User login
50.6 million tobacco users are not a homogeneous group
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
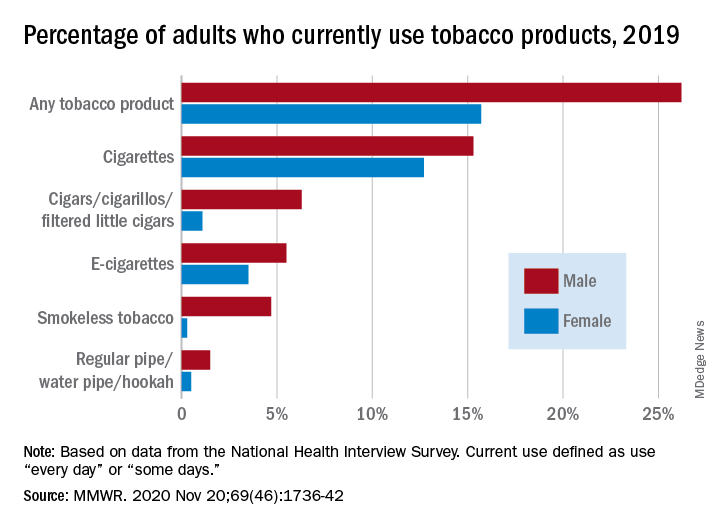
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
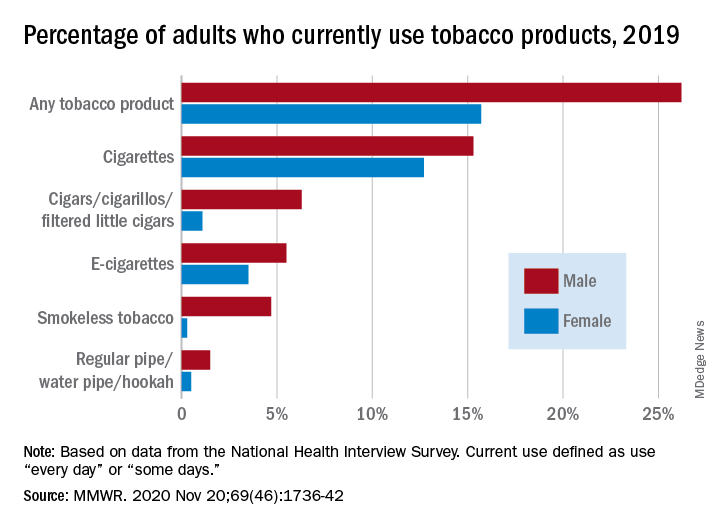
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
Cigarettes are still the product of choice among U.S. adults who use tobacco, but the youngest adults are more likely to use e-cigarettes than any other product, according to data from the 2019 National Health Interview Survey.
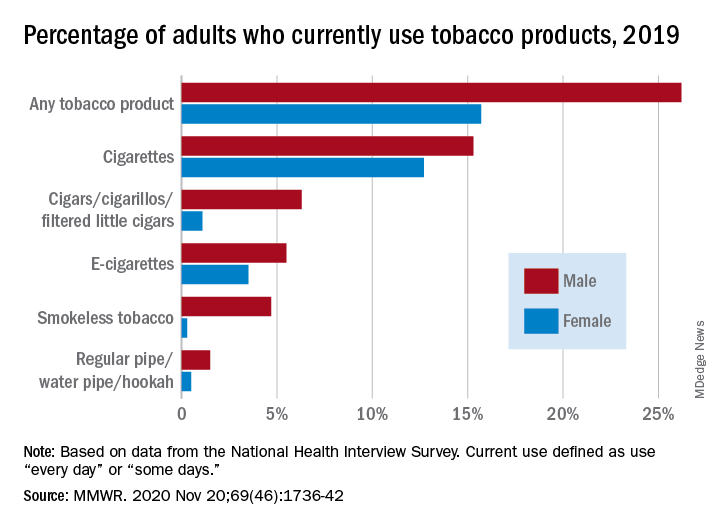
with cigarette use reported by the largest share of respondents (14.0%) and e-cigarettes next at 4.5%, Monica E. Cornelius, PhD, and associates said in the Morbidity and Mortality Weekly Report.
Among adults aged 18-24 years, however, e-cigarettes were used by 9.3% of respondents in 2019, compared with 8.0% who used cigarettes every day or some days. Current e-cigarette use was 6.4% in 25- to 44-year-olds and continued to diminish with increasing age, said Dr. Cornelius and associates at the Centers for Disease Control and Prevention’s National Center for Chronic Disease Prevention and Health Promotion.
Men were more likely than women to use e-cigarettes (5.5% vs. 3.5%), and to use any tobacco product (26.2% vs. 15.7%). Use of other products, including cigarettes (15.3% for men vs. 12.7% for women), followed the same pattern to varying degrees, the national survey data show.
“Differences in prevalence of tobacco use also were also seen across population groups, with higher prevalence among those with a [high school equivalency degree], American Indian/Alaska Natives, uninsured adults and adults with Medicaid, and [lesbian, gay, or bisexual] adults,” the investigators said.
Among those groups, overall tobacco use and cigarette use were highest in those with an equivalency degree (43.8%, 37.1%), while lesbian/gay/bisexual individuals had the highest prevalence of e-cigarette use at 11.5%, they reported.
“As part of a comprehensive approach” to reduce tobacco-related disease and death, Dr. Cornelius and associates suggested, “targeted interventions are also warranted to reach subpopulations with the highest prevalence of use, which might vary by tobacco product type.”
SOURCE: Cornelius ME et al. MMWR. 2020 Nov 20;69(46);1736-42.
FROM MMWR
New findings on ‘exceptional responders’ to cancer therapies
An ongoing research project is studying why some patients have exceptional responses. The researchers have found particular molecular features in the tumors of about a quarter of these patients. In some cases, there are multiple rare genetic changes in the tumor genome. In other cases, the tumors are infiltrated with certain types of immune cells.
The findings were published online November 19 in Cancer Cell. They come from a genomic analysis of tumor biopsy specimens from 111 patients who were identified by the National Cancer Institute’s (NCI’s) Exceptional Responders Initiative, a national project launched in 2014.
An exceptional responder is defined as an individual who achieves a partial or complete response to a treatment that would be effective in fewer than 10% of similar patients. For exceptional response, the duration of response is at least three times longer than the usual median response time.
In this study of 111 such patients, about one quarter (24%, n = 26 patients) were found to have tumors in which there were molecular features that could potentially explain exceptional responses to treatment.
“We won’t be able to identify, in every patient, which particular drugs will be beneficial,” said Louis Staudt, MD, PhD, director of the NCI’s Center for Cancer Genomics, who co-led the study. “We are nowhere near that. But what it does say is that we have identified particular mutations, some of which we knew about in some types of cancer but can also occur less commonly in other cancer types.”
Staudt noted that these mutations can “illuminate” the path that the cancer will take — and potentially can be used to predict whether the cancer will be aggressive and will require treatment or could be managed with surveillance. This is why this research can be useful in the short term, he said.
“In the longer term, this is the kind of research that inspires future work,” he told Medscape Medical News. “That would encompass clinical trials involving drugs that target some of the pathways we found to be genetically inactivated in some of these responders.”
These results support the use of genetic testing in routine clinical care, he said.
Earlier this year, the NCI team published the results of a pilot study that affirmed the feasibility of this approach. Of the more than 100 cases that were analyzed, six were identified as involving potentially clinically actionable germline mutations.
‘Curiosity drove the research’
“We had these wonderful and gratifying experiences with our patients, so we were immediately curious how that happened, so it was pretty much that curiosity that drove a lot of this work,” said Staudt.
In the current study, Staudt and colleagues used multiple genomic methodologies to detect mutations, copy number changes, aberrant methylation, outlier gene expression, and the cellular makeup of the tumor microenvironment.
The hypothesized mechanisms for exceptional responses were broadly divided into the following four categories: DNA damage response (n = 15), intracellular signaling pathway (n = 9), prognostic genetics (n = 9), and immunologic engagement (n = 16). For many patients, two or more of these mechanisms were involved.
The authors note that the “predominance of plausible DNA damage response mechanisms parallels the frequent use of cytotoxic chemotherapy in routine cancer treatment reflected in this cohort.”
Twenty-six patients were identified as exceptional responders. Among these patients, a variety of cancer types was represented: brain (8); gastrointestinal tract (6); breast (4); cholangiocarcinoma (2); lung (2); pancreas, endometrium, ovarian, and bladder (1 each). Many of these patients (65%, n = 17) were treated with chemotherapy that included DNA-damaging agents. For more than half (54%, n = 14), targeted therapies were used, and some patients received both.
The authors highlight several patients as examples of exceptional responders:
- One patient with glioblastoma multiforme (GBM) was treated sequentially with surgery, localized carmustine, and radiotherapy. When the cancer recurred, temozolomide was administered. This induced a complete response that has lasted for more than a decade.
- A patient with metastatic colon adenocarcinoma has had an ongoing and nearly complete response that has lasted 45 months (last follow-up) after receiving temozolomide in combination with the investigational drug TRC102 (methoxyamine, under development by Tracon) in a phase 1 clinical trial. TRC102 is an inhibitor of the DNA base excision repair pathway, which is a pathway that causes resistance to alkylating and antimetabolite chemotherapeutics.
- A patient with metastatic, estrogen receptor–positive breast cancer received trastuzumab because of a high-level ERBB2 amplification, together with anastrozole. This resulted in an ongoing 2.4-year partial response.
- Although the patient was clinically HER2 positive, her tumor had exceedingly low expression of ERBB2 mRNA. Molecular profiling had classified the tumor as of the basal-like subtype rather than the HER2-enriched subtype. This meant that it was unlikely that trastuzumab contributed to the exceptional response, the authors note. Because the patient was estrogen-receptor positive, she received anastrozole, an inhibitor of aromatase (CYP19A), which converts testosterone into estradiol.
- A patient who had a gastrointestinal stromal tumor with a deletion of KIT exon 11 experienced relapse after an initial response to imatinib, which targets KIT and other tyrosine kinases, but then achieved a complete response with sunitinib. Gene expression profiling revealed high expression not only of KIT but also of genes encoding several tyrosine kinases that are targeted by sunitinib (KDR, FLT1, and FLT3). This may have accounted for the patient’s response.
Favorable genomic characteristics
The authors defined a “prognostic genetics” category of tumors, characterized by genetic lesions that are now known to be associated with a favorable prognosis but that were not addressed through routine care that these patients received when they were first diagnosed. Although the patients experienced relapse after first-line treatment, their exceptional survival after salvage therapy could be linked to favorable genomic characteristics.
For example, several of the patients with high-grade GBMs and astrocytomas had genetic lesions that are generally more common in low-grade glioma and that have been associated with an indolent clinical course following standard therapy.
The authors also assessed immune response. Examining immune cell infiltration in responder tumors in comparison with control cases, the team found that signatures of B cells and activated (CD56dim) natural killer cells were higher in exceptional-responder tumors.
In one patient with metastatic urothelial cancer who experienced disease progression after chemotherapy, radiotherapy, and surgery, treatment with nivolumab produced a complete response that lasted 7 months. Such an outcome occurs in only about 3% of bladder cancer patients. The tumor expressed high mRNA levels of PDCD1, which encodes the nivolumab target PD-1, and CD274, which encodes the PD-1 ligand PD-L1. There was also a high level of amplification of IFNG, which encodes interferon-gamma, a cytokine that has been linked to favorable response to immune checkpoint blockade.
Moving to precision medicine
“It is very valuable to be tested up front and again when the disease progresses, because there may have been some genetic changes, and this may change the treatment,” said co–lead author S. Percy Ivy, MD, of the NCI’s Division of Cancer Treatment and Diagnosis.
“The goal of this study was to understand what was unique about these patients and their genetic makeup that led them to be classified as exceptional responders, and hopefully we will be able to tease that out,” she added.
“As researchers, we have a lot to learn from these patients, and they have a lot to teach us,” she added. “In the future, they will help us as we move closer to the goal of delivering precision oncology to all of our patients. We’re not there yet, but every time we study more deeply and learn more, we are able to provide better care.”
To encourage participation in this effort by investigators around the world, the NCI team and their colleagues have made their molecular profiling results and clinical information publicly available in the NCI Genomic Data Commons.
The study was supported by the NCI’s Intramural Research Program, the National Institutes of Health, the Center for Cancer Research, and the NCI’s Center for Cancer Genomics. Staudt and Ivy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
An ongoing research project is studying why some patients have exceptional responses. The researchers have found particular molecular features in the tumors of about a quarter of these patients. In some cases, there are multiple rare genetic changes in the tumor genome. In other cases, the tumors are infiltrated with certain types of immune cells.
The findings were published online November 19 in Cancer Cell. They come from a genomic analysis of tumor biopsy specimens from 111 patients who were identified by the National Cancer Institute’s (NCI’s) Exceptional Responders Initiative, a national project launched in 2014.
An exceptional responder is defined as an individual who achieves a partial or complete response to a treatment that would be effective in fewer than 10% of similar patients. For exceptional response, the duration of response is at least three times longer than the usual median response time.
In this study of 111 such patients, about one quarter (24%, n = 26 patients) were found to have tumors in which there were molecular features that could potentially explain exceptional responses to treatment.
“We won’t be able to identify, in every patient, which particular drugs will be beneficial,” said Louis Staudt, MD, PhD, director of the NCI’s Center for Cancer Genomics, who co-led the study. “We are nowhere near that. But what it does say is that we have identified particular mutations, some of which we knew about in some types of cancer but can also occur less commonly in other cancer types.”
Staudt noted that these mutations can “illuminate” the path that the cancer will take — and potentially can be used to predict whether the cancer will be aggressive and will require treatment or could be managed with surveillance. This is why this research can be useful in the short term, he said.
“In the longer term, this is the kind of research that inspires future work,” he told Medscape Medical News. “That would encompass clinical trials involving drugs that target some of the pathways we found to be genetically inactivated in some of these responders.”
These results support the use of genetic testing in routine clinical care, he said.
Earlier this year, the NCI team published the results of a pilot study that affirmed the feasibility of this approach. Of the more than 100 cases that were analyzed, six were identified as involving potentially clinically actionable germline mutations.
‘Curiosity drove the research’
“We had these wonderful and gratifying experiences with our patients, so we were immediately curious how that happened, so it was pretty much that curiosity that drove a lot of this work,” said Staudt.
In the current study, Staudt and colleagues used multiple genomic methodologies to detect mutations, copy number changes, aberrant methylation, outlier gene expression, and the cellular makeup of the tumor microenvironment.
The hypothesized mechanisms for exceptional responses were broadly divided into the following four categories: DNA damage response (n = 15), intracellular signaling pathway (n = 9), prognostic genetics (n = 9), and immunologic engagement (n = 16). For many patients, two or more of these mechanisms were involved.
The authors note that the “predominance of plausible DNA damage response mechanisms parallels the frequent use of cytotoxic chemotherapy in routine cancer treatment reflected in this cohort.”
Twenty-six patients were identified as exceptional responders. Among these patients, a variety of cancer types was represented: brain (8); gastrointestinal tract (6); breast (4); cholangiocarcinoma (2); lung (2); pancreas, endometrium, ovarian, and bladder (1 each). Many of these patients (65%, n = 17) were treated with chemotherapy that included DNA-damaging agents. For more than half (54%, n = 14), targeted therapies were used, and some patients received both.
The authors highlight several patients as examples of exceptional responders:
- One patient with glioblastoma multiforme (GBM) was treated sequentially with surgery, localized carmustine, and radiotherapy. When the cancer recurred, temozolomide was administered. This induced a complete response that has lasted for more than a decade.
- A patient with metastatic colon adenocarcinoma has had an ongoing and nearly complete response that has lasted 45 months (last follow-up) after receiving temozolomide in combination with the investigational drug TRC102 (methoxyamine, under development by Tracon) in a phase 1 clinical trial. TRC102 is an inhibitor of the DNA base excision repair pathway, which is a pathway that causes resistance to alkylating and antimetabolite chemotherapeutics.
- A patient with metastatic, estrogen receptor–positive breast cancer received trastuzumab because of a high-level ERBB2 amplification, together with anastrozole. This resulted in an ongoing 2.4-year partial response.
- Although the patient was clinically HER2 positive, her tumor had exceedingly low expression of ERBB2 mRNA. Molecular profiling had classified the tumor as of the basal-like subtype rather than the HER2-enriched subtype. This meant that it was unlikely that trastuzumab contributed to the exceptional response, the authors note. Because the patient was estrogen-receptor positive, she received anastrozole, an inhibitor of aromatase (CYP19A), which converts testosterone into estradiol.
- A patient who had a gastrointestinal stromal tumor with a deletion of KIT exon 11 experienced relapse after an initial response to imatinib, which targets KIT and other tyrosine kinases, but then achieved a complete response with sunitinib. Gene expression profiling revealed high expression not only of KIT but also of genes encoding several tyrosine kinases that are targeted by sunitinib (KDR, FLT1, and FLT3). This may have accounted for the patient’s response.
Favorable genomic characteristics
The authors defined a “prognostic genetics” category of tumors, characterized by genetic lesions that are now known to be associated with a favorable prognosis but that were not addressed through routine care that these patients received when they were first diagnosed. Although the patients experienced relapse after first-line treatment, their exceptional survival after salvage therapy could be linked to favorable genomic characteristics.
For example, several of the patients with high-grade GBMs and astrocytomas had genetic lesions that are generally more common in low-grade glioma and that have been associated with an indolent clinical course following standard therapy.
The authors also assessed immune response. Examining immune cell infiltration in responder tumors in comparison with control cases, the team found that signatures of B cells and activated (CD56dim) natural killer cells were higher in exceptional-responder tumors.
In one patient with metastatic urothelial cancer who experienced disease progression after chemotherapy, radiotherapy, and surgery, treatment with nivolumab produced a complete response that lasted 7 months. Such an outcome occurs in only about 3% of bladder cancer patients. The tumor expressed high mRNA levels of PDCD1, which encodes the nivolumab target PD-1, and CD274, which encodes the PD-1 ligand PD-L1. There was also a high level of amplification of IFNG, which encodes interferon-gamma, a cytokine that has been linked to favorable response to immune checkpoint blockade.
Moving to precision medicine
“It is very valuable to be tested up front and again when the disease progresses, because there may have been some genetic changes, and this may change the treatment,” said co–lead author S. Percy Ivy, MD, of the NCI’s Division of Cancer Treatment and Diagnosis.
“The goal of this study was to understand what was unique about these patients and their genetic makeup that led them to be classified as exceptional responders, and hopefully we will be able to tease that out,” she added.
“As researchers, we have a lot to learn from these patients, and they have a lot to teach us,” she added. “In the future, they will help us as we move closer to the goal of delivering precision oncology to all of our patients. We’re not there yet, but every time we study more deeply and learn more, we are able to provide better care.”
To encourage participation in this effort by investigators around the world, the NCI team and their colleagues have made their molecular profiling results and clinical information publicly available in the NCI Genomic Data Commons.
The study was supported by the NCI’s Intramural Research Program, the National Institutes of Health, the Center for Cancer Research, and the NCI’s Center for Cancer Genomics. Staudt and Ivy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
An ongoing research project is studying why some patients have exceptional responses. The researchers have found particular molecular features in the tumors of about a quarter of these patients. In some cases, there are multiple rare genetic changes in the tumor genome. In other cases, the tumors are infiltrated with certain types of immune cells.
The findings were published online November 19 in Cancer Cell. They come from a genomic analysis of tumor biopsy specimens from 111 patients who were identified by the National Cancer Institute’s (NCI’s) Exceptional Responders Initiative, a national project launched in 2014.
An exceptional responder is defined as an individual who achieves a partial or complete response to a treatment that would be effective in fewer than 10% of similar patients. For exceptional response, the duration of response is at least three times longer than the usual median response time.
In this study of 111 such patients, about one quarter (24%, n = 26 patients) were found to have tumors in which there were molecular features that could potentially explain exceptional responses to treatment.
“We won’t be able to identify, in every patient, which particular drugs will be beneficial,” said Louis Staudt, MD, PhD, director of the NCI’s Center for Cancer Genomics, who co-led the study. “We are nowhere near that. But what it does say is that we have identified particular mutations, some of which we knew about in some types of cancer but can also occur less commonly in other cancer types.”
Staudt noted that these mutations can “illuminate” the path that the cancer will take — and potentially can be used to predict whether the cancer will be aggressive and will require treatment or could be managed with surveillance. This is why this research can be useful in the short term, he said.
“In the longer term, this is the kind of research that inspires future work,” he told Medscape Medical News. “That would encompass clinical trials involving drugs that target some of the pathways we found to be genetically inactivated in some of these responders.”
These results support the use of genetic testing in routine clinical care, he said.
Earlier this year, the NCI team published the results of a pilot study that affirmed the feasibility of this approach. Of the more than 100 cases that were analyzed, six were identified as involving potentially clinically actionable germline mutations.
‘Curiosity drove the research’
“We had these wonderful and gratifying experiences with our patients, so we were immediately curious how that happened, so it was pretty much that curiosity that drove a lot of this work,” said Staudt.
In the current study, Staudt and colleagues used multiple genomic methodologies to detect mutations, copy number changes, aberrant methylation, outlier gene expression, and the cellular makeup of the tumor microenvironment.
The hypothesized mechanisms for exceptional responses were broadly divided into the following four categories: DNA damage response (n = 15), intracellular signaling pathway (n = 9), prognostic genetics (n = 9), and immunologic engagement (n = 16). For many patients, two or more of these mechanisms were involved.
The authors note that the “predominance of plausible DNA damage response mechanisms parallels the frequent use of cytotoxic chemotherapy in routine cancer treatment reflected in this cohort.”
Twenty-six patients were identified as exceptional responders. Among these patients, a variety of cancer types was represented: brain (8); gastrointestinal tract (6); breast (4); cholangiocarcinoma (2); lung (2); pancreas, endometrium, ovarian, and bladder (1 each). Many of these patients (65%, n = 17) were treated with chemotherapy that included DNA-damaging agents. For more than half (54%, n = 14), targeted therapies were used, and some patients received both.
The authors highlight several patients as examples of exceptional responders:
- One patient with glioblastoma multiforme (GBM) was treated sequentially with surgery, localized carmustine, and radiotherapy. When the cancer recurred, temozolomide was administered. This induced a complete response that has lasted for more than a decade.
- A patient with metastatic colon adenocarcinoma has had an ongoing and nearly complete response that has lasted 45 months (last follow-up) after receiving temozolomide in combination with the investigational drug TRC102 (methoxyamine, under development by Tracon) in a phase 1 clinical trial. TRC102 is an inhibitor of the DNA base excision repair pathway, which is a pathway that causes resistance to alkylating and antimetabolite chemotherapeutics.
- A patient with metastatic, estrogen receptor–positive breast cancer received trastuzumab because of a high-level ERBB2 amplification, together with anastrozole. This resulted in an ongoing 2.4-year partial response.
- Although the patient was clinically HER2 positive, her tumor had exceedingly low expression of ERBB2 mRNA. Molecular profiling had classified the tumor as of the basal-like subtype rather than the HER2-enriched subtype. This meant that it was unlikely that trastuzumab contributed to the exceptional response, the authors note. Because the patient was estrogen-receptor positive, she received anastrozole, an inhibitor of aromatase (CYP19A), which converts testosterone into estradiol.
- A patient who had a gastrointestinal stromal tumor with a deletion of KIT exon 11 experienced relapse after an initial response to imatinib, which targets KIT and other tyrosine kinases, but then achieved a complete response with sunitinib. Gene expression profiling revealed high expression not only of KIT but also of genes encoding several tyrosine kinases that are targeted by sunitinib (KDR, FLT1, and FLT3). This may have accounted for the patient’s response.
Favorable genomic characteristics
The authors defined a “prognostic genetics” category of tumors, characterized by genetic lesions that are now known to be associated with a favorable prognosis but that were not addressed through routine care that these patients received when they were first diagnosed. Although the patients experienced relapse after first-line treatment, their exceptional survival after salvage therapy could be linked to favorable genomic characteristics.
For example, several of the patients with high-grade GBMs and astrocytomas had genetic lesions that are generally more common in low-grade glioma and that have been associated with an indolent clinical course following standard therapy.
The authors also assessed immune response. Examining immune cell infiltration in responder tumors in comparison with control cases, the team found that signatures of B cells and activated (CD56dim) natural killer cells were higher in exceptional-responder tumors.
In one patient with metastatic urothelial cancer who experienced disease progression after chemotherapy, radiotherapy, and surgery, treatment with nivolumab produced a complete response that lasted 7 months. Such an outcome occurs in only about 3% of bladder cancer patients. The tumor expressed high mRNA levels of PDCD1, which encodes the nivolumab target PD-1, and CD274, which encodes the PD-1 ligand PD-L1. There was also a high level of amplification of IFNG, which encodes interferon-gamma, a cytokine that has been linked to favorable response to immune checkpoint blockade.
Moving to precision medicine
“It is very valuable to be tested up front and again when the disease progresses, because there may have been some genetic changes, and this may change the treatment,” said co–lead author S. Percy Ivy, MD, of the NCI’s Division of Cancer Treatment and Diagnosis.
“The goal of this study was to understand what was unique about these patients and their genetic makeup that led them to be classified as exceptional responders, and hopefully we will be able to tease that out,” she added.
“As researchers, we have a lot to learn from these patients, and they have a lot to teach us,” she added. “In the future, they will help us as we move closer to the goal of delivering precision oncology to all of our patients. We’re not there yet, but every time we study more deeply and learn more, we are able to provide better care.”
To encourage participation in this effort by investigators around the world, the NCI team and their colleagues have made their molecular profiling results and clinical information publicly available in the NCI Genomic Data Commons.
The study was supported by the NCI’s Intramural Research Program, the National Institutes of Health, the Center for Cancer Research, and the NCI’s Center for Cancer Genomics. Staudt and Ivy have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Immunotherapy could fill unmet need in leptomeningeal metastases
Results from the trial were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Unfortunately, when patients present with leptomeningeal disease, they usually have a poor prognosis. Their median survival is measured at 6-24 weeks,” commented lead study author Jarushka Naidoo, MBBCh, an adjunct assistant professor of oncology at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore, and a consultant medical oncologist at Beaumont Hospital in Dublin.
“While there may be some standard approaches for how we treat leptomeningeal disease, there are no universal standard therapies that are efficacious across solid tumor types,” Dr. Naidoo added.
With this in mind, Dr. Naidoo and colleagues tested systemic pembrolizumab in a trial of patients with leptomeningeal metastases from solid tumors.
The trial closed early because of poor accrual, after enrolling 13 patients: 5 with breast carcinoma, 3 with high-grade glioma, 3 with non–small cell lung cancer, 1 with squamous cell carcinoma of the skin, and 1 with head and neck squamous carcinoma. Nine patients (69%) had received at least two prior lines of systemic therapy.
Response, safety, and biomarkers
Overall, five patients (38%) had a central nervous system response, as ascertained from radiologic response on MRI, cytologic response in cerebrospinal fluid (CSF), and/or clinical response in neurologic symptoms, Dr. Naidoo reported.
Two patients had a complete CNS response: a patient with squamous cell carcinoma of the skin, who was still alive at 3 years, and a patient with non–small cell lung cancer, who survived 9 months but succumbed to metastases elsewhere.
For the entire cohort, median CNS progression-free survival was 2.9 months, and median overall survival was 4.9 months.
“This is consistent with published prospective studies of systemic agents for leptomeningeal disease,” Dr. Naidoo pointed out. “Notably, even though numbers are small, we do see the tail-on-the-curve phenomenon in both of these survival curves, which is consistent with immune checkpoint blockade prospective studies.”
The rate of grade 3 or higher treatment-related adverse events was 15.4%, and there were no grade 3 or higher immune-related adverse events.
The number of patients was too small for formal correlational testing, but both patients who achieved a complete response developed immune-related adverse events.
The trial’s biomarker analyses showed that an aneuploidy assay using CSF tumor-derived DNA performed well at detecting leptomeningeal metastases, with sensitivity of 84.6%, compared with just 53.8% for CSF cytopathology (the current preferred method).
A multiplex assay of CSF cytokines identified similar baseline profiles for patients who went on to have responses and showed similar changes in profile (notably a reduction in proinflammatory cytokines) for the two patients who had complete responses.
Given the trial’s 38% CNS response rate, pembrolizumab “needs to be studied in larger populations of patients to confirm this result, but it could be used as a potential treatment option for patients with leptomeningeal disease from solid tumors,” Dr. Naidoo concluded. “Reassuringly, pembrolizumab was well tolerated, and this is extremely important in a patient population that is traditionally quite frail and in which other standard therapies that are used, such as high-dose methotrexate or intrathecal chemotherapy, are associated with far higher rates of toxicity.”
An unmet need
“Leptomeningeal metastasis is a strong unmet need, although its occurrence is fortunately quite rare,” commented Kim Margolin, MD, a clinical professor and medical oncologist at City of Hope National Medical Center in Duarte, Calif., who was not involved in this study.
The trial is noteworthy for showing activity of programmed death–1 (PD-1) blockade given only systemically and not with additional intrathecal therapy (as has been done in a concurrent study at MD Anderson Cancer Center) and for providing insight into various biomarkers, Dr. Margolin said in an interview.
“I cannot take a stand on author conclusions other than to agree it warrants further evaluation in carefully selected patients, and it would be great to compare something like peripheral PD-1 blockade alone versus in combination with intrathecal therapy versus a combination such as CTLA4 blockade plus PD-1 blockade such as our group and others have shown to have increased activity in CNS metastases over PD-1 block alone,” Dr. Margolin said.
“The drugs in this class are already approved, so there is no reason not to try them,” she noted.
However, patients with leptomeningeal metastases of melanoma, for example, are likely to have already received anti-PD-1 immunotherapy.
“So the settings in which off-the-shelf PD-1 blockade would be useful are extremely limited,” she concluded.
The current trial was funded by Merck, the National Institutes of Health, the Lung Cancer Foundation of America, the International Association for the Study of Lung Cancer, and Johns Hopkins University Seed Grants. Dr. Naidoo disclosed relationships with AstraZeneca, Merck, Bristol Myers Squibb, and Roche/Genentech. Dr. Margolin disclosed no relevant conflicts of interest.
SOURCE: Naidoo J et al. SITC 2020, Abstract 788.
Results from the trial were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Unfortunately, when patients present with leptomeningeal disease, they usually have a poor prognosis. Their median survival is measured at 6-24 weeks,” commented lead study author Jarushka Naidoo, MBBCh, an adjunct assistant professor of oncology at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore, and a consultant medical oncologist at Beaumont Hospital in Dublin.
“While there may be some standard approaches for how we treat leptomeningeal disease, there are no universal standard therapies that are efficacious across solid tumor types,” Dr. Naidoo added.
With this in mind, Dr. Naidoo and colleagues tested systemic pembrolizumab in a trial of patients with leptomeningeal metastases from solid tumors.
The trial closed early because of poor accrual, after enrolling 13 patients: 5 with breast carcinoma, 3 with high-grade glioma, 3 with non–small cell lung cancer, 1 with squamous cell carcinoma of the skin, and 1 with head and neck squamous carcinoma. Nine patients (69%) had received at least two prior lines of systemic therapy.
Response, safety, and biomarkers
Overall, five patients (38%) had a central nervous system response, as ascertained from radiologic response on MRI, cytologic response in cerebrospinal fluid (CSF), and/or clinical response in neurologic symptoms, Dr. Naidoo reported.
Two patients had a complete CNS response: a patient with squamous cell carcinoma of the skin, who was still alive at 3 years, and a patient with non–small cell lung cancer, who survived 9 months but succumbed to metastases elsewhere.
For the entire cohort, median CNS progression-free survival was 2.9 months, and median overall survival was 4.9 months.
“This is consistent with published prospective studies of systemic agents for leptomeningeal disease,” Dr. Naidoo pointed out. “Notably, even though numbers are small, we do see the tail-on-the-curve phenomenon in both of these survival curves, which is consistent with immune checkpoint blockade prospective studies.”
The rate of grade 3 or higher treatment-related adverse events was 15.4%, and there were no grade 3 or higher immune-related adverse events.
The number of patients was too small for formal correlational testing, but both patients who achieved a complete response developed immune-related adverse events.
The trial’s biomarker analyses showed that an aneuploidy assay using CSF tumor-derived DNA performed well at detecting leptomeningeal metastases, with sensitivity of 84.6%, compared with just 53.8% for CSF cytopathology (the current preferred method).
A multiplex assay of CSF cytokines identified similar baseline profiles for patients who went on to have responses and showed similar changes in profile (notably a reduction in proinflammatory cytokines) for the two patients who had complete responses.
Given the trial’s 38% CNS response rate, pembrolizumab “needs to be studied in larger populations of patients to confirm this result, but it could be used as a potential treatment option for patients with leptomeningeal disease from solid tumors,” Dr. Naidoo concluded. “Reassuringly, pembrolizumab was well tolerated, and this is extremely important in a patient population that is traditionally quite frail and in which other standard therapies that are used, such as high-dose methotrexate or intrathecal chemotherapy, are associated with far higher rates of toxicity.”
An unmet need
“Leptomeningeal metastasis is a strong unmet need, although its occurrence is fortunately quite rare,” commented Kim Margolin, MD, a clinical professor and medical oncologist at City of Hope National Medical Center in Duarte, Calif., who was not involved in this study.
The trial is noteworthy for showing activity of programmed death–1 (PD-1) blockade given only systemically and not with additional intrathecal therapy (as has been done in a concurrent study at MD Anderson Cancer Center) and for providing insight into various biomarkers, Dr. Margolin said in an interview.
“I cannot take a stand on author conclusions other than to agree it warrants further evaluation in carefully selected patients, and it would be great to compare something like peripheral PD-1 blockade alone versus in combination with intrathecal therapy versus a combination such as CTLA4 blockade plus PD-1 blockade such as our group and others have shown to have increased activity in CNS metastases over PD-1 block alone,” Dr. Margolin said.
“The drugs in this class are already approved, so there is no reason not to try them,” she noted.
However, patients with leptomeningeal metastases of melanoma, for example, are likely to have already received anti-PD-1 immunotherapy.
“So the settings in which off-the-shelf PD-1 blockade would be useful are extremely limited,” she concluded.
The current trial was funded by Merck, the National Institutes of Health, the Lung Cancer Foundation of America, the International Association for the Study of Lung Cancer, and Johns Hopkins University Seed Grants. Dr. Naidoo disclosed relationships with AstraZeneca, Merck, Bristol Myers Squibb, and Roche/Genentech. Dr. Margolin disclosed no relevant conflicts of interest.
SOURCE: Naidoo J et al. SITC 2020, Abstract 788.
Results from the trial were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Unfortunately, when patients present with leptomeningeal disease, they usually have a poor prognosis. Their median survival is measured at 6-24 weeks,” commented lead study author Jarushka Naidoo, MBBCh, an adjunct assistant professor of oncology at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins University, Baltimore, and a consultant medical oncologist at Beaumont Hospital in Dublin.
“While there may be some standard approaches for how we treat leptomeningeal disease, there are no universal standard therapies that are efficacious across solid tumor types,” Dr. Naidoo added.
With this in mind, Dr. Naidoo and colleagues tested systemic pembrolizumab in a trial of patients with leptomeningeal metastases from solid tumors.
The trial closed early because of poor accrual, after enrolling 13 patients: 5 with breast carcinoma, 3 with high-grade glioma, 3 with non–small cell lung cancer, 1 with squamous cell carcinoma of the skin, and 1 with head and neck squamous carcinoma. Nine patients (69%) had received at least two prior lines of systemic therapy.
Response, safety, and biomarkers
Overall, five patients (38%) had a central nervous system response, as ascertained from radiologic response on MRI, cytologic response in cerebrospinal fluid (CSF), and/or clinical response in neurologic symptoms, Dr. Naidoo reported.
Two patients had a complete CNS response: a patient with squamous cell carcinoma of the skin, who was still alive at 3 years, and a patient with non–small cell lung cancer, who survived 9 months but succumbed to metastases elsewhere.
For the entire cohort, median CNS progression-free survival was 2.9 months, and median overall survival was 4.9 months.
“This is consistent with published prospective studies of systemic agents for leptomeningeal disease,” Dr. Naidoo pointed out. “Notably, even though numbers are small, we do see the tail-on-the-curve phenomenon in both of these survival curves, which is consistent with immune checkpoint blockade prospective studies.”
The rate of grade 3 or higher treatment-related adverse events was 15.4%, and there were no grade 3 or higher immune-related adverse events.
The number of patients was too small for formal correlational testing, but both patients who achieved a complete response developed immune-related adverse events.
The trial’s biomarker analyses showed that an aneuploidy assay using CSF tumor-derived DNA performed well at detecting leptomeningeal metastases, with sensitivity of 84.6%, compared with just 53.8% for CSF cytopathology (the current preferred method).
A multiplex assay of CSF cytokines identified similar baseline profiles for patients who went on to have responses and showed similar changes in profile (notably a reduction in proinflammatory cytokines) for the two patients who had complete responses.
Given the trial’s 38% CNS response rate, pembrolizumab “needs to be studied in larger populations of patients to confirm this result, but it could be used as a potential treatment option for patients with leptomeningeal disease from solid tumors,” Dr. Naidoo concluded. “Reassuringly, pembrolizumab was well tolerated, and this is extremely important in a patient population that is traditionally quite frail and in which other standard therapies that are used, such as high-dose methotrexate or intrathecal chemotherapy, are associated with far higher rates of toxicity.”
An unmet need
“Leptomeningeal metastasis is a strong unmet need, although its occurrence is fortunately quite rare,” commented Kim Margolin, MD, a clinical professor and medical oncologist at City of Hope National Medical Center in Duarte, Calif., who was not involved in this study.
The trial is noteworthy for showing activity of programmed death–1 (PD-1) blockade given only systemically and not with additional intrathecal therapy (as has been done in a concurrent study at MD Anderson Cancer Center) and for providing insight into various biomarkers, Dr. Margolin said in an interview.
“I cannot take a stand on author conclusions other than to agree it warrants further evaluation in carefully selected patients, and it would be great to compare something like peripheral PD-1 blockade alone versus in combination with intrathecal therapy versus a combination such as CTLA4 blockade plus PD-1 blockade such as our group and others have shown to have increased activity in CNS metastases over PD-1 block alone,” Dr. Margolin said.
“The drugs in this class are already approved, so there is no reason not to try them,” she noted.
However, patients with leptomeningeal metastases of melanoma, for example, are likely to have already received anti-PD-1 immunotherapy.
“So the settings in which off-the-shelf PD-1 blockade would be useful are extremely limited,” she concluded.
The current trial was funded by Merck, the National Institutes of Health, the Lung Cancer Foundation of America, the International Association for the Study of Lung Cancer, and Johns Hopkins University Seed Grants. Dr. Naidoo disclosed relationships with AstraZeneca, Merck, Bristol Myers Squibb, and Roche/Genentech. Dr. Margolin disclosed no relevant conflicts of interest.
SOURCE: Naidoo J et al. SITC 2020, Abstract 788.
FROM SITC 2020
Risk factors for severe immune-related AEs identified
The first nationwide study of severe immune-related adverse events among cancer patients treated with immune checkpoint inhibitors helps identify those at elevated risk. The findings were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Immune-related adverse events are a very serious side effect of immune checkpoint inhibitor therapy, and as this therapy has become more common for treating advanced cancers, the incidence of immune-related adverse events has increased as well,” said presenting author William Murphy, a dual MD and MBA student at Harvard Medical School and Harvard Business School, both in Boston.
“However, because there is no ICD code for immune-related adverse events, it’s very difficult to study them at a population level. Most of the current literature around the incidence of immune-related adverse events and factors that are predictive of incidence are based on clinical trials and small studies,” Mr. Murphy noted.
He and his colleagues analyzed claims data from a U.S. nationwide health insurance plan for 14,378 patients who had a primary cancer and received at least one administration of an immune checkpoint inhibitor – an inhibitor of PD-1, PD-L1, or CTLA4 – during 2011-2019.
Over 19,117 patient-years of follow-up, 504 patients (3.5%) developed a severe immune-related adverse event (irAE), defined as one occurring within 2 years of their treatment and requiring inpatient hospitalization and new immunosuppression.
The incidence of severe irAEs per patient treatment year was 2.6% overall, rising from 0% in 2011 to 3.7% in 2016.
In multivariate analysis, patients had an elevated risk of severe irAEs if they received combination immunotherapy as compared with monotherapy (odds ratio, 2.44; P < .001).
On the other hand, risk fell with advancing age (OR, 0.98 per additional year; P < .001). And risk was lower for patients with melanoma (OR, 0.70; P = .01), renal cell carcinoma (OR, 0.71; P = .03), and other cancers (OR, 0.50; P < .001), compared with lung cancer.
Sex, geographic region, income, employment status, and comorbidity were not significantly associated with the risk of severe irAEs.
“We hope that patients and providers can use this evidence from a nationwide study of severe irAEs to guide treatment and management decisions,” Mr. Murphy concluded.
Real-world evidence
“As the use of immune checkpoint inhibitors increases for patients with a variety of different tumor types, there is increasing need for population-level evidence for patients treated outside of clinical trials,” said Allison Betof Warner, MD, PhD, an assistant attending physician with the melanoma service at Memorial Sloan Kettering Cancer Center in New York.
“This is a well-conducted study with an innovative approach to using real-world evidence to examine immune-related adverse events,” she added.
To her knowledge, it is the first study to look at multiple cancers for which immunotherapy is approved, Dr. Betof Warner said. This approach resulted in a large patient sample, giving power to detect differences between groups.
“The authors’ finding that combination immunotherapy is associated with more severe irAEs is in line with our clinical experience and other data sets, and the data regarding increased odds of severe irAEs in younger patients and those with lung cancer raise interesting biological questions about the etiology of irAEs,” Dr. Betof Warner noted.
However, certain factors complicate interpretation of the study’s findings, she cautioned. One such factor is requiring hospitalization to define an irAE.
“Practice patterns regarding hospitalization vary quite widely from center to center. For example, in some centers, all patients with immune-mediated colitis are hospitalized, whereas in others, these patients are managed predominantly in the outpatient setting, even in cases of high-grade toxicity,” she explained. “Practice patterns have also changed drastically over time as oncologists have grown more comfortable managing immune-related adverse events.”
Another factor is potential confounding. For example, patients with melanoma are more likely to receive combination immunotherapy given its longstanding approval for this cancer, whereas it is comparatively new for other cancers. Also, age may differ across cancers.
“The data the authors have provided are a great starting point, but I think further analysis is needed before these observations can be validated and integrated into practice,” Dr. Betof Warner concluded.
This study did not receive any specific funding. Mr. Murphy and Dr. Betof Warner disclosed no relevant conflicts of interest.
SOURCE: Murphy W et al. SITC 2020, Abstract 854.
The first nationwide study of severe immune-related adverse events among cancer patients treated with immune checkpoint inhibitors helps identify those at elevated risk. The findings were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Immune-related adverse events are a very serious side effect of immune checkpoint inhibitor therapy, and as this therapy has become more common for treating advanced cancers, the incidence of immune-related adverse events has increased as well,” said presenting author William Murphy, a dual MD and MBA student at Harvard Medical School and Harvard Business School, both in Boston.
“However, because there is no ICD code for immune-related adverse events, it’s very difficult to study them at a population level. Most of the current literature around the incidence of immune-related adverse events and factors that are predictive of incidence are based on clinical trials and small studies,” Mr. Murphy noted.
He and his colleagues analyzed claims data from a U.S. nationwide health insurance plan for 14,378 patients who had a primary cancer and received at least one administration of an immune checkpoint inhibitor – an inhibitor of PD-1, PD-L1, or CTLA4 – during 2011-2019.
Over 19,117 patient-years of follow-up, 504 patients (3.5%) developed a severe immune-related adverse event (irAE), defined as one occurring within 2 years of their treatment and requiring inpatient hospitalization and new immunosuppression.
The incidence of severe irAEs per patient treatment year was 2.6% overall, rising from 0% in 2011 to 3.7% in 2016.
In multivariate analysis, patients had an elevated risk of severe irAEs if they received combination immunotherapy as compared with monotherapy (odds ratio, 2.44; P < .001).
On the other hand, risk fell with advancing age (OR, 0.98 per additional year; P < .001). And risk was lower for patients with melanoma (OR, 0.70; P = .01), renal cell carcinoma (OR, 0.71; P = .03), and other cancers (OR, 0.50; P < .001), compared with lung cancer.
Sex, geographic region, income, employment status, and comorbidity were not significantly associated with the risk of severe irAEs.
“We hope that patients and providers can use this evidence from a nationwide study of severe irAEs to guide treatment and management decisions,” Mr. Murphy concluded.
Real-world evidence
“As the use of immune checkpoint inhibitors increases for patients with a variety of different tumor types, there is increasing need for population-level evidence for patients treated outside of clinical trials,” said Allison Betof Warner, MD, PhD, an assistant attending physician with the melanoma service at Memorial Sloan Kettering Cancer Center in New York.
“This is a well-conducted study with an innovative approach to using real-world evidence to examine immune-related adverse events,” she added.
To her knowledge, it is the first study to look at multiple cancers for which immunotherapy is approved, Dr. Betof Warner said. This approach resulted in a large patient sample, giving power to detect differences between groups.
“The authors’ finding that combination immunotherapy is associated with more severe irAEs is in line with our clinical experience and other data sets, and the data regarding increased odds of severe irAEs in younger patients and those with lung cancer raise interesting biological questions about the etiology of irAEs,” Dr. Betof Warner noted.
However, certain factors complicate interpretation of the study’s findings, she cautioned. One such factor is requiring hospitalization to define an irAE.
“Practice patterns regarding hospitalization vary quite widely from center to center. For example, in some centers, all patients with immune-mediated colitis are hospitalized, whereas in others, these patients are managed predominantly in the outpatient setting, even in cases of high-grade toxicity,” she explained. “Practice patterns have also changed drastically over time as oncologists have grown more comfortable managing immune-related adverse events.”
Another factor is potential confounding. For example, patients with melanoma are more likely to receive combination immunotherapy given its longstanding approval for this cancer, whereas it is comparatively new for other cancers. Also, age may differ across cancers.
“The data the authors have provided are a great starting point, but I think further analysis is needed before these observations can be validated and integrated into practice,” Dr. Betof Warner concluded.
This study did not receive any specific funding. Mr. Murphy and Dr. Betof Warner disclosed no relevant conflicts of interest.
SOURCE: Murphy W et al. SITC 2020, Abstract 854.
The first nationwide study of severe immune-related adverse events among cancer patients treated with immune checkpoint inhibitors helps identify those at elevated risk. The findings were reported at the Society for Immunotherapy of Cancer’s 35th Anniversary Annual Meeting.
“Immune-related adverse events are a very serious side effect of immune checkpoint inhibitor therapy, and as this therapy has become more common for treating advanced cancers, the incidence of immune-related adverse events has increased as well,” said presenting author William Murphy, a dual MD and MBA student at Harvard Medical School and Harvard Business School, both in Boston.
“However, because there is no ICD code for immune-related adverse events, it’s very difficult to study them at a population level. Most of the current literature around the incidence of immune-related adverse events and factors that are predictive of incidence are based on clinical trials and small studies,” Mr. Murphy noted.
He and his colleagues analyzed claims data from a U.S. nationwide health insurance plan for 14,378 patients who had a primary cancer and received at least one administration of an immune checkpoint inhibitor – an inhibitor of PD-1, PD-L1, or CTLA4 – during 2011-2019.
Over 19,117 patient-years of follow-up, 504 patients (3.5%) developed a severe immune-related adverse event (irAE), defined as one occurring within 2 years of their treatment and requiring inpatient hospitalization and new immunosuppression.
The incidence of severe irAEs per patient treatment year was 2.6% overall, rising from 0% in 2011 to 3.7% in 2016.
In multivariate analysis, patients had an elevated risk of severe irAEs if they received combination immunotherapy as compared with monotherapy (odds ratio, 2.44; P < .001).
On the other hand, risk fell with advancing age (OR, 0.98 per additional year; P < .001). And risk was lower for patients with melanoma (OR, 0.70; P = .01), renal cell carcinoma (OR, 0.71; P = .03), and other cancers (OR, 0.50; P < .001), compared with lung cancer.
Sex, geographic region, income, employment status, and comorbidity were not significantly associated with the risk of severe irAEs.
“We hope that patients and providers can use this evidence from a nationwide study of severe irAEs to guide treatment and management decisions,” Mr. Murphy concluded.
Real-world evidence
“As the use of immune checkpoint inhibitors increases for patients with a variety of different tumor types, there is increasing need for population-level evidence for patients treated outside of clinical trials,” said Allison Betof Warner, MD, PhD, an assistant attending physician with the melanoma service at Memorial Sloan Kettering Cancer Center in New York.
“This is a well-conducted study with an innovative approach to using real-world evidence to examine immune-related adverse events,” she added.
To her knowledge, it is the first study to look at multiple cancers for which immunotherapy is approved, Dr. Betof Warner said. This approach resulted in a large patient sample, giving power to detect differences between groups.
“The authors’ finding that combination immunotherapy is associated with more severe irAEs is in line with our clinical experience and other data sets, and the data regarding increased odds of severe irAEs in younger patients and those with lung cancer raise interesting biological questions about the etiology of irAEs,” Dr. Betof Warner noted.
However, certain factors complicate interpretation of the study’s findings, she cautioned. One such factor is requiring hospitalization to define an irAE.
“Practice patterns regarding hospitalization vary quite widely from center to center. For example, in some centers, all patients with immune-mediated colitis are hospitalized, whereas in others, these patients are managed predominantly in the outpatient setting, even in cases of high-grade toxicity,” she explained. “Practice patterns have also changed drastically over time as oncologists have grown more comfortable managing immune-related adverse events.”
Another factor is potential confounding. For example, patients with melanoma are more likely to receive combination immunotherapy given its longstanding approval for this cancer, whereas it is comparatively new for other cancers. Also, age may differ across cancers.
“The data the authors have provided are a great starting point, but I think further analysis is needed before these observations can be validated and integrated into practice,” Dr. Betof Warner concluded.
This study did not receive any specific funding. Mr. Murphy and Dr. Betof Warner disclosed no relevant conflicts of interest.
SOURCE: Murphy W et al. SITC 2020, Abstract 854.
FROM SITC 2020
Using telehealth to deliver palliative care to cancer patients
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Traditional delivery of palliative care to outpatients with cancer is associated with many challenges.
Telehealth can eliminate some of these challenges but comes with issues of its own, according to results of the REACH PC trial.
Jennifer S. Temel, MD, of Massachusetts General Hospital in Boston, discussed the use of telemedicine in palliative care, including results from REACH PC, during an educational session at the ASCO Virtual Quality Care Symposium 2020.
Dr. Temel noted that, for cancer patients, an in-person visit with a palliative care specialist can cost time, induce fatigue, and increase financial burden from transportation and parking expenses.
For caregivers and family, an in-person visit may necessitate absence from family and/or work, require complex scheduling to coordinate with other office visits, and result in additional transportation and/or parking expenses.
For health care systems, to have a dedicated palliative care clinic requires precious space and financial expenditures for office personnel and other resources.
These issues make it attractive to consider whether telehealth could be used for palliative care services.
Scarcity of palliative care specialists
In the United States, there is roughly 1 palliative care physician for every 20,000 older adults with a life-limiting illness, according to research published in Annual Review of Public Health in 2014.
In its 2019 state-by-state report card, the Center to Advance Palliative Care noted that only 72% of U.S. hospitals with 50 or more beds have a palliative care team.
For patients with serious illnesses and those who are socioeconomically or geographically disadvantaged, palliative care is often inaccessible.
Inefficiencies in the current system are an additional impediment. Palliative care specialists frequently see patients during a portion of the patient’s routine visit to subspecialty or primary care clinics. This limits the palliative care specialist’s ability to perform comprehensive assessments and provide patient-centered care efficiently.
Special considerations regarding telehealth for palliative care
As a specialty, palliative care involves interactions that could make the use of telehealth problematic. For example, conveyance of interest, warmth, and touch are challenging or impossible in a video format.
Palliative care specialists engage with patients regarding relatively serious topics such as prognosis and end-of-life preferences. There is uncertainty about how those discussions would be received by patients and their caregivers via video.
Furthermore, there are logistical impediments such as prescribing opioids with video or across state lines.
Despite these concerns, the ENABLE study showed that supplementing usual oncology care with weekly (transitioning to monthly) telephone-based educational palliative care produced higher quality of life and mood than did usual oncology care alone. These results were published in JAMA in 2009.
REACH PC study demonstrates feasibility of telehealth model
Dr. Temel described the ongoing REACH PC trial in which palliative care is delivered via video visits and compared with in-person palliative care for patients with advanced non–small cell lung cancer.
The primary aim of REACH PC is to determine whether telehealth palliative care is equivalent to traditional palliative care in improving quality of life as a supplement to routine oncology care.
Currently, REACH PC has enrolled 581 patients at its 20 sites, spanning a geographically diverse area. Just over half of patients approached about REACH PC agreed to enroll in it. Ultimately, 1,250 enrollees are sought.
Among patients who declined to participate, 7.6% indicated “discomfort with technology” as the reason. Most refusals were due to lack of interest in research (35.1%) and/or palliative care (22.9%).
Older adults were prominent among enrollees. More than 60% were older than 60 years of age, and more than one-third were older than 70 years.
Among patients who began the trial, there were slightly more withdrawals in the telehealth participants, in comparison with in-person participants (13.6% versus 9.1%).
When palliative care clinicians were queried about video visits, 64.3% said there were no challenges. This is comparable to the 65.5% of clinicians who had no challenges with in-person visits.
When problems occurred with video visits, they were most frequently technical (19.1%). Only 1.4% of clinicians reported difficulty addressing topics that felt uncomfortable over video, and 1.5% reported difficulty establishing rapport.
The success rates of video and in-person visits were similar. About 80% of visits accomplished planned goals.
‘Webside’ manner
Strategies such as reflective listening and summarizing what patients say (to verify an accurate understanding of the patient’s perspective) are key to successful palliative care visits, regardless of the setting.
For telehealth visits, Dr. Temel described techniques she defined as “webside manner,” to compensate for the inability of the clinician to touch a patient. These techniques include leaning in toward the camera, nodding, and pausing to be certain the patient has finished speaking before the clinician speaks again.
Is telehealth the future of palliative care?
I include myself among those oncologists who have voiced concern about moving from face-to-face to remote visits for complicated consultations such as those required for palliative care. Nonetheless, from the preliminary results of the REACH PC trial, it appears that telehealth could be a valuable tool.
To minimize differences between in-person and remote delivery of palliative care, practical strategies for ensuring rapport and facilitating a trusting relationship should be defined further and disseminated.
In addition, we need to be vigilant for widening inequities of care from rapid movement to the use of technology (i.e., an equity gap). In their telehealth experience during the COVID-19 pandemic, investigators at Houston Methodist Cancer Center found that patients declining virtual visits tended to be older, lower-income, and less likely to have commercial insurance. These results were recently published in JCO Oncology Practice.
For the foregoing reasons, hybrid systems for palliative care services will probably always be needed.
Going forward, we should heed the advice of Alvin Toffler in his book Future Shock. Mr. Toffler said, “The illiterate of the 21st century will not be those who cannot read and write, but those who cannot learn, unlearn, and relearn.”
The traditional model for delivering palliative care will almost certainly need to be reimagined and relearned.
Dr. Temel disclosed institutional research funding from Pfizer.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
FROM ASCO QUALITY CARE SYMPOSIUM 2020
Lung cancer: Proton beam radiotherapy likely reduces cardiovascular events
The findings were reported at the American Society for Radiation Oncology Annual Meeting 2020.
Patients with lung cancer often have underlying cardiac risk factors, noted lead investigator Timothy Kegelman, MD, PhD, of University of Pennsylvania in Philadelphia.
“The dose to the heart correlates with adverse cardiovascular events following radiation therapy. One strategy to minimize dose to the heart is proton beam radiation,” Dr. Kegelman said.
He and his colleagues retrospectively studied consecutive patients with locally advanced non–small cell lung cancer (NSCLC) treated with chemotherapy plus either proton beam radiotherapy or conventional photon radiotherapy.
The team used electronic health records to ascertain incidence of six cardiovascular events: MI, atrial fibrillation, coronary artery disease, heart failure, stroke, and transient ischemic attack. Patients who had previously experienced an event were not considered as part of the at-risk population for that specific event after radiotherapy.
Analyses were based on 98 patients who received proton beam radiotherapy and 104 patients who received conventional photon radiotherapy.
At baseline, the proton cohort was older, had a heavier smoking history, and had a higher prevalence of previous cardiovascular events (46.9% vs. 31.7%; P = .03).
The total median radiation dose was identical for the proton and photon groups (66.6 Gy), but the former group had significantly lower measures of cardiac radiation dose, including roughly half the mean dose to the heart (6.9 vs. 13.3 Gy).
Outcomes and next steps
At a median follow-up of 29 months, the proton beam radiotherapy group had a significantly lower incidence of transient ischemic attack, compared with the photon radiotherapy group (1.1% vs. 8.2%; P = .04).
The proton group also had numerically lower incidences of MI (2.3% vs. 9.0%; P = .06) and stroke (3.2% vs. 6.1%; P = .50).
The proton and photon groups were similar as far as the incidence of total cardiovascular events (53.1% vs. 47.1%; P = .48) and the 3-year overall survival rate (38.8% vs. 42.1%; P = .99).
“Our future studies aim to examine the potential relationships between grade of cardiac event and type of radiotherapy and dose to cardiac substructures,” Dr. Kegelman commented.
In addition, his institution is participating in RTOG 1308, a phase 3 trial comparing photon and proton beam radiotherapy in patients with inoperable lung cancer that will better assess cardiac-related morbidity and mortality. The trial is expected to be completed by the end of 2025.
Accumulating evidence
“This study adds to a growing body of evidence about the potential importance of heart dose in any radiation modality,” said Daniel Gomez, MD, MBA, of Memorial Sloan Kettering Cancer Center in New York, who was not involved in the study.
The RTOG 0617 trial and the Lung ART trial previously showed correlations between lower radiation dose to the heart and better survival in patients with lung cancer, Dr. Gomez noted.
“It’s been well established that protons can improve heart dose, and therefore it’s been inferred that they may improve outcomes, but the exact mechanisms remain unclear,” Dr. Gomez said.
Proton beam radiotherapy performed well in a single-arm, phase 2 trial among patients with unresectable NSCLC.
“The ongoing phase 3 trial is using a more modern proton technique and has a larger population, with a randomized study design. It will be much more informative,” Dr. Gomez predicted.
The current study did not receive specific funding. Dr. Kegelman disclosed no relevant conflicts of interest. Dr. Gomez disclosed honoraria from Varian.
SOURCE: Kegelman TP et al. ASTRO 2020, Abstract 1046.
The findings were reported at the American Society for Radiation Oncology Annual Meeting 2020.
Patients with lung cancer often have underlying cardiac risk factors, noted lead investigator Timothy Kegelman, MD, PhD, of University of Pennsylvania in Philadelphia.
“The dose to the heart correlates with adverse cardiovascular events following radiation therapy. One strategy to minimize dose to the heart is proton beam radiation,” Dr. Kegelman said.
He and his colleagues retrospectively studied consecutive patients with locally advanced non–small cell lung cancer (NSCLC) treated with chemotherapy plus either proton beam radiotherapy or conventional photon radiotherapy.
The team used electronic health records to ascertain incidence of six cardiovascular events: MI, atrial fibrillation, coronary artery disease, heart failure, stroke, and transient ischemic attack. Patients who had previously experienced an event were not considered as part of the at-risk population for that specific event after radiotherapy.
Analyses were based on 98 patients who received proton beam radiotherapy and 104 patients who received conventional photon radiotherapy.
At baseline, the proton cohort was older, had a heavier smoking history, and had a higher prevalence of previous cardiovascular events (46.9% vs. 31.7%; P = .03).
The total median radiation dose was identical for the proton and photon groups (66.6 Gy), but the former group had significantly lower measures of cardiac radiation dose, including roughly half the mean dose to the heart (6.9 vs. 13.3 Gy).
Outcomes and next steps
At a median follow-up of 29 months, the proton beam radiotherapy group had a significantly lower incidence of transient ischemic attack, compared with the photon radiotherapy group (1.1% vs. 8.2%; P = .04).
The proton group also had numerically lower incidences of MI (2.3% vs. 9.0%; P = .06) and stroke (3.2% vs. 6.1%; P = .50).
The proton and photon groups were similar as far as the incidence of total cardiovascular events (53.1% vs. 47.1%; P = .48) and the 3-year overall survival rate (38.8% vs. 42.1%; P = .99).
“Our future studies aim to examine the potential relationships between grade of cardiac event and type of radiotherapy and dose to cardiac substructures,” Dr. Kegelman commented.
In addition, his institution is participating in RTOG 1308, a phase 3 trial comparing photon and proton beam radiotherapy in patients with inoperable lung cancer that will better assess cardiac-related morbidity and mortality. The trial is expected to be completed by the end of 2025.
Accumulating evidence
“This study adds to a growing body of evidence about the potential importance of heart dose in any radiation modality,” said Daniel Gomez, MD, MBA, of Memorial Sloan Kettering Cancer Center in New York, who was not involved in the study.
The RTOG 0617 trial and the Lung ART trial previously showed correlations between lower radiation dose to the heart and better survival in patients with lung cancer, Dr. Gomez noted.
“It’s been well established that protons can improve heart dose, and therefore it’s been inferred that they may improve outcomes, but the exact mechanisms remain unclear,” Dr. Gomez said.
Proton beam radiotherapy performed well in a single-arm, phase 2 trial among patients with unresectable NSCLC.
“The ongoing phase 3 trial is using a more modern proton technique and has a larger population, with a randomized study design. It will be much more informative,” Dr. Gomez predicted.
The current study did not receive specific funding. Dr. Kegelman disclosed no relevant conflicts of interest. Dr. Gomez disclosed honoraria from Varian.
SOURCE: Kegelman TP et al. ASTRO 2020, Abstract 1046.
The findings were reported at the American Society for Radiation Oncology Annual Meeting 2020.
Patients with lung cancer often have underlying cardiac risk factors, noted lead investigator Timothy Kegelman, MD, PhD, of University of Pennsylvania in Philadelphia.
“The dose to the heart correlates with adverse cardiovascular events following radiation therapy. One strategy to minimize dose to the heart is proton beam radiation,” Dr. Kegelman said.
He and his colleagues retrospectively studied consecutive patients with locally advanced non–small cell lung cancer (NSCLC) treated with chemotherapy plus either proton beam radiotherapy or conventional photon radiotherapy.
The team used electronic health records to ascertain incidence of six cardiovascular events: MI, atrial fibrillation, coronary artery disease, heart failure, stroke, and transient ischemic attack. Patients who had previously experienced an event were not considered as part of the at-risk population for that specific event after radiotherapy.
Analyses were based on 98 patients who received proton beam radiotherapy and 104 patients who received conventional photon radiotherapy.
At baseline, the proton cohort was older, had a heavier smoking history, and had a higher prevalence of previous cardiovascular events (46.9% vs. 31.7%; P = .03).
The total median radiation dose was identical for the proton and photon groups (66.6 Gy), but the former group had significantly lower measures of cardiac radiation dose, including roughly half the mean dose to the heart (6.9 vs. 13.3 Gy).
Outcomes and next steps
At a median follow-up of 29 months, the proton beam radiotherapy group had a significantly lower incidence of transient ischemic attack, compared with the photon radiotherapy group (1.1% vs. 8.2%; P = .04).
The proton group also had numerically lower incidences of MI (2.3% vs. 9.0%; P = .06) and stroke (3.2% vs. 6.1%; P = .50).
The proton and photon groups were similar as far as the incidence of total cardiovascular events (53.1% vs. 47.1%; P = .48) and the 3-year overall survival rate (38.8% vs. 42.1%; P = .99).
“Our future studies aim to examine the potential relationships between grade of cardiac event and type of radiotherapy and dose to cardiac substructures,” Dr. Kegelman commented.
In addition, his institution is participating in RTOG 1308, a phase 3 trial comparing photon and proton beam radiotherapy in patients with inoperable lung cancer that will better assess cardiac-related morbidity and mortality. The trial is expected to be completed by the end of 2025.
Accumulating evidence
“This study adds to a growing body of evidence about the potential importance of heart dose in any radiation modality,” said Daniel Gomez, MD, MBA, of Memorial Sloan Kettering Cancer Center in New York, who was not involved in the study.
The RTOG 0617 trial and the Lung ART trial previously showed correlations between lower radiation dose to the heart and better survival in patients with lung cancer, Dr. Gomez noted.
“It’s been well established that protons can improve heart dose, and therefore it’s been inferred that they may improve outcomes, but the exact mechanisms remain unclear,” Dr. Gomez said.
Proton beam radiotherapy performed well in a single-arm, phase 2 trial among patients with unresectable NSCLC.
“The ongoing phase 3 trial is using a more modern proton technique and has a larger population, with a randomized study design. It will be much more informative,” Dr. Gomez predicted.
The current study did not receive specific funding. Dr. Kegelman disclosed no relevant conflicts of interest. Dr. Gomez disclosed honoraria from Varian.
SOURCE: Kegelman TP et al. ASTRO 2020, Abstract 1046.
FROM ASTRO 2020
New cancer drugs may have saved more than 1.2 million Americans
Reductions in mortality were most notable for tumor types with relatively more approvals, including lung and breast cancer, melanoma, lymphoma, and leukemia.
A report from the American Cancer Society (ACS) estimated that, from 1991 to 2017, there were 2,902,200 total cancer deaths avoided from improvements in mortality from all potential sources.
The new findings, reported in the Journal of Medical Economics, suggest that drugs approved between 2000 and 2016 to treat the 15 most common cancer types helped to reduce mortality by 24% per 100,000 people.
“This study provides evidence that a significant share of that reduction from 2000 to 2016 was associated with the introduction of new therapies. The ACS report and other studies demonstrate that the improvements in lung cancer specifically are likely due to new treatments,” said lead study author Joanna P. MacEwan, MD, of PRECISIONheor in Los Angeles.
The findings contribute to a better understanding of whether increased spending on cancer drugs are worth the investment, according to the study authors.
“We provide evidence that the gains in survival measured in clinical trials are translating into health benefits for patients in the real world and confirm previous research that has also shown that new pharmaceutical treatments are associated with improved real-world survival outcomes for patients,” Dr. MacEwan said.
Full effect not yet observed
The researchers used a series of national data sets from sources including the Centers for Disease Control and Prevention; the U.S. Mortality Files by the National Center of Health Statistics; Survival, Epidemiology and End Results program; and United States Cancer Statistics.
The team calculated age-adjusted cancer mortality rates per year for the 15 most common tumor types and also looked at incident cases of cancer by tumor type, represented as per 100,000 people, for all ages, races, and genders.
The researchers then translated the change in cancer mortality in the U.S. from 2000 to 2016 associated with treatment stocks in each year into deaths averted per year.
Across the 16 years, mortality was down by 1,291,769 deaths. The following cancers had significant reductions in mortality: breast (n = 127,874), colorectal (n = 46,705), lung (n = 375,256), prostate (n = 476,210), gastric (n = 758), and renal (n = 739) cancers, as well as non-Hodgkin lymphoma (n = 48,836) and leukemia (n = 4,011).
Estimated mortality increased by 825 deaths in patients with thyroid cancer and 7,768 deaths for those with bladder cancer. These rises are likely due to the result of sparse drug approvals during this period – five for thyroid cancer and three for bladder cancer – Dr. MacEwan said. There were no approvals in liver or uterine cancer and few approvals in pancreatic and oral cancer.
The full effect of new drug introductions may not have been observed yet, Dr. MacEwan noted.
“There are fewer patients using the treatments for drugs approved in the later years of our study and less follow-up time to measure outcomes,” she said. “Over time, utilization of the newer therapies will likely increase and the full effect on mortality will be observed.”
Other factors at play
Multiple factors have led to the declines in mortality, said William G. Cance, MD, chief medical and scientific officer for the ACS, who was not involved in this study. “We are slowly sorting out the explanations in greater granularity.”
Dr. MacEwan said improved cancer screening may partially explain the decline in mortality in some tumor types.
“If screening in a particular tumor type improved during the study period and tumors were diagnosed earlier, then mortality for that tumor type may decline,” she said. “However, we did not find strong evidence to suggest that there were significant changes in screening during our study period. Breast cancer screening rates, for example, were stable over our study period.”
Cancer screening is not as strong an influence as it should be, Dr. Cance said.
“The lung cancer screening rate is low. In breast and colorectal cancers, we need to double down on earlier screening,” he said, noting that less than one-quarter of adults between ages 45 and 50 years are currently screened for colorectal cancer. The ACS recommends that people at average risk of colorectal cancer start regular screening at age 45.
More research is necessary to evaluate the relationship between drug approvals and cancer mortality, Dr. MacEwan said.
“Research directly linking utilization of new therapies to improved survival or reduced mortality in the real-world setting would more definitively demonstrate the impact of new treatments,” she said. “New therapies have improved outcomes for many patients and should continue to be considered as key elements of cancer treatment.”
“We need to continue to reduce tobacco smoking and improve on modifiable behaviors at the same time as we work on getting new drugs to cancer patients,” Dr. Cance said. “We are coming into an era of multiple new therapeutics, including targeted therapies, immunotherapies, and cellular therapies. Clinicians need to look closely at the trial data of new drugs and pay close attention to those that have the most mortality impact.”
“We also need equitable distribution of newer drugs,” Dr. Cance added. “They should be distributed to everybody who deserves them. Mortality is often impacted by social determinants of health.”
Funding for this research was provided by Pfizer. Study authors disclosed relationships, including employment, with Pfizer. Dr. Cance had no disclosures.
SOURCE: MacEwan JP et al. J Med Econ. 2020 Nov 9;1-12.
Reductions in mortality were most notable for tumor types with relatively more approvals, including lung and breast cancer, melanoma, lymphoma, and leukemia.
A report from the American Cancer Society (ACS) estimated that, from 1991 to 2017, there were 2,902,200 total cancer deaths avoided from improvements in mortality from all potential sources.
The new findings, reported in the Journal of Medical Economics, suggest that drugs approved between 2000 and 2016 to treat the 15 most common cancer types helped to reduce mortality by 24% per 100,000 people.
“This study provides evidence that a significant share of that reduction from 2000 to 2016 was associated with the introduction of new therapies. The ACS report and other studies demonstrate that the improvements in lung cancer specifically are likely due to new treatments,” said lead study author Joanna P. MacEwan, MD, of PRECISIONheor in Los Angeles.
The findings contribute to a better understanding of whether increased spending on cancer drugs are worth the investment, according to the study authors.
“We provide evidence that the gains in survival measured in clinical trials are translating into health benefits for patients in the real world and confirm previous research that has also shown that new pharmaceutical treatments are associated with improved real-world survival outcomes for patients,” Dr. MacEwan said.
Full effect not yet observed
The researchers used a series of national data sets from sources including the Centers for Disease Control and Prevention; the U.S. Mortality Files by the National Center of Health Statistics; Survival, Epidemiology and End Results program; and United States Cancer Statistics.
The team calculated age-adjusted cancer mortality rates per year for the 15 most common tumor types and also looked at incident cases of cancer by tumor type, represented as per 100,000 people, for all ages, races, and genders.
The researchers then translated the change in cancer mortality in the U.S. from 2000 to 2016 associated with treatment stocks in each year into deaths averted per year.
Across the 16 years, mortality was down by 1,291,769 deaths. The following cancers had significant reductions in mortality: breast (n = 127,874), colorectal (n = 46,705), lung (n = 375,256), prostate (n = 476,210), gastric (n = 758), and renal (n = 739) cancers, as well as non-Hodgkin lymphoma (n = 48,836) and leukemia (n = 4,011).
Estimated mortality increased by 825 deaths in patients with thyroid cancer and 7,768 deaths for those with bladder cancer. These rises are likely due to the result of sparse drug approvals during this period – five for thyroid cancer and three for bladder cancer – Dr. MacEwan said. There were no approvals in liver or uterine cancer and few approvals in pancreatic and oral cancer.
The full effect of new drug introductions may not have been observed yet, Dr. MacEwan noted.
“There are fewer patients using the treatments for drugs approved in the later years of our study and less follow-up time to measure outcomes,” she said. “Over time, utilization of the newer therapies will likely increase and the full effect on mortality will be observed.”
Other factors at play
Multiple factors have led to the declines in mortality, said William G. Cance, MD, chief medical and scientific officer for the ACS, who was not involved in this study. “We are slowly sorting out the explanations in greater granularity.”
Dr. MacEwan said improved cancer screening may partially explain the decline in mortality in some tumor types.
“If screening in a particular tumor type improved during the study period and tumors were diagnosed earlier, then mortality for that tumor type may decline,” she said. “However, we did not find strong evidence to suggest that there were significant changes in screening during our study period. Breast cancer screening rates, for example, were stable over our study period.”
Cancer screening is not as strong an influence as it should be, Dr. Cance said.
“The lung cancer screening rate is low. In breast and colorectal cancers, we need to double down on earlier screening,” he said, noting that less than one-quarter of adults between ages 45 and 50 years are currently screened for colorectal cancer. The ACS recommends that people at average risk of colorectal cancer start regular screening at age 45.
More research is necessary to evaluate the relationship between drug approvals and cancer mortality, Dr. MacEwan said.
“Research directly linking utilization of new therapies to improved survival or reduced mortality in the real-world setting would more definitively demonstrate the impact of new treatments,” she said. “New therapies have improved outcomes for many patients and should continue to be considered as key elements of cancer treatment.”
“We need to continue to reduce tobacco smoking and improve on modifiable behaviors at the same time as we work on getting new drugs to cancer patients,” Dr. Cance said. “We are coming into an era of multiple new therapeutics, including targeted therapies, immunotherapies, and cellular therapies. Clinicians need to look closely at the trial data of new drugs and pay close attention to those that have the most mortality impact.”
“We also need equitable distribution of newer drugs,” Dr. Cance added. “They should be distributed to everybody who deserves them. Mortality is often impacted by social determinants of health.”
Funding for this research was provided by Pfizer. Study authors disclosed relationships, including employment, with Pfizer. Dr. Cance had no disclosures.
SOURCE: MacEwan JP et al. J Med Econ. 2020 Nov 9;1-12.
Reductions in mortality were most notable for tumor types with relatively more approvals, including lung and breast cancer, melanoma, lymphoma, and leukemia.
A report from the American Cancer Society (ACS) estimated that, from 1991 to 2017, there were 2,902,200 total cancer deaths avoided from improvements in mortality from all potential sources.
The new findings, reported in the Journal of Medical Economics, suggest that drugs approved between 2000 and 2016 to treat the 15 most common cancer types helped to reduce mortality by 24% per 100,000 people.
“This study provides evidence that a significant share of that reduction from 2000 to 2016 was associated with the introduction of new therapies. The ACS report and other studies demonstrate that the improvements in lung cancer specifically are likely due to new treatments,” said lead study author Joanna P. MacEwan, MD, of PRECISIONheor in Los Angeles.
The findings contribute to a better understanding of whether increased spending on cancer drugs are worth the investment, according to the study authors.
“We provide evidence that the gains in survival measured in clinical trials are translating into health benefits for patients in the real world and confirm previous research that has also shown that new pharmaceutical treatments are associated with improved real-world survival outcomes for patients,” Dr. MacEwan said.
Full effect not yet observed
The researchers used a series of national data sets from sources including the Centers for Disease Control and Prevention; the U.S. Mortality Files by the National Center of Health Statistics; Survival, Epidemiology and End Results program; and United States Cancer Statistics.
The team calculated age-adjusted cancer mortality rates per year for the 15 most common tumor types and also looked at incident cases of cancer by tumor type, represented as per 100,000 people, for all ages, races, and genders.
The researchers then translated the change in cancer mortality in the U.S. from 2000 to 2016 associated with treatment stocks in each year into deaths averted per year.
Across the 16 years, mortality was down by 1,291,769 deaths. The following cancers had significant reductions in mortality: breast (n = 127,874), colorectal (n = 46,705), lung (n = 375,256), prostate (n = 476,210), gastric (n = 758), and renal (n = 739) cancers, as well as non-Hodgkin lymphoma (n = 48,836) and leukemia (n = 4,011).
Estimated mortality increased by 825 deaths in patients with thyroid cancer and 7,768 deaths for those with bladder cancer. These rises are likely due to the result of sparse drug approvals during this period – five for thyroid cancer and three for bladder cancer – Dr. MacEwan said. There were no approvals in liver or uterine cancer and few approvals in pancreatic and oral cancer.
The full effect of new drug introductions may not have been observed yet, Dr. MacEwan noted.
“There are fewer patients using the treatments for drugs approved in the later years of our study and less follow-up time to measure outcomes,” she said. “Over time, utilization of the newer therapies will likely increase and the full effect on mortality will be observed.”
Other factors at play
Multiple factors have led to the declines in mortality, said William G. Cance, MD, chief medical and scientific officer for the ACS, who was not involved in this study. “We are slowly sorting out the explanations in greater granularity.”
Dr. MacEwan said improved cancer screening may partially explain the decline in mortality in some tumor types.
“If screening in a particular tumor type improved during the study period and tumors were diagnosed earlier, then mortality for that tumor type may decline,” she said. “However, we did not find strong evidence to suggest that there were significant changes in screening during our study period. Breast cancer screening rates, for example, were stable over our study period.”
Cancer screening is not as strong an influence as it should be, Dr. Cance said.
“The lung cancer screening rate is low. In breast and colorectal cancers, we need to double down on earlier screening,” he said, noting that less than one-quarter of adults between ages 45 and 50 years are currently screened for colorectal cancer. The ACS recommends that people at average risk of colorectal cancer start regular screening at age 45.
More research is necessary to evaluate the relationship between drug approvals and cancer mortality, Dr. MacEwan said.
“Research directly linking utilization of new therapies to improved survival or reduced mortality in the real-world setting would more definitively demonstrate the impact of new treatments,” she said. “New therapies have improved outcomes for many patients and should continue to be considered as key elements of cancer treatment.”
“We need to continue to reduce tobacco smoking and improve on modifiable behaviors at the same time as we work on getting new drugs to cancer patients,” Dr. Cance said. “We are coming into an era of multiple new therapeutics, including targeted therapies, immunotherapies, and cellular therapies. Clinicians need to look closely at the trial data of new drugs and pay close attention to those that have the most mortality impact.”
“We also need equitable distribution of newer drugs,” Dr. Cance added. “They should be distributed to everybody who deserves them. Mortality is often impacted by social determinants of health.”
Funding for this research was provided by Pfizer. Study authors disclosed relationships, including employment, with Pfizer. Dr. Cance had no disclosures.
SOURCE: MacEwan JP et al. J Med Econ. 2020 Nov 9;1-12.
FROM JOURNAL OF MEDICAL ECONOMICS
‘Test all patients with cancer’: One in eight have inherited mutations
These findings come from the largest study of its kind so far, conducted in nearly 3,000 patients with a wide range of cancer stages and types, including breast, colorectal, lung, ovarian, pancreatic, bladder, prostate, and endometrial cancers.
“This study tells us that the clinical practice guidelines are not very sensitive for identifying who does or doesn’t have a genetic mutation that is predisposing them to cancer,” commented first author Niloy Jewell Samadder, MD, director of the high-risk cancer clinic at the Mayo Clinic in Phoenix.
Finding a genetic mutation can alter clinical management of the cancer.
“This really does open up treatment and management options that might not have been accessible to these patients,” Dr. Samadder emphasized.
The results were published online on Oct. 30 in JAMA Oncology and were presented simultaneously at the American Society of Human Genetics. Dr. Samadder discussed details of the study in a video posted on YouTube.
A clinician not involved in the study said the new results should lead to changes in practice.
“For cancer patients, I think the debate is over. We should test everybody,” Peter Beitsch, MD, surgical oncologist at the Dallas Surgical Group, said in an interview.
The Mayo Clinic is changing its daily practice at all four of its cancer centers. The changes will begin in the first quarter of 2021 at its Arizona campus.
“Every cancer patient who comes to Mayo Clinic will be offered genomic evaluation that includes genetic testing to identify if they have an underlying genetic mutation that predisposes to their cancer and [helps physicians decide] how to incorporate that knowledge into designing the best surgical and treatment options for that patient and their family,” Dr. Samadder said.
Study details
The study included 2,984 patients with cancer who were receiving care for a variety of solid tumor cancers at Mayo Clinic cancer centers in Arizona, Florida, Minnesota, and a community cancer center in Wisconsin.
Patients were tested for about 84 genes using next-generation sequencing provided by Invitae.
Among participants, 13.3% (n = 397) tested positive for pathogenic mutations. Of these, about 70% (282 of 397 patients) carried moderate- and high-penetrance genes that increased their risk for cancer. For almost 28.2% (n = 42) of patients with high-penetrance mutations, changes were made in treatment as a result of genetic testing. These included changes in surgical management, immunotherapy, chemotherapy, or enrollment in a clinical trial for which they may otherwise have not been eligible.
Researchers also compared their universal testing approach with targeted testing recommended in guidelines from the National Comprehensive Cancer Network, the National Society of Genetic Counselors, and the American College of Medical Genetics.
They identified pathogenic mutations in 192 patients whose mutations would have been missed using guideline-recommended criteria, such as tumor pathology or family history. This represents 6.4% of all participants in the study (192 of 2,984 patients) and 48.4% of patients who tested positive for pathogenic mutations (397 of 2,984 patients).
“Genetic testing is underutilized in cancer care, both for patients and for their families, often due to outdated guidelines that restrict testing to a narrow group of high-risk patients. All cancer patients should have access to complete genetic information that can guide their care and inform their families’ health,” coauthor Robert Nussbaum, MD, chief medical officer of Invitae, said in a statement.
Some clinicians have been pushing for genetic testing of all patients with cancer, including Dr. Beitsch, who was lead author of a similar study in breast cancer patients published last year in the Journal of Oncology. That article made waves when the authors concluded that all breast cancer patients should have expanded panel genetic testing.
This new Mayo Clinic study extends the findings in breast cancer to “all cancer patients, not just breast cancer patients,” Dr. Beitsch said in an interview.
Long-running debate
The new findings and opinions add to a long-running debate in oncology over the role of genetic testing and screening for pathogenic mutations.
Part of the debate about genetic testing has hinged on the question of costs, said Dr. Beitsch. When genetic testing first became available, it was conducted by hand, and costs were often prohibitive. Since then, genetic testing has been automated using next-generation sequencing, and the cost has decreased considerably.
“The Invitae cash price for an 80-plus gene panel is $250. That’s [the cost of] a mani-pedi in Dallas. I don’t discount that it’s a lot of money for a lot of people. Yes, it’s expensive, but it’s a lot less expensive than it used to be,” Dr. Beitsch said.
Another issue is that doctors are not entirely sure how to manage variants of uncertain significance (VUSs) when they are found. In the Mayo Clinic study, about half (47.4%; n = 1415) of participants had VUSs. The authors noted that these results are consistent with past studies.
Dr. Beitsch said that VUSs are a matter of education. To date, only about 2% of VUSs have been associated with cancer. The remainder, about 98%, do not affect treatment for patients who have already been diagnosed with cancer.
“We all have VUSs. They’re just minor variations in a gene. The vast majority of them have no consequence and don’t alter the function of the gene,” he said. “I tell everybody to ignore the VUSs [when found in patients with cancer]. Do not act on them at all. We just need to educate everybody to make sure they don’t get stressed about it.”
These comments echo guidance from the American Society of Breast Surgeons, which says that VUSs are DNA sequences that are not clinically actionable. This type of result needs to be considered as inconclusive, and patient management should not be influenced by such results.
However, VUSs are more significant if they are found in individuals who do not have cancer but who have a strong family history of cancer. In such cases, clinicians should be more aware, Dr. Beitsch emphasized.
“Patients who have a VUS and don’t have a cancer should absolutely pay more attention to their health. They got tested for a reason, and that reason is usually strong family history,” Dr. Beitsch said.
He added that a major advantage of genetic testing is that it can enable cascade genetic testing of family members. Identifying pathogenic mutations in family members can lead them to undergo screening to detect early cancers, and preventive measures can be taken that may be lifesaving.
In the Mayo Clinic study, researchers offered genetic testing to family members of patients who tested positive for a pathogenic mutation. Testing was available free of charge for up to 90 days after a participant tested positive. In addition, family members were shown an educational video.
Nevertheless, only 17.6% (n = 70) of patients with pathogenic mutations had family members who underwent testing. Among these, 45% (79 of 176) of family members who were tested were found to carry pathogenic mutations.
“This really told us that financial barriers are not the only barrier to families understanding and undergoing preventive testing,” Dr. Samadder said. “There are probably a number of other barriers – socioeconomic or emotional – that we have to deal with.”
Genetic testing was provided by Invitae. The study was supported by several grants, including a Mayo Transform the Practice Grant, and by Mayo Clinic’s Center for Individualized Medicine. Two coauthors are employees of Invitae. Dr. Beitsch reported participating in a study 2 years ago that was funded by Invitae. He currently receives no financial support from Invitae. Several authors report receiving fees from one or more of the following companies: Pfizer, Maze Therapeutics, Genome Medical, Astellas, and Merck.
This article first appeared on Medscape.com.
These findings come from the largest study of its kind so far, conducted in nearly 3,000 patients with a wide range of cancer stages and types, including breast, colorectal, lung, ovarian, pancreatic, bladder, prostate, and endometrial cancers.
“This study tells us that the clinical practice guidelines are not very sensitive for identifying who does or doesn’t have a genetic mutation that is predisposing them to cancer,” commented first author Niloy Jewell Samadder, MD, director of the high-risk cancer clinic at the Mayo Clinic in Phoenix.
Finding a genetic mutation can alter clinical management of the cancer.
“This really does open up treatment and management options that might not have been accessible to these patients,” Dr. Samadder emphasized.
The results were published online on Oct. 30 in JAMA Oncology and were presented simultaneously at the American Society of Human Genetics. Dr. Samadder discussed details of the study in a video posted on YouTube.
A clinician not involved in the study said the new results should lead to changes in practice.
“For cancer patients, I think the debate is over. We should test everybody,” Peter Beitsch, MD, surgical oncologist at the Dallas Surgical Group, said in an interview.
The Mayo Clinic is changing its daily practice at all four of its cancer centers. The changes will begin in the first quarter of 2021 at its Arizona campus.
“Every cancer patient who comes to Mayo Clinic will be offered genomic evaluation that includes genetic testing to identify if they have an underlying genetic mutation that predisposes to their cancer and [helps physicians decide] how to incorporate that knowledge into designing the best surgical and treatment options for that patient and their family,” Dr. Samadder said.
Study details
The study included 2,984 patients with cancer who were receiving care for a variety of solid tumor cancers at Mayo Clinic cancer centers in Arizona, Florida, Minnesota, and a community cancer center in Wisconsin.
Patients were tested for about 84 genes using next-generation sequencing provided by Invitae.
Among participants, 13.3% (n = 397) tested positive for pathogenic mutations. Of these, about 70% (282 of 397 patients) carried moderate- and high-penetrance genes that increased their risk for cancer. For almost 28.2% (n = 42) of patients with high-penetrance mutations, changes were made in treatment as a result of genetic testing. These included changes in surgical management, immunotherapy, chemotherapy, or enrollment in a clinical trial for which they may otherwise have not been eligible.
Researchers also compared their universal testing approach with targeted testing recommended in guidelines from the National Comprehensive Cancer Network, the National Society of Genetic Counselors, and the American College of Medical Genetics.
They identified pathogenic mutations in 192 patients whose mutations would have been missed using guideline-recommended criteria, such as tumor pathology or family history. This represents 6.4% of all participants in the study (192 of 2,984 patients) and 48.4% of patients who tested positive for pathogenic mutations (397 of 2,984 patients).
“Genetic testing is underutilized in cancer care, both for patients and for their families, often due to outdated guidelines that restrict testing to a narrow group of high-risk patients. All cancer patients should have access to complete genetic information that can guide their care and inform their families’ health,” coauthor Robert Nussbaum, MD, chief medical officer of Invitae, said in a statement.
Some clinicians have been pushing for genetic testing of all patients with cancer, including Dr. Beitsch, who was lead author of a similar study in breast cancer patients published last year in the Journal of Oncology. That article made waves when the authors concluded that all breast cancer patients should have expanded panel genetic testing.
This new Mayo Clinic study extends the findings in breast cancer to “all cancer patients, not just breast cancer patients,” Dr. Beitsch said in an interview.
Long-running debate
The new findings and opinions add to a long-running debate in oncology over the role of genetic testing and screening for pathogenic mutations.
Part of the debate about genetic testing has hinged on the question of costs, said Dr. Beitsch. When genetic testing first became available, it was conducted by hand, and costs were often prohibitive. Since then, genetic testing has been automated using next-generation sequencing, and the cost has decreased considerably.
“The Invitae cash price for an 80-plus gene panel is $250. That’s [the cost of] a mani-pedi in Dallas. I don’t discount that it’s a lot of money for a lot of people. Yes, it’s expensive, but it’s a lot less expensive than it used to be,” Dr. Beitsch said.
Another issue is that doctors are not entirely sure how to manage variants of uncertain significance (VUSs) when they are found. In the Mayo Clinic study, about half (47.4%; n = 1415) of participants had VUSs. The authors noted that these results are consistent with past studies.
Dr. Beitsch said that VUSs are a matter of education. To date, only about 2% of VUSs have been associated with cancer. The remainder, about 98%, do not affect treatment for patients who have already been diagnosed with cancer.
“We all have VUSs. They’re just minor variations in a gene. The vast majority of them have no consequence and don’t alter the function of the gene,” he said. “I tell everybody to ignore the VUSs [when found in patients with cancer]. Do not act on them at all. We just need to educate everybody to make sure they don’t get stressed about it.”
These comments echo guidance from the American Society of Breast Surgeons, which says that VUSs are DNA sequences that are not clinically actionable. This type of result needs to be considered as inconclusive, and patient management should not be influenced by such results.
However, VUSs are more significant if they are found in individuals who do not have cancer but who have a strong family history of cancer. In such cases, clinicians should be more aware, Dr. Beitsch emphasized.
“Patients who have a VUS and don’t have a cancer should absolutely pay more attention to their health. They got tested for a reason, and that reason is usually strong family history,” Dr. Beitsch said.
He added that a major advantage of genetic testing is that it can enable cascade genetic testing of family members. Identifying pathogenic mutations in family members can lead them to undergo screening to detect early cancers, and preventive measures can be taken that may be lifesaving.
In the Mayo Clinic study, researchers offered genetic testing to family members of patients who tested positive for a pathogenic mutation. Testing was available free of charge for up to 90 days after a participant tested positive. In addition, family members were shown an educational video.
Nevertheless, only 17.6% (n = 70) of patients with pathogenic mutations had family members who underwent testing. Among these, 45% (79 of 176) of family members who were tested were found to carry pathogenic mutations.
“This really told us that financial barriers are not the only barrier to families understanding and undergoing preventive testing,” Dr. Samadder said. “There are probably a number of other barriers – socioeconomic or emotional – that we have to deal with.”
Genetic testing was provided by Invitae. The study was supported by several grants, including a Mayo Transform the Practice Grant, and by Mayo Clinic’s Center for Individualized Medicine. Two coauthors are employees of Invitae. Dr. Beitsch reported participating in a study 2 years ago that was funded by Invitae. He currently receives no financial support from Invitae. Several authors report receiving fees from one or more of the following companies: Pfizer, Maze Therapeutics, Genome Medical, Astellas, and Merck.
This article first appeared on Medscape.com.
These findings come from the largest study of its kind so far, conducted in nearly 3,000 patients with a wide range of cancer stages and types, including breast, colorectal, lung, ovarian, pancreatic, bladder, prostate, and endometrial cancers.
“This study tells us that the clinical practice guidelines are not very sensitive for identifying who does or doesn’t have a genetic mutation that is predisposing them to cancer,” commented first author Niloy Jewell Samadder, MD, director of the high-risk cancer clinic at the Mayo Clinic in Phoenix.
Finding a genetic mutation can alter clinical management of the cancer.
“This really does open up treatment and management options that might not have been accessible to these patients,” Dr. Samadder emphasized.
The results were published online on Oct. 30 in JAMA Oncology and were presented simultaneously at the American Society of Human Genetics. Dr. Samadder discussed details of the study in a video posted on YouTube.
A clinician not involved in the study said the new results should lead to changes in practice.
“For cancer patients, I think the debate is over. We should test everybody,” Peter Beitsch, MD, surgical oncologist at the Dallas Surgical Group, said in an interview.
The Mayo Clinic is changing its daily practice at all four of its cancer centers. The changes will begin in the first quarter of 2021 at its Arizona campus.
“Every cancer patient who comes to Mayo Clinic will be offered genomic evaluation that includes genetic testing to identify if they have an underlying genetic mutation that predisposes to their cancer and [helps physicians decide] how to incorporate that knowledge into designing the best surgical and treatment options for that patient and their family,” Dr. Samadder said.
Study details
The study included 2,984 patients with cancer who were receiving care for a variety of solid tumor cancers at Mayo Clinic cancer centers in Arizona, Florida, Minnesota, and a community cancer center in Wisconsin.
Patients were tested for about 84 genes using next-generation sequencing provided by Invitae.
Among participants, 13.3% (n = 397) tested positive for pathogenic mutations. Of these, about 70% (282 of 397 patients) carried moderate- and high-penetrance genes that increased their risk for cancer. For almost 28.2% (n = 42) of patients with high-penetrance mutations, changes were made in treatment as a result of genetic testing. These included changes in surgical management, immunotherapy, chemotherapy, or enrollment in a clinical trial for which they may otherwise have not been eligible.
Researchers also compared their universal testing approach with targeted testing recommended in guidelines from the National Comprehensive Cancer Network, the National Society of Genetic Counselors, and the American College of Medical Genetics.
They identified pathogenic mutations in 192 patients whose mutations would have been missed using guideline-recommended criteria, such as tumor pathology or family history. This represents 6.4% of all participants in the study (192 of 2,984 patients) and 48.4% of patients who tested positive for pathogenic mutations (397 of 2,984 patients).
“Genetic testing is underutilized in cancer care, both for patients and for their families, often due to outdated guidelines that restrict testing to a narrow group of high-risk patients. All cancer patients should have access to complete genetic information that can guide their care and inform their families’ health,” coauthor Robert Nussbaum, MD, chief medical officer of Invitae, said in a statement.
Some clinicians have been pushing for genetic testing of all patients with cancer, including Dr. Beitsch, who was lead author of a similar study in breast cancer patients published last year in the Journal of Oncology. That article made waves when the authors concluded that all breast cancer patients should have expanded panel genetic testing.
This new Mayo Clinic study extends the findings in breast cancer to “all cancer patients, not just breast cancer patients,” Dr. Beitsch said in an interview.
Long-running debate
The new findings and opinions add to a long-running debate in oncology over the role of genetic testing and screening for pathogenic mutations.
Part of the debate about genetic testing has hinged on the question of costs, said Dr. Beitsch. When genetic testing first became available, it was conducted by hand, and costs were often prohibitive. Since then, genetic testing has been automated using next-generation sequencing, and the cost has decreased considerably.
“The Invitae cash price for an 80-plus gene panel is $250. That’s [the cost of] a mani-pedi in Dallas. I don’t discount that it’s a lot of money for a lot of people. Yes, it’s expensive, but it’s a lot less expensive than it used to be,” Dr. Beitsch said.
Another issue is that doctors are not entirely sure how to manage variants of uncertain significance (VUSs) when they are found. In the Mayo Clinic study, about half (47.4%; n = 1415) of participants had VUSs. The authors noted that these results are consistent with past studies.
Dr. Beitsch said that VUSs are a matter of education. To date, only about 2% of VUSs have been associated with cancer. The remainder, about 98%, do not affect treatment for patients who have already been diagnosed with cancer.
“We all have VUSs. They’re just minor variations in a gene. The vast majority of them have no consequence and don’t alter the function of the gene,” he said. “I tell everybody to ignore the VUSs [when found in patients with cancer]. Do not act on them at all. We just need to educate everybody to make sure they don’t get stressed about it.”
These comments echo guidance from the American Society of Breast Surgeons, which says that VUSs are DNA sequences that are not clinically actionable. This type of result needs to be considered as inconclusive, and patient management should not be influenced by such results.
However, VUSs are more significant if they are found in individuals who do not have cancer but who have a strong family history of cancer. In such cases, clinicians should be more aware, Dr. Beitsch emphasized.
“Patients who have a VUS and don’t have a cancer should absolutely pay more attention to their health. They got tested for a reason, and that reason is usually strong family history,” Dr. Beitsch said.
He added that a major advantage of genetic testing is that it can enable cascade genetic testing of family members. Identifying pathogenic mutations in family members can lead them to undergo screening to detect early cancers, and preventive measures can be taken that may be lifesaving.
In the Mayo Clinic study, researchers offered genetic testing to family members of patients who tested positive for a pathogenic mutation. Testing was available free of charge for up to 90 days after a participant tested positive. In addition, family members were shown an educational video.
Nevertheless, only 17.6% (n = 70) of patients with pathogenic mutations had family members who underwent testing. Among these, 45% (79 of 176) of family members who were tested were found to carry pathogenic mutations.
“This really told us that financial barriers are not the only barrier to families understanding and undergoing preventive testing,” Dr. Samadder said. “There are probably a number of other barriers – socioeconomic or emotional – that we have to deal with.”
Genetic testing was provided by Invitae. The study was supported by several grants, including a Mayo Transform the Practice Grant, and by Mayo Clinic’s Center for Individualized Medicine. Two coauthors are employees of Invitae. Dr. Beitsch reported participating in a study 2 years ago that was funded by Invitae. He currently receives no financial support from Invitae. Several authors report receiving fees from one or more of the following companies: Pfizer, Maze Therapeutics, Genome Medical, Astellas, and Merck.
This article first appeared on Medscape.com.
One-month delay in cancer treatment linked to increase in mortality
In light of the treatment delays resulting from the pandemic, Canadian and U.K. researchers carried out a review and analysis of relevant studies published between January 2000 and April 2020.
Included studies examined data on surgical interventions, systemic therapy, or radiotherapy for seven forms of cancer – bladder, breast, colon, rectum, lung, cervix, and head and neck. Delays were measured from diagnosis to the first treatment or from the completion of one treatment to the start of the next.
The search identified 34 suitable studies for 17 indications, with data from more than 1.2 million patients. The analysis identified a significant association between delay and increased mortality for 13 of the 17 indications (P < .05).
For surgery, there was a 6%-8% increase in the risk of death for every 4-week treatment delay. Estimates for systemic treatment varied (hazard ratio range, 1.01-1.28). Four-week delays in radiotherapy were for radical radiotherapy for head and neck cancer (HR, 1.09; 95% confidence interval, 1.05-1.14), adjuvant radiotherapy after breast-conserving surgery (HR, 0.98; 95% CI, 0.88-1.09), and cervical cancer adjuvant radiotherapy (HR, 1.23; 95% CI, 1.00-1.50).
Delays of up to 8 and 12 weeks further increased mortality. An 8-week delay in breast cancer surgery was linked to a 17% increased mortality, and a 12-week delay would increase mortality by 26%.
A surgical delay of 12 weeks for patients with breast cancer continuing for 1 year – which is likely to be the case as the pandemic continues – would lead to 1,400 excess deaths in the United Kingdom.
The authors said the results of this study could be used to guide policy making on the organization of cancer services, particularly as the pandemic continues and further delays are expected.
This article originally appeared on Univadis, part of the Medscape Professional Network.
In light of the treatment delays resulting from the pandemic, Canadian and U.K. researchers carried out a review and analysis of relevant studies published between January 2000 and April 2020.
Included studies examined data on surgical interventions, systemic therapy, or radiotherapy for seven forms of cancer – bladder, breast, colon, rectum, lung, cervix, and head and neck. Delays were measured from diagnosis to the first treatment or from the completion of one treatment to the start of the next.
The search identified 34 suitable studies for 17 indications, with data from more than 1.2 million patients. The analysis identified a significant association between delay and increased mortality for 13 of the 17 indications (P < .05).
For surgery, there was a 6%-8% increase in the risk of death for every 4-week treatment delay. Estimates for systemic treatment varied (hazard ratio range, 1.01-1.28). Four-week delays in radiotherapy were for radical radiotherapy for head and neck cancer (HR, 1.09; 95% confidence interval, 1.05-1.14), adjuvant radiotherapy after breast-conserving surgery (HR, 0.98; 95% CI, 0.88-1.09), and cervical cancer adjuvant radiotherapy (HR, 1.23; 95% CI, 1.00-1.50).
Delays of up to 8 and 12 weeks further increased mortality. An 8-week delay in breast cancer surgery was linked to a 17% increased mortality, and a 12-week delay would increase mortality by 26%.
A surgical delay of 12 weeks for patients with breast cancer continuing for 1 year – which is likely to be the case as the pandemic continues – would lead to 1,400 excess deaths in the United Kingdom.
The authors said the results of this study could be used to guide policy making on the organization of cancer services, particularly as the pandemic continues and further delays are expected.
This article originally appeared on Univadis, part of the Medscape Professional Network.
In light of the treatment delays resulting from the pandemic, Canadian and U.K. researchers carried out a review and analysis of relevant studies published between January 2000 and April 2020.
Included studies examined data on surgical interventions, systemic therapy, or radiotherapy for seven forms of cancer – bladder, breast, colon, rectum, lung, cervix, and head and neck. Delays were measured from diagnosis to the first treatment or from the completion of one treatment to the start of the next.
The search identified 34 suitable studies for 17 indications, with data from more than 1.2 million patients. The analysis identified a significant association between delay and increased mortality for 13 of the 17 indications (P < .05).
For surgery, there was a 6%-8% increase in the risk of death for every 4-week treatment delay. Estimates for systemic treatment varied (hazard ratio range, 1.01-1.28). Four-week delays in radiotherapy were for radical radiotherapy for head and neck cancer (HR, 1.09; 95% confidence interval, 1.05-1.14), adjuvant radiotherapy after breast-conserving surgery (HR, 0.98; 95% CI, 0.88-1.09), and cervical cancer adjuvant radiotherapy (HR, 1.23; 95% CI, 1.00-1.50).
Delays of up to 8 and 12 weeks further increased mortality. An 8-week delay in breast cancer surgery was linked to a 17% increased mortality, and a 12-week delay would increase mortality by 26%.
A surgical delay of 12 weeks for patients with breast cancer continuing for 1 year – which is likely to be the case as the pandemic continues – would lead to 1,400 excess deaths in the United Kingdom.
The authors said the results of this study could be used to guide policy making on the organization of cancer services, particularly as the pandemic continues and further delays are expected.
This article originally appeared on Univadis, part of the Medscape Professional Network.
Guideline Concordance with Durvalumab in Unresectable Stage III Non-Small Cell Lung Cancer: A Single Center Veterans Hospital Experience
The US Food and Drug Administration (FDA) approved the use of durvalumab for patients with unresectable stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (CRT).1 After 2 randomized phase 3 studies in 2017 and 2018 showed significant progression-free and overall survival respectively,2,3 durvalumab became a category 1 recommendation for the above indication per National Comprehensive Cancer Network (NCCN) guidelines.4 Adherence to guidelines have been shown to improve patient survival across several cancer types.5-7 However, guideline adherence rates have been variable across health institutions. Therefore, further study is warranted to evaluate nonadherent practices with the goal of improving the quality of cancer care delivery.8,9
Stage III NSCLC is associated with poor survival rates.10 Concurrent CRT remains the standard of care in patients with good performance status based on clinical trial populations.4 Lung cancer remains a disease of the elderly, with a median age at diagnosis of 70 years.11 Discrepancies in the treatment of lung cancer in older adults can vary widely due to a lack of evidence surrounding the treatment in those who have comorbidities and poor performance status, widening the gap between clinical trial and real-world populations.11
A recent review by Passaro and colleagues revealed that at least 11 pivotal randomized controlled trials have shown the activity of immune checkpoint inhibitors (ICI) in locally advanced and metastatic lung cancer. However, these studies have mostly excluded patients with a performance status of the Eastern Cooperative Oncology Group (ECOG) level ≥ 2.11
Durvalumab is one of many new therapies to enter clinical practice to demonstrate survival benefit, but its use among veterans with stage III NSCLC in adherence with National Comprehensive Cancer Network (NCCN) guidelines was not robust at the Birmingham Veterans Affairs Medical Center (VAMC) in Alabama. Therefore, we decided to study the level of adherence and to identify barriers to conformity to the category 1 NCCN recommendations.
Methods
The Birmingham VAMC Outpatient Oncology Clinic billing data identified all individuals diagnosed with lung cancer treated between October 2017 and August 2019. Patients who did not have NSCLC that was stage III and unresectable were excluded from our study. Patients who did not receive a majority of their treatment at US Department of Veterans Affairs (VA) facilities were excluded as well. Each patient’s demographic, functional level, and tumor characteristics during the treatment planning phase and follow-up visits were obtained. Two investigators who evaluated health care provider documentation using the VA Computerized Patient Record System (CPRS) conducted chart reviews.
The primary outcomes were the proportion of patients who received concurrent CRT and the proportion who received durvalumab consolidation. Our chart review also categorized reasons for nonreceipt of concurrent CRT and subsequent durvalumab. Documented reasons for guideline discordancy were generated empirically and broadly. We noted if documentation was unclear and included reasons for why a veteran was not a candidate for CRT, the presence of toxicities associated with CRT, and a patient’s refusal for therapy despite medical advice. Descriptive data were analyzed for all clinical or demographic characteristics and outcomes.
This was considered an internal quality improvement initiative. As such, Birmingham VAMC did not require institutional review board approval for the study. The facility is accredited by the American College of Surgeons Commission on Cancer.
Results
A total of 41 veterans with stage III NSCLC were identified to have established care in the Birmingham VAMC Oncology Clinic between October 2017 and August 2019. Of these, 7 received the majority of their treatment from community-based non-VA facilities and 14 were not candidates for CRT and were excluded from this study.
The mean (SD) age of study participants was 70.0 (8.4) years (range, 57 to 92 years). Most of the study veterans (33; 97.1%) were male and 20 (58.8%) were African American (Table). Eighteen (53%) of study participants had clinical stage IIIa NSCLC; 19 (56%) showed a squamous subtype of NSCLC. A majority (53%) of the veterans studied were evaluated to be functionally fit with an ECOG status of 0 to 1, although documentation of ECOG status was lacking in 5 (14.7%) patients in the initial treatment planning visit records. It was unclear if performance status had been reevaluated and changes noted over the course of concurrent CRT.
CRT Patients
The relative distribution of veterans who underwent CRT for stage III NSCLC plus the reasons they did not receive guideline-based treatment with durvalumab is shown in the Figure. Fourteen patients (41%) were inappropriate candidates for CRT; the most common reason for this was their poor performance status upon initial evaluation and 3 patients (8.8%) in the study had extensive disease or were upstaged upon follow-up clinic visit.
Twenty (59%) veterans in the study initiated CRT. However, only 16 (47.1%) completed CRT. Those who dropped out of CRT did so because of toxicities that included various cytopenia, gastrointestinal toxicities due to radiation and/or chemotherapy, or failure to thrive.
Durvalumab Treatment
After initiation of CRT, 9 (26.5%) patients did not go on to receive durvalumab. Three patients (8.8%) suffered toxicities during CRT. One study patient was found to have a severe respiratory infection requiring intensive care unit admission. Another study patient was found to have a new sternal lesion on follow-up positron emission tomography. One declined because of a history of severe antineutrophil cytoplasmic antibodies vasculitis, which made durvalumab use unsafe. Three patients (8.8%) declined treatment with CRT or durvalumab because of personal preference. Documentation was unclear as to why durvalumab was prescribed to one patient who had completed CRT.
Discussion
NCCN guidelines on the use of durvalumab in NSCLC are based on the phase 3 PACIFIC placebo-controlled randomized clinical trial. This trial, which included only patients with documented performance status of ECOG 0 or 1, reported that grade 3 or 4 events occurred in 30.5% of patients randomized to consolidative durvalumab. Treatment was discontinued in 15.4% of patients due to adverse events.3
Our study examined consolidation therapy with durvalumab in patients with unresectable stage III NSCLC with an ECOG performance status of 0 to 1 who had not progressed after 2 or more cycles of definitive concurrent CRT.4 Patients with previous exposure to immunotherapy, a history of immunodeficiency, active infection, unresolved toxicity from CRT, autoimmune disease, and patients who received sequential CRT were excluded.2 Surprisingly, the adherence rate to guidelines was close to 100% with appropriate documentation and justification of CRT initiation and durvalumab use. Five (14.7%) of veterans with unresectable stage III NSCLC did not have clear documentation of ECOG status on initial visit and only 1 veteran who completed CRT did not have clear documentation as to why durvalumab was not provided. Unfortunately, 23 (68.6%) veterans in the study were unable to receive durvalumab, a potentially disease-modifying drug; nearly one-third (10) of veterans were deemed poor candidates for concurrent CRT despite the fact that 52.9% (18) of veterans in the study had a documented ECOG of 0 or 1 on initial evaluation.
Clinical Trials vs Real World
The heterogeneity between anticipated study populations, those who were able to receive durvalumab in the PACIFIC trial, compared with our observed real-world veteran population, likely stems from the lack of information about how comorbidity and fitness can affect the choice of therapeutic intervention in patients with lung cancer.12 In addition, older adults who participated in randomized controlled trials (RCTs) are not representative of the average older adult who presents to medical oncology clinics, making the application of guideline concordant care difficult.13
Similar real-world observations parallel to our analyses have confirmed, complemented and/or refuted findings of RCTs, and have helped impact the treatment of multiple acute and chronic conditions including influenza, cardiovascular disease, and diabetes.14
A component of socioeconomic barriers and access to supportive care played roles in the decisions of certain patients who chose not to undergo concurrent CRT despite medical advice. These 2 obstacles also affected the decision making for some in the study when considering the use of durvalumab (administered by a 60-minute IV infusion every 2 weeks for 1 year) per recommended guidelines.1 These hurdles need further study in the context of their effect on quality of life and the difficulties generated by various social determinants of health.
Limitations
Study limitations included the biased and confounding factors previously described about retrospective and nonrandomized observational studies that are controlled for during RCTs.15 Electronic health record data may have been incorrectly collected resulting in missing or wrong data points that affect the validity of our conclusion. Recall bias with regard to documentation by health care providers describing reasons why CRT or durvalumab were not initiated or the patient’s ability to recall previous treatments and report ECOG status or toxicities also may have impacted our findings. Comorbidities and poor performance status, frequently occurring among veterans, negatively impact cancer treatment decisions and may result in a detection bias. For example, tobacco use, cardiovascular disease, including heart failure, and chronic obstructive pulmonary disease, are notoriously higher in the US veteran population when compared with civilian cohorts.16-18 Also, veterans with poorly controlled depression and posttraumatic stress disorder resulting in functional impairment are a factor.19 Steps were taken to address some of these biases by performing repeat checks of tabulated data and employing 2 independent reviewers to evaluate all relevant clinical documentation, compare results, and reach a consensus.
Conlcusions
This retrospective analysis of adherence to category 1 NCCN guidelines for durvalumab use among patients at the Birmingham VAMC Oncology Clinic reinforced our practice and identified minor deficiencies in documentation that would impact future clinical visits. More importantly, it depicted the massive disparity in treatment candidacy among Birmingham veterans compared with clinical trial populations. Efforts will be made to address factors impacting a veteran’s candidacy for CRT and explore other variables such as socioeconomic barriers to treatment. Multiple complementary tools to assess patients’ frailty, such as the Charlson Comorbidity Index (CCI), are now being used for a variety of disorders including cancers. More robust data and standardization are needed to validate the use of these assessments in predicting response to immune checkpoint inhibitors.
Immune checkpoint inhibitors are currently being evaluated in stage III NSCLC studies and may be implemented as routine practice in the future.12 It is important to distinguish fit from frail veterans with lung cancer for treatment selection. We would like to see the expansion of the eligibility criteria for clinical trials to include patients with a performance status of ECOG 2 in order for results to be truly generalizable to the real-world population. Our hope is that such work will improve not only the quality of lung cancer care, but also the quality of care across multiple tumor types.
1. US Food and Drug Administration. FDA approves durvalumab after chemoradiation for unresectable stage II. Published February 20, 2018. Accessed October 9, 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-durvalumab-after-chemoradiation-unresectable-stage-iii-nsclc
2. Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919-1929. doi:10.1056/NEJMoa1709937
3. Antonia SJ, Villegas A, Daniel D, et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med. 2018;379(24):2342-2350. doi:10.1056/NEJMoa1809697
4. Ettinger DS, Wood DE, Aisner DL et al. NCCN clinical practice guidelines in oncology: non-small cell lung cancer. Version8.2020. Updated September 15, 2020. Accessed October 9, 2020. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
5. Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H. Impact of National Cancer Institute Comprehensive Cancer Centers on ovarian cancer treatment and survival. J Am Coll Surg. 2015;220(5):940-950. doi:10.1016/j.jamcollsurg.2015.01.056
6. Boland GM, Chang GJ, Haynes AB, et al. Association between adherence to National Comprehensive Cancer Network treatment guidelines and improved survival in patients with colon cancer. Cancer. 2013;119(8):1593-1601. doi:10.1002/cncr.27935
7. Schwentner L, Wöckel A, König J, et al. Adherence to treatment guidelines and survival in triple-negative breast cancer: a retrospective multi-center cohort study with 9,156 patients. BMC Cancer. 2013;13:487. Published 2013 Oct 21. doi:10.1186/1471-2407-13-487
8. Jazieh A, Alkaiyat MO, Ali Y, Hashim MA, Abdelhafiz N, Al Olayan A. Improving adherence to lung cancer guidelines: a quality improvement project that uses chart review, audit and feedback approach. BMJ Open Qual. 2019;8(3):e000436. Published 2019 Aug 26. doi:10.1136/bmjoq-2018-000436
9. Shaverdian N, Offin MD, Rimner A, et al. Utilization and factors precluding the initiation of consolidative durvalumab in unresectable stage III non-small cell lung cancer. Radiother Oncol. 2020;144:101-104. doi:10.1016/j.radonc.2019.11.015
10. National Cancer Institute. SEER cancer statistics review, 1975-2015, Table 15.1 cancer of the lung and bronchus. Accessed October 19, 2020 https://seer.cancer.gov/archive/csr/1975_2015/results_merged/sect_15_lung_bronchus.pdf. Updated September 10, 2018
11. Passaro A, Spitaleri G, Gyawali B, de Marinis F. Immunotherapy in non-small-cell lung cancer patients with performance status 2: clinical decision making with scant evidence. J Clin Oncol. 2019;37(22):1863-1867. doi:10.1200/JCO.18.02118
12. Driessen EJM, Janssen-Heijnen MLG, Maas HA, Dingemans AC, van Loon JGM. Study protocol of the NVALT25-ELDAPT trial: selecting the optimal treatment for older patients with stage III non-small-cell lung cancer. Clin Lung Cancer. 2018;19(6):e849-e852. doi:10.1016/j.cllc.2018.07.003
13. Schulkes KJ, Nguyen C, van den Bos F, van Elden LJ, Hamaker ME. Selection of Patients in Ongoing Clinical Trials on Lung Cancer. Lung. 2016;194(6):967-974. doi:10.1007/s00408-016-9943-7
14. Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35(11):1763-1774. doi:10.1007/s12325-018-0805-y
15. Garrison LP Jr, Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value Health. 2007;10(5):326-335. doi:10.1111/j.1524-4733.2007.00186.x
16. Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014;5(6):703-709.
17. Shahoumian TA, Phillips BR, Backus LI. Cigarette smoking, reduction and quit attempts: prevalence among veterans with coronary heart disease. Prev Chronic Dis. 2016;13:E41. Published 2016 Mar 24. doi:10.5888/pcd13.150282
18. Murphy DE, Chaudhry Z, Almoosa KF, Panos RJ. High prevalence of chronic obstructive pulmonary disease among veterans in the urban midwest. Mil Med. 2011;176(5):552-560. doi:10.7205/milmed-d-10-00377
19. Kozel FA, Didehbani N, DeLaRosa B, et al. Factors impacting functional status in veterans of recent conflicts with PTSD. J Neuropsychiatry Clin Neurosci. 2016;28(2):112-117. doi:10.1176/appi.neuropsych.15070183
The US Food and Drug Administration (FDA) approved the use of durvalumab for patients with unresectable stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (CRT).1 After 2 randomized phase 3 studies in 2017 and 2018 showed significant progression-free and overall survival respectively,2,3 durvalumab became a category 1 recommendation for the above indication per National Comprehensive Cancer Network (NCCN) guidelines.4 Adherence to guidelines have been shown to improve patient survival across several cancer types.5-7 However, guideline adherence rates have been variable across health institutions. Therefore, further study is warranted to evaluate nonadherent practices with the goal of improving the quality of cancer care delivery.8,9
Stage III NSCLC is associated with poor survival rates.10 Concurrent CRT remains the standard of care in patients with good performance status based on clinical trial populations.4 Lung cancer remains a disease of the elderly, with a median age at diagnosis of 70 years.11 Discrepancies in the treatment of lung cancer in older adults can vary widely due to a lack of evidence surrounding the treatment in those who have comorbidities and poor performance status, widening the gap between clinical trial and real-world populations.11
A recent review by Passaro and colleagues revealed that at least 11 pivotal randomized controlled trials have shown the activity of immune checkpoint inhibitors (ICI) in locally advanced and metastatic lung cancer. However, these studies have mostly excluded patients with a performance status of the Eastern Cooperative Oncology Group (ECOG) level ≥ 2.11
Durvalumab is one of many new therapies to enter clinical practice to demonstrate survival benefit, but its use among veterans with stage III NSCLC in adherence with National Comprehensive Cancer Network (NCCN) guidelines was not robust at the Birmingham Veterans Affairs Medical Center (VAMC) in Alabama. Therefore, we decided to study the level of adherence and to identify barriers to conformity to the category 1 NCCN recommendations.
Methods
The Birmingham VAMC Outpatient Oncology Clinic billing data identified all individuals diagnosed with lung cancer treated between October 2017 and August 2019. Patients who did not have NSCLC that was stage III and unresectable were excluded from our study. Patients who did not receive a majority of their treatment at US Department of Veterans Affairs (VA) facilities were excluded as well. Each patient’s demographic, functional level, and tumor characteristics during the treatment planning phase and follow-up visits were obtained. Two investigators who evaluated health care provider documentation using the VA Computerized Patient Record System (CPRS) conducted chart reviews.
The primary outcomes were the proportion of patients who received concurrent CRT and the proportion who received durvalumab consolidation. Our chart review also categorized reasons for nonreceipt of concurrent CRT and subsequent durvalumab. Documented reasons for guideline discordancy were generated empirically and broadly. We noted if documentation was unclear and included reasons for why a veteran was not a candidate for CRT, the presence of toxicities associated with CRT, and a patient’s refusal for therapy despite medical advice. Descriptive data were analyzed for all clinical or demographic characteristics and outcomes.
This was considered an internal quality improvement initiative. As such, Birmingham VAMC did not require institutional review board approval for the study. The facility is accredited by the American College of Surgeons Commission on Cancer.
Results
A total of 41 veterans with stage III NSCLC were identified to have established care in the Birmingham VAMC Oncology Clinic between October 2017 and August 2019. Of these, 7 received the majority of their treatment from community-based non-VA facilities and 14 were not candidates for CRT and were excluded from this study.
The mean (SD) age of study participants was 70.0 (8.4) years (range, 57 to 92 years). Most of the study veterans (33; 97.1%) were male and 20 (58.8%) were African American (Table). Eighteen (53%) of study participants had clinical stage IIIa NSCLC; 19 (56%) showed a squamous subtype of NSCLC. A majority (53%) of the veterans studied were evaluated to be functionally fit with an ECOG status of 0 to 1, although documentation of ECOG status was lacking in 5 (14.7%) patients in the initial treatment planning visit records. It was unclear if performance status had been reevaluated and changes noted over the course of concurrent CRT.
CRT Patients
The relative distribution of veterans who underwent CRT for stage III NSCLC plus the reasons they did not receive guideline-based treatment with durvalumab is shown in the Figure. Fourteen patients (41%) were inappropriate candidates for CRT; the most common reason for this was their poor performance status upon initial evaluation and 3 patients (8.8%) in the study had extensive disease or were upstaged upon follow-up clinic visit.
Twenty (59%) veterans in the study initiated CRT. However, only 16 (47.1%) completed CRT. Those who dropped out of CRT did so because of toxicities that included various cytopenia, gastrointestinal toxicities due to radiation and/or chemotherapy, or failure to thrive.
Durvalumab Treatment
After initiation of CRT, 9 (26.5%) patients did not go on to receive durvalumab. Three patients (8.8%) suffered toxicities during CRT. One study patient was found to have a severe respiratory infection requiring intensive care unit admission. Another study patient was found to have a new sternal lesion on follow-up positron emission tomography. One declined because of a history of severe antineutrophil cytoplasmic antibodies vasculitis, which made durvalumab use unsafe. Three patients (8.8%) declined treatment with CRT or durvalumab because of personal preference. Documentation was unclear as to why durvalumab was prescribed to one patient who had completed CRT.
Discussion
NCCN guidelines on the use of durvalumab in NSCLC are based on the phase 3 PACIFIC placebo-controlled randomized clinical trial. This trial, which included only patients with documented performance status of ECOG 0 or 1, reported that grade 3 or 4 events occurred in 30.5% of patients randomized to consolidative durvalumab. Treatment was discontinued in 15.4% of patients due to adverse events.3
Our study examined consolidation therapy with durvalumab in patients with unresectable stage III NSCLC with an ECOG performance status of 0 to 1 who had not progressed after 2 or more cycles of definitive concurrent CRT.4 Patients with previous exposure to immunotherapy, a history of immunodeficiency, active infection, unresolved toxicity from CRT, autoimmune disease, and patients who received sequential CRT were excluded.2 Surprisingly, the adherence rate to guidelines was close to 100% with appropriate documentation and justification of CRT initiation and durvalumab use. Five (14.7%) of veterans with unresectable stage III NSCLC did not have clear documentation of ECOG status on initial visit and only 1 veteran who completed CRT did not have clear documentation as to why durvalumab was not provided. Unfortunately, 23 (68.6%) veterans in the study were unable to receive durvalumab, a potentially disease-modifying drug; nearly one-third (10) of veterans were deemed poor candidates for concurrent CRT despite the fact that 52.9% (18) of veterans in the study had a documented ECOG of 0 or 1 on initial evaluation.
Clinical Trials vs Real World
The heterogeneity between anticipated study populations, those who were able to receive durvalumab in the PACIFIC trial, compared with our observed real-world veteran population, likely stems from the lack of information about how comorbidity and fitness can affect the choice of therapeutic intervention in patients with lung cancer.12 In addition, older adults who participated in randomized controlled trials (RCTs) are not representative of the average older adult who presents to medical oncology clinics, making the application of guideline concordant care difficult.13
Similar real-world observations parallel to our analyses have confirmed, complemented and/or refuted findings of RCTs, and have helped impact the treatment of multiple acute and chronic conditions including influenza, cardiovascular disease, and diabetes.14
A component of socioeconomic barriers and access to supportive care played roles in the decisions of certain patients who chose not to undergo concurrent CRT despite medical advice. These 2 obstacles also affected the decision making for some in the study when considering the use of durvalumab (administered by a 60-minute IV infusion every 2 weeks for 1 year) per recommended guidelines.1 These hurdles need further study in the context of their effect on quality of life and the difficulties generated by various social determinants of health.
Limitations
Study limitations included the biased and confounding factors previously described about retrospective and nonrandomized observational studies that are controlled for during RCTs.15 Electronic health record data may have been incorrectly collected resulting in missing or wrong data points that affect the validity of our conclusion. Recall bias with regard to documentation by health care providers describing reasons why CRT or durvalumab were not initiated or the patient’s ability to recall previous treatments and report ECOG status or toxicities also may have impacted our findings. Comorbidities and poor performance status, frequently occurring among veterans, negatively impact cancer treatment decisions and may result in a detection bias. For example, tobacco use, cardiovascular disease, including heart failure, and chronic obstructive pulmonary disease, are notoriously higher in the US veteran population when compared with civilian cohorts.16-18 Also, veterans with poorly controlled depression and posttraumatic stress disorder resulting in functional impairment are a factor.19 Steps were taken to address some of these biases by performing repeat checks of tabulated data and employing 2 independent reviewers to evaluate all relevant clinical documentation, compare results, and reach a consensus.
Conlcusions
This retrospective analysis of adherence to category 1 NCCN guidelines for durvalumab use among patients at the Birmingham VAMC Oncology Clinic reinforced our practice and identified minor deficiencies in documentation that would impact future clinical visits. More importantly, it depicted the massive disparity in treatment candidacy among Birmingham veterans compared with clinical trial populations. Efforts will be made to address factors impacting a veteran’s candidacy for CRT and explore other variables such as socioeconomic barriers to treatment. Multiple complementary tools to assess patients’ frailty, such as the Charlson Comorbidity Index (CCI), are now being used for a variety of disorders including cancers. More robust data and standardization are needed to validate the use of these assessments in predicting response to immune checkpoint inhibitors.
Immune checkpoint inhibitors are currently being evaluated in stage III NSCLC studies and may be implemented as routine practice in the future.12 It is important to distinguish fit from frail veterans with lung cancer for treatment selection. We would like to see the expansion of the eligibility criteria for clinical trials to include patients with a performance status of ECOG 2 in order for results to be truly generalizable to the real-world population. Our hope is that such work will improve not only the quality of lung cancer care, but also the quality of care across multiple tumor types.
The US Food and Drug Administration (FDA) approved the use of durvalumab for patients with unresectable stage III non-small cell lung cancer (NSCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy (CRT).1 After 2 randomized phase 3 studies in 2017 and 2018 showed significant progression-free and overall survival respectively,2,3 durvalumab became a category 1 recommendation for the above indication per National Comprehensive Cancer Network (NCCN) guidelines.4 Adherence to guidelines have been shown to improve patient survival across several cancer types.5-7 However, guideline adherence rates have been variable across health institutions. Therefore, further study is warranted to evaluate nonadherent practices with the goal of improving the quality of cancer care delivery.8,9
Stage III NSCLC is associated with poor survival rates.10 Concurrent CRT remains the standard of care in patients with good performance status based on clinical trial populations.4 Lung cancer remains a disease of the elderly, with a median age at diagnosis of 70 years.11 Discrepancies in the treatment of lung cancer in older adults can vary widely due to a lack of evidence surrounding the treatment in those who have comorbidities and poor performance status, widening the gap between clinical trial and real-world populations.11
A recent review by Passaro and colleagues revealed that at least 11 pivotal randomized controlled trials have shown the activity of immune checkpoint inhibitors (ICI) in locally advanced and metastatic lung cancer. However, these studies have mostly excluded patients with a performance status of the Eastern Cooperative Oncology Group (ECOG) level ≥ 2.11
Durvalumab is one of many new therapies to enter clinical practice to demonstrate survival benefit, but its use among veterans with stage III NSCLC in adherence with National Comprehensive Cancer Network (NCCN) guidelines was not robust at the Birmingham Veterans Affairs Medical Center (VAMC) in Alabama. Therefore, we decided to study the level of adherence and to identify barriers to conformity to the category 1 NCCN recommendations.
Methods
The Birmingham VAMC Outpatient Oncology Clinic billing data identified all individuals diagnosed with lung cancer treated between October 2017 and August 2019. Patients who did not have NSCLC that was stage III and unresectable were excluded from our study. Patients who did not receive a majority of their treatment at US Department of Veterans Affairs (VA) facilities were excluded as well. Each patient’s demographic, functional level, and tumor characteristics during the treatment planning phase and follow-up visits were obtained. Two investigators who evaluated health care provider documentation using the VA Computerized Patient Record System (CPRS) conducted chart reviews.
The primary outcomes were the proportion of patients who received concurrent CRT and the proportion who received durvalumab consolidation. Our chart review also categorized reasons for nonreceipt of concurrent CRT and subsequent durvalumab. Documented reasons for guideline discordancy were generated empirically and broadly. We noted if documentation was unclear and included reasons for why a veteran was not a candidate for CRT, the presence of toxicities associated with CRT, and a patient’s refusal for therapy despite medical advice. Descriptive data were analyzed for all clinical or demographic characteristics and outcomes.
This was considered an internal quality improvement initiative. As such, Birmingham VAMC did not require institutional review board approval for the study. The facility is accredited by the American College of Surgeons Commission on Cancer.
Results
A total of 41 veterans with stage III NSCLC were identified to have established care in the Birmingham VAMC Oncology Clinic between October 2017 and August 2019. Of these, 7 received the majority of their treatment from community-based non-VA facilities and 14 were not candidates for CRT and were excluded from this study.
The mean (SD) age of study participants was 70.0 (8.4) years (range, 57 to 92 years). Most of the study veterans (33; 97.1%) were male and 20 (58.8%) were African American (Table). Eighteen (53%) of study participants had clinical stage IIIa NSCLC; 19 (56%) showed a squamous subtype of NSCLC. A majority (53%) of the veterans studied were evaluated to be functionally fit with an ECOG status of 0 to 1, although documentation of ECOG status was lacking in 5 (14.7%) patients in the initial treatment planning visit records. It was unclear if performance status had been reevaluated and changes noted over the course of concurrent CRT.
CRT Patients
The relative distribution of veterans who underwent CRT for stage III NSCLC plus the reasons they did not receive guideline-based treatment with durvalumab is shown in the Figure. Fourteen patients (41%) were inappropriate candidates for CRT; the most common reason for this was their poor performance status upon initial evaluation and 3 patients (8.8%) in the study had extensive disease or were upstaged upon follow-up clinic visit.
Twenty (59%) veterans in the study initiated CRT. However, only 16 (47.1%) completed CRT. Those who dropped out of CRT did so because of toxicities that included various cytopenia, gastrointestinal toxicities due to radiation and/or chemotherapy, or failure to thrive.
Durvalumab Treatment
After initiation of CRT, 9 (26.5%) patients did not go on to receive durvalumab. Three patients (8.8%) suffered toxicities during CRT. One study patient was found to have a severe respiratory infection requiring intensive care unit admission. Another study patient was found to have a new sternal lesion on follow-up positron emission tomography. One declined because of a history of severe antineutrophil cytoplasmic antibodies vasculitis, which made durvalumab use unsafe. Three patients (8.8%) declined treatment with CRT or durvalumab because of personal preference. Documentation was unclear as to why durvalumab was prescribed to one patient who had completed CRT.
Discussion
NCCN guidelines on the use of durvalumab in NSCLC are based on the phase 3 PACIFIC placebo-controlled randomized clinical trial. This trial, which included only patients with documented performance status of ECOG 0 or 1, reported that grade 3 or 4 events occurred in 30.5% of patients randomized to consolidative durvalumab. Treatment was discontinued in 15.4% of patients due to adverse events.3
Our study examined consolidation therapy with durvalumab in patients with unresectable stage III NSCLC with an ECOG performance status of 0 to 1 who had not progressed after 2 or more cycles of definitive concurrent CRT.4 Patients with previous exposure to immunotherapy, a history of immunodeficiency, active infection, unresolved toxicity from CRT, autoimmune disease, and patients who received sequential CRT were excluded.2 Surprisingly, the adherence rate to guidelines was close to 100% with appropriate documentation and justification of CRT initiation and durvalumab use. Five (14.7%) of veterans with unresectable stage III NSCLC did not have clear documentation of ECOG status on initial visit and only 1 veteran who completed CRT did not have clear documentation as to why durvalumab was not provided. Unfortunately, 23 (68.6%) veterans in the study were unable to receive durvalumab, a potentially disease-modifying drug; nearly one-third (10) of veterans were deemed poor candidates for concurrent CRT despite the fact that 52.9% (18) of veterans in the study had a documented ECOG of 0 or 1 on initial evaluation.
Clinical Trials vs Real World
The heterogeneity between anticipated study populations, those who were able to receive durvalumab in the PACIFIC trial, compared with our observed real-world veteran population, likely stems from the lack of information about how comorbidity and fitness can affect the choice of therapeutic intervention in patients with lung cancer.12 In addition, older adults who participated in randomized controlled trials (RCTs) are not representative of the average older adult who presents to medical oncology clinics, making the application of guideline concordant care difficult.13
Similar real-world observations parallel to our analyses have confirmed, complemented and/or refuted findings of RCTs, and have helped impact the treatment of multiple acute and chronic conditions including influenza, cardiovascular disease, and diabetes.14
A component of socioeconomic barriers and access to supportive care played roles in the decisions of certain patients who chose not to undergo concurrent CRT despite medical advice. These 2 obstacles also affected the decision making for some in the study when considering the use of durvalumab (administered by a 60-minute IV infusion every 2 weeks for 1 year) per recommended guidelines.1 These hurdles need further study in the context of their effect on quality of life and the difficulties generated by various social determinants of health.
Limitations
Study limitations included the biased and confounding factors previously described about retrospective and nonrandomized observational studies that are controlled for during RCTs.15 Electronic health record data may have been incorrectly collected resulting in missing or wrong data points that affect the validity of our conclusion. Recall bias with regard to documentation by health care providers describing reasons why CRT or durvalumab were not initiated or the patient’s ability to recall previous treatments and report ECOG status or toxicities also may have impacted our findings. Comorbidities and poor performance status, frequently occurring among veterans, negatively impact cancer treatment decisions and may result in a detection bias. For example, tobacco use, cardiovascular disease, including heart failure, and chronic obstructive pulmonary disease, are notoriously higher in the US veteran population when compared with civilian cohorts.16-18 Also, veterans with poorly controlled depression and posttraumatic stress disorder resulting in functional impairment are a factor.19 Steps were taken to address some of these biases by performing repeat checks of tabulated data and employing 2 independent reviewers to evaluate all relevant clinical documentation, compare results, and reach a consensus.
Conlcusions
This retrospective analysis of adherence to category 1 NCCN guidelines for durvalumab use among patients at the Birmingham VAMC Oncology Clinic reinforced our practice and identified minor deficiencies in documentation that would impact future clinical visits. More importantly, it depicted the massive disparity in treatment candidacy among Birmingham veterans compared with clinical trial populations. Efforts will be made to address factors impacting a veteran’s candidacy for CRT and explore other variables such as socioeconomic barriers to treatment. Multiple complementary tools to assess patients’ frailty, such as the Charlson Comorbidity Index (CCI), are now being used for a variety of disorders including cancers. More robust data and standardization are needed to validate the use of these assessments in predicting response to immune checkpoint inhibitors.
Immune checkpoint inhibitors are currently being evaluated in stage III NSCLC studies and may be implemented as routine practice in the future.12 It is important to distinguish fit from frail veterans with lung cancer for treatment selection. We would like to see the expansion of the eligibility criteria for clinical trials to include patients with a performance status of ECOG 2 in order for results to be truly generalizable to the real-world population. Our hope is that such work will improve not only the quality of lung cancer care, but also the quality of care across multiple tumor types.
1. US Food and Drug Administration. FDA approves durvalumab after chemoradiation for unresectable stage II. Published February 20, 2018. Accessed October 9, 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-durvalumab-after-chemoradiation-unresectable-stage-iii-nsclc
2. Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919-1929. doi:10.1056/NEJMoa1709937
3. Antonia SJ, Villegas A, Daniel D, et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med. 2018;379(24):2342-2350. doi:10.1056/NEJMoa1809697
4. Ettinger DS, Wood DE, Aisner DL et al. NCCN clinical practice guidelines in oncology: non-small cell lung cancer. Version8.2020. Updated September 15, 2020. Accessed October 9, 2020. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
5. Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H. Impact of National Cancer Institute Comprehensive Cancer Centers on ovarian cancer treatment and survival. J Am Coll Surg. 2015;220(5):940-950. doi:10.1016/j.jamcollsurg.2015.01.056
6. Boland GM, Chang GJ, Haynes AB, et al. Association between adherence to National Comprehensive Cancer Network treatment guidelines and improved survival in patients with colon cancer. Cancer. 2013;119(8):1593-1601. doi:10.1002/cncr.27935
7. Schwentner L, Wöckel A, König J, et al. Adherence to treatment guidelines and survival in triple-negative breast cancer: a retrospective multi-center cohort study with 9,156 patients. BMC Cancer. 2013;13:487. Published 2013 Oct 21. doi:10.1186/1471-2407-13-487
8. Jazieh A, Alkaiyat MO, Ali Y, Hashim MA, Abdelhafiz N, Al Olayan A. Improving adherence to lung cancer guidelines: a quality improvement project that uses chart review, audit and feedback approach. BMJ Open Qual. 2019;8(3):e000436. Published 2019 Aug 26. doi:10.1136/bmjoq-2018-000436
9. Shaverdian N, Offin MD, Rimner A, et al. Utilization and factors precluding the initiation of consolidative durvalumab in unresectable stage III non-small cell lung cancer. Radiother Oncol. 2020;144:101-104. doi:10.1016/j.radonc.2019.11.015
10. National Cancer Institute. SEER cancer statistics review, 1975-2015, Table 15.1 cancer of the lung and bronchus. Accessed October 19, 2020 https://seer.cancer.gov/archive/csr/1975_2015/results_merged/sect_15_lung_bronchus.pdf. Updated September 10, 2018
11. Passaro A, Spitaleri G, Gyawali B, de Marinis F. Immunotherapy in non-small-cell lung cancer patients with performance status 2: clinical decision making with scant evidence. J Clin Oncol. 2019;37(22):1863-1867. doi:10.1200/JCO.18.02118
12. Driessen EJM, Janssen-Heijnen MLG, Maas HA, Dingemans AC, van Loon JGM. Study protocol of the NVALT25-ELDAPT trial: selecting the optimal treatment for older patients with stage III non-small-cell lung cancer. Clin Lung Cancer. 2018;19(6):e849-e852. doi:10.1016/j.cllc.2018.07.003
13. Schulkes KJ, Nguyen C, van den Bos F, van Elden LJ, Hamaker ME. Selection of Patients in Ongoing Clinical Trials on Lung Cancer. Lung. 2016;194(6):967-974. doi:10.1007/s00408-016-9943-7
14. Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35(11):1763-1774. doi:10.1007/s12325-018-0805-y
15. Garrison LP Jr, Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value Health. 2007;10(5):326-335. doi:10.1111/j.1524-4733.2007.00186.x
16. Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014;5(6):703-709.
17. Shahoumian TA, Phillips BR, Backus LI. Cigarette smoking, reduction and quit attempts: prevalence among veterans with coronary heart disease. Prev Chronic Dis. 2016;13:E41. Published 2016 Mar 24. doi:10.5888/pcd13.150282
18. Murphy DE, Chaudhry Z, Almoosa KF, Panos RJ. High prevalence of chronic obstructive pulmonary disease among veterans in the urban midwest. Mil Med. 2011;176(5):552-560. doi:10.7205/milmed-d-10-00377
19. Kozel FA, Didehbani N, DeLaRosa B, et al. Factors impacting functional status in veterans of recent conflicts with PTSD. J Neuropsychiatry Clin Neurosci. 2016;28(2):112-117. doi:10.1176/appi.neuropsych.15070183
1. US Food and Drug Administration. FDA approves durvalumab after chemoradiation for unresectable stage II. Published February 20, 2018. Accessed October 9, 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-durvalumab-after-chemoradiation-unresectable-stage-iii-nsclc
2. Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med. 2017;377(20):1919-1929. doi:10.1056/NEJMoa1709937
3. Antonia SJ, Villegas A, Daniel D, et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med. 2018;379(24):2342-2350. doi:10.1056/NEJMoa1809697
4. Ettinger DS, Wood DE, Aisner DL et al. NCCN clinical practice guidelines in oncology: non-small cell lung cancer. Version8.2020. Updated September 15, 2020. Accessed October 9, 2020. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
5. Bristow RE, Chang J, Ziogas A, Campos B, Chavez LR, Anton-Culver H. Impact of National Cancer Institute Comprehensive Cancer Centers on ovarian cancer treatment and survival. J Am Coll Surg. 2015;220(5):940-950. doi:10.1016/j.jamcollsurg.2015.01.056
6. Boland GM, Chang GJ, Haynes AB, et al. Association between adherence to National Comprehensive Cancer Network treatment guidelines and improved survival in patients with colon cancer. Cancer. 2013;119(8):1593-1601. doi:10.1002/cncr.27935
7. Schwentner L, Wöckel A, König J, et al. Adherence to treatment guidelines and survival in triple-negative breast cancer: a retrospective multi-center cohort study with 9,156 patients. BMC Cancer. 2013;13:487. Published 2013 Oct 21. doi:10.1186/1471-2407-13-487
8. Jazieh A, Alkaiyat MO, Ali Y, Hashim MA, Abdelhafiz N, Al Olayan A. Improving adherence to lung cancer guidelines: a quality improvement project that uses chart review, audit and feedback approach. BMJ Open Qual. 2019;8(3):e000436. Published 2019 Aug 26. doi:10.1136/bmjoq-2018-000436
9. Shaverdian N, Offin MD, Rimner A, et al. Utilization and factors precluding the initiation of consolidative durvalumab in unresectable stage III non-small cell lung cancer. Radiother Oncol. 2020;144:101-104. doi:10.1016/j.radonc.2019.11.015
10. National Cancer Institute. SEER cancer statistics review, 1975-2015, Table 15.1 cancer of the lung and bronchus. Accessed October 19, 2020 https://seer.cancer.gov/archive/csr/1975_2015/results_merged/sect_15_lung_bronchus.pdf. Updated September 10, 2018
11. Passaro A, Spitaleri G, Gyawali B, de Marinis F. Immunotherapy in non-small-cell lung cancer patients with performance status 2: clinical decision making with scant evidence. J Clin Oncol. 2019;37(22):1863-1867. doi:10.1200/JCO.18.02118
12. Driessen EJM, Janssen-Heijnen MLG, Maas HA, Dingemans AC, van Loon JGM. Study protocol of the NVALT25-ELDAPT trial: selecting the optimal treatment for older patients with stage III non-small-cell lung cancer. Clin Lung Cancer. 2018;19(6):e849-e852. doi:10.1016/j.cllc.2018.07.003
13. Schulkes KJ, Nguyen C, van den Bos F, van Elden LJ, Hamaker ME. Selection of Patients in Ongoing Clinical Trials on Lung Cancer. Lung. 2016;194(6):967-974. doi:10.1007/s00408-016-9943-7
14. Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and impact of real-world clinical data for the practicing clinician. Adv Ther. 2018;35(11):1763-1774. doi:10.1007/s12325-018-0805-y
15. Garrison LP Jr, Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value Health. 2007;10(5):326-335. doi:10.1111/j.1524-4733.2007.00186.x
16. Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014;5(6):703-709.
17. Shahoumian TA, Phillips BR, Backus LI. Cigarette smoking, reduction and quit attempts: prevalence among veterans with coronary heart disease. Prev Chronic Dis. 2016;13:E41. Published 2016 Mar 24. doi:10.5888/pcd13.150282
18. Murphy DE, Chaudhry Z, Almoosa KF, Panos RJ. High prevalence of chronic obstructive pulmonary disease among veterans in the urban midwest. Mil Med. 2011;176(5):552-560. doi:10.7205/milmed-d-10-00377
19. Kozel FA, Didehbani N, DeLaRosa B, et al. Factors impacting functional status in veterans of recent conflicts with PTSD. J Neuropsychiatry Clin Neurosci. 2016;28(2):112-117. doi:10.1176/appi.neuropsych.15070183