaining Treatment Decisions Initiative (LSTDI). Updated March 2024. Accessed September 12, 2024. https://marketplace.va.gov/innovations/life-sustaining-treatment-decisions-initiative
- U.S. Department of Veterans Affairs. Center for Health Equity Research and Promotion: Surgical Pause Saving Veterans Lives. Updated September 22, 2021. Accessed September 9, 2024. https://www.cherp.research.va.gov/features/Surgical_Pause_Saving_Veterans_Lives.asp
- Munro S, Church K, Berner C, et al. Implementation of an agefriendly template in the Veterans Health Administration electronic health record. J Inform Nurs. 2023;8(3):6-11.
- Burns JM. Transforming Leadership: A New Pursuit of Happiness. Grove Press; 2003.
- US Department of Veterans Affairs, Veterans Health Administration. Whole Health: Circle of Health Overview. Updated May 20, 2024. Accessed September 12, 2024. https://www.va.gov/WHOLEHEALTH/circle-of-health/index.asp
How Psychedelic Drugs Can Aid Patients at the End of Life
Palliative care has proven to be one of the most promising fields for research on interventions with psychedelic substances. One of the most prominent researchers in this area was the American psychopharmacologist Roland Griffiths, PhD.
In 2016, Dr. Griffiths and his team at Johns Hopkins University in Baltimore, Maryland, published one of the most relevant contributions to the field by demonstrating in a placebo-controlled study that psilocybin can reduce depressive and anxiety symptoms in patients with cancer. The study, conducted with 51 patients diagnosed with advanced-stage cancer, compared the effects of a low dose and a high dose of psilocybin, showing that the high dose resulted in improvements in mood, quality of life, and sense of life, reducing death-related anxiety.
In 2021, after a routine examination, Dr. Griffiths himself was diagnosed with advanced colon cancer. Unexpectedly, the researcher found himself in the position of his research subjects. In an interview with The New York Times in April 2023, he stated that, after some resistance, he agreed to undergo an LSD session.
In the conversation, he revealed that he had a 50% chance of being alive by Halloween. Despite the diagnosis, he showed no discouragement. “As a scientist, I feel like a kid in a candy store, considering all the research and questions that need to be answered about psychedelics and the theme of human flourishing,” he said.
In his last months of life, in the various appearances and interviews he gave, Dr. Griffiths demonstrated a perception of life uncommon in people facing death. “I’m excited to communicate, to shake off the dust and tell people: ‘Come on, wake up!’ ”
He passed away on October 16, 2023, at age 77 years, opening new horizons for clinical research with psychedelics and becoming an example of the therapeutic potential of these substances.
Innovative Treatments
“I believe this will be one of the next conditions, if not the next condition, to be considered for the designation of innovative treatment in future psilocybin regulation in the United States, where the field is more advanced,” said Lucas Maia, PhD, a psychopharmacologist and researcher affiliated with the Advanced Center for Psychedelic Medicine (CAMP) at the Federal University of Rio Grande do Norte (UFRN) and the Interdisciplinary Cooperation for Ayahuasca Research and Outreach (ICARO) at the State University of Campinas in São Paulo, Brazil.
Currently, MDMA (for the treatment of posttraumatic stress disorder), psilocybin (for depressive disorder), and MM120 (an LSD analogue used to treat generalized anxiety disorder) are the only psychedelic substances that have received the designation of innovative treatment by the Food and Drug Administration (FDA).
In 2022, Dr. Maia and a colleague from ICARO, Ana Cláudia Mesquita Garcia, PhD, a professor at the School of Nursing at the Federal University of Alfenas in Brazil and leader of the Interdisciplinary Center for Studies in Palliative Care, published a systematic review in the Journal of Pain and Symptom Management that evaluated the use of psychedelic-assisted treatments for symptom control in patients with serious or terminal illnesses.
Of the 20 articles reviewed, 9 (45%) used LSD, 5 (25%) psilocybin, 2 (10%) dipropyltryptamine (DPT), 1 (5%) used ketamine, and 1 (5%) used MDMA. In 10% of the studies, LSD and DPT were combined. Altogether, 347 participants (54%) received LSD, 116 (18%) psilocybin, 81 (13%) LSD and DPT, 64 (10%) DPT, 18 (3%) MDMA, and 14 (2%) ketamine.
The conclusion of the study is that psychedelics provide therapeutic effects on physical, psychological, social, and existential outcomes. They are associated with a reduction in pain and improvement in sleep. A decrease in depressive and anxiety symptoms is also observed; such symptoms are common in patients with serious diseases. In addition, interpersonal relationships become closer and more empathetic. Finally, there is a reduction in the fear of death and suffering, an increase in acceptance, and a redefinition of the disease.
In 55% of the studies, the adverse effects were mild to moderate and transient. They included nausea, vomiting, dry mouth, and fatigue, as well as anxiety, panic, and hallucinations. The researchers concluded that the scarcity and difficulty of access to professional training in psychedelic-assisted treatments represent a significant challenge for the advancement of these interventions, especially in countries in the Global South.
Another systematic review and meta-analysis published in July by researchers at the University of Michigan in Ann Arbor, Michigan, included seven studies with 132 participants and showed significant improvements in quality of life, pain control, and anxiety relief after psychedelic-assisted psychotherapy with psilocybin. The combined effects indicated statistically significant reductions in anxiety symptoms after 4.0-4.5 months and after 6.0-6.5 months post administration, compared with the initial evaluations.
One of the most advanced research studies currently being conducted is led by Stephen Ross, MD, a psychiatrist affiliated with New York University’s Langone Medical Center, New York City. The phase 2b clinical study is randomized, double blind, and placebo controlled, and involves 300 participants. The study aims to evaluate the effects of psilocybin-assisted psychotherapy on psychiatric and existential distress in patients with advanced cancer. Its expected completion date is in 2027.
“We still lack effective interventions in minimizing psychological, spiritual, and existential suffering,” said Dr. Garcia. “In this sense, respecting the contraindications of a physical nature (including pre-existing illnesses at study initiation, disease staging, patient functionality level, comorbidities, concurrent pharmacological treatments, etc) and of a psychiatric nature for the use of psychedelics, depending on the clinical picture, end-of-life patients facing existential crises and psychological suffering will likely benefit more from psychedelic-assisted psychotherapy, which highlights the need for more research and the integration of this treatment into clinical practice.”
Changing Perceptions
Since 2021, the Cancer Institute of the State of São Paulo (Icesp) has been providing palliative treatment with ketamine — an atypical psychedelic — following a rigorous and carefully monitored clinical protocol. The substance is already used off label to treat refractory depressive disorder. In addition, in 2020, Brazil’s National Health Surveillance Agency approved the use of Spravato, an intranasal antidepressant based on the ketamine derivative esketamine.
Icesp has hospice beds for clinical oncology patients, and a pain management team evaluates which patients meet the inclusion criteria for ketamine use. In addition to difficult-to-control pain, it is important that the patient present emotional, existential, or spiritual symptoms that amplify that pain.
After this evaluation, a psychoeducation process takes place, in which the patient receives clear information about the treatment, its potential benefits and risks, and understands how ketamine can be a viable option for managing their symptoms. Finally, it is essential that the patient accept the referral and demonstrate a willingness to participate in the treatment, agreeing to the proposed terms.
The treatment takes place in a hospital environment, with an ambiance that aims to provide comfort and safety. Clinicians consider not only the substance dose (such as 0.5 mg/kg) but also the emotional state (“set”) and the treatment environment (“setting”). The experience is facilitated through psychological support for the patient during and after treatment.
According to Alessandro Campolina, MD, PhD, a researcher at the Center for Translational Oncology Research at Icesp, it is important to highlight that quality of life is intrinsically linked to the patient’s self-perception, including how they see themselves in terms of health and in the context in which they live.
The doctor explains that psychedelic interventions can provide a “window of opportunity,” allowing a qualified clinician to help the patient explore new perspectives based on their experiences.
“Often, although the intensity of pain remains the same, the way the patient perceives it can change significantly. For example, a patient may report that, despite the pain, they now feel less concerned about it because they were able to contemplate more significant aspects of their life,” said Dr. Campolina.
“This observation shows that treatment is not limited to addressing the pain or primary symptoms, but also addresses the associated suffering. While some patients have profound insights, many others experience more subtle changes that, under the guidance of a competent therapist, can turn into valuable clinical insights, thus improving quality of life and how they deal with their pathologies.”
Dr. Griffiths exemplified this in the interview with the Times when he reflected on his own cancer. He came to believe, as if guided an external observer, that “there is a meaning and a purpose in this [disease] that go beyond your understanding, and the way you are dealing with it is exactly how you should.”
Toshio Chiba, MD, chief physician of the Palliative Care Service at Icesp, emphasized that ketamine is already in use. “It is not feasible to wait years for the approval of psilocybin or for the FDA’s decision on MDMA, especially if the patient needs immediate care,” he said.
Furthermore, recreational and therapeutic uses are distinct. “It is essential to note that responsibilities are shared between the professional and the patient,” said Dr. Chiba. “In the therapeutic setting, there is an ethical and civil responsibility of the medical professional, as well as the patient actively engaging in treatment.”
Early palliative care can also facilitate the establishment of care goals. “I prefer to avoid terms like ‘coping’ or ‘fighting the disease,’” said Dr. Chiba. “Nowadays, dealing with cancer is more about coexisting with the disease properly, as treatments can last for years.
“Of course, there are still highly lethal tumors. However, for neoplasms like breast, colorectal, and prostate cancers, we often talk about 5, 10, or even 15 years of coexistence [with the condition]. The lack of this information [about the disease, treatments, and existential issues] can generate distress in some patients, who end up excessively worrying about the future,” he added.
But palliative treatment with psychedelics as a panacea, he said.
In addition, Marcelo Falchi, MD, medical director of CAMP at UFRN, also emphasized that psychedelics are not a risk-free intervention. Substances like LSD and psilocybin, for example, can cause increases in blood pressure and tachycardia, which, may limit their use for patients at high cardiovascular risk. Crises of anxiety or dissociative symptoms also may occur, and they require mitigation strategies such as psychological support and attention to set and setting.
“But research seems to agree that the risks can be managed effectively through a diligent process, allowing for the responsible exploration of the therapeutic potential of psychedelics,” said Dr. Falchi, who is responsible for CAMP’s postgraduate course in psychedelic therapies. The program provides training in substances used in Brazil, such as ketamine and ibogaine.
The use of psychedelics in palliative care requires a significant shift in how professionals relate to patients.
Unlike in traditional practice, where the prescription is followed by quick consultations, palliative care with psychedelics requires deep and continuous involvement, as Dr. Campolina pointed out. “We joke that it’s not a high-tech specialty, but ‘high touch,’ because it demands the constant presence of the doctor or therapist with the patient. This can involve sessions of several hours, with frequent monitoring and regular contact after sessions. This dynamic emphasizes the importance of human touch and connection during the process, reflecting a new way of practicing medicine.”
In his last months of life, Dr. Griffiths sought to emphasize this point, suggesting that, from a broader perspective, doctors and patients face the same fundamental questions. “We all know we are terminal,” he said. “Essentially, we shouldn’t need a stage 4 cancer diagnosis to awaken to this reality.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Palliative care has proven to be one of the most promising fields for research on interventions with psychedelic substances. One of the most prominent researchers in this area was the American psychopharmacologist Roland Griffiths, PhD.
In 2016, Dr. Griffiths and his team at Johns Hopkins University in Baltimore, Maryland, published one of the most relevant contributions to the field by demonstrating in a placebo-controlled study that psilocybin can reduce depressive and anxiety symptoms in patients with cancer. The study, conducted with 51 patients diagnosed with advanced-stage cancer, compared the effects of a low dose and a high dose of psilocybin, showing that the high dose resulted in improvements in mood, quality of life, and sense of life, reducing death-related anxiety.
In 2021, after a routine examination, Dr. Griffiths himself was diagnosed with advanced colon cancer. Unexpectedly, the researcher found himself in the position of his research subjects. In an interview with The New York Times in April 2023, he stated that, after some resistance, he agreed to undergo an LSD session.
In the conversation, he revealed that he had a 50% chance of being alive by Halloween. Despite the diagnosis, he showed no discouragement. “As a scientist, I feel like a kid in a candy store, considering all the research and questions that need to be answered about psychedelics and the theme of human flourishing,” he said.
In his last months of life, in the various appearances and interviews he gave, Dr. Griffiths demonstrated a perception of life uncommon in people facing death. “I’m excited to communicate, to shake off the dust and tell people: ‘Come on, wake up!’ ”
He passed away on October 16, 2023, at age 77 years, opening new horizons for clinical research with psychedelics and becoming an example of the therapeutic potential of these substances.
Innovative Treatments
“I believe this will be one of the next conditions, if not the next condition, to be considered for the designation of innovative treatment in future psilocybin regulation in the United States, where the field is more advanced,” said Lucas Maia, PhD, a psychopharmacologist and researcher affiliated with the Advanced Center for Psychedelic Medicine (CAMP) at the Federal University of Rio Grande do Norte (UFRN) and the Interdisciplinary Cooperation for Ayahuasca Research and Outreach (ICARO) at the State University of Campinas in São Paulo, Brazil.
Currently, MDMA (for the treatment of posttraumatic stress disorder), psilocybin (for depressive disorder), and MM120 (an LSD analogue used to treat generalized anxiety disorder) are the only psychedelic substances that have received the designation of innovative treatment by the Food and Drug Administration (FDA).
In 2022, Dr. Maia and a colleague from ICARO, Ana Cláudia Mesquita Garcia, PhD, a professor at the School of Nursing at the Federal University of Alfenas in Brazil and leader of the Interdisciplinary Center for Studies in Palliative Care, published a systematic review in the Journal of Pain and Symptom Management that evaluated the use of psychedelic-assisted treatments for symptom control in patients with serious or terminal illnesses.
Of the 20 articles reviewed, 9 (45%) used LSD, 5 (25%) psilocybin, 2 (10%) dipropyltryptamine (DPT), 1 (5%) used ketamine, and 1 (5%) used MDMA. In 10% of the studies, LSD and DPT were combined. Altogether, 347 participants (54%) received LSD, 116 (18%) psilocybin, 81 (13%) LSD and DPT, 64 (10%) DPT, 18 (3%) MDMA, and 14 (2%) ketamine.
The conclusion of the study is that psychedelics provide therapeutic effects on physical, psychological, social, and existential outcomes. They are associated with a reduction in pain and improvement in sleep. A decrease in depressive and anxiety symptoms is also observed; such symptoms are common in patients with serious diseases. In addition, interpersonal relationships become closer and more empathetic. Finally, there is a reduction in the fear of death and suffering, an increase in acceptance, and a redefinition of the disease.
In 55% of the studies, the adverse effects were mild to moderate and transient. They included nausea, vomiting, dry mouth, and fatigue, as well as anxiety, panic, and hallucinations. The researchers concluded that the scarcity and difficulty of access to professional training in psychedelic-assisted treatments represent a significant challenge for the advancement of these interventions, especially in countries in the Global South.
Another systematic review and meta-analysis published in July by researchers at the University of Michigan in Ann Arbor, Michigan, included seven studies with 132 participants and showed significant improvements in quality of life, pain control, and anxiety relief after psychedelic-assisted psychotherapy with psilocybin. The combined effects indicated statistically significant reductions in anxiety symptoms after 4.0-4.5 months and after 6.0-6.5 months post administration, compared with the initial evaluations.
One of the most advanced research studies currently being conducted is led by Stephen Ross, MD, a psychiatrist affiliated with New York University’s Langone Medical Center, New York City. The phase 2b clinical study is randomized, double blind, and placebo controlled, and involves 300 participants. The study aims to evaluate the effects of psilocybin-assisted psychotherapy on psychiatric and existential distress in patients with advanced cancer. Its expected completion date is in 2027.
“We still lack effective interventions in minimizing psychological, spiritual, and existential suffering,” said Dr. Garcia. “In this sense, respecting the contraindications of a physical nature (including pre-existing illnesses at study initiation, disease staging, patient functionality level, comorbidities, concurrent pharmacological treatments, etc) and of a psychiatric nature for the use of psychedelics, depending on the clinical picture, end-of-life patients facing existential crises and psychological suffering will likely benefit more from psychedelic-assisted psychotherapy, which highlights the need for more research and the integration of this treatment into clinical practice.”
Changing Perceptions
Since 2021, the Cancer Institute of the State of São Paulo (Icesp) has been providing palliative treatment with ketamine — an atypical psychedelic — following a rigorous and carefully monitored clinical protocol. The substance is already used off label to treat refractory depressive disorder. In addition, in 2020, Brazil’s National Health Surveillance Agency approved the use of Spravato, an intranasal antidepressant based on the ketamine derivative esketamine.
Icesp has hospice beds for clinical oncology patients, and a pain management team evaluates which patients meet the inclusion criteria for ketamine use. In addition to difficult-to-control pain, it is important that the patient present emotional, existential, or spiritual symptoms that amplify that pain.
After this evaluation, a psychoeducation process takes place, in which the patient receives clear information about the treatment, its potential benefits and risks, and understands how ketamine can be a viable option for managing their symptoms. Finally, it is essential that the patient accept the referral and demonstrate a willingness to participate in the treatment, agreeing to the proposed terms.
The treatment takes place in a hospital environment, with an ambiance that aims to provide comfort and safety. Clinicians consider not only the substance dose (such as 0.5 mg/kg) but also the emotional state (“set”) and the treatment environment (“setting”). The experience is facilitated through psychological support for the patient during and after treatment.
According to Alessandro Campolina, MD, PhD, a researcher at the Center for Translational Oncology Research at Icesp, it is important to highlight that quality of life is intrinsically linked to the patient’s self-perception, including how they see themselves in terms of health and in the context in which they live.
The doctor explains that psychedelic interventions can provide a “window of opportunity,” allowing a qualified clinician to help the patient explore new perspectives based on their experiences.
“Often, although the intensity of pain remains the same, the way the patient perceives it can change significantly. For example, a patient may report that, despite the pain, they now feel less concerned about it because they were able to contemplate more significant aspects of their life,” said Dr. Campolina.
“This observation shows that treatment is not limited to addressing the pain or primary symptoms, but also addresses the associated suffering. While some patients have profound insights, many others experience more subtle changes that, under the guidance of a competent therapist, can turn into valuable clinical insights, thus improving quality of life and how they deal with their pathologies.”
Dr. Griffiths exemplified this in the interview with the Times when he reflected on his own cancer. He came to believe, as if guided an external observer, that “there is a meaning and a purpose in this [disease] that go beyond your understanding, and the way you are dealing with it is exactly how you should.”
Toshio Chiba, MD, chief physician of the Palliative Care Service at Icesp, emphasized that ketamine is already in use. “It is not feasible to wait years for the approval of psilocybin or for the FDA’s decision on MDMA, especially if the patient needs immediate care,” he said.
Furthermore, recreational and therapeutic uses are distinct. “It is essential to note that responsibilities are shared between the professional and the patient,” said Dr. Chiba. “In the therapeutic setting, there is an ethical and civil responsibility of the medical professional, as well as the patient actively engaging in treatment.”
Early palliative care can also facilitate the establishment of care goals. “I prefer to avoid terms like ‘coping’ or ‘fighting the disease,’” said Dr. Chiba. “Nowadays, dealing with cancer is more about coexisting with the disease properly, as treatments can last for years.
“Of course, there are still highly lethal tumors. However, for neoplasms like breast, colorectal, and prostate cancers, we often talk about 5, 10, or even 15 years of coexistence [with the condition]. The lack of this information [about the disease, treatments, and existential issues] can generate distress in some patients, who end up excessively worrying about the future,” he added.
But palliative treatment with psychedelics as a panacea, he said.
In addition, Marcelo Falchi, MD, medical director of CAMP at UFRN, also emphasized that psychedelics are not a risk-free intervention. Substances like LSD and psilocybin, for example, can cause increases in blood pressure and tachycardia, which, may limit their use for patients at high cardiovascular risk. Crises of anxiety or dissociative symptoms also may occur, and they require mitigation strategies such as psychological support and attention to set and setting.
“But research seems to agree that the risks can be managed effectively through a diligent process, allowing for the responsible exploration of the therapeutic potential of psychedelics,” said Dr. Falchi, who is responsible for CAMP’s postgraduate course in psychedelic therapies. The program provides training in substances used in Brazil, such as ketamine and ibogaine.
The use of psychedelics in palliative care requires a significant shift in how professionals relate to patients.
Unlike in traditional practice, where the prescription is followed by quick consultations, palliative care with psychedelics requires deep and continuous involvement, as Dr. Campolina pointed out. “We joke that it’s not a high-tech specialty, but ‘high touch,’ because it demands the constant presence of the doctor or therapist with the patient. This can involve sessions of several hours, with frequent monitoring and regular contact after sessions. This dynamic emphasizes the importance of human touch and connection during the process, reflecting a new way of practicing medicine.”
In his last months of life, Dr. Griffiths sought to emphasize this point, suggesting that, from a broader perspective, doctors and patients face the same fundamental questions. “We all know we are terminal,” he said. “Essentially, we shouldn’t need a stage 4 cancer diagnosis to awaken to this reality.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Palliative care has proven to be one of the most promising fields for research on interventions with psychedelic substances. One of the most prominent researchers in this area was the American psychopharmacologist Roland Griffiths, PhD.
In 2016, Dr. Griffiths and his team at Johns Hopkins University in Baltimore, Maryland, published one of the most relevant contributions to the field by demonstrating in a placebo-controlled study that psilocybin can reduce depressive and anxiety symptoms in patients with cancer. The study, conducted with 51 patients diagnosed with advanced-stage cancer, compared the effects of a low dose and a high dose of psilocybin, showing that the high dose resulted in improvements in mood, quality of life, and sense of life, reducing death-related anxiety.
In 2021, after a routine examination, Dr. Griffiths himself was diagnosed with advanced colon cancer. Unexpectedly, the researcher found himself in the position of his research subjects. In an interview with The New York Times in April 2023, he stated that, after some resistance, he agreed to undergo an LSD session.
In the conversation, he revealed that he had a 50% chance of being alive by Halloween. Despite the diagnosis, he showed no discouragement. “As a scientist, I feel like a kid in a candy store, considering all the research and questions that need to be answered about psychedelics and the theme of human flourishing,” he said.
In his last months of life, in the various appearances and interviews he gave, Dr. Griffiths demonstrated a perception of life uncommon in people facing death. “I’m excited to communicate, to shake off the dust and tell people: ‘Come on, wake up!’ ”
He passed away on October 16, 2023, at age 77 years, opening new horizons for clinical research with psychedelics and becoming an example of the therapeutic potential of these substances.
Innovative Treatments
“I believe this will be one of the next conditions, if not the next condition, to be considered for the designation of innovative treatment in future psilocybin regulation in the United States, where the field is more advanced,” said Lucas Maia, PhD, a psychopharmacologist and researcher affiliated with the Advanced Center for Psychedelic Medicine (CAMP) at the Federal University of Rio Grande do Norte (UFRN) and the Interdisciplinary Cooperation for Ayahuasca Research and Outreach (ICARO) at the State University of Campinas in São Paulo, Brazil.
Currently, MDMA (for the treatment of posttraumatic stress disorder), psilocybin (for depressive disorder), and MM120 (an LSD analogue used to treat generalized anxiety disorder) are the only psychedelic substances that have received the designation of innovative treatment by the Food and Drug Administration (FDA).
In 2022, Dr. Maia and a colleague from ICARO, Ana Cláudia Mesquita Garcia, PhD, a professor at the School of Nursing at the Federal University of Alfenas in Brazil and leader of the Interdisciplinary Center for Studies in Palliative Care, published a systematic review in the Journal of Pain and Symptom Management that evaluated the use of psychedelic-assisted treatments for symptom control in patients with serious or terminal illnesses.
Of the 20 articles reviewed, 9 (45%) used LSD, 5 (25%) psilocybin, 2 (10%) dipropyltryptamine (DPT), 1 (5%) used ketamine, and 1 (5%) used MDMA. In 10% of the studies, LSD and DPT were combined. Altogether, 347 participants (54%) received LSD, 116 (18%) psilocybin, 81 (13%) LSD and DPT, 64 (10%) DPT, 18 (3%) MDMA, and 14 (2%) ketamine.
The conclusion of the study is that psychedelics provide therapeutic effects on physical, psychological, social, and existential outcomes. They are associated with a reduction in pain and improvement in sleep. A decrease in depressive and anxiety symptoms is also observed; such symptoms are common in patients with serious diseases. In addition, interpersonal relationships become closer and more empathetic. Finally, there is a reduction in the fear of death and suffering, an increase in acceptance, and a redefinition of the disease.
In 55% of the studies, the adverse effects were mild to moderate and transient. They included nausea, vomiting, dry mouth, and fatigue, as well as anxiety, panic, and hallucinations. The researchers concluded that the scarcity and difficulty of access to professional training in psychedelic-assisted treatments represent a significant challenge for the advancement of these interventions, especially in countries in the Global South.
Another systematic review and meta-analysis published in July by researchers at the University of Michigan in Ann Arbor, Michigan, included seven studies with 132 participants and showed significant improvements in quality of life, pain control, and anxiety relief after psychedelic-assisted psychotherapy with psilocybin. The combined effects indicated statistically significant reductions in anxiety symptoms after 4.0-4.5 months and after 6.0-6.5 months post administration, compared with the initial evaluations.
One of the most advanced research studies currently being conducted is led by Stephen Ross, MD, a psychiatrist affiliated with New York University’s Langone Medical Center, New York City. The phase 2b clinical study is randomized, double blind, and placebo controlled, and involves 300 participants. The study aims to evaluate the effects of psilocybin-assisted psychotherapy on psychiatric and existential distress in patients with advanced cancer. Its expected completion date is in 2027.
“We still lack effective interventions in minimizing psychological, spiritual, and existential suffering,” said Dr. Garcia. “In this sense, respecting the contraindications of a physical nature (including pre-existing illnesses at study initiation, disease staging, patient functionality level, comorbidities, concurrent pharmacological treatments, etc) and of a psychiatric nature for the use of psychedelics, depending on the clinical picture, end-of-life patients facing existential crises and psychological suffering will likely benefit more from psychedelic-assisted psychotherapy, which highlights the need for more research and the integration of this treatment into clinical practice.”
Changing Perceptions
Since 2021, the Cancer Institute of the State of São Paulo (Icesp) has been providing palliative treatment with ketamine — an atypical psychedelic — following a rigorous and carefully monitored clinical protocol. The substance is already used off label to treat refractory depressive disorder. In addition, in 2020, Brazil’s National Health Surveillance Agency approved the use of Spravato, an intranasal antidepressant based on the ketamine derivative esketamine.
Icesp has hospice beds for clinical oncology patients, and a pain management team evaluates which patients meet the inclusion criteria for ketamine use. In addition to difficult-to-control pain, it is important that the patient present emotional, existential, or spiritual symptoms that amplify that pain.
After this evaluation, a psychoeducation process takes place, in which the patient receives clear information about the treatment, its potential benefits and risks, and understands how ketamine can be a viable option for managing their symptoms. Finally, it is essential that the patient accept the referral and demonstrate a willingness to participate in the treatment, agreeing to the proposed terms.
The treatment takes place in a hospital environment, with an ambiance that aims to provide comfort and safety. Clinicians consider not only the substance dose (such as 0.5 mg/kg) but also the emotional state (“set”) and the treatment environment (“setting”). The experience is facilitated through psychological support for the patient during and after treatment.
According to Alessandro Campolina, MD, PhD, a researcher at the Center for Translational Oncology Research at Icesp, it is important to highlight that quality of life is intrinsically linked to the patient’s self-perception, including how they see themselves in terms of health and in the context in which they live.
The doctor explains that psychedelic interventions can provide a “window of opportunity,” allowing a qualified clinician to help the patient explore new perspectives based on their experiences.
“Often, although the intensity of pain remains the same, the way the patient perceives it can change significantly. For example, a patient may report that, despite the pain, they now feel less concerned about it because they were able to contemplate more significant aspects of their life,” said Dr. Campolina.
“This observation shows that treatment is not limited to addressing the pain or primary symptoms, but also addresses the associated suffering. While some patients have profound insights, many others experience more subtle changes that, under the guidance of a competent therapist, can turn into valuable clinical insights, thus improving quality of life and how they deal with their pathologies.”
Dr. Griffiths exemplified this in the interview with the Times when he reflected on his own cancer. He came to believe, as if guided an external observer, that “there is a meaning and a purpose in this [disease] that go beyond your understanding, and the way you are dealing with it is exactly how you should.”
Toshio Chiba, MD, chief physician of the Palliative Care Service at Icesp, emphasized that ketamine is already in use. “It is not feasible to wait years for the approval of psilocybin or for the FDA’s decision on MDMA, especially if the patient needs immediate care,” he said.
Furthermore, recreational and therapeutic uses are distinct. “It is essential to note that responsibilities are shared between the professional and the patient,” said Dr. Chiba. “In the therapeutic setting, there is an ethical and civil responsibility of the medical professional, as well as the patient actively engaging in treatment.”
Early palliative care can also facilitate the establishment of care goals. “I prefer to avoid terms like ‘coping’ or ‘fighting the disease,’” said Dr. Chiba. “Nowadays, dealing with cancer is more about coexisting with the disease properly, as treatments can last for years.
“Of course, there are still highly lethal tumors. However, for neoplasms like breast, colorectal, and prostate cancers, we often talk about 5, 10, or even 15 years of coexistence [with the condition]. The lack of this information [about the disease, treatments, and existential issues] can generate distress in some patients, who end up excessively worrying about the future,” he added.
But palliative treatment with psychedelics as a panacea, he said.
In addition, Marcelo Falchi, MD, medical director of CAMP at UFRN, also emphasized that psychedelics are not a risk-free intervention. Substances like LSD and psilocybin, for example, can cause increases in blood pressure and tachycardia, which, may limit their use for patients at high cardiovascular risk. Crises of anxiety or dissociative symptoms also may occur, and they require mitigation strategies such as psychological support and attention to set and setting.
“But research seems to agree that the risks can be managed effectively through a diligent process, allowing for the responsible exploration of the therapeutic potential of psychedelics,” said Dr. Falchi, who is responsible for CAMP’s postgraduate course in psychedelic therapies. The program provides training in substances used in Brazil, such as ketamine and ibogaine.
The use of psychedelics in palliative care requires a significant shift in how professionals relate to patients.
Unlike in traditional practice, where the prescription is followed by quick consultations, palliative care with psychedelics requires deep and continuous involvement, as Dr. Campolina pointed out. “We joke that it’s not a high-tech specialty, but ‘high touch,’ because it demands the constant presence of the doctor or therapist with the patient. This can involve sessions of several hours, with frequent monitoring and regular contact after sessions. This dynamic emphasizes the importance of human touch and connection during the process, reflecting a new way of practicing medicine.”
In his last months of life, Dr. Griffiths sought to emphasize this point, suggesting that, from a broader perspective, doctors and patients face the same fundamental questions. “We all know we are terminal,” he said. “Essentially, we shouldn’t need a stage 4 cancer diagnosis to awaken to this reality.”
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Alzheimer’s and Comorbidities: Implications for Patient Care
Alzheimer’s disease (AD), the most common cause of dementia, is the fifth leading cause of death in the United States. An estimated 6.9 million Americans aged 65 years or older have AD. Comorbid conditions in AD may exacerbate the progression of dementia and negatively affect overall health.
Although the exact mechanisms remain unclear, systemic inflammation is thought to play a significant role in the development of many common comorbidities associated with AD. Among the most frequently observed comorbid conditions are hypertension, diabetes, and depression. The presence of these comorbidities affects the treatment and management of AD, underscoring the need to understand the mechanisms of their interrelationship and develop effective management strategies.
Hypertension
Hypertension is a well-established risk factor for numerous health conditions, including AD. A comprehensive review of five meta-analyses and 52 primary studies revealed that elevated systolic blood pressure (SBP) correlates with an 11 % increased risk of developing AD, raising the question of whether early intervention and control of blood pressure would mitigate the risk for AD later in life.
Findings from the Northern Manhattan Study suggest that although elevated SBP contributes to cognitive decline in older patients, the use of antihypertensive medications can neutralize the effects of high SBP on certain cognitive functions. Furthermore, a systematic review and meta-analysis comprising 12 trials (92,135 participants) demonstrated a significant reduction in the risk for dementia and cognitive impairment with antihypertensive treatment.
Notably, a retrospective cohort study involving 69,081 participants treated with beta-blockers for hypertension found that beta-blockers with high blood-brain barrier permeability were associated with a reduced risk for AD compared with those with low blood-brain barrier permeability. Additionally, a secondary analysis of the SPRINT trial found antihypertensive medications that stimulate vs inhibit type 2 and 4 angiotensin II receptors were associated with a lower incidence of cognitive impairment. Although further clinical trials are necessary to directly assess specific medications, these findings emphasize the potential of antihypertensive treatment as a strategic approach to reduce the risk for AD.
Type 2 Diabetes
The connection between AD and type 2 diabetes is such that AD is sometimes referred to as “type 3 diabetes.” Both diseases share some of the same underlying pathophysiologic mechanisms, particularly the development of insulin resistance and oxidative stress. A prospective cohort study of 10,095 participants showed that diabetes was significantly associated with a higher risk of developing dementia; this risk is even greater in patients who develop diabetes at an earlier age.
In an interview with this news organization, Alvaro Pascual-Leone, MD, PhD, a professor of neurology at Harvard Medical School, Boston, said, “In addition to being a comorbidity factor, diabetes appears to be a predisposing risk factor for AD.” This is supported by a comprehensive literature review showing an increased progression from mild cognitive impairment (MCI) to dementia in patients with diabetes, prediabetes, or metabolic syndrome, with a pooled odds ratio for dementia progression in individuals with diabetes of 1.53.
Owing to the overlapping pathophysiologic mechanisms in AD and diabetes, treating one condition may have beneficial effects on the other. A systematic umbrella review and meta-analysis that included 10 meta-analyses across nine classes of diabetes drugs found a protective effect against dementia with the use of metformin, thiazolidinediones (including pioglitazone), glucagon-like peptide 1 receptor agonists, and sodium-glucose cotransporter 2 inhibitors. Moreover, a cohort study of 12,220 patients who discontinued metformin early (ie, stopped using metformin without a prior history of abnormal kidney function) and 29,126 patients considered routine users found an increased risk for dementia in the early terminator group. Although further research is warranted, the concurrent treatment of AD and diabetes with antidiabetic agents holds considerable promise.
Depression and Anxiety
Anxiety and depression are significant risk factors for AD, and conversely, AD increases the likelihood of developing these psychiatric conditions. A systematic review of 14,760 studies showed dysthymia often emerges during the early stages of AD as an emotional response to cognitive decline.
Data from the Australian Imaging Biomarkers and Lifestyle study showed a markedly elevated risk for AD and MCI among individuals with preexisting anxiety or depression. This study also found that age, sex, and marital status are important determinants, with men and single individuals with depression being particularly susceptible to developing AD. Conversely, a cohort study of 129,410 AD patients with AD, 390,088 patients with all-cause dementia, and 3,900,880 age-matched controls without a history of depression showed a cumulative incidence of depression of 13% in the AD group vs 3% in the control group, suggesting a heightened risk for depression following an AD diagnosis.
These findings underscore the importance of targeted screening and assessment for patients with anxiety and depression who may be at risk for AD or those diagnosed with AD who are at risk for subsequent depression and anxiety. Although antidepressants are effective in treating depression in general, their efficacy in AD-related depression is of variable quality, probably owing to differing pathophysiologic mechanisms of the disease. Further research is necessary to explore both pharmacologic and nonpharmacologic interventions for treating depression in AD patients. Some studies have found that cognitive behavioral-therapy can be effective in improving depression in patients with AD.
Sleep Disorders
Research has shown a strong correlation between AD and sleep disorders, particularly obstructive sleep apnea, insomnia, and circadian rhythm disruptions. Additionally, studies suggest that insomnia and sleep deprivation contribute to increased amyloid beta production and tau pathology, hallmark features of AD. A scoping review of 70 studies proposed that this relationship is mediated by the glymphatic system (glial-dependent waste clearance pathway in the central nervous system), and that sleep deprivation disrupts its function, leading to protein accumulation and subsequent neurologic symptoms of AD. Another study showed that sleep deprivation triggers glial cell activation, initiating an inflammatory cascade that accelerates AD progression.
Given that the gold standard treatment for obstructive sleep apnea is continuous positive airway pressure (CPAP), it has been hypothesized that CPAP could also alleviate AD symptoms owing to shared pathophysiologic mechanisms of these conditions. A large systemic review found that CPAP use improved AD symptoms in patients with mild AD or MCI, though other sleep interventions, such as cognitive-behavioral therapy and melatonin supplementation, have yielded mixed outcomes. However, most studies in this area are small in scale, and there remains a paucity of research on treating sleep disorders in AD patients, indicating a need for further investigation.
Musculoskeletal Disorders
Although no direct causative link has been established, research indicates an association between osteoarthritis (OA) and dementia, likely because of similar pathophysiologic mechanisms, including systemic inflammation. Longitudinal analyses of data from the Alzheimer’s Disease Neuroimaging Initiative study found cognitively normal older individuals with OA experience more rapid declines in hippocampal volumes compared to those without OA, suggesting that OA may elevate the risk of cognitive impairment. Current treatments for OA, such as nonsteroidal anti-inflammatory drugs, glucocorticoids, and disease-modifying OA drugs, might also help alleviate AD symptoms related to inflammation, though the research in this area is limited.
AD has also been linked to osteoporosis. In a longitudinal follow-up study involving 78,994 patients with osteoporosis and 78,994 controls, AD developed in 5856 patients with osteoporosis compared with 3761 patients in the control group. These findings represent a 1.27-fold higher incidence of AD in patients with osteoporosis than in the control group, suggesting that osteoporosis might be a risk factor for AD.
Additionally, research has identified a relationship between AD and increased fracture risk and decreased bone mineral density, with AD patients exhibiting a significantly higher likelihood of bone fractures compared with those without AD. “Falls and fractures, aside from the risk they pose in all geriatric patients, in individuals with cognitive impairment — whether due to AD or another cause — have higher risk to cause delirium and that can result in greater morbidity and mortality and a lasting increase in cognitive disability,” stated Dr. Pascual-Leone. Current recommendations emphasize exercise and fall prevention strategies to reduce fracture risk in patients with AD, but there is a lack of comprehensive research on the safety and efficacy of osteoporosis medications in this population.
Implications for Clinical Practice
The intricate interplay between AD and its comorbidities highlights the need for a comprehensive and integrated approach to patient care. The overlapping pathophysiologic mechanisms suggest that these comorbidities can contribute to the evolution and progression of AD. Likewise, AD can exacerbate comorbid conditions. As such, a holistic assessment strategy that prioritizes early detection and management of comorbid conditions to mitigate their impact on AD progression would be beneficial. Dr. Pascual-Leone added, “The presence of any of these comorbidities suggests a need to screen for MCI earlier than might otherwise be indicated or as part of the treatment for the comorbid condition. In many cases, patients can make lifestyle modifications that improve not only the comorbid condition but also reduce its effect on dementia.” In doing so, healthcare providers can help improve patient outcomes and enhance the overall quality of life for individuals living with AD.
Alissa Hershberger, Professor of Nursing, University of Central Missouri, Lee’s Summit, Missouri, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alzheimer’s disease (AD), the most common cause of dementia, is the fifth leading cause of death in the United States. An estimated 6.9 million Americans aged 65 years or older have AD. Comorbid conditions in AD may exacerbate the progression of dementia and negatively affect overall health.
Although the exact mechanisms remain unclear, systemic inflammation is thought to play a significant role in the development of many common comorbidities associated with AD. Among the most frequently observed comorbid conditions are hypertension, diabetes, and depression. The presence of these comorbidities affects the treatment and management of AD, underscoring the need to understand the mechanisms of their interrelationship and develop effective management strategies.
Hypertension
Hypertension is a well-established risk factor for numerous health conditions, including AD. A comprehensive review of five meta-analyses and 52 primary studies revealed that elevated systolic blood pressure (SBP) correlates with an 11 % increased risk of developing AD, raising the question of whether early intervention and control of blood pressure would mitigate the risk for AD later in life.
Findings from the Northern Manhattan Study suggest that although elevated SBP contributes to cognitive decline in older patients, the use of antihypertensive medications can neutralize the effects of high SBP on certain cognitive functions. Furthermore, a systematic review and meta-analysis comprising 12 trials (92,135 participants) demonstrated a significant reduction in the risk for dementia and cognitive impairment with antihypertensive treatment.
Notably, a retrospective cohort study involving 69,081 participants treated with beta-blockers for hypertension found that beta-blockers with high blood-brain barrier permeability were associated with a reduced risk for AD compared with those with low blood-brain barrier permeability. Additionally, a secondary analysis of the SPRINT trial found antihypertensive medications that stimulate vs inhibit type 2 and 4 angiotensin II receptors were associated with a lower incidence of cognitive impairment. Although further clinical trials are necessary to directly assess specific medications, these findings emphasize the potential of antihypertensive treatment as a strategic approach to reduce the risk for AD.
Type 2 Diabetes
The connection between AD and type 2 diabetes is such that AD is sometimes referred to as “type 3 diabetes.” Both diseases share some of the same underlying pathophysiologic mechanisms, particularly the development of insulin resistance and oxidative stress. A prospective cohort study of 10,095 participants showed that diabetes was significantly associated with a higher risk of developing dementia; this risk is even greater in patients who develop diabetes at an earlier age.
In an interview with this news organization, Alvaro Pascual-Leone, MD, PhD, a professor of neurology at Harvard Medical School, Boston, said, “In addition to being a comorbidity factor, diabetes appears to be a predisposing risk factor for AD.” This is supported by a comprehensive literature review showing an increased progression from mild cognitive impairment (MCI) to dementia in patients with diabetes, prediabetes, or metabolic syndrome, with a pooled odds ratio for dementia progression in individuals with diabetes of 1.53.
Owing to the overlapping pathophysiologic mechanisms in AD and diabetes, treating one condition may have beneficial effects on the other. A systematic umbrella review and meta-analysis that included 10 meta-analyses across nine classes of diabetes drugs found a protective effect against dementia with the use of metformin, thiazolidinediones (including pioglitazone), glucagon-like peptide 1 receptor agonists, and sodium-glucose cotransporter 2 inhibitors. Moreover, a cohort study of 12,220 patients who discontinued metformin early (ie, stopped using metformin without a prior history of abnormal kidney function) and 29,126 patients considered routine users found an increased risk for dementia in the early terminator group. Although further research is warranted, the concurrent treatment of AD and diabetes with antidiabetic agents holds considerable promise.
Depression and Anxiety
Anxiety and depression are significant risk factors for AD, and conversely, AD increases the likelihood of developing these psychiatric conditions. A systematic review of 14,760 studies showed dysthymia often emerges during the early stages of AD as an emotional response to cognitive decline.
Data from the Australian Imaging Biomarkers and Lifestyle study showed a markedly elevated risk for AD and MCI among individuals with preexisting anxiety or depression. This study also found that age, sex, and marital status are important determinants, with men and single individuals with depression being particularly susceptible to developing AD. Conversely, a cohort study of 129,410 AD patients with AD, 390,088 patients with all-cause dementia, and 3,900,880 age-matched controls without a history of depression showed a cumulative incidence of depression of 13% in the AD group vs 3% in the control group, suggesting a heightened risk for depression following an AD diagnosis.
These findings underscore the importance of targeted screening and assessment for patients with anxiety and depression who may be at risk for AD or those diagnosed with AD who are at risk for subsequent depression and anxiety. Although antidepressants are effective in treating depression in general, their efficacy in AD-related depression is of variable quality, probably owing to differing pathophysiologic mechanisms of the disease. Further research is necessary to explore both pharmacologic and nonpharmacologic interventions for treating depression in AD patients. Some studies have found that cognitive behavioral-therapy can be effective in improving depression in patients with AD.
Sleep Disorders
Research has shown a strong correlation between AD and sleep disorders, particularly obstructive sleep apnea, insomnia, and circadian rhythm disruptions. Additionally, studies suggest that insomnia and sleep deprivation contribute to increased amyloid beta production and tau pathology, hallmark features of AD. A scoping review of 70 studies proposed that this relationship is mediated by the glymphatic system (glial-dependent waste clearance pathway in the central nervous system), and that sleep deprivation disrupts its function, leading to protein accumulation and subsequent neurologic symptoms of AD. Another study showed that sleep deprivation triggers glial cell activation, initiating an inflammatory cascade that accelerates AD progression.
Given that the gold standard treatment for obstructive sleep apnea is continuous positive airway pressure (CPAP), it has been hypothesized that CPAP could also alleviate AD symptoms owing to shared pathophysiologic mechanisms of these conditions. A large systemic review found that CPAP use improved AD symptoms in patients with mild AD or MCI, though other sleep interventions, such as cognitive-behavioral therapy and melatonin supplementation, have yielded mixed outcomes. However, most studies in this area are small in scale, and there remains a paucity of research on treating sleep disorders in AD patients, indicating a need for further investigation.
Musculoskeletal Disorders
Although no direct causative link has been established, research indicates an association between osteoarthritis (OA) and dementia, likely because of similar pathophysiologic mechanisms, including systemic inflammation. Longitudinal analyses of data from the Alzheimer’s Disease Neuroimaging Initiative study found cognitively normal older individuals with OA experience more rapid declines in hippocampal volumes compared to those without OA, suggesting that OA may elevate the risk of cognitive impairment. Current treatments for OA, such as nonsteroidal anti-inflammatory drugs, glucocorticoids, and disease-modifying OA drugs, might also help alleviate AD symptoms related to inflammation, though the research in this area is limited.
AD has also been linked to osteoporosis. In a longitudinal follow-up study involving 78,994 patients with osteoporosis and 78,994 controls, AD developed in 5856 patients with osteoporosis compared with 3761 patients in the control group. These findings represent a 1.27-fold higher incidence of AD in patients with osteoporosis than in the control group, suggesting that osteoporosis might be a risk factor for AD.
Additionally, research has identified a relationship between AD and increased fracture risk and decreased bone mineral density, with AD patients exhibiting a significantly higher likelihood of bone fractures compared with those without AD. “Falls and fractures, aside from the risk they pose in all geriatric patients, in individuals with cognitive impairment — whether due to AD or another cause — have higher risk to cause delirium and that can result in greater morbidity and mortality and a lasting increase in cognitive disability,” stated Dr. Pascual-Leone. Current recommendations emphasize exercise and fall prevention strategies to reduce fracture risk in patients with AD, but there is a lack of comprehensive research on the safety and efficacy of osteoporosis medications in this population.
Implications for Clinical Practice
The intricate interplay between AD and its comorbidities highlights the need for a comprehensive and integrated approach to patient care. The overlapping pathophysiologic mechanisms suggest that these comorbidities can contribute to the evolution and progression of AD. Likewise, AD can exacerbate comorbid conditions. As such, a holistic assessment strategy that prioritizes early detection and management of comorbid conditions to mitigate their impact on AD progression would be beneficial. Dr. Pascual-Leone added, “The presence of any of these comorbidities suggests a need to screen for MCI earlier than might otherwise be indicated or as part of the treatment for the comorbid condition. In many cases, patients can make lifestyle modifications that improve not only the comorbid condition but also reduce its effect on dementia.” In doing so, healthcare providers can help improve patient outcomes and enhance the overall quality of life for individuals living with AD.
Alissa Hershberger, Professor of Nursing, University of Central Missouri, Lee’s Summit, Missouri, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alzheimer’s disease (AD), the most common cause of dementia, is the fifth leading cause of death in the United States. An estimated 6.9 million Americans aged 65 years or older have AD. Comorbid conditions in AD may exacerbate the progression of dementia and negatively affect overall health.
Although the exact mechanisms remain unclear, systemic inflammation is thought to play a significant role in the development of many common comorbidities associated with AD. Among the most frequently observed comorbid conditions are hypertension, diabetes, and depression. The presence of these comorbidities affects the treatment and management of AD, underscoring the need to understand the mechanisms of their interrelationship and develop effective management strategies.
Hypertension
Hypertension is a well-established risk factor for numerous health conditions, including AD. A comprehensive review of five meta-analyses and 52 primary studies revealed that elevated systolic blood pressure (SBP) correlates with an 11 % increased risk of developing AD, raising the question of whether early intervention and control of blood pressure would mitigate the risk for AD later in life.
Findings from the Northern Manhattan Study suggest that although elevated SBP contributes to cognitive decline in older patients, the use of antihypertensive medications can neutralize the effects of high SBP on certain cognitive functions. Furthermore, a systematic review and meta-analysis comprising 12 trials (92,135 participants) demonstrated a significant reduction in the risk for dementia and cognitive impairment with antihypertensive treatment.
Notably, a retrospective cohort study involving 69,081 participants treated with beta-blockers for hypertension found that beta-blockers with high blood-brain barrier permeability were associated with a reduced risk for AD compared with those with low blood-brain barrier permeability. Additionally, a secondary analysis of the SPRINT trial found antihypertensive medications that stimulate vs inhibit type 2 and 4 angiotensin II receptors were associated with a lower incidence of cognitive impairment. Although further clinical trials are necessary to directly assess specific medications, these findings emphasize the potential of antihypertensive treatment as a strategic approach to reduce the risk for AD.
Type 2 Diabetes
The connection between AD and type 2 diabetes is such that AD is sometimes referred to as “type 3 diabetes.” Both diseases share some of the same underlying pathophysiologic mechanisms, particularly the development of insulin resistance and oxidative stress. A prospective cohort study of 10,095 participants showed that diabetes was significantly associated with a higher risk of developing dementia; this risk is even greater in patients who develop diabetes at an earlier age.
In an interview with this news organization, Alvaro Pascual-Leone, MD, PhD, a professor of neurology at Harvard Medical School, Boston, said, “In addition to being a comorbidity factor, diabetes appears to be a predisposing risk factor for AD.” This is supported by a comprehensive literature review showing an increased progression from mild cognitive impairment (MCI) to dementia in patients with diabetes, prediabetes, or metabolic syndrome, with a pooled odds ratio for dementia progression in individuals with diabetes of 1.53.
Owing to the overlapping pathophysiologic mechanisms in AD and diabetes, treating one condition may have beneficial effects on the other. A systematic umbrella review and meta-analysis that included 10 meta-analyses across nine classes of diabetes drugs found a protective effect against dementia with the use of metformin, thiazolidinediones (including pioglitazone), glucagon-like peptide 1 receptor agonists, and sodium-glucose cotransporter 2 inhibitors. Moreover, a cohort study of 12,220 patients who discontinued metformin early (ie, stopped using metformin without a prior history of abnormal kidney function) and 29,126 patients considered routine users found an increased risk for dementia in the early terminator group. Although further research is warranted, the concurrent treatment of AD and diabetes with antidiabetic agents holds considerable promise.
Depression and Anxiety
Anxiety and depression are significant risk factors for AD, and conversely, AD increases the likelihood of developing these psychiatric conditions. A systematic review of 14,760 studies showed dysthymia often emerges during the early stages of AD as an emotional response to cognitive decline.
Data from the Australian Imaging Biomarkers and Lifestyle study showed a markedly elevated risk for AD and MCI among individuals with preexisting anxiety or depression. This study also found that age, sex, and marital status are important determinants, with men and single individuals with depression being particularly susceptible to developing AD. Conversely, a cohort study of 129,410 AD patients with AD, 390,088 patients with all-cause dementia, and 3,900,880 age-matched controls without a history of depression showed a cumulative incidence of depression of 13% in the AD group vs 3% in the control group, suggesting a heightened risk for depression following an AD diagnosis.
These findings underscore the importance of targeted screening and assessment for patients with anxiety and depression who may be at risk for AD or those diagnosed with AD who are at risk for subsequent depression and anxiety. Although antidepressants are effective in treating depression in general, their efficacy in AD-related depression is of variable quality, probably owing to differing pathophysiologic mechanisms of the disease. Further research is necessary to explore both pharmacologic and nonpharmacologic interventions for treating depression in AD patients. Some studies have found that cognitive behavioral-therapy can be effective in improving depression in patients with AD.
Sleep Disorders
Research has shown a strong correlation between AD and sleep disorders, particularly obstructive sleep apnea, insomnia, and circadian rhythm disruptions. Additionally, studies suggest that insomnia and sleep deprivation contribute to increased amyloid beta production and tau pathology, hallmark features of AD. A scoping review of 70 studies proposed that this relationship is mediated by the glymphatic system (glial-dependent waste clearance pathway in the central nervous system), and that sleep deprivation disrupts its function, leading to protein accumulation and subsequent neurologic symptoms of AD. Another study showed that sleep deprivation triggers glial cell activation, initiating an inflammatory cascade that accelerates AD progression.
Given that the gold standard treatment for obstructive sleep apnea is continuous positive airway pressure (CPAP), it has been hypothesized that CPAP could also alleviate AD symptoms owing to shared pathophysiologic mechanisms of these conditions. A large systemic review found that CPAP use improved AD symptoms in patients with mild AD or MCI, though other sleep interventions, such as cognitive-behavioral therapy and melatonin supplementation, have yielded mixed outcomes. However, most studies in this area are small in scale, and there remains a paucity of research on treating sleep disorders in AD patients, indicating a need for further investigation.
Musculoskeletal Disorders
Although no direct causative link has been established, research indicates an association between osteoarthritis (OA) and dementia, likely because of similar pathophysiologic mechanisms, including systemic inflammation. Longitudinal analyses of data from the Alzheimer’s Disease Neuroimaging Initiative study found cognitively normal older individuals with OA experience more rapid declines in hippocampal volumes compared to those without OA, suggesting that OA may elevate the risk of cognitive impairment. Current treatments for OA, such as nonsteroidal anti-inflammatory drugs, glucocorticoids, and disease-modifying OA drugs, might also help alleviate AD symptoms related to inflammation, though the research in this area is limited.
AD has also been linked to osteoporosis. In a longitudinal follow-up study involving 78,994 patients with osteoporosis and 78,994 controls, AD developed in 5856 patients with osteoporosis compared with 3761 patients in the control group. These findings represent a 1.27-fold higher incidence of AD in patients with osteoporosis than in the control group, suggesting that osteoporosis might be a risk factor for AD.
Additionally, research has identified a relationship between AD and increased fracture risk and decreased bone mineral density, with AD patients exhibiting a significantly higher likelihood of bone fractures compared with those without AD. “Falls and fractures, aside from the risk they pose in all geriatric patients, in individuals with cognitive impairment — whether due to AD or another cause — have higher risk to cause delirium and that can result in greater morbidity and mortality and a lasting increase in cognitive disability,” stated Dr. Pascual-Leone. Current recommendations emphasize exercise and fall prevention strategies to reduce fracture risk in patients with AD, but there is a lack of comprehensive research on the safety and efficacy of osteoporosis medications in this population.
Implications for Clinical Practice
The intricate interplay between AD and its comorbidities highlights the need for a comprehensive and integrated approach to patient care. The overlapping pathophysiologic mechanisms suggest that these comorbidities can contribute to the evolution and progression of AD. Likewise, AD can exacerbate comorbid conditions. As such, a holistic assessment strategy that prioritizes early detection and management of comorbid conditions to mitigate their impact on AD progression would be beneficial. Dr. Pascual-Leone added, “The presence of any of these comorbidities suggests a need to screen for MCI earlier than might otherwise be indicated or as part of the treatment for the comorbid condition. In many cases, patients can make lifestyle modifications that improve not only the comorbid condition but also reduce its effect on dementia.” In doing so, healthcare providers can help improve patient outcomes and enhance the overall quality of life for individuals living with AD.
Alissa Hershberger, Professor of Nursing, University of Central Missouri, Lee’s Summit, Missouri, has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.