User login
Living liver donation safety supported in single-center study
SCOTTSDALE, ARIZ. – A single-center analysis of complications following living liver donation found a low rate of severe complications, and a high quality of life among donors. The results are similar to what has been seen in a previous multicenter study in the United States, and the authors hope that the results can help inform potential donors and their physicians.
There is a significant shortage of deceased liver donors, leading to the death of about 3,500 liver transplant hopefuls in 2016, compared with about 2,900 who received a transplant. Living donor transplant was developed and first attempted in 1996 as an attempt to counter this shortage, and for a brief period it was popular, peaking at 500 donor surgeries in 2001. But that year the death of a donor occurred in New York and received widespread publicity.
Overall, though, the study showed relatively few complications, and that donors reported good quality of life. “There was a slight dip in health-related quality of life at 5 years and 10 years, but at all times the donors had significantly better quality of life compared to the standard population,” said Dr. Chinnakotla, clinical director of pediatric transplantation at the University of Minnesota, Minneapolis.
The researchers examined long-term complications and quality of life among 176 liver donors who underwent surgery between 1997 and 2016 at the University of Minnesota. At total of 140 donors underwent a right-lobe hepatectomy without middle hepatic vein, 14 underwent right lobe with middle hepatic vein, 4 underwent left lobe, and 18 underwent left lateral segmentectomy.
The researchers then analyzed complications graded by the Clavien scale. They found that 59.1% of right-lobe donors experienced no complications at all; 5.8% had Clavien scale 1 complications, meaning something abnormal occurred but required no intervention; and 27.3% had a Clavien 2 complication, requiring pharmaceutical treatment, a blood transfusion, or parenteral nutrition. Clavien 3a complications, which required an intervention without general anesthesia, occurred in 1.9% of cases, and Clavien 3b complications, which required anesthesia, occurred in 5.8%.
A total of 81.8% of left-lobe donors experienced no complications, 4.5% had a Clavien 1 complication, and 13.6% a Clavien 2. There were no Clavien 3 or 4 complications in left-lobe donors.
Overall, the incidence of Clavien grade 3 or higher complications was 7%, there were no complications involving organ failure, and there were no deaths.
Quality of life, as measured by the 36-item Short Form Health Survey and an internally designed donor-specific survey, was higher among recipients than in the general population at all time points. The primary long-term complaints were incisional discomfort, which ranged from about 23% to 38% in frequency, and intolerance to fatty meals, which had a frequency of 20%-30%, and is likely attributable to accompanying cholecystectomy, according to Dr. Chinnakotla.
“The overall results appear to have been excellent,” said William C. Chapman, MD, who was invited by the meeting organizers to review and comment on the study. Dr. Chapman is surgical director of transplant surgery at Washington University in St. Louis.
Dr. Chapman also noted that some studies in Asia have looked at reducing complications in donors, while avoiding a small-for-size graft, by using two left-lobe grafts from separate living donors (Liver Transpl 2015;21[11]1438-48). “We haven’t been brave enough to do that in the United States, but I think that is a strategy we can look forward to in the future,” said Dr. Chinnakotla.
No funding source was disclosed.
SCOTTSDALE, ARIZ. – A single-center analysis of complications following living liver donation found a low rate of severe complications, and a high quality of life among donors. The results are similar to what has been seen in a previous multicenter study in the United States, and the authors hope that the results can help inform potential donors and their physicians.
There is a significant shortage of deceased liver donors, leading to the death of about 3,500 liver transplant hopefuls in 2016, compared with about 2,900 who received a transplant. Living donor transplant was developed and first attempted in 1996 as an attempt to counter this shortage, and for a brief period it was popular, peaking at 500 donor surgeries in 2001. But that year the death of a donor occurred in New York and received widespread publicity.
Overall, though, the study showed relatively few complications, and that donors reported good quality of life. “There was a slight dip in health-related quality of life at 5 years and 10 years, but at all times the donors had significantly better quality of life compared to the standard population,” said Dr. Chinnakotla, clinical director of pediatric transplantation at the University of Minnesota, Minneapolis.
The researchers examined long-term complications and quality of life among 176 liver donors who underwent surgery between 1997 and 2016 at the University of Minnesota. At total of 140 donors underwent a right-lobe hepatectomy without middle hepatic vein, 14 underwent right lobe with middle hepatic vein, 4 underwent left lobe, and 18 underwent left lateral segmentectomy.
The researchers then analyzed complications graded by the Clavien scale. They found that 59.1% of right-lobe donors experienced no complications at all; 5.8% had Clavien scale 1 complications, meaning something abnormal occurred but required no intervention; and 27.3% had a Clavien 2 complication, requiring pharmaceutical treatment, a blood transfusion, or parenteral nutrition. Clavien 3a complications, which required an intervention without general anesthesia, occurred in 1.9% of cases, and Clavien 3b complications, which required anesthesia, occurred in 5.8%.
A total of 81.8% of left-lobe donors experienced no complications, 4.5% had a Clavien 1 complication, and 13.6% a Clavien 2. There were no Clavien 3 or 4 complications in left-lobe donors.
Overall, the incidence of Clavien grade 3 or higher complications was 7%, there were no complications involving organ failure, and there were no deaths.
Quality of life, as measured by the 36-item Short Form Health Survey and an internally designed donor-specific survey, was higher among recipients than in the general population at all time points. The primary long-term complaints were incisional discomfort, which ranged from about 23% to 38% in frequency, and intolerance to fatty meals, which had a frequency of 20%-30%, and is likely attributable to accompanying cholecystectomy, according to Dr. Chinnakotla.
“The overall results appear to have been excellent,” said William C. Chapman, MD, who was invited by the meeting organizers to review and comment on the study. Dr. Chapman is surgical director of transplant surgery at Washington University in St. Louis.
Dr. Chapman also noted that some studies in Asia have looked at reducing complications in donors, while avoiding a small-for-size graft, by using two left-lobe grafts from separate living donors (Liver Transpl 2015;21[11]1438-48). “We haven’t been brave enough to do that in the United States, but I think that is a strategy we can look forward to in the future,” said Dr. Chinnakotla.
No funding source was disclosed.
SCOTTSDALE, ARIZ. – A single-center analysis of complications following living liver donation found a low rate of severe complications, and a high quality of life among donors. The results are similar to what has been seen in a previous multicenter study in the United States, and the authors hope that the results can help inform potential donors and their physicians.
There is a significant shortage of deceased liver donors, leading to the death of about 3,500 liver transplant hopefuls in 2016, compared with about 2,900 who received a transplant. Living donor transplant was developed and first attempted in 1996 as an attempt to counter this shortage, and for a brief period it was popular, peaking at 500 donor surgeries in 2001. But that year the death of a donor occurred in New York and received widespread publicity.
Overall, though, the study showed relatively few complications, and that donors reported good quality of life. “There was a slight dip in health-related quality of life at 5 years and 10 years, but at all times the donors had significantly better quality of life compared to the standard population,” said Dr. Chinnakotla, clinical director of pediatric transplantation at the University of Minnesota, Minneapolis.
The researchers examined long-term complications and quality of life among 176 liver donors who underwent surgery between 1997 and 2016 at the University of Minnesota. At total of 140 donors underwent a right-lobe hepatectomy without middle hepatic vein, 14 underwent right lobe with middle hepatic vein, 4 underwent left lobe, and 18 underwent left lateral segmentectomy.
The researchers then analyzed complications graded by the Clavien scale. They found that 59.1% of right-lobe donors experienced no complications at all; 5.8% had Clavien scale 1 complications, meaning something abnormal occurred but required no intervention; and 27.3% had a Clavien 2 complication, requiring pharmaceutical treatment, a blood transfusion, or parenteral nutrition. Clavien 3a complications, which required an intervention without general anesthesia, occurred in 1.9% of cases, and Clavien 3b complications, which required anesthesia, occurred in 5.8%.
A total of 81.8% of left-lobe donors experienced no complications, 4.5% had a Clavien 1 complication, and 13.6% a Clavien 2. There were no Clavien 3 or 4 complications in left-lobe donors.
Overall, the incidence of Clavien grade 3 or higher complications was 7%, there were no complications involving organ failure, and there were no deaths.
Quality of life, as measured by the 36-item Short Form Health Survey and an internally designed donor-specific survey, was higher among recipients than in the general population at all time points. The primary long-term complaints were incisional discomfort, which ranged from about 23% to 38% in frequency, and intolerance to fatty meals, which had a frequency of 20%-30%, and is likely attributable to accompanying cholecystectomy, according to Dr. Chinnakotla.
“The overall results appear to have been excellent,” said William C. Chapman, MD, who was invited by the meeting organizers to review and comment on the study. Dr. Chapman is surgical director of transplant surgery at Washington University in St. Louis.
Dr. Chapman also noted that some studies in Asia have looked at reducing complications in donors, while avoiding a small-for-size graft, by using two left-lobe grafts from separate living donors (Liver Transpl 2015;21[11]1438-48). “We haven’t been brave enough to do that in the United States, but I think that is a strategy we can look forward to in the future,” said Dr. Chinnakotla.
No funding source was disclosed.
AT WSA 2017
Statin didn’t slow hepatic steatosis in HIV patients
SAN DIEGO – Statin therapy wasn’t effective against a rising rate of hepatic steatosis in HIV patients, and may increase nonalcoholic fatty liver disease (NAFLD) risk, according to a small study.
The findings are contrary to the limited data currently available, which suggest statins can have a beneficial effect on hepatic steatosis, according to the study’s investigators.
NAFLD is one of the leading causes of mortality and morbidity in people living with HIV, said Vanessa El Kamari, MD, of Case Western Reserve University, Cleveland, and rates are continuing to increase. With a lack of therapeutic interventions for NAFLD in patients with HIV, finding effective treatments is a major concern for providers.
Dr. El Kamari and her colleagues conducted a secondary analysis of the SATURN-HIV trial, a randomized, placebo-controlled trial of 147 patients with HIV who were on stable antiretroviral therapy (ART) with LDL cholesterol levels at or below 130 mg/dL. Patients were either treated with 10 mg rosuvastatin or placebo.
Patients in the treatment and placebo arms were an average age of 45 years, most patients were male (81% and 76%, respectively), and a majority was African American (69% and 67%, respectively). The two groups reported average CD4+ counts of 644 and 636, respectively.
Investigators used validated scores to determine hepatic steatosis in patients, although researchers acknowledged that liver biopsy is the gold standard for hepatic steatosis measurement.
“We understand liver fat score has its limitation,” said Dr. El Kamari in a question and answer session following the presentation at an annual scientific meeting on infectious diseases. “Further studies are needed in this area in order to detect, in noninvasive ways, hepatic steatosis.”
Liver fat scores (LFS) were measured on entry, at week 48, and week 96.
After 96 weeks, investigators saw significant increases in LFS in both the placebo and rosuvastatin groups (P = .01 and P less than .01, respectively). Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Studying predictors for LFS changes, a trend toward insignificance among the randomization group led investigators to the conclusion that statin may have negatively affected the liver fat score of patients over the 96-week time period.
The study researchers identified 92 patients who did not have hepatic steatosis at baseline to study how statins influenced the development of hepatic steatosis.
Of the 13 patients who developed steatosis during the trial period, 10 were part of the rosuvastatin group, while only 3 were from the placebo group.
Increases in LFS were associated with increases in insulin resistance, detected presence of HIV-1 RNA, and higher interferon-inducible proteins, according to Dr. El Kamari.
While increased homeostatic assessment of insulin resistance was associated with increased hepatic homeostasis, Dr. El Kamari was not able to determine if statins that are not associated with insulin resistance will have different outcomes.
The investigators cautioned that the findings may not be generalizable to the entire HIV population due to the overwhelming majority of African American patients with increased inflammation, as well as the study patients’ LDL cholesterol levels of less than or equal to 130 mg/dL.
The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
SAN DIEGO – Statin therapy wasn’t effective against a rising rate of hepatic steatosis in HIV patients, and may increase nonalcoholic fatty liver disease (NAFLD) risk, according to a small study.
The findings are contrary to the limited data currently available, which suggest statins can have a beneficial effect on hepatic steatosis, according to the study’s investigators.
NAFLD is one of the leading causes of mortality and morbidity in people living with HIV, said Vanessa El Kamari, MD, of Case Western Reserve University, Cleveland, and rates are continuing to increase. With a lack of therapeutic interventions for NAFLD in patients with HIV, finding effective treatments is a major concern for providers.
Dr. El Kamari and her colleagues conducted a secondary analysis of the SATURN-HIV trial, a randomized, placebo-controlled trial of 147 patients with HIV who were on stable antiretroviral therapy (ART) with LDL cholesterol levels at or below 130 mg/dL. Patients were either treated with 10 mg rosuvastatin or placebo.
Patients in the treatment and placebo arms were an average age of 45 years, most patients were male (81% and 76%, respectively), and a majority was African American (69% and 67%, respectively). The two groups reported average CD4+ counts of 644 and 636, respectively.
Investigators used validated scores to determine hepatic steatosis in patients, although researchers acknowledged that liver biopsy is the gold standard for hepatic steatosis measurement.
“We understand liver fat score has its limitation,” said Dr. El Kamari in a question and answer session following the presentation at an annual scientific meeting on infectious diseases. “Further studies are needed in this area in order to detect, in noninvasive ways, hepatic steatosis.”
Liver fat scores (LFS) were measured on entry, at week 48, and week 96.
After 96 weeks, investigators saw significant increases in LFS in both the placebo and rosuvastatin groups (P = .01 and P less than .01, respectively). Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Studying predictors for LFS changes, a trend toward insignificance among the randomization group led investigators to the conclusion that statin may have negatively affected the liver fat score of patients over the 96-week time period.
The study researchers identified 92 patients who did not have hepatic steatosis at baseline to study how statins influenced the development of hepatic steatosis.
Of the 13 patients who developed steatosis during the trial period, 10 were part of the rosuvastatin group, while only 3 were from the placebo group.
Increases in LFS were associated with increases in insulin resistance, detected presence of HIV-1 RNA, and higher interferon-inducible proteins, according to Dr. El Kamari.
While increased homeostatic assessment of insulin resistance was associated with increased hepatic homeostasis, Dr. El Kamari was not able to determine if statins that are not associated with insulin resistance will have different outcomes.
The investigators cautioned that the findings may not be generalizable to the entire HIV population due to the overwhelming majority of African American patients with increased inflammation, as well as the study patients’ LDL cholesterol levels of less than or equal to 130 mg/dL.
The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
SAN DIEGO – Statin therapy wasn’t effective against a rising rate of hepatic steatosis in HIV patients, and may increase nonalcoholic fatty liver disease (NAFLD) risk, according to a small study.
The findings are contrary to the limited data currently available, which suggest statins can have a beneficial effect on hepatic steatosis, according to the study’s investigators.
NAFLD is one of the leading causes of mortality and morbidity in people living with HIV, said Vanessa El Kamari, MD, of Case Western Reserve University, Cleveland, and rates are continuing to increase. With a lack of therapeutic interventions for NAFLD in patients with HIV, finding effective treatments is a major concern for providers.
Dr. El Kamari and her colleagues conducted a secondary analysis of the SATURN-HIV trial, a randomized, placebo-controlled trial of 147 patients with HIV who were on stable antiretroviral therapy (ART) with LDL cholesterol levels at or below 130 mg/dL. Patients were either treated with 10 mg rosuvastatin or placebo.
Patients in the treatment and placebo arms were an average age of 45 years, most patients were male (81% and 76%, respectively), and a majority was African American (69% and 67%, respectively). The two groups reported average CD4+ counts of 644 and 636, respectively.
Investigators used validated scores to determine hepatic steatosis in patients, although researchers acknowledged that liver biopsy is the gold standard for hepatic steatosis measurement.
“We understand liver fat score has its limitation,” said Dr. El Kamari in a question and answer session following the presentation at an annual scientific meeting on infectious diseases. “Further studies are needed in this area in order to detect, in noninvasive ways, hepatic steatosis.”
Liver fat scores (LFS) were measured on entry, at week 48, and week 96.
After 96 weeks, investigators saw significant increases in LFS in both the placebo and rosuvastatin groups (P = .01 and P less than .01, respectively). Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Studying predictors for LFS changes, a trend toward insignificance among the randomization group led investigators to the conclusion that statin may have negatively affected the liver fat score of patients over the 96-week time period.
The study researchers identified 92 patients who did not have hepatic steatosis at baseline to study how statins influenced the development of hepatic steatosis.
Of the 13 patients who developed steatosis during the trial period, 10 were part of the rosuvastatin group, while only 3 were from the placebo group.
Increases in LFS were associated with increases in insulin resistance, detected presence of HIV-1 RNA, and higher interferon-inducible proteins, according to Dr. El Kamari.
While increased homeostatic assessment of insulin resistance was associated with increased hepatic homeostasis, Dr. El Kamari was not able to determine if statins that are not associated with insulin resistance will have different outcomes.
The investigators cautioned that the findings may not be generalizable to the entire HIV population due to the overwhelming majority of African American patients with increased inflammation, as well as the study patients’ LDL cholesterol levels of less than or equal to 130 mg/dL.
The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
AT IDWEEK 2017
Key clinical point:
Major finding: Progression from nonsteatosis at baseline to steatosis over 96 weeks was greater in patients given rosuvastatin than in those given placebo (odds ratio, 4.3; P = .03).
Data source: A randomized, placebo-controlled study of 147 patients with HIV on stable ART.
Disclosures: The National Institutes of Health funded the study. Dr. El Kamari had no disclosures.
FDA approves first two-dose HBV vaccine
When the Food and Drug Administration approved Heplisav-B Nov. 9, it marked the first new vaccine for hepatitis B virus (HBV) to be sanctioned in over 25 years.
Heplisav-B is the only two-dose regimen that protects against all known subtypes of HBV in adults 18 years and older, according to a statement released by Dynavax Technologies, the creator of the drug.
“Heplisav-B is the first FDA-approved product for Dynavax and demonstrates our ability to develop innovative products and progress them from discovery to commercialization,” according to Eddie Gray, chief executive officer of Dynavax. “We expect that it will become an essential tool in the public health community’s fight to prevent hepatitis B [infection], and we look forward to making Heplisav-B available to clinicians and their adult patients.”
Incidence of HBV has increased sharply from 2012 to 2015 in the United States, with reported cases rising from 2,895 to 3,370, according to the Centers for Disease Control and Prevention.
From 2014 to 2015, acute HBV infection increased 20.7%, according to the CDC report.
The new vaccine’s approval came after review of safety and efficacy data from three phase 3 trials comparing Heplisav-B with Engerix-B, another HBV vaccine currently available, that is given in a three-dose regimen.
In one study of 2,032 patients between the ages of 18 and 55 years, seroprotection rate in the Heplisav-B group (1,511) was 95%, compared with 81.5% in the Engerix-B group (521).
Heplisav-B patients were given a two-dose regimen of the drug at 0 and 1 months, followed by a placebo at 6 months, while investigators administered Engerix-B at all three intervals in the comparator subjects.
The FDA’s decision to green-light the new vaccine follows a recommendation for approval from the FDA’s Vaccines and Related Biological Products Advisory Committee, held at the end of July this year.
During the advisory committee meeting, members were concerned about an increased relative risk for acute myocardial infarction of 6.97 in Heplisav-B patients (14), compared with Engerix-B patients (1).
The recommendation for approval came with the caveat of conducting postmarketing analysis for the risk of AMI in Heplisav-B patients, which Dynavax is conducting through the Kaiser Permanente system in California.
“To evaluate the risk of AMIs, the study will enroll 25,000 Heplisav-B patients and 25,000 Engerix-B patients over approximately 10 months and follow them for 1 year after vaccination,” according to a statement from Dynavax. “In addition we will evaluate the rate of immune-mediated diseases in these patients in an additional 5,000 Heplisav-B recipients and 5,000 Engerix-B recipients.”
Dynavax is currently set to introduce Heplisav-B commercially in the United States in 2018, with the cost of the drug set to be released soon.
“Dynavax is in the process of finalizing the price of a two-dose series of Heplisav-B, and they plan to disclose it shortly after approval,” according to the company. “Their pricing and access strategy will be aimed at ensuring that populations at risk of infection are able to access this new vaccine, while recognizing the value it brings to the health care system with a two-dose regimen and higher rates of protection compared to Engerix-B.”
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
When the Food and Drug Administration approved Heplisav-B Nov. 9, it marked the first new vaccine for hepatitis B virus (HBV) to be sanctioned in over 25 years.
Heplisav-B is the only two-dose regimen that protects against all known subtypes of HBV in adults 18 years and older, according to a statement released by Dynavax Technologies, the creator of the drug.
“Heplisav-B is the first FDA-approved product for Dynavax and demonstrates our ability to develop innovative products and progress them from discovery to commercialization,” according to Eddie Gray, chief executive officer of Dynavax. “We expect that it will become an essential tool in the public health community’s fight to prevent hepatitis B [infection], and we look forward to making Heplisav-B available to clinicians and their adult patients.”
Incidence of HBV has increased sharply from 2012 to 2015 in the United States, with reported cases rising from 2,895 to 3,370, according to the Centers for Disease Control and Prevention.
From 2014 to 2015, acute HBV infection increased 20.7%, according to the CDC report.
The new vaccine’s approval came after review of safety and efficacy data from three phase 3 trials comparing Heplisav-B with Engerix-B, another HBV vaccine currently available, that is given in a three-dose regimen.
In one study of 2,032 patients between the ages of 18 and 55 years, seroprotection rate in the Heplisav-B group (1,511) was 95%, compared with 81.5% in the Engerix-B group (521).
Heplisav-B patients were given a two-dose regimen of the drug at 0 and 1 months, followed by a placebo at 6 months, while investigators administered Engerix-B at all three intervals in the comparator subjects.
The FDA’s decision to green-light the new vaccine follows a recommendation for approval from the FDA’s Vaccines and Related Biological Products Advisory Committee, held at the end of July this year.
During the advisory committee meeting, members were concerned about an increased relative risk for acute myocardial infarction of 6.97 in Heplisav-B patients (14), compared with Engerix-B patients (1).
The recommendation for approval came with the caveat of conducting postmarketing analysis for the risk of AMI in Heplisav-B patients, which Dynavax is conducting through the Kaiser Permanente system in California.
“To evaluate the risk of AMIs, the study will enroll 25,000 Heplisav-B patients and 25,000 Engerix-B patients over approximately 10 months and follow them for 1 year after vaccination,” according to a statement from Dynavax. “In addition we will evaluate the rate of immune-mediated diseases in these patients in an additional 5,000 Heplisav-B recipients and 5,000 Engerix-B recipients.”
Dynavax is currently set to introduce Heplisav-B commercially in the United States in 2018, with the cost of the drug set to be released soon.
“Dynavax is in the process of finalizing the price of a two-dose series of Heplisav-B, and they plan to disclose it shortly after approval,” according to the company. “Their pricing and access strategy will be aimed at ensuring that populations at risk of infection are able to access this new vaccine, while recognizing the value it brings to the health care system with a two-dose regimen and higher rates of protection compared to Engerix-B.”
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
When the Food and Drug Administration approved Heplisav-B Nov. 9, it marked the first new vaccine for hepatitis B virus (HBV) to be sanctioned in over 25 years.
Heplisav-B is the only two-dose regimen that protects against all known subtypes of HBV in adults 18 years and older, according to a statement released by Dynavax Technologies, the creator of the drug.
“Heplisav-B is the first FDA-approved product for Dynavax and demonstrates our ability to develop innovative products and progress them from discovery to commercialization,” according to Eddie Gray, chief executive officer of Dynavax. “We expect that it will become an essential tool in the public health community’s fight to prevent hepatitis B [infection], and we look forward to making Heplisav-B available to clinicians and their adult patients.”
Incidence of HBV has increased sharply from 2012 to 2015 in the United States, with reported cases rising from 2,895 to 3,370, according to the Centers for Disease Control and Prevention.
From 2014 to 2015, acute HBV infection increased 20.7%, according to the CDC report.
The new vaccine’s approval came after review of safety and efficacy data from three phase 3 trials comparing Heplisav-B with Engerix-B, another HBV vaccine currently available, that is given in a three-dose regimen.
In one study of 2,032 patients between the ages of 18 and 55 years, seroprotection rate in the Heplisav-B group (1,511) was 95%, compared with 81.5% in the Engerix-B group (521).
Heplisav-B patients were given a two-dose regimen of the drug at 0 and 1 months, followed by a placebo at 6 months, while investigators administered Engerix-B at all three intervals in the comparator subjects.
The FDA’s decision to green-light the new vaccine follows a recommendation for approval from the FDA’s Vaccines and Related Biological Products Advisory Committee, held at the end of July this year.
During the advisory committee meeting, members were concerned about an increased relative risk for acute myocardial infarction of 6.97 in Heplisav-B patients (14), compared with Engerix-B patients (1).
The recommendation for approval came with the caveat of conducting postmarketing analysis for the risk of AMI in Heplisav-B patients, which Dynavax is conducting through the Kaiser Permanente system in California.
“To evaluate the risk of AMIs, the study will enroll 25,000 Heplisav-B patients and 25,000 Engerix-B patients over approximately 10 months and follow them for 1 year after vaccination,” according to a statement from Dynavax. “In addition we will evaluate the rate of immune-mediated diseases in these patients in an additional 5,000 Heplisav-B recipients and 5,000 Engerix-B recipients.”
Dynavax is currently set to introduce Heplisav-B commercially in the United States in 2018, with the cost of the drug set to be released soon.
“Dynavax is in the process of finalizing the price of a two-dose series of Heplisav-B, and they plan to disclose it shortly after approval,” according to the company. “Their pricing and access strategy will be aimed at ensuring that populations at risk of infection are able to access this new vaccine, while recognizing the value it brings to the health care system with a two-dose regimen and higher rates of protection compared to Engerix-B.”
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
Clinical hepatology debrief wraps up 2017 Liver Meeting
WASHINGTON – Research into alcoholic liver disease, drug-induced liver injury, the complications of chronic liver disease, and cholestatic liver diseases were among the clinical hepatology highlights presented at the annual meeting of the American Association for the Study of Liver Diseases.
This year’s debrief was given by Kris V. Kowdley, MD, of Swedish Medical Center in Seattle.
Over a median of 1.6 years of follow-up, 27% of patients resumed alcohol consumption post transplant with a median time to alcohol of 160 days, according to Brian Lee, MD, of the University of California, San Francisco. Younger age and lack of complete acceptance of their alcoholic hepatitis diagnosis were significant predictors of alcohol use post transplant while factors such as length of abstinence, race/ethnicity, insurance status, history of illicit drug use, and history of failed rehab attempts were not. Further, heavy drinking at presentation (more than 10 drinks per day), any alcohol use post transplant, and sustained alcohol use post transplant were significant predictors of posttransplant death.
Alcoholic hepatitis now “appears to be affecting more and more younger women, who present with a higher level of acuity,” Dr. Kowdley noted. He added that, while recent advances have decreased the absolute number of hepatitis C patients with decompensated liver disease who are listed for liver transplant, “the number is increasing rapidly in alcoholic liver disease, approaching the rate of patients being listed for hepatitis C.”
Unknown ingredients in herbal and dietary supplements continue to be of concern, Dr. Kowdley noted, as highlighted by Victor J. Navarro, MD, of Einstein Healthcare Network, Philadelphia, and his colleagues at the Drug-Induced Liver Injury Network (DILIN).
Investigators collected herbal and dietary supplements from patients enrolled in the DILIN prospective study and had chemical analysis performed by an outside laboratory. Labeled contents could not be verified in over half of the supplements collected and several unlabeled hepatotoxic ingredients were identified, Dr. Navarro and colleagues found (abstract 264).
“Even though we collect the supplements and review them with the patients, it’s not clear that we even know what it is that they are taking,” Dr. Kowdley commented.
Another DILIN study, this one presented by Jawad Ahmad, MD, of the Icahn School of Medicine at Mount Sinai, New York, “provided an opportunity for pause,” Dr. Kowdley said.
Dr. Ahmad and colleagues looked at hepatitis C virus (HCV) testing in DILIN patients and were able to correlate anti-HCV test results with HCV RNA tests results in more than 95% of 1,500 patients (abstract 16). About 7% of patients were HCV positive, and 23 cases of acute hepatitis were identified (16 with anti-HCV antibodies and HCV RNA, 7 with HCV RNA alone, and none with anti-HCV antibodies alone).
“So the take-home message here for me is, even if we think the patient has drug-induced liver injury, if they have not been tested for hepatitis C, especially if in the hospitalized setting … it is important to check not only the antibody test but also the RNA test,” Dr. Kowdley said.
Finally, in children, minocycline and valproate were the most commonly indicated agents in pediatric drug-induced liver injury, according to Frank DiPaola, MD, of the University of Michigan, and colleagues, on behalf of DILIN (abstract 13).
Dr. Kowdley also highlighted a couple of studies that addressed the complications of chronic liver disease.
The ADAPT-1 and ADAPT-2 trials (abstract 217) studied the use of avatrombopag, a thrombopoietin (TPO)–receptor agonist, to reduce severe thrombocytopenia in patients with chronic liver disease. Platelet transfusion is the current standard of care to reduce the risk of bleeding during invasive procedures in these patients; currently there are no drugs approved for this indication, Dr. Kowdley said.
Avatrombopag is an oral, small molecule TPO-receptor agonist, he said. “Because it binds to a different site on the TPO receptor than endogenous TPO, the effects are additive.”
In the phase 3 ADAPT-1 and ADAPT-2, the proportion of patients who did not require platelet transfusion or any rescue procedure for bleeding was significantly less in avatrombopag-treated patients than those receiving placebo. The effect was the same for patients with a low baseline platelet count (less than 40,000 platelets per mcL) as well as those with a high baseline platelet count (between 40,000/mcL and 50,000/mcL). Further, the proportion of patients who by procedure day achieved platelet count of at least 50,000/mcL was significantly higher in patients on the study drug.
Data on lusutrombopag, another TPO-receptor agonist, was presented as a late-breaker at the meeting, with very similar results in avoiding platelet transfusion, Dr. Kowdley noted.Two abstracts (502 and 219) focused on reducing ammonia levels in hospitalized cirrhosis patients with hepatic encephalitis.
Patients in the STOP-HE trial were randomized to either physician’s choice for standard of care or standard of care plus continuous infusion of ornithine phenylacetate for up to 5 days. Patients were assigned to one of three dosing groups (20 g, 15 g, or 10 g), based on severity of underlying liver disease; those with the most severe disease received the lowest dose.
Reduction in plasma ammonia levels correlated significantly with clinical improvement. At 48 hours, meaningful clinical improvement occurred in 84% of patients on ornithine phenylacetate, compared with 58% of placebo patients, according to Robert S. Rahimi, MD, of Baylor University, Dallas, and his colleagues.
“So, this may be an option for our hepatic encephalopathy patients who are admitted to the hospital and need acute treatment,” Dr. Kowdley said.
Dr. Kowdley finished up with two studies on primary biliary cholangitis (PBC).
Carla Murillo Perez, MD, of Toronto General Hospital and her colleagues in the Global PBC Study Group investigated the role of serum bilirubin in predicting transplant-free survival in patients with PBC (abstract 70).
When serum bilirubin levels from a previous study were input into a Cox regression analysis as a cubic spline function, then adjusted for factors such as age, sex, treatment with ursodeoxycholic acid, and year of diagnosis, the investigators found that patients with serum bilirubin levels of 0.7 times the upper limit of normal had a significantly increased risk of liver transplantation or death.
“We may want to be more sensitive in looking at bilirubin levels,” Dr. Kowdley said.
Another small but notable study presented by Gideon M. Hirschfield, MD, of the University of Birmingham (England), looked into whether a lower dose of seladelpar would safely and effectively lower alkaline phosphatase (AP) levels in PBC patients. A previous study of seladelpar at 50 mg and 200 mg doses indicated the drug’s effectiveness; however, the study was stopped because of the development of grade 3 alanine aminotransferase increases in a number of patients (Lancet Gastroenterol Hepatol. 2017;2;716-26).
Dr. Hirschfield and colleagues enrolled 24 patients and randomized 12 to seladelpar 5 mg and another 12 to 10 mg. The study cohort was mostly female, with an average age of 58 years. Most were either intolerant of or inadequately treated by ursodeoxycholic acid. AP levels were reduced significantly over time in both groups; however, differences between the groups were not significant, the investigators noted.
The Liver Meeting will be held in San Francisco in 2018, taking place Nov. 9-13. Many investigators in these trials reported relevant conflicts of interest; information is available (open access) in a supplement to Hepatology.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
WASHINGTON – Research into alcoholic liver disease, drug-induced liver injury, the complications of chronic liver disease, and cholestatic liver diseases were among the clinical hepatology highlights presented at the annual meeting of the American Association for the Study of Liver Diseases.
This year’s debrief was given by Kris V. Kowdley, MD, of Swedish Medical Center in Seattle.
Over a median of 1.6 years of follow-up, 27% of patients resumed alcohol consumption post transplant with a median time to alcohol of 160 days, according to Brian Lee, MD, of the University of California, San Francisco. Younger age and lack of complete acceptance of their alcoholic hepatitis diagnosis were significant predictors of alcohol use post transplant while factors such as length of abstinence, race/ethnicity, insurance status, history of illicit drug use, and history of failed rehab attempts were not. Further, heavy drinking at presentation (more than 10 drinks per day), any alcohol use post transplant, and sustained alcohol use post transplant were significant predictors of posttransplant death.
Alcoholic hepatitis now “appears to be affecting more and more younger women, who present with a higher level of acuity,” Dr. Kowdley noted. He added that, while recent advances have decreased the absolute number of hepatitis C patients with decompensated liver disease who are listed for liver transplant, “the number is increasing rapidly in alcoholic liver disease, approaching the rate of patients being listed for hepatitis C.”
Unknown ingredients in herbal and dietary supplements continue to be of concern, Dr. Kowdley noted, as highlighted by Victor J. Navarro, MD, of Einstein Healthcare Network, Philadelphia, and his colleagues at the Drug-Induced Liver Injury Network (DILIN).
Investigators collected herbal and dietary supplements from patients enrolled in the DILIN prospective study and had chemical analysis performed by an outside laboratory. Labeled contents could not be verified in over half of the supplements collected and several unlabeled hepatotoxic ingredients were identified, Dr. Navarro and colleagues found (abstract 264).
“Even though we collect the supplements and review them with the patients, it’s not clear that we even know what it is that they are taking,” Dr. Kowdley commented.
Another DILIN study, this one presented by Jawad Ahmad, MD, of the Icahn School of Medicine at Mount Sinai, New York, “provided an opportunity for pause,” Dr. Kowdley said.
Dr. Ahmad and colleagues looked at hepatitis C virus (HCV) testing in DILIN patients and were able to correlate anti-HCV test results with HCV RNA tests results in more than 95% of 1,500 patients (abstract 16). About 7% of patients were HCV positive, and 23 cases of acute hepatitis were identified (16 with anti-HCV antibodies and HCV RNA, 7 with HCV RNA alone, and none with anti-HCV antibodies alone).
“So the take-home message here for me is, even if we think the patient has drug-induced liver injury, if they have not been tested for hepatitis C, especially if in the hospitalized setting … it is important to check not only the antibody test but also the RNA test,” Dr. Kowdley said.
Finally, in children, minocycline and valproate were the most commonly indicated agents in pediatric drug-induced liver injury, according to Frank DiPaola, MD, of the University of Michigan, and colleagues, on behalf of DILIN (abstract 13).
Dr. Kowdley also highlighted a couple of studies that addressed the complications of chronic liver disease.
The ADAPT-1 and ADAPT-2 trials (abstract 217) studied the use of avatrombopag, a thrombopoietin (TPO)–receptor agonist, to reduce severe thrombocytopenia in patients with chronic liver disease. Platelet transfusion is the current standard of care to reduce the risk of bleeding during invasive procedures in these patients; currently there are no drugs approved for this indication, Dr. Kowdley said.
Avatrombopag is an oral, small molecule TPO-receptor agonist, he said. “Because it binds to a different site on the TPO receptor than endogenous TPO, the effects are additive.”
In the phase 3 ADAPT-1 and ADAPT-2, the proportion of patients who did not require platelet transfusion or any rescue procedure for bleeding was significantly less in avatrombopag-treated patients than those receiving placebo. The effect was the same for patients with a low baseline platelet count (less than 40,000 platelets per mcL) as well as those with a high baseline platelet count (between 40,000/mcL and 50,000/mcL). Further, the proportion of patients who by procedure day achieved platelet count of at least 50,000/mcL was significantly higher in patients on the study drug.
Data on lusutrombopag, another TPO-receptor agonist, was presented as a late-breaker at the meeting, with very similar results in avoiding platelet transfusion, Dr. Kowdley noted.Two abstracts (502 and 219) focused on reducing ammonia levels in hospitalized cirrhosis patients with hepatic encephalitis.
Patients in the STOP-HE trial were randomized to either physician’s choice for standard of care or standard of care plus continuous infusion of ornithine phenylacetate for up to 5 days. Patients were assigned to one of three dosing groups (20 g, 15 g, or 10 g), based on severity of underlying liver disease; those with the most severe disease received the lowest dose.
Reduction in plasma ammonia levels correlated significantly with clinical improvement. At 48 hours, meaningful clinical improvement occurred in 84% of patients on ornithine phenylacetate, compared with 58% of placebo patients, according to Robert S. Rahimi, MD, of Baylor University, Dallas, and his colleagues.
“So, this may be an option for our hepatic encephalopathy patients who are admitted to the hospital and need acute treatment,” Dr. Kowdley said.
Dr. Kowdley finished up with two studies on primary biliary cholangitis (PBC).
Carla Murillo Perez, MD, of Toronto General Hospital and her colleagues in the Global PBC Study Group investigated the role of serum bilirubin in predicting transplant-free survival in patients with PBC (abstract 70).
When serum bilirubin levels from a previous study were input into a Cox regression analysis as a cubic spline function, then adjusted for factors such as age, sex, treatment with ursodeoxycholic acid, and year of diagnosis, the investigators found that patients with serum bilirubin levels of 0.7 times the upper limit of normal had a significantly increased risk of liver transplantation or death.
“We may want to be more sensitive in looking at bilirubin levels,” Dr. Kowdley said.
Another small but notable study presented by Gideon M. Hirschfield, MD, of the University of Birmingham (England), looked into whether a lower dose of seladelpar would safely and effectively lower alkaline phosphatase (AP) levels in PBC patients. A previous study of seladelpar at 50 mg and 200 mg doses indicated the drug’s effectiveness; however, the study was stopped because of the development of grade 3 alanine aminotransferase increases in a number of patients (Lancet Gastroenterol Hepatol. 2017;2;716-26).
Dr. Hirschfield and colleagues enrolled 24 patients and randomized 12 to seladelpar 5 mg and another 12 to 10 mg. The study cohort was mostly female, with an average age of 58 years. Most were either intolerant of or inadequately treated by ursodeoxycholic acid. AP levels were reduced significantly over time in both groups; however, differences between the groups were not significant, the investigators noted.
The Liver Meeting will be held in San Francisco in 2018, taking place Nov. 9-13. Many investigators in these trials reported relevant conflicts of interest; information is available (open access) in a supplement to Hepatology.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
WASHINGTON – Research into alcoholic liver disease, drug-induced liver injury, the complications of chronic liver disease, and cholestatic liver diseases were among the clinical hepatology highlights presented at the annual meeting of the American Association for the Study of Liver Diseases.
This year’s debrief was given by Kris V. Kowdley, MD, of Swedish Medical Center in Seattle.
Over a median of 1.6 years of follow-up, 27% of patients resumed alcohol consumption post transplant with a median time to alcohol of 160 days, according to Brian Lee, MD, of the University of California, San Francisco. Younger age and lack of complete acceptance of their alcoholic hepatitis diagnosis were significant predictors of alcohol use post transplant while factors such as length of abstinence, race/ethnicity, insurance status, history of illicit drug use, and history of failed rehab attempts were not. Further, heavy drinking at presentation (more than 10 drinks per day), any alcohol use post transplant, and sustained alcohol use post transplant were significant predictors of posttransplant death.
Alcoholic hepatitis now “appears to be affecting more and more younger women, who present with a higher level of acuity,” Dr. Kowdley noted. He added that, while recent advances have decreased the absolute number of hepatitis C patients with decompensated liver disease who are listed for liver transplant, “the number is increasing rapidly in alcoholic liver disease, approaching the rate of patients being listed for hepatitis C.”
Unknown ingredients in herbal and dietary supplements continue to be of concern, Dr. Kowdley noted, as highlighted by Victor J. Navarro, MD, of Einstein Healthcare Network, Philadelphia, and his colleagues at the Drug-Induced Liver Injury Network (DILIN).
Investigators collected herbal and dietary supplements from patients enrolled in the DILIN prospective study and had chemical analysis performed by an outside laboratory. Labeled contents could not be verified in over half of the supplements collected and several unlabeled hepatotoxic ingredients were identified, Dr. Navarro and colleagues found (abstract 264).
“Even though we collect the supplements and review them with the patients, it’s not clear that we even know what it is that they are taking,” Dr. Kowdley commented.
Another DILIN study, this one presented by Jawad Ahmad, MD, of the Icahn School of Medicine at Mount Sinai, New York, “provided an opportunity for pause,” Dr. Kowdley said.
Dr. Ahmad and colleagues looked at hepatitis C virus (HCV) testing in DILIN patients and were able to correlate anti-HCV test results with HCV RNA tests results in more than 95% of 1,500 patients (abstract 16). About 7% of patients were HCV positive, and 23 cases of acute hepatitis were identified (16 with anti-HCV antibodies and HCV RNA, 7 with HCV RNA alone, and none with anti-HCV antibodies alone).
“So the take-home message here for me is, even if we think the patient has drug-induced liver injury, if they have not been tested for hepatitis C, especially if in the hospitalized setting … it is important to check not only the antibody test but also the RNA test,” Dr. Kowdley said.
Finally, in children, minocycline and valproate were the most commonly indicated agents in pediatric drug-induced liver injury, according to Frank DiPaola, MD, of the University of Michigan, and colleagues, on behalf of DILIN (abstract 13).
Dr. Kowdley also highlighted a couple of studies that addressed the complications of chronic liver disease.
The ADAPT-1 and ADAPT-2 trials (abstract 217) studied the use of avatrombopag, a thrombopoietin (TPO)–receptor agonist, to reduce severe thrombocytopenia in patients with chronic liver disease. Platelet transfusion is the current standard of care to reduce the risk of bleeding during invasive procedures in these patients; currently there are no drugs approved for this indication, Dr. Kowdley said.
Avatrombopag is an oral, small molecule TPO-receptor agonist, he said. “Because it binds to a different site on the TPO receptor than endogenous TPO, the effects are additive.”
In the phase 3 ADAPT-1 and ADAPT-2, the proportion of patients who did not require platelet transfusion or any rescue procedure for bleeding was significantly less in avatrombopag-treated patients than those receiving placebo. The effect was the same for patients with a low baseline platelet count (less than 40,000 platelets per mcL) as well as those with a high baseline platelet count (between 40,000/mcL and 50,000/mcL). Further, the proportion of patients who by procedure day achieved platelet count of at least 50,000/mcL was significantly higher in patients on the study drug.
Data on lusutrombopag, another TPO-receptor agonist, was presented as a late-breaker at the meeting, with very similar results in avoiding platelet transfusion, Dr. Kowdley noted.Two abstracts (502 and 219) focused on reducing ammonia levels in hospitalized cirrhosis patients with hepatic encephalitis.
Patients in the STOP-HE trial were randomized to either physician’s choice for standard of care or standard of care plus continuous infusion of ornithine phenylacetate for up to 5 days. Patients were assigned to one of three dosing groups (20 g, 15 g, or 10 g), based on severity of underlying liver disease; those with the most severe disease received the lowest dose.
Reduction in plasma ammonia levels correlated significantly with clinical improvement. At 48 hours, meaningful clinical improvement occurred in 84% of patients on ornithine phenylacetate, compared with 58% of placebo patients, according to Robert S. Rahimi, MD, of Baylor University, Dallas, and his colleagues.
“So, this may be an option for our hepatic encephalopathy patients who are admitted to the hospital and need acute treatment,” Dr. Kowdley said.
Dr. Kowdley finished up with two studies on primary biliary cholangitis (PBC).
Carla Murillo Perez, MD, of Toronto General Hospital and her colleagues in the Global PBC Study Group investigated the role of serum bilirubin in predicting transplant-free survival in patients with PBC (abstract 70).
When serum bilirubin levels from a previous study were input into a Cox regression analysis as a cubic spline function, then adjusted for factors such as age, sex, treatment with ursodeoxycholic acid, and year of diagnosis, the investigators found that patients with serum bilirubin levels of 0.7 times the upper limit of normal had a significantly increased risk of liver transplantation or death.
“We may want to be more sensitive in looking at bilirubin levels,” Dr. Kowdley said.
Another small but notable study presented by Gideon M. Hirschfield, MD, of the University of Birmingham (England), looked into whether a lower dose of seladelpar would safely and effectively lower alkaline phosphatase (AP) levels in PBC patients. A previous study of seladelpar at 50 mg and 200 mg doses indicated the drug’s effectiveness; however, the study was stopped because of the development of grade 3 alanine aminotransferase increases in a number of patients (Lancet Gastroenterol Hepatol. 2017;2;716-26).
Dr. Hirschfield and colleagues enrolled 24 patients and randomized 12 to seladelpar 5 mg and another 12 to 10 mg. The study cohort was mostly female, with an average age of 58 years. Most were either intolerant of or inadequately treated by ursodeoxycholic acid. AP levels were reduced significantly over time in both groups; however, differences between the groups were not significant, the investigators noted.
The Liver Meeting will be held in San Francisco in 2018, taking place Nov. 9-13. Many investigators in these trials reported relevant conflicts of interest; information is available (open access) in a supplement to Hepatology.
dfulton@frontlinemedcom.com
On Twitter @denisefulton
AT THE LIVER MEETING 2017
Study examines intestinal microbiota role post liver transplant
WASHINGTON – During and after liver transplant, the reaction of the intestinal microbiota may be a critical determinant of outcomes; preliminary data from a cohort study may provide some clarification of what modulates gut microbiota post transplantation and shed light on predictive factors.
Anna-Catrin Uhlemann, MD, PhD, of Columbia University Medical Center, New York, noted that several studies in recent years sought to clarify influences on gut microbiota in people receiving liver transplants, but “there are still a number of important gaps in knowledge, including what exactly is the longitudinal evolution of the host transplant microbiome and what is the predictive value of pre- and early posttransplant dysbiosis on outcomes and complications.”
The researchers collected more than 1,000 samples to screen for colonization by the following MDR organisms: carbapenem-resistant Enterobacteriaceae (CRE), Enterobacteriaceae resistant to third-generation cephalosporins (ESBL), and vancomycin-resistant enterococci (VRE). Over the 1-year follow-up period, 19% (P =.031) of patients had CRE colonization associated with subsequent infection, 41% (P = .003) had ESBL colonization, and 46% (P = .021) had VRE colonization, Dr. Uhlemann said at the annual meeting of the American Association for the Study of Liver Diseases. The researchers then selected 484 samples for sequencing of the 16S ribosomal RNA gene to determine the composition of gut microbiota.
The study used two indexes to determine the alpha diversity of microbiota: the Chao index to estimate richness and the Shannon diversity index to determine the abundance of species in different settings. “We observed dynamic temporal evolution of alpha diversity and taxa abundance over the 1-year follow-up period,” Dr. Uhlemann said. “The diagnosis, the Child-Pugh class, and changes in perioperative antibiotics were important predictors of posttransplant alpha diversity.”
The study also found that Enterobacteriaceae and enterococci increased post transplant in general and as MDR organisms, and that a patient’s MDR status was an important modulator of the posttransplant microbiome, as was the lack of protective operational taxonomic units (OTUs).
The researchers evaluated the relative abundance of taxa and beta diversity. For example, pretransplant patients with a Model for End-stage Liver Disease (MELD) score greater than 25 showed enrichment of Enterobacteriaceae as well as different taxa of the Bacteroidiaceae, while those with MELD scores below 25 showed enrichment of Veillonellaceae. “The significance of this is not clear yet,” Dr. Uhlemann said.
Liver disease severity can also influence gut microbes. Those with Child-Pugh class C disease have the highest numbers in terms of richness and lowest in terms of diversity, Dr. Uhlemann said. “However, at the moment when we are looking at the differential abundance of the taxa, we don’t see quite as clear a pattern, although we noticed in the high group a higher abundance of Bacteroidiaceae,” she said.
Hepatitis B and C patients also presented divergent microbiota profiles. Hepatitis B virus patients “in general are always relatively healthy, and we actually see that these indices are relatively preserved,” Dr. Uhlemann said. “When we look at hepatitis C, however, we see that these patients are starting off quite low and then have an increase in alpha-diversity measures at around month 6.” A subset of patients with alcoholic liver disease also didn’t reach higher Chao and Shannon levels until 6 months after transplant.
“We also find that adjustment of periodic antibiotics for allergy or history of prior infection is significantly associated with a decrease in alpha diversity several months into the posttransplant course,” said Dr. Uhlemann. This is driven by an increase in the abundance of Enterococcaceae and Enterobacteriaceae. “And when we look at MDR colonization as a predictor of alpha diversity, we see that those who have MDR colonization, irrespective of the species, also have the lower alpha diversity.”
The researchers also started to look at pretransplant alpha diversity as a predictor of transplant outcomes, and while the analysis is still in progress, the Shannon indices were significantly different between patients who died and those who survived a year. “There was a trend for significant differences for posttransplant infection and the length of the hospital stay,” Dr. Uhlemann said. “However, we did not see any association with posttransplant ICU readmission, rejection, or VRE complications.”
She added that future analyses are needed to further evaluate the interaction between the clinical comorbidities in the microbiome and vice versa.
Dr. Uhlemann disclosed links to Merck.
WASHINGTON – During and after liver transplant, the reaction of the intestinal microbiota may be a critical determinant of outcomes; preliminary data from a cohort study may provide some clarification of what modulates gut microbiota post transplantation and shed light on predictive factors.
Anna-Catrin Uhlemann, MD, PhD, of Columbia University Medical Center, New York, noted that several studies in recent years sought to clarify influences on gut microbiota in people receiving liver transplants, but “there are still a number of important gaps in knowledge, including what exactly is the longitudinal evolution of the host transplant microbiome and what is the predictive value of pre- and early posttransplant dysbiosis on outcomes and complications.”
The researchers collected more than 1,000 samples to screen for colonization by the following MDR organisms: carbapenem-resistant Enterobacteriaceae (CRE), Enterobacteriaceae resistant to third-generation cephalosporins (ESBL), and vancomycin-resistant enterococci (VRE). Over the 1-year follow-up period, 19% (P =.031) of patients had CRE colonization associated with subsequent infection, 41% (P = .003) had ESBL colonization, and 46% (P = .021) had VRE colonization, Dr. Uhlemann said at the annual meeting of the American Association for the Study of Liver Diseases. The researchers then selected 484 samples for sequencing of the 16S ribosomal RNA gene to determine the composition of gut microbiota.
The study used two indexes to determine the alpha diversity of microbiota: the Chao index to estimate richness and the Shannon diversity index to determine the abundance of species in different settings. “We observed dynamic temporal evolution of alpha diversity and taxa abundance over the 1-year follow-up period,” Dr. Uhlemann said. “The diagnosis, the Child-Pugh class, and changes in perioperative antibiotics were important predictors of posttransplant alpha diversity.”
The study also found that Enterobacteriaceae and enterococci increased post transplant in general and as MDR organisms, and that a patient’s MDR status was an important modulator of the posttransplant microbiome, as was the lack of protective operational taxonomic units (OTUs).
The researchers evaluated the relative abundance of taxa and beta diversity. For example, pretransplant patients with a Model for End-stage Liver Disease (MELD) score greater than 25 showed enrichment of Enterobacteriaceae as well as different taxa of the Bacteroidiaceae, while those with MELD scores below 25 showed enrichment of Veillonellaceae. “The significance of this is not clear yet,” Dr. Uhlemann said.
Liver disease severity can also influence gut microbes. Those with Child-Pugh class C disease have the highest numbers in terms of richness and lowest in terms of diversity, Dr. Uhlemann said. “However, at the moment when we are looking at the differential abundance of the taxa, we don’t see quite as clear a pattern, although we noticed in the high group a higher abundance of Bacteroidiaceae,” she said.
Hepatitis B and C patients also presented divergent microbiota profiles. Hepatitis B virus patients “in general are always relatively healthy, and we actually see that these indices are relatively preserved,” Dr. Uhlemann said. “When we look at hepatitis C, however, we see that these patients are starting off quite low and then have an increase in alpha-diversity measures at around month 6.” A subset of patients with alcoholic liver disease also didn’t reach higher Chao and Shannon levels until 6 months after transplant.
“We also find that adjustment of periodic antibiotics for allergy or history of prior infection is significantly associated with a decrease in alpha diversity several months into the posttransplant course,” said Dr. Uhlemann. This is driven by an increase in the abundance of Enterococcaceae and Enterobacteriaceae. “And when we look at MDR colonization as a predictor of alpha diversity, we see that those who have MDR colonization, irrespective of the species, also have the lower alpha diversity.”
The researchers also started to look at pretransplant alpha diversity as a predictor of transplant outcomes, and while the analysis is still in progress, the Shannon indices were significantly different between patients who died and those who survived a year. “There was a trend for significant differences for posttransplant infection and the length of the hospital stay,” Dr. Uhlemann said. “However, we did not see any association with posttransplant ICU readmission, rejection, or VRE complications.”
She added that future analyses are needed to further evaluate the interaction between the clinical comorbidities in the microbiome and vice versa.
Dr. Uhlemann disclosed links to Merck.
WASHINGTON – During and after liver transplant, the reaction of the intestinal microbiota may be a critical determinant of outcomes; preliminary data from a cohort study may provide some clarification of what modulates gut microbiota post transplantation and shed light on predictive factors.
Anna-Catrin Uhlemann, MD, PhD, of Columbia University Medical Center, New York, noted that several studies in recent years sought to clarify influences on gut microbiota in people receiving liver transplants, but “there are still a number of important gaps in knowledge, including what exactly is the longitudinal evolution of the host transplant microbiome and what is the predictive value of pre- and early posttransplant dysbiosis on outcomes and complications.”
The researchers collected more than 1,000 samples to screen for colonization by the following MDR organisms: carbapenem-resistant Enterobacteriaceae (CRE), Enterobacteriaceae resistant to third-generation cephalosporins (ESBL), and vancomycin-resistant enterococci (VRE). Over the 1-year follow-up period, 19% (P =.031) of patients had CRE colonization associated with subsequent infection, 41% (P = .003) had ESBL colonization, and 46% (P = .021) had VRE colonization, Dr. Uhlemann said at the annual meeting of the American Association for the Study of Liver Diseases. The researchers then selected 484 samples for sequencing of the 16S ribosomal RNA gene to determine the composition of gut microbiota.
The study used two indexes to determine the alpha diversity of microbiota: the Chao index to estimate richness and the Shannon diversity index to determine the abundance of species in different settings. “We observed dynamic temporal evolution of alpha diversity and taxa abundance over the 1-year follow-up period,” Dr. Uhlemann said. “The diagnosis, the Child-Pugh class, and changes in perioperative antibiotics were important predictors of posttransplant alpha diversity.”
The study also found that Enterobacteriaceae and enterococci increased post transplant in general and as MDR organisms, and that a patient’s MDR status was an important modulator of the posttransplant microbiome, as was the lack of protective operational taxonomic units (OTUs).
The researchers evaluated the relative abundance of taxa and beta diversity. For example, pretransplant patients with a Model for End-stage Liver Disease (MELD) score greater than 25 showed enrichment of Enterobacteriaceae as well as different taxa of the Bacteroidiaceae, while those with MELD scores below 25 showed enrichment of Veillonellaceae. “The significance of this is not clear yet,” Dr. Uhlemann said.
Liver disease severity can also influence gut microbes. Those with Child-Pugh class C disease have the highest numbers in terms of richness and lowest in terms of diversity, Dr. Uhlemann said. “However, at the moment when we are looking at the differential abundance of the taxa, we don’t see quite as clear a pattern, although we noticed in the high group a higher abundance of Bacteroidiaceae,” she said.
Hepatitis B and C patients also presented divergent microbiota profiles. Hepatitis B virus patients “in general are always relatively healthy, and we actually see that these indices are relatively preserved,” Dr. Uhlemann said. “When we look at hepatitis C, however, we see that these patients are starting off quite low and then have an increase in alpha-diversity measures at around month 6.” A subset of patients with alcoholic liver disease also didn’t reach higher Chao and Shannon levels until 6 months after transplant.
“We also find that adjustment of periodic antibiotics for allergy or history of prior infection is significantly associated with a decrease in alpha diversity several months into the posttransplant course,” said Dr. Uhlemann. This is driven by an increase in the abundance of Enterococcaceae and Enterobacteriaceae. “And when we look at MDR colonization as a predictor of alpha diversity, we see that those who have MDR colonization, irrespective of the species, also have the lower alpha diversity.”
The researchers also started to look at pretransplant alpha diversity as a predictor of transplant outcomes, and while the analysis is still in progress, the Shannon indices were significantly different between patients who died and those who survived a year. “There was a trend for significant differences for posttransplant infection and the length of the hospital stay,” Dr. Uhlemann said. “However, we did not see any association with posttransplant ICU readmission, rejection, or VRE complications.”
She added that future analyses are needed to further evaluate the interaction between the clinical comorbidities in the microbiome and vice versa.
Dr. Uhlemann disclosed links to Merck.
AT THE LIVER MEETING 2017
Key clinical point: The presence or lack of specific modulators of gut microbiota may influence outcomes of liver transplantation.
Major finding: Over a 1-year follow-up period, 19% of patients had colonization with carbapenem-resistant Enterobacteriaceae, 41% had Enterobacteriaceae resistant to third-generation cephalosporins, and 46% had vancomycin-resistant enterococci associated with subsequent infections.
Data source: A prospective longitudinal cohort study of 323 patients, 125 of whom completed 1 year of follow-up.
Disclosures: Dr. Uhlemann disclosed receiving research funding from Merck.
Nivolumab may extend survival in HCC patients
WASHINGTON – A multinational clinical trial has found that the metastatic cancer agent nivolumab can improve long-term survival and durable tumor responses in patients with advanced hepatocellular carcinoma (HCC) whether or not they’ve had previous treatment with a chemotherapy agent already approved for advanced primary liver cancer, a principal investigator reported at the annual meeting of the American Association for the Study of Liver Diseases.
“Nivolumab has demonstrated clinically meaningful efficacy across etiologies in sorafenib-naive and -experienced patients with extended follow-up,” Bruno Sangro, MD, of the University of Navarra in Pamplona, Spain, said in reporting results of the CheckMate-040 trial. “The median overall survival is 15 and 15.6 months in patients who were sorafenib-experienced in both the dose-escalation and expansion cohorts.”
The dose-escalation cohort received 0.1 to 10 mg/kg of nivolumab (Opdivo) while the dose-expansion group received a steady dose of 3 mg/kg. In all, 262 patients participated in the trial, 80 of whom had never been on sorafenib (Nexavar) therapy. The survival outcome in these subgroups, Dr. Sangro said, “really speaks for the consistency and the robustness of the results.”
Trial participants had inoperable, usually metastatic HCC, with Child-Pugh scores up to and including 7 in the escalation group or up to and including 6 in the expansion group. Most of them were progressing to treatment with one or more prior systemic therapies, including sorafenib. Their aspartate aminotransferase and alanine aminotransferase scores were in the upper limits of normal, and bilirubin was less than or equal to 3 mg/dL. If they had hepatitis B (HBV), their viral load had to be less than 100 IU/mL and they had to be on effective antiviral therapy. Any history of hepatic encephalopathy or clinically significant ascites and an active HBV and hepatitis C (HCV) coinfection were grounds for exclusion.
“Most patients had to discontinue nivolumab because of disease progression,” Dr. Sangro noted, so that only 36 patients, or 14%, were continuing treatment at the time of this analysis. Thirteen patients in the total population that discontinued nivolumab did so because of toxicity, he said.
“Around 20% of patients achieved an objective remission that included complete responses in all subgroups of patients; 15% of progressors and 23% of sorafenib-intolerant patients had an objective response,” Dr. Sangro said. In terms of overall response, about half of all patients in the sorafenib-experienced subgroups had a complete or partial response or stable disease: 51% in the dose-escalation subgroup and 54% in the dose-expansion subgroup.
Although tumor responses were associated with declines in alpha-fetoprotein levels, “it’s unlikely that these biomarkers will be useful either for monitoring or selecting patients for treatment,” he added. “Indeed, baseline alpha-fetoprotein levels were comparable between responders and nonresponders to nivolumab” Dr. Sangro said.
“We also showed there was some impact on HCV viral kinetics in infected individuals,” Dr. Sangro noted. “The overall safety profile for the HCC population is consistent with other tumor types in which nivolumab is approved; these include patients who are infected with hepatitis B or C viruses.”
The study showed that 36% (19/53) of HCV infected patients had a greater than 1 log decrease in viral load. No signs of additional antiviral activity were detected among HBV-infected patients already on effective antiviral treatment: only 5% (3/59) posted a up to 1 log decrease in HB surface antigen levels, and 11% (7/64) of patients had increases in viral load. “These increases occurred in the setting of low-level viremia.” Dr. Sangro said. “They were asymptomatic and [nivolumab] did not result in changes in hepatic parameters or other serious adverse events.”
With regard to adverse events (AEs), 77% of all patients had some treatment-related AEs, ranging from fatigue to rash to dry mouth to increased lab levels, but only 20% were grade 3 or 4, and 88% of those resolved in an average of 8 weeks, Dr. Sangro said.
More research into nivolumab for HCC is needed, Dr. Sangro said. “Ongoing and future studies in patients with advanced tumors will evaluate nivolumab in the first-line setting or in combination with other agents,” he said.
Dr. Sangro disclosed relationships with Bayer Schering Pharma, Onxeo, Astra Zeneca, and Bristol-Myers Squibb. Bristol-Myers Squibb funded the trial, and Chrysalis Medical Communications assisted in reporting the study results.
WASHINGTON – A multinational clinical trial has found that the metastatic cancer agent nivolumab can improve long-term survival and durable tumor responses in patients with advanced hepatocellular carcinoma (HCC) whether or not they’ve had previous treatment with a chemotherapy agent already approved for advanced primary liver cancer, a principal investigator reported at the annual meeting of the American Association for the Study of Liver Diseases.
“Nivolumab has demonstrated clinically meaningful efficacy across etiologies in sorafenib-naive and -experienced patients with extended follow-up,” Bruno Sangro, MD, of the University of Navarra in Pamplona, Spain, said in reporting results of the CheckMate-040 trial. “The median overall survival is 15 and 15.6 months in patients who were sorafenib-experienced in both the dose-escalation and expansion cohorts.”
The dose-escalation cohort received 0.1 to 10 mg/kg of nivolumab (Opdivo) while the dose-expansion group received a steady dose of 3 mg/kg. In all, 262 patients participated in the trial, 80 of whom had never been on sorafenib (Nexavar) therapy. The survival outcome in these subgroups, Dr. Sangro said, “really speaks for the consistency and the robustness of the results.”
Trial participants had inoperable, usually metastatic HCC, with Child-Pugh scores up to and including 7 in the escalation group or up to and including 6 in the expansion group. Most of them were progressing to treatment with one or more prior systemic therapies, including sorafenib. Their aspartate aminotransferase and alanine aminotransferase scores were in the upper limits of normal, and bilirubin was less than or equal to 3 mg/dL. If they had hepatitis B (HBV), their viral load had to be less than 100 IU/mL and they had to be on effective antiviral therapy. Any history of hepatic encephalopathy or clinically significant ascites and an active HBV and hepatitis C (HCV) coinfection were grounds for exclusion.
“Most patients had to discontinue nivolumab because of disease progression,” Dr. Sangro noted, so that only 36 patients, or 14%, were continuing treatment at the time of this analysis. Thirteen patients in the total population that discontinued nivolumab did so because of toxicity, he said.
“Around 20% of patients achieved an objective remission that included complete responses in all subgroups of patients; 15% of progressors and 23% of sorafenib-intolerant patients had an objective response,” Dr. Sangro said. In terms of overall response, about half of all patients in the sorafenib-experienced subgroups had a complete or partial response or stable disease: 51% in the dose-escalation subgroup and 54% in the dose-expansion subgroup.
Although tumor responses were associated with declines in alpha-fetoprotein levels, “it’s unlikely that these biomarkers will be useful either for monitoring or selecting patients for treatment,” he added. “Indeed, baseline alpha-fetoprotein levels were comparable between responders and nonresponders to nivolumab” Dr. Sangro said.
“We also showed there was some impact on HCV viral kinetics in infected individuals,” Dr. Sangro noted. “The overall safety profile for the HCC population is consistent with other tumor types in which nivolumab is approved; these include patients who are infected with hepatitis B or C viruses.”
The study showed that 36% (19/53) of HCV infected patients had a greater than 1 log decrease in viral load. No signs of additional antiviral activity were detected among HBV-infected patients already on effective antiviral treatment: only 5% (3/59) posted a up to 1 log decrease in HB surface antigen levels, and 11% (7/64) of patients had increases in viral load. “These increases occurred in the setting of low-level viremia.” Dr. Sangro said. “They were asymptomatic and [nivolumab] did not result in changes in hepatic parameters or other serious adverse events.”
With regard to adverse events (AEs), 77% of all patients had some treatment-related AEs, ranging from fatigue to rash to dry mouth to increased lab levels, but only 20% were grade 3 or 4, and 88% of those resolved in an average of 8 weeks, Dr. Sangro said.
More research into nivolumab for HCC is needed, Dr. Sangro said. “Ongoing and future studies in patients with advanced tumors will evaluate nivolumab in the first-line setting or in combination with other agents,” he said.
Dr. Sangro disclosed relationships with Bayer Schering Pharma, Onxeo, Astra Zeneca, and Bristol-Myers Squibb. Bristol-Myers Squibb funded the trial, and Chrysalis Medical Communications assisted in reporting the study results.
WASHINGTON – A multinational clinical trial has found that the metastatic cancer agent nivolumab can improve long-term survival and durable tumor responses in patients with advanced hepatocellular carcinoma (HCC) whether or not they’ve had previous treatment with a chemotherapy agent already approved for advanced primary liver cancer, a principal investigator reported at the annual meeting of the American Association for the Study of Liver Diseases.
“Nivolumab has demonstrated clinically meaningful efficacy across etiologies in sorafenib-naive and -experienced patients with extended follow-up,” Bruno Sangro, MD, of the University of Navarra in Pamplona, Spain, said in reporting results of the CheckMate-040 trial. “The median overall survival is 15 and 15.6 months in patients who were sorafenib-experienced in both the dose-escalation and expansion cohorts.”
The dose-escalation cohort received 0.1 to 10 mg/kg of nivolumab (Opdivo) while the dose-expansion group received a steady dose of 3 mg/kg. In all, 262 patients participated in the trial, 80 of whom had never been on sorafenib (Nexavar) therapy. The survival outcome in these subgroups, Dr. Sangro said, “really speaks for the consistency and the robustness of the results.”
Trial participants had inoperable, usually metastatic HCC, with Child-Pugh scores up to and including 7 in the escalation group or up to and including 6 in the expansion group. Most of them were progressing to treatment with one or more prior systemic therapies, including sorafenib. Their aspartate aminotransferase and alanine aminotransferase scores were in the upper limits of normal, and bilirubin was less than or equal to 3 mg/dL. If they had hepatitis B (HBV), their viral load had to be less than 100 IU/mL and they had to be on effective antiviral therapy. Any history of hepatic encephalopathy or clinically significant ascites and an active HBV and hepatitis C (HCV) coinfection were grounds for exclusion.
“Most patients had to discontinue nivolumab because of disease progression,” Dr. Sangro noted, so that only 36 patients, or 14%, were continuing treatment at the time of this analysis. Thirteen patients in the total population that discontinued nivolumab did so because of toxicity, he said.
“Around 20% of patients achieved an objective remission that included complete responses in all subgroups of patients; 15% of progressors and 23% of sorafenib-intolerant patients had an objective response,” Dr. Sangro said. In terms of overall response, about half of all patients in the sorafenib-experienced subgroups had a complete or partial response or stable disease: 51% in the dose-escalation subgroup and 54% in the dose-expansion subgroup.
Although tumor responses were associated with declines in alpha-fetoprotein levels, “it’s unlikely that these biomarkers will be useful either for monitoring or selecting patients for treatment,” he added. “Indeed, baseline alpha-fetoprotein levels were comparable between responders and nonresponders to nivolumab” Dr. Sangro said.
“We also showed there was some impact on HCV viral kinetics in infected individuals,” Dr. Sangro noted. “The overall safety profile for the HCC population is consistent with other tumor types in which nivolumab is approved; these include patients who are infected with hepatitis B or C viruses.”
The study showed that 36% (19/53) of HCV infected patients had a greater than 1 log decrease in viral load. No signs of additional antiviral activity were detected among HBV-infected patients already on effective antiviral treatment: only 5% (3/59) posted a up to 1 log decrease in HB surface antigen levels, and 11% (7/64) of patients had increases in viral load. “These increases occurred in the setting of low-level viremia.” Dr. Sangro said. “They were asymptomatic and [nivolumab] did not result in changes in hepatic parameters or other serious adverse events.”
With regard to adverse events (AEs), 77% of all patients had some treatment-related AEs, ranging from fatigue to rash to dry mouth to increased lab levels, but only 20% were grade 3 or 4, and 88% of those resolved in an average of 8 weeks, Dr. Sangro said.
More research into nivolumab for HCC is needed, Dr. Sangro said. “Ongoing and future studies in patients with advanced tumors will evaluate nivolumab in the first-line setting or in combination with other agents,” he said.
Dr. Sangro disclosed relationships with Bayer Schering Pharma, Onxeo, Astra Zeneca, and Bristol-Myers Squibb. Bristol-Myers Squibb funded the trial, and Chrysalis Medical Communications assisted in reporting the study results.
AT THE LIVER MEETING 2017
Key clinical point: Nivolumab demonstrated long-term survival, durable tumor responses, and manageable overall and hepatic safety profiles, regardless of prior sorafenib treatment, in patients with advanced hepatocellular carcinoma.
Major finding: The 18-month overall survival rate was 57% in sorafenib-naive patients and 46% (dose-escalation) and 44% (dose-expansion) in sorafenib-experienced patients.
Data source: CheckMate-040 phase 1/2 dose-escalation and -expansion trial of 262 patients.
Disclosures: Dr. Sangro disclosed relationships with Bayer Schering Pharma, Onxeo, Astra Zeneca, and Bristol-Myers Squibb. Bristol-Myers Squibb funded the trial, and Chrysalis Medical Communications assisted in reporting the study results.
Case study suggests maternal inheritance of PBC susceptibility
A case report involving a family with four sisters with primary biliary cholangitis (PBC) suggests that there may be a maternal inheritance of susceptibility, according to Saeam Shin, MD, and associates at Hallym University in Seoul, South Korea.
In the first case, a 56-year-old woman was diagnosed with PBC, and afterwards, her three sisters, her brother, and her half-sister born to a different mother were evaluated for PBC as well. The second and fourth sisters showed no symptoms, but they were antimitochondrial-antibody (AMA) positive and were diagnosed with PBC. The third sister had been admitted to a different hospital for acute hepatitis of unknown origin – after receiving a positive AMA test, she also was diagnosed with PBC.
The brother and half-sister evaluated for PBC showed no symptoms and had negative AMA tests. The four sisters diagnosed showed good response to ursodeoxycholic acid in liver biochemistry tests and have continued on that medication without complication.
“If one patient is diagnosed with PBC, screening with AMA and liver function tests should be recommended to other family members for the early detection and management of this condition, especially for female relatives,” the investigators wrote.
Find the full case report in the World Journal of Gastroenterology (doi: 10.3748/wjg.v23.i39.7191).
A case report involving a family with four sisters with primary biliary cholangitis (PBC) suggests that there may be a maternal inheritance of susceptibility, according to Saeam Shin, MD, and associates at Hallym University in Seoul, South Korea.
In the first case, a 56-year-old woman was diagnosed with PBC, and afterwards, her three sisters, her brother, and her half-sister born to a different mother were evaluated for PBC as well. The second and fourth sisters showed no symptoms, but they were antimitochondrial-antibody (AMA) positive and were diagnosed with PBC. The third sister had been admitted to a different hospital for acute hepatitis of unknown origin – after receiving a positive AMA test, she also was diagnosed with PBC.
The brother and half-sister evaluated for PBC showed no symptoms and had negative AMA tests. The four sisters diagnosed showed good response to ursodeoxycholic acid in liver biochemistry tests and have continued on that medication without complication.
“If one patient is diagnosed with PBC, screening with AMA and liver function tests should be recommended to other family members for the early detection and management of this condition, especially for female relatives,” the investigators wrote.
Find the full case report in the World Journal of Gastroenterology (doi: 10.3748/wjg.v23.i39.7191).
A case report involving a family with four sisters with primary biliary cholangitis (PBC) suggests that there may be a maternal inheritance of susceptibility, according to Saeam Shin, MD, and associates at Hallym University in Seoul, South Korea.
In the first case, a 56-year-old woman was diagnosed with PBC, and afterwards, her three sisters, her brother, and her half-sister born to a different mother were evaluated for PBC as well. The second and fourth sisters showed no symptoms, but they were antimitochondrial-antibody (AMA) positive and were diagnosed with PBC. The third sister had been admitted to a different hospital for acute hepatitis of unknown origin – after receiving a positive AMA test, she also was diagnosed with PBC.
The brother and half-sister evaluated for PBC showed no symptoms and had negative AMA tests. The four sisters diagnosed showed good response to ursodeoxycholic acid in liver biochemistry tests and have continued on that medication without complication.
“If one patient is diagnosed with PBC, screening with AMA and liver function tests should be recommended to other family members for the early detection and management of this condition, especially for female relatives,” the investigators wrote.
Find the full case report in the World Journal of Gastroenterology (doi: 10.3748/wjg.v23.i39.7191).
FROM THE WORLD JOURNAL OF GASTROENTEROLOGY
Emerging oral agent reduces ALT in NAFLD
WASHINGTON – Limited treatment options for nonalcoholic steatohepatitis (NASH) in nonalcoholic fatty liver disease mean that NASH is the fastest-growing reason for liver transplants in the United States, but preclinical and, now, phase 2 clinical results have shown that treatment with 24-nor-ursodeoxycholic acid, otherwise known as norUDCA, can improve steatosis and liver stiffness in selected patients, a principal investigator in a European study of the treatment reported at the 2017 annual meeting of the American Association for the Study of Liver Diseases.
“The norUDCA dose of 1,500 mg resulted in significant reduction of ALT [alanine aminotransferase] within 12 weeks,” said Michael Trauner, MD, head of the division of gastroenterology and hepatology at the Medical University of Vienna, a coinventor of the drug. “The results are supported by improvement in liver stiffness and steatosis in the subsets analyzed.”
The 1,500-mg group had an average reduction in ALT of 17.4% whereas those in the 500-mg group only had a 4.2% reduction and placebo actually had an increase of 10.4%. “The reduction of the 500-mg dose was not significant,” Dr. Trauner said. “And this was emphasized in the proportion of patients reaching ALT less than 0.8 x ULN (upper limits of normal) at the end of treatment, with about 17% of patients reaching this endpoint in the higher dose group.” Among patients in the 500-mg group, 15% achieved that level, as did 5% in the placebo group.
The therapy also had an effect on lipid levels, Dr. Trauner noted. “Surprisingly, we saw a slight increase in LDL levels, with the highest in the 1,500-mg dose,” he said. “There were no significant changes in triglycerides and HDL levels, although there were some trends for reduced triglycerides and increased HDL.” Triglycerides decreased 14.6 mg/dL on average and HDL increased 2.8 mg/dL. The slight rise in LDL, 14.6 mg/dL on average, occurred in the first 2 weeks of treatment and continued through the treatment period, but then receded after discontinuation of therapy, said Dr. Trauner. “Please note that HDL cholesterol also increased in time, and the HDL-LDL ratio remained unchanged in these patients,” he added.
During the discussion, Dr. Trauner offered a possible explanation for the change in lipid levels. “One possibility could be that a slight repression of endogenous bile acid biosynthesis and subsequent upregulation of the LDL receptor,” he said, “but the changes are really very mild and subtle.”
He also noted that liver stiffness improved in a higher proportion of patients in the treatment groups than in the placebo group – 25% and 21% of patients in the 1,500- and 500-mg groups vs. 9% under placebo. Hepatic fat fraction values also improved from 21.3% to 16.3% (relative reduction of 23.5%) from baseline to end of treatment in the 1,500-mg group in a subset of patients undergoing more extensive MRI and spectroscopy studies – a degree of reduction that other studies have shown to be predictive of histologic improvement, Dr. Trauner said. Patients in this exploratory study did not have liver biopsies.
Overall, the drug was well tolerated, Dr. Trauner said. “There were slightly higher potentially adverse drug reactions in the 1,500-mg group, mainly due to higher rate of headache, nausea, and rash,” he said. Based on these results, a phase 2b study with histologic endpoints is underway, he added.
Dr. Trauner disclosed relationships with Gilead, Albireo, Takeda, Falk Pharma, Genfit, Intercept, MSD, Novartis, Roche, and Phenex.
WASHINGTON – Limited treatment options for nonalcoholic steatohepatitis (NASH) in nonalcoholic fatty liver disease mean that NASH is the fastest-growing reason for liver transplants in the United States, but preclinical and, now, phase 2 clinical results have shown that treatment with 24-nor-ursodeoxycholic acid, otherwise known as norUDCA, can improve steatosis and liver stiffness in selected patients, a principal investigator in a European study of the treatment reported at the 2017 annual meeting of the American Association for the Study of Liver Diseases.
“The norUDCA dose of 1,500 mg resulted in significant reduction of ALT [alanine aminotransferase] within 12 weeks,” said Michael Trauner, MD, head of the division of gastroenterology and hepatology at the Medical University of Vienna, a coinventor of the drug. “The results are supported by improvement in liver stiffness and steatosis in the subsets analyzed.”
The 1,500-mg group had an average reduction in ALT of 17.4% whereas those in the 500-mg group only had a 4.2% reduction and placebo actually had an increase of 10.4%. “The reduction of the 500-mg dose was not significant,” Dr. Trauner said. “And this was emphasized in the proportion of patients reaching ALT less than 0.8 x ULN (upper limits of normal) at the end of treatment, with about 17% of patients reaching this endpoint in the higher dose group.” Among patients in the 500-mg group, 15% achieved that level, as did 5% in the placebo group.
The therapy also had an effect on lipid levels, Dr. Trauner noted. “Surprisingly, we saw a slight increase in LDL levels, with the highest in the 1,500-mg dose,” he said. “There were no significant changes in triglycerides and HDL levels, although there were some trends for reduced triglycerides and increased HDL.” Triglycerides decreased 14.6 mg/dL on average and HDL increased 2.8 mg/dL. The slight rise in LDL, 14.6 mg/dL on average, occurred in the first 2 weeks of treatment and continued through the treatment period, but then receded after discontinuation of therapy, said Dr. Trauner. “Please note that HDL cholesterol also increased in time, and the HDL-LDL ratio remained unchanged in these patients,” he added.
During the discussion, Dr. Trauner offered a possible explanation for the change in lipid levels. “One possibility could be that a slight repression of endogenous bile acid biosynthesis and subsequent upregulation of the LDL receptor,” he said, “but the changes are really very mild and subtle.”
He also noted that liver stiffness improved in a higher proportion of patients in the treatment groups than in the placebo group – 25% and 21% of patients in the 1,500- and 500-mg groups vs. 9% under placebo. Hepatic fat fraction values also improved from 21.3% to 16.3% (relative reduction of 23.5%) from baseline to end of treatment in the 1,500-mg group in a subset of patients undergoing more extensive MRI and spectroscopy studies – a degree of reduction that other studies have shown to be predictive of histologic improvement, Dr. Trauner said. Patients in this exploratory study did not have liver biopsies.
Overall, the drug was well tolerated, Dr. Trauner said. “There were slightly higher potentially adverse drug reactions in the 1,500-mg group, mainly due to higher rate of headache, nausea, and rash,” he said. Based on these results, a phase 2b study with histologic endpoints is underway, he added.
Dr. Trauner disclosed relationships with Gilead, Albireo, Takeda, Falk Pharma, Genfit, Intercept, MSD, Novartis, Roche, and Phenex.
WASHINGTON – Limited treatment options for nonalcoholic steatohepatitis (NASH) in nonalcoholic fatty liver disease mean that NASH is the fastest-growing reason for liver transplants in the United States, but preclinical and, now, phase 2 clinical results have shown that treatment with 24-nor-ursodeoxycholic acid, otherwise known as norUDCA, can improve steatosis and liver stiffness in selected patients, a principal investigator in a European study of the treatment reported at the 2017 annual meeting of the American Association for the Study of Liver Diseases.
“The norUDCA dose of 1,500 mg resulted in significant reduction of ALT [alanine aminotransferase] within 12 weeks,” said Michael Trauner, MD, head of the division of gastroenterology and hepatology at the Medical University of Vienna, a coinventor of the drug. “The results are supported by improvement in liver stiffness and steatosis in the subsets analyzed.”
The 1,500-mg group had an average reduction in ALT of 17.4% whereas those in the 500-mg group only had a 4.2% reduction and placebo actually had an increase of 10.4%. “The reduction of the 500-mg dose was not significant,” Dr. Trauner said. “And this was emphasized in the proportion of patients reaching ALT less than 0.8 x ULN (upper limits of normal) at the end of treatment, with about 17% of patients reaching this endpoint in the higher dose group.” Among patients in the 500-mg group, 15% achieved that level, as did 5% in the placebo group.
The therapy also had an effect on lipid levels, Dr. Trauner noted. “Surprisingly, we saw a slight increase in LDL levels, with the highest in the 1,500-mg dose,” he said. “There were no significant changes in triglycerides and HDL levels, although there were some trends for reduced triglycerides and increased HDL.” Triglycerides decreased 14.6 mg/dL on average and HDL increased 2.8 mg/dL. The slight rise in LDL, 14.6 mg/dL on average, occurred in the first 2 weeks of treatment and continued through the treatment period, but then receded after discontinuation of therapy, said Dr. Trauner. “Please note that HDL cholesterol also increased in time, and the HDL-LDL ratio remained unchanged in these patients,” he added.
During the discussion, Dr. Trauner offered a possible explanation for the change in lipid levels. “One possibility could be that a slight repression of endogenous bile acid biosynthesis and subsequent upregulation of the LDL receptor,” he said, “but the changes are really very mild and subtle.”
He also noted that liver stiffness improved in a higher proportion of patients in the treatment groups than in the placebo group – 25% and 21% of patients in the 1,500- and 500-mg groups vs. 9% under placebo. Hepatic fat fraction values also improved from 21.3% to 16.3% (relative reduction of 23.5%) from baseline to end of treatment in the 1,500-mg group in a subset of patients undergoing more extensive MRI and spectroscopy studies – a degree of reduction that other studies have shown to be predictive of histologic improvement, Dr. Trauner said. Patients in this exploratory study did not have liver biopsies.
Overall, the drug was well tolerated, Dr. Trauner said. “There were slightly higher potentially adverse drug reactions in the 1,500-mg group, mainly due to higher rate of headache, nausea, and rash,” he said. Based on these results, a phase 2b study with histologic endpoints is underway, he added.
Dr. Trauner disclosed relationships with Gilead, Albireo, Takeda, Falk Pharma, Genfit, Intercept, MSD, Novartis, Roche, and Phenex.
AT THE LIVER MEETING 2017
Key clinical point: Treatment with oral 24-nor-ursodeoxycholic acid (norUDCA) resulted in a significant reduction of alanine aminotransferase (ALT) levels in nonalcoholic fatty liver disease.
Major finding: Mean value of hepatic fat fraction decreased 23.5% in a subset of patients treated with 1,500 mg norUDCA.
Data source: Double-blind, randomized, placebo-controlled, proof-of-concept phase 2 dose-finding study of 198 patients receiving treatment over 12 weeks.
Disclosures: Dr. Trauner disclosed relationships with Gilead, Albireo, Takeda, Falk Pharma, Genfit, Intercept, MSD, Novartis, Roche, and Phenex, and is listed as a coinventor on patents filed for the medical use of 24-nor-ursodeoxycholic acid.
Novel metabolite may be key in NAFLD
WASHINGTON – A newly identified metabolite of the gut microbiome may be a potentially useful biomarker in determining the severity of nonalcoholic fatty liver disease (NAFLD) and may provide a new treatment target, according to results of an analysis of serum metabolites isolated from 100 pairs of twins presented at the annual meeting of the American Association for the Study of Liver Diseases.
The researchers at the NAFLD Research Center at the University of California at San Diego isolated a metabolite derived from the gut microbiome, known as 3-(4-hydroxyphenyl)lactate, from 713 serum metabolites they analyzed, 440 of which were identified as heritable, said Cyrielle Caussy, MD, PhD. The researchers further winnowed that pool down to 94 associated with fibrosis alone and 170 associated with hepatic steatosis alone, 56 of which overlapped to have a shared gene effect with both hepatic steatosis and fibrosis, six of which derived from the gut microbiome.
Of the four heritable serum metabolites the researchers found to be significantly associated with NAFLD after adjustment for age, sex and Hispanic ethnicity, 3-(4-hydroxyphenyl)lactate had the highest odds ratio (95% confidence interval): 4.29 (1.87-9.81, P = .0006) vs. phenyllactate (OR 2.12, 1.09-4.10, P = .0258), palmitic acid (2.58, 1.31-5.17, P = .0065) and gamma-glutamylisoleucine (2.98, 1.36-6.51, P = .0062).
Dr. Caussy noted that previous studies have found a strong correlation between bacterial species in the gut and advanced fibrosis in NAFLD (Cell Metab. 2017;25:1054-62). This latest research takes those findings to the next level, Dr. Caussy said. “This metabolite could be a useful biomarker of the severity of NAFLD and may be a target for future treatment of NAFLD and could be used to monitor a treatment response,” she added.
The goal of the study was to determine if any serum metabolites have a shared genetic effect with hepatic steatosis and fibrosis, Dr. Caussy said. “The heritability of serum metabolites associated with NAFLD and their shared gene effect with hepatic steatosis and fibrosis have not been assessed yet,” she noted. The researchers isolated the serum metabolites from a cohort of 100 pairs of twins and 56 other relatives in the Southern California Twins Register, and validated the data in a cohort of 156 patients who had biopsy-proven NAFLD.
Dr. Caussy reported having no financial disclosures.
WASHINGTON – A newly identified metabolite of the gut microbiome may be a potentially useful biomarker in determining the severity of nonalcoholic fatty liver disease (NAFLD) and may provide a new treatment target, according to results of an analysis of serum metabolites isolated from 100 pairs of twins presented at the annual meeting of the American Association for the Study of Liver Diseases.
The researchers at the NAFLD Research Center at the University of California at San Diego isolated a metabolite derived from the gut microbiome, known as 3-(4-hydroxyphenyl)lactate, from 713 serum metabolites they analyzed, 440 of which were identified as heritable, said Cyrielle Caussy, MD, PhD. The researchers further winnowed that pool down to 94 associated with fibrosis alone and 170 associated with hepatic steatosis alone, 56 of which overlapped to have a shared gene effect with both hepatic steatosis and fibrosis, six of which derived from the gut microbiome.
Of the four heritable serum metabolites the researchers found to be significantly associated with NAFLD after adjustment for age, sex and Hispanic ethnicity, 3-(4-hydroxyphenyl)lactate had the highest odds ratio (95% confidence interval): 4.29 (1.87-9.81, P = .0006) vs. phenyllactate (OR 2.12, 1.09-4.10, P = .0258), palmitic acid (2.58, 1.31-5.17, P = .0065) and gamma-glutamylisoleucine (2.98, 1.36-6.51, P = .0062).
Dr. Caussy noted that previous studies have found a strong correlation between bacterial species in the gut and advanced fibrosis in NAFLD (Cell Metab. 2017;25:1054-62). This latest research takes those findings to the next level, Dr. Caussy said. “This metabolite could be a useful biomarker of the severity of NAFLD and may be a target for future treatment of NAFLD and could be used to monitor a treatment response,” she added.
The goal of the study was to determine if any serum metabolites have a shared genetic effect with hepatic steatosis and fibrosis, Dr. Caussy said. “The heritability of serum metabolites associated with NAFLD and their shared gene effect with hepatic steatosis and fibrosis have not been assessed yet,” she noted. The researchers isolated the serum metabolites from a cohort of 100 pairs of twins and 56 other relatives in the Southern California Twins Register, and validated the data in a cohort of 156 patients who had biopsy-proven NAFLD.
Dr. Caussy reported having no financial disclosures.
WASHINGTON – A newly identified metabolite of the gut microbiome may be a potentially useful biomarker in determining the severity of nonalcoholic fatty liver disease (NAFLD) and may provide a new treatment target, according to results of an analysis of serum metabolites isolated from 100 pairs of twins presented at the annual meeting of the American Association for the Study of Liver Diseases.
The researchers at the NAFLD Research Center at the University of California at San Diego isolated a metabolite derived from the gut microbiome, known as 3-(4-hydroxyphenyl)lactate, from 713 serum metabolites they analyzed, 440 of which were identified as heritable, said Cyrielle Caussy, MD, PhD. The researchers further winnowed that pool down to 94 associated with fibrosis alone and 170 associated with hepatic steatosis alone, 56 of which overlapped to have a shared gene effect with both hepatic steatosis and fibrosis, six of which derived from the gut microbiome.
Of the four heritable serum metabolites the researchers found to be significantly associated with NAFLD after adjustment for age, sex and Hispanic ethnicity, 3-(4-hydroxyphenyl)lactate had the highest odds ratio (95% confidence interval): 4.29 (1.87-9.81, P = .0006) vs. phenyllactate (OR 2.12, 1.09-4.10, P = .0258), palmitic acid (2.58, 1.31-5.17, P = .0065) and gamma-glutamylisoleucine (2.98, 1.36-6.51, P = .0062).
Dr. Caussy noted that previous studies have found a strong correlation between bacterial species in the gut and advanced fibrosis in NAFLD (Cell Metab. 2017;25:1054-62). This latest research takes those findings to the next level, Dr. Caussy said. “This metabolite could be a useful biomarker of the severity of NAFLD and may be a target for future treatment of NAFLD and could be used to monitor a treatment response,” she added.
The goal of the study was to determine if any serum metabolites have a shared genetic effect with hepatic steatosis and fibrosis, Dr. Caussy said. “The heritability of serum metabolites associated with NAFLD and their shared gene effect with hepatic steatosis and fibrosis have not been assessed yet,” she noted. The researchers isolated the serum metabolites from a cohort of 100 pairs of twins and 56 other relatives in the Southern California Twins Register, and validated the data in a cohort of 156 patients who had biopsy-proven NAFLD.
Dr. Caussy reported having no financial disclosures.
AT THE LIVER MEETING 2017
Key clinical point: Researchers have identified a novel serum metabolite that may be the key to linking the role of the gut microbiome with the presence of nonalcoholic fatty liver disease (NAFLD)–related fibrosis.
Major finding: An analysis of 713 serum metabolites identified a novel, gut microbiome–derived serum metabolite known as 3-(4-hydroxyphenyl)lactate that had an odds ratio of 4.29 for NAFLD.
Data source: Cross-sectional analysis of a prospective cohort of 156 subjects in the Southern California Twin Study Cohort.
Disclosures: Dr. Caussy reported having no financial disclosures.
Hispanics bear brunt of NAFLD disease burden
WASHINGTON — Significant racial and ethnic disparities exist in nonalcoholic fatty liver disease prevalence and severity in the United States, with Hispanics at highest risk and blacks at the lowest, but the risk of death from NAFLD is highest in whites, according to a meta-analysis of 34 studies presented at the annual meeting of the American Association for the Study of Liver Diseases.
The findings are based on a meta-analysis of studies in the MEDLINE, EMBASE, and Cochrane databases from inception through August 2016 that included 368,569 unique patients that characterized disparities in NAFLD prevalence, severity, or prognosis, Dr. Rich said.
When the researchers drilled down into the data, they found the disparities dissipated somewhat. “When we looked at the severity of NAFLD we looked at two things: whether there was NASH (nonalcoholic steatohepatitis) present, or if there was the presence of advanced fibrosis,” Dr. Rich said. “We found there was no significant difference in the risk of NASH in Hispanic patients, compared to white patients; however, the proportion of Hispanic NAFLD patients that had NASH was 45.4%, compared to 32.2% in whites.” The pooled relative risk was 1.09.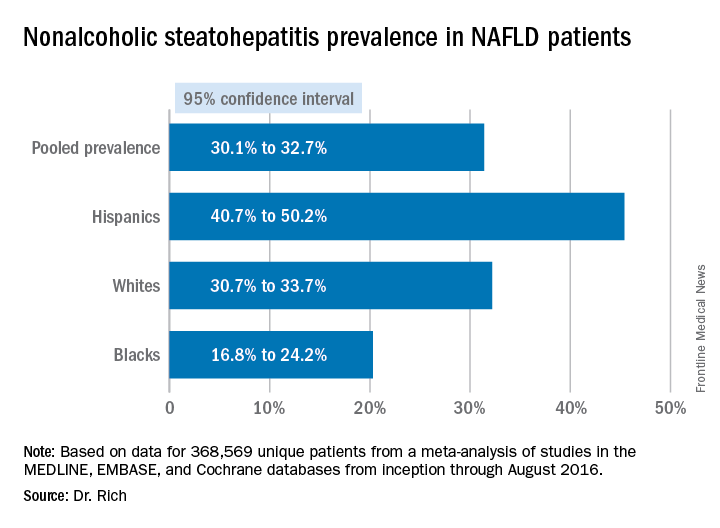
The meta-analysis tended to attenuate the disparities found in disease severity, compared with the disparities the researchers found in prevalence, Dr. Rich said. “Data are limited and discordant on racial and ethnic differences in NAFLD prognosis and outcomes,” she said. “In the current literature the studies have notable limitations, highlighting the need for future high-quality data in this area, and further studies are needed to determine the need and pathways to reduce NAFLD disparities in the future,” she said.
Dr. Rich had no financial relationships to disclose.
WASHINGTON — Significant racial and ethnic disparities exist in nonalcoholic fatty liver disease prevalence and severity in the United States, with Hispanics at highest risk and blacks at the lowest, but the risk of death from NAFLD is highest in whites, according to a meta-analysis of 34 studies presented at the annual meeting of the American Association for the Study of Liver Diseases.
The findings are based on a meta-analysis of studies in the MEDLINE, EMBASE, and Cochrane databases from inception through August 2016 that included 368,569 unique patients that characterized disparities in NAFLD prevalence, severity, or prognosis, Dr. Rich said.
When the researchers drilled down into the data, they found the disparities dissipated somewhat. “When we looked at the severity of NAFLD we looked at two things: whether there was NASH (nonalcoholic steatohepatitis) present, or if there was the presence of advanced fibrosis,” Dr. Rich said. “We found there was no significant difference in the risk of NASH in Hispanic patients, compared to white patients; however, the proportion of Hispanic NAFLD patients that had NASH was 45.4%, compared to 32.2% in whites.” The pooled relative risk was 1.09.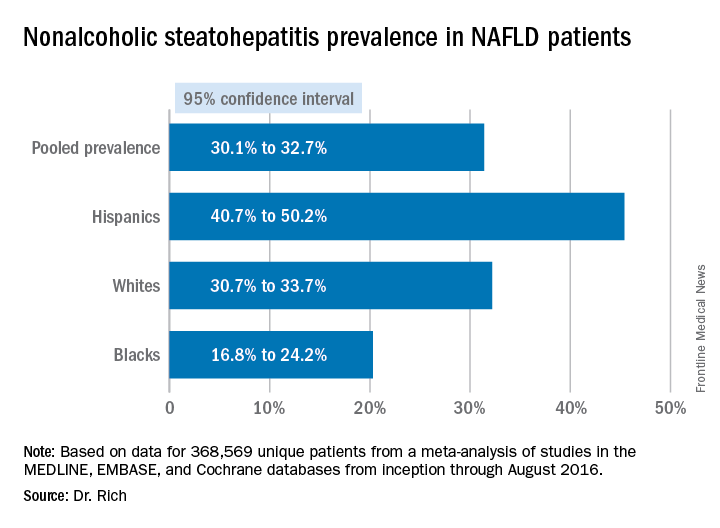
The meta-analysis tended to attenuate the disparities found in disease severity, compared with the disparities the researchers found in prevalence, Dr. Rich said. “Data are limited and discordant on racial and ethnic differences in NAFLD prognosis and outcomes,” she said. “In the current literature the studies have notable limitations, highlighting the need for future high-quality data in this area, and further studies are needed to determine the need and pathways to reduce NAFLD disparities in the future,” she said.
Dr. Rich had no financial relationships to disclose.
WASHINGTON — Significant racial and ethnic disparities exist in nonalcoholic fatty liver disease prevalence and severity in the United States, with Hispanics at highest risk and blacks at the lowest, but the risk of death from NAFLD is highest in whites, according to a meta-analysis of 34 studies presented at the annual meeting of the American Association for the Study of Liver Diseases.
The findings are based on a meta-analysis of studies in the MEDLINE, EMBASE, and Cochrane databases from inception through August 2016 that included 368,569 unique patients that characterized disparities in NAFLD prevalence, severity, or prognosis, Dr. Rich said.
When the researchers drilled down into the data, they found the disparities dissipated somewhat. “When we looked at the severity of NAFLD we looked at two things: whether there was NASH (nonalcoholic steatohepatitis) present, or if there was the presence of advanced fibrosis,” Dr. Rich said. “We found there was no significant difference in the risk of NASH in Hispanic patients, compared to white patients; however, the proportion of Hispanic NAFLD patients that had NASH was 45.4%, compared to 32.2% in whites.” The pooled relative risk was 1.09.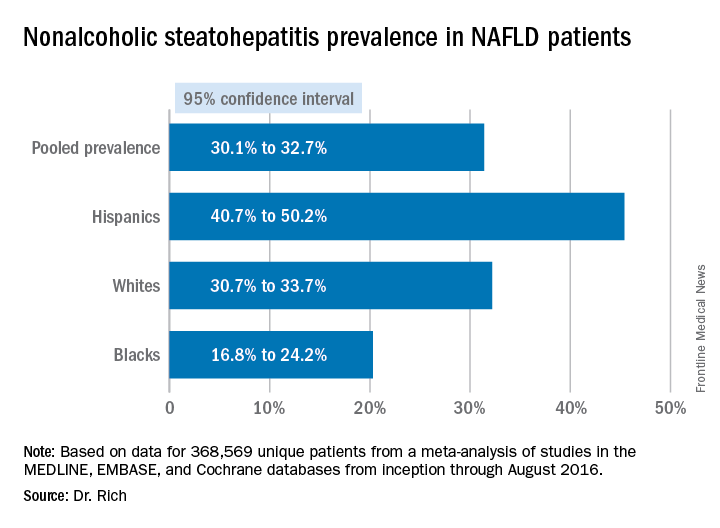
The meta-analysis tended to attenuate the disparities found in disease severity, compared with the disparities the researchers found in prevalence, Dr. Rich said. “Data are limited and discordant on racial and ethnic differences in NAFLD prognosis and outcomes,” she said. “In the current literature the studies have notable limitations, highlighting the need for future high-quality data in this area, and further studies are needed to determine the need and pathways to reduce NAFLD disparities in the future,” she said.
Dr. Rich had no financial relationships to disclose.
AT THE LIVER MEETING 2017
Key clinical point: Hispanics have a much higher incidence of fatty liver disease than other ethnic groups.
Major finding: NAFLD prevalence is highest in Hispanics and lower in blacks, compared with whites, although differences between groups are smaller in high-risk cohorts (range, 47.6%-55.5%) than in population-based cohorts (range, 13.0%-22.9%).
Data source: Meta-analysis of 34 studies in the MEDLINE, EMBASE, and Cochrane databases from inception through August 2016 that involved 368,569 patients.
Disclosures: Dr. Rich had no financial relationships to disclose.