User login
Nodding Off While Feeding an Infant
In a recent survey of 1259 mothers published in the journal Pediatrics, 28% reported they had fallen asleep while feeding their babies, and 83% of those mothers reported that the sleep was unplanned. Although the study sample was small, the investigators found that sociodemographic factors did not increase the odds that a mother would fall asleep while feeding.
These numbers are not surprising, but nonetheless they are concerning because co-sleeping is a known risk factor for sudden unexplained infant death (SUID). Every parent will tell you during the first 6 months of their adventure in parenting they didn’t get enough sleep. In fact some will tell you that sleep deprivation was their chronic state for the child’s first year.
Falling asleep easily at times and places not intended for sleep is the primary symptom of sleep deprivation. SUID is the most tragic event associated with parental sleep deprivation, but it is certainly not the only one. Overtired parents are more likely to be involved in accidents and are more likely to make poor decisions, particularly those regarding how to respond to a crying or misbehaving child.
The investigators found that 24% of mothers who reported that their usual nighttime feeding location was a chair or sofa (14%). Not surprisingly, mothers who fed in chairs were less likely to fall asleep while feeding. Many of these mothers reported that they chose the chair because they thought they would be less likely to fall asleep and/or disturb other family members. One wonders how we should interpret these numbers in light of other research that has found it is “relatively less hazardous to fall asleep with an infant in the adult bed than on a chair or sofa.” Had these chair feeding mothers made the better choice under the circumstances? It would take a much larger and more granular study to answer that question.
Mothers who exclusively breastfed were more likely to fall asleep feeding than were those who partially breastfed or used formula. The investigators postulated that the infants of mothers who exclusively breastfed may have required more feedings because breast milk is more easily and quickly digested. I know this is a common explanation, but in my experience I have found that exclusively breastfed infants often use nursing as pacification and a sleep trigger and spend more time at the breast regardless of how quickly they emptied their stomachs.
This study also examined the effect of repeated educational interventions and support and found that mothers who received an intervention based on safe sleep practices were less likely to fall asleep while feeding than were the mothers who had received the intervention focused on exclusive breastfeeding value and barriers to its adoption.
Education is one avenue, particularly when it includes the mother’s partner who can play an important role as standby lifeguard to make sure the mother doesn’t fall asleep. Obviously, this is easier said than done because when there is a new baby in the house sleep deprivation is usually a shared experience.
Although I believe that my family is on the verge of gifting me a smartwatch to protect me from my own misadventures, I don’t have any personal experience with these wonders of modern technology. However, I suspect with very little tweaking a wearable sensor could be easily programmed to detect when a mother is beginning to fall asleep while she is feeding her infant. A smartwatch would be an expensive intervention and is unlikely to filter down to economically challenged families. On the other hand, this paper has reinforced our suspicions that sleep-deprived infant feeding is a significant problem. A subsidized loaner program for those families that can’t afford a smartwatch is an option that should be considered.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In a recent survey of 1259 mothers published in the journal Pediatrics, 28% reported they had fallen asleep while feeding their babies, and 83% of those mothers reported that the sleep was unplanned. Although the study sample was small, the investigators found that sociodemographic factors did not increase the odds that a mother would fall asleep while feeding.
These numbers are not surprising, but nonetheless they are concerning because co-sleeping is a known risk factor for sudden unexplained infant death (SUID). Every parent will tell you during the first 6 months of their adventure in parenting they didn’t get enough sleep. In fact some will tell you that sleep deprivation was their chronic state for the child’s first year.
Falling asleep easily at times and places not intended for sleep is the primary symptom of sleep deprivation. SUID is the most tragic event associated with parental sleep deprivation, but it is certainly not the only one. Overtired parents are more likely to be involved in accidents and are more likely to make poor decisions, particularly those regarding how to respond to a crying or misbehaving child.
The investigators found that 24% of mothers who reported that their usual nighttime feeding location was a chair or sofa (14%). Not surprisingly, mothers who fed in chairs were less likely to fall asleep while feeding. Many of these mothers reported that they chose the chair because they thought they would be less likely to fall asleep and/or disturb other family members. One wonders how we should interpret these numbers in light of other research that has found it is “relatively less hazardous to fall asleep with an infant in the adult bed than on a chair or sofa.” Had these chair feeding mothers made the better choice under the circumstances? It would take a much larger and more granular study to answer that question.
Mothers who exclusively breastfed were more likely to fall asleep feeding than were those who partially breastfed or used formula. The investigators postulated that the infants of mothers who exclusively breastfed may have required more feedings because breast milk is more easily and quickly digested. I know this is a common explanation, but in my experience I have found that exclusively breastfed infants often use nursing as pacification and a sleep trigger and spend more time at the breast regardless of how quickly they emptied their stomachs.
This study also examined the effect of repeated educational interventions and support and found that mothers who received an intervention based on safe sleep practices were less likely to fall asleep while feeding than were the mothers who had received the intervention focused on exclusive breastfeeding value and barriers to its adoption.
Education is one avenue, particularly when it includes the mother’s partner who can play an important role as standby lifeguard to make sure the mother doesn’t fall asleep. Obviously, this is easier said than done because when there is a new baby in the house sleep deprivation is usually a shared experience.
Although I believe that my family is on the verge of gifting me a smartwatch to protect me from my own misadventures, I don’t have any personal experience with these wonders of modern technology. However, I suspect with very little tweaking a wearable sensor could be easily programmed to detect when a mother is beginning to fall asleep while she is feeding her infant. A smartwatch would be an expensive intervention and is unlikely to filter down to economically challenged families. On the other hand, this paper has reinforced our suspicions that sleep-deprived infant feeding is a significant problem. A subsidized loaner program for those families that can’t afford a smartwatch is an option that should be considered.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
In a recent survey of 1259 mothers published in the journal Pediatrics, 28% reported they had fallen asleep while feeding their babies, and 83% of those mothers reported that the sleep was unplanned. Although the study sample was small, the investigators found that sociodemographic factors did not increase the odds that a mother would fall asleep while feeding.
These numbers are not surprising, but nonetheless they are concerning because co-sleeping is a known risk factor for sudden unexplained infant death (SUID). Every parent will tell you during the first 6 months of their adventure in parenting they didn’t get enough sleep. In fact some will tell you that sleep deprivation was their chronic state for the child’s first year.
Falling asleep easily at times and places not intended for sleep is the primary symptom of sleep deprivation. SUID is the most tragic event associated with parental sleep deprivation, but it is certainly not the only one. Overtired parents are more likely to be involved in accidents and are more likely to make poor decisions, particularly those regarding how to respond to a crying or misbehaving child.
The investigators found that 24% of mothers who reported that their usual nighttime feeding location was a chair or sofa (14%). Not surprisingly, mothers who fed in chairs were less likely to fall asleep while feeding. Many of these mothers reported that they chose the chair because they thought they would be less likely to fall asleep and/or disturb other family members. One wonders how we should interpret these numbers in light of other research that has found it is “relatively less hazardous to fall asleep with an infant in the adult bed than on a chair or sofa.” Had these chair feeding mothers made the better choice under the circumstances? It would take a much larger and more granular study to answer that question.
Mothers who exclusively breastfed were more likely to fall asleep feeding than were those who partially breastfed or used formula. The investigators postulated that the infants of mothers who exclusively breastfed may have required more feedings because breast milk is more easily and quickly digested. I know this is a common explanation, but in my experience I have found that exclusively breastfed infants often use nursing as pacification and a sleep trigger and spend more time at the breast regardless of how quickly they emptied their stomachs.
This study also examined the effect of repeated educational interventions and support and found that mothers who received an intervention based on safe sleep practices were less likely to fall asleep while feeding than were the mothers who had received the intervention focused on exclusive breastfeeding value and barriers to its adoption.
Education is one avenue, particularly when it includes the mother’s partner who can play an important role as standby lifeguard to make sure the mother doesn’t fall asleep. Obviously, this is easier said than done because when there is a new baby in the house sleep deprivation is usually a shared experience.
Although I believe that my family is on the verge of gifting me a smartwatch to protect me from my own misadventures, I don’t have any personal experience with these wonders of modern technology. However, I suspect with very little tweaking a wearable sensor could be easily programmed to detect when a mother is beginning to fall asleep while she is feeding her infant. A smartwatch would be an expensive intervention and is unlikely to filter down to economically challenged families. On the other hand, this paper has reinforced our suspicions that sleep-deprived infant feeding is a significant problem. A subsidized loaner program for those families that can’t afford a smartwatch is an option that should be considered.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Fibrosis Risk High in Young Adults With Both Obesity and T2D
TOPLINE:
METHODOLOGY:
- Researchers aimed to assess the prevalence of hepatic steatosis and clinically significant fibrosis (stage ≥ 2) in young adults without a history of metabolic dysfunction–associated steatotic liver disease (MASLD), hypothesizing that the rates would be comparable with those in older adults, especially in the presence of cardiometabolic risk factors.
- Overall, 1420 participants aged 21-79 years with or without T2D (63% or 37%, respectively) were included from outpatient clinics at the University of Florida, Gainesville, Florida, and divided into two age groups: < 45 years (n = 243) and ≥ 45 years (n = 1177).
- All the participants underwent assessment of liver stiffness via transient elastography, with magnetic resonance elastography (MRE) or liver biopsy recommended when indicated.
- Participants also underwent a medical history review, physical examination, and fasting blood tests to rule out secondary causes of liver disease.
TAKEAWAY:
- Overall, 52% of participants had hepatic steatosis, and 9.5% had clinically significant fibrosis.
- There were no significant differences in the frequencies of hepatic steatosis (50.2% vs 52.7%; P = .6) or clinically significant hepatic fibrosis (7.5% vs 9.9%; P = .2) observed between young and older adults.
- The presence of either T2D or obesity was linked to an increased prevalence of both hepatic steatosis and fibrosis in both the age groups (P < .01).
- In young and older adults, the presence of both T2D and obesity led to the highest rates of both hepatic steatosis and clinically significant fibrosis, with the latter rate being statistically similar between the groups (15.7% vs 17.3%; P = .2).
- The presence of T2D and obesity was the strongest risk factors for hepatic fibrosis in young adults (odds ratios, 4.33 and 1.16, respectively; P < .05 for both).
IN PRACTICE:
“The clinical implication is that young adults with obesity and T2D carry a high risk of future cirrhosis, possibly as high as older adults, and must be aggressively screened at the first visit and carefully followed,” the authors wrote.
SOURCE:
This study, led by Anu Sharma, University of Florida College of Medicine, Gainesville, was published online in Obesity.
LIMITATIONS:
The diagnosis of clinically significant hepatic fibrosis was confirmed via MRE and/or liver biopsy in only 30% of all participants. The study population included a slightly higher proportion of young adults with obesity, T2D, and other cardiometabolic risk factors than that in national averages, which may have limited its generalizability. Genetic variants associated with MASLD were not included in this study.
DISCLOSURES:
This study was funded partly by grants from the National Institutes of Health and Echosens. One author disclosed receiving research support and serving as a consultant for various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers aimed to assess the prevalence of hepatic steatosis and clinically significant fibrosis (stage ≥ 2) in young adults without a history of metabolic dysfunction–associated steatotic liver disease (MASLD), hypothesizing that the rates would be comparable with those in older adults, especially in the presence of cardiometabolic risk factors.
- Overall, 1420 participants aged 21-79 years with or without T2D (63% or 37%, respectively) were included from outpatient clinics at the University of Florida, Gainesville, Florida, and divided into two age groups: < 45 years (n = 243) and ≥ 45 years (n = 1177).
- All the participants underwent assessment of liver stiffness via transient elastography, with magnetic resonance elastography (MRE) or liver biopsy recommended when indicated.
- Participants also underwent a medical history review, physical examination, and fasting blood tests to rule out secondary causes of liver disease.
TAKEAWAY:
- Overall, 52% of participants had hepatic steatosis, and 9.5% had clinically significant fibrosis.
- There were no significant differences in the frequencies of hepatic steatosis (50.2% vs 52.7%; P = .6) or clinically significant hepatic fibrosis (7.5% vs 9.9%; P = .2) observed between young and older adults.
- The presence of either T2D or obesity was linked to an increased prevalence of both hepatic steatosis and fibrosis in both the age groups (P < .01).
- In young and older adults, the presence of both T2D and obesity led to the highest rates of both hepatic steatosis and clinically significant fibrosis, with the latter rate being statistically similar between the groups (15.7% vs 17.3%; P = .2).
- The presence of T2D and obesity was the strongest risk factors for hepatic fibrosis in young adults (odds ratios, 4.33 and 1.16, respectively; P < .05 for both).
IN PRACTICE:
“The clinical implication is that young adults with obesity and T2D carry a high risk of future cirrhosis, possibly as high as older adults, and must be aggressively screened at the first visit and carefully followed,” the authors wrote.
SOURCE:
This study, led by Anu Sharma, University of Florida College of Medicine, Gainesville, was published online in Obesity.
LIMITATIONS:
The diagnosis of clinically significant hepatic fibrosis was confirmed via MRE and/or liver biopsy in only 30% of all participants. The study population included a slightly higher proportion of young adults with obesity, T2D, and other cardiometabolic risk factors than that in national averages, which may have limited its generalizability. Genetic variants associated with MASLD were not included in this study.
DISCLOSURES:
This study was funded partly by grants from the National Institutes of Health and Echosens. One author disclosed receiving research support and serving as a consultant for various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Researchers aimed to assess the prevalence of hepatic steatosis and clinically significant fibrosis (stage ≥ 2) in young adults without a history of metabolic dysfunction–associated steatotic liver disease (MASLD), hypothesizing that the rates would be comparable with those in older adults, especially in the presence of cardiometabolic risk factors.
- Overall, 1420 participants aged 21-79 years with or without T2D (63% or 37%, respectively) were included from outpatient clinics at the University of Florida, Gainesville, Florida, and divided into two age groups: < 45 years (n = 243) and ≥ 45 years (n = 1177).
- All the participants underwent assessment of liver stiffness via transient elastography, with magnetic resonance elastography (MRE) or liver biopsy recommended when indicated.
- Participants also underwent a medical history review, physical examination, and fasting blood tests to rule out secondary causes of liver disease.
TAKEAWAY:
- Overall, 52% of participants had hepatic steatosis, and 9.5% had clinically significant fibrosis.
- There were no significant differences in the frequencies of hepatic steatosis (50.2% vs 52.7%; P = .6) or clinically significant hepatic fibrosis (7.5% vs 9.9%; P = .2) observed between young and older adults.
- The presence of either T2D or obesity was linked to an increased prevalence of both hepatic steatosis and fibrosis in both the age groups (P < .01).
- In young and older adults, the presence of both T2D and obesity led to the highest rates of both hepatic steatosis and clinically significant fibrosis, with the latter rate being statistically similar between the groups (15.7% vs 17.3%; P = .2).
- The presence of T2D and obesity was the strongest risk factors for hepatic fibrosis in young adults (odds ratios, 4.33 and 1.16, respectively; P < .05 for both).
IN PRACTICE:
“The clinical implication is that young adults with obesity and T2D carry a high risk of future cirrhosis, possibly as high as older adults, and must be aggressively screened at the first visit and carefully followed,” the authors wrote.
SOURCE:
This study, led by Anu Sharma, University of Florida College of Medicine, Gainesville, was published online in Obesity.
LIMITATIONS:
The diagnosis of clinically significant hepatic fibrosis was confirmed via MRE and/or liver biopsy in only 30% of all participants. The study population included a slightly higher proportion of young adults with obesity, T2D, and other cardiometabolic risk factors than that in national averages, which may have limited its generalizability. Genetic variants associated with MASLD were not included in this study.
DISCLOSURES:
This study was funded partly by grants from the National Institutes of Health and Echosens. One author disclosed receiving research support and serving as a consultant for various pharmaceutical companies.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Satisfaction With Department of Veterans Affairs Prosthetics and Support Services as Reported by Women and Men Veterans
Satisfaction With Department of Veterans Affairs Prosthetics and Support Services as Reported by Women and Men Veterans
Limb loss is a significant and growing concern in the United States. Nearly 2 million Americans are living with limb loss, and up to 185,000 people undergo amputations annually.1-4 Of these patients, about 35% are women.5 The Veterans Health Administration (VHA) provides about 10% of US amputations.6-8 Between 2015 and 2019, the number of prosthetic devices provided to female veterans increased from 3.3 million to 4.6 million.5,9,10
Previous research identified disparities in prosthetic care between men and women, both within and outside the VHA. These disparities include slower prosthesis prescription and receipt among women, in addition to differences in self-reported mobility, satisfaction, rates of prosthesis rejection, and challenges related to prosthesis appearance and fit.5,10,11 Recent studies suggest women tend to have worse outcomes following amputation, and are underrepresented in amputation research.12,13 However, these disparities are poorly described in a large, national sample. Because women represent a growing portion of patients with limb loss in the VHA, understanding their needs is critical.14
The Johnny Isakson and David P. Roe, MD Veterans Health Care and Benefits Improvement Act of 2020 was enacted, in part, to improve the care provided to women veterans.15 The law required the VHA to conduct a survey of ≥ 50,000 veterans to assess the satisfaction of women veterans with prostheses provided by the VHA. To comply with this legislation and understand how women veterans rate their prostheses and related care in the VHA, the US Department of Veterans Affairs (VA) Center for Collaborative Evaluation (VACE) conducted a large national survey of veterans with limb loss that oversampled women veterans. This article describes the survey results, including characteristics of female veterans with limb loss receiving care from the VHA, assesses their satisfaction with prostheses and prosthetic care, and highlights where their responses differ from those of male veterans.
Methods
We conducted a cross-sectional, mixedmode survey of eligible amputees in the VHA Support Service Capital Assets Amputee Data Cube. We identified a cohort of veterans with any major amputation (above the ankle or wrist) or partial hand or foot amputation who received VHA care between October 1, 2019, and September 30, 2020. The final cohort yielded 46,646 potentially eligible veterans. Thirty-three had invalid contact information, leaving 46,613 veterans who were asked to participate, including 1356 women.
Survey
We created a survey instrument de novo that included questions from validated instruments, including the Trinity Amputation Prosthesis and Experience Scales to assess prosthetic device satisfaction, the Prosthesis Evaluation Questionnaire to assess quality of life (QOL) satisfaction, and the Orthotics Prosthetics Users Survey to assess prosthesis-related care satisfaction. 16-18 Additional questions were incorporated from a survey of veterans with upper limb amputation to assess the importance of cosmetic considerations related to the prosthesis and comfort with prosthesis use in intimate relationships.19 Questions were also included to assess amputation type, year of amputation, if a prosthesis was currently used, reasons for ceasing use of a prosthesis, reasons for never using a prosthesis, the types of prostheses used, intensity of prosthesis use, satisfaction with time required to receive a prosthetic limb, and if the prosthesis reflected the veteran’s selfidentified gender. Veterans were asked to answer questions based on their most recent amputation.
We tested the survey using cognitive interviews with 6 veterans to refine the survey and better understand how veterans interpreted the questions. Pilot testers completed the survey and participated in individual interviews with experienced interviewers (CL and RRK) to describe how they selected their responses.20 This feedback was used to refine the survey. The online survey was programmed using Qualtrics Software and manually translated into Spanish.
Given the multimodal design, surveys were distributed by email, text message, and US Postal Service (USPS). Surveys were emailed to all veterans for whom a valid email address was available. If emails were undeliverable, veterans were contacted via text message or the USPS. Surveys were distributed by text message to all veterans without an email address but with a cellphone number. We were unable to consistently identify invalid numbers among all text message recipients. Invitations with a survey URL and QR code were sent via USPS to veterans who had no valid email address or cellphone number. Targeted efforts were made to increase the response rate for women. A random sample of 200 women who had not completed the survey 2 weeks prior to the closing date (15% of women in sample) was selected to receive personal phone calls. Another random sample of 400 women was selected to receive personalized outreach emails. The survey data were confidential, and responses could not be traced to identifying information.
Data Analyses
We conducted a descriptive analysis, including percentages and means for responses to variables focused on describing amputation characteristics, prosthesis characteristics, and QOL. All data, including missing values, were used to document the percentage of respondents for each question. Removing missing data from the denominator when calculating percentages could introduce bias to the analysis because we cannot be certain data are missing at random. Missing variables were removed to avoid underinflation of mean scores.
We compared responses across 2 groups: individuals who self-identified as men and individuals who self-identified as women. For each question, we assessed whether each of these groups differed significantly from the remaining sample. For example, we examined whether the percentage of men who answered affirmatively to a question was significantly higher or lower than that of individuals not identifying as male, and whether the percentage of women who answered affirmatively was significantly higher or lower than that of individuals not identifying as female. We utilized x2 tests to determine significant differences for percentage calculations and t tests to determine significant differences in means across gender.
Since conducting multiple comparisons within a dataset may result in inflating statistical significance (type 1 errors), we used a more conservative estimate of statistical significance (α = 0.01) and high significance (α = 0.001). This study was deemed quality improvement by the VHA Rehabilitation and Prosthetic Services (12RPS) and acknowledged by the VA Research Office at Eastern Colorado Health Care System and was not subject to institutional review board review.
Results
Surveys were distributed to 46,613 veterans and were completed by 4981 respondents for a 10.7% overall response rate. Survey respondents were generally similar to the eligible population invited to participate, but the proportion of women who completed the survey was higher than the proportion of women eligible to participate (2.0% of eligible population vs 16.7% of respondents), likely due to specific efforts to target women. Survey respondents were slightly younger than the general population (67.3 years vs 68.7 years), less likely to be male (97.1% vs 83.3%), showed similar representation of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans (4.4% vs 4.1%), and were less likely to have diabetes (58.0% vs 52.7% had diabetes) (Table 1).
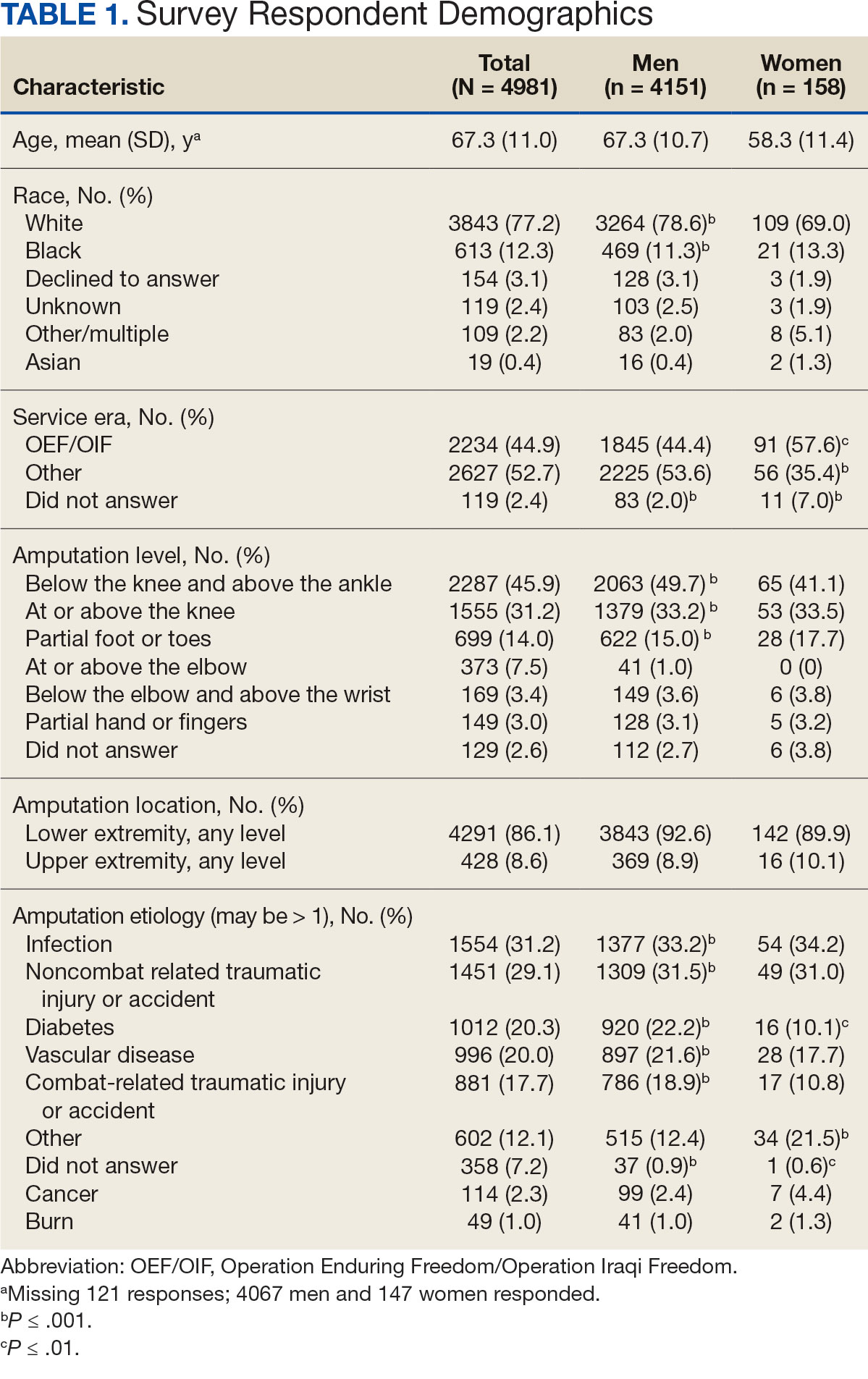
The mean age of male respondents was 67.3 years, while the mean age of female respondents was 58.3 years. The majority of respondents were male (83.3%) and White (77.2%). Female respondents were less likely to have diabetes (35.4% of women vs 53.5% of men) and less likely to report that their most recent amputation resulted from diabetes (10.1% of women vs 22.2% of men). Women respondents were more likely to report an amputation due to other causes, such as adverse results of surgery, neurologic disease, suicide attempt, blood clots, tumors, rheumatoid arthritis, and revisions of previous amputations. Most women respondents did not serve during the OEF or OIF eras. The most common amputation site for women respondents was lower limb, either below the knee and above the ankle or above the knee.
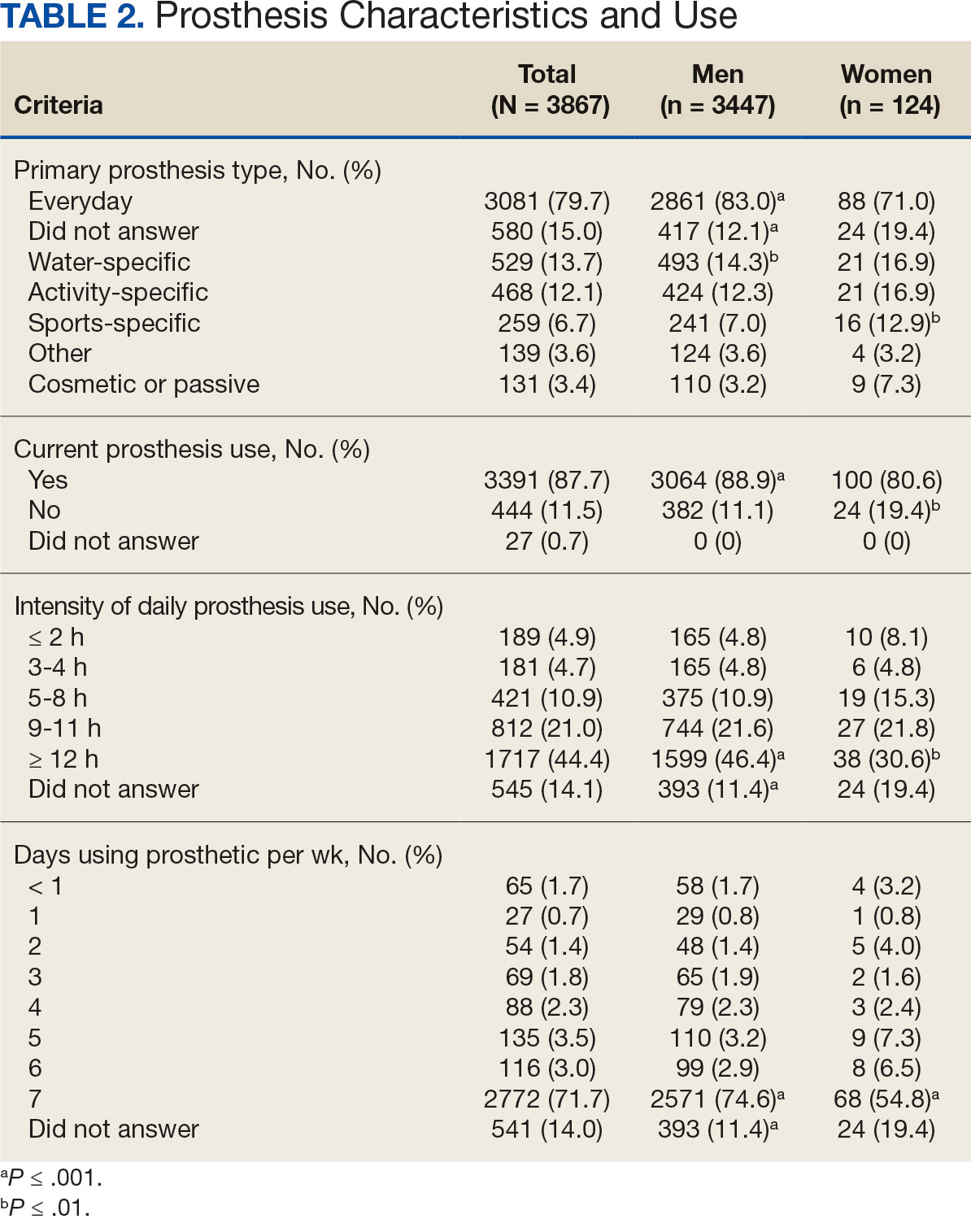
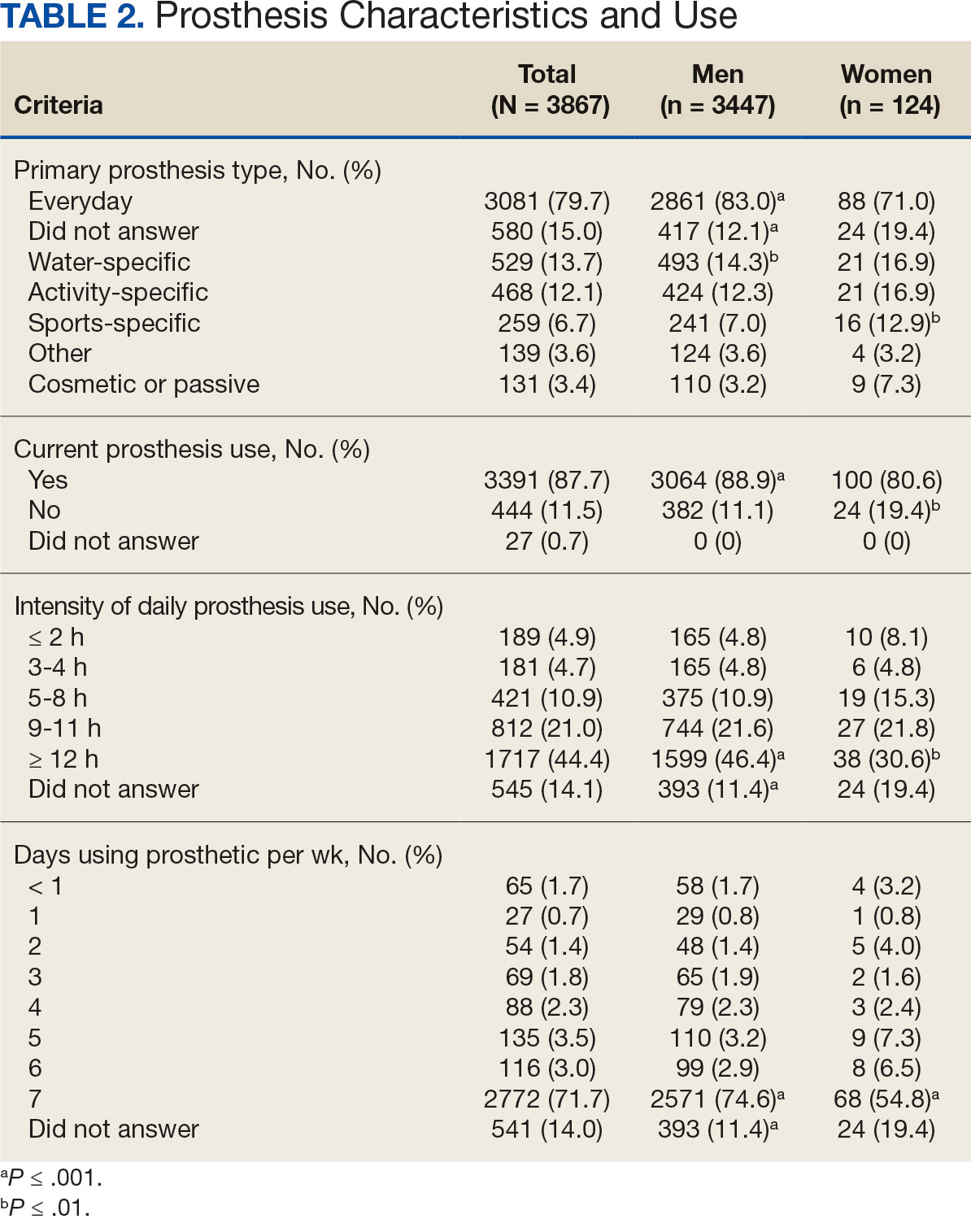
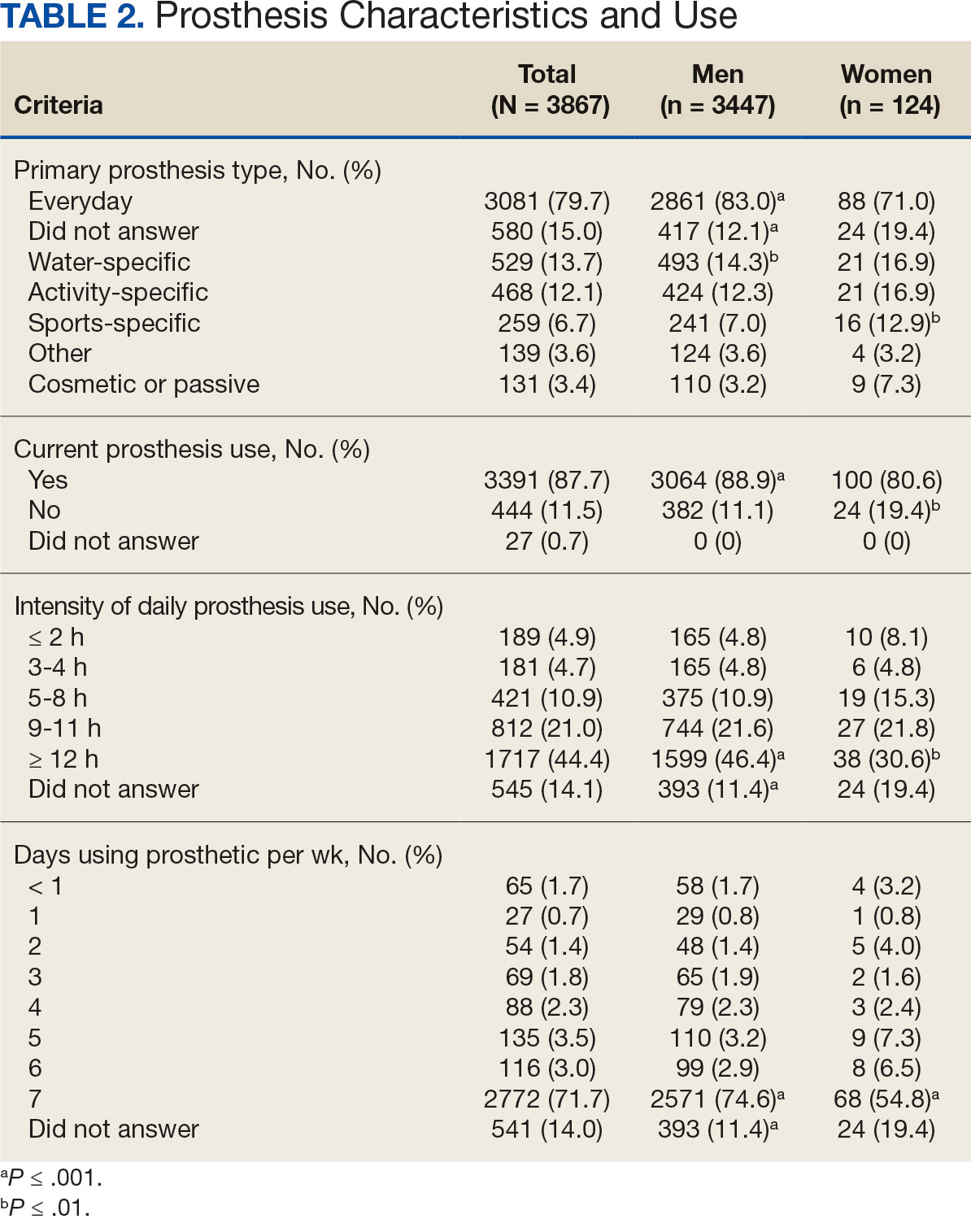
Most participants use an everyday prosthesis, but women were more likely to report using a sports-specific prosthesis (Table 2). Overall, most respondents report using a prosthesis (87.7%); however, women were more likely to report not using a prosthesis (19.4% of women vs 11.1% of men; P ≤ .01). Additionally, a lower proportion of women report using a prosthesis for < 12 hours per day (30.6% of women vs 46.4% of men; P ≤ .01) or using a prosthesis every day (54.8% of women vs 74.6% of men; P ≤ .001).
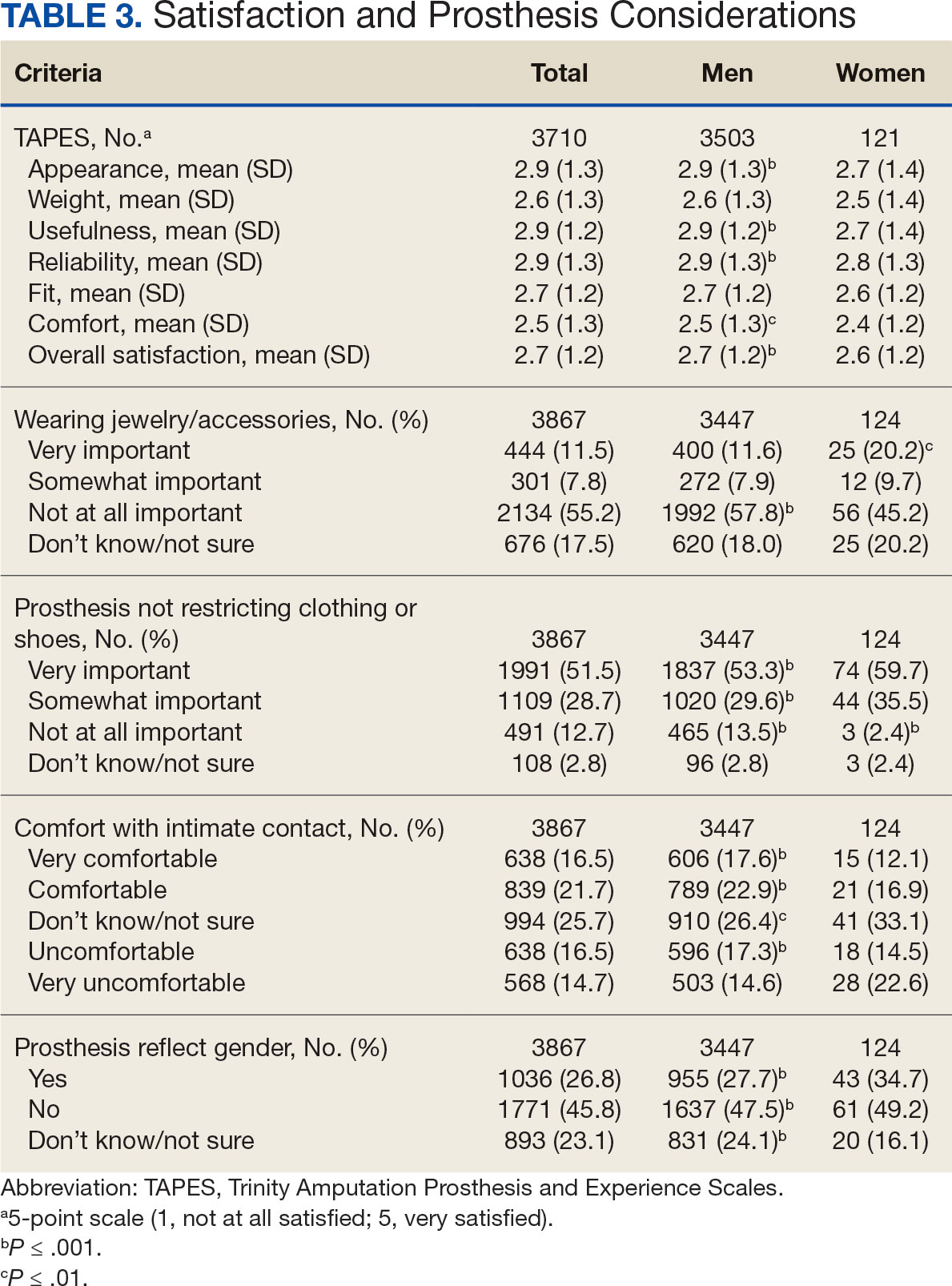
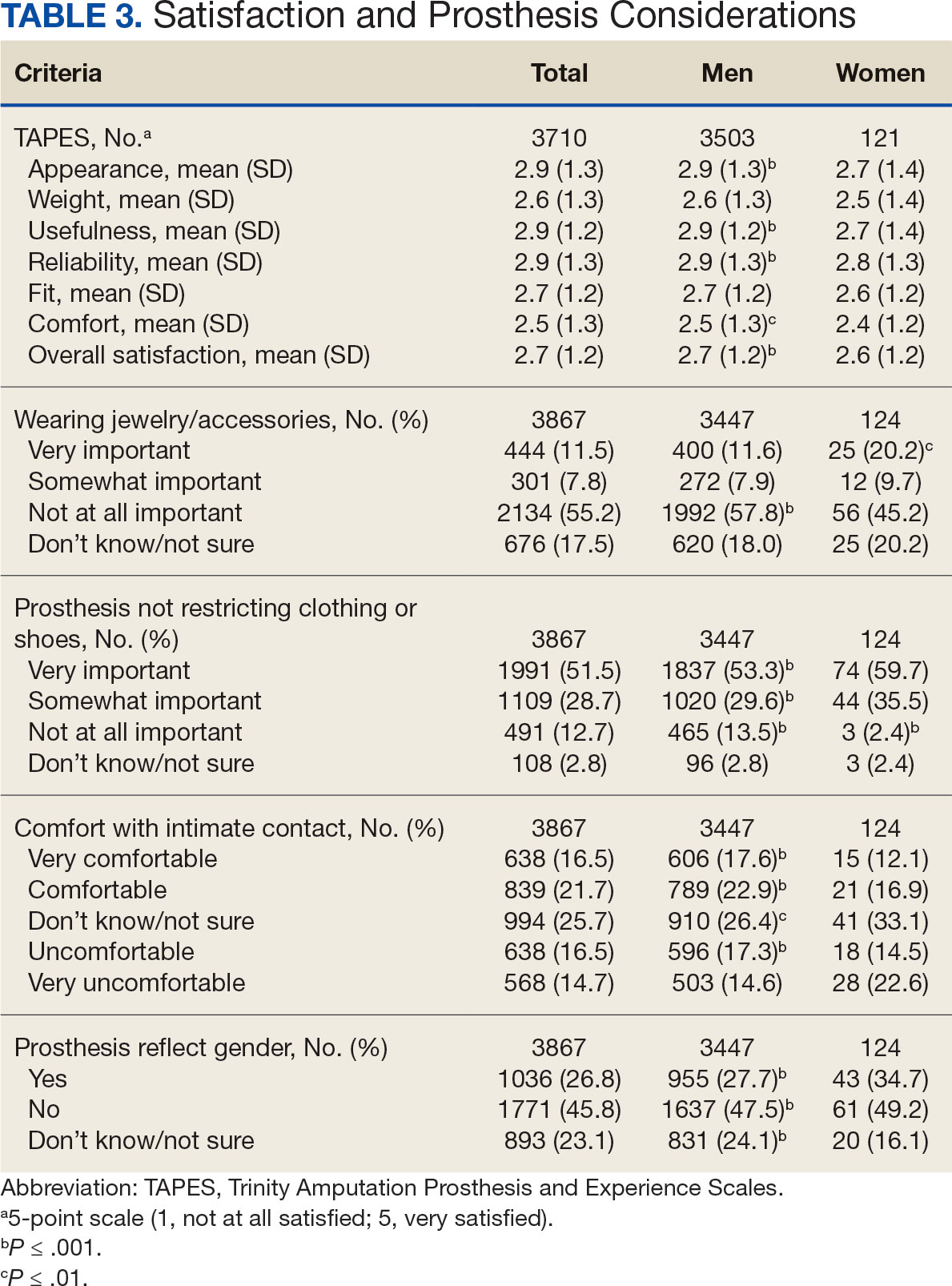
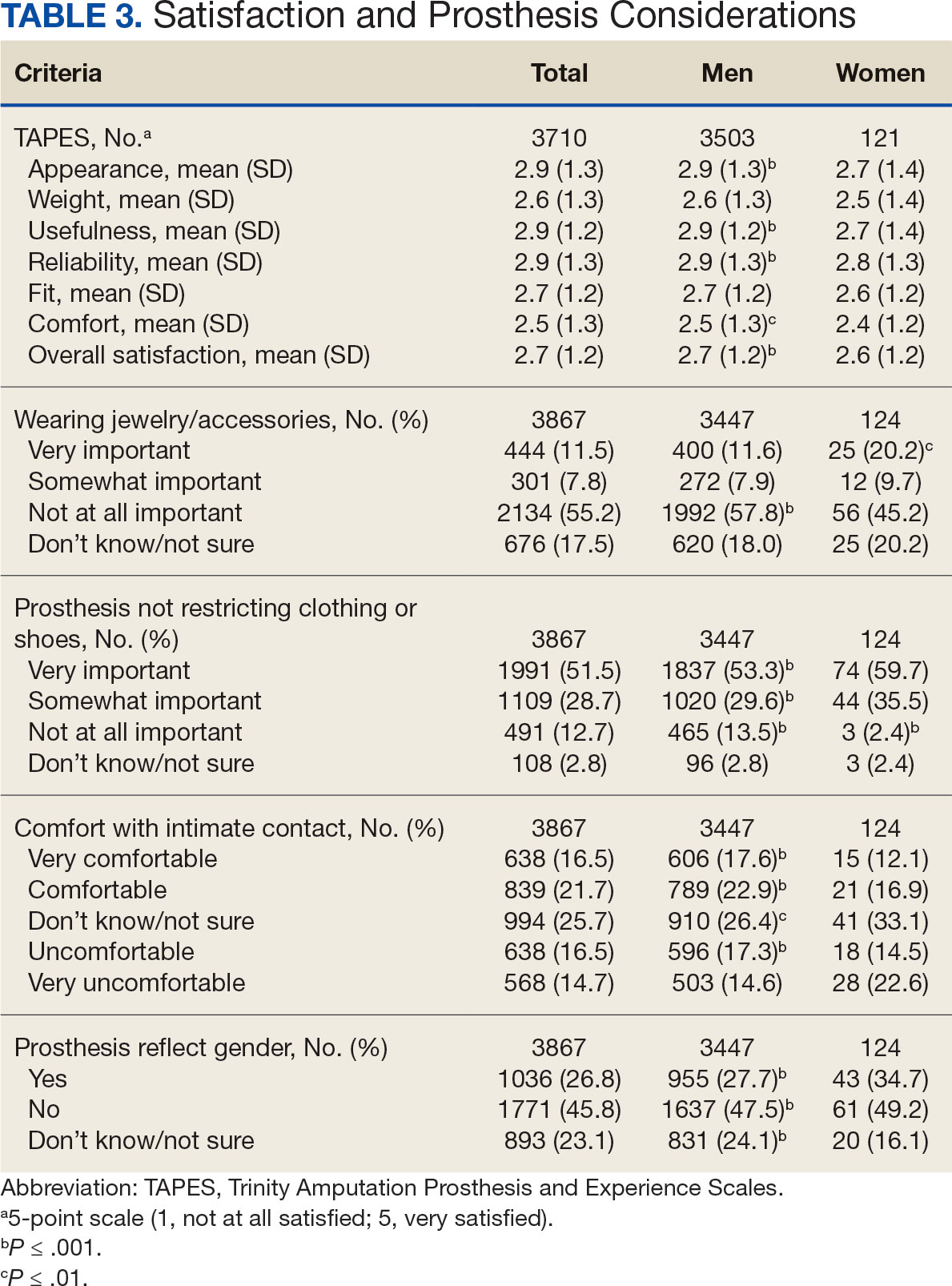
In the overall sample, the mean satisfaction score with a prosthesis was 2.7 on a 5-point scale, and women had slightly lower overall satisfaction scores (2.6 for women vs 2.7 for men; P ≤ .001) (Table 3). Women also had lower satisfaction scores related to appearance, usefulness, reliability, and comfort. Women were more likely to indicate that it was very important to be able to wear jewelry and accessories (20.2% of women vs 11.6% of men; P ≤ .01), while men were less likely to indicate that it was somewhat or very important that the prosthesis not restrict clothing or shoes (95.2% of women vs 82.9% of men; P ≤ .001). Men were more likely than women to report being comfortable or very comfortable using their prosthesis in intimate contact: 40.5% vs 29.0%, respectively (P ≤ .001).
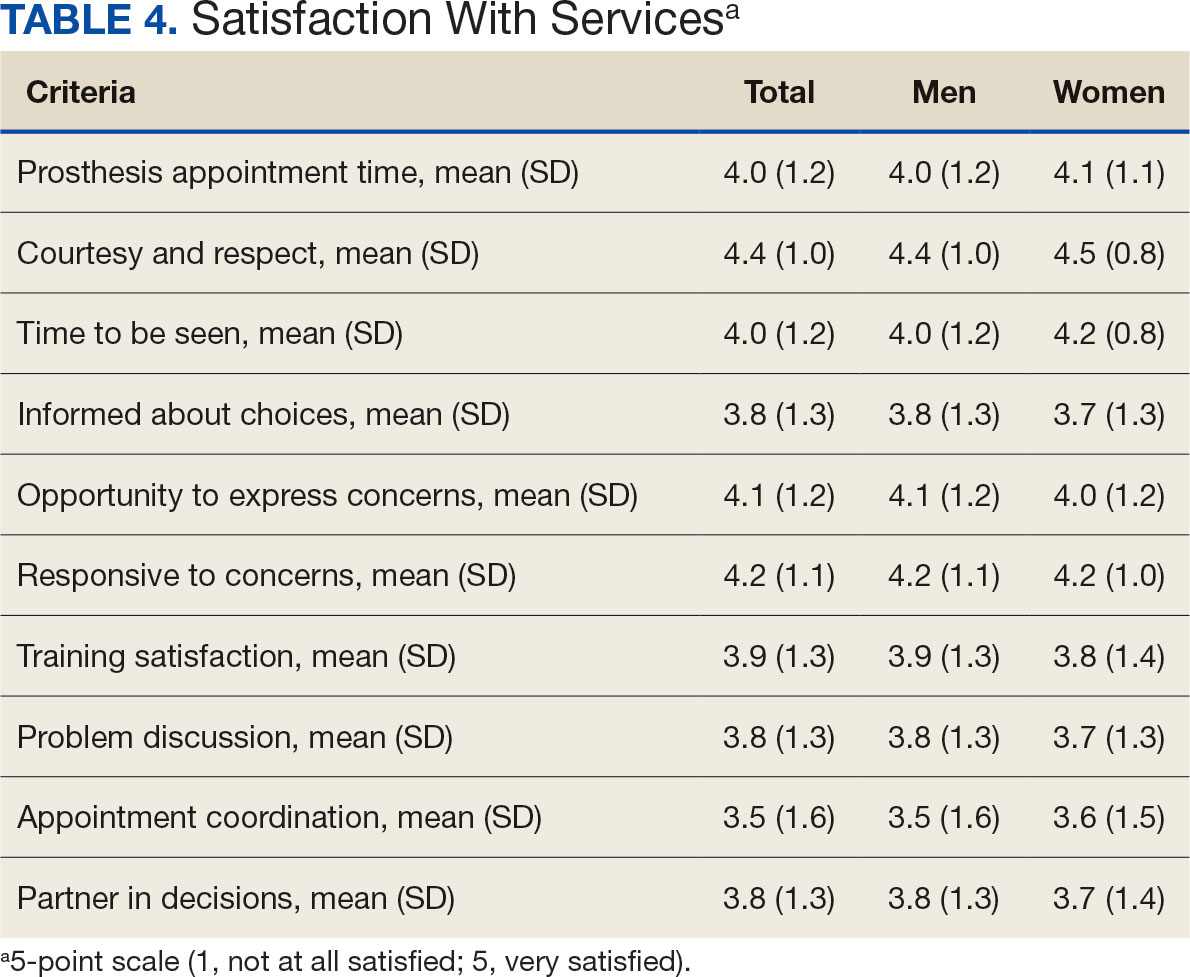
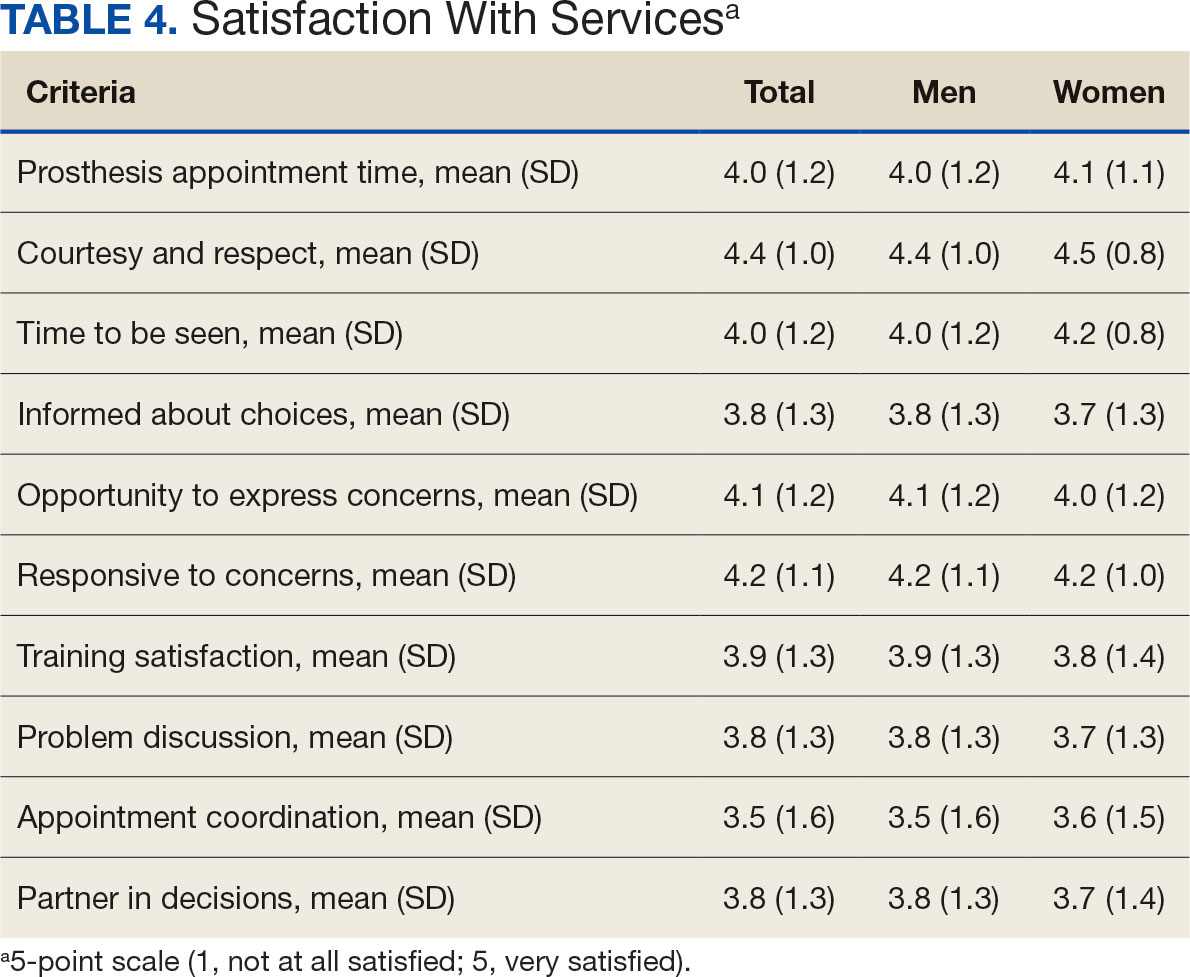
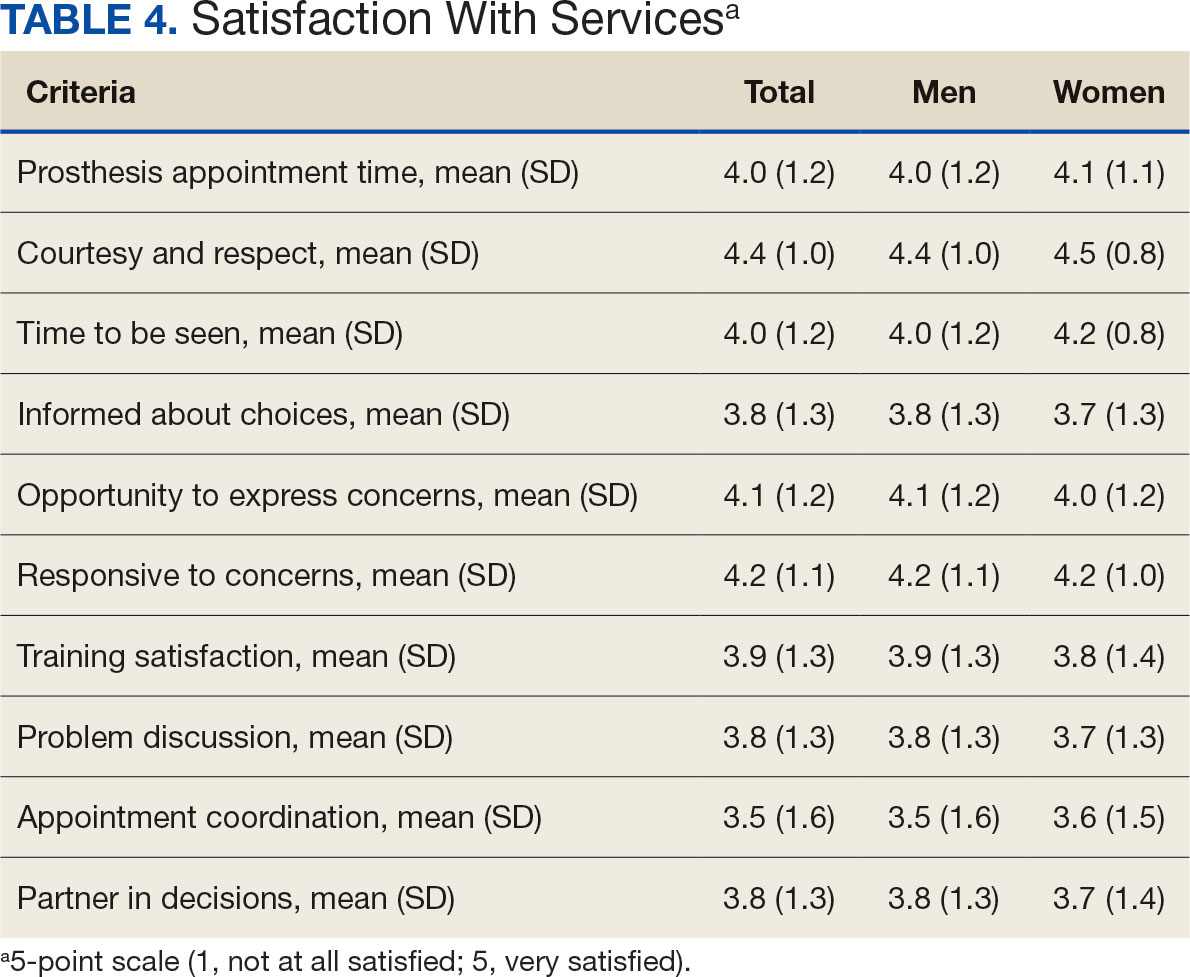
Overall, participants reported high satisfaction with appointment times, wait times, courteous treatment, opportunities to express concerns, and staff responsiveness. Men were slightly more likely than women to be satisfied with training (P ≤ 0.001) and problem discussion (P ≤ 0.01) (Table 4). There were no statistically significant differences in satisfaction or QOL ratings between women and men. The overall sample rated both QOL and satisfaction with QOL 6.7 on a 10-point scale.
Discussion
The goal of this study was to characterize the experience of veterans with limb loss receiving care in the VHA and assess their satisfaction with prostheses and prosthetic care. We received responses from nearly 5000 veterans, 158 of whom were women. Women veteran respondents were slightly younger and less likely to have an amputation due to diabetes. We did not observe significant differences in amputation level between men and women but women were less likely to use a prosthesis, reported lower intensity of prosthesis use, and were less satisfied with certain aspects of their prostheses. Women may also be less satisfied with prosthesis training and problem discussion. However, we found no differences in QOL ratings between men and women.
Findings indicating women were more likely to report not using a prosthesis and that a lower proportion of women report using a prosthesis for > 12 hours a day or every day are consistent with previous research. 21,22 Interestingly, women were more likely to report using a sports-specific prosthesis. This is notable because prior research suggests that individuals with amputations may avoid participating in sports and exercise, and a lack of access to sports-specific prostheses may inhibit physical activity.23,24 Women in this sample were slightly less satisfied with their prostheses overall and reported lower satisfaction scores regarding appearance, usefulness, reliability, and comfort, consistent with previous findings.25
A lower percentage of women in this sample reported being comfortable or very comfortable using their prosthesis during intimate contact. Previous research on prosthesis satisfaction suggests individuals who rate prosthesis satisfaction lower also report lower body image across genders. 26 While women in this sample did not rate their prosthesis satisfaction lower than men, they did report lower intensity of prosthesis use, suggesting potential issues with their prostheses this survey did not evaluate. Women indicated the importance of prostheses not restricting jewelry, accessories, clothing, or shoes. These results have significant clinical and social implications. A recent qualitative study emphasizes that women veterans feel prostheses are primarily designed for men and may not work well with their physiological needs.9 Research focused on limbs better suited to women’s bodies could result in better fitting sockets, lightweight limbs, or less bulky designs. Additional research has also explored the difficulties in accommodating a range of footwear for patients with lower limb amputation. One study found that varying footwear heights affect the function of adjustable prosthetic feet in ways that may not be optimal.27
Ratings of satisfaction with prosthesisrelated services between men and women in this sample are consistent with a recent study showing that women veterans do not have significant differences in satisfaction with prosthesis-related services.28 However, this study focused specifically on lower limb amputations, while the respondents of this study include those with both upper and lower limb amputations. Importantly, our findings that women are less likely to be satisfied with prosthesis training and problem discussions support recent qualitative findings in which women expressed a desire to work with prosthetists who listen to them, take their concerns seriously, and seek solutions that fit their needs. We did not observe a difference in QOL ratings between men and women in the sample despite lower satisfaction among women with some elements of prosthesis-related services. Previous research suggests many factors impact QOL after amputation, most notably time since amputation.16,29
Limitations
This survey was deployed in a short timeline that did not allow for careful sample selection or implementing strategies to increase response rate. Additionally, the study was conducted among veterans receiving care in the VHA, and findings may not be generalizable to limb loss in other settings. Finally, the discrepancy in number of respondents who identified as men vs women made it difficult to compare differences between the 2 groups.
Conclusions
This is the largest sample of survey respondents of veterans with limb loss to date. While the findings suggest veterans are generally satisfied with prosthetic-related services overall, they also highlight several areas for improvement with services or prostheses. Given that most veterans with limb loss are men, there is a significant discrepancy between the number of women and men respondents. Additional studies with more comparable numbers of men and women have found similar ratings of satisfaction with prostheses and services.28 Further research specifically focused on improving the experiences of women should focus on better characterizing their experiences and identifying how they differ from those of male veterans. For example, understanding how to engage female veterans with limb loss in prosthesis training and problem discussions may improve their experience with their care teams and improve their use of prostheses. Understanding experiences and needs that are specific to women could lead to the development of processes, resources, or devices that are tailored to the unique requirements of women with limb loss.
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422-429. doi:10.1016/j.apmr.2007.11.005
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the united states. South Med J. 2002;95(8):875-883. doi:10.1097/00007611-200208000-00018
- Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehabil. 2005;86(3):480-486. doi:10.1016/j.apmr.2004.06.072
- Centers for Disease Control and Prevention. Ambulatory and inpatient procedures in the United States. Accessed September 30, 2024. https://www.cdc.gov/nchs/pressroom/98facts/ambulat.htm
- Ljung J, Iacangelo A. Identifying and acknowledging a sex gap in lower-limb prosthetics. JPO. 2024;36(1):e18-e24. doi:10.1097/JPO.0000000000000470
- Feinglass J, Brown JL, LoSasso A, et al. Rates of lower-extremity amputation and arterial reconstruction in the united states, 1979 to 1996. Am J Public Health. 1999;89(8):1222- 1227. doi:10.2105/ajph.89.8.1222
- Mayfield JA, Reiber GE, Maynard C, Czerniecki JM, Caps MT, Sangeorzan BJ. Trends in lower limb amputation in the Veterans Health Administration, 1989-1998. J Rehabil Res Dev. 2000;37(1):23-30.
- Feinglass J, Pearce WH, Martin GJ, et al. Postoperative and late survival outcomes after major amputation: findings from the department of veterans affairs national surgical quality improvement program. Surgery. 2001;130(1):21-29. doi:10.1067/msy.2001.115359
- Lehavot K, Young JP, Thomas RM, et al. Voices of women veterans with lower limb prostheses: a qualitative study. J Gen Intern Med. 2022;37(3):799-805. doi:10.1007/s11606-022-07572-8
- US Government Accountability Office. COVID-19: Opportunities to improve federal response. GAO-21-60. Published November 12, 2020. Accessed September 30, 2024. https://www.gao.gov/products/gao-21-60
- Littman AJ, Peterson AC, Korpak A, et al. Differences in prosthetic prescription between men and women veterans after transtibial or transfemoral lowerextremity amputation: a longitudinal cohort study. Arch Phys Med Rehabil. 2023;104(8)1274-1281. doi:10.1016/j.amjsurg.2023.02.011
- Cimino SR, Vijayakumar A, MacKay C, Mayo AL, Hitzig SL, Guilcher SJT. Sex and gender differences in quality of life and related domains for individuals with adult acquired lower-limb amputation: a scoping review. Disabil Rehabil. 2022 Oct 23;44(22):6899-6925. doi:10.1080/09638288.2021.1974106
- DadeMatthews OO, Roper JA, Vazquez A, Shannon DM, Sefton JM. Prosthetic device and service satisfaction, quality of life, and functional performance in lower limb prosthesis clients. Prosthet Orthot Int. 2024;48(4):422-430. doi:10.1097/PXR.0000000000000285
- Hamilton AB, Schwarz EB, Thomas HN, Goldstein KM. Moving women veterans’ health research forward: a special supplement. J Gen Intern Med. 2022;37(Suppl3):665– 667. doi:10.1007/s11606-022-07606-1
- US Congress. Public Law 116-315: An Act to Improve the Lives of Veterans, S 5108 (2) (F). 116th Congress; 2021. Accessed September 30, 2024. https://www.congress.gov/116/plaws/publ315/PLAW-116publ315.pdf
- Gallagher P, MacLachlan M. The Trinity amputation and prosthesis experience scales and quality of life in people with lower-limb amputation. Arch Phys Med Rehabil. 2004;85(5):730-736. doi:10.1016/j.apmr.2003.07.009
- Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931-938. doi:10.1016/s0003-9993(98)90090-9
- Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931-938. doi:10.1016/s0003-9993(98)90090-9
- Heinemann AW, Bode RK, O’Reilly C. Development and measurement properties of the orthotics and prosthetics users’ survey (OPUS): a comprehensive set of clinical outcome instruments. Prosthet Orthot Int. 2003;27(3):191-206. doi:10.1080/03093640308726682
- Resnik LJ, Borgia ML, Clark MA. A national survey of prosthesis use in veterans with major upper limb amputation: comparisons by gender. PM R. 2020;12(11):1086-1098. doi:10.1002/pmrj.12351
- Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12(3):229-238. doi:10.1023/a:1023254226592
- Østlie K, Lesjø IM, Franklin RJ, Garfelt B, Skjeldal OH, Magnus P. Prosthesis rejection in acquired major upper-limb amputees: a population-based survey. Disabil Rehabil Assist Technol. 2012;7(4):294-303. doi:10.3109/17483107.2011.635405
- Pezzin LE, Dillingham TR, MacKenzie EJ, Ephraim P, Rossbach P. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil. 2004;85(5):723-729. doi:10.1016/j.apmr.2003.06.002
- Deans S, Burns D, McGarry A, Murray K, Mutrie N. Motivations and barriers to prosthesis users participation in physical activity, exercise and sport: a review of the literature. Prosthet Orthot Int. 2012;36(3):260-269. doi:10.1177/0309364612437905
- McDonald CL, Kahn A, Hafner BJ, Morgan SJ. Prevalence of secondary prosthesis use in lower limb prosthesis users. Disabil Rehabil. 2023;46(5):1016-1022. doi:10.1080/09638288.2023.2182919
- Baars EC, Schrier E, Dijkstra PU, Geertzen JHB. Prosthesis satisfaction in lower limb amputees: a systematic review of associated factors and questionnaires. Medicine (Baltimore). 2018;97(39):e12296. doi:10.1097/MD.0000000000012296
- Murray CD, Fox J. Body image and prosthesis satisfaction in the lower limb amputee. Disabil Rehabil. 2002;24(17):925–931. doi:10.1080/09638280210150014
- Major MJ, Quinlan J, Hansen AH, Esposito ER. Effects of women’s footwear on the mechanical function of heel-height accommodating prosthetic feet. PLoS One. 2022;17(1). doi:10.1371/journal.pone.0262910.
- Kuo PB, Lehavot K, Thomas RM, et al. Gender differences in prosthesis-related outcomes among veterans: results of a national survey of U.S. veterans. PM R. 2024;16(3):239- 249. doi:10.1002/pmrj.13028
- Asano M, Rushton P, Miller WC, Deathe BA. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int. 2008;32(2):231-243. doi:10.1080/03093640802024955
Limb loss is a significant and growing concern in the United States. Nearly 2 million Americans are living with limb loss, and up to 185,000 people undergo amputations annually.1-4 Of these patients, about 35% are women.5 The Veterans Health Administration (VHA) provides about 10% of US amputations.6-8 Between 2015 and 2019, the number of prosthetic devices provided to female veterans increased from 3.3 million to 4.6 million.5,9,10
Previous research identified disparities in prosthetic care between men and women, both within and outside the VHA. These disparities include slower prosthesis prescription and receipt among women, in addition to differences in self-reported mobility, satisfaction, rates of prosthesis rejection, and challenges related to prosthesis appearance and fit.5,10,11 Recent studies suggest women tend to have worse outcomes following amputation, and are underrepresented in amputation research.12,13 However, these disparities are poorly described in a large, national sample. Because women represent a growing portion of patients with limb loss in the VHA, understanding their needs is critical.14
The Johnny Isakson and David P. Roe, MD Veterans Health Care and Benefits Improvement Act of 2020 was enacted, in part, to improve the care provided to women veterans.15 The law required the VHA to conduct a survey of ≥ 50,000 veterans to assess the satisfaction of women veterans with prostheses provided by the VHA. To comply with this legislation and understand how women veterans rate their prostheses and related care in the VHA, the US Department of Veterans Affairs (VA) Center for Collaborative Evaluation (VACE) conducted a large national survey of veterans with limb loss that oversampled women veterans. This article describes the survey results, including characteristics of female veterans with limb loss receiving care from the VHA, assesses their satisfaction with prostheses and prosthetic care, and highlights where their responses differ from those of male veterans.
Methods
We conducted a cross-sectional, mixedmode survey of eligible amputees in the VHA Support Service Capital Assets Amputee Data Cube. We identified a cohort of veterans with any major amputation (above the ankle or wrist) or partial hand or foot amputation who received VHA care between October 1, 2019, and September 30, 2020. The final cohort yielded 46,646 potentially eligible veterans. Thirty-three had invalid contact information, leaving 46,613 veterans who were asked to participate, including 1356 women.
Survey
We created a survey instrument de novo that included questions from validated instruments, including the Trinity Amputation Prosthesis and Experience Scales to assess prosthetic device satisfaction, the Prosthesis Evaluation Questionnaire to assess quality of life (QOL) satisfaction, and the Orthotics Prosthetics Users Survey to assess prosthesis-related care satisfaction. 16-18 Additional questions were incorporated from a survey of veterans with upper limb amputation to assess the importance of cosmetic considerations related to the prosthesis and comfort with prosthesis use in intimate relationships.19 Questions were also included to assess amputation type, year of amputation, if a prosthesis was currently used, reasons for ceasing use of a prosthesis, reasons for never using a prosthesis, the types of prostheses used, intensity of prosthesis use, satisfaction with time required to receive a prosthetic limb, and if the prosthesis reflected the veteran’s selfidentified gender. Veterans were asked to answer questions based on their most recent amputation.
We tested the survey using cognitive interviews with 6 veterans to refine the survey and better understand how veterans interpreted the questions. Pilot testers completed the survey and participated in individual interviews with experienced interviewers (CL and RRK) to describe how they selected their responses.20 This feedback was used to refine the survey. The online survey was programmed using Qualtrics Software and manually translated into Spanish.
Given the multimodal design, surveys were distributed by email, text message, and US Postal Service (USPS). Surveys were emailed to all veterans for whom a valid email address was available. If emails were undeliverable, veterans were contacted via text message or the USPS. Surveys were distributed by text message to all veterans without an email address but with a cellphone number. We were unable to consistently identify invalid numbers among all text message recipients. Invitations with a survey URL and QR code were sent via USPS to veterans who had no valid email address or cellphone number. Targeted efforts were made to increase the response rate for women. A random sample of 200 women who had not completed the survey 2 weeks prior to the closing date (15% of women in sample) was selected to receive personal phone calls. Another random sample of 400 women was selected to receive personalized outreach emails. The survey data were confidential, and responses could not be traced to identifying information.
Data Analyses
We conducted a descriptive analysis, including percentages and means for responses to variables focused on describing amputation characteristics, prosthesis characteristics, and QOL. All data, including missing values, were used to document the percentage of respondents for each question. Removing missing data from the denominator when calculating percentages could introduce bias to the analysis because we cannot be certain data are missing at random. Missing variables were removed to avoid underinflation of mean scores.
We compared responses across 2 groups: individuals who self-identified as men and individuals who self-identified as women. For each question, we assessed whether each of these groups differed significantly from the remaining sample. For example, we examined whether the percentage of men who answered affirmatively to a question was significantly higher or lower than that of individuals not identifying as male, and whether the percentage of women who answered affirmatively was significantly higher or lower than that of individuals not identifying as female. We utilized x2 tests to determine significant differences for percentage calculations and t tests to determine significant differences in means across gender.
Since conducting multiple comparisons within a dataset may result in inflating statistical significance (type 1 errors), we used a more conservative estimate of statistical significance (α = 0.01) and high significance (α = 0.001). This study was deemed quality improvement by the VHA Rehabilitation and Prosthetic Services (12RPS) and acknowledged by the VA Research Office at Eastern Colorado Health Care System and was not subject to institutional review board review.
Results
Surveys were distributed to 46,613 veterans and were completed by 4981 respondents for a 10.7% overall response rate. Survey respondents were generally similar to the eligible population invited to participate, but the proportion of women who completed the survey was higher than the proportion of women eligible to participate (2.0% of eligible population vs 16.7% of respondents), likely due to specific efforts to target women. Survey respondents were slightly younger than the general population (67.3 years vs 68.7 years), less likely to be male (97.1% vs 83.3%), showed similar representation of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans (4.4% vs 4.1%), and were less likely to have diabetes (58.0% vs 52.7% had diabetes) (Table 1).
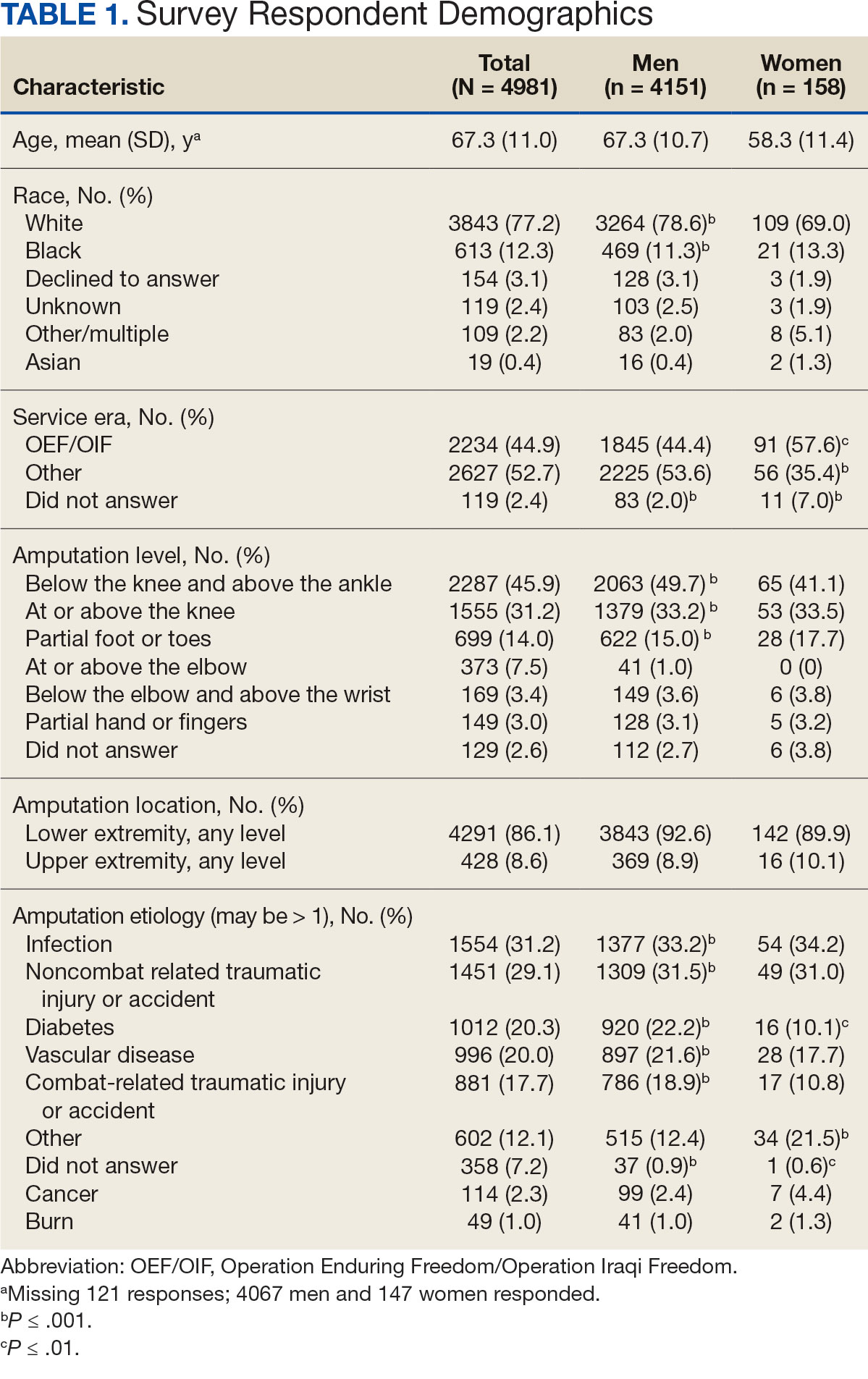
The mean age of male respondents was 67.3 years, while the mean age of female respondents was 58.3 years. The majority of respondents were male (83.3%) and White (77.2%). Female respondents were less likely to have diabetes (35.4% of women vs 53.5% of men) and less likely to report that their most recent amputation resulted from diabetes (10.1% of women vs 22.2% of men). Women respondents were more likely to report an amputation due to other causes, such as adverse results of surgery, neurologic disease, suicide attempt, blood clots, tumors, rheumatoid arthritis, and revisions of previous amputations. Most women respondents did not serve during the OEF or OIF eras. The most common amputation site for women respondents was lower limb, either below the knee and above the ankle or above the knee.
Most participants use an everyday prosthesis, but women were more likely to report using a sports-specific prosthesis (Table 2). Overall, most respondents report using a prosthesis (87.7%); however, women were more likely to report not using a prosthesis (19.4% of women vs 11.1% of men; P ≤ .01). Additionally, a lower proportion of women report using a prosthesis for < 12 hours per day (30.6% of women vs 46.4% of men; P ≤ .01) or using a prosthesis every day (54.8% of women vs 74.6% of men; P ≤ .001).
In the overall sample, the mean satisfaction score with a prosthesis was 2.7 on a 5-point scale, and women had slightly lower overall satisfaction scores (2.6 for women vs 2.7 for men; P ≤ .001) (Table 3). Women also had lower satisfaction scores related to appearance, usefulness, reliability, and comfort. Women were more likely to indicate that it was very important to be able to wear jewelry and accessories (20.2% of women vs 11.6% of men; P ≤ .01), while men were less likely to indicate that it was somewhat or very important that the prosthesis not restrict clothing or shoes (95.2% of women vs 82.9% of men; P ≤ .001). Men were more likely than women to report being comfortable or very comfortable using their prosthesis in intimate contact: 40.5% vs 29.0%, respectively (P ≤ .001).
Overall, participants reported high satisfaction with appointment times, wait times, courteous treatment, opportunities to express concerns, and staff responsiveness. Men were slightly more likely than women to be satisfied with training (P ≤ 0.001) and problem discussion (P ≤ 0.01) (Table 4). There were no statistically significant differences in satisfaction or QOL ratings between women and men. The overall sample rated both QOL and satisfaction with QOL 6.7 on a 10-point scale.
Discussion
The goal of this study was to characterize the experience of veterans with limb loss receiving care in the VHA and assess their satisfaction with prostheses and prosthetic care. We received responses from nearly 5000 veterans, 158 of whom were women. Women veteran respondents were slightly younger and less likely to have an amputation due to diabetes. We did not observe significant differences in amputation level between men and women but women were less likely to use a prosthesis, reported lower intensity of prosthesis use, and were less satisfied with certain aspects of their prostheses. Women may also be less satisfied with prosthesis training and problem discussion. However, we found no differences in QOL ratings between men and women.
Findings indicating women were more likely to report not using a prosthesis and that a lower proportion of women report using a prosthesis for > 12 hours a day or every day are consistent with previous research. 21,22 Interestingly, women were more likely to report using a sports-specific prosthesis. This is notable because prior research suggests that individuals with amputations may avoid participating in sports and exercise, and a lack of access to sports-specific prostheses may inhibit physical activity.23,24 Women in this sample were slightly less satisfied with their prostheses overall and reported lower satisfaction scores regarding appearance, usefulness, reliability, and comfort, consistent with previous findings.25
A lower percentage of women in this sample reported being comfortable or very comfortable using their prosthesis during intimate contact. Previous research on prosthesis satisfaction suggests individuals who rate prosthesis satisfaction lower also report lower body image across genders. 26 While women in this sample did not rate their prosthesis satisfaction lower than men, they did report lower intensity of prosthesis use, suggesting potential issues with their prostheses this survey did not evaluate. Women indicated the importance of prostheses not restricting jewelry, accessories, clothing, or shoes. These results have significant clinical and social implications. A recent qualitative study emphasizes that women veterans feel prostheses are primarily designed for men and may not work well with their physiological needs.9 Research focused on limbs better suited to women’s bodies could result in better fitting sockets, lightweight limbs, or less bulky designs. Additional research has also explored the difficulties in accommodating a range of footwear for patients with lower limb amputation. One study found that varying footwear heights affect the function of adjustable prosthetic feet in ways that may not be optimal.27
Ratings of satisfaction with prosthesisrelated services between men and women in this sample are consistent with a recent study showing that women veterans do not have significant differences in satisfaction with prosthesis-related services.28 However, this study focused specifically on lower limb amputations, while the respondents of this study include those with both upper and lower limb amputations. Importantly, our findings that women are less likely to be satisfied with prosthesis training and problem discussions support recent qualitative findings in which women expressed a desire to work with prosthetists who listen to them, take their concerns seriously, and seek solutions that fit their needs. We did not observe a difference in QOL ratings between men and women in the sample despite lower satisfaction among women with some elements of prosthesis-related services. Previous research suggests many factors impact QOL after amputation, most notably time since amputation.16,29
Limitations
This survey was deployed in a short timeline that did not allow for careful sample selection or implementing strategies to increase response rate. Additionally, the study was conducted among veterans receiving care in the VHA, and findings may not be generalizable to limb loss in other settings. Finally, the discrepancy in number of respondents who identified as men vs women made it difficult to compare differences between the 2 groups.
Conclusions
This is the largest sample of survey respondents of veterans with limb loss to date. While the findings suggest veterans are generally satisfied with prosthetic-related services overall, they also highlight several areas for improvement with services or prostheses. Given that most veterans with limb loss are men, there is a significant discrepancy between the number of women and men respondents. Additional studies with more comparable numbers of men and women have found similar ratings of satisfaction with prostheses and services.28 Further research specifically focused on improving the experiences of women should focus on better characterizing their experiences and identifying how they differ from those of male veterans. For example, understanding how to engage female veterans with limb loss in prosthesis training and problem discussions may improve their experience with their care teams and improve their use of prostheses. Understanding experiences and needs that are specific to women could lead to the development of processes, resources, or devices that are tailored to the unique requirements of women with limb loss.
Limb loss is a significant and growing concern in the United States. Nearly 2 million Americans are living with limb loss, and up to 185,000 people undergo amputations annually.1-4 Of these patients, about 35% are women.5 The Veterans Health Administration (VHA) provides about 10% of US amputations.6-8 Between 2015 and 2019, the number of prosthetic devices provided to female veterans increased from 3.3 million to 4.6 million.5,9,10
Previous research identified disparities in prosthetic care between men and women, both within and outside the VHA. These disparities include slower prosthesis prescription and receipt among women, in addition to differences in self-reported mobility, satisfaction, rates of prosthesis rejection, and challenges related to prosthesis appearance and fit.5,10,11 Recent studies suggest women tend to have worse outcomes following amputation, and are underrepresented in amputation research.12,13 However, these disparities are poorly described in a large, national sample. Because women represent a growing portion of patients with limb loss in the VHA, understanding their needs is critical.14
The Johnny Isakson and David P. Roe, MD Veterans Health Care and Benefits Improvement Act of 2020 was enacted, in part, to improve the care provided to women veterans.15 The law required the VHA to conduct a survey of ≥ 50,000 veterans to assess the satisfaction of women veterans with prostheses provided by the VHA. To comply with this legislation and understand how women veterans rate their prostheses and related care in the VHA, the US Department of Veterans Affairs (VA) Center for Collaborative Evaluation (VACE) conducted a large national survey of veterans with limb loss that oversampled women veterans. This article describes the survey results, including characteristics of female veterans with limb loss receiving care from the VHA, assesses their satisfaction with prostheses and prosthetic care, and highlights where their responses differ from those of male veterans.
Methods
We conducted a cross-sectional, mixedmode survey of eligible amputees in the VHA Support Service Capital Assets Amputee Data Cube. We identified a cohort of veterans with any major amputation (above the ankle or wrist) or partial hand or foot amputation who received VHA care between October 1, 2019, and September 30, 2020. The final cohort yielded 46,646 potentially eligible veterans. Thirty-three had invalid contact information, leaving 46,613 veterans who were asked to participate, including 1356 women.
Survey
We created a survey instrument de novo that included questions from validated instruments, including the Trinity Amputation Prosthesis and Experience Scales to assess prosthetic device satisfaction, the Prosthesis Evaluation Questionnaire to assess quality of life (QOL) satisfaction, and the Orthotics Prosthetics Users Survey to assess prosthesis-related care satisfaction. 16-18 Additional questions were incorporated from a survey of veterans with upper limb amputation to assess the importance of cosmetic considerations related to the prosthesis and comfort with prosthesis use in intimate relationships.19 Questions were also included to assess amputation type, year of amputation, if a prosthesis was currently used, reasons for ceasing use of a prosthesis, reasons for never using a prosthesis, the types of prostheses used, intensity of prosthesis use, satisfaction with time required to receive a prosthetic limb, and if the prosthesis reflected the veteran’s selfidentified gender. Veterans were asked to answer questions based on their most recent amputation.
We tested the survey using cognitive interviews with 6 veterans to refine the survey and better understand how veterans interpreted the questions. Pilot testers completed the survey and participated in individual interviews with experienced interviewers (CL and RRK) to describe how they selected their responses.20 This feedback was used to refine the survey. The online survey was programmed using Qualtrics Software and manually translated into Spanish.
Given the multimodal design, surveys were distributed by email, text message, and US Postal Service (USPS). Surveys were emailed to all veterans for whom a valid email address was available. If emails were undeliverable, veterans were contacted via text message or the USPS. Surveys were distributed by text message to all veterans without an email address but with a cellphone number. We were unable to consistently identify invalid numbers among all text message recipients. Invitations with a survey URL and QR code were sent via USPS to veterans who had no valid email address or cellphone number. Targeted efforts were made to increase the response rate for women. A random sample of 200 women who had not completed the survey 2 weeks prior to the closing date (15% of women in sample) was selected to receive personal phone calls. Another random sample of 400 women was selected to receive personalized outreach emails. The survey data were confidential, and responses could not be traced to identifying information.
Data Analyses
We conducted a descriptive analysis, including percentages and means for responses to variables focused on describing amputation characteristics, prosthesis characteristics, and QOL. All data, including missing values, were used to document the percentage of respondents for each question. Removing missing data from the denominator when calculating percentages could introduce bias to the analysis because we cannot be certain data are missing at random. Missing variables were removed to avoid underinflation of mean scores.
We compared responses across 2 groups: individuals who self-identified as men and individuals who self-identified as women. For each question, we assessed whether each of these groups differed significantly from the remaining sample. For example, we examined whether the percentage of men who answered affirmatively to a question was significantly higher or lower than that of individuals not identifying as male, and whether the percentage of women who answered affirmatively was significantly higher or lower than that of individuals not identifying as female. We utilized x2 tests to determine significant differences for percentage calculations and t tests to determine significant differences in means across gender.
Since conducting multiple comparisons within a dataset may result in inflating statistical significance (type 1 errors), we used a more conservative estimate of statistical significance (α = 0.01) and high significance (α = 0.001). This study was deemed quality improvement by the VHA Rehabilitation and Prosthetic Services (12RPS) and acknowledged by the VA Research Office at Eastern Colorado Health Care System and was not subject to institutional review board review.
Results
Surveys were distributed to 46,613 veterans and were completed by 4981 respondents for a 10.7% overall response rate. Survey respondents were generally similar to the eligible population invited to participate, but the proportion of women who completed the survey was higher than the proportion of women eligible to participate (2.0% of eligible population vs 16.7% of respondents), likely due to specific efforts to target women. Survey respondents were slightly younger than the general population (67.3 years vs 68.7 years), less likely to be male (97.1% vs 83.3%), showed similar representation of Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans (4.4% vs 4.1%), and were less likely to have diabetes (58.0% vs 52.7% had diabetes) (Table 1).
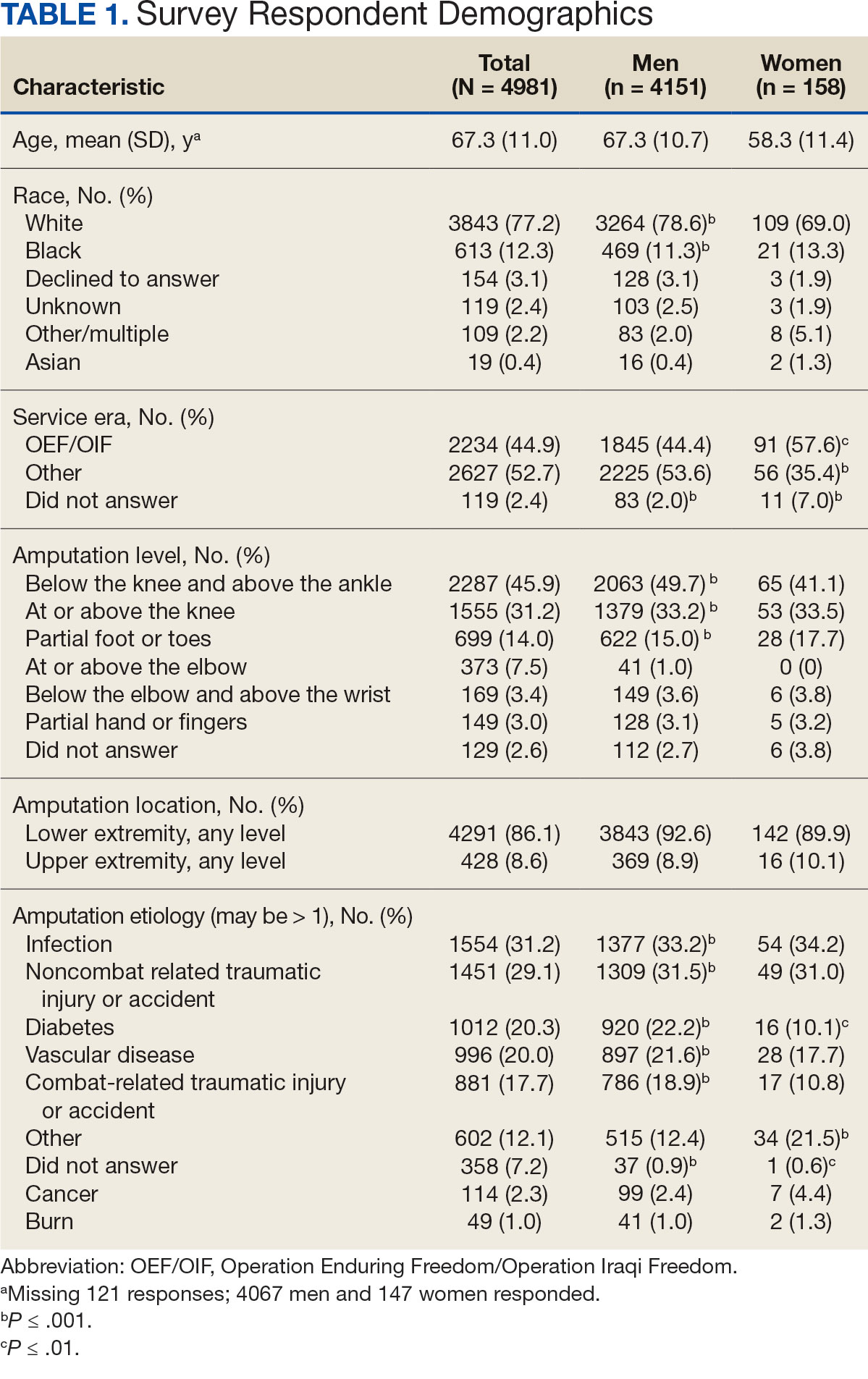
The mean age of male respondents was 67.3 years, while the mean age of female respondents was 58.3 years. The majority of respondents were male (83.3%) and White (77.2%). Female respondents were less likely to have diabetes (35.4% of women vs 53.5% of men) and less likely to report that their most recent amputation resulted from diabetes (10.1% of women vs 22.2% of men). Women respondents were more likely to report an amputation due to other causes, such as adverse results of surgery, neurologic disease, suicide attempt, blood clots, tumors, rheumatoid arthritis, and revisions of previous amputations. Most women respondents did not serve during the OEF or OIF eras. The most common amputation site for women respondents was lower limb, either below the knee and above the ankle or above the knee.
Most participants use an everyday prosthesis, but women were more likely to report using a sports-specific prosthesis (Table 2). Overall, most respondents report using a prosthesis (87.7%); however, women were more likely to report not using a prosthesis (19.4% of women vs 11.1% of men; P ≤ .01). Additionally, a lower proportion of women report using a prosthesis for < 12 hours per day (30.6% of women vs 46.4% of men; P ≤ .01) or using a prosthesis every day (54.8% of women vs 74.6% of men; P ≤ .001).
In the overall sample, the mean satisfaction score with a prosthesis was 2.7 on a 5-point scale, and women had slightly lower overall satisfaction scores (2.6 for women vs 2.7 for men; P ≤ .001) (Table 3). Women also had lower satisfaction scores related to appearance, usefulness, reliability, and comfort. Women were more likely to indicate that it was very important to be able to wear jewelry and accessories (20.2% of women vs 11.6% of men; P ≤ .01), while men were less likely to indicate that it was somewhat or very important that the prosthesis not restrict clothing or shoes (95.2% of women vs 82.9% of men; P ≤ .001). Men were more likely than women to report being comfortable or very comfortable using their prosthesis in intimate contact: 40.5% vs 29.0%, respectively (P ≤ .001).
Overall, participants reported high satisfaction with appointment times, wait times, courteous treatment, opportunities to express concerns, and staff responsiveness. Men were slightly more likely than women to be satisfied with training (P ≤ 0.001) and problem discussion (P ≤ 0.01) (Table 4). There were no statistically significant differences in satisfaction or QOL ratings between women and men. The overall sample rated both QOL and satisfaction with QOL 6.7 on a 10-point scale.
Discussion
The goal of this study was to characterize the experience of veterans with limb loss receiving care in the VHA and assess their satisfaction with prostheses and prosthetic care. We received responses from nearly 5000 veterans, 158 of whom were women. Women veteran respondents were slightly younger and less likely to have an amputation due to diabetes. We did not observe significant differences in amputation level between men and women but women were less likely to use a prosthesis, reported lower intensity of prosthesis use, and were less satisfied with certain aspects of their prostheses. Women may also be less satisfied with prosthesis training and problem discussion. However, we found no differences in QOL ratings between men and women.
Findings indicating women were more likely to report not using a prosthesis and that a lower proportion of women report using a prosthesis for > 12 hours a day or every day are consistent with previous research. 21,22 Interestingly, women were more likely to report using a sports-specific prosthesis. This is notable because prior research suggests that individuals with amputations may avoid participating in sports and exercise, and a lack of access to sports-specific prostheses may inhibit physical activity.23,24 Women in this sample were slightly less satisfied with their prostheses overall and reported lower satisfaction scores regarding appearance, usefulness, reliability, and comfort, consistent with previous findings.25
A lower percentage of women in this sample reported being comfortable or very comfortable using their prosthesis during intimate contact. Previous research on prosthesis satisfaction suggests individuals who rate prosthesis satisfaction lower also report lower body image across genders. 26 While women in this sample did not rate their prosthesis satisfaction lower than men, they did report lower intensity of prosthesis use, suggesting potential issues with their prostheses this survey did not evaluate. Women indicated the importance of prostheses not restricting jewelry, accessories, clothing, or shoes. These results have significant clinical and social implications. A recent qualitative study emphasizes that women veterans feel prostheses are primarily designed for men and may not work well with their physiological needs.9 Research focused on limbs better suited to women’s bodies could result in better fitting sockets, lightweight limbs, or less bulky designs. Additional research has also explored the difficulties in accommodating a range of footwear for patients with lower limb amputation. One study found that varying footwear heights affect the function of adjustable prosthetic feet in ways that may not be optimal.27
Ratings of satisfaction with prosthesisrelated services between men and women in this sample are consistent with a recent study showing that women veterans do not have significant differences in satisfaction with prosthesis-related services.28 However, this study focused specifically on lower limb amputations, while the respondents of this study include those with both upper and lower limb amputations. Importantly, our findings that women are less likely to be satisfied with prosthesis training and problem discussions support recent qualitative findings in which women expressed a desire to work with prosthetists who listen to them, take their concerns seriously, and seek solutions that fit their needs. We did not observe a difference in QOL ratings between men and women in the sample despite lower satisfaction among women with some elements of prosthesis-related services. Previous research suggests many factors impact QOL after amputation, most notably time since amputation.16,29
Limitations
This survey was deployed in a short timeline that did not allow for careful sample selection or implementing strategies to increase response rate. Additionally, the study was conducted among veterans receiving care in the VHA, and findings may not be generalizable to limb loss in other settings. Finally, the discrepancy in number of respondents who identified as men vs women made it difficult to compare differences between the 2 groups.
Conclusions
This is the largest sample of survey respondents of veterans with limb loss to date. While the findings suggest veterans are generally satisfied with prosthetic-related services overall, they also highlight several areas for improvement with services or prostheses. Given that most veterans with limb loss are men, there is a significant discrepancy between the number of women and men respondents. Additional studies with more comparable numbers of men and women have found similar ratings of satisfaction with prostheses and services.28 Further research specifically focused on improving the experiences of women should focus on better characterizing their experiences and identifying how they differ from those of male veterans. For example, understanding how to engage female veterans with limb loss in prosthesis training and problem discussions may improve their experience with their care teams and improve their use of prostheses. Understanding experiences and needs that are specific to women could lead to the development of processes, resources, or devices that are tailored to the unique requirements of women with limb loss.
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422-429. doi:10.1016/j.apmr.2007.11.005
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the united states. South Med J. 2002;95(8):875-883. doi:10.1097/00007611-200208000-00018
- Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehabil. 2005;86(3):480-486. doi:10.1016/j.apmr.2004.06.072
- Centers for Disease Control and Prevention. Ambulatory and inpatient procedures in the United States. Accessed September 30, 2024. https://www.cdc.gov/nchs/pressroom/98facts/ambulat.htm
- Ljung J, Iacangelo A. Identifying and acknowledging a sex gap in lower-limb prosthetics. JPO. 2024;36(1):e18-e24. doi:10.1097/JPO.0000000000000470
- Feinglass J, Brown JL, LoSasso A, et al. Rates of lower-extremity amputation and arterial reconstruction in the united states, 1979 to 1996. Am J Public Health. 1999;89(8):1222- 1227. doi:10.2105/ajph.89.8.1222
- Mayfield JA, Reiber GE, Maynard C, Czerniecki JM, Caps MT, Sangeorzan BJ. Trends in lower limb amputation in the Veterans Health Administration, 1989-1998. J Rehabil Res Dev. 2000;37(1):23-30.
- Feinglass J, Pearce WH, Martin GJ, et al. Postoperative and late survival outcomes after major amputation: findings from the department of veterans affairs national surgical quality improvement program. Surgery. 2001;130(1):21-29. doi:10.1067/msy.2001.115359
- Lehavot K, Young JP, Thomas RM, et al. Voices of women veterans with lower limb prostheses: a qualitative study. J Gen Intern Med. 2022;37(3):799-805. doi:10.1007/s11606-022-07572-8
- US Government Accountability Office. COVID-19: Opportunities to improve federal response. GAO-21-60. Published November 12, 2020. Accessed September 30, 2024. https://www.gao.gov/products/gao-21-60
- Littman AJ, Peterson AC, Korpak A, et al. Differences in prosthetic prescription between men and women veterans after transtibial or transfemoral lowerextremity amputation: a longitudinal cohort study. Arch Phys Med Rehabil. 2023;104(8)1274-1281. doi:10.1016/j.amjsurg.2023.02.011
- Cimino SR, Vijayakumar A, MacKay C, Mayo AL, Hitzig SL, Guilcher SJT. Sex and gender differences in quality of life and related domains for individuals with adult acquired lower-limb amputation: a scoping review. Disabil Rehabil. 2022 Oct 23;44(22):6899-6925. doi:10.1080/09638288.2021.1974106
- DadeMatthews OO, Roper JA, Vazquez A, Shannon DM, Sefton JM. Prosthetic device and service satisfaction, quality of life, and functional performance in lower limb prosthesis clients. Prosthet Orthot Int. 2024;48(4):422-430. doi:10.1097/PXR.0000000000000285
- Hamilton AB, Schwarz EB, Thomas HN, Goldstein KM. Moving women veterans’ health research forward: a special supplement. J Gen Intern Med. 2022;37(Suppl3):665– 667. doi:10.1007/s11606-022-07606-1
- US Congress. Public Law 116-315: An Act to Improve the Lives of Veterans, S 5108 (2) (F). 116th Congress; 2021. Accessed September 30, 2024. https://www.congress.gov/116/plaws/publ315/PLAW-116publ315.pdf
- Gallagher P, MacLachlan M. The Trinity amputation and prosthesis experience scales and quality of life in people with lower-limb amputation. Arch Phys Med Rehabil. 2004;85(5):730-736. doi:10.1016/j.apmr.2003.07.009
- Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931-938. doi:10.1016/s0003-9993(98)90090-9
- Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931-938. doi:10.1016/s0003-9993(98)90090-9
- Heinemann AW, Bode RK, O’Reilly C. Development and measurement properties of the orthotics and prosthetics users’ survey (OPUS): a comprehensive set of clinical outcome instruments. Prosthet Orthot Int. 2003;27(3):191-206. doi:10.1080/03093640308726682
- Resnik LJ, Borgia ML, Clark MA. A national survey of prosthesis use in veterans with major upper limb amputation: comparisons by gender. PM R. 2020;12(11):1086-1098. doi:10.1002/pmrj.12351
- Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12(3):229-238. doi:10.1023/a:1023254226592
- Østlie K, Lesjø IM, Franklin RJ, Garfelt B, Skjeldal OH, Magnus P. Prosthesis rejection in acquired major upper-limb amputees: a population-based survey. Disabil Rehabil Assist Technol. 2012;7(4):294-303. doi:10.3109/17483107.2011.635405
- Pezzin LE, Dillingham TR, MacKenzie EJ, Ephraim P, Rossbach P. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil. 2004;85(5):723-729. doi:10.1016/j.apmr.2003.06.002
- Deans S, Burns D, McGarry A, Murray K, Mutrie N. Motivations and barriers to prosthesis users participation in physical activity, exercise and sport: a review of the literature. Prosthet Orthot Int. 2012;36(3):260-269. doi:10.1177/0309364612437905
- McDonald CL, Kahn A, Hafner BJ, Morgan SJ. Prevalence of secondary prosthesis use in lower limb prosthesis users. Disabil Rehabil. 2023;46(5):1016-1022. doi:10.1080/09638288.2023.2182919
- Baars EC, Schrier E, Dijkstra PU, Geertzen JHB. Prosthesis satisfaction in lower limb amputees: a systematic review of associated factors and questionnaires. Medicine (Baltimore). 2018;97(39):e12296. doi:10.1097/MD.0000000000012296
- Murray CD, Fox J. Body image and prosthesis satisfaction in the lower limb amputee. Disabil Rehabil. 2002;24(17):925–931. doi:10.1080/09638280210150014
- Major MJ, Quinlan J, Hansen AH, Esposito ER. Effects of women’s footwear on the mechanical function of heel-height accommodating prosthetic feet. PLoS One. 2022;17(1). doi:10.1371/journal.pone.0262910.
- Kuo PB, Lehavot K, Thomas RM, et al. Gender differences in prosthesis-related outcomes among veterans: results of a national survey of U.S. veterans. PM R. 2024;16(3):239- 249. doi:10.1002/pmrj.13028
- Asano M, Rushton P, Miller WC, Deathe BA. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int. 2008;32(2):231-243. doi:10.1080/03093640802024955
- Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422-429. doi:10.1016/j.apmr.2007.11.005
- Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the united states. South Med J. 2002;95(8):875-883. doi:10.1097/00007611-200208000-00018
- Dillingham TR, Pezzin LE, Shore AD. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch Phys Med Rehabil. 2005;86(3):480-486. doi:10.1016/j.apmr.2004.06.072
- Centers for Disease Control and Prevention. Ambulatory and inpatient procedures in the United States. Accessed September 30, 2024. https://www.cdc.gov/nchs/pressroom/98facts/ambulat.htm
- Ljung J, Iacangelo A. Identifying and acknowledging a sex gap in lower-limb prosthetics. JPO. 2024;36(1):e18-e24. doi:10.1097/JPO.0000000000000470
- Feinglass J, Brown JL, LoSasso A, et al. Rates of lower-extremity amputation and arterial reconstruction in the united states, 1979 to 1996. Am J Public Health. 1999;89(8):1222- 1227. doi:10.2105/ajph.89.8.1222
- Mayfield JA, Reiber GE, Maynard C, Czerniecki JM, Caps MT, Sangeorzan BJ. Trends in lower limb amputation in the Veterans Health Administration, 1989-1998. J Rehabil Res Dev. 2000;37(1):23-30.
- Feinglass J, Pearce WH, Martin GJ, et al. Postoperative and late survival outcomes after major amputation: findings from the department of veterans affairs national surgical quality improvement program. Surgery. 2001;130(1):21-29. doi:10.1067/msy.2001.115359
- Lehavot K, Young JP, Thomas RM, et al. Voices of women veterans with lower limb prostheses: a qualitative study. J Gen Intern Med. 2022;37(3):799-805. doi:10.1007/s11606-022-07572-8
- US Government Accountability Office. COVID-19: Opportunities to improve federal response. GAO-21-60. Published November 12, 2020. Accessed September 30, 2024. https://www.gao.gov/products/gao-21-60
- Littman AJ, Peterson AC, Korpak A, et al. Differences in prosthetic prescription between men and women veterans after transtibial or transfemoral lowerextremity amputation: a longitudinal cohort study. Arch Phys Med Rehabil. 2023;104(8)1274-1281. doi:10.1016/j.amjsurg.2023.02.011
- Cimino SR, Vijayakumar A, MacKay C, Mayo AL, Hitzig SL, Guilcher SJT. Sex and gender differences in quality of life and related domains for individuals with adult acquired lower-limb amputation: a scoping review. Disabil Rehabil. 2022 Oct 23;44(22):6899-6925. doi:10.1080/09638288.2021.1974106
- DadeMatthews OO, Roper JA, Vazquez A, Shannon DM, Sefton JM. Prosthetic device and service satisfaction, quality of life, and functional performance in lower limb prosthesis clients. Prosthet Orthot Int. 2024;48(4):422-430. doi:10.1097/PXR.0000000000000285
- Hamilton AB, Schwarz EB, Thomas HN, Goldstein KM. Moving women veterans’ health research forward: a special supplement. J Gen Intern Med. 2022;37(Suppl3):665– 667. doi:10.1007/s11606-022-07606-1
- US Congress. Public Law 116-315: An Act to Improve the Lives of Veterans, S 5108 (2) (F). 116th Congress; 2021. Accessed September 30, 2024. https://www.congress.gov/116/plaws/publ315/PLAW-116publ315.pdf
- Gallagher P, MacLachlan M. The Trinity amputation and prosthesis experience scales and quality of life in people with lower-limb amputation. Arch Phys Med Rehabil. 2004;85(5):730-736. doi:10.1016/j.apmr.2003.07.009
- Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931-938. doi:10.1016/s0003-9993(98)90090-9
- Legro MW, Reiber GD, Smith DG, del Aguila M, Larsen J, Boone D. Prosthesis evaluation questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil. 1998;79(8):931-938. doi:10.1016/s0003-9993(98)90090-9
- Heinemann AW, Bode RK, O’Reilly C. Development and measurement properties of the orthotics and prosthetics users’ survey (OPUS): a comprehensive set of clinical outcome instruments. Prosthet Orthot Int. 2003;27(3):191-206. doi:10.1080/03093640308726682
- Resnik LJ, Borgia ML, Clark MA. A national survey of prosthesis use in veterans with major upper limb amputation: comparisons by gender. PM R. 2020;12(11):1086-1098. doi:10.1002/pmrj.12351
- Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12(3):229-238. doi:10.1023/a:1023254226592
- Østlie K, Lesjø IM, Franklin RJ, Garfelt B, Skjeldal OH, Magnus P. Prosthesis rejection in acquired major upper-limb amputees: a population-based survey. Disabil Rehabil Assist Technol. 2012;7(4):294-303. doi:10.3109/17483107.2011.635405
- Pezzin LE, Dillingham TR, MacKenzie EJ, Ephraim P, Rossbach P. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil. 2004;85(5):723-729. doi:10.1016/j.apmr.2003.06.002
- Deans S, Burns D, McGarry A, Murray K, Mutrie N. Motivations and barriers to prosthesis users participation in physical activity, exercise and sport: a review of the literature. Prosthet Orthot Int. 2012;36(3):260-269. doi:10.1177/0309364612437905
- McDonald CL, Kahn A, Hafner BJ, Morgan SJ. Prevalence of secondary prosthesis use in lower limb prosthesis users. Disabil Rehabil. 2023;46(5):1016-1022. doi:10.1080/09638288.2023.2182919
- Baars EC, Schrier E, Dijkstra PU, Geertzen JHB. Prosthesis satisfaction in lower limb amputees: a systematic review of associated factors and questionnaires. Medicine (Baltimore). 2018;97(39):e12296. doi:10.1097/MD.0000000000012296
- Murray CD, Fox J. Body image and prosthesis satisfaction in the lower limb amputee. Disabil Rehabil. 2002;24(17):925–931. doi:10.1080/09638280210150014
- Major MJ, Quinlan J, Hansen AH, Esposito ER. Effects of women’s footwear on the mechanical function of heel-height accommodating prosthetic feet. PLoS One. 2022;17(1). doi:10.1371/journal.pone.0262910.
- Kuo PB, Lehavot K, Thomas RM, et al. Gender differences in prosthesis-related outcomes among veterans: results of a national survey of U.S. veterans. PM R. 2024;16(3):239- 249. doi:10.1002/pmrj.13028
- Asano M, Rushton P, Miller WC, Deathe BA. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int. 2008;32(2):231-243. doi:10.1080/03093640802024955
Satisfaction With Department of Veterans Affairs Prosthetics and Support Services as Reported by Women and Men Veterans
Satisfaction With Department of Veterans Affairs Prosthetics and Support Services as Reported by Women and Men Veterans
Key Updates in Resuscitation Procedure After Drowning
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
From Pediatrics
Caregiver Surveys on Firearms, Suicide Offer Pediatricians Prevention Opportunities
ORLANDO, FLORIDA — , according to researchers who presented their findings at the American Academy of Pediatrics (AAP) 2024 National Conference.
An estimated 4.6 million US homes with children have firearms that are loaded and unlocked, a risk factor for youth suicide, yet only about half of parents of suicidal children had been screened for gun ownership in the hospital even as most would be receptive to both firearm screening and counseling, found one study in Texas.
In another study in Colorado, nearly all firearm owners believed that securely storing guns reduces the risk for firearm injury or death, but owners were less likely than non-owners to believe suicide is preventable or that removing a gun from the home reduces the risk for injury or death.
“Previous studies have shown that when pediatricians discuss the importance of armed safe storage guidance with families, families are actually more likely to go home and store firearms safely — storing them locked, unloaded, and separate from the ammunition,” said study author Taylor Rosenbaum, MD, a former pediatric fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston and now an assistant professor at Children’s Hospital University of Miami. “However, previous studies have also shown that pediatricians really are not discussing firearm safe storage with our patients and their families, and we see this both in the outpatient setting, but especially in the inpatient setting for youth suicides, which have risen since 2020 and now are the second leading cause of death for those who are 10-24 years old in the United States.”
Firearm Safety Is a Necessary Conversation
The leading cause of death among children and teens aged 1-19 years is actually firearms, which are also the most fatal method for suicide. While only 4% of all suicide attempts in youth are fatal, 90% of those attempted with a firearm are fatal, Dr. Rosenbaum said. In addition, she said, 80% of the guns used in attempted suicide by children and teens belonged to a family member, and an estimated 70% of firearm-related suicides in youth can be prevented with safe storage of guns.
“This really gives us, as pediatricians, something actionable to do during these hospitalizations” for suicidal ideation or attempts, Dr. Rosenbaum said. “We know that when pediatricians discuss the importance of firearm safe storage guidance with families, they’re more likely to store their firearm safely,” Dr. Rosenbaum said. “We also know that families are not being screened for firearm ownership, that caregivers of youth who are in the hospital for suicidal thoughts or actions want their healthcare team to be screening for firearms, to be giving them information on how to safely secure their firearms, and to be providing free firearm blocks.”
Nathan Boonstra, MD, a general pediatrician at Blank Children’s Hospital, Des Moines, Iowa, said these findings are encouraging in terms of the opportunity pediatricians have.
“There is so much politicization around even basic firearm safety that pediatricians might shy away from the topic, but this research is reassuring that parents are receptive to our advice on safe gun storage,” said Dr. Boonstra, who was not involved in any of this presented research. “It’s especially important for pediatricians to address home firearms when their patient has a history of suicidal ideation or an attempt.”
Reducing the Risk
The Colorado findings similarly reinforce the opportunity physicians have to help caregivers reduce suicide risk, according to Maya Haasz, MD, an associate professor of pediatrics and emergency medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colorado.
“Only 60% of firearm owners believed that removing firearms from the home in times of mental health crisis can decrease the risk of suicide,” she said. “These findings are really concerning, but what we found on the flip side was that 93% of firearm owners actually believe that secure storage can overall decrease the risk for firearm injury and death. So overall, we are underestimating the risk for suicide in our community, and we’re also underestimating our ability to prevent it.”
That presents an opportunity, Dr. Haasz said, “to educate families both about the preventability of suicide but also to have specific strategies, like secure storage and temporary removable requirements from the home, that can prevent suicide.”
Dr. Boonstra found it “disheartening that so many children live in a house with an unlocked and even loaded firearm when the evidence is so clear that this is a significant risk factor for youth suicide,” he said. “It’s also disheartening, though not too surprising, that families with a firearm are less likely to think that youth suicide can be prevented.”
Survey Results
Dr. Rosenbaum’s team conducted the survey in Houston with caregivers whose children were 8-21 years old and hospitalized for suicidal ideation or attempts at a large children’s hospital and two nearby community hospitals between June 2023 and May 2024. The respondents were 46% White and 23% Black, and 47% of the population were Hispanic, all but three of whom were not gun owners.
Among 244 potential participants, only 150 were eligible and approached, and 100 of these completed the surveys, including 26% firearm owners and 68% non-owners. Most of the youth (74%) were aged 14-17 years, and about three in four respondents were their mothers. Only half of the respondents (51%) said the healthcare provider had asked them whether they owned a gun.
One of the key findings Dr. Rosenbaum highlighted was the receptiveness of firearm-owning caregivers to advice from healthcare providers about ownership. If the healthcare team advised parents not to have any guns in the home for the safety of their child with self-arm, 58% of the firearm owners would follow the advice and 27% would consider it, with none saying they would be offended by it.
Among the firearm owners, 81% said their guns were safely secured where they did not believe their child could access it, which meant one in five youth had unsecured access to firearms. Most of the gun owners (77%), like the non-owners (70%), were “not at all worried” about their child getting ahold of a gun in the home, though 11.5% of the firearm owners were “very worried” about it. Interestingly, more gun owners (19%) were very worried about their children accessing a gun outside their home, a concern shared by 37% of non-owners. Nearly twice as many gun owners (46%) as non-owners (25%) were not at all worried about their child getting a gun outside the home.
The vast majority of respondents — 88% of gun owners and 91% of non-owners — felt it was “very important for the healthcare team to ask parents of children with suicidal ideation/attempts about firearms in the home.” Similarly, high proportions believed it was important for the healthcare team to counsel those parents on safe gun storage. Although only 69% of firearm owners believed it was important to distribute firearm locks in the hospital, 81% would be interested in receiving a free one. Significantly more of the non-owners (80%; P = .02) believed free lock distribution was important, and 72% of non-owners would also be interested in one.
About half the respondents (55%) preferred to hear firearm counseling one-on-one from a provider, whereas 31% would like written information and 27% would be interested in a video. In terms of what information parents preferred to receive, a little over half of owners (54%) and non-owners (56%) were interested in how or when (50% and 40%, respectively) to discuss the topic with their child. Only about a third (35% owners and 37% non-owners) wanted information on how to discuss the topic with the parents of their child’s friends.
The survey’s biggest limitations after its small size were the selection bias of those willing to complete the survey and potential response bias from the self-reported data.
The study of Colorado caregivers, just published in Pediatrics, surveyed 512 Colorado caregivers in April-May 2023 to learn about their beliefs and perceptions regarding firearms, firearm storage and risk, and youth suicide (2024 Oct 1;154[4]:e2024066930. doi: 10.1542/peds.2024-066930). Just over half the respondents (52%) had grown up in a household with firearms, and 44% currently lived in a household with a gun. The sample was 43% men and 88% White, predominantly non-Hispanic (75%), with 11% living in rural areas and 19% who currently or previously served in the military. Most (79%) had a child age 12 or younger in the home.
Only about one in four caregivers (24%) correctly answered that suicide is the leading cause of firearm death in Colorado, with similar rates of correct responses among both firearm owners and non-firearm owners. Both groups were also similarly likely (64% overall) to be concerned about youth suicide in their community, though those from homes with firearms were less likely to be concerned about youth suicide in their own family (28%) than those from homes without firearms (39%; P = .013).
In addition, caregivers from homes with versus without firearms were considerably less likely to believe suicide can be prevented (48% vs 69%) and were less likely to believe that temporarily removing a firearm from the home reduces the risk for gun injury or death (60% vs 78%; P < .001 for both comparisons).
Firearm owners were also much less likely than non-owners to believe keeping a gun in the home makes it more dangerous (7% vs 29%) and over twice as likely to think keeping a firearm makes their home safer (52% vs 22%; P < .001). The vast majority of respondents (89%) believed secure storage of guns reduces the risk for injury or death, though the response was higher for firearm owners (93%) than for non-owners (86%; P < .001).
“Our finding that most firearm owners believe that secure firearm storage is protective against firearm injury is a promising messaging strategy,” the authors wrote. “It presents a preventive education opportunity for adults living with children who have mental health concerns, who may benefit most from secure in-home storage and/or temporary and voluntary storage of firearms away from home.”
Firearm Injuries
A separate study at the AAP conference underscored the devastating impact of firearm injuries even among those who survive, whether self-inflicted or not, and the potential for reducing healthcare treatment and costs from effective prevention efforts. A national analysis of pediatric inpatient data from 2017 to 2020 calculated how much greater the burden of healthcare treatment and costs is for firearm injuries of any kind compared with penetrating traumas and blunt traumas.
“As a surgical resident, I have seen these patients who make it into the trauma bed that we are then faced to care for,” said Colleen Nofi, DO, PhD, MBA, a general surgery resident at Cohen Children’s Medical Center at Northwell Health in New York. “Anecdotally, we understand that the devastation and injury caused by bullets far outweighs the injuries caused by other trauma mechanisms,” but the actual calculation of the burden hasn’t been studied.
Among 6615 firearm injuries, 9787 penetrating traumas and 66,003 blunt traumas examined from the National Inpatient Sample Healthcare Cost and Utilization Project Database, 11% of firearm traumas required a transfusion of red blood cells, compared with 1.4% of penetrating traumas and 3% of blunt traumas (P < .001). Patients with firearm injuries also had a longer length of stay — 10.8 days compared with 8.3 for patients with penetrating trauma and 9.8 for those with blunt trauma — and significantly higher rates of CPR, pericardiotomy, chest tube, exploratory laparotomy and/or thoracotomy, colorectal surgery, small bowel surgery, ostomy formation, splenectomy, hepatic resection, tracheostomy, and feeding tube placement.
Pulmonary complications were higher for firearm injuries (4.9%) than for penetrating trauma (0.6%) or blunt trauma (2.9%), and septicemia rates were also higher (1.7% vs 0.2% and 1%, respectively). Cardiac, neurologic, and urinary complications were also significantly and substantially higher for firearm injuries, 6.9% of which resulted in death compared with 0.2% of penetrating traumas and 1.2% of blunt traumas.
The costs from firearm injuries were also significantly higher than the costs from other traumas; “firearm injury remained independently predictive of greater hospital costs, even when controlling for injury severity as well as age, sex, race, insurance, region, hospital type, and household income.
“These findings underscore the urgent need for targeted prevention, supportive measures, and resource allocation to mitigate the devastating impact of firearm injuries on children and healthcare systems alike,” Dr. Nofi said.
The Colorado study was funded by the Colorado Department of Public Health and Environment and a National Institutes of Health grant to Dr. Haasz. The Texas study and the one from Northwell Health did not note any external funding. Dr. Haasz, Dr. Rosenbaum, Dr. Boonstra, and Dr. Nofi had no disclosures.
A version of this article appeared on Medscape.com.
ORLANDO, FLORIDA — , according to researchers who presented their findings at the American Academy of Pediatrics (AAP) 2024 National Conference.
An estimated 4.6 million US homes with children have firearms that are loaded and unlocked, a risk factor for youth suicide, yet only about half of parents of suicidal children had been screened for gun ownership in the hospital even as most would be receptive to both firearm screening and counseling, found one study in Texas.
In another study in Colorado, nearly all firearm owners believed that securely storing guns reduces the risk for firearm injury or death, but owners were less likely than non-owners to believe suicide is preventable or that removing a gun from the home reduces the risk for injury or death.
“Previous studies have shown that when pediatricians discuss the importance of armed safe storage guidance with families, families are actually more likely to go home and store firearms safely — storing them locked, unloaded, and separate from the ammunition,” said study author Taylor Rosenbaum, MD, a former pediatric fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston and now an assistant professor at Children’s Hospital University of Miami. “However, previous studies have also shown that pediatricians really are not discussing firearm safe storage with our patients and their families, and we see this both in the outpatient setting, but especially in the inpatient setting for youth suicides, which have risen since 2020 and now are the second leading cause of death for those who are 10-24 years old in the United States.”
Firearm Safety Is a Necessary Conversation
The leading cause of death among children and teens aged 1-19 years is actually firearms, which are also the most fatal method for suicide. While only 4% of all suicide attempts in youth are fatal, 90% of those attempted with a firearm are fatal, Dr. Rosenbaum said. In addition, she said, 80% of the guns used in attempted suicide by children and teens belonged to a family member, and an estimated 70% of firearm-related suicides in youth can be prevented with safe storage of guns.
“This really gives us, as pediatricians, something actionable to do during these hospitalizations” for suicidal ideation or attempts, Dr. Rosenbaum said. “We know that when pediatricians discuss the importance of firearm safe storage guidance with families, they’re more likely to store their firearm safely,” Dr. Rosenbaum said. “We also know that families are not being screened for firearm ownership, that caregivers of youth who are in the hospital for suicidal thoughts or actions want their healthcare team to be screening for firearms, to be giving them information on how to safely secure their firearms, and to be providing free firearm blocks.”
Nathan Boonstra, MD, a general pediatrician at Blank Children’s Hospital, Des Moines, Iowa, said these findings are encouraging in terms of the opportunity pediatricians have.
“There is so much politicization around even basic firearm safety that pediatricians might shy away from the topic, but this research is reassuring that parents are receptive to our advice on safe gun storage,” said Dr. Boonstra, who was not involved in any of this presented research. “It’s especially important for pediatricians to address home firearms when their patient has a history of suicidal ideation or an attempt.”
Reducing the Risk
The Colorado findings similarly reinforce the opportunity physicians have to help caregivers reduce suicide risk, according to Maya Haasz, MD, an associate professor of pediatrics and emergency medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colorado.
“Only 60% of firearm owners believed that removing firearms from the home in times of mental health crisis can decrease the risk of suicide,” she said. “These findings are really concerning, but what we found on the flip side was that 93% of firearm owners actually believe that secure storage can overall decrease the risk for firearm injury and death. So overall, we are underestimating the risk for suicide in our community, and we’re also underestimating our ability to prevent it.”
That presents an opportunity, Dr. Haasz said, “to educate families both about the preventability of suicide but also to have specific strategies, like secure storage and temporary removable requirements from the home, that can prevent suicide.”
Dr. Boonstra found it “disheartening that so many children live in a house with an unlocked and even loaded firearm when the evidence is so clear that this is a significant risk factor for youth suicide,” he said. “It’s also disheartening, though not too surprising, that families with a firearm are less likely to think that youth suicide can be prevented.”
Survey Results
Dr. Rosenbaum’s team conducted the survey in Houston with caregivers whose children were 8-21 years old and hospitalized for suicidal ideation or attempts at a large children’s hospital and two nearby community hospitals between June 2023 and May 2024. The respondents were 46% White and 23% Black, and 47% of the population were Hispanic, all but three of whom were not gun owners.
Among 244 potential participants, only 150 were eligible and approached, and 100 of these completed the surveys, including 26% firearm owners and 68% non-owners. Most of the youth (74%) were aged 14-17 years, and about three in four respondents were their mothers. Only half of the respondents (51%) said the healthcare provider had asked them whether they owned a gun.
One of the key findings Dr. Rosenbaum highlighted was the receptiveness of firearm-owning caregivers to advice from healthcare providers about ownership. If the healthcare team advised parents not to have any guns in the home for the safety of their child with self-arm, 58% of the firearm owners would follow the advice and 27% would consider it, with none saying they would be offended by it.
Among the firearm owners, 81% said their guns were safely secured where they did not believe their child could access it, which meant one in five youth had unsecured access to firearms. Most of the gun owners (77%), like the non-owners (70%), were “not at all worried” about their child getting ahold of a gun in the home, though 11.5% of the firearm owners were “very worried” about it. Interestingly, more gun owners (19%) were very worried about their children accessing a gun outside their home, a concern shared by 37% of non-owners. Nearly twice as many gun owners (46%) as non-owners (25%) were not at all worried about their child getting a gun outside the home.
The vast majority of respondents — 88% of gun owners and 91% of non-owners — felt it was “very important for the healthcare team to ask parents of children with suicidal ideation/attempts about firearms in the home.” Similarly, high proportions believed it was important for the healthcare team to counsel those parents on safe gun storage. Although only 69% of firearm owners believed it was important to distribute firearm locks in the hospital, 81% would be interested in receiving a free one. Significantly more of the non-owners (80%; P = .02) believed free lock distribution was important, and 72% of non-owners would also be interested in one.
About half the respondents (55%) preferred to hear firearm counseling one-on-one from a provider, whereas 31% would like written information and 27% would be interested in a video. In terms of what information parents preferred to receive, a little over half of owners (54%) and non-owners (56%) were interested in how or when (50% and 40%, respectively) to discuss the topic with their child. Only about a third (35% owners and 37% non-owners) wanted information on how to discuss the topic with the parents of their child’s friends.
The survey’s biggest limitations after its small size were the selection bias of those willing to complete the survey and potential response bias from the self-reported data.
The study of Colorado caregivers, just published in Pediatrics, surveyed 512 Colorado caregivers in April-May 2023 to learn about their beliefs and perceptions regarding firearms, firearm storage and risk, and youth suicide (2024 Oct 1;154[4]:e2024066930. doi: 10.1542/peds.2024-066930). Just over half the respondents (52%) had grown up in a household with firearms, and 44% currently lived in a household with a gun. The sample was 43% men and 88% White, predominantly non-Hispanic (75%), with 11% living in rural areas and 19% who currently or previously served in the military. Most (79%) had a child age 12 or younger in the home.
Only about one in four caregivers (24%) correctly answered that suicide is the leading cause of firearm death in Colorado, with similar rates of correct responses among both firearm owners and non-firearm owners. Both groups were also similarly likely (64% overall) to be concerned about youth suicide in their community, though those from homes with firearms were less likely to be concerned about youth suicide in their own family (28%) than those from homes without firearms (39%; P = .013).
In addition, caregivers from homes with versus without firearms were considerably less likely to believe suicide can be prevented (48% vs 69%) and were less likely to believe that temporarily removing a firearm from the home reduces the risk for gun injury or death (60% vs 78%; P < .001 for both comparisons).
Firearm owners were also much less likely than non-owners to believe keeping a gun in the home makes it more dangerous (7% vs 29%) and over twice as likely to think keeping a firearm makes their home safer (52% vs 22%; P < .001). The vast majority of respondents (89%) believed secure storage of guns reduces the risk for injury or death, though the response was higher for firearm owners (93%) than for non-owners (86%; P < .001).
“Our finding that most firearm owners believe that secure firearm storage is protective against firearm injury is a promising messaging strategy,” the authors wrote. “It presents a preventive education opportunity for adults living with children who have mental health concerns, who may benefit most from secure in-home storage and/or temporary and voluntary storage of firearms away from home.”
Firearm Injuries
A separate study at the AAP conference underscored the devastating impact of firearm injuries even among those who survive, whether self-inflicted or not, and the potential for reducing healthcare treatment and costs from effective prevention efforts. A national analysis of pediatric inpatient data from 2017 to 2020 calculated how much greater the burden of healthcare treatment and costs is for firearm injuries of any kind compared with penetrating traumas and blunt traumas.
“As a surgical resident, I have seen these patients who make it into the trauma bed that we are then faced to care for,” said Colleen Nofi, DO, PhD, MBA, a general surgery resident at Cohen Children’s Medical Center at Northwell Health in New York. “Anecdotally, we understand that the devastation and injury caused by bullets far outweighs the injuries caused by other trauma mechanisms,” but the actual calculation of the burden hasn’t been studied.
Among 6615 firearm injuries, 9787 penetrating traumas and 66,003 blunt traumas examined from the National Inpatient Sample Healthcare Cost and Utilization Project Database, 11% of firearm traumas required a transfusion of red blood cells, compared with 1.4% of penetrating traumas and 3% of blunt traumas (P < .001). Patients with firearm injuries also had a longer length of stay — 10.8 days compared with 8.3 for patients with penetrating trauma and 9.8 for those with blunt trauma — and significantly higher rates of CPR, pericardiotomy, chest tube, exploratory laparotomy and/or thoracotomy, colorectal surgery, small bowel surgery, ostomy formation, splenectomy, hepatic resection, tracheostomy, and feeding tube placement.
Pulmonary complications were higher for firearm injuries (4.9%) than for penetrating trauma (0.6%) or blunt trauma (2.9%), and septicemia rates were also higher (1.7% vs 0.2% and 1%, respectively). Cardiac, neurologic, and urinary complications were also significantly and substantially higher for firearm injuries, 6.9% of which resulted in death compared with 0.2% of penetrating traumas and 1.2% of blunt traumas.
The costs from firearm injuries were also significantly higher than the costs from other traumas; “firearm injury remained independently predictive of greater hospital costs, even when controlling for injury severity as well as age, sex, race, insurance, region, hospital type, and household income.
“These findings underscore the urgent need for targeted prevention, supportive measures, and resource allocation to mitigate the devastating impact of firearm injuries on children and healthcare systems alike,” Dr. Nofi said.
The Colorado study was funded by the Colorado Department of Public Health and Environment and a National Institutes of Health grant to Dr. Haasz. The Texas study and the one from Northwell Health did not note any external funding. Dr. Haasz, Dr. Rosenbaum, Dr. Boonstra, and Dr. Nofi had no disclosures.
A version of this article appeared on Medscape.com.
ORLANDO, FLORIDA — , according to researchers who presented their findings at the American Academy of Pediatrics (AAP) 2024 National Conference.
An estimated 4.6 million US homes with children have firearms that are loaded and unlocked, a risk factor for youth suicide, yet only about half of parents of suicidal children had been screened for gun ownership in the hospital even as most would be receptive to both firearm screening and counseling, found one study in Texas.
In another study in Colorado, nearly all firearm owners believed that securely storing guns reduces the risk for firearm injury or death, but owners were less likely than non-owners to believe suicide is preventable or that removing a gun from the home reduces the risk for injury or death.
“Previous studies have shown that when pediatricians discuss the importance of armed safe storage guidance with families, families are actually more likely to go home and store firearms safely — storing them locked, unloaded, and separate from the ammunition,” said study author Taylor Rosenbaum, MD, a former pediatric fellow at Baylor College of Medicine/Texas Children’s Hospital in Houston and now an assistant professor at Children’s Hospital University of Miami. “However, previous studies have also shown that pediatricians really are not discussing firearm safe storage with our patients and their families, and we see this both in the outpatient setting, but especially in the inpatient setting for youth suicides, which have risen since 2020 and now are the second leading cause of death for those who are 10-24 years old in the United States.”
Firearm Safety Is a Necessary Conversation
The leading cause of death among children and teens aged 1-19 years is actually firearms, which are also the most fatal method for suicide. While only 4% of all suicide attempts in youth are fatal, 90% of those attempted with a firearm are fatal, Dr. Rosenbaum said. In addition, she said, 80% of the guns used in attempted suicide by children and teens belonged to a family member, and an estimated 70% of firearm-related suicides in youth can be prevented with safe storage of guns.
“This really gives us, as pediatricians, something actionable to do during these hospitalizations” for suicidal ideation or attempts, Dr. Rosenbaum said. “We know that when pediatricians discuss the importance of firearm safe storage guidance with families, they’re more likely to store their firearm safely,” Dr. Rosenbaum said. “We also know that families are not being screened for firearm ownership, that caregivers of youth who are in the hospital for suicidal thoughts or actions want their healthcare team to be screening for firearms, to be giving them information on how to safely secure their firearms, and to be providing free firearm blocks.”
Nathan Boonstra, MD, a general pediatrician at Blank Children’s Hospital, Des Moines, Iowa, said these findings are encouraging in terms of the opportunity pediatricians have.
“There is so much politicization around even basic firearm safety that pediatricians might shy away from the topic, but this research is reassuring that parents are receptive to our advice on safe gun storage,” said Dr. Boonstra, who was not involved in any of this presented research. “It’s especially important for pediatricians to address home firearms when their patient has a history of suicidal ideation or an attempt.”
Reducing the Risk
The Colorado findings similarly reinforce the opportunity physicians have to help caregivers reduce suicide risk, according to Maya Haasz, MD, an associate professor of pediatrics and emergency medicine at the University of Colorado Anschutz Medical Campus, Aurora, Colorado.
“Only 60% of firearm owners believed that removing firearms from the home in times of mental health crisis can decrease the risk of suicide,” she said. “These findings are really concerning, but what we found on the flip side was that 93% of firearm owners actually believe that secure storage can overall decrease the risk for firearm injury and death. So overall, we are underestimating the risk for suicide in our community, and we’re also underestimating our ability to prevent it.”
That presents an opportunity, Dr. Haasz said, “to educate families both about the preventability of suicide but also to have specific strategies, like secure storage and temporary removable requirements from the home, that can prevent suicide.”
Dr. Boonstra found it “disheartening that so many children live in a house with an unlocked and even loaded firearm when the evidence is so clear that this is a significant risk factor for youth suicide,” he said. “It’s also disheartening, though not too surprising, that families with a firearm are less likely to think that youth suicide can be prevented.”
Survey Results
Dr. Rosenbaum’s team conducted the survey in Houston with caregivers whose children were 8-21 years old and hospitalized for suicidal ideation or attempts at a large children’s hospital and two nearby community hospitals between June 2023 and May 2024. The respondents were 46% White and 23% Black, and 47% of the population were Hispanic, all but three of whom were not gun owners.
Among 244 potential participants, only 150 were eligible and approached, and 100 of these completed the surveys, including 26% firearm owners and 68% non-owners. Most of the youth (74%) were aged 14-17 years, and about three in four respondents were their mothers. Only half of the respondents (51%) said the healthcare provider had asked them whether they owned a gun.
One of the key findings Dr. Rosenbaum highlighted was the receptiveness of firearm-owning caregivers to advice from healthcare providers about ownership. If the healthcare team advised parents not to have any guns in the home for the safety of their child with self-arm, 58% of the firearm owners would follow the advice and 27% would consider it, with none saying they would be offended by it.
Among the firearm owners, 81% said their guns were safely secured where they did not believe their child could access it, which meant one in five youth had unsecured access to firearms. Most of the gun owners (77%), like the non-owners (70%), were “not at all worried” about their child getting ahold of a gun in the home, though 11.5% of the firearm owners were “very worried” about it. Interestingly, more gun owners (19%) were very worried about their children accessing a gun outside their home, a concern shared by 37% of non-owners. Nearly twice as many gun owners (46%) as non-owners (25%) were not at all worried about their child getting a gun outside the home.
The vast majority of respondents — 88% of gun owners and 91% of non-owners — felt it was “very important for the healthcare team to ask parents of children with suicidal ideation/attempts about firearms in the home.” Similarly, high proportions believed it was important for the healthcare team to counsel those parents on safe gun storage. Although only 69% of firearm owners believed it was important to distribute firearm locks in the hospital, 81% would be interested in receiving a free one. Significantly more of the non-owners (80%; P = .02) believed free lock distribution was important, and 72% of non-owners would also be interested in one.
About half the respondents (55%) preferred to hear firearm counseling one-on-one from a provider, whereas 31% would like written information and 27% would be interested in a video. In terms of what information parents preferred to receive, a little over half of owners (54%) and non-owners (56%) were interested in how or when (50% and 40%, respectively) to discuss the topic with their child. Only about a third (35% owners and 37% non-owners) wanted information on how to discuss the topic with the parents of their child’s friends.
The survey’s biggest limitations after its small size were the selection bias of those willing to complete the survey and potential response bias from the self-reported data.
The study of Colorado caregivers, just published in Pediatrics, surveyed 512 Colorado caregivers in April-May 2023 to learn about their beliefs and perceptions regarding firearms, firearm storage and risk, and youth suicide (2024 Oct 1;154[4]:e2024066930. doi: 10.1542/peds.2024-066930). Just over half the respondents (52%) had grown up in a household with firearms, and 44% currently lived in a household with a gun. The sample was 43% men and 88% White, predominantly non-Hispanic (75%), with 11% living in rural areas and 19% who currently or previously served in the military. Most (79%) had a child age 12 or younger in the home.
Only about one in four caregivers (24%) correctly answered that suicide is the leading cause of firearm death in Colorado, with similar rates of correct responses among both firearm owners and non-firearm owners. Both groups were also similarly likely (64% overall) to be concerned about youth suicide in their community, though those from homes with firearms were less likely to be concerned about youth suicide in their own family (28%) than those from homes without firearms (39%; P = .013).
In addition, caregivers from homes with versus without firearms were considerably less likely to believe suicide can be prevented (48% vs 69%) and were less likely to believe that temporarily removing a firearm from the home reduces the risk for gun injury or death (60% vs 78%; P < .001 for both comparisons).
Firearm owners were also much less likely than non-owners to believe keeping a gun in the home makes it more dangerous (7% vs 29%) and over twice as likely to think keeping a firearm makes their home safer (52% vs 22%; P < .001). The vast majority of respondents (89%) believed secure storage of guns reduces the risk for injury or death, though the response was higher for firearm owners (93%) than for non-owners (86%; P < .001).
“Our finding that most firearm owners believe that secure firearm storage is protective against firearm injury is a promising messaging strategy,” the authors wrote. “It presents a preventive education opportunity for adults living with children who have mental health concerns, who may benefit most from secure in-home storage and/or temporary and voluntary storage of firearms away from home.”
Firearm Injuries
A separate study at the AAP conference underscored the devastating impact of firearm injuries even among those who survive, whether self-inflicted or not, and the potential for reducing healthcare treatment and costs from effective prevention efforts. A national analysis of pediatric inpatient data from 2017 to 2020 calculated how much greater the burden of healthcare treatment and costs is for firearm injuries of any kind compared with penetrating traumas and blunt traumas.
“As a surgical resident, I have seen these patients who make it into the trauma bed that we are then faced to care for,” said Colleen Nofi, DO, PhD, MBA, a general surgery resident at Cohen Children’s Medical Center at Northwell Health in New York. “Anecdotally, we understand that the devastation and injury caused by bullets far outweighs the injuries caused by other trauma mechanisms,” but the actual calculation of the burden hasn’t been studied.
Among 6615 firearm injuries, 9787 penetrating traumas and 66,003 blunt traumas examined from the National Inpatient Sample Healthcare Cost and Utilization Project Database, 11% of firearm traumas required a transfusion of red blood cells, compared with 1.4% of penetrating traumas and 3% of blunt traumas (P < .001). Patients with firearm injuries also had a longer length of stay — 10.8 days compared with 8.3 for patients with penetrating trauma and 9.8 for those with blunt trauma — and significantly higher rates of CPR, pericardiotomy, chest tube, exploratory laparotomy and/or thoracotomy, colorectal surgery, small bowel surgery, ostomy formation, splenectomy, hepatic resection, tracheostomy, and feeding tube placement.
Pulmonary complications were higher for firearm injuries (4.9%) than for penetrating trauma (0.6%) or blunt trauma (2.9%), and septicemia rates were also higher (1.7% vs 0.2% and 1%, respectively). Cardiac, neurologic, and urinary complications were also significantly and substantially higher for firearm injuries, 6.9% of which resulted in death compared with 0.2% of penetrating traumas and 1.2% of blunt traumas.
The costs from firearm injuries were also significantly higher than the costs from other traumas; “firearm injury remained independently predictive of greater hospital costs, even when controlling for injury severity as well as age, sex, race, insurance, region, hospital type, and household income.
“These findings underscore the urgent need for targeted prevention, supportive measures, and resource allocation to mitigate the devastating impact of firearm injuries on children and healthcare systems alike,” Dr. Nofi said.
The Colorado study was funded by the Colorado Department of Public Health and Environment and a National Institutes of Health grant to Dr. Haasz. The Texas study and the one from Northwell Health did not note any external funding. Dr. Haasz, Dr. Rosenbaum, Dr. Boonstra, and Dr. Nofi had no disclosures.
A version of this article appeared on Medscape.com.
From AAP 2024
Heat-Related Pediatric ED Visits More Than Double
ORLANDO – according to research presented at the annual meeting of the American Academy of Pediatrics (AAP).
“Our study really highlights the adverse effects that can come from extreme heat, and how increasing heat-related illness is affecting our children,” Taylor Merritt, MD, a pediatric resident at the University of Texas Southwestern Medical Center and Children’s Health in Dallas, said during a press briefing.
Underestimating the Problem?
Lori Byron, MD, a pediatrician from Red Lodge, Montana, who heads the AAP Chapter Climate Advocates program and was not involved in this research, was not surprised by the findings. “If anything, we’re vastly underestimating it because when people come in with heat exhaustion or heat smoke, that gets coded correctly, but when people come in with heart attacks, asthma attacks, strokes, and other exacerbations of chronic disease, it very rarely gets coded as a heat-related illness.”
Record-breaking summer temperatures from the changing climate have led to increased heat-related morbidity and mortality. Past research suggests that children and teens make up nearly half of all those affected by heat-related illnesses, she noted. 2023, for example, was the hottest year on record, and 2024 is predicted to be hotter, Dr. Merritt said.
A Sharp Increase in Cases
The retrospective study examined emergency department diagnoses during May-September from 2012-2023 at two large children’s hospitals within a north Texas pediatric health care system. The researchers compared heat-specific conditions with rhabdomyolysis encounters based on ICD-10 coding.
Heat-specific conditions include heatstroke/sunstroke, exertion heatstroke, heat syncope, heat crap, heat exhaustion, heat fatigue, heat edema, and exposure to excessive natural heat. Rhabdomyolysis encounters included both exertional and nonexertional rhabdomyolysis as well as non-traumatic rhabdomyolysis and elevated creatine kinase (CK) levels.
Among 542 heat-related encounters, 77% had heat-specific diagnoses and 24% had a rhabdomyolysis diagnosis. Combined, heat-related encounters increased 170% from 2012 to 2023, from 4.3 per 10,000 to 11.6 per 10,000 (P = .1). Summer months with higher peak temperatures were also associated with higher heat-related volume in the emergency department (P < .001).
Teenage boys were most likely to have rhabdomyolysis, with 82% of the cases occurring in boys and 70% in ages 12-18 (P < .001). “Compared to the rhabdomyolysis group, the heat-specific group was more likely to be younger, Hispanic, use government-based insurance, and live in an area with a lower Child Opportunity Index,” Dr. Merritt reported. “Most heat-specific encounters resulted in an ED discharge (96%), while most rhabdomyolysis encounters resulted in hospital admission (63%)” (P < .001).
”Thankfully, pediatric heat-related illness is still relatively rare,” Dr. Merritt said. “However, given the context of increasing temperatures, this is important for us all to know, anyone who cares for children, whether that be families or parents or pediatricians.”
Prevention Is Key
Dr. Byron noted that about half of AAP chapters now have climate committees, many of which have created educational materials on heat and wildfire smoke and on talking with athletes about risk of heat-related illnesses.
“A lot of the state high school sports associations are actually now adopting guidelines on when it’s safe to practice and when it’s safe to play for heat and for smoke, so that’s definitely something that we can talk to parents about and kids about,” Dr. Byron said. “Otherwise, you still have a lot of coaches and a lot of kids out there that think you’re just supposed to be tough and barrel through it.”
Rhabdomyolysis and heat stroke are both potentially deadly illnesses, so the biggest focus needs to be on prevention, Dr. Byron said. “Not just working with individuals in your office, but working within your school or within your state high school sports association is totally within the lane of a pediatrician to get involved.”
The research had no external funding. Dr. Merritt and Dr. Byron had no disclosures.
ORLANDO – according to research presented at the annual meeting of the American Academy of Pediatrics (AAP).
“Our study really highlights the adverse effects that can come from extreme heat, and how increasing heat-related illness is affecting our children,” Taylor Merritt, MD, a pediatric resident at the University of Texas Southwestern Medical Center and Children’s Health in Dallas, said during a press briefing.
Underestimating the Problem?
Lori Byron, MD, a pediatrician from Red Lodge, Montana, who heads the AAP Chapter Climate Advocates program and was not involved in this research, was not surprised by the findings. “If anything, we’re vastly underestimating it because when people come in with heat exhaustion or heat smoke, that gets coded correctly, but when people come in with heart attacks, asthma attacks, strokes, and other exacerbations of chronic disease, it very rarely gets coded as a heat-related illness.”
Record-breaking summer temperatures from the changing climate have led to increased heat-related morbidity and mortality. Past research suggests that children and teens make up nearly half of all those affected by heat-related illnesses, she noted. 2023, for example, was the hottest year on record, and 2024 is predicted to be hotter, Dr. Merritt said.
A Sharp Increase in Cases
The retrospective study examined emergency department diagnoses during May-September from 2012-2023 at two large children’s hospitals within a north Texas pediatric health care system. The researchers compared heat-specific conditions with rhabdomyolysis encounters based on ICD-10 coding.
Heat-specific conditions include heatstroke/sunstroke, exertion heatstroke, heat syncope, heat crap, heat exhaustion, heat fatigue, heat edema, and exposure to excessive natural heat. Rhabdomyolysis encounters included both exertional and nonexertional rhabdomyolysis as well as non-traumatic rhabdomyolysis and elevated creatine kinase (CK) levels.
Among 542 heat-related encounters, 77% had heat-specific diagnoses and 24% had a rhabdomyolysis diagnosis. Combined, heat-related encounters increased 170% from 2012 to 2023, from 4.3 per 10,000 to 11.6 per 10,000 (P = .1). Summer months with higher peak temperatures were also associated with higher heat-related volume in the emergency department (P < .001).
Teenage boys were most likely to have rhabdomyolysis, with 82% of the cases occurring in boys and 70% in ages 12-18 (P < .001). “Compared to the rhabdomyolysis group, the heat-specific group was more likely to be younger, Hispanic, use government-based insurance, and live in an area with a lower Child Opportunity Index,” Dr. Merritt reported. “Most heat-specific encounters resulted in an ED discharge (96%), while most rhabdomyolysis encounters resulted in hospital admission (63%)” (P < .001).
”Thankfully, pediatric heat-related illness is still relatively rare,” Dr. Merritt said. “However, given the context of increasing temperatures, this is important for us all to know, anyone who cares for children, whether that be families or parents or pediatricians.”
Prevention Is Key
Dr. Byron noted that about half of AAP chapters now have climate committees, many of which have created educational materials on heat and wildfire smoke and on talking with athletes about risk of heat-related illnesses.
“A lot of the state high school sports associations are actually now adopting guidelines on when it’s safe to practice and when it’s safe to play for heat and for smoke, so that’s definitely something that we can talk to parents about and kids about,” Dr. Byron said. “Otherwise, you still have a lot of coaches and a lot of kids out there that think you’re just supposed to be tough and barrel through it.”
Rhabdomyolysis and heat stroke are both potentially deadly illnesses, so the biggest focus needs to be on prevention, Dr. Byron said. “Not just working with individuals in your office, but working within your school or within your state high school sports association is totally within the lane of a pediatrician to get involved.”
The research had no external funding. Dr. Merritt and Dr. Byron had no disclosures.
ORLANDO – according to research presented at the annual meeting of the American Academy of Pediatrics (AAP).
“Our study really highlights the adverse effects that can come from extreme heat, and how increasing heat-related illness is affecting our children,” Taylor Merritt, MD, a pediatric resident at the University of Texas Southwestern Medical Center and Children’s Health in Dallas, said during a press briefing.
Underestimating the Problem?
Lori Byron, MD, a pediatrician from Red Lodge, Montana, who heads the AAP Chapter Climate Advocates program and was not involved in this research, was not surprised by the findings. “If anything, we’re vastly underestimating it because when people come in with heat exhaustion or heat smoke, that gets coded correctly, but when people come in with heart attacks, asthma attacks, strokes, and other exacerbations of chronic disease, it very rarely gets coded as a heat-related illness.”
Record-breaking summer temperatures from the changing climate have led to increased heat-related morbidity and mortality. Past research suggests that children and teens make up nearly half of all those affected by heat-related illnesses, she noted. 2023, for example, was the hottest year on record, and 2024 is predicted to be hotter, Dr. Merritt said.
A Sharp Increase in Cases
The retrospective study examined emergency department diagnoses during May-September from 2012-2023 at two large children’s hospitals within a north Texas pediatric health care system. The researchers compared heat-specific conditions with rhabdomyolysis encounters based on ICD-10 coding.
Heat-specific conditions include heatstroke/sunstroke, exertion heatstroke, heat syncope, heat crap, heat exhaustion, heat fatigue, heat edema, and exposure to excessive natural heat. Rhabdomyolysis encounters included both exertional and nonexertional rhabdomyolysis as well as non-traumatic rhabdomyolysis and elevated creatine kinase (CK) levels.
Among 542 heat-related encounters, 77% had heat-specific diagnoses and 24% had a rhabdomyolysis diagnosis. Combined, heat-related encounters increased 170% from 2012 to 2023, from 4.3 per 10,000 to 11.6 per 10,000 (P = .1). Summer months with higher peak temperatures were also associated with higher heat-related volume in the emergency department (P < .001).
Teenage boys were most likely to have rhabdomyolysis, with 82% of the cases occurring in boys and 70% in ages 12-18 (P < .001). “Compared to the rhabdomyolysis group, the heat-specific group was more likely to be younger, Hispanic, use government-based insurance, and live in an area with a lower Child Opportunity Index,” Dr. Merritt reported. “Most heat-specific encounters resulted in an ED discharge (96%), while most rhabdomyolysis encounters resulted in hospital admission (63%)” (P < .001).
”Thankfully, pediatric heat-related illness is still relatively rare,” Dr. Merritt said. “However, given the context of increasing temperatures, this is important for us all to know, anyone who cares for children, whether that be families or parents or pediatricians.”
Prevention Is Key
Dr. Byron noted that about half of AAP chapters now have climate committees, many of which have created educational materials on heat and wildfire smoke and on talking with athletes about risk of heat-related illnesses.
“A lot of the state high school sports associations are actually now adopting guidelines on when it’s safe to practice and when it’s safe to play for heat and for smoke, so that’s definitely something that we can talk to parents about and kids about,” Dr. Byron said. “Otherwise, you still have a lot of coaches and a lot of kids out there that think you’re just supposed to be tough and barrel through it.”
Rhabdomyolysis and heat stroke are both potentially deadly illnesses, so the biggest focus needs to be on prevention, Dr. Byron said. “Not just working with individuals in your office, but working within your school or within your state high school sports association is totally within the lane of a pediatrician to get involved.”
The research had no external funding. Dr. Merritt and Dr. Byron had no disclosures.
FROM AAP 2024
Identifying Child Abuse Through Oral Health: What Every Clinician Should Know
TOPLINE:
Researchers detail best practices for pediatricians in evaluating dental indications of child abuse and how to work with other physicians to detect and report these incidents.
METHODOLOGY:
- Approximately 323,000 children in the United States were identified as having experienced physical abuse in 2006, the most recent year evaluated, according to the Fourth National Incidence Study of Child Abuse and Neglect.
- One in seven children in the United States are abused or neglected each year; craniofacial, head, face, and neck injuries occur in more than half of child abuse cases.
- Children with orofacial and torso bruising who are younger than age 4 years are at risk for future, more serious abuse.
- Child trafficking survivors are twice as likely to have dental issues due to poor nutrition and inadequate care.
TAKEAWAY:
- In cases of possible oral sexual abuse, physicians should test for sexually transmitted infections and document incidents to support forensic investigations.
- Pediatricians should consult with forensic pediatric dentists or child abuse specialists for assistance in evaluating bite marks or any other indications of abuse.
- If a parent fails to seek treatment for a child’s oral or dental disease after detection, pediatricians should report the case to child protective services regarding concerns of dental neglect.
- Because trafficked children may receive medical or dental care while in captivity, physicians should use screening tools to identify children at risk of trafficking, regardless of gender.
- Physicians should be mindful of having a bias against reporting because of sharing a similar background to the parents or other caregivers of a child who is suspected of experiencing abuse.
IN PRACTICE:
“Pediatric dentists and oral and maxillofacial surgeons, whose advanced education programs include a mandated child abuse curriculum, can provide valuable information and assistance to other health care providers about oral and dental aspects of child abuse and neglect,” the study authors wrote.
SOURCE:
The study was led by Anupama Rao Tate, DMD, MPH, of the American Academy of Pediatrics, and was published online in Pediatrics.
LIMITATIONS:
No limitations were reported.
DISCLOSURES:
Susan A. Fischer-Owens reported financial connections with Colgate. No other disclosures were reported.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Researchers detail best practices for pediatricians in evaluating dental indications of child abuse and how to work with other physicians to detect and report these incidents.
METHODOLOGY:
- Approximately 323,000 children in the United States were identified as having experienced physical abuse in 2006, the most recent year evaluated, according to the Fourth National Incidence Study of Child Abuse and Neglect.
- One in seven children in the United States are abused or neglected each year; craniofacial, head, face, and neck injuries occur in more than half of child abuse cases.
- Children with orofacial and torso bruising who are younger than age 4 years are at risk for future, more serious abuse.
- Child trafficking survivors are twice as likely to have dental issues due to poor nutrition and inadequate care.
TAKEAWAY:
- In cases of possible oral sexual abuse, physicians should test for sexually transmitted infections and document incidents to support forensic investigations.
- Pediatricians should consult with forensic pediatric dentists or child abuse specialists for assistance in evaluating bite marks or any other indications of abuse.
- If a parent fails to seek treatment for a child’s oral or dental disease after detection, pediatricians should report the case to child protective services regarding concerns of dental neglect.
- Because trafficked children may receive medical or dental care while in captivity, physicians should use screening tools to identify children at risk of trafficking, regardless of gender.
- Physicians should be mindful of having a bias against reporting because of sharing a similar background to the parents or other caregivers of a child who is suspected of experiencing abuse.
IN PRACTICE:
“Pediatric dentists and oral and maxillofacial surgeons, whose advanced education programs include a mandated child abuse curriculum, can provide valuable information and assistance to other health care providers about oral and dental aspects of child abuse and neglect,” the study authors wrote.
SOURCE:
The study was led by Anupama Rao Tate, DMD, MPH, of the American Academy of Pediatrics, and was published online in Pediatrics.
LIMITATIONS:
No limitations were reported.
DISCLOSURES:
Susan A. Fischer-Owens reported financial connections with Colgate. No other disclosures were reported.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Researchers detail best practices for pediatricians in evaluating dental indications of child abuse and how to work with other physicians to detect and report these incidents.
METHODOLOGY:
- Approximately 323,000 children in the United States were identified as having experienced physical abuse in 2006, the most recent year evaluated, according to the Fourth National Incidence Study of Child Abuse and Neglect.
- One in seven children in the United States are abused or neglected each year; craniofacial, head, face, and neck injuries occur in more than half of child abuse cases.
- Children with orofacial and torso bruising who are younger than age 4 years are at risk for future, more serious abuse.
- Child trafficking survivors are twice as likely to have dental issues due to poor nutrition and inadequate care.
TAKEAWAY:
- In cases of possible oral sexual abuse, physicians should test for sexually transmitted infections and document incidents to support forensic investigations.
- Pediatricians should consult with forensic pediatric dentists or child abuse specialists for assistance in evaluating bite marks or any other indications of abuse.
- If a parent fails to seek treatment for a child’s oral or dental disease after detection, pediatricians should report the case to child protective services regarding concerns of dental neglect.
- Because trafficked children may receive medical or dental care while in captivity, physicians should use screening tools to identify children at risk of trafficking, regardless of gender.
- Physicians should be mindful of having a bias against reporting because of sharing a similar background to the parents or other caregivers of a child who is suspected of experiencing abuse.
IN PRACTICE:
“Pediatric dentists and oral and maxillofacial surgeons, whose advanced education programs include a mandated child abuse curriculum, can provide valuable information and assistance to other health care providers about oral and dental aspects of child abuse and neglect,” the study authors wrote.
SOURCE:
The study was led by Anupama Rao Tate, DMD, MPH, of the American Academy of Pediatrics, and was published online in Pediatrics.
LIMITATIONS:
No limitations were reported.
DISCLOSURES:
Susan A. Fischer-Owens reported financial connections with Colgate. No other disclosures were reported.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
How Common Is Pediatric Emergency Mistriage?
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
FROM JAMA PEDIATRICS
E-Bikes: The Good ... and the Ugly
Bicycles have been woven into my life since I first straddled a hand-me-down with a fan belt drive when I was 3. At age 12 my friend Ricky and I took a 250 mile–plus 2-night adventure on our 3-speed “English” style bikes. We still marvel that our parents let us do it when neither cell phones nor GPS existed.
I have always bike commuted to work, including the years when that involved a perilous navigation into Boston from the suburbs. In our mid-50s my wife and I biked from Washington state back here to Maine with another couple unsupported. We continue to do at least one self-guided cycle tour out of the country each year.
Not surprisingly, I keep a close eye on what’s happening in the bicycle market. For decades the trends have shifted back and forth between sleek road models and beefier off-roaders. There have been boom years here and there for the dealers and manufacturers, but nothing like what the bike industry is experiencing now with the arrival of e-bikes on the market. Driven primarily by electrification, micromobility ridership (which includes conventional bikes and scooters) has grown more than 50-fold over the last 10 years. Projections suggest the market’s value will be $300 billion by 2030.
It doesn’t take an MBA with a major in marketing to understand the broad appeal of electrification. Most adults have ridden a bicycle as children, but several decades of gap years has left many of them with a level of fitness that makes pedaling against the wind or up any incline difficult and unappealing. An e-bike can put even the least fitness conscious back in the saddle and open the options for outdoor recreation they haven’t dreamed of since childhood.
In large part the people flocking to e-bikes are retiree’s who thought they were “over the hill.” They are having so much fun they don’t care if the Lycra-clad “serious” cyclists notice the battery bulge in the frame on their e-bikes. Another group of e-bike adopters are motivated by the “greenness” of a fossil-fuel–free electric powered transportation which, with minimal compromise, can be used as they would a car around town and for longer commutes than they would have considered on a purely pedal-powered bicycle.
Unfortunately, there is a growing group of younger e-bike riders who are motivated and uninhibited by the potential that the power boost of a small electric motor can provide. And here is where the ugliness begins to intrude on what was otherwise a beautiful and expanding landscape. However, it is the young who are, not surprisingly, drawn to the speed, and with any vehicle – motorized or conventional – as speed increases so does the frequency and seriousness of accidents.
The term e-bike covers a broad range of vehicles, from those designated class 1, which require pedaling and are limited to 20 miles per hour, to class 3, which may have a throttle and unmodified can hit 28 mph. Class 2 bikes have a throttle that will allow the rider to reach 20 mph without pedaling. Modifying any class of e-bike can substantially increase its speed, but this is more common in classes 2 and 3. As an example, some very fast micromobiles are considered unclassified e-bikes and avoid being labeled motorcycles simply because they have pedals.
One has to give some credit to the e-bike industry for eventually adopting this classification system. But, we must give the rest of us, including parents and public safety officials, a failing grade for doing a poor job of translating these scores into enforceable regulations to protect both riders and pedestrians from serious injury.
On the governmental side only a little more than half of US states have used the three category classification to craft their regulations. Many jurisdictions have failed to differentiate between streets, sidewalks, and trails. Regulations vary from state to state, and many states leave it up to local communities. From my experience chairing our town’s Bicycle and Pedestrian Advisory Committee, I can tell you that even “progressive” communities are struggling to decide who can ride what where. The result has been that people of all ages, but mostly adolescents, are traveling on busy streets and sidewalks at speeds that put themselves and pedestrians at risk.
On the parental side of the problem are families that have either allowed or enabled their children to ride class 2 and 3 e-bikes without proper safety equipment or consideration for the safety of the rest of the community. Currently, this is not much of a problem here in Maine thanks to the weather and the high price of e-bikes. However, I frequently visit an affluent community in the San Francisco Bay Area, where it is not uncommon to see middle school children speeding along well in excess of 20 mph.
Unfortunately this is another example, like television and cell phone, in which our society has been unable to keep up with technology by molding the behavior of our children and/or creating enforceable rules that allow us to reap the benefits of new discoveries while minimizing the collateral damage that can accompany them.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Bicycles have been woven into my life since I first straddled a hand-me-down with a fan belt drive when I was 3. At age 12 my friend Ricky and I took a 250 mile–plus 2-night adventure on our 3-speed “English” style bikes. We still marvel that our parents let us do it when neither cell phones nor GPS existed.
I have always bike commuted to work, including the years when that involved a perilous navigation into Boston from the suburbs. In our mid-50s my wife and I biked from Washington state back here to Maine with another couple unsupported. We continue to do at least one self-guided cycle tour out of the country each year.
Not surprisingly, I keep a close eye on what’s happening in the bicycle market. For decades the trends have shifted back and forth between sleek road models and beefier off-roaders. There have been boom years here and there for the dealers and manufacturers, but nothing like what the bike industry is experiencing now with the arrival of e-bikes on the market. Driven primarily by electrification, micromobility ridership (which includes conventional bikes and scooters) has grown more than 50-fold over the last 10 years. Projections suggest the market’s value will be $300 billion by 2030.
It doesn’t take an MBA with a major in marketing to understand the broad appeal of electrification. Most adults have ridden a bicycle as children, but several decades of gap years has left many of them with a level of fitness that makes pedaling against the wind or up any incline difficult and unappealing. An e-bike can put even the least fitness conscious back in the saddle and open the options for outdoor recreation they haven’t dreamed of since childhood.
In large part the people flocking to e-bikes are retiree’s who thought they were “over the hill.” They are having so much fun they don’t care if the Lycra-clad “serious” cyclists notice the battery bulge in the frame on their e-bikes. Another group of e-bike adopters are motivated by the “greenness” of a fossil-fuel–free electric powered transportation which, with minimal compromise, can be used as they would a car around town and for longer commutes than they would have considered on a purely pedal-powered bicycle.
Unfortunately, there is a growing group of younger e-bike riders who are motivated and uninhibited by the potential that the power boost of a small electric motor can provide. And here is where the ugliness begins to intrude on what was otherwise a beautiful and expanding landscape. However, it is the young who are, not surprisingly, drawn to the speed, and with any vehicle – motorized or conventional – as speed increases so does the frequency and seriousness of accidents.
The term e-bike covers a broad range of vehicles, from those designated class 1, which require pedaling and are limited to 20 miles per hour, to class 3, which may have a throttle and unmodified can hit 28 mph. Class 2 bikes have a throttle that will allow the rider to reach 20 mph without pedaling. Modifying any class of e-bike can substantially increase its speed, but this is more common in classes 2 and 3. As an example, some very fast micromobiles are considered unclassified e-bikes and avoid being labeled motorcycles simply because they have pedals.
One has to give some credit to the e-bike industry for eventually adopting this classification system. But, we must give the rest of us, including parents and public safety officials, a failing grade for doing a poor job of translating these scores into enforceable regulations to protect both riders and pedestrians from serious injury.
On the governmental side only a little more than half of US states have used the three category classification to craft their regulations. Many jurisdictions have failed to differentiate between streets, sidewalks, and trails. Regulations vary from state to state, and many states leave it up to local communities. From my experience chairing our town’s Bicycle and Pedestrian Advisory Committee, I can tell you that even “progressive” communities are struggling to decide who can ride what where. The result has been that people of all ages, but mostly adolescents, are traveling on busy streets and sidewalks at speeds that put themselves and pedestrians at risk.
On the parental side of the problem are families that have either allowed or enabled their children to ride class 2 and 3 e-bikes without proper safety equipment or consideration for the safety of the rest of the community. Currently, this is not much of a problem here in Maine thanks to the weather and the high price of e-bikes. However, I frequently visit an affluent community in the San Francisco Bay Area, where it is not uncommon to see middle school children speeding along well in excess of 20 mph.
Unfortunately this is another example, like television and cell phone, in which our society has been unable to keep up with technology by molding the behavior of our children and/or creating enforceable rules that allow us to reap the benefits of new discoveries while minimizing the collateral damage that can accompany them.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Bicycles have been woven into my life since I first straddled a hand-me-down with a fan belt drive when I was 3. At age 12 my friend Ricky and I took a 250 mile–plus 2-night adventure on our 3-speed “English” style bikes. We still marvel that our parents let us do it when neither cell phones nor GPS existed.
I have always bike commuted to work, including the years when that involved a perilous navigation into Boston from the suburbs. In our mid-50s my wife and I biked from Washington state back here to Maine with another couple unsupported. We continue to do at least one self-guided cycle tour out of the country each year.
Not surprisingly, I keep a close eye on what’s happening in the bicycle market. For decades the trends have shifted back and forth between sleek road models and beefier off-roaders. There have been boom years here and there for the dealers and manufacturers, but nothing like what the bike industry is experiencing now with the arrival of e-bikes on the market. Driven primarily by electrification, micromobility ridership (which includes conventional bikes and scooters) has grown more than 50-fold over the last 10 years. Projections suggest the market’s value will be $300 billion by 2030.
It doesn’t take an MBA with a major in marketing to understand the broad appeal of electrification. Most adults have ridden a bicycle as children, but several decades of gap years has left many of them with a level of fitness that makes pedaling against the wind or up any incline difficult and unappealing. An e-bike can put even the least fitness conscious back in the saddle and open the options for outdoor recreation they haven’t dreamed of since childhood.
In large part the people flocking to e-bikes are retiree’s who thought they were “over the hill.” They are having so much fun they don’t care if the Lycra-clad “serious” cyclists notice the battery bulge in the frame on their e-bikes. Another group of e-bike adopters are motivated by the “greenness” of a fossil-fuel–free electric powered transportation which, with minimal compromise, can be used as they would a car around town and for longer commutes than they would have considered on a purely pedal-powered bicycle.
Unfortunately, there is a growing group of younger e-bike riders who are motivated and uninhibited by the potential that the power boost of a small electric motor can provide. And here is where the ugliness begins to intrude on what was otherwise a beautiful and expanding landscape. However, it is the young who are, not surprisingly, drawn to the speed, and with any vehicle – motorized or conventional – as speed increases so does the frequency and seriousness of accidents.
The term e-bike covers a broad range of vehicles, from those designated class 1, which require pedaling and are limited to 20 miles per hour, to class 3, which may have a throttle and unmodified can hit 28 mph. Class 2 bikes have a throttle that will allow the rider to reach 20 mph without pedaling. Modifying any class of e-bike can substantially increase its speed, but this is more common in classes 2 and 3. As an example, some very fast micromobiles are considered unclassified e-bikes and avoid being labeled motorcycles simply because they have pedals.
One has to give some credit to the e-bike industry for eventually adopting this classification system. But, we must give the rest of us, including parents and public safety officials, a failing grade for doing a poor job of translating these scores into enforceable regulations to protect both riders and pedestrians from serious injury.
On the governmental side only a little more than half of US states have used the three category classification to craft their regulations. Many jurisdictions have failed to differentiate between streets, sidewalks, and trails. Regulations vary from state to state, and many states leave it up to local communities. From my experience chairing our town’s Bicycle and Pedestrian Advisory Committee, I can tell you that even “progressive” communities are struggling to decide who can ride what where. The result has been that people of all ages, but mostly adolescents, are traveling on busy streets and sidewalks at speeds that put themselves and pedestrians at risk.
On the parental side of the problem are families that have either allowed or enabled their children to ride class 2 and 3 e-bikes without proper safety equipment or consideration for the safety of the rest of the community. Currently, this is not much of a problem here in Maine thanks to the weather and the high price of e-bikes. However, I frequently visit an affluent community in the San Francisco Bay Area, where it is not uncommon to see middle school children speeding along well in excess of 20 mph.
Unfortunately this is another example, like television and cell phone, in which our society has been unable to keep up with technology by molding the behavior of our children and/or creating enforceable rules that allow us to reap the benefits of new discoveries while minimizing the collateral damage that can accompany them.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
Consider Risks, Toxicity of Some Topical Ingredients in Infants, Young Children
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
TORONTO — Lawrence A. Schachner, MD, would like pediatric dermatologists to adopt a “toxic agent of the year” to raise awareness about the potential harm related to certain topical treatments in babies and young children.
Dr. Schachner, director of the Division of Pediatric Dermatology in the Department of Dermatology & Cutaneous Surgery at the University of Miami, Coral Gables, Florida, said he got the idea from the American Contact Dermatitis Society, which annually names the “Allergen of the Year.”
, said Dr. Schachner, professor of pediatrics and dermatology at the University of Miami.
“Any one of those would be excellent toxic substances of the year” that could be the focus of an educational campaign, he told this news organization following his presentation on “Toxicology of Topical Ingredients in Pediatric Dermatology” at the annual meeting of the Society for Pediatric Dermatology on July 14.
Benzene might also be a good candidate for the list, although the jury seems to be still out on its toxicity, said Dr. Schachner.
He talked about the “four Ps” of poisoning — the physician, pharmacy, parents, and pharmaceutical manufacturing — which all have some responsibility for errors that lead to adverse outcomes but can also take steps to prevent them.
During his presentation, Dr. Schachner discussed how babies are especially sensitive to topical therapies, noting that a baby’s skin is thinner and more permeable than that of an adult. And children have a greater body surface-to-weight ratio, so they absorb more substances through their skin.
He also noted that babies lack natural moisturizing factors, and their skin barrier isn’t mature until about age 3-5 years, stressing the need for extreme care when applying a topical agent to a baby’s skin.
Tragic Stories
Dr. Schachner pointed to some instances of mishaps related to toxic topical substances in children. There was the outbreak in the early 1980s of accidental hexachlorophene poisoning among children in France exposed to talc “baby powder.” Of the 204 affected children, 36 died.
The cause was a manufacturing error; the product contained 6.3% hexachlorophene, as opposed to the 0.1% limit recommended by the US Food and Drug Administration (FDA).
Local anesthetics, including lidocaine, dibucaine, and prilocaine, can cause local anesthetic systemic toxicity, a syndrome with symptoms that include central nervous system depression, seizures, and cardiotoxicity. Dr. Schachner described the case of a 3-year-old who developed methemoglobinemia, with seizures, after treatment with an excessive amount of eutectic mixture of local anesthetics (EMLA) cream, which contains both lidocaine and prilocaine.
EMLA shouldn’t be used with methemoglobinemia-inducing agents, such as some antimalarials, analgesics, anesthetics, and antineoplastic agents. It’s not recommended in neonates or for those under 12 months if receiving methemoglobinemia-inducing agents, “and I would keep an eye on it after 12 months of age,” said Dr. Schachner.
He cited a retrospective review of topical lidocaine toxicity in pediatric patients reported to the National Poison Data System from 2000 to 2020. It found 37 cases of toxicity, the most common from application prior to dermatologic procedures (37.5%), which led to two deaths.
Not Benign Agents
“These are not benign agents; we have to use them correctly,” Dr. Schachner stressed. When discussing alcohols and antiseptics, he noted that phenol is found in a variety of household disinfectants, gargling products, ointments, and lip balms. Phenol can be used as a chemical peel and is the antiseptic component of Castellani paint. He also referred to cases of alcohol intoxication linked to umbilical care in newborns.
Benzene at elevated levels has been found in some topical benzoyl peroxide acne products and in some sunscreens. There have been suggestions, not strongly substantiated, that benzene may increase the risk for cancer, especially leukemias.
But there is sparse data on the absorption and toxicity of benzene exposure with sunscreen use. The data, he said, include an analysis of National Health and Nutrition Examination Survey data, which found that people who regularly used sunscreens were less likely to have elevated benzene levels compared with those who didn’t use sunscreens.
Turning to insecticides, Dr. Schachner discussed N,N-diethyl-m-toluamide (DEET), the active ingredient in many insect repellents. It helps avoid “some terrible diseases,” including mosquito-borne illnesses such as malaria and tick-borne conditions such as Lyme disease, and is available in several convenient formulations, he said.
When used on children, the American Academy of Pediatrics (AAP) recommends products with no more than 30% DEET. And insect repellents are not recommended for children younger than 2 months, or under clothing or damaged skin, he said.
Dr. Schachner referred to a case series of 18 children who developed DEET-induced encephalopathy; 13 (72%) involved dermal exposure. Three of those with cutaneous exposure died, mostly from neurologic, respiratory, and cardiac issues. “What’s very striking is that 55% of the kids were exposed to DEET of 20% or less, even though the AAP approves DEET at 30%, so maybe that’s something we have to look at,” he said.
Medication Patches
With medication patches, especially fentanyl transdermal patches, much can go wrong when it comes to children. This was highlighted by the cases Schachner cited, including an infant who developed acute cytotoxic cerebellar edema from fentanyl patch intoxication.
In another case, emergency room staff found a fentanyl patch stuck to the back of a 3-year-old girl. A CT scan showed global cerebral edema, and the patient progressed to brain death. “This is not a unique case; there have been over 10 such cases in the United States,” said Dr. Schachner. “We should be doing better with fentanyl.”
Nicotine patches can also be dangerous to children, he added. As for other topical agents, there have been reports of toxicity and deaths linked to salicylic acid, commonly used by dermatologists because of its bacteriostatic, fungicidal, keratolytic, and photoprotective properties.
Dr. Schachner cited the case of a 2-month-old where the pediatrician prescribed 50% salicylic acid for seborrheic dermatitis of the scalp, under occlusion. “It’s amazing this child survived; that’s clearly a physician error,” he said.
Henna, a reddish-brown dye derived from the crushed leaves of Lawsonia alba, is used cosmetically for the hair, skin, and nails. Many henna products are mixed with additives, including para-phenylenediamine, which has been associated with dermatitis, asthma, renal failure, and permanent vision loss.
Asked to comment on the presentation, Sheilagh Maguiness, MD, professor of dermatology and pediatrics and chair of pediatric dermatology at the University of Minnesota, Minneapolis, recalled a particularly concerning story in 2008, when the FDA issued a warning about Mommy’s Bliss, a cream containing chlorphenesin and phenoxyethanol as preservatives, promoted to nursing mothers for soothing cracked nipples. There were reports of the cream causing respiratory distress, vomiting, and diarrhea in nursing infants.
Dr. Schachner is chair of Stiefel Laboratories and is an investigator with: Astellas, Berg Pharma, Celgene, Ferndale Labs, Lilly, Medimetriks Pharmaceuticals, Novartis, Organogenesis, Pfizer, Sciton; is a consultant for: Alphyn, Amryt Pharma, Beiersdorf, Brickell, Cutanea, Hoth, Lexington, Mustela, TopMD, Noble Pharma; a speaker for: Novartis, Sanofi-Regeneron, CeraVe; is on the advisory boards of: Almirall, Alphyn, Apogee, Aslan, Biofrontera, CeraVe, Krystal Biotech, Mustela, Noble Pharma, Pfizer, Pierre Fabre, Sanofi-Regeneron; and owns stocks in: TopMD and Alphyn. Dr. Maguiness had no relevant conflicts of interest.
A version of this article appeared on Medscape.com.
FROM SPD 2024








