User login
FDA approves first twice-yearly antipsychotic for schizophrenia
The U.S. Food and Drug Administration has approved a 6-month injection form of the long-acting atypical antipsychotic paliperidone palmitate (Invega Hafyera, Janssen Pharmaceuticals) for the treatment of schizophrenia in adults, the company has announced.
This marks the “first-and-only twice-yearly injectable” approved for treating schizophrenia, the company added in a press release.
Before transitioning to the 6-month form, patients must be adequately treated for a minimum of 4 months with the company’s 1-month formulation of paliperidone (Invega Sustenna), or with the 3-month version (Invega Trinza) for at least one 3-month injection cycle.
The FDA approved the twice-yearly formulation on the basis of results from a 12-month, randomized, double-blind, phase 3 study that enrolled 702 adults with schizophrenia from 20 countries.
“The phase 3 trial results provide compelling evidence that 6-month paliperidone palmitate offers longer-term symptom control with the fewest doses per year, which may support greater patient adherence,” Gustavo Alva, MD, medical director at ATP Clinical Research, Costa Mesa, Calif., and 6-month paliperidone palmitate clinical trial investigator, said in the release.
Noninferiority results
In the phase 3 trial, the twice-yearly version of the drug proved noninferior to the 3-month version on the primary endpoint of time to first relapse at the end of 12 months, with 92.5% and 95% of patients, respectively, relapse-free at 12 months.
Relapse was defined as psychiatric hospitalization, increase in Positive and Negative Syndrome Scale (PANSS) total score, increase in individual PANSS item scores, self-injury, violent behavior, or suicidal/homicidal ideation.
The safety profile observed in the trial was in line with prior studies of the 1-month and 3-month versions, with no new safety signals, the researchers note.
The most common adverse reactions affecting at least 5% of participants in the clinical trial receiving twice-year paliperidone were upper respiratory tract infection (12%), injection site reaction (11%), weight gain (9%), headache (7%), and parkinsonism (5%).
Relapse is common in adults with schizophrenia, often because of missed doses of medication, the company said in the news release.
, while research continues to demonstrate that stronger medication adherence means better patient outcomes,” Dr. Alva said.
Recently updated evidence-based guidelines from the American Psychiatric Association recommend consideration of long-acting injectables for appropriate adults living with schizophrenia.
“Long-acting injectable treatments offer a number of advantages, compared to oral medication for schizophrenia, including relief from needing to remember to take medication daily, lower discontinuation rates, and sustained treatment over longer periods,” Bill Martin, PhD, with Janssen Research & Development, said in the release.
“Today’s approval enables us to rethink how we manage this chronic disease by offering patients and caregivers the potential for a life less defined by schizophrenia medication,” Dr. Martin added.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a 6-month injection form of the long-acting atypical antipsychotic paliperidone palmitate (Invega Hafyera, Janssen Pharmaceuticals) for the treatment of schizophrenia in adults, the company has announced.
This marks the “first-and-only twice-yearly injectable” approved for treating schizophrenia, the company added in a press release.
Before transitioning to the 6-month form, patients must be adequately treated for a minimum of 4 months with the company’s 1-month formulation of paliperidone (Invega Sustenna), or with the 3-month version (Invega Trinza) for at least one 3-month injection cycle.
The FDA approved the twice-yearly formulation on the basis of results from a 12-month, randomized, double-blind, phase 3 study that enrolled 702 adults with schizophrenia from 20 countries.
“The phase 3 trial results provide compelling evidence that 6-month paliperidone palmitate offers longer-term symptom control with the fewest doses per year, which may support greater patient adherence,” Gustavo Alva, MD, medical director at ATP Clinical Research, Costa Mesa, Calif., and 6-month paliperidone palmitate clinical trial investigator, said in the release.
Noninferiority results
In the phase 3 trial, the twice-yearly version of the drug proved noninferior to the 3-month version on the primary endpoint of time to first relapse at the end of 12 months, with 92.5% and 95% of patients, respectively, relapse-free at 12 months.
Relapse was defined as psychiatric hospitalization, increase in Positive and Negative Syndrome Scale (PANSS) total score, increase in individual PANSS item scores, self-injury, violent behavior, or suicidal/homicidal ideation.
The safety profile observed in the trial was in line with prior studies of the 1-month and 3-month versions, with no new safety signals, the researchers note.
The most common adverse reactions affecting at least 5% of participants in the clinical trial receiving twice-year paliperidone were upper respiratory tract infection (12%), injection site reaction (11%), weight gain (9%), headache (7%), and parkinsonism (5%).
Relapse is common in adults with schizophrenia, often because of missed doses of medication, the company said in the news release.
, while research continues to demonstrate that stronger medication adherence means better patient outcomes,” Dr. Alva said.
Recently updated evidence-based guidelines from the American Psychiatric Association recommend consideration of long-acting injectables for appropriate adults living with schizophrenia.
“Long-acting injectable treatments offer a number of advantages, compared to oral medication for schizophrenia, including relief from needing to remember to take medication daily, lower discontinuation rates, and sustained treatment over longer periods,” Bill Martin, PhD, with Janssen Research & Development, said in the release.
“Today’s approval enables us to rethink how we manage this chronic disease by offering patients and caregivers the potential for a life less defined by schizophrenia medication,” Dr. Martin added.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved a 6-month injection form of the long-acting atypical antipsychotic paliperidone palmitate (Invega Hafyera, Janssen Pharmaceuticals) for the treatment of schizophrenia in adults, the company has announced.
This marks the “first-and-only twice-yearly injectable” approved for treating schizophrenia, the company added in a press release.
Before transitioning to the 6-month form, patients must be adequately treated for a minimum of 4 months with the company’s 1-month formulation of paliperidone (Invega Sustenna), or with the 3-month version (Invega Trinza) for at least one 3-month injection cycle.
The FDA approved the twice-yearly formulation on the basis of results from a 12-month, randomized, double-blind, phase 3 study that enrolled 702 adults with schizophrenia from 20 countries.
“The phase 3 trial results provide compelling evidence that 6-month paliperidone palmitate offers longer-term symptom control with the fewest doses per year, which may support greater patient adherence,” Gustavo Alva, MD, medical director at ATP Clinical Research, Costa Mesa, Calif., and 6-month paliperidone palmitate clinical trial investigator, said in the release.
Noninferiority results
In the phase 3 trial, the twice-yearly version of the drug proved noninferior to the 3-month version on the primary endpoint of time to first relapse at the end of 12 months, with 92.5% and 95% of patients, respectively, relapse-free at 12 months.
Relapse was defined as psychiatric hospitalization, increase in Positive and Negative Syndrome Scale (PANSS) total score, increase in individual PANSS item scores, self-injury, violent behavior, or suicidal/homicidal ideation.
The safety profile observed in the trial was in line with prior studies of the 1-month and 3-month versions, with no new safety signals, the researchers note.
The most common adverse reactions affecting at least 5% of participants in the clinical trial receiving twice-year paliperidone were upper respiratory tract infection (12%), injection site reaction (11%), weight gain (9%), headache (7%), and parkinsonism (5%).
Relapse is common in adults with schizophrenia, often because of missed doses of medication, the company said in the news release.
, while research continues to demonstrate that stronger medication adherence means better patient outcomes,” Dr. Alva said.
Recently updated evidence-based guidelines from the American Psychiatric Association recommend consideration of long-acting injectables for appropriate adults living with schizophrenia.
“Long-acting injectable treatments offer a number of advantages, compared to oral medication for schizophrenia, including relief from needing to remember to take medication daily, lower discontinuation rates, and sustained treatment over longer periods,” Bill Martin, PhD, with Janssen Research & Development, said in the release.
“Today’s approval enables us to rethink how we manage this chronic disease by offering patients and caregivers the potential for a life less defined by schizophrenia medication,” Dr. Martin added.
A version of this article first appeared on Medscape.com.
Neuropsychiatry affects pediatric OCD treatment
Treatment of pediatric obsessive-compulsive disorder (OCD) has evolved in recent years, with more attention given to some of the neuropsychiatric underpinnings of the condition and how they can affect treatment response.
At the Focus on Neuropsychiatry 2021 meeting, Jeffrey Strawn, MD, outlined some of the neuropsychiatry affecting disease and potential mechanisms to help control obsessions and behaviors, and how they may fit with some therapeutic regimens.
Dr. Strawn discussed the psychological construct of cognitive control, which can provide patients an “out” from the cycle of obsession/fear/worry and compulsion/avoidance. In the face of distress, compulsion and avoidance lead to relief, which reinforces the obsession/fear/worry; this in turn leads to more distress.
“We have an escape door for this circuit” in the form of cognitive control, said Dr. Strawn, who is an associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center.
Cognitive control is linked to insight, which can in turn increase adaptive behaviors that help the patient resist the compulsion. Patients won’t eliminate distress, but they can be helped to make it more tolerable. Therapists can then help them move toward goal-directed thoughts and behaviors. Cognitive control is associated with several neural networks, but Dr. Strawn focused on two: the frontoparietal network, associated with top-down regulation; and the cingular-opercular network. Both of these are engaged during cognitive control processes, and play a role inhibitory control and error monitoring.
Dr. Strawn discussed a recent study that explored the neurofunctional basis of treatment. It compared the effects of a stress management therapy and cognitive-behavioral therapy (CBT) in children and adults with OCD at 6 and 12 weeks. The study found similar symptom reductions in both adults and adolescents in both intervention groups.
Before initiating treatment, the researchers conducted functional MRI scans of participants while conducting an incentive flanker task, which reveals brain activity in response to cognitive control and reward processing.
A larger therapeutic response was found in the CBT group among patients who had a larger pretreatment activation within the right temporal lobe and rostral anterior cingulate cortex during cognitive control, as well as those with more activation within the medial prefrontal, orbitofrontal, lateral prefrontal, and amygdala regions during reward processing. On the other hand, within the stress management therapy group, treatment responses were better among those who had lower pretreatment activation among overlapping regions.
“There was a difference in terms of the neurofunctional predictors of treatment response. One of the key regions is the medial prefrontal cortex as well as the rostral anterior cingulate,” said Dr. Strawn, at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
On the neuropharmacology side, numerous medications have been approved for OCD. Dr. Strawn highlighted some studies to illustrate general OCD treatment concepts. That included the 2004 Pediatric OCD Treatment Study, which was one of the only trials to compare placebo with an SSRI, CBT, and the combination of SSRI and CBT. It showed the best results with combination therapy, and the difference appeared early in the treatment course.
That study had aggressive dosing, which led to some issues with sertraline tolerability. Dr. Strawn showed results of a study at his institution which showed that the drug levels of pediatric patients treated with sertraline depended on CYP2C19 metabolism, which affects overall exposure and peak dose concentration. In pediatric populations, some SSRIs clear more slowly and can have high peak concentrations. SSRIs have more side effects than serotonin and norepinephrine reuptake inhibitors in both anxiety disorders and OCD. A key difference between the two is that SSRI treatment is associated with greater frequency of activation, which is difficult to define, but includes restlessness and agitation and insomnia in the beginning stages of treatment.
SSRIs also lead to improvement early in the course of treatment, which was shown in a meta-analysis of nine trials. However, the same study showed that clomipramine is associated with a faster and greater magnitude of improvement, compared with SSRIs, even when the latter are dosed aggressively.
Clomipramine is a potent inhibitor of both serotonin and norepinephrine reuptake. It is recommended to monitor clomipramine levels in pediatric OCD patients, and Dr. Strawn suggested that monitoring should include both the parent drug and its primary metabolite, norclomipramine. At a given dose, there can be a great deal of variation in drug level. The clomipramine/norclomipramine ratio can provide information about the patient’s metabolic state, as well as drug adherence.
Dr. Strawn noted that peak levels occur around 1-3 hours after the dose, “and we really do want at least a 12-hour trough level.” EKGs should be performed at baseline and after any titration of clomipramine dose.
He also discussed pediatric OCD patients with OCD and tics. About one-third of Tourette syndrome patients experience OCD at some point. Tics often improve, whereas OCD more often persists. Tics that co-occur with OCD are associated with a lesser response to SSRI treatment, but not CBT treatment. Similarly, patients with hoarding tendencies are about one-third less likely to respond to SSRIs, CBT, or combination therapy.
Dr. Strawn discussed the concept of accommodation, in which family members cope with a patient’s behavior by altering routines to minimize distress and impairment. This may take the form of facilitating rituals, providing reassurance about a patient’s fears, acquiescing to demands, reducing the child’s day-to-day responsibilities, or helping the child complete tasks. Such actions are well intentioned, but they undermine cognitive control, negatively reinforce symptom engagement, and are associated with functional impairment. Reassurance is the most important behavior, occurring in more than half of patients, and it’s measurable. Parental involvement with rituals is also a concern. “This is associated with higher levels of child OCD severity, as well as parental psychopathology, and lower family cohesion. So
New developments in neurobiology and neuropsychology have changed the view of exposure. The old model emphasized the child’s fear rating as an index of corrective learning. The idea was that habituation would decrease anxiety and distress from future exposures. The new model revolves around inhibitory learning theory, which focuses on the variability of distress and aims to increase tolerance of distress. Another goal is to develop new, non-threat associations.
Finally, Dr. Strawn pointed out predictors of poor outcomes in pediatric OCD, including factors such as compulsion severity, oppositional behavior, frequent handwashing, functional impairment, lack of insight, externalizing symptoms, and possibly hoarding. Problematic family characteristics include higher levels of accommodation, parental anxiety, low family cohesion, and high levels of conflict. “The last three really represent a very concerning triad of family behaviors that may necessitate specific family work in order to facilitate the recovery of the pediatric patient,” Dr. Strawn said.
During the question-and-answer session after the talk, Dr. Strawn was asked whether there might be an inflammatory component to OCD, and whether pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) might be a prodromal condition. He noted that some studies have shown a relationship, but results have been mixed, with lots of heterogeneity within the studied populations. To be suspicious that a patient had OCD resulting from PANDAS would require a high threshold, including an acute onset of symptoms. “This is a situation also where I would tend to involve consultation with some other specialties, including neurology. And obviously there would be follow-up in terms of the general workup,” he said.
Dr. Strawn has received research funding from Allergan, Otsuka, and Myriad Genetics. He has consulted for Myriad Genetics, and is a speaker for CMEology and the Neuroscience Education Institute.
Treatment of pediatric obsessive-compulsive disorder (OCD) has evolved in recent years, with more attention given to some of the neuropsychiatric underpinnings of the condition and how they can affect treatment response.
At the Focus on Neuropsychiatry 2021 meeting, Jeffrey Strawn, MD, outlined some of the neuropsychiatry affecting disease and potential mechanisms to help control obsessions and behaviors, and how they may fit with some therapeutic regimens.
Dr. Strawn discussed the psychological construct of cognitive control, which can provide patients an “out” from the cycle of obsession/fear/worry and compulsion/avoidance. In the face of distress, compulsion and avoidance lead to relief, which reinforces the obsession/fear/worry; this in turn leads to more distress.
“We have an escape door for this circuit” in the form of cognitive control, said Dr. Strawn, who is an associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center.
Cognitive control is linked to insight, which can in turn increase adaptive behaviors that help the patient resist the compulsion. Patients won’t eliminate distress, but they can be helped to make it more tolerable. Therapists can then help them move toward goal-directed thoughts and behaviors. Cognitive control is associated with several neural networks, but Dr. Strawn focused on two: the frontoparietal network, associated with top-down regulation; and the cingular-opercular network. Both of these are engaged during cognitive control processes, and play a role inhibitory control and error monitoring.
Dr. Strawn discussed a recent study that explored the neurofunctional basis of treatment. It compared the effects of a stress management therapy and cognitive-behavioral therapy (CBT) in children and adults with OCD at 6 and 12 weeks. The study found similar symptom reductions in both adults and adolescents in both intervention groups.
Before initiating treatment, the researchers conducted functional MRI scans of participants while conducting an incentive flanker task, which reveals brain activity in response to cognitive control and reward processing.
A larger therapeutic response was found in the CBT group among patients who had a larger pretreatment activation within the right temporal lobe and rostral anterior cingulate cortex during cognitive control, as well as those with more activation within the medial prefrontal, orbitofrontal, lateral prefrontal, and amygdala regions during reward processing. On the other hand, within the stress management therapy group, treatment responses were better among those who had lower pretreatment activation among overlapping regions.
“There was a difference in terms of the neurofunctional predictors of treatment response. One of the key regions is the medial prefrontal cortex as well as the rostral anterior cingulate,” said Dr. Strawn, at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
On the neuropharmacology side, numerous medications have been approved for OCD. Dr. Strawn highlighted some studies to illustrate general OCD treatment concepts. That included the 2004 Pediatric OCD Treatment Study, which was one of the only trials to compare placebo with an SSRI, CBT, and the combination of SSRI and CBT. It showed the best results with combination therapy, and the difference appeared early in the treatment course.
That study had aggressive dosing, which led to some issues with sertraline tolerability. Dr. Strawn showed results of a study at his institution which showed that the drug levels of pediatric patients treated with sertraline depended on CYP2C19 metabolism, which affects overall exposure and peak dose concentration. In pediatric populations, some SSRIs clear more slowly and can have high peak concentrations. SSRIs have more side effects than serotonin and norepinephrine reuptake inhibitors in both anxiety disorders and OCD. A key difference between the two is that SSRI treatment is associated with greater frequency of activation, which is difficult to define, but includes restlessness and agitation and insomnia in the beginning stages of treatment.
SSRIs also lead to improvement early in the course of treatment, which was shown in a meta-analysis of nine trials. However, the same study showed that clomipramine is associated with a faster and greater magnitude of improvement, compared with SSRIs, even when the latter are dosed aggressively.
Clomipramine is a potent inhibitor of both serotonin and norepinephrine reuptake. It is recommended to monitor clomipramine levels in pediatric OCD patients, and Dr. Strawn suggested that monitoring should include both the parent drug and its primary metabolite, norclomipramine. At a given dose, there can be a great deal of variation in drug level. The clomipramine/norclomipramine ratio can provide information about the patient’s metabolic state, as well as drug adherence.
Dr. Strawn noted that peak levels occur around 1-3 hours after the dose, “and we really do want at least a 12-hour trough level.” EKGs should be performed at baseline and after any titration of clomipramine dose.
He also discussed pediatric OCD patients with OCD and tics. About one-third of Tourette syndrome patients experience OCD at some point. Tics often improve, whereas OCD more often persists. Tics that co-occur with OCD are associated with a lesser response to SSRI treatment, but not CBT treatment. Similarly, patients with hoarding tendencies are about one-third less likely to respond to SSRIs, CBT, or combination therapy.
Dr. Strawn discussed the concept of accommodation, in which family members cope with a patient’s behavior by altering routines to minimize distress and impairment. This may take the form of facilitating rituals, providing reassurance about a patient’s fears, acquiescing to demands, reducing the child’s day-to-day responsibilities, or helping the child complete tasks. Such actions are well intentioned, but they undermine cognitive control, negatively reinforce symptom engagement, and are associated with functional impairment. Reassurance is the most important behavior, occurring in more than half of patients, and it’s measurable. Parental involvement with rituals is also a concern. “This is associated with higher levels of child OCD severity, as well as parental psychopathology, and lower family cohesion. So
New developments in neurobiology and neuropsychology have changed the view of exposure. The old model emphasized the child’s fear rating as an index of corrective learning. The idea was that habituation would decrease anxiety and distress from future exposures. The new model revolves around inhibitory learning theory, which focuses on the variability of distress and aims to increase tolerance of distress. Another goal is to develop new, non-threat associations.
Finally, Dr. Strawn pointed out predictors of poor outcomes in pediatric OCD, including factors such as compulsion severity, oppositional behavior, frequent handwashing, functional impairment, lack of insight, externalizing symptoms, and possibly hoarding. Problematic family characteristics include higher levels of accommodation, parental anxiety, low family cohesion, and high levels of conflict. “The last three really represent a very concerning triad of family behaviors that may necessitate specific family work in order to facilitate the recovery of the pediatric patient,” Dr. Strawn said.
During the question-and-answer session after the talk, Dr. Strawn was asked whether there might be an inflammatory component to OCD, and whether pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) might be a prodromal condition. He noted that some studies have shown a relationship, but results have been mixed, with lots of heterogeneity within the studied populations. To be suspicious that a patient had OCD resulting from PANDAS would require a high threshold, including an acute onset of symptoms. “This is a situation also where I would tend to involve consultation with some other specialties, including neurology. And obviously there would be follow-up in terms of the general workup,” he said.
Dr. Strawn has received research funding from Allergan, Otsuka, and Myriad Genetics. He has consulted for Myriad Genetics, and is a speaker for CMEology and the Neuroscience Education Institute.
Treatment of pediatric obsessive-compulsive disorder (OCD) has evolved in recent years, with more attention given to some of the neuropsychiatric underpinnings of the condition and how they can affect treatment response.
At the Focus on Neuropsychiatry 2021 meeting, Jeffrey Strawn, MD, outlined some of the neuropsychiatry affecting disease and potential mechanisms to help control obsessions and behaviors, and how they may fit with some therapeutic regimens.
Dr. Strawn discussed the psychological construct of cognitive control, which can provide patients an “out” from the cycle of obsession/fear/worry and compulsion/avoidance. In the face of distress, compulsion and avoidance lead to relief, which reinforces the obsession/fear/worry; this in turn leads to more distress.
“We have an escape door for this circuit” in the form of cognitive control, said Dr. Strawn, who is an associate professor of pediatrics at Cincinnati Children’s Hospital Medical Center.
Cognitive control is linked to insight, which can in turn increase adaptive behaviors that help the patient resist the compulsion. Patients won’t eliminate distress, but they can be helped to make it more tolerable. Therapists can then help them move toward goal-directed thoughts and behaviors. Cognitive control is associated with several neural networks, but Dr. Strawn focused on two: the frontoparietal network, associated with top-down regulation; and the cingular-opercular network. Both of these are engaged during cognitive control processes, and play a role inhibitory control and error monitoring.
Dr. Strawn discussed a recent study that explored the neurofunctional basis of treatment. It compared the effects of a stress management therapy and cognitive-behavioral therapy (CBT) in children and adults with OCD at 6 and 12 weeks. The study found similar symptom reductions in both adults and adolescents in both intervention groups.
Before initiating treatment, the researchers conducted functional MRI scans of participants while conducting an incentive flanker task, which reveals brain activity in response to cognitive control and reward processing.
A larger therapeutic response was found in the CBT group among patients who had a larger pretreatment activation within the right temporal lobe and rostral anterior cingulate cortex during cognitive control, as well as those with more activation within the medial prefrontal, orbitofrontal, lateral prefrontal, and amygdala regions during reward processing. On the other hand, within the stress management therapy group, treatment responses were better among those who had lower pretreatment activation among overlapping regions.
“There was a difference in terms of the neurofunctional predictors of treatment response. One of the key regions is the medial prefrontal cortex as well as the rostral anterior cingulate,” said Dr. Strawn, at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
On the neuropharmacology side, numerous medications have been approved for OCD. Dr. Strawn highlighted some studies to illustrate general OCD treatment concepts. That included the 2004 Pediatric OCD Treatment Study, which was one of the only trials to compare placebo with an SSRI, CBT, and the combination of SSRI and CBT. It showed the best results with combination therapy, and the difference appeared early in the treatment course.
That study had aggressive dosing, which led to some issues with sertraline tolerability. Dr. Strawn showed results of a study at his institution which showed that the drug levels of pediatric patients treated with sertraline depended on CYP2C19 metabolism, which affects overall exposure and peak dose concentration. In pediatric populations, some SSRIs clear more slowly and can have high peak concentrations. SSRIs have more side effects than serotonin and norepinephrine reuptake inhibitors in both anxiety disorders and OCD. A key difference between the two is that SSRI treatment is associated with greater frequency of activation, which is difficult to define, but includes restlessness and agitation and insomnia in the beginning stages of treatment.
SSRIs also lead to improvement early in the course of treatment, which was shown in a meta-analysis of nine trials. However, the same study showed that clomipramine is associated with a faster and greater magnitude of improvement, compared with SSRIs, even when the latter are dosed aggressively.
Clomipramine is a potent inhibitor of both serotonin and norepinephrine reuptake. It is recommended to monitor clomipramine levels in pediatric OCD patients, and Dr. Strawn suggested that monitoring should include both the parent drug and its primary metabolite, norclomipramine. At a given dose, there can be a great deal of variation in drug level. The clomipramine/norclomipramine ratio can provide information about the patient’s metabolic state, as well as drug adherence.
Dr. Strawn noted that peak levels occur around 1-3 hours after the dose, “and we really do want at least a 12-hour trough level.” EKGs should be performed at baseline and after any titration of clomipramine dose.
He also discussed pediatric OCD patients with OCD and tics. About one-third of Tourette syndrome patients experience OCD at some point. Tics often improve, whereas OCD more often persists. Tics that co-occur with OCD are associated with a lesser response to SSRI treatment, but not CBT treatment. Similarly, patients with hoarding tendencies are about one-third less likely to respond to SSRIs, CBT, or combination therapy.
Dr. Strawn discussed the concept of accommodation, in which family members cope with a patient’s behavior by altering routines to minimize distress and impairment. This may take the form of facilitating rituals, providing reassurance about a patient’s fears, acquiescing to demands, reducing the child’s day-to-day responsibilities, or helping the child complete tasks. Such actions are well intentioned, but they undermine cognitive control, negatively reinforce symptom engagement, and are associated with functional impairment. Reassurance is the most important behavior, occurring in more than half of patients, and it’s measurable. Parental involvement with rituals is also a concern. “This is associated with higher levels of child OCD severity, as well as parental psychopathology, and lower family cohesion. So
New developments in neurobiology and neuropsychology have changed the view of exposure. The old model emphasized the child’s fear rating as an index of corrective learning. The idea was that habituation would decrease anxiety and distress from future exposures. The new model revolves around inhibitory learning theory, which focuses on the variability of distress and aims to increase tolerance of distress. Another goal is to develop new, non-threat associations.
Finally, Dr. Strawn pointed out predictors of poor outcomes in pediatric OCD, including factors such as compulsion severity, oppositional behavior, frequent handwashing, functional impairment, lack of insight, externalizing symptoms, and possibly hoarding. Problematic family characteristics include higher levels of accommodation, parental anxiety, low family cohesion, and high levels of conflict. “The last three really represent a very concerning triad of family behaviors that may necessitate specific family work in order to facilitate the recovery of the pediatric patient,” Dr. Strawn said.
During the question-and-answer session after the talk, Dr. Strawn was asked whether there might be an inflammatory component to OCD, and whether pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) might be a prodromal condition. He noted that some studies have shown a relationship, but results have been mixed, with lots of heterogeneity within the studied populations. To be suspicious that a patient had OCD resulting from PANDAS would require a high threshold, including an acute onset of symptoms. “This is a situation also where I would tend to involve consultation with some other specialties, including neurology. And obviously there would be follow-up in terms of the general workup,” he said.
Dr. Strawn has received research funding from Allergan, Otsuka, and Myriad Genetics. He has consulted for Myriad Genetics, and is a speaker for CMEology and the Neuroscience Education Institute.
FROM FOCUS ON NEUROPSYCHIATRY 2021
EDs saw more benzodiazepine overdoses, but fewer patients overall, in 2020
In a year when emergency department visits dropped by almost 18%, visits for benzodiazepine overdoses did the opposite, according to a report from the Centers for Disease Control and Prevention.
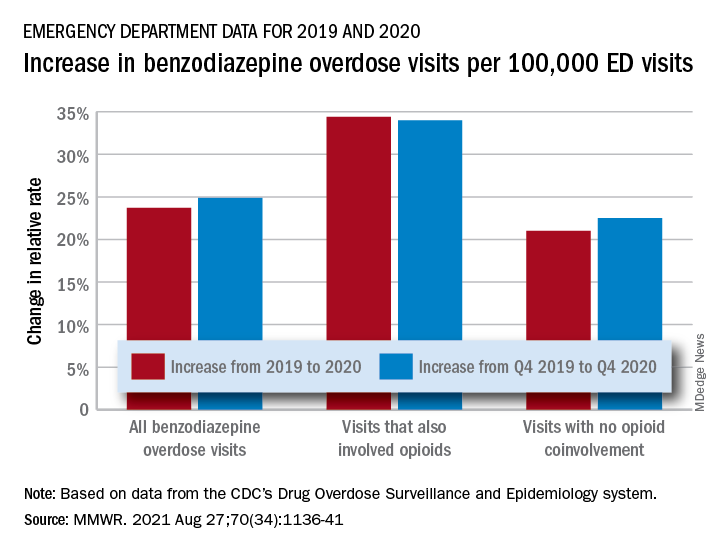
The actual increase in the number of overdose visits for benzodiazepine overdoses was quite small – from 15,547 in 2019 to 15,830 in 2020 (1.8%) – but the 11 million fewer ED visits magnified its effect, Stephen Liu, PhD, and associates said in the Morbidity and Mortality Weekly Report.
The rate of benzodiazepine overdose visits to all visits increased by 23.7% from 2019 (24.22 per 100,000 ED visits) to 2020 (29.97 per 100,000), with the larger share going to those involving opioids, which were up by 34.4%, compared with overdose visits not involving opioids (21.0%), the investigators said, based on data reported by 32 states and the District of Columbia to the CDC’s Drug Overdose Surveillance and Epidemiology system. All of the rate changes are statistically significant.
The number of overdose visits without opioid coinvolvement actually dropped, from 2019 (12,276) to 2020 (12,218), but not by enough to offset the decline in total visits, noted Dr. Liu, of the CDC’s National Center for Injury Prevention and Control and associates.
The number of deaths from benzodiazepine overdose, on the other hand, did not drop in 2020. Those data, coming from 23 states participating in the CDC’s State Unintentional Drug Overdose Reporting System, were available only for the first half of the year.
In those 6 months, The first quarter of 2020 also showed an increase, but exact numbers were not provided in the report. Overdose deaths rose by 22% for prescription forms of benzodiazepine and 520% for illicit forms in Q2 of 2020, compared with 2019, the researchers said.
Almost all of the benzodiazepine deaths (93%) in the first half of 2020 also involved opioids, mostly in the form of illicitly manufactured fentanyls (67% of all deaths). Between Q2 of 2019 and Q2 of 2020, involvement of illicit fentanyls in benzodiazepine overdose deaths increased from almost 57% to 71%, Dr. Liu and associates reported.
“Despite progress in reducing coprescribing [of opioids and benzodiazepines] before 2019, this study suggests a reversal in the decline in benzodiazepine deaths from 2017 to 2019, driven in part by increasing involvement of [illicitly manufactured fentanyls] in benzodiazepine deaths and influxes of illicit benzodiazepines,” they wrote.
In a year when emergency department visits dropped by almost 18%, visits for benzodiazepine overdoses did the opposite, according to a report from the Centers for Disease Control and Prevention.
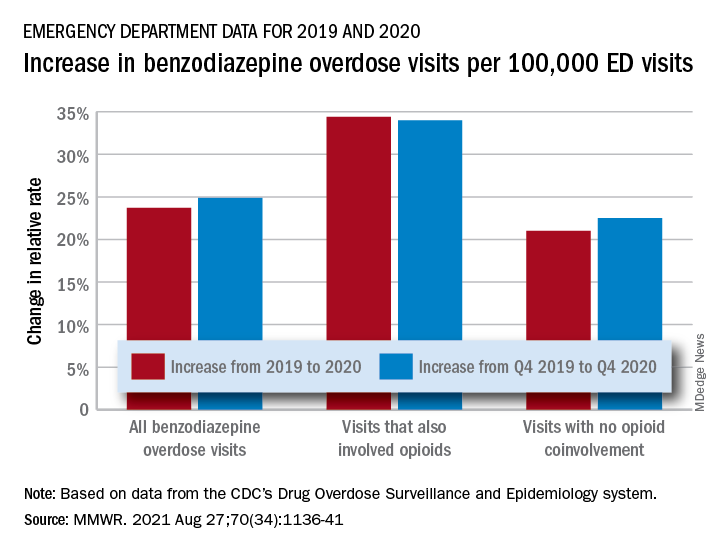
The actual increase in the number of overdose visits for benzodiazepine overdoses was quite small – from 15,547 in 2019 to 15,830 in 2020 (1.8%) – but the 11 million fewer ED visits magnified its effect, Stephen Liu, PhD, and associates said in the Morbidity and Mortality Weekly Report.
The rate of benzodiazepine overdose visits to all visits increased by 23.7% from 2019 (24.22 per 100,000 ED visits) to 2020 (29.97 per 100,000), with the larger share going to those involving opioids, which were up by 34.4%, compared with overdose visits not involving opioids (21.0%), the investigators said, based on data reported by 32 states and the District of Columbia to the CDC’s Drug Overdose Surveillance and Epidemiology system. All of the rate changes are statistically significant.
The number of overdose visits without opioid coinvolvement actually dropped, from 2019 (12,276) to 2020 (12,218), but not by enough to offset the decline in total visits, noted Dr. Liu, of the CDC’s National Center for Injury Prevention and Control and associates.
The number of deaths from benzodiazepine overdose, on the other hand, did not drop in 2020. Those data, coming from 23 states participating in the CDC’s State Unintentional Drug Overdose Reporting System, were available only for the first half of the year.
In those 6 months, The first quarter of 2020 also showed an increase, but exact numbers were not provided in the report. Overdose deaths rose by 22% for prescription forms of benzodiazepine and 520% for illicit forms in Q2 of 2020, compared with 2019, the researchers said.
Almost all of the benzodiazepine deaths (93%) in the first half of 2020 also involved opioids, mostly in the form of illicitly manufactured fentanyls (67% of all deaths). Between Q2 of 2019 and Q2 of 2020, involvement of illicit fentanyls in benzodiazepine overdose deaths increased from almost 57% to 71%, Dr. Liu and associates reported.
“Despite progress in reducing coprescribing [of opioids and benzodiazepines] before 2019, this study suggests a reversal in the decline in benzodiazepine deaths from 2017 to 2019, driven in part by increasing involvement of [illicitly manufactured fentanyls] in benzodiazepine deaths and influxes of illicit benzodiazepines,” they wrote.
In a year when emergency department visits dropped by almost 18%, visits for benzodiazepine overdoses did the opposite, according to a report from the Centers for Disease Control and Prevention.
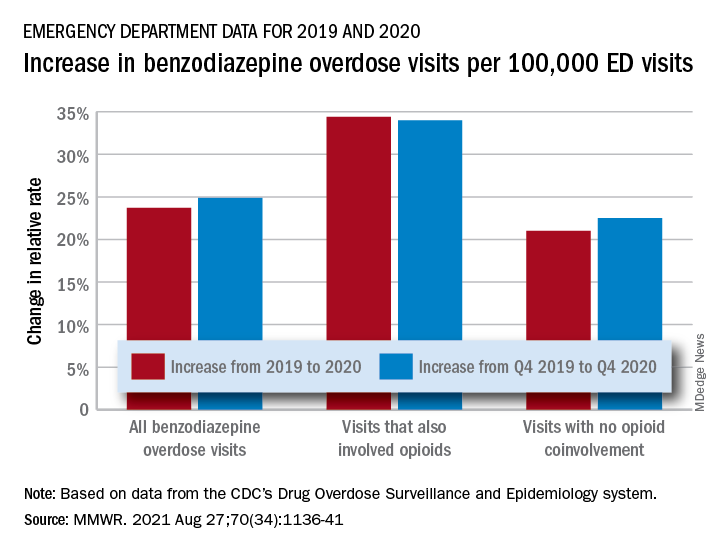
The actual increase in the number of overdose visits for benzodiazepine overdoses was quite small – from 15,547 in 2019 to 15,830 in 2020 (1.8%) – but the 11 million fewer ED visits magnified its effect, Stephen Liu, PhD, and associates said in the Morbidity and Mortality Weekly Report.
The rate of benzodiazepine overdose visits to all visits increased by 23.7% from 2019 (24.22 per 100,000 ED visits) to 2020 (29.97 per 100,000), with the larger share going to those involving opioids, which were up by 34.4%, compared with overdose visits not involving opioids (21.0%), the investigators said, based on data reported by 32 states and the District of Columbia to the CDC’s Drug Overdose Surveillance and Epidemiology system. All of the rate changes are statistically significant.
The number of overdose visits without opioid coinvolvement actually dropped, from 2019 (12,276) to 2020 (12,218), but not by enough to offset the decline in total visits, noted Dr. Liu, of the CDC’s National Center for Injury Prevention and Control and associates.
The number of deaths from benzodiazepine overdose, on the other hand, did not drop in 2020. Those data, coming from 23 states participating in the CDC’s State Unintentional Drug Overdose Reporting System, were available only for the first half of the year.
In those 6 months, The first quarter of 2020 also showed an increase, but exact numbers were not provided in the report. Overdose deaths rose by 22% for prescription forms of benzodiazepine and 520% for illicit forms in Q2 of 2020, compared with 2019, the researchers said.
Almost all of the benzodiazepine deaths (93%) in the first half of 2020 also involved opioids, mostly in the form of illicitly manufactured fentanyls (67% of all deaths). Between Q2 of 2019 and Q2 of 2020, involvement of illicit fentanyls in benzodiazepine overdose deaths increased from almost 57% to 71%, Dr. Liu and associates reported.
“Despite progress in reducing coprescribing [of opioids and benzodiazepines] before 2019, this study suggests a reversal in the decline in benzodiazepine deaths from 2017 to 2019, driven in part by increasing involvement of [illicitly manufactured fentanyls] in benzodiazepine deaths and influxes of illicit benzodiazepines,” they wrote.
FROM MMWR
Number of global deaths by suicide increased over 30 years
The overall global number of deaths by suicide increased by almost 20,000 during the past 30 years, new research shows.
The increase occurred despite a significant decrease in age-specific suicide rates from 1990 through 2019, according to data from the Global Burden of Disease Study 2019.
Population growth, population aging, and changes in population age structure may explain the increase in number of suicide deaths, the investigators note.
“As suicide rates are highest among the elderly (70 years or above) for both genders in almost all regions of the world, the rapidly aging population globally will pose huge challenges for the reduction in the number of suicide deaths in the future,” write the researchers, led by Paul Siu Fai Yip, PhD, of the HKJC Center for Suicide Research and Prevention, University of Hong Kong, China.
The findings were published online Aug. 16 in Injury Prevention.
Global public health concern
Around the world, approximately 800,000 individuals die by suicide each year, while many others attempt suicide. Yet suicide has not received the same level of attention as other global public health concerns, such as HIV/AIDS and cancer, the investigators write.
They examined data from the Global Burden of Disease Study 2019 to assess how demographic and epidemiologic factors contributed to the number of suicide deaths during the past 30 years.
The researchers also analyzed relationships between population growth, population age structure, income level, and gender- and age-specific suicide rates.
The Global Burden of Disease Study 2019 includes information from 204 countries about 369 diseases and injuries by age and gender. The dataset also includes population estimates for each year by location, age group, and gender.
In their analysis, the investigators looked at changes in suicide rates and the number of suicide deaths from 1990 to 2019 by gender and age group in the four income level regions defined by the World Bank. These categories include low-income, lower-middle–income, upper-middle–income, and high-income regions.
Number of deaths versus suicide rates
The number of deaths was 738,799 in 1990 and 758,696 in 2019.
The largest increase in deaths occurred in the lower-middle–income region, where the number of suicide deaths increased by 72,550 (from 232,340 to 304,890).
Population growth (300,942; 1,512.5%) was the major contributor to the overall increase in total number of suicide deaths. The second largest contributor was population age structure (189,512; 952.4%).
However, the effects of these factors were offset to a large extent by the effect of reduction in overall suicide rates (−470,556; −2,364.9%).
Interestingly, the overall suicide rate per 100,000 population decreased from 13.8 in 1990 to 9.8 in 2019.
The upper-middle–income region had the largest decline (−6.25 per 100,000), and the high-income region had the smallest decline (−1.77 per 100,000). Suicide rates also decreased in lower-middle–income (−2.51 per 100,000) and low-income regions (−1.96 per 100,000).
Reasons for the declines across all regions “have yet to be determined,” write the investigators. International efforts coordinated by the United Nations and World Health Organization likely contributed to these declines, they add.
‘Imbalance of resources’
The overall reduction in suicide rate of −4.01 per 100,000 “was mainly due” to reduction in age-specific suicide rates (−6.09; 152%), the researchers report.
This effect was partly offset, however, by the effect of the changing population age structure (2.08; −52%). In the high-income–level region, for example, the reduction in age-specific suicide rate (−3.83; 216.3%) was greater than the increase resulting from the change in population age structure (2.06; −116.3%).
“The overall contribution of population age structure mainly came from the 45-64 (565.2%) and 65+ (528.7%) age groups,” the investigators write. “This effect was observed in middle-income– as well as high-income–level regions, reflecting the global effect of population aging.”
They add that world populations will “experience pronounced and historically unprecedented aging in the coming decades” because of increasing life expectancy and declining fertility.
Men, but not women, had a notable increase in total number of suicide deaths. The significant effect of male population growth (177,128; 890.2% vs. 123,814; 622.3% for women) and male population age structure (120,186; 604.0% vs. 69,325; 348.4%) were the main factors that explained this increase, the investigators note.
However, from 1990 to 2019, the overall suicide rate per 100,000 men decreased from 16.6 to 13.5 (–3.09). The decline in overall suicide rate was even greater for women, from 11.0 to 6.1 (–4.91).
This finding was particularly notable in the upper-middle–income region (–8.12 women vs. –4.37 men per 100,000).
“This study highlighted the considerable imbalance of the resources in carrying out suicide prevention work, especially in low-income and middle-income countries,” the investigators write.
“It is time to revisit this situation to ensure that sufficient resources can be redeployed globally to meet the future challenges,” they add.
The study was funded by a Humanities and Social Sciences Prestigious Fellowship, which Dr. Yip received. He declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The overall global number of deaths by suicide increased by almost 20,000 during the past 30 years, new research shows.
The increase occurred despite a significant decrease in age-specific suicide rates from 1990 through 2019, according to data from the Global Burden of Disease Study 2019.
Population growth, population aging, and changes in population age structure may explain the increase in number of suicide deaths, the investigators note.
“As suicide rates are highest among the elderly (70 years or above) for both genders in almost all regions of the world, the rapidly aging population globally will pose huge challenges for the reduction in the number of suicide deaths in the future,” write the researchers, led by Paul Siu Fai Yip, PhD, of the HKJC Center for Suicide Research and Prevention, University of Hong Kong, China.
The findings were published online Aug. 16 in Injury Prevention.
Global public health concern
Around the world, approximately 800,000 individuals die by suicide each year, while many others attempt suicide. Yet suicide has not received the same level of attention as other global public health concerns, such as HIV/AIDS and cancer, the investigators write.
They examined data from the Global Burden of Disease Study 2019 to assess how demographic and epidemiologic factors contributed to the number of suicide deaths during the past 30 years.
The researchers also analyzed relationships between population growth, population age structure, income level, and gender- and age-specific suicide rates.
The Global Burden of Disease Study 2019 includes information from 204 countries about 369 diseases and injuries by age and gender. The dataset also includes population estimates for each year by location, age group, and gender.
In their analysis, the investigators looked at changes in suicide rates and the number of suicide deaths from 1990 to 2019 by gender and age group in the four income level regions defined by the World Bank. These categories include low-income, lower-middle–income, upper-middle–income, and high-income regions.
Number of deaths versus suicide rates
The number of deaths was 738,799 in 1990 and 758,696 in 2019.
The largest increase in deaths occurred in the lower-middle–income region, where the number of suicide deaths increased by 72,550 (from 232,340 to 304,890).
Population growth (300,942; 1,512.5%) was the major contributor to the overall increase in total number of suicide deaths. The second largest contributor was population age structure (189,512; 952.4%).
However, the effects of these factors were offset to a large extent by the effect of reduction in overall suicide rates (−470,556; −2,364.9%).
Interestingly, the overall suicide rate per 100,000 population decreased from 13.8 in 1990 to 9.8 in 2019.
The upper-middle–income region had the largest decline (−6.25 per 100,000), and the high-income region had the smallest decline (−1.77 per 100,000). Suicide rates also decreased in lower-middle–income (−2.51 per 100,000) and low-income regions (−1.96 per 100,000).
Reasons for the declines across all regions “have yet to be determined,” write the investigators. International efforts coordinated by the United Nations and World Health Organization likely contributed to these declines, they add.
‘Imbalance of resources’
The overall reduction in suicide rate of −4.01 per 100,000 “was mainly due” to reduction in age-specific suicide rates (−6.09; 152%), the researchers report.
This effect was partly offset, however, by the effect of the changing population age structure (2.08; −52%). In the high-income–level region, for example, the reduction in age-specific suicide rate (−3.83; 216.3%) was greater than the increase resulting from the change in population age structure (2.06; −116.3%).
“The overall contribution of population age structure mainly came from the 45-64 (565.2%) and 65+ (528.7%) age groups,” the investigators write. “This effect was observed in middle-income– as well as high-income–level regions, reflecting the global effect of population aging.”
They add that world populations will “experience pronounced and historically unprecedented aging in the coming decades” because of increasing life expectancy and declining fertility.
Men, but not women, had a notable increase in total number of suicide deaths. The significant effect of male population growth (177,128; 890.2% vs. 123,814; 622.3% for women) and male population age structure (120,186; 604.0% vs. 69,325; 348.4%) were the main factors that explained this increase, the investigators note.
However, from 1990 to 2019, the overall suicide rate per 100,000 men decreased from 16.6 to 13.5 (–3.09). The decline in overall suicide rate was even greater for women, from 11.0 to 6.1 (–4.91).
This finding was particularly notable in the upper-middle–income region (–8.12 women vs. –4.37 men per 100,000).
“This study highlighted the considerable imbalance of the resources in carrying out suicide prevention work, especially in low-income and middle-income countries,” the investigators write.
“It is time to revisit this situation to ensure that sufficient resources can be redeployed globally to meet the future challenges,” they add.
The study was funded by a Humanities and Social Sciences Prestigious Fellowship, which Dr. Yip received. He declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The overall global number of deaths by suicide increased by almost 20,000 during the past 30 years, new research shows.
The increase occurred despite a significant decrease in age-specific suicide rates from 1990 through 2019, according to data from the Global Burden of Disease Study 2019.
Population growth, population aging, and changes in population age structure may explain the increase in number of suicide deaths, the investigators note.
“As suicide rates are highest among the elderly (70 years or above) for both genders in almost all regions of the world, the rapidly aging population globally will pose huge challenges for the reduction in the number of suicide deaths in the future,” write the researchers, led by Paul Siu Fai Yip, PhD, of the HKJC Center for Suicide Research and Prevention, University of Hong Kong, China.
The findings were published online Aug. 16 in Injury Prevention.
Global public health concern
Around the world, approximately 800,000 individuals die by suicide each year, while many others attempt suicide. Yet suicide has not received the same level of attention as other global public health concerns, such as HIV/AIDS and cancer, the investigators write.
They examined data from the Global Burden of Disease Study 2019 to assess how demographic and epidemiologic factors contributed to the number of suicide deaths during the past 30 years.
The researchers also analyzed relationships between population growth, population age structure, income level, and gender- and age-specific suicide rates.
The Global Burden of Disease Study 2019 includes information from 204 countries about 369 diseases and injuries by age and gender. The dataset also includes population estimates for each year by location, age group, and gender.
In their analysis, the investigators looked at changes in suicide rates and the number of suicide deaths from 1990 to 2019 by gender and age group in the four income level regions defined by the World Bank. These categories include low-income, lower-middle–income, upper-middle–income, and high-income regions.
Number of deaths versus suicide rates
The number of deaths was 738,799 in 1990 and 758,696 in 2019.
The largest increase in deaths occurred in the lower-middle–income region, where the number of suicide deaths increased by 72,550 (from 232,340 to 304,890).
Population growth (300,942; 1,512.5%) was the major contributor to the overall increase in total number of suicide deaths. The second largest contributor was population age structure (189,512; 952.4%).
However, the effects of these factors were offset to a large extent by the effect of reduction in overall suicide rates (−470,556; −2,364.9%).
Interestingly, the overall suicide rate per 100,000 population decreased from 13.8 in 1990 to 9.8 in 2019.
The upper-middle–income region had the largest decline (−6.25 per 100,000), and the high-income region had the smallest decline (−1.77 per 100,000). Suicide rates also decreased in lower-middle–income (−2.51 per 100,000) and low-income regions (−1.96 per 100,000).
Reasons for the declines across all regions “have yet to be determined,” write the investigators. International efforts coordinated by the United Nations and World Health Organization likely contributed to these declines, they add.
‘Imbalance of resources’
The overall reduction in suicide rate of −4.01 per 100,000 “was mainly due” to reduction in age-specific suicide rates (−6.09; 152%), the researchers report.
This effect was partly offset, however, by the effect of the changing population age structure (2.08; −52%). In the high-income–level region, for example, the reduction in age-specific suicide rate (−3.83; 216.3%) was greater than the increase resulting from the change in population age structure (2.06; −116.3%).
“The overall contribution of population age structure mainly came from the 45-64 (565.2%) and 65+ (528.7%) age groups,” the investigators write. “This effect was observed in middle-income– as well as high-income–level regions, reflecting the global effect of population aging.”
They add that world populations will “experience pronounced and historically unprecedented aging in the coming decades” because of increasing life expectancy and declining fertility.
Men, but not women, had a notable increase in total number of suicide deaths. The significant effect of male population growth (177,128; 890.2% vs. 123,814; 622.3% for women) and male population age structure (120,186; 604.0% vs. 69,325; 348.4%) were the main factors that explained this increase, the investigators note.
However, from 1990 to 2019, the overall suicide rate per 100,000 men decreased from 16.6 to 13.5 (–3.09). The decline in overall suicide rate was even greater for women, from 11.0 to 6.1 (–4.91).
This finding was particularly notable in the upper-middle–income region (–8.12 women vs. –4.37 men per 100,000).
“This study highlighted the considerable imbalance of the resources in carrying out suicide prevention work, especially in low-income and middle-income countries,” the investigators write.
“It is time to revisit this situation to ensure that sufficient resources can be redeployed globally to meet the future challenges,” they add.
The study was funded by a Humanities and Social Sciences Prestigious Fellowship, which Dr. Yip received. He declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alcohol use by young adolescents drops during pandemic
The restrictions resulting from the COVID-19 pandemic altered patterns of substance use by early adolescents to less alcohol use and greater use and misuse of nicotine and prescription drugs, based on data from more than 7,000 youth aged 10-14 years.
Substance use in early adolescence is a function of many environmental factors including substance availability, parent and peer use, and family function, as well as macroeconomic factors, William E. Pelham III, PhD, of the University of California, San Diego, and colleagues wrote. “Thus, it is critical to evaluate how substance use during early adolescence has been impacted by the coronavirus disease 2019 (COVID-19) pandemic, a source of large and sustained disruptions to adolescents’ daily lives in terms of education, contact with family/friends, and health behaviors.”
In a prospective, community-based cohort study, published in the Journal of Adolescent Health, the researchers conducted a three-wave assessment of substance use between May 2020 and August 2020, and reviewed prepandemic assessments from 2018 to 2019. The participants included 7,842 adolescents with an average age of 12 years who were initially enrolled in the Adolescent Brain Cognitive Development (ABCD) study at age 9-10 years. At the start of the study, 48% of the participants were female, 20% were Hispanic, 15% were Black, and 2% were Asian. Participants completed three online surveys between May 2020 and August 2020.
Each survey included the number of days in the past 30 days in which the adolescents drank alcohol; smoked cigarettes; used electronic nicotine delivery systems; smoked a cigar, hookah, or pipe; used smokeless tobacco products; used a cannabis product; abused prescription drugs; used inhalants; or used any other drugs. The response scale was 0 days to 10-plus days.
The overall prevalence of substance use among young adolescents was similar between prepandemic and pandemic periods; however fewer respondents reported using alcohol, but more reported using nicotine or misusing prescription medications.
Across all three survey periods, 7.4% of youth reported any substance use, 3.4% reported ever using alcohol, and 3.2% reported ever using nicotine. Of those who reported substance use, 79% reported 1-2 days of use in the past month, and 87% reported using a single substance.
In comparing prepandemic and pandemic substance use, the prevalence of alcohol use in the past 30 days decreased significantly, from 2.1% to 0.8%. However, use of nicotine increased significantly from 0% to 1.3%, and misuse of prescription drugs increased significantly from 0% to 0.6%. “Changes in the rates of use of any substance, cannabis, or inhalants were not statistically significant,” the researchers wrote.
Sex and ethnicity were not associated with substance use during the pandemic, but rates of substance use were higher among youth whose parents were unmarried or had lower levels of education, and among those with preexisting externalizing and internalizing behaviors. Youth who reported higher levels of uncertainty related to COVID-19 were significantly more likely to report substance use; additionally, stress, anxiety, and depressive symptoms were positively association with any substance use during the pandemic survey periods. Youth whose parents experienced hardship or whose parents used alcohol or drugs also were more likely to report substance use.
“Stability in the overall rate of substance use in this cohort is reassuring given that the pandemic has brought increases in teens’ unoccupied time, stress, and loneliness, reduced access to support services, and disruptions to routines and family/parenting practices, all of which might be expected to have increased youth substance use,” the researchers noted. The findings do not explain the decreased alcohol use, but the researchers cited possible reasons for reduced alcohol use including lack of contact with friends and social activities, and greater supervision by parents.
The study findings were limited by several factors including the comparison of prepandemic and pandemic substance use in younger adolescents, which may not reflect changes in substance use in older adolescents. The study also could not establish causality, and did not account for the intensity of substance use, such as number of drinks, the researchers wrote. However, the results were strengthened by the longitudinal design and large, diverse study population, and the use of prepandemic assessments that allowed evaluation of changes over time.
Overall, the results highlight the importance of preexisting and acute risk protective factors in mitigating substance use in young adolescents, and suggest the potential of economic support for families and emotional support for youth as ways to reduce risk, the researchers concluded.
Predicting use and identifying risk factors
“It was important to conduct research at this time so we know how trends have changed during the pandemic,” Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview. The research helps clinicians “so we can better predict which substances our patients may be using, especially those with preexisting psychological conditions and those at socioeconomic disadvantage.
“I was surprised by the increased prescription drug use, but it make sense, as adolescents are at home more and may be illicitly using their parents medications,” Dr. Kinsella noted. “I think as they go back to school, trends will shift back to where they were as they will be spending more time with friends.” The take-home message to clinicians is the increased use of nicotine and prescription drugs during the pandemic, and future research should focus on substance use trends in 14- to 20-year-olds.
The ABCD study was supported by the National Institutes of Health, and the current study also received support from the National Science Foundation and Children and Screens: Institute of Digital Media and Child Development. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
The restrictions resulting from the COVID-19 pandemic altered patterns of substance use by early adolescents to less alcohol use and greater use and misuse of nicotine and prescription drugs, based on data from more than 7,000 youth aged 10-14 years.
Substance use in early adolescence is a function of many environmental factors including substance availability, parent and peer use, and family function, as well as macroeconomic factors, William E. Pelham III, PhD, of the University of California, San Diego, and colleagues wrote. “Thus, it is critical to evaluate how substance use during early adolescence has been impacted by the coronavirus disease 2019 (COVID-19) pandemic, a source of large and sustained disruptions to adolescents’ daily lives in terms of education, contact with family/friends, and health behaviors.”
In a prospective, community-based cohort study, published in the Journal of Adolescent Health, the researchers conducted a three-wave assessment of substance use between May 2020 and August 2020, and reviewed prepandemic assessments from 2018 to 2019. The participants included 7,842 adolescents with an average age of 12 years who were initially enrolled in the Adolescent Brain Cognitive Development (ABCD) study at age 9-10 years. At the start of the study, 48% of the participants were female, 20% were Hispanic, 15% were Black, and 2% were Asian. Participants completed three online surveys between May 2020 and August 2020.
Each survey included the number of days in the past 30 days in which the adolescents drank alcohol; smoked cigarettes; used electronic nicotine delivery systems; smoked a cigar, hookah, or pipe; used smokeless tobacco products; used a cannabis product; abused prescription drugs; used inhalants; or used any other drugs. The response scale was 0 days to 10-plus days.
The overall prevalence of substance use among young adolescents was similar between prepandemic and pandemic periods; however fewer respondents reported using alcohol, but more reported using nicotine or misusing prescription medications.
Across all three survey periods, 7.4% of youth reported any substance use, 3.4% reported ever using alcohol, and 3.2% reported ever using nicotine. Of those who reported substance use, 79% reported 1-2 days of use in the past month, and 87% reported using a single substance.
In comparing prepandemic and pandemic substance use, the prevalence of alcohol use in the past 30 days decreased significantly, from 2.1% to 0.8%. However, use of nicotine increased significantly from 0% to 1.3%, and misuse of prescription drugs increased significantly from 0% to 0.6%. “Changes in the rates of use of any substance, cannabis, or inhalants were not statistically significant,” the researchers wrote.
Sex and ethnicity were not associated with substance use during the pandemic, but rates of substance use were higher among youth whose parents were unmarried or had lower levels of education, and among those with preexisting externalizing and internalizing behaviors. Youth who reported higher levels of uncertainty related to COVID-19 were significantly more likely to report substance use; additionally, stress, anxiety, and depressive symptoms were positively association with any substance use during the pandemic survey periods. Youth whose parents experienced hardship or whose parents used alcohol or drugs also were more likely to report substance use.
“Stability in the overall rate of substance use in this cohort is reassuring given that the pandemic has brought increases in teens’ unoccupied time, stress, and loneliness, reduced access to support services, and disruptions to routines and family/parenting practices, all of which might be expected to have increased youth substance use,” the researchers noted. The findings do not explain the decreased alcohol use, but the researchers cited possible reasons for reduced alcohol use including lack of contact with friends and social activities, and greater supervision by parents.
The study findings were limited by several factors including the comparison of prepandemic and pandemic substance use in younger adolescents, which may not reflect changes in substance use in older adolescents. The study also could not establish causality, and did not account for the intensity of substance use, such as number of drinks, the researchers wrote. However, the results were strengthened by the longitudinal design and large, diverse study population, and the use of prepandemic assessments that allowed evaluation of changes over time.
Overall, the results highlight the importance of preexisting and acute risk protective factors in mitigating substance use in young adolescents, and suggest the potential of economic support for families and emotional support for youth as ways to reduce risk, the researchers concluded.
Predicting use and identifying risk factors
“It was important to conduct research at this time so we know how trends have changed during the pandemic,” Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview. The research helps clinicians “so we can better predict which substances our patients may be using, especially those with preexisting psychological conditions and those at socioeconomic disadvantage.
“I was surprised by the increased prescription drug use, but it make sense, as adolescents are at home more and may be illicitly using their parents medications,” Dr. Kinsella noted. “I think as they go back to school, trends will shift back to where they were as they will be spending more time with friends.” The take-home message to clinicians is the increased use of nicotine and prescription drugs during the pandemic, and future research should focus on substance use trends in 14- to 20-year-olds.
The ABCD study was supported by the National Institutes of Health, and the current study also received support from the National Science Foundation and Children and Screens: Institute of Digital Media and Child Development. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
The restrictions resulting from the COVID-19 pandemic altered patterns of substance use by early adolescents to less alcohol use and greater use and misuse of nicotine and prescription drugs, based on data from more than 7,000 youth aged 10-14 years.
Substance use in early adolescence is a function of many environmental factors including substance availability, parent and peer use, and family function, as well as macroeconomic factors, William E. Pelham III, PhD, of the University of California, San Diego, and colleagues wrote. “Thus, it is critical to evaluate how substance use during early adolescence has been impacted by the coronavirus disease 2019 (COVID-19) pandemic, a source of large and sustained disruptions to adolescents’ daily lives in terms of education, contact with family/friends, and health behaviors.”
In a prospective, community-based cohort study, published in the Journal of Adolescent Health, the researchers conducted a three-wave assessment of substance use between May 2020 and August 2020, and reviewed prepandemic assessments from 2018 to 2019. The participants included 7,842 adolescents with an average age of 12 years who were initially enrolled in the Adolescent Brain Cognitive Development (ABCD) study at age 9-10 years. At the start of the study, 48% of the participants were female, 20% were Hispanic, 15% were Black, and 2% were Asian. Participants completed three online surveys between May 2020 and August 2020.
Each survey included the number of days in the past 30 days in which the adolescents drank alcohol; smoked cigarettes; used electronic nicotine delivery systems; smoked a cigar, hookah, or pipe; used smokeless tobacco products; used a cannabis product; abused prescription drugs; used inhalants; or used any other drugs. The response scale was 0 days to 10-plus days.
The overall prevalence of substance use among young adolescents was similar between prepandemic and pandemic periods; however fewer respondents reported using alcohol, but more reported using nicotine or misusing prescription medications.
Across all three survey periods, 7.4% of youth reported any substance use, 3.4% reported ever using alcohol, and 3.2% reported ever using nicotine. Of those who reported substance use, 79% reported 1-2 days of use in the past month, and 87% reported using a single substance.
In comparing prepandemic and pandemic substance use, the prevalence of alcohol use in the past 30 days decreased significantly, from 2.1% to 0.8%. However, use of nicotine increased significantly from 0% to 1.3%, and misuse of prescription drugs increased significantly from 0% to 0.6%. “Changes in the rates of use of any substance, cannabis, or inhalants were not statistically significant,” the researchers wrote.
Sex and ethnicity were not associated with substance use during the pandemic, but rates of substance use were higher among youth whose parents were unmarried or had lower levels of education, and among those with preexisting externalizing and internalizing behaviors. Youth who reported higher levels of uncertainty related to COVID-19 were significantly more likely to report substance use; additionally, stress, anxiety, and depressive symptoms were positively association with any substance use during the pandemic survey periods. Youth whose parents experienced hardship or whose parents used alcohol or drugs also were more likely to report substance use.
“Stability in the overall rate of substance use in this cohort is reassuring given that the pandemic has brought increases in teens’ unoccupied time, stress, and loneliness, reduced access to support services, and disruptions to routines and family/parenting practices, all of which might be expected to have increased youth substance use,” the researchers noted. The findings do not explain the decreased alcohol use, but the researchers cited possible reasons for reduced alcohol use including lack of contact with friends and social activities, and greater supervision by parents.
The study findings were limited by several factors including the comparison of prepandemic and pandemic substance use in younger adolescents, which may not reflect changes in substance use in older adolescents. The study also could not establish causality, and did not account for the intensity of substance use, such as number of drinks, the researchers wrote. However, the results were strengthened by the longitudinal design and large, diverse study population, and the use of prepandemic assessments that allowed evaluation of changes over time.
Overall, the results highlight the importance of preexisting and acute risk protective factors in mitigating substance use in young adolescents, and suggest the potential of economic support for families and emotional support for youth as ways to reduce risk, the researchers concluded.
Predicting use and identifying risk factors
“It was important to conduct research at this time so we know how trends have changed during the pandemic,” Karalyn Kinsella, MD, a pediatrician in private practice in Cheshire, Conn., said in an interview. The research helps clinicians “so we can better predict which substances our patients may be using, especially those with preexisting psychological conditions and those at socioeconomic disadvantage.
“I was surprised by the increased prescription drug use, but it make sense, as adolescents are at home more and may be illicitly using their parents medications,” Dr. Kinsella noted. “I think as they go back to school, trends will shift back to where they were as they will be spending more time with friends.” The take-home message to clinicians is the increased use of nicotine and prescription drugs during the pandemic, and future research should focus on substance use trends in 14- to 20-year-olds.
The ABCD study was supported by the National Institutes of Health, and the current study also received support from the National Science Foundation and Children and Screens: Institute of Digital Media and Child Development. The researchers had no financial conflicts to disclose. Dr. Kinsella had no financial conflicts to disclose, but serves on the editorial advisory board of Pediatric News.
FROM THE JOURNAL OF ADOLESCENT HEALTH
Antidepressant helps prevent hospitalization in COVID patients: Study
A handful of studies have suggested that for newly infected COVID-19 patients, risk for serious illness may be reduced with a short course of fluvoxamine (Luvox), a decades-old pill typically prescribed for depression or obsessive-compulsive disorder (OCD). But those were small studies involving just a few hundred people.
This week, researchers reported promising data from a large, randomized phase 3 trial that enrolled COVID-19 patients from 11 sites in Brazil. In this study, in which 1,472 people were assigned to receive either a 10-day course of fluvoxamine or placebo pills, the antidepressant cut emergency department and hospital admissions by 29%.
Findings from the new study, which have not yet been peer reviewed, were published August 23 in MedRxiv.
Around the globe, particularly in countries without access to vaccines, “treatment options that are cheap and available and supported by good-quality evidence are the only hope we’ve got to reduce mortality within high-risk populations,” said Edward Mills, PhD, professor in the department of health research methods, evidence, and impact, McMaster University, Hamilton, Ont.
The new findings came from TOGETHER, a large platform trial coordinated by Dr. Mills and colleagues to evaluate the use of fluvoxamine and other repurposed drug candidates for symptomatic, high-risk, adult outpatients with confirmed cases of COVID-19.
The trial’s adaptive format allows multiple agents to be added and tested alongside placebo in a single master protocol – similar to the United Kingdom’s Recovery trial, which found that the common steroid dexamethasone could reduce deaths among hospitalized COVID-19 patients.
In platform trials, treatment arms can be dropped for futility, as was the case with hydroxychloroquine and lopinavir-ritonavir, neither of which did better than placebo at preventing hospitalization in an earlier TOGETHER trial analysis.
Study details
In the newly reported analysis, patients were randomly assigned to receive fluvoxamine or placebo between January and August 2021. Participants took fluvoxamine 100 mg twice daily for 10 days. By comparison, the U.S. Food and Drug Administration recommends a maximum daily dose of 300 mg of fluvoxamine for patients with OCD; full psychiatric benefits occur after 6 weeks.
For the primary outcome, the investigators assessed whether the conditions of patients with COVID worsened over a 28-day period so as to require either hospitalization or observation in the emergency department for more than 6 hours. In the placebo group, 108 of 733 patients’ conditions deteriorated to this extent (14.7%); by contrast, only 77 of 739 patients in the fluvoxamine group (10.4%) met these primary criteria – a relative risk reduction of 29%.
The treatment effect was greater (34%) in the per protocol analysis of participants who completed their course of pills.
The investigators also collected data on vital signs, including temperature and oxygen saturation, as well as adverse events reported at clinic visits or through video conferencing, phone calls, or social media applications. Side effects were mild, most commonly nausea and fatigue, and did not differ significantly between active treatment and control groups, Dr. Mills said in an interview.
Amid scores of studies evaluating repurposed drugs for COVID-19, the data on fluvoxamine are “looking much more favorable than anyone could have guessed – at least anyone in infectious disease,” said Paul Sax, MD, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The new TOGETHER trial results augment supportive data published in JAMA last November from a phase 2 randomized trial that was small but “very well done,” Dr. Sax told this news organization.
Those results got a boost from a subsequent study of 65 racetrack workers who chose to take fluvoxamine during a COVID-19 outbreak in the San Francisco Bay area. Forty-eight persons opted against taking the drug. In this small, nonrandomized study, “the people who chose to be treated with fluvoxamine were sicker [at baseline] than the people who didn’t go on it, and yet the [treated group] ended up better,” said Dr. Sax, who discussed accumulating data on the use of fluvoxamine for COVID-19 in a recent New England Journal of Medicine blog post.
Anti-inflammatory effect?
After reviewing the new findings, Frank Domino, MD, professor of family medicine and community health at the University of Massachusetts, Worcester, said he would encourage patients with high-risk COVID-19 to consider taking fluvoxamine to lower their risk of being hospitalized. “But I would make it clear this was not a ‘cure,’ “ he said, “and we are unsure how it helps.”
At this point, U.S. treatment guidelines do not recommend fluvoxamine as the standard of care for nonhospitalized COVID-19 patients, but the National Institutes of Health is “very aware of the data,” Dr. Sax told this news organization.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) – a class of drugs that includes the more commonly prescribed antidepressant fluoxetine (Prozac). If prescribed off-label to COVID-19 patients, fluvoxamine should not be used within 2 weeks of starting treatment with other SSRI or monoamine oxidase inhibitor antidepressants and should be used with caution with other QT-interval prolonging medications, Dr. Sax said.
In addition, fluvoxamine can enhance the effect of antiplatelet and anticoagulant drugs, potentially triggering bleeding.
On the basis of in vitro and mouse studies of fluvoxamine, “we think it has an anti-inflammatory effect,” said child psychiatrist Angela Reiersen, MD, of Washington University, St. Louis, who came up with the idea for testing fluvoxamine in last year’s phase 2 trial and coauthored a recent article describing the drug’s potential mechanisms of action in COVID-19.
She and other researchers believe fluvoxamine’s anti-inflammatory effects derive from the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, which regulates cellular responses to stress and infection.
Fluvoxamine also inhibits the activation of platelets. “In COVID-19, there does seem to be a problem with hyperactivation of platelets and excessive blood clots forming, so it is possible this could be another mechanism where it might be helping,” Dr. Reiersen said.
If sigma-1 activation turns out to be the main mechanism underlying fluvoxamine’s benefits in COVID-19, other sigma-1 agonists, such as fluoxetine, may also help. In a retrospective analysis of thousands of adults hospitalized for COVID-19 in France early in the pandemic, those who were taking antidepressants had a 44% lower risk for intubation or death.
And in a study under review, researchers at Stanford (Calif.) University and the University of California, San Francisco, analyzed electronic health records to explore a potential link between fluoxetine use and COVID outcomes among more than 80,000 patients from over 80 institutions across the United States. Other research suggests that antipsychotics could also have protective effects for patients with COVID-19.
Long COVID, long-term challenges
On the basis of its potential mechanisms of action, fluvoxamine may be able to prevent or treat long COVID, Dr. Reiersen said. That possibility will be assessed among other secondary endpoints in two ongoing studies of repurposed drugs: the NIH’s ACTIV-6, and the University of Minnesota’s COVID-OUT, an at-home trial of ivermectin, metformin, and fluvoxamine.
Dr. Reiersen and Washington University colleagues are also analyzing longer-term outcomes of participants in their own phase 3 trial of fluvoxamine (Stop COVID 2), which was discontinued when enrollment slowed to a trickle during the U.S. vaccine rollout. Logistical hurdles and scant funding have greatly hampered efforts to test the use of off-patent drugs for COVID-19 outpatients during the pandemic.
U.S. efforts face other obstacles as well. Elsewhere in the world – including Brazil, where the TOGETHER trial was run – vaccines are scarce, and there are no monoclonal antibodies.
“People have a great sense of community duty, and they’re participating in the trials,” Dr. Mills said. “You’re in a much more political environment in the U.S. on these outpatient trials.”
The TOGETHER trial was funded by Fast Grants and the Rainwater Foundation. Dr. Reiersen is an inventor on a patent application related to methods of treating COVID-19, which was filed by Washington University, St. Louis. Dr. Mills, Dr. Domino, and Dr. Sax report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A handful of studies have suggested that for newly infected COVID-19 patients, risk for serious illness may be reduced with a short course of fluvoxamine (Luvox), a decades-old pill typically prescribed for depression or obsessive-compulsive disorder (OCD). But those were small studies involving just a few hundred people.
This week, researchers reported promising data from a large, randomized phase 3 trial that enrolled COVID-19 patients from 11 sites in Brazil. In this study, in which 1,472 people were assigned to receive either a 10-day course of fluvoxamine or placebo pills, the antidepressant cut emergency department and hospital admissions by 29%.
Findings from the new study, which have not yet been peer reviewed, were published August 23 in MedRxiv.
Around the globe, particularly in countries without access to vaccines, “treatment options that are cheap and available and supported by good-quality evidence are the only hope we’ve got to reduce mortality within high-risk populations,” said Edward Mills, PhD, professor in the department of health research methods, evidence, and impact, McMaster University, Hamilton, Ont.
The new findings came from TOGETHER, a large platform trial coordinated by Dr. Mills and colleagues to evaluate the use of fluvoxamine and other repurposed drug candidates for symptomatic, high-risk, adult outpatients with confirmed cases of COVID-19.
The trial’s adaptive format allows multiple agents to be added and tested alongside placebo in a single master protocol – similar to the United Kingdom’s Recovery trial, which found that the common steroid dexamethasone could reduce deaths among hospitalized COVID-19 patients.
In platform trials, treatment arms can be dropped for futility, as was the case with hydroxychloroquine and lopinavir-ritonavir, neither of which did better than placebo at preventing hospitalization in an earlier TOGETHER trial analysis.
Study details
In the newly reported analysis, patients were randomly assigned to receive fluvoxamine or placebo between January and August 2021. Participants took fluvoxamine 100 mg twice daily for 10 days. By comparison, the U.S. Food and Drug Administration recommends a maximum daily dose of 300 mg of fluvoxamine for patients with OCD; full psychiatric benefits occur after 6 weeks.
For the primary outcome, the investigators assessed whether the conditions of patients with COVID worsened over a 28-day period so as to require either hospitalization or observation in the emergency department for more than 6 hours. In the placebo group, 108 of 733 patients’ conditions deteriorated to this extent (14.7%); by contrast, only 77 of 739 patients in the fluvoxamine group (10.4%) met these primary criteria – a relative risk reduction of 29%.
The treatment effect was greater (34%) in the per protocol analysis of participants who completed their course of pills.
The investigators also collected data on vital signs, including temperature and oxygen saturation, as well as adverse events reported at clinic visits or through video conferencing, phone calls, or social media applications. Side effects were mild, most commonly nausea and fatigue, and did not differ significantly between active treatment and control groups, Dr. Mills said in an interview.
Amid scores of studies evaluating repurposed drugs for COVID-19, the data on fluvoxamine are “looking much more favorable than anyone could have guessed – at least anyone in infectious disease,” said Paul Sax, MD, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The new TOGETHER trial results augment supportive data published in JAMA last November from a phase 2 randomized trial that was small but “very well done,” Dr. Sax told this news organization.
Those results got a boost from a subsequent study of 65 racetrack workers who chose to take fluvoxamine during a COVID-19 outbreak in the San Francisco Bay area. Forty-eight persons opted against taking the drug. In this small, nonrandomized study, “the people who chose to be treated with fluvoxamine were sicker [at baseline] than the people who didn’t go on it, and yet the [treated group] ended up better,” said Dr. Sax, who discussed accumulating data on the use of fluvoxamine for COVID-19 in a recent New England Journal of Medicine blog post.
Anti-inflammatory effect?
After reviewing the new findings, Frank Domino, MD, professor of family medicine and community health at the University of Massachusetts, Worcester, said he would encourage patients with high-risk COVID-19 to consider taking fluvoxamine to lower their risk of being hospitalized. “But I would make it clear this was not a ‘cure,’ “ he said, “and we are unsure how it helps.”
At this point, U.S. treatment guidelines do not recommend fluvoxamine as the standard of care for nonhospitalized COVID-19 patients, but the National Institutes of Health is “very aware of the data,” Dr. Sax told this news organization.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) – a class of drugs that includes the more commonly prescribed antidepressant fluoxetine (Prozac). If prescribed off-label to COVID-19 patients, fluvoxamine should not be used within 2 weeks of starting treatment with other SSRI or monoamine oxidase inhibitor antidepressants and should be used with caution with other QT-interval prolonging medications, Dr. Sax said.
In addition, fluvoxamine can enhance the effect of antiplatelet and anticoagulant drugs, potentially triggering bleeding.
On the basis of in vitro and mouse studies of fluvoxamine, “we think it has an anti-inflammatory effect,” said child psychiatrist Angela Reiersen, MD, of Washington University, St. Louis, who came up with the idea for testing fluvoxamine in last year’s phase 2 trial and coauthored a recent article describing the drug’s potential mechanisms of action in COVID-19.
She and other researchers believe fluvoxamine’s anti-inflammatory effects derive from the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, which regulates cellular responses to stress and infection.
Fluvoxamine also inhibits the activation of platelets. “In COVID-19, there does seem to be a problem with hyperactivation of platelets and excessive blood clots forming, so it is possible this could be another mechanism where it might be helping,” Dr. Reiersen said.
If sigma-1 activation turns out to be the main mechanism underlying fluvoxamine’s benefits in COVID-19, other sigma-1 agonists, such as fluoxetine, may also help. In a retrospective analysis of thousands of adults hospitalized for COVID-19 in France early in the pandemic, those who were taking antidepressants had a 44% lower risk for intubation or death.
And in a study under review, researchers at Stanford (Calif.) University and the University of California, San Francisco, analyzed electronic health records to explore a potential link between fluoxetine use and COVID outcomes among more than 80,000 patients from over 80 institutions across the United States. Other research suggests that antipsychotics could also have protective effects for patients with COVID-19.
Long COVID, long-term challenges
On the basis of its potential mechanisms of action, fluvoxamine may be able to prevent or treat long COVID, Dr. Reiersen said. That possibility will be assessed among other secondary endpoints in two ongoing studies of repurposed drugs: the NIH’s ACTIV-6, and the University of Minnesota’s COVID-OUT, an at-home trial of ivermectin, metformin, and fluvoxamine.
Dr. Reiersen and Washington University colleagues are also analyzing longer-term outcomes of participants in their own phase 3 trial of fluvoxamine (Stop COVID 2), which was discontinued when enrollment slowed to a trickle during the U.S. vaccine rollout. Logistical hurdles and scant funding have greatly hampered efforts to test the use of off-patent drugs for COVID-19 outpatients during the pandemic.
U.S. efforts face other obstacles as well. Elsewhere in the world – including Brazil, where the TOGETHER trial was run – vaccines are scarce, and there are no monoclonal antibodies.
“People have a great sense of community duty, and they’re participating in the trials,” Dr. Mills said. “You’re in a much more political environment in the U.S. on these outpatient trials.”
The TOGETHER trial was funded by Fast Grants and the Rainwater Foundation. Dr. Reiersen is an inventor on a patent application related to methods of treating COVID-19, which was filed by Washington University, St. Louis. Dr. Mills, Dr. Domino, and Dr. Sax report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A handful of studies have suggested that for newly infected COVID-19 patients, risk for serious illness may be reduced with a short course of fluvoxamine (Luvox), a decades-old pill typically prescribed for depression or obsessive-compulsive disorder (OCD). But those were small studies involving just a few hundred people.
This week, researchers reported promising data from a large, randomized phase 3 trial that enrolled COVID-19 patients from 11 sites in Brazil. In this study, in which 1,472 people were assigned to receive either a 10-day course of fluvoxamine or placebo pills, the antidepressant cut emergency department and hospital admissions by 29%.
Findings from the new study, which have not yet been peer reviewed, were published August 23 in MedRxiv.
Around the globe, particularly in countries without access to vaccines, “treatment options that are cheap and available and supported by good-quality evidence are the only hope we’ve got to reduce mortality within high-risk populations,” said Edward Mills, PhD, professor in the department of health research methods, evidence, and impact, McMaster University, Hamilton, Ont.
The new findings came from TOGETHER, a large platform trial coordinated by Dr. Mills and colleagues to evaluate the use of fluvoxamine and other repurposed drug candidates for symptomatic, high-risk, adult outpatients with confirmed cases of COVID-19.
The trial’s adaptive format allows multiple agents to be added and tested alongside placebo in a single master protocol – similar to the United Kingdom’s Recovery trial, which found that the common steroid dexamethasone could reduce deaths among hospitalized COVID-19 patients.
In platform trials, treatment arms can be dropped for futility, as was the case with hydroxychloroquine and lopinavir-ritonavir, neither of which did better than placebo at preventing hospitalization in an earlier TOGETHER trial analysis.
Study details
In the newly reported analysis, patients were randomly assigned to receive fluvoxamine or placebo between January and August 2021. Participants took fluvoxamine 100 mg twice daily for 10 days. By comparison, the U.S. Food and Drug Administration recommends a maximum daily dose of 300 mg of fluvoxamine for patients with OCD; full psychiatric benefits occur after 6 weeks.
For the primary outcome, the investigators assessed whether the conditions of patients with COVID worsened over a 28-day period so as to require either hospitalization or observation in the emergency department for more than 6 hours. In the placebo group, 108 of 733 patients’ conditions deteriorated to this extent (14.7%); by contrast, only 77 of 739 patients in the fluvoxamine group (10.4%) met these primary criteria – a relative risk reduction of 29%.
The treatment effect was greater (34%) in the per protocol analysis of participants who completed their course of pills.
The investigators also collected data on vital signs, including temperature and oxygen saturation, as well as adverse events reported at clinic visits or through video conferencing, phone calls, or social media applications. Side effects were mild, most commonly nausea and fatigue, and did not differ significantly between active treatment and control groups, Dr. Mills said in an interview.
Amid scores of studies evaluating repurposed drugs for COVID-19, the data on fluvoxamine are “looking much more favorable than anyone could have guessed – at least anyone in infectious disease,” said Paul Sax, MD, clinical director of the Division of Infectious Diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, Boston.
The new TOGETHER trial results augment supportive data published in JAMA last November from a phase 2 randomized trial that was small but “very well done,” Dr. Sax told this news organization.
Those results got a boost from a subsequent study of 65 racetrack workers who chose to take fluvoxamine during a COVID-19 outbreak in the San Francisco Bay area. Forty-eight persons opted against taking the drug. In this small, nonrandomized study, “the people who chose to be treated with fluvoxamine were sicker [at baseline] than the people who didn’t go on it, and yet the [treated group] ended up better,” said Dr. Sax, who discussed accumulating data on the use of fluvoxamine for COVID-19 in a recent New England Journal of Medicine blog post.
Anti-inflammatory effect?
After reviewing the new findings, Frank Domino, MD, professor of family medicine and community health at the University of Massachusetts, Worcester, said he would encourage patients with high-risk COVID-19 to consider taking fluvoxamine to lower their risk of being hospitalized. “But I would make it clear this was not a ‘cure,’ “ he said, “and we are unsure how it helps.”
At this point, U.S. treatment guidelines do not recommend fluvoxamine as the standard of care for nonhospitalized COVID-19 patients, but the National Institutes of Health is “very aware of the data,” Dr. Sax told this news organization.
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) – a class of drugs that includes the more commonly prescribed antidepressant fluoxetine (Prozac). If prescribed off-label to COVID-19 patients, fluvoxamine should not be used within 2 weeks of starting treatment with other SSRI or monoamine oxidase inhibitor antidepressants and should be used with caution with other QT-interval prolonging medications, Dr. Sax said.
In addition, fluvoxamine can enhance the effect of antiplatelet and anticoagulant drugs, potentially triggering bleeding.
On the basis of in vitro and mouse studies of fluvoxamine, “we think it has an anti-inflammatory effect,” said child psychiatrist Angela Reiersen, MD, of Washington University, St. Louis, who came up with the idea for testing fluvoxamine in last year’s phase 2 trial and coauthored a recent article describing the drug’s potential mechanisms of action in COVID-19.
She and other researchers believe fluvoxamine’s anti-inflammatory effects derive from the molecule’s binding to the sigma-1 receptor in the endoplasmic reticulum, which regulates cellular responses to stress and infection.
Fluvoxamine also inhibits the activation of platelets. “In COVID-19, there does seem to be a problem with hyperactivation of platelets and excessive blood clots forming, so it is possible this could be another mechanism where it might be helping,” Dr. Reiersen said.
If sigma-1 activation turns out to be the main mechanism underlying fluvoxamine’s benefits in COVID-19, other sigma-1 agonists, such as fluoxetine, may also help. In a retrospective analysis of thousands of adults hospitalized for COVID-19 in France early in the pandemic, those who were taking antidepressants had a 44% lower risk for intubation or death.
And in a study under review, researchers at Stanford (Calif.) University and the University of California, San Francisco, analyzed electronic health records to explore a potential link between fluoxetine use and COVID outcomes among more than 80,000 patients from over 80 institutions across the United States. Other research suggests that antipsychotics could also have protective effects for patients with COVID-19.
Long COVID, long-term challenges
On the basis of its potential mechanisms of action, fluvoxamine may be able to prevent or treat long COVID, Dr. Reiersen said. That possibility will be assessed among other secondary endpoints in two ongoing studies of repurposed drugs: the NIH’s ACTIV-6, and the University of Minnesota’s COVID-OUT, an at-home trial of ivermectin, metformin, and fluvoxamine.
Dr. Reiersen and Washington University colleagues are also analyzing longer-term outcomes of participants in their own phase 3 trial of fluvoxamine (Stop COVID 2), which was discontinued when enrollment slowed to a trickle during the U.S. vaccine rollout. Logistical hurdles and scant funding have greatly hampered efforts to test the use of off-patent drugs for COVID-19 outpatients during the pandemic.
U.S. efforts face other obstacles as well. Elsewhere in the world – including Brazil, where the TOGETHER trial was run – vaccines are scarce, and there are no monoclonal antibodies.
“People have a great sense of community duty, and they’re participating in the trials,” Dr. Mills said. “You’re in a much more political environment in the U.S. on these outpatient trials.”
The TOGETHER trial was funded by Fast Grants and the Rainwater Foundation. Dr. Reiersen is an inventor on a patent application related to methods of treating COVID-19, which was filed by Washington University, St. Louis. Dr. Mills, Dr. Domino, and Dr. Sax report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Four police suicides in the aftermath of the Capitol siege: What can we learn?
Officer Scott Davis is a passionate man who thinks and talks quickly. As a member of the Special Events Team for Montgomery County, Maryland, he was already staging in Rockville, outside of Washington, D.C., when the call came in last Jan. 6 to move their unit to the U.S. Capitol.

“It was surreal,” said Mr. Davis. “There were people from all different groups at the Capitol that day. Many people were trying to get out, but others surrounded us. They called us ‘human race traitors.’ And then I heard someone say, ‘It’s good you brought your shields, we’ll carry your bodies out on them.’”
Mr. Davis described hours of mayhem during which he was hit with bear spray, a brick, a chair, and a metal rod. One of the members of Mr. Davis’ unit remains on leave with a head injury nearly 9 months after the siege.
“It went on for 3 hours, but it felt like 15 minutes. Then, all of a sudden, it was over.”
For the members of law enforcement at the Capitol that day, the repercussions are still being felt, perhaps most notably in the case of the four officers who subsequently died of suicide. Three of the officers were with the Metropolitan Police Department of the District of Columbia and one worked for the Capitol Police Department.
Police officers are subjected to traumas on a regular basis and often placed in circumstances where their lives are in danger. Yet four suicides within a short time – all connected to a single event – is particularly shocking and tragic, even more so for how little attention it has garnered to date.
What contributes to the high rate of suicide among officers?
Scott Silverii, PhD, a former police officer and author of Broken and Blue: A Policeman’s Guide to Health, Hope, and Healing, commented that he “wouldn’t be surprised if there are more suicides to come.” This stems not only from the experiences of that day but also the elevated risk for suicide that law enforcement officers already experienced prior to the Capitol riots. Suicide remains a rare event, with a national all-population average of 13.9 per 100,000 citizens. But as Dr. Silverii noted, more officers die by suicide each year than are killed in the line of duty.
“Suicide is a big part of police culture – officers are doers and fixers, and it is seen as being more honorable to take yourself out of the equation than it is to ask for help,” he said. “Most officers come in with past pain, and this is a situation where they are being overwhelmed and under-respected. At the same time, police culture is a closed culture, and it is not friendly to researchers.”
Another contributor is the frequency with which law enforcement officers are exposed to trauma, according to Vernon Herron, Director of Officer Safety and Wellness for the Baltimore City Police.
Mr. Herron said, citing the psychiatric and addiction issues that officers commonly experience.
Protecting the protectors
Mr. Herron and others are working to address these problems head-on.
“We are trying to identify employees exposed to trauma and to offer counseling and intervention,” he said, “Otherwise, everything else will fall short.”
Yet implementing such measures is no easy task, given the lack of a central oversight organization for law enforcement, said Sheldon Greenberg, PhD, a former police officer and professor of management in the School of Education at Johns Hopkins University, Baltimore.
“In the United States there is no such thing as ‘The Police.’ There is no one in a position to set policy, standards, or training mandates nationally,” he said. “There are approximately 18,000 police and sheriff departments in the country, and many of them are small. No one can compel law enforcement agencies to implement officer wellness and suicide prevention programs, make counseling available to officers, or train supervisors and peers to identify suicide ideation.”
Dr. Greenberg said a further barrier to helping police officers considering self-harm is posed by the fact that even if they do seek out counseling, there is no guarantee that it will remain confidential.
“Support personnel have an obligation to report an officer who is thinking about committing suicide,” he said. “Many officers are concerned about this lack of confidentiality and that they may be branded if they seek help.”
Although Dr. Greenberg said many police officers are self-professed “action junkies,” even their unusually high capacity for stress is often tested by the realities of the job.
“Increasing demands for service, shortages of personnel, misinformation about police, COVID-19, talk about restructuring policing with little concrete direction, increased exposure to violence, greater numbers of vulnerable people, and more take a toll over time,” he lamented. “In addition, we are in a recruiting crisis in law enforcement, and there are no standards to ensure the quality of psychological screening provided to applicants. Many officers will go through their entire career and never be screened again. We know little about the stresses and strains that officers bring to the job.”
After the siege
It is not clear how many police officers were present at the Capitol on Jan. 6. During the chaos of the day, reinforcements to the Capitol Police Department arrived from Washington D.C., Maryland, and Virginia, but no official numbers on responders were obtained; Mr. Davis thought it was likely that there were at least 1,000 law enforcement officers present. Those who did respond sustained an estimated 100 injuries, including an officer who died the next day. Of the officers who died by suicide, one died 3 days after, another died 9 days later, and two more died in July – numbers that contradict the notion that this is some coincidence. Officer Alexander Kettering, a colleague of Mr. Davis who has been with Montgomery County Police for 15 years, was among those tasked with protecting the Capitol on Jan. 6. The chaos, violence, and destruction of the day has stuck with him and continues to occupy his thoughts.
“I had a front-row seat to the whole thing. It was overwhelming, and I’ve never seen people this angry,” said Mr. Kettering. “There were people up on the veranda and on the scaffolding set up for the inauguration. They were smashing windows and throwing things into the crowd. It was insane. There were decent people coming up to us and saying they would pray for us, then others calling us traitors, telling us to stand down and join them.”
In the aftermath of the Capitol siege, Mr. Kettering watched in dismay as the narrative of the day’s events began to warp.
“At first there was a consensus that what happened was so wrong, and then the politics took over. People were saying it wasn’t as bad as the media said, that it really wasn’t that violent and those speaking out are traitors or political operatives. I relive it every day, and it’s hard to escape, even in casual conversation.”
He added that the days’ events were compounded by the already heightened tensions surrounding the national debate around policing.
“It’s been 18 months of stress, of anti-police movements, and there is a fine line between addressing police brutality and being anti-police,” Mr. Kettering said, noting that the aforementioned issues have all contributed to the ongoing struggles his fellow officers are experiencing.
“It’s not a thing for cops to talk about how an event affected them,” he said. “A lot of officers have just shut down. People have careers and pensions to protect, and every time we stop a motorist, something could go wrong, even if we do everything right. There are mixed signals: They tell us, ‘Defend but don’t defend.’”
His colleague, Mr. Davis, said that officers “need more support from politicians,” noting that he felt particularly insulted by a comment made by a Montgomery County public official who accused the officers present at the Capitol of racism. “And finally, we feel a little betrayed by the public.”
More questions than answers from the Capitol’s day of chaos
What about the events of Jan. 6 led to the suicides of four law enforcement officers and what can be done to prevent more deaths in the future? There are the individual factors of each man’s personal history, circumstances, and vulnerabilities, including the sense of being personally endangered, witnessing trauma, and direct injury – one officer who died of suicide had sustained a head injury that day.
We don’t know if the officers went into the event with preexisting mental illness or addiction or if the day’s events precipitated psychiatric episodes. And with all the partisan anger surrounding the presidential election, we don’t know if each officer’s political beliefs amplified his distress over what occurred in a social media climate where police are being faulted by all sides.
When multiple suicides occur in a community, there is always concern about a “copycat” phenomena. These concerns are made more difficult to address, however, given the police culture of taboo and stigma associated with getting professional help, difficulty accessing care, and career repercussions for speaking openly about suicidal thoughts and mental health issues.
Finally, there is the current political agenda that leaves officers feeling unsupported, fearful of negative outcomes, and unappreciated. The Capitol siege in particular embodied a great deal of national distress and confusion over basic issues of truth, justice, and perceptions of reality in our polarized society.
Can we move to a place where those who enforce laws have easy access to treatment, free from stigma? Can we encourage a culture that does not tolerate brutality or racism, while also refusing to label all police as bad and lending support to their mission? Can we be more attuned to the repercussions of circumstances where officers are witnesses to trauma, are endangered themselves, and would benefit from acknowledgment of their distress?
Time will tell if our anti-police pendulum swings back. In the meantime, these four suicides among people defending our country remain tragically overlooked.
Dinah Miller, MD, is coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016). She has a private practice in Baltimore and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University. A version of this article first appeared on Medscape.com.
Officer Scott Davis is a passionate man who thinks and talks quickly. As a member of the Special Events Team for Montgomery County, Maryland, he was already staging in Rockville, outside of Washington, D.C., when the call came in last Jan. 6 to move their unit to the U.S. Capitol.

“It was surreal,” said Mr. Davis. “There were people from all different groups at the Capitol that day. Many people were trying to get out, but others surrounded us. They called us ‘human race traitors.’ And then I heard someone say, ‘It’s good you brought your shields, we’ll carry your bodies out on them.’”
Mr. Davis described hours of mayhem during which he was hit with bear spray, a brick, a chair, and a metal rod. One of the members of Mr. Davis’ unit remains on leave with a head injury nearly 9 months after the siege.
“It went on for 3 hours, but it felt like 15 minutes. Then, all of a sudden, it was over.”
For the members of law enforcement at the Capitol that day, the repercussions are still being felt, perhaps most notably in the case of the four officers who subsequently died of suicide. Three of the officers were with the Metropolitan Police Department of the District of Columbia and one worked for the Capitol Police Department.
Police officers are subjected to traumas on a regular basis and often placed in circumstances where their lives are in danger. Yet four suicides within a short time – all connected to a single event – is particularly shocking and tragic, even more so for how little attention it has garnered to date.
What contributes to the high rate of suicide among officers?
Scott Silverii, PhD, a former police officer and author of Broken and Blue: A Policeman’s Guide to Health, Hope, and Healing, commented that he “wouldn’t be surprised if there are more suicides to come.” This stems not only from the experiences of that day but also the elevated risk for suicide that law enforcement officers already experienced prior to the Capitol riots. Suicide remains a rare event, with a national all-population average of 13.9 per 100,000 citizens. But as Dr. Silverii noted, more officers die by suicide each year than are killed in the line of duty.
“Suicide is a big part of police culture – officers are doers and fixers, and it is seen as being more honorable to take yourself out of the equation than it is to ask for help,” he said. “Most officers come in with past pain, and this is a situation where they are being overwhelmed and under-respected. At the same time, police culture is a closed culture, and it is not friendly to researchers.”
Another contributor is the frequency with which law enforcement officers are exposed to trauma, according to Vernon Herron, Director of Officer Safety and Wellness for the Baltimore City Police.
Mr. Herron said, citing the psychiatric and addiction issues that officers commonly experience.
Protecting the protectors
Mr. Herron and others are working to address these problems head-on.
“We are trying to identify employees exposed to trauma and to offer counseling and intervention,” he said, “Otherwise, everything else will fall short.”
Yet implementing such measures is no easy task, given the lack of a central oversight organization for law enforcement, said Sheldon Greenberg, PhD, a former police officer and professor of management in the School of Education at Johns Hopkins University, Baltimore.
“In the United States there is no such thing as ‘The Police.’ There is no one in a position to set policy, standards, or training mandates nationally,” he said. “There are approximately 18,000 police and sheriff departments in the country, and many of them are small. No one can compel law enforcement agencies to implement officer wellness and suicide prevention programs, make counseling available to officers, or train supervisors and peers to identify suicide ideation.”
Dr. Greenberg said a further barrier to helping police officers considering self-harm is posed by the fact that even if they do seek out counseling, there is no guarantee that it will remain confidential.
“Support personnel have an obligation to report an officer who is thinking about committing suicide,” he said. “Many officers are concerned about this lack of confidentiality and that they may be branded if they seek help.”
Although Dr. Greenberg said many police officers are self-professed “action junkies,” even their unusually high capacity for stress is often tested by the realities of the job.
“Increasing demands for service, shortages of personnel, misinformation about police, COVID-19, talk about restructuring policing with little concrete direction, increased exposure to violence, greater numbers of vulnerable people, and more take a toll over time,” he lamented. “In addition, we are in a recruiting crisis in law enforcement, and there are no standards to ensure the quality of psychological screening provided to applicants. Many officers will go through their entire career and never be screened again. We know little about the stresses and strains that officers bring to the job.”
After the siege
It is not clear how many police officers were present at the Capitol on Jan. 6. During the chaos of the day, reinforcements to the Capitol Police Department arrived from Washington D.C., Maryland, and Virginia, but no official numbers on responders were obtained; Mr. Davis thought it was likely that there were at least 1,000 law enforcement officers present. Those who did respond sustained an estimated 100 injuries, including an officer who died the next day. Of the officers who died by suicide, one died 3 days after, another died 9 days later, and two more died in July – numbers that contradict the notion that this is some coincidence. Officer Alexander Kettering, a colleague of Mr. Davis who has been with Montgomery County Police for 15 years, was among those tasked with protecting the Capitol on Jan. 6. The chaos, violence, and destruction of the day has stuck with him and continues to occupy his thoughts.
“I had a front-row seat to the whole thing. It was overwhelming, and I’ve never seen people this angry,” said Mr. Kettering. “There were people up on the veranda and on the scaffolding set up for the inauguration. They were smashing windows and throwing things into the crowd. It was insane. There were decent people coming up to us and saying they would pray for us, then others calling us traitors, telling us to stand down and join them.”
In the aftermath of the Capitol siege, Mr. Kettering watched in dismay as the narrative of the day’s events began to warp.
“At first there was a consensus that what happened was so wrong, and then the politics took over. People were saying it wasn’t as bad as the media said, that it really wasn’t that violent and those speaking out are traitors or political operatives. I relive it every day, and it’s hard to escape, even in casual conversation.”
He added that the days’ events were compounded by the already heightened tensions surrounding the national debate around policing.
“It’s been 18 months of stress, of anti-police movements, and there is a fine line between addressing police brutality and being anti-police,” Mr. Kettering said, noting that the aforementioned issues have all contributed to the ongoing struggles his fellow officers are experiencing.
“It’s not a thing for cops to talk about how an event affected them,” he said. “A lot of officers have just shut down. People have careers and pensions to protect, and every time we stop a motorist, something could go wrong, even if we do everything right. There are mixed signals: They tell us, ‘Defend but don’t defend.’”
His colleague, Mr. Davis, said that officers “need more support from politicians,” noting that he felt particularly insulted by a comment made by a Montgomery County public official who accused the officers present at the Capitol of racism. “And finally, we feel a little betrayed by the public.”
More questions than answers from the Capitol’s day of chaos
What about the events of Jan. 6 led to the suicides of four law enforcement officers and what can be done to prevent more deaths in the future? There are the individual factors of each man’s personal history, circumstances, and vulnerabilities, including the sense of being personally endangered, witnessing trauma, and direct injury – one officer who died of suicide had sustained a head injury that day.
We don’t know if the officers went into the event with preexisting mental illness or addiction or if the day’s events precipitated psychiatric episodes. And with all the partisan anger surrounding the presidential election, we don’t know if each officer’s political beliefs amplified his distress over what occurred in a social media climate where police are being faulted by all sides.
When multiple suicides occur in a community, there is always concern about a “copycat” phenomena. These concerns are made more difficult to address, however, given the police culture of taboo and stigma associated with getting professional help, difficulty accessing care, and career repercussions for speaking openly about suicidal thoughts and mental health issues.
Finally, there is the current political agenda that leaves officers feeling unsupported, fearful of negative outcomes, and unappreciated. The Capitol siege in particular embodied a great deal of national distress and confusion over basic issues of truth, justice, and perceptions of reality in our polarized society.
Can we move to a place where those who enforce laws have easy access to treatment, free from stigma? Can we encourage a culture that does not tolerate brutality or racism, while also refusing to label all police as bad and lending support to their mission? Can we be more attuned to the repercussions of circumstances where officers are witnesses to trauma, are endangered themselves, and would benefit from acknowledgment of their distress?
Time will tell if our anti-police pendulum swings back. In the meantime, these four suicides among people defending our country remain tragically overlooked.
Dinah Miller, MD, is coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016). She has a private practice in Baltimore and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University. A version of this article first appeared on Medscape.com.
Officer Scott Davis is a passionate man who thinks and talks quickly. As a member of the Special Events Team for Montgomery County, Maryland, he was already staging in Rockville, outside of Washington, D.C., when the call came in last Jan. 6 to move their unit to the U.S. Capitol.

“It was surreal,” said Mr. Davis. “There were people from all different groups at the Capitol that day. Many people were trying to get out, but others surrounded us. They called us ‘human race traitors.’ And then I heard someone say, ‘It’s good you brought your shields, we’ll carry your bodies out on them.’”
Mr. Davis described hours of mayhem during which he was hit with bear spray, a brick, a chair, and a metal rod. One of the members of Mr. Davis’ unit remains on leave with a head injury nearly 9 months after the siege.
“It went on for 3 hours, but it felt like 15 minutes. Then, all of a sudden, it was over.”
For the members of law enforcement at the Capitol that day, the repercussions are still being felt, perhaps most notably in the case of the four officers who subsequently died of suicide. Three of the officers were with the Metropolitan Police Department of the District of Columbia and one worked for the Capitol Police Department.
Police officers are subjected to traumas on a regular basis and often placed in circumstances where their lives are in danger. Yet four suicides within a short time – all connected to a single event – is particularly shocking and tragic, even more so for how little attention it has garnered to date.
What contributes to the high rate of suicide among officers?
Scott Silverii, PhD, a former police officer and author of Broken and Blue: A Policeman’s Guide to Health, Hope, and Healing, commented that he “wouldn’t be surprised if there are more suicides to come.” This stems not only from the experiences of that day but also the elevated risk for suicide that law enforcement officers already experienced prior to the Capitol riots. Suicide remains a rare event, with a national all-population average of 13.9 per 100,000 citizens. But as Dr. Silverii noted, more officers die by suicide each year than are killed in the line of duty.
“Suicide is a big part of police culture – officers are doers and fixers, and it is seen as being more honorable to take yourself out of the equation than it is to ask for help,” he said. “Most officers come in with past pain, and this is a situation where they are being overwhelmed and under-respected. At the same time, police culture is a closed culture, and it is not friendly to researchers.”
Another contributor is the frequency with which law enforcement officers are exposed to trauma, according to Vernon Herron, Director of Officer Safety and Wellness for the Baltimore City Police.
Mr. Herron said, citing the psychiatric and addiction issues that officers commonly experience.
Protecting the protectors
Mr. Herron and others are working to address these problems head-on.
“We are trying to identify employees exposed to trauma and to offer counseling and intervention,” he said, “Otherwise, everything else will fall short.”
Yet implementing such measures is no easy task, given the lack of a central oversight organization for law enforcement, said Sheldon Greenberg, PhD, a former police officer and professor of management in the School of Education at Johns Hopkins University, Baltimore.
“In the United States there is no such thing as ‘The Police.’ There is no one in a position to set policy, standards, or training mandates nationally,” he said. “There are approximately 18,000 police and sheriff departments in the country, and many of them are small. No one can compel law enforcement agencies to implement officer wellness and suicide prevention programs, make counseling available to officers, or train supervisors and peers to identify suicide ideation.”
Dr. Greenberg said a further barrier to helping police officers considering self-harm is posed by the fact that even if they do seek out counseling, there is no guarantee that it will remain confidential.
“Support personnel have an obligation to report an officer who is thinking about committing suicide,” he said. “Many officers are concerned about this lack of confidentiality and that they may be branded if they seek help.”
Although Dr. Greenberg said many police officers are self-professed “action junkies,” even their unusually high capacity for stress is often tested by the realities of the job.
“Increasing demands for service, shortages of personnel, misinformation about police, COVID-19, talk about restructuring policing with little concrete direction, increased exposure to violence, greater numbers of vulnerable people, and more take a toll over time,” he lamented. “In addition, we are in a recruiting crisis in law enforcement, and there are no standards to ensure the quality of psychological screening provided to applicants. Many officers will go through their entire career and never be screened again. We know little about the stresses and strains that officers bring to the job.”
After the siege
It is not clear how many police officers were present at the Capitol on Jan. 6. During the chaos of the day, reinforcements to the Capitol Police Department arrived from Washington D.C., Maryland, and Virginia, but no official numbers on responders were obtained; Mr. Davis thought it was likely that there were at least 1,000 law enforcement officers present. Those who did respond sustained an estimated 100 injuries, including an officer who died the next day. Of the officers who died by suicide, one died 3 days after, another died 9 days later, and two more died in July – numbers that contradict the notion that this is some coincidence. Officer Alexander Kettering, a colleague of Mr. Davis who has been with Montgomery County Police for 15 years, was among those tasked with protecting the Capitol on Jan. 6. The chaos, violence, and destruction of the day has stuck with him and continues to occupy his thoughts.
“I had a front-row seat to the whole thing. It was overwhelming, and I’ve never seen people this angry,” said Mr. Kettering. “There were people up on the veranda and on the scaffolding set up for the inauguration. They were smashing windows and throwing things into the crowd. It was insane. There were decent people coming up to us and saying they would pray for us, then others calling us traitors, telling us to stand down and join them.”
In the aftermath of the Capitol siege, Mr. Kettering watched in dismay as the narrative of the day’s events began to warp.
“At first there was a consensus that what happened was so wrong, and then the politics took over. People were saying it wasn’t as bad as the media said, that it really wasn’t that violent and those speaking out are traitors or political operatives. I relive it every day, and it’s hard to escape, even in casual conversation.”
He added that the days’ events were compounded by the already heightened tensions surrounding the national debate around policing.
“It’s been 18 months of stress, of anti-police movements, and there is a fine line between addressing police brutality and being anti-police,” Mr. Kettering said, noting that the aforementioned issues have all contributed to the ongoing struggles his fellow officers are experiencing.
“It’s not a thing for cops to talk about how an event affected them,” he said. “A lot of officers have just shut down. People have careers and pensions to protect, and every time we stop a motorist, something could go wrong, even if we do everything right. There are mixed signals: They tell us, ‘Defend but don’t defend.’”
His colleague, Mr. Davis, said that officers “need more support from politicians,” noting that he felt particularly insulted by a comment made by a Montgomery County public official who accused the officers present at the Capitol of racism. “And finally, we feel a little betrayed by the public.”
More questions than answers from the Capitol’s day of chaos
What about the events of Jan. 6 led to the suicides of four law enforcement officers and what can be done to prevent more deaths in the future? There are the individual factors of each man’s personal history, circumstances, and vulnerabilities, including the sense of being personally endangered, witnessing trauma, and direct injury – one officer who died of suicide had sustained a head injury that day.
We don’t know if the officers went into the event with preexisting mental illness or addiction or if the day’s events precipitated psychiatric episodes. And with all the partisan anger surrounding the presidential election, we don’t know if each officer’s political beliefs amplified his distress over what occurred in a social media climate where police are being faulted by all sides.
When multiple suicides occur in a community, there is always concern about a “copycat” phenomena. These concerns are made more difficult to address, however, given the police culture of taboo and stigma associated with getting professional help, difficulty accessing care, and career repercussions for speaking openly about suicidal thoughts and mental health issues.
Finally, there is the current political agenda that leaves officers feeling unsupported, fearful of negative outcomes, and unappreciated. The Capitol siege in particular embodied a great deal of national distress and confusion over basic issues of truth, justice, and perceptions of reality in our polarized society.
Can we move to a place where those who enforce laws have easy access to treatment, free from stigma? Can we encourage a culture that does not tolerate brutality or racism, while also refusing to label all police as bad and lending support to their mission? Can we be more attuned to the repercussions of circumstances where officers are witnesses to trauma, are endangered themselves, and would benefit from acknowledgment of their distress?
Time will tell if our anti-police pendulum swings back. In the meantime, these four suicides among people defending our country remain tragically overlooked.
Dinah Miller, MD, is coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016). She has a private practice in Baltimore and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins University. A version of this article first appeared on Medscape.com.
Pups for veterans with PTSD: Biden signs PAWS act into law
Service members with posttraumatic stress disorder and other mental health conditions may eventually have expanded access to service dogs through legislation recently signed into law by President Joseph R. Biden.
The Puppies Assisting Wounded Servicemembers (PAWS) for Veterans Therapy Act (HR 1448) orders the Department of Veterans Affairs to begin a pilot program that over the course of 5 years will examine the utility and effectiveness of service dogs for improving the mental health of military veterans.
The legislation does not set a specific start date for the pilot program, but Rory Diamond, CEO of K9s for Warriors, a nonprofit organization based in Ponte Vedra, Fla., noted that K9s for Warriors and other organizations will be pushing the VA to start in 2022.
“We commend the White House for supporting this bill as a critical step in combating veteran suicide, and we’re confident in the path ahead for service dogs ultimately becoming a covered VA benefit to veterans with PTSD,” Mr. Diamond said in a statement provided to this news organization.
“For servicemembers relying on task-trained service dogs for PTSD, the HR 1448 is a giant leap towards supporting veterans and their service dogs in an equitable way,” Canine Companions, a national nonprofit organization that trains and provides service dogs, said in its own statement.
“It might mean the difference between having a veteran who won’t be here tomorrow and having one that will,” the group added.
Invisible wounds of war
In another statement, Bill McCabe, legislative affairs director at the Enlisted Association, said that “now, more than ever, veterans suffering from invisible wounds of war need access to trained service dogs, which have been scientifically proven to help alleviate symptoms of posttraumatic stress,” as well as traumatic brain injuries (TBIs) and military sexual trauma.
“We thank President Biden for recognizing veterans need every possible option when seeking mental health treatments, and look forward to working with the Department of Veterans Affairs to implement this important program,” Mr. McCabe said.
A recent VA report showed that in 2014, 40% of veterans had mental health conditions such as PTSD and substance use. An average of 20 veterans per day died by suicide that year.
Veterans with problems regarding mobility, hearing, and sight, as well as some mental health problems, have been eligible to have costs of veterinary care for service dogs paid by the VA, although the VA has not paid for the training of the animals.
The PAWS Act, which was bipartisan legislation introduced by U.S. Senators Thom Tillis (R-N.C.), Kyrsten Sinema (D-Ariz.), Kevin Cramer (R-N.D.), and Dianne Feinstein (D-Calif.), aims to expand eligibility to those with any mental health problems.
For at least a decade, various service dog and veterans’ organizations have pushed to have the VA expand the service dog benefit. This new law is a “first step,” said Mr. Diamond. “We had to kick open the door,” he said, adding that “the VA has essentially said no for almost 15 years.”
Mr. Diamond noted that there is “overwhelming” evidence showing that service dogs improve quality of life and reduce distress for veterans with PTSD and other diagnoses.
‘No excuse’
Results from a VA study showed that suicidal ideation was reduced in veterans who were paired with service dogs, compared with veterans paired with emotional support dogs. The study, which was made public in March, found no reduction in overall disability, according to a report by Military.com.
K9s for Warriors cites numerous other studies, published in peer-reviewed journals, that have shown that service dogs reduce PTSD symptoms, especially hypervigilance.
“There really is no excuse not to have the VA engaged in helping veterans suffering from posttraumatic stress who are extremely high risk of suicide to get a lifesaving service dog,” Mr. Diamond said.
His organization has paired 700 veterans suffering from TBI, PTSD, or military sexual trauma with a service dog. The organization provides a 3-week training program for the veteran and his or her dog.
Although about 200 of the graduates have been eligible to receive coverage from the VA for veterinary care for the dogs, it requires a lot of paperwork, and the criteria for who can be certified to receive that benefit are somewhat vague, Mr. Diamond noted.
Under current policy, the dog and veteran must have successfully completed a training program offered by an organization accredited by Assistance Dogs International or the International Guide Dog Federation.
The new pilot program will enable eligible veterans to receive dog training instruction from accredited nonprofit service dog training organizations, and it will give them the opportunity to adopt a dog that they actively assisted in training.
A version of this article first appeared on Medscape.com.
Service members with posttraumatic stress disorder and other mental health conditions may eventually have expanded access to service dogs through legislation recently signed into law by President Joseph R. Biden.
The Puppies Assisting Wounded Servicemembers (PAWS) for Veterans Therapy Act (HR 1448) orders the Department of Veterans Affairs to begin a pilot program that over the course of 5 years will examine the utility and effectiveness of service dogs for improving the mental health of military veterans.
The legislation does not set a specific start date for the pilot program, but Rory Diamond, CEO of K9s for Warriors, a nonprofit organization based in Ponte Vedra, Fla., noted that K9s for Warriors and other organizations will be pushing the VA to start in 2022.
“We commend the White House for supporting this bill as a critical step in combating veteran suicide, and we’re confident in the path ahead for service dogs ultimately becoming a covered VA benefit to veterans with PTSD,” Mr. Diamond said in a statement provided to this news organization.
“For servicemembers relying on task-trained service dogs for PTSD, the HR 1448 is a giant leap towards supporting veterans and their service dogs in an equitable way,” Canine Companions, a national nonprofit organization that trains and provides service dogs, said in its own statement.
“It might mean the difference between having a veteran who won’t be here tomorrow and having one that will,” the group added.
Invisible wounds of war
In another statement, Bill McCabe, legislative affairs director at the Enlisted Association, said that “now, more than ever, veterans suffering from invisible wounds of war need access to trained service dogs, which have been scientifically proven to help alleviate symptoms of posttraumatic stress,” as well as traumatic brain injuries (TBIs) and military sexual trauma.
“We thank President Biden for recognizing veterans need every possible option when seeking mental health treatments, and look forward to working with the Department of Veterans Affairs to implement this important program,” Mr. McCabe said.
A recent VA report showed that in 2014, 40% of veterans had mental health conditions such as PTSD and substance use. An average of 20 veterans per day died by suicide that year.
Veterans with problems regarding mobility, hearing, and sight, as well as some mental health problems, have been eligible to have costs of veterinary care for service dogs paid by the VA, although the VA has not paid for the training of the animals.
The PAWS Act, which was bipartisan legislation introduced by U.S. Senators Thom Tillis (R-N.C.), Kyrsten Sinema (D-Ariz.), Kevin Cramer (R-N.D.), and Dianne Feinstein (D-Calif.), aims to expand eligibility to those with any mental health problems.
For at least a decade, various service dog and veterans’ organizations have pushed to have the VA expand the service dog benefit. This new law is a “first step,” said Mr. Diamond. “We had to kick open the door,” he said, adding that “the VA has essentially said no for almost 15 years.”
Mr. Diamond noted that there is “overwhelming” evidence showing that service dogs improve quality of life and reduce distress for veterans with PTSD and other diagnoses.
‘No excuse’
Results from a VA study showed that suicidal ideation was reduced in veterans who were paired with service dogs, compared with veterans paired with emotional support dogs. The study, which was made public in March, found no reduction in overall disability, according to a report by Military.com.
K9s for Warriors cites numerous other studies, published in peer-reviewed journals, that have shown that service dogs reduce PTSD symptoms, especially hypervigilance.
“There really is no excuse not to have the VA engaged in helping veterans suffering from posttraumatic stress who are extremely high risk of suicide to get a lifesaving service dog,” Mr. Diamond said.
His organization has paired 700 veterans suffering from TBI, PTSD, or military sexual trauma with a service dog. The organization provides a 3-week training program for the veteran and his or her dog.
Although about 200 of the graduates have been eligible to receive coverage from the VA for veterinary care for the dogs, it requires a lot of paperwork, and the criteria for who can be certified to receive that benefit are somewhat vague, Mr. Diamond noted.
Under current policy, the dog and veteran must have successfully completed a training program offered by an organization accredited by Assistance Dogs International or the International Guide Dog Federation.
The new pilot program will enable eligible veterans to receive dog training instruction from accredited nonprofit service dog training organizations, and it will give them the opportunity to adopt a dog that they actively assisted in training.
A version of this article first appeared on Medscape.com.
Service members with posttraumatic stress disorder and other mental health conditions may eventually have expanded access to service dogs through legislation recently signed into law by President Joseph R. Biden.
The Puppies Assisting Wounded Servicemembers (PAWS) for Veterans Therapy Act (HR 1448) orders the Department of Veterans Affairs to begin a pilot program that over the course of 5 years will examine the utility and effectiveness of service dogs for improving the mental health of military veterans.
The legislation does not set a specific start date for the pilot program, but Rory Diamond, CEO of K9s for Warriors, a nonprofit organization based in Ponte Vedra, Fla., noted that K9s for Warriors and other organizations will be pushing the VA to start in 2022.
“We commend the White House for supporting this bill as a critical step in combating veteran suicide, and we’re confident in the path ahead for service dogs ultimately becoming a covered VA benefit to veterans with PTSD,” Mr. Diamond said in a statement provided to this news organization.
“For servicemembers relying on task-trained service dogs for PTSD, the HR 1448 is a giant leap towards supporting veterans and their service dogs in an equitable way,” Canine Companions, a national nonprofit organization that trains and provides service dogs, said in its own statement.
“It might mean the difference between having a veteran who won’t be here tomorrow and having one that will,” the group added.
Invisible wounds of war
In another statement, Bill McCabe, legislative affairs director at the Enlisted Association, said that “now, more than ever, veterans suffering from invisible wounds of war need access to trained service dogs, which have been scientifically proven to help alleviate symptoms of posttraumatic stress,” as well as traumatic brain injuries (TBIs) and military sexual trauma.
“We thank President Biden for recognizing veterans need every possible option when seeking mental health treatments, and look forward to working with the Department of Veterans Affairs to implement this important program,” Mr. McCabe said.
A recent VA report showed that in 2014, 40% of veterans had mental health conditions such as PTSD and substance use. An average of 20 veterans per day died by suicide that year.
Veterans with problems regarding mobility, hearing, and sight, as well as some mental health problems, have been eligible to have costs of veterinary care for service dogs paid by the VA, although the VA has not paid for the training of the animals.
The PAWS Act, which was bipartisan legislation introduced by U.S. Senators Thom Tillis (R-N.C.), Kyrsten Sinema (D-Ariz.), Kevin Cramer (R-N.D.), and Dianne Feinstein (D-Calif.), aims to expand eligibility to those with any mental health problems.
For at least a decade, various service dog and veterans’ organizations have pushed to have the VA expand the service dog benefit. This new law is a “first step,” said Mr. Diamond. “We had to kick open the door,” he said, adding that “the VA has essentially said no for almost 15 years.”
Mr. Diamond noted that there is “overwhelming” evidence showing that service dogs improve quality of life and reduce distress for veterans with PTSD and other diagnoses.
‘No excuse’
Results from a VA study showed that suicidal ideation was reduced in veterans who were paired with service dogs, compared with veterans paired with emotional support dogs. The study, which was made public in March, found no reduction in overall disability, according to a report by Military.com.
K9s for Warriors cites numerous other studies, published in peer-reviewed journals, that have shown that service dogs reduce PTSD symptoms, especially hypervigilance.
“There really is no excuse not to have the VA engaged in helping veterans suffering from posttraumatic stress who are extremely high risk of suicide to get a lifesaving service dog,” Mr. Diamond said.
His organization has paired 700 veterans suffering from TBI, PTSD, or military sexual trauma with a service dog. The organization provides a 3-week training program for the veteran and his or her dog.
Although about 200 of the graduates have been eligible to receive coverage from the VA for veterinary care for the dogs, it requires a lot of paperwork, and the criteria for who can be certified to receive that benefit are somewhat vague, Mr. Diamond noted.
Under current policy, the dog and veteran must have successfully completed a training program offered by an organization accredited by Assistance Dogs International or the International Guide Dog Federation.
The new pilot program will enable eligible veterans to receive dog training instruction from accredited nonprofit service dog training organizations, and it will give them the opportunity to adopt a dog that they actively assisted in training.
A version of this article first appeared on Medscape.com.
Genetic link may tie cannabis use disorder to severe COVID-19
The same genetic variations may boost susceptibility to both severe COVID-19 and cannabis use disorder (CUD), a new study suggests. The research does not confirm a genetic link, but the lead author said the signs of an association are still “troubling.”
“Reducing cannabis use among heavy users may potentially provide protection against severe COVID-19 presentations,” Alexander S. Hatoum, PhD, a postdoctoral scholar at Washington University, St. Louis, said in an interview. “Outside of individual risk, these data also have important implications for policy regarding vaccination as well as treatment prioritization in an overly taxed medical system.”
The study was published in the journal Biological Psychiatry Global Open Science.
Dr. Hatoum and colleagues launched the study to gain insight into whether CUD might be a risk factor for severe COVID-19 presentations.
As defined by the DSM-5, people with CUD suffer from impairment or distress because of their cannabis use and meet at least 2 of 11 criteria over a 12-month period, such as cravings, cannabis tolerance, and withdrawal symptoms. According to a 2020 study that examined 2008-2016 data, 2.72% of children aged 12-17 showed signs of CUD, as did 1.23% of those aged over 26.
The primary reasons for hospitalization and death related to COVID-19 are respiratory symptoms. “And we have observed that genetic vulnerability to CUD is shared with respiratory disease, even after tobacco use is considered,” Dr. Hatoum said.
He and his colleagues examined data from genomewide association studies and searched for genetic correlations between CUD (14,080 cases, 343,726 controls) and COVID-19 hospitalization (9,373 cases, 1,197,256 controls). “Genetic vulnerability to COVID-19 was correlated with genetic liability to CUD (P = 1.33e–6),” the researchers wrote. “This association remained when accounting for genetic liability to related risk factors and covariates (P = .012-.049).”
According to Dr. Hatoum, the researchers found inconclusive evidence that CUD might worsen COVID-19 cases. “We applied statistical causal models, which found an effect consistent with causality, but it was nonsignificant,” he said.
Despite the absence of causality, the study findings could prove useful for clinicians and policy makers.
“Those struggling with CUD may be prioritized for vaccination and vaccination boosters to mitigate their higher likelihood of a severe COVID-19 presentation,” Dr. Hatoum said. “When testing positive for COVID-19, they may also be prioritized for earlier treatment.”
The study authors also added that the findings “urge caution” in regard to the wave of U.S. states legalizing cannabis. “Our data suggest that heavy cannabis use, but not lifetime cannabis use, represents a risk factor for severe COVID-19 presentations,” Dr. Hatoum said.
In an interview, Danielle Dick, PhD, who was not involved with the study, said it applies “cutting-edge methods to an important research question” and offers a “hint” of a genetic risk factor that makes some people more likely to be hospitalized for COVID-19. However, “the study does not tell us what those underlying genetically influenced processes might be,” added Dr. Dick, professor of psychology, and human and molecular genetics at Virginia Commonwealth University, Richmond. “And it’s an important caveat to point out that the results from this study are limited in that they are based on data from people from European descent – so they can’t necessarily be applied to address the harm experienced by so many people of color from the COVID pandemic. That’s an unfortunate limitation.”
As for the idea that the study findings should prompt caution about marijuana legalization, Dr. Dick said it’s true that increased acceptability of drug use “increases the likelihood that individuals who are genetically vulnerable will develop problems. There is robust evidence of this.”
However, Dr. Dick said, “the legalization of marijuana is a complex topic because the health consequences aren’t the only consideration when it comes to legalization. The other side of the coin is the huge harm that has been caused to communities of color through marijuana criminalization. Legalization will hopefully lead to decreased harm on that front. So it’s a double-edged sword.”
Dr. Hatoum, his colleagues, and Dr. Dick reported no relevant disclosures.
The same genetic variations may boost susceptibility to both severe COVID-19 and cannabis use disorder (CUD), a new study suggests. The research does not confirm a genetic link, but the lead author said the signs of an association are still “troubling.”
“Reducing cannabis use among heavy users may potentially provide protection against severe COVID-19 presentations,” Alexander S. Hatoum, PhD, a postdoctoral scholar at Washington University, St. Louis, said in an interview. “Outside of individual risk, these data also have important implications for policy regarding vaccination as well as treatment prioritization in an overly taxed medical system.”
The study was published in the journal Biological Psychiatry Global Open Science.
Dr. Hatoum and colleagues launched the study to gain insight into whether CUD might be a risk factor for severe COVID-19 presentations.
As defined by the DSM-5, people with CUD suffer from impairment or distress because of their cannabis use and meet at least 2 of 11 criteria over a 12-month period, such as cravings, cannabis tolerance, and withdrawal symptoms. According to a 2020 study that examined 2008-2016 data, 2.72% of children aged 12-17 showed signs of CUD, as did 1.23% of those aged over 26.
The primary reasons for hospitalization and death related to COVID-19 are respiratory symptoms. “And we have observed that genetic vulnerability to CUD is shared with respiratory disease, even after tobacco use is considered,” Dr. Hatoum said.
He and his colleagues examined data from genomewide association studies and searched for genetic correlations between CUD (14,080 cases, 343,726 controls) and COVID-19 hospitalization (9,373 cases, 1,197,256 controls). “Genetic vulnerability to COVID-19 was correlated with genetic liability to CUD (P = 1.33e–6),” the researchers wrote. “This association remained when accounting for genetic liability to related risk factors and covariates (P = .012-.049).”
According to Dr. Hatoum, the researchers found inconclusive evidence that CUD might worsen COVID-19 cases. “We applied statistical causal models, which found an effect consistent with causality, but it was nonsignificant,” he said.
Despite the absence of causality, the study findings could prove useful for clinicians and policy makers.
“Those struggling with CUD may be prioritized for vaccination and vaccination boosters to mitigate their higher likelihood of a severe COVID-19 presentation,” Dr. Hatoum said. “When testing positive for COVID-19, they may also be prioritized for earlier treatment.”
The study authors also added that the findings “urge caution” in regard to the wave of U.S. states legalizing cannabis. “Our data suggest that heavy cannabis use, but not lifetime cannabis use, represents a risk factor for severe COVID-19 presentations,” Dr. Hatoum said.
In an interview, Danielle Dick, PhD, who was not involved with the study, said it applies “cutting-edge methods to an important research question” and offers a “hint” of a genetic risk factor that makes some people more likely to be hospitalized for COVID-19. However, “the study does not tell us what those underlying genetically influenced processes might be,” added Dr. Dick, professor of psychology, and human and molecular genetics at Virginia Commonwealth University, Richmond. “And it’s an important caveat to point out that the results from this study are limited in that they are based on data from people from European descent – so they can’t necessarily be applied to address the harm experienced by so many people of color from the COVID pandemic. That’s an unfortunate limitation.”
As for the idea that the study findings should prompt caution about marijuana legalization, Dr. Dick said it’s true that increased acceptability of drug use “increases the likelihood that individuals who are genetically vulnerable will develop problems. There is robust evidence of this.”
However, Dr. Dick said, “the legalization of marijuana is a complex topic because the health consequences aren’t the only consideration when it comes to legalization. The other side of the coin is the huge harm that has been caused to communities of color through marijuana criminalization. Legalization will hopefully lead to decreased harm on that front. So it’s a double-edged sword.”
Dr. Hatoum, his colleagues, and Dr. Dick reported no relevant disclosures.
The same genetic variations may boost susceptibility to both severe COVID-19 and cannabis use disorder (CUD), a new study suggests. The research does not confirm a genetic link, but the lead author said the signs of an association are still “troubling.”
“Reducing cannabis use among heavy users may potentially provide protection against severe COVID-19 presentations,” Alexander S. Hatoum, PhD, a postdoctoral scholar at Washington University, St. Louis, said in an interview. “Outside of individual risk, these data also have important implications for policy regarding vaccination as well as treatment prioritization in an overly taxed medical system.”
The study was published in the journal Biological Psychiatry Global Open Science.
Dr. Hatoum and colleagues launched the study to gain insight into whether CUD might be a risk factor for severe COVID-19 presentations.
As defined by the DSM-5, people with CUD suffer from impairment or distress because of their cannabis use and meet at least 2 of 11 criteria over a 12-month period, such as cravings, cannabis tolerance, and withdrawal symptoms. According to a 2020 study that examined 2008-2016 data, 2.72% of children aged 12-17 showed signs of CUD, as did 1.23% of those aged over 26.
The primary reasons for hospitalization and death related to COVID-19 are respiratory symptoms. “And we have observed that genetic vulnerability to CUD is shared with respiratory disease, even after tobacco use is considered,” Dr. Hatoum said.
He and his colleagues examined data from genomewide association studies and searched for genetic correlations between CUD (14,080 cases, 343,726 controls) and COVID-19 hospitalization (9,373 cases, 1,197,256 controls). “Genetic vulnerability to COVID-19 was correlated with genetic liability to CUD (P = 1.33e–6),” the researchers wrote. “This association remained when accounting for genetic liability to related risk factors and covariates (P = .012-.049).”
According to Dr. Hatoum, the researchers found inconclusive evidence that CUD might worsen COVID-19 cases. “We applied statistical causal models, which found an effect consistent with causality, but it was nonsignificant,” he said.
Despite the absence of causality, the study findings could prove useful for clinicians and policy makers.
“Those struggling with CUD may be prioritized for vaccination and vaccination boosters to mitigate their higher likelihood of a severe COVID-19 presentation,” Dr. Hatoum said. “When testing positive for COVID-19, they may also be prioritized for earlier treatment.”
The study authors also added that the findings “urge caution” in regard to the wave of U.S. states legalizing cannabis. “Our data suggest that heavy cannabis use, but not lifetime cannabis use, represents a risk factor for severe COVID-19 presentations,” Dr. Hatoum said.
In an interview, Danielle Dick, PhD, who was not involved with the study, said it applies “cutting-edge methods to an important research question” and offers a “hint” of a genetic risk factor that makes some people more likely to be hospitalized for COVID-19. However, “the study does not tell us what those underlying genetically influenced processes might be,” added Dr. Dick, professor of psychology, and human and molecular genetics at Virginia Commonwealth University, Richmond. “And it’s an important caveat to point out that the results from this study are limited in that they are based on data from people from European descent – so they can’t necessarily be applied to address the harm experienced by so many people of color from the COVID pandemic. That’s an unfortunate limitation.”
As for the idea that the study findings should prompt caution about marijuana legalization, Dr. Dick said it’s true that increased acceptability of drug use “increases the likelihood that individuals who are genetically vulnerable will develop problems. There is robust evidence of this.”
However, Dr. Dick said, “the legalization of marijuana is a complex topic because the health consequences aren’t the only consideration when it comes to legalization. The other side of the coin is the huge harm that has been caused to communities of color through marijuana criminalization. Legalization will hopefully lead to decreased harm on that front. So it’s a double-edged sword.”
Dr. Hatoum, his colleagues, and Dr. Dick reported no relevant disclosures.
FROM BIOLOGICAL PSYCHIATRY GLOBAL OPEN SCIENCE
Neurodegenerative nature of schizophrenia makes case for LAIs
Schizophrenia is a complex disease caused by dysfunction in specific brain regions or circuits. In fact, schizophrenia is not a single disease but several hundred different diseases, according to Henry A. Nasrallah, MD, who spoke on the topic at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
The underlying causes of schizophrenia can be either genetic or environmental, but all involve changes in brain development in the fetus or newborn. Psychosis can occur in a range of disorders, including epilepsy, Parkinson’s disease, cerebral tumors, and narcolepsy, to name just a few. Although it starts out as a neurodevelopmental disorder, schizophrenia becomes neurodegenerative after onset, with each new psychotic episode leading to further damage, said Dr. Nasrallah, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati. Further damage leaves patients with greater and greater disability over time, said Dr. Nasrallah at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
The course of illness in some ways resembles the cascading disability associated with strokes. Schizophrenia relapses lead to subcortical atrophy, ventricular enlargement, and further loss of white matter. The accumulating damage is a result of microglia activation, which leads to neuroinflammation and oxidative stress. Mitochondria may also produce insufficient amounts of the antioxidant glutathione.
“The main reason for relapse in schizophrenia is poor adherence to antipsychotic medications, due to anosognosia, memory impairment, avolition, and substance use. It is absolutely necessary to realize that, while oral antipsychotics are effective in the hospital due to enforced compliance by the nursing staff, patients should be switched to long-acting injectable antipsychotics (LAIs) upon discharge from the first episode, which astonishingly is rarely done by 99% of clinicians,” said Dr. Nasrallah in an interview.
That frequent failure leads to further neurodegeneration and increasing disability, which in turn can lead to high rates of homelessness, suicide, and as well as incarceration, because many state hospitals that used to provide medical care for relapsing individuals have been closed down. All of these consequences place great financial and emotional burdens on families and loved ones.
Reconceptualizing the illness
Dr. Nasrallah also advocated that schizophrenia should be classified as a neurologic disorder instead of a psychiatric disorder. He said that the neuropsychiatric mechanisms behind these related diseases support that classification, and neurologic disorders receive much more insurance coverage.
The neuroinflammatory mechanisms underlying schizophrenia suggest that therapies such as omega-3 fatty acids could provide benefit during the prodromal stages of illness. Antioxidants like N-acetyl cysteine could potentially be useful during psychotic episodes, since it boosts levels of glutathione to reduce damaging free radicals. Other approaches could prevent microglia activation, which appears to initiate neurodegeneration.
Another consequence of psychosis is programmed cell death, or apoptosis, in response to reduced levels of neurotropic agents. That could potentially be countered using agents to prevent apoptosis.
Dr. Nasrallah believes clinicians should not use first-generation antipsychotics such as haloperidol, because research has shown that those drugs, while effective, also destroy neurons. Second-generation antipsychotics (SGAs) are safer and avoid that neurotoxicity, and they also have a neuroprotective effect. The SGAs may owe their improved efficacy and safety to the fact that they don’t bind as strongly to dopamine receptors, and they are stronger 5-hydroxytryptamine2A antagonists, according to Dr. Nasrallah. A meta-analysis of 18 studies showed that patients on SGAs maintained gray matter volume, and may even achieve increases in the hippocampus and the prefrontal cortex.
In the Q&A session after the presentation, Dr. Nasrallah was asked whether treatment should be kept up for the rest of the patient’s life, or whether medication should be tapered – and perhaps stopped. He likened treatment of schizophrenia to diabetes or high blood pressure.
“It’s an illness. A lot of medical disorders require lifetime treatment, and there is no difference between psychiatry and the rest of medicine,” he said. “You have to continue the medication at the dose that worked in the acute episode, hopefully the lowest possible dose.”
Dr. Nasrallah did concede that it can be challenging to get patients to accept permanent treatment, and he shared his own strategy to achieve that outcome. “I don’t tell the patient, ‘You’re going to take this the rest of your life.’ It depresses them. So I say, ‘Let’s keep this on board for a year, and I’ll see you regularly, and I’ll monitor you, and we’ll see how it goes, and then we will make another decision at the end of the year.’ ”
During that year, Dr. Nasrallah educates the patient and develops a rapport. “I will show them a lot of data and information about the illness and the hazards of stopping [treatment]. And by the end of the year, most of my patients say: ‘Yeah, I agree. Let’s continue the good thing and let’s not fix something that’s not broken.’ ”
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has also served on a speaker’s bureau for most of those companies, in addition to that of Noven.
Schizophrenia is a complex disease caused by dysfunction in specific brain regions or circuits. In fact, schizophrenia is not a single disease but several hundred different diseases, according to Henry A. Nasrallah, MD, who spoke on the topic at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
The underlying causes of schizophrenia can be either genetic or environmental, but all involve changes in brain development in the fetus or newborn. Psychosis can occur in a range of disorders, including epilepsy, Parkinson’s disease, cerebral tumors, and narcolepsy, to name just a few. Although it starts out as a neurodevelopmental disorder, schizophrenia becomes neurodegenerative after onset, with each new psychotic episode leading to further damage, said Dr. Nasrallah, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati. Further damage leaves patients with greater and greater disability over time, said Dr. Nasrallah at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
The course of illness in some ways resembles the cascading disability associated with strokes. Schizophrenia relapses lead to subcortical atrophy, ventricular enlargement, and further loss of white matter. The accumulating damage is a result of microglia activation, which leads to neuroinflammation and oxidative stress. Mitochondria may also produce insufficient amounts of the antioxidant glutathione.
“The main reason for relapse in schizophrenia is poor adherence to antipsychotic medications, due to anosognosia, memory impairment, avolition, and substance use. It is absolutely necessary to realize that, while oral antipsychotics are effective in the hospital due to enforced compliance by the nursing staff, patients should be switched to long-acting injectable antipsychotics (LAIs) upon discharge from the first episode, which astonishingly is rarely done by 99% of clinicians,” said Dr. Nasrallah in an interview.
That frequent failure leads to further neurodegeneration and increasing disability, which in turn can lead to high rates of homelessness, suicide, and as well as incarceration, because many state hospitals that used to provide medical care for relapsing individuals have been closed down. All of these consequences place great financial and emotional burdens on families and loved ones.
Reconceptualizing the illness
Dr. Nasrallah also advocated that schizophrenia should be classified as a neurologic disorder instead of a psychiatric disorder. He said that the neuropsychiatric mechanisms behind these related diseases support that classification, and neurologic disorders receive much more insurance coverage.
The neuroinflammatory mechanisms underlying schizophrenia suggest that therapies such as omega-3 fatty acids could provide benefit during the prodromal stages of illness. Antioxidants like N-acetyl cysteine could potentially be useful during psychotic episodes, since it boosts levels of glutathione to reduce damaging free radicals. Other approaches could prevent microglia activation, which appears to initiate neurodegeneration.
Another consequence of psychosis is programmed cell death, or apoptosis, in response to reduced levels of neurotropic agents. That could potentially be countered using agents to prevent apoptosis.
Dr. Nasrallah believes clinicians should not use first-generation antipsychotics such as haloperidol, because research has shown that those drugs, while effective, also destroy neurons. Second-generation antipsychotics (SGAs) are safer and avoid that neurotoxicity, and they also have a neuroprotective effect. The SGAs may owe their improved efficacy and safety to the fact that they don’t bind as strongly to dopamine receptors, and they are stronger 5-hydroxytryptamine2A antagonists, according to Dr. Nasrallah. A meta-analysis of 18 studies showed that patients on SGAs maintained gray matter volume, and may even achieve increases in the hippocampus and the prefrontal cortex.
In the Q&A session after the presentation, Dr. Nasrallah was asked whether treatment should be kept up for the rest of the patient’s life, or whether medication should be tapered – and perhaps stopped. He likened treatment of schizophrenia to diabetes or high blood pressure.
“It’s an illness. A lot of medical disorders require lifetime treatment, and there is no difference between psychiatry and the rest of medicine,” he said. “You have to continue the medication at the dose that worked in the acute episode, hopefully the lowest possible dose.”
Dr. Nasrallah did concede that it can be challenging to get patients to accept permanent treatment, and he shared his own strategy to achieve that outcome. “I don’t tell the patient, ‘You’re going to take this the rest of your life.’ It depresses them. So I say, ‘Let’s keep this on board for a year, and I’ll see you regularly, and I’ll monitor you, and we’ll see how it goes, and then we will make another decision at the end of the year.’ ”
During that year, Dr. Nasrallah educates the patient and develops a rapport. “I will show them a lot of data and information about the illness and the hazards of stopping [treatment]. And by the end of the year, most of my patients say: ‘Yeah, I agree. Let’s continue the good thing and let’s not fix something that’s not broken.’ ”
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has also served on a speaker’s bureau for most of those companies, in addition to that of Noven.
Schizophrenia is a complex disease caused by dysfunction in specific brain regions or circuits. In fact, schizophrenia is not a single disease but several hundred different diseases, according to Henry A. Nasrallah, MD, who spoke on the topic at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
The underlying causes of schizophrenia can be either genetic or environmental, but all involve changes in brain development in the fetus or newborn. Psychosis can occur in a range of disorders, including epilepsy, Parkinson’s disease, cerebral tumors, and narcolepsy, to name just a few. Although it starts out as a neurodevelopmental disorder, schizophrenia becomes neurodegenerative after onset, with each new psychotic episode leading to further damage, said Dr. Nasrallah, professor of psychiatry, neurology, and neuroscience at the University of Cincinnati. Further damage leaves patients with greater and greater disability over time, said Dr. Nasrallah at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
The course of illness in some ways resembles the cascading disability associated with strokes. Schizophrenia relapses lead to subcortical atrophy, ventricular enlargement, and further loss of white matter. The accumulating damage is a result of microglia activation, which leads to neuroinflammation and oxidative stress. Mitochondria may also produce insufficient amounts of the antioxidant glutathione.
“The main reason for relapse in schizophrenia is poor adherence to antipsychotic medications, due to anosognosia, memory impairment, avolition, and substance use. It is absolutely necessary to realize that, while oral antipsychotics are effective in the hospital due to enforced compliance by the nursing staff, patients should be switched to long-acting injectable antipsychotics (LAIs) upon discharge from the first episode, which astonishingly is rarely done by 99% of clinicians,” said Dr. Nasrallah in an interview.
That frequent failure leads to further neurodegeneration and increasing disability, which in turn can lead to high rates of homelessness, suicide, and as well as incarceration, because many state hospitals that used to provide medical care for relapsing individuals have been closed down. All of these consequences place great financial and emotional burdens on families and loved ones.
Reconceptualizing the illness
Dr. Nasrallah also advocated that schizophrenia should be classified as a neurologic disorder instead of a psychiatric disorder. He said that the neuropsychiatric mechanisms behind these related diseases support that classification, and neurologic disorders receive much more insurance coverage.
The neuroinflammatory mechanisms underlying schizophrenia suggest that therapies such as omega-3 fatty acids could provide benefit during the prodromal stages of illness. Antioxidants like N-acetyl cysteine could potentially be useful during psychotic episodes, since it boosts levels of glutathione to reduce damaging free radicals. Other approaches could prevent microglia activation, which appears to initiate neurodegeneration.
Another consequence of psychosis is programmed cell death, or apoptosis, in response to reduced levels of neurotropic agents. That could potentially be countered using agents to prevent apoptosis.
Dr. Nasrallah believes clinicians should not use first-generation antipsychotics such as haloperidol, because research has shown that those drugs, while effective, also destroy neurons. Second-generation antipsychotics (SGAs) are safer and avoid that neurotoxicity, and they also have a neuroprotective effect. The SGAs may owe their improved efficacy and safety to the fact that they don’t bind as strongly to dopamine receptors, and they are stronger 5-hydroxytryptamine2A antagonists, according to Dr. Nasrallah. A meta-analysis of 18 studies showed that patients on SGAs maintained gray matter volume, and may even achieve increases in the hippocampus and the prefrontal cortex.
In the Q&A session after the presentation, Dr. Nasrallah was asked whether treatment should be kept up for the rest of the patient’s life, or whether medication should be tapered – and perhaps stopped. He likened treatment of schizophrenia to diabetes or high blood pressure.
“It’s an illness. A lot of medical disorders require lifetime treatment, and there is no difference between psychiatry and the rest of medicine,” he said. “You have to continue the medication at the dose that worked in the acute episode, hopefully the lowest possible dose.”
Dr. Nasrallah did concede that it can be challenging to get patients to accept permanent treatment, and he shared his own strategy to achieve that outcome. “I don’t tell the patient, ‘You’re going to take this the rest of your life.’ It depresses them. So I say, ‘Let’s keep this on board for a year, and I’ll see you regularly, and I’ll monitor you, and we’ll see how it goes, and then we will make another decision at the end of the year.’ ”
During that year, Dr. Nasrallah educates the patient and develops a rapport. “I will show them a lot of data and information about the illness and the hazards of stopping [treatment]. And by the end of the year, most of my patients say: ‘Yeah, I agree. Let’s continue the good thing and let’s not fix something that’s not broken.’ ”
Dr. Nasrallah has consulted for Acadia, Alkermes, Allergan, Boehringer-Ingelheim, Indivior, Intra-Cellular, Janssen, Neurocrine, Otsuka, Sunovion, and Teva. He has also served on a speaker’s bureau for most of those companies, in addition to that of Noven.
REPORTING FROM FOCUS ON NEUROPSYCHIATRY 2021









