User login
Vulvar intraepithelial neoplasia: Changing terms and therapy trends
Vulvar intraepithelial neoplasia is a premalignant lesion of the vulva frequently encountered by gynecologic providers. There has been an increase in the incidence of VIN in younger women in recent decades thought be to be secondary to human papillomavirus infection, cigarette smoking, and sexual behavior (J Reprod Med. 2000 Aug;45[8]:613-5).
Data from the Surveillance Epidemiology and End Results (SEER) database were significant for a 411% increase in the incidence of in situ carcinoma and a 20% increase in invasive vulvar carcinoma from 1973 to 2000 (Obstet Gynecol. 2006 May;107[5]:1018-22). In addition, younger age groups are seeing an increase of in situ disease until age 49. Vulvar cancer however, continues to be a disease of older age.
Terminology
Previously, the term vulvar intraepithelial neoplasia followed the cervical intraepithelial neoplasia (CIN) designation in the 1960s. Conventions for grading these lesions have changed over time. Most recently, in 2004, the International Society for the Study of Vulvar Disease (ISSVD), composed of dermatologists, pathologists, and gynecologists, agreed to change the classification of squamous VIN from the previous VIN 1-3 classification system. The committee described VIN in two forms, “usual type” and “differentiated type” (J Reprod Med 2005;50:807-10).
In making this transition, it was recognized that VIN 1 is not in fact an oncogenic lesion and is now solely referred to as condyloma acuminatum. Grade 2 and 3 are now collectively referred to as VIN. These changes made by the ISSVD reflect the current literature on grading of VIN. In addition to VIN 1 not having any progression to malignancy, it is a diagnosis that is difficult to reproduce and may, at times, reflect reactive changes or other dermatosis. VIN 2 and 3 are not discriminated from each other in a reproducible manner and clinically have no reason for individual distinction (J Low Genit Tract Dis. 2006 Jul;10[3]:161-9).
VIN, usual type is the most common intraepithelial lesion and is historically referred to as classic VIN or Bowen’s disease. This type is associated with HPV infection and includes the formerly described warty type, basaloid type, and mixed type. The carcinogenic subtypes of HPV, 16, 18, 31, and 33 are the most common HPV subtypes responsible. It should be noted, however, that diagnosis is morphological and not based on HPV testing. Usual type is also traditionally thought to be more closely associated with risk factors such as smoking and immunocompromised states.
VIN, differentiated type is not associated with the HPV virus and is frequently found in older women. This lesion is often associated with other dermatologic conditions such as lichen sclerosis and lichen simplex chronicus. Diagnosis is also made by histology with abnormal cells being confined to the parabasal and basal portion of the rete pegs. This type also finds genetic alterations that are seen in invasive squamous cell carcinoma (Appl Immunohistochem Mol Morphol 2001;9:150-63). Differentiated type is thought to be a precursor for HPV-negative keratinizing squamous cell carcinoma of the vulva (Am J Surg Pathol. 2000 Mar;24[3]:429-41).
As awareness of this distinct form of VIN increases and more is learned about the precursors of HPV-negative squamous cell carcinoma, physicians are encouraged to closely follow up hyperplastic lesions and lichen sclerosis with biopsies and excision. The diagnosis of differentiated VIN is rarely made at present; however, this distinction by the ISSVD may improve the ability of clinicians and pathologists to recognize this HPV-negative precursor before squamous cell carcinoma is present.
The Lower Anogenital Squamous Terminology project of the College of American Pathology and the American Society for Colposcopy and Cervical Pathology advocates for more consistent terminology across lower anogenital tract lesions. This terminology applies only to HPV-related lesions (usual type) and considers the VIN 1 or condyloma accuminatum to be a low-grade lesion (LSIL), and VIN 2-3 or usual type to be high-grade lesions (HSIL) (Int J Gynecol Pathol. 2013 Jan;32[1]:76-115).
Many clinicians and pathologists have not adopted this most recent terminology; however, there is evidence that the ISSVD classification is the most clinically relevant.
Diagnosis
The majority of patients with any VIN will present with complaints of vulvar pruritus. However, women can also present with pain, burning, or dysuria, or can have an asymptomatic lesion found on pelvic exam. There are no recommended screening strategies to diagnose early VIN. Cytologic testing is complicated by the keratinization of the vulva, making this an unreliable diagnostic assessment.
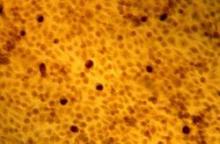
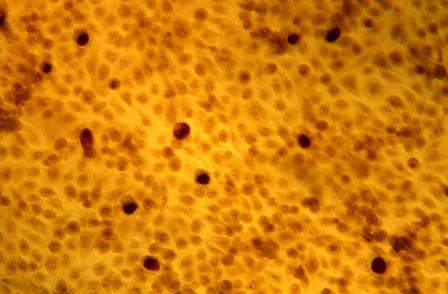
On physical exam, VIN can have a heterogeneous presentation including papules, plaques, color variations, or ulcer. Differentiated type is thought to have a more defined appearance that frequently develops in the setting of other vulvar dermatosis. These are distinct, solitary lesions that are commonly raised, can have an overlying scale, and have ill-defined borders. A distinct lesion with ulceration or erosion is concerning for invasion.
Diagnosis is ultimately made by biopsy. Physicians should have a low threshold to biopsy any suspicious lesions or those unresponsive to therapy. Colposcopy is a frequent adjunct to the physical exam. Acetic acid 3%-5% soaked gauze is allowed to rest on the vulva for several minutes prior to observation with a colposcope or hand-held magnifying glass. Colposcopic findings are usually those of focal “white” epithelium. Vascular changes seen on the cervix (punctuation and mosaicism) are rarely seen on the vulva.
The entire anogenital region shares the same susceptibility to the HPV virus, thus squamous intraepithelial lesions are frequently multifocal. Physicians should have a heightened awareness of other lesions, such as cervical, vaginal, or anal, when managing a patient with VIN (Gynecol Oncol. 1995 Feb;56[2]:276-9). Appropriate cervical screening should be strictly adhered to and a thorough exam done at the time of vulvar colposcopy or exam.
Treatment
The goals of treatment include preventing carcinoma and improving symptoms while maintaining function and preserving anatomy. Treatment options for both types of VIN include excision, ablation, or medical therapy pending an evaluation of concurrent risk factors.
Premalignant disease was traditionally treated surgically. While surgical excision is still the mainstay of therapy, less aggressive techniques and medical therapy are more readily utilized. The goal of surgical excision for VIN is both diagnostic and therapeutic. When an excision for high-grade dysplasia is done (formerly VIN 3), detection of occult carcinoma was found in up to 3.2% in one large review (Gynecol Oncol. 2005;97:645-51).
Using a wide local excision to completely remove lesions with a pathologically clear margin reduces a patient’s risk of recurrence for disease compared to those excisions with positive margins (Obstet Gynecol. 1998;92:962-6). It is therefore critical that physicians carefully counsel patients who desire conservative therapy for VIN.
With any treatment, however, patients and physicians should be aware of the risk of recurrence; for vulvectomy, partial vulvectomy, local excision, and laser ablation, recurrences were seen at rates of 19%, 18%, 22%, and 23%, respectively, in a review of 3,322 patients (Gynecol Oncol. 2005;97:645-51).
CO2 laser ablation has been used for single lesions as well as multifocal or confluent disease. Many physicians advocate for its use in patients with multifocal lesions as well as those with disease around the clitoris or anus, where excisional therapy is less desirable as laser therapy results in less scarring.
A 2015 Cochrane Database Review of medical therapy for high-grade dysplasia (usual-type VIN, VIN 2/3, or high-grade VIN) found that topical imiquimod can be used as a safe and effective option for high-grade VIN. Physicians should, however, be aware of unfavorable side effects that may require dose reductions. Cidofovir may be an alternative to imiquimod pending more evidence on long-term response and progression (Cochrane Database Syst Rev. 2015 Aug 18;8:CD007924). Topical 5-fluorouracil has fallen out of favor for VIN given its significant chemical desquamation, however response rates are thought to be favorable if tolerated.
As the use of VIN terminology solidifies and information emerges on medical therapy to treat VIN, it is critical that physicians remain current when counseling and providing treatment recommendations for vulvar intraepithelial neoplasia.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. Dr. Sullivan is a fellow in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at obnews@frontlinemedcom.com.
Vulvar intraepithelial neoplasia is a premalignant lesion of the vulva frequently encountered by gynecologic providers. There has been an increase in the incidence of VIN in younger women in recent decades thought be to be secondary to human papillomavirus infection, cigarette smoking, and sexual behavior (J Reprod Med. 2000 Aug;45[8]:613-5).
Data from the Surveillance Epidemiology and End Results (SEER) database were significant for a 411% increase in the incidence of in situ carcinoma and a 20% increase in invasive vulvar carcinoma from 1973 to 2000 (Obstet Gynecol. 2006 May;107[5]:1018-22). In addition, younger age groups are seeing an increase of in situ disease until age 49. Vulvar cancer however, continues to be a disease of older age.
Terminology
Previously, the term vulvar intraepithelial neoplasia followed the cervical intraepithelial neoplasia (CIN) designation in the 1960s. Conventions for grading these lesions have changed over time. Most recently, in 2004, the International Society for the Study of Vulvar Disease (ISSVD), composed of dermatologists, pathologists, and gynecologists, agreed to change the classification of squamous VIN from the previous VIN 1-3 classification system. The committee described VIN in two forms, “usual type” and “differentiated type” (J Reprod Med 2005;50:807-10).
In making this transition, it was recognized that VIN 1 is not in fact an oncogenic lesion and is now solely referred to as condyloma acuminatum. Grade 2 and 3 are now collectively referred to as VIN. These changes made by the ISSVD reflect the current literature on grading of VIN. In addition to VIN 1 not having any progression to malignancy, it is a diagnosis that is difficult to reproduce and may, at times, reflect reactive changes or other dermatosis. VIN 2 and 3 are not discriminated from each other in a reproducible manner and clinically have no reason for individual distinction (J Low Genit Tract Dis. 2006 Jul;10[3]:161-9).
VIN, usual type is the most common intraepithelial lesion and is historically referred to as classic VIN or Bowen’s disease. This type is associated with HPV infection and includes the formerly described warty type, basaloid type, and mixed type. The carcinogenic subtypes of HPV, 16, 18, 31, and 33 are the most common HPV subtypes responsible. It should be noted, however, that diagnosis is morphological and not based on HPV testing. Usual type is also traditionally thought to be more closely associated with risk factors such as smoking and immunocompromised states.
VIN, differentiated type is not associated with the HPV virus and is frequently found in older women. This lesion is often associated with other dermatologic conditions such as lichen sclerosis and lichen simplex chronicus. Diagnosis is also made by histology with abnormal cells being confined to the parabasal and basal portion of the rete pegs. This type also finds genetic alterations that are seen in invasive squamous cell carcinoma (Appl Immunohistochem Mol Morphol 2001;9:150-63). Differentiated type is thought to be a precursor for HPV-negative keratinizing squamous cell carcinoma of the vulva (Am J Surg Pathol. 2000 Mar;24[3]:429-41).
As awareness of this distinct form of VIN increases and more is learned about the precursors of HPV-negative squamous cell carcinoma, physicians are encouraged to closely follow up hyperplastic lesions and lichen sclerosis with biopsies and excision. The diagnosis of differentiated VIN is rarely made at present; however, this distinction by the ISSVD may improve the ability of clinicians and pathologists to recognize this HPV-negative precursor before squamous cell carcinoma is present.
The Lower Anogenital Squamous Terminology project of the College of American Pathology and the American Society for Colposcopy and Cervical Pathology advocates for more consistent terminology across lower anogenital tract lesions. This terminology applies only to HPV-related lesions (usual type) and considers the VIN 1 or condyloma accuminatum to be a low-grade lesion (LSIL), and VIN 2-3 or usual type to be high-grade lesions (HSIL) (Int J Gynecol Pathol. 2013 Jan;32[1]:76-115).
Many clinicians and pathologists have not adopted this most recent terminology; however, there is evidence that the ISSVD classification is the most clinically relevant.
Diagnosis
The majority of patients with any VIN will present with complaints of vulvar pruritus. However, women can also present with pain, burning, or dysuria, or can have an asymptomatic lesion found on pelvic exam. There are no recommended screening strategies to diagnose early VIN. Cytologic testing is complicated by the keratinization of the vulva, making this an unreliable diagnostic assessment.
On physical exam, VIN can have a heterogeneous presentation including papules, plaques, color variations, or ulcer. Differentiated type is thought to have a more defined appearance that frequently develops in the setting of other vulvar dermatosis. These are distinct, solitary lesions that are commonly raised, can have an overlying scale, and have ill-defined borders. A distinct lesion with ulceration or erosion is concerning for invasion.
Diagnosis is ultimately made by biopsy. Physicians should have a low threshold to biopsy any suspicious lesions or those unresponsive to therapy. Colposcopy is a frequent adjunct to the physical exam. Acetic acid 3%-5% soaked gauze is allowed to rest on the vulva for several minutes prior to observation with a colposcope or hand-held magnifying glass. Colposcopic findings are usually those of focal “white” epithelium. Vascular changes seen on the cervix (punctuation and mosaicism) are rarely seen on the vulva.
The entire anogenital region shares the same susceptibility to the HPV virus, thus squamous intraepithelial lesions are frequently multifocal. Physicians should have a heightened awareness of other lesions, such as cervical, vaginal, or anal, when managing a patient with VIN (Gynecol Oncol. 1995 Feb;56[2]:276-9). Appropriate cervical screening should be strictly adhered to and a thorough exam done at the time of vulvar colposcopy or exam.
Treatment
The goals of treatment include preventing carcinoma and improving symptoms while maintaining function and preserving anatomy. Treatment options for both types of VIN include excision, ablation, or medical therapy pending an evaluation of concurrent risk factors.
Premalignant disease was traditionally treated surgically. While surgical excision is still the mainstay of therapy, less aggressive techniques and medical therapy are more readily utilized. The goal of surgical excision for VIN is both diagnostic and therapeutic. When an excision for high-grade dysplasia is done (formerly VIN 3), detection of occult carcinoma was found in up to 3.2% in one large review (Gynecol Oncol. 2005;97:645-51).
Using a wide local excision to completely remove lesions with a pathologically clear margin reduces a patient’s risk of recurrence for disease compared to those excisions with positive margins (Obstet Gynecol. 1998;92:962-6). It is therefore critical that physicians carefully counsel patients who desire conservative therapy for VIN.
With any treatment, however, patients and physicians should be aware of the risk of recurrence; for vulvectomy, partial vulvectomy, local excision, and laser ablation, recurrences were seen at rates of 19%, 18%, 22%, and 23%, respectively, in a review of 3,322 patients (Gynecol Oncol. 2005;97:645-51).
CO2 laser ablation has been used for single lesions as well as multifocal or confluent disease. Many physicians advocate for its use in patients with multifocal lesions as well as those with disease around the clitoris or anus, where excisional therapy is less desirable as laser therapy results in less scarring.
A 2015 Cochrane Database Review of medical therapy for high-grade dysplasia (usual-type VIN, VIN 2/3, or high-grade VIN) found that topical imiquimod can be used as a safe and effective option for high-grade VIN. Physicians should, however, be aware of unfavorable side effects that may require dose reductions. Cidofovir may be an alternative to imiquimod pending more evidence on long-term response and progression (Cochrane Database Syst Rev. 2015 Aug 18;8:CD007924). Topical 5-fluorouracil has fallen out of favor for VIN given its significant chemical desquamation, however response rates are thought to be favorable if tolerated.
As the use of VIN terminology solidifies and information emerges on medical therapy to treat VIN, it is critical that physicians remain current when counseling and providing treatment recommendations for vulvar intraepithelial neoplasia.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. Dr. Sullivan is a fellow in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at obnews@frontlinemedcom.com.
Vulvar intraepithelial neoplasia is a premalignant lesion of the vulva frequently encountered by gynecologic providers. There has been an increase in the incidence of VIN in younger women in recent decades thought be to be secondary to human papillomavirus infection, cigarette smoking, and sexual behavior (J Reprod Med. 2000 Aug;45[8]:613-5).
Data from the Surveillance Epidemiology and End Results (SEER) database were significant for a 411% increase in the incidence of in situ carcinoma and a 20% increase in invasive vulvar carcinoma from 1973 to 2000 (Obstet Gynecol. 2006 May;107[5]:1018-22). In addition, younger age groups are seeing an increase of in situ disease until age 49. Vulvar cancer however, continues to be a disease of older age.
Terminology
Previously, the term vulvar intraepithelial neoplasia followed the cervical intraepithelial neoplasia (CIN) designation in the 1960s. Conventions for grading these lesions have changed over time. Most recently, in 2004, the International Society for the Study of Vulvar Disease (ISSVD), composed of dermatologists, pathologists, and gynecologists, agreed to change the classification of squamous VIN from the previous VIN 1-3 classification system. The committee described VIN in two forms, “usual type” and “differentiated type” (J Reprod Med 2005;50:807-10).
In making this transition, it was recognized that VIN 1 is not in fact an oncogenic lesion and is now solely referred to as condyloma acuminatum. Grade 2 and 3 are now collectively referred to as VIN. These changes made by the ISSVD reflect the current literature on grading of VIN. In addition to VIN 1 not having any progression to malignancy, it is a diagnosis that is difficult to reproduce and may, at times, reflect reactive changes or other dermatosis. VIN 2 and 3 are not discriminated from each other in a reproducible manner and clinically have no reason for individual distinction (J Low Genit Tract Dis. 2006 Jul;10[3]:161-9).
VIN, usual type is the most common intraepithelial lesion and is historically referred to as classic VIN or Bowen’s disease. This type is associated with HPV infection and includes the formerly described warty type, basaloid type, and mixed type. The carcinogenic subtypes of HPV, 16, 18, 31, and 33 are the most common HPV subtypes responsible. It should be noted, however, that diagnosis is morphological and not based on HPV testing. Usual type is also traditionally thought to be more closely associated with risk factors such as smoking and immunocompromised states.
VIN, differentiated type is not associated with the HPV virus and is frequently found in older women. This lesion is often associated with other dermatologic conditions such as lichen sclerosis and lichen simplex chronicus. Diagnosis is also made by histology with abnormal cells being confined to the parabasal and basal portion of the rete pegs. This type also finds genetic alterations that are seen in invasive squamous cell carcinoma (Appl Immunohistochem Mol Morphol 2001;9:150-63). Differentiated type is thought to be a precursor for HPV-negative keratinizing squamous cell carcinoma of the vulva (Am J Surg Pathol. 2000 Mar;24[3]:429-41).
As awareness of this distinct form of VIN increases and more is learned about the precursors of HPV-negative squamous cell carcinoma, physicians are encouraged to closely follow up hyperplastic lesions and lichen sclerosis with biopsies and excision. The diagnosis of differentiated VIN is rarely made at present; however, this distinction by the ISSVD may improve the ability of clinicians and pathologists to recognize this HPV-negative precursor before squamous cell carcinoma is present.
The Lower Anogenital Squamous Terminology project of the College of American Pathology and the American Society for Colposcopy and Cervical Pathology advocates for more consistent terminology across lower anogenital tract lesions. This terminology applies only to HPV-related lesions (usual type) and considers the VIN 1 or condyloma accuminatum to be a low-grade lesion (LSIL), and VIN 2-3 or usual type to be high-grade lesions (HSIL) (Int J Gynecol Pathol. 2013 Jan;32[1]:76-115).
Many clinicians and pathologists have not adopted this most recent terminology; however, there is evidence that the ISSVD classification is the most clinically relevant.
Diagnosis
The majority of patients with any VIN will present with complaints of vulvar pruritus. However, women can also present with pain, burning, or dysuria, or can have an asymptomatic lesion found on pelvic exam. There are no recommended screening strategies to diagnose early VIN. Cytologic testing is complicated by the keratinization of the vulva, making this an unreliable diagnostic assessment.
On physical exam, VIN can have a heterogeneous presentation including papules, plaques, color variations, or ulcer. Differentiated type is thought to have a more defined appearance that frequently develops in the setting of other vulvar dermatosis. These are distinct, solitary lesions that are commonly raised, can have an overlying scale, and have ill-defined borders. A distinct lesion with ulceration or erosion is concerning for invasion.
Diagnosis is ultimately made by biopsy. Physicians should have a low threshold to biopsy any suspicious lesions or those unresponsive to therapy. Colposcopy is a frequent adjunct to the physical exam. Acetic acid 3%-5% soaked gauze is allowed to rest on the vulva for several minutes prior to observation with a colposcope or hand-held magnifying glass. Colposcopic findings are usually those of focal “white” epithelium. Vascular changes seen on the cervix (punctuation and mosaicism) are rarely seen on the vulva.
The entire anogenital region shares the same susceptibility to the HPV virus, thus squamous intraepithelial lesions are frequently multifocal. Physicians should have a heightened awareness of other lesions, such as cervical, vaginal, or anal, when managing a patient with VIN (Gynecol Oncol. 1995 Feb;56[2]:276-9). Appropriate cervical screening should be strictly adhered to and a thorough exam done at the time of vulvar colposcopy or exam.
Treatment
The goals of treatment include preventing carcinoma and improving symptoms while maintaining function and preserving anatomy. Treatment options for both types of VIN include excision, ablation, or medical therapy pending an evaluation of concurrent risk factors.
Premalignant disease was traditionally treated surgically. While surgical excision is still the mainstay of therapy, less aggressive techniques and medical therapy are more readily utilized. The goal of surgical excision for VIN is both diagnostic and therapeutic. When an excision for high-grade dysplasia is done (formerly VIN 3), detection of occult carcinoma was found in up to 3.2% in one large review (Gynecol Oncol. 2005;97:645-51).
Using a wide local excision to completely remove lesions with a pathologically clear margin reduces a patient’s risk of recurrence for disease compared to those excisions with positive margins (Obstet Gynecol. 1998;92:962-6). It is therefore critical that physicians carefully counsel patients who desire conservative therapy for VIN.
With any treatment, however, patients and physicians should be aware of the risk of recurrence; for vulvectomy, partial vulvectomy, local excision, and laser ablation, recurrences were seen at rates of 19%, 18%, 22%, and 23%, respectively, in a review of 3,322 patients (Gynecol Oncol. 2005;97:645-51).
CO2 laser ablation has been used for single lesions as well as multifocal or confluent disease. Many physicians advocate for its use in patients with multifocal lesions as well as those with disease around the clitoris or anus, where excisional therapy is less desirable as laser therapy results in less scarring.
A 2015 Cochrane Database Review of medical therapy for high-grade dysplasia (usual-type VIN, VIN 2/3, or high-grade VIN) found that topical imiquimod can be used as a safe and effective option for high-grade VIN. Physicians should, however, be aware of unfavorable side effects that may require dose reductions. Cidofovir may be an alternative to imiquimod pending more evidence on long-term response and progression (Cochrane Database Syst Rev. 2015 Aug 18;8:CD007924). Topical 5-fluorouracil has fallen out of favor for VIN given its significant chemical desquamation, however response rates are thought to be favorable if tolerated.
As the use of VIN terminology solidifies and information emerges on medical therapy to treat VIN, it is critical that physicians remain current when counseling and providing treatment recommendations for vulvar intraepithelial neoplasia.
Dr. Gehrig is professor and director of gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Clarke-Pearson is the chair and the Robert A. Ross Distinguished Professor of Obstetrics and Gynecology and professor in the division of gynecologic oncology at the university. Dr. Sullivan is a fellow in the division of gynecologic oncology at the university. They reported having no relevant financial disclosures. Email them at obnews@frontlinemedcom.com.
FDA panel set to vet Essure safety
On Sept. 24, the Food and Drug Administration’s Obstetrics and Gynecology Devices Panel will meet in Silver Spring, Md., to discuss the future of Bayer’s Essure permanent female sterilization coil.
FDA officials have asked the 19-member advisory panel to evaluate the currently available scientific data on the safety and effectiveness of the Essure system and make recommendations on appropriate use, product labeling, and the potential need for additional postmarket clinical studies.
Since Essure’s approval in 2002, the FDA has received more than 5,000 complaints about Essure. Most concern chronic pain, perforation, dyspareunia, device migration, menstrual problems, and possible allergic reactions to the nickel in Essure, but more than 100 adverse symptoms have been reported to the agency, according to newly posted meeting materials.
The complaints have been filed mostly in the past 2 years by patients who have organized online to share their stories and lobby to have Essure taken off the market; some are involved in legal action against Bayer. Meanwhile, Bayer maintains that, for most of the approximately 750,000 women who have received Essure, the device is safe and effective.
Advisory panel members will have their work cut out for them as they sort through the issues. The FDA has released a new 89-page review of Essure, and Bayer has submitted its own lengthy review document. Testimony is expected from Bayer, FDA reviewers, patients, and others. The meeting is scheduled to run almost 12 hours, from 8 a.m. to 7:30 p.m. Eastern time, at the agency’s White Oak Campus in Silver Spring, Md., and will be broadcast live online.
FDA noted in its review that it has been monitoring social media with automated software that scours Twitter, Facebook, patient forums, and other websites for “posts with resemblance to adverse events” or “Proto-AEs.” The program picked up 350,000 references to Essure between September 2013 and July 2015 and classified more than 20,000 as Proto-AEs, mostly related to pain, hysterectomy, malaise, pregnancy, and device removal. The social media data, however, are preliminary since the FDA has yet to remove duplications and retweets.
On Sept. 24, the Food and Drug Administration’s Obstetrics and Gynecology Devices Panel will meet in Silver Spring, Md., to discuss the future of Bayer’s Essure permanent female sterilization coil.
FDA officials have asked the 19-member advisory panel to evaluate the currently available scientific data on the safety and effectiveness of the Essure system and make recommendations on appropriate use, product labeling, and the potential need for additional postmarket clinical studies.
Since Essure’s approval in 2002, the FDA has received more than 5,000 complaints about Essure. Most concern chronic pain, perforation, dyspareunia, device migration, menstrual problems, and possible allergic reactions to the nickel in Essure, but more than 100 adverse symptoms have been reported to the agency, according to newly posted meeting materials.
The complaints have been filed mostly in the past 2 years by patients who have organized online to share their stories and lobby to have Essure taken off the market; some are involved in legal action against Bayer. Meanwhile, Bayer maintains that, for most of the approximately 750,000 women who have received Essure, the device is safe and effective.
Advisory panel members will have their work cut out for them as they sort through the issues. The FDA has released a new 89-page review of Essure, and Bayer has submitted its own lengthy review document. Testimony is expected from Bayer, FDA reviewers, patients, and others. The meeting is scheduled to run almost 12 hours, from 8 a.m. to 7:30 p.m. Eastern time, at the agency’s White Oak Campus in Silver Spring, Md., and will be broadcast live online.
FDA noted in its review that it has been monitoring social media with automated software that scours Twitter, Facebook, patient forums, and other websites for “posts with resemblance to adverse events” or “Proto-AEs.” The program picked up 350,000 references to Essure between September 2013 and July 2015 and classified more than 20,000 as Proto-AEs, mostly related to pain, hysterectomy, malaise, pregnancy, and device removal. The social media data, however, are preliminary since the FDA has yet to remove duplications and retweets.
On Sept. 24, the Food and Drug Administration’s Obstetrics and Gynecology Devices Panel will meet in Silver Spring, Md., to discuss the future of Bayer’s Essure permanent female sterilization coil.
FDA officials have asked the 19-member advisory panel to evaluate the currently available scientific data on the safety and effectiveness of the Essure system and make recommendations on appropriate use, product labeling, and the potential need for additional postmarket clinical studies.
Since Essure’s approval in 2002, the FDA has received more than 5,000 complaints about Essure. Most concern chronic pain, perforation, dyspareunia, device migration, menstrual problems, and possible allergic reactions to the nickel in Essure, but more than 100 adverse symptoms have been reported to the agency, according to newly posted meeting materials.
The complaints have been filed mostly in the past 2 years by patients who have organized online to share their stories and lobby to have Essure taken off the market; some are involved in legal action against Bayer. Meanwhile, Bayer maintains that, for most of the approximately 750,000 women who have received Essure, the device is safe and effective.
Advisory panel members will have their work cut out for them as they sort through the issues. The FDA has released a new 89-page review of Essure, and Bayer has submitted its own lengthy review document. Testimony is expected from Bayer, FDA reviewers, patients, and others. The meeting is scheduled to run almost 12 hours, from 8 a.m. to 7:30 p.m. Eastern time, at the agency’s White Oak Campus in Silver Spring, Md., and will be broadcast live online.
FDA noted in its review that it has been monitoring social media with automated software that scours Twitter, Facebook, patient forums, and other websites for “posts with resemblance to adverse events” or “Proto-AEs.” The program picked up 350,000 references to Essure between September 2013 and July 2015 and classified more than 20,000 as Proto-AEs, mostly related to pain, hysterectomy, malaise, pregnancy, and device removal. The social media data, however, are preliminary since the FDA has yet to remove duplications and retweets.
Individualizing treatment of menopausal symptoms
Menopause experts Andrew M. Kaunitz, MD, and JoAnn E. Manson, MD, DrPH, provide a comprehensive review of various treatments for menopausal symptoms in an article recently published ahead of print in Obstetrics and Gynecology.1 They discuss hormonal and nonhormonal options to treat vasomotor symptoms, genitourinary syndrome of menopause (GSM), and considerations for the use of hormone therapy in special populations: women with early menopause, women with a history of breast cancer and those who carry the BRCA gene mutation, and women with a history of venous thrombosis.1
The authors write that, “given the lower rates of adverse events on HT among women close to menopause onset and at lower baseline risk of cardiovascular disease, risk stratification and personalized risk assessment appear to represent a sound strategy for optimizing the benefit–risk profile and safety of HT.”1 They suggest that instead of stopping systemic HT at age 65 years, the length of treatment be individualized based on a woman’s risk profile and preferences. The authors encourage gynecologists and other clinicians to use benefit–risk profile tools for both hormonal and nonhormonal options to help women make sound decisions on treating menopausal symptoms.1
Readthe full Clinical Expert Series here.
Reference
- Kaunitz AM, Manson JE. Management of menopausal symptoms [published online ahead of print September 3, 2015]. Obstet Gynecol. doi: 10.1097/AOG.0000000000001058. Accessed September 18, 2015.
Menopause experts Andrew M. Kaunitz, MD, and JoAnn E. Manson, MD, DrPH, provide a comprehensive review of various treatments for menopausal symptoms in an article recently published ahead of print in Obstetrics and Gynecology.1 They discuss hormonal and nonhormonal options to treat vasomotor symptoms, genitourinary syndrome of menopause (GSM), and considerations for the use of hormone therapy in special populations: women with early menopause, women with a history of breast cancer and those who carry the BRCA gene mutation, and women with a history of venous thrombosis.1
The authors write that, “given the lower rates of adverse events on HT among women close to menopause onset and at lower baseline risk of cardiovascular disease, risk stratification and personalized risk assessment appear to represent a sound strategy for optimizing the benefit–risk profile and safety of HT.”1 They suggest that instead of stopping systemic HT at age 65 years, the length of treatment be individualized based on a woman’s risk profile and preferences. The authors encourage gynecologists and other clinicians to use benefit–risk profile tools for both hormonal and nonhormonal options to help women make sound decisions on treating menopausal symptoms.1
Readthe full Clinical Expert Series here.
Menopause experts Andrew M. Kaunitz, MD, and JoAnn E. Manson, MD, DrPH, provide a comprehensive review of various treatments for menopausal symptoms in an article recently published ahead of print in Obstetrics and Gynecology.1 They discuss hormonal and nonhormonal options to treat vasomotor symptoms, genitourinary syndrome of menopause (GSM), and considerations for the use of hormone therapy in special populations: women with early menopause, women with a history of breast cancer and those who carry the BRCA gene mutation, and women with a history of venous thrombosis.1
The authors write that, “given the lower rates of adverse events on HT among women close to menopause onset and at lower baseline risk of cardiovascular disease, risk stratification and personalized risk assessment appear to represent a sound strategy for optimizing the benefit–risk profile and safety of HT.”1 They suggest that instead of stopping systemic HT at age 65 years, the length of treatment be individualized based on a woman’s risk profile and preferences. The authors encourage gynecologists and other clinicians to use benefit–risk profile tools for both hormonal and nonhormonal options to help women make sound decisions on treating menopausal symptoms.1
Readthe full Clinical Expert Series here.
Reference
- Kaunitz AM, Manson JE. Management of menopausal symptoms [published online ahead of print September 3, 2015]. Obstet Gynecol. doi: 10.1097/AOG.0000000000001058. Accessed September 18, 2015.
Reference
- Kaunitz AM, Manson JE. Management of menopausal symptoms [published online ahead of print September 3, 2015]. Obstet Gynecol. doi: 10.1097/AOG.0000000000001058. Accessed September 18, 2015.
Which is the more effective treatment for uncomplicated skin infections—clindamycin or trimethoprim-sulfamethoxazole?
Miller and colleagues conducted their study in adults as well as children. Patients were included if they had either a discrete skin abscess or cellulitis, or both. They were excluded if they had one of the following:
- impetigo
- perirectal, genital, or hand infection
- a human or animal bite at the site of infection
- temperature of 38.5° C or higher
- immunocompromise
- morbid obesity
- prosthetic device at the site of infection.
The remaining patients then were stratified into one of 2 groups:
- those with a larger abscess (>5 cm in maximum diameter in adults, proportionally smaller in children) and/or cellulitis
- those who had a smaller abscess.
This study by Miller and colleagues focuses only on the patients in the former group.
Details of the trial
All discrete abscesses were incised and drained, and patients were randomly assigned to either:
- clindamycin, 300 mg 3 times daily for 10 days
- trimethoprim-sulfamethoxazole, 2 single-strength tablets orally twice daily for 10 days.
The primary endpoint was clinical cure at 7 to 10 days after completion of antibiotic therapy.
The study enrolled 524 patients—264 in the clindamycin group and 260 in the trimethoprim-sulfamethoxazole group. Approximately 30% of the patients were children. One hundred sixty patients (30.5%) had a discrete abscess, 280 (53.4%) had cellulitis, and 82 (15.6%) had both an abscess and cellulitis. An incision and drainage procedure was performed in 44.5% of patients. Slightly more than 50% of patients had a microbiological culture.
The most common organism isolated was S aureus (217 of 524 patients, or 41.4%), of which 167 (77%) were methicillin-resistant S aureus (MRSA). Of the 217 isolates identified as S aureus, 27 (12.4%) were resistant to clindamycin, and only one (0.5%) was resistant to trimethoprim-sulfamethoxazole.
Of the 466 patients who were fully evaluable, the rate of cure was 89.5% in the clindamycin group (95% confidence interval [CI], 85.2–93.7) and 88.2% in the trimethoprim-sulfamethoxazole group (95% CI, 83.7–92.7). The difference in the observed rate of clinical cure was not statistically significant.
Eleven of 15 patients in the clindamycin group who had clindamycin-resistant isolates were cured, compared with 77 of 84 patients with susceptible isolates (73.3% vs 91.7%; P = .06). At 1 month after treatment, cure rates remained similar. The overall rates of adverse effects in the 2 groups were similar, at 19%. No patient developed Clostridium difficile-associated diarrhea.
Skin infections can be life-threatening
Skin and skin-structure infections are common—and can influence the decision of when to perform a cesarean delivery, how to prepare the skin before surgery, and where to place the surgical incision. In some patients, these infections can be quite debilitating, even life-threatening. When a discrete abscess (furuncle, carbuncle) is present, the most likely organism is S aureus, and the majority of strains are MRSA. When cellulitis is present, S aureus is less likely, and the dominant organisms are usually streptococci, particularly Streptococcus pyogenes.
Abscesses of any size need incision and drainage and, in most cases, systemic antibiotic therapy. When cellulitis without a discrete abscess is present, the key to treatment is antibiotic therapy.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
For uncomplicated skin and skin-structure infections in immunocompetent women, oral clindamycin and oral trimethoprim-sulfamethoxazole are equally effective; both achieve cures in approximately 90% of patients.
Given that more strains of S aureus were resistant to clindamycin, trimethoprim-sulfamethoxazole may be the preferred agent. It also is less expensive and, in theory at least, less likely to cause drug-induced diarrhea.
Affected patients need to be followed closely because recurrences are common and, in isolated instances, serious complications such as sepsis can develop.
—Patrick Duff, MD
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Miller and colleagues conducted their study in adults as well as children. Patients were included if they had either a discrete skin abscess or cellulitis, or both. They were excluded if they had one of the following:
- impetigo
- perirectal, genital, or hand infection
- a human or animal bite at the site of infection
- temperature of 38.5° C or higher
- immunocompromise
- morbid obesity
- prosthetic device at the site of infection.
The remaining patients then were stratified into one of 2 groups:
- those with a larger abscess (>5 cm in maximum diameter in adults, proportionally smaller in children) and/or cellulitis
- those who had a smaller abscess.
This study by Miller and colleagues focuses only on the patients in the former group.
Details of the trial
All discrete abscesses were incised and drained, and patients were randomly assigned to either:
- clindamycin, 300 mg 3 times daily for 10 days
- trimethoprim-sulfamethoxazole, 2 single-strength tablets orally twice daily for 10 days.
The primary endpoint was clinical cure at 7 to 10 days after completion of antibiotic therapy.
The study enrolled 524 patients—264 in the clindamycin group and 260 in the trimethoprim-sulfamethoxazole group. Approximately 30% of the patients were children. One hundred sixty patients (30.5%) had a discrete abscess, 280 (53.4%) had cellulitis, and 82 (15.6%) had both an abscess and cellulitis. An incision and drainage procedure was performed in 44.5% of patients. Slightly more than 50% of patients had a microbiological culture.
The most common organism isolated was S aureus (217 of 524 patients, or 41.4%), of which 167 (77%) were methicillin-resistant S aureus (MRSA). Of the 217 isolates identified as S aureus, 27 (12.4%) were resistant to clindamycin, and only one (0.5%) was resistant to trimethoprim-sulfamethoxazole.
Of the 466 patients who were fully evaluable, the rate of cure was 89.5% in the clindamycin group (95% confidence interval [CI], 85.2–93.7) and 88.2% in the trimethoprim-sulfamethoxazole group (95% CI, 83.7–92.7). The difference in the observed rate of clinical cure was not statistically significant.
Eleven of 15 patients in the clindamycin group who had clindamycin-resistant isolates were cured, compared with 77 of 84 patients with susceptible isolates (73.3% vs 91.7%; P = .06). At 1 month after treatment, cure rates remained similar. The overall rates of adverse effects in the 2 groups were similar, at 19%. No patient developed Clostridium difficile-associated diarrhea.
Skin infections can be life-threatening
Skin and skin-structure infections are common—and can influence the decision of when to perform a cesarean delivery, how to prepare the skin before surgery, and where to place the surgical incision. In some patients, these infections can be quite debilitating, even life-threatening. When a discrete abscess (furuncle, carbuncle) is present, the most likely organism is S aureus, and the majority of strains are MRSA. When cellulitis is present, S aureus is less likely, and the dominant organisms are usually streptococci, particularly Streptococcus pyogenes.
Abscesses of any size need incision and drainage and, in most cases, systemic antibiotic therapy. When cellulitis without a discrete abscess is present, the key to treatment is antibiotic therapy.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
For uncomplicated skin and skin-structure infections in immunocompetent women, oral clindamycin and oral trimethoprim-sulfamethoxazole are equally effective; both achieve cures in approximately 90% of patients.
Given that more strains of S aureus were resistant to clindamycin, trimethoprim-sulfamethoxazole may be the preferred agent. It also is less expensive and, in theory at least, less likely to cause drug-induced diarrhea.
Affected patients need to be followed closely because recurrences are common and, in isolated instances, serious complications such as sepsis can develop.
—Patrick Duff, MD
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Miller and colleagues conducted their study in adults as well as children. Patients were included if they had either a discrete skin abscess or cellulitis, or both. They were excluded if they had one of the following:
- impetigo
- perirectal, genital, or hand infection
- a human or animal bite at the site of infection
- temperature of 38.5° C or higher
- immunocompromise
- morbid obesity
- prosthetic device at the site of infection.
The remaining patients then were stratified into one of 2 groups:
- those with a larger abscess (>5 cm in maximum diameter in adults, proportionally smaller in children) and/or cellulitis
- those who had a smaller abscess.
This study by Miller and colleagues focuses only on the patients in the former group.
Details of the trial
All discrete abscesses were incised and drained, and patients were randomly assigned to either:
- clindamycin, 300 mg 3 times daily for 10 days
- trimethoprim-sulfamethoxazole, 2 single-strength tablets orally twice daily for 10 days.
The primary endpoint was clinical cure at 7 to 10 days after completion of antibiotic therapy.
The study enrolled 524 patients—264 in the clindamycin group and 260 in the trimethoprim-sulfamethoxazole group. Approximately 30% of the patients were children. One hundred sixty patients (30.5%) had a discrete abscess, 280 (53.4%) had cellulitis, and 82 (15.6%) had both an abscess and cellulitis. An incision and drainage procedure was performed in 44.5% of patients. Slightly more than 50% of patients had a microbiological culture.
The most common organism isolated was S aureus (217 of 524 patients, or 41.4%), of which 167 (77%) were methicillin-resistant S aureus (MRSA). Of the 217 isolates identified as S aureus, 27 (12.4%) were resistant to clindamycin, and only one (0.5%) was resistant to trimethoprim-sulfamethoxazole.
Of the 466 patients who were fully evaluable, the rate of cure was 89.5% in the clindamycin group (95% confidence interval [CI], 85.2–93.7) and 88.2% in the trimethoprim-sulfamethoxazole group (95% CI, 83.7–92.7). The difference in the observed rate of clinical cure was not statistically significant.
Eleven of 15 patients in the clindamycin group who had clindamycin-resistant isolates were cured, compared with 77 of 84 patients with susceptible isolates (73.3% vs 91.7%; P = .06). At 1 month after treatment, cure rates remained similar. The overall rates of adverse effects in the 2 groups were similar, at 19%. No patient developed Clostridium difficile-associated diarrhea.
Skin infections can be life-threatening
Skin and skin-structure infections are common—and can influence the decision of when to perform a cesarean delivery, how to prepare the skin before surgery, and where to place the surgical incision. In some patients, these infections can be quite debilitating, even life-threatening. When a discrete abscess (furuncle, carbuncle) is present, the most likely organism is S aureus, and the majority of strains are MRSA. When cellulitis is present, S aureus is less likely, and the dominant organisms are usually streptococci, particularly Streptococcus pyogenes.
Abscesses of any size need incision and drainage and, in most cases, systemic antibiotic therapy. When cellulitis without a discrete abscess is present, the key to treatment is antibiotic therapy.
WHAT THIS EVIDENCE MEANS FOR PRACTICE
For uncomplicated skin and skin-structure infections in immunocompetent women, oral clindamycin and oral trimethoprim-sulfamethoxazole are equally effective; both achieve cures in approximately 90% of patients.
Given that more strains of S aureus were resistant to clindamycin, trimethoprim-sulfamethoxazole may be the preferred agent. It also is less expensive and, in theory at least, less likely to cause drug-induced diarrhea.
Affected patients need to be followed closely because recurrences are common and, in isolated instances, serious complications such as sepsis can develop.
—Patrick Duff, MD
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Debunking five myths about minilaparoscopy
NEW YORK – The next big advance in gynecologic minimally invasive surgery could be the wider adoption of minilaparoscopy using newer, frictionless instruments.
Minilaparoscopy is commonly used in cholecystectomy, but is making inroads in gynecology. Minilaparoscopy performed with the newer, smaller instruments is especially well suited for fertility procedures and endometriosis surgery, according to Dr. Gustavo Carvalho, a pioneer in minilaparoscopy. Gynecologists are using minilaparoscopy successfully in hysterectomy as well, but the mini-instruments are not strong enough to survive many hysterectomies, he added.
“Traditional laparoscopy is suited for brutal procedures, such as hysterectomy, but minilap is better for delicate procedures requiring precise, tiny instruments,” Dr. Carvalho said at the meeting.
Despite the promise of utilizing the newer instruments, many surgeons have misconceptions about them.
“This is partly related to instruments used in older procedures called minilap. But after they try it with these newer instruments and learn how to do it, they actually prefer it for many procedures,” Dr. Carvalho, an associate professor of general surgery at Pernambuco University, Recife, Brazil, said in an interview.
Dr. Carvalho debunked the following “myths” about minilaparoscopy:
1. Single-port laparoscopy is cosmetically superior to minilaparoscopy. That’s not the case, Dr. Carvalho said. The few published papers on this subject compared single-port laparoscopy with older, high-friction instruments for minilaparoscopy, he said.
2. Minilaparoscopy should not be performed on obese patients. That’s false, Dr. Carvalho said. “Using newer instruments, we can move around better and see better for delicate operations in obese patients, but surgeons need special training,” he said.
3. Patients don’t want minilaparoscopy. The only published paper looking at patient preference did not offer patients minilaparoscopy with the newer instruments, Dr. Carvalho said. He and his colleagues plans to publish a paper based on research showing that 47% of patients prefer minilaparoscopy, compared with 27% who preferred single-port procedures. “There is a role for single-port procedures,” he added.
4. Minilaparoscopy hurts more than single-port laparoscopy. “No one can prove that minilap hurts less, but it is obvious and intuitive that smaller trocars and instruments cause less pain,” Dr. Carvalho said. “Surgeons want randomized trials, but they won’t be done because this is obvious.”
5. Surgeons lose dexterity and precision with minilaparoscopy. In new research that will be published in the Journal of the Society Laparoendoscopic Surgeons, Dr. Caravalho and his colleagues demonstrate that newer minilaparoscopy instruments are better than larger instruments for delicate tasks. In this study, 22 medical students and 22 surgical residents were given one gross task and three delicate tasks to perform randomly with a 3-mm frictionless trocar, a 3-mm high-friction trocar, and a 5-mm trocar. The larger instruments were significantly better for the gross task, while the smaller instruments were significantly better for the delicate tasks, Dr. Carvalho said. “This study shows the utility of precise, delicate instruments for delicate procedures,” he said.
Dr. Caravalho reported that he is an unpaid consultant for Karl Storz on the development of minilaparoscopic low-friction trocars.
NEW YORK – The next big advance in gynecologic minimally invasive surgery could be the wider adoption of minilaparoscopy using newer, frictionless instruments.
Minilaparoscopy is commonly used in cholecystectomy, but is making inroads in gynecology. Minilaparoscopy performed with the newer, smaller instruments is especially well suited for fertility procedures and endometriosis surgery, according to Dr. Gustavo Carvalho, a pioneer in minilaparoscopy. Gynecologists are using minilaparoscopy successfully in hysterectomy as well, but the mini-instruments are not strong enough to survive many hysterectomies, he added.
“Traditional laparoscopy is suited for brutal procedures, such as hysterectomy, but minilap is better for delicate procedures requiring precise, tiny instruments,” Dr. Carvalho said at the meeting.
Despite the promise of utilizing the newer instruments, many surgeons have misconceptions about them.
“This is partly related to instruments used in older procedures called minilap. But after they try it with these newer instruments and learn how to do it, they actually prefer it for many procedures,” Dr. Carvalho, an associate professor of general surgery at Pernambuco University, Recife, Brazil, said in an interview.
Dr. Carvalho debunked the following “myths” about minilaparoscopy:
1. Single-port laparoscopy is cosmetically superior to minilaparoscopy. That’s not the case, Dr. Carvalho said. The few published papers on this subject compared single-port laparoscopy with older, high-friction instruments for minilaparoscopy, he said.
2. Minilaparoscopy should not be performed on obese patients. That’s false, Dr. Carvalho said. “Using newer instruments, we can move around better and see better for delicate operations in obese patients, but surgeons need special training,” he said.
3. Patients don’t want minilaparoscopy. The only published paper looking at patient preference did not offer patients minilaparoscopy with the newer instruments, Dr. Carvalho said. He and his colleagues plans to publish a paper based on research showing that 47% of patients prefer minilaparoscopy, compared with 27% who preferred single-port procedures. “There is a role for single-port procedures,” he added.
4. Minilaparoscopy hurts more than single-port laparoscopy. “No one can prove that minilap hurts less, but it is obvious and intuitive that smaller trocars and instruments cause less pain,” Dr. Carvalho said. “Surgeons want randomized trials, but they won’t be done because this is obvious.”
5. Surgeons lose dexterity and precision with minilaparoscopy. In new research that will be published in the Journal of the Society Laparoendoscopic Surgeons, Dr. Caravalho and his colleagues demonstrate that newer minilaparoscopy instruments are better than larger instruments for delicate tasks. In this study, 22 medical students and 22 surgical residents were given one gross task and three delicate tasks to perform randomly with a 3-mm frictionless trocar, a 3-mm high-friction trocar, and a 5-mm trocar. The larger instruments were significantly better for the gross task, while the smaller instruments were significantly better for the delicate tasks, Dr. Carvalho said. “This study shows the utility of precise, delicate instruments for delicate procedures,” he said.
Dr. Caravalho reported that he is an unpaid consultant for Karl Storz on the development of minilaparoscopic low-friction trocars.
NEW YORK – The next big advance in gynecologic minimally invasive surgery could be the wider adoption of minilaparoscopy using newer, frictionless instruments.
Minilaparoscopy is commonly used in cholecystectomy, but is making inroads in gynecology. Minilaparoscopy performed with the newer, smaller instruments is especially well suited for fertility procedures and endometriosis surgery, according to Dr. Gustavo Carvalho, a pioneer in minilaparoscopy. Gynecologists are using minilaparoscopy successfully in hysterectomy as well, but the mini-instruments are not strong enough to survive many hysterectomies, he added.
“Traditional laparoscopy is suited for brutal procedures, such as hysterectomy, but minilap is better for delicate procedures requiring precise, tiny instruments,” Dr. Carvalho said at the meeting.
Despite the promise of utilizing the newer instruments, many surgeons have misconceptions about them.
“This is partly related to instruments used in older procedures called minilap. But after they try it with these newer instruments and learn how to do it, they actually prefer it for many procedures,” Dr. Carvalho, an associate professor of general surgery at Pernambuco University, Recife, Brazil, said in an interview.
Dr. Carvalho debunked the following “myths” about minilaparoscopy:
1. Single-port laparoscopy is cosmetically superior to minilaparoscopy. That’s not the case, Dr. Carvalho said. The few published papers on this subject compared single-port laparoscopy with older, high-friction instruments for minilaparoscopy, he said.
2. Minilaparoscopy should not be performed on obese patients. That’s false, Dr. Carvalho said. “Using newer instruments, we can move around better and see better for delicate operations in obese patients, but surgeons need special training,” he said.
3. Patients don’t want minilaparoscopy. The only published paper looking at patient preference did not offer patients minilaparoscopy with the newer instruments, Dr. Carvalho said. He and his colleagues plans to publish a paper based on research showing that 47% of patients prefer minilaparoscopy, compared with 27% who preferred single-port procedures. “There is a role for single-port procedures,” he added.
4. Minilaparoscopy hurts more than single-port laparoscopy. “No one can prove that minilap hurts less, but it is obvious and intuitive that smaller trocars and instruments cause less pain,” Dr. Carvalho said. “Surgeons want randomized trials, but they won’t be done because this is obvious.”
5. Surgeons lose dexterity and precision with minilaparoscopy. In new research that will be published in the Journal of the Society Laparoendoscopic Surgeons, Dr. Caravalho and his colleagues demonstrate that newer minilaparoscopy instruments are better than larger instruments for delicate tasks. In this study, 22 medical students and 22 surgical residents were given one gross task and three delicate tasks to perform randomly with a 3-mm frictionless trocar, a 3-mm high-friction trocar, and a 5-mm trocar. The larger instruments were significantly better for the gross task, while the smaller instruments were significantly better for the delicate tasks, Dr. Carvalho said. “This study shows the utility of precise, delicate instruments for delicate procedures,” he said.
Dr. Caravalho reported that he is an unpaid consultant for Karl Storz on the development of minilaparoscopic low-friction trocars.
EXPERT ANALYSIS FROM MINIMALLY INVASIVE SURGERY WEEK
Internet-based service increases access to STI testing
BRISBANE, AUSTRALIA – An internet-based testing referral service for sexually transmitted infections could take the pressure off overloaded clinics and reduce barriers to testing, according to new research.
Researchers reported data from a Vancouver-based pilot study of a virtual extension of clinic services called GetCheckedOnline.com. The service was offered to patients who were unable to get an immediate appointment at an STI clinic.
The service, which is being piloted in three clinic settings in Vancouver, is aimed at individuals who are asymptomatic and have not had STI contact.
It enables them to print out a requisition for a test for chlamydia, gonorrhea, syphilis, HIV, or hepatitis C, after completing a sexual history questionnaire.
Negative results are made available through the same website, but individuals who have positive results are asked to contact the clinic to receive their results. The clinic is also notified to ensure follow-up.
Devon Haag of the British Columbia Centre for Disease Control said the pilot was initiated in an attempt to address the long wait times for clinic appointments, with many patients unable to get an appointment for 3-4 weeks.
“We’ve been seeing increasing rates of STIs and at the same time a limited ability and availability of clinical services to meet the demands for timely testing and diagnosis,” Ms. Haag said at the World STI & HIV Congress 2015.
Analysis of data from the first month of the pilot study found that uptake and completion of testing varied considerably across test sites and the source of referral.
Among the 37 individuals who were given access codes to the website after being turned away from the provincial STI clinic – which is located within the BC Centre for Disease Control – 12 individuals went on to create an account on the site, and 10 of those got tested.
Among 108 individuals who contacted that same clinic by telephone and were referred to the service, 80 individuals (74%) created an account, and 62 of them (78%) were tested.
However, uptake was much lower at the two other clinics, with only 7 (19%) of those referred to the website creating an account. Ms. Haag said this may have been due to the nature of the two clinics, which were both located in nonprofit, community-based organizations in an area with a large population of gay men.
“We’ve heard anecdotally from both frontline clinicians and clients, that the clients are really happy with the services that they’re receiving at these clinics and actually would prefer to just come back into the clinic,” she said.
Overall, the pilot resulted in two positive test results and achieved a 2.9% increase in capacity at the provincial clinic.
“We demonstrated that referring clinic turnaways to GetCheckedOnline was feasible and in fact led to new STI diagnoses, so proof of concept was established,” Ms. Haag said.
The researchers also looked at the impact of promotional campaigns aimed at men who have sex with men, finding that these did achieve a significant increase in the number of people creating accounts, but this effect dropped off after the campaign ended.
Ms. Haag said that some clinic patients are now asking to use the online service rather than having to come into the clinic to get tested.
An audience member asked about the number of people who might have dropped out at the sexual health questionnaire stage of the process. While the 1-year data were yet to be analyzed, they do suggest that the questionnaire stage was associated with drop-offs, Ms. Haag said.
She reported having no financial disclosures.
BRISBANE, AUSTRALIA – An internet-based testing referral service for sexually transmitted infections could take the pressure off overloaded clinics and reduce barriers to testing, according to new research.
Researchers reported data from a Vancouver-based pilot study of a virtual extension of clinic services called GetCheckedOnline.com. The service was offered to patients who were unable to get an immediate appointment at an STI clinic.
The service, which is being piloted in three clinic settings in Vancouver, is aimed at individuals who are asymptomatic and have not had STI contact.
It enables them to print out a requisition for a test for chlamydia, gonorrhea, syphilis, HIV, or hepatitis C, after completing a sexual history questionnaire.
Negative results are made available through the same website, but individuals who have positive results are asked to contact the clinic to receive their results. The clinic is also notified to ensure follow-up.
Devon Haag of the British Columbia Centre for Disease Control said the pilot was initiated in an attempt to address the long wait times for clinic appointments, with many patients unable to get an appointment for 3-4 weeks.
“We’ve been seeing increasing rates of STIs and at the same time a limited ability and availability of clinical services to meet the demands for timely testing and diagnosis,” Ms. Haag said at the World STI & HIV Congress 2015.
Analysis of data from the first month of the pilot study found that uptake and completion of testing varied considerably across test sites and the source of referral.
Among the 37 individuals who were given access codes to the website after being turned away from the provincial STI clinic – which is located within the BC Centre for Disease Control – 12 individuals went on to create an account on the site, and 10 of those got tested.
Among 108 individuals who contacted that same clinic by telephone and were referred to the service, 80 individuals (74%) created an account, and 62 of them (78%) were tested.
However, uptake was much lower at the two other clinics, with only 7 (19%) of those referred to the website creating an account. Ms. Haag said this may have been due to the nature of the two clinics, which were both located in nonprofit, community-based organizations in an area with a large population of gay men.
“We’ve heard anecdotally from both frontline clinicians and clients, that the clients are really happy with the services that they’re receiving at these clinics and actually would prefer to just come back into the clinic,” she said.
Overall, the pilot resulted in two positive test results and achieved a 2.9% increase in capacity at the provincial clinic.
“We demonstrated that referring clinic turnaways to GetCheckedOnline was feasible and in fact led to new STI diagnoses, so proof of concept was established,” Ms. Haag said.
The researchers also looked at the impact of promotional campaigns aimed at men who have sex with men, finding that these did achieve a significant increase in the number of people creating accounts, but this effect dropped off after the campaign ended.
Ms. Haag said that some clinic patients are now asking to use the online service rather than having to come into the clinic to get tested.
An audience member asked about the number of people who might have dropped out at the sexual health questionnaire stage of the process. While the 1-year data were yet to be analyzed, they do suggest that the questionnaire stage was associated with drop-offs, Ms. Haag said.
She reported having no financial disclosures.
BRISBANE, AUSTRALIA – An internet-based testing referral service for sexually transmitted infections could take the pressure off overloaded clinics and reduce barriers to testing, according to new research.
Researchers reported data from a Vancouver-based pilot study of a virtual extension of clinic services called GetCheckedOnline.com. The service was offered to patients who were unable to get an immediate appointment at an STI clinic.
The service, which is being piloted in three clinic settings in Vancouver, is aimed at individuals who are asymptomatic and have not had STI contact.
It enables them to print out a requisition for a test for chlamydia, gonorrhea, syphilis, HIV, or hepatitis C, after completing a sexual history questionnaire.
Negative results are made available through the same website, but individuals who have positive results are asked to contact the clinic to receive their results. The clinic is also notified to ensure follow-up.
Devon Haag of the British Columbia Centre for Disease Control said the pilot was initiated in an attempt to address the long wait times for clinic appointments, with many patients unable to get an appointment for 3-4 weeks.
“We’ve been seeing increasing rates of STIs and at the same time a limited ability and availability of clinical services to meet the demands for timely testing and diagnosis,” Ms. Haag said at the World STI & HIV Congress 2015.
Analysis of data from the first month of the pilot study found that uptake and completion of testing varied considerably across test sites and the source of referral.
Among the 37 individuals who were given access codes to the website after being turned away from the provincial STI clinic – which is located within the BC Centre for Disease Control – 12 individuals went on to create an account on the site, and 10 of those got tested.
Among 108 individuals who contacted that same clinic by telephone and were referred to the service, 80 individuals (74%) created an account, and 62 of them (78%) were tested.
However, uptake was much lower at the two other clinics, with only 7 (19%) of those referred to the website creating an account. Ms. Haag said this may have been due to the nature of the two clinics, which were both located in nonprofit, community-based organizations in an area with a large population of gay men.
“We’ve heard anecdotally from both frontline clinicians and clients, that the clients are really happy with the services that they’re receiving at these clinics and actually would prefer to just come back into the clinic,” she said.
Overall, the pilot resulted in two positive test results and achieved a 2.9% increase in capacity at the provincial clinic.
“We demonstrated that referring clinic turnaways to GetCheckedOnline was feasible and in fact led to new STI diagnoses, so proof of concept was established,” Ms. Haag said.
The researchers also looked at the impact of promotional campaigns aimed at men who have sex with men, finding that these did achieve a significant increase in the number of people creating accounts, but this effect dropped off after the campaign ended.
Ms. Haag said that some clinic patients are now asking to use the online service rather than having to come into the clinic to get tested.
An audience member asked about the number of people who might have dropped out at the sexual health questionnaire stage of the process. While the 1-year data were yet to be analyzed, they do suggest that the questionnaire stage was associated with drop-offs, Ms. Haag said.
She reported having no financial disclosures.
FROM THE WORLD STI & HIV CONGRESS 2015
Key clinical point: An internet-based testing referral service for sexually transmitted infections could increase testing capacity.
Major finding: The Internet-based service achieved a 2.9% increase in capacity for one STI clinic.
Data source: Pilot study at three Vancouver STI clinics.
Disclosures: Ms. Haag reported having no financial disclosures.
Point-of-care chlamydia, gonorrhea assay as good as lab test
BRISBANE, AUSTRALIA - A molecular-based, point-of-care test for chlamydia and gonorrhea has shown similar accuracy to laboratory-based testing in a primary care setting, according to new data.
The GeneXpert Chlamydia trachomatis and Neisseria gonorrhea assay was tested in 1,995 individuals participating in the Test, Treat and Go (TTANGO) randomized, cross-over trial in regional and remote Australian primary health care services.
Researchers showed that the assay – which delivers results in 90 minutes – achieved 99.4% concordance with conventional laboratory nucleic acid amplification testing for chlamydia, and 99.9% concordance for gonorrhea.
The GeneXpert system is largely found in hospital laboratories or specialist clinical settings to test for tuberculosis, and this is the first time it has been applied to test for sexually transmitted infections and has been used in a primary care setting, according to Dr. Louise Causer of the Kirby Institute at the University of New South Wales, Sydney.
The results represent a significant improvement on existing lateral flow tests for chlamydia and gonorrhea, which have a high error rate, Dr. Causer said at the World STI & HIV Congress 2015.
“Particularly with chlamydia and gonorrhea, the new technology has allowed for these highly accurate results, whereas before people didn’t use the [lateral flow] tests, even though they were simple and cheap,” she said in an interview.
Of the 14 discordant results, 12 were for chlamydia and 10 of these were a positive point-of-care test, but negative laboratory results. The two discordant gonorrhea results were also both false positives.
Dr. Causer said the discordant results may have been caused by a lower organism load that was close to the limits of test detection.
While staff were trained in using the point-of-care system as part of the trial, Dr. Causer said there were several initial invalid results, which were mostly attributable to the staff getting used to the pipette technique. There was also one incidence of cartridge failure with the device, which resulted in a batch of invalid results.
GeneXpert is already used to test for infections such as tuberculosis, influenza, MRSA, and norovirus, and Dr. Causer said an assay for Trichomonas vaginalis also was being developed.
“It’s the idea that if you invest in the actual platform, you have the potential to adapt it to whatever setting, whatever epidemic is going on,” Dr. Causer said, suggesting there was potential to expand the assay to include other sexually transmitted infections such as HIV and human papillomavirus.
She told attendees at the conference that there is a particular need for rapid point-of-care testing in regional and remote communities, where it can take up to a week for laboratory results to be received, resulting in long delays to treatment and patients being lost to follow-up.
The study received in-kind support from GeneXpert manufacturer Cepheid.
BRISBANE, AUSTRALIA - A molecular-based, point-of-care test for chlamydia and gonorrhea has shown similar accuracy to laboratory-based testing in a primary care setting, according to new data.
The GeneXpert Chlamydia trachomatis and Neisseria gonorrhea assay was tested in 1,995 individuals participating in the Test, Treat and Go (TTANGO) randomized, cross-over trial in regional and remote Australian primary health care services.
Researchers showed that the assay – which delivers results in 90 minutes – achieved 99.4% concordance with conventional laboratory nucleic acid amplification testing for chlamydia, and 99.9% concordance for gonorrhea.
The GeneXpert system is largely found in hospital laboratories or specialist clinical settings to test for tuberculosis, and this is the first time it has been applied to test for sexually transmitted infections and has been used in a primary care setting, according to Dr. Louise Causer of the Kirby Institute at the University of New South Wales, Sydney.
The results represent a significant improvement on existing lateral flow tests for chlamydia and gonorrhea, which have a high error rate, Dr. Causer said at the World STI & HIV Congress 2015.
“Particularly with chlamydia and gonorrhea, the new technology has allowed for these highly accurate results, whereas before people didn’t use the [lateral flow] tests, even though they were simple and cheap,” she said in an interview.
Of the 14 discordant results, 12 were for chlamydia and 10 of these were a positive point-of-care test, but negative laboratory results. The two discordant gonorrhea results were also both false positives.
Dr. Causer said the discordant results may have been caused by a lower organism load that was close to the limits of test detection.
While staff were trained in using the point-of-care system as part of the trial, Dr. Causer said there were several initial invalid results, which were mostly attributable to the staff getting used to the pipette technique. There was also one incidence of cartridge failure with the device, which resulted in a batch of invalid results.
GeneXpert is already used to test for infections such as tuberculosis, influenza, MRSA, and norovirus, and Dr. Causer said an assay for Trichomonas vaginalis also was being developed.
“It’s the idea that if you invest in the actual platform, you have the potential to adapt it to whatever setting, whatever epidemic is going on,” Dr. Causer said, suggesting there was potential to expand the assay to include other sexually transmitted infections such as HIV and human papillomavirus.
She told attendees at the conference that there is a particular need for rapid point-of-care testing in regional and remote communities, where it can take up to a week for laboratory results to be received, resulting in long delays to treatment and patients being lost to follow-up.
The study received in-kind support from GeneXpert manufacturer Cepheid.
BRISBANE, AUSTRALIA - A molecular-based, point-of-care test for chlamydia and gonorrhea has shown similar accuracy to laboratory-based testing in a primary care setting, according to new data.
The GeneXpert Chlamydia trachomatis and Neisseria gonorrhea assay was tested in 1,995 individuals participating in the Test, Treat and Go (TTANGO) randomized, cross-over trial in regional and remote Australian primary health care services.
Researchers showed that the assay – which delivers results in 90 minutes – achieved 99.4% concordance with conventional laboratory nucleic acid amplification testing for chlamydia, and 99.9% concordance for gonorrhea.
The GeneXpert system is largely found in hospital laboratories or specialist clinical settings to test for tuberculosis, and this is the first time it has been applied to test for sexually transmitted infections and has been used in a primary care setting, according to Dr. Louise Causer of the Kirby Institute at the University of New South Wales, Sydney.
The results represent a significant improvement on existing lateral flow tests for chlamydia and gonorrhea, which have a high error rate, Dr. Causer said at the World STI & HIV Congress 2015.
“Particularly with chlamydia and gonorrhea, the new technology has allowed for these highly accurate results, whereas before people didn’t use the [lateral flow] tests, even though they were simple and cheap,” she said in an interview.
Of the 14 discordant results, 12 were for chlamydia and 10 of these were a positive point-of-care test, but negative laboratory results. The two discordant gonorrhea results were also both false positives.
Dr. Causer said the discordant results may have been caused by a lower organism load that was close to the limits of test detection.
While staff were trained in using the point-of-care system as part of the trial, Dr. Causer said there were several initial invalid results, which were mostly attributable to the staff getting used to the pipette technique. There was also one incidence of cartridge failure with the device, which resulted in a batch of invalid results.
GeneXpert is already used to test for infections such as tuberculosis, influenza, MRSA, and norovirus, and Dr. Causer said an assay for Trichomonas vaginalis also was being developed.
“It’s the idea that if you invest in the actual platform, you have the potential to adapt it to whatever setting, whatever epidemic is going on,” Dr. Causer said, suggesting there was potential to expand the assay to include other sexually transmitted infections such as HIV and human papillomavirus.
She told attendees at the conference that there is a particular need for rapid point-of-care testing in regional and remote communities, where it can take up to a week for laboratory results to be received, resulting in long delays to treatment and patients being lost to follow-up.
The study received in-kind support from GeneXpert manufacturer Cepheid.
AT THE WORLD STI & HIV CONGRESS 2015
Key clinical point:A molecular-based, point of care test for chlamydia and gonorrhea has similar accuracy to laboratory-based testing.
Major finding: The GeneXpert molecular-based, point-of-care test achieves 99.4% concordance for chlamydia and 99.9% concordance for gonorrhea.
Data source: Randomized, cross-over, point-of-care trial in 1,995 individuals (TTANGO).
Disclosures: The study received in-kind support from GeneXpert manufacturer Cepheid.
Uterine size not linked to increased surgical complications
NEW YORK – Uterine size does not appear to increase the risk of surgical complications in patients who undergo type VII total laparoscopic hysterectomy, but both uterine size and the number of prior pelvic surgeries increased surgical time in a linear manner, according to a retrospective case-control analysis.
“There is insufficient evidence to determine a statistical correlation between uterine size and presence of surgical complications. Therefore, type VII [total laparoscopic hysterectomy] seems to be a feasible and safe surgical procedure, resulting in a short hospital stay, minimal blood loss, minimal operating time, and a low complication rate regardless of uterine weight,” Dr. Carlos Hernández Nieto said at the annual Minimally Invasive Surgery Week.
Type VII total laparoscopic hysterectomy consists of completing all surgical dissection, ligations, and sutures through trocars, including vaginal closure.
The study was based on 235 consecutive patients undergoing type VII total laparoscopic hysterectomy at two hospitals between January 2008 and December 2014. Sufficient information was available on 211 patients.
The mean age of women in the study was 45 years, with a mean body mass index of 25.3 kg/m2. The mean number of prior births was two; the mean number of prior pelvic surgeries was two; the mean number of days in hospital was three; the mean surgical time was 140 minutes; and the mean uterine weight was 142 grams. Mean blood loss during surgery was 100 cc.
Surgical complications occurred in 14 patients (6.6%); two had bleeding which led to conversion to laparotomy and 12 had fever. The mean uterine weight in the group with complications was 161.8 grams, according to Dr. Hernández Nieto of TEC Salud Health Care System, Monterrey, Mexico.
A logistical regression analysis showed that the only factor significantly related to complications was the mean surgical time (170 minutes in this group of patients; P = .003). Uterine weight was not significantly related to complications.
Uterine weight was, however, significantly associated with increased surgical time. Surgical time increased from 0.02 to 1 minute for each additional gram of weight (P = .002), Dr. Hernández Nieto said. The number of prior pelvic surgeries also significantly increased surgical time. For each prior pelvic surgery, surgical time increased from 1.62 to 8.72 minutes (P = .006).
Dr. Hernández Nieto reported having no financial disclosures.
NEW YORK – Uterine size does not appear to increase the risk of surgical complications in patients who undergo type VII total laparoscopic hysterectomy, but both uterine size and the number of prior pelvic surgeries increased surgical time in a linear manner, according to a retrospective case-control analysis.
“There is insufficient evidence to determine a statistical correlation between uterine size and presence of surgical complications. Therefore, type VII [total laparoscopic hysterectomy] seems to be a feasible and safe surgical procedure, resulting in a short hospital stay, minimal blood loss, minimal operating time, and a low complication rate regardless of uterine weight,” Dr. Carlos Hernández Nieto said at the annual Minimally Invasive Surgery Week.
Type VII total laparoscopic hysterectomy consists of completing all surgical dissection, ligations, and sutures through trocars, including vaginal closure.
The study was based on 235 consecutive patients undergoing type VII total laparoscopic hysterectomy at two hospitals between January 2008 and December 2014. Sufficient information was available on 211 patients.
The mean age of women in the study was 45 years, with a mean body mass index of 25.3 kg/m2. The mean number of prior births was two; the mean number of prior pelvic surgeries was two; the mean number of days in hospital was three; the mean surgical time was 140 minutes; and the mean uterine weight was 142 grams. Mean blood loss during surgery was 100 cc.
Surgical complications occurred in 14 patients (6.6%); two had bleeding which led to conversion to laparotomy and 12 had fever. The mean uterine weight in the group with complications was 161.8 grams, according to Dr. Hernández Nieto of TEC Salud Health Care System, Monterrey, Mexico.
A logistical regression analysis showed that the only factor significantly related to complications was the mean surgical time (170 minutes in this group of patients; P = .003). Uterine weight was not significantly related to complications.
Uterine weight was, however, significantly associated with increased surgical time. Surgical time increased from 0.02 to 1 minute for each additional gram of weight (P = .002), Dr. Hernández Nieto said. The number of prior pelvic surgeries also significantly increased surgical time. For each prior pelvic surgery, surgical time increased from 1.62 to 8.72 minutes (P = .006).
Dr. Hernández Nieto reported having no financial disclosures.
NEW YORK – Uterine size does not appear to increase the risk of surgical complications in patients who undergo type VII total laparoscopic hysterectomy, but both uterine size and the number of prior pelvic surgeries increased surgical time in a linear manner, according to a retrospective case-control analysis.
“There is insufficient evidence to determine a statistical correlation between uterine size and presence of surgical complications. Therefore, type VII [total laparoscopic hysterectomy] seems to be a feasible and safe surgical procedure, resulting in a short hospital stay, minimal blood loss, minimal operating time, and a low complication rate regardless of uterine weight,” Dr. Carlos Hernández Nieto said at the annual Minimally Invasive Surgery Week.
Type VII total laparoscopic hysterectomy consists of completing all surgical dissection, ligations, and sutures through trocars, including vaginal closure.
The study was based on 235 consecutive patients undergoing type VII total laparoscopic hysterectomy at two hospitals between January 2008 and December 2014. Sufficient information was available on 211 patients.
The mean age of women in the study was 45 years, with a mean body mass index of 25.3 kg/m2. The mean number of prior births was two; the mean number of prior pelvic surgeries was two; the mean number of days in hospital was three; the mean surgical time was 140 minutes; and the mean uterine weight was 142 grams. Mean blood loss during surgery was 100 cc.
Surgical complications occurred in 14 patients (6.6%); two had bleeding which led to conversion to laparotomy and 12 had fever. The mean uterine weight in the group with complications was 161.8 grams, according to Dr. Hernández Nieto of TEC Salud Health Care System, Monterrey, Mexico.
A logistical regression analysis showed that the only factor significantly related to complications was the mean surgical time (170 minutes in this group of patients; P = .003). Uterine weight was not significantly related to complications.
Uterine weight was, however, significantly associated with increased surgical time. Surgical time increased from 0.02 to 1 minute for each additional gram of weight (P = .002), Dr. Hernández Nieto said. The number of prior pelvic surgeries also significantly increased surgical time. For each prior pelvic surgery, surgical time increased from 1.62 to 8.72 minutes (P = .006).
Dr. Hernández Nieto reported having no financial disclosures.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: A larger-size uterus is not associated with an increased rate of complications following type VII total laparoscopic hysterectomy.
Major finding: The only factor significantly associated with surgical complications was the mean surgical time (170 minutes among patients with complications; P = .003).
Data source: A case-control retrospective study of 235 women.
Disclosures: Dr. Hernández Nieto reported having no financial disclosures.
Survey: Most gyn surgeons don’t use power morcellation
NEW YORK – More than a year after the Food and Drug Administration first warned physicians and patients about the risks of disseminating unsuspected cancer with electric power morcellation, most minimally invasive gynecologic surgeons are not using the technology.
But rather than convert to open laparotomy for fibroid removal, many surgeons are using conventional and robotic-assisted laparoscopic techniques, Dr. Farr Nezhat said at the annual Minimally Invasive Surgery Week.
“The controversy over electric power morcellation demonstrates the difficulty with surgical innovation. The risks and balances of morcellation must be balanced. The current debate demonstrates the power of public opinion,” said Dr. Nezhat, who is director of minimally invasive surgery and gynecologic robotics at Mount Sinai Roosevelt and Mount Sinai St. Luke’s hospitals, New York. “The good news is that the majority of respondents have not converted to laparotomy.”
Dr. Nezhat and his colleagues sent a survey to 3,505 members of the Society of Laparoendoscopic Surgeons and received 518 responses. Surgeons were queried on their beliefs about morcellation and current practices for fibroid removal.
Sixty-one percent of respondents said they do not currently use a power morcellator. Of those who do not use the device, nearly half said it was because power morcellation was banned by their hospital, while others responded that they were not comfortable using it or that their hospital didn’t have power morcellation equipment.
A total of 60% said they believe morcellation affects survival, and 66% said that morcellation also disseminates benign pathology. Additionally, 48% reported that they have encountered a diagnosis of unsuspected uterine carcinoma in their practices.
So what are surgeons doing instead of power morcellation? About three-quarters of respondents currently perform open laparotomy in fewer than 25% of their cases. Their responses indicated that they mostly use laparoscopic and robotic procedures.
“It is encouraging that they did not go back to open laparotomy and that they have obviously found alternatives,” Dr. Nezhat said at the meeting sponsored by the Society of Laparoendoscopic Surgeons and affiliated societies.
Dr. Nezhat and his colleagues are planning a second survey to get details on the type of approaches that ob.gyns. are now using: vaginal morcellation, minilaparoscopy, or posterior colostomy, as well as and whether they perform morcellation in a bag.
“I have stopped using electric morcellation, and now we use a bag,” he said.
Dr. Nezhat reported having no relevant financial disclosures.
NEW YORK – More than a year after the Food and Drug Administration first warned physicians and patients about the risks of disseminating unsuspected cancer with electric power morcellation, most minimally invasive gynecologic surgeons are not using the technology.
But rather than convert to open laparotomy for fibroid removal, many surgeons are using conventional and robotic-assisted laparoscopic techniques, Dr. Farr Nezhat said at the annual Minimally Invasive Surgery Week.
“The controversy over electric power morcellation demonstrates the difficulty with surgical innovation. The risks and balances of morcellation must be balanced. The current debate demonstrates the power of public opinion,” said Dr. Nezhat, who is director of minimally invasive surgery and gynecologic robotics at Mount Sinai Roosevelt and Mount Sinai St. Luke’s hospitals, New York. “The good news is that the majority of respondents have not converted to laparotomy.”
Dr. Nezhat and his colleagues sent a survey to 3,505 members of the Society of Laparoendoscopic Surgeons and received 518 responses. Surgeons were queried on their beliefs about morcellation and current practices for fibroid removal.
Sixty-one percent of respondents said they do not currently use a power morcellator. Of those who do not use the device, nearly half said it was because power morcellation was banned by their hospital, while others responded that they were not comfortable using it or that their hospital didn’t have power morcellation equipment.
A total of 60% said they believe morcellation affects survival, and 66% said that morcellation also disseminates benign pathology. Additionally, 48% reported that they have encountered a diagnosis of unsuspected uterine carcinoma in their practices.
So what are surgeons doing instead of power morcellation? About three-quarters of respondents currently perform open laparotomy in fewer than 25% of their cases. Their responses indicated that they mostly use laparoscopic and robotic procedures.
“It is encouraging that they did not go back to open laparotomy and that they have obviously found alternatives,” Dr. Nezhat said at the meeting sponsored by the Society of Laparoendoscopic Surgeons and affiliated societies.
Dr. Nezhat and his colleagues are planning a second survey to get details on the type of approaches that ob.gyns. are now using: vaginal morcellation, minilaparoscopy, or posterior colostomy, as well as and whether they perform morcellation in a bag.
“I have stopped using electric morcellation, and now we use a bag,” he said.
Dr. Nezhat reported having no relevant financial disclosures.
NEW YORK – More than a year after the Food and Drug Administration first warned physicians and patients about the risks of disseminating unsuspected cancer with electric power morcellation, most minimally invasive gynecologic surgeons are not using the technology.
But rather than convert to open laparotomy for fibroid removal, many surgeons are using conventional and robotic-assisted laparoscopic techniques, Dr. Farr Nezhat said at the annual Minimally Invasive Surgery Week.
“The controversy over electric power morcellation demonstrates the difficulty with surgical innovation. The risks and balances of morcellation must be balanced. The current debate demonstrates the power of public opinion,” said Dr. Nezhat, who is director of minimally invasive surgery and gynecologic robotics at Mount Sinai Roosevelt and Mount Sinai St. Luke’s hospitals, New York. “The good news is that the majority of respondents have not converted to laparotomy.”
Dr. Nezhat and his colleagues sent a survey to 3,505 members of the Society of Laparoendoscopic Surgeons and received 518 responses. Surgeons were queried on their beliefs about morcellation and current practices for fibroid removal.
Sixty-one percent of respondents said they do not currently use a power morcellator. Of those who do not use the device, nearly half said it was because power morcellation was banned by their hospital, while others responded that they were not comfortable using it or that their hospital didn’t have power morcellation equipment.
A total of 60% said they believe morcellation affects survival, and 66% said that morcellation also disseminates benign pathology. Additionally, 48% reported that they have encountered a diagnosis of unsuspected uterine carcinoma in their practices.
So what are surgeons doing instead of power morcellation? About three-quarters of respondents currently perform open laparotomy in fewer than 25% of their cases. Their responses indicated that they mostly use laparoscopic and robotic procedures.
“It is encouraging that they did not go back to open laparotomy and that they have obviously found alternatives,” Dr. Nezhat said at the meeting sponsored by the Society of Laparoendoscopic Surgeons and affiliated societies.
Dr. Nezhat and his colleagues are planning a second survey to get details on the type of approaches that ob.gyns. are now using: vaginal morcellation, minilaparoscopy, or posterior colostomy, as well as and whether they perform morcellation in a bag.
“I have stopped using electric morcellation, and now we use a bag,” he said.
Dr. Nezhat reported having no relevant financial disclosures.
AT MINIMALLY INVASIVE SURGERY WEEK
Key clinical point: Abandoning the power morcellator has not led to an increase in laparotomy.
Major finding: A total of 61% of ob.gyns. who perform minimally invasive surgery do not use a power morcellator.
Data source: Survey of 3,505 members of Society of Laparoendoscopic Surgeons with 518 responses.
Disclosures: Dr. Nezhat reported having no relevant financial disclosures.
Attack PCOS in adolescents hard
ESTES PARK, COLO. – The sweet spot for intervention in polycystic ovary syndrome occurs early: in the adolescent who doesn’t yet desire pregnancy and who is just starting to experience the classic PCOS progressive weight gain.
“The obstetricians don’t want to see these patients when they’re already 220 lb and they’re trying to induce ovulation. It’s our job to pick them up in their adolescence. You want to clamp the hormones – suppress the androgens – so that things will be better down the road,” Dr. Margaret E. Wierman urged at a conference on internal medicine sponsored by the University of Colorado.
Aggressive treatment at this stage will reduce the risk of a host of potential health problems later. In addition to infertility issues, these include increased long-term risks of diabetes, hypertension, dyslipidemia, metabolic syndrome, endometrial cancer, obstructive sleep apnea, and nonalcoholic fatty liver disease, noted Dr. Wierman, professor of medicine, ob.gyn., and physiology at the university and chief of endocrinology at the Denver VA Medical Center.
PCOS is by far the most common cause of hyperandrogenic anovulation. Indeed, 6%-8% of all women in their childbearing years have PCOS. The condition is defined by clinical and/or biochemical hyperandrogenism, oligomenorrhea or amenorrhea, and the presence of ovarian cysts or increased ovarian volume on ultrasound.
In the adolescent with PCOS who doesn’t desire pregnancy, Dr. Wierman takes a three-pronged treatment approach: regularize menses with a less androgenic oral contraceptive, such as one containing norethindrone, or by using cyclic progesterone; treat hirsutism with spironolactone at 50-100 mg once daily coupled with electrolysis for local control; and consider using short-acting metformin as an insulin-sensitizing agent.
The use of metformin in treating PCOS is controversial. It is off-label therapy. There have been no prospective, randomized, placebo-controlled, double-blind studies supporting this application of the drug. Nevertheless, Dr. Wierman is a believer.
“If you take these adolescent girls, especially as they’re beginning to start the weight gain, and you give them metformin, it will stop the weight gain, improve their androgen level and their insulin resistance, and it will help them when they’re ready to have kids later on. I use metformin, and I call it Antabuse for fat: You cheat, you pay. You have no side effects if you eat healthy. If you eat fatty foods, you will have nausea and diarrhea,” she explained.
The endocrinologist added that she finds metformin works best in the adolescent with PCOS who has a family history of diabetes, is gaining weight, but is not yet diabetic herself.
“And that’s based on clinical experience, no prospective studies,” Dr. Wierman emphasized.
She reported having no financial conflicts regarding her presentation.
ESTES PARK, COLO. – The sweet spot for intervention in polycystic ovary syndrome occurs early: in the adolescent who doesn’t yet desire pregnancy and who is just starting to experience the classic PCOS progressive weight gain.
“The obstetricians don’t want to see these patients when they’re already 220 lb and they’re trying to induce ovulation. It’s our job to pick them up in their adolescence. You want to clamp the hormones – suppress the androgens – so that things will be better down the road,” Dr. Margaret E. Wierman urged at a conference on internal medicine sponsored by the University of Colorado.
Aggressive treatment at this stage will reduce the risk of a host of potential health problems later. In addition to infertility issues, these include increased long-term risks of diabetes, hypertension, dyslipidemia, metabolic syndrome, endometrial cancer, obstructive sleep apnea, and nonalcoholic fatty liver disease, noted Dr. Wierman, professor of medicine, ob.gyn., and physiology at the university and chief of endocrinology at the Denver VA Medical Center.
PCOS is by far the most common cause of hyperandrogenic anovulation. Indeed, 6%-8% of all women in their childbearing years have PCOS. The condition is defined by clinical and/or biochemical hyperandrogenism, oligomenorrhea or amenorrhea, and the presence of ovarian cysts or increased ovarian volume on ultrasound.
In the adolescent with PCOS who doesn’t desire pregnancy, Dr. Wierman takes a three-pronged treatment approach: regularize menses with a less androgenic oral contraceptive, such as one containing norethindrone, or by using cyclic progesterone; treat hirsutism with spironolactone at 50-100 mg once daily coupled with electrolysis for local control; and consider using short-acting metformin as an insulin-sensitizing agent.
The use of metformin in treating PCOS is controversial. It is off-label therapy. There have been no prospective, randomized, placebo-controlled, double-blind studies supporting this application of the drug. Nevertheless, Dr. Wierman is a believer.
“If you take these adolescent girls, especially as they’re beginning to start the weight gain, and you give them metformin, it will stop the weight gain, improve their androgen level and their insulin resistance, and it will help them when they’re ready to have kids later on. I use metformin, and I call it Antabuse for fat: You cheat, you pay. You have no side effects if you eat healthy. If you eat fatty foods, you will have nausea and diarrhea,” she explained.
The endocrinologist added that she finds metformin works best in the adolescent with PCOS who has a family history of diabetes, is gaining weight, but is not yet diabetic herself.
“And that’s based on clinical experience, no prospective studies,” Dr. Wierman emphasized.
She reported having no financial conflicts regarding her presentation.
ESTES PARK, COLO. – The sweet spot for intervention in polycystic ovary syndrome occurs early: in the adolescent who doesn’t yet desire pregnancy and who is just starting to experience the classic PCOS progressive weight gain.
“The obstetricians don’t want to see these patients when they’re already 220 lb and they’re trying to induce ovulation. It’s our job to pick them up in their adolescence. You want to clamp the hormones – suppress the androgens – so that things will be better down the road,” Dr. Margaret E. Wierman urged at a conference on internal medicine sponsored by the University of Colorado.
Aggressive treatment at this stage will reduce the risk of a host of potential health problems later. In addition to infertility issues, these include increased long-term risks of diabetes, hypertension, dyslipidemia, metabolic syndrome, endometrial cancer, obstructive sleep apnea, and nonalcoholic fatty liver disease, noted Dr. Wierman, professor of medicine, ob.gyn., and physiology at the university and chief of endocrinology at the Denver VA Medical Center.
PCOS is by far the most common cause of hyperandrogenic anovulation. Indeed, 6%-8% of all women in their childbearing years have PCOS. The condition is defined by clinical and/or biochemical hyperandrogenism, oligomenorrhea or amenorrhea, and the presence of ovarian cysts or increased ovarian volume on ultrasound.
In the adolescent with PCOS who doesn’t desire pregnancy, Dr. Wierman takes a three-pronged treatment approach: regularize menses with a less androgenic oral contraceptive, such as one containing norethindrone, or by using cyclic progesterone; treat hirsutism with spironolactone at 50-100 mg once daily coupled with electrolysis for local control; and consider using short-acting metformin as an insulin-sensitizing agent.
The use of metformin in treating PCOS is controversial. It is off-label therapy. There have been no prospective, randomized, placebo-controlled, double-blind studies supporting this application of the drug. Nevertheless, Dr. Wierman is a believer.
“If you take these adolescent girls, especially as they’re beginning to start the weight gain, and you give them metformin, it will stop the weight gain, improve their androgen level and their insulin resistance, and it will help them when they’re ready to have kids later on. I use metformin, and I call it Antabuse for fat: You cheat, you pay. You have no side effects if you eat healthy. If you eat fatty foods, you will have nausea and diarrhea,” she explained.
The endocrinologist added that she finds metformin works best in the adolescent with PCOS who has a family history of diabetes, is gaining weight, but is not yet diabetic herself.
“And that’s based on clinical experience, no prospective studies,” Dr. Wierman emphasized.
She reported having no financial conflicts regarding her presentation.
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM